- TX: primary tumor cannot be assessed
- T0: no evidence of primary tumor
- Tis: carcinoma in situ / high grade dysplasia
- T1: tumor invades the bile duct wall with a depth less than 5 mm
- T2: tumor invades the bile duct wall with a depth of 5 - 12 mm
- T3: tumor invades the bile duct wall with a depth greater than 12 mm
- T4: tumor invades the celiac axis, superior mesenteric artery or common hepatic artery
- Notes: careful perpendicular or longitudinal sections of the bile duct wall must be taken in order for accurate measurements of invasion to be made
- 90% of cases
- Mean age 60 years, 60% women
- Abdominal pain, right upper quadrant tenderness, nausea, vomiting, fever, leukocytosis, mild jaundice
- 50% of those with jaundice have coexisting choledocholithiasis
- Due to stone impaction, versus biliary colic, which is due to intermittent obstruction
- 50% have bacterial infection (E. coli, Enterobacter, Enterococcus, Klebsiella, Clostridium, Peptostreptococcus, Bacteroides)
- 1% mortality
- Perforation unlikely if early operation
- Chronic obstruction causes increased intraluminal pressure, vascular compromise, stasis and concentration of bile within lumen, mucosal damage, release of cellular enzymes, release of inflammatory mediators such as lysolecithin and prostagladins
- Gall bladder volume increases as acute cholecystitis progresses to gangrene or empyema
- Gallstone formation is associated with poorer contractility and larger volume in gallbladders that contain stones (World J Gastroenterol 2010;16:4341)
- As the weight, volume and size of the stone increases, gall bladder mucosa changes from cholecystitis, hyperplasia, metaplasia, dysplasia, to carcinoma (Trop Gastroenterol 2012;33:39)
- Eosinophils accumulate in gallbladder mucosa in young patients (Pol J Pathol 2011;62:41)
- Abrupt destructive process of gallbladder
- Not typical inflammation; neutrophils often absent
- Most often due to stones blocking cystic duct
- ~50% of cases complicated by aerobic bacterial infection
- Inflammation of gallbladder induced by choleliths, ischemia or substances
- Gallbladder wall thickening and pericholecystic fluid seen on transabdominal ultrasound
- Complications, such as perforation, seen most often in acalculous cholecystitis
- Cholecystectomy within 72 hours is typically curative
- ICD-9:
- 574.00 - calculus of gallbladder with acute cholecystitis, without mention of obstruction
- 574.01 - calculus of gallbladder with acute cholecystitis with obstruction
- 574.30 - calculus of bile duct with acute cholecystitis, without mention of obstruction
- 574.31 - calculus of bile duct with acute cholecystitis with obstruction
- 574.60 - calculus of gallbladder and bile duct with acute cholecystitis, without mention of obstruction
- 574.61 - calculus of gallbladder and bile duct with acute cholecystitis, with obstruction
- 575.0 - acute cholecystitis
- Reference: Gastroenterol Rep (Oxf) 2017;5:36
- 10 - 15% of American population
- Native American women have highest rates
- As high as 73% in women > 30 years (Surg Clin North Am 2014;94:455)
- Gallbladder
- Calculous
- Blockage of neck or cystic duct
- Typically by gallstones or biliary sludge
- Continued production of mucus by gallbladder with no outlet
- Increased pressure within gallbladder
- Venous stasis
- Arterial stasis
- Gallbladder ischemia and necrosis (Surg Clin North Am 2014;94:455)
- Blockage of neck or cystic duct
- Acalculous
- Bile stasis and ischemia not provoked by a physical blockade of cystic duct
- Ischemia due to:
- Activated factor XII
- No collateral blood supply; complete reliance on cystic artery (Surg Clin North Am 2014;94:455)
- Ischemia due to:
- Bile stasis and ischemia not provoked by a physical blockade of cystic duct
- Calculous
- Due to stones physically blocking cystic duct
- Acalculous
- 2 - 15% of cases (Histopathology 2005;47:485)
- Greater complication risk
- More likely to get gangrenous cholecystitis and subsequent perforation (Infect Dis Clin North Am 2010;24:885)
- AIDS related
- Similar clinical picture
- Due to cytomegalovirus, cryptosporidia or microsporidia
- Cocaine induced (Mills: Sternberg's Diagnostic Surgical Pathology 5th Edition, 2012)
- Seen in young, healthy patients
- Suspect when concurrent vascular thrombosis
- Classic: right upper quadrant pain, nausea, vomiting, anorexia, fever
- Combination of history, physical, laboratory and imaging findings (Surg Clin North Am 2014;94:455)
- Leukocytosis
- Hyperbilirubinemia and elevated liver function tests
- May indicate choledocholithiasis (Surg Clin North Am 2014;94:455)
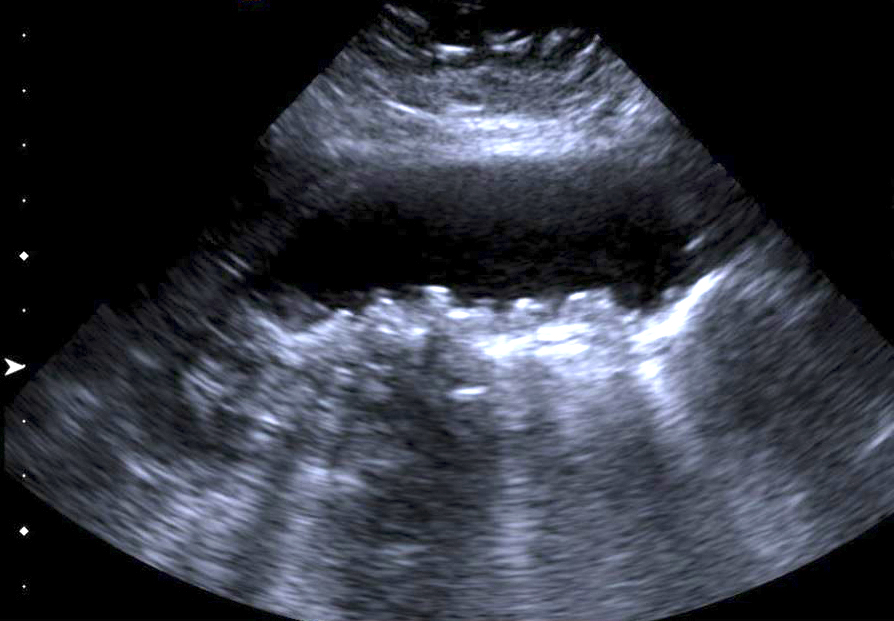
- Transabdominal ultrasound
- Gallbladder wall > 4 mm
- Pericholecystic fluid
- Cholescintigraphy
- Hepatic 2,6-dimethyl-iminodiacetic acid (HIDA) injected intravenously
- Gallbladder not visualized (Surg Clin North Am 2014;94:455)
- Complications
- Perforation, pericholecystic abscess, fistula
- Mortality from untreated complications is 20% (BMJ Clin Evid 2008;2008:0411)
- 53 and 58 year old women with empyematous cholecystitis and a 75 year old man with perforated cholecystitis, who were treated with robotic cholecystectomy in the emergency setting (Medicine (Baltimore) 2019;98:e16010)
- 59 year old man with COVID-19 pneumonia and ischemic gangrenous cholecystitis (World J Emerg Surg 2020;15:43)
- 66 year old man with COVID-19 pneumonia and acute acalculous cholecystitis (Ann Med Surg (Lond) 2020;58:73)
- 68 year old woman with COVID-19 pneumonia and concurrent acute cholecystitis (BMC Infect Dis 2020;20:437)
- Antibiotics
- Cholecystectomy
- Within 72 hours preferred for surgical candidates
- Cholecystostomy drain for critically ill, poor candidates (Infect Dis Clin North Am 2010;24:885)
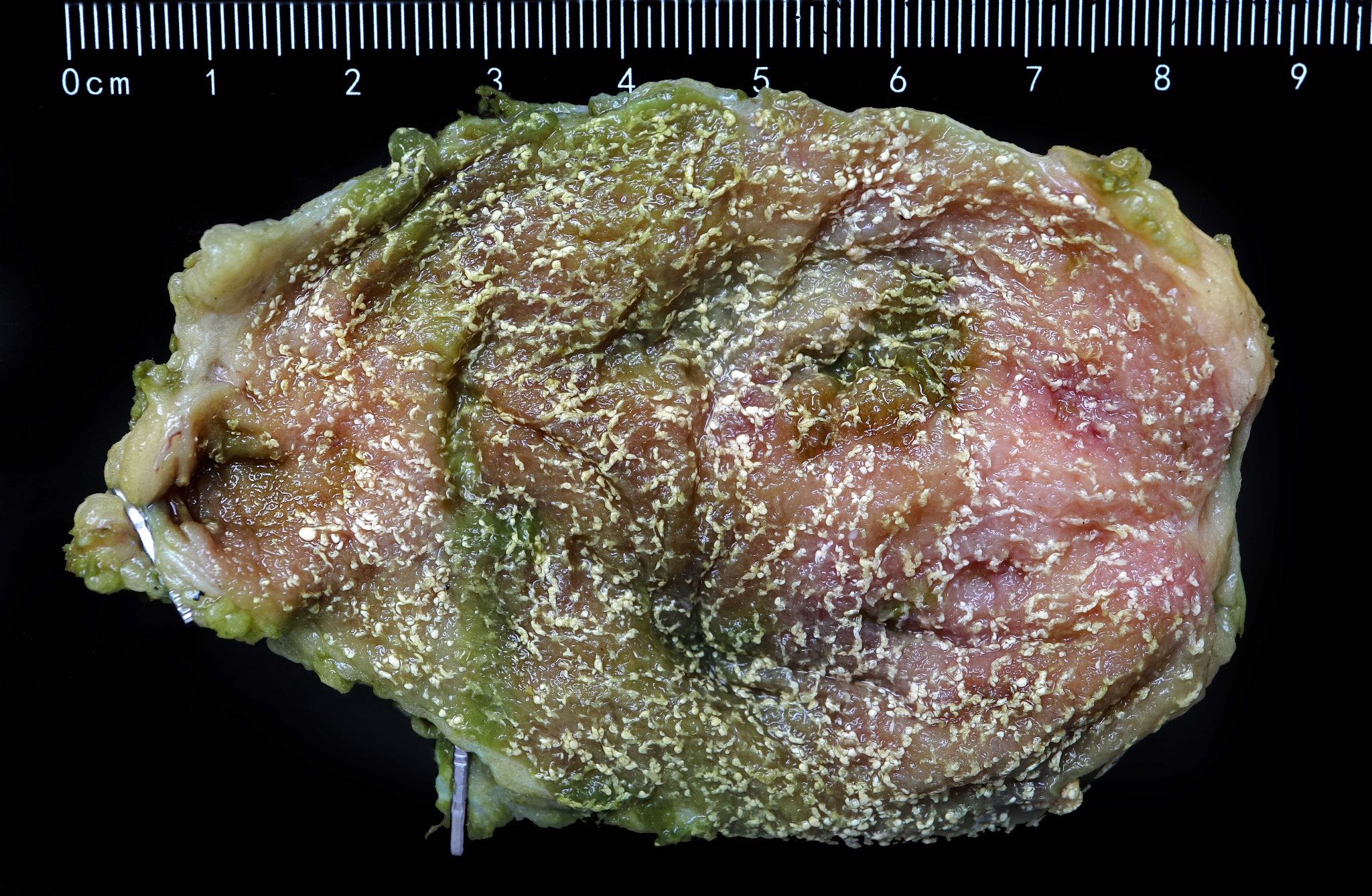
- Distention / edema of gallbladder
- Serosa
- Exudate
- Color alteration
- Hemorrhagic
- Wall
- Thickened up to 2 cm
- Edematous
- Hemorrhagic
- Mucosa
- May see ulcers
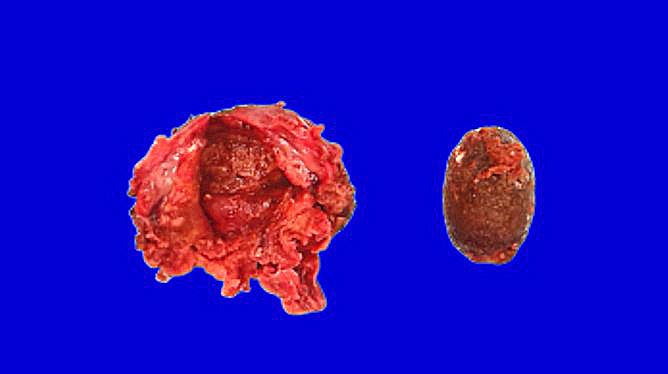
- Cholelith(s)
- In neck or cystic duct
- Lumen
- May see bile, hemorrhage, fluid mixture of cholesterol and calcium carbonate (J Hepatobiliary Pancreat Surg 2007;14:15)
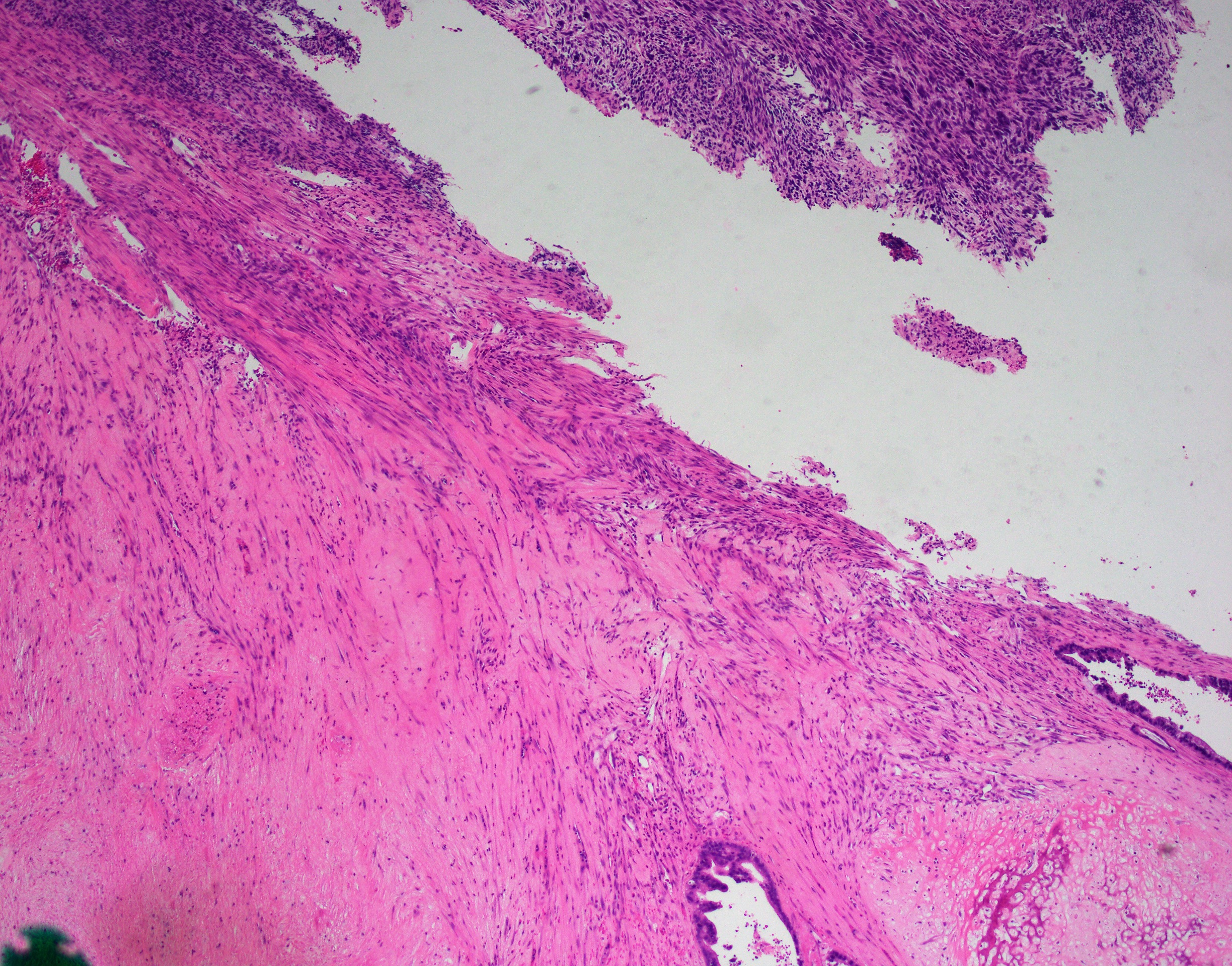
- May not see acute inflammatory cells unless there is a secondary bacterial infection or choledocholelithiasis
- Erosion of mucosa
- Edema
- Myofibroblasts, lymphocytes, plasma cells, eosinophils and pigment laden macrophages
- Fibrin
- Thrombi in small veins
- Sometimes fibrinoid necrosis (Int J Clin Exp Pathol 2013;6:91)
Overview of acute cholecystitis
Imaging findings in cholelithiasis and acute cholecystitis
- Gallbladder, cholecystectomy:
- Acute calculous cholecystitis
- Gallbladder cancer:
- Frozen section analysis during cholcystectomy if suspected (Hepatobiliary Pancreat Dis Int 2015;14:300)
Comment Here
Reference: Acute cholecystitis
Comment Here
Reference: Acute cholecystitis
What factors make the pictured organ susceptible to ischemia necessitating removal, even in the absence of physical blockade of the duct?
- Location in zone 3, furthest from the hepatic artery
- Location within a watershed zone
- No collateral blood supply
- Sensitivity to atherosclerosis of the inferior mesenteric artery
Comment Here
Reference: Acute cholecystitis
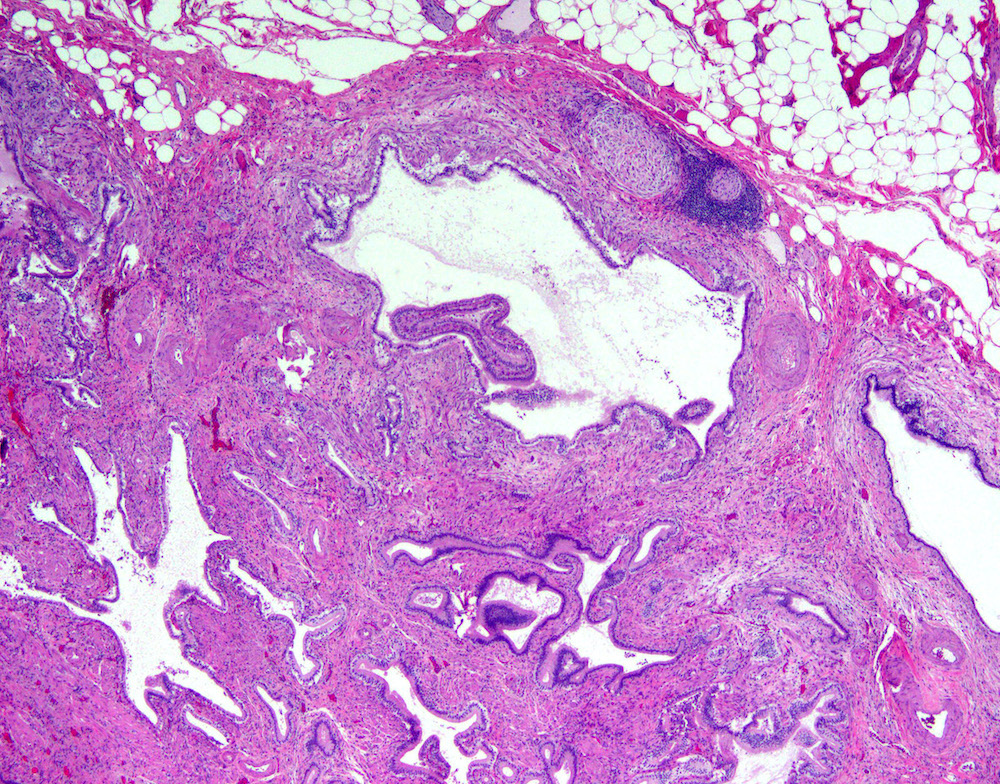
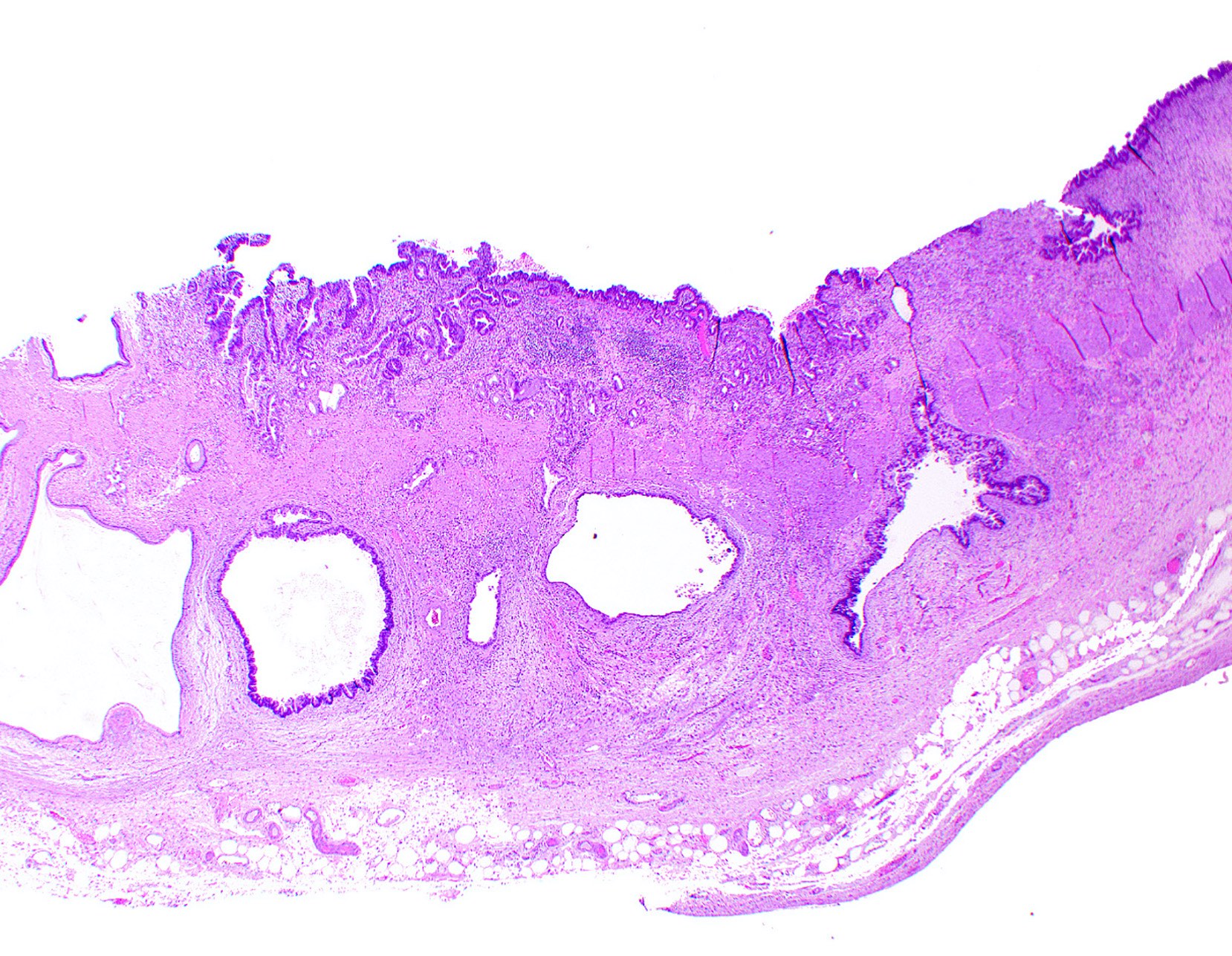
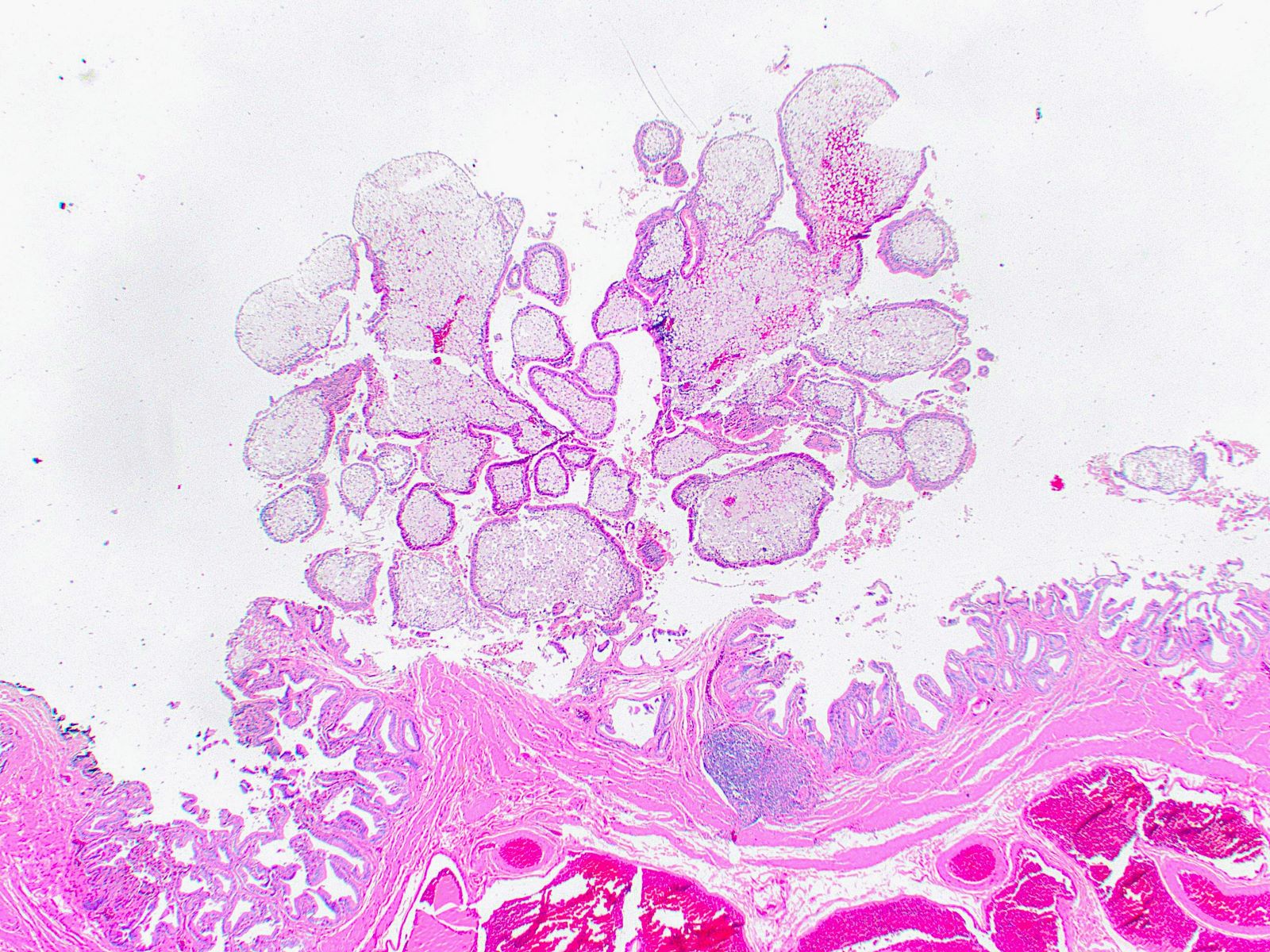
- Benign reactive nonneoplastic lesion of the gallbladder
- Associated with chronic inflammation / injury (cholecystitis, cholelithiasis) (StatPearls: Adenomyomatosis [Accessed 26 January 2021])
- Most common benign gallbladder polypoid lesion after cholesterol polyps (Euroasian J Hepatogastroenterol 2019;9:40)
- May form tumor-like lesions (adenomyomatous nodules) (Am J Surg Pathol 2020;44:1649)
- Most patients thought to be asymptomatic; right upper quadrant pain can be seen (StatPearls: Adenomyomatosis [Accessed 26 January 2021])
- Reported frequency: up to 10% of cholecystectomy specimens (Burt: MacSween's Pathology of the Liver, 7th Edition, 2017, StatPearls: Adenomyomatosis [Accessed 26 January 2021])
- May also represent diverticular change or hamartomatous malformation (Burt: MacSween's Pathology of the Liver, 7th Edition, 2017, Korean J Gastroenterol 2016;67:332)
- Usually found in the gallbladder but may rarely occur in extrahepatic bile ducts (Korean J Gastroenterol 2016;67:332)
- Rarely develops dysplasia and carcinoma (Am J Surg Pathol 2020;44:1649, Burt: MacSween's Pathology of the Liver, 7th Edition, 2017)
- Also called adenomyoma, adenomyomatosis (Korean J Gastroenterol 2016;67:332)
- Generalized, segmental or localized types
- Generalized:
- Diffuse wall thickening (up to 5x normal) with intramural diverticula resembling cystic spaces within the wall
- Also called adenomyomatosis, adenomyosis
- Localized:
- Fundus has nodules from 0.5 to 2.5 cm with grayish white cut surface containing multiple cysts
- May cause gallbladder inversion
- Also called adenomyoma
- Generalized:
- F:M = 3:1; some authors report similar prevalence between sexes (StatPearls: Adenomyomatosis [Accessed 26 January 2021])
- Wide age range of patients; most are diagnosed in their 50s (StatPearls: Adenomyomatosis [Accessed 26 January 2021])
- Rare in children (World J Clin Pediatr 2016;5:223)
- Gallbladder (fundus if localized), rarely extrahepatic bile ducts
- Associated with chronic inflammation / injury (cholecystitis, cholelithiasis) (StatPearls: Adenomyomatosis [Accessed 26 January 2021])
- May also represent diverticular change or hamartomatous malformation (Burt: MacSween's Pathology of the Liver, 7th Edition, 2017, Korean J Gastroenterol 2016;67:332)
- Usually diagnosed by microscopic evaluation of hematoxylin and eosin stained slides
- Ultrasound is the most commonly used imaging modality; CT or MRI may also be used (HPB (Oxford) 2016;18:129)
- 17 year boy with adenomyomatosis of the gallbladder (Arch Argent Pediatr 2020;118:e43)
- 81 year old woman with right upper quadrant pain (BMC Gastroenterol 2010;10:41)
- 3 cases with fundal variant (J Clin Med Res 2010;2:150)
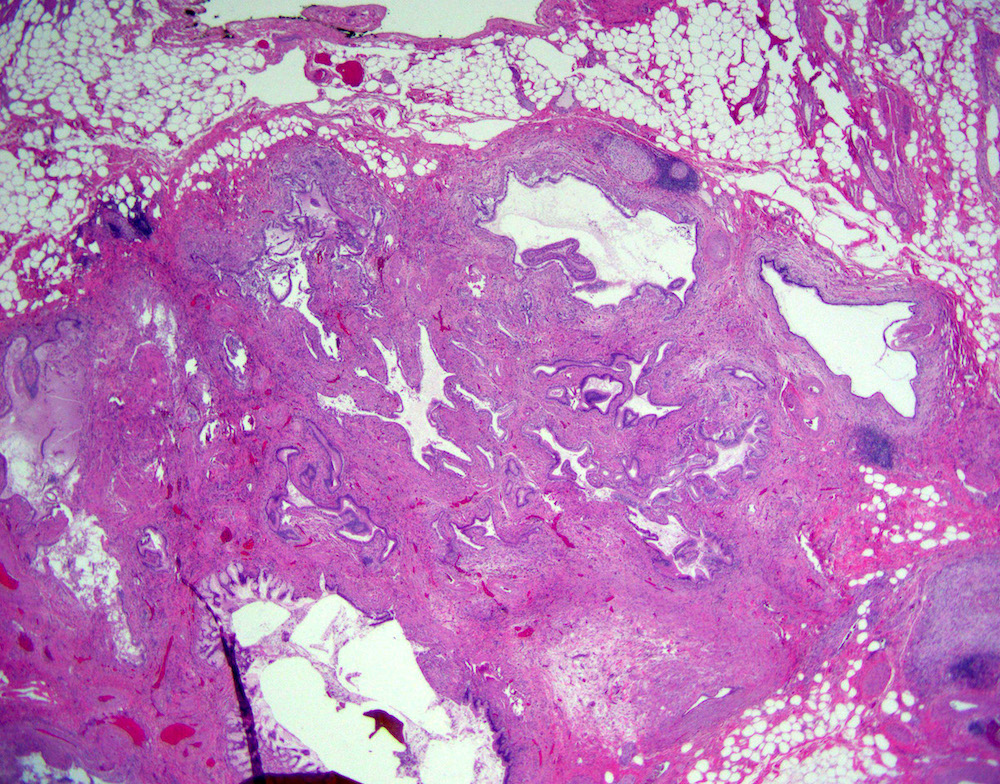
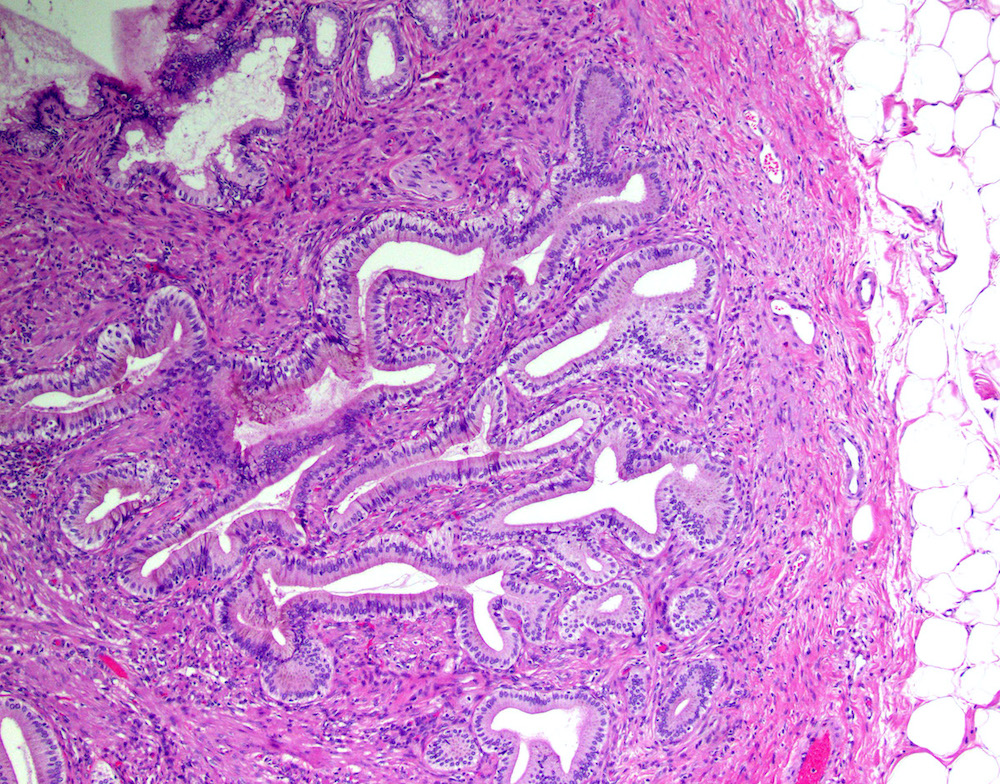
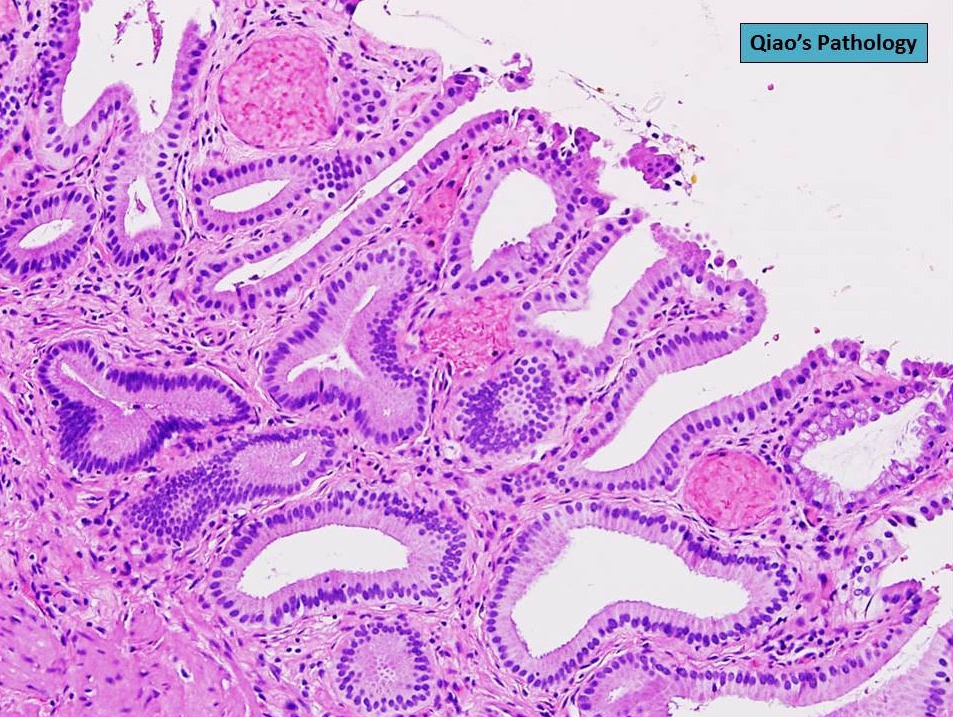
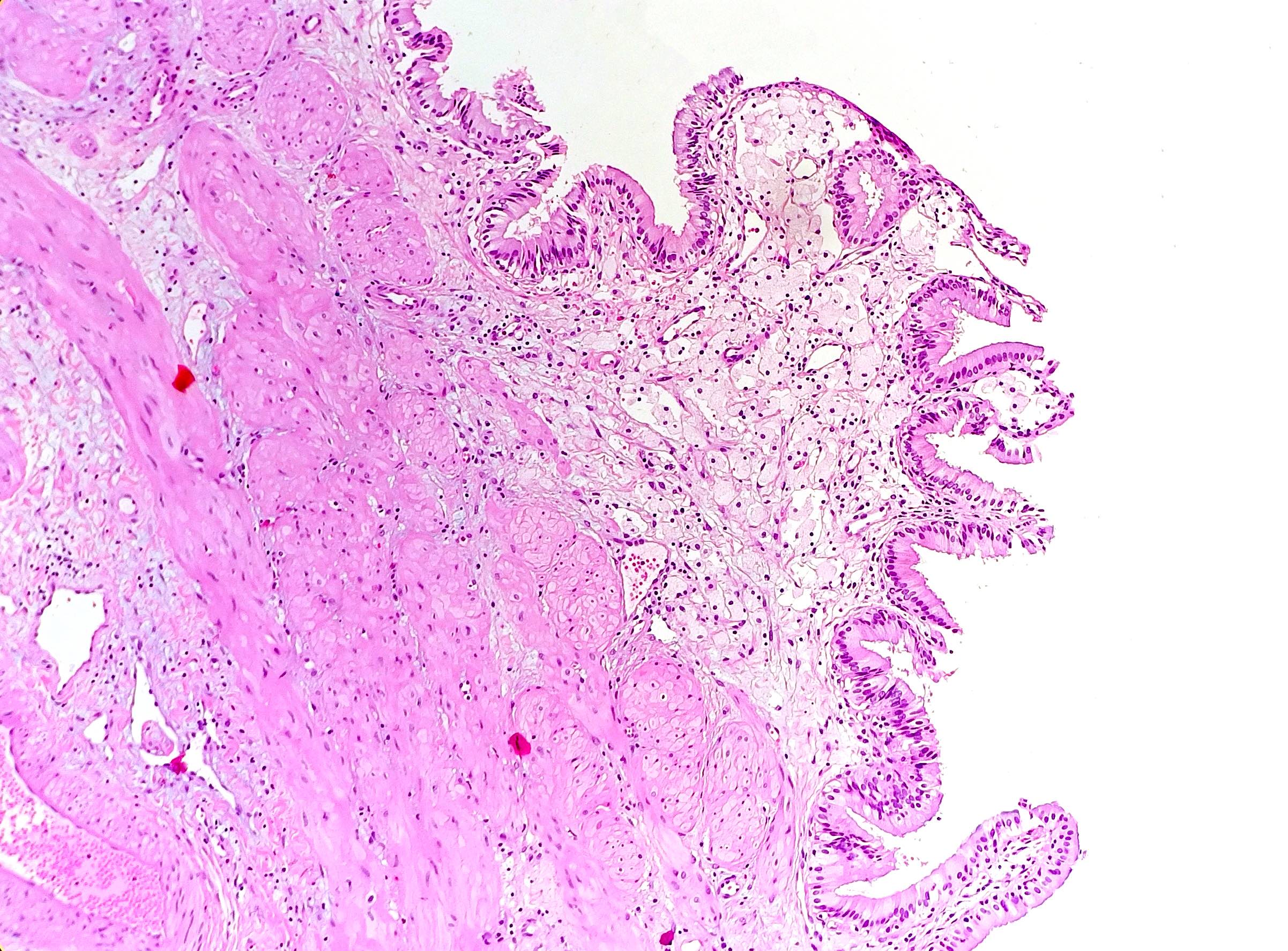
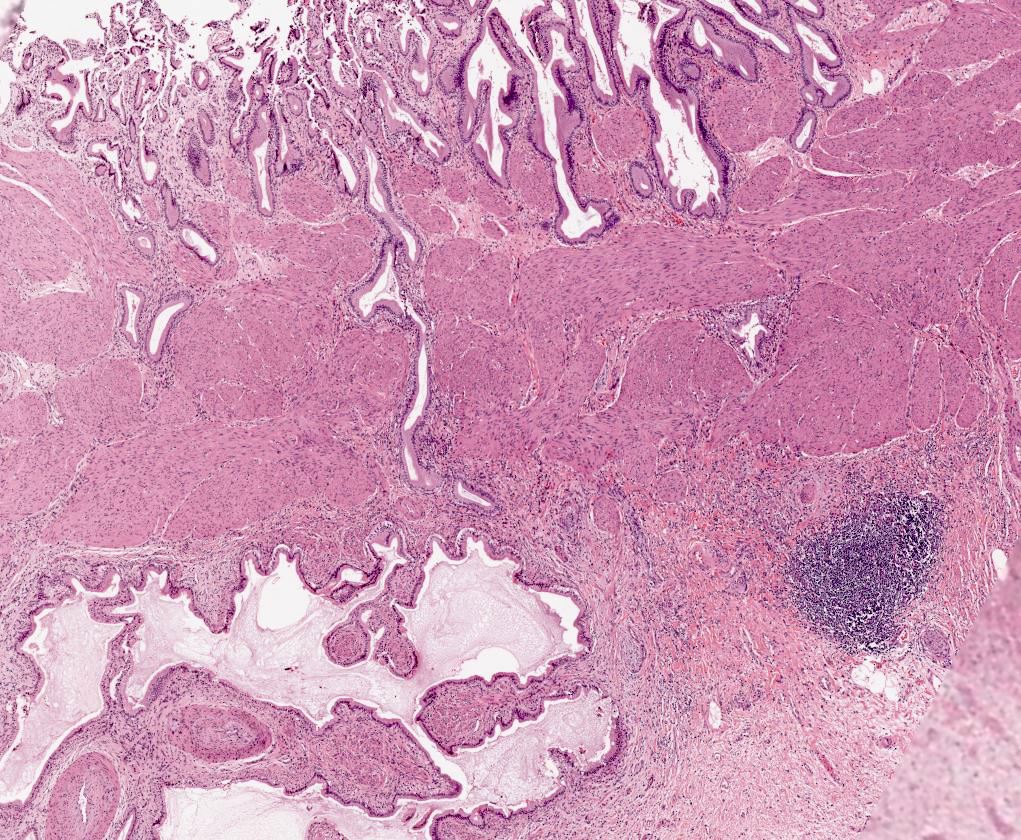
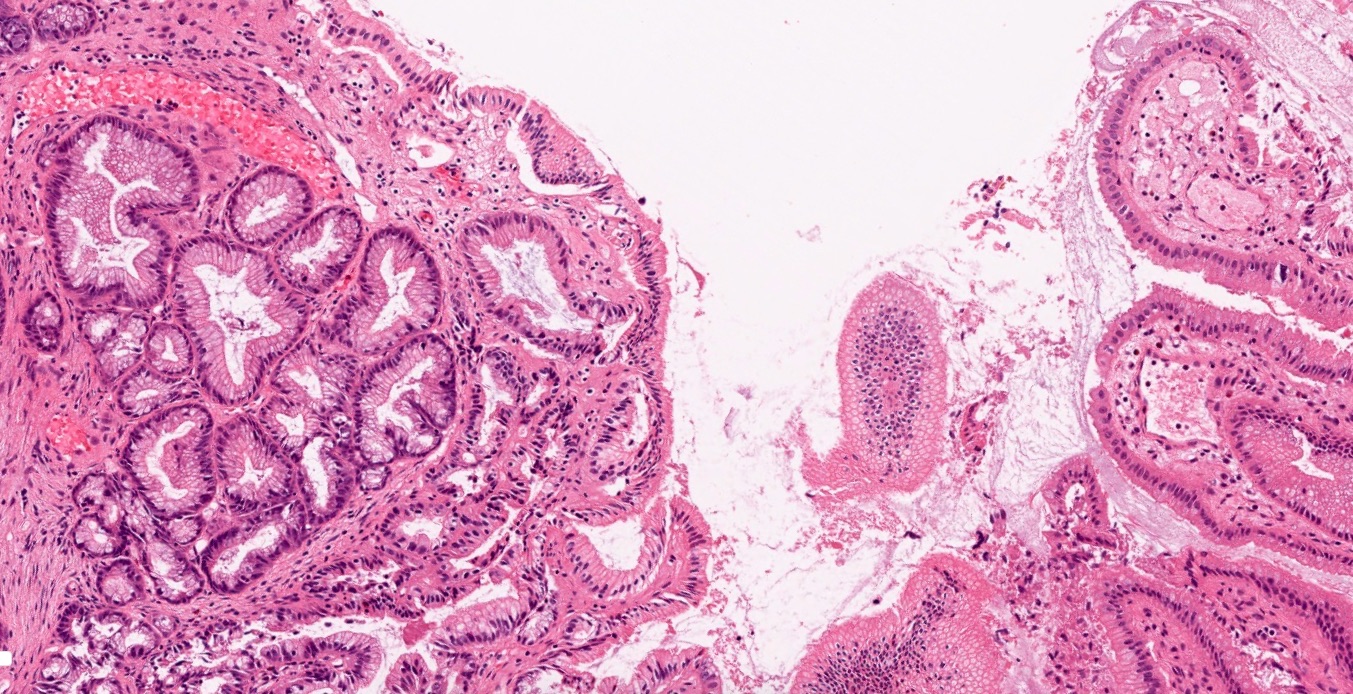
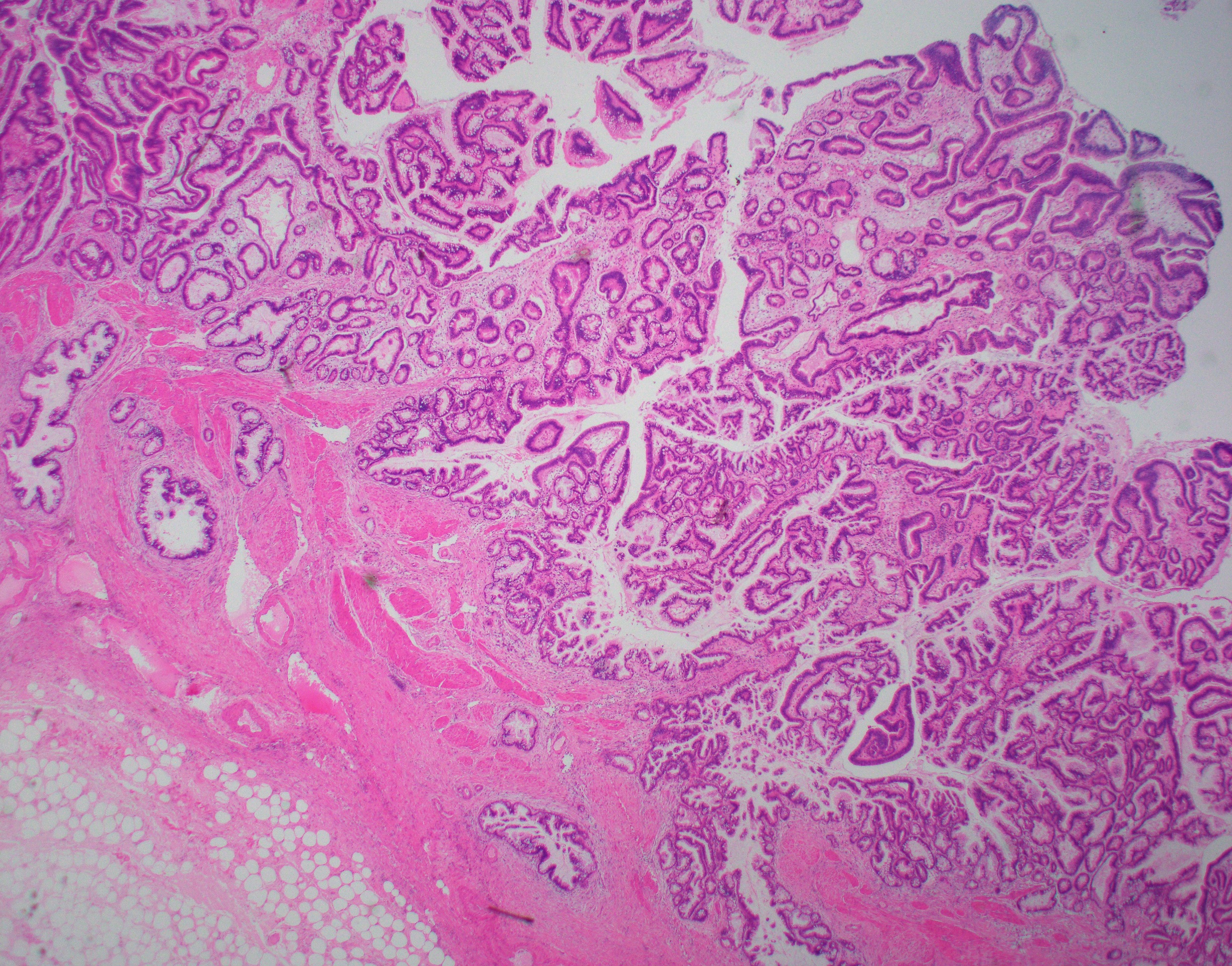
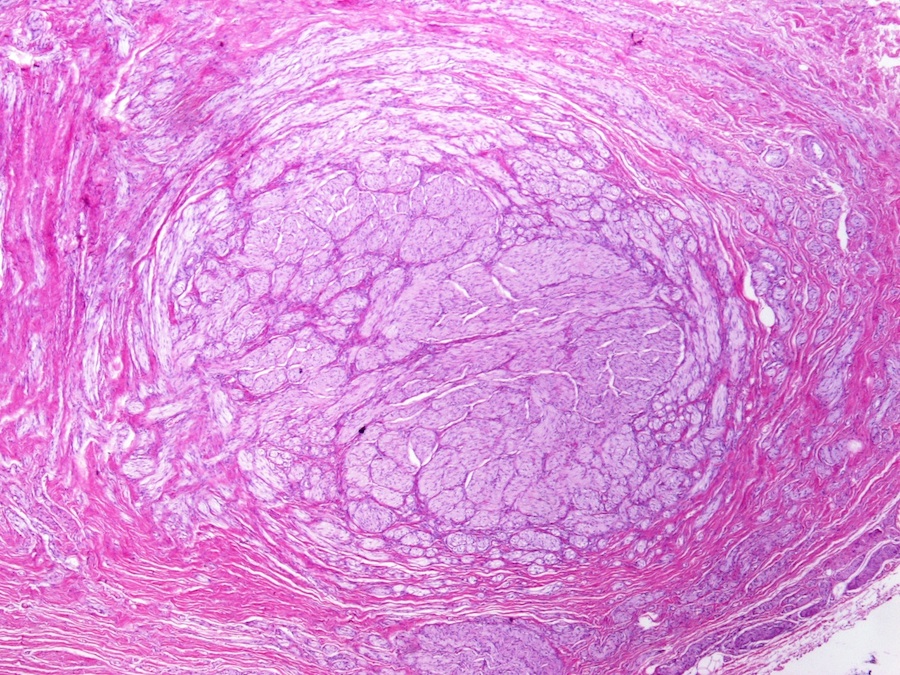
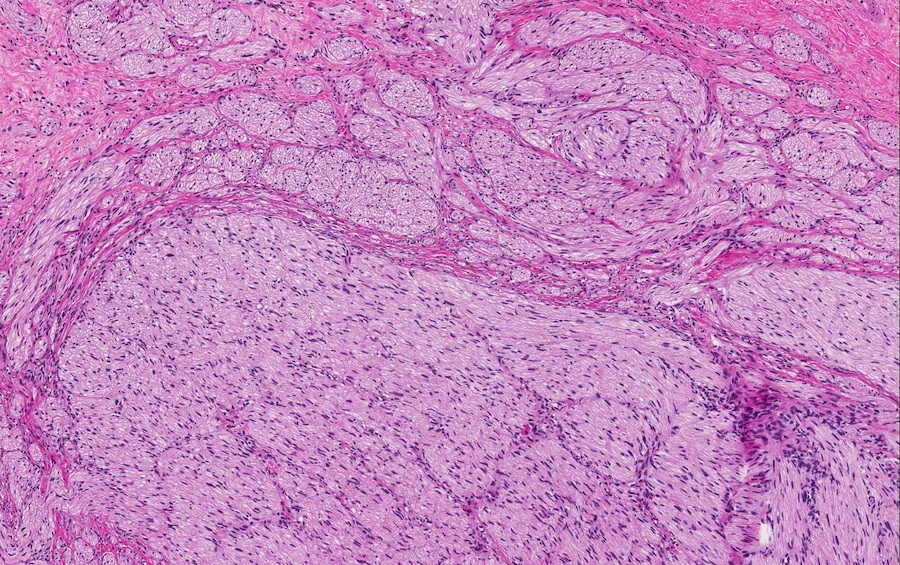
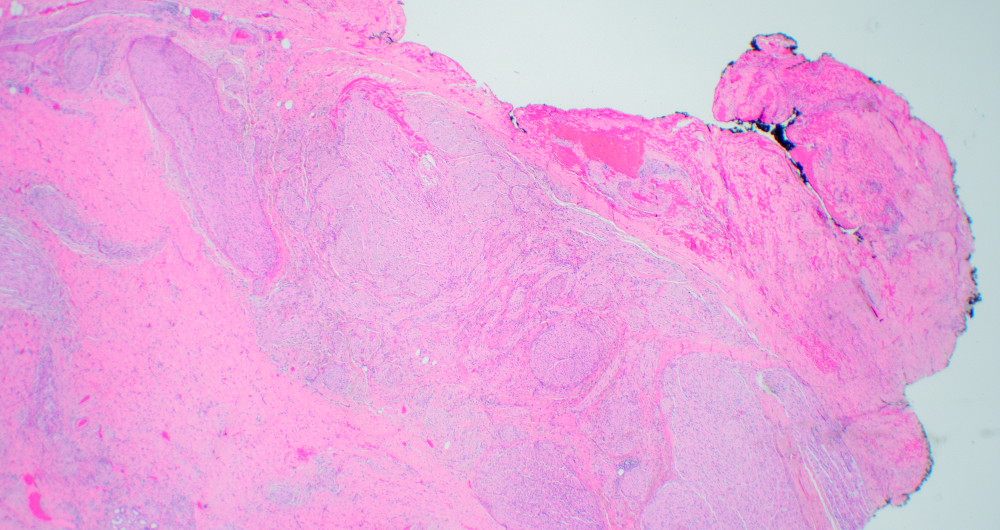
- Cystically dilated benign biliary glands accompanied by smooth muscle hypertrophy of gallbladder wall, thickened / fibrotic subserosa (StatPearls: Adenomyomatosis [Accessed 26 January 2021])
- Glands are distinct from the Rokitansky-Aschoff sinuses, which are epithelial diverticula, usually multifocal and occur throughout gallbladder secondary to injury, versus adenomyomatous nodule (distinct localized lesion of the gallbladder wall, 1 - 1.5 cm mural nodule in the fundus) (Am J Surg Pathol 2020;44:1649)
- May have reactive epithelial changes, papillary change and intestinal metaplasia (StatPearls: Adenomyomatosis [Accessed 26 January 2021])
- Rarely, benign glands are seen in proximity to nerves, appearing as perineural and intraneural invasion only in the subserosal layer (benign gland-like structures may migrate into nerves due to chemotactic factors or signaling substances with activation of cell receptors) (Am J Surg Pathol 2007;31:1598)
- Adenomyomatous nodules may rarely show dysplastic / carcinomatous transformation, whereas dysplasia in Rokitansky-Aschoff sinuses appears to be more common; however, the true association between adenomyomatous nodules and neoplasia has not yet been determined (Am J Surg Pathol 2020;44:1649)
- Recently, papillary dysplastic lesions of adenomyomas have been identified (intracholecystic neoplasms of adenomyomas), demonstrating cystic and solid areas with papillary projections that show biliary, gastric and intestinal phenotypes, with low or high grade dysplasia (Am J Surg Pathol 2020;44:1649)
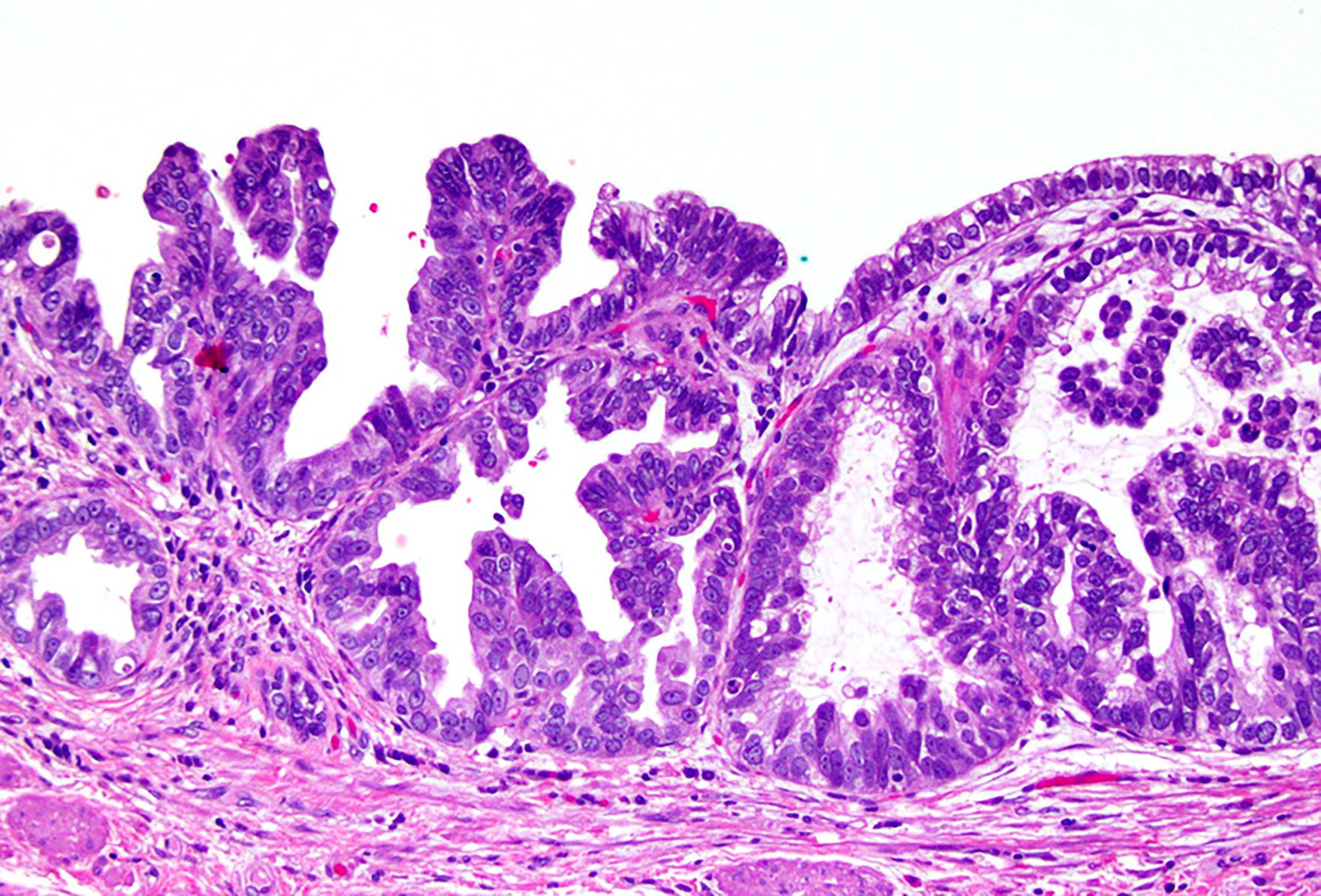
- In general, biliary dysplasia (biliary intraepithelial neoplasia [BilIN]) can be either low grade or high grade and is recognized by the abrupt transition from normal mucosa with nuclear hyperchromasia, overlapping and enlargement in low grade, with the inclusion of those features as well as loss of nuclear polarity/nuclear stratification seen in high grade dysplasia
Contributed by Monica T. Garcia-Buitrago, M.D.
- Gallbladder, cholecystectomy:
- Chronic cholecystitis and cholelithiasis with adenomyomatous hyperplasia
- Adenocarcinoma:
- Glands and tubules lined by cuboidal to columnar epithelium
- Cytologic atypia
- Prominent nucleoli
- Increased mitotic activity
- Desmoplastic stroma
- Chronic cholecystitis:
- Lymphoplasmacytic infiltrates in lamina propria, may extend deeper, occasionally form lymphoid aggregates / follicles, occasionally may contain eosinophils
- May contain Rokitansky-Aschoff sinuses: epithelial diverticula that can occur throughout gallbladder secondary to injury
- Thickened wall with mural fibrosis
- May have smooth muscle hyperplasia
- Acute cholecystitis
- Biliary intraepithelial neoplasia
- Chronic biliary epithelial inflammation / injury (chronic cholecystitis, cholelithiasis)
- Invasive adenocarcinoma
- Involvement of extrahepatic bile ducts
Comment Here
Reference: Adenomyomatous hyperplasia
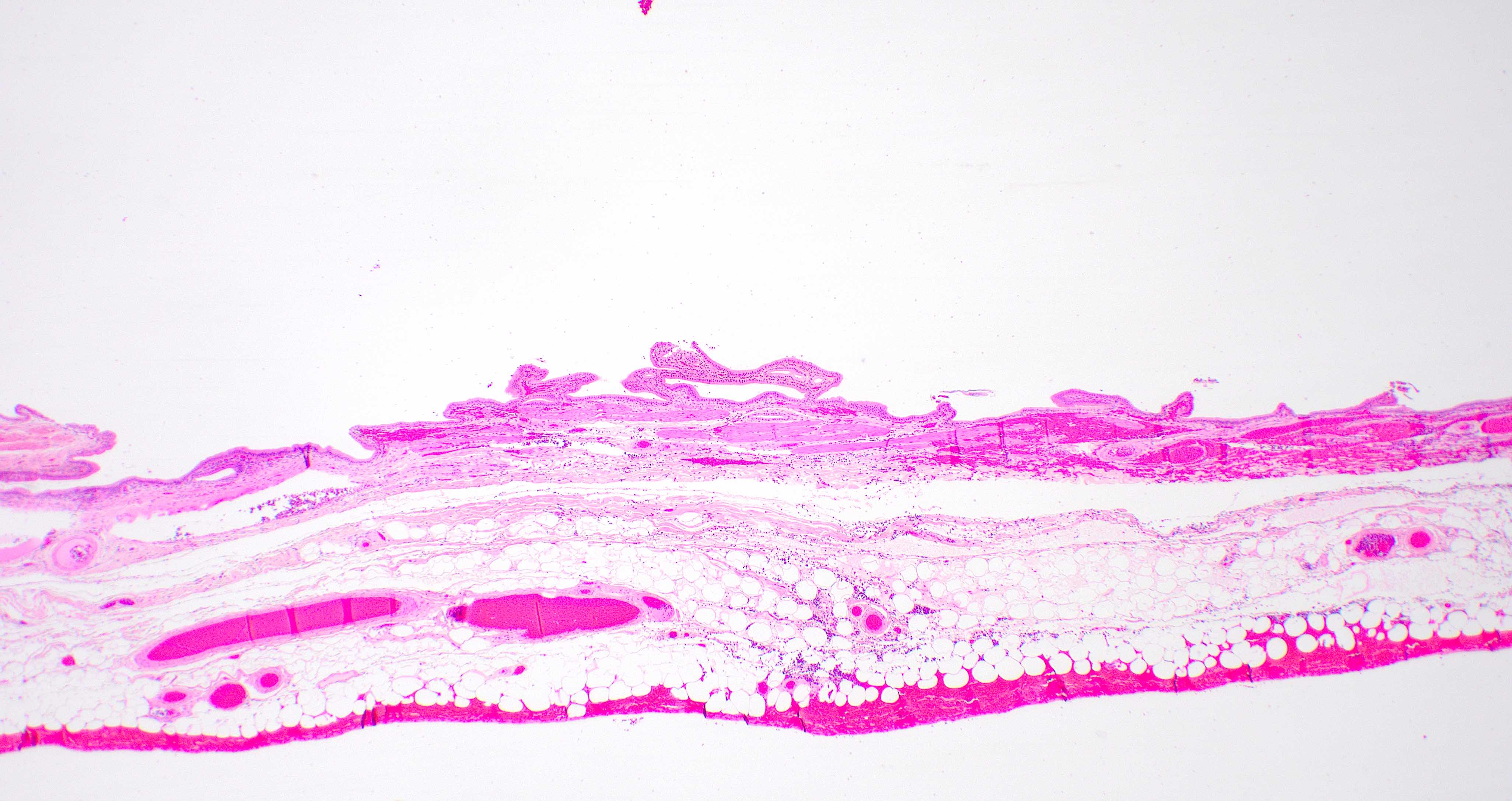
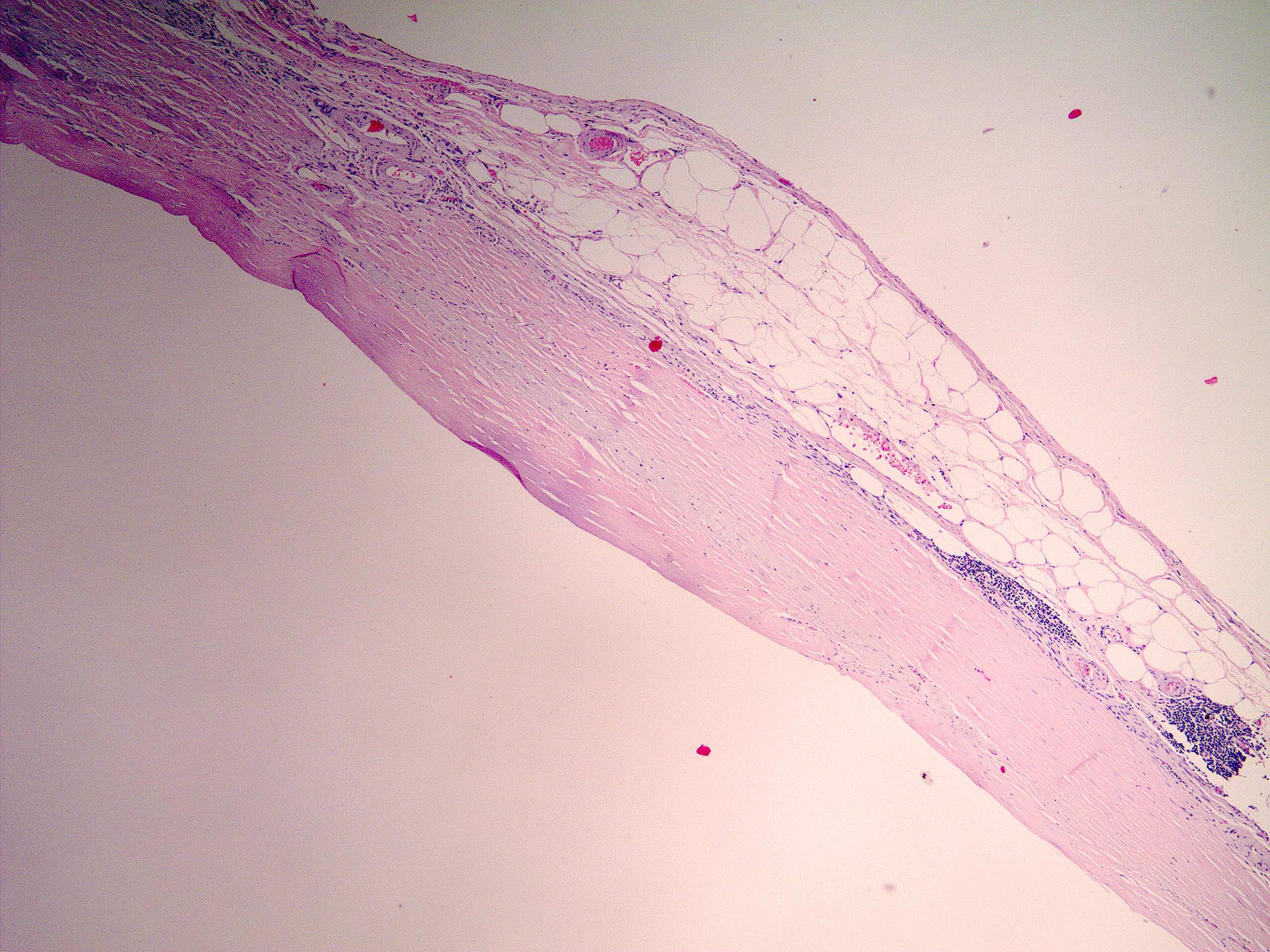
- The gallbladder is a pear shaped saccular organ connected to the extrahepatic biliary system via the cystic duct
- Gallbladder wall is 1 - 2 mm thick and composed of mucosa, muscularis propria and serosa
- No muscularis mucosae or submucosa is present
- With the exception of the common bile duct and the cystic duct at the junction with the gallbladder, the extrahepatic bile ducts do not have a muscle layer
- Gallbladder:
- Pear shaped saccular structure located on the inferior surface of the right hepatic lobe
- Wall thickness: 1 - 2 mm
- Composed of fundus, body and neck
- Distal fundus: extends beyond the anterior liver margin
- Central body: most of the gallbladder
- Neck: narrows as it joins the cystic duct
- Extrahepatic biliary tree:
- Right and left hepatic ducts:
- Join to form common hepatic duct (CHD) in the porta hepatis (hilum of liver)
- Common hepatic duct:
- Joins cystic duct to form common bile duct
- Cystic duct:
- Connects gallbladder to common hepatic duct (CHD)
- Has spiral valve of Heister (mucosal folds that avoid collapse)
- Common bile duct:
- Results from the fusion of CHD and cystic duct
- 2 - 9 cm long; passes posterior to the first portion of duodenum, traverses the head of pancreas, enters the second part of duodenum through the ampulla of Vater and discharges gallbladder contents into the duodenal lumen
- 60% of the population have common channel for pancreatic duct and common bile duct
- Remainder of the population have 2 ducts in parallel
- Right and left hepatic ducts:
- Gallbladder stores and releases bile
- Gallbladder empties into cystic duct, which connects it to the extrahepatic biliary tree
- Extrahepatic biliary tree serves as conduit for bile flow
- Bile excretion is normally 500 - 1000 mL/day
- Bile is concentrated 5 - 10x via active absorption of electrolytes accompanied by passive movement of water
- Cholecystokinin causes gallbladder contraction and release of stored bile into the gut
- Bile is critical for intestinal absorption of dietary fat but the gallbladder is not
- Bile is 66% bile salts, is bicarbonate rich and has 3% organic solutes
- 95% of secreted bile salts are reabsorbed in the ileum and are subsequently returned to the liver via portal blood (called enterohepatic circulation of bile salts)
- Cholesterol is eliminated via loss of 0.5 g of bile salts per day
- Bile salts:
- Cholates, chenodeoxycholates, deoxycholates, lithocholates, ursodeoxycholates
- Major hepatic products of cholesterol metabolism
- Family of water soluble sterols with carboxylated side chains
- Highly effective detergents, solubilize water insoluble lipids secreted by the liver (usually lecithin) into the biliary tree and promote dietary lipid absorption within the gut
- Lecithin (phosphatidylcholine):
- Hydrophobic, nonaqueous
- Has minimal solubility in water
- Gallbladder:
- Microscopic layers: mucosa, muscular wall, perimuscular subserosal connective tissue and serosa; muscularis mucosae and submucosa are not present
- Mucosa:
- Branching folds composed of surface epithelium and lamina propria
- Cores of lamina propria are lined by a single layer of columnar epithelial cells
- Epithelial cells have eosinophilic cytoplasm with variably present apical vacuoles; nuclei are basally oriented, oval and uniform, with inconspicuous nucleoli
- There are also inconspicuous scattered basal epithelial cells located above the basement membrane
- Tubuloalveolar mucus glands are present only in the neck region; true glands are not present outside the neck in normal gallbladder
- Goblet cells are not present in normal gallbladder epithelium
- Lamina propria is composed of loose connective tissue, blood vessels and lymphatics; few lymphocytes, plasma cells, mast cells and histiocytes are usually present (Mills: Histology for Pathologists, 3rd Edition, 2007)
- Muscular wall:
- Loose bundles of smooth muscle fibers without well formed distinct layers
- Resembles muscularis mucosae
- Adjacent to lamina propria without an intervening submucosa
- Perimuscular subserosal connective tissue (adventitia):
- Perimuscular connective tissue composed of collagen, elastic tissue, fat, vessels, lymphatics and nerves
- May contain lymph nodes and paraganglia
- Serosa:
- Peritoneum covers the portion of gallbladder that is not connected to the liver
- Aberrant bile ducts (ducts of Luschka):
- Present in 10% of cholecystectomy specimens, often buried in gallbladder wall adjacent to liver, may contain a collar of fibrous tissue, may communicate with intrahepatic bile ducts
- Histologically composed of lobular aggregates of small ductules lined by bland cuboidal to columnar biliary type epithelium (Am J Surg Pathol 2011;35:883)
- Rokitansky-Aschoff sinuses:
- Outpouchings of gallbladder mucosa that penetrate the muscle wall
- May be acquired herniations
- Ectopic or heterotopic tissue:
- Variety of ectopic tissues can be found in the gallbladder wall and biliary tract, namely liver, pancreas, adrenal, gastric, thyroid and cartilage, resulting in tumor-like lesions (Zimmermann: Ectopias and Heterotopies as Tumor-like Lesions of the Hepatobiliary Tract [Accessed 17 February 2022], Medicine (Baltimore) 2019;98:e18293, Case Rep Gastroenterol 2018;12:170, Cases J 2009;2:6786, Medicine (Baltimore) 2018;97:e0058)
- Endometriosis can also occur in the gallbladder wall and cause occult bleeding
- Extrahepatic bile ducts:
- Epithelial layer:
- Single layer of columnar cells with round, basally located nuclei
- Subepithelial stroma:
- Composed of fibroblasts, collagen, small vessels and scattered inflammatory cells
- Muscle layer:
- Present along the common bile duct and at the junction of the cystic duct and gallbladder
- Peribiliary connective tissue:
- Consists of adipose tissue, vessels, nerves and ganglion cells
- Epithelial layer:
- Peribiliary mucous glands:
- Considered a local progenitor cell niche in extrahepatic biliary epithelium (Liver Int 2012;32:554)
- Unevenly distributed within large intrahepatic ducts and all extrahepatic bile ducts
- Lobular architecture; are surrounded by fibroconnective tissue (important in distinguishing from well differentiated carcinoma)
- Gallbladder lacks muscularis mucosae and submucosa
- Goblet cells are present in normal gallbladder epithelium
- Muscle layer is not present along the common bile duct and at the junction of the cystic duct and gallbladder
- Tubuloalveolar mucus glands are present throughout the entire gallbladder
Comment Here
Reference: Gallbladder & extrahepatic bile ducts - Anatomy, histology & embryology
Comment Here
Reference: Gallbladder & extrahepatic bile ducts - Anatomy, histology & embryology
- Angiodysplasia is a term describing distinct gastrointestinal mucosal vascular ectasias which are not associated with:
- Cutaneous lesions
- Systemic vascular disease or
- Familial syndrome
- Angiodysplasia of the gallbladder is extremely rare
- Pathogenesis of angiodysplasia of the gallbladder is unknown
- It is usually an incidental finding on histopathological examination of the excised gallbladder
- It is usually asymptomatic but has the potential to bleed
- Laparoscopic cholecystectomy is a definitive cure
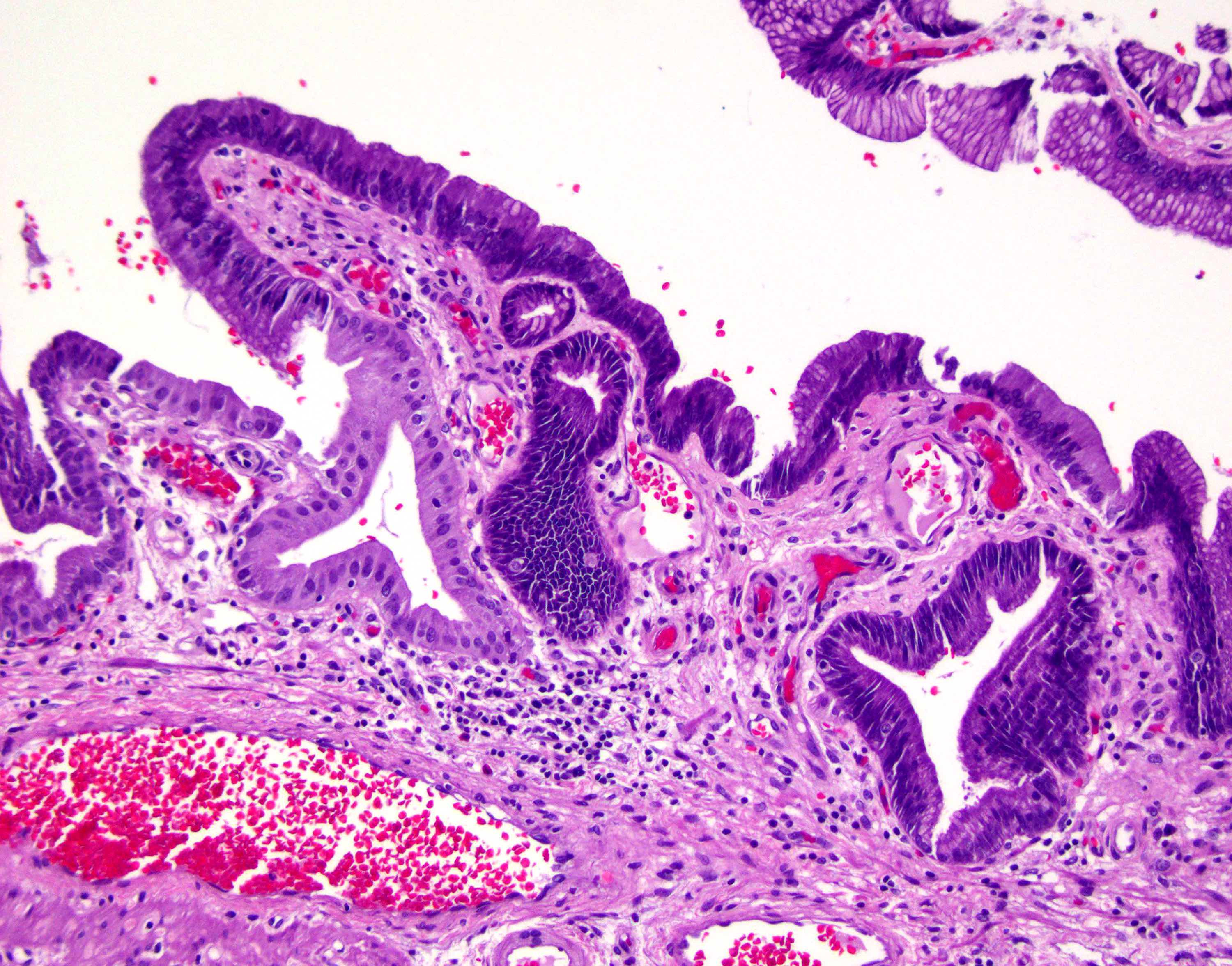
- Vascular ectasia
- Angiodysplasia of the gallbladder occurs in a wide age range (30s - 70s), in both men and women
- Proposed etiology similar to colonic vascular ectasia
- Likely due to gallbladder distention and contraction, causing intermittent obstruction of blood vessels
- Obstruction subsequently leads to dilatation and tortuosity of the vessels
- Usually asymptomatic
- Incidental finding during histologic examination of excised gallbladder
- 36 year old woman with a history of dyspepsia and right upper quadrant abdominal pain (Int J Surg Case Rep 2011;2:256)
- Laparoscopic cholecystectomy is curative
- Distended gallbladder with gallstones
- Gallbladder mucosal ulceration
- Dilated mucosal capillary sized vessels
- Disorganized dilated veins
- Thick arteries in muscularis propria
- Angiodysplasia of the gallbladder is extremely rare.
- Angiodysplasia of the gallbladder is usually asymptomatic.
- The pathogenesis of angiodysplasia of the gallbladder is unknown.
- Laparoscopic cholecystectomy is usually curative.
Which of the above statements are true?
- 1, 2, 3
- 1, 3
- 2, 4
- All of the above
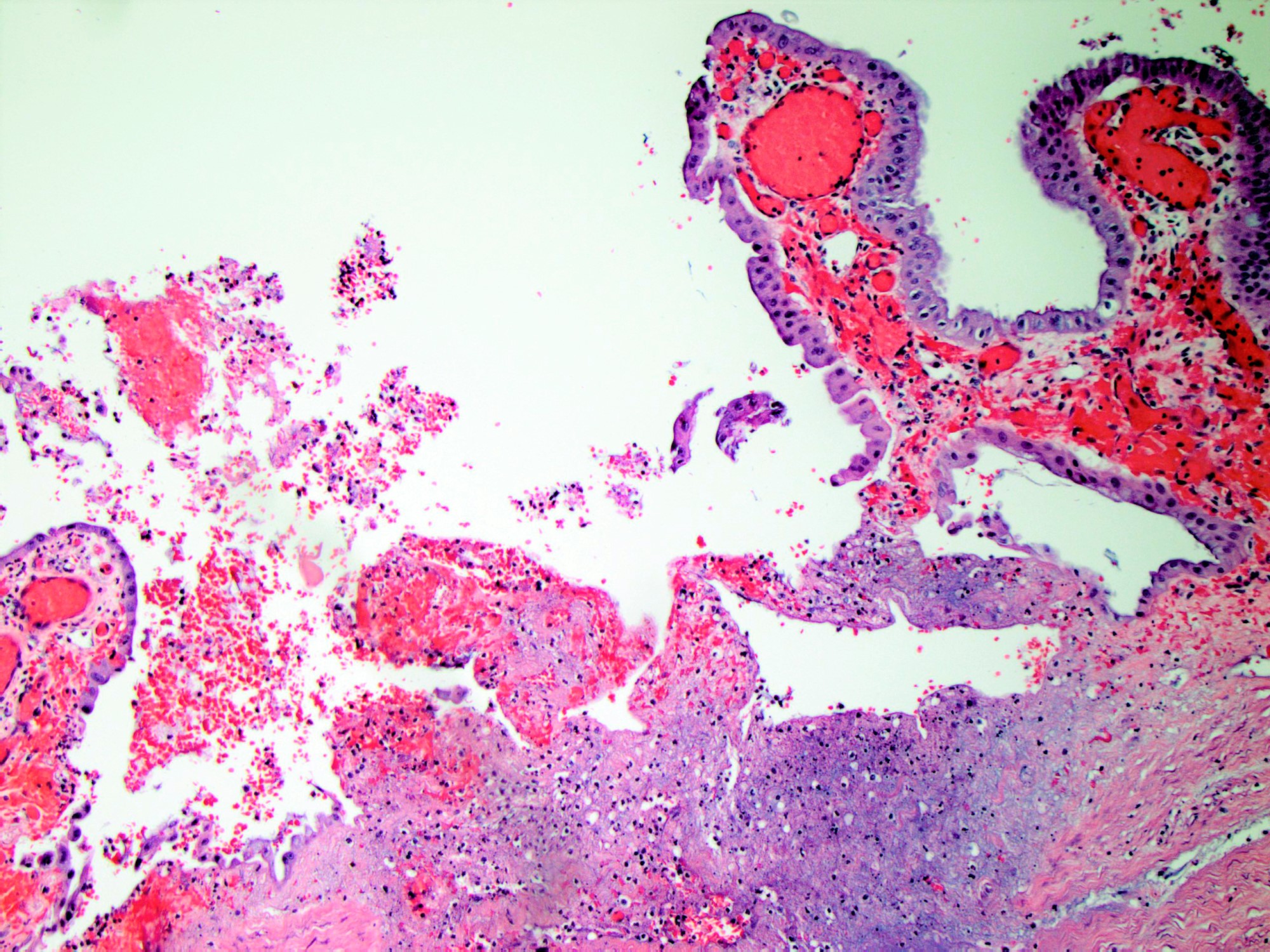
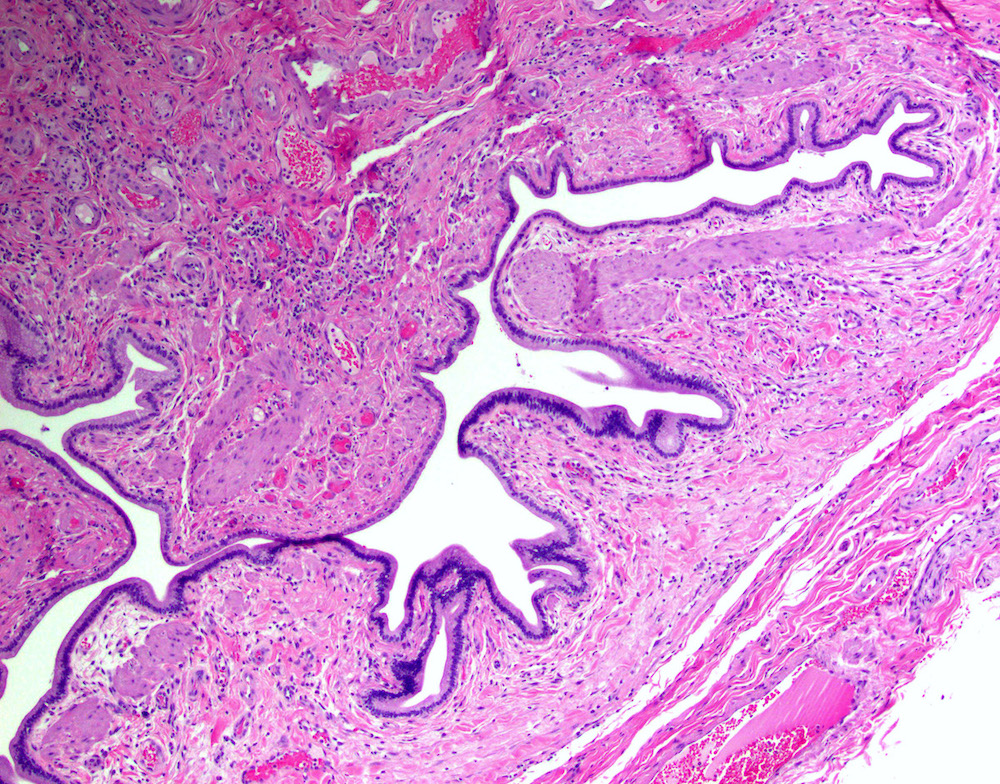
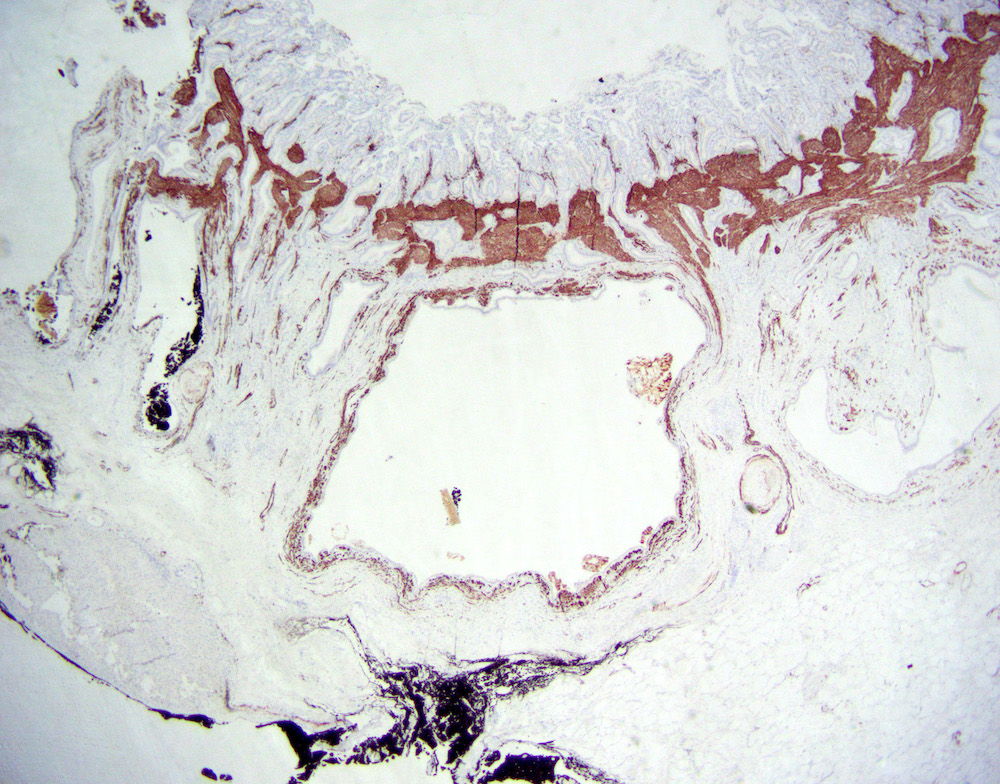
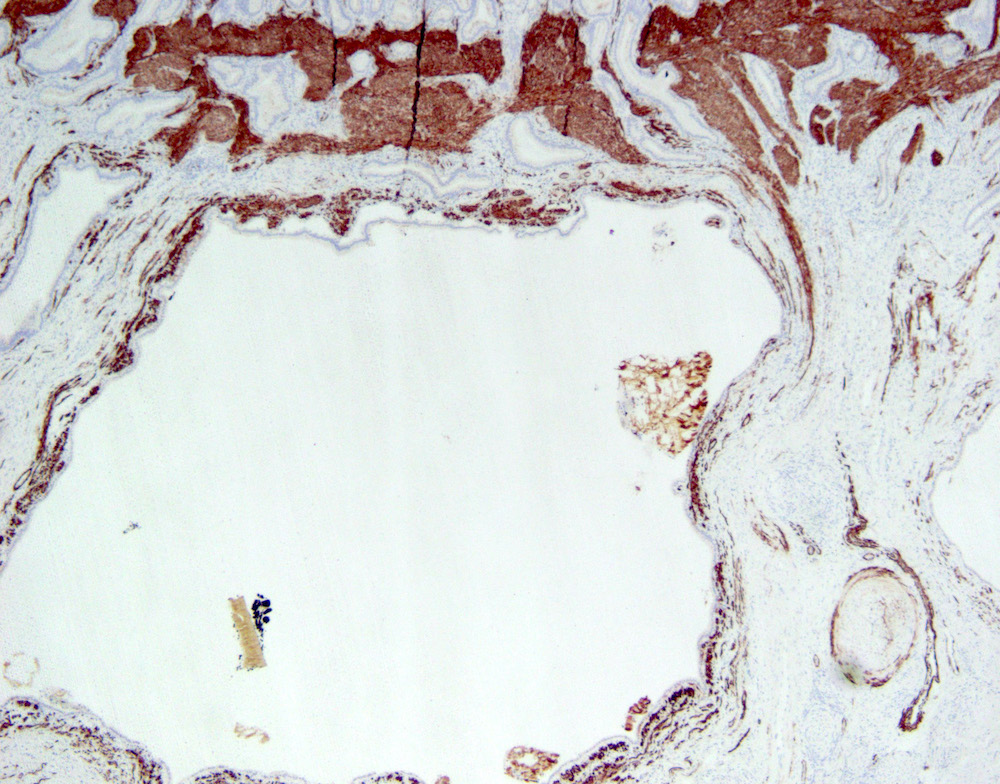
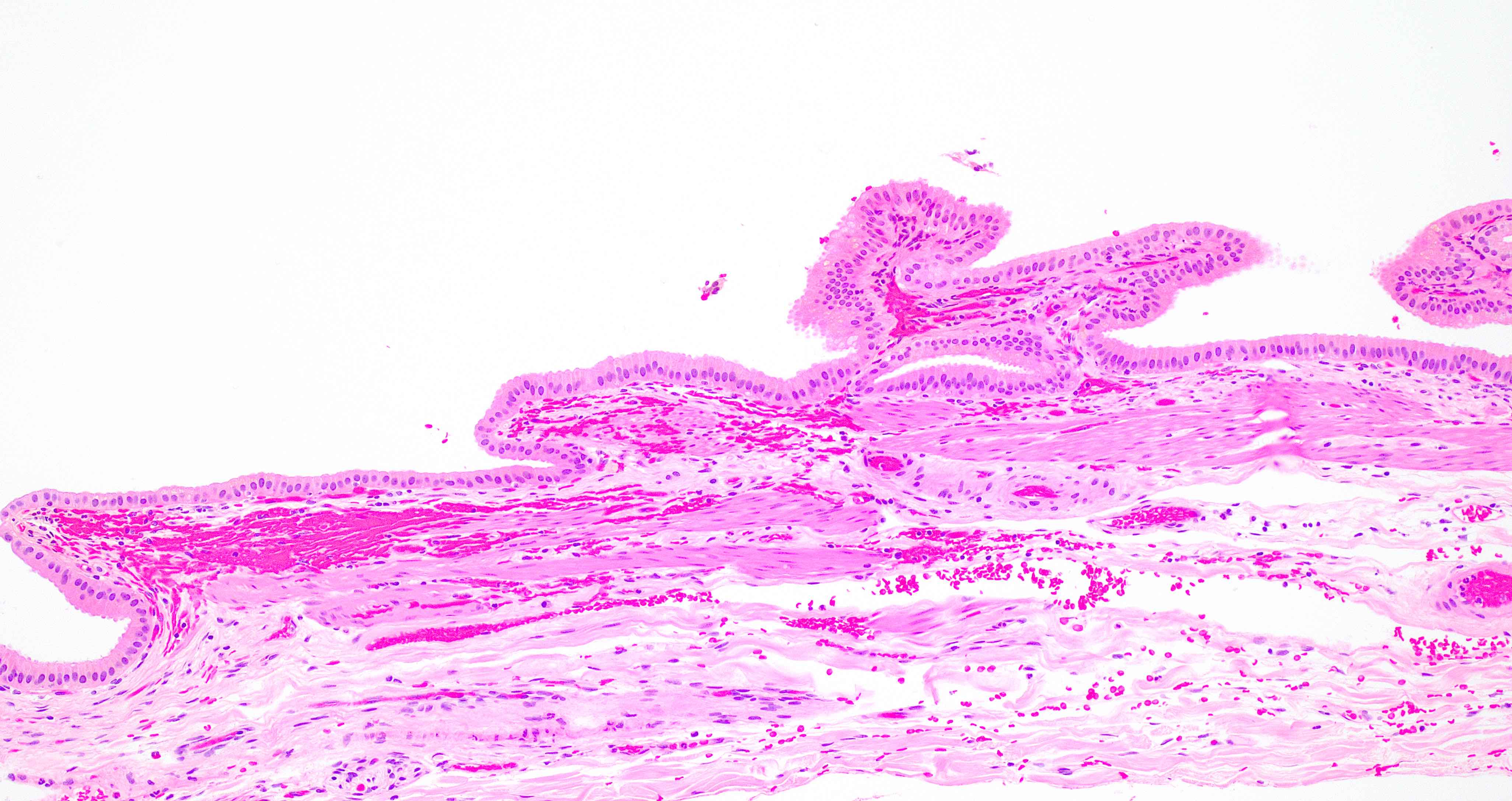
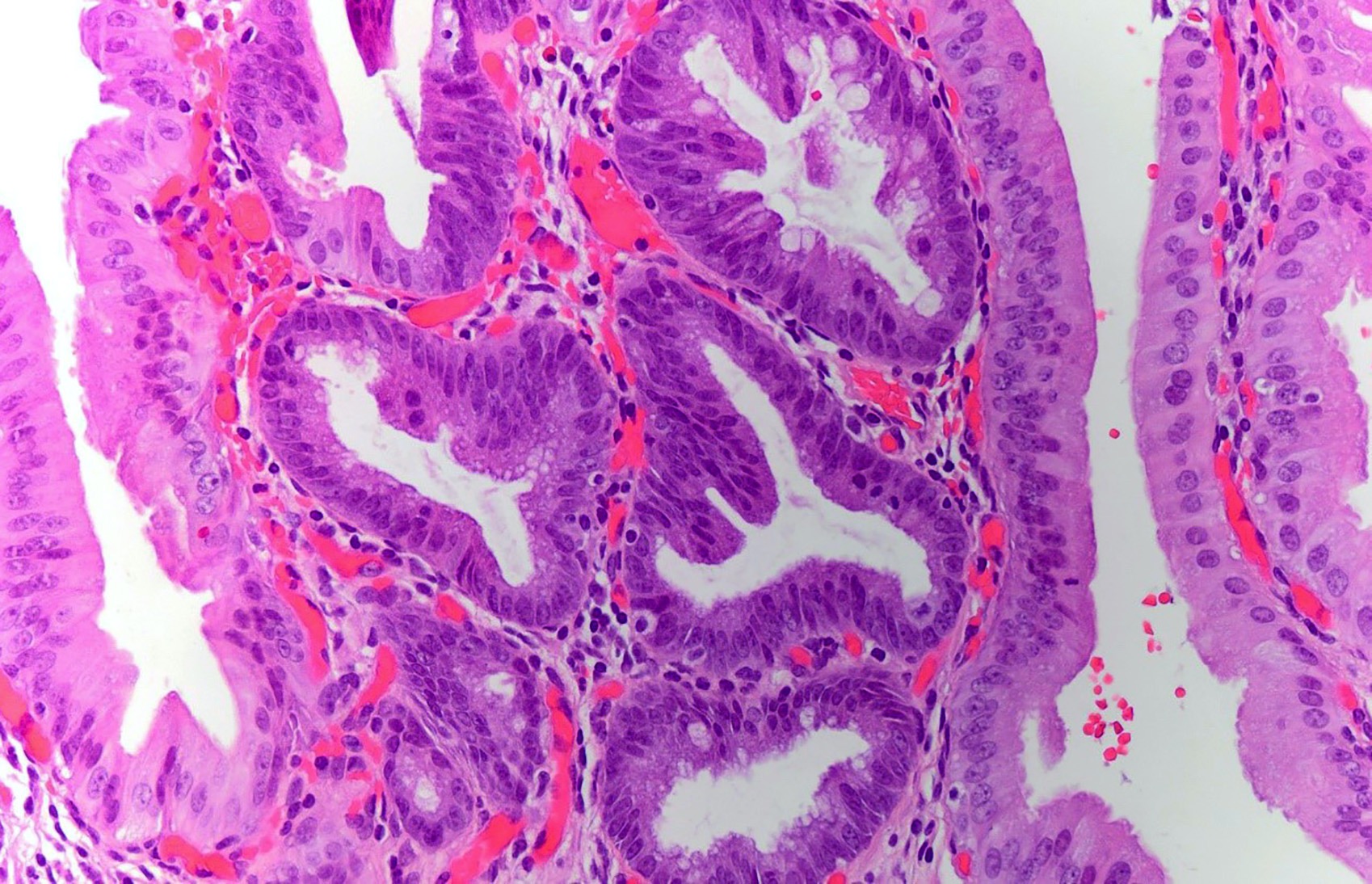
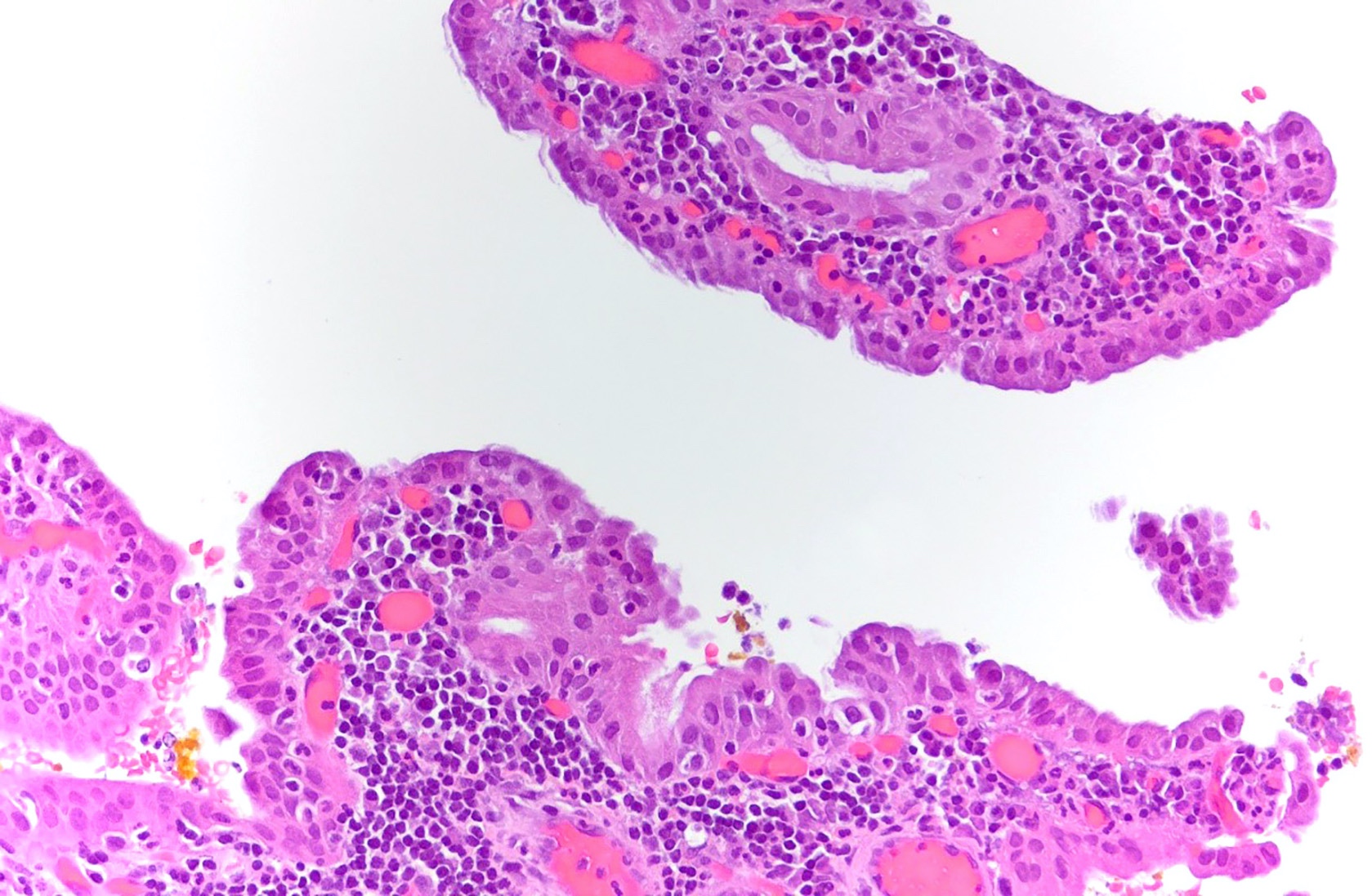
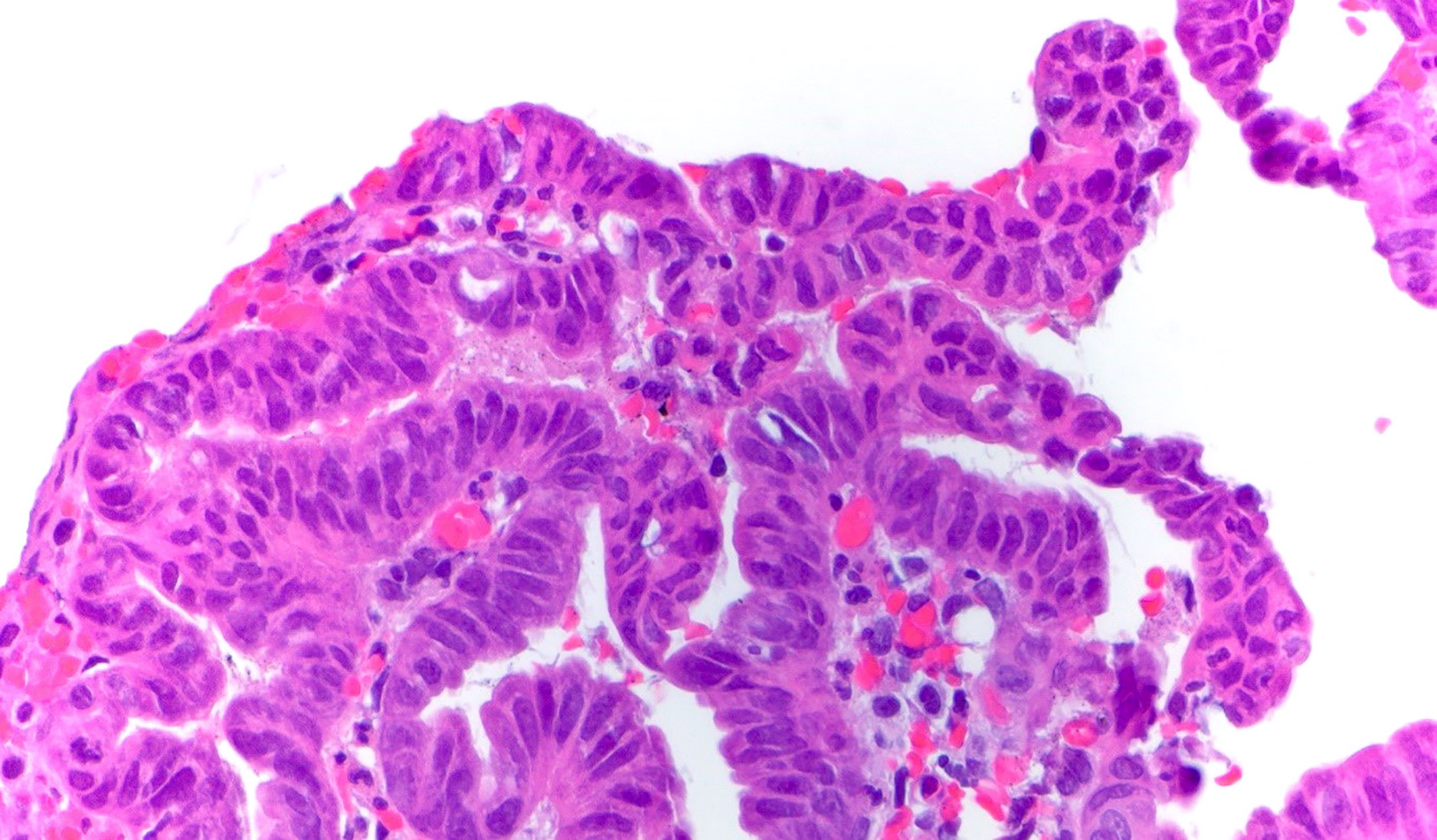
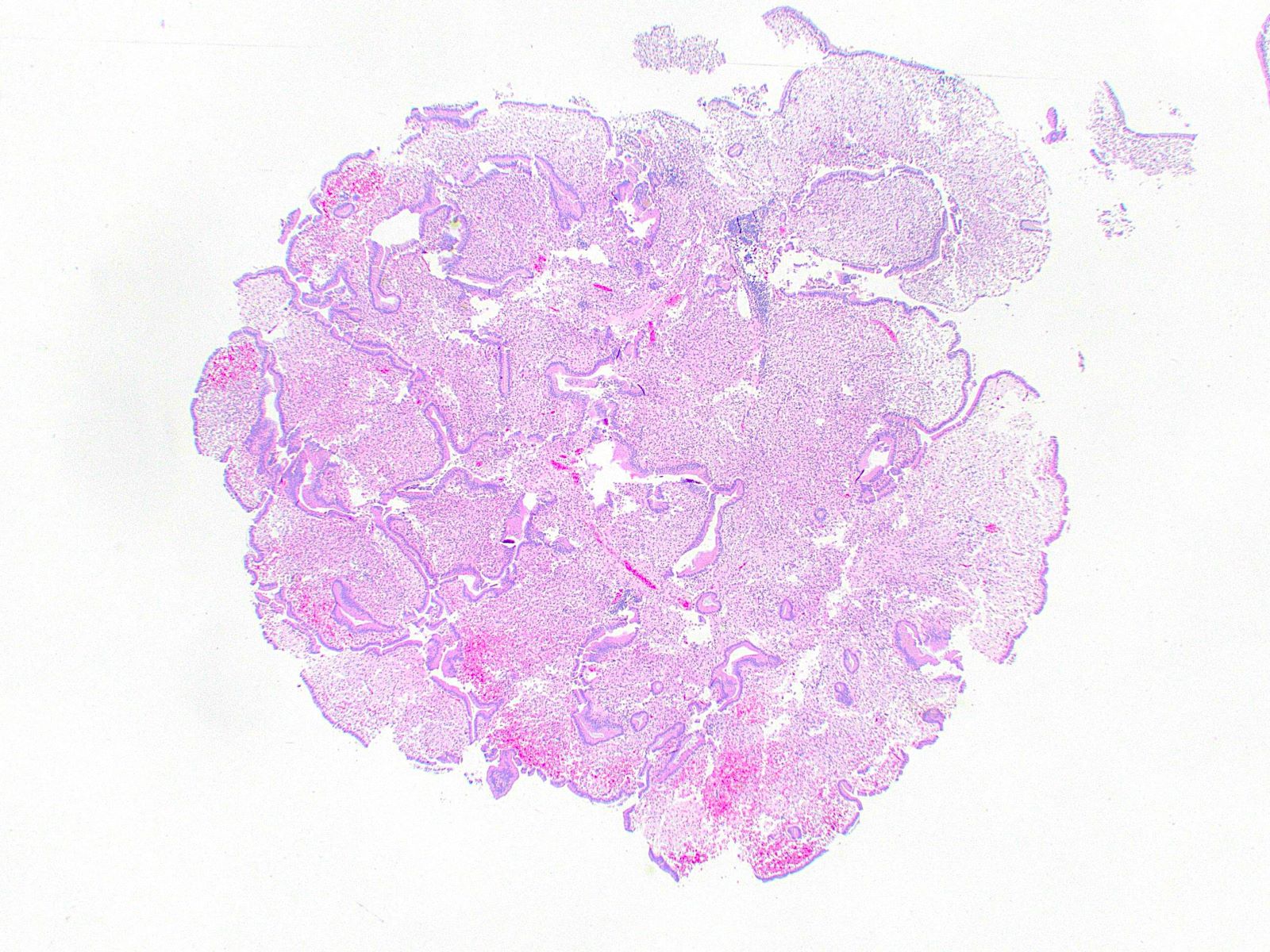
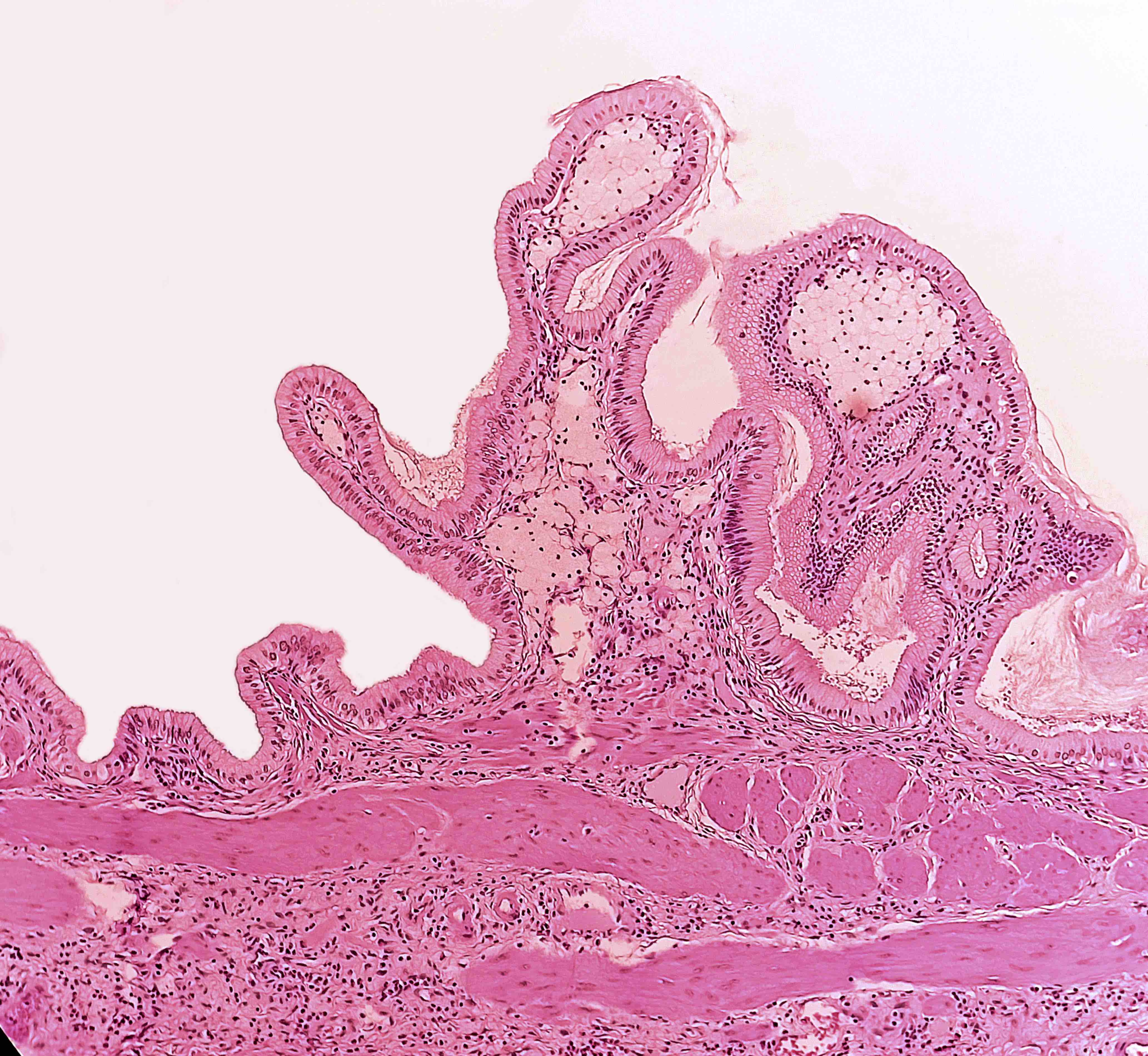
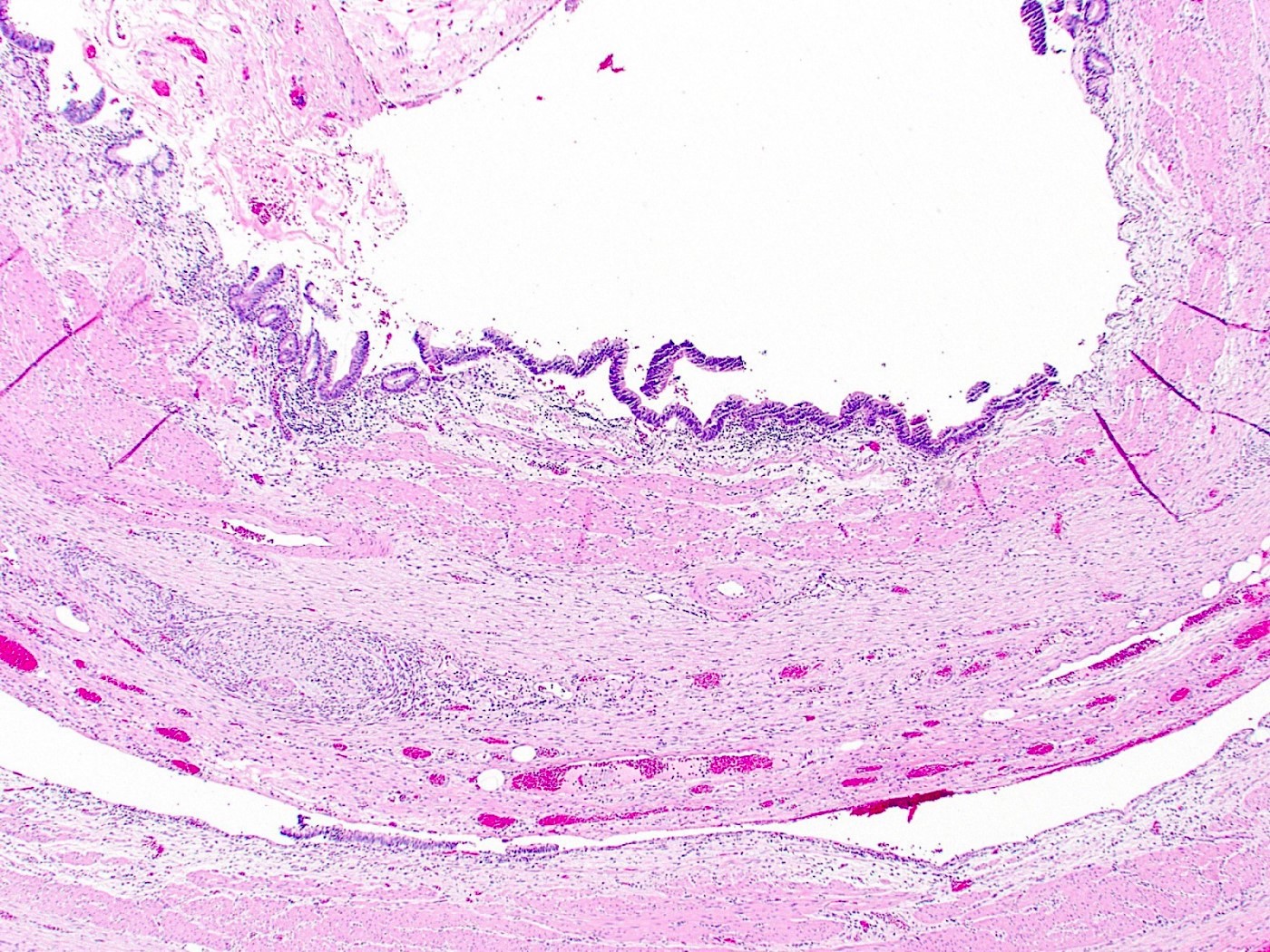
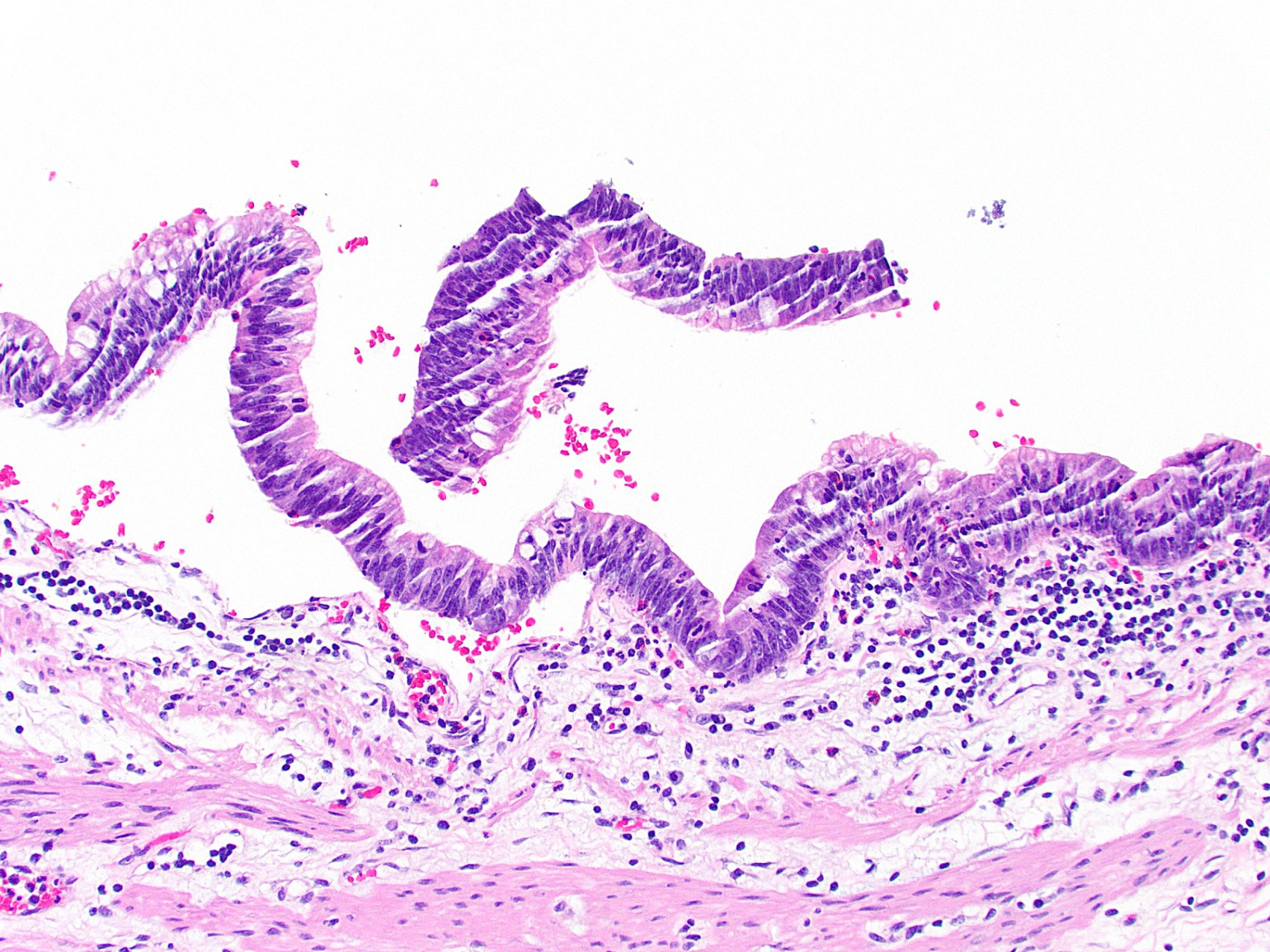
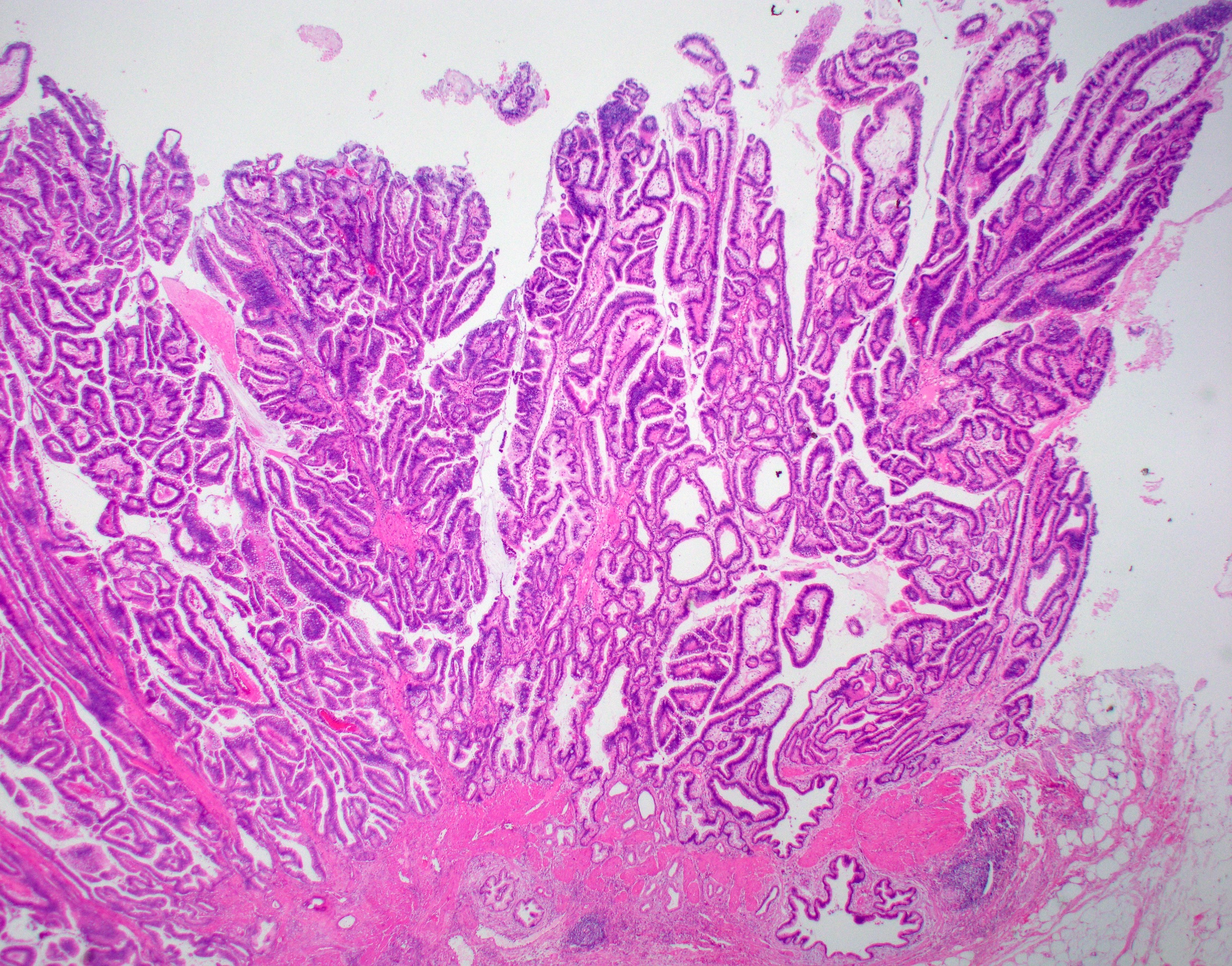
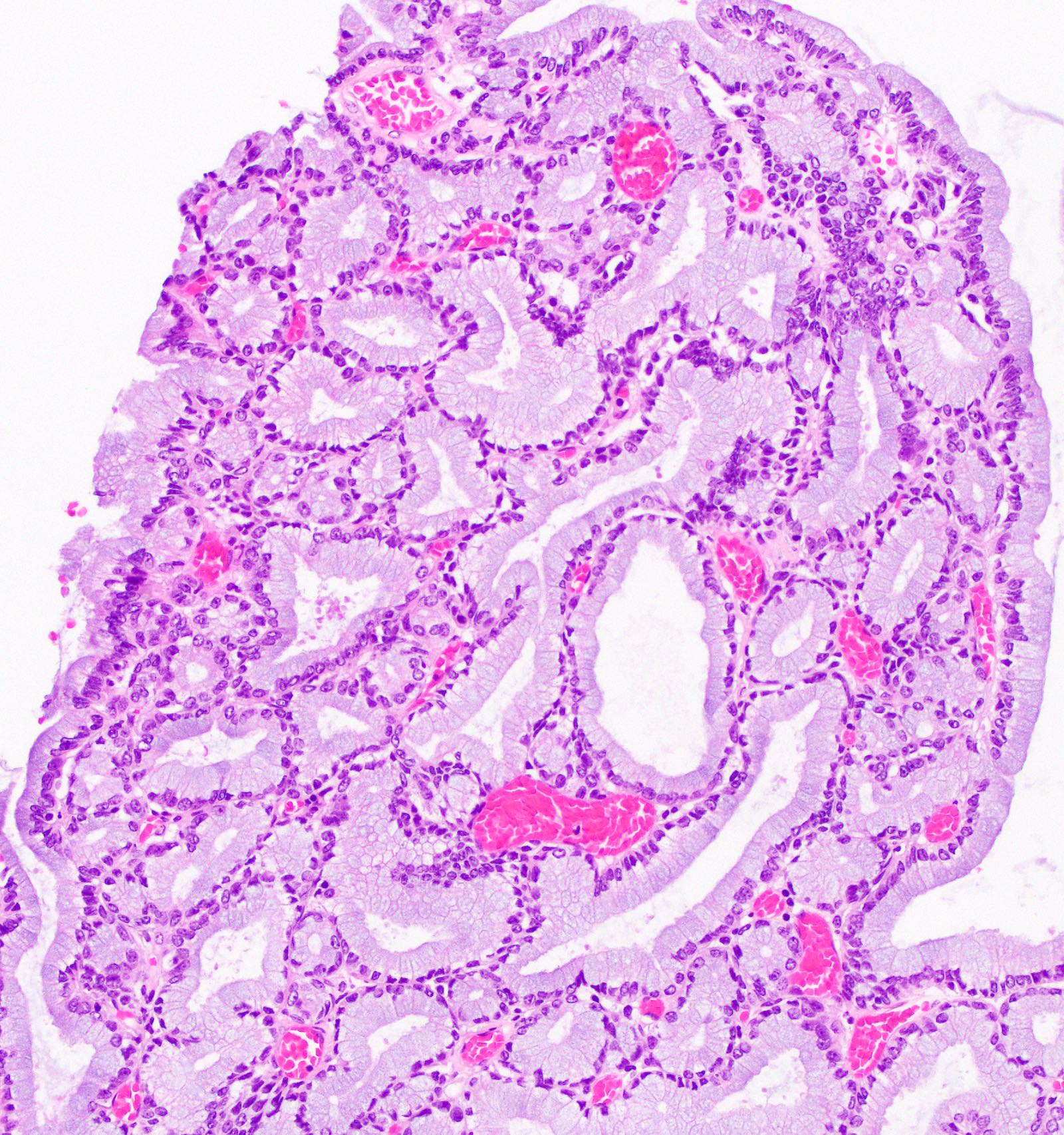
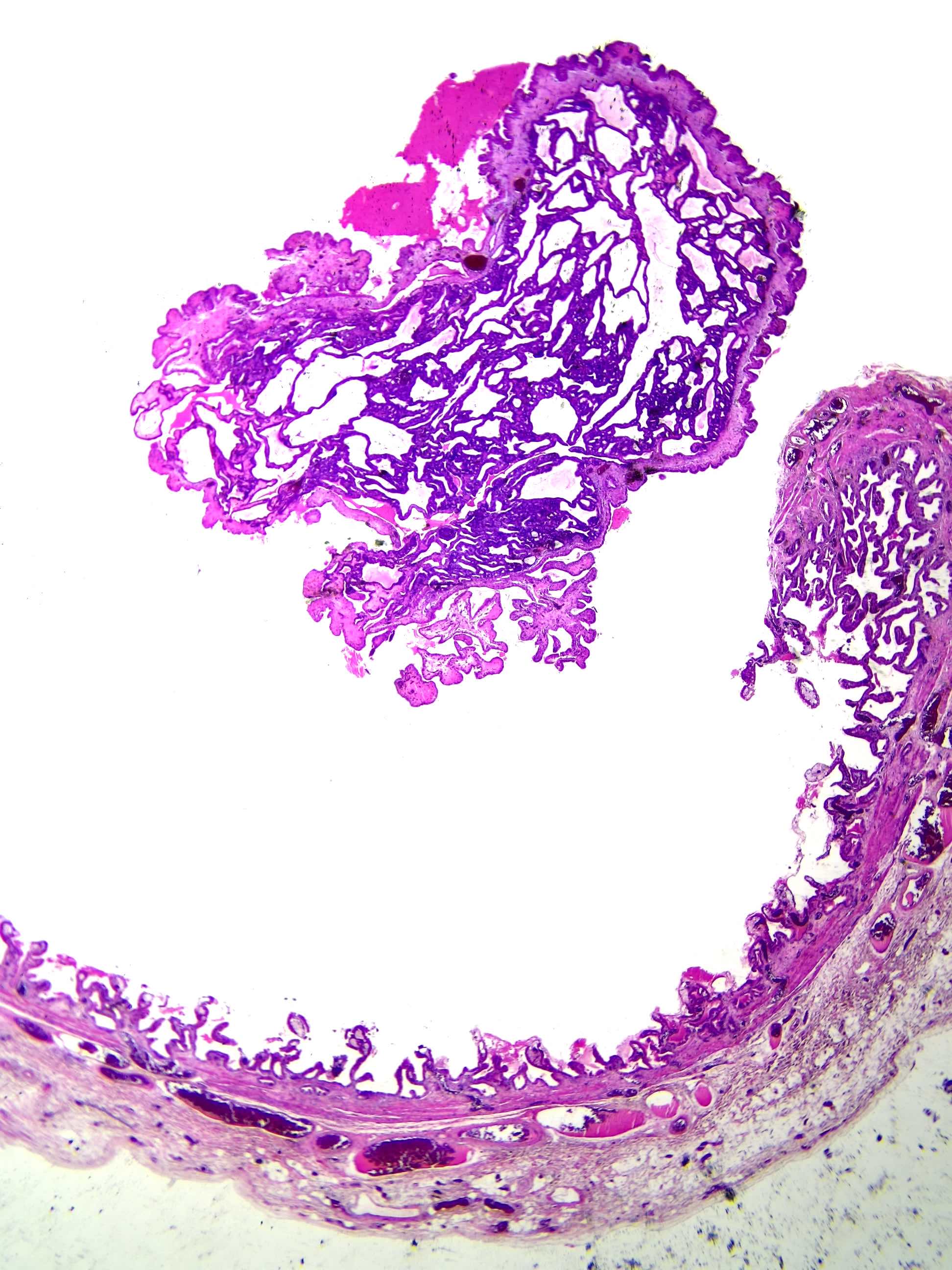
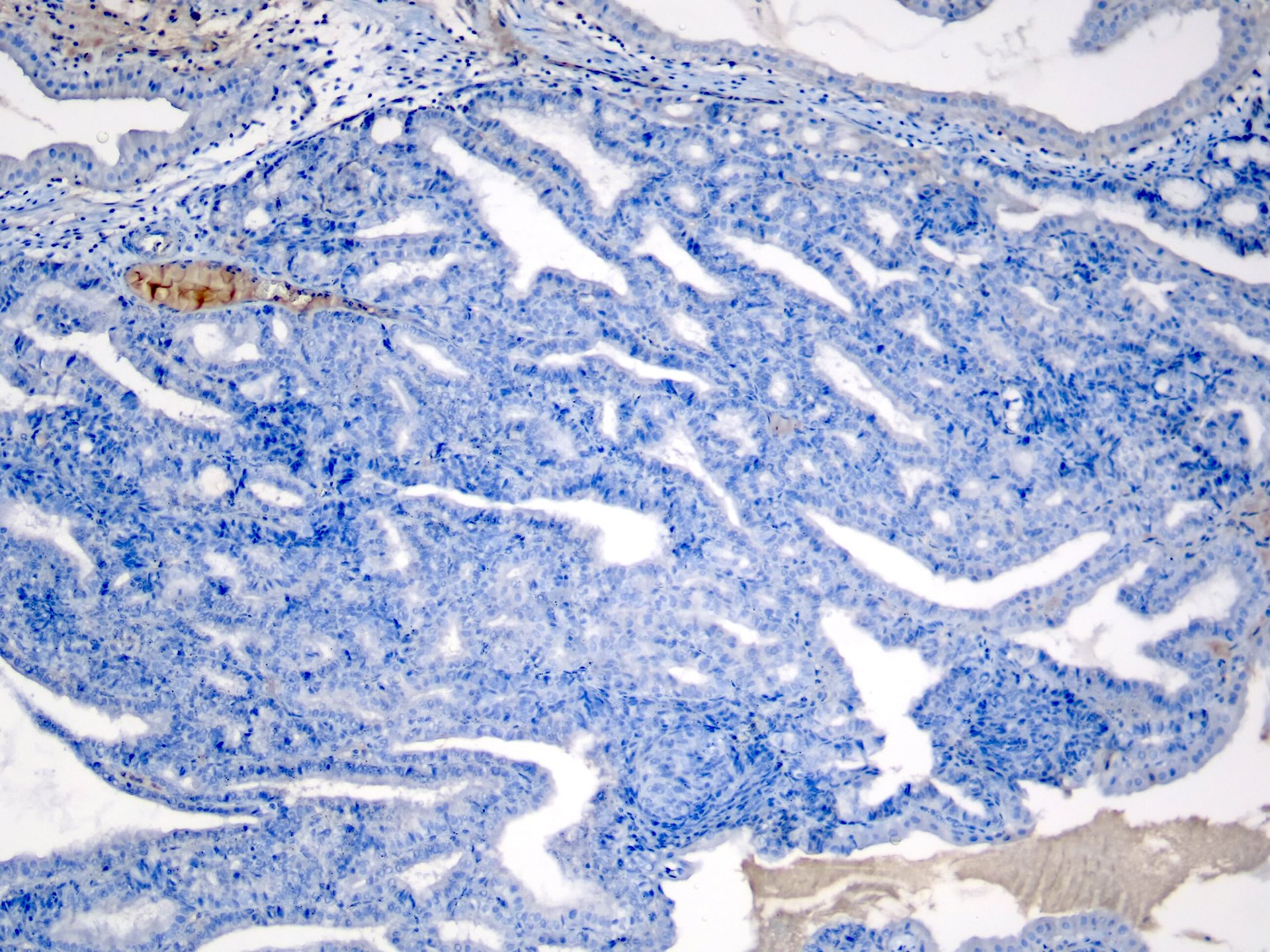
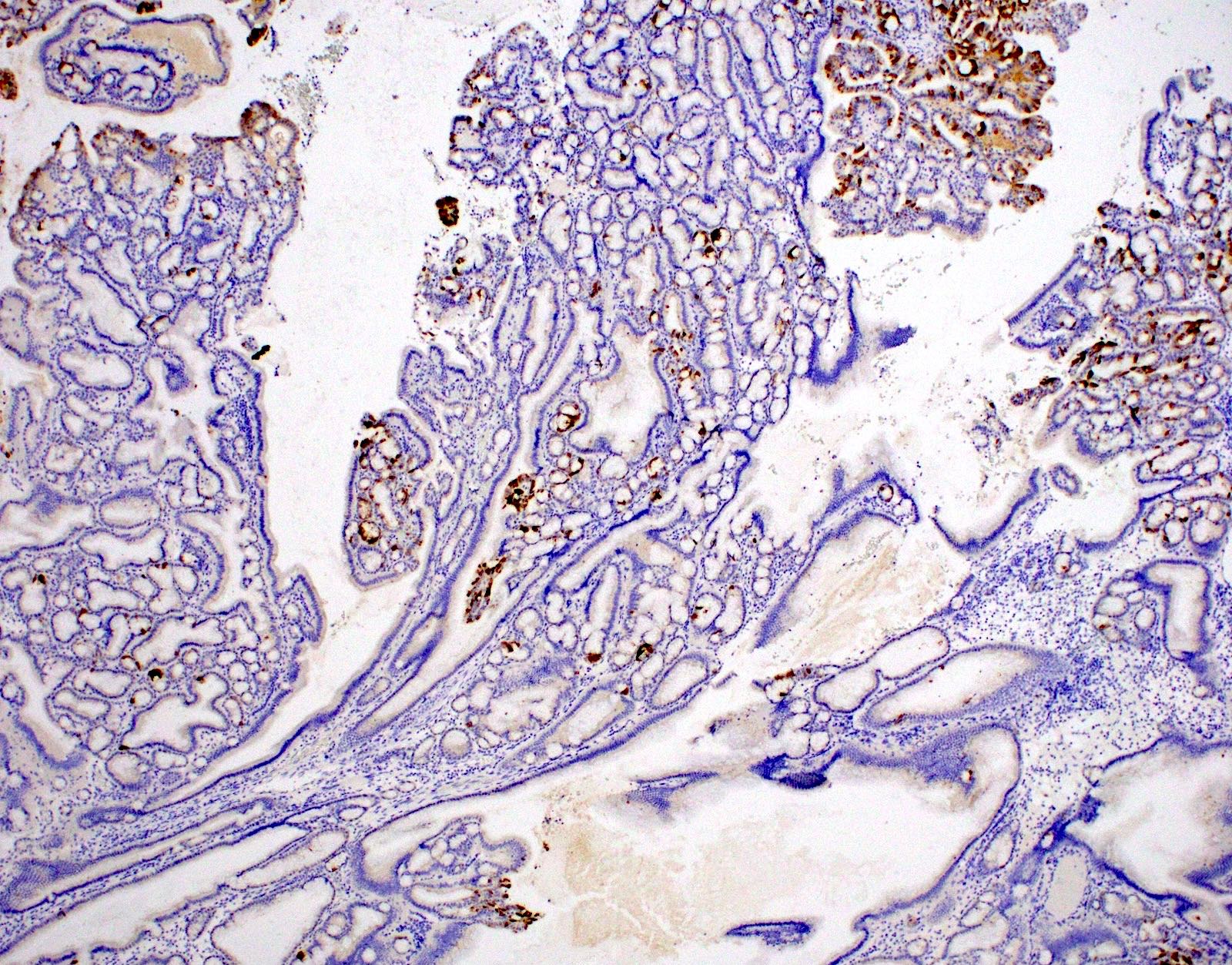
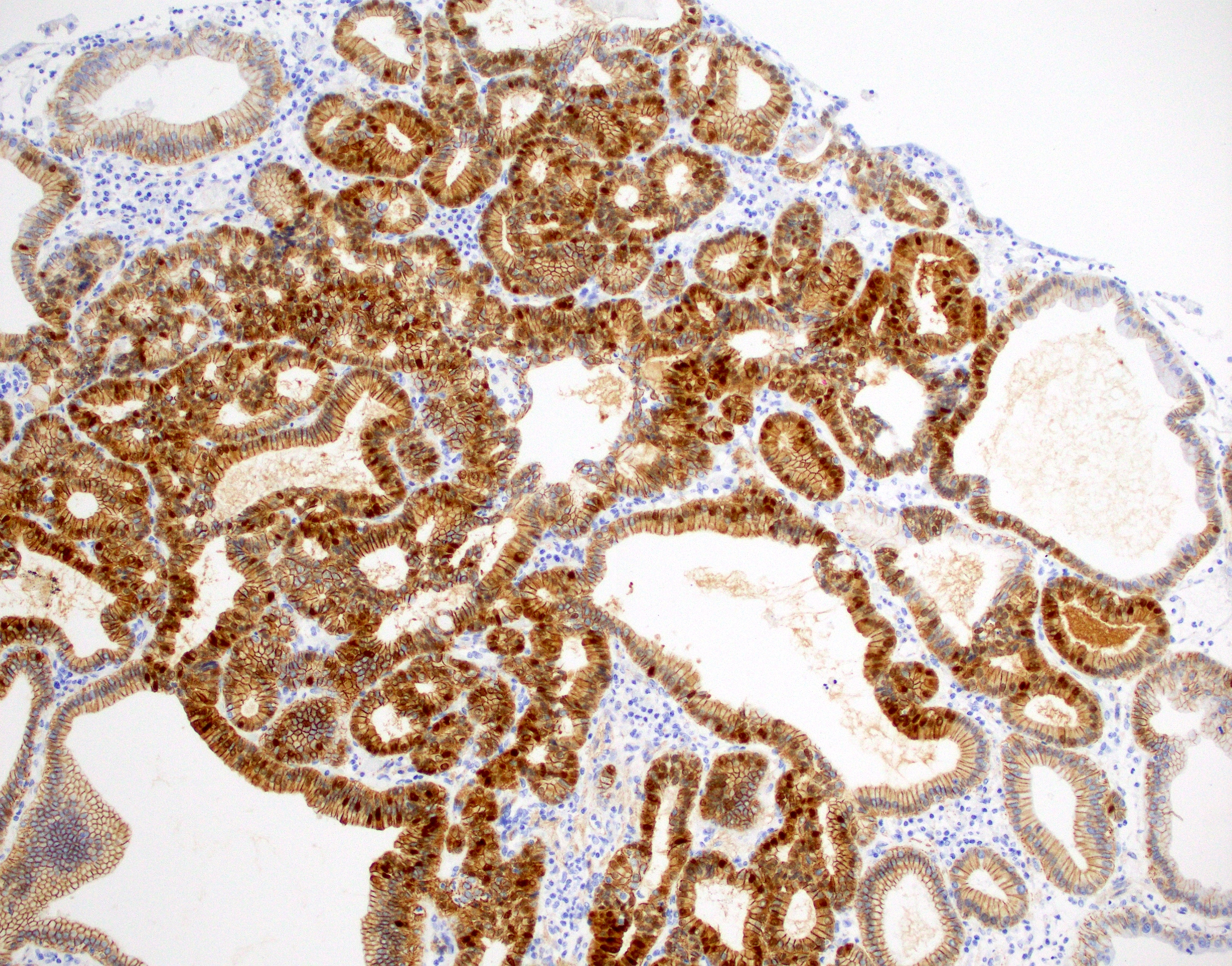
- Biliary intraepithelial neoplasia (BilIN) is a microscopic, premalignant, noninvasive neoplastic lesion of gallbladder or bile duct
- Classification is based on highest degree of cytologic atypia
- BilIN represents the biliary counterpart of pancreatic intraepithelial neoplasia (PanIN)
- Non mass forming lesions
- Microscopically flat or micropapillary lesion with low or high grade dysplasia (Mod Pathol 2007;20:701)
- Commonly associated with lithiasis
- Mostly found incidentally in elective cholecystectomy specimens
- Favorable outcome as most high grade dysplasia can be cured by surgical resection
- Biliary dysplasia or carcinoma in situ
- Approximately 1 - 3.5% of cholecystectomies are found to have incidental BilIN
- No gender predilection
- Reference: J Surg Oncol 2006;93:615
- Gallbladder
- Intrahepatic and extrahepatic biliary tree
- Persistent chronic inflammation and cytokine stimulation to biliary epithelium induces neoplastic changes, with involvement of different molecular pathways (Histopathology 2011;59:867)
- KRAS mutations are an early event in biliary carcinogenesis and are present in almost 33% of BilINs, while TP53 mutations occur as a late molecular event (Cancer 2013;119:1669)
- Risk factors: lithiasis, primary sclerosing cholangitis, choledochal cysts (Mod Pathol 2007;20:701)
- Anomalous arrangement of pancreaticobiliary ductal system (J Gastroenterol 2007;42:211)
- Does not manifest clinically
- These lesions are identified in mucosa that is adjacent to invasive carcinoma
- Microscopic examination is required for diagnosis
- Cytology alone is not sufficient to distinguish between reactive changes, preinvasive and invasive lesions (J Gastroenterol 2014;49:64)
- Non mass forming lesions, not detectable by imaging studies (J Gastroenterol 2014;49:64)
- Extensive disease, involvement of Rokitansky-Aschoff sinuses and positive margin status increase the risk of recurrence (Virchows Arch 2013;463:651)
- 21 year old woman with a giant choledochal cyst (Medicine (Baltimore) 2021;100:e24022)
- 64 year old man with abdominal pain and anorexia (World J Surg Oncol 2019;17:191)
- 70 year old woman with general weakness (Korean J Hepatol 2011;17:328)
- 72 year old man with obstructive jaundice (J Gastroenterol 2021;14:297)
- 84 year old man with epigastric pain and a short irregular stricture in the cystic duct (Intern Med 2021;60:47)
- Most high grade BilIN of gallbladder can be cured by cholecystectomy
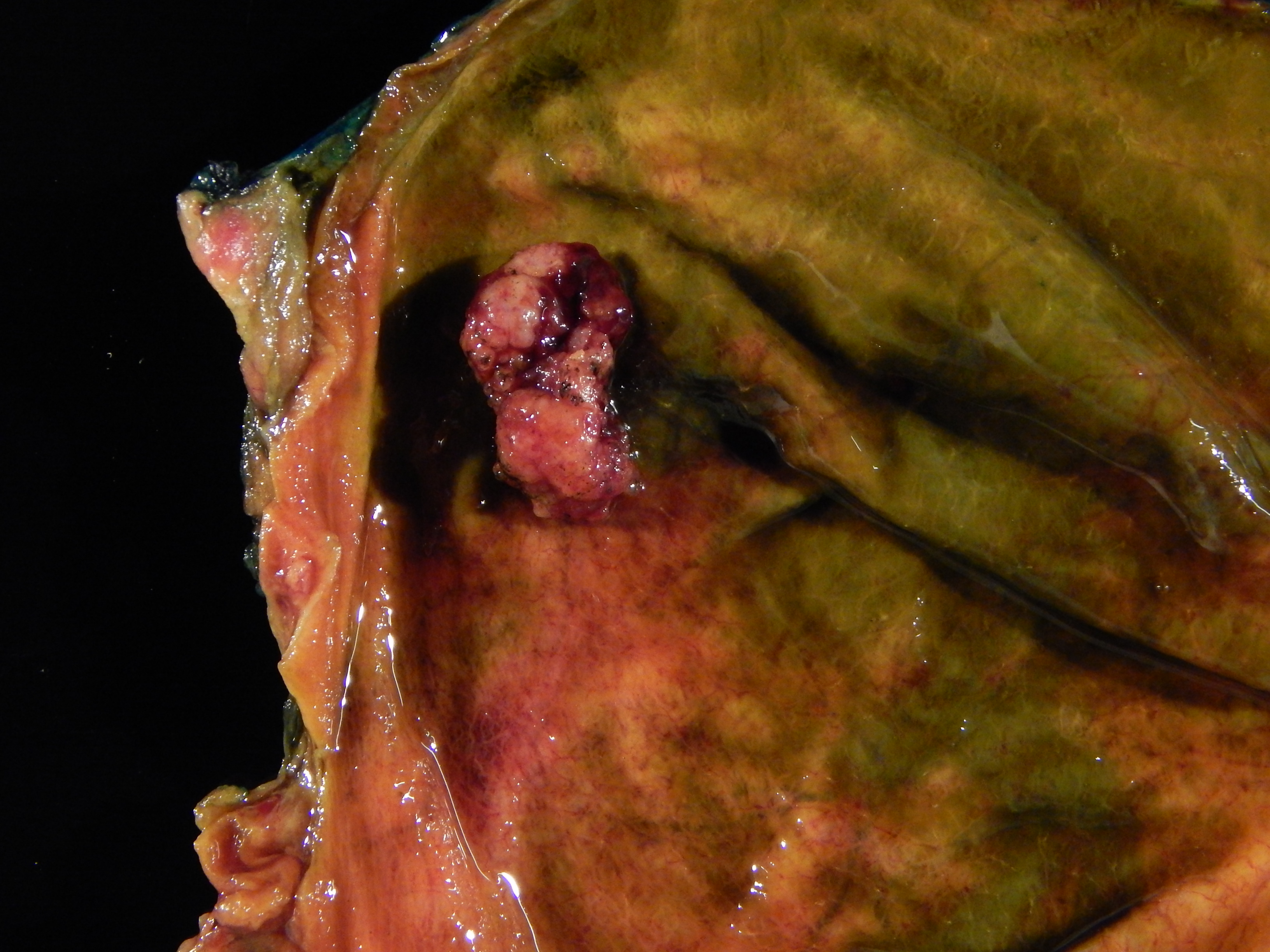
- No grossly identifiable lesion
- Granular velvety mucosa
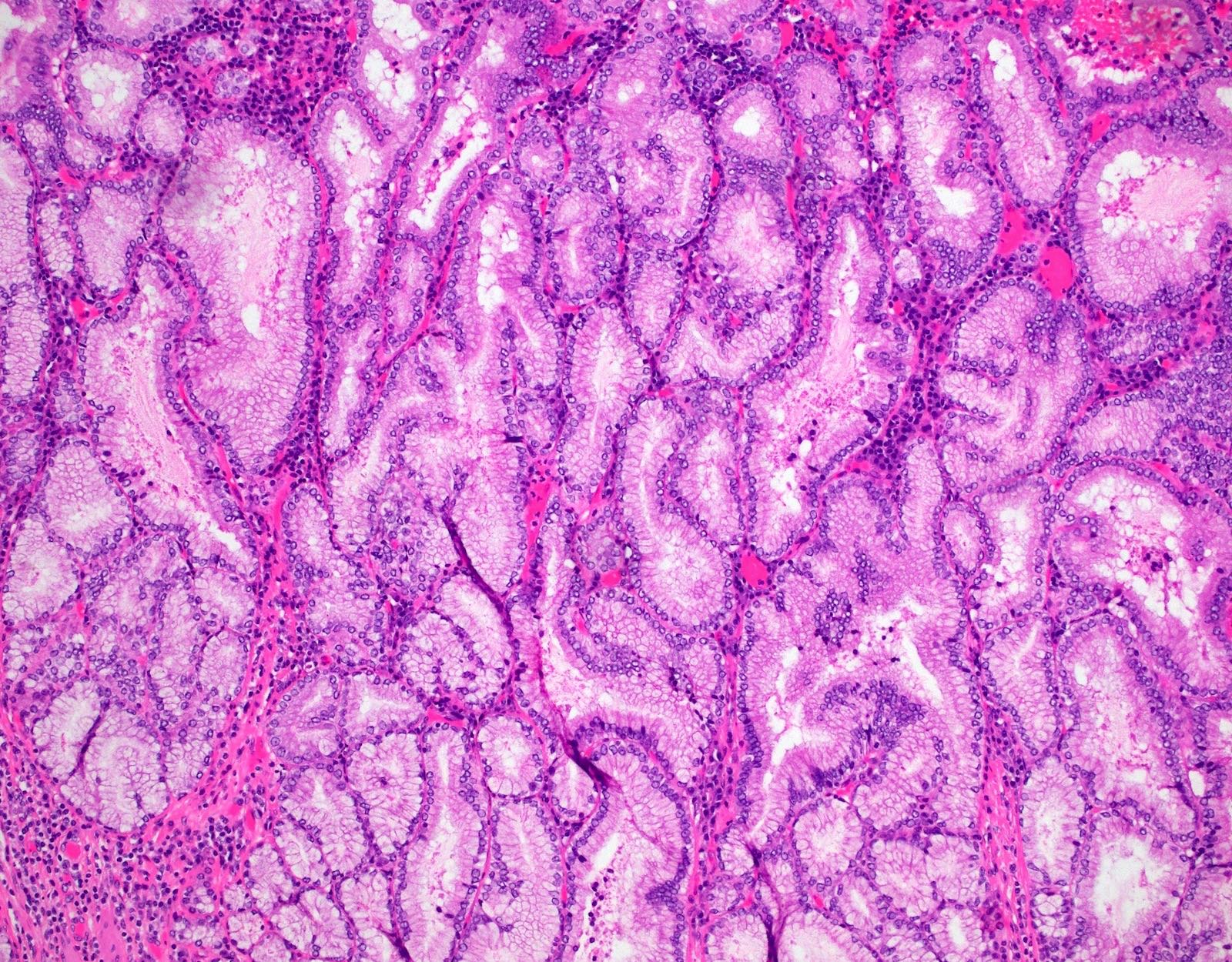
- Predominantly flat, micropapillary or pseudopapillary architecture
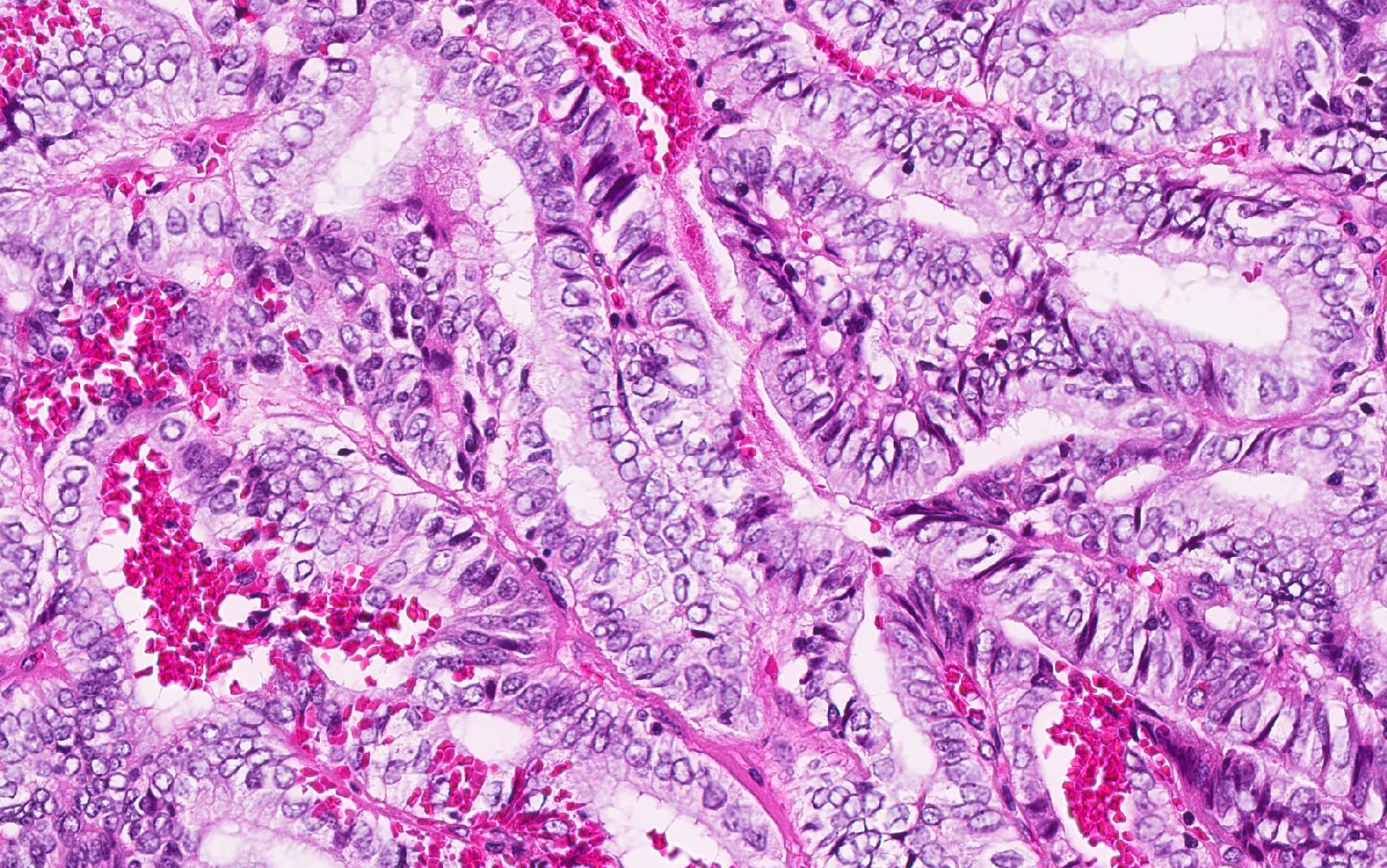
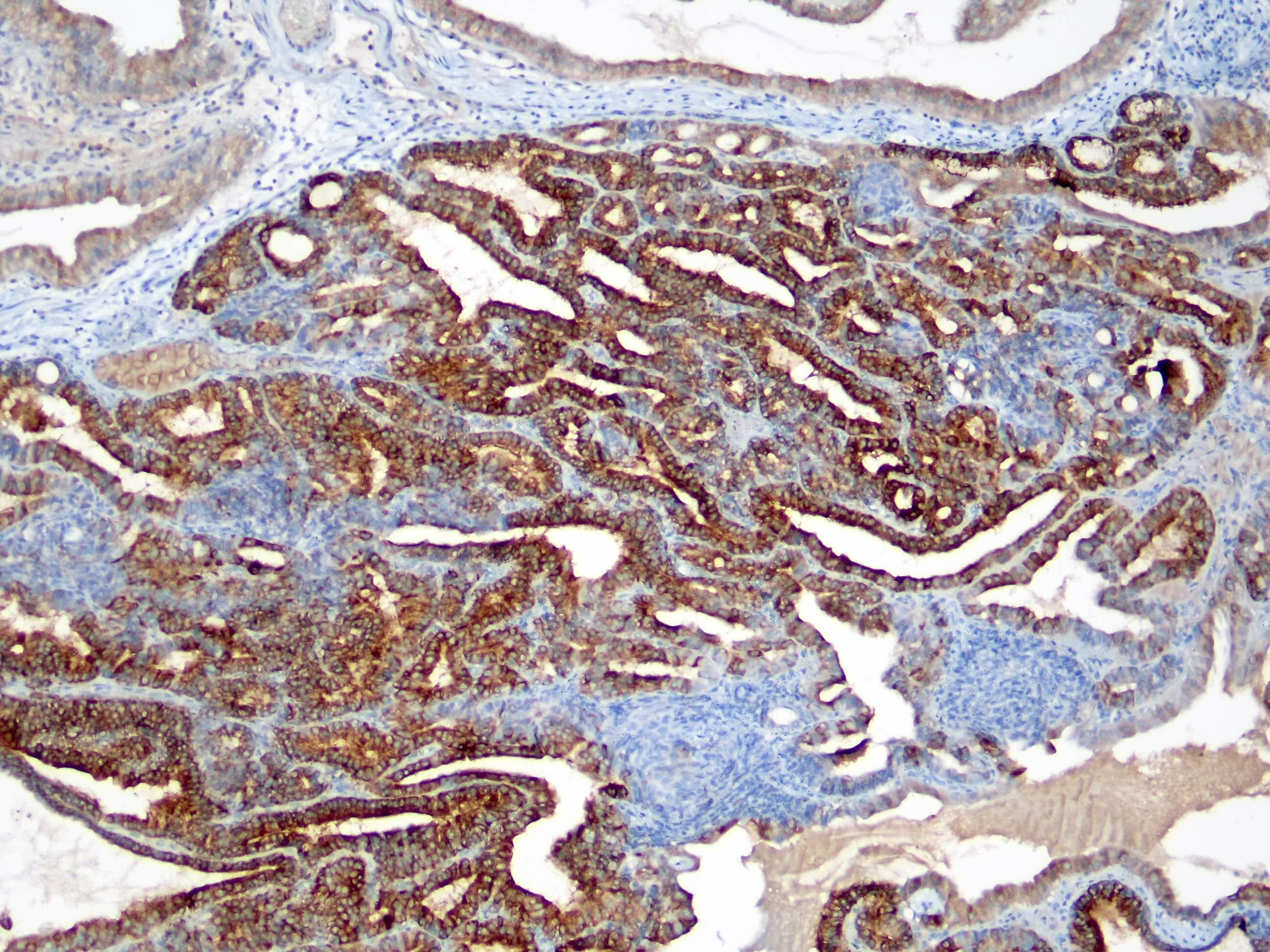
- Low grade BilIN
- Involves relatively small areas and does not involve peribiliary glands
- Hyperchromatic nucleus with relatively regular nuclear membrane
- Increased nuclear to cytoplasmic ratio
- Nuclear stratification
- Preserved nuclear polarity
- Mild to moderately increased Ki67 proliferative index
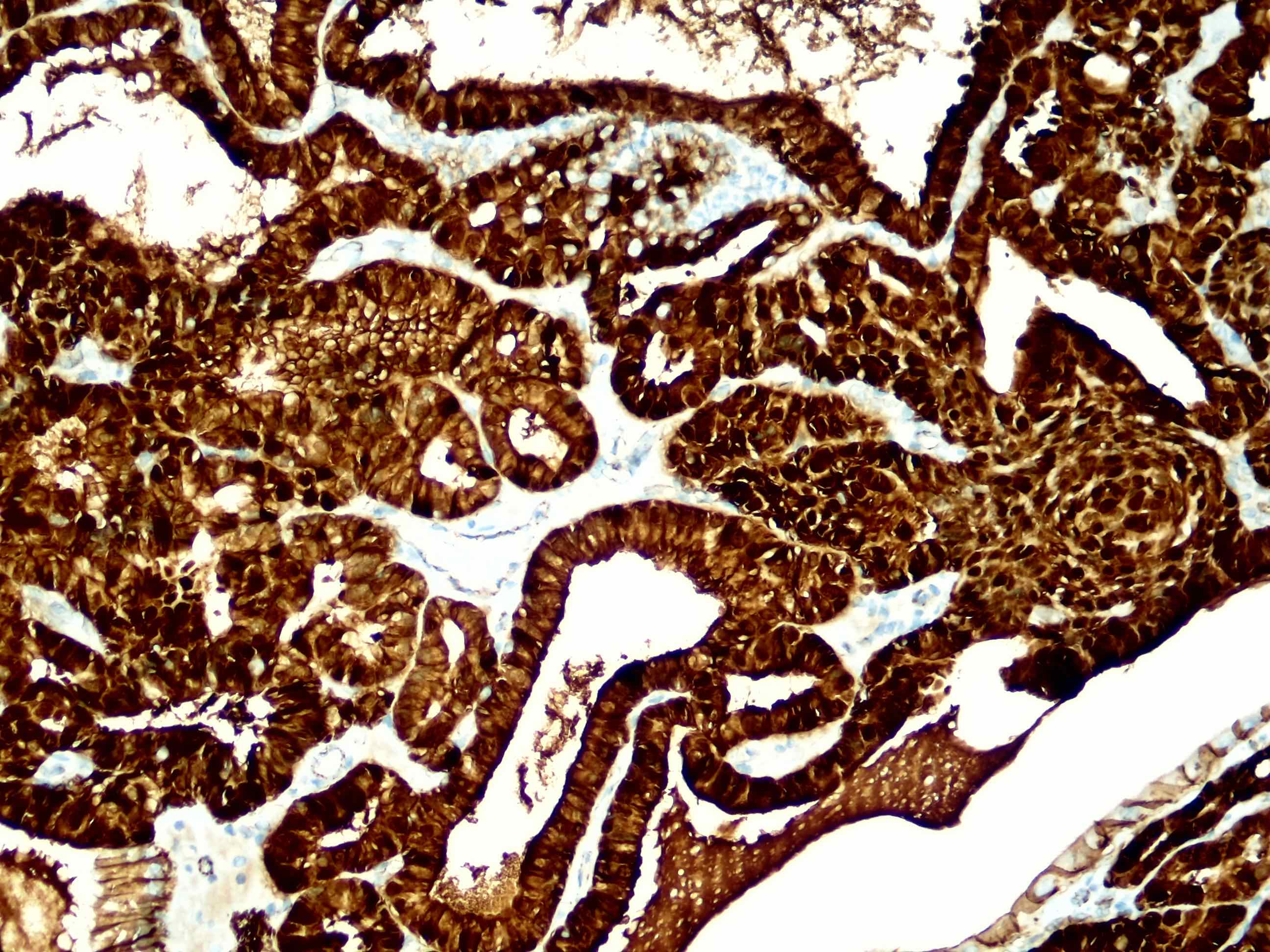
- High grade BilIN
- Involves extensive areas, including peribiliary glands
- Hyperchromatic nucleus with irregular nuclear membrane
- Very high nuclear to cytoplasmic ratio
- Relatively extensive degree of polymorphism and prominent nuclear atypia
- Complex nuclear stratification
- Loss of nuclear polarity
- Markedly increased Ki67 proliferative index
- Reference: Pathol Int 2005;55:180
- BilINs are microscopic, non mass forming lesions; not amenable to sampling via fine needle aspiration
- Bile duct brushing cytology: increased nuclear to cytoplasmic ratio, nucleomegaly, anisonucleosis, nuclear border irregularity, hyperchromasia, visible or prominent nucleoli are associated with next generation sequencing (NGS) positivity (clonal somatic mutations) (J Am Soc Cytopatol 2020;9:520)
- Approximately 33% of BilIN lesions show KRAS mutations, which occur as an early molecular event during the progression of BilIN; p53 overexpression occurs as a late molecular event (Surg Oncol Clin N Am 2009;18:215)
- p21, p53, cyclin D1 and DPC4 are involved in BilIN carcinogenesis (Hum Pathol 2008;39:1153)
- Gallbladder, cholecystectomy:
- Multifocal high grade biliary intraepithelial lesion (BilIN3), extending to Rokitansky-Aschoff sinuses (see comment)
- Comment: The specimen is entirely submitted for microscopic examination. No invasive carcinoma is identified. Cystic duct margin is negative for dysplasia.
- Gallbladder, cholecystectomy:
- Chronic cholecystitis with cholelithiasis and focal low grade biliary intraepithelial lesion (BilIN) (see comment)
- Comment: The specimen is entirely submitted for microscopic examination. No invasive carcinoma is identified. Cystic duct margin is negative for dysplasia.
- Reactive changes:
- Background acute and chronic inflammation present
- Gradual transition between benign epithelium and reactive epithelium
- Adenocarcinoma:
- Presence of invasive component
- Desmoplastic stroma
Comment Here
Reference: Biliary intraepithelial neoplasia
- Advanced age
- Extensive lesion with Rokitansky-Aschoff sinus involvement
- Female gender
- Granular velvety mucosa
- Radiologically identifiable mass
Comment Here
Reference: Biliary intraepithelial neoplasia
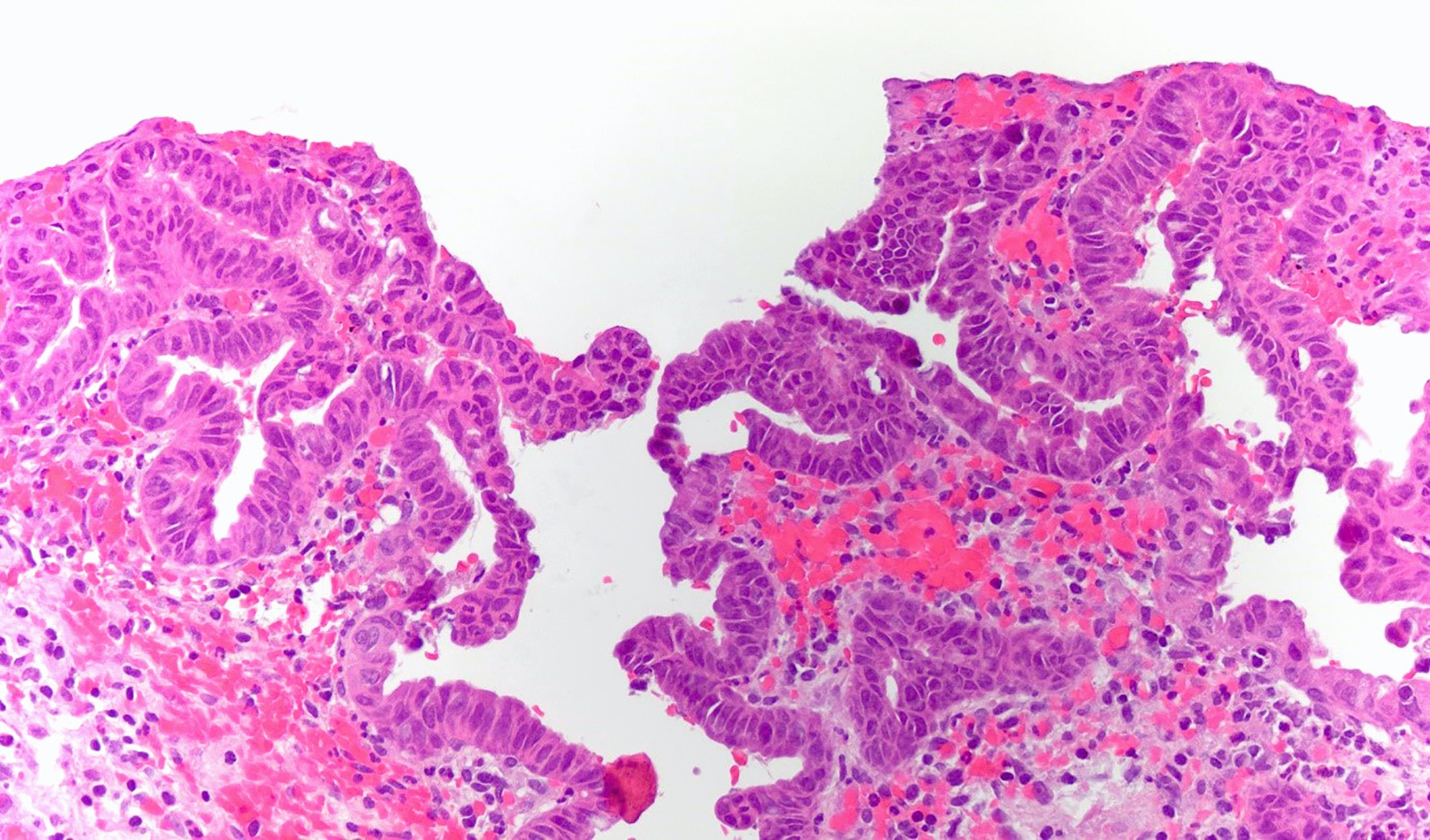
- Rare malignant adenocarcinoma arising from extrahepatic bile ducts
- Biliary adenocarcinomas (cholangiocarcinomas) typically divided into intrahepatic bile duct origin, gallbladder origin, perihilar bile origin (this topic) and distal extrahepatic bile duct origin (this topic), including right and left hepatic ducts, common hepatic duct and common bile duct
- Adenocarcinoma arising from the biliary system outside the liver, with several risk factors
- Histology is similar to intrahepatic cholangiocarcinoma, particularly large duct type
- Poor prognosis
- Some prefer to restrict the term cholangiocarcinoma to intrahepatic adenocarcinomas only but others use the term for any adenocarcinoma of the biliary system
- Klatskin tumor refers to a hilar cholangiocarcinoma arising at the bifurcation of the right and left hepatic ducts
- 0.53 - 2 per 100,000 in population
- Incidence is decreasing in recent years (StatPearls: Biliary Tract Cholangiocarcinoma [Accessed 17 November 2023])
- Slight male predominance due to primary sclerosing cholangitis being more common in men (StatPearls: Biliary Tract Cholangiocarcinoma [Accessed 17 November 2023], Ann Hepatobiliary Pancreat Surg 2023;27:151)
- Occurs primarily in sixth and seventh decades of life (Ann Hepatobiliary Pancreat Surg 2023;27:151)
- Can develop at any level of the extrahepatic biliary tree, including within the pancreas
- Bismuth-Corlette classification relates to extent of infiltration of ducts
- Risk factors such as infections, genetics and primary sclerosing cholangitis can play a role in disease pathogenesis (StatPearls: Biliary Tract Cholangiocarcinoma [Accessed 17 November 2023])
- Often arises from precursor lesions, namely biliary intraepithelial neoplasia and intraductal papillary neoplasm of the bile ducts
- Various mutations in oncogenes and tumor suppressor genes transform normal epithelium into premalignant lesions
- Several risk factors exist for development of extrahepatic cholangiocarcinoma (Liver Int 2019;39:19)
- Choledochal cyst
- Primary sclerosing cholangitis
- Parasites (Opisthorchis viverrini and Clonorchis sinensis)
- Caroli disease
- Cholelithiasis
- Chronic pancreatitis
- May arise de novo, without risk factors being present
- Signs of biliary obstruction may occur, including jaundice (most characteristic and common symptom), pruritis, acholic stools and dark urine (Liver Int 2019;39:98)
- Patients can present with nonspecific symptoms, including abdominal pain, nausea / vomiting, anorexia, weight loss and malaise (Liver Int 2019;39:98)
- Many patients present with unresectable disease
- Early diagnosis is challenging and is often delayed due to asymptomatic early stage disease (World J Hepatol 2021;13:166)
- Lack of a standardized screening protocol
- MRI and magnetic resonance cholangiopancreatography (MRCP) can assess size and extent of tumor
- Endoscopic ultrasound (EUS) and EUS guided FNA can be utilized in the diagnosis and staging of cholangiocarcinoma
- Intraductal ultrasound is suggested for patients with obstructive jaundice for local tumor staging and bile duct stricture assessment
- Elevated serum CA 19-9, CEA-M, CA125 (BJS Open 2021;5:zrab127)
- May form a mass or cause thickening of bile duct walls
- CT and MRI (Liver Int 2019;39:98)
- Duct wall thickening and lumen obliteration, indicating infiltration
- Mass lesion
- Ultrasound (Liver Int 2019;39:98)
- Duct dilation, indicating obstruction
- Endoscopic retrograde cholangiopancreatography (ERCP)
- Stricture of the bile duct
- Favorable prognostic factors
- Absence of comorbidities and presence of dysplasia are favorable prognostic factors (Hepatobiliary Pancreat Dis Int 2020;19:153)
- Increase in albumin and a decrease in total bilirubin improve the prognosis of patients with hilar cholangiocarcinoma (Hepatobiliary Pancreat Dis Int 2020;19:153)
- Intrapancreatic cases have a better prognosis than pancreatic ductal adenocarcinoma but a worse prognosis than ampullary adenocarcinoma (Mod Pathol 2016;29:1358)
- Prognostic biomarkers
- Albumin, ALT, CA 19-9 and CEA are independent prognostic biomarkers for overall survival (Cancers (Basel) 2022;14:1026, Medicine (Baltimore) 2019;98:e14556)
- Preoperative C reactive protein to albumin ratio (CAR) is an accurate prognostic biomarker, predicting overall survival and disease free survival (J Surg Oncol 2020;122:1516)
- CAR is the most valuable prognostic biomarker in patients with resected extrahepatic cholangiocarcinoma (Dig Surg 2022;39:65)
- Lymph node metastasis is one of the most important prognostic factors (J Surg Oncol 2020;122:1516)
- Presence of venous, lymphatic and perineural invasion indicate a worse prognosis (J Surg Oncol 2020;122:1516)
- pT category staging for extrahepatic cases is based on depth of invasion into bile duct wall (Am J Surg Pathol 2007;31:199)
- 17 year old boy with perihilar mass in an explanted liver (Pathol Int 2020;70:888)
- 57 year old man with obstructive jaundice (Front Oncol 2022;12:948799)
- 71 year old woman with extrahepatic cholangiocarcinoma and thigh mass (Front Surg 2022;9:922834)
- Surgical resection is the only hope for long term survival (Rozhl Chir 2022;101:416)
- Chemotherapy can be used as adjuvant treatment or for palliation in unresectable cases (J Clin Oncol 2019;37:1015)
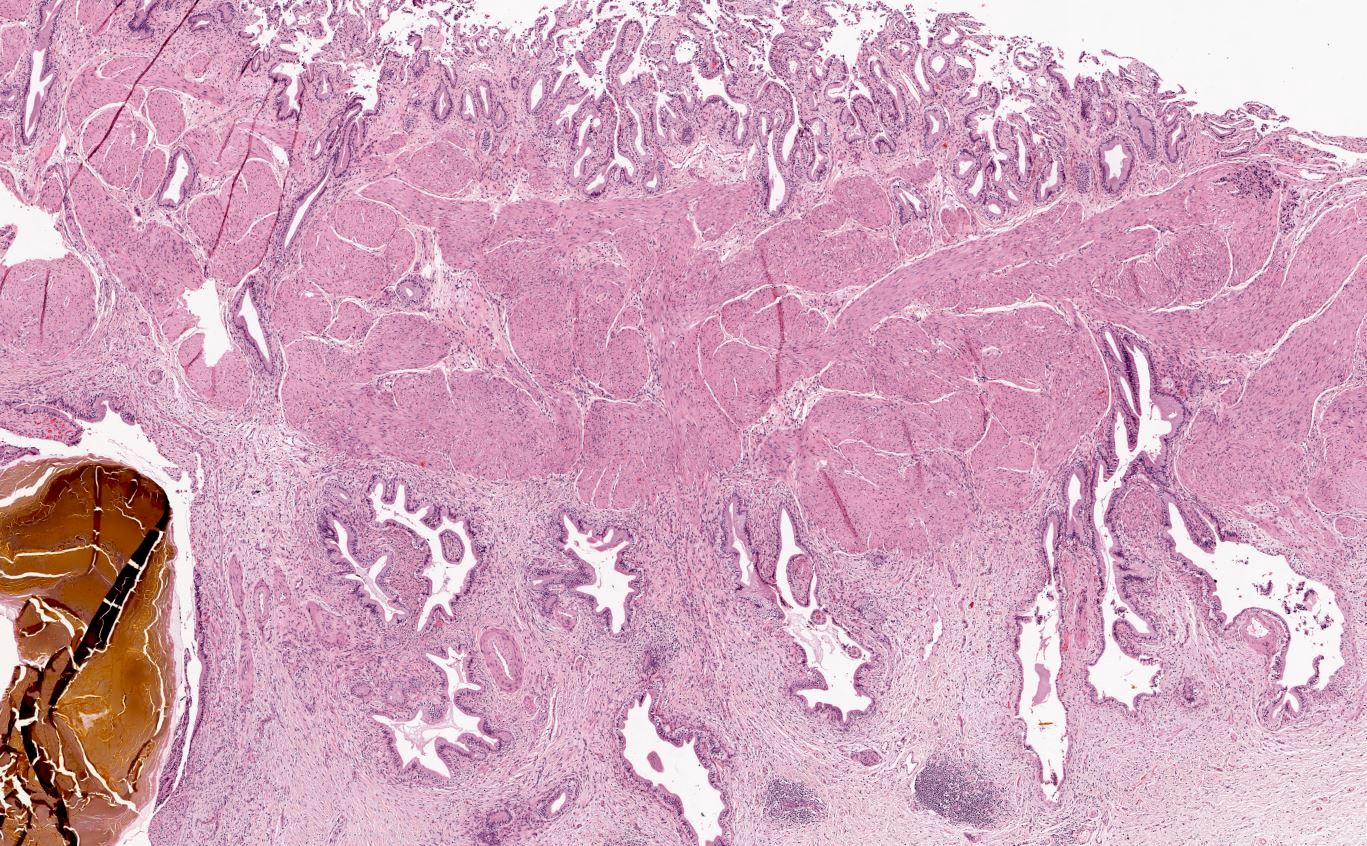
- Various configurations possible, including stenotic, nodular, polypoid, sclerosing and diffusely infiltrating
- Mass forming cases have a firm, white, gritty cut surface
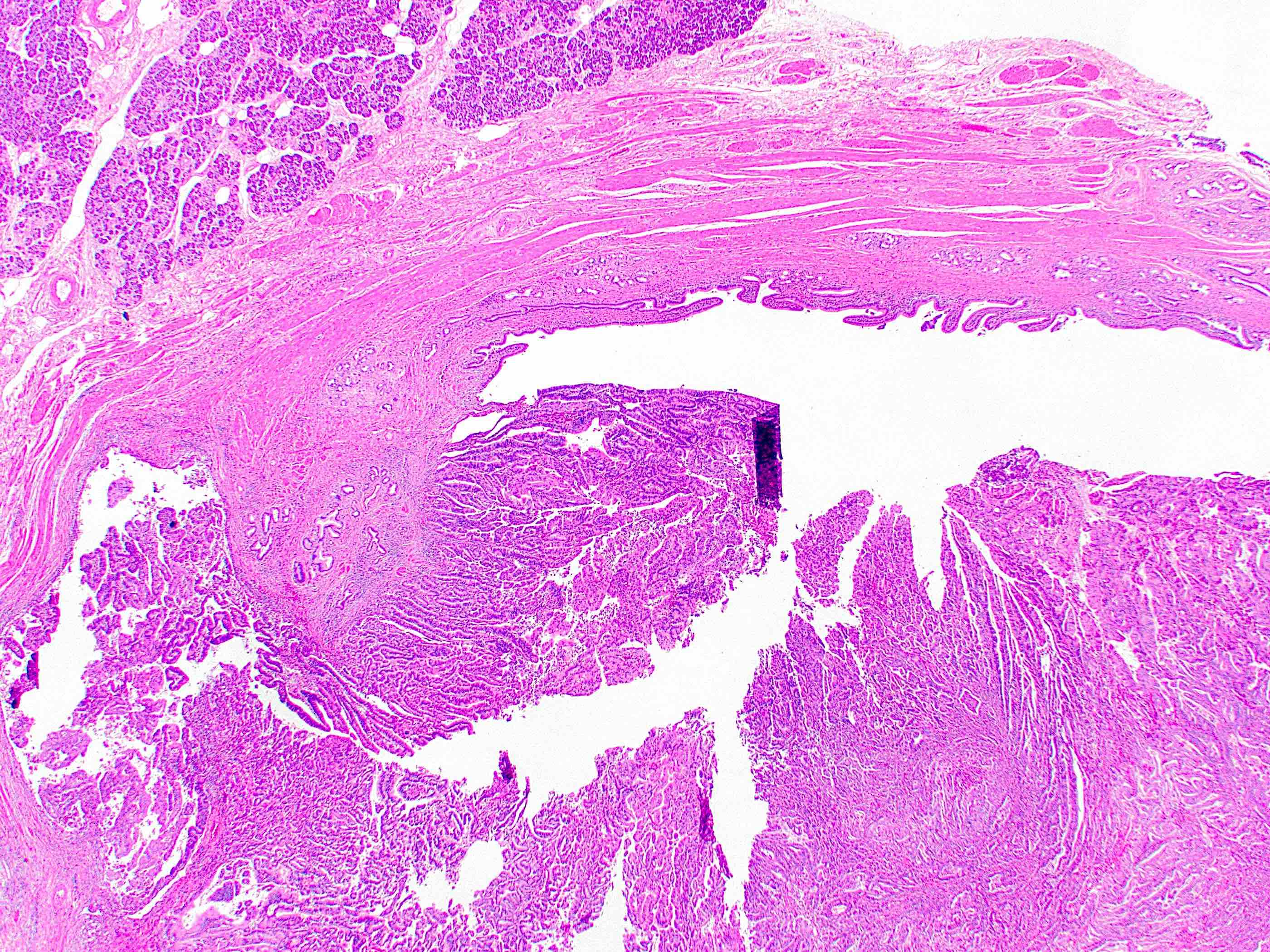
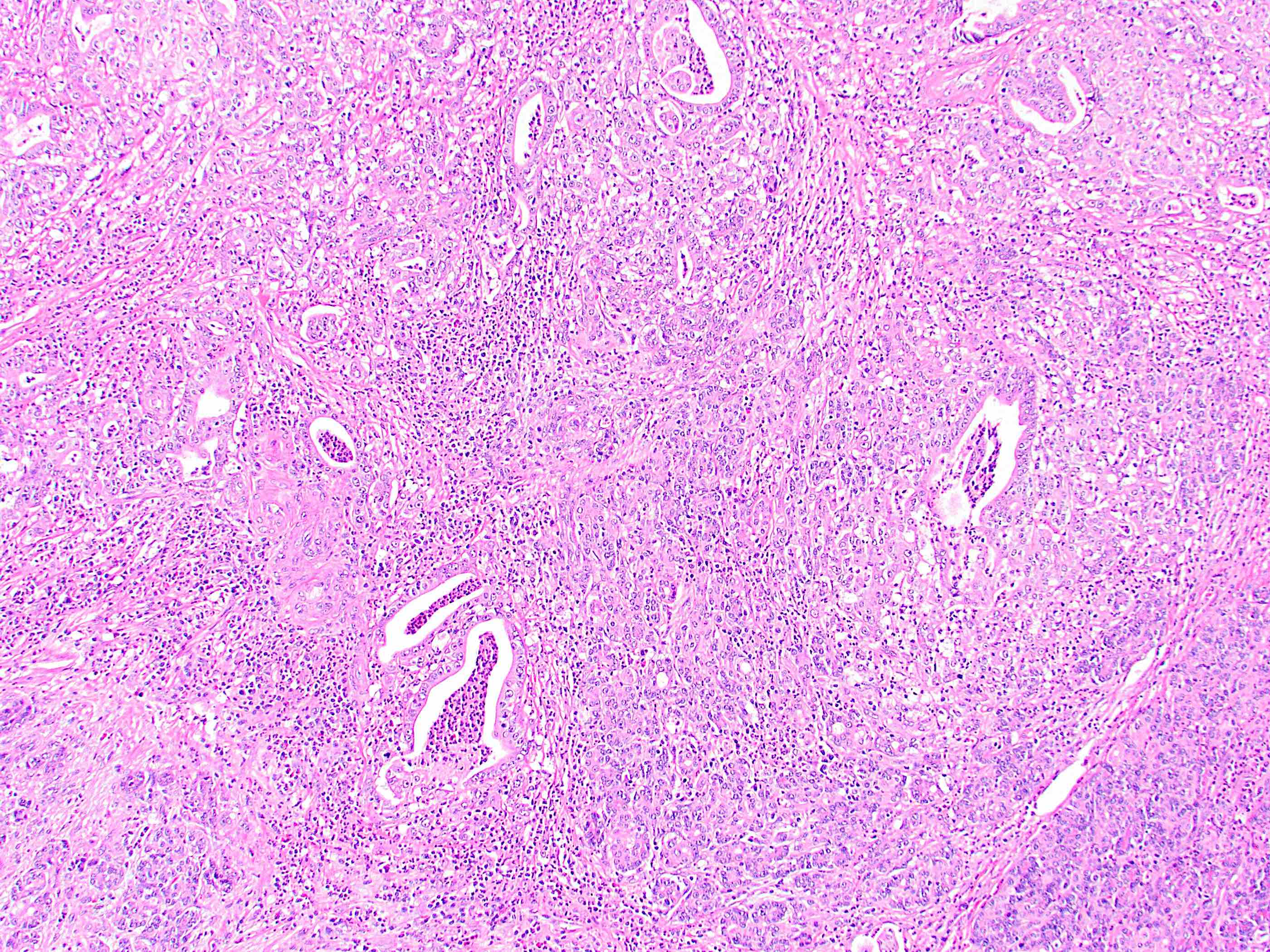
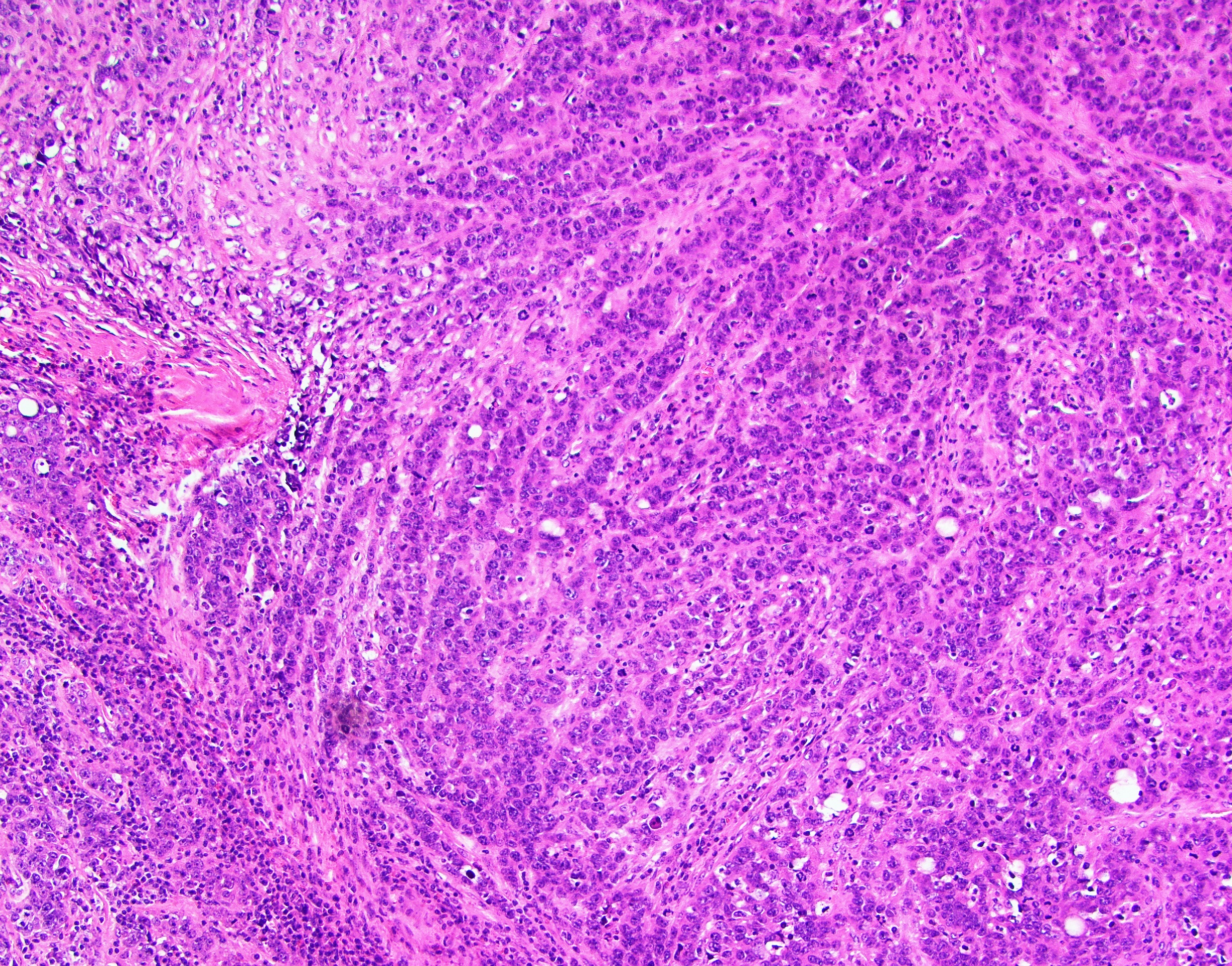
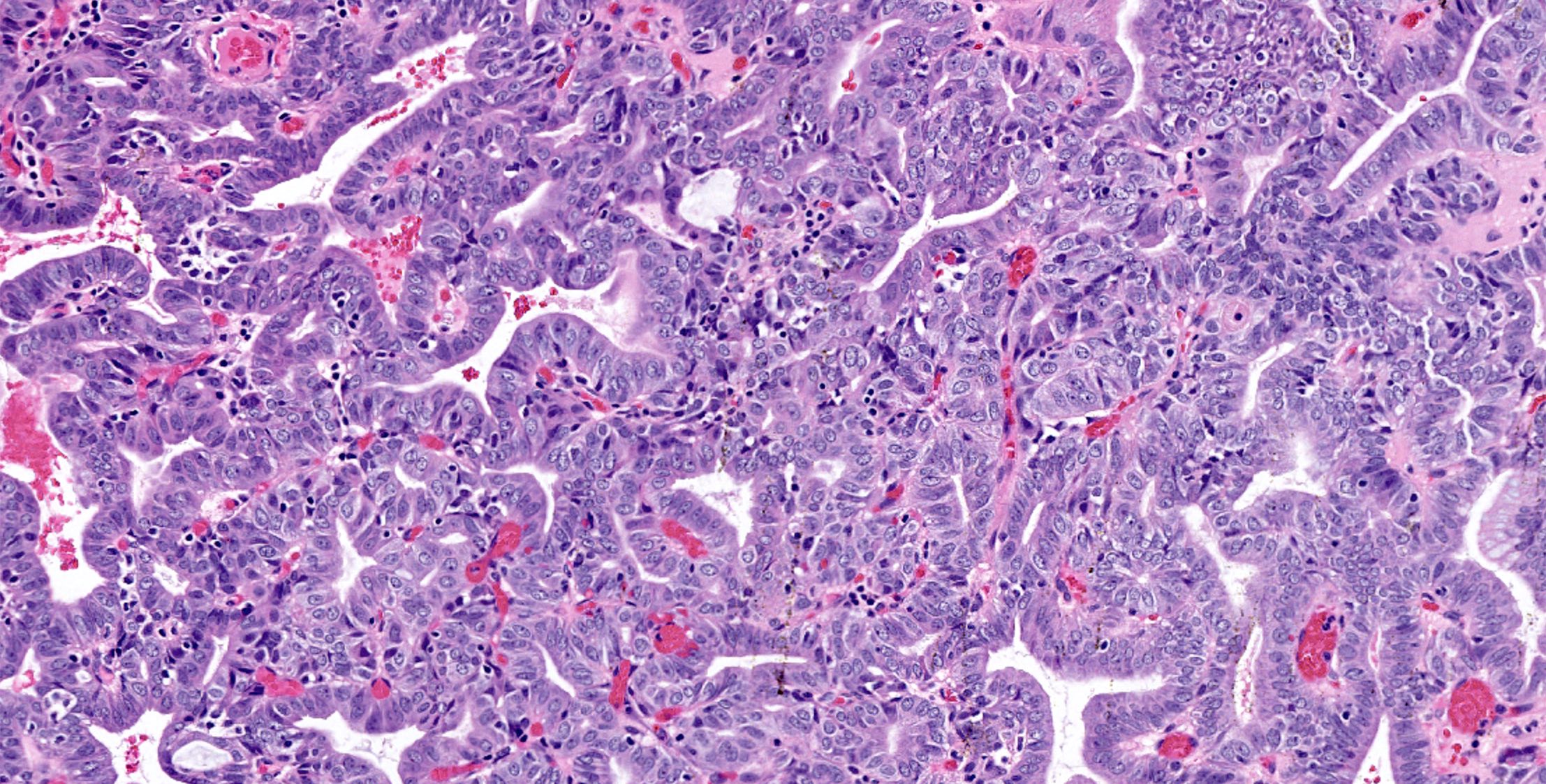
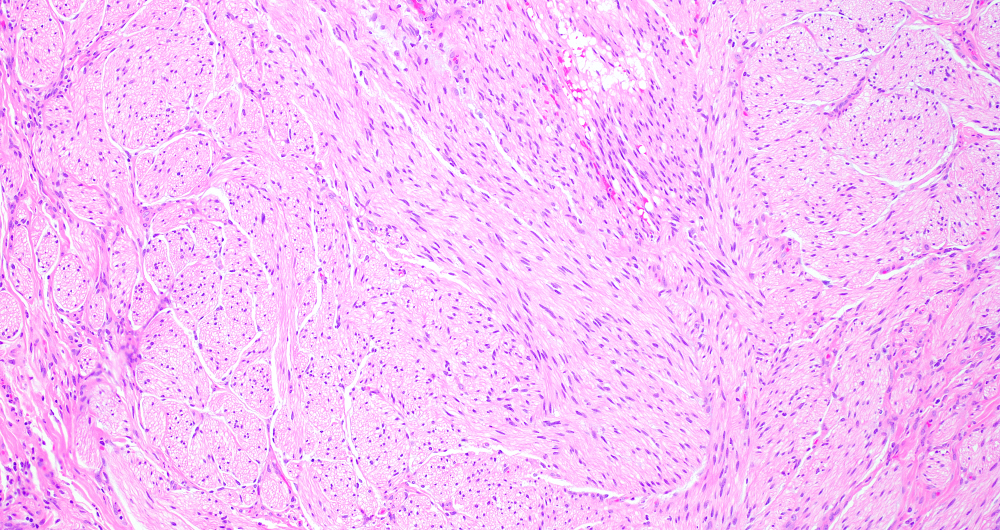
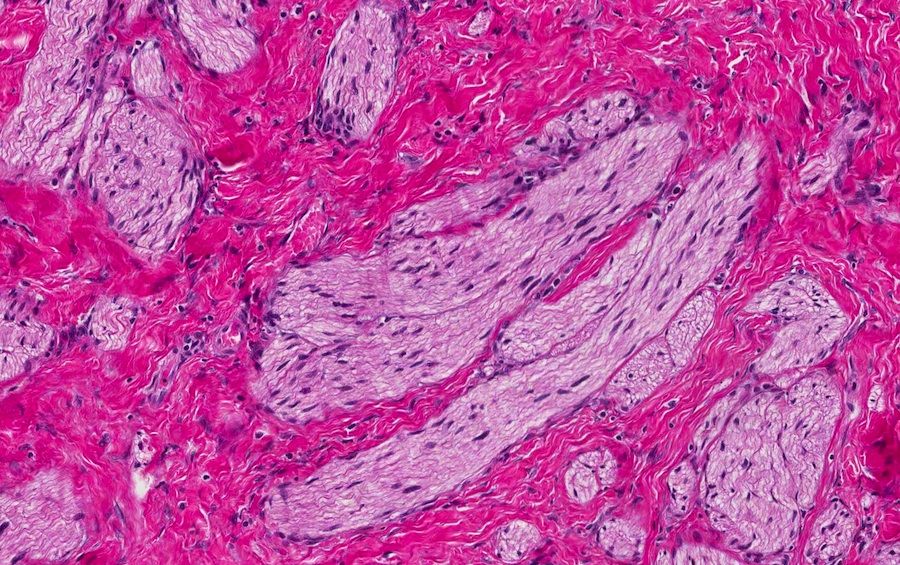
- Generally resembles the large duct type of intrahepatic cholangiocarcinoma (Mod Pathol 2014;27:1163)
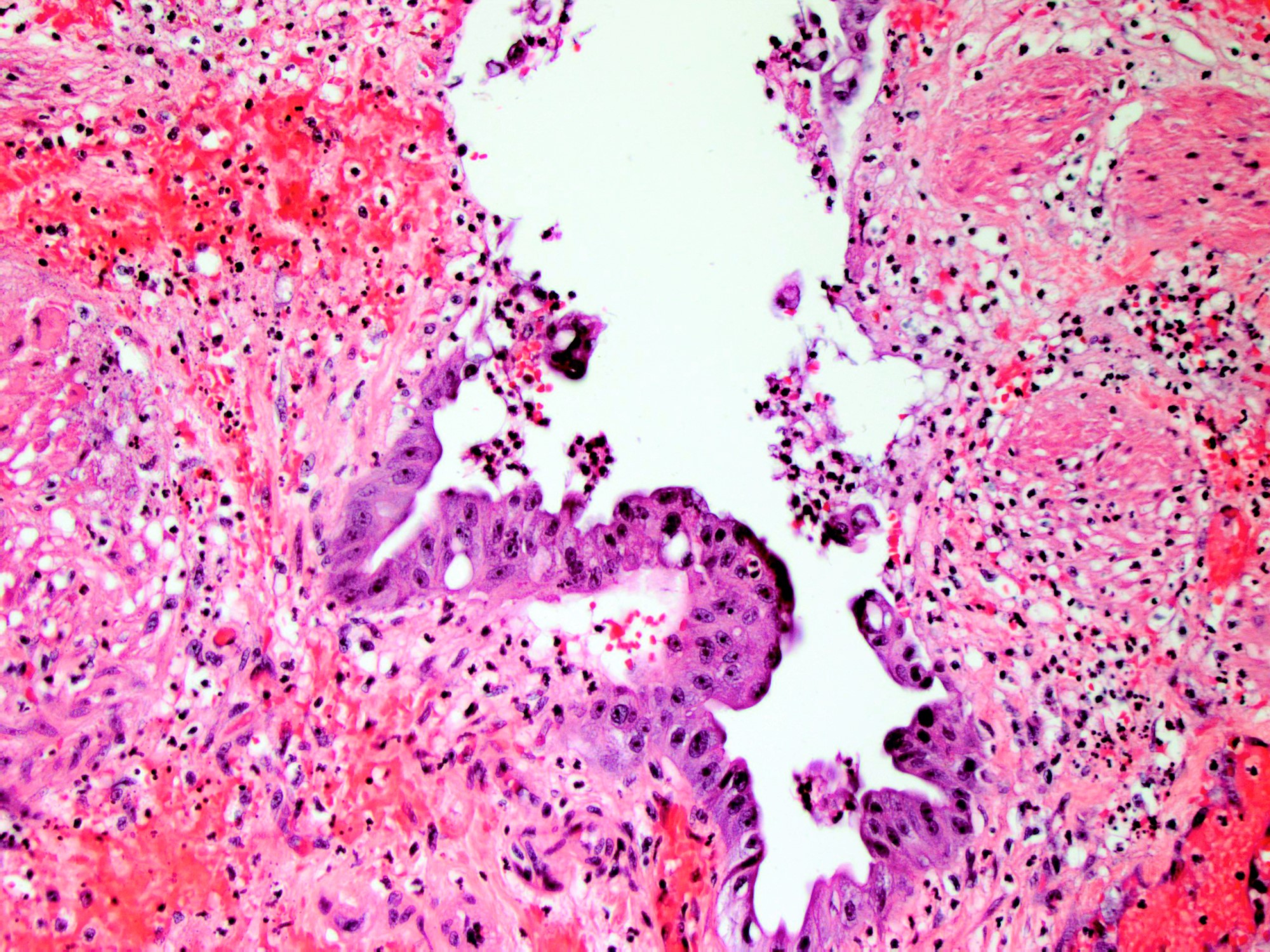
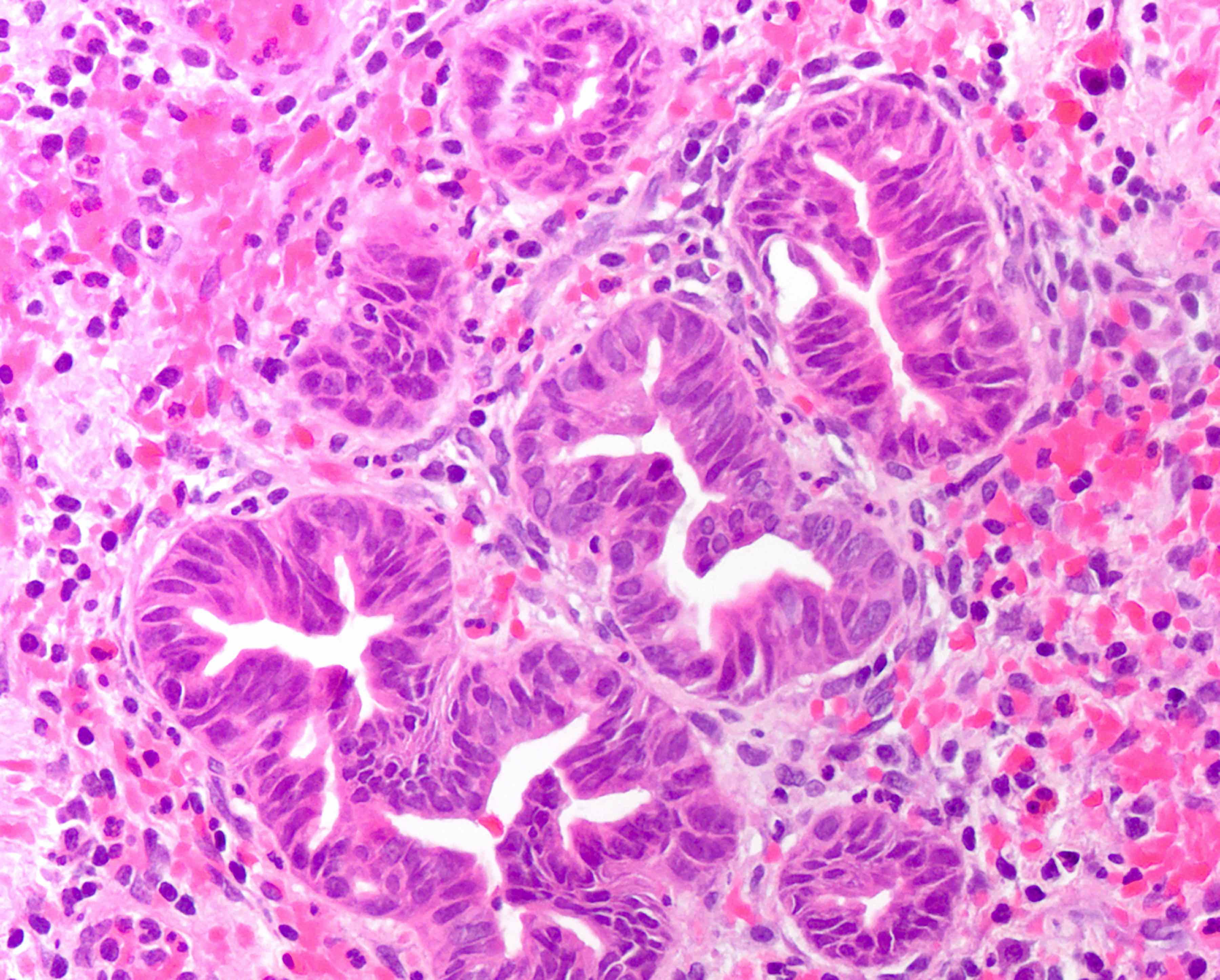
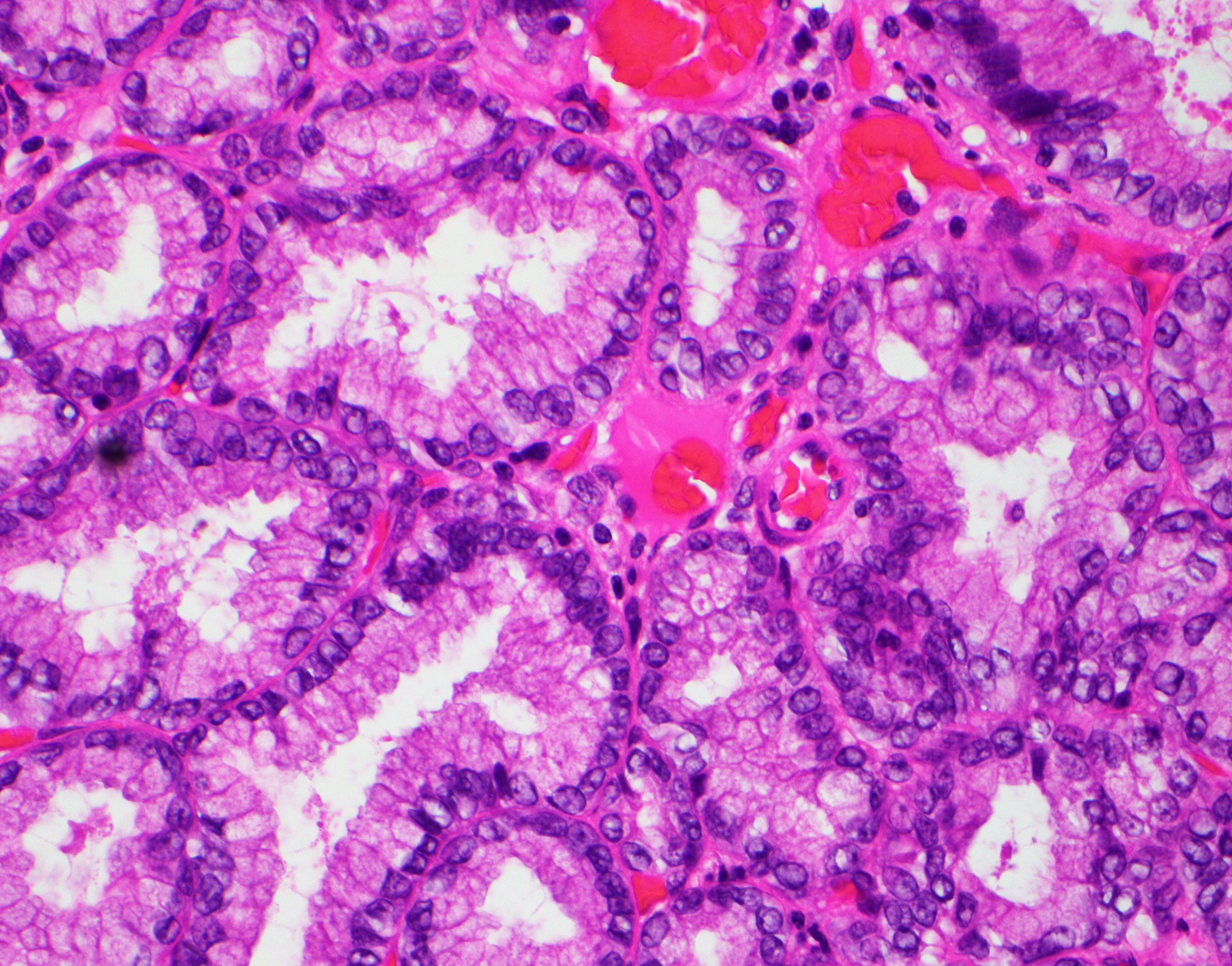
- Invasive malignant adenocarcinoma with variable nuclear and cytologic pleomorphism (World J Gastrointest Oncol 2022;14:607)
- Widely spaced glands haphazardly infiltrate duct wall
- Glands may be well formed, irregular, solid, cord-like, cribriform, abortive or forming papillary structures
- Individual infiltrating cells
- Variable necrosis can be present
- Often a prominent associated neutrophilic infiltrate
- May show intraductal growth with papillary, tubular or superficial spreading patterns (World J Gastrointest Oncol 2022;14:607)
- Precursor lesion may be visible (biliary intraepithelial neoplasia, intraductal papillary neoplasm of the bile ducts)
- Cytologic features include (Cytopathology 2022;33:257)
- Irregular, variably sized sheets of atypical to malignant glandular cells
- Peripheral palisading nuclei
- Branching tapered columns (resembling bile duct epithelium)
- Disorderly growth with crowding and piling up
- Loss of nuclear polarity (drunken honeycomb appearance)
- CK20 (Surg Case Rep 2020;6:264)
- Generally negative for markers indicating origin in other organ systems (e.g., TTF1, GATA3, PAX8)
- KRAS, TP53, ARID1A and SMAD4 mutations most common (J Hepatol 2020;73:315)
- 4 molecular classes have been proposed: metabolic class, proliferation class, mesenchymal class and immune class
- Extrahepatic bile duct, excision:
- Segment of bile duct with extrahepatic cholangiocarcinoma (2.5 cm), extending 0.7 cm into bile duct wall (pT2) (see synoptic report)
- Margins of resection unremarkable
- Lymphovascular and perineural invasion present
- One lymph node positive for carcinoma (1/1)
- Background bile duct with acute and chronic inflammation
- Secondary involvement of pancreatic ductal adenocarcinoma or ampullary carcinoma (Cancers (Basel) 2023;15:1454):
- Most relevant in pancreatoduodenectomy specimens
- Requires careful gross examination and correlation with clinical and imaging findings
- May be impossible to definitively determine for advanced lesions
- Reactive change:
- Can involve biliary surface epithelium or peribiliary glands
- On cytology specimens, features of malignancy include 3 dimensional clusters, pleomorphism, 2 cell population and chromatin pattern changes (Mod Pathol 2017;30:1273)
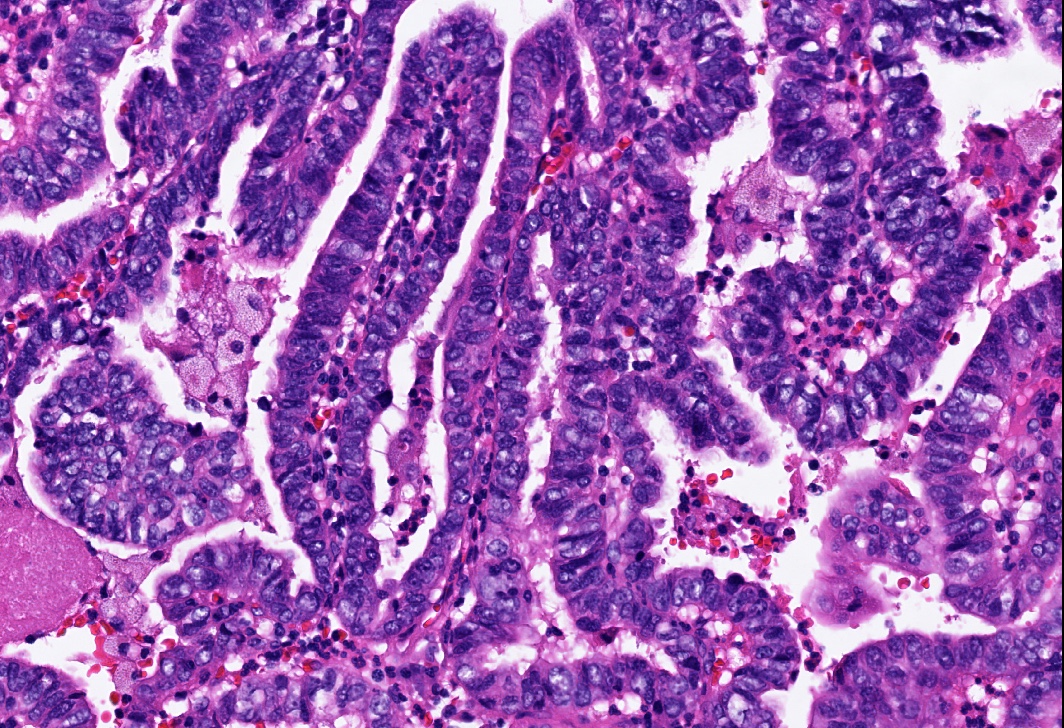
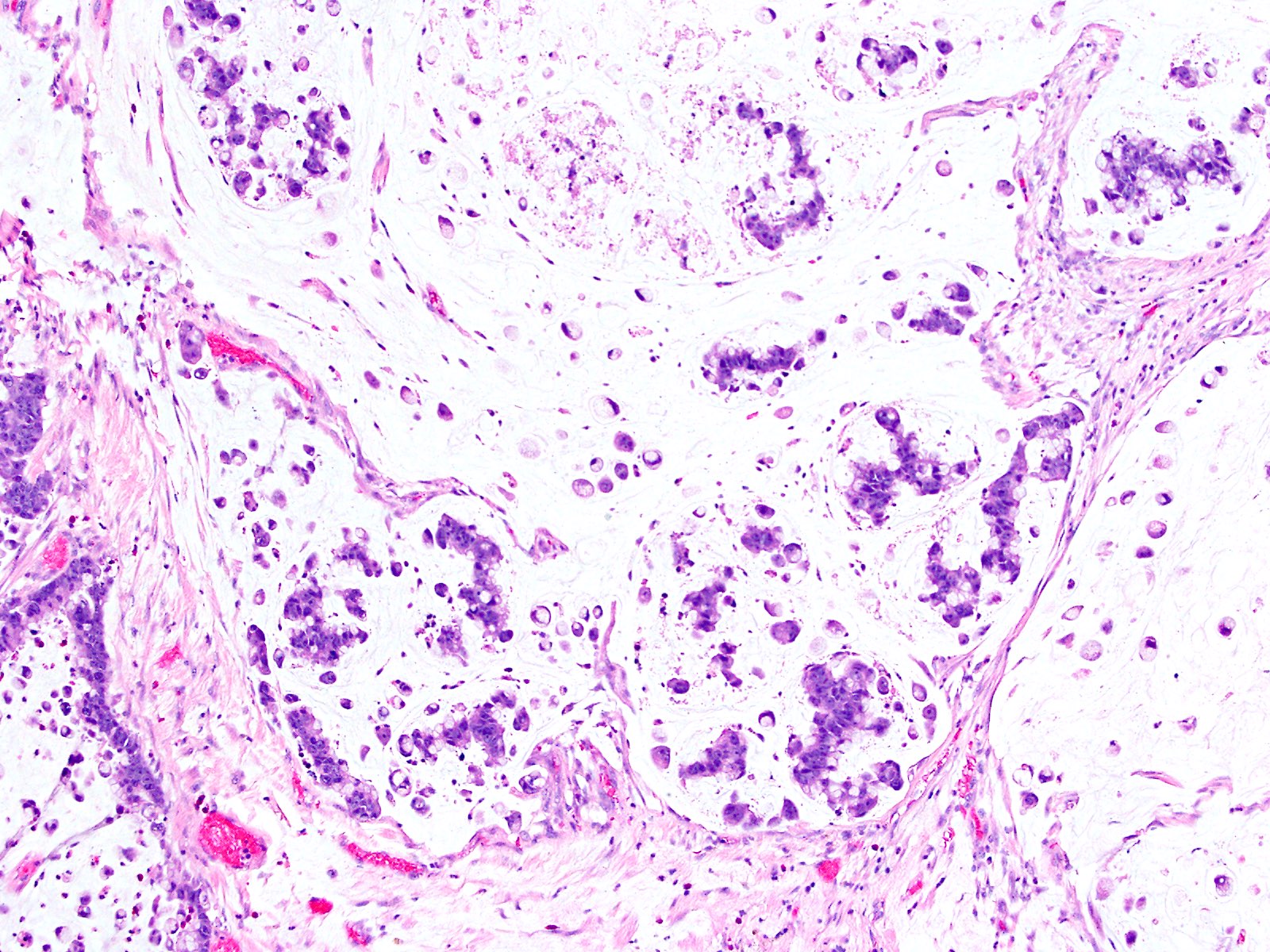
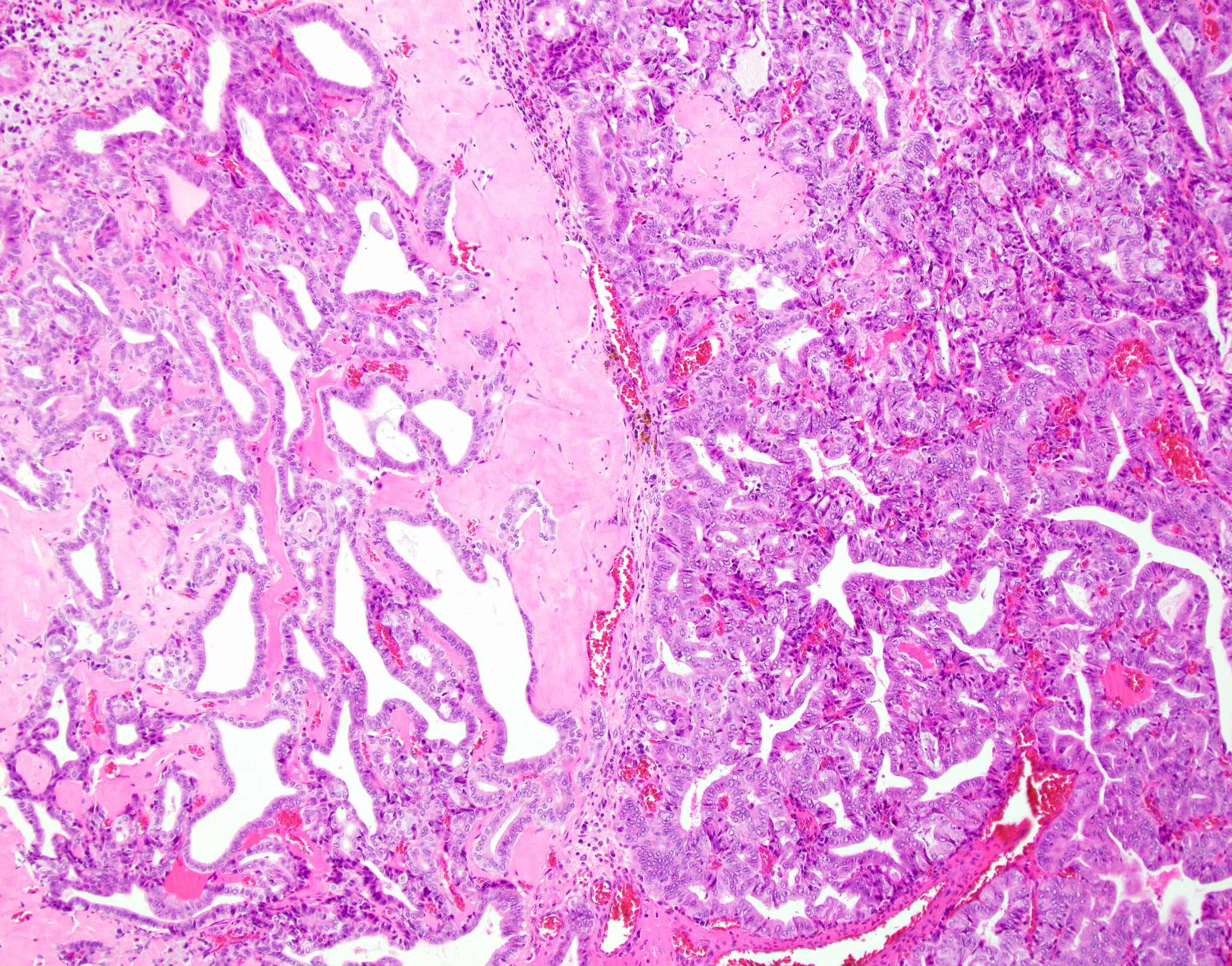
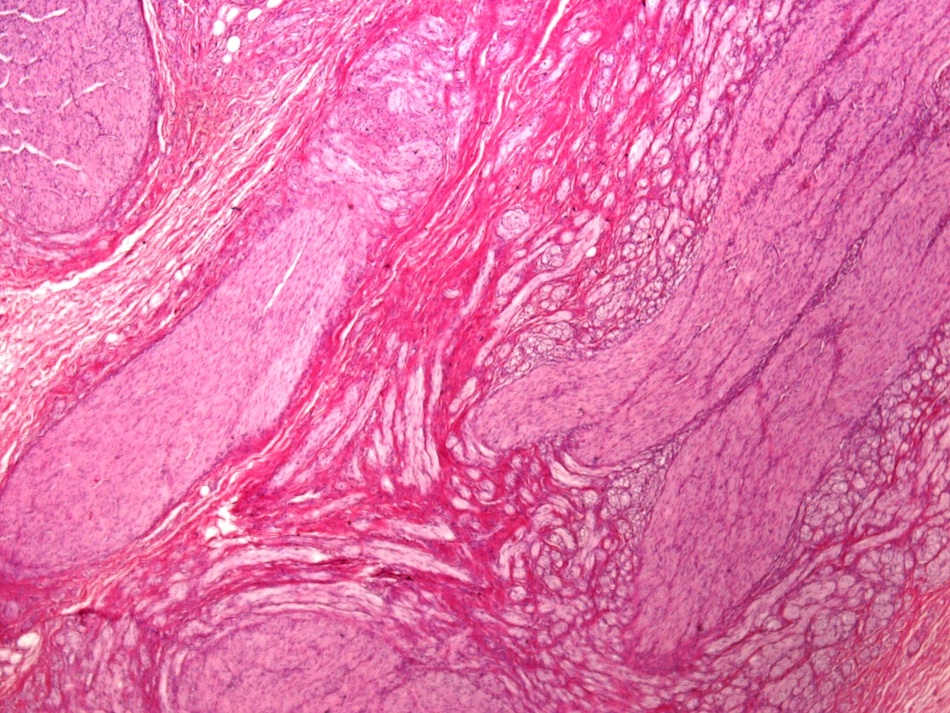
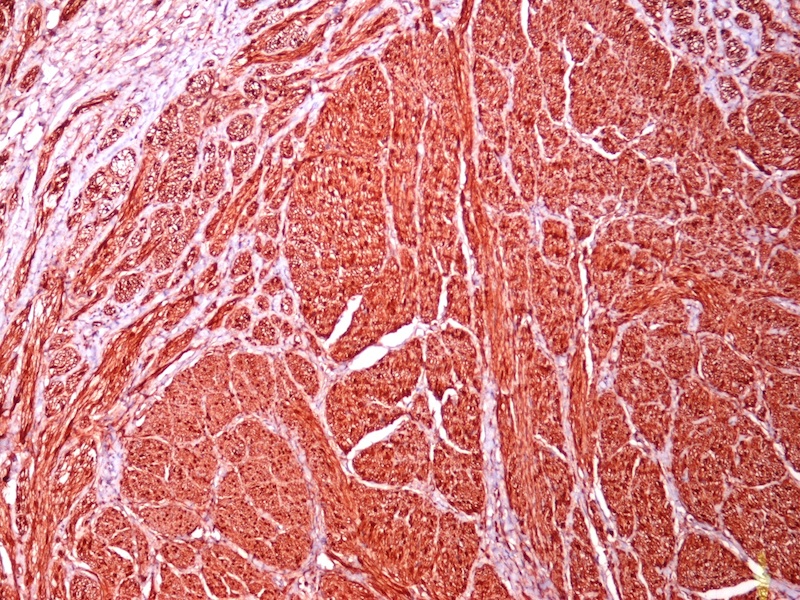
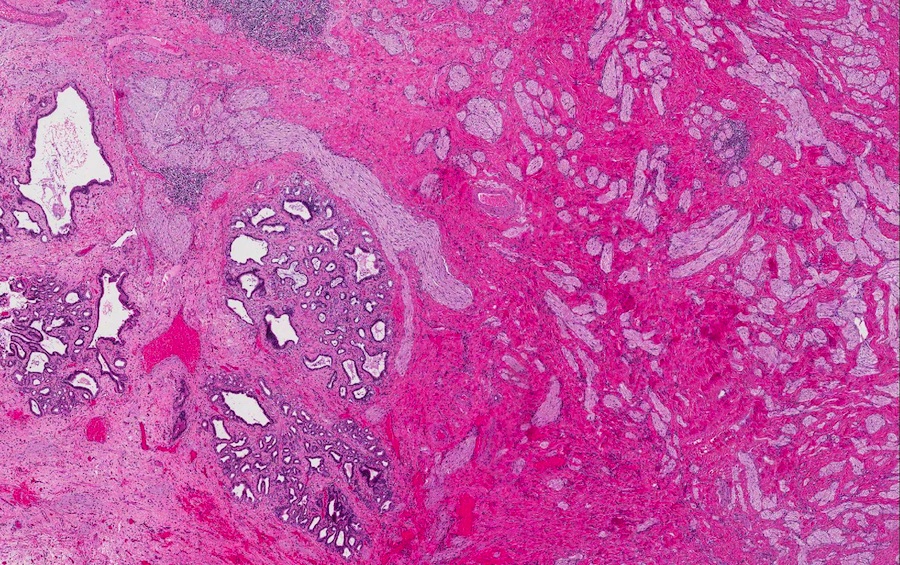
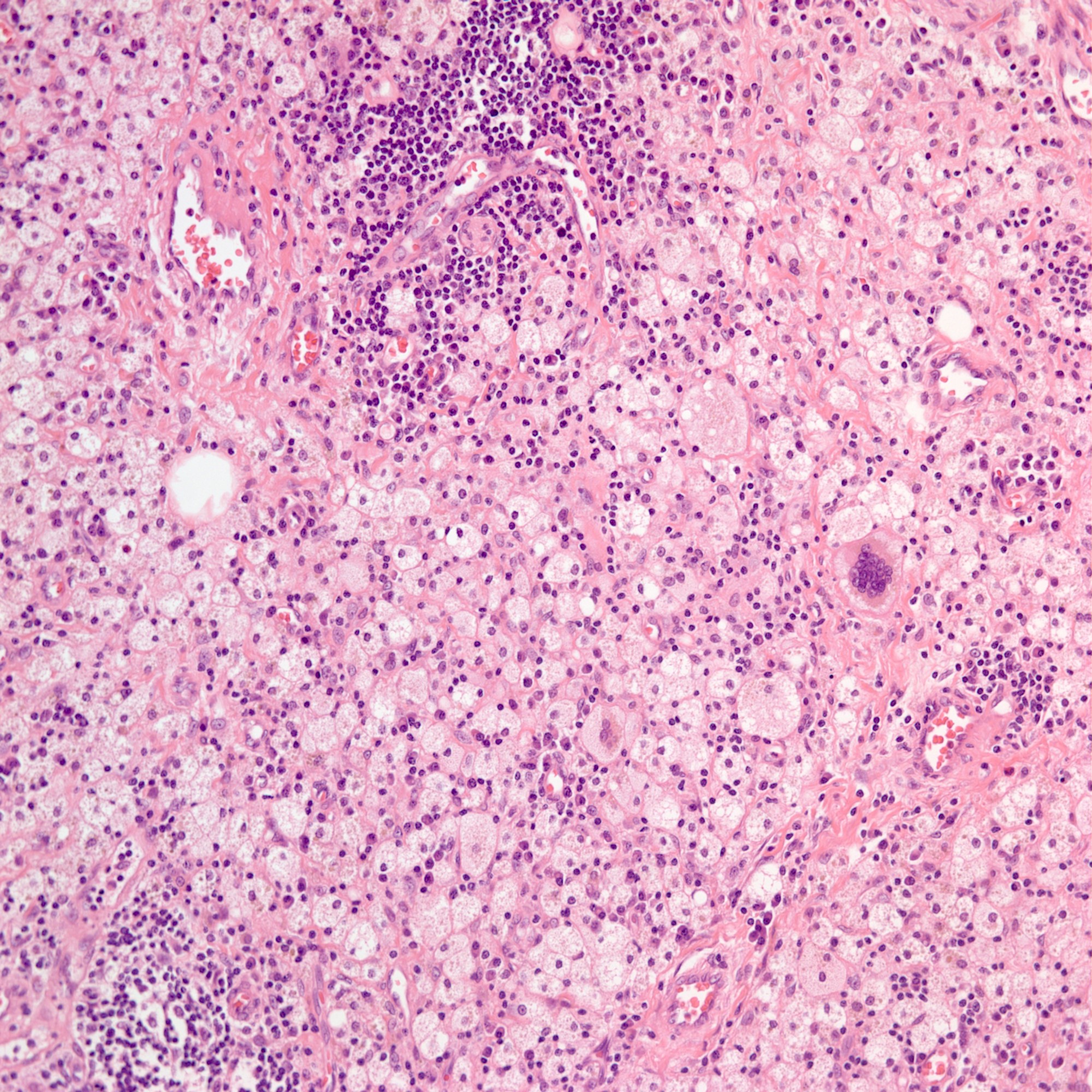
This image shows a cholangiocarcinoma arising within the pancreas. Which of the following is true regarding extrahepatic cholangiocarcinoma?
- It has a good prognosis
- It often shows a prominent neutrophilic infiltrate
- It resembles the small duct type of intrahepatic cholangiocarcinoma
- Peak onset is in the third decade of life
- Primary biliary cholangitis is a risk factor
B. It often shows a prominent neutrophilic infiltrate. This finding is often seen in pancreatobiliary adenocarcinomas in general, including extrahepatic cholangiocarcinoma. Answer A is incorrect because this disease has a poor prognosis. Answer D is incorrect because peak onset is in the sixth and seventh decades of life. Answer E is incorrect because primary sclerosing cholangitis is a risk factor, not primary biliary cholangitis. Answer C is incorrect because histologically, it most resembles the large duct type of intrahepatic cholangiocarcinoma.
Comment Here
Reference: Carcinoma of extrahepatic bile ducts
- CDX2
- CK7
- CK20
- PAX8
- TTF1
Comment Here
Reference: Carcinoma of extrahepatic bile ducts
- Associated with other hepatobiliary tract abnormalities
- May rupture spontaneously, be associated with reflux of pancreatic enzymes into bile duct
- Associated with stones in 1 - 30% of cases
- Not actually a cyst but a dilation of common bile duct which may secondarily obstruct other biliary ducts or the duodenum
- 2 - 8% develop biliary tract carcinoma (20x normal risk) at mean age 34 years, lower risk if surgery earlier in life (age 10 years or less), carcinoma may develop within wall of cyst, within gallbladder or bile ducts
- In Korea, usually type I or IVa (Arch Surg 2011;146:1178)
- Type 1: segmental or diffuse fusiform dilation of common bile duct (50 - 90%)
- Type 2: diverticulum of common bile duct
- Type 3: dilation of intraduodenal common bile duct (choledochocele)
- Type 4: multiple cysts of extrahepatic bile ducts with (4A) or without (4B) cysts of intrahepatic ducts
- Type 5: one or more cysts of intrahepatic ducts (Caroli disease)
- 1 per 13,000 live births in U.S. vs. 1 per 1,000 in Japan
- 75% girls
- Most common cause of obstructive jaundice in infants beyond infancy but may be found at any age
- 11 year old boy (Hum Pathol 2003;34:99)
- 34 year old man with adenosquamous carcinoma in congenital choledochal cyst associated with pancreaticobiliary maljunction (Pathol Int 2009;59:482)
- 41 year old woman with squamous cell carcinoma arising within choledochal cyst (Dig Dis Sci 2008;53:2822)
- Type IV A choledochal cyst with cystic duct cyst (HPB (Oxford) 2010;12:285)
- Complete cyst removal with biliary reconstruction, usually with Roux-en-Y hepaticojejunostomy
- Contain 1 - 2 liters of bile, up to 15 cm in diameter
- Wall is fibrous, variable calcification, 2 - 10 mm thick
- Focal columnar epithelium (more intact in infants)
- Walls composed of dense fibrous tissue, scattered smooth muscle and elastic fibers
- Variable chronic inflammatory infiltrate (increases with age)
- Variable hyperplasia, metaplasia, dysplasia
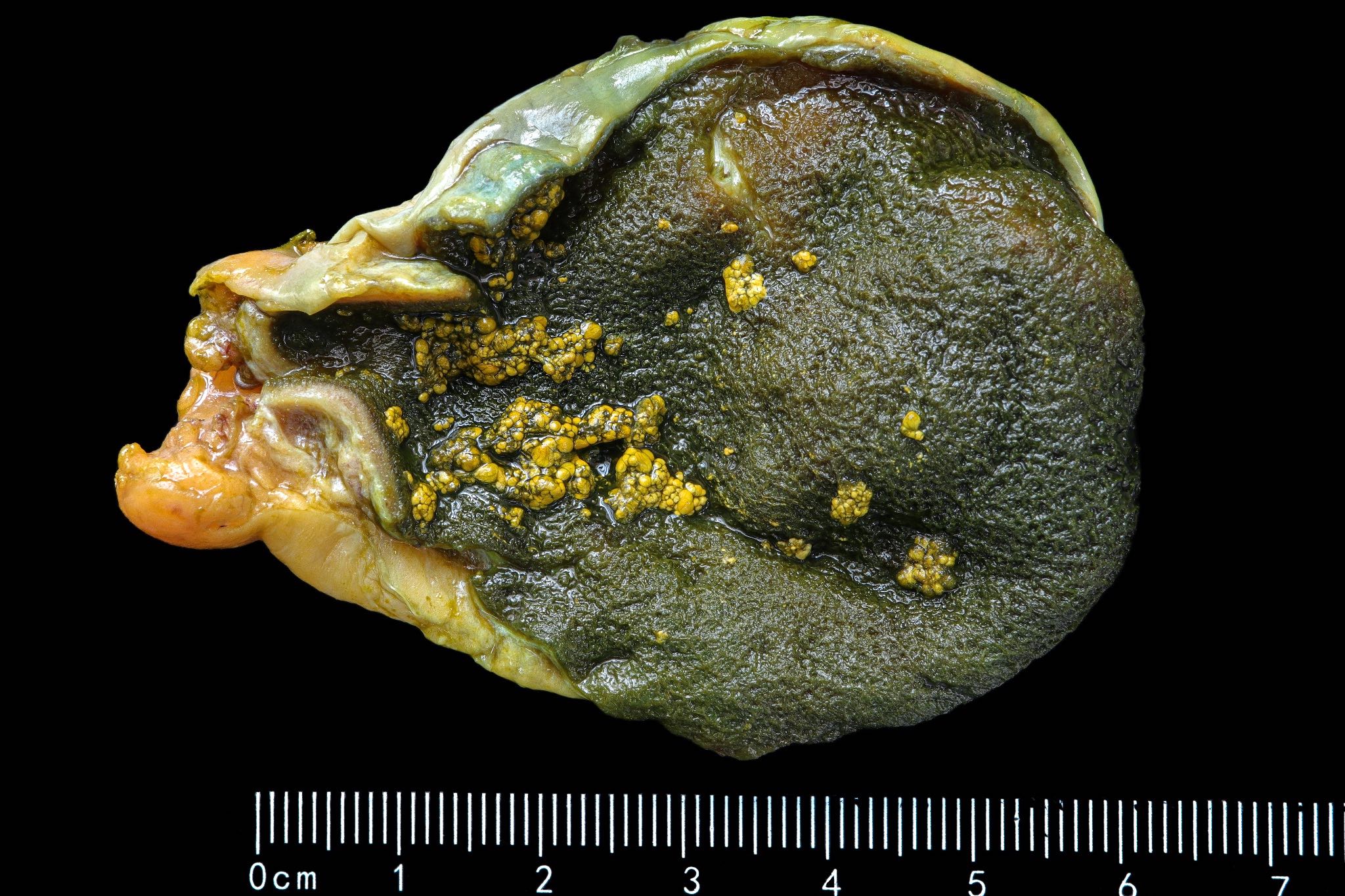
- Also called gallstones
- Accounts for 1% of national heath care budget
- Affects 10% of adults in developed countries (80% are silent) vs. < 1% of children
- 80% of gallstones in West are cholesterol stones with 50% or more crystalline cholesterol monohydrate
- 20% of gallstones in West are pigment stones composed of bilirubin calcium salts
- Gallstones impact at neck just proximal to cystic duct
- Typically within lumen but may be intramural
Risk factors:
- Pima, Hopi or Navajo (75% of stones are pure cholesterol vs. 25% in industrialized vs. minimal in developing countries), also Scandinavians, Chileans, Mexican Americans, increasing age (> 50% risk by age 80)
- Fat, fertile [multiple pregnancies], forty, female, obesity (Korean J Gastroenterol 2012;59:27), rapid weight loss, gallbladder stasis, genetic disorders that impair bile salt synthesis / secretion or increase cholesterol levels (serum or biliary), low HDL levels
- May be influenced by Apolipoprotein E genotype (Ann Epidemiol 2006;16:763)
- Biliary sludge typically occurs before gallstones
- Estrogens from birth control pills or pregnancy increase expression of hepatic LDL receptors, which increase cholesterol uptake, which stimulate HMG CoA reductase, which synthesizes cholesterol
- Pigment stone risk factors are increased unconjugated bilirubin (from hemolytic syndromes, ileal dysfunction / bypass, bacterial contamination of biliary tree)
Clofibrate:
- Anticholesterol drug that increases HMG CoA reductase activity and decreases conversion of cholesterol to bile acids by reducing cholesterol 7 alpha hydroxylase activity, causes excess biliary secretion of cholesterol
Symptoms:
- Usually none but may have biliary colic (severe, right upper quadrant pain)
Complications:
- 1 - 2% have acute or chronic cholecystitis, choledocholithiasis, cholangitis, empyema, gallstone ileus, acute pancreatitis
Mirizzi syndrome:
- Rare
- Stone impacting in cystic duct or gallbladder neck causes extrinsic compression or obstruction of common bile duct, causing jaundice
Report:
- Presence of biliary sludge, number, size and type of gallstones
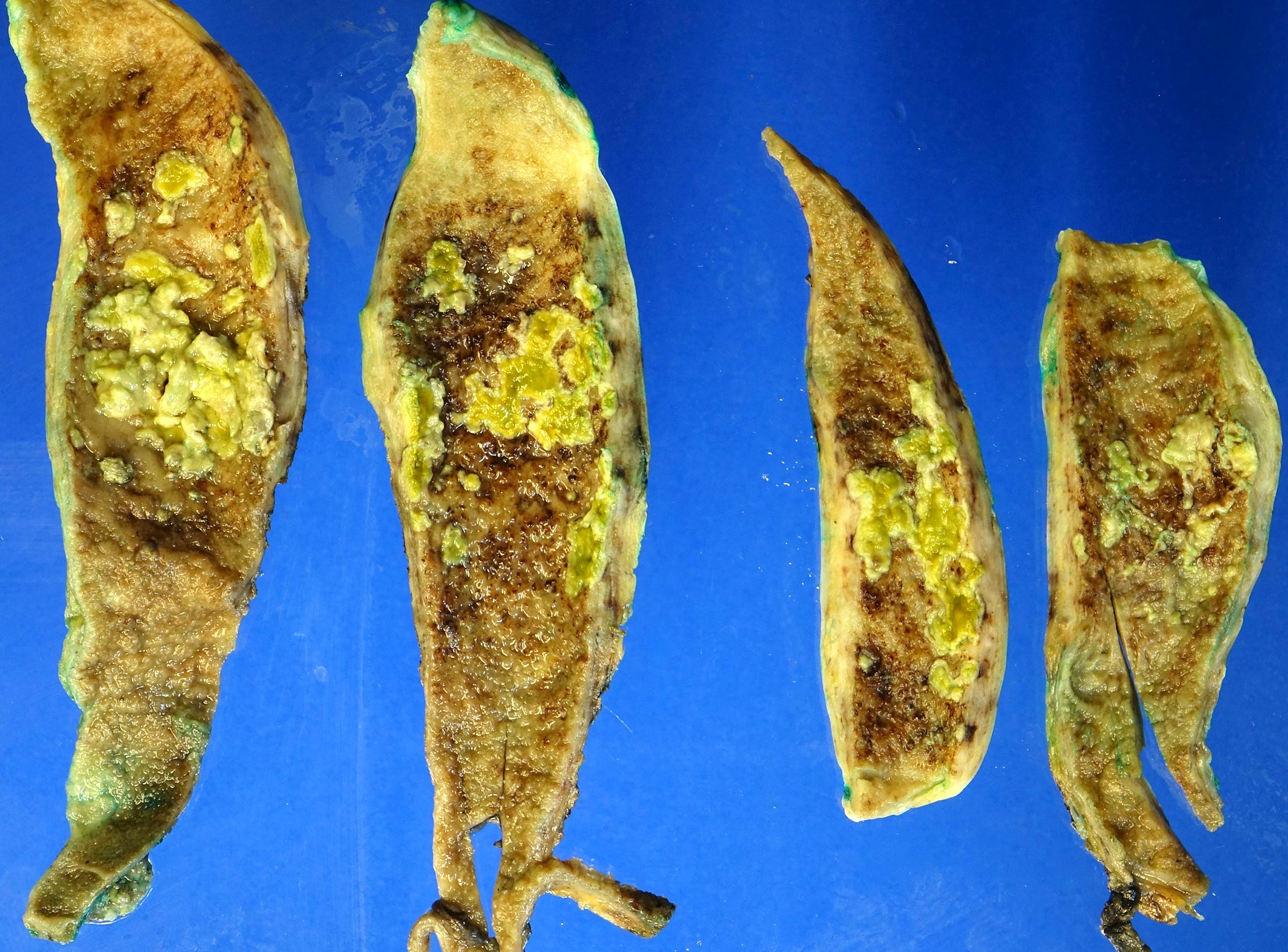
- Gallstones are composed of insoluble bile components: cholesterol, calcium bilirubinate, calcium salts (organic and inorganic), bile salts, mucin glycoproteins
- In U.S., 75 - 85% are cholesterol stones, 15 - 25% are pigment stones
- Larger stones are associated with carcinoma (Trop Gastroenterol 2012;33:39); also cholesterol, not pigment stones (Aust N Z J Surg 2000;70:667)
- Calcium stones are gray white and amorphous; very uncommon
- Calcium carbonate may fill lumen as thick, inspissated, cream gray to yellow green putty-like material
- Choledocholithiasis: stones in common bile duct
- 40% of common bile duct stones are brown stones, usually associated with recurrent pyogenic cholangitis and older age (J Int Med Res 2009;37:1220)
- Primary: originate in common bile duct
- Secondary: originate in gallbladder
- ERCP (95% sensitive and specific), ultrasound is only 50% sensitive
- 75 - 85% of all gallstones
- Only 10% are pure (at least 90% cholesterol), the remainder are mixtures with at least 60% cholesterol by weight
- Cholesterol monohydrate precipitates when no longer soluble in bile
- Initially bile supersaturation with cholesterol occurs
- Then nucleation (initial crystallization), then stone growth facilitated by bile stasis and mucin hypersecretion
- Pure and mixed occur predominantly in women
- Also associated with increasing age, obesity, rapid weight loss, diabetes, ileal disease, multiple pregnancies, total parenteral nutrition, various drugs, specific ethnic groups
- Adenomatous hyperplasia and Rokitansky-Aschoff sinuses:associated with mixed and cholesterol stones; not associated with pigment stones (Trop Gastroenterol 2002;23:25)
- 15 - 25% of all gallstones
- Associated with increasing age
- Less than 25 - 35% cholesterol
- Composed of calcium bilirubinate, calcium salts, mucin glycoprotein
- Brown (not black) stones associated with infected bile (usually E. coli) due to acute cholecystitis or choledocholithiasis with cholangitis
- Black stones associated with older age, chronic hemolysis, cirrhosis, sclerosing cholangitis (increased unconjugated bilirubin in bile)
- Ultrasound (95% sensitive and specific for gallstones 2 mm or larger or gallbladder sludge), Xrays detect 10 - 25% of gallstones that are radiopaque due to calcium
- Laparoscopic cholecystectomy if symptomatic or in children, Native Americans, patients with sickle cell disease or porcelain gallbladder, stones 3 cm or larger
- 85% are 2 cm or less
- Cholesterol stones: < 1 cm to 4 cm; single or multiple; white yellow, round / oval with crystalline cut surface
- Pigmen stones: multiple shiny black stones, 0.2 to 5 cm, rarely brown in U.S. (more commonly brown in Japan)
- Minimal / mild lymphocytic mucosal inflammation, Rokitansky-Aschoff sinuses, fibrosis, thickening of muscularis propria, cholesterolosis, focal epithelial metaplasia (pyloric / gastric mucin cell metaplasia or intestinal metaplasia) (Am J Surg Pathol 2003;27:1313)
- Benign polypoid variant of cholesterolosis
- Polypoid variant of cholesterolosis
- Cauliflower-like architecture with core of foamy lipid laden macrophages
- Benign
- Cholesterol polyps are the most common type of gallbladder polyp, constituting 60 - 90% of all polyps (N Am J Med Sci 2012;4:203)
- Slightly more common in women (F:M = 2.2:1)
- Associated with metabolic syndrome, high BMI and young age (40 - 50 years) (N Am J Med Sci 2012;4:203, Lipids Health Dis 2021;20:26, Am J Surg Pathol 2020;44:467)
- Almost always arises in gallbladder
- Possible in the common bile duct but very rare
- Lipids deposit inside macrophages, resulting in the formation of a distinct polyp
- Etiologic mechanism is not clear
- Suggested etiologies include dyslipidemia, high bile viscosity and increased expression of mucin genes (Lipids Health Dis 2021;20:26, Int J Biol Markers 2016;31:e73, BMC Gastroenterol 2020;20:268, Gut Liver 2016;10:851)
- Most are asymptomatic
- May detach and behave like gallstones, causing biliary colic, obstruction, nausea, vomiting and rarely pancreatitis (N Am J Med Sci 2012;4:203)
- Incidental finding during abdominal ultrasound or on histopathologic examination following cholecystectomy
- Definitive diagnosis requires microscopic examination (J Ultrasound 2021;24:131)
- Risk factors for cholesterol polyp formation are closely related to lipid metabolism (Lipids Health Dis 2021;20:26)
- Usually multiple, pedunculated, small (< 1 cm) (J Ultrasound 2021;24:131)
- Transabdominal ultrasound
- Homogeneous, slightly more hyperechoic than liver parenchyma
- Immobile / fixed despite positional change
- Posterior acoustic shadowing is absent
- Benign with no malignant potential (Lipids Health Dis 2021;20:26)
- 39 year old man with acute cholecystitis (J Nippon Med Sch 2001;68:259)
- 53 year old woman with polyps in the distal common bile duct (Medicine (Baltimore) 2016;95:e5374)
- 62 year old man with large cholesterol polyp clinically mimicking carcinoma (Abdom Imaging 2004;29:100)
- Asymptomatic polyps diagnosed incidentally can be managed by clinical follow up
- If symptomatic, cholecystectomy
- Yellow rounded polyps with smooth contours
- Up to 67% of cases are associated with cholesterolosis (Am J Surg Pathol 2020;44:467)
- Cauliflower-like architecture is a distinctive / pathognomonic feature present in all cases and is generally not seen in other polyps
- Connected to the gallbladder via very thin stalks; hence, they may detach from the surface
- Foamy lipid laden macrophages generally make up the wide and edematous core of the polyp
- 15% of cholesterol polyps may lack these lipid laden macrophages
- Lined by a single layer of normal gallbladder epithelium
- No epithelial elements in the core of the polyp and no dysplasia
- Cholesterol polyps can be found in gallbladders devoid of any significant chronic changes (Am J Surg Pathol 2020;44:467)
- Gallbladder, cholecystectomy:
- Cholesterol polyps (see comment)
- Comment: Multiple yellowish round polyps are present in the body of the gallbladder, with the largest measuring 0.5 cm.
- Cholesterolosis:
- Foamy lipid laden macrophages in the lamina propria and the villi (focal or diffuse)
- Affected areas do not have distinct polyp structures or cauliflower-like architecture
- Xanthogranulomatous cholecystitis:
- Foamy lipid laden macrophages associated with inflammatory cells
- Intracholecystic papillary neoplasm:
- Resorption of the macrophages in a cholesterol polyp leaves behind edematous acellular stroma that might mimic neoplastic polyps (Am J Surg Pathol 2020;44:467)
- True neoplastic polyps demonstrate dysplastic epithelium
Comment Here
Reference: Cholesterol polyp
- Most are > 1 cm
- Most are sessile
- The surface exhibits a gritty texture
- They are usually solitary
- They exhibit a yellowish color
Comment Here
Reference: Cholesterol polyp
- Accumulation of lipids (triglycerides, cholesterol precursors and cholesterol esters) within subepithelial macrophages in the lamina propria of the gallbladder (J Ultrasound 2021;24:131)
- Can be focal, diffuse or polypoid (also known as cholesterol polyps) (Minerva Gastroenterol Dietol 2003;49:217)
- Second most common histopathological finding in resected gallbladders (most common being chronic cholecystitis) (JSLS 2020;24:e2020.00052, Rev Col Bras Cir 2020;46:e20192279)
- Due to accumulation of lipids in macrophages in the lamina propria
- Demographic: females, high BMI
- Focal, diffuse or polypoid (polypoid cholesterolosis = cholesterol polyps)
- Gross feature: focal or diffuse flat yellowish dots on the lining of the gallbladder
- When diffuse, resembles a strawberry, hence the name strawberry gallbladder
- Microscopic features: subepithelial lipid laden macrophages in the lamina propria and inside villi
- Also known as strawberry gallbladder
- Seen in 10 - 30% of cholecystectomies (Rev Col Bras Cir 2020;46:e20192279, Cureus 2020;12:e9627)
- Occurs in female patients 75% of the time (Niger J Clin Pract 2019;22:1002)
- Associated with high BMI (Niger J Clin Pract 2019;22:1002)
- Gallbladder
- Bile is supersaturated with cholesterol in both cholesterolosis and gallstone disease, perhaps due to excess bile production
- Patients who are unable to fully solubilize cholesterol will form cholesterol gallstones
- Patients who are able to keep cholesterol fully solubilized may have increased mucosal cholesterol uptake and develop cholesterolosis (J Clin Pathol 1987;40:524)
- This likely occurs in patients with increased acyl-CoA cholesterol ester acyltransferase activity in gallbladder mucosa (Am J Gastroenterol 1998;93:1518)
- The enzyme causes increased synthesis of cholesterol esters, which accumulate in mucosal macrophages (Am J Gastroenterol 1998;93:1518)
- Asymptomatic (J Ultrasound 2021;24:131, Semin Gastrointest Dis 2003;14:178)
- Noninflammatory (is usually an isolated finding) (Rev Col Bras Cir 2020;46:e20192279)
- No malignant potential (Rev Col Bras Cir 2020;46:e20192279)
- Incidentally found during abdominal sonography (appears as a pseudopolyp; see Radiology description for details) or diagnosed on histopathology of surgical specimens (J Ultrasound 2021;24:131)
- Microscopic examination provides the definitive diagnosis
- Serum cholesterol may be normal or elevated
- Ultrasound cannot reliably detect cholesterolosis (Semin Gastrointest Dis 2003;14:178)
- Cholesterolosis may form pseudopolyps that appear as single or multiple hyperechoic parietal foci generating comet tail artifacts (J Ultrasound 2021;24:131)
- 22 year old pregnant woman with persistent abdominal pain and vomiting (BMJ Case Rep 2019;12:e227826)
- 55 year old woman with acute pancreatitis (Proc (Bayl Univ Med Cent) 2018;31:324)
- 78 year old woman with a cholesterol polyp with osseous metaplasia (Cureus 2020;12:e12357)
- Cholecystectomy (Saudi Med J 2004;25:1226)
- Diffuse or focal flat yellow dots on the lining of the gallbladder
- In the diffuse form, the dots on the mucosa / lining resemble a strawberry (J Hepatol 2004;40:8)
- Foamy lipid laden macrophages expanding the lamina propria
- Mucosal villous hyperplasia and hypertrophy (Semin Gastrointest Dis 2003;14:178, Cureus 2020;12:e9627)
- Usually isolated, with no signs of inflammation
- When cholesterolosis is not an isolated finding, most common association would be chronic cholecystitis (Rev Col Bras Cir 2020;46:e20192279)
Contributed by Reem Hamasha, M.D., Faris Alshammas, M.D., Andrey Bychkov, M.D., Ph.D. and Jijgee Munkhdelger, M.D., Ph.D.
- Gallbladder, cholecystectomy:
- Chronic cholecystitis and cholesterolosis
- Cholesterol polyp:
- Essentially a variant of cholesterolosis that forms a distinct polyp
- Xanthogranulomatous cholecystitis:
- A variant of chronic cholecystitis, with lipid laden macrophages and acute and chronic inflammatory cells in the wall of the gallbladder (World J Radiol 2016;8:183)
- Hyperplastic polyp:
- Poorly defined benign entity characterized by mucosal hyperplasia including elongated villi, sometimes with metaplastic changes but never with dysplasia; macrophages are not part of this process
Comment Here
Reference: Cholesterolosis
- Increased synthesis and deposition of cholesterol esters
- Infiltration of macrophages due to subclinical infection
- Mucosal irritation due to longstanding inflammation
- Slow degradation and absorption of gallstones
Comment Here
Reference: Cholesterolosis
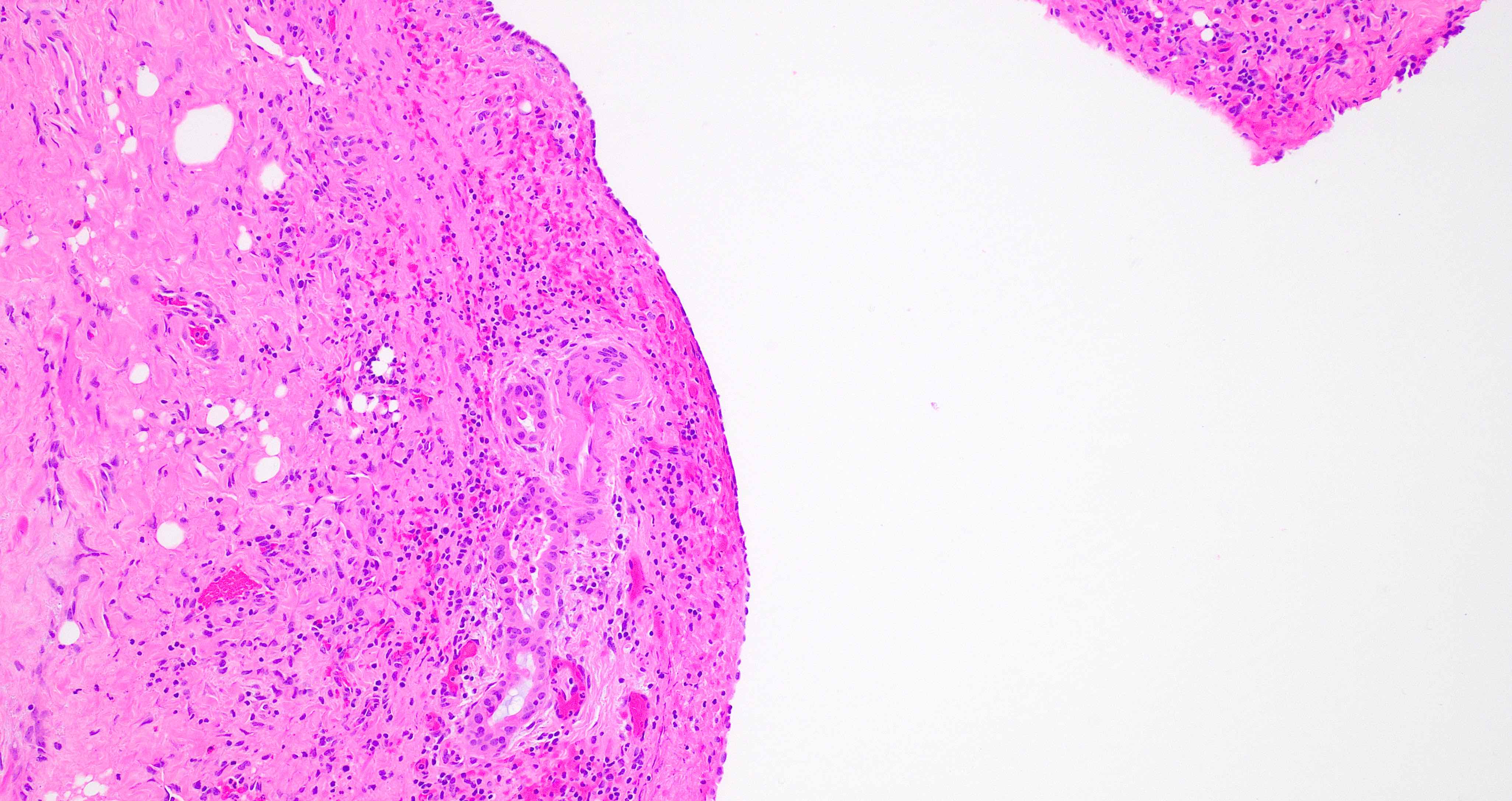
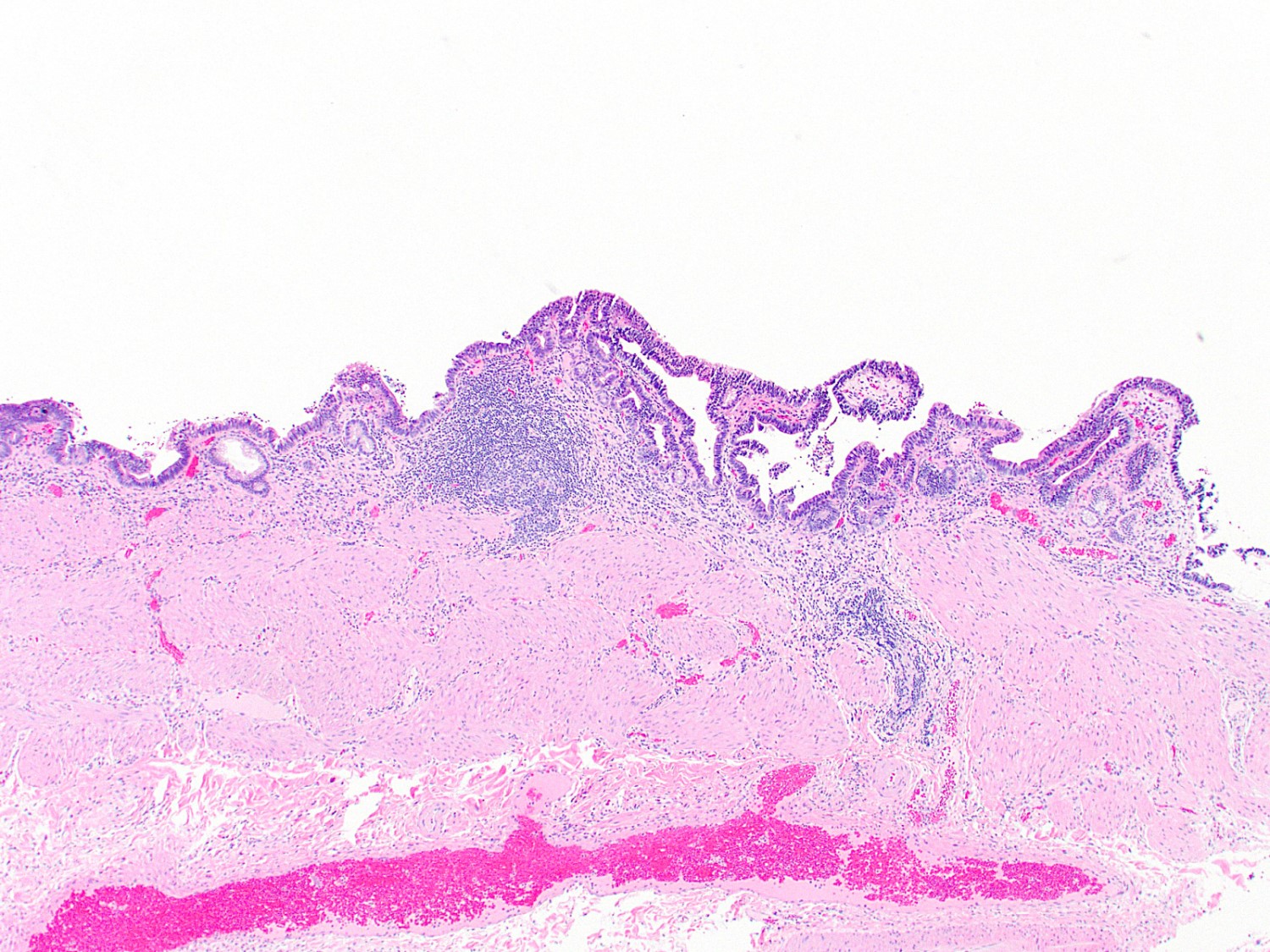
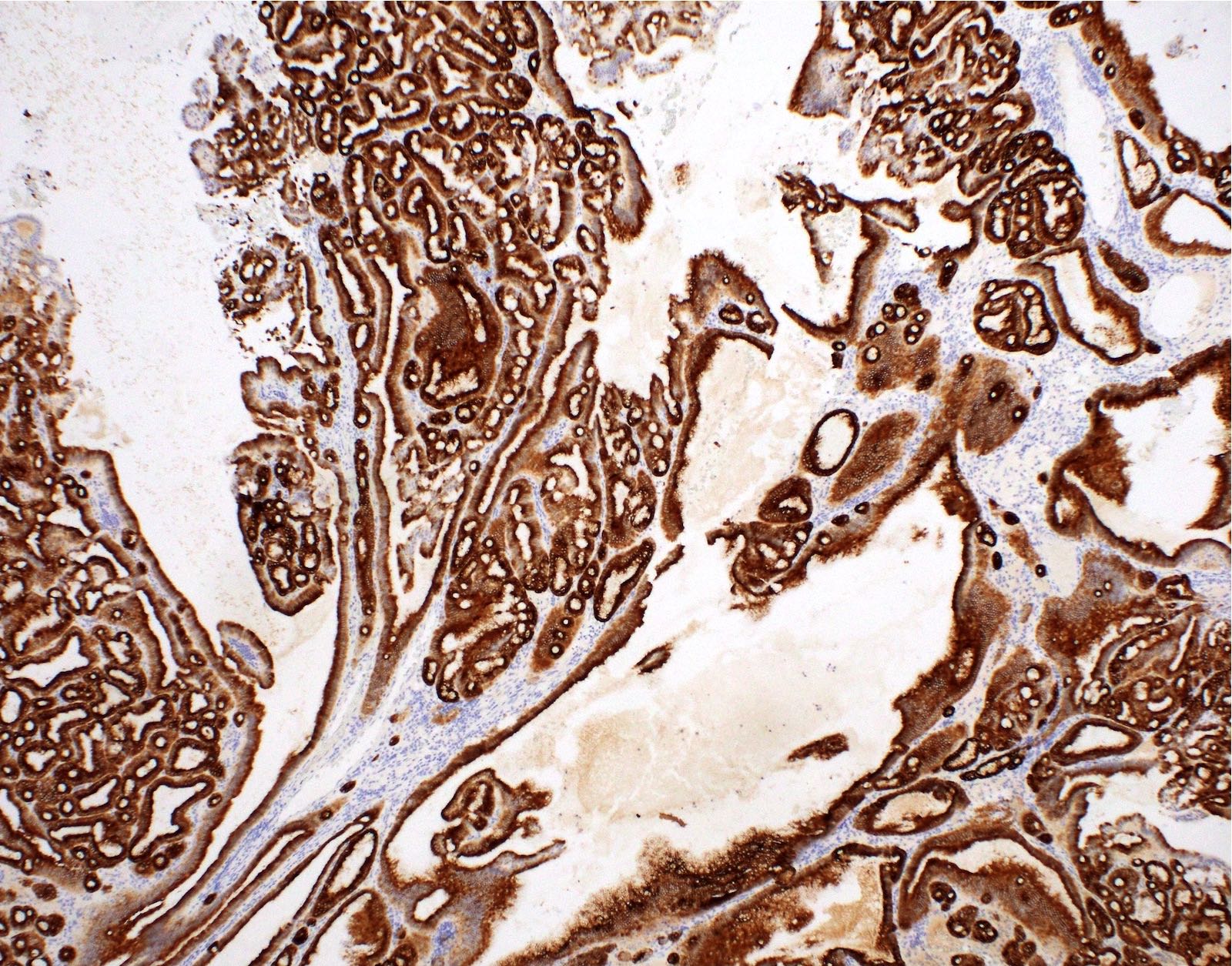
- Chronic inflammation of the gallbladder, typically secondary to gallstones
- The most common disease of the gallbladder, typically secondary to cholelithiasis
- Variety of histologic findings, including variable amounts of mononuclear cell predominant inflammation, mucosal changes including metaplasia, muscular hypertrophy and transmural fibrosis
- Rokitansky-Aschoff sinuses and ducts of Luschka should not be mistaken for invasive adenocarcinoma
- Female predominance (StatPearls: Chronic Cholecystitis [Accessed 19 February 2020])
- Associated with cholelithiasis in > 90% of cases
- Can be a sequela of recurrent acute cholecystitis
- Typically related to cholelithiasis, either through direct mucosal irritation or via intermittent mechanical obstruction with associated alteration of bile chemistry
- Altered mechanics of gallbladder emptying plays crucial role
- Up to 33% of patients have bile cultures positive for bacteria (e.g. Escherichia coli, enterococci, Helicobacter pylori, etc.), the significance of which is uncertain (Br J Surg 2010;97:532, Scand J Gastroenterol 2005;40:96, Helicobacter 2018;23:e12457)
- Cholelithiasis, though severity of disease poorly correlates with stone burden (In Vivo 2008;22:269)
- Risk factors correspond to those that increase risk of cholelithiasis: female sex, obesity, rapid weight loss, pregnancy, advanced age (Gastroenterol Nurs 2016;39:297)
- Does not always cause clinical symptoms
- Can present with dull right upper quadrant pain that radiates to mid back or right scapula (StatPearls: Chronic Cholecystitis [Accessed 19 February 2020])
- Murphy sign: right upper abdominal pain with deep palpation
- Abdominal discomfort often related to fatty food ingestion
- Nausea, vomiting, bloating, flatulence
- Abdominal ultrasound (StatPearls: Chronic Cholecystitis [Accessed 19 February 2020])
- Abdominal CT with contrast
- HIDA (hepatobiliary iminodiacetic acid) scan demonstrating a reduced ejection fraction (< 35%)
- Gallbladder wall thickening with associated cholelithiasis
- Gallbladder may appear contracted or distended (Medicine (Baltimore) 2018;97:e11851)
- Majority of uncomplicated cases have an excellent outcome (Am J Surg 2003;185:91)
- With elective cholecystectomy, bile duct injuries do occur with regular frequency (Endoscopy 2018;50:577)
- Biliary leakage reported in up to 3% of cases (Visc Med 2017;33:184)
- Generally, a very low risk (< 0.5%) of associated incidental carcinoma (Rev Col Bras Cir 2020;46:e20192279, Surgery 2001;129:699)
- 44 year old man with gallstones and chronic cholecystitis revealing metachronous gallbladder metastasis from renal clear cell carcinoma (ANZ J Surg 2019 Jun 23 [Epub ahead of print])
- 45 year old woman with porcelain gallbladder secondary to chronic cholecystitis, without adenocarcinoma (Mymensingh Med J 2019;28:694)
- 53 year old man with history of colorectal adenocarcinoma with progressively elevating CEA secondary to chronic cholecystitis (J Surg Case Rep 2019;2019:rjz138)
- 70 year old man with chronic cholecystitis secondary to biliary taeniasis (Am J Trop Med Hyg 2019;100:135)
- Elective cholecystectomy (Am J Surg 2003;185:91)
- Nearly normal to thickened gallbladder wall (StatPearls: Chronic Cholecystitis [Accessed 19 February 2020])
- Gallbladder may appear shrunken due to marked fibrosis
- Severe cases show adhesions to adjacent organs
- Variable mucosal appearance: can be granular, ulcerated, polypoid
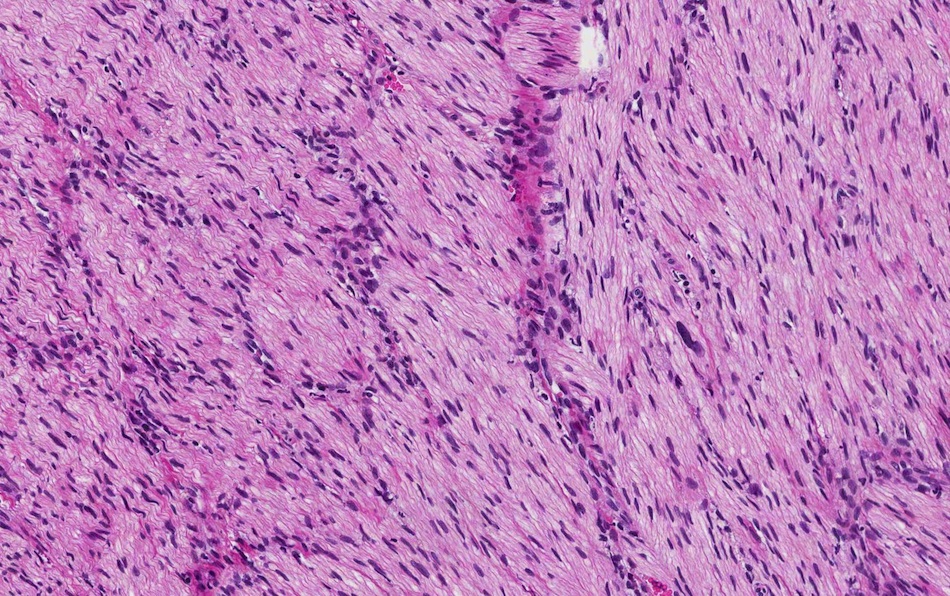
- Variable amounts of predominantly mononuclear inflammatory infiltrate in lamina propria, which may extend into the muscularis and pericholecystic tissues
- Inflammatory infiltrate predominantly consists of T lymphocytes, with some plasma cells, histiocytes and occasional eosinophils (Ann Diagn Pathol 2003;7:147)
- Inflammation typically rather minimal; occasional lymphoid follicles may be seen in lamina propria
- Hypertrophy of muscularis and variable degrees of mural fibrosis, elastosis, neural hyperplasia
- Accentuation of Rokitansky-Aschoff sinuses (pseudodiverticula)
- Adenomyomatous hyperplasia may occur
- Variable mucosal changes: normal, atrophic, ulcerated, hyperplastic
- Metaplastic changes common: foveolar metaplasia, pyloric gland metaplasia, intestinal metaplasia
- Hyalinizing variant: dense paucicellular hyalinizing fibrosis effacing ≥ 80% of normal histologic structures, resulting in a thinned gallbladder wall with (porcelain gallbladder) or without dystrophic calcification
- Increased frequency of associated carcinoma (Sultan Qaboos Univ Med J 2016;16:e416, Am J Surg Pathol 2011;35:1104)
- IgG4 associated variant: increased frequency of transmural lymphoplasmacytic inflammatory infiltrates, extramural inflammatory nodules, increased eosinophils, phlebitis and increased IgG4 plasma cells by immunostain
- Associated with autoimmune pancreatitis (Dig Dis Sci 2011;56:1290)
- 2 patterns of inflammation associated with idiopathic inflammatory bowel disease: marked chronic cholecystitis (ulcerative colitis or Crohn's disease) and nodular lymphoid aggregates (Crohn's disease > ulcerative colitis) (J Crohns Colitis 2012;6:895)
- Beware of invasive adenocarcinoma mimics: adenomyoma, Luschka ducts
- In rare instances, reactive / hyperplastic ducts of Luschka can be seen isolated to the gallbladder adventitia (Am J Surg Pathol 2011;35:883)
- Gallbladder, cholecystectomy:
- Chronic cholecystitis and cholelithiasis
- Normal gallbladder:
- Lacks significant expansion of the lamina propria by an inflammatory infiltrate, thickened muscularis or mural fibrosis
- Lymphoma:
- Lymphoma of the gallbladder is exceedingly rare (0.1 - 0.2% of cholecystectomies) and is generally identified as part of a systemic disease
- The most common primary lymphoma of the gallbladder is MALT lymphoma (BMJ Case Rep 2017;2017:bcr2017220161)
- Primary MALT lymphoma of gallbladder is typically identified on presurgical imaging as gallbladder wall thickening or a polypoid lesion
- Lymphoplasmacytic cholecystitis:
- Plasma cell rich inflammatory infiltrate that diffusely involves the mucosa and is primarily confined to the lamina propria (Am J Surg Pathol 2003;27:1313)
- Typically but not always associated with autoimmune disorders (e.g. ulcerative colitis, primary sclerosing cholangitis, autoimmune pancreatitis) (Am J Clin Pathol 2014;142:209)
- Also termed sclerosing cholangitis, as it is believed to fall within the spectrum of IgG4 related autoimmune disorders
- AIDS related cholecystitis:
- Typically presents as acalculous cholecystitis; > 50% of cases are idiopathic (Clin Infect Dis 1995;21:852)
- Can be related to infectious agents, particularly cytomegalovirus and cryptosporidia
- In cryptosporidia related cases, associated inflammation may be minimal
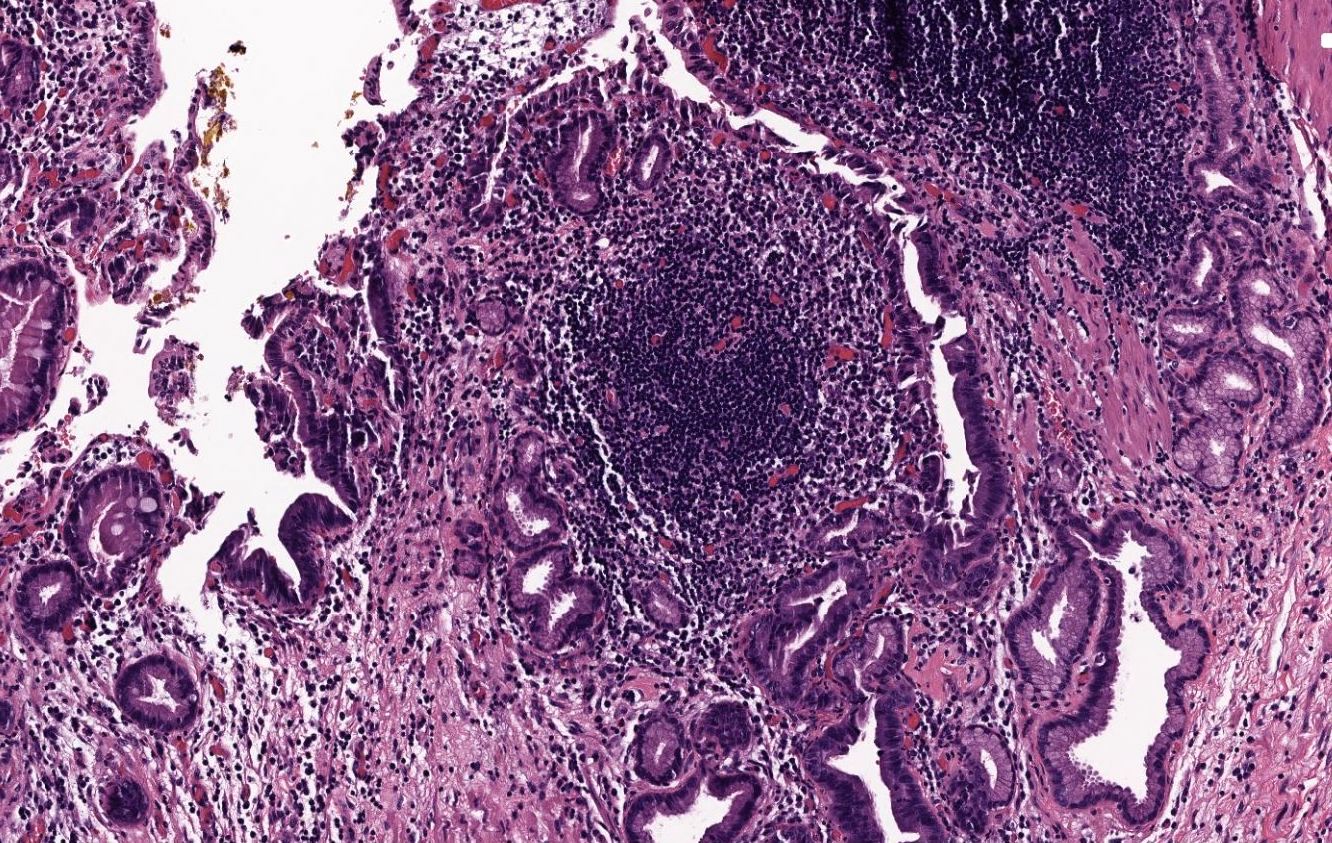
- Follicular cholecystitis:
- Numerous prominent lymphoid follicles in lamina propria throughout gallbladder
- Rare and accounts for < 0.1% of cholecystectomies (Hum Pathol 2019;88:1)
- Up to 5% of otherwise ordinary chronic cholecystitis may show scattered, occasional follicle formation
- Eosinophilic cholecystitis:
- Massive infiltration of the gallbladder by sheets of eosinophils with few, if any, other intervening inflammatory cells (Am J Surg Pathol 1994;18:215)
- Common to see eosinophils as part of the mixed inflammatory milieu of chronic (and acute) cholecystitis
- Xanthogranulomatous cholecystitis:
- Prominent proliferation of foamy macrophages, in addition to admixed lymphocytes, plasma cells and foreign body type giant cells
- Thought to be secondary to mucosal ulceration or rupture of Rokitansky-Aschoff sinuses with bile extravasation
- Grossly, may display diffuse plaque-like thickening of gallbladder wall or a discrete mass lesion (pseudotumor)
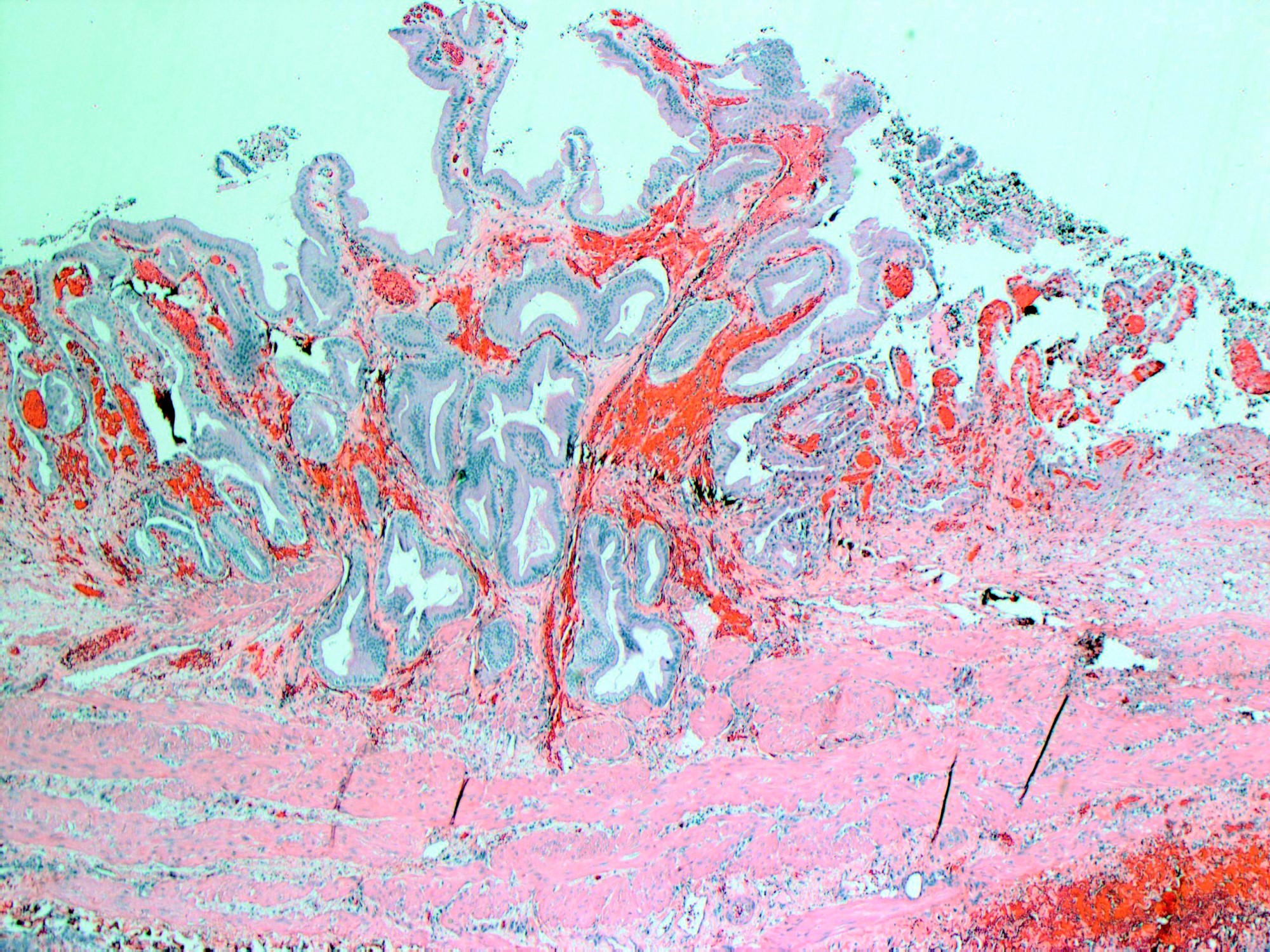
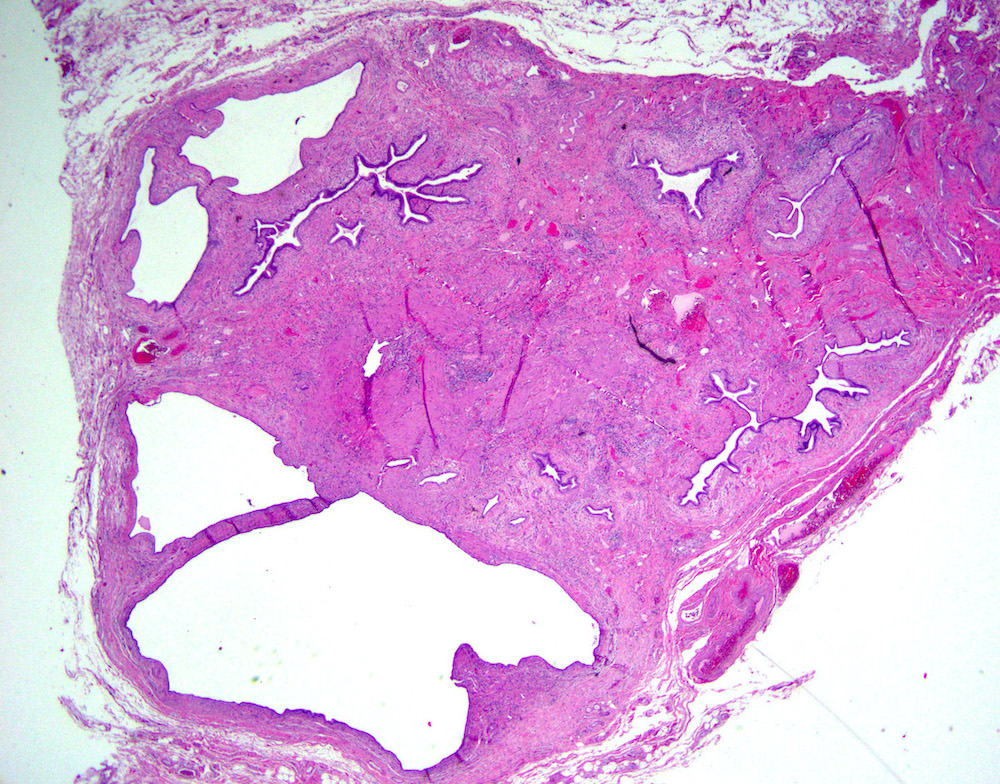
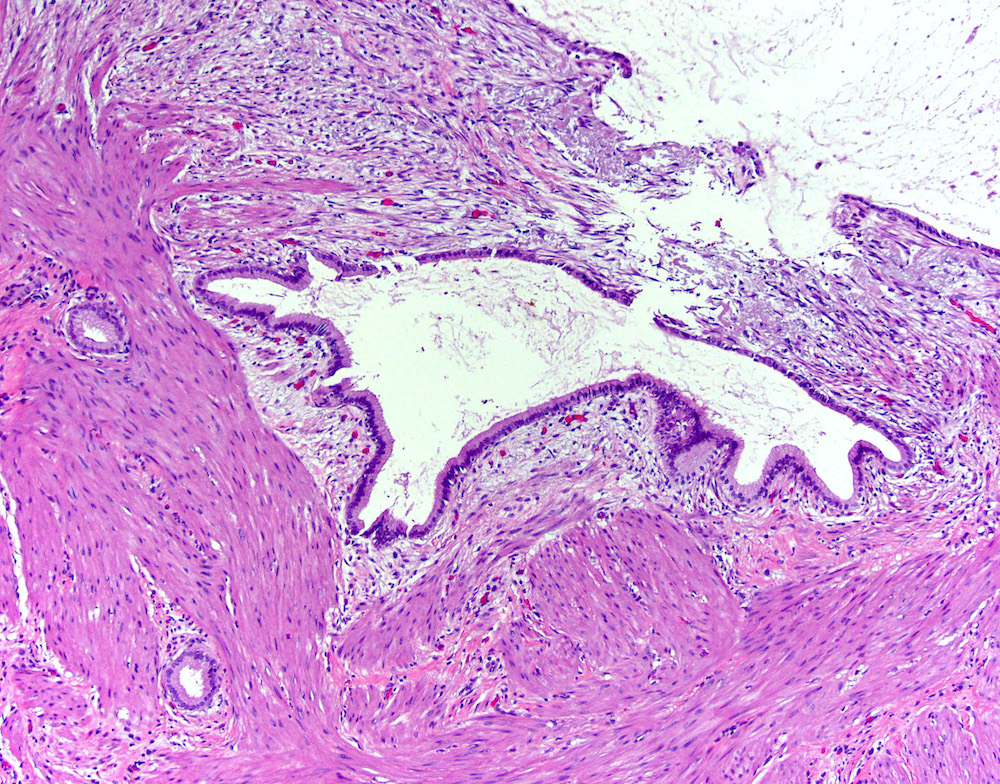
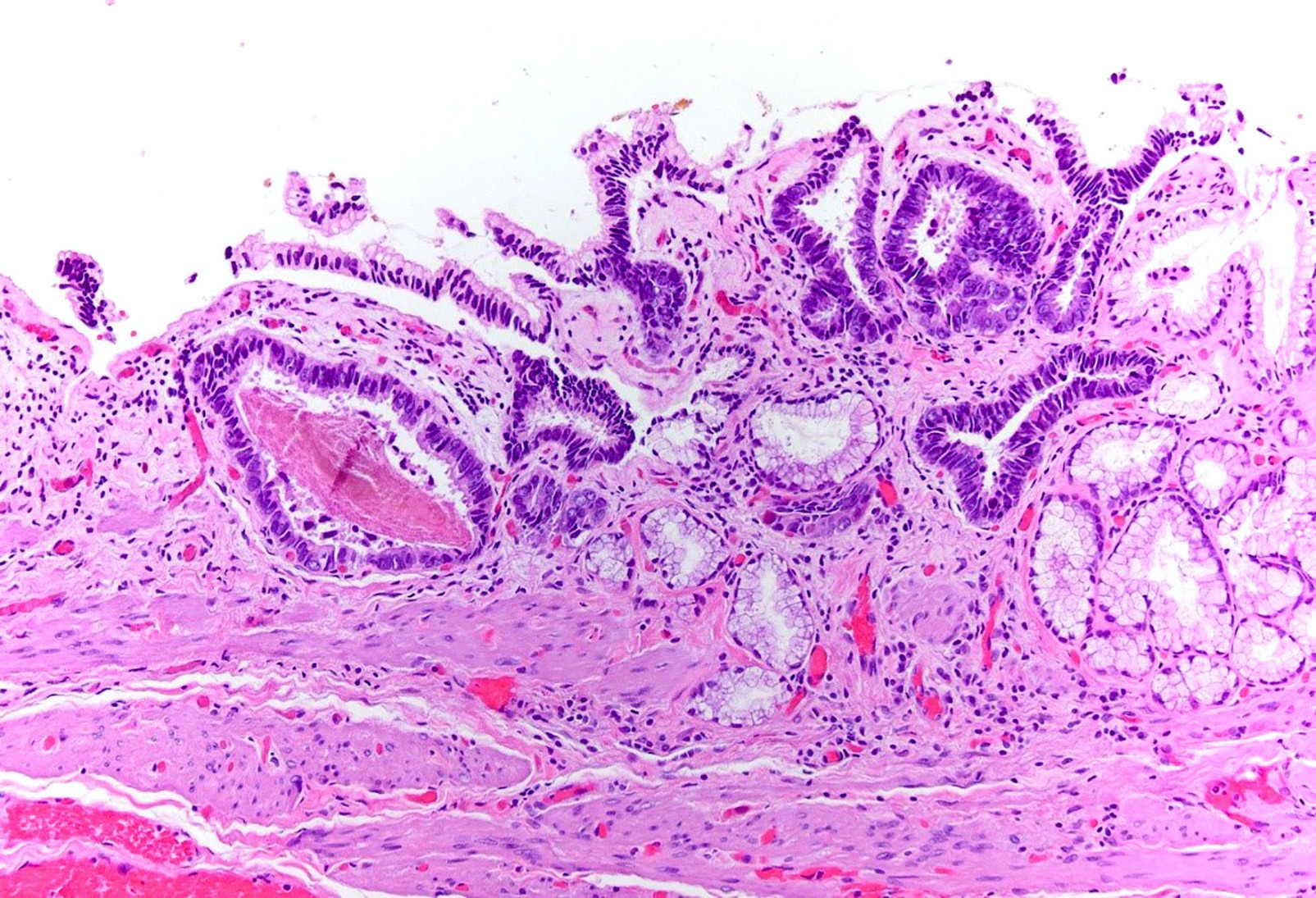
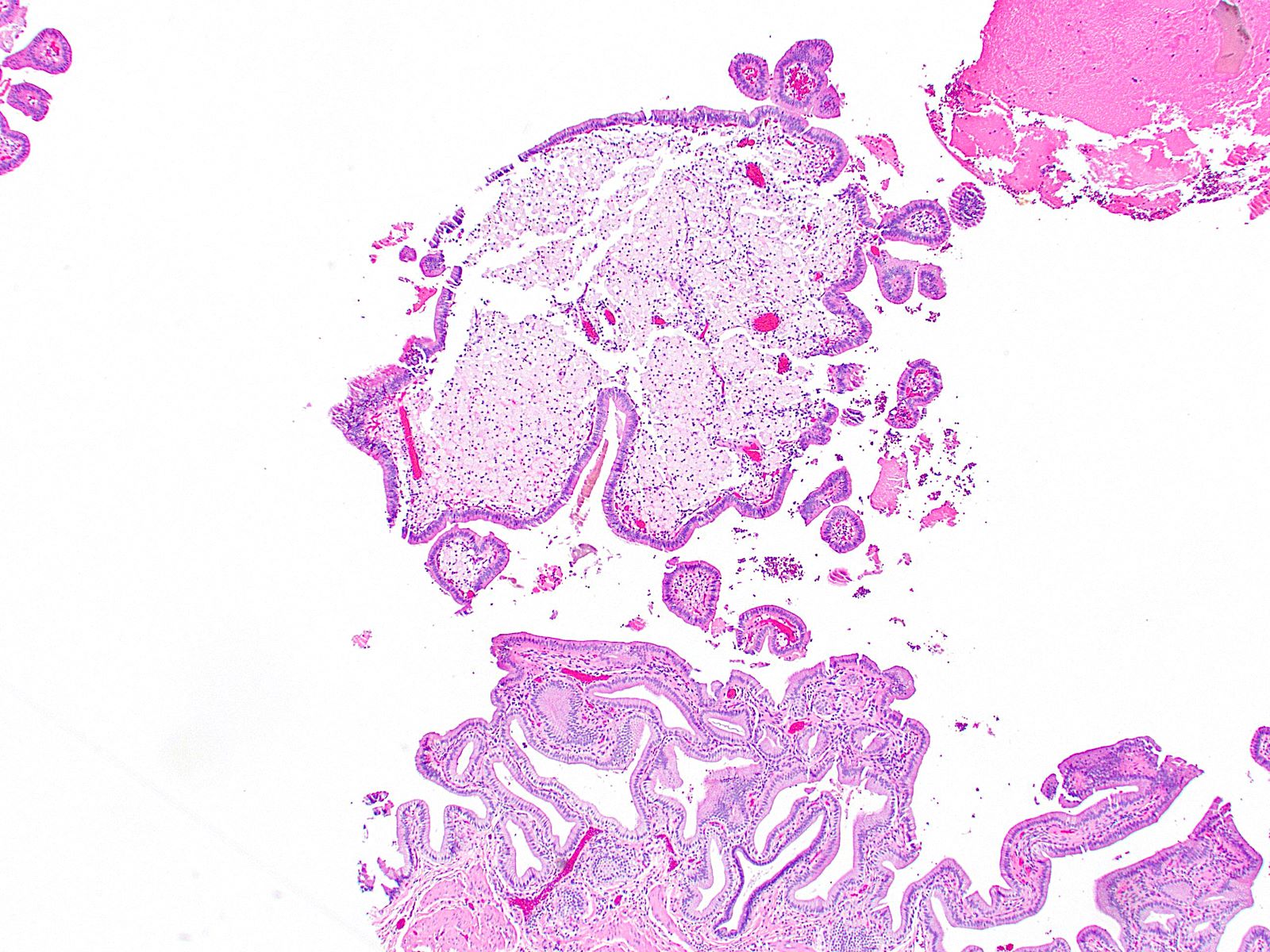
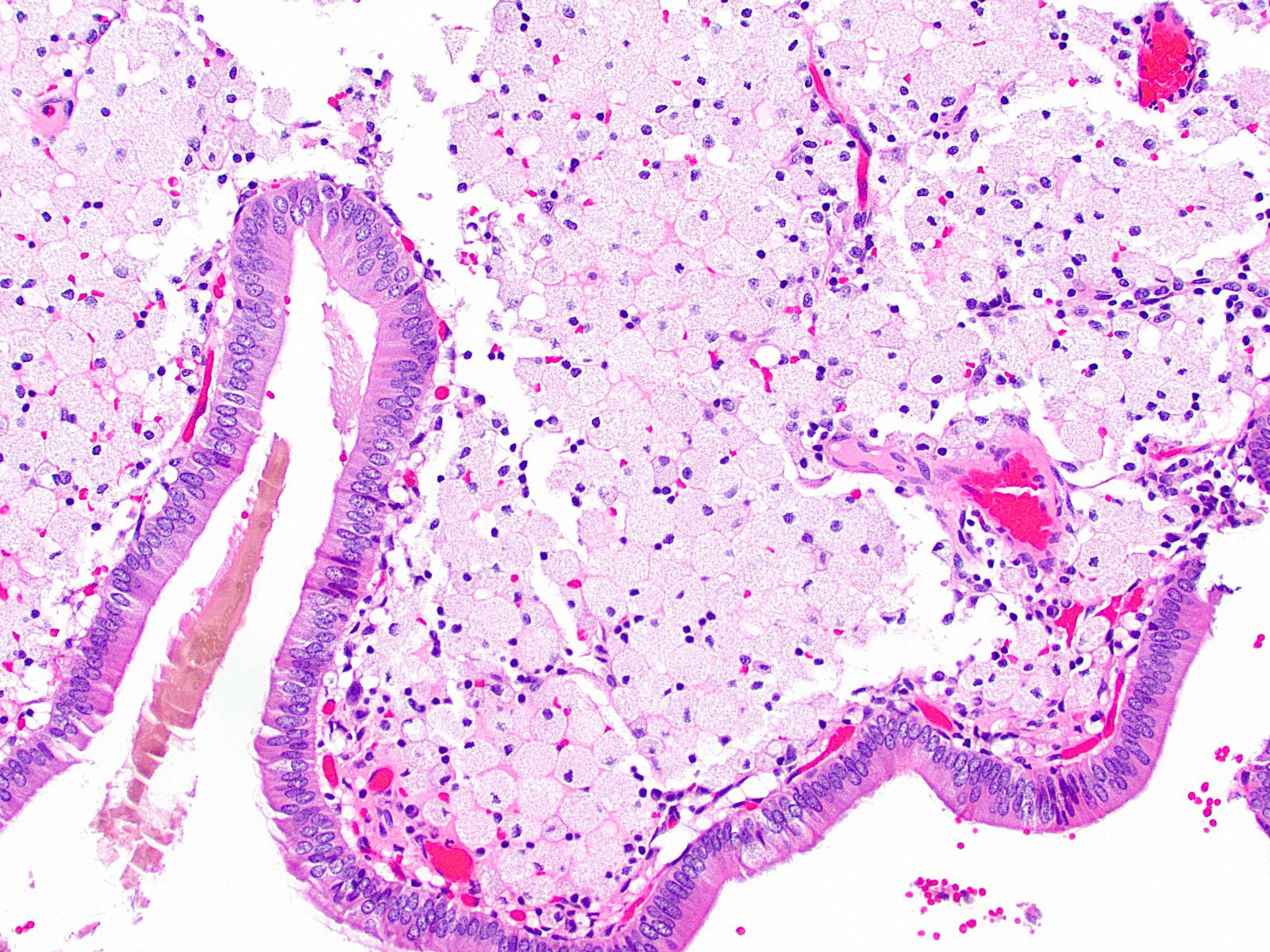
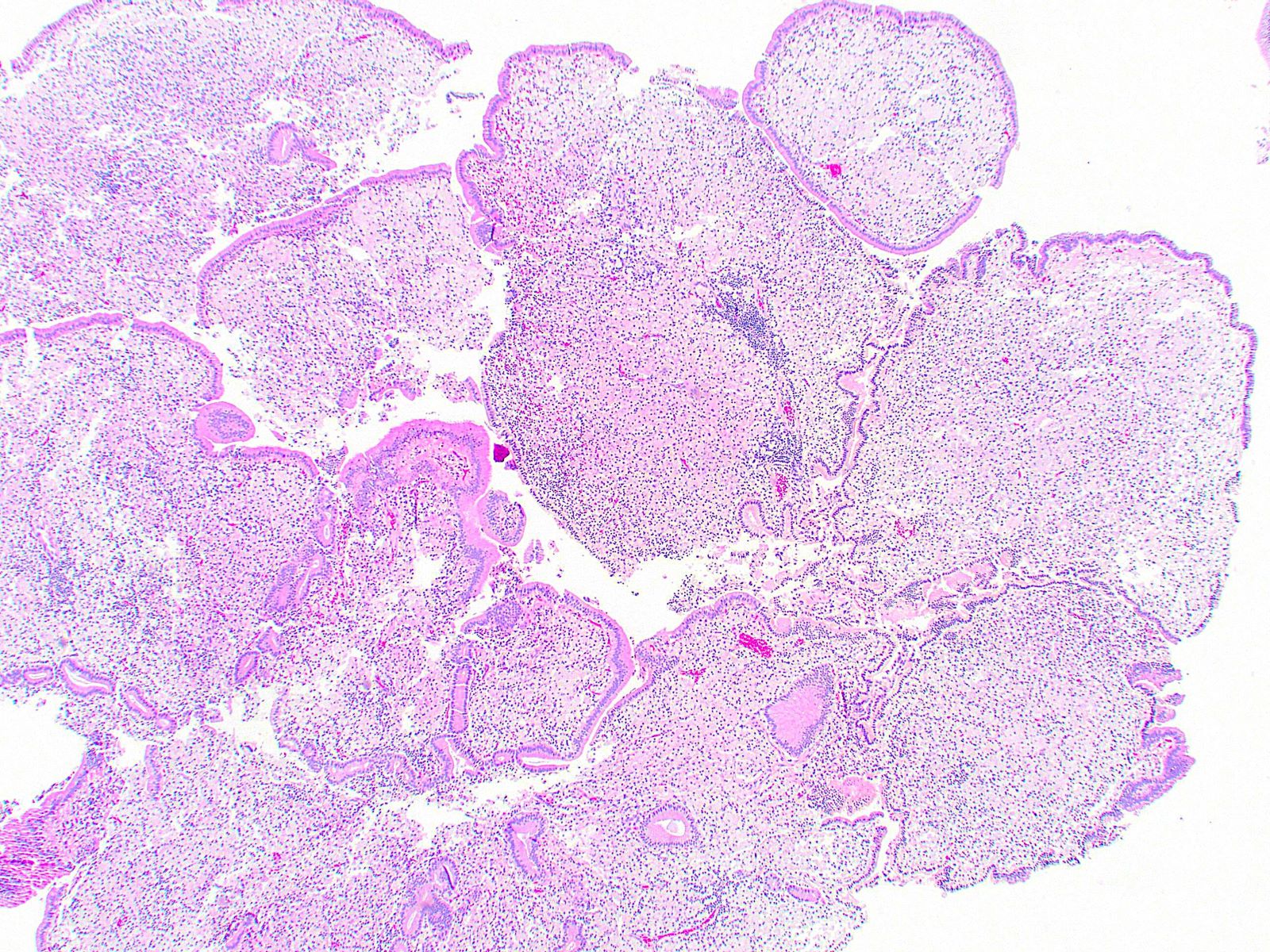
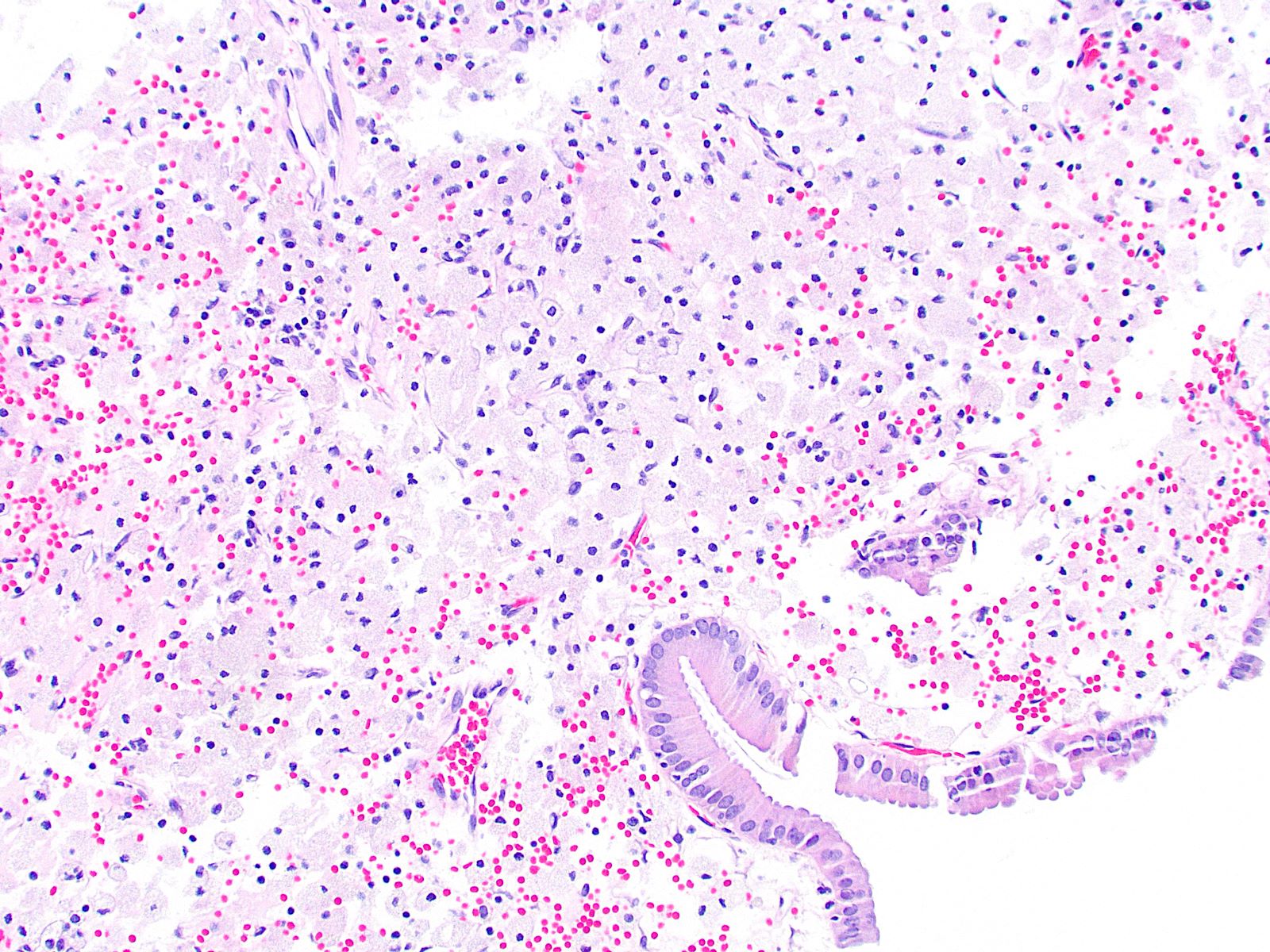
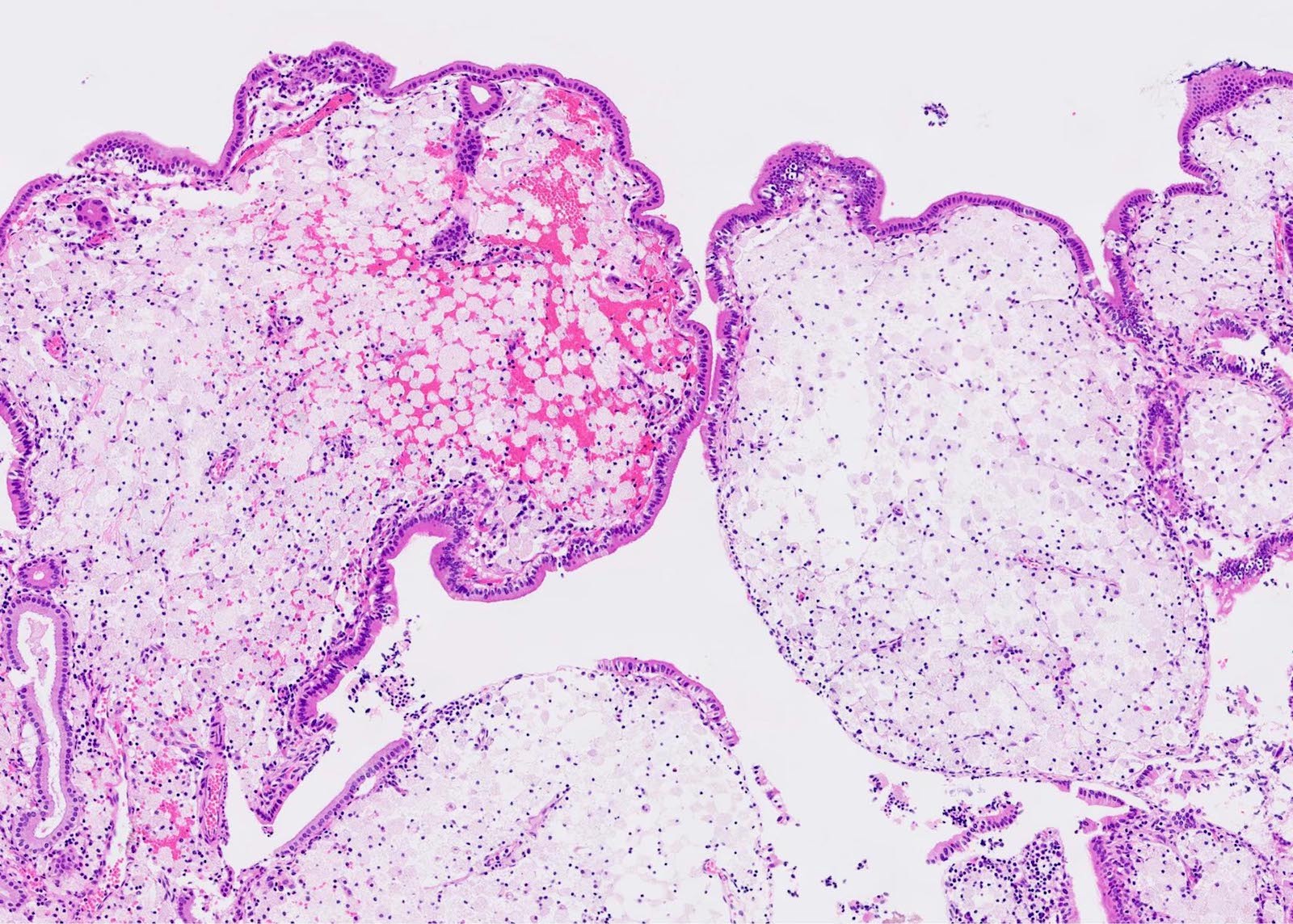
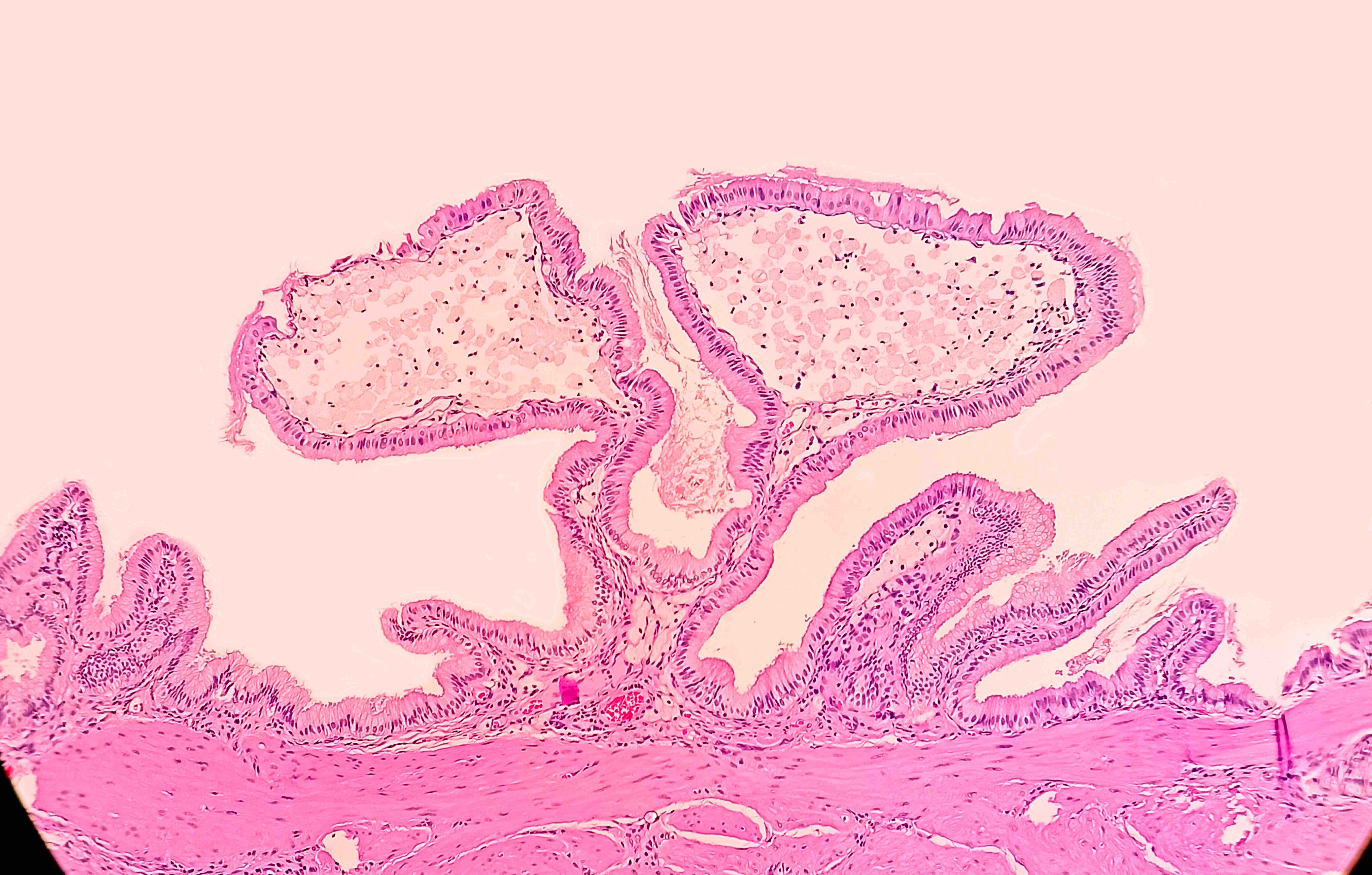
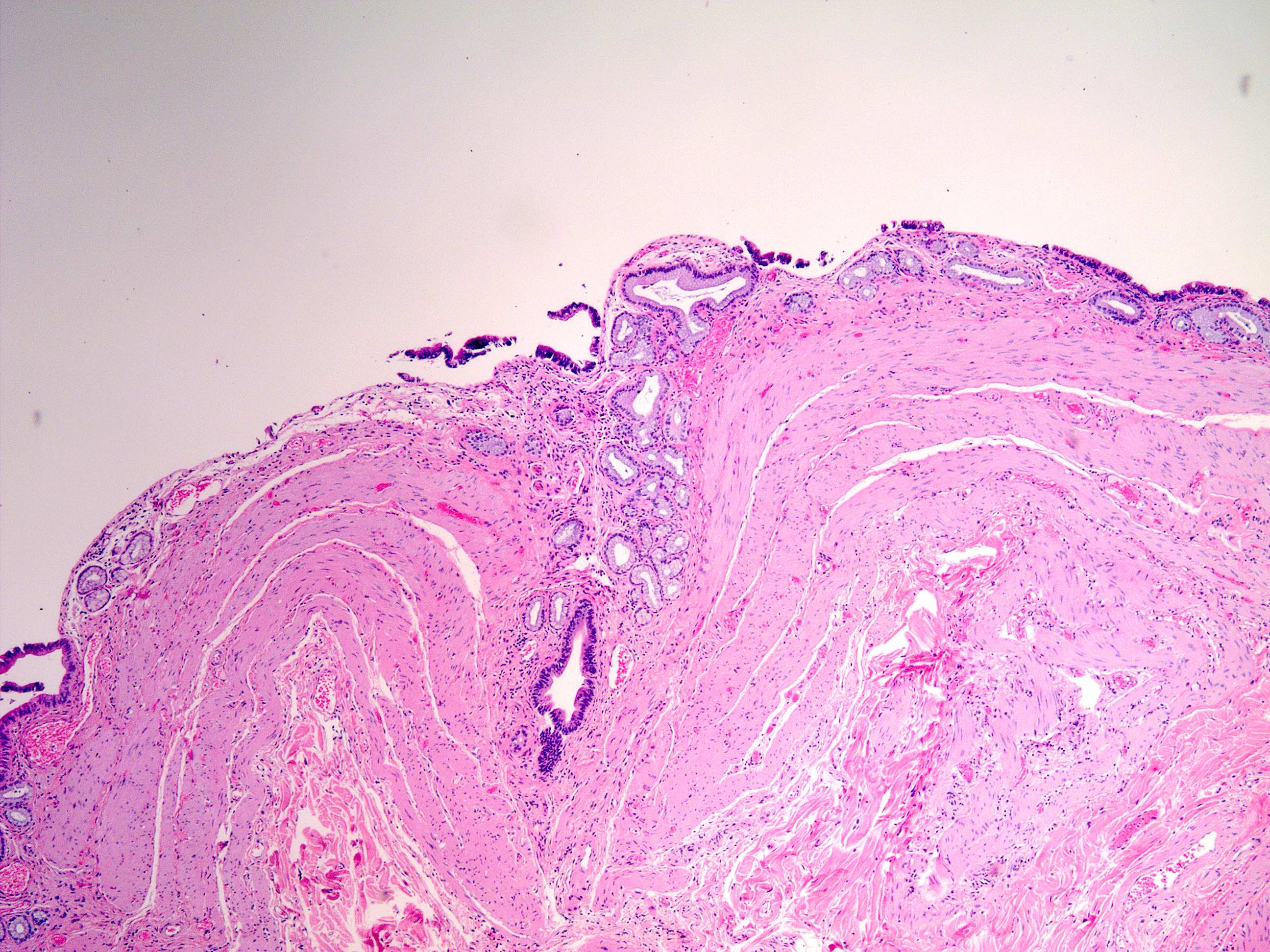
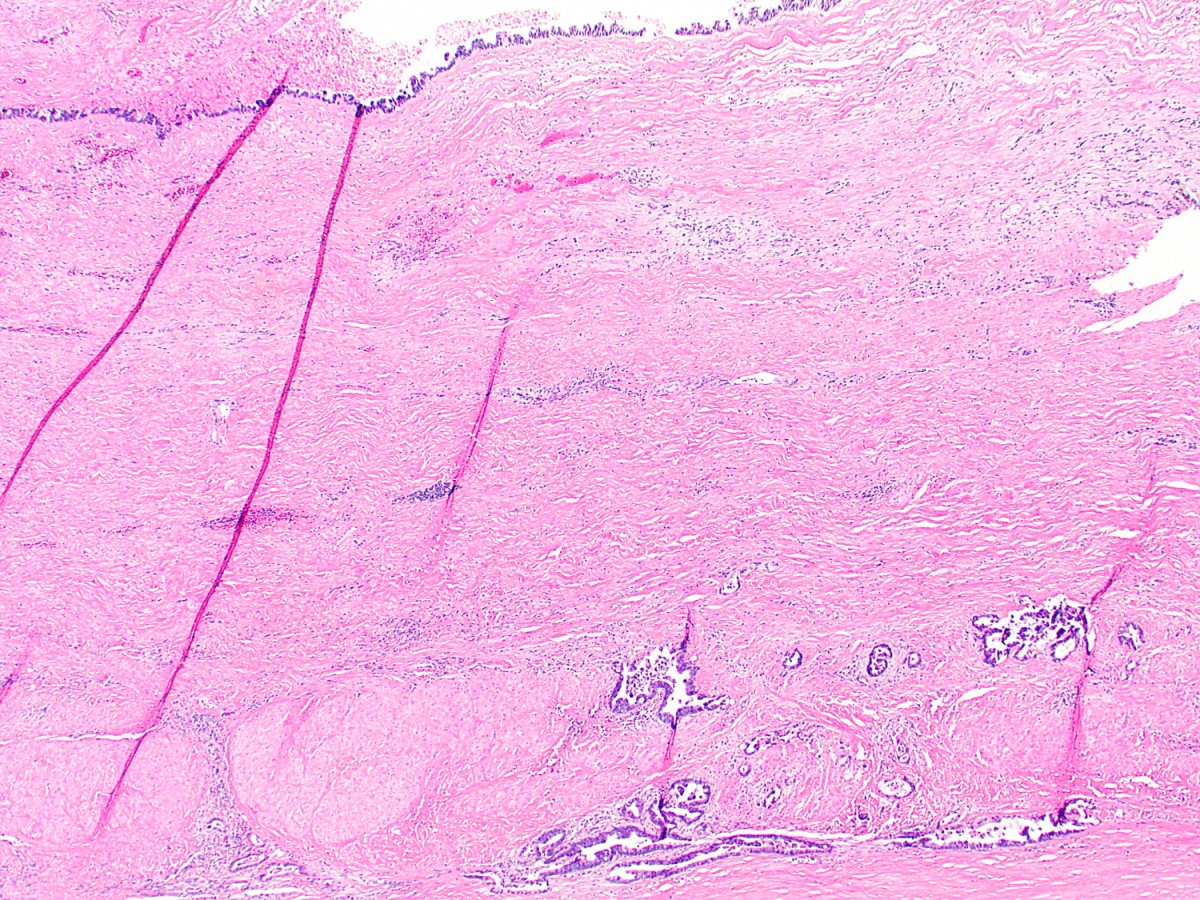
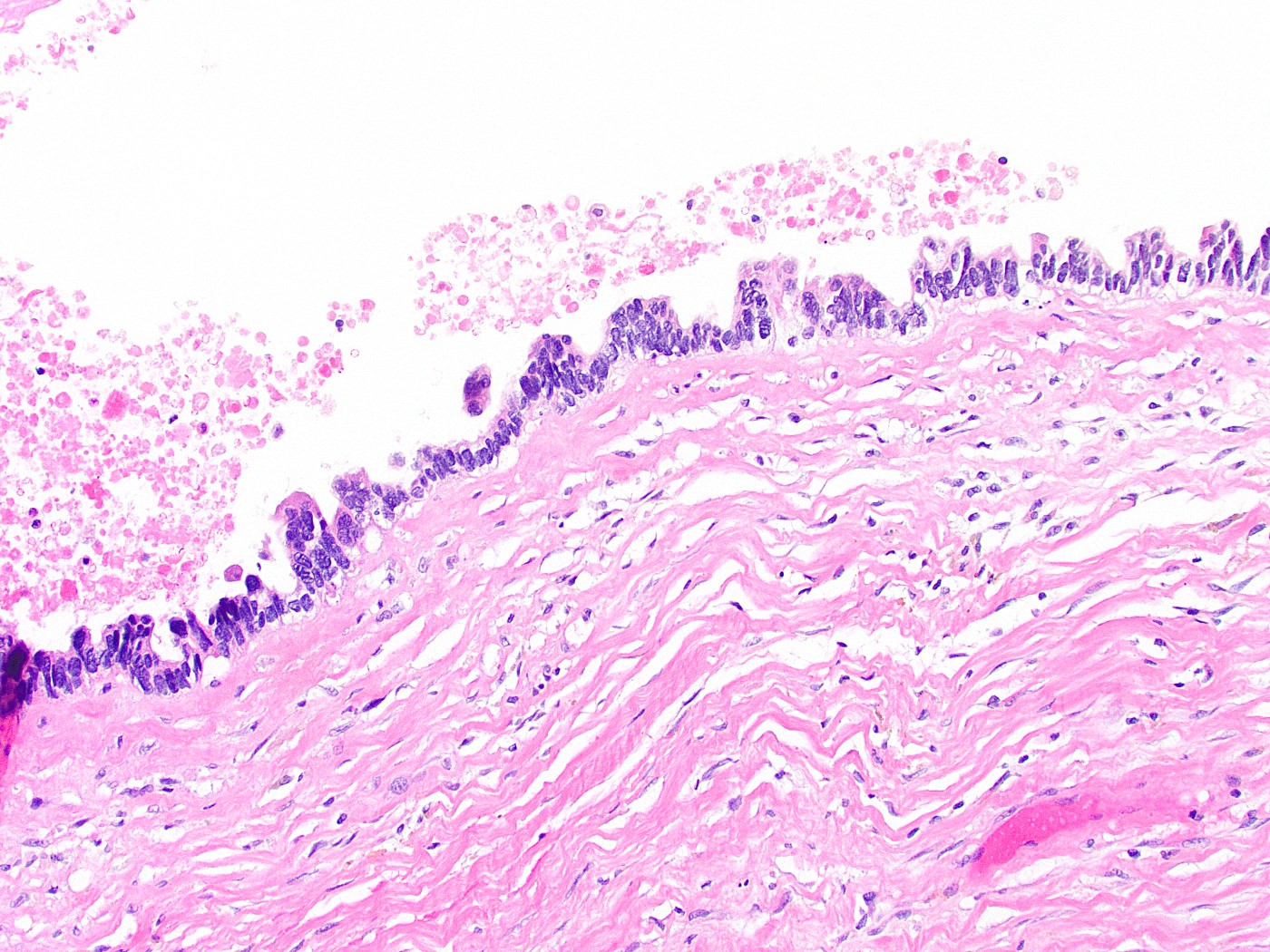
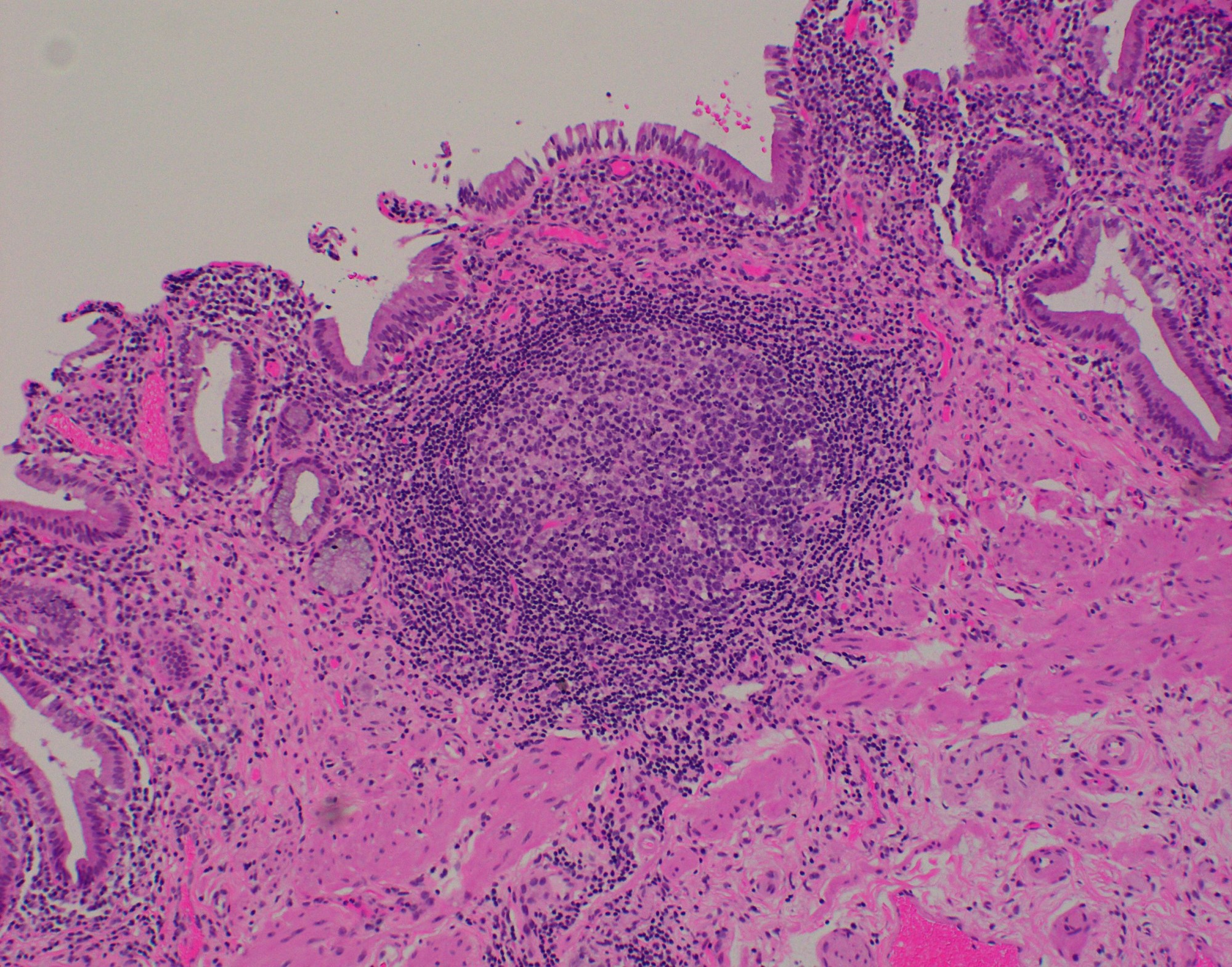
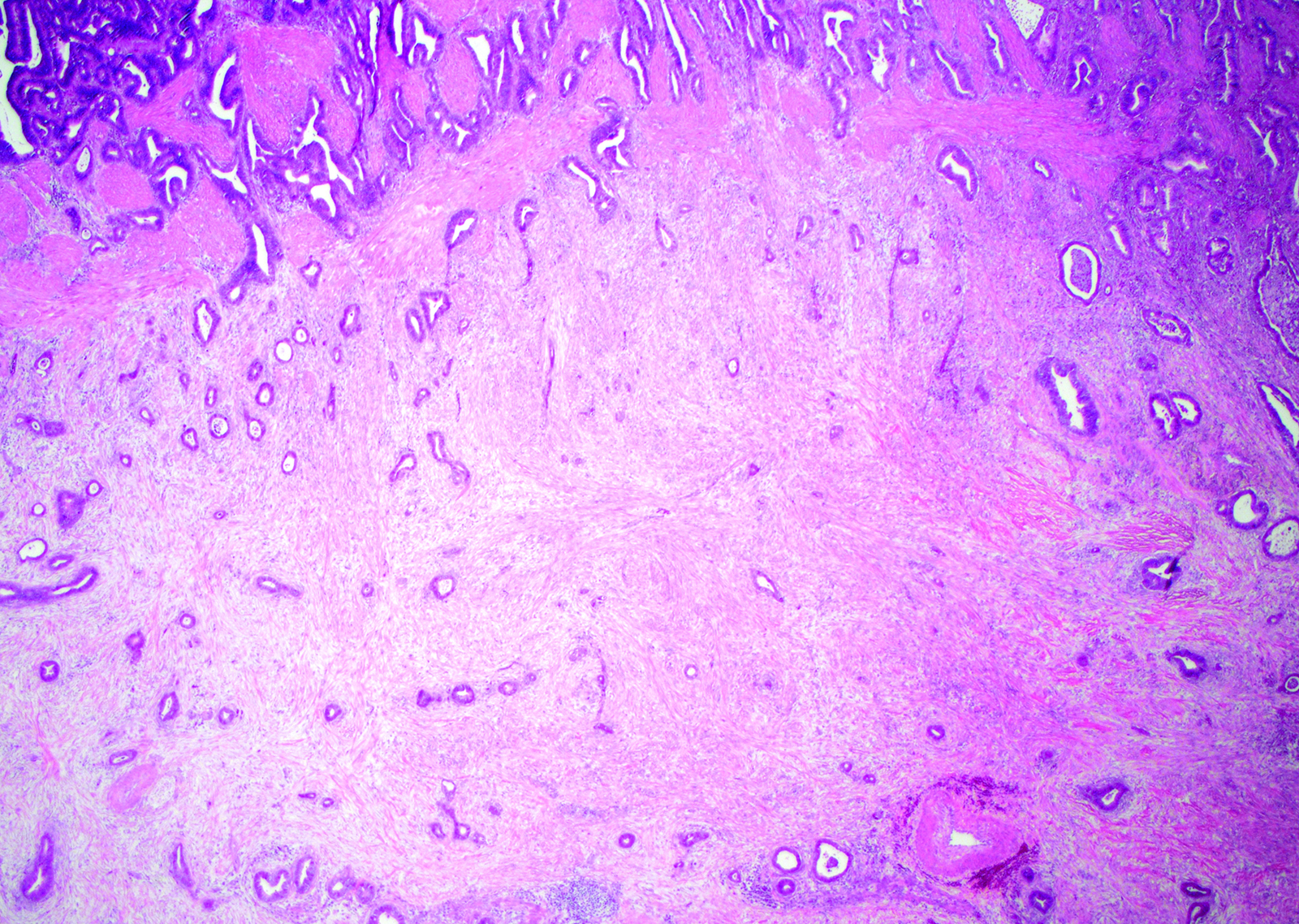
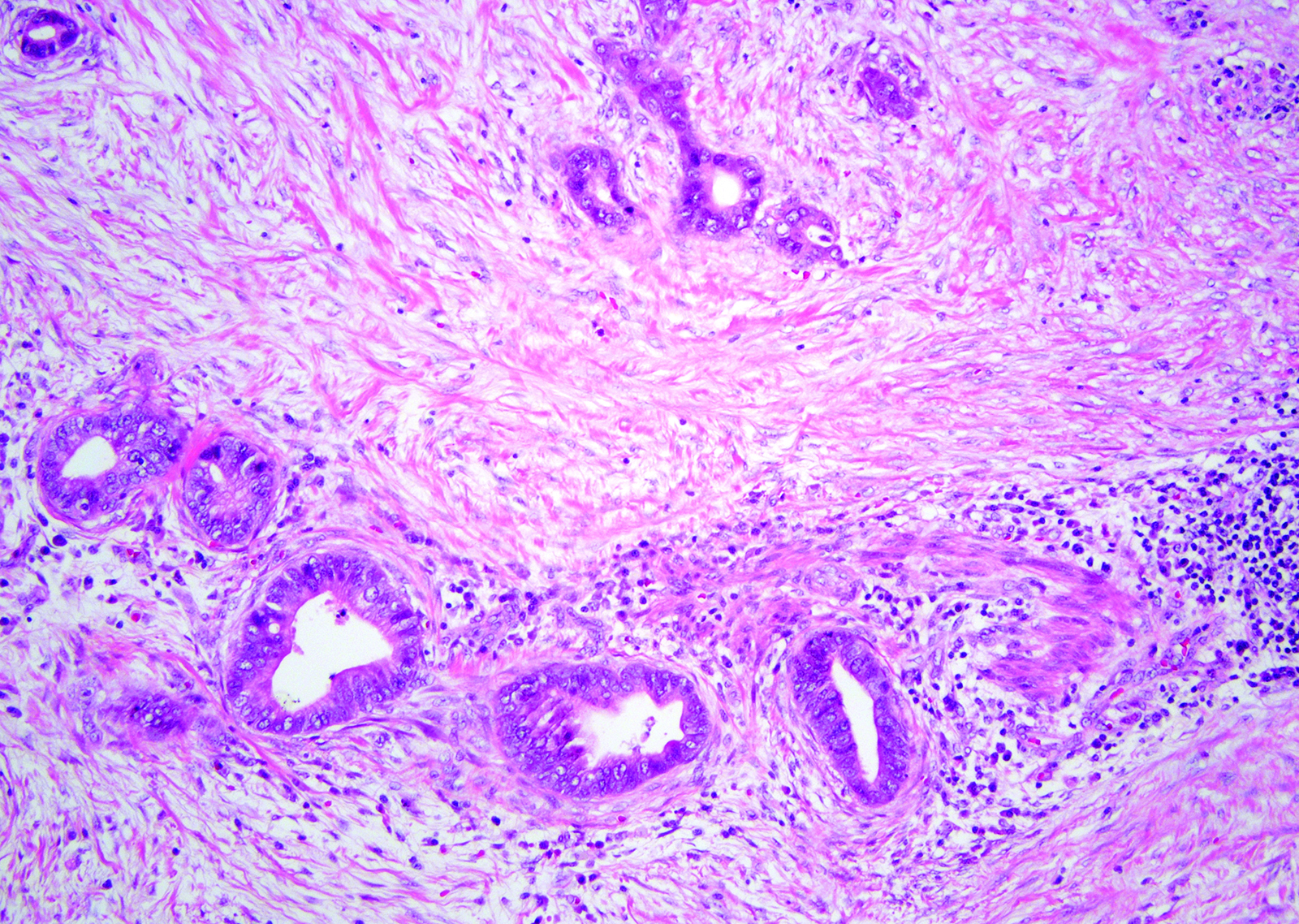
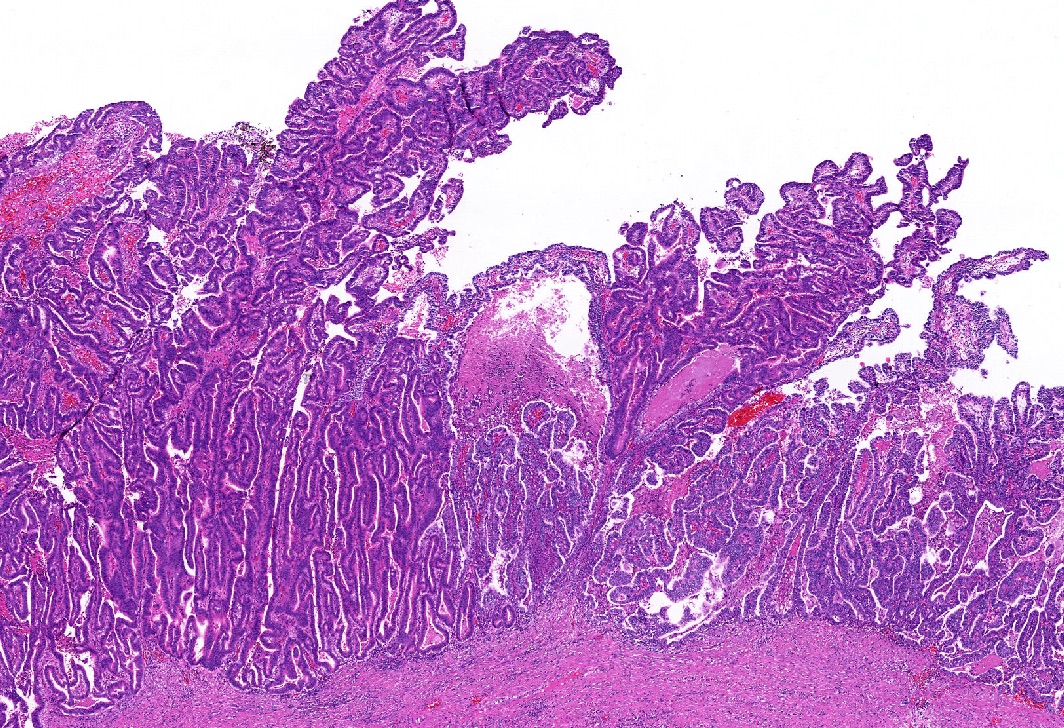
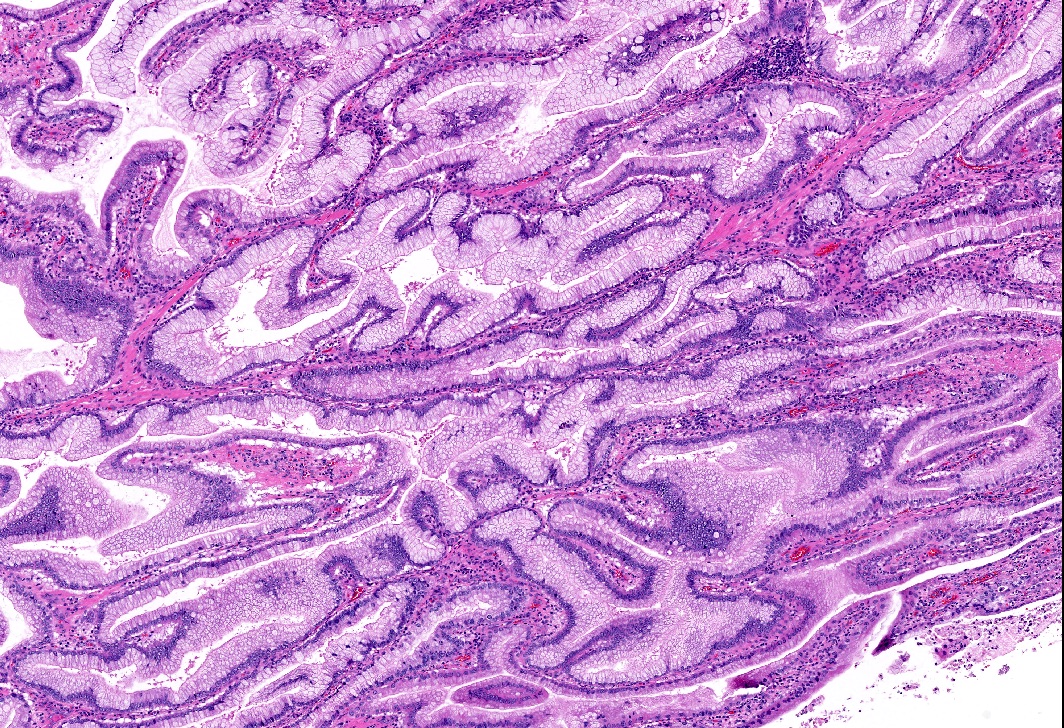
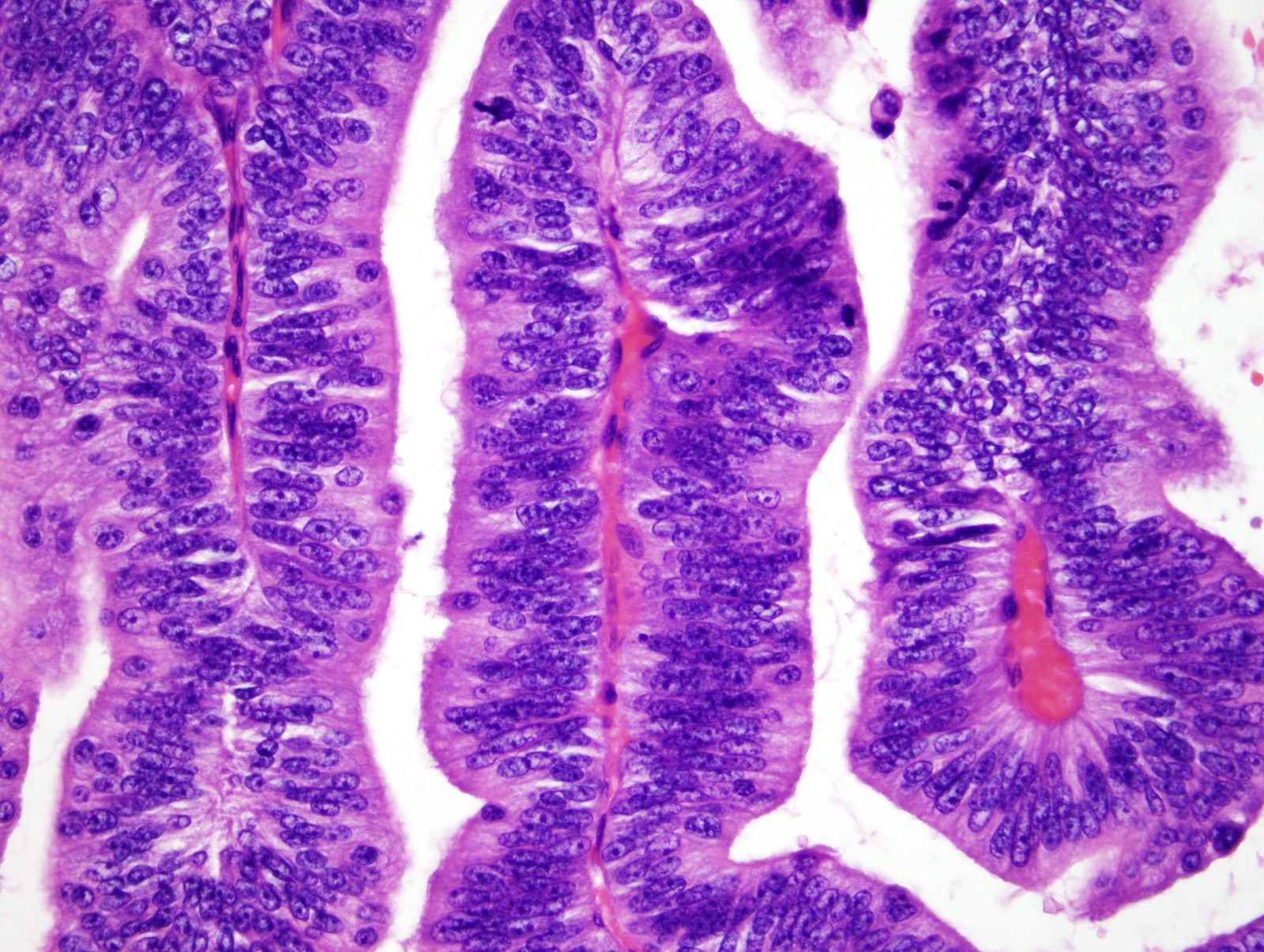
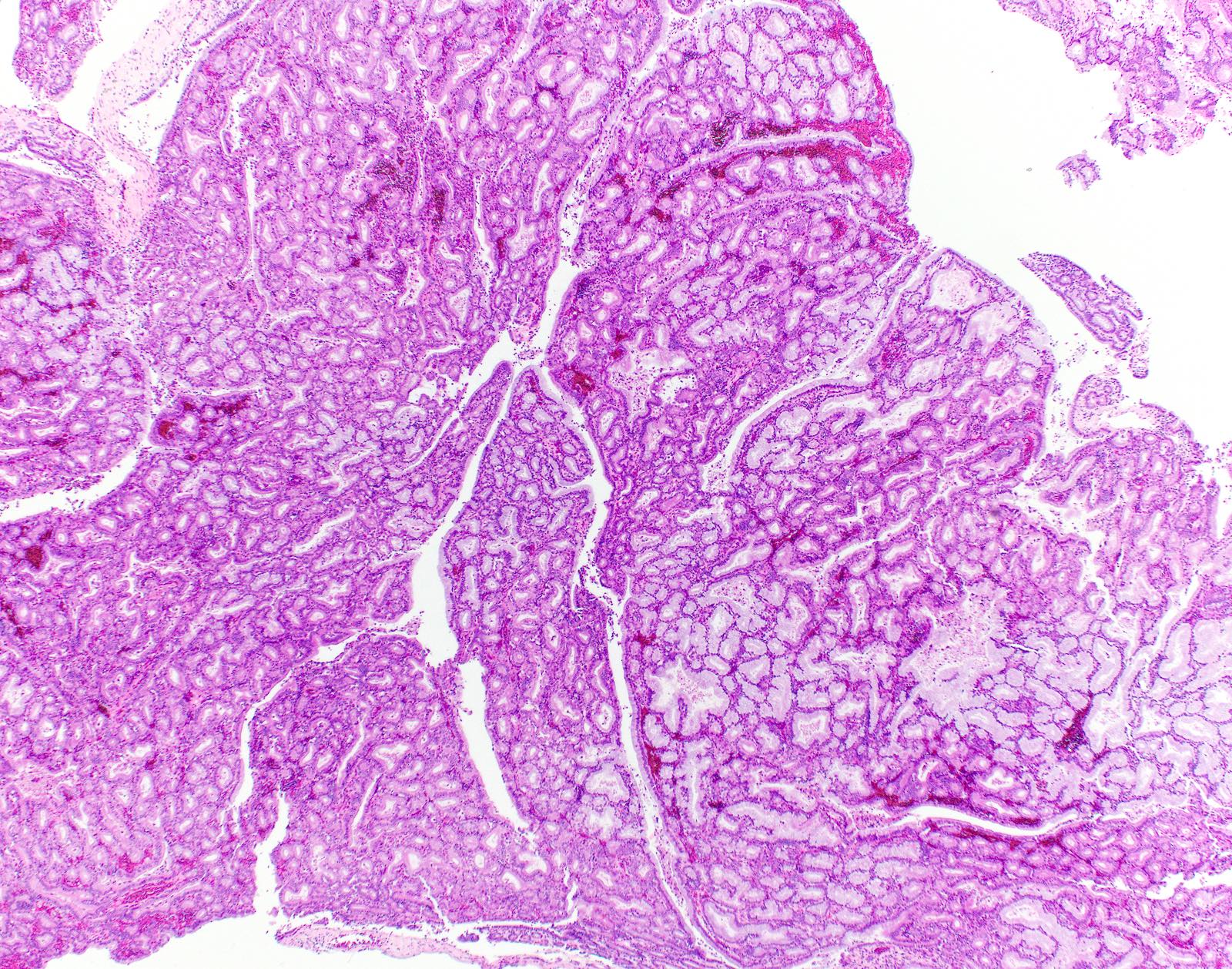
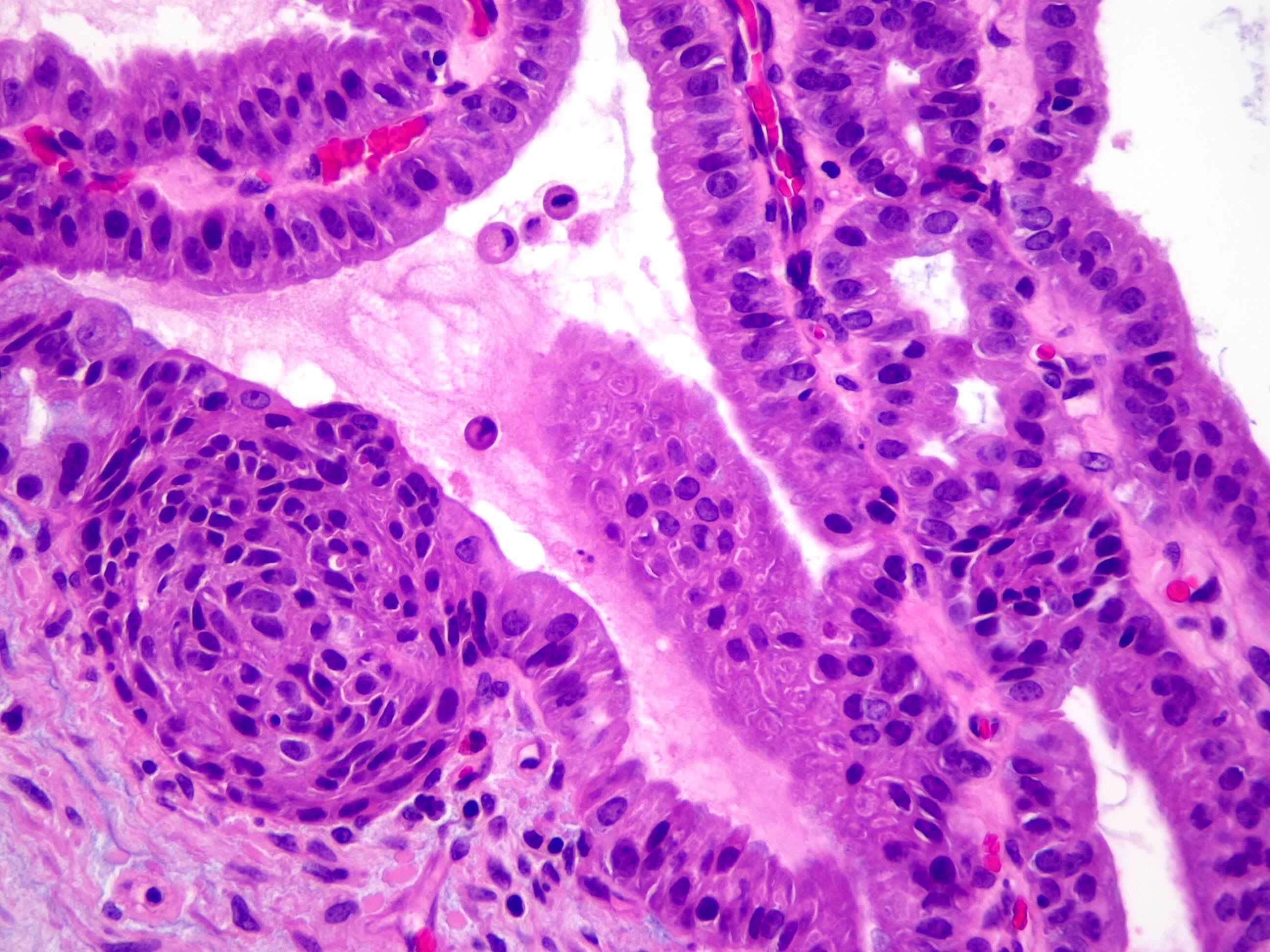
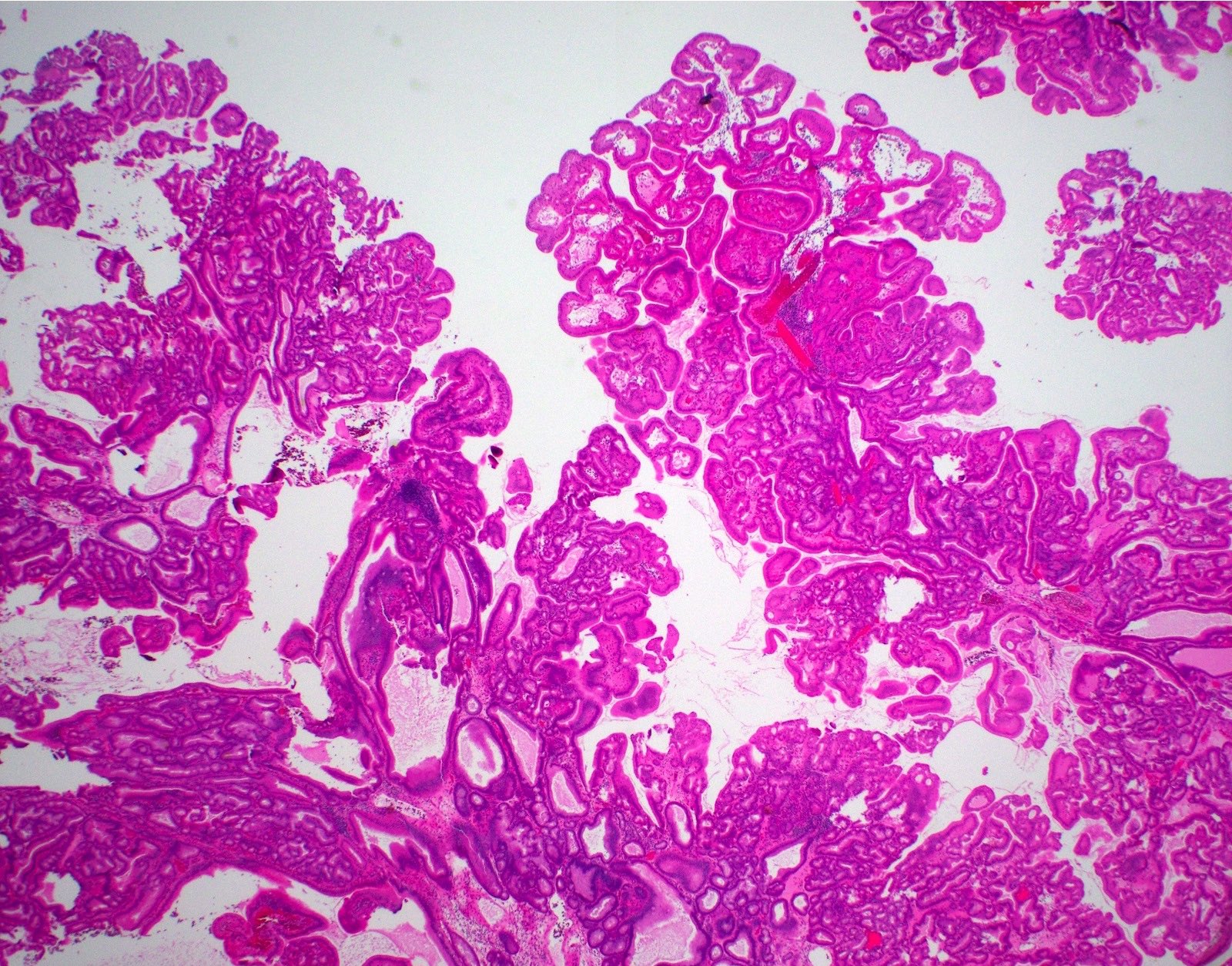
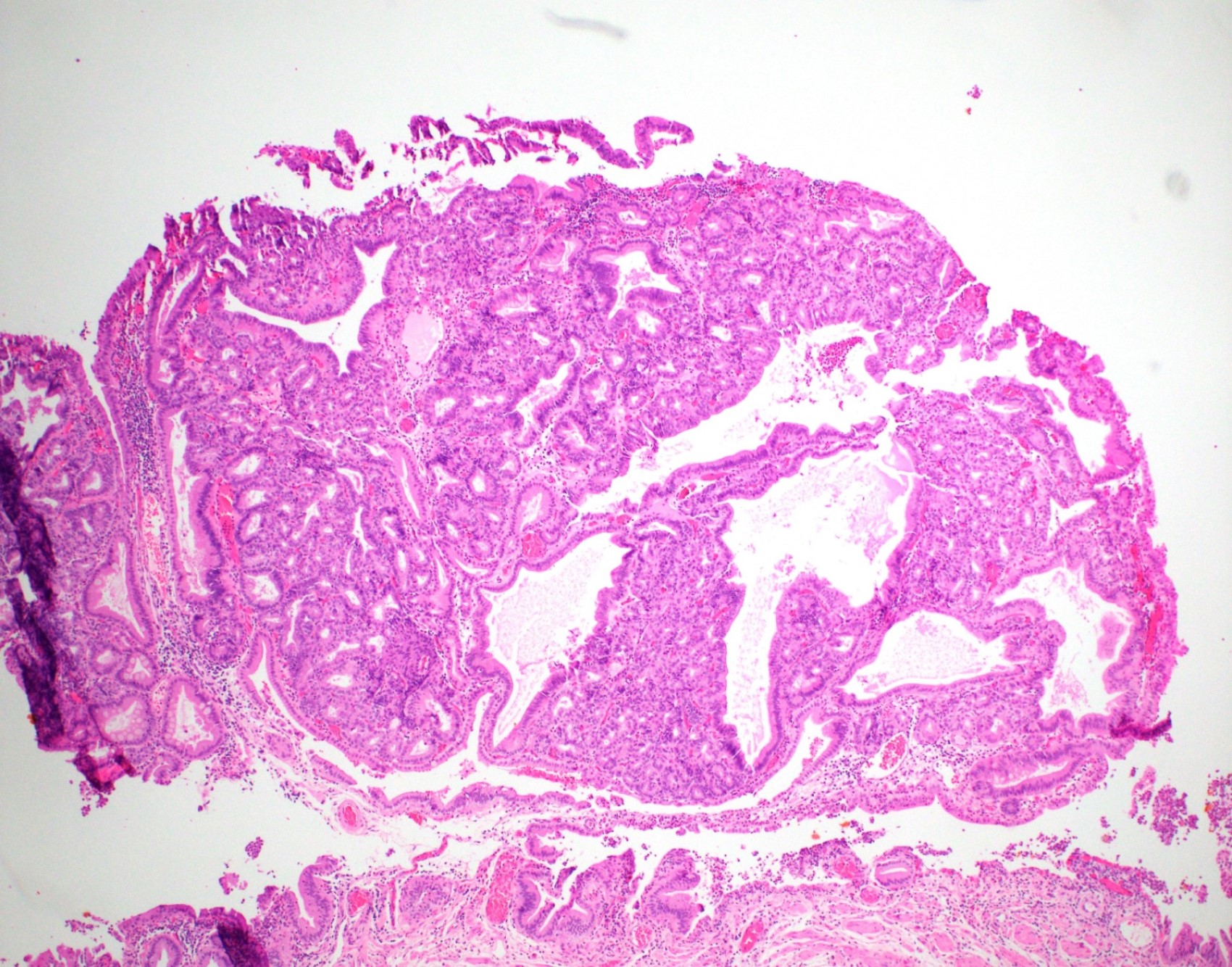
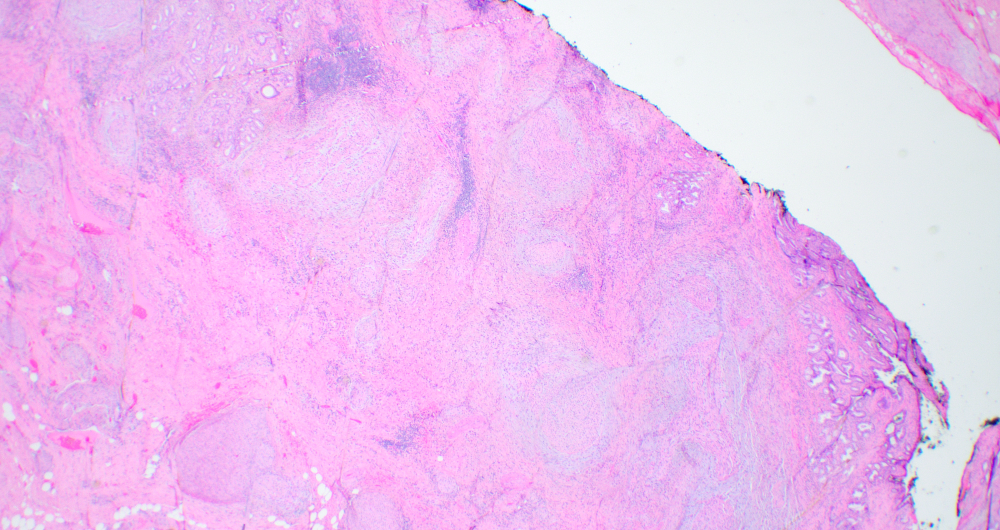
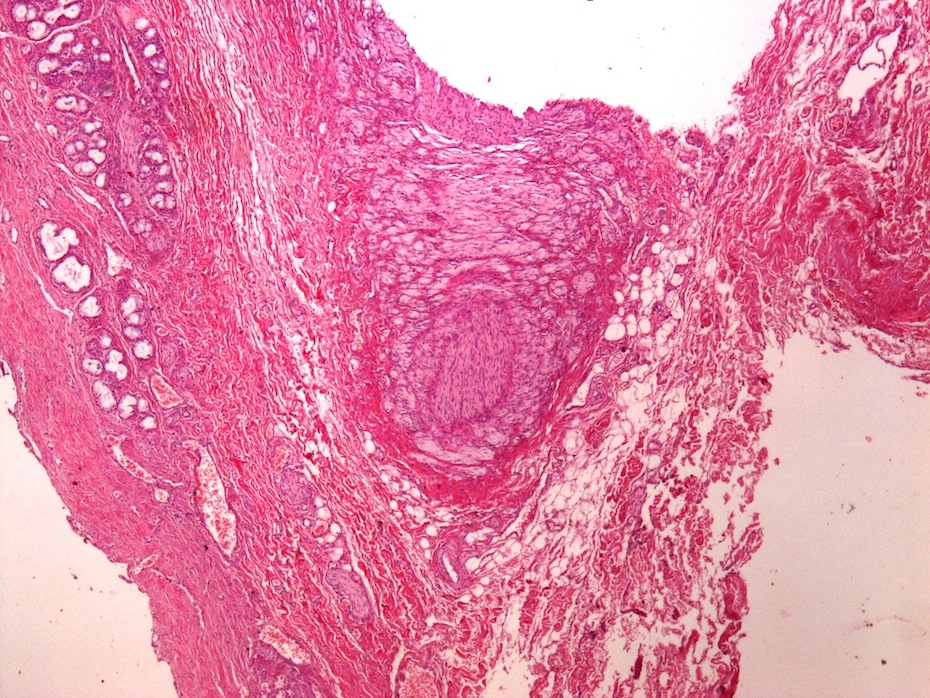
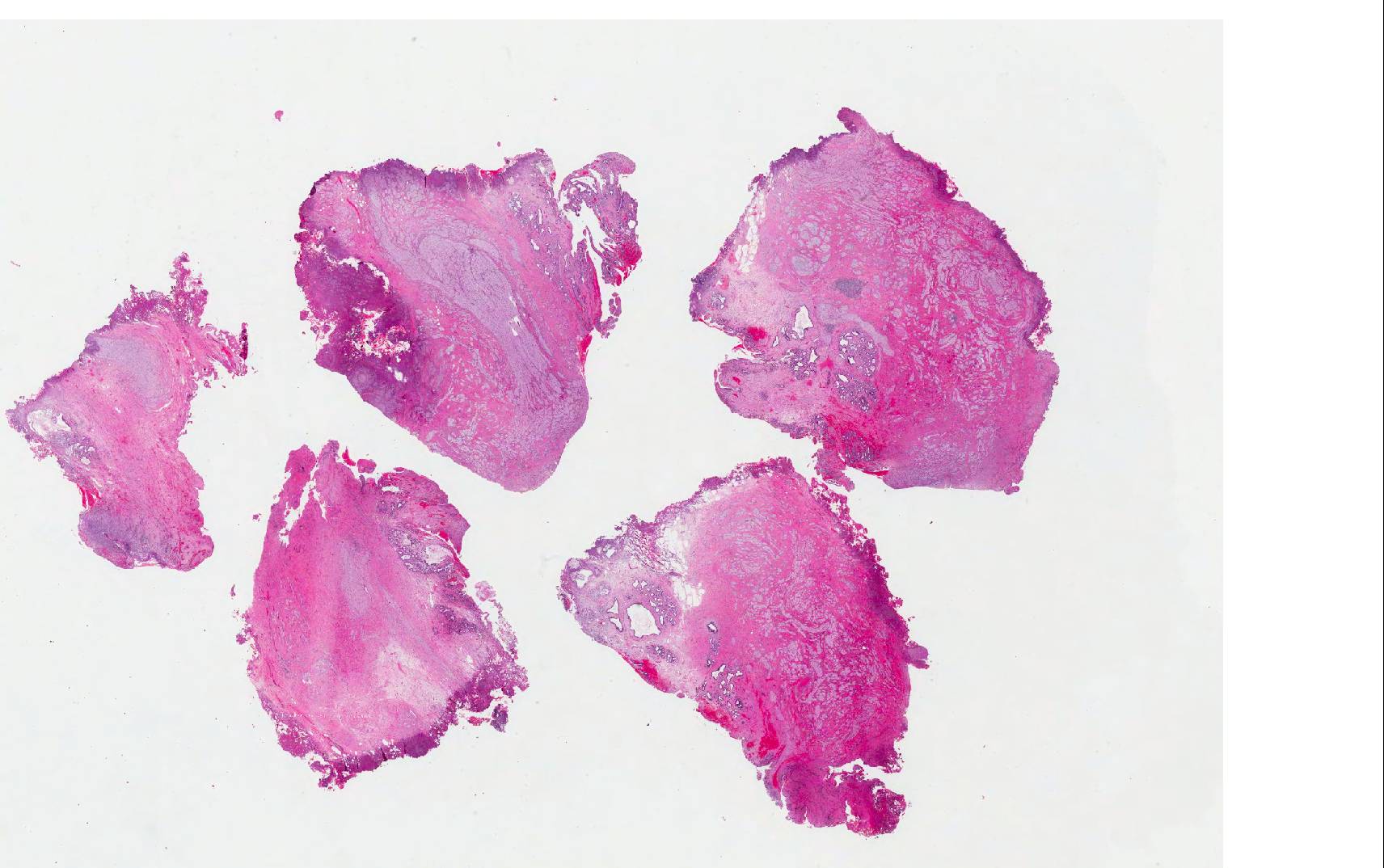
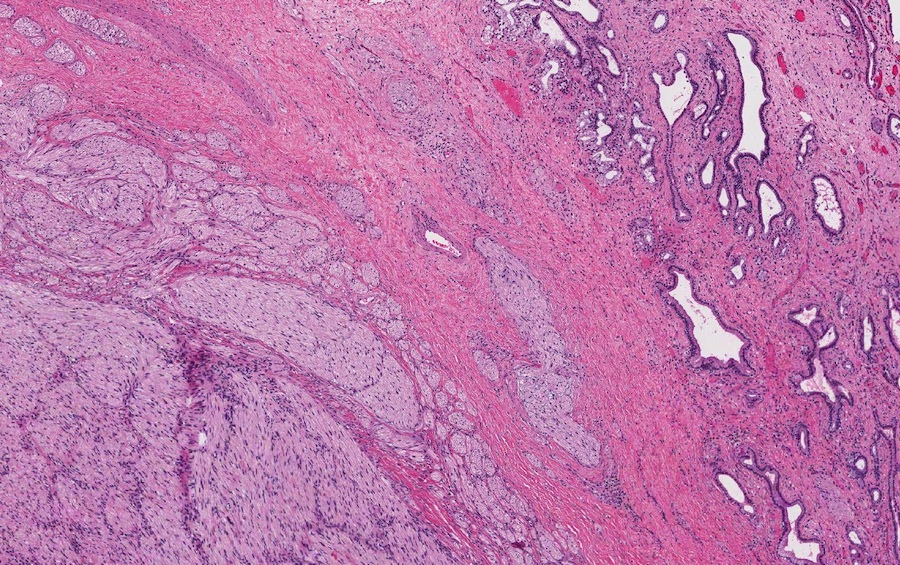
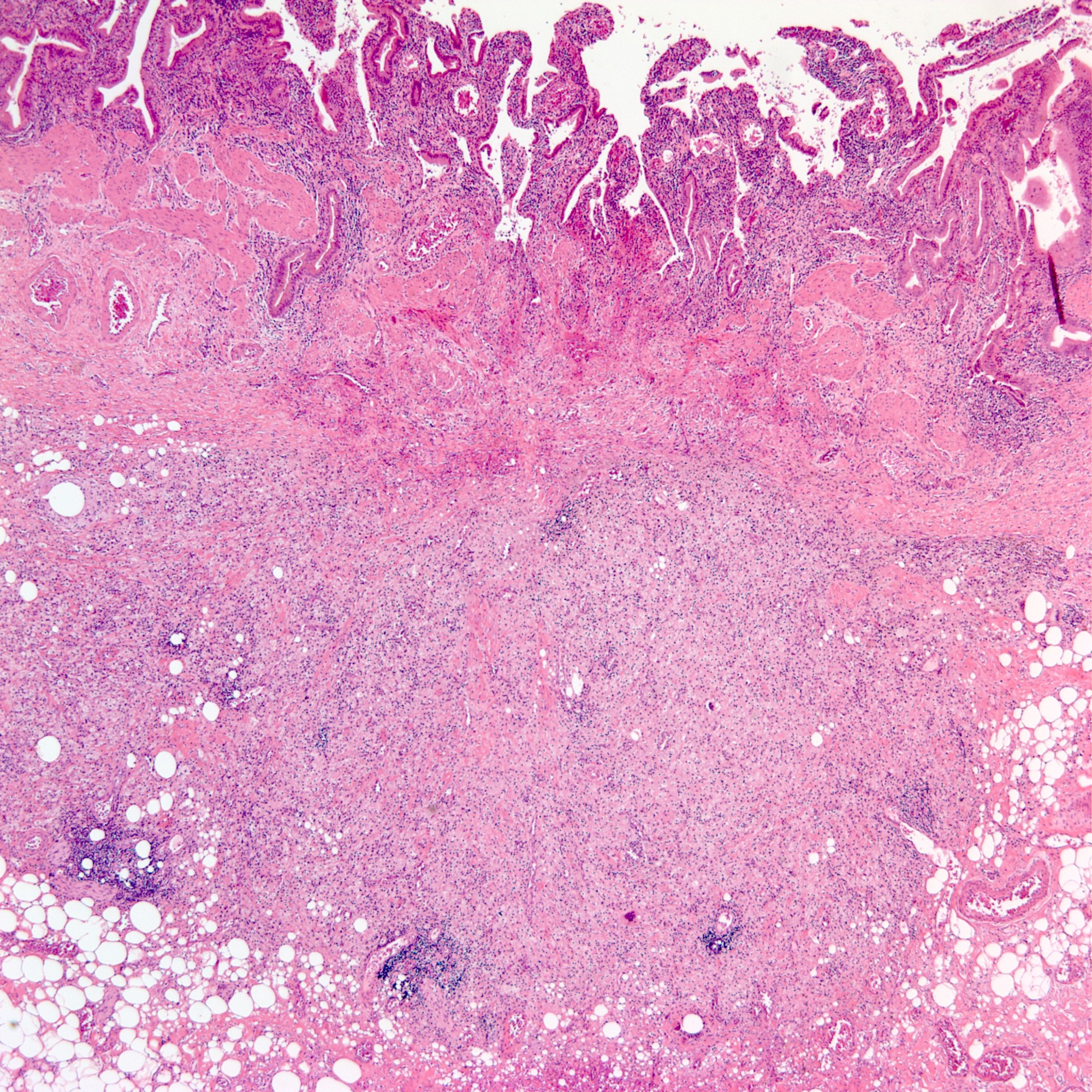
A 40 year old woman with a BMI of 36 undergoes cholecystectomy for intermittent, dull right upper quadrant abdominal pain, reproducible on physical examination with deep palpation. Sections of gallbladder wall show the following
What is the best interpretation of these findings?
- Chronic cholecystitis
- Cystadenocarcinoma
- Dilated ducts of Luschka
- Intracholecystic papillary tubular neoplasm (ICPN)
- Invasive adenocarcinoma
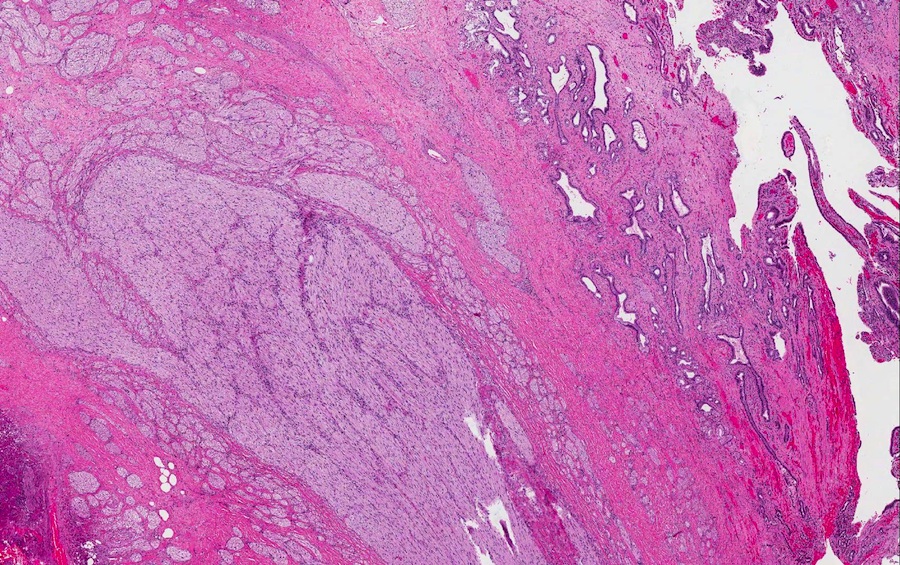
- Acute cholecystitis
- Chronic cholecystitis
- Eosinophilic cholecystitis
- Follicular cholecystitis
- Xanthogranulomatous cholecystitis
- Adenomyomatous chronic cholecystitis
- Diffuse lymphoplasmacytic cholecystitis
- Follicular cholecystitis
- Hyalinizing cholecystitis
- IgG4 associated cholecystitis
- Biliary intraepithelial neoplasia (BilIN) arising in the gallbladder
- Precursor lesion to gallbladder carcinoma with high risk of progression
- Almost always found incidentally in cholecystectomy specimens
- Indicates an increased risk for carcinoma of the gallbladder and elsewhere in the biliary tract
- High grade dysplasia is found concurrently in 40 - 100% of patients with invasive carcinoma
- There remains a lack of consensus regarding the appropriate extent of grossing and histologic examination
- Biliary intraepithelial neoplasia, low grade and high grade dysplasia, carcinoma in situ
- ICD-10: K82.9 - disease of gallbladder, unspecified
- Rare; found incidentally in 1 - 5% of cholecystectomies (Ann Diagn Pathol 2018;37:7)
- Follows gallbladder carcinoma trends but with slightly younger age (early sixth decade) (J Surg Res 2014;189:17, Ann Diagn Pathol 2018;37:7)
- More common in women (F:M = 3:1) and in India, Chile, Mexico and Japan (Histopathology 2021;79:2, J Surg Res 2014;189:17)
- Incidence of gallbladder dysplasia in the United States appears comparatively low (Arch Pathol Lab Med 2005;129:386, Am J Clin Pathol 2012;138:374, Ann Diagn Pathol 2018;37:7)
- In Western countries, reportedly more common among native American, Hispanic and Asian populations (J Surg Res 2014;189:17, Histopathology 2021;79:2)
- Risk factors include anything leading to chronic inflammation (Histopathology 2021;79:2)
- Cholelithiasis (most common); patients may have larger gallstones (Ann Diagn Pathol 2014;18:181)
- Chronic cholecystitis
- Chronic bacterial or parasitic infection (e.g., Salmonella typhi)
- Aflatoxin B1
- Primary sclerosing cholangitis
- Porcelain gallbladder
- Pancreaticobiliary maljunction
- Fundus (most common) > body > neck (least common) (Hum Pathol 2018;82:87)
- Low grade dysplasia is usually focal
- Dysplasia is unlikely to cover > 20% of the gallbladder in patients without carcinoma (Hum Pathol 2018;82:87)
- Chronic inflammation leads to epithelial metaplasia (most commonly intestinal metaplasia), then low grade dysplasia, then high grade dysplasia and finally invasive carcinoma (Arch Pathol Lab Med 2005;129:386, Hum Pathol 2018;82:87)
- Ranges from asymptomatic to vague, nonspecific signs and symptoms
- Clinical presentation can overlap with cholelithiasis / cholecystitis (Histopathology 2021;79:2)
- True neoplastic symptoms (right upper quadrant [RUQ] pain, fever, weight loss) rare in premalignant lesions
- Almost always detected incidentally in cholecystectomy specimens or in the background of frankly invasive gallbladder carcinoma
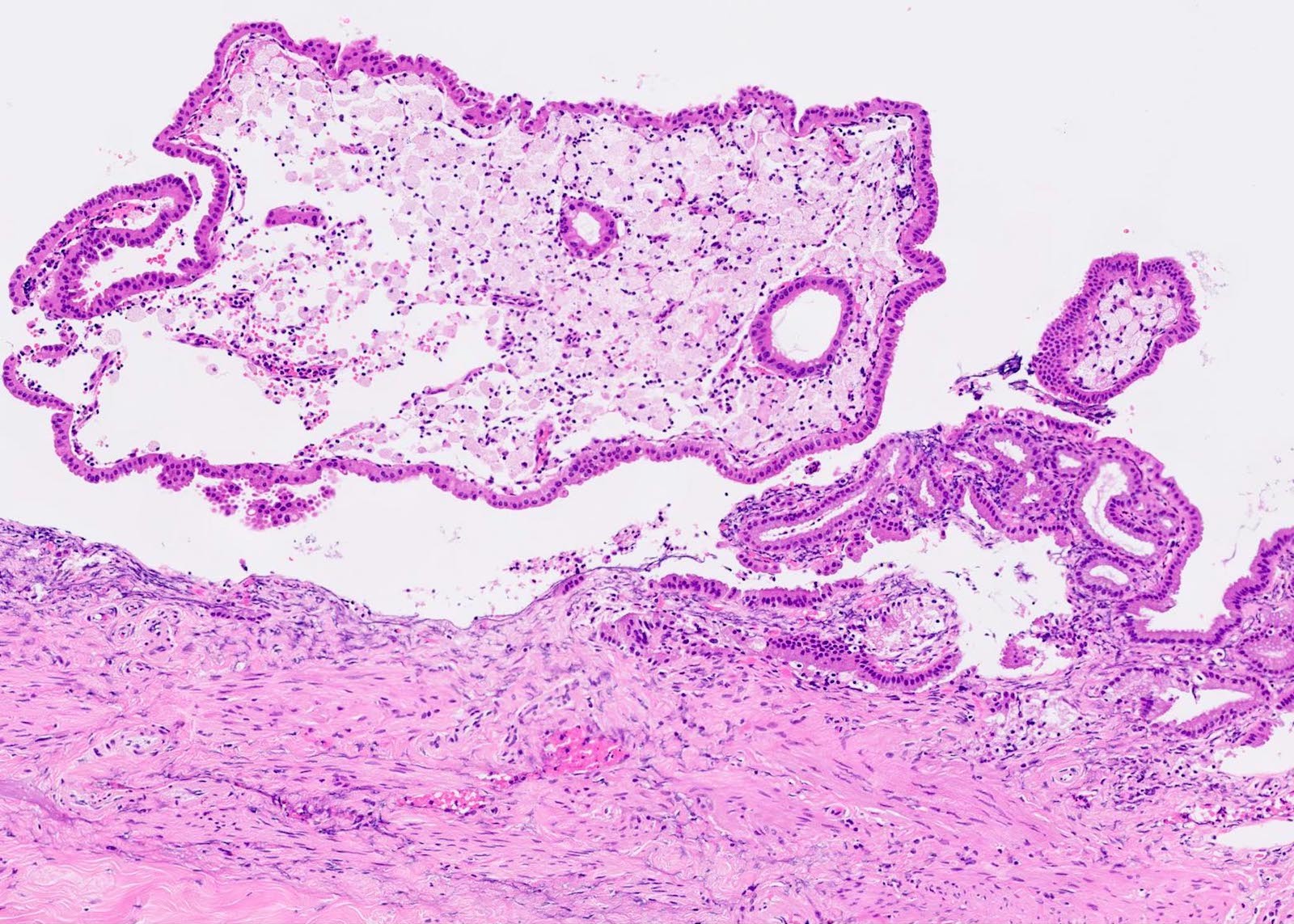
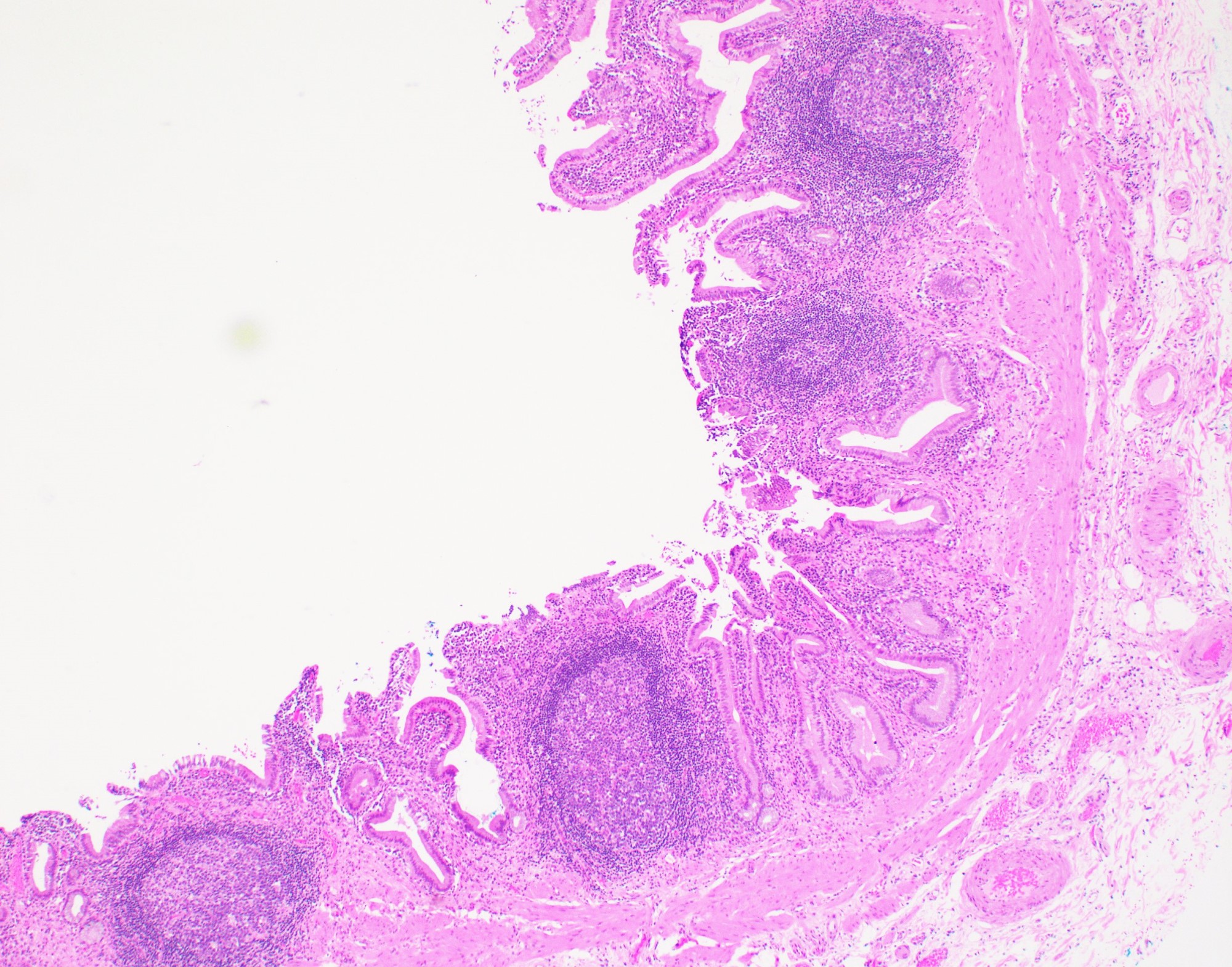
- Finding incidental dysplasia in initial sections should prompt further careful assessment with additional sampling, though specific recommendations vary (Am J Clin Pathol 2012;138:374, HPB (Oxford) 2015;17:681, Ann Diagn Pathol 2018;37:7, Am J Surg Pathol 2019;43:1668)
- Intestinal metaplasia: 4 additional sections (Am J Clin Pathol 2013;140:278)
- Low grade dysplasia: 4 additional sections (consider more in high risk patients or populations)
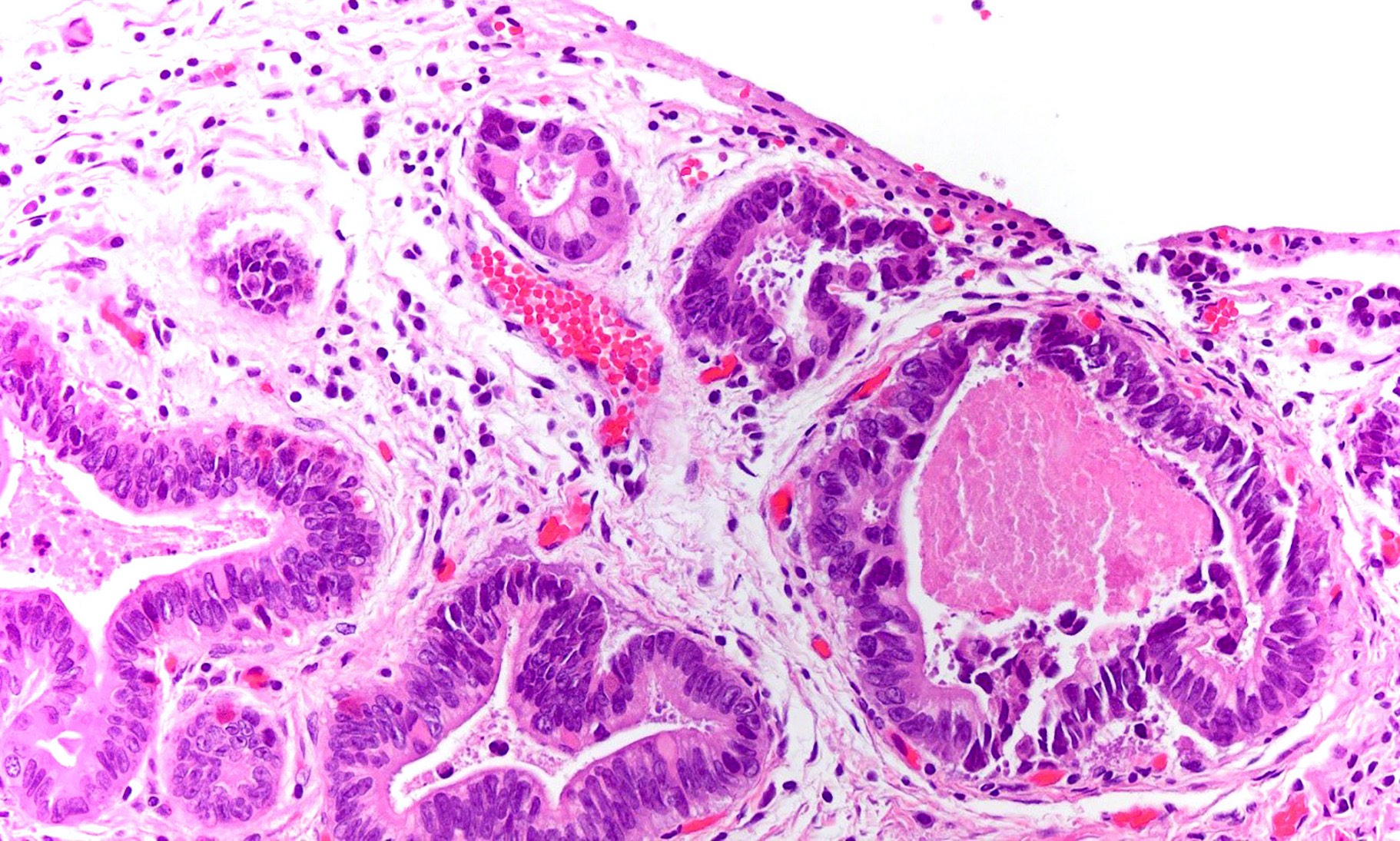
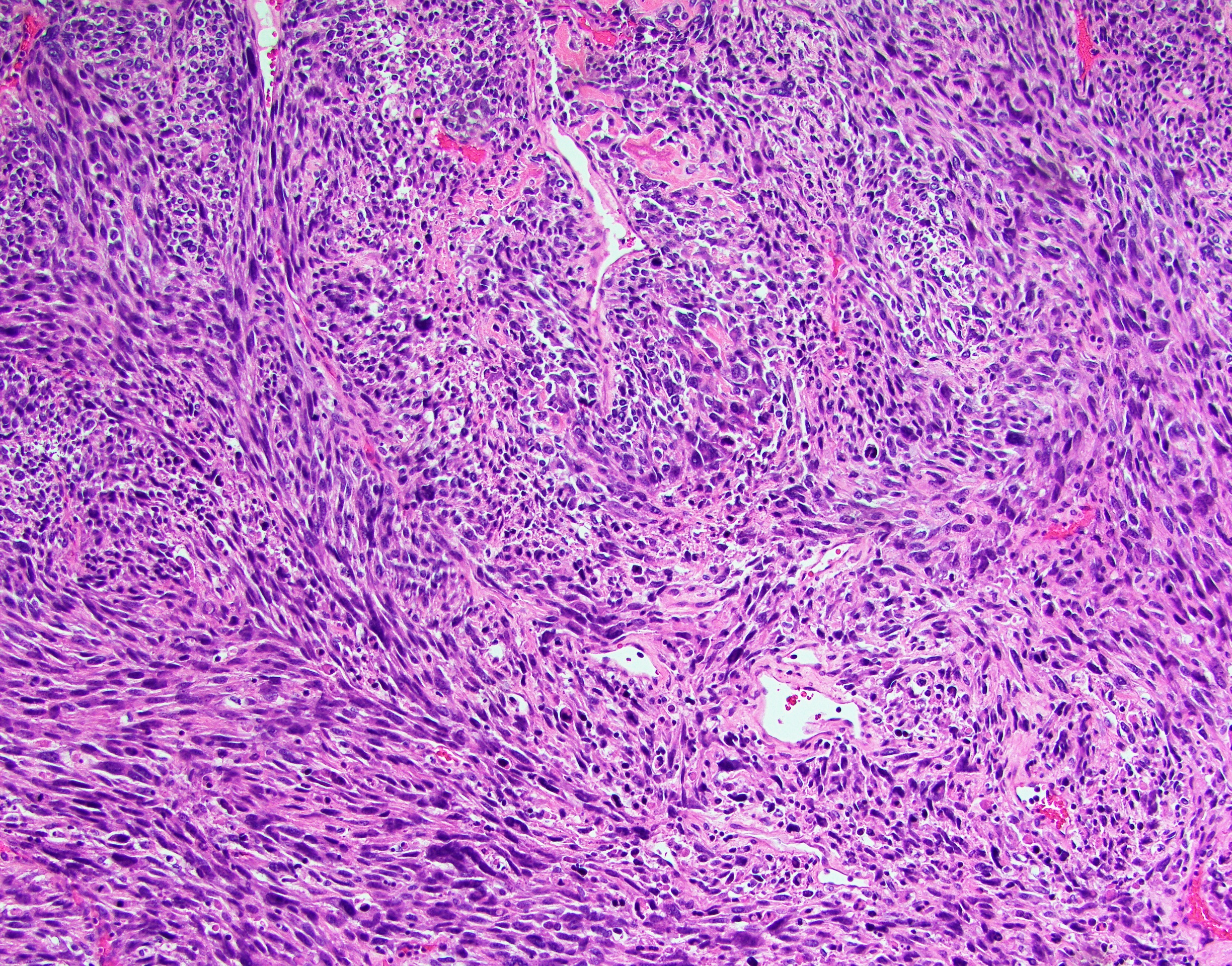
- High grade dysplasia: at least 4 additional sections but strongly consider submitting entire remaining gallbladder (high risk of malignancy elsewhere in gallbladder)
- Usually no findings
- US, CT or MRI can show nonspecific focal or diffuse gallbladder wall thickening or a space occupying lesion (Ann Diagn Pathol 2018;37:7)
- Increases risk for carcinoma of the gallbladder and elsewhere in the pancreatobiliary tract (J Gastrointest Surg 2019;23:686)
- 36 year old woman with gallstone pancreatitis (BMJ Case Rep 2017;2017:bcr2016218994)
- 44 year old man with RUQ pain (Chin Clin Oncol 2019;8:34)
- 59 year old man with adenomyomatosis and gallbladder cancer (Surg Laparosc Endosc Percutan Tech 2019;29:290)
- 61 year old woman with pancreatobiliary reflux (J Gastroenterol 2005;40:756)
- Unlike gallbladder carcinoma, which likely necessitates further treatment, isolated gallbladder dysplasia is cured by cholecystectomy
- If cystic duct margin is involved, imaging and further surgery may be considered (HPB (Oxford) 2011;13:865)
- Gallbladder almost always appears grossly normal (Hum Pathol 2018;82:87)
- Rarely shows nonspecific changes, such as a poorly defined area of mucosal thickening and induration (Ann Diagn Pathol 2018;37:7, Histopathology 2021;79:2)
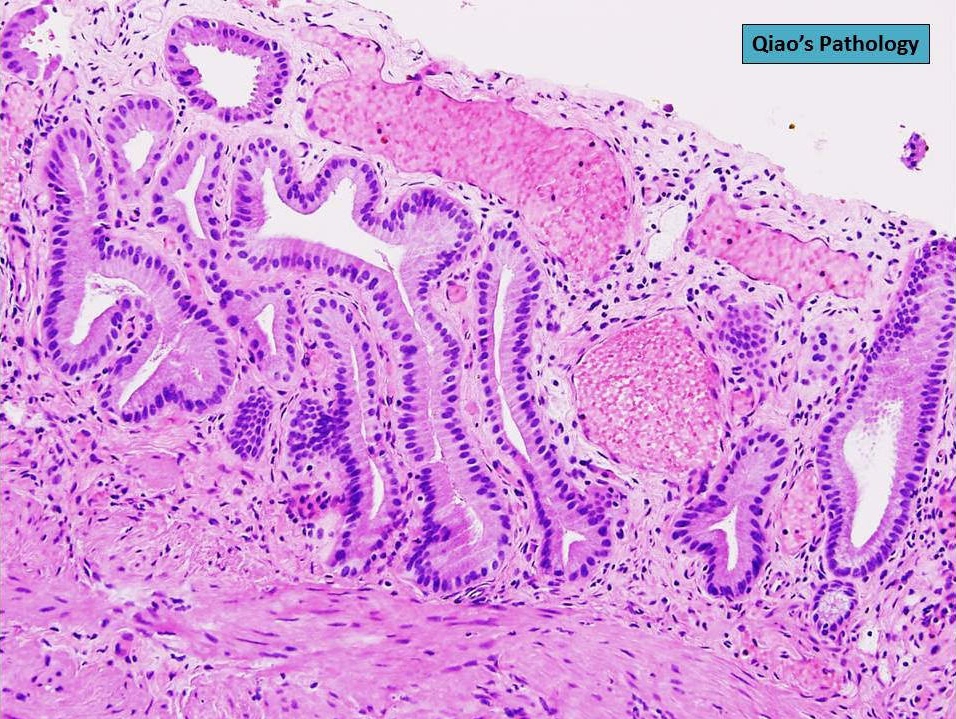
- Gallbladder dysplasia can be difficult to reproducibly define, in particular low grade dysplasia (Histopathology 2021;79:2)
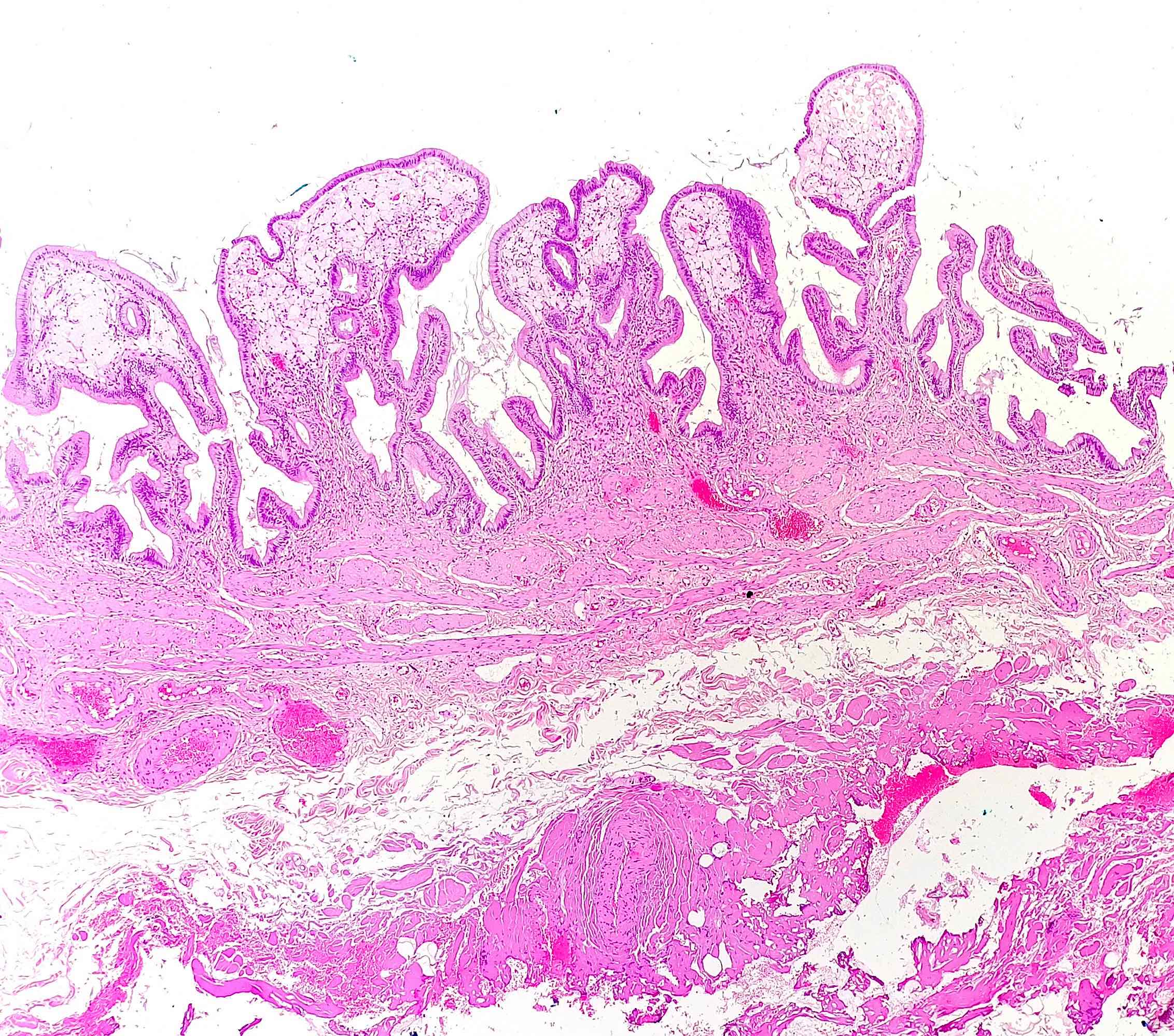
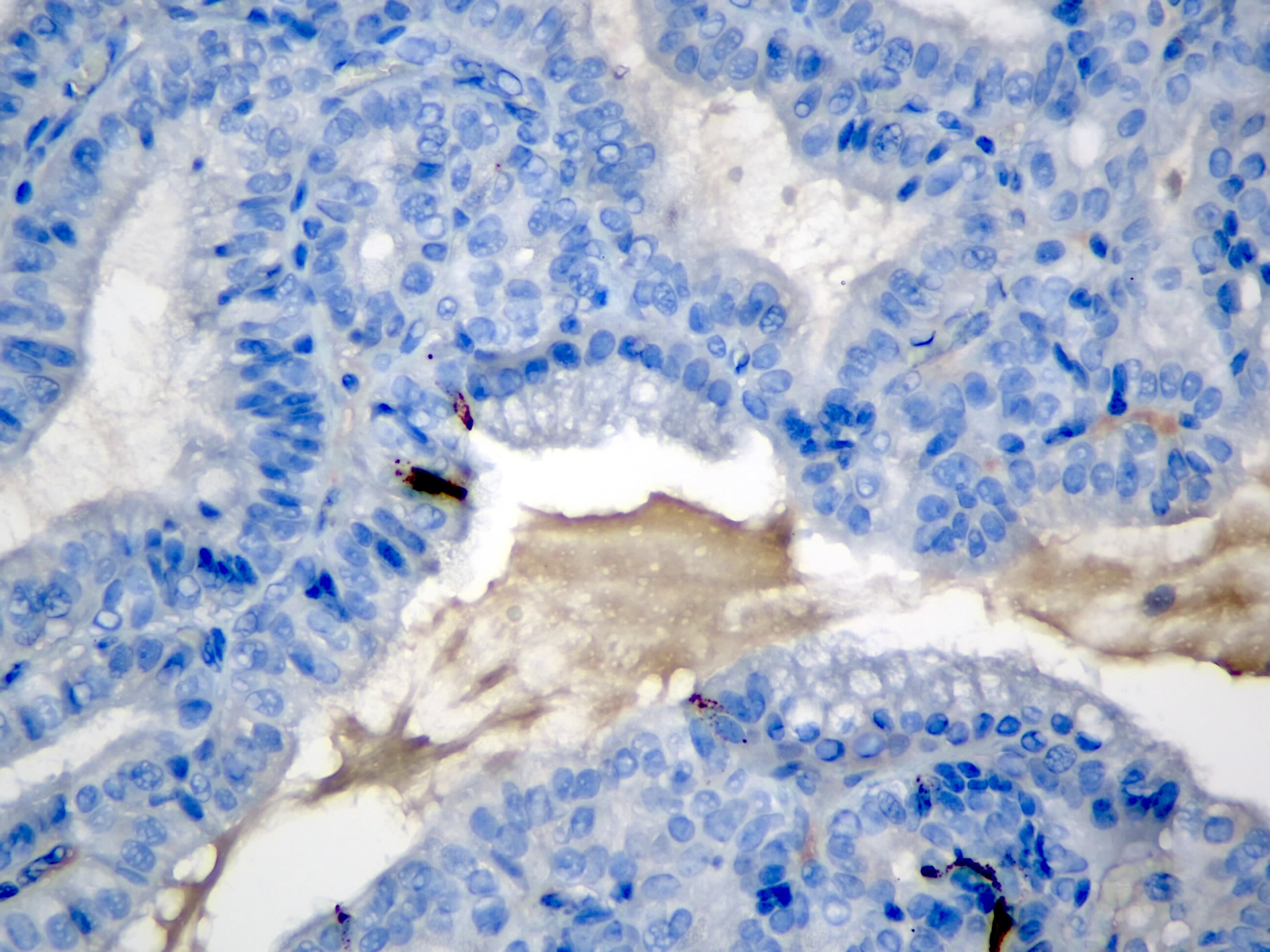
- Low grade dysplasia
- Elongated (pencillate) hyperchromatic nuclei that may show pseudostratification but still maintain basal polarity, with moderate N:C ratios
- Mucosal surface often remains flat
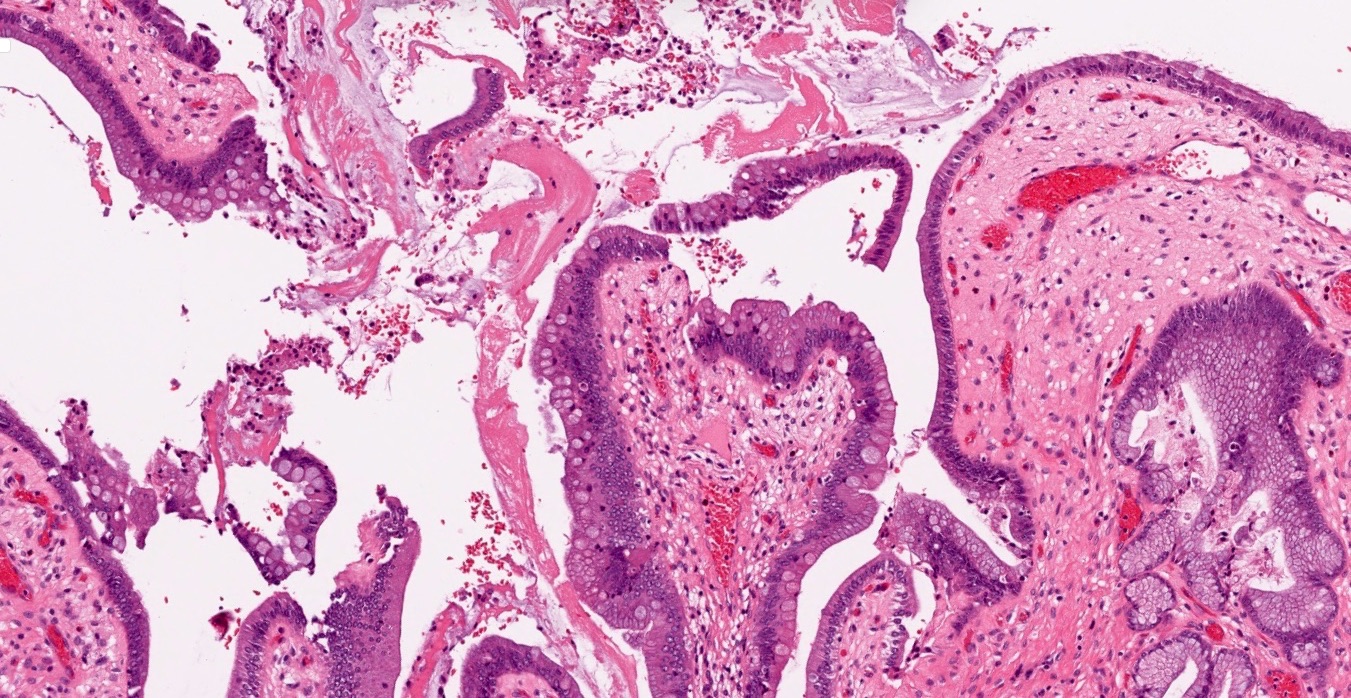
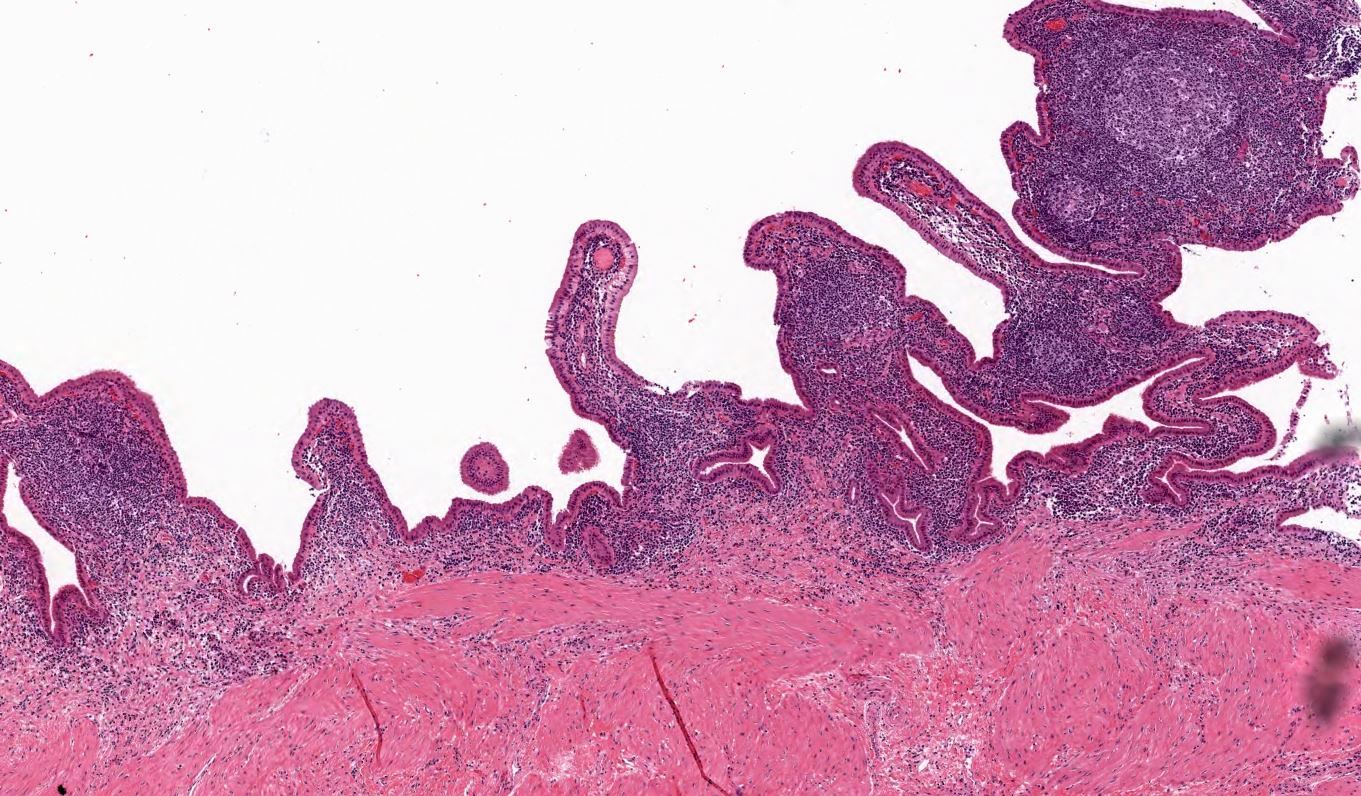
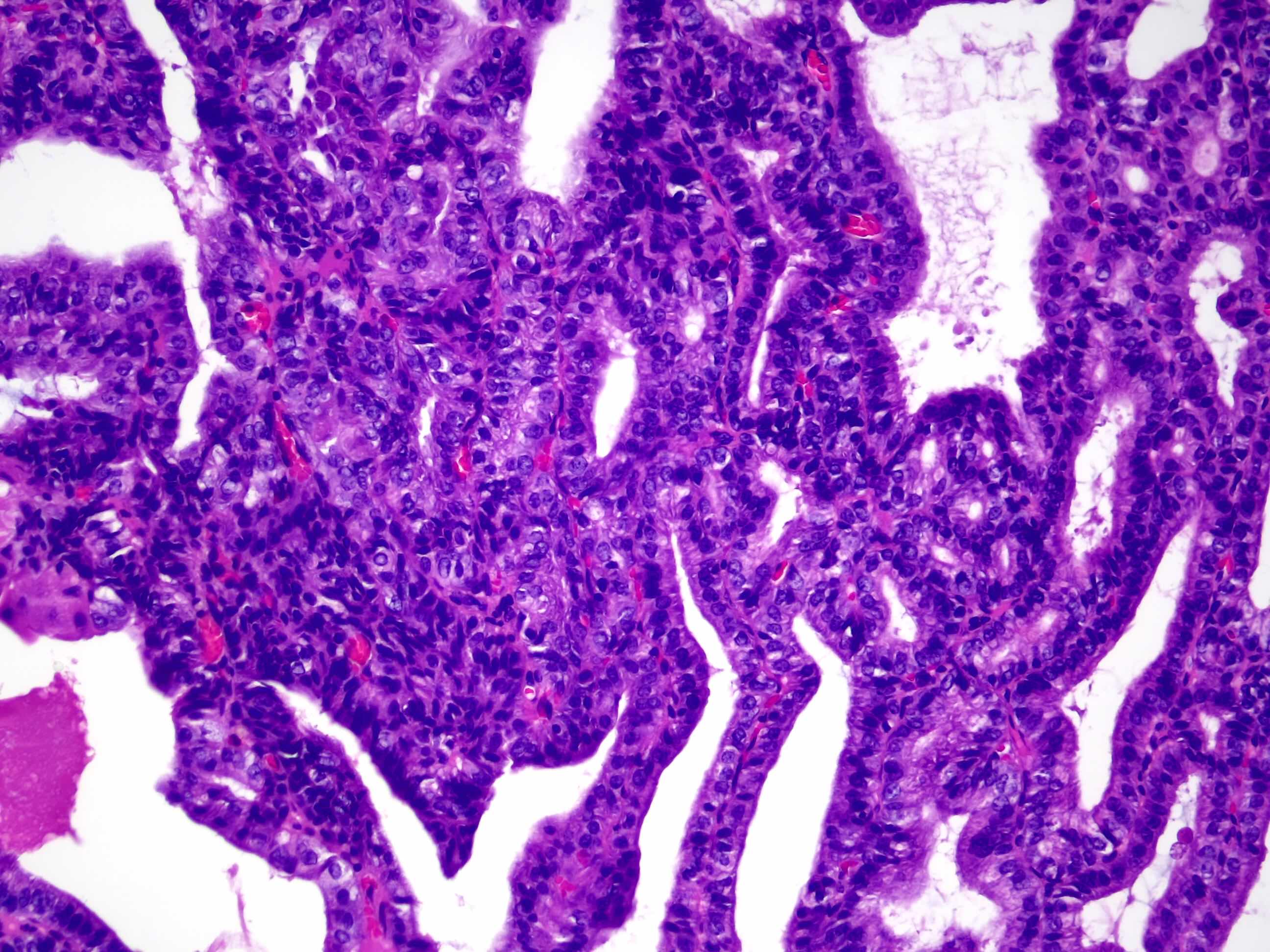
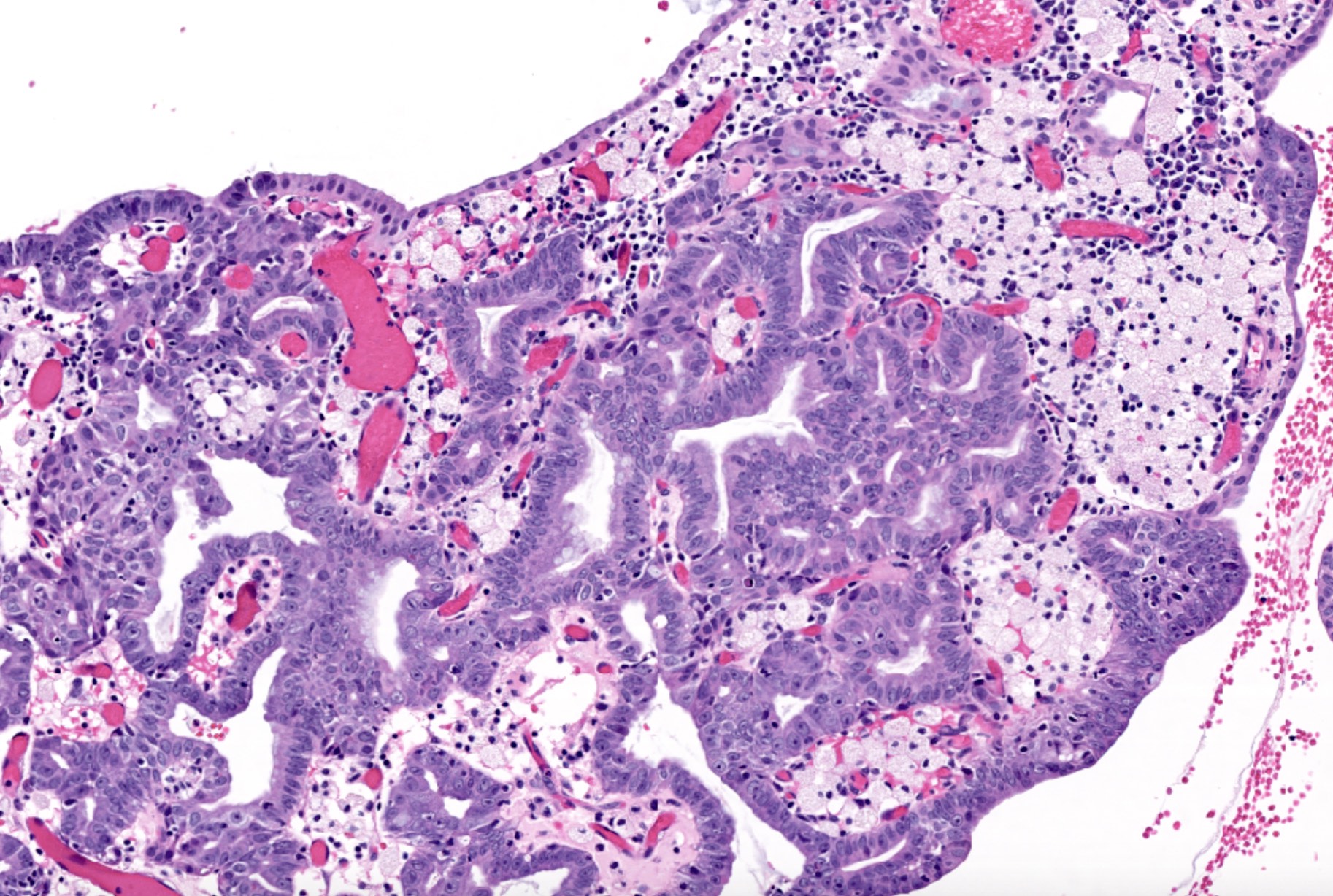
- High grade dysplasia
- Markedly atypical nuclei with rounding, nucleoli and loss of polarity, with high N:C ratios and more complex surface architecture
- Low grade dysplasia often accompanies high grade dysplasia
- Intestinal metaplasia is often present in the background
- Neutrophils (acute inflammation) may be present in dysplastic epithelium, raising consideration for reactive atypia but erosion or ulceration is uncommon
- Interobserver variability exists for these diagnoses; strict diagnostic criteria have been proposed to address this (Mod Pathol 2007;20:701)
- May show p53 overexpression and increased Ki67 index (Hum Pathol 1996;27:360, Rev Med Chir Soc Med Nat Iasi 2007;111:734)
Gallbladder and bile duct pathology by Dr. Adsay
- Gallbladder, cholecystectomy:
- Multifocal, flat, high grade dysplasia arising in chronic cholecystitis and cholelithiasis (see comment)
- Negative for invasive malignancy
- Cystic duct margin negative for dysplasia
- Comment: The entire gallbladder was submitted for microscopic examination.
- Reactive atypia:
- Often occurs in the setting of prominent acute cholecystitis
- Nuclei have lower N:C ratios and less striking hyperchromasia
- Atypia may gradually transition into adjacent normal mucosa, rather than a clear cutoff
- Intestinal metaplasia:
- Defined by the presence of goblet cells
- Cells also show mild nuclear hyperchromasia and amphophilic cytoplasm
- Intracholecystic papillary tubular neoplasm:
- Dysplastic process that forms a discrete polypoid lesion, rather than remaining relatively flat
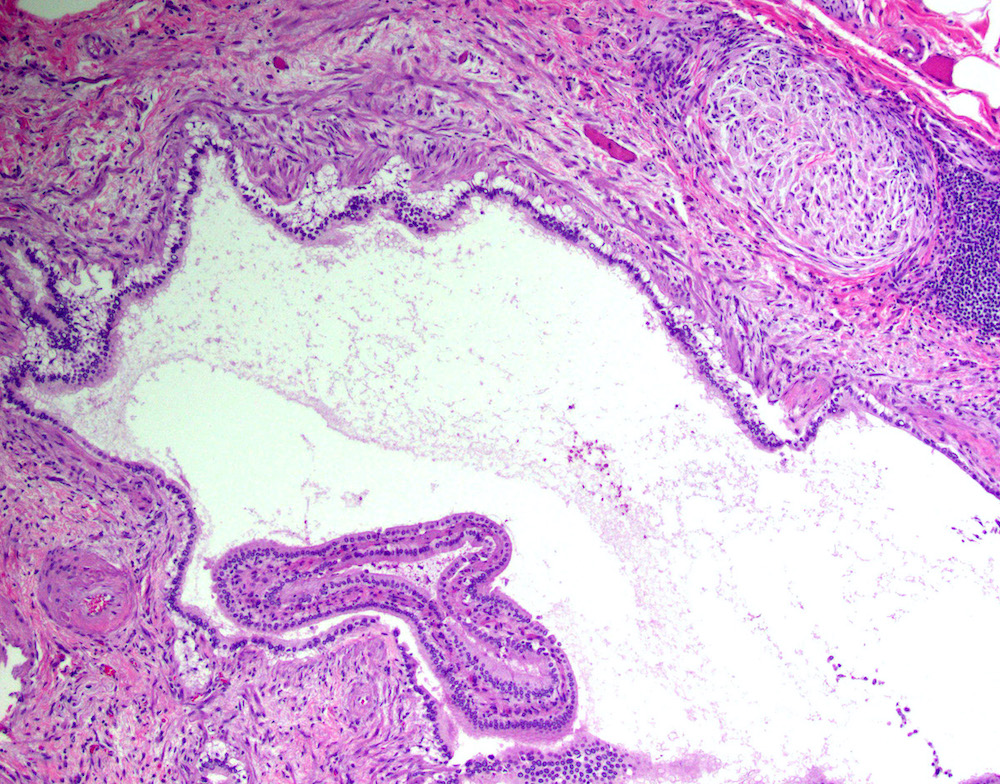
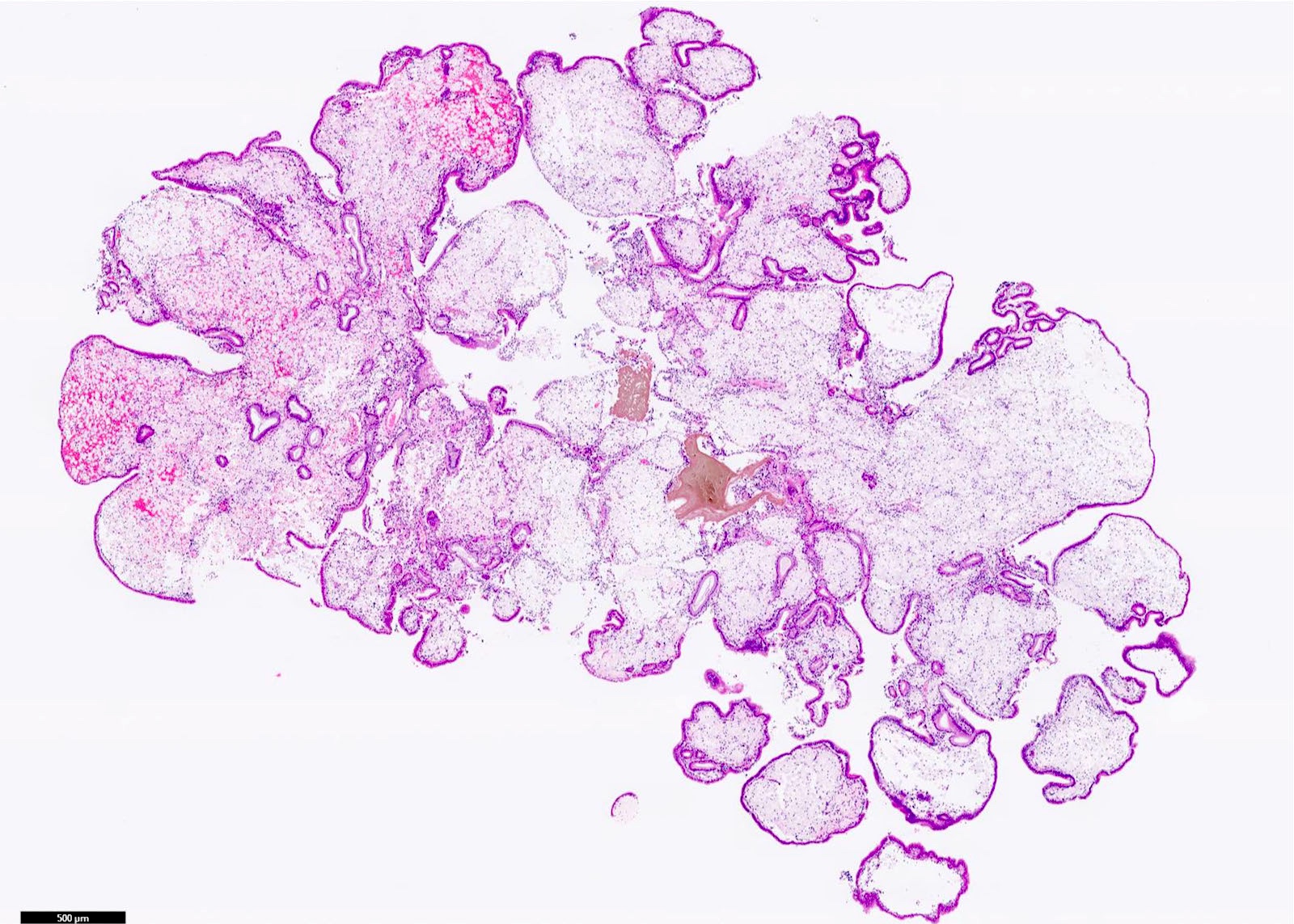
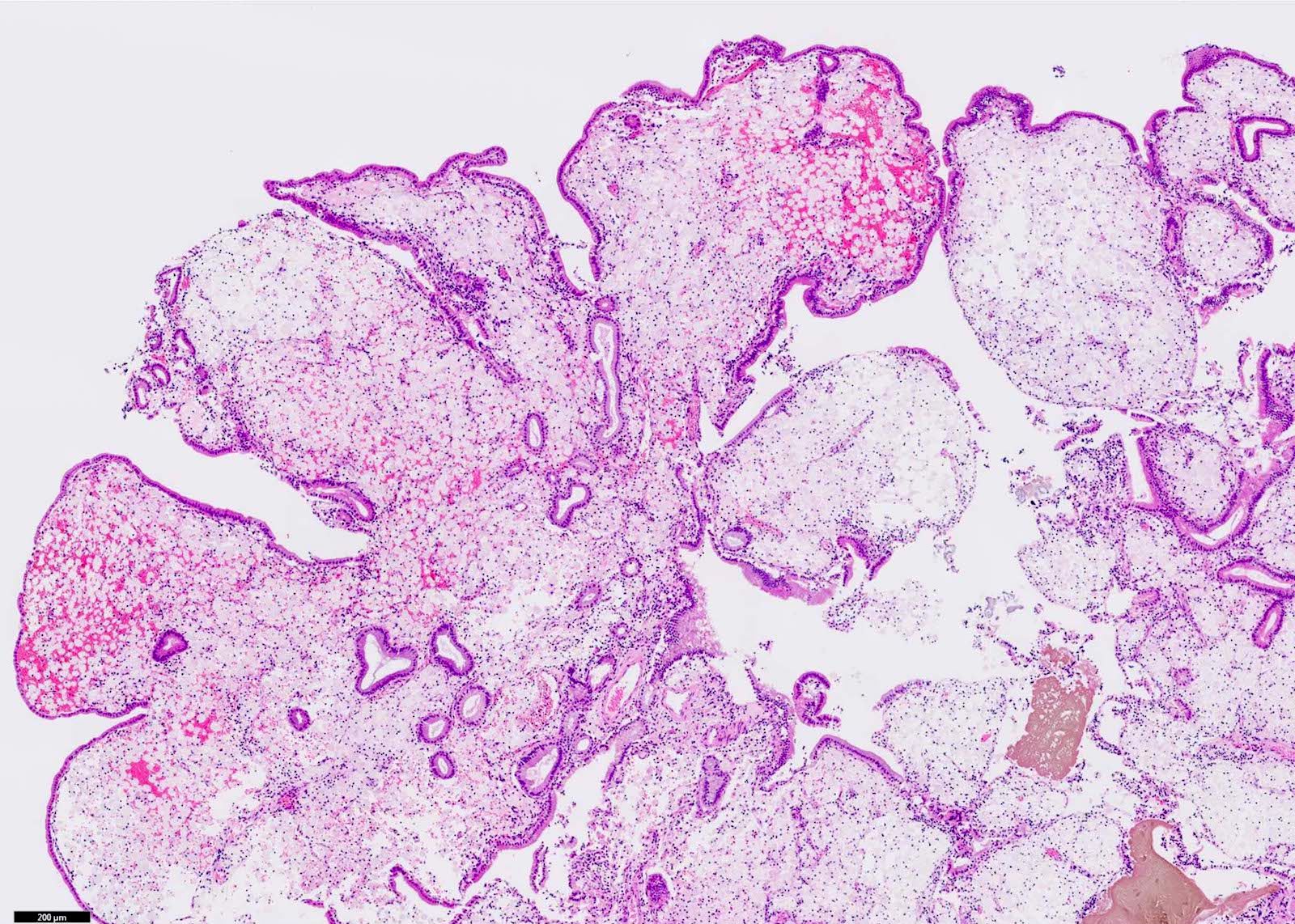
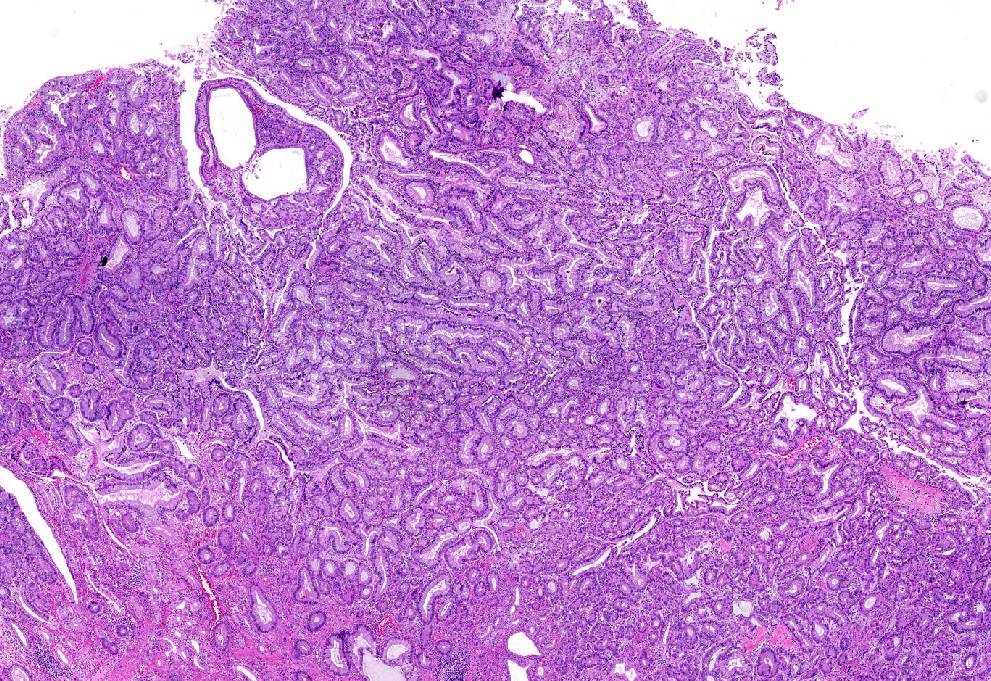
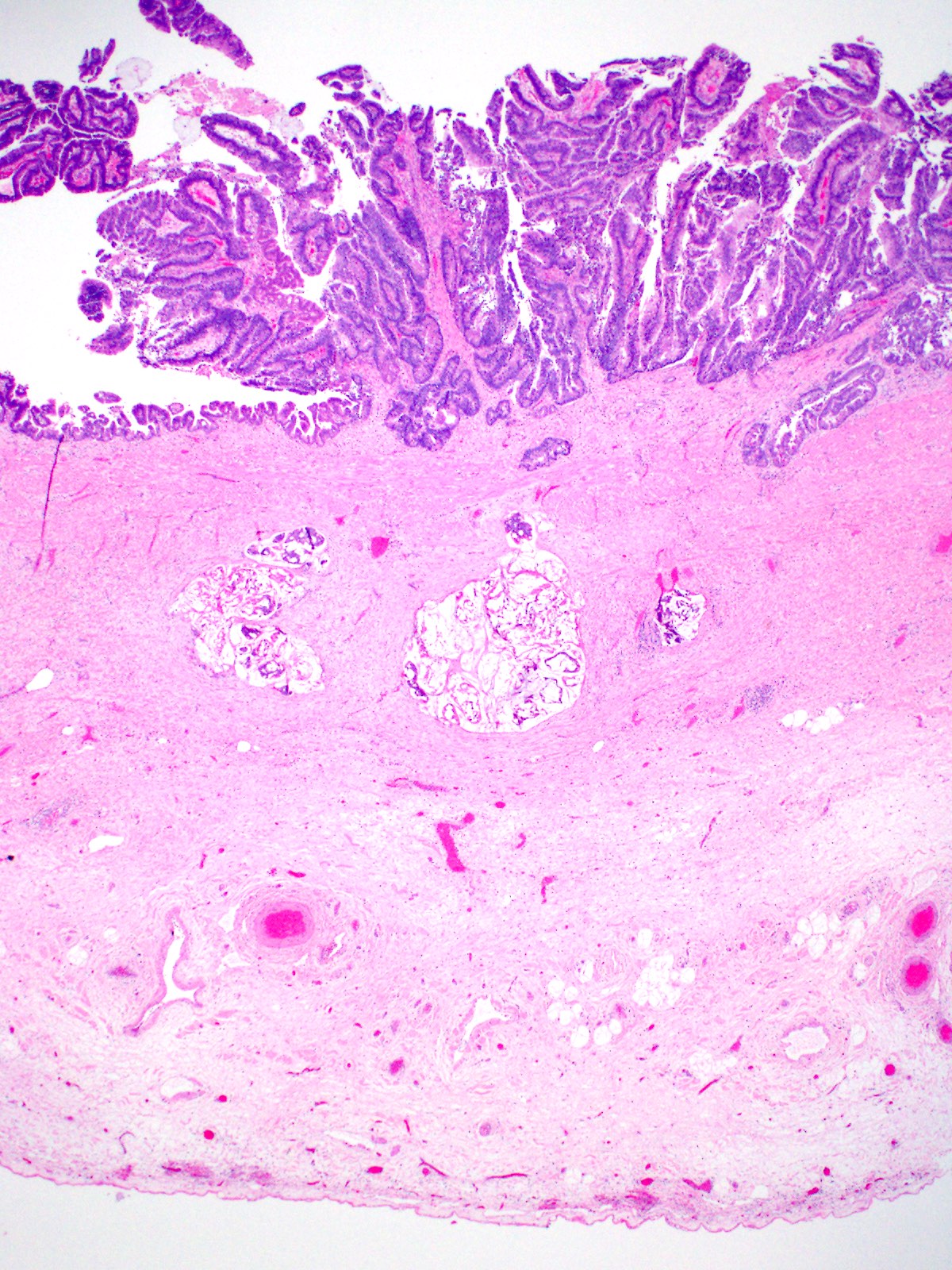
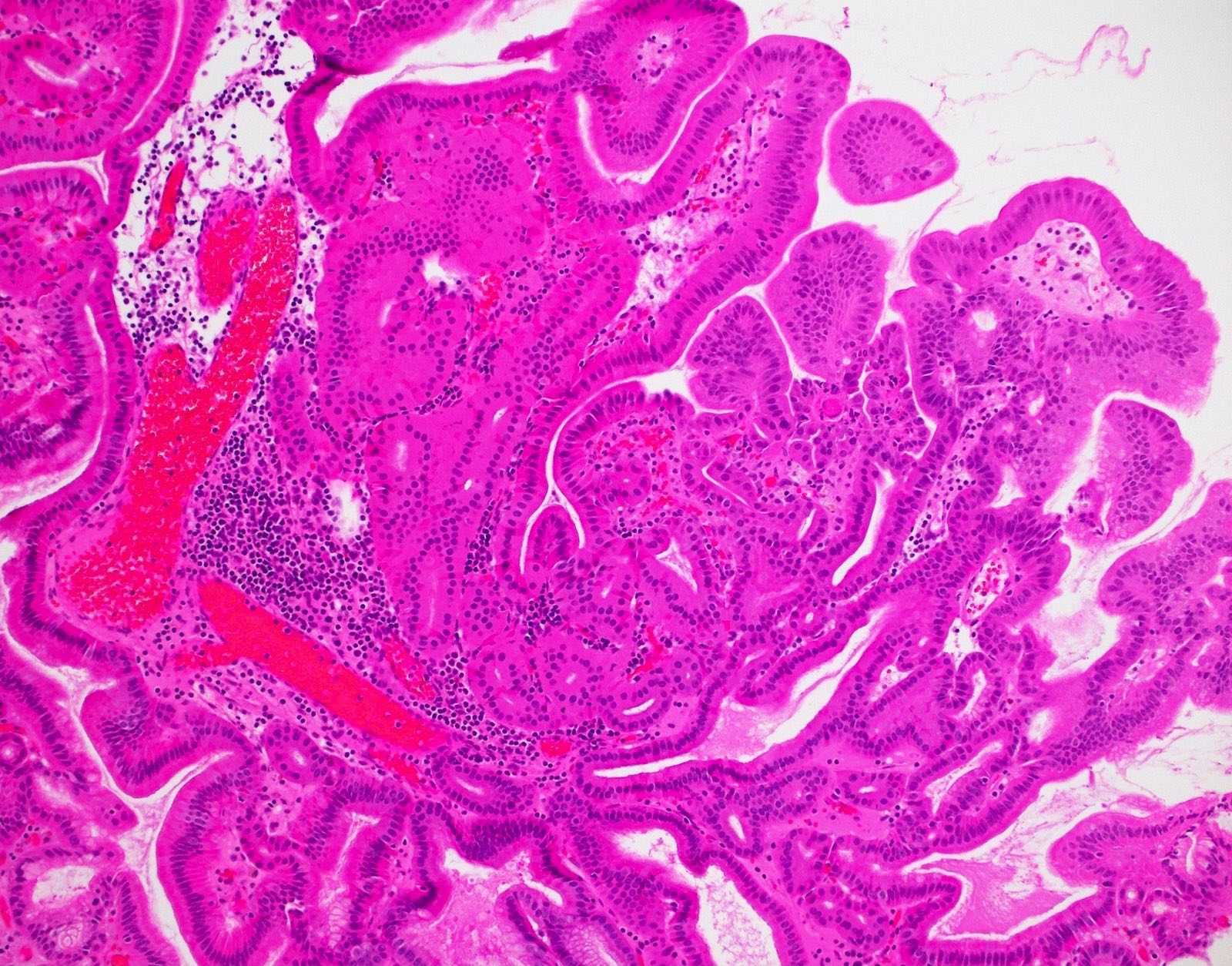
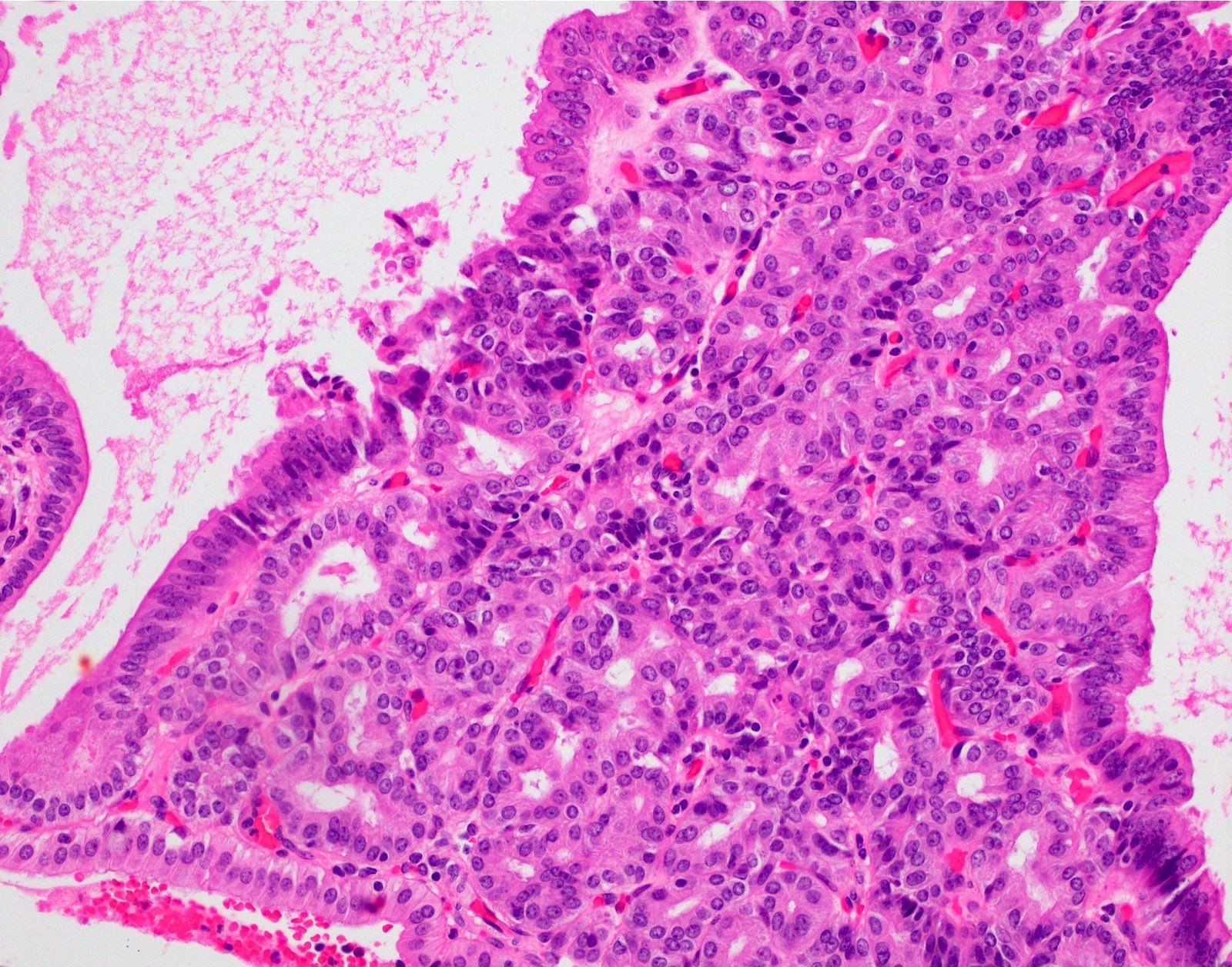
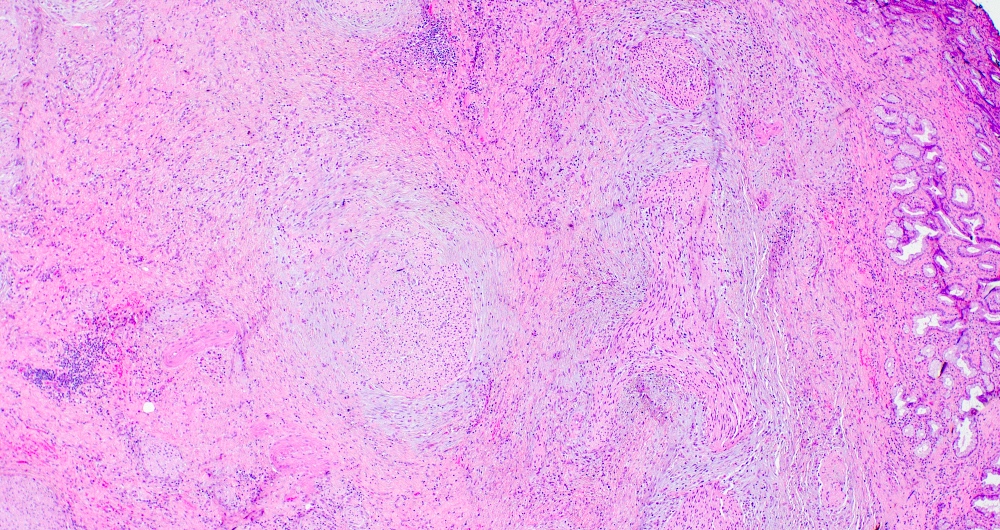
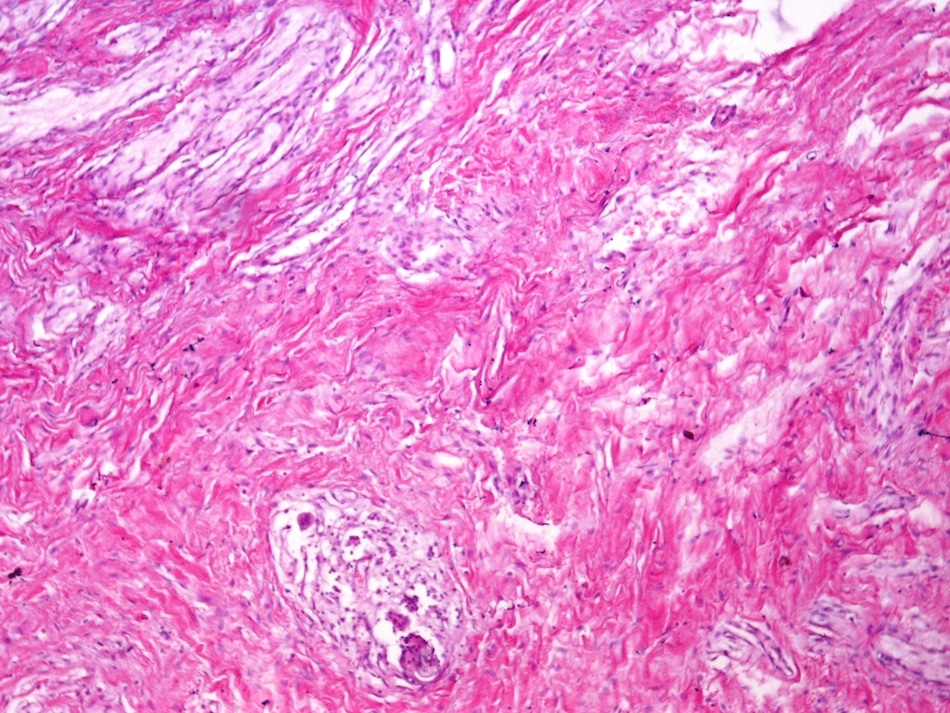
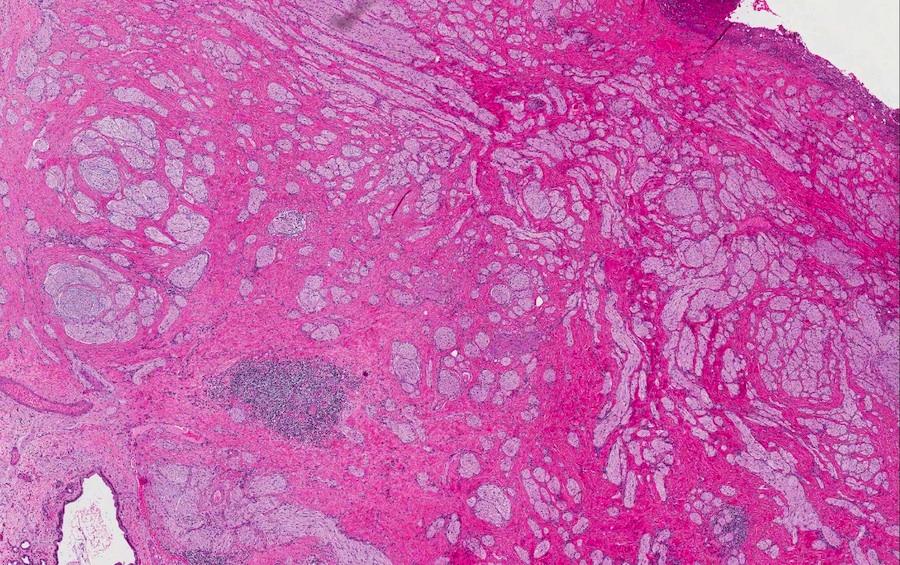
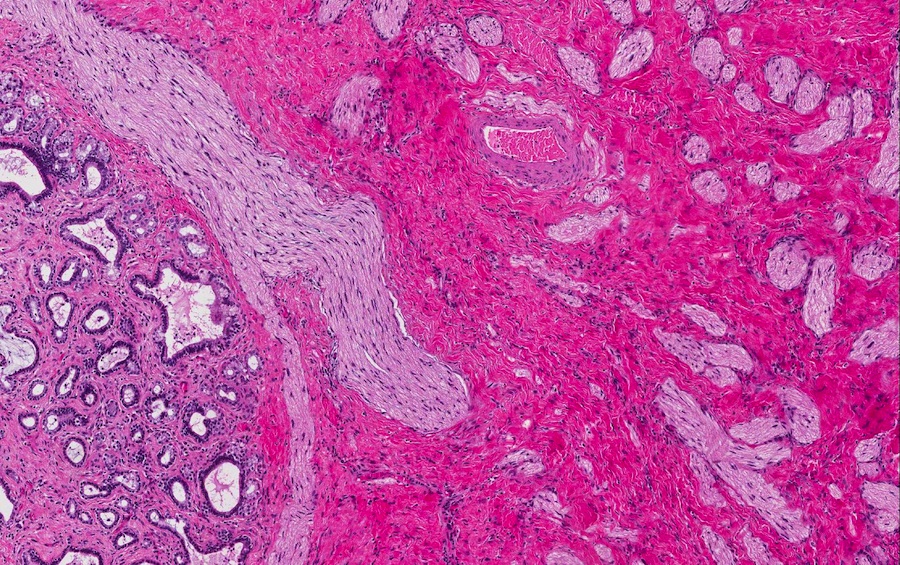
A 72 year old woman presented to the emergency department with symptoms of cholecystitis and underwent laparoscopic cholecystectomy. The gallbladder grossly looked normal but the one routine section submitted for histology showed the changes seen in the image above. What is the most appropriate next step in the workup of this case?
- Sign out the pathology report
- Submit 1 - 2 additional cassettes
- Submit the entire gallbladder
- Tell the surgeon the patient needs urgent hepatectomy
Comment Here
Reference: Gallbladder & extrahepatic bile ducts - Dysplasia
- Chile
- India
- Japan
- United States
Comment Here
Reference: Gallbladder & extrahepatic bile ducts - Dysplasia
- Rare form of acute cholecystitis with gas in gallbladder wall, associated with diabetes and peripheral atherosclerotic disease
- 2/3 men, usually 50 - 70 years old, diagnosed with ultrasonographic studies
- May be due to vascular compromise of cystic artery
- Associated with acalculous disease, gallbladder perforation, Clostridium welchii and E. coli infection
Contributed by @RaulSGonzalezMD on Twitter
 Contributed by @RaulSGonzalezMD on Twitter (see original post here)">
Contributed by @RaulSGonzalezMD on Twitter (see original post here)">
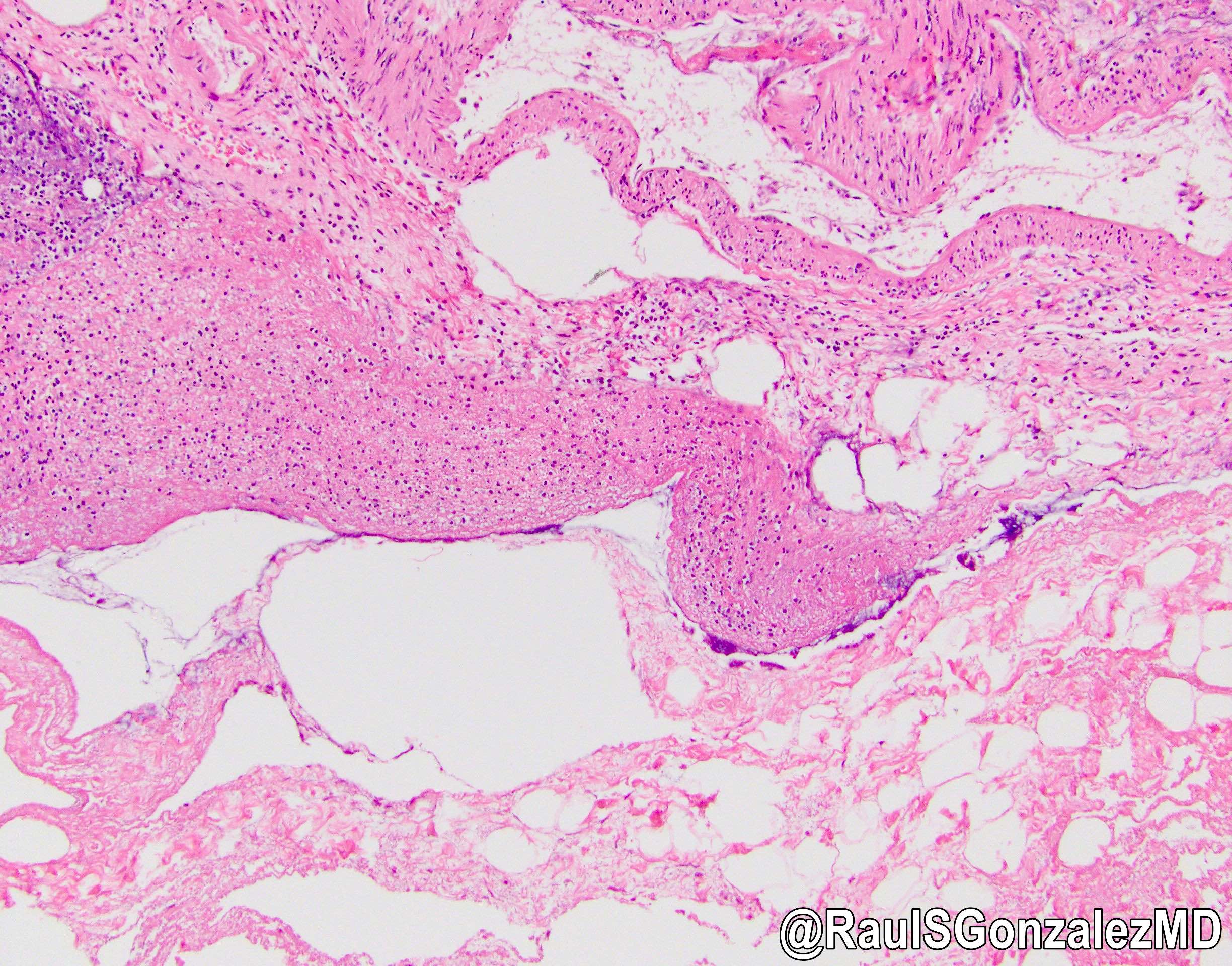
Emphysematous cholecystitis
- Well formed germinal centers throughout gallbladder wall
- Also called lymphoid polyp
- May grossly resemble polyps up to several mm
- Associated with typhoid fever, primary sclerosing cholangitis, gram negative bacterial infection of bile (Acta Pathol Jpn 1979;29:67)
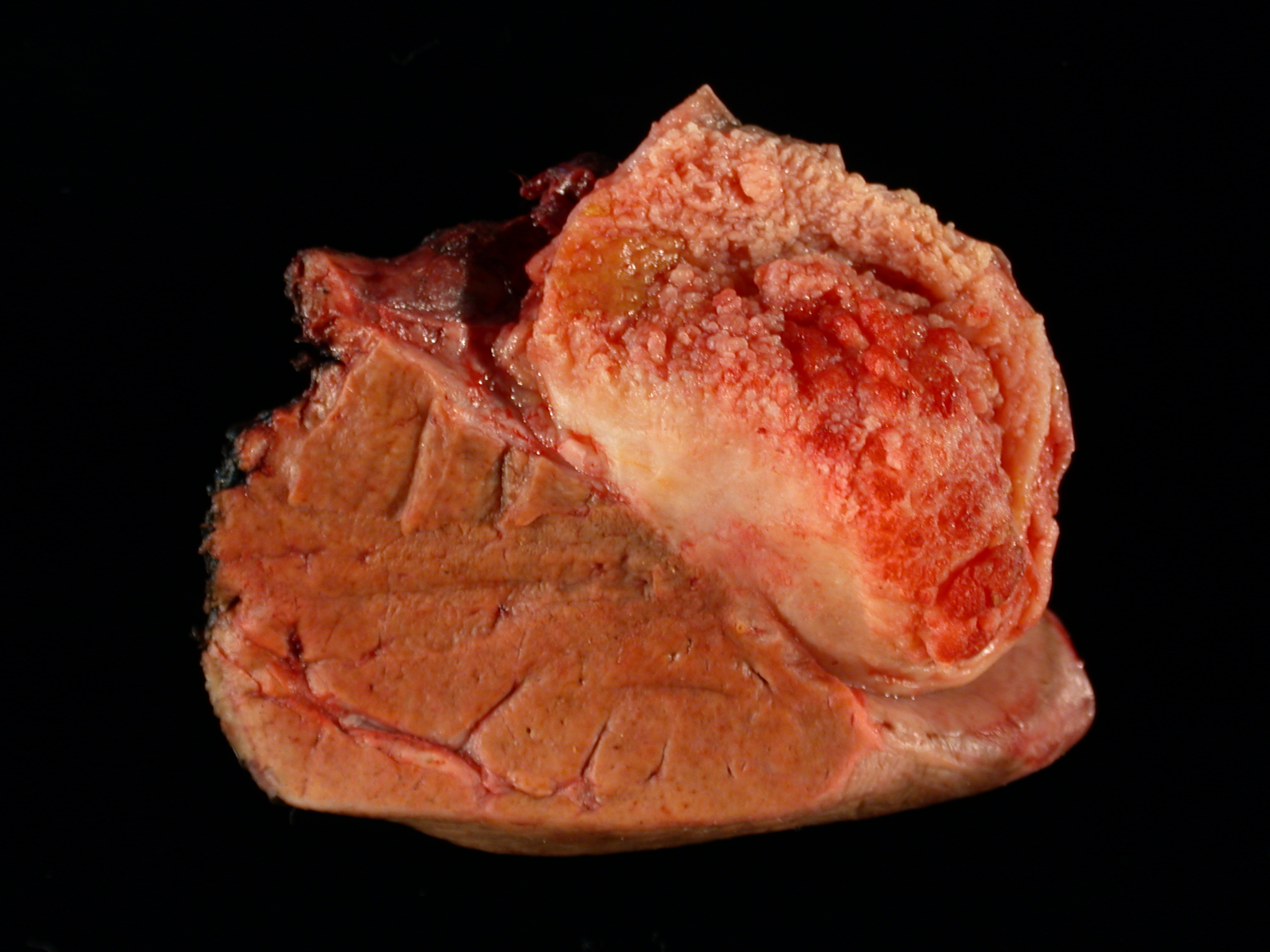
- Carcinoma arising from the gallbladder epithelium (WHO Classification of Tumours Editorial Board: Digestive System Tumours (Medicine), 5th Edition, 2019)
- Aggressive cancer, with an overall 5 year survival rate of < 10%
- Cholelithiasis is a major risk factor
- Up to 50% are detected incidentally in routine cholecystectomy specimens due to absence of gross abnormalities; systematic sampling of these specimens is therefore crucial to detect incidental gallbladder adenocarcinomas (Am J Surg Pathol 2019;43:1668)
- Carcinoma of gallbladder; adenocarcinoma of gallbladder; malignant epithelial neoplasm of gallbladder
- Commonly occurs in the sixth and seventh decades
- F:M = 3:1
- Highest incidence in women from Chile (27.3/100 000), India (21.5/100 000), Pakistan (13.8/100 000) and Ecuador (12.9/100 000) (Int J Cancer 2010;127:2446, Histopathology 2009;55:218)
- Incidence 1.1 per 100,000 in the United States (Cancer Epidemiol Biomarkers Prev 2015;24:1319)
- Overall 5 year survival rate of < 10%
- Primarily affects the fundus (60%), body (30%) or neck (10%) of gallbladder
- Advanced tumors involve the liver and extrahepatic biliary tree
- Longstanding cholelithiasis and cholecystitis give rise to metaplastic changes (intestinal or pseudopyloric types) in the gallbladder mucosa (Cancer 1993;72:1878)
- Metaplasia (especially intestinal type) gives rise to epithelial dysplasia and carcinoma in situ (J Hepatobiliary Pancreat Surg 2000;7:556)
- Progression from dysplasia to advanced gallbladder carcinoma takes around 15 years (Gastroenterology 1996;111:232)
- Risk factors include:
- Cholelithiasis (major risk factor)
- Chronic cholecystitis, especially hyalinizing cholecystitis
- Obesity
- Infections (esp. Salmonella and Opisthorchis viverrini)
- Porcelain gallbladder
- Primary sclerosing cholangitis
- Pancreaticobiliary maljunction (supra-Oddi union of common bile duct with the main pancreatic duct)
- Occasionally occurs in patients with Lynch syndrome or familial adenomatous polyposis (FAP)
- Asymptomatic in a large majority of patients
- Symptoms when present are vague
- Right upper quadrant pain (most common)
- Weight loss
- Fever
- Disease is usually advanced by the time patient develops symptoms
- 50% are diagnosed incidentally on routine cholecystectomy specimens
- Finding a thickened gallbladder wall or polypoid lesions in the gallbladder on imaging done for other reasons should prompt surgical resection
- Elevated alkaline phosphatase in advanced cancers (HPB (Oxford) 2008;10:446)
- CEA only has 50% sensitivity (Int J Cancer 1990;45:821)
- Imaging findings are variable from subtle (in early disease) to obvious (in late disease)
- Thickening of the gallbladder wall
- Raised / polypoid lesion in the gallbladder wall / lumen
- Mass occupying or replacing the gallbladder lumen
- Gallbladder mass invading the liver (in advanced disease)
- Ultrasound is the primary imaging modality for screening purposes in suspected cases
- Abnormal findings on ultrasound are further investigated by CT and MRI that provide detailed information, including staging parameters
- Noninvasive papillary carcinomas, regardless of size and differentiation, do not metastasize
- Invasive papillary carcinomas have the most favorable prognosis (Arch Pathol Lab Med 2005;129:905)
- Prognosis of adenocarcinoma, NOS depends on tumor stage:
- Superficially invasive cancers limited to the lamina propria (pT1a) have excellent prognosis as they are completely cured by cholecystectomy (Ann Surg 2017;266:625)
- Advanced cancers (i.e. muscle invasive and beyond; pT1b - pT4) have a higher chance of recurrence and have poorer outcomes (J Gastrointest Surg 2007;11:631, Ann Surg 2011;254:320)
- High histologic grade (poor differentiation) and vascular invasion have adverse outcomes (Cancer 1992;70:1493)
- Rokitansky-Aschoff sinus involvement by carcinoma and cystic duct margin status are suspected predictors of progression (Am J Clin Pathol 2014;141:675)
- 22 year old man with primary signet ring cell carcinoma of gallbladder in the absence of choleliths (Int J Surg Pathol 2010;18:358)
- 56 year old woman with clear cell carcinoma of the gallbladder (Int J Surg Case Rep 2017;32:36)
- 59 year old woman with hepatoid carcinoma of the gallbladder (World J Surg Oncol 2011;9:103)
- 62 year old man with carcinosarcoma of the gallbladder with chondroid differentiation (Int J Clin Exp Pathol 2015;8:7464)
- Cholecystectomy with a negative cystic duct margin is curative in pT1a tumors (Ann Surg 2017;266:625)
- Hilar / portal lymphadenectomy, plus resection of hepatic bed and the common bile duct to achieve negative margins, is necessary for tumors that extend into a muscle or beyond (pT1b - pT3) (HPB (Oxford) 2015;17:681)
- Chemotherapy or radiation for metastatic tumors
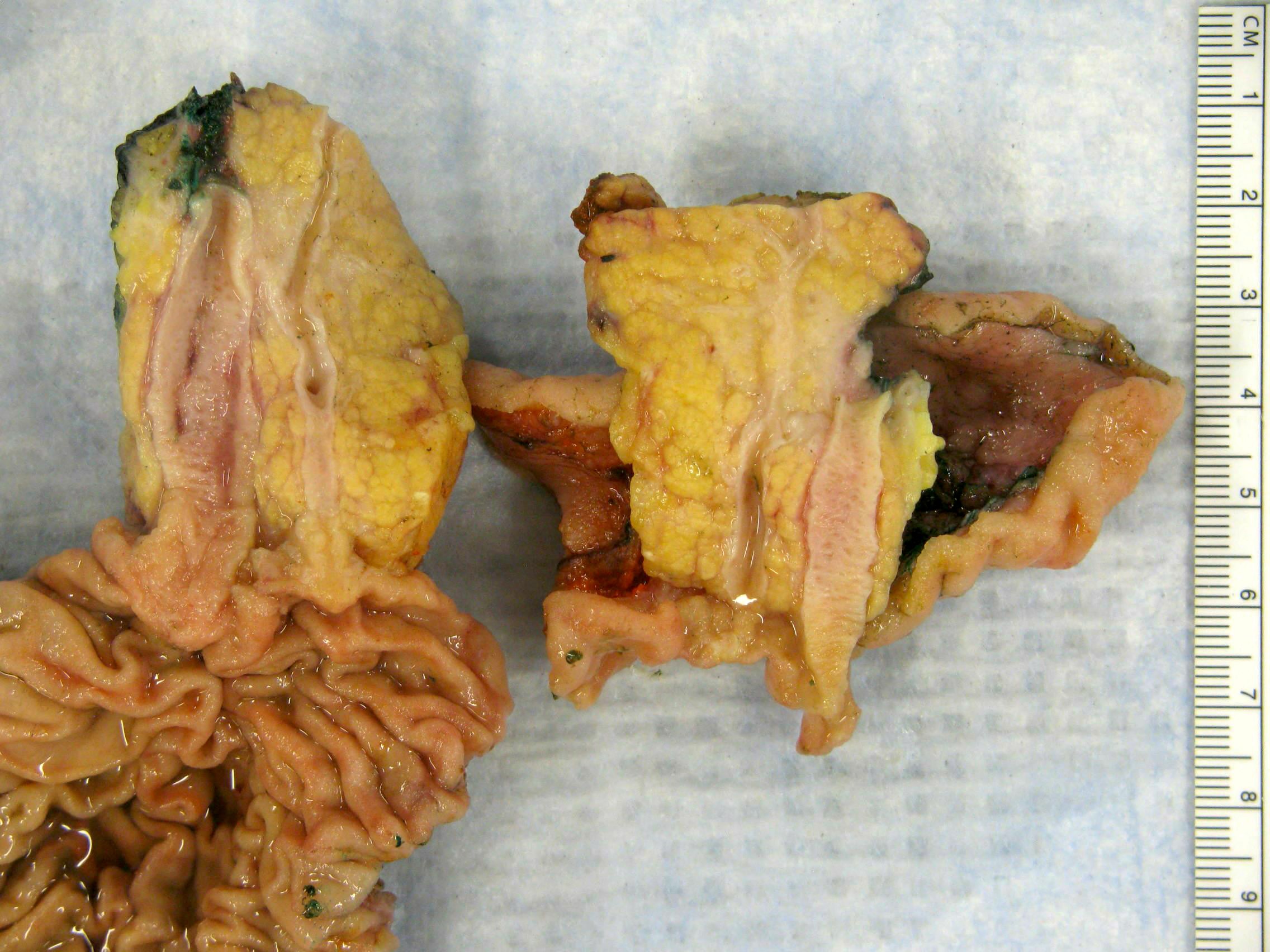
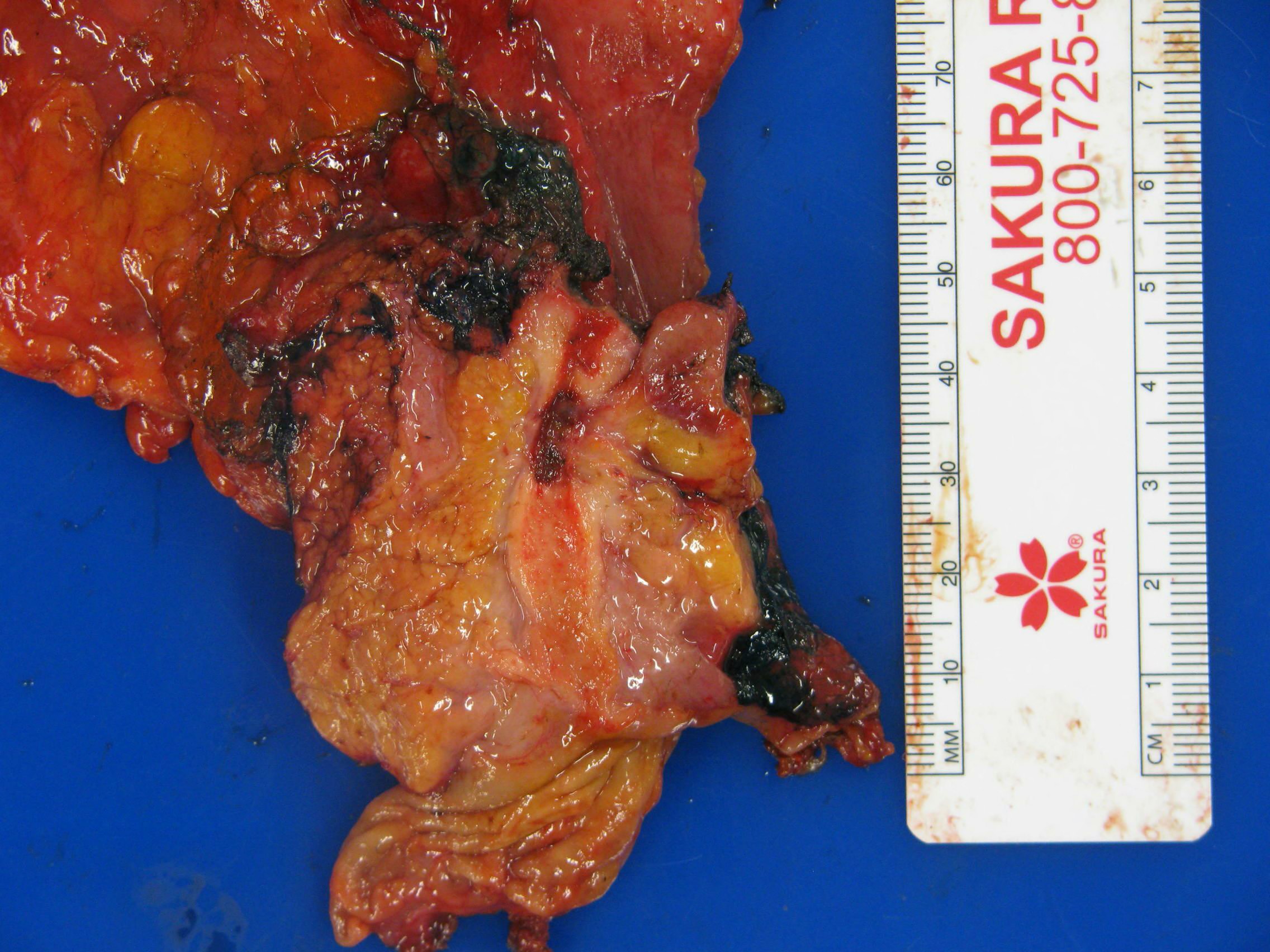
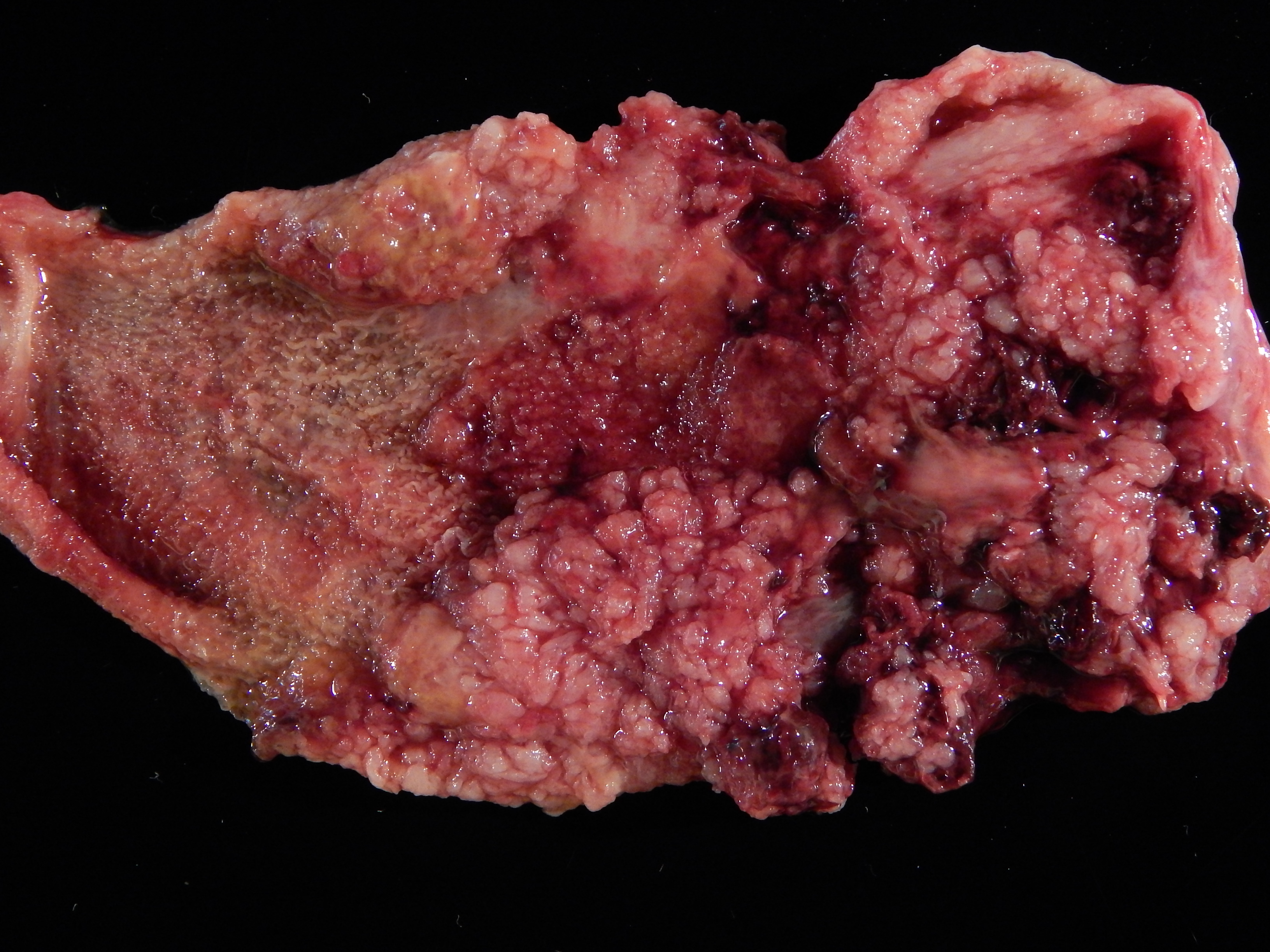
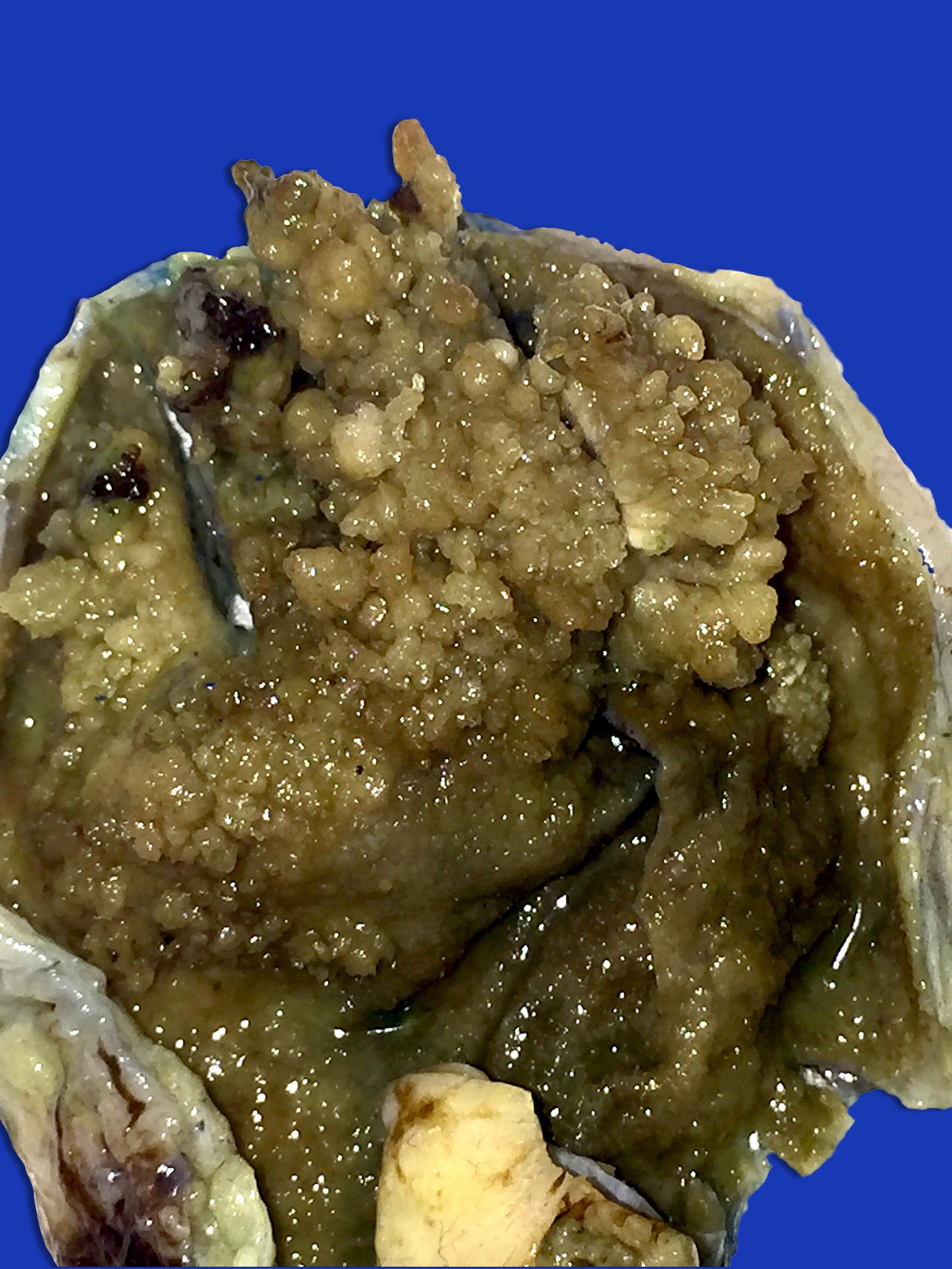
- Incidental gallbladder cancer in routine cholecystectomy specimens can be grossly subtle, with areas of mucosal granularity / irregularity, minimally raised / polypoid mucosal lesions or focally thickened fundus / body (Am J Surg Pathol 2019;43:1668)
- Frank tumors may have one or more of the following features:
- Thickened and indurated gallbladder wall
- Exophytic or polypoid friable mucosal lesions (especially those arising from intracholecystic papillary neoplasm)
- Firm, gritty, tan-white to yellow-gray cut surface
- Histologic variants recognized by WHO include:
- Biliary type adenocarcinoma (~75%):
- Similar to pancreatic ductal adenocarcinoma
- Includes adenocarcinoma, NOS (most common), papillary, micropapillary
- Composed of tubules (lined by cuboidal to columnar cells) embedded in a desmoplastic stroma
- Moderately differentiated is more common but has a wide histologic spectrum, from deceptively bland to poorly differentiated
- Intestinal type adenocarcinoma:
- Tubules lined by columnar cells with elongated hyperchromatic nuclei, very similar to colonic adenocarcinomas
- Mucinous carcinoma:
- Comprised of > 50% extracellular mucin
- Clear cell carcinoma:
- Sheets of clear cells in an alveolar arrangement separated by blood vessels, similar in appearance to metastatic clear cell renal carcinoma
- Signet ring cell carcinoma:
- Signet ring cells are the predominant or exclusive component
- Hepatoid carcinoma:
- > 50% with abundant eosinophilic cytoplasm, enlarged nuclei and prominent nucleoli arranged in a trabecular pattern
- Sarcomatoid carcinoma (carcinosarcoma):
- Predominant spindle cell morphology with or without heterologous differentiation (e.g. skeletal muscle, bone and cartilage)
- Biliary type adenocarcinoma (~75%):
- Differentiation
- Well differentiated:
- Well formed glands lined by columnar cells with minimal cytologic abnormality
- Glands in perimuscular connective tissue, nuclear irregularities and mitoses may be the only clues
- Desmoplasia may be subtle
- Moderately differentiated:
- Irregular / angulated glands lined by polygonal tumor cells with enlarged nuclei showing vesicular chromatin, prominent nucleoli and increased mitoses
- Desmoplasia is usually prominent
- Poorly differentiated:
- Incomplete or poorly formed tubules / glands, single cells or sheets of pleomorphic tumor cells with bizarre nuclei
- Well differentiated:
- CK7 (strong and diffuse) (Arch Pathol Lab Med 2000;124:1196), p53 (majority), CEA and CA19-9 (70 - 90%), IMP3 (80%) (Arch Pathol Lab Med 2017;141:1155), Maspin (60 - 100%), S100P and MUC1 (75%), HER2 (> 60%), CK20 and CDX2 (focal)
- Hep par1 and alpha-fetoprotein (AFP) (Positive in hepatoid variant)
- p16 (not expressed in a majority of cases akin to normal gallbladder) (Hepatogastroenterology 2010;57:18)
- PAX8, CD10 and CAIX
- Common genetic alterations include TP53 (seen in > 50% of cases), CDKN2A (20%), ARID1A (13%), PIK3CA (10%) and CTNNB1 (10%) (WHO Classification of Tumours Editorial Board: Digestive System Tumours (Medicine), 5th Edition, 2019)
- Amplifications of ERBB2 (HER2) have been reported in 16% of cases and microsatellite instability (MSI) in 10% of cancers, both of which have therapeutic implications (Cancer 2016;122:3838, Histopathology 2009;55:218)
- A higher KRAS mutation rate is noted in lesions related to pancreatobiliary maljunction (Hum Pathol 1999;30:21)
Extended cholecystectomy
- Gallbladder; cholecystectomy:
- Invasive adenocarcinoma, moderately differentiated, biliary type (2.7 cm in largest dimension), arising in a background of extensive high grade biliary intraepithelial neoplasia (BilIN).
- Adenocarcinoma invades perimuscular connective tissue on the peritoneal side, without involvement of the serosa (visceral peritoneum).
- Cystic duct margin is free from biliary intraepithelial neoplasia (BilIN) or carcinoma.
- One lymph node, negative for carcinoma (0/1).
- Lymphovascular invasion is not identified.
- pT2a, N0, M-not applicable (AJCC 8th edition). Please see synoptic report
- Background gallbladder with chronic cholecystitis.
- Cholelithiasis.
- Pancreatic ductal adenocarcinoma:
- Cholangiocarcinoma (both intrahepatic and extrahepatic):
- Epicenter in the bile ducts; CK19+
- Colonic adenocarcinoma:
- Epicenter in the colon, intestinal phenotype, CK20 strong and diffuse
- A 58 year old woman presents with right upper quadrant pain. Imaging reveals a polypoid lesion in the gallbladder. Patient undergoes cholecystectomy. Pathology shows the finding seen in the image above. Which of the following is true about this entity?
- Has aggressive dissemination potential
- Has a more favorable prognosis than conventional nonpapillary gallbladder adenocarcinomas
- Immunoreactive to hepatocellular markers
- Is not detected early on imaging
Comment Here
Reference: Gallbladder carcinoma
- What is the amount of extracellular mucin needed to diagnose a mucinous adenocarcinoma of the gallbladder?
- > 25%
- > 30%
- > 50%
- > 90%
- What are actionable molecular targets in the treatment of advanced GBCs?
- HER2 and MSI
- KRAS and ARID1A
- TP53 and CDKN2A
- PIK3CA and CTNNB1 (beta-catenin)
- p16
- Occurs in 15% of acute cholecystitis cases
- Mural infarction, with perforation in 25%
- Associated with Clostridium perfringens and air in gallbladder (pneumobilia)
- High mortality rate
- 79 year old man with acute cholecystitis (J Med Case Rep 2011;5:199)
- Crohn's disease, fungi, Mycobacterium tuberculosis (Indian J Pathol Microbiol 2008;51:175), parasites, primary biliary cirrhosis
- 26 year old woman with abdominal and epigastric pain (Ann Saudi Med 2010;30:244)
- 33 year old woman with panperitonitis due to intestinal perforation and cholecystitis (World J Gastroenterol 2006;12:977)
-
Larger masses / carcinoma:
- Sample tumor thoroughly, margins, normal bile duct
- Submit several full thickness sections, including areas of deepest penetration
- Cystic duct margin, hepatic margin, extent of penetration into liver (if applicable)
- May want to submit entire specimen
- Submit margins separately, including hepatic margin (if liver tissue present)
Extrahepatic bile ducts:
- Click here for the frozen section procedure topic
- Optimally should have clinical data and serum AFP levels available
- Should know if specimen is from a mass
- Indication: presence of a polypoid mucosal lesion or a suspicious thickening of the gallbladder wall (Arch Pathol Lab Med 2005;129:1610)
- Tumor size and location
- Tumor histologic type and pattern
- Depth of invasion
- Number and size of tumor nodules
- Tumor extension to adjacent structures
- Status of resection margins (cystic duct, liver bed, other)
- Cystic duct involvement
- Liver bed involvement
- Regional lymph nodes: number identified, number with tumor
- Angiolymphatic invasion
- Perineural invasion
- Presence of carcinoma in situ or dysplasia
Additional pathologic findings to report:
- Chronic cholecystitis, metaplasia (squamous, pyloric gland, intestinal metaplasia), inflammatory bowel disease, porcelain gall bladder, presence or absence of stones (gallbladder cancer occurring without stones may be caused by anomalous choledochopancreatic junction or associated with chronic inflammatory bowel disease, Arch Pathol Lab Med 2000;124:37)
- Bile duct wall thickness, external surface, obstruction, stones
- Tumor size and location
- Tumor histologic type, pattern and grade
- Depth of invasion
- Number and size of tumor nodules
- Tumor extension to adjacent structures
- Status of resection margins
- Regional lymph nodes: number identified, number with tumor
- Angiolymphatic invasion
- Perineural invasion
- Presence of carcinoma in situ or dysplasia
- References: Arch Pathol Lab Med 2000;124:26, Arch Pathol Lab Med 2010;134:e8, CAP: Protocol for the Examination of Specimens From Patients With Carcinoma of the Distal Extrahepatic Bile Ducts [Accessed 8 February 2018]
- Distended gallbladder containing clear and watery (hydrops) or mucoid secretions (mucocele), instead of bile
- Adult cases almost always due to impacted stones in ampulla or cystic duct
- Rarely due to regional tumors causing compression
- Pediatric cases associated with Kawasaki syndrome or other inflammatory narrowing of cystic duct
- Mucoceles that perforate may cause pseudomyxoma peritonei
- 24 year old man with right upper quadrant pain with a palpable mass (Prilozi 2011;32:207)
- 31 year old woman with 10 year history of mild, episodic abdominal pain (N Engl J Med 2011;364:e43)
- Massive hydrops mimicking a choledochal cyst (J Pediatr Surg 2011;46:1015)
- Thickened gallbladder wall
- Fibrous replacement of muscular wall
- Rarely muciphages simulating signet ring cell adenocarcinoma
Children:
- Thin wall with flattened epithelium and sparse inflammation
- 15% of benign polyps
- Associated with chronic cholecystitis
- 69 year old man with inflammatory polyp mimicking early polypoid carcinoma (Case Rep Gastroenterol 2009;3:255)
- 3 - 15 mm, red gray brown, usually sessile and single
- Sessile mucosal projections with a surface of columnar epithelial cells covering a fibrous stroma with chronic inflammatory cells and lipid laden macrophages in granulation type tissue
- Grossly visible, mass forming, noninvasive epithelial neoplasm arising in the mucosa and projecting into the lumen of the gallbladder (Am J Surg Pathol 2012;36:1279, HPB (Oxford) 2015;17:811)
- First described in 2012 by Adsay et al. (Am J Surg Pathol 2012;36:1279)
- 2019 WHO recognizes as a distinct type of preinvasive neoplasm of gallbladder under the name of intracholecystic papillary neoplasm (ICPN)
- Exhibits many similarities to pancreatic intraductal papillary mucosal neoplasms as they demonstrate a spectrum of variable configurations, different cell lineages (often in a mixture) and dysplastic changes as well
- Seen in < 1% of all cholecystectomies (Am J Surg Pathol 2012;36:1279, Ann Diagn Pathol 2019;40:88, Int J Surg Pathol 2016;24:504, Best Pract Res Clin Gastroenterol 2013;27:285)
- Usually measures ≥ 1 cm in diameter
- Microscopically reveals papillary, tubular or tubulopapillary growth patterns
- 4 morphologic patterns (biliary, intestinal, gastric and oncocytic) are described
- May be associated with an invasive carcinoma
- Has relatively favorable overall outcome even if it is associated with an invasive carcinoma (Am J Surg Pathol 2012;36:1279, Ann Diagn Pathol 2019;40:88, Mol Clin Oncol 2019;11:488)
- Older terms (not recommended) are biliary adenoma, papillary adenoma, tubulopapillary adenoma, intracystic papillary neoplasm, intracholecystic papillary tubular neoplasm or papillary carcinoma
- Mean age is 61 (Am J Surg Pathol 2012;36:1279)
- F:M = 2:1 (Am J Surg Pathol 2012;36:1279)
- Seen in < 1% of all cholecystectomies (Am J Surg Pathol 2012;36:1279, Ann Diagn Pathol 2019;40:88; Int J Surg Pathol 2016;24:504, Best Pract Res Clin Gastroenterol 2013;27:285)
- More common in the fundus and body of the gallbladder (Int J Surg Pathol 2016;24:504, Ann Diagn Pathol 2019;40:88)
- No known etiologic factor
- No association with gallbladder stones
- Some are incidentally detected (Am J Surg Pathol 2012;36:1279, Ann Diagn Pathol 2019;40:88, Abdom Radiol (NY) 2018;43:1535)
- Others present with right upper quadrant pain (Am J Surg Pathol 2012;36:1279, Ann Diagn Pathol 2019;40:88)
- Characteristic imaging findings include contrast enhanced tumor on CT image and on MR cholangiopancreatography examination a tumor-like defect within the gallbladder with dilatation of the upstream bile duct (Clin J Gastroenterol 2019;12:197)
- Radiologically, half of them are misdiagnosed as gallbladder cancer (Am J Surg Pathol 2012;36:1279)
- Even ICPN associated invasive carcinomas are relatively indolent neoplasms with significantly better prognosis compared with conventional (pancreatobiliary type) gallbladder carcinomas (Am J Surg Pathol 2012;36:1279)
- Papillary configuration, biliary or foveolar phenotype and especially presence of high grade dysplasia are considered significant pathologic risk factors for associated invasive carcinoma (Am J Surg Pathol 2012;36:1279, Indian J Pathol Microbiol 2018;61:516)
- 58 year old woman with jaundice (Intern Med 2014;53:2313)
- 58 year old woman with fever (Mol Clin Oncol 2019;11:488)
- 59 year old man with anorexia (Clin J Gastroenterol 2019;12:197)
- 64 year old man with upper abdominal pain (Surg Case Rep 2016;2:62)
- 70 year old man with elevated liver function tests (Surg Case Rep 2018;4:124)
- Treated primarily by surgical resection
- Prominent exophytic growth within the gallbladder or granular, friable soft tan excrescences
- Friable excrescences loosely attached to the lumen may be mistaken as sludge or debris in the lumen and not adequately sampled during initial macroscopic examination
- Median tumor size is 2.2 cm
- May be solitary or multifocal
- Reference: Am J Surg Pathol 2012;36:1279
- Back to back epithelial units in papillary, tubular or tubulopapillary configuration with limited stroma (Am J Surg Pathol 2012;36:1279, Best Pract Res Clin Gastroenterol 2013;27:285)
- 4 morphologic patterns are recognized (Am J Surg Pathol 2012;36:1279, Hum Pathol 2012;43:1506, Appl Immunohistochem Mol Morphol 2020;28:57):
- Biliary phenotype: most common phenotype characterized by papillae lined by cuboidal cells with clear to eosinophilic cytoplasm and enlarged nuclei with distinct nucleoli; carries the highest risk for associated invasive carcinoma
- Gastric phenotype:
- Pyloric type:
- Intracholecystic neoplasms characterized by back to back mucinous glands with features characteristic of gastric pyloric glands were originally described as one of the subtypes of ICPN
- However, current (2019) WHO classifies these neoplasms as a distinct entity (i.e. pyloric gland adenoma)
- These carry the lowest risk for associated invasive carcinoma
- Foveolar type: large elongated glands lined by tall columnar mucinous epithelium with pale cytoplasm
- Pyloric type:
- Intestinal phenotype: morphologically similar to colonic adenoma showing pseudostratified cigar shaped nuclei and overall basophilia
- Oncocytic phenotype: least common subtype characterized by arborizing papillae that are lined by oncocytic cells (large, granular cytoplasm and prominent, large, eccentric nucleoli) with atypia
- 4 morphologic patterns are recognized (Am J Surg Pathol 2012;36:1279, Hum Pathol 2012;43:1506, Appl Immunohistochem Mol Morphol 2020;28:57):
- Mixed phenotypes are common
- Lesions histologically characterized by abundant cytoplasm, small and uniform nuclei and distinct nucleoli are classified as low grade dysplasia; those with architectural complexity as well as nuclear atypia have high grade dysplasia (Am J Surg Pathol 2012;36:1279)
- For the noninvasive cases, it is important to assess the presence and amount of high grade dysplasia
- Associated invasive carcinoma is detected in more than half of the cases at the time of diagnosis, mostly in lesions with biliary phenotype and high grade dysplasia (Am J Surg Pathol 2012;36:1279, Ann Diagn Pathol 2019;40:88)
- Associated invasive carcinoma is mostly pancreatobiliary type adenocarcinoma but other types of carcinomas, such as colloid or poorly differentiated neuroendocrine carcinoma, may also be seen (GE Port J Gastroenterol 2019;26:356, Surg Case Rep 2016;2:62)
- Invasive carcinoma may be grossly inapparent and may even occur away from the ICPN, therefore thorough sampling and careful microscopic evaluation are extremely important (Semin Diagn Pathol 2012;29:127)
- KRAS mutation is common (Hum Pathol 1999;30:21, Appl Immunohistochem Mol Morphol 2011;19:133)
- STK11, CTNNB1 and APC mutations are identified (Am J Surg Pathol 2019;43:783)
- TP53 and GNAS mutations are rare
- Gallbladder, cholecystectomy:
- Intracholecystic papillary neoplasm of gallbladder (ICPN), biliary type, with extensive high grade dysplasia (> 75% of the tumor) (see comment)
- Comment: The gallbladder was submitted entirely for microscopic evaluation and no invasive carcinoma is identified. The ICPN measures 3.5 cm in greatest dimension. Cystic duct margin is free of ICPN.
- Gallbladder, cholecystectomy:
- Invasive adenocarcinoma, moderately differentiated, colloid type, arising in an intracholecystic papillary neoplasm (ICPN), intestinal type, with high grade dysplasia (see comment)
- Comment: The entire tumor is 5.3 cm in greatest dimension; the invasive carcinoma component is 1.5 cm in greatest dimension. The carcinoma invades through the muscularis layer (pT2). Cystic duct margin is free of invasive carcinoma but reveals high grade dysplasia.
- Pyloric gland metaplasia:
- Not visible by gross examination or is smaller than 0.5 cm in greatest dimension
- Microscopically not well demarcated from surrounding mucosa
- Intracholecystic tubular nonmucinous neoplasms (ICTNs):
- Another type of preinvasive neoplasm of gallbladder, recently described by Pehlivanoglu et al. (Virchows Arch 2020 [Online ahead of print])
- Presents as a mass forming gallbladder neoplasm characterized by cauliflower-like architecture and is comprised of compact, back to back, small tubular units showing variable complexity
- Tubules are lined by low cuboidal, nonmucinous epithelium
- Nuclei are either round and have visible nucleoli or are more ovoid, overlapping and have optically clear chromatin, creating a picture highly reminiscent of papillary thyroid carcinoma
- Squamoid / meningothelial-like morules and neuroendocrine cell clusters are frequent
- Despite their cytoarchitectural complexity, they are not associated with invasive carcinoma
- Positive for MUC1 and MUC6 while negative for MUC2, CDX2 and MUC5AC
Which of the following is true about intracholecystic neoplasms of the gallbladder (ICPNs)?
- Jaundice is one of most common symptoms
- KRAS mutation is common
- Oncocytic phenotype is the most common subtype
- They are commonly seen in male patients
- They have a significantly worse prognosis compared with conventional gallbladder carcinomas
- CK7
- MUC1
- MUC2
- MUC5AC
- MUC6
- Noninvasive epithelial neoplasm of the gallbladder that forms pedunculated polyps composed exclusively of small, nonmucinous tubules, often with squamoid morules (Virchows Arch 2021;478:435)
- Despite the cytoarchitectural complexity that warrants high grade dysplasia diagnosis, almost never associated with invasion (Virchows Arch 2021;478:435)
- Pedunculated, typically solitary polyps with cauliflower architecture composed of lobules of back to back small acinar-like tubular units; possible association with cholesterol polyps
- Morules are common but can be subtle; they can be highlighted by beta catenin nuclear labeling
- Usually no dysplasia in the background gallbladder, uninvolved gallbladder is typically devoid of inflammation or chronic changes
- Virtually no association with invasive carcinoma (unlike other preinvasive neoplasia of the gallbladder) (Virchows Arch 2021;478:435)
- Does not appear to have field effect risk for biliary tract
- Previously regarded as complex pyloric nonmucinous type of intracholecystic papillary tubular neoplasms (Am J Surg Pathol 2012;36:1279, Ann Diagn Pathol 2019;40:88, Mod Pathol 2014;27:446A)
- Considered as a type of pyloric gland adenoma by some authors, along with pure and possibly hybrid (with both mucinous and nonmucinous components) pyloric gland adenomas (Am J Surg Pathol 2018;42:1237, Appl Immunohistochem Mol Morphol 2020;28:57, Virchows Arch 2008;453:521)
- Not defined as a distinct entity in WHO 2019; mentioned as intracholecystic papillary neoplasm showing gastric pyloric, nonmucinous morphology or presumably included in pyloric gland adenoma category
- Use of older terms, such as biliary adenoma, tubulopapillary adenoma or papillary carcinoma is not recommended
- No specific ICD code present; can be regarded under adenoma or intracholecystic papillary neoplasms
- ICD-O: 8503/2 - intracystic papillary neoplasm with high grade intraepithelial neoplasia
- Mean age = 51 (Virchows Arch 2021;478:435)
- F:M = 0.9:1 (Virchows Arch 2021;478:435)
- Detected in < 1% of cholecystectomies (Ann Diagn Pathol 2019;40:88, Am J Surg Pathol 2012;36:1279)
- Specific to gallbladder; neoplasms with some similarities occur in the pancreatobiliary tract and are called intraductal tubulopapillary neoplasms (Mod Pathol 2015;28:1249, Am J Surg Pathol 2017;41:313)
- Considering the WNT / beta catenin alterations along with the common presence of morules, may be regarded as a part of the so called BROCN family tumors (morule forming with biotin rich optically clear nuclei, namely fetal type pulmonary adenocarcinoma, pancreatoblastoma, cribriform morular thyroid carcinomas and some endometrial adenocarcinomas) (Mod Pathol 2003;16:1124, Mod Pathol 2002;15:617, J Pathol 2001;194:59, Am J Pathol 2001;159:1619)
- May be arising from cholesterol polyps (Virchows Arch 2021;478:435)
- No association with chronic cholecystitis or gallstones
- Discovered incidentally or may present with abdominal pain (Virchows Arch 2021;478:435)
- Polyp identified on imaging studies; histology is confirmed after resection
- Features suggestive of a gallbladder polyp / mass or mimicking gallstones (Virchows Arch 2021;478:435)
- Excellent prognosis (Virchows Arch 2021;478:435)
- Hybrid lesions with both ICTN morphology and mucinous areas may be associated with invasive carcinoma (Am J Surg Pathol 2012;36:1279)
- Should be classified as intracholecystic papillary neoplasm
- Proper sampling to exclude associated lesions or invasive carcinoma is warranted regardless, although both are rare
- 15 year old girl with recurrent right upper quadrant pain (J Pediatr Surg Case Rep 2017;25:46)
- 40 and 53 year old men presented with > 1 cm gallbladder polyps (J Gastrointest Oncol 2016;7:S81)
- 44 year old man with a polyp in the gallbladder (Gastroenterology 2011;141:e3)
- 61 year old woman with a pedunculated polyp in the gallbladder (Pathol Res Pract 1996;192:963)
- Simple cholecystectomy is deemed adequate for this tumor, follow up may be appropriate (Virchows Arch 2021;478:435, Am J Surg Pathol 2012;36:1279)
- Radical cholecystectomy is not indicated (Virchows Arch 2021;478:435)
- Most observed as detached intraluminal nodules or hemorrhagic debris / fibrin
- Typically present as pedunculated polyps with thin stalks
- Cauliflower architecture resembling cholesterol polyps
- Reference: Virchows Arch 2021;478:435
- Pedunculated polyps; nodular lesion in the lumen; the nodules often have normal epithelial covering
- Predominantly tubular, occasionally tubulopapillary architecture
- Compact, back to back small tubular units with minimal lumen
- Neoplastic cells have round nuclei with prominent nucleoli and scant cytoplasm
- Some show nuclei with washed out chromatin resembling papillary thyroid carcinoma
- Squamoid / meningothelial-like morules (> 60%)
- Amorphous amyloid-like hyalinization zones may be present in the stroma
- Cholesterolosis in the polyp and often in the uninvolved gallbladder
- Scattered neuroendocrine cells
- High grade dysplasia (HGD) by default of complexity but the background mucosa is typically devoid of any pathology, including dysplasia
- Usually no significant inflammation in the remaining gallbladder
- Lesions with a mucinous component should be evaluated separately
- Reference: Virchows Arch 2021;478:435
Contributed by Burcin Pehlivanoglu, M.D. and Volkan Adsay, M.D.
- MUC6: in virtually all cases and diffuse strong
- MUC1: variable, often focal
- Beta catenin: nuclear expression typically highlights squamoid morules and occasionally is diffuse in the lesional cells
- CDX2: occasionally positive, especially in squamoid morules (Virchows Arch 2021;478:435, Virchows Arch 2008;453:521)
- MUC5AC (rarely positive) (Virchows Arch 2021;478:435)
- MUC2
- Remains to be fully elucidated but may be associated with CTNNB1 mutations or pathway (Lab Invest 2018;98:687, Mod Pathol 2019;32:44, Virchows Arch 2021;478:435)
- Gallbladder, cholecystectomy:
- Intracholecystic tubular nonmucinous neoplasm (ICTN) (see comment)
- No dysplasia identified in the remainder of the gallbladder
- No invasive carcinoma is identified
- Cholesterolosis (if present)
- Comment: Although there is high grade dysplasia within the lesion, intracholecystic tubular nonmucinous neoplasm (ICTN) typically has an innocuous behavior and does not seem to bear any risk for invasive carcinoma in the gallbladder or biliary tract.
- Pyloric gland adenoma:
- Composed of mucinous cells forming glands, such as gastric pyloric type or Brunner-like mucinous glands
- Often multifocal and can be associated with invasive carcinoma
- Intracholecystic papillary neoplasm:
- Papillary configuration and in areas with tubule formation, which are common, either has mucinous characteristics or intestinal phenotype; cytologically different than ICTNs (Am J Surg Pathol 2012;36:1279, Best Pract Res Clin Gastroenterol 2013;27:285)
- May be of biliary, gastric, intestinal, oncocytic or mixed type (Am J Surg Pathol 2012;36:1279, Hum Pathol 2012;43:1506, Appl Immunohistochem Mol Morphol 2020;28:57)
- May show MUC5AC or MUC2 expression
- More than 50% have associated invasive carcinoma at the time of diagnosis (Am J Surg Pathol 2012;36:1279, Ann Diagn Pathol 2019;40:88, Int J Surg Pathol 2016;24:504)
Which of the following is true about intracholecystic tubular nonmucinous neoplasm (ICTN) of the gallbladder?
- Characterized by intestinal type neoplastic glands similar to colonic adenomas
- Commonly associated with diffuse high grade dysplasia in the background gallbladder; connotes high risk for entire biliary tract
- Squamoid morules that show beta catenin nuclear labeling are common
- Typically associated with invasive carcinoma
- Usually seen in gallbladders with severe chronic inflammation
Comment Here
Reference: Intracholecystic tubular nonmucinous neoplasm (ICTN)
- Intestinal differentiation
- Prominent papillary architecture
- Salt and pepper chromatin
- Squamoid or meningothelial-like morules
- Tubule forming cells with abundant mucin
Comment Here
Reference: Intracholecystic tubular nonmucinous neoplasm (ICTN)
- Uncommon
- Solitary or may spread along biliary tree to cystic duct or duodenal papilla
- May resemble intrapapillary mucinous neoplasms of pancreas as both arise within a dilated duct system and demonstrate predominantly intraductal growth
- Risk factor for cholangiocarcinoma, biliary obstruction, recurring ascending cholangitis
- Are often carcinomas (HPB (Oxford) 2009;11:684)
- p21, p53, cyclin D1, DPC4 are involved in neoplastic progression (Hum Pathol 2008;39:1153)
- Preinavsive neoplasms at least 1 cm (Am J Surg Pathol 2012;36:1279)
- Analogous to pancreatic (IPMN) and biliary counterparts
- Show variable cellular lineages with a spectrum of dysplasia, mixture of papillary or tubular growth patterns
- Relatively indolent behavior - better prognosis than pancreatobiliary type gallbladder carcinoma
- 67 year old woman with polypoid mass (Pathol Int 2010;60:516)
- Either polypoid, cast-like growth, superficial spreading or cystic type but does not correlate with prognosis (Abdom Imaging 2011;36:438)
- Papillary fronds with fine vascular cores
- Epithelial cells are either biliary type or have gastric or intestinal differentiation with goblet cells and Paneth cells
- Production of extracellular intraductal mucin less common than papillary IPMN
- Variants have oncocytic changes or cysts (Mod Pathol 2006;19:1243)
- Borderline tumor: mild to moderate nuclear atypia and nuclear pseudostratification limited to basal 2/3 of the epithelium
- Carcinoma: severe cytological atypia, loss of nuclear polarity or architectural cribriforming / papillary fusion is present
- MUC5AC, MUC6, claudin18 and HepPar1
- Variable CK20 (Hum Pathol 2002;33:503)
- Tumors with oncocytic changes have gastric phenotype (Hum Pathol 2009;40:1543), express Wnt pathway proteins beta catenin and E-cadherin (Pathology 2007;39:413)
- KRAS activating mutations (29%), 18q- (31%) but no loss of DPC4
- Often has microsatellite instability (Mod Pathol 2002;15:1309)
- Usually gastric or intestinal, rarely squamous
- Associated with older age, gallstones
- 53 year old woman with abdominal pain (South Med J 2009;102:322)
- Bone metaplasia in the gallbladder wall (Eksp Klin Gastroenterol 2011;(8):86)
- Infant with extrahepatic biliary atresia with cartilaginous metaplasia (J Clin Pathol 2008;61:965)
- 66 - 84% of cholecystectomy specimens
- Pyloric, antral or mucous glands
- Glands usually scattered in lamina propria but may extend into muscular layer
- May form polyps
- Don't call adenoma unless dysplasia present
Microscopic (histologic) images
Images hosted on other servers:
Positive stains
- Acid mucin positive (Acta Gastroenterol Latinoam 2007;37:11)
- Very common finding in cholecystectomy specimens (up to 86%, Sao Paulo Med J 2008;126:220)
- Goblet cells, endocrine cells, Paneth cells, absorptive cells
- Also pyloric gland metaplasia
- Rarely forms polyps
Case reports
- Case reports: 78 year old man and 62 year old woman (Gut 2001;48:719)
Microscopic (histologic) images
Images hosted on other servers:
Additional references
- 47 year old woman with gastric heterotopia and squamous metaplasia (Acta Gastroenterol Latinoam 2007;37:164)
- 56 year old woman with pseudoepidermoid cyst arising from exuberant squamous metaplasia (Arch Pathol Lab Med 2005;129:e138)
- Usually secondary to inflammatory disorders (chronic cholecystitis [5 - 20%] or cholelithiasis, adenomyomatous hyperplasia, primary sclerosing cholangitis, ulcerative colitis), cholesterolosis (up to 100%) or anomalous arrangement of pancreaticobiliary duct (40 - 90%)
- Diffuse or focal
- 12 year old girl with biliary colic (J Pediatr Surg 2001;36:1584)
- Primary diffuse papillary hyperplasia of gallbladder (Pathology 2006;38:591)
- Single layer of columnar epithelium in papillary mucosal folds, may be villiform
- Basal nuclei, no atypia
- Dense, paucicellular hyaline fibrosis transforming gallbladder wall into relatively thin and uniform band
- Diffusely effaces most of normal structure, some cases show calcifications
- Also called hyalinizing cholecystitis
- 0.5% of cholecystectomies - 20% of cases associated with gallbladder carcinoma
- Pearly white appearance due to dystrophic calcification
- Widely scattered and bland appearing glands embedded in thin band of hyaline stroma, commonly showing a disappearing lining, leaving behind granular, necrotic intraluminal debris (regression) with or without calcification (Am J Surg Pathol 2011;35:1104)
- Surface epithelium, if preserved, typically shows carcinoma in situ of either denuding or micropapillary types
- Glandular elements in wall should raise suspicion of carcinoma, since benign glands are usually sparse
- Carcinoma of gallbladder:
- Glands have longitudinal axis parallel to the surface, irregular contours, clear cytoplasm with distinct borders, nuclear irregularities, washed out chromatin
- Chronic cholestatic disorder of unknown origin (possibly autoimmune) involving entire biliary tract from ampulla of Vater to small intrahepatic bile ducts or gallbladder
- Much less common than secondary sclerosing cholangitis
- Rule of 70s: 70% men, 70% have chronic inflammatory bowel disease (particularly ulcerative colitis which is usually detected first; only 4% with ulcerative colitis have primary sclerosing cholangitis, which is unaffected by colectomy), 70% younger than age 45
- Also associated with chronic pancreatitis (15 - 25%), Riedel thyroiditis, retroperitoneal and mediastinal fibrosis, orbital pseudotumor, Sjögren syndrome, angioimmunoblastic lymphadenopathy
- End stage disease is associated with hyperplasia of glands of extrahepatic bile ducts, with low incidence of dysplasia and adenocarcinoma (Am J Surg Pathol 2003;27:349)
- Bile ducts in PSC show two distinct pathways of dysplasia-carcinoma, based on differences in cell morphology, growth patterns, immunophenotypes and grade of malignancy (Histopathology 2011;59:1100)
- Symptoms: fatigue, jaundice, pruritis
Complications:
- Biliary cirrhosis and liver failure in all cases with median survival 9 - 12 years
- Cholangiocarcinoma (10 - 43%), colon carcinoma
Staging:
- Inflammation without expansion of portal tracts or piecemeal necrosis
- Piecemeal necrosis or fibrosis without bridging
- Bridging necrosis or fibrosis
- Cirrhosis
- Elevated serum alkaline phosphatase, IgM, IgG
- Variable bilirubin
- May be pANCA positive
- Xray: beading of barium column in cholangiogram due to irregular strictures and dilations of affected bile ducts
- 17 year old boy (Diagn Cytopathol 2012;40:337)
- Liver transplant (Hum Pathol 2003;34:1127, Am J Surg Pathol 2007;31:907) since no effective medical therapy
- Periductal portal tract fibrosis, segmental stenosis of extrahepatic and intrahepatic bile ducts
- Fibrosing cholangitis of intra and extrahepatic bile ducts with lymphocytic infiltration
- Progressive atrophy of bile duct epithelium and obliteration of the lumen, diffuse bile ductular proliferation
- "Onion skin" fibrosis around affected ducts, which later disappear, leaving cord-like fibrous scar
- Remaining ducts are ectatic and inflamed
- Mild to florid hyperplasia often noted
- Recurrence after transplant exhibits bile duct structuring and nonspecific autoimmune hepatitis with variable fibrosis
- Variable portal eosinophils
- Sclerosing, well differentiated adenocarcinoma
- Grossly visible, noninvasive neoplasm of the gallbladder composed of uniform back to back mucinous glands arranged in a tubular configuration
- WHO classification
- Architecture is often complex
- Glands are bland looking pyloric type or Brunner gland-like
- There is minimal cytological atypia in most of the lesions
- By definition, the cytologic atypia is sufficient for low grade dysplasia
- Foci of high grade dysplasia can be seen in larger lesions
- If lesion is > 1 cm with dysplasia present, classification as intracholecystic papillary (tubular) neoplasm is recommended by some authors (Am J Surg Pathol 2012;36:1279)
- Grossly visible, complex, back to back, uniform mucinous glands of pyloric type or Brunner gland-like
- Usually > 0.5 cm and < 2 cm
- < 0.5 cm should be distinguished from nodular pyloric gland metaplasia, which by definition bears no cytologic atypia or dysplasia
- > 1 cm with dysplasia may be classified as intracholecystic papillary (tubular) neoplasm
- Intracholecystic papillary tubular neoplasm, gastric pyloric, simple mucinous type
- Found in 0.1 - 10% of gallbladders removed for cholelithiasis or chronic cholecystitis (Diagnostics (Basel) 2022;12:341, PLoS One 2020;15:e0237979, Adv Med 2018;2018:7539694)
- Accounts for ~82% of gallbladder adenomas (Hum Pathol 2012;43:1506)
- M = F (Am J Surg Pathol 2018;42:1237)
- Mean age of 62.8 years (Am J Surg Pathol 2018;42:1237)
- No specific site preference reported
- Can occur in the cystic duct with malignant transformation (BMC Cancer 2012;12:570)
- 50 - 65% associated with cholelithiasis (Hum Pathol 2012;43:1506)
- Commonly associated with pyloric gland metaplasia, which is possibly a precursor
- Usually asymptomatic and is an incidental finding
- When arising in the gallbladder neck, can lead to gallbladder distension and right upper quadrant pain
- Abdominal ultrasound is usually performed and shows polyps within the gallbladder (J Gastrointest Oncol 2016;7:S81)
- If invasive carcinoma is ruled out, pyloric gland adenoma is cured by cholecystectomy, even when high grade dysplasia is present
- 37 year old woman with dyspeptic complaints found to have a 2 cm polypoid lesion (Turk J Gastroenterol 2014;25:234)
- 40 and 53 year old men each presented with a 1 cm polyp (J Gastrointest Oncol 2016;7:S81)
- 44 year old man with upper abdominal pain found to have a 2 cm polyp (Gastroenterology 2011;141:e3)
- 62 year old man with a 2 cm tumor with transition into well differentiated adenocarcinoma and high grade biliary intraepithelial neoplasia (BMC Cancer 2012;12:570)
- Surgery (cholecystectomy) is indicated for any polypoid lesions ≥ 1 cm
- < 2 cm, sessile or pedunculated
- Usually single but can be multiple
- Tightly packed, bland looking pyloric type or Brunner gland-like glands (Histopathology 2018;72:1007)
- Lined by cuboidal or columnar mucus secreting cells with apical mucinous cytoplasm
- Round or oval, relatively small, hyperchromatic, basally located nuclei with a small round conspicuous nucleolus
- Slight nuclear overlapping and increased N:C ratios when compared to background normal glands
- High grade dysplasia features more complex architecture, prominent nucleoli and loss of nuclear polarity
- Some glands may be cystically dilated
- There is minimal or no intervening stroma
- Paneth cells and neuroendocrine cells are often present
- CK7 and MUC6 (diffuse and strong)
- Nuclear beta catenin reported (Am J Surg Pathol 2018;42:1237)
- MUC2, MUC5AC and CDX2 usually negative or only focally positive (Am J Surg Pathol 2018;42:1237)
- CTNNB1 mutations detected in 60% and 100% in 2 separate studies (Hum Pathol 1999;30:21, Am J Surg Pathol 2018;42:1237)
- KRAS mutation reported in a subset (Hum Pathol 1999;30:21, Am J Surg Pathol 2018;42:1237)
- TP53 and GNAS mutations usually not identified
- Gallbladder, cholecystectomy:
- Pyloric gland adenoma
- Gallbladder, cholecystectomy:
- Pyloric gland adenoma with focal high grade dysplasia
- Pyloric gland metaplasia:
- Size is the most important criteria; metaplasia is usually < 0.5 cm and does not form a discrete mass
- Intracholecystic papillary (tubular) neoplasm:
- Considered an umbrella term for any neoplastic polyps, adenomas and papillary neoplasms that are ≥ 1 cm
- Can be further divided into several categories by morphology
- Biliary, gastric, intestinal and oncocytic
- Pyloric gland adenoma is currently not included under this umbrella
- However, terms may be interchangeable between intracholecystic papillary (tubular) neoplasm and pyloric gland adenomas that are ≥ 1 cm with invasive carcinoma
A polypoid lesion of the gallbladder is identified by ultrasound and is resected. Based on the photomicrograph above, which of the following statements is true?
- Aberrant expression of CDX2 is a frequent feature
- Frequently shows MUC5AC positivity
- It is a precursor lesion for most of the gallbladder adenocarcinomas
- Occurs predominantly in males
- Usually CK7 positive
Comment Here
Reference: Pyloric gland adenoma
- Frequently shows p53 aberrant expression
- Lesions > 1 cm can be reclassified as intracholecystic papillary neoplasm
- They are not associated with chronic cholecystitis
- Those are benign lesions and never progress to cancer
Comment Here
Reference: Pyloric gland adenoma
- All carcinomas of the distal common bile duct (with an epicenter between the cystic duct / common hepatic duct confluence and the ampulla of Vater), including poorly differentiated neuroendocrine carcinomas, are covered by this staging system
- Cystic duct lesions are staged using the gallbladder template and common hepatic duct lesions are staged using the perihilar template
- AJCC, 7th Edition staging was sunset on December 31, 2017; as of January 1, 2018, use of the AJCC, 8th Edition, 2018 is mandatory
- These lesions are generally referred to as adenocarcinoma, rather than cholangiocarcinoma
- C24.0: malignant neoplasm of extrahepatic bile duct
- NX: regional lymph nodes cannot be assessed
- N0: no regional lymph node metastasis
- N1: metastasis in one to three regional lymph nodes
- N2: metastasis in four or more regional lymph nodes
- Notes: regional lymph nodes include the common bile duct, hepatic artery, anterior and posterior pancreaticoduodenal and right lateral superior mesenteric artery nodes
- M0: no distant metastasis
- M1: distant metastasis
- Stage 0:Tis N0 M0
- Stage I:T1 N0 M0
- Stage IIA:T1 N1 M0
- T2 N0 M0
- Stage IIB:T2 N1 M0
- T3 N0 - 1 M0
- Stage IIIA:T1 - 3 N2 M0
- Stage IIIB:T4 N0 - 2 M0
- Stage IVB:any T any N M1
- Tumor location: cystic duct, perihilar bile ducts or distal bile duct
- CEA
- CA19-9
- GX: grade cannot be assessed
- G1: well differentiated
- G2: moderately differentiated
- G3: poorly differentiated
- Adenocarcinoma, biliary type
- Adenocarcinoma, intestinal type
- Adenocarcinoma, gastric foveolar type
- Mucinous adenocarcinoma
- Clear cell adenocarcinoma
- Signet ring cell carcinoma
- Squamous cell carcinoma
- Adenosquamous carcinoma
- Undifferentiated carcinoma
- Neuroendocrine carcinoma
- Small cell neuroendocrine carcinoma
- Large cell neuroendocrine carcinoma
- Mixed adenoneuroendocrine carcinoma
- Intraductal papillary neoplasm with an associated invasive component
- Mucinous cystic neoplasm with an associated invasive component
- R0: complete resection with grossly and microscopically negative margins of resection
- R1: grossly negative but microscopically positive margins of resection
- R2: grossly and microscopically positive margins of resection
- pT1
- pT2
- pT3
- pT4
- All carcinomas of the gallbladder and cystic duct, including poorly differentiated neuroendocrine carcinomas, are covered by this staging system
- Well differentiated neuroendocrine tumors at this location are extremely rare and have no AJCC staging system
- AJCC 7th edition staging was sunset on December 31, 2017; as of January 1, 2018, use of the 8th edition is mandatory
- C23: Malignant neoplasm of gallbladder
- TX: primary tumor cannot be assessed
- T0: no evidence of primary tumor
- Tis: carcinoma in situ
- T1: tumor invades lamina propria or muscular layer
- T1a: tumor invades lamina propria
- T1b: tumor invades muscular layer
- T2: tumor invades the perimuscular connective tissue on the peritoneal side, without involvement of the serosa (visceral peritoneum) or tumor invades the perimuscular connective tissue on the hepatic side, with no extension into the liver
- T2a: tumor invades the perimuscular connective tissue on the peritoneal side, without involvement of the serosa (visceral peritoneum)
- T2b: tumor invades the perimuscular connective tissue on the hepatic side, with no extension into the liver
- T3: tumor perforates the serosa (visceral peritoneum) or directly invades the liver or one other adjacent organ or structure, such as the stomach, duodenum, colon, pancreas, omentum or extrahepatic bile ducts
- T4: tumor invades the main portal vein or hepatic artery or invades two or more extrahepatic organs or structures
- NX: Regional lymph nodes cannot be assessed
- N0: No regional lymph node metastasis
- N1: Metastasis in 1 - 3 regional lymph nodes
- N2: Metastasis in 4 or more regional lymph nodes
Note:
- Regional lymph nodes include the common bile duct, hepatic artery, portal vein and cystic duct nodes
- M0: no distant metastasis
- M1: distant metastasis
| Stage 0: | Tis | N0 | M0 | |
| Stage I: | T1 | N0 | M0 | |
| Stage IIA: | T2a | N0 | M0 | |
| Stage IIB: | T2b | N0 | M0 | |
| Stage IIIA: | T3 | N0 | M0 | |
| Stage IIIB: | T1-3 | N1 | M0 | |
| Stage IVA: | T4 | N0-1 | M0 | |
| Stage IVB: | any T | N2 | M0 | |
| any T | any N | M1 |
- Specimen type
- Extent of liver resection
- Free peritoneal side versus hepatic side for T2 tumors
- GX: grade cannot be assessed
- G1: well differentiated
- G2: moderately differentiated
- G3: poorly differentiated
- Adenocarcinoma, biliary type
- Adenocarcinoma, intestinal type
- Adenocarcinoma, gastric foveolar type
- Mucinous adenocarcinoma
- Clear cell adenocarcinoma
- Signet ring cell carcinoma
- Squamous cell carcinoma
- Adenosquamous carcinoma
- Undifferentiated carcinoma
- Neuroendocrine carcinoma
- Small cell neuroendocrine carcinoma
- Large cell neuroendocrine carcinoma
- Mixed adenoneuroendocrine carcinoma
- Intraductal papillary neoplasm with an associated invasive component
- Mucinous cystic neoplasm with an associated invasive component
- R0: complete resection with grossly and microscopically negative margins of resection
- R1: grossly negative but microscopically positive margins of resection
- R2: grossly and microscopically positive margins of resection
- pT1
- pT2
- pT3
- pT4
- All carcinomas of the perihilar bile ducts (arising predominantly in the main lobar extrahepatic bile ducts, distal to segmental bile ducts and proximal to the cystic duct), including poorly differentiated neuroendocrine carcinomas, are covered by this staging system
- Cystic duct lesions are staged using the gallbladder template and common bile duct lesions are staged using the distal bile duct template
- AJCC, 7th Edition staging was sunset on December 31, 2017; as of January 1, 2018, use of the AJCC, 8th Edition, 2018 is mandatory
- AJCC advocates the term cholangiocarcinoma for adenocarcinomas of this region
- C24.0: malignant neoplasm of extrahepatic bile duct
- TX: primary tumor cannot be assessed
- T0: no evidence of primary tumor
- Tis: carcinoma in situ / high grade dysplasia
- T1: tumor confined to the bile duct, with extension up to the muscle layer or fibrous tissue
- T2: tumor invades beyond the wall of the bile duct to surrounding adipose tissue or tumor invades adjacent hepatic parenchyma
- T2a: tumor invades beyond the wall of the bile duct to surrounding adipose tissue
- T2b: tumor invades adjacent hepatic parenchyma
- T3: tumor invades unilateral branches of the portal vein or hepatic artery
- T4: tumor invades the main portal vein or its branches bilaterally or the common hepatic artery; or unilateral second order biliary radicles with contralateral portal vein or hepatic artery involvement
- NX: regional lymph nodes cannot be assessed
- N0: no regional lymph node metastasis
- N1: one to three positive lymph nodes typically involving the hilar, cystic duct, common bile duct (choledochal), hepatic artery, posterior pancreatoduodenal and portal vein lymph nodes
- N2: four or more positive lymph nodes from the sites described for N1
- Notes: regional lymph nodes are listed above, in the N1 criteria
- M0: no distant metastasis
- M1: distant metastasis
- Stage 0:Tis N0 M0
- Stage I:T1 N0 M0
- Stage II:T2a - b N0 M0
- Stage IIIA:T3 N0 M0
- Stage IIIB:T4 N0 M0
- Stage IIIC:any T N1 M0
- Stage IVA:any T N2 M0
- Stage IVB:any T any N M1
- Tumor location and extent according to Bismuth-Corlette classification:
- I: tumor is limited to the common hepatic duct, below the level of the confluence of the right and left hepatic ducts
- II: tumor involves the confluence of the right and left hepatic ducts
- IIIa: tumor with type II involvement plus extension to the right second order ducts
- IIIb: tumor with type II involvement plus extension to the left second order ducts
- IV: tumor extends into both right and left second order ducts
- Papillary histology (improved prognosis)
- Primary sclerosing cholangitis
- GX: grade cannot be assessed
- G1: well differentiated
- G2: moderately differentiated
- G3: poorly differentiated
- Adenocarcinoma, biliary type
- Adenocarcinoma, intestinal type
- Adenocarcinoma, gastric foveolar type
- Mucinous adenocarcinoma
- Clear cell adenocarcinoma
- Signet ring cell carcinoma
- Squamous cell carcinoma
- Adenosquamous carcinoma
- Undifferentiated carcinoma
- Neuroendocrine carcinoma
- Small cell neuroendocrine carcinoma
- Large cell neuroendocrine carcinoma
- Intraductal papillary neoplasm with an associated invasive component
- Mucinous cystic neoplasm with an associated invasive component
- R0: complete resection with grossly and microscopically negative margins of resection
- R1: grossly negative but microscopically positive margins of resection
- R2: grossly and microscopically positive margins of resection
- Clear cell
- Mucinous
- Papillary
- Tubular
- Nonneoplastic, disorganized proliferation of normal nerve components at the site of previously damaged peripheral nerves
- Commonly seen after gallbladder surgery (i.e., cholecystectomy)
- Usually asymptomatic but can present with obstructive jaundice and a solitary mass, mimicking malignancy
- Appears as firm, gray-white mass or multiple nodules at the nerve stump
- Histologically, appears as haphazard proliferation of normal nerve components
- Amputation neuroma
- Patients who have had prior gallbladder or biliary surgery
- No predilection for gender or age
- Found incidentally in up to 10% of autopsies with prior cholecystectomy (Am Surg 1999;65:47)
- Gallbladder
- Extrahepatic bile ducts
- Commonly seen in cystic duct stump
- Gallbladder or bile duct nerve fibers become damaged after procedures, inflammatory processes or trauma
- Proximal and distal stumps of nerves are not reapproximated or a distal nerve stump is not present (Goldblum: Enzinger and Weiss's Soft Tissue Tumors, 7th Edition, 2020)
- Proximal nerve stump attempts to regenerate resulting in disorganized proliferation of normal nerve components, including nerve fibers, Schwann cells and perineural cells arranged in fascicles
- Presents after surgery or procedure (i.e., laparoscopic or open cholecystectomy, biliary surgery for cholangiocarcinoma, liver transplantation, gallbladder biopsy)
- Can arise without prior surgery (e.g., inflammation) (Acta Med Okayama 1996;50:273)
- Most are asymptomatic without any specific physical examination findings
- Can present with right upper quadrant pain, obstructive jaundice, ascending biliary cholangitis (upper abdominal pain, fever, jaundice) and mass (Ann Hepatobiliary Pancreat Surg 2019;23:282)
- Symptoms can present decades after the initial injury
- Abdominal ultrasound (Abdom Imaging 2008;33:560)
- CT
- MRI
- Magnetic resonance cholangiopancreatography (MRCP)
- Endoscopic retrograde cholangiopancreatography (ERCP) / endoscopic ultrasound
- Normal liver transaminases, bilirubin and tumor markers
- If causing obstructive jaundice, may have elevated bilirubin
- Can have elevated CA19-9, raising concern for biliary malignancy (South Med J 2003;96:89)
- Leukocytosis, elevated bilirubin if associated with ascending cholangitis (Ann Hepatobiliary Pancreat Surg 2019;23:282)
- Abdominal ultrasound: mildly echogenic mass (Abdom Imaging 2008;33:560)
- Contrast enhanced CT: enhancing mass near bile ducts, can increase in size compared to prior exams
- T2 weighted MRI: high intensity nodule with low intensity capsule, dilatation of bile ducts
- T1 weighted MRI: homogenously enhanced nodule isointense to aorta
- Solitary mass or multiple nodules if nerve plexus is affected
- May see biliary structure with proximal dilatation of ducts
- Radiographically similar to cholangiocarcinoma, periampullary tumors, metastatic lymph nodes if at level of hilum (Int J Surg Case Rep 2017;39:123)
- Favorable prognosis
- Symptoms usually resolve after surgical resection
- 41 year old man with acute cholangitis 10 years after open cholecystectomy (Ann Hepatobiliary Pancreat Surg 2019;23:282)
- 69 year old woman with hilar traumatic neuroma masquerading as Klatskin tumor (Trop Gastroenterol 2015;36:54)
- 72 year old man with traumatic neuroma of cystic duct mimicking duodenal subepithelial tumor (World J Clin Cases 2020;8:3821)
- 76 year old man with obstructive jaundice 1 year after cholecystectomy (Clin Case Rep 2021;9:e04619)
- Surgical resection is curative
- Circumscribed, firm gray-white rubbery mass (Goldblum: Enzinger and Weiss's Soft Tissue Tumors, 7th Edition, 2020)
- Solitary mass or multiple nodules if nerve plexus is affected
- < 5 cm in diameter
- Located at end of proximal nerve
- Disordered proliferation of nerve fascicles composed of axons, surrounded by Schwann cells and perineural cells within collagenous stroma (Goldblum: Enzinger and Weiss's Soft Tissue Tumors, 7th Edition, 2020)
- Fascicles are less myelinated than normal nerve
- Collagenous stroma may demonstrate inflammatory or myxoid change if subjected to repeat trauma or infection
- Perineural fibrosis
Contributed by Naziheh Assarzadegan, M.D., Saba Hassan, M.B.B.S. and Kristin Olson, M.D. (Case #329)
- EMA and GLUT1: perineural cells (Mod Pathol 2003;16:293)
- CD34: endoneurium
- S100: stains surrounding Schwann cells
- Bile duct, excision:
- Portion of bile duct with benign traumatic neuroma; no malignancy seen (see comment)
- Comment: The patient's history of obstructive jaundice, biliary stricture, perihilar mass and previous cholecystectomy is noted. Histological examination reveals a benign haphazard proliferation of nerve fascicles in the fibromuscular layer of the bile duct, features consistent with a postcholecystectomy traumatic neuroma. The lesion focally displays areas of nuclear palisading and we considered the possibility of a benign nerve sheath tumor such as plexiform schwannoma. However, the lesion lacks encapsulation and has interspersed, normal appearing nerves. Immunostains show that the lesional cells are immunoreactive with S100 protein and SOX10. Ki67 proliferation index is not increased. EMA highlights the perineurium. CD34 highlights the myofibroblasts. Traumatic neuromas are a rare, nonneoplastic cause of long distance bile duct stenosis and progressive jaundice; in particular, in patients with a history of cholecystectomy or surgical history in this abdominal region.
- References: Hepatogastroenterology 2004;51:39, Visc Med 2021;37:226
- Cholangiocarcinoma:
- Both can present with biliary stricture and obstructive jaundice
- Composed of malignant glands, not normal components of peripheral nerve
- Schwannoma (Stanford University: Traumatic Neuroma [Accessed 5 May 2022]):
- No prior trauma or surgery
- Encapsulated
- Proliferation of Schwann cells and axons
- Rare axons, which are subcapsular
- Antoni A and Antoni B areas
- Verocay bodies
- Neurofibroma:
- No prior trauma or surgery
- Infiltrates into soft tissue
- Proliferation of Schwann cells and axons
- Rare axons
Comment Here
Reference: Traumatic neuroma
- Large, heterogeneous mass with fascicles of uniform spindle cells with frequent mitoses and areas of coagulative necrosis in vascularized, myxoid to collagenous stroma
- Well circumscribed, encapsulated, tan-gray mass with spindle cells arranged in biphasic hypercellular and hypocellular areas with diffuse staining of S100 and SOX10
- Well circumscribed, gray-white mass with haphazard proliferation of benign nerve fascicles
- Well circumscribed, nonencapsulated, tan-gray mass with haphazard spindle cells, mast cells, rare axons in shredded carrot collagenous stroma with hypocellular and myxoid areas
Comment Here
Reference: Traumatic neuroma
- WHO classification of tumors of the gallbladder and extrahepatic bile ducts
- Currently on 5th edition, published in 2019
- Based on histologic appearance, not molecular characteristics
-
Benign epithelial tumors and precursors ICD-O codes
- Adenoma, NOS 8140/0
- Biliary intraepithelial neoplasia, low grade 8148/0
- Biliary intraepithelial neoplasia, high grade 8148/2
- Intracystic papillary neoplasm with low grade intraepithelial neoplasia 8503/0
- Intracystic papillary neoplasm with high grade intraepithelial neoplasia 8503/2
- Intracystic papillary neoplasm with associated invasive carcinoma 8503/3
- Intraductal papillary neoplasm with low grade intraepithelial neoplasia 8503/0
- Intraductal papillary neoplasm with high grade intraepithelial neoplasia 8503/2
- Intraductal papillary neoplasm with associated invasive carcinoma 8503/3
-
Malignant epithelial tumors ICD-O codes
- Adenocarcinoma, NOS: gallbladder extrahepatic bile ducts8140/3
- Adenocarcinoma, intestinal type 8144/3
- Clear cell adenocarcinoma, NOS 8310/3
- Mucinous cystic neoplasm with associated invasive carcinoma 8470/3
- Mucinous adenocarcinoma 8480/3
- Poorly cohesive carcinoma 8490/3
- Intracystic papillary neoplasm with associated invasive carcinoma 8503/3
- Squamous cell carcinoma, NOS 8070/3
- Carcinoma, undifferentiated, NOS 8020/3
- Adenosquamous carcinoma 8560/3
- Cholangiocarcinoma 8160/3
- Neuroendocrine tumor, NOS 8240/3
- Neuroendocrine tumor, grade 1 8240/3
- Neuroendocrine tumor, grade 2 8249/3
- Neuroendocrine tumor, grade 3 8249/3
- Neuroendocrine carcinoma, NOS 8246/3
- Large cell neuroendocrine carcinoma 8013/3
- Small cell neuroendocrine carcinoma 8041/3
- Mixed neuroendocrine - nonneuroendocrine neoplasm (MiNEN) 8154/3
- Unusual histologic variant of chronic cholecystitis
- Infiltration of foamy histiocytes and fibrosis in the background of chronic active inflammation
- Xanthogranulomatous cholecystitis (XGC), in clinical and radiologic findings, can frequently mimic gallbladder cancer
- Pathologic findings are quite characteristic with foamy histiocytes, fibrosis and chronic active inflammation; when XGC is confused with gallbladder cancer, frozen examination can be useful in excluding malignancy
- 0.7 - 10% of examined resected gallbladders (Gastroenterol Res Pract 2014;2014:253645)
- Usually ages 60 - 70; rarely children and young adults (World J Radiol 2016;8:183)
- Typically associated with gallstones (Lancet 1988;2:931)
- Increased intraluminal pressure due to obstruction of bile flow (various etiologies: gallstone, cancer, etc.) ⇢ rupture of Rokinstanky-Aschoff sinuses ⇢ bile spillage ⇢ inflammatory reaction (Gastroenterol Res Pract 2014;2014:253645, World J Radiol 2016;8:183)
- Gallstones
- Patients' symptoms manifest as acute cholecystitis
- XGC is usually diagnosed with histopathologic examination
- Radiologic imaging, including computed tomography, ultrasonography and magnetic resonance imaging, can be helpful but are limited for diagnosis
- 15 year old boy with abdominal pain (Clin Gastroenterol Hepatol 2016;14:A29)
- 63 year old woman with suspected gallbladder tumor (Int J Surg Case Rep 2014;5:138)
- 64 year old man with multiple liver abscesses (J Surg Case Rep 2018;2018:rjy337)
- Cholecystectomy
- Irregular thickening of the gallbladder wall with multiple yellow nodules
- Round to spindled shaped, lipid laden macrophages, giant cells and proliferative fibrosis in the background of chronic active inflammation (lymphocytes, plasma cells, neutrophils and eosinophils)
- Transmural inflammation, mural and extramural inflammatory nodule
- Small foci of xanthomatous inflammation associated with chronic cholecystitis cannot be qualified as XGC
- Reference: World J Radiol 2016;8:183
- Cytokeratin may be needed to exclude carcinoma of the gallbladder
- Gallbladder, cholecystectomy:
- Xanthogranulomatous cholecystitis
- Gallbladder adenocarcinoma with signet ring cell features:
- Cytokeratin staining is helpful
- Malakoplakia:
- Histiocytes with Michaelis-Gutmann bodies that are positive for PAS and von Kossa stains (Odze: Surgical Pathology of the GI Tract, Liver, Biliary Tract and Pancreas, 3rd Edition, 2014)
- Hemophagocytosis
- Malakoplakia
- Rosai-Dorfmann disease
- Signet ring cell carcinoma
- Xathogranulomatous cholecystitis
Comment Here
Reference: Xanthogranulomatous cholecystitis
A 63 year old patient visited the hospital with upper quadrant abdominal pain. Gallbladder cancer was strongly suspected in preoperative computed tomography. After the operation, histologic examination showed the findings in the image above. What is the best diagnosis?
- Acute emphysematous cholecystitis
- IgG4 related cholecystitis
- Mycobacterial infection
- Signet ring cell carcinoma
- Xanthogranulomatous cholecystitis
Comment Here
Reference: Xanthogranulomatous cholecystitis
Find related Pathology books: GI, liver