Superpage
Superpage Topics
STK11 adnexal tumor (pending)
Adenomyoma (pending)
Adenosarcoma (pending)
Adenosarcoma (pending)
Adrenocortical remnants (pending)
Anatomy, histology, embryology & features to report
Anatomy, histology, embryology & features to report
Chronic salpingitis
Developmental cysts
Ectopic / tubal pregnancy
Endometrioid adenocarcinoma
High grade serous carcinoma
Leiomyoma (pending)
Leiomyosarcoma (pending)
Mesonephric duct remnants
Metaplastic changes
Metaplastic papillary lesion
Mucinous metaplasia (pending)
Papillary cystadenoma of mesosalpinx
Paratubal cysts
Placental site nodule
Prolapse
Salpingitis isthmica nodosa
Serous adenofibroma and papilloma
Serous borderline tumor
Serous borderline tumor (pending)
Serous tubal intraepithelial carcinoma
STK11 adnexal tumor
Teratoma (pending)
Tubal hyperplasia
Tubo-ovarian abscess
Walthard cell nests
WHO classification
Wolffian tumor / Female adnexal tumor of probable Wolffian originSTK11 adnexal tumor (pending)
[Pending]
Adenomyoma (pending)
[Pending]
Adenosarcoma (pending)
[Pending]
Adenosarcoma (pending)
[Pending]
Adrenocortical remnants (pending)
[Pending]
Anatomy, histology, embryology & features to report
Table of Contents
Definition / general | Essential features | Terminology | Physiology | Diagrams / tables | Clinical features | Laboratory | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Videos | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Fallopian tube represents an anatomic bridge between the ovary and the uterus in which fertilization of an egg by sperm may occur followed by delivery of the zygote to the uterus; it also provides the environment needed to sustain the gametes and prevent rejection of the zygote by the body
Essential features
- Fallopian tube is divided into several anatomic regions (i.e., intramural, isthmus, ampulla and infundibulum) and comprises mucosal, muscular and serosal layers
- Mucosa is composed of 4 cell types that can be readily recognized on H&E staining; however, more cell subtypes can be identified immunohistochemically and molecularly
- Composition of these cell types varies based on location, phase of the menstrual cycle and menopausal status
- A complex immune system moderates tolerance to a fertilized egg, fights infection and plays a role in cancer surveillance
Terminology
- Other historically used names include tuba uteri, oviduct, uterine tube or tube (J Reprod Fertil 1988;82:843)
Physiology
- Ciliated cells move egg toward the ampulloisthmic junction
- Ampulloisthmic junction is the site of fertilization
- Growth is encouraged by estradiol
- Deciliation is encouraged by progesterone
- Prolonged exposure to progesterone or removal of estrogen causes epithelial atrophy (Mills: Histology for Pathologists, 5th Edition, 2019)
- Motile cilia beat to provide fluid flow (Int J Gynecol Cancer 2018;28:1535)
- Control gamete and embryo movement (Dev Cell 2022;57:914)
- Secretory cells
- Secrete oviduct fluid
- Complex mixture of materials derived from plasma and proteins specifically formed by the tubal epithelium
- Function of tubal fluid (J Reprod Fertil 1988;82:843)
- Moisturizes surface epithelium
- Bacteriostatic function
- Electrolyte balances may influence the development of embryos into blastocysts, the motility of sperm and the health of the ovum
- Contains nutrients for spermatozoa, oocytes and zygotes and promotes the capacitation of sperm by removing glycoproteins and other molecules from the plasma membrane
- Major constituents are calcium, sodium, chloride, glucose, proteins, bicarbonates, amylase, lactic acid (J Reprod Fertil 1988;82:843)
- Bicarbonates and lactic acid are vital to the sperm's use of oxygen; they also help with postfertilization egg development
- Tubal fluid flows against the action of cilia (i.e., toward the fimbriated end) (J Reprod Fertil 1988;82:843)
- Formation of fallopian tubal fluid (Reproduction 2001;121:339)
- Secrete oviduct fluid
- Intercalated cells are either secretory cells or a form of reserve cells
- After menopause, the lining will contract and the epithelial cells will decrease in number, leading to blunting of the plica
- During pregnancy
- Inactive during gestation
- Mild decidual change in the endosalpingeal stroma during the later half of pregnancy
- Epithelial atrophy
- Birth control pills and tubal ligation can cause changes in morphology (Mills: Histology for Pathologists, 5th Edition, 2019)
- Molecular and transcriptional alterations occur throughout the menstrual cycle and after menopause (medRxiv 2023 Nov 23 [Preprint], Cell Rep 2022;41:111838)
- Immune system (Int J Gynecol Pathol 2014;33:581)
- Prevents infection
- Helps develop tolerance to the zygote
Diagrams / tables
Clinical features
- Fallopian tubes can be evaluated with hysterosalpingography (Fertil Steril 2022;118:19)
- Dye is injected into the uterus that can be visualized using Xray
- Flow of the dye is visualized to assess the patency of the fallopian tubes
Laboratory
- CA125 can be used to screen for ovarian / fallopian tube cancer (J Ovarian Res 2019;12:28)
- More useful in postmenopausal women
- False positive results are associated with endometriosis, pelvic inflammatory disease and uterine fibroids
Gross description
- Bilateral hollow, tubular structures, measuring 8 - 12 cm in length and 0.5 - 1.2 cm in diameter
- Lined by a single layer of mucosal epithelium with many folds (plicae), which are most obvious in the ampulla where they subsequently merge with fimbriae
- Extend laterally from the posterior superior uterine fundus and lead to the ovaries
- Connected to broad ligament by mesosalpinx (double fold of peritoneum), to uterine cornu by utero-ovarian ligament and to lateral pelvic sidewall by infundibulopelvic (suspensory) ligament
- Arterial supply is from branches of uterine and ovarian arteries, located within mesosalpinx
- Nerve supply from both sympathetic and parasympathetic fibers
- Sensory fibers run from T11 - T12 and L1
- Lymphatic drainage to para-aortic, internal iliac, external iliac, common iliac and inguinal lymph nodes
- Segments
- Intramural (within wall of uterus)
- Isthmus (thick walled, narrower opening, ~2 cm in length)
- Ampulla (thin walled, major portion, typical site of fertilization)
- Infundibulum (trumpet shaped end lined by fimbriae, attaches to ovary)
- Tubal ostium is an opening to the peritoneal cavity
- Uterotubal junction is an entrance to the uterine cavity
- Reference: StatPearls: Anatomy, Abdomen and Pelvis - Fallopian Tube [Accessed 18 April 2024]
Frozen section description
- Fallopian tube specimen is most often received for frozen section as a part of a salpingo-oophorectomy specimen (Hui: Atlas of Intraoperative Frozen Section Diagnosis in Gynecologic Pathology, 1st Edition, 2015)
- Frozen section is not usually performed on grossly identifiable and unremarkable fallopian tubes; however, adherent fallopian tube tissue may occasionally be submitted for intraoperative consultation
- Morphologic features are consistent with normal fallopian tube as described below
Frozen section images
Not applicable
Microscopic (histologic) description
Embryologic histology
Adult histology
- Third week
- Following migration of primordial germ cells from yolk sac, genital ridge forms from intermediate mesoderm and cloaca forms
- Fourth week
- Müllerian (paramesonephric) ducts form from coelomic epithelium invaginating ventrolaterally into Wolffian (mesonephric) duct and genital mesentery
- This site of invagination later becomes the tubal ostium in which the fimbriae develop and septation of the cloaca occurs
- Fifth to eighth weeks
- Unfused cephalic part of Müllerian ducts form fallopian tube
- Fused part forms uterus and upper vagina
- In a female fetus (or male without functioning testes) (Bhatnagar: Essentials of Human Embryology, 3rd Edition, 2000)
- Müllerian structures persist and Wolffian (mesonephric) duct regresses; vestiges may persist as epithelial inclusions
- Development is affected by clomiphene, tamoxifen and to a lesser extent, diethylstilbestrol (DES) (Hum Pathol 1987;18:1132, Hum Pathol 1982;13:190)
Adult histology
- Fallopian tube wall is composed of mucosal, muscular and serosal layers
- Mucosa comprises luminal epithelium and underlying lamina propria (stroma)
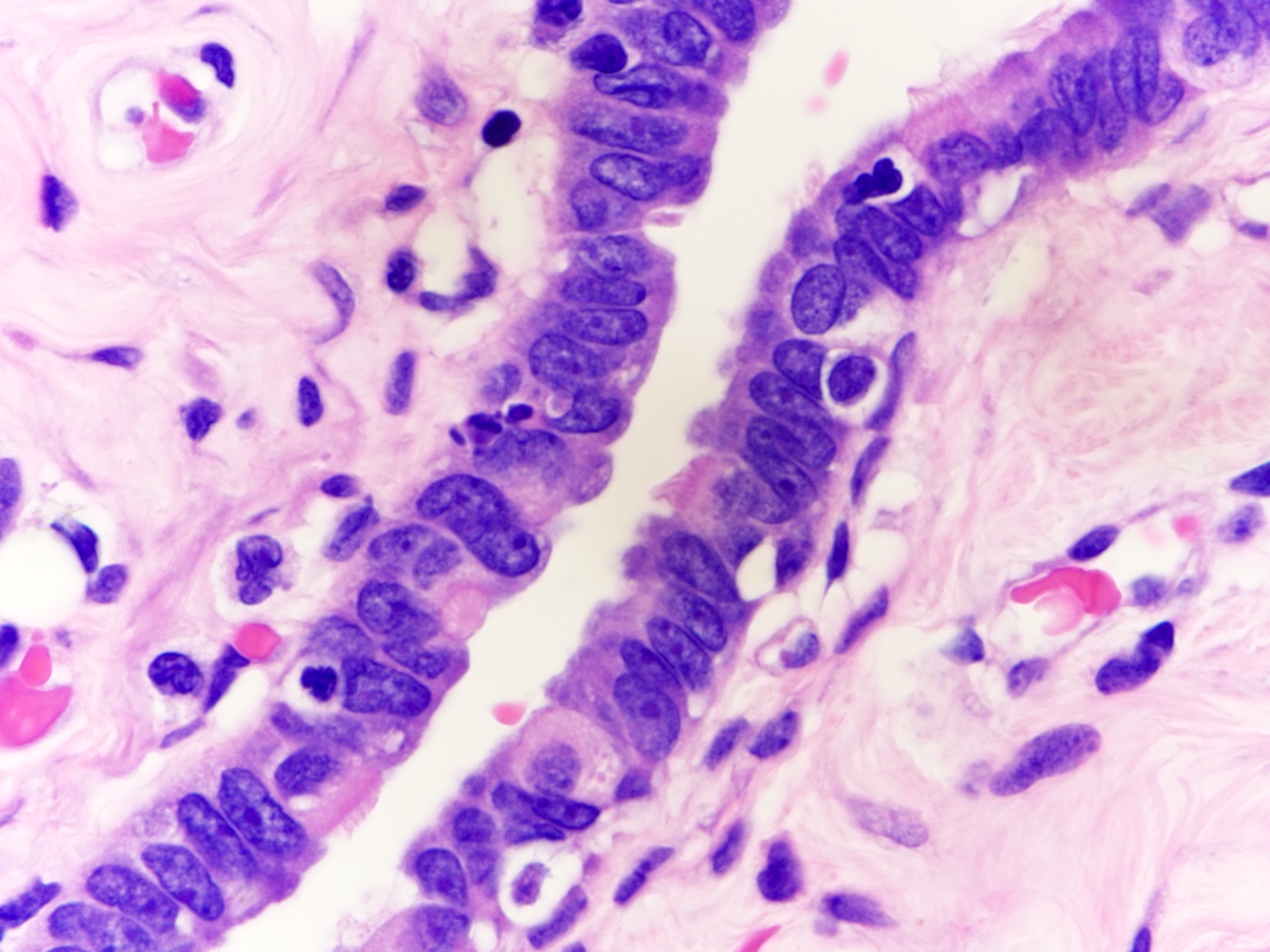
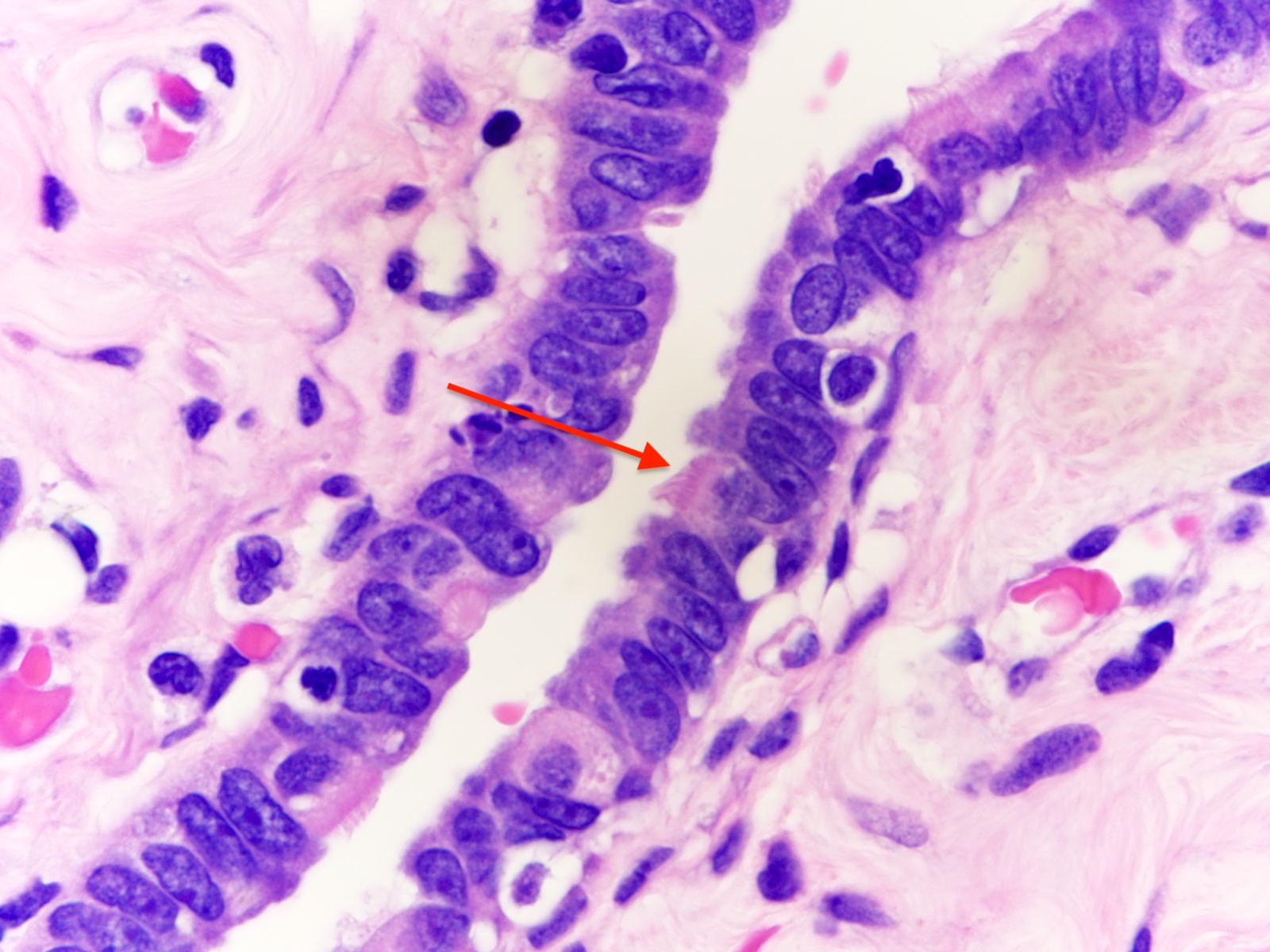
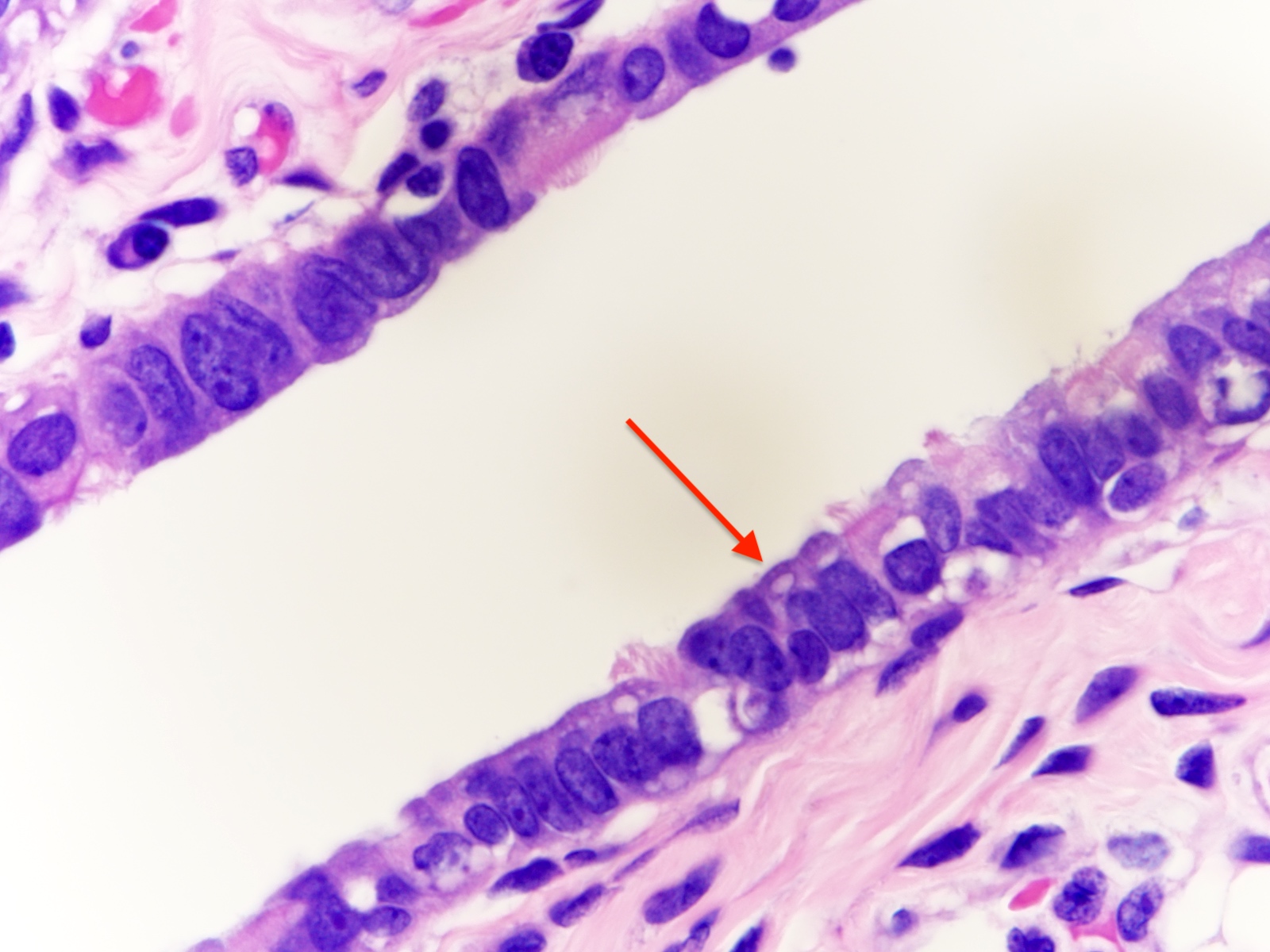
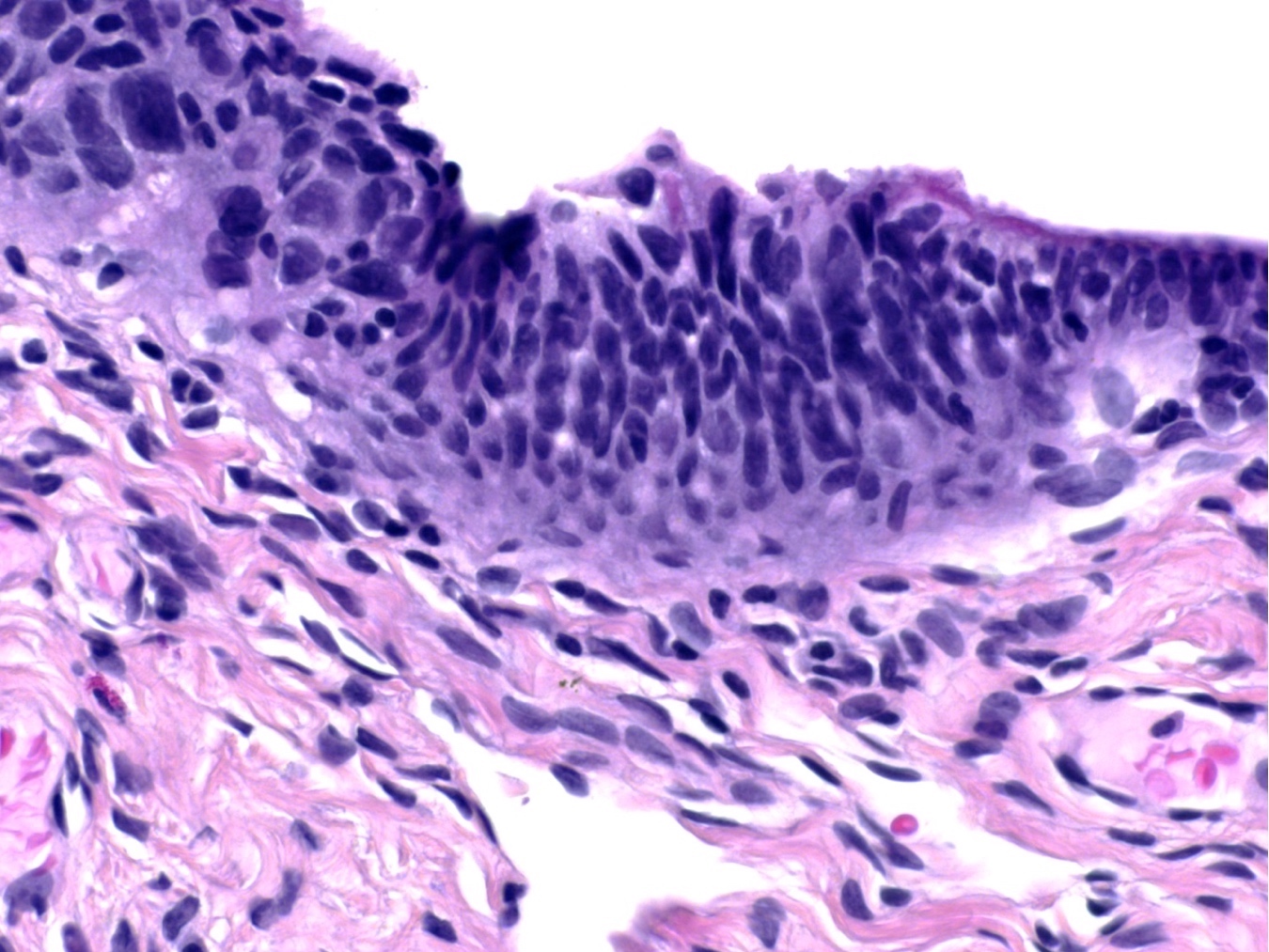
- Luminal epithelium consists of the following cells (Mills: Histology for Pathologists, 5th Edition, 2019)
- Ciliated columnar cells (~25%)
- Most abundant in infundibulum and ampulla
- Estrogen increases production of cilia
- Most often seen at the apex of mucosal folds
- Most common at the ovarian end of the tube, especially in fimbriae
- Most common during midcycle and decrease to the minimum number at menstruation
- Decrease during gestation
- Secretory cells (~60%)
- Nonciliated, containing apical granules and producing tubular fluid
- Exhibit ovoid, dense nuclei
- Most common at the proximal segment of the fallopian tube
- Increase in number in response to progesterone
- Height and secretory activity increase in response to estrogen
- Menstruation cycle changes cell height and appearance
- May exhibit nonmotile primary cilia
- Contain sensory organelles
- React to cilia mediated stimuli and are fully capable of affecting cilia mediated signaling pathways
- Lost in serous tubal intraepithelial carcinoma (Int J Gynecol Cancer 2018;28:1535)
- Peg (intercalated) cells (< 10%)
- Exhibit thin dense nuclei and little cytoplasm
- Hypothesized to be stem / progenitor cells (J Reprod Immunol 2022;152:103646)
- A stage in the cyclic variation during the menstrual cycle of the secretory cells
- Basal cells (Dev Cell 2022;57:914)
- Exhibit round nuclei and a cytoplasmic ring
- Ciliated columnar cells (~25%)
- Lamina propria (stroma) (Dev Cell 2022;57:914)
- Stromal cells resembling fibroblasts, surrounded by dense reticulin network
- Blood vessels
- Possibly Cajal-like cells (Dev Cell 2022;57:914)
- Muscle layer comprising 3 sublayers
- Innermost (obliquely arranged)
- Middle (circular)
- Outermost (longitudinal, extending into fimbriae)
- Serosal layer
- Lined by mesothelium of visceral peritoneum
- Often contains Walthard rests with transitional type epithelium
- Immune cells
- Lymphocytes may be observed in epithelium, lamina propria and muscular wall (Int J Gynecol Pathol 2014;33:581)
- Occasional lymphoid follicles may be seen
- Other immune cells include CD163+ macrophages, CD11c+ dendritic cells, CD8+ T cells and a minor populations CD56+ NK cells, CD4+ T helpers, CD20+ B cells, TCRγδ+ T cells, CD207+ (langerin) Langerhans cells, mast cells (Int J Gynecol Pathol 2014;33:581, Dev Cell 2022;57:914)
- Distribution varies according to menopausal status; T helper and B cells are more common in postmenopausal women, while macrophages are more abundant in premenopausal women (Int J Gynecol Pathol 2014;33:581)
- Play a role in cancer immune surveillance (Int J Gynecol Pathol 2014;33:581)
- Normal histologic variations
- Intramuscular edema in 12.5% of specimens, most frequently postpartum
- Plical fibrosis (35.5%), epithelial vacuolization (6.6%) and epithelial tufting / stratification (3.5%) correlated with increased patient age (Arch Pathol Lab Med 2002;126:951)
- Rare mitotic figures
- Metaplasia, including mucinous, endometrioid or transitional cell (Walthard rests)
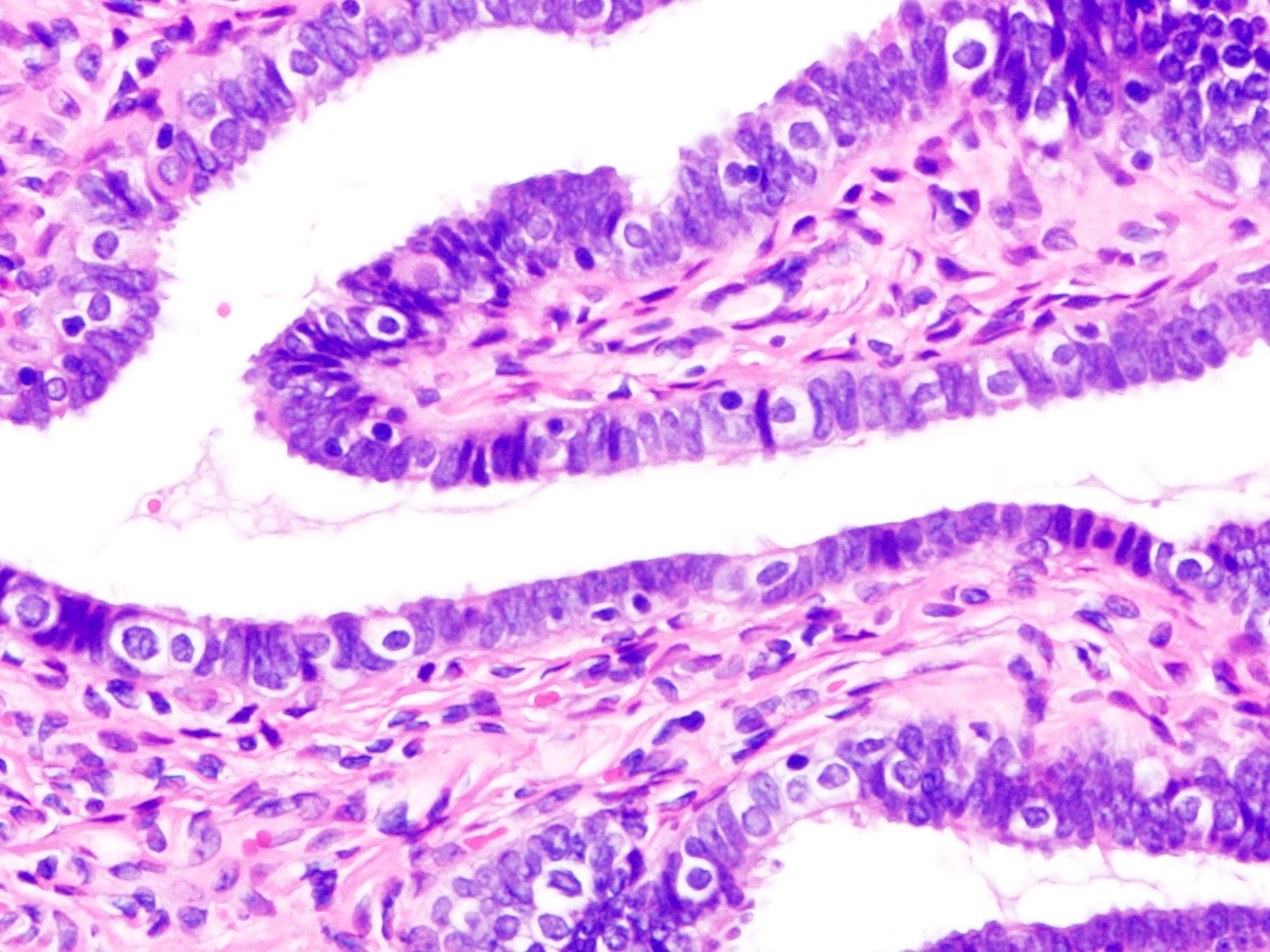
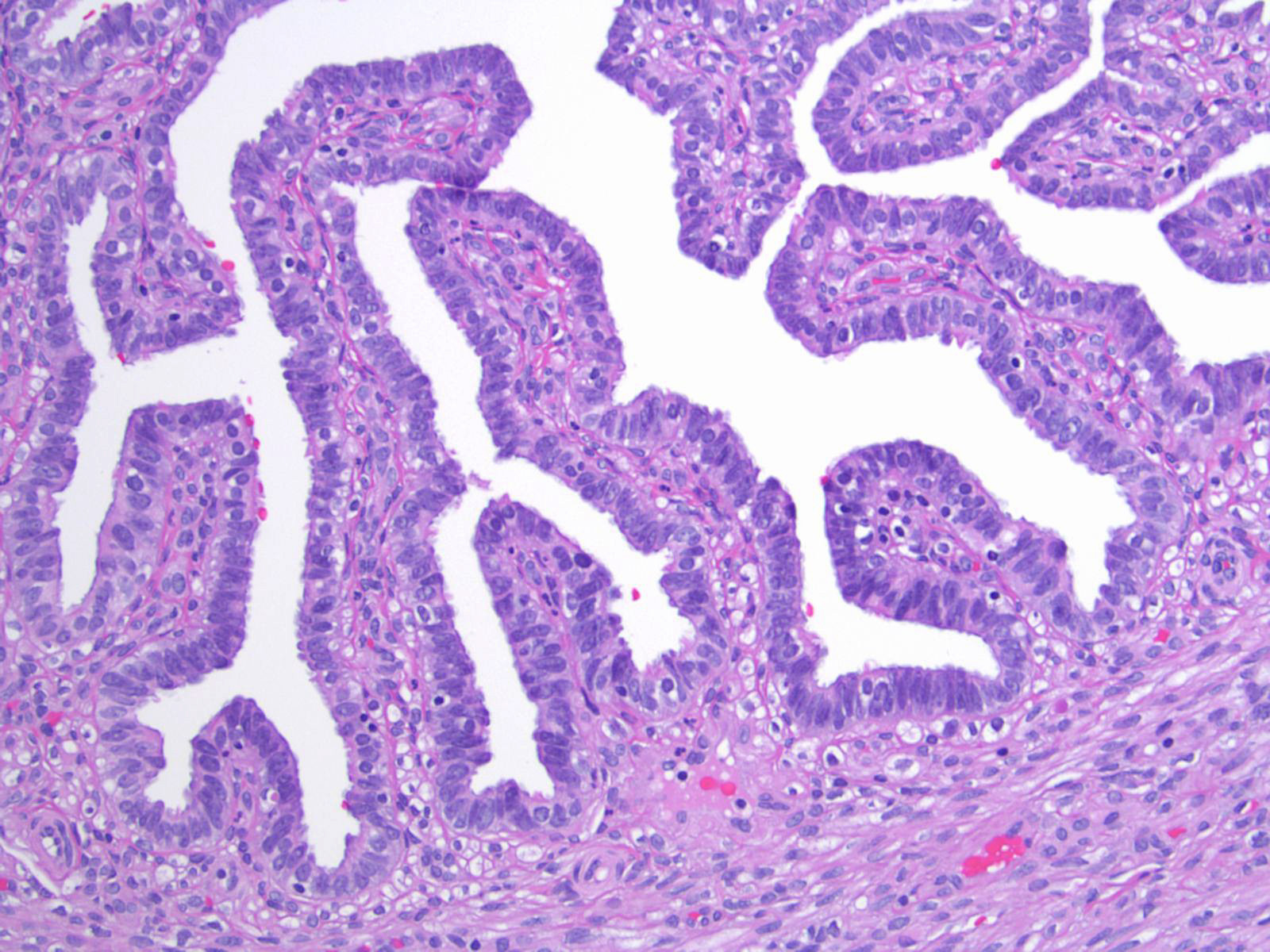
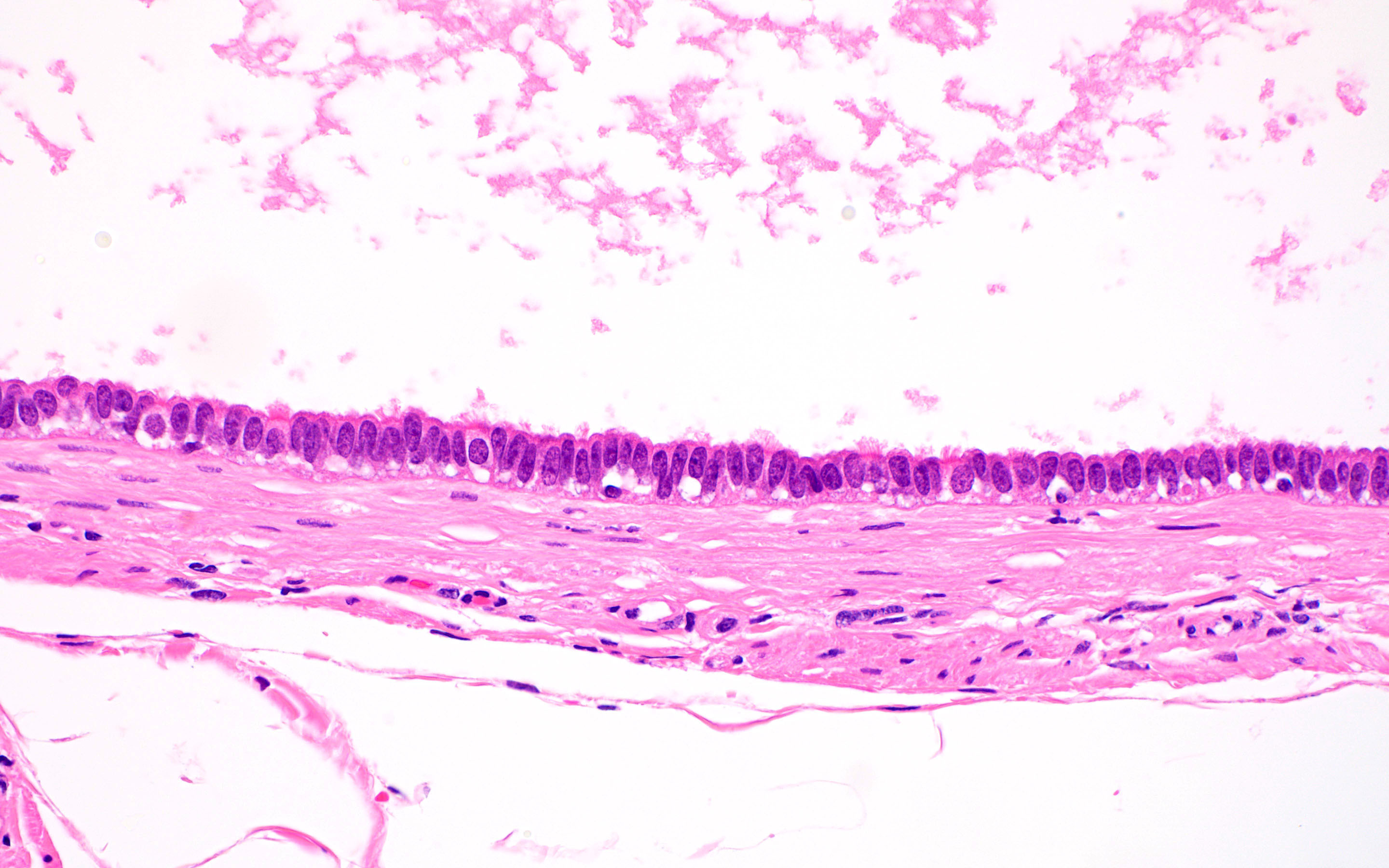
Microscopic (histologic) images
Contributed by Brandon D. Metcalf, M.D. and Nicole D. Riddle, M.D.
Virtual slides
Not applicable
Cytology description
- Ciliated cells in clustered arrangements with round or oval nuclei, hyperchromatic chromatin and mild nuclear membrane irregularity
- Honeycomb / monolayered sheets
- Spindled appearance is not characteristic (Cytojournal 2018;15:28)
- Utility of minimally invasive laparoscopic screening of fallopian tubes in patients at high risk for high grade serous carcinoma is being investigated (J Vis Exp 2017;125:55887, J Am Soc Cytopathol 2023;12:368)
Positive stains
- Ciliated cells (Dev Cell 2022;57:914, Stem Cells 2012;30:2487, Cancer Cell 2020;37:226)
- FOXJ1
- CAPS
- B tubulin
- TUBB4
- CCdC17
- CCDC78
- Secretory cells (Dev Cell 2022;57:914, Stem Cells 2012;30:2487)
- Peg cells (Dev Cell 2022;57:914)
- Basal cells (Dev Cell 2022;57:914)
- Stromal cells
- In postmenopausal fallopian tubes (Cell Rep 2022;41:111838)
- PAX8 in secretory cells
- FOXJ1, adiponectin, estrogen, insulin and oxytocin in ciliated cells (Cell Rep 2022;41:111838)
- EpCAM mainly in the ampulla and fimbriae (Cell Rep 2022;41:111838)
- AR, ER and PR in stromal cells (Cell Rep 2022;41:111838)
- Dual PolyGlut-tubulin / DNAH5 stain
- Distinguishes motile cilia from primary cilia (Int J Gynecol Cancer 2018;28:1535)
Negative stains
Not applicable
Electron microscopy description
- Variations during menstrual cycle (Physiol Res 2022;71:S137)
- Postmenstrual
- Ciliation is separated by fields of nonciliated flat cells with indistinct cell borders
- Preovulatory epithelium
- Swelling of nonciliated polyhedral cells
- Still maintain overall distribution of ciliated and nonciliated cells.
- Clusters of nonciliated cells bulge up to the height of the cilia tips
- Imparts a more uniform appearance of the surface epithelium
- Ovulatory epithelium
- Nonciliated cells show disrupted membranes after releasing their secretions
- Premenstrual period
- Nonciliated cells
- Regress below the level of the ciliary tips
- Become flattened
- Regain their distinct boundaries
- Clear boundaries: classic feature for differentiating the premenstrual / luteal phase from the postmenstrual phase
- Ciliated cells
- May cluster in elongated fields called tracts
- May form small ciliated clumps
- Nonciliated cells
- Postmenstrual
- Menopausal (Physiol Res 2022;71:S137)
- Surface epithelium is similar to the luteal phase of premenopausal women
- Mucosal folds with tracts of ciliated cells alternate with stretched clumps of ciliated cells
- Postmenopausal (Physiol Res 2022;71:S137)
- More nonciliated cells
- Frequently turn into dome shaped giant cells
- Observe delicate microplicae-like structures (Histol Histopathol 2006;21:219)
- Gradual shortening of microvilli
- More nonciliated cells
Electron microscopy images
Videos
Shotgun histology: fallopian tube
UB medical: oviduct histology
Additional references
Board review style question #1
Board review style answer #1
B. Ciliated cell and movement of the egg. The ciliated cell contains motile cilia which beat in a wave-like fashion to move the egg. Answer D is incorrect because secretory cells are not responsible for the movement of the egg. Answer A is incorrect because basal cells do not produce tubal fluid and are found at the basal aspect of the epithelium. Answer C is incorrect because ciliated cells do not produce tubal fluid.
Comment Here
Reference: Fallopian tubes & broad ligament - Anatomy, histology, embryology & features to report
Comment Here
Reference: Fallopian tubes & broad ligament - Anatomy, histology, embryology & features to report
Board review style question #2
Board review style answer #2
D. PAX8 stains secretory cells. Answers A and B are incorrect because CD44 and EpCAM stain peg cells. Answer C is incorrect because FOXJ1 stains ciliated cells.
Comment Here
Reference: Fallopian tubes & broad ligament - Anatomy, histology, embryology & features to report
Comment Here
Reference: Fallopian tubes & broad ligament - Anatomy, histology, embryology & features to report
Anatomy, histology, embryology & features to report
Table of Contents
Definition / general | Embryology | Features to report | Diagrams / tables | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Additional referencesDefinition / general
- Also known as oviducts, uterine tubes, salpinges (singular salpinx means 'trumpet')
- Named after their discoverer, the 16th century Italian anatomist Gabriele Falloppio
Embryology
- 3rd week:
- Migration of primordial germ cells from yolk sac, genital ridge forms from intermediate mesoderm, cloaca forms
- 4th week:
- Müllerian (paramesonephric) ducts form from coelomic epithelium invaginating venterolaterally into Wolffian (mesonephric) duct and genital mesentery
- This site of invagination later becomes the tubal ostium in which the fimbriae develop; septation of the cloaca occurs
- 5th - 8th weeks:
- Unfused cephalic part of Müllerian ducts form fallopian tube
- Fused part forms uterus and upper vagina
- In a female fetus (or male without functioning testis):
- Müllerian structures persist and Wolffian (mesonephric) duct regresses; vestiges may persist as epithelial inclusions
- Development affected by clomiphene, tamoxifen and to a lesser extent diethylstilbestrol (DES) (Hum Pathol 1987;18:1132, Hum Pathol 1982;13:190)
- In a male fetus:
- Testes produce Müllerian inhibitory substance, which causes regression of Müllerian ducts and persistence of paired Wolffian (mesonephric) ducts, which form epididymis and vas deferens
- The Müllerian remant is the rudimentary appendix testis
- Reference: Bhatnagar: Essentials of Human Embryology, Third Edition, 2000
Features to report
Gross description
- Hollow, tubular structures, bilateral, 8 - 12 cm long and 0.5 - 1.2 cm in diameter, lined by a single layer of mucosal epithelium with many folds (plica)
- Extends from posterior superior uterine fundus laterally and leads to ovaries
- Connected to broad ligament by mesosalpinx (double fold of peritoneum), to uterine cornu by utero ovarian ligament, to lateral pelvic sidewall by infundibulopelvic (suspensory) ligament
- Arterial supply from branches of uterine and ovarian arteries, located within mesosalpinx
- Nerve supply from both sympathetic and parasympathetic fibers
- Sensory fibers run from T11 - T12 and L1
- Lymphatic drainage to para aortic, internal iliac, external iliac, common iliac and inguinal nodes
- Segments: intramural (within wall of uterus), isthmus (thick walled, narrower opening, ~ 2 cm in length), ampulla (thin walled, major portion of lateral tube, typically where fertilization occurs), infundibulum (trumpet shaped end lined by fimbriae, attaches to ovary)
- Tubal ostium: opening to peritoneal cavity
- Uterotubal junction: entrance to uterine cavity
Gross images
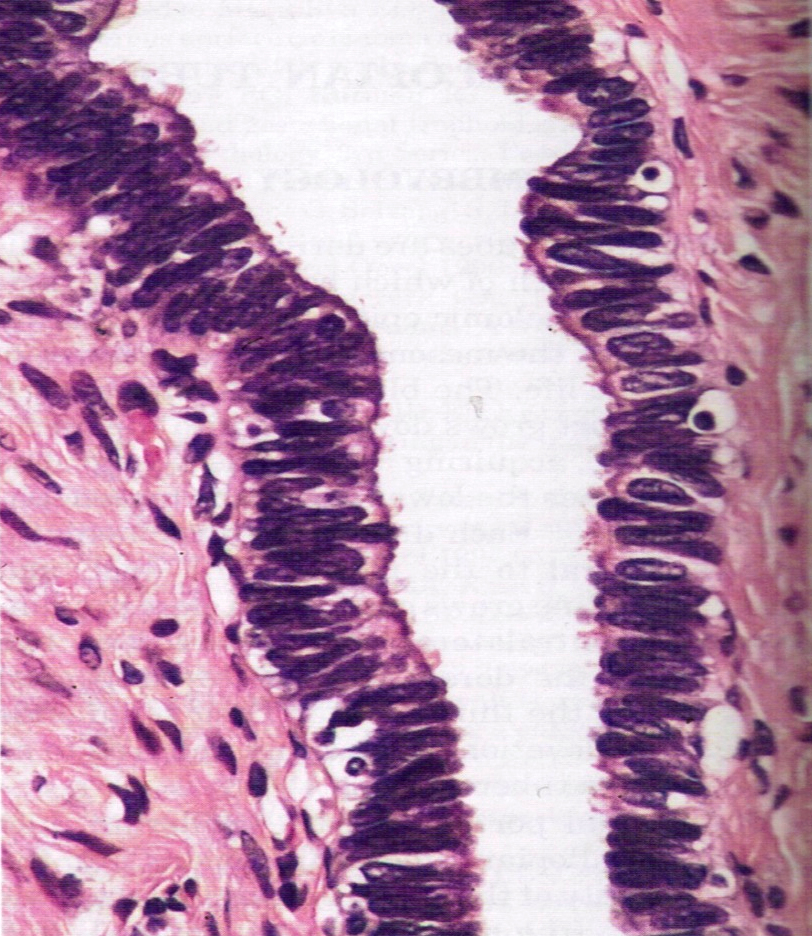
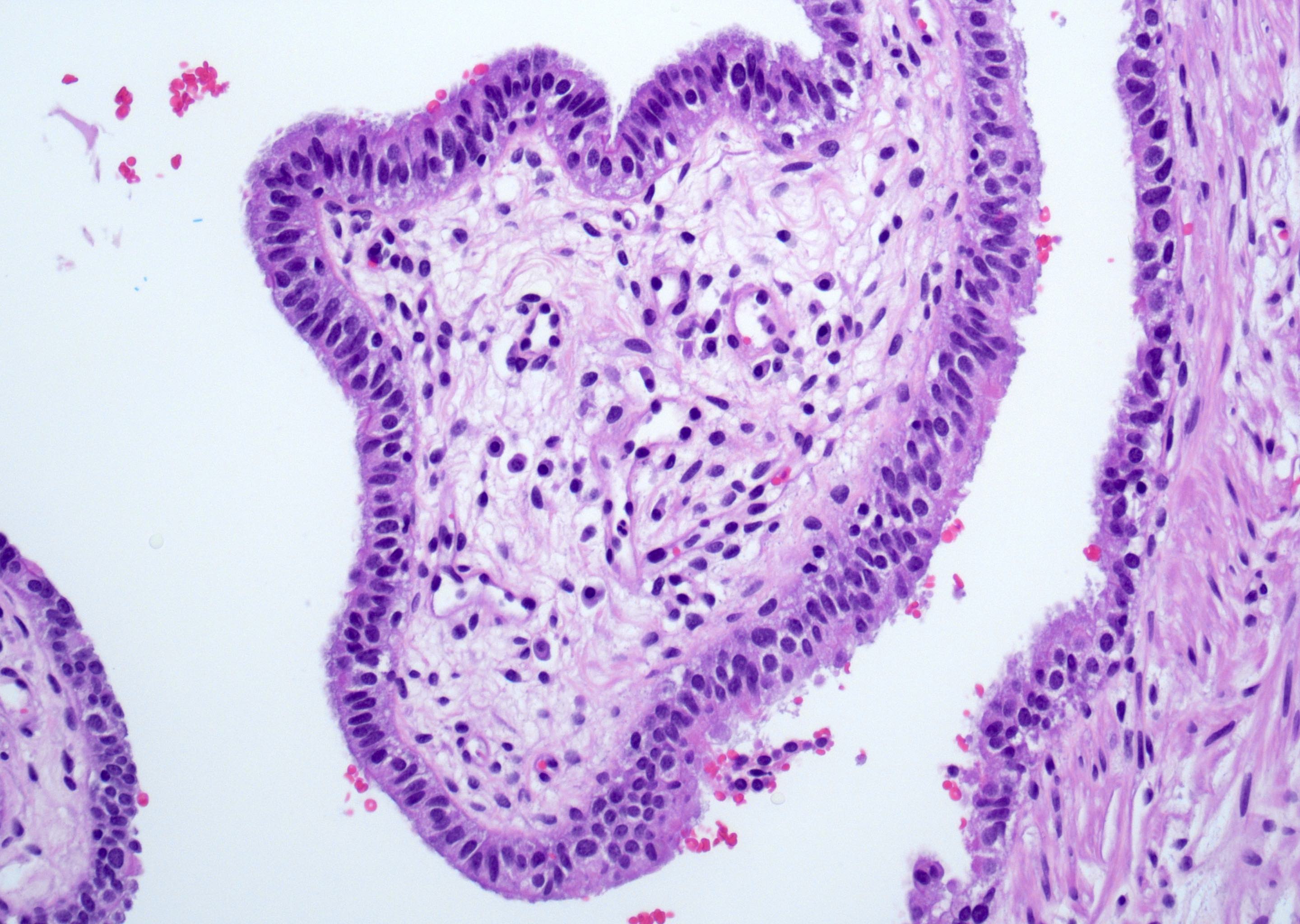
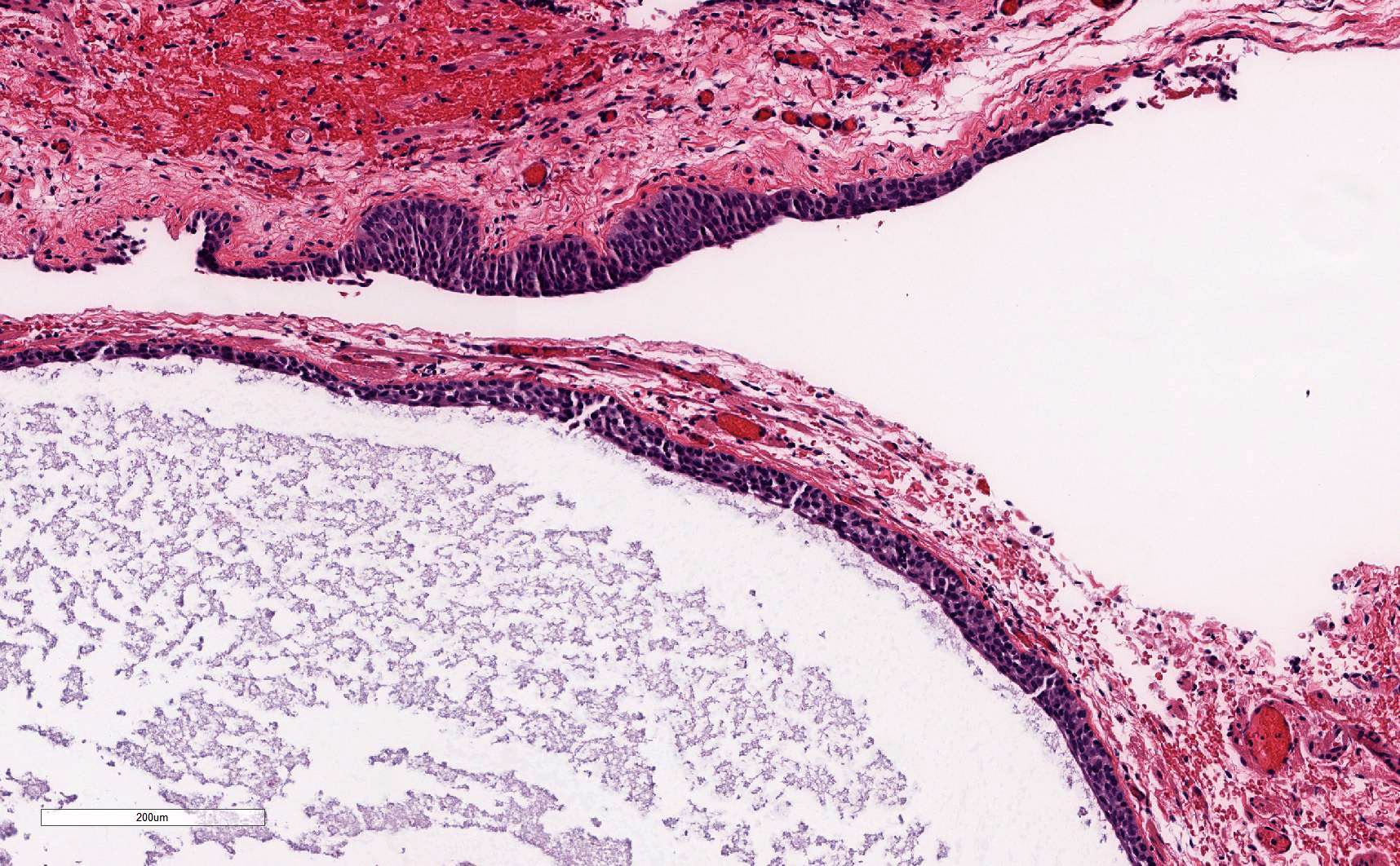
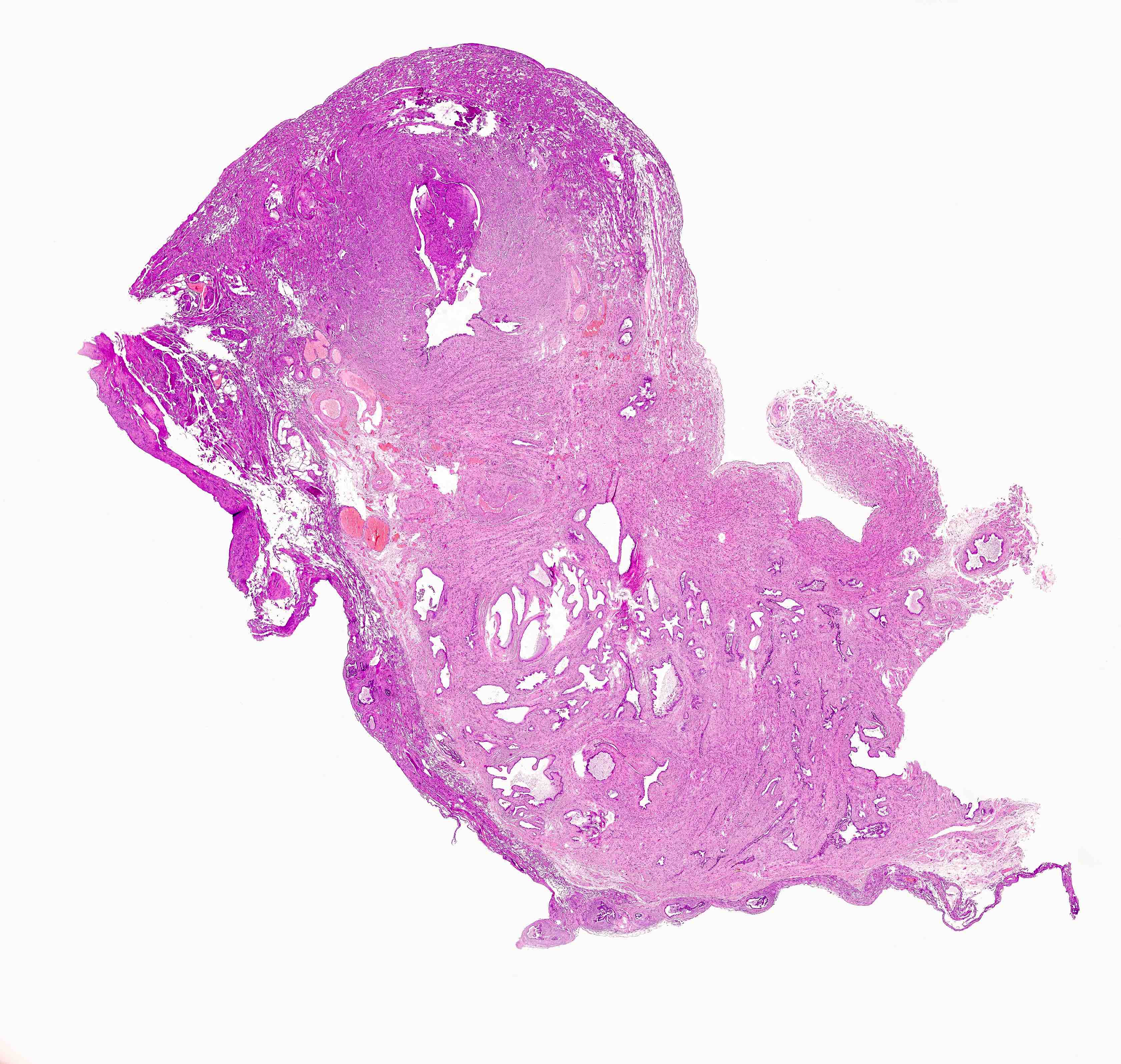
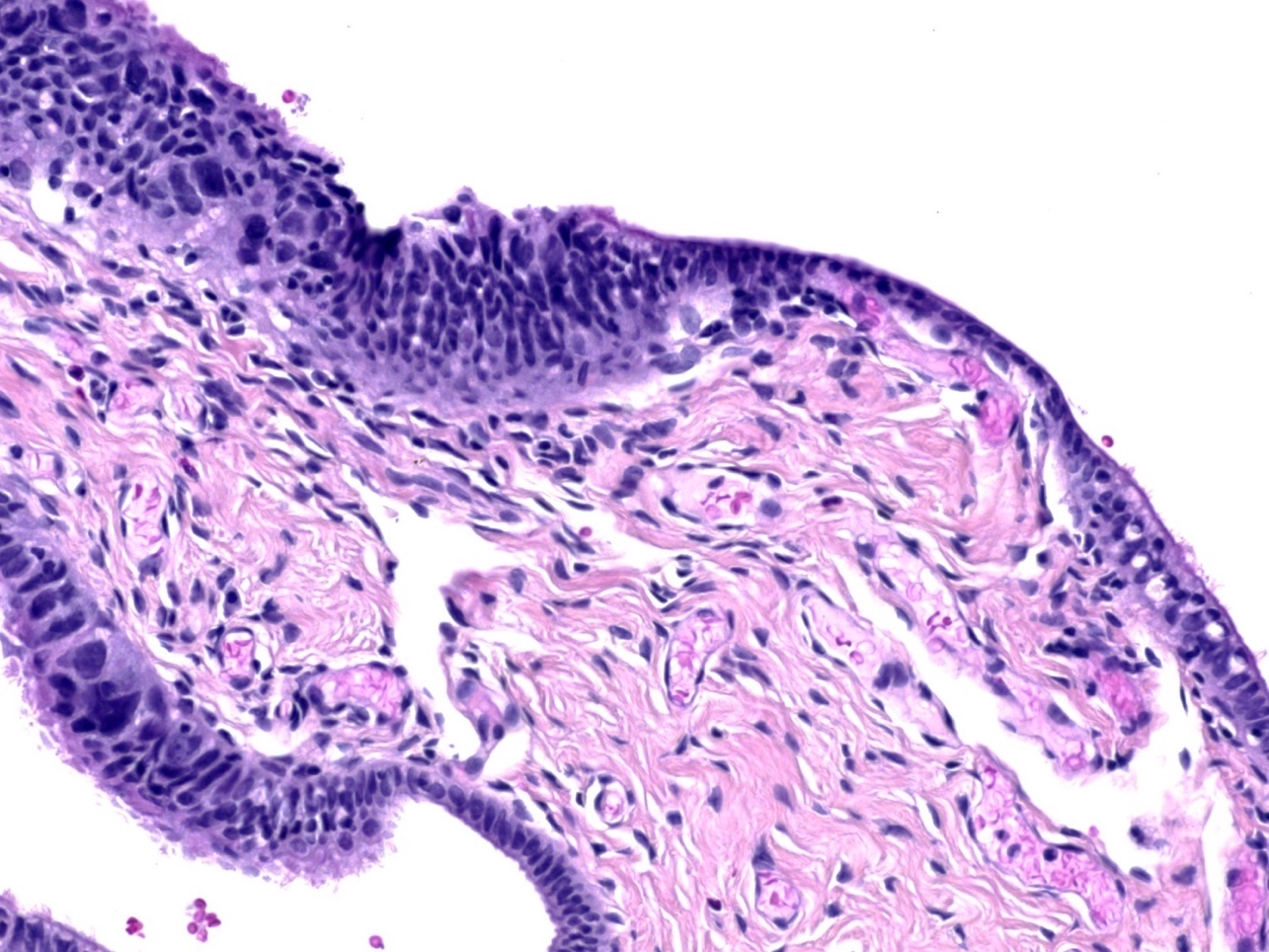
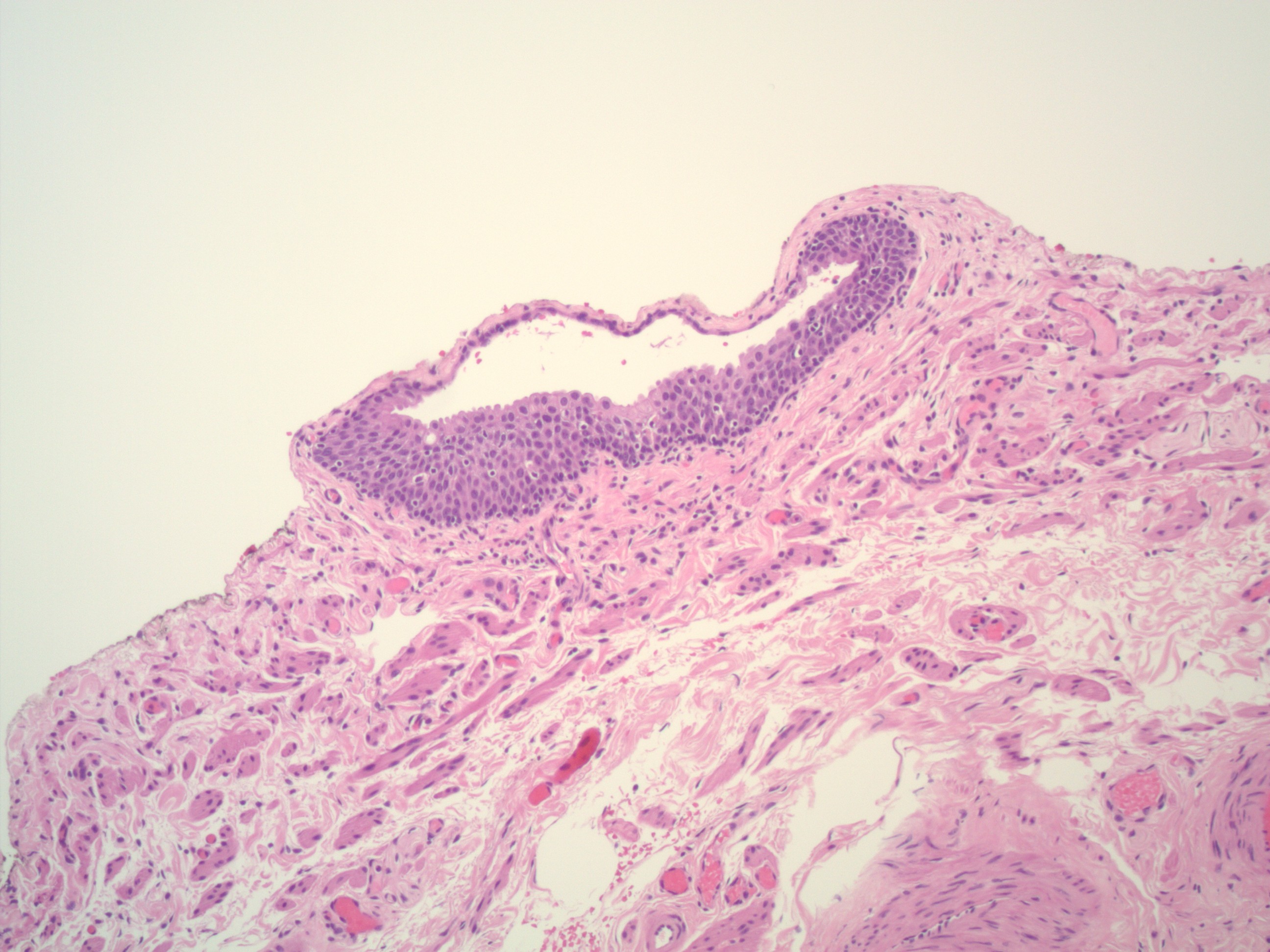
Microscopic (histologic) description
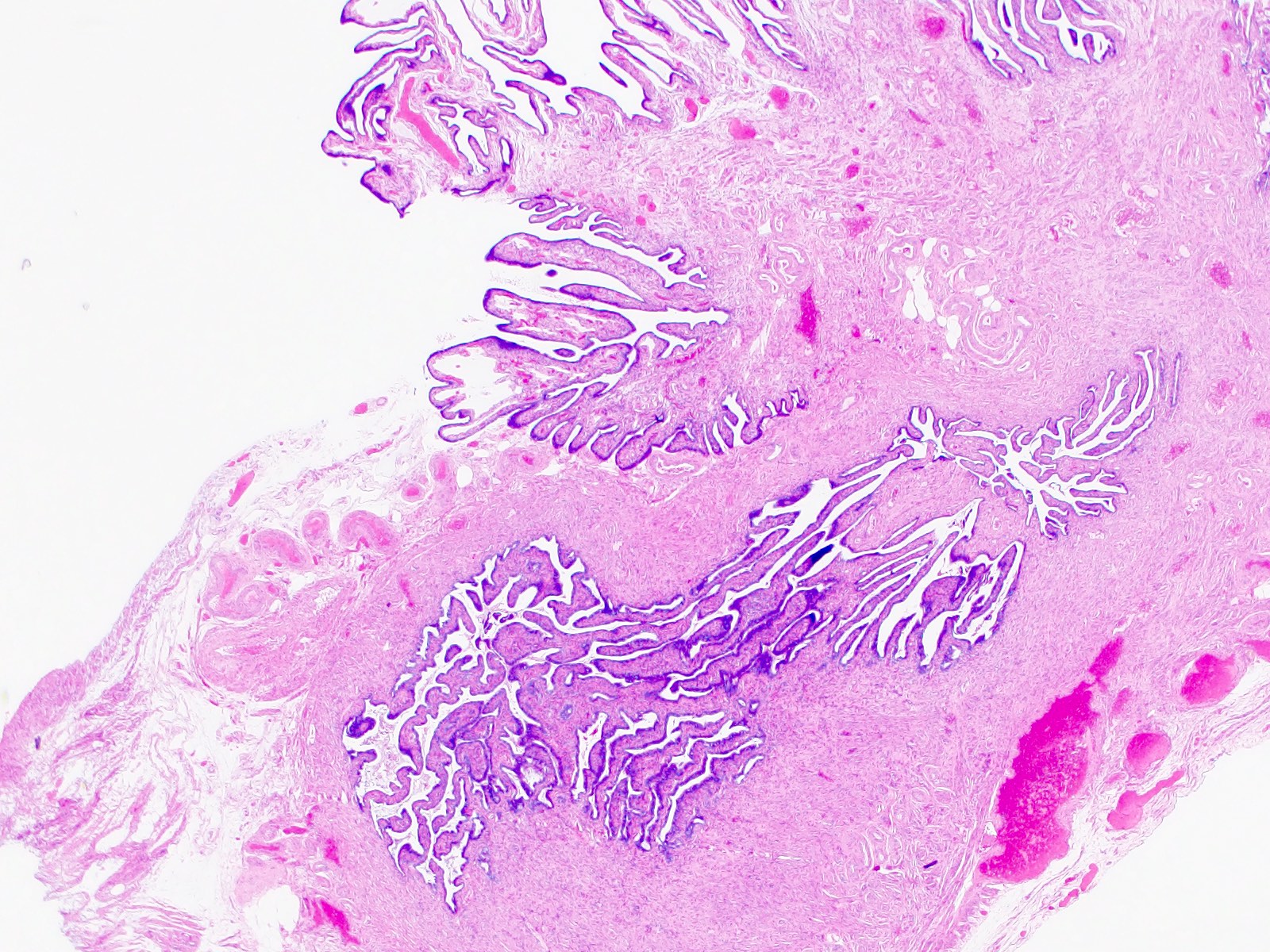
- Plica: delicate folds of mucosa on inner aspect of tube, most evident in ampulla, merge with fimbriae
- Mucosa: consists predominately of single layer of cells including:
- Ciliated columnar cells (~25%), most abundant in infundibulum and ampulla, estrogen increases production of cilia
- Secretory cells (~60%), nonciliated, contain apical granules and produce tubular fluid, progesterone increases their number while estrogen increases their height and secretory activity
- Intercalated cells (peg cells, < 10%), which may be inactive secretory cells
- Tubal fluid:
- Contains nutrients for spermatozoa, oocytes and zygotes and promotes the capacitation of sperm by removing glycoproteins and other molecules from the plasma membrane
- Major constituents are calcium, sodium, chloride, glucose, proteins, bicarbonates, amylase, lactic acid
- Bicarbonates and lactic acid are vital to sperm's use of oxygen; also help egg develop postfertilization
- Tubal fluid flows against action of cilia; i.e. toward the fimbriated end
- Formation of fallopian tubal fluid: see Reproduction 2001;121:339
- Muscle layer: 3 smooth muscle layers:
- Innermost - obliquely arranged
- Middle - circular
- Outermost - longitudinal, extends into fimbriae
- Serosal surface: mesothelium of visceral peritoneum
- Stroma:
- Resembles fibroblasts, whorled / storiform pattern, surrounded by dense reticulin network
- Positive for SMA and desmin
- Normal histologic variations:
- Intramuscular edema in 12.5% of specimens, most frequently in postpartum women
- Plical fibrosis (35.5%), epithelial vacuolization (6.6%), and epithelial tufting / stratification (3.5%) correlated with increased patient age
- Inflammatory cells are common; intramuscular mast cells (~70% of cases), plasma cells (~20%), neutrophils (10.5%), and lymphoid follicles (2.1%) (Arch Pathol Lab Med 2002;126:951)
Microscopic (histologic) images
Additional references
Chronic salpingitis
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagnosis | Radiology description | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Chronic inflammation of fallopian tube with lymphoplasmacytic infiltrate and with or without foamy histiocytes and granulomas
Essential features
- Presence of plasma cells and lymphocytes in the submucosa
- Plicae are fibrotic, fused, short and thick
- May be associated with epithelial hyperplasia
Terminology
- Chronic salpingitis, follicular salpingitis, granulomatous salpingitis, ligneous salpingitis, pseudoxanthomatous salpingitis and xanthomatous salpingitis
Epidemiology
- Women of reproductive age
- Occurs in up to 50% of ectopic pregnancies
Sites
- Fallopian tube, unilateral or bilateral
Pathophysiology
- May be associated with active or prior history of infection (pelvic inflammatory disease) (Fertil Steril 2000;74:152)
- May be seen in association with endometriosis or tubal ectopic pregnancy
- Other associations include inflammatory bowel disease (with pulse granulomas) or other infectious processes (tuberculosis, sarcoidosis) (Int J Gynecol Pathol 2015;34:275)
Etiology
- Several bacterial organisms (Neisseria gonorrhoeae, Chlamydia trachomatis, Mycoplasma), foreign body (lubricants, mineral oil, starch), endometriosis
Diagnosis
- Usually an incidental finding on microscopic examination
- May be associated with pelvic pain, especially in the setting of pelvic inflammatory disease, endometriosis or tubal ectopic pregnancy
Radiology description
- May show hydrosalpinx, unilateral or bilateral
Case reports
- 2 year old girl with xanthogranulomatous inflammation (Case Rep Obstet Gynecol 2015;2015:237250)
- 32 year old woman with bilateral tubal gestation (Case Rep Obstet Gynecol 2014;2014:674514)
- 55 year old woman with tuberculous salpingitis (J Clin Diagn Res 2013;7:1186)
Treatment
- Treating the underlying infection / inflammation if there is concurrent acute salpingitis
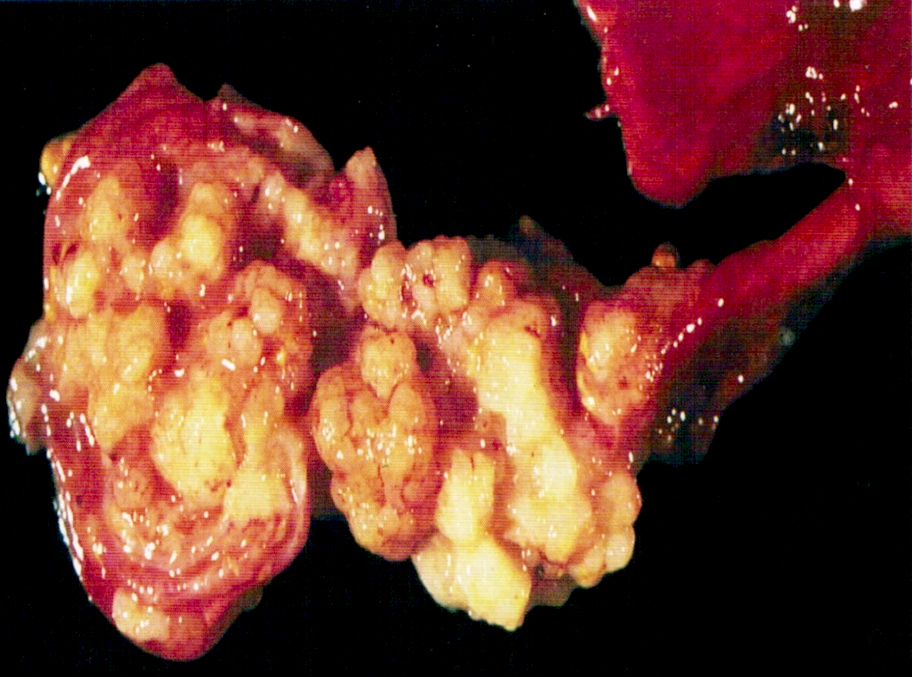
Gross description
- Fused fimbriae, causing blunted end (clubbed tube)
- May form significant tubo-ovarian adhesions and a conglomerated mass
- May show marked tubal dilation (hydrosalpinx)
- May show areas of hemorrhage if associated with endometriosis
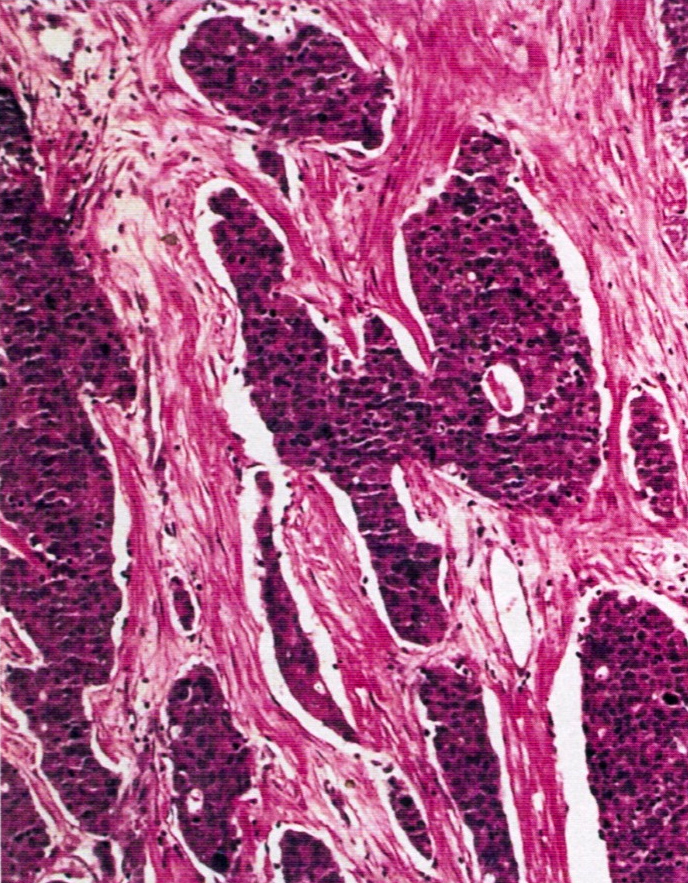
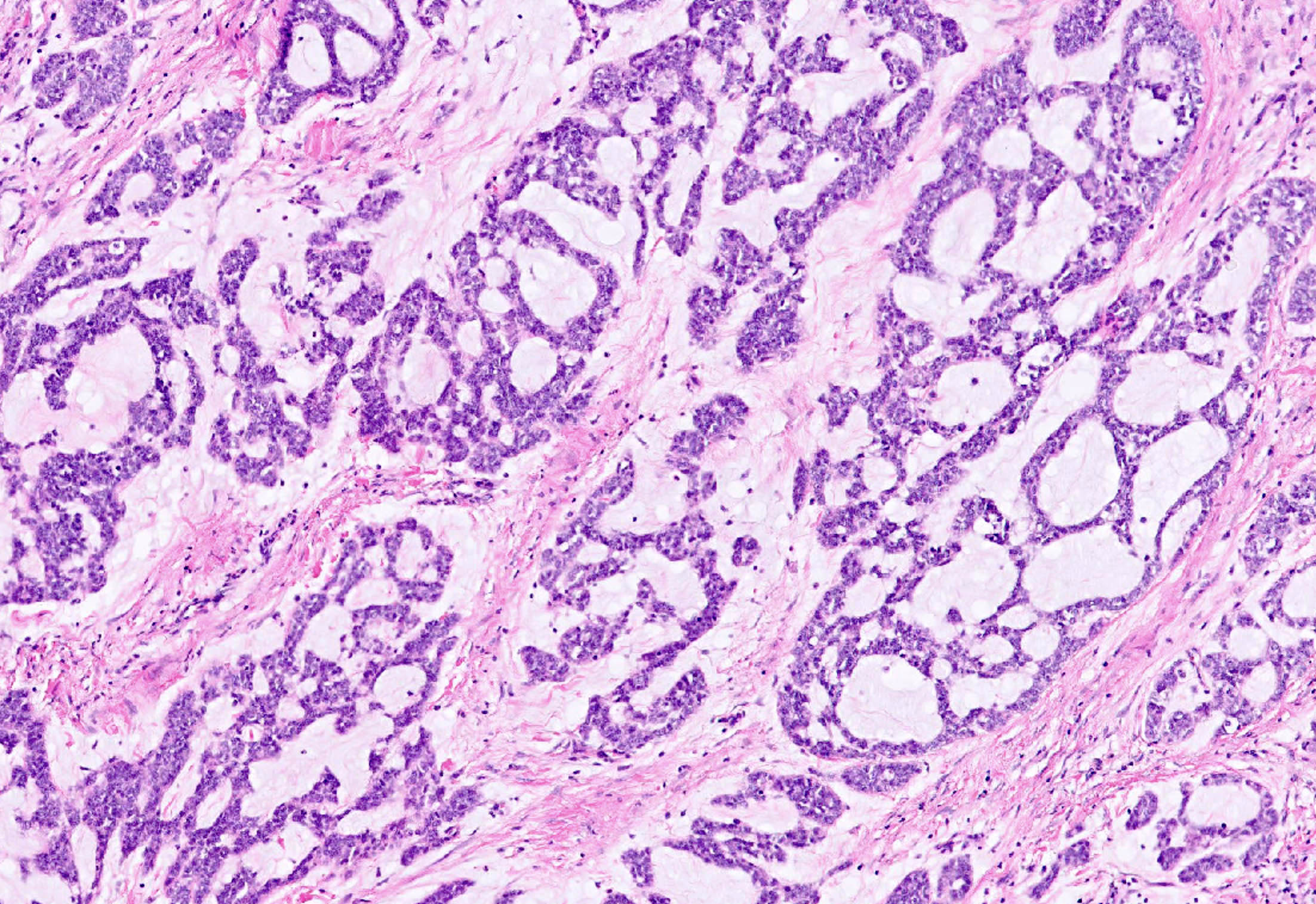
Microscopic (histologic) description
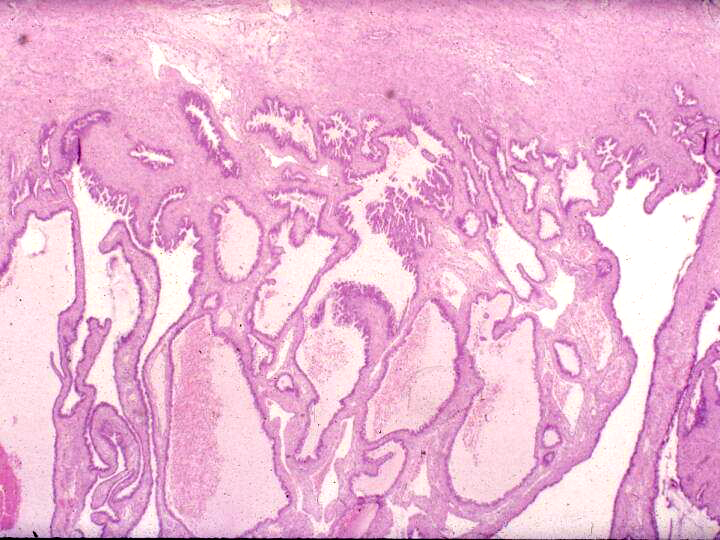
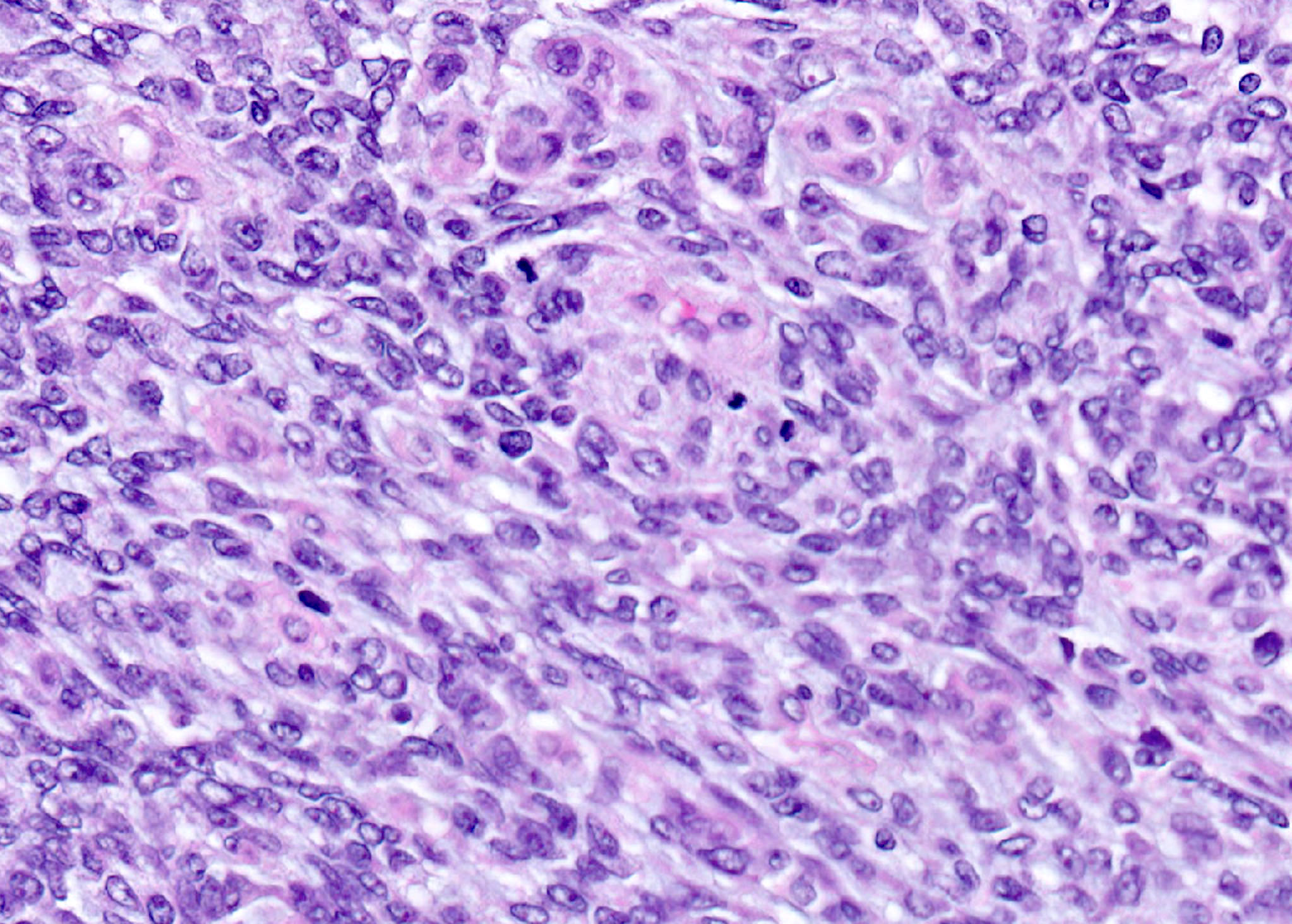
- Chronic salpingitis (Fertil Steril 2000;74:152):
- Usually short, thick plicae with fibrous stroma, lymphocytes, plasma cells or both in the mucosa
- Hydrosalpinx may or may not be seen
- Plicae may look normal or fused
- Epithelial hyperplasia may be seen
- Granulomas, either necrotizing or nonnecrotizing, suggest infection (especially tuberculosis), sarcoidosis or other autoimmune disease (e.g., inflammatory bowel disease)
- Pseudoxanthomatous salpingitis (Int J Gynecol Pathol 2015;34:275):
- Abundant hemosiderin laden macrophages within fallopian tube lamina propria with associated lymphoplasmacytic infiltrate
- Endometriosis in the tubal subserosa or ovarian tissue
- Xanthogranulomatous salpingitis:
- Foamy histiocytes, granulomas and chronic inflammation in the fallopian tube submucosa (Int J Gynecol Pathol 2002;21:56)
- May be associated with pelvic inflammatory disease
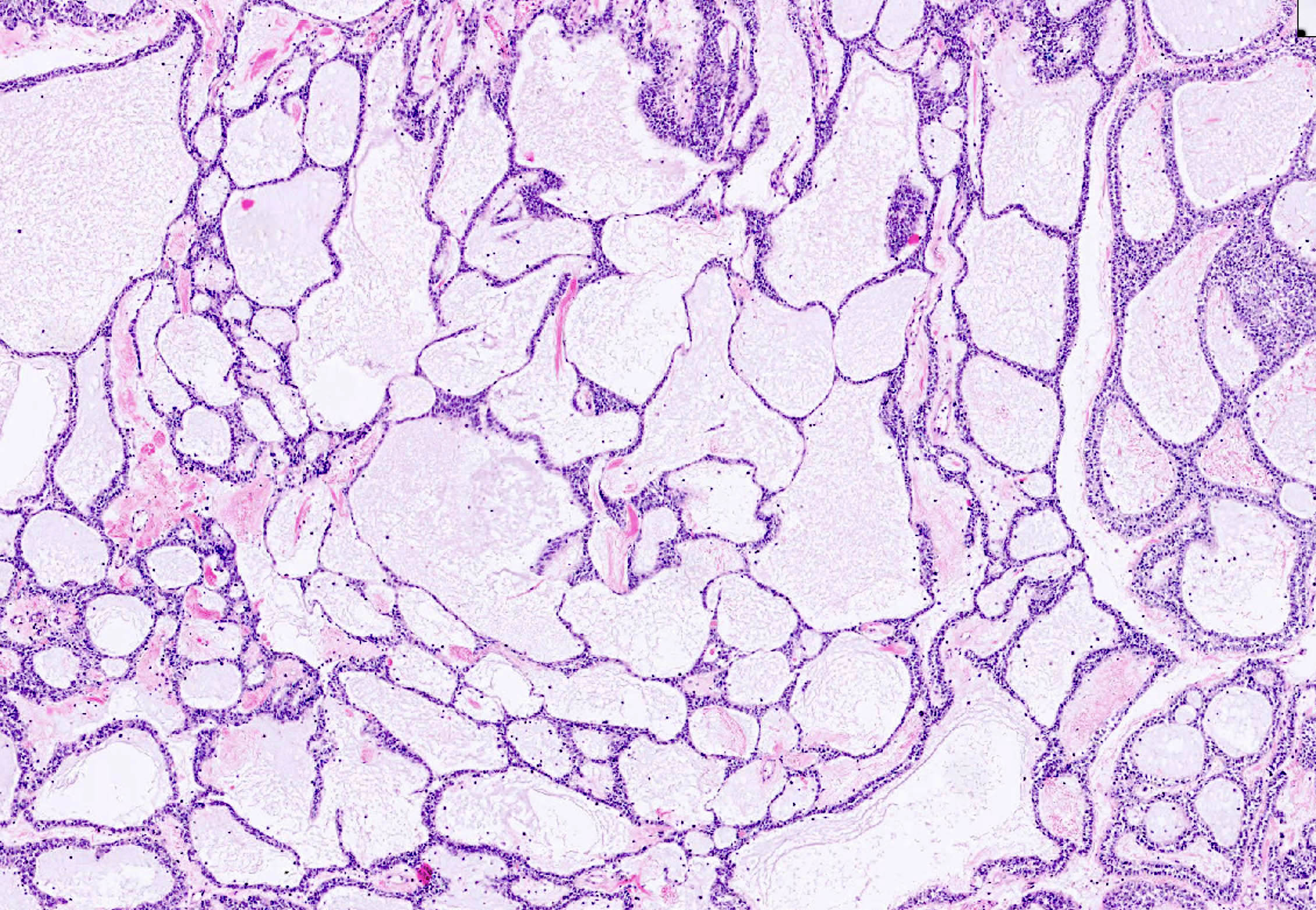
- Follicular salpingitis (misnomer): later stage of chronic salpingitis with fusing plicae, mimicking a pattern of thyroid follicles
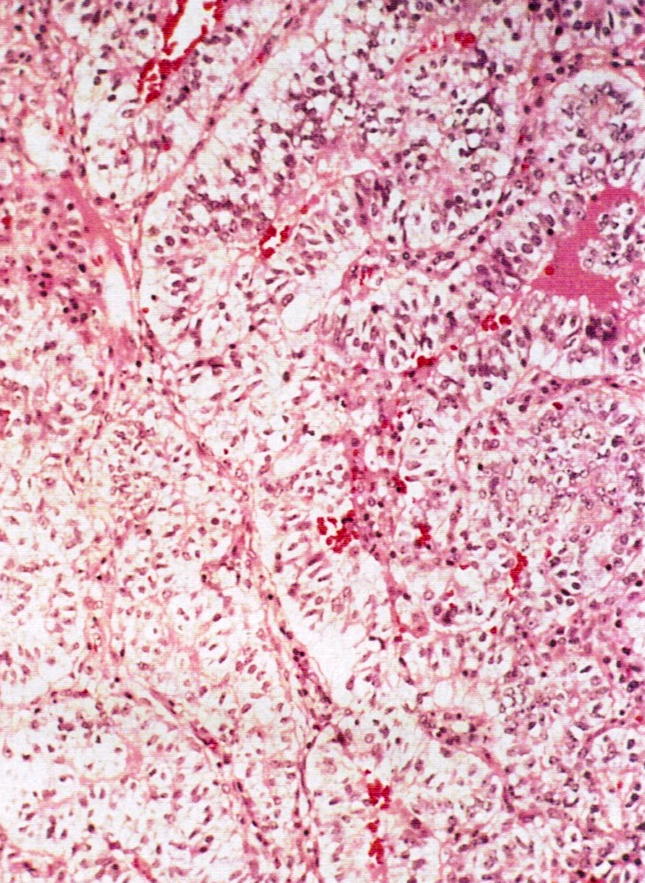
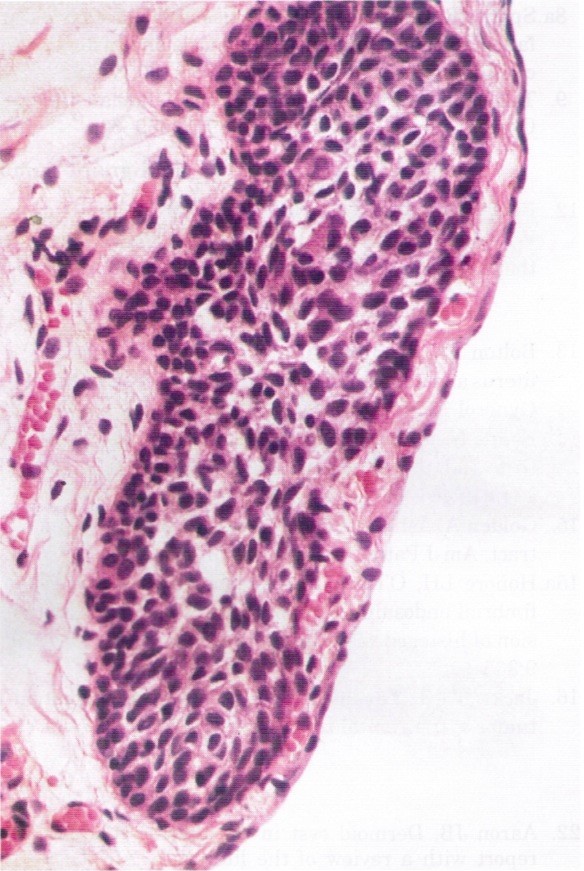
Microscopic (histologic) images
Sample pathology report
- Fallopian tube, salpingectomy:
- Chronic salpingitis, xanthogranulomatous salpingitis or pseudoxanthomatous salpingitis
Differential diagnosis
- Fibrotic plica:
- A normal physiologic change in postmenopausal women
- Inflammatory infiltrate is absent
- Physiologic salpingitis during menses:
- Only minimal neutrophilic infiltrate is seen
- Salpingitis isthmica nodosa:
- Nodular thickening of fallopian tube with cystically dilated glands within muscular layer
- No associated inflammation
- Serous tubal intraepithelial carcinoma (STIC):
- Older women
- Cytologic atypia and loss of ciliation
- Abnormal (mutant) pattern of p53 expression by immunohistochemistry
Board review style question #1
Which of the following is the most common finding associated with pseudoxanthomatous salpingitis?
- Endometriosis
- History of prior pelvic surgery
- Inflammatory bowel disease and diverticulosis
- Pelvic tuberculosis
Board review style answer #1
A. Endometriosis. Answer B is incorrect because prior pelvic surgery is not associated with pseudoxanthomatous salpingitis. Answer C is incorrect because inflammatory bowel disease and diverticulosis can be seen in association with pulse granuloma and chronic salpingitis. Answer D is incorrect because pelvic tuberculosis is associated with granulomatous salpingitis.
Comment Here
Reference: Chronic salpingitis
Comment Here
Reference: Chronic salpingitis
Board review style question #2
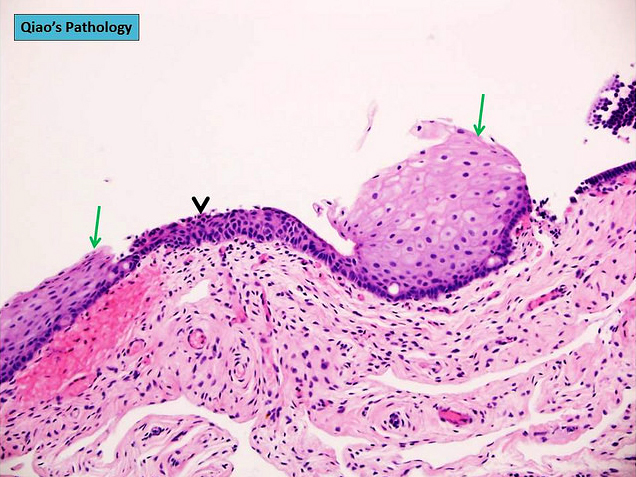
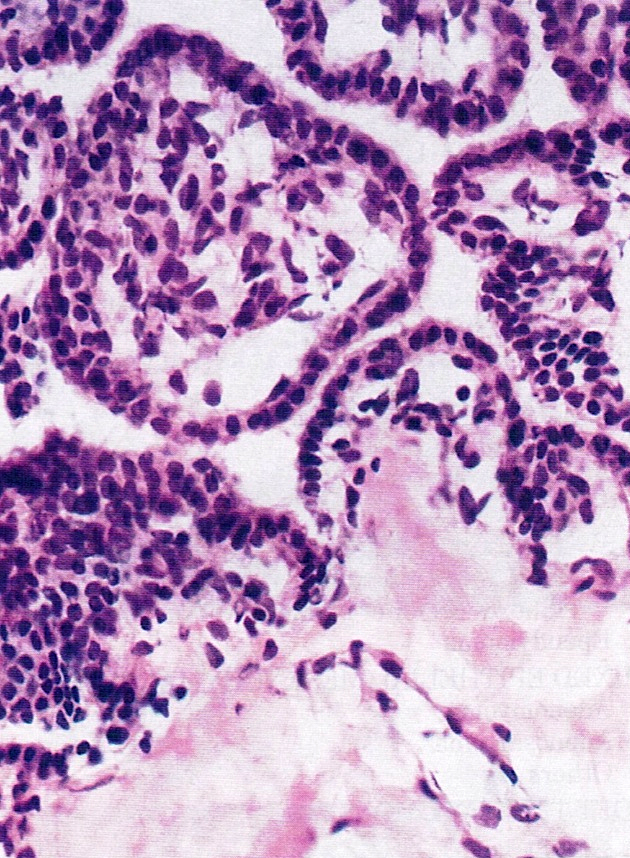
Which of the following statements is true regarding the photomicrograph above?
- Associated hydrosalpinx is uncommon
- Rarely seen in ectopic tubal pregnancy
- The most common inflammatory infiltrates are neutrophils and eosinophils
- When associated with endometriosis, it has distinct gross and microscopic findings
Board review style answer #2
D. When associated with endometriosis, it has distinct gross and microscopic findings. Answer A is incorrect because hydrosalpinx is common.
Answer B is incorrect because this can be seen in half of ectopic tubal pregnancy. Answer C is incorrect because plasma cells and lymphocytes are usually present in the submucosa.
Comment Here
Reference: Chronic salpingitis
Comment Here
Reference: Chronic salpingitis
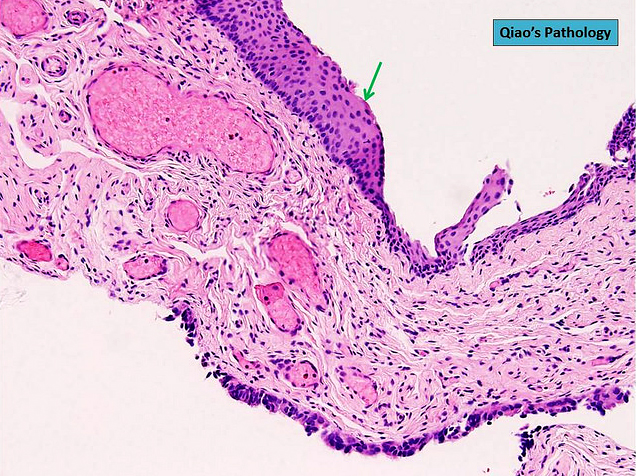
Developmental cysts
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Definition / general
- Benign developmental cysts arising from remnants of Müllerian and Wolffian ducts as well as from mesothelium
Essential features
- Benign, fluid filled cysts located adjacent to the adnexa (fallopian tube or ovary)
- Cysts are lined by non-stratified epithelium, which can be ciliated (paramesonephric cyst) or flat, cuboidal (mesothelial and mesonephric cysts)
- Usually are incidental findings
Terminology
- Paratubal cysts, paraovarian cysts, mesothelial (or simple) cyst
- Hydatid cyst of Morgagni (no longer recommended): typically refers to pedunculated cyst located near tubal fimbria (Arch Gynecol Obstet 2012;285:1563)
ICD coding
Epidemiology
- ~10% of all adnexal masses (Arch Gynecol Obstet 2012;285:1563)
- Vast majority are Müllerian (paramesonephric) cysts, commonly known as paratubal cysts
- < 2% are Wolffian (mesonephric) cysts (Am J Obstet Gynecol 1977;129:873)
Sites
- Adjacent to the adnexa, along broad ligament, between the fallopian tube and the ovary
Pathophysiology
- Müllerian (paramesonephric) and Wolffian (mesonephric) ducts grow mostly in parallel during development
- Müllerian ducts eventually fuse
- Fusion of Müllerian ducts creates a transverse fold, which becomes the broad ligament
- Broad ligament contains Müllerian and Wolffian duct remnants, which can then become cystic
- Reference: Kurman: Blaustein's Pathology of the Female Genital Tract, 7th Edition, 2019
Etiology
- Thought to originate from remnants of Müllerian and Wolffian ducts as well as from mesothelium (Am J Obstet Gynecol 1977;129:873, Gynecol Obstet Invest 1981;12:1)
Clinical features
- Usually asymptomatic and incidentally found
- Large cysts can be painful, bleed, rupture or cause ovarian torsion (Arch Gynecol Obstet 2012;285:1563)
Diagnosis
- Incidental finding
- If symptomatic, usually diagnosed by ultrasound
Radiology description
- Ultrasound findings: majority are unilocular cysts without papillations (Ultrasound Obstet Gynecol 2006;28:330)
- Presence of papillary projections / solid nodule typically indicates neoplastic cysts
Prognostic factors
- Benign
- May rarely give rise to serous borderline tumor and carcinoma (Gynecol Oncol Rep 2020;32:100559, Appl Immunohistochem Mol Morphol 2017;25:e21)
Case reports
- 13 year old girl with bilateral paraovarian cysts (Sultan Qaboos Univ Med J 2021;21:e308)
- 31 year old woman with giant paratubal cyst presented with adnexal torsion (Case Rep Womens Health 2020;27:e00222)
- 85 year old woman with serous borderline tumor arising from a paratubal cyst (Gynecol Oncol Rep 2020;32:100559)
Treatment
- Surgical excision if large or symptomatic
Clinical images
Gross description
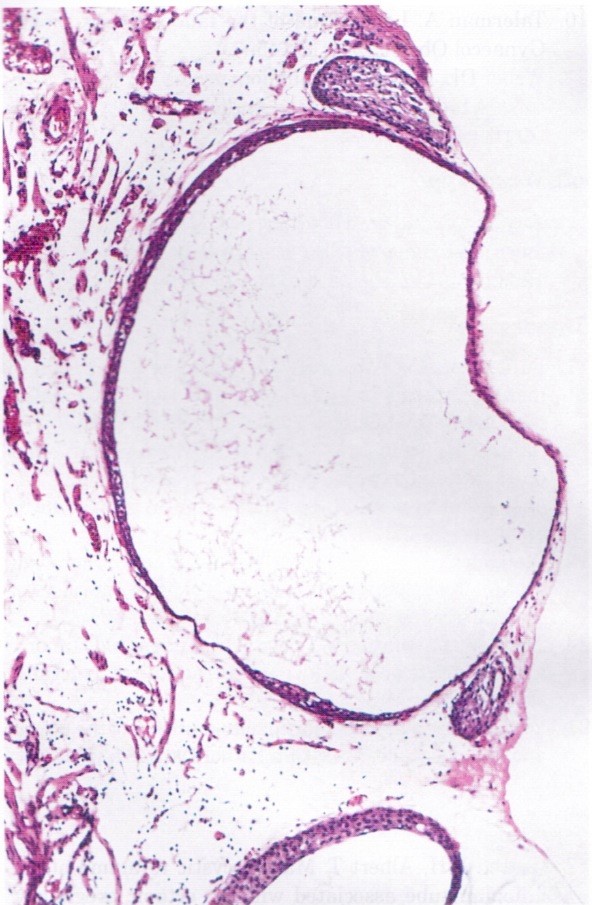
- Thin walled, fluid filled cyst(s) located adjacent to fallopian tube or ovary
Microscopic (histologic) description
- Paramesonephric cysts are lined by single layer of bland ciliated tubal epithelium
- Mesonephric cysts are lined by single layer of low cuboidal, nonciliated epithelium with occasional clear cells (rare) (Am J Obstet Gynecol 1977;129:873)
- Mesothelial cysts are lined by single layer of flat or cuboidal, nonciliated cells, which may show transitional cell metaplasia (see Walthard cell nests)
- Distinction between the types of cyst may be difficult but has no clinical implications
Microscopic (histologic) images
Sample pathology report
- Not essential to include in report, particularly if cysts are small and incidental
- Right fallopian tube, salpingectomy:
- Fallopian tube with paratubal cysts
Differential diagnosis
- Serous cystadenoma:
- Presence of dense collagenized cyst wall
- Absence of rudimentary plicae
- Hydrosalpinx:
- Presence of well developed, smooth muscle wall
- Presence of occasional branching plicae with columnar epithelium containing histologic normal ciliated and secretory cells
- Direct communication with nondilated portion of fallopian tube
Additional references
Board review style question #1
A 45 year old patient underwent total hysterectomy and bilateral salpingo-oophorectomy for a myomatous uterus. The left adnexa showed the finding in the image above. What is the next step in management regarding this finding?
- Computed tomography (CT) of the chest
- Germline testing
- No additional therapy
- Serial serum CA-125 levels
- Surgical staging
Board review style answer #1
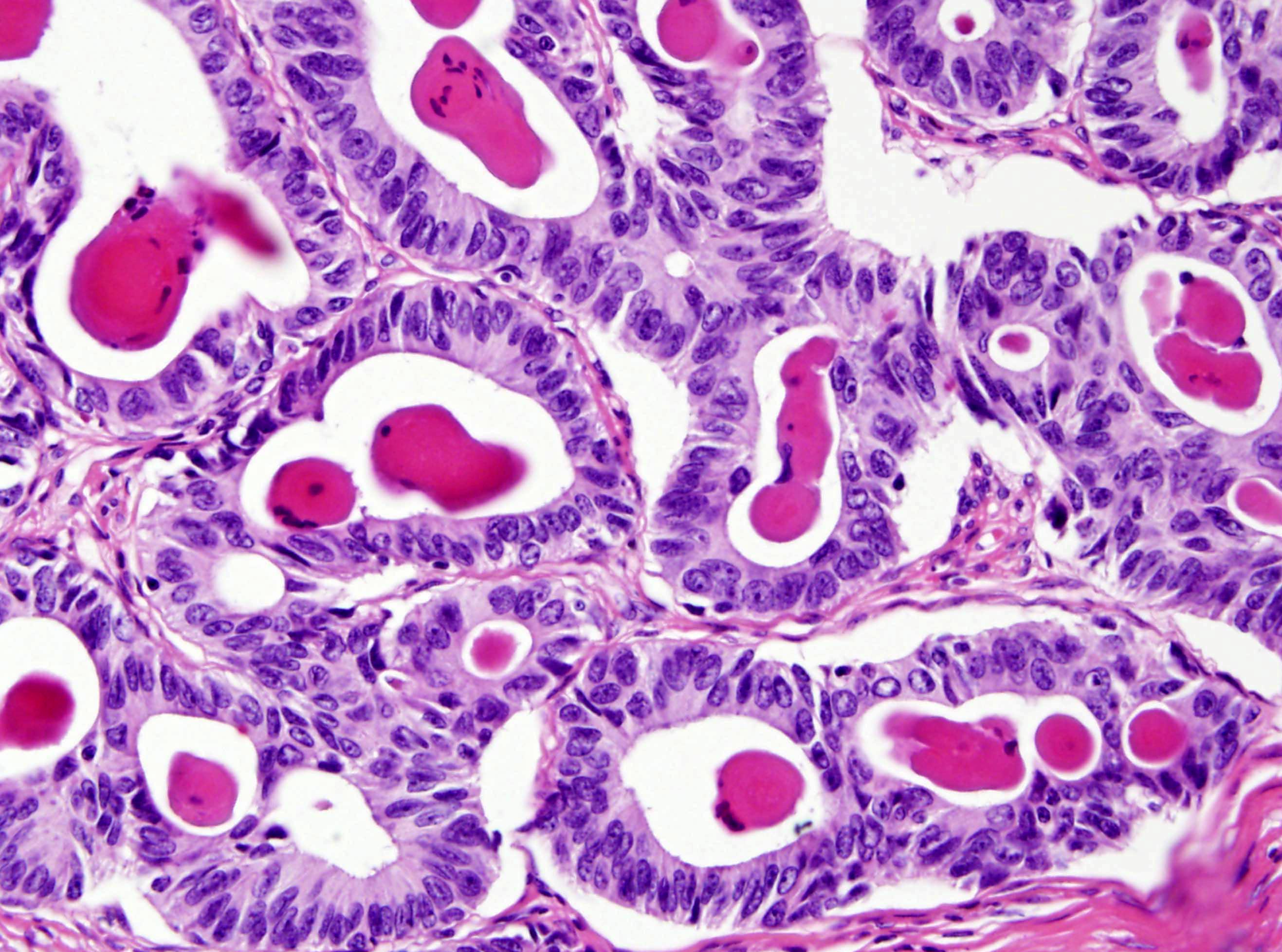
Ectopic / tubal pregnancy
Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Definition / general
- Extrauterine implantation of a fertilized egg
Essential features
- Extrauterine implantation of a fertilized egg
- > 95% occur in the fallopian tube
- Diagnosis based on visualization of an extrauterine gestational sac by transvaginal ultrasound (TVUS) or histologic confirmation
ICD coding
Epidemiology
- Approximately 2% of all reported pregnancies in the United States are ectopic (MMWR Morb Mortal Wkly Rep 1995;44:46, Fertil Steril 2014;102:1671, Obstet Gynecol 2010;115:495)
- 2.7% of pregnancy related mortalities attributed to ruptured ectopic (Obstet Gynecol 2017;130:366)
- Diagnosis increases with age: 0.29% (15 - 19 years old), ~0.5% (20 - 24 years old), ~0.58% (25 - 29 years old), ~0.7% (30 - 34 years old) and ~0.89% (35 - 44 years old) (South Med J 2017;110:18)
Sites
- Fallopian tube accounts for 95.5% of extrauterine implantation sites: 2.4% interstitial, 11.1% fimbrial, 12.0% isthmic and 70% ampullary (Hum Reprod 2002;17:3224)
- 4.5% are extratubal: 3.2% ovarian and 1.3% abdominal (Hum Reprod 2002;17:3224)
- May implant at any place on the abdominal viscera or peritoneal surface (Radiographics 2015;35:946):
- Cervix (J Emerg Med 2019;56:e123)
- Liver (Pathology 2018;50:478)
- Spleen (BMJ Case Rep 2016;2016:bcr2016218291)
- Prior cesarean scars (Clin Imaging 2020;66:26)
Pathophysiology
- 4 possible mechanisms of ectopic implantation (Sex Transm Infect 2020;96:322):
- Anatomic obstruction preventing passage of the zygote
- Abnormal conceptus
- Tubal motility abnormalities
- Zygote transperitoneal migration
Etiology
- Pelvic inflammatory disease
- Disruption of tubal anatomy caused by infection is the most likely cause; inflammation of the tube is present in up to 90% of tubal pregnancies, which is 6x more common than in normal tubes
- Cigarette smoking
- Prior fallopian tube pathology
- Infertility
- Intrauterine device
- Previous fallopian tube surgery
- Previous ectopic pregnancy
- Approximately half of ectopic pregnancy patients do not have any identifiable risk factors
- References: Clin Obstet Gynecol 2012;55:376, Fertil Steril 1996;65:1093, Obstet Gynecol 2018;131:e91
Clinical features
- Most common clinical presentationis first trimester vaginal bleeding or abdominal pain
- Symptoms usually appear 6 - 8 weeks after the patient’s last menstrual period but may occur even later, particularly if the pregnancy occurs outside of the fallopian tube
- No confirmed intrauterine pregnancy
Diagnosis
- Positive pregnancy test and visualization of an extrauterine gestational sac, with or without an embryo on transvaginal ultrasound
- Visualization at surgery with histologic confirmation
Laboratory
- Positive beta hCG
Radiology description
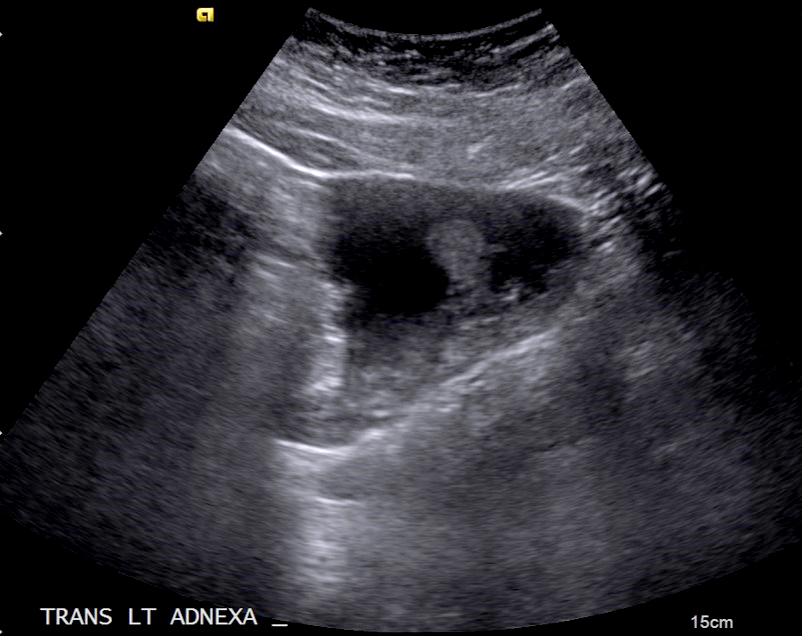
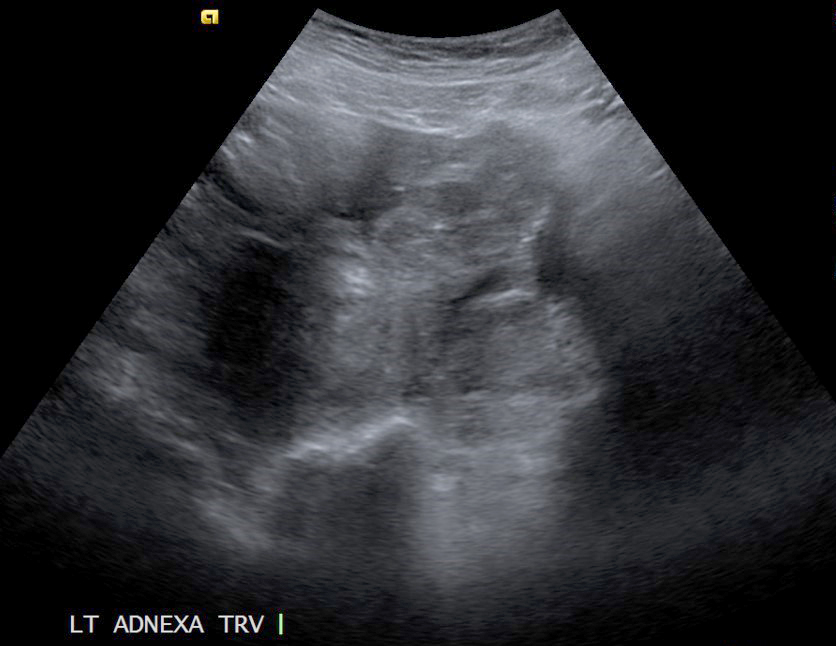
- Extrauterine gestational sac, with or without an embryo on transvaginal ultrasound
Prognostic factors
- Significant risk of morbidity and mortality if not promptly recognized and treated
- Patients with earlier ectopic pregnancies and relatively modest beta hCG levels are more likely to have successful treatment with single dose methotrexate therapy (Clin Obstet Gynecol 2012;55:376)
- Following methotrexate therapy, patients not exhibiting at least a 15% decrease in beta hCG from day 4 - 7 are more likely to experience treatment failure (Reprod Biomed Online 2017;34:383)
Case reports
- 29 year old woman with vaginal bleeding and discharge (Radiol Case Rep 2019;14:354)
- 30 year old woman with abdominal ectopic pregnancy after in vitro fertilization and single embryo transfer (Reprod Biol Endocrinol 2016;14:69)
- 38 year old woman with acute onset of lower abdominal pain associated with a history of amenorrhea (Cureus 2020;12:e10993)
Treatment
- Surgical management (typically salpingectomy or salpingotomy) for hemodynamically unstable patients
- Methotrexate may be administrated for hemodynamically stable patients (Clin Obstet Gynecol 2012;55:376)
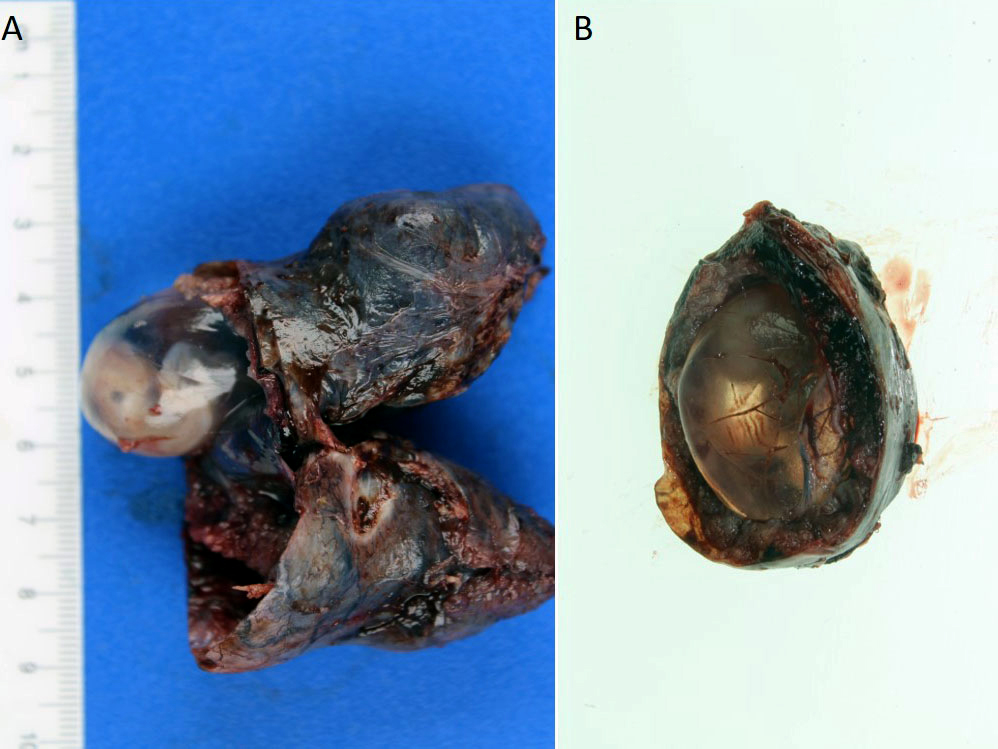
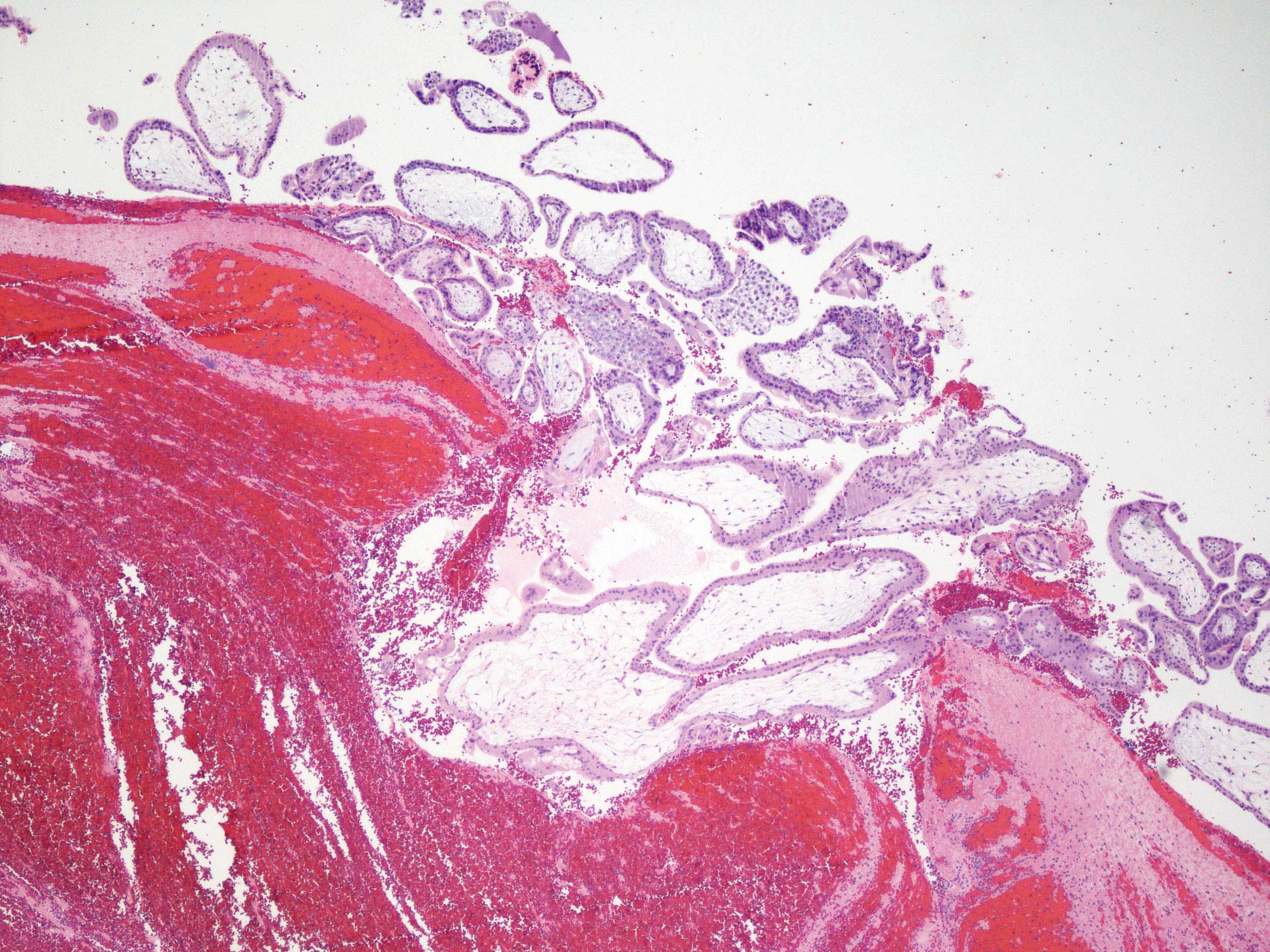
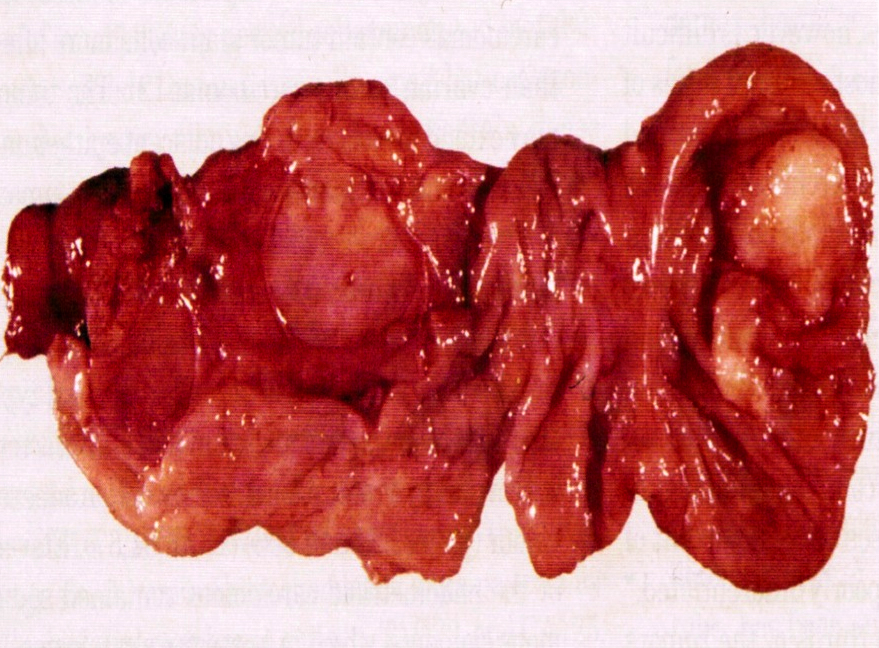
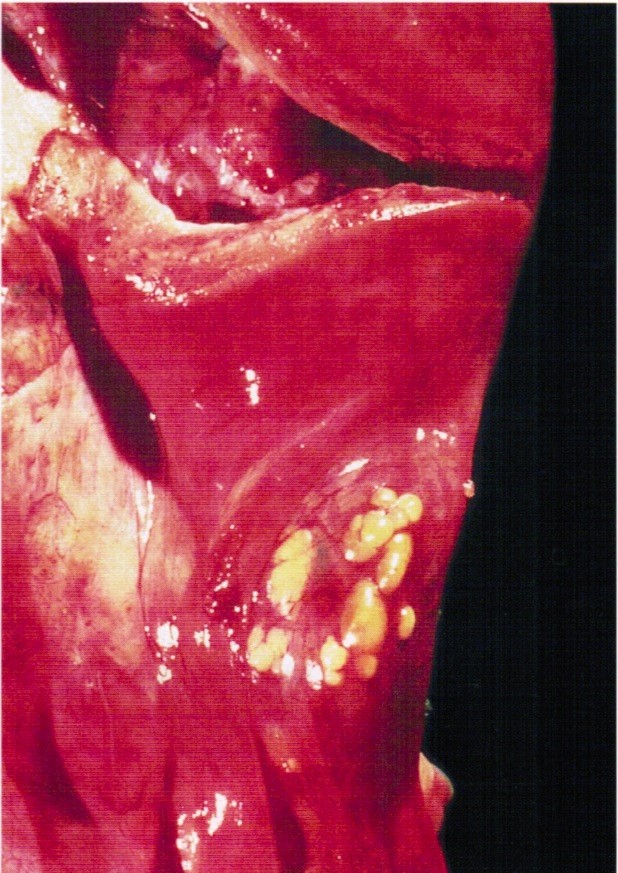
Gross description
- Dilated tube with distended wall, with or without rupture
- Lumen contains blood clot, embryo, chorionic villi
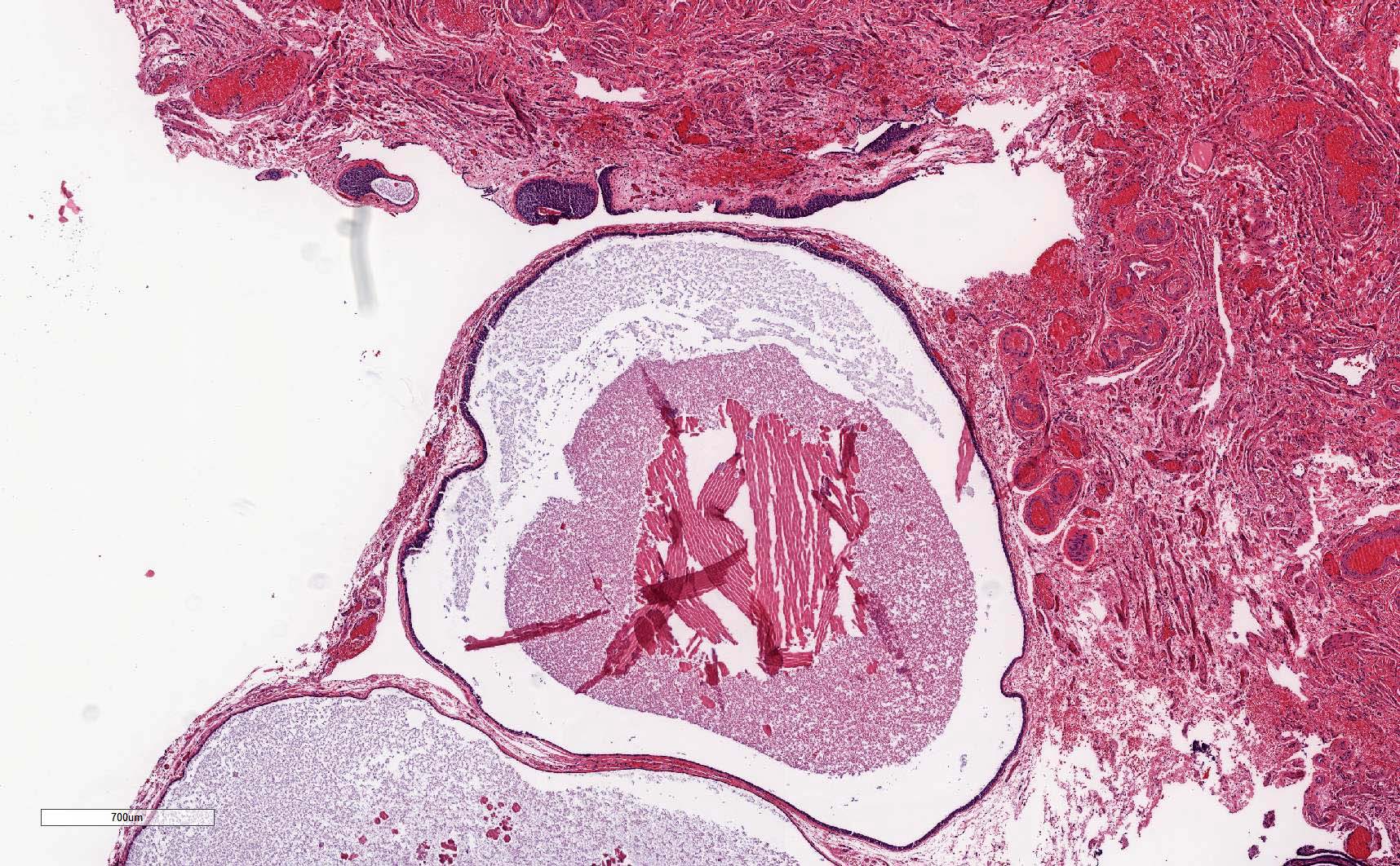
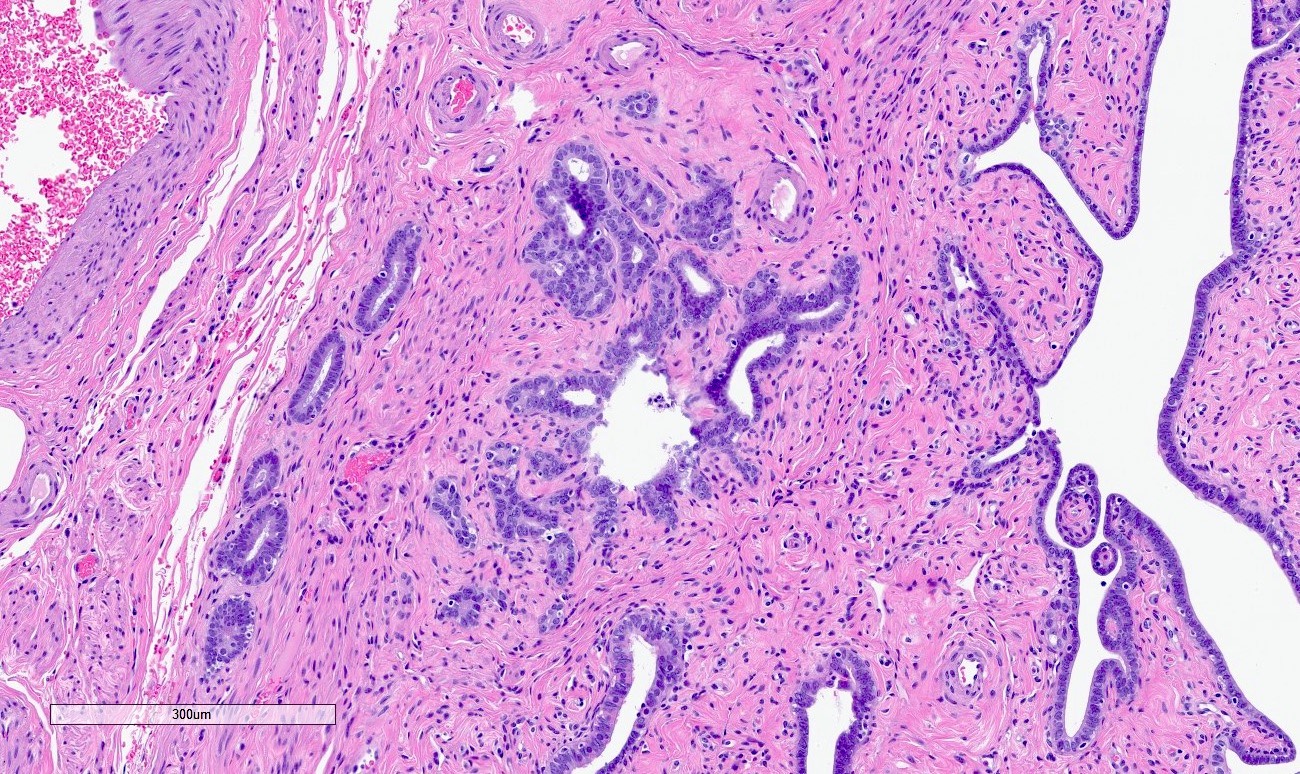
Microscopic (histologic) description
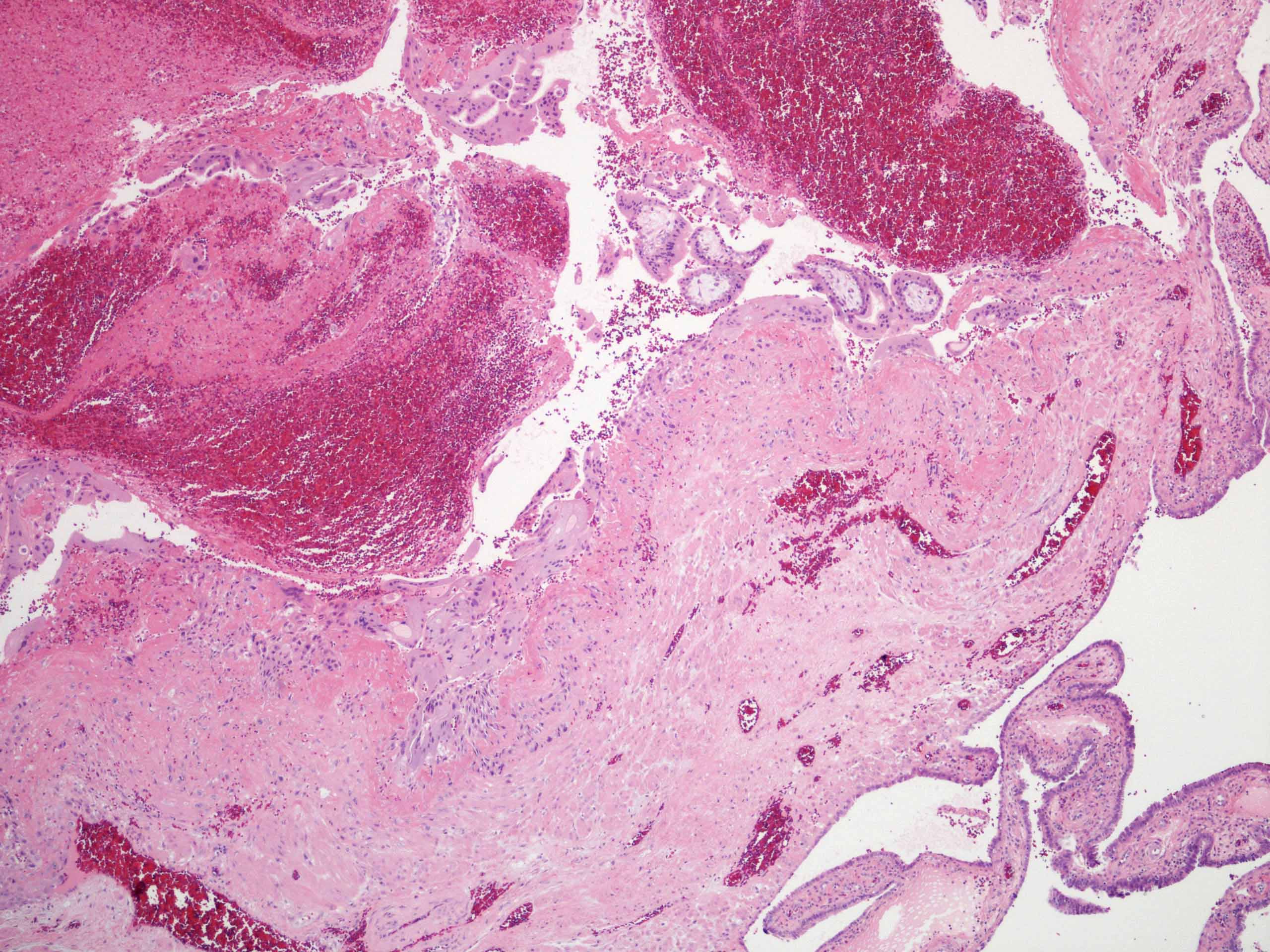
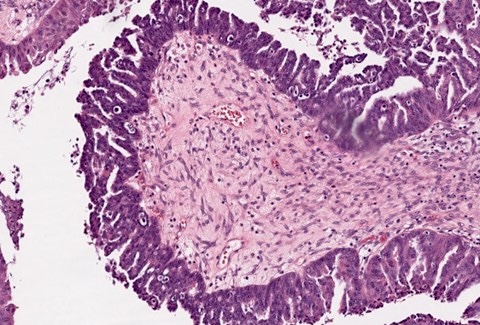
- Presence of extrauterine chorionic villi or extravillous trophoblast is needed for diagnosis
- Fetal tissue may be present
- Endometrial stromal decidualization in isolation is not diagnostic of ectopic pregnancy
- Mesothelial reactive changes, often reactive mesothelial proliferation, may be present (on the surface of the fallopian tube or the closest peritoneum to the site of the ectopic pregnancy); of note, the exaggerated cytological changes and mesothelial proliferation should not be confused with atypical mesothelial proliferation
Microscopic (histologic) images
Sample pathology report
- Fallopian tube, salpingectomy:
- Fallopian tube with intraluminal immature chorionic villi, consistent with ectopic (tubal) pregnancy
Differential diagnosis
- Spontaneous abortion:
- Identification of product of conceptions in expelled uterine tissue or endometrial curettage tissue
- Lack of evidence of extrauterine gestational sac / embryo by either transvaginal ultrasound or histological confirmation
Board review style question #1
The most common site of ectopic tubal pregnancy is
- Ampulla
- Fimbria
- Interstitial
- Isthmic
Board review style answer #1
A. Ampulla. 70% of tubal pregnancies are ampullary, followed by isthmic (12.0%), fimbrial (11%) and interstitial (2.4%).
Comment Here
Reference: Ectopic / tubal pregnancy
Comment Here
Reference: Ectopic / tubal pregnancy
Board review style question #2
The most common cause of ectopic pregnancy is
- Idiopathic
- Infertility
- Intrauterine device
- Pelvic inflammatory disease
Board review style answer #2
A. Idiopathic. Approximately half of ectopic pregnancy patients do not have any identifiable risk factors.
Comment Here
Reference: Ectopic / tubal pregnancy
Comment Here
Reference: Ectopic / tubal pregnancy
Board review style question #3
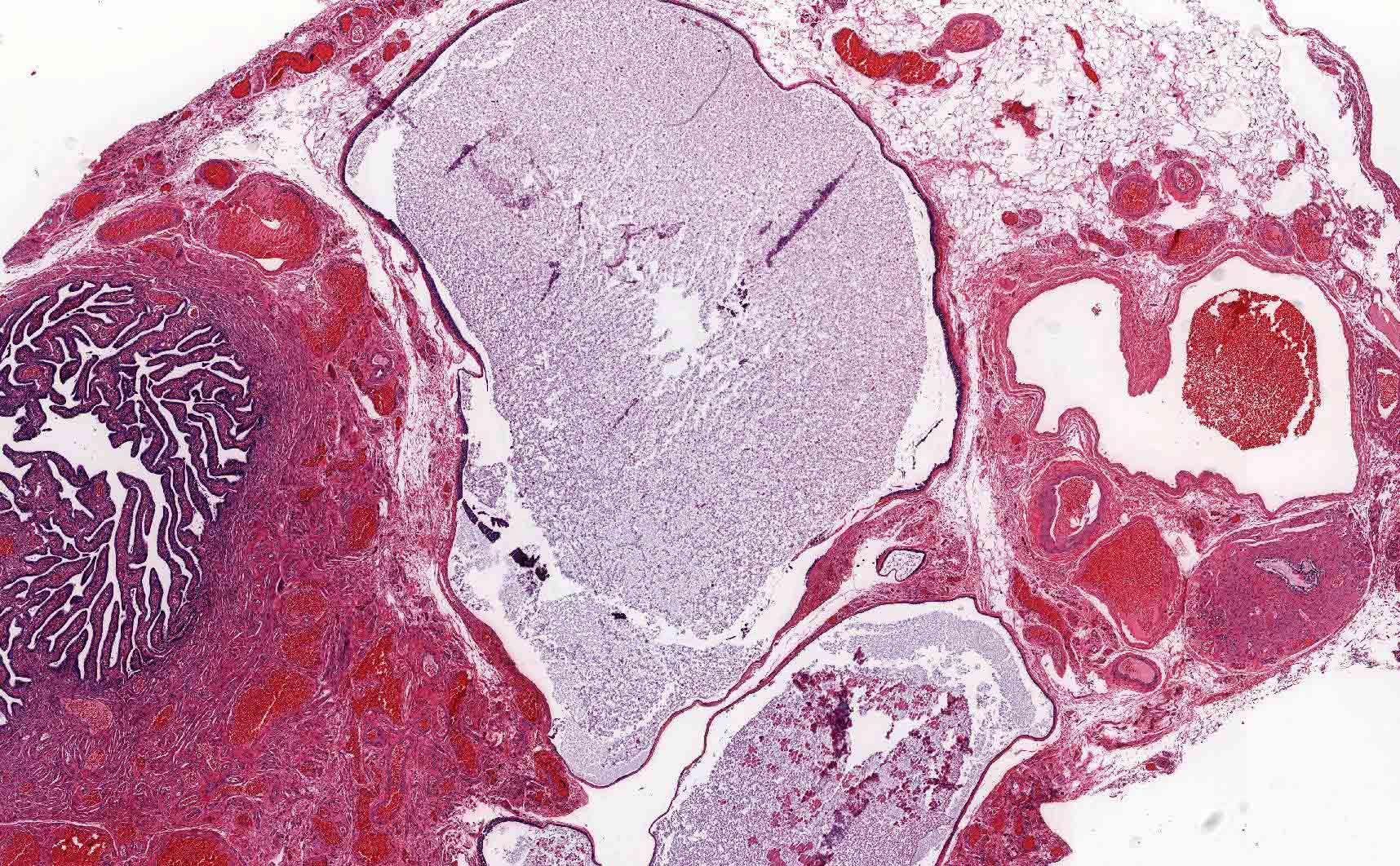
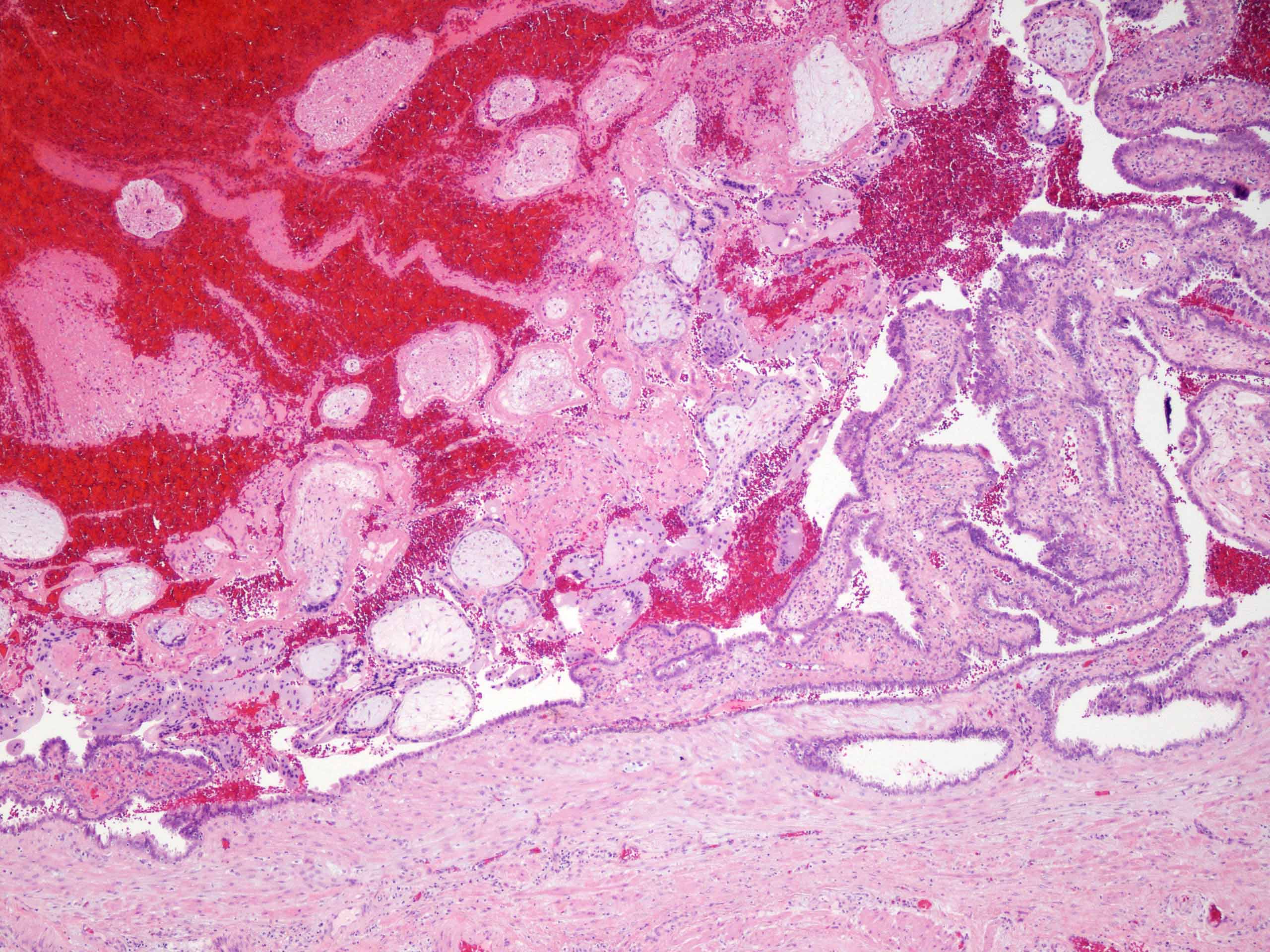
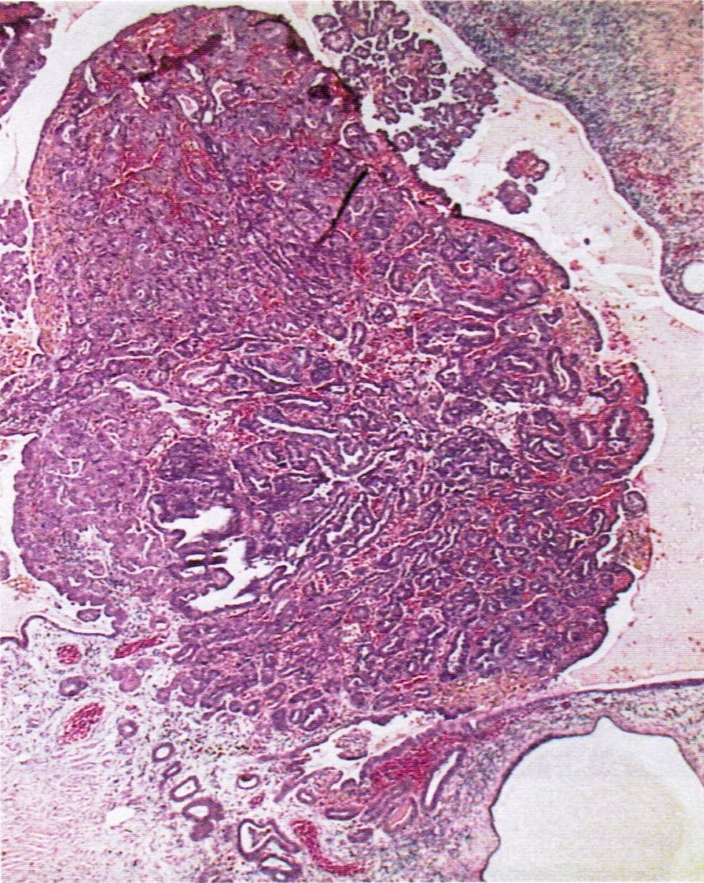
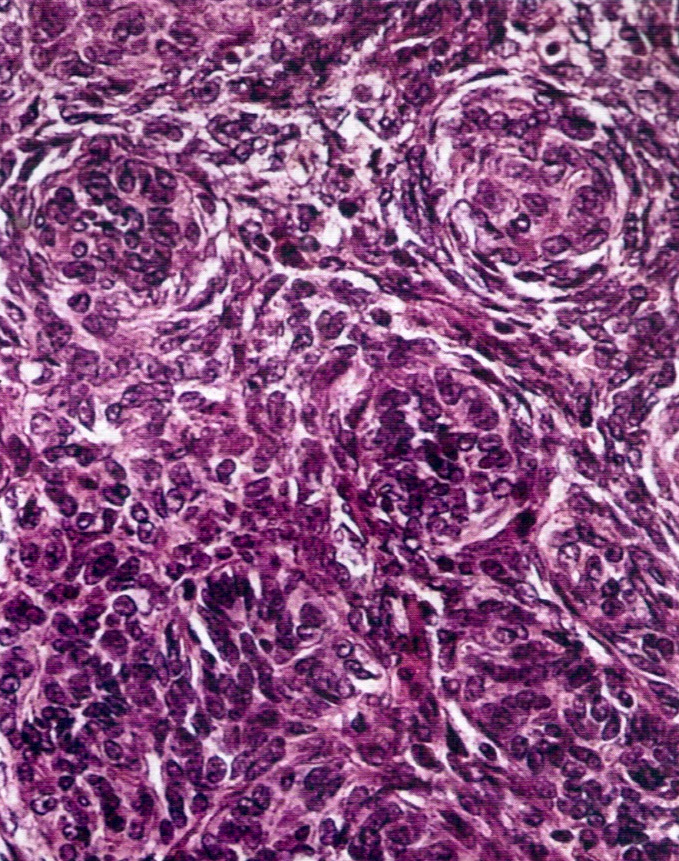
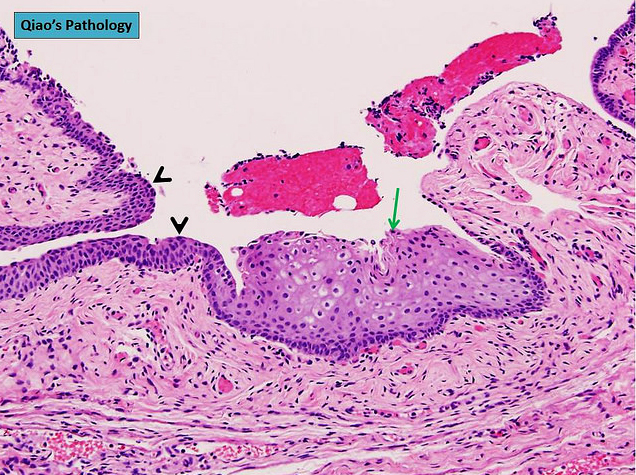
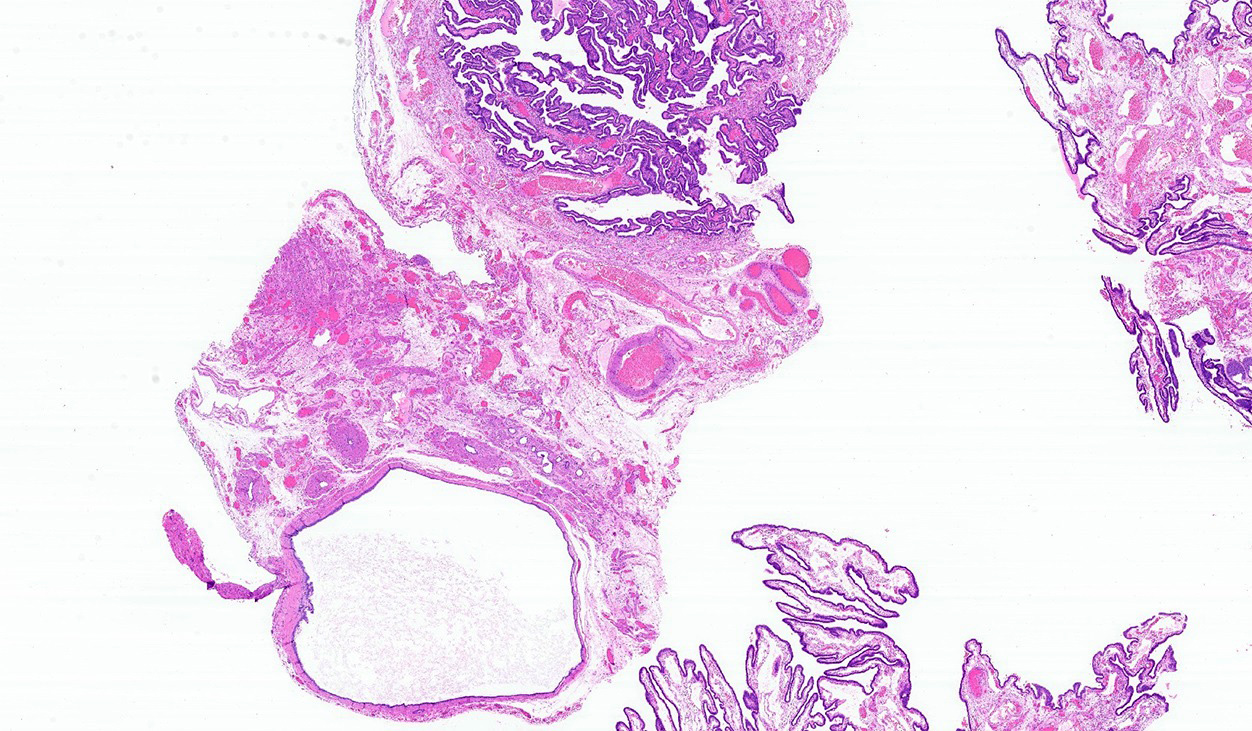
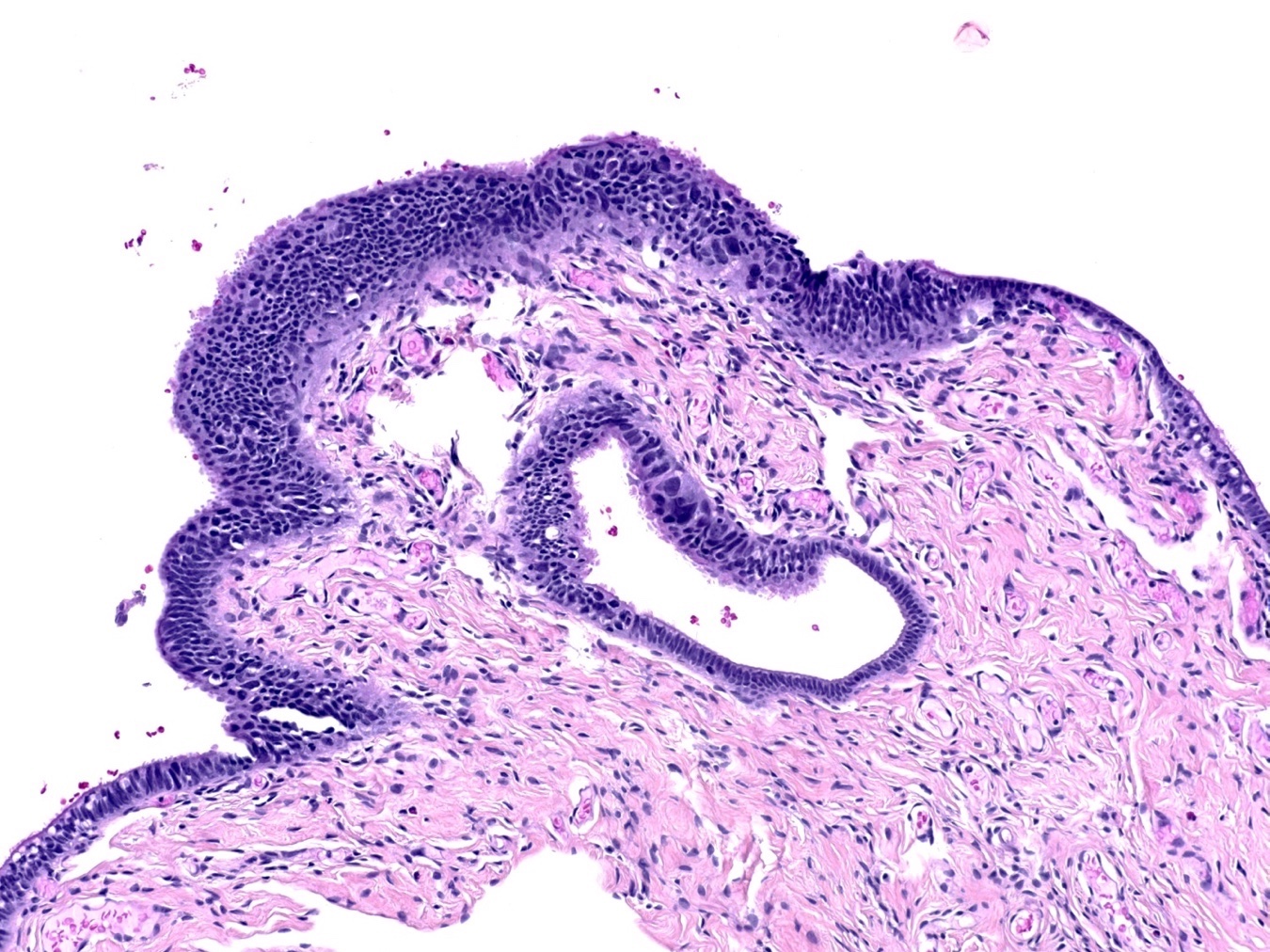
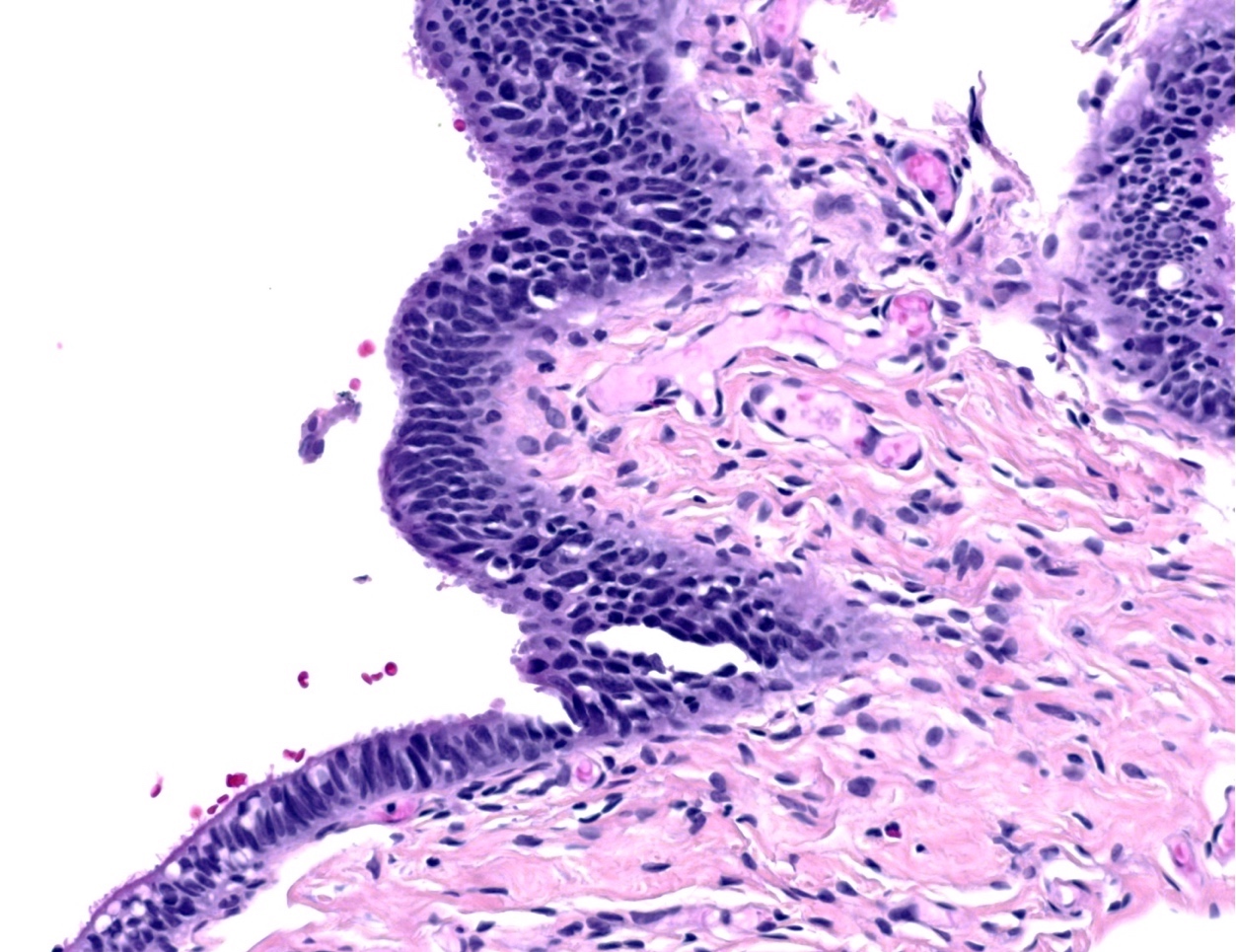
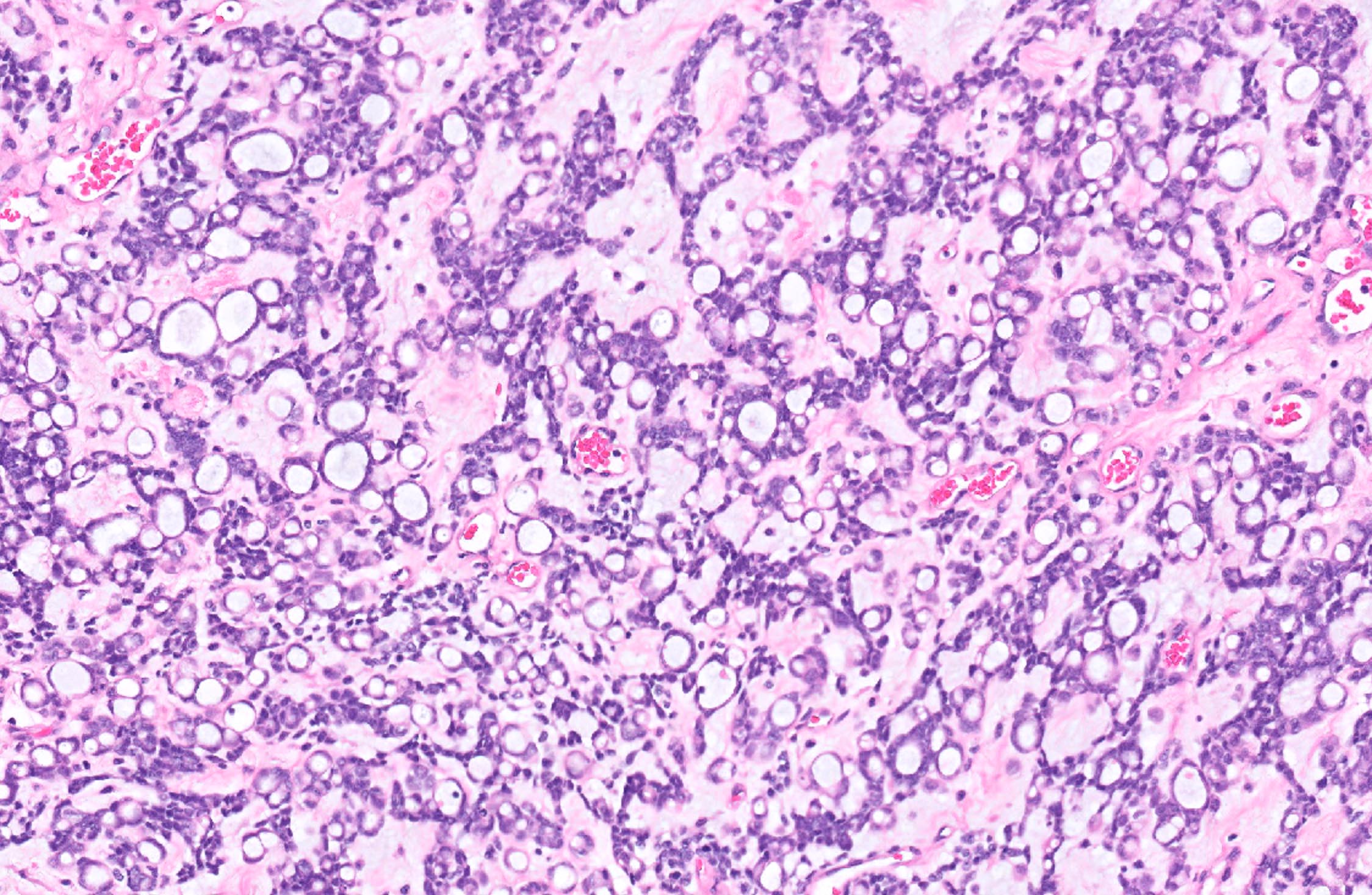
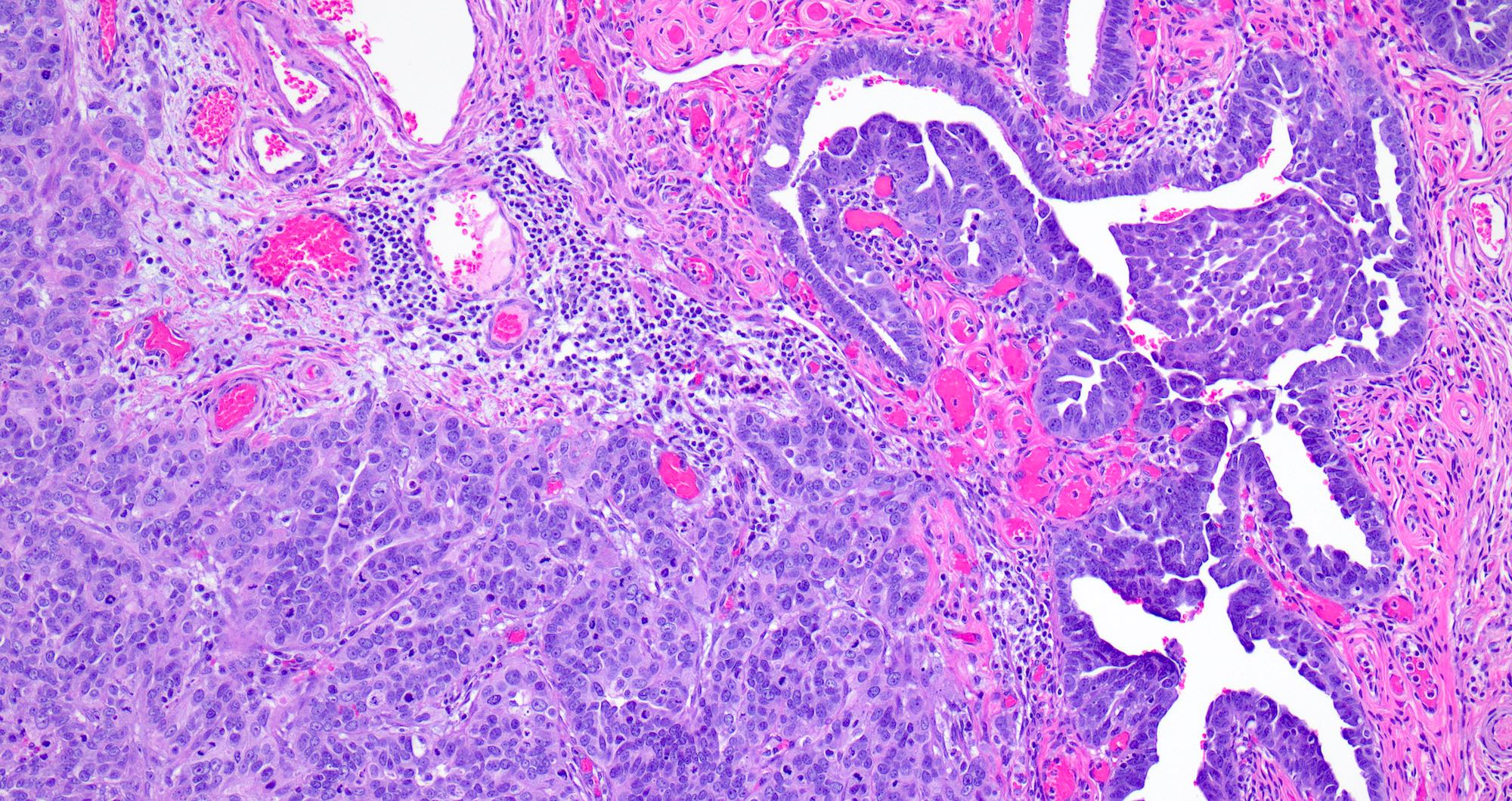
A 28 year old woman presented with acute onset abdominal pain and vaginal bleeding. Pregnancy test was positive. Transvaginal ultrasound showed left adnexal mass. Left salpingectomy was performed. The histological findings were as showed in the above image. The diagnosis is
- Chronic salpingitis
- Ectopic tubal pregnancy
- Tubo-ovarian abscess
- Tubo-ovarian torsion
Board review style answer #3
B. Ectopic tubal pregnancy. Intraluminal chorionic villi, implantation site (upper left). Of note, tubal epithelia is located at lower right corner.
Comment Here
Reference: Ectopic / tubal pregnancy
Comment Here
Reference: Ectopic / tubal pregnancy
Endometrioid adenocarcinoma
Table of Contents
Definition / general | Clinical features | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) imagesDefinition / general
- Rare, 0.3 to 1.0% of genital tract malignancies
- Mean age 57 years, rarely teenagers; usually incorrect preoperative diagnosis
- High stage with pelvic extension or positive peritoneal cytology
- To call primary in fallopian tube, should arise from mucosa (endosalpinx), have tubal histologic pattern, involve the lumen, uterus and ovaries must be normal or have foci of malignancy that resemble metastases or independent primaries; if tubal wall is involved, should detect a transition between benign and malignant tubal epithelium
Clinical features
- 5 year survival: stage 1 - 77%, stage 3 - 20%; usually recur intra-abdominally
- Associated with BRCA1 and BRCA2 mutations; for patients with known mutation or family history of breast or ovarian cancer, should submit entire fallopian tube and ovary for microscopic examination (Am J Surg Pathol 2002;26:171, Am J Surg Pathol 2001;25:1283)
- Carcinomas at this site: 50% serous, 25% endometrioid, 20% transitional or undifferentiated
- Symptoms: vaginal bleeding or discharge (2/3), pain, adnexal mass (triad in 50%); endometrial smear positive in 10%
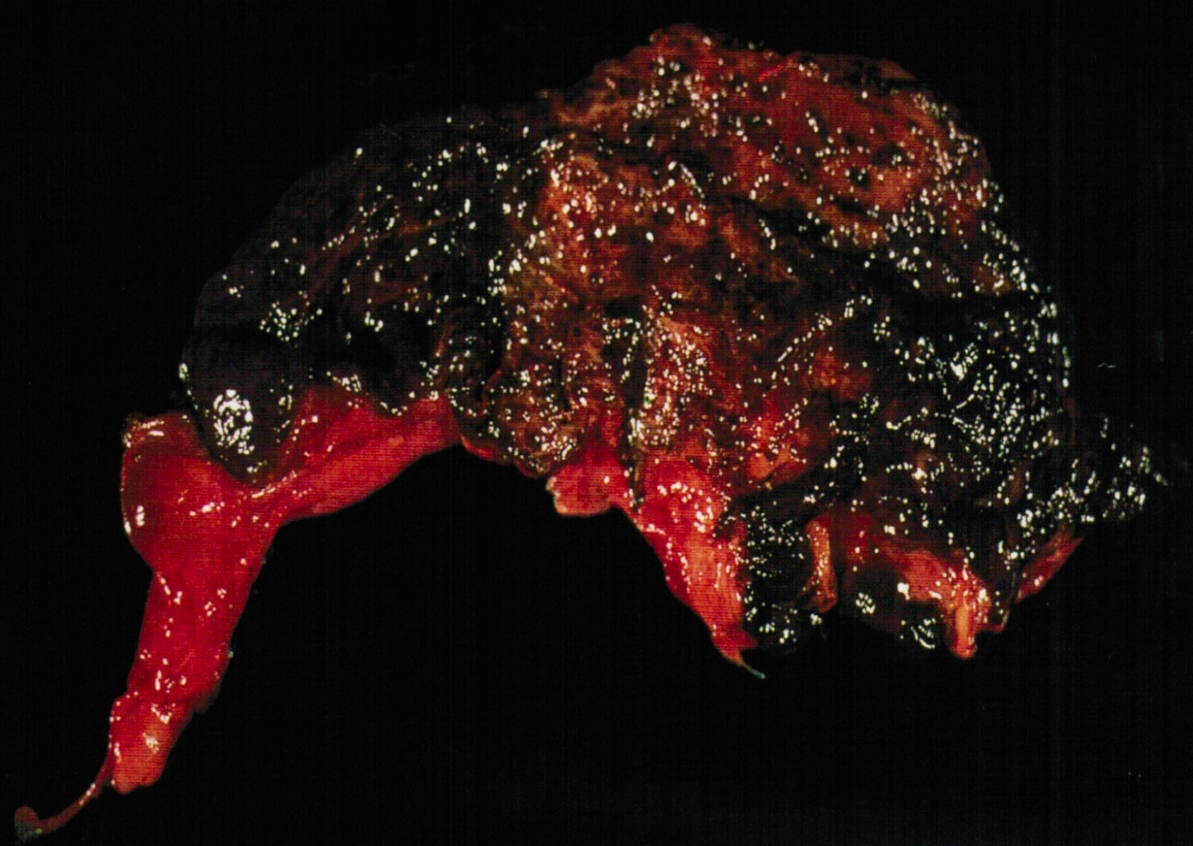
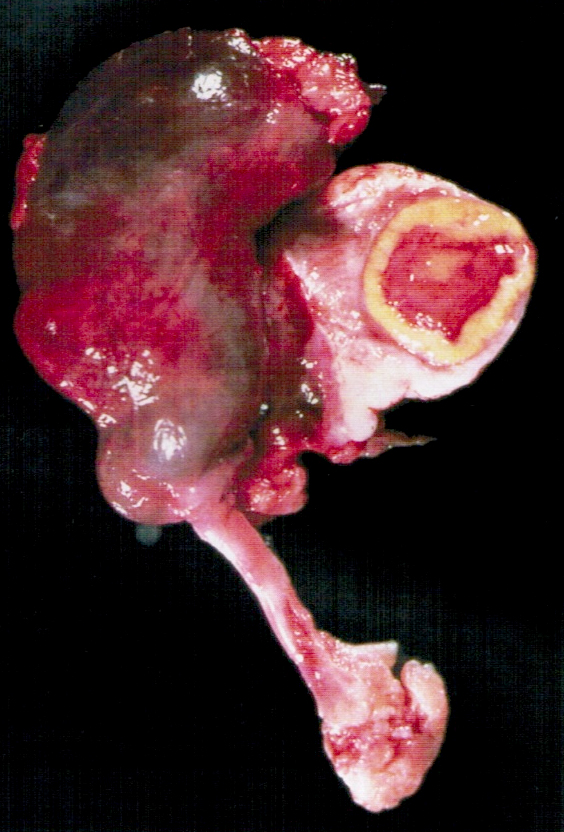
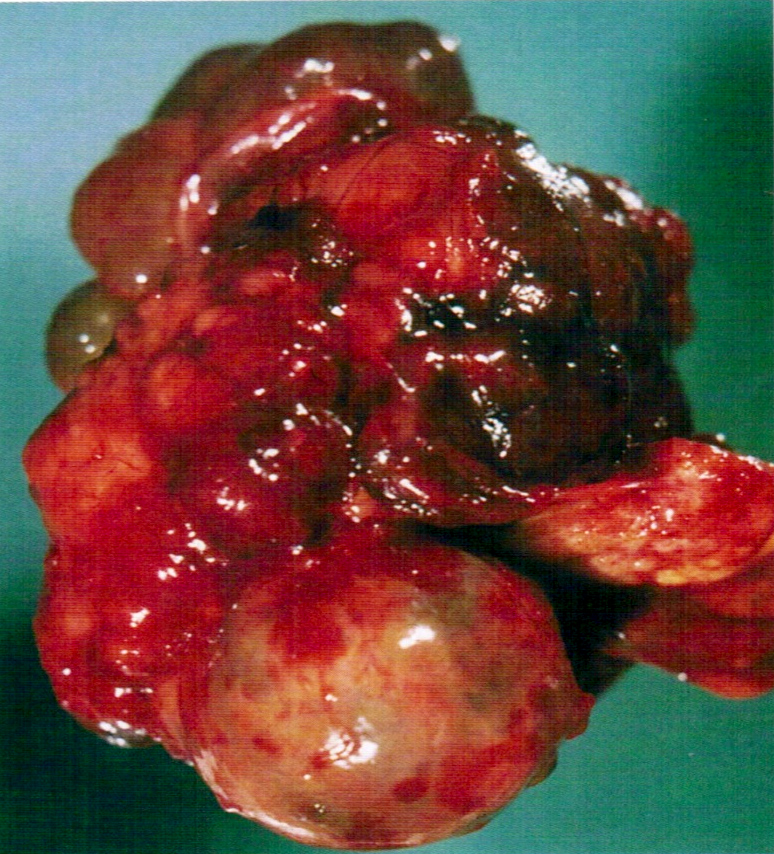
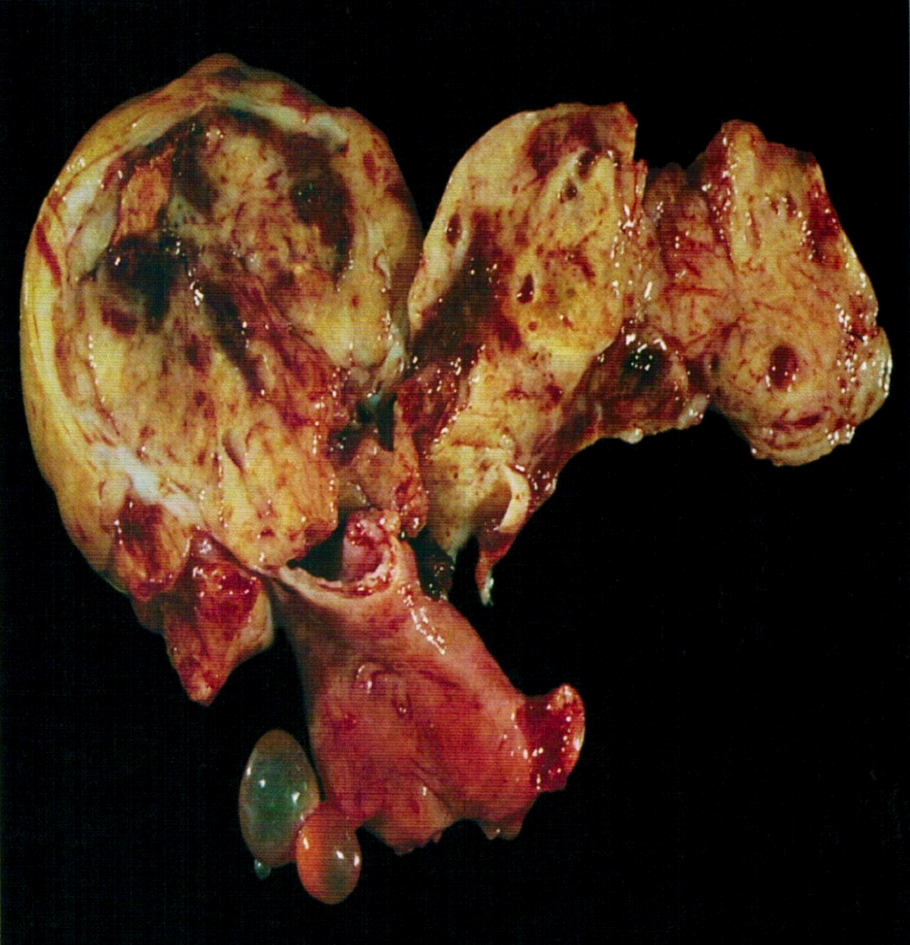
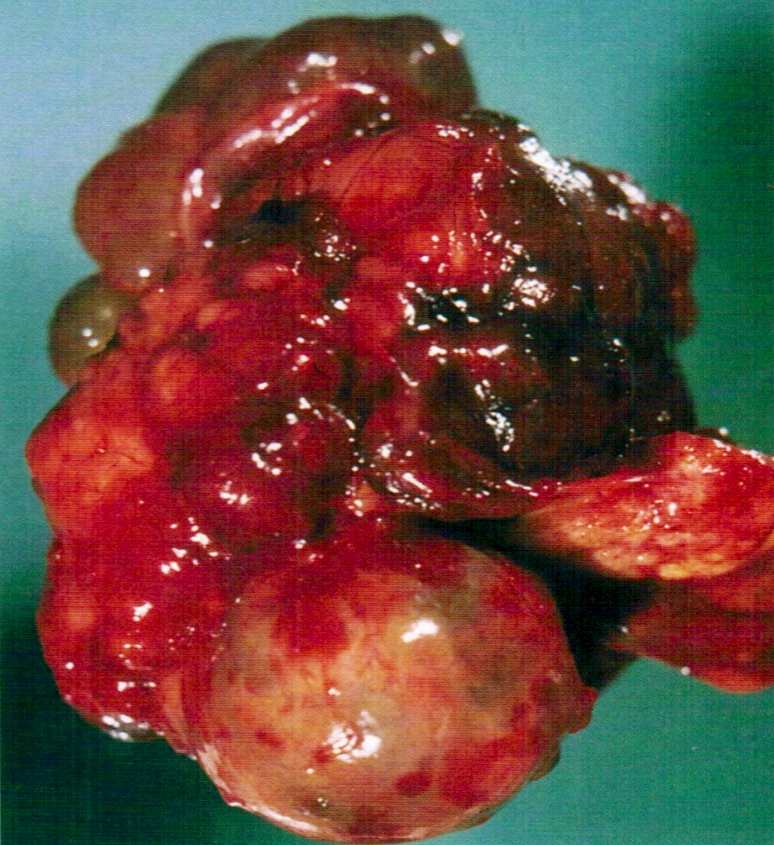
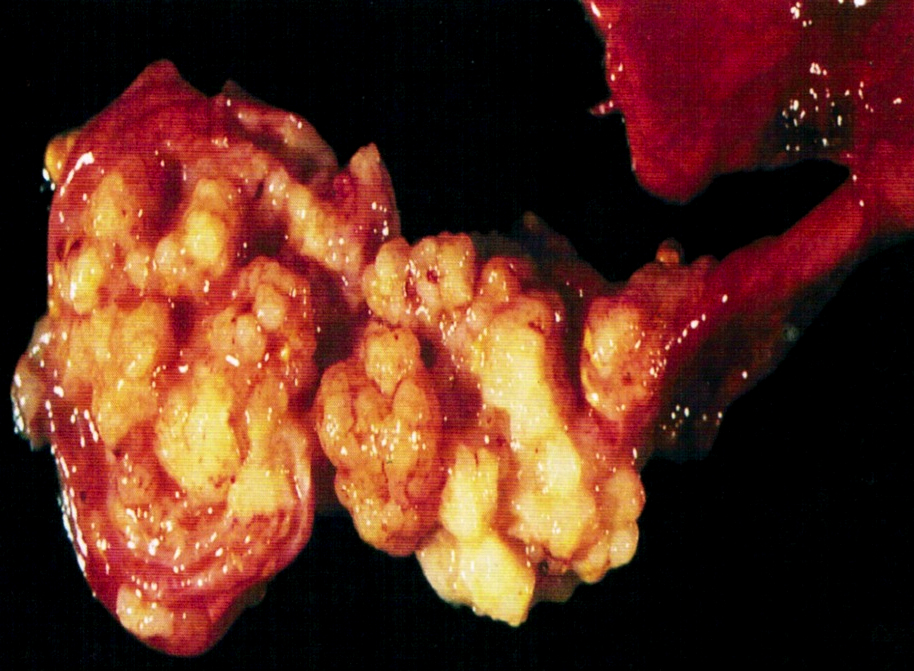
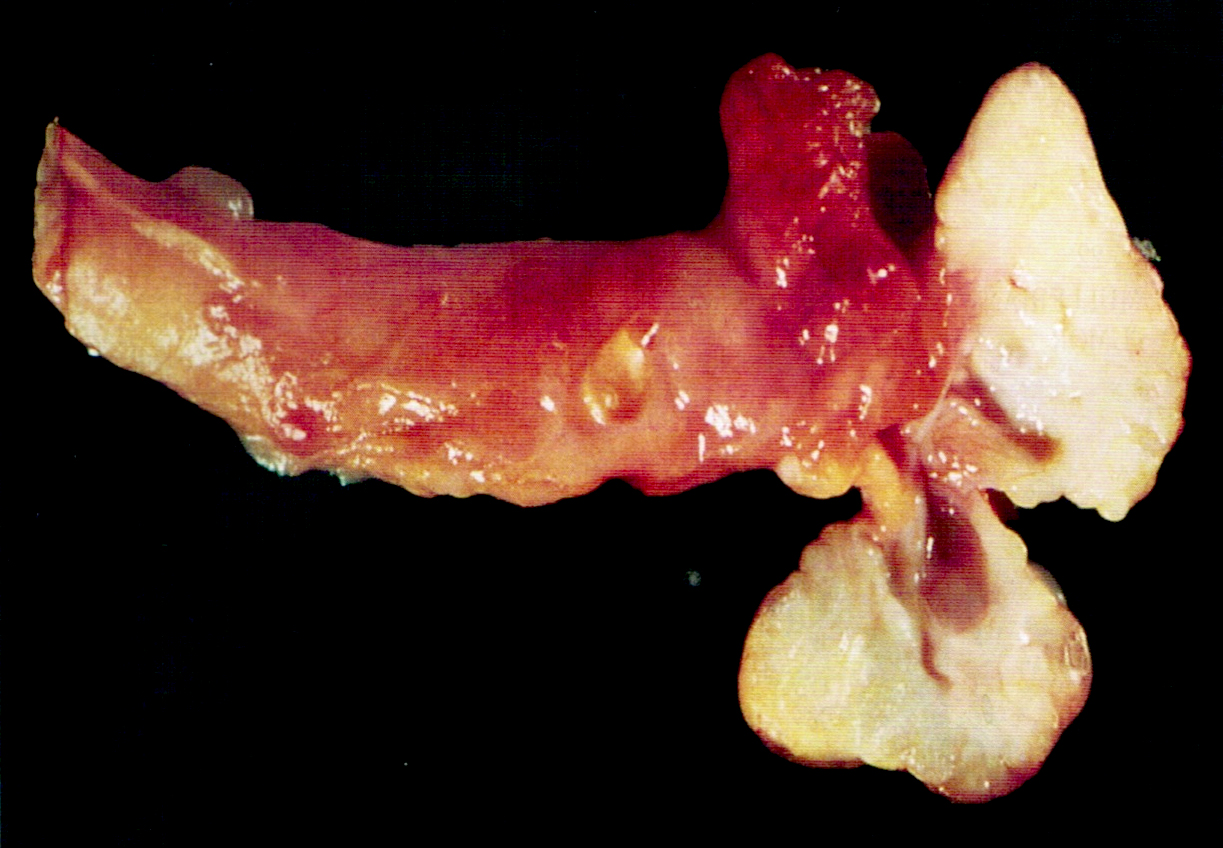
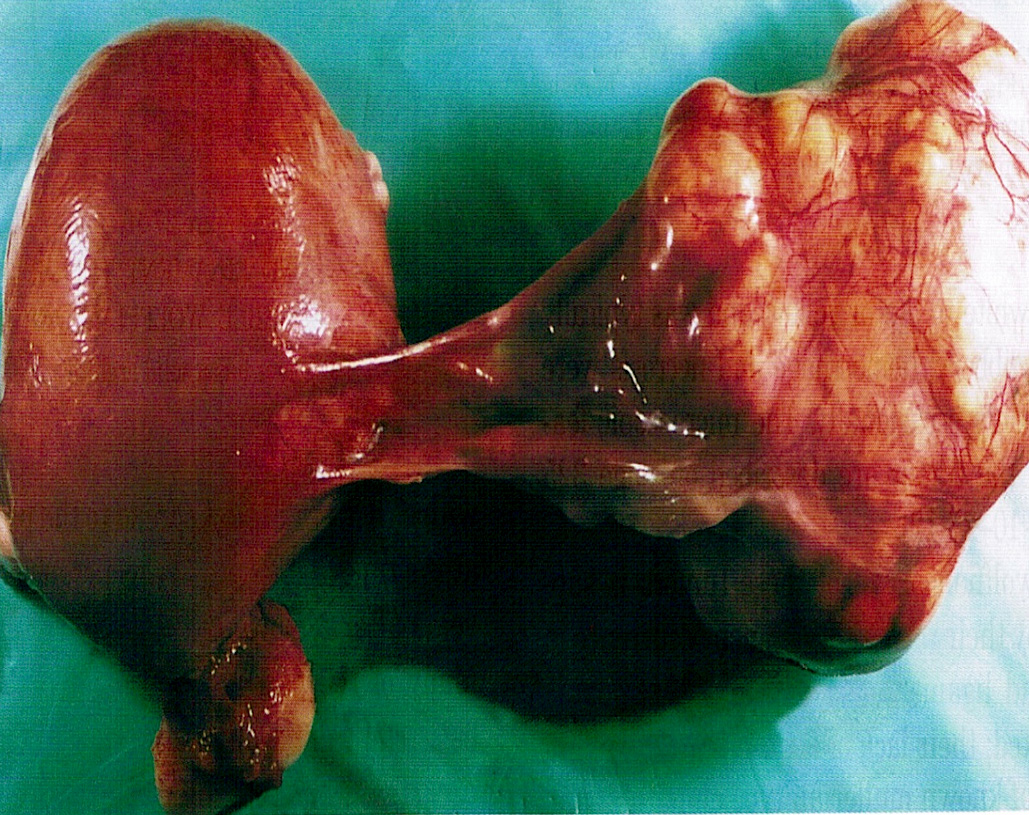
Gross description
- Enlarged tube, with solid or papillary tumor filling the lumen
- Tumors occasionally are primary in the fimbriae
- 80 - 97% unilateral; hemorrhage, necrosis and cysts common
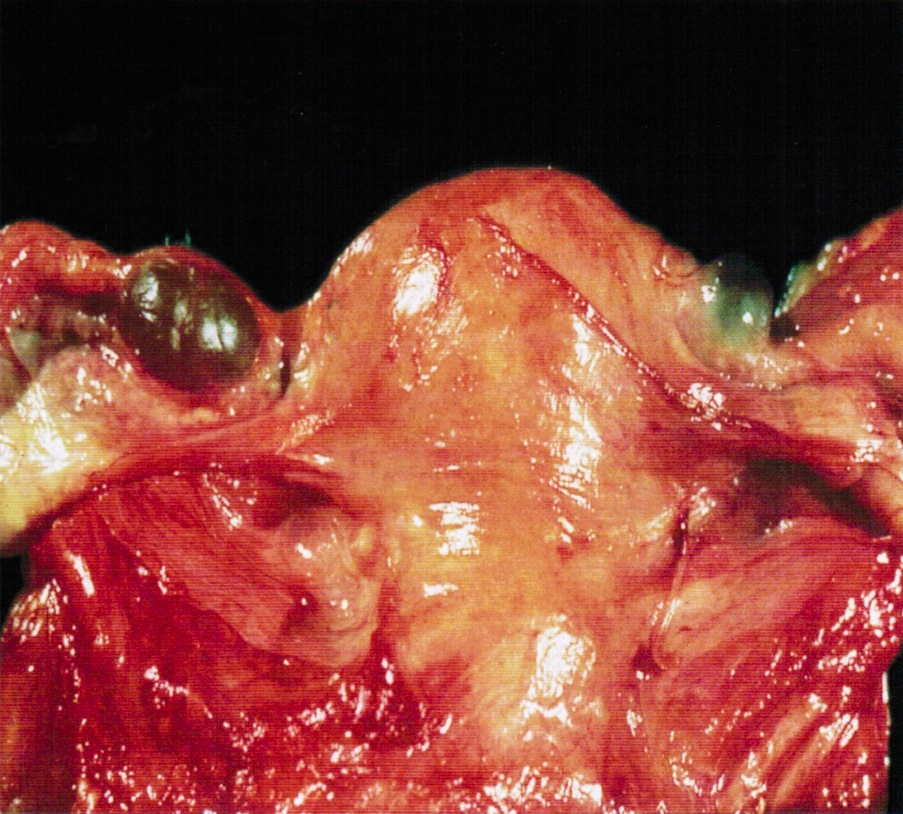
Gross images
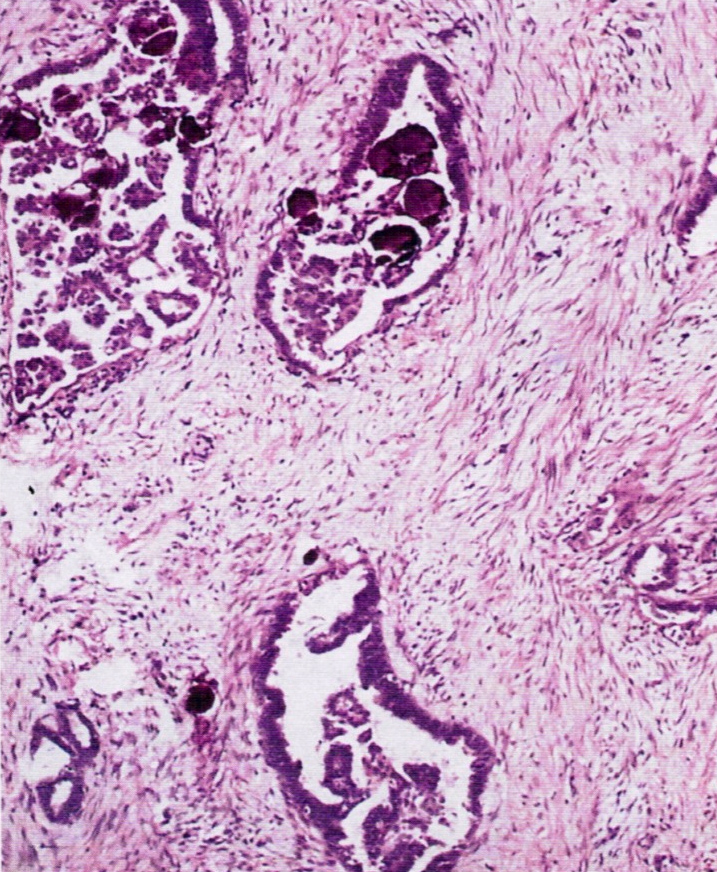
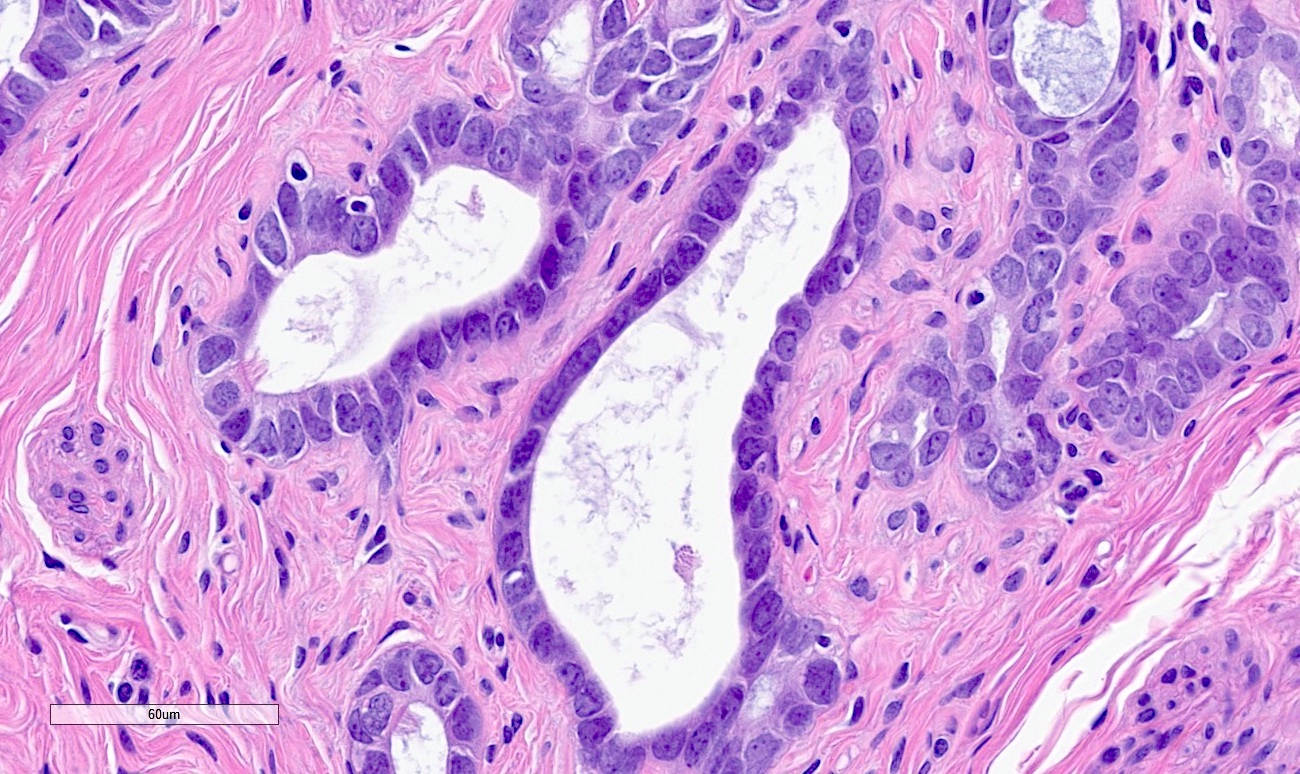
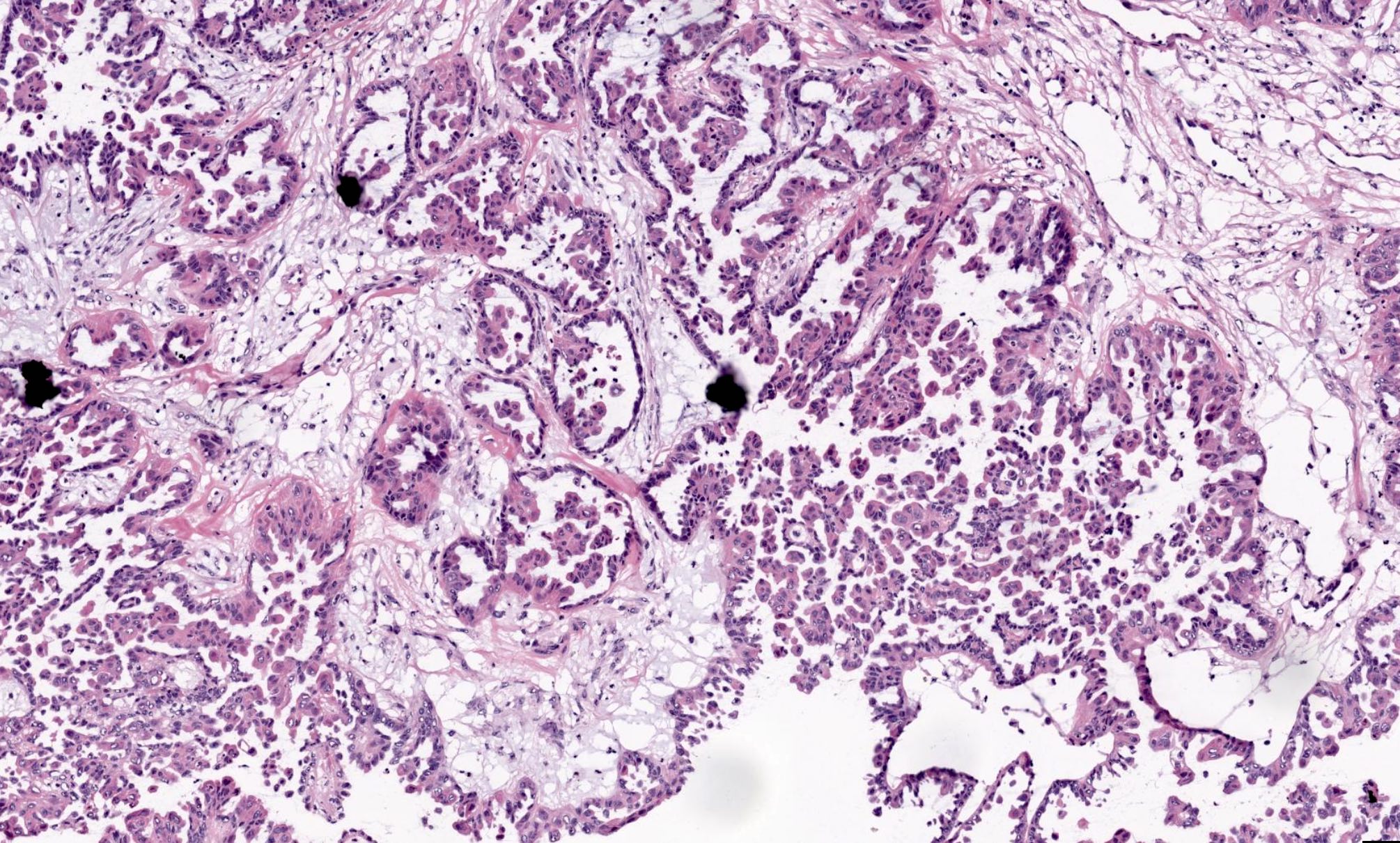
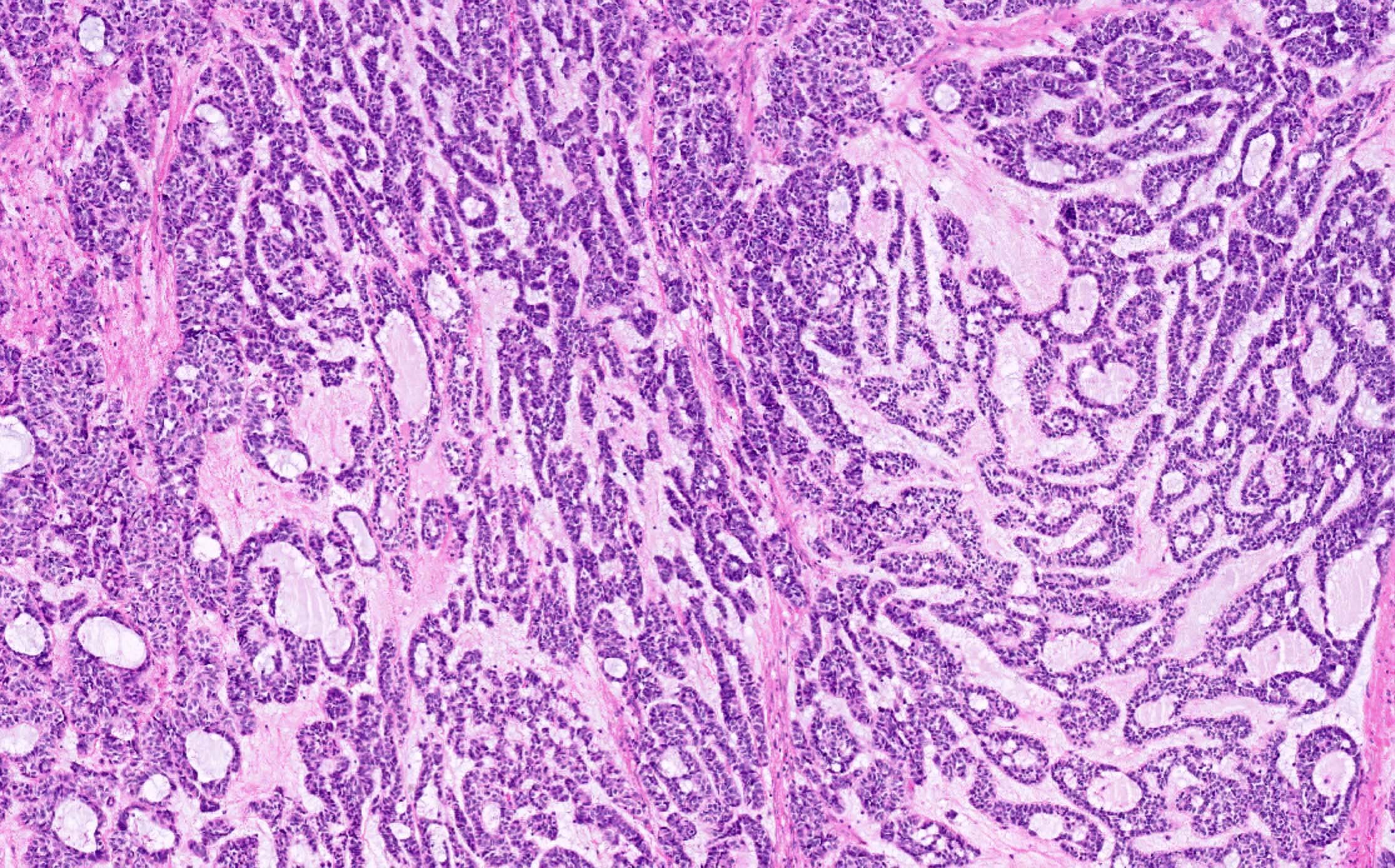
Microscopic (histologic) description
- Endometrioid tumors may be noninvasive, have squamous metaplasia, be associated with endometriosis and contain spindled epithelial cells
- May have small, closely packed cells with numerous glandular spaces of varying sizes, containing PAS+ dense colloid-like secretion, resembling female adnexal tumor of probable Wolffian origin (FATWO), but usually intraluminal, typical endometrioid carcinoma elsewhere, more mitotic activity and atypia, mucin present
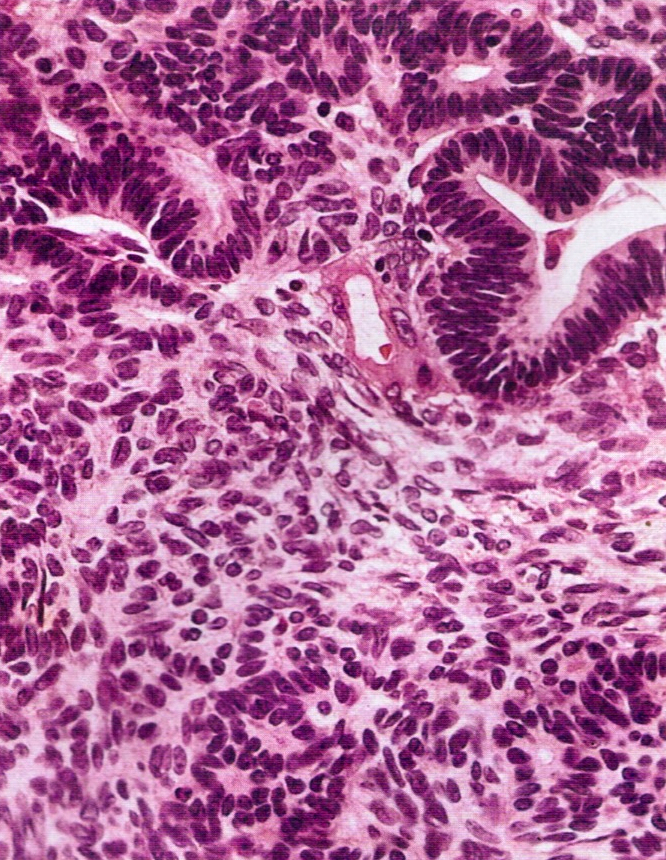
Microscopic (histologic) images
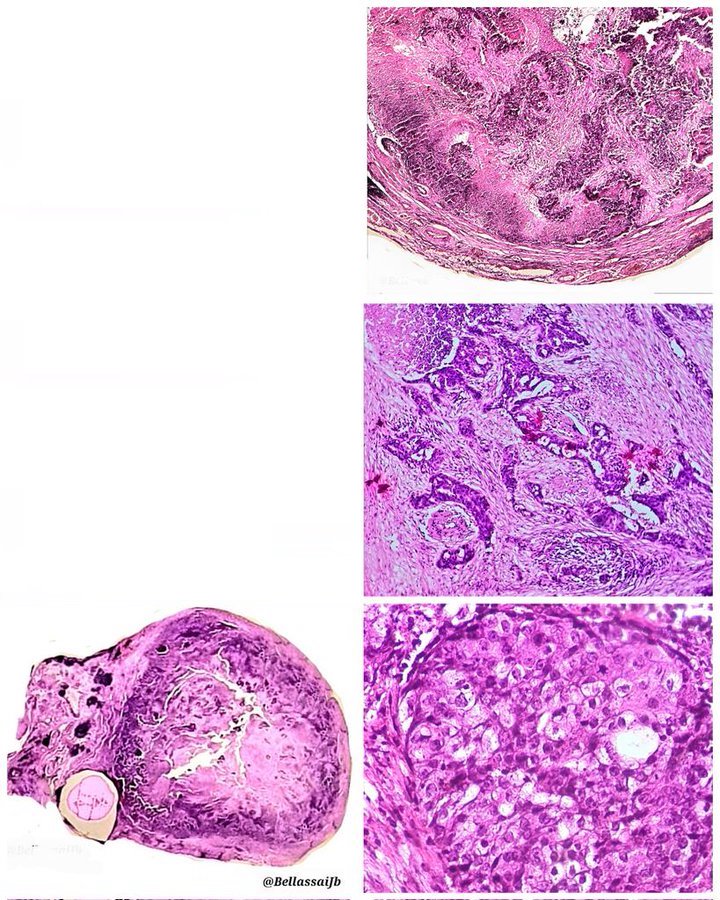
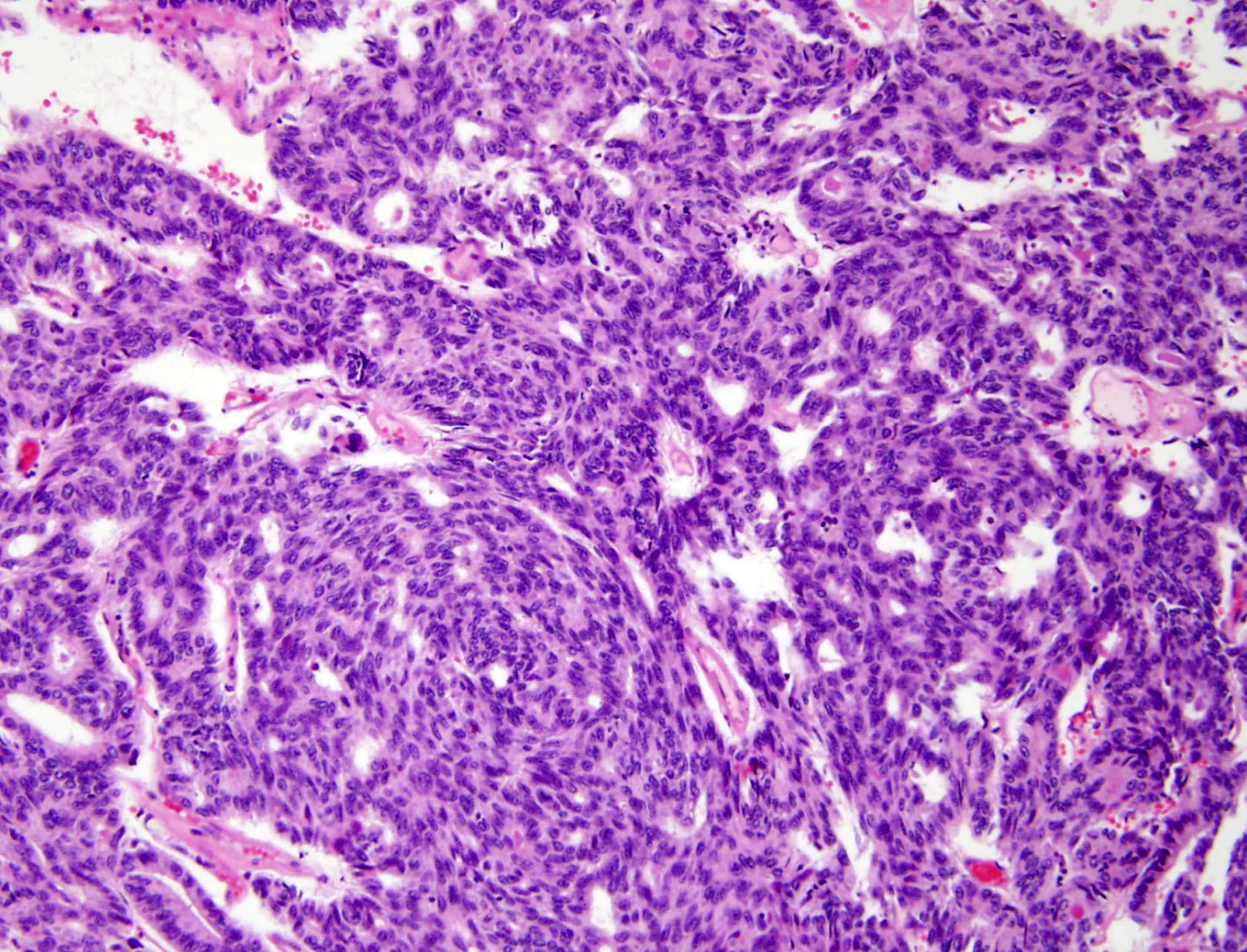
High grade serous carcinoma
Table of Contents
Definition / general | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) imagesDefinition / general
- High stage with pelvic extension or positive peritoneal cytology
- To call primary in fallopian tube, should arise from mucosa (endosalpinx), have tubal histologic pattern, involve the lumen, uterus and ovaries must be normal or have foci of malignancy that resemble metastases or independent primaries; if tubal wall is involved, should detect a transition between benign and malignant tubal epithelium
- 5 year survival: stage 1 - 77%, stage 3 - 20%; usually recur intra-abdominally
- Associated with BRCA1 and BRCA2 mutations; for patients with known mutation or family history of breast or ovarian cancer, should submit entire fallopian tube and ovary for microscopic examination (Am J Surg Pathol 2002;26:171, Am J Surg Pathol 2001;25:1283)
- 50% serous, 25% endometrioid, 20% transitional or undifferentiated
- Symptoms: vaginal bleeding or discharge (2/3), pain, adnexal mass (triad in 50%); endometrial smear positive in 10%
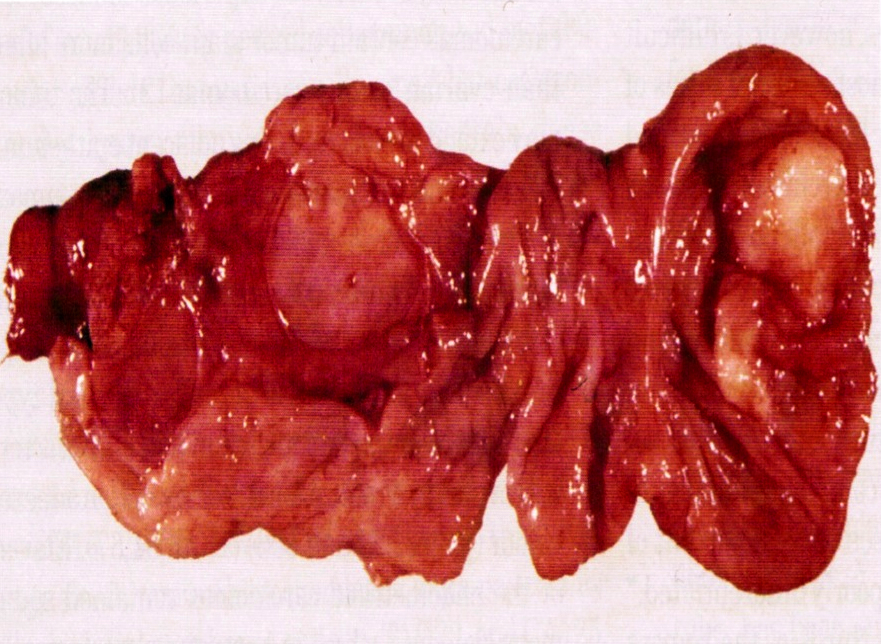
Gross description
- Enlarged tube, with solid or papillary tumor filling the lumen
- Tumors occasionally are primary in the fimbriae
- 80 - 97% unilateral; hemorrhage, necrosis and cysts common
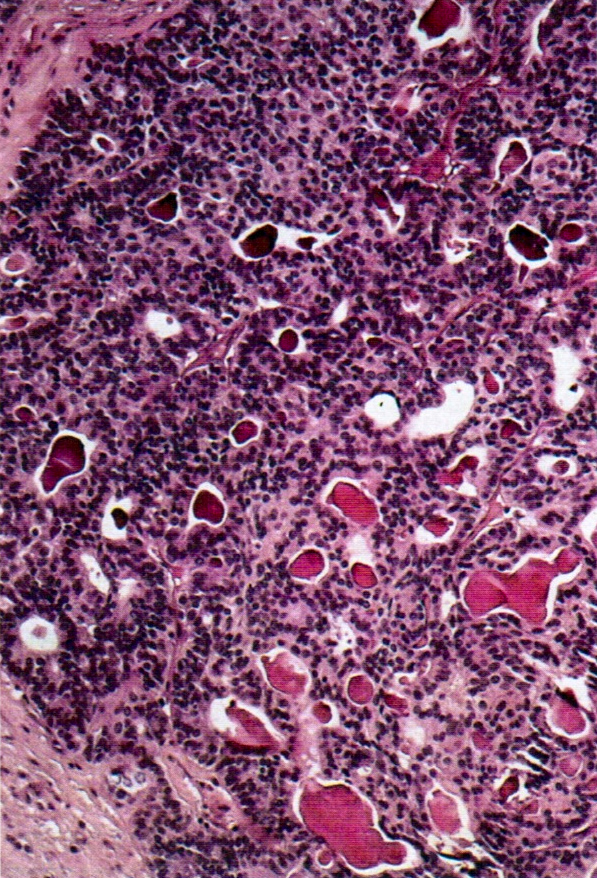
Gross images
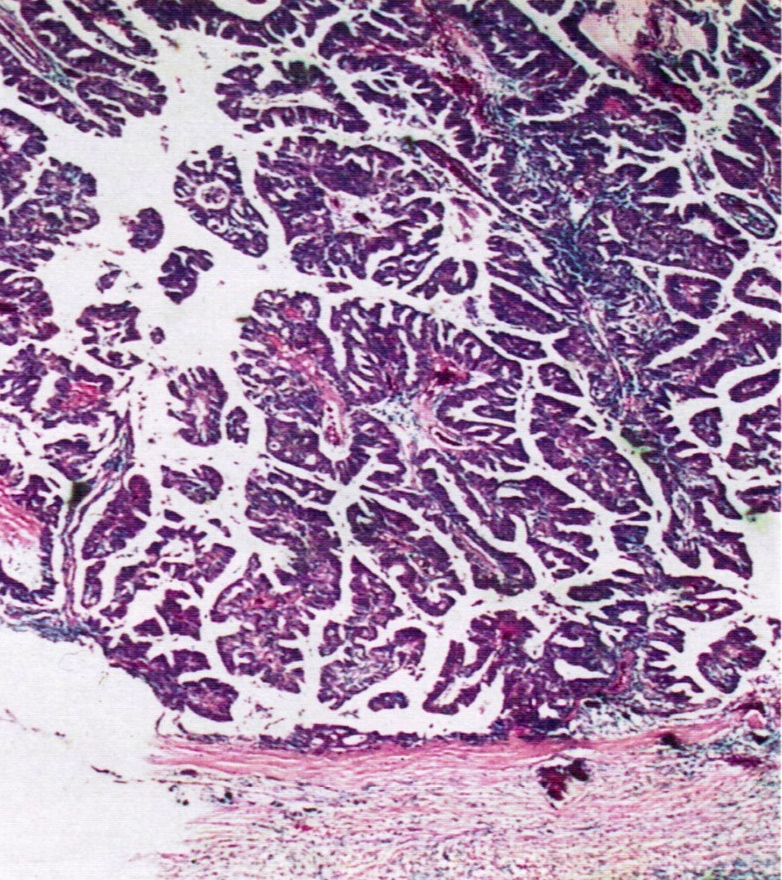
Microscopic (histologic) description
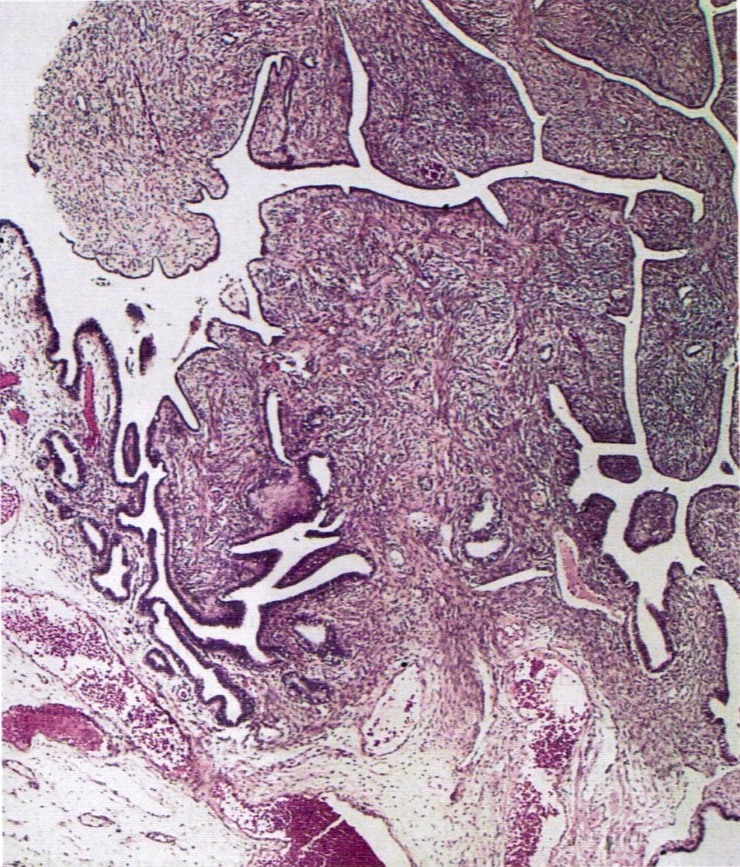
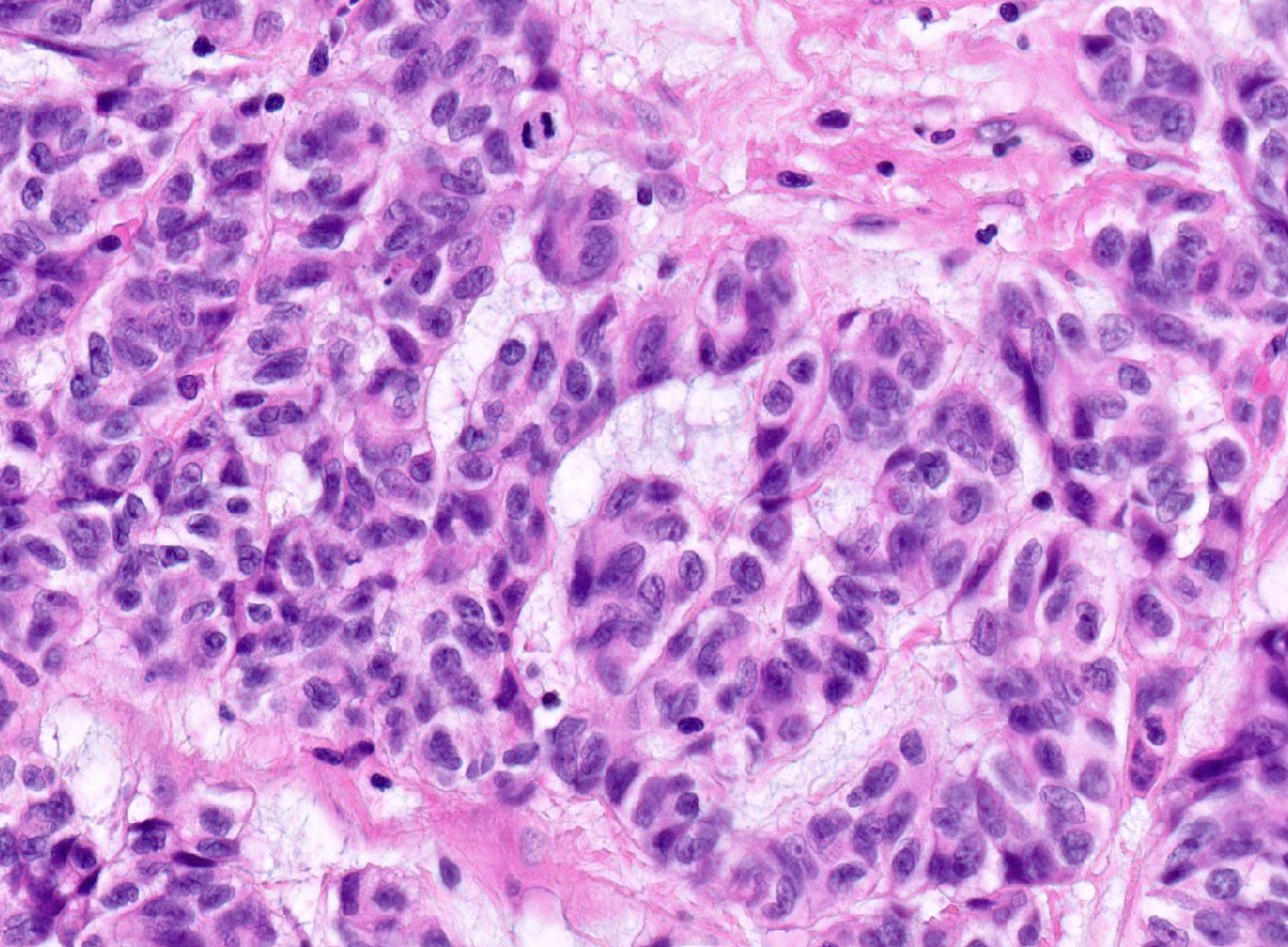
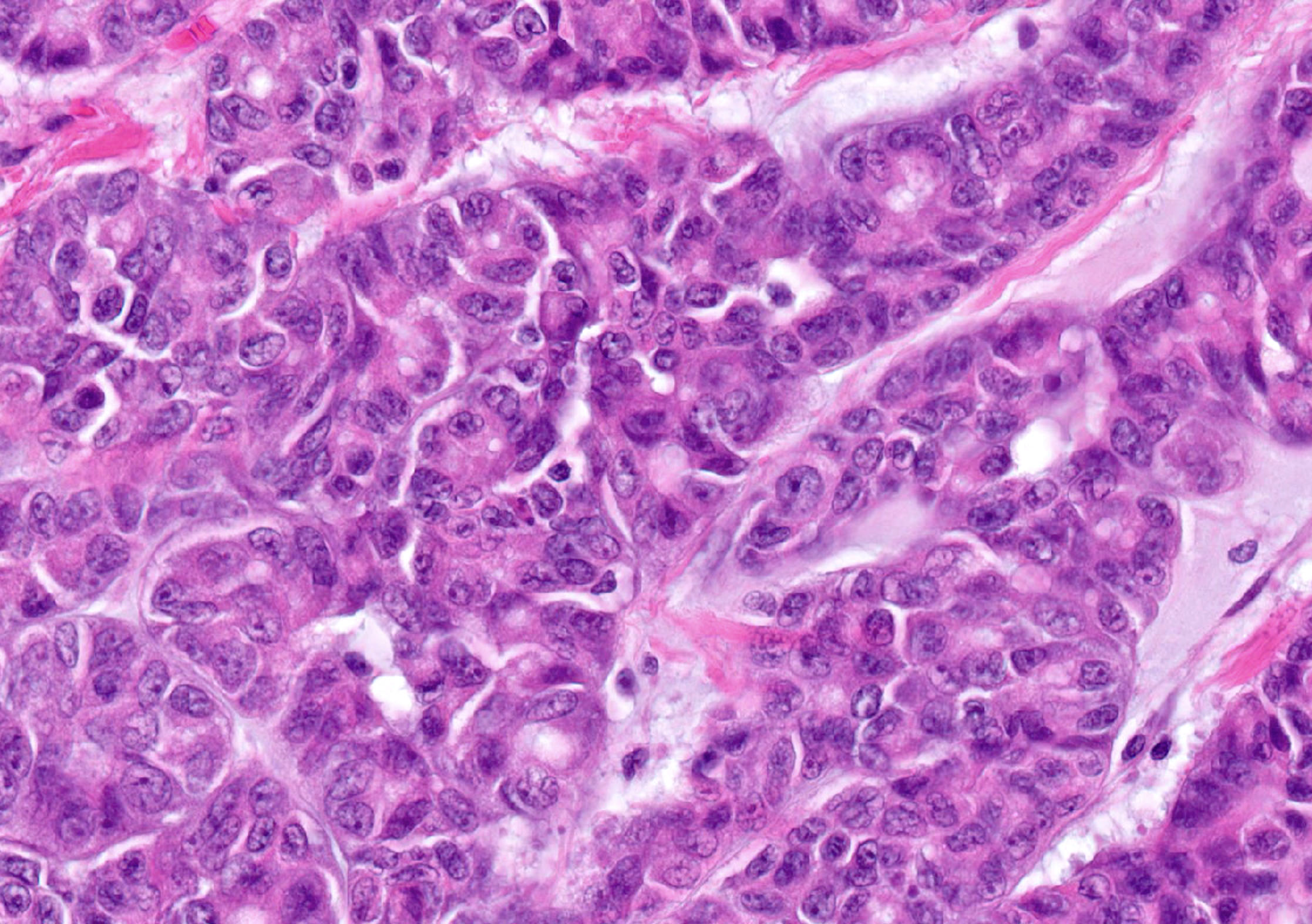
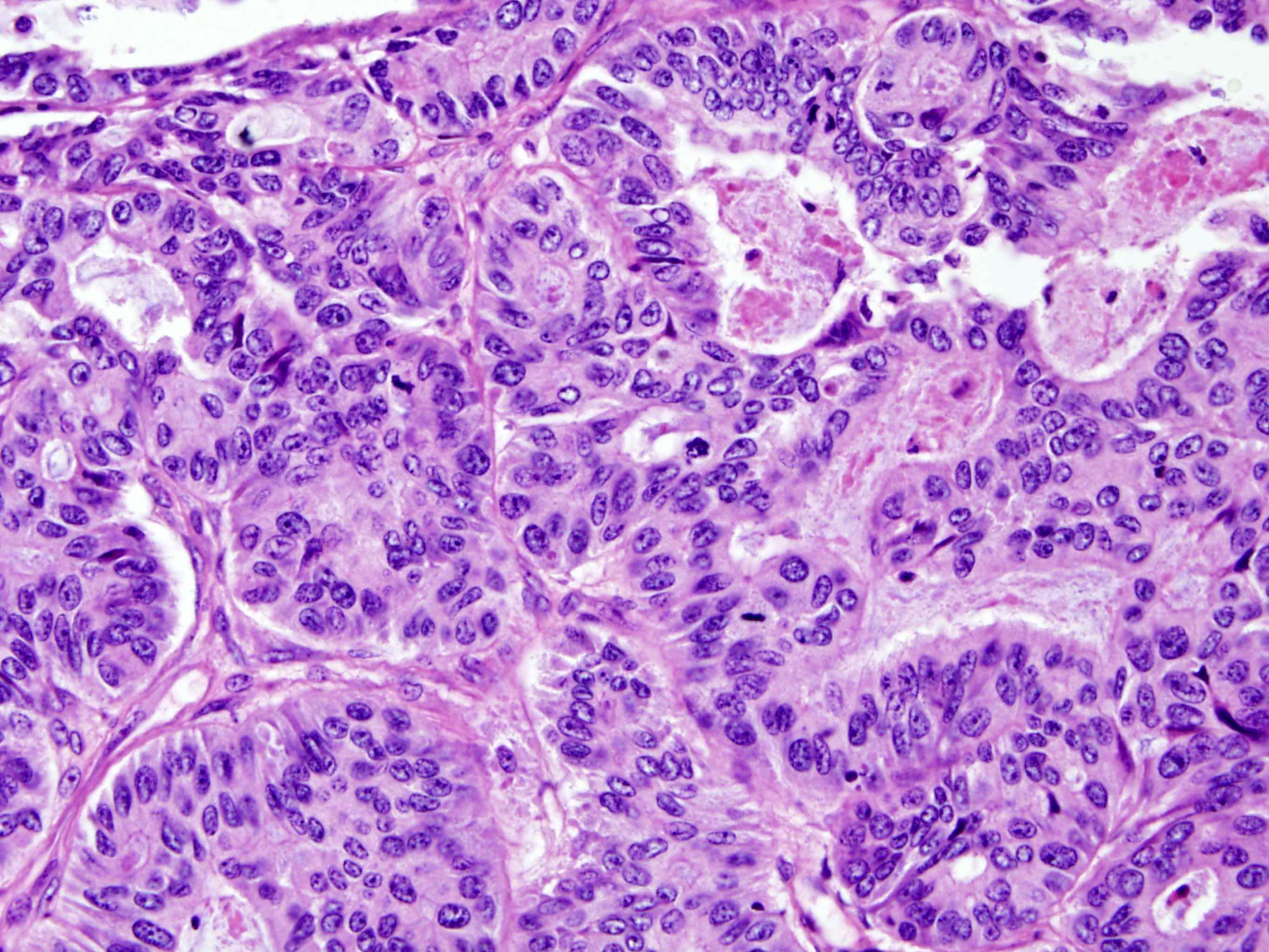
- Invasive papillary adenocarcinoma; may resemble ovarian serous adenocarcinoma with complex papillary architecture
Microscopic (histologic) images
Leiomyoma (pending)
[Pending]
Leiomyosarcoma (pending)
[Pending]
Mesonephric duct remnants
Table of Contents
Definition / general | Terminology | Epidemiology | Sites | Etiology | Treatment | Gross description | Microscopic (histologic) description | Positive stains | Negative stains | Differential diagnosisDefinition / general
- Mesonephric duct is paired organ present during embryogenesis connecting primitive kidney to cloaca, which becomes part of male reproductive organs (Wikipedia: Mesonephric Duct [Accessed 20 December 2018])
- In women, duct regresses but normal remnants remain; however, "abnormal" ductular remnants may remain and cause confusion as they appear as glands "out of place"
Terminology
- Also known as Wolffian duct, archinephric duct, Leydig duct, nephric duct
Epidemiology
- Embryological remnant which occurs in all women of any age
- No known predisposing factors
Sites
- Anywhere in pelvic cavity, including broad ligament, cervix (20% of women), fallopian tube, lymph nodes, ovary
Etiology
- In early development, mesonephric and paramesonephric ducts coexist
- Mesonephric ducts develops in bladder trigone in both sexes
- In men, under influence of testosterone, mesonephric duct develops into epididymis, vas deferens, seminal vesicle
- In women, absence of testosterone causes duct regression; this may be incomplete and inclusions / remnants may persist
- Gartners ducts are paired remnants that may give rise to cysts and are typically located lateral to vaginal wall in broad ligament
- Epoophoron (also known as organ of Rosenmüller or parovarium) is analogous to male epididymis; most cranial portion of remnant, located in lateral broad ligament, between ovary and fallopian tube; may communicate with Gartner ducts
- Paraoophoron is analogous to male paradidymis, usually located in medial broad ligament
Treatment
- None needed
Gross description
- Usually no significant gross findings, incidental on microscopy, unless cyst formation
Microscopic (histologic) description
- Small tubules lined by low columnar to cuboidal cells without cilia; surrounded by prominent smooth muscle; may be cystic
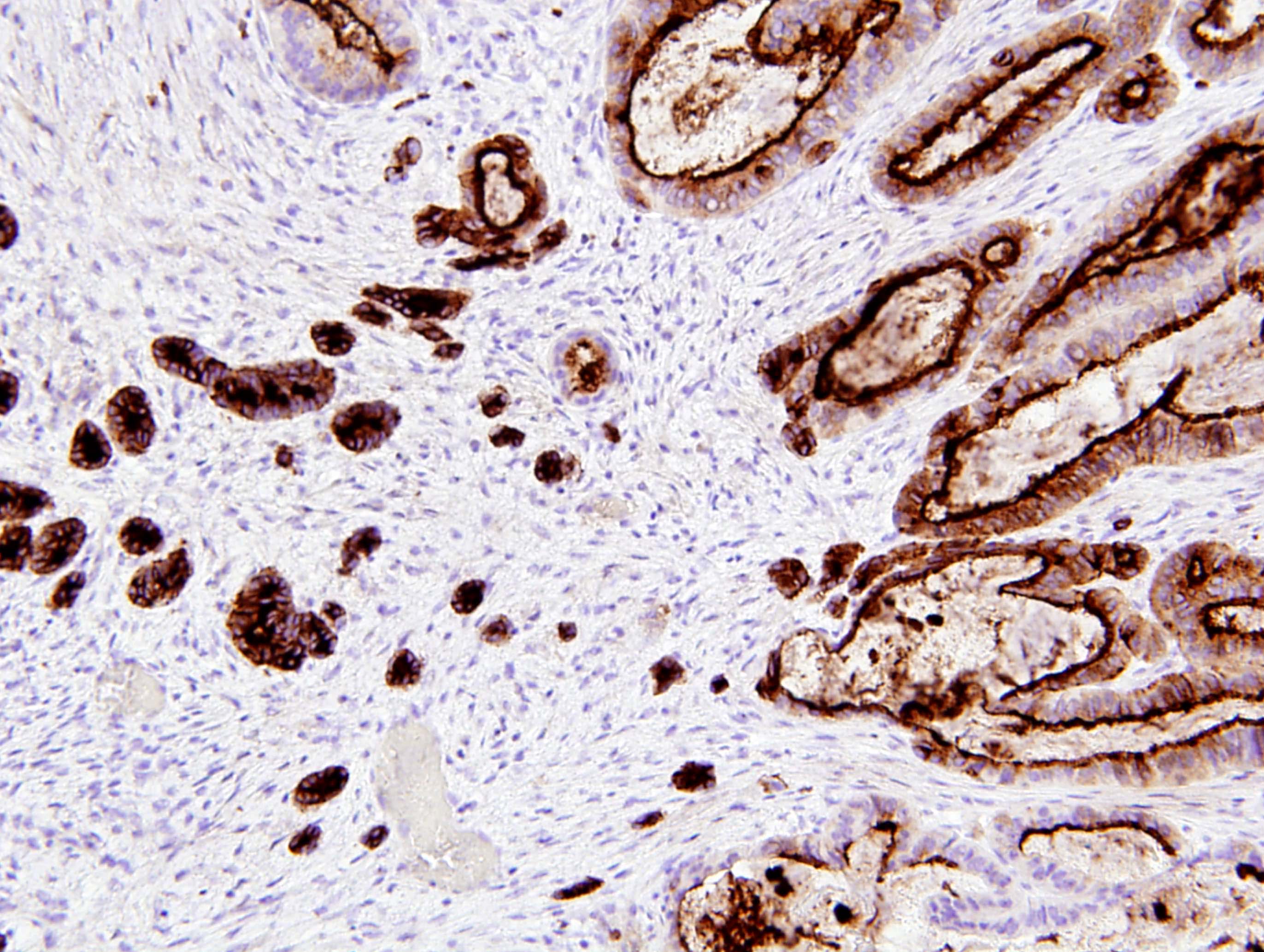
Positive stains
- CK903 (may be focal), CD10 (luminal, patchy), vimentin, p16 (Arch Pathol Lab Med 2008;132:402)
- Calretinin (2/3 of mesonephric adenocarcinomas, Histopathology 2003;43:144)
Negative stains
- ER, PR, CEA, p63 (rare focal positivity), PSA in males (Am J Surg Pathol 2011;35:1054)
- Calretinin (benign ducts)
Differential diagnosis
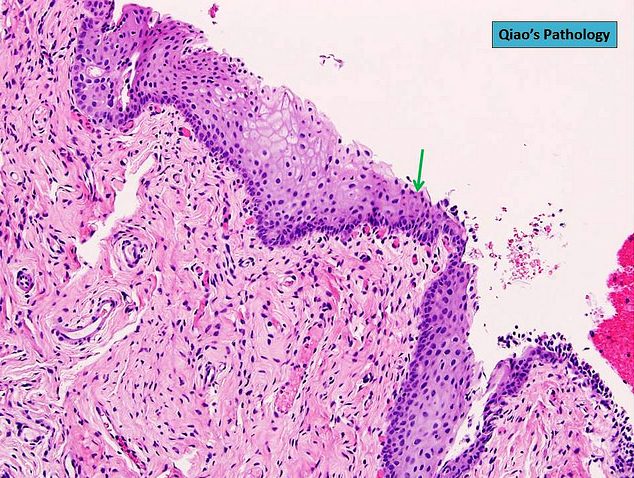
Metaplastic changes
Table of Contents
Definition / general | Essential features | Epidemiology | Sites | Etiology | Diagnosis | Prognostic factors | Case reports | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Negative stains | Differential diagnosis | Board review style question #1 | Board review style answer #1Definition / general
- Defined as alteration in which the normal tubal epithelium is replaced by metaplastic cells resembling benign transitional (urothelial) cells of urinary bladder (Am J Surg Pathol 2009;33:111)
Essential features
- Transitional cell metaplasia is a benign epithelial alteration but is underrecognized in the tubal fimbriae, where it may mimic serous tubal intraepithelial neoplasm / carcinoma
- It is increasing found because over the past two decades, risk reducing salpingo-oophorectomy (RRSO) for BRCA1 and BRCA2 mutation patients is being performed to identify epithelial atypia and early intraepithelial carcinoma in the distal fallopian tube / fimbriae
- Opportunistic salpingectomy is a viable alternative to salpingo-oophorectomy for BRCA+ women, which reduces the risk of serous carcinoma while preserving ovarian function
Epidemiology
- Present in 26% of all RRSO specimens
- Usually multifocal, with involvement of tip, edges or base of the fimbrial plicae
- Average size of a metaplastic focus is 1.3 mm (ranging from 0.1 to 10 mm)
- Also due to fallopian tube prolapse or peritoneal dialysis (squamous) (Int J Gynecol Pathol 2008;27:465)
- Also associated with ovarian mucinous tumors, Peutz-Jeghers syndrome, endometriosis within fallopian tube
Sites
- Distal fallopian tube / fimbriae
Etiology
- Unclear: it is possible that transitional cell metaplasia of the fimbriae is a reaction to mechanical irritation, inflammation or infection
- Findings that only the distal fimbriae are involved and not the isthmus, ampulla or infundibulum supports the notion of a reaction to peritoneal based stimulus
- Prior pregnancy is a potential inciting incident
Diagnosis
- Diagnosis of transitional cell metaplasia of fimbriae is only possible after salpingectomy by microscopic examination of distal fallopian tube / fimbriae
Prognostic factors
- Clinical followup of transitional cell metaplasia of the fimbriae shows no biologic significance
Case reports
- 45 year old woman with prolapsed fallopian tube with squamous metaplasia (J Postgrad Med 2002;48:241)
- 52 year old woman with papillary syncytial metaplasia of fallopian tube endometriosis (Arch Pathol Lab Med 2013;137:126)
Gross description
- Generally, such lesions are undetectable grossly and are only identified by careful histologic examination of sections of fallopian tubes; thus, fallopian tubes have to be submitted entirely in serial cross sections whereas fimbriae have to be submitted entirely in longitudinal sections
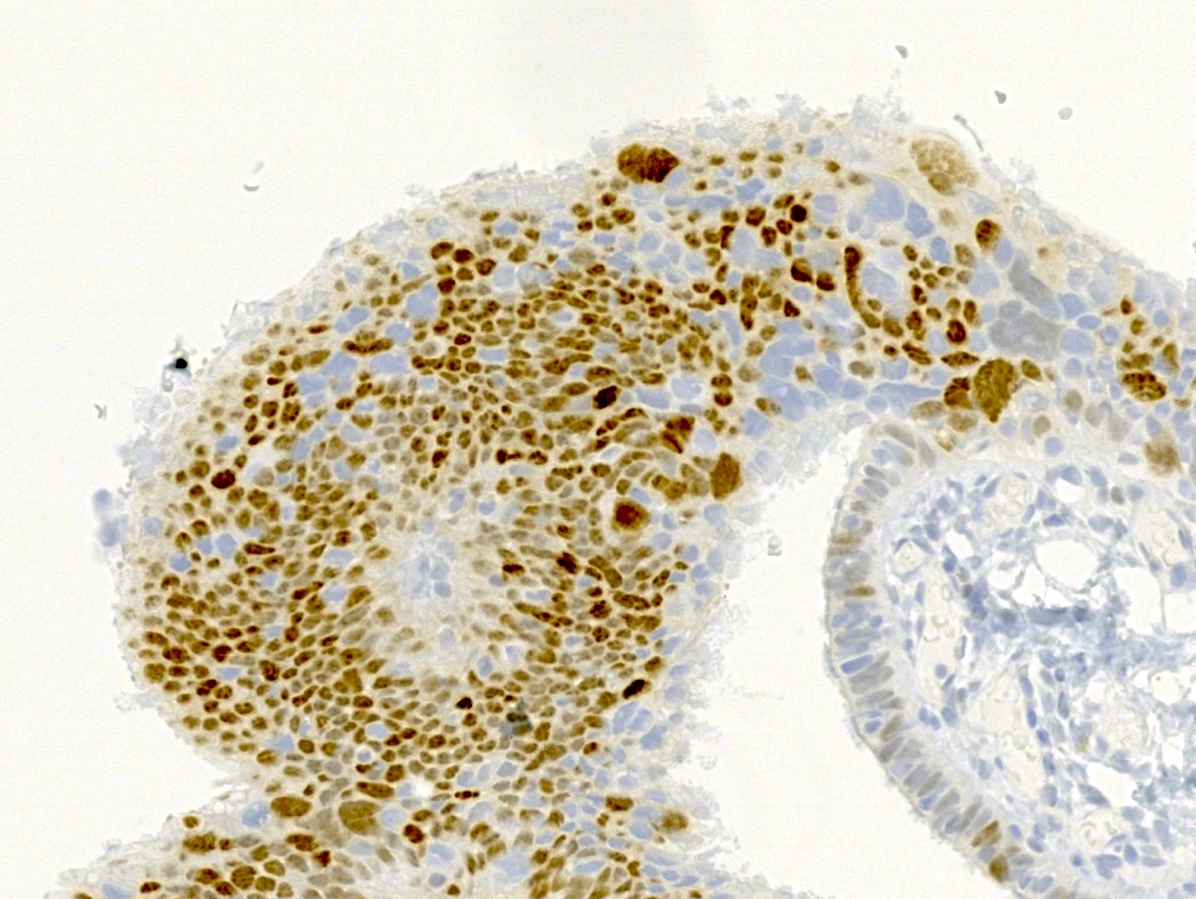
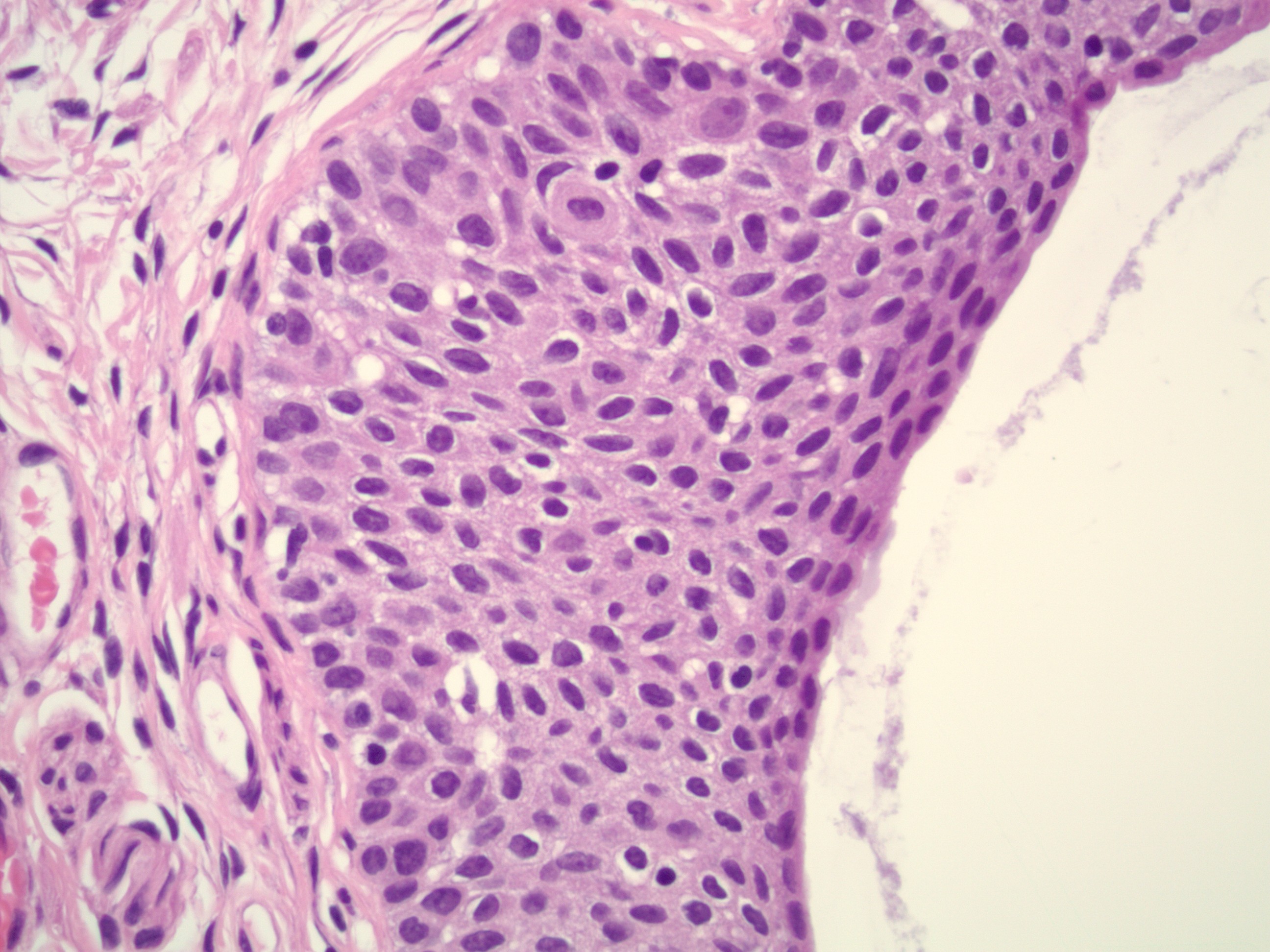
Microscopic (histologic) description
- Mostly commonly mucinous metaplasia; urethelial and squamous metaplasia less common
- Characteristic features of transitional cell metaplasia are the presence of uniform nuclei with pale chromatin and nuclear grooves and abundant cytoplasm; these features are not seen in serous tubal intraepithelial neoplasia, including serous tubal intraepithelial carcinoma (STIC) and serous tubal epithelial proliferation of uncertain significance
- Careful histologic examination, attention to cytologic details and p53 and Ki67 staining will help prevent the misinterpretation of transitional cell metaplasia as malignancy
Microscopic (histologic) images
Negative stains
Differential diagnosis
- Serous tubal epithelial proliferation of uncertain significance: nuclear enlargement, increased N/C ratio and polarity is preserved; evidence of TP53 mutation ("p53 signature") by immunohistochemistry; Ki67 index is variably increased (Mod Pathol 2017;30:710)
- Serous tubal intraepithelial carcinoma (STIC): nuclear enlargement, increased N/C ratio, lost cellular polarity, irregular nuclear stacking, small detached papillary clusters, horizontally oriented surface nuclei and intraepithelial fractures; evidence of TP53 mutation by immunohistochemistry; Ki67 index is variably increased (Mod Pathol 2017;30:710)
Board review style question #1
The following statements about transitional cell metaplasia of the fimbriae are correct, except
- Cells of transitional cell metaplasia show uniform nuclei, pale chromatin and nuclear grooves
- Clinical followup of transitional cell metaplasia of the fimbriae shows no biological significance
- p53 signature and increased Ki67 are usually present in transitional cell metaplasia of the fimbriae
- Transitional cell metaplasia is undetectable by gross examination
- Transitional cell metaplasia shows no evidence of nuclear enlargement, loss of cellular polarity or irregular nuclear stacking
Board review style answer #1
C. p53 signature and increased Ki67 are not associated with transitional cell metaplasia of distal fimbriae but are characteristic of serous tubal intraepithelial carcinoma and serous tubal epithelial proliferation of uncertain significance.
Comment Here
Reference: Metaplastic changes
Comment Here
Reference: Metaplastic changes
Metaplastic papillary lesion
Table of Contents
Definition / general | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosisDefinition / general
- A rare, benign, incidental lesion that is usually found during pregnancy or postpartum
Case reports
- Metaplastic papillary tumor of fallopian tube (Arch Pathol Lab Med 1989;113:545)
- Metaplastic papillary tumor of salpinx (Int J Gynecol Pathol 2011;30:532)
Treatment
- Not needed
Gross description
- Usually incidental microscopic finding
Microscopic (histologic) description
- Eosinophilic or mucinous papillae with small cysts
- Large vesicular nuclei with minimal stratification, no crowding or atypia
- Rare mitoses
Differential diagnosis
- May mimic carcinoma
Mucinous metaplasia (pending)
[Pending]
Papillary cystadenoma of mesosalpinx
Definition / general
- Associated with von Hippel-Lindau disease
Microscopic (histologic) images
Paratubal cysts
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Fluid filled cyst with ciliated lining adjacent to fallopian tube
Essential features
- Ciliated cyst adjacent to fallopian tube
- Typically asymptomatic
- Almost always benign, with rare reports of borderline tumor
Terminology
- Paraovarian cyst
- Hydatid cyst
- Not recommended: hydatid of Morgagni
ICD coding
- ICD-10: N83.8 - other noninflammatory disorders of ovary, fallopian tube and broad ligament
Epidemiology
- Common benign incidental finding (~7 - 10% of women) (J Pediatr Surg 2011;46:2161)
- All age groups, most commonly third to fifth decade
Sites
- Paratubal (between fallopian tube and ovary)
Pathophysiology
- Unknown
Etiology
- Believed to originate from mesothelium or be remnant of Müllerian duct or Wolffian duct
Clinical features
- Most cysts are small and asymptomatic (< 1 to 8 cm; rarely, 20+ cm)
- Size of paratubal cysts may correlate with obesity (J Pediatr Adolesc Gynecol 2017;30:571)
- May be found during surgery or incidentally on radiological study performed for another reason
- Larger lesions may become symptomatic, causing pressure or pain (J Pediatr Surg 2011;46:2161)
- May lead to torsion of adnexa, resulting in acute pain (J Pediatr Surg 2011;46:2161)
Diagnosis
- Typically noted incidentally on intraoperative or gross examination
Radiology description
- While not often diagnosed on imaging, paratubal cysts are unilocular and anechoic or hypoechoic on ultrasound (J Clin Endocrinol Metab 2000;85:1021)
Prognostic factors
- Paratubal cysts are benign
- Rarely gives rise to serous borderline tumor or even more rarely malignancy (Appl Immunohistochem Mol Morphol 2017;25:e21)
Case reports
- 15 year old girl with giant paratubal serous cystadenoma (J Pediatr Adolesc Gynecol 2020;33:438)
- 17 year old girl with paratubal borderline tumor (J Pediatr Adolesc Gynecol 2016;29:74)
- 34 year old nulligravid woman with paratubal cyst and bilateral hydrosalpinges diagnosed during evaluation of infertility (Taiwan J Obstet Gynecol 2014;53:239)
Treatment
- Surgical excision of the paratubal cyst represents definitive treatment for symptomatic patients (J Clin Endocrinol Metab 2000;85:1021)
- Benign follow up is expected; treatment is not required for asymptomatic patients
Gross description
- Simple fluid filled cyst(s) near fallopian tube
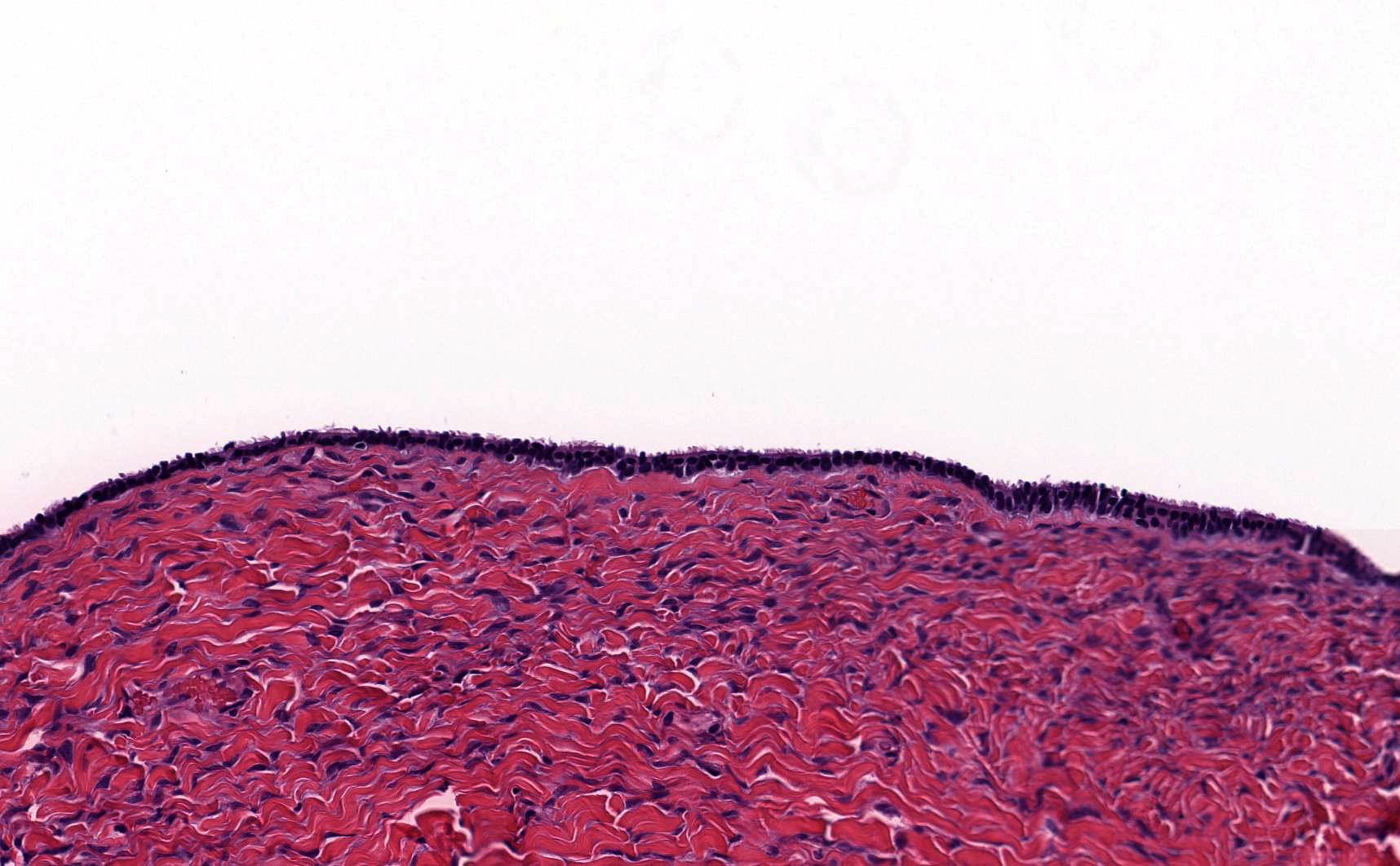
Microscopic (histologic) description
- Simple fluid filled cyst lined by ciliated tubal type epithelium
- Focal papillary projections may be seen
Microscopic (histologic) images
Sample pathology report
- Fallopian tubes, bilateral salpingectomy:
- Benign fallopian tubes with paratubal cysts
Differential diagnosis
- Endometriotic cyst:
- Associated with endometrial type stroma with or without hemosiderin laden macrophages
- Serous cystadenoma:
- Histologically identical to paratubal cyst but > 1 cm in size
- Hydrosalpinx:
- Dilation of the fallopian tube lumen with attenuation of the tubal epithelium with or without diminished plicae
- Distinction based largely on location of the cystic space within rather than near the fallopian tube
Board review style question #1
Board review style answer #1
Board review style question #2
Which of the following is true about paratubal cysts?
- Large paratubal cysts may cause torsion
- Large paratubal cysts often progress to borderline tumors
- Paratubal cysts are frequently diagnosed on MRI
- Paratubal cysts are an unusual finding
Board review style answer #2
Placental site nodule
Prolapse
Table of Contents
Definition / general | Epidemiology | Clinical features | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Differential diagnosisDefinition / general
- Turning of tubes inside out, back into vaginal vault or even more rarely into bladder or uterine cavity
Epidemiology
- Rare (less than 100 cases reported), ~80% occur after vaginal hysterectomy (0.5% incidence), presumed due to nonclosure of vaginal vault
- 0.06% incidence after abdominal hystertecomy, less frequent with interposition or colpotomy
- Associated factors include postoperative fever, hematoma formation / failure to maintain adequate hemostasis, poor physical condition, insufficient preoperative vaginal preparation, difficultly with surgical procedure, use of intraperitoneal vaginal drains and packs
Clinical features
- Occurs two months to eight years after surgery
- May present with watery vaginal discharge, lower abdominal pain, dyspareunia
Case reports
- 27 year old woman with peritoneovaginal fistula (Can J Urol 2010;17:5117)
- 35 year old woman (J Midlife Health 2012;3:40)
- Prolapse of fallopian tube into urinary bladder, resembling carcinoma (Arch Pathol Lab Med 1983;107:613)
Treatment
- Surgical excision
Gross description
- Polypoid mass resembling granulation tissue, visible at vaginal apex
Microscopic (histologic) description
- Normal ciliated fallopian tube epithelium with variable surrounding fibrosis, edema, chronic inflammation
Microscopic (histologic) images
Cytology description
- May be seen on Pap smears
- Columnar cells with cilia and sheets of cells with small granular uniform nuclei in an orderly arrangement; also inflammatory cells and reactive atypia (Diagn Cytopathol 2013;41:146)
Differential diagnosis
- Carcinoma (well differentiated): has glands at odd locations
- Cysts of mesonephric and paramesonephric duct
- Endometriosis
- Vaginal adenosis
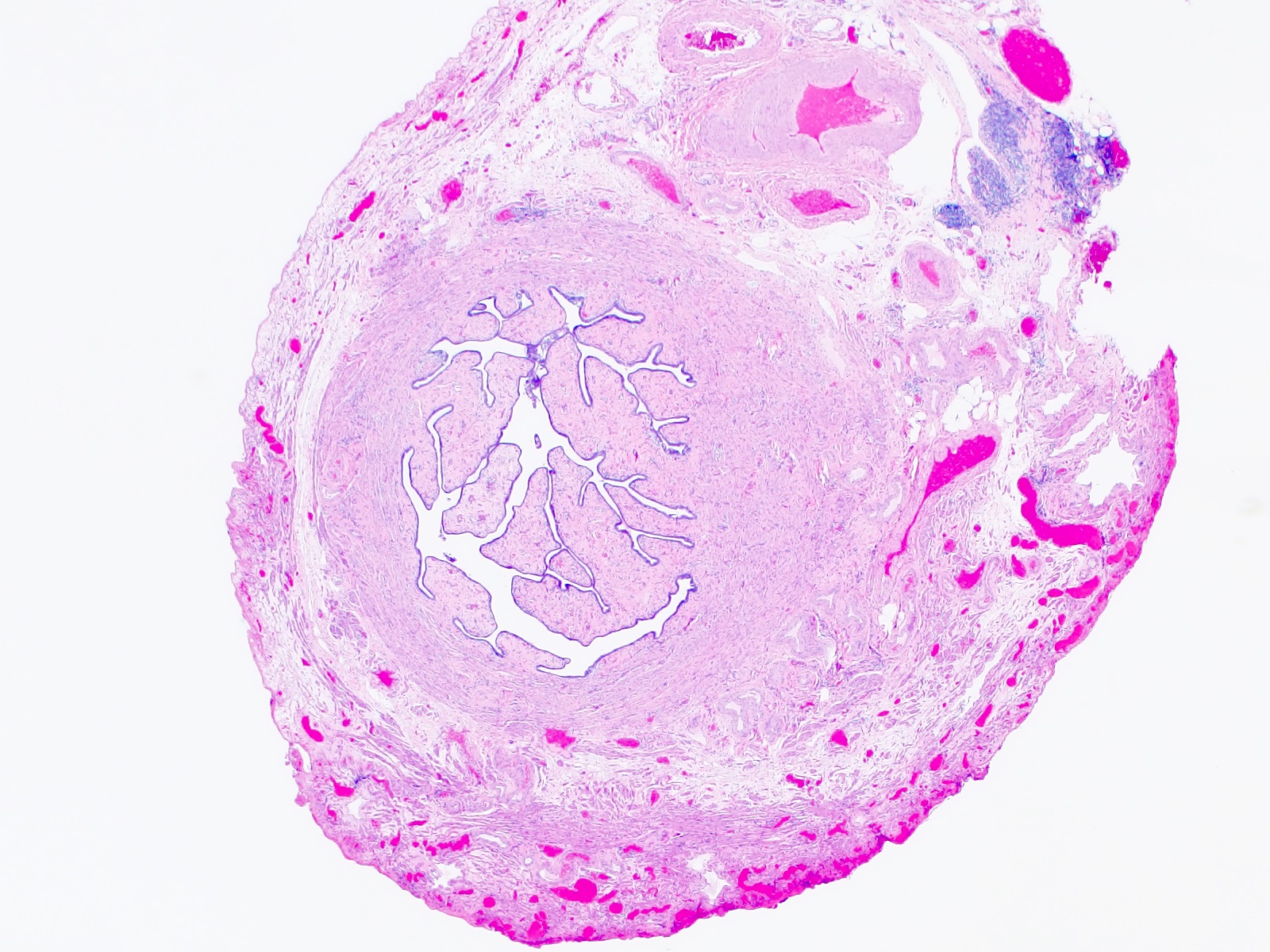
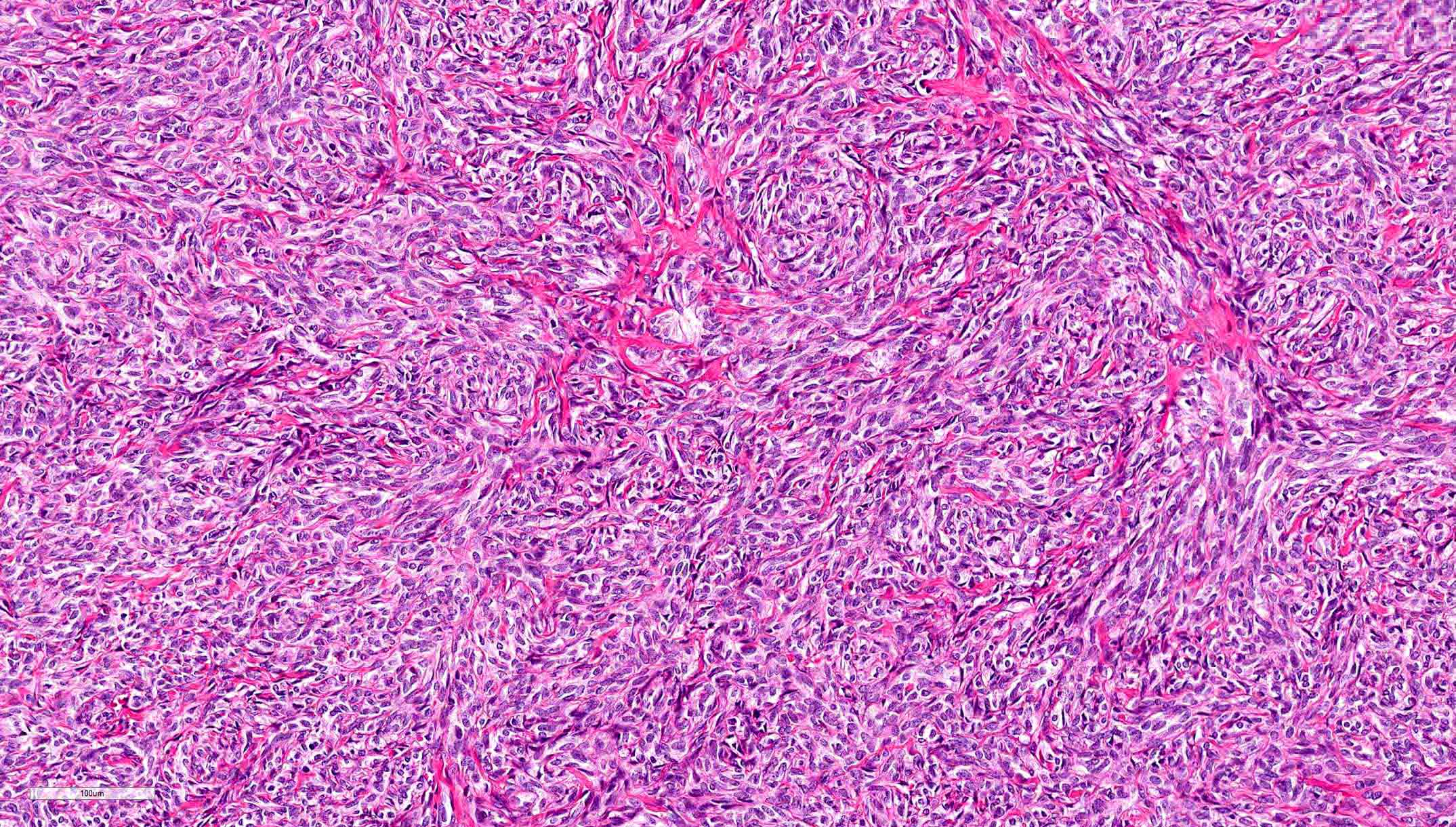
Salpingitis isthmica nodosa
Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
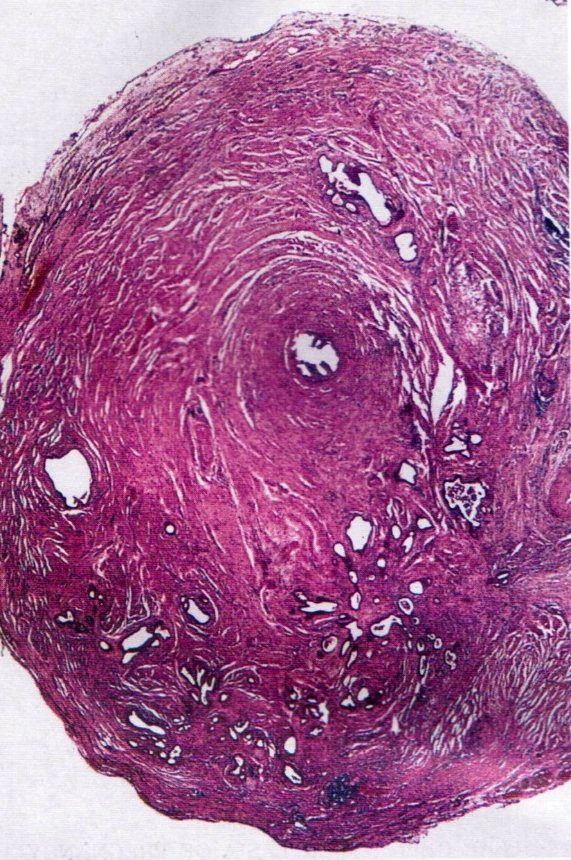
- Salpingitis isthmica nodosa (SIN) is an outpouching of the fallopian tube epithelium into the smooth muscle wall (adenomyosis of the tube)
- Multiple discrete lumina are enveloped in smooth muscle and in severe cases, the tubal lumen may be completely obstructed
- SIN can lead to infertility or ectopic pregnancy
Essential features
- Adenomyosis of the fallopian tube
- Nodular swelling of the isthmic segment of the fallopian tube
- Multiple glands lined by bland tubal epithelium within the tubal wall, separated and surrounded by smooth muscle
- Associated with infertility and ectopic pregnancy
Terminology
- Diverticulosis of the fallopian tube
- Tubal adenomyosis
Epidemiology
- 0.6 - 11% of healthy fertile women (StatPearls: Salpingitis Isthmica Nodosa [Accessed 22 June 2023], Fertil Steril 1993;60:599)
- Incidence is ~1% in the white female population (Fertil Steril 1978;29:164)
- Primarily affects young women of reproductive age (mean: 26 years)
- 10% incidence in cases of ectopic tubular pregnancies (Gynecol Obstet Invest 1992;34:202)
Sites
- Fallopian tubes, predominantly the isthmus
Pathophysiology
- Invasion of the epithelium into the smooth muscle may lead to muscular hypertrophy, generating the nodular appearance of the lesion
Etiology
- Unclear but early theories include inflammatory or congenital causes (Radiology 1985;154:597)
- Other controversial hypotheses include
- Origination in Wolffian rests or mesonephric rests due to SIN occurring at the location in which these ducts cross during embryologic development (Clin Radiol 1987;38:207)
- Acquired etiology with some studies suggesting diethylstilbestrol exposure; chronic tubal spasm due to increased intramural pressure / weakness in the wall at the site of vasculature (Clin Obstet Gynecol 1987;30:181)
- Infectious etiology due to chronic infection or inflammation
Clinical features
- More common in the background of ectopic pregnancy and infertility
- Associated with infertility in 50% of patients but its presence may not actually affect the number of births (Hum Reprod 1991;6:828)
- Incidence in healthy, fertile women ranges from 0.6 to 11% (Fertil Steril 1993;60:599)
- May be unilateral or bilateral
Diagnosis
- Incidental finding during evaluation for pelvic pain or infertility (hysterosalpingogram [HSG], laparotomy, laparoscopy)
- Tubal evaluation for primary infertility may reveal gross lesion
- HSG can demonstrate the nodular swellings (Fertil Steril 1993;60:599)
- No pathognomonic clinical symptomatology
Radiology description
- Hysterosalpingography (HSG)
- Globular 2 mm diameter collections of contrast medium in isthmus
- Tubal occlusion and hydrosalpinx may be observed
Radiology images
Prognostic factors
- Smooth muscle hypertrophy can cause near complete occlusion of the tubal lumen and increase the risk of secondary infection, infertility or ectopic pregnancy
Case reports
- 29 year old woman with subfertility (Eur J Obstet Gynecol Reprod Biol 2015;184:73)
- 33 year old woman with ruptured salpingitis isthmica nodosum (BMJ Case Rep 2021;14:e237860)
- 42 year old woman with abdominal pain and amenorrhea (J Clin Diagn Res 2013;7:2581)
Treatment
- Recanalization using interventional radiology (Fertil Steril 1995;63:715)
- Microsurgical tubocornual anastomosis (Fertil Steril 1993;60:599)
- Assisted reproductive technology (ART) for infertility (Eur J Obstet Gynecol Reprod Biol 2015;184:73)
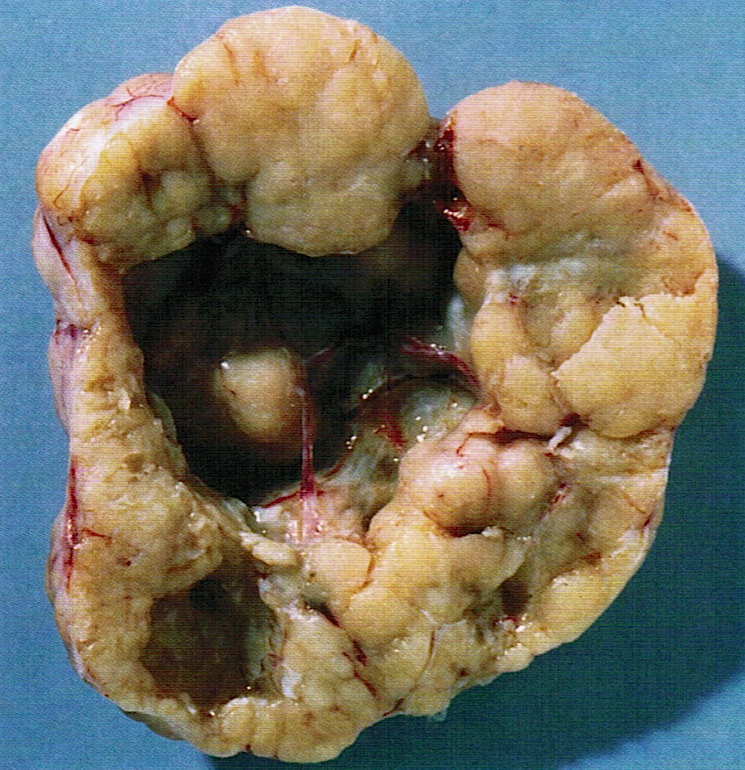
Gross description
- Firm, nodular swellings of the fallopian tube, ranging in size up to 2 cm in greatest dimension (Br J Radiol 2021;94:20201386)
- May be unilateral or bilateral
- Smooth, intact serosal covering
- Cross section of the nodules reveal gray, yellow or brown tissue punctuated by small cysts that surround the original tubal lumen (StatPearls: Salpingitis Isthmica Nodosa [Accessed 22 June 2023])
- Nodosity of the isthmus may give the uterus a horned appearance
Gross images
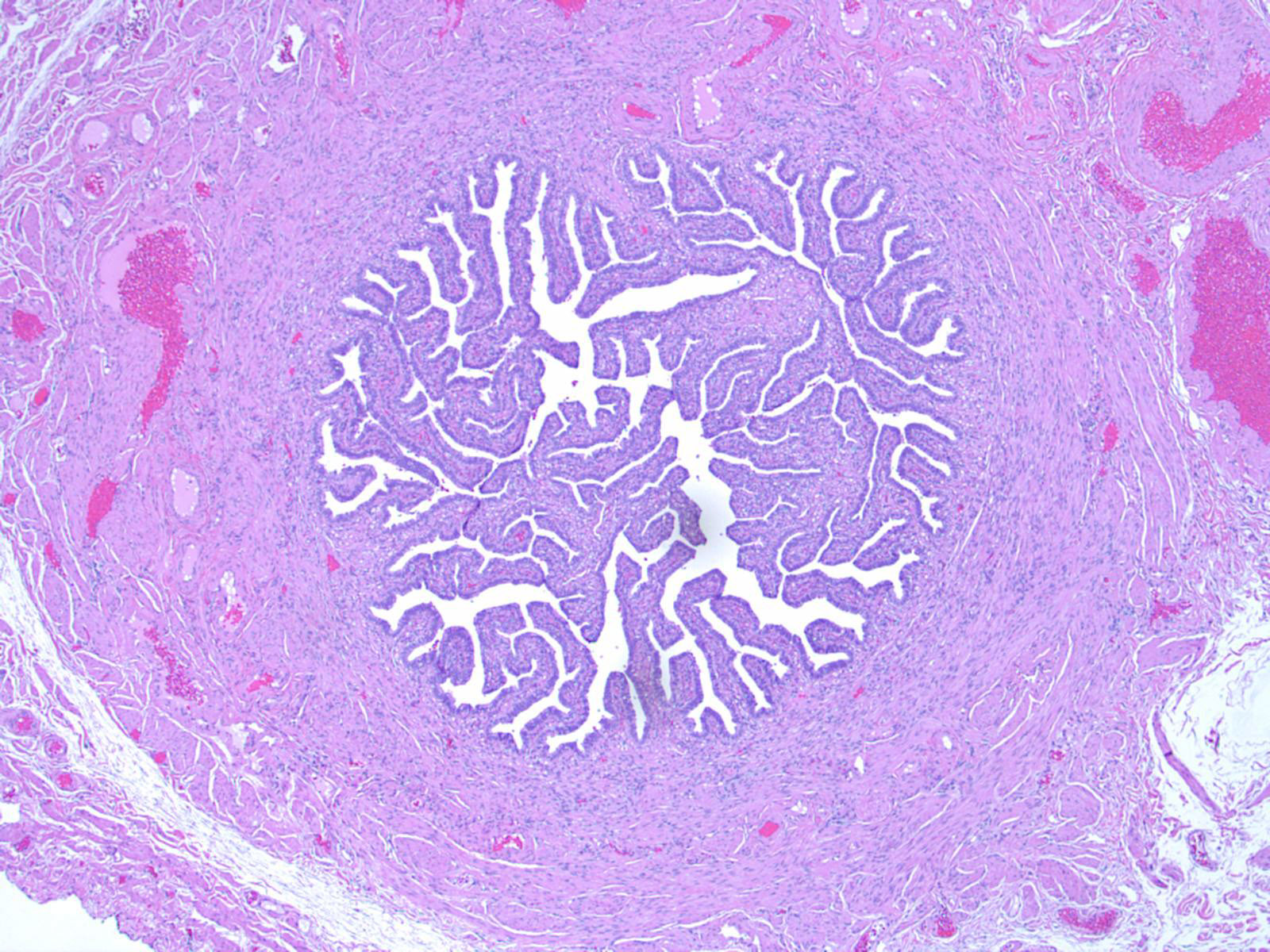
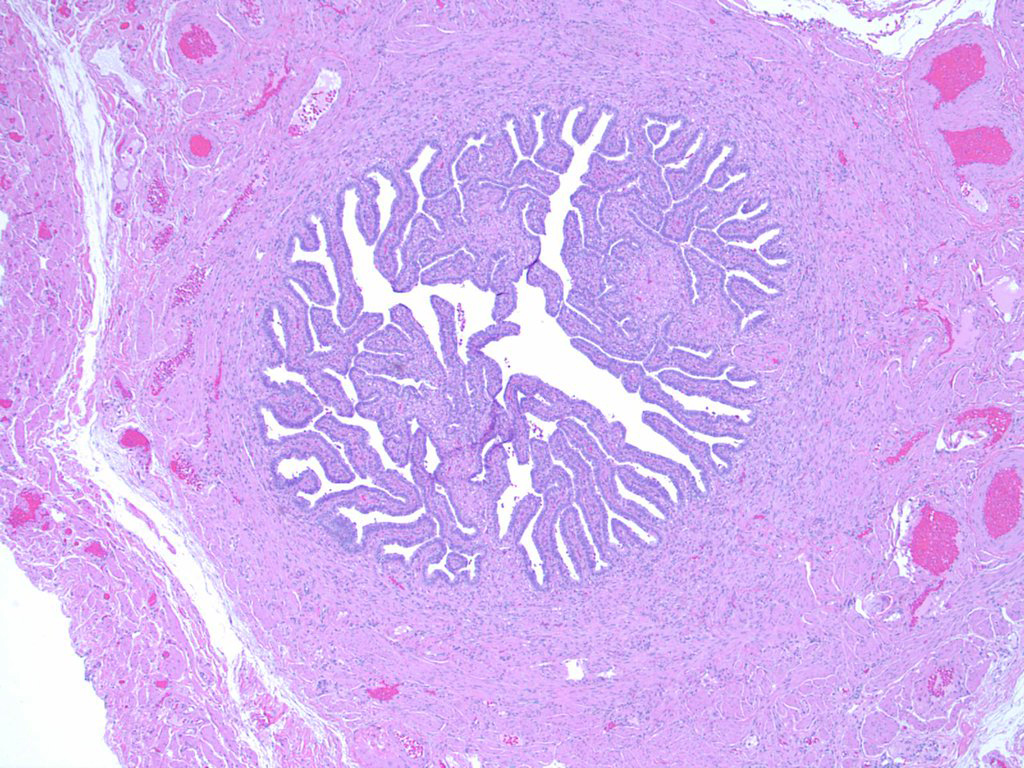
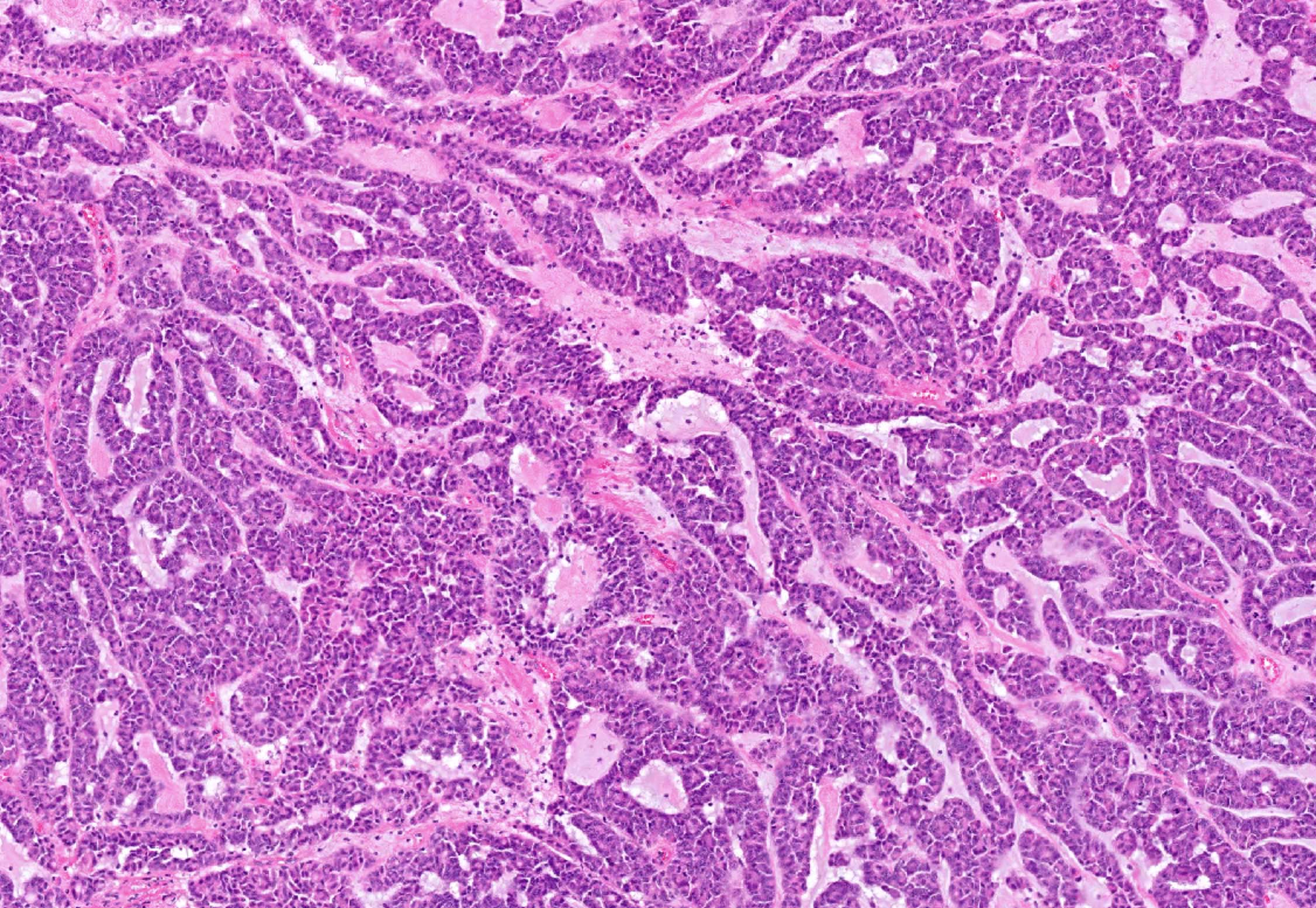
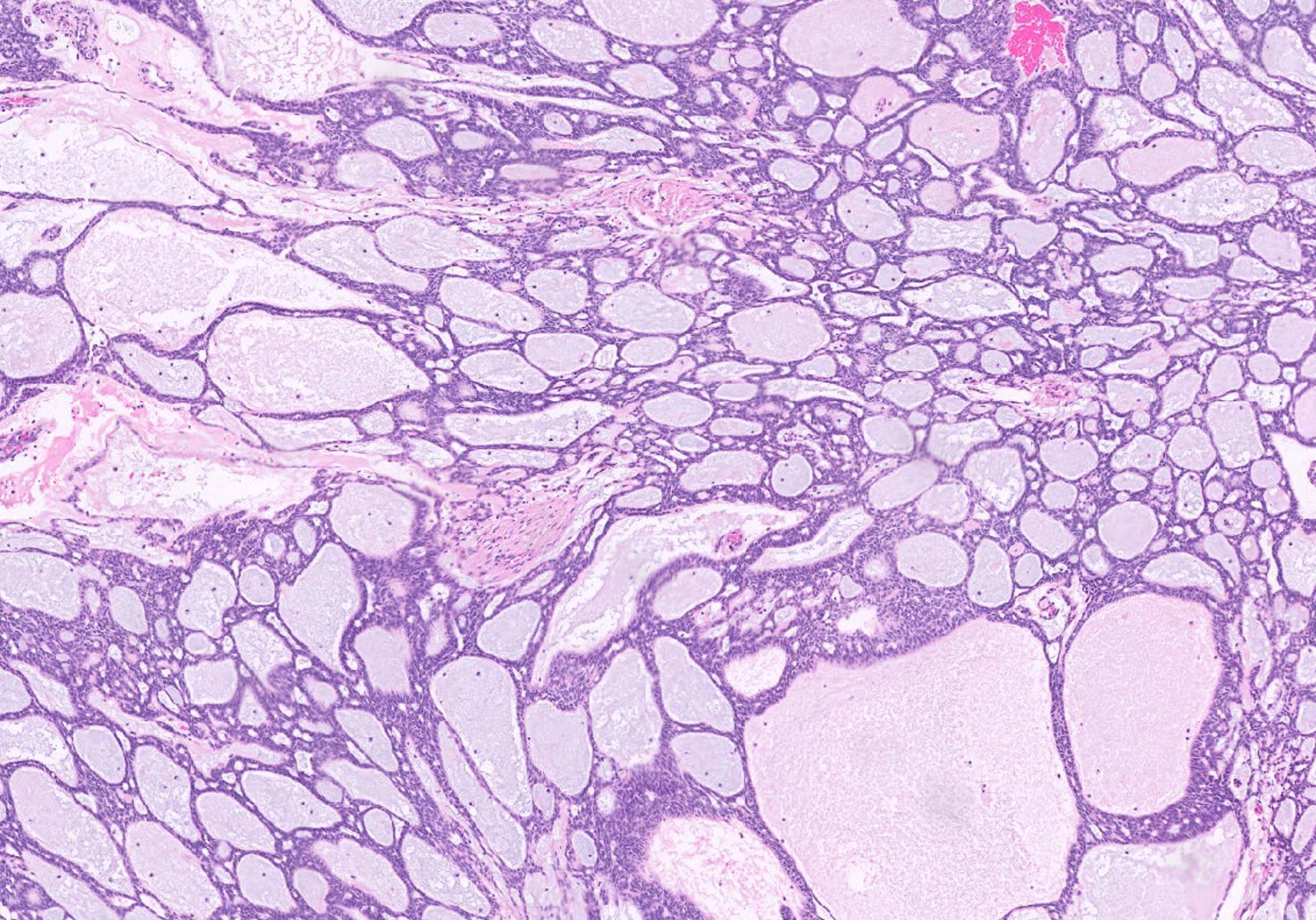
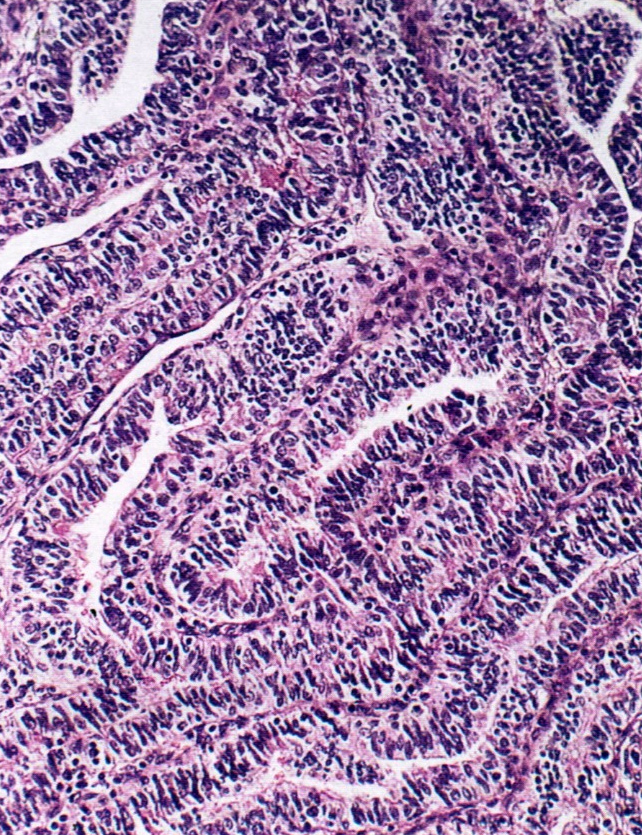
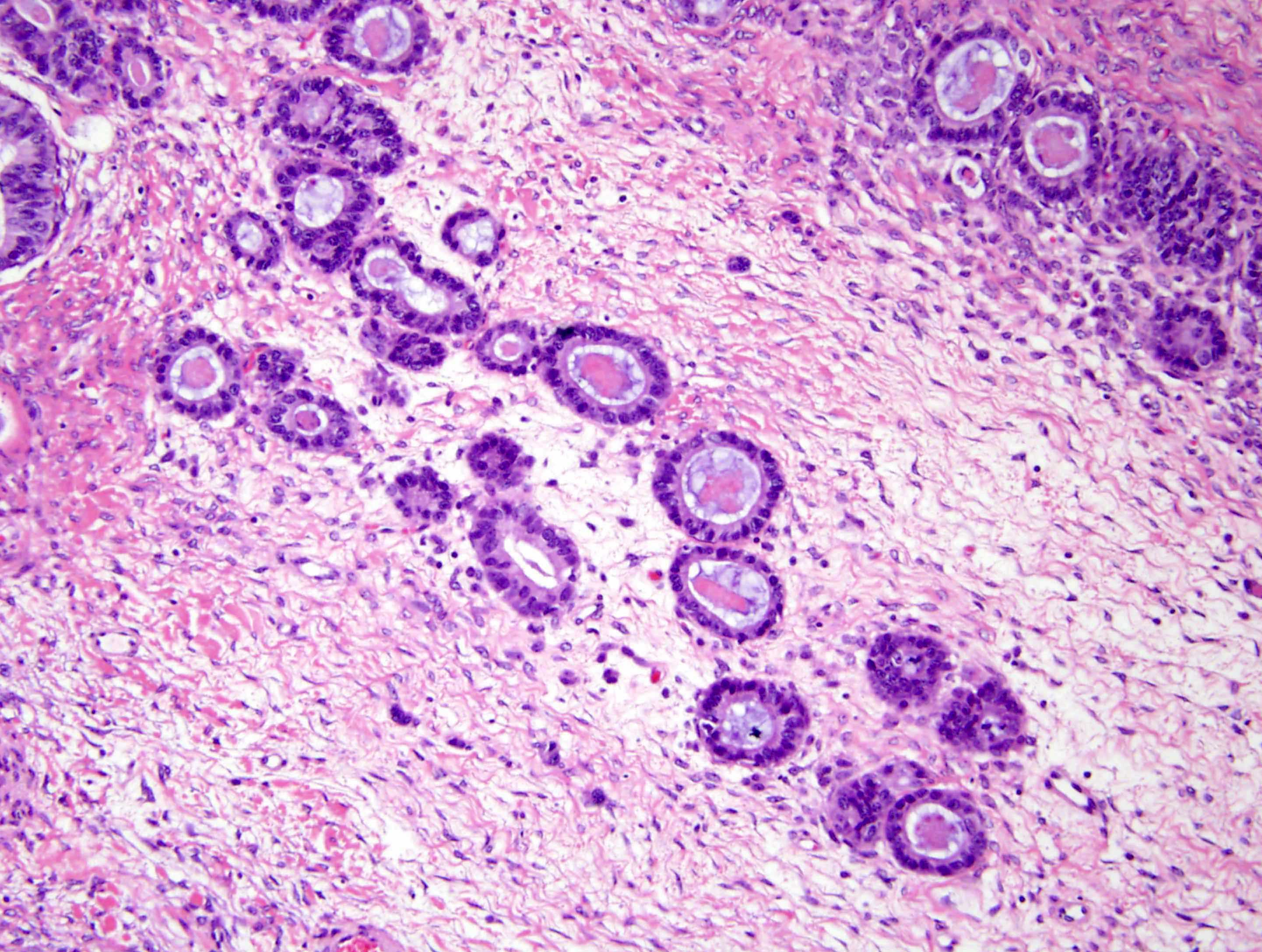
Microscopic (histologic) description
- Regularly spaced glands lined by normal appearing tubal epithelium surrounded by smooth muscle or fibrous tissue
- Tubal lumina are true diverticula that communicate with the central tubal lumen but do not connect with the serosa
- Glands can become cystically dilated (Am J Clin Pathol 1951;21:212)
- No significant atypia, scarring or associated inflammatory / stromal response
- Absence of endometrial stroma differentiates this entity from tubal endometriosis
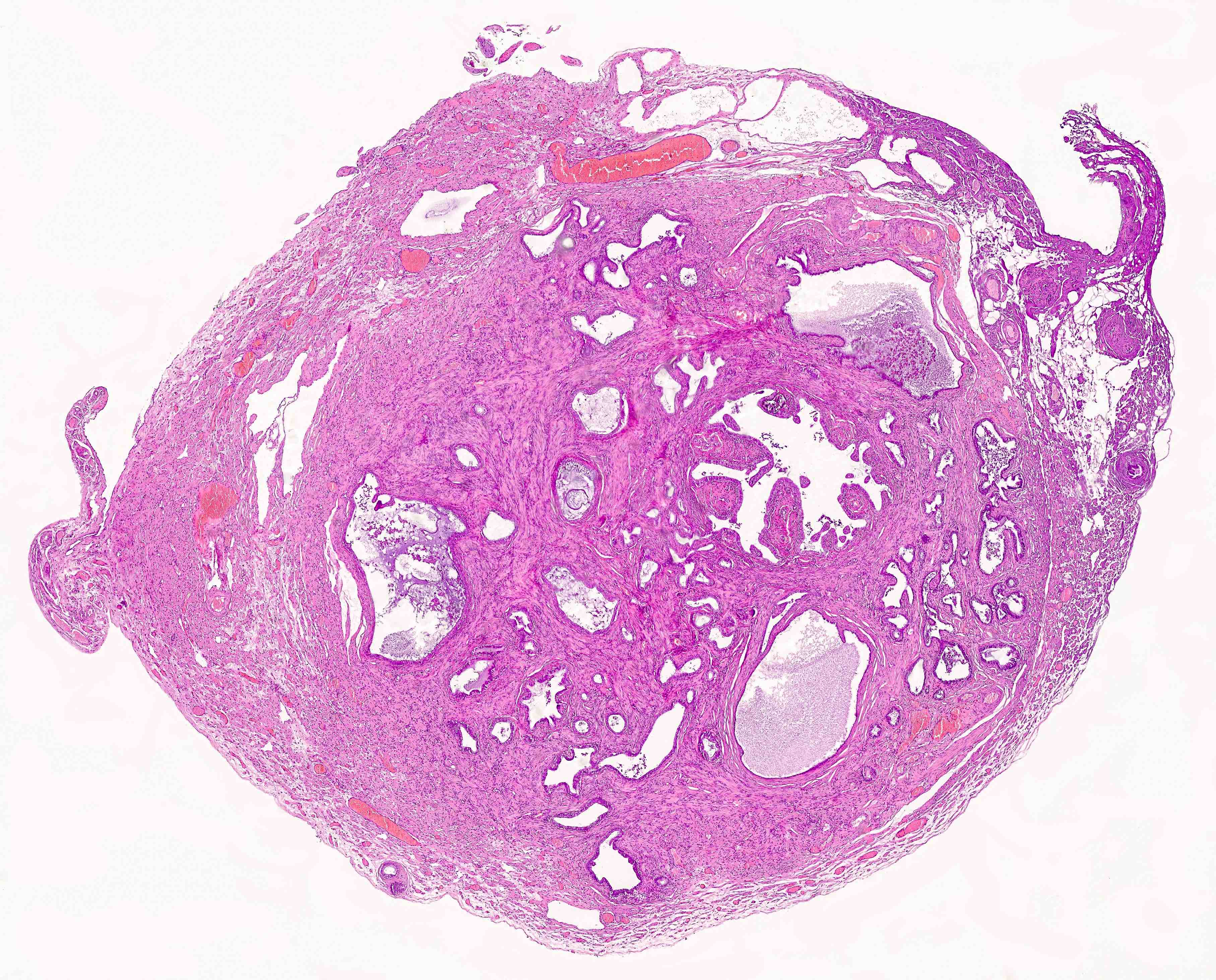
Microscopic (histologic) images
Sample pathology report
- Right fallopian tube, salpingectomy:
- Salpingitis isthmica nodosa
Differential diagnosis
- Endometriosis:
- Glands are surrounded by endometrial stroma with or without hemosiderin laden macrophages
- Adenocarcinoma:
- Desmoplastic or inflammatory response and prominent cytologic atypia
- Adenomatoid tumor:
- Slit-like glands with thin, tapered septa lined by bland flattened to cuboidal cells
Additional references
Board review style question #1
What is the most common clinical sequela associated with salpingitis isthmica nodosa?
- Ectopic pregnancy
- Endometrioid adenocarcinoma
- Endometriosis
- Fitz-Hugh-Curtis syndrome
- Serous tubal intraepithelial carcinoma (STIC)
Board review style answer #1
A. Ectopic pregnancy. The most commonly documented and reported clinical sequela of salpingitis isthmica nodosa (SIN) is ectopic pregnancy. Answers E and B are incorrect because SIN is not a premalignant or malignant lesion. Answer C is incorrect because endometriosis is not a known clinical consequence of SIN. Answer D is incorrect because Fitz-Hugh-Curtis syndrome results from pelvic inflammatory disease, which may be seen in patients with SIN.
Comment Here
Reference: Salpingitis isthmica nodosa
Comment Here
Reference: Salpingitis isthmica nodosa
Board review style question #2
A 48 year old woman with a history of infertility undergoes a hysterectomy with bilateral salpingectomy for abnormal uterine bleeding. What is the most likely diagnosis in her right fallopian tube?
- Endometrioid adenocarcinoma
- Endometriosis
- Endosalpingiosis
- Salpingitis isthmica nodosa (SIN)
- Serous cystadenofibroma
Board review style answer #2
D. Salpingitis isthmica nodosa (SIN). SIN is the correct answer with multiple cystically dilated glands in the muscular wall of the tube and is common in patients with a history of infertility. Answer A is incorrect because endometrioid adenocarcinoma will have nuclear atypia and glandular complexity. Answer B is incorrect because endometriosis may appear as dilated glands in the muscular wall but will contain surrounding endometrial stroma, differentiating this entity from SIN (which does not contain associated endometrial stroma). Answer C is incorrect because endosalpingiosis is usually found in the peritoneum. Answer E is incorrect because serous cystadenofibroma will be grossly described as a cystic mass lesion, more commonly found on the ovary.
Comment Here
Reference: Salpingitis isthmica nodosa
Comment Here
Reference: Salpingitis isthmica nodosa
Serous adenofibroma and papilloma
Definition / general
- Similar to ovarian counterpart
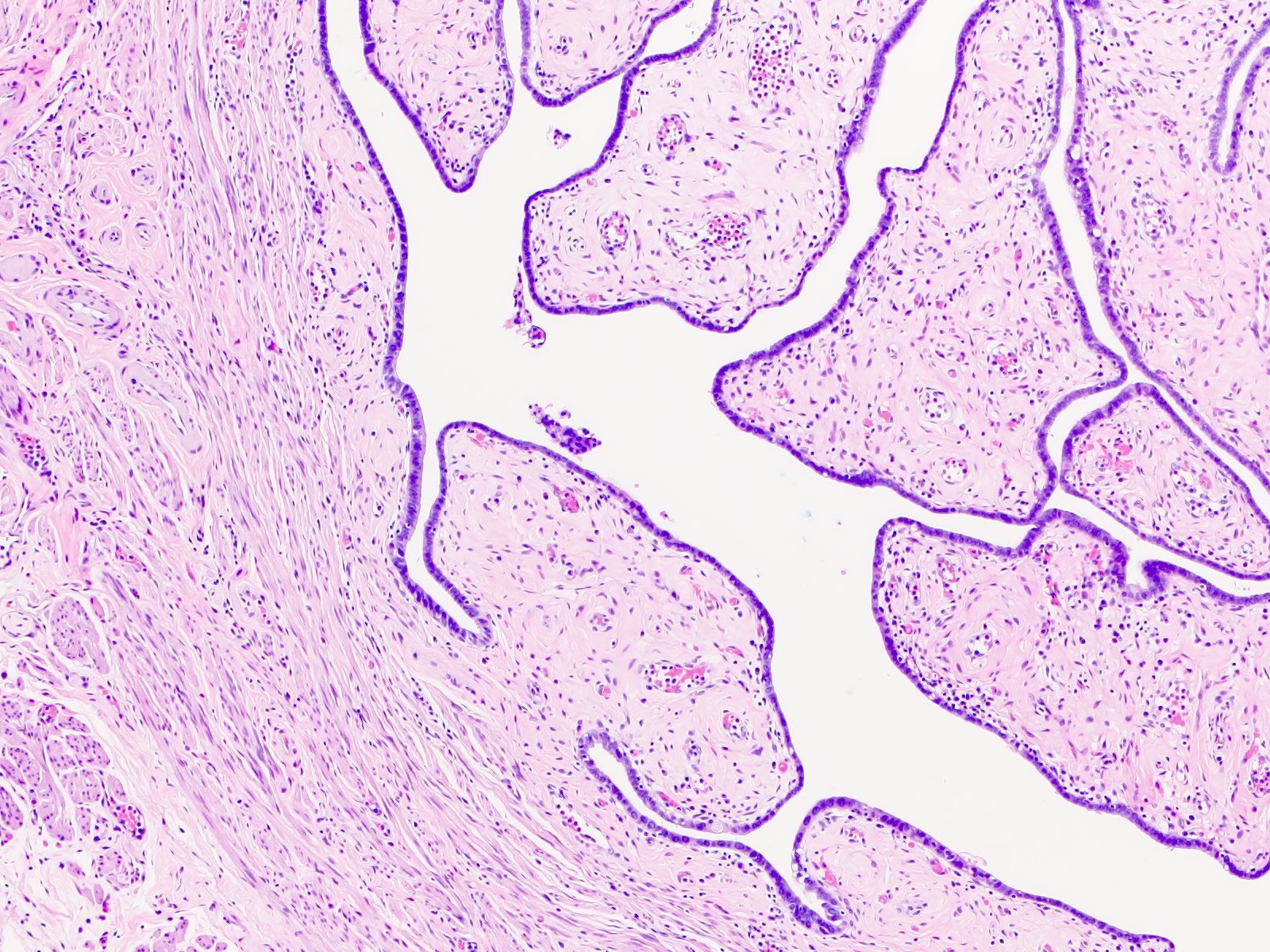
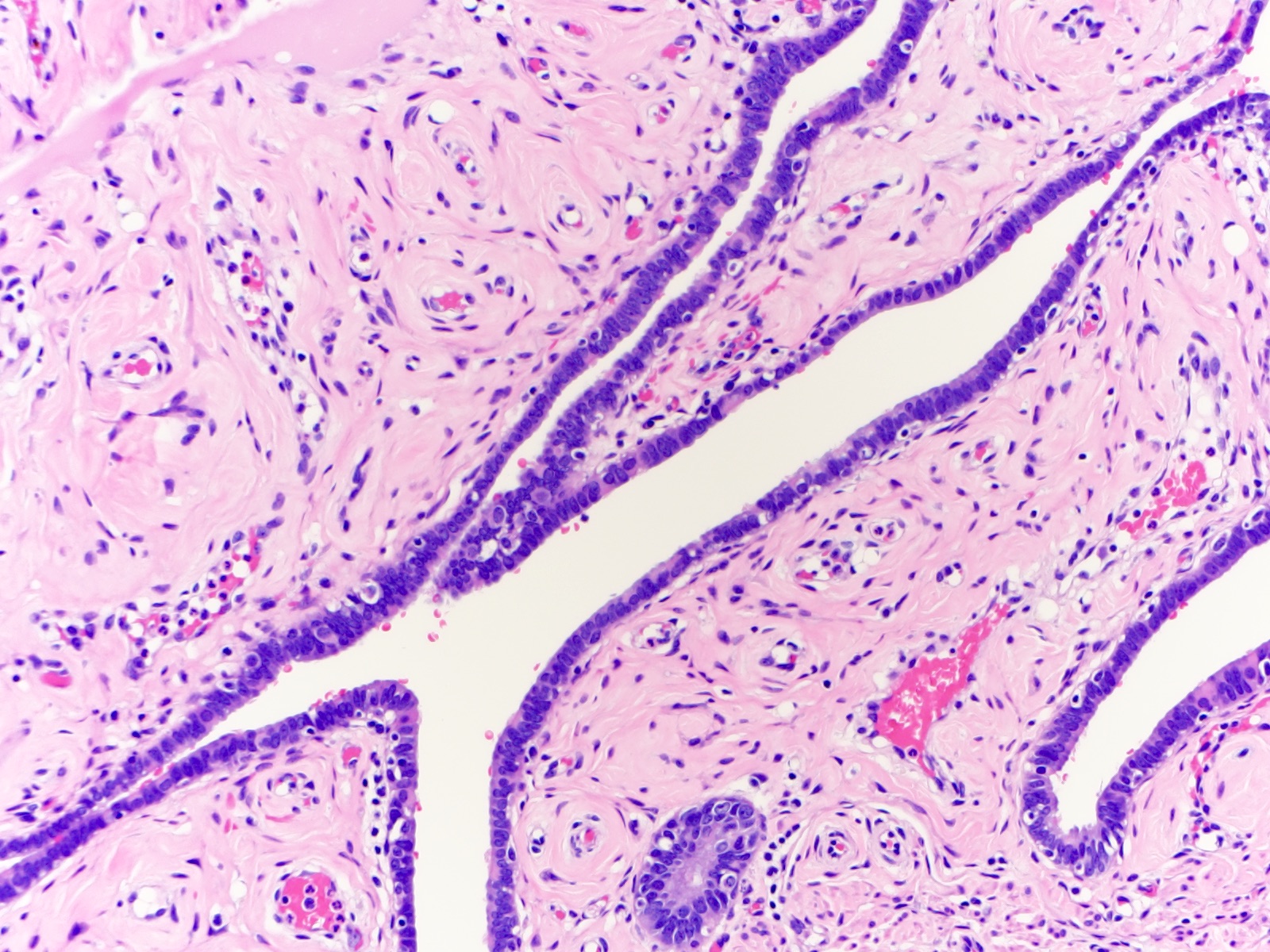
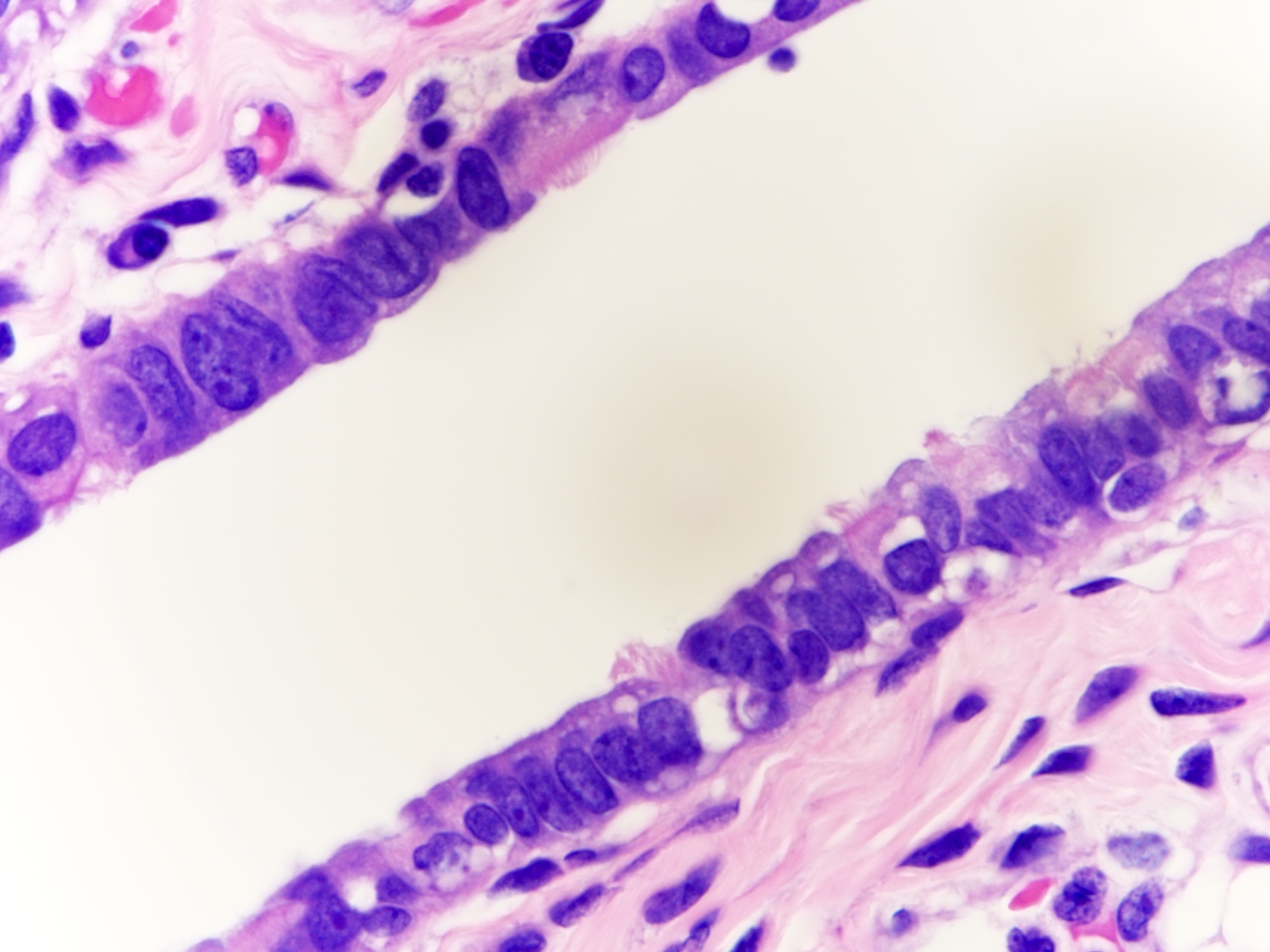
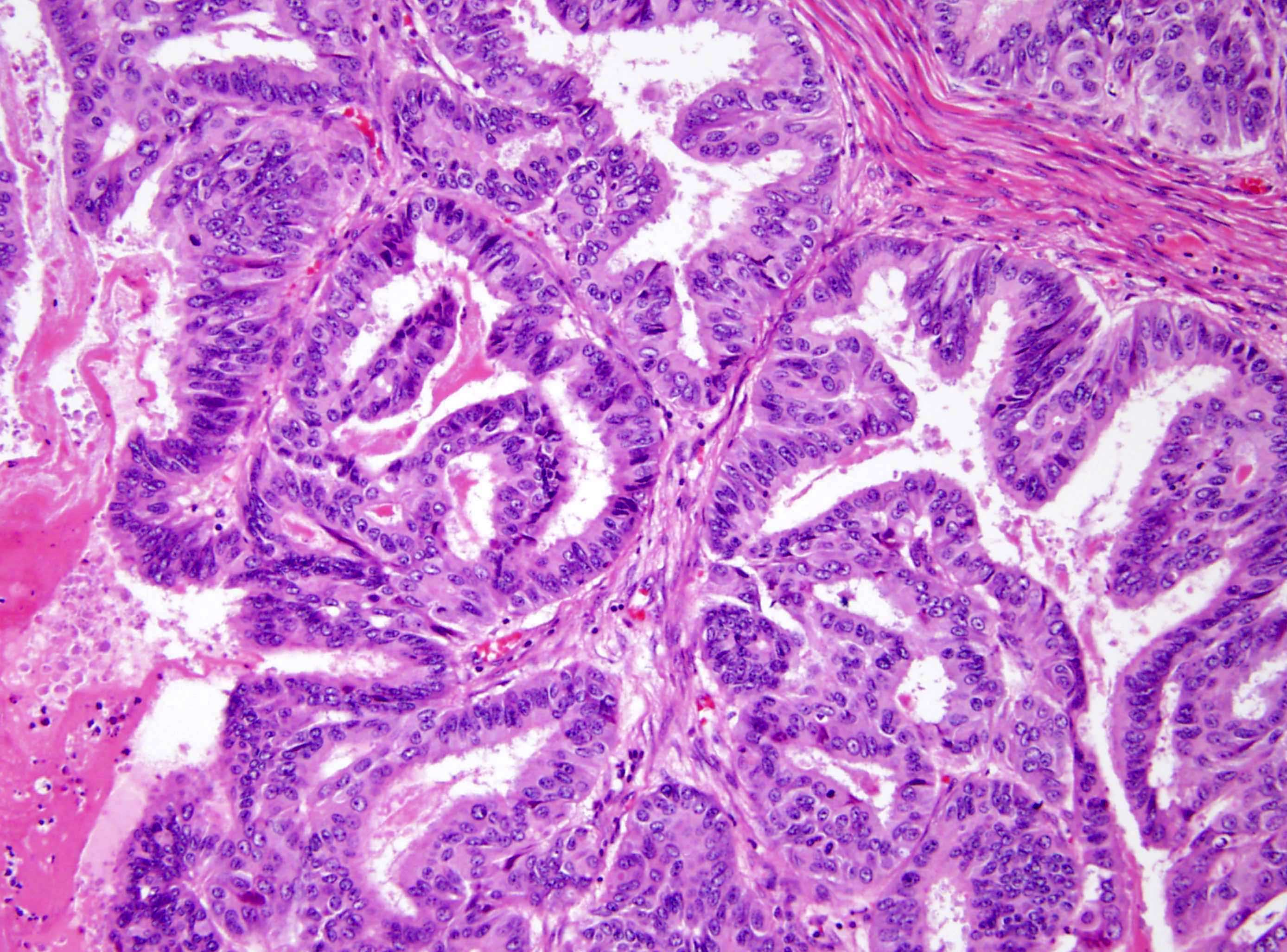
Serous borderline tumor
Table of Contents
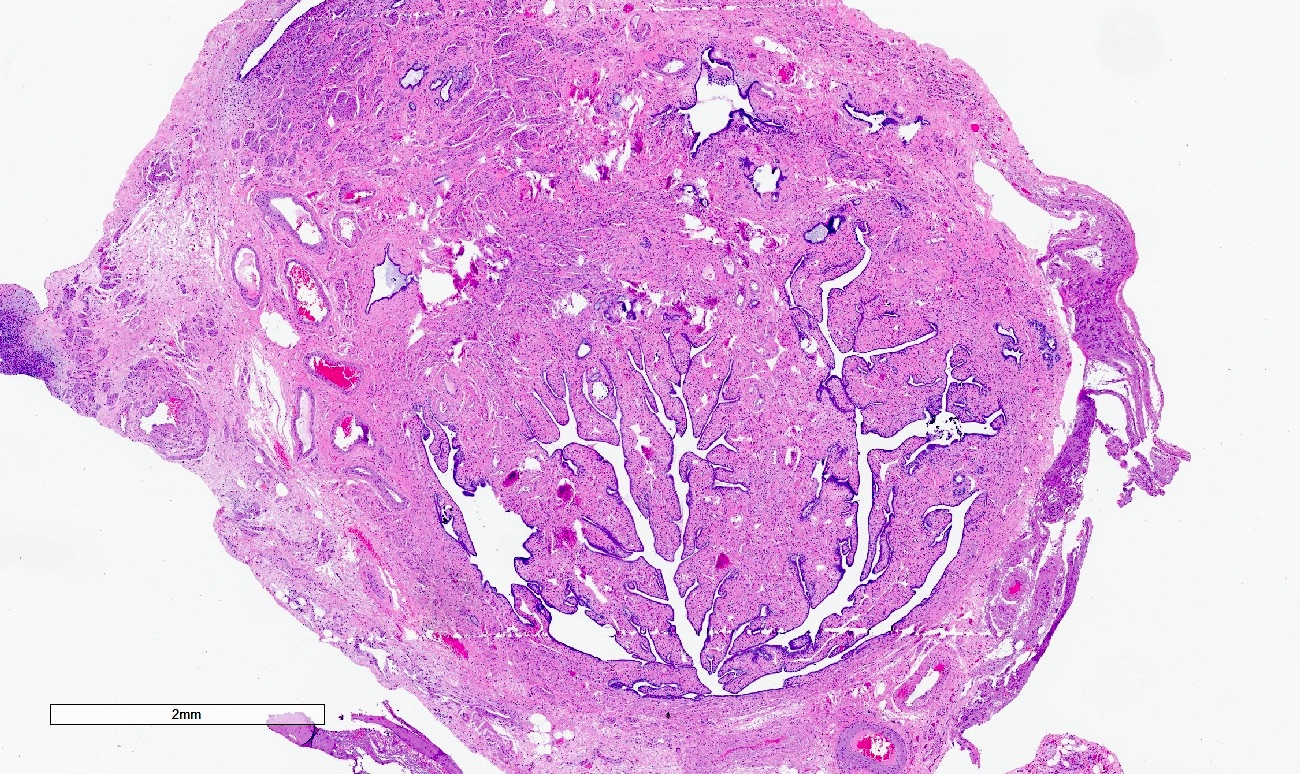
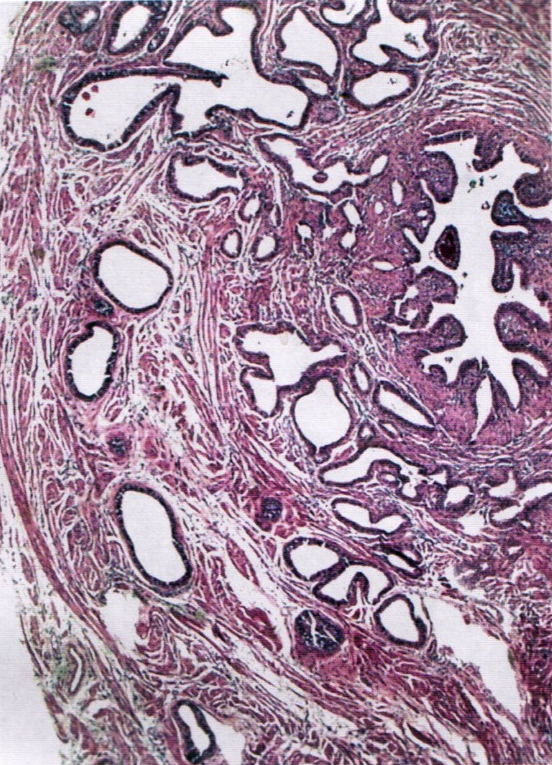
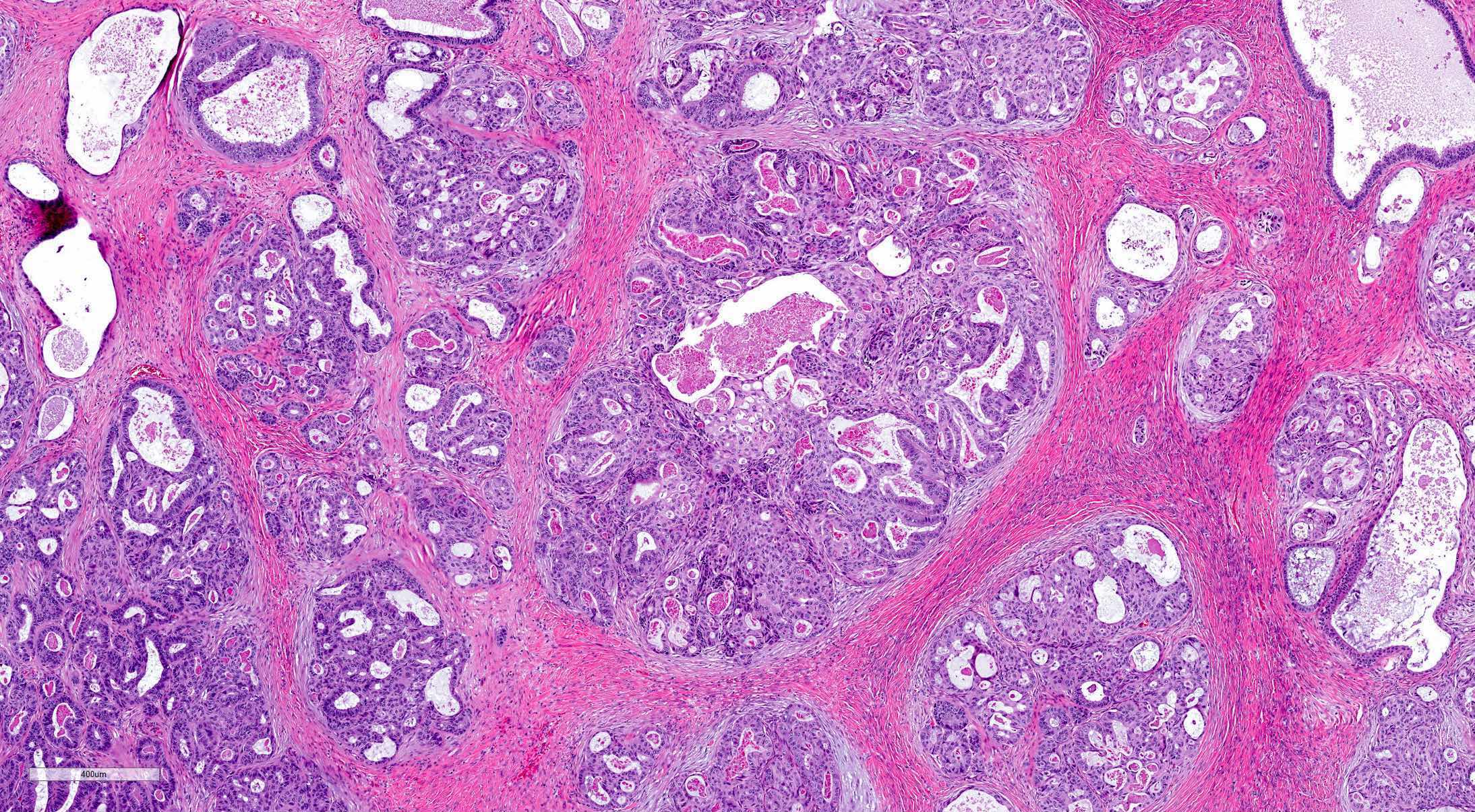
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Immunofluorescence description | Immunofluorescence images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Definition / general
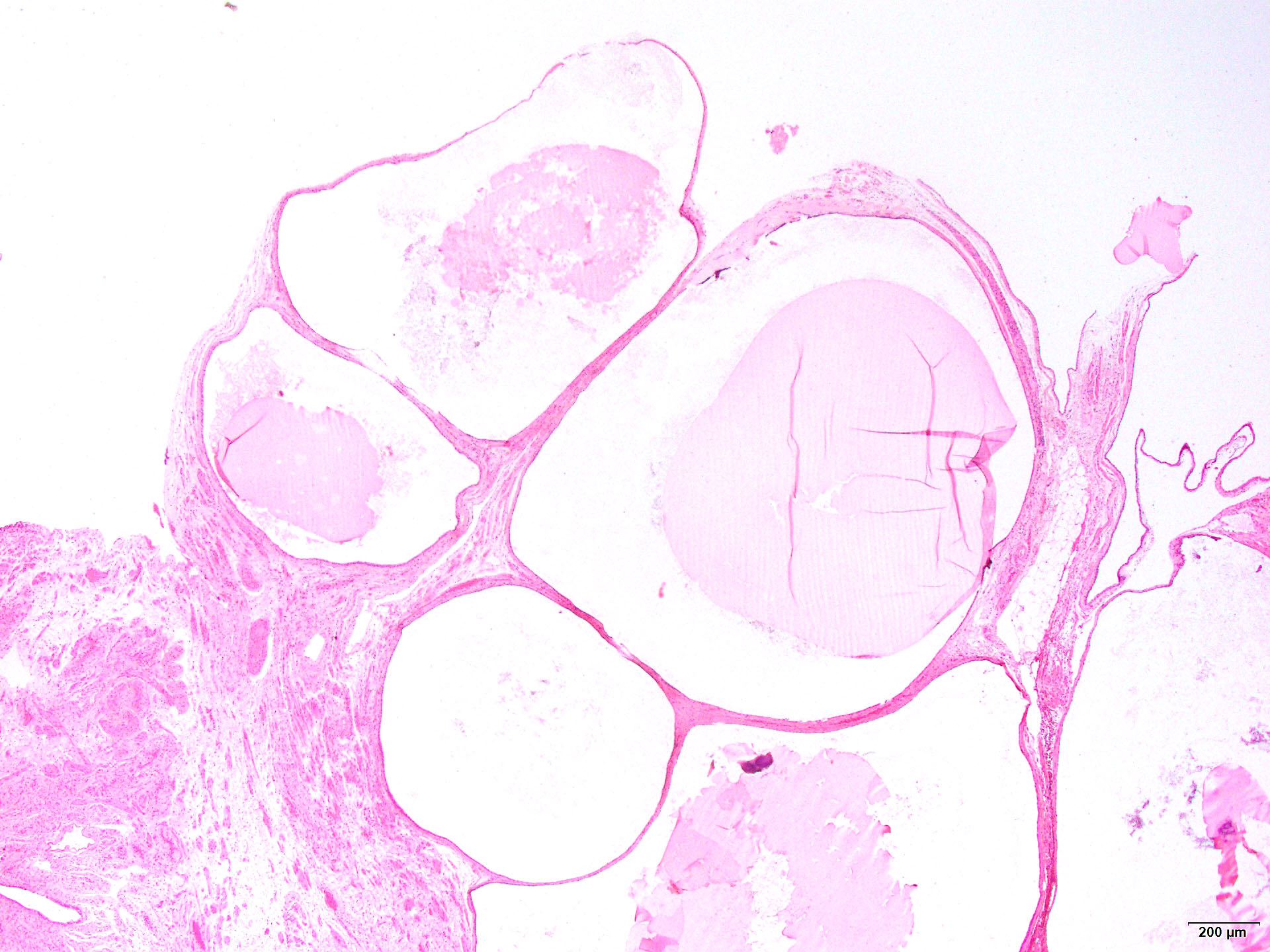
- Serous borderline tumor (SBT) of the fallopian tube is a proliferative epithelial neoplasm that is by definition noninvasive (Pan Afr Med J 2019;32:129)
Essential features
- Serous borderline tumor arising in the fallopian tube is a rare entity with fewer than 20 cases in the literature
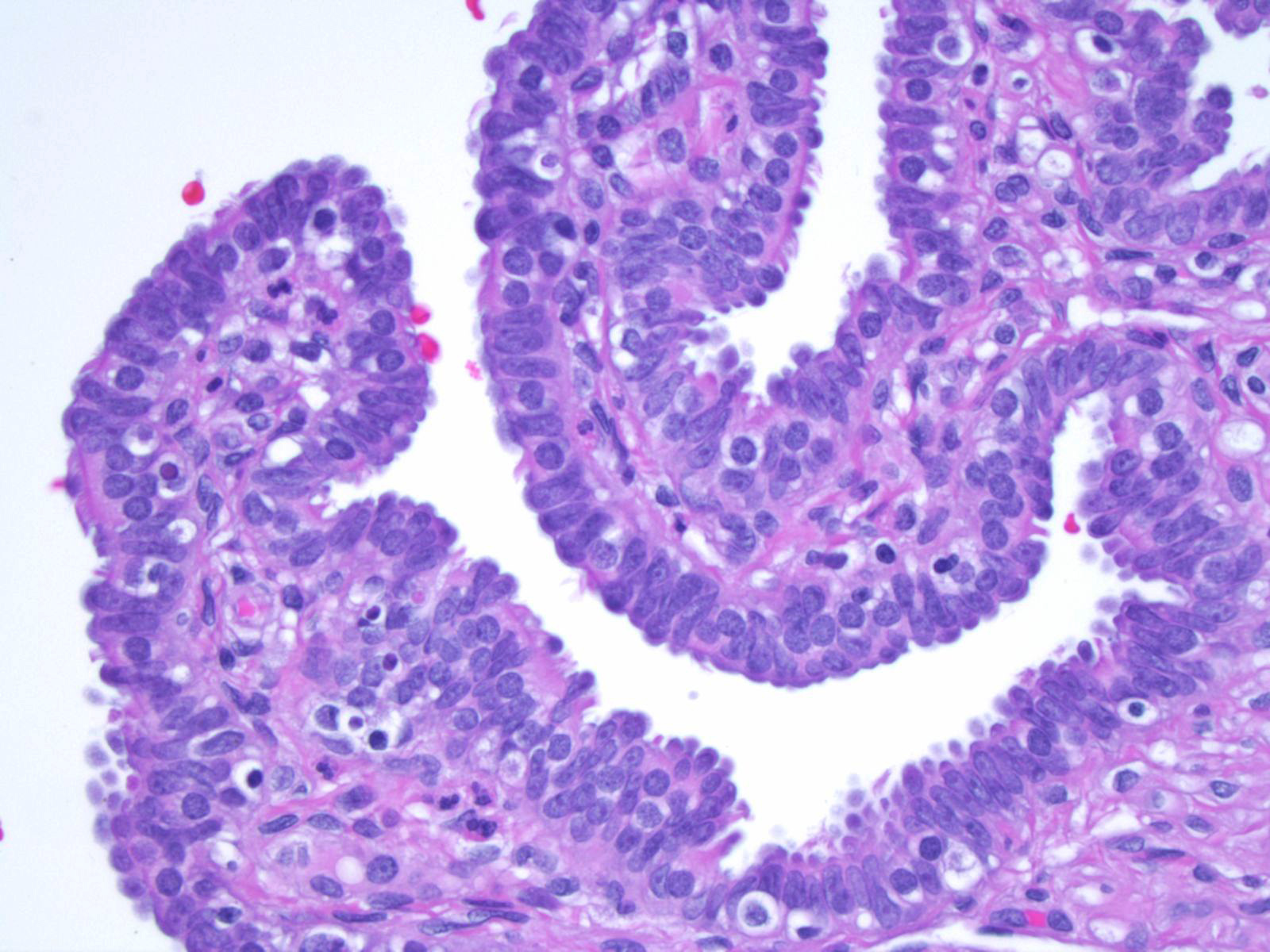
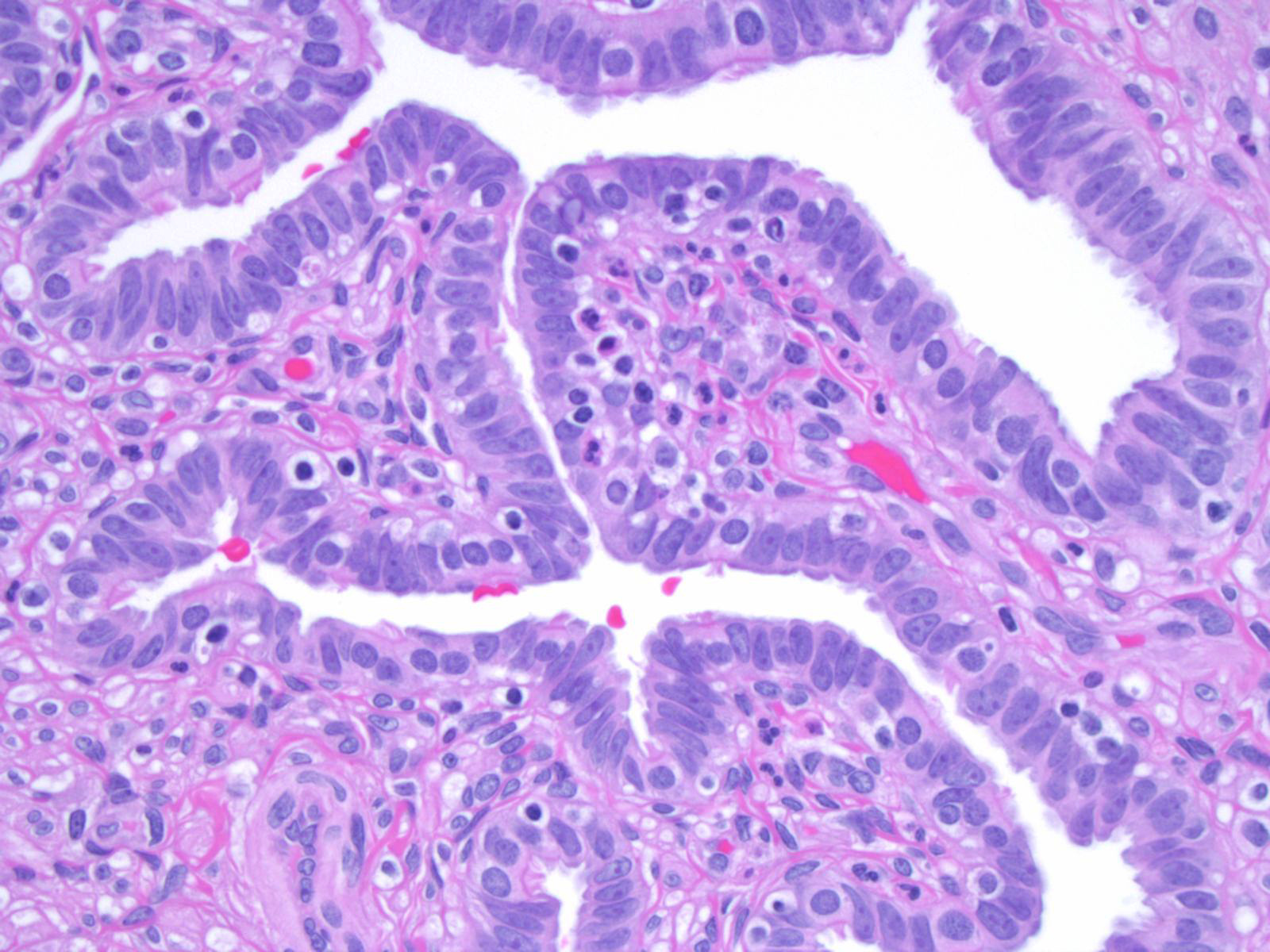
- Microscopically similar to SBT arising in the ovary, with numerous papillae of varying size arborizing down to smaller papillae
- Hobnailing may also be present
Terminology
- Serous borderline tumor is currently the sole recommended term for primary fallopian tumors
- Not recommended: atypical proliferative serous tumor (Am J Surg Pathol 2011;35:1605)
ICD coding
- ICD-O: 8442/1 - serous borderline tumor, NOS
- ICD-11: 2C74.Y & XH3ZK9 - other specified malignant neoplasms of fallopian tube & serous cystadenoma, borderline malignancy
Epidemiology
- Serous borderline tumor of the fallopian tube is a rare neoplasm with fewer than 20 cases reported in the literature (Arch Gynecol Obstet 2011;283:349)
- Age range is broad, from 22 to 83 years (BMC Cancer 2005;5:129)
Sites
- Fallopian tube
Pathophysiology
- Theorized to arise from papillary hyperplasia of the fallopian tube
- May similarly be related to BRAF V600E mutation as in serous borderline tumor of the ovary (J Natl Cancer Inst 2003;95:484)
Etiology
- Unknown
Diagrams / tables
NA
Clinical features
- Nonspecific, may be asymptomatic or may have abdominal pain (Obstet Gynecol Sci 2014;57:334)
Diagnosis
- Adnexal mass may be noted on routine gynecologic exam
- Ultrasound findings may reveal cystic mass near ovary
- On laparoscopy, dilated fallopian tube or hematosalpinx may be noted (BMC Cancer 2005;5:129)
Laboratory
- Generally, CA125 levels are normal (Pan Afr Med J 2019;32:129)
Radiology description
- Hypoechogenic cystic mass on ultrasound, sometimes with intramural papillary projections (Pan Afr Med J 2019;32:129)
Prognostic factors
- Prognosis is excellent with surgical removal (Clin Case Rep 2023;11:e7140)
Case reports
- 25 year old woman with lower abdominal pain and abdominal mass (Obstet Gynecol Sci 2014;57:334)
- 30 year old woman with a 1 year history of pelvic pain (Clin Case Rep 2023;11:e7140)
- 61 year old woman with a left fallopian paratubal cyst (Pan Afr Med J 2019;32:129)
Treatment
- Too few cases to determine optimal treatment, however, most commonly treated through conservative surgical management via salpingectomy or salpingo-oophorectomy for fertility preservation purposes
- At times includes hysterectomy for staging (Obstet Gynecol Sci 2014;57:334)
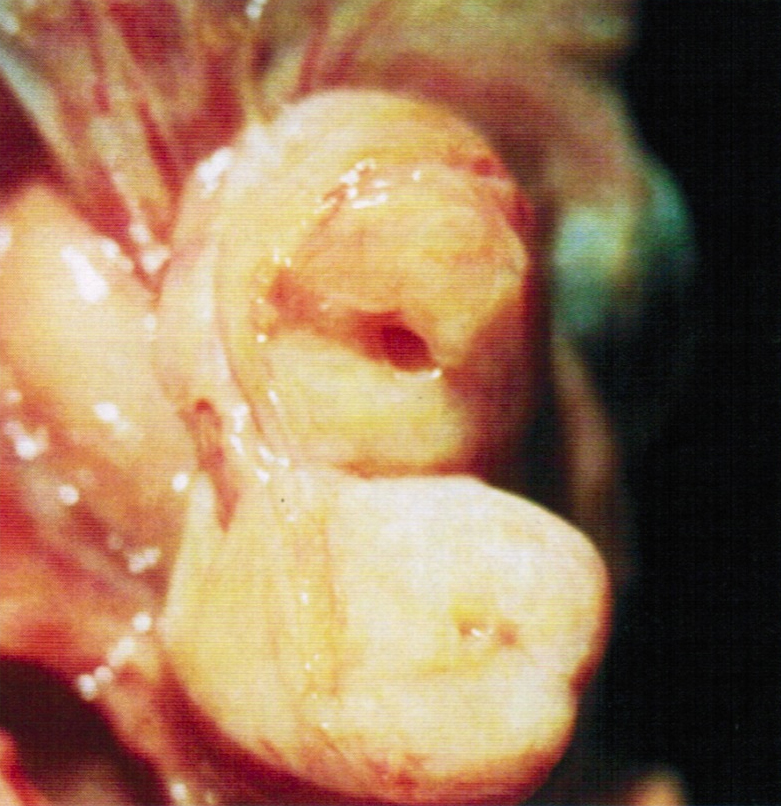
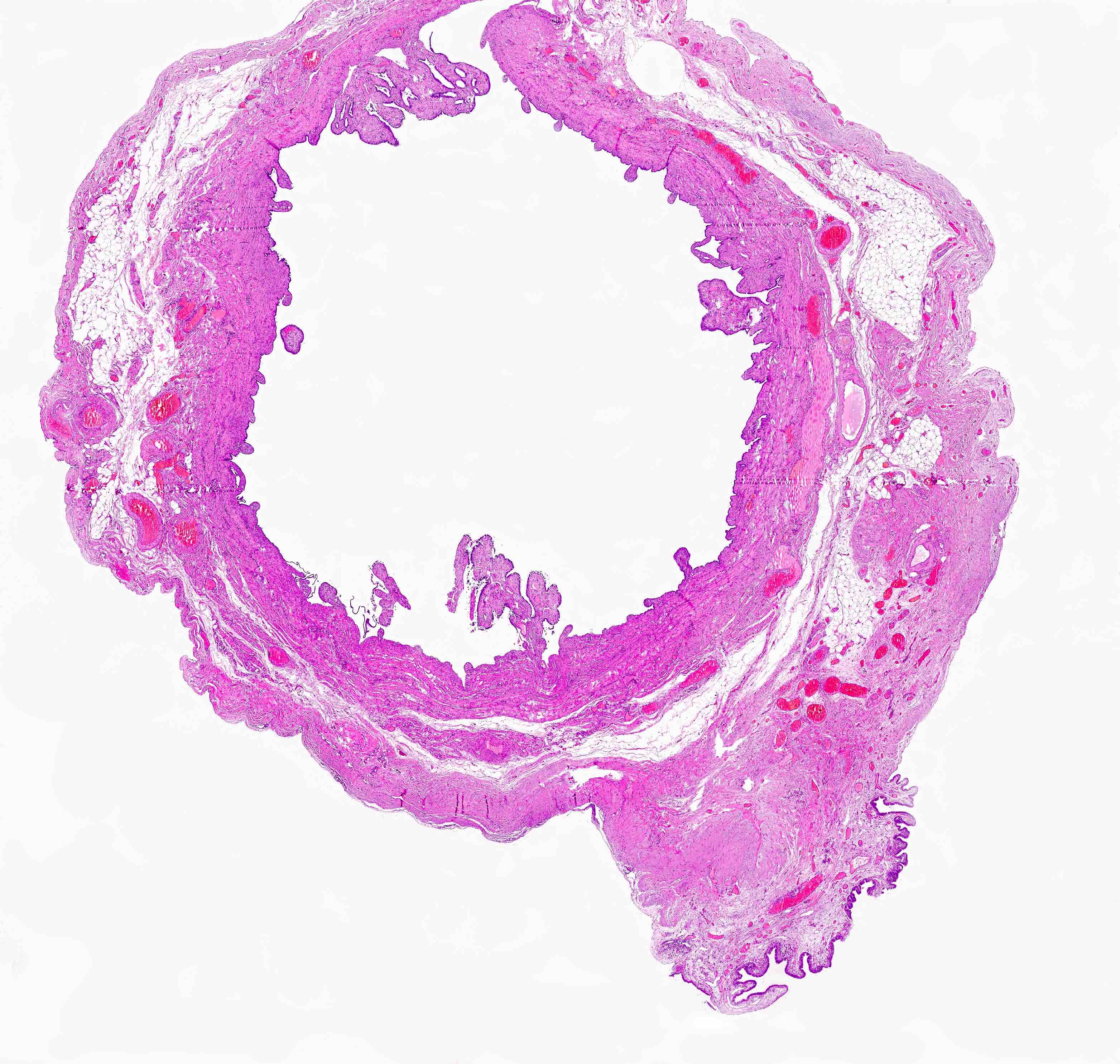
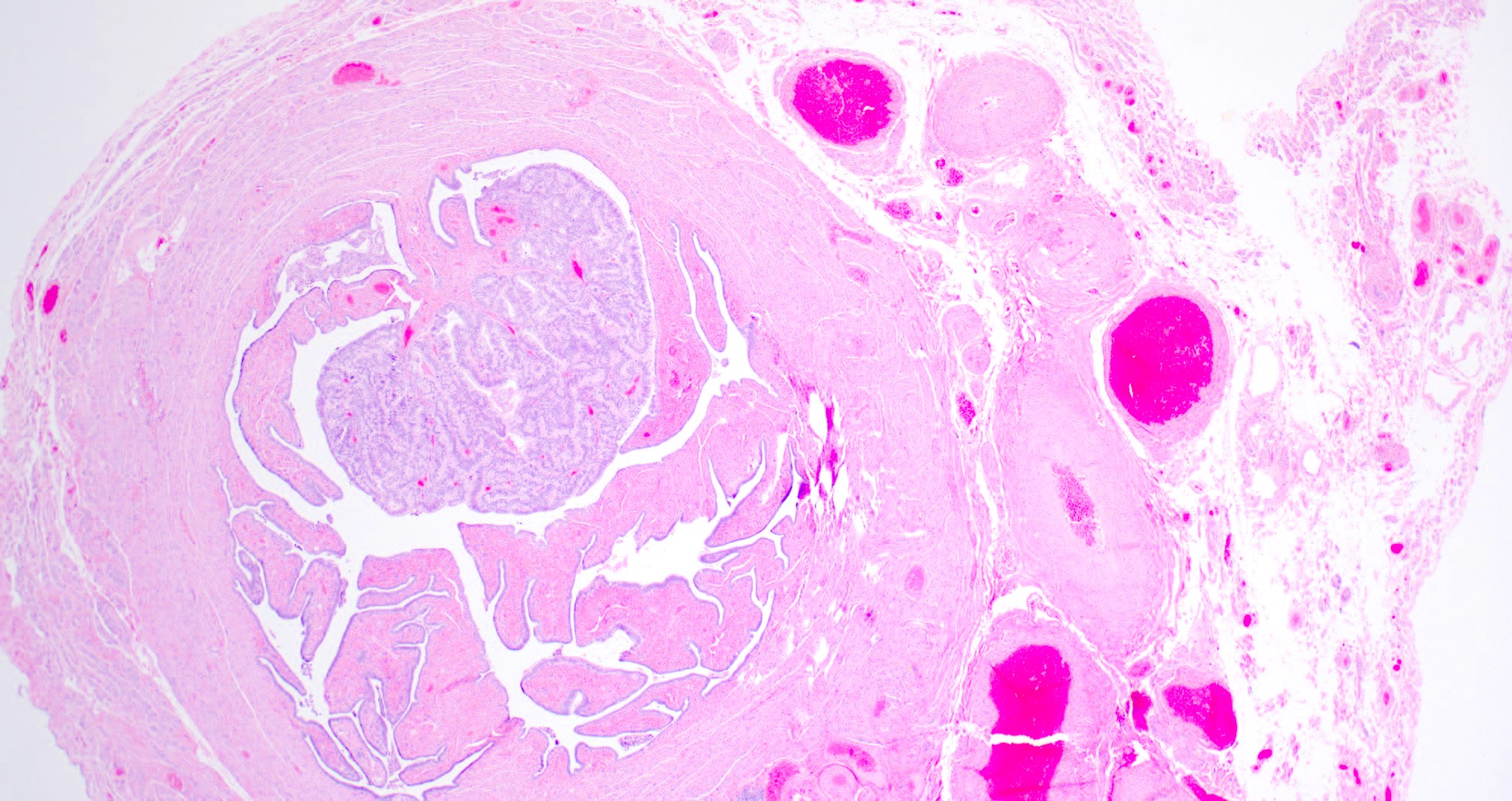
Gross description
- Received from surgery as cystic mass or distended fallopian tube
- Cut surface
- Multiloculated cystic mass
- Intralocular papillary projections
- Filled with serous fluid
Frozen section description
- Gross intraoperative evaluation
- Solid areas and papillary excrescences should be evaluated histologically
- Histologic intraoperative evaluation
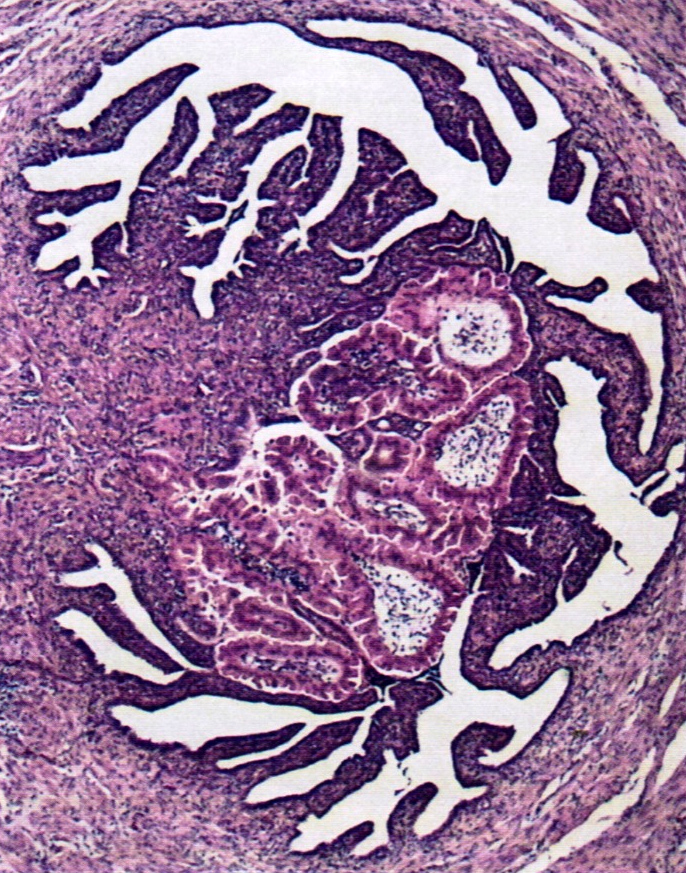
- Bulbous papillae branching into smaller papillae on lower power
- Hobnailing or epithelial tufting
- Comparable to serous borderline tumor of the ovary
Frozen section images
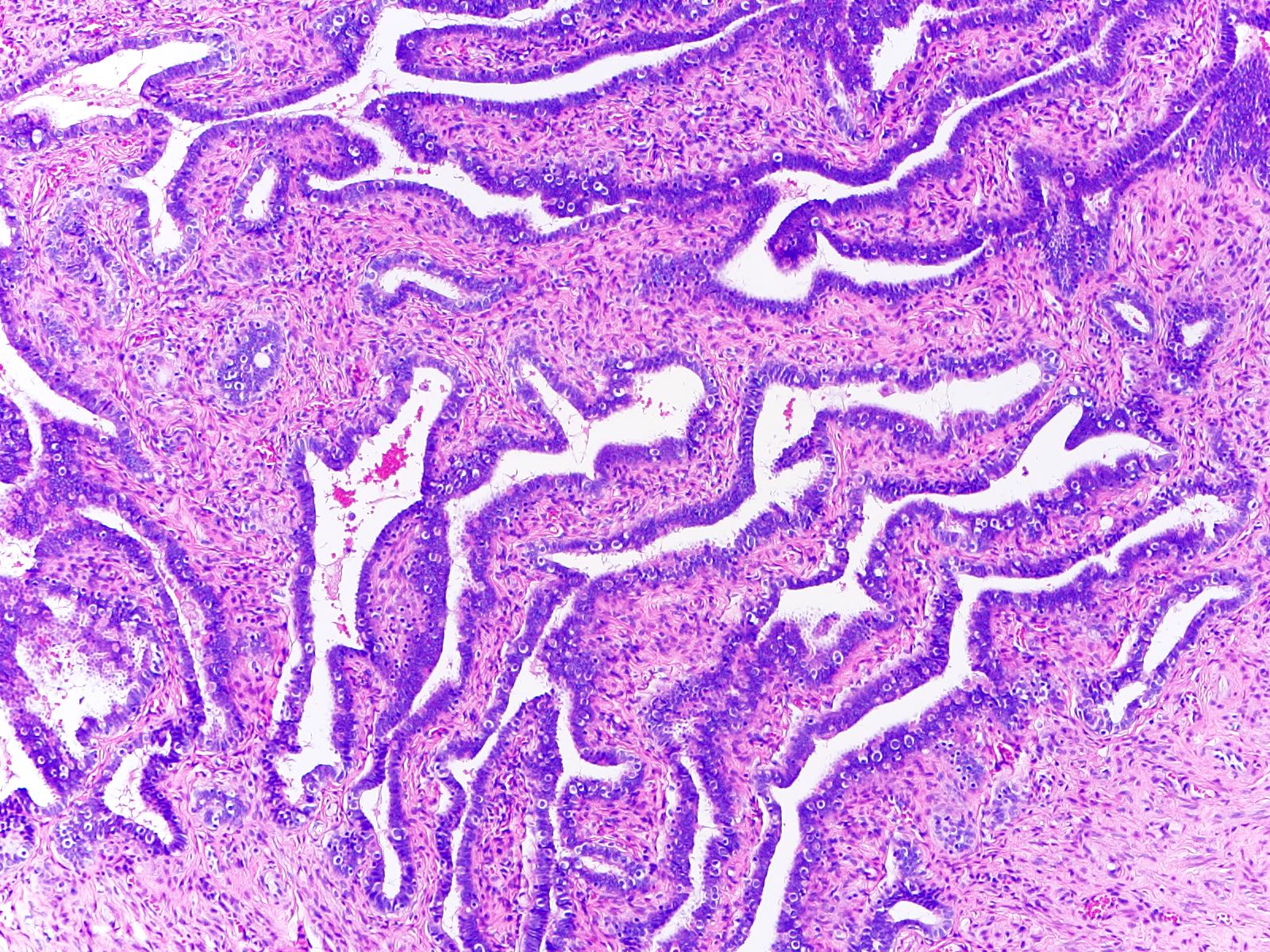
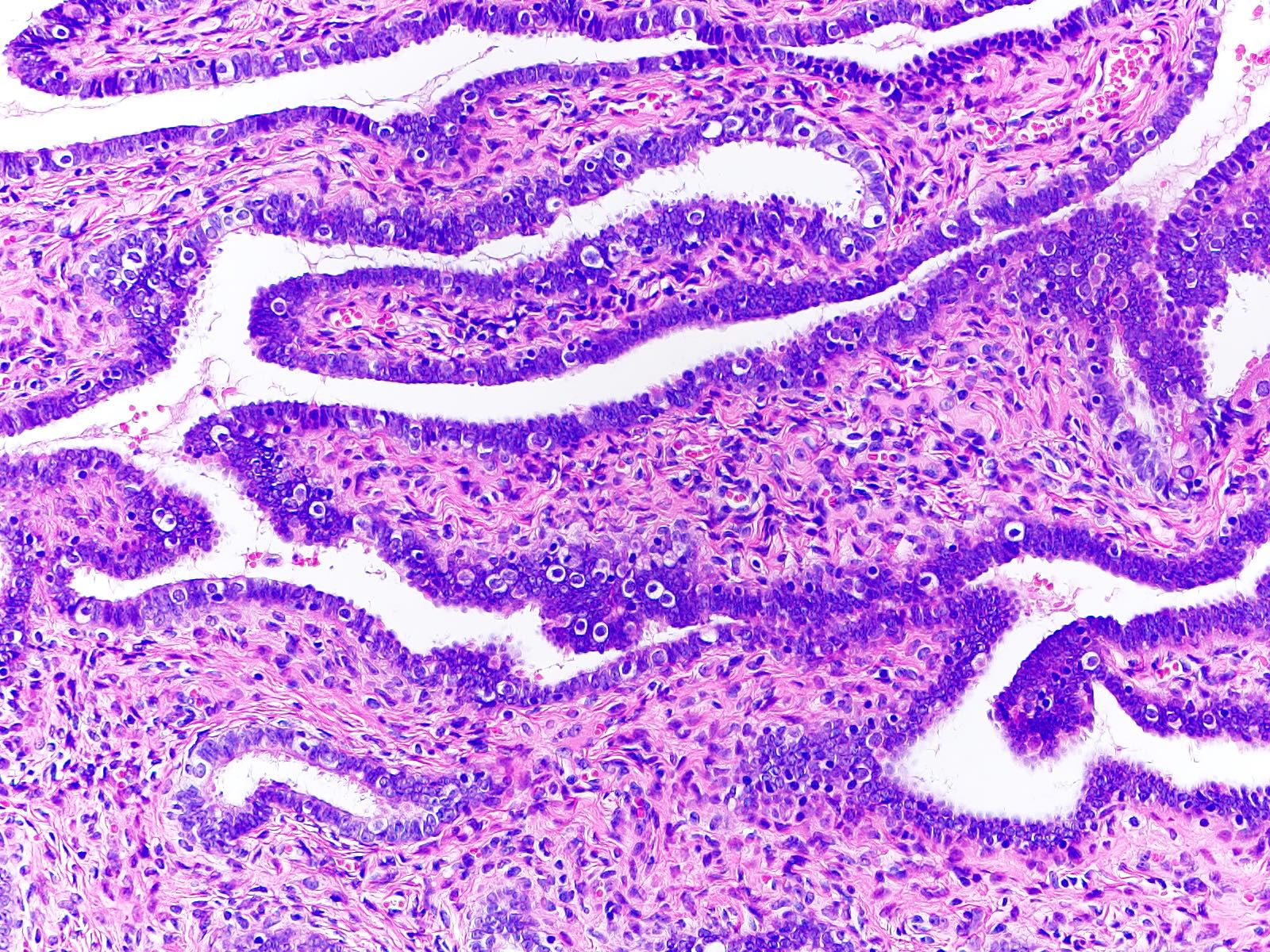
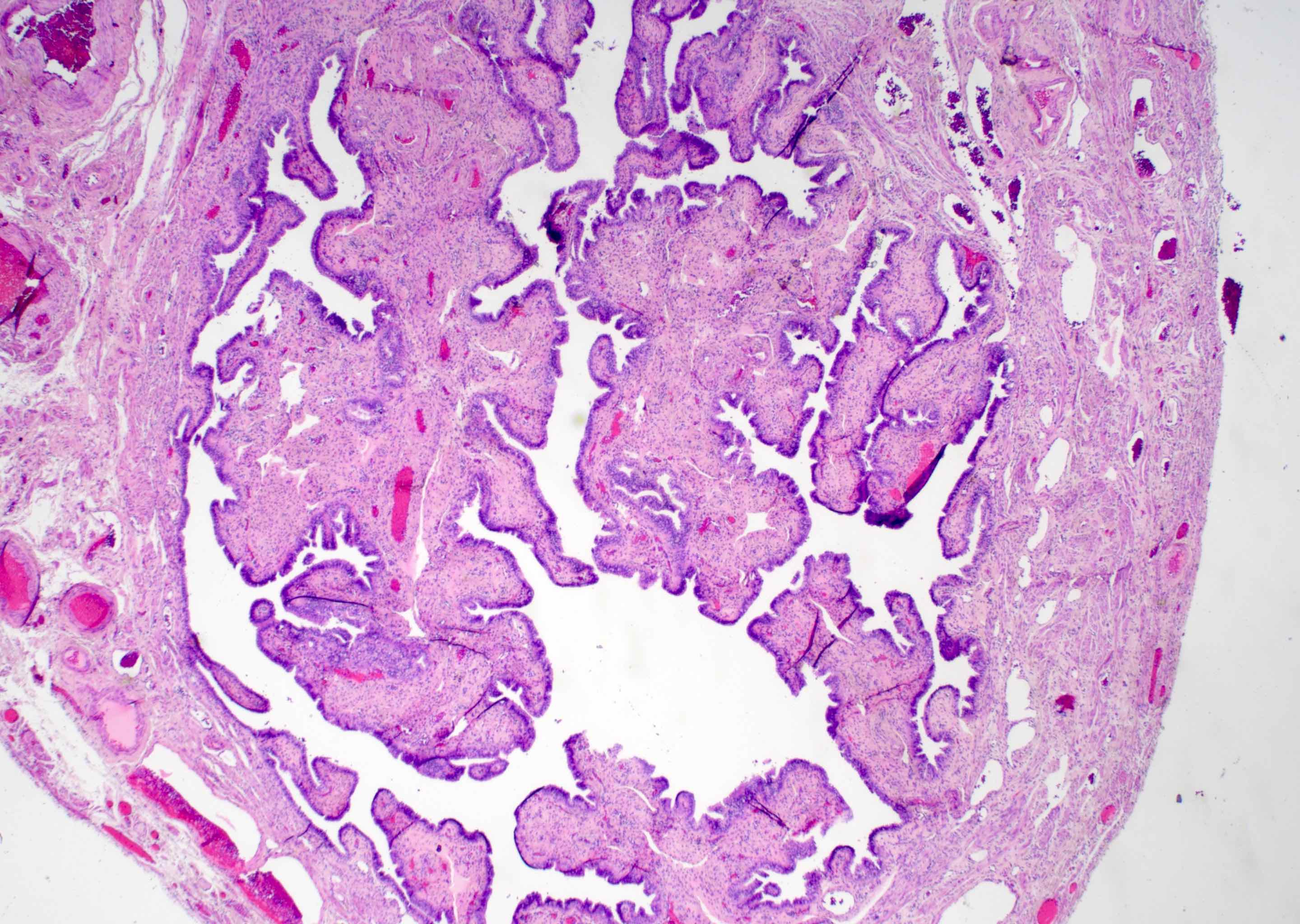
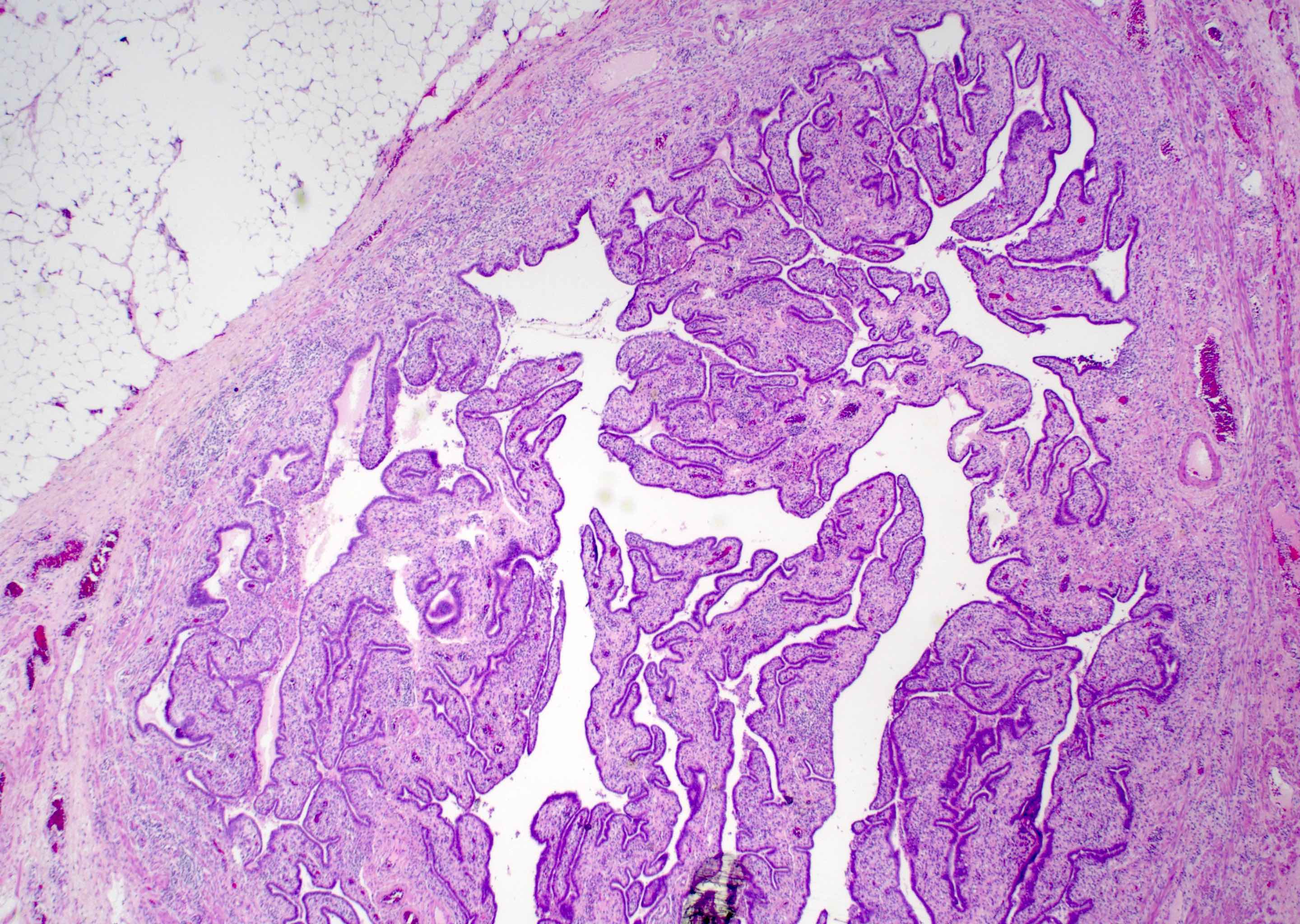
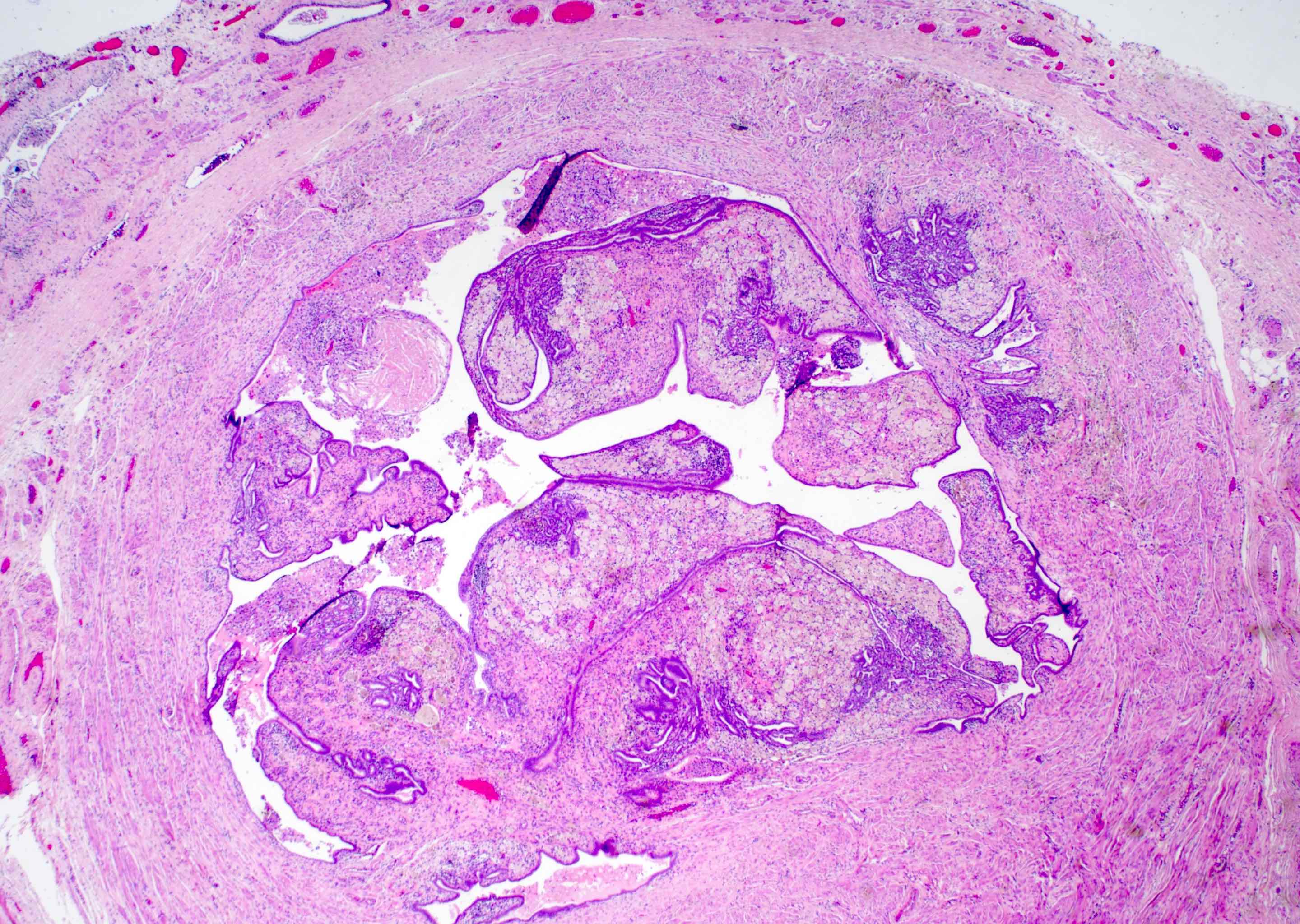
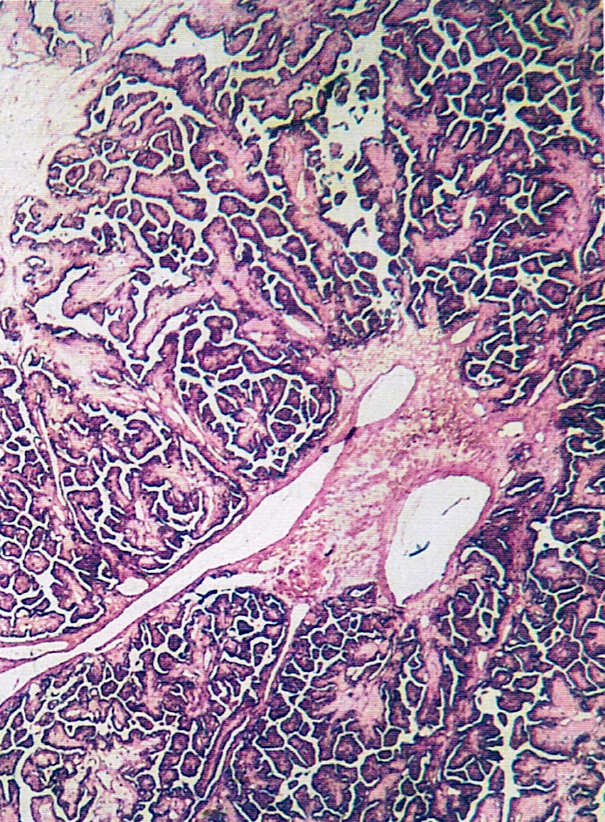
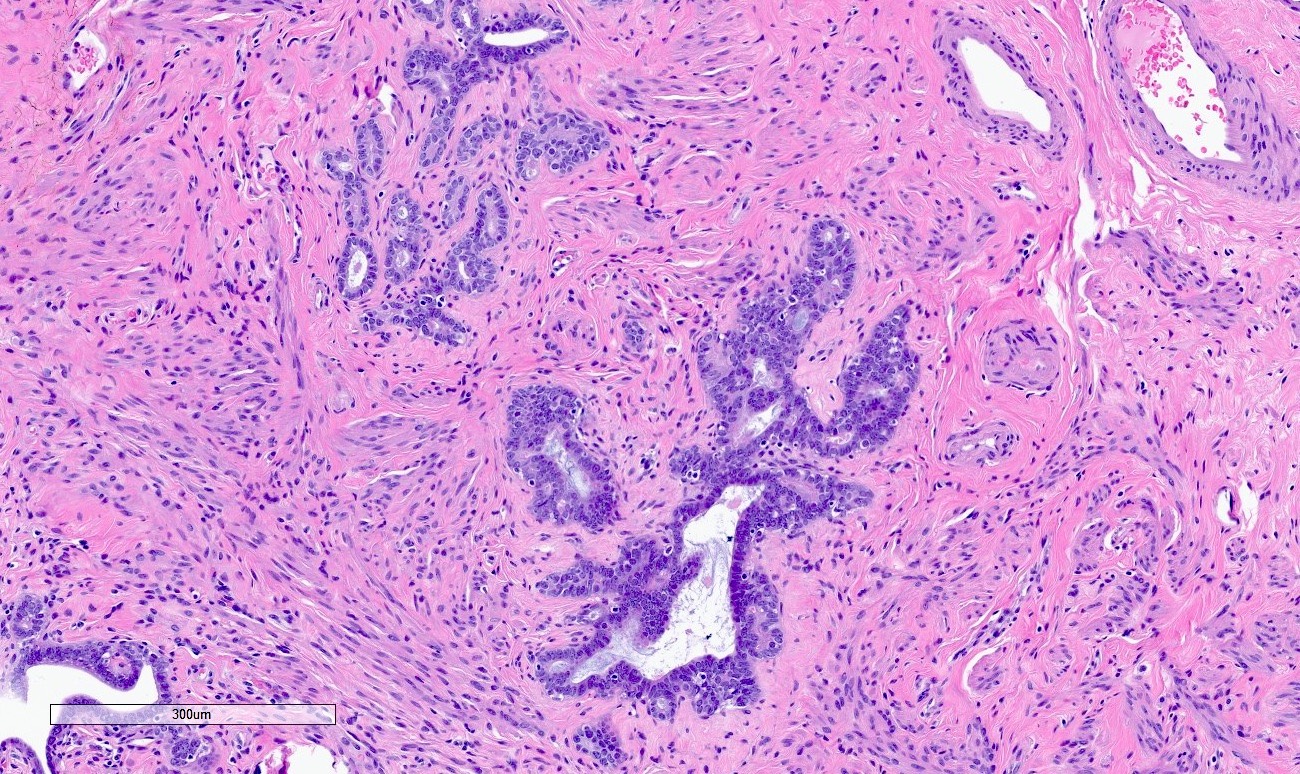
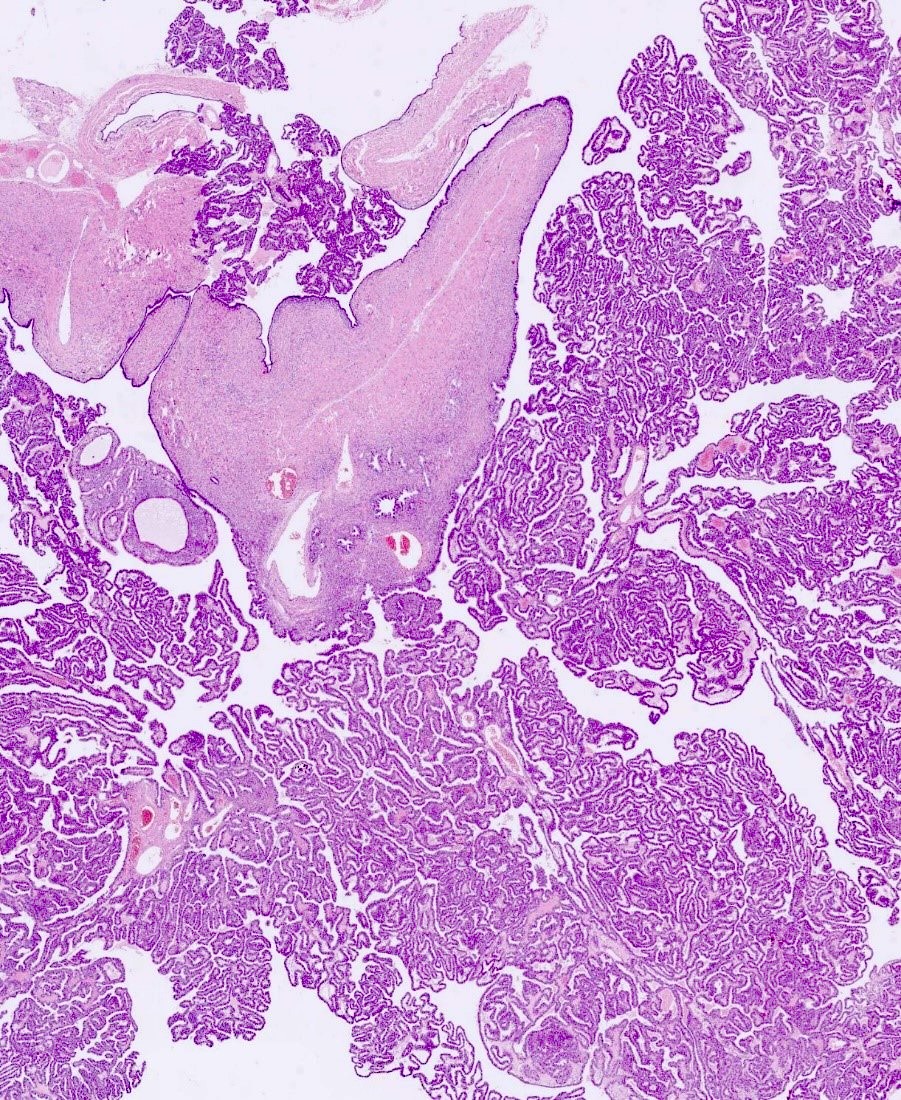
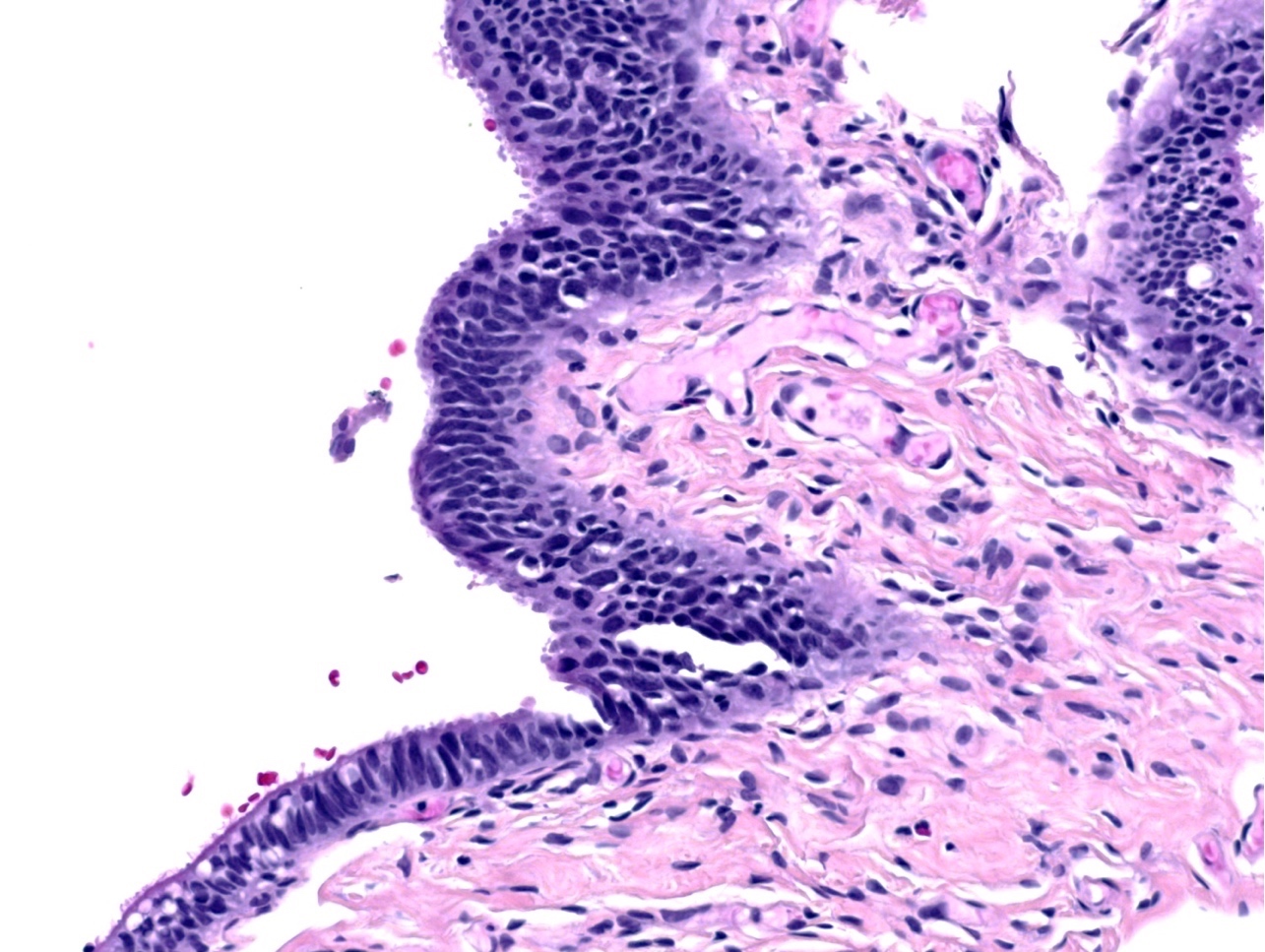
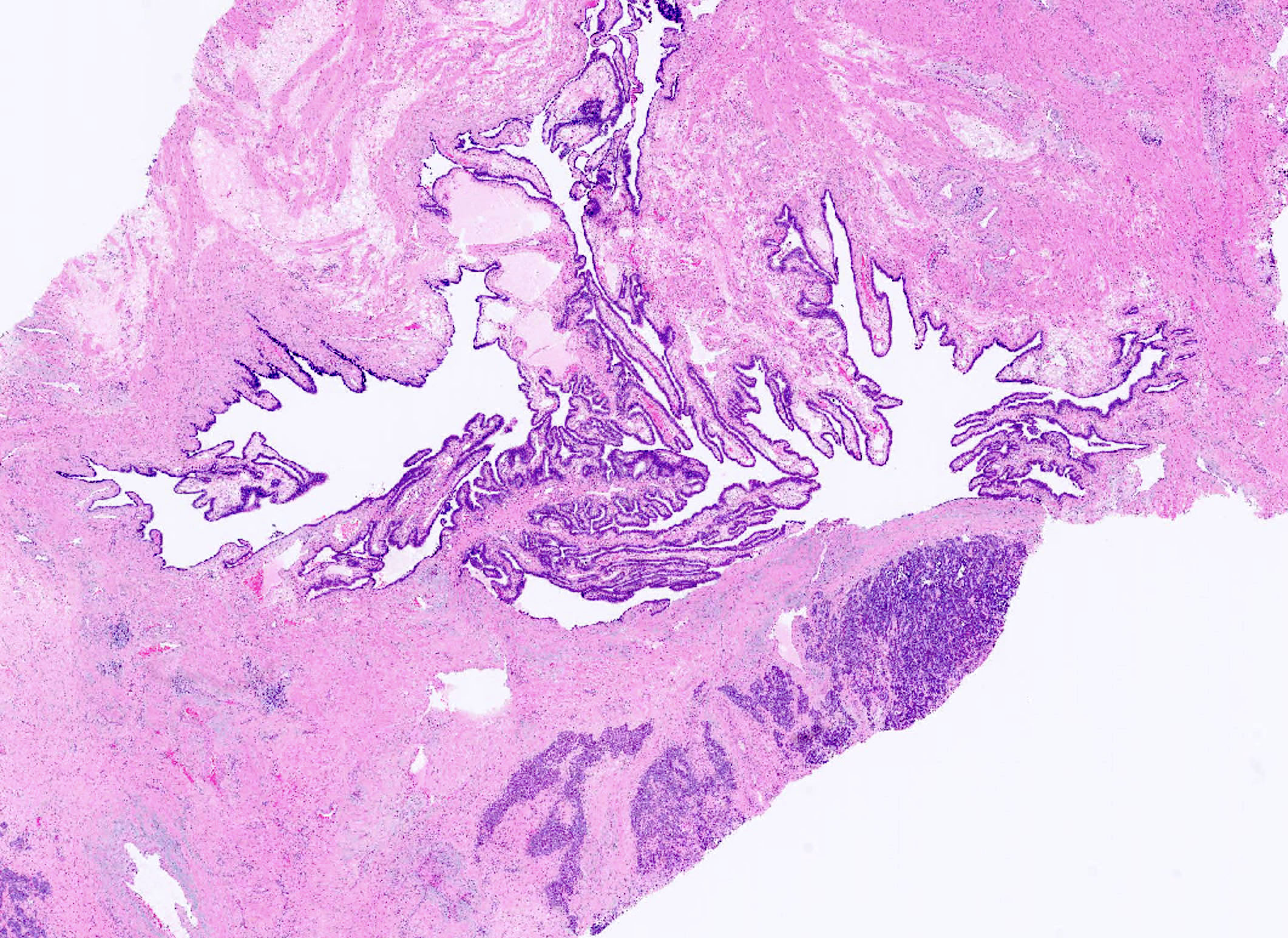
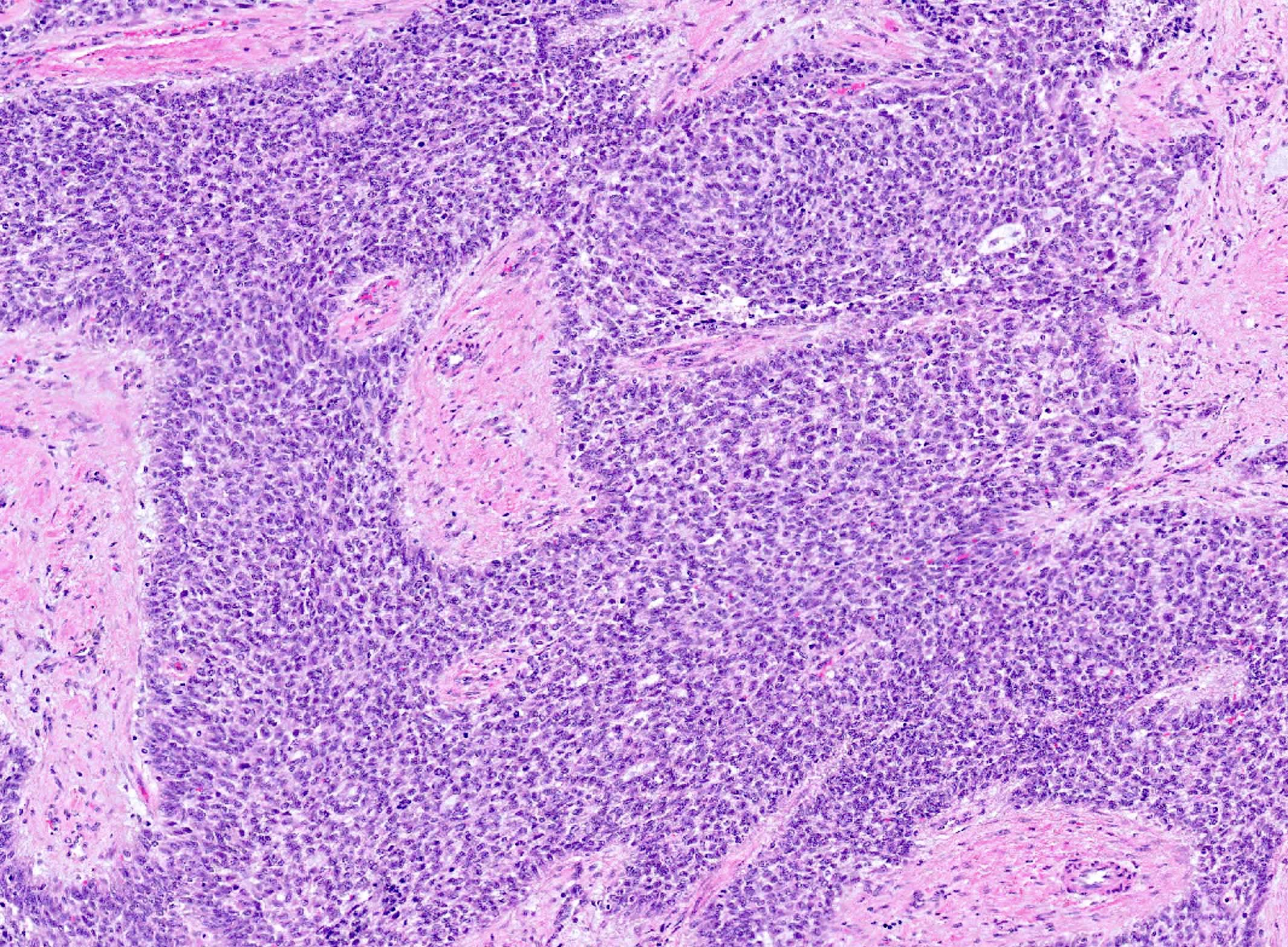
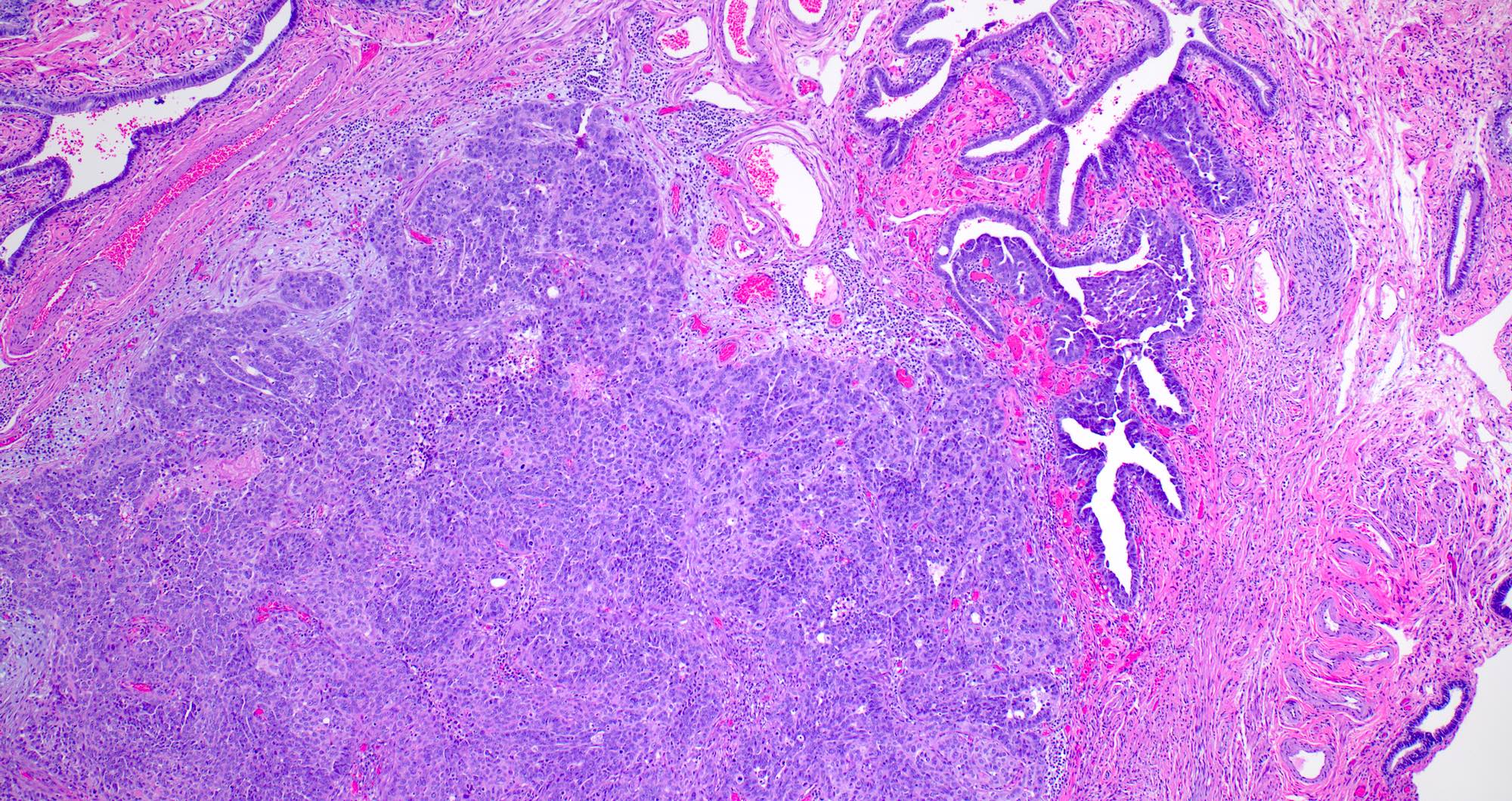
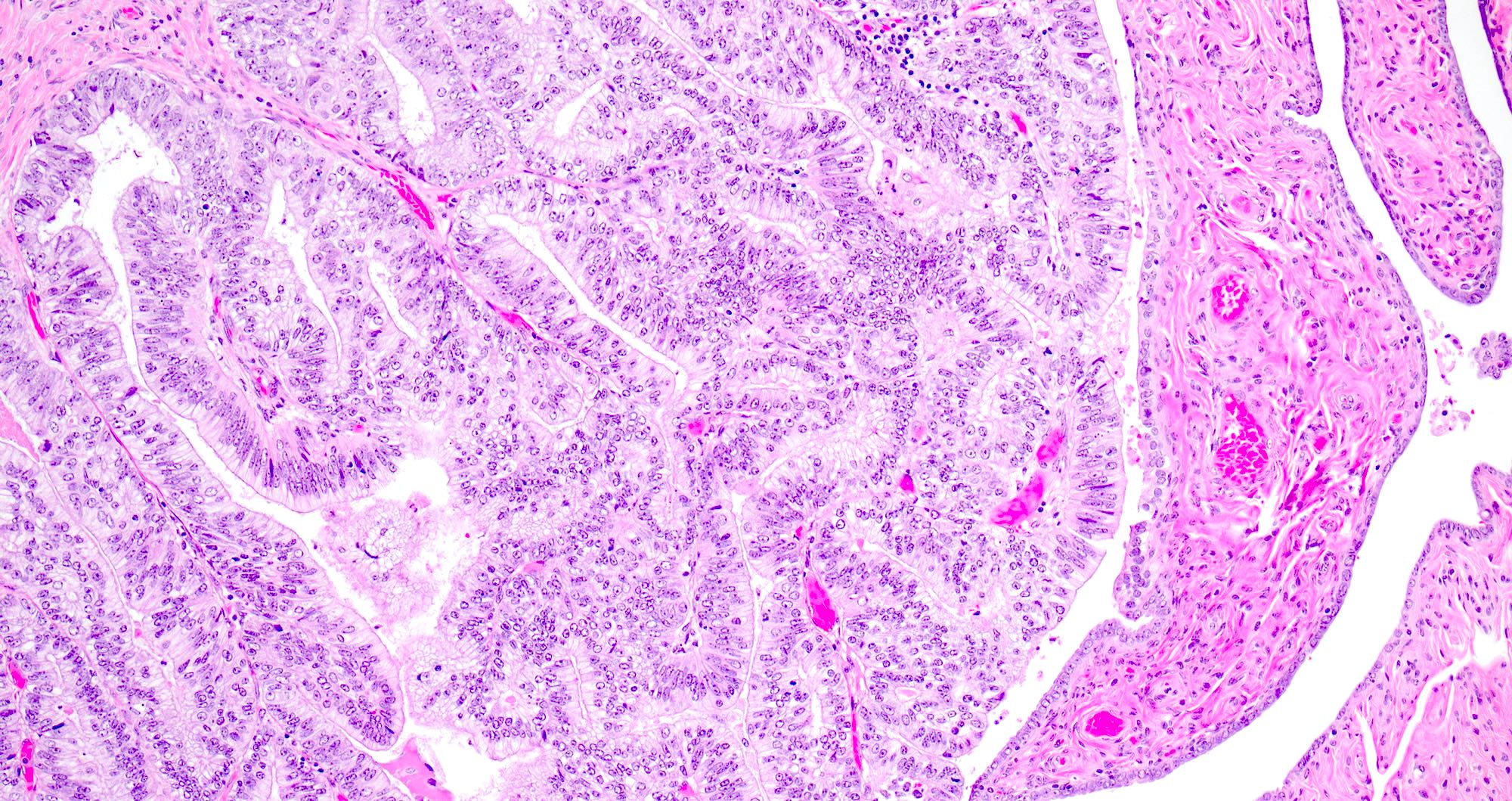
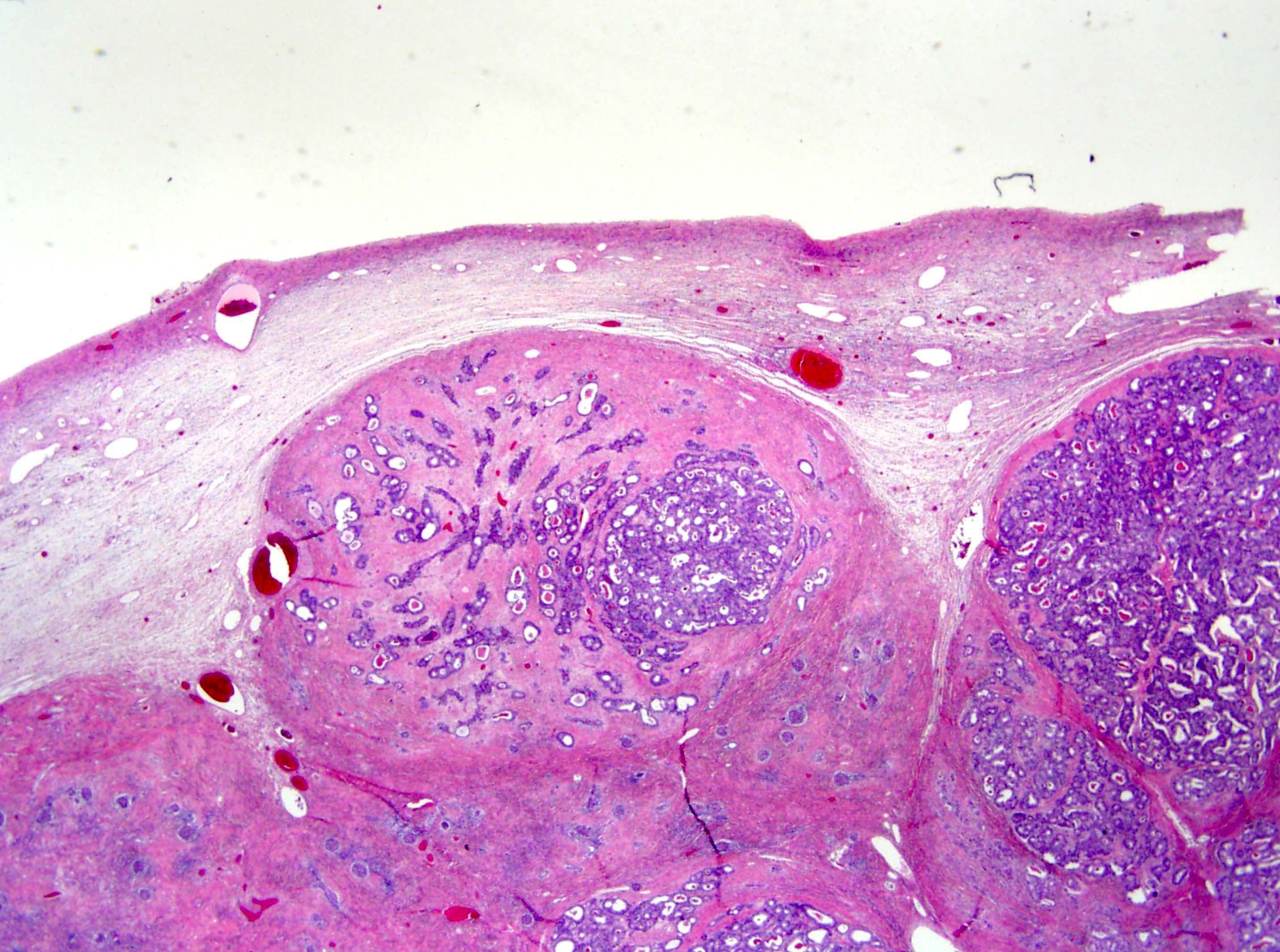
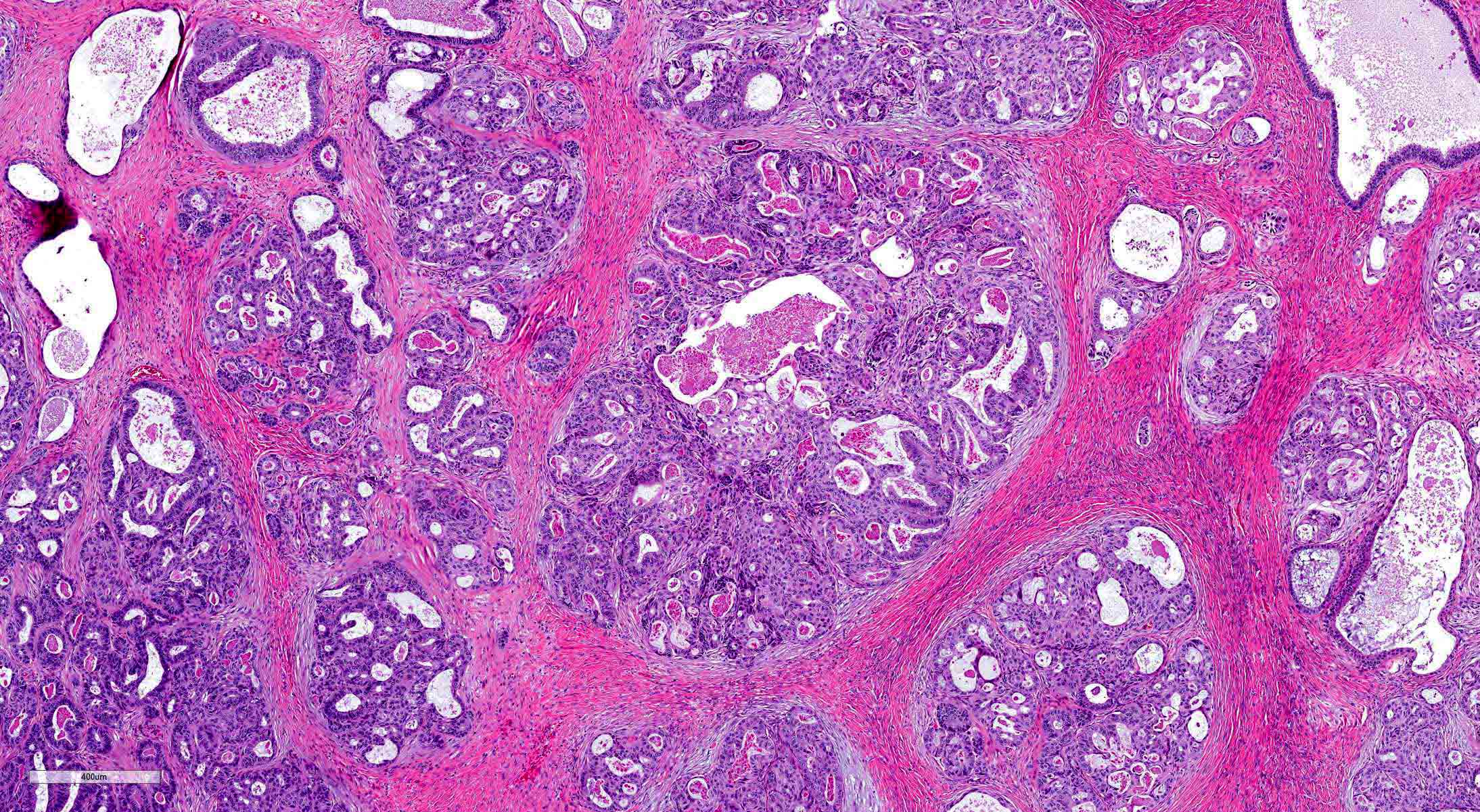
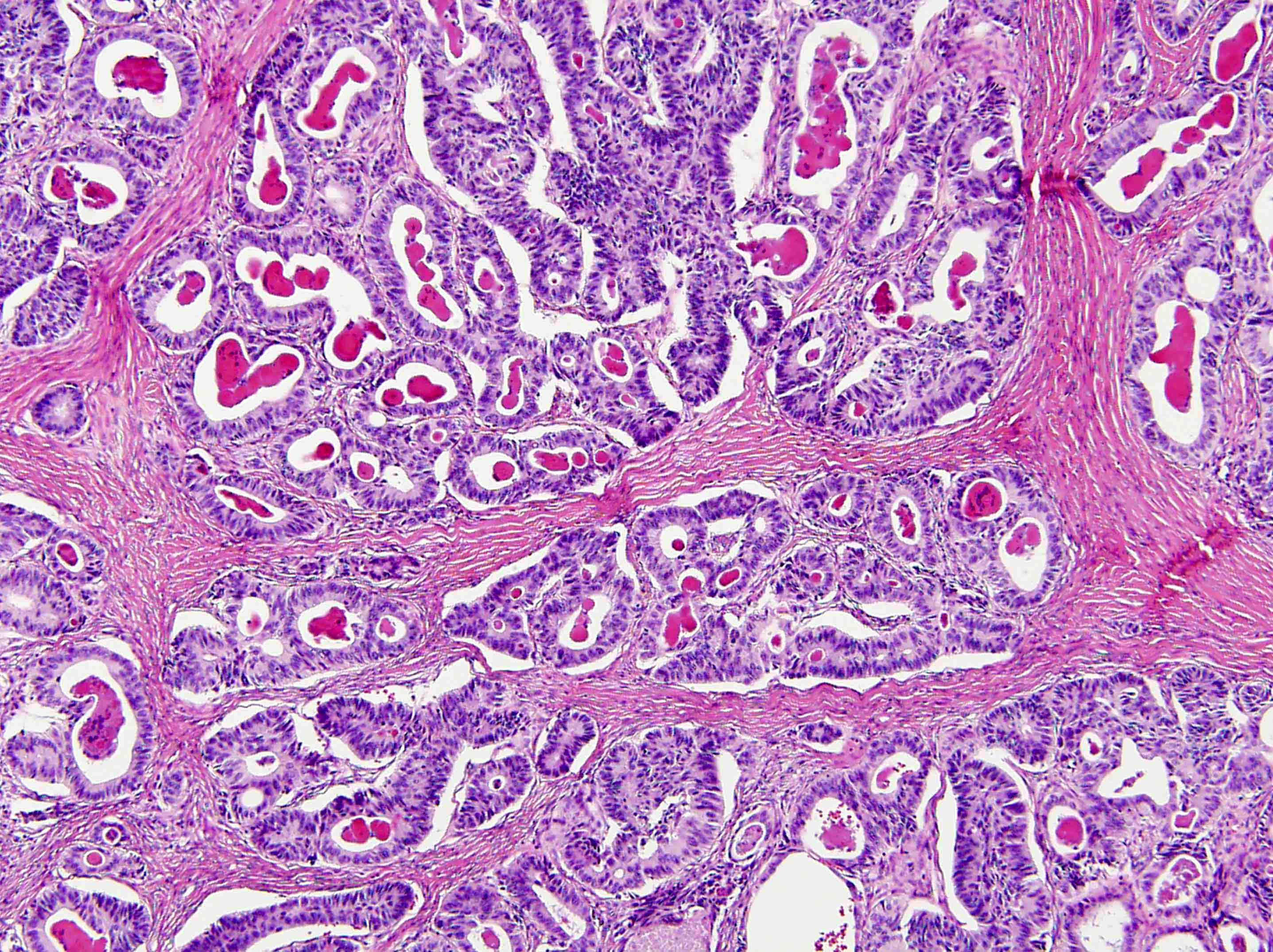
Microscopic (histologic) description
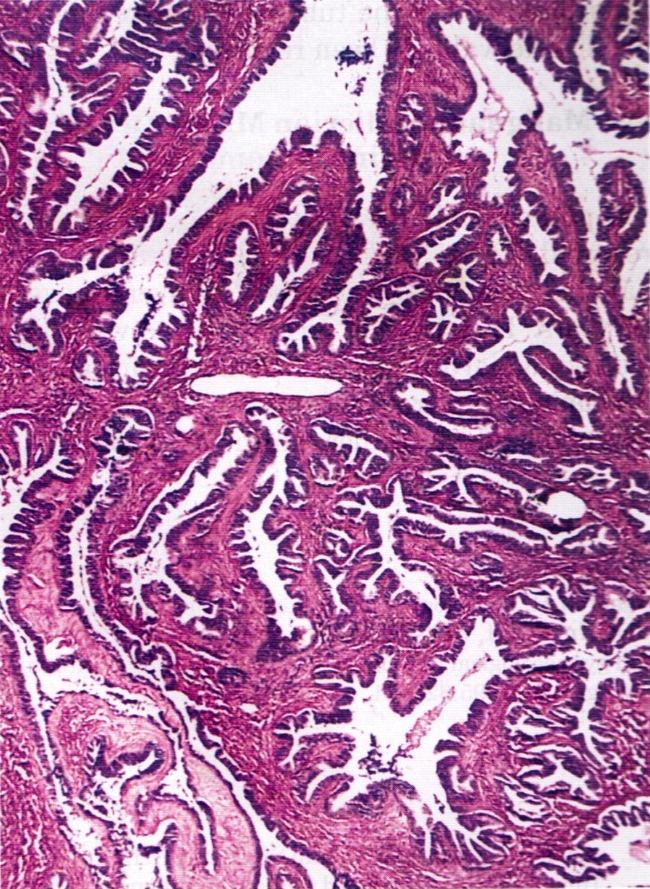
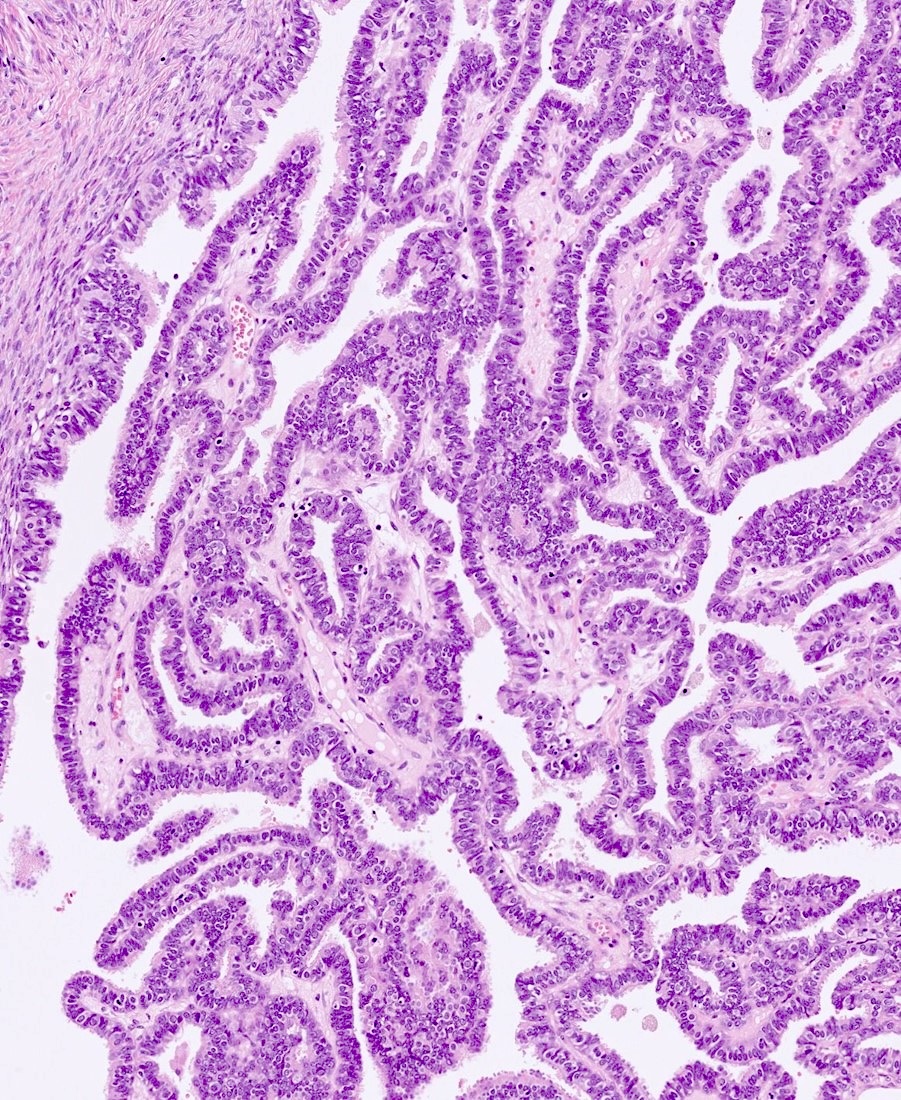
- Serous borderline tumors of the fallopian tube closely resemble their ovarian counterparts
- Architecture
- Numerous papillae of variable size and width (Obstet Gynecol Sci 2014;57:334)
- These papillae occupy a variable extent of a cyst lined by pseudostratified epithelium
- Larger papillae arborize down to smaller papillae which terminate in epithelial clusters or single cells
- Hobnailing or epithelial tufting
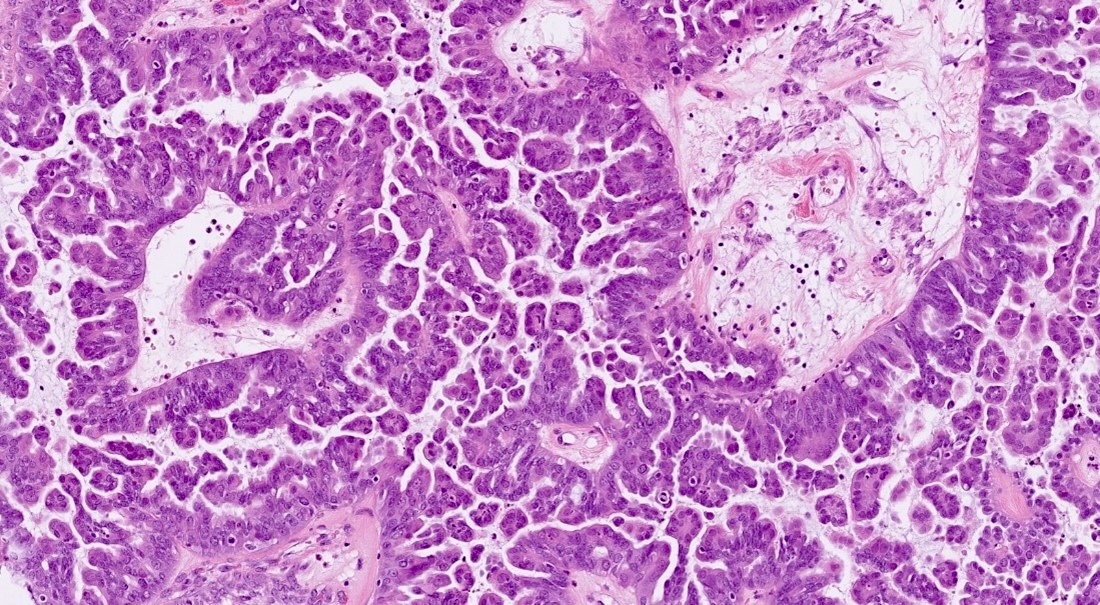
- Cytologic features
- Ciliated cells that are cuboidal to columnar
- Up to moderate atypia - cellular enlargement, coarse chromatin, small nucleoli may be present, minimal mitotic activity
Microscopic (histologic) images
Cytology description
NA
Cytology images
NA
Immunofluorescence description
NA
Immunofluorescence images
NA
Electron microscopy description
NA
Electron microscopy images
NA
Molecular / cytogenetics description
NA
Molecular / cytogenetics images
NA
Videos
NA
Sample pathology report
- Right fallopian tube and ovary, salpingo-oophorectomy:
- Borderline tumor of the fallopian tube (see comment)
- Procedure: unilateral salpingo-oopherectomy, lymphadenectomy
- Specimen integrity: serosa intact
- Surface involvement: absent
- Tumor site: right fallopian tube
- Tumor size: 8.5 cm
- Additional dimensions: 7 x 5 cm
- Histologic type: serous borderline tumor
- Implants: not identified
- Other organ involvement: not identified
- Peritoneal fluid: not submitted
- Regional lymph nodes: all lymph nodes negative for tumor cells
- Number of lymph nodes examined: 4
- Specify sites: right pelvic
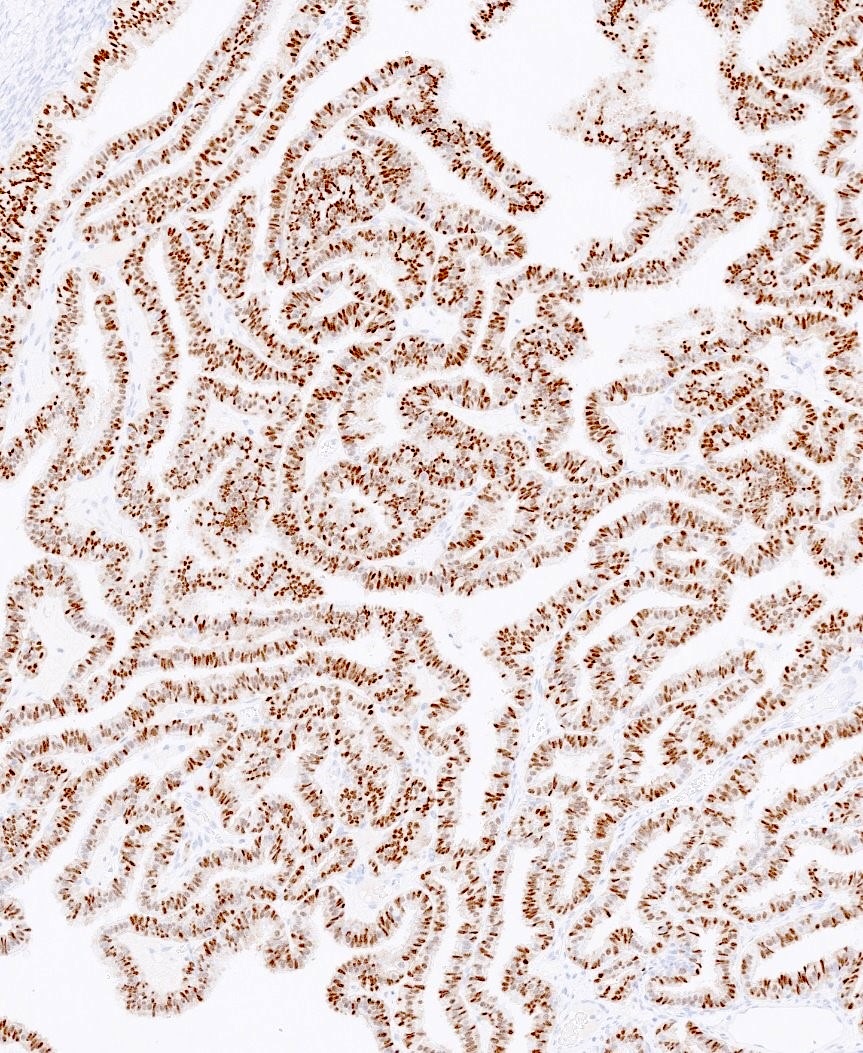
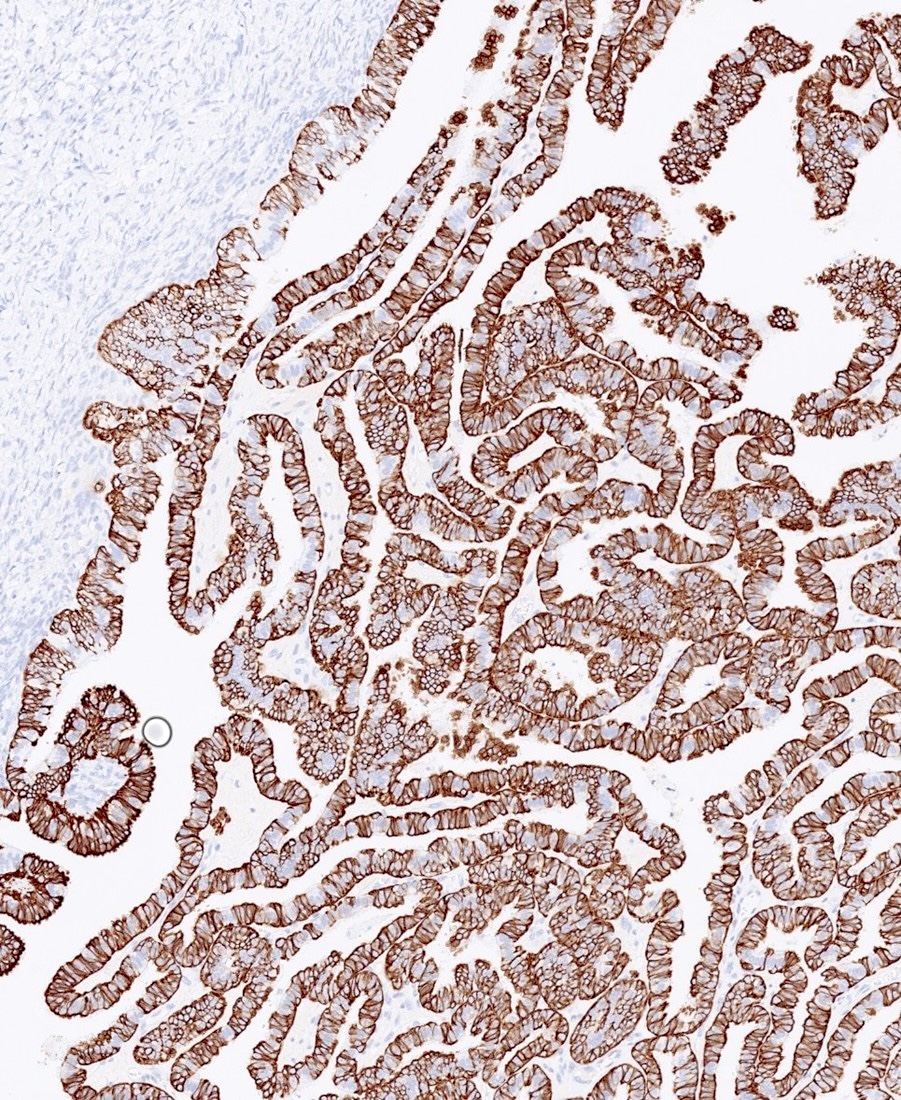
- Pathologic stage: pT1, pN0
- FIGO stage: IA
- Comment: Microscopically this lesion shows numerous papillae of varying size and width. These papillae arborize down into smaller papillae. On higher power there is hobnailing, the epithelial cells are cuboidal to columnar and are ciliated. Immunohistochemical stains performed with adequate controls on sections of the right fallopian tube tumor show the tumor cells to be diffusely positive for PAX8, WT1, ER and PR, with focal / weak expression of p53 (wild type expression) and patchy positivity for p16. The combined morphologic and immunohistochemical findings support the above diagnosis (CAP: Protocol for the Examination of Specimens From Patients With Primary Tumors of the Ovary, Fallopian Tube, or Peritoneum [Accessed 19 April 2024]).
Differential diagnosis
- Endosalpingiosis:
- Minimal architectural complexity or cytologic atypia
- Psammomatous calcifications may be present; rarely larger than a few millimeters
- Serous cystadenoma / cystadenofibroma:
- No architectural complexity, e.g., papillae, micropapillae, cribriforming or nesting
- If there is architectural complexity but it constitutes < 10% of overall tumor then it is a serous cystadenoma / cystadenofibroma with focal epithelial proliferation
- Heterogenous population of ciliated and secretory cells but without atypia or mitoses
- Serous borderline tumor with intraepithelial / microinvasive carcinoma:
- Significant cytologic atypia and or evidence of invasion of stroma
- Usually micropapillary
- Clear cell carcinoma:
- Clear cytoplasm
- High grade nuclei
- Napsin A positivity, loss of hormonal markers
Additional references
NA
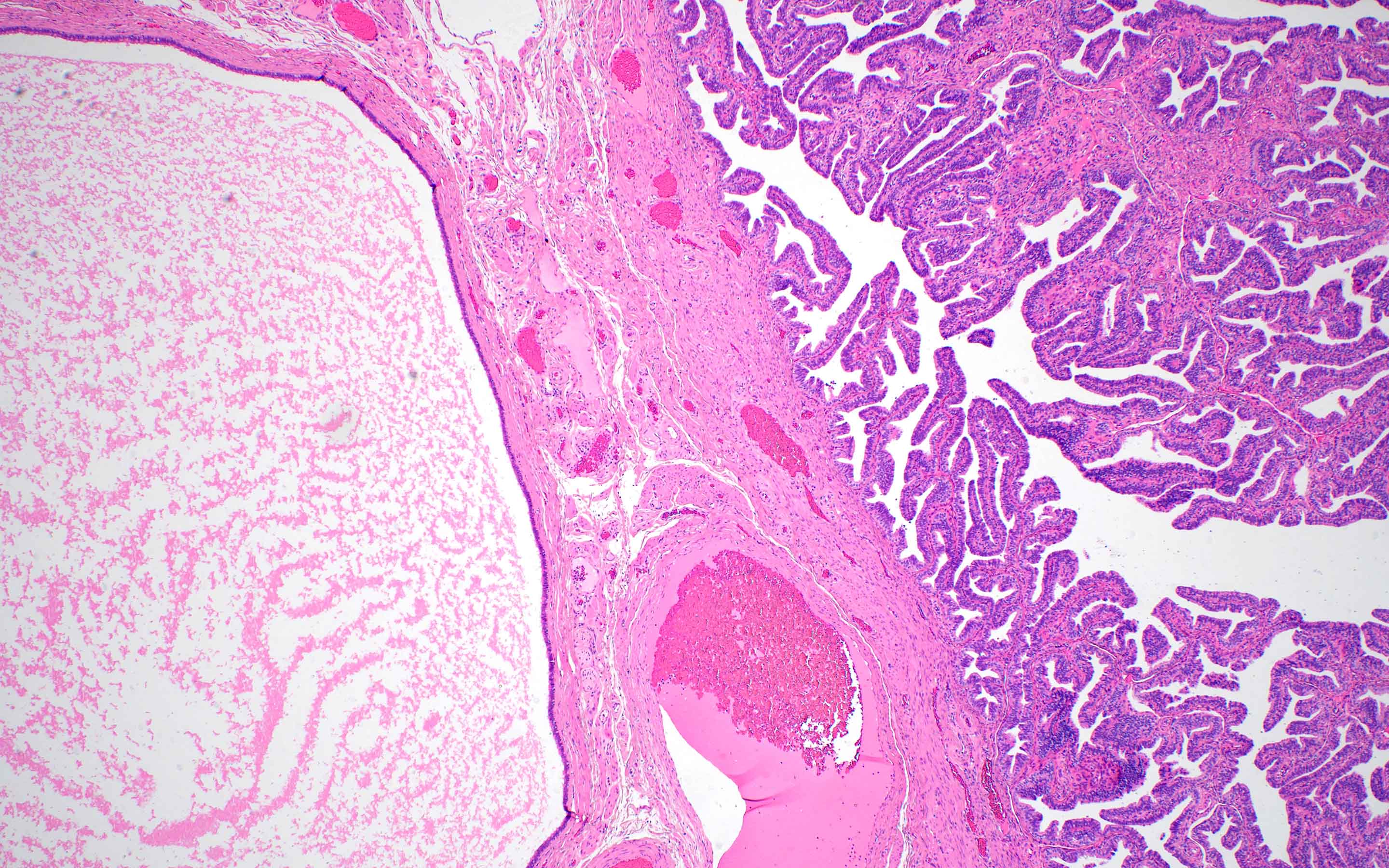
Board review style question #1
Board review style answer #1
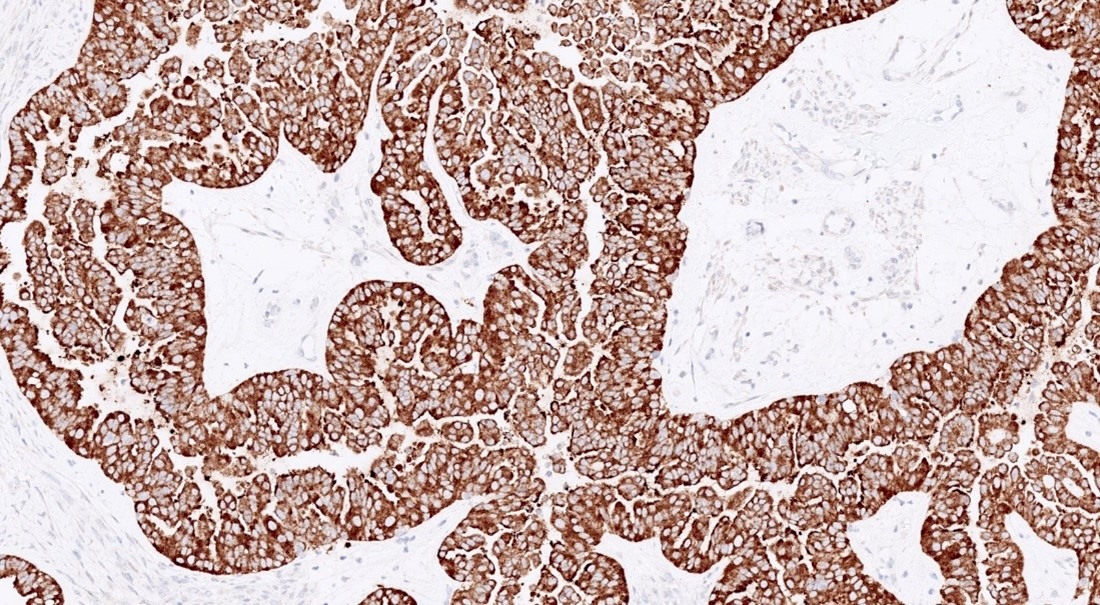
D. Serous borderline tumor arising from the fallopian tube. Serous borderline tumor is far more commonly located in the ovary; however, it can also arise in the fallopian tube. Answer A is incorrect because the image does not display high grade features. Answers B, C and E are incorrect because the histology findings are more consistent with those of a serous borderline tumor.
Comment Here
Reference: Serous borderline tumor
Comment Here
Reference: Serous borderline tumor
Serous borderline tumor (pending)
[Pending]
Serous tubal intraepithelial carcinoma
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Lesion that is limited to the fallopian tube epithelium and a precursor to extrauterine (pelvic) high grade serous carcinoma
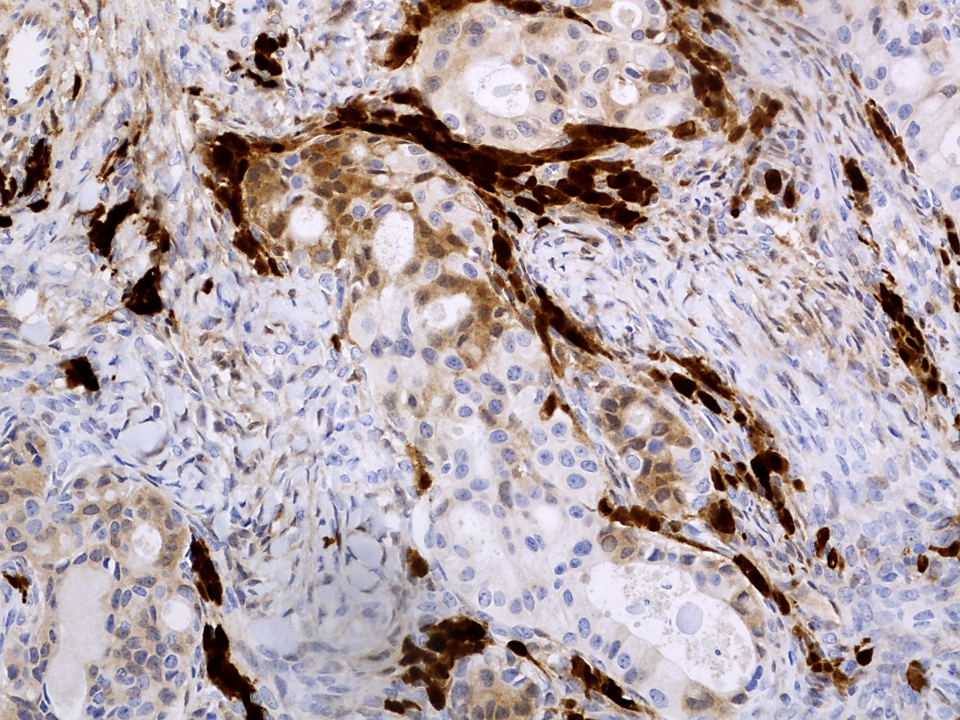
Essential features
- Confined to epithelium
- Histologic features: significant atypia, architectural alterations, high proliferative index and mutant pattern of p53 staining
- Important precursor lesion to recognize, as it is a criterion for assigning fallopian tube as primary site of high grade tubo-ovarian serous carcinoma irrespective of presence and size of ovarian and peritoneal disease (Histopathology 2015;67:331)
Terminology
- Various terms used to describe a spectrum of tubal epithelial alterations:
- Secretory cell outgrowths (SCOUTs): secretory cell expansion with variable ciliation (type 1 / tubal differentiation and type 2 / endometrioid differentiation), wild type p53 staining
- p53 signature: histologically normal epithelium (at least 12 cells) with mutant pattern p53 staining and low proliferation index (MIB1) (typically less than 10%)
- Serous tubal intraepithelial lesion (STIL): abnormal histology (high N/C but preserved polarity), mutant p53 and variable MIB1; STIL is regarded as a lesion of uncertain significance and diagnostic features fall short of STIC
- Serous tubal intraepithelial carcinoma (STIC): abnormal histology (high N/C, loss of polarity, lack of ciliated cells), mutant pattern p53 staining and high proliferation index (MIB1)
ICD coding
- ICD-10: N83.9 - fallopian tube disorder
Epidemiology
- Patients with hereditary BRCA mutation have a high risk of high grade serous carcinoma
- Incidence of STIC in risk reducing salpingo-oophorectomies in BRCA+ women is 5 - 8% (Gynecol Oncol 2006;100:58)
Sites
- Fallopian tube fimbria is the most common site of origin
Pathophysiology
- Secretory epithelium of fallopian tube is postulated as the cell of origin (Adv Anat Pathol 2010;17:293)
Clinical features
- Usually discovered incidentally during routine surgery or risk reducing prophylactic salpingo-oophorectomies
- May be seen adjacent to invasive carcinoma
- Reference: Gynecol Oncol 2017;146:69
Diagnosis
- Careful morphologic evaluation is key to the diagnosis; immunohistochemistry (p53 and MIB1) is only supportive
- Gross protocol (sectioning and extensively examining the fimbria [SEE-FIM]) influences ability to diagnose (Am J Surg Pathol 2006;30:230):
- Amputation and longitudinal sectioning of the infundibulum and fimbrial segment (distal 2 cm) allows maximal exposure of the tubal plicae; isthmus and ampulla are cut transversely at 2 - 3 mm intervals
- Entire fallopian tube should be submitted for evaluation in women with BRCA mutations or strong family history of ovarian carcinoma
- Extensively examine the fimbriated end
- Controversial role of multiple levels with 1 study finding no impact and another study reporting 25% missed with a single section (Am J Surg Pathol 2009;33:1878, Int J Gynecol Pathol 2013;32:353)
- STIC is staged as pathologic stage pT1
Case reports
- 48 year old woman with STIC in cervical smears (Diagn Cytopathol 2018;46:945)
- 51 year old postmenopausal woman with STIC and BRCA1 mutation (Jpn J Clin Oncol 2014;44:597)
- 55 year old woman with synchronous papillary serous carcinoma of ovary and endometrium and STIC (Indian J Pathol Microbiol 2017;60:125)
- 56 year old woman with incidental STIC (Case Rep Obstet Gynecol 2015;2015:760429)
- 58 year old woman with retroperitoneal high grade serous carcinoma and STIC (Diagn Pathol 2019;14:17)
Treatment
- No current consensus among gynecologic oncologists regarding appropriate management of incidental STIC
- Patients have been managed by surgical staging / peritoneal washings / chemotherapy or follow up without additional intervention
- Yield of surgical staging is low and short term clinical outcomes are favorable
- Individualized management is warranted until additional data become available (Int J Gynecol Cancer 2013;23:1603)
Gross description
- Not evident on gross examination
Microscopic (histologic) description
- Epithelial stratification
- Lack of ciliated cells (Mod Pathol 2017;30:710)
- High N/C ratio
- Nuclear pleomorphism, hyperchromasia, prominent nucleoli
- Loss of polarity (may be focal)
- Epithelial fractures (Adv Anat Pathol 2010;17:293)
- Exfoliation of small epithelial clusters
Microscopic (histologic) images
Virtual slides
Cytology description
- Brush cytology shows clusters of cells with haphazard pleomorphic nuclei, high N/C ratio and lack of cilia (Cancer Cytopathol 2019;127:192)
Positive stains
- p53: mutant pattern of staining (diffusely positive (nuclear), completely negative (null type) or less commonly, cytoplasmic staining)
- Ki67 / MIB index: high (suggested cutoff of 10%) (Am J Surg Pathol 2011;35:1766, Int J Gynecol Pathol 2012;31:243)
Sample pathology report
- Bilateral fallopian tubes, salpingectomy:
- Right fallopian tube with serous tubal intraepithelial carcinoma (see comment)
- Left fallopian tube with no pathologic change
- Comment: Immunostain for p53 is diffusely and strongly positive in the lesional cells. Ki67 index is > 10%.
Differential diagnosis
- p53 signature:
- Precursor lesion which shows normal histology with p53 mutant pattern of staining
- Transitional cell metaplasia:
- Uniform cells with nuclear grooves; p53 wild type (Am J Surg Pathol 2009;33:111)
- Florid epithelial hyperplasia and reactive atypia associated with acute salpingitis:
- Has a background of inflammation, retained polarity and presence of ciliated cells; p53 wild type
- Intramucosal fallopian tube metastasis from uterine serous carcinoma:
- May closely mimic STIC; usually WT1 negative (Am J Surg Pathol 2017;41:161)
Additional references
- Front Biosci (Elite Ed) 2011;3:625, Int J Gynecol Pathol 2010;29:310, Mod Pathol 2009;22:985, Curr Opin Obstet Gynecol 2007;19:3, Adv Anat Pathol 2006;13:1, CAP: Protocol for the Examination of Specimens from Patients with Primary Tumors of the Ovary, Fallopian Tube or Peritoneum [Accessed 5 January 2022]
Board review style question #1
Which fallopian tube lesion appears normal on histology but shows a mutant pattern of p53 immunostaining?
- p53 signature
- Reactive atypia
- Secretory cell outgrowth (SCOUT)
- Serous tubal intraepithelial carcinoma (STIC)
Board review style answer #1
Board review style question #2
The grossing protocol for examination of the fallopian tube to identify the diagnosis in the photomicrograph should
- Ensure complete evaluation of the fallopian tube in all cases
- Increase detection of precursor lesions in at risk women
- Require multistep levels in at risk women
- Require tangential sectioning of the infundibulum and fimbrial segment to allow maximal exposure
Board review style answer #2
B. Increase detection of precursor lesions in at risk women. Serous tubal intraepithelial carcinoma is shown in the photomicrograph.
Comment Here
Reference: Serous tubal intraepithelial carcinoma
Comment Here
Reference: Serous tubal intraepithelial carcinoma
STK11 adnexal tumor
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Immunofluorescence description | Immunofluorescence images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Aggressive tumor that arises in paratubal / paraovarian soft tissues, has variable morphology and immunohistochemistry and harbors pathognomonic alterations in STK11
Essential features
- Associated with Peutz-Jeghers syndrome in ~50% of cases
- STK11 alterations
- Adnexal or paratubal mass
Terminology
Not relevant to this topic
ICD coding
- ICD-10: C57.4 - malignant neoplasm of uterine adnexa, unspecified
Epidemiology
- Age: wide range from middle age to elderly (mean: 40 years old) (Am J Surg Pathol 2021;45:1061)
- Rare pediatric case (16 years old) has been reported (Pediatr Dev Pathol 2023;26:486)
Sites
- Paratubal (most common)
- Fallopian tubes
- Ovaries
- Uterine serosa
- Less commonly, the abdomen and pelvis
- Reference: Am J Surg Pathol 2021;45:1061
Pathophysiology
- Associated with Peutz-Jeghers syndrome in ~50% of cases
- Can be sporadic
- Histogenesis of this tumor (Wolffian versus sex cord stromal versus epithelial or mesothelial origins) remains uncertain (Am J Surg Pathol 2021;45:1061)
- Reference: Pediatr Dev Pathol 2023;26:486
Etiology
Repetitive with Molecular / cytogenetics description and Pathophysiology headings
Diagrams / tables
Not relevant to this topic
Clinical features
- Abdominal / pelvic pain or mass
- Abdominal distension
- Urinary tract symptoms
- Abnormal uterine bleeding
- Can be incidental finding
- Metastatic tumor at presentation (50%)
- Reference: Am J Surg Pathol 2021;45:1061
Diagnosis
- Pelvic ultrasound or MRI and histopathologic diagnosis
Laboratory
Not relevant to this topic
Radiology description
Not relevant to this topic
Radiology images
Not provided
Prognostic factors
- Recurrences at 3 - 79 months (mean: 29) after initial diagnosis, most commonly in the omentum, abdominal wall, peritoneum and pelvis
- Metastasis: most commonly to omentum and uterine serosa; less commonly to bladder peritoneum, anterior abdominal wall, small bowel, liver, paraaortic lymph node and pouch of Douglas
- Reference: Am J Surg Pathol 2021;45:1061
Case reports
- 16 year old girl with large, bilateral, solid and cystic adnexal masses (Pediatr Dev Pathol 2023;26:486)
- 29 year old woman peritubal neoplastic lesion with STK11 mutation and response to mTOR inhibitor (Gynecol Oncol Rep 2021;37:100838)
- 22 cases of paratubal adnexal tumors that harbored STK11 alterations (Am J Surg Pathol 2021;45:1061)
Treatment
- Surgery with or without chemotherapy or radiation (Gynecol Oncol Rep 2021;37:100838)
Gross description
- Adnexal mass that ranges from 4.5 to 25.5 cm in size (mean: 12.4 cm)
- Solid, cystic or both
- Variable in color (tan, white, gray, yellow, pink)
- Hemorrhage and necrosis are often present
- Reference: Am J Surg Pathol 2021;45:1061
Gross images
First image not free to access; second image moved to Clinical images
Frozen section description
Not relevant to this topic
Frozen section images
Not provided
Microscopic (histologic) description
- Mixed architectural patterns are characteristically present within a single tumor and may be key to recognition
- Architecture
- Interanastomosing cords and trabeculae that can form tubular, cystic, cribriform or microacinar architecture
- Solid growth, large nests, broad columns or nodules of varying sizes
- Whorling tumor cells with vaguely glomeruloid appearance
- Focal macrofollicular pattern, pseudofollicular, papillary or pseudopapillary growth
- Villoglandular configuration
- Focally dilated glands or salivary gland type
- Basophilic secretions
- Stroma
- Prominent myxoid stroma (Am J Surg Pathol 2021;45:1061)
- Other ranges from scant to abundant and is either edematous, loosely collagenous or rarely hyalinized
- Cell morphology
- Mostly, columnar to cuboidal cells but a spindled morphology can be seen
- Nuclei are round to ovoid with irregular, often angulated contours and vesicular chromatin
- Prominent nucleoli and inconspicuous nuclear grooves
- Cytoplasm can be eosinophilic, finely vacuolated or clear
- Rarely, squamoid or signet ring-like appearance
- No overt pleomorphism
- Other
- Mitoses range from 2 to 20 (mean: 10) per 10 high power fields
- Incidental findings: sex cord tumor with annular tubules
- References: Pediatr Dev Pathol 2023;26:486, Am J Surg Pathol 2021;45:1061
Microscopic (histologic) images
Cytology description
Not relevant to this topic
Cytology images
Not relevant to this topic
Immunofluorescence description
Not relevant to this topic
Immunofluorescence images
Not relevant to this topic
Positive stains
- Strong CAM5.2 (94%), strong AE1 / AE3 (93%) and focal CK7 (60%)
- Inhibin (90%), calretinin (100%), WT1 (100%)
- AR (93%), ER (80%), PR (76%)
- Variable D2-40 (75%)
- Focal CD10 (81%)
- Reference: Pediatr Dev Pathol 2023;26:486, Am J Surg Pathol 2021;45:1061
Negative stains
- Claudin4
- FOXL2
- TTF1
- Focal SF1 (30% positive) (Am J Surg Pathol 2021;45:1061)
- Focal PAX8 (25% positive) (Am J Surg Pathol 2021;45:1061)
- Weak focal GATA3 (5% positive)
- Weak to moderate EMA staining (Am J Surg Pathol 2021;45:1061)
- Rare p63 (< 1% positive)
- Reference: Pediatr Dev Pathol 2023;26:486
Electron microscopy description
Not relevant to this topic
Electron microscopy images
Not relevant to this topic
Molecular / cytogenetics description
- STK11 alterations
- Pathogenic mutations (most commonly loss of heterozygosity [LOH] event)
- Variants of uncertain significance
- STK11 deletions
- References: Am J Surg Pathol 2021;45:1061, Jpn J Cancer Res 1999;90:629
Molecular / cytogenetics images
Not relevant to this topic
Videos
Pathology of fallopian tube
Sample pathology report
- Uterus, bilateral fallopian tubes and ovaries:
- Other histologic type: STK11 adnexal tumor (see synoptic summary)
- Clinical history: Peutz-Jehgers syndrome
- Specimen: total hysterectomy with bilateral tubes and ovaries, robotic assisted laparoscopic
- Specimen integrity: not applicable
- Tumor site: right adnexa
- Tumor size: 15 cm; other dimensions: 10 x 9 cm
- Histologic type: other, STK11 adnexal tumor
- Tumor grade: not applicable
- Surface involvement: not identified
- Implants: not identified
- Other tissue involvement: not identified
- Peritoneal fluid involvement: not submitted
- Lymph nodes: none submitted
- Distant metastatic sites: not applicable
- Stage: pT1a pN not assigned; pM not assigned
- FIGO stage: IA
- Note: Tumor can be confidently called stage 1A if the staging biopsies and such are all found to be negative. On the other hand, peritoneal cancers are all classified as stage II. A single adnexal tumor falls conveniently in between these two somewhere but overall, it would still be staged as 1A if all the staging biopsies were negative and if it is a single mass with no surface involvement.
Differential diagnosis
- Female adnexal tumor of probable Wolffian origin (FATWO):
- Sex cord stromal tumor:
- Müllerian adenocarcinoma, endometrioid carcinoma:
- Mesothelioma:
- Diffuse or plaque-like growth
- Rarely, the pleura may harbor STK11 mutations but in association with other alterations (BAP1 mutations or CDKN2A / CDKN2B deletions)
- Loss of BAP1
- Mesonephric adenocarcinoma and mesonephric-like carcinoma:
- Tubular pattern with back to back round tubules with or without eosinophilic secretions
- Uniform nuclei with mild to (at most) moderate cytologic atypia and variable mitotic activity
- AR and inhibin positive in ~33%
- GATA3 and TTF1 positive
- ER / PR, WT1 negative and PAX8 positive
- Positive EMA, claudin4
- KRAS, NRAS mutations
- ARID1A, ARID1B or SMARCA4 mutations ~60%
- Rarely, ovarian adenoid cystic carcinoma:
- Dual population of cells (epithelial / ductal and myoepithelial)
Additional references
Board review style question #1
A 45 year old woman presents with a 10 cm adnexal mass demonstrating the pattern of cystic spaces surrounded by cuboidal epithelium shown above. The tumor shows the following immunophenotype: ER / PR positive, CK7 positive, PAX8 positive, GATA3 negative, inhibin positive, TTF1 negative, FOXL2 negative, p53 wild type. Which of the following is the best diagnosis for this tumor?
- Female adnexal tumor of probable Wolffian origin (FATWO)
- High grade serous carcinoma
- Mesonephric adenocarcinoma
- STK11 adnexal neoplasm
- Sex cord stromal tumor, NOS
Board review style answer #1
D. STK11 adnexal neoplasm. The immunophenotype and microscopic appearance are characteristic of STK11 adnexal tumor. Answer A is incorrect because FATWO is typically negative for hormonal markers. Answer B is incorrect because high grade serous carcinoma tumors uniformly harbor TP53 mutations, reflected in abnormal p53 staining patterns. Answer C is incorrect because mesonephric adenocarcinoma tumors are typically TTF1 and GATA3 positive. Answer E is incorrect because sex cord stromal tumors, while manifesting positive stromal markers like inhibin, are also FOXL2 positive.
Comment Here
Reference: STK11 adnexal tumor
Comment Here
Reference: STK11 adnexal tumor
Board review style question #2
A patient with Peutz-Jeghers syndrome may manifest which of the following components?
- Cutaneous dermatofibromas with hyperpigmentation
- Desmoid type fibromatoses
- Juvenile polyps of the intestinal tract
- Sertoli-Leydig tumors of the ovary or testis
- STK11 adnexal tumors
Board review style answer #2
E. STK11 adnexal tumors. Peutz-Jeghers syndrome is associated with STK11 in 50% of cases. Answer C is incorrect because Peutz-Jeghers syndrome is associated with distinctive hamartomatous polyps not of the juvenile type. Answer D is incorrect because Sertoli-Leydig tumors are associated with DICER1 syndrome. Answer A is incorrect because the pigmented lesions of Peutz-Jeghers syndrome are lentiginous hyperpigmentation only. Answer B is incorrect because desmoid fibromas are characteristic of familial adenomatous polyposis or Gardner syndrome.
Comment Here
Reference: STK11 adnexal tumor
Comment Here
Reference: STK11 adnexal tumor
Teratoma (pending)
[Pending]
Tubal hyperplasia
Table of Contents
Definition / general | Terminology | Epidemiology | Clinical features | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosisDefinition / general
- Hyperplasia of tubal epithelium, variable atypia
Terminology
- Also known as pseudocarcinomatous hyperplasia
Epidemiology
- Typically present in women with estrogen producing ovarian tumors (Int J Gynecol Pathol 1989;8:214)
- May also be associated with salpingitis and PID (Am J Surg Pathol 1994;18:1125)
Clinical features
- Often incidental finding
Gross description
- No specific gross findings
Microscopic (histologic) description
- Papillary, gland-like or cribriform patterns, lined by epithelial cells with mild to moderate nuclear pleomorphism, loss of polarity, stratification, crowding, hyperchromasia and scattered mitotic figures; no invasion
- May be associated with severe inflammation and scarring mimicking adenocarcinoma
Microscopic (histologic) images
Differential diagnosis
- Carcinoma: typically grossly evident, older age, solid epithelial proliferation, brisk mitotic activity, severe atypia, possible invasion
Tubo-ovarian abscess
Table of Contents
Definition / general | Terminology | Epidemiology | Etiology | Clinical features | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosis | Additional referencesDefinition / general
- Inflammation of fallopian tube, most commonly sexually transmitted due to chlamydia and gonorrhea
Terminology
- Part of spectrum of pelvic inflammatory disease (PID)
Epidemiology
- > 1 million cases of acute salpingitis reported annually in US but actual number probably larger due to incomplete and untimely reporting
- For women 16 - 25 years, salpingitis is most common serious infection; affects 11% of females of reproductive age, 12% of women before age 20
- Salpingitis has higher incidence among lower socioeconomic classes, possibly due to earlier sex debut, multiple partners, poorer health care
- Highest risk for people aged 15 - 24 years, possibly due to multiple partners, less awareness of symptoms, reduced willingness to use protective contraceptives
- Infection also occurs via childbirth, abortion (therapeutic or elective), endometrial biopsy, IUD insertion, miscarriage
- In 2005, World Health Organization (WHO) estimated 448 million new cases of curable STIs occur annually in individuals aged 15 - 49 years
Etiology
- Bacteria most associated with salpingitis are: actinomyces, Chlamydia trachomatis, enteric gram - negative rods (eg. E. coli), Gardnerella vaginalis, Haemophilus influenza, Mycoplasma, Neisseria gonorrhoeae, rarely other anaerobic and aerobic bacteria, Staphylococcus, Streptococcus, Trichomonos vaginalis, Ureaplasma urealyticum
- Also Herpes and CMV, fungi, parasites
- 30 - 40% are polymicrobial
- In US, chlamydia is #1 most reported sexually transmitted disease associated with PID, N. gonorrhoeae is #2
- 10 - 20% of untreated chlamydial or gonorrheal infections progress to PID
Clinical features
- Symptoms usually appear after a menstrual period; most commonly abdominal pain, abnormal smell and color of vaginal discharge, bloating, fever, lower back pain, nausea, pain during ovulation, pain during periods, pain during sexual intercourse, vomiting
- Tubo-ovarian abscess in 1/3 of women hospitalized for PID
- Often asymptomatic, may be diagnosed clinically by pelvic examination, blood tests, vaginal or cervical swab
- PID has 3 principal complications: chronic pelvic pain (~25%), infertility, ectopic pregnancy (15 - 50%)
- Impaired fertility is major concern; infection and inflammation can lead to scarring and adhesions within tubal lumens
- Of women with tubal factor infertility, 50% have no history of PID but have scarring of fallopian tubes and exhibit antibodies to C. trachomatis
- May lead to tubule ovarian abscess, pelvic peritonitis, Fitz-Hugh-Curtis syndrome (perihepatitis)
- Taiwanese studies of > 60,000 women diagnosed with PID found that PID was independent risk factor for myocardial infarction in women > age 55 (Int J Cardiol 2013;167:416), with increased risk of stroke for 3 years following PID (Stroke 2011;42:2074); also increased risk of ovarian cancer, particularly in women with 5+ episodes of PID (Lancet Oncol 2011;12:900)
Case reports
- 46 year old woman with S. pneumonia (Hum Pathol 1990;21:1288)
- 50 year old woman with focally calcified cysticercus larva (Hum Pathol 1982;13:665)
Treatment
- Antibiotics or antifungals
Gross description
- Pyosalpinx (pus), hematosalpinx
- Enlarged, erythematous, edematous
- May have fibrinous exudate
- Tubo-ovarian abscess common
Microscopic (histologic) description
- Marked neutrophilic infiltrate, congestion and edema
- Mucosal ulceration
- Reactive epithelial changes
- Variable abscess formation, variable presence of microorganisms
Differential diagnosis
- Ectopic pregnancy
- Hydrosalpinx: transudate, follows purulent salpingitis
- Menstruation / pregnancy: neutrophils common but usually don't invade muscularis, no necrosis, no ulceration, no chronic inflammatory infiltrate
Additional references
Walthard cell nests
Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Case reports | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Nests, plaques or cysts (with eosinophilic luminal material) of metaplastic transitional epithelium involving the serosal surface of fallopian tube, mesosalpinx and mesovarium
- Benign common incidental finding
Essential features
- Benign incidental finding in the subserosa of tubal, paratubal and paraovarian soft tissue
- Bland transitional type epithelium forming small nests / cysts
- CK7+, GATA3+, P63+, PAX8-, CK20- and uroplakin-
ICD coding
Epidemiology
- Common incidental finding
Sites
- Serosa of fallopian tube, including fimbriated end, fimbrial peritoneal junction, mesosalpinx and meso-ovarium
Pathophysiology
- Nests or cysts, including mesothelial cells from the tubal and paratubal serosa, that undergo transitional cell metaplasia
Etiology
- Unknown
Clinical features
- Suggested association between Walthard cell nests and Brenner tumors or mucinous tumors of the ovary (stronger association with the former, though unexplained) (Arch Pathol Lab Med 2008;132:1753)
- Walthard cell nests can be the origin for rare examples of Brenner tumors outside the ovarian parenchyma (Diagn Pathol 2020;15:22)
- Histologically, presence of nests of bland, metaplastic transitional type cells on the serosal surface is diagnostic of Walthard nests
- Pelvic tuberculosis is characterized by granulomatous peritonitis whereas endometriosis will show endometrial type glands and stroma within the serosal surface of adnexal tissue
- Disseminated carcinomatosis shows malignant cells with stromal reaction in the serosal nodules / plaques
- Clinically, Walthard cells are benign asymptomatic and incidental findings, whereas the other differential diagnosis usually presents with abdominal pain, mass, constitutional symptoms or ascites
- Clinically can be mistaken for pelvic tuberculosis (diagnosed based on the presence of granulomas on the tissue along with patient's clinical symptoms) or disseminated tumor (diagnosed based on the presence of malignant tumor cells along with patient's clinical presentation such as abdominal pain / mass, ascites or elevated serum tumor markers)
Case reports
- 10 year old girl with acute appendicitis and urothelial rests (Fetal Pediatr Pathol 2021 Aug 2 [Epub ahead of print])
- 53 year old postmenopausal woman with extraovarian Brenner tumor of the uterus (Diagn Pathol 2020;15:22)
Gross description
- Small 1 - 2 mm yellow-white nodules beneath the serosa of the fallopian tube and paratubal soft tissue
Microscopic (histologic) description
- Small solid nests or cysts of transitional type epithelium with relatively uniform nuclei with irregular borders and nuclear grooves, located beneath the serosa of tubal / paratubal / paraovarian tissue
- Cystic lesions may have eosinophilic luminal secretions
- Rare or no mitotic figures
Microscopic (histologic) images
Immunofluorescence description
- Dual staining for α tubulin and γ tubulin shows attenuated and patchy distribution of cilia in the metaplastic cells of Walthard cell nests and Brenner tumor, suggesting a common origin from tubal epithelium (Eur J Cancer 2013;49:3839)
Positive stains
Negative stains
Sample pathology report
- These are benign, incidental findings and are typically not included within the pathology report
Differential diagnosis
- Benign Brenner tumors:
- Endometriosis:
- Presence of endometrial glands, endometrial stroma or hemosiderin laden macrophages
- 2 out of 3 required for the diagnosis
- Paratubal cysts:
- No solid component
- Lined by ciliated tubal type epithelium
- Endosalpingiosis:
- Glands lined by ciliated tubal type epithelium
Additional references
Board review style question #1
How does the immunohistochemical profile of Walthard cell rests differ from benign Brenner tumor?
- Benign Brenner tumors are P63+, GATA3+, uroplakin+, whereas Walthard cell nests are P63+, GATA+ and uroplakin-
- They share the same IHC phenotype
- Walthard cell nests are PAX2 / PAX8- but benign Brenner tumors show diffuse and strong staining with PAX2 / PAX8+
- Walthard cell nests are positive for uroplakin and GATA3; Brenner tumors are positive for GATA3 but negative for uroplakin
Board review style answer #1
A. Walthard cell nests are positive with P63, GATA3, CK7 and are negative with CK20, uroplakin and PAX2 / PAX8 (focal weak)
Comment Here
Reference: Walthard cell nests
Comment Here
Reference: Walthard cell nests
Board review style question #2
Which of the following is true about the pathologic finding in the image shown above?
- If bilateral, they are associated with higher risk for malignant Brenner tumor
- They are usually GATA3- and PAX8+
- They can mimic peritoneal carcinomatosis by imaging and intraoperatively
- They can only be found on the fallopian tube serosal surface
Board review style answer #2
C. Walthard cell nests are benign incidental findings and can mimic peritoneal carcinomatosis by both imaging and intraoperative examination
Comment Here
Reference: Walthard cell nests
Comment Here
Reference: Walthard cell nests
WHO classification
Table of Contents
Definition / general | Major updates | WHO (2020) - fallopian tube | WHO (2020) - broad ligament and other uterine ligaments | Microscopic (histologic) images | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- WHO classification of tumors of the female genital tract
- Currently on 5th edition, published in 2020
Major updates
- No major updates, mostly refined definitions
- Most high grade serous carcinomas of the ovary arise at the fimbriated end of the fallopian tube from a precursor lesion known as serous tubal intraepithelial carcinoma (STIC) (Pathology 2015;47:423, Mod Pathol 2015;28:1101)
- Undifferentiated carcinoma of the fallopian tube is no longer a separate category
WHO (2020) - fallopian tube
-
Epithelial tumors ICD-O
- Serous adenofibroma, NOS9014/0
- Serous borderline tumor, NOS8442/1
- High grade serous carcinoma8461/3
- Endometrioid adenocarcinoma, NOS 8380/3
- Carcinosarcoma, NOS8980/3
-
Tumor-like lesions
- Paratubal cysts
- Tubal hyperplasia
- Tubo-ovarian abscess
- Salpingitis isthmica nodosa
- Metaplastic papillary lesion
- Placental site nodule
- Mucinous metaplasia
- Endosalpingiosis
-
Mixed epithelial and mesenchymal tumors
- Adenosarcoma8933/3
-
Germ cell tumors
- Mature teratoma, NOS9080/0
- Immature teratoma, NOS9080/3
WHO (2020) - broad ligament and other uterine ligaments
-
Mesenchymal and mixed tumors ICD-O
- Leiomyoma, NOS8890/0
- Adenomyoma, NOS8932/0
- Adenosarcoma8933/3
- Leiomyosarcoma, NOS8890/3
-
Miscellaneous tumors
- Wolffian tumor9110/1
- Papillary cystadenoma, NOS8450/0
- Ependymoma, NOS9391/3
-
Tumor-like lesions
- Adrenocortical remnants
Microscopic (histologic) images
Additional references
Board review style question #1
What is a precursor lesion of most high grade serous carcinomas?
- Low grade serous carcinoma
- Ovarian cortical inclusion cysts
- Paratubal cyst
- Serous borderline tumor
- Serous tubal intraepithelial carcinoma (STIC)
Board review style answer #1
E. Serous tubal intraepithelial carcinoma (STIC)
Comment Here
Reference: Fallopian tubes & broad ligament - WHO classification
Comment Here
Reference: Fallopian tubes & broad ligament - WHO classification
Board review style question #2
Board review style answer #2
C. High grade serous carcinoma and serous tubal intraepithelial carcinoma (STIC)
Comment Here
Reference: Fallopian tubes & broad ligament - WHO classification
Comment Here
Reference: Fallopian tubes & broad ligament - WHO classification
Wolffian tumor / Female adnexal tumor of probable Wolffian origin
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Adnexal tumor arising from remnants of Wolffian (mesonephric) duct
Essential features
- Adnexal tumor arising from mesonephric (Wolffian duct) remnants
- Heterogeneous histologic appearance
- Diagnosis based predominantly on the anatomical site and morphology
Terminology
- Wolffian tumor
- Female adnexal tumor of probable Wolffian origin (FATWO)
- Wolffian adnexal tumor (WAT)
- Wolffian adenoma
- Retiform Wolffian adenoma
- Mesonephric tumor, NOS
ICD coding
- ICD-O: 9110/1 - mesonephric tumor, NOS
- ICD-11: 2F33.Y & XH2WJ5 - benign neoplasm of other or unspecified female genital organs & Wolffian tumor
Epidemiology
- Rare, approximately 130 cases reported (Oncol Lett 2017;14:5167)
- Median age 50 years, range 15 - 87 years (Int J Surg Pathol 2008;16:222)
Sites
- Broad ligament (most common site) (Hum Pathol 1999;30:856)
- Ovaries (Am J Surg Pathol 1983;7:125)
- Mesosalpinx, fallopian tubes
- Paravaginal (Am J Clin Pathol 1994;101:275)
- Peritoneum
Pathophysiology
- Believed to originate from mesonephric (Wolffian) duct remnants
- Arises along the trajectory of the Wolffian duct: from the ovarian hilum, along mesosalpinx, broad ligament, lateral aspects of the uterus and cervix, to the outer third of the vagina (Hum Pathol 1999;30:856)
Etiology
- Unknown
Clinical features
- Adnexal mass with nonspecific symptoms or an incidental finding
- Complaints include lower abdominal pain / distention, pelvic mass, abnormal vaginal bleeding or ascites
- Most tumors are hormonally inert; rare tumors are hormonally active, causing endometrial hyperplasia (Gynecol Oncol 1995;59:304)
- Most tumors are unilateral; rarely bilateral
Diagnosis
- Tumor location
- Surgical specimen: gross and microscopic examination
Radiology description
- Well defined, encapsulated, lobulated or ovoid mass, often separate from ovaries, tubes and uterus
- May demonstrate solid and cystic areas
- Low signal intensity rim around the tumor on T2 weighted MRI images; might be a characteristic feature (J Obstet Gynaecol Res 2016;42:1046)
Prognostic factors
- Low malignant potential; most tumors behave in a benign fashion
- Recurrence or metastases occur in 11 - 20% of cases; median of 48 months to recurrence (range 13 - 96 months) (Gynecol Oncol 2002;86:225)
- Adverse prognostic factors: large size (> 10 cm), capsular invasion and rupture with tumor implants (Histopathology 2005;46:716)
- Aggressive behavior includes intra-abdominal spread, recurrence or distant metastasis, typically to the liver and lungs (Gynecol Oncol 2002;86:225)
- High cellularity, nuclear pleomorphism and high mitotic activity are associated with worse prognosis but tumors with minimal nuclear atypia and low mitotic rate may recur; no single feature is predictive of malignant behavior (Tohoku J Exp Med 1997;181:371)
Case reports
- 28 year old woman with left paratubal cyst (Gynecol Oncol Rep 2021;36:100726)
- 30 year old woman with an incidental ovarian mass (Gynecol Oncol Rep 2014;10:22)
- 37 year old woman with abdominal pain and adnexal mass (Oncol Lett 2017;13:3403)
- 50 year old woman with bilateral adnexal masses (Int J Gynecol Pathol 2018;37:331)
- 70 year old woman with an abdominal mass (Indian J Pathol Microbiol 2014;57:620)
- Series of 11 cases of FATWO (Arch Pathol Lab Med 2022;146:166)
- Series of 15 tumors of FATWO (Mod Pathol 2020;33:734)
Treatment
- Hysterectomy and bilateral salpingo-oophorectomy; tumor debulking
- Role of adjuvant chemotherapy or radiation therapy is unknown
- For recurrent / metastatic KIT (CD117) expressing tumors, tyrosine kinase inhibitor Gleevac (STI571) is a treatment option (Int J Gynecol Cancer 2004;14:546)
Gross description
- Size from < 1 cm to 30 cm
- Encapsulated mass, often nodular, lobulated appearance
- Often centered within or hanging from broad ligament or fallopian tube by a pedicle
- Solid or partially cystic; may have spongy appearance
- Cut surface is rubbery, variegated, pale yellow, gray-white or tan
- May be hemorrhagic or necrotic
- References: Cancer 1973;31:671, Am J Surg Pathol 1983;7:125, Hum Pathol 1999;30:856
Gross images
Frozen section description
- May be mistaken for adenocarcinoma, sex cord stromal tumor or mesonephric carcinoma
- If the tumor is extraovarian, the tumor location (e.g., broad ligament, mesosalpinx) may help to include FATWO in the differential diagnosis during intraoperative consultation
- Variety of patterns may aid with a differential diagnosis, although this may be difficult to appreciate during frozen section due to limited sampling
Microscopic (histologic) description
- Cribriform, tubular, cystic, tubulocystic, sieve-like, solid cords and diffuse growth patterns
- Usually a single pattern predominates but several architectural patterns may coexist (Am J Surg Pathol 1983;7:125)
- Solid sheets of spindle or polygonal cells may be the dominant morphology
- Fibrous stroma varies from scant to large areas of hyalinization
- Intraluminal, bright eosinophilic secretions are often present
- Cells are columnar or cuboidal, may have scant clear cytoplasm, flat or hobnail appearance
- Large cytoplasmic vacuoles and signet ring cell-like forms may be seen (Int J Surg Pathol 2008;16:222)
- Uniform, round or oval nuclei with pale, evenly dispersed chromatin; may have nuclear grooves
- Nuclear atypia is mild to moderate
- Mitotic activity is typically low (up to 1/10 - 3/10 high power fields)
- Malignant tumors have been suggested to present as undifferentiated carcinoma with high cellularity, pleomorphic nuclei or increased mitoses (up to 16/10 high power fields); however, a recent literature review of tumors classified as malignant FATWO indicates that many represent STK11 adnexal tumor or endometrioid carcinoma with unusual features (Am J Surg Pathol 1983;7:125, Histopathology 2022;81:280)
Microscopic (histologic) images
Contributed by Elena Lucas, M.D. and Wenxin Zheng, M.D.
Positive stains
- Pancytokeratin (AE1 / AE3, CAM5.2), CK7, CK19
- Variable: CD10 (50 - 100%), calretinin, inhibin, MelanA, CD99, WT1, ER, PR, androgen receptor, EMA, GATA3, CD117 (KIT), vimentin, SMA (in spindle cell areas)
- References: Hum Pathol 1999;30:856, Int J Gynecol Pathol 2019;38:543, Mod Pathol 2020;33:734, Am J Surg Pathol 2015;39:1411, Arch Pathol Lab Med 2022;146:166
Negative stains
- PAX8 (negative in majority of cases, although focal positivity has been rarely reported) (Mod Pathol 2020;33:734)
- EMA (typically negative; may show focal weak staining)
- CK20, CEA, TTF1, SF1 (Int J Gynecol Pathol 2016;35:167)
Electron microscopy description
- Distinct basal laminae, desmosomal junctions and poorly developed cytoplasmic organelles (Pathol Int 2006;56:95)
- No / minimal cilia, no secretory granules (Pathol Int 2006;56:95)
Molecular / cytogenetics description
- No disease defining molecular alterations identified
- Rare tumors harbor APC and MBD4 mutations; KMT2D mutations (Mod Pathol 2020;33:734, Int J Gynecol Pathol 2019;38:543)
- Tumors previously classified as FATWOs with recurring STK11 mutations are now known to represent STK11 adnexal tumors (Histopathology 2022;81:280)
- Despite CD117 positivity in some tumors, no KIT mutations have been detected (Pathol Int 2006;56:95)
Sample pathology report
- Right adnexal mass, right salpingo-oophorectomy:
- Female adnexal tumor of probable Wolffian origin (FATWO), 6.0 cm (see synoptic report and comment)
- Comment: FATWO (also known as Wolffian tumor) is a rare tumor of low malignant potential. These tumors are thought to arise from mesonephric remnants. Most tumors behave in a benign fashion, although some tumors exhibit aggressive behavior. Although features known to be associated with adverse prognosis (e.g., large size, capsular invasion, rupture, high cellularity, nuclear pleomorphism, high mitotic activity) are absent in this case, cases without these features may also recur. Clinical correlation and follow up are recommended.
Differential diagnosis
- Endometrioid carcinoma:
- Glandular pattern with variable squamous differentiation
- Nuclear atypia
- May show intraluminal mucin
- Positive for PAX8
- High grade serous carcinoma:
- Clear cell carcinoma:
- High grade nuclear features
- Typical architectural patterns (papillary, tubulocystic, solid)
- Positive for PAX8
- Sertoli cell tumor (SCT) and Sertoli-Leydig cell tumors (SLCT):
- Androgenic or estrogenic manifestations; presence of Leydig cells (in SLCT)
- Negative for CD10
- Positive for SF1 and FOXL2
- DICER1 mutation in moderately and poorly differentiated SLCT (Am J Surg Pathol 2017;41:1178)
- Adult granulosa cell tumor:
- Typically solid pattern
- Pale, angulated cells with nuclear grooves
- Hyperestrogenism
- Negative for CD10
- FOXL2 mutation (FOXL2 immunohistochemistry is not specific for mutation status) (N Engl J Med 2009;360:2719)
- STK11 tumors:
- Interanastomosing cords and trabeculae, salivary gland tumor-like growth, tubular, cystic, cribriform, microacinar, nested, nodular, papillary, follicular and solid
- Myxoid, collagenous or hyalinized stroma
- Nuclear atypia with prominent nucleoli, variable mitoses
- Basophilic intraluminal secretions
- Association with Peutz-Jeghers syndrome in ~50%
- Recurrent STK11 alterations (Histopathology 2022;81:280)
- Mesonephric carcinoma:
- Predominantly in the cervix
- May arise in a background of mesonephric hyperplasia
- Mesonephric-like carcinoma:
- Adenomatoid tumor:
- Small, unencapsulated tumor
- Lacks variety of patterns within the same tumor
- Negative for CD10
- Mesothelioma:
- Metastatic carcinoma:
- Higher nuclear grade
- Typically lacks variety of patterns
- Often shows necrosis
- Often positive for CEA
Additional references
Board review style question #1
A 48 year old woman is diagnosed with a 6 cm adnexal mass arising from the broad ligament. She undergoes salpingo-oophorectomy. Microscopically, the tumor has a nodular appearance with low grade cells arranged in a sieve-like pattern and tightly packed tubules with eosinophilic secretions. No necrosis is seen. Mitotic activity is 1/10 high power fields. The tumor cells are negative for PAX8 and positive for CD10. Which of the following is likely to be true?
- Final diagnosis is based on ancillary studies
- Minimal nuclear atypia and low mitotic rate are predictive of benign behavior
- Patients often have virilizing symptoms
- Tumor likely originated from mesonephric embryological remnants
- Tumor originated from paramesonephric embryological remnants
Board review style answer #1
D. Tumor likely originated from mesonephric embryological remnants
Comment Here
Reference: Female adnexal tumor of probable Wolffian origin
Comment Here
Reference: Female adnexal tumor of probable Wolffian origin
Board review style question #2
This image is from a 50 year old woman with an encapsulated adnexal mass, found incidentally. Which of the following statements is true?
- Calretinin and inhibin immunostains help to differentiate it from sex cord stromal tumors
- CD117+ tumors harbor KIT mutation
- ER and PR immunostains help to differentiate it from endometrioid carcinoma
- FOXL2 mutation is present in the majority of tumors
- Tumor is typically positive for pancytokeratin and CD10
Board review style answer #2
E. Tumor is typically positive for pancytokeratin and CD10. This is a female adnexal tumor of probable Wolffian origin (FATWO), which is typically positive for pancytokeratin and CD10.
Comment Here
Reference: Female adnexal tumor of probable Wolffian origin
Comment Here
Reference: Female adnexal tumor of probable Wolffian origin
Recent Fallopian tubes & broad ligament Pathology books
Find related Pathology books: gynecologic