27 February 2019 - Case of the Week #476
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Week page. To subscribe or unsubscribe to Case of the Week or our other email lists, click here.
Thanks to Dr. Ayesha Azam, University Hospital Coventry & Warwickshire (UK) for contributing this case; Dr. Akira Yoshikawa, Kameda Medical Center, Kamogawa City, Chiba (Japan) for writing the discussion; and Dr. Andrey Bychkov, Kameda Medical Center, Kamogawa City, Chiba (Japan) for the Editorial Board review. To contribute a Case of the Week, first make sure that we are currently accepting cases, then follow the guidelines on our main Case of the Week page.
Case of the Week #476
Clinical history:
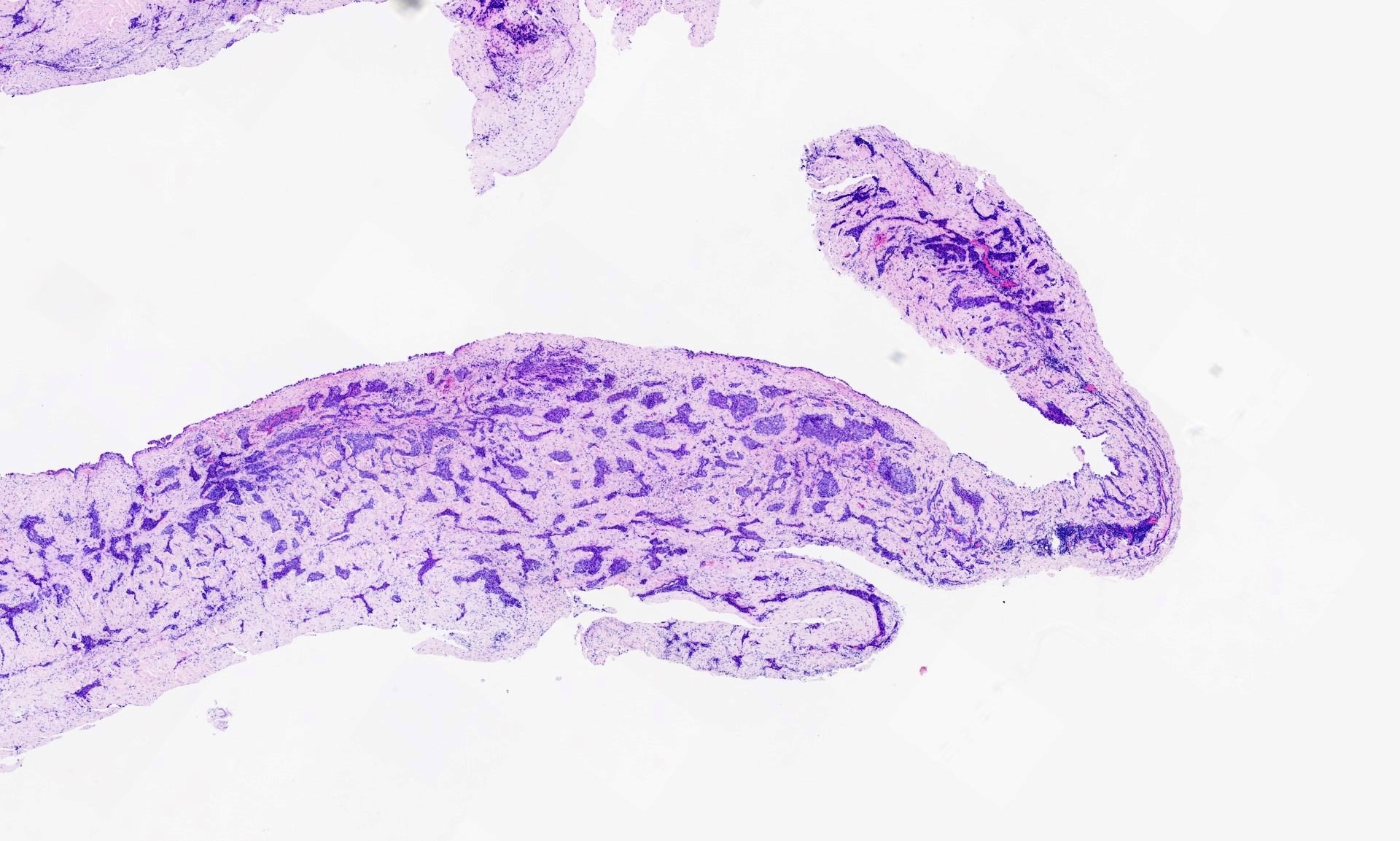
A 73 year old man with shortness of breath had bilateral pleural effusions, lung nodules and pleural thickening. A pleural biopsy was obtained. The specimen was 45 x 15 x 28 mm, and was a sheet of membranous pale grey tissue.
Histopathology images:
What is your diagnosis?
Diagnosis:
Epithelioid mesothelioma
Test question (answer at the end):
Which set of antibodies is useful for distinguishing pleural malignant mesothelioma from lung adenocarcinoma?
A. WT1, CA125, BerEP4 (EpCAM)
B. CA125, BerEP4, Calretinin
C. BerEP4, Calretinin, AE1/AE3
D. WT1, BerEP4, Calretinin
E. WT1, BerEP4, AE1/AE3
Stains:
Discussion:
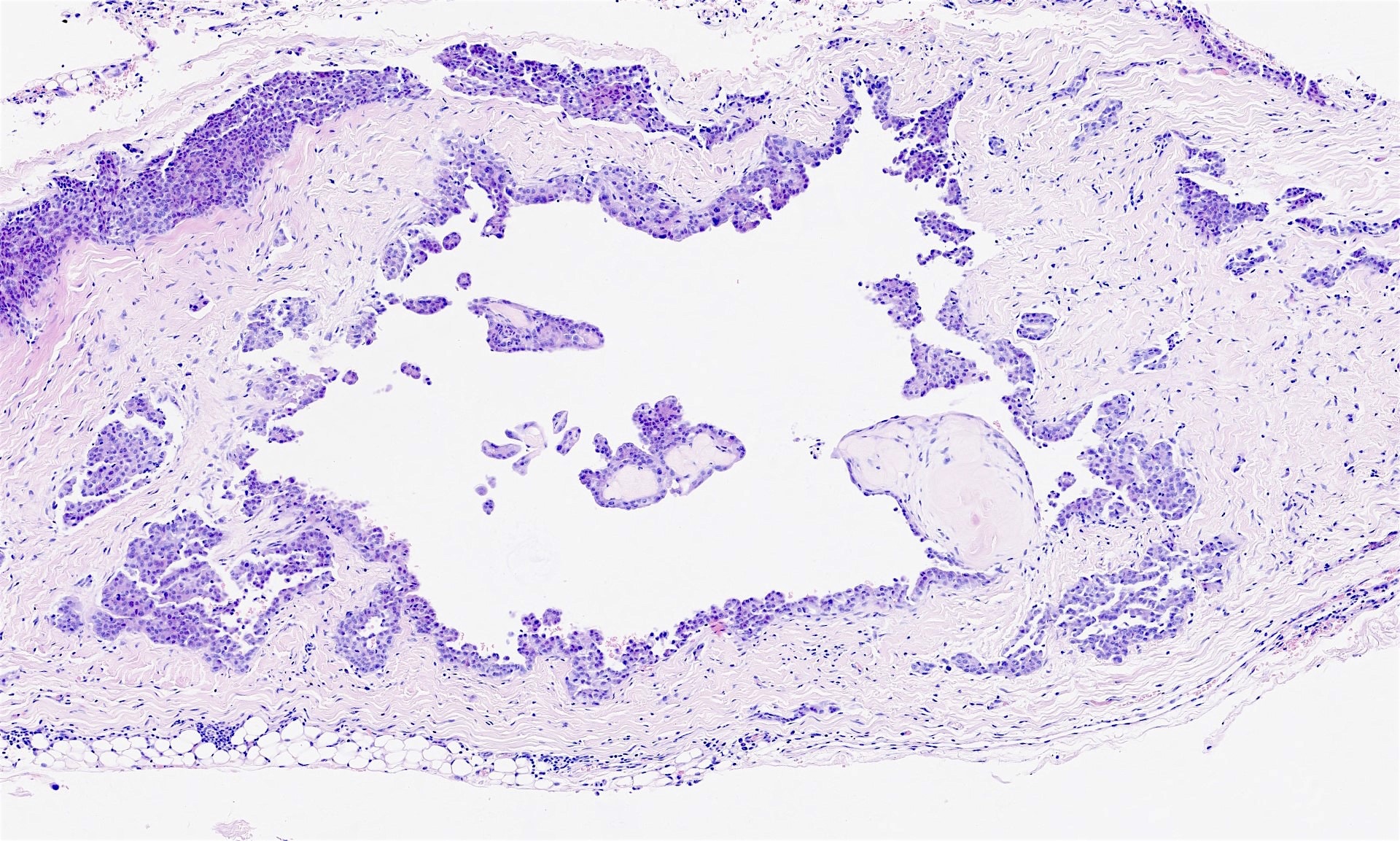
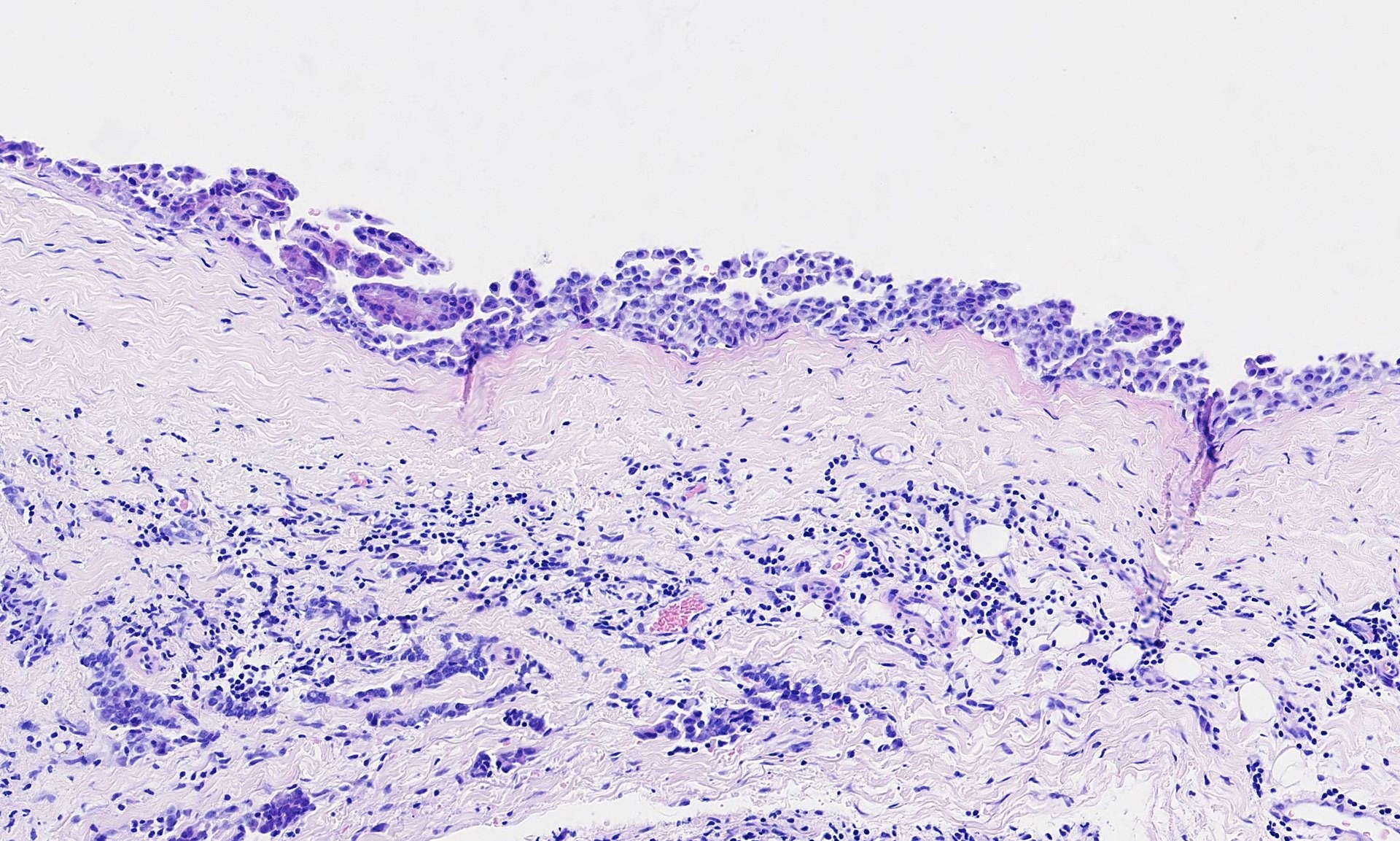
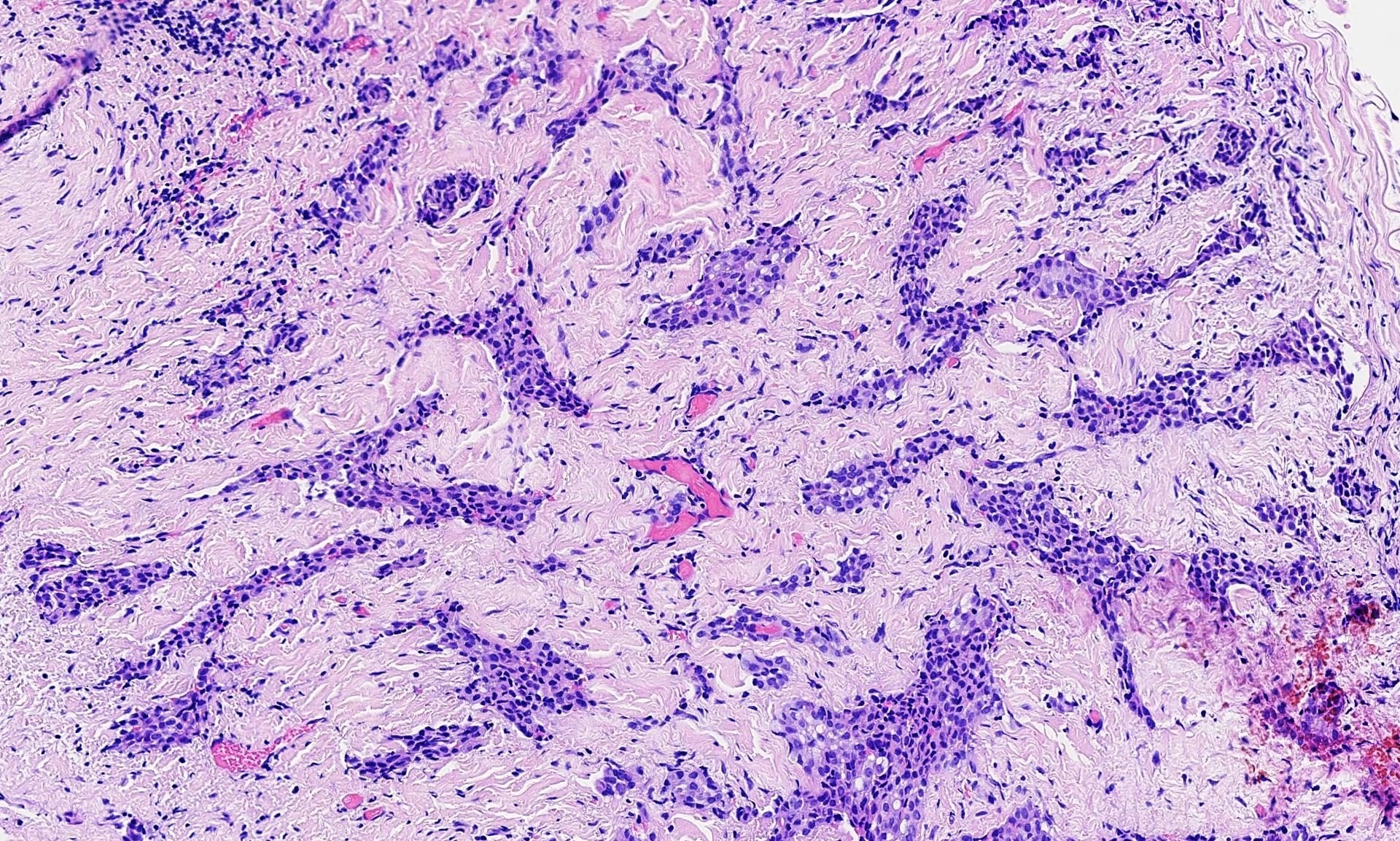
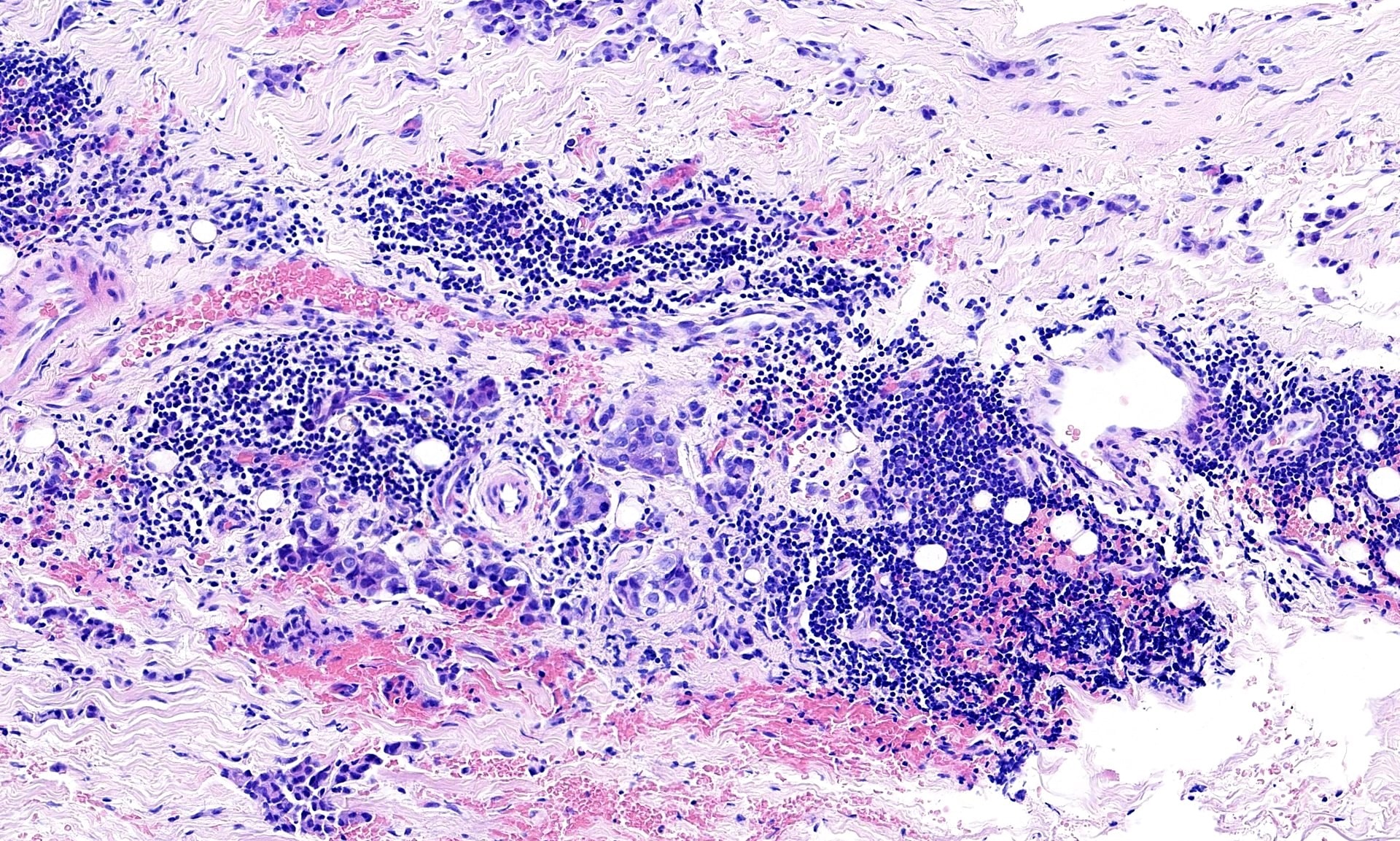
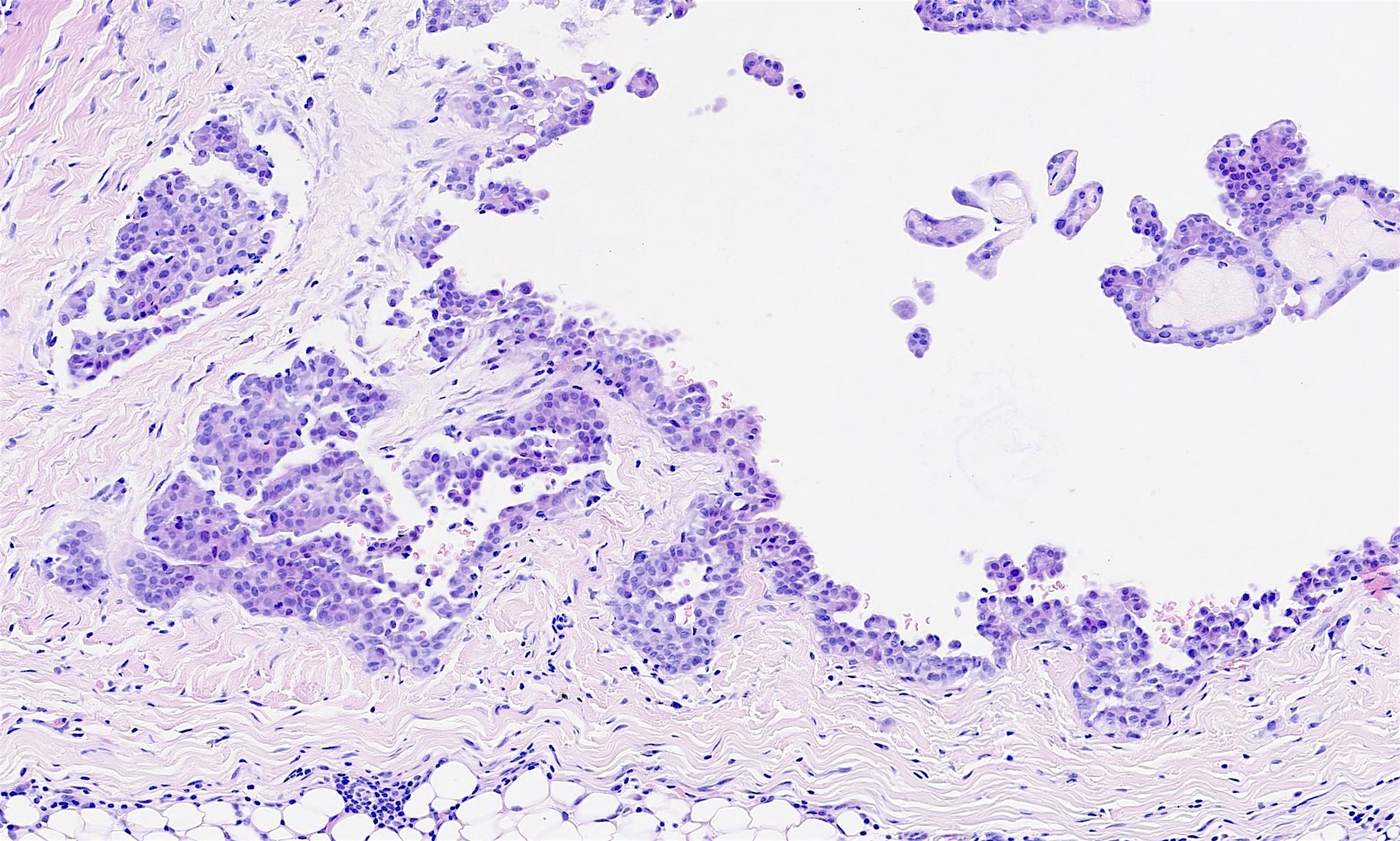
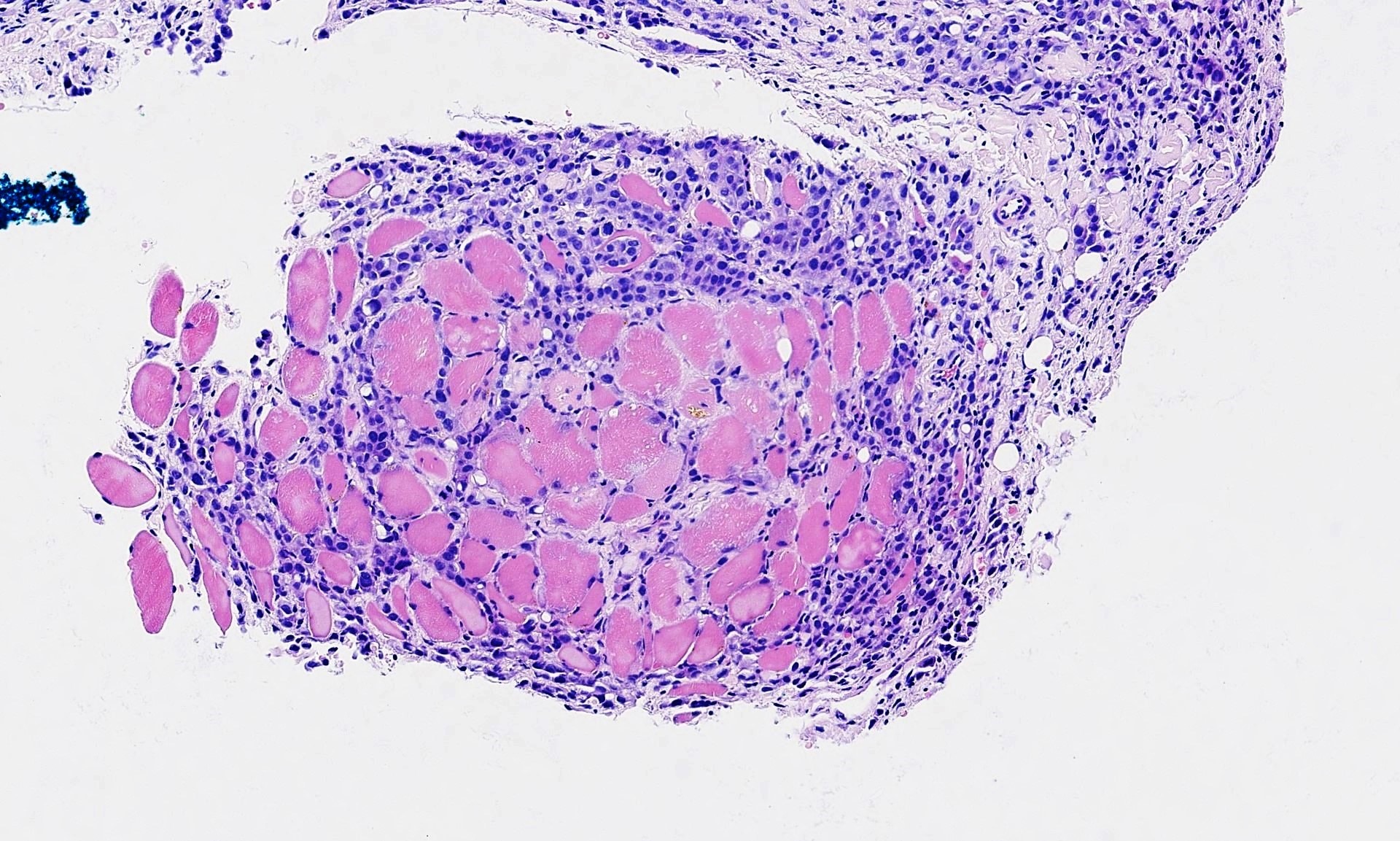
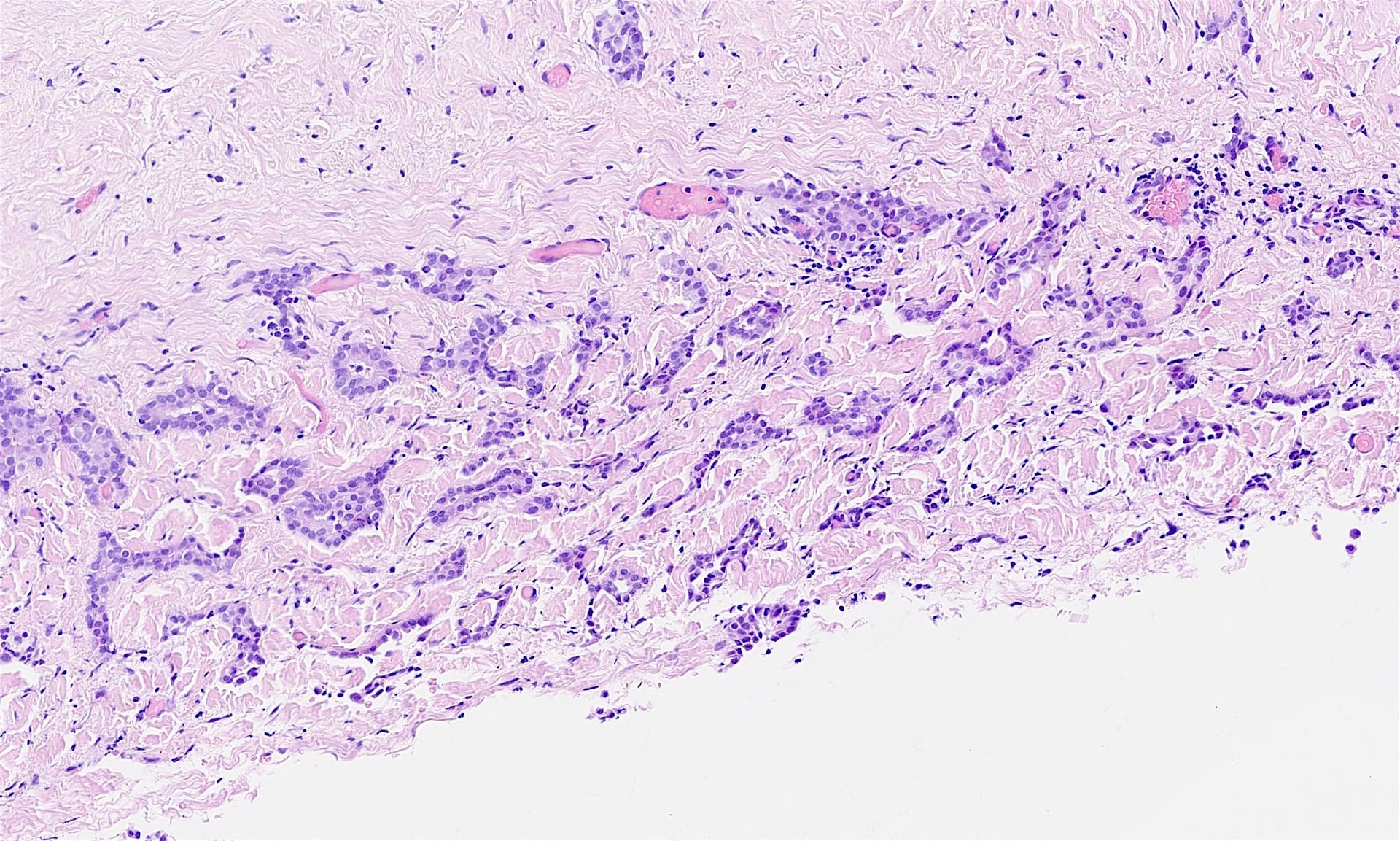
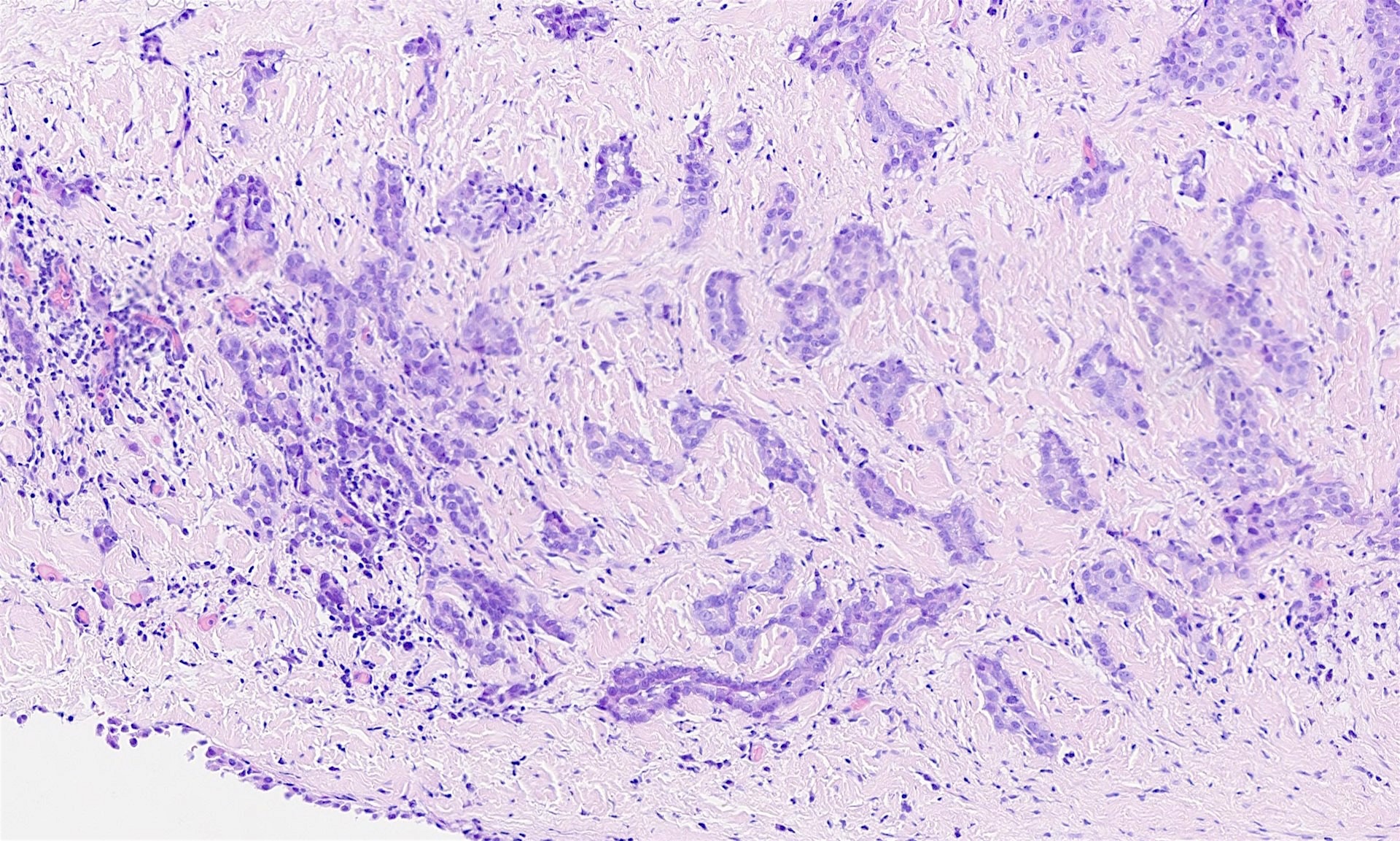
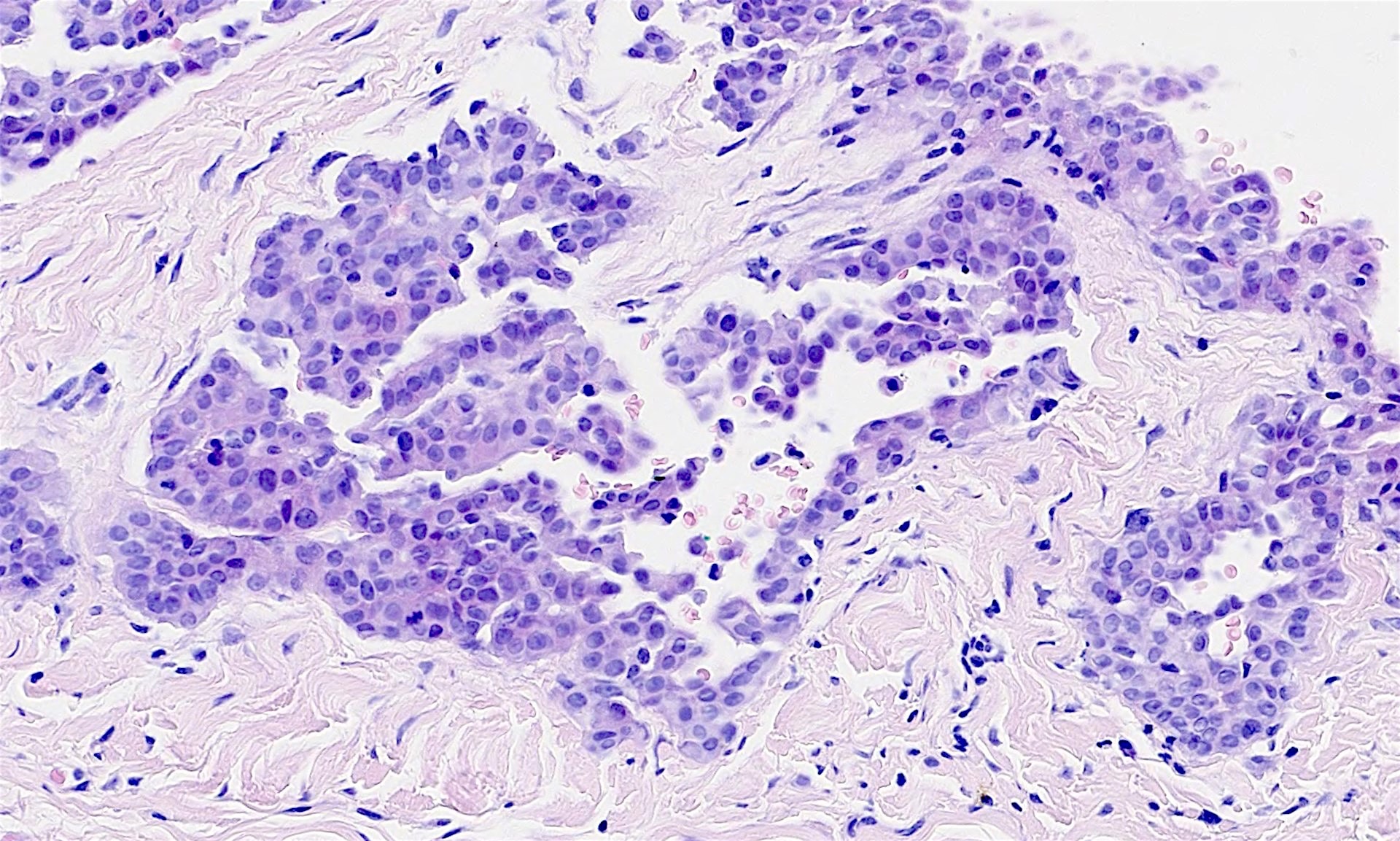
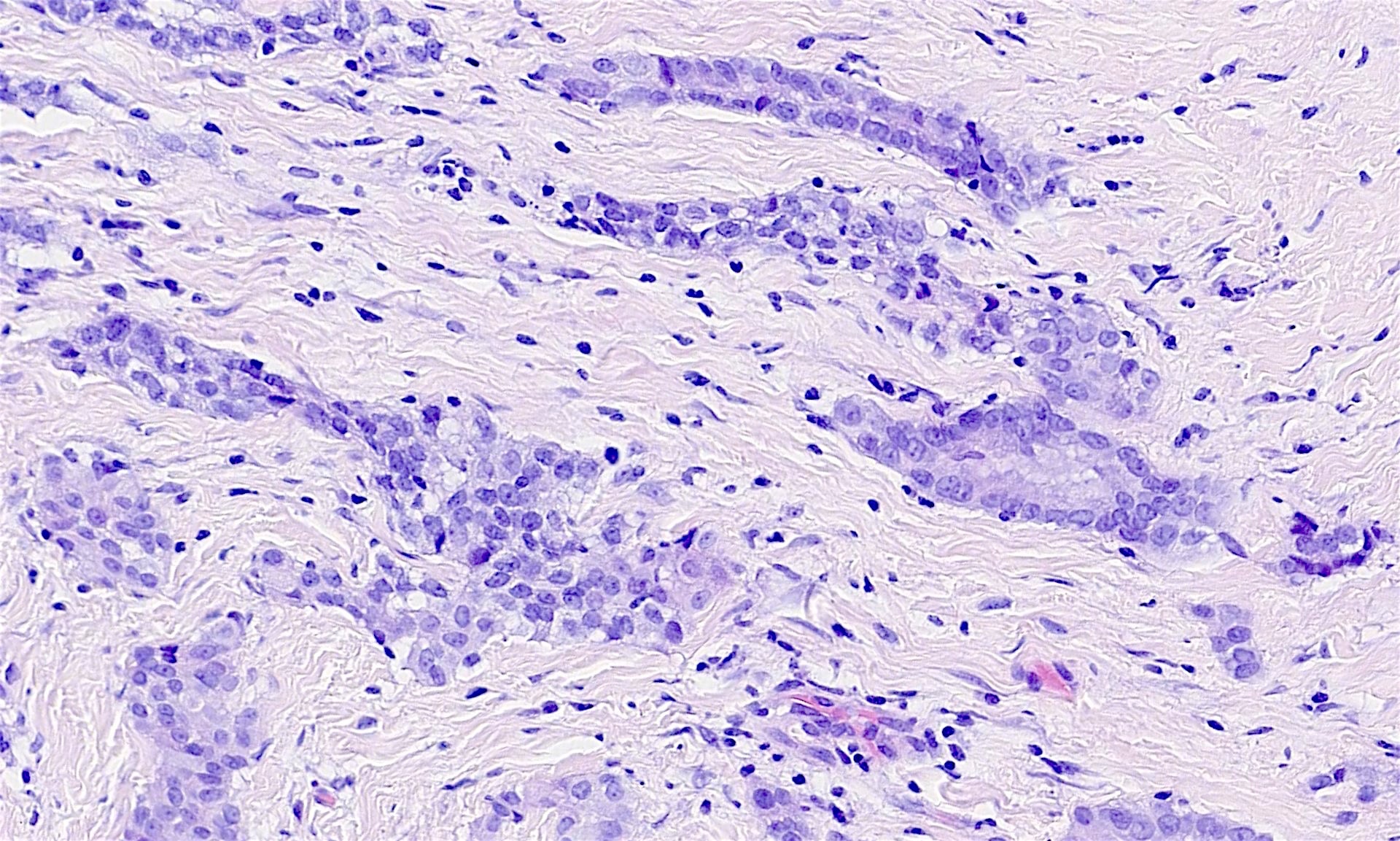
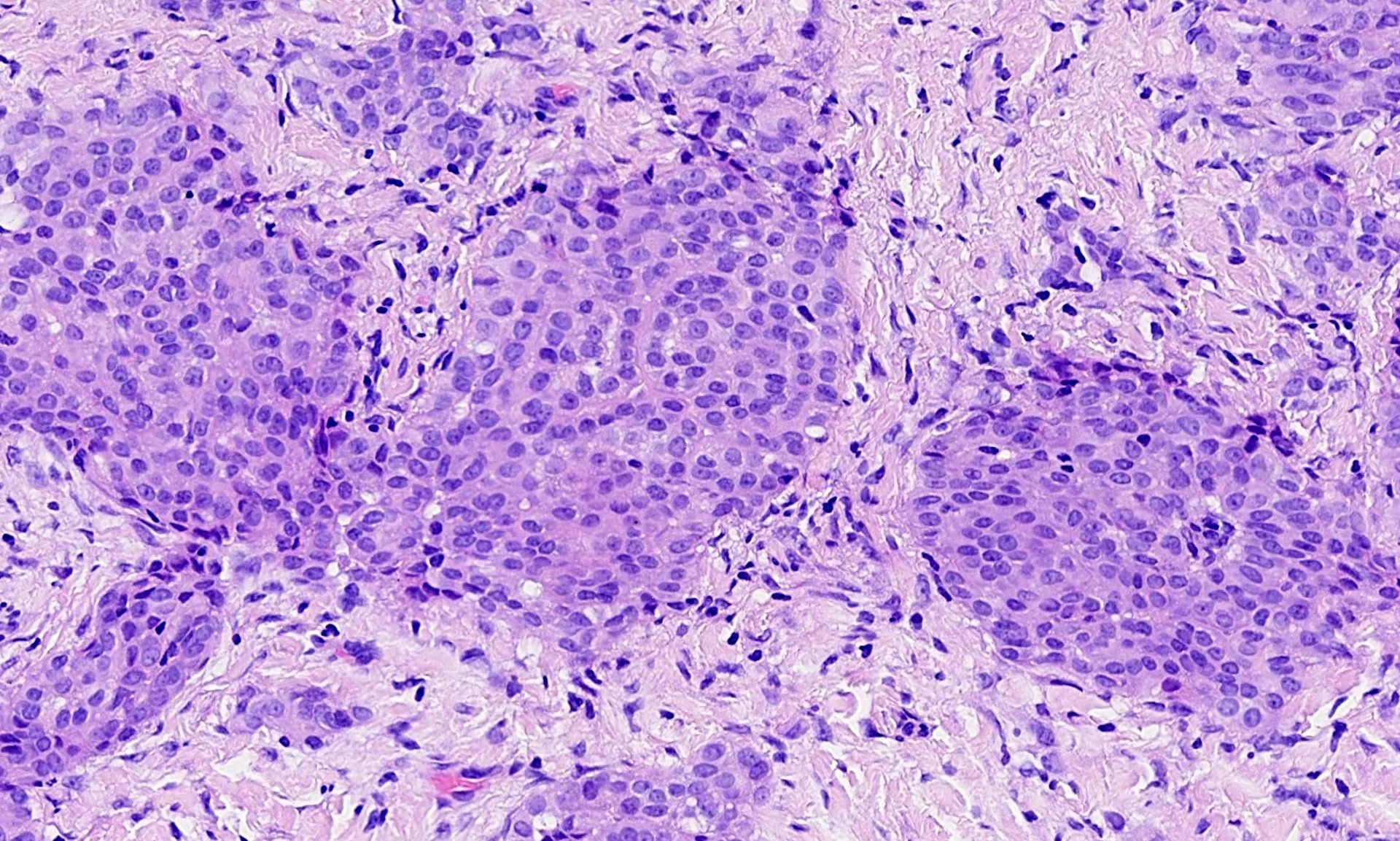
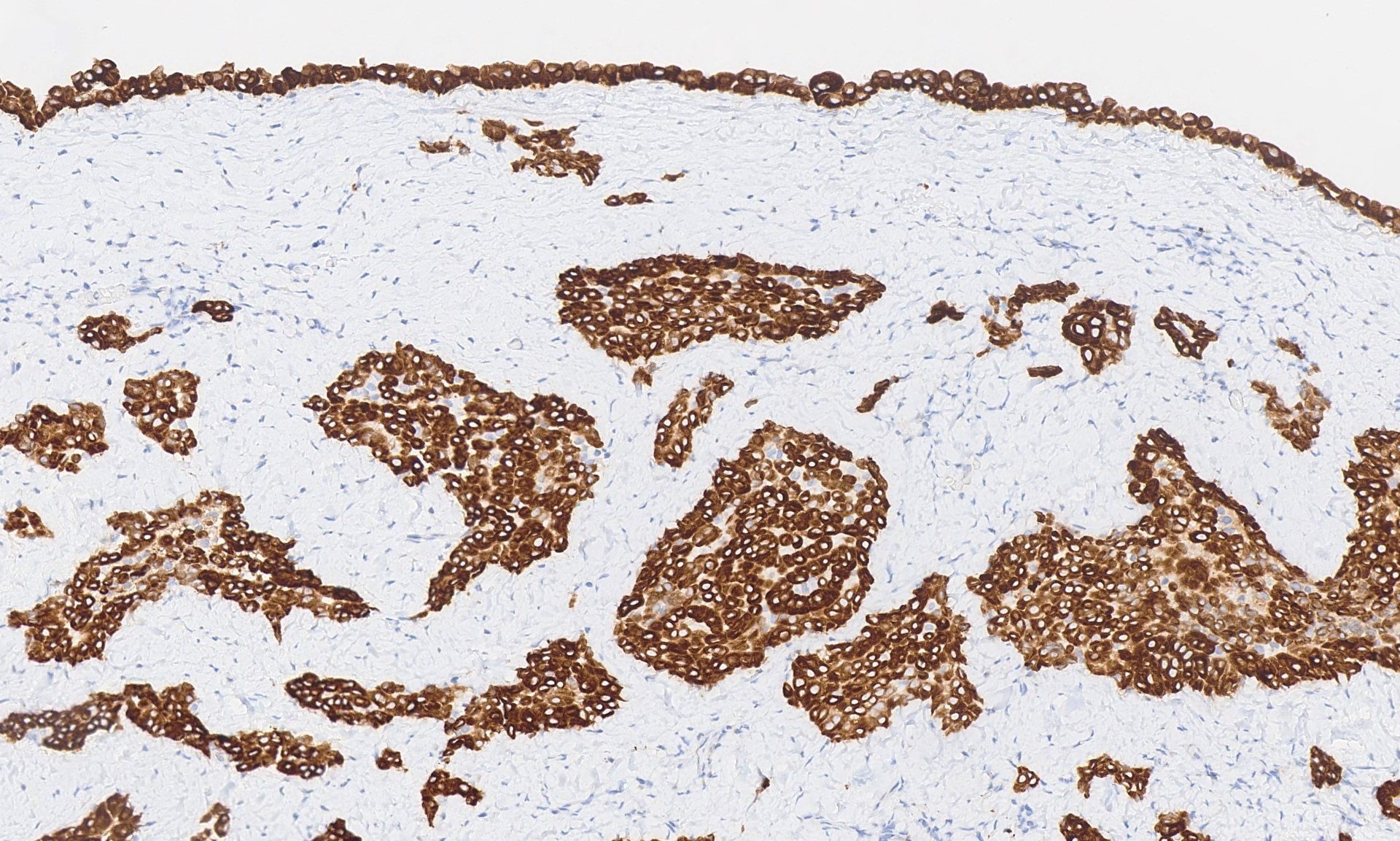
The pleural biopsy is heavily infiltrated by a malignant epithelioid neoplasm. Tumor cells are arranged in small nests, irregular strands and tubular gland-like structures surrounded by fibrous tissue. There is moderate cytological atypia with nuclear shape variation, increased nuclear-cytoplasmic ratio, some prominent nucleoli and a few intracytoplasmic vacuoles. The tumor focally infiltrates into adipose and underlying skeletal muscle. The overlying mesothelial lining shows nuclear atypia, multilayering and papillary architecture.
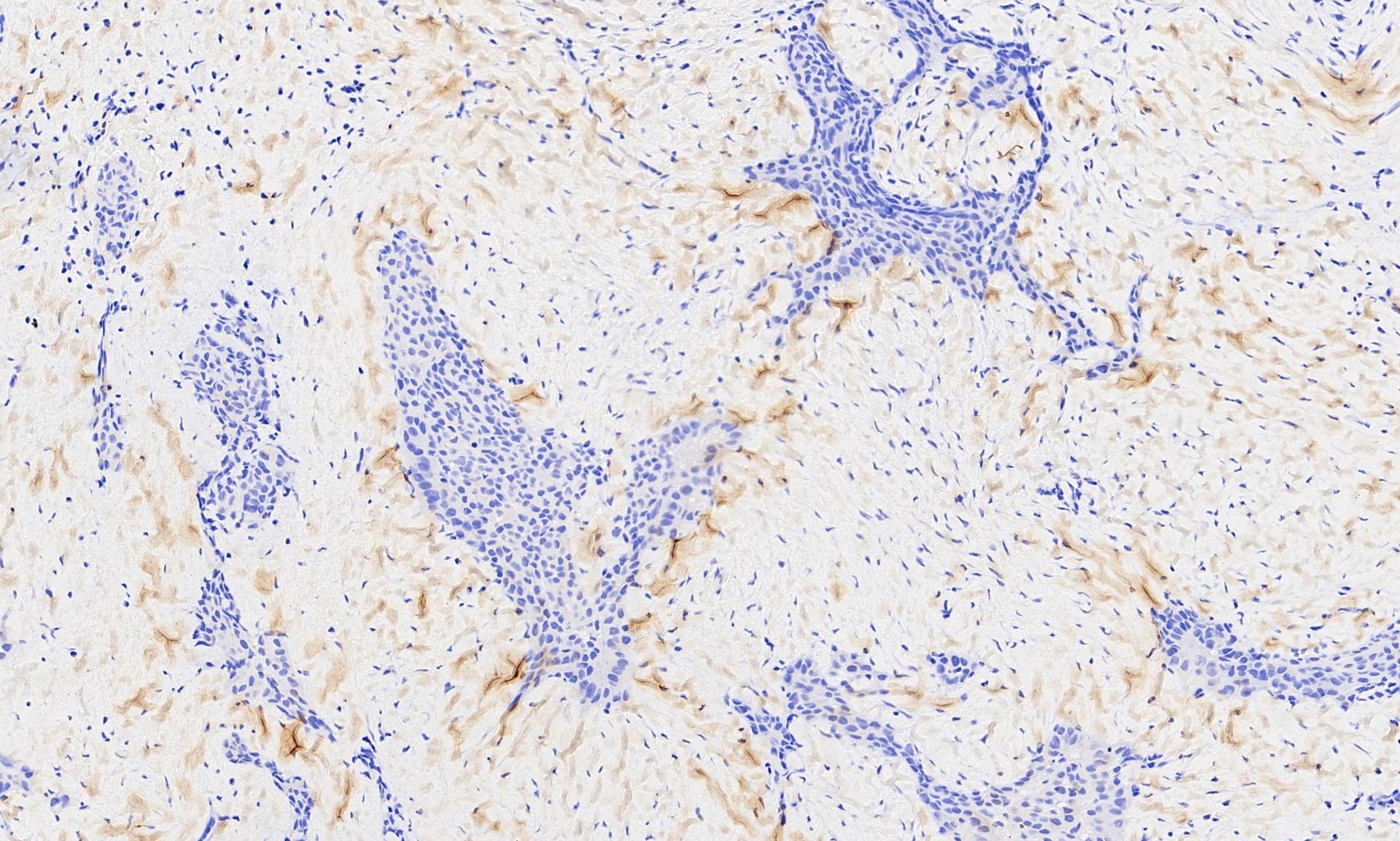
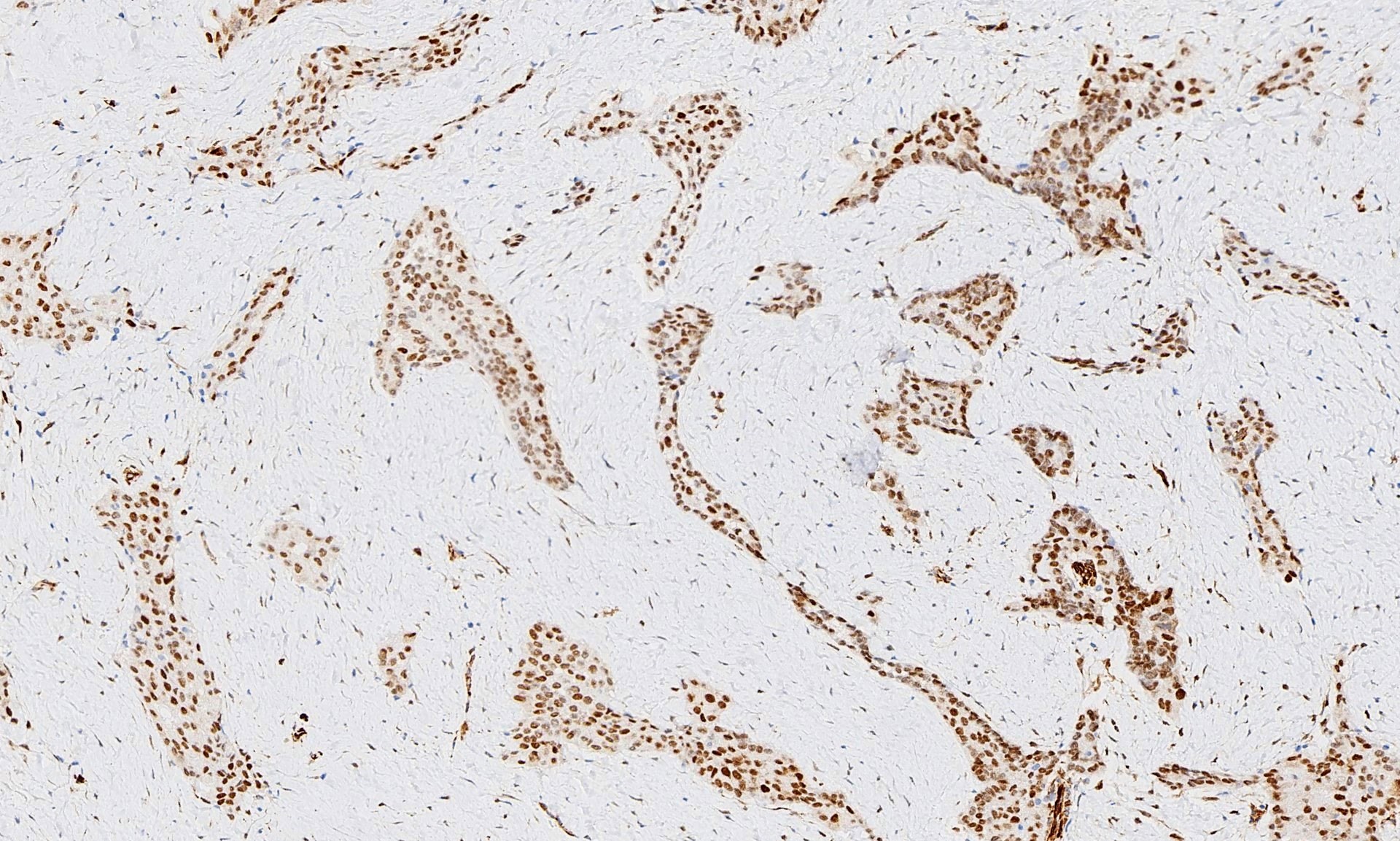
Immunohistochemistry was positive for WT1, CK5/CK6 and calretinin and negative for BerEP4, MOC31, synaptophysin, chromogranin and CD56 (occasional cells positive). The morphologic features and immunoprofile are consistent with malignant mesothelioma – epithelioid type. No spindle cell areas (sarcomatoid component) are seen. Correlation with radiological and clinical features is advised in these cases.
Pleural malignant mesothelioma is a rare tumor of the thoracic cavity with a very poor prognosis. It is difficult to treat early because of lack of symptoms or nonspecific symptoms including cough, dyspnea and chest pain. Most patients are age 60 or older with male predominance (M:F = 4:1). Its major risk factor is asbestos exposure (J Toxicol Environ Health B Crit Rev 2016;19:250). CT shows diffuse pleural thickening or nodules with effusion. Cytology of pleural effusion is often sensitive enough for diagnosis but some cases require pleural biopsy for definite diagnosis (Cytojournal 2015;12:26).
Two year survival varies from 46% (stage IA) to 17% (stage IV, American Cancer Society: Survival Statistics for Mesothelioma [Accessed 25 February 2019]). Treatment may include resection (extrapleural pneumonectomy and pneumonectomy/decortication), chemotherapy and radiotherapy.
Malignant mesothelioma has three subtypes: epithelioid, sarcomatoid and biphasic (mixed) (WHO Classification of Tumours of the Lung, Pleura, Thymus and Heart, 4th edition [Accessed 25 February 2019]). The epithelioid subtype is the most common, and has cuboidal cells in glandular, tubular or papillary clusters. The sarcomatoid subtype has spindle cells but may contain heterogenous features such as histiocytic, rhabromyosarcomatous and osteosarcomatous figures (Arch Pathol Lab Med 2018;142:89).
Immunohistochemistry and molecular studies play an important role in differentiating malignant mesothelioma from its morphological mimics. Immunohistochemistry for WT1, calretinin, CK 5/6 and D2-40 is positive in epithelioid malignant mesothelioma and typically negative in lung adenocarcinoma (Arch Pathol Lab Med 2018;142:89). Combined testing of BAP1 immunohistochemistry and p16 FISH differentiates malignant mesothelioma (BAP negative with homozygous deletion for p16) and benign mesothelial proliferation (Am J Surg Pathol 2015;39:977). HEG1, 5-hmC, MET, MTAP and EZH2 are reported by recent studies to be potentially useful diagnostic and prognostic markers (Lung Cancer 2019;127:69, Histopathology 2017;70:722, Arch Pathol Lab Med 2018;142:1549, Mod Pathol 2018 [Epub ahead of print]).
Test question answer:
D. WT1 and calretinin are specific for mesothelial cells and BerEP4 is specific for lung adenocarcinoma. CA125 and AE1/AE3 are immunoreactive in both mesothelioma and adenocarcinoma.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Week page. To subscribe or unsubscribe to Case of the Week or our other email lists, click here.
Thanks to Dr. Ayesha Azam, University Hospital Coventry & Warwickshire (UK) for contributing this case; Dr. Akira Yoshikawa, Kameda Medical Center, Kamogawa City, Chiba (Japan) for writing the discussion; and Dr. Andrey Bychkov, Kameda Medical Center, Kamogawa City, Chiba (Japan) for the Editorial Board review. To contribute a Case of the Week, first make sure that we are currently accepting cases, then follow the guidelines on our main Case of the Week page.
Case of the Week #476
Clinical history:
A 73 year old man with shortness of breath had bilateral pleural effusions, lung nodules and pleural thickening. A pleural biopsy was obtained. The specimen was 45 x 15 x 28 mm, and was a sheet of membranous pale grey tissue.
Histopathology images:
What is your diagnosis?
Diagnosis:
Epithelioid mesothelioma
Test question (answer at the end):
Which set of antibodies is useful for distinguishing pleural malignant mesothelioma from lung adenocarcinoma?
A. WT1, CA125, BerEP4 (EpCAM)
B. CA125, BerEP4, Calretinin
C. BerEP4, Calretinin, AE1/AE3
D. WT1, BerEP4, Calretinin
E. WT1, BerEP4, AE1/AE3
Stains:
Discussion:
The pleural biopsy is heavily infiltrated by a malignant epithelioid neoplasm. Tumor cells are arranged in small nests, irregular strands and tubular gland-like structures surrounded by fibrous tissue. There is moderate cytological atypia with nuclear shape variation, increased nuclear-cytoplasmic ratio, some prominent nucleoli and a few intracytoplasmic vacuoles. The tumor focally infiltrates into adipose and underlying skeletal muscle. The overlying mesothelial lining shows nuclear atypia, multilayering and papillary architecture.
Immunohistochemistry was positive for WT1, CK5/CK6 and calretinin and negative for BerEP4, MOC31, synaptophysin, chromogranin and CD56 (occasional cells positive). The morphologic features and immunoprofile are consistent with malignant mesothelioma – epithelioid type. No spindle cell areas (sarcomatoid component) are seen. Correlation with radiological and clinical features is advised in these cases.
Pleural malignant mesothelioma is a rare tumor of the thoracic cavity with a very poor prognosis. It is difficult to treat early because of lack of symptoms or nonspecific symptoms including cough, dyspnea and chest pain. Most patients are age 60 or older with male predominance (M:F = 4:1). Its major risk factor is asbestos exposure (J Toxicol Environ Health B Crit Rev 2016;19:250). CT shows diffuse pleural thickening or nodules with effusion. Cytology of pleural effusion is often sensitive enough for diagnosis but some cases require pleural biopsy for definite diagnosis (Cytojournal 2015;12:26).
Two year survival varies from 46% (stage IA) to 17% (stage IV, American Cancer Society: Survival Statistics for Mesothelioma [Accessed 25 February 2019]). Treatment may include resection (extrapleural pneumonectomy and pneumonectomy/decortication), chemotherapy and radiotherapy.
Malignant mesothelioma has three subtypes: epithelioid, sarcomatoid and biphasic (mixed) (WHO Classification of Tumours of the Lung, Pleura, Thymus and Heart, 4th edition [Accessed 25 February 2019]). The epithelioid subtype is the most common, and has cuboidal cells in glandular, tubular or papillary clusters. The sarcomatoid subtype has spindle cells but may contain heterogenous features such as histiocytic, rhabromyosarcomatous and osteosarcomatous figures (Arch Pathol Lab Med 2018;142:89).
Immunohistochemistry and molecular studies play an important role in differentiating malignant mesothelioma from its morphological mimics. Immunohistochemistry for WT1, calretinin, CK 5/6 and D2-40 is positive in epithelioid malignant mesothelioma and typically negative in lung adenocarcinoma (Arch Pathol Lab Med 2018;142:89). Combined testing of BAP1 immunohistochemistry and p16 FISH differentiates malignant mesothelioma (BAP negative with homozygous deletion for p16) and benign mesothelial proliferation (Am J Surg Pathol 2015;39:977). HEG1, 5-hmC, MET, MTAP and EZH2 are reported by recent studies to be potentially useful diagnostic and prognostic markers (Lung Cancer 2019;127:69, Histopathology 2017;70:722, Arch Pathol Lab Med 2018;142:1549, Mod Pathol 2018 [Epub ahead of print]).
Test question answer:
D. WT1 and calretinin are specific for mesothelial cells and BerEP4 is specific for lung adenocarcinoma. CA125 and AE1/AE3 are immunoreactive in both mesothelioma and adenocarcinoma.