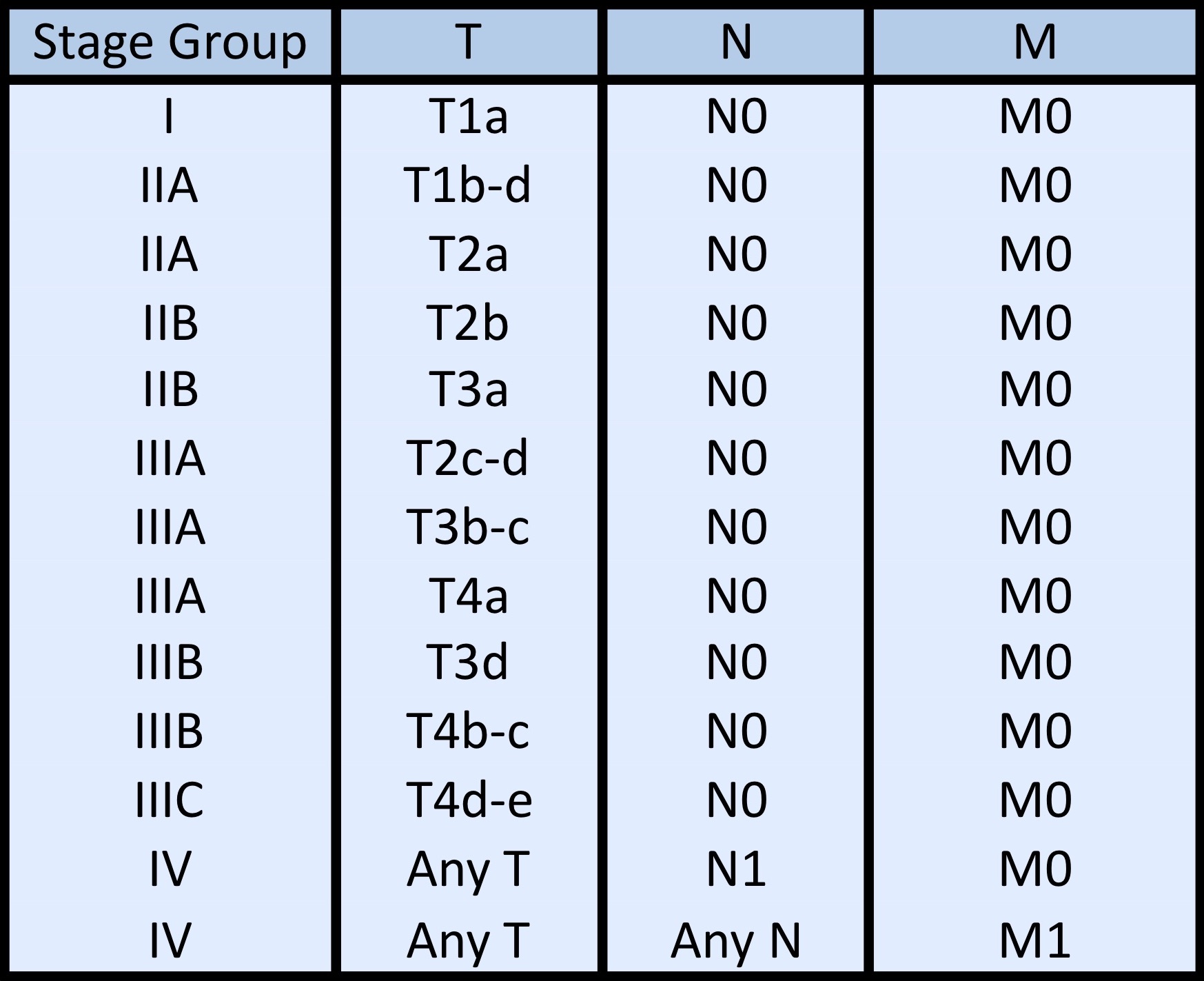
- TX: Primary tumor cannot be assessed
- T0: No evidence of primary tumor
- Tis: Carcinoma in situ
- T1: Tumor 5 mm or less in greatest dimension
- T2: Tumor more than 5 mm in greatest dimension, without invasion of adjacent structures
- T3: Tumor invades adjacent structures, excluding the orbit
- T4: Tumor invades the orbit with or without further extension
- T4a: Tumor invades orbital soft tissues, without bone invasion
- T4b: Tumor invades bone
- T4c: Tumor invades adjacent paranasal sinuses
- T4d: Tumor invades brain
Superpage
Superpage Topics
Acanthamoeba keratitis
Actinic keratopathy
Actinic keratosis
Acute hemorrhagic conjunctivitis
Adenocarcinoma-eyelid
Adenocarcinoma-lacrimal gland / sac
Adenocarcinoma-retinal pigment epithelium
Adenoid cystic carcinoma
Anatomy & histology-ciliary body
Anatomy & histology-conjunctiva
Anatomy & histology-cornea
Anatomy & histology-eyelid
Anatomy & histology-other
Anatomy & histology-retina
Astrocytic tumor
Benign epithelial melanosis of the conjunctiva
Blue nevus
Bullous keratopathy
CCN Test
Calcific band keratopathy
Carcinoma ex pleomorphic adenoma
Cataract
Chalazion
Choroid
Cicatrizing conjunctivitis
Ciliary body adenoma
Coats disease
Coloboma
Conjunctival intraepithelial neoplasia
Conjunctival melanocytic intraepithelial lesions (CMIL)
Conjunctival oncocytoma
Conjunctivitis and variants
Corneal dystrophy
Corneal transplantation & graft failure
Cysts-conjunctiva
Dacryoadenitis
Dacryocystitis / canaliculitis
Dacryolithiasis
Dermoid cyst-orbit
Detachment of retina
Diabetes mellitus
Dysthyroid ophthalmopathy
Epibulbar choristoma
Epithelial cyst-orbit
Eyelid cysts
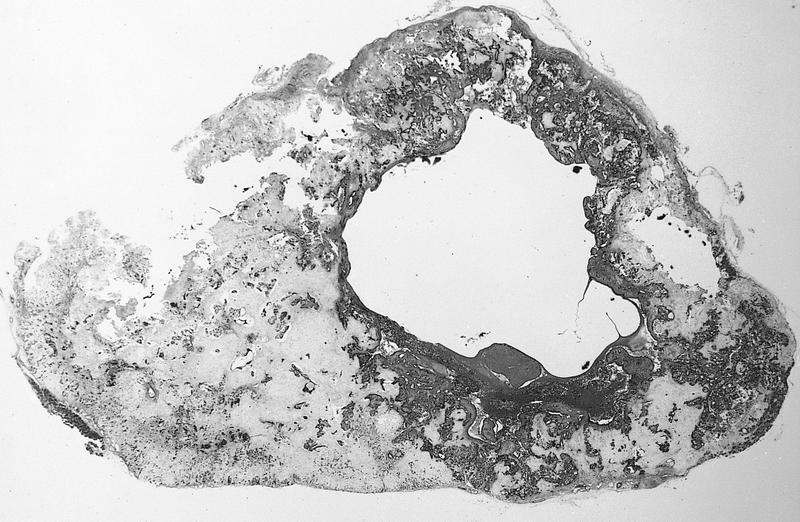
Glaucoma
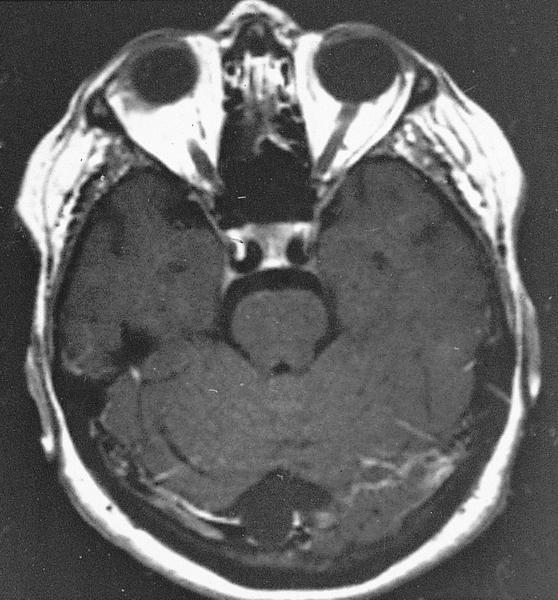
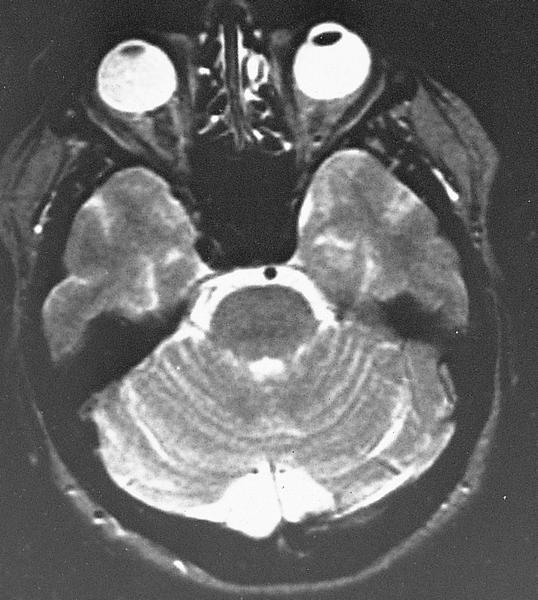
Glioma-optic nerve
Graft versus host disease
Granulomatous conjunctivitis
Grossing & features to report
Hereditary benign intraepithelial dyskeratosis
IgG4 related disease
Infectious keratitis
Inflamed juvenile conjunctival nevus
Iris
Kaposi sarcoma-eyelid
Keratoconus
Keratomalacia
Lattice degeneration
Ligneous conjunctivitis
Lisch nodule
Lymphoma-conjunctiva
Lymphoma-orbit
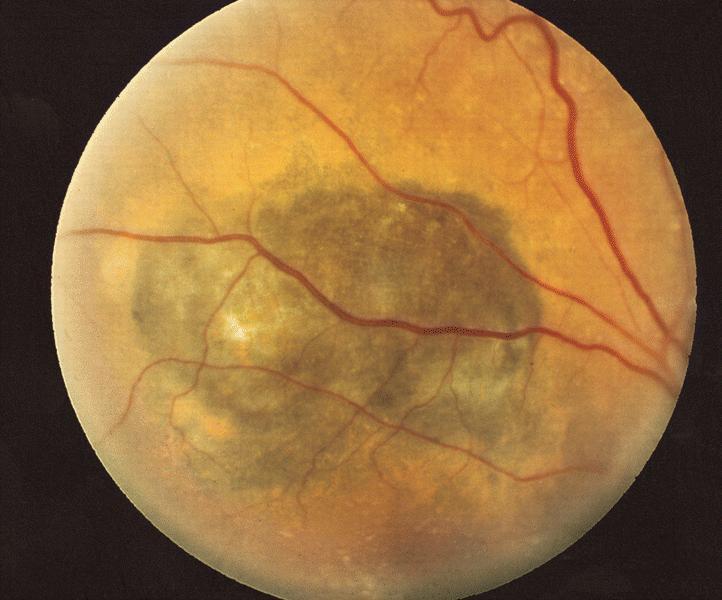
Macular degeneration
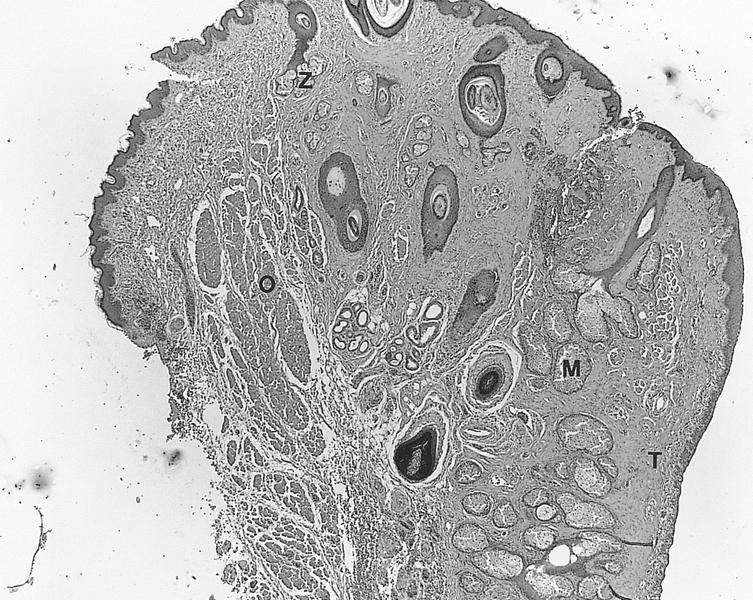
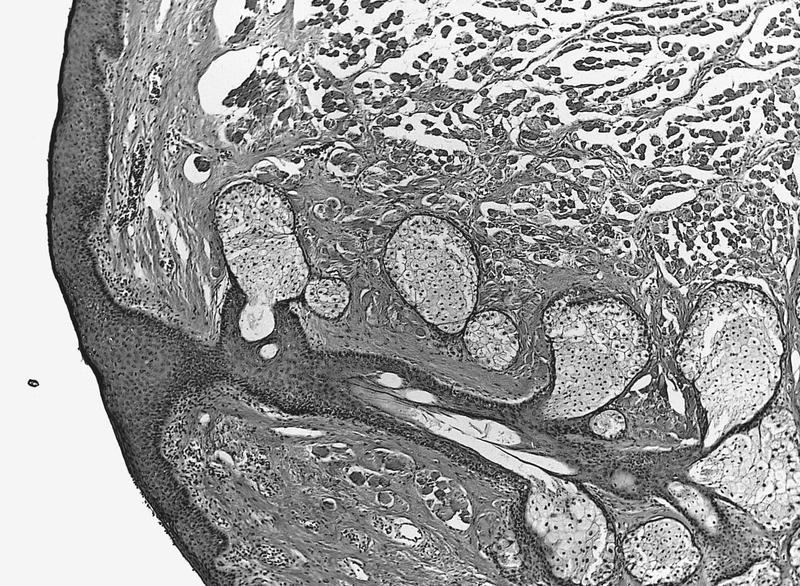
Medulloepithelioma
Melanocytoma
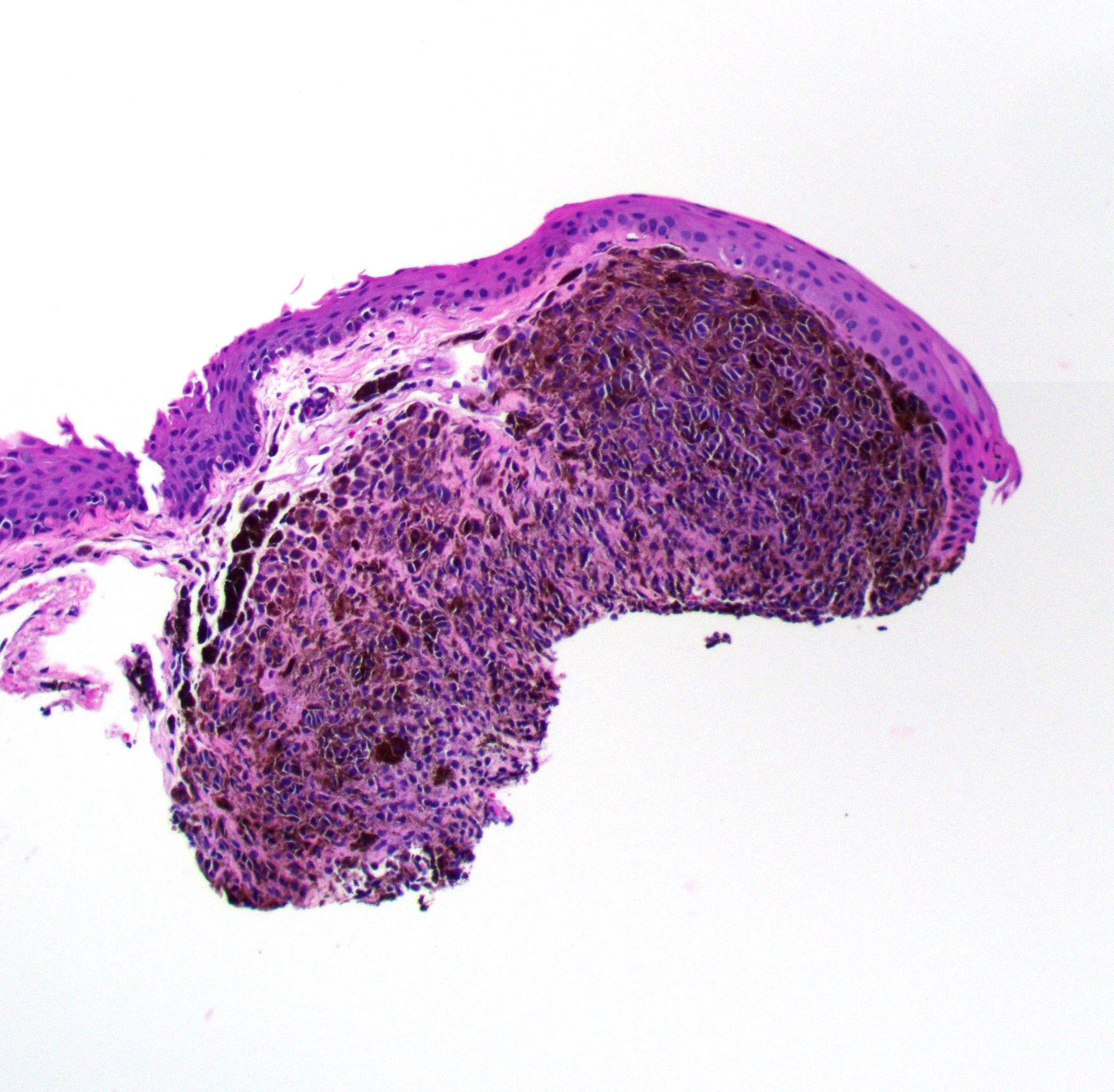
Melanoma-conjunctiva
Melanoma-eyelid
Melanoma-uvea
Melanosis oculi-eyelid
Melanosis oculi-uvea
Meningioma
Merkel cell carcinoma
Mikulicz disease
Molluscum contagiosum
Mucocele-lacrimal sac
Mucocele-orbit
Myxoma-eyelid
Necrobiotic xanthogranuloma with paraproteinemia
Nevi-choroid or iris
Nevi-conjunctiva
Nevi-eyelid
Nevus of Ota-eyelid
Nodular & massive retinal gliosis
Nonspecific responses-cornea
Ocular cicatricial pemphigoid
Oncocytoma-lacrimal duct
Optic atrophy
Papilloma-lacrimal duct
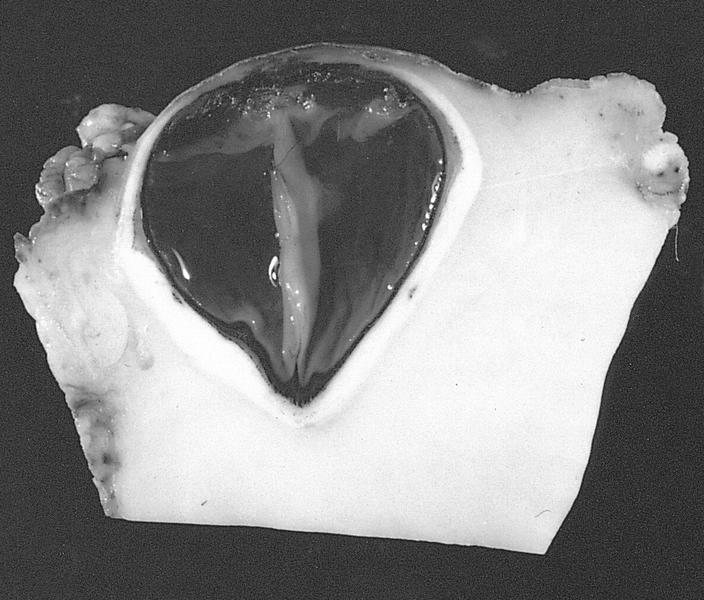
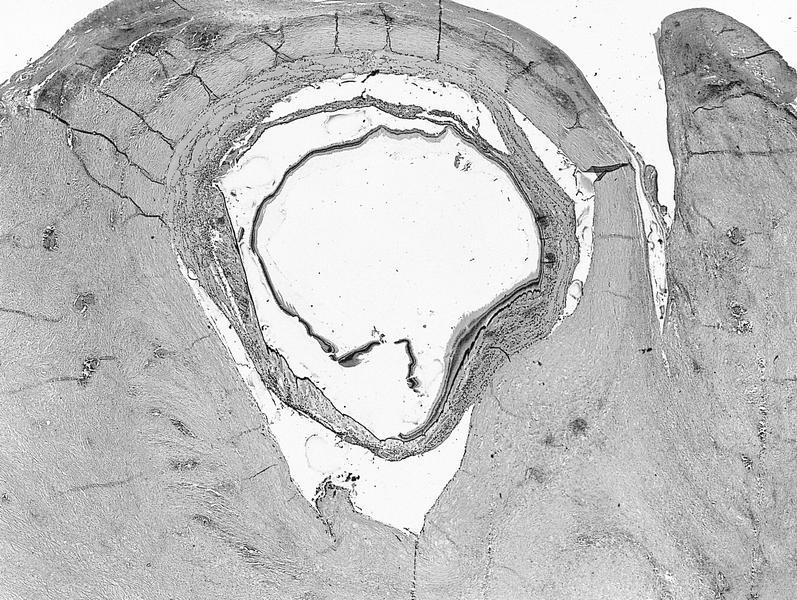
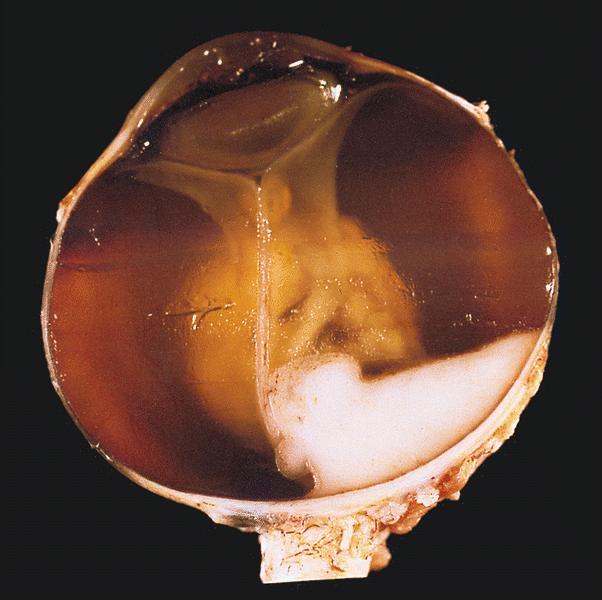
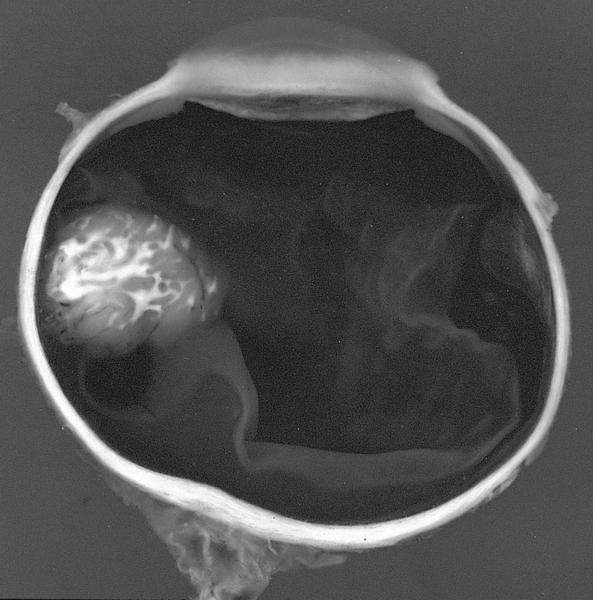
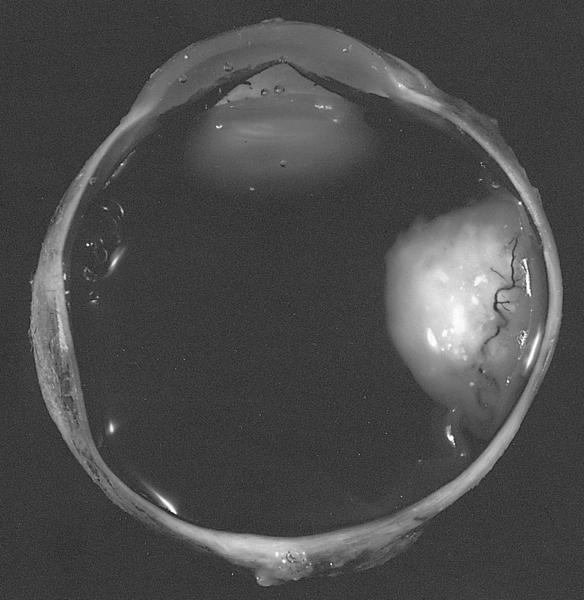
Persistent hyperplastic primary vitreous
Phacoanaphylactic endophthalmitis
Phakomatous choristoma
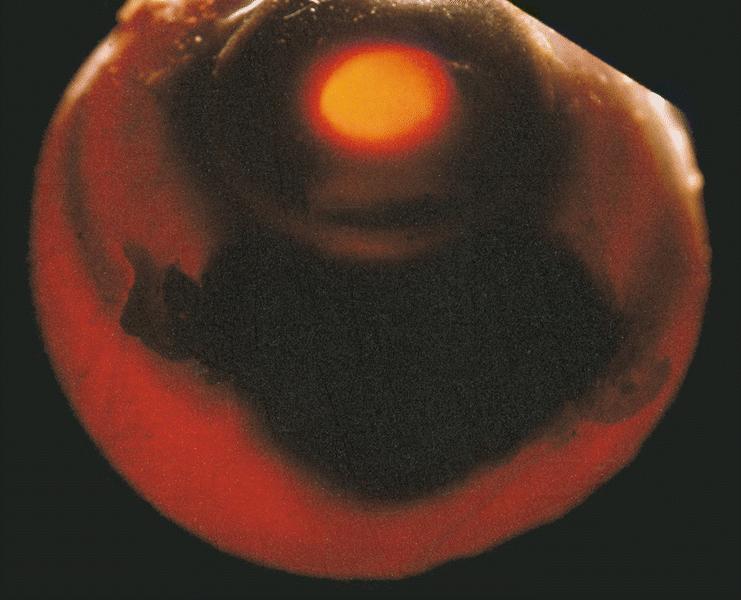
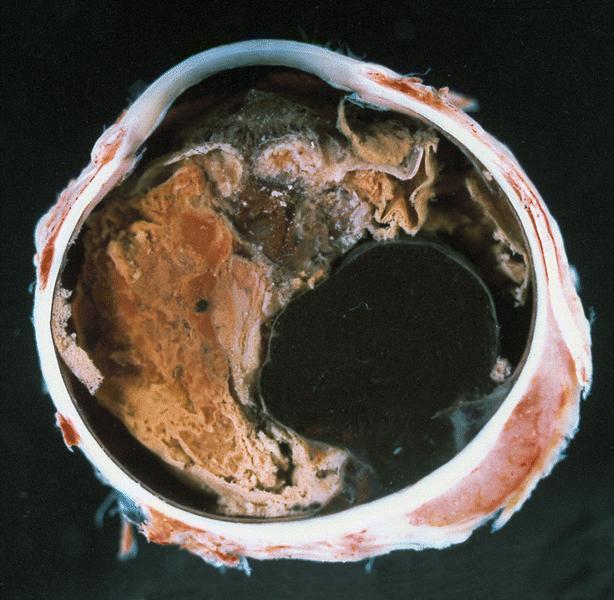
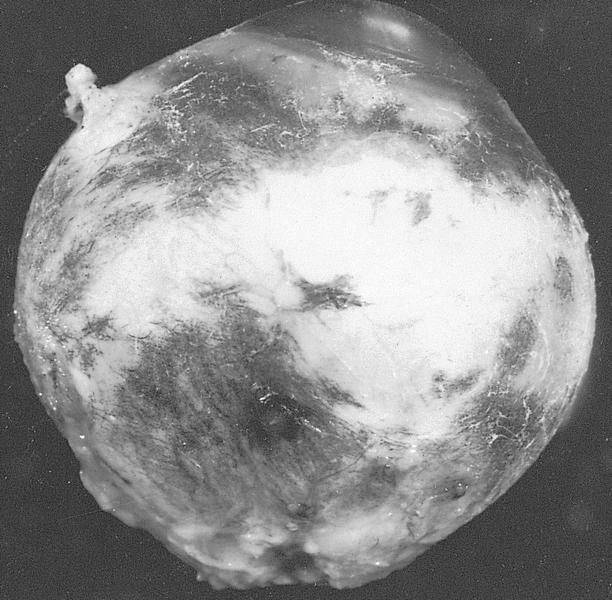
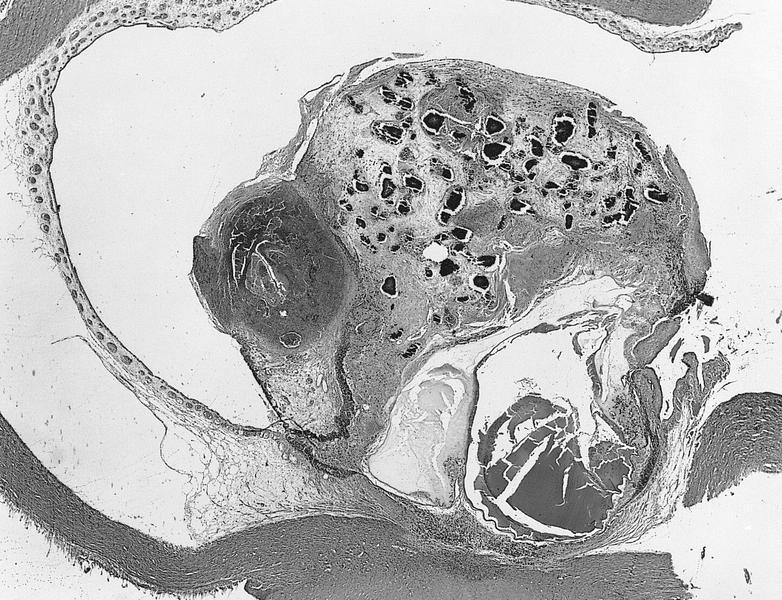
Phthisis bulbi
Pinguecula
Pleomorphic adenoma-lacrimal duct
Posterior polymorphous dystrophy
Primary choroidal lymphoma (pending)
Primary vitreoretinal large B cell lymphoma (pending)
Pseudorheumatoid nodules
Pterygium
Pyogenic granuloma-eyelid
Retinitis pigmentosa
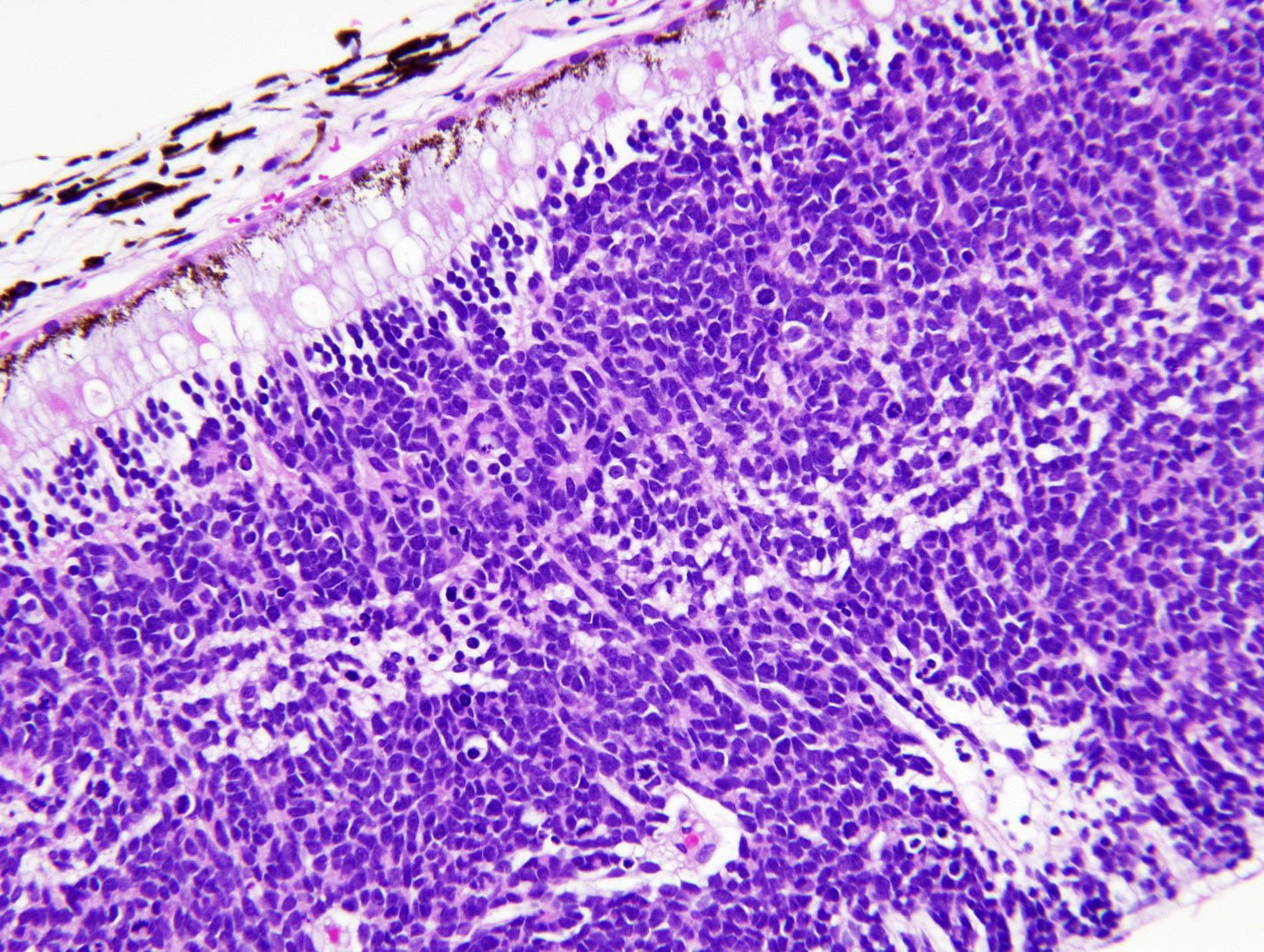
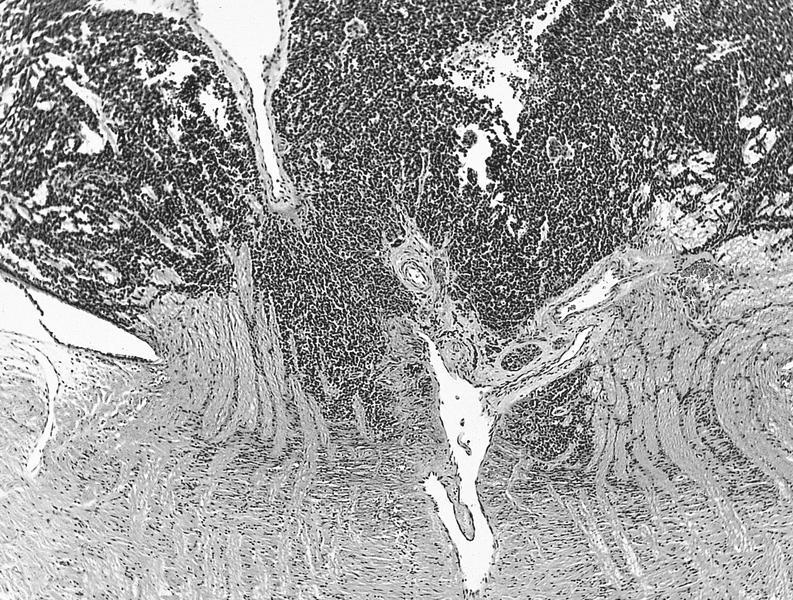
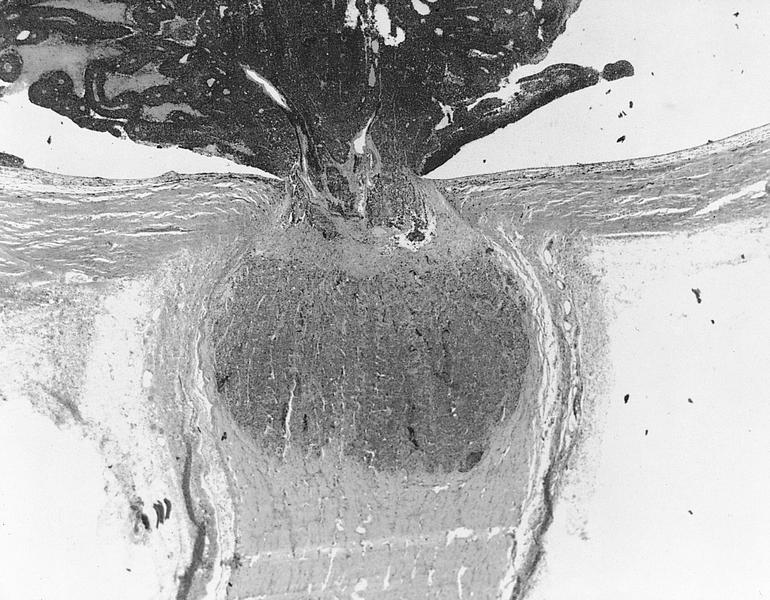
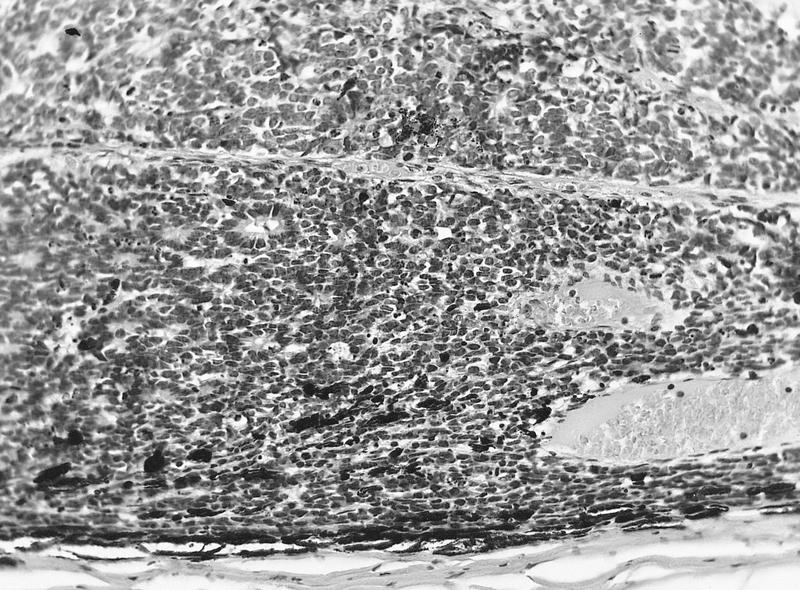
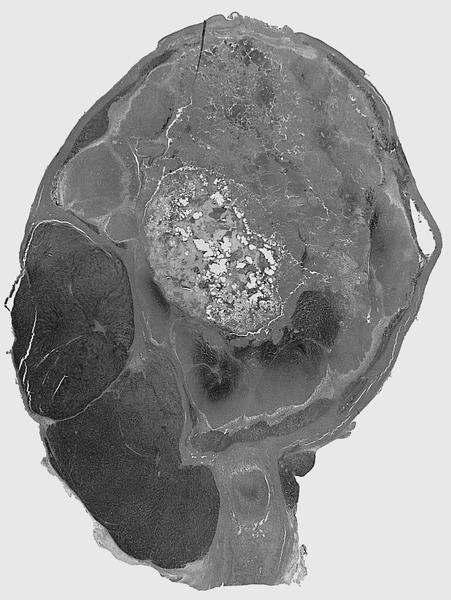
Retinoblastoma
Retinocytoma
Retrolental fibroplasia
Rhabdomyosarcoma-orbit
Schnabel cavernous degeneration
Sclera
Seborrheic keratosis
Silica granuloma
Solitary fibrous tumor-orbit
Squamous cell carcinoma-conjunctiva
Squamous cell carcinoma-eyelid
Squamous cell carcinoma-lacrimal duct
Squamous papilloma-conjunctiva
Squamous papilloma-eyelid
Staging-conjunctiva carcinoma
Staging-conjunctiva melanoma
Staging-eyelid
Staging-lacrimal duct
Staging-ocular adnexal lymphoma
Staging-orbital sarcoma
Staging-retinoblastoma
Staging-uvea melanoma
Steatocystoma simplex
Stye
Subconjunctival herniated orbital fat
Sweat gland carcinoma
Temporal arteritis
Trachoma
Tumors general-eyelid
Uveitis
Visceral larva migrans
Vitreous humor pathology
WHO classification of tumors of the conjunctiva and caruncle
WHO classification of tumors of the conjunctiva and caruncle (pending)
XanthelasmaAcanthamoeba keratitis
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Electron microscopy description | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Rare, serious parasitic infection of the cornea occurring mostly in contact lens wearers
- Acanthamoeba are free living, ubiquitous protozoa found in soil and freshwater (tap water, hot tubs, swimming pools)
Essential features
- Clinically has a waxing and waning course and may be difficult to diagnose and treat
- Direct correlation with contact lens wearing or corneal trauma with exposure to soil or contaminated water (Parasite 2015:22:10)
- Microscopic features include ulceration, necrosis, heavy neutrophilic and macrophage infiltrates
- Encysted forms may be highlighted with PAS or GMS stains (Hum Pathol 2013;44:918)
Terminology
- Amebic keratitis
Epidemiology
- 85% of cases occur in contact lens wearers (CDC: Sources of Infection and Risk Factors [Accessed 17 November 2023])
- Risk factors include poor contact lens hygiene (e.g., wearing lenses overnight or during swimming / showering) and orthokeratology (specially fitted lenses) (J Clin Med 2021;10:942)
Sites
- Cornea, typically unilateral but can be bilateral (Am J Ophthalmol 2008;145:193)
- Sclera or conjunctiva
- In prolonged cases, chorioretinitis
Pathophysiology
- Breaching of the surface epithelium
- Keratocyte depletion by the invading trophozoites
- Neutrophilic inflammatory response
- Stromal necrosis (leukocytoclastic) (Br J Ophthalmol 1993;77:366, Pathogens 2021;10:323)
Etiology
- Direct correlation with contact lens wearing (Parasite 2015:22:10)
- Corneal trauma with exposure to soil or contaminated water (Parasite 2015:22:10, Folia Parasitol (Praha) 2003;50:97, J Infect Public Health 2023;16:841)
- Most common infectious species are Acanthamoeba castellani and Acanthamoeba polyphaga (Pathogens 2021;10:323)
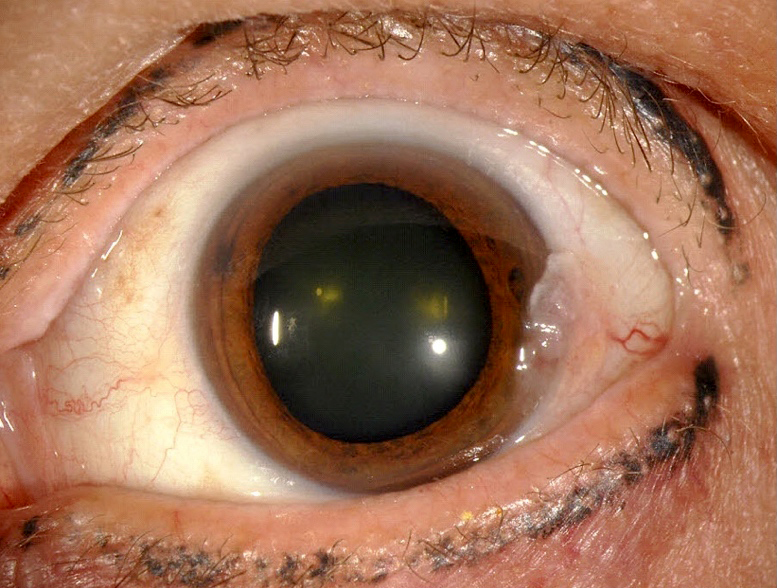
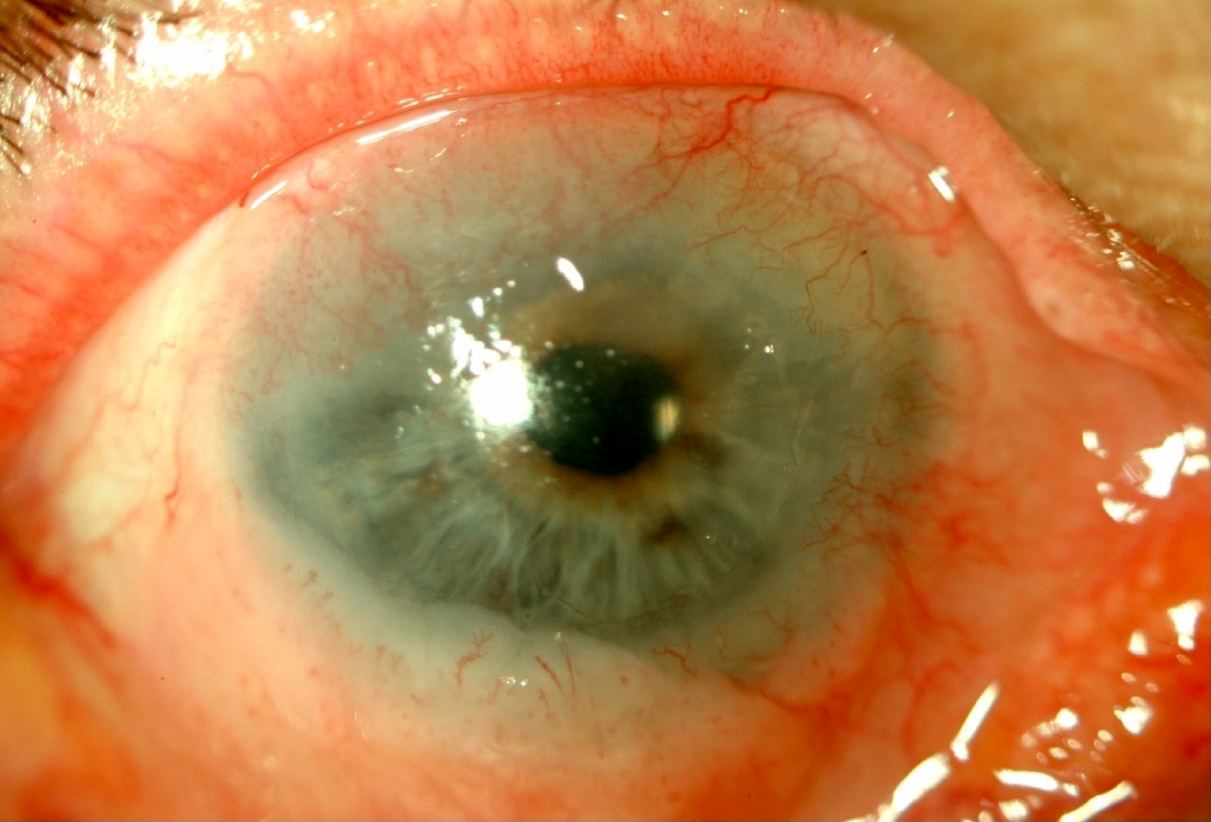
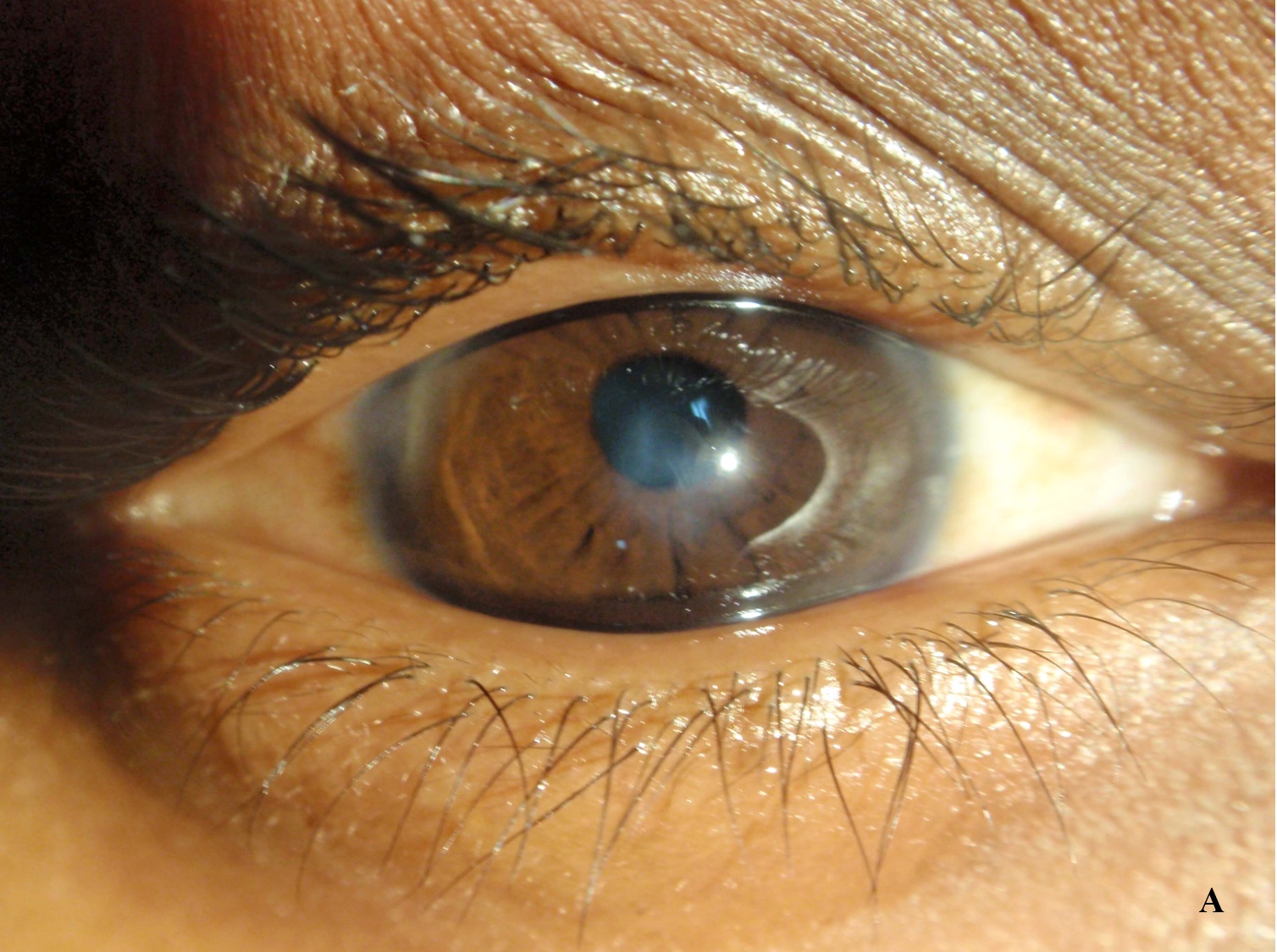
Clinical features
- Waxing and waning course
- Classically severe pain disproportionate to the clinical picture (Br J Ophthalmol 1995;79:1078)
- However, can also be painless, leading to diagnostic uncertainties (Diagnostics (Basel) 2023;13:2655)
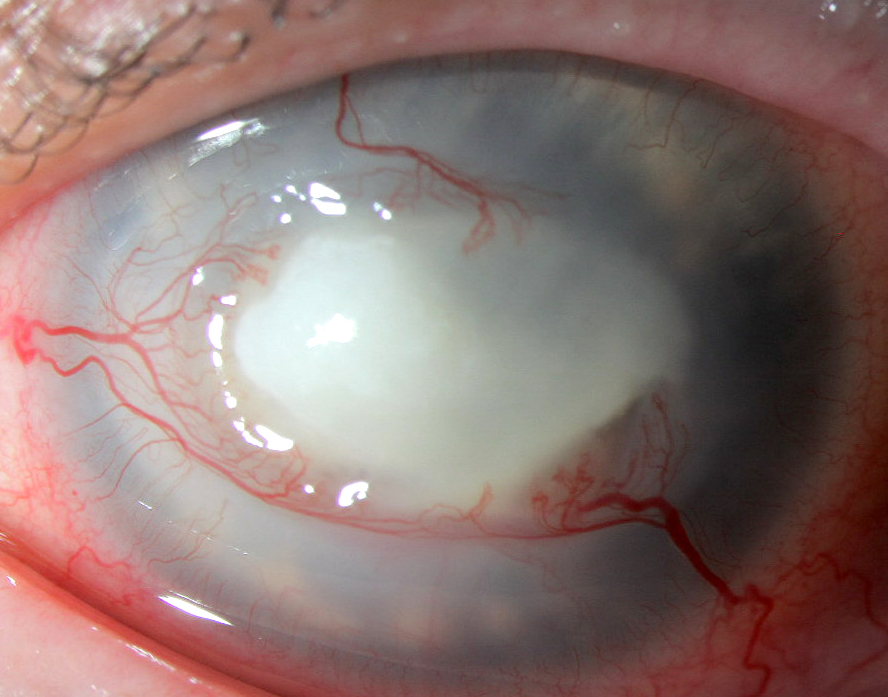
- Pattern of radial perineural infiltrates on ophthalmic exam (may lead to misdiagnosis as herpes simplex keratitis) (Br J Ophthalmol 1995;79:1078)
- Late: ring shaped stromal infiltrate and central ulcer on slit lamp exam (Diagnostics (Basel) 2023;13:2655)
Diagnosis
- Slit lamp examination with or without fluorescein application (Parasite 2015:22:10, J Infect Public Health 2023;16:841)
- Anterior segment optical coherence tomography (Diagnostics (Basel) 2023;13:2655)
- Corneal scraping for microbiological culture and PCR
- Note: culture may require up to 10 days of incubation, which can delay the diagnosis and treatment (Diagnostics (Basel) 2023;13:2655)
- Corneal biopsy following negative scrape
Laboratory
- Amoebic cyst walls identified by direct microscopy on calcofluor white (CFW) and potassium hydroxide (KOH) wet mount (Diagnostics (Basel) 2023;13:2655, J Infect Public Health 2023;16:841)
Prognostic factors
- Poor outcomes associated with both delayed diagnosis and the use of corticosteroids before therapy (Br J Ophthalmol 2018;102:1431)
- Older age is associated with worse outcome (Br J Ophthalmol 2018;102:1431)
Case reports
- 20 year old man with orthokeratology contact lenses, right eye pain and redness for 2 days and dendrite-like anterior stromal keratitis coinfected with Acanthamoeba and Pseudomonas (Taiwan J Ophthalmol 2019;9:131)
- 26 year old woman with history of immunocompetence and contact lens use presented with severe pain, photophobia, tearing and decreased visual acuity of her left eye for 2 months (Parasitol Res 2021;120:1121)
- 53 year old woman with contact lens use and a 2 month history of a persistent left corneal ulcer (Hum Pathol 2013;44:918)
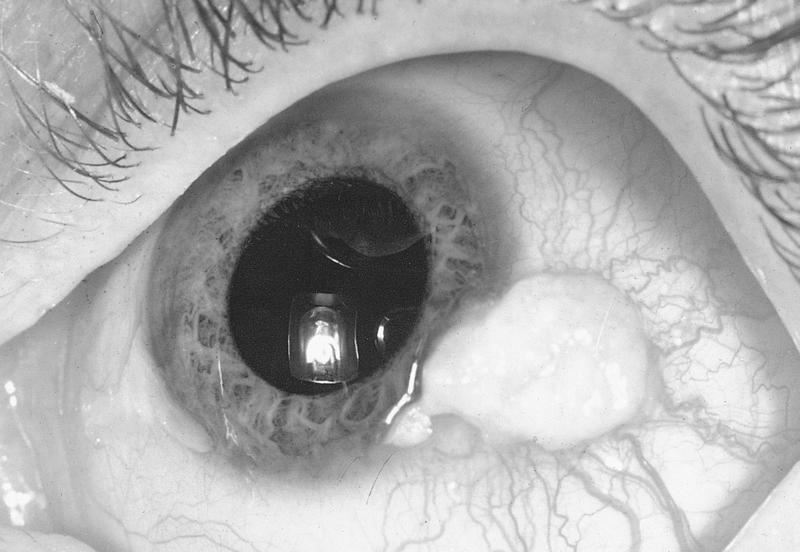
- 65 year old man presented with a 10 year history of bilateral uveitis, scleritis and eventual complete loss of vision and severe pain in both eyes (bilateral enucleation) (Am J Ophthalmol Case Rep 2020:20:100970)
- 74 year old woman with history of extended soft contact lens use and intense painful ring corneal ulcer refractory to conventional antibiotics (Pathogens 2021;10:323)
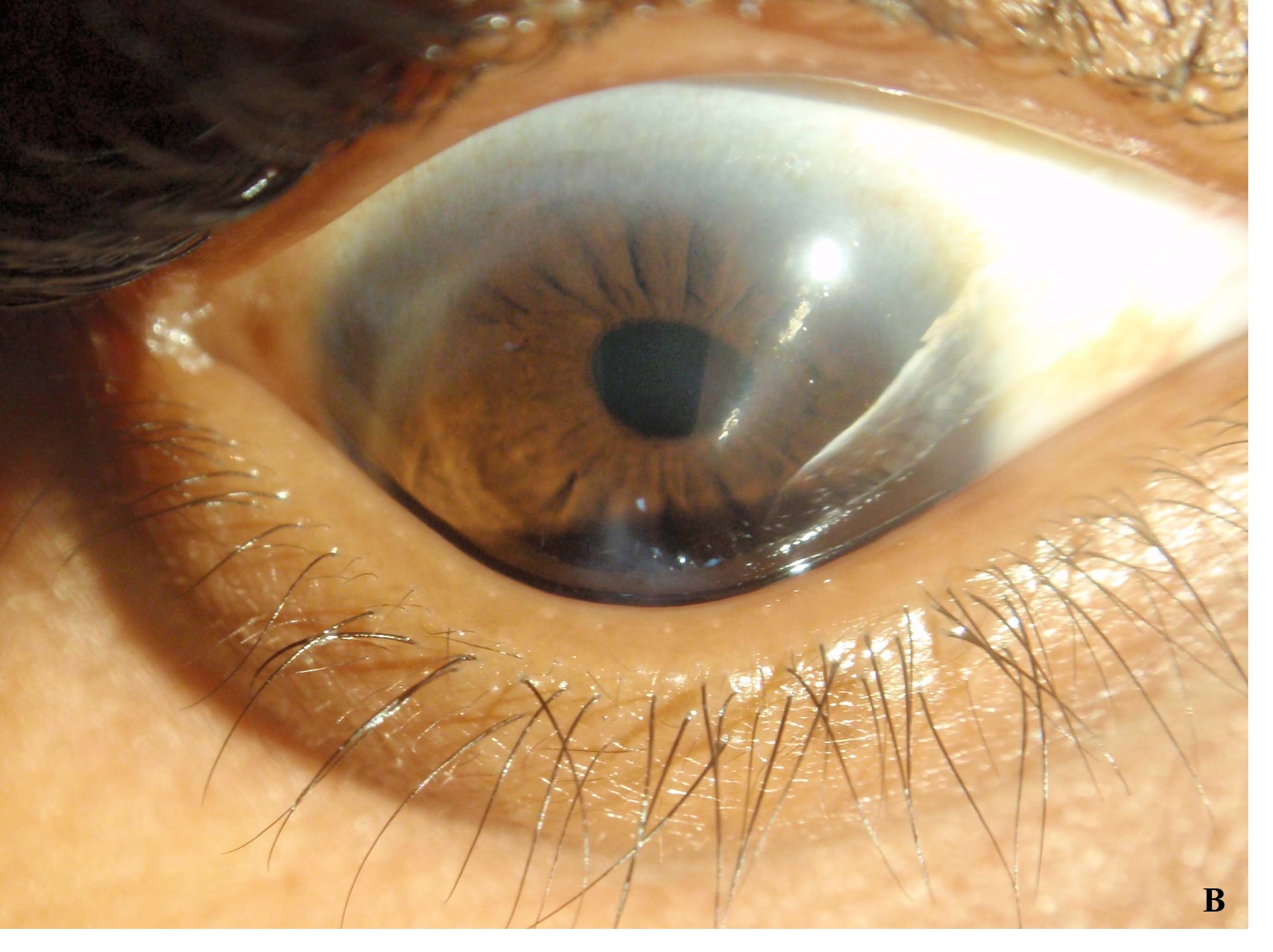
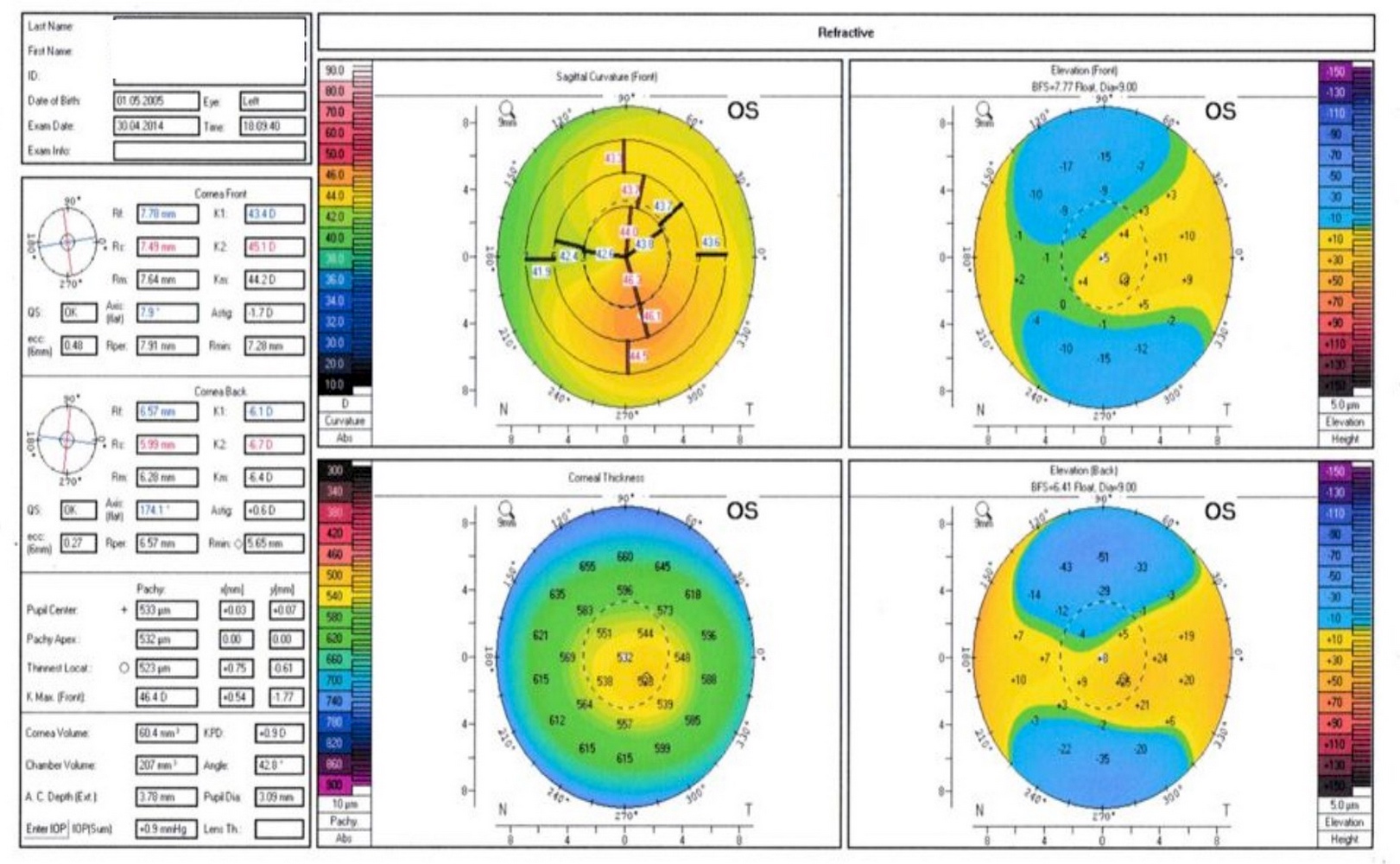
- 76 year old man with rigid gas permeable lens use in the setting of keratoconus presented after a 4 month history of corneal ulcer of the left eye (BMJ Case Rep 2021;14:e241864)
Treatment
- Acanthamoeba trophozoite form is susceptible but the cystic form is highly drug resistant and may persist for months
- Principal initial treatment is topical biguanide, such as polyhexamethylene biguanide (PHMB) 0.02 - 0.08% or chlorhexidine 0.02 - 0.06% (J Clin Med 2021;10:942)
- PHMB 0.08% monotherapy (Ophthalmology 2023 Oct 4 [Epub ahead of print])
- In severe cases, therapeutic keratoplasty
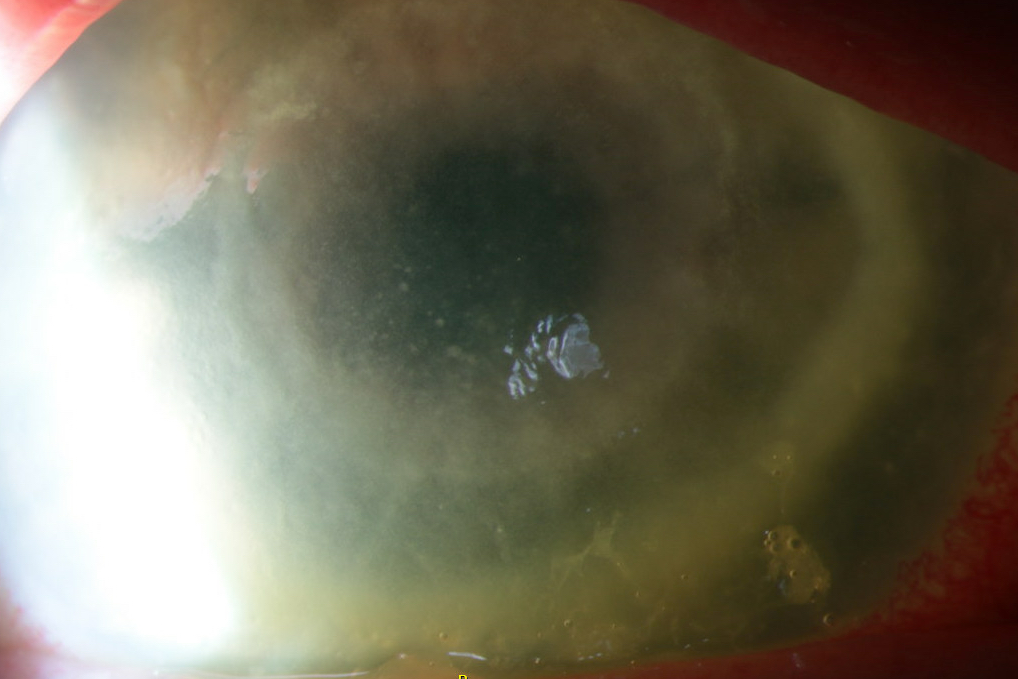
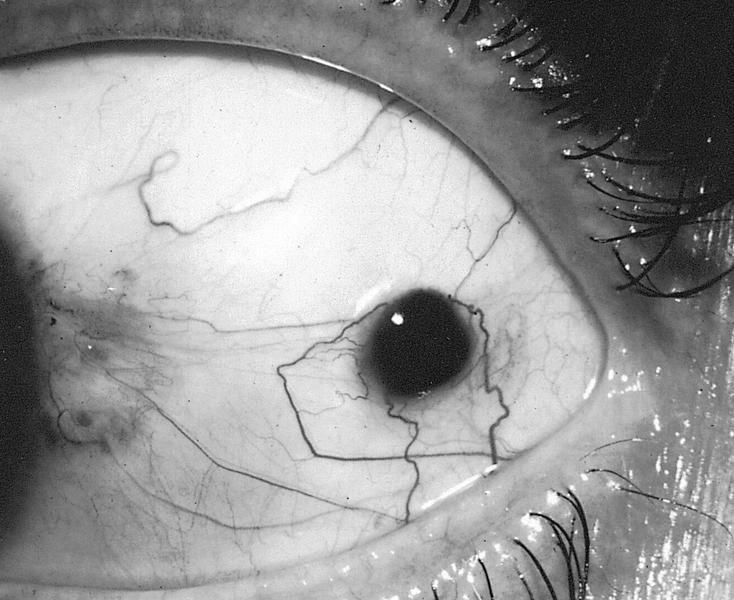
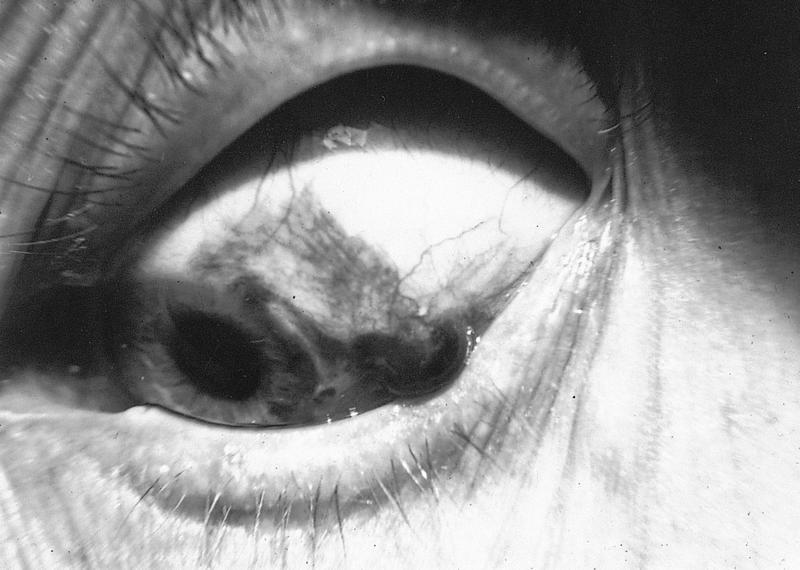
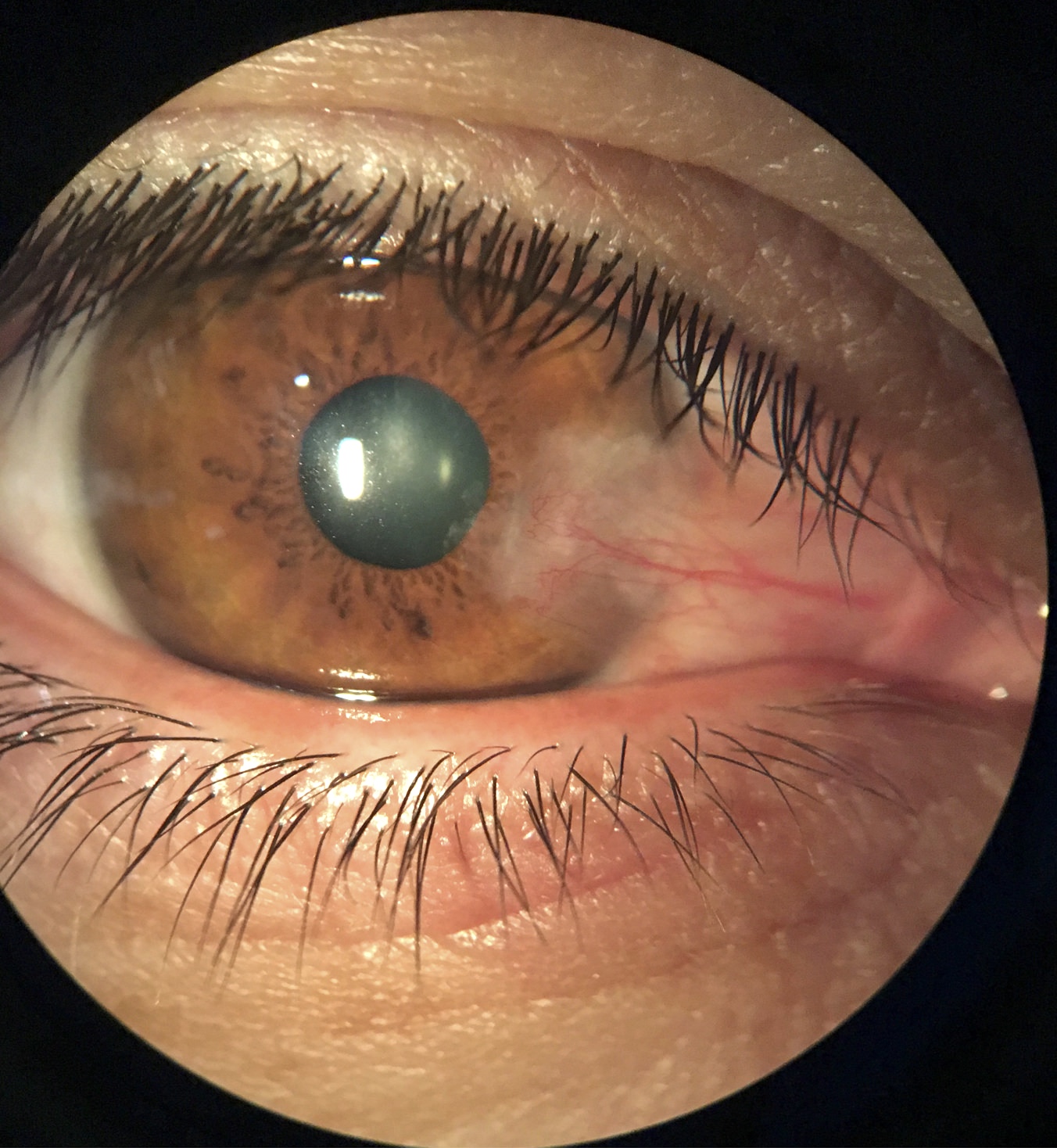
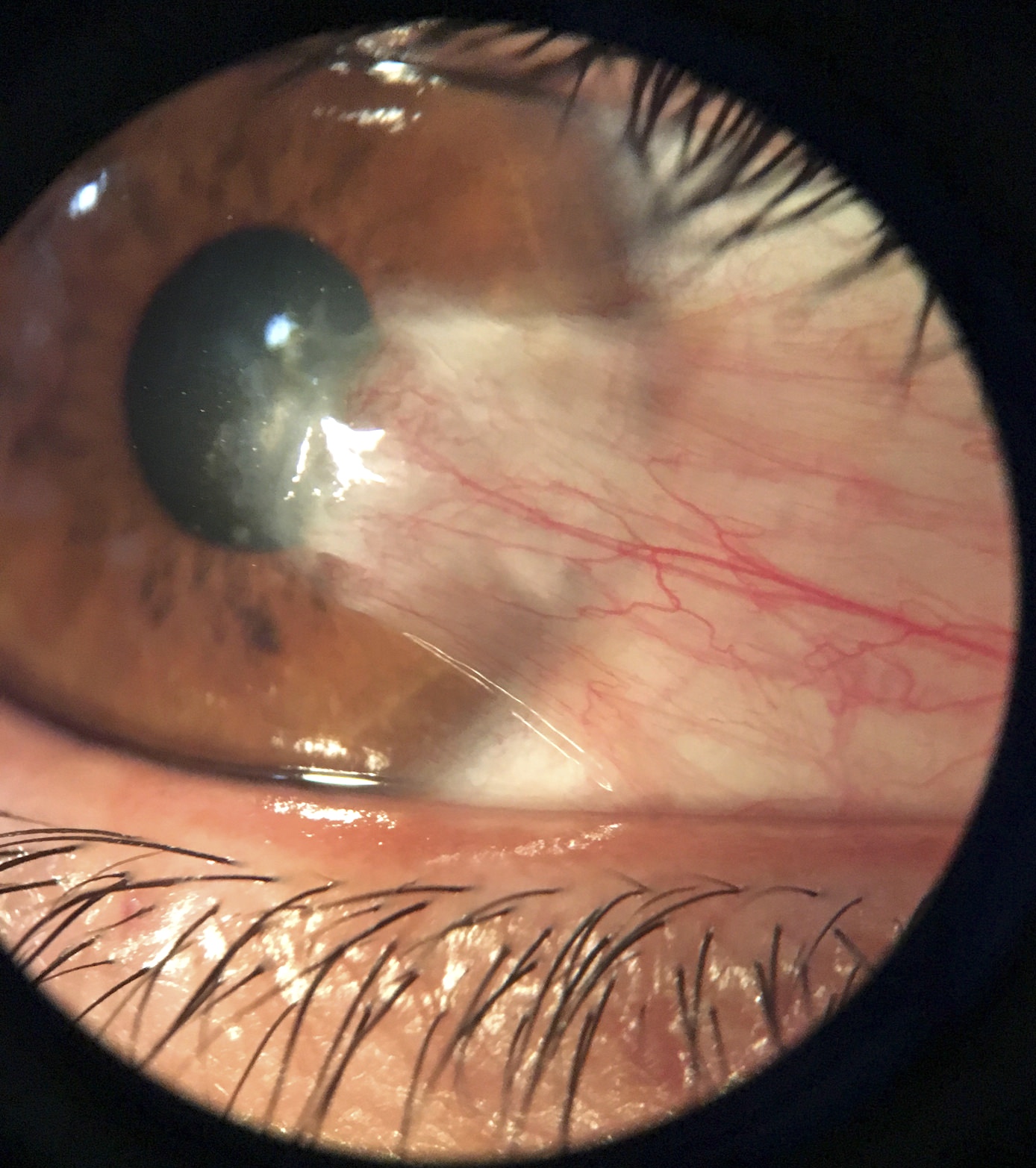
Clinical images
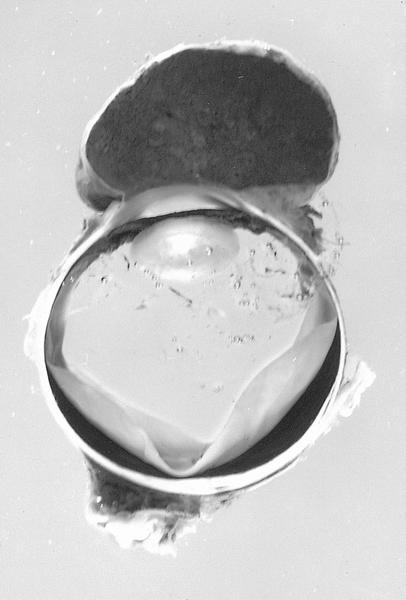
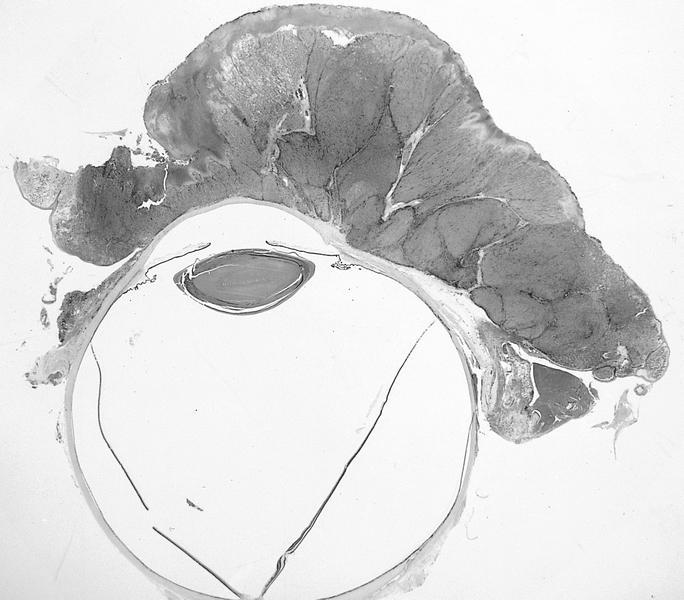
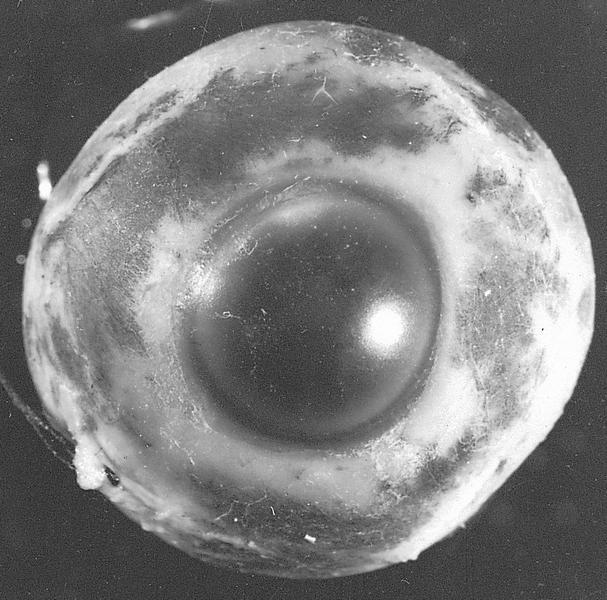
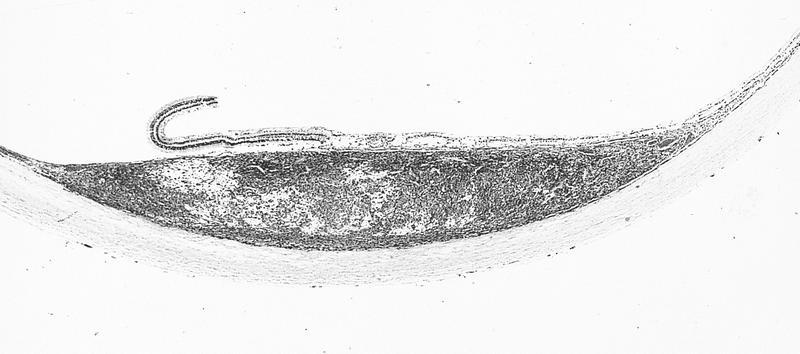
Gross description
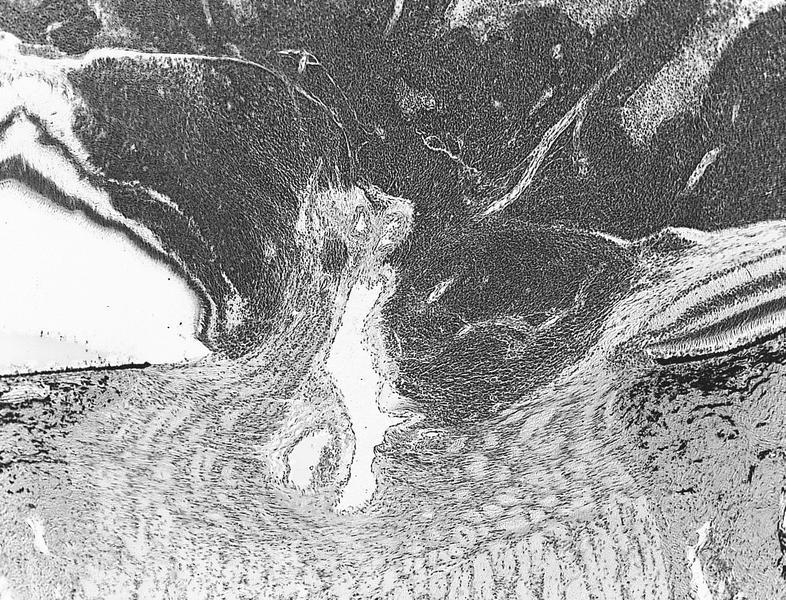
- Transparent to opacified / cloudy disc shaped tissue
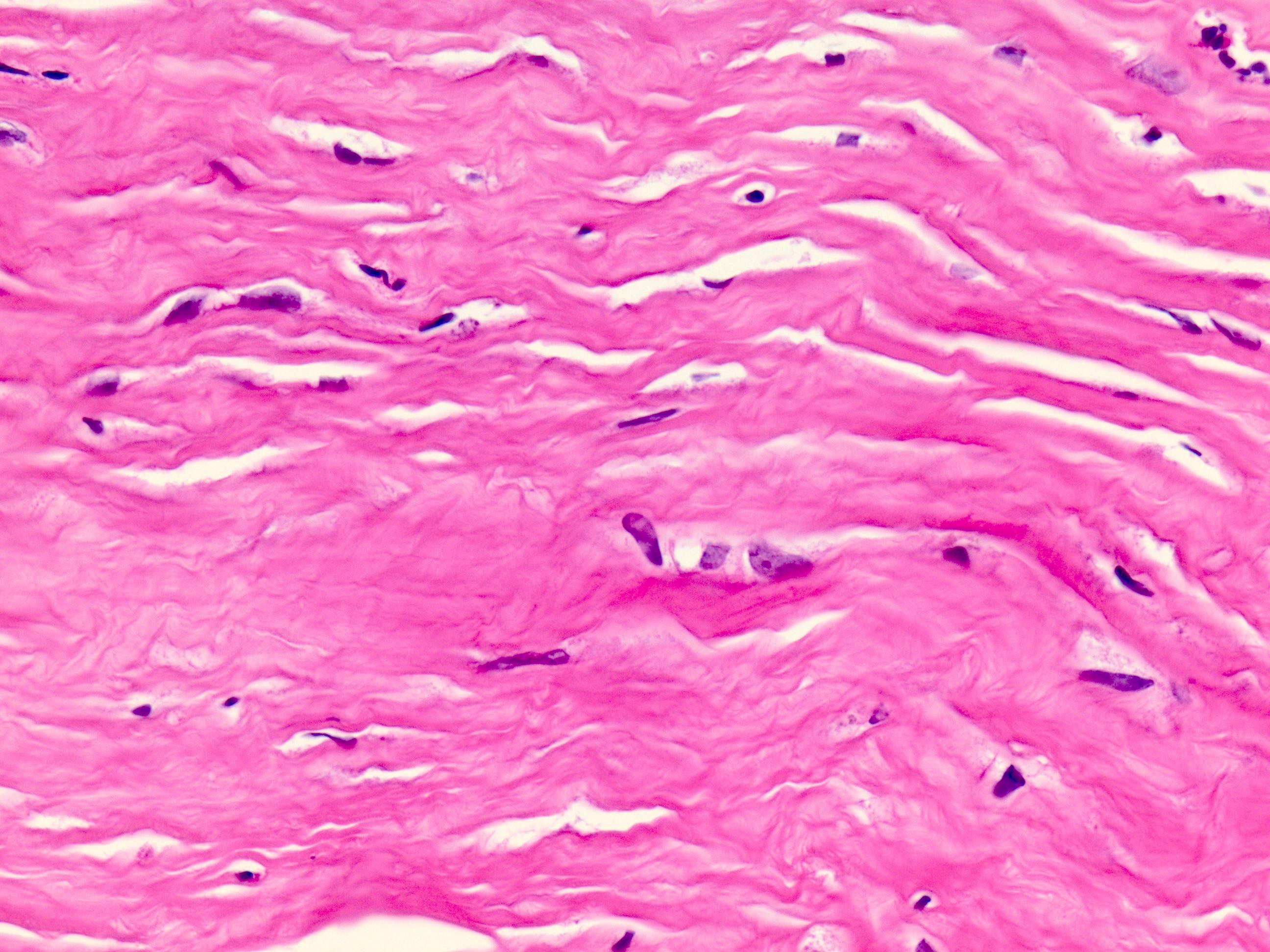
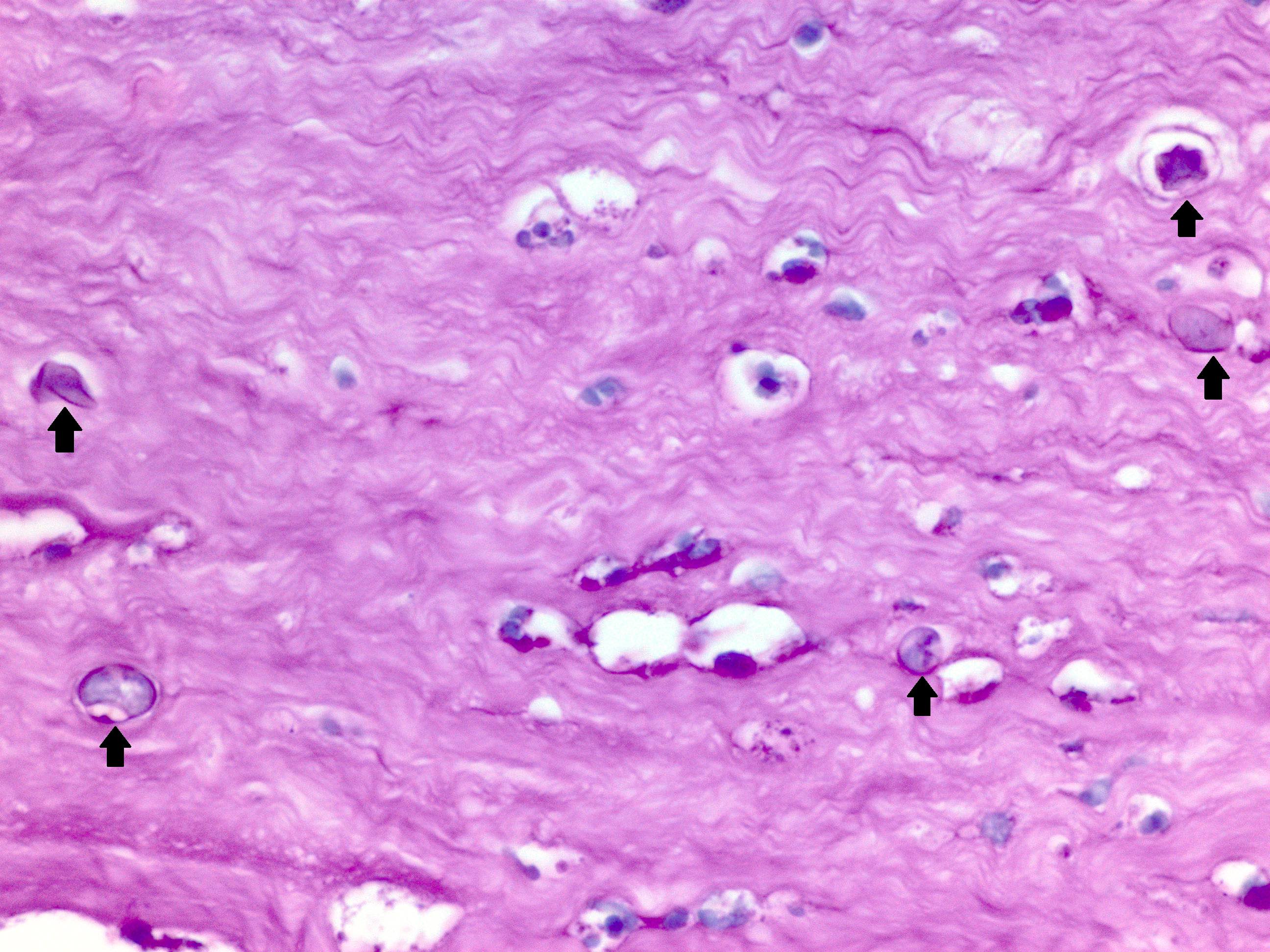
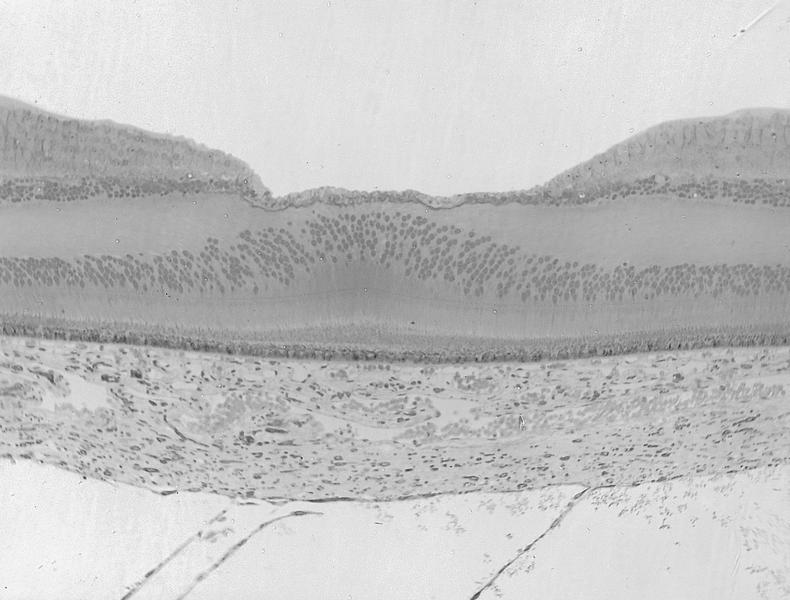
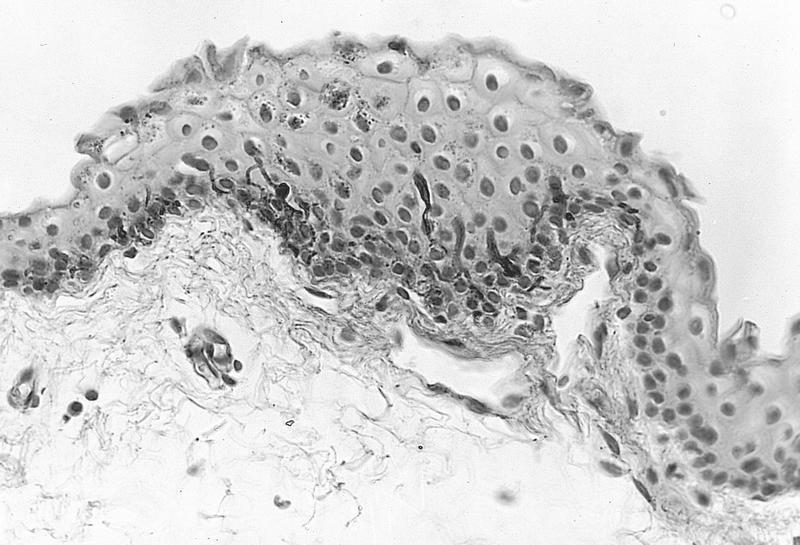
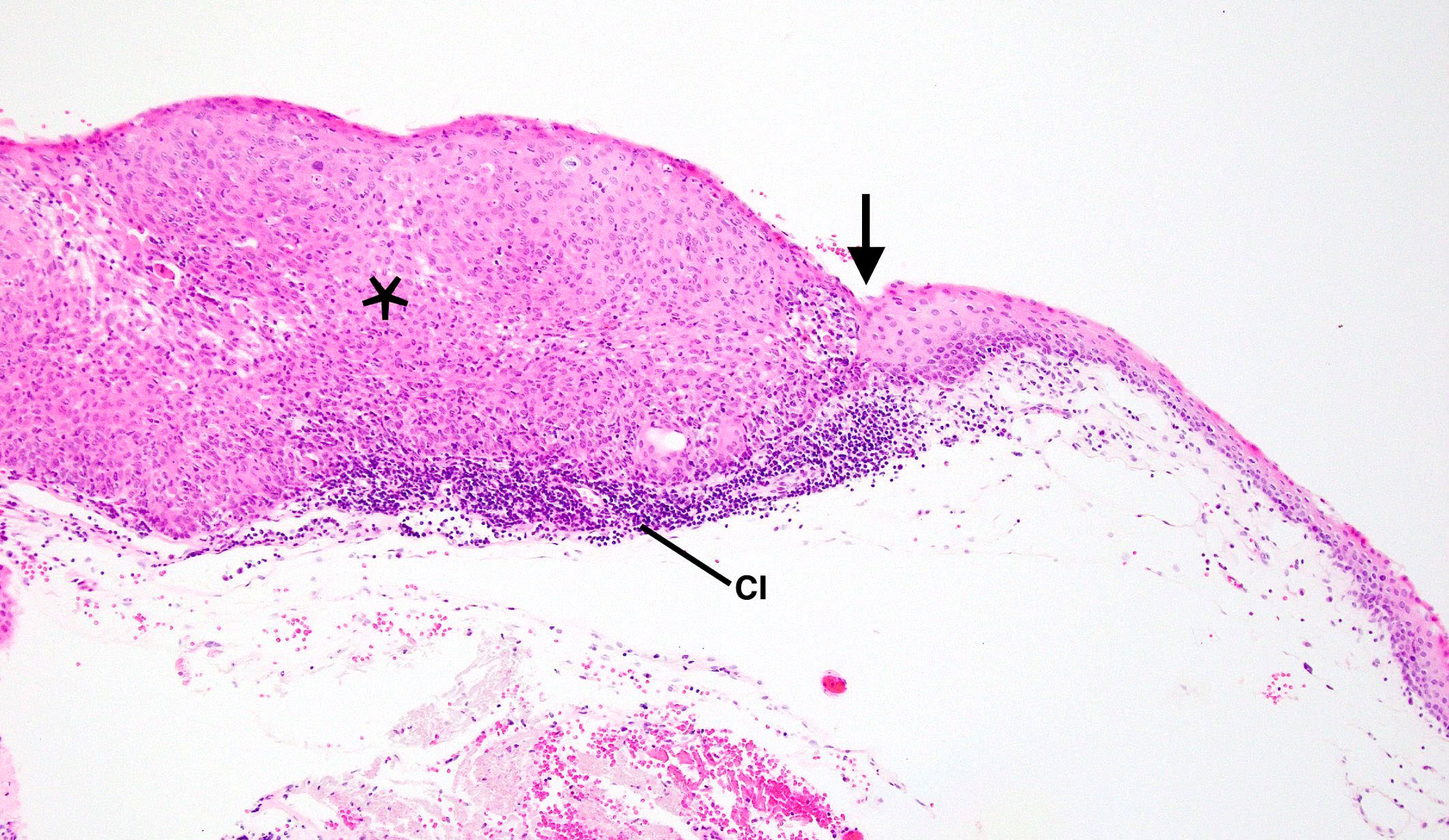
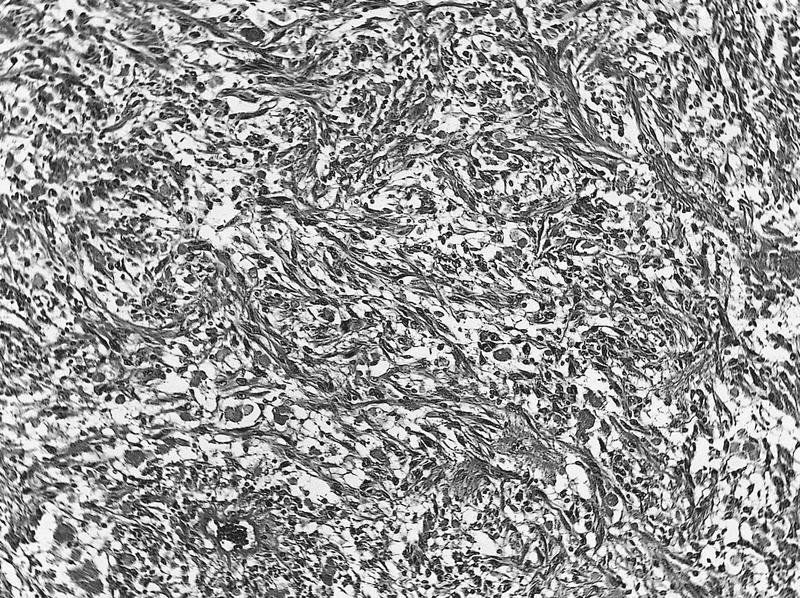
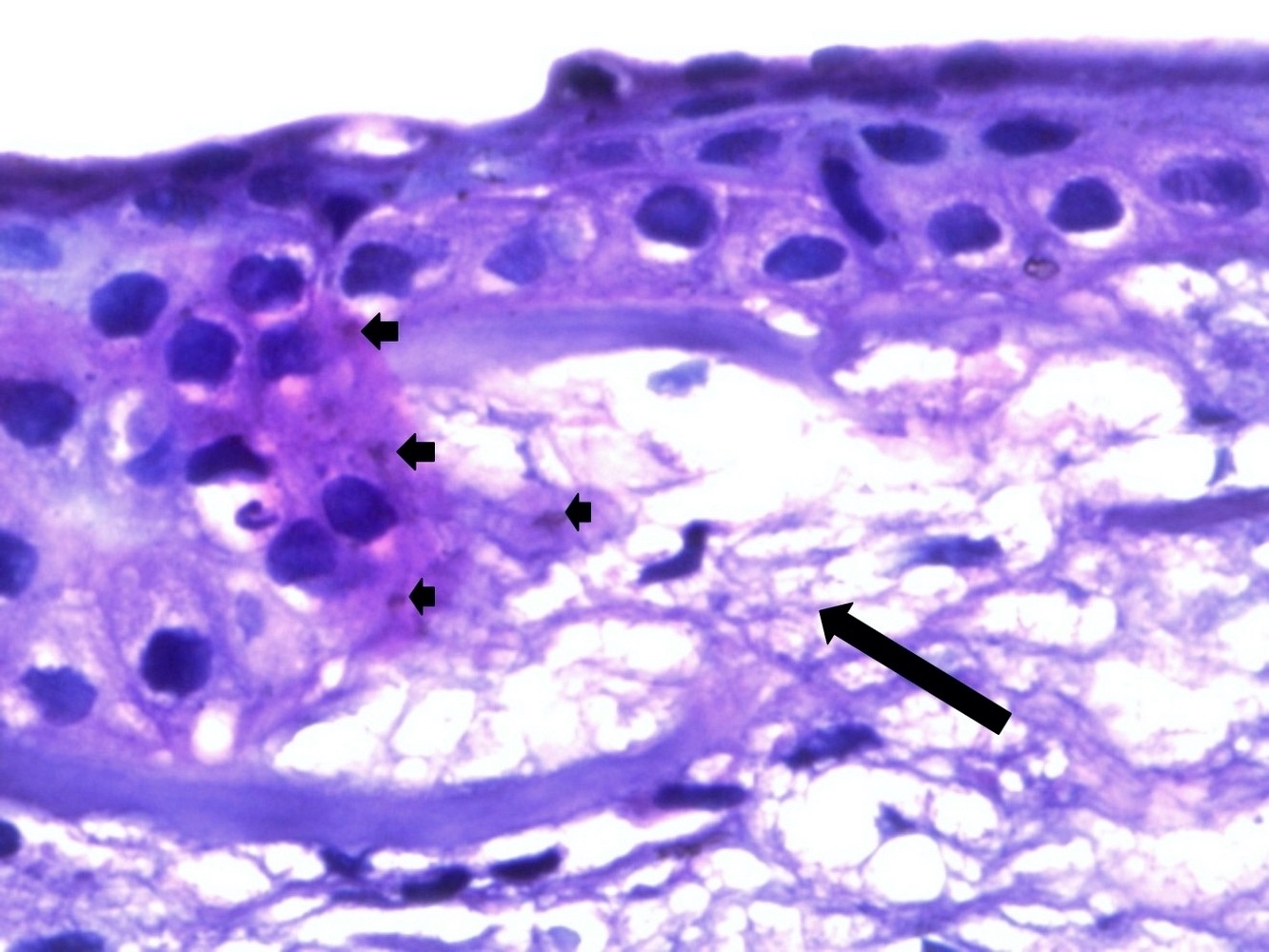
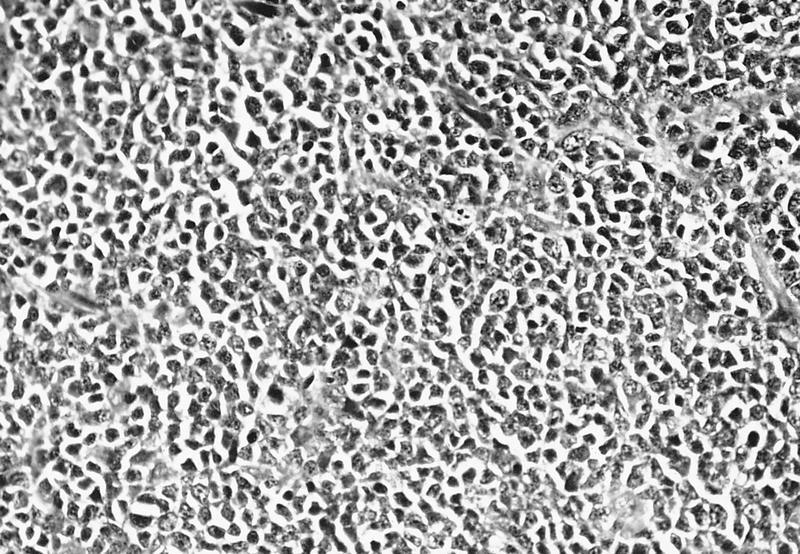
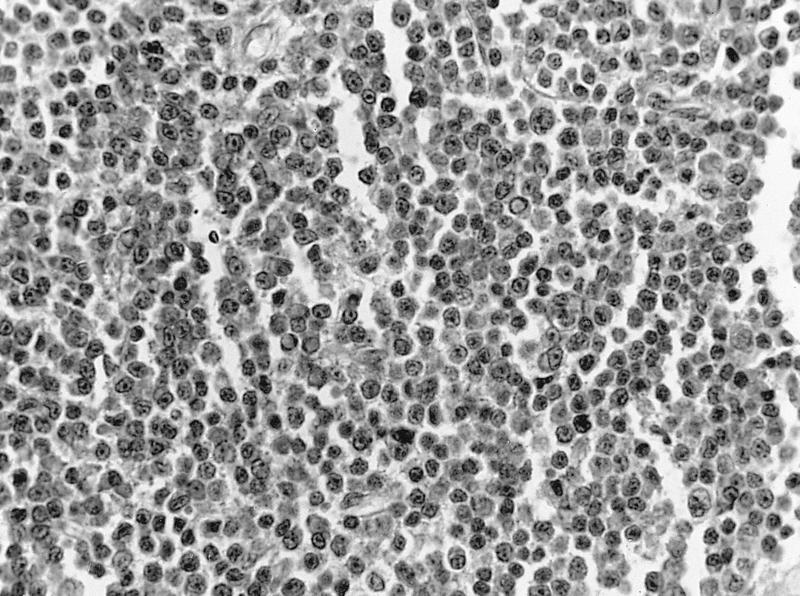
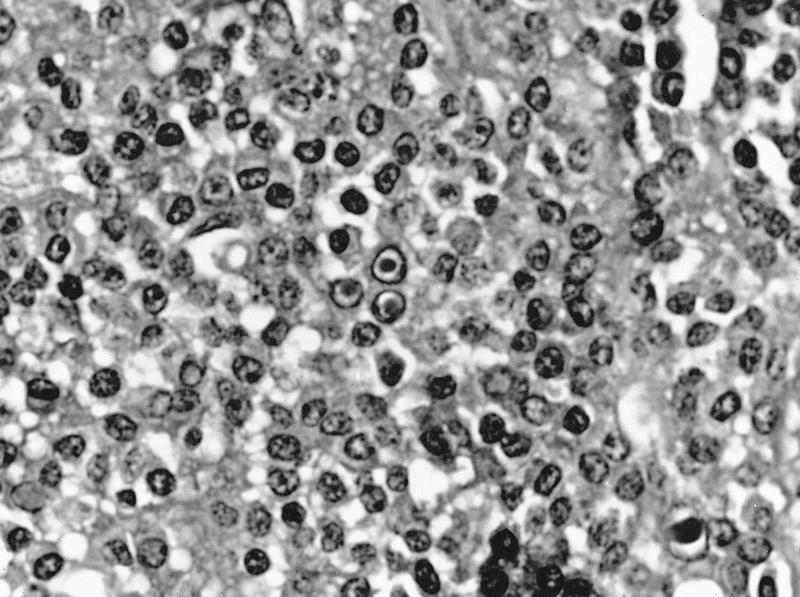
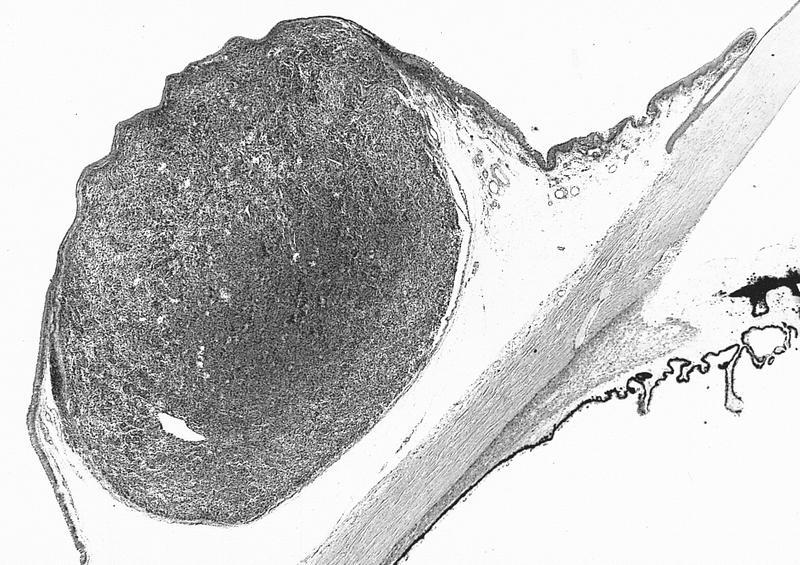
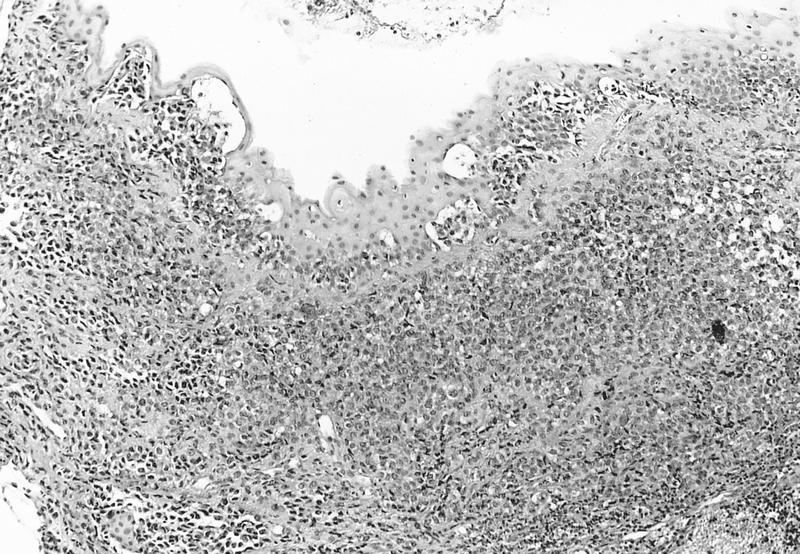
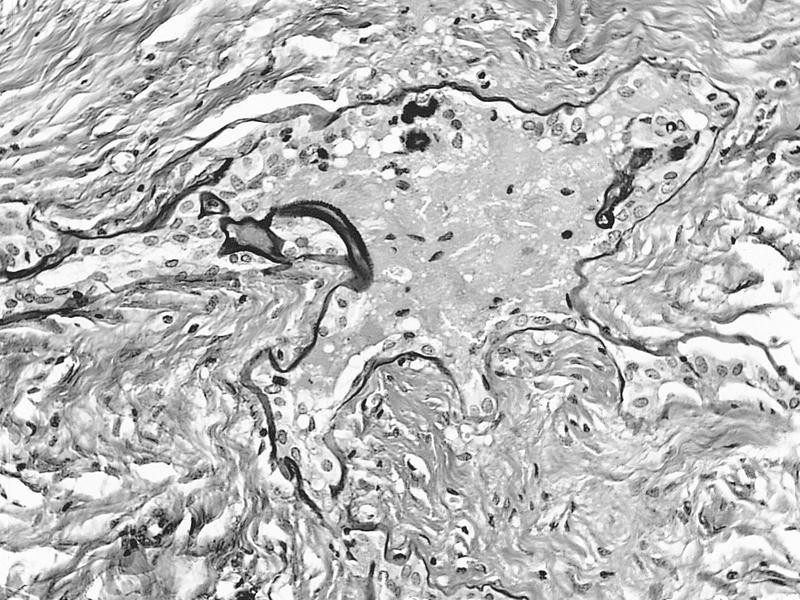
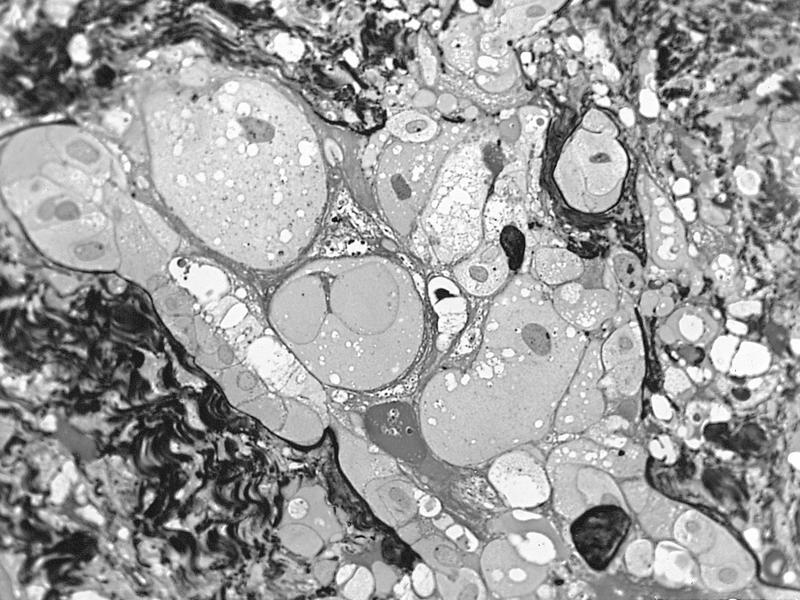
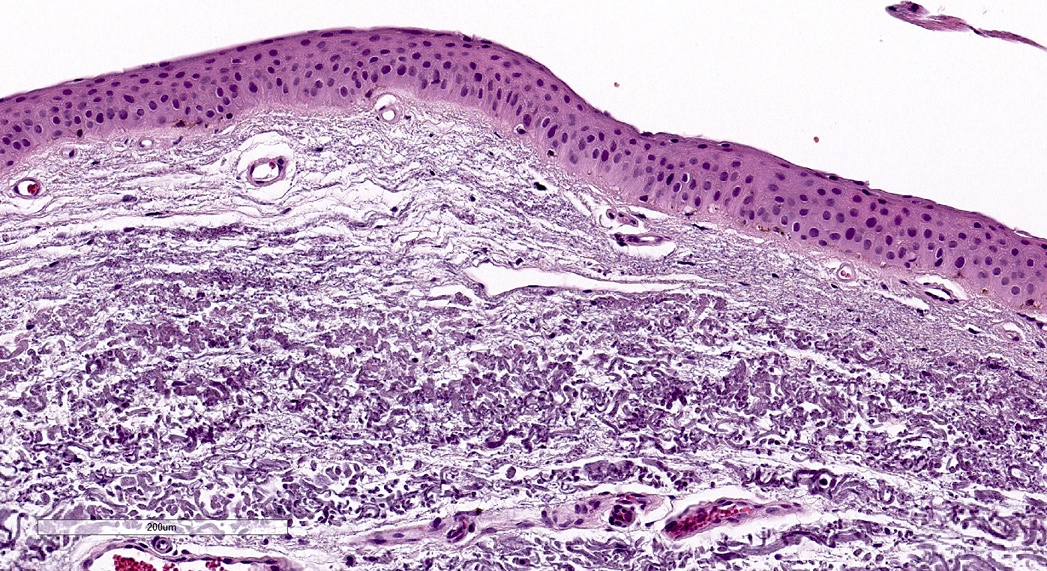
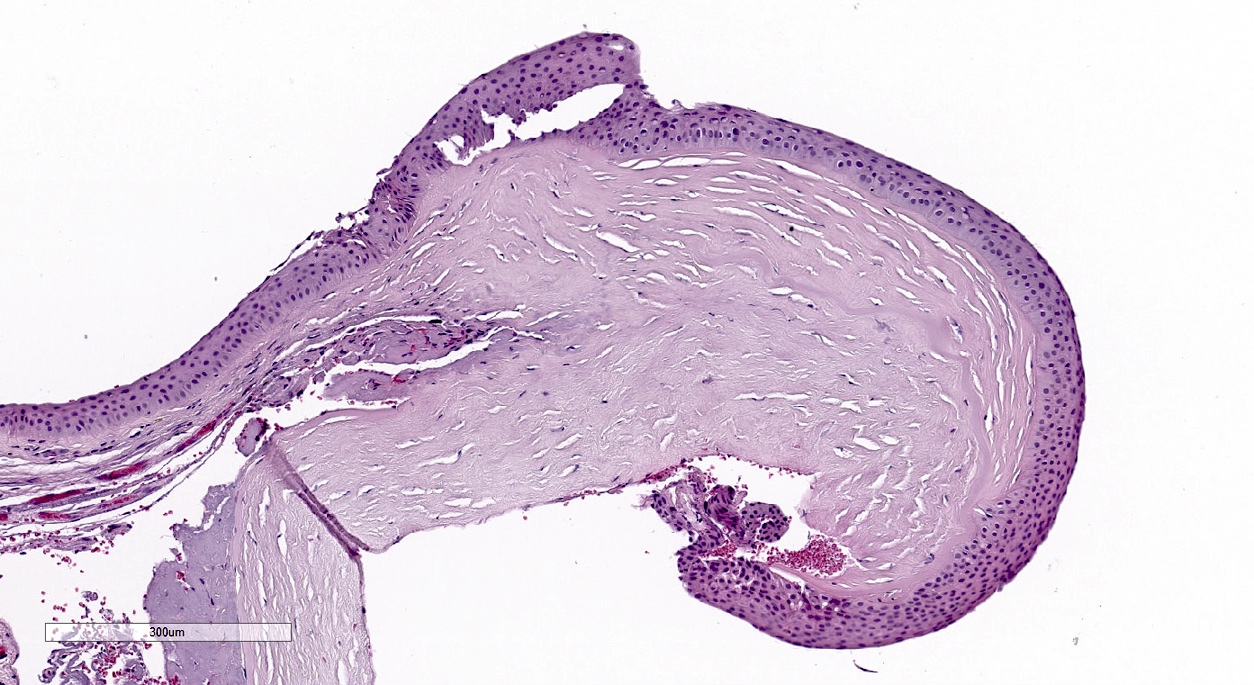
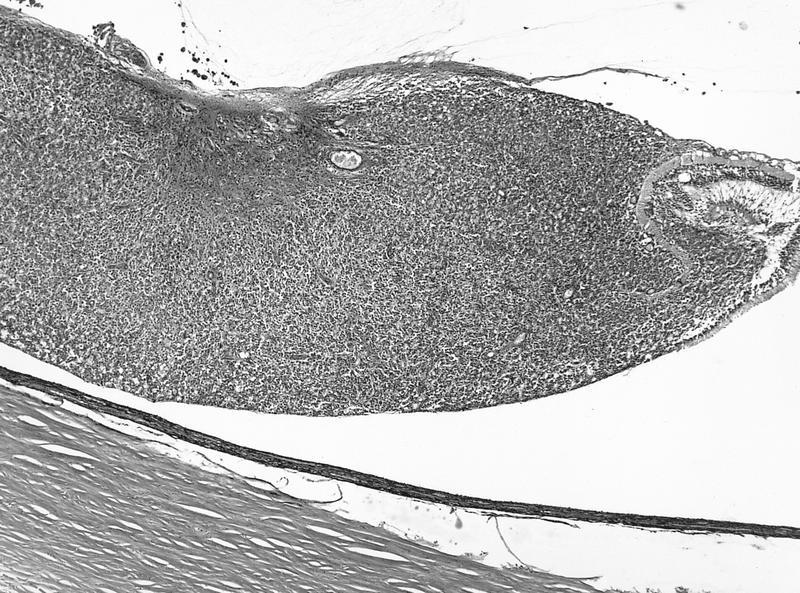
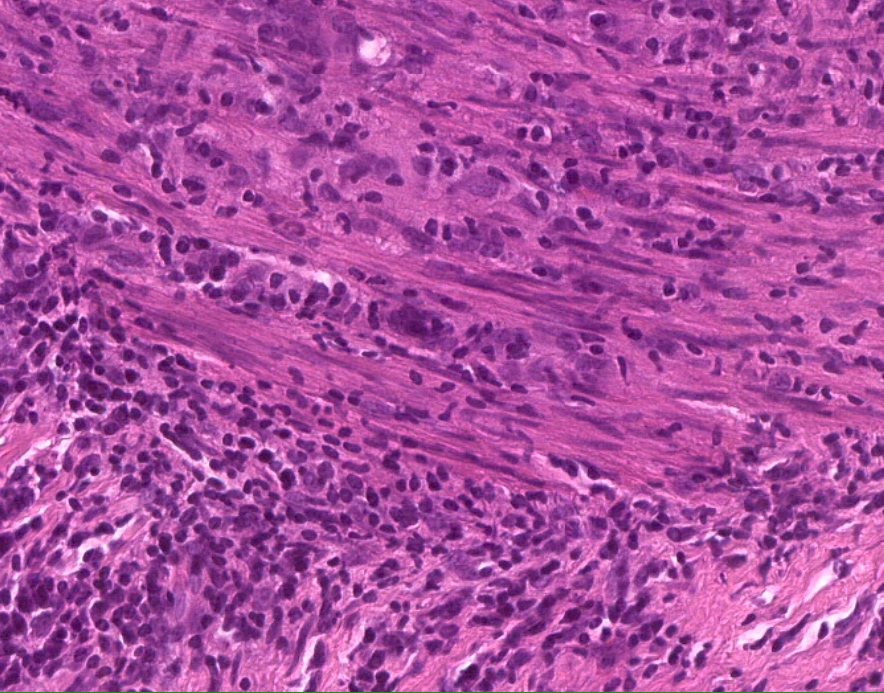
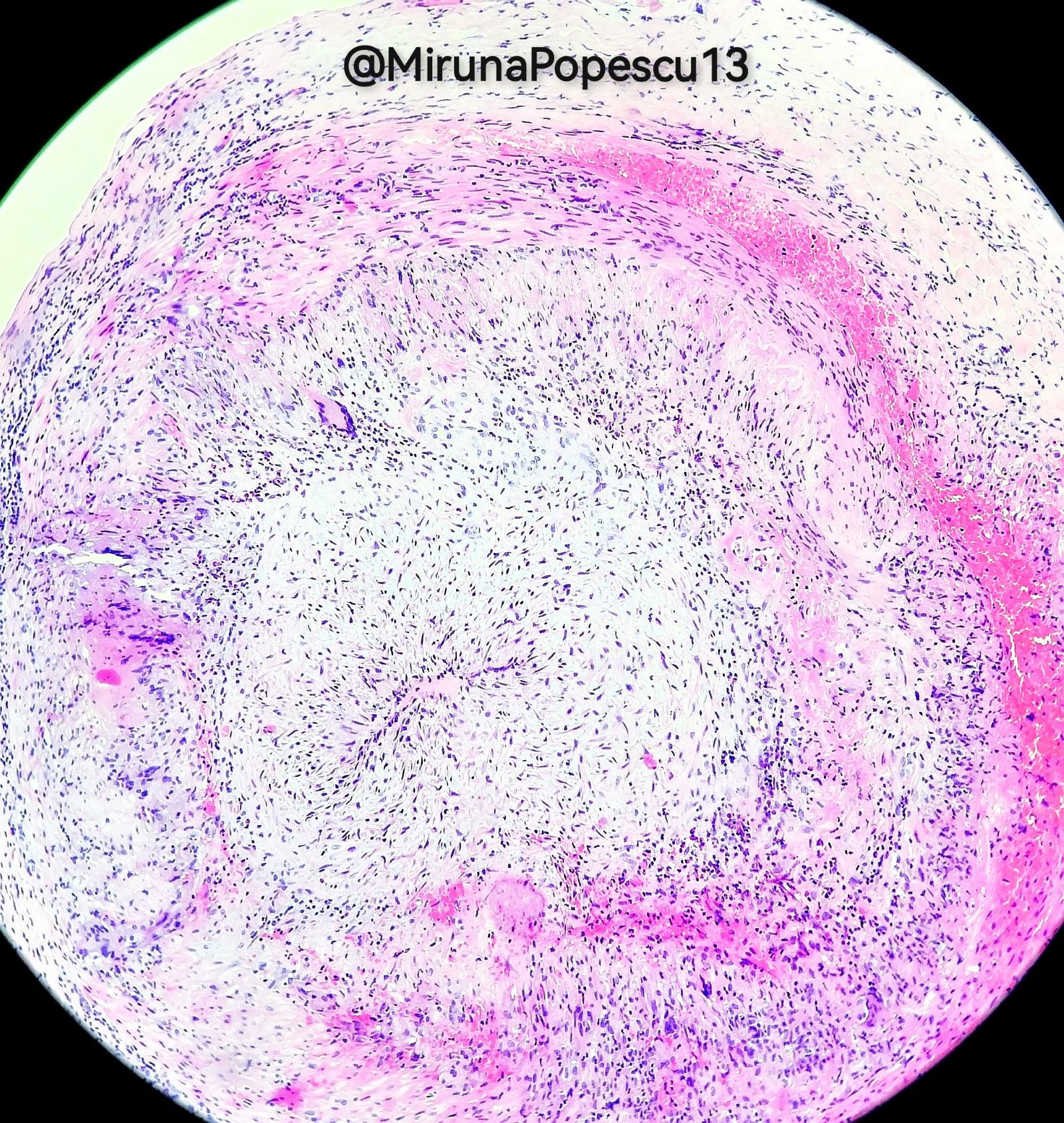
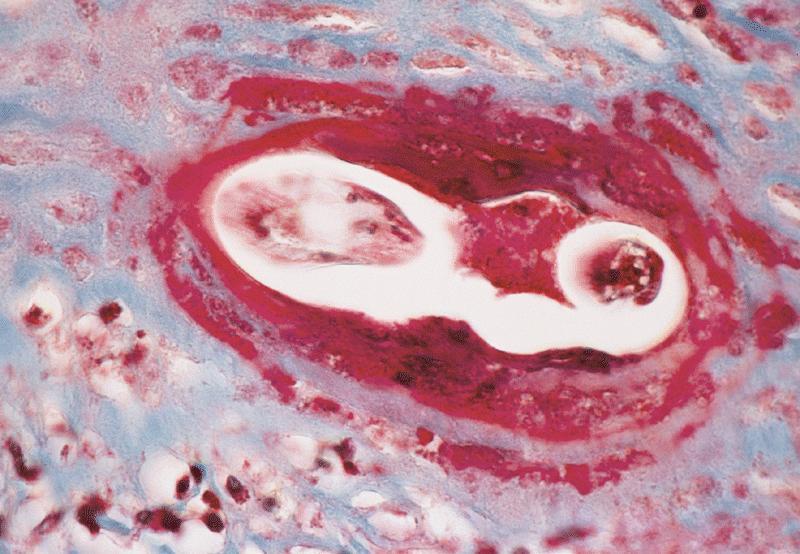
Microscopic (histologic) description
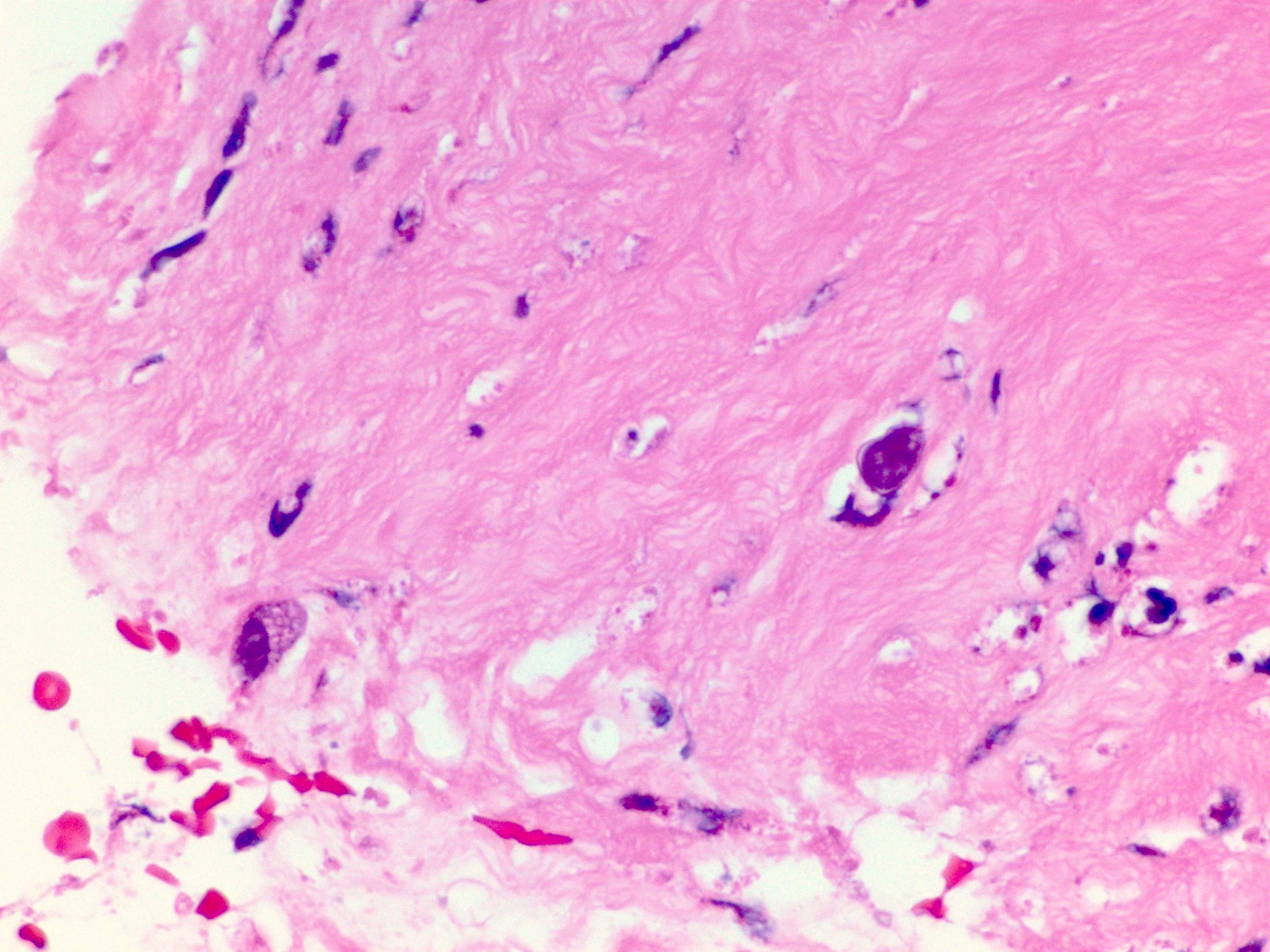
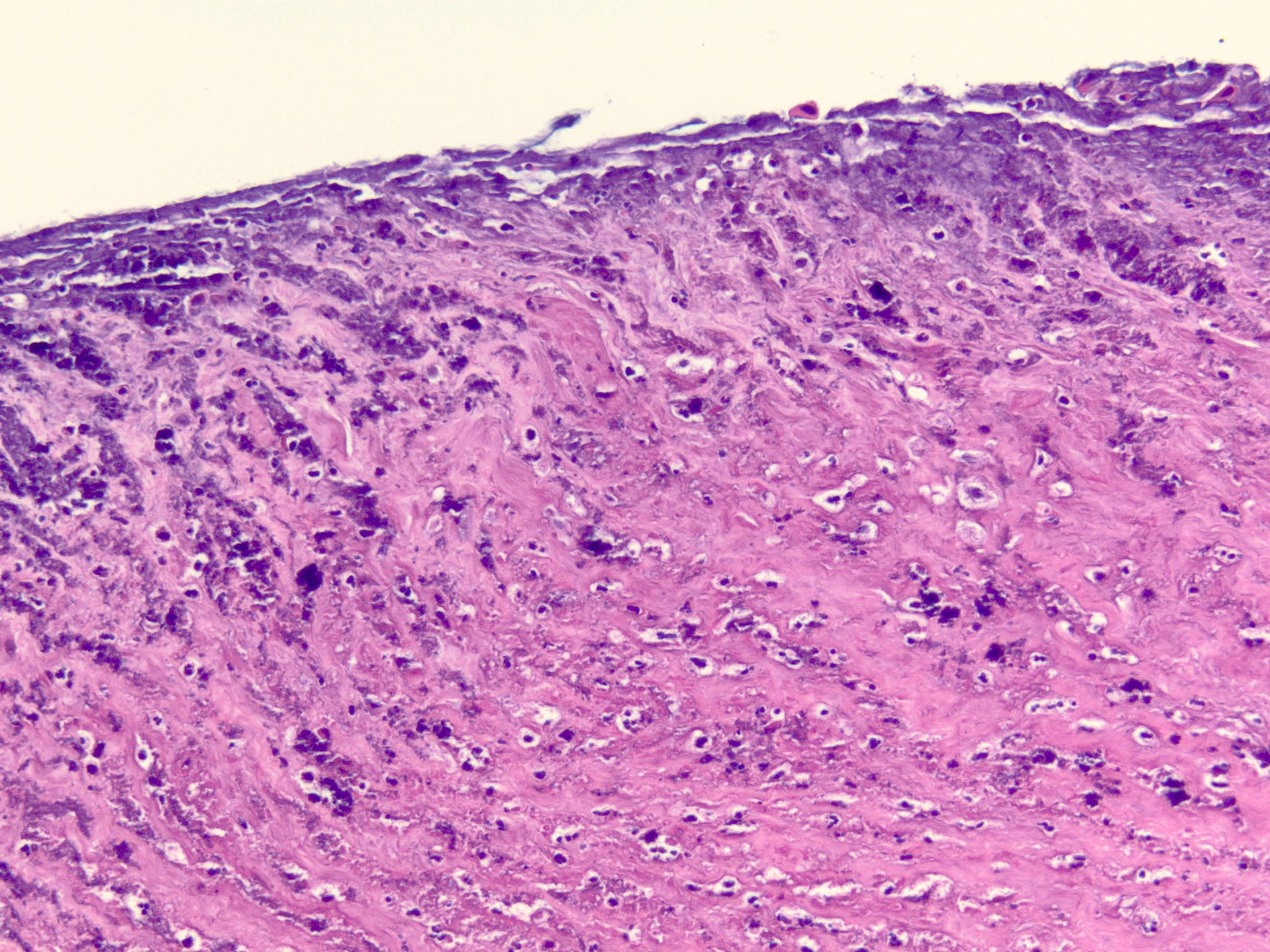
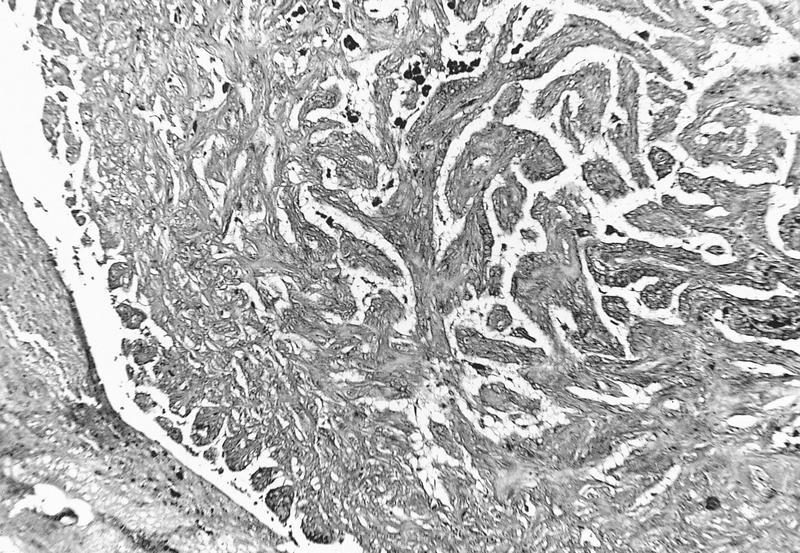
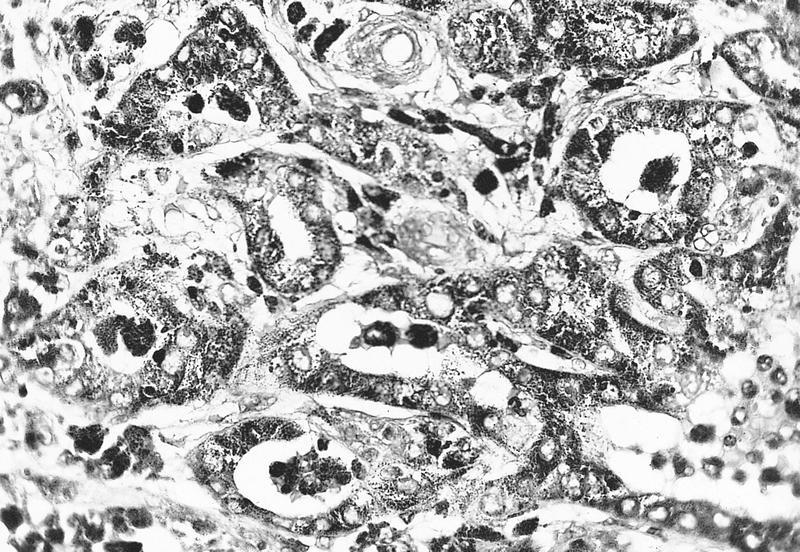
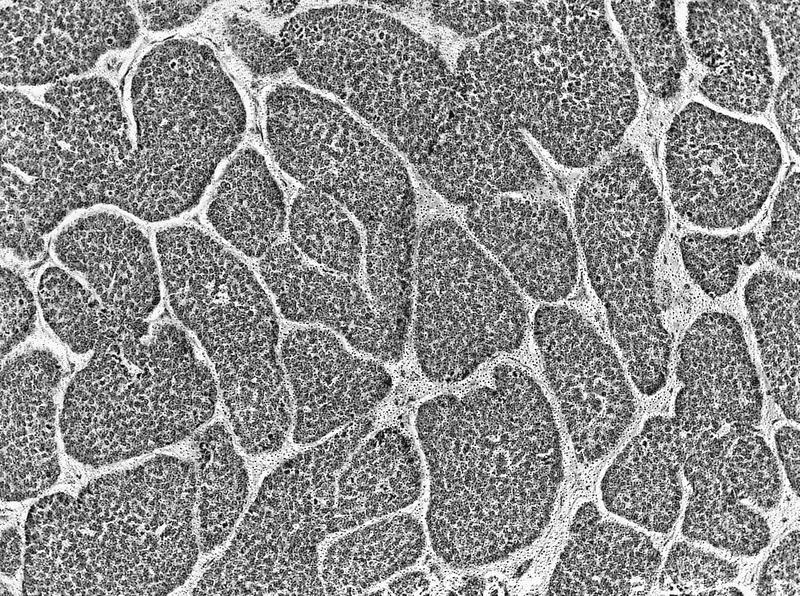
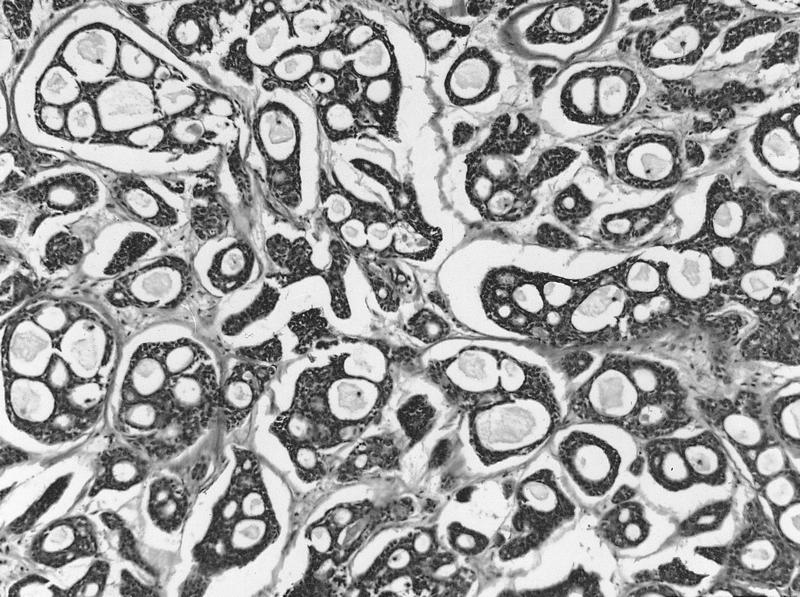
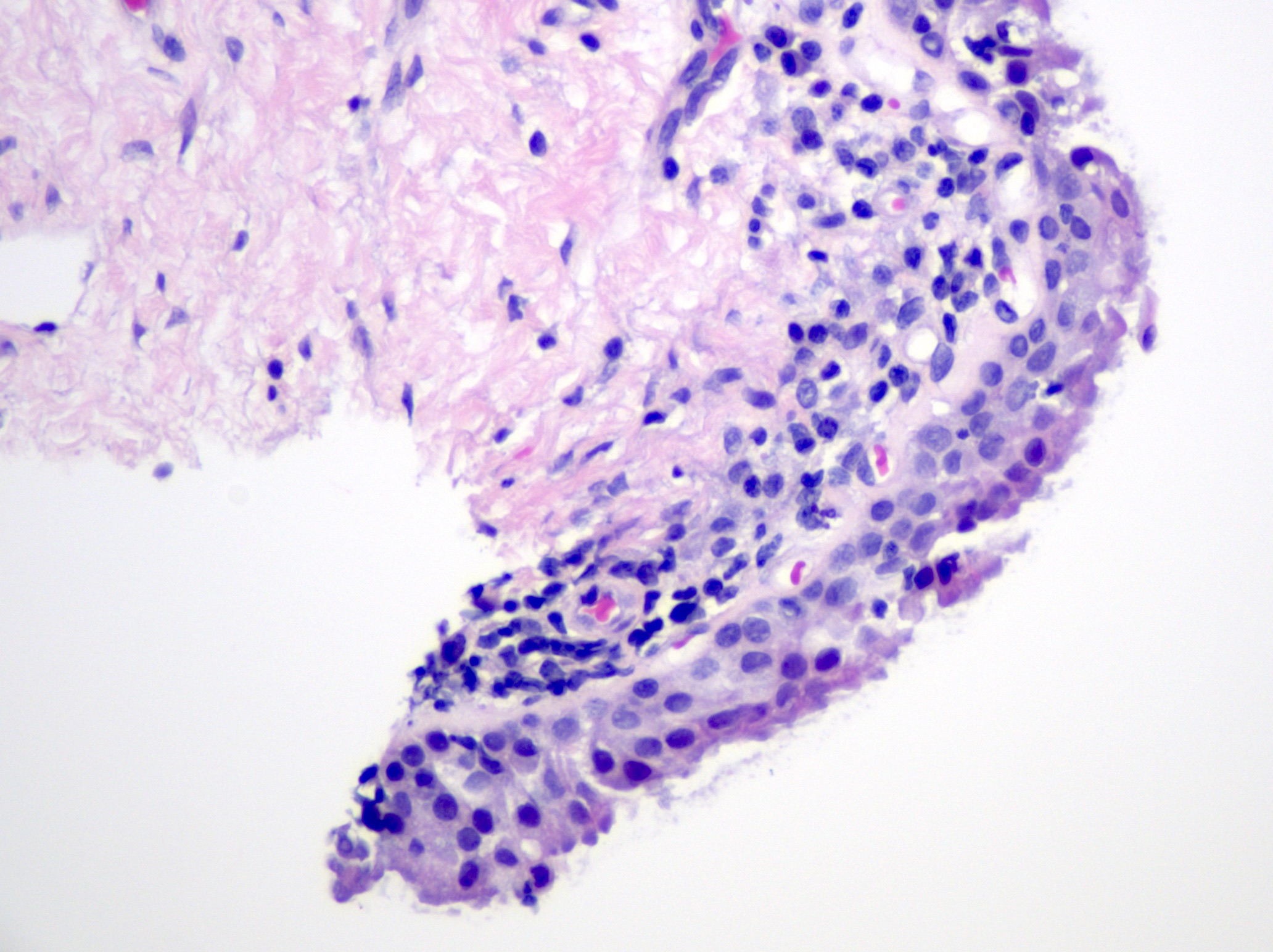
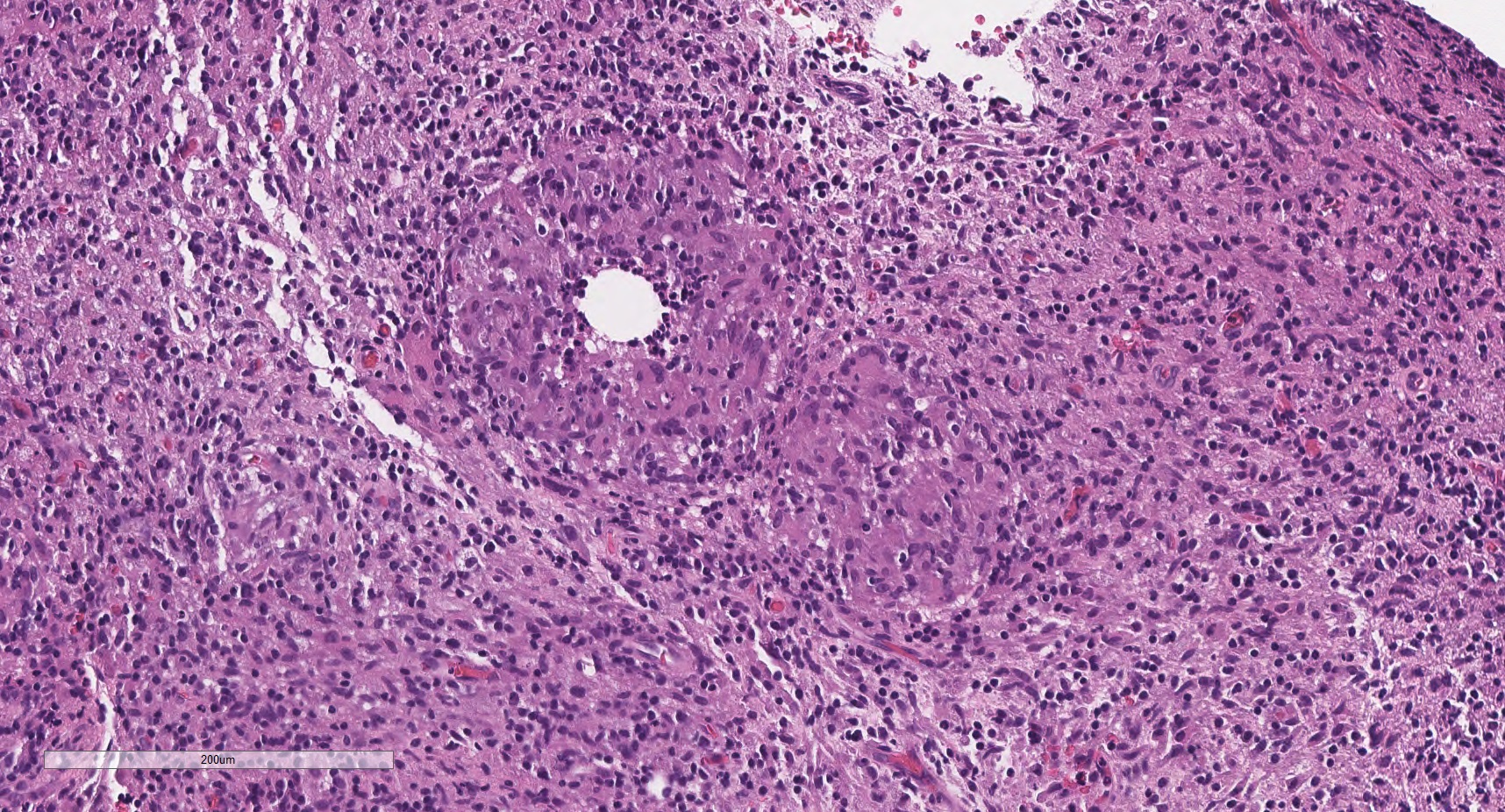
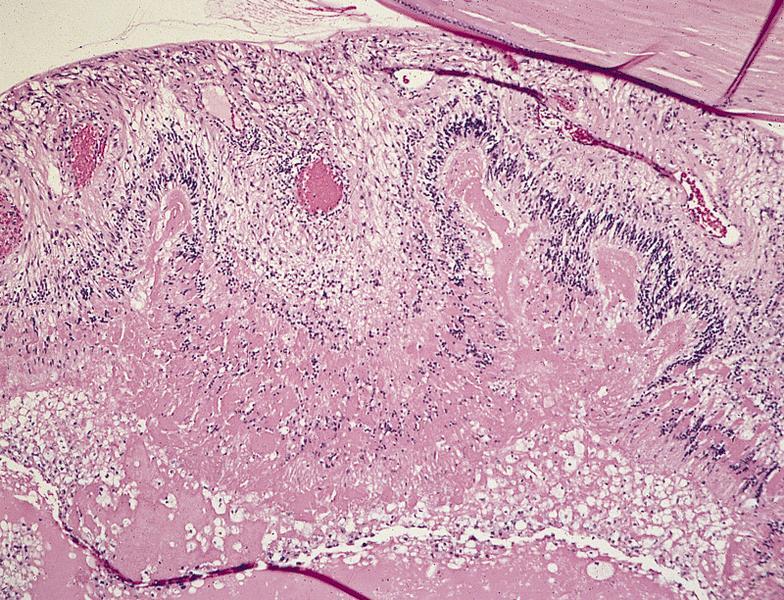
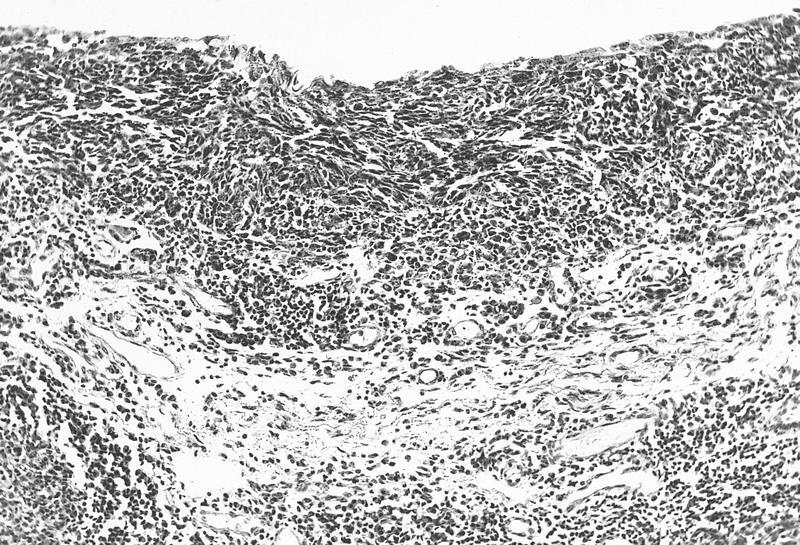
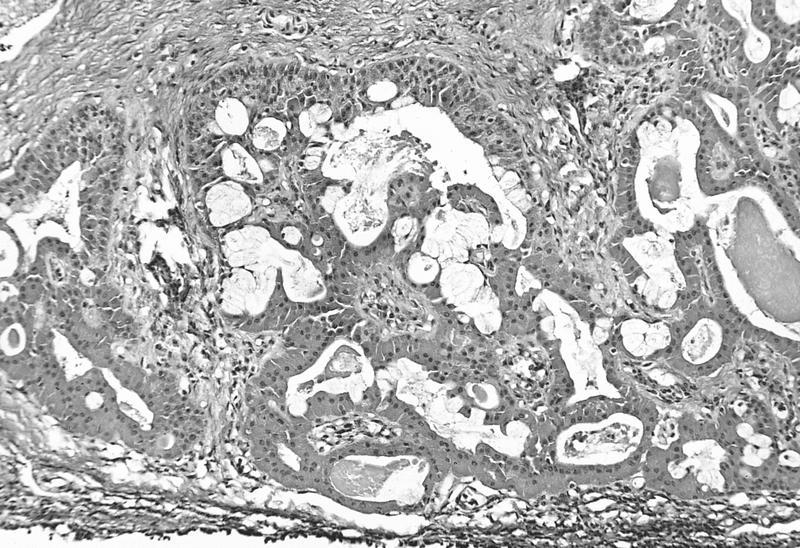
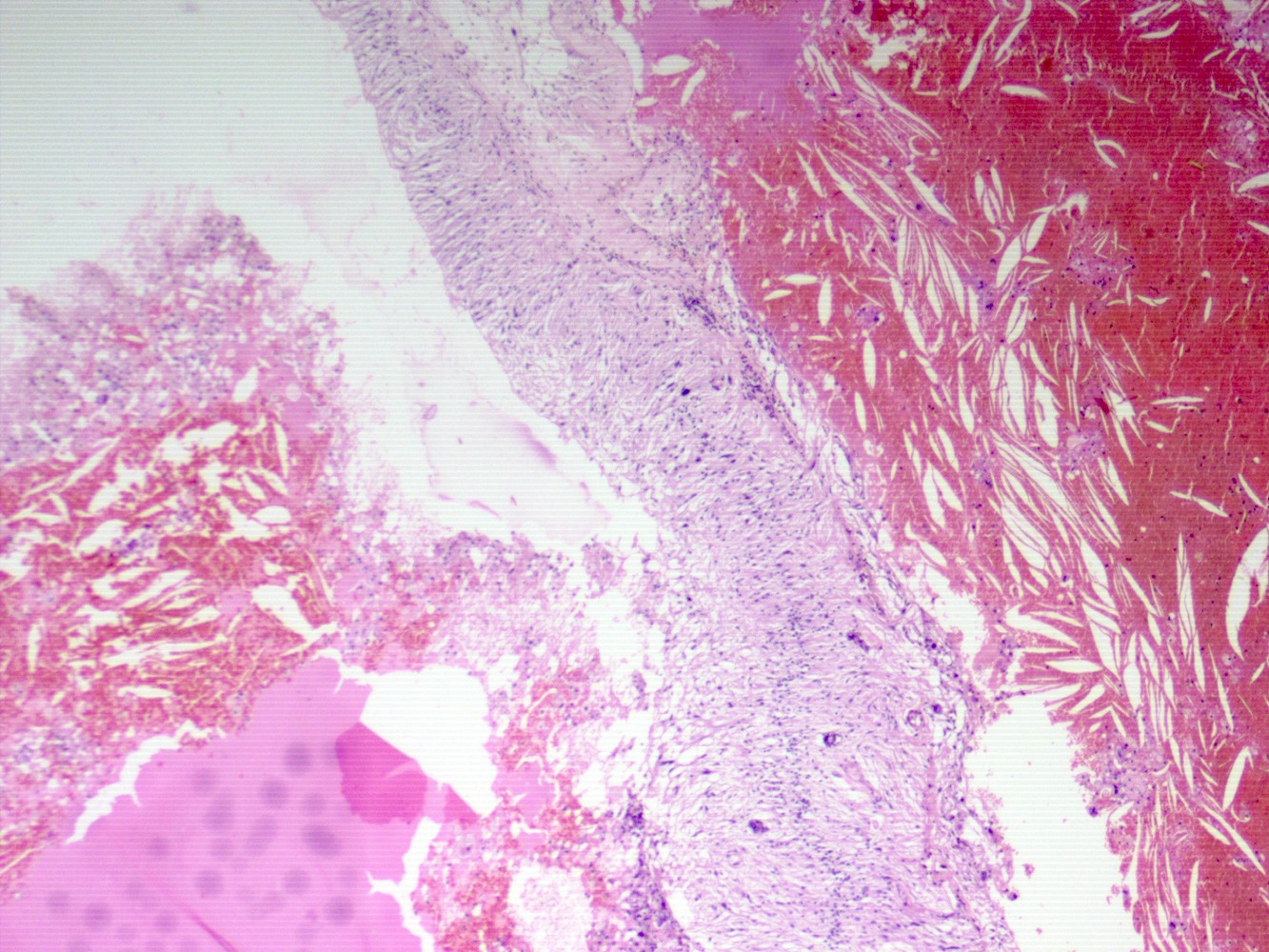
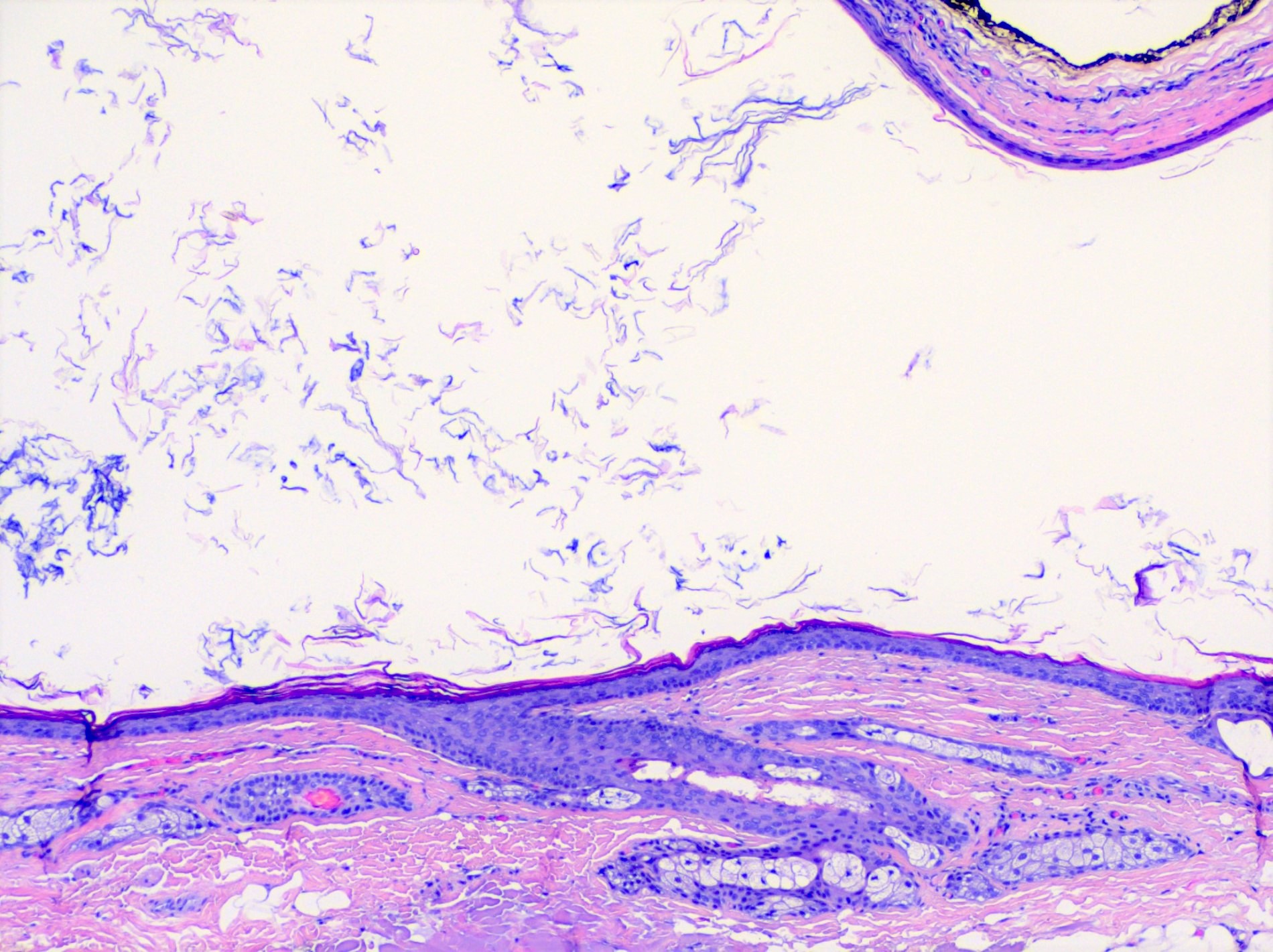
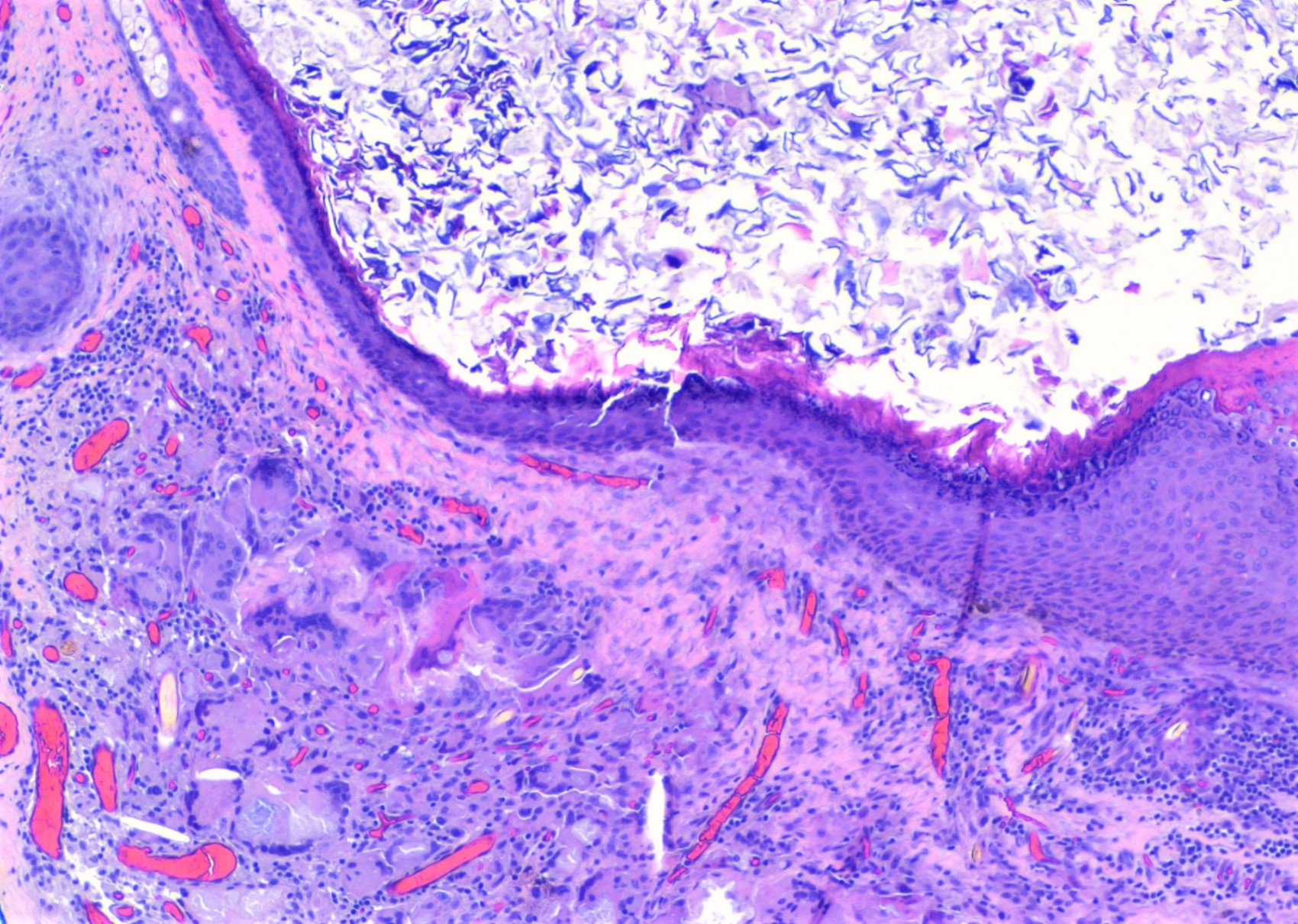
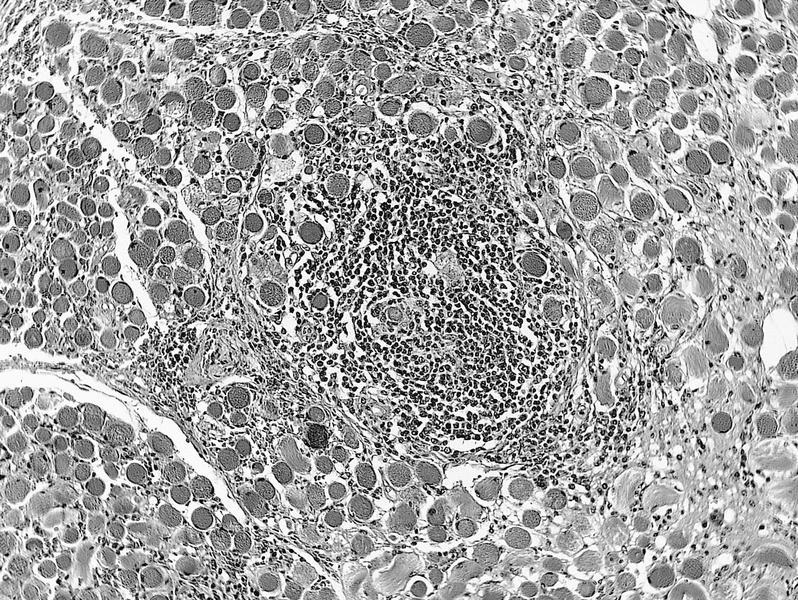
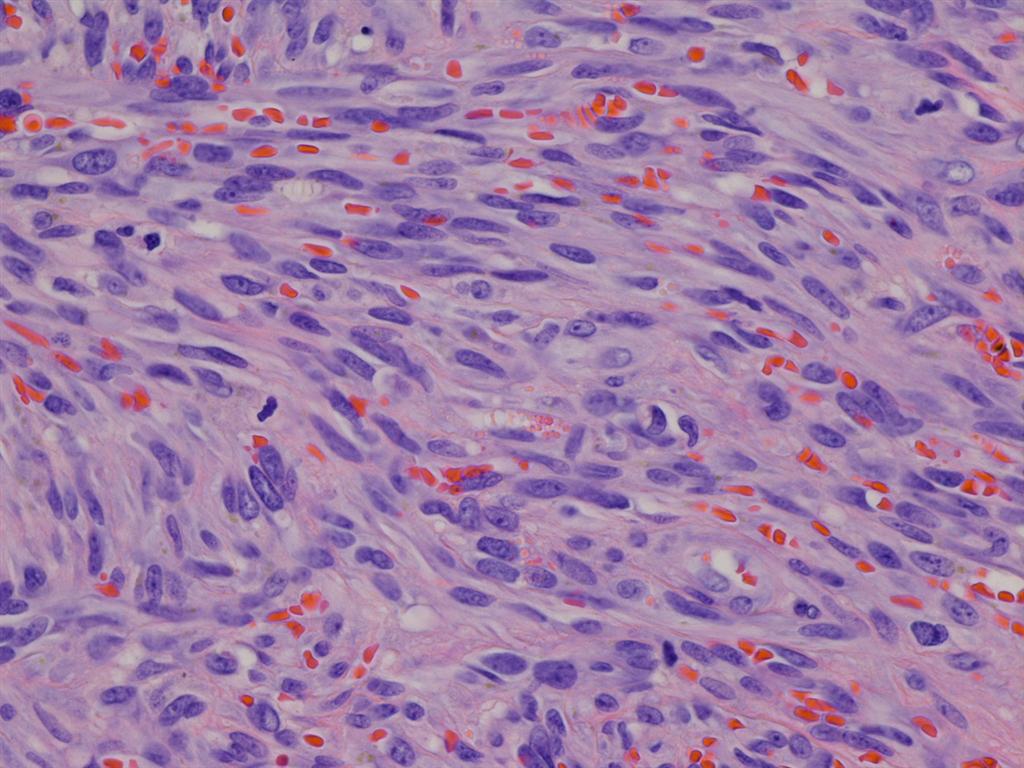
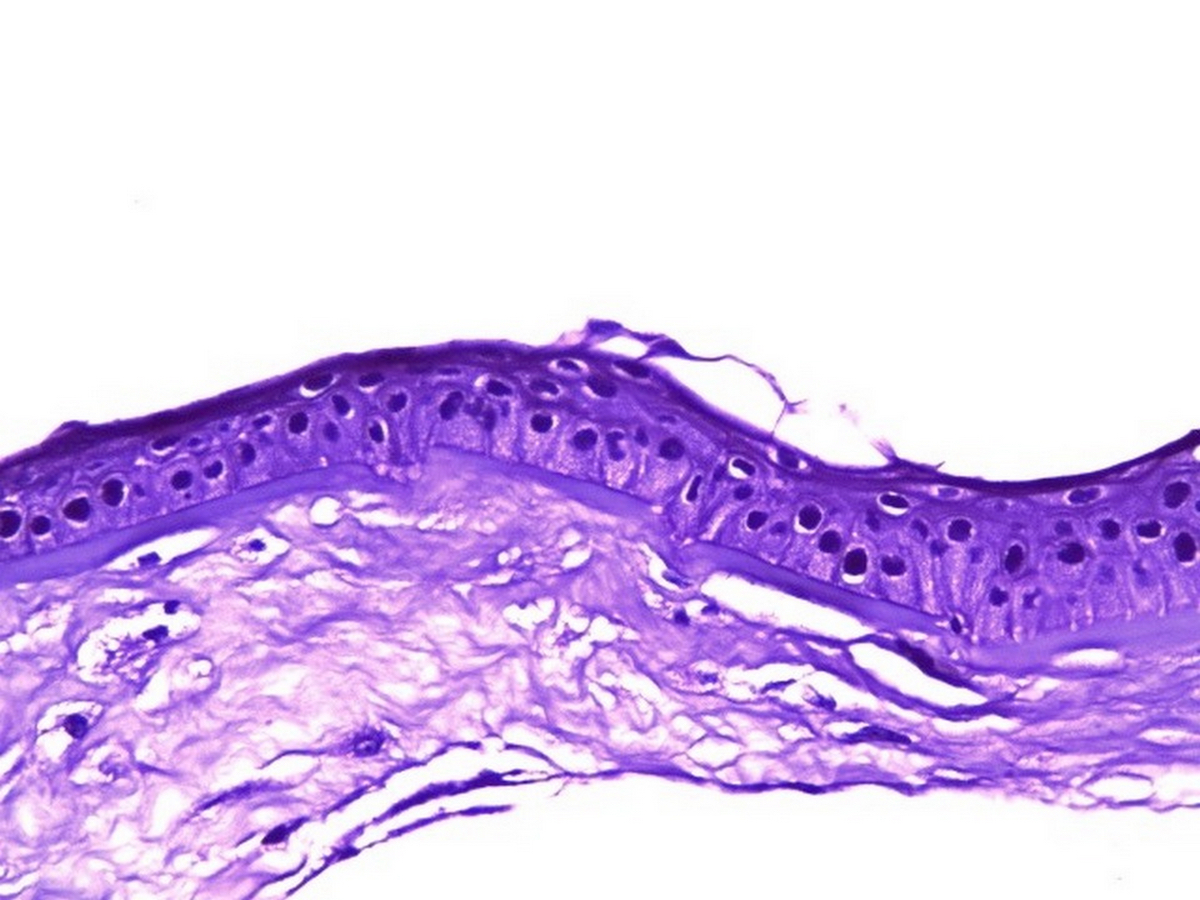
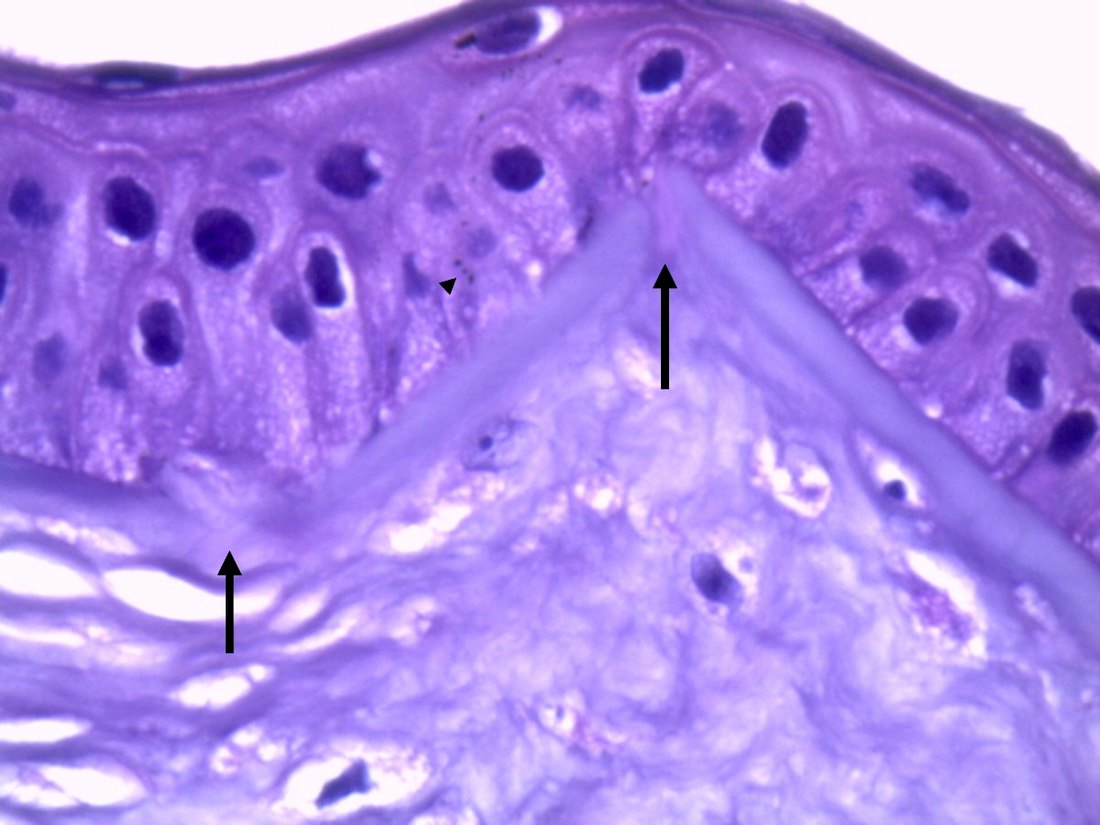
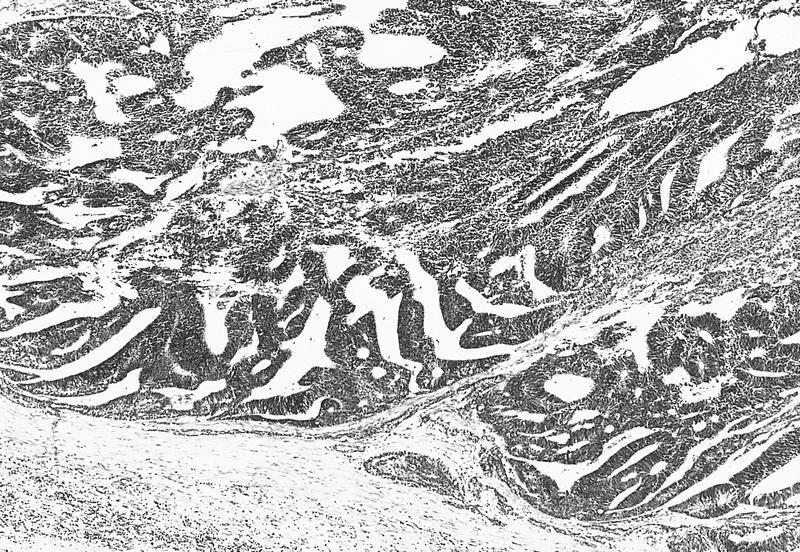
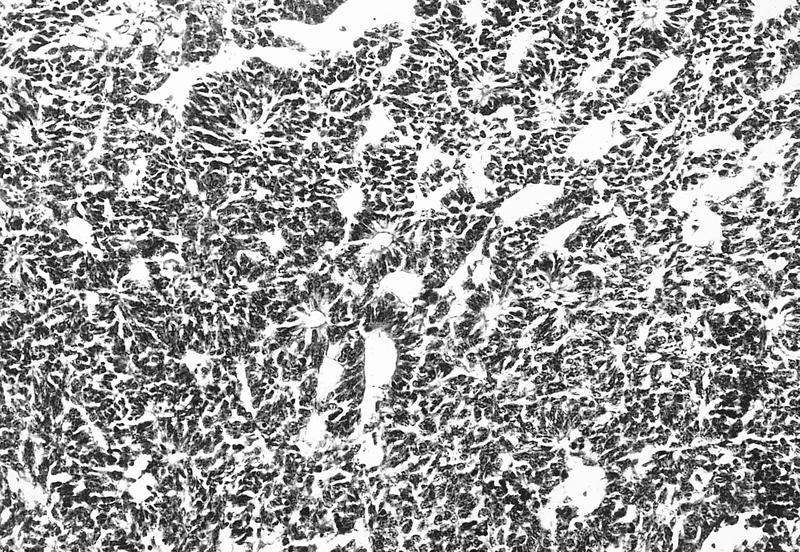
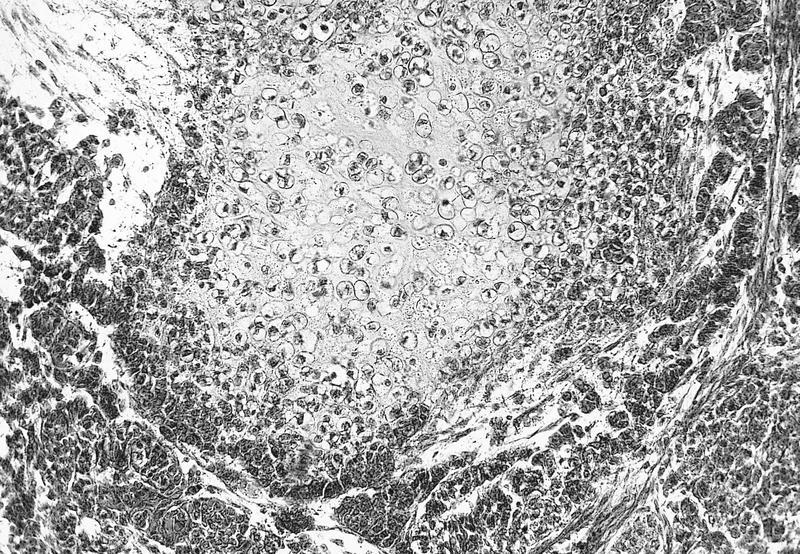
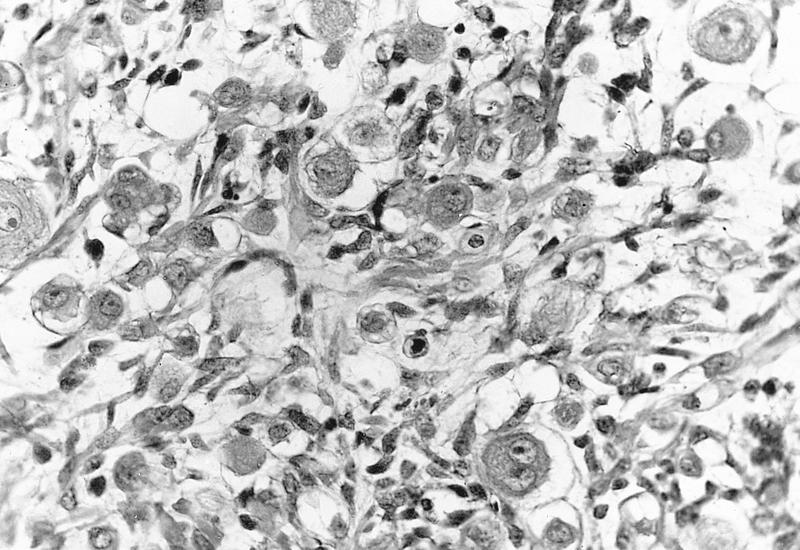
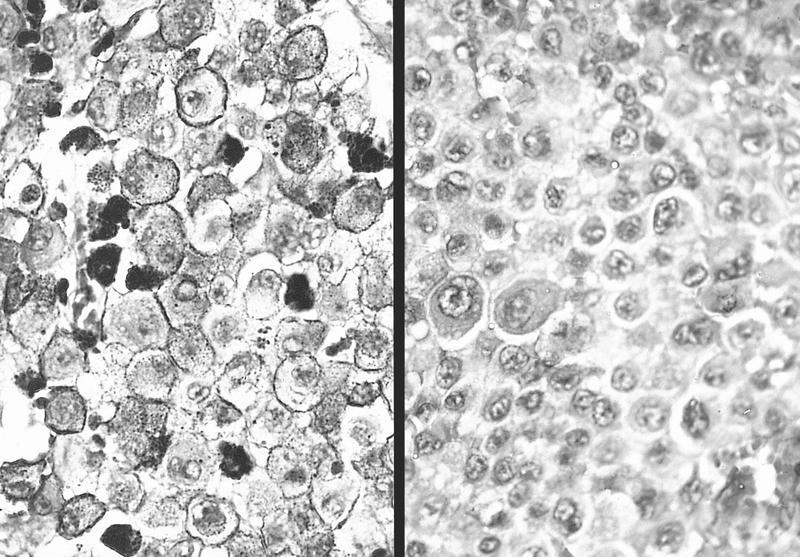
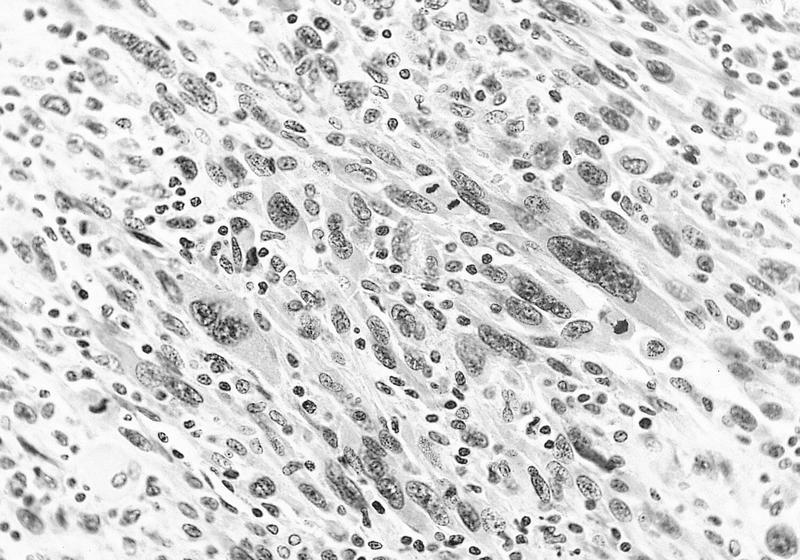
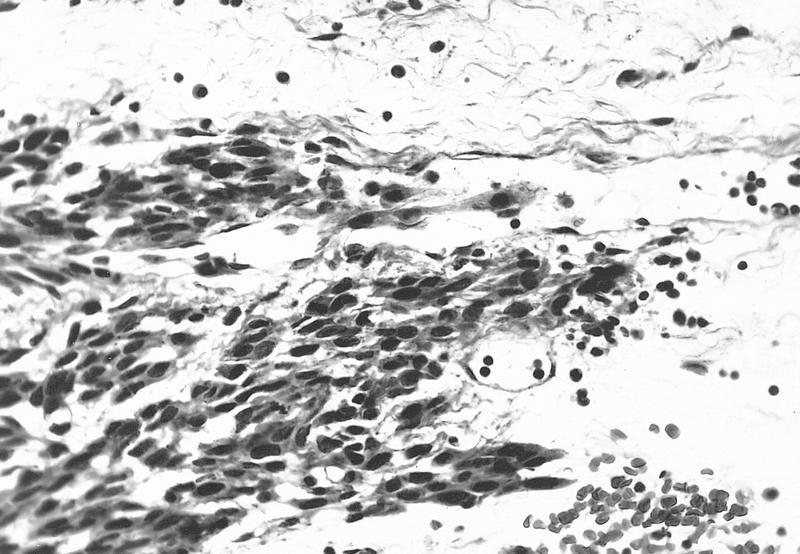
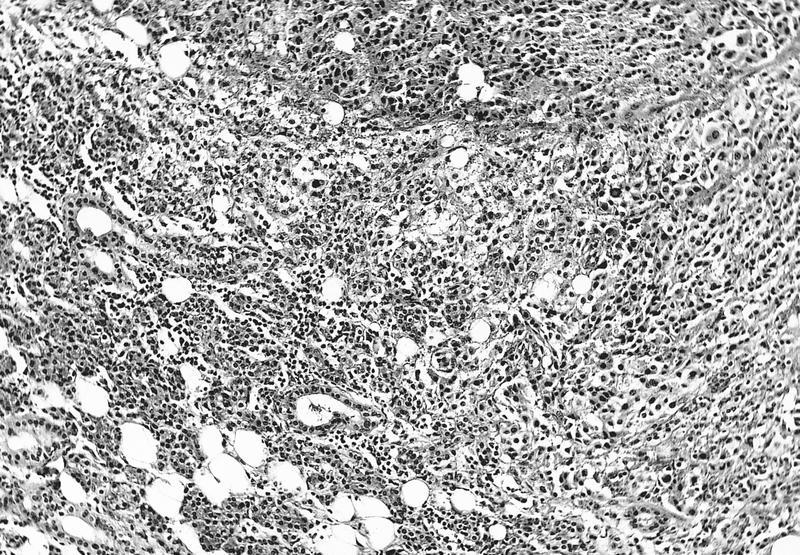
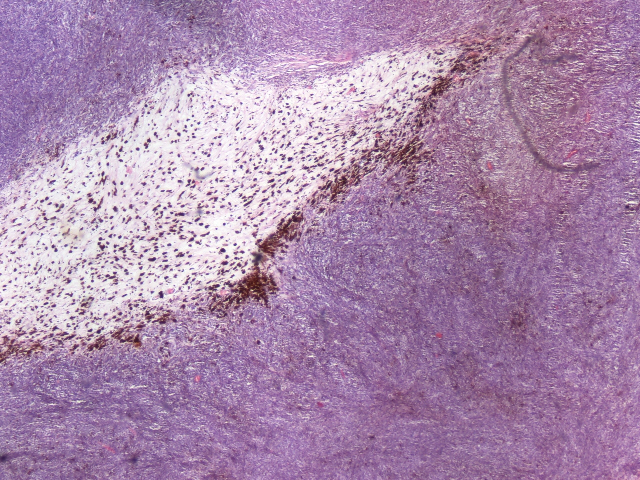
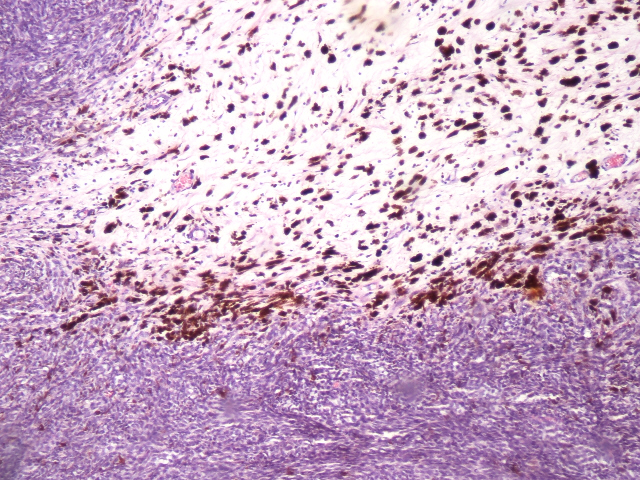
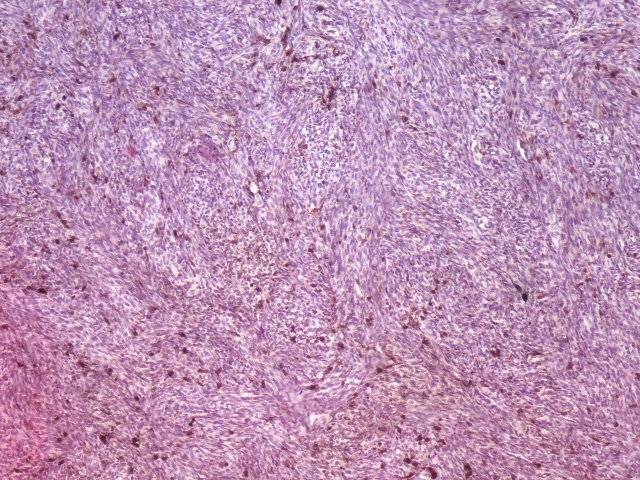
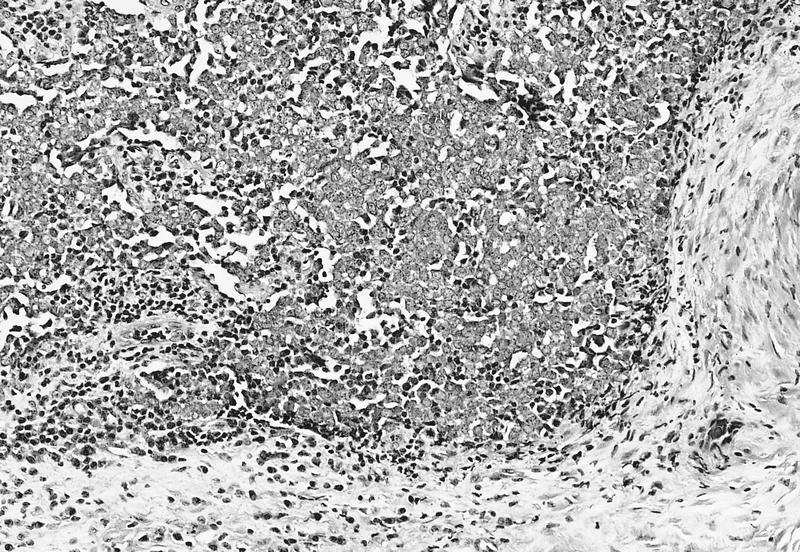
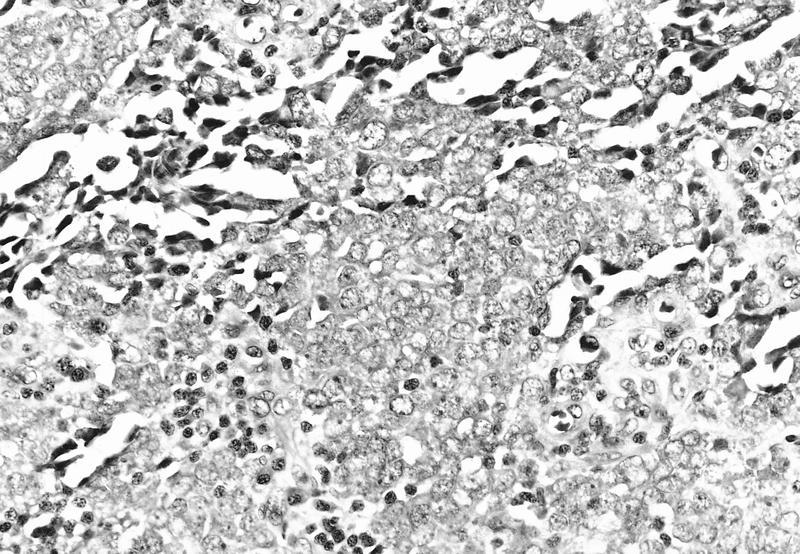
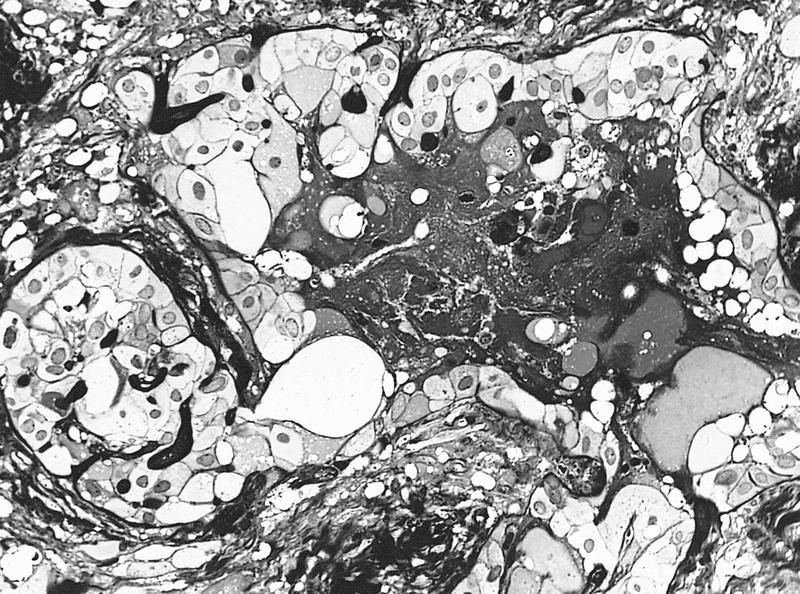
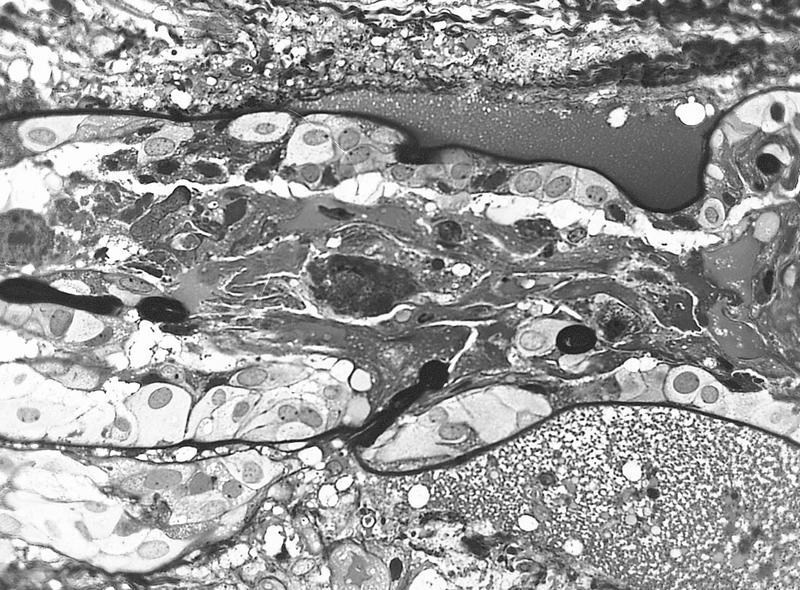
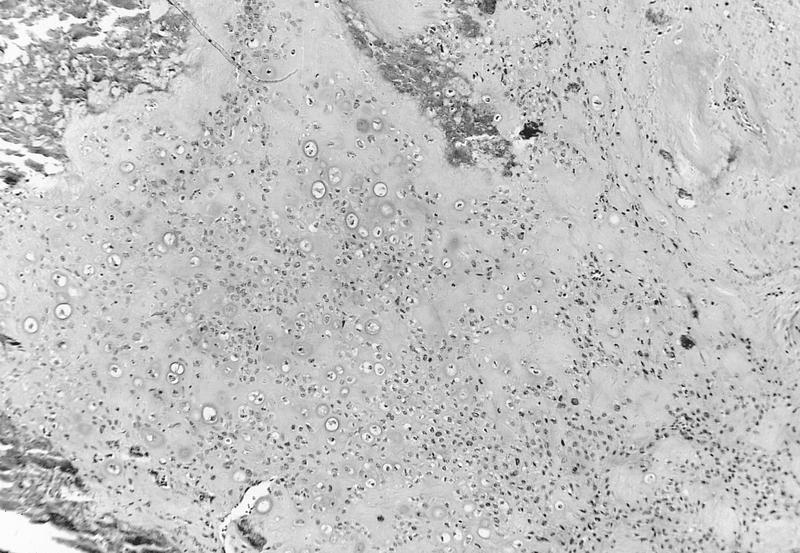
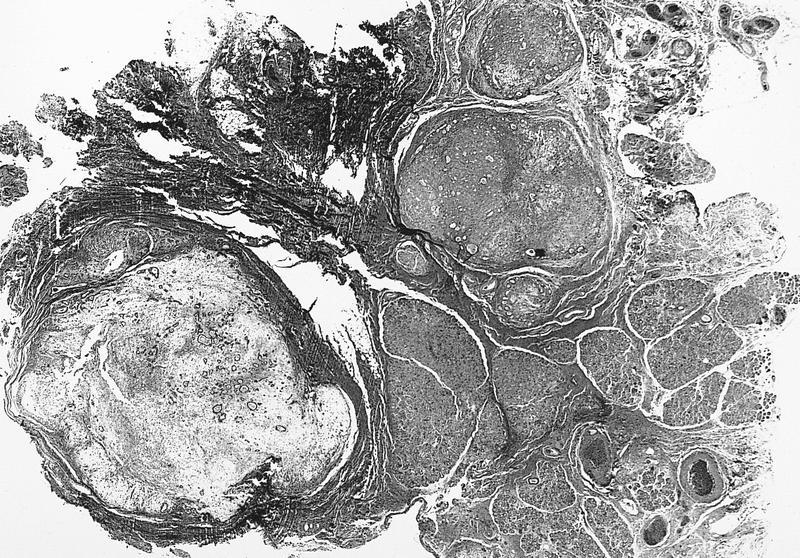
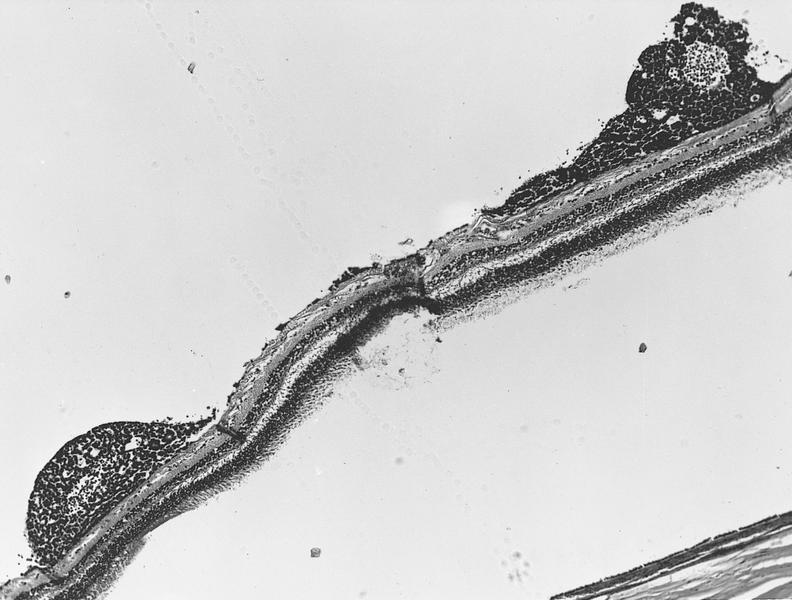
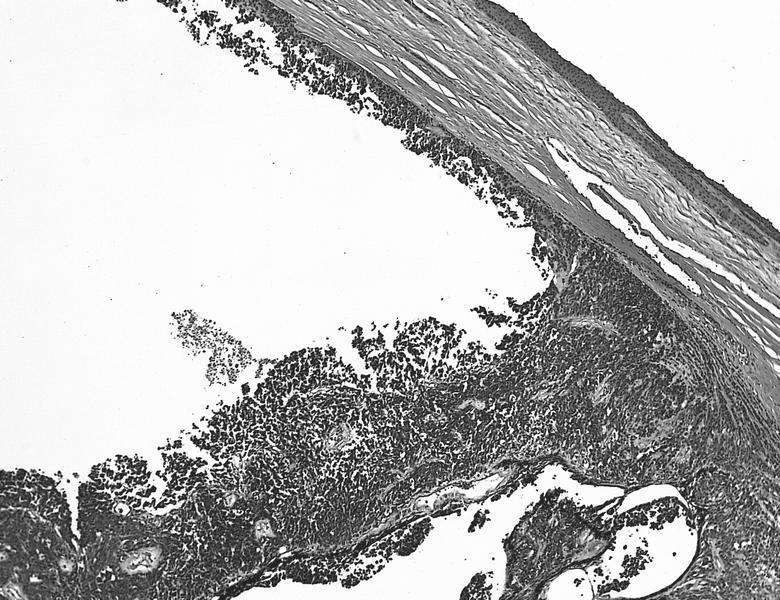
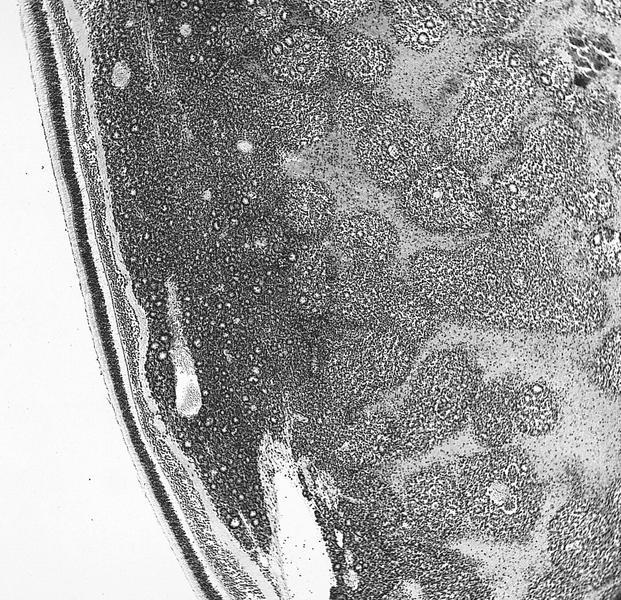
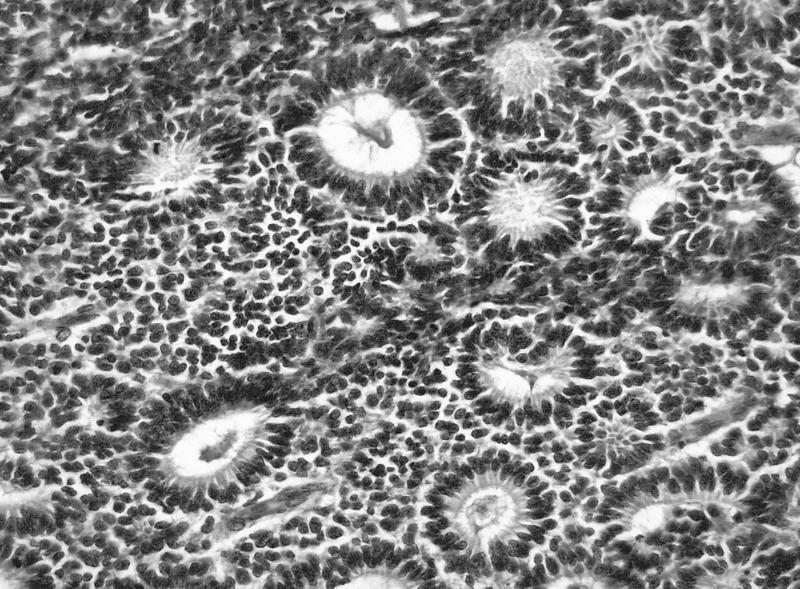
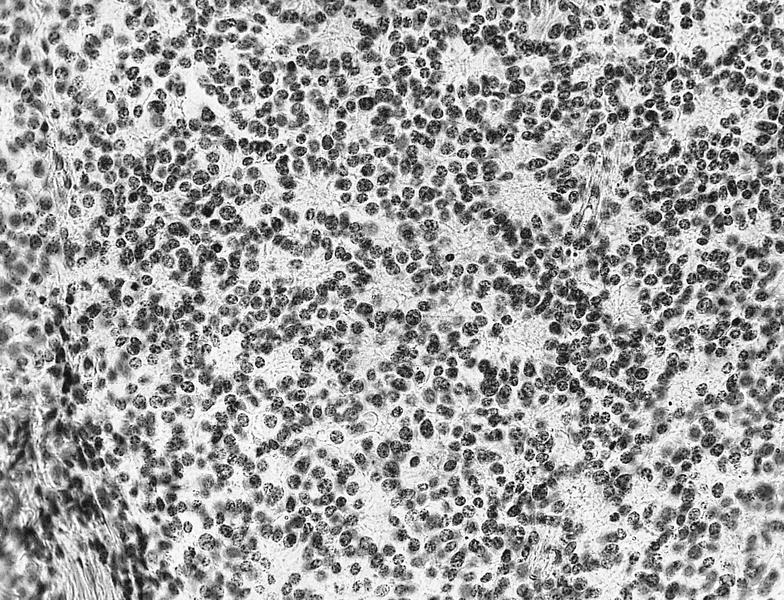
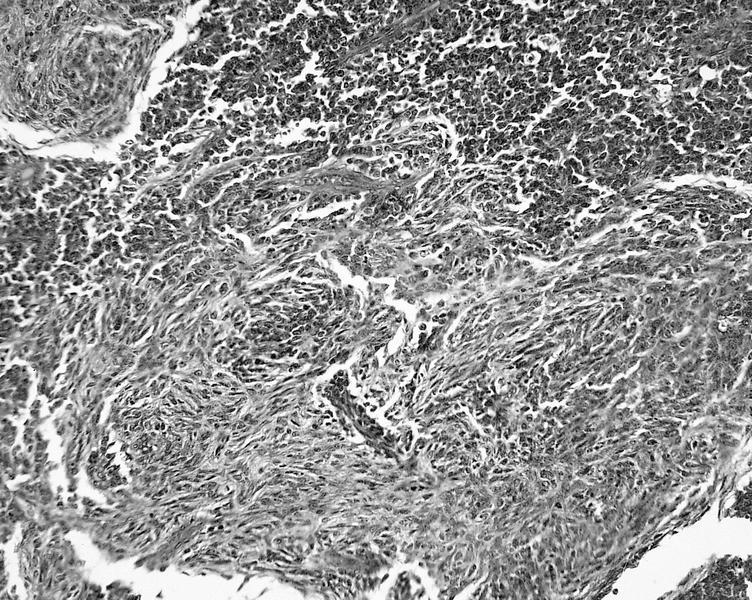
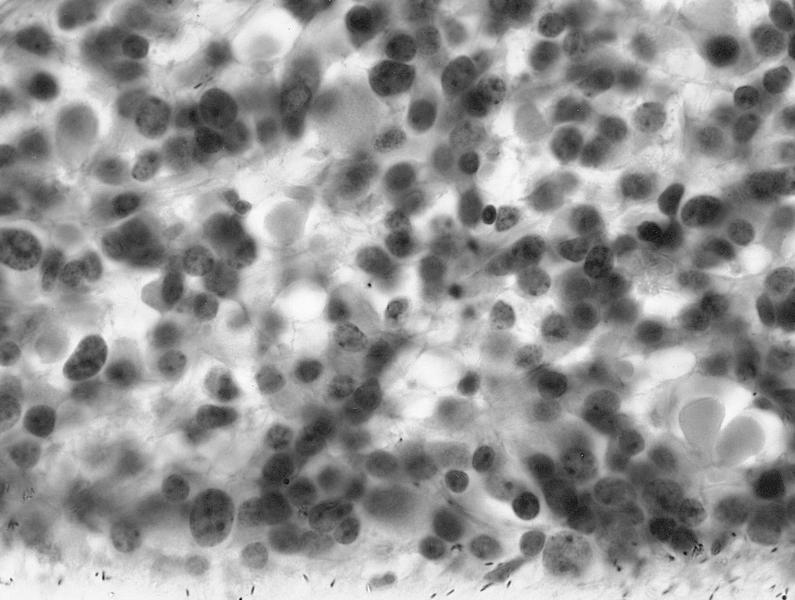
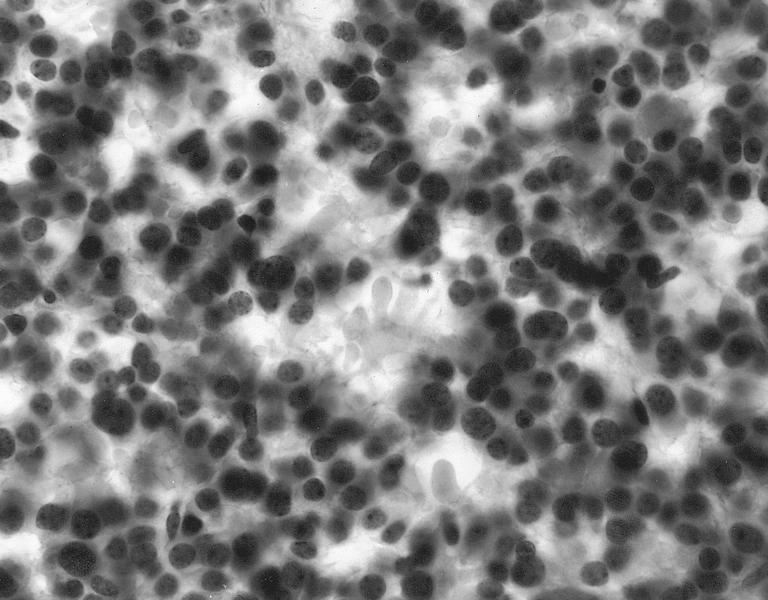
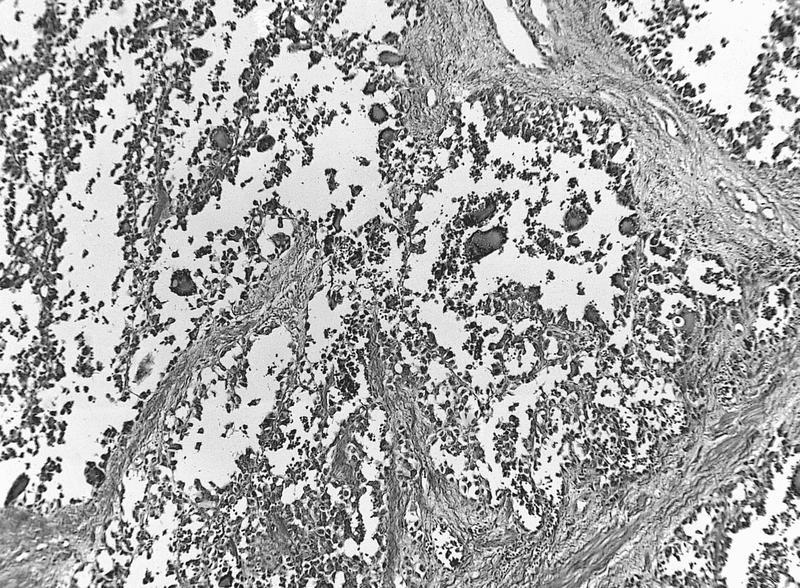
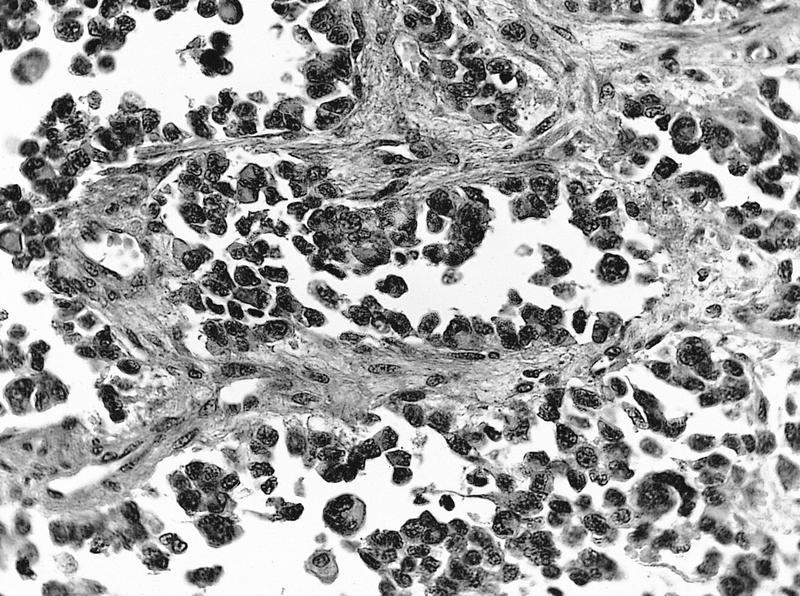
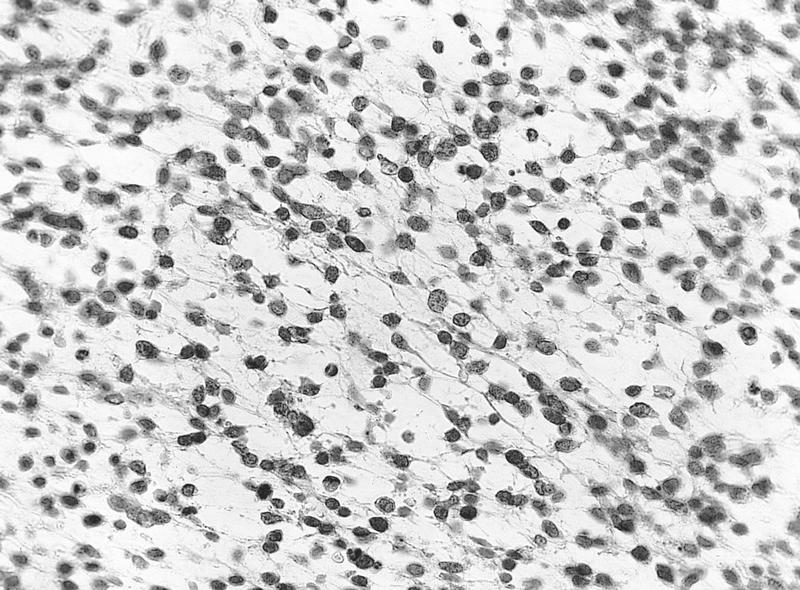
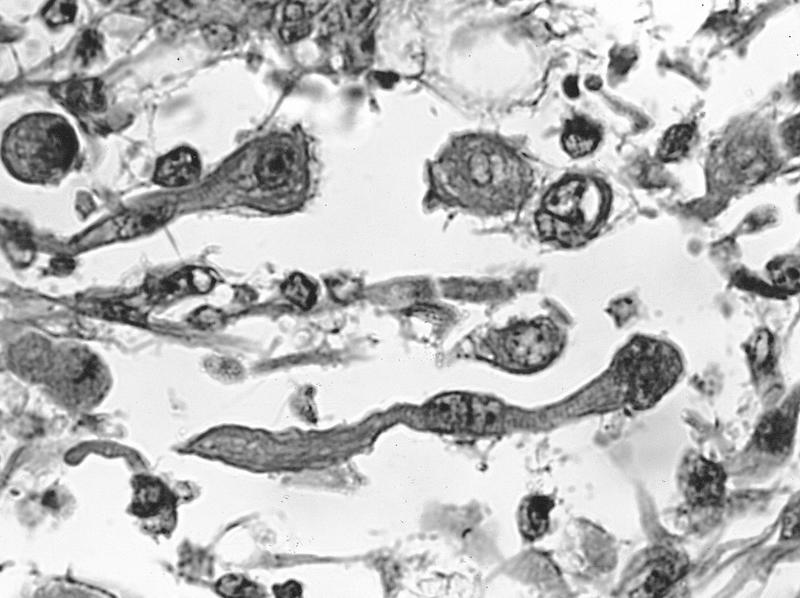
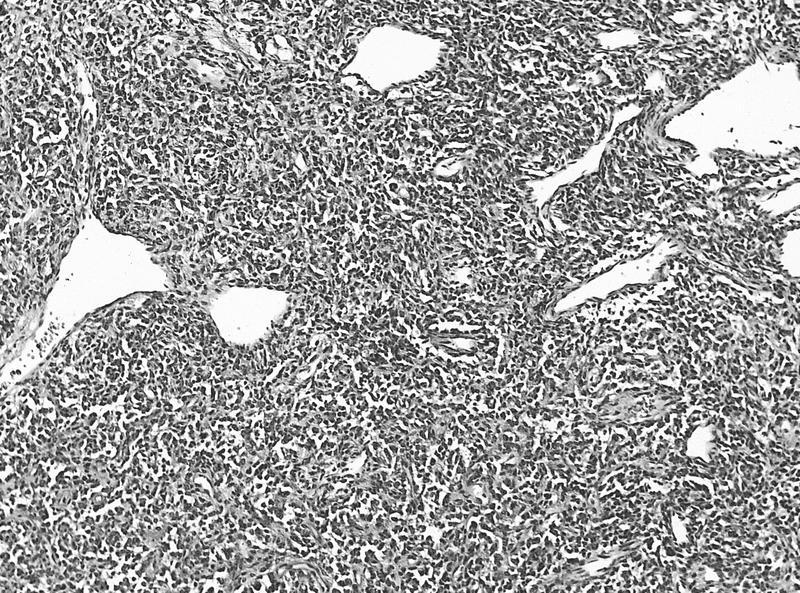
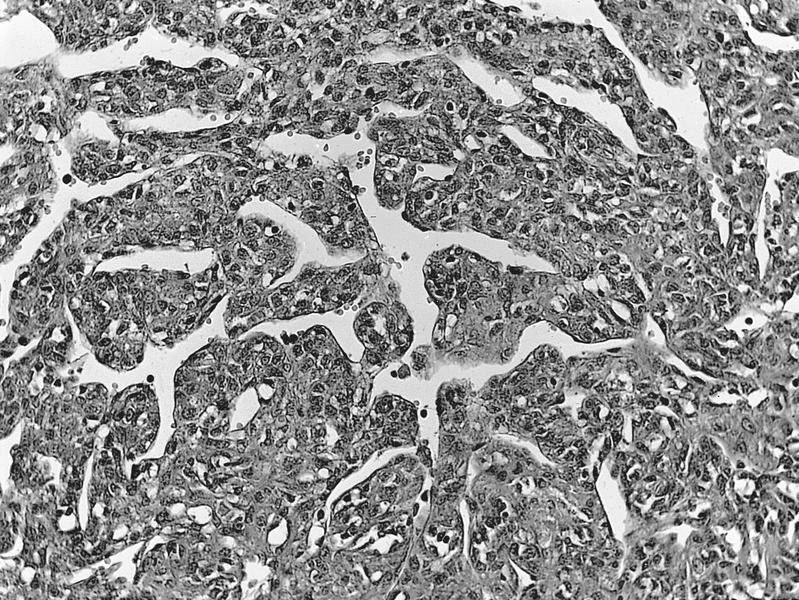
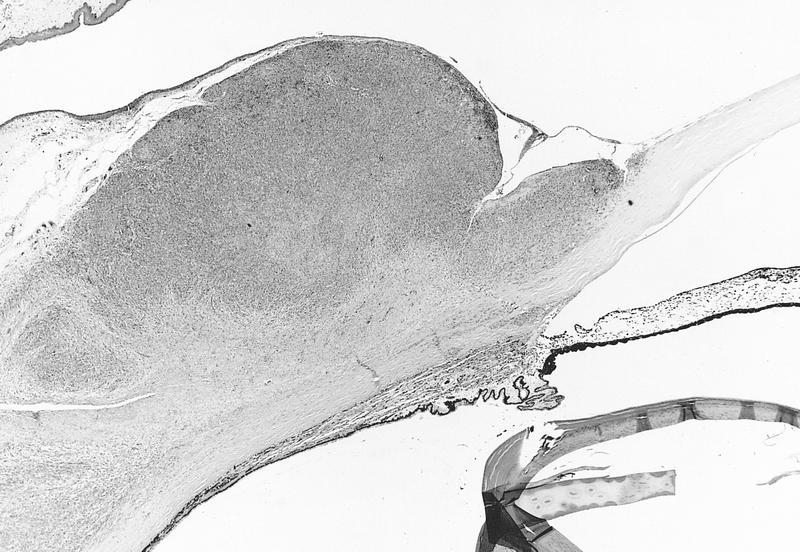
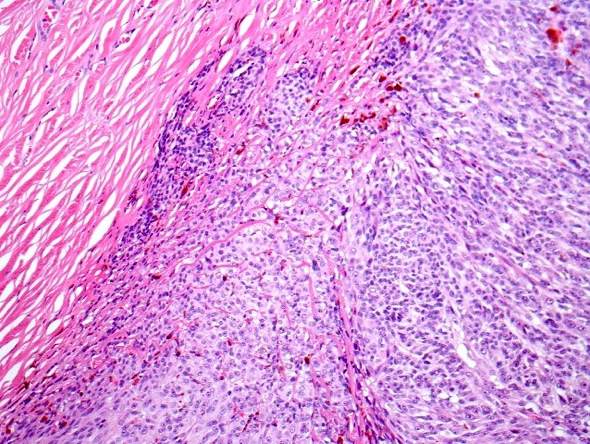
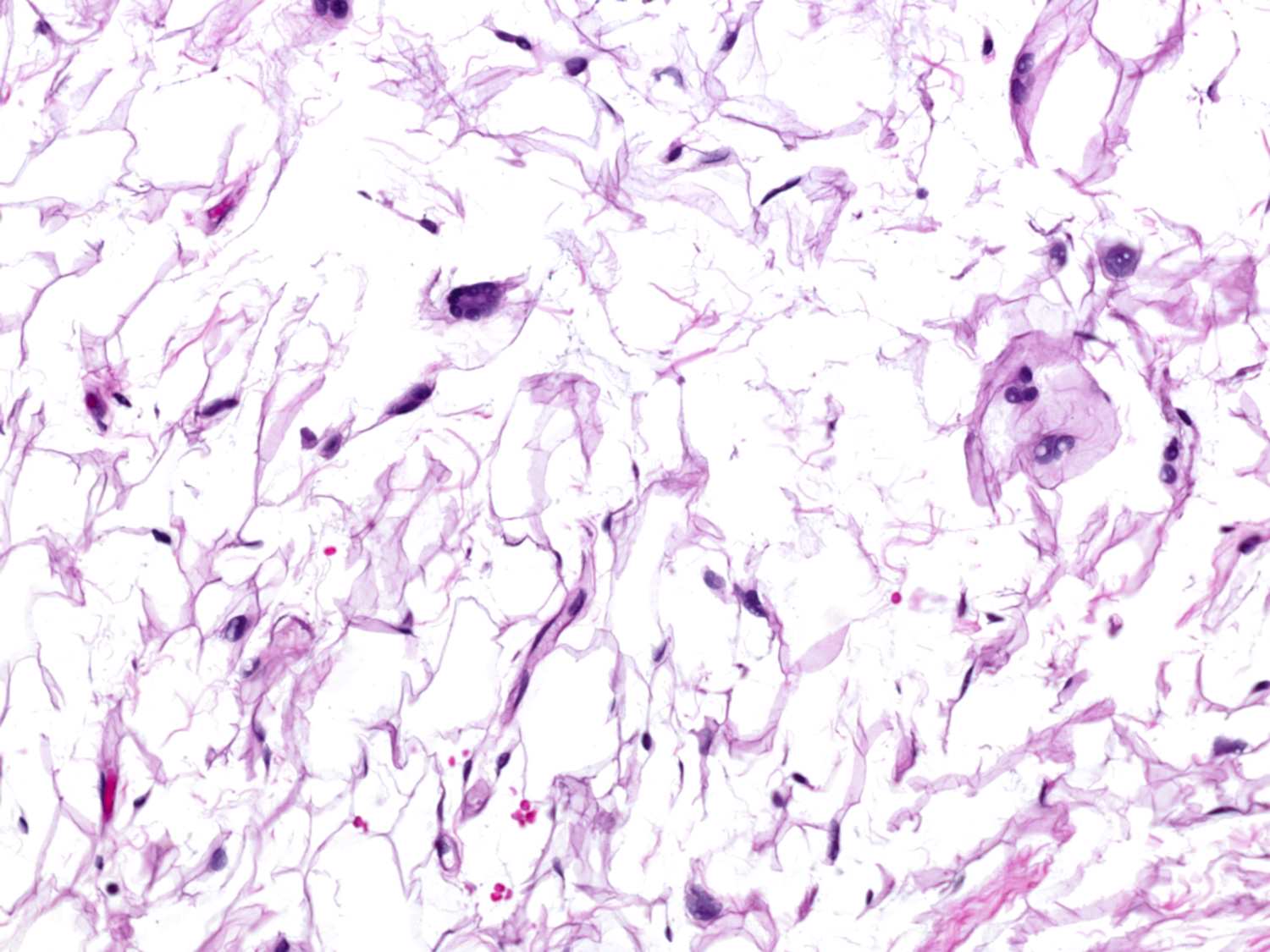
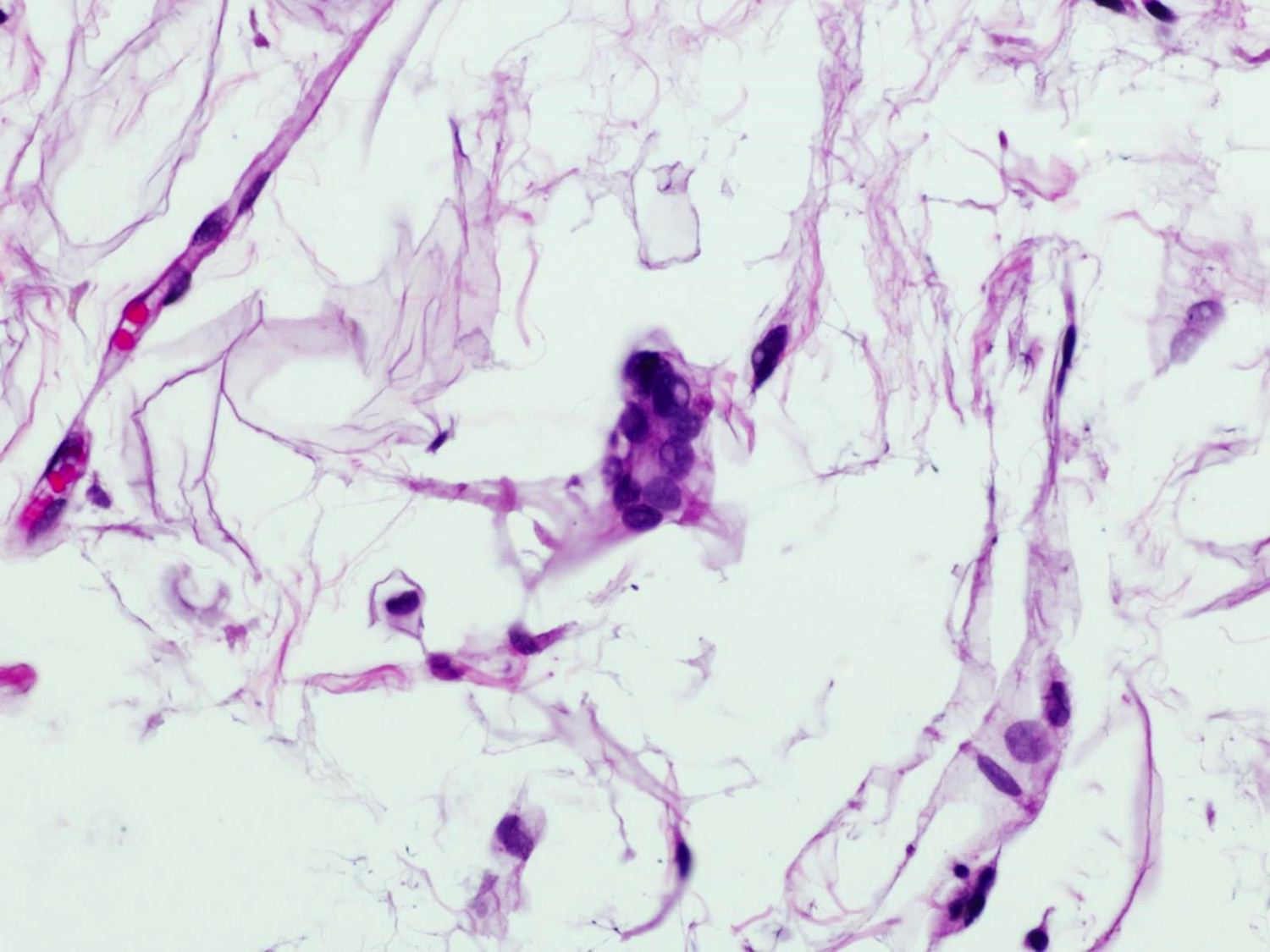
- Ulceration, necrosis, heavy neutrophil and macrophage infiltrates
- May have granulomatous inflammation
- Encysted forms
- Typically, absence of lymphocytes (Hum Pathol 2013;44:918)
Microscopic (histologic) images
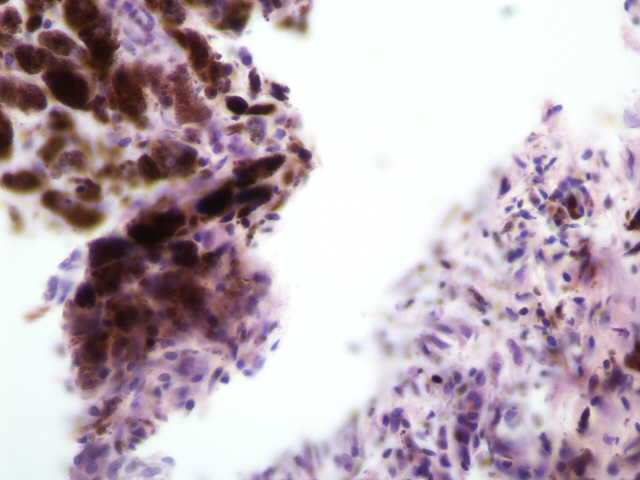
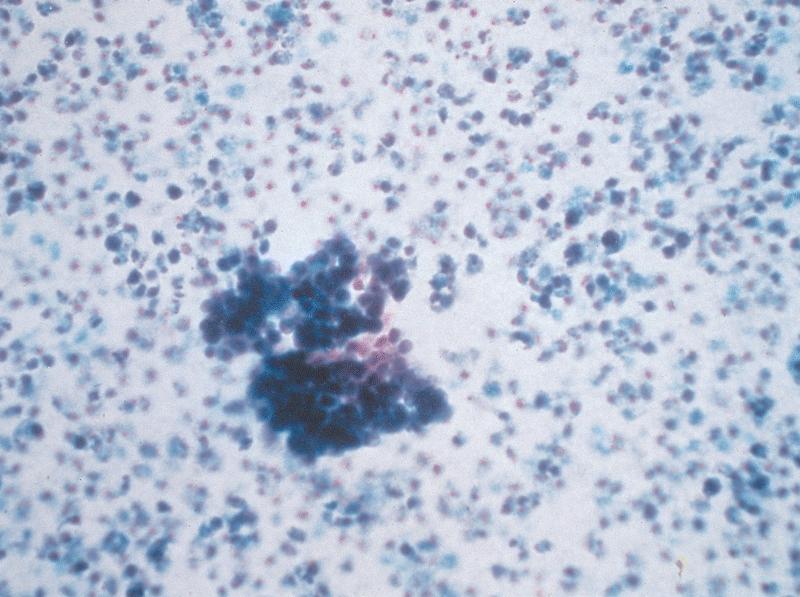
Cytology description
- Impression cytology with double walled Acanthamoeba cysts and occasional trophozoites scattered among corneal epithelia (Pathogens 2021;10:323)
- Acanthamoeba cysts identified as unstained, hollow structures on Diff-Quik stain (Diagn Cytopathol 2023;51:98)
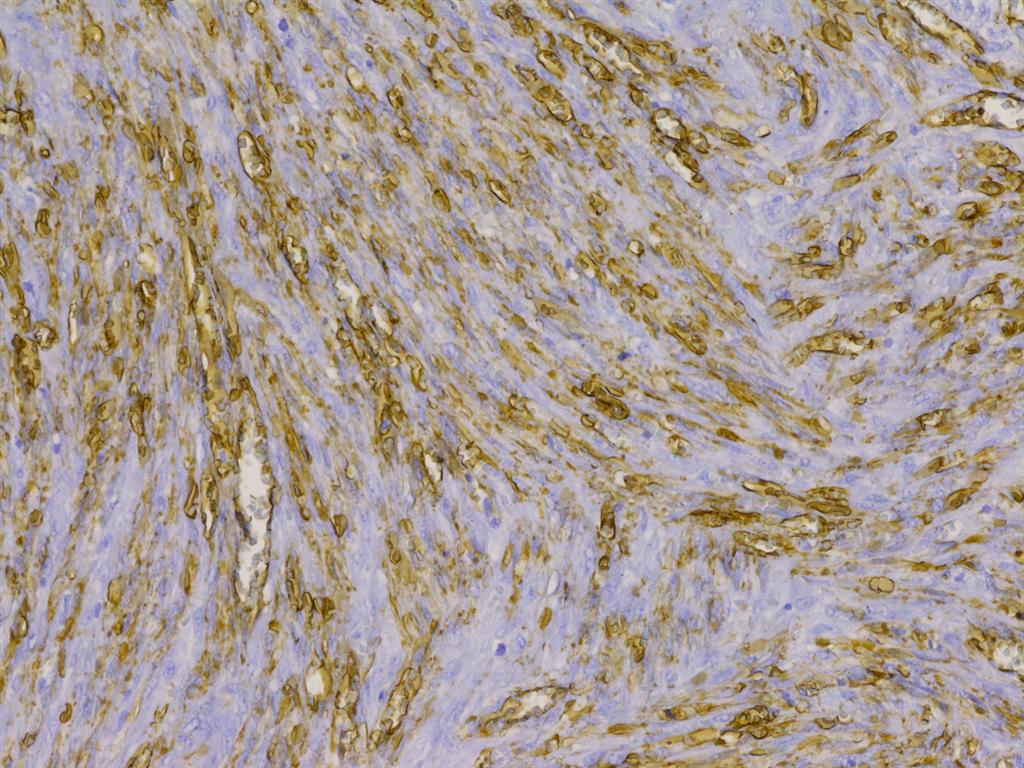
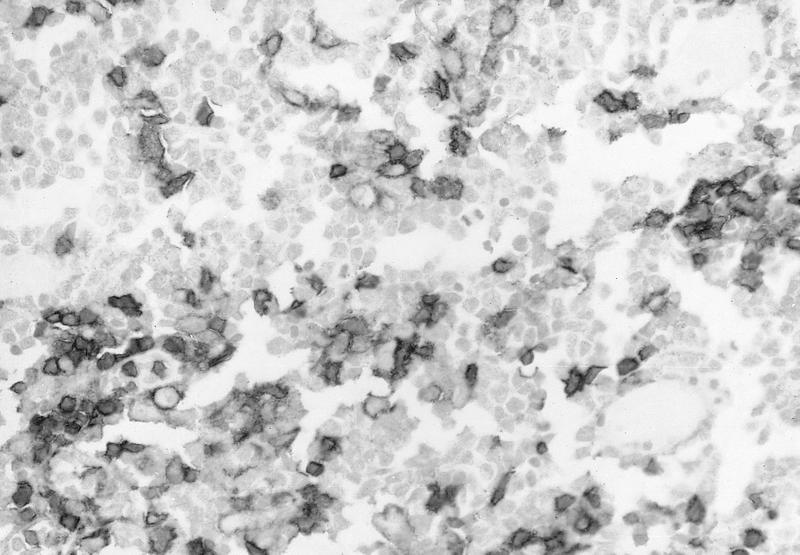
Positive stains
- GMS highlights walls of amoebic cysts (silver / black)
- PAS highlights walls of amoebic cysts
- Immunohistochemical stains for Acanthamoeba spp. exist but are not readily available in most clinical settings (Mod Pathol 2007;20:1230)
Negative stains
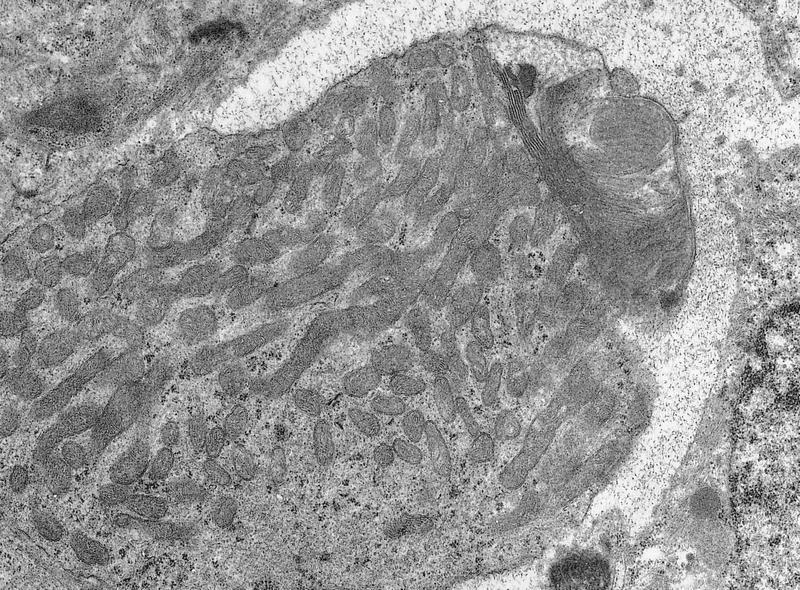
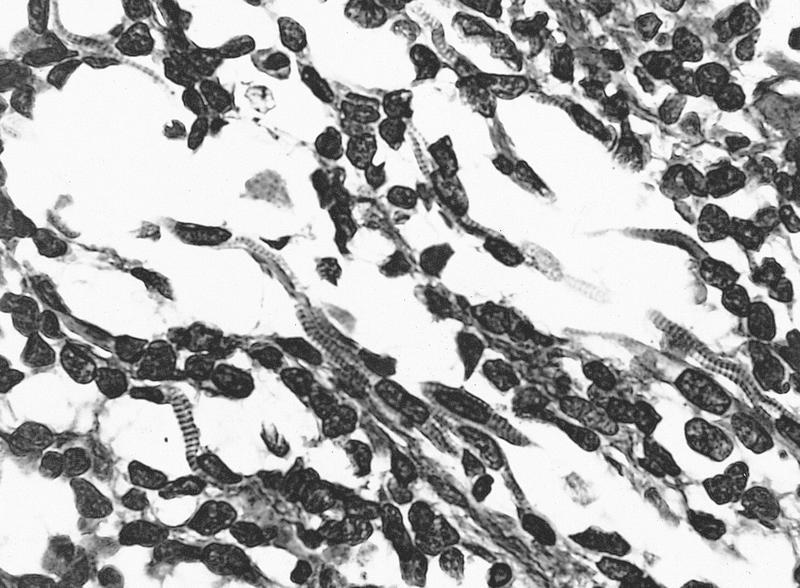
Electron microscopy description
- Typically for education / research rather than diagnosis: transmission electron micrograph showing an encysted Acanthamoeba organism with outer ectocyst layer, mitochondria, lipid vacuoles and lysosomes; adjacent neutrophils (Am J Ophthalmol 1987;103:626)
Videos
Clinical presentation of Acanthamoeba keratitis
Sample pathology report
- Eye, (side) cornea, biopsy or keratoplasty:
- Acanthamoeba keratitis (see comment)
- Comment: The cornea is ulcerated with necrosis and neutrophils. PAS and GMS stains highlight amoebic forms. PAS also highlights the Descemet membrane.
Differential diagnosis
- Herpetic keratitis:
- Ulceration, may or may not have Cowdry A intranuclear inclusions in corneal epithelium at edge of ulcer (may be IHC HSV1 / HSV2 positive)
- Lymphocytes, plasma cells, vascularization
- Multinucleated giant cells around Descemet membrane
- Mycotic (fungal) keratitis:
Board review style question #1
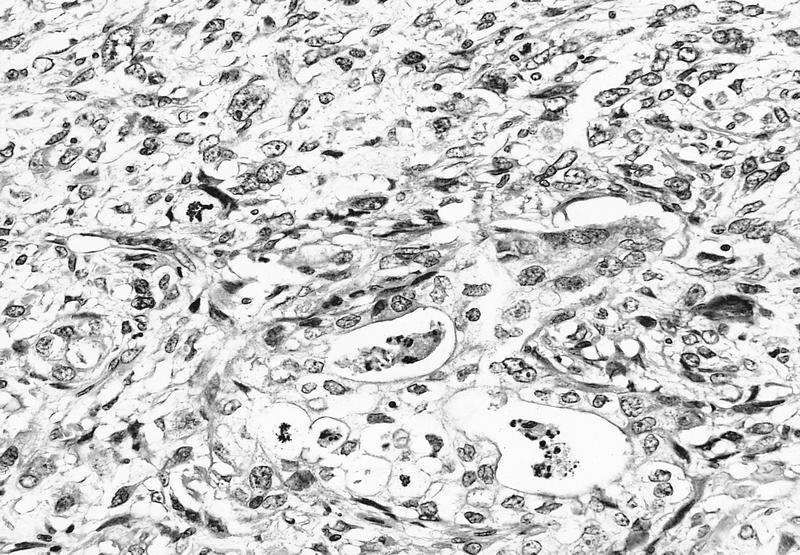
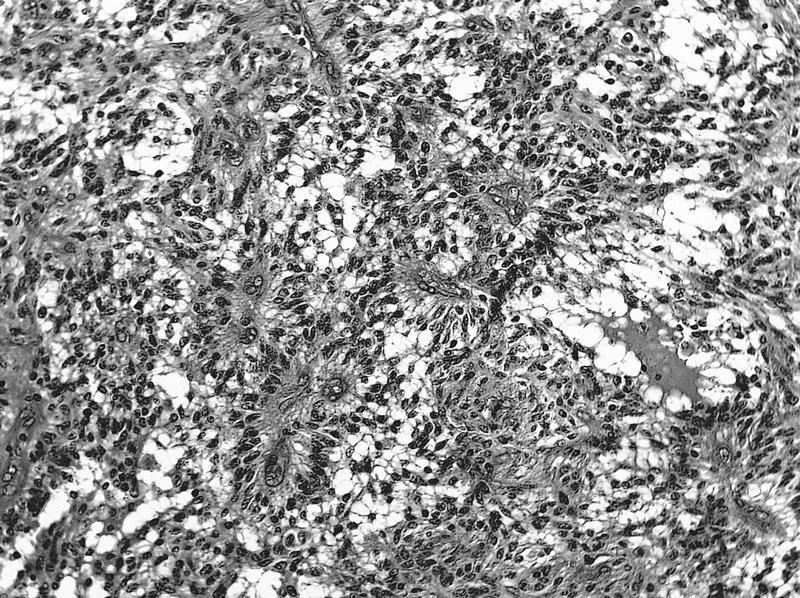
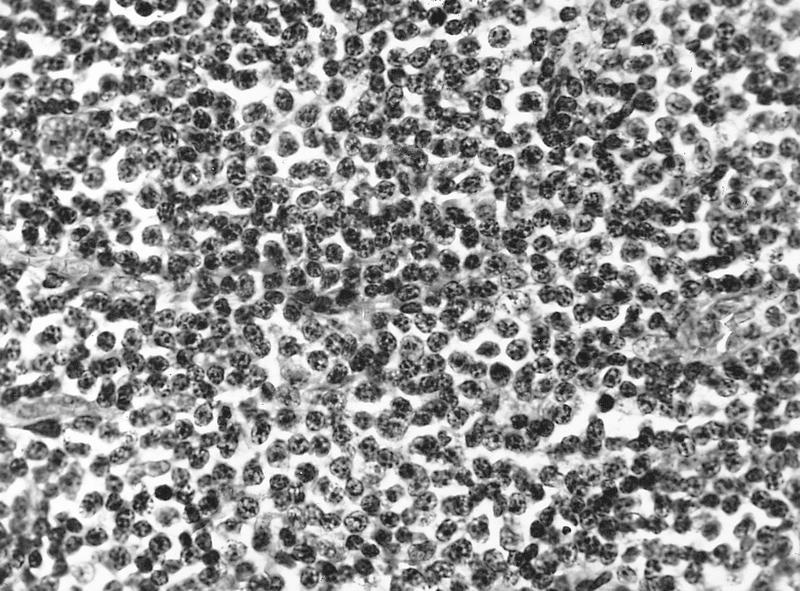
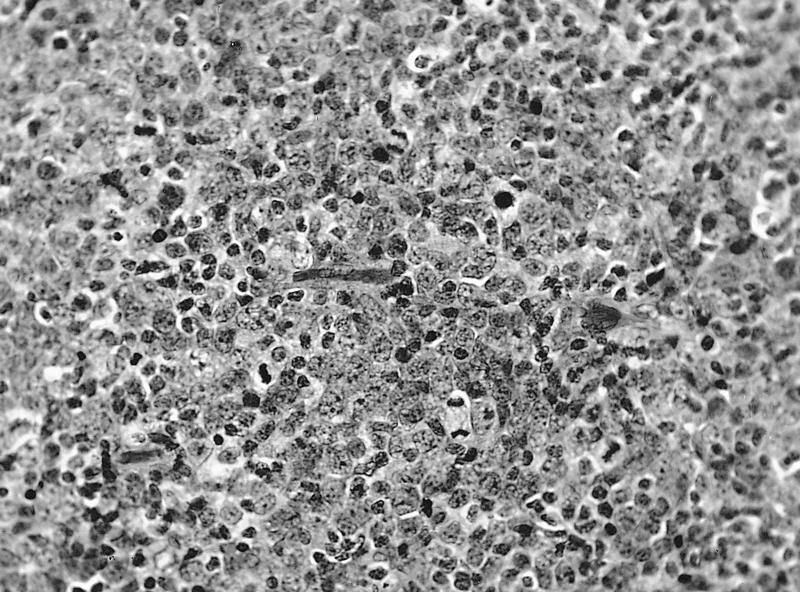
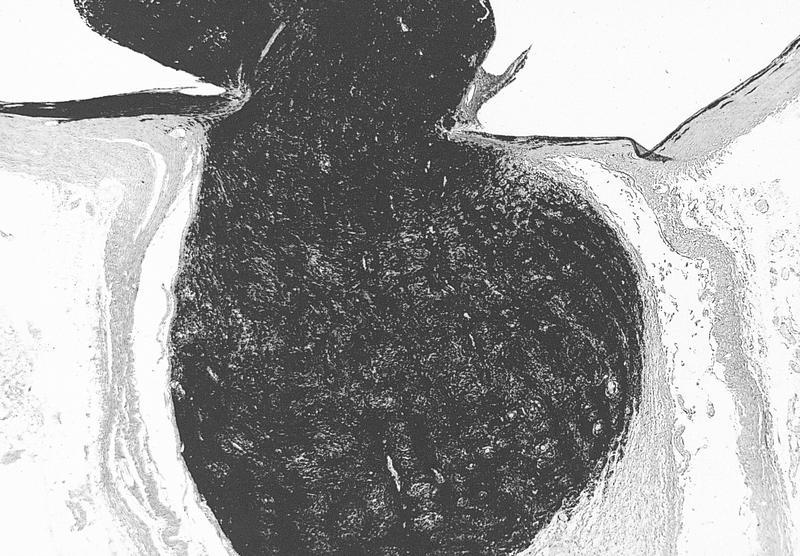
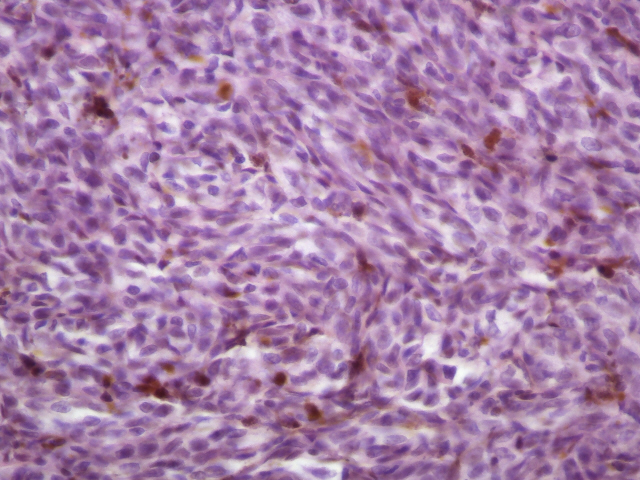
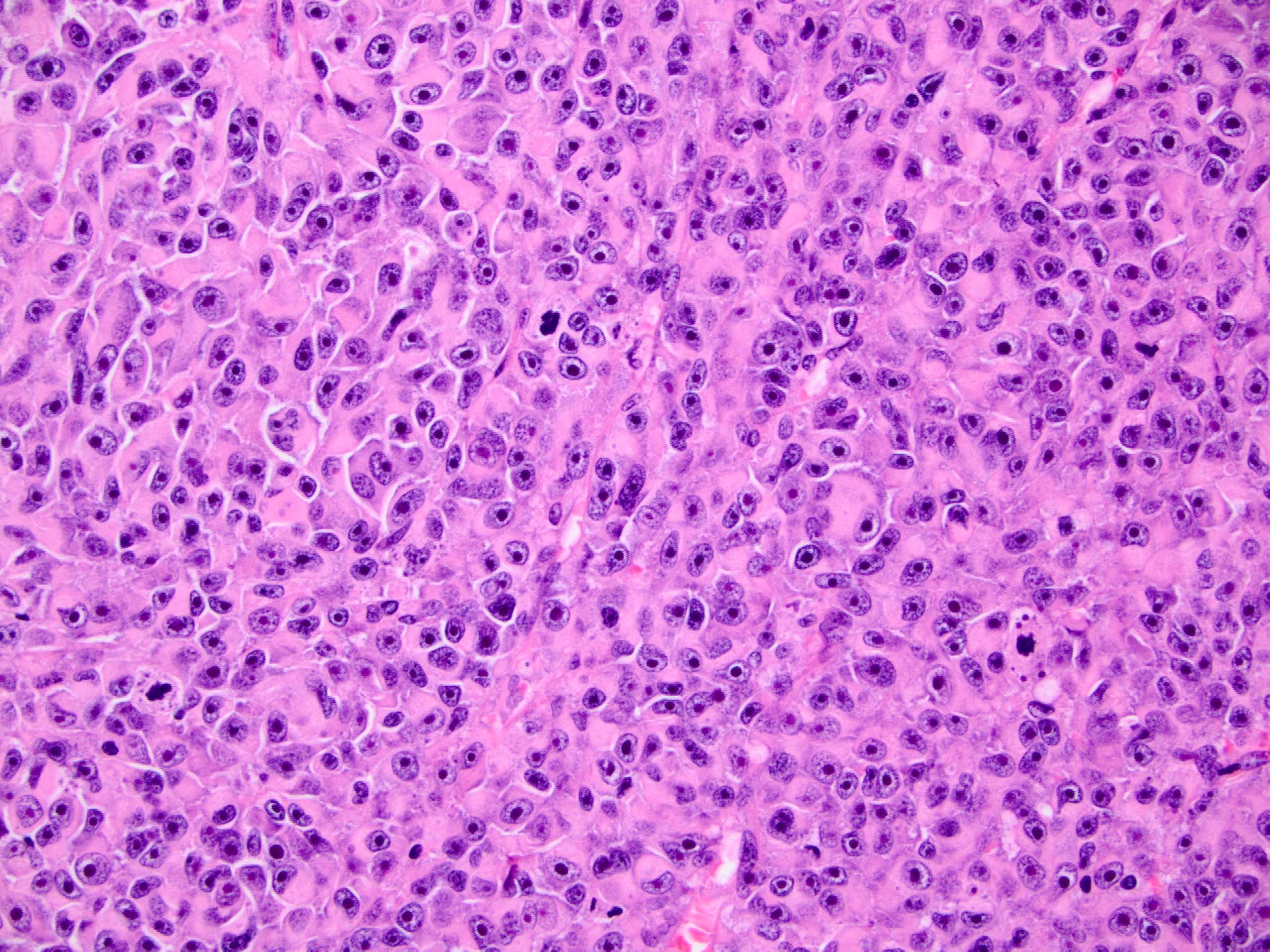
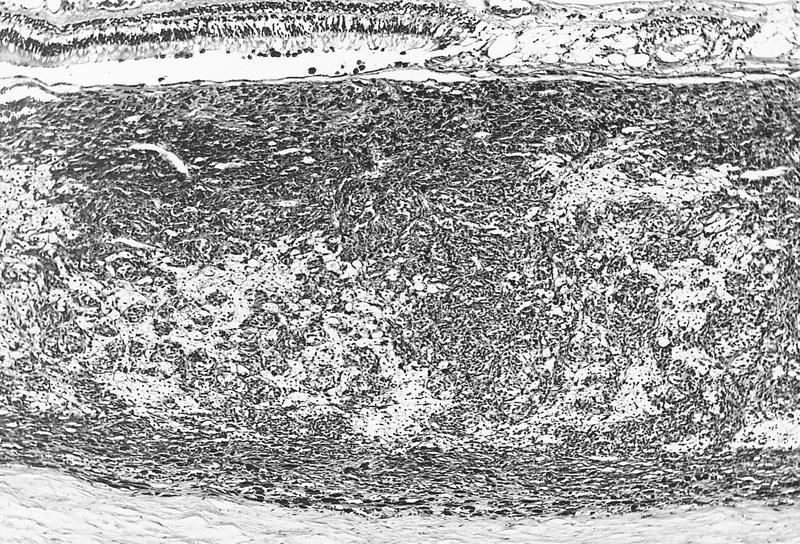
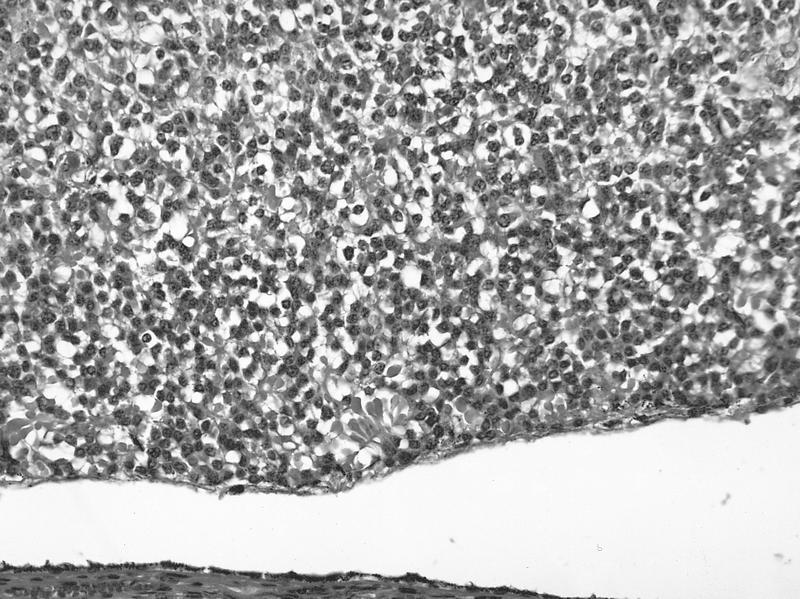
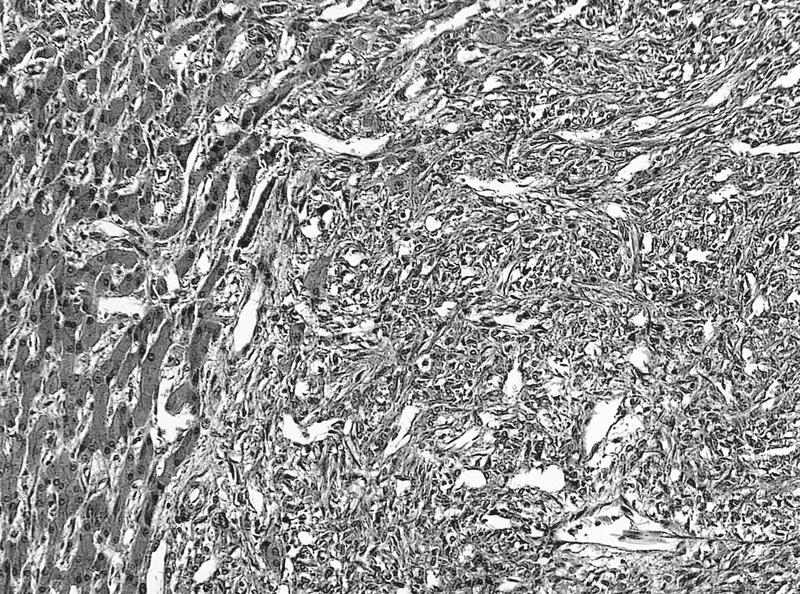
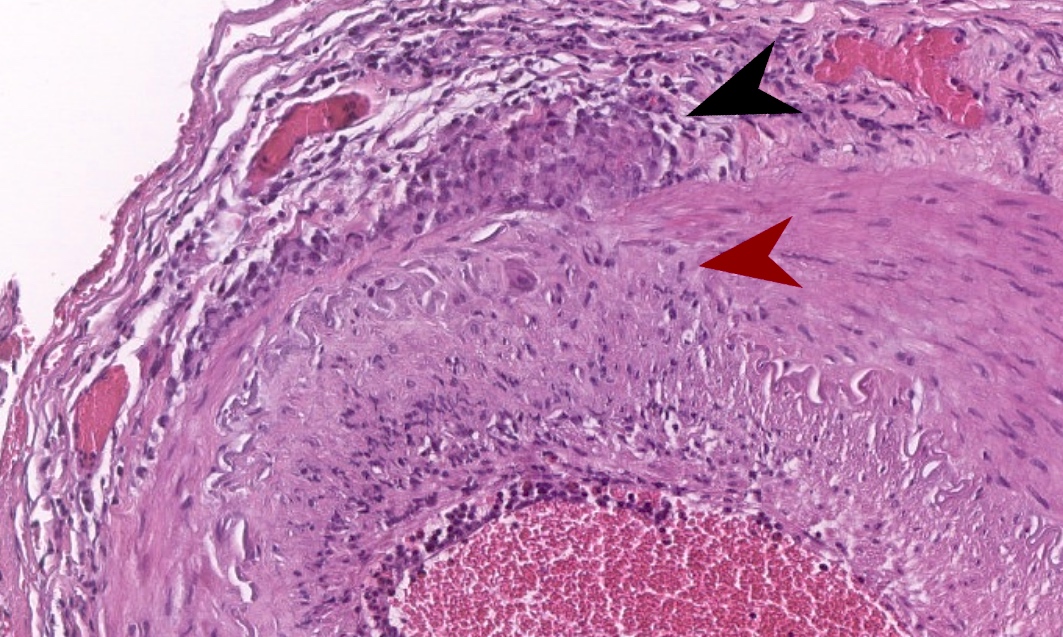
A 25 year old man with orthokeratology (specially fitted lenses) presents with severe pain in his left eye. The slit lamp examination shows a pattern of radial perineural and ring infiltrate in cornea. Corneal biopsy following negative direct smear examination on corneal scrapes shows focal ulceration of the surface with loss of epithelium; infiltrate of inflammatory cells, mainly polymorphonuclear cells and macrophages, are shown in the image above. What is the most likely diagnosis?
- Acanthamoeba keratitis
- Bacterial keratitis
- Herpetic keratitis
- Mycotic (fungal) keratitis
Board review style answer #1
A. Acanthamoeba keratitis. H&E sections at high power show several Acanthamoeba infiltrating corneal stroma in varying states of degeneration. Microscopic features on corneal biopsy also include ulceration, necrosis, neutrophilic and macrophage infiltrates; may show nonnecrotizing granulomatous inflammation. Encysted forms may be highlighted with PAS or GMS stains. Answer C is incorrect because a corneal biopsy for herpetic keratitis shows inflammatory infiltrates of mainly lymphocytes, plasma cells with stromal vascularization on H&E sections. Multinucleated giant cells around Descemet membrane are also identified. Answer D is incorrect because a corneal biopsy for mycotic (fungal) keratitis shows granulomatous, chronic nongranulomatous or rarely purulent inflammation on H&E sections; PAS or GMS positive for yeast or hyphal forms. Answer B is incorrect because microscopic findings of infiltration of the stroma by polymorphonuclear leukocytes occur in acute bacterial keratitis. The endothelium is often damaged and may have associated hypopyon and corneal perforation. Gram stain often shows bacteria in the stroma bordering the inflammatory infiltrate.
Comment Here
Reference: Acanthamoeba keratitis
Comment Here
Reference: Acanthamoeba keratitis
Board review style question #2
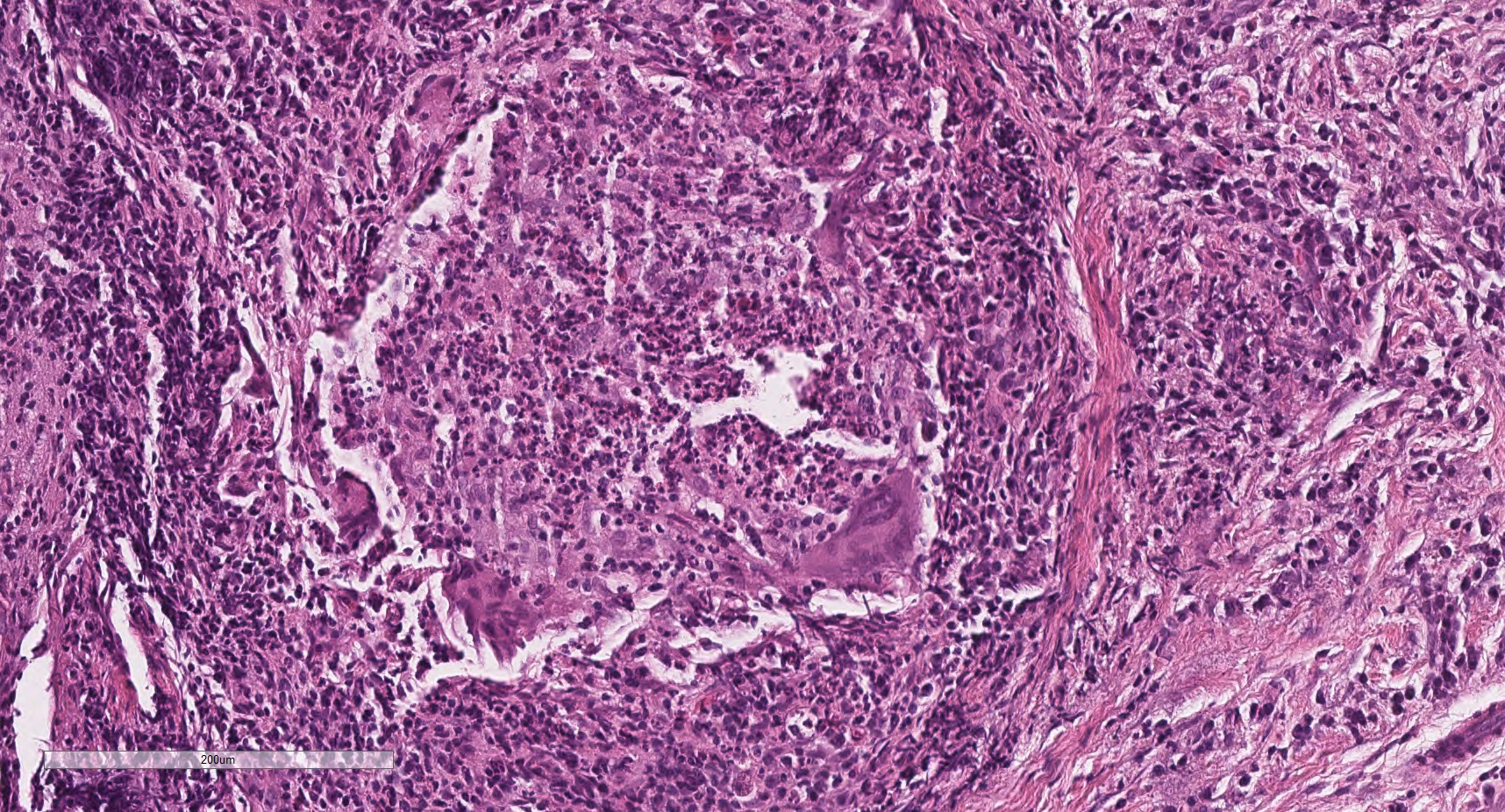
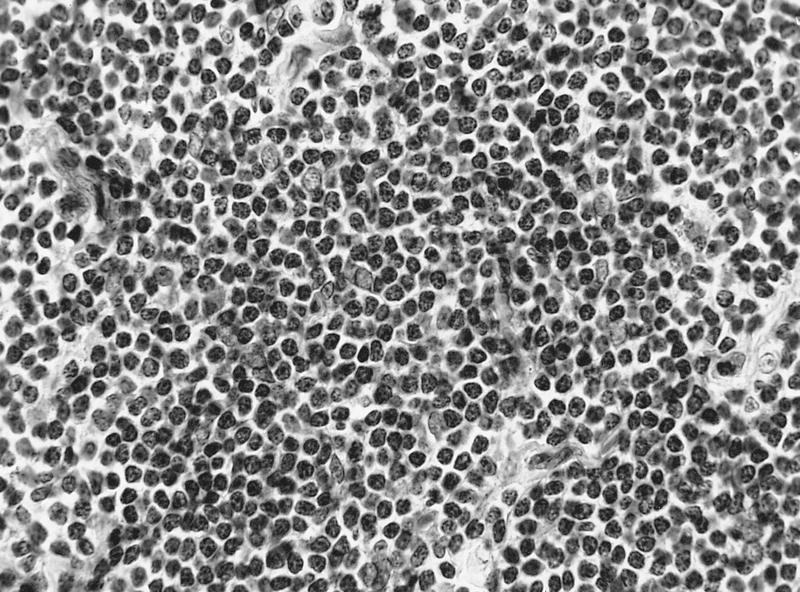
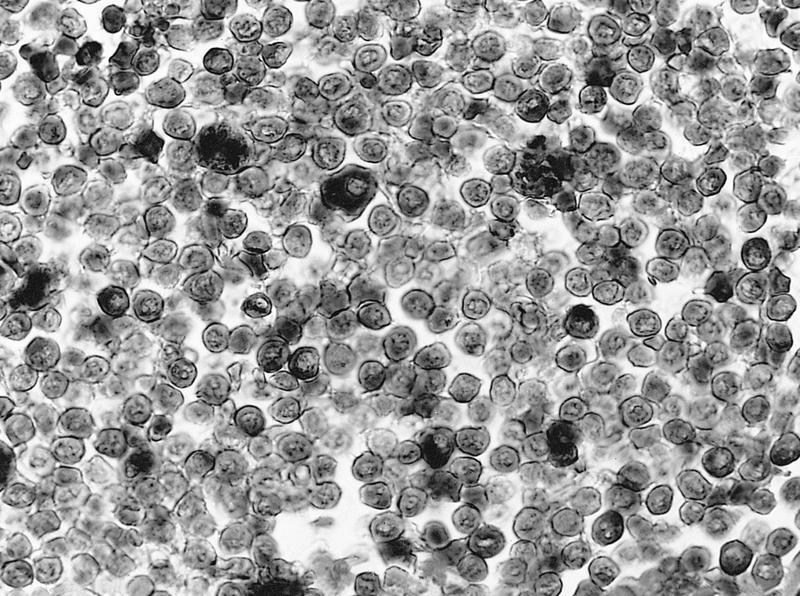
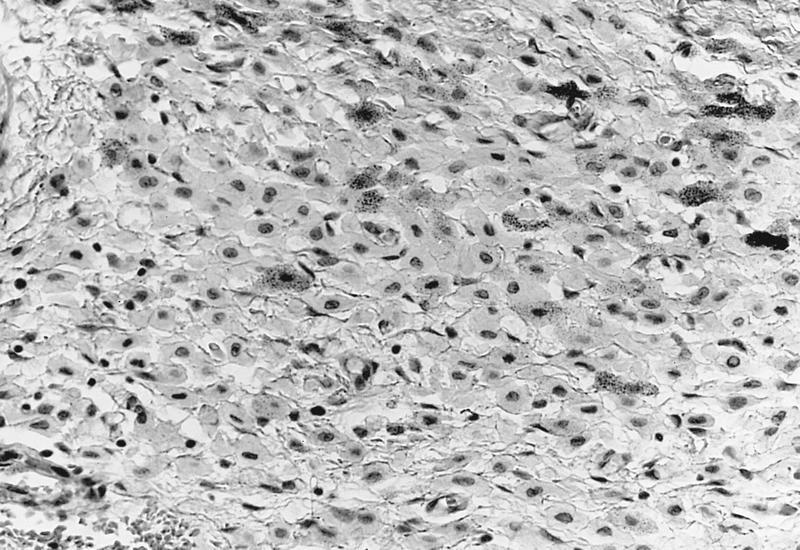
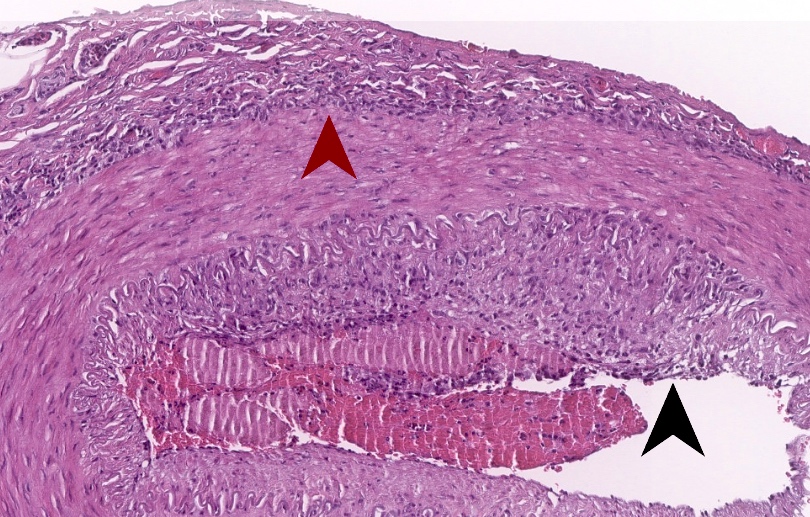
A 52 year old man who is a soft contact lens wearer presents with left eye pain and vision changes. Ophthalmic exam shows a ring shaped corneal stromal defect. Corneal biopsy reveals necrosis, neutrophilic infiltrates as shown in the image above. Which of the following is the best choice of stain to confirm the diagnosis?
- AFB Fite
- AFB Ziehl-Neelsen
- GMS
- Gram
- Mucicarmine
Board review style answer #2
C. GMS. GMS staining will highlight the encysted forms of amoeba in this description of Acanthamoeba keratitis. Answer A is incorrect because AFB Fite is used for Nocardia and would not stain amoebic forms. Answer B is incorrect because AFB Ziehl-Neelsen identifies acid fast organisms such as tuberculosis but would not stain amoebic forms. Answer D is incorrect because Gram stain is typically for bacterial organisms and would not be helpful in amoebic keratitis. Answer E is incorrect because mucicarmine is a stain for mucin and highlights cryptococcal forms, for example but is not helpful in this case of Acanthamoeba keratitis.
Comment Here
Reference: Acanthamoeba keratitis
Comment Here
Reference: Acanthamoeba keratitis
Actinic keratopathy
Actinic keratopathy
Definition / general
Gross description
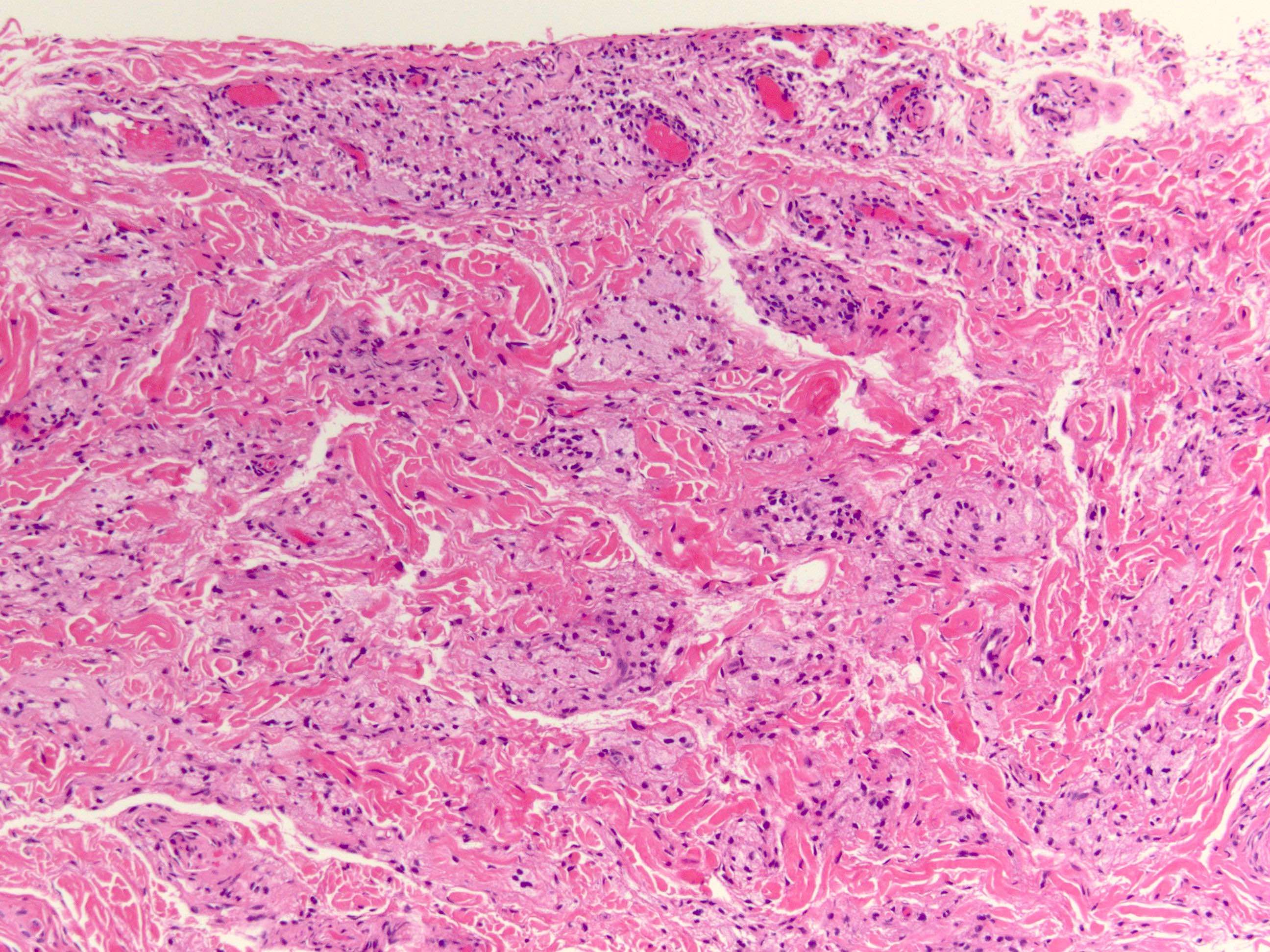
- Extensive solar elastosis in superficial layers of corneal collagen in band-like area of interpalpebral fissure
- Due to chronic high levels of ultraviolet light
Gross description
- Yellow due to solar elastosis
Chronic actinic keratopathy
Definition / general
Microscopic (histologic) description
Differential diagnosis
- Also called climatic droplet keratopathy or spheroidal degeneration
- Initially involves periphery of cornea, increases in severity and incidence with age
- Associated with long term exposure to excessive ultraviolet light
Microscopic (histologic) description
- Amorphous globules of protein accumulate in superficial stroma of interpalpebral portion of cornea
Differential diagnosis
- Other disorders produce similar globules
Actinic keratosis
Table of Contents
Definition / general | Case reports | Drawings | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosisDefinition / general
- Also called leukoplakic lesions, ultraviolet light related lesions
- Usually limbal conjunctiva at advancing head of pterygium
Case reports
- 42 year old man with conjunctival mass (Indian J Ophthalmol 2004;52:154)
- 61 year old man with bilateral limbus lesions (J Fr Ophtalmol 1992;15:65)
- 73 year old man with slowly progressive and whitish limbal conjunctival tumor (J Fr Ophtalmol 1998;21:458)
Drawings
Gross description
- Thickened conjunctiva with leukoplakia
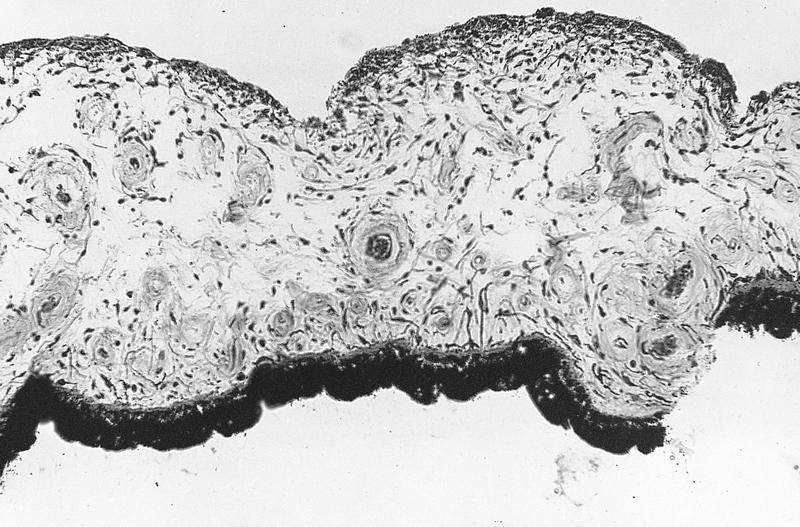
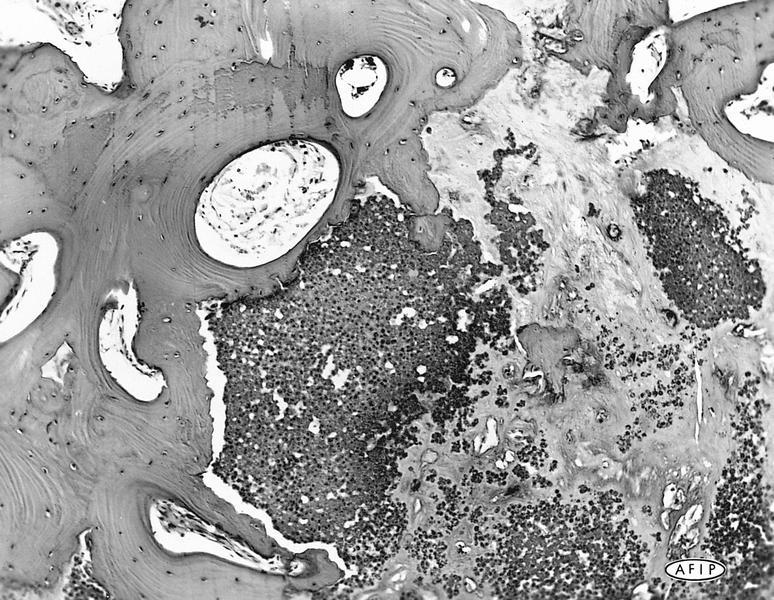
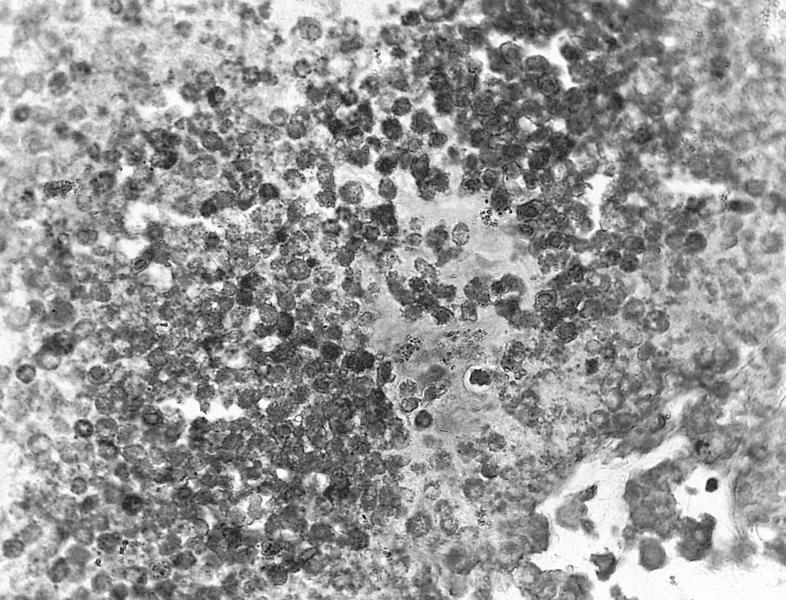
Microscopic (histologic) description
- Sharply demarcated
- Mild atypia of epithelium, acanthosis, parakeratosis, hyperkeratosis but normal polarity, normal maturation
- Elastotic degeneration and lymphocytes in substantia propria
Microscopic (histologic) images
AFIP images
Images hosted on other servers:
Differential diagnosis
- Carcinoma in situ
- Dysplasia: more diffuse and gelatinous (Can J Ophthalmol 1995;30:312)
Acute hemorrhagic conjunctivitis
Table of Contents
Terminology | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Treatment | Clinical images | Microscopic (histologic) descriptionTerminology
- Also known as Apollo disease
Epidemiology
- First described in Ghana in 1969
- Most common in developing countries, may affect > 50% of local population
Sites
- Palpebral conjunctiva; cornea may be involved with a fine punctate keratopathy and rarely subepithelial opacities (eMedicine: Acute Hemorrhagic Conjunctivitis [Accessed 24 April 2018])
Pathophysiology
- Epidemic form is rapidly progressive and highly contagious
Etiology
- Most commonly human coxsackievirus A24 variant (CV-A24v, Arch Virol 2007;152:2005, J Med Virol 2007;79:748, MMWR Morb Mortal Wkly Rep 2004;53:632, Virol J 2013;10:96) or human enterovirus 70 (EV-70, Emerg Infect Dis 1999;5(2)); less frequently adenovirus serotype 11
Clinical features
- Ocular pain, eyelid swelling, tearing, foreign body sensation or irritation, photophobia and conjunctival hemorrhages
- Associated with polio-like paralysis
Diagnosis
- RT-PCR (J Virol Methods 2007;142:89, J Clin Microbiol 2005;43:1069), culture
Laboratory
- Eye mucous swab samples
Treatment
- Symptomatic, usually self-limited after 5 - 7 days with no sequelae
- Patient education to avoid spread
Microscopic (histologic) description
- Palpebral conjunctival follicular reaction
- Subconjunctival hemorrhage ranging from petechiae to large areas, and congestion
- Fine pinpoint epithelial keratitis
Adenocarcinoma-eyelid
Table of Contents
Definition / generalDefinition / general
- Malignant sweat gland tumor, often mucinous
- Similar to adenocystic carcinoma of skin at other sites
- Local recurrences are common, rarely distant metastases
Adenocarcinoma-lacrimal gland / sac
Table of Contents
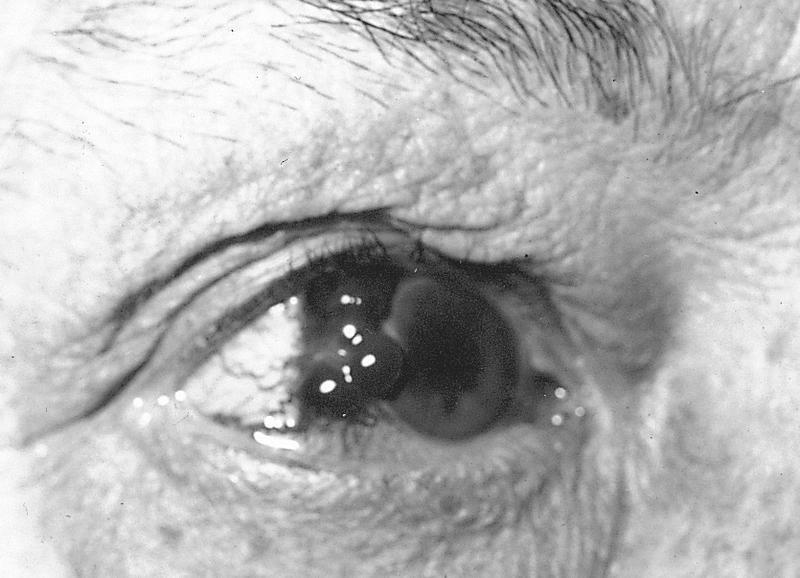
Microscopic (histologic) imagesAdenocarcinoma-retinal pigment epithelium
Definition / general
- Rare, < 50 cases reported
- More common in women
- Often diagnosed as atypical choroidal melanoma clinically
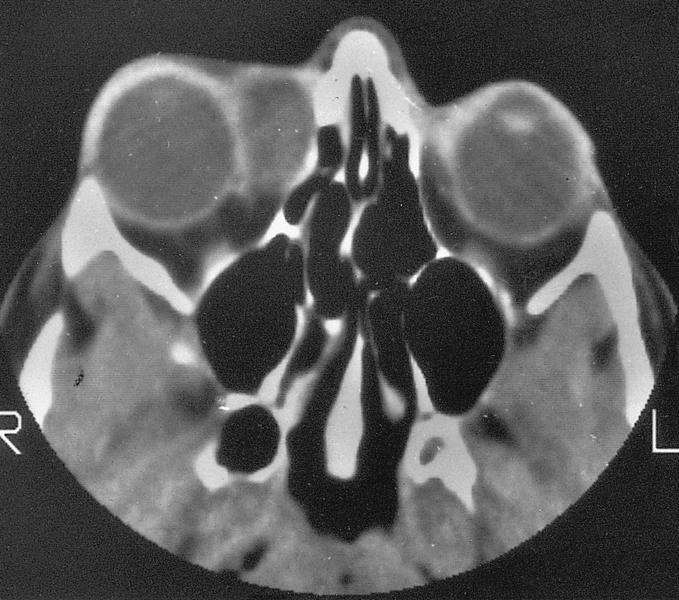
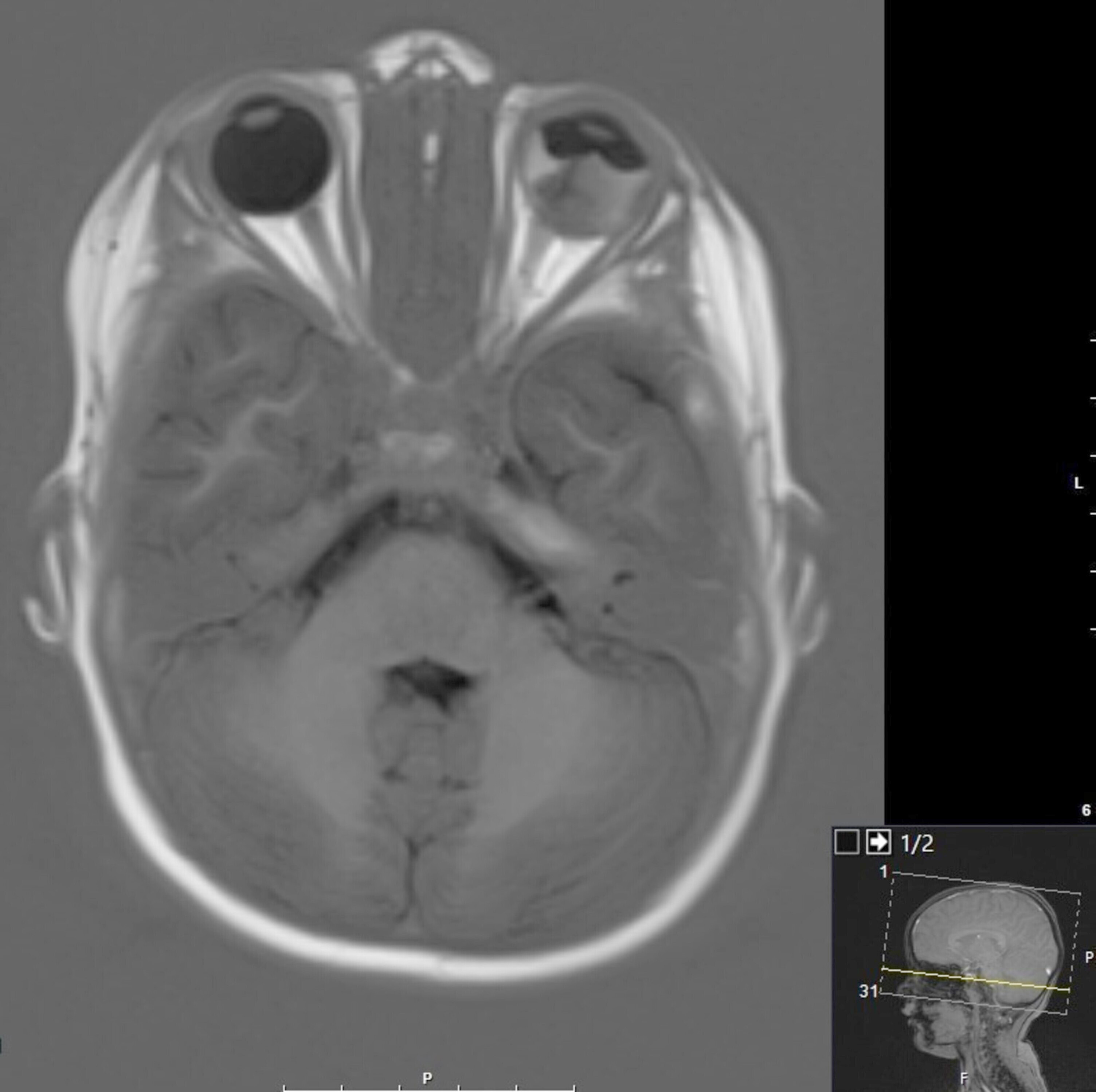
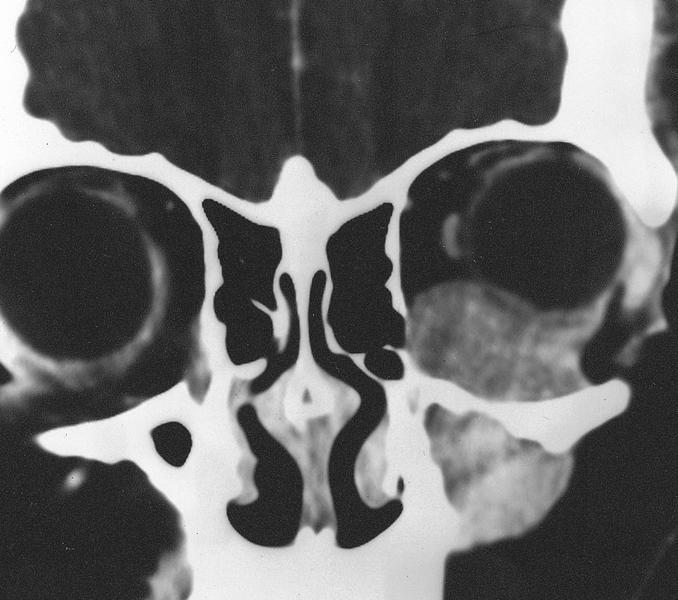
Adenoid cystic carcinoma
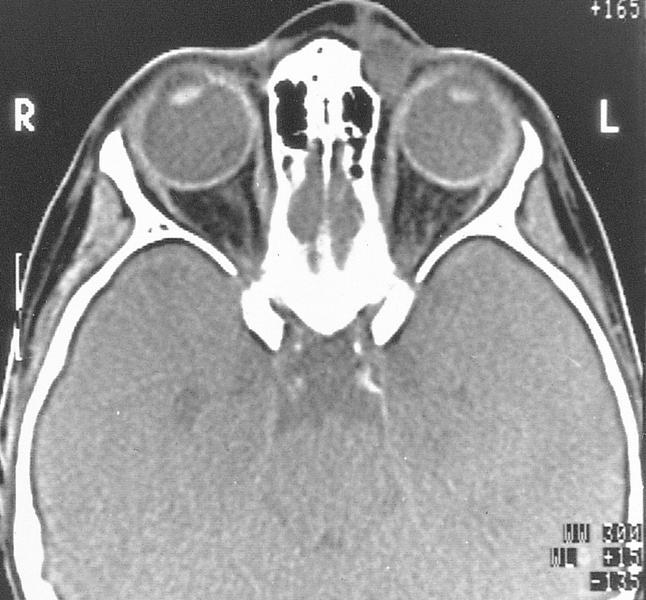
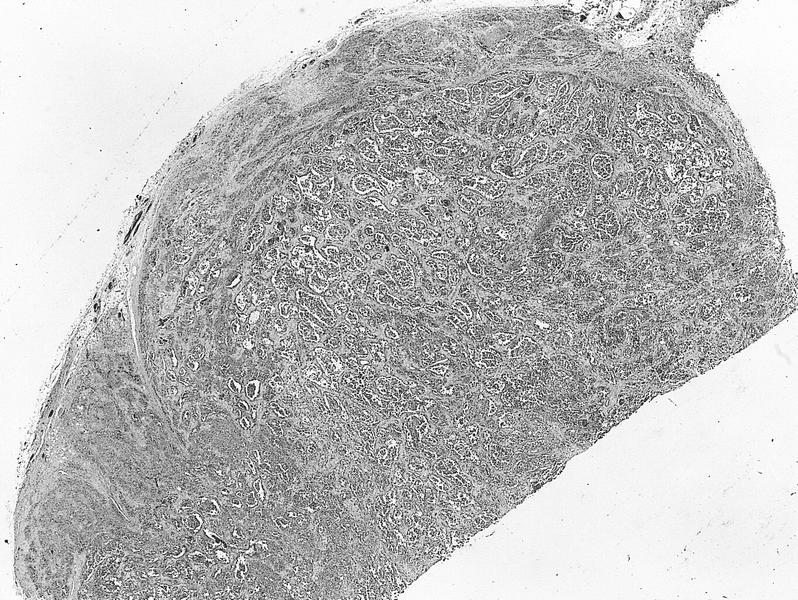
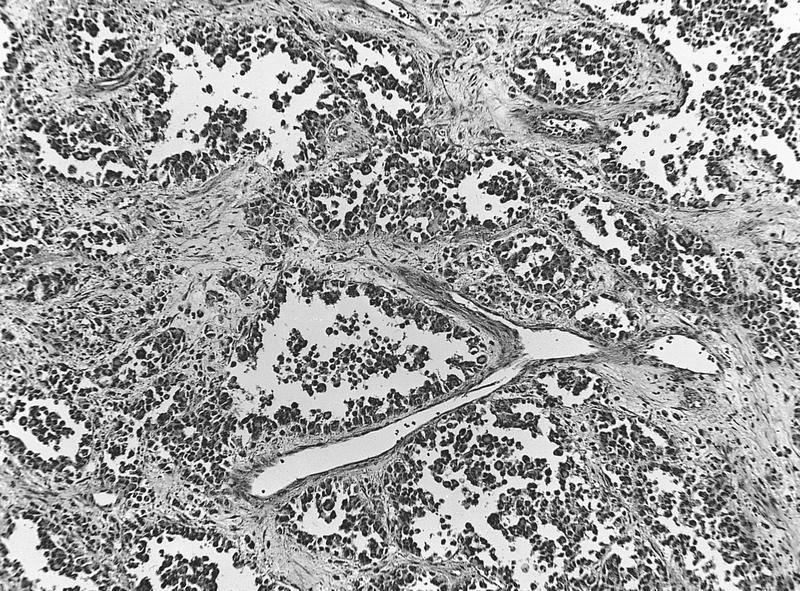
Table of Contents
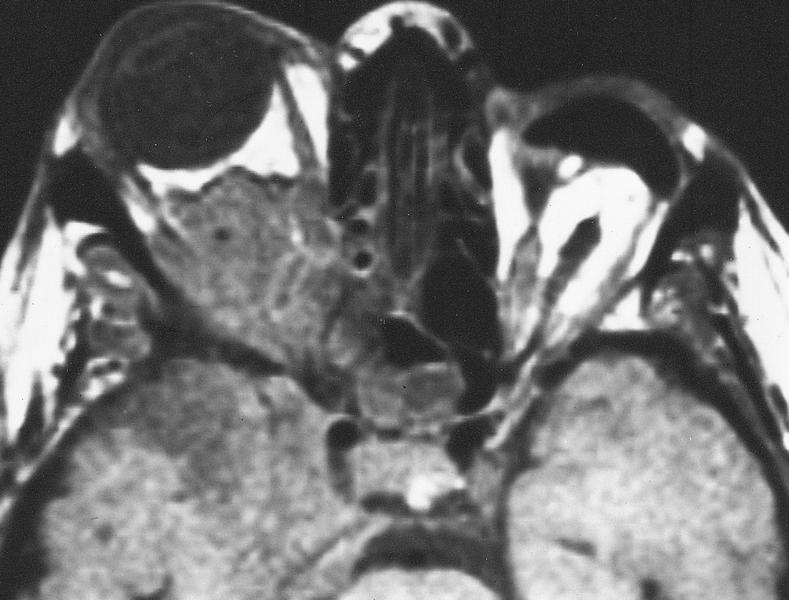
Definition / general | Radiology images | Microscopic (histologic) description | Microscopic (histologic) imagesDefinition / general
- 20 - 30% of lacrimal gland tumors
- Most common malignant tumor of lacrimal gland
- Aggressive, may infiltrate eyelid or brain
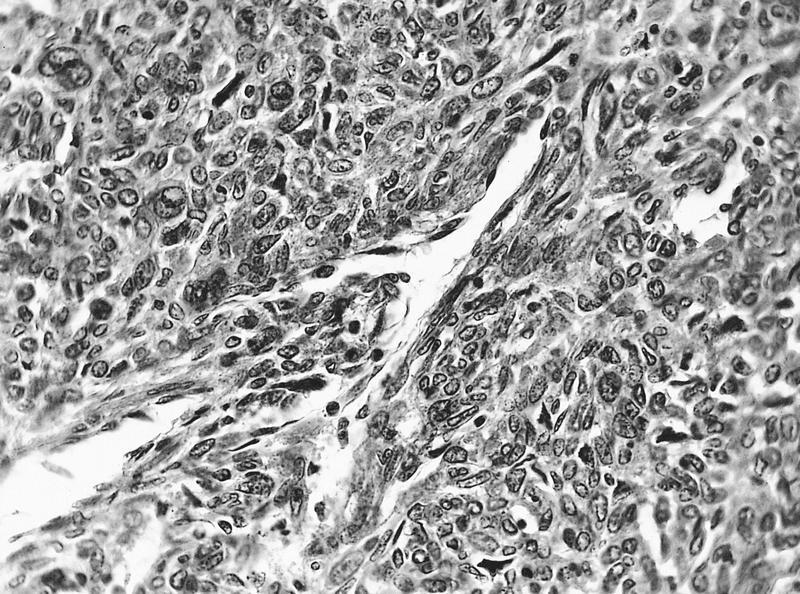
Microscopic (histologic) description
- Basaloid growth with cribriform change
- Relatively bland cytology
- Perineural invasion, focal tumor necrosis
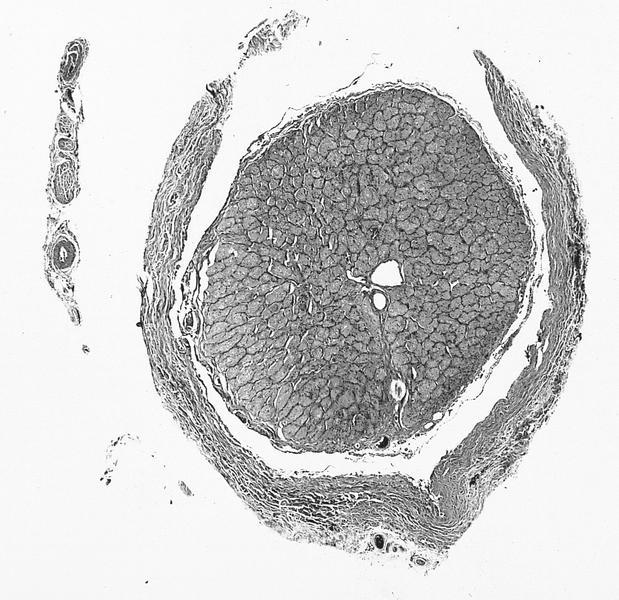
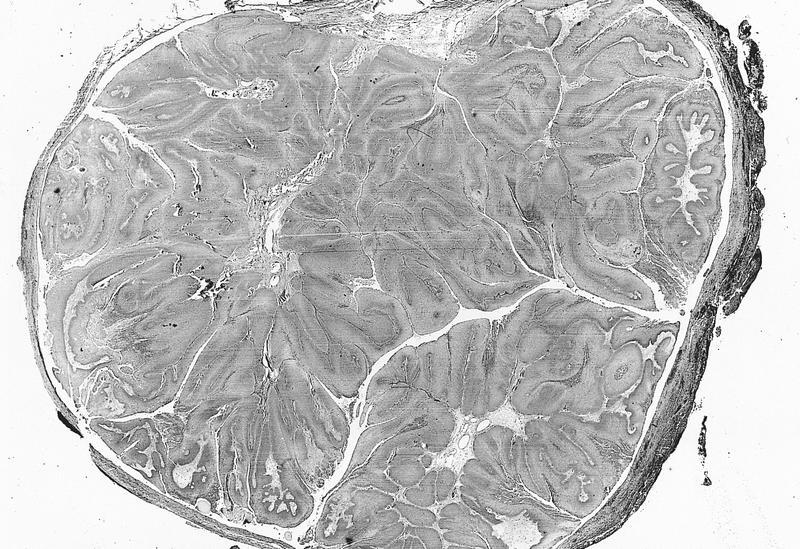
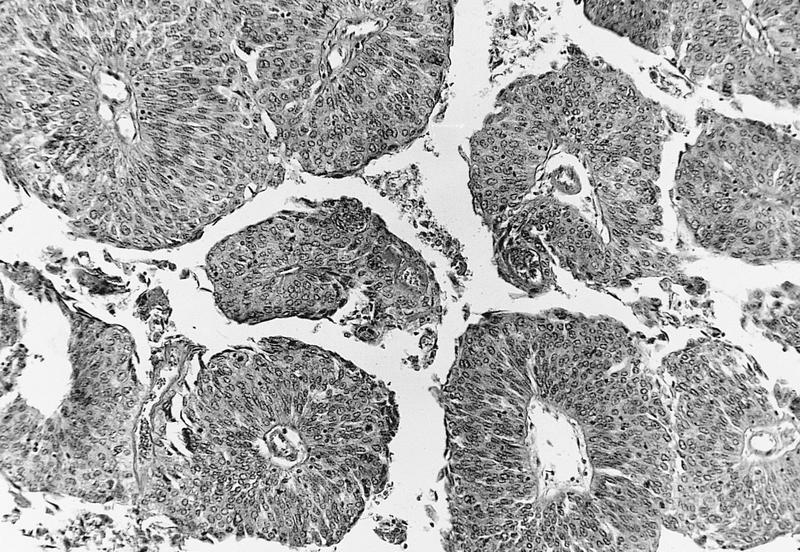
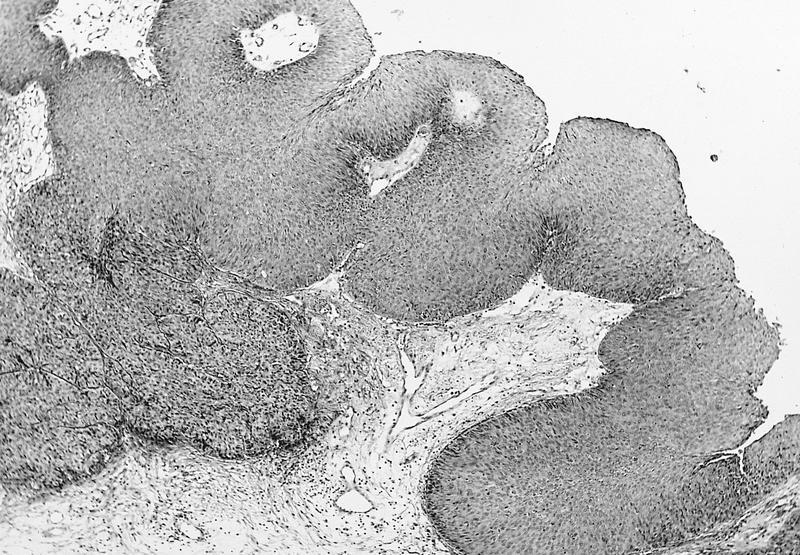
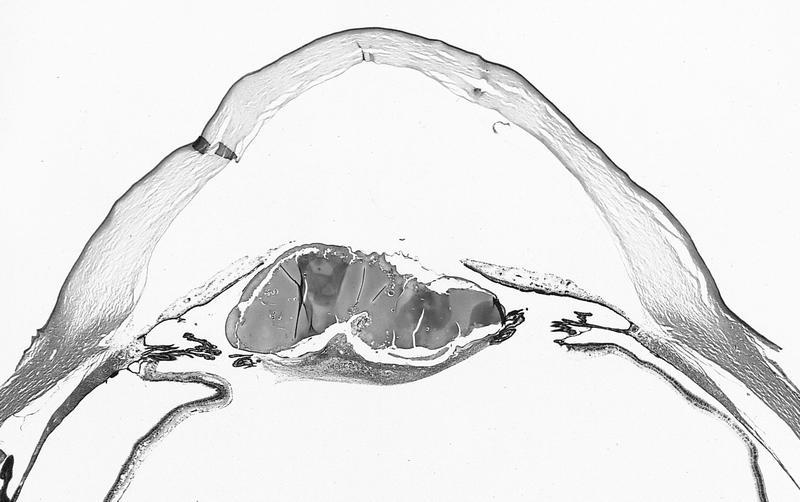
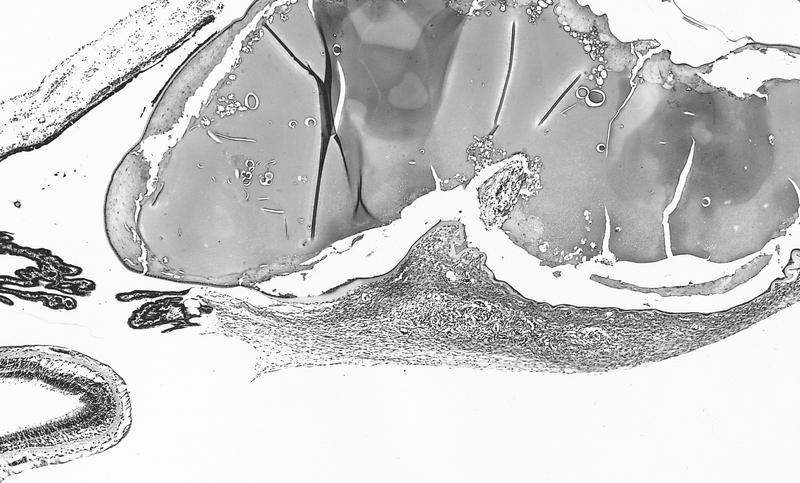
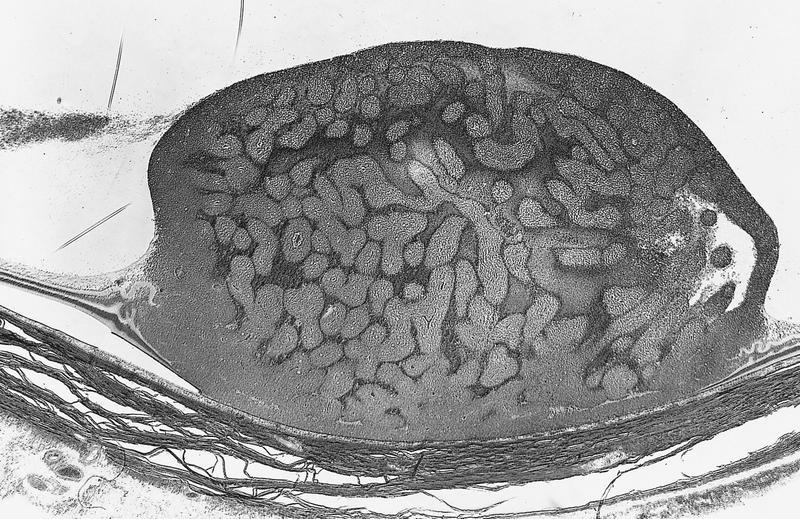
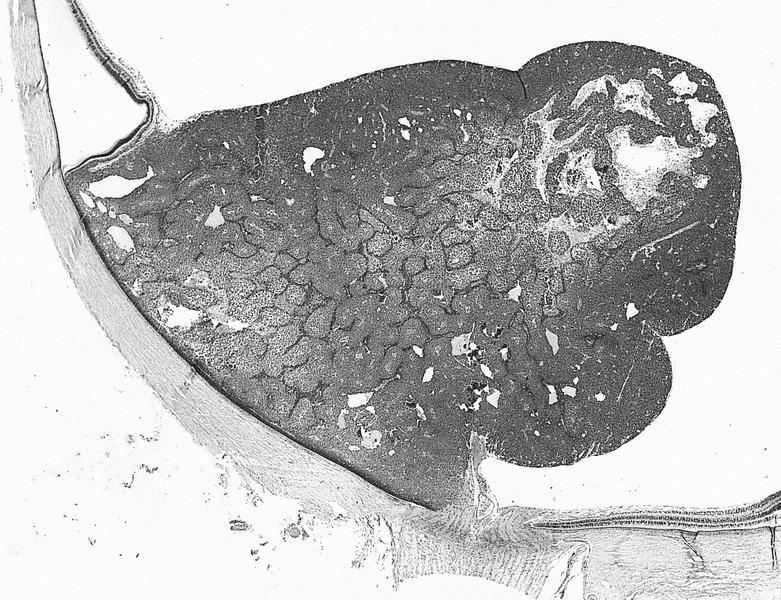
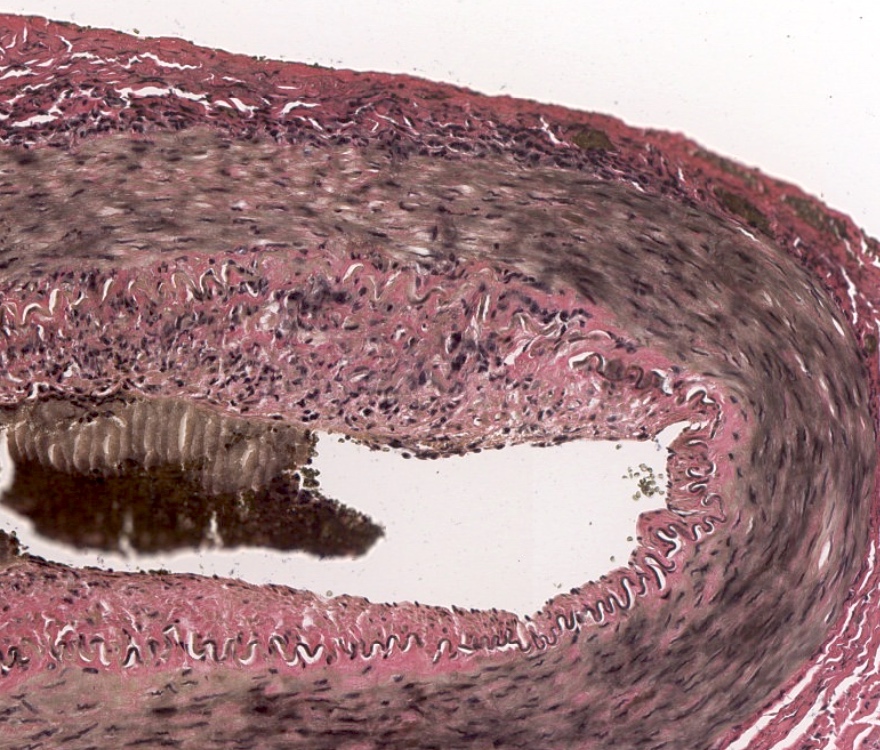
Anatomy & histology-ciliary body
Definition / general
- Middle segment of uveal tract, between iris and choroid
- Composed of pars plicata and pars plana
- Holds lens in place
- Cyclectomy: resecting portion of ciliary body containing tumor; may also include other surrounding structures
- Pars plicata: 70 sagitally oriented folds or ciliary processes that gradually merge with posterior flat pars plana, which merges posteriorly with serrated, anterior border of retina (ora serrata)
- Ciliary epithelium composed of inner epithelial layer (nonpigmented, contiguous with aqueous of posterior chamber) and outer epithelial layer (pigmented, unites with retinal pigment epithelium at ora serrata)
- Outer epithelial layer overlies PAS+ basal lamina that thickens in diabetes mellitus
- Zonules: acellular fibers that attach crests of nonpigmented ciliary epithelium in pars plicata to capsule of crystalline lens
- Ciliary body has 3 distinct bundles of smooth muscle which assist in accommodation; as muscle contacts, ciliary body extends forward, reducing pressure on zonules, enabling lens to become less concave, thereby increasing its refractive power
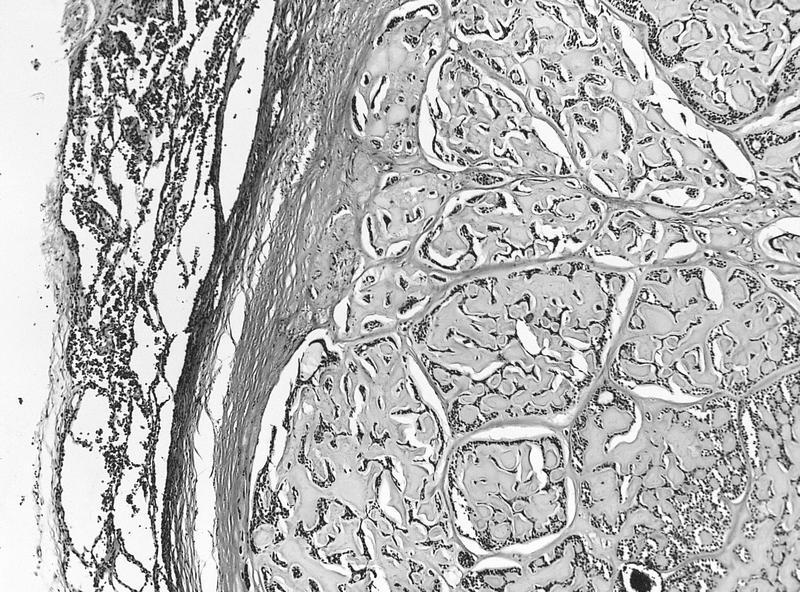
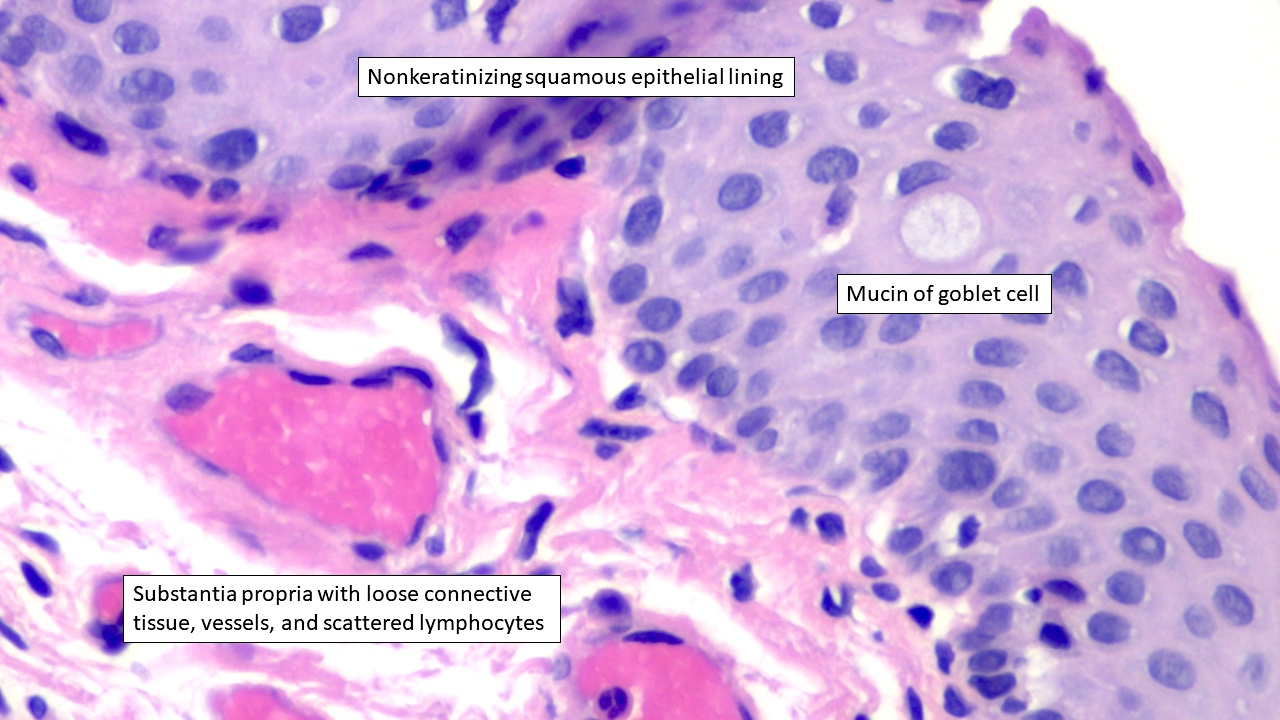
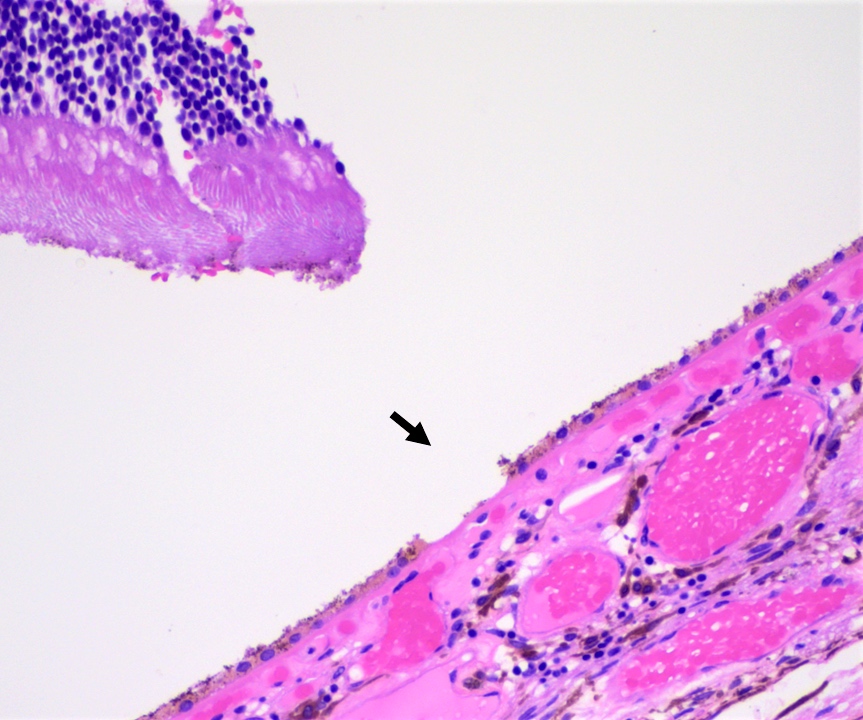
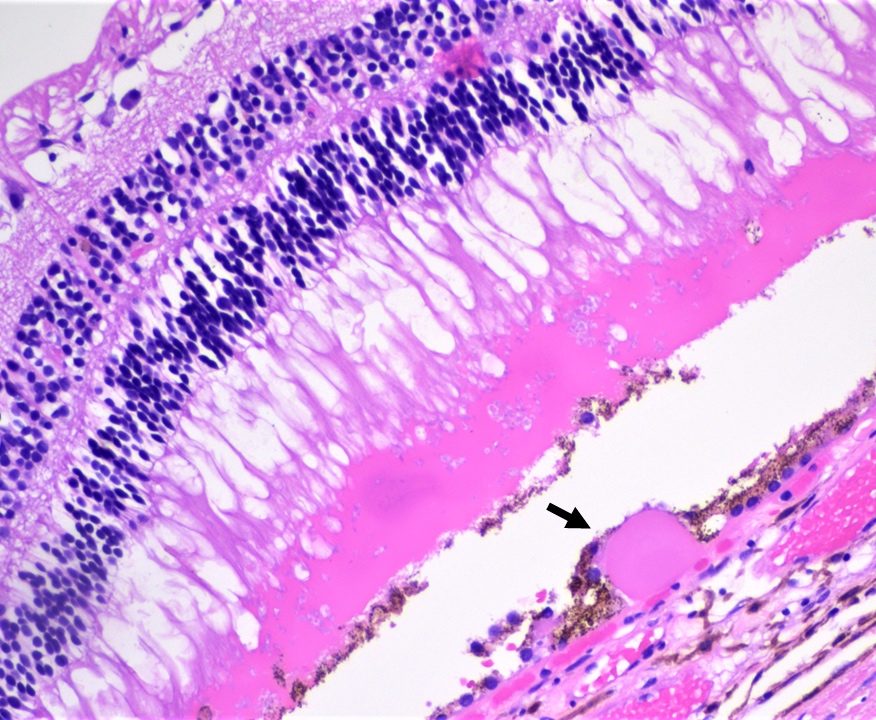
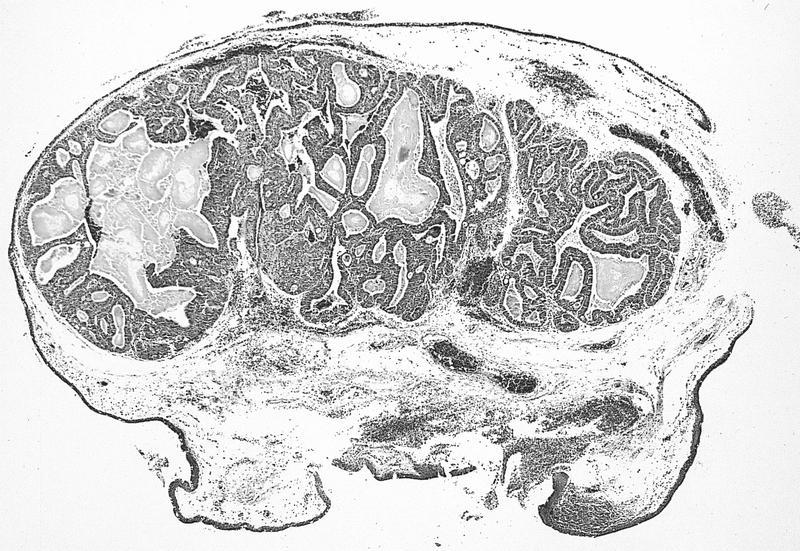
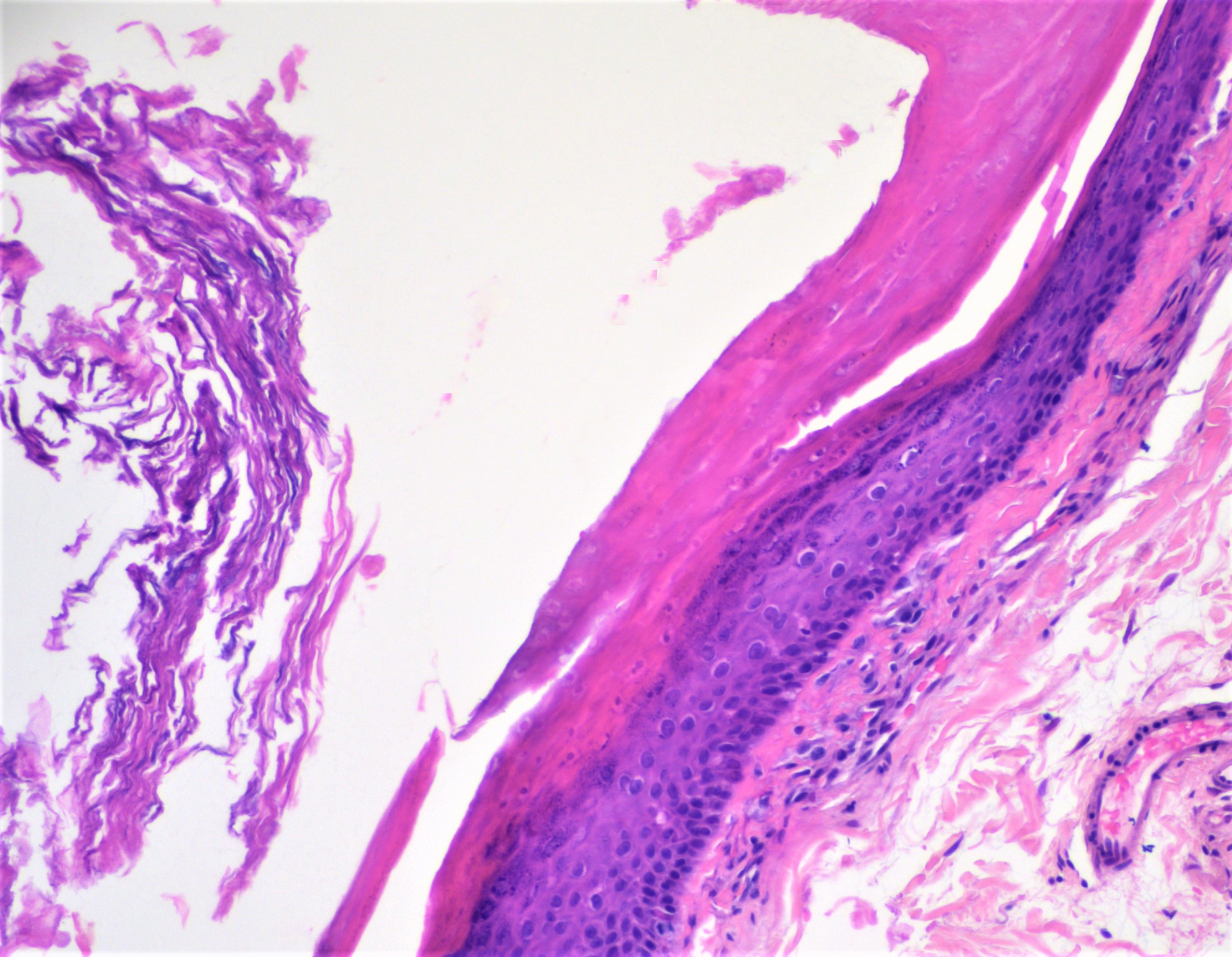
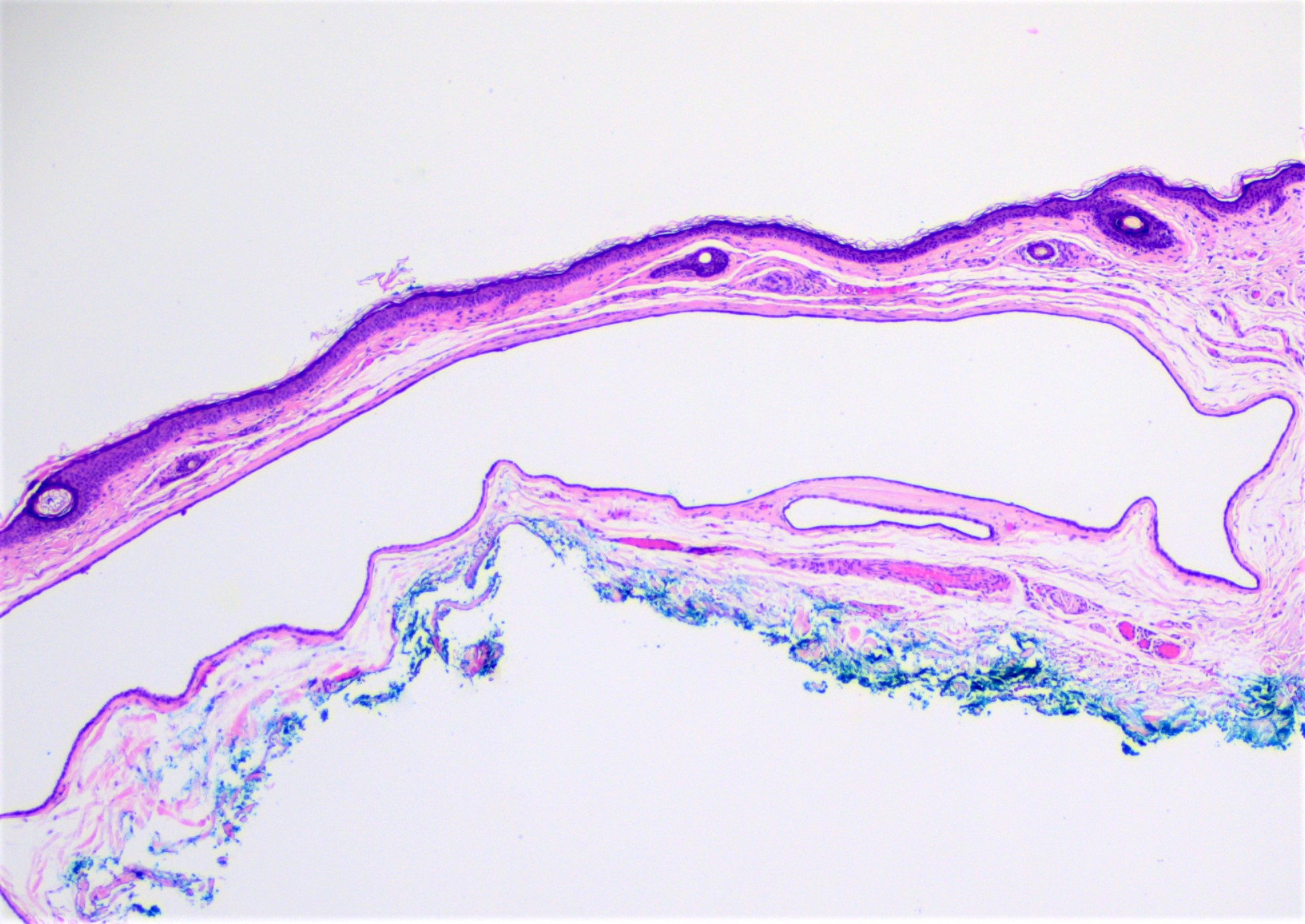
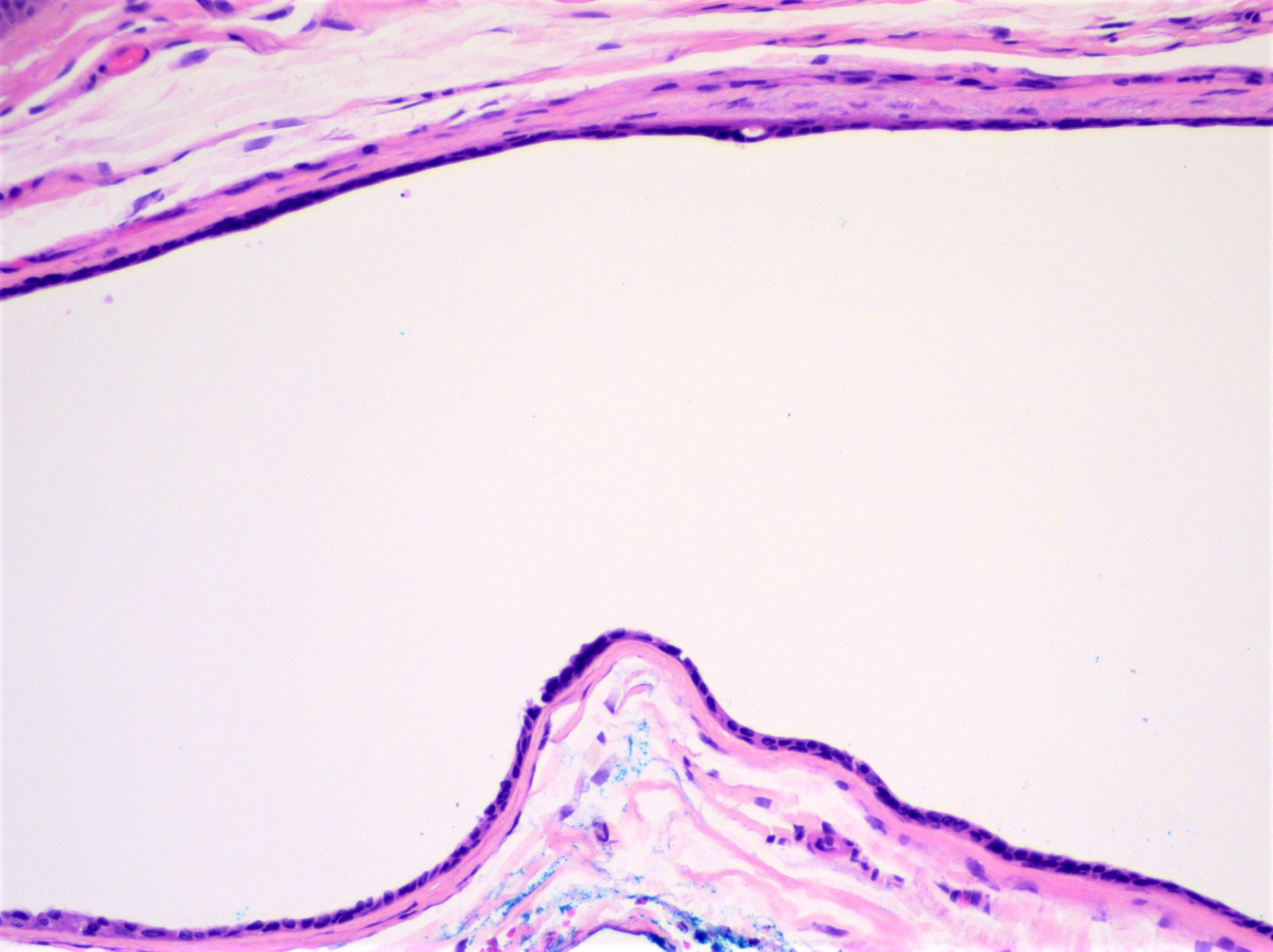
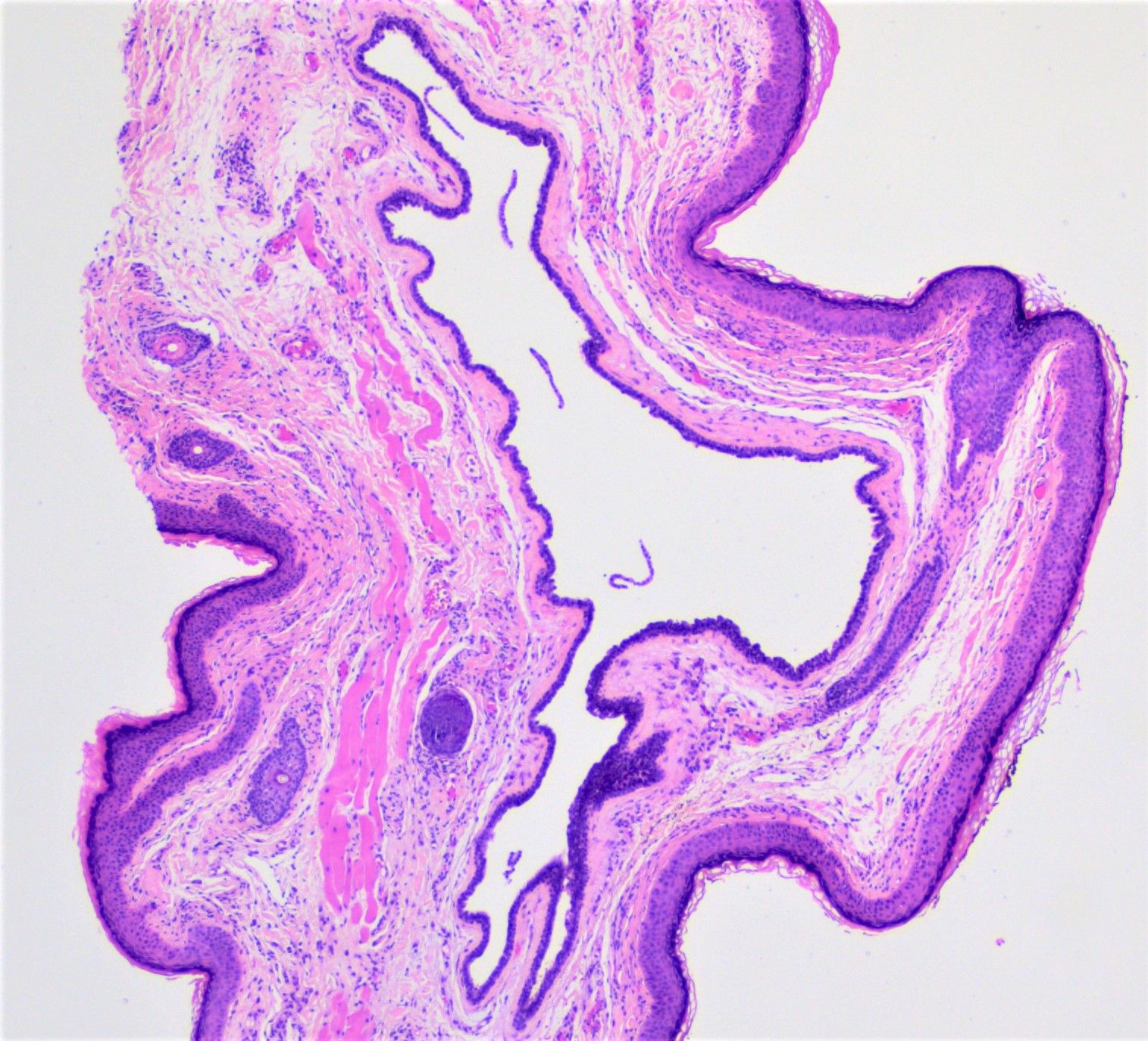
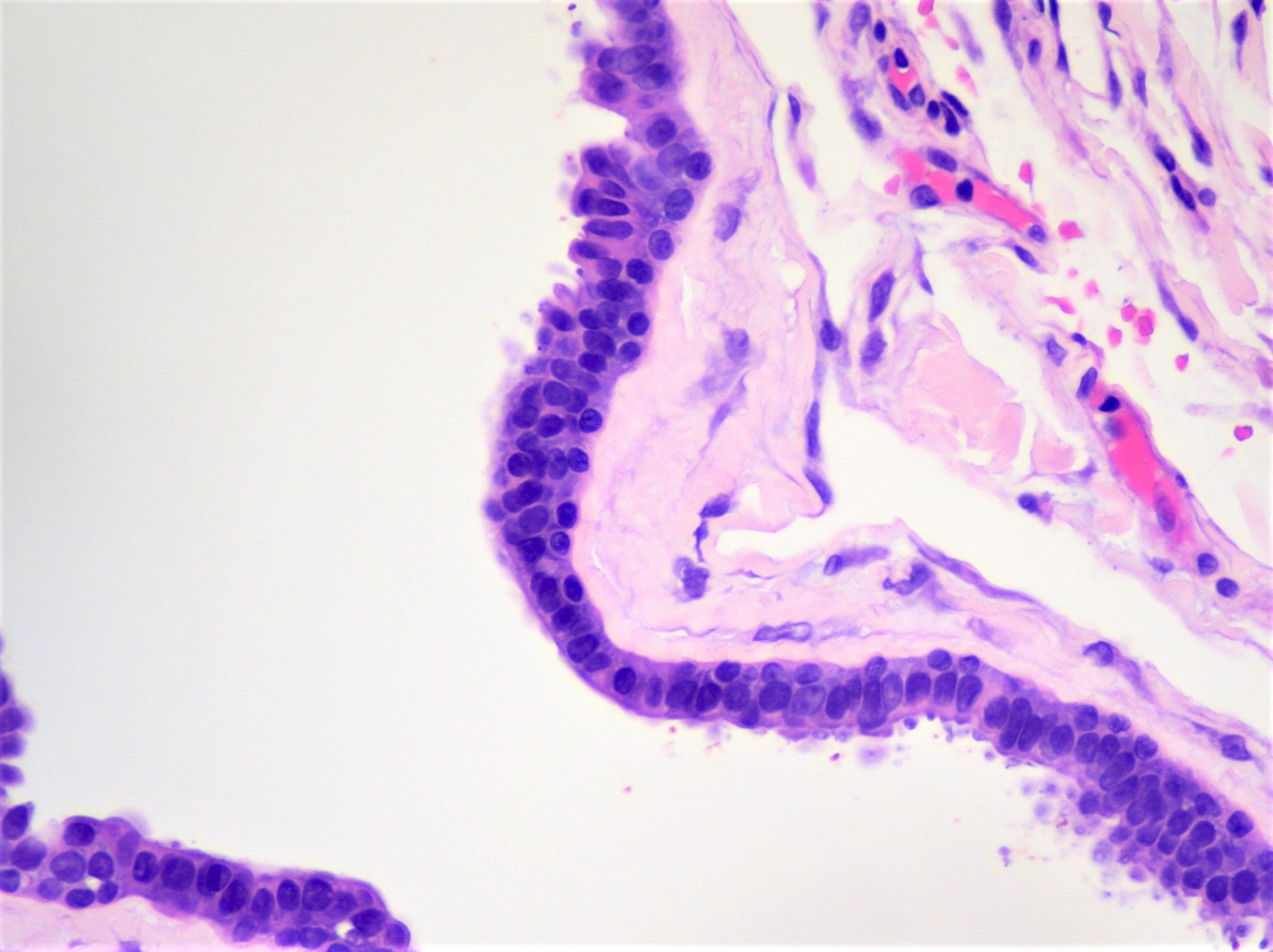
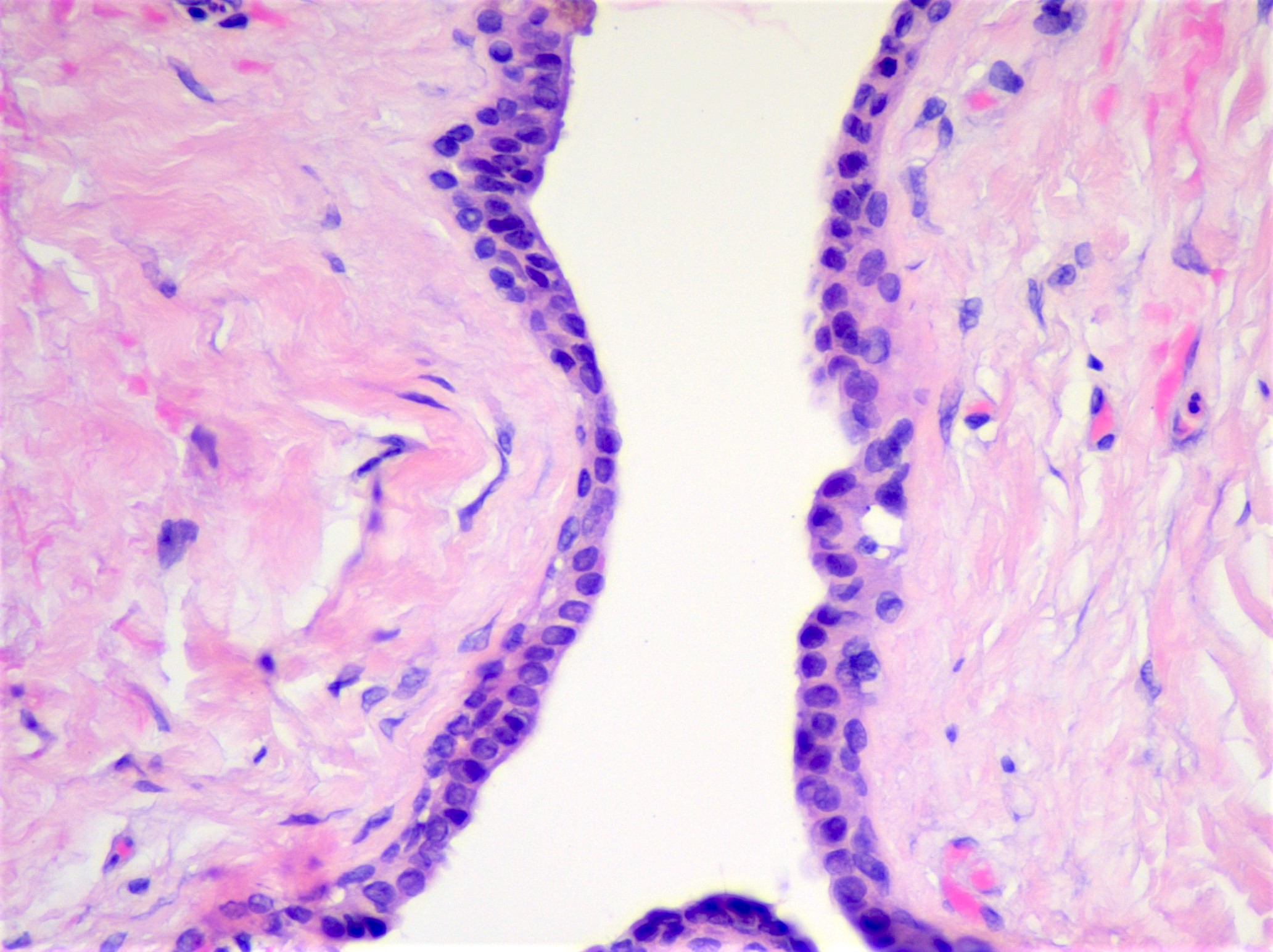
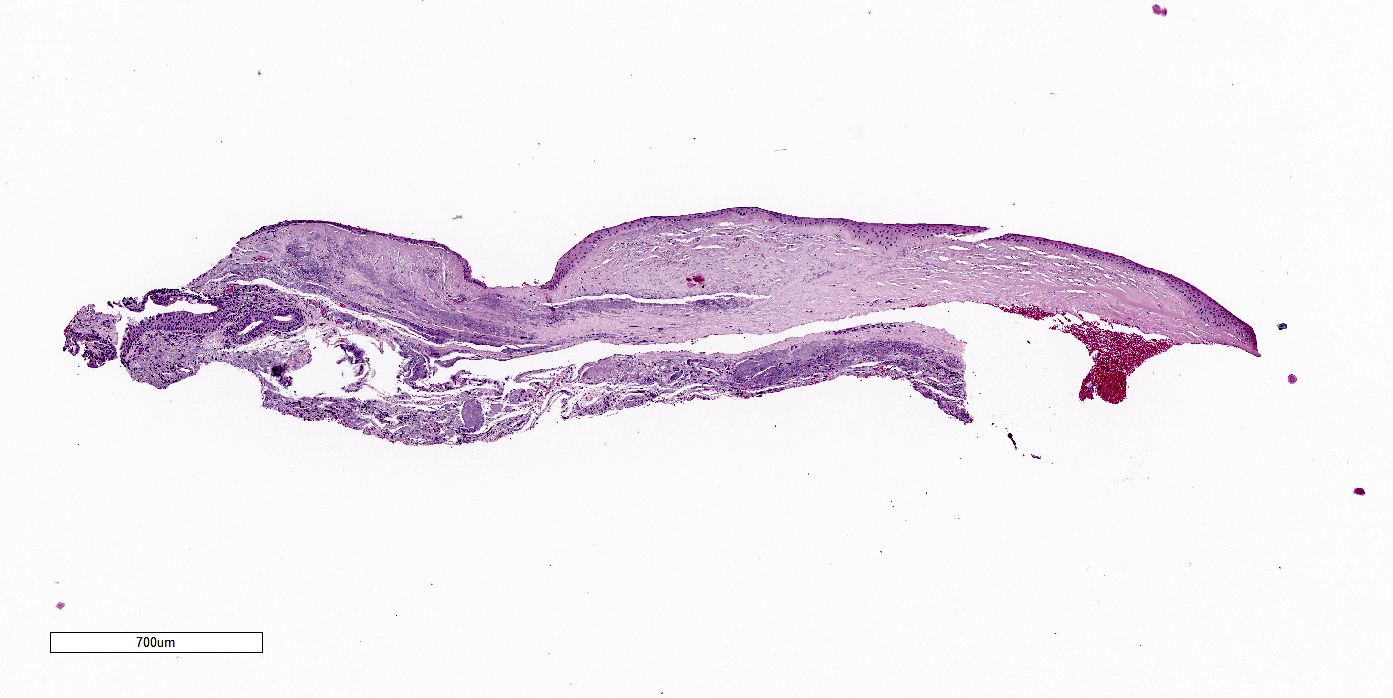
Anatomy & histology-conjunctiva
Table of Contents
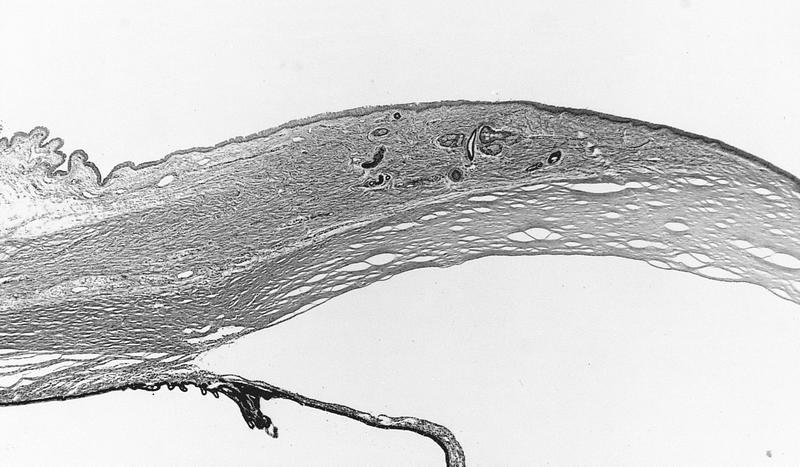
Definition / general | Essential features | Terminology | Embryology and physiology | Diagrams / tables | Clinical features | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Videos | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Mucous membrane that covers, protects and lubricates the posterior surface of the eyelids (palpebral, also known as tarsal, conjunctiva) and anterior surface of the globe (bulbar conjunctiva) as well as provides redundant folds (forniceal conjunctiva) to aid eye movement
Essential features
- Nonkeratinizing squamous epithelium with goblet cells overlying loose connective tissue
- Aids in protecting and lubricating the eye
- Bulbar conjunctiva covers the anterior globe
- Palpebral conjunctiva covers the posterior surface of the eyelids
- Forniceal conjunctiva forms redundant folds to aid eye movement
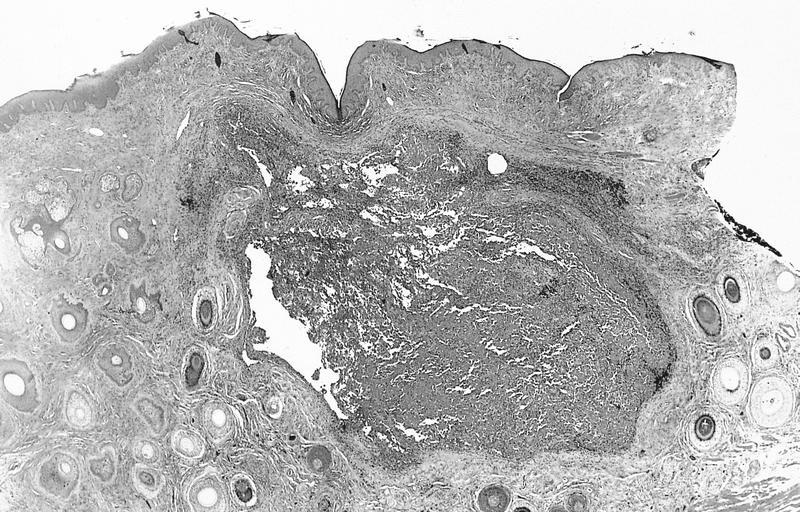
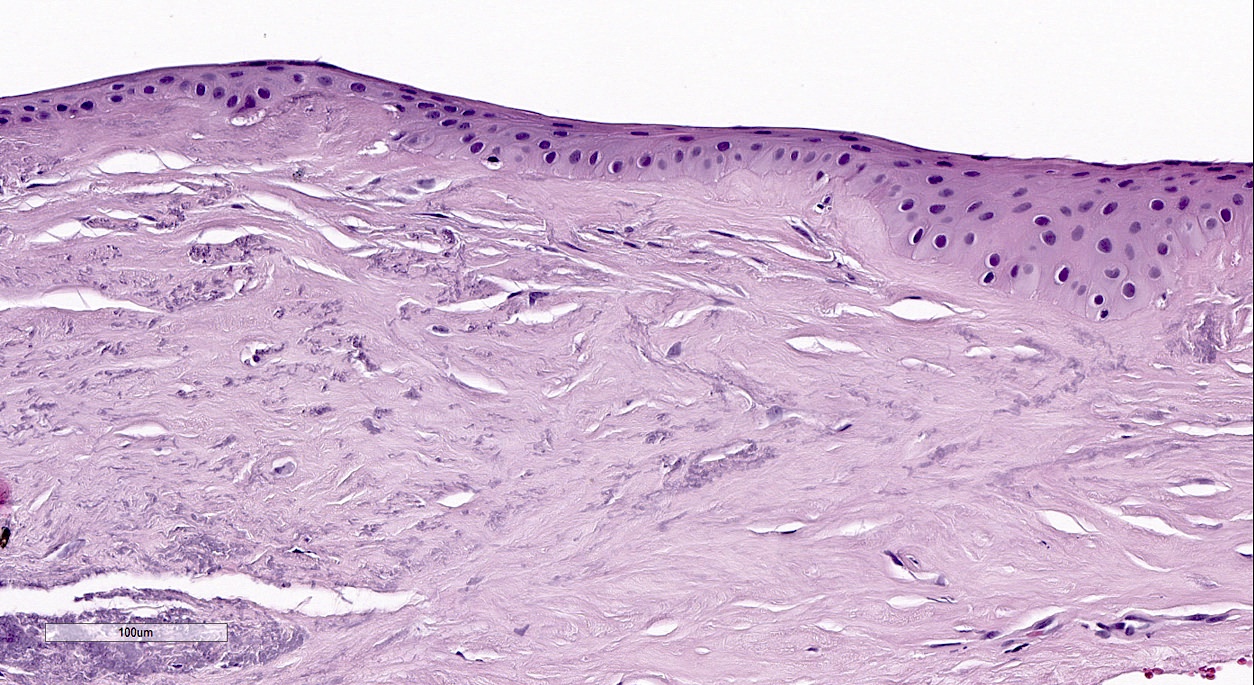
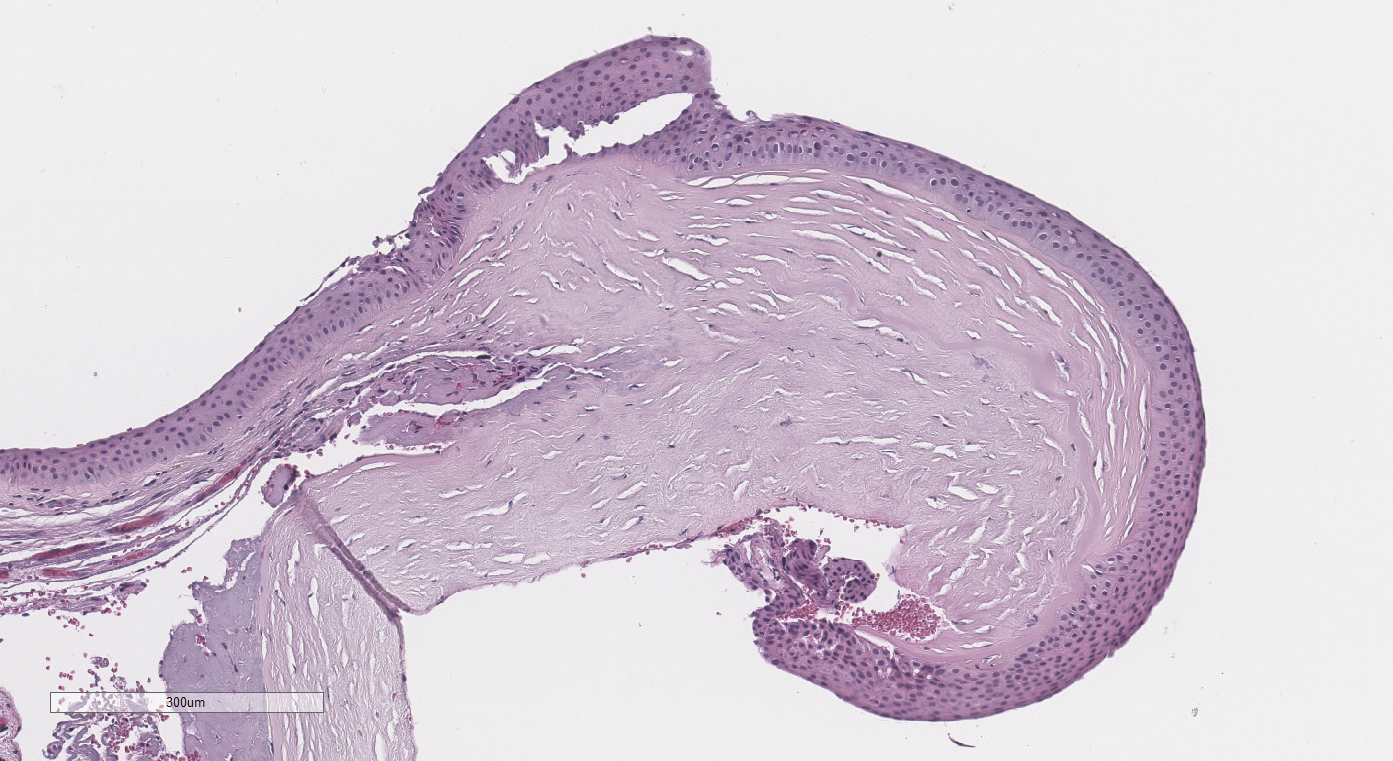
Terminology
- Palpebral (tarsal) conjunctiva covers the posterior surface of the eyelid and is associated with the tarsal plate and sebaceous (Meibomian) glands
- Tarsal plate is the thick fibroconnective tissue that provides structural support to the eyelid and houses sebaceous (Meibomian) glands (J Anat 2005;206:37)
- Palpebral accessory lacrimal glands of Wolfring are present in the palpebral conjunctiva (Invest Ophthalmol Vis Sci 2012;53:6738)
- Meibomian glands are sebaceous glands of the tarsal plate that secrete meibum through holocrine secretion (Ophthalmology 2017;124:S20)
- Bulbar conjunctiva covers the anterior globe (excluding the cornea) and can be further divided into scleral conjunctiva, limbal conjunctiva and plica semilunaris
- Scleral conjunctiva covers the sclera, the dense, fibrous connective tissue of the eye
- Limbal conjunctiva forms an annular rim around the cornea
- Plica semilunaris is a fold of conjunctiva lateral to the caruncle
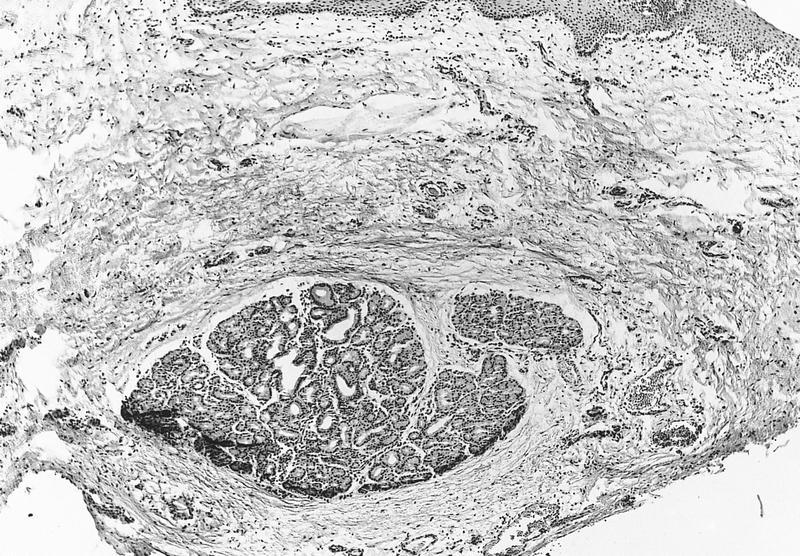
- Limbus includes the border between the corneal and conjunctival epithelium and is an important location for multipotent stem cells (Eye (Lond) 1989;3:101)
- Characterized by fibrovascular ridges that exist in a radial orientation, known as the palisades of Vogt, which are interspaced by limbal epithelial crypts that house stem cells that mediate corneal epithelial regeneration and superficial wound healing (Trans Am Ophthalmol Soc 1982;80:155, Br J Ophthalmol 2005;89:529)
- Caruncle is the fleshy pink prominence at the medial aspect of the eye; it contains conjunctiva, skin, hair follicles and other adnexal structures (Eye (Lond) 2009;23:1004)
- Forniceal conjunctiva forms redundant folds in the cul de sac of the upper and lower fornices (the areas where the bulbar and palpebral conjunctivas meet) and allows for movement of the globe and eyelids (StatPearls: Mucous Membrane Graft [Accessed 28 June 2023])
- Pseudoglands of Henle are infoldings, invaginations or tangentially sectioned conjunctival epithelium that resemble glands, often in the context of chronic inflammation (Ophthalmology 2001;108:135)
- Conjunctival vascular supply
- Conjunctival blood supply is primarily derived from the ophthalmic artery and its branches, such as the anterior ciliary arteries (Eye (Lond) 1988;2:533)
- Conjunctival lymphatic drainage
- Conjunctiva drains to the preauricular and submandibular lymph nodes (Plast Reconstr Surg 2017;139:628e)
- Conjunctival innervation
- Sensory innervation of the conjunctiva is derived from the infratrochlear, infraorbital, lacrimal and long ciliary nerves (StatPearls: Anatomy, Head and Neck, Eye Conjunctiva [Accessed 28 June 2023])
Embryology and physiology
- Conjunctiva arises from the surface ectoderm, while the tarsal plate originates from mesenchyme (Ophthalmic Plast Reconstr Surg 2016;32:407)
- Tarsal plate originates from mesenchyme and neural crest cells (Ophthalmic Plast Reconstr Surg 2016;32:407)
- Additional mesenchyme and neural crest derivatives include connective tissue and pericytes (Ophthalmic Plast Reconstr Surg 2016;32:407)
- Sebaceous (Meibomian) glands and hair follicles are of mixed origin with contributions from the surface ectoderm (Ophthalmic Plast Reconstr Surg 2016;32:407)
- Key functions of the conjunctiva include production of tear constituents and the maintenance of ocular surface homeostasis (Acta Biomater 2018;67:259)
Clinical features
- Pterygium appears as a wing-like lesion of encroaching bulbar conjunctiva over the cornea (see Pterygium) (Am J Pathol 2011;178:817)
- Pinguecula appears as a yellow to brown nodular lesion of the bulbar conjunctiva near the limbus without extension over the cornea (see Pinguecula) (Graefes Arch Clin Exp Ophthalmol 2006;244:104)
- Inflammation of the conjunctiva (conjunctivitis) manifests as eye redness with watery discharge associated with viral and allergic etiologies and purulent discharge, a sign of bacterial infection (see Chronic conjunctivitis, Infectious conjunctivitis, Conjunctivitis-general) (StatPearls: Conjunctivitis (Nursing) [Accessed 31 July 2023])
Gross description
- Routine surgical specimens of benign conjunctiva are typically small, unoriented fragments of tan-pink tissue
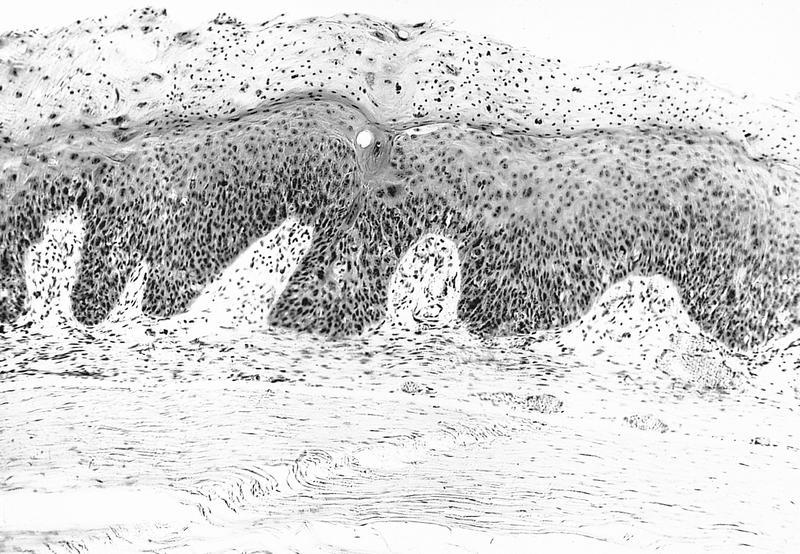
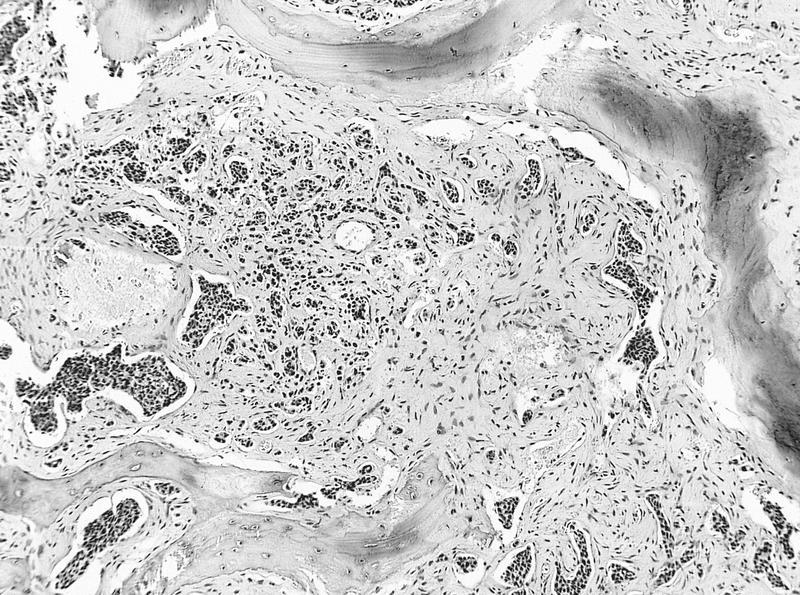
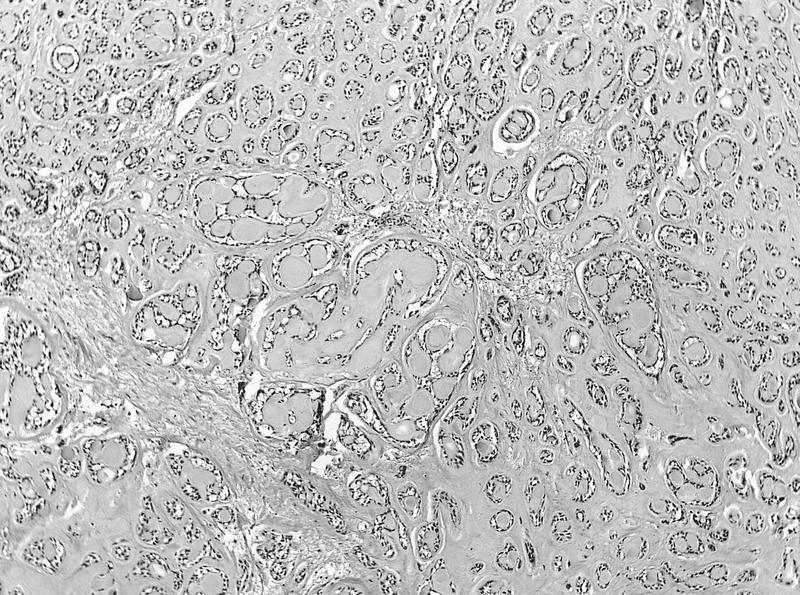
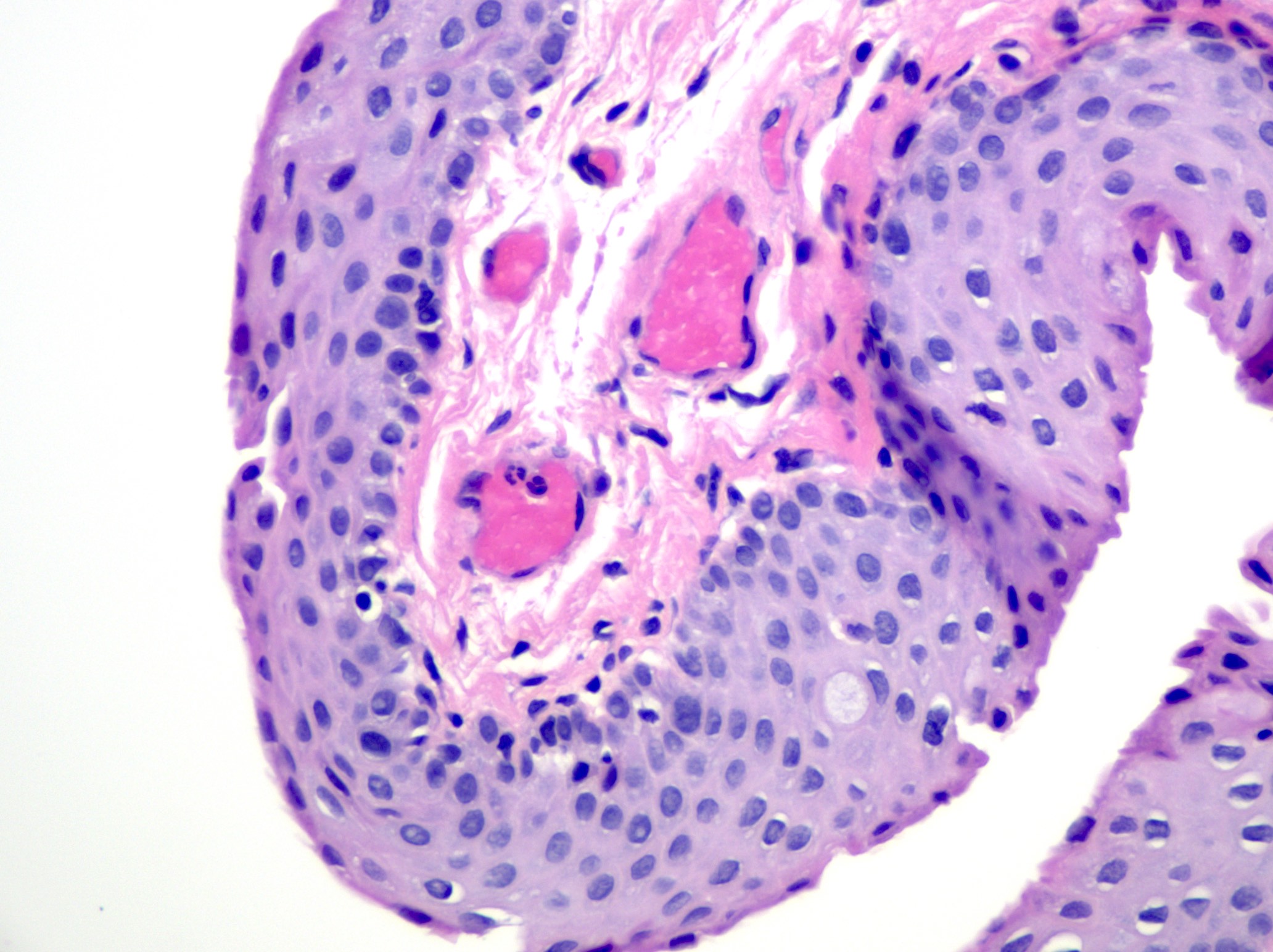
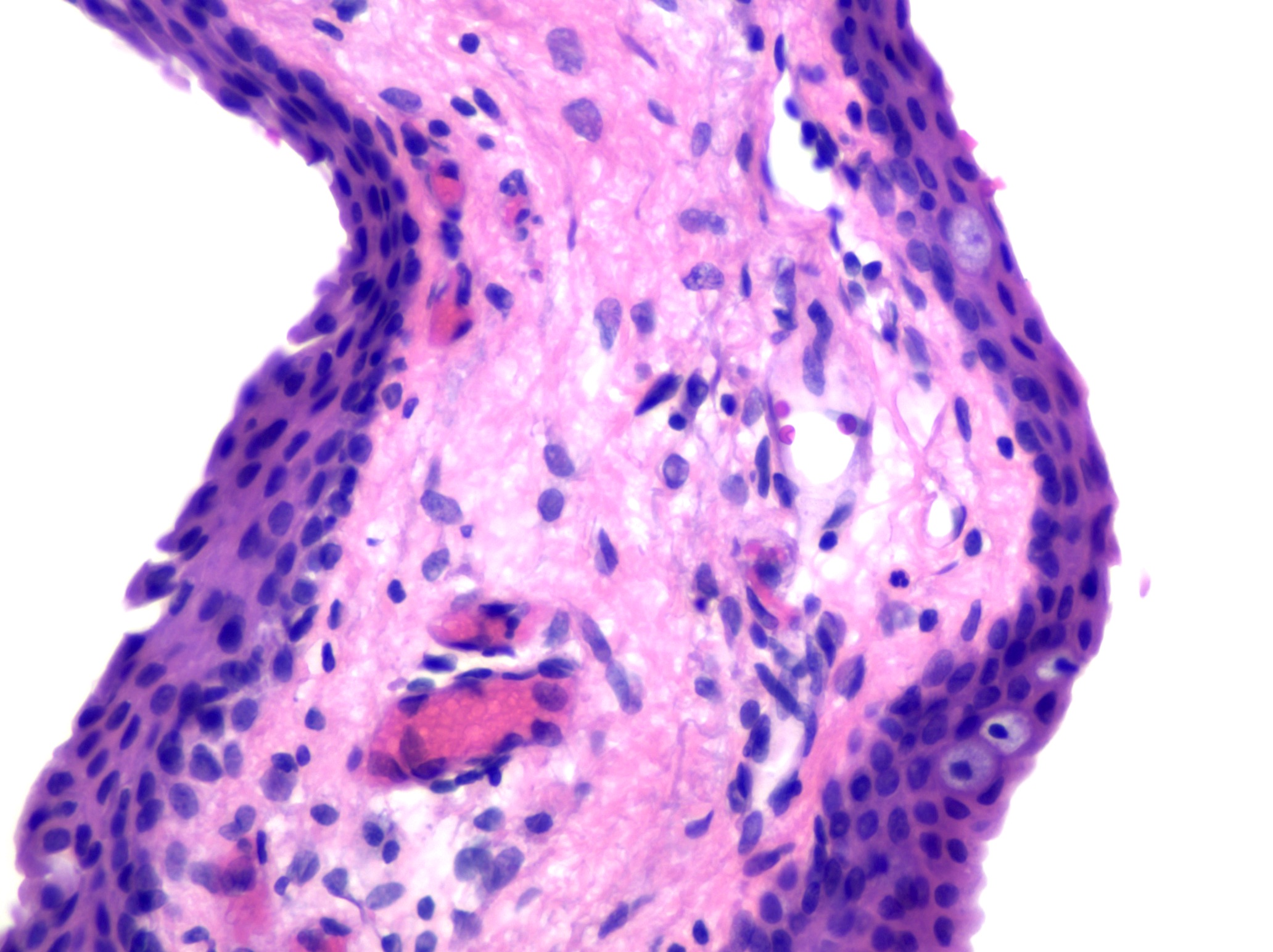
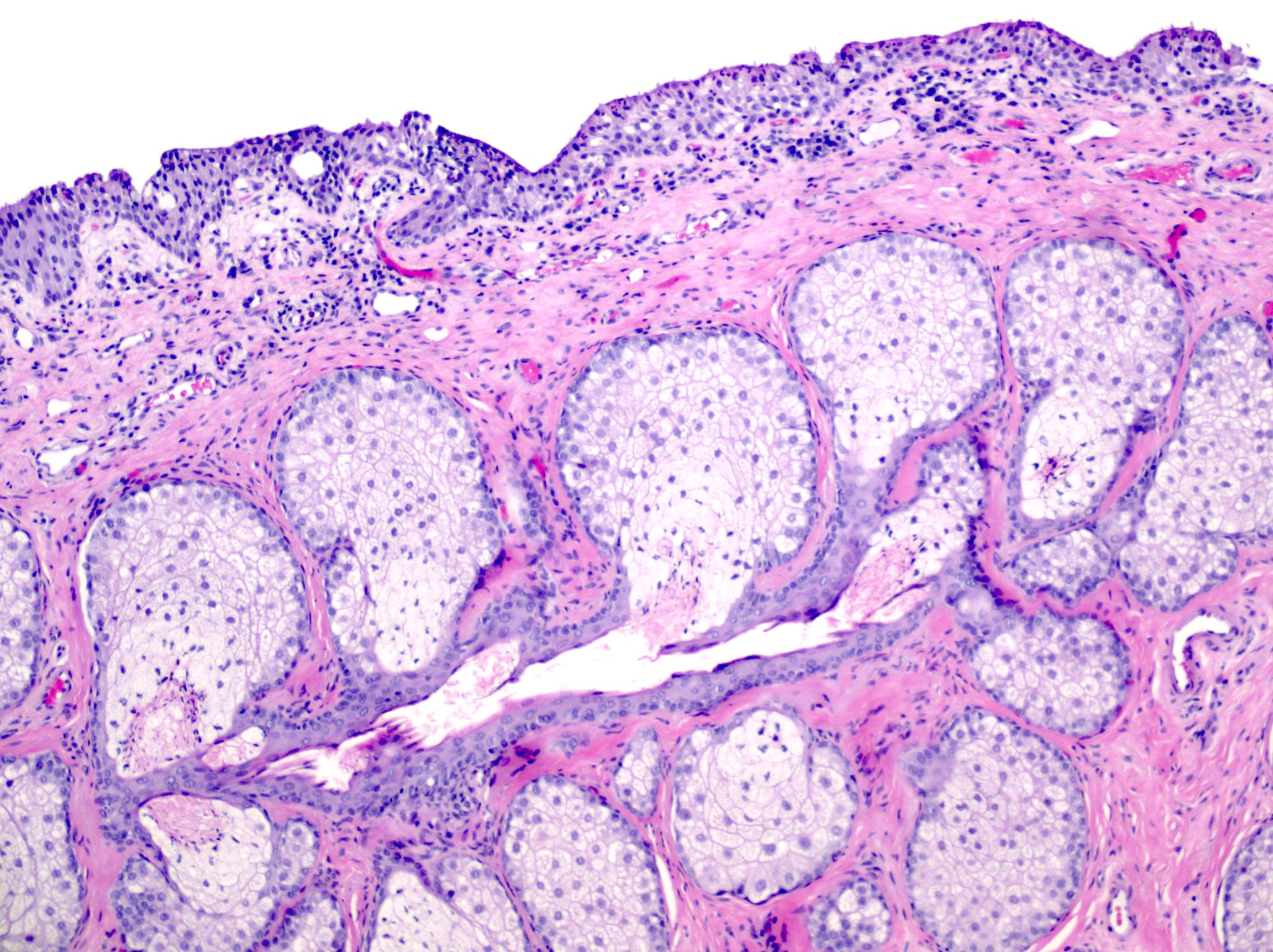
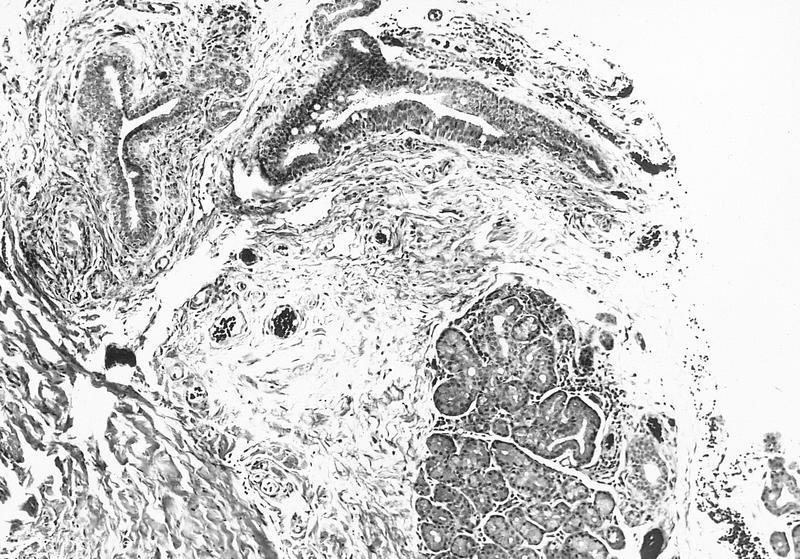
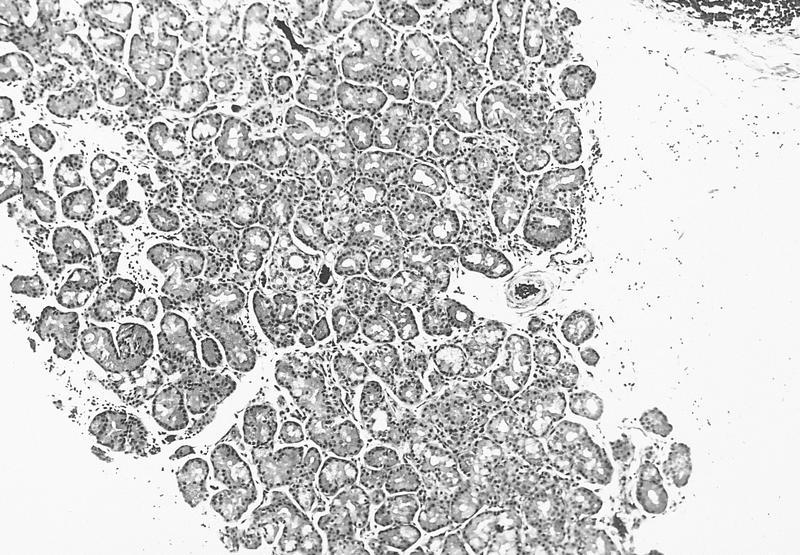
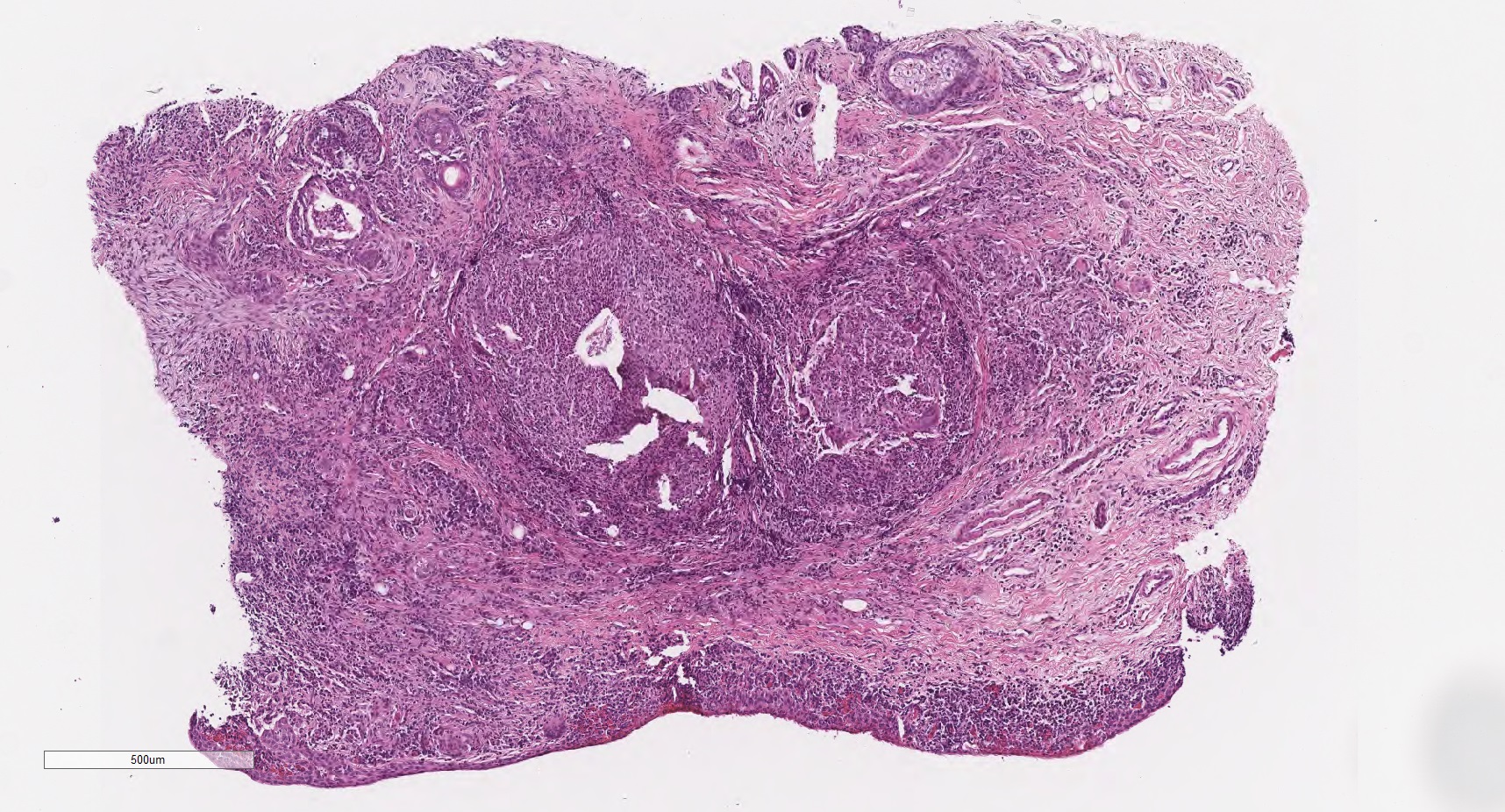
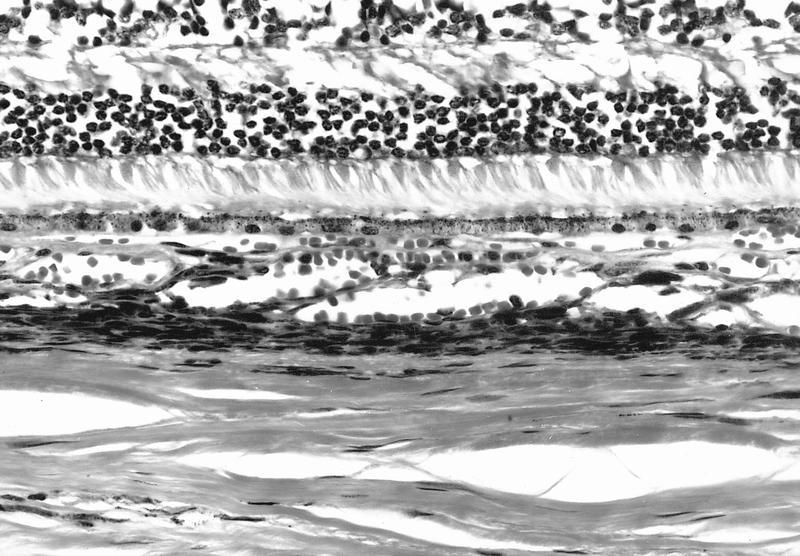
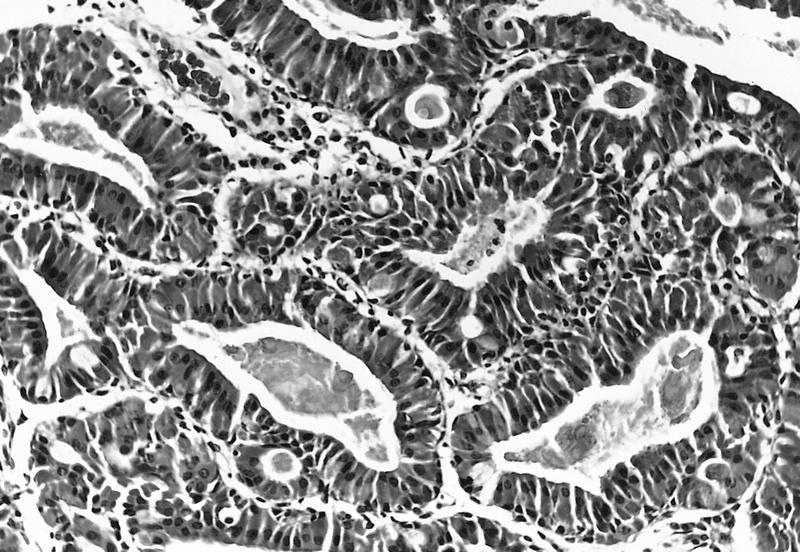
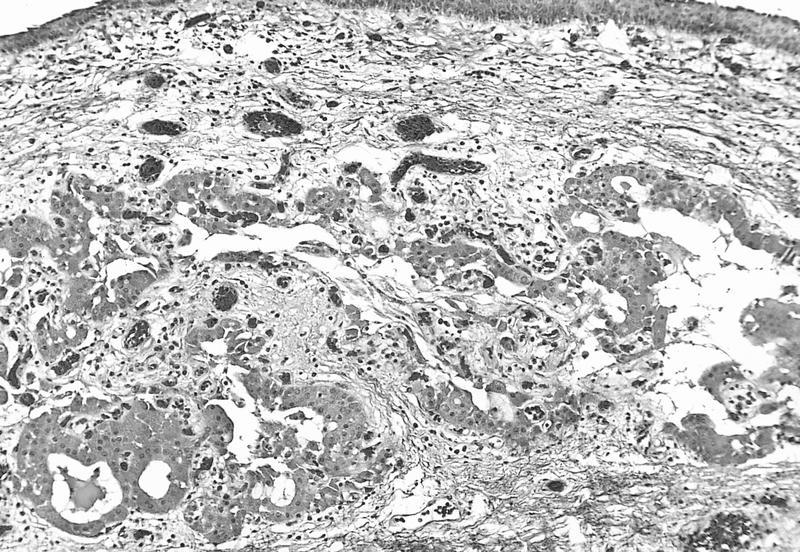
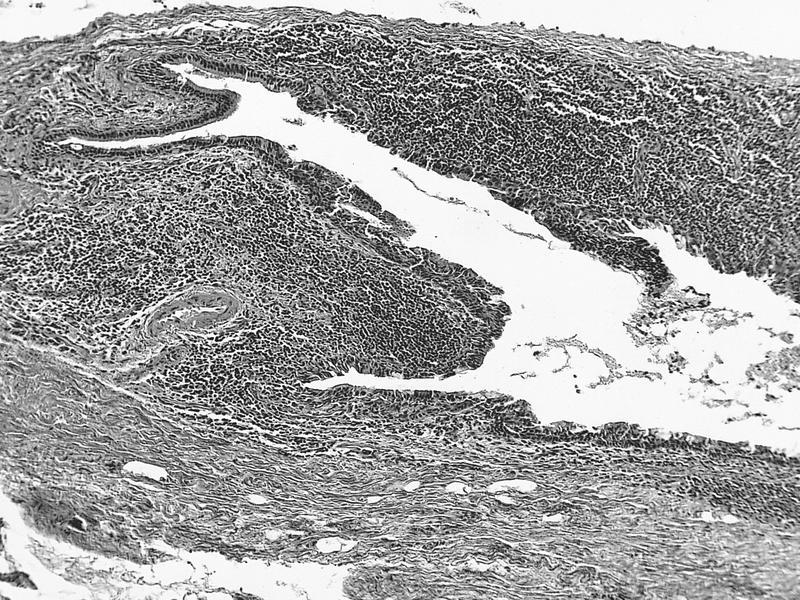
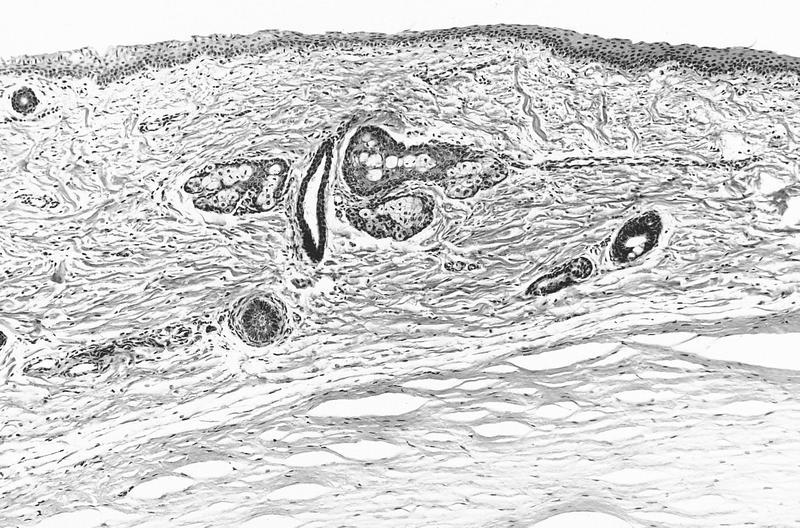
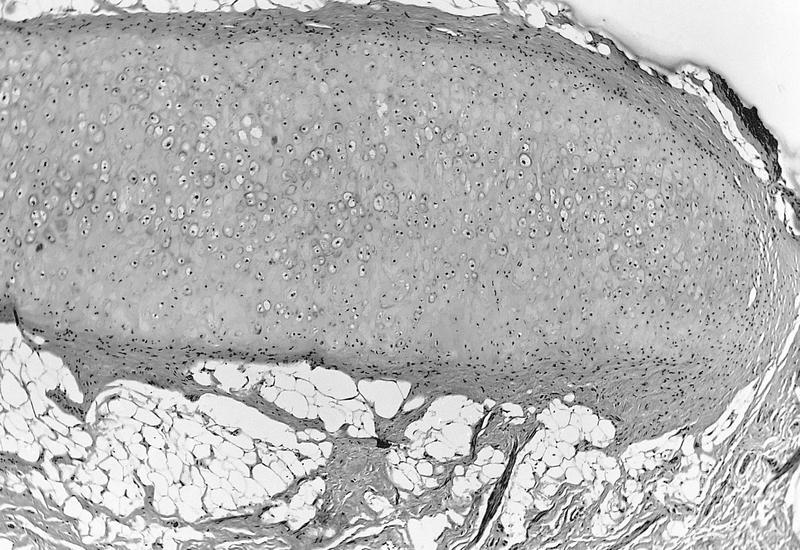
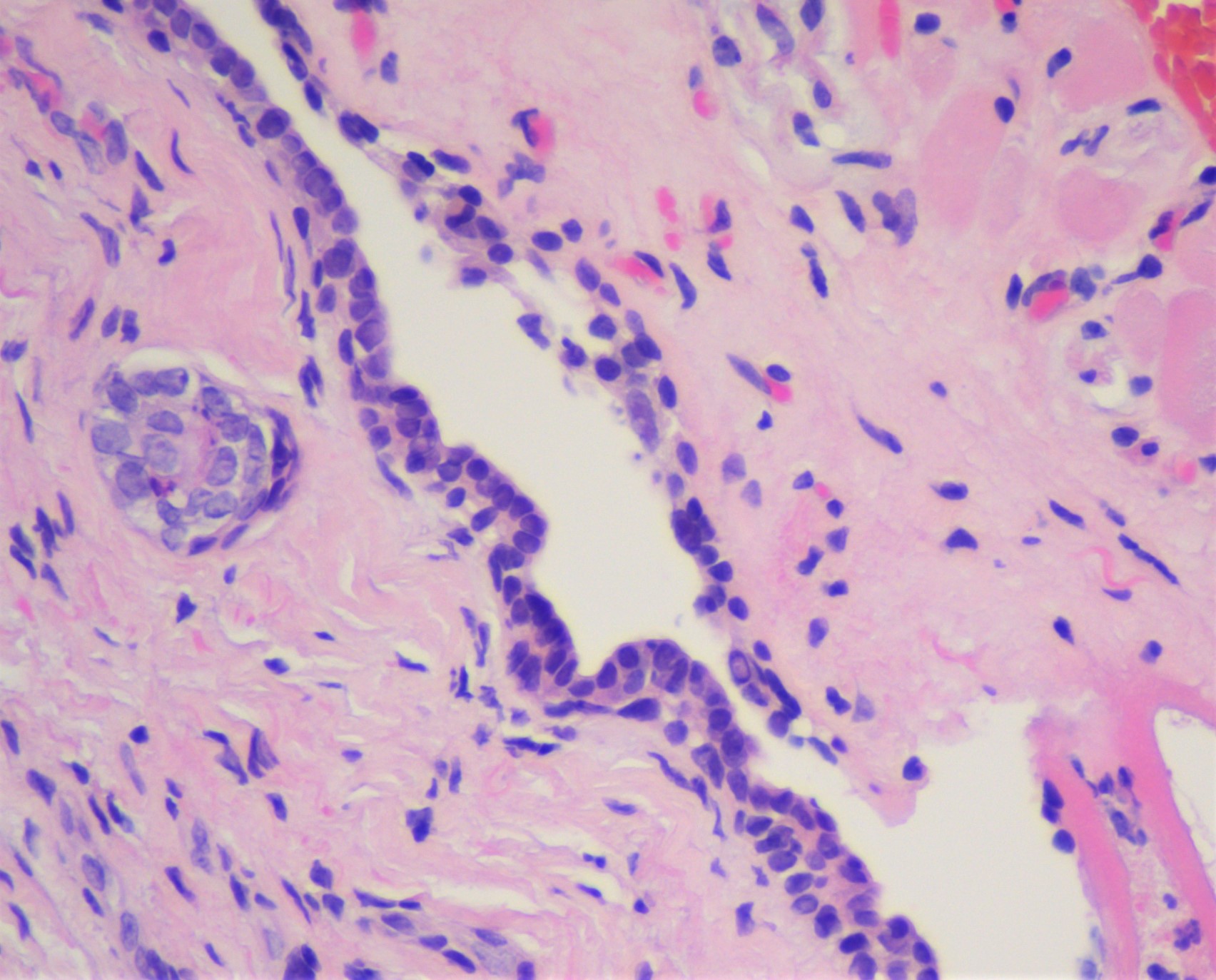
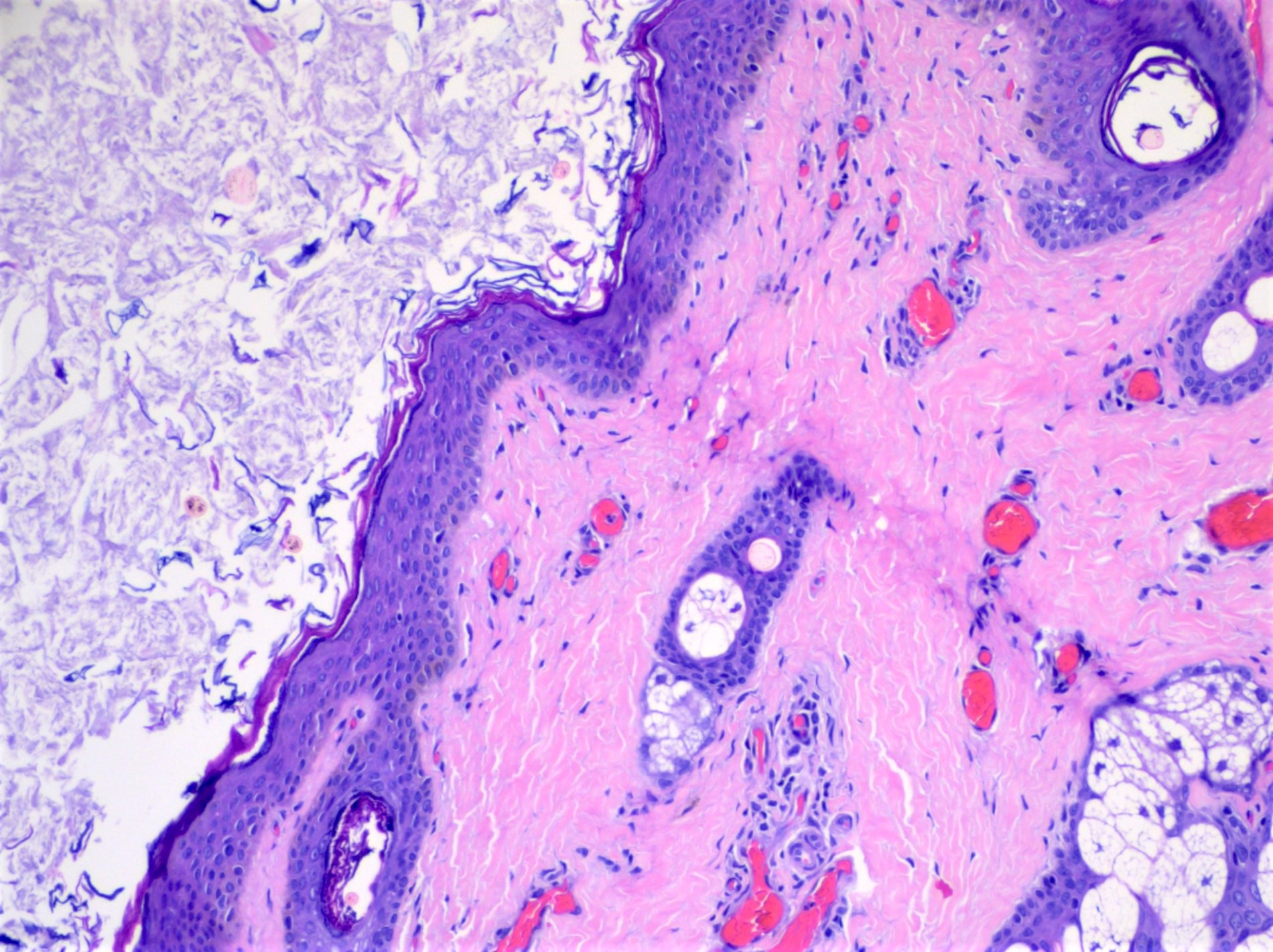
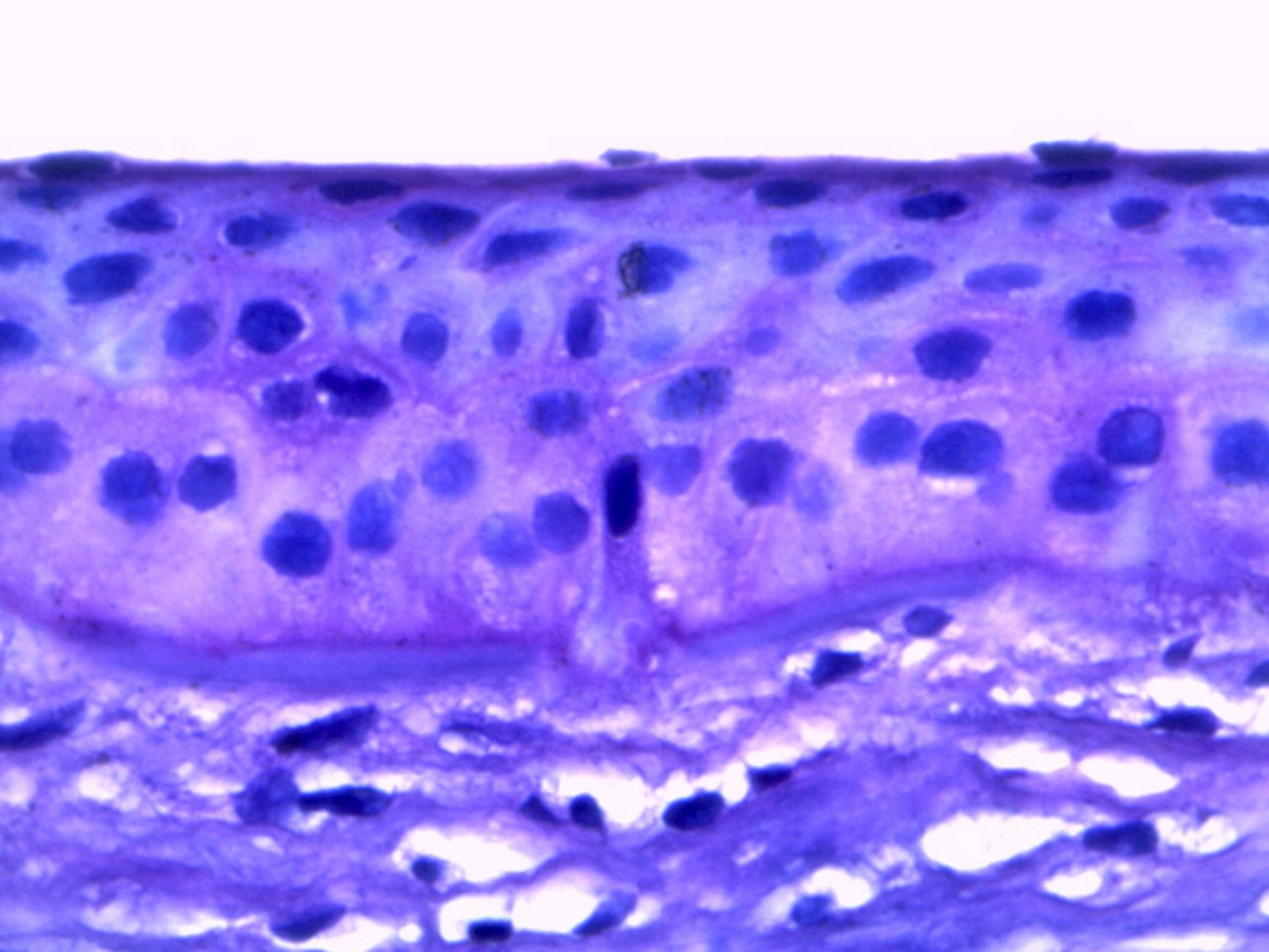
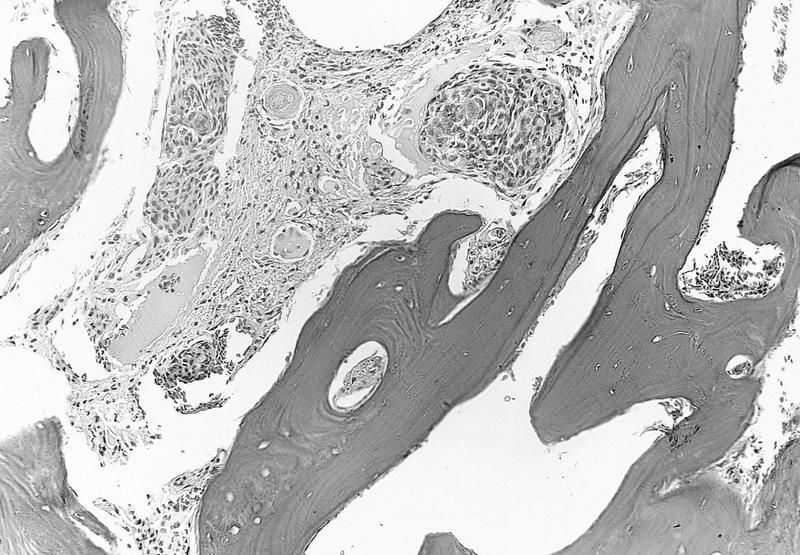
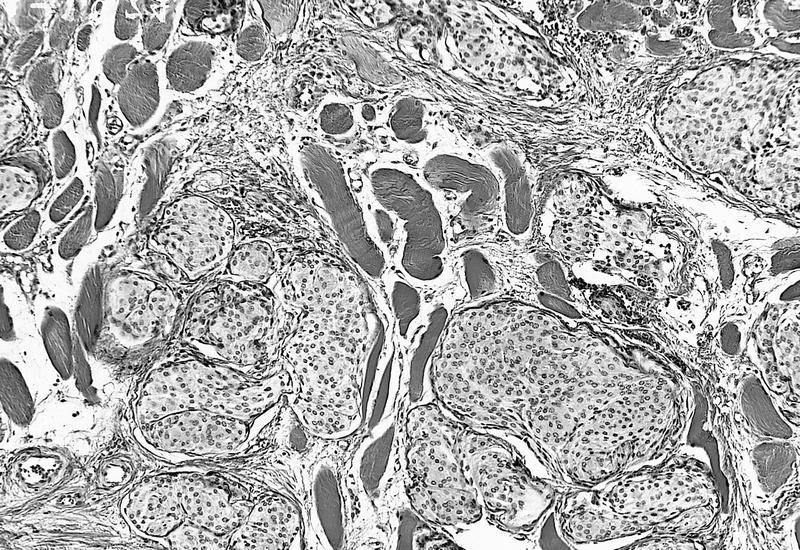
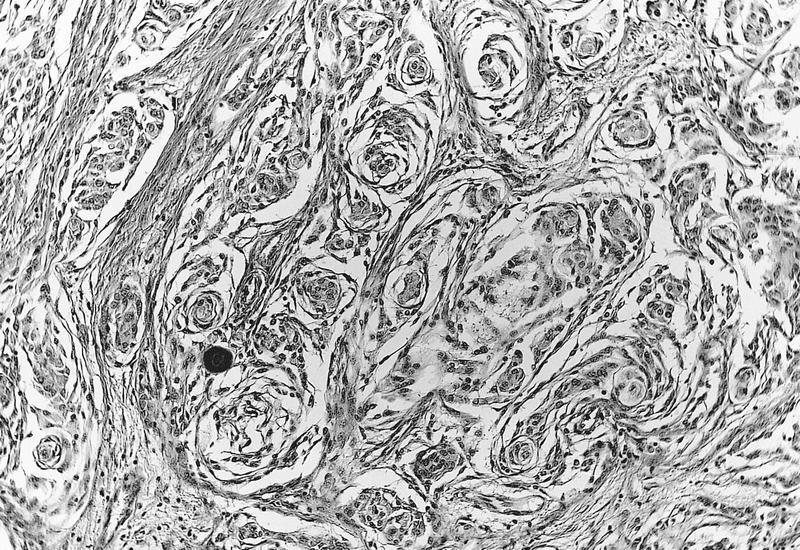
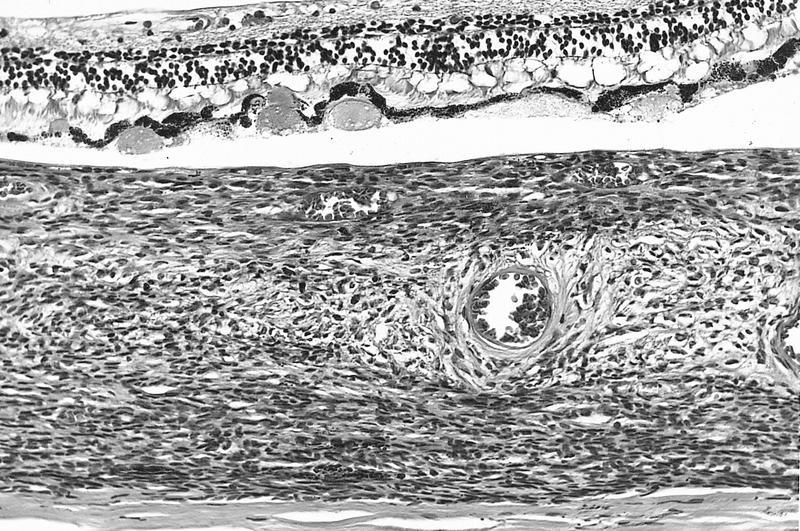
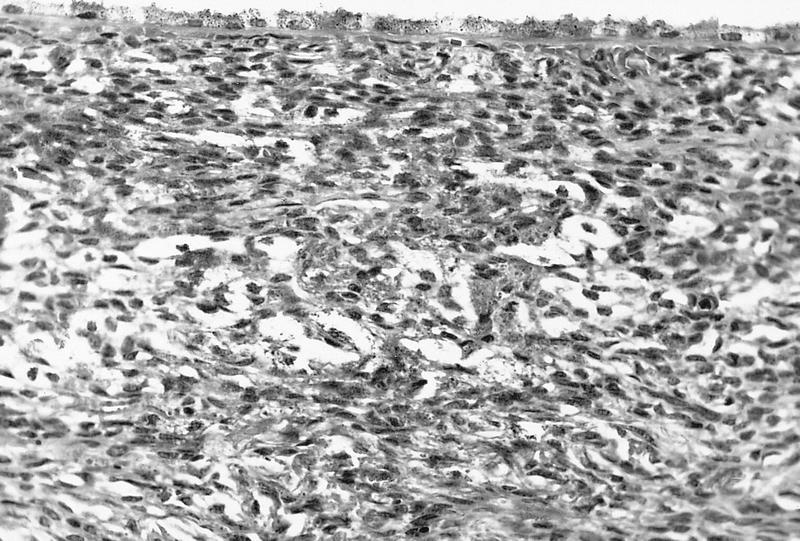
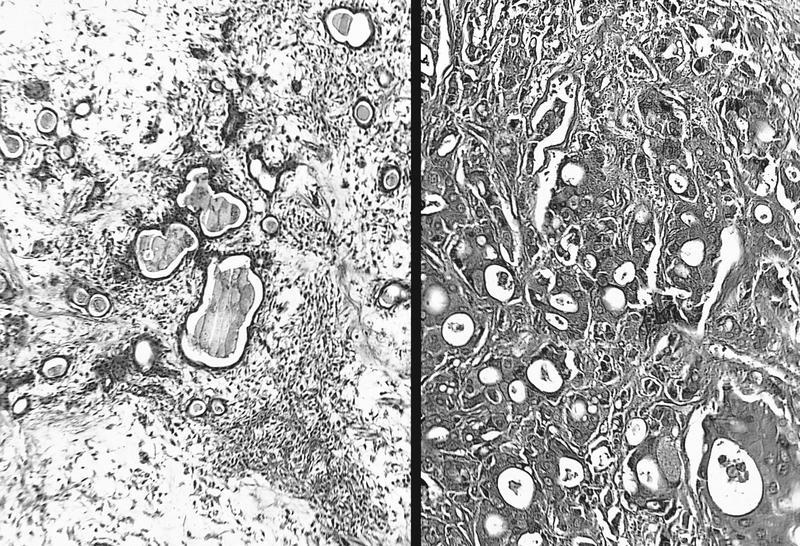
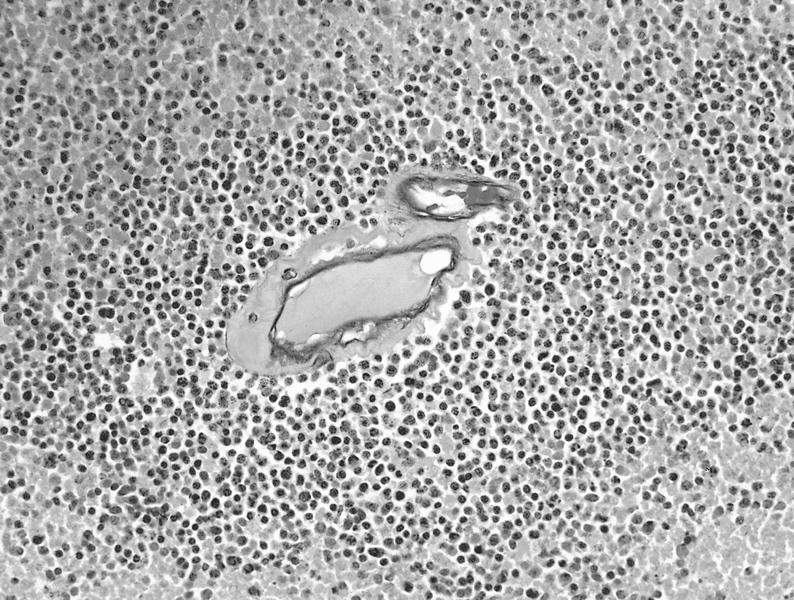
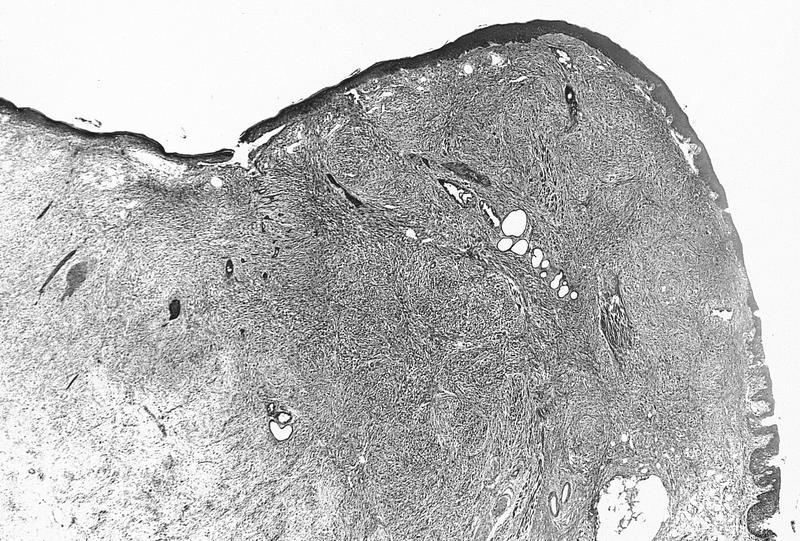
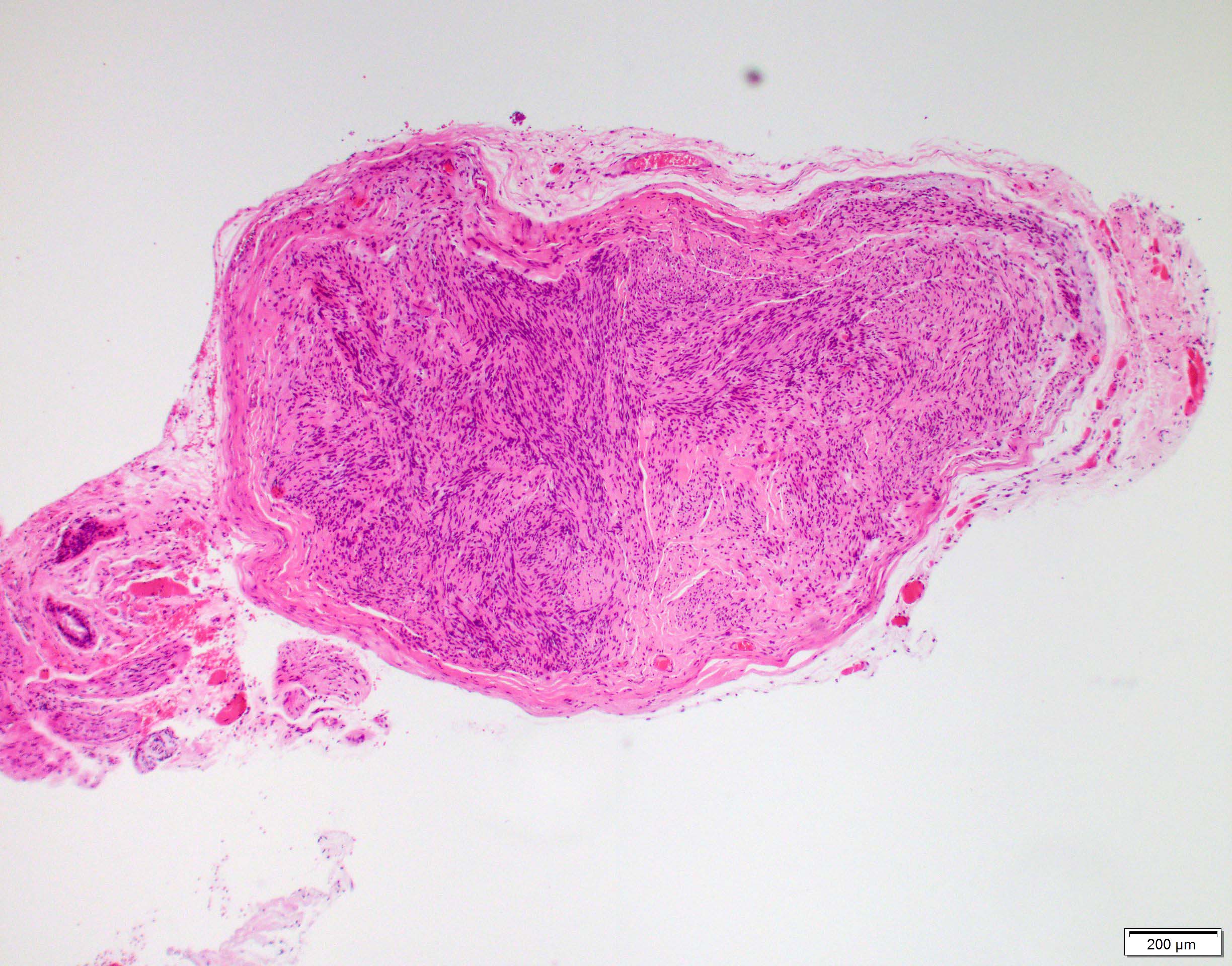
Microscopic (histologic) description
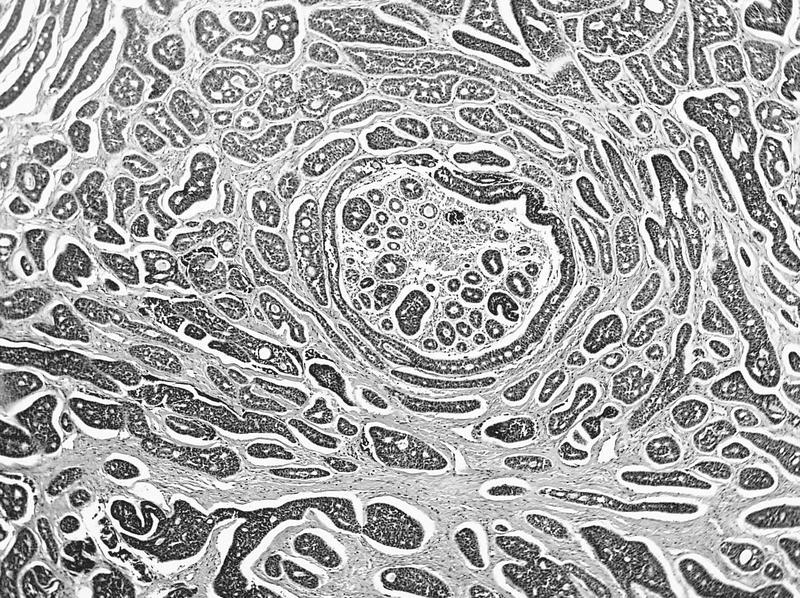
- Nonkeratinizing squamous epithelium with scattered goblet cells overlying loose connective tissue of the substantia propria with limited chronic inflammation (including lymphocytes and plasma cells) and subepithelial glands, such as sebaceous (Meibomian) glands in the vicinity of the tarsal plate (Exp Eye Res 2014;129:172, Invest Ophthalmol Vis Sci 2011;52:1938)
- Tarsal plate is identified by dense fibroconnective tissue in association with sebaceous (Meibomian) glands (J Anat 2005;206:37)
- Infoldings of conjunctival epithelium, particularly in the context of chronic conjunctivitis, may mimic glandular tissue, a histologic appearance known as pseudoglands of Henle (Ophthalmology 2001;108:135)
- Caruncle is identified by the presence of adnexal structures in addition to conjunctiva
- Degenerative changes related to the conjunctiva include pterygium and pinguecula; both are caused by ultraviolet light damage
- Pterygium histologically appears as benign conjunctival epithelium with corneal Bowman membrane, underlying elastotic (solar) degeneration and neovascularization (see Pterygium) (Am J Pathol 2011;178:817)
- Pinguecula histologically demonstrates solar elastotic degeneration with variably present, hyalinized and amorphous material (see Pinguecula) (Graefes Arch Clin Exp Ophthalmol 2006;244:104)
- Inflammatory changes may also be encountered
- Follicular conjunctivitis is comprised of lymphocytic nodules in the substantia propria and causes a bulge of the overlying epithelium; etiologies include infections, drug reaction, manifestations of systemic diseases and idiopathic causes
- Papillary conjunctivitis is a polygonal distortion of the epithelium, often affecting tarsal conjunctiva and may be caused by chronic mechanical irritation, allergy, topical drugs and as a complication of contact lenses (Ocul Surf 2020;18:396)
- Granulomatous conjunctivitis may be caused by foreign material, infection, systemic diseases or sarcoidosis (see Granulomatous conjunctivitis)
Microscopic (histologic) images
Positive stains
- Though stains are not routinely used in practice, the normal conjunctiva is positive for pancytokeratins (AE1 / AE3) and CK7 (Invest Ophthalmol Vis Sci 1997;38:142)
Videos
Pathology lecture: conjunctiva
Additional references
Board review style question #1
Board review style answer #1
E. Palpebral conjunctiva. The presence of dense fibroconnective tissue constituting the tarsal plate and sebaceous (Meibomian) glands is helpful for identifying the palpebral (tarsal) conjunctiva. Answer B is incorrect because the caruncle is identified by the presence of adnexal structures, such as pilosebaceous units. Answer C is incorrect because the cornea features corneal epithelium, Bowman membrane, corneal stroma, Descemet membrane and endothelium. Answers A and D are incorrect because the bulbar and forniceal conjunctivas are not seen in association with the tarsal plate.
Comment Here
Reference: Anatomy & histology-conjunctiva
Comment Here
Reference: Anatomy & histology-conjunctiva
Board review style question #2
Board review style answer #2
B. Caruncle. The caruncle is identified by the presence of adnexal structures, such as the pilosebaceous unit seen in this histologic image. Answer E is incorrect because thick fibroconnective tissue of the tarsal plate and sebaceous (Meibomian) glands would be helpful for identifying the palpebral conjunctiva. Answer C is incorrect because the cornea features corneal epithelium, Bowman membrane, corneal stroma, Descemet membrane and endothelium. Answers A and D are incorrect because the bulbar and forniceal conjunctivas would not feature an associated pilosebaceous unit.
Comment Here
Reference: Anatomy & histology-conjunctiva
Comment Here
Reference: Anatomy & histology-conjunctiva
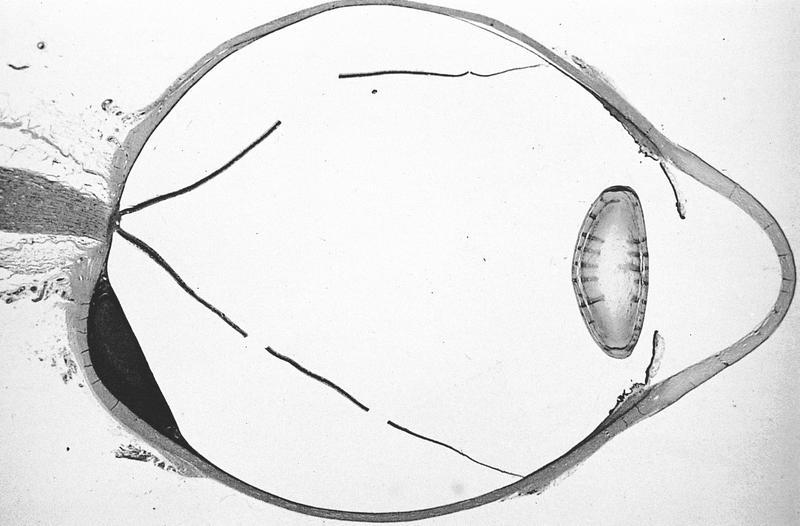
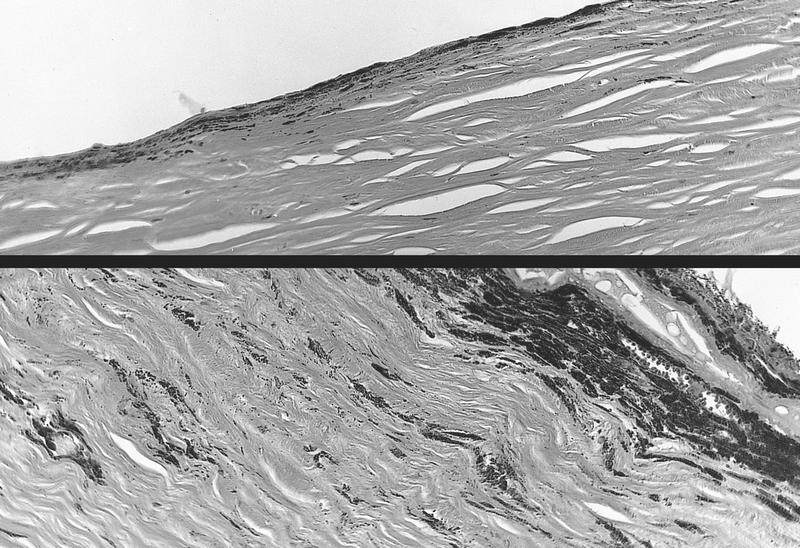
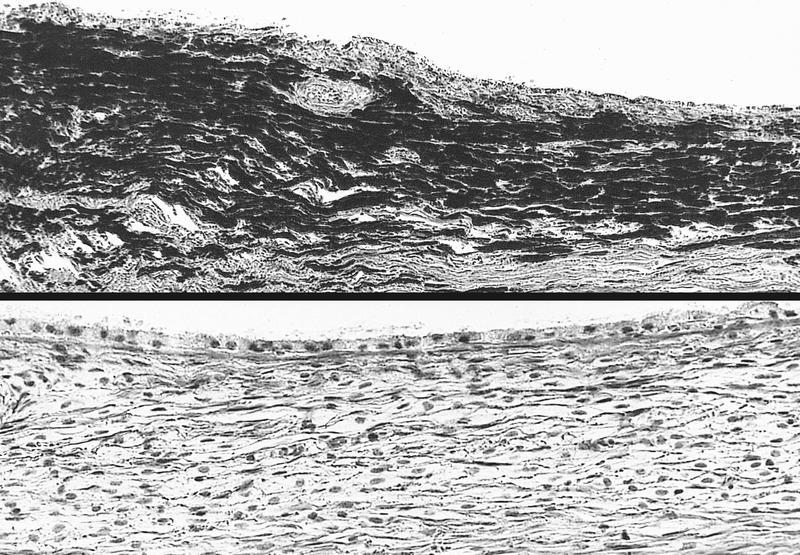
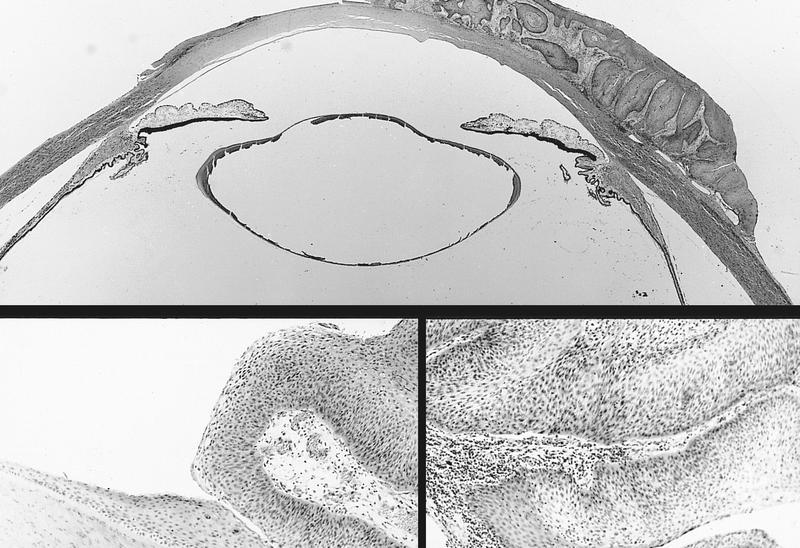
Anatomy & histology-cornea
Table of Contents
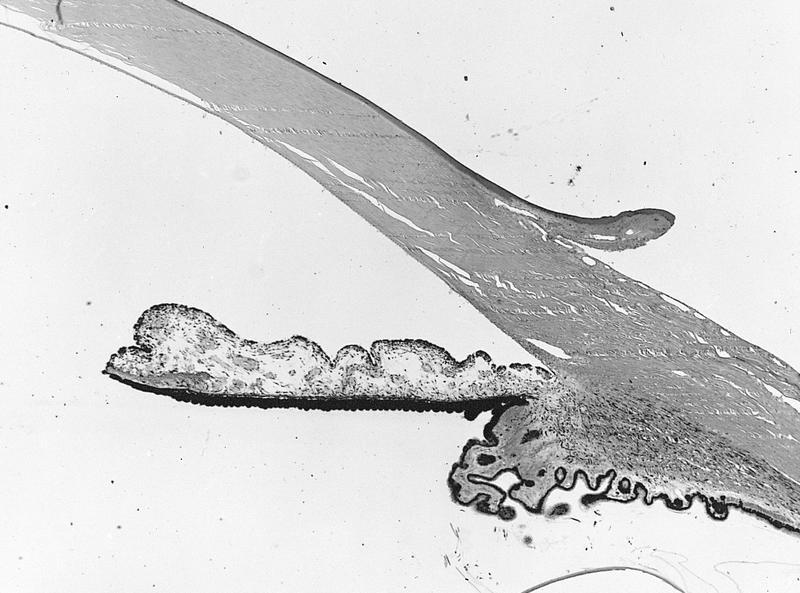
Definition / general | Hasall-Henle bodies (warts) | Hyperopia | Laser assisted in situ keratomileusis (LASIK) | Limbus | Myopia | Schlemm canal and trabecular meshwork | Vasculature | Microscopic (histologic) images | Drawings | Positive stains | Negative stains | Electron microscopy description | Additional referencesDefinition / general
- Wider than tall (11.7 mm horizontally vs. 10.6 mm vertically)
- Thickness varies from 0.5 mm (central) to 0.67 mm (peripheral)
- Cornea and overlying tear film are major refractive surface of eye, not the lens
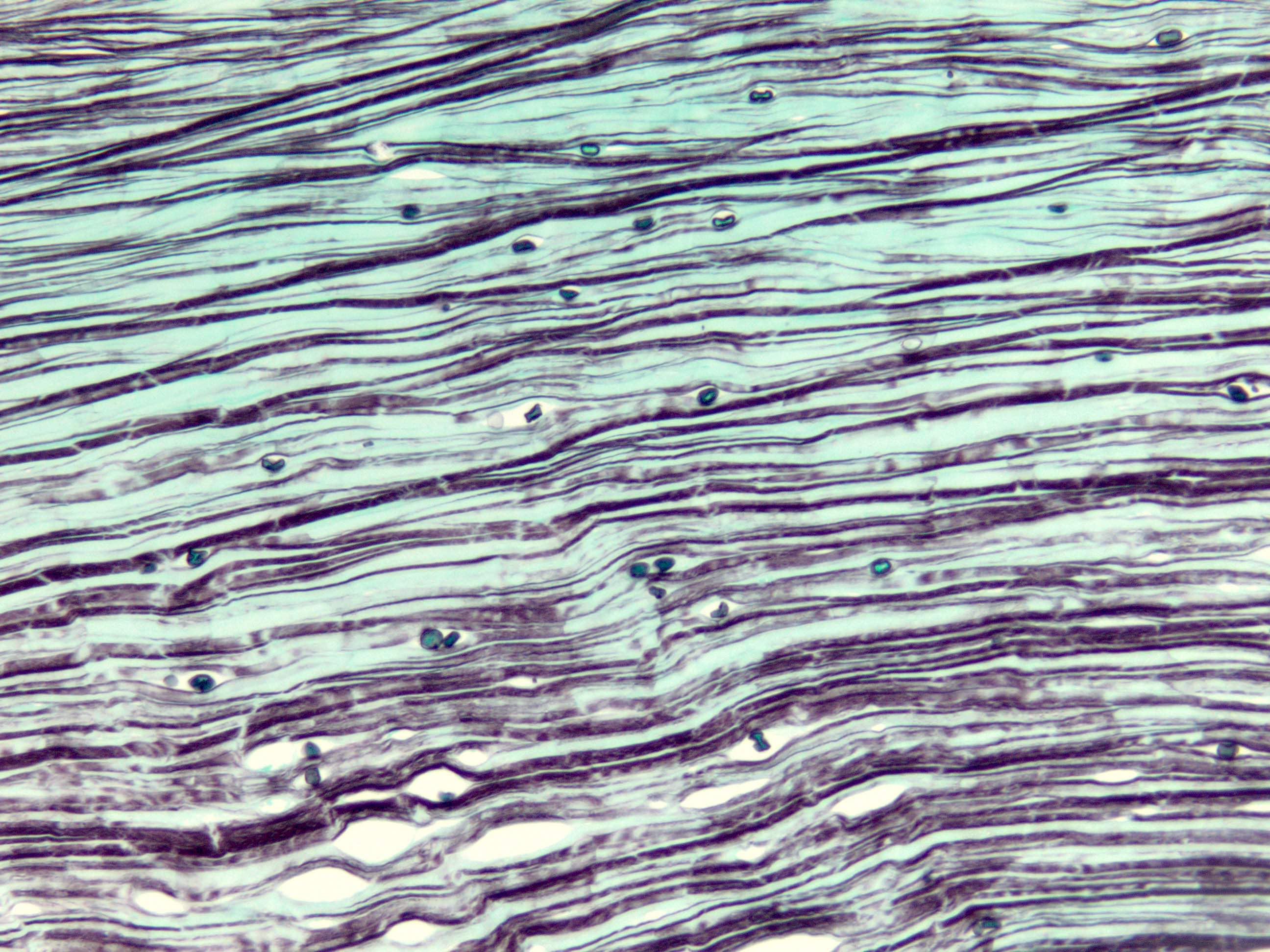
- 6 distinct layers (outside to inside):
- Outer epithelium: stratified squamous, nonkeratinized, 5 layers thick centrally, thicker peripherally, polygonal at basal layer but flatten as they approach surface; basal cells may have mitotic figures; Langerhans cells are CD1a+; note: layers often rubbed off while grossing specimen
- Epithelial basal lamina (basement membrane): highlighted with PAS stain
- Bowman layer: most anterior stroma, acellular, 8 - 14 microns thick, not a true basement membrane, composed of randomly oriented delicate collagen fibers, does not regenerate
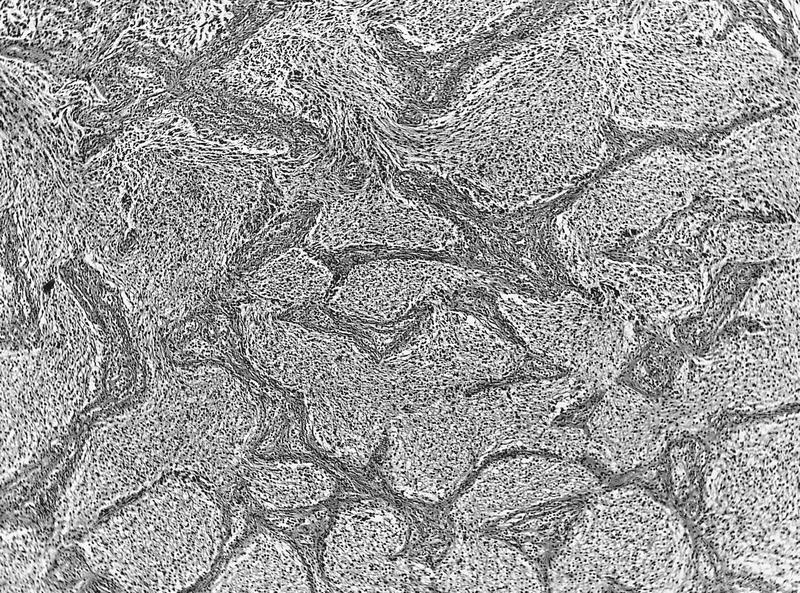
- Stroma: also called substantia propria, no blood vessels or lymphatics, 90% of cornea's thickness, contains regularly spaced collagen fibrils; normally separated by glycoprotein and mucoprotein which makes cornea transparent; normally see stromal lamellae separated by clefts, a processing artifact, absence of clefts is caused by stroma edema (causes corneal clouding), due to damage of endothelium
- Descemet [pronounced DEZMET] membrane: a true basal lamina produced by underlying corneal endothelial cells; 3 - 4 microns at birth, 10 - 12 microns in adults; does not regenerate; site of copper deposition in Kayser-Fleisher ring of Wilson disease
- "Endothelium": single layer of very flat cells, does not regenerate, functions as pump to keeps cornea dehydrated and transparent
- Neural crest origin (S100+); does not line blood vessels or lymphatic spaces; directly contacts aqueous humor of anterior chamber, often rubbed off while grossing specimen
Hasall-Henle bodies (warts)
- Focal excrescences that form on peripheral Descemet membrane with normal aging
- Not seen in surgically excised corneal buttons because are too peripheral in location
Hyperopia
- Eye too short for its refractive power
Laser assisted in situ keratomileusis (LASIK)
- Sculpt cornea and change its refractive properties to eliminate need for glasses
Limbus
- Junction of peripheral cornea and anterior sclera, 1.5 to 2.0 mm wide
- Not a distinct anatomic site but a significant clinical landmark
- Composed of conjunctiva (epithelium and stroma), cornea and scleral stroma, episclera, Tenon capsule (fibrous tissue that covers the globe)
- Descemet membrane terminates at limbus and gives rise to Schwalbe ring
- 15% have prominent area of thickening at this site
- Contains trabecular meshwork and Schlemm canal
- Site of incisions for surgery on anterior eye
- Restricts deeper extension of superficial tumors
Myopia
- Eye too long for its refractive power
Schlemm canal and trabecular meshwork
- Schlemm canal
- Anterior and superficial to trabecular meshwork
- Endothelial lined venous canal that completely encircles limbus
- Separated from trabecular meshwork by thin connective tissue and separate endothelial linings
- Trabecular meshwork
- With Schlemm canal, are apparatus for removal of aqueous from eye
- Collection of finely branching and delicately pigmented connective tissue bands
- Lining cells are continuous with corneal endothelium
- Posteriorly, trabecular meshwork extends to scleral connective tissue called scleral spur
Vasculature
- No blood vessels or lymphatics within cornea
- Arterial plexus is present at junction of cornea and sclera
- Is also nourished by aqueous humor of anterior chamber
Microscopic (histologic) images
Positive stains
Negative stains
Electron microscopy description
- Schlemm canal endothelial cells contain giant cytoplasmic vacuoles
Additional references
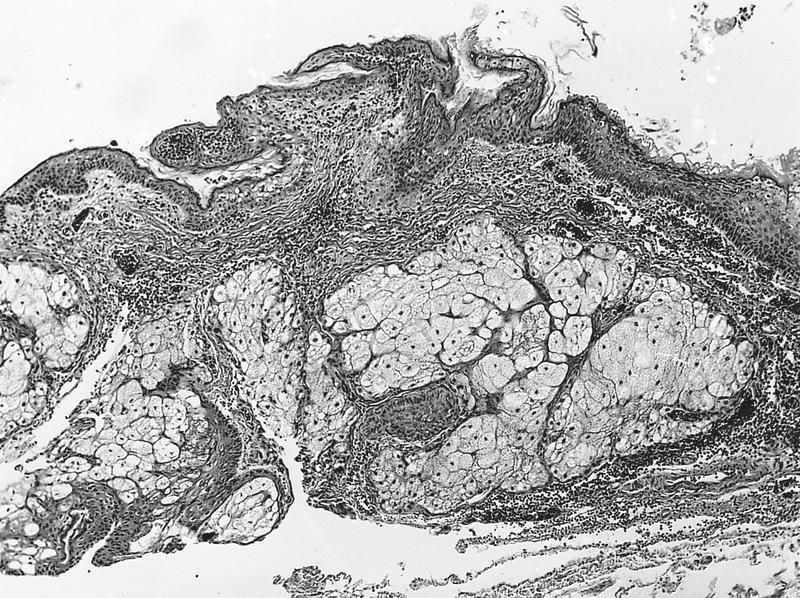
Anatomy & histology-eyelid
Table of Contents
Definition / general | Pathophysiology | Gray line | Drawings | Microscopic (histologic) imagesDefinition / general
- Has cutaneous and conjunctival portion
- Palpebral (tarsal) conjunctiva lines interior of eyelid
- Very thin
- Continuous with bulbar conjunctiva that covers the sclera
- Becomes papillary with allergic or bacterial conjunctivitis
- Contains eccrine and apocrine glands (glands of Moll) and sebaceous glands
- Sebaceous glands (Meibomian glands within eyelid fibrous tarsus and glands of Zeis associated with eyelashes) create lipid layer of tear film which retards evaporation of tears
- The orifices of Meibomian glands open just in front of the posterior edge of the lid margin and are separated from the more anteriorly placed eyelashes by a gray line
- Muscular layer is composed primary of orbicularis oculi muscle
Pathophysiology
- Specimens received are often from cosmetic blepharoplasty or other reparative surgery with no abnormalities
- Other lesions are similar to those in skin
- Creates tear film via accessory lacrimal glands embedded above fibrous tarsus of eyelid
- Helps to protect and lubricate the globe
- Tumors may prevent complete closure of eyelid, leading to exposure and ulceration of cornea
Gray line
- Divides the eyelid into anterior and posterior parts
- It corresponds with the position of the pretarsal orbicularis muscle
Anatomy & histology-other
Table of Contents
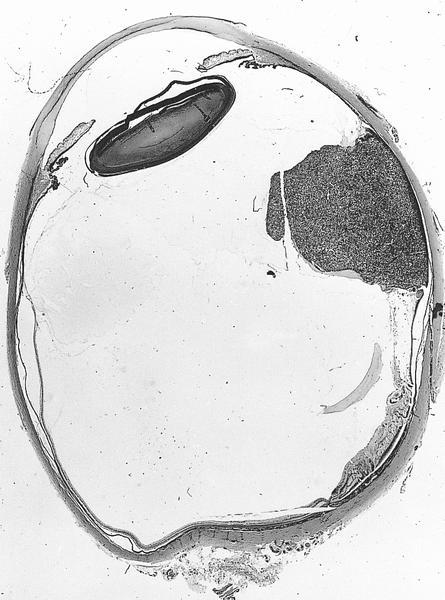
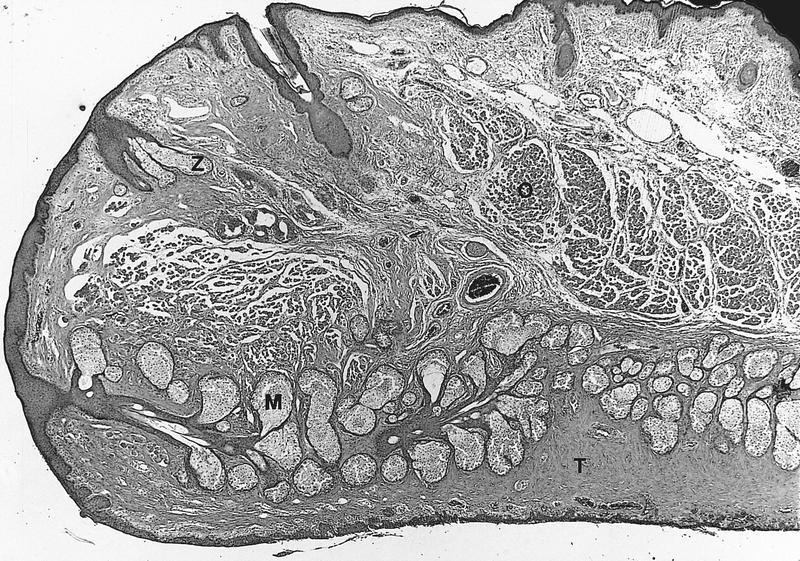
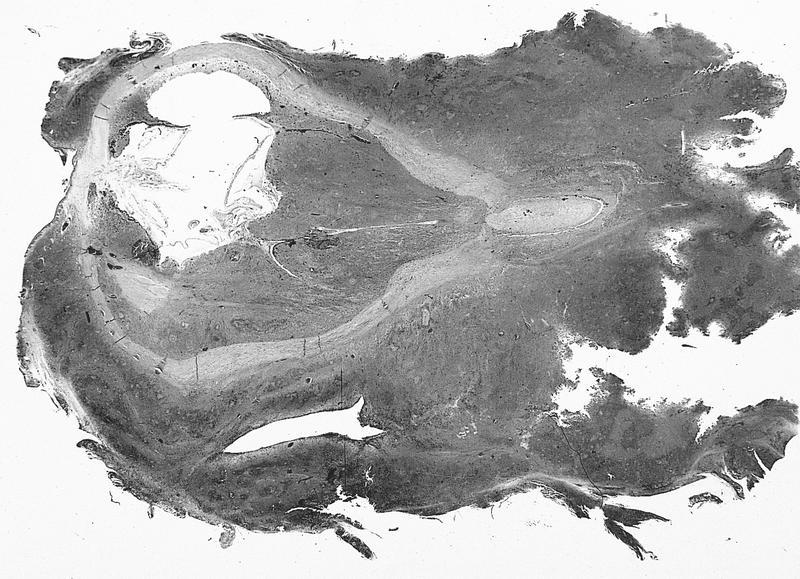
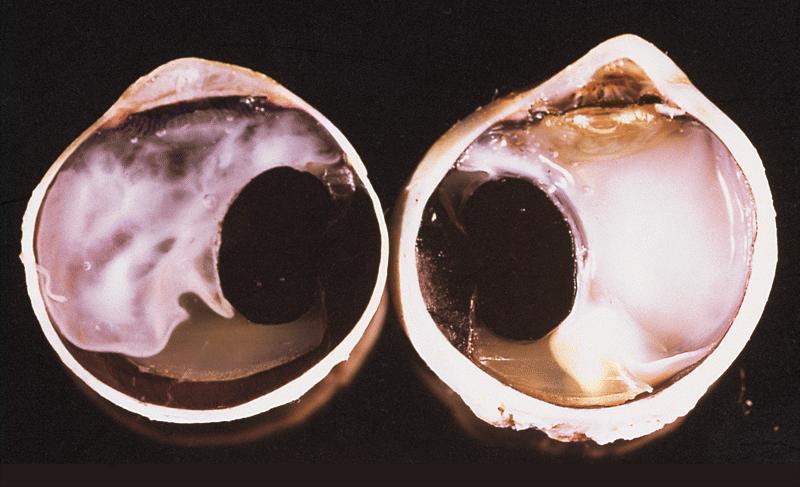
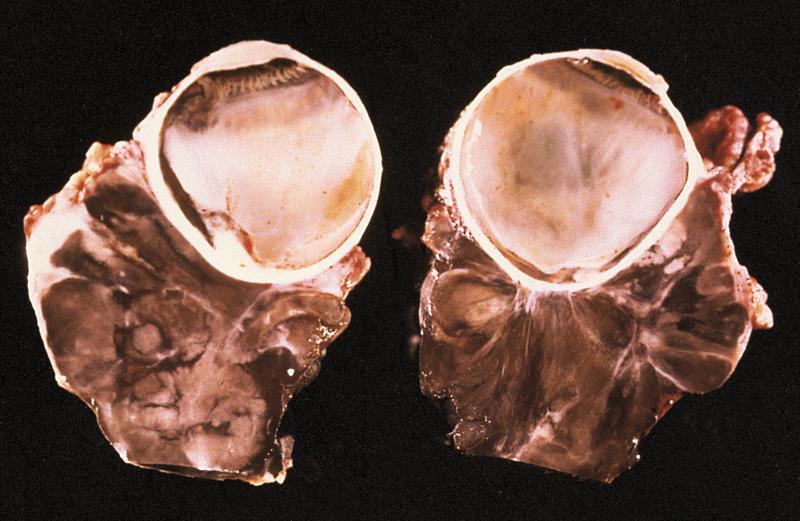
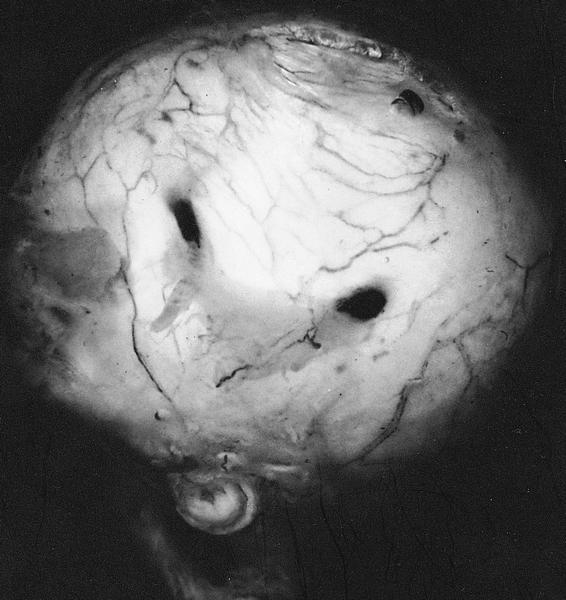
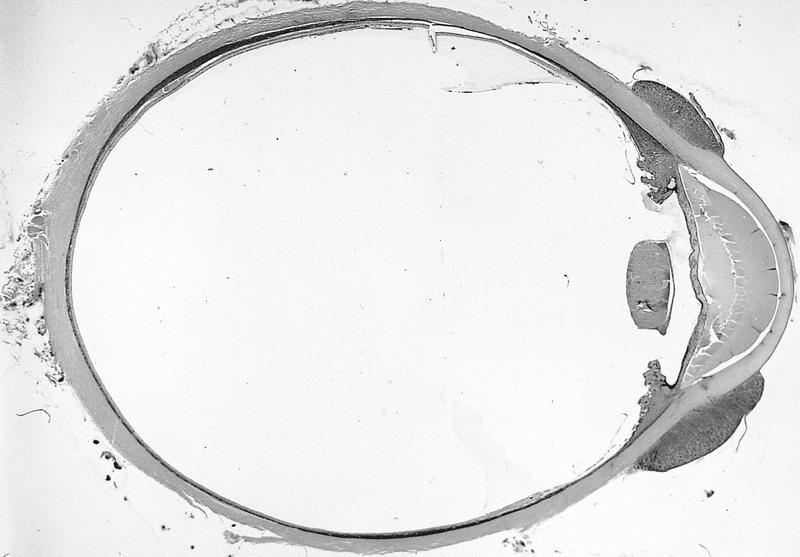
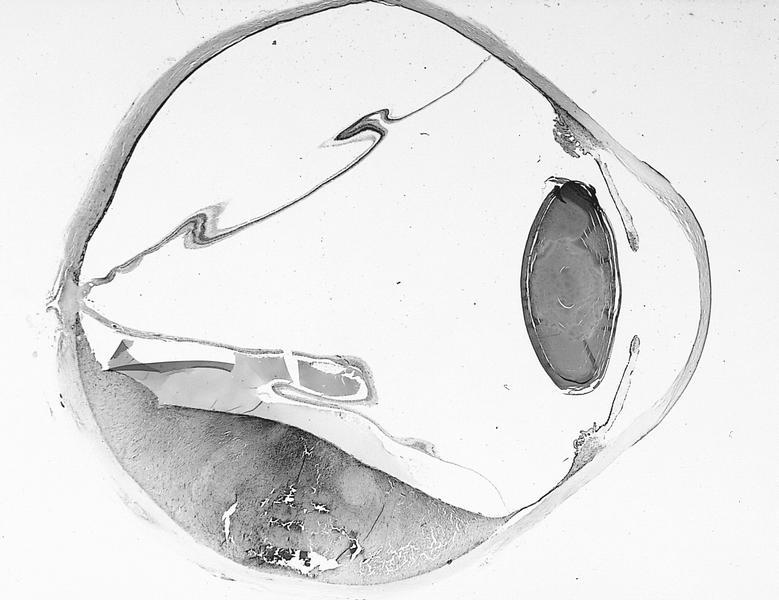
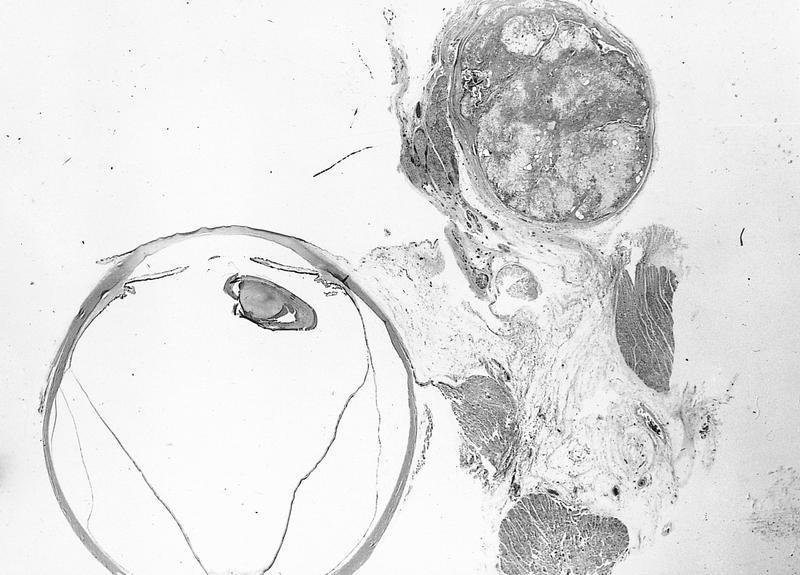
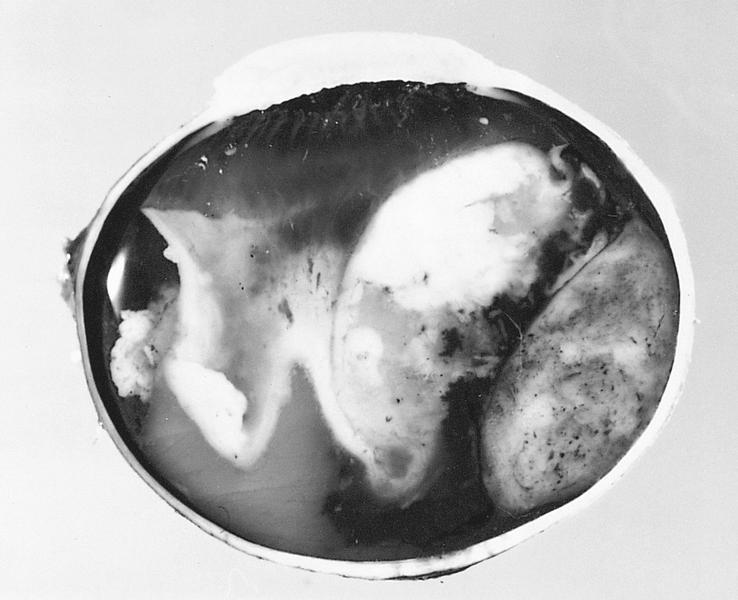
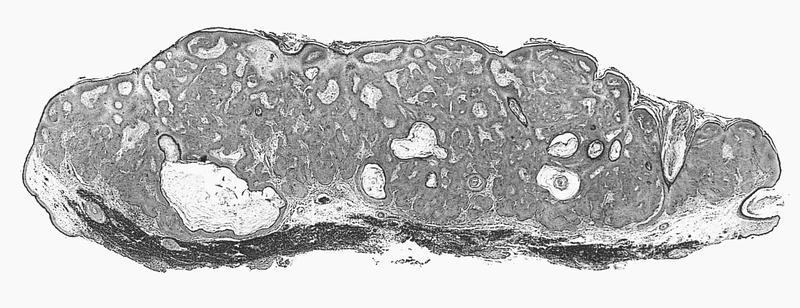
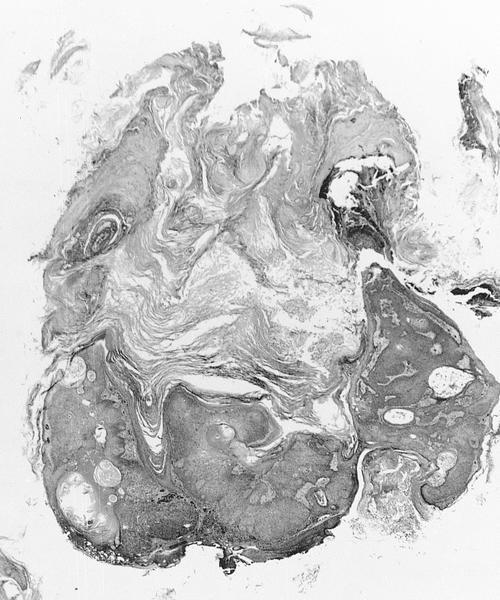
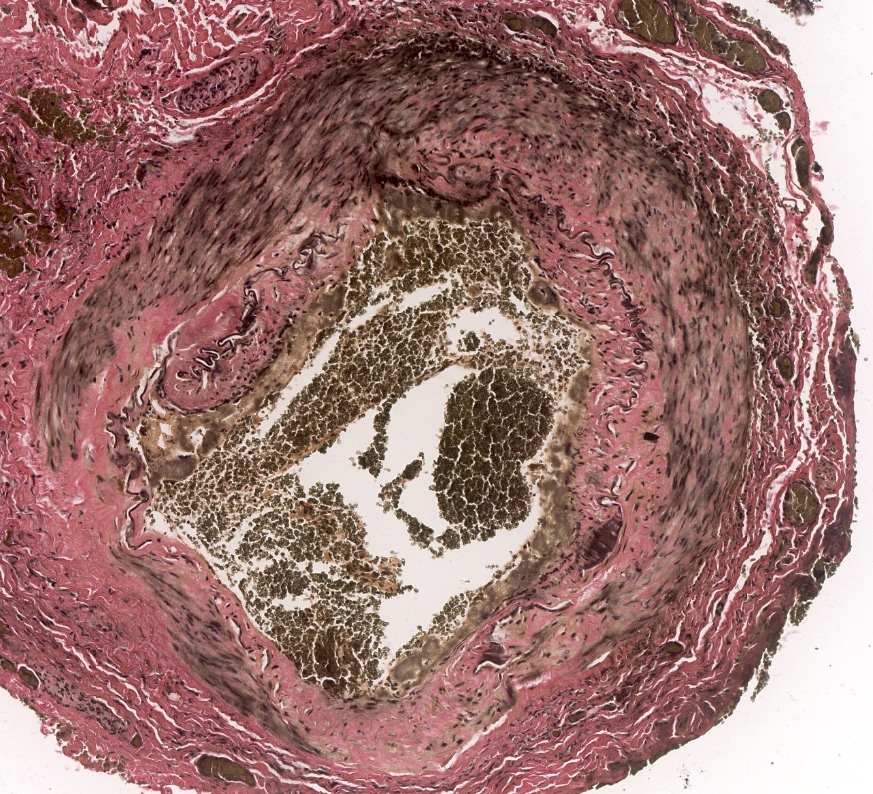
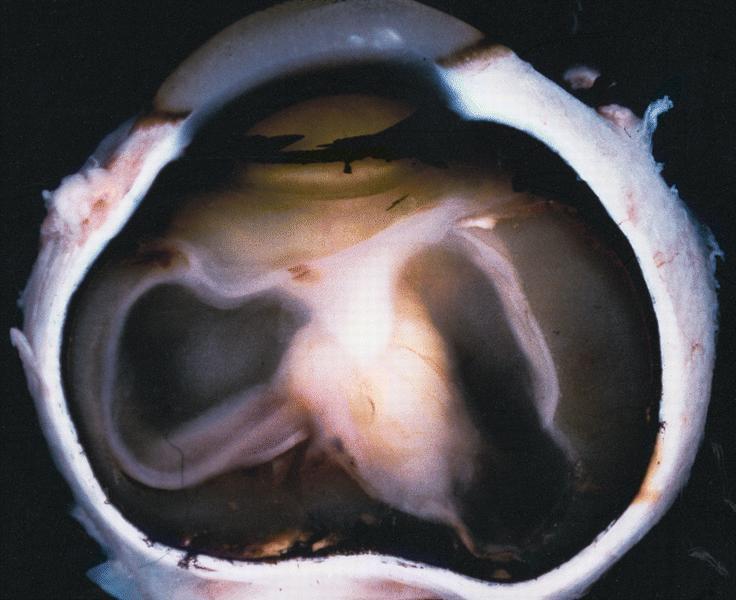
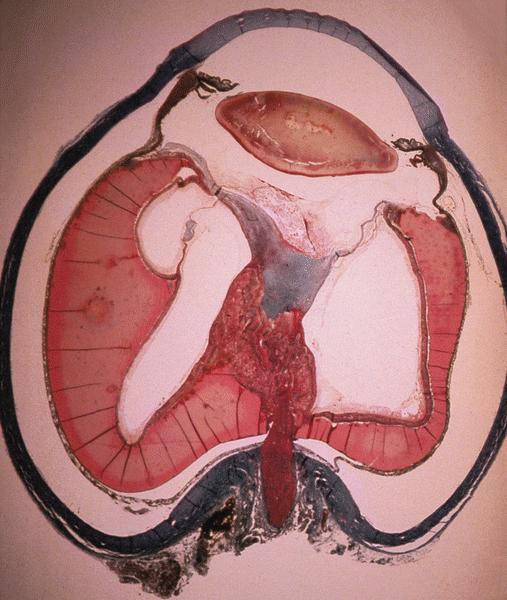
Globe | Lacrimal duct & gland | Lens | Orbit & optic nerve | Radiology images | Drawings | Microscopic (histologic) description | Microscopic (histologic) imagesGlobe
- Defined as eyeball itself plus intraocular tissues, or eye proper without its appendages
- Dimensions: anterior-posterior 24 mm, vertical and horizontal dimensions are both 23 to 23.5 mm
- Six extraocular muscles:
- 4 rectus and 2 oblique muscles
- Arise in posterior orbit from fibrous ring called annulus of Zinn, and insert into sclera
- Muscles are surrounded by fascia
- Inferior oblique inserts on sclera, other muscles insert on tendons
- Equator: midway between anterior and posterior poles
- Specimen is the result of enucleation, performed because eye is nonfunctional, painful, unsightly, infectious, contains neoplasm, post-trauma (may be removed to prevent sympathetic uveitis) or has chronic glaucoma
- Globe usually intact but free of extraocular muscles and orbital fat
- Globe may be eviscerated, with only fragments available for microscopic study
- Initial pathologic processes may be obscured by subsequent pathologic processes
- Enucleation: due to tumor (48%, usually melanoma), glaucoma (13%), phthisis bulbi (12%), recent trauma (11%)
- Specimens also received after evisceration (10%) or exenteration (9%) to manage malignant orbital tumors (Am J Clin Pathol 2003;119:594)
- During 1990 to 2000, decrease in percentages due to neoplasms, increase due to glaucoma and phthisis bulbi
Lacrimal duct & gland
- Lacrimal gland located in superiotemporal aspect of orbit, not palpable
- Contributes secretions to tear film including IgA
- Accessory lacrimal glands are embedded above fibrous tarsus of eyelid and in conjunctival fornix
- Serous with minor mucinous component
- Larger ducts have myoepithelial layer
- Normally may have lymphocytes and plasma cells
- Drainage apparatus is composed of puncta, canaliculi, lacrimal sac and nasolacrimal duct
- Tears drain toward medial canthus, then through lacrimal punctum into lacrimal canaliculi, then nasolacrimal sac, then nasolacrimal duct, then nose
- Puncta:
- Opening in medial aspect of eyelid where tear fluid drains
- Canaliculi (lacrimal duct):
- Tubular structures 0.5 mm in diameter where puncta drains
- Nonkeratinizing squamous epithelium surrounded by fibrous tissue
- Lacrimal sac:
- Merging of canaliculi, encased by bones of orbit
- Stratified columnar epithelium with goblet cells
- Nasolacrimal duct:
- Drains lacrimal sac, 1 cm long, connects to inferior meatus of nose
- Stratified columnar epithelium with goblet cells
- Lacrimal duct disorders often cause epiphora (tears flow over lid margin onto cheek), induration, inflammation of lower eyelid
- Tumors tend to displace eye downward because adjacent orbit restricts growth
- Tumors are difficult to resect completely leading to high recurrence rate
- Lacrimal gland is considered a minor salivary gland for tumor reporting
- Regional lymph nodes are preauricular (parotid), submandibular and cervical
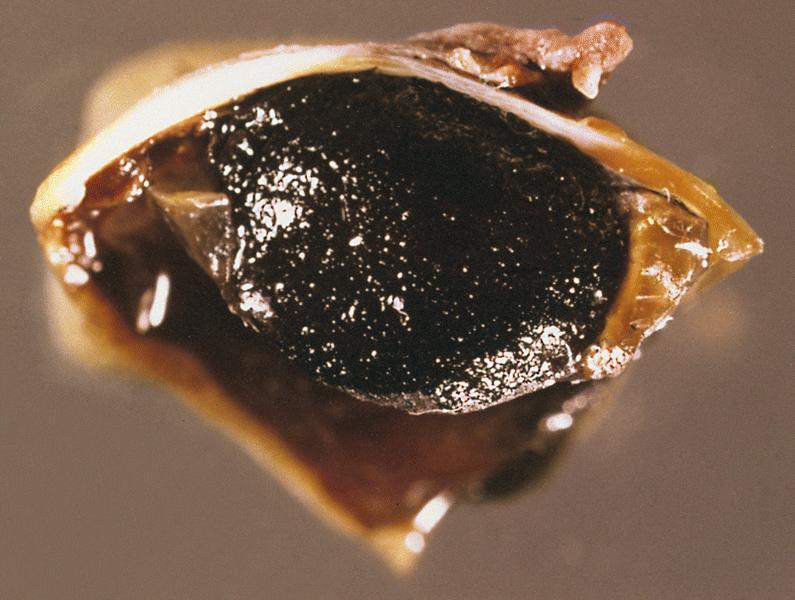
Lens
- Most surgical specimens are cataracts or prosthetic intraocular lens
- Normal lens is biconvex, behind pupil / iris, in front of vitreous, in posterior chamber
- 10 mm in diameter by 4 - 5 mm in width
- Usually Gross Examination Only (report as transparent - Yes or No), don't section
- Anterior lens capsule is eosinophilic acellular band overlying single layer of epithelial cells
- Lens capsule is strongly PAS+, holds lens in place
- Lens has thinner capsule posteriorly, without epithelial cells
- Lens in held in place by zonules that connect to pars plicata of ciliary body
- Lens normally opacifies with age due to globules of degenerate lens fibers
- Is a closed epithelial system with lens capsule (epithelium) that totally envelops the lens
- Vitreous humor:
- Avascular
- Extends from lens to sensory retina
- Contains gel-like material composed of water, protein, hyaluronic acid and "hyalocytes"
- Gel consistency is due to randomly oriented collagen fibrils
- May appear as amorphous material on H&E
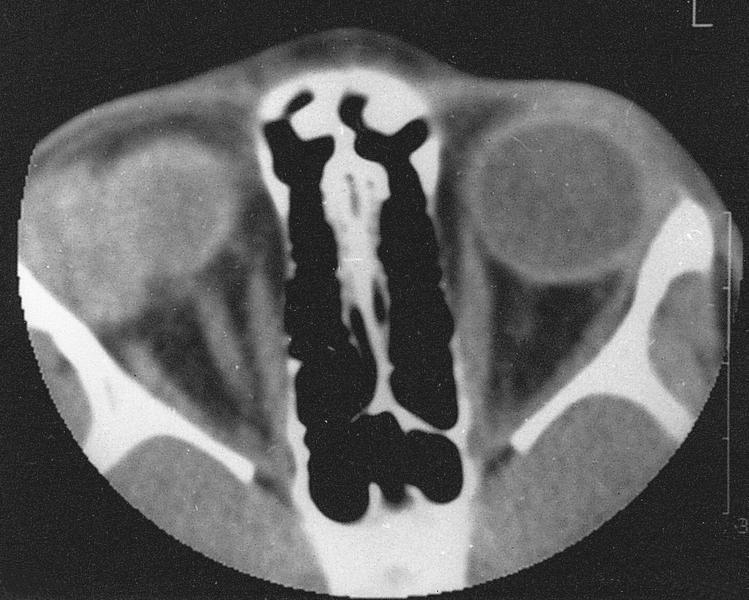
Orbit & optic nerve
- Orbit contains globe and its fibrous covering (Tenon capsule), lacrimal gland, optic nerve and its meningeal covering, extraocular muscles, cartilaginous trochlea, blood vessels and delicate fibroadipose connective tissue
- Floor of orbit is roof of maxillary sinus
- Medial wall of orbit (lamina papyracea) separates orbit from ethmoidal sinuses
- Proptosis: forward displacement of eyeball (or other organs), due to any disease that increases orbital contents, since orbit is closed medially, laterally and posteriorly
- Exophthalmos: abnormal protrusion of eyeball
- Common symptom of orbital disease, although often due to thyroid disease and not biopsied
- Other common causes of exophthalmos are mucocele from paranasal sinus, hemangioma, inflammatory pseudotumor
- Optic nerve:
- Surrounded by meninges; part of central nervous system
- Not usually biopsied
- Often has psammoma bodies or drusen (calcified acellular globular concretions of nerve fibers)
- Site of convergence of one million axons from retinal nerve fiber layer
- Nerve head accounts for physiologic blind spot in normal visual field
- Receives blood supply from branches of ophthalmic artery
- Surrounded on both sides by short posterior ciliary arteries
- Lamina cribrosa:
- Site of myelination of optic nerve axons
- Highlighted with Luxol fast blue or other myelin stains
- Trochlea:
- Arc shaped structure through which tendon of superior oblique muscle passes before insertion upon eyeball
- The only cartilaginous structure in normal orbit
- Tumors should be reported using formats published for their counterparts elsewhere in body
- Drainage through submandibular, parotid and cervical lymph nodes through vascular anastomosis
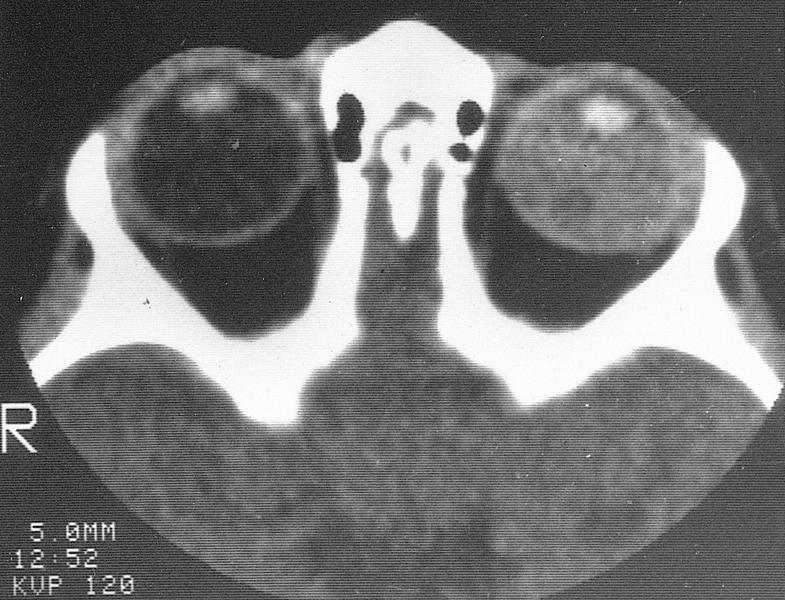
Radiology images
Drawings
Microscopic (histologic) description
- Anterior but not posterior lens has single epithelial layer
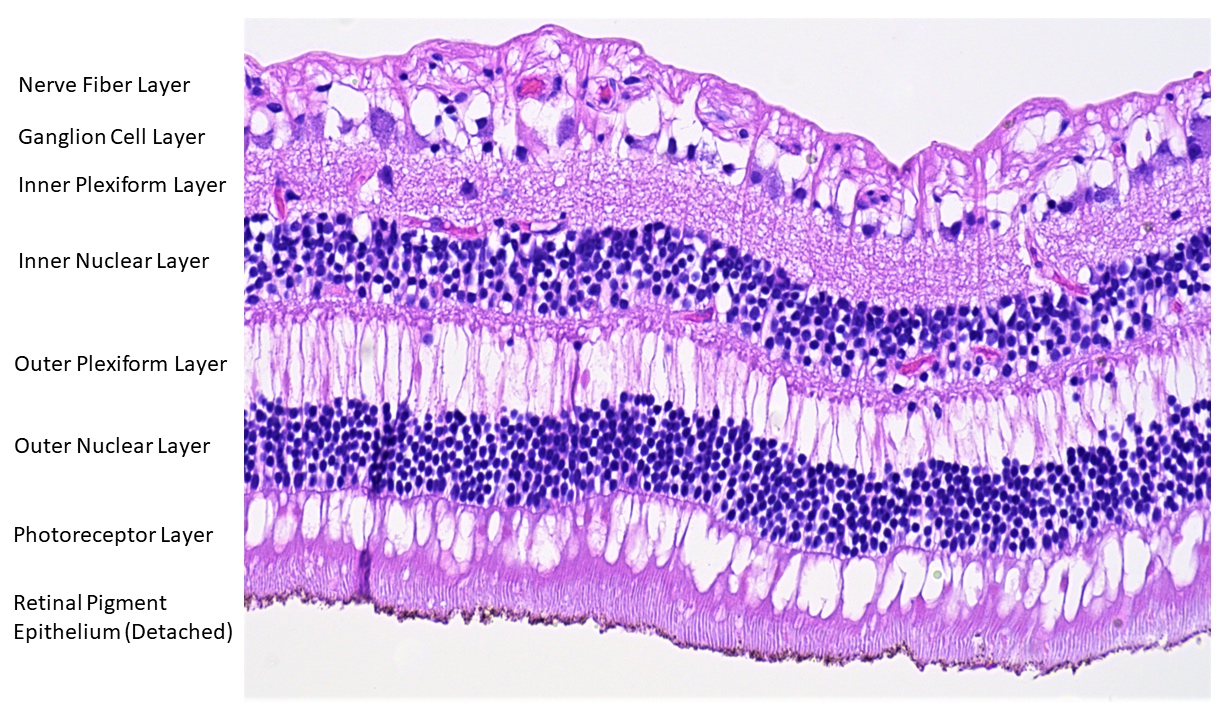
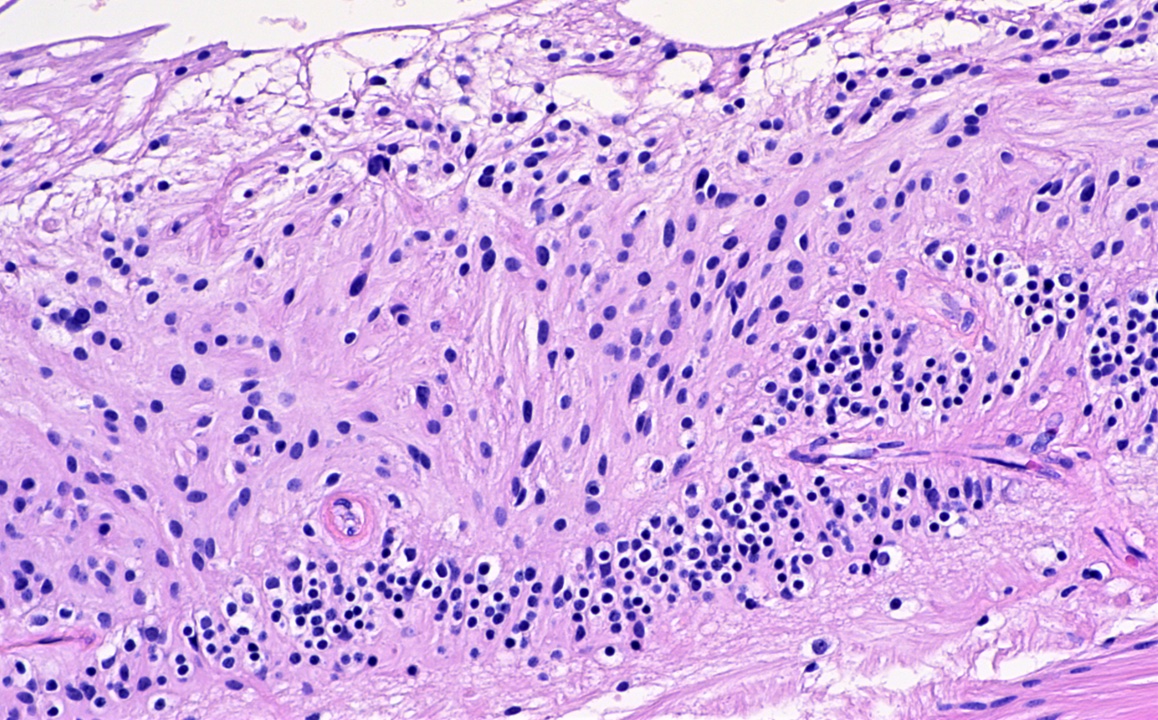
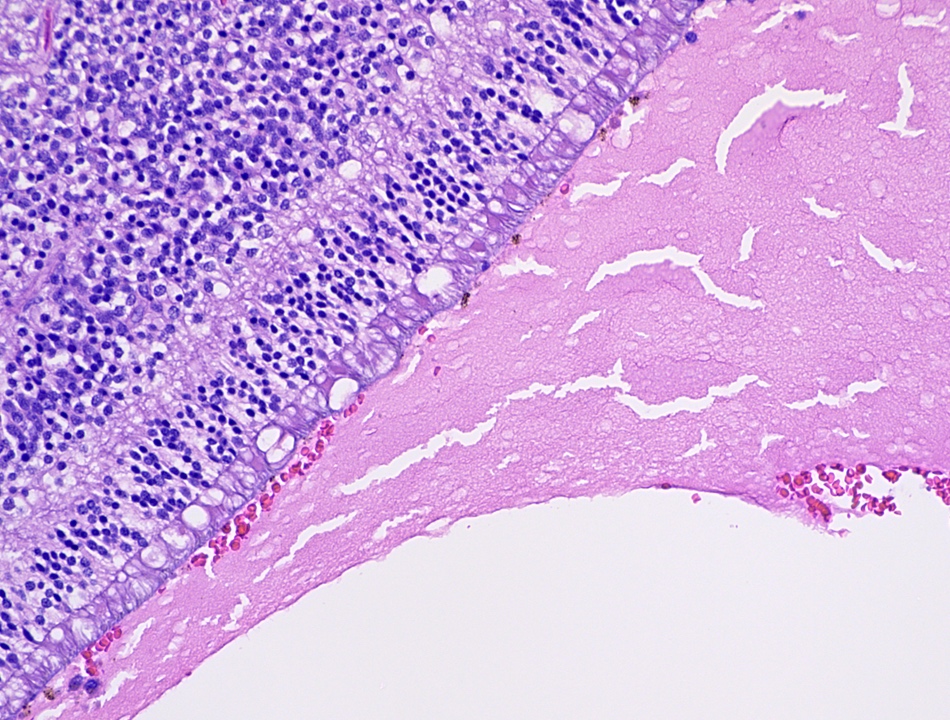
Anatomy & histology-retina
Table of Contents
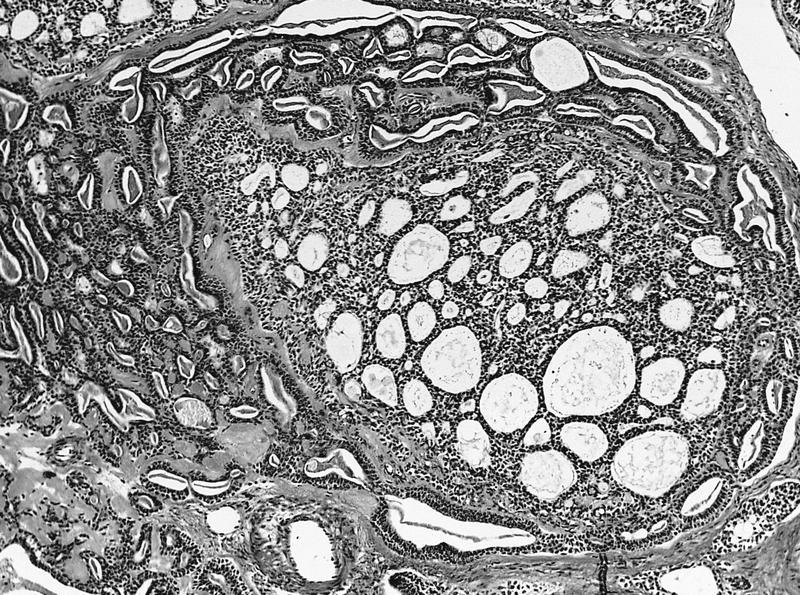
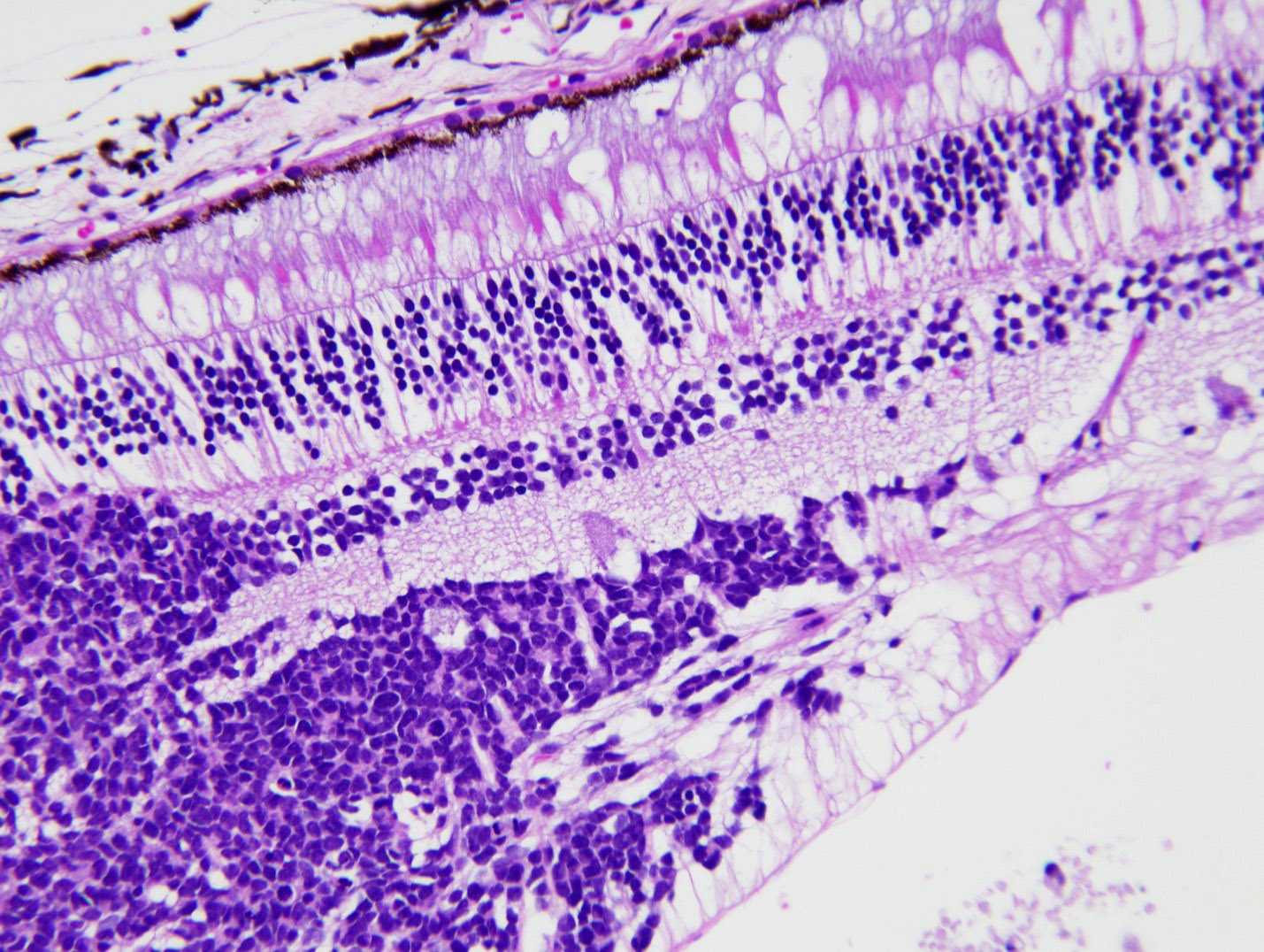
Definition / general | Essential features | Terminology | Anatomy and physiology | Diagrams / tables | Clinical features | Microscopic (histologic) description | Microscopic (histologic) images | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Specialized nervous tissue of the posterior eye that is responsible for the detection of light
Essential features
- Embryologic derivative of the optic vesicle, which arises from the diencephalon and enables detection of light (Dev Biol 2007;305:1)
- Composed of photoreceptors, first order neurons, second order neurons and glia (including Müller cells), the latter of which account for gliotic reaction
- Lines the innermost layer (or coat) of the eye, extending posteriorly from the ora serrata and situated between the vitreous body and choroid
Terminology
- Macula: highest density of photoreceptors and ganglion cells, responsible for high acuity vision and identified histologically by an increased number of ganglion cells and increased layer thickness
- Fovea centralis: small depression located in the center of the macula that is responsible for highest acuity vision, lacks rods and blood vessels, and relies on choroidal circulation (StatPearls: Anatomy, Head and Neck, Eye Fovea [Accessed 6 April 2022])
- Ora serrata: point of transition between anterior ciliary body and posterior retina
- Bruch membrane (not part of retina): separates choroid from overlying retinal pigment epithelium and features a 5 layer structure (basement membrane of retinal pigment epithelium, inner collagenous layer, elastin layer, outer collagenous layer and basement membrane of choriocapillaris); thickens with age and acquires focal extracellular deposits known as drusen (Prog Retin Eye Res 2010;29:1)
Anatomy and physiology
- Light is detected by the rods and cones of the photoreceptor layer and signals are transmitted through the layered retina to the optic nerve
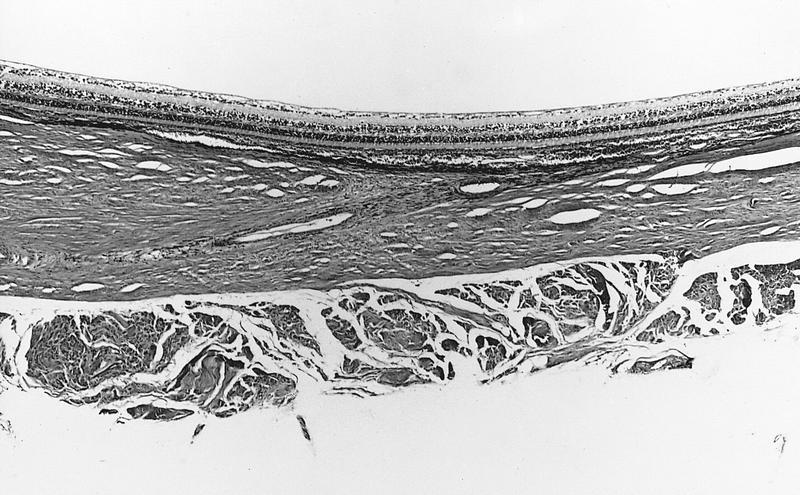
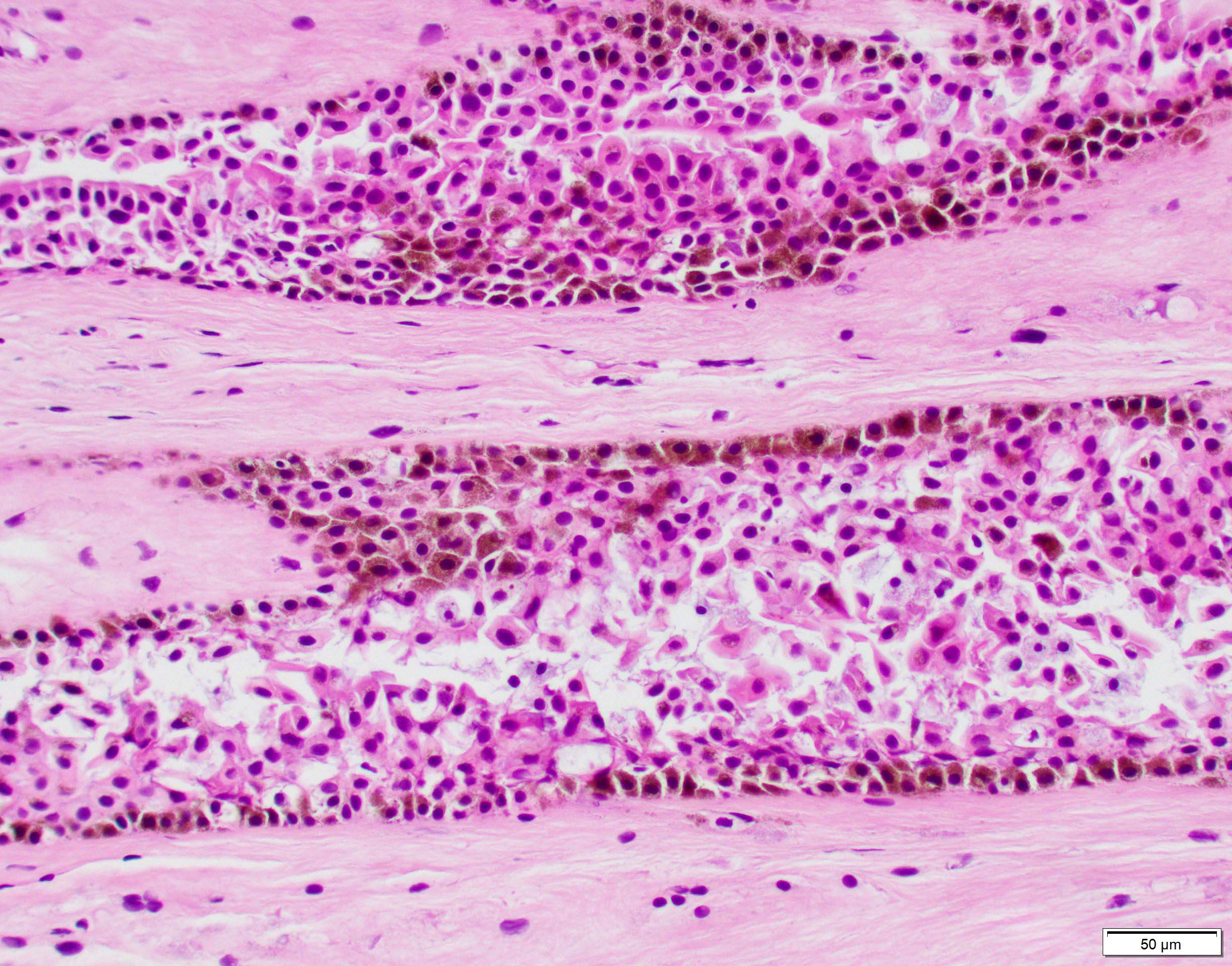
- Anatomical structure of retina and surrounding structures (outer to inner):
- Orientation
- Outer: nearest the limits of the globe (sclera)
- Inner: nearest the center of the globe (vitreous body)
- Retinal pigment epithelium: single layer of microvillous, cuboidal cells containing melanosomes that aid in light absorption by melanin, nutrient and fluid transport and phagocytosis that assists in photoreceptor turnover; forms the outer limit of the retina adjacent to Bruch membrane (Curr Mol Med 2010;10:802)
- Photoreceptor (rods and cones) layer: composed of the outer segments of the rods and cones (the photoreceptors that convert light into signal impulses) (J Cell Sci 2015;128:4039)
- External (outer) limiting membrane: permeable adherent junctions between photoreceptors and Müller cells (J Comp Neurol 1990;295:155)
- Outer nuclear layer: contains the photoreceptor nuclei
- Outer plexiform layer: located between the outer nuclear and inner nuclear layers and contains axons and dendrites of photoreceptors and bipolar cells (first order neurons), including Henle fibers (photoreceptor axons) that are prominent in the perifoveolar region and features a line of synapses known as the middle limiting membrane (Dev Ophthalmol 2016;55:7)
- Inner nuclear layer: contains bipolar cells, horizontal cells, amacrine cells and Müller cells (Invest Ophthalmol Vis Sci 2021;62:22, Physiol Rev 2019;99:1527)
- Inner plexiform layer: network of neuronal processes between the inner nuclear layer and the ganglion cell layer
- Ganglion cell layer: accommodates the ganglion cells, varying in thickness and density up to 5 - 8 layers in the macula; it is responsible for various functions in the relaying of received visual information out of the retina (Front Neurol 2021;12:661938)
- Nerve fiber layer: comprised of the axons of ganglion cells
- Internal limiting membrane: the only true basement membrane of the retina; it is located adjacent to the vitreous body where it serves as an anchor point for collagen fibers of the vitreous cortex (Exp Eye Res 2021;206:108545)
- Orientation
- Relevant vasculature to the retina:
- Central retinal artery: a branch of the ophthalmic artery that supplies the inner retina, including the nerve fiber layer, ganglion cell layer, inner plexiform layer and a portion of the inner nuclear layer
- Choriocapillaris: supplies the outer retina, including the photoreceptor layer and the innermost portion of the choroid adjacent to Bruch membrane (Prog Retin Eye Res 2022;87:100997)
- Central retinal vein and branches: drain the inner retina
- Retina lacks lymphatics
Clinical features
- Central retinal artery occlusion: often presents with sudden, painless vision loss and damage to the inner aspect of the retina (Eye (Lond) 2013;27:688)
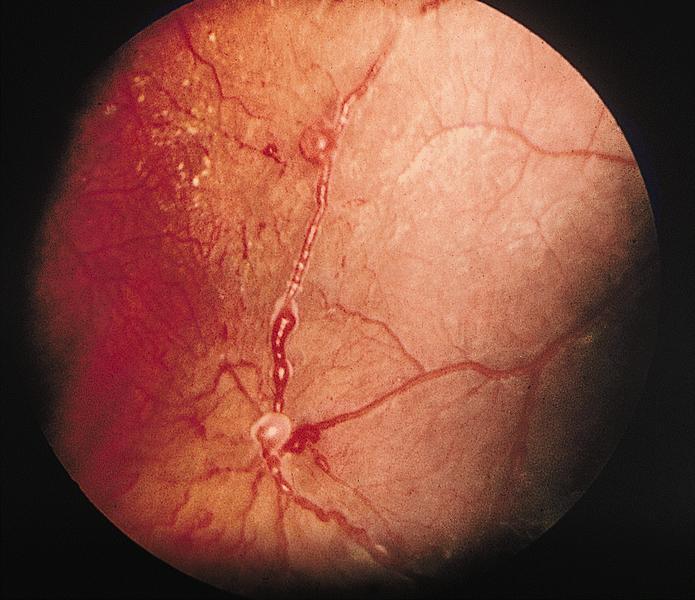
- Central retinal vein or branch occlusion: features cystoid macular edema as well as superficial and deep retinal hemorrhages, and in chronic cases, gliosis and inner ischemic retinal atrophy (Eagle: Eye Pathology - An Atlas and Text, 2nd Edition, 2011, Trans Am Ophthalmol Soc 1981;79:371)
- Hemorrhages of the nerve fiber layer appear streaked or flame shaped, while hemorrhages of deeper layers appear dot-like or blot-like on ophthalmoscopic examination (Pediatr Emerg Care 2018;34:665)
Microscopic (histologic) description
- Gliotic reaction due to the presence of glia (including Müller cells) are seen as a hypercellularity of variably spindled cells with oblong nuclei
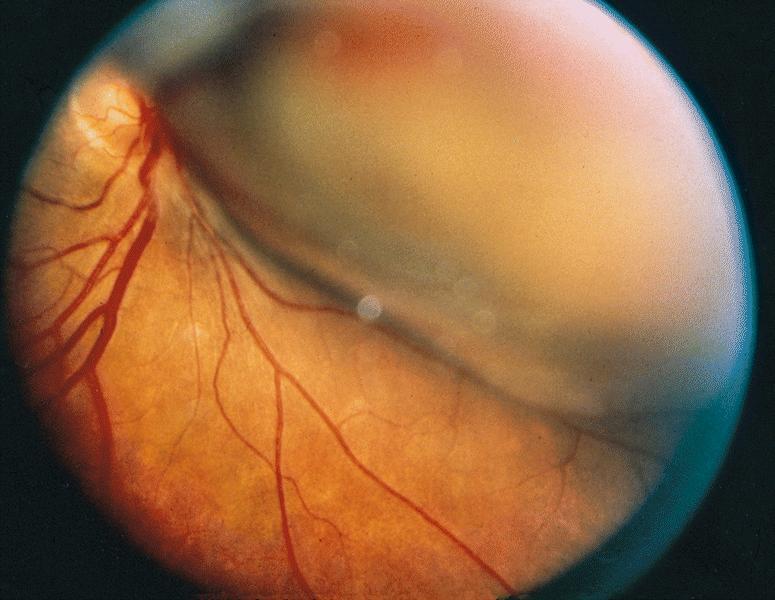
- Retinal detachment: separation of neurosensory retina (rods and cones) from retinal pigment epithelium
- Artifactual retinal detachment: common artifact of processing and lacks the subretinal proteinaceous fluid or hemorrhage found in true retinal detachments (Eagle: Eye Pathology - An Atlas and Text, 2nd Edition, 2011)
- Peripheral microcystoid degeneration: commonly encountered cystoid spaces of the outer plexiform layer near the ora serrata in adults > 20 years of age
- Hard drusen are eosinophilic nodules that are observed between the retinal pigment epithelium and Bruch membrane and are encountered in aging
Microscopic (histologic) images
Additional references
Board review style question #1
Board review style answer #1
C. Müller cells. Glial cells, including Müller cells, cause retinal gliosis in response to injury.
Comment Here
Reference: Anatomy & histology-retina
Comment Here
Reference: Anatomy & histology-retina
Board review style question #2
A patient with sudden, painless vision loss is diagnosed with central retinal artery occlusion. What layer of the retina would be expected to be affected?
- Ganglion cell layer
- Outer nuclear layer
- Outer plexiform layer
- Photoreceptor layer
Board review style answer #2
A. Ganglion cell layer. The central retinal artery supplies the inner layers of the retina, including much of the inner nuclear layer, the inner plexiform layer, the ganglion cell layer and the nerve fiber layer.
Comment Here
Reference: Anatomy & histology-retina
Comment Here
Reference: Anatomy & histology-retina
Astrocytic tumor
Definition / general
- Associated with tuberous sclerosis (57%), neurofibromatosis (14%), or no syndrome (29%)
- Tuberous sclerosis patients usually have multiple, peripheral retinal tumors with giant astrocytes vs. disc based tumors in non tuberous sclerosis patients
- Usually benign and extremely rare in retina
- References: Arch Pathol Lab Med 1984;108:160
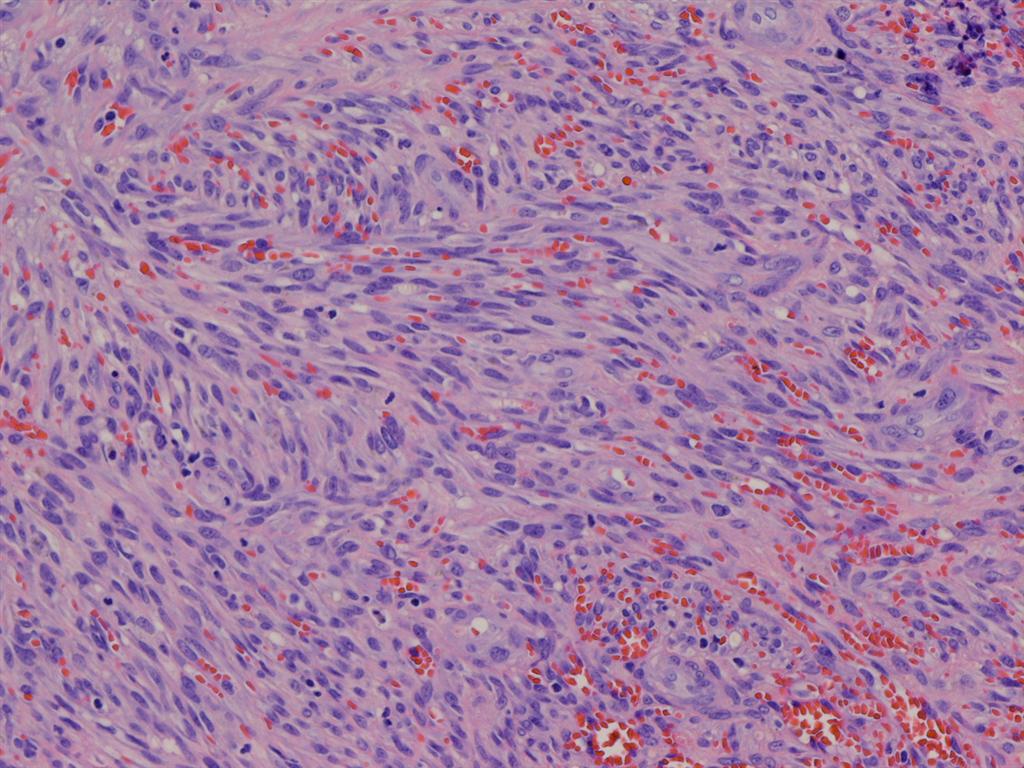
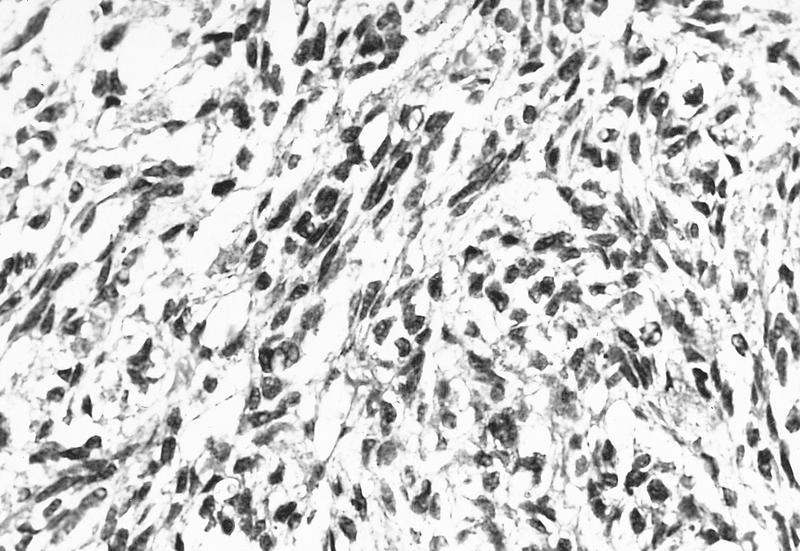
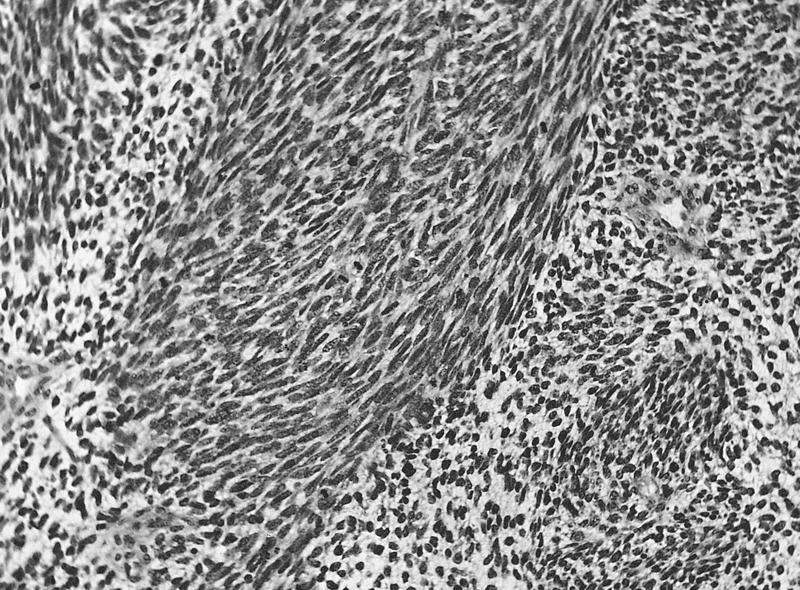
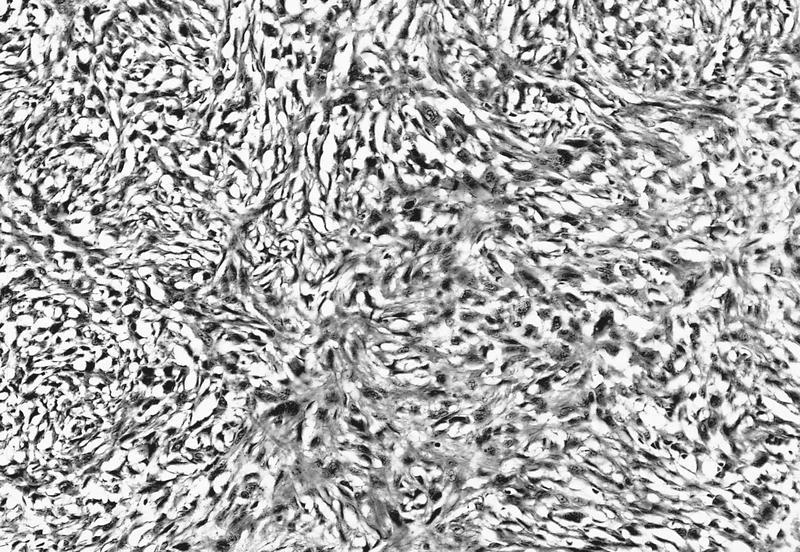
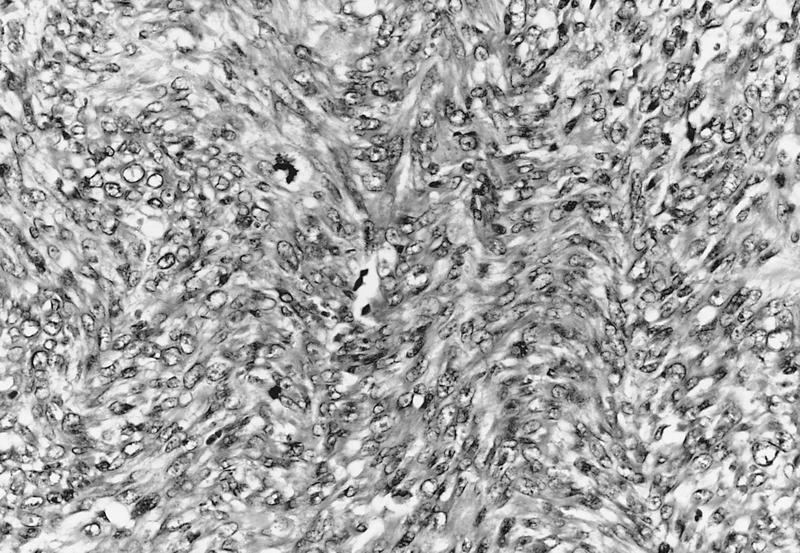
Microscopic (histologic) description
- Interlacing, spindle shaped astrocytes
Benign epithelial melanosis of the conjunctiva
Table of Contents
Definition / general | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Negative stains | Differential diagnosisDefinition / general
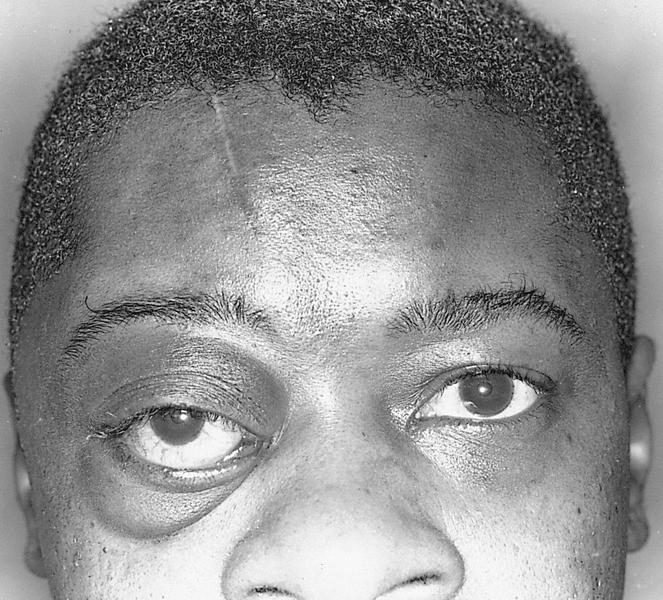
- Pigmented thickening of conjunctival epithelium, may be normal finding in dark skinned individuals - bilateral, continues throughout life (Surv Ophthalmol 2004;49:3)
- Present in 92% of blacks, 36% of Asians, 28% of Hispanics, 5% of whites
- Uncommon finding in Laugier-Hunziker syndrome (Arch Dermatol 2007;143:631)
- Can be cystic (Cornea 2012;31:1273)
Clinical images
Microscopic (histologic) description
- Dense pigmentation at basal layer of epithelium but normal number of melanocytes
- Cystic variant has epithelial lined cysts with goblet cells in substantia propria
Microscopic (histologic) images
Negative stains
- HMB45 in racial melanosis (Histopathology 2001;39:426)
Differential diagnosis
- Early primary acquired melanosis:
- Melanocytic proliferation is present
- Iron containing foreign bodies
- Medications:
- Epinephrine, tetracycline, silver containing products
- Melanocyte migration associated with inflammation or trauma
- Ochronosis
- Ocular melanocytosis:
- Pigmentation of ocular structures due to abnormal migration of melanocytes during development
Blue nevus
Table of Contents
Definition / general | Case reports | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) imagesDefinition / general
- Combined nevus: combination of nevocytic and blue nevus (Trans Am Ophthalmol Soc 1999;97:170)
Case reports
- 41 year old man with blue nevus giving rise to melanoma (Arch Ophthalmol 2000;118:1581)
- 54 year old man with multifocal pigmentations (Klin Monatsbl Augenheilkd 1994;205:242)
- 55 year old woman with multifocal blue nevus (Surv Ophthalmol 2008;53:41)
- 71 year old woman with slow growing lesion (Ophthalmology 1992;99:1714)
Gross description
- Blue-brown due to superficial location, lack of dermal collagen and numerous pigmented nevus cells
Microscopic (histologic) description
- Spindled and dendritic melanocytes in epithelium and collagenous stroma
- Melanocytes have coarsely clumped melanin granules
Bullous keratopathy
Bullous keratopathy
Definition / general
Microscopic (histologic) description
- Injury to endothelium (does not regenerate) which normally pumps fluid out from corneal stroma
- Leads to chronic edema of stroma and epithelium, subepithelial bullae, pain, eventually diffuse scarring and reduced vision
- Called aphakic bullous keratopathy if after cataract extraction
- Causes include
- Immunologic rejection of corneal endothelium
- Fuchs dystrophy
- Implantation of prosthetic intraocular lens
Microscopic (histologic) description
- Intraepithelial vesicles
- Bullae between epithelium and Bowman layer
- Fewer endothelial cells than normal
- Increased corneal thickness with loss of normal artifactual clefts between collagen lamellae
Aphakic bullous keratopathy
Definition / general
Microscopic (histologic) description
- Secondary endothelial compensation, often after cataract extraction (with or without an intraocular lens)
- Resembles Fuchs dystrophy
- Causes severe visual loss and astigmatism
Microscopic (histologic) description
- Corneal edema with bullae between corneal epithelium and Bowman layer
- Late changes are replacement of bullous cavity with fibrous tissue
- No / attenuated endothelium
CCN Test
ccn testCalcific band keratopathy
Table of Contents
Definition / general | Gross description | Microscopic (histologic) description | Positive stainsDefinition / general
- Due to chronic inflammation, calcium and phosphate disorders
- May complicate chronic uveitis, especially in patients with juvenile rheumatoid arthritis
Gross description
- Brown staining material in anterior cornea within palpebral fissure
Microscopic (histologic) description
- Calcium deposition in Bowman layer and superficial corneal stroma
- May be associated pannus formation
Positive stains
- Calcium (von Kossa stain)
Carcinoma ex pleomorphic adenoma
Definition / general
- 5 - 10% of lacrimal gland tumors
Case reports
- Lacrimal gland tumor developing after 8 recurrences of pleomorphic adenoma over 32 years (Am J Surg Pathol 1979;3:457)
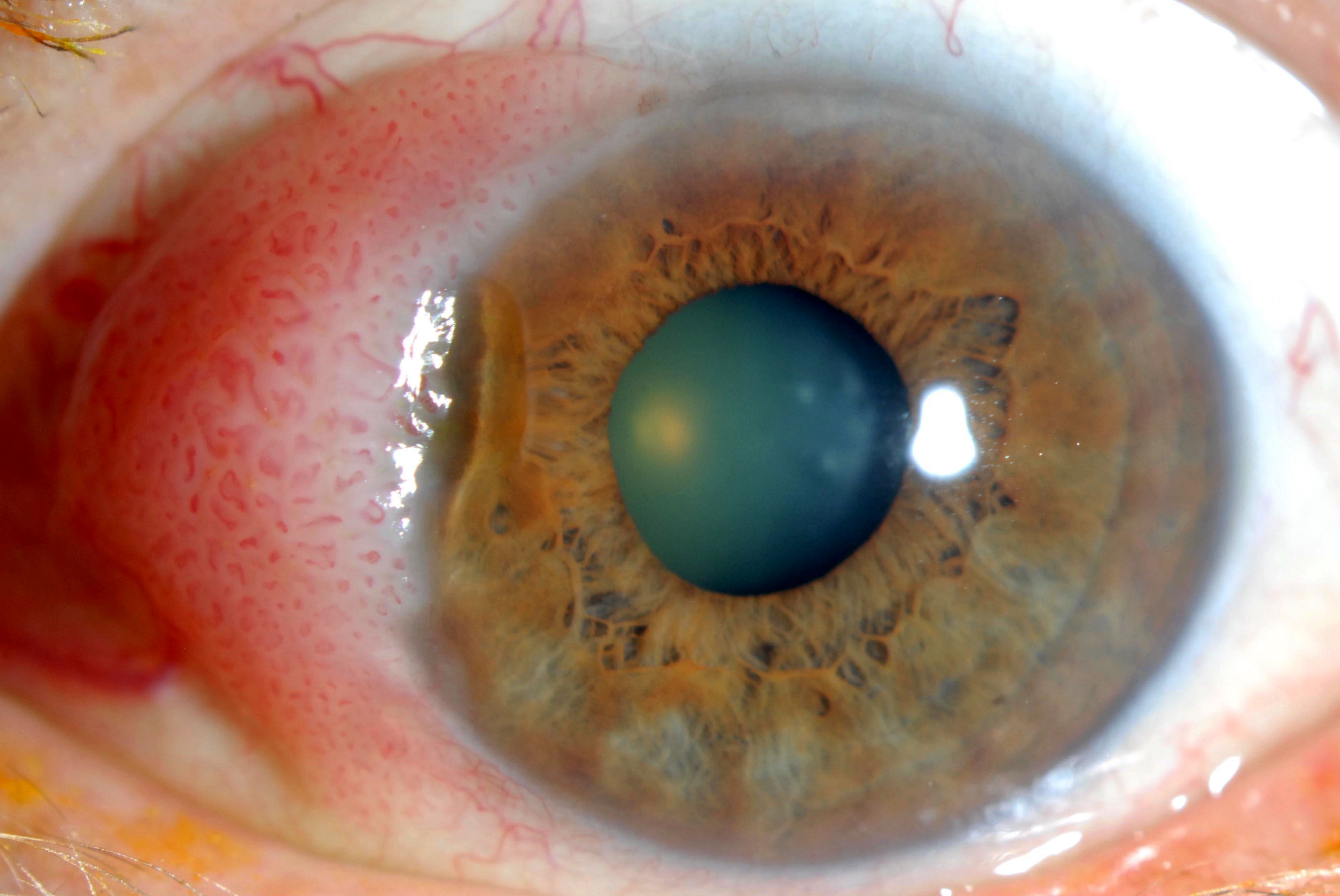
Cataract
Table of Contents
Definition / general | Treatment | Gross description | Microscopic (histologic) descriptionDefinition / general
- Defined as progressive opacity of crystalline lens that decreases visual acuity
- Usually develops in older individuals, rarely in infancy or childhood
- Associated with systemic diseases (galactosemia, diabetes mellitus, Wilson disease, atopic dermatitis), corticosteroids, radiation (ultraviolet light or radiation therapy), trauma, glaucoma, uveitis, retinitis pigmentosa, steroids
- Age related cataract is due to opacification of lens nucleus, which becomes brown and distorts perception of blue color
- Changes occur in lens nucleus, cortex and subcapsular regions
- Nuclear changes due to progressive crosslinking and insolubility of crystalline proteins
- Cortical changes begin as small peripheral water clefts and diffuse degenerative changes that coalesce into dense bands of opaque cortical material
- Anterior lens epithelial cells may undergo fibrous metaplasia, creating a thick fibrous plaque between the anterior lens capsule and the anterior epithelial cells
- Congenital cataract:
- Becomes apparent within first 6 months of life
- Posterior subcapsular cataract:
- Migration of lens epithelium posterior to lens equator
- Morgagnian cataract:
- Long standing cataract that undergoes liquefaction of lens cortex with sinking of nucleus into fluid filled sac and clinical brown nucleus
- Soemmering ring cataract:
- Peripheral donut or ring shape due to loss of lens nucleus and much of anterior and posterior cortex
- Also proliferating lens epithelial cells in periphery and equatorial region of lens
Treatment
- Often high frequency sound waves are used to disintegrate the lens (phacoemulsification), then lens contents aspirated and disposed of (not submitted for examination)
- Lens capsule is intact
- Then placement of prosthetic intraocular lens
Gross description
- Senile cataracts are yellow-brown
Microscopic (histologic) description
- Homogenous eosinophilic lens fibers, vacuolization of superficial cortical fibers, extracellular clefts and eosinophilic globules of variable size (morgagnian globules) between lens fibers
Chalazion
Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Very common, inflammatory eyelid lesion, characterized by granulomatous inflammation with lipogranulomas
- All specimens with tissue should be submitted to rule out malignant neoplasms and other masquerading conditions; most of the time they are not submitted
Essential features
- Very frequent inflammatory eyelid lesion
- More frequent in the upper eyelid
- Broad histopathological spectrum from acute to more chronic findings
- Lipogranulomas, suppurated granulomas, granulation tissue and fibrosing inflammation
- Can masquerade as neoplastic process
ICD coding
- ICD-10: H00.19 - chalazion unspecified eye, unspecified eyelid
Epidemiology
- More common in younger adults than in children, uncommon in late life
Sites
- Eyelid
Pathophysiology
- Probably due to obstruction or nonspecific inflammation (blepharitis) surrounding sebaceous gland ducts, leading to discharge of sebaceous material into surrounding tissue and resulting in intense foreign body granulomatous inflammatory reaction
- Superficial chalazion from Zeis gland
- Deep chalazion from Meibomian gland
- May erupt through conjunctival surface of eyelid (internal chalazion)
Etiology
- More significant: history of chalazion and blepharitis
- Less significant: rosacea, gastritis, anxiety and smoking (Cornea 2011;30:1376)
- There is no evidence that cosmetics in the eyelid causes, aggravates or protects from this condition
Clinical features
- Upper eyelid > lower eyelid
- Slowly growing mass with variability in size on a day to day basis
- Solitary, nontender nodule; eversion helps to identify the lesion
- Clinically may masquerade as sebaceous carcinoma and other neoplasms (Eye (Lond) 2004;18:135)
Diagnosis
- Typically suspected upon clinical examination
- Histologic examination of resected tissue can confirm the diagnosis
Treatment
- Medical treatment includes applying of heat and massage at least twice a day
- No benefit with antibacterial topical preparations except when infected (hordoleum) (BMJ 2010; 341 :c4044)
- Surgical management using incision and curettage is a second line of treatment
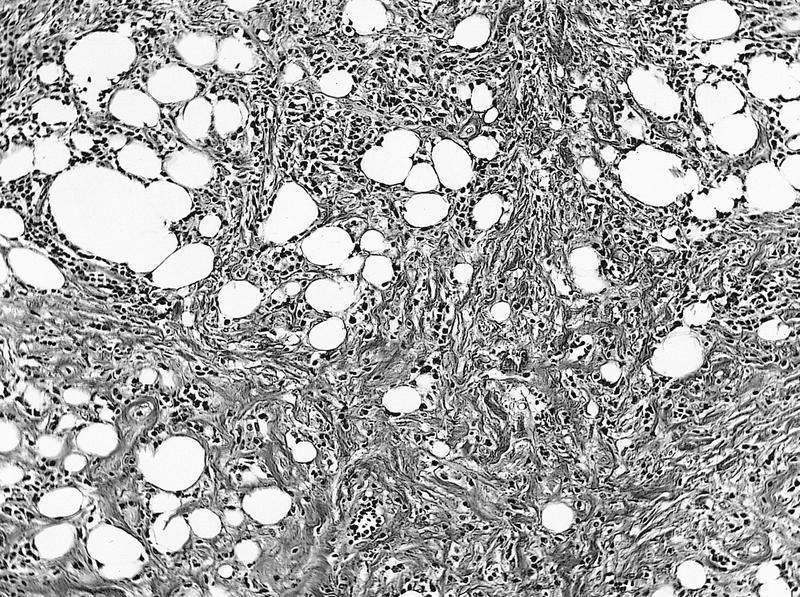
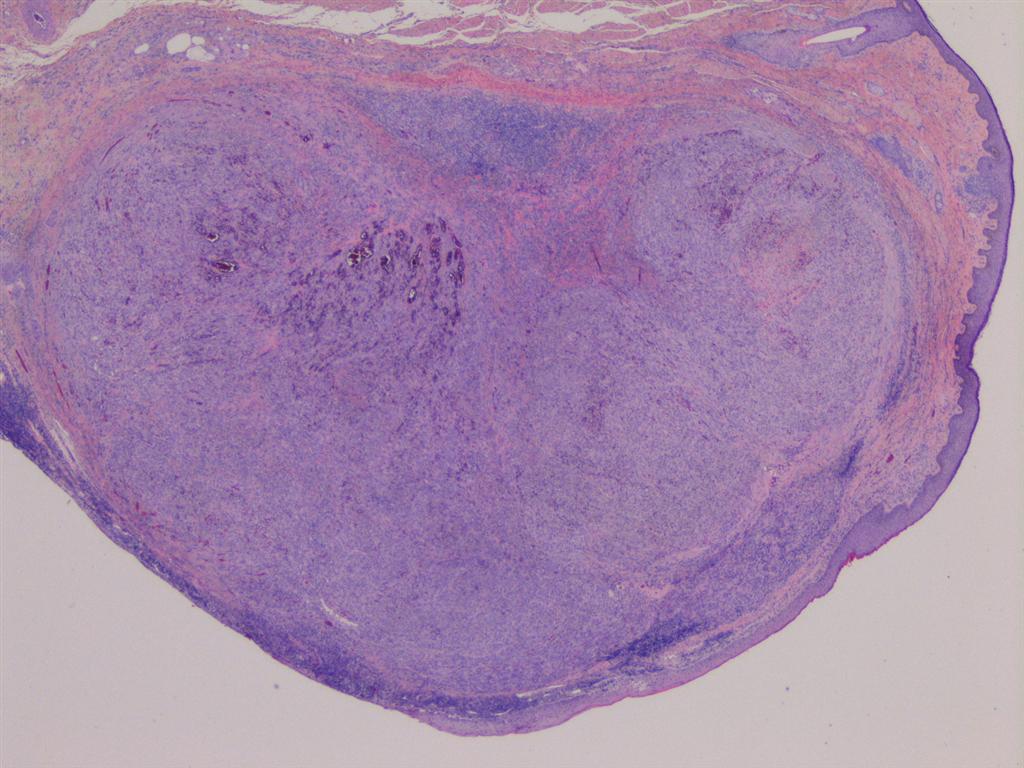
Microscopic (histologic) description
- Lipogranuloma (empty spaces surrounded by epithelioid and foamy histiocytes with multinucleated foreign body and or Touton type giant cells)
- Some lesions have granulation tissue, fibrosis or suppurative inflammation
- Early lesions can have necrotizing (neutrophilic) granulomas
- Conchoidal bodies and asteroid bodies can be observed
Microscopic (histologic) images
Positive stains
- Oil Red O: positive in the lipid droplets (central clearings)
Negative stains
- Grocott methenamine stain (GMS) and Ziehl-Neelsen could be helpful to rule out microorganisms when suspected
Sample pathology report
- Right eyelid, nodule, excision:
- Chalazion (lipogranulomas) (see comment)
- Comment: There is no sign of malignancy.
Differential diagnosis
- Steatocystoma:
- Cystic lesion lined by pluristratified epithelium without granular stratum wavy keratin
- Some sebaceous gland can be present attached to the cyst
- Sebaceous carcinoma:
- Basal cell carcinoma:
- Basaloid neoplasm with palisades and stromal clefts
- IHC: EMA-
- Hematolymphoid neoplasms:
- Myeloid sarcoma:
- Large cells with large cytoplasm and blastoid nucleus
- IHC: lysozyme+
- Histiocytic neoplasm (Langerhans and non-Langerhans):
- Neoplastic process of large cells with reniform nuclei (non-Langerhans) or grooved nuclei (Langerhans)
- Lymphoma:
- Myeloid sarcoma:
- Infectious granulomas:
- Necrotizing or caseiform granulomas
- Ziehl-Neelsen or Kinyoun+ when mycobacteria present
- GMS+ for fungal granulomas
- Autoimmune inflammation:
- Granulomatosis with polyangiitis:
- Necrosis, granulomas and angeitis present
- IgG4 related disease:
- Lymphoplasmacytic infiltrate with storiform fibrosis
- Lymphoid aggregates
- Obliterative phlebitis
- IgG4/IgGt ratio higher than 60%
- Granulomatosis with polyangiitis:
Board review style question #1
Board review style answer #1
C. Lipogranulomas. This is the key morphological finding in chalazion. The granulomas are usually nonnecrotizing. All the other changes such as lymphoplasmacytic chronic inflammation of the tarsal plate, exuberant granulation tissue and fibrosing chronic inflammation could be present but are nonspecific.
Comment Here
Reference: Chalazion of eyelid
Comment Here
Reference: Chalazion of eyelid
Board review style question #2
What is the most common location of a chalazion?
- External canthus
- Inner canthus
- Lower eyelid
- Upper eyelid
Board review style answer #2
D. Upper eyelid. The most common site of a chalazion is the upper eyelid, followed by the lower eyelid. Canthal location is rare.
Comment Here
Reference: Chalazion of eyelid
Comment Here
Reference: Chalazion of eyelid
Choroid
Definition / general
- Middle layer of globe between outer sclera and inner retina
- Highly vascular but no lymphatics
- Extends from ciliary body to optic nerve
- Inner aspect is adherent to retinal pigment epithelium; outer surface is loosely attached to overlying sclera
- Stroma contains abundant pigmented melanocytes
- Bruch membrane: separates choroid from overlying retinal pigment epithelium, is 2 - 4 microns thick, has 5 distinct layers (basal lamina of overlying retinal pigment epithelium, collagenous layer, elastic fiber rich layer, collagenous layer and basal lamina of endothelial cells of choriocapillaris), thickens with age, has focal excrescences known as drusen
- Choriocapillaris: in innermost choroidal stroma adjacent to Bruch membrane, connects with arterial and venous channels from vessels in outer choroidal stroma to nourish outer retinal layers
Cicatrizing conjunctivitis
Table of Contents
Definition / general | Etiology | Clinical features | Diagnosis | Treatment | Microscopic (histologic) descriptionDefinition / general
- Cicatrizing: causing a scar and possibly affecting vision
- Conjunctival fibrosis due to chronic inflammation, leading to alterations of conjunctival architecture
Etiology
- Numerous causes (Curr Opin Ophthalmol 2001;12:250)
- Atopic keratoconjunctivitis
- Burns
- Discoid lupus erythematosus (Ocul Immunol Inflamm 2002;10:287)
- Epidermolysis bullosa acquisita (Arch Ophthalmol 2006;124:1615)
- Lichen planus (Am J Ophthalmol 2003;136:239)
- Ocular cicatricial pemphigoid
- Ocular rosacea (Cornea 2004;23:630)
- Paraneoplastic syndrome associated with lung tumors (Cornea 2006;25:611)
- Porphyria cutaneous tarda (Am J Ophthalmol 2002;134:619)
- Post-infectious
- Sarcoidosis (Ann Ophthalmol 1989;21:92)
- Sjögren syndrome
- Stevens-Johnson syndrome
- Systemic sclerosis
- Trachoma
- Granulomatosis with polyangiitis (Wegener's) (Nephrol Dial Transplant 2006;21:3342)
Clinical features
- Dry eyes
- Loss of transparency and vision
Diagnosis
- Positive direct immunofluorescence with IgA, IgM, IgG, complement C3, complement C4, and fibrinogen in autoimmune diseases
Treatment
- Medical management varies according to specific causes
Microscopic (histologic) description
- Fibrosis and inflammation consisting of neutrophils, lymphocytes, plasma cells
- Keratinization of superficial layer, hyperplasia of basal layers
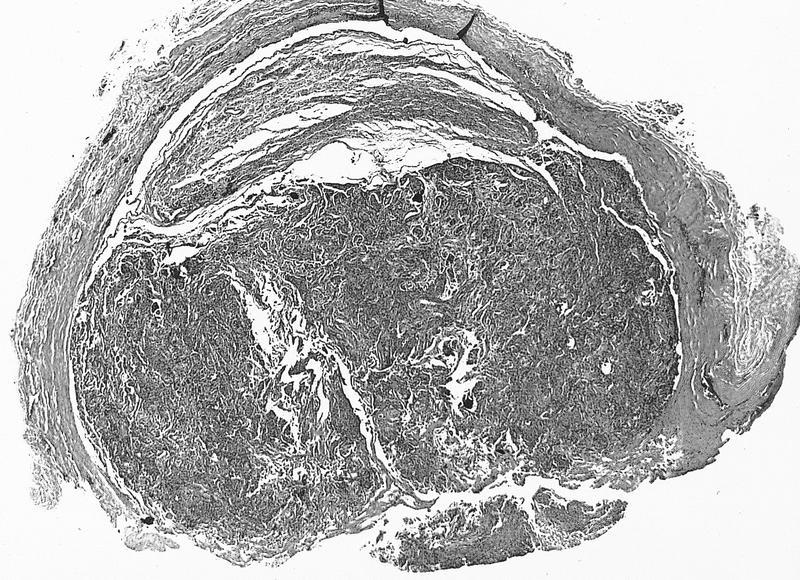
Ciliary body adenoma
Definition / general
- Also called benign ciliary epithelioma, coronal adenoma
- Benign tumor of ciliary body
- Usually incidental finding in enucleated eye or at autopsy
Microscopic (histologic) description
- Interlacing trabeculae of uniform, nonpigmented ciliary epithelial cells, surrounded by amorphous and PAS+ hyaline material
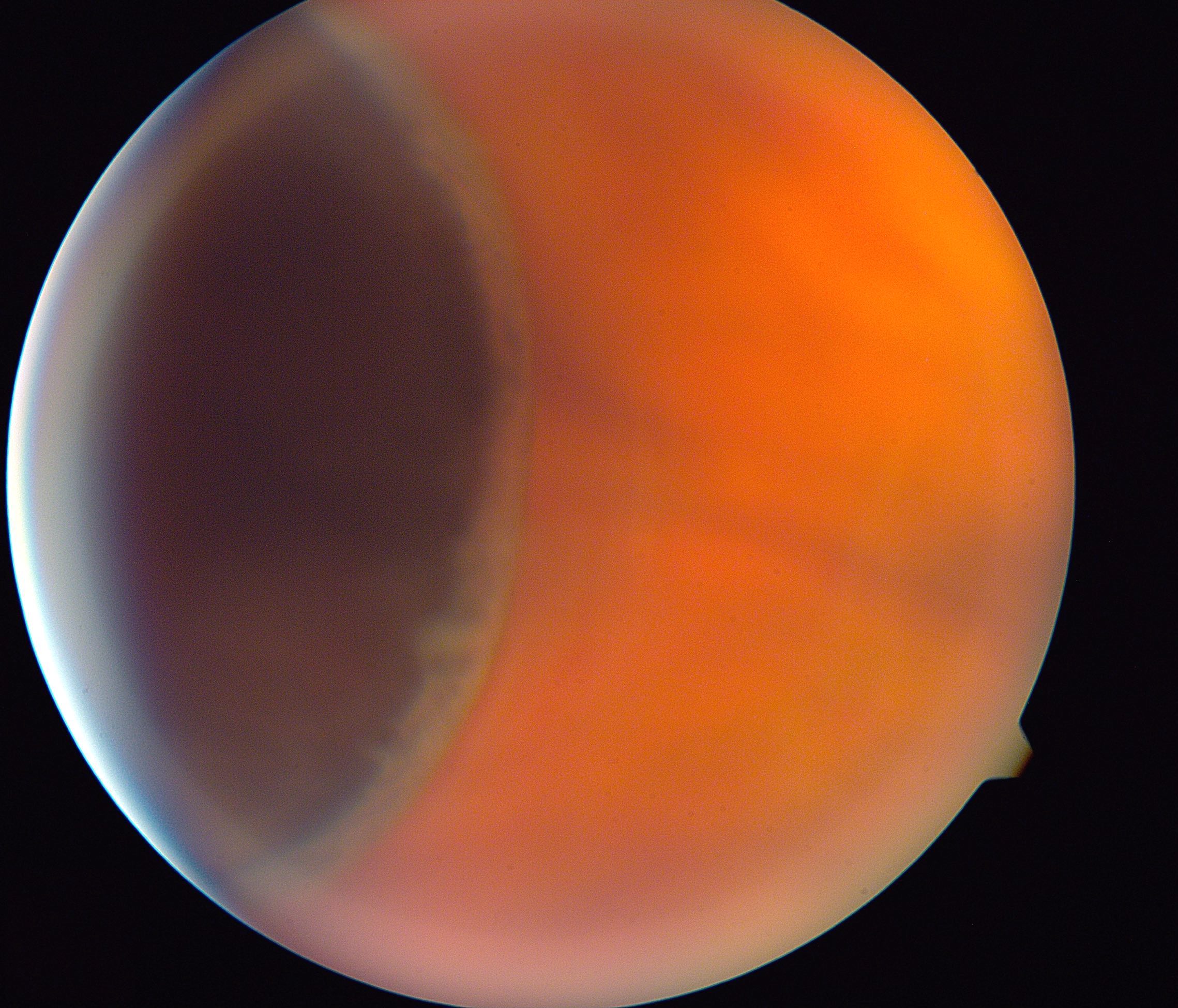
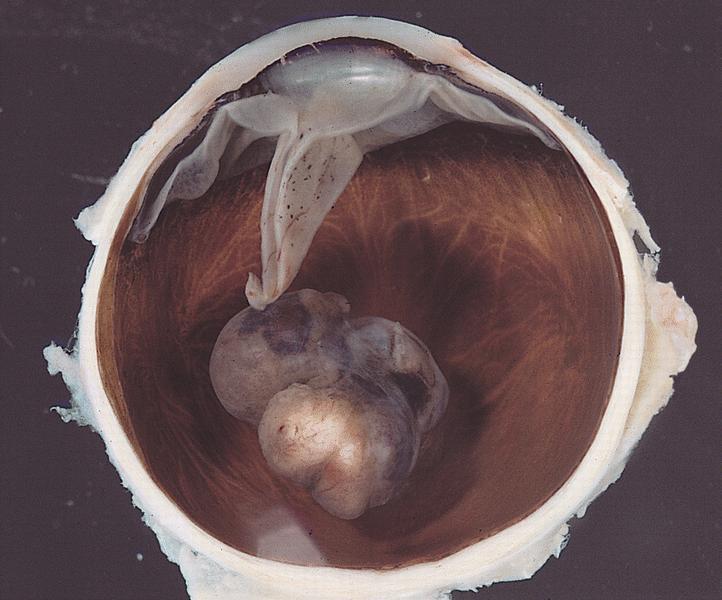
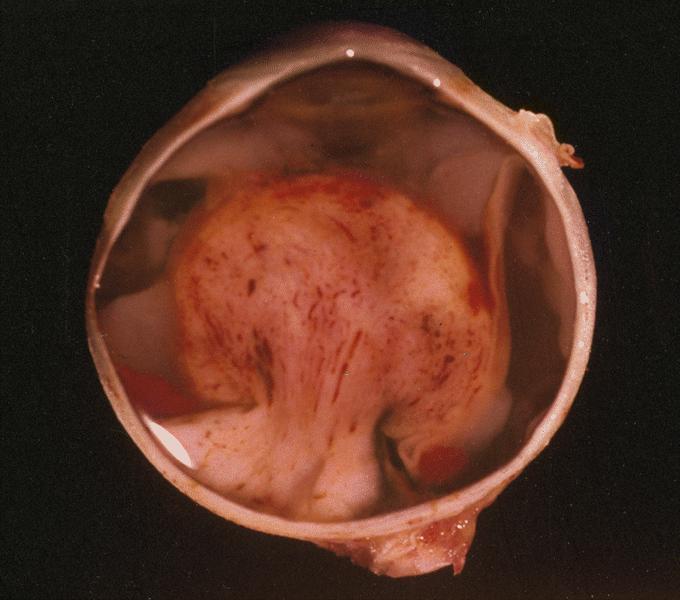
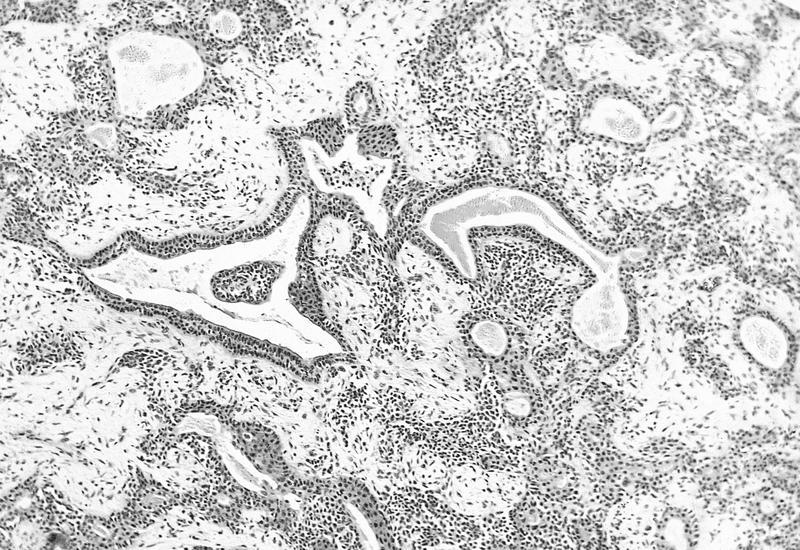
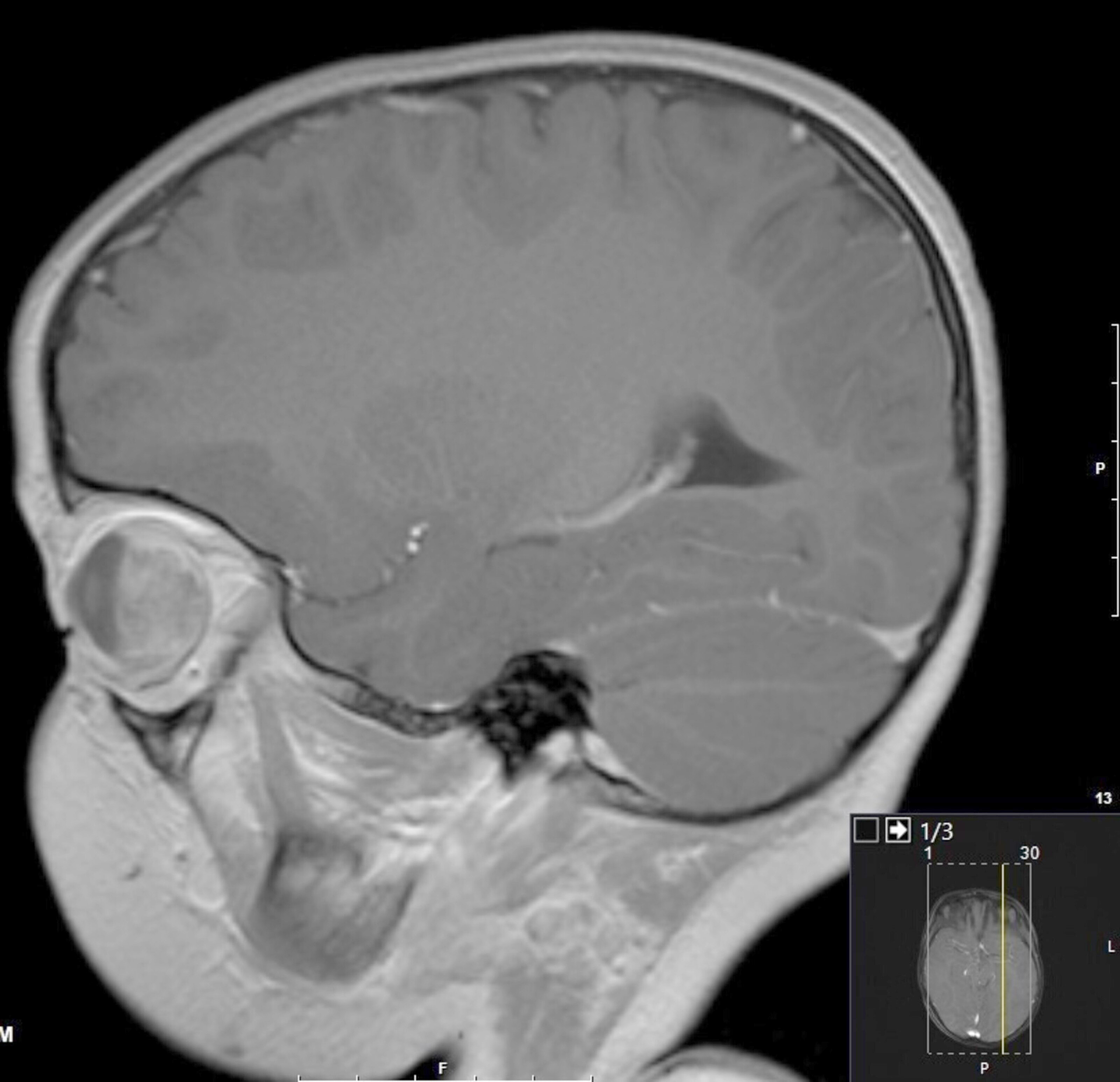
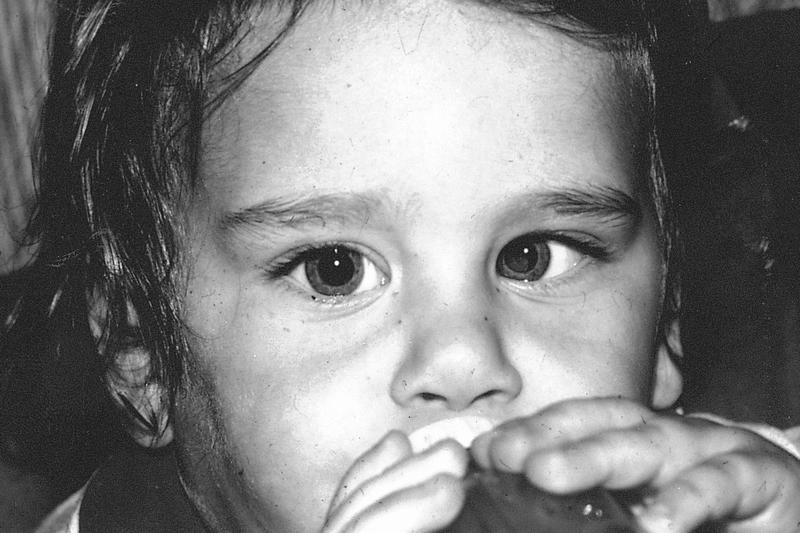
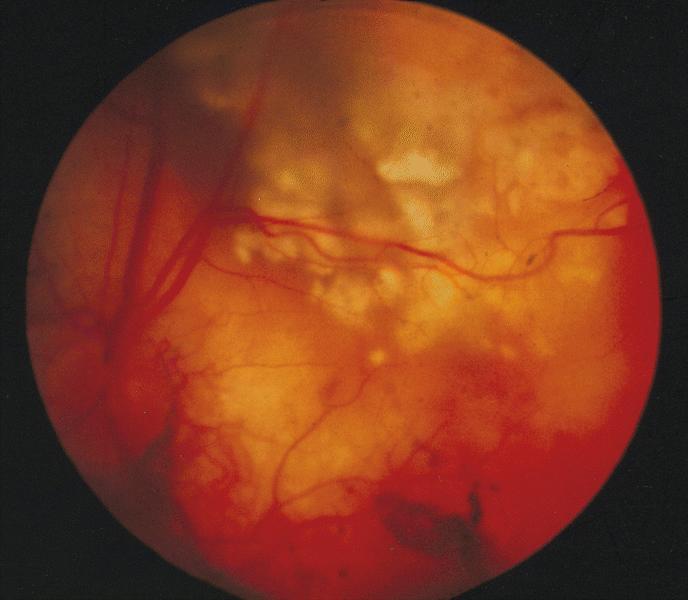
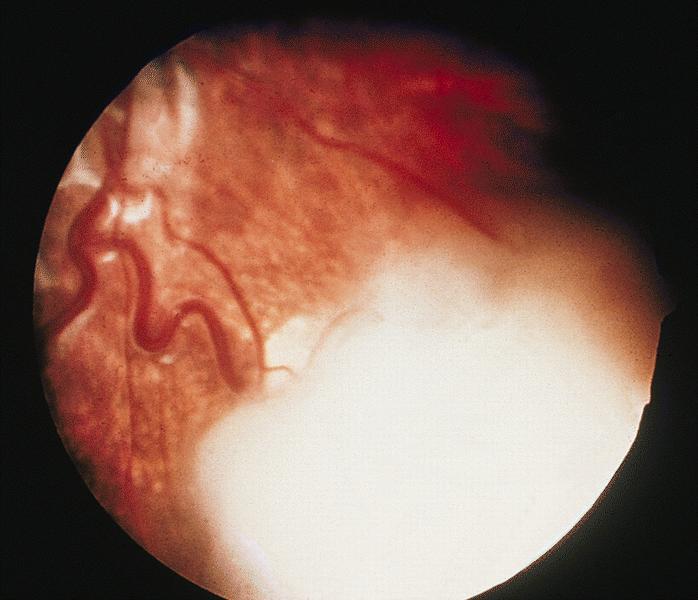
Coats disease
Table of Contents
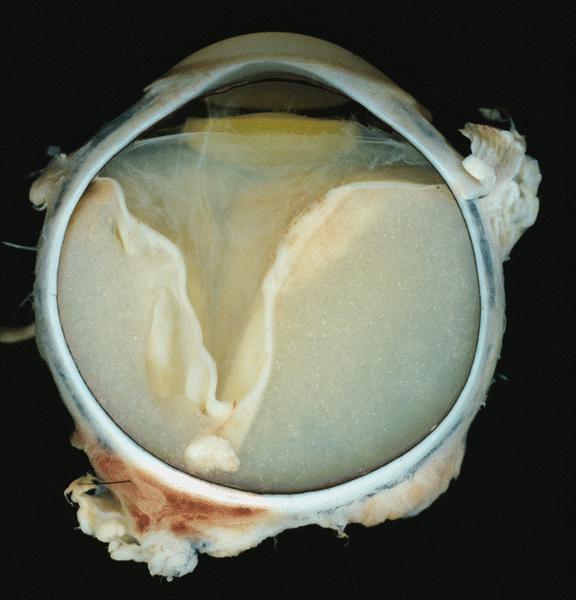
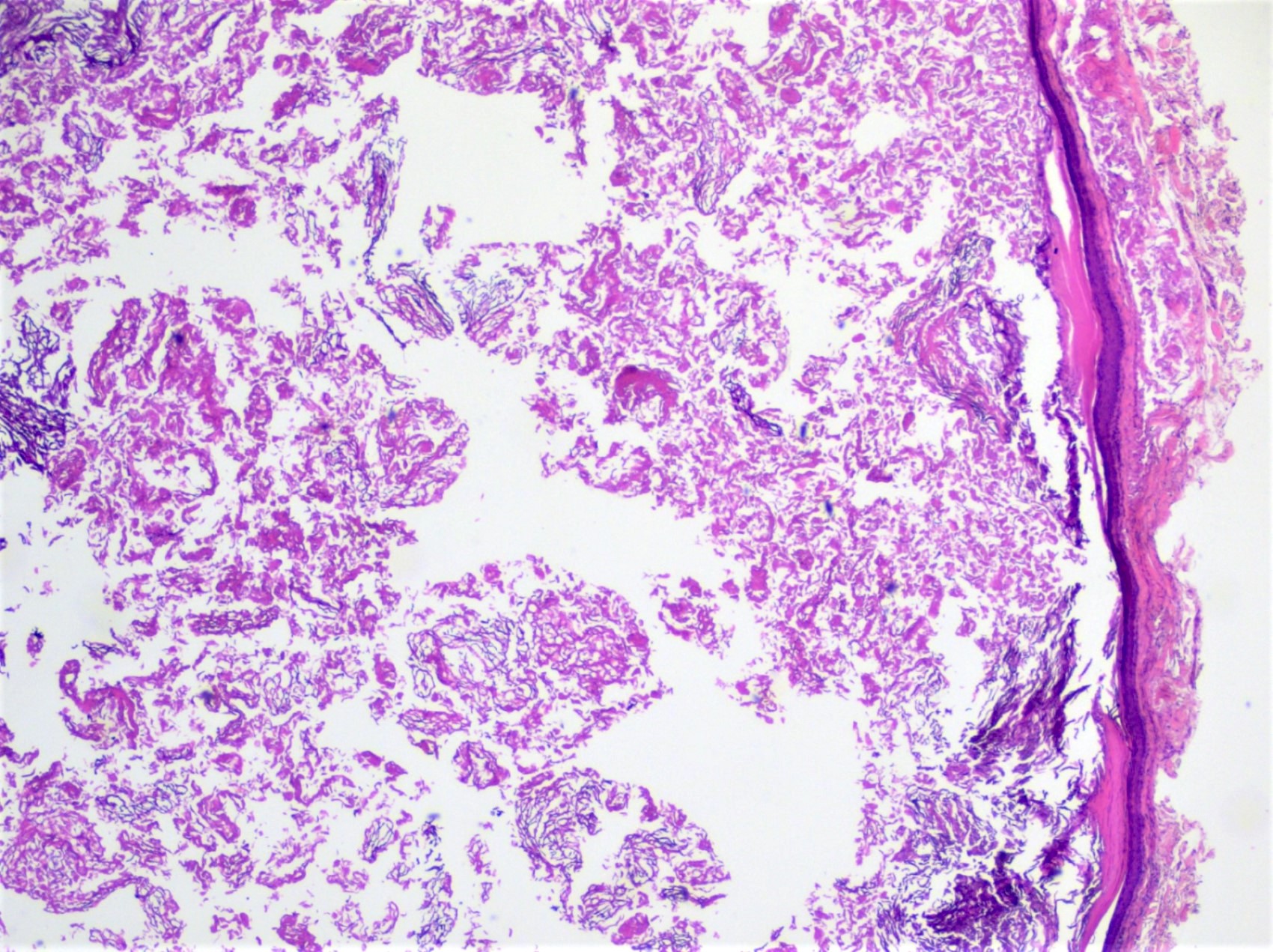
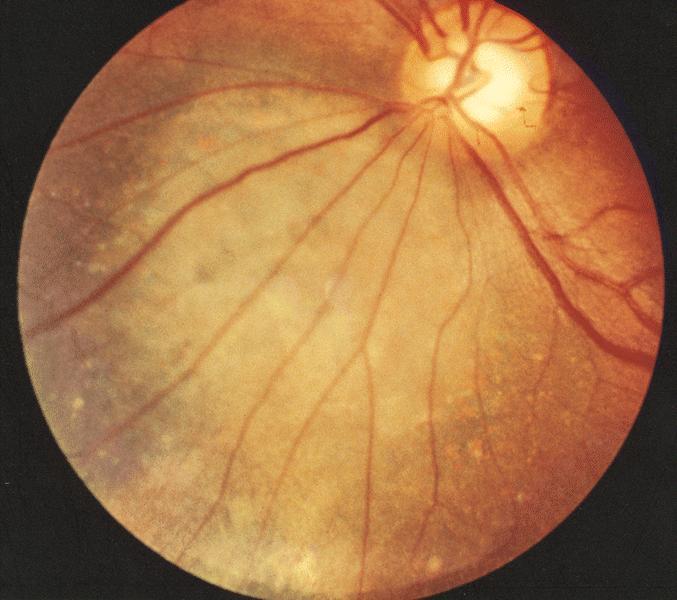
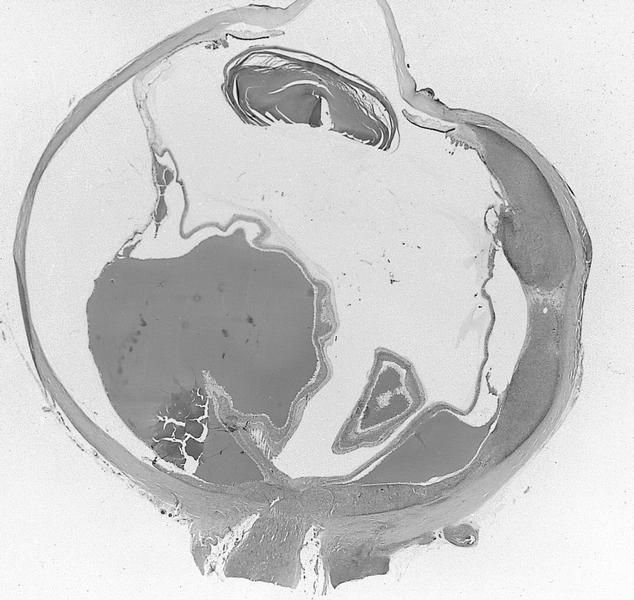
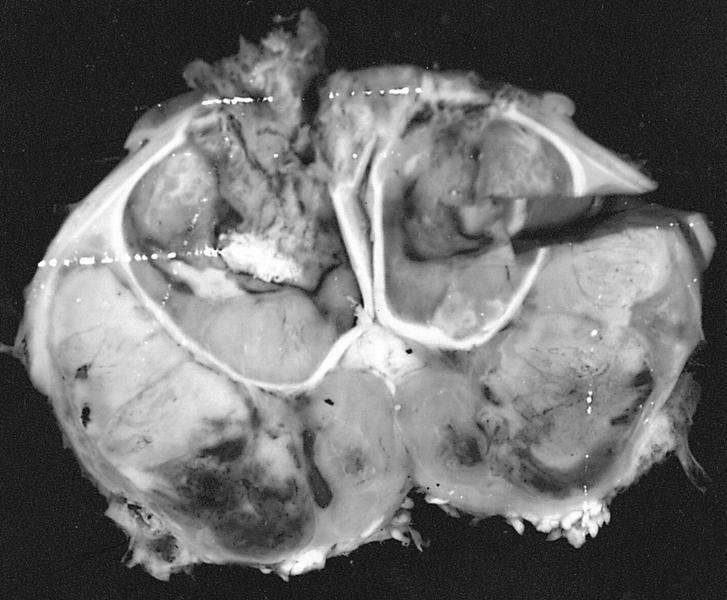
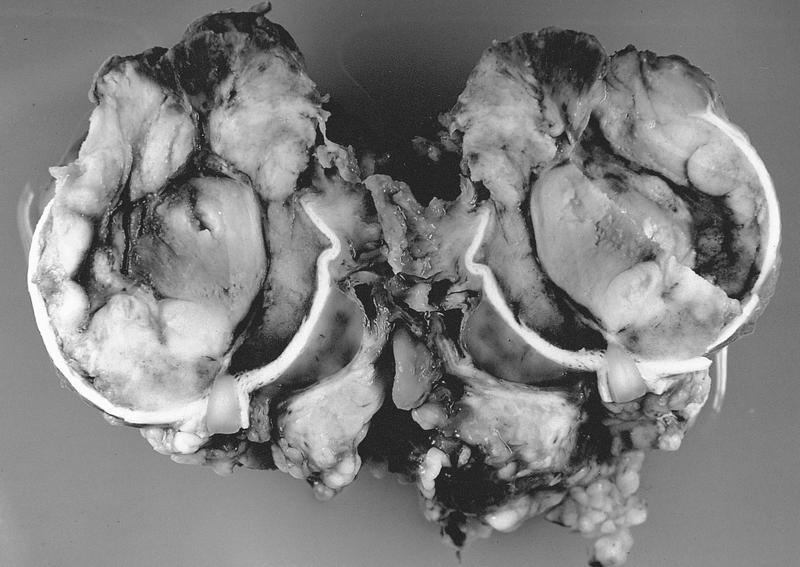
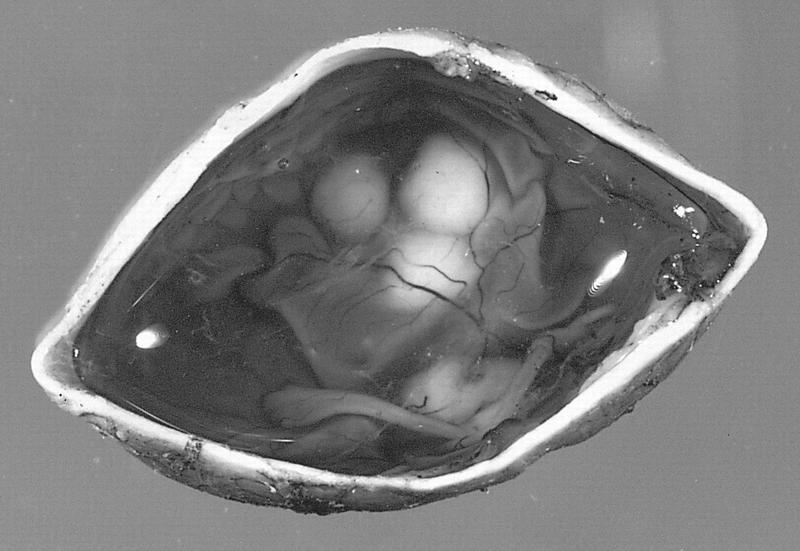
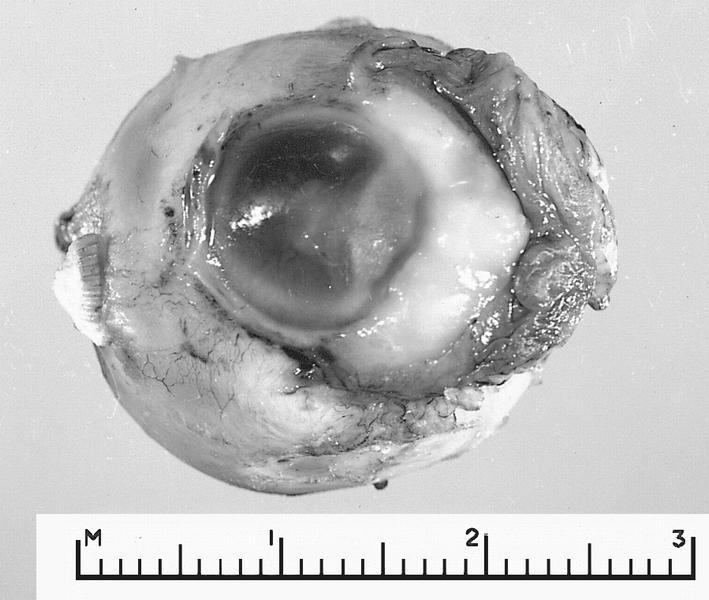
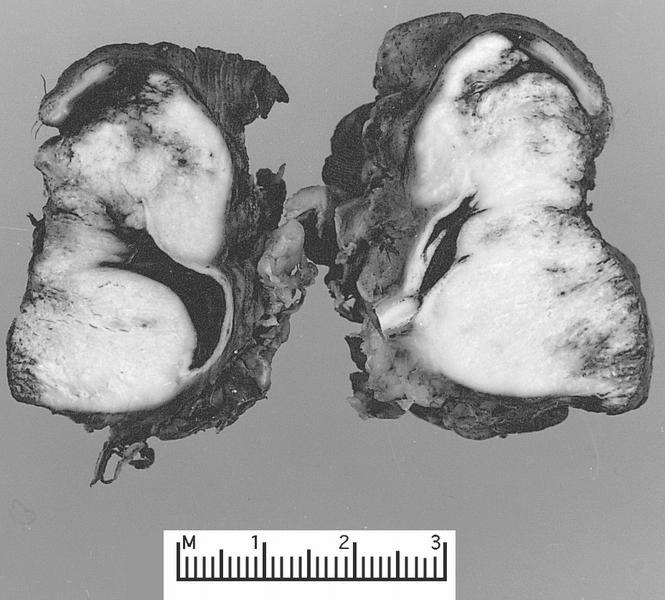
Definition / general | Radiology images | Clinical images | Gross images | Microscopic (histologic) imagesDefinition / general
- Exudative retinopathy associated with retinal detachment and telangiectatic retinal vessels
- Usually unilateral, young children and male predominant
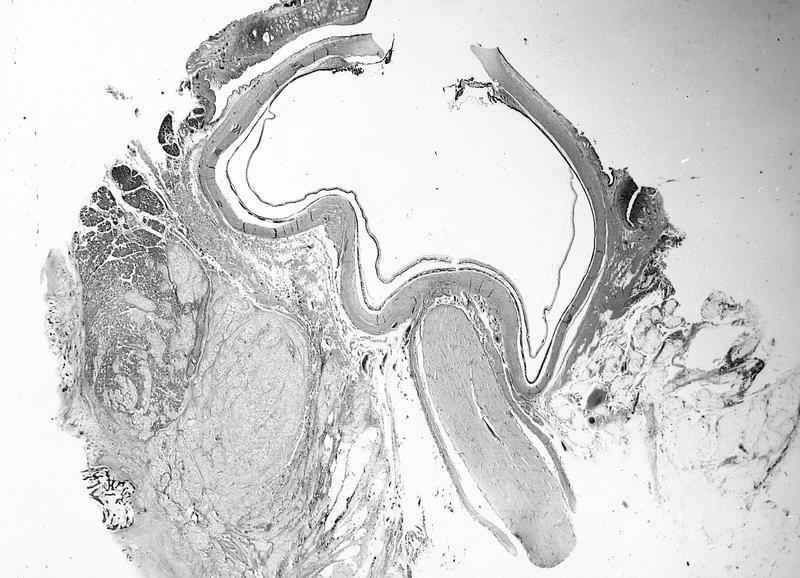
Coloboma
Definition / general
- Unilateral abnormality of optic nerve head, of congenital origin
- Complete coloboma may form large hole or posterior protrusion near optic nerve
Microscopic (histologic) description
- Large defect with mostly bare sclera, lined by fibrous or glial tissue
- May involve retina and choroid along its edges
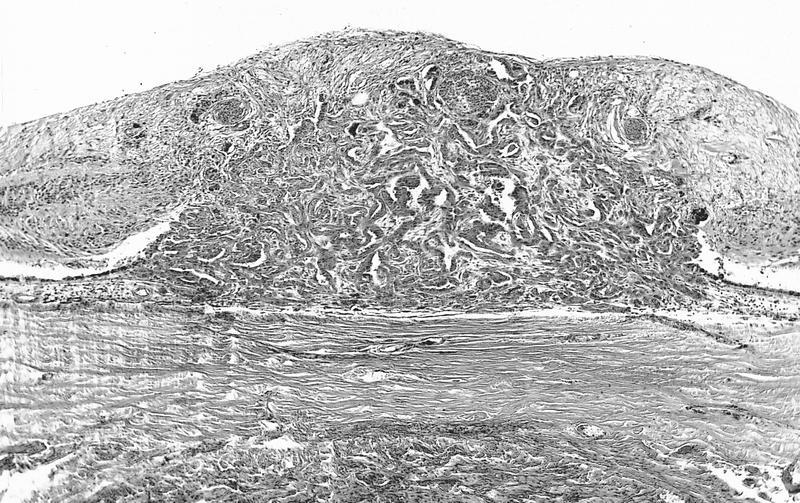
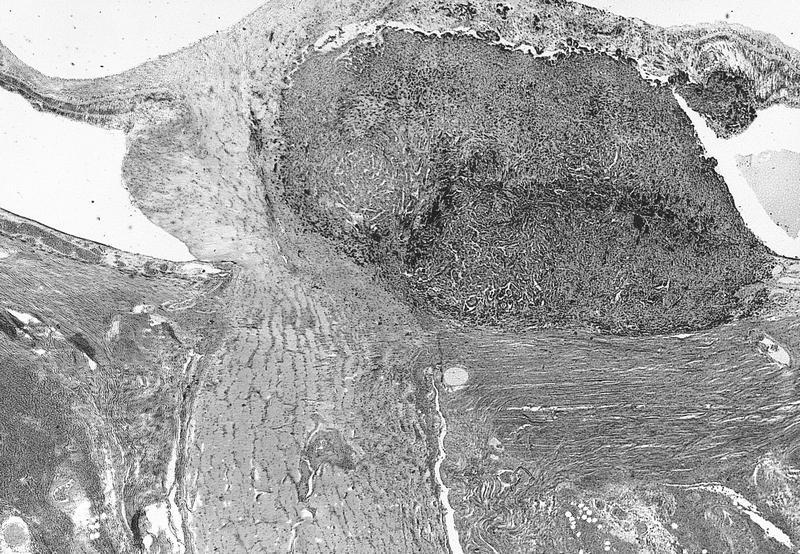
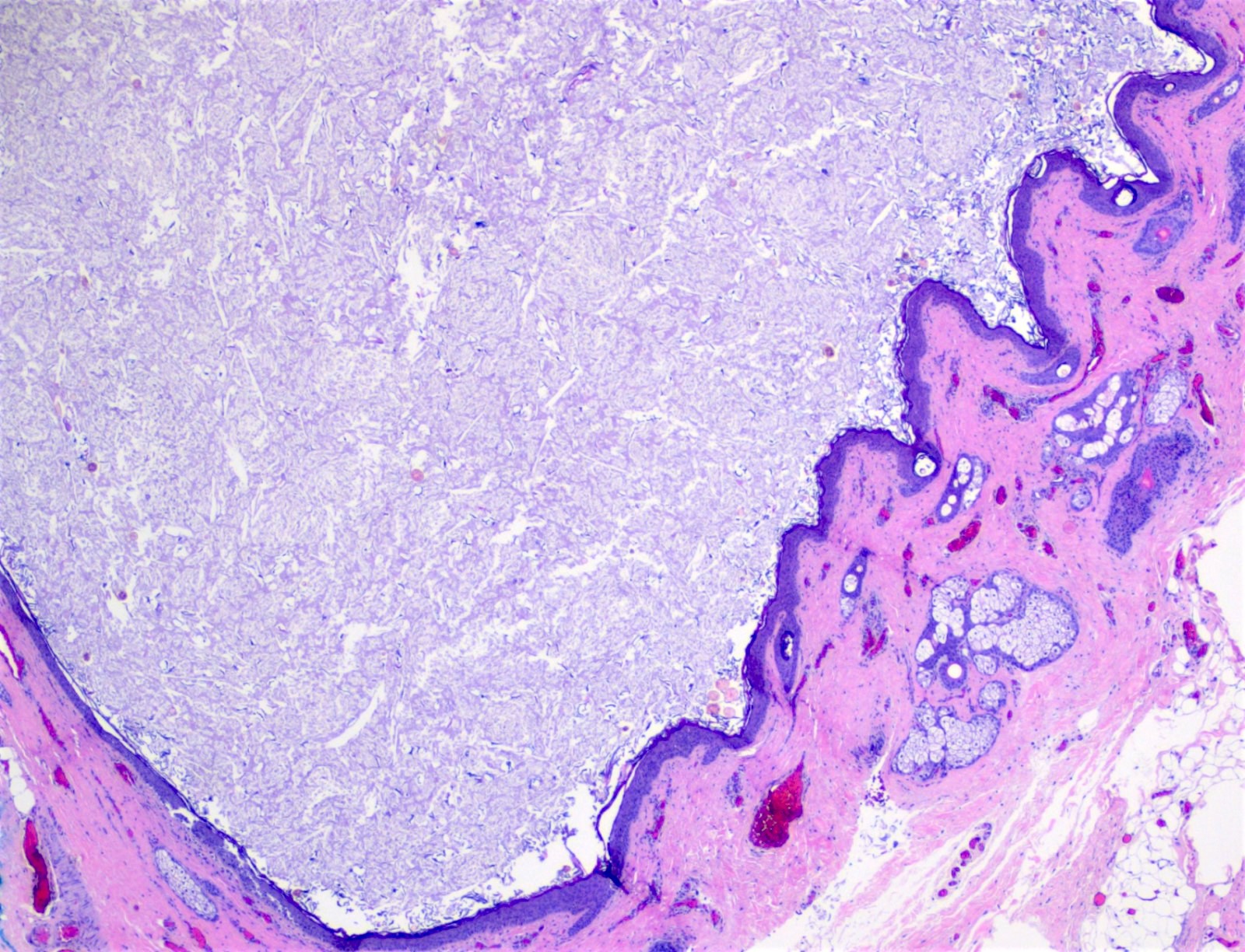
Conjunctival intraepithelial neoplasia
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
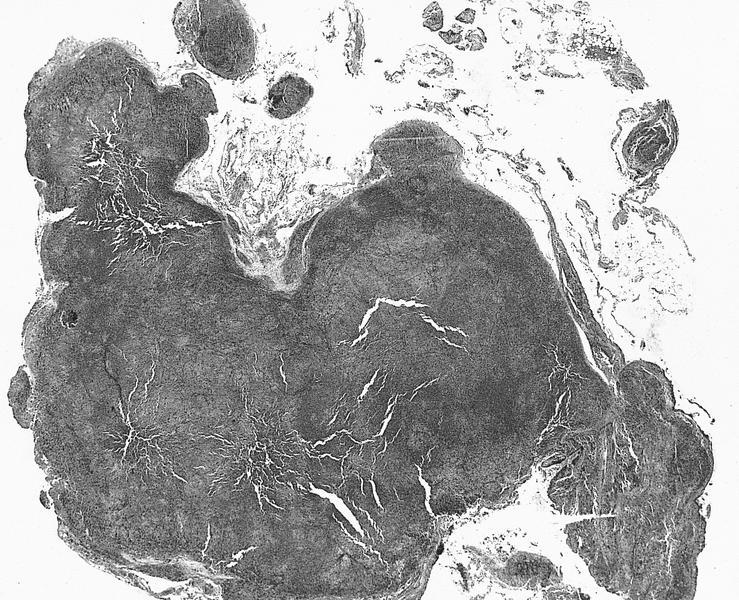
- Spectrum of abnormal growth of atypical squamous epithelial cells of the conjunctiva; graded based on thickness of epithelial involvement
- Noninvasive; epithelial basement membrane remains intact
- Considered to be a premalignant lesion that can progress to invasive squamous cell carcinoma
Essential features
- Dysplastic changes of conjunctiva
- Precursor to squamous cell carcinoma
- Typical clinical presentation is a lesion at the limbus within the interpalpebral fissure
Terminology
- Conjunctival intraepithelial neoplasia (1, 2 or 3)
- Also called conjunctival dysplasia (mild, moderate or severe), conjunctival epithelial dyskeratosis, Bowen disease
- Falls within the broad spectrum of ocular surface squamous neoplasia (OSSN), which encompasses neoplastic squamous abnormalities of the conjunctival, limbal and corneal epithelium, including squamous cell carcinoma
ICD coding
Epidemiology
- Estimated incidence is 17 - 20 cases per 1 million person years (Arch Ophthalmol 1992;110:525)
- Incidence rate varies worldwide; highest rates in Africa (3.4 cases per 100,000 per year in Zimbabwe) (Trop Med Int Health 2013;18:1424)
- Reported incidence of OSSN was 0.53 cases/million/year (conjunctival intraepithelial neoplasia: 0.43 cases/million/year; squamous cell carcinoma: 0.08 cases/million/year) in the United Kingdom (Eye (Lond) 2019;33:283)
- Third most common conjunctival lesion in adults (after pterygium and nevus) (Cornea 1987;6:78)
- 2 disease patterns:
- In northern high latitude areas, mostly affects elderly males
- Close to the equator, males and females are equally affected at a younger age; also associated with HIV
- Occurs at a younger age and with more aggressive clinical course in patients with xeroderma pigmentosum and HIV (Graefes Arch Clin Exp Ophthalmol 2011;249:1217, Ophthalmology 2015;122:1688)
- HIV testing should be considered in patients < 40 years old with no other risk factors
- Risk factors include exposure to UV light, especially in light skinned individuals, human papillomavirus infection (HPV 16 / 18), immunosuppression, tobacco use, vitamin A deficiency, ocular surface injury and exposure to petroleum products (Ophthalmology 1994;101:360, Ophthalmology 2002;109:542, Cornea 2003;22:687)
Sites
- Typically occurs in the bulbar conjunctiva in the interpalpebral fissure (sun exposed area) arising at the limbus (where stem cells reside)
- Can spread onto the cornea
- Occasionally occurs in the forniceal or palpebral conjunctiva
- Reference: Am J Ophthalmol 2017;173:106
Pathophysiology
- Arises from conjunctival epithelial cells that originate from the ocular surface ectoderm
- Preferred limbal location suggests that most cases arise from limbal stem cells; limbal stem cells are sensitive to oncogenic factors and are susceptible to DNA alterations secondary to UV light
- Reference: Exp Eye Res 2014;129:172
Etiology
- Appears to be multifactorial, involving a variety of environmental factors in a susceptible host
- Acquired condition linked to chronic ultraviolet B radiation exposure
- Deficiency of DNA repair in xeroderma pigmentosum confers an increased risk
- Reference: Asia Pac J Ophthalmol (Phila) 2017;6:109
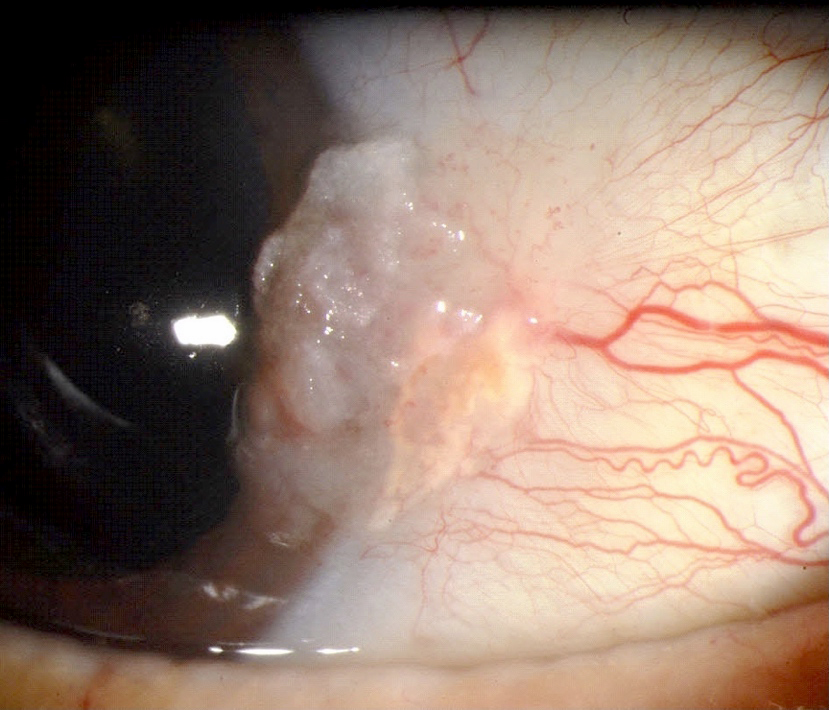
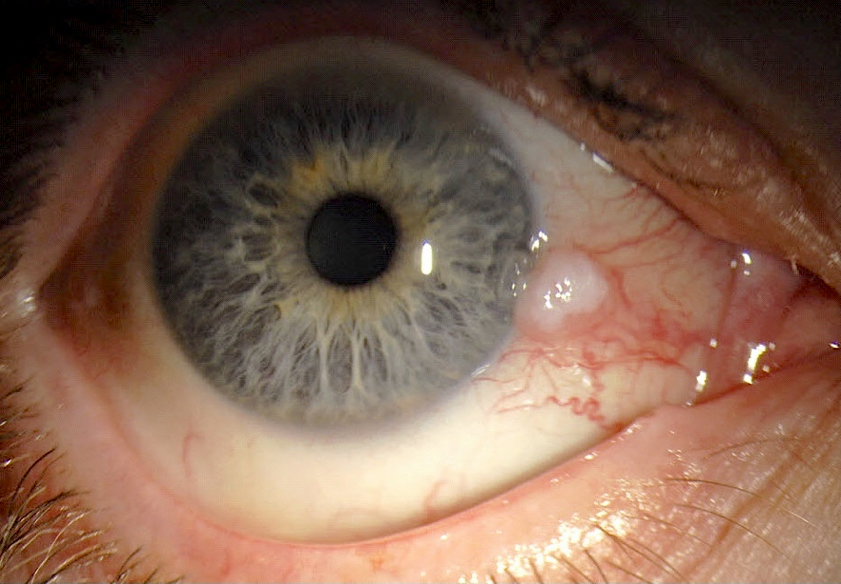
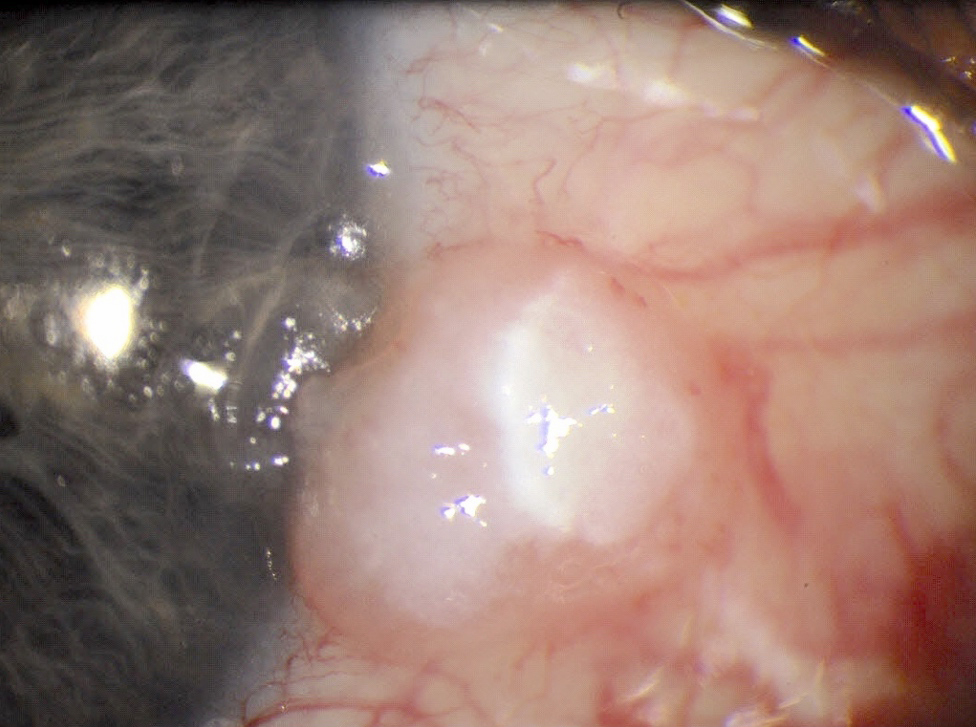
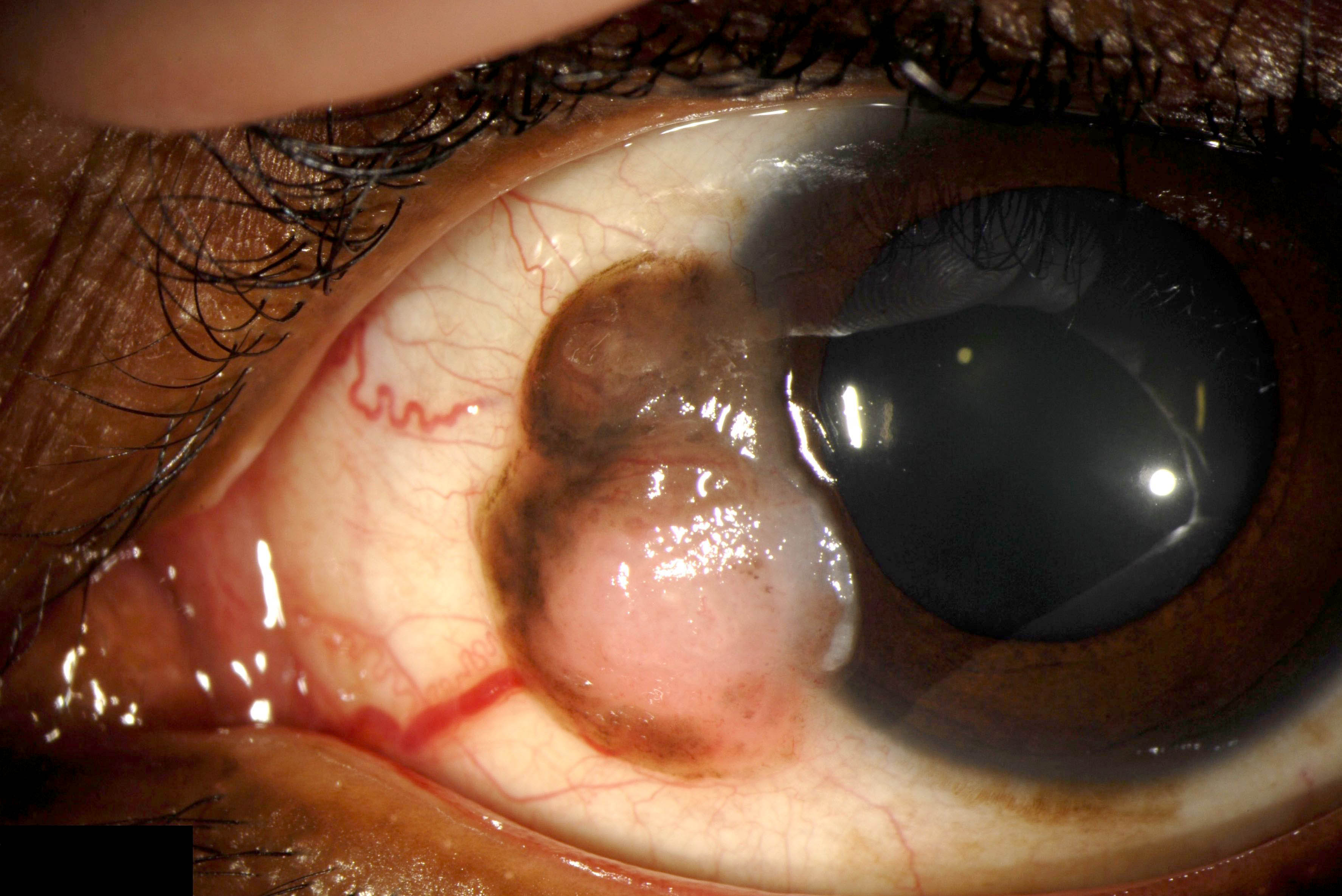
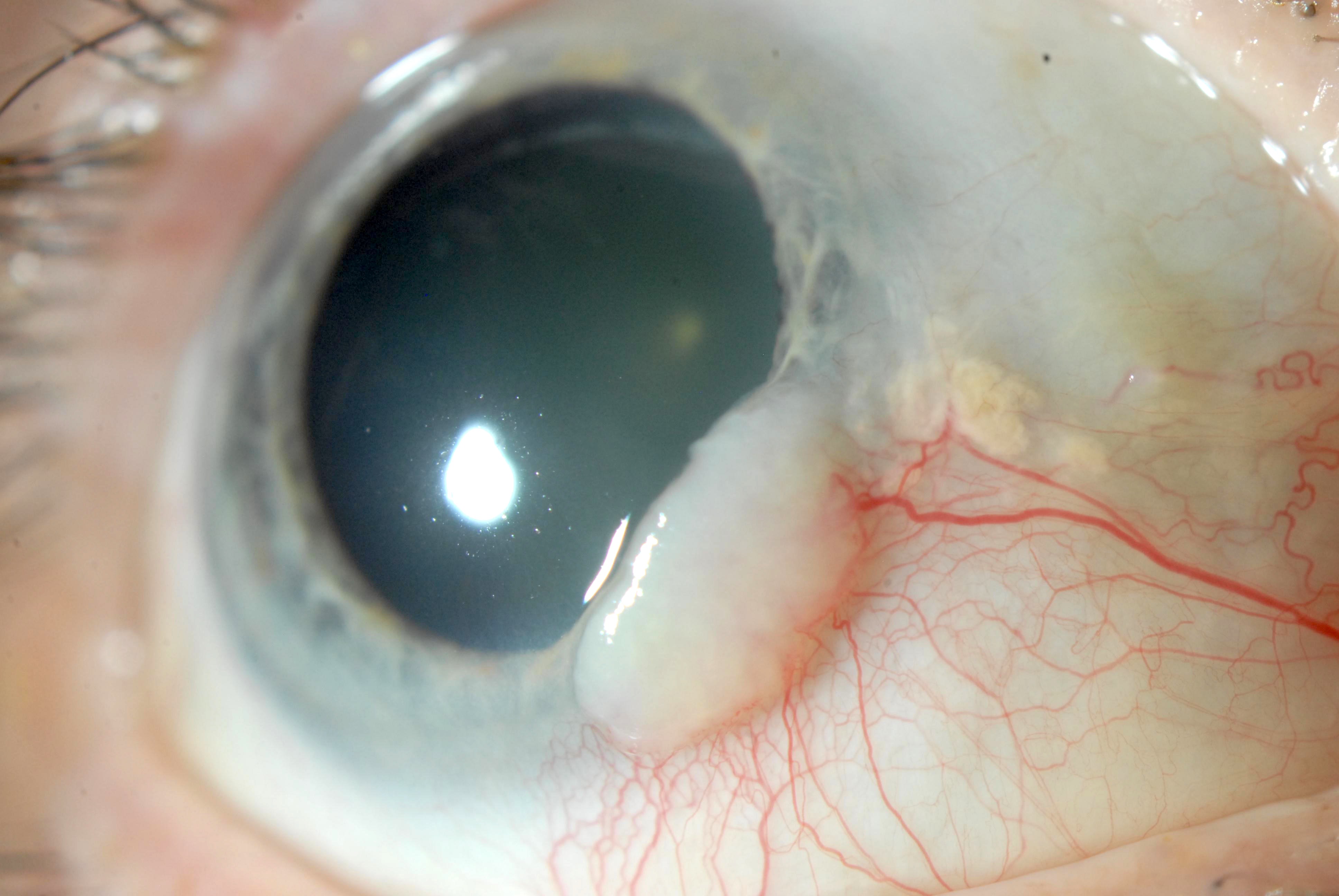
Clinical features
- Fleshy, gray or white conjunctival lesion
- May be elevated or flat
- May appear gelatinous, leukoplakic, papilliform or diffuse (Optometry 2011;82:15)
- Lesions commonly have associated feeder vessels
- Lesions may be pigmented and resemble melanoma due to intratumoral pigmented dendritic melanocytes (Ophthalmology 2008;115:1673)
- Moves freely over the underlying episclera, unlike invasive carcinoma, which is fixed (Optometry 2011;82:15)
Diagnosis
- Histopathologic evaluation of excised tissue to confirm the diagnosis
- Exfoliative cytology and in vivo confocal microscopy are safe, noninvasive and effective diagnostic tools (Am J Ophthalmol 2009;148:772, Eye (Lond) 2012;26:781, Am J Ophthalmol 2011;151:238)
Prognostic factors
- Recurrence associated with higher grade lesions, tumors and positive margins (Ophthalmology 2012;119:1974, Ophthalmology 2012;119:233)
- Recurrence rate 5 - 33% with negative margins and 53 - 56% with positive margins (Ophthalmology 1986;93:176, Ophthalmology 1997;104:485)
- Actinic keratosis growth pattern has a good prognosis while diffuse growth pattern has poorer prognosis with more recurrences because tumoral margin is not well defined
Case reports
- 41 year old HIV positive man with low CD4 counts presented with conjunctival epithelial dysplasia and viral retinitis (Indian J Ophthalmol 2019;67:116)
- 45 year old woman with a history of HPV 16 presented with bilateral conjunctival squamous cell carcinoma in situ (Ophthalmic Plast Reconstr Surg 2018;34:e1)
- 48 year old white man with a leukoplakic conjunctival growth 3 months after total body phototherapy for mycosis fungoides (MF) (Am J Ophthalmol Case Rep 2019;14:98)
- 56 year old woman with conjunctival intraepithelial neoplasia presented as a pigmented conjunctival lesion (Case Rep Ophthalmol 2021;12:77)
- Man with conjunctival lesion and history of basal cell carcinoma (Ophthalmology 2015;122:1039)
Treatment
- Surgical excision using a no touch technique with 2 - 4 mm margins, alcohol application and supplemental surgical margin cryotherapy (Arch Ophthalmol 1997;115:808)
- Topical interferon alpha 2b, mitomycin or 5-fluorouracil (Ophthalmology 2008;115:1291, Ophthalmology 2007;114:976, Br J Ophthalmol 2017;101:1094)
Clinical images
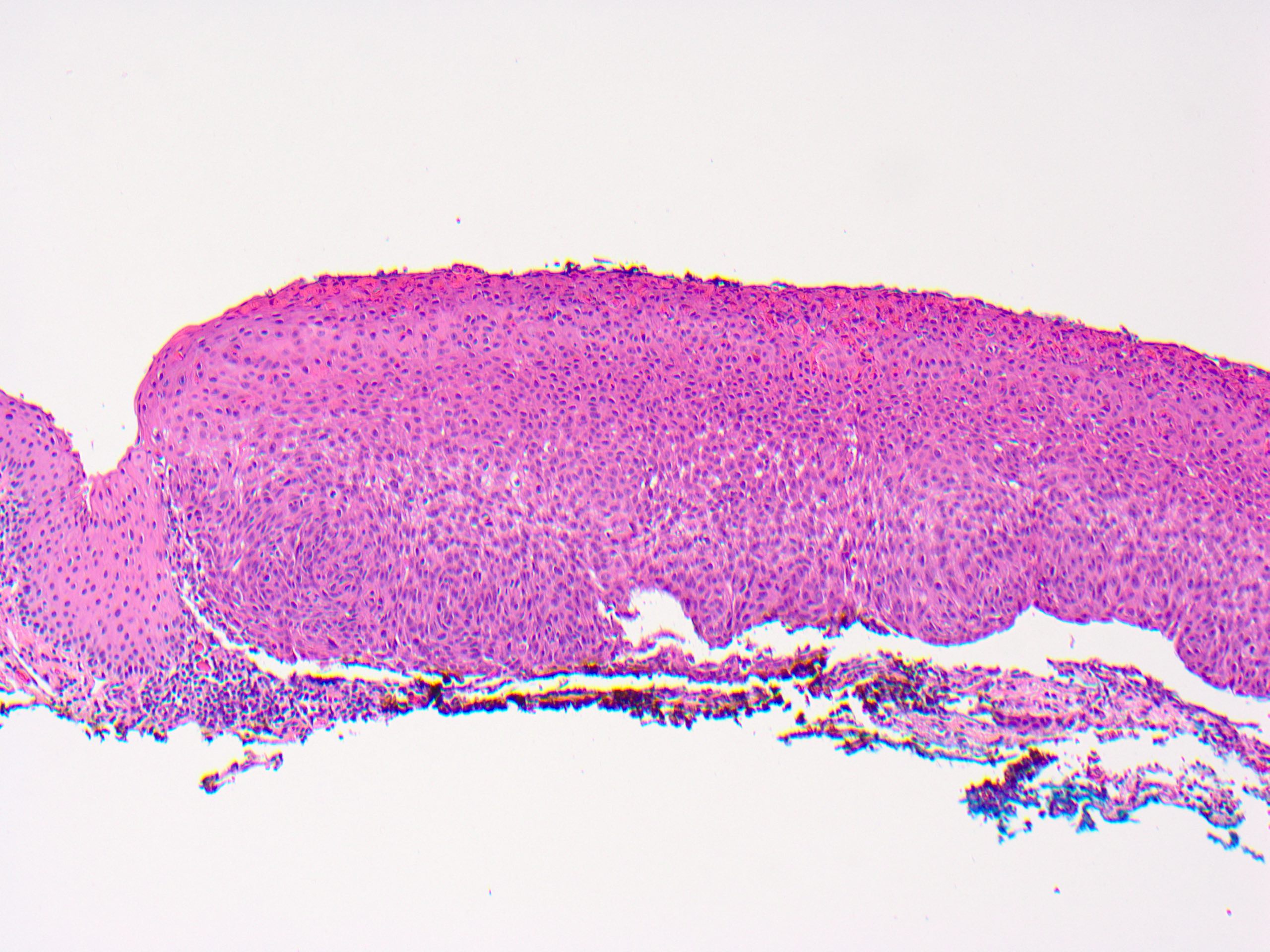
Gross description
- Gelatinous, translucent or granular appearance of conjunctiva
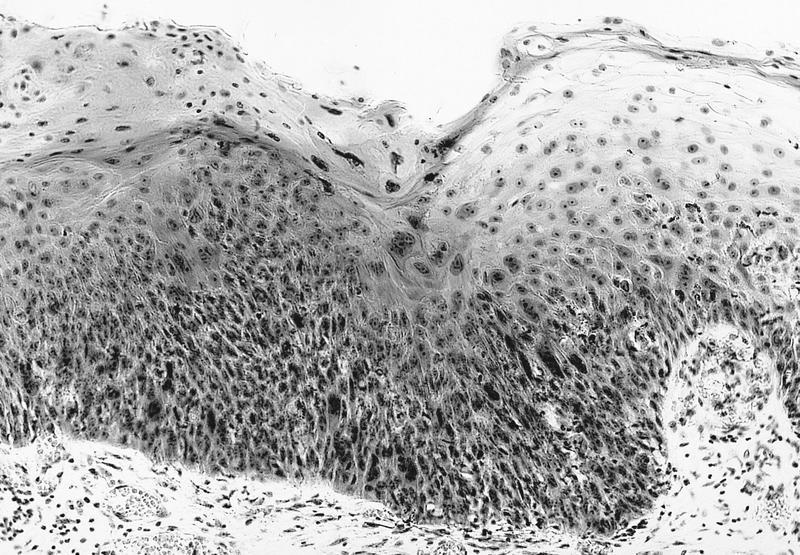
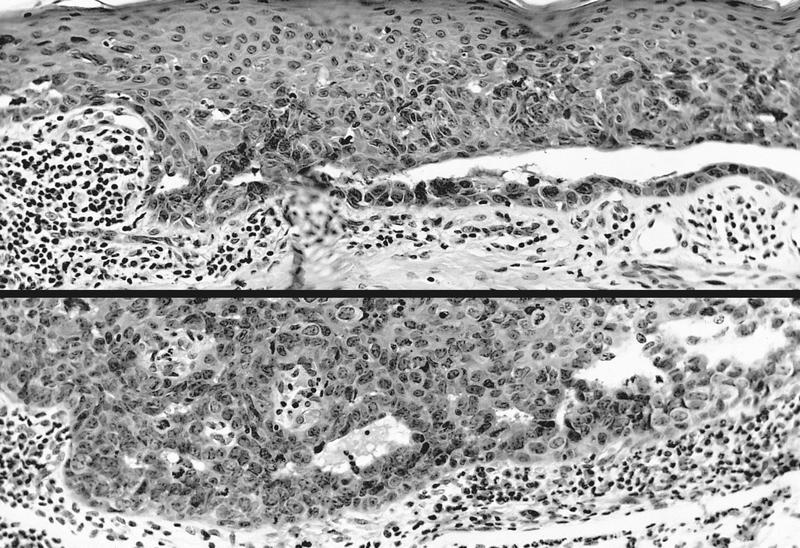
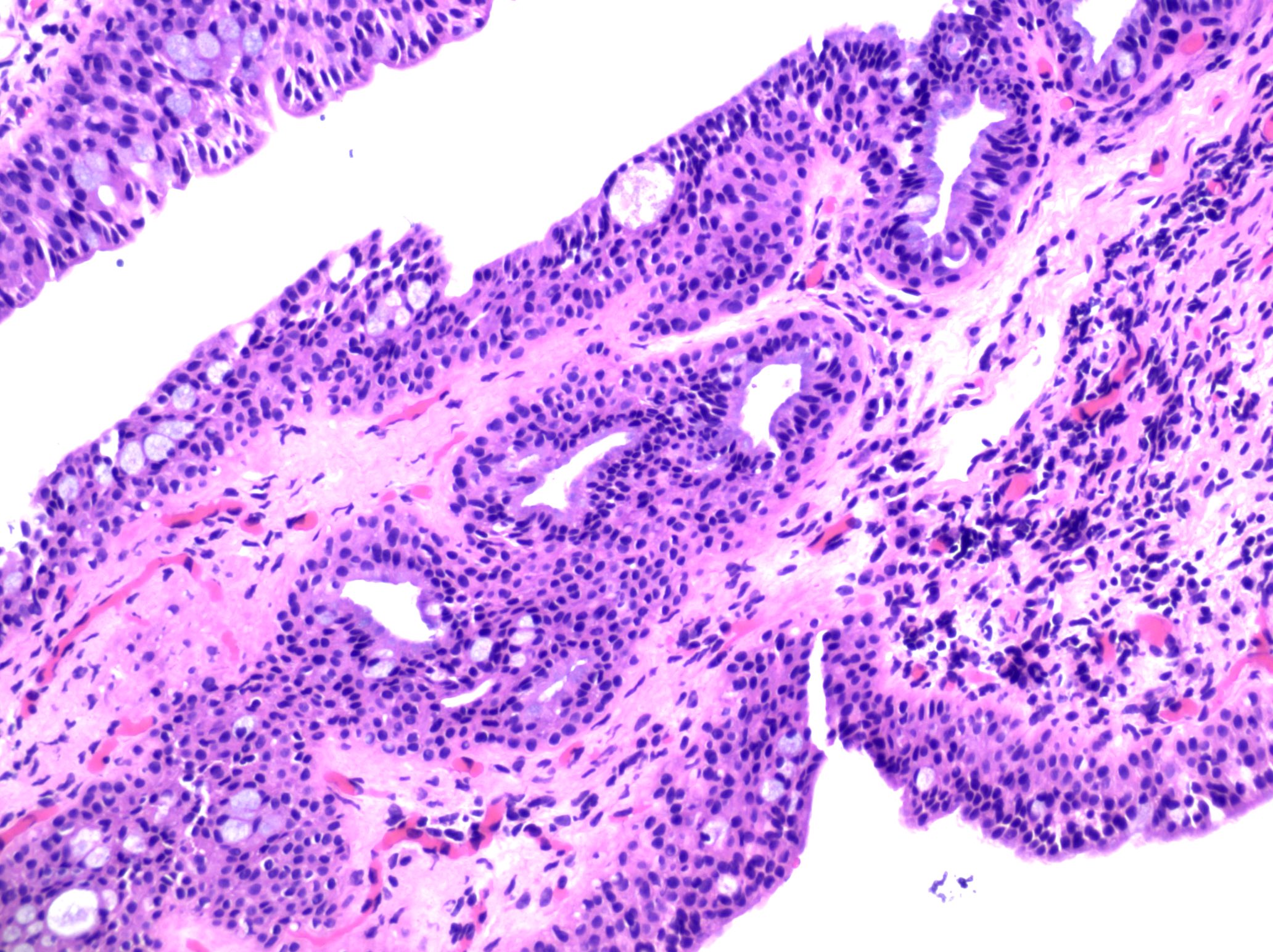
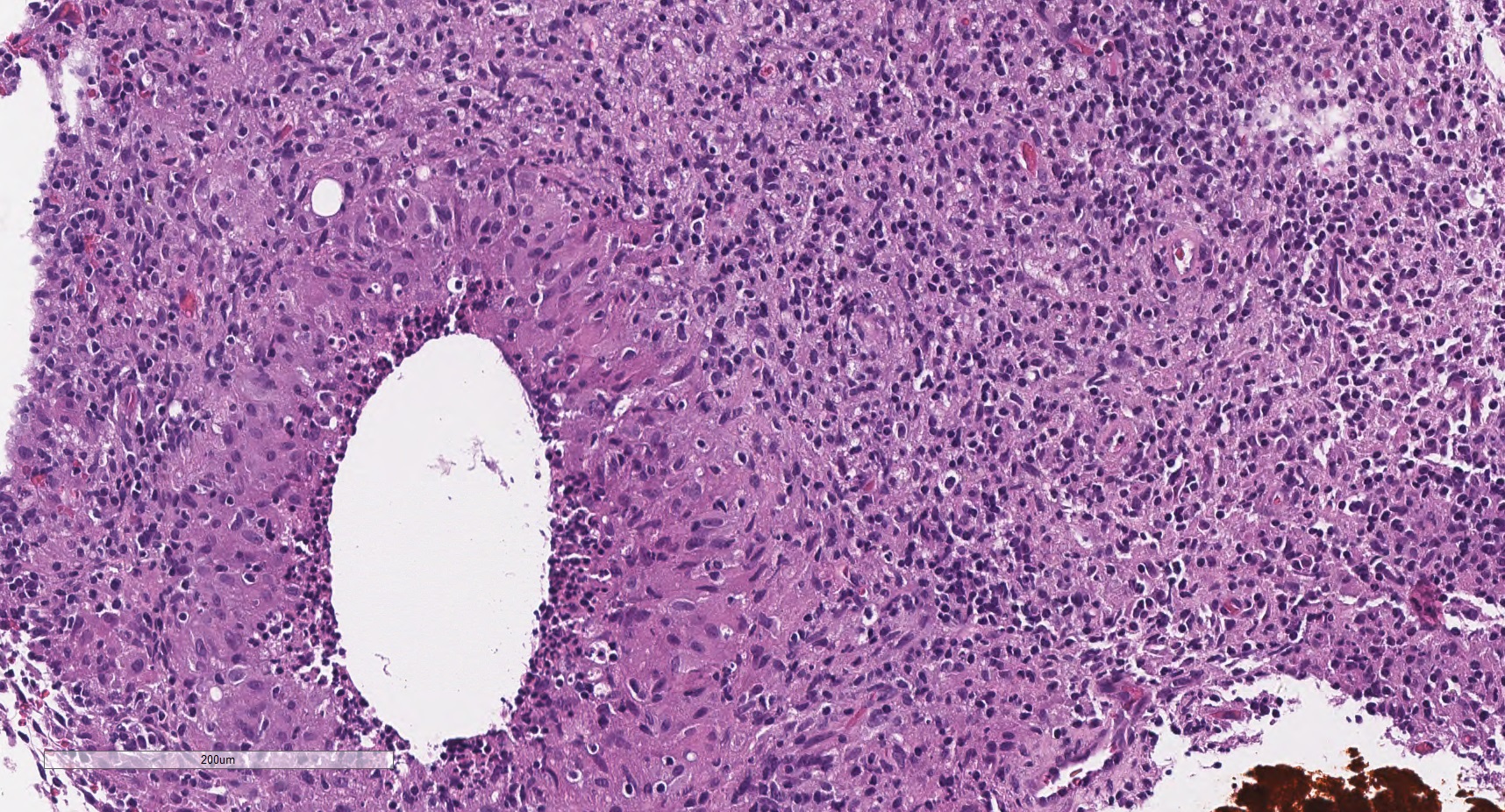
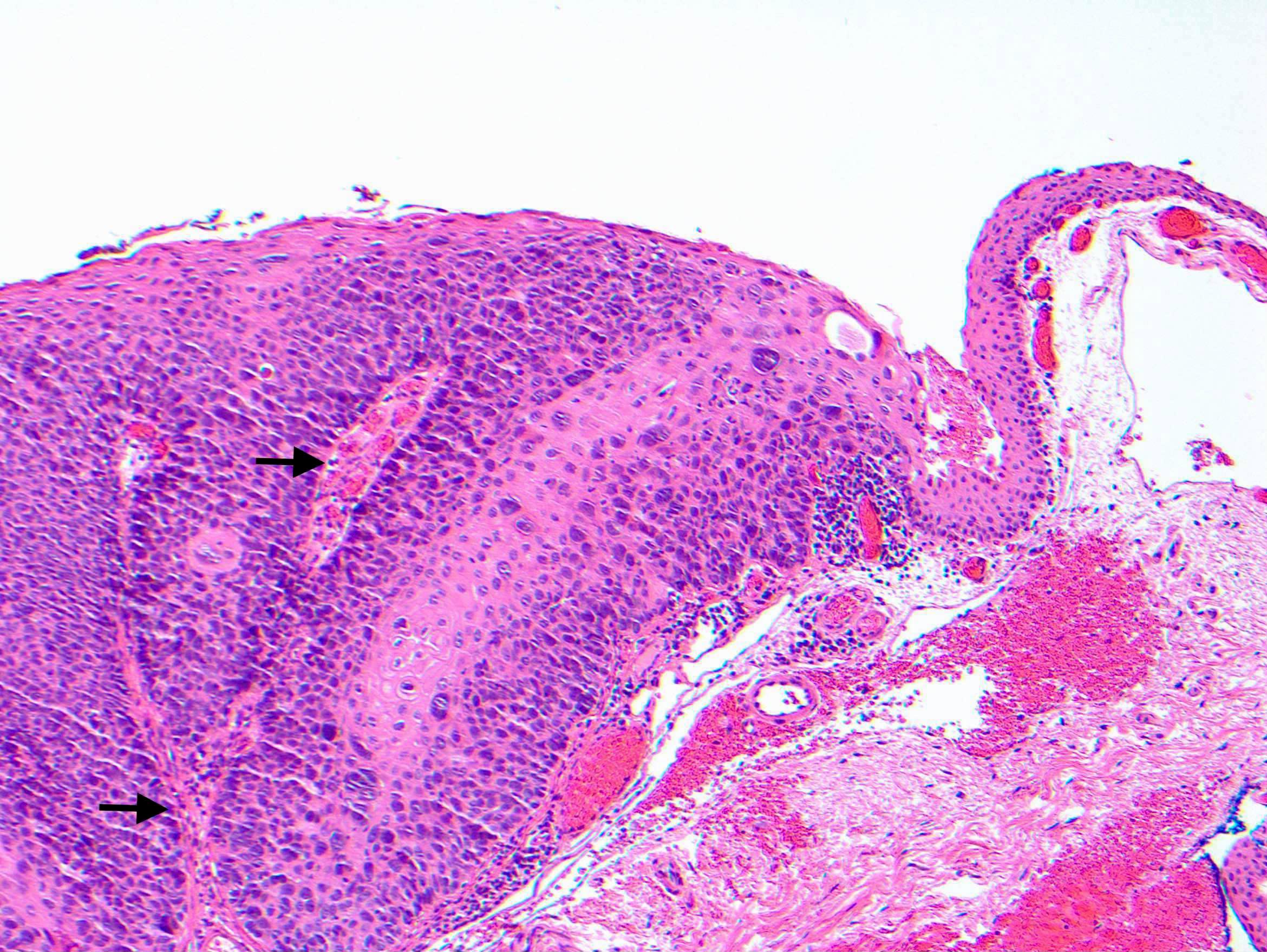
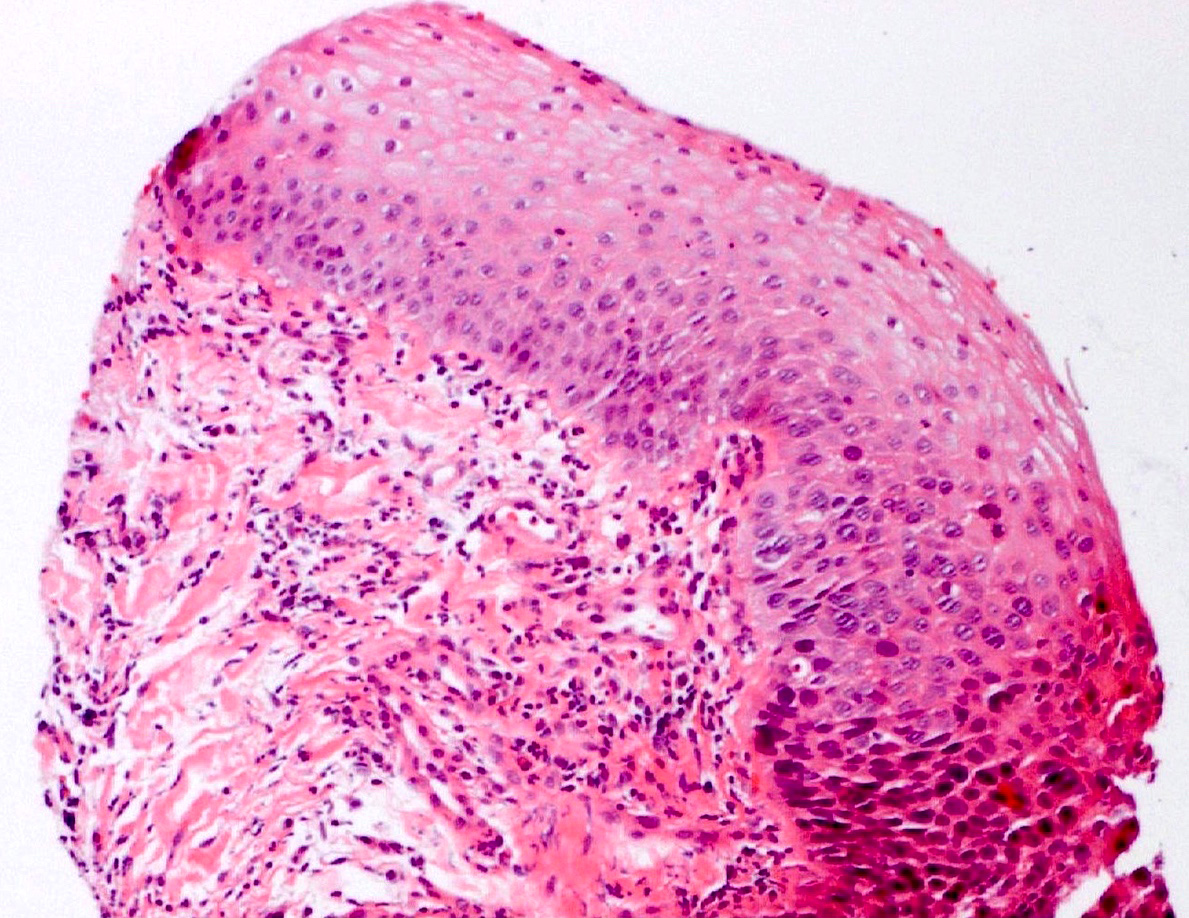
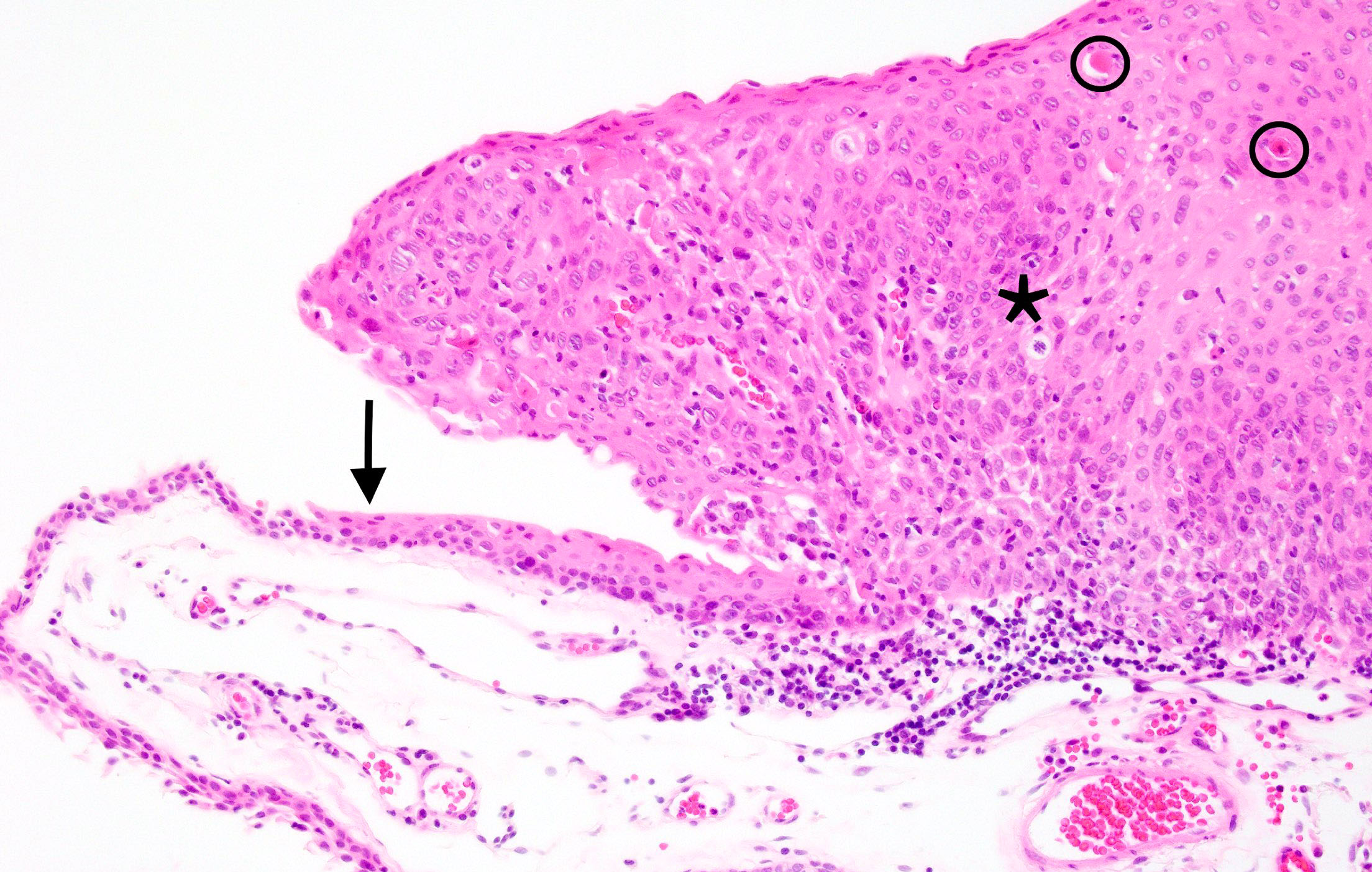
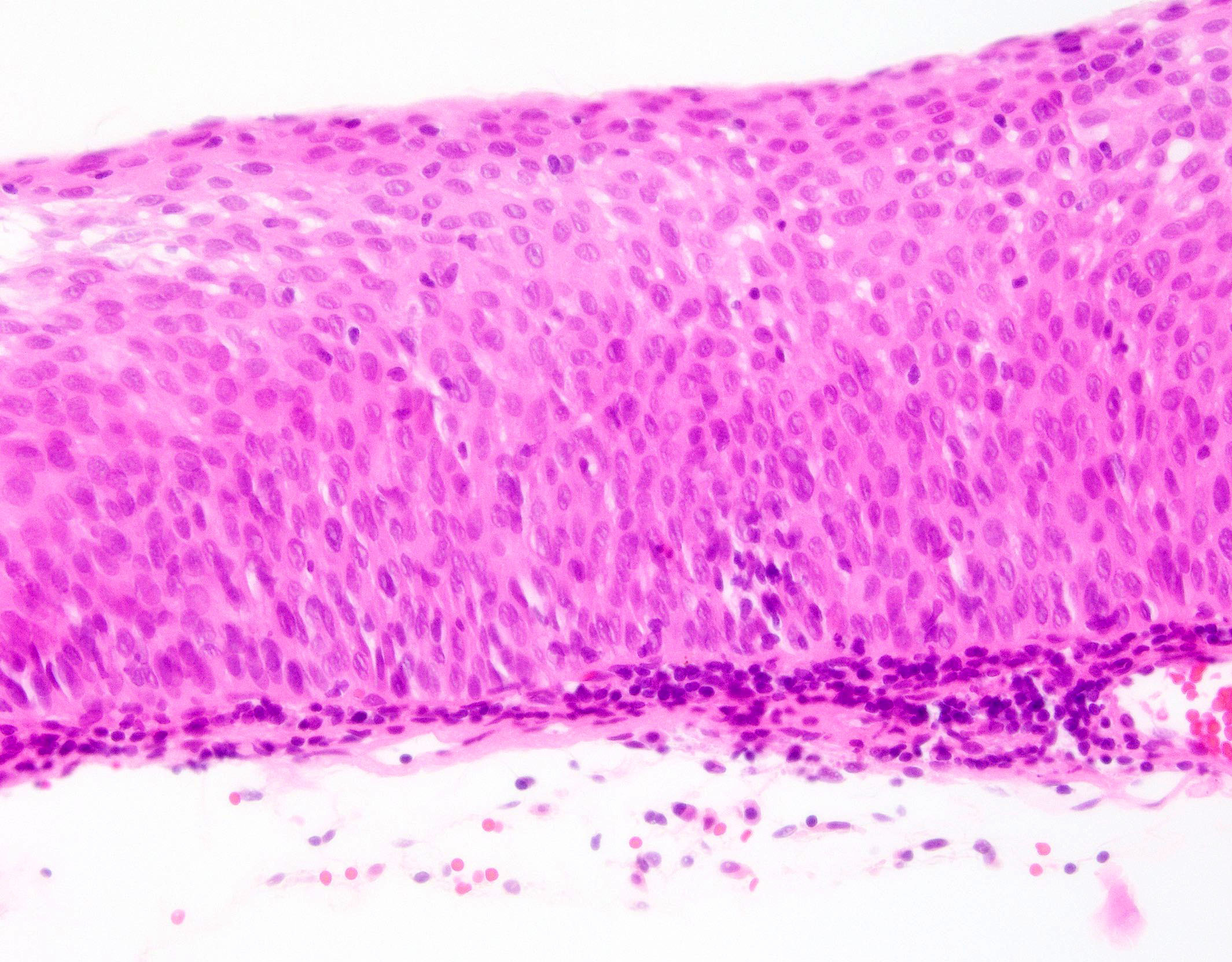
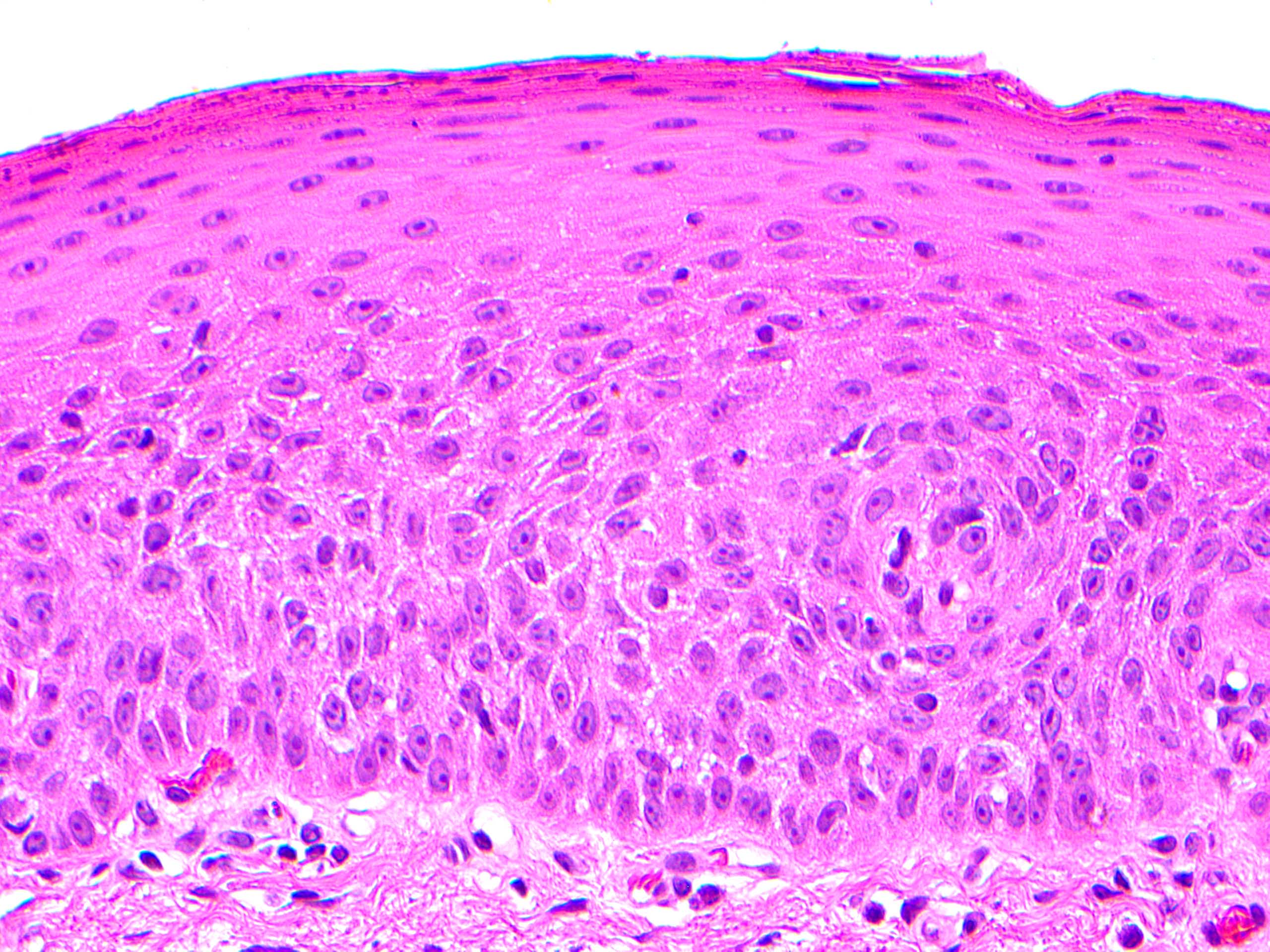
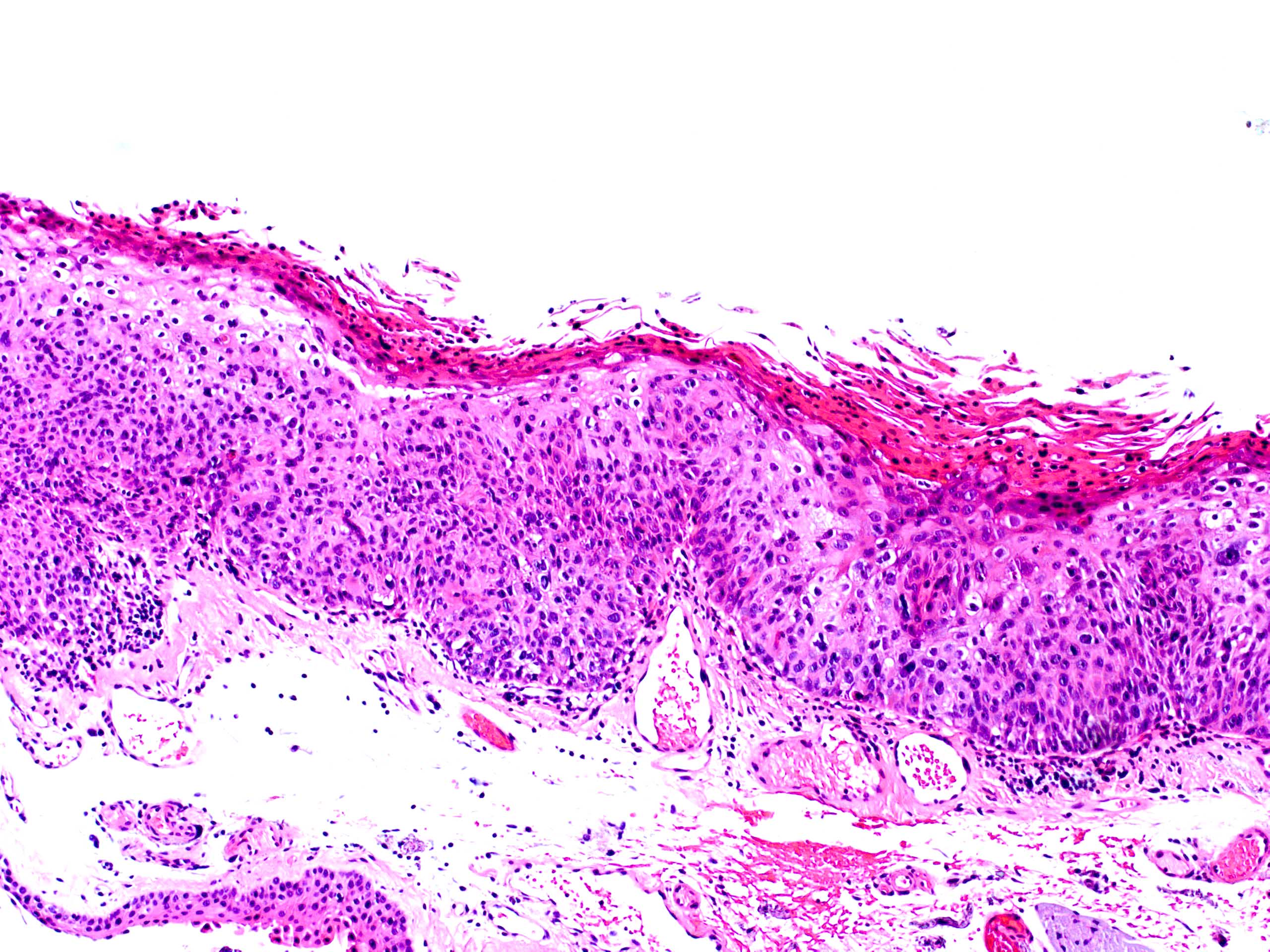
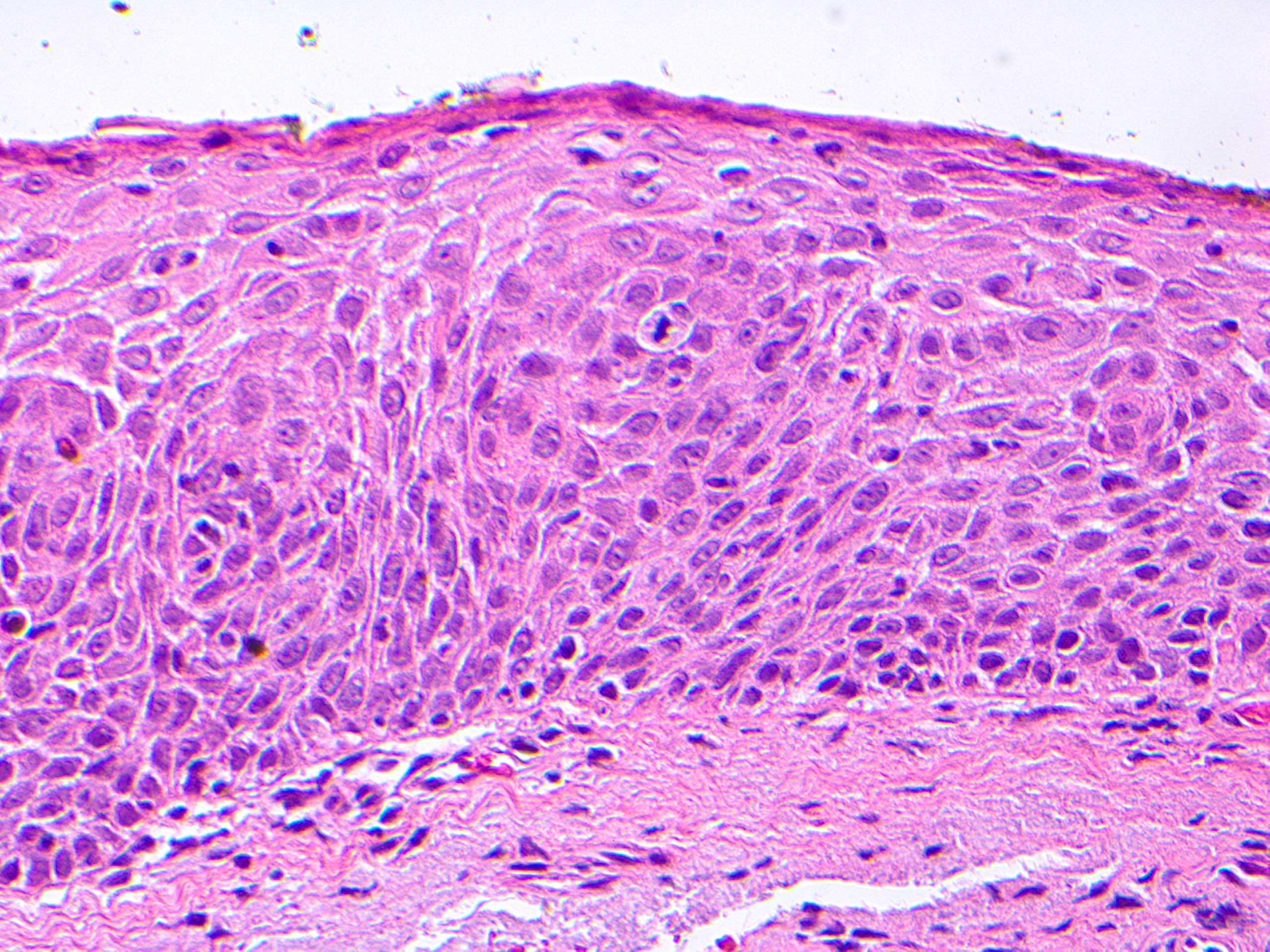
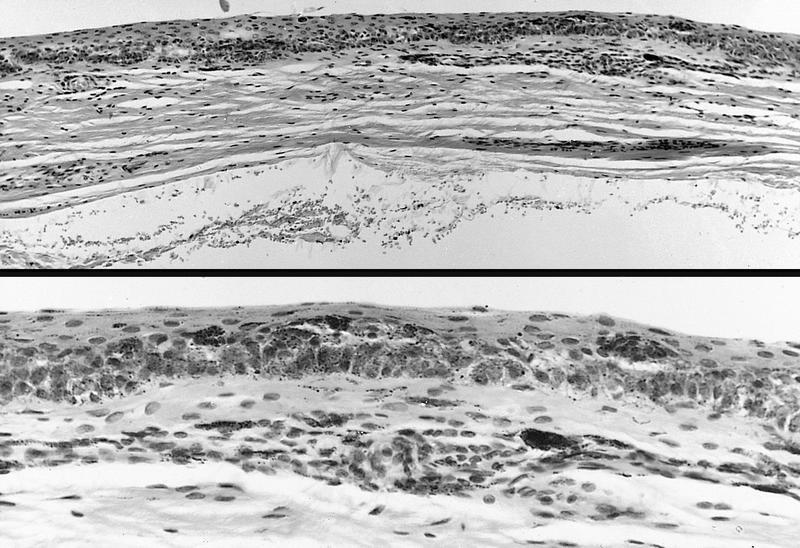
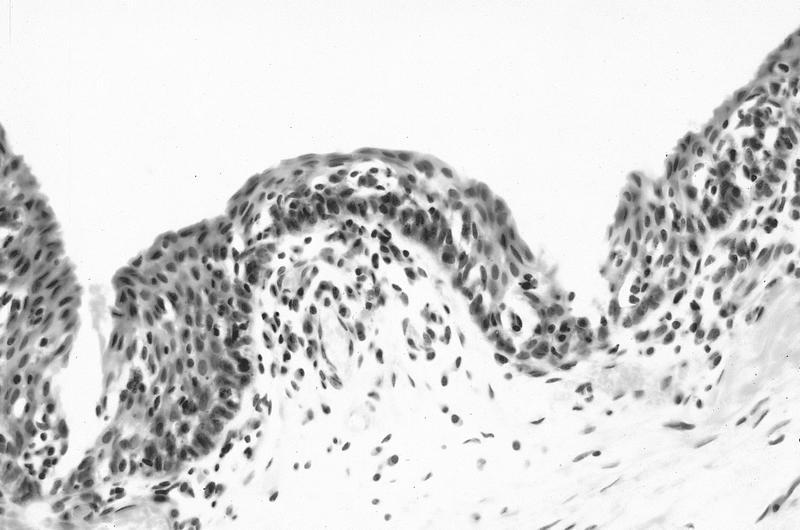
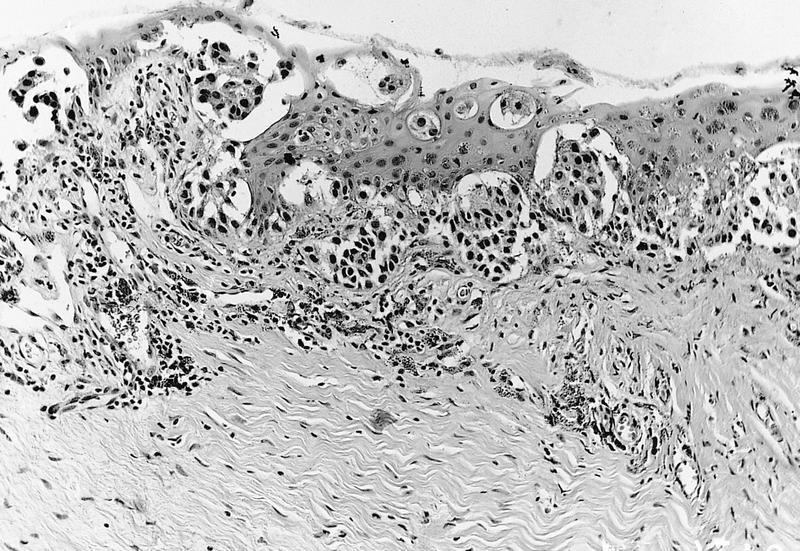
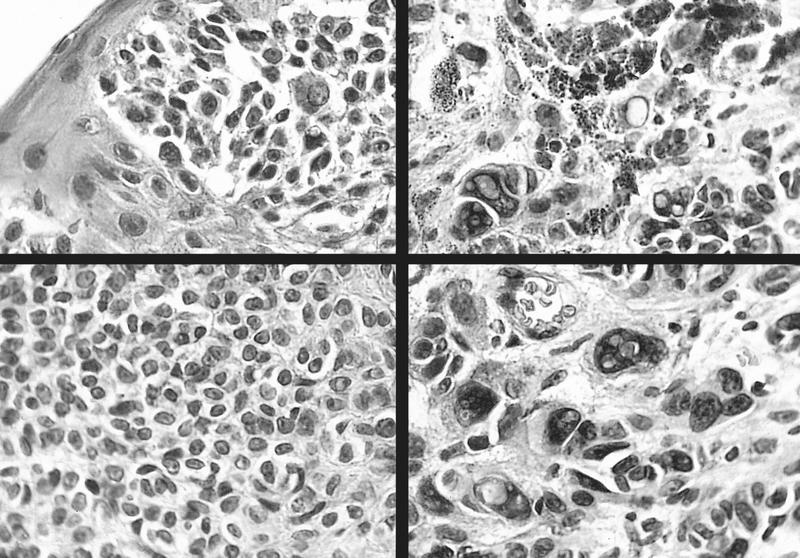
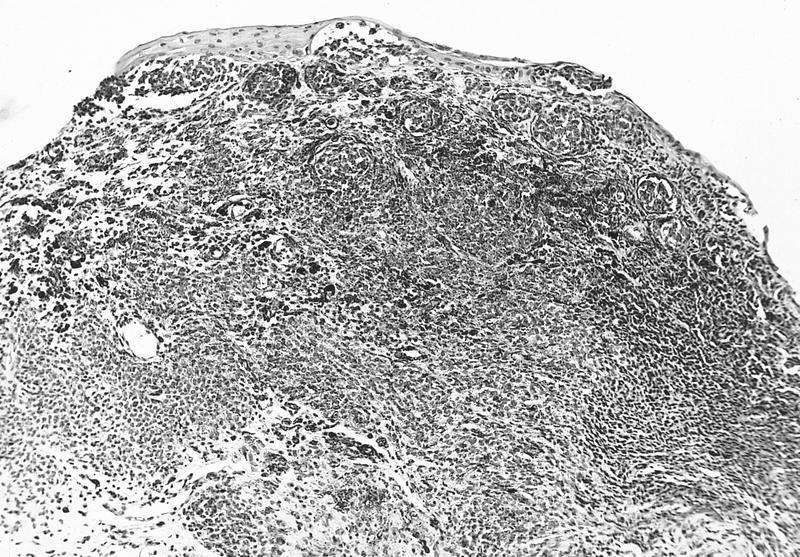
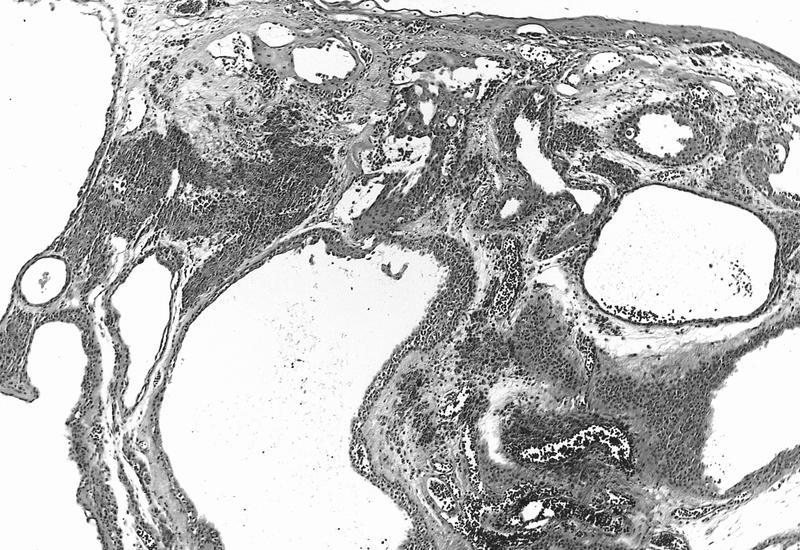
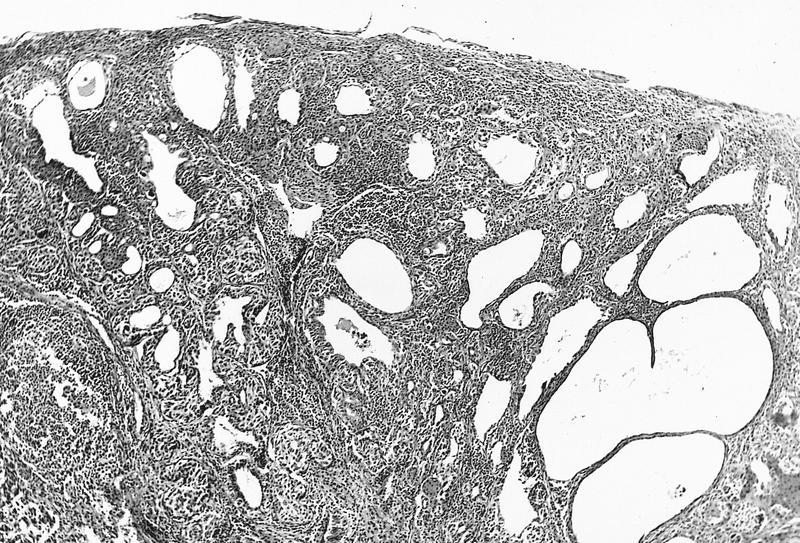
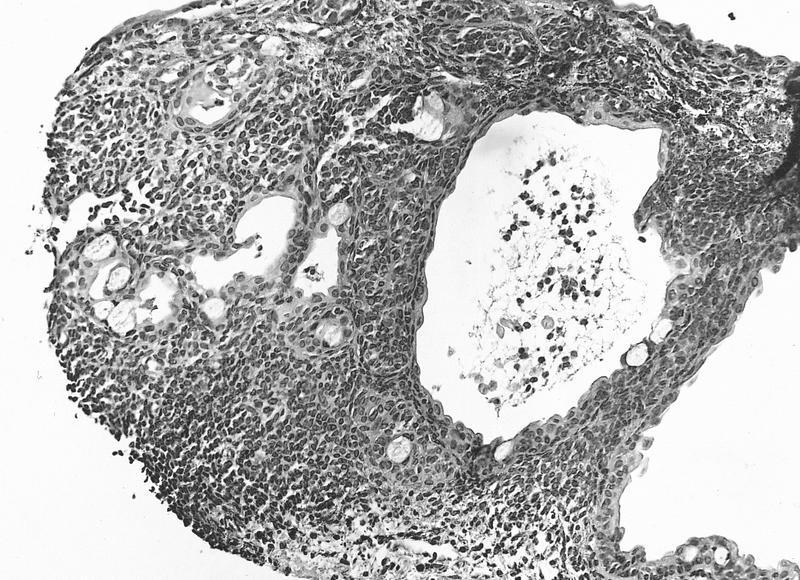
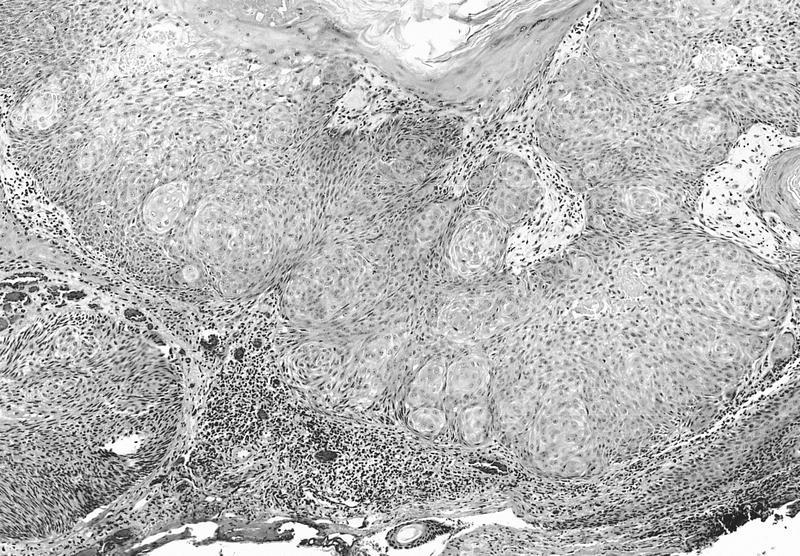
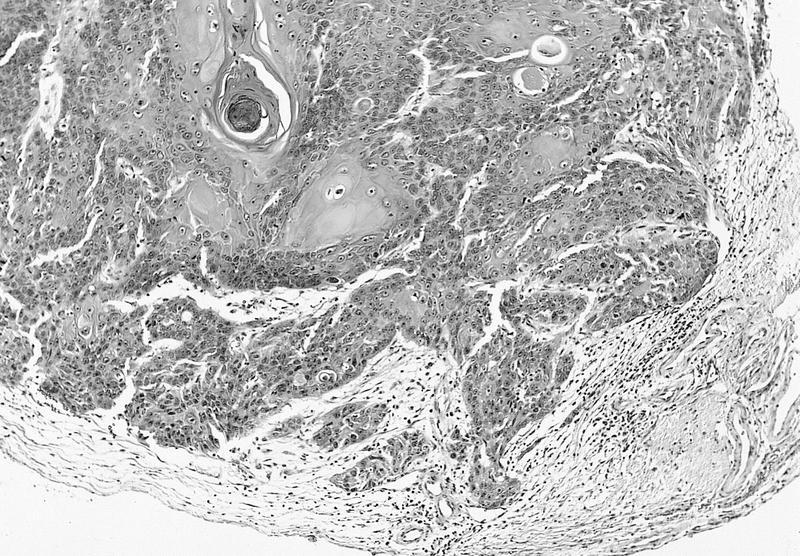
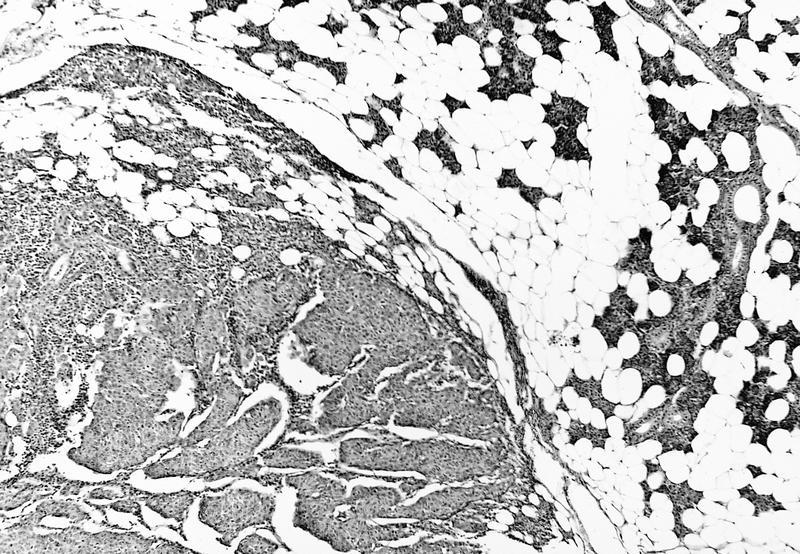
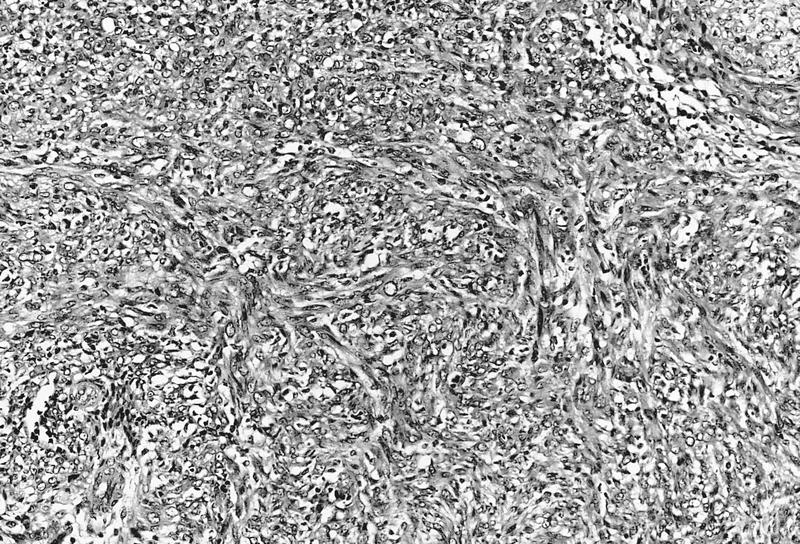
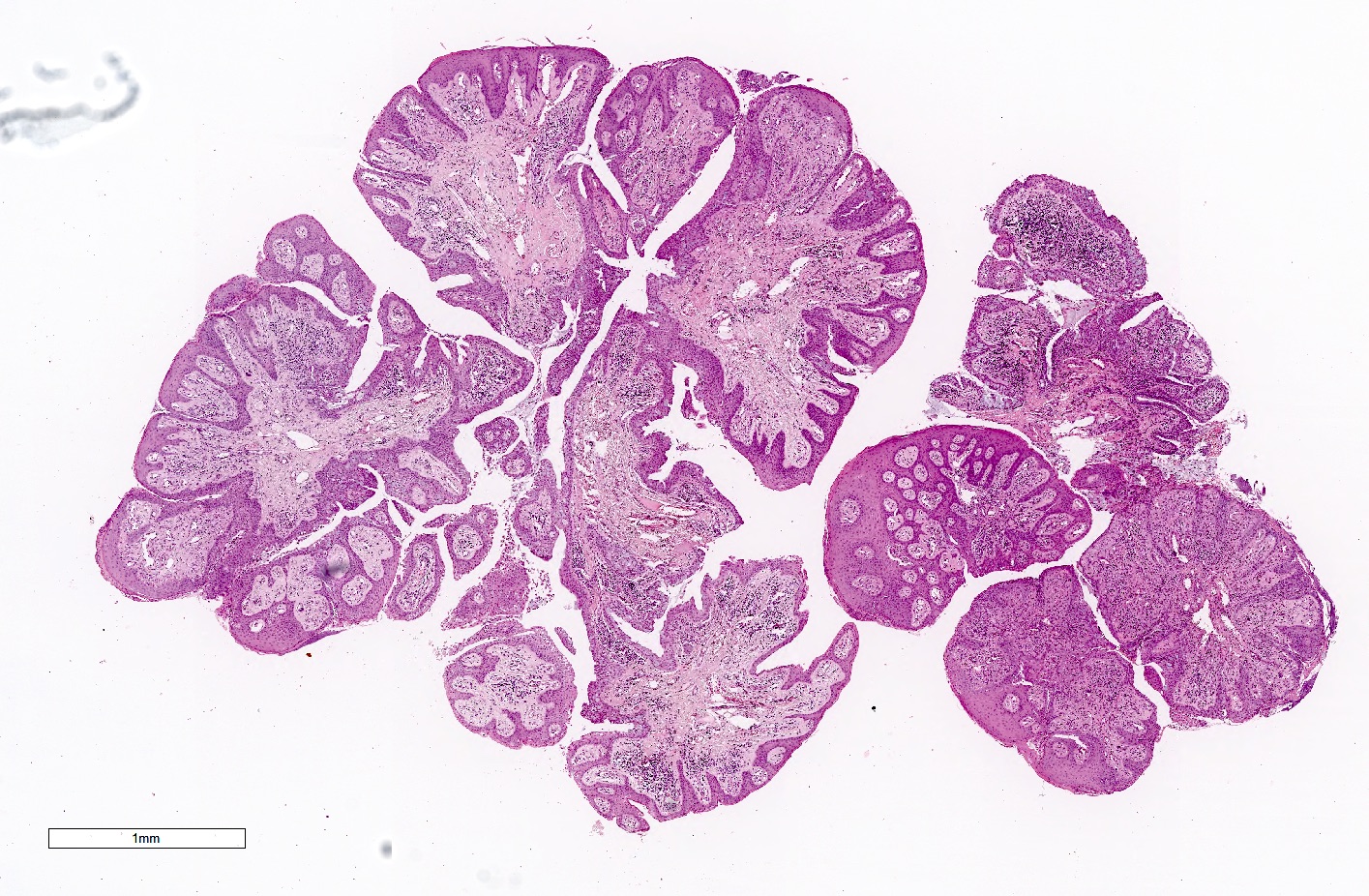
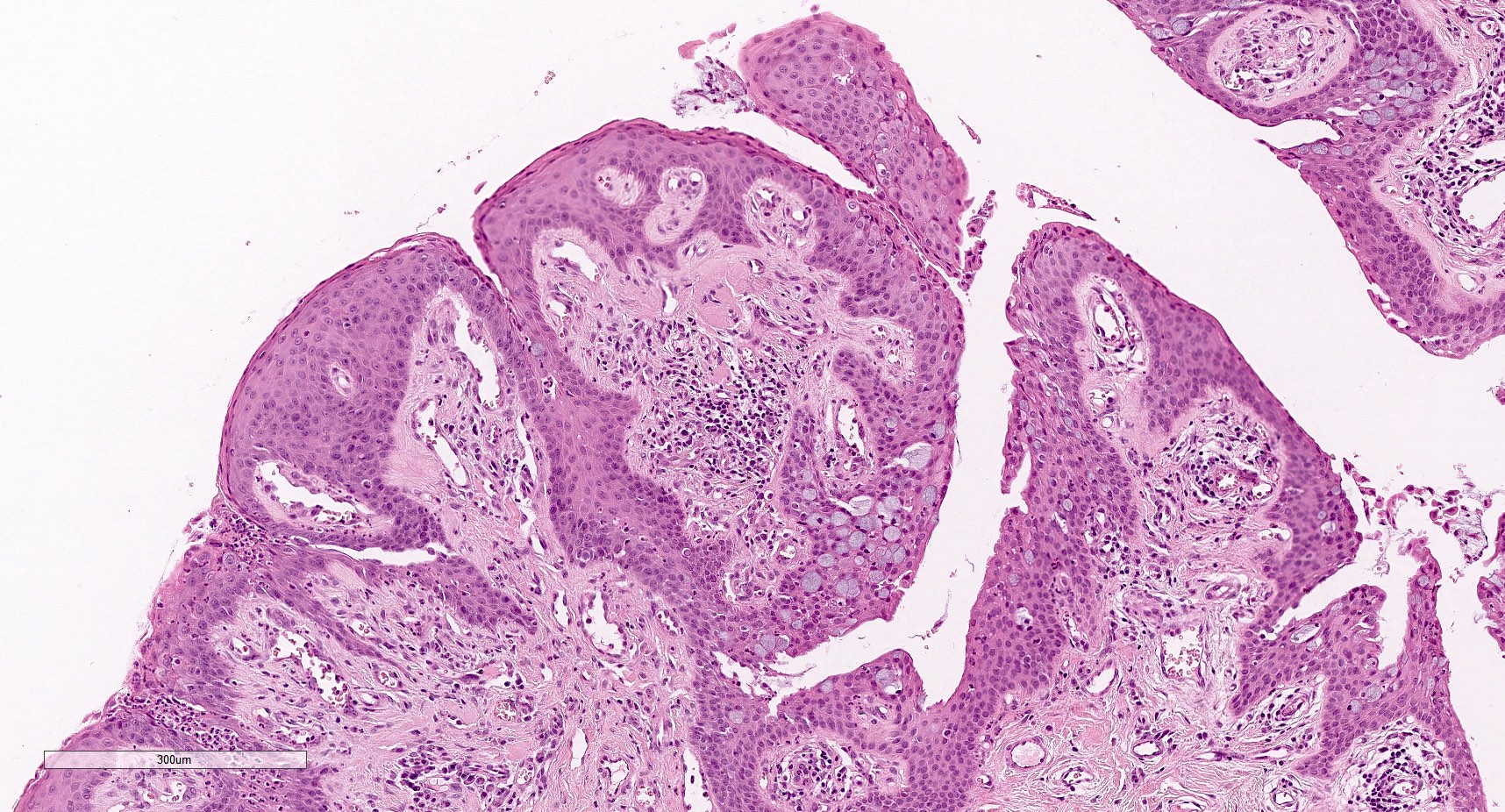
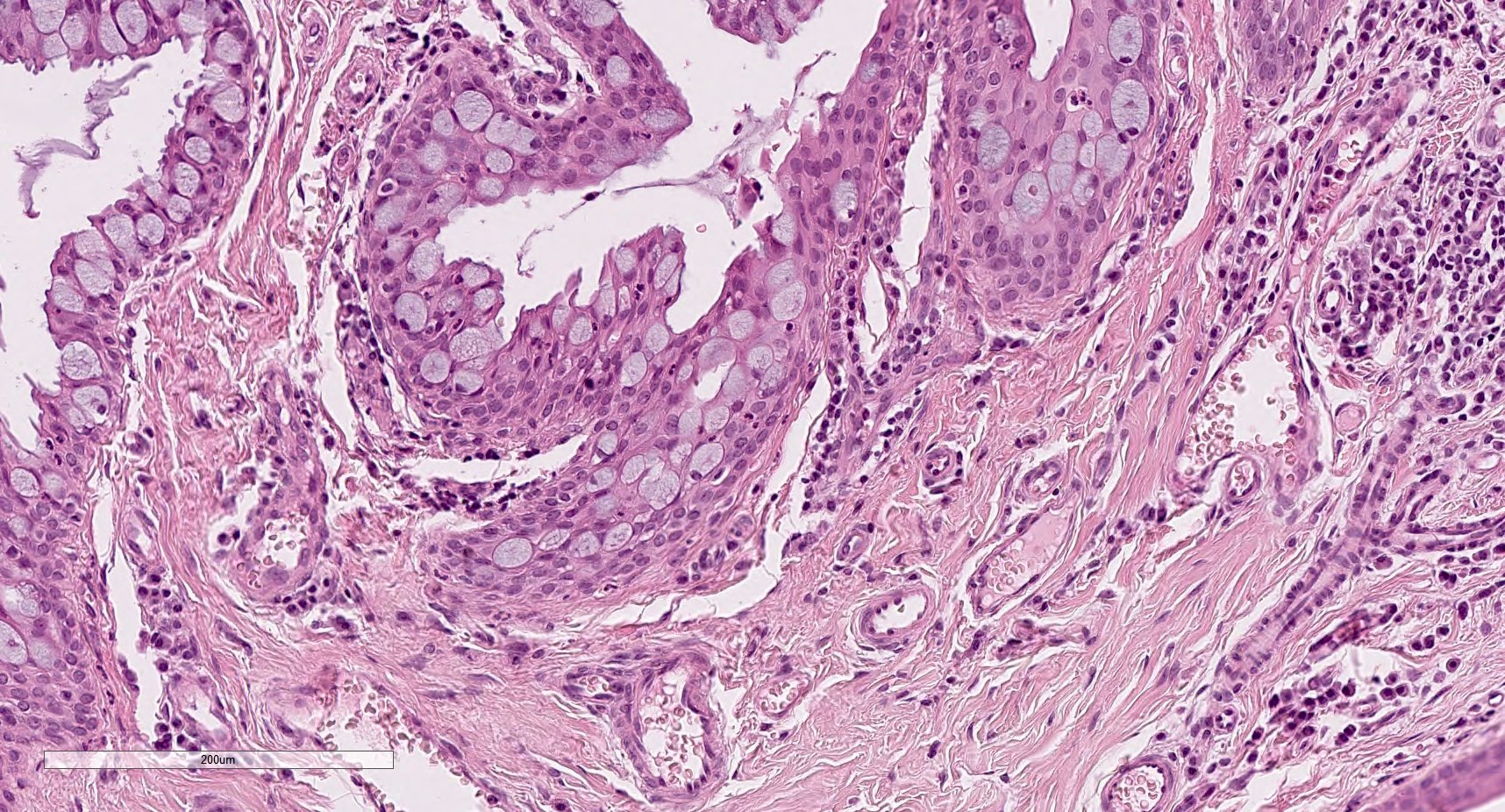
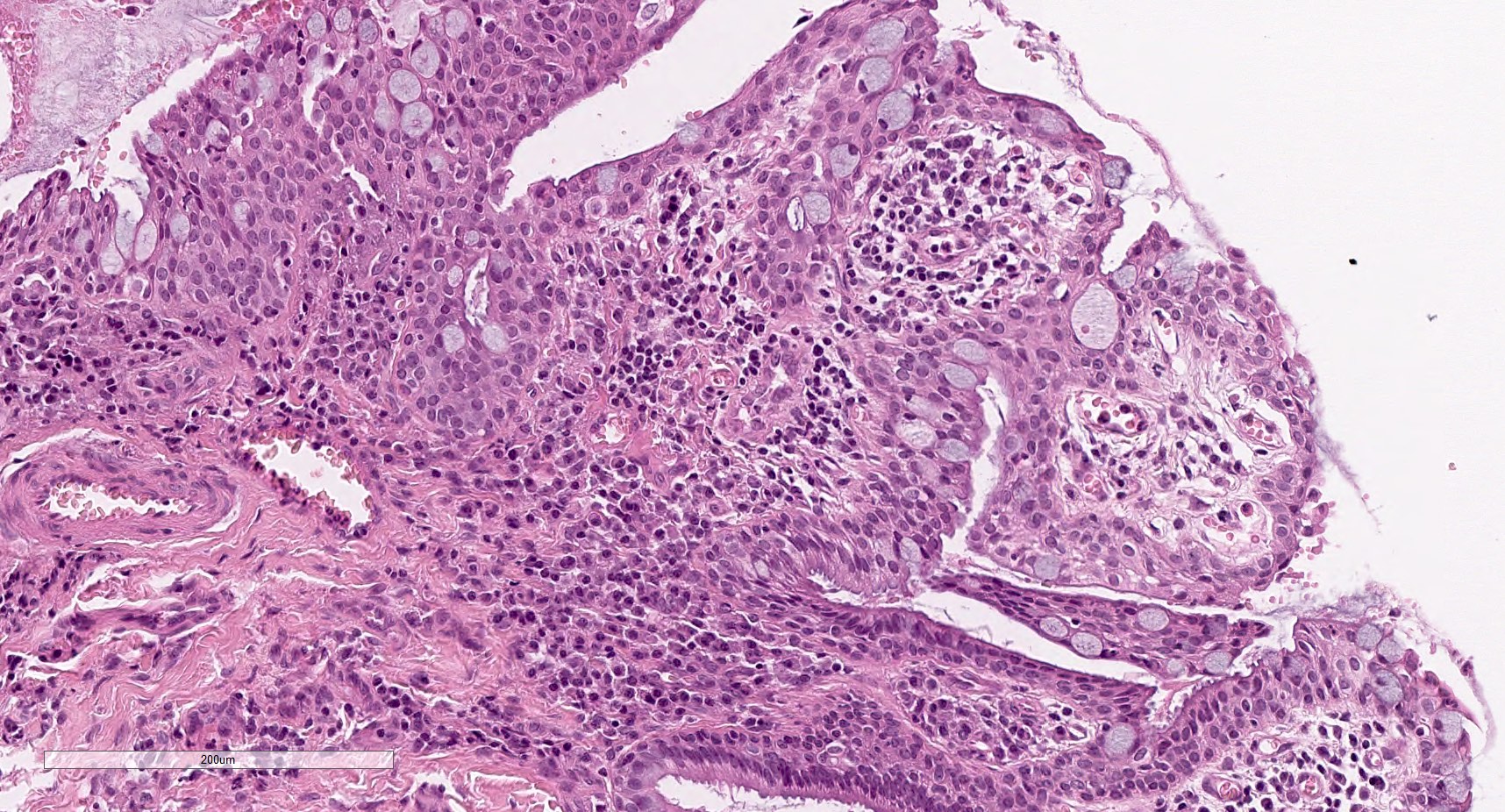
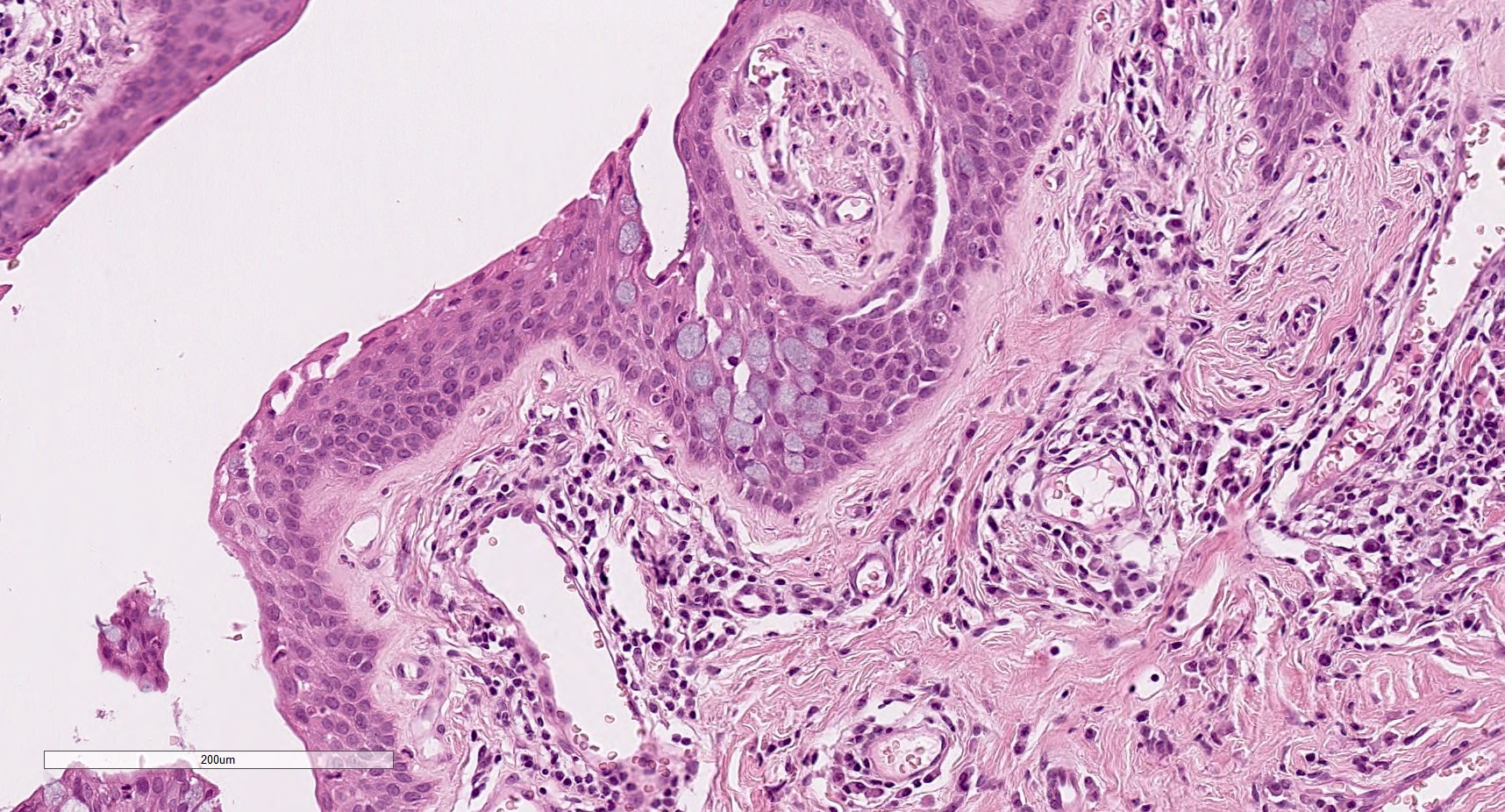
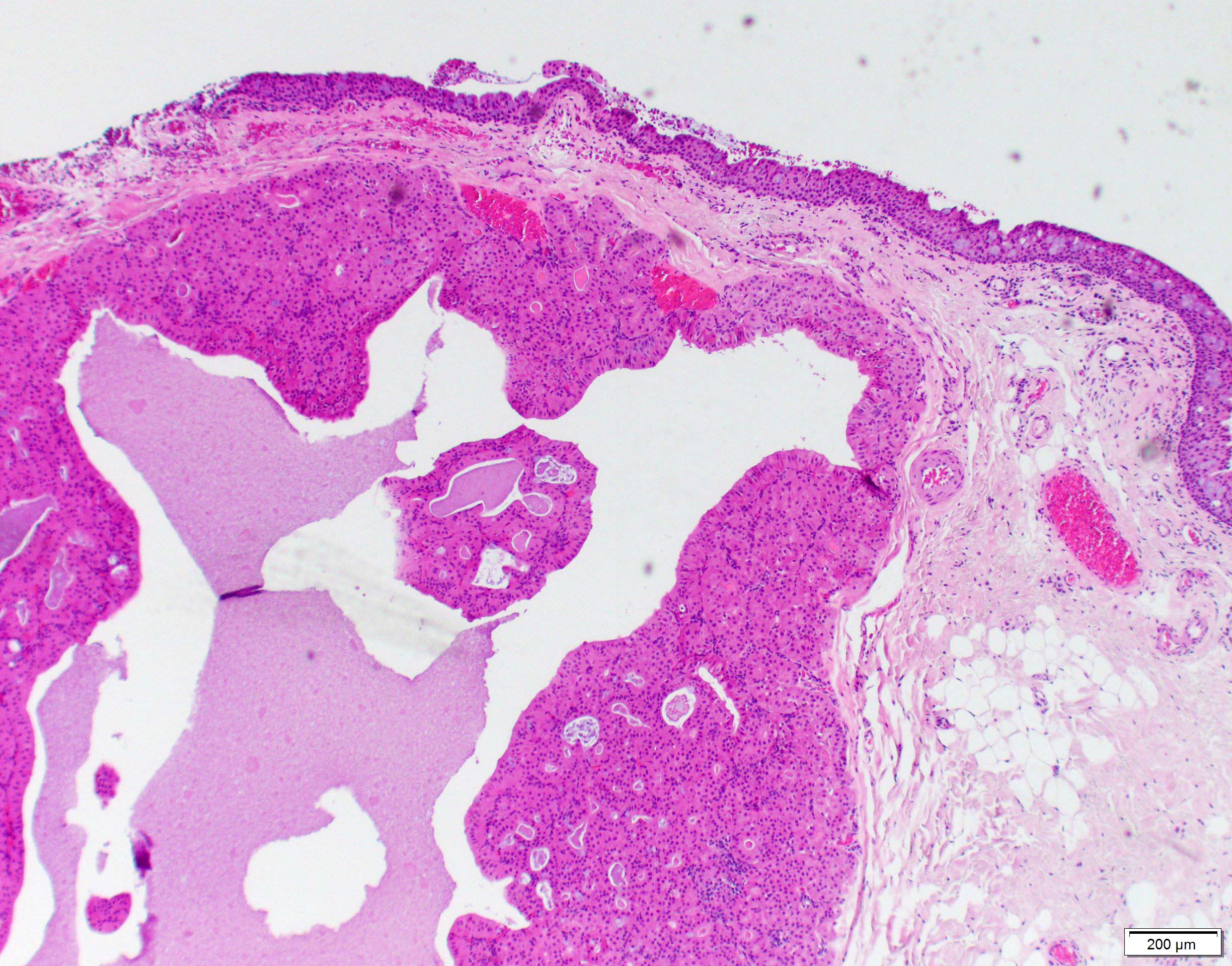
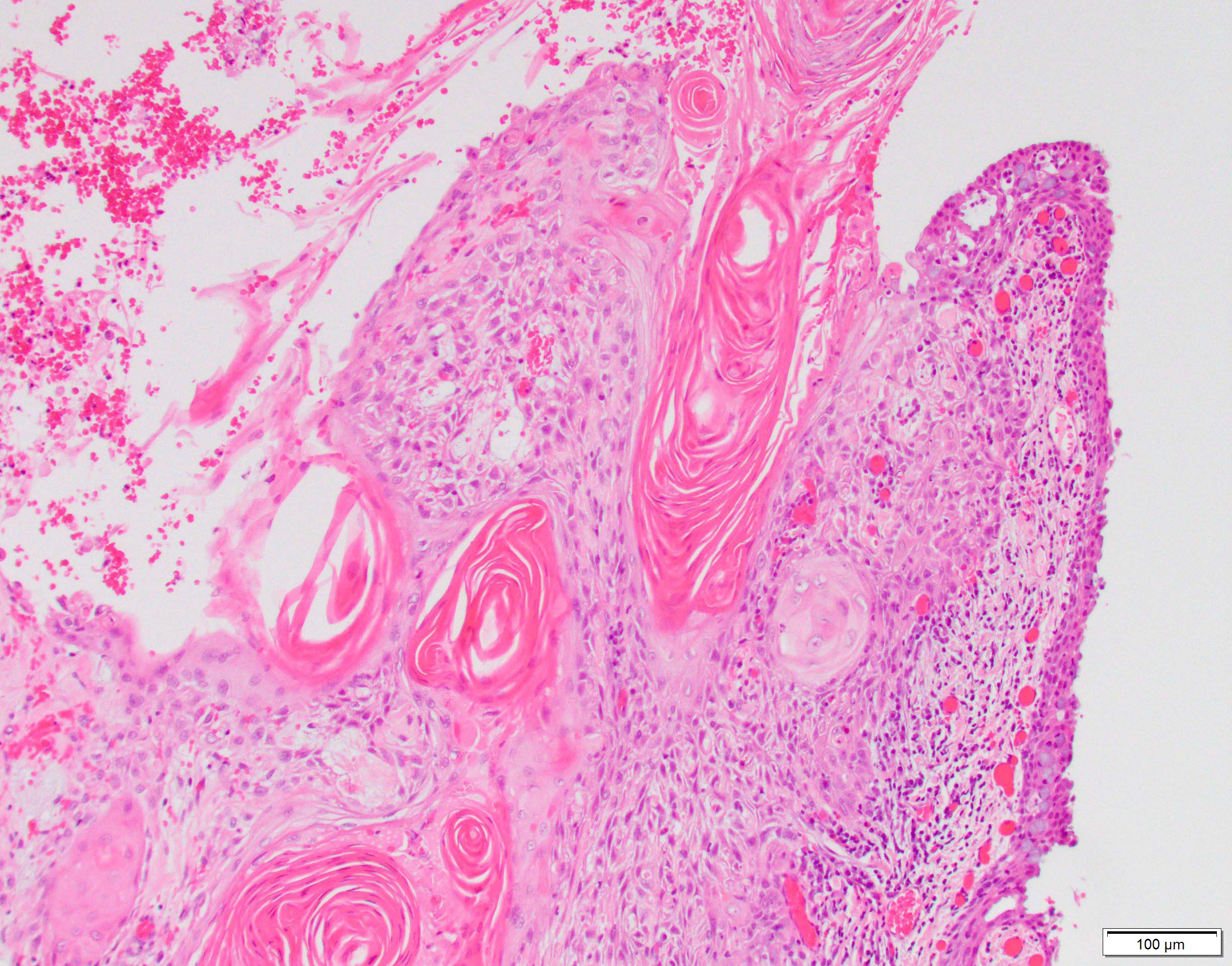
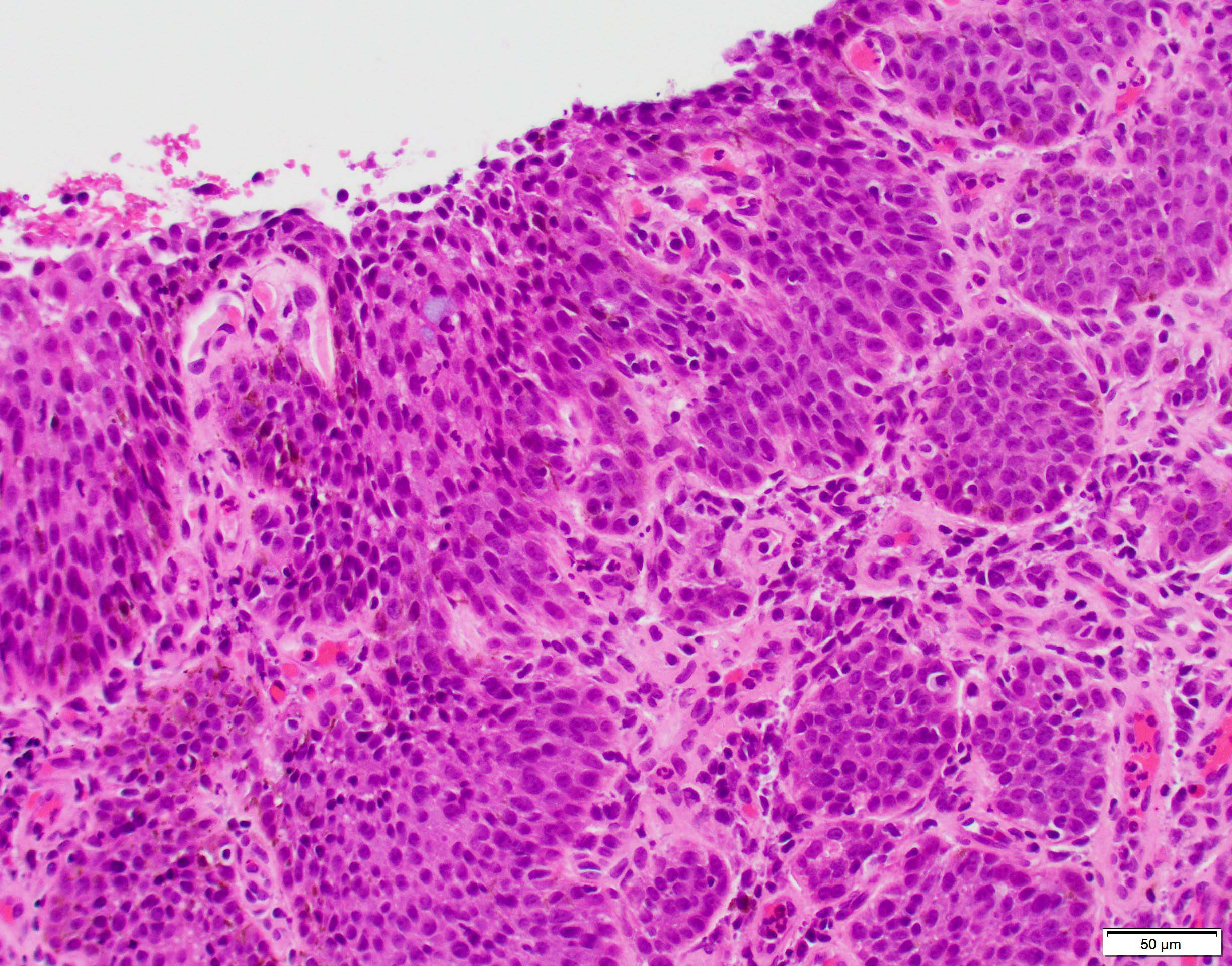
Microscopic (histologic) description
- Grading:
- Depends on thickness of conjunctival epithelial involvement by dysplasia:
- Conjunctival intraepithelial neoplasia 1 (mild dysplasia): involves lower third of epithelial thickness
- Conjunctival intraepithelial neoplasia 2 (moderate dysplasia): involves lower two - thirds
- Conjunctival intraepithelial neoplasia 3 (severe dysplasia): involves > two - thirds of thickness; surface maturation still present
- Carcinoma in situ: involves entire epithelium (full thickness); no more surface maturation (surface epithelium replaced by dysplastic cells)
- Depends on thickness of conjunctival epithelial involvement by dysplasia:
- Architectural features:
- Thickened epithelium (acanthosis); increased cellularity
- Loss of normal maturation sequence; disorganization
- Dysplasia begins in basal layers and extends toward surface
- Noninvasive; epithelial basement membrane is intact
- May have sharp demarcation between normal and abnormal epithelium
- Chronic inflammatory infiltrate in underlying stroma may be present
- Can have surface keratinization
- Papillary configuration with intralesional vessels and occasionally fibrovascular cores
- Intratumoral pigmented dendritic melanocytes can give rise to pigmented lesions resembling melanoma (Ophthalmology 2008;115:1673)
- Varieties (Can J Ophthalmol 1995;30:312):
- Actinic keratosis variety:
- Arises in epithelium covered areas of solar elastosis
- Usually leukoplakic due to surface keratinization
- Focal and well delineated
- Diffuse variety:
- Arises in non sun exposed epithelium
- Usually gelatinous
- Diffuse and poorly delineated
- Actinic keratosis variety:
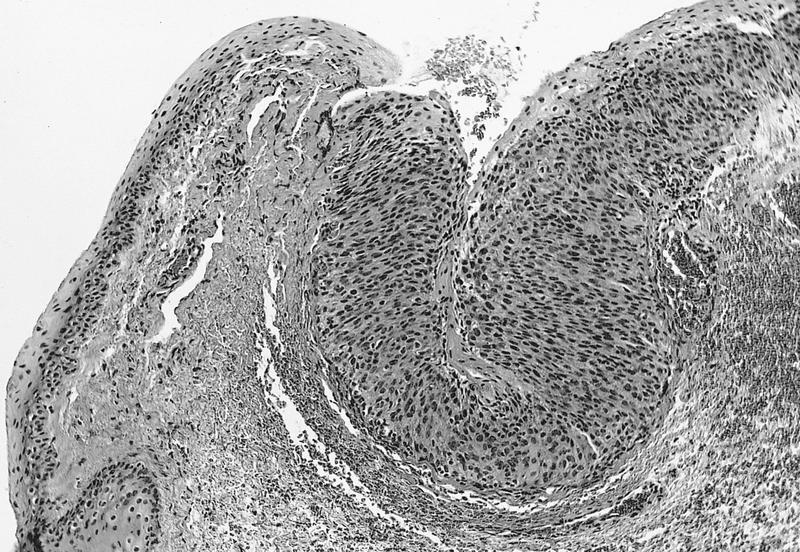
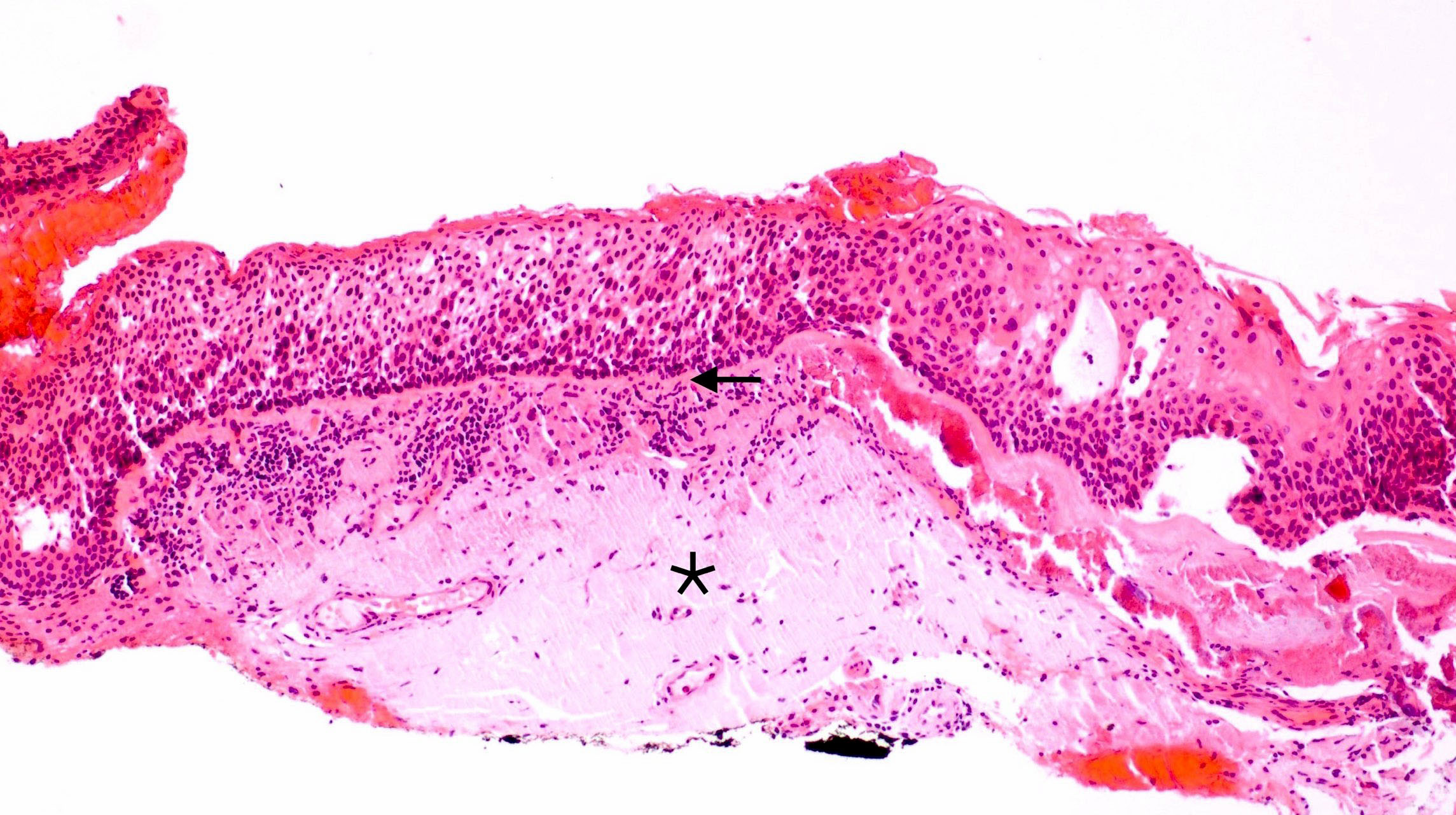
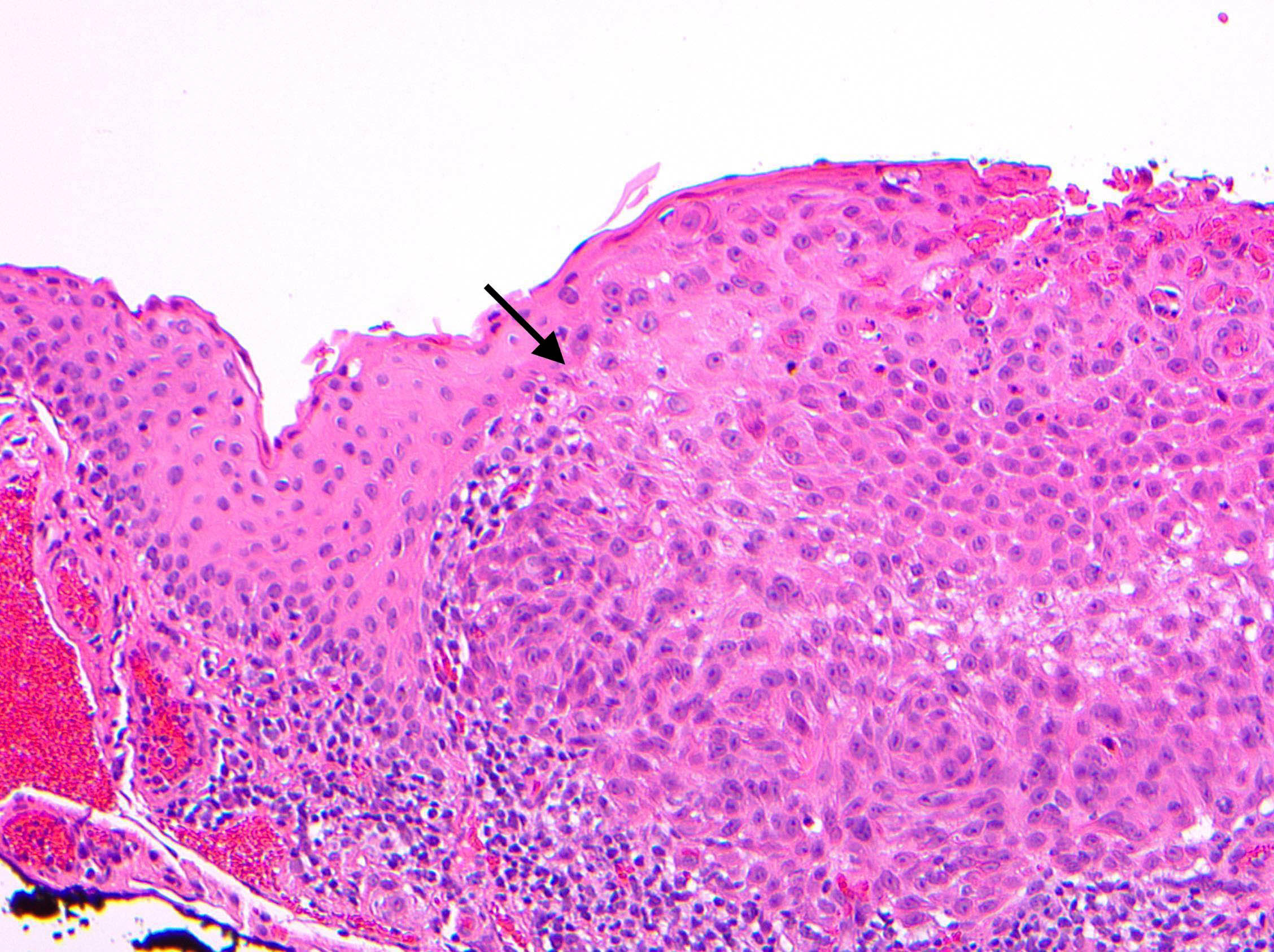
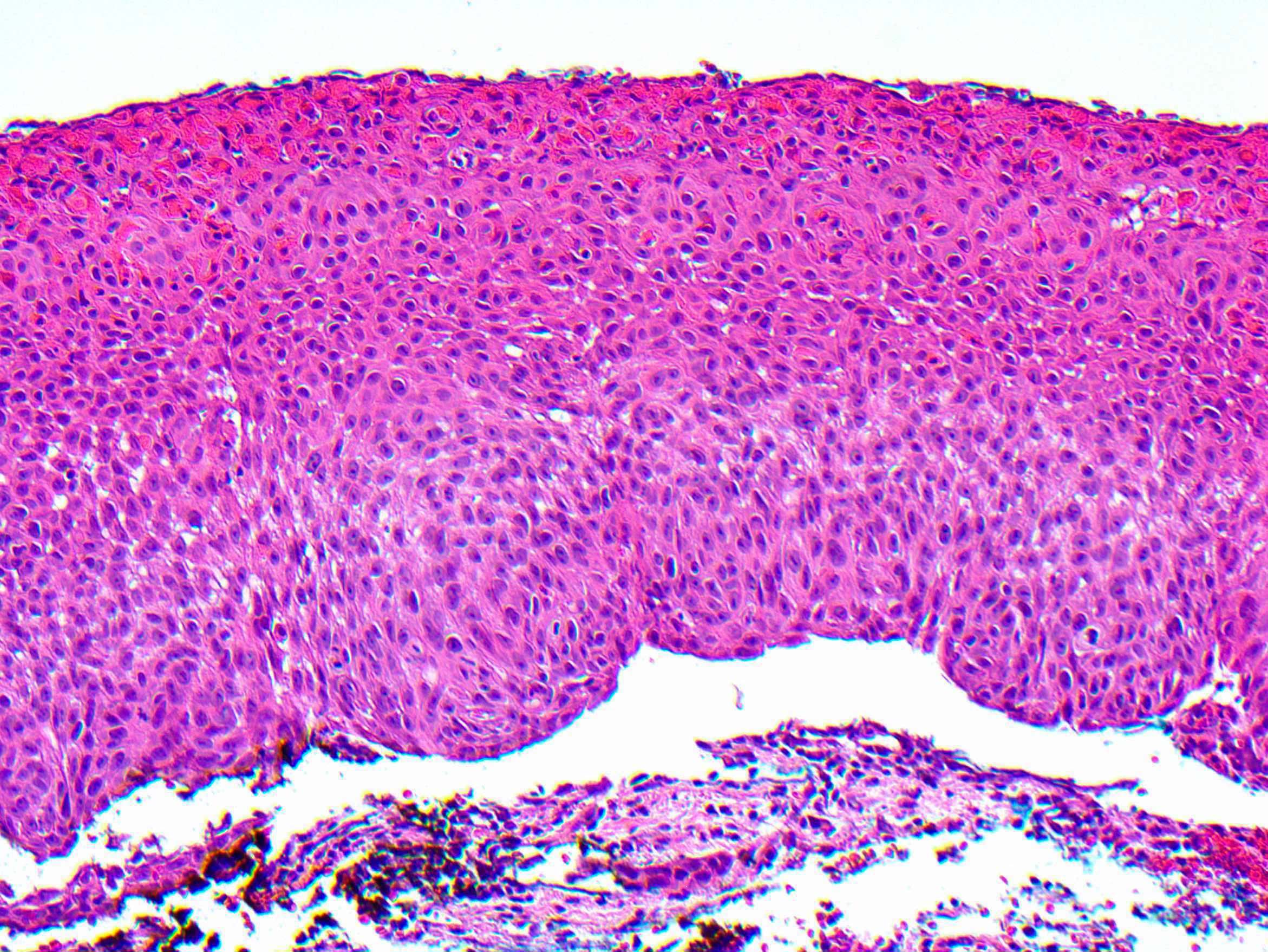
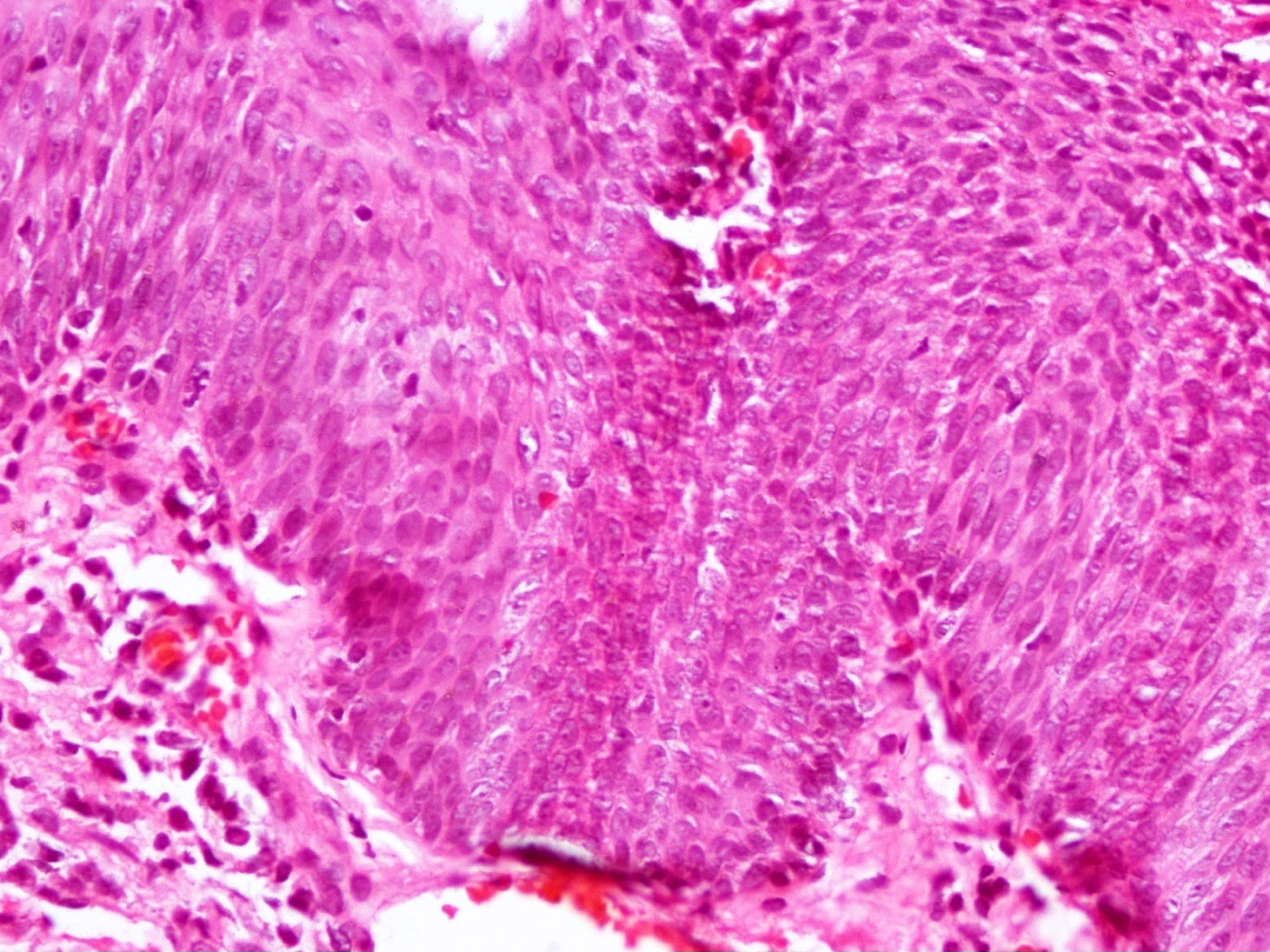
Microscopic (histologic) images
Contributed by Pia Mendoza, M.D.
Contributed by Frederick A. Jakobiec, M.D., D.Sc., Deepali Jain, M.D. and Hans Grossniklaus, M.D.
Cytology description
- Increased N/C ratio
- Nuclear hyperchromasia
- Pleomorphism
- May have prominent nucleoli
- May have dyskeratosis
- Rarely has HPV related / koilocytic changes
- Reference: Am J Ophthalmol 2009;148:772
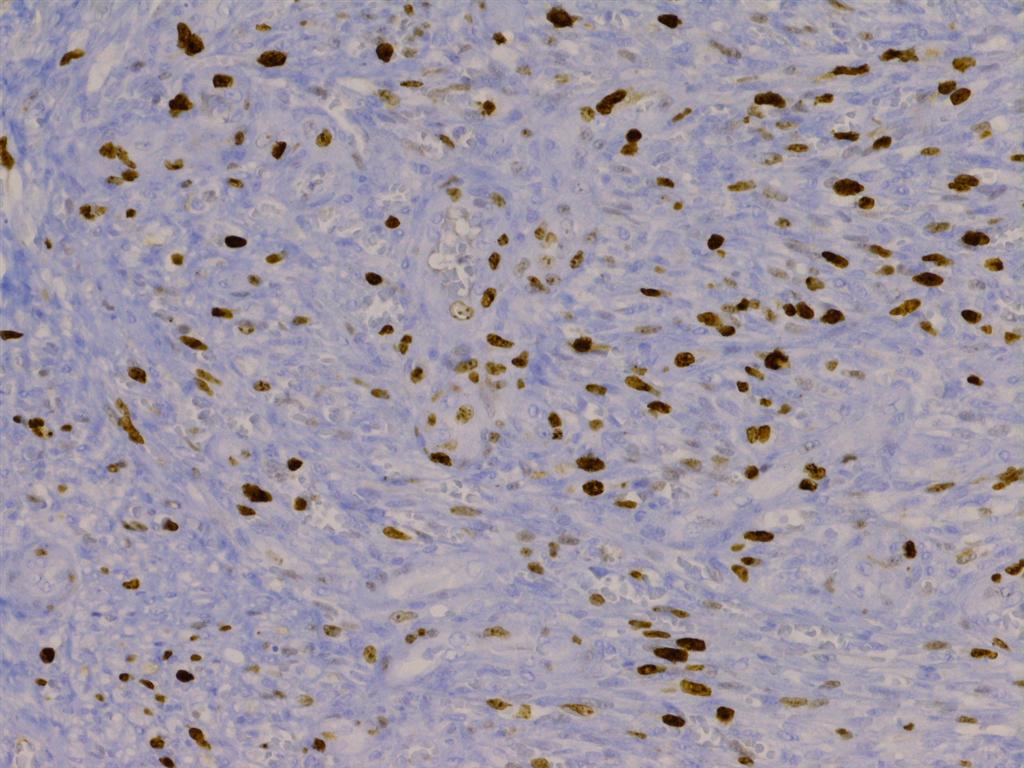
Positive stains
- p53: increased immunoreactivity in dysplasia (Am J Ophthalmol 2013;156:830)
- Ki67: increased proliferation rates in suprabasal epithelium in dysplasia (Am J Ophthalmol 2013;156:830)
- p16: greater intensity and percentage staining in high grade dysplasia (Am J Dermatopathol 2018;40:486)
Negative stains
- CK7: loss of expression in dysplasia (expressed in normal conjunctiva and squamous papillomas) (Am J Ophthalmol 2013;156:830)
- Periodic acid Schiff (PAS): negative in dysplasia due to loss of goblet cells (highlights goblet cells in normal conjunctiva and squamous papillomas)
Molecular / cytogenetics description
- Somatic TP53 mutations have been reported (Cornea 2000;19:159)
- Frequent TERT promoter mutations consistent with UV radiation induced damage (Invest Ophthalmol Vis Sci 2015;56:5854)
Sample pathology report
- Right eye, conjunctiva, excision:
- Conjunctival intraepithelial neoplasia 2 / moderate dysplasia (see comment)
- Comment: Surgical margins are negative for intraepithelial neoplasia. Negative for invasive carcinoma.
Differential diagnosis
- Conjunctival squamous papilloma:
- Pterygium:
- Wing-like, fleshy conjunctival lesion
- Epithelium without dysplasia
- Underlying stromal fibrovascular tissue with solar elastosis
- Pyogenic granuloma:
- Lobulated capillary proliferation with acute and chronic inflammation
- Sebaceous gland carcinoma:
- Primarily an eyelid tumor, with extension into the conjunctiva
- Large anaplastic cells with finely vacuolated cytoplasm spreading in pagetoid fashion to the conjunctiva
- Adipophilin+
- Pinguecula:
- Whitish yellow elevated conjunctival lesion in interpalpebral zone near limbus
- Goblet cell containing epithelium with various degrees of acanthosis or keratinizing metaplasia without dysplasia
- Subepithelial solar elastosis
Additional references
Board review style question #1
Board review style answer #1
A. Conjunctival intraepithelial neoplasia grade 3.
The patient is an older, light skinned man, likely with significant UV exposure, putting him at higher risk for the conditions listed in the choices. The clinical image shows a gelatinous conjunctival lesion with feeder vessels at the limbus in the interpalpebral zone. The biopsy shows thickened conjunctival epithelium with loss of the normal maturation sequence. There is a proliferation of dysplastic squamous cells with high N/C ratios, mitotic activity, hyperchromatic and pleomorphic nuclei involving > two - thirds of the epithelial thickness (conjunctival intraepithelial neoplasia 3 / severe dysplasia). The basement membrane is intact.
Primary acquired melanosis (choice B) is a proliferation of intraepithelial melanocytes that typically grow in a nested pattern. Pterygium (choice C) would present clinically as a wing-like, fleshy conjunctival lesion. Histopathology would show thin epithelium without dysplasia and underlying stromal fibrovascular tissue with solar elastosis. Conjunctival intraepithelial neoplasia is a precursor of squamous cell carcinoma (choice D). In squamous cell carcinoma, dysplastic cells invade beyond the basement membrane.
Comment Here
Reference: Conjunctival intraepithelial neoplasia
Primary acquired melanosis (choice B) is a proliferation of intraepithelial melanocytes that typically grow in a nested pattern. Pterygium (choice C) would present clinically as a wing-like, fleshy conjunctival lesion. Histopathology would show thin epithelium without dysplasia and underlying stromal fibrovascular tissue with solar elastosis. Conjunctival intraepithelial neoplasia is a precursor of squamous cell carcinoma (choice D). In squamous cell carcinoma, dysplastic cells invade beyond the basement membrane.
Comment Here
Reference: Conjunctival intraepithelial neoplasia
Board review style question #2
Which of the following is a feature of conjunctival intraepithelial neoplasia?
- Association with HPV 6 and 11
- Goblet cell containing epithelium without dysplasia
- Positivity for CK7 and periodic acid Schiff (PAS)
- Proliferation of atypical squamous cells, which may be a precursor to squamous cell carcinoma
Board review style answer #2
D. Proliferation of atypical squamous cells, which may be a precursor to squamous cell carcinoma.
Conjunctival intraepithelial neoplasia is characterized by a proliferation of neoplastic squamous cells showing cellular atypia. It is considered a premalignant lesion that may progress to invasive squamous cell carcinoma.
HPV 6 and 11 (choice A) are associated with squamous papilloma. HPV 16 and 18 are associated with conjunctival intraepithelial neoplasia. Goblet cell containing epithelium without dysplasia (choice B) is seen in other entities that may mimic conjunctival intraepithelial neoplasia, such as pterygium, pingueculae and squamous papilloma. CK7 (choice C) is expressed in normal conjunctiva and squamous papillomas but usually negative in dysplasia. PAS is positive in normal conjunctiva and squamous papillomas due to presence of goblet cells; however, goblet cells are usually lacking in conjunctival intraepithelial neoplasia.
Comment Here
Reference: Conjunctival intraepithelial neoplasia
HPV 6 and 11 (choice A) are associated with squamous papilloma. HPV 16 and 18 are associated with conjunctival intraepithelial neoplasia. Goblet cell containing epithelium without dysplasia (choice B) is seen in other entities that may mimic conjunctival intraepithelial neoplasia, such as pterygium, pingueculae and squamous papilloma. CK7 (choice C) is expressed in normal conjunctiva and squamous papillomas but usually negative in dysplasia. PAS is positive in normal conjunctiva and squamous papillomas due to presence of goblet cells; however, goblet cells are usually lacking in conjunctival intraepithelial neoplasia.
Comment Here
Reference: Conjunctival intraepithelial neoplasia
Conjunctival melanocytic intraepithelial lesions (CMIL)
Table of Contents
Definition / general | Terminology | Conjunctival melanocytic intra-epithelial neoplasia (C-MIN) | Clinical features | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Differential diagnosisDefinition / general
- See also benign melanosis
- 11% of conjunctival melanocytic proliferations (Arch Pathol Lab Med 2010;134:1785)
- Called melanoma in situ by some, although cases without atypia don't progress (Mod Pathol 1991;4:253)
- Variable biologic behavior from benign to locally spreading to malignant
- Usually ages 40+ years, whites
- Presents as gradual appearance of golden brown pigmented lesion of bulbar conjunctiva
- May be associated with Addison disease
- May be contiguous with lentigo maligna (similar histology but with rete pegs) of adjacent eyelid skin
- May involve pseudoglands of Henle in palpebral conjunctiva and resemble invasive melanoma
Terminology
- Also called primary acquired melanosis (PAM)
Conjunctival melanocytic intra-epithelial neoplasia (C-MIN)
- Conjunctival melanosis now differentiated histologically into hypermelanosis and conjunctival melanocytic intra-epithelial neoplasia (C-MIN)
- Cases formerly classified as PAM are now classified as C-MIN:
- C-MIN score of 0 is melanosis only
- C-MIN score of 1 is PAM with mild atypia
- C-MIN score of 2 - 3 is PAM with moderate atypia
- C-MIN score of 4 is PAM with severe atypia
- C-MIN score of 5+ is Conjunctival melanoma in situ
- Scoring of C-MIN based on pattern of horizontal epithelial involvement, vertical depth of melanocytic infiltration, degree of cellular atypia (Eye (Lond) 2013;27:142, Clin Experiment Ophthalmol 2008;36:786)
Clinical features
- Unilateral, flat, acquired, brown pigmentation, rarely amelanotic, fair skinned individual
Prognostic factors
- Cases without atypia have no / minimal risk of progression to melanoma
- 46% with atypia do progress to melanoma (Hum Pathol 1985;16:129)
- Extent in clock hours is significant factor for recurrence and progression (Ophthalmology 2008;115:511)
- Was predisposing lesion in 13 - 75% cases of melanoma (Int J Surg Pathol 2010;18:60, Trans Am Ophthalmol Soc 2007;105:61)
Case reports
- 30 year old woman with conjunctival melanoma arising from diffuse primary acquired melanosis (Cornea 2005;24:352)
- Associated benign pigmented nodule (Orbit 2007;26:57)
Treatment
- Excision or cryotherapy
- Also topical mitomycin C (Clin Experiment Ophthalmol 2006;34:708, Graefes Arch Clin Exp Ophthalmol 2005;243:1108) or 5-FU
- Cases with atypia usually recur or develop new foci
Gross description
- Diffuse granular conjunctival pigmentation, usually in bulbar conjunctiva, also cornea, palpebral conjunctiva, eyelid skin
Microscopic (histologic) description
- See C-MIN scoring system above
- Intraepithelial proliferation of abnormal melanocytes with variable atypia
- Early: pigmentation of basilar epithelium only
- Later:
- Basilar melanocytic hyperplasia with nests, resembling Paget disease
- Cells have retracted cytoplasm, larger nuclei than neighboring cells, clumped chromatin and prominent basophilic nucleoli
- Cells may be small with scant cytoplasm and small round nuclei
- Classification: with or without atypia
- High risk of progression: atypia plus epithelioid features including abundant cytoplasm, vesicular nuclei, prominent nucleoli, may be mixed with low risk areas (almost all are associated with invasion, Am J Surg Pathol 2007;31:185)
- Low risk of progression: atypia plus primarily single cell lentinginous growth, small / medium size, high N/C ratio, small / medium hyperchromatic nuclei, no nucleoli, 15% risk of invasion
- Pitfalls: don't interpret melanophages as invasive tumor cells
- Sine pigmento: melanocytes without pigment
- Post-topical chemotherapy changes: epithelial atrophy, dyskeratosis, pyknosis, focal keratinization
Microscopic (histologic) images
Electron microscopy description
- Grade 1: melanocytes with dendritic processes and transferred melanin in epithelial cells
- Grade 2: melanocytes have short dendritic processes, incomplete melanin transfer and immature melanosomes, irregular nuclei with clumped chromatin and large nucleoli
- Grade 3: epithelioid cells, no cytoplasmic processes, large irregular nuclei with large prominent nucleoli and abnormal melanin transfer
Differential diagnosis
- Cystic benign melanosis:
- Epithelial lined cysts in substantia propria, goblet cells and secondary pigmentation of basilar keratinocytes (Cornea 2012;31:1273)
- Hypermelanosis:
- Freckle or complexion melanosis
- Bilateral, does not change over time
- Junctional nevus:
- Children, no irregular epithelial involvement, no melanocytic nests, no polygonal cells, no atypia
- Melanoma:
- Invasion
- Secondary melanosis:
- Due to Addison disease, pigmented squamous cell carcinoma
- Subconjunctival pigmentation:
- Congenital ocular melanocytosis
Conjunctival oncocytoma
Table of Contents
Definition / general | Case reports | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics descriptionDefinition / general
- Usually caruncle (Arch Ophthalmol 1977;95:474, Ophthal Plast Reconstr Surg 2012;28:14)
- Often elderly (mean age 73), more common in women
- Proposed origin from lacrimal and accessory lacrimal glands based on cytokeratin profile (Acta Ophthalmol 2011;89:263)
Case reports
- 51 year old woman with tumor of caruncle (Int Ophthalmol 2004;25:321)
- 60 year old woman with tumor of caruncle (Klin Monatsbl Augenheilkd 2005;222:733)
- 72 year old woman with tumor of bulbar conjunctiva (Klin Monatsbl Augenheilkd 1996;209:176)
- 75 year old woman with tumor of caruncle (Indian J Ophthalmol 2002;50:60)
Gross description
- Red-orange or yellow-tan mass
Microscopic (histologic) description
- Solid nests and cords of polyhedral cells with abundant, finely granular acidophilic cytoplasm and round / oval paracentral nuclei, usually with one prominent nucleolus
- May have microcystic areas with occasional goblet cells (Am J Dermatopathol 2007;29:279), may have malignant histology and behavior
Microscopic (histologic) images
AFIP images
Images hosted on other servers:
Negative stains
Electron microscopy description
- Large numbers of mitochondria (Br J Ophthalmol 1980;64:935)
Molecular / cytogenetics description
- Mitochondrial DNA mutations (Arch Ophthalmol 2011;129:664)
Conjunctivitis and variants
Table of Contents
Allergic conjunctivitis | Chronic conjunctivitis | Giant papillary conjunctivitis | Infectious conjunctivitis | Papillary and follicular conjunctivitis (pending)Allergic conjunctivitis
Epidemiology
Sites
Pathophysiology
Clinical features
Diagnosis
Treatment
Clinical images
Images hosted on other servers:
Microscopic (histologic) description
Cytology description
Differential diagnosis
- Prevalence of 15 - 40% (Curr Opin Allergy Clin Immunol 2011;11:471)
Sites
- Unilateral or bilateral; affects palpebral and bulbar conjunctiva
Pathophysiology
- Ocular surface inflammation (usually mast cell driven) is associated with type 1 hypersensitivity reactions (eMedicine: Allergic Conjunctivitis [Accessed 24 April 2018])
- May be part of systemic atopic reaction to a systemic allergen
- Most prevalent types (95%) are perennial and seasonal (hay fever eyes) (Curr Opin Allergy Clin Immunol 2013;13:543)
- Most frequent allergens are tree and grass pollens
- More severe forms
- Chronic vernal keratoconjunctivitis: more common in spring (vernal); conjunctival scarring, eyelid thickening, ptosis, corneal neovascularization, ulceration, thinning, infection, keratoconus, and vision loss
- Atopic keratoconjunctivitis: eyelid tightening, loss of eyelashes, cataracts
- Giant papillary conjunctivitis: eyelid inflammation and ptosis
Clinical features
- History of allergy, asthma, or eczema
- Itching (pruritus), chemosis, tearing and redness with or without sneezing and nasal discharge
- 2 - 3 times increased risk for herpetic infection (Curr Eye Res 2006;31:721)
Diagnosis
- Cobblestoning (vernal) or papillary hypertrophy (giant papillary) of upper tarsal conjunctiva in chronic forms
Treatment
- Allergy type medications; topical cyclosporine if severe (Cornea 2007;26:1035)
- Patient education, lifestyle modification and topical medications (antihistamines, mast cell stabilizers, corticosteroids, immunomodulators)
Clinical images
Images hosted on other servers:
Microscopic (histologic) description
- May have eosinophils in conjunctival scraping (Acta Ophthalmol (Copenh) 1988;66:381)
Cytology description
- Consistent with clinical diagnosis (Indian J Pathol Microbiol 1992;35:118)
Differential diagnosis
- Atopic keratoconjunctivitis
- Giant papillary keratoconjunctivitis:
- Lymphocyte and eosinophil predominant, versus predominance of mast cells and eosinophils in allergic cases
- Vernal keratoconjunctivitis
Chronic conjunctivitis
Pathophysiology
Etiology
Clinical features
Diagnosis
Case reports
Treatment
Clinical images
Images hosted on other servers:
Microscopic (histologic) description
Cytology description
Molecular / cytogenetics description
Differential diagnosis
Additional references
- Conjunctivitis that persists for 4+ weeks
Etiology
- Unilateral:
- Due to keratitis, nasolacrimal duct obstruction, occult foreign body, neoplasm, tuberculosis, phthiriasis palpebrarum (due to lice, Int Ophthalmol 2012;32:467)
- Bilateral:
- Due to bacteria, tuberculosis (Int Ophthalmol 2014;34:655), virus, trachoma, other microorganisms
- Also allergic or chemical causes, inflammation of meibomian glands of eyelid
- Tarsoconjunctival crypts containing bacteria (Am J Ophthalmol 2012;154:527)
- Giant fornix syndrome (Ophthal Plast Reconstr Surg 2012;28:4)
- Vitamin A deficiency
Clinical features
- Insidious onset; slow progression of ocular discomfort, conjunctival injection, discharge
Diagnosis
- Conjunctival scrapings and culture are useful for diagnosis (Eur J Ophthalmol 1997;7:19)
Case reports
- 50 year old woman with relapsing polychondritis and obliterative microangiopathy (Cornea 2006;25:621)
- Boy with X linked hypogammaglobulinemia and bilateral inflammation (J Paediatr Child Health 1996;32:463)
Treatment
- Antibiotics, artificial tears, topical medications
Clinical images
Images hosted on other servers:
Microscopic (histologic) description
- 2 basic patterns:
- Chronic follicular conjunctivitis (associated with cosmetics, infectious mononucleosis, molluscum contagiosum, moraxella, phthiriasis palpebrarum, psittacosis, topical medications, trachoma)
- Chronic papillary conjunctivitis (tarsal conjunctiva)
- Numerous goblet cells and papillary folds
- Chronic inflammatory cells (lymphoid follicles and plasma cells)
- Isolated islands of epithelium may form retention cysts that calcify
- Late changes are epithelial atrophy, keratinization and stromal scarring
- Note that lymphocytes are common within normal conjunctiva
Cytology description
- Scrapings may yield more specific findings than impression cytology in chronic conjunctivitis (Eur J Ophthalmol 1997;7:19)
Molecular / cytogenetics description
- PCR is gold standard for chlamydia related conjunctivitis (Semin Ophthalmol 2013;28:216)
Differential diagnosis
Additional references
Giant papillary conjunctivitis
Definition / general
Terminology
Epidemiology
Etiology
Clinical features
Diagnosis
Treatment
Clinical images
Images hosted on other servers:
Microscopic (histologic) description
Cytology description
Differential diagnosis
Additional references
- Noninfectious inflammatory disorder due to mechanical and immunologic processes (type I and type IV hypersensitivity)
Terminology
- Also known as contact lens induced papillary conjunctivitis
Epidemiology
- Young adults with history of atopy
- 1 - 5% of soft contact lens wearers
- Average onset after 10 - 20 months of contact lens use
Etiology
- Associated with soft, hydrogel contact lenses (Trans Am Ophthalmol Soc 1999;97:205)
- Also exposed sutures, prostheses, rigid lenses (incidence only 10% of soft lenses) (Clin Experiment Ophthalmol 2007;35:535, Cont Lens Anterior Eye 2008;31:41)
- Also ocular surgery, foreign body, cyanoacrylate glue
Clinical features
- Itching, burning, foreign body sensation, redness
- Mucus accumulating in inner canthus noticed in morning
- Blurred vision, contact lens coating
- Usually bilateral (10% unilateral)
Diagnosis
- Upper tarsal conjunctiva has inflammation and papules (usually > 0.3 mm)
Treatment
- Change contact lenses more frequently (Eye Contact Lens 2003;29:S37)
- Mast cell stabilizers
- Olopatadine and fluorometholone (Eye Contact Lens 2010;36:210)
Clinical images
Images hosted on other servers:
Microscopic (histologic) description
- Thickened and irregular epithelium
- Epithelial cells show polymorphism with greater number of conjunctival goblet cells
- Upper tarsal conjunctival biopsies show mast cells, eosinophils and basophils in epithelium and substantia propria
Cytology description
- Impression cytology: honeycomb pattern consistent with giant papillae, increased inflammation and mucous strands (Ophthal Plast Reconstr Surg 2005;21:39)
Differential diagnosis
- Allergic conjunctivitis
- Toxic conjunctivitis
Additional references
Infectious conjunctivitis
Definition / general
Epidemiology
Sites
Etiology
Clinical features
Case reports
Clinical images
Images hosted on other servers:
Microscopic (histologic) description
Additional references
- See also Granulomatous conjunctivitis, Trachoma, Infectious keratitis
- Often due to inadequate personnel hygiene
Epidemiology
- In children, bacterial conjunctivitis is more common than viral
- Viral conjunctivitis is highly contagious
Sites
- Bulbar and palpebral conjunctiva
Etiology
- Most bacterial conjunctivitis is acute; chronic bacterial conjunctivitis is often caused by Chlamydia, rarely by Moraxella
- Adenovirus conjunctivitis:
- Most common cause of viral conjunctivitis (Arch Soc Esp Oftalmol 2013;88:108)
- 60% of ER conjunctivitis patients in Florida
- Detected by PCR (Optometry 2007;78:236)
- Other viruses:
- Herpes simplex virus
- Varicella zoster virus
- Enterovirus 70
- Coxsackie A24
- Molluscum contagiosum
- Vaccinia
- Human immunodeficiency virus
- Alcaligenes xylosoxidans conjunctivitis:
- Rare; can cause chronic conjunctivitis (Cornea 2007;26:868)
- Conjunctivitis within first 4 weeks of life
- Usually S. aureus, S. epidermidis, S. pneumoniae, M. catarrhalis
- Also C. trachomatis, N. gonorrhoeae, herpes simplex virus (HSV)
- Mothers with untreated chlamydial infections have a 30 - 40% chance of transmission to newborns
- Unilateral or bilateral (Pediatr Rev 2010;31:196)
- Bacterial conjunctivitis in children:
- Should exclude infected children from school until asymptomatic (J Pediatr Ophthalmol Strabismus 2007;44:101)
- Local antibiotics may not be necessary (Prescrire Int 2007;16:120)
- Often due to H. influenzae and Streptococcus pneumoniae (Ophthalmology 2008;115:51)
- S. aureus is uncommon in children (Acad Emerg Med 2007;14:1)
- Bacterial conjunctivitis in adults:
- Often due to Staphylococcus aureus, may be methicillin resistant
- Streptococcus pneumoniae is associated with outbreaks (Pediatr Infect Dis J 2006;25:906)
- Delayed use of antibiotics may be appropriate (BMJ 2006;333:321)
- Hyperacute conjunctivitis:
- Rapid onset
- Due to Neisseria gonorrhoeae or N. meningitides (Pediatr Rev 2010;31:196)
- Other bacteria are Pneumococcus species, Pseudomonas (Infection 2012;40:579)
- Gonococcal conjunctivitis:
- Due to autoinoculation
- Rare in developed countries (J Fr Ophtalmol 2007;30:e18)
- May cause corneal perforation (Med J Malaysia 2006;61:366)
- Influenza A virus conjunctivitis:
- Outbreak from poultry (Proc Natl Acad Sci U S A 2004;101:1356)
Clinical features
- Bacterial: itching, tearing, redness, purulent discharge, matting of eyelids
- Viral: irritation, photophobia, watery discharge
Case reports
- Child with acute conjunctivitis caused by Ewingella americana (J Pediatr Ophthalmol Strabismus 2012;49)
- 23 year old woman with conjunctivitis due to Achromobacter xylosoxidans (Arq Bras Oftalmol 2009;72:261)
Clinical images
Images hosted on other servers:
Microscopic (histologic) description
- Neutrophils on Gram stain if bacterial; lymphocytes in viral conjunctivitis
Additional references
Papillary and follicular conjunctivitis (pending)
Vernal
[Pending]
Atopic
[Pending]
Viral
[Pending]
Inclusion variants
[Pending]
[Pending]
Atopic
[Pending]
Viral
[Pending]
Inclusion variants
[Pending]
Corneal dystrophy
Table of Contents
Definition / general | Site of damage and types of corneal dystrophy | Types of corneal dystrophy | Microscopic (histologic) images | Differential diagnosisDefinition / general
- Heterogeneous group of inherited, bilateral, symmetric corneal disorders
- Most common is Fuchs dystrophy
- Also macular, lattice and granular corneal dystrophy
- Cause severe visual loss reparable by corneal transplantation
Site of damage and types of corneal dystrophy
- Epithelium:
- Meesman dystrophy
- Microcystic
- Map dot and fingerprint dystrophy
- Bowman layer and superficial stroma:
- Granular corneal dystrophy type III
- Thiel-Behnke dystrophy
- Familial subepithelial amyloidosis
- Stroma:
- Granular corneal dystrophy types I and II
- Macular corneal dystrophy
- Central stromal crystalline dystrophy
- Endothelium:
- Fuchs dystrophy (see below)
- Posterior polymorphous dystrophy
- Congenital hereditary endothelial dystrophy
Types of corneal dystrophy
- Central stromal crystalline dystrophy:
- Also called Schnyder corneal dystrophy
- Disease maps to 1p34-p32
- Crystals of cholesterol ester in anterior stroma
- Congenital hereditary endothelial dystrophy:
- Autosomal dominant (maps to 20q12-q13.1) or autosomal recessive
- Edematous epithelium with lack of Bowman layer
- Thickened stroma and Descemet membrane
- Diminished number of endothelial cells
- Familial subepithelial amyloidosis:
- Also called primary gelatinous droplike dystrophy
- Bowman layer and superficial stroma dystrophy
- Autosomal recessive
- Usually due to mutation in M1S1 gene at 1p
- Has subepithelial amyloid deposits that contain lactoferrin
- Fleck dystrophy:
- Also called speckled, cloudy dystrophy
- Subepithelial and stromal amyloid deposits
- Autosomal dominant
- Maps to 2q35
- Stains with colloidal iron and Alcian blue
- Granular corneal dystrophy type I:
- Stromal dystrophy
- Autosomal dominant
- Usually due to R555W mutation in TGFB1 gene at 5q31
- Discrete deposits of mutated protein appear red with Masson trichrome stain
- Granular corneal dystrophy type II:
- Also called Avellino corneal dystrophy
- Autosomal dominant
- Due to R124H mutation in TGFB1 gene at 5q31
- Corneal deposits similar to granular corneal dystrophy type I plus amyloid
- Granular corneal dystrophy type III:
- Also called Reis-Bucklers dystrophy
- Bowman layer and superficial stroma dystrophy
- Autosomal dominant
- Due to R124L mutation in TGFB1 gene at 5q31
- Lattice dystrophy:
- Irregular linear subepithelial and stromal amyloid deposits
- Normal Descemet membrane and endothelium
- Birefringent amyloid with Congo Red stain
- Lattice type I:
- Autosomal dominant
- Usually due to R124C mutation in TGFB1 at 5q31
- Lesions limited to cornea
- Often recurrent epithelial erosions and subepithelial amyloid or collagenous plaques
- Lattice type II:
- Autosomal dominant
- Mutation in GSN gene at 9q34
- Associated with familial amyloid polyneuropathy
- Amyloid is derived from fragment of mutated gelsolin
- Lattice type III:
- Autosomal recessive
- Amyloid deposits thicker than in types I and II
- Identity of amyloid unknown
- Lattice type IIIA:
- Autosomal dominant
- Amyloid deposits resemble type III
- Mutation in TGFB1 gene at 5q31
- Lattice type I:
- Macular corneal dystrophy:
- Autosomal recessive
- Due to mutation in CHST6 gene at 16q22.1
- Deficiency in carbohydrate sulfotransferase
- Causes deposits of low sulfated keratan sulfate related glycosaminoglycan throughout stroma
- Descemet membrane and endothelium
- Also corneal guttae
- Deposits are positive for colloidal iron and Alcian blue
- Macular type I:
- No / low serum keratan sulfate
- Keratocytes don't react to keratan sulfate antibodies
- Macular type IA:
- No / low serum keratan sulfate
- Keratocytes DO react to keratan sulfate antibodies
- Macular type II:
- Normal serum keratan sulfate
- Keratocytes DO react to keratan sulfate antibodies
- Macular type I:
- Meesmann dystrophy:
- Epithelium dystrophy
- Autosomal dominant
- Mutation in keratin KRT3 (12q) or KRT12 gene (17q)
- Intraepithelial microcysts
- Microcystic, map dot and fingerprint dystrophy:
- Epithelium dystrophy with nonspecific features
- Intraepithelial basement membrane and microcysts
- Posterior polymorphous dystrophy:
- Endothelial dystrophy
- Autosomal dominant (may be due to mutation in COL8A2 at 1p34.3-p32.3), or autosomal recessive
- May also map to 20q12-q13
- Abnormal Descemet membrane
- Has multilayered epithelial cells in posterior cornea
- Thiel-Behnke dystrophy:
- Transmission EM shows subepithelial "curly" fibers
- Due to R555Q mutation in TGFB1 gene at 5q31 or 10q23-q24
- Focal loss of epithelial basement membrane and Bowman layer
Differential diagnosis
- Amyloid due to trauma
- Glaucoma
- Keratoconus
- Retrolental fibroplasia
- Sympathetic ophthalmia
- Trachoma
- Uveitis
Corneal transplantation & graft failure
Corneal transplantation
- Keratoplasty (corneal transplantation):
- Produces button 8 mm in diameter
- Indications for keratoplasty:
- Primary and secondary endothelial decompensation (dystrophy)
- Fibrosis
- Vascularization
- Keratoconus
- Failed prior grafts
- Interstitial keratitis
- Penetrating keratoplasty:
- Full thickness corneal graft
- 8 mm in diameter
- Lamellar keratoplasty:
- Partial thickness corneal graft
- Donor corneal scleral rim:
- Want to check for endothelial damage
Graft failure
- Most corneal transplants are successful and provide long term improvement in visual acuity
- Matching of donor and recipient tissue is not necessary for corneal transplants since no lymphatics or blood vessels in corneal stroma
- Graft failure may be due to surgical damage of endothelium, immunologic rejection (uncommon) or recurrence of dystrophy
Microscopic (histologic) description
Graft failure:
- Fibrosis, vascularization, inflammatory cell infiltrate
- Full thickness scars from prior surgery are present at edge of specimen
- 50% have fibrous retrocorneal membrane
Cysts-conjunctiva
Definition / general
- See also steatocystoma simplex
- Most are acquired due to surgery (Ophthalmology 2006;113:1049), trauma (Br J Anaesth 2005;95:825), foreign bodies or chronic inflammation
- Also due to parasites, vernal keratoconjunctivitis (Korean J Ophthalmol 2007;21:251)
- Usually on nasal conjunctiva and lower fornix
- Most (65%) conjunctival nevi are also cystic (Curr Opin Ophthalmol 2007;18:351); some tumors such as lymphangioma can be highly cystic
- Cyst may be injected with Healon V and trypan blue to facilitate visualization and excision
(Cornea 2005;24:759)
- Dermoid cysts or 'conjunctivoid':
- See also dermoid tumor
- Young adults in contrast to skin dermoid
- Usually located in nasal or superonasal deep orbit
- Lined by stratified squamous epithelium, contains cutaneous adnexae (Ophthal Plast Reconstr Surg 2006;22:137)
- Rarely lipogranulomas from cyst rupture
- May have oncocytic differentiation (Ophthal Plast Reconstr Surg 2008;24:69)
- Inclusion cysts:
- One or two cell lining of nonkeratinized epithelium containing goblet cells
- May have apocrine snouts resembling apocrine glands
- May be associated with Stevens-Johnson syndrome (Ophthal Plast Reconstr Surg 2006;22:475)
Case reports
- 41 year old (Cornea 2013;32:513) and 54 year old men with keratinous cyst of the palpebral conjunctiva that represents trichilemmal keratinization (Ophthal Plast Reconstr Surg 2009;25:337)
Gross description
- Usually translucent to light blue
Dacryoadenitis
Table of Contents
Definition / generalDefinition / general
- Inflammation of lacrimal gland due to obstruction of lacrimal ducts by dacryoliths
Dacryocystitis / canaliculitis
Definition / general
- Often obscure origin; may be due to inflammatory spread from nose or conjunctiva
- Acute or chronic inflammation with suppurative, granulomatous or necrotizing features
- Fistulous tracts may form to skin below eyelid near base of nose
Terminology
- Canaliculitis: inflammation of lacrimal duct
- Dacryocystitis: inflammation of lacrimal sac
- Acute: ducts filled with purulent exudate
- Chronic: lacrimal canal narrows due to inflammatory thickening, epithelial hyperplasia
Dacryolithiasis
Definition / general
- Stone (dacryolith) in lacrimal canal
- Probably due to low grade inflammation, including mycoses (Arachnia propionica)
Microscopic (histologic) description
- Laminated concretions in lacrimal sac
- May contain degenerating epithelial cells and neutrophils, often fungi
Dermoid cyst-orbit
Table of Contents
Definition / general | Radiology images | Gross description | Microscopic (histologic) description | Microscopic (histologic) imagesDefinition / general
- Congenital but may not be clinically evident until age 20 years
- Most common in superior temporal orbit, also eyelid
Gross description
- Soft, nontender, round / oval cyst with thickened wall, 1 cm or less
- Contain yellow, cheesy material
Microscopic (histologic) description
- Encapsulated, lined by well differentiated epidermis and dermis, lumen filled with keratinous debris, hair, sebum
- May have foreign body inflammatory reaction if cyst ruptures
Detachment of retina
Table of Contents
Definition / general | Gross images | Whole mount images | Microscopic (histologic) description | Microscopic (histologic) imagesDefinition / general
- Separation of neurosensory retina (rods and cone and more superficial layers) from retinal pigment epithelium
- Rhegmatogenous ("due to a rupture or fracture") detachment: associated with full thickness retinal defect, such as collapse of vitreous, causing traction on retinal internal limiting membrane, causing tears and seepage of vitreous between neurosensory layer and retinal pigment epithelium; treated by relieving vitreous traction
- Nonrhegmatogenous detachment: no retinal break; due to significant exudates or conditions causing leakage of fluid from choroidal circulation beneath the retina, such as choroidal tumors and malignant hypertension
- Chronic retinal detachment may cause loss of photoreceptor outer segments, gliosis and development of microcystic spaces in detached retina
Microscopic (histologic) description
- Early changes are degeneration of outer retinal layers and photoreceptors with subretinal exudates
- Late changes are disruption and atrophy of retinal architecture with marked gliosis and proliferative vitreoretinopathy
Diabetes mellitus
Definition / general
- Common cause of blindness in Western society
- Classified as background, preproliferative or proliferative retinopathy
- Background retinopathy: initial lesion is capillary microangiopathy
- Preproliferative retinopathy: changes of background diabetic retinopathy plus significant venous dilation / beading, cotton wool spots (due to focal infarcts in nerve fiber layer), extensive formation of intraretinal microvascular abnormalities (due to vascular shunts) and extensive ischemia
- Proliferative retinopathy: growth of neovascular tissue from inner surface of retina into vitreous; causes retinal detachment, treat with laser photocoagulation; may occur without clinically visible background diabetic retinopathy
- Retinopathy is associated with duration of diabetes - 60% at 15 years
- May cause rubeosis iridis (neovascularization of iris) and secondary glaucoma
- Also causes thickening of basement membrane of pars plicata of ciliary body
- Also causes vacuolization of iris pigment epithelium with glycogen containing vacuoles related to blood glucose level at time of enucleation
Microscopic (histologic) description
- Background retinopathy: retinal capillary microaneurysms and cotton wool spots (due to hypoxia from microvascular obstructions and nonperfusion) with PAS+ deposits on endothelium, basement membrane thickening, loss of pericytes; also venous anomalies, hemorrhage (flame shaped between fibers of nerve fiber layer), exudates (hard, yellow, waxy protein and lipid of outer plexiform layer appears eosinophilic) and edema
- Proliferative retinopathy: new vessels that sprout from existing vessels on surface of optic nerve head or retina and penetrate the internal limiting membrane of the retina; thickened basement membrane, reduction in number of pericytes (causes microaneurysms and arteriovenous shunts)
Dysthyroid ophthalmopathy
Table of Contents
Definition / general | Gross description | Clinical images | Microscopic (histologic) descriptionDefinition / general
- Most common cause of orbital disease and exophthalmos
- Associated with hyperthyroidism or thyroid related treatment, although patient may be hyper, hypo or euthyroid at the time
- Usually bilateral but may be unilateral
- Most cases are not biopsied
Gross description
- Marked enlargement of extraocular muscles
Clinical images
Microscopic (histologic) description
- Severe edema and chronic inflammation of orbital tissues
- Degeneration and hyalinization of extraocular muscles with increase in interstitial connective tissue in muscles and other orbital tissue
Epibulbar choristoma
Table of Contents
Definition / general | Diagrams / tables | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) imagesDefinition / general
- A type of choristoma (congenital, nonneoplastic lesion composed of cytologically normal tissue not normally found at that location), often at limbus
- Mainly children
- No malignant potential
- May be associated with colobomas of iris and ciliary body, Goldenhar syndrome (ocular dermoid tumors, extra-auricular appendages, vertebral anomalies, East Afr Med J 2002;79:502), organoid nevus syndrome (also called linear nevus sebaceus of Jadassohn, Br J Ophthalmol 1987;71:268)
Gross description
- Bulbar tumors are firm, localized, elevated, opaque, yellow-white masses at limbus
Microscopic (histologic) description
- Dermoid:
- Solid (not cystic) choristoma mass with surface epithelium resembling epidermis and dermis and containing a few hairs, overlying thick bundles of collagen, which make up bulk of mass (eMedicine: Limbal Dermoid [Accessed 17 April 2018])
- Complex choristoma:
- Cartilage, lacrimal tissue, smooth muscle, adipose tissue, neural tissue (Ophthalmology 1987;94:1249)
- May be confused with prolapsed lacrimal gland (Acta Ophthalmol Scand 2005;83:100); teeth (odontogenic choristoma, Am J Ophthalmol 2009;147:531)
- Osseous choristoma:
- More than 70% female
- Small, solid, circumscribed, red-white bony lesion behind limbus and between superior and lateral rectus muscles
- Composed of compact lamellar bone surrounded by dense, collagenous bone (Br J Ophthalmol 1979;63:173, Ophthalmic Surg Lasers 2002;33:410)
- Dermolipoma (lipodermoid):
- Superotemporal most common site
- Abundant adipose tissue but minimal skin adnexae, usually in upper outer fornix; only superficial portion is excised as deep portion is attached to rectus muscles and fascia (The Internet Journal of Ophthalmology and Visual Science 2006;4:Number 1, Arch Ophthalmol 1994;112:1114)
- Resembles subconjunctival herniated orbital fat (Aust N Z J Ophthalmol 1999;27:33)
- Smooth muscle hamartoma:
- Gray, cyst-like appearance
- Spindled smooth muscle, fibrous stroma, lobules of adipose tissue (Am J Ophthalmol 1999;128:643, Ophthal Plast Reconstr Surg 2012;28:e102)
Microscopic (histologic) images
AFIP images
Complex choristoma:
Images hosted on other servers:
Epithelial cyst-orbit
Table of Contents
Case reportsCase reports
- 57 year old woman with primary conjunctival epithelial cyst of the orbit (Int Ophthalmol 2007;27:269)
Eyelid cysts
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Etiology | Clinical features | Diagnosis | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Benign cystic lesions of the eyelid, most of which are caused by blockages of ducts (hidrocystomas) or hair follicles (epidermal cyst) or are consequence of entrapped benign, embryologic tissue (dermoid cyst)
- Includes epidermal cyst, dermoid cyst, eccrine hidrocystoma and apocrine hidrocytoma, all of which are generally cured by excision
Essential features
- Epidermal cysts feature a lining of benign keratinizing stratified squamous epithelium with a granular layer (in the absence of adnexal structures) and contain keratinaceous debris
- Dermoid cysts are embryologically derived lesions histologically identified by the presence of adnexal structures in conjunction with benign, stratified squamous epithelial cyst lining
- Eccrine hidrocystomas are caused by obstruction of eccrine sweat glands and are histologically identified by a dual layer of bland, cuboidal epithelial cells
- Apocrine hidrocystomas are caused by obstruction of apocrine sweat glands and are histologically identified by the presence of an inner layer of elongated, epithelial cells with apical snouts and decapitation secretions
Terminology
- Epidermal (infundibular) cyst, epidermal inclusion cyst, follicular cyst, infundibular type, epidermoid cyst, clinical sebaceous cyst
- Hidrocystoma, sudoriferous cyst, sweat ductal cyst
ICD coding
- ICD-10:
- H02.82 - cysts of eyelid
- H02.821 - cysts of right upper eyelid
- H02.822 - cysts of right lower eyelid
- H02.823 - cysts of right eye, unspecified eyelid
- H02.824 - cysts of left upper eyelid
- H02.825 - cysts of left lower eyelid
- H02.826 - cysts of left eye, unspecified eyelid
- H02.829 - cysts of unspecified eye, unspecified eyelid
- ICD-11:
Epidemiology
- Epidermal cysts are common, sporadic lesions that typically affect adults with a slight male predominance (StatPearls: Epidermoid Cyst [Accessed 18 August 2022])
- Periocular dermoid cysts are most often encountered in pediatric patients, with many cases arising in the superotemporal region within the first year of life (Ophthalmic Epidemiol 2019;26:117)
- Eccrine hidrocytomas generally arise along the medial or lateral eyelid in middle aged to older adults (Eye (Lond) 2005;19:77)
- Apocrine hidrocystomas often occur near the canthus in middle aged and older adults but may rarely be seen in the pediatric population (MedGenMed 2006;8:57)
Etiology
- Most epidermal cysts are thought to arise secondary to occlusion of hair follicles (Arch Ophthalmol 1988;106:270)
- Dermoid cysts are caused by entrapment of embryologic epithelium (Otolaryngol Head Neck Surg 2005;132:938)
- Eccrine hidrocystomas occur secondary to blockages of eccrine sweat glands (Eye (Lond) 2005;19:77)
- Apocrine hidrocystomas result from blockages of apocrine sweat glands (MedGenMed 2006;8:57)
Clinical features
- Epidermal cysts typically present as solitary, subcutaneous nodules and keratinaceous contents may appear cheese-like (StatPearls: Epidermal Inclusion Cyst [Accessed 18 August 2022])
- Dermoid cysts present as subcutaneous nodules, often superotemporally in the vicinity of the zygomaticofrontal suture (Int Ophthalmol 2011;31:93)
- Most hidrocystomas appear as single, dome shaped lesions with varying tints (including transparent, skin colored, brown, blue and blue-black hues) though examples of multiple hidrocystomas do occur (MedGenMed 2006;8:57)
Diagnosis
- Histopathologic examination of excised tissue
Case reports
- 8 and 11 month old boys with upper eyelid lesions (Ophthalmic Plast Reconstr Surg 2009;25:146)
- 15 month old boy with a right upper eyelid mass (Saudi J Ophthalmol 2015;29:312)
- 9 year old girl with drooping of the right upper eyelid (Indian J Ophthalmol 2017;65:884)
- 35 year old man with a large right upper eyelid swelling over a period of 10 years (Indian J Ophthalmol 2012;60:211)
- 70 year old man with a large, cystic swelling of the forehead (Indian J Otolaryngol Head Neck Surg 2019;71:59)
Treatment
- Excision is usually curative
Gross description
- Benign eyelid cysts are often received as small excisions with nodules, papules or grossly identifiable cysts
- Keratinaceous cyst contents in epidermal and dermoid cysts may appear yellow to white, cheese-like or chalky (StatPearls: Epidermal Inclusion Cyst [Accessed 18 August 2022])
- Hidrocystomas are thin walled and usually contain clear cyst contents (MedGenMed 2006;8:57)
Microscopic (histologic) description
- Epidermal cyst:
- Bland, keratinizing stratified squamous epithelial cyst lining with a granular layer of keratohyaline granules in the absence of adnexal structures
- Keratinaceous debris cyst contents
- Rupture of cyst may induce an inflammatory response, including a foreign body giant cell reaction
- Dermoid cyst:
- Features adnexal structures, such as hair follicles and sebaceous glands, in conjunction with bland, stratified squamous epithelial cyst lining
- Keratinaceous debris in cyst contents
- Like epidermal cysts, rupture may lead to an inflammatory response and a foreign body giant cell reaction
- Conjunctivoid dermoid cysts with nonkeratinizing squamous epithelium and goblet cells may rarely be encountered in addition to other rare features, such as oncocytic and basaloid differentiation (Ophthalmic Plast Reconstr Surg 2008;24:69, J Eur Acad Dermatol Venereol 2001;15:268)
- Eccrine hidrocystoma:
- Subepithelial cyst with dual lining of variably attenuated, cuboidal cells
- Unilocular or multilocular
- Cyst cavity may appear clear / empty or contain eosinophilic, proteinaceous material
- Apocrine hidrocystoma:
- Subepithelial cyst with an inner epithelial lining of elongated (columnar), eosinophilic cells with apical snouts and decapitation secretions
- Unilocular or multilocular
- Like eccrine hidrocystomas, the cyst cavity may appear clear / empty or contain eosinophilic, proteinaceous material
Microscopic (histologic) images
Contributed by J. Stephen Nix, M.D.
Videos
Hidrocystoma: 5 minute pathology pearls by Dr. Jared Gardner
Dermoid cyst: 5 minute pathology pearls by Dr. Jared Gardner
Sample pathology report
- Eyelid, left upper, excision:
- Epidermal cyst (see comment)
- Comment: Histologic examination shows a cyst with a bland keratinizing squamous epithelial lining with a granular layer and keratinaceous cyst contents in the absence of adnexal structures.
- Periocular nodule, excision:
- Dermoid cyst (see comment)
- Comment: Histologic examination shows a cyst with a bland keratinizing squamous epithelial lining and adjoining adnexal structures.
- Eyelid, right upper, excision:
- Apocrine hidrocystoma (see comment)
- Comment: Histologic examination shows a subepithelial cyst that features an inner layer of elongated, eosinophilic cells with apical snouts and decapitation secretions.
- Eyelid, left lower, excision:
- Eccrine hidrocystoma (see comment)
- Comment: Histologic examination shows a subepithelial cyst with an epithelial lining composed of a dual layer of flattened, cuboidal cells.
- Eyelid, left upper, excision:
- Epidermal cyst (see comment)
- Comment: Histologic examination shows a cyst with a bland keratinizing squamous epithelial lining with a granular layer and keratinaceous cyst contents in the absence of adnexal structures.
- Periocular nodule, excision:
- Dermoid cyst (see comment)
- Comment: Histologic examination shows a cyst with a bland keratinizing squamous epithelial lining and adjoining adnexal structures.
- Eyelid, right upper, excision:
- Apocrine hidrocystoma (see comment)
- Comment: Histologic examination shows a subepithelial cyst that features an inner layer of elongated, eosinophilic cells with apical snouts and decapitation secretions.
- Eyelid, left lower, excision:
- Eccrine hidrocystoma (see comment)
- Comment: Histologic examination shows a subepithelial cyst with an epithelial lining composed of a dual layer of flattened, cuboidal cells.
Differential diagnosis
- Chalazion:
- Lipogranulomatous inflammation that lacks an epithelial cyst lining
- Typically presents as a tender eyelid nodule
Additional references
Board review style question #1
A 68 year old man presents with a skin colored nodule of the lateral left lower eyelid. Based on the histologic image, what is the most likely etiology of the lesion?
- Blockage of an apocrine sweat gland
- Blockage of an eccrine sweat gland
- Entrapped embryologic tissue
- Obstruction of a pilosebaceous unit
Board review style answer #1
B. Blockage of an eccrine sweat gland. The histologic image shows an epithelial lining composed of a dual layer of cuboidal cells, consistent with the diagnosis of eccrine hidrocystoma. Eccrine hidrocystomas are caused by blockages of eccrine sweat glands. Apocrine hidrocystomas result from blockages of apocrine sweat glands (A). Entrapped embryonal tissue is encountered in a dermoid cyst (C) and obstruction of a pilosebaceous unit may result in an epidermal cyst (D).
Comment Here
Reference: Eyelid cysts
Comment Here
Reference: Eyelid cysts
Board review style question #2
Board review style answer #2
B. Dermoid cyst. Periocular dermoid cysts most often occur in pediatric patients and are diagnosed histologically by the presence of adnexal structures in association with a bland stratified squamous epithelial cyst lining. Apocrine hidrocystomas demonstrate a cyst lining with an inner layer of elongated, eosinophilic cells with apical snouts and decapitation secretions (A). Eccrine hidrocystomas feature a cyst lining composed of a dual layer of cuboidal cells (C). Epidermal cysts have a cyst lining of bland keratinizing stratified squamous epithelium with a granular layer in the absence of adnexal structures (D).
Comment Here
Reference: Eyelid cysts
Comment Here
Reference: Eyelid cysts
Glaucoma
Table of Contents
Definition / general | Normal circulation of aqueous humor | Drawings | Microscopic (histologic) imagesDefinition / general
- Diverse etiologies, causes widespread degeneration of ocular tissue
- Defined as optic neuropathy with distinct excavation of optic nerve head and incremental loss of visual field sensitivity
- Almost always due to increased intraocular pressure (due to impaired outflow of aqueous humor) which causes optic nerve damage and degenerative changes below
Normal circulation of aqueous humor
- Aqueous humor is produced by pars plicata of ciliary body, discharged into posterior chamber, flows between lens and iris, through pupil, into anterior chamber, then through trabecular meshwork (in deep layers of peripheral cornea just in front of angle of anterior chamber), into Schlemm canal, leaves eye via plexus of intrascleral and episcleral veins along limbus
Glioma-optic nerve
Table of Contents
Definition / general | Radiology description | Radiology images | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) imagesDefinition / general
- Relatively rare
- Slow growing tumor within orbital segment of optic nerve
- Usually ages 0 - 9 years with symptoms of minimal exophthalmos, optic nerve atrophy or papilledema
- Associated with neurofibromatosis type 1
Radiology description
- Thickening of nerve on CT scan
- May enlarge optic canal
Treatment
- Resection for tumors limited to optic nerve
- Also radiation therapy for more extensive lesions
Gross description
- Small tumors are limited to optic nerve
- Larger tumors form bulbous enlargement of nerve, often infiltrate pia causing arachnoid thickening
Microscopic (histologic) description
- Variable cytology and cellularity, even within same tumor, but usually are low grade pilocytic astrocytomas similar to cerebellar and third ventricle tumors with round to spindled nuclei and dendrite-like cytoplasmic processes
- Often Rosenthal fibers (fusiform, cigar shaped eosinophilic structures within astrocyte cytoplasmic processes, are a nonspecific degenerative change)
- Rarely are hypercellular with brisk mitotic activity, marked pleomorphism, necrosis and vascular proliferation
- Difficult to differentiate reactive vs. neoplastic resection margins
- Typically has intense mucinous degeneration with tumor cells in pools of mucin
- Infiltrating tumor may cause reactive proliferation of arachnoid cells resembling meningioma
Graft versus host disease
Table of Contents
Definition / general | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Electron microscopy imagesDefinition / general
- Occurs in up to 80% of chronic graft versus host disease patients with allogeneic hematopoietic transplants
- Most commonly affects conjunctiva, lacrimal gland, meibomian glands; also cornea, choroid
- Bulbar conjunctiva is biopsied for diagnosis
- Conjunctival and lacrimal gland fibrosis may be due to epithelial mesenchymal transition (Am J Pathol 2009;175:2372)
- Modified Lerner classification of bulbar GVHD seems to have prognostic value (Graefes Arch Clin Exp Ophthalmol 2007;245:1001)
Microscopic (histologic) description
- Reduced goblet cells (Eur J Ophthalmol 2006;16:17)
- Pseudomembrane due to loss of conjunctival epithelium
- May have keratinization
- Increased ICAM-1 expression (Eur J Ophthalmol 2006;16:17)
- Reduced mucosal microvilli (Bone Marrow Transplant 2012;47:416)
Microscopic (histologic) images
Cytology description
- Conjunctival scrape cytology:
- Atypical epithelial cells
- Loss of goblet cells
- Epithelial cells with vacuolated or coarse, granular cytoplasm
- Squamous metaplasia
- Prominent inflammatory background (Acta Cytol 2010;54:272)
- Expression of Th1-associated chemokines (Bone Marrow Transplant 2010;45:1340)
Electron microscopy images
Granulomatous conjunctivitis
Table of Contents
Sites | Etiology | Clinical features | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) imagesSites
- Unilateral or bilateral (in systemic diseases)
- Palpebral conjunctiva and upper lid more often in tuberculosis
Etiology
- Usually associated with systemic disease
- Conjunctival granulomata form in response to foreign body, allergen, infectious organism or as part of systemic disease
- With necrosis:
- Tuberculosis (Int Ophthalmol 2014;34:655)
- Parinaud oculoglandular syndrome due to cat scratch fever (Ugeskr Laeger 1995;157:4137) or tularemia (Am J Ophthalmol 2001;131:283)
- Granulomatosis with polyangiitis (Wegener's) (Ophthalmology 2003;110:1770)
- Without necrosis:
- Crohn's disease (Br J Ophthalmol 1984;68:901)
- Foreign bodies (ophthalmia nodosa due to hair of caterpillar, surgical talc) (J AAPOS 2007;11:402)
- Hodgkin lymphoma (Am J Ophthalmol 2001;131:796)
- Sarcoidosis
- Syphilis
- Other:
- Acid fast bacilli
- Actinic granulomas (Ophthalmology 2013;120:1786)
- Churg-Strauss syndrome (Arch Ophthalmol 2012;130:1228)
- Drugs (brimonidine-timolol fixed combination) (Int Ophthalmol 2013;33:557, Br J Ophthalmol 2007;91:691)
- HIV (Ocul Immunol Inflamm 2006;14:309)
- Ocular rosacea in children
- Parasites (Ophthalmology 2001;108:1223)
- Ulcerative colitis (Eye (Lond) 2013;27:567)
Clinical features
- Eye discharge, watering, redness and itching
- Often regional lymphadenopathy
Case reports
- 2 and 5 year old girls with conjunctivitis due to synthetic fibers from teddy bears (BMC Ophthalmol 2011;11:17)
- 34 year old male cattle farmer with no history of trauma (Cornea 2002;21:831)
- 62 year old woman with bulbar conjunctival sporotrichosis presenting as tumor (Cornea 2010;29:573)
- Two women with Sporothrix schenckii (Cornea 2005;24:491)
Treatment
- Varies by etiology
- Tuberculosis: anti-tuberculosis therapy, topical prednisolone
- Excision in systemic conditions
Gross description
- Sarcoidosis: (EyeWiki: Conjunctival Biopsy in the Diagnosis of Ocular Sarcoidosis [Accessed 25 April 2018])
- Small, tan conjunctival nodules
- Tuberculosis: ulcerative, nodular, hypertrophic granulomatous and pedunculated
Microscopic (histologic) description
- Chronic inflammatory infiltrate with epitheloid histiocytes and giant cells
- Elastolysis and granulomatous inflammation in actinic granuloma
Grossing & features to report
Table of Contents
Conjunctiva | Cornea | Eyelid tumors | Globe - description | Globe - sectioning | Retina tumors (retinoblastoma) | Uvea tumorsConjunctiva
Grossing
- Specimens are thin and tend to fold when placed in fixative
- Surgeon should spread lesion onto filter paper, allow to dry for a few seconds, then place in specimen container
- Relevant landmarks should be labeled
- For lesions that extend to limbus, cut so sections are perpendicular to limbus
- Don't use methylene blue or toluidine blue ink for margins as they bleed into sample
- Don't place specimens on sponges which expand in fixative and distort specimen
Conjunctiva tumors - features to report
- Histologic type
- Degree of differentiation
- Precise anatomic location: bulbar by quadrant, palpebral (superior or inferior), fornix (superior or inferior), caruncle, plica semilunaris, limbus, cornea
- Tumor size
- Involvement of corneal stroma, episclera, orbital fat
- Involvement (noninvolvement) of other tissues present
- Margins (deep and lateral, minimum clearance)
- Presence of angiolymphatic, perineural, intraocular or intraorbital invasion
- Presence of ulceration
- For melanomas, also indicate thickness (from top of epithelium to deepest tumor cell in substantia propria using ocular micrometer) and mitotic activity
- Reference: Am J Surg Pathol 2003;27:999
Cornea
Grossing
- Don't pick up with forceps
- Bisect at center with sharp razor to see papillary excrescences or other lesions of interest
- Embed "on edge"
- Routine stains are hematoxylin & eosin and PAS (highlights basal lamina)
Cornea tumors - features to report
- Precise anatomic location - limbus by clock hour
- Histologic type
- Tumor size
- Involvement (noninvolvement) of other tissues present
- Margins (minimum clearance)
- Angiolymphatic invasion
- Presence of ulceration
Eyelid tumors
Features to report
- Precise anatomic location - upper or lower eyelid, medial or lateral canthus
- Histologic type and differentiation
- Tumor size(s) and gland of origin (Meibomian vs. Zeis)
- Presence of infiltrative growth pattern
- Presence of pagetoid spread
- Involvement (noninvolvement) of other tissues present
- Margins (minimum clearance); includes conjunctival margins and resection margin of optic nerve if specimen includes the globe
- Angiolymphatic invasion
- Perineural invasion
- Presence of ulceration
- For melanomas, indicate thickness and mitotic activity
Globe - description
Grossing
- Measure dimensions of the eye (anterior-posterior, horizontal, vertical)
- Measure length and diameter of optic nerve
- Measure cornea in mm (horizontal and vertical and anterioposterior)
- Look for sites of trauma (accidental or surgical)
- Examine eye surface for gross evidence of extraocular extension of tumor
- Describe the following:
- Corneal clarity
- Shape and diameter of pupil
- Color of iris, lesions
- Presence of lens
- Anterior chamber depth, configuration of anterior chamber angle
- Condition of ciliary body, lens, choroid, retina, vitreous body, optic disc
- Presence of foreign bodies (in traumatic specimens)
- For tumors, describe location, dimensions, shape, ulceration, color, consistency, hemorrhage, necrosis, calcification, ocular structures involved, extension into optic nerve, tumor distance to optic nerve and limbus, rupture of Bruch membrane
- Transillumination findings
Globe - sectioning
Grossing
- Enucleation: globe and part of optic nerve are removed from orbit
- For retinoblastoma, may need fresh tissue for genetic studies:
- Identify tumor location by transillumination
- Submit optic nerve margin separately before cut into globe
- Cut small window in sclera overlying tumor and obtain small tumor sample
- Try to avoid seeding of tumor cells onto optic nerve or elsewhere
- Fix in formalin (300 ml of 10% neutral buffered formalin) for 24 - 48 hours before sectioning
- Do not open or puncture the eye
- Wash in running tap water for 5 - 15 minutes
- Optionally place in 60 - 70% ethyl alcohol for 1 - 2 hours (firms up eye and restores color of vessels)
- Review clinical history and results of ophthalmologic examination prior to sectioning
- "Temporal" is same as lateral; "nasal" is same as medial
- Orient globe based on:
- Cornea is wider than tall by 1 mm
- Optic nerve distance to limbus (junction of cornea and sclera) is less medially than laterally (i.e. optic nerve is medial (nasal) to posterior pole)
- Superior oblique muscle tendon inserts in upper outer quadrant of posterior globe behind superior rectus muscle insertion and insertion points towards anterior nasal eye
- Inferior oblique muscle has muscular insertion in lower outer (temporal) quadrant of sclera and fibers run posteriorly and medially
- Long posterior ciliary arteries are in horizontal plane
- Four vortex veins exit posterior sclera
- Transilluminate globe to find tumor and cut accordingly
- Can use a substage microscope lamp in a dark room
- Rotate globe over light, mark abnormal shadows on sclera with indelible pencil
- Take Xray before opening globe if foreign body or retinoblastoma is suspected
- If choroidal melanoma is suspected, sample at least one vortex vein from each of four quadrants and submit separately
- Central section is called "pupil-optic nerve" section; other fragments are called calottes
- Try to include optic nerve, pupil, cornea, lens and large cut surface of tumor in same section, about 8 mm thick
- Use sharp razor to cut, holding globe with nondominant hand, cornea down against cutting block using blade between thumb and middle finger of dominant hand
- Open eye with sawing motion from back (adjacent to optic nerve) to front (1 mm inside limbus through peripheral cornea)
- If no tumor, cut globe at superior and inferior edges of iris in horizontal plane from back to front (5 mm above and below the optic nerve, missing the lens)
- Quick freeze first in liquid nitrogen to minimize artifacts
- Obtain cross section of optic nerve
Retina tumors (retinoblastoma)
Features to report
- Tumor location
- Number, size and location of lesion(s)
- Differentiation (poorly differentiated, Flexner-Wintersteiner rosettes, Homer-Wright rosettes, fleurettes)
- Growth pattern (diffuse, unifocal, multifocal)
- Extraocular extension or choroidal invasion
- Presence or absence of vitreous seeding
- Presence of absence of retinal detachment
- Invasion into optic nerve (prelaminar, to lamina cribrosa, retrolaminar, posterior resection margin)
- Involvement or noninvolvement of other structures submitted
- Margins (minimum clearance)
- Angiolymphatic invasion
- Tumor necrosis, calcification, DNA deposition around blood vessels, anterior chamber seeding, retinal or iris neovascularization
Uvea tumors
Features to report
- Histologic type
- Cell types present (for melanomas)
- Precise anatomic location (iris, ciliary body, choroid), relative to clock hour
- Tumor size
- Extraocular extension
- Growth pattern (diffuse, ring, focal)
- Dimension of largest diameter in contact with sclera
- Color of surface lesion and cut surface of lesion
- Involvement or noninvolvement of other structures present
- Margins (minimum clearance)
- Mitotic figures per 40 high power fields
- Presence of absence of 100 tumor infiltrating lymphocytes per 40 high power fields
- Presence of matrix rich microcirculation associated loops, networks or parallel with cross linking structures
- Angiolymphatic invasion
- Presence of retinal detachment or hemorrhage
- Involvement of intrascleral emissary channels
- For melanomas, indicate thickness and mitotic activity, color of surface lesion
- Other features present: drusen, neovascularization, nevi, etc.
- Reference: Arch Pathol Lab Med 2001;125:1177
Hereditary benign intraepithelial dyskeratosis
Table of Contents
Definition / general | Treatment | Gross description | Microscopic (histologic) description | Electron microscopy description | Molecular / cytogenetics description | Molecular / cytogenetics images | Differential diagnosisDefinition / general
- Also called Witkop von Sallman syndrome, red eye disease
- Acanthotic and dyskeratotic epithelium of conjunctiva and oral mucosa
- Rare, autosomal dominant disease with incomplete penetrance that usually appears in first decade of life
- Originally described in Haliwa Indians in North Carolina (USA), also elsewhere in US and Europe
- Bilateral lesions of conjunctiva; also oral lesions (J Am Acad Dermatol 2001;45:634)
Treatment
- Excision, but lesions commonly recur; no malignant transformation
Gross description
- Gray-white, inflamed, horseshoe shaped elevated lesions of conjunctiva and oral mucosa; bilateral corneal involvement (Cornea 2011;30:1481)
Microscopic (histologic) description
- Acanthotic and dyskeratotic epithelium of conjunctiva and oral mucosa
- Overlying multilayered parakeratotic mantle with pyknotic nuclei and epithelial ghosts, middle and superficial layers have large squamous cells and dyskeratotic cells but no atypia
- Subepithelial lymphoid infiltrate (Arch Pathol Lab Med 2008;132:1325)
Electron microscopy description
- Numerous vesicular bodies in immature dyskeratotic cells
- Densely packed tonofilaments fill mature dyskeratotic cells which lack cellular interdigitations and desmosomes (Oral Surg Oral Med Oral Pathol 1977;44:567)
Molecular / cytogenetics description
- Associated with 4q35 telomeric region (Am J Hum Genet 2001;68:491)
Differential diagnosis
- Conjunctival dysplasia: atypia, no family history, not bilateral, no oral mucosal involvement
IgG4 related disease
Inflammatory pseudotumor
Definition / general
Case reports
Treatment
Gross description
Gross images
AFIP images
Microscopic (histologic) description
Whole mount images
AFIP images
Microscopic (histologic) images
AFIP images
Positive stains
Differential diagnosis
- May not be a specific disease process, but due to various causes (paranasal sinus tumors, Rosai-Dorfman disease, inflammatory fibrosclerosis, dysthyroid ophthalmopathy, cholesterol or keratin granulomas, traumatic fat necrosis, prior hemorrhage or abscess)
- More common than infectious granulomas
- Usually ages 20 - 49 years with good health and sudden onset of exophthalmos with variable lid or conjunctival edema
Case reports
- 50 year old man with intraocular inflammatory myofibroblastic tumor with ALK overexpression (Arch Pathol Lab Med 2004;128:e5)
Treatment
- Steroids (alleviate signs and symptoms)
- Excision
Gross description
- Indurated orbital mass, often surrounding optic nerve and enveloping extraocular muscles
Gross images
AFIP images
Microscopic (histologic) description
- General:
- Edematous tissue with excessive production of ground substance, chronic inflammatory cells, vascular proliferation and hyperplastic connective tissue
- May have periphlebitis with tissue eosinophilia
- Inflammatory myofibroblastic tumor:
- Combinations of fibroblasts and myofibroblasts in background of plasma cells and other inflammatory cells
- Rosai-Dorfman related:
- Large histiocytes, some with lymphocytophagocytosis, lymphocytes and plasma cells, often with prominent fibrosis
Whole mount images
AFIP images
Microscopic (histologic) images
AFIP images
Positive stains
- Inflammatory myofibroblastic tumor: smooth muscle actin, variable ALK
Differential diagnosis
Idiopathic sclerosing inflammation
Definition / general
Microscopic (histologic) description
- Insidious, chronic and progressive fibrosing process
- Damages orbital structures by entrapment and mass effect
- May have cell mediated pathogenesis, similar to retroperitoneal fibrosis (Mod Pathol 1993;6:581)
Microscopic (histologic) description
- Desmoplasia, sparse lymphocytes (usually T cells), histiocytes, plasma cells, neutrophils, eosinophils
Other
[Pending]
Infectious keratitis
Table of Contents
Definition / general | Granulomatous keratitis | Herpes keratitis | Microscopic (histologic) descriptionDefinition / general
- Contact lens wearers are susceptible to Pseudomonas and Acanthamoeba
- Keratitis caused by microfilaria of Onchocerca volvulus is the leading cause of blindness worldwide, outside US
Granulomatous keratitis
- Due to HSV1, juvenile xanthogranuloma, leprosy, sarcoidosis
Herpes keratitis
- Most common cause of corneal ulcers
- Usually unilateral, may recur
- Usually HSV1
- Diagnosis difficult in recurrent cases; may need EM, PCR, ISH or immunohistochemistry since cultures are usually negative and inclusions are rarely identified
Microscopic (histologic) description
- Similar histologic findings for all organisms
- Destruction of corneal epithelium, Bowman layer and stroma
- Necrosis and prominent neutrophils
- Discontinuities of Descemet membrane with corneal perforation
- Crystal-like stromal opacities with Streptococcus viridans
- May need special stains to detect organisms
Herpes keratitis:
- Diffuse epithelial edema causing bullae between epithelium and Bowman layer
- Also patchy loss of Bowman layer
- Irregular epithelium
- Infiltration of anterior stroma by lymphocytes and plasma cells with stromal fibrosis and neovascularization
- Severe cases have granulomatous reaction surrounding Descemet membrane
- Herpetic inclusions are rare
Inflamed juvenile conjunctival nevus
Table of Contents
Definition / general | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosis | Additional referencesDefinition / general
- Benign, inflammatory juxtalimbal lesion characterized by marked eosinophils
- Children and teenagers
- May grow rapidly and cause congestion, and clinically resemble melanoma
- Associated with systemic allergies and bilateral papillary conjunctivitis (Br J Ophthalmol 2002;86:28)
Treatment
- Excision and close follow up
Microscopic (histologic) description
- Confluent growth pattern and a lack of maturation
- Epithelial cysts and solid islands composed of benign nevus cells
- Also prominent eosinophils and mast cells (some degranulated)
- Often lymphocytes (52%) and lymphoid follicles (Invest Ophthalmol Vis Sci 2002;43:1850) and plasma cells
- MUC5AC in enlarging cysts (Jpn J Ophthalmol 2012;56:107)
Microscopic (histologic) images
Differential diagnosis
Additional references
Iris
Definition / general
- Thin diaphragm of tissue with central opening (pupil)
- Forms boundary of anterior and posterior chamber
- Highly textured with folds and crypts
- Part of middle layer of eye (also ciliary body and choroid)
- Normally rests gently upon lens and bulges slightly forward
- Consists of stroma and posterior epithelial lining (two closely apposed epithelial layers, with numerous melanosomes); contains sphincter muscle within stroma that controls pupil
- Anterior iris lacks a cellular lining
- Color is due to number of stromal melanocytes; blue irises have few stromal melanocytes; brown irises have numerous melanocytes
- Blood vessels are usually surrounded by a thick collar of collagen fibers, resembling arteriolosclerosis
- Fewer melanosomes and melanocytes in patients with ocular and oculocutaneous albinism
- Regulates amount of light reaching pupil; muscles of iris dilate or constrict pupil in response to parasympathetic or sympathetic nerve impulses; normal diameter of pupil is 1 - 8 mm
- Iridectomy: excision of small segment of iris; place on filter paper to avoid folding
- Ectropion uveae: fibrovascular tissue on anterior surface of iris everts the papillary margin and pulls pigmented epithelia onto anterior surface of iris
Kaposi sarcoma-eyelid
Table of Contents
Definition / general | Case reports | Gross description | Microscopic (histologic) images | Differential diagnosisDefinition / general
- Develops in eyelid or conjunctiva of AIDS patients
- Appears purple in eyelid due to deep location in dermis, but red in conjunctiva since superficial
Case reports
- 96 year old woman with eyelid lesion (Case #368)
Gross description
- Thickening of conjunctiva
Microscopic (histologic) images
Differential diagnosis
- Hemorrhage
Keratoconus
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Complex, genetically heterogeneous multifactorial degenerative disorder
- Prevalence ranges between 1/2,000 and 1/50,000 in the general population
- Characterized by corneal ectasia and thinning
- Visual acuity decreases due to progressive myopia, irregular astigmatism and often, corneal apical opacification
Essential features
- Bilateral, progressive ectatic disease of the cornea that becomes cone shaped
- Leading indicator for corneal transplantation
- Complex disorder with both genetic and environmental factors
- Disease progression of keratoconus affects the epithelium, Bowman layer, stroma and Descemet membrane of the cornea but not the corneal endothelium
- Reference: StatPearls: Keratoconus [Accessed 30 September 2021]
Terminology
- Conical cornea
- KC (keratoconus)
- KCN (keratoconus)
ICD coding
Epidemiology
- Black and Latino > Caucasian
- M:F = 6:1
- Presents at puberty and progresses until the third to fourth decades of life but can occur or progress at any age
- Progresses more rapidly in young patients and stabilizes approximately 20 years after initial onset
- Reference: eMedicine: Keratoconus [Accessed 24 September 2021]
Sites
- Often affects both eyes
- Can lead to very different vision between the eyes
- Reference: American Academy of Ophthalmology: Keratoconus Symptoms [Accessed 24 September 2021]
Pathophysiology
- All layers of the cornea are believed to be affected
- Characteristic structural changes include:
- Epithelial basement membrane fragmentation and scarring
- Breaks in the anterior limiting lamina (i.e. Bowman membrane)
- Axial stromal thinning and scarring
- Deposition of iron in the basal epithelial cells forms Fleischer rings
- Breaks and folds close to the Descemet membrane form commonly seen striae and rarely, acute hydrops when aqueous humor enters corneal stroma
- Keratoconic corneas have been shown to have:
- Altered antioxidant enzymes, accumulations of cytotoxic reactive oxygen / nitrogen species, activated caspase pathways and mitochondrial DNA damage
- Abnormal oxidative stress related properties that can induce activation of degradative enzymes and degradation of tissue inhibitors of metalloproteinases
- Genomic deletion in the superoxide dismutase 1 (SOD1) gene has also been associated with the disease
- Some data suggests an inflammatory component (Eye (Lond) 2014;28:189)
Etiology
- Family history: increased chance of getting keratoconus; patient's children's eyes should be checked for signs starting around age 10
- Age: starts in teenage years; might show earlier in childhood and can less commonly affect people 40 and older
- Certain disorders: Down syndrome, Ehlers-Danlos syndrome, osteogenesis imperfecta and retinitis pigmentosa
- Inflammation: allergies, asthma or atopic eye disease can break down the tissue of the cornea
- Hard eye rubbing over time can break down the cornea; it can also make keratoconus progress faster if already present
- Race: people who are black or Latino are ~50% more likely to get it than people who are white
- Reference: WebMD: What Is Keratoconus? [Accessed 24 September 2021]
Clinical features
- Blurred or distorted vision, classical perception of multiple ghost images known as monocular polyopia
- Increased sensitivity to bright light and glare, which can cause problems with night driving
- Need for frequent changes in eyeglass prescriptions
- Sudden worsening or clouding of vision
- Reference: Clin Ophthalmol 2013;7:2019
Diagnosis
- Physical examination
- Medical history
- Eye examination with measuring corneal curvature using a manual keratometer
- Slit lamp examination:
- Fleischer ring: a ring of yellow-brown to olive-green pigmentation
- Vogt striae: fine stress lines within the cornea caused by stretching and thinning
- Munson sign: V shaped indentation in the lower eyelid when the person's gaze is directed downwards is highly pronounced
- Handheld keratoscope: for noninvasive visualization of the surface of the cornea by projecting series of concentric rings of light onto the cornea
- Corneal topography provides map indicating any distortions or scarring in the cornea, including steepening of curvature that is usually below the centerline of the eye; helps in detection at early stages
- Reference: Wikipedia: Keratoconus [Accessed 24 September 2021]
Prognostic factors
- Severe vision threatening disorder that commonly indicates corneal transplantation
Case reports
- 17 year old girl, 21 year old man and 22 year old man with rare complications of stromal thinning up to Descemet membrane 3 - 6 years post corneal collagen crosslinking (CXL) (Indian J Ophthalmol 2020;68:224)
- 19 year old man presenting with an unusual case of hydrops in keratoconus (Indian J Ophthalmol 2018;66:309)
- 25 year old man with epithelial remodeling masquerading as keratoconus progression (Indian J Ophthalmol 2020;68:3053)
Treatment
- In the early stages, eyeglasses or soft contact lenses
- As the disorder progresses and the cornea continues to thin and change shape, rigid gas permeable (RGP) contact lenses
- Corneal crosslinking
- Corneal transplantation
- In severe cases, due to scarring, extreme thinning or contact lens intolerance
- Keratoconus cornea is replaced with healthy donor tissue
- Reference: StatPearls: Keratoconus [Accessed 30 September 2021]
Clinical images
Gross description
- Wrinkled corneal button after transplantation
- Cornea is cone shaped
- Often has Fleischer ring (brown, stainable intraepithelial iron arc surrounds conical portion of cornea)
- Reference: StatPearls: Keratoconus [Accessed 30 September 2021]
Microscopic (histologic) description
- In vitro study of fixed, processed corneas with light microscopy shows 2 microscopic patterns:
- Typical pattern (identified in > 80%): both stromal and central epithelial thinning with multiple Bowman layer breaks
- Atypical pattern: lacks breaks in Bowman layer and has less thinning of the central epithelium
- Alterations in different layers of cornea are:
- Epithelium: cellular enlargement with irregular arrangement and apoptosis
- Stroma: loss in collagenous lamella, reduction in keratocyte density with appearance of nonkeratocyte cells
- Descemet membrane: morphological folds and irregularities; its rupture with entering of aqueous humor into corneal epithelium and stroma is a serious complication for keratoconus known as acute corneal hydrops
- Endothelium: does not exhibit any changes during keratoconus progression
- Using optical coherence tomography (OCT) for in vivo examining cornea, Sandali et al. proposed a classification system for keratoconus with 5 distinct stages (Ophthalmology 2013;120:2403):
- Stage 1: thinner corneal epithelium and stroma at the conus than control
- Stage 2: hyperreflective anomalies in Bowman layer are noticed with thickening epithelium and opaque stroma
- Stage 3: increased epithelial thickening and stromal thinning with disruptions in Bowman layer
- Stage 4: shows panstromal scarring
- Stage 5: considered as the acute form of keratoconus (hydrops) with Descemet membrane rupture and total corneal scar
- Reference: Biomed Res Int 2017;2017:7803029
Microscopic (histologic) images
Sample pathology report
- Cornea, keratoplasty:
- Keratoconus (see comment)
- Comment: Sections in keratoconus cornea show stromal and central epithelial thinning with multiple Bowman layer breaks. Brown iron deposits are seen within basal layer of corneal epithelium.
Differential diagnosis
- Pellucid marginal degeneration:
- Often considered a variant of keratoconus
- Corneal thinning occurs about 1 mm above the inferior limbus, resulting in advanced against the rule corneal astigmatism that may be observed on corneal topography or tomography
- Terrien marginal corneal degeneration:
- Slowly progressive noninflammatory, unilateral or asymmetrically bilateral peripheral corneal thinning
- Associated with corneal neovascularization, opacification and lipid deposition
- Keratoglobus:
- Extremely rare corneal disease in which the entire cornea thins from limbus to limbus, sometimes to the point where spontaneous perforation becomes possible
- Contact lens induced corneal warpage:
- Corneas swell (rather than thin) from hypoxia
- Stromal striations similar to Vogt striae occur
- Corneal ectasia postrefractive laser treatment
Additional references
Board review style question #1
A 25 year old woman complaining of blurred vision and polyopia comes to the ophthalmology department. On examination, a bilateral V shaped indentation in the lower eyelids is apparent when she looks downwards and corneal topography shows steeping of corneal curvature. She undergoes keratoplasty and the removed cornea is sent for pathological examination. What is the most likely diagnosis?
- Calcific band keratopathy
- Corneal dystrophy
- Keratitis
- Keratoconus
Board review style answer #1
Board review style question #2
Board review style answer #2
Keratomalacia
Table of Contents
Definition / generalDefinition / general
- Severe form of Vitamin A deficiency with diffuse, severe keratinization of mucous membrane epithelia, including corneal and conjunctiva epithelia (xerophthalmia)
- Leading cause of blindness in developing world
- Associated with secondary bacterial infection, corneal ulceration / necrosis, which causes corneal perforation and panophthalmitis
Lattice degeneration
Definition / general
- Bilateral condition that involves retina peripherally between ora serrata and equator
- Associated with hyperpigmentation, condensed overlying vitreous forming adhesions to margins of lattice degeneration that may cause subsequent retinal detachment
- Fundoscopy: circumferential area of involvement with small criss-crossing white lattice lines (thickened hyalinized blood vessels)
Microscopic (histologic) description
- Atrophic and thinned retina with superficial gliosis
- Thickened and hyalinized retinal vessels
- Overlying liquefaction of vitreous with vitroretinal adhesions at edge of lattice lesion
Ligneous conjunctivitis
Table of Contents
Definition / general | Terminology | Epidemiology | Sites | Etiology | Clinical features | Laboratory | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy images | Differential diagnosis | Additional referencesDefinition / general
- Chronic relapsing pseudomembranous conjunctivitis with woody induration of eyelid and tarsal conjunctiva and pseudomembrane on tarsal conjunctiva
- Also affects other mucosa
Terminology
- "Ligneous" means resembling wood
- Liesegang rings:
- Rings of precipitated iron and calcium (a phenomenon of chemical systems) seen in conjunctiva and eyelid, associated with inflammation, necrosis, fibrosis or cysts
- May resemble helminth eggs, larvae or adults (Am J Surg Pathol 1987;11:598, Wikipedia: Liesegang rings [Accessed 26 April 2018])
Epidemiology
- Usually children (median age 5 years), but can occur in adults
Sites
- Unilateral or bilateral
- Palpebral most common but also limbal and bulbar conjunctiva
Etiology
- Due to mutations in plasminogen PLG gene at 6q26 / plasminogen deficiency (J Thromb Haemost 2007;5:2315)
- Autosomal recessive
- Triggered with external irritants, fever, antifibrinolytic therapy and ocular surgery
Clinical features
- Mild discomfort with redness, woody induration of conjunctiva
- Similar lesions in mouth and upper respiratory tract, female genital tract or other mucosal surfaces
- May threaten sight
- Pseudomembrane typically separates from underlying epithelium without bleeding
- Corneal scarring, vascularization, infection or melting in advanced cases
Laboratory
- Decreased serum level of plasminogen type I
Case reports
- 7 month old boy with "sticky eye" (Digital Journal of Ophthalmology 2006;12(3))
- 20 year old woman with prosthetic eye (Int Ophthalmol 2011;31:25)
- 27 year old woman with Crohn's disease (Clin Ophthalmol 2008;2:203)
Treatment
- Excision, but pseudomembrane recurs (Virchows Arch 2007;451:815)
- Topical and systemic FFP treatment and conjunctival membrane excision (Cornea 2008;27:501)
- Topical or systemic plasminogen
- Topical heparin and steroids
Gross description
- Woody accumulation of fibrin
Microscopic (histologic) description
- Membrane contains large hyaline masses of fibrin and immunoglobulin but resembling amyloid
- Also T cells and B cells
- Conjunctival epithelium is thin and replaced focally with necrotic tissue
- Pink eosinophilic amorphous material within subepithelial tissue mimics amyloid
Microscopic (histologic) images
Positive stains
- Fibrinogen
Differential diagnosis
- Adenovirus infection
- Chlamydia
- Graft versus host disease: see Hum Pathol 1996;27:307
- Klebsiella
- Streptococcus
- Toxic epidermal necrolysis
Additional references
Lisch nodule
Table of Contents
Definition / general | Clinical images | Microscopic (histologic) description | Positive stains | Differential diagnosisDefinition / general
- Pigmented iris hamartomas
- Associated with neurofibromatosis type 1, also familial angiolipomatosis, a benign condition with no malignant potential (Arch Pathol Lab Med 1999;123:946)
Microscopic (histologic) description
- Dome shaped papules on anterior surface of iris consisting of aggregates of ovoid to round cells
Differential diagnosis
- Iris melanoma
- Neurofibromatosis
- Nevi
- Trauma
Lymphoma-conjunctiva
Table of Contents
Definition / general | Diagnosis | Case reports | Treatment | Gross description | Microscopic (histologic) description | Molecular / cytogenetics description | Additional referencesDefinition / general
- Usually indolent MALT lymphomas - difficult to predict malignant potential
- Often remains an isolated lesion
- May be preceded by apparently reactive lymphoid hyperplasia
- Mantle cell lymphomas have more aggressive behavior with median survival of 3 - 5 years
Diagnosis
- H&E for high grade lesions
- For low grade lesions, need fresh tissue for flow cytometry or gene rearrangement studies
- Immunohistochemistry (light chain restriction)
Case reports
- 8 year old boy with posttransplant lymphoproliferative disorder (Am J Ophthalmol 2007;143:1050)
- 53 year old woman with T cell lymphoma (Cornea 2007;26:1147)
- 55 year old man with primary diffuse large B cell lymphoma of palpebral conjunctiva (Can J Ophthalmol 2007;42:630)
- 72 year old woman with T cell lymphoma (Arch Ophthalmol 2002;120:508)
- CD5+ low grade marginal zone B cell lymphoma (Am J Surg Pathol 1998;22:201)
Treatment
- MALT: chemoradiation therapy (Virchows Arch 2006;448:506), possibly antibiotics (Am J Ophthalmol 2005;140:729)
Gross description
- Salmon colored mass or masses
Microscopic (histologic) description
- MALT: well differentiated, monoclonal small B lymphocytes, occasionally exhibits overt monocytoid cytology, prominent plasmacytic features or lymphoepithelial lesions (Am J Surg Pathol 2007;31:792)
Molecular / cytogenetics description
- MALT may have t(14;18)(q32;q21) involving IgH and MALT1 genes
- B cell clonality in 55% of MALT and 60% of diffuse large B cell lymphomas (Mod Pathol 2001;14:641)
Additional references
Lymphoma-orbit
Table of Contents
Definition / general | Radiology images | Case reports | Clinical images | Microscopic (histologic) images | Positive stains | Differential diagnosisDefinition / general
- Tumors composed of small lymphocytic proliferations confined to orbit are usually indolent and associated with long survival, even with minimal treatment
- MALT lymphoma:
- Uniform and monotonous proliferation of small lymphocytes infiltrating into orbital fat, blood vessels and nerves
- May have plasmacytoid features with Dutcher bodies (intranuclear inclusions) and serum paraproteinemia
- Light chain restriction
Case reports
- 5 year old girl with an angiocentric orbital lesion with an immature natural killer cell immunophenotype (Hum Pathol 2001;32:339)
- Nasal-type NK/T cell lymphoma of the orbit with distant metastases (Hum Pathol 2003;34:290)
Microscopic (histologic) images
AFIP images
Low grade tumor
Positive stains
- Monotypic immunoglobulins
Differential diagnosis
- Lymphoid hyperplasia:
- Polymorphic lymphocytes, vascular proliferation, prominent follicles with germinal centers
Macular degeneration
Definition / general
- Age related (senile) macular degeneration is the most common cause of irreversible visual loss in US
- Causes loss of central portion of vision
- May be due to vascular disease in choriocapillaris and retinal pigment epithelium
- Non-disciform (atrophic, dry type) causes slow, bilateral visual loss in elderly with atrophy and degeneration of retinal pigment epithelium and choriocapillaris; also drusen
- Disciform (wet, exudative type) is associated with more severe and acute vision loss; often after non-disciform degenerative changes and due to hemorrhagic retinal detachment secondary to neovascularization, as vessels from choriocapillaris penetrate through Bruch membrane beneath the retinal pigment epithelium and leak fluid / blood which organizes into macular scars
Microscopic (histologic) description
- Small macular scars
Medulloepithelioma
Melanocytoma
Melanoma-conjunctiva
Table of Contents
Definition / general | Epidemiology | Prognostic factors | Clinical features | Case reports | Treatment | Clinical images | Gross description | Gross images | Whole mount images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology images | Positive stains | Negative stains | Differential diagnosis | Additional referencesDefinition / general
- #2 malignancy of conjunctiva after squamous cell carcinoma
- 2% of ocular malignancies, 5% of ocular melanomas
- Due to primary acquired melanosis, nevi (20 - 30%) or no apparent precursor lesion (18 - 25%)
- Usually fair complexioned individuals age 40+ years
- Be wary of diagnosis in children as it is very rare (J Pediatr Ophthalmol Strabismus 2007;44:277)
Epidemiology
- 0.012 cases/100K in US, 0.024/100K in Sweden, 0.052/100K in Denmark
- Rare in blacks
Prognostic factors
- Excellent if small, localized and bulbar
- Intermediate if diffuse and bulbar
- Poor prognostic factors:
- Fornix, caruncle, plica semilunaris or palpebral conjunctiva
- Tumor thickness > 4 mm
- Epithelioid cells or 5+ mitotic figures / 10 HPF (Br J Ophthalmol 1994;78:252)
- Prognosis not related to nature of initial lesion, although acquired melanosis cases are often multicentric
Clinical features
- Metastases to parotid or submandibular lymph nodes, but uncommon if primary tumor less than 1.5 cm
- May extend directly into orbit, eyelids, sinuses, anterior chamber (Graefes Arch Clin Exp Ophthalmol 2007;245:431)
- Often recurs locally
- Overall mortality 25% - 32% (J Fr Ophtalmol 1999;22:315)
Case reports
- 32 year old man with amelanotic tumor (Cutis 2006;77:377)
- 61 year old woman with prior primary acquired melanosis (University of Iown Health Care: Conjunctival Melanoma arising from PAM [Accessed 30 April 2018])
- 79 year old man with metastasis to parotid gland (Br J Ophthalmol 2003;87:1428)
Treatment
- Complete excision or radical surgery, depending on extent of disease
- Cryotherapy for margins and base
- Also topical mitomycin C
- Recommended to avoid incisional biopsy (Trans Am Ophthalmol Soc 2000;98:471)
Clinical images
Gross description
- Vascular, pigmented, nodular
Microscopic (histologic) description
- Invasion of atypical melanocytes into epithelial connective tissue
- Usually thin surface epithelium
- Bizarre polygonal epithelioid cells with eosinophilic cytoplasm, large atypical nuclei, prominent eosinophilic nuclei
- Also spindle cells, smaller cells, balloon cells containing lipid
- Often lymphocytes at base or tumor margins
- Report: presence of primary acquired melanosis or nevi, presence of pagetoid spread at edge of excision, atypical intraepithelial melanocytes, nevus cells; also tumor thickness from surface of lesion to deepest margin using calibrated micrometer
Microscopic (histologic) images
Differential diagnosis
- Extension of extraocular melanoma
- Metastatic melanoma: clinical history of melanoma, more circumscribed, no intraepithelial tumor
- Spindle cell carcinoma
Melanoma-eyelid
Definition / general
- Rare
- May originate from nevus, acquired melanosis or de novo
- Poor prognosis due to early metastasis via lymphatics or bloodstream
- Sentinel lymph node biopsy has been used for melanoma of eyelid
Microscopic (histologic) description
- Resembles skin tumors more than globe tumors
- Spindled or epithelioid cells with marked atypia and invasion into dermis
Melanoma-uvea
Table of Contents
Definition / general | Essential features | Epidemiology | Pathophysiology | Clinical features | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Whole mount images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Malignant neoplasm of melanocytes within uveal tract, including iris, ciliary body and choroid
Essential features
- Tumor center located in iris, ciliary body or choroid (Methods Mol Biol 2014;1102:397)
- Approximately half metastasize, almost exclusively to liver (Methods Mol Biol 2014;1102:397)
- Tumor size, location and cell type are the most important histopathologic prognostic factors but molecular testing plays an increasing clinical role in prognostication
Epidemiology
- Most common primary intraocular malignancy in adults (PDQ Cancer Information Summaries: Intraocular (Uveal) Melanoma Treatment [Accessed 7 August 2018])
- Incidence is 5.1 new cases per million people in United States, which is low compared to other countries (Ophthalmol Clin North Am 2005;18:75)
- Mean age at diagnosis is 61 years (Br J Ophthalmol 2015;99:1550)
- Risk factors include light skin, Caucasian race, light eye color, inability to tan; weak association with sunlight exposure (Cancer Causes Control 2003;14:251, Ophthalmol Clin North Am 2005;18:75)
Pathophysiology
- May arise from preexisting uveal nevi or de novo (Arch Ophthalmol 2009;127:981)
Clinical features
- Half of cases are asymptomatic and discovered on exam; half present with visual disturbance
- Melanoma of iris: presents as elevated mass with variable pigmentation, often with distortion of pupil and prominent vessels
- Melanoma of choroid: irregular, slate gray, solid, choroidal tumor that may extend through Bruch membrane into retina and vitreous producing retinal detachment, macular edema, choroidal hemorrhage; occasionally spreads along scleral canals into orbit, rarely invades optic nerve
- Melanoma of ciliary body: may interfere with accommodation or cause localized cataract
- Tends to spread through scleral emissary canal
- Up to half of cases metastasize
- Distant metastases nearly exclusively to liver (95%), sometimes to lung and bone (Methods Mol Biol 2014;1102:397)
- Lymphatic spread uncommon due to lack of lymphatic channels in eye
Prognostic factors
- Size of tumor
- Ciliary body involvement
- Extension outside of orbit, metastasis and recurrence have very poor prognosis (Ophthalmology 1991;98:383)
- Cytogenetic abnormalities, particularly monosomy 3 and gain of 8q (Cancer Control 2016;23:93)
- Gene expression profiling (class 1A, 1B and 2) (Ophthalmology 2012;119:1596, Clin Cancer Res 2007;13:1466, Ophthalmology 2014;121:1281, JAMA Ophthalmol 2016;134:734)
- Histologic features: mitoses, cell type (spindle B versus epithelioid), extravascular matrix loops, tumor infiltrating lymphocytes and macrophages (PDQ Cancer Information Summaries: Intraocular (Uveal) Melanoma Treatment [Accessed 7 August 2018])
Case reports
- 19 year old man with melanoma of anterior chamber presenting as pigmentary glaucoma (Surv Ophthalmol 2017;62:670)
- 60 year old woman with sudden ocular pain (Indian J Ophthalmol 2018;66:1059)
- 63 year old woman with extension of choroidal melanoma after brachytherapy (Ophthalmology 2017;124:1503)
- 74 year old man with metastases treated with ipilimumab and nivolumab (Pigment Cell Melanoma Res 2017;30:558)
Treatment
- Episcleral brachytherapy utilizing radioactive seeds is the mainstay of eye sparing treatment and yields equivalent survival rates to enucleation (Arch Ophthalmol 2001;119:969, Clin Ophthalmol 2018;12:925)
- Location and size of tumor affect ability to use this mode of treatment (Brachytherapy 2014;13:1)
- Local resection for select tumors of the iris and ciliary body
- Enucleation reserved for large tumors (PDQ Cancer Information Summaries: Intraocular (Uveal) Melanoma Treatment [Accessed 7 August 2018])
- Rarely evisceration is necessary
Clinical images
Gross description
- Small uveal melanomas may be difficult to distinguish from a nevus clinically; size criteria are used
- Gross findings suspicious for melanoma include:
- Orange pigment
- Subretinal fluid
- Tumor thickness > 2 mm
- Low internal reflectivity on ultrasound examination
Gross images
Contributed by Lynn R. Schoenfield, M.D. and AFIP images
Whole mount images
Microscopic (histologic) description
- There are 2 distinct cell types and most tumors contain a combination of the 2:
- Spindle B cells: spindle shaped cells with large oval nuclei and distinct nucleoli
- Epithelioid cells: large polygonal cells with atypical nuclei, 1 or more prominent nucleoli and sometimes intranuclear pseudoinclusions
- Note that spindle A cells also exist, which are spindle shaped cells with slender nuclei that lack visible nucleoli; these are typically benign and are the melanocytes of uveal nevi
Microscopic (histologic) images
Positive stains
- HMB45: specific and sensitive
- S100: sensitive
- Vimentin, MelanA, MITF1 (Arch Pathol Lab Med 1996;120:497, Invest Ophthalmol Vis Sci 2002;43:2533, Methods Mol Biol 2014;1102:397)
- SOX10: highly sensitive for melanocytic proliferation
- Ki67 and pHH3: used to estimate proliferation rate but not for clinical management
Negative stains
- Cytokeratin markers should be negative but may sometimes stain focally
Molecular / cytogenetics description
- Monosomy 3, 8q gain and expression profiling (Invest Ophthalmol Vis Sci 2001;42:313, Clin Cancer Res 2007;13:1466)
Differential diagnosis
- Metastatic carcinoma (especially if amelanotic):
- Nevi:
- Small uveal melanomas may be difficult to distinguish from a nevus clinically; size criteria are used
- Clinical findings suspicious for melanoma include:
- Orange pigment
- Subretinal fluid
- Tumor thickness > 2 mm
- Low internal reflectivity on ultrasound examination
Board review style question #1
Which feature is suspicious for uveal melanoma as opposed to choroidal nevus?
- High internal reflectivity on ultrasound examination
- Lack of subretinal fluid
- Orange pigment
- Tumor thickness of 1.5 mm
Board review style answer #1
Board review style question #2
Board review style answer #2
Melanosis oculi-eyelid
Table of Contents
Definition / generalDefinition / general
- Also called ocular melanocytosis
- Rare congenital anomaly with variable hyperpigmentation of conjunctiva, episclera, sclera, uveal tract, possibly optic nerve
- May be variant of nevus of Ota
- Associated with ocular melanoma
- Sclera appears blue due to deep uveal pigmentation (see Tyndall effect)
Melanosis oculi-uvea
Meningioma
Table of Contents
Definition / general | Radiology images | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosisDefinition / general
- Arise from meninges of optic nerve or extension of cranial meninges
- Less common than intracranial tumor
- Associated with hearing loss, optic atrophy and exophthalmos
- Also papilledema if arises near inner sphenoidal ridge
Microscopic (histologic) description
- Meningothelial pattern of whorled spindle cells, psammoma bodies
Microscopic (histologic) images
Differential diagnosis
- Exuberant arachnoid hyperplasia
- Fibrous histiocytoma
- Juvenile ossifying fibroma
- Metastatic carcinoma
- Solitary fibrous tumor / hemangiopericytoma
Merkel cell carcinoma
Definition / general
- Resembles skin tumor
- Usually upper eyelid
- Often presents as large, nontender, red or violet mass
Mikulicz disease
Mikulicz disease
- Lymphocytic infiltration and formation of lymphoepithelial lesions
- Most common cause of Mikulicz syndrome
Mikulicz syndrome
- Chronic dacryoadenitis associated with enlargement of salivary glands
- Causes include:
- Mikulicz disease
- Sarcoidosis
- Tuberculosis
- Syphilis
- Mumps
- Lymphoma
- Leukemia
- Graves disease
Sjögren syndrome
- Usually postmenopausal women
- Mikulicz disease, with failure of lacrimal and conjunctival secretions and keratoconjunctivitis sicca
Molluscum contagiosum
Table of Contents
Definition / general | Treatment | Gross description | Microscopic (histologic) descriptionDefinition / general
- Poxvirus that produces small nodules on eyelid
- See Skin nontumor chapter
Treatment
- Excision if on eyelid margin to prevent infection of ocular surface
Gross description
- Multiple raised skin nodules with umbilicated centers
Microscopic (histologic) description
- Lobules of acanthotic epithelium that surround intracytoplasmic eosinophilic inclusion bodies (molluscum bodies) which become larger as they reach superficial epithelium
Mucocele-lacrimal sac
Definition / general
- Complication of chronic inflammation of lacrimal sac, with distention of sac due to low grade obstructive lesion or hypersecreting mucosa
- Cyst contents may be clear, milky, gelatinous, fibrinous or flocculent
- May be sterile or infected
Microscopic (histologic) description
- Cyst wall is atrophic with degenerative changes
- Also hyperplasia and chronic inflammatory infiltrate
Mucocele-orbit
Definition / general
- Due to chronic inflammation of frontal or ethmoid sinus
- Lesion erodes sinus wall, produces downward and lateral displacement of globe
- Insidious onset with slow and asymptomatic enlargement
Microscopic (histologic) description
- Cystic mass lined by ciliated, mucus-secreting columnar epithelium with scarring and inflammation
Myxoma-eyelid
Table of Contents
Definition / generalDefinition / general
- Rare
- May be part of Carney syndrome (spotty pigmentation of skin, overactive endocrine glands, myxoma of heart)
Necrobiotic xanthogranuloma with paraproteinemia
Definition / general
- Multiple nodules or plaques in periorbital areas and elsewhere in body
- Patients always have IgG paraprotein dysproteinemia
Microscopic (histologic) description
- Granulomas with collagen necrobiosis, foamy macrophages, Touton giant cells
Nevi-choroid or iris
Definition / general
- Common
- Detected during ophthalmic exams
- Most do not progress; at risk for malignancy if thick or enlarging circumference
- Iris nevi are elevated on iris surface
Nevi-conjunctiva
Table of Contents
Definition / general | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Differential diagnosis | Additional referencesDefinition / general
- See also Nevus of Ota in eyelid
- Most common tumor of conjunctiva
- Rarely invades cornea, appears in fornix or over palpebral conjunctiva
- Rarely involves bulbar conjunctiva, caruncle, or plica semilunaris
- May be observed at birth or later
- May enlarge and become more pigmented at puberty or during pregnancy
- About half of excised pigmented lesions are nevi, remainder are melanomas or primary acquired melanosis
Case reports
- 11 year old girl with balloon cell nevus (Arch Pediatr Adolesc Med 2001;155:93)
Treatment
- Excision or watchful waiting, only rarely transforms (1 per 150K)
- Excise if newly acquired in adults, clinical growth, change in pigmentation, cosmetic reasons
Clinical images
Gross description
- Discrete, flat or slightly elevated; circumscribed, pink, yellow-tan, brown or nonpigmented, in interpalpebral zone near limbus; 1/3 are amelanotic
Microscopic (histologic) description
- Nevomelanocytes organized into intraepithelial nests of oval cells (type A), sheets of oval to cuboidal cells (type B), and spindled cells in subepithelium (type C)
- Often (50%) with solid and prominent cystic inclusions of conjunctival epithelium and chronic inflammatory infiltrate
- May have atypical features and mitotic figures during growth periods
- Compound (70 - 78%):
- Most common, nevi cells in epithelium and subepithelial connective tissue
- Cells have cysts lined by cuboidal and goblet cells and intranuclear inclusions
- May have large pigmented cells with prominent basophilic nucleoli
- Usually mixed inflammatory cells
- Junctional (5%):
- Contiguous nests of round / spindle melanocytes near basal cell region with oval nuclei, small nucleoli
- Nucleoli may be basophilic and prominent but no atypia
- Uncommon except in young children
- Resembles primary acquired melanosis with atypia
- Subepithelial (9%):
- Nevus cells only in subepithelial connective tissue, no pigment, bland nuclei
- May have clear cytoplasm due to lipid and central round nucleus (balloon cell nevus)
Microscopic (histologic) images
AFIP images
Cystic compound nevus:
Images hosted on other servers:
Balloon cell:
Positive stains
Differential diagnosis
- Melanoma: cysts are rare, atypical intraepithelial component, atypical mitotic figures, necrosis, WT1+, HMB45+ (Arch Ophthalmol 2009;127:964), cytogenetic aberrations of 6p25, 6q23, 11q13, centromere 6 (J Cutan Pathol 2010;37:196, Br J Ophthalmol 2013;97:40)
Additional references
Nevi-eyelid
Definition / general
- On cutaneous or conjunctival surface, commonly on lid margin
- Usually junctional (nests of nevus cells at border of epidermis and dermis) or compound (nests at junction and within dermis)
- Usually acquired
- Rarely give rise to melanoma
Microscopic (histologic) description
- Nevus cells with bland nuclei
- May be multinucleated
- No / rare atypia, no / rare mitotic figures
Nevus of Ota-eyelid
Definition / general
- Also called congenital oculodermal melanosis
- More common in Asians and blacks
- A form of extrasacral mongolian spot involving the distribution of the first and second branches of trigeminal nerve in face
- Diffuse and deeply seated melanocytic lesion
- Slight risk of uveal melanoma if skin of eyelid or periorbital area is affected
Nodular & massive retinal gliosis
Table of Contents
Definition / general | Case reports | Microscopic (histologic) description | Positive stainsDefinition / general
- Relatively uncommon
- Large elevated scar near disc and posterior pole after hemorrhage or inflammation
- Polyclonal - not a neoplasm
Case reports
- 32 year old woman born with bilateral microphthalmia (Hum Pathol 2005;36:702)
Microscopic (histologic) description
- Vitreous body replaced by massively proliferating spindle cells containing fibrillary cytoplasm but no nuclear atypia
Nonspecific responses-cornea
Definition / general
- Corneal edema may lead to intraepithelial vesicles and bullae between epithelium and Bowman layer
- Aberrant basal lamina may develop within corneal epithelium in response to some injuries
- Collagenous tissue (pannus) may accumulate between corneal epithelium and Bowman layer
- Blood vessels may be present in superficial or deep stroma after inflammatory conditions (normally cornea is avascular)
- Irregular thickening of Descemet membrane occurs with aging
Blood staining
- Due to chronic anterior chamber hemorrhage or hyphema, caused by trauma or increased intraocular pressure
- Hemoglobin and other red blood cell breakdown products may diffuse into and stain cornea
- May eventually clear, beginning in periphery
- Microscopic (histologic) description: small pink-brown globules or spheres in corneal lamellae
Epithelial ingrowth
- Occurs after penetrating corneal injury (trauma, surgery)
- Epibulbar squamous epithelium grows through wound into anterior chamber of eye and may replace corneal epithelium and cause bullous keratopathy
- May cause intractable glaucoma if epithelium invades trabecular meshwork
- Microscopic (histologic) description: squamous epithelium in cornea instead of single layered corneal epithelium
- Positive stains: keratin
Pannus
Ulceration
- Due to any process that causes uneven distribution of the tear film across cornea
- Bacterial ulcers often destroy epithelium and Bowman layer with variable stromal destruction; due to Staphylococcus aureus, Streptococcus pneumoniae, E. coli, Klebsiella, Pseudomonas
- Complications include corneal perforation and scarring
- Fungal ulcers occur 8 - 15 days after trauma, usually involving vegetative matter; due to Candida, Aspergillus, Cephalosporium, Fusarium
- Satellite lesions are also present
- Rarely due to ocular cicatricial pemphigoid (Eur J Ophthalmol 2007;17:121)
- Case reports: 47 year old man with Exserohilum longirostratum (dematiaceous fungus) after trauma (Am J Clin Pathol 1994;101:452)
- Microscopic (histologic) description: eosinophils and granulomas with fungal infection
Ocular cicatricial pemphigoid
Table of Contents
Definition / general | Grossing | Diagnosis | Case reports | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Electron microscopy description | Differential diagnosis | Additional referencesDefinition / general
- Also called mucus membrane pemphigoid of conjunctiva
- Mucocutaneous autoimmune disorder
- Bilateral; only rarely unilateral (Cornea 2010;29:1462)
- Usually age 50+ years, more common in women
- 50% of cases involve conjunctiva, usually 10 years or more after onset of cutaneous or other mucosal disease; may occasionally demonstrate purely ocular disease (Ophthalmology 1999;106:355)
- Uncontrolled cases are associated with infection (Cornea 2004;23:819)
- Rarely presents with corneal ulceration (Eur J Ophthalmol 2007;17:121)
Grossing
- Impression cytology may be useful for diagnosis (Arch Soc Esp Oftalmol 2004;79:67)
- Divide sample in two - one for formalin, one in transport media for immunofluorescent studies
Diagnosis
- Compatible clinical picture plus linear deposition of IgA and IgG along conjunctival basal lamina or circulating anti-basement membrane antibodies (Ophthalmology 2004;111:45)
- Autoantibodies targeting α-6 and β-4 integrins (Clin Dermatol 2012;30:34)
- Fragmented and lumpy basement membrane fibrinogen on immunofluroscence (Am J Dermatopathol 2011;33:786)
Case reports
- 62 year old woman with anti-laminin 5 antibodies (Clin Exp Dermatol 2005;30:679)
- 2 case reports associated with Lyell syndrome in 80 and 60 year old patients (Ophthalmology 2012;119:688)
Clinical images
Microscopic (histologic) description
- Early - epithelial erosions and bullae
- Late - epithelial and stromal scarring, perivascular lymphocytes and plasma cells
Microscopic (histologic) images
Positive stains
- Local overexpression of IL6, IL12, IL17 (Invest Ophthalmol Vis Sci. 2012;53:8112)
Electron microscopy description
- EM has only limited usefulness in diagnosis (Ophthalmology 2006;113:1651)
Differential diagnosis
- Epidermolysis bullosa acquisita (Arch Ophthalmol 2006;124:1615)
- Paraneoplastic syndrome from nonocular carcinoma (Br J Ophthalmol 2007;91:1562)
Oncocytoma-lacrimal duct
Definition / general
- Develops in lacrimal sac or caruncle
- Usually elderly women
Treatment
- Excision is curative
Optic atrophy
Definition / general
- Loss of function of optic nerve with gliosis, loss of capillaries and loss of axonal tissue
- Due to damage from within the eye (optic neuritis, papilledema, glaucoma, retina-choroid lesions), to optic nerve or brain (trauma, tumor, demyelinating disorders, hydrocephalus) or congenital (Leber optic atrophy)
Gross description
- White, pale disc
Microscopic (histologic) description
- Loss of substance of optic nerve due to degeneration of myelin sheaths and axons
- Dura appears redundant due to loss of substance
- Gliosis within nerve
Papilloma-lacrimal duct
Table of Contents
Definition / general | Radiology images | Microscopic (histologic) description | Microscopic (histologic) imagesDefinition / general
- Similar to conjunctival papilloma
Microscopic (histologic) description
- Papillary aggregates of benign transitional epithelial cells with infiltrating neutrophils
- May have pseudoepitheliomatous hyperplasia
Persistent hyperplastic primary vitreous
Table of Contents
Definition / general | Radiology images | Gross images | Clinical images | Microscopic (histologic) description | Whole mount images | Microscopic (histologic) images | Differential diagnosisDefinition / general
- Congenital, due to incomplete regression of fetal vasculature of vitreous humor, producing a retrolental mass
- Usually unilateral
- Associated with small eye, white reflex behind pupil (leukokoria), fibrous tissue behind lens, often cataract
- Retina normal or with retinal dysplasia
Microscopic (histologic) description
- Dense fibrovascular retrolental mass containing elongated ciliary processes and part of hyaloid vascular system
Differential diagnosis
- Retinoblastoma:
- Also produces white reflex
Phacoanaphylactic endophthalmitis
Definition / general
- Usually occurs after penetrating injuries to lens
- Rarely due to spontaneous rupture of swollen lens with a cataract
- Granulomatous reaction may be due to acquired hypersensitivity to lens proteins
- May coexist with sympathetic uveitis
Microscopic (histologic) description
- Granulomatous inflammation surrounding area of lens perforation, with zonal pattern of central neutrophils around disintegrating lens fibers and peripheral macrophages, epithelioid cells and giant cells
- Posterior synechiae usually present
- Usually perivasculitis of retinal vessels
- Variable plasma cells in iris
Phakomatous choristoma
Table of Contents
Microscopic (histologic) imagesPhthisis bulbi
Table of Contents
Definition / general | Microscopic (histologic) description | Microscopic (histologic) imagesDefinition / general
- Degenerative change of globe involving all tissues
- Usually takes several years to develop
- Often due to accidental or post-surgical trauma
- Also found in eyes removed for blindness, pain, glaucoma, inflammation
- Due to reduced production of aqueous humor causing reduced intraocular pressure (hypotony) and shrinkage of globe
- Also due to organization of inflammatory exudate
- Degenerative changes and degree of shrinkage are variable in different tissues
- May be calcification and ossification with bone marrow
- Note: must decalcify globe
Microscopic (histologic) description
- Typically disorganization of intraocular contents, opaque media, corneal scars, exudate in anterior and posterior chambers, advanced cataracts, destruction of vitreous, scleral thickening, cyclitic membrane extends from one ciliary body behind the lens to the other ciliary body, complete detachment of retina; also ossification or bone formation
- Usually histology does not disclose initial condition leading to phthisis bulbi
- Occasionally occult melanoma or lymphoma is found
Pinguecula
Table of Contents
Definition / general | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) imagesDefinition / general
- Common bilateral degenerative process associated with sun damage and age; also advanced glycation end products (Graefes Arch Clin Exp Ophthalmol 2006;244:104) and diabetes mellitus (Cornea 2012;31:264)
- Not progressive
- Usually not biopsied
- May cause uneven distribution of tear film, leading to focal dehydration and saucer like depression in corneal tissue ("dellen"); associated with conjunctivochalasis (Acta Ophthalmol 2012;90:773) and contact lens induced subconjunctial hemorrhage (Am J Ophthalmol 2010;150:656)
Treatment
- Excision for cosmetic reasons or to remove mild irritation; otherwise no treatment
Gross description
- Elevated yellow lesion (due to solar elastosis) in bulbar conjunctiva in interpalpebral region near nasal limbus; conjunctiva is atrophic or thickened
Microscopic (histologic) description
- Band of subepithelial actinic elastosis with variable hyalinization and calcification
- May have acanthosis or dyskeratosis resembling carcinoma
- May have foreign body giant cell reaction around elastotic material (actinic granuloma)
Microscopic (histologic) images
Pleomorphic adenoma-lacrimal duct
Table of Contents
Definition / general | Treatment | Microscopic (histologic) description | Microscopic (histologic) imagesDefinition / general
- 50 - 60% of lacrimal gland tumors
- Resemble salivary gland tumors of same type
Treatment
- Excisional biopsy with negative margins to prevent recurrence and implantation within the orbit
Microscopic (histologic) description
- Usually encapsulated, composed of benign epithelial and myxoid mesenchymal elements
- Often prominent component of S100+ hyaline cells (presumed myoepithelial origin) with diffuse eosinophilic staining
- May have squamous metaplasia, bone, cartilage or fat
Microscopic (histologic) images
AFIP images
With carcinoma
Posterior polymorphous dystrophy
Table of Contents
Definition / general | Gross description | Microscopic (histologic) description | Differential diagnosisDefinition / general
- Type of primary endothelial dystrophy or endothelial decompensation
- Most common endothelial dystrophy and common indication for corneal transplantation in US
- Damage (decompensation) to endothelium, which normally pumps out fluid from corneal stroma, leads to chronic edema of stroma and epithelium, pain from rupture of epithelial bullae, eventually diffuse scarring and reduced vision
- Women ages 50+
- Some cases are autosomal dominant
- Some cases are due to mutation in COL8A2 at 1p34.3-p32.3
Gross description
- Bilateral
- Often asymmetric
Microscopic (histologic) description
- Corneal edema and cysts due to endothelial damage with paucity of endothelial cells and thickening of Descemet membrane
- Epithelium is separated from Bowman layer
- Papillary excrescences (guttae) in middle of cornea (must bisect cornea at equator and embed at equator to see)
- If severe, may see edema of basal cells, bullae formation and pannus formation (fibrovascular ingrowth between Bowman layer and epithelium)
Differential diagnosis
- Interstitial keratitis: inconspicuous ghost vessels in most posterior corneal stroma
Primary choroidal lymphoma (pending)
[Pending]
Primary vitreoretinal large B cell lymphoma (pending)
[Pending]
Pseudorheumatoid nodules
Table of Contents
Definition / generalDefinition / general
- Also called deep granuloma annulare
- May involve eyelid and eyebrow
Pterygium
Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Frequent, degenerative ocular surface lesion, characterized by invasion of the cornea by a fibrovascular tissue originating from the bulbar conjunctiva (Surv Ophthalmol 2018;63:719)
- Most frequent in the interpalpebral area, nasal side
- Thought to be UV light associated; not associated with human papillomavirus (HPV) (Br J Ophthalmol 200;91:1016)
- Develops from limbal epithelial progenitors; may be a stem cell disorder with possible premalignant features (Am J Pathol 2011;178:817)
Essential features
- Frequent, degenerative ocular surface lesion
- Similar to pinguecula but with corneal infiltration
- UV related
- Can masquerade as a neoplastic process
- Fibrovascular connective tissue that migrates to cornea
ICD coding
- ICD-10: H11.0 - pterygium of eye
Epidemiology
- Prevalence of 12%, with a geographic variation of 53% in China and 0.07% in Saudi Arabia (Surv Ophthalmol 2018;63:719)
Sites
- Corneoconjunctival limbus and cornea
Pathophysiology
- There are many hypotheses but its pathogenesis is still unknown
- Environmental factors have been suggested, due to high prevalence in hot and dry climates
- UV radiation has been proposed, due to the similarity with the histopathology of solar elastosis
- Other proposed hypotheses are corneal stem cell deficiency, inflammation, angiogenic disregulation, ultraviolet albedo (reflected, scattered light) in the anterior eye (Br J Ophthalmol 1993;77:734)
Etiology
- Older age, M > F, rurality, outdoor activities, prolonged exposure to UV light and alcohol consumption are known risk factors (Surv Ophthalmol 2018;63:719)
Clinical features
- Causes significant changes in corneal refractive status that increases with grade of pterygia (Indian J Ophthalmol 2007;55:383)
- High prevalence (18%) in those older than 40 living at high altitude in Mongolia (Eye (Lond) 2009;23:421)
- Clinically, may resemble ocular surface squamous neoplasia or melanoma
- Not related to multiple pterygium (webbing) syndrome (Am J Hum Genet 2006;79:390)
- Recurs in ~15% of patients and may masquerade as a neoplastic process
Diagnosis
- Diagnosis is performed when the typical clinical appearance is observed
Prognostic factors
- Recurrence rate is lower than 1/1,000 surgical procedures
Case reports
- 33 year old woman with growth in her eye (Am Fam Physician 2018;97:337)
- 40 year old man with mitomycin C excision and adjuvant extracellular matrix placement (Digit J Ophthalmol 2017;23:15)
- 60 year old man with corneal perforation associated with dellen after excision (BMJ Case Rep 2015;2015:bcr2015213319)
- 65 year old man with recurrent lesion treated with small incision lenticule extraction (J Int Med Res 2018;46:2474)
Treatment
- Treatment for cosmetic reasons, visual impairment, recurrent inflammation, mild irritation
- Medical therapy:
- Symptoms can be alleviated using over the counter vasoconstrictor drops and lubricating agents such as ointments or drops
- Corneal extension should be followed to determine the growth ratio to the visual axis
- Surgery:
- Excision with adjunctive therapies (radiotherapy, mitomycin C or fluorouracil [5FU]): low recurrence and fast but can have complication secondary to the use of the adjunctive agents
- Conjunctival flap or graft: considered the gold standard with recurrence as low as 1/1,000 with autografts; it is a lengthier procedure and technically more difficult
- References: Ther Adv Ophthalmol 2021;13:25158414211020152, J Curr Ophthalmol 2022;33:367
Clinical images
Gross description
- Fleshy
- Grossing tip: always bisect the tissue from the conjunctiva to the cornea
Microscopic (histologic) description
- Stromal changes:
- Fibrovascular connective tissue that migrates from the conjunctiva to cornea, dissecting into plane of Bowman layer, leading to fragmentation
- Fibrovascular core is composed of collagen mixed with basophilic fibrillar structures and blood vessels, all in variable amounts
- Variable acute and chronic inflammatory infiltrate
- Epithelial changes:
- May cause squamous metaplasia with goblet cell loss
- Acanthosis or atrophy
- Conjunctival intraepithelial neoplasia, primary acquired melanosis and nevus may coexist with pterygium (Saudi J Ophthalmol 2016;30:113, Histopathology 2006;48:387)
Microscopic (histologic) images
Positive stains
- Abnormal expression of HSP90 and Ki67 (Diagn Pathol 2013;8:32)
- Stromal plaques: E-cadherin and beta catenin (Br J Ophthalmol 2007;91:1209)
Negative stains
- HSP90 negativity may be useful to rule out ocular surface squamous neoplasia (Am J Clin Pathol 2016;145:385)
Sample pathology report
- Right eye, excision:
- Pterygium
Differential diagnosis
- Pinguecula:
- Histologically similar but there is no corneal invasion clinically or pathologically
- Superior limbic keratoconjunctivitis:
- Originates from the upper limbus
- Conjunctival intraepithelial neoplasia:
- Epithelial dysplasia; can coexist and be overlooked
Board review style question #1
Board review style answer #1
B. Elastosis of the lamina propria with corneal invasion. Elastosis is the key morphological finding in pterygia. The infiltration of the corneal stroma is important to be able to differentiate it from a pinguecula when there is no clinical information. Epithelial atrophy with goblet cell loss is nonspecific and can be seen in dry eye syndrome or superior limbic
keratoconjunctivitis. Neovascularization is present in most of pterygia but is also seen in many other
conjunctival inflammatory processes. Fragmentation of the Bowman layer may be present but is
also seen in keratoconus and other chronic keratitis.
Comment Here
Reference: Pterygium
Comment Here
Reference: Pterygium
Board review style question #2
Which of the following is the most important risk factor of pterygium?
- Chlamydia psittaci infection
- Human papillomavirus
- Sun exposure
- Tobacco and alcohol consumption
Board review style answer #2
C. Sun exposure is the most important risk factor. Human papillomavirus is not strongly associated with either pterygium or conjunctival intraepithelial neoplasia. Chlamydia psittaci has been associated with some MALT lymphomas but has not been associated with pterygium. Alcohol and tobacco have been listed as possible predisposing factors but are not as prevalent as sun exposure.
Comment Here
Reference: Pterygium
Comment Here
Reference: Pterygium
Pyogenic granuloma-eyelid
Definition / general
- Post-traumatic or post-surgical
Gross description
- Red, fleshy, often pedunculated
Microscopic (histologic) description
- Inflammatory lesion composed of granulation tissue with mixed inflammatory infiltrate
Retinitis pigmentosa
Definition / general
- Various inherited retinal disorders that are not actually inflammatory
- Common (incidence of 1/3600) with variable inheritance or as part of Refsum disease
- Usually causes loss of rods and cones to apoptosis and focal proliferation of retinal pigment epithelium
- Loss of rods causes early night blindness and restricted visual fields (bilateral loss of peripheral vision)
- Loss of cones affects central visual acuity
- Retinal atrophy causes constriction of retinal vessels, optic nerve head atrophy and accumulation of retinal pigment around blood vessels
Microscopic (histologic) description
- Migration of macrophages and retinal pigment epithelial cells with melanin into retina, particularly around vessels
- Also atrophy of photoreceptors in retina and choriocapillaris
Retinoblastoma
Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Whole mount images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Retinoblastoma is the most common intraocular malignancy in children characterized by hyperchromatic small round blue cells with scant cytoplasm arranged in sheets, nests and trabeculae
- Prognosis dependent on many factors; histopathological evaluation determines metastatic risk, including tumor invasion into anterior chamber, significant invasion into choroid (at least 3 mm) and postlaminar optic nerve invasion
- Retinoma / retinocytoma is the benign form of retinoblastoma
Essential features
- Most common intraocular malignancy of childhood (1 in 16,000 - 18,000 births) (Nat Rev Dis Primers 2015;1:15021)
- Often due to loss or inactivation of both alleles of the retinoblastoma 1 gene (RB1) (Knudson 2 hit hypothesis)
- Hyperchromatic small round blue cells with scant cytoplasm arranged in sheets, nests and trabeculae, often with calcifications and necrosis
- Most often has presurgical diagnosis by radiological and clinical features
- Localized chemotherapy is first line treatment, followed by systemic therapy and surgery
ICD coding
Epidemiology
- Most common intraocular malignancy of childhood (1 in 16,000 - 18,000 births) (Nat Rev Dis Primers 2015;1:15021)
- > 40% of cases are located in 6 countries in Asia-Pacific region (Eye (Lond) 2019;33:87)
- Approximately 90% in middle and low income countries (Nat Rev Dis Primers 2015;1:15021)
Sites
- Sporadic retinoblastoma usually unilateral eye
- Inherited retinoblastoma often bilateral eyes
- Can be trilateral (pineoblastoma) or very rarely quadrilateral (pineoblastoma and suprasellar primitive neuroectodermal tumor) (Pediatr Blood Cancer 2010;55:570)
Pathophysiology
- Loss or inactivation of both alleles of the retinoblastoma 1 gene (RB1)
- Tumor suppressor gene located at 13q14.2 locus
- Encodes RB1 protein
- Knudson 2 hit hypothesis
- Results from 2 separate mutations:
- First mutation is somatic or germline
- Second mutation is somatic
- Results from 2 separate mutations:
- Germline mutations in RB1 lead to inherited / familial retinoblastoma
- Earlier age of onset (J Neurosci Res 2019;97:29)
- Often bilateral involvement but can be trilateral or quadrilateral (Pediatr Blood Cancer 2010;55:570)
- Predisposes to development of other malignancies including osteosarcoma and melanoma (Pneumologie 1990;44:327)
- Reference: Annu Rev Pathol 2015;10:547
Etiology
- Inherited germline mutation of RB1
Clinical features
- Leukocoria (white reflex) of affected eye (late presenting sign) (J Neurosci Res 2019;97:29, J Ophthalmol 2020;2020:9315784)
- Glaucoma
- Strabismus (second most common sign)
- Eye pain
- Decreased visual acuity
- Retinal detachment
Diagnosis
- Diagnosis is almost always made clinically and radiologically
- High resolution MRI used for preoperative planning
- Can reliably detect optic nerve invasion, choroid and extrascleral invasion (Egypt J Radiol Nucl Med 2020;51:28)
- Can be diagnosed histopathologically post surgery
- Controversial use of FNA / cytology with concern for tumor seeding
- Can be done safely in select cases where imaging is not definitive (Int J Ophthalmol 2016;9:1233)
Radiology description
- Most often diagnosed via imaging
- Ultrasound:
- Does not require sedation or exposure to radiation
- Can visualize tumor calcification (J Neurosci Res 2019;97:29)
- Variably heterogeneous, echogenic soft tissue mass (AJR Am J Roentgenol 2000;175:495)
- Helps monitor tumor in treatment
- MRI:
- Modality of choice for pretreatment staging and surgical planning
- Helps correlate calcifications on ultrasound to confirm diagnosis
- T2 hypointense compared with surrounding vitreous
- Variable sensitivity for detecting high risk features (Ophthalmology 2014;121:1109)
- Optic nerve (59%), choroidal (74%) and scleral invasion (88%)
- CT:
- Exposure to radiation not preferred, especially in patients with RB1 germline predisposed to a second malignancy
- Contrast enhancing retrolental mass with calcifications
Radiology images
Prognostic factors
- > 95% survival in high income countries and ~30% survival in low income countries (Nat Rev Dis Primers 2015;1:15021, Cancer Lett 2014;351:59, Can J Ophthalmol 2009;44:S1)
- Risk of metastatic spread evaluated by histology post enucleation
- High risk histopathological features
- Involvement of optic nerve, choroid or anterior ocular structures (Oncogene 2018;37:1551, Arch Ophthalmol 2011;129:1422)
- High risk histopathological features
- International Intraocular Retinoblastoma Classification
- Classifies tumors into 5 groups based on clinical and radiological features:
- Group A (tumor ≤ 3 mm away from the fovea and disk)
- Group B (larger tumor without dissemination)
- Group C (local tumor dissemination)
- Group D (diffuse tumor dissemination)
- Group E (unsalvageable eye)
- Classifies tumors into 5 groups based on clinical and radiological features:
Case reports
- 23 year old man treated with primary intra-arterial and intravitreal chemotherapy (Oman J Ophthalmol 2019;12:119)
- 55 year old woman with late stage intraocular mass, diagnosed with FNA (J Cytol 2018;35:120)
- 3 sets of twins with retinoblastoma discordance (Indian J Ophthalmol 2019;67:436)
Treatment
- Evolved significantly from enucleation to vision sparing, localized chemotherapy
- Intraophthalmic artery / nerve chemotherapy
- Increased concentration within eye with less systemic effect
- Cured 85% of group D high risk cases in one trial (PLoS One 2016;11:e0151343)
- Systemic chemotherapy
- Second choice following targeted chemotherapy
- Increased systemic side effects and less effective
- Adjuvant in very high risk cases treats any micrometastases
- Role for primary enucleation in some high risk and all very high risk cases and in low income countries (Br J Ophthalmol 2018;102:265, Oncogene 2018;37:1551)
- Single curative procedure with low recurrence
Clinical images
Gross description
- Creamy white with chalky areas of calcification and yellow necrotic areas
- May grow inward (endophytic) or outward toward choroid (exophytic)
- Rarely are diffusely infiltrative; typically seeds intraocularly
- References: Int J Ophthalmol 2018;11:2011, Turk Patoloji Derg 2015;31:45
Gross images
Contributed by Marta Couce, M.D., Ph.D. and AFIP images
Frozen section description
- Cluster of partially crushed, small round blue cells
- Touch prep helpful in evaluating optic nerve margin
Microscopic (histologic) description
- Hyperchromatic small round blue cells with scant cytoplasm arranged in sheets, nests and trabeculae (Ophthalmology 2012;119:850)
- Variable differentiation
- Calcification and perivascular ischemic necrosis common
- Flexner-Wintersteiner rosettes (most common)
- Central lumen with basally located nuclei
- Analogous to outer limiting membrane of normal retina
- Homer Wright rosettes (less common in retinoblastoma)
- Lack of central lumen
- Tumor nuclei displaced away from eosinophilic center
- Fleurettes
- Tumor cells arranged side by side with central lumen
- Resembles fleur de lis
- Tumor cells arranged side by side with central lumen
- Photoreceptor differentiation
- Histological high risk features (tumor involving any of the following structures) (Community Eye Health 2018;31:17)
- Anterior chamber
- Iris
- Trabecular meshwork
- Schlemm canal
- Ciliary body
- Choroid
- Sclera
- Extraocular structures
- Retrolaminar optic nerve
- Histologic grade:
- G1: tumor with areas of retinocytoma (fleurettes or neuronal differentiation accounting for more than half of tumor)
- G2: tumor with many rosettes, Flexner-Wintersteiner or Homer Wright rosettes accounting for more than half of tumor
- G3: tumor with occasional rosettes, Flexner-Wintersteiner or Homer Wright rosettes accounting for less than half of tumor
- G4: tumor with poorly differentiated cells without rosettes or with extensive areas of anaplasia
Microscopic (histologic) images
Contributed by Marta Couce, M.D., Ph.D.
AFIP images
Whole mount images
Cytology description
- Variably cellular
- Small round cells with scant cytoplasm
- Clusters and rosettes
- PAS positive granules
- Must have mitosis and apoptosis
- Reference: J Cytol 2018;35:120
Cytology images
Positive stains
Negative stains
Molecular / cytogenetics description
- Recurrent chromosomal abnormalities (Annu Rev Pathol 2015;10:547)
- Isochromosome 6p (45%)
- E2F3 and DEK genes
- Gain of regions of chromosome 1q (44%)
- zsKIF14 and MDM4 genes
- Monosomy 16 (18%)
- CDH11 gene
- Gain of 1p (13%)
- Less common - loss of sex chromosomes and alterations in 17 and 19
- Isochromosome 6p (45%)
- Whole genome sequencing revealed recurrent BCOR mutations in 13% of retinoblastomas (Nature 2012;481:329)
- Sonic hedgehog signaling proteins (J Clin Pathol 2015;68:6)
- SHH (98.7%), GLI1 (85.9%) and GLI2 (92.2%) frequently expressed in retinoblastoma
- 26.6% of 79 cases had strong SHH expression
- High SHH expression closely related to advanced disease
- SHH (98.7%), GLI1 (85.9%) and GLI2 (92.2%) frequently expressed in retinoblastoma
- Non-RB1 mutated retinoblastomas (2.7%)
- Vast majority MYCN mutated
- Also has role in controlled E2F1, E2F2 and E2F3 genes
- Frequent gain of 19p, 17p/q and 2p and telomeric end of 9q
- Very small percentage have RB1 inactivated by chromothriptic event in chromosome 13
- Vast majority MYCN mutated
Sample pathology report
- Eye, right, enucleation:
- Retinoblastoma (follow College of American Pathologists: Protocol for the Examination of Specimens From Patients With Retinoblastoma [Accessed 11 October 2021])
- Case summary: retinoblastoma
- AJCC-UICC 8
- Case summary report
- No known preoperative therapy
- Procedure
- Enucleation
- Total length of optic nerve
- Less than 1 mm
- Tumor sampling for molecular studies
- Yes
- Specimen laterality
- Right
- Tumor
- Tumor site (macroscopic examination / transillumination)
- Superotemporal quadrant of globe
- Tumor site after sectioning
- Superotemporal
- Tumor size after sectioning
- Greatest basal diameter of tumor
- Exact measurement: 6 mm
- Basal diameter at cut edge of tumor
- Exact measurement: 2 mm
- Greatest thickness of tumor
- Exact measurement: 3 mm
- Percentage of vitreous cavity occupied by tumor
- Specify percentage: 15%
- Distance from anterior edge of tumor to limbus at cut edge
- Exact distance: 7 mm
- Distance from posterior margin of tumor base to edge of optic disc
- Exact distance: 6 mm
- Greatest basal diameter of tumor
- Tumor growth pattern
- Exophytic
- Histologic grade
- G2 (tumor with many rosettes [Flexner-Wintersteiner or Homer Wright rosettes accounting for more than half of tumor])
- Anaplasia grade
- Mild
- Histopathologic features suggesting MYCN amplification
- Not identified
- Extent of optic nerve invasion
- None identified
- Tumor site (macroscopic examination / transillumination)
- Margins
- Margin status (select all that apply)
- All margins negative for tumor
- Margin status (select all that apply)
- Regional lymph nodes
- Regional lymph node status
- Not applicable (no regional lymph nodes submitted or found)
- Regional lymph node status
- Pathologic stage classification (pTNM, AJCC 8th edition)
- TNM descriptors (select all that apply)
- Not applicable
- pT category
- pT1: intraocular tumor without any local invasion, focal choroidal invasion or prelaminar or intralaminar involvement of the optic nerve head
- pN category
- pN not assigned (no nodes submitted or found)
- pM category (required only if confirmed pathologically)
- Not applicable - pM cannot be determined from the submitted specimen(s)
- TNM descriptors (select all that apply)
Differential diagnosis
- Astrocytoma:
- Generally not small, round blue cell pattern
- GFAP positive
- Leukemia / lymphoma:
- Massive retinal gliosis:
- No rosettes or fleurettes
- No necrosis or calcifications
Board review style question #1
An 8 year old girl had an enucleation that showed a white, chalky intraocular tumor. A histologic image is shown above. Which of the following statements is true regarding this entity?
- Enucleation remains the best initial treatment
- Involvement of the optic nerve is not considered a significant prognostic factor
- Majority of these tumors have MYCN mutations
- Recommended initial treatment paradigm is chemoreduction
- Strabismus is never seen in patients with this tumor
Board review style answer #1
Board review style question #2
Retinoblastomas can occur both in sporadic and familial forms. Which of the following features is more indicative of a sporadic tumor?
- Bilateral retinoblastomas
- Development of subsequent melanoma or osteosarcoma
- Early age of onset
- Germline mutation of Rb gene
- Late age of onset
Board review style answer #2
E. Late age of onset. Familial tumors result from germline mutations in the Rb gene and are more likely to be bilateral or trilateral. They have an early age of onset and are prone to the development of other malignancies, including osteosarcoma, melanoma, sarcoma and breast cancer.
Comment Here
Reference: Retinoblastoma
Comment Here
Reference: Retinoblastoma
Retinocytoma
Table of Contents
Microscopic (histologic) imagesRetrolental fibroplasia
Definition / general
- Also called retinopathy of prematurity
- Previously was leading cause of blindness in US
- Occurs in premature infants given oxygen therapy; related to level and duration of oxygen, degree of prematurity at birth and status as carrier for defect in Norrie disease gene
- Immature vessels of premature infants are damaged by high or even physiologic oxygen; rarely occurs in term infants
Pathophysiology
- Oxygen therapy causes vasoconstriction and obliteration of immature retinal vessels in lateral (temporal) retina which causes ischemia and failure of retina to vascularize
- Then vasoproliferative phase and angiogenesis
- Vessels grow into vitreous or leak serum or fluid, 25% have associated scarring which causes retinal detachment
Rhabdomyosarcoma-orbit
Table of Contents
Definition / general | Radiology images | Clinical images | Whole mount images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology images | Positive stains | Negative stainsDefinition / general
- Most common orbital sarcoma in childhood
- Usually embryonal and alveolar subtypes (alveolar more aggressive)
- Often rapid onset of unilateral proptosis
- May occur after radiation therapy for retinoblastoma, close to previously irradiated fields
- Tumors in retinoblastoma patients may have rosette-like structures
- References: Am J Surg Pathol 1998;22:1351 (postradiation therapy for bilateral retinoblastoma)
Microscopic (histologic) description
- Syncytium of strap cells with abundant eosinophilic cytoplasm
- Also closely packed small round cells with scanty cytoplasm, coarse nuclear chromatin and increased mitotic activity
- Many have minimal rhabdomyoblastic differentiation except in occasional mature strap cells with cross striations
- Alveolar pattern has fibrovascular septa resembling lung alveoli
Microscopic (histologic) images
AFIP images
Cytology images
Positive stains
- Myogenin, desmin, muscle specific actin (HHF35), vimentin and neurofilament
Schnabel cavernous degeneration
Table of Contents
Definition / generalDefinition / general
- Defined as formation of cavernous spaces in retrolaminar portion of proximal optic nerve due to focal loss of myelin and axons and accumulation of hyaluronic acid
- Present in < 0.1% of eyes at autopsy; 80% are women, mean age 88 years (range 54 - 103 years)
- Associated with severe vascular anomalies (75%), glaucoma (24%)
- Grading of cavernous degeneration: I - clearly present but < 10% of diameter of optic nerve at point of most severe involvement; II - 10 - 25%; III - 50 - 75%; IV - > 75%
- References: Arch Pathol Lab Med 2003;127:1314, Klin Monbl Augenheilkd 1990;197:162
Sclera
Table of Contents
Definition / generalDefinition / general
- 80% of surface area of eye
- Begins at periphery of cornea, extends posteriorly to optic nerve
- Relatively rigid; protects eye from trauma and maintains intraocular pressure
- Visible anteriorly under transparent conjunctiva; white in adults
- Thickness varies; 0.3 mm at insertion of rectus muscles, 0.8 mm at limbus and 1.0 mm at insertion of optic nerve
- Weakly attached to underlying choroid by thin collagen fibers
- Heals poorly due to few blood vessels or fibroblasts
- Aging related changes include calcification between collagen fibers, senile scleral plaques
- Composed of episclera, stroma and lamina fusca
- Episclera: most superficial part of sclera, located between fibrous structure that envelopes the globe (Tenon capsule) and scleral stroma; composed of loose collagen fibers and fibroblasts with numerous vessels, occasional melanocytes and mononuclear white blood cells
- Stroma: largest component of sclera, randomly arranged bands of collagen with occasional elastic fibers and fibroblasts; minimal blood vessels except in perforating emissiary canals, accompanied by nerves and scattered melanocytes; rarely contains a prominent nerve (nerve loop of Axenfeld) in an emissiarial canal near limbus, which may mimic a neurofibroma; anterior ciliary arteries perforate sclera near insertion of rectus muscles, posterior ciliary arteries pass through sclera near optic nerve; vortex veins exit sclera posterior to equator of eye
- Lamina fusca: innermost layer of sclera with loose collagen fibers, fibroblasts and scattered melanocytes
Seborrheic keratosis
Table of Contents
Gross description | Microscopic (histologic) description | Microscopic (histologic) imagesGross description
- Elevated irregular lesions, often crusty or greasy appearing
- Often pigmented
Microscopic (histologic) description
- Acanthosis with marked hyperkeratosis and keratin filled cysts
- Also increased pigmentation in basal layer
- No atypia
Silica granuloma
Table of Contents
Definition / generalDefinition / general
- Noncaseating, composed of epithelioid cells, multinucleated giant cells and birefringent silica crystals, surrounded by fibrosis
Solitary fibrous tumor-orbit
Table of Contents
Definition / general | Prognosis and treatment | Case reports | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Differential diagnosisDefinition / general
- Usually benign but may be aggressive
- Lipomatous hemangiopericytoma may be variants of solitary fibrous tumor (Hum Pathol 2000;31:1108)
- References: Am J Surg Pathol 1994;18:281
Prognosis and treatment
- 30% recur, 15% metastasize (lung, liver, bone, regional lymph nodes), usually late
- Histology does not predict behavior (Hum Pathol 1982;13:210)
Case reports
- 58 year old man with t(9;22)(q31;p13) and orbital tumor (Arch Pathol Lab Med 2000;124:756)
- 66 year old woman with left eye proptosis, ptosis, and blindness (Arch Pathol Lab Med 2002;126:1555)
- Myxoid variant (Mod Pathol 1999;12:463)
Microscopic (histologic) description
- Usually encapsulated
- Random pattern of polygonal and rounded cells with ill defined cytoplasm, variable nucleoli
- Staghorn vascular pattern and perivascular collagen, dense pericellular reticulin, occasional mitotic figures
- Must rule out other tumors with this pattern
Microscopic (histologic) images
Positive stains
Negative stains
Differential diagnosis
- Fibrous histiocytoma:
- Predominant storiform pattern
- Foam cells and giant cells present
- Meningiomas:
- EMA positive
- Complex interdigitating processes and desmosomes by EM, deletions of #22
- Solitary fibrous tumor:
- CD34 strongly positive
Squamous cell carcinoma-conjunctiva
Table of Contents
Definition / general | Clinical features | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Molecular / cytogenetics description | Differential diagnosis | Additional referencesDefinition / general
- See also mucoepidermoid carcinoma
- Rare but more common than basal cell carcinoma at this site
- In U.S., precancerous lesions are excised, so invasive carcinoma is uncommon
- Rates: 0.03 per 100,000 in U.S., 3.5 per 100,000 in Uganda
- Mainly adults
- In U.S., commonly 60+ years, 55 - 70% men (Can J Ophthalmol 2002;37:14)
- Associated with sunlight exposure, actinic keratosis; also xeroderma pigmentosum, albinism, toxins, HPV 16/18 (55%), possibly atopic eczema (Cornea 2003;22:135)
- May invade anterior chamber of globe or orbit but only rarely metastasizes or causes death
Clinical features
- HIV / AIDS patients
- Rising incidence with 8% prevalence in Kenya (East Afr Med J 2006;83:267)
- Recommended to screen HIV / AIDS patients for conjunctival lesions
- Mean age is 35 years
- Usually affects women
- Patients present late with advanced disease
- More aggressive with high recurrence rates
Case reports
- 6 year old boy with 2 conjunctival tumors, atypical fibroxanthoma and xeroderma pigmentosum (Pediatr Dev Pathol 2007;10:149)
- 38 year old woman with AIDS with multifocal disease and intraocular penetration (Cornea 2006;25:745)
- 65 year old man with prosthetic eye (J Postgrad Med 2006;52:234)
- 71 year old man with bony metastases (Klin Monbl Augenheilkd 2002;219:813)
Treatment
- Complete excision of superficial tumors
- Radical surgery for deeply invasive tumors
- 6% recur
- Rarely metastasize to lymph nodes (more common if large or multiple recurrences)
Gross description
- Papillary or exophytic gray-white mass, often at limbus
- Occasionally jet black resembling melanoma (in heavily pigmented individuals)
- Surrounded by inflamed conjunctiva
Gross images
Microscopic (histologic) description
- Atypia throughout full thickness of epithelium (conjunctival intraepithelial neoplasia) with individual tumor cells or nests extending into underlying stroma
- Dense sclera usually limits deepest margins
- Epithelium may be keratinized
- Cells have eosinophilic or clear cytoplasm, intercellular bridges, dyskeratosis, coarse chromatin, prominent nucleoli
- May have pigment within benign and malignant cells in heavily pigmented patients (Ophthalmic Surg Lasers Imaging 2003;34:406)
Microscopic (histologic) images
AFIP images
Images hosted on other servers:
Positive stains
- High molecular weight keratin, EMA, EGFR (tumor and normal) (Ophthal Plast Reconstr Surg 2006;22:113)
Molecular / cytogenetics description
- Usually aneuploid
Differential diagnosis
Additional references
Squamous cell carcinoma-eyelid
Table of Contents
Definition / general | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosisDefinition / general
- 10% of carcinomas in eyelid
- Usually lower lid
- Rarely are adenoid (pseudoglandular)
- Rarely invade eye or orbit or metastasize
Gross description
- Elevated and thickened areas of eyelid, may be ulcerated or friable
Microscopic (histologic) description
- Invasion of malignant squamous cells into dermis
- Cells are large and eosinophilic with marked atypia
- Often abnormal deep keratinization, may have keratin pearls
Microscopic (histologic) images
Differential diagnosis
- Actinic keratosis
- Inverted follicular keratosis
- Keratoacanthoma
- Pseudoepitheliomatous hyperplasia
- Seborrheic keratosis
- Squamous papilloma
Squamous cell carcinoma-lacrimal duct
Definition / general
- Uncommon; usually moderately differentiated
- Similar to nasal or conjunctival squamous cell carcinoma
- Often spreads along surfaces as well as infiltrating
- Lung is most common site for metastases, then bone and remote viscera
Microscopic (histologic) description
- Often papillary projections into lumen
Squamous papilloma-conjunctiva
Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Benign tumor characterized by an outgrowth of epithelial and stromal elements of the conjunctiva
- High recurrence rate
Essential features
- Benign epithelial tumor
- Strong association with human papillomavirus (HPV 6 and 11)
- Grossly classified as sessile or pedunculated
- Location: plica semilunaris or caruncle in younger patients and limbal area in older patients; less frequent in fornix or palpebral conjunctiva
Epidemiology
- Incidence unknown
- Approximately 1% of epibulbar cases in children and 11% in adults (JAMA Ophthalmol 2013;131:585)
- More common in 20 - 30 year olds
- High association with human papillomavirus 6 and 11 (low risk subtype) in nonlimbal papilloma
Etiology
- Human papillomavirus 6 and 11 (low risk subtype) in nonlimbal papilloma
- UV exposure in limbal papilloma
- Reference: Br J Ophthalmol 2007;91:1014
Clinical features
- Younger patients
- No decrease or loss of visual acuity
- Single lesion that is soft and has classic finger-like projections
- Siblings may be affected
- Association with cutaneous warts
- Reference: JAMA Ophthalmol 2013;131:585
Diagnosis
- Performed under ophthalmologic examination; slit lamp observation usually aids in the differential diagnosis
- Biomicroscopy and optical coherence tomography (OCT) imaging may help to identify intraocular extension in cases where malignancy is suspected
- Reference: Eye Vis (Lond) 2019;6:18
Prognostic factors
- High recurrence rate: younger patients > older patients
- HPV positive cases
Case reports
- 5 year old girl with a disfiguring right eye lesion that recurred several times (AMA Ophthalmol 2020;138:e190930)
- 28 year old woman with a caruncular mass (Bezmialem Science 2018;6:160)
- 49 year old woman with a limbal mass treated with interferon alpha 2b eye drops (Medicine (Baltimore) 2020;99:e19181)
- 54 year old woman with a rapidly growing eyelid tumor (Case Rep Ophthalmol Med 2019;2019:5830493)
Treatment
- Observation and follow up can be used, as some of these lesions regress
- Medical treatment includes cryotherapy, CO2 laser, mitomycin C, cimetidine and interferon
- Excision recommended in adult limbal cases to rule out dysplasia; in children, if discomfort is present or for aesthetic reasons
- Reference: Eye Vis (Lond) 2019;6:18
Clinical images
Gross description
- Fragment of whitish / reddish sessile / pedunculated papillomatous tissue measuring 2 mm to 1 cm
Microscopic (histologic) description
- Exophytic:
- Finger-like projection of an acanthotic epithelium with numerous goblet cells without dysplasia
- Stroma is composed of a fibrovascular core, usually containing inflammatory cells
- Occasionally, koilocytosis is present
- Limbal squamous cell papilloma:
- Characterized by squamous cells with mild atypia
- Contains only a few goblet cells
- Solar elastosis is usually present within the stroma
- Papillomatosis in this location is less striking
- Sessile papillomas can be more frequently associated with dysplastic changes than pedunculated papillomas
- Reference: Acta Ophthalmol Scand 2000;78:663
Microscopic (histologic) images
Cytology description
- Conjunctival impression cytology:
- Squamous cells with numerous goblet cells
- Dysplasia can be seen in limbal lesions
- If no dysplasia is observed, is similar to conjunctiva with mild to moderate squamous metaplasia
Positive stains
- Often p53, Ki67, BCL2 (Ann N Y Acad Sci 2004;1030:419)
- Ki67: mostly basilar cells but many higher level cells positive
- p53: weakly and focally positive (10 - 20%) (Surv Ophthalmol 2015;60:263)
- CK7: full thickness staining
- CK14: basilar positive (Am J Ophthalmol 2013;156:830)
Negative stains
Molecular / cytogenetics description
- HPV 6 in 80% (Clin Ophthalmol 2012;6:1553)
- Also HPV 11; rarely HPV 45 (Br J Ophthalmol 2007;91:1014)
- Rarely HPV 13 (Diagn Microbiol Infect Dis 2005;53:71)
- Note: koilocytosis is often lacking even when HPV is present (Br J Ophthalmol 2001;85:785)
Sample pathology report
- Right eye, excision:
- Conjunctival squamous papilloma (see comment)
- Comment: There is no sign of malignancy in this particular specimen.
Differential diagnosis
- Ocular surface squamous neoplasia:
- Dysplasia is present within the squamous epithelium
- If the basement membrane is infiltrated, squamous cell carcinoma is the diagnosis
- Pyogenic granuloma:
- Usually erosion is present at the surface and there is no acanthotic epithelium
- Granulation tissue is exuberant
- Clinically, with a history of trauma or previous surgery
- Follicular conjunctivitis:
- Dense lymphoplasmacytic infiltrate is present with germinal center formation
- Epithelium is thin
Board review style question #1
Board review style answer #1
B. Goblet cells are classically observed in these cases. Sometimes they are very numerous and they are characteristically slightly basophilic. Pagetoid spread of sebaceous cells is represented by malignant cells with atypical nuclei and optically empty vacuolated cytoplasm. Amelanotic spread of melanoma cells must show malignant features of the nuclei and is usually centrally located. An artifact will not be structured as observed in the cells here.
Comment Here
Reference: Squamous papilloma-conjunctiva
Comment Here
Reference: Squamous papilloma-conjunctiva
Board review style question #2
Squamous papilloma is more frequently associated with
- Herpex simplex virus
- Human papillomavirus 6 and 11
- Human papillomavirus 16 and 18
- Sun exposure
Board review style answer #2
B. The most frequent associations are with HPV 6 and 11. Sun exposure is an important association in limbal papillomas but is less frequent than HPV. Herpes virus is not associated with squamous papilloma. HPV 16 and 18 are associated with ocular surface squamous neoplasia.
Comment Here
Reference: Squamous papilloma-conjunctiva
Comment Here
Reference: Squamous papilloma-conjunctiva
Squamous papilloma-eyelid
Gross description
- Resemble skin tags
Microscopic (histologic) description
- Acanthotic epithelium with hyperkeratosis, papillary projections with inner fibrovascular core
Staging-conjunctiva carcinoma
Table of Contents
Definition / general | Primary tumor (T) | Regional lymph nodes (N) | Distant metastasis (M) | Stage groupingPathologic TNM staging of carcinoma of conjunctiva, AJCC 7th edition
Definition / general
- Applies to clinical and pathologic staging
- Excludes melanoma and malignancies other than carcinoma
Primary tumor (T)
Regional lymph nodes (N)
- NX: Regional lymph nodes cannot be assessed
- N0: No regional lymph node metastasis
- N1: Regional lymph node metastasis
Distant metastasis (M)
- M0: No distant metastasis
- M1: Distant metastasis
Stage grouping
- No stage grouping is presently recommended by AJCC
Staging-conjunctiva melanoma
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Primary tumor (pT) | Regional lymph nodes (pN) | Distant metastasis (pM) | Prefixes | AJCC prognostic stage groups | Registry data collection variables | Histologic grade (G) | Histopathologic type | Board review style question #1 | Board review style answer #1Definition / general
- Based on AJCC 8th edition staging system
- Used for melanomas arising from bulbar and palpebral conjunctiva, the caruncle and the fornices
- Not applicable to primary eyelid skin melanomas
- Not applicable to uveal melanomas with secondary involvement of conjunctiva
Essential features
- AJCC 7th edition staging was sunset on December 31, 2017; as of January 1, 2018, use of the 8th edition is mandatory
Terminology
- Bulbar conjunctiva is the mucosal epithelium lining the surface of the eye
- Palpebral conjunctiva is the mucosal epithelium lining the inner surface of the eyelid
- Caruncle is the fleshy protuberance in the inner corner (canthus) of the eye
- Fornix (plural fornices) is the loose fold of conjunctiva at the reflection from the bulbar to the palpebral conjunctiva, present superiorly and inferiorly
ICD coding
- ICD-10: C69.0 - Conjunctiva
Primary tumor (pT)
- pTX: primary tumor cannot be assessed
- pT0: no evidence of primary tumor
- pT1: tumor of the bulbar conjunctiva
- pT1a: tumor of the bulbar conjunctiva with ≤ 2 mm of invasion of substantia propria
- pT1b: tumor of the bulbar conjunctiva with > 2 mm of invasion of substantia propria
- pT2: tumor of nonbulbar conjunctiva (i.e. palpebral, forniceal or caruncle)
- pT2a: tumor of the nonbulbar conjunctiva with ≤ 2 mm of invasion of substantia propria
- pT2b: tumor of the nonbulbar conjunctiva with > 2 mm of invasion of substantia propria
- pT3: tumor of any size with local invasion
- pT3a: invasion of the globe
- pT3b: invasion of the eyelid
- pT3c: invasion of the orbit
- pT3d: invasion of the nasolacrimal duct, lacrimal sac or paranasal sinuses
- pT4: tumor of any size with invasion of the central nervous system
Regional lymph nodes (pN)
- pNX: regional lymph nodes cannot be assessed
- pN0: no regional lymph node metastasis
- pN1: regional lymph node metastasis
Notes:
- Regional lymph nodes are the preauricular, parotid, postauricular, submandibular and cervical
Distant metastasis (pM)
- pM0: no distant metastasis
- pM1: distant metastasis
Prefixes
- y: preoperative radiotherapy or chemotherapy
- r: recurrent tumor stage
AJCC prognostic stage groups
- There are currently no proposed prognostic groups
Registry data collection variables
- Tumor thickness: depth of invasion measure in millimeters into substantia propria from the surface of the conjunctiva
- Presence or absence of epithelioid cytology
- Mitotic count: number of mitoses per square millimeter
- Margin status
- Presence or absence of
- Ulceration
- Epithelioid cytology
- Growth regression
- Lymphatic invasion
- Angioinvasion
- Perineural invasion
- Conjunctival melanoma in situ
- Conjunctival nevus
- Microsatellites / in transit metastases
Histologic grade (G)
- Grading is not performed
Histopathologic type
- Spindle cell
- Epithelioid
- Anaplastic
Board review style question #1
The AJCC 8th edition staging for the conjunctiva should be used for which of these tumors
- Caruncle melanoma
- Eyelid melanoma
- Uveal melanomas with secondary involvement of conjunctiva
- Metastatic melanoma
Board review style answer #1
A. Caruncle melanoma
This staging should be used for melanomas arising from bulbar and palpebral conjunctiva, the caruncle and the fornices but not for primary eyelid skin melanomas or uveal melanomas with secondary involvement of conjunctiva. Although not specifically described in this topic, primary staging systems in general should not be used for metastases.
Comment Here
Reference: Staging-conjunctiva melanoma
This staging should be used for melanomas arising from bulbar and palpebral conjunctiva, the caruncle and the fornices but not for primary eyelid skin melanomas or uveal melanomas with secondary involvement of conjunctiva. Although not specifically described in this topic, primary staging systems in general should not be used for metastases.
Comment Here
Reference: Staging-conjunctiva melanoma
Staging-eyelid
Table of Contents
Definition / general | Primary tumor (T) | Regional lymph nodes (N) | Distant metastasis (M) | Stage grouping of eyelid carcinomaPathologic TNM staging of carcinoma of the eyelid, AJCC 7th edition
Definition / general
- Applies to clinical and pathologic staging
- Note: excludes melanoma and malignancies other than carcinoma
Primary tumor (T)
- TX: Primary tumor cannot be assessed
- T0: No evidence of primary tumor
- Tis: Carcinoma in situ
- T1: Tumor 5 mm or less in greatest dimension, not invading the tarsal plate or eyelid margin
- T2a: Tumor more than 5 mm, but not more than 10 mm in greatest dimension, or any tumor that invades the tarsal plate or eyelid margin
- T2b: Tumor more than 10 mm, but not more than 20 mm in greatest dimension, or involving the full thickness eyelid
- T3a: Tumor more than 20 mm in greatest dimension, or any tumor that invades adjacent ocular or orbital structures, or any T with perineural tumor invasion
- T3b: Complete tumor resection requires enucleation, exenteration or bone resection
- T4: Tumor is not resectable due to extensive invasion of ocular, orbital, craniofacial structures or brain
Regional lymph nodes (N)
- NX: Regional lymph nodes cannot be assessed
- cN0: No regional lymph node metastasis, based on clinical evaluation or imaging
- pN0: No regional lymph node metastasis, based on lymph node biopsy
- N1: Regional lymph node metastasis
Distant metastasis (M)
- M0: No distant metastasis
- M1: Distant metastasis
Stage grouping of eyelid carcinoma
- 0: Tis N0 M0
- IA: T1 N0 M0
- IB: T2a N0 M0
- IC: T2b N0 M0
- II: T3a N0 M0
- IIIA: T3b N0 M0
- IIIB: Any T N1 M0
- IIIC: T4 Any N M0
- IV: Any T any N, M1
Staging-lacrimal duct
Table of Contents
Definition / general | Primary tumor (T) | Regional lymph nodes (N) | Distant metastasis (M) | Stage groupingPathologic TNM staging of lacrimal gland carcinoma, AJCC 7th edition
Definition / general
- Applies to both clinical and pathologic staging
Primary tumor (T)
- TX: Primary tumor cannot be assessed
- T0: No evidence of primary tumor
- T1: Tumor 2 cm or less in greatest dimension, with or without extraglandular extension into the orbital soft tissue
- T2: Tumor more than 2 cm but not more than 4 cm in greatest dimension
- T3: Tumor more than 4 cm in greatest dimension
- T4: Tumor invades periosteum or orbital bone or adjacent structures
- T4a: Tumor invades periosteum
- T4b: Tumor invades orbital bone
- T4c: Tumor invades adjacent structures (brain, sinus, pterygoid fossa or temporal fossa)
- Notes:
- As the maximum size of the lacrimal gland is 2 cm, T2 and greater tumors will usually extend into the orbital soft tissue
Regional lymph nodes (N)
- NX: Regional lymph nodes cannot be assessed
- N0: No regional lymph node metastasis
- N1: Regional lymph node metastasis
Distant metastasis (M)
- M0: No distant metastasis
- M1: Distant metastasis
Stage grouping
- No stage grouping is presently recommended by AJCC 7th edition
Staging-ocular adnexal lymphoma
Table of Contents
Primary tumor (T) | Regional lymph nodes (N) | Distant metastasis (M) | Stage groupingPathologic TNM staging of ocular adnexal lymphoma, AJCC 7th edition
Primary tumor (T)
- TX: lymphoma extent not specified
- T0: no evidence of lymphoma
- T1: lymphoma involving the conjunctiva alone without orbital involvement
- T1a: bulbar conjunctiva alone
- T1b: palpebral conjunctiva, +/- fornix, +/- caruncle
- T1c: extensive conjunctival involvement
- T2: lymphoma with orbital involvement +/- any conjunctival involvement
- T2a: anterior orbital involvement (+/- any conjunctival involvement)
- T2b: anterior orbital involvement (+/- any conjunctival involvement but with lacrimal involvement)
- T2c: posterior orbital involvement (+/- any conjunctival involvement, +/- anterior involvement, +/- any extraocular muscle involvement)
- T2d: nasolacrimal drainage system involvement (+/- conjunctival involvement but not including nasopharynx)
- T3: lymphoma with preseptal eyelid involvement (infiltrates preseptal tissues such as dermis or orbicularis muscle of anterior eyelid skin) +/- orbital involvement, +/- any conjunctival involvement
- T4: orbital adnexal lymphoma extending beyond orbit to adjacent structures such as bone and brain
- T4a: involvement of nasopharynx
- T4b: osseous involvement (including periosteum)
- T4c: involvement of maxillofacial, ethmoidal or frontal sinuses
- T4d: intracranial spread
Regional lymph nodes (N)
- NX: involvement of lymph nodes not assessed
- N0: no evidence of lymph node involvement
- N1: involvement of ipsilateral regional lymph nodes
- N2: involvement of contralateral or bilateral regional lymph nodes
- N3: involvement of peripheral lymph nodes not draining ocular adnexal region
- N4: involvement of central lymph nodes
- Notes: regional lymph nodes include preauricular (parotid), submandibular and cervical
Distant metastasis (M)
- M0: no evidence of involvement of other extranodal sites
- M1a: noncontiguous involvement of tissues or organs external to the ocular adnexa (e.g. parotid glands, submandibular gland, lung, liver, spleen, kidney, breast, etc.)
- M1b: lymphomatous involvement of the bone marrow
- M1c: both M1a and M1b involvement
Stage grouping
- No stage grouping is presently recommended by AJCC 7th edition
Staging-orbital sarcoma
Table of Contents
Definition / general | Primary tumor (T) | Regional lymph nodes (N) | Distant metastasis (M) | Stage groupingPathologic TNM staging of sarcoma of the orbit, AJCC 7th edition
Definition / general
- Includes rhabdomyosarcoma, osteogenic sarcoma, leiomyosarcoma, etc
Primary tumor (T)
- TX: primary tumor cannot be assessed
- T0: no evidence of primary tumor
- T1: tumor 15 mm or less in greatest dimension
- T2: tumor more than 15 mm in greatest dimension without invasion of globe or bony wall
- T3: tumor of any size with invasion of orbital tissues or bony walls
- T4: tumor invasion of globe or periorbital structure, such as eyelids, temporal fossa, nasal cavity and paranasal sinuses, or central nervous system
Regional lymph nodes (N)
- NX: regional lymph nodes cannot be assessed
- N0: no regional lymph node metastasis
- N1: regional lymph node metastasis
Distant metastasis (M)
- M0: no distant metastasis
- M1: distant metastasis
Stage grouping
- No stage grouping is presently recommended by AJCC 7th edition
Staging-retinoblastoma
Pathologic TNM staging of retinoblastoma, AJCC 7th edition
Primary tumor (T)
- pTX: primary tumor cannot be assessed
- pT0: no evidence of primary tumor
- pT1: tumor confined to eye with no optic nerve or choroidal invasion
- pT2: tumor with minimal optic nerve or choroidal invasion
- pT2a: tumor superficially invades optic nerve head but does not extend past lamina cribrosa OR tumor exhibits focal choroidal invasion, but not both
- pT2b: tumor superficially invades optic nerve head but does not extend past lamina cribrosa AND exhibits focal choroidal invasion
- pT3: tumor with significant optic nerve or choroidal invasion
- pT3a: tumor invades optic nerve past lamina cribrosa but not to surgical resection line OR tumor exhibits massive choroidal invasion, but not both
- pT3b: tumor invades optic nerve past lamina cribrosa but not to surgical resection line AND exhibits massive choroidal invasion
- pT4: tumor invades optic nerve to resection line OR exhibits extraocular extension elsewhere, but not both
- pT4a: tumor invades optic nerve to resection line but no extraocular extension identified
- pT4b: tumor invades optic nerve to resection line AND extraocular extension identified
Regional lymph nodes (N)
- pNX: regional lymph nodes cannot be assessed
- pN0: no regional lymph node involvement
- pN1: regional lymph node involvement (preauricular, cervical)
- N2: distant lymph node involvement
Metastasis (M)
- cM0: no metastasis
- pM1: metastasis to sites other than CNS
- pM1a: single lesion
- pM1b: multiple lesions
- pM1c: CNS metastasis
- pM1d: discrete mass(es) without leptomeningeal or CSF involvement
- pM1e: leptomeningeal or CSF involvement
Stage grouping
- No stage grouping is presently recommended by AJCC 7th edition
Staging-uvea melanoma
Table of Contents
Definition / general | Essential features | ICD coding | Diagrams / tables | Primary tumor (pT) | Regional lymph nodes (pN) | Distant metastasis (pM) | Prefixes | AJCC prognostic stage groups | Registry data collection variables | Histologic grade (G) / histopathologic type | Gross images | Whole mount images | Microscopic (histologic) images | Board review style question #1 | Board review style answer #1Definition / general
- Based on AJCC 8th edition staging system
- Uveal tract is the middle layer of the eye, between sclera and retina
- Uveal tract consists of the iris, ciliary body and the choroid
Essential features
- AJCC 7th edition staging was sunset on December 31, 2017; as of January 1, 2018, use of the 8th edition is mandatory
- There are 2 separate pT classification systems for uveal melanomas: one for the iris and one for the ciliary body and choroid melanomas
- Tumors with < 50% of their volume located in the iris should be categorized using the ciliary body and the choroid pT classification
- Clinical and pathological T categories are the same
- Some patients with iris melanoma experience a secondary open angle glaucoma caused by the tumor cells and tumor pigment laden macrophages becoming trapped in and obstructing the trabecular meshwork
Primary tumor (pT)
Iris:
Ciliary body and choroid:
Notes:
- pTX: primary tumor cannot be assessed
- pT0: no evidence of primary tumor
- pT1: tumor limited to the iris
- pT1a: tumor limited to the iris, not more than 3 clock hours in size
- pT1b: tumor limited to the iris, more than 3 clock hours in size
- pT1c: tumor limited to the iris, with secondary glaucoma
- pT2: tumor extending into the ciliary body, choroid or both
- pT2a: tumor extending into the ciliary body, without secondary glaucoma
- pT2b: tumor extending into the ciliary body and choroid, without secondary glaucoma
- pT2c: tumor extending into the ciliary body, choroid or both, with secondary glaucoma
- pT3: tumor extending into the ciliary body, choroid or both, with scleral extension (but without extrascleral extension)
- pT4: tumor with extrascleral extension
- pT4a: tumor with extrascleral extension ≤ 5 mm in largest diameter
- pT4b: tumor with extrascleral extension > 5 mm in largest diameter
Ciliary body and choroid:
- pT1: tumor size category 1
- pT1a: tumor size category 1 without ciliary body involvement or extraocular extension
- pT1b: tumor size category 1 with ciliary body involvement
- pT1c: tumor size category 1 without ciliary body involvement but with extraocular extension ≤ 5 mm in largest diameter
- pT1d: tumor size category 1 with ciliary body involvement and extraocular extension ≤ 5 mm in largest diameter
- pT2: tumor size category 2
- pT2a: tumor size category 2 without ciliary body involvement or extraocular extension
- pT2b: tumor size category 2 with ciliary body involvement
- pT2c: tumor size category 2 without ciliary body involvement but with extraocular extension ≤ 5 mm in largest diameter
- pT2d: tumor size category 2 with ciliary body involvement and extraocular extension ≤ 5 mm in largest diameter
- pT3: tumor size category 3
- pT3a: tumor size category 3 without ciliary body involvement or extraocular extension
- pT3b: tumor size category 3 with ciliary body involvement
- pT3c: tumor size category 3 without ciliary body involvement but with extraocular extension ≤ 5 mm in largest diameter
- pT3d: tumor size category 3 with ciliary body involvement and extraocular extension ≤ 5 mm in largest diameter
- pT4: tumor size category 4 or any tumor with extraocular extension > 5 mm
- pT4a: tumor size category 4 without ciliary body involvement or extraocular extension
- pT4b: tumor size category 4 with ciliary body involvement
- pT4c: tumor size category 4 without ciliary body involvement but with extraocular extension ≤ 5 mm in largest diameter
- pT4d: tumor size category 4 with ciliary body involvement and extraocular extension ≤ 5 mm in diameter
- pT4e: any tumor size category with extraocular extension > 5 mm in largest diameter
Notes:
- Largest basal diameter and tumor thickness are used to determine size category (see table above), required to assign pT category to melanomas of the ciliary body and choroid
- Proper grossing technique is required to obtain largest basal diameter and tumor thickness in enucleation specimens
- Globe should be transilluminated with strong light source to map out the tumor shadow on the sclera in order to determine the best orientation of pupil-optic nerve section
- Pupil-optic nerve section should capture the largest basal diameter based on the shadow
- In clinical practice, largest basal diameter may be estimated in optic disc diameters (dd) (average 1 dd = 1.5 mm) and tumor thickness may be estimated in diopters (average 3 diopters = 1 mm)
Regional lymph nodes (pN)
- pNX: regional lymph nodes cannot be assessed
- pN0: no regional lymph node metastasis
- pN1: regional lymph node metastasis or discrete orbital tumor deposits
- pN1a: metastasis in one or more regional lymph nodes
- pN1b: discrete orbital tumor deposits discontinuous with the globe without regional lymph node metastases
Notes:
- Regional lymph nodes include preauricular, submandibular and cervical
Distant metastasis (pM)
- pM0: no distant metastasis
- pM1: distant metastasis
- pM1a: largest diameter of the largest metastasis is ≤ 3 cm
- pM1b: largest diameter of the largest metastasis is 3.1 - 8.0 cm
- pM1c: largest diameter of the largest metastasis is > 8 cm
Prefixes
- y: preoperative radiotherapy or chemotherapy
- r: recurrent tumor stage
AJCC prognostic stage groups
| Stage group I: | T1a | N0 | M0 |
| Stage group IIA: | T1b - d | N0 | M0 |
| Stage group IIA: | T2a | N0 | M0 |
| Stage group IIB: | T2b | N0 | M0 |
| Stage group IIB: | T3a | N0 | M0 |
| Stage group IIIA: | T2c - d | N0 | M0 |
| Stage group IIIA: | T3b - c | N0 | M0 |
| Stage group IIIA: | T4a | N0 | M0 |
| Stage group IIIB: | T3d | N0 | M0 |
| Stage group IIIB: | T4b - c | N0 | M0 |
| Stage group IIIC: | T4d - e | N0 | M0 |
| Stage group IV: | any T | N1 | M0 |
| Stage group IV: | any T | any N | M1 |
Registry data collection variables
- Patient age, gender
- Prior treatment
- Tumor site: iris, ciliary body, choroid
- Largest basal diameter and thickness
- Scleral and optic nerve invasion
- Extraocular extension
- Histologic type: spindle, mixed, epithelioid
- Mitotic count
- Vascular invasion
- Extravascular matrix pattern
- Molecular results (if known):
- Chromosome 3 and 8 loss / gain
- BAP1 status
- Gene expression profile
- Multiplex ligation dependent probe amplification (MLPA) analysis
Histologic grade (G) / histopathologic type
- G1: spindle (> 90% spindle cells)
- G2: mixed (> 10% epithelioid cells and < 90% spindle cells)
- G3: epithelioid (> 90% epithelioid cells)
Notes:
- There is a lack of agreement on the proportions needed for the diagnosis of spindle cell and epithelioid types; 10% and 90% are provided for guidance only
Microscopic (histologic) images
Board review style question #1
Uveal melanoma involving 2 mm of iris, all of ciliary body and 9 mm of the choroid has a thickness of 12 mm and largest basal diameter of 16 mm. There is no extraocular extension present and no glaucoma. The pT category is
- pT2b
- pT2d
- pT3b
- pT3d
Board review style answer #1
Steatocystoma simplex
Table of Contents
Definition / general | Etiology | Clinical features | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosis | Additional referencesDefinition / general
- Rare benign adnexal tumor, usually in caruncle
- Steatocystoma simplex if solitary; steatocystoma multiplex if multiple cysts
- Due to nevoid malformation of pilosebaceous duct junction
Etiology
- Autosomal dominant trait in multiplex
Clinical features
- Typically affects individuals younger than 30 years; contains yellow sebum associated with hairs
Case reports
- 26 year old woman with tumor of caruncle (Br J Ophthalmol 2003;87:240)
- 42 year old man with tumor of caruncle (Can J Ophthalmol 2006;41:83)
- 57 year old man and 85 year old man with intratarsal keratinous cysts of the meibomian gland (Am J Dermatopathol 2011;33:624)
Treatment
- Simple excision with removal of cyst wall intact
Gross description
- Flesh colored or yellowish, well circumscribed, soft, mobile, and non-tender
- On incision contains oily sebum
Microscopic (histologic) description
- Cystic space lined by nonkeratinizing squamous epithelium with an eosinophilic cuticle and sebaceous lobules within the cyst wall, but no granular layer
Microscopic (histologic) images
Differential diagnosis
- Keratinous cyst:
- Older adults, no sebaceous glands in or adjoining wall
Additional references
Stye
Definition / general
- Also called hordeolum, chalazion (by some)
- Acute suppurative inflammation of sebaceous glands or follicles of eyelid
- Usually due to Staphylococcal infection
- Internal: affects meibomian glands
- External: affects glands of Moll or Zeis and adjacent hair follicles and cilia
Treatment
- Medical
Subconjunctival herniated orbital fat
Table of Contents
Definition / general | Essential features | Case reports | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Differential diagnosis | Board review style question #1 | Board review style answer #1Definition / general
- Rare entity; first described in path literature in 2007 (Am J Surg Pathol 2007;31:193)
- Prolapsed intraconal fat due to dehiscence of tenon capsule precipitated by age, disease, trauma or surgery
- Typically occurs in elderly obese men
- Presents as small (up to 2.5 cm), raised, convex, yellow, compressible mass in the superotemporal quadrant of the eye (Optom Vis Sci 2015;92:1021, Figure 1 & 2)
- Unilateral or bilateral
- Low recurrence rate after simple excision
Essential features
- Rare entity, caused by forward movement of intraconal fat due to dehiscence of tenon capsule precipitated by age, disease, trauma or surgery
- Typically presents in elderly obese men as a small, raised, yellow, compressible mass in the superotemporal quadrant of the eye
- Composed of an admixture of mature adipocytes, delicate fibrovascular septae, Lochkern cells and floret-like giant cells
- Principal differential diagnosis includes pleomorphic lipoma and atypical lipomatous tumor
Case reports
- An infant with a yellowish subconjunctival lesion (Eur J Pediatr 2010;169:1427)
- An elderly man presented with a 1.5 cm "orbital" mass (Case of the Week #426)
Microscopic (histologic) description
- Composed of uniformly shaped mature adipocytes separated by a delicate fibrovascular septae
- Scattered Lochkern cells (adipocytes with enlarged nuclei containing intranuclear vacuoles) and floret-like giant cells (multinucleated giant cells with a wreath like arrangement of bland, uniform, often vacuolated nuclei)
- Varying numbers of inflammatory cells, including lymphocytes, plasma cells, histiocytes and mast cells
Differential diagnosis
- Pleomorphic lipoma:
- Different location; PL often involves soft tissues of back and shoulder of elderly men
- Areas typical of spindle cell lipomas, including variably myxoid stroma, wire-like collagen and bland spindle cell proliferation are focally present
- Floret-like giant cells show notable nuclear enlargement and hyperchromasia
- Well differentiated liposarcoma:
- May rarely involve the orbit (Ann Diagn Pathol 2001 Oct;5:255)
- Similar to other sites, will contain enlarged hyperchromatic cells within fibrous septae
- MDM2 amplification
Board review style question #1
Regarding subconjunctival herniated orbital fat, which of the following statements is true?
- Associated with MDM2 amplification
- Floret-like giant cells with nuclear hyperchromasia and pleomorphism are typically seen in SHOF
- Nuclei of Lochkern cells and floret-like giant cells are highlighted by CD34 immunohistochemistry
- Has an aggressive course and the management includes radiation therapy
Board review style answer #1
C. The nuclei of Lochkern cells and floret-like giant cells in SHOF are highlighted by CD34 immunohistochemistry (although not necessary for diagnosis)
Comment Here
Reference: Subconjunctival herniated orbital fat
Comment Here
Reference: Subconjunctival herniated orbital fat
Sweat gland carcinoma
Case reports
- 2 cases: endocrine mucin-producing sweat gland carcinoma (Am J Surg Pathol 1997;21:1501)
Microscopic (histologic) description
- Resembles solid papillary carcinoma of breast
Temporal arteritis
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Temporal (or giant cell) arteritis is a systemic and discontinuous nonnecrotizing, granulomatous vasculitis of elastic and muscular arteries
Essential features
- Presents in patients in the sixth decade of life or older with new onset headache
- Risk of permanent vision loss if left untreated
- Diagnosis requires morphologic confirmation (biopsy is the preferred modality)
- Classic findings include lymphocytes and macrophages arranged in concentric rings surrounding the external and internal elastic lamina as well as an association with intimal hyperplasia and loss / fragmentation of elastic fibers
- Useful stains: elastic stain, CD3 and CD68
Terminology
- Temporal arteritis
- Giant cell arteritis
- Horton disease
- Horton giant cell arteritis
- Cranial arteritis
ICD coding
Epidemiology
- Most common systemic / primary vasculitis (Semin Arthritis Rheum 2020;50:1040)
- Age: > 50 years; mean: 70 years; peak: 71 - 80 years
- Gender: F:M = 3:1
- Race / ethnicity: more common in Caucasians; rare in Asian and African American patients
- Incidence (ACR classification criteria)
- Northern Europe (Norway): 29 - 32.8 / 100,000 (J Rheumatol 1997;24:1739, J Rheumatol 2000;27:2624)
- U.S. (Minnesota): 19.8 / 100,000 (Scand J Rheumatol 2015;44:215)
- Southern Europe (Spain): 2.2 - 10.2 / 100,000 (Clin Exp Rheumatol 2015;33:S-11, Rheum Dis Clin North Am 2001;27:729)
- Seasonal variation: there is no seasonal influence (RMD Open 2017;3:e000531)
- Mortality (Rheumatology (Oxford) 2022;61:1195)
- All cause mortality
- 6.4% at 1 year (relative risk 1.49 ± 0.13); 45% at 10 years (relative risk 1.03 ± 0.02)
- Cause specific mortality
- Compared to the general population, there is increased mortality due to infectious, endocrine, cardiovascular and gastrointestinal diseases
- This increased mortality may be corticosteroid related (J Rheumatol 2017;44:84)
- All cause mortality
Sites
- Cranial arteries: temporal artery, occipital artery and intraorbital branches (ophthalmic and posterior ciliary)
- Extracranial arteries are compromised in 20 - 67% of cases (angiography) (Arthritis Care Res (Hoboken) 2020;72:1615)
- Most common sites: carotid, subclavian, axillary and thoracic aorta
- Bilateral axillary artery compromise is common
Pathophysiology
- Immunopathological model as described by Greigert et al. (J Clin Med 2022;11:2905)
- Phase 1: loss of tolerance and activation of the adventitia resident dendritic cells
- Dendritic cells acquire mature phenotype and produce IL12, IL23, IL6 and IL1β
- Phase 2: recruitment, activation and polarization of CD4+ T cells
- CD4+ T cells polarize to Th1 and Th17 phenotypes
- Phase 3: recruitment of CD8+ T cells and monocytes
- Phase 4: vascular remodeling
- Macrophages release several factors, such as reactive oxygen species and matrix metalloproteinases, which mediate internal elastic lamina destruction
- Vascular smooth muscle cells migrate to the intima and acquire a myofibroblast phenotype
- Myofibroblasts produce intimal hyperplasia, which then causes vessel occlusion and subsequent ischemia
- Phase 1: loss of tolerance and activation of the adventitia resident dendritic cells
Etiology
- Immune mediated disease of unknown etiology
- Postulated genetic predisposing factors (Sci Rep 2017;7:43953):
- Major histocompatibility class II genes (HLA-DRB1*04 alleles)
- IL12B locus
Clinical features
- Headache (73%)
- Tender temporal artery (31%)
- Scalp tenderness (44%)
- Jaw claudication (45%) (best predictor of positive biopsy)
- Can be elicited by the chewing gum test (N Engl J Med 2016;374:1794)
- Visual disturbances
- Blurred vision (18%)
- Transient vision loss (5%)
- Permanent vision loss (6%), due to ischemic optic neuropathy
- Fever (16%)
- Weight loss (25%)
- 25% of patients can be asymptomatic
- Comorbidities
- Polymyalgia rheumatica (PMR) (Rheumatology (Oxford) 2017;56:506)
- 40 - 60% of patients with giant cell arteritis have signs and symptoms of polymyalgia rheumatica
- 16 - 21% of patients with polymyalgia rheumatica develop giant cell arteritis
- Symptomatic thoracic aneurysm: 10 - 15% of giant cell arteritis patients develop symptomatic thoracic aneurysms
- Polymyalgia rheumatica (PMR) (Rheumatology (Oxford) 2017;56:506)
- Reference: Semin Arthritis Rheum 2021;51:1193
Diagnosis
- Diagnosis requires morphologic confirmation
- EULAR 2018: diagnostic confirmation can be performed by imaging or histology (Ann Rheum Dis 2020;79:19)
- ACR / Vasculitis Foundation 2021: temporal artery biopsy is the preferred modality for diagnostic confirmation (Arthritis Rheumatol 2021;73:1349)
- Ultrasonography: offers good sensitivity and specificity in treatment naive patients (up to 4 days of treatment)
- Temporal artery biopsy (TAB): offers good sensitivity and specificity within 2 - 4 weeks of glucocorticoid treatment (BMC Musculoskelet Disord 2016;17:363)
- Optimal length of biopsy: > 1 cm with at least 1.5 cm preferred by some groups (ANZ J Surg 2018;88:191)
- Unilateral temporal artery biopsy is the preferred modality as an initial approach over bilateral biopsies, though bilateral biopsies are recommended by some groups due to possible discordant findings (J Vasc Surg 2022;76:1704, Can J Ophthalmol 2014;49:157)
Laboratory
- Elevated erythrocyte sedimentation rate
- Elevated C reactive protein
Radiology description
- High frequency Doppler ultrasound
- Halo sign (sensitivity 80%, specificity 80%): hypoechoic halo surrounding temporal artery lumen (J Ultrasound 2022;25:837)
- Compression sign (sensitivity 85%, specificity 65%): compression of the temporal artery produces contrasting echogenicity in the surrounding tissue (Clin Exp Rheumatol 2015;33:S-113)
Prognostic factors
- Predictors associated with reduced risk of permanent visual loss
- Fever
- Rheumatic symptoms
- Predictors associated with increased risk of permanent visual loss
- Age
- History of transient visual ischemic symptoms
- Jaw claudication
- Reference: J Rheumatol 2016;43:1393
Case reports
- 68 year old woman with tongue necrosis (Case Rep Med 2017;2017:6327437)
- 71 year old woman with headache and normal inflammatory markers (Clin Med (Lond) 2020;20:224)
- 72 year old man with an aortic aneurysm (Radiol Case Rep 2021;16:3734)
- 79 year old man with vision loss (Rheumatol Int 2022;42:1855)
- 81 year old woman with scalp ulceration (BMJ Case Rep 2019;12:e230795)
Treatment
- High dose glucocorticoids
Gross description
- Segment of muscular artery with thickened, nodular and rubbery wall
- Grossing and processing differ between institutions but should be thorough and account for the possibility of skip lesions or the uneven distribution of pathologic changes
- Serially section vessel at 3 mm intervals
- Embed in cross section (ink may be used to indicate which surface should be embedded to ensure uniform examination along the entire length of the artery)
- Some prefer cutting 30 levels with 1 H&E slide performed every third level, leaving intervening unstained slides for additional stains as needed
- Others recommend cutting 4 leveled groups with 1 H&E, 1 elastin stain and 1 unstained slide per group (Westra: Surgical Pathology Dissection - An Illustrated Guide, 2nd Edition, 2003, J Clin Pathol 2000;53:137)
Microscopic (histologic) description
- Classic giant cell arteritis (77% of cases) (Am J Surg Pathol 2014;38:1360)
- Transmural inflammation pattern with lymphocytes and macrophages arranged in concentric rings, surrounding the external and internal elastic lamina and associated with intimal hyperplasia and loss of elastic fibers
- 50 - 70% of cases exhibit giant cells but giant cells are not required for the diagnosis
- Neutrophils are uncommon (1.8%)
- Unusual findings include necrosis, well formed granulomas and thrombosis
- Transmural inflammation pattern with lymphocytes and macrophages arranged in concentric rings, surrounding the external and internal elastic lamina and associated with intimal hyperplasia and loss of elastic fibers
- Borderline arteritis - lymphocytic and histiocytic infiltrate restricted to the following localizations
- Vasa vasorum vasculitis (6.5% of cases): inflammation of vasa vasorum in the absence of medial inflammation
- Inflammation limited to the adventitia (7% of cases): crescent shaped configuration limited to the adventitia and external elastic lamina, with sparing of the media
- Small vessel vasculitis (9% of cases): inflammatory lymphocytic infiltrate surrounding (cuffing) small periadventitial vessels
- Healed arteritis - fibrotic changes without inflammatory lymphocytic infiltrate
- Marked intimal thickening
- Intimal, medial and adventitial fibrosis and scarring, with neovascularization
- Loss of elastic fibers
Microscopic (histologic) images
Virtual slides
Positive stains
Videos
Vasculitis Foundation giant cell arteritis webinar
Giant cell arteritis
by Nicholas J. Volpe,
European Society of Ophthalmology
Temporal artery biopsy technique
Giant cell arteritis (temporal arteritis) pathology by Jerad Gardner, M.D.
Sample pathology report
- Right temporal artery, biopsy:
- Morphological findings consistent with temporal arteritis (see comment)
- Comment: There is lymphocytic and macrophagic infiltration within the vascular wall. Multinucleated giant cell phagocytizing elastic fibers (elastic stain) are observed, supporting the diagnosis.
- Gross description: Specimen A is received in formalin in a container and labeled with the patient’s name and specimen number and designated right temporal artery. The specimen consists of a tan, tubular structure, consistent with a muscular artery, that measures 1.5 cm in length and is notable for nodularity and thickening. The specimen is serially cross sectioned at 3 mm intervals, placed between sponges and submitted entirely in a cassette.
Differential diagnosis
- Age related changes:
- Intimal hyperplasia, duplication of the elastic inner lamina, adventitial fibrosis
- Absence of mononuclear infiltration of the arterial wall
- Another vasculitis (up to 5% of cases):
- Neutrophil infiltration, abundant fibrinoid necrosis, microthrombi and leukocytoclasis
- AL amyloidosis (< 1%) (Mod Rheumatol Case Rep 2020;4:90):
- Intramural amorphous eosinophilic material deposits
- Light chain immunofixation in urine
- Congo red+ with green dichroism
- Calciphylaxis (< 1%) (J Neuroophthalmol 2022;42:e362):
- Calcium deposition in vessels
- Numerous thrombi
- Necrosis of distal territories
- Atherosclerosis (< 1%) (J Neuroophthalmol 2022;42:e359):
- Intimal hyperplasia, foamy macrophages (early)
- Intimal fibrosis, cholesterol cleft and variable inflammatory cell infiltration within the intima (chronic)
- No medial inflammation, no phagocytosis of elastic fibers
- Mönckeberg medial calcific sclerosis of the temporal artery (< 1%) (Cureus 2020;12:e9210):
- Annular calcification within media
- No thrombus
- No inflammatory infiltrate
Additional references
Board review style question #1
In addition to special staining to evaluate elastic fibers, which of the following antibody panels is most useful for evaluating temporal arteritis?
- CD3 / CD68
- CD4 / CD8
- CD20 / CD138
- CD34 / CD68
Board review style answer #1
A. CD3 / CD68. The hallmark of temporal arteritis is a transmural lymphocytic (T cells) and macrophagic infiltrate, which can be demonstrated with antibodies against CD3 and CD68, respectively. Answer C is incorrect because B cells (CD20+) and plasma cells (CD138+) are not diagnostic findings. Answer D is incorrect because the combination of CD34 and CD68 highlights histiocytes, myofibroblasts and small blood vessels but excludes T cells. Answer B is incorrect because although CD4+ and CD8+ are T cell markers, this panel does not stain macrophages.
Comment Here
Reference: Temporal arteritis
Comment Here
Reference: Temporal arteritis
Board review style question #2
Board review style answer #2
B. Loss of elastic fibers. The Verhoeff-Van Gieson stain is a special stain used to demonstrate elastic fibers. In the setting of temporal arteritis, it can be used to evaluate areas of loss and disorganization of elastic fibers. Answer A is incorrect because intimal hyperplasia is visible with H&E and does not require special stains. Answer D is incorrect because tunica media fibrosis is a nonspecific finding and can be observed in the scenario of healed arteritis. Answer C is incorrect because myxoid degeneration is not a characteristic finding of temporal arteritis.
Comment Here
Reference: Temporal arteritis
Comment Here
Reference: Temporal arteritis
Trachoma
Table of Contents
Epidemiology | Sites | Etiology | Clinical features | WHO grading system | Laboratory | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) imagesEpidemiology
- Major cause of blindness outside US (Wikipedia: Trachoma [Accessed 26 April 2018], eMedicine: Trachoma [Accessed 26 April 2018])
- 40 million people affected worldwide (WHO); 1.2 billion people live in endemic areas
- Associated with poverty, overcrowding, direct contact, flies and poor hygiene
Sites
- Entire conjunctiva but most prominent on upper tarsus
Etiology
- Caused by Chlamydia trachomatis, serovars A, B, Ba, and C of Chlamydia trachomatis
- Serovars D-K associated with adult inclusion conjunctivitis
- Causes scarring of corneal tissue
Clinical features
- Active trachoma:
- Most common in preschool children
- Mixed follicular / papillary conjunctivitis associated with a mucopurulent discharge
- Superior epithelial keratitis and pannus
- Cicatricial trachoma:
- Most common in middle age adults
- Linear or stellate conjunctival scars (mild cases)
- Broad confluent scars or Arlt lines in severe cases
- Adult inclusion conjunctivitis:
- Acute mucopurulent conjunctival infection
- Superior limbal follicles may resolve to leave a row of shallow depressions (Herbert pits)
- Trichiasis, distichiasis, corneal vascularization and cicatricial entropion
- Corneal opacification
- Dry eye
WHO grading system
- TF:
- 5 or more follicles on the upper conjunctiva
- Follicles must be at least 0.5 mm in diameter and are round, white, paler than surrounding conjunctiva
- TI:
- Intense trachomatous inflammation
- Tarsal conjunctiva appears red, rough and thickened, obscuring more than half of the normal, deep, tarsal vessels
- Numerous follicles are partially covered by thickened conjunctiva
- TS:
- Scarring and fibrosis of tarsal conjunctiva due to severe or chronic trachoma
- Also called cicatricial trachoma
- Scars are visible as white lines, bands or sheets
- TT:
- Trichiasis defined as at least one eyelash that rubs on eyeball due to entropion of lid
- CO:
- Corneal opacity
- Eyelashes have abraded and damaged cornea, causing corneal opacity and visual loss
Laboratory
- Dacron swab culture
- RNA and DNA based nucleic acid amplification tests (Curr Opin Ophthalmol 2012;23:288)
Treatment
- World Health Organization has instituted its SAFE (surgery, antibiotics, facial cleanliness, and environmental improvement) program (Trop Med Int Health 2010;15:673, Lancet 2008;371:1945)
Clinical images
Microscopic (histologic) description
- Stage I:
- Conjunctival inflammatory infiltrates (lymphoid follicles and diffuse infiltrates)
- Followed by pannus formation (fibrovascular tissue in conjunctival and corneal stroma) with Chlamydia elementary bodies and larger basophilic initial bodies seen
- Also lymphocytes, plasma cells, neutrophils
- Stage II:
- Florid inflammation, more follicles, epithelial thickening, severe pannus
- Macrophages with ingested debris (Leber cells) in conjunctiva
- Stage III:
- Scarring
- No follicles
- Cicatricial entropion (inversion of upper lid)
- Misdirected lashes (trichiasis)
- Stage IV:
- Arrest of disease due to entropion and trichiasis but with continuing corneal damage and infection
Tumors general-eyelid
Table of Contents
Definition / generalDefinition / general
- Consist of epithelial tumors originating in skin and conjunctival surfaces (squamous cell and basal cell carcinoma), glandular tumors originating from sebaceous, sweat and apocrine glands and hair follicles
- Also lymphoid and melanocytic tumors
- Occasionally Kaposi sarcoma, fibrous histiocytoma and other sarcomas
- Regional lymph nodes are pretarsal and posttarsal plexuses, which are anastamosed
- Lateral 2/3 of upper eyelid and lateral 1/3 of lower eyelid drain into preauricular nodes
- Remaining lymphatics drain into submandibular nodes
- Local extension includes soft tissue of orbit, lacrimal gland and globe
- Frozen section (Mohs technique) useful to minimize size of excised tissue
- Metastases to cervical, axillary and mediastinal lymph nodes, lung, liver and other viscera
Uveitis
Table of Contents
Definition / generalDefinition / general
-
Anterior uveitis (iridocyclitis):
- Diffuse infiltration by plasma cells, occasionally nodular lymphocytic infiltrates
- Associated with obliteration of anterior chamber and adherence of iris to cornea
- May be seen in juvenile rheumatoid arthritis
- Diffuse, focal or scattered chronic inflammatory infiltrate, often involving retina
- May form cyclitic membrane that contracts, leading to detachment of retina and ciliary body
- Not painful, so enucleation often not necessary
- Enucleation if recurrence leads to adhesions between iris and cornea (anterior synechiae) or iris and anterior surface of lens (posterior synechiae) causing secondary glaucoma
- Cause usually cannot be determined; known causes are herpes zoster, Behcet's disease (obliterative vasculitis of retinal vessels), Pneumocystis carinii
- May be due to sarcoidosis
- Also tuberculosis, leprosy, syphilis, tularemia, CMV, varicella zoster virus, fungi and parasites
Posterior uveitis (choroiditis, chorioretinitis):
Granulomatous uveitis:
Visceral larva migrans
Definition / general
- A type of nematodiasis (parasitic disease)
- Somewhat common in US and Great Britain
- Usually produced by Toxocara canis in children ages 3 - 14 years without systemic disease
- Single migrating larva enters eye hematogenously and rests in vitreous or inner surface of retina with accompanying acute and chronic inflammatory cells and intense eosinophilia
- Late changes are scarring, retinal detachment and leukokoria, simulating retinoblastoma
- Dead larvae may cause minute granulomas, found with serial sectioning
Vitreous humor pathology
Definition / general
- Hemorrhage (from trauma or retinal neovascularization) causes opacification
- Calcium soaps produce particulate matter called asteroid hyalosis since resembles stars when viewed with ophthalmoscope
- Amyloid deposits may reduce vision significantly
- Age related collapse may product floaters or detachment from neurosecretory retina
WHO classification of tumors of the conjunctiva and caruncle
Table of Contents
Definition / general | Major updates | WHO (2023) | Diagrams / tables | Microscopic (histologic) images | Additional references | Board review style question #1 | Board review style answer #1Definition / general
- WHO classification of tumors of conjunctiva and caruncle
- Currently on 5th edition (to be published in 2023; beta version now available online)
Major updates
- 5th edition is now available online in beta form
- This edition contains updated information on molecular pathology, expression profiling and molecular classification of tumors; however, the focus remains on morphologic classification
- Additional classification and incorporation of tumor lineage (e.g., epithelial, adnexal, melanocytic) has been emphasized.
- Selected entities reclassified in this edition
- Phakomatous choristoma has been removed (now classified under eyelid)
- Sebaceous carcinoma has been removed (now classified under eyelid)
- Spitz nevus has been removed (now classified under eyelid)
- Keratoacanthoma of the conjunctiva is no longer listed as a separate tumor type
- Spindle squamous cell carcinoma and squamous cell carcinoma with mucinous differentiation are included within the broader group of squamous cell carcinoma
- WNT activated deep penetrating / plexiform melanocytoma has been included as a new entity in the WHO 5th edition
- Includes an update on pathogenesis and molecular genetics of melanocytic conjunctival lesions
- Within the melanocytic lesions, nomenclature for premalignant and malignant lesions has been updated.
- Nonneoplastic pterygium and pinguecula were added as tumor-like lesions to delineate them from conjunctival squamous intraepithelial neoplasia
- Soft tissue tumors, hematolymphoid neoplasms and secondary tumors of the conjunctiva are discussed in separate chapters
WHO (2023)
-
Tumor-like lesions and choristomas of the conjunctiva
- Cysts of the conjunctiva and caruncle (ICD-10: H11. 449)
- Epithelial conjunctival inclusion cyst
- Reactive, epithelial and degenerative conjunctival lesions
- Reactive epithelial hyperplasia of the conjunctiva
- Papillary and follicular conjunctivitis
- Pterygium and pinguecula
- Choristomas of the conjunctiva
- Epibulbar choristoma (dermoid; dermolipoma; complex choriostoma)
- Epibulbar osseous choristoma
- Benign epithelial conjunctival tumors
- Premalignant and malignant epithelial tumors of the conjunctiva
- Conjunctival squamous intraepithelial neoplasia (conjunctival intraepithelial neoplasia and carcinoma in situ) 8077/2
- Conjunctival squamous cell carcinoma 8070/3, 8076/2, 8071/3
- Adenosquamous carcinoma 8560/3
- Benign melanocytic conjunctival tumors
- Benign epithelial melanosis of the conjunctiva
- Junctional, compound and subepithelial conjunctival nevi (8740/0, 8760/0, 8750/)
- Inflamed juvenile conjunctival nevus 8770/0
- Blue nevus of the conjunctiva 8780/0
- WNT activated deep penetrating / plexiform melanocytoma (nevus)
- Combined nevus of the conjunctiva
- Premalignant and malignant melanocytic conjunctival tumors
Epithelial tumors of the conjunctiva
Melanocytic conjunctival tumors
Diagrams / tables
No information provided
Microscopic (histologic) images
Contributed by Marta Couce, M.D., Ph.D.
Additional references
Board review style question #1
Among melanocytic lesions of the conjunctiva, which of the following statements is true about the lesion shown in the above image?
- It has a high risk for transformation into malignant melanoma
- It is best treated by enucleation
- It is commonly found as a poorly defined, pigmented mass
- It is most commonly found in ages 70 - 90 years
- It is the most common melanocytic lesion of the conjunctiva
Board review style answer #1
E. It is the most common melanocytic lesion of the conjunctiva. This is a conjunctival melanocytic nevus, which accounts for up to 53% of all conjunctival neoplasms. Differentials include primary acquired melanosis, racial melanosis, ocular melanocytosis and malignant melanoma. Answer A is incorrect because conjunctival nevi have a low rate of conversion to conjunctival melanoma (less than 1%). Answer B is incorrect because treatment is usually for cosmetic reasons; conjunctival melanocytic nevus is typically managed by periodic observation and serial photographic comparison. Answer C is incorrect because the morphology is usually a well defined, slightly elevated mass. The classic location is the interpalpebral bulbar conjunctiva, caruncle or plica semilunaris. Answer D is incorrect because most often these lesions are apparent within the first or second decade of life as a discrete, pigmented lesion.
Comment Here
Reference: WHO classification of tumors of the conjunctiva and caruncle
Comment Here
Reference: WHO classification of tumors of the conjunctiva and caruncle
WHO classification of tumors of the conjunctiva and caruncle (pending)
[Pending]
Xanthelasma
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Xanthelasma is a soft yellow, lipid laden plaque occurring bilaterally on the medial aspect of eyelid skin
- It may occur in association with primary hypercholesterolemia
Essential features
- Yellow, lipid laden plaques occur symmetrically on bilateral medial upper and lower eyelids
- Typically occurs in middle aged to elderly patients; occurs in women more than men (Plast Reconstr Surg 2002;110:1310)
- About half of patients have hyperlipidemia (Plast Reconstr Surg 2002;110:1310)
- Histopathology reveals foamy histiocytes in the superficial dermis
Terminology
- Xanthelasma palpebrarum
- Cutaneous xanthoma
ICD coding
Epidemiology
- F > M (Plast Reconstr Surg 2002;110:1310)
- Age of onset: 15 - 73 years; peak: 30 - 50 years (Clin Cosmet Investig Dermatol 2017;11:1)
- ~Half of patients with hyperlipidemia (Plast Reconstr Surg 2002;110:1310)
- Increased likelihood of familial hyperlipidemia if presentation occurs at < 40 years of age (Plast Reconstr Surg 2002;110:1310)
- May be associated with atherosclerosis, diabetes mellitus and thyroid disease (Plast Reconstr Surg Glob Open 2023;11:e4982)
Sites
- Symmetric on eyelids
Pathophysiology
- Intracellular cholesterol rich deposition (Clin Cosmet Investig Dermatol 2017;11:1)
Etiology
- Primary hyperlipidemias (especially type 2a) (Plast Reconstr Surg 2002;110:1310)
- Low high density lipoprotein (HDL) levels (Clin Cosmet Investig Dermatol 2017;11:1)
- Secondary hyperlipidemias, such as hypothyroidism, diabetes mellitus, drugs (glucocorticoids, estrogens, etc.) (Plast Reconstr Surg 2002;110:1310)
- Diet rich in saturated fats, cholesterol and alcohol (Clin Cosmet Investig Dermatol 2017;11:1)
Clinical features
- Thin, yellow papules and plaques symmetrically distributed on the medial upper or lower eyelids
- May be associated with cirrhosis, thyroid disorder, nephrotic syndrome
- Periorbital hyperpigmentation noted in > 80% of women with xanthelasma (J Clin Aesthet Dermatol 2016;9:52)
Diagnosis
- Clinical diagnosis based on characteristic appearance
- Biopsy not usually required
Laboratory
- Lipid panel to evaluate for hypercholesterolemia
Prognostic factors
- Increased risk of recurrence with the following (Plast Reconstr Surg 2002;110:1310)
- All 4 eyelids are involved
- Underlying hyperlipidemia
- Prior recurrence
Case reports
- 29 and 40 year old women with xanthelasma palpebrarum arising as a side effect of nilotinib (BMJ Case Rep 2016;2016:bcr2015213511)
- 45 year old White man with a several year history of xanthelasma of the bilateral medial canthal area (Plast Reconstr Surg Glob Open 2023;11:e4982)
- 46 year old Japanese woman with a 1 year history of asymptomatic yellowish papules on the neck and elbow (J Dermatol 2019;46:e362)
- 66 year old man presented with longstanding lesions on the 4 eyelids for several years, recently becoming larger and heavily pigmented (Am J Dermatopathol 2023;45:646)
- 70 year old man with bilateral extensive nodular xanthelasma palpebrarum (Int Ophthalmol 2018;38:803)
Treatment
- Conservative, as nodules often recur
- Excision, laser ablation or topical treatment for cosmesis
- Lipid lowering agent (Ann Intern Med 2020;172:701)
- References: Plast Reconstr Surg Glob Open 2023;11:e4982, Dermatol Surg 2020;46:847
Microscopic (histologic) description
- Lipid laden foamy histiocytes in superficial dermis, clustering around blood vessel walls
Microscopic (histologic) images
Positive stains
- Additional stains are not required
- Oil red O
- CD68
- CD163
- Reference: Arch Pathol Lab Med 2009;133:1994
Negative stains
- BRAF V600E (wild type)
- CD1a
- Langerin
- Reference: Arch Pathol Lab Med 2009;133:1994
Videos
Xanthelasma (xanthoma of eyelid)
Sample pathology report
- Skin, eyelid, shave biopsy:
- Xanthelasma
Differential diagnosis
- Periorbital Erdheim-Chester disease:
- Similar but more abundant sheets of foamy histiocytes forming mass lesion
- Widespread, mulitfocal disorder involving viscera and bones, BRAF V600E
- Periorbital Langerhans cell histiocytosis:
- Injected foreign material, poly-L lactic acid (tissue filler) paraffinoma (J Cutan Pathol 2008;35:536):
- Paraffinoma features: look for empty pseudocystic spaces
Additional references
Board review style question #1
Board review style answer #1
E. Xanthelasma is correct because there are abundant foamy histiocytes in the superficial dermis. Answer A is incorrect because chalazion typically shows mixed acute and chronic inflammation with extracellular lipid deposits; it is sometimes granulomatous. Answer B is incorrect because Erdheim-Chester is a non-Langerhans histiocytosis with intermixed lymphocytes, which may involve the orbit but also has involvement of other organ systems: bone, CNS, pituitary. Answer C is incorrect because there is not an abundant mixed inflammatory infiltrate with histiocytes showing grooved nuclei. Answer D is incorrect because ruptured epidermal inclusion cyst would show portions of epithelial lines cyst with a surrounding mixed inflammatory infiltrate, often with keratin debris and foreign body giant cells, many of which may contain keratin fragments.
Comment Here
Reference: Xanthelasma
Comment Here
Reference: Xanthelasma
Board review style question #2
A 50 year old woman presents with bilateral medial upper eyelid yellow plaques. Which systemic medical condition is most likely associated with this pathology?
- Acromegaly
- Atherosclerosis
- Breast cancer
- Colon cancer
Board review style answer #2
B. Atherosclerosis. Xanthelasma characteristically presents with symmetric medial upper eyelid yellow plaques. It may be associated with cirrhosis, atherosclerosis, thyroid disorders, nephrotic syndrome, primary hyperlipidemias (especially type 2a) and diabetes mellitus. Answer A is incorrect because acromegaly is growth hormone overproduction and is not associated with xanthelasma. Answer C is incorrect because breast cancer is not associated with xanthelasma. Metastatic breast cancer can cause enophthalmos but not yellow plaques. Answer D is incorrect because colon cancer is not associated with xanthelasma.
Comment Here
Reference: Xanthelasma
Comment Here
Reference: Xanthelasma
Recent Eye Pathology books
Find related Pathology books: eye, head & neck/endocrine