All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Lina Hu, SUNY Downstate Medical Center, Brooklyn, New York, for contributing this case; Dr. Akira Yoshikawa, Kameda Medical Center, Kamogawa City, Chiba (Japan), for writing the discussion; and Dr. Andrey Bychkov, Kameda Medical Center and Dr. Debra Zynger, The Ohio State University, for the Editorial Board review. To contribute a Case of the Month, first make sure that we are currently accepting cases, then follow the guidelines on our main Case of the Month page.

Chief of Pathology / Laboratory Medical Director
MINNEAPOLIS, MINNESOTA (USA).
The Department of Pathology and Laboratory Medicine at Children's Minnesota is seeking Chief of Pathology/Laboratory Medical Director. The successful candidate must have an MD or DO degree, be eligible for licensing in Minnesota, be Board eligible or Board certified in Anatomic and Clinical Pathology and/or Fellowship trained in Pediatric Pathology. The successful candidate will have strong diagnostic and consultative skills in both Anatomic Pathology and Clinical Pathology, proven leadership skills and a track record of collegiality and excellence in clinical service.
At Children's Minnesota, we don't simply care for kids, we care for the most amazing people on earth. For more than 90 years, we have proudly served our community as an independent and not-for-profit system dedicated to providing health care exclusively to children, from before birth to young adulthood. We are looking for an individual who is driven to join us in our mission to champion the special health needs of children and their families. Children's Minnesota is a 420 bed pediatric health care system that includes outpatient clinics, surgical care centers, and two tertiary care hospitals in the Minneapolis/St Paul metropolitan area. We provide extraordinary patient care to the surrounding five state region. The Department of Pathology and Laboratory Medicine has a very close consultative relationship with all clinical and surgical services.
Qualifications:
• Must have an MD, DO or equivalent degree from another country with a current Minnesota Medical License or eligible to obtain one
• Board certified/Board eligible in Anatomic and Clinical Pathology and/or Fellowship trained in Pediatric Pathology
• Ability to be successfully credentialed by both the hospital and 3rd party payers
• Demonstrated history of positive relations with colleagues, support staff, administrators, patients and families
The candidate should submit CV and references to:
Ryan Berreth, FASPR
Children's Minnesota
Email: Ryan.Berreth@childrensmn.org
Telephone: 952-992-5317
Case of the Month #479
Clinical history:
A 47 year old Asian woman presented with malaise, weight loss, chest pain and shortness of breath. CT scan showed an anterior mediastinal mass with irregular, ill defined and infiltrative borders, measuring up to 8.3 x 7.1 x 8.2 cm. A biopsy was performed.
CT scan:
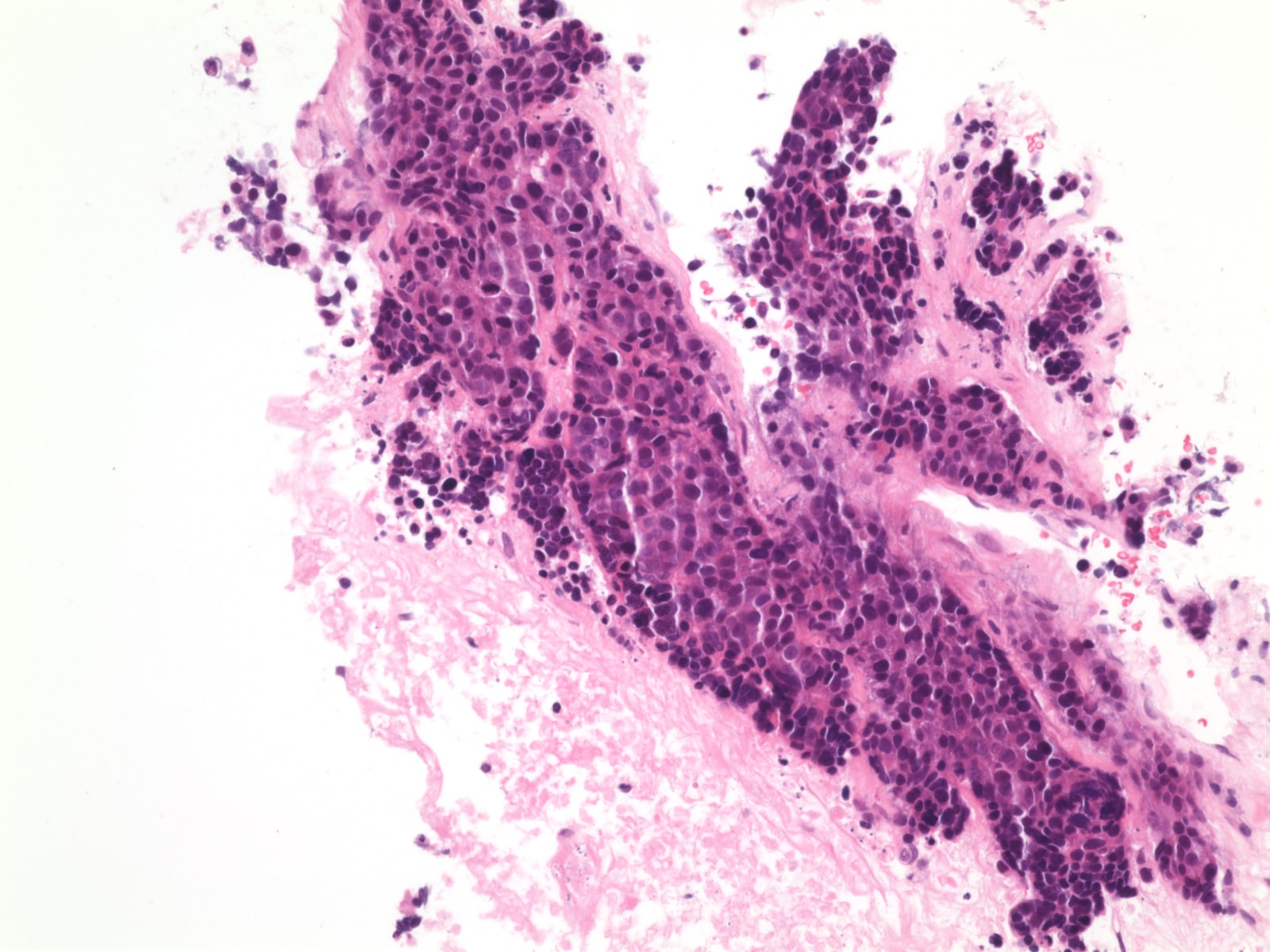
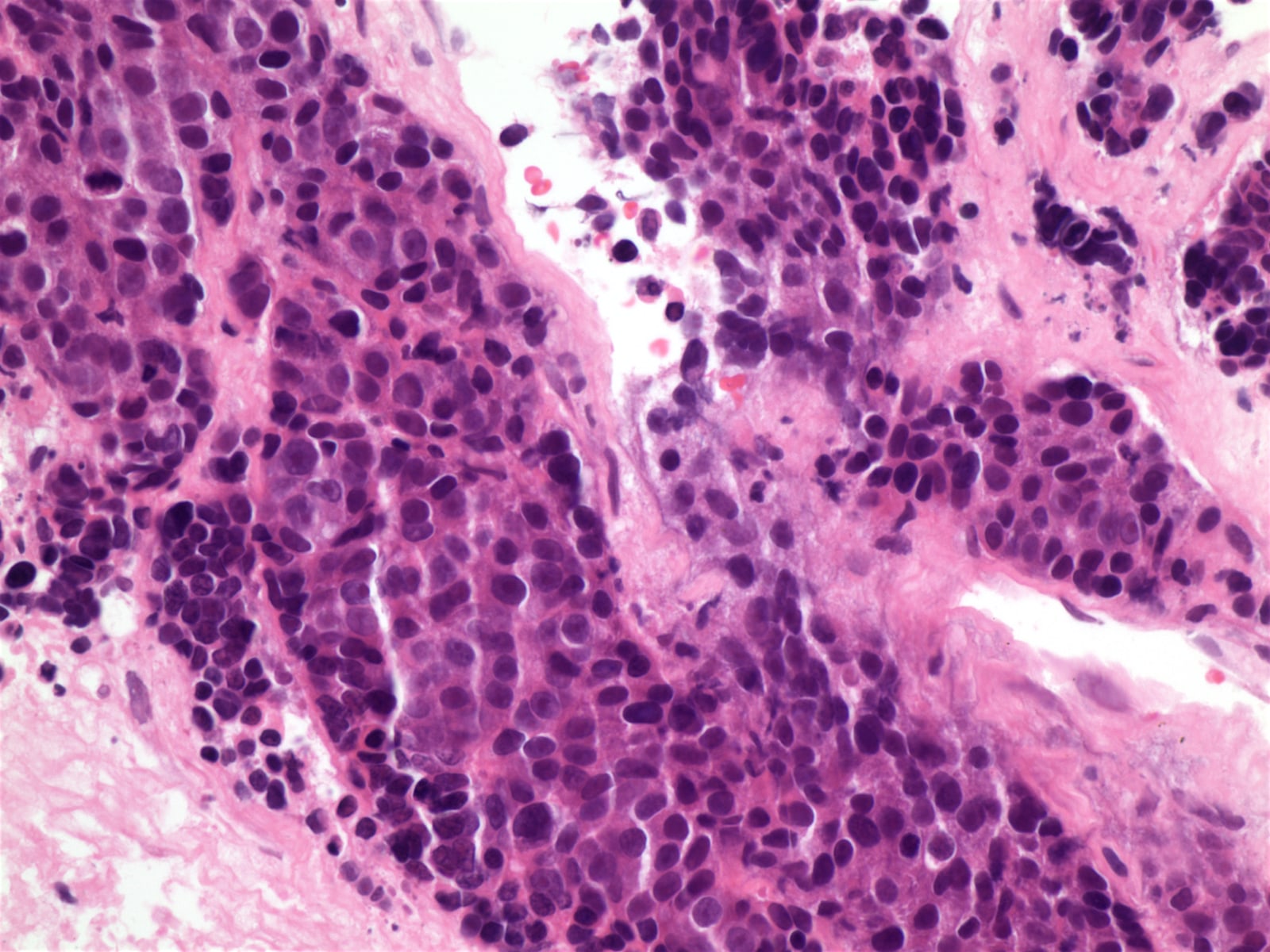
Histopathology images:
What is your diagnosis?
Diagnosis:
Thymic carcinoma
Test question (answer at the end):
Which two antibodies are most helpful in diagnosing thymic carcinoma?
A. CK5/6, 34bE12
B. CD5, p63
C. CEA, synaptophysin
D. p63, p40
E. KIT / CD117, INSM1
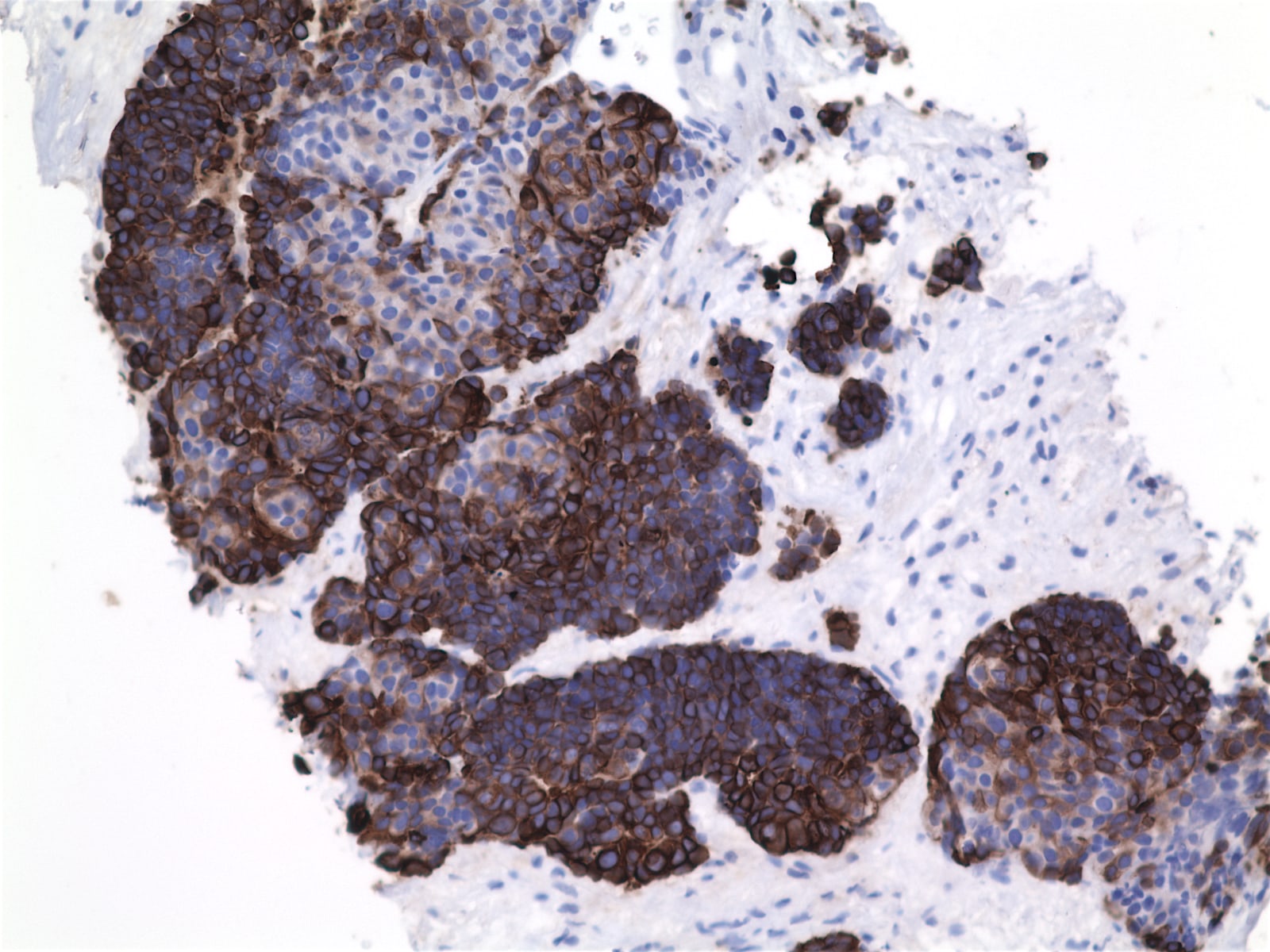
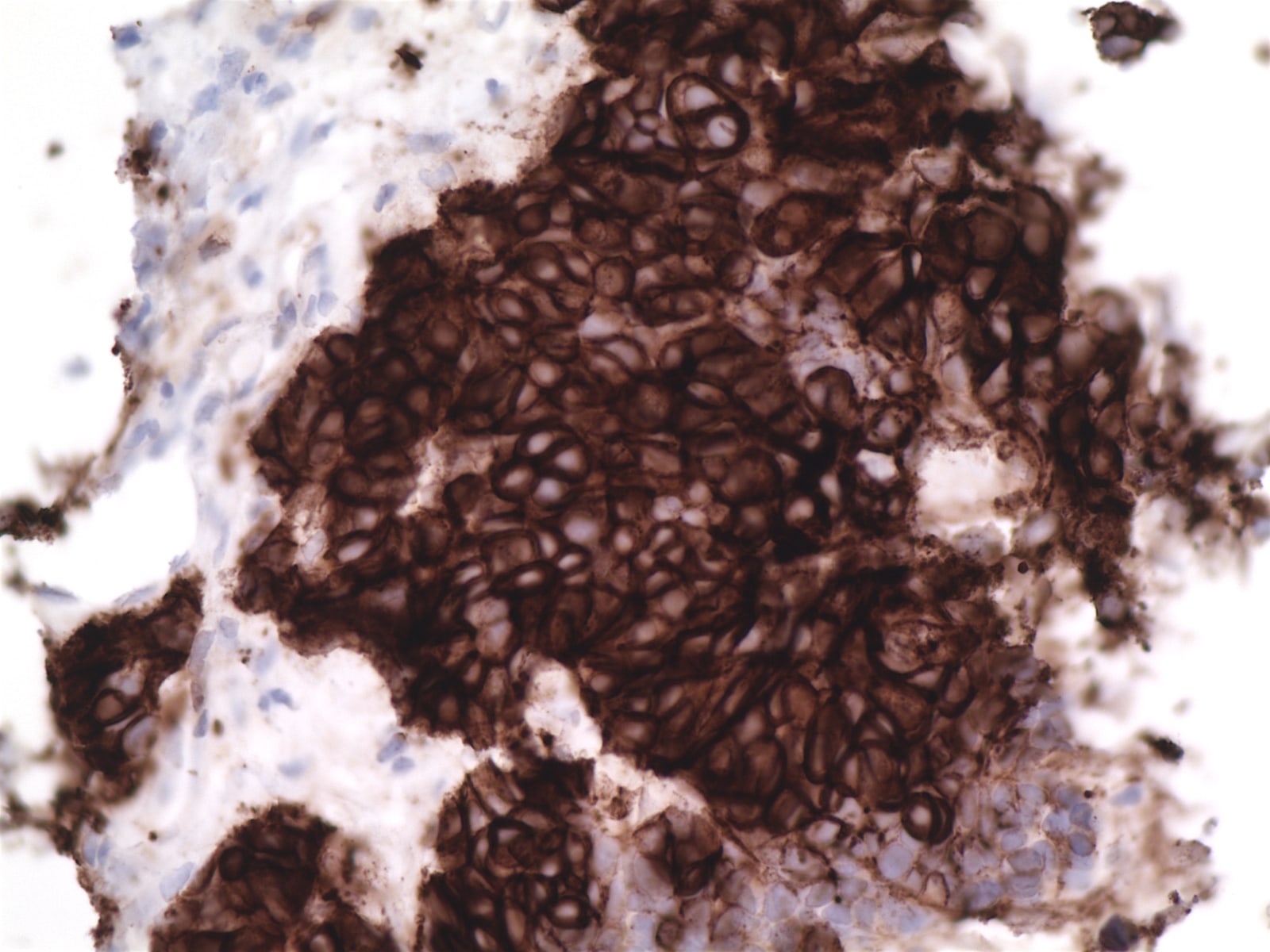
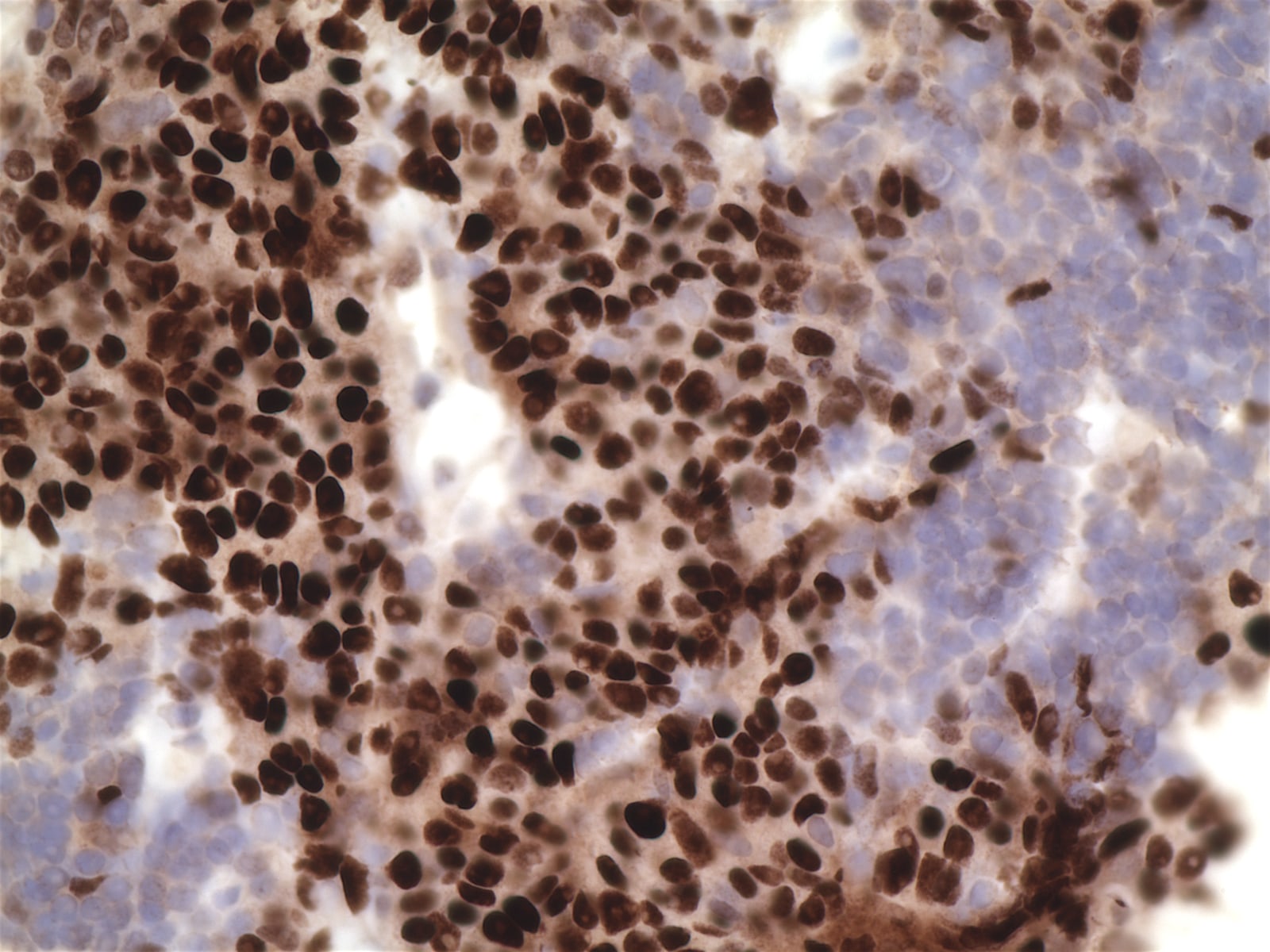
Stains:
Discussion:
The biopsy showed nests of infiltrating tumor cells with frequent atypical mitoses, hyperchromasia, occasionally prominent nucleoli, scant eosinophilic cytoplasm and no distinct cell borders. IHC was strongly positive for p63, CK7 and KIT / CD117 (> 60% tumor cells), focally positive for chromogranin, p40 and E-cadherin and negative for TTF1, CK20, CD56, synaptophysin, ER and PR. The final diagnosis was thymic carcinoma, most likely squamous cell carcinoma subtype.
Thymic carcinoma is a rare malignancy in the mediastinum (< 1% of all thymic tumors), comprised of a heterogeneous group of thymic epithelial tumors. Thymic carcinoma is more common in middle aged adults, with a slight male predominance (M:F = 3:2) (Lung Cancer 2017;108:161). Most patients present with cough, malaise, fever and chest pain. It may be accompanied by myasthenia gravis, pure red cell aplasia, immunodeficiency or other autoimmune diseases but only when thymoma transforms into thymic carcinoma.
Thymic carcinoma is classified into subtypes based on histologic, immunohistochemical and genetic features, including squamous cell carcinoma (90% of cases), basaloid carcinoma, mucoepidermoid carcinoma, lymphoepithelioma-like carcinoma, clear cell carcinoma, sarcomatoid carcinoma, adenocarcinoma, NUT carcinoma and undifferentiated carcinoma (WHO Classification of Tumours of the Lung, Pleura, Thymus and Heart, 4th Edition).
Histologically, thymic squamous cell carcinoma shows islands or sheets of large polygonal cells with eosinophilic cytoplasm, hyperchromatic nuclei and distinct nucleoli. Keratinization and Hassall's corpuscles can be seen. Lymphocytic background is variable. Unlike squamous cell carcinoma at other sites, tumors in the thymis tend to infiltrate with smooth contours. Invasion of vessels, lung, pleura and pericardium is common.
The main immunohistochemical markers are CD5 (membranous staining), KIT / CD117 and p63 (nuclear staining). PAX8 is positive in most cases. Epithelial neoplastic cells are positive for various keratins, e.g. pancytokeratin, high molecular weight cytokeratin 34 beta E12, CK5 / 6, CK7 and others. Neuroendocrine markers (chromogranin and synaptophysin) are expressed in scattered cells.
The differential diagnosis includes other mediastinal primaries and invasion and metastases from lung, esophagus or elsewhere. Compared with thymoma (especially type B3), thymic squamous cell carcinoma tends to have more cytologic atypia and mitoses and less lymphocytic infiltration, although there are no clear criteria. Immunohistochemistry deemed useful for distinguishing thymic carcinoma from thymoma includes GLUT1, MUC1 and KIT / CD117 (Appl Immunohistochem Mol Morphol 2014;22:479, Int J Clin Exp Pathol 2015;8:5354). In the differentiation from metastatic carcinoma, CD5 and KIT / CD117 are specifically positive in squamous cell carcinoma of thymic primary (Diagn Pathol 2015;10:210, Appl Immunohistochem Mol Morphol 2003;11:107). Genetic studies on thymic epithelial tumors show that mutation of the tyrosine kinase KIT gene is the only known targetable alteration in thymic carcinoma but it is present in only 6 - 12% of cases (Lung Cancer 2008;62:316, Ann Oncol 2012;23:2409). Exome and targeted gene sequencing have identified common mutations in TP53 and the tumor suppressor CDKN2A (Pathol Oncol Res 2017;23:551, Sci Rep 2014;4:7336).
AJCC/TNM stage is determined primarily by extent of invasion into surrounding mediastinal structures (T classification), while nodal involvement and metastatic spread are much rarer (Amin et al: AJCC Cancer Staging Manual, 8th Edition, 2017). Treatment is surgical resection with postoperative radiotherapy or chemotherapy (J Thorac Oncol 2017;12:734, Lung Cancer 2017;108:161). Overall five year survival is approximately 55%.
Test question answer:
B. CD5 combined with p63 are helpful thymic markers.