14 March 2018 - Case of the Week #451
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Week page. To subscribe or unsubscribe to Case of the Week or our other email lists, click here.
Thanks to Drs. Aysha Mubeen and Raafat Makary, University of Florida College of Medicine, Jacksonville, Florida (USA) for contributing this case and Dr. Ayse Ayhan, Hamamatsu University School of Medicine and Seirei Mikatahara Hospital (Japan) for editing the discussion. This case was reviewed in May 2020 by Dr. Jennifer Bennett, University of Chicago and Dr. Carlos Parra-Herran, University of Toronto. To contribute a Case of the Week, first make sure that we are currently accepting cases, then follow the guidelines on our main Case of the Week page.
 Advertisement
Advertisement
Website news:
(1) Congratulations to the winners of our top author awards for 2017 at PathologyOutlines.com:
Top staff author:
• Nicole K. Andeen, M.D., Assistant Professor, Oregon Health & Science University
Top trainee authors:
• Daniel Anderson, M.D., MBA, Resident, University of Washington
• Akira Yoshikawa, M.D., Medical Student, Nagasaki University School of Medicine
• Anthony Martinez, M.D., Fellow, Mayo Clinic, Rochester, MN
We appreciate their hard work and dedication in improving topics with thorough research, careful writing, high quality images and following our procedures. The award was based on nominations by our Editorial Board and staff. Read more...
(2) February may have been a short month, but we had a record number of 29,472 sessions per day. This is a 34% increase from February 2017. To see our other traffic statistics please visit: http://www.pathologyoutlines.com/monthlystats.php.
Visit and follow our Blog to see recent updates to the website.
Case of the Week #451
Clinical history:
A 45 year old woman presented with postmenopausal bleeding. She had a history of invasive cervical carcinoma treated with radiotherapy 20 years ago. She underwent an endometrial curettage followed by hysterectomy with bilateral salpingo-oophorectomy:
Gross image:
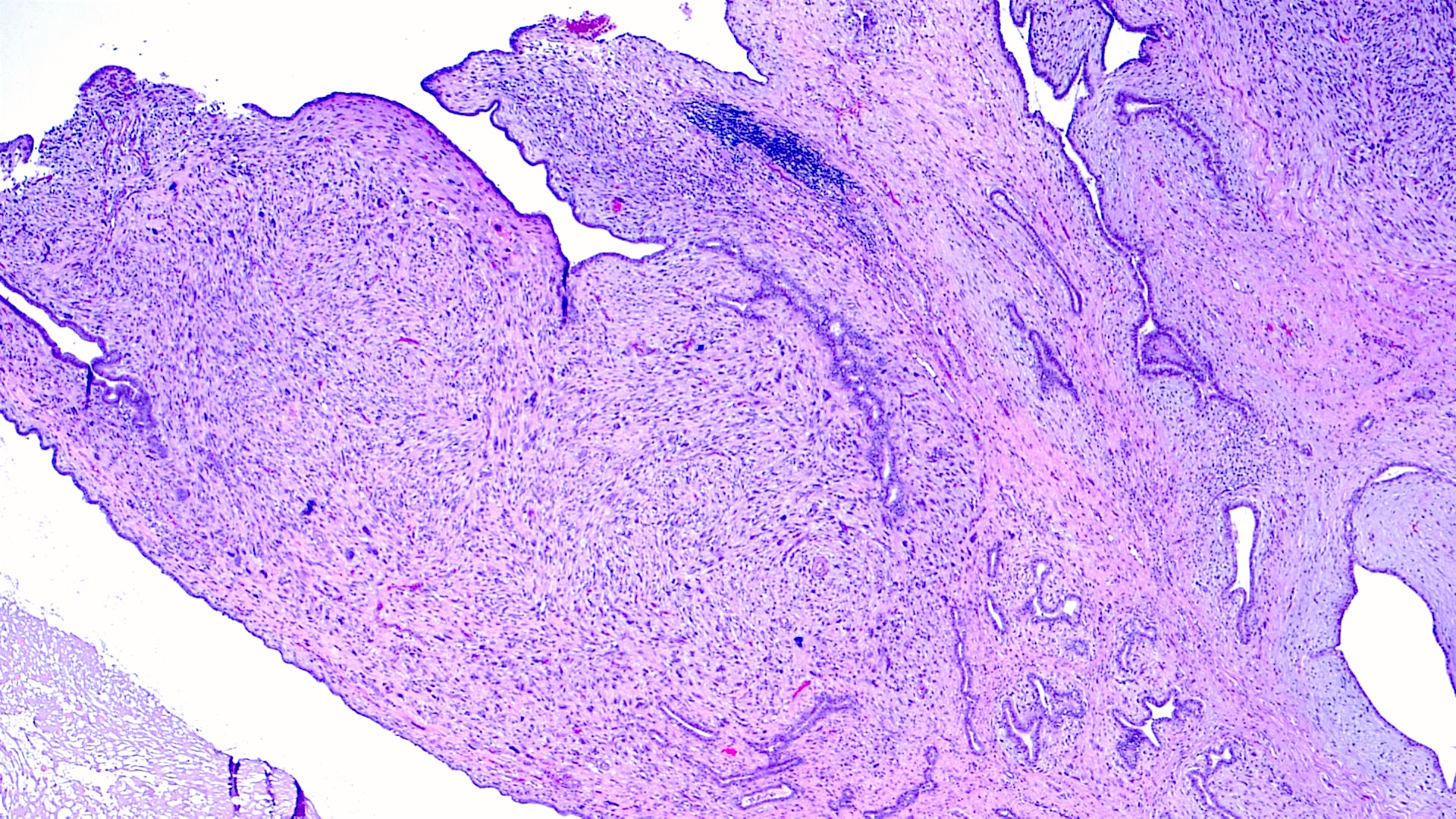
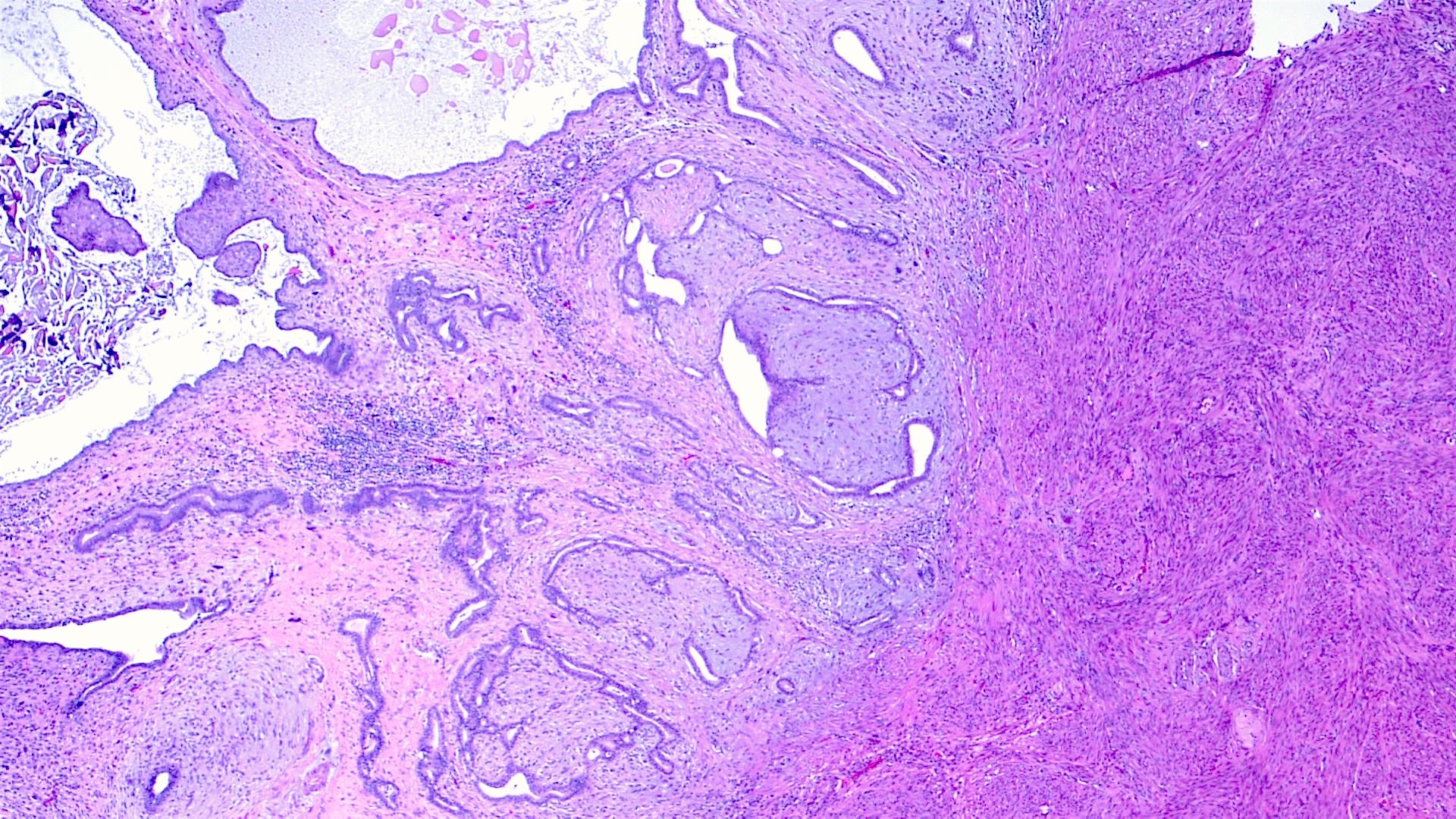
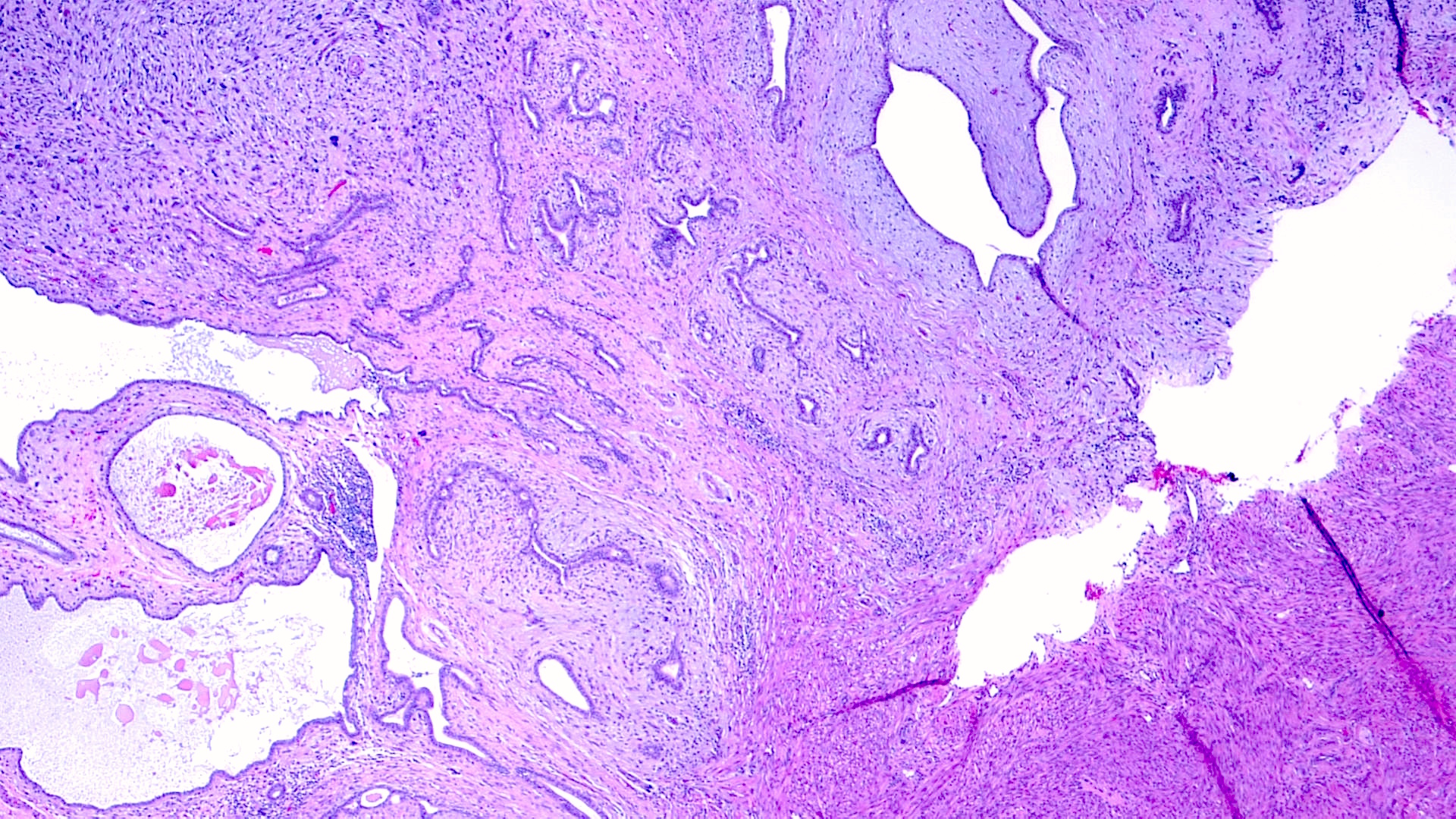
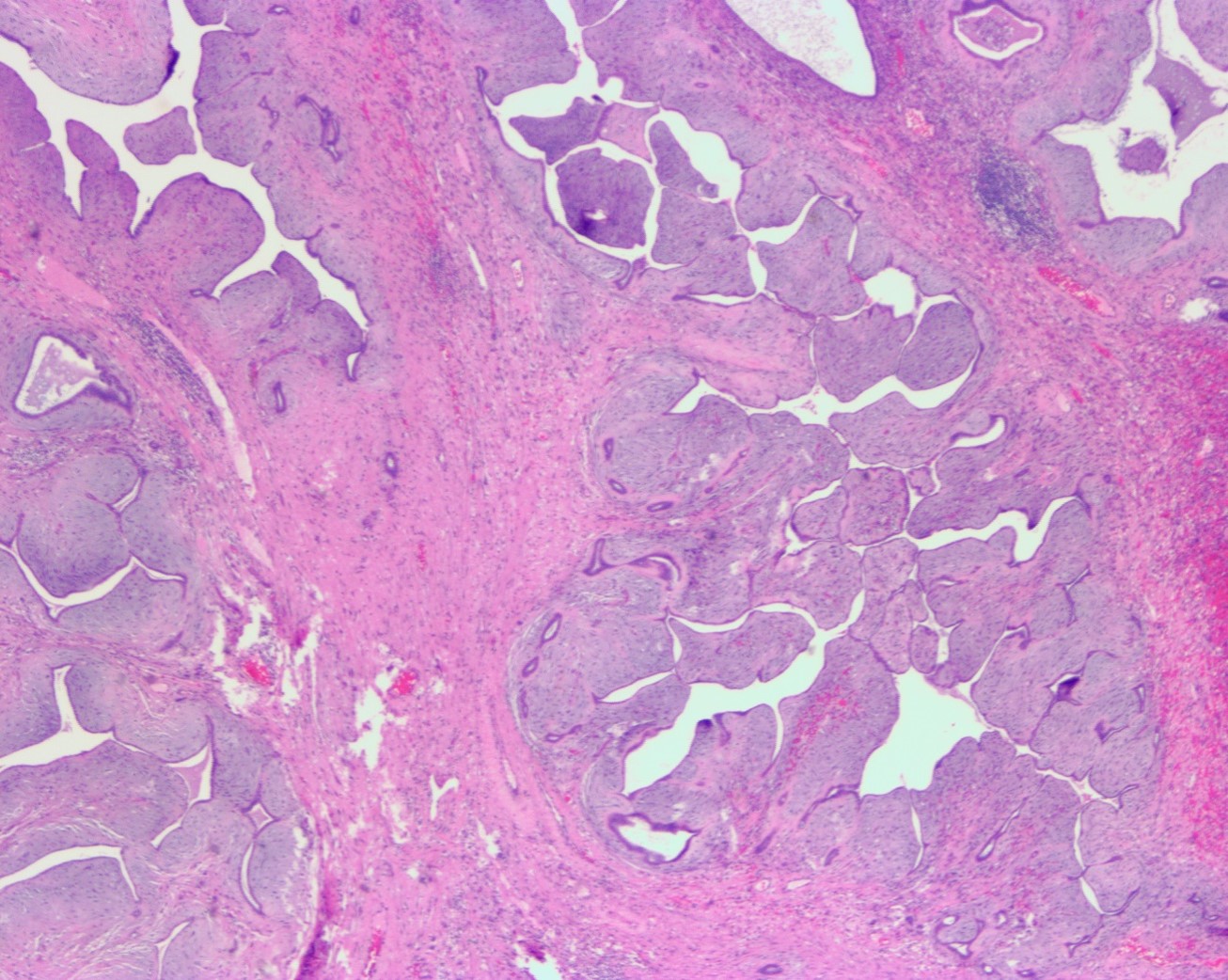
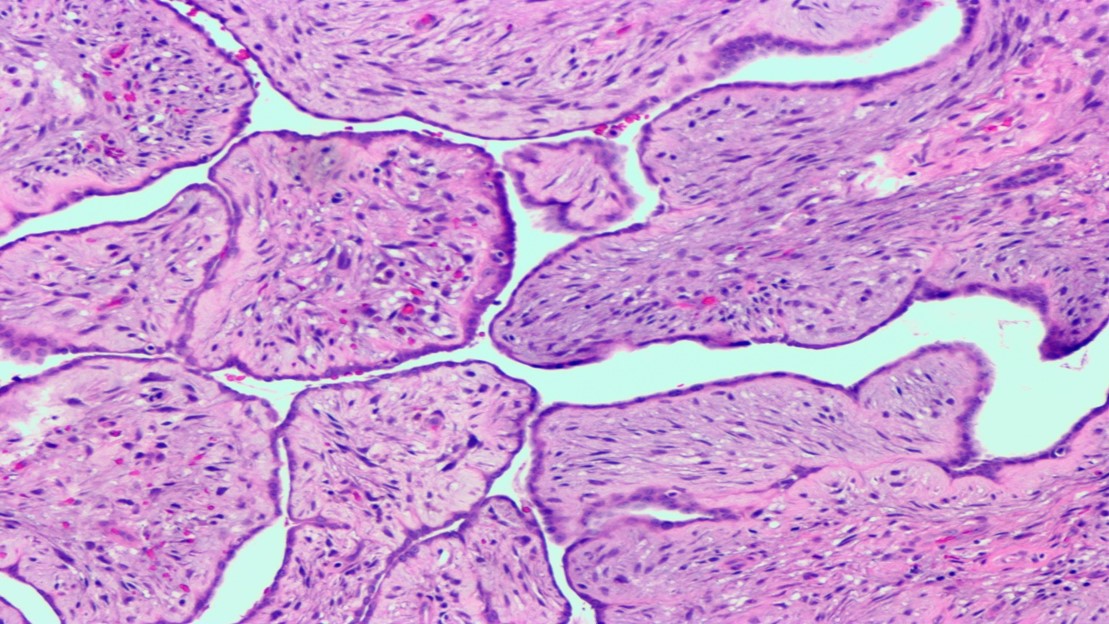
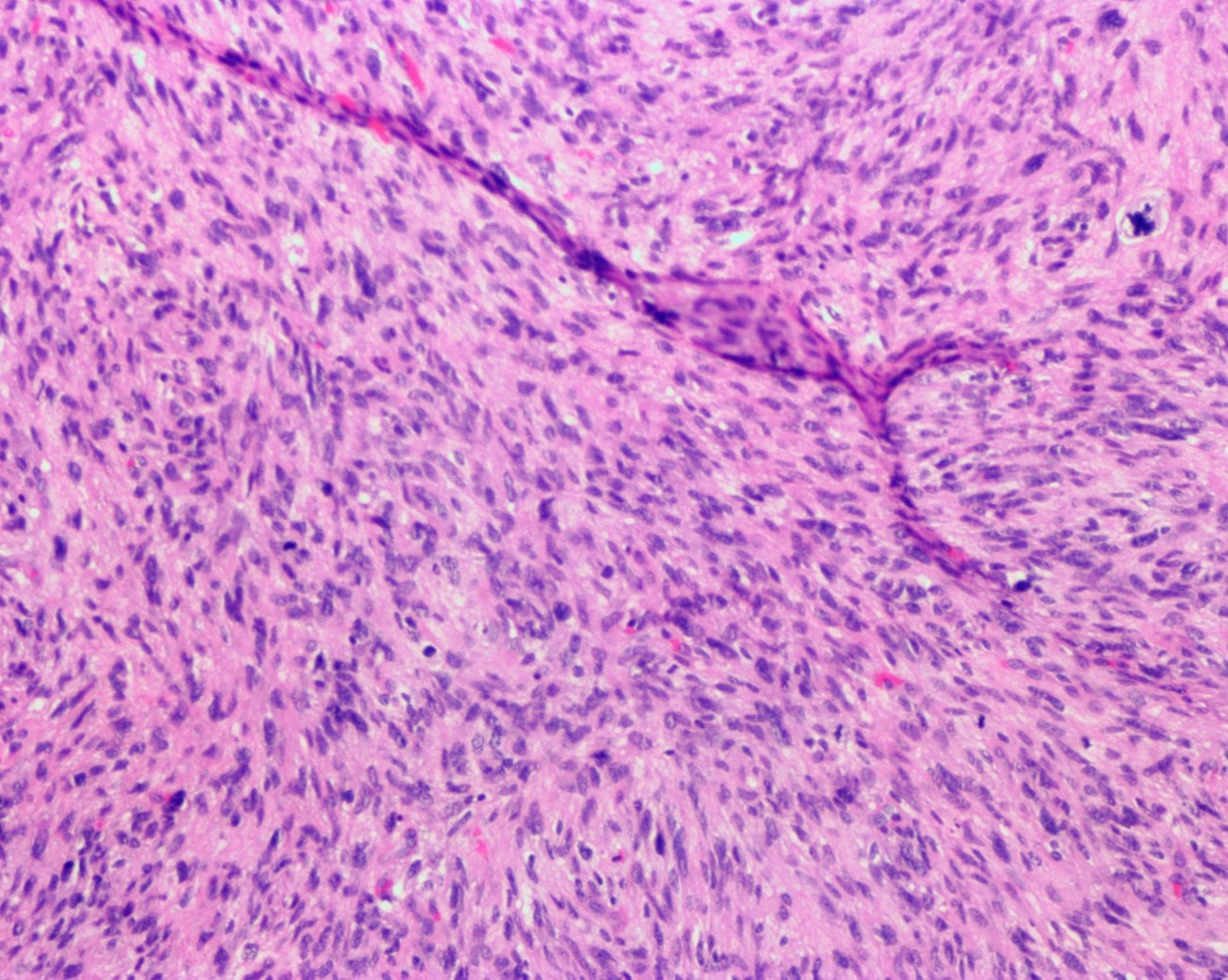
Histopathology images:
What is your diagnosis?
Diagnosis:
Adenosarcoma of the uterus
Test question (answer at the end):
Which of the following is a poor prognostic factor for uterine adenosarcoma?
A. Sarcomatous overgrowth
B. Increased mitotic activity and presence of tumor necrosis
C. Tumor cell necrosis
D. Anatomic location (endometrium versus cervix)
Discussion:
Adenosarcoma is an uncommon biphasic tumor composed of malignant stromal and benign epithelial components. It usually affects postmenopausal women, presenting with pelvic pain or vaginal bleeding. The corpus of the uterus is the most common site. It usually carries a good prognosis unless accompanied by deep myometrial invasion, stromal overgrowth or high-grade nuclear atypia. Grossly, these tumors are usually polypoid and exophytic. Histologic examination shows a leaf-like architecture reminiscent of phyllodes tumor of the breast. Benign glands are compressed to slit-like spaces by the growth of the malignant stromal component. There is usually periglandular condensation of stroma.
Sarcomatous overgrowth is seen in about 10% of the cases. It is defined as the presence of pure sarcoma (without any epithelial component) comprising at least 25% of the tumor (Am J Surg Pathol 1989;13:28). High grade in the sarcomatous component is another adverse prognostic factor; it is defined as significant nuclear pleomorphism appreciable at low power magnification (Am J Surg Pathol 2017;41:1513). Sarcomatous overgrowth and high grade atypia are usually seen together. Heterologous differentiation (rhabdomyosarcoma, liposarcoma, chondrosarcoma) occurs in a minority of lesions, typically those that are high-grade.
The main differential diagnoses are endometrial polyp, adenomyoma, carcinosarcoma, leiomyosarcoma and endometrial stromal tumor (Arch Pathol Lab Med 2016;140:286).
Our case highlights that adenosarcoma, although uncommon, should be considered in the differential diagnosis of a biphasic uterine tumor. The previous history of radiation also suggests that this is a radiation induced sarcoma, namely a tumor at least 5 years post radiation with a different histologic type but within the field of irradiation (WHO Classification of Tumours of Female Reproductive organs, 2014, p.149).
For this patient, no chemotherapy was given. After 5 months, she was readmitted with abdominal pain. Pelvic CT showed a large peripherally enhancing central fluid density measuring 9 cm. Image guided drainage revealed hypocellular material with blood elements but no malignant cells. At surgery, a large pelvic mass was noted in the right lower quadrant consisting of friable, hemorrhagic, straw colored gelatinous material. The mass was unresectable, but a biopsy was reported as recurrent high grade adenosarcoma with extensive necrosis, no epithelial component present. She succumbed to her illness a month later.
Test Question Answer:
A.
Poor prognostic factors include the presence of sarcomatous overgrowth, deep myometrial invasion and high nuclear grade. Other histologic features such as increased mitoses and necrosis are helpful in the diagnosis of adenosarcoma, but do not stratify adenosarcoma cases prognostically.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Week page. To subscribe or unsubscribe to Case of the Week or our other email lists, click here.
Thanks to Drs. Aysha Mubeen and Raafat Makary, University of Florida College of Medicine, Jacksonville, Florida (USA) for contributing this case and Dr. Ayse Ayhan, Hamamatsu University School of Medicine and Seirei Mikatahara Hospital (Japan) for editing the discussion. This case was reviewed in May 2020 by Dr. Jennifer Bennett, University of Chicago and Dr. Carlos Parra-Herran, University of Toronto. To contribute a Case of the Week, first make sure that we are currently accepting cases, then follow the guidelines on our main Case of the Week page.
Website news:
(1) Congratulations to the winners of our top author awards for 2017 at PathologyOutlines.com:
Top staff author:
• Nicole K. Andeen, M.D., Assistant Professor, Oregon Health & Science University
Top trainee authors:
• Daniel Anderson, M.D., MBA, Resident, University of Washington
• Akira Yoshikawa, M.D., Medical Student, Nagasaki University School of Medicine
• Anthony Martinez, M.D., Fellow, Mayo Clinic, Rochester, MN
We appreciate their hard work and dedication in improving topics with thorough research, careful writing, high quality images and following our procedures. The award was based on nominations by our Editorial Board and staff. Read more...
(2) February may have been a short month, but we had a record number of 29,472 sessions per day. This is a 34% increase from February 2017. To see our other traffic statistics please visit: http://www.pathologyoutlines.com/monthlystats.php.
Visit and follow our Blog to see recent updates to the website.
Case of the Week #451
Clinical history:
A 45 year old woman presented with postmenopausal bleeding. She had a history of invasive cervical carcinoma treated with radiotherapy 20 years ago. She underwent an endometrial curettage followed by hysterectomy with bilateral salpingo-oophorectomy:
Gross image:
Histopathology images:
What is your diagnosis?
Diagnosis:
Adenosarcoma of the uterus
Test question (answer at the end):
Which of the following is a poor prognostic factor for uterine adenosarcoma?
A. Sarcomatous overgrowth
B. Increased mitotic activity and presence of tumor necrosis
C. Tumor cell necrosis
D. Anatomic location (endometrium versus cervix)
Discussion:
Adenosarcoma is an uncommon biphasic tumor composed of malignant stromal and benign epithelial components. It usually affects postmenopausal women, presenting with pelvic pain or vaginal bleeding. The corpus of the uterus is the most common site. It usually carries a good prognosis unless accompanied by deep myometrial invasion, stromal overgrowth or high-grade nuclear atypia. Grossly, these tumors are usually polypoid and exophytic. Histologic examination shows a leaf-like architecture reminiscent of phyllodes tumor of the breast. Benign glands are compressed to slit-like spaces by the growth of the malignant stromal component. There is usually periglandular condensation of stroma.
Sarcomatous overgrowth is seen in about 10% of the cases. It is defined as the presence of pure sarcoma (without any epithelial component) comprising at least 25% of the tumor (Am J Surg Pathol 1989;13:28). High grade in the sarcomatous component is another adverse prognostic factor; it is defined as significant nuclear pleomorphism appreciable at low power magnification (Am J Surg Pathol 2017;41:1513). Sarcomatous overgrowth and high grade atypia are usually seen together. Heterologous differentiation (rhabdomyosarcoma, liposarcoma, chondrosarcoma) occurs in a minority of lesions, typically those that are high-grade.
The main differential diagnoses are endometrial polyp, adenomyoma, carcinosarcoma, leiomyosarcoma and endometrial stromal tumor (Arch Pathol Lab Med 2016;140:286).
Our case highlights that adenosarcoma, although uncommon, should be considered in the differential diagnosis of a biphasic uterine tumor. The previous history of radiation also suggests that this is a radiation induced sarcoma, namely a tumor at least 5 years post radiation with a different histologic type but within the field of irradiation (WHO Classification of Tumours of Female Reproductive organs, 2014, p.149).
For this patient, no chemotherapy was given. After 5 months, she was readmitted with abdominal pain. Pelvic CT showed a large peripherally enhancing central fluid density measuring 9 cm. Image guided drainage revealed hypocellular material with blood elements but no malignant cells. At surgery, a large pelvic mass was noted in the right lower quadrant consisting of friable, hemorrhagic, straw colored gelatinous material. The mass was unresectable, but a biopsy was reported as recurrent high grade adenosarcoma with extensive necrosis, no epithelial component present. She succumbed to her illness a month later.
Test Question Answer:
A.
Poor prognostic factors include the presence of sarcomatous overgrowth, deep myometrial invasion and high nuclear grade. Other histologic features such as increased mitoses and necrosis are helpful in the diagnosis of adenosarcoma, but do not stratify adenosarcoma cases prognostically.