
Advertisement
Board Review Questions
Revised: 17 July 2018
Copyright: (c) 2003-2018, PathologyOutlines.com, Inc.
Note: since these questions are being incorporated into our new Board Review page, this page will soon disappear.
Recently Added Questions
- The image shown below is a Wright-Giemsa stained bone marrow aspirate smear from a child who presented with a 5 cm abdominal mass. Which of the following answer choices, if present, would result in an improved prognosis for the patient? The child is 6 months old.

- The child is less than age 1 year old
- The child is male
- Molecular diagnostic testing shows N-myc amplification
- FISH shows loss of chromosome 1p
- FISH shows loss of chromosome 11q
The bone marrow aspirate shows clusters of small, round, blue cells with smudged chromatin and nuclear molding; given the history of a child with an abdominal mass, this is consistent with metastatic neuroblastoma in the bone marrow. If the patient is less than 1 year old and has metastatic disease limited to skin, liver and bone marrow, the tumor would be staged as 4S, which has a good prognosis. In contrast, N-myc amplification and loss of chromosomes 1p and 11q are associated with a worse prognosis.
b. Incorrect. Gender does not significantly affect prognosis in neuroblastoma.
c. Incorrect. See answer explanation above.
d. Incorrect. See answer explanation above.
e. Incorrect. See answer explanation above.
Source: BoardVitals, 2/5/2014
Questions from January 31, 2014
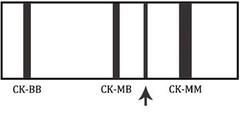
- This is an image of a creatinine kinase electrophoresis. Which of the following patients would likely have this electrophoretic pattern?
- A 55 year old male with acute onset chest pain
- A 32 year old healthy male who just finished a marathon
- A 45 year old female with widely metastatic breast cancer
- A 78 year old asymptomatic female
This is the CK electrophoretic pattern seen in macro-CK, a benign finding in healthy, elderly females. Macro-CK is a result of a CK-antibody conjugate and typically appears between CK-MM and CK-MB. Choices 'a' and 'b' would not have a macro-CK band. A 45 year old female (c) may have an additional band that migrates to the right of CK-MM. This band is mitochondrial CK and is seen in patients with widely metastatic disease.
Source: BoardVitals, 1/31/2014
- Which of the following is an advantage of the capillary electrophoresis (CE) analytical method?
- The ability of the method to detect non-volatile compounds
- The ability of the method to use hydrostatic pressure, rather than voltage, to promote separation
- The ability of the machine to perform separations based on differing physicochemical principles without having to make changes to the instrument's hardware
- a and c
- None of the above
a. Incorrect. Liquid chromatography-mass spectroscopy is the method of choice for detecting non-volatile compounds.
b. Incorrect. CE uses voltage to drive separation. High-performance liquid chromatography is a method that uses hydrostatic pressure.
c. Correct. The ability of the machine to perform separations based on differing physicochemical principles without having to make changes to the instrument's hardware is the primary advantage of this method.
d. Incorrect.
e. Incorrect.
Citation: Henry's Clinical Diagnosis and Management by Laboratory Methods (Chapter 23)
Source: BoardVitals, 1/31/2014
- In what disease will HbA1C levels be reliable?
- Hereditary spherocytosis
- G6PD deficiency
- Sickle cell anemia
- Iron-deficiency anemia
Any condition which shortens red blood cell survival or requires frequent blood transfusions will lower the accuracy and reliability of hemoglobin-A1C.
a. Incorrect. RBCs in HS are prone to intravascular hemolysis due to their fragility.
b. Incorrect. G6PD deficiency results in increased RBC death to oxidative stress after exposure to many compounds (including fava beans, sulfa drugs, aspirin, nitrofurantoin, isoniazid and others).
c. Incorrect. Sickle cells are prone to hemolysis. Additionally, many sickle cell patients require blood transfusions.
d. Correct. Iron deficiency anemia is a defect in red blood cell production with no significant changes in the lifespan of the RBC. HbA1C testing remains accurate in this setting.
e. Incorrect. Though beta-thalassemia minor can be subclinical and often untreated, this hemoglobinopathy does result in decreased RBC survival.
Citation: Henry's Clinical Diagnosis and Management by Laboratory Methods (Chapter 16)
Source: BoardVitals, 1/31/2014
- A laboratory notices that it is consistently reporting physiologically impossible potassium concentrations on all patient samples one morning including controls. Which of the following is the most likely cause?
- Defects in the perm-selective membrane
- Buildup of counter voltages from liquid junction potentials present at the salt bridge
- Protein buildup on the electrodes
- Improper sample storage
- Sample hemolysis
a. Correct. Defects in the perm-selective membrane allow other ions to arrive at the measuring electrode, falsely elevating the results. It is the most common malfunction of an ion-selective electrode.
b. Incorrect. This is the second most common cause, and it occurs over time to all electrodes, falsely lowering the results and necessitating timely replacement.
c. Incorrect. This is the third most common, and results in unpredictable changes. It can be avoided by proper electrode washing.
d. Incorrect. Hyperkalemia can be caused by allowing a sample to warm to ambient temperature. However, it would likely not affect controls, nor should it affect all patient samples consistently.
e. Incorrect. A hemolyzed sample will cause spurious hyperkalemia, but this will affect individual samples, not a generalized ion-selective electrode malfunction.
Citation: Henry's Clinical Diagnosis and Management by Laboratory Methods (Chapter 27)
Source: BoardVitals, 1/31/2014
- After being involved as the unrestrained passenger in a motor vehicle crash, a patient has persistent rhinorrhea. Which of the following is most helpful in identifying this fluid as CSF?
- Protein level
- Glucose level
- Transferrin immunofixation
- Fluid cytology
- Corticotropin level
a. Incorrect. Protein levels, even calibrated with other body fluids, are nonspecific.
b. Incorrect. Glucose levels, even calibrated with other body fluids, are nonspecific.
c. Correct. Two transferrin isoforms are present in CSF. B1 Transferrin is present in all body fluids. B2 Transferrin is found only in the CNS (and is converted from B1 by neuraminidase). Protein electrophoresis with transferrin immunofixation can distinguish the two isoforms, with the presence of the B2 confirming the fluid as CSF.
d. Incorrect. Cytology is often used to diagnose malignancy but is not helpful in determining the origin of the unknown fluid.
e. Incorrect. Pituitary hormones (ACTH, GH, FSH, LH, TSH) may be lower in the CSF of patients with pituitary dysfunction or malignancy, but their level is not used diagnostically to identify CSF.
Citation: Henry's Clinical Diagnosis and Management by Laboratory Methods (Chapter 29)
Source: BoardVitals, 1/31/2014
Questions from December 7, 2013
- A 58 year old man with hypertension, asthma and a long history of "acid reflux" presents at the request of multiple family members with a complaint of "skin turning yellow," and weight loss. The patient has a long history of noncompliance, but his family became alarmed when they noticed his appearance at a recent family gathering. Imaging reveals a 1.5 cm mass obstructing the ampulla of Vater. Subsequent studies reveal elevated gastrin excretion. A mutation in which of the following genes is most likely responsible for this patient's symptoms?
- RET
- APC
- MENIN
- MLH1
- MSH2
a. Incorrect. The RET proto-oncogene mutations are responsible for Multiple Endocrine Neoplasia (MEN) Type 2. Neither MEN2A nor MEN2B include gastrinoma.
b. Incorrect. The autosomal dominant APC gene mutation is responsible for Familial Adenomatous Polyposis (FAP). This condition causes multiple adenomatous polyps in the colon of affected individuals.
c. Correct. This patient presents with symptoms of obstruction related to a duodenal carcinoid tumor. Additionally, his history of acid reflux indicates oversecretion of gastrin, likely due to a gastrinoma. Gastrinomas are often found as part of Multiple Endocrine Neoplasia Type 1, and are caused by a mutation in the MENIN gene. The syndrome is comprised of pituitary, parathyroid and pancreatic islet cell tumors.
d. Incorrect. MLH1 is one of the mismatch-repair gene mutations that have been implicated in the development of Hereditary Non-Polyposis Colon Cancer (Lynch) Syndrome. This patient's presentation is not consistent with colon cancer.
e. Incorrect. MSH2 is one of the mismatch-repair gene mutations that have been implicated in the development of Hereditary Non-Polyposis Colon Cancer (Lynch) Syndrome. This patient's presentation is not consistent with colon cancer.
Citation: "Intestinal Neoplasms." Sternberg's Diagnostic Surgical Pathology. 4th ed. 2004. Print.
Source: BoardVitals, 12/7/2013
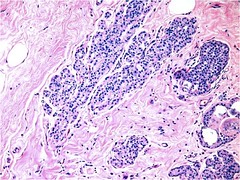
- A 65 year old woman with a history of hypertension, diabetes and rheumatoid arthritis presents with three months of constipation and rectal bleeding. She initially attributed the bleeding to hemorrhoids, but the symptoms continued to worsen. She has never had a colonoscopy, but states that her mother died of "bad colon cancer." Vital signs are stable, and physical examination is notable only for a palpable rectal mass. Laboratory examination reveals anemia. The patient undergoes colonoscopic biopsy of the lesion. Which of the following histopathologic findings is consistent with the diagnosis seen below?

- Invasive neoplasm with squamous pearl formation, foci of keratinization and areas of granular necrosis
- Invasive glandular and tubular structures lined by uniform mucus-producing columnar epithelium
- Invasive lesion composed of nested, pigmented epithelioid cells exhibiting positivity for S100, HMB45 and Melan A
- Dilated, thick-walled submucosal vessels and sinusoidal spaces with adjacent hemorrhage
- Spindle-shaped cells with large and hyperchromatic nuclei, eosinophilic cytoplasm and positivity for S100, vimentin and cytokeratin and negativity for CEA
a. Incorrect. This is the microscopic appearance of squamous cell carcinoma of the anus. Squamous cell carcinoma is prognosticated based upon depth of invasion, state of regional lymph nodes and presence of distant metastases. Condyloma, squamous cell dysplasias and carcinoma in situ have been identified adjacent to identified cancers, and may be precursor lesions. Other risk factors for the development of anal cancers include increased age, receptive anal intercourse, smoking, history of sexually transmitted diseases, immunosuppression and presence of concurrent lower genital tract neoplasia.
b. Incorrect. This is the microscopic appearance of mucinous adenocarcinoma of the rectum. These lesions may occur either as primary carcinoma of the anal canal or as a result of downward extension of a more proximal colonic tumor. Risk factors for the development of these lesions include the presence of perianal disease, including fistulae, abscesses and previous surgeries. Prognosis after definitive resection is favorable.
c. Incorrect. This is the microscopic appearance of malignant melanoma of the anus. Malignant melanoma of the anus is a rare condition that presents in a clinical fashion similar to that of other rectal mass lesions; however, they are usually advanced lesions at the time of diagnosis. Prognosis is poor.
d. Incorrect. This is the microscopic appearance of an anal hemorrhoid, a benign deterioration of the connective tissue and smooth muscle anchoring the anal and submucosal sinusoids.
e. Correct. This is the microscopic appearance of sarcomatoid carcinoma of the anus, a rare neoplasm consisting of proliferations of both epithelial and mesenchymal elements. The clinical presentation and treatment of this condition is identical to that of other rectal cancers.
Citation: "Anus and Perianal Area." Sternberg's Diagnostic Surgical Pathology. 4th ed. 2004. Print.
Source: BoardVitals, 12/7/2013
- Which of the following describes all of the tests that must be performed when an obstetric panel is ordered?
- CBC, CMP, qualitative syphilis test, ABO blood typing, Rh blood typing, Hep B surface antigen, rubella antibody
- CBC, Hep B surface antigen, rubella antibody, qualitative Syphilis test, RBC antibody screen, ABO blood typing, Rh blood typing
- CBC, BMP, TSH, Hep B surface antigen, qualitative Syphilis test, RBC antibody screen, ABO blood typing, Rh blood typing
- CBC, Hep B surface antigen, rubella antibody, qualitative Syphilis test, HIV test, RBC antibody screen, ABO blood typing, Rh blood typing
- CBC, BMP, TSH, Hep B surface antigen, HIV test, RBC antibody screen, ABO blood typing, Rh blood typing
All of these tests are included in the obstetric panel. Tests such as CMP, BMP, HIV test and TSH are all not part of this panel (under CPT code 80055 as of 2009).
Citation: Henry's Clinical Diagnosis and Management by Laboratory Methods
Source: BoardVitals, 12/7/2013
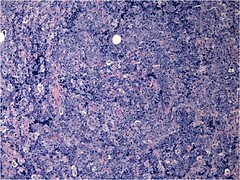
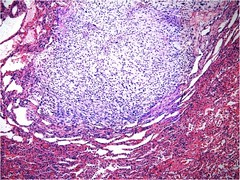
- 61 year old male with history of hypertension presents with abdominal pain, hip pain and hematuria. Upon further questioning, he also notes that he has experienced a 20-lb weight loss and night sweats during the past 3 months. Imaging of the hip reveals several lesions and laboratory studies reveal anemia, increased erythrocyte sedimentation rate, elevated BUN and creatinine, and hypercalcemia. The patient undergoes biopsy of the bone, which is seen in the image below. A mutation in which of the following is most likely to be identified in this specimen?


- Von Hippel-Lindau gene
- TFE3 gene
- Chromosome 1
- Chromosome 7
- Chromosome Y
a. Correct. This patient presents with classic signs, symptoms, clinical and pathologic signs of clear cell renal carcinoma. This neoplasm is the most common of all renal cancers. It is characterized by loss of genetic material of the short arm of chromosome 3, and by mutations in the von-Hippel Lindau gene, even in sporadic, unilateral and unifocal tumors.
b. Incorrect. Papillary renal cell carcinoma is a rare renal cell carcinoma, which is histologically composed of discrete papillary fronds lined by neoplastic epithelial cells and a central fibrovascular core. These neoplasms are associated with trisomies of chromosomes 7, 17 and loss of chromosome Y. The translocation t (x; 1)(p11:q21) has also been observed, and results in the fusion of the TFE3 gene on chromosome X to the PRCC gene on chromosome 1.
c. Incorrect. Chromophobe renal cell carcinoma is clinically very similar to clear cell renal carcinoma, however they grossly exhibit a homogenous beige or pink cut surface with a central scar. Histologically, they are nonencapsulated and demonstrate a solid growth pattern and perinuclear cytoplasmic clearing. They are associated with loss of chromosomes 1 and Y, as well as mutations in chromosomes 1, 6, 10, 13, 17 and 21.
d. Incorrect. Trisomy of chromosome 7 is associated with papillary renal cell carcinoma.
e. Incorrect. Loss of chromosome Y is associated both with papillary renal cell carcinoma and chromophobe renal cell carcinoma.
Citation: "Adult Renal Tumors." Sternberg's Diagnostic Surgical Pathology. 4th ed. 2004. Print.
Source: BoardVitals, 12/7/2013
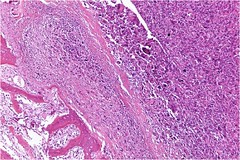
- A 25 year old male with no significant past medical history presents with six months of progressive headache, dizziness, nausea, vomiting and trouble seeing. He has been taking acetaminophen and non-steroidal anti-inflammatory agents without relief. Physical exam is notable for papilledema, positive Rhomberg sign and ataxic gait. Laboratory studies are unremarkable. Imaging studies demonstrate a poorly defined, homogeneous, low-density mass without contrast enhancement within the cerebellum. Patient undergoes neurosurgical resection of the mass, seen below. Which of the following histologic findings, if present, would suggest a pilocytic astrocytoma?


- Bipolar neoplastic cells with elongated, hairlike processes projecting from either end and other neoplastic cells with multiple processes
- Mixture of cellular processes and nuclei of greater angularity and density than those of the surrounding CNS parenchyma
- Presence of plump cells containing hyaline pink cytoplasm and lacking Nissl substance
- Increased cell density with pleomorphism of nuclei in glial fibrillary acidic protein-positivity and increased mitotic figures
- Huge cells with large, round nuclei and abundant finely granular cytoplasm mingling with bright pink cellular processes
a. Correct. This patient presents with signs and symptoms of a mass lesion located within the central nervous system. Imaging studies are characteristic of astrocytoma, a central nervous system neoplasm derived from immortalized astrocytes. These lesions occur most frequently in the second decade of life. There are several types of astrocytomas, which are differentiated based both on grading and structural differences. Pilocytic astrocytomas carry the most favorable prognosis of all subtypes of astrocytoma, especially when located in easily resectable regions, such as the cerebellum.
b. Incorrect. These are the typical histopathologic findings in diffuse fibrillar astrocytoma. These tumors closely mimic oligodendrogliomas. Their diffuse nature of growth and infiltration explain their low cure rate.
c. Incorrect. This is the characteristic appearance of gemistocytic cells, observed in gemistocytic astrocytoma. Gemistocytic cells must be differentiated from reactive astrocytes. These tumors are highly aggressive and carry a poor prognosis.
d. Incorrect. This is the histologic appearance of anaplastic astrocytoma. These tumors need to be differentiated from oligodendrogliomas and ependymomas. Forty percent of anaplastic astrocytomas demonstrate loss of DNA from the long arm of chromosome 19. These are high-grade lesions that carry the poorest prognosis of all astrocytomas.
e. Incorrect. This is the histologic appearance of subependymal giant cell astrocytoma, which is associated with tuberous sclerosis complex and mutations in the TSC1 gene.
Citation: "Astrocytomas." Sternberg's Diagnostic Surgical Pathology. 4th ed. 2004. Print.
Source: BoardVitals, 12/7/2013
Questions from November 12, 2013
- All of the following can affect response to antibiotic treatment EXCEPT:
- Route of antibiotic administration
- Renal function of the patient
- Pharmacokinetics of the antibiotic
- Anatomic site of bacterial infection
- All of the above can affect response to antibiotic treatment
a. Incorrect. The route of antibiotic administration can affect response to antibiotic treatment. However, the other responses are also correct.
b. Incorrect. The renal function of the patient can affect response to antibiotic treatment. However, the other responses are also correct.
c. Incorrect. The pharmacokinetics of the antibiotic can affect response to treatment. However, the other responses are also correct.
d. Incorrect. The anatomic site of bacterial infection can affect response to antiobiotic treatment. However, the other responses are also correct.
e. Correct. All of the above can affect response to antibiotic treatment.
Citation: Henry's Clinical Diagnosis and Management by Laboratory Methods
Source: BoardVitals, 11/12/2013
- How can you differentiate between acute lymphoblastic leukemia and lymphocytic leukemoid reactions with immature lymphocytes (such as infectious mononucleosis)?
- Cytochemical stains to differentiate malignant cells, from reactive lymphocytes
- It depends on the lymphocyte count. If it is more than 100 x 109/L, it is an acute lymphoblastic leukemia
- Flow cytometric studies of the peripheral blood will reveal a non-clonal lymphocytosis in the case of a lymphocytic leukemoid reaction
- Repeat the full blood count in 7 days, if the lymphocyte count decrease, it is a leukamoid reaction
- Do a C-reactive protein. If it is raised, it indicates a reactive lymphocytosis
a. Incorrect. Cytochemical stains are not helpful to differentiate reactive lymphocytosis from malignant cells.
b. Incorrect. The absolute lymphocyte count does not indicate whether the lymphocytes is malignant or not. Both infective mononucleosis and ALL may have very high counts.
c. Correct. Immunophenotyping will show normal distribution of lymphocyte surface markers with no clonal populations.
d. Incorrect. If an ALL is suspected, treatment should be started as soon as possible and a delay in testing is not advised.
e. Incorrect. A CRP may be raised in both conditions, and wont give a definitive diagnosis.
Citation: Henry's Clinical Diagnosis and Management by Laboratory Methods
Source: BoardVitals, 11/12/2013
- There is an error rate of 1 in 100 base pairs for in vitro solid base oligonucleotide synthesis. In vivo, human DNA repair mechanisms reduce the rate of base pair mismatches to which of the following?
- 1 in 1,000
- 1 in 10,000
- 1in 100,000
- 1 in 1 million
- 1 in 10 million
a. Incorrect.
b. Incorrect.
c. Incorrect.
d. Incorrect.
e. Correct.
Citation: Henry's Clinical Diagnosis and Management by Laboratory Methods
Source: BoardVitals, 11/12/2013
- Which of the following accurately describes collecting duct carcinoma?
- It is the least common of the renal cell carcinomas
- It arises from the intercalated cells of the collecting ducts
- Histologically, there are nests of malignant cells entangled in a prominent fibrotic stroma
- Sarcomatoid changes portend a good prognosis
- A, B, C
- A and C
- None of the above
Both statements A and C accurately describe collecting duct carcinoma. It accounts for less than 1% of renal cell carcinomas. The histology has irregular channels and nests with a prominent fibrotic stroma.
b. Incorrect. This statement is not true. Chromophobe renal carcinoma is believed to grow from the intercalated cells of collecting ducts. Collecting duct carcinoma is believed to arise from the collecting duct cells of the medulla.
c. Incorrect. Sarcomatoid changes may be seen in all types of renal cell carcinoma and they indicate a poor prognosis.
Citation: Robbins & Cotran Pathologic Basis of Disease
Source: BoardVitals, 11/12/2013
- A 67 year old male with a history of asthma presents to his primary care physician with dyspnea. A chest X-ray is performed which shows an ill-defined mass in the lower lobe of the left lung. Fine needle aspiration of the mass is performed, and H&E-stained and Gomori methenamine silver-stained images of the cell block preparation are shown. Gram and acid-fast stains were negative. The organism seen in the images is most likely to be:


- Pneumocystis jiroveci
- Aspergillus fumigatus
- Histoplasma capsulatum
- Coccidioides immitis
- Blastomyces dermatitidis
The H&E and silver stains show fungal yeast forms with diameter 20-30 microns (compare to the surrounding erythrocytes with diameter 6-7 microns) and broad-based budding. These findings are typical of blastomycosis.
a. Incorrect. Pneumocystis organisms are seen on cytologic preparations as cup-shaped cysts with diameter similar to that of a red cell.
b. Incorrect. Aspergillus organisms are filamentous and show narrow-angle branching.
c. Incorrect. This is the chief differential diagnostic consideration in this case. However, histoplasma organisms are smaller (8-15 microns vs. 20-30) and show narrow-based, not broad-based, budding.
d. Incorrect. The large spherules (structures 60 or more microns in diameter, containing numerous fungal spores) characteristic of coccidiomycosis are not present here.
Source: BoardVitals, 11/12/2013
- A 70 year old female has had gradually worsening anemia for the past five years. Recently, she has developed thrombocytopenia as well and complains of abdominal discomfort. Physical examination reveals a spleen palpable 6 cm below the costal margin. A bone marrow biopsy is performed; the image shows an H&E stained section of the core biopsy (the aspirate was a "dry tap" and was non-contributory). Which of the following ancillary studies would be most useful in confirming the diagnosis?

- PCR for JAK2 V617F mutation
- PCR for C-KIT D816V mutation
- PCR for BRAF V600E mutation
- FISH for t(9;22)
- FISH for del(5q)
The core biopsy shows architectural distortion and numerous megakaryocyte clusters with atypical, hyperlobulated nuclei. In the context of the clinical history of progressive pancytopenia and splenomegaly, these findings are consistent with primary myelofibrosis (PMF). Although not as common as in polycythemia vera, the JAK2 V617F mutation will be present in approximately 50% of cases and supports the diagnosis.
b. Incorrect. This mutation is seen in systemic mastocytosis.
c. Incorrect. This mutation is seen in hairy cell leukemia.
d. Incorrect. This translocation is seen in CML and in a subset of ALL.
e. Incorrect. This deletion is seen in a subset of MDS characterized by small, hypolobated megakaryocytes and therapeutic response to lenalidomide.
Source: BoardVitals, 11/12/2013
- A 23 year old Latino male presents in severe pain. He reports that he has "sickle cell anemia" and has been transfusion dependent since birth. CBC is remarkable for a hemoglobin of 7.8, hematocrit of 24, normal MCV and a markedly elevated RDW. Iron studies are entirely within normal limits. The patients Wright-Giemsa stained peripheral blood smear is shown. A Sickledex (sickle solubility) test is positive. Hemoglobin electrophoresis shows two bands of approximately equal intensity, one co-migrating with hemoglobin S and one co-migrating with hemoglobin A2. What is the diagnosis?

- Sickle cell disease (hemoglobin SS)
- Compound heterozygosity for hemoglobin S and alpha thalassemia
- Compound heterozygosity for hemoglobin S and beta thalassemia
- Hemoglobin E trait
- Compound heterozygosity for hemoglobin S and hemoglobin C
The blood smear shows marked anisocytosis and poikilocytosis with numerous target cells. In the context of a normal MCV, these findings are suggestive of the presence of hemoglobin C (particularly the presence of numerous target cells). Hemoglobin C co-migrates with hemoglobin A2 on cellulose acetate electrophoresis at alkaline pH, as does hemoglobin E. Since the patient is symptomatic and has a positive Sickledex test, hemoglobin SC is the correct diagnosis.
a. Incorrect. This would be expected to show mostly hemoglobin S on electrophoresis, with an elevated HbF and some HbA resulting from transfusion.
b. Incorrect. This would show microcytosis with variable HbA and HbS (depending on the extent of thalassemia), and normal to reduced HbA2.
c. Incorrect. This would show microcytosis with variable HbA and HbS (depending on the extent of thalassemia), and increased HbA2.
d. Incorrect. This could give the electrophoresis results described in the question. However, because HbE is unstable, it is associated with a thalassemic presentation, not sickle cell disease.
Source: BoardVitals, 11/12/2013
- A 75 year old male presents to his primary care physician complaining of progressive fatigue and reduced exercise tolerance over the past 6 months. He is otherwise healthy and is on no medications. On examination, he is tachycardic and appears pale. Laboratory workup reveals the following:
Hemoglobin 9.5
Hematocrit 29
MCV 80
Reticulocytes 6%
Leukocyte and platelet counts are within normal limits. Coombs test is positive, at 37C, against all cells in the screen. All of the following are true EXCEPT:
- The patient has warm autoimmune hemolytic anemia (AIHA)
- The patient should be worked up for an underlying lymphoma
- The patients autoantibody is most likely IgM
- The patients autoantibody most likely reacts with Rh antigens
- The patients relatively indolent presentation increases the likelihood of an underlying malignancy
This is a classic presentation of warm autoimmune hemolytic anemia (WAIHA), which is caused by IgG (not IgM) autoantibodies, the majority of which are reactive to Rh antigens. Approximately 70% of cases are secondary, and any WAIHA should raise suspicion of an underlying malignancy (often hematolymphoid).
a. Incorrect (true statement). See explanation above.
b. Incorrect (true statement). See explanation above.
d. Incorrect (true statement). See explanation above.
e. Incorrect (true statement). Patients who present with acute, severe symptomatic anemia are less likely to have an underlying malignancy.
Source: BoardVitals, 11/12/2013
- In 2010, the American Diabetes Association recommended the HbA1c test for the diagnosis of diabetes. Which concentration of HbA1c is diagnostic of diabetes when the testing is performed by a clinical laboratory method (certified by the National Glycohemoglobin Standardization Program)?
- HbA1c of > 3.5%
- HbA1c of > 4.5%
- HbA1c of > 5.5%
- HbA1c of > 6.5%
- HbA1c of > 7.5%
Currently, the HbA1c assay methods are not standardized. Global standardization of HbA1c assay methods is a high priority for several organizations including the American Association of Clinical Chemistry - National Glycohemoglobin Standardization Program and the Working Group of the HbA1c Assay (American Diabetes, European Association for the Study of Diabetes and the International Diabetes Federation).
Source: BoardVitals, 11/12/2013
- A 38 year old female presents with a small, painless soft tissue mass just lateral of the tibial tuberosity. The mass is completely excised and a representative photomicrograph is shown below. What is the diagnosis?

- Low-grade fibromyxoid sarcoma
- Angiomyofibroblastoma
- Juxta-articular myxoma
- Myxoid liposarcoma
J-AM typically presents as a well-circumscribed mass adjacent to large joints; the knee being the most common. This benign mass is cured by complete excision. This example is hypovascular and hypocellular with prominent myxoid change. The cells are spindled and small without nucleoli. An Alcian-blue stain if performed, would highlight the background myxoid material.
J-AM superficially resemble low-grade fibromyxoid sarcoma (a). Low-grade fibromyxoid sarcomas typically present as a deep, slow-growing mass in the limbs and trunk. The histopathology of low-grade fibromyxoid sarcoma shows alternating cellular collagenous and myxoid areas. The curvilinear vasculature pattern is characteristic. In addition, this sarcoma shows a reciprocal t(7;16) FUS-CREB3L2.
Angiomyofibroblastoma (b) is a benign mass that presents in the region of the vulva or scrotum characterized by a proliferation of small-medium sized vessels, surrounded by myofibroblasts, in a background of loose stroma.
Myxoid liposarcoma (d) is a malignant tumor that typically occurs in the limbs. Microscopic sections show a hypocellular, eosinophilic myxoid background with intermixed small, bland-appearing, spindled cells, fat vacuoles and "chicken wire" vasculature. Myxoid liposarcoma carries a t(12;16).
Source: BoardVitals, 11/12/2013
Questions from September 4, 2013
- A large 12 x 8 x 6 cm mass in the body of the pancreas was incidentally discovered in a 27 year old female. A representative photomicrograph is shown below. The tumor is strongly positive for the progesterone receptor. What is the diagnosis?

- Pancreatoblastoma
- Serous cystadenoma
- Solid-pseudopapillay neoplasm
- Intraductal papillary mucinous neoplasm
This is an example of solid pseudopapillary (SPP) tumor, which is a low-grade malignancy. 90% of SPP tumors occur in females with an average age of 28 years. Tumor size at presentation can be quite large. Grossly, SPP tumors are variably solid and cystic, with associated hemorrhage and necrosis. Microscopic evaluation demonstrates sheets of uniform tumor cells which can become discohesive in necrotic areas, resulting in a pseudo-papillary appearance. Cholesterol clefts with surrounding foreign body giant cells are commonly encountered. PAS positive, diastase resistant hyaline globules can be seen by H&E as both intra- and extracellular eosinophilic globules. SPP neoplasms are frequently positive for cyclin D1, beta-catenin, vimentin, CD10, NSE, galectin 3, alpha-1-antitrypsin, alpha-chymotrypsin, progesterone receptor and occasionally synaptophysin. Chromogranin is negative in these tumors. Tumor positivity for CD10 and beta-catenin effectively rule out a pancreatic endocrine neoplasm. Patients with SPP neoplasms have an excellent prognosis if completely excised, which is the case approximately 90% of the time.
Pancreatoblastoma is usually seen in the pediatric population, but has been reported in adults as well. Histologically, it is a cellular tumor comprised of sheets / nests of acini and squamoid corpuscles. Cystic areas with pseudopapillae argue against this diagnosis.
Serous cystadenoma is a tumor seen predominantly in females with the gross appearance of a sponge. Microscopically, small cystic spaces are seen with a PAS positive (due to glycogen), plump, cuboidal lining.
Intraductal papillary mucinous neoplasm (IPMN) is most commonly seen in elderly men in the head of the pancreas. It is important to grossly determine if it involves either the main pancreatic duct or one of the branches of the pancreatic duct, as a higher rate of high grade invasive carcinoma is associated with main duct compared to branch duct involvement. Microscopically, complex papillary fronds comprised of mucinous epithelium are seen, without the presence of ovarian-type stroma (differentiating it from mucinous cystic neoplasm). It is associated with Peutz-Jegher syndrome.
Source: BoardVitals, 9/4/2013
- In the case of QC failure, what step would be taken after checking instruments and reagents with repeat controls (assuming QC fails again)?
- Assay new control
- Evaluate if near limits and for trends
- Further technical investigation is warranted
- Recalibrate or verify calibration
- Send patient samples to a new lab for testing
The correct sequence is assay new control; check instruments and reagents and repeat controls; recalibrate or verify calibration and repeat controls; further technical investigation. This is assuming the instrument fails QC at every step.
Citation: Henry's Clinical Diagnosis and Management by Laboratory Methods
Source: BoardVitals, 9/4/2013
- A 24 year old female presents to her dermatologist complaining of a painful lesion on her left-lateral ring finger. The pain is exacerbated when her hands are cold. The lesion is 1.3 cm and has a slight bluish hue. During the excision there was a moderate amount of bleeding. A representative low and high power photomicrograph are shown below. What is the diagnosis?

- Aggressive digital papillary adenoma
- Epithelioid sarcoma
- Glomangioma
- Cylindroma
This is a glomangioma, which is similar to a glomus tumor except it typically is less painful, and histologically demonstrates increased vascular spaces and fewer glomus cells. Glomangiomas / glomus tumors are painful red to purple nodules or macules (when subungual). Microscopically, sheets of glomus cells are seen surrounding vascular structures. Glomus cells are monomorphic with eosinophillic cytoplasm as can be seen above. The stroma surrounding the tumor is fibrous with pale staining nuclei. Glomus cells are positive for SMA and negative for CD31.
Aggressive digital papillary adenoma, also called digital papillary eccrine adenoma, generally occurs on the digits, and has a distinct appearance of ductal and tubuloalveolar stuctures with papillary projections (these tumors cannot be reliably differentiated histologically from aggressive digital papillary adenocarcinoma). Epithelioid sarcoma occurs most commonly on the distal extremities, but is usually painless. Microscopically, geographic central necrosis is typically seen with surrounding tumor cells with frequent mitoses Cylindromas are solitary nodules of the head and neck that microscopically are characterized by irregular basaloid nests that fit together in a "jigsaw" fashion.
Source: BoardVitals, 9/4/2013
- A 65 year old male patient with type II Diabetes Mellitus and COPD is brought to care by his wife, who has noted intermittent trouble speaking and personality changes. The patient is otherwise well, and does not recognize when these episodes occur. There is no personal or family history of stroke. Physical examination reveals papilledema and normal mental status examination. Imaging studies reveal a lack of cerebral infarction, but demonstrate a low-density mass with calcifications within the left frontal lobe. Further work up reveals lack of additional lesions. The patient undergoes neurosurgical resection, seen below. Histologically, in areas, there is a prominent thin walled vascular component between the cells with a "fried egg" appearance. Which of the following histopathologic staining patterns is expected in this diagnosis?


- Vimentin, EMA, reticulin positivity
- Leu 7, S100 positivity
- GFAP positivity
- Cytokeratin, EMA positivity
- Melanin, HMB45 antigen positivity
a. Incorrect. This is the histologic staining pattern observed in meningiomas. Meningiomas are primary central nervous system neoplasms composed of whorls, psammoma bodies, interdigitating cell processes and desmosomes. These lesions are generally attached to the dura.
b. Correct. This patient presents with clinical signs, symptoms and imaging findings suspicious for oligodendroglioma. These neoplasms often involve a 1p/19q codeletion, and histologically possess round cells and nuclei with prominent perinuclear halos and nests of cells between delicate vessels.
c. Incorrect. This is the histologic staining pattern observed in ependymomas and astrocytomas. These lesions are glial neoplasms composed of masses of fibrillar cells. Additionally, subtypes of each of these neoplasms possess their own characteristic immunohistochemical staining patterns.
d. Incorrect. This is the histologic staining pattern observed in metastatic carcinoma. Cytokeratin positivity is an important immunohistochemical marker for distinguishing primary central nervous system lesions from metastases. Additionally, this patient does not have evidence of a primary tumor site.
e. Incorrect. This is the histologic staining pattern observed in metastatic melanoma. This patient has no evidence of a primary focus of malignant melanoma.
Citation: "The Brain, Spinal Cord, and Meninges." Sternberg's Diagnostic Surgical Pathology. 4th ed. 2004. Print.
Source: BoardVitals, 9/4/2013
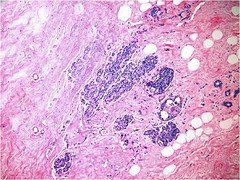
- A 60 year old woman with history of hypertension presents for routine screening mammography. The woman has no complaints and feels well. There is no family or personal history of breast cancer. Mammography reveals microcalcifications in both breasts. The patient subsequently undergoes needle-guided biopsy of the area (seen below). Which of the following histopathologic findings is expected in this diagnosis?

- Distended and distorted acini
- Presence of comedo necrosis
- Complete luminal obliteration
- Pagetoid spread into duct-like structures
- Involvement of a portion of the lobular unit
a-d. Incorrect. Answer choices a-d are all histopathologic findings that suggest lobular carcinoma in situ. Lobular carcinoma in situ is a malignant proliferation of lobular epithelial cells. This condition is characterized by preservation of the lobular architecture, which may be distorted and distended. Lobular carcinoma in situ must be differentiated from cancerization of lobules by ductal carcinoma in situ. In addition, ductal carcinoma in situ and lobular carcinoma in situ may occur side by side within the same lesion. Incidence of bilateral disease is frequent.
e. Correct. This patients findings on mammography are suspicious for breast cancer. Atypical lobular hyperplasia is a non-neoplastic proliferation of lobular epithelial cells that mimics, but does not possess all the histologic characteristics of lobular carcinoma in situ. Atypical lobular hyperplasia is thus characterized by less distorted and distended acini, involvement of a portion of the lobular unit, incomplete luminal obliteration and more cellular cohesion. Both atypical lobular hyperplasia and lobular carcinoma in situ are most commonly identified on screening mammography.
Citation: "Lobular Neoplasia (Atypical Lobular Hyperplasia and Lobular Carcinoma in Situ)." Sternberg's Diagnostic Surgical Pathology. 4th ed. 2004. Print.
Source: BoardVitals, 9/4/2013
Questions from July 30, 2013
- A 68 year-old male presents with recent-onset of hypertension and after an extensive workup is found to have a solitary renal cortical tumor measuring 2.8 x 2.5 x 2.1 cm. Grossly, the tumor is well-circumscribed with a faint-yellow hue. A diagnosis of juxtaglomerular cell tumor is rendered. Which of the following is true about this patient?
- The patient is hypernatremic
- The patient is hypokalemic
- This tumor produces aldosterone
- This tumor is HMB-45 positive
Juxtaglomerular cell tumors produce renin which cleaves angiotensinogen to angiotensin I. In the lungs angiotensin I is converted to angiotensin II which causes arteriole constriction and stimulates the zona glomerulosa in the adrenal cortex to produce the mineralocorticoid aldosterone. Aldosterone acts on the distal tubules and collecting ducts of the nephron causing the retention of sodium (hypernatremia) and excretion of potassium (hypokalemia). This process is called the renin-angiotensin-aldosterone system which increases blood pressure in two ways: constricting arterioles and the retention of sodium. The patient would be hypokalemic (B). Unlike angiomyolipomas, juxtaglomerular cell tumors are negative for HMB-45.
Source: BoardVitals, 7/30/2013
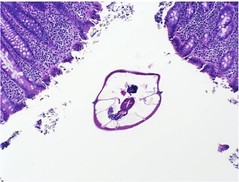
- This is an incidental finding in a colon biopsy of a 50 year-old female day-care worker. What is the diagnosis?
- Entamoeba histolytica
- Isospora belli
- Tropheryma whipplei
- Enterobius vermicularis
This is Enterobius vermicularis (pinworm). Pinworm is the most common nematode infection in the United States and affects persons of all ages. It is spread by the fecal-oral route. Children in daycare and preschool as well as those who care for them are at risk for contracting this helminth. Many individuals who contract pinworm experience intense anal itching, especially at night.
Adult pinworms live in the ileum or cecum and after several weeks, the female migrate through the colon and at night, emerge from the anus to deposit her eggs. The eggs irritate the anus and cause the intense nocturnal anal itching. Since the eggs are deposited on the anus, scotch tape can be applied to the anus and then applied to a glass slide for microscopic evaluation. The eggs are oval with one flat side and are approximately 50 um in size. A cross section of the worm (as seen here) shows several internal strictures. The adult worms do not invade the colonic mucosa, but occasionally can cause appendicitis.
Entamoeba histolytica (A) is a protozoan parasite that is transmitted by a fecal-oral route. Entamoeba histolitica can cause amoebic dysentery, amoeboma and amoebic liver abscesses. Symptoms of amoebic dysentery include bloody diarrhea, weight loss and abdominal pain. An amoeboma is a colonic mass that can mimic colon cancer. The patient presents with diarrhea or constipation, a CT-scan shows a large, semi/circumferential colonic mass. Colonoscopy confirms a mass that is often ulcerated. Biopsies show E. histolytica organisms and histiocytes.
Amoebic liver abscesses are often described as having the consistency of "anchovy paste". E. histolytica is an amoebic parasite, the image shows a nematode.
Whipple's disease (C) is a bacterial infection caused by T. whipplei. It affects middle-aged men who present with malabsorption, diarrhea, joint pain and abdominal lymphadenopathy. A small bowel biopsy shows villi distended and blunted by an infiltrate of foamy histiocytes containing PAS positive bacilli.
Isospora belli (B) is a parasite that typically infects immunocompromised patients and causes, non-bloody diarrhea, malabsorption and abdominal pain. It invades the colonic epithelium and is found at the apical cytoplasm of the mucosal cells. Morphologically, it is elongate and contains 1 or 2 round, centrally placed nuclei. I. belli is not a nematode (as seen in this example), invades the epithelial cells and is much smaller than E. vermicularis.
Source: BoardVitals, 7/30/2013
- A 5-year-old African American male presents with weight loss, fevers, and a painless swelling in the area of his jaw. The patient has no significant past medical history, and was adopted as an infant. CBC reveals anemia and lymphocytosis. Biopsy findings are seen in image below. Which of the following is true of this patients condition?

- A bcl-2 mutation may be present
- Cells are generally CD5+
- The most common genetic rearrangement is t(14;18) (q32;q21)
- C-myc gene translocation is unique to this patient's condition
- The endemic form of this patients condition is associated with Epstein-Barr virus positivity.
- Incorrect. Bcl-2 mutations are characteristic of diffuse large B-cell lymphomas. Although diffuse large-B cell lymphoma may mimic Burkitt Lymphoma, this patients presentation and histologic findings are more consistent with Burkitt Lymphoma.
- Incorrect. Burkitt lymphoma cells are typically CD5-.
- Incorrect. This is the most common genetic rearrangement responsible for the translocation that is characteristic of follicular lymphoma. While this is the most common genetic translocation, it is important to note that other variants are possible.
- Incorrect. While characteristic of Burkitt Lymphoma, The c-myc gene mutation can also be found in certain diffuse large B-cell lymphomas.
- Correct. The endemic form of Burkitt Lymphoma is associated with Epstein-Barr virus positivity.
- A patient with hypogonadism presents with an inability to smell. His dermatological exam in negative. Chromosome analysis reveals a deletion at Xp22.3. What is the diagnosis and which gene is affected?
- Kallman syndrome, KAL1 gene
- Ichthyosis, STS gene
- Retinoblastoma, Rb1 gene
- Prader-Willi syndrome, SNRPN gene
- Lissencephaly, LIS1 gene
- Correct. Kallman syndrome is consistent with this presentation and chromosome result.
- Incorrect. Ichthyosis presents with scaly skin, short stature, hypogonadism, and intellectual disability, and is associated with a deletion at Xp22.32.
- Incorrect. Retinoblastoma is an eye tumor associated with deletion at 13q14.1-q14.2.
- Incorrect. Prader-Willi syndrome can present with hypogonadism but a different spectrum of clinical signs and symptoms. This disorder is most commonly caused by a deletion in the paternal copy of 15q11.2.
- Incorrect. Lissencephaly presents with a "smooth brain," profound intellectual disabilities, and seizures and is associated with deletion at 17p13.3 (the same locus as Miller-Dieker syndrome, which tends to also affect genes contiguous to the LIS1 gene).
- A 60-year old woman with history of hypertension presents for routine screening mammography. The woman has no complaints and feels well. There is no family or personal history of breast cancer. Mammography reveals microcalcifications in both breasts. The patient subsequently undergoes needle-guided biopsy of the area (seen below). Which of the following histopathologic findings is expected in this diagnosis?
- Distended and distorted acini
- Presence of comedo necrosis
- Complete luminal obliteration
- Pagetoid spread into ductlike structures
- Involvement of a portion of the lobular unit
- a-d. Incorrect. Answer choices a-d are all histopathologic findings that suggest lobular carcinoma in situ. Lobular carcinoma in situ is a malignant proliferation of lobular epithelial cells. This condition is characterized by preservation of the lobular architecture, which may be distorted and distended. Lobular carcinoma in situ must be differentiated from cancerization of lobules by ductal carcinoma in situ. In addition, ductal carcinoma in situ and lobular carcinoma in situ may occur side by side within the same lesion. Incidence of bilateral disease is frequent.
- e. Correct. This patients findings on mammography are suspicious for breast cancer. Atypical lobular hyperplasia is a non-neoplastic proliferation of lobular epithelial cells that mimics, but does not possess all the histologic characteristics of lobular carcinoma in situ. Atypical lobular hyperplasia is thus characterized by less distorted and distended acini, involvement of a portion of the lobular unit, incomplete luminal obliteration, and more cellular cohesion. Both atypical lobular hyperplasia and lobular carcinoma in situ are most commonly identified on screening mammography.
End of Recently Added Questions
Questions from June 19, 2013
- A 64-year old African American male with history of hypertension and COPD presents for evaluation of an itchy skin rash of several years duration. He has been evaluated for this rash several times, and has previously had many inconclusive biopsies. He has failed treatment with multiple courses of steroids as well as other topical medications. On physical examination, there are multiple patches and, plaques, as well as generalized erythroderma located in the bathing trunk distribution. The patient undergoes biopsy of one of the skin lesions, which can be seen below. Which of the following immunophenotypes is most consistent with this diagnosis?


- CD2+, CD3+, CD5+, and CD7-
- CD2-, CD3-, CD5 -, and CD7-
- CD2+, CD3+, CD5-, and CD7+
- CD2-, CD3+, CD5+, and CD7+
- CD2+, CD3-, CD5+, and CD7+
- a. Correct. This clinical vignette describes the typical patient presentation concerning for mycosis fungoides, a mature T cell non-Hodgkin lymphoma. Although the most common presentation involves dermal involvement, there may also be involvement of the nodes, blood, and viscera. There may be a period of misdiagnosis, and the condition may wax and wane. Microscopically, these lesions may include the presence of Pautrier's abscesses, haloed lymphocytes, exocytosis, disproportionate epidermotropism, epidermal lymphocytes that are larger than dermal lymphocytes, hyperconvoluted intraepidermal lymphocytes, and lymphocytes aligned within the basal layer. Immunophenotyping can distinguish mycosis fungoides from other disorders involving immature T cells. The immunophenotype of mature T cells includes expression of CD2, CD3, CD5.
- d-e. Incorrect. Mature T cell markers include CD2, CD3, CD5. Lack of any one or more of these markers suggests the presence of immature T cells and is concerning for lymphoma.
Source: BoardVitals, 6/18/2013
- Which of the following is true regarding renal cell carcinoma?
- Collecting duct carcinoma is more common than chromophobe renal carcinoma
- Chromophobe carcinoma is more common than papillary carcinoma
- Papillary carcinoma is more common than collecting duct carcinoma
- All of the above
- None of the above
- c. Correct: Papillary carcinoma accounts for 10-15% or renal cancers. Chromophobe renal carcinoma accounts for 5% of renal cancers, collecting duct carcinoma accounts for less than 1% or renal epithelial neoplasms. The most common type is clear cell carcinoma, which accounts for 70-80% of cases.
- a. Incorrect: this statement is false. Collecting duct carcinoma is a rare tumor and the least common of the renal carcinomas.
- b. Incorrect: Papillary carcinoma accounts for 10-15% or renal cancers. Chromophobe renal carcinoma accounts for 5% of renal cancers.
Source: BoardVitals, 6/18/2013
- A 21-year-old male with no significant past medical history presents with fatigue, shortness of breath, weight loss, and leg pain. He had previously been diagnosed with growing pains, six months ago, but the pain has failed to remit since that time. Plain radiographs of the chest as well as a subsequent CT scan of the chest are abnormal. A lung biopsy is performed and is seen in the image below. Alkaline phosphatase, vimentin, variable smooth muscle actin and desmin are positive; EMA and keratin are negative. Which of the following histologic characteristics are typical for this diagnosis?
- Osteoid composed of fine, lacelike pink matrix
- Spaces separated by septa composed of highly malignant cells
- Purely spindle cell growth with only a small foci of matrix
- Malignant-appearing cartilage with hyperchromasia and hypercellularity with spindling at the periphery of cartilage lobules
- Predominance of benign giant cells
- Incorrect. This is the microscopic appearance of osteoblastic osteosarcoma.
- Incorrect. This is the microscopic appearance of telangiectatic osteosarcoma. Telangiectatic osteosarcoma differs from classic osteosarcoma in that radiographically appears as a purely lytic destructive lesion resembling and aneurismal bone cyst.
- Correct. This patient presents with signs, symptoms, and radiologic findings of metastatic osteosarcoma. The three primary types of osteosarcoma are osteoblastic, fibroblastic, and chondroblastic, which are classified based upon the predominant matrix.
- Incorrect. This is the classic microscopic appearance of chondroblastic osteosarcoma.
- Incorrect. This is another possible microscopic appearance of chondroblastic osteosarcoma. The finding of a giant cell tumor n the metaphysis of a young patient should suggest osteosarcoma.
Source: BoardVitals, 6/18/2013
- Which of these methods can reduce the incidence of transfusion transmitted disease?
- Donor selection
- Infectious disease testing
- Leukocyte reduction
- Diverting the first 8 ml of blood at venipuncture
- All of the above
- Correct. Criteria for donor selection are laid down by regulatory bodies and aim to protect both donor and recipient. Strict compliance with these regulations can limit the transmission of infectious diseases.
- Correct. Improvements in infectious disease testing has significantly reduced the transfusion-transmitted disease risk over the past 2 decades.
- Correct. Although leukocyte reduction is done to reduce the incidence of HLA immunization, it has been shown that leukocyte reduced blood components are as effective as seronegative components in reducing the risk of CMV transmission.
- Correct. Diverting the first 8 ml of blood at venipuncture reduces the risk of bacterial contamination by skin flora by 50%.
Source: BoardVitals, 6/18/2013
- Blood centers and transfusion services are regulated by the U.S.Food and Drug Administration. Criteria for acceptance of blood donors are all defined by the FDA. In which of the following clinical situations, a donor must avoid donating blood for 3 years?
- Malaria
- Pregnancy
- Recipient of blood transfusion
- Clinical laboratory evidence of HIV
- Recipient of toxoid vaccine
- Correct- In a confirmed diagnosis of malaria, deferment for donating blood is for 3 years after becoming asymptomatic.
- Deferred for 6 months in pregnancy.
- If a donor had received blood transfusion recently, donating blood should be deferred for 12 months.
- Clinical evidence of HIV infection indicates an indefinite deferral.
- There is no deferral with toxoid vaccine.
Source: BoardVitals, 6/18/2013
Questions from February 25, 2013
- A 25-year-old female with no significant past medical history presents with progressive pain and swelling of her left shin. She is concerned because she has been trying to lose weight for some time, but is unable to keep a regular exercise routine because of the pain. She denies a history of trauma and constitutional symptoms. Plain x-rays reveal a large lesion in the shaft of the tibia, which appears to be composed of areas of both sclerosis and lucency. Further imagining studies reveal no additional skeletal, intra-abdominal, or intra-thoracic lesions. Biopsy of the lesion is seen below. A biopsy of this diagnosis is most likely to reveal which of the following pathologic findings?

- Well-circumscribed lesion composed of anastomosing bony trabeculae
- Hypocellular proliferation of plump spindle cells with metaplastic bone formation
- Clusters of spindle cells with focal squamous differentiation
- High-grade spindle cells producing a fine, pink osteoid matrix
- Doubly nucleated cells and moderate areas of atypia permeating preexisting trabecular bone and filling the marrow space
- Incorrect: This is the histologic appearance of osteoid osteoma. Osteoid osteoma typically occurs in the second decade of life with a male predominance and involves the metaphysis of long bones. Its appearance on plain x-ray is that of a radiolucent nidus surrounded by an extensive sclerotic zone.
- Incorrect: This is the microscopic appearance of fibrous dysplasia. Fibrous dysplasia is developmental defect of bone formation that appears as a well-defined area of rarefaction with a sclerotic rim on plain x-rays. It is usually seen in patients less than 30 years of age, and affects the jawbones, skill, ribs, or proximal femur. It may be associated with Albright syndrome (skin pigmentation, endocrine dysfunction, and precocious puberty) or Mazabraud syndrome (intramuscular myxomas).
- Correct: This is the microscopic appearance of adamantinoma. Adamantinoma is an epithelial-appearing neoplasm of bone with predilection for the tibia that affects young men and woman equally. Patients often present with pain and swelling that may progress over a period of years. X-rays demonstrate large areas of sclerosis interspersed with areas of lucency in the shaft of the bone affecting both the cortex and medullary cavity.
- Incorrect: This is the histologic appearance of conventional osteoscarcoma. Conventional osteosarcoma is a high-grade malignant neoplasm that occurs in the metaphysis of the long bones of adolescents and young adults. Patients present with pain and swelling of the affected area, which appears as an area of destruction with extension into soft tissues and reactive new bone formation, known as Codman Triangle.
- Incorrect: This is the appearance of conventional chondrosarcoma. Conventional chondrosarcoma is the most common variant of a malignant bone neoplasm, which predominantly affects the axial skeletons of adult patients. Patients present with swelling and pain, and plain x-ray demonstrates erosion of markedly thickened cortices.
Source: BoardVitals, 2/25/2013
- A 65-year old man with hypertension and emphysema presents for the results of a recent biopsy of the lump under my jaw. He has a long history of smoking, chewing tobacco, and working outside as a farmer. He is concerned because a neighbor recently developed skin cancer, and he would like to stick around to see my grandkids run around on the farm. The biopsy results are consistent with adenoid cystic carcinoma. Which of the following statements most correctly describe the means of prognosticating this mans diagnosis?
- Predominant Ki-67 antigen activity indicates a greater likelihood of responding to treatment
- C-kit activity is demonstrated in both malignant and benign salivary glands and is not useful in prognosis of adenoid cystic carcinoma
- The p53 oncogene is found more frequently in recurrent tumors, and indicates the presence of a late-stage tumor
- Lung metastasis indicate aggressive, end-stage disease
- Clinical staging is a unreliable indicator of response to treatment
- Incorrect: Ki-67 antigen activity is seen most frequently in cases of adenoid cystic carcinoma that have failed to respond to treatment.
- Incorrect: C-kit expression is demonstrated in the majority of malignant cases of adenoid cystic carcinoma, but not normal glands. It has been implicated in the development of malignancy.
- Correct: The p53 oncogene is a marker of late-stage disease, and can this be used as an adverse prognostic factor.
- Incorrect: The most common site of metastasis of adenoid cystic carcinoma is the lung. Although lung metastases affect clinical staging of adenoid cystic carcinoma, they may remain stable for years.
- Incorrect: The clinical staging of adenoid cystic carcinoma, including tumor size and presence of metastases, is the most reliable prognostic factor.
Source: BoardVitals, 2/25/2013
- A 3 year old boy with developmental delay presents to a clinical geneticist with the following dysmorphic features: microcephaly, epicanthal folds, arched eyebrows, long nose, and micrognathia. Neurological history is significant for seizures and physical exam for hypotonia. Chromosome analysis reveals a karyotype of 46, XY, del(4)(p16). What is the diagnosis?
- Wolf-Hirschorn syndrome
- Cri du chat syndrome
- Angelman syndrome
- Miller-Dieker syndrome
- Langer-Giedion syndrome
- Correct: This clinical presentation and karyotype are consistent with Wolf-Hirschorn syndrome, also known as 4p- syndrome.
- Incorrect: This syndrome is associated with a deletion at 5p15.
- Incorrect: This syndrome is most commonly associated with a deletion at 15q11.2.
- Incorrect: This syndrome is associated with a deletion at 17p13.3.
- Incorrect: This syndrome is associated with a deletion at 8q24.11-24.13.
Source: BoardVitals, 2/25/2013
- A 29-year-old male with history of asthma presents with a painless swelling in the back of his thigh. On examination, the area is soft, non-erythematous, and a bruit is heard over the area. Excisional biopsy grossly reveals a soft, shelled out tumor, which microscopically demonstrates a thin microvasculature surrounding nests of PAS-positive polygonal cells with prominent nuclei and abundant cytoplasm. Which of the following chromosomal abnormalities has been implicated in the development of this tumor?
- t(1:22)
- +8, +12
- t(12:22)(q13;q12)
- t(12;14)
- t(11:22); +1q
- Incorrect: This is the chromosomal mutation responsible for neurofibroma, an unencapsulated nerve sheath lesion, which appears microscopically as uniformly cellular and slightly myxoid with an undulating fibrillar background and nuclear atypia.
- Correct: This vignette describes the typical presentation and pathologic appearance of alveolar soft part sarcoma.
- Incorrect: This is the chromosomal mutation responsible for clear cell sarcoma, which microscopically forms nests of clear cells that are surrounded by pink collagen bands, which stain with reticulin.
- Incorrect: This is the chromosomal mutation responsible for leiomyosarcoma, a malignant smooth muscle tumor that histologically appears as an alternating fascicle pattern with blunt-ended nuclei and a prominent mitotic rate.
- Incorrect: This is the chromosomal mutation responsible for neuroepithelioma (PNET), which microscopically demonstrates sheets of small, uniform cells with a bubbly appearance; it may be PAS-positive.
Source: BoardVitals, 2/25/2013
- A previously healthy 15-year-old male presents with recurrent fevers, weight loss, and an enlarging, painless lump in his groin for the last six months. Blood work reveals pancytopenia, and a reflex smear demonstrates large, pleomorphic cells with lobulated nuclei, prominent nucleoli and basophilic, vacuolated cytoplasm. Imaging reveals diffuse lymphadenopathy, with no obvious primary lesions. The lymph node biopsy is seen in the image below. Presence of which of the following is both diagnostic and prognostic for this condition?

- Epstein-Barr Virus positivity
- CD30 positivity
- Keratin positivity
- Anaplastic lymphoma kinase positivity
- Leukocyte common antigen positivity
- Incorrect: Epstein-Barr virus positivity would be expected if in lymphomatoid graulomatosis.
- Incorrect: CD30 positivity may be expected in both typical Hodgkins Lymphoma and Anaplastic Large Cell Lymphoma (ALCL). However, although present in ALCL, it cannot be used to guide treatment or to prognosticate.
- Incorrect: Keratin positivity would be expected in a pleomorphic carcinoma. This patients imaging studies did not reveal any primary tumor, nor is the cytologic appearance typical for carcinoma. It cannot be used for prognostication.
- Correct: This is the typical presentation of Anaplastic Large Cell Lymphoma (ALCL). The presence of anaplastic lymphoma kinase can be used to distinguish cutaneous from systemic ALCL, guide treatment, and also corresponds with a higher likelihood of response to chemotherapy.
- Incorrect: Leukocyte common antigen is a non-specific marker for conditions that may histologically mimic Hodgkins Lymphoma in bone marrow aspirates. It cannot be used for prognostication.
Source: BoardVitals, 2/25/2013
Questions from January 30, 2013
General Surgical Pathology
1. What lymphomas are common in the stomach?
A) Follicular Lymphoma and T cell lymphoma
B) Diffuse Large B Cell Lymphoma and MALT lymphoma
C) Hodgkins Lymphoma and Burkitts lymphoma
D) Lymphoplasmacytic Lymphoma and Anaplastic lymphoma
Answer: Diffuse Large B Cell Lymphoma and MALT lymphoma
Source: Ann Oncol 2008;19:1992, also Stomach chapter of PathologyOutlines.com
Contributor: Crystal L. Rose MD, MS, Ball Memorial Hospital, Indiana
2. What is the most common hereditary kidney abnormality?
A) Autosomal dominant polycystic kidney disease
B) Autosomal recessive polycystic kidney disease
C) Renal manifestions of tuberous sclerosis
D) Caroli's syndrome
Answer: Autosomal dominant polycystic kidney disease. It primarily affects adults, and has an incidence of 1-2 per 1000 live births, compared to 1 per 6,000 to 20,000 live births for autosomal recessive polycystic kidney disease, 1 per 10,000 for tuberous sclerosis (with or without renal disease, Neurology 1985;35:600) and 1 per 1,000,000 for Carolis disease, which primarily affects the intrahepatic bile ducts (eMedicine)
Source: Rosai (9th edition), page 959, Kidney tumor chapter of PathologyOutlines.com
Contributor: Crystal L. Rose MD, MS, Ball Memorial Hospital, Indiana
3. Tuberous sclerosis is associated with all of the following tumors except:
A) Clear cell sarcoma of soft parts
B) Angiomyolipoma of the kidney
C) Lymphangiomyomatosis of the lung
D) Cortical tuber of the brain
Answer: Clear cell sarcoma of soft parts. Tuberous sclerosis is caused by mutations in the TSC1 or TSC2 genes, although many cases are sporadic. It is associated with tubers of the brain cortex and lymphangiomyomatosis of the lung. It is also associated with renal angiomyolipoma and renal clear cell carcinoma, but not with renal clear cell sarcoma of soft parts, which is due to the t(12;22)(q13;q12) translocation.
Source: Kidney tumor chapter of PathologyOutlines.com
Contributor: Crystal L. Rose MD, MS, Ball Memorial Hospital, Indiana
Questions from January 2012
Transfusion Medicine
1. What is the shelf life of platelets?
A) 5 days
B) 6 days
C) 7 days
D) 8 days
E) 10 days
Answer: 5 days
Source: AABB Technical Manual
Contributor: Crystal L. Rose MD, MS, Ball Memorial Hospital, Indiana
2. How soon must a full written report regarding a transfusion related death be submitted to the FDA?
A) 24 hours
B) Five business days
C) Seven business days
D) Seven days
E) One month
Answer: Seven Days
Source: AABB Technical Manual
Contributor: Crystal L. Rose MD, MS, Ball Memorial Hospital, Indiana
3. What are Howell-Jolly bodies composed of?
A) RNA
B) DNA
C) Ribosomes
D) Keratin
E) All of the above
Answer: DNA
Source: Robbins (7th ed); image
Contributor: Crystal L. Rose MD, MS, Ball Memorial Hospital, Indiana
4. What are Pappenheimer bodies composed of?
A) RNA
B) DNA
C) Microtubules
D) Iron
E) Keratin
Answer: Iron
Contributor: Crystal L. Rose MD, MS, Ball Memorial Hospital, Indiana
5. Hereditary hemochromatosis is inherited in what pattern and physiologic disruption:
A) Autosomal Dominant, inability to excrete iron adequately
B) Autosomal Recessive, inability to excrete iron adequately
C) Autosomal Dominant, excess iron absorption
D) Autosomal Recessive, excess iron absorption
E) Mitochondrial, inability to excrete iron adequately
Answer: Autosomal Recessive, excess iron absorption
Source: PathologyOutlines.com-Liver nontumor chapter, also Foundations in Diagnostic Pathology: Gastrointestinal and Liver Pathology, page 503
Contributor: Crystal L. Rose MD, MS, Ball Memorial Hospital, Indiana
6. What is the most common mutation for hereditary hemochromatosis?
A) S65C
B) H63D
C) C282Y
D) H85Y
E) HFE
Answer: C282Y
Source: PathologyOutlines.com-Liver nontumor chapter, also Foundations in Diagnostic Pathology: Gastrointestinal and Liver Pathology, page 503. Up to 85% of clinically recognized cases in Northern and Western Europeans are homozygotes for the C282Y mutation, a missense mutation. S65C and H63D are other HH mutations but are not the most common. HFE is the gene located on chromosome 6p.
Contributor: Crystal L. Rose MD, MS, Ball Memorial Hospital, Indiana
7. What is the most common genetic disorder in Caucasians?
A) Cystic fibrosis
B) Hereditary hemochromatosis
C) Tuberous sclerosis
D) Sickle Cell Anemia
E) Tay Sachs
Answer: Hereditary hemochromatosis
Source: PathologyOutlines.com-Liver nontumor chapter, also Foundations in Diagnostic Pathology: Gastrointestinal and Liver Pathology, page 503; also Human Genome Project
Prevalence in homozygous state is 1 in 200 whites with carrier frequency between 1 in 10 and 1 in 20.
Contributor: Crystal L. Rose MD, MS, Ball Memorial Hospital, Indiana
End of Board Review Questions

