Superpage - Images
Superpage Topics
4 factor PCC
Acquired thrombophilia - general
Activated protein C resistance / Factor V Leiden
Algorithm for workup of hereditary bleeding disorders
D-dimer / dimerized plasmin fragment D
Dabigatran
Disseminated intravascular coagulation (DIC)
Factor II (prothrombin) deficiency
Factor VIII deficiency (hemophilia A)
Factor XI deficiency
Factor XII deficiency
Factor XIII deficiency
Heparin
Heparin - low molecular weight
Heparin induced thrombocytopenia
Heparin induced thrombocytopenia (HIT)
Hyperhomocysteinemia
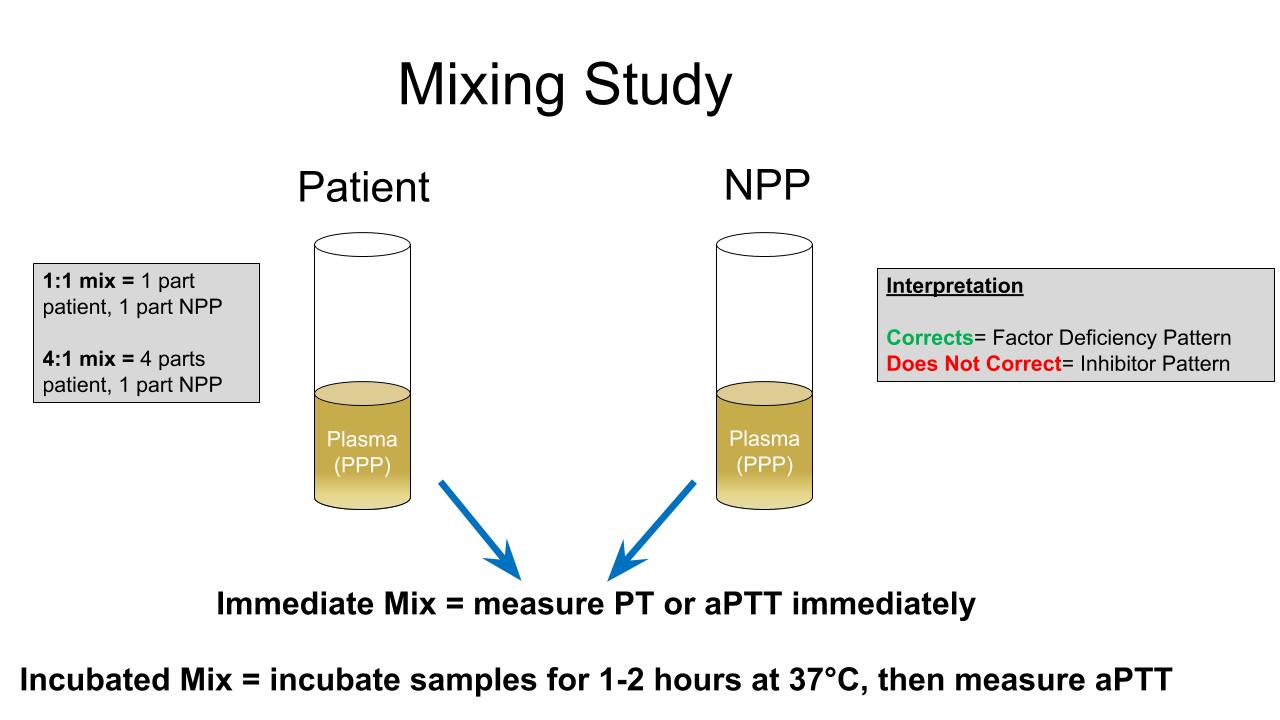
Mixing studies
Physiology
Protein C deficiency
Viscoelastic hemostatic assays
von Willebrand disease and testing4 factor PCC
Diagrams / tables
None
Videos
None
Acquired thrombophilia - general
Activated protein C resistance / Factor V Leiden
Algorithm for workup of hereditary bleeding disorders
Diagrams / tables
| Bleeding disorder | Prevalence | Inheritance pattern | ||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Factor I (fibrinogen) deficiency
| More than 200 cases reported
|
| Autosomal recessive Autosomal dominant or recessive Autosomal dominant or recessive Factor II (prothrombin) deficiency
| Less than 100 cases reported
| Autosomal recessive
| Factor V deficiency
| Less than 1 in 1,000,000
| Autosomal recessive
| Factor VII deficiency
| 1 in 500,000
| Autosomal recessive
| Factor VIII deficiency
| 1 in 5000 male births
| X-linked recessive
| Factor IX deficiency
| 1 in 30,000 male births
| X-linked recessive
| Factor X deficiency
| 1 in 500,000
| Autosomal recessive
| Factor XI deficiency
| 4% in Ashkenazi Jews, otherwise rare
| Autosomal recessive
| Factor XIII deficiency
| More than 200 cases reported
| Autosomal recessive
| Combined factor deficiencies
|
| > 30 families reported < 15 families reported
| Autosomal recessive Autosomal recessive
a2-antiplasmin deficiency
| > 10 families reported
| Autosomal recessive
| a1-antitrypsin Pittsburgh deficiency
| Only 3 cases reported
| Autosomal dominant
| von Willebrand Disease (VWD)
|
1 in 100
|
| Autosomal dominant Autosomal dominant Autosomal recessive Glanzmann thrombasthenia
| 1 in 1,000,000
| Autosomal recessive
| Bernard-Soulier syndrome
| < 1 in 1,000,000
| Autosomal recessive
| Gray platelet syndrome
| Rare
| Autosomal dominant, recessive or X-linked recessive
| Wiskott-Aldrich syndrome
| 1 in 1,000,000
| X-linked recessive
| |
| Disorders of Primary Hemostasis |
|---|
| von Willebrand disease |
| Glanzmann thrombasthenia |
| Bernard-Soulier syndrome |
| Platelet storage pool disease |
| Gray platelet syndrome |
| Wiskott-Aldrich syndrome |
| Disorders of Secondary Hemostasis | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Factor I (fibrinogen) abnormalities
| Factor II (prothrombin) deficiency
| Factor V deficiency
| Factor VII deficiency
| Factor VIII deficiency (Hemophilia A)
| Factor IX deficiency (Hemophilia B)
| Factor X deficiency
| Factor XI deficiency
| Factor XIII deficiency
| Combined factor deficiencies
| a2-antiplasmin deficiency
| a1-antitrypsin deficiency
| Ehlers-Danlos syndrome
| Osler-Weber-Rendu syndrome
| Scurvy (vitamin C deficiency) | |
D-dimer / dimerized plasmin fragment D
Dabigatran
Diagrams / tables
Disseminated intravascular coagulation (DIC)
Diagrams / tables
Images hosted on other servers:
Table 1: secondary causes
| Severe infectious diseases | Gram positive or negative organisms, malaria, hemorrhagic fevers |
| Malignancy | Solid tumors (e.g. adenocarcinomas), acute promyelocytic leukemia or monocytic leukemia |
| Trauma | Multitrauma, brain injury, burns |
| Obstetrical complications | Abruptio placentae, amniotic fluid embolism |
| Vascular malformations | Kasabach-Merrit syndrome, giant hemangiomas Other vascular malformations, large aortic aneurysms |
| Severe immunologic reactions | Transfusion reaction |
| Heat stroke | |
| Postcardiopulmonary resuscitation |
Table 2: DIC scoring systems by the JAAM and the ISTH (AMIA Annu Symp Proc 2015;2015:804)
| SIRS* criteria | |
| ≥ 3 | +1 |
| 0 to 2 | 0 |
| Platelet count | |
| < 80 × 109/L or > 50% decrease within 24 hours | +3 |
| ≥ 80 < 120 × 109/L or > 30% decrease within 24 hours | +1 |
| ≥ 120 × 109/L | 0 |
| Prothrombin time (value of patient / normal value) | |
| ≥ 1.2 | +1 |
| < 1.2 | 0 |
| Fibrin / fibrinogen degradation products | |
| ≥ 25 mg/L | +3 |
| ≥ 10 < 25 mg/L | +1 |
| < 10 mg/L | 0 |
| Diagnosis: if ≥ 4, there is positive diagnosis of DIC | |
| *Systemic inflammatory response syndrome | |
| Platelet count | |
| < 50 × 109/L | +2 |
| ≥ 50 < 100 × 109/L | +1 |
| ≥ 100 × 109/L | 0 |
| Elevated fibrin related marker | |
| Strong increase | +3 |
| Moderate increase | +2 |
| No increase | 0 |
| Prolonged prothrombin time | |
| ≥ 6 seconds | +2 |
| ≥ 3 < 6 seconds | +1 |
| < 3 seconds | 0 |
| Fibrinogen level | |
| < 100 g/mL | +1 |
| ≥ 100 g/mL | 0 |
| Diagnosis: if > 5, there is positive diagnosis of overt DIC; if < 5, suggestive (not affirmative) of nonovert DIC | |
Factor II (prothrombin) deficiency
Factor VIII deficiency (hemophilia A)
Factor XI deficiency
Factor XII deficiency
Diagrams / tables
Factor XIII deficiency
Heparin
Heparin - low molecular weight
Heparin induced thrombocytopenia
Heparin induced thrombocytopenia (HIT)
Hyperhomocysteinemia
Mixing studies
Diagrams / tables
Contributed by Tori Seasor, M.D. and Karen A. Moser, M.D.
| Differential diagnosis of prolonged PT or aPTT incorporating mixing study results (correction versus noncorrection) | ||
| Clotting time prolonged | Mixing study result | Key differential diagnoses |
| Prothrombin time (PT) | Corrects |
|
| Does not correct |
| |
| Activated partial thromboplastin time (aPTT) | Corrects |
|
| Does not correct |
| |
| PT and aPTT | Corrects |
|
| Does not correct |
| |
Physiology
Diagrams / tables
Protein C deficiency
Viscoelastic hemostatic assays
Diagrams / tables
von Willebrand disease and testing
Diagrams / tables
Table 1: Clinical characteristics of vWD subtypes (Clin Appl Thromb Hemost 2017;23:900)
| Condition | Inheritance pattern | Common mutation domain | Defect | Clinical presentation |
| Type 1 | Autosomal dominant | Throughout vWF gene (OMIM: Von Willebrand Disease, Type 1 [Accessed 3 August 2022]) | Decreased concentration of functionally normal vWF | Mild to moderate mucocutaneous bleeding |
| Type 2A | Autosomal dominant (OMIM: Von Willebrand Disease, Type 2 [Accessed 3 August 2022]) | A1, A2 | Enhanced susceptibility to cleavage by ADAMTS13 | Moderate to severe mucocutaneous bleeding |
| CK | Impaired dimer assembly | |||
| D1, D2 | Impaired multimer assembly | |||
| A1, A2, D3 | Impaired secretion of vWF, with enhanced intracellular retention | |||
| Type 2B | Autosomal dominant (OMIM: Von Willebrand Disease, Type 2 [Accessed 3 August 2022]) | A1 | Increased affinity of GPIb binding site on vWF for the GPIb receptor | Moderate to severe mucocutaneous bleeding |
| Type 2M | Autosomal dominant (OMIM: Von Willebrand Disease, Type 2 [Accessed 3 August 2022]) | A1 | Reduced affinity of GPIbα binding site on vWF for the GPIb receptor | Moderate to severe mucocutaneous bleeding |
| A3 | Reduced affinity of vWF for collagen | |||
| Type 2N | Autosomal recessive (OMIM: Von Willebrand Disease, Type 2 [Accessed 3 August 2022]) | D' - D3 | Reduced affinity of vWF for FVIII | Moderate to severe hemophilia-like bleeding |
| Type 3 | Autosomal recessive (OMIM: Von Willebrand Disease, Type 3 [Accessed 3 August 2022]) | Throughout vWF gene | Null alleles result in virtual absence of vWF | Severe mucocutaneous bleeding and hemophilia-like bleeding |
| Rare: D1 - D2 | Impaired dimer formation and intracellular retention |
Table 2: Laboratory characteristics of subtypes of vWD (Clin Appl Thromb Hemost 2017;23:900, Teruya: Management of Bleeding Patients, 2nd Edition, 2021)
| Condition | vWF antigen level (vWF:Ag) in % | vWF activity (vWF:Act) in % | vWF:Act / vWF:Ag | Factor VIII (FVIII) | Multimers |
| Type 1 | < 30 | < 30 | > 0.7 | Low, normal | All low |
| Type 2A | Mildly low | Low | < 0.7 | Normal, mildly low | Absent high and intermediate multimers |
| Type 2B | Normal, low | Low | < 0.7 | Normal, mildly low | Absent high multimers |
| Type 2M | Normal, low | Low | < 0.7 | Normal, mildly low | Normal |
| Type 2N | Normal, low | Normal, low | > 0.7 | Low | Normal |
| Type 3 | < 3 | < 3 | Not applicable | Low | Absent |
| Low vWF | 30 - 50 | Normal, low | > 0.7 | Normal | Normal |
| Normal | 50 - 200 | 50 - 200 | > 0.7 | Normal | Normal |
Recent Coagulation Pathology books
Find related Pathology books: hematopathology, lab medicine, other, transfusion, management