15 July 2020 - Case of the Month #493
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Kelly Magliocca, Emory University, Atlanta, Georgia (USA), for contributing this case and writing the discussion.
Advertisement Register for the webcast here
Case of the Month #493
Clinical history:
A 26 year old man presented with refractory AML and sinus pain. The patient underwent debridement of non-viable tissue from the nasal septum and turbinates.
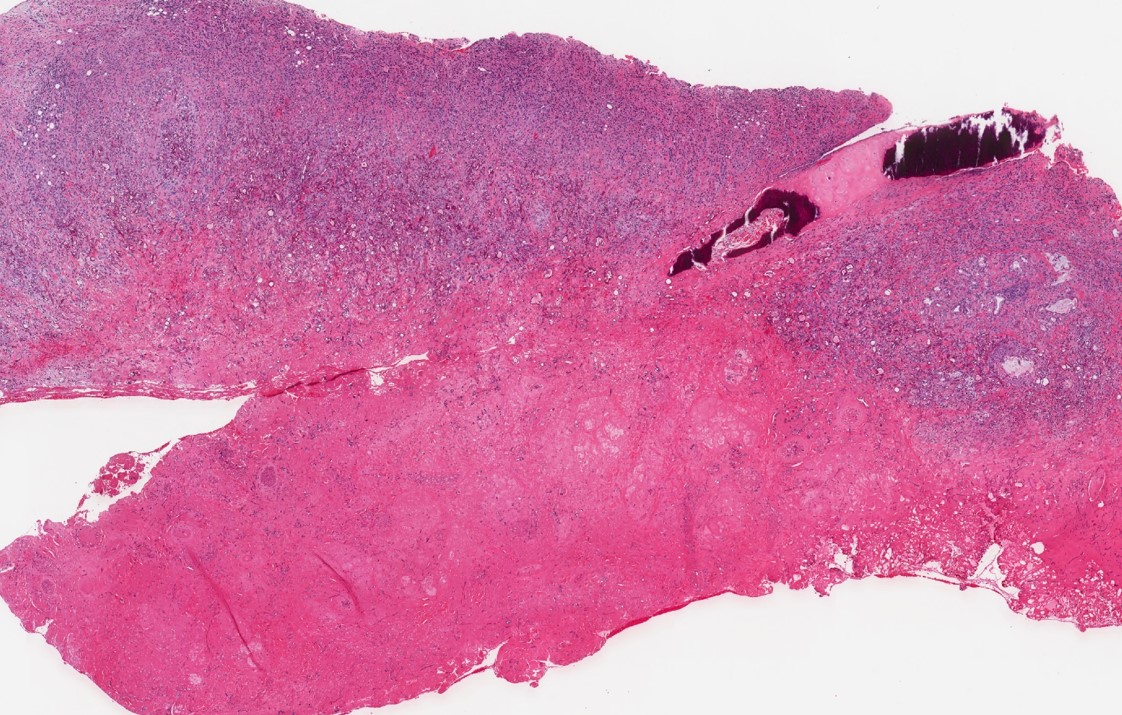
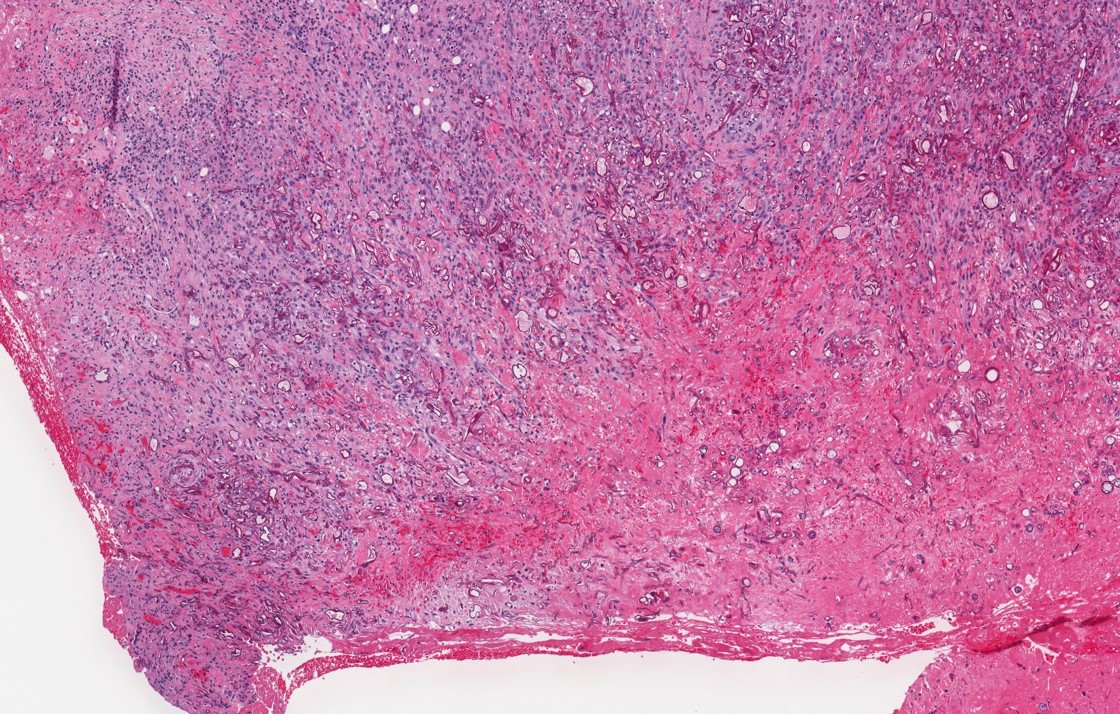
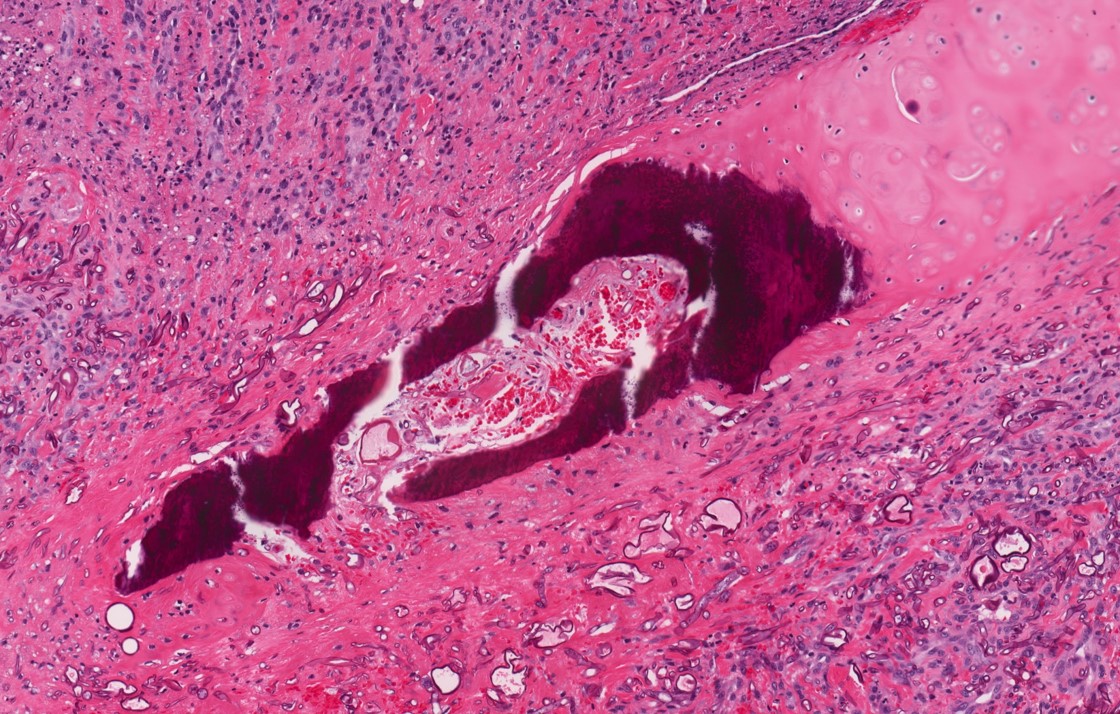
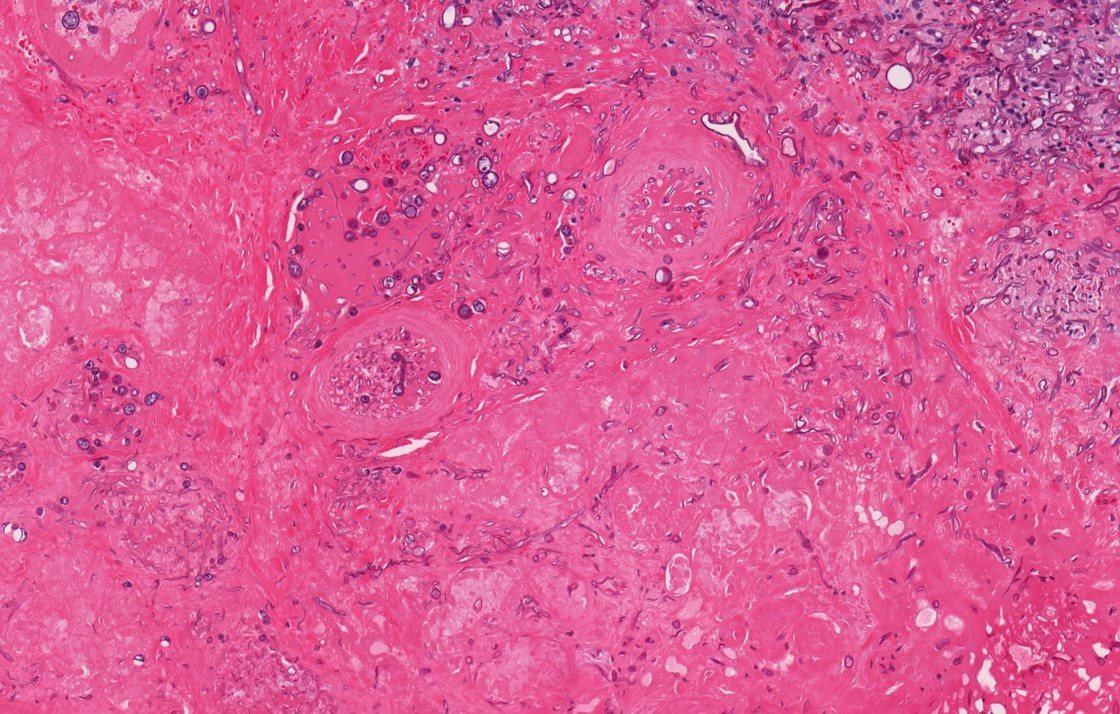
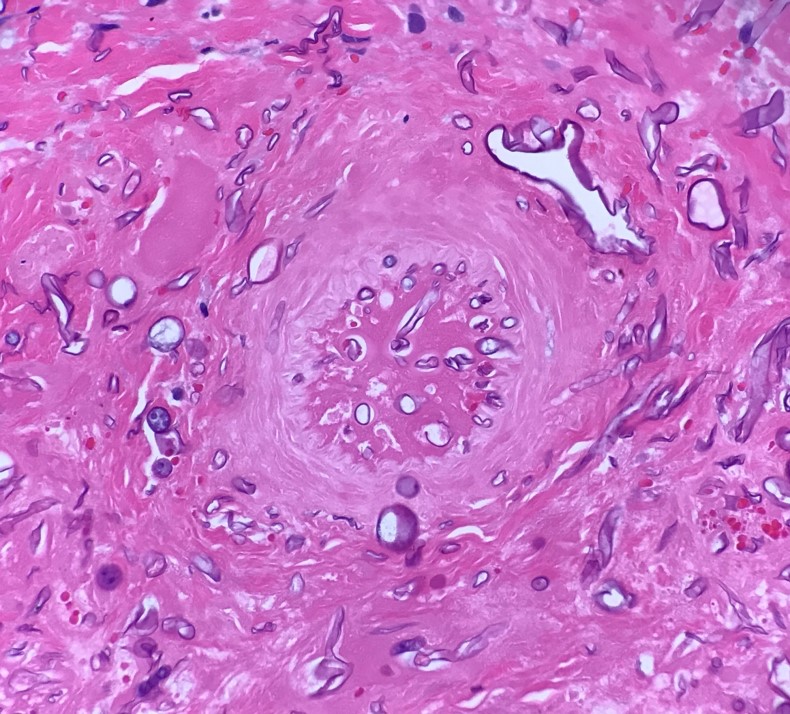
Histopathology images:
What is your diagnosis?
Diagnosis: Acute invasive fungal sinusitis (microbiology culture studies demonstrated Rhizopus species)
Test question (answer at the end):
Which of the following anatomic sites is most commonly involved in acute invasive fungal sinusitis?
A. Nasal septum
B. Inferior turbinate
C. Ethmoid sinus
D. Middle turbinate
Stains:
Discussion:
Acute invasive fungal sinusitis (AIFS), also referred to as acute fulminant invasive fungal sinusitis, is an important condition because it is a potentially life threatening infection typically occurring in immunocompromised patients. Organisms ubiquitous in the environment such as Aspergillus species and those within the Mucorales genera are most commonly associated with AIFS.
Early clinical signs and symptoms are nonspecific and include fever, headache, facial pain and nasal congestion. Nasal endoscopic evaluation may reveal areas of mucosal pallor, crusting or necrosis, involving the middle turbinate, nasal septum or floor of the nasal cavity, with the middle turbinate most commonly involved.
Given the urgent nature of acute fulminant invasive fungal sinusitis and the importance of early diagnosis, bedside or intraoperative evaluation of biopsy material may be requested. Frozen section (FS) analysis has been shown to be a sensitive (87%) and specific (100%) method of identifying fungal forms in AIFS (Otolaryngol Head Neck Surg 2017;157:314) with a high positive predictive value (100% when fungal forms are identified on FS). The low negative predictive value (NPV) of 65% underscores the importance of clinical suspicion and intraoperative decision making based on endoscopic findings when negative FS results are encountered (Int Forum Allergy Rhinol 2017;7:502). Importantly, permanent pathology is still the gold standard for final diagnosis of AIFS. Microbiology culture studies remain the gold standard for speciation.
Microscopic evaluation reveals necrosis, hemorrhage and tissue invasion by organisms. Angioinvasion and perineural and bone invasion may be present. While acute and chronic inflammation are present, the degree of inflammation may be sparse, particularly in patients with underlying neutropenia. Hyphal forms of Aspergillus spp. are uniform in appearance and are septate with acute angle branching, whereas elements of the Mucorales genera are characterized by pauciseptate, folded or ribbon-like hyphae that tend to branch irregularly, including at right angles. Special stains such as Grocott-Gomori Methenamine Silver (GMS) or Periodic Acid-Schiff (PAS) delineate the fungal forms on permanent slide sections. While these two groups of fungi have morphologies which frequently enable them to be differentiated with reasonable accuracy, if hyphae degenerate or are aerated, they may become swollen, form prominent vesicles and, in general, show morphologic distortion. For this reason, culture material is necessary for definitive organism identification. Culture results may also allow for further optimization of medical therapy (Clin Microbiol Rev 2011;24:247).
The management of AIFS is multimodal: antifungal therapy, optimal management of the predisposing condition (i.e., neutropenia, ketoacidosis, etc.) and surgical debridement.
Test question answer:
D. The middle turbinate is most commonly involved among the anatomic sites listed.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Kelly Magliocca, Emory University, Atlanta, Georgia (USA), for contributing this case and writing the discussion.
Advertisement Register for the webcast here
Case of the Month #493
Clinical history:
A 26 year old man presented with refractory AML and sinus pain. The patient underwent debridement of non-viable tissue from the nasal septum and turbinates.
Histopathology images:
What is your diagnosis?
Click here for diagnosis, test question and discussion:
Diagnosis: Acute invasive fungal sinusitis (microbiology culture studies demonstrated Rhizopus species)
Test question (answer at the end):
Which of the following anatomic sites is most commonly involved in acute invasive fungal sinusitis?
A. Nasal septum
B. Inferior turbinate
C. Ethmoid sinus
D. Middle turbinate
Stains:
Discussion:
Acute invasive fungal sinusitis (AIFS), also referred to as acute fulminant invasive fungal sinusitis, is an important condition because it is a potentially life threatening infection typically occurring in immunocompromised patients. Organisms ubiquitous in the environment such as Aspergillus species and those within the Mucorales genera are most commonly associated with AIFS.
Early clinical signs and symptoms are nonspecific and include fever, headache, facial pain and nasal congestion. Nasal endoscopic evaluation may reveal areas of mucosal pallor, crusting or necrosis, involving the middle turbinate, nasal septum or floor of the nasal cavity, with the middle turbinate most commonly involved.
Given the urgent nature of acute fulminant invasive fungal sinusitis and the importance of early diagnosis, bedside or intraoperative evaluation of biopsy material may be requested. Frozen section (FS) analysis has been shown to be a sensitive (87%) and specific (100%) method of identifying fungal forms in AIFS (Otolaryngol Head Neck Surg 2017;157:314) with a high positive predictive value (100% when fungal forms are identified on FS). The low negative predictive value (NPV) of 65% underscores the importance of clinical suspicion and intraoperative decision making based on endoscopic findings when negative FS results are encountered (Int Forum Allergy Rhinol 2017;7:502). Importantly, permanent pathology is still the gold standard for final diagnosis of AIFS. Microbiology culture studies remain the gold standard for speciation.
Microscopic evaluation reveals necrosis, hemorrhage and tissue invasion by organisms. Angioinvasion and perineural and bone invasion may be present. While acute and chronic inflammation are present, the degree of inflammation may be sparse, particularly in patients with underlying neutropenia. Hyphal forms of Aspergillus spp. are uniform in appearance and are septate with acute angle branching, whereas elements of the Mucorales genera are characterized by pauciseptate, folded or ribbon-like hyphae that tend to branch irregularly, including at right angles. Special stains such as Grocott-Gomori Methenamine Silver (GMS) or Periodic Acid-Schiff (PAS) delineate the fungal forms on permanent slide sections. While these two groups of fungi have morphologies which frequently enable them to be differentiated with reasonable accuracy, if hyphae degenerate or are aerated, they may become swollen, form prominent vesicles and, in general, show morphologic distortion. For this reason, culture material is necessary for definitive organism identification. Culture results may also allow for further optimization of medical therapy (Clin Microbiol Rev 2011;24:247).
The management of AIFS is multimodal: antifungal therapy, optimal management of the predisposing condition (i.e., neutropenia, ketoacidosis, etc.) and surgical debridement.
Test question answer:
D. The middle turbinate is most commonly involved among the anatomic sites listed.