19 December 2018 - Case of the Week #471 (revised 15 June 2020)
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Week page. To subscribe or unsubscribe to Case of the Week or our other email lists, click here.
Thanks to Dr. Jaya Bajaj, PBM Laboratories, Lewisville, Texas (USA) for contributing this case and Dr. Raul S. Gonzalez, Beth Israel Deaconess Medical Center, Boston, Massachusetts (USA) for writing the discussion. This case was reviewed in May 2020 by Dr. Jennifer Bennett, University of Chicago and Dr. Carlos Parra-Herran, University of Toronto.
Advertisement
Case of the Week #471
Clinical history:
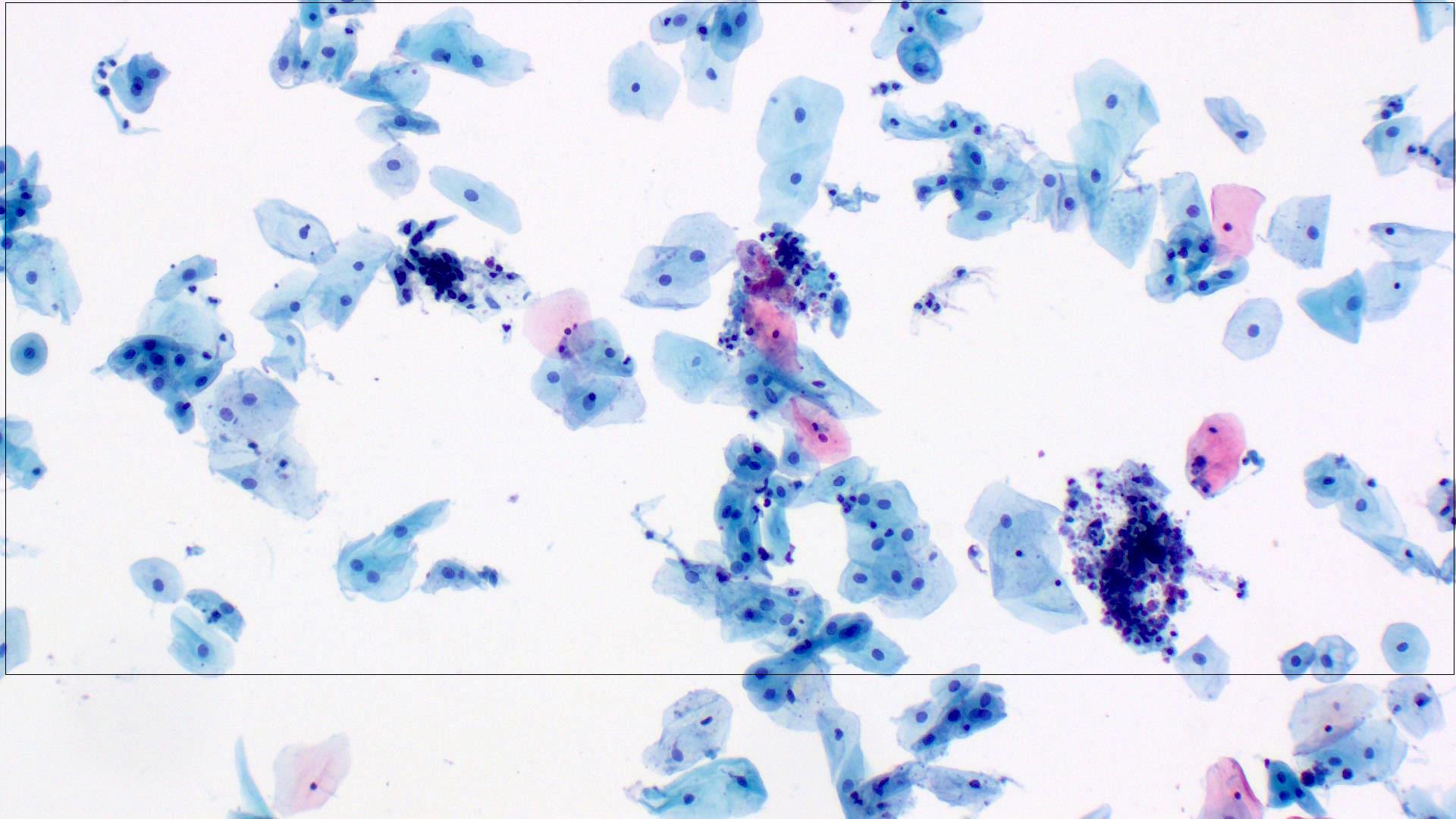
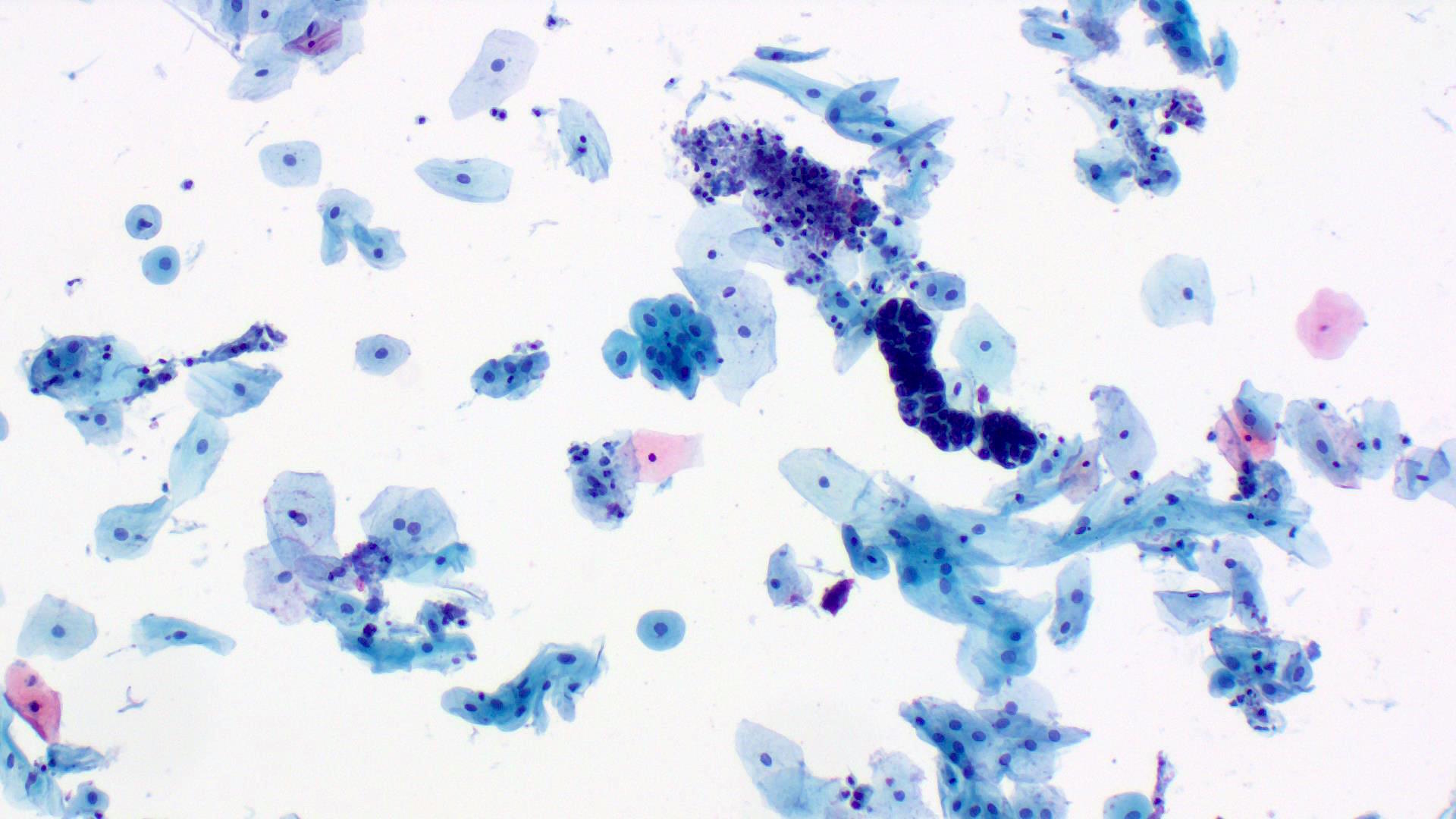
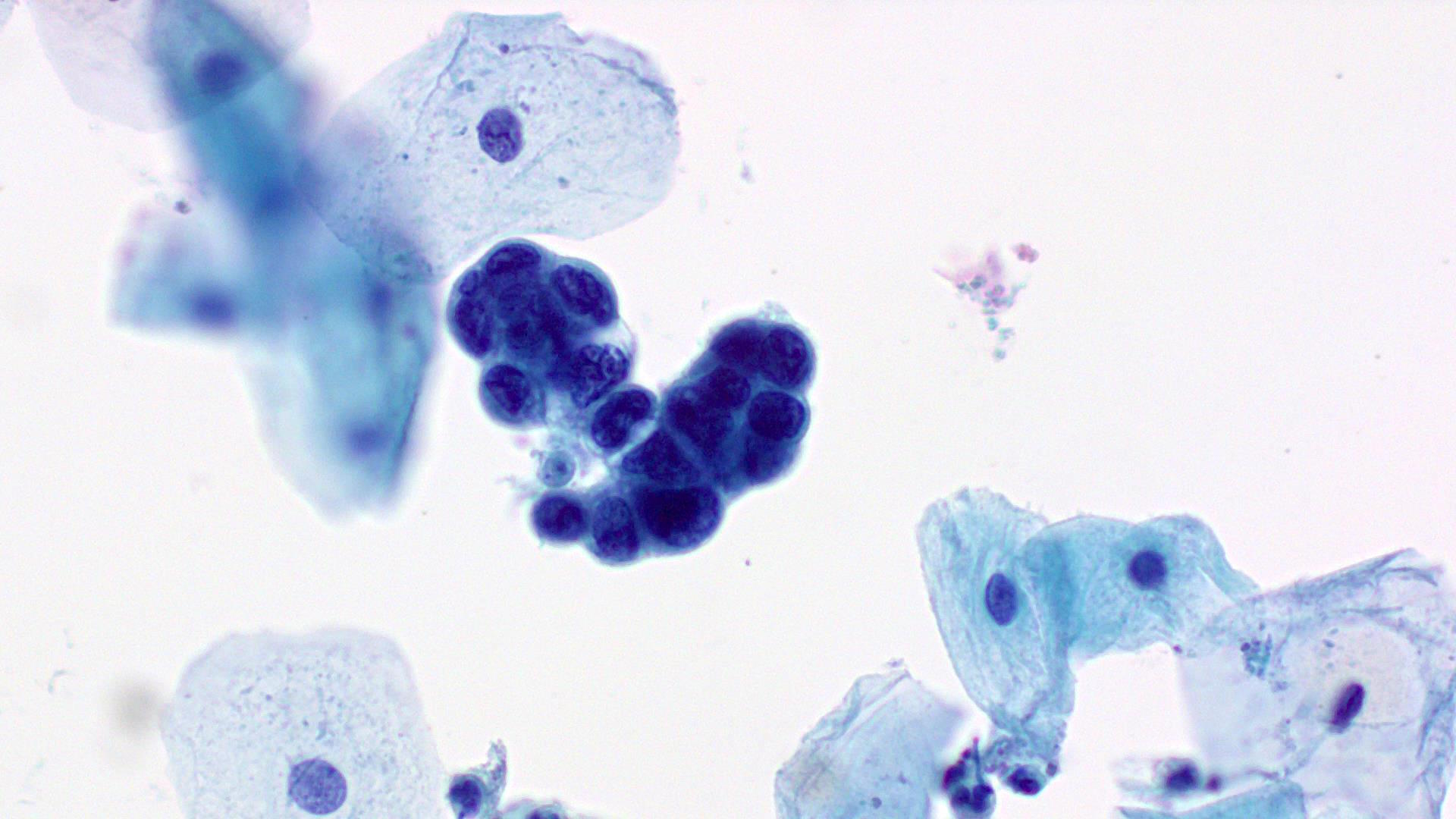
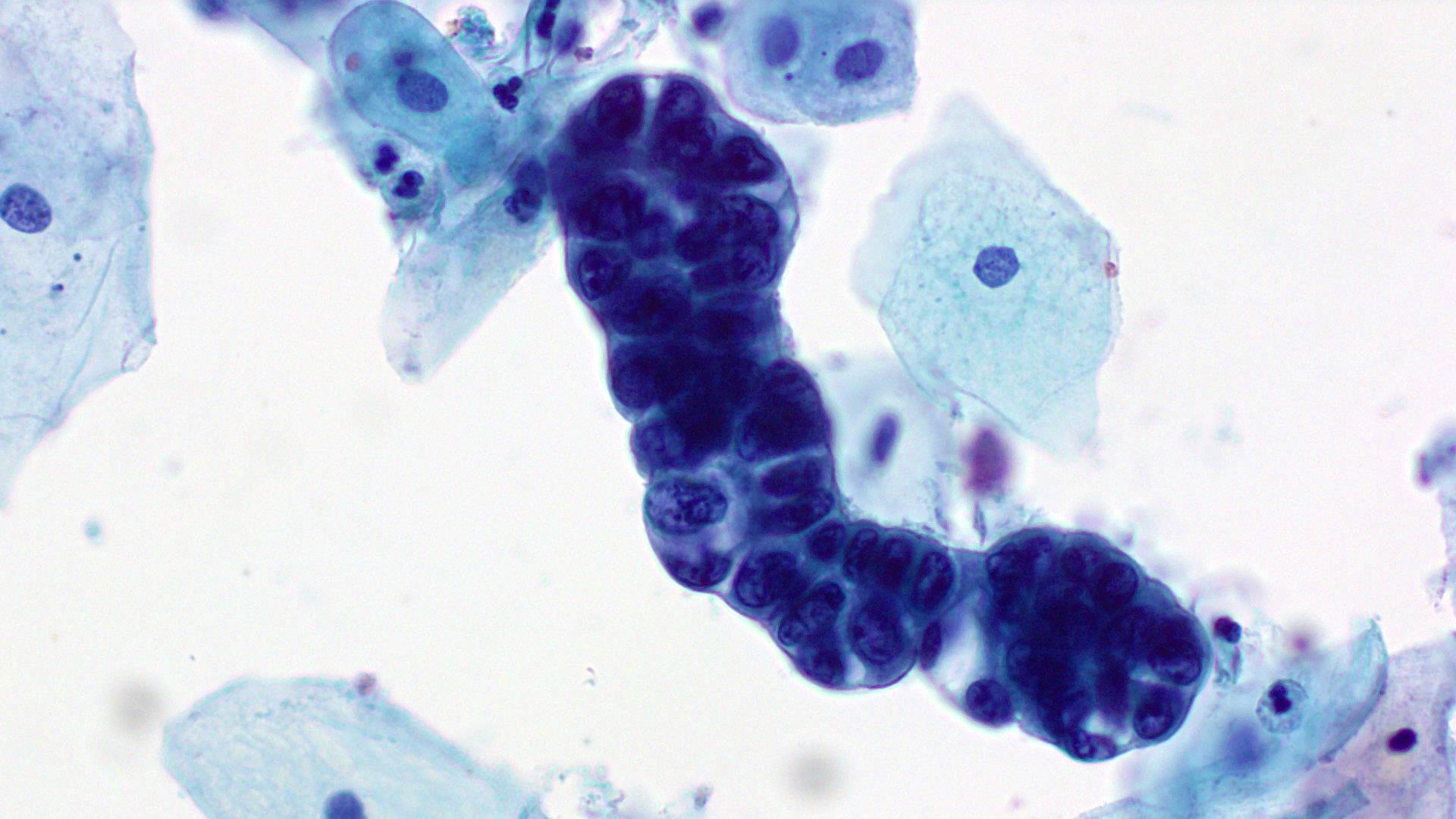
A 72 year old woman with no significant prior medical history presented with a vaginal mass. A Pap smear and biopsy were performed.
Cytology images:
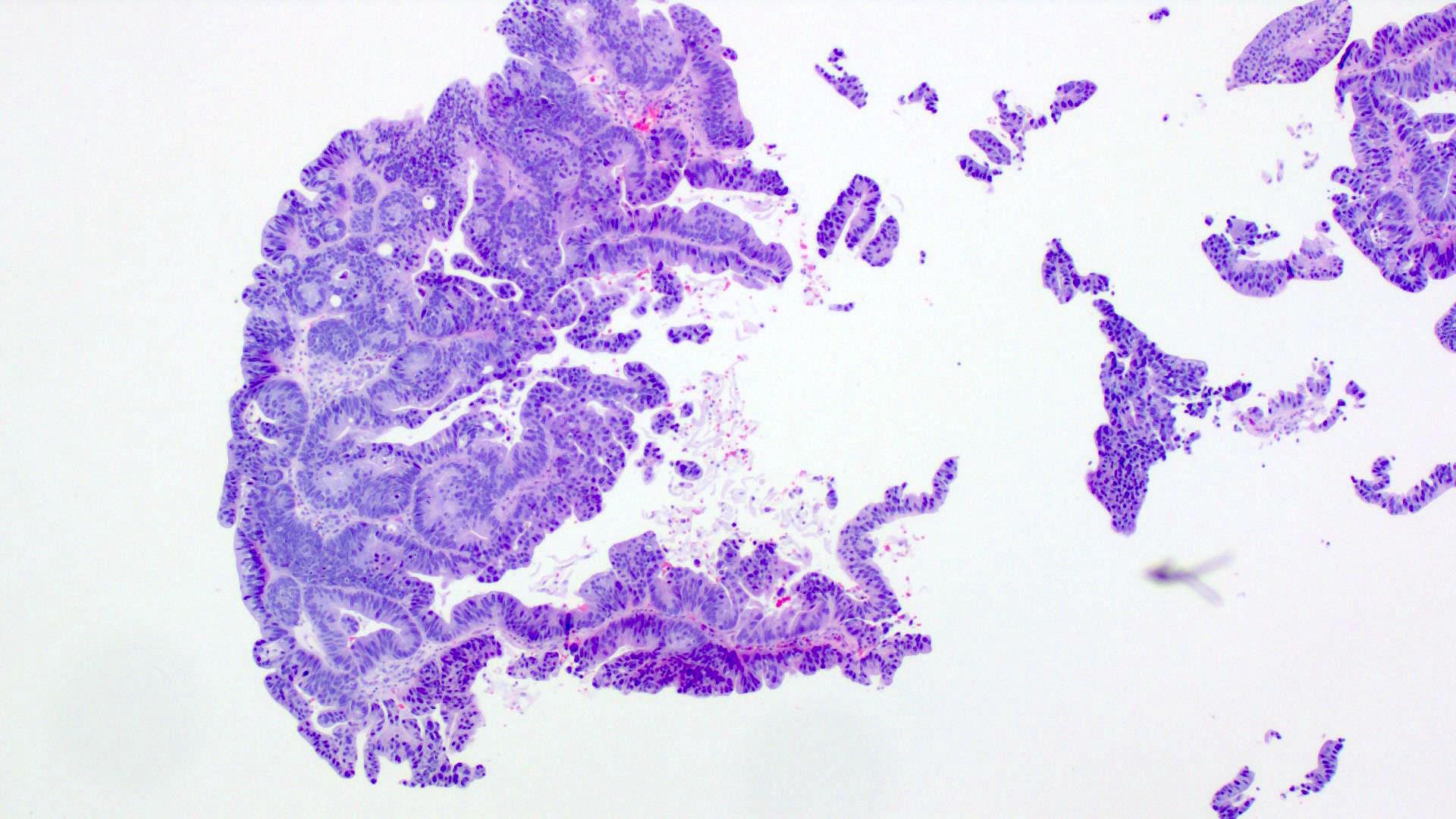
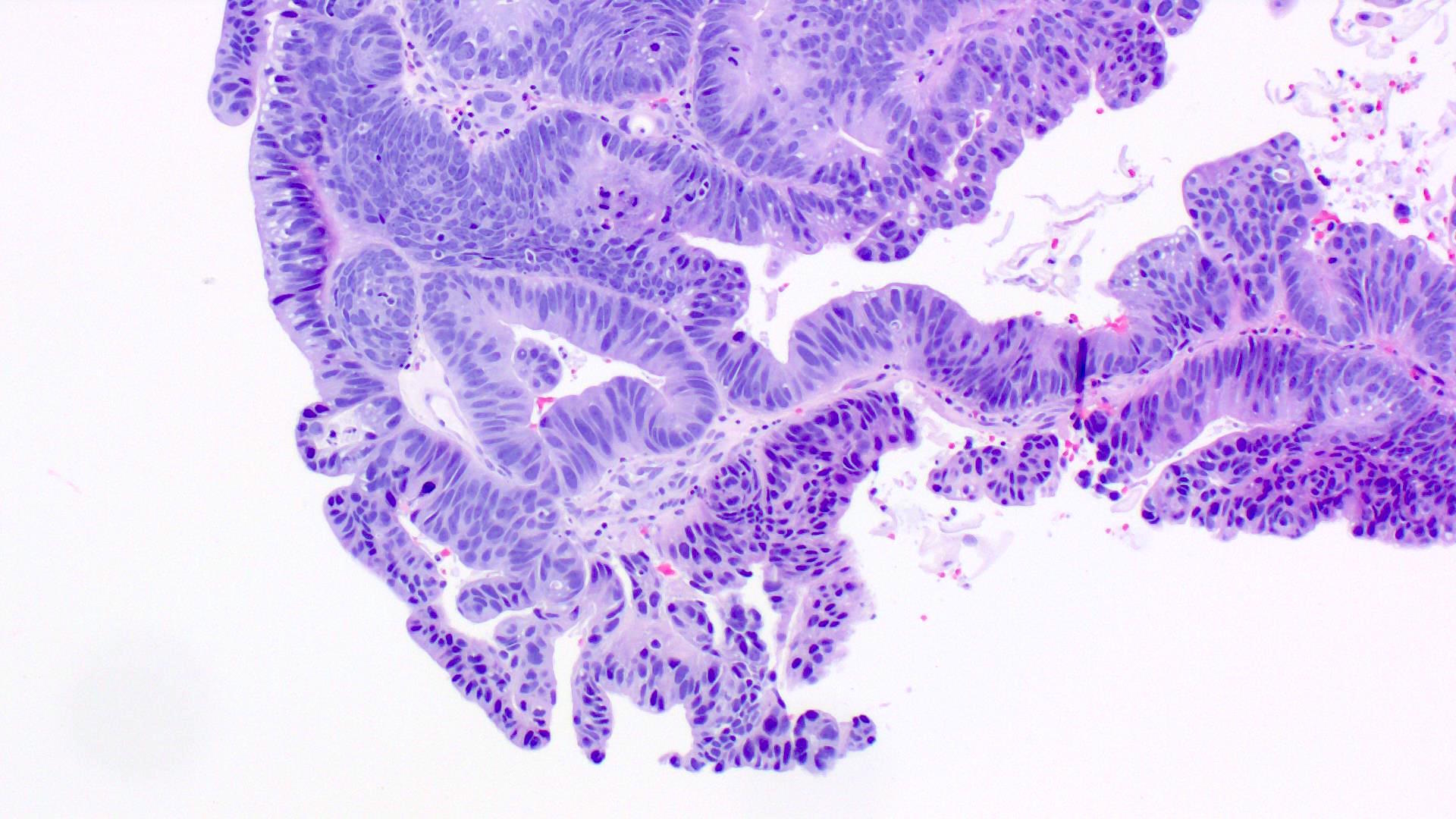
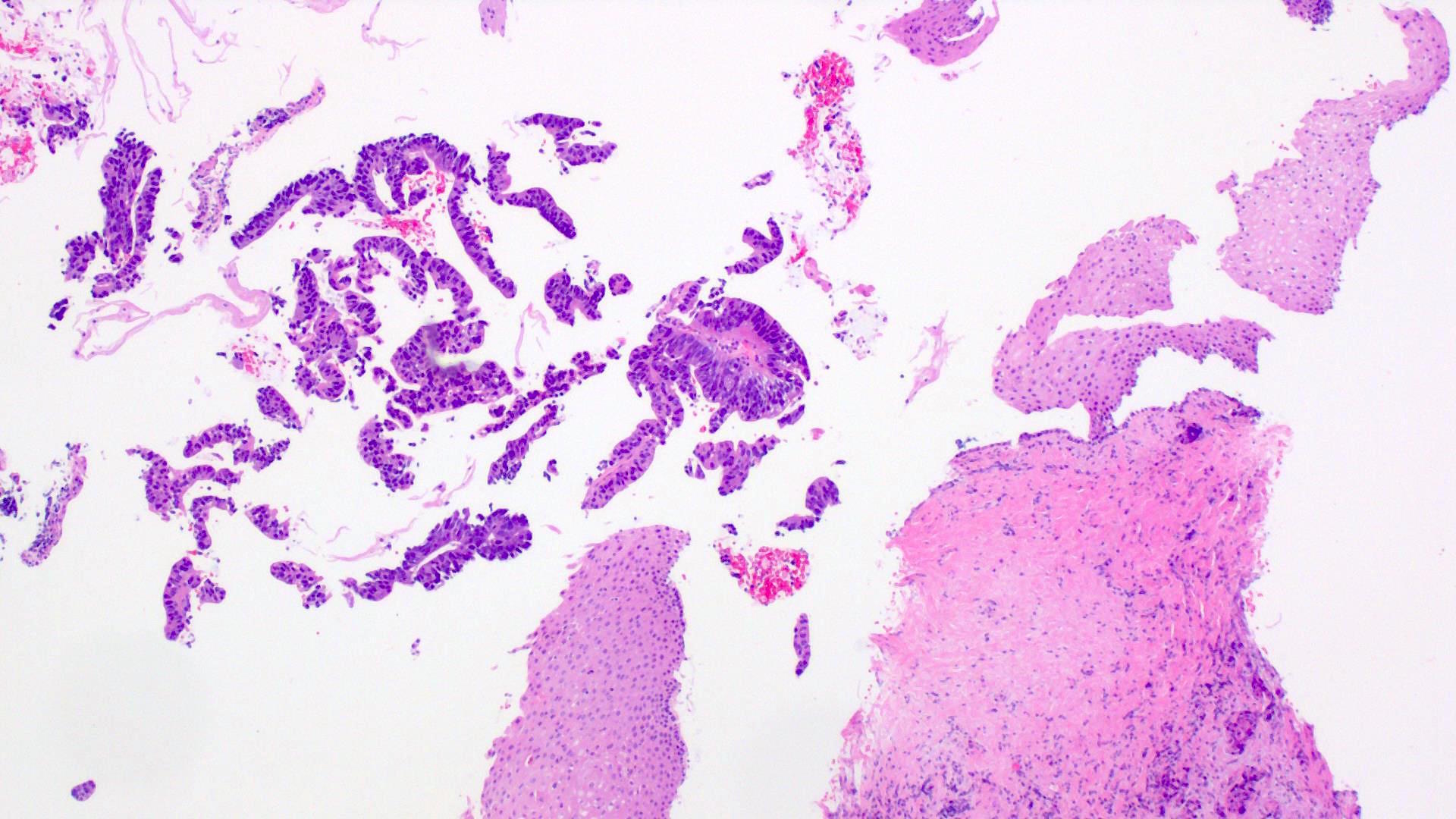
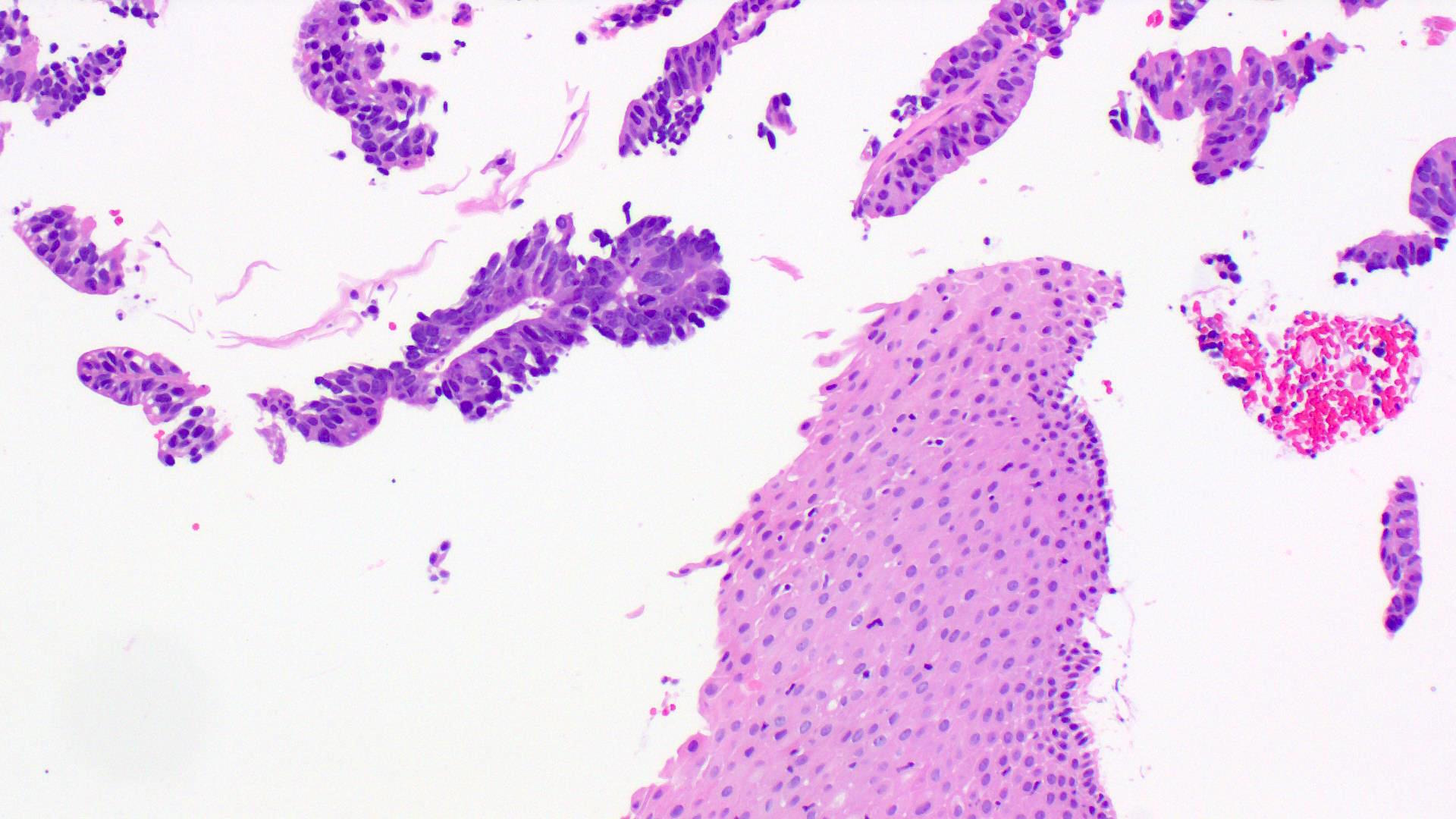
Histopathology images:
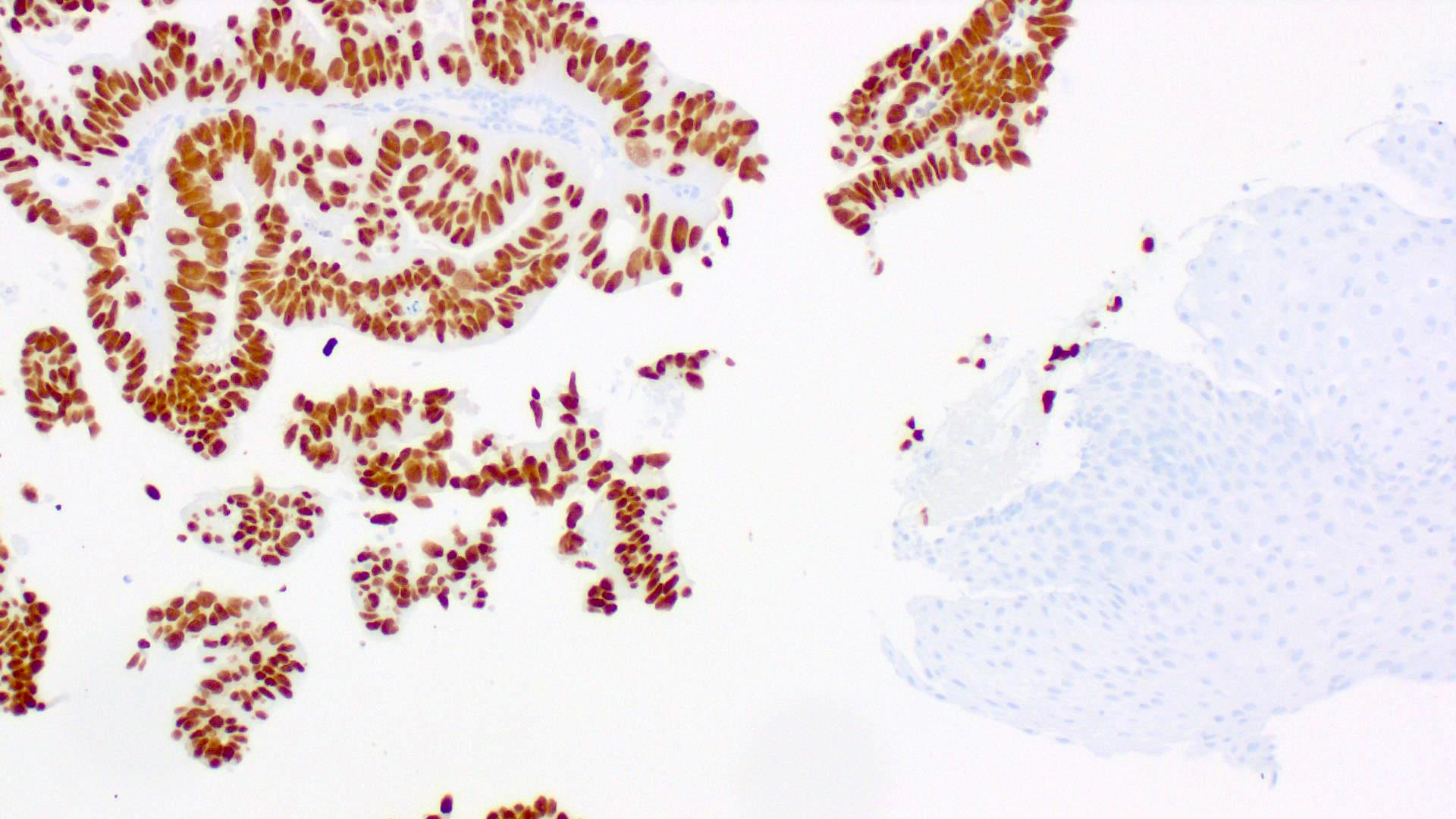
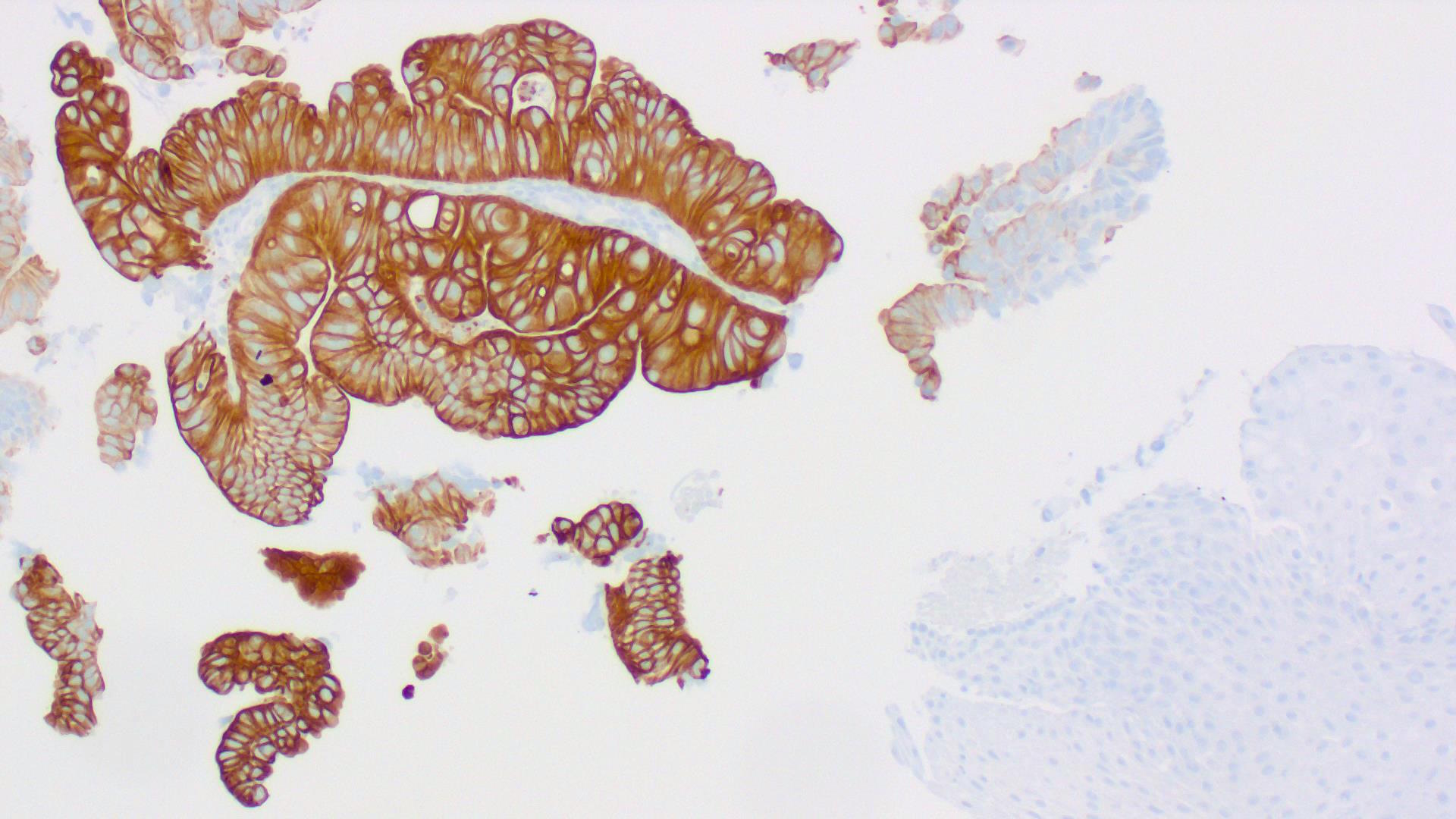
Special stains:
What is your diagnosis?
Diagnosis:
Metastatic colon carcinoma
Test question (answer at the end):
Roughly what percentage of vaginal adenocarcinomas are primary, rather than metastatic?
A. 5%
B. 20%
C. 50%
D. 75%
Discussion:
Adenocarcinomas in the vagina are distinctly uncommon, in contrast to squamous cell carcinoma. No more than 20% of vaginal adenocarcinomas are primary at this site (Nucci, Parra-Herran: Gynecologic Pathology - Foundations in Diagnostic Pathology, 2nd Ed., 2020), so a metastases needs to be ruled out. In fact, the vagina is one of the most common gynecologic organs targeted by metastatic disease (Cancer 1984;53:1978). Possible sites of origin for vaginal metastases include cervix, endometrium, ovary, kidney and colon. The patient often has a known carcinoma, but the metastasis may also represent the initial presentation.
Only a few dozen colorectal carcinomas metastatic to the vagina have been characterized in the literature (Int J Surg 2013;11:1048). Average patient age is about 60 years. Vaginal bleeding is the most common presenting symptom and roughly one third of patients have widely metastatic disease.
Most tumors show typical morphology with variable mucin production, atypical columnar cells with hyperchromatic nuclei, brisk mitoses and central "dirty" necrosis filling the glandular lumens. Immunohistochemistry is confirmatory, with metastatic colorectal carcinoma being positive for CK20 and CDX2 and negative for CK7 (as in this case). In general, primary vaginal adenocarcinomas show the opposite pattern (positive for CK7, negative for CK20 and CDX2).
Most primary vaginal adenocarcinomas are either clear cell adenocarcinomas or endometrioid adenocarcinoma. Clear cell adenocarcinomas are often seen in patients with a history of intrauterine diethylstilbestrol exposure. These patients are young (average age around 20 years), while patients without this exposure history are generally middle-aged or older. Histology shows tubulocystic, papillary or solid patterns and cells with hobnail nuclei and eosinophilic to clear cytoplasm. Endometrioid adenocarcinoma of the vagina usually arises from endometriosis and can be very difficult to distinguish from a uterine metastasis without careful clinical workup.
Rare types of vaginal adenocarcinoma include mesonephric adenocarcinoma (glands are eosinophilic and often cribriform) and mucinous adenocarcinoma (similar to cervical counterpart, and may arise from endocervicosis). Gastric-type adenocarcinoma, typically a well differentiated variant of cervical cancer, has recently been reported to arise in the vagina (Am J Surg Pathol 2018;42:958). It is CDX2 positive, and usually CK7 positive and CK20 negative. It may mimic vaginal adenosis.
Test question answer:
B. 20%
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Week page. To subscribe or unsubscribe to Case of the Week or our other email lists, click here.
Thanks to Dr. Jaya Bajaj, PBM Laboratories, Lewisville, Texas (USA) for contributing this case and Dr. Raul S. Gonzalez, Beth Israel Deaconess Medical Center, Boston, Massachusetts (USA) for writing the discussion. This case was reviewed in May 2020 by Dr. Jennifer Bennett, University of Chicago and Dr. Carlos Parra-Herran, University of Toronto.
Advertisement
Case of the Week #471
Clinical history:
A 72 year old woman with no significant prior medical history presented with a vaginal mass. A Pap smear and biopsy were performed.
Cytology images:
Histopathology images:
Special stains:
What is your diagnosis?
Diagnosis:
Metastatic colon carcinoma
Test question (answer at the end):
Roughly what percentage of vaginal adenocarcinomas are primary, rather than metastatic?
A. 5%
B. 20%
C. 50%
D. 75%
Discussion:
Adenocarcinomas in the vagina are distinctly uncommon, in contrast to squamous cell carcinoma. No more than 20% of vaginal adenocarcinomas are primary at this site (Nucci, Parra-Herran: Gynecologic Pathology - Foundations in Diagnostic Pathology, 2nd Ed., 2020), so a metastases needs to be ruled out. In fact, the vagina is one of the most common gynecologic organs targeted by metastatic disease (Cancer 1984;53:1978). Possible sites of origin for vaginal metastases include cervix, endometrium, ovary, kidney and colon. The patient often has a known carcinoma, but the metastasis may also represent the initial presentation.
Only a few dozen colorectal carcinomas metastatic to the vagina have been characterized in the literature (Int J Surg 2013;11:1048). Average patient age is about 60 years. Vaginal bleeding is the most common presenting symptom and roughly one third of patients have widely metastatic disease.
Most tumors show typical morphology with variable mucin production, atypical columnar cells with hyperchromatic nuclei, brisk mitoses and central "dirty" necrosis filling the glandular lumens. Immunohistochemistry is confirmatory, with metastatic colorectal carcinoma being positive for CK20 and CDX2 and negative for CK7 (as in this case). In general, primary vaginal adenocarcinomas show the opposite pattern (positive for CK7, negative for CK20 and CDX2).
Most primary vaginal adenocarcinomas are either clear cell adenocarcinomas or endometrioid adenocarcinoma. Clear cell adenocarcinomas are often seen in patients with a history of intrauterine diethylstilbestrol exposure. These patients are young (average age around 20 years), while patients without this exposure history are generally middle-aged or older. Histology shows tubulocystic, papillary or solid patterns and cells with hobnail nuclei and eosinophilic to clear cytoplasm. Endometrioid adenocarcinoma of the vagina usually arises from endometriosis and can be very difficult to distinguish from a uterine metastasis without careful clinical workup.
Rare types of vaginal adenocarcinoma include mesonephric adenocarcinoma (glands are eosinophilic and often cribriform) and mucinous adenocarcinoma (similar to cervical counterpart, and may arise from endocervicosis). Gastric-type adenocarcinoma, typically a well differentiated variant of cervical cancer, has recently been reported to arise in the vagina (Am J Surg Pathol 2018;42:958). It is CDX2 positive, and usually CK7 positive and CK20 negative. It may mimic vaginal adenosis.
Test question answer:
B. 20%