Preparing for the Merit-Based Incentive Payment System (and its effect on your bottom line)
11 May 2016
By: Alex Mitchell, Director of Information and Content, Stark Medical Auditing / Vachette Pathology
Medicare Part B providers throughout the country should be actively preparing to have their
performance graded by the new Merit-Based Incentive Payment System starting next year. The scoring
system -- which is calculated by combining three existing CMS qualitative measurements and one new
one under a single roof -- will reward the highest-scoring physicians with incentives of up to 4 percent of
Part B baseline payments starting in 2019, while the lowest performers will pay fines of up to 4 percent
of Part B.
- Providers preparing for MIPS should initially focus efforts on existing components of the system they perform well in since all MIPS participants will be competing for the same dollars.
- Work to ensure management of your existing performance programs is coordinated under a single roof, both to manage administrative costs and understands the capabilities and possible shortcomings of your practice’s EHR system.
- CMS is expected to release a draft of MIPS rules sometime this summer. Keep up with the latest information on MIPS at www.vachettepathology.com/latest-news and www.starkmedicalauditing.com/latest-news.
The performance program comes as a result of the passage of the Medicare Access and CHIP Reauthorization Act (MACRA) that was signed into law in April 2015. While the law abolished the highly unpopular Sustainable Growth Rate adjustments, it also created a new learning curve by introducing MIPS.
In essence, MIPS continues the move away from fee-for-service billing and toward bundled or value-based Alternative Payment Models by offering substantial incentives to providers already participating in APMs and exempting a handful of "qualifying providers" (QPs) who receive a certain percentage of patient payments through APMs that already base payments on quality metrics comparable to MIPS. Providers determined to be QPs by CMS will earn a 5 percent lump sum bonus payment each year from 2019 to 2024 and will receive a higher Medicare fee schedule in 2026 and in future years, meaning MIPS eligible providers (EPs) should be taking a hard look at how integrating an APM could put them ahead of their peers.
The program also does not apply to first-year Medicare participants, providers that do not meet the low volume threshold or hospitals and facilities, according to CMS.
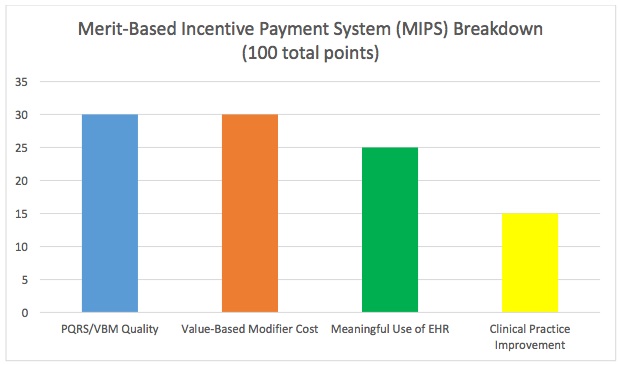
While the majority of Part B providers will be subject to MIPS, the system won't start tracking performance until 2017, meaning there's still time to prepare for this major shift. Once installed, MIPS participants will be able to earn a maximum of 100 points annually across four categories: meaningful use of EHR (25 points), quality measurements/PQRS (30 points), resource use determined by the Value-Based Payment Modifier (30 points), and clinical practice improvement (15 points).
But exactly how are points in each of these categories earned? Good question. That information won't be released until CMS unveils its final MIPS rules sometime this fall. However, a draft of the rules that should give some insight into the scoring process is scheduled to be released this summer.
Breakdown
Since how each of MIPS four categories will add up to make a whole is still a mystery, here is a quick refresher on the key points of each performance measurement:
- PQRS: Providers participating in this CMS initiative are required to send data to the agency each year regarding quality measurements performed during the care of Medicare patients. While it was initially viewed as a voluntary incentive, physicians who fail to report PQRS in 2016 will automatically receive a 2 percent reduction in their 2018 Medicare reimbursement for 2018. Despite the penalty, just roughly 61 percent of physicians complied with PQRS requirements during the most recent performance year.
- VBM: First established under the ACA as a way for CMS to offer varying levels of payment to physicians operating under the Medicare fee schedule based on quality of care compared to cost of care provided to Medicare patients. The measurement, which is tied to PQRS, essentially seeks to reward providers offering a higher quality of services at a lower cost than competitors. For the 2016 reporting year, providers in groups of 10 or more physicians can gain or lose up to 4 percent of their Medicare reimbursements in 2018 based on their VBM scores (providers in groups of fewer than 10 physicians face just a 2 percent adjustment). This means providers who fail to properly comply with PQRS will also fail their VBM requirement and will see a 6 percent reduction in Medicare reimbursements in 2018.
- EHR Meaningful Use: Enacted in 2011, the EHR Incentive Program offers incentive payments to providers that meaningfully use EHRs to capture clinical data and provide patients with electronic copies of health information, among other objectives. Conversely, providers that are determined not to be making optimal use of their EHRs will see a negative Medicare payment adjustment.
- Clinical Practice Improvement: This new category will seek to measure providers in areas such as offering timely appointments, monitoring the health of their patient population, utilizing clinical checklists to assess your practice and patient safety and use of alternative payment models. While this category should be further defined when a draft of MIPS rule are released this summer, the MACRA bill notes practices certified as patient-centered medical homes or similar specialty practice will earn the maximum 15 points. Additionally, simply participating in an eligible APM will net the provider a minimum of 7.5 points. Examples of eligible APMs include the Medicare Shared Savings Program or incorporating an Accountable Care Organization model.
MIPS scoring
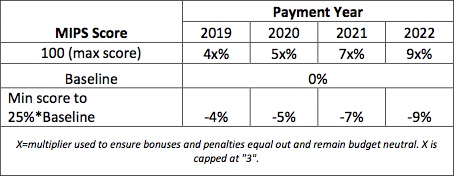
Each year, a baseline threshold for performance will be defined by CMS. So, if the agency chooses to set the benchmark at 55 points, a score of 56 would earn a slight incentive, while a score of 54 would net a slight penalty. The bonuses and penalties increase as the provider's score moves further from the baseline score.
Here's the rub: CMS designed the program to be budget neutral, meaning incentives will be drawn from the same pot low performers pay into. But, that doesn't mean there will be an equal number of winners and losers, as evidenced by the fact that CMS is including a "scaling factor" to multiply performance bonuses by in case incentive payouts don't initially match the penalty fees taken in. That scaling factor is currently capped at "3", meaning a provider could earn up to a 12 percent bonus (4%*3) in 2019 if enough EPs don't meet the baseline performance threshold. The adjustments are set to increase each year through 2022 when they will be capped at +/- 9 percent -- with the conversion factor allowing bonuses to reach a maximum of 27 percent.
This move represents a significant deviation from the existing EHR Meaningful Use and VBM programs where providers can avoid penalties by scoring within a large median range. MIPS ensures providers throughout the country will be forced to compete with each other for the same dollars.
Financial implications aside, it's also important for physicians to note their MIPS score will be publicly listed on the CMS Physician Compare website, meaning the score could have a direct effect on how patients view various providers. While it will likely take patients some time to become familiar with exactly what a MIPS score quantifies in relation to the quality of their provider, there's little doubt a negative score could impact a physician's perceived quality in the eyes of his/her patients.
Still, there are numerous details that must be ironed out by CMS before MIPS launches next year. These include determining the process for reporting data to CMS and ruling on whether providers will be allowed to earn partial credit in the MIPS categories. There is expected to be at least a two-month window between the release of the final MIPS rules and the launch of the program in January 2017, which will leave EPs scrambling to adjust to the rules on the fly. Vachette and Stark will work with their clients to ensure compliance in preparation for MIPS.
Providers attempting to prepare for MIPS should be realistic about the challenges of adjusting to a new performance measurement and attempt target the components of the system in which they are most accomplished and are performing well. While it may be difficult to score well against peers in all four categories, physicians can outperform others and reach the baseline performance threshold by emphasizing strengths and minimizing weaknesses.
It's also key to ensure existing performance programs are being managed in concert with one another - both to effectively manage administrative costs and understand the demands this could place on your EHR system.
Summary
- MIPS performance grading kicks into effect for physicians in 2017, however, payments and penalties won't start being levied until 2019.
- During the 2019 payment year, EPs could face Medicare payment penalties of up to 4 percent and bonuses of up to 12 percent. These adjustments will increase gradually each year until they're capped in 2022 at a 9 percent penalty and 27 percent bonus.
- Providers participating in APMs will receive varying levels of automatic bonuses, and a small number of qualified APM participants will be exempt from MIPS. It may be time to discuss if utilizing an APM could benefit your practice.
This isn't a change your practice must face alone. Contact Mick Raich, President of Vachette Pathology and Stark Medical Auditing, at 517-486-4262 or at mraich@vachettepathology.com or visit www.vachettepathology.com for further information.
Sources:
- https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value- Based-Programs/MACRA-MIPS-and-APMs/MACRA-LAN-PPT.pdf
- https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value- Based-Programs/MACRA-MIPS-and-APMs/MACRA-MIPS-and-APMs.html
- http://www.saignite.com/resources/faq-about-merit-based-incentive-payment-mips
Terms of Use:
All rights reserved. No part of this report may be reproduced or retransmitted in any form or by any means, electronic or mechanical, including photocopying, recording, faxing, emailing, posting online, or by any information storage or retrieval system, without written permission from the Publisher.
All trademarks and brands referred to herein are the property of their respective owner.
Legal Notices:
While all attempts have been made to verify information provided in this publication, neither the author nor the publisher assumes any responsibility for error, omission or contrary interpretations of the subject matter contained herein.
The purchaser or reader of this publication assumes responsibility for the use of these materials and information. Adherence to all applicable laws and regulations, both federal and state and local, governing professional licensing, business practice, advertising, and all other aspects of doing business in the United States or any other jurisdiction, is the sole responsibility of the purchase or reader. The author and publisher assume no responsibility or liability whatsoever on the behalf of any purchaser or reader of these materials.
Any perceived slights of specific people or organizations are unintentional.

