17 April 2019 - Case of the Month #478
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Nay Myo Wai, Grand Mandalay Hospital, Mandalay (Myanmar) for contributing this case and Dr. Katrina Krogh Northwestern University McGaw Medical Center and Feinberg School of Medicine, Chicago, Illinois (USA), for writing the discussion. To contribute a Case of the Month, first make sure that we are currently accepting cases, then follow the guidelines on our main Case of the Month page.
Advertisement
Case of the Month #478
Clinical history:
A 79 year old woman presented with a painful 4 x 3 x 3 cm left breast lump for one year, no regional lymph node enlargement or nipple discharge. Excisional biopsy was done.
Gross image:
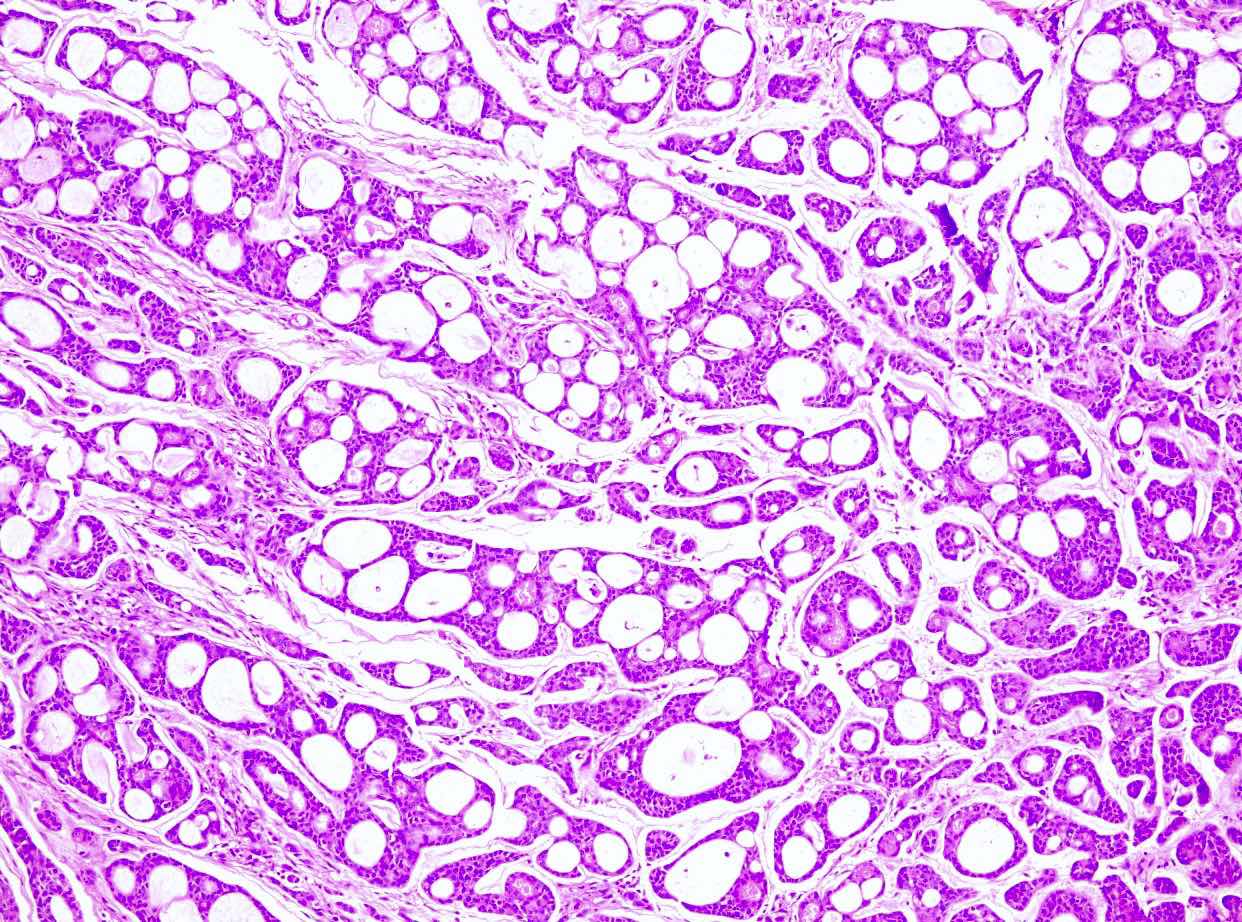
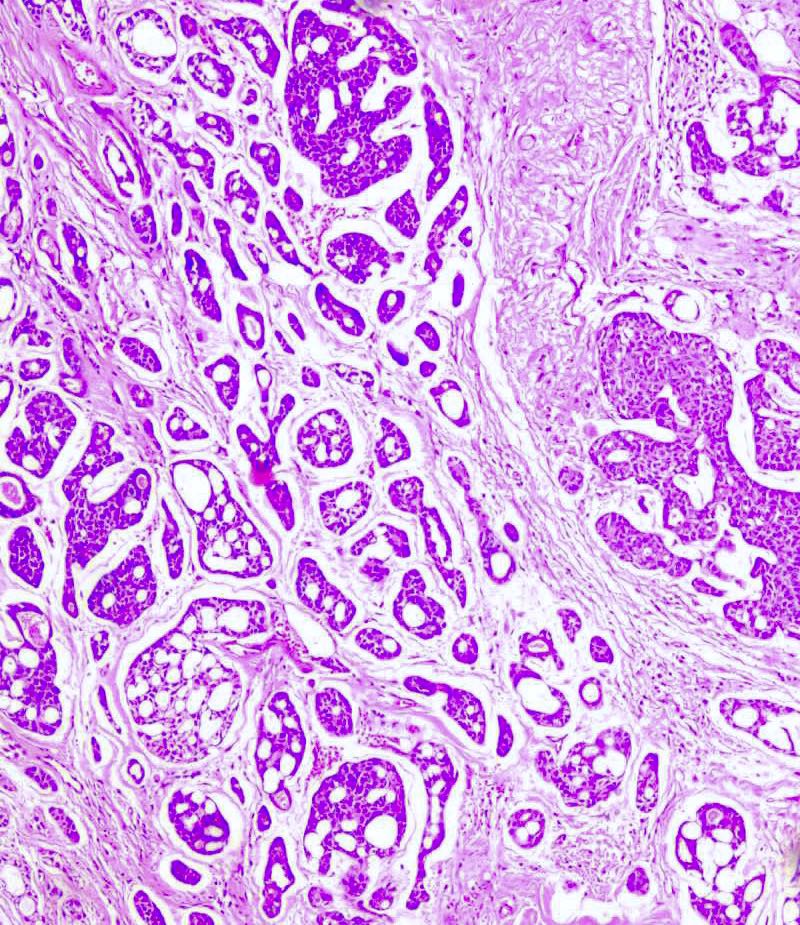
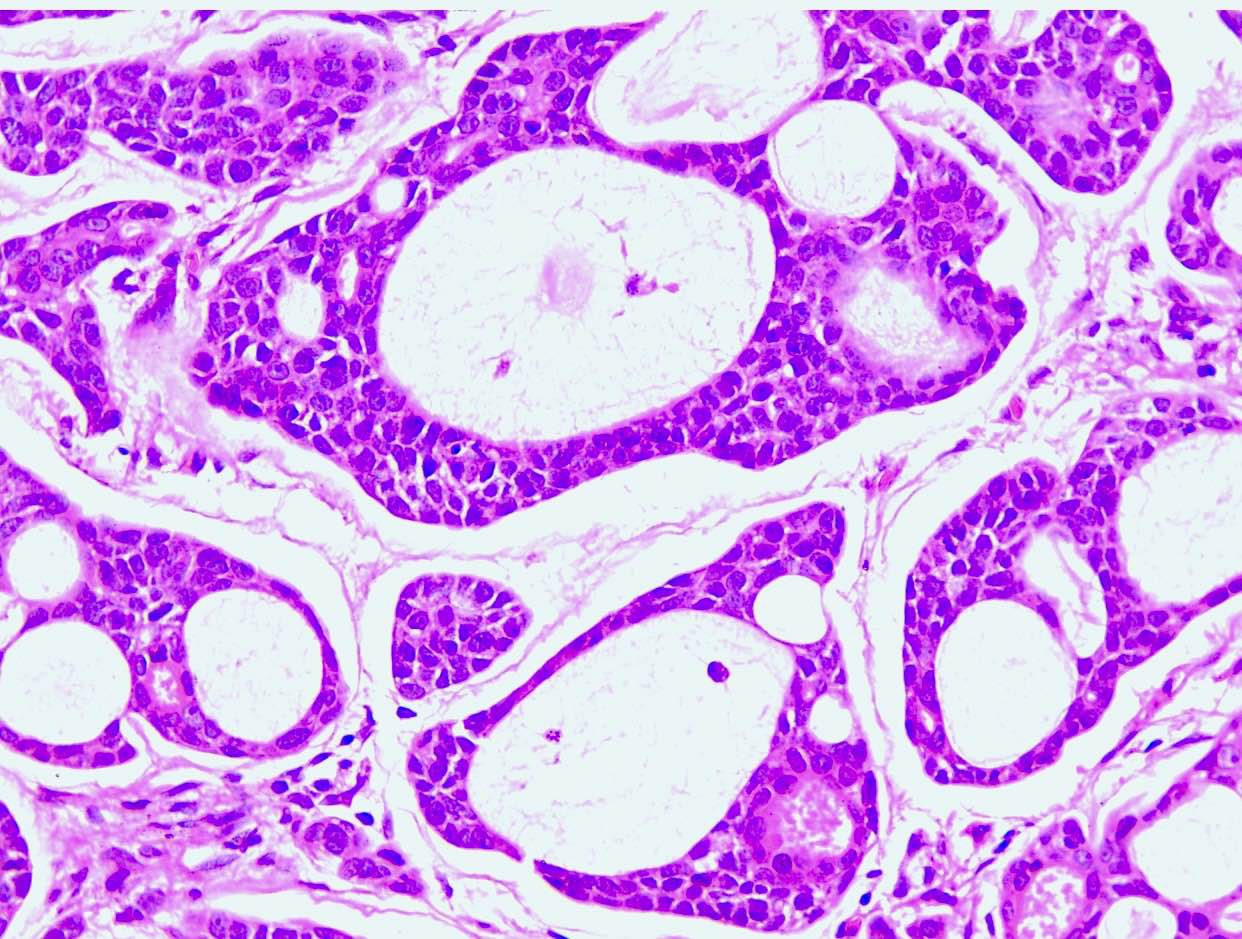
Histopathology images:
What is your diagnosis?
Diagnosis:
Adenoid cystic carcinoma
Test question (answer at the end):
Which of the following is true about adenoid cystic carcinoma of the breast?
A. Primary adenoid cystic carcinomas of the breast are more likely to have regional lymph node metastases than invasive ductal carcinoma, NOS.
B. The incidence of adenoid cystic carcinoma of the breast is widely accepted to be ~5%.
C. Adenoid cystic carcinoma of the breast is likely underdiagnosed.
D. HER2 positivity is common in adenoid cystic carcinoma of the breast.
E. Like adenoid cystic carcinoma of the salivary gland, CD117/KIT is positive in luminal-like cells in adenoid cystic carcinoma of the breast.
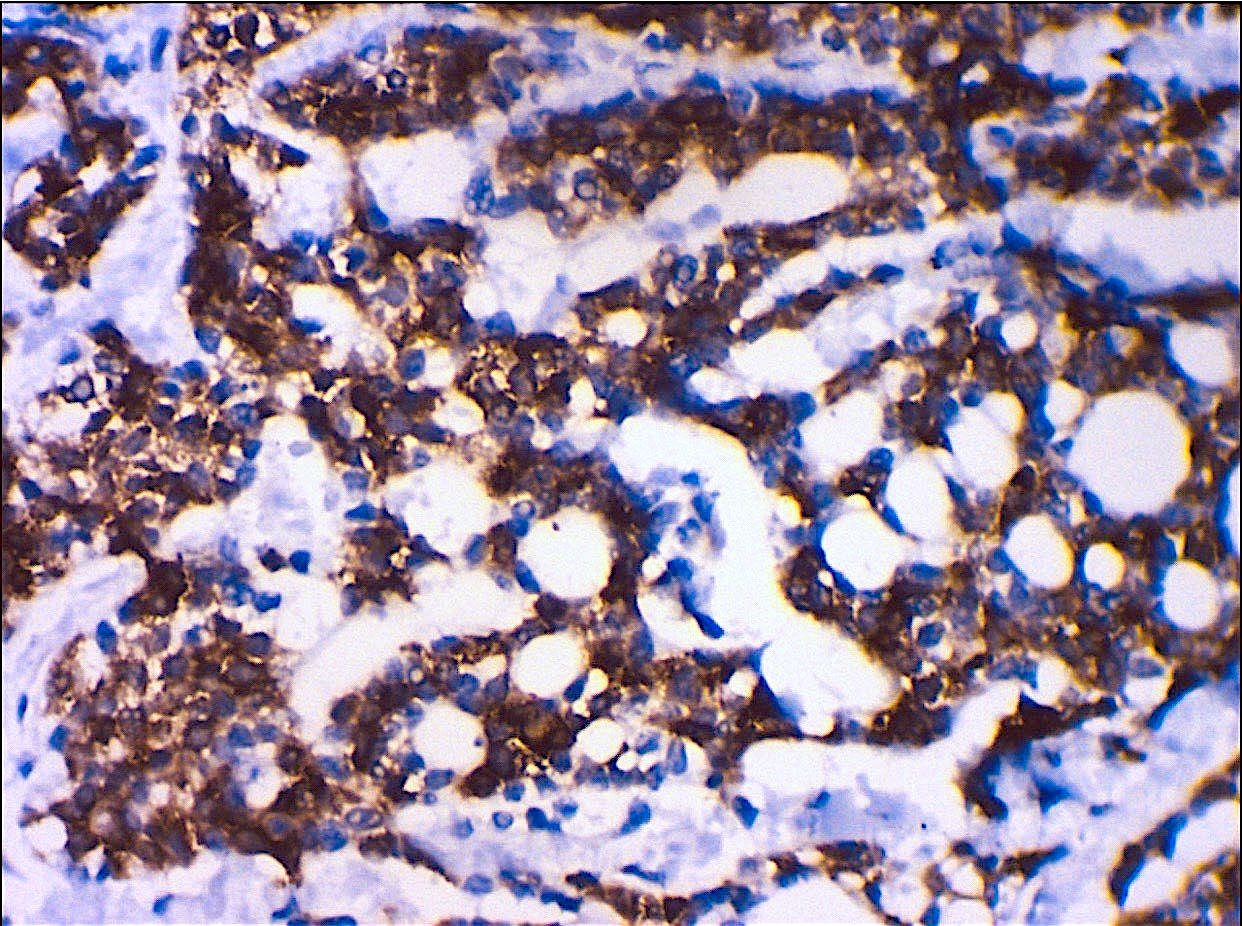
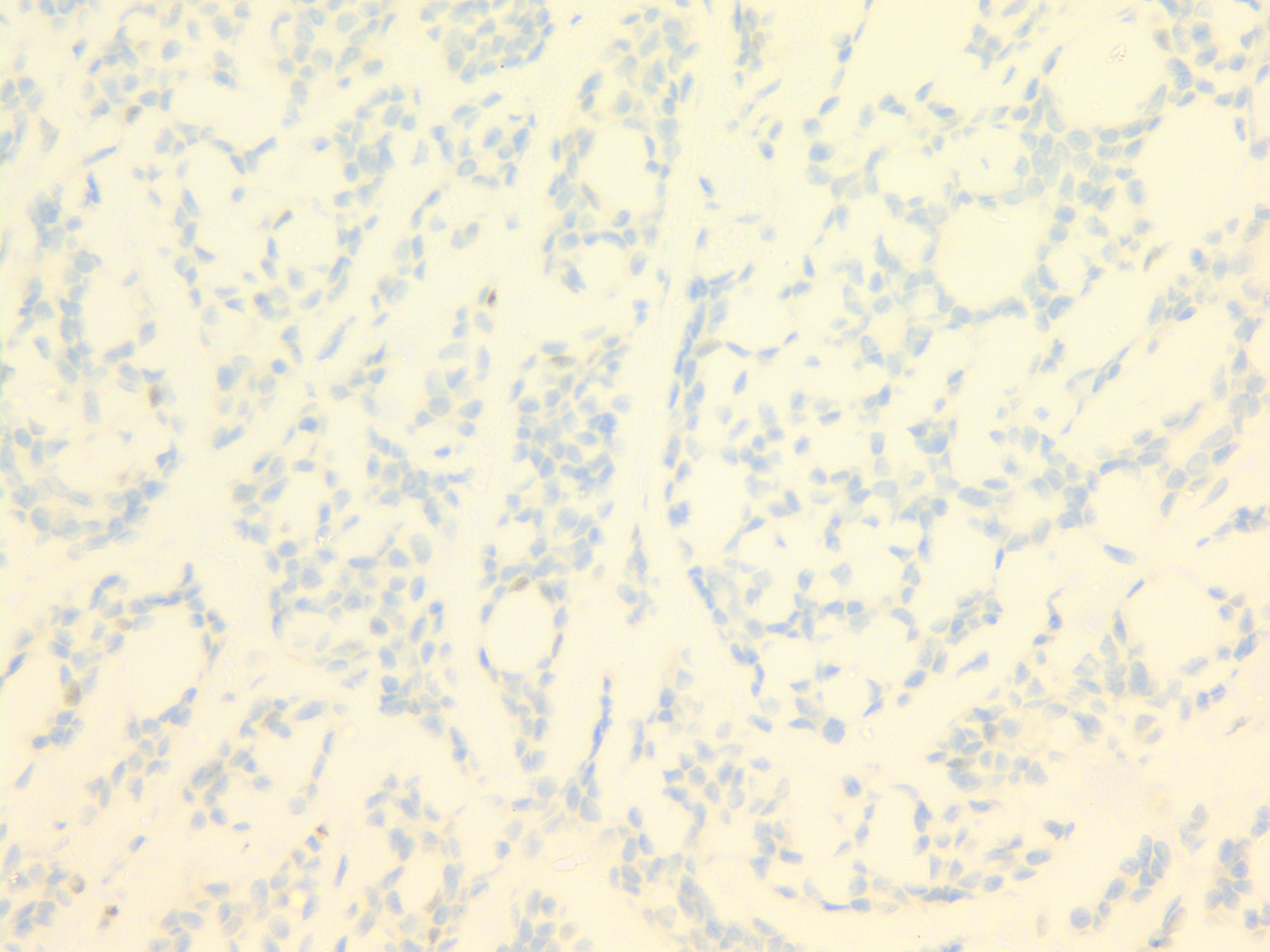
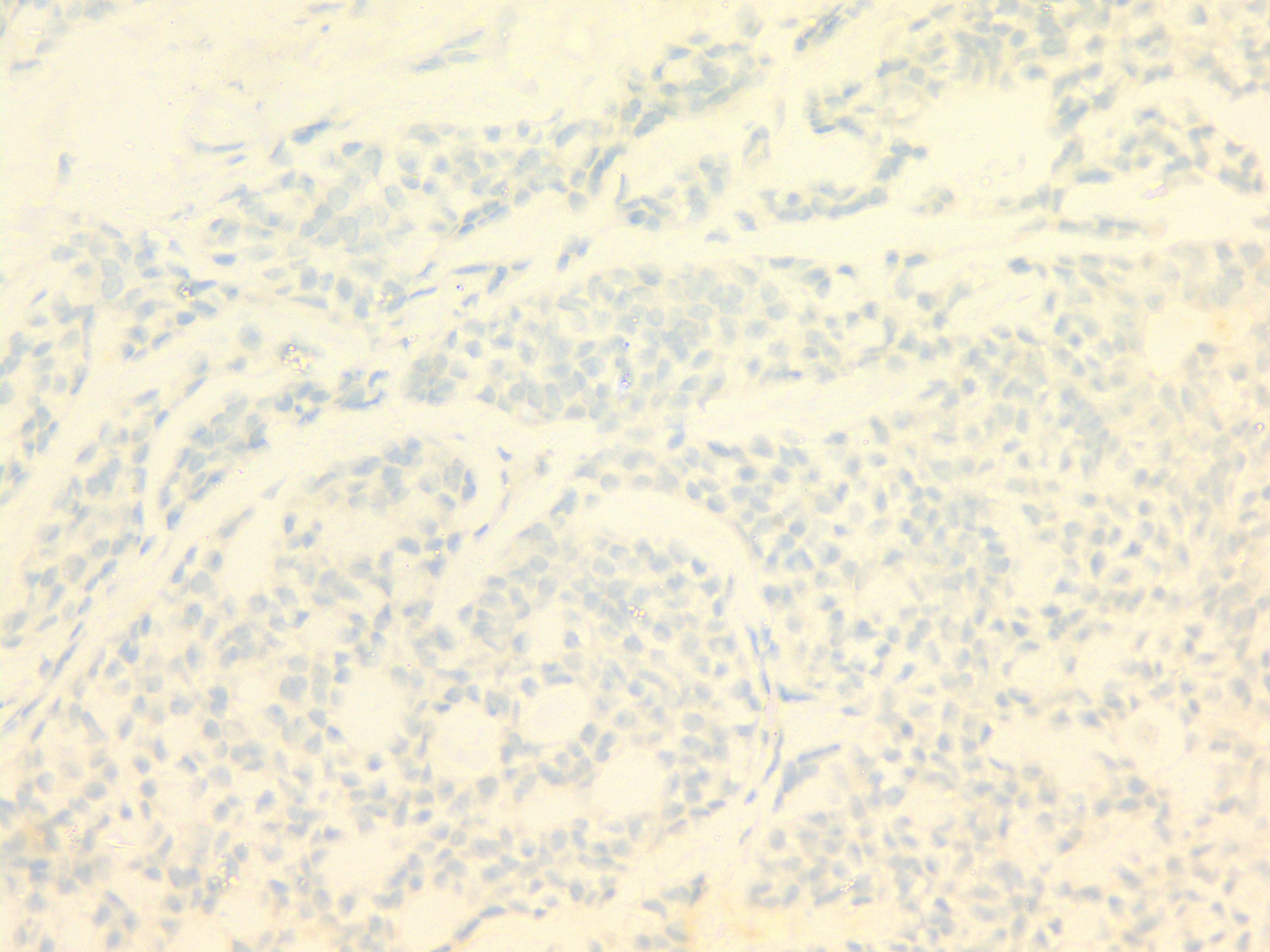
Stains:
Discussion:
Adenoid cystic carcinoma (ACC) of the breast is a low grade malignant tumor that is extremely rare (< 0.1% of all primary breast carcinomas) (Am J Surg 2002;183:646). Patients typically present with a palpable mass below the nipple that has been present for several years. The mass can be painless or tender and rarely presents as a mass on mammogram; when it does, it can appear lobulated or irregular. ACC of the breast usually occurs in women 50 - 65 years of age (range 30 - 97), though up to 1% of cases occur in males.
As in the salivary gland, ACC of the breast is composed of two neoplastic populations - luminal-like cells and myoepithelial-like cells. A small number of cases are associated with adenomyoepithelioma (Diagn Pathol 2014;9:148) or microglandular adenosis (Am J Surg Pathol 2003;27:1052) and while ACC may coincidentally arise in these lesions, most do not have an identifiable precursor lesion.
Ancillary studies, including immunohistochemistry and molecular testing, are useful for the diagnosis of ACC of the breast, which has the same translocation as ACC of the salivary gland, namely t(6;9)(q22-23;p23-24), resulting in a MYB-NFIB fusion gene (~ 90%) (J Pathol 2012;226:84). This leads to overexpression of MYB protein, causing overexpression of CD117/KIT in luminal-like cells (Mod Pathol 2005;18:1623). This translocation can be detected with FISH break apart probes and is generally not present in other basal-like breast carcinomas. In addition, hormone receptors are negative in ACC of the breast. The myoepithelial-like cells show positivity for p63, SMA, CK5/CK6, CK14, CK17 and calponin. The luminal-like cells show positivity for CK7, EMA, CEA and CD117/KIT.
Three histologic patterns are described in ACC of the breast: cribriform (most common), reticular-tubular (predominant stromal component surrounding tumor cells) and basaloid (solid, predominantly myoepithelial cells with few luminal-type cells). Of the three patterns, the basaloid pattern is most reported to result in lymph node metastases. Current histology grading correlates well with the prognosis, though some pathologists grade lesions based on the percentage of solid component. The prognosis in general is excellent (90 - 100% survival at 10 years) (Breast Cancer Res 2010;12:R54). Histologic subtype is more important than gene expression profile in predicting prognosis.
The differential diagnosis for ACC of the breast includes invasive cribriform carcinoma, ductal carcinoma in situ, cribriform type and collagenous spherulosis. Collagenous spherulosis is only a diagnostic consideration in small core needle biopsies. Both entities have two distinct cell populations and form basement membrane material from a myoepithelial cell population. In low to intermediate nuclear grade invasive cribriform carcinoma and ductal carcinoma in situ, tumor cells are usually positive for ER and PR and are negative for CD117/KIT.
ACC of the breast may be overdiagnosed, with up to 20% of reported cases not fulfilling the criteria. This can result in the incorrect treatment for patients with triple negative cancers and may account for the very rare cases reporting aggressive behavior. Distant metastasis and death are rare (~ 2%) (J Med Case Rep 2017;11:303) but when present most metastases occur in the lung. In addition, the tumor can recur after resection with a prolonged clinical course. It is important to note that unlike some primary breast carcinomas, patients with ACC of the breast do not have an increased risk of developing a second malignancy compared with the general population. ACC of the breast is usually cured with complete resection. In addition, local adjuvant radiotherapy can be used as a treatment.
Test question answer:
E. Specific MYB-NFIB gene fusion defines majority of ACC of the breast (~ 90%). This causes overexpression of the MYB gene, which causes overexpression of CD117 (c-kit) in luminal-like cells.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Nay Myo Wai, Grand Mandalay Hospital, Mandalay (Myanmar) for contributing this case and Dr. Katrina Krogh Northwestern University McGaw Medical Center and Feinberg School of Medicine, Chicago, Illinois (USA), for writing the discussion. To contribute a Case of the Month, first make sure that we are currently accepting cases, then follow the guidelines on our main Case of the Month page.

AP/CP Board Certified Pathologist
BOSTON, MASSACHUSETTS (USA) / GENERAL USA.
This is an exciting part-time opportunity for a pathologist with strong surgical pathology skills to provide pathology interpretation services for research and development efforts at PathAI (www.PathAI.com), based in Cambridge, Massachusetts. The part-time services can be performed remotely and over evenings/weekends, depending on your schedule and existing employment commitments. Candidates applying for this position must be certified by the American Board of Pathology and eligible to work in the US.
If interested in learning more, please send an email with your CV to Jobs@PathAI.com.
Case of the Month #478
Clinical history:
A 79 year old woman presented with a painful 4 x 3 x 3 cm left breast lump for one year, no regional lymph node enlargement or nipple discharge. Excisional biopsy was done.
Gross image:
Histopathology images:
What is your diagnosis?
Diagnosis:
Adenoid cystic carcinoma
Test question (answer at the end):
Which of the following is true about adenoid cystic carcinoma of the breast?
A. Primary adenoid cystic carcinomas of the breast are more likely to have regional lymph node metastases than invasive ductal carcinoma, NOS.
B. The incidence of adenoid cystic carcinoma of the breast is widely accepted to be ~5%.
C. Adenoid cystic carcinoma of the breast is likely underdiagnosed.
D. HER2 positivity is common in adenoid cystic carcinoma of the breast.
E. Like adenoid cystic carcinoma of the salivary gland, CD117/KIT is positive in luminal-like cells in adenoid cystic carcinoma of the breast.
Stains:
Discussion:
Adenoid cystic carcinoma (ACC) of the breast is a low grade malignant tumor that is extremely rare (< 0.1% of all primary breast carcinomas) (Am J Surg 2002;183:646). Patients typically present with a palpable mass below the nipple that has been present for several years. The mass can be painless or tender and rarely presents as a mass on mammogram; when it does, it can appear lobulated or irregular. ACC of the breast usually occurs in women 50 - 65 years of age (range 30 - 97), though up to 1% of cases occur in males.
As in the salivary gland, ACC of the breast is composed of two neoplastic populations - luminal-like cells and myoepithelial-like cells. A small number of cases are associated with adenomyoepithelioma (Diagn Pathol 2014;9:148) or microglandular adenosis (Am J Surg Pathol 2003;27:1052) and while ACC may coincidentally arise in these lesions, most do not have an identifiable precursor lesion.
Ancillary studies, including immunohistochemistry and molecular testing, are useful for the diagnosis of ACC of the breast, which has the same translocation as ACC of the salivary gland, namely t(6;9)(q22-23;p23-24), resulting in a MYB-NFIB fusion gene (~ 90%) (J Pathol 2012;226:84). This leads to overexpression of MYB protein, causing overexpression of CD117/KIT in luminal-like cells (Mod Pathol 2005;18:1623). This translocation can be detected with FISH break apart probes and is generally not present in other basal-like breast carcinomas. In addition, hormone receptors are negative in ACC of the breast. The myoepithelial-like cells show positivity for p63, SMA, CK5/CK6, CK14, CK17 and calponin. The luminal-like cells show positivity for CK7, EMA, CEA and CD117/KIT.
Three histologic patterns are described in ACC of the breast: cribriform (most common), reticular-tubular (predominant stromal component surrounding tumor cells) and basaloid (solid, predominantly myoepithelial cells with few luminal-type cells). Of the three patterns, the basaloid pattern is most reported to result in lymph node metastases. Current histology grading correlates well with the prognosis, though some pathologists grade lesions based on the percentage of solid component. The prognosis in general is excellent (90 - 100% survival at 10 years) (Breast Cancer Res 2010;12:R54). Histologic subtype is more important than gene expression profile in predicting prognosis.
The differential diagnosis for ACC of the breast includes invasive cribriform carcinoma, ductal carcinoma in situ, cribriform type and collagenous spherulosis. Collagenous spherulosis is only a diagnostic consideration in small core needle biopsies. Both entities have two distinct cell populations and form basement membrane material from a myoepithelial cell population. In low to intermediate nuclear grade invasive cribriform carcinoma and ductal carcinoma in situ, tumor cells are usually positive for ER and PR and are negative for CD117/KIT.
ACC of the breast may be overdiagnosed, with up to 20% of reported cases not fulfilling the criteria. This can result in the incorrect treatment for patients with triple negative cancers and may account for the very rare cases reporting aggressive behavior. Distant metastasis and death are rare (~ 2%) (J Med Case Rep 2017;11:303) but when present most metastases occur in the lung. In addition, the tumor can recur after resection with a prolonged clinical course. It is important to note that unlike some primary breast carcinomas, patients with ACC of the breast do not have an increased risk of developing a second malignancy compared with the general population. ACC of the breast is usually cured with complete resection. In addition, local adjuvant radiotherapy can be used as a treatment.
Test question answer:
E. Specific MYB-NFIB gene fusion defines majority of ACC of the breast (~ 90%). This causes overexpression of the MYB gene, which causes overexpression of CD117 (c-kit) in luminal-like cells.