Superpage
Superpage Topics
Acute antibody mediated rejection including hyperacute rejection
Acute hepatitis-general
Acute T cell mediated rejection
Adenovirus hepatitis
Alagille syndrome
Alcoholic liver disease
Alpha-1 antitrypsin deficiency
Amiodarone
Anatomy
Angiomyolipoma
Angiosarcoma
Arterial disorders
Ascending cholangitis
Ascites
Autoimmune cholangitis
Autoimmune hepatitis
Benign recurrent intrahepatic cholestasis
Bile duct adenoma
Biliary adenofibroma
Biopsy
Budd-Chiari syndrome
Calcifying nested stromal epithelial tumor
Cardiac (congestive) hepatopathy and Fontan associated liver disease
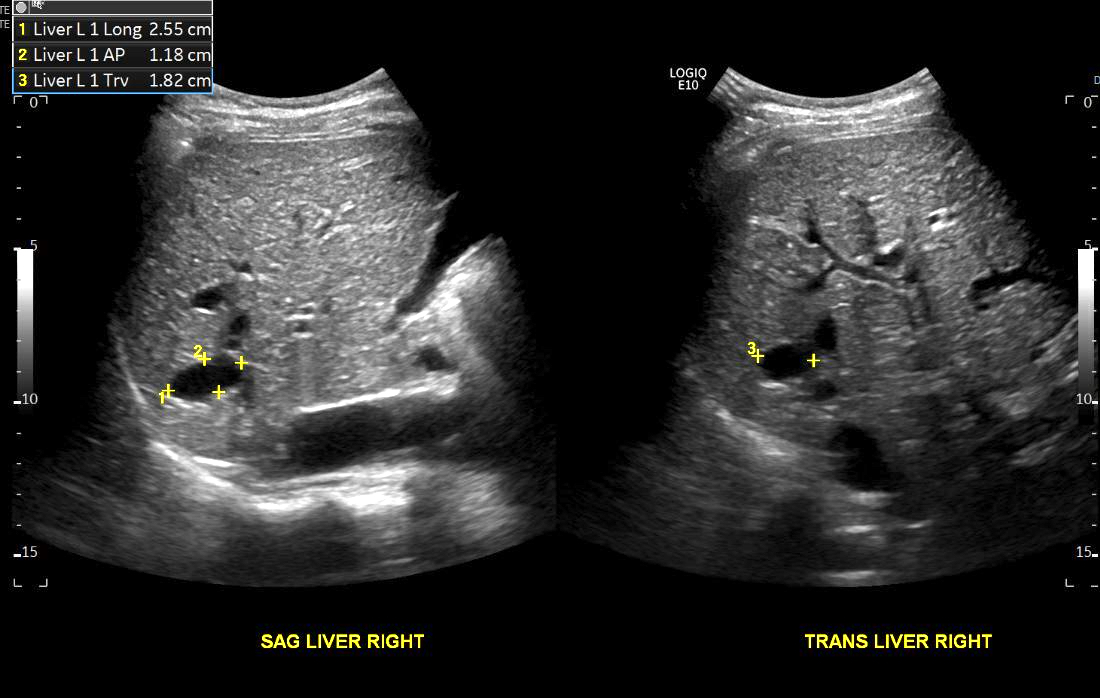
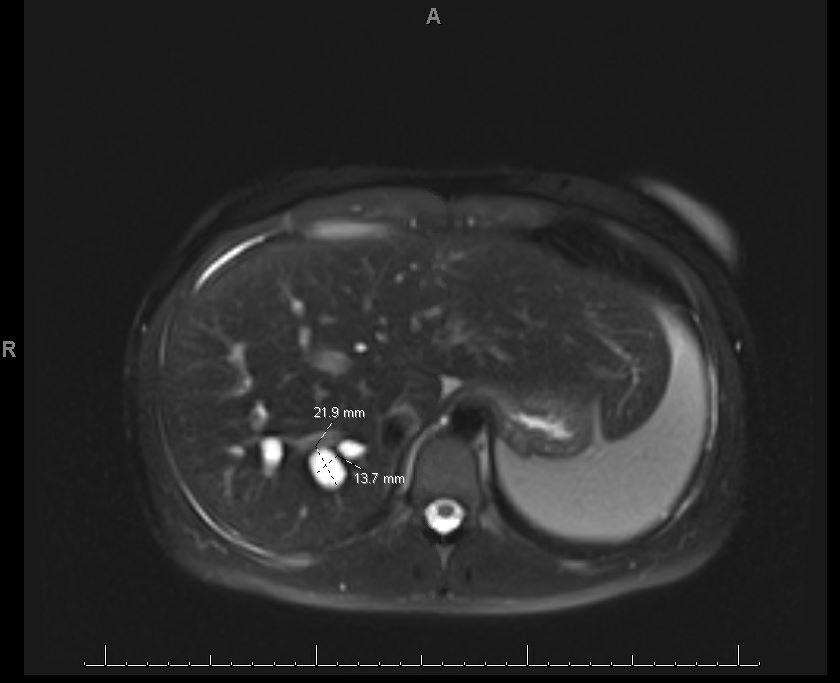
Caroli disease
Checkpoint inhibitor associated hepatitis
Cholangitis lenta / sepsis
Choledochal cyst
Cholestasis
Chronic antibody mediated rejection
Chronic ductopenic rejection (pending)
Chronic hepatitis
Chronic hepatitis-grading / staging
Chronic viral hepatitis
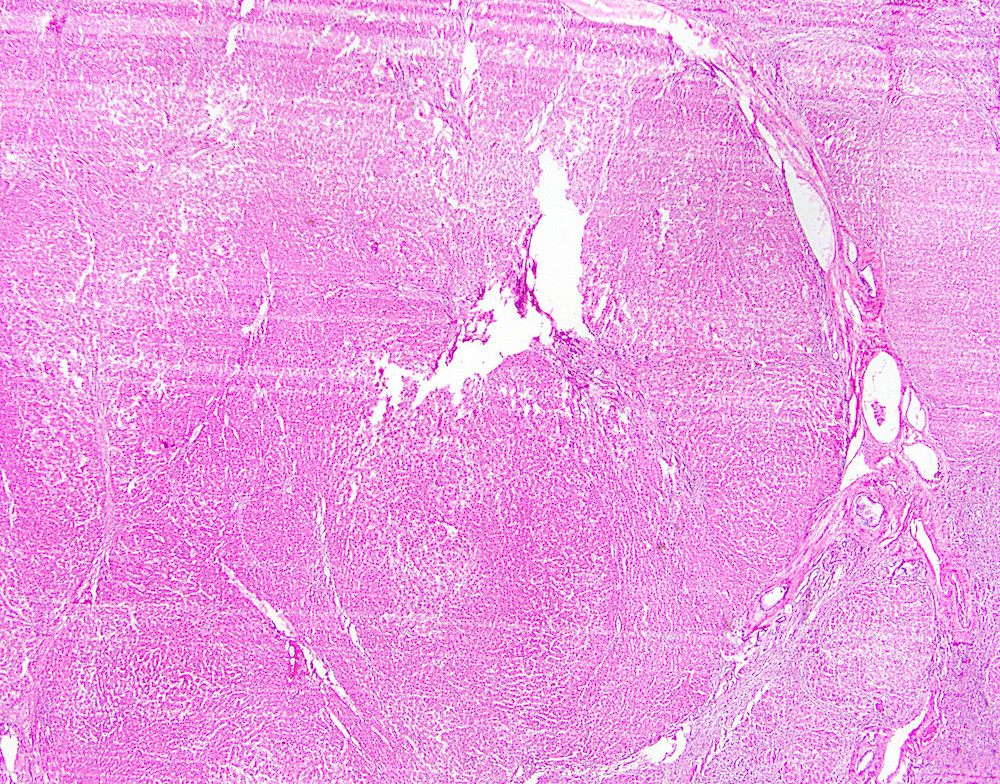
Cirrhosis
Combined hepatocellular carcinoma-cholangiocarcinoma
Congenital hepatic fibrosis
COVID-19
Cystic fibrosis
Cytomegalovirus hepatitis
Diagnostic patterns-differential diagnosis
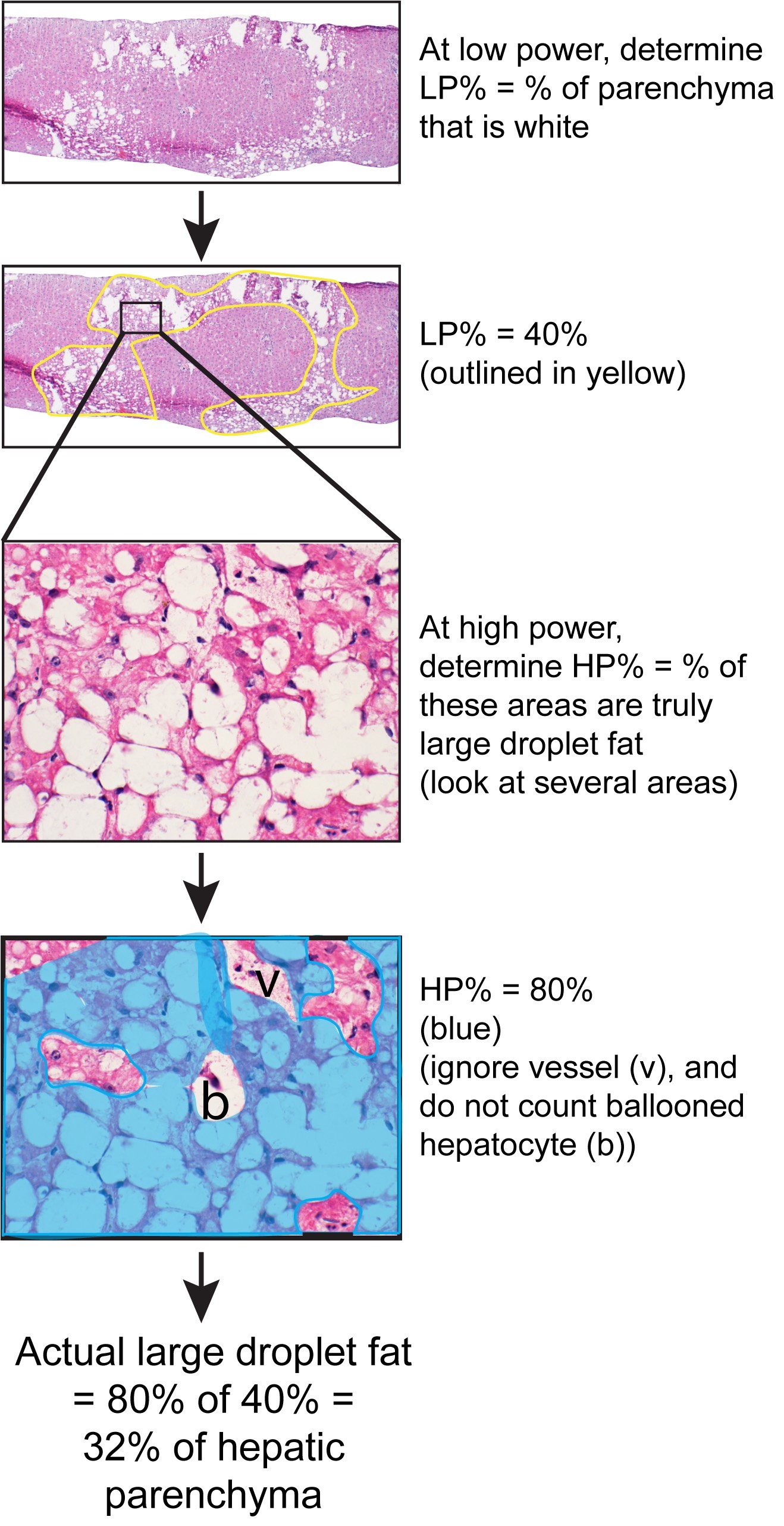
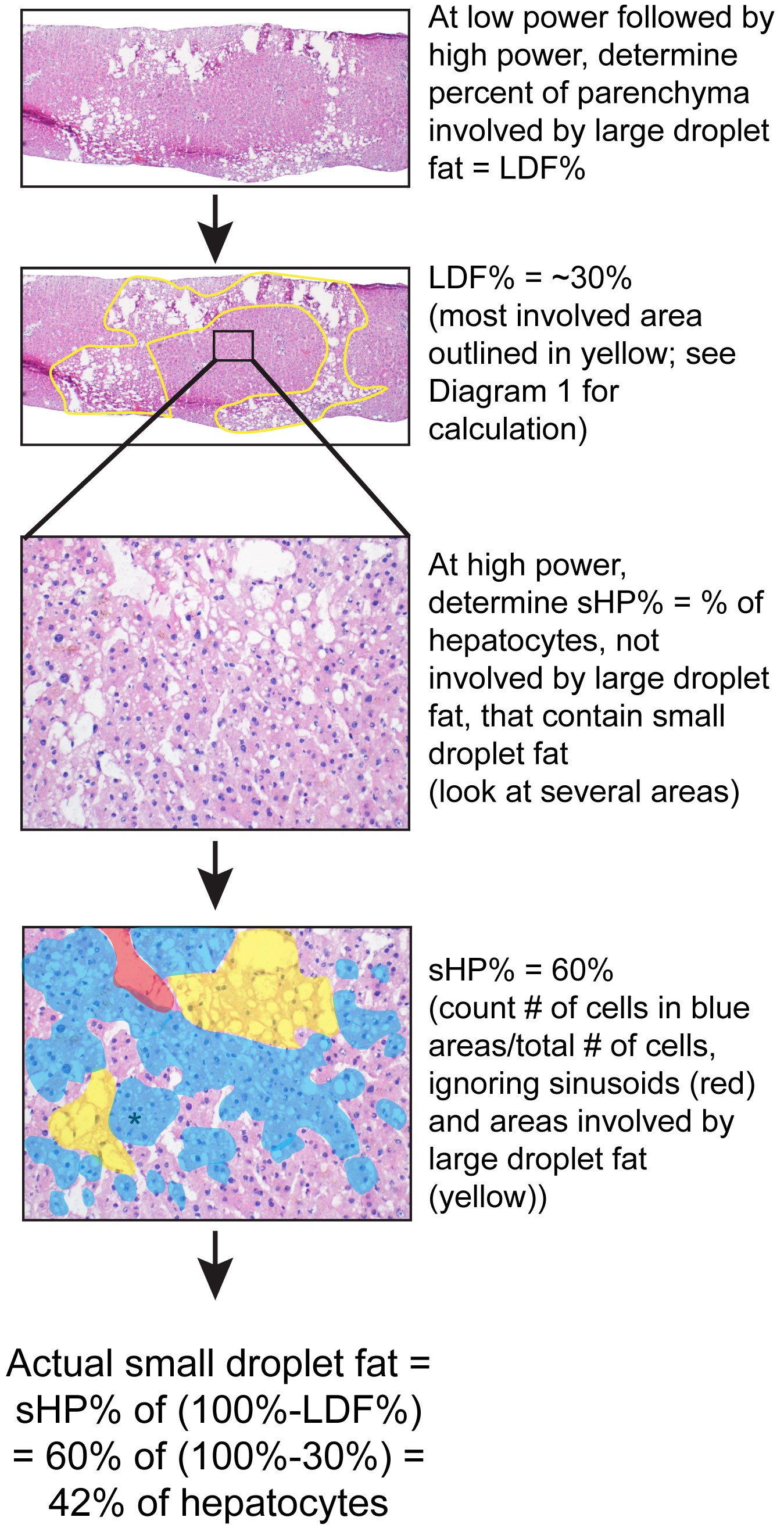
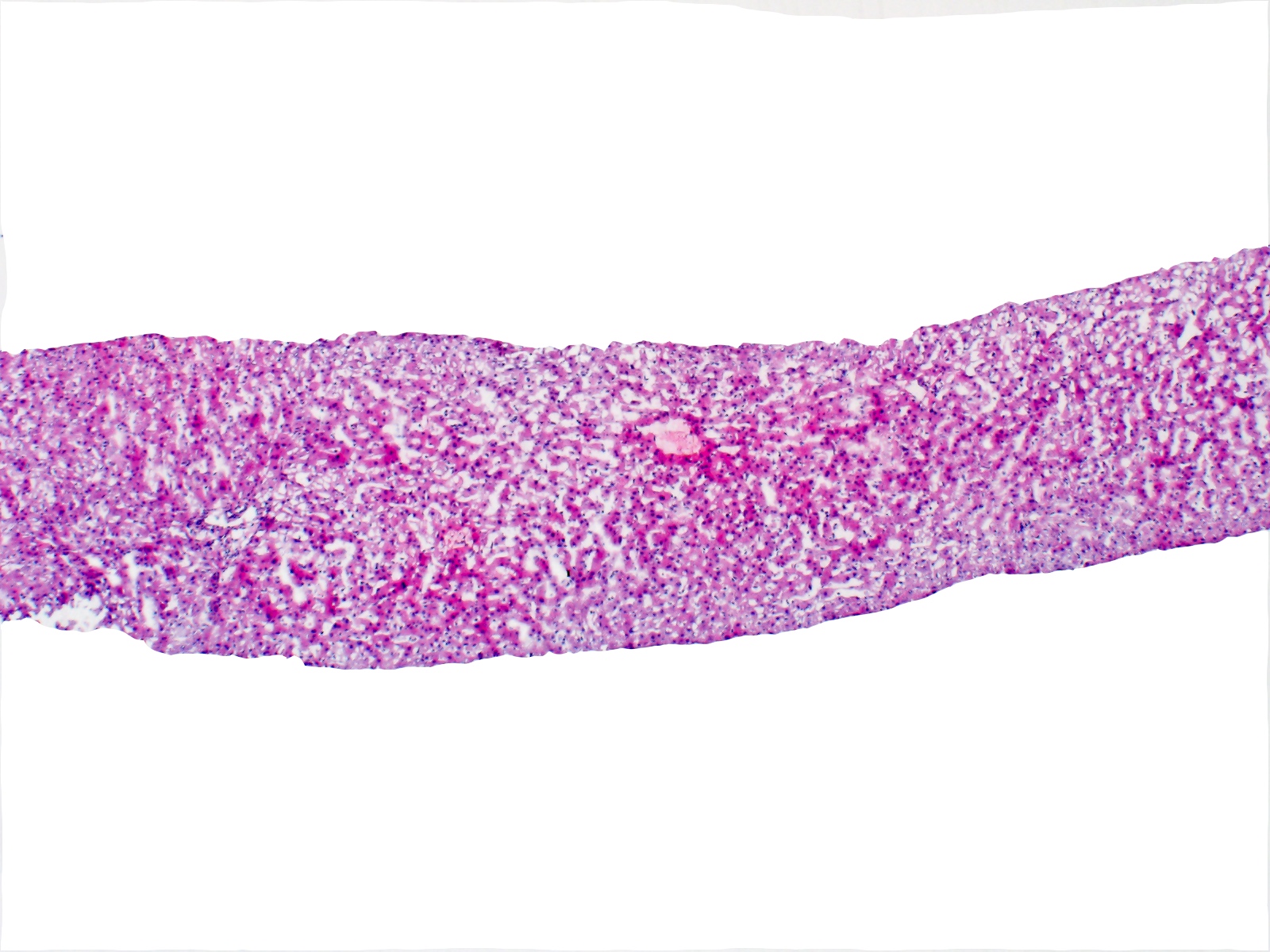
Donor liver frozen section evaluation
Drug / toxin induced hepatitis (DILI)-general
Drug / toxin induced hepatitis-acetaminophen
Ductular reaction
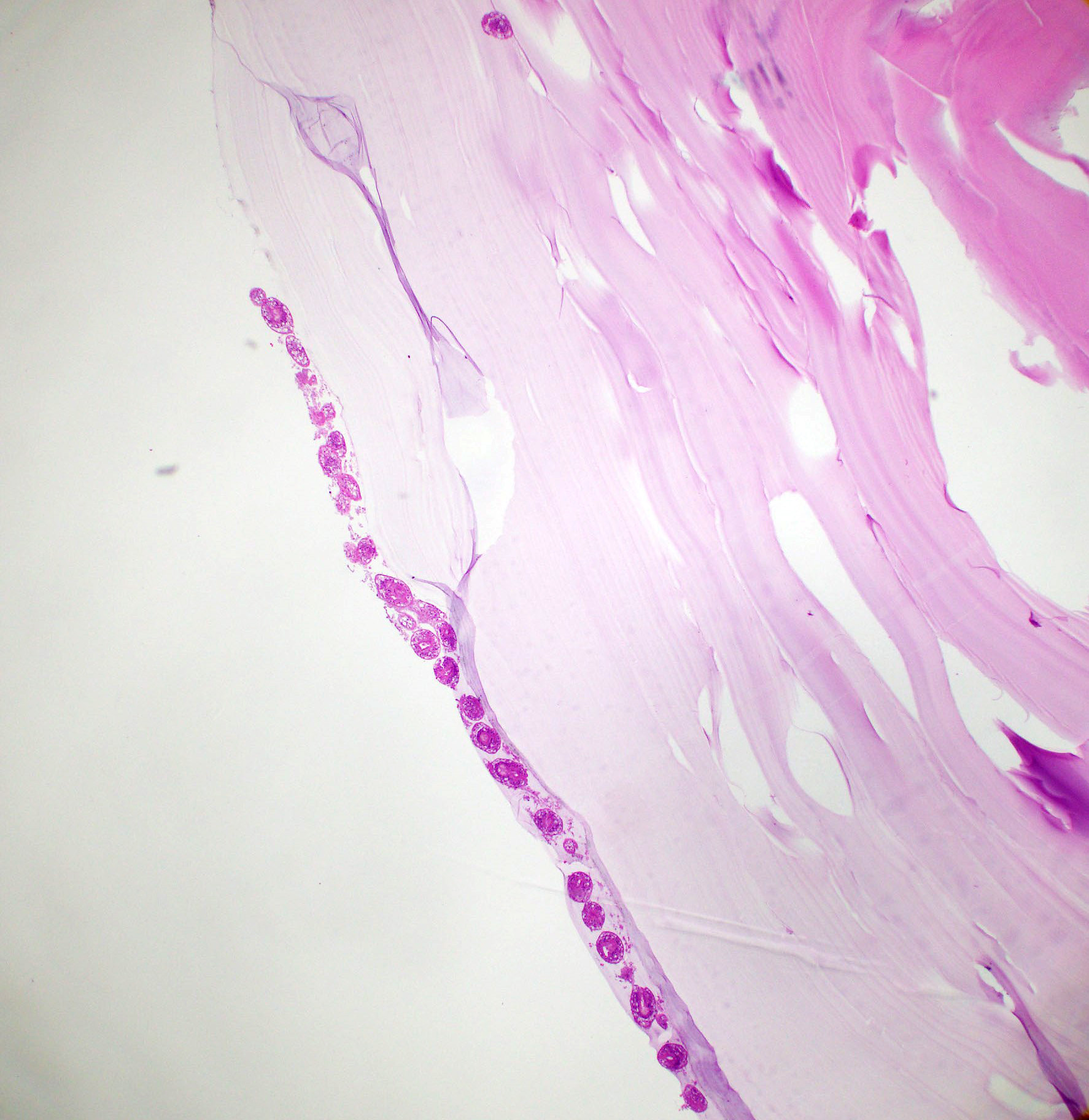
Echinococcal cyst
Entamoeba histolytica abscess
Epithelioid hemangioendothelioma
Epstein-Barr virus hepatitis
Erythropoietic protoporphyria
Extrahepatic biliary atresia
Extramedullary hematopoiesis
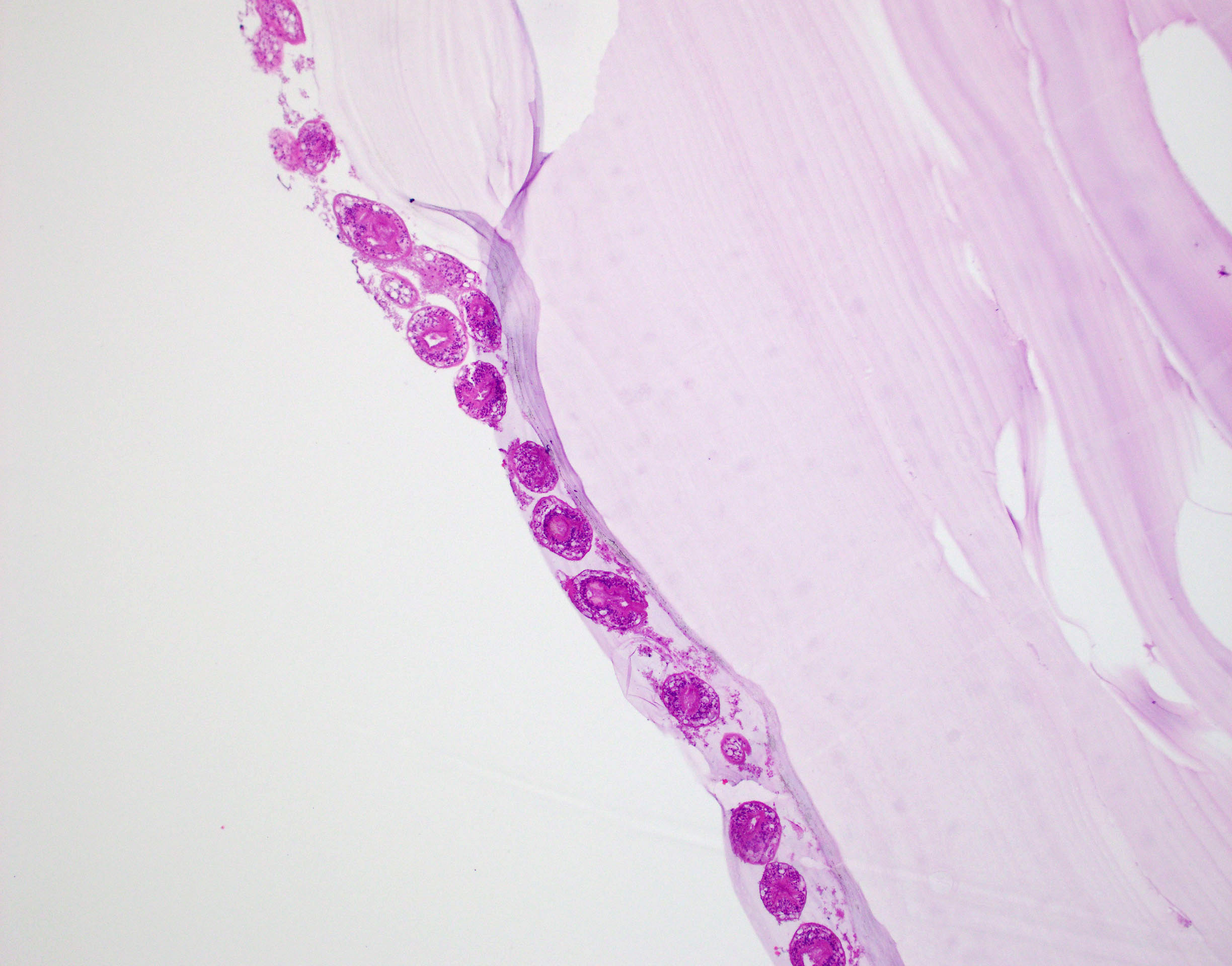
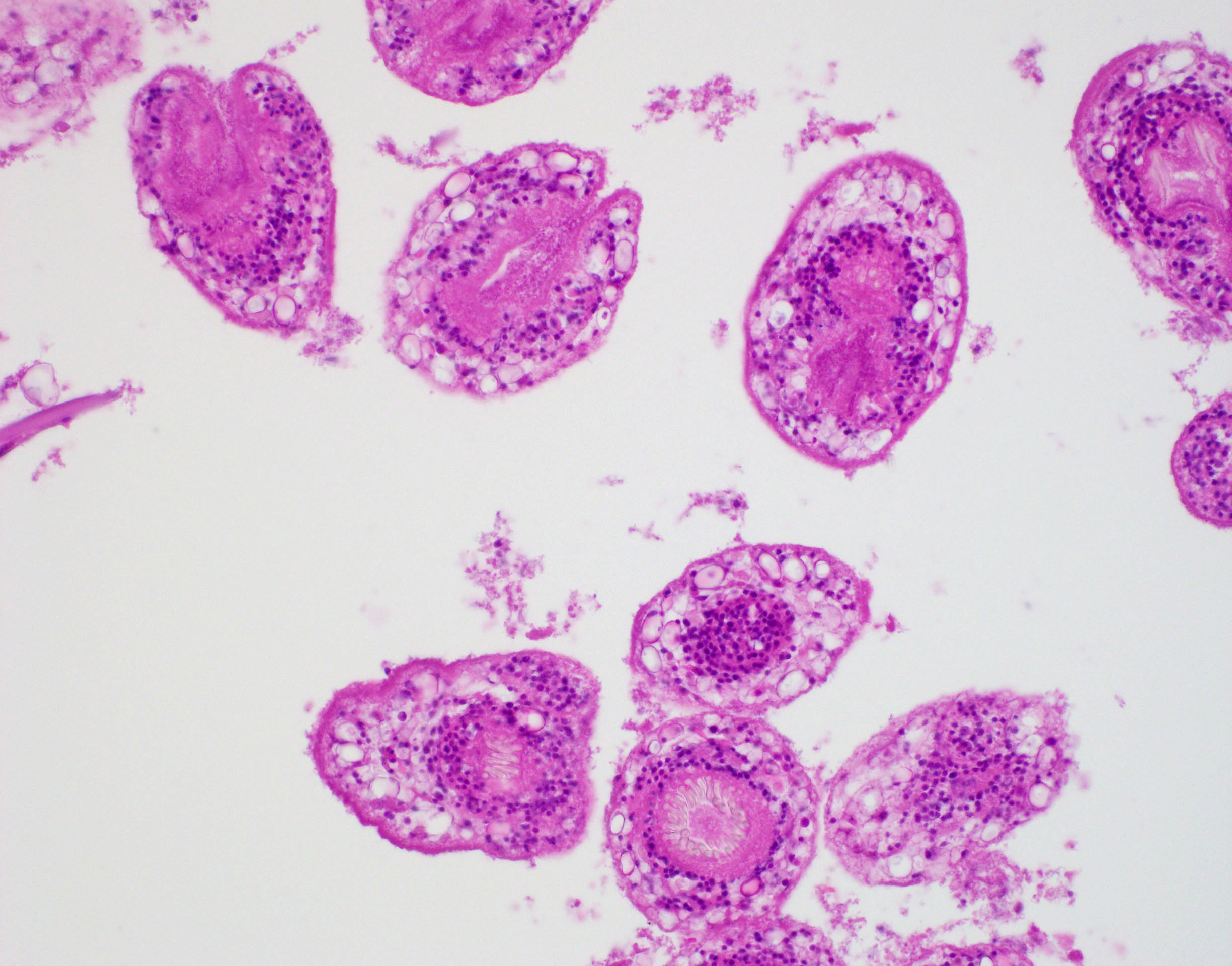
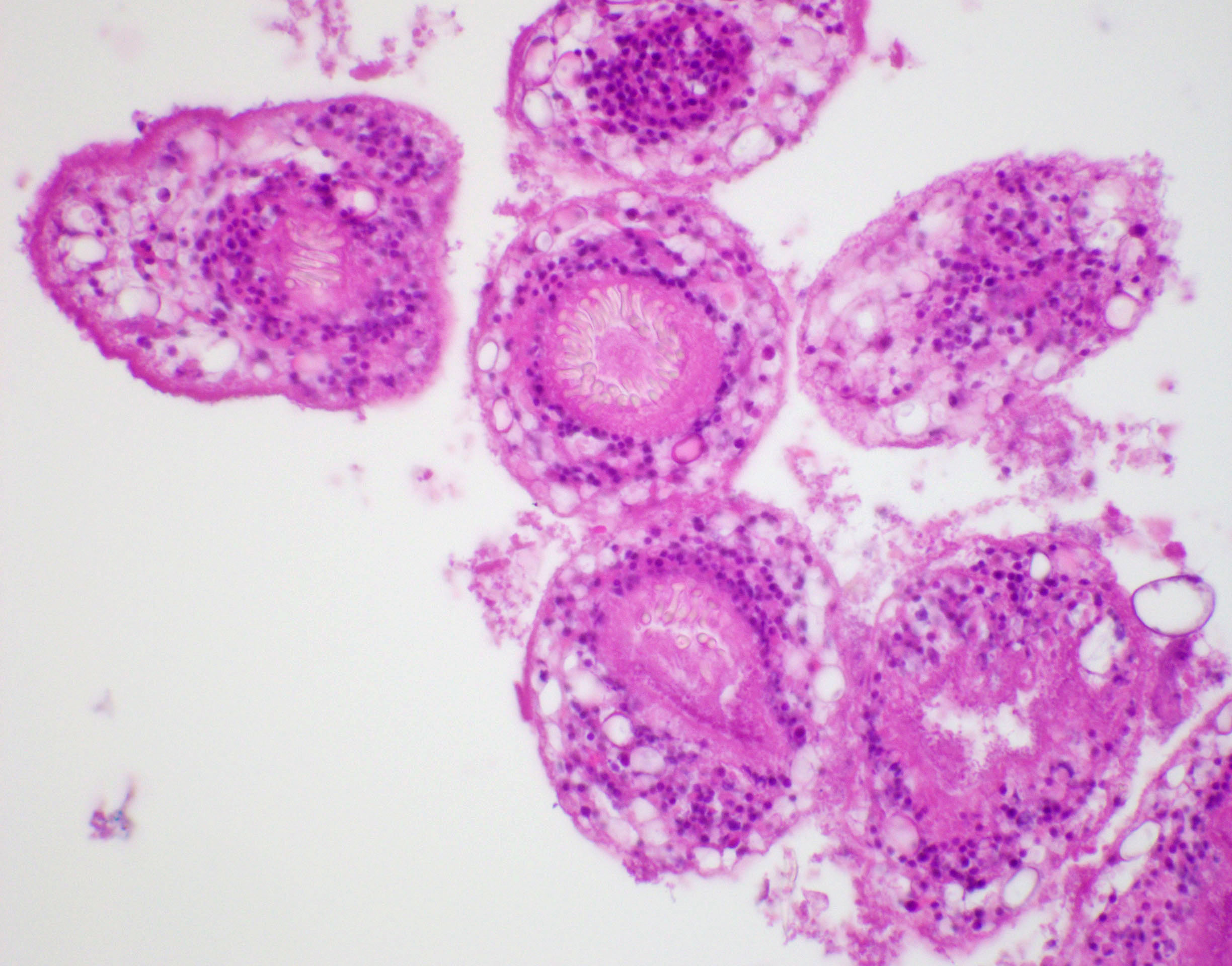
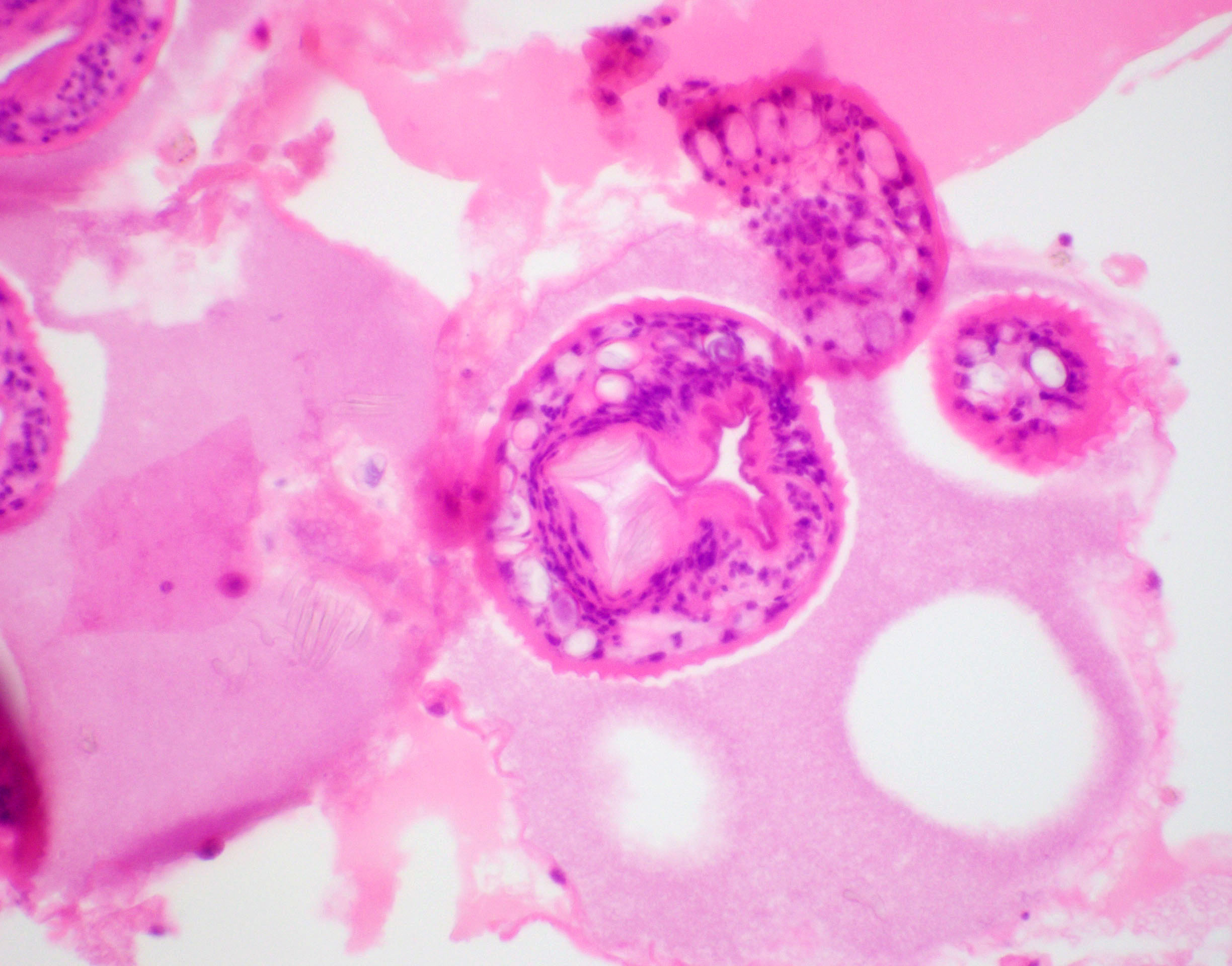
Fasciola hepatica
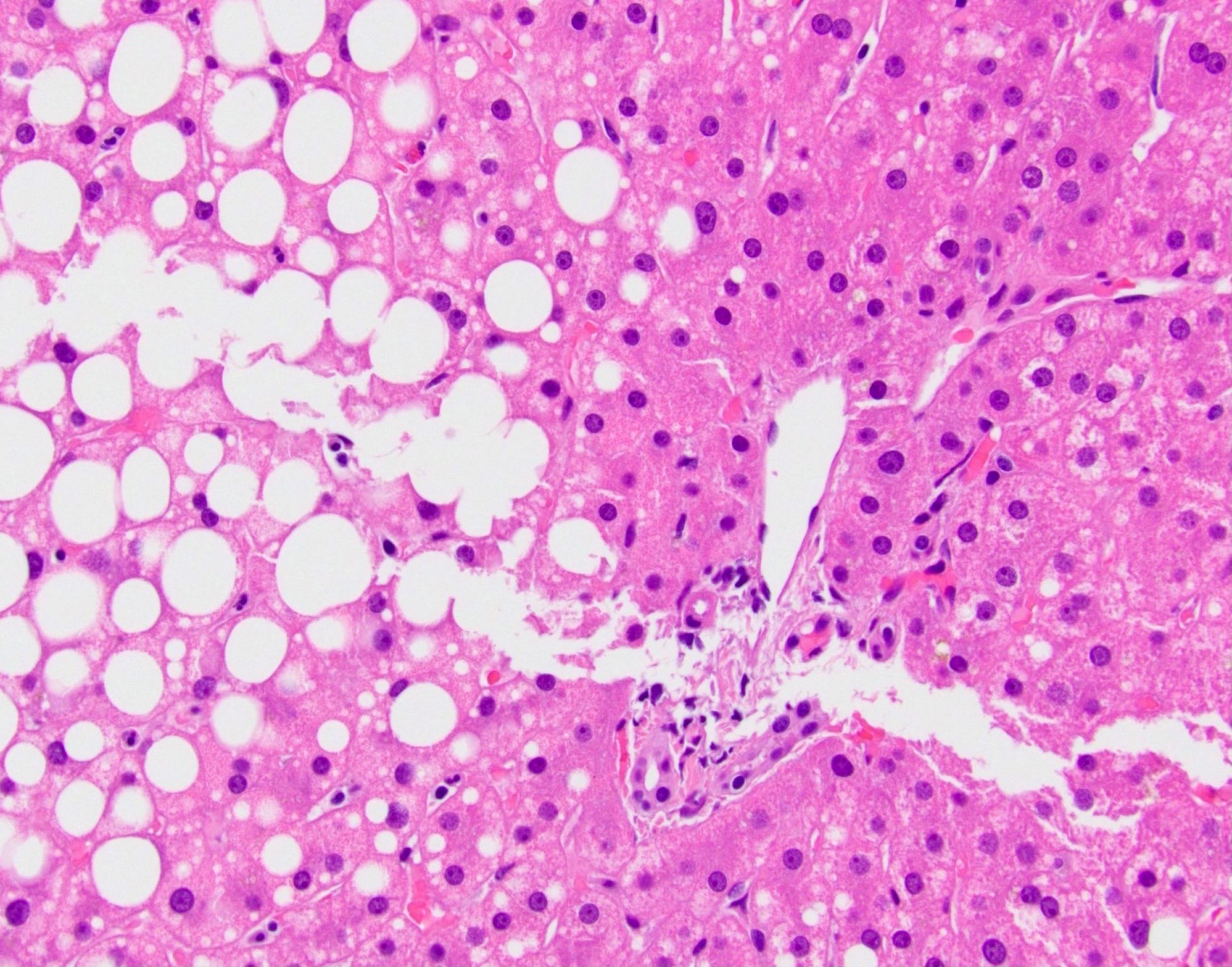
Focal fatty change
Focal nodular hyperplasia
Foregut cyst
Forms of hepatic injury
Gaucher disease
Glycogen storage diseases
Glycogenic hepatopathy
Granulomatous hepatitis
Grossing, frozen section & features to report
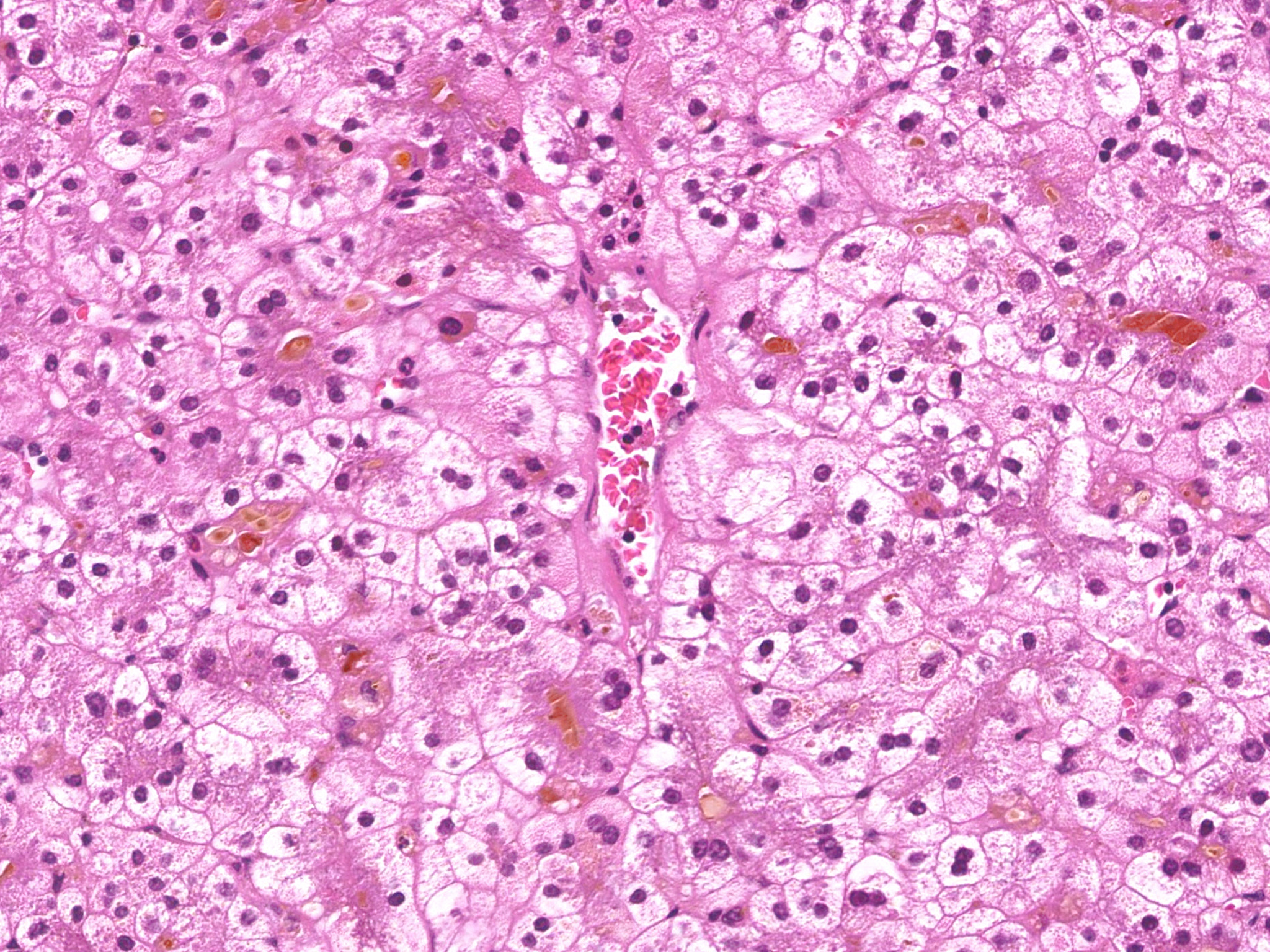
HCC - clear cell variant
HCC - cytology
HCC - fibrolamellar variant
HCC - lymphocyte rich
HCC - macrotrabecular massive
HCC - sarcomatoid variant
HCC - scirrhous type
HCC - steatohepatitic
HCC - undifferentiated variant
Hemangioma
Hemochromatosis
Hepatic failure
Hepatic failure
Hepatic infantile hemangioma
Hepatic small vessel neoplasm
Hepatitis (acute and chronic)-general
Hepatitis A virus (HAV)
Hepatitis B virus (HBV)
Hepatitis B virus (HBV)
Hepatitis C virus (HCV)
Hepatoblastoma
Hepatocellular adenoma
Hepatocellular carcinoma overview
Hepatoportal sclerosis
Hereditary hemorrhagic telangiectasia
Herpes simplex virus hepatitis
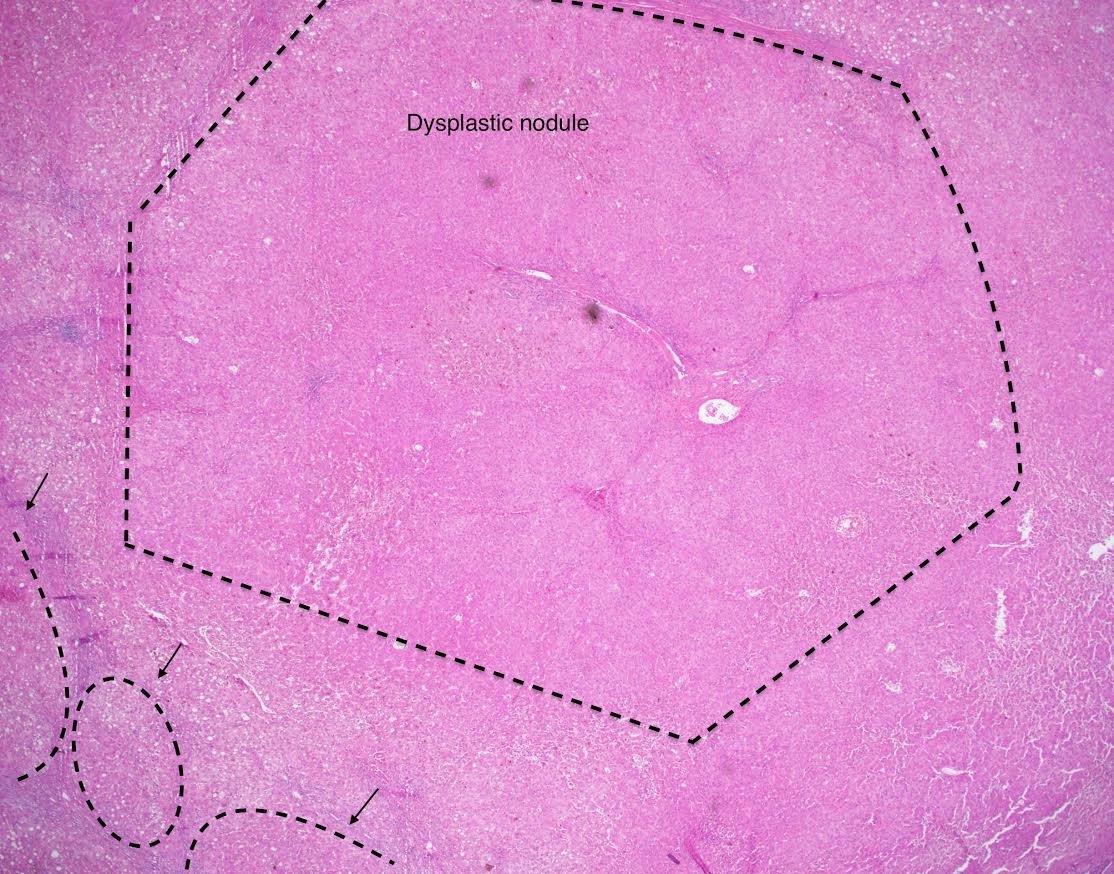
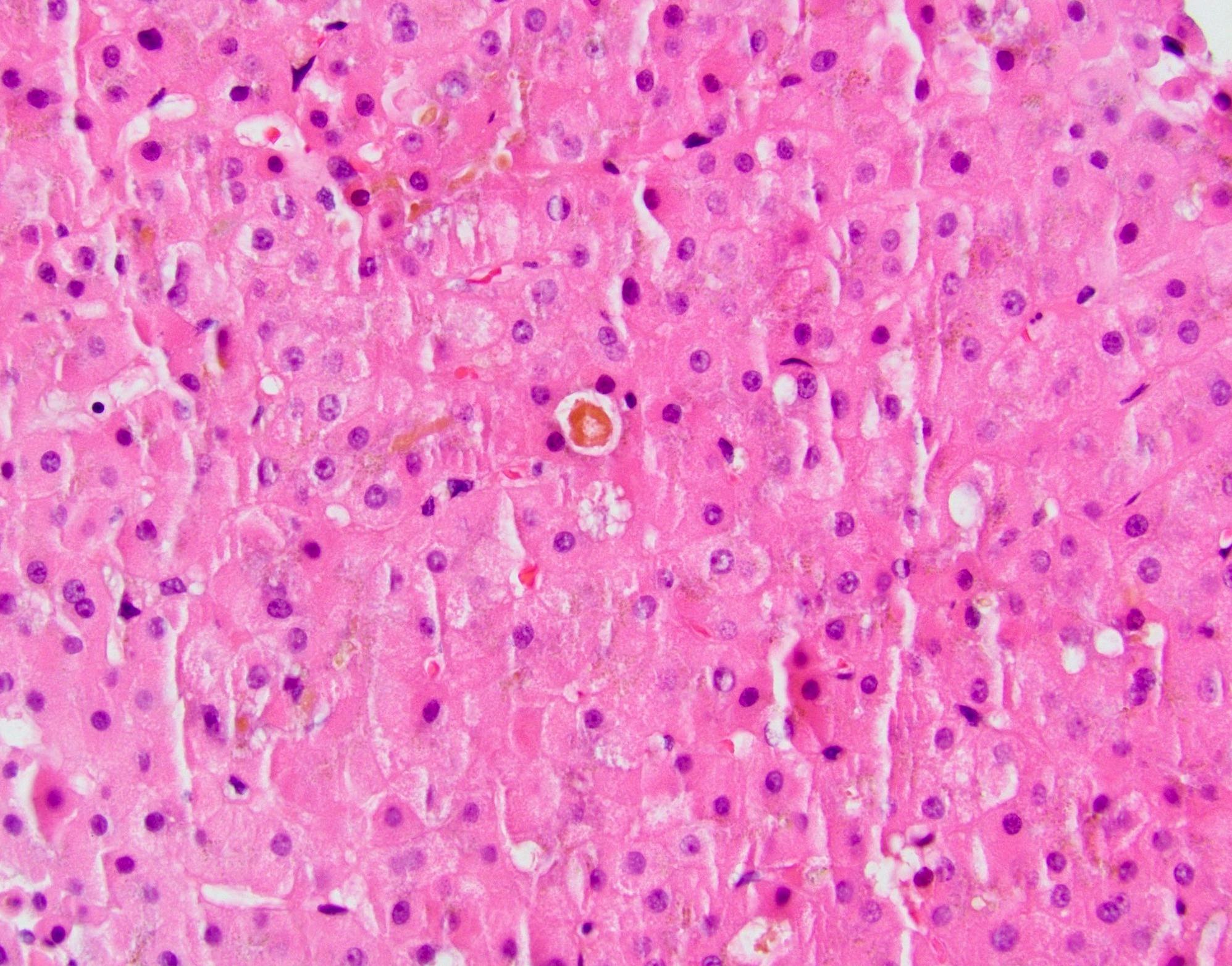
High grade dysplastic nodule
Histology
Infantile hemangioendothelioma / hemangioma
Intraductal papillary neoplasm of the bile ducts
Intrahepatic biliary atresia
Intrahepatic cholangiocarcinoma (small and large duct types)
Lafora disease
Large duct obstruction
Large regenerative nodule
Late T cell mediated (cellular) rejection
Late T cell mediated (cellular) rejection (pending)
Liver cell dysplasia
Liver transplantation overview
Low grade dysplastic nodule
Macroregenerative nodule
Malnutrition (total parenteral nutrition)
Mesenchymal hamartoma
Metastases
Methotrexate
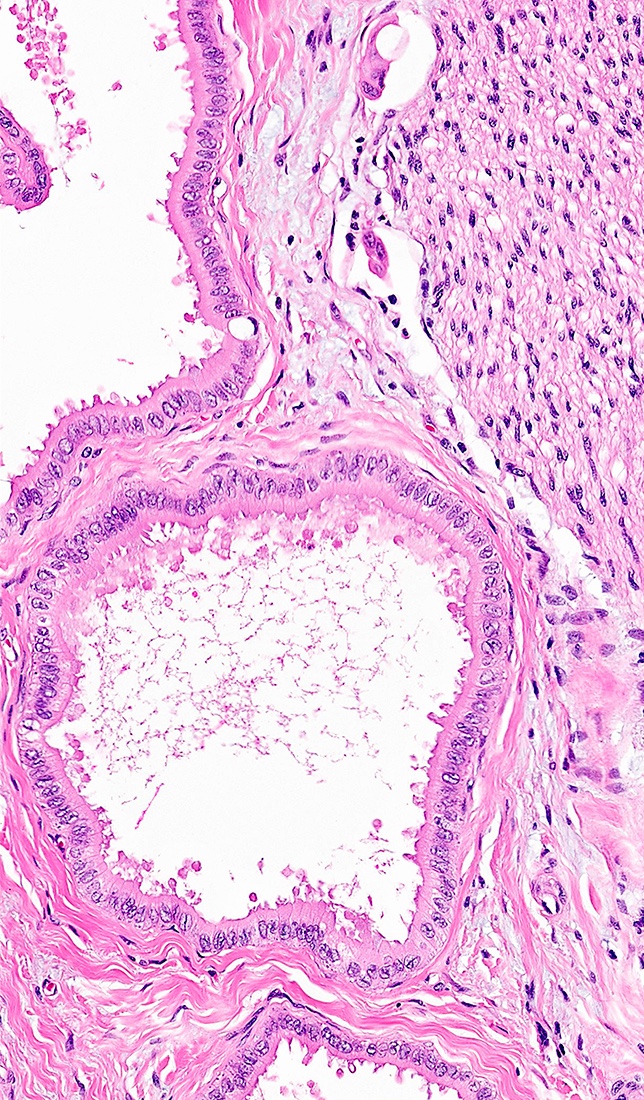
Mucinous cystic neoplasm
Navajo hepatopathy
Neonatal hepatitis
Neuroendocrine carcinoma
Niemann-Pick disease
Nodular regenerative hyperplasia
Nonalcoholic fatty liver disease / nonalcoholic steatohepatitis (NASH)
Other flukes (Clonorchis / Opisthorchis) (pending)
Peliosis hepatis
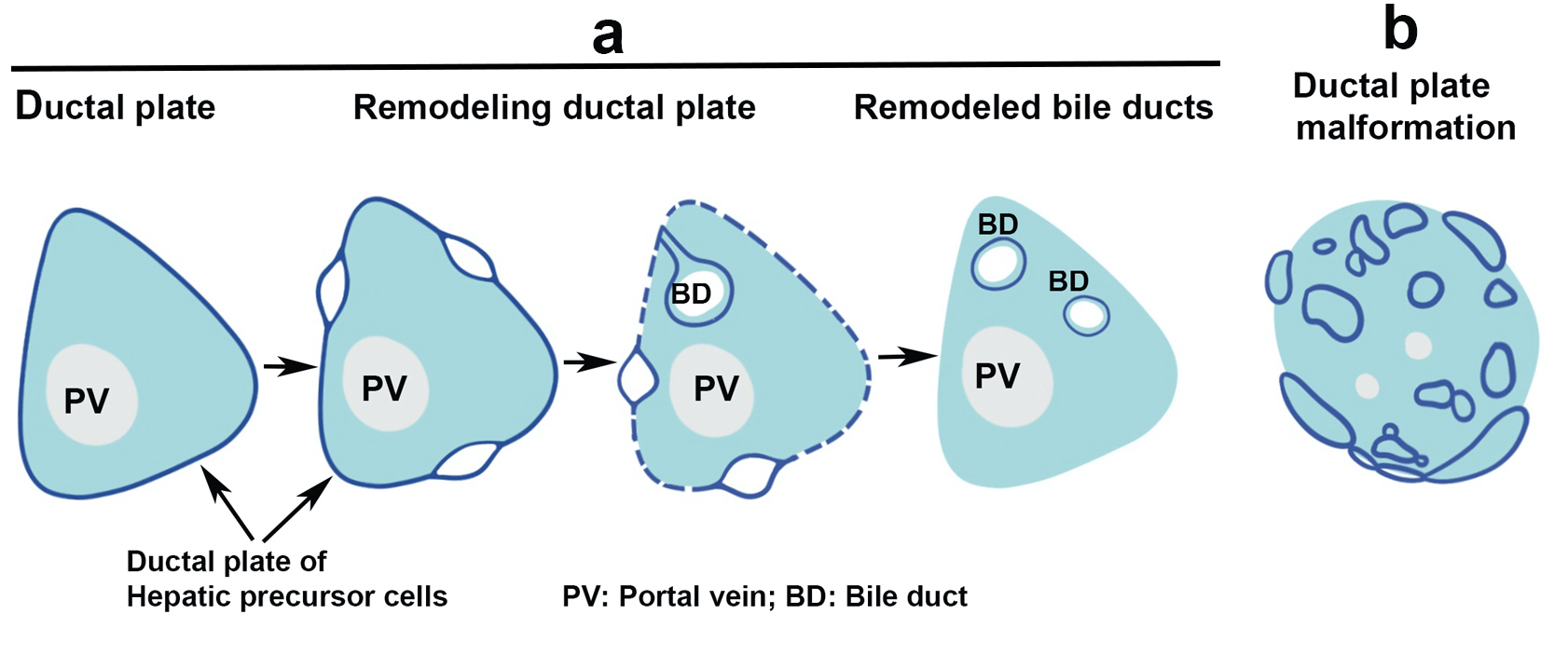
Polycystic liver disease / duct plate malformation
Portal hypertension
Portal vein obstruction
Pregnancy
Primary biliary cholangitis
Primary hyperoxaluria
Primary sclerosing cholangitis
Progressive familial intrahepatic cholestasis
Pyogenic abscess
Q fever
Reactive lymphoid hyperplasia / pseudolymphoma
Recurrent disease
Recurrent pyogenic cholangitis
Reye syndrome
Schistosomiasis
Secondary biliary cirrhosis
Segmental atrophy
Simple biliary cyst
Sinusoidal obstruction syndrome / venoocclusive disease (SOS / VOD)
Staging-cholangiocarcinoma
Staging-hepatocellular carcinoma
Transplantation - surgical / vascular complications
Undifferentiated embryonal sarcoma
Vascular disorders-general
Von Meyenburg complex
Well differentiated neuroendocrine tumor
WHO classification
Wilson diseaseAcute antibody mediated rejection including hyperacute rejection
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Antibody mediated immune injury to liver allografts with short and long term consequences
- 3 distinct subtypes:
- Hyperacute rejection (rare / mostly eliminated)
- Acute antibody mediated rejection (aAMR)
- Chronic active antibody mediated rejection (cAMR), see separate section
Essential features
- Hyperacute rejection is extremely rare nowadays and is predominantly limited to era of ABO incompatible transplants without desensitization
- Acute antibody mediated rejection is associated with circulating donor specific antibodies (human leukocyte antigen (HLA) and non-HLA), microvascular injury (capillaritis) and complement split products (C4d)
- Acute antibody mediated rejection may occur early posttransplantation in patients with preformed antibodies or late in patients with low immunosuppression compliance who may harbor preformed / memory antibodies or develop de novo antibodies
- Plasma cell rich rejection in patients with original disease other than autoimmune hepatitis (de novo autoimmune hepatitis / plasma cell hepatitis) is an atypical form of rejection, likely representing mixed T cell mediated rejection (TCMR) and aAMR etiology
Terminology
- Preferred terminology: antibody mediated rejection (AMR)
- Old terminology: humoral rejection (Am J Transplant 2016;16:2816)
- Preferred terminology: plasma cell rich rejection
- Old terminology: de novo autoimmune hepatitis / plasma cell hepatitis (Am J Transplant 2016;16:2816)
ICD coding
- ICD-10: T86.41 - liver transplant rejection
Epidemiology
- Hyperacute rejection:
- Now exceedingly rare; occurred during era of ABO incompatible transplantation without pretreatment (Surg Today 2011;41:317)
- Incidence: 60% without efforts to mitigate isoagglutinin titers, which must be kept below 1:16 (Semin Liver Dis 1992;12:51)
- Acute antibody mediated rejection:
- Estimated incidence is 5 - 20% in sensitized recipients with positive crossmatch (Am J Transplant 2012;12:171, Hepatology 1992;16:671)
- Plasma cell rich rejection variant is uncommon (3 - 5%) and is generally seen in patients with hepatitis C virus (HCV), primary sclerosing cholangitis (PSC) and primary biliary cholangitis (PBC), among other primary diseases (Am J Transplant 2016;16:2816)
- F > M
- Reduced size or living donor allografts > whole organs (Clin Transplant 2001;15:309)
Sites
- Liver allografts
- Also occurs in other solid organ allografts such as kidney and heart (Am J Transplant 2017;17:28, J Heart Lung Transplant 2005;24:1710)
Pathophysiology
- Can be caused by HLA and non-HLA donor specific antibodies (e.g. HLA, ABO isoagglutinins, AT1R, glutathione S-transferase, etc.) (Liver Transpl 2011;17:779, Liver Transpl 2004;10:1166, Transplantation 2020 Feb 25 [Epub ahead of print])
- Antibodies bind allograft endothelial cells and fix complement; this triggers the complement cascade with direct endothelial cell damage
- Donor specific antibody (DSA) binding also facilitates antibody dependent cellular cytotoxicity (ADCC), which is the basis for some of the histologic features of AMR, such as capillaritis and microvascular inflammation (Am J Transplant 2016;16:1653)
Etiology
- Transplantation in setting of ABO mismatch
- Presensitized patients with positive crossmatch
- Non compliance with immunosuppression regimen (particularly in late presentations of acute AMR)
Clinical features
- Hyperacute rejection:
- Begins immediately
- Allograft dysfunction evolves over a period of hours to days
- Coagulopathy, thrombocytopenia and increased need for blood products (Semin Liver Dis 1992;12:51)
- Acute antibody mediated rejection:
- Persistent elevation in transaminases alanine aminotransferase (ALT) / Aspartate transaminase (AST) and bilirubin
- Refractory thrombocytopenia
- Low serum complement levels
- Persistent circulating DSA
Diagnosis
- Criteria and categories for diagnosis of aAMR were defined by the Banff working group based on a combination of clinical, histopathological and serological findings (Am J Transplant 2016;16:2816):
Definitive for acute / active AMR (all 4 criteria required) A Histopathological pattern of injury consistent with acute AMR: e.g portal
microvascular endothelial cell hypertrophy, portal capillary and inlet venule
dilatation and portal microvasculitis (see microscopic description below for
h scoring and other associated pathological features)B Positive serum DSA (mean fluorescence intensity [MFI] usually > 5,000) C Diffuse microvascular endothelial C4d deposition (C4d score = 3) on formalin
fixed or frozen tissue in ABO compatible or portal stromal C4d in ABO
incompatible allografts (see positive stains below for C4d scoring)D Reasonable exclusion of other insults that might cause a similar pattern of injury
Suspicious for AMR (both criteria required)A DSA is positive B Nonzero h score with (C4d score + h score = 3 or 4) (see microscopic
description below for scoring parameters)
Indeterminate for AMR (requires a + b and c or d)A C4d score + h score ≥ 2 B DSA not available, equivocal or negative C C4d staining not available, equivocal or negative D Coexisting insult might be contributing to the injury
Laboratory
- ABO incompatible: isoagglutinins titer > 1:64
- HLA-DSA particularly against class II, frequently against multiple specificities, MFI usually > 5,000
- C1q binding capabilities
- Elevated AST, ALT, alkaline phosphatase, gamma glutamyl transpeptidase, bilirubin
Radiology description
- Helpful for ruling out other causes of dysfunction, such as biliary and vascular etiologies
Prognostic factors
- DSA are associated with:
- Decreased 5 year graft and patient survival
- Increased incidence of TCMR and plasma cell rich rejection
- Increased incidence of allograft fibrosis and chronic rejection (Am J Transplant 2014;14:779, J Immunol Res 2017;2017:3234906)
Case reports
- 23 year old woman with severe aAMR treated with plasmapheresis and mycophenolate mofetil (Transpl Int 2005;18:1298)
- 27 year old man with portal vein thrombosis and antibody mediated rejection (Transplant Proc 2008;40:870)
- 50 year old woman with isolated aAMR post-ABO compatible liver transplantation (Am J Transplant 2006;6:3022)
Treatment
- Usually consists of steroids and tacrolimus
- Thymoglobulin helps by disrupting T and B cell interaction
- Plasmapheresis and IVIG are used to deplete circulating antibodies in patients with severe aAMR (Curr Opin Organ Transplant 2016;21:209)
- Bortezomib, proteasome inhibitors and rituximab have also been used (Am J Transplant 2012;12:2526, World J Gastroenterol 2009;15:3426)
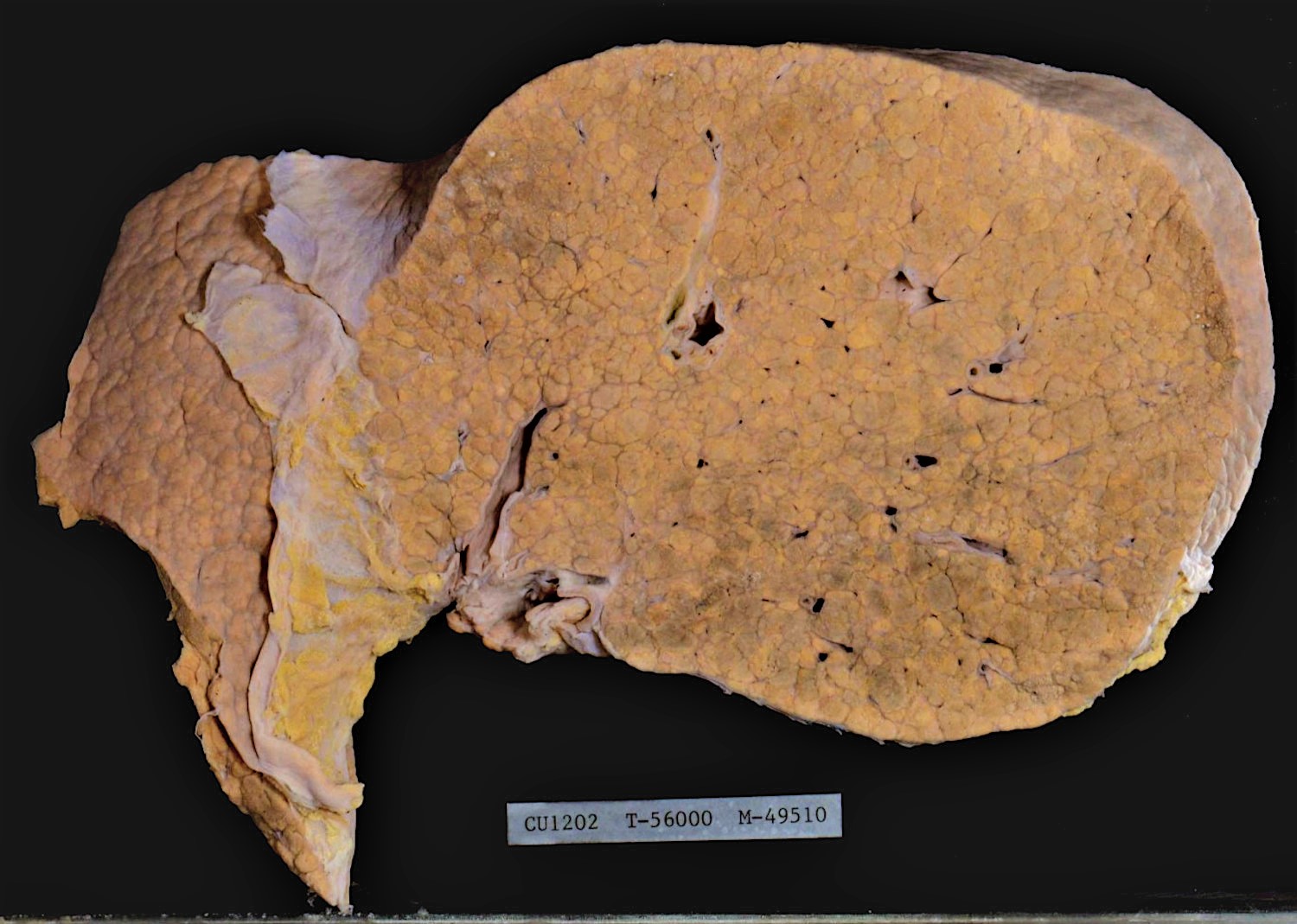
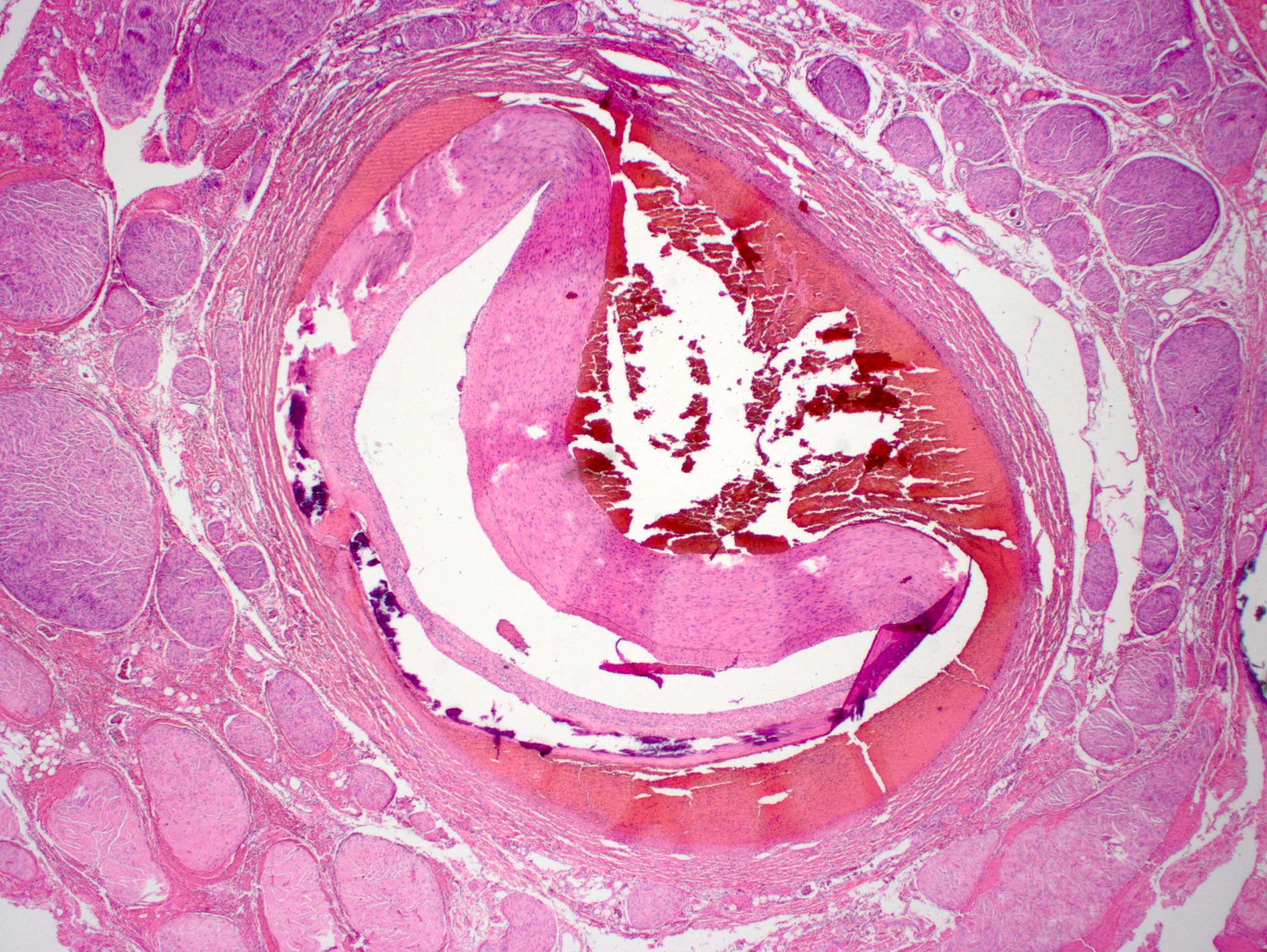
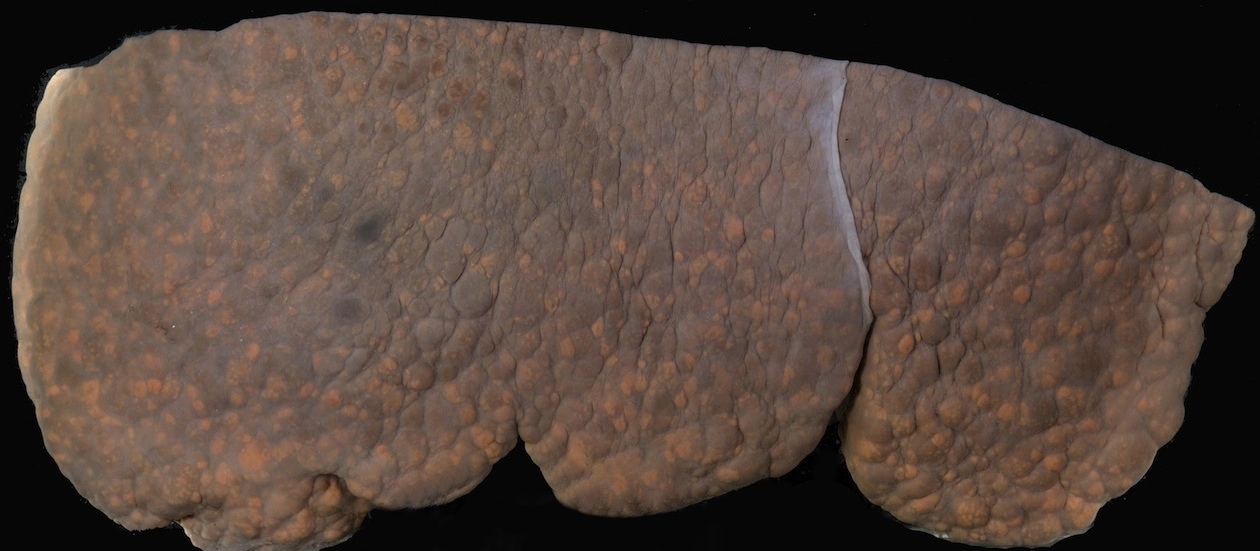
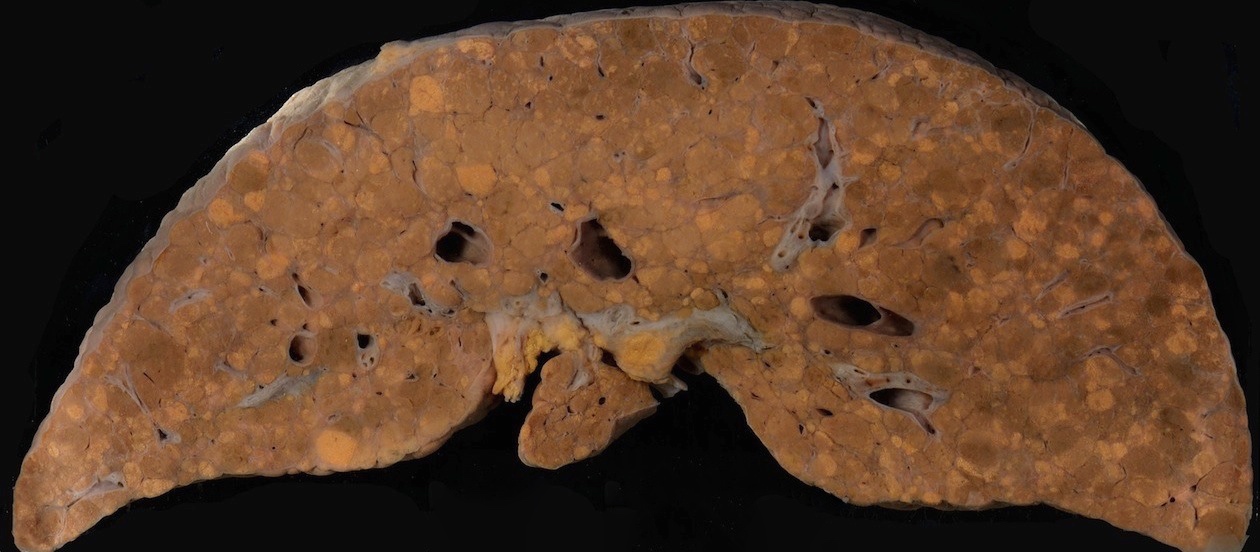
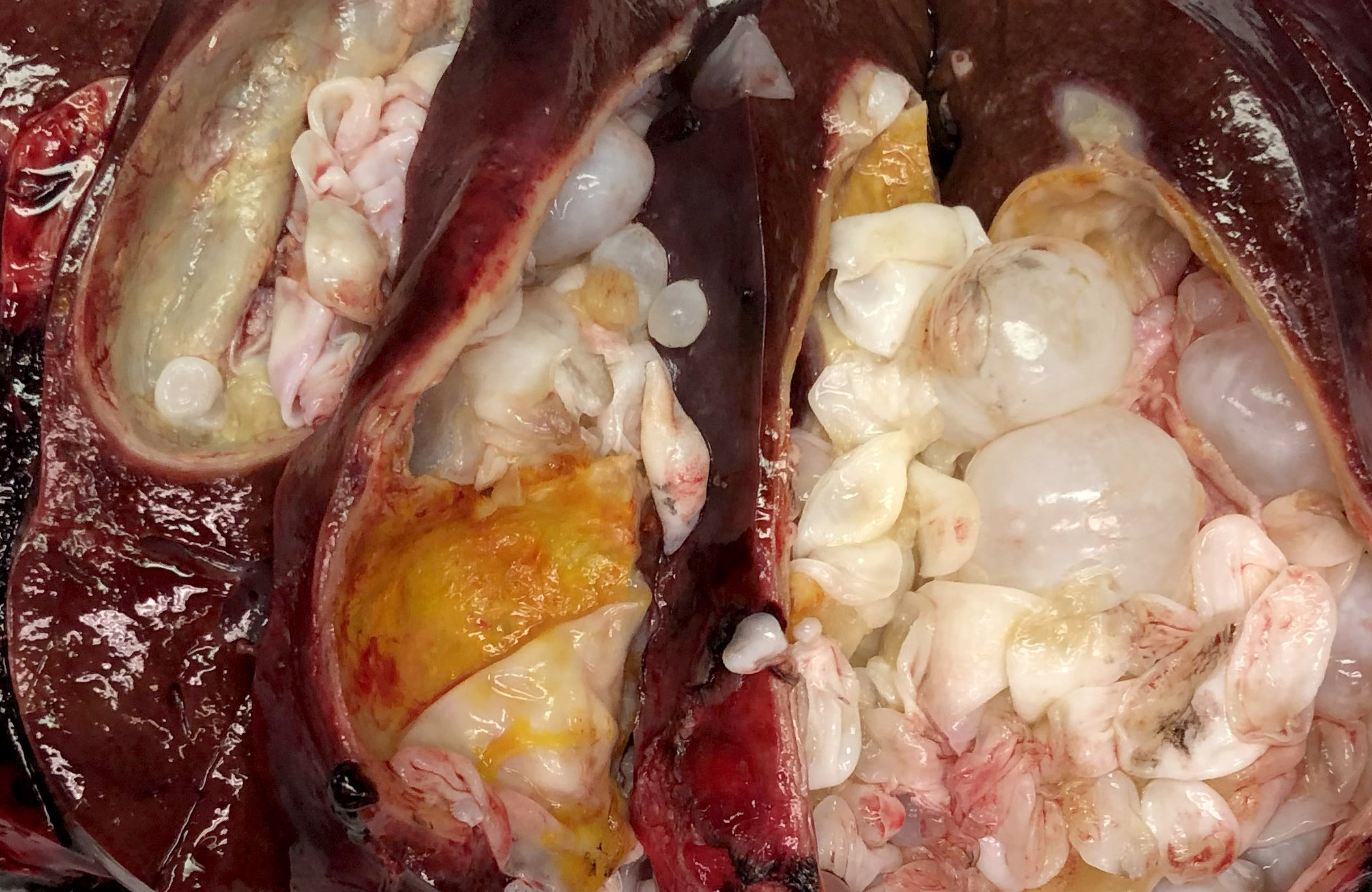
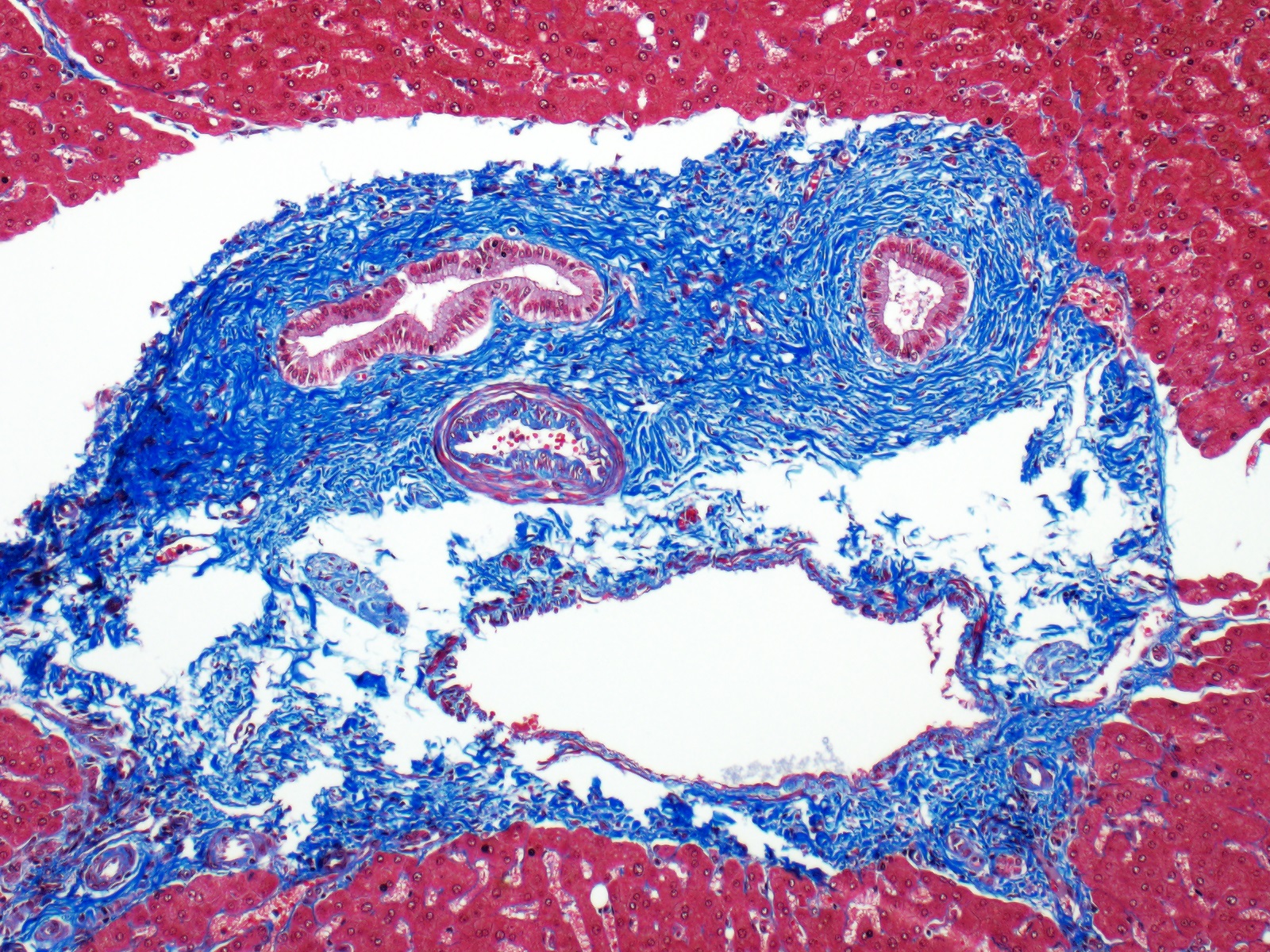
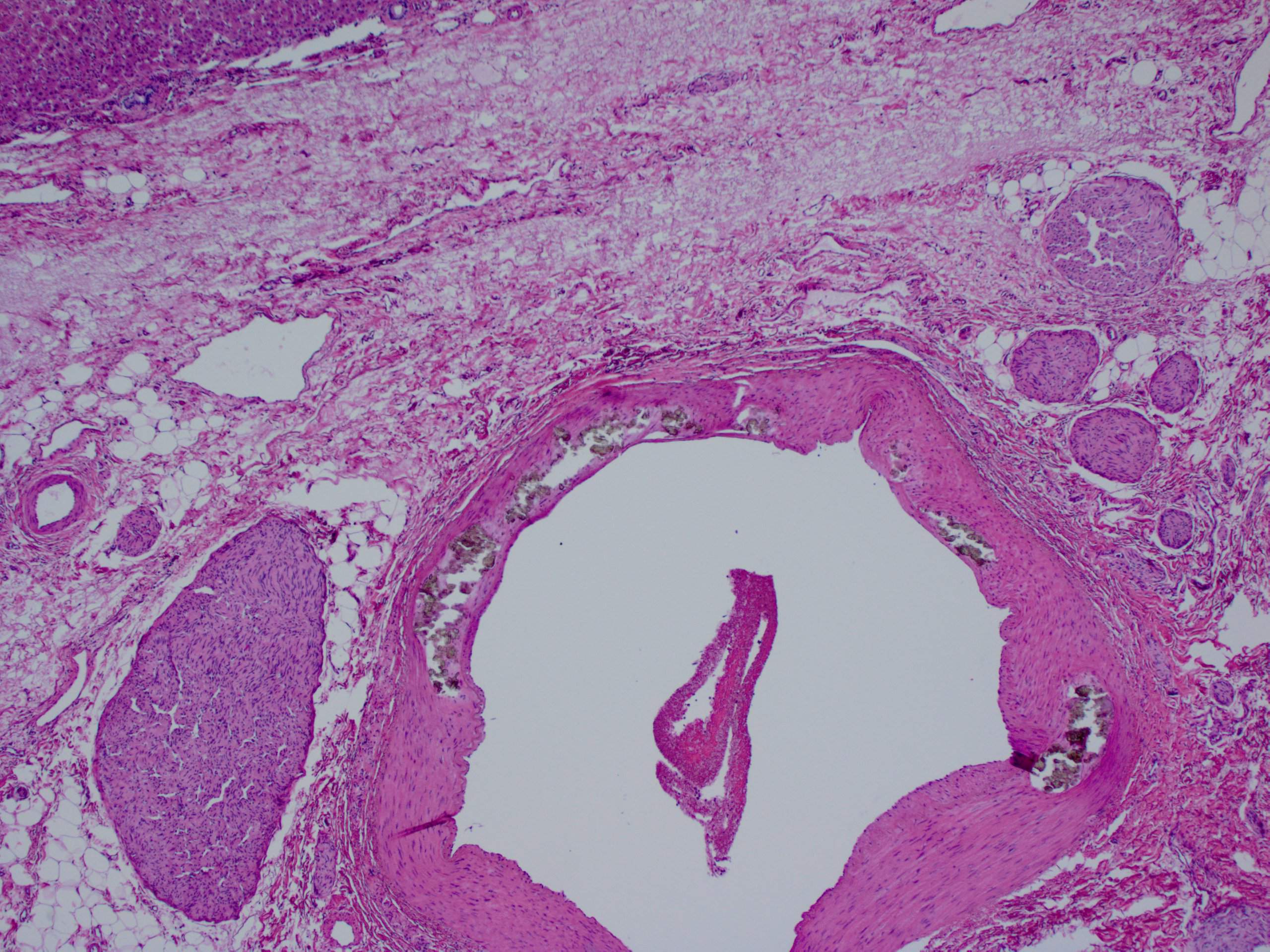
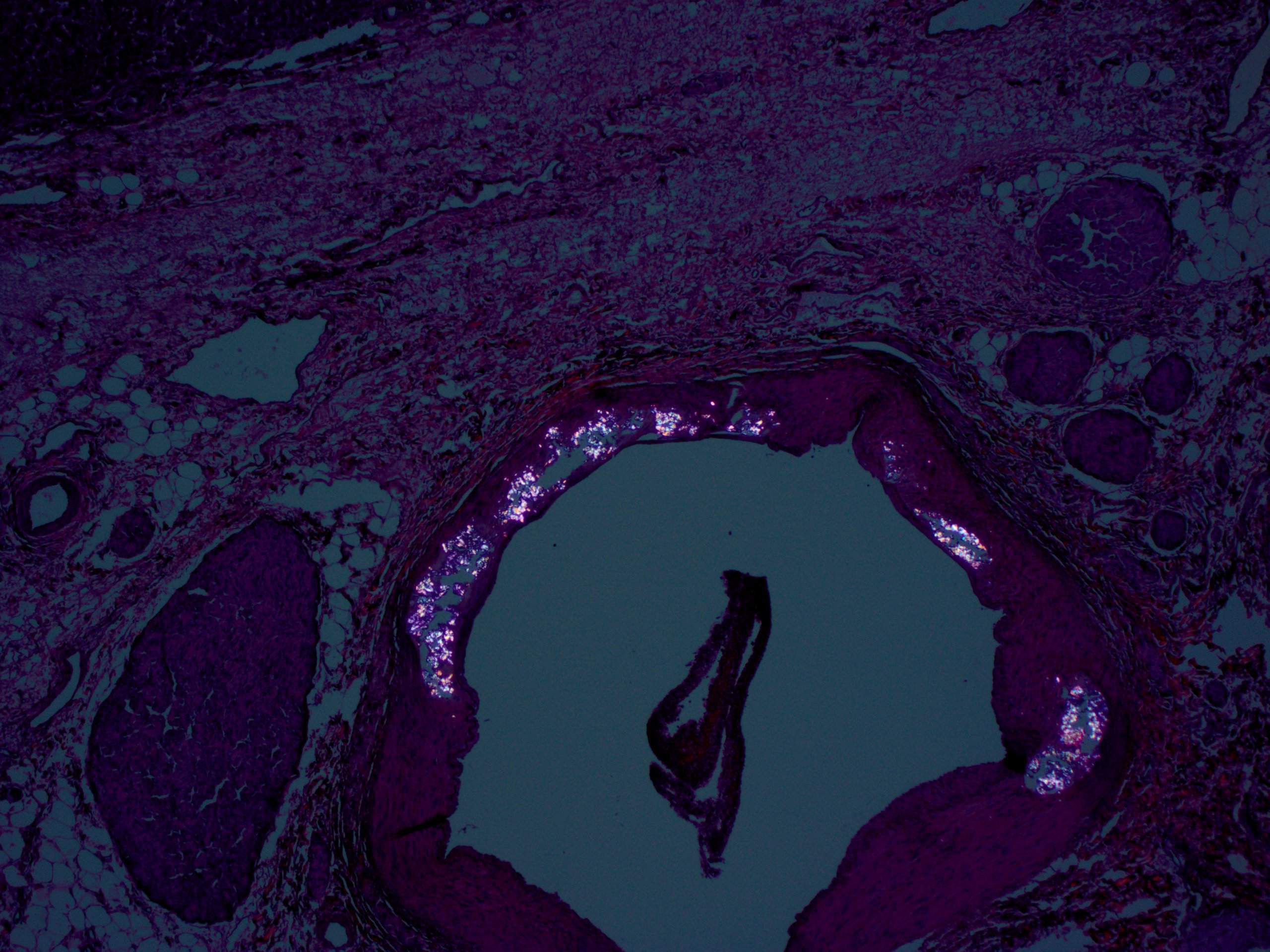
Gross description
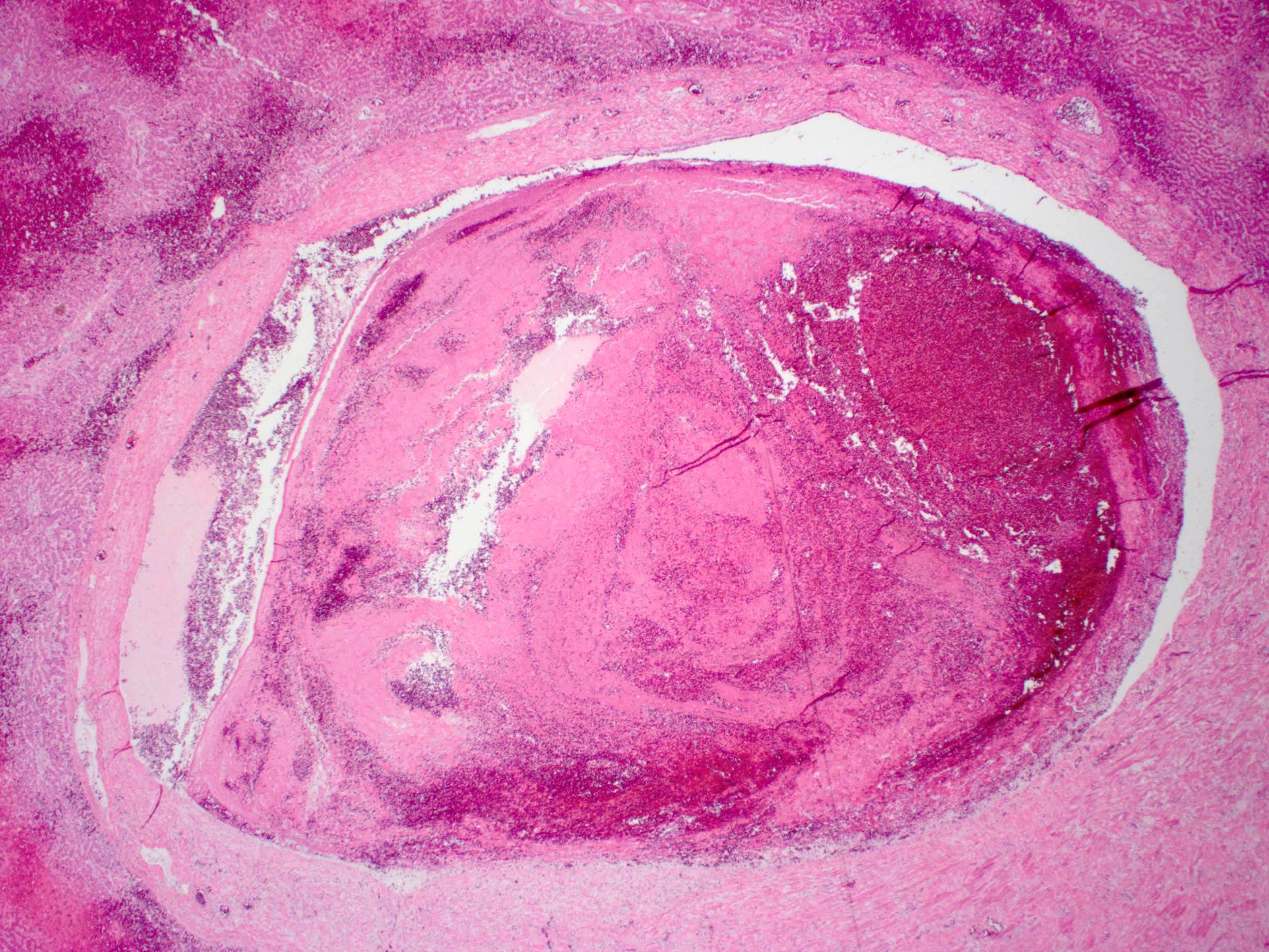
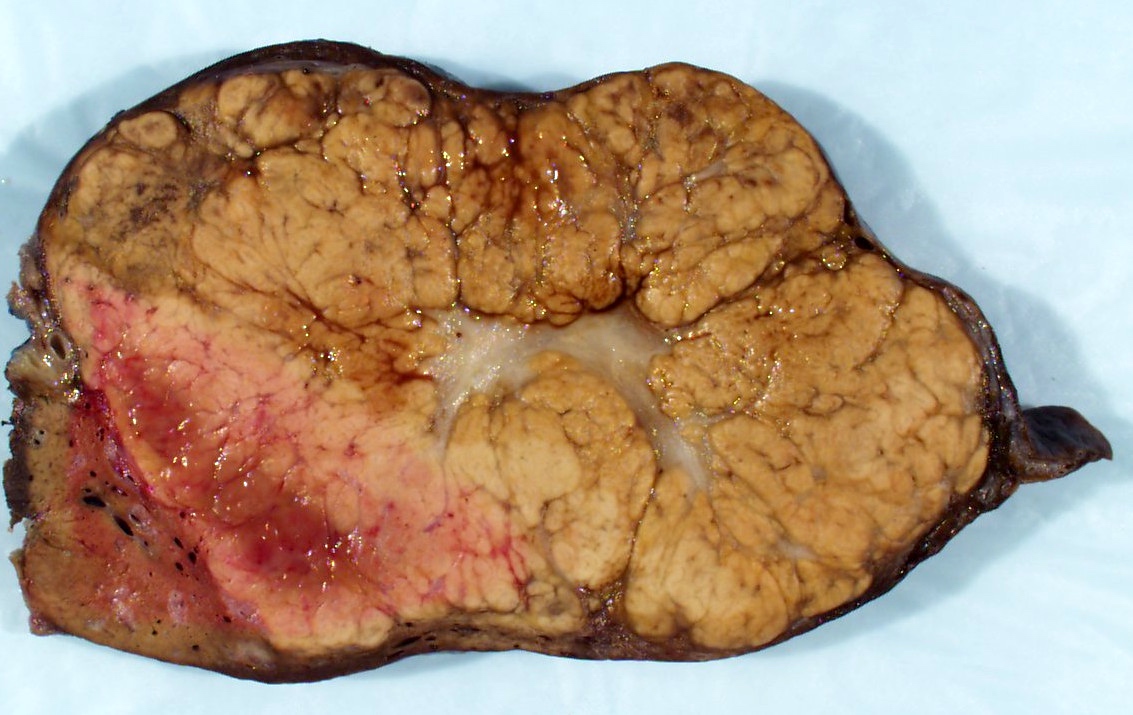
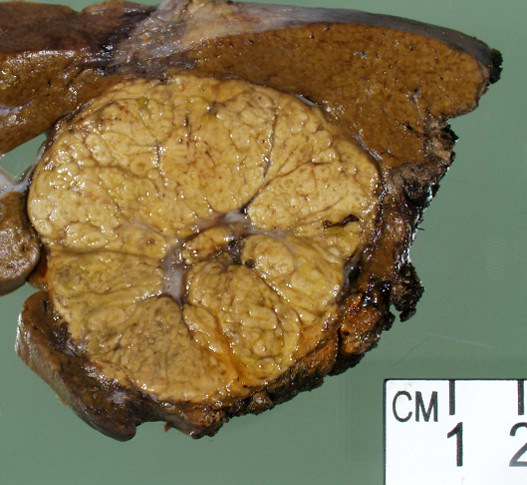
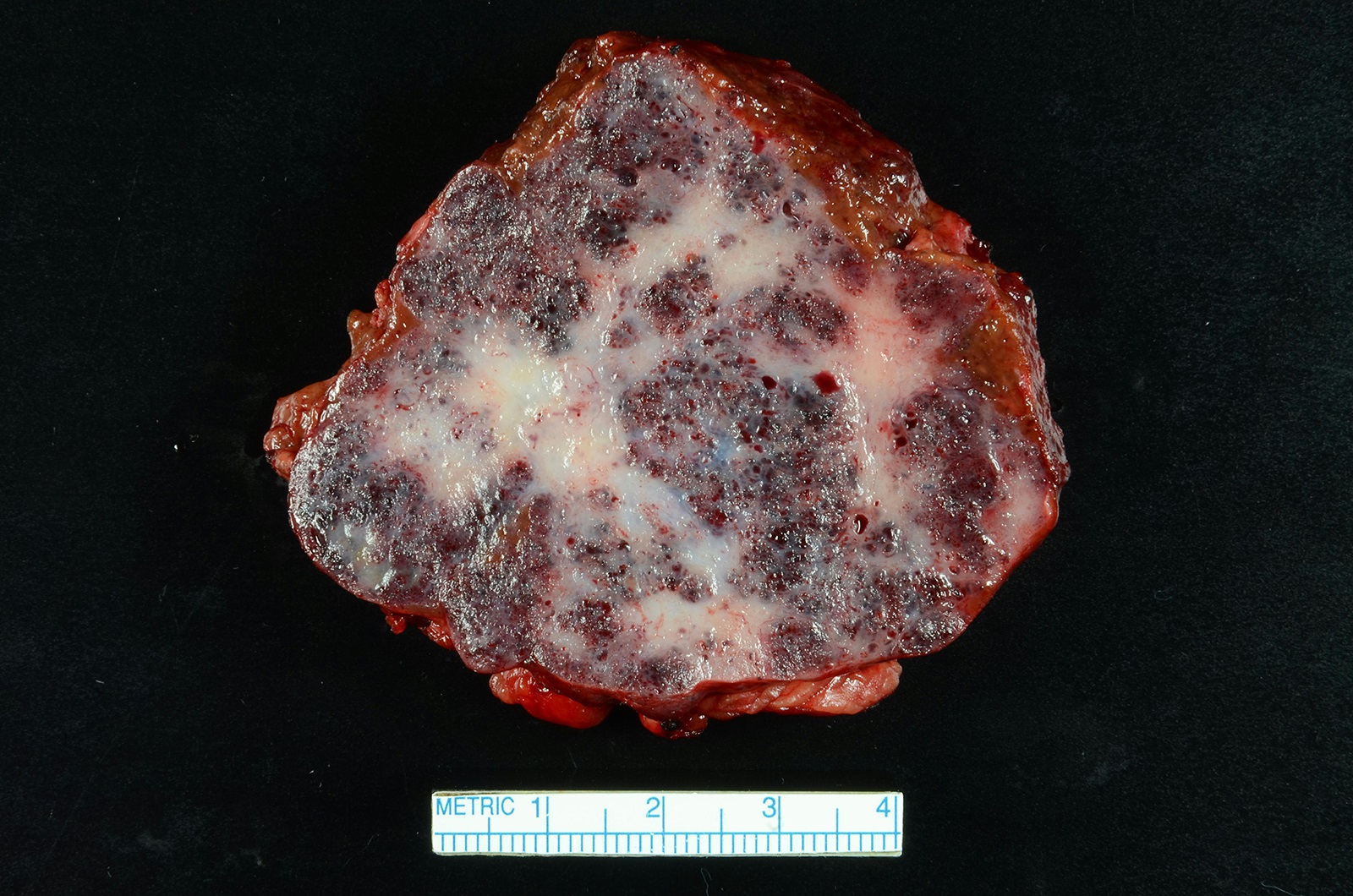
- In hyperacute rejection:
- Explanted organs are grossly enlarged and mottled areas of geographic necrosis
- Hepatic artery and portal vein thrombosis
- Capsular rupture
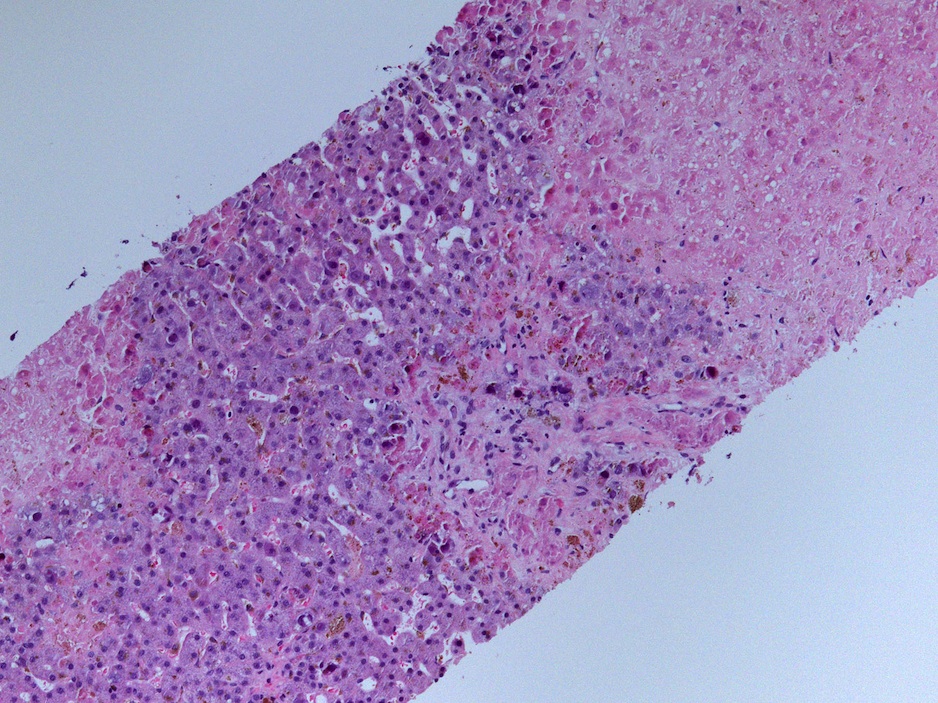
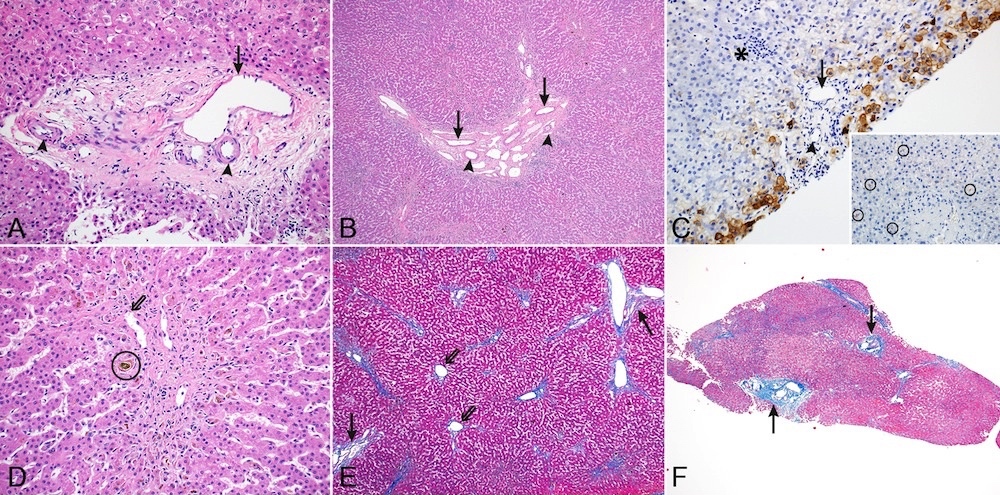
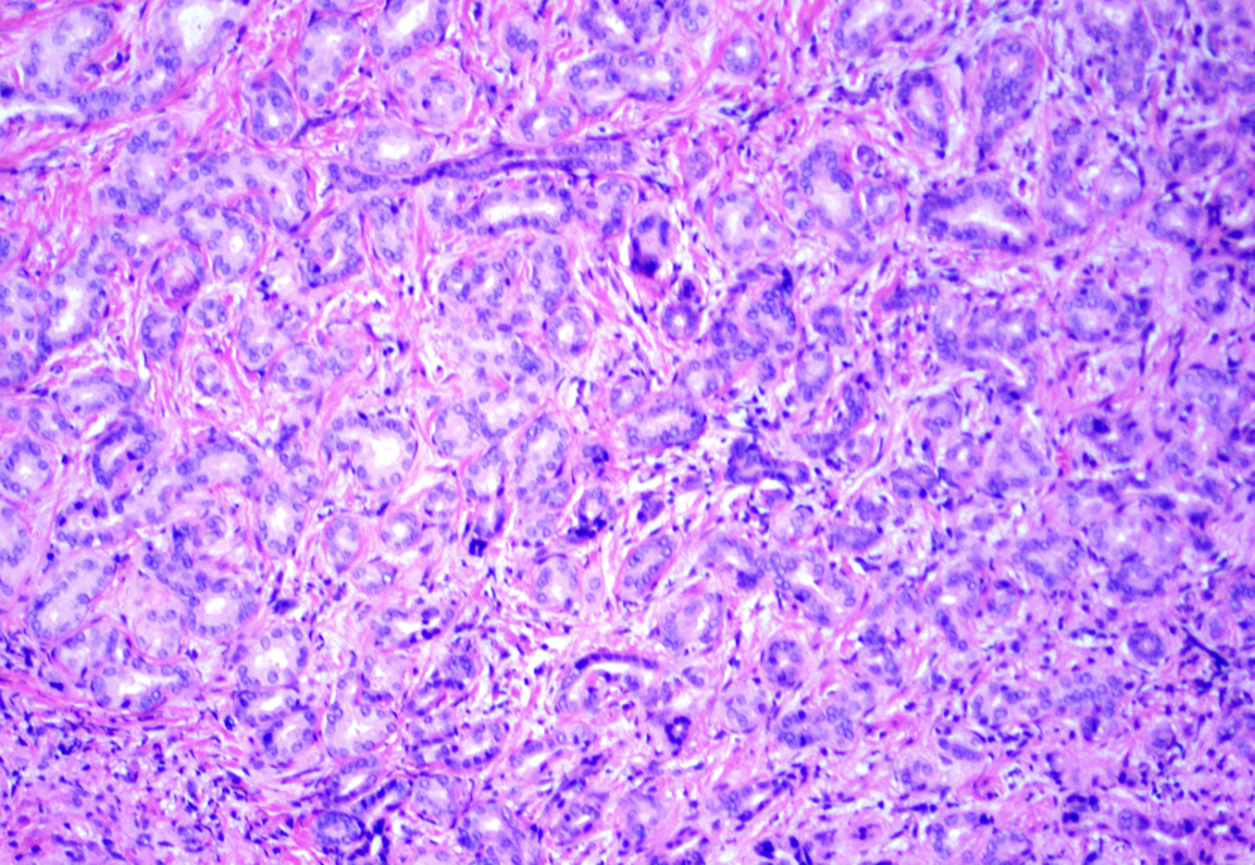
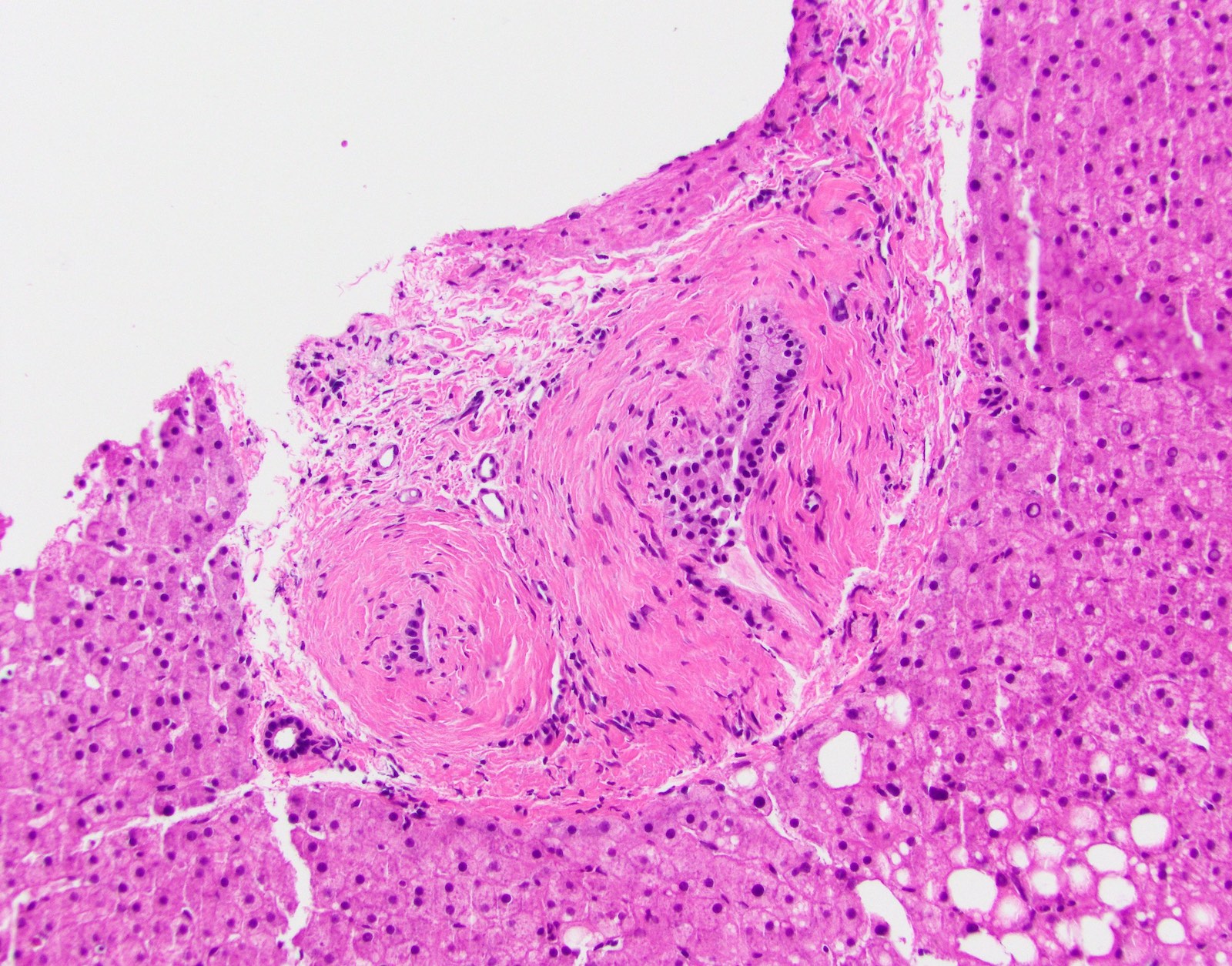
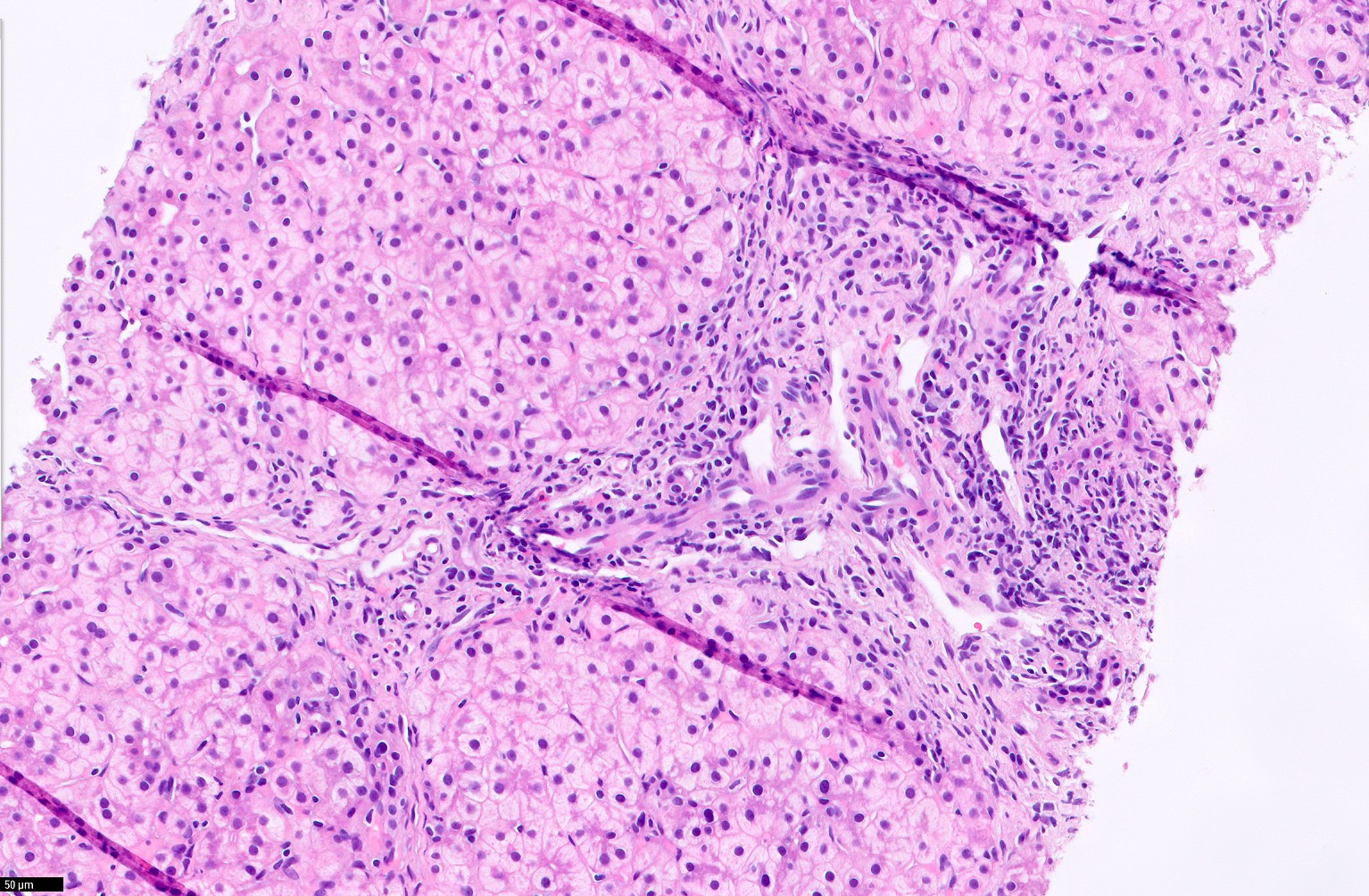
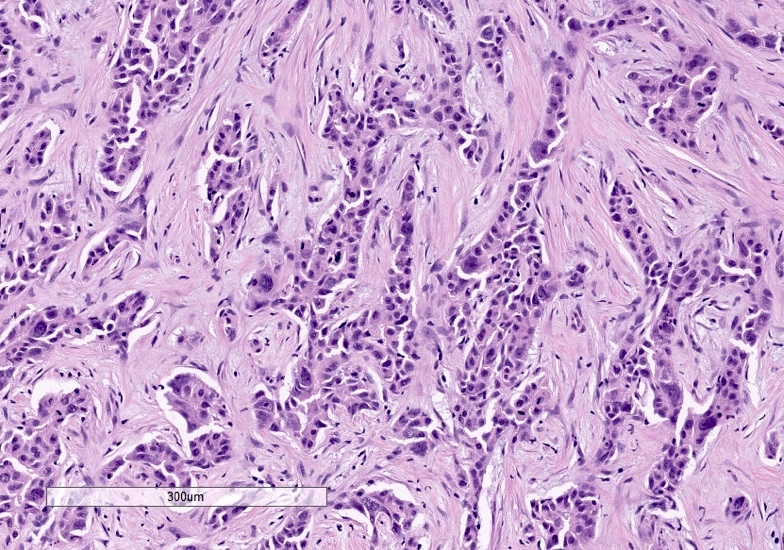
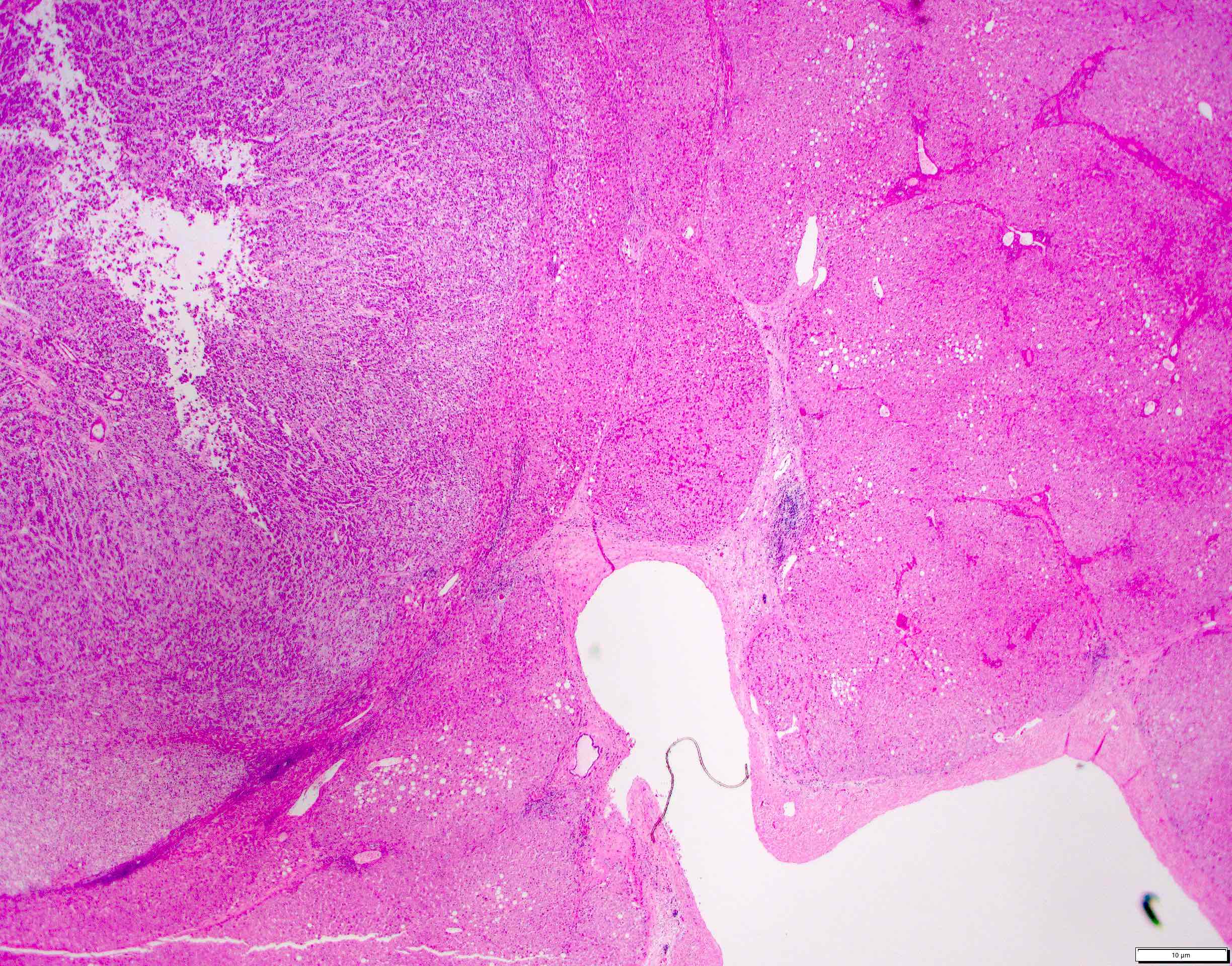
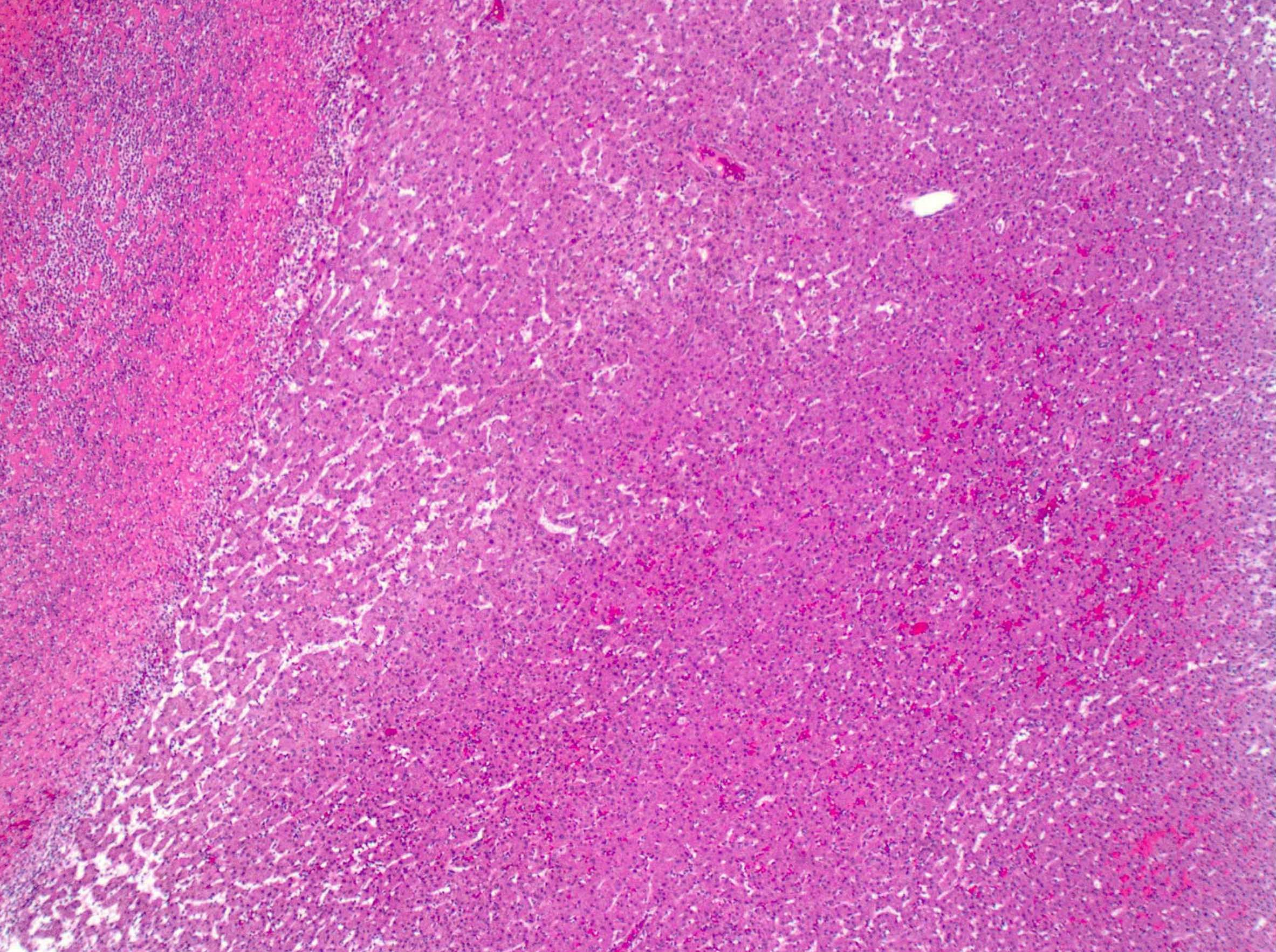
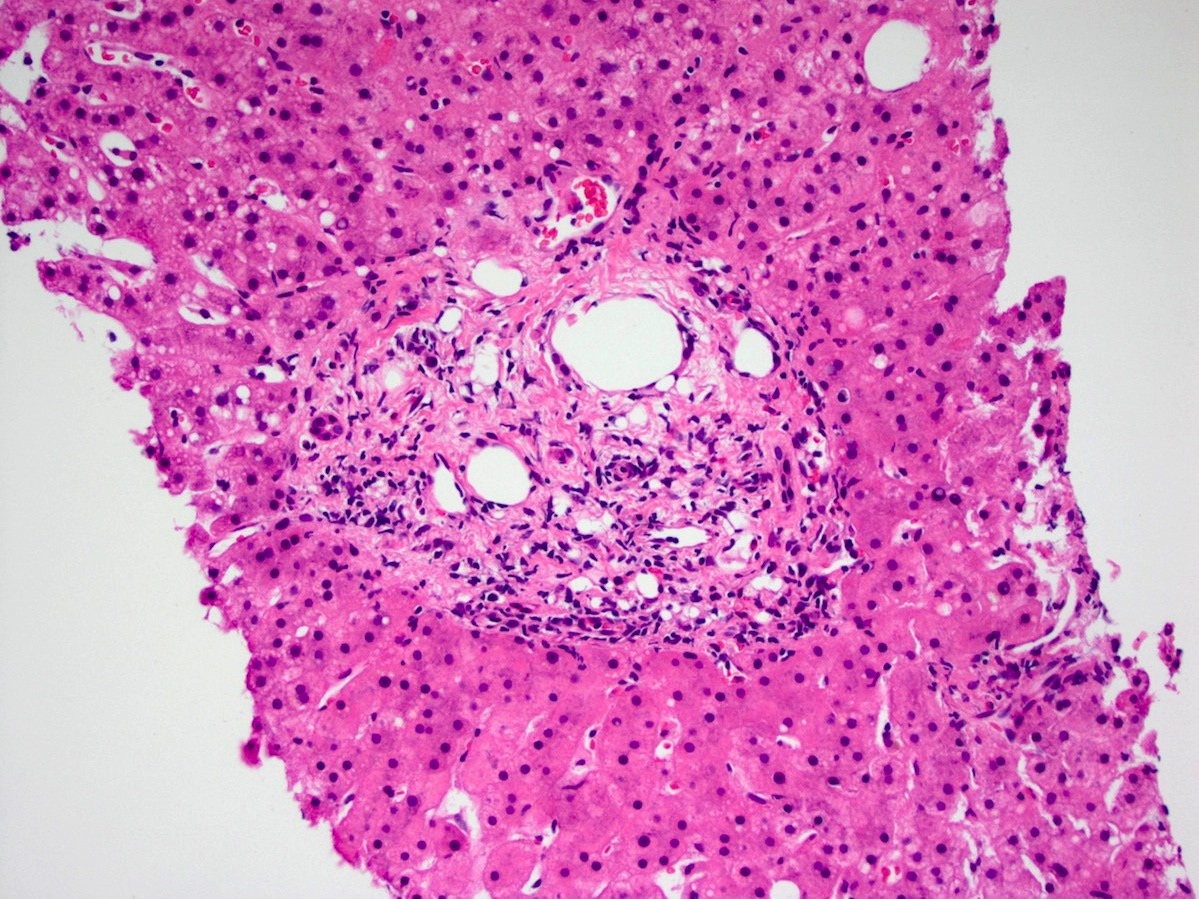
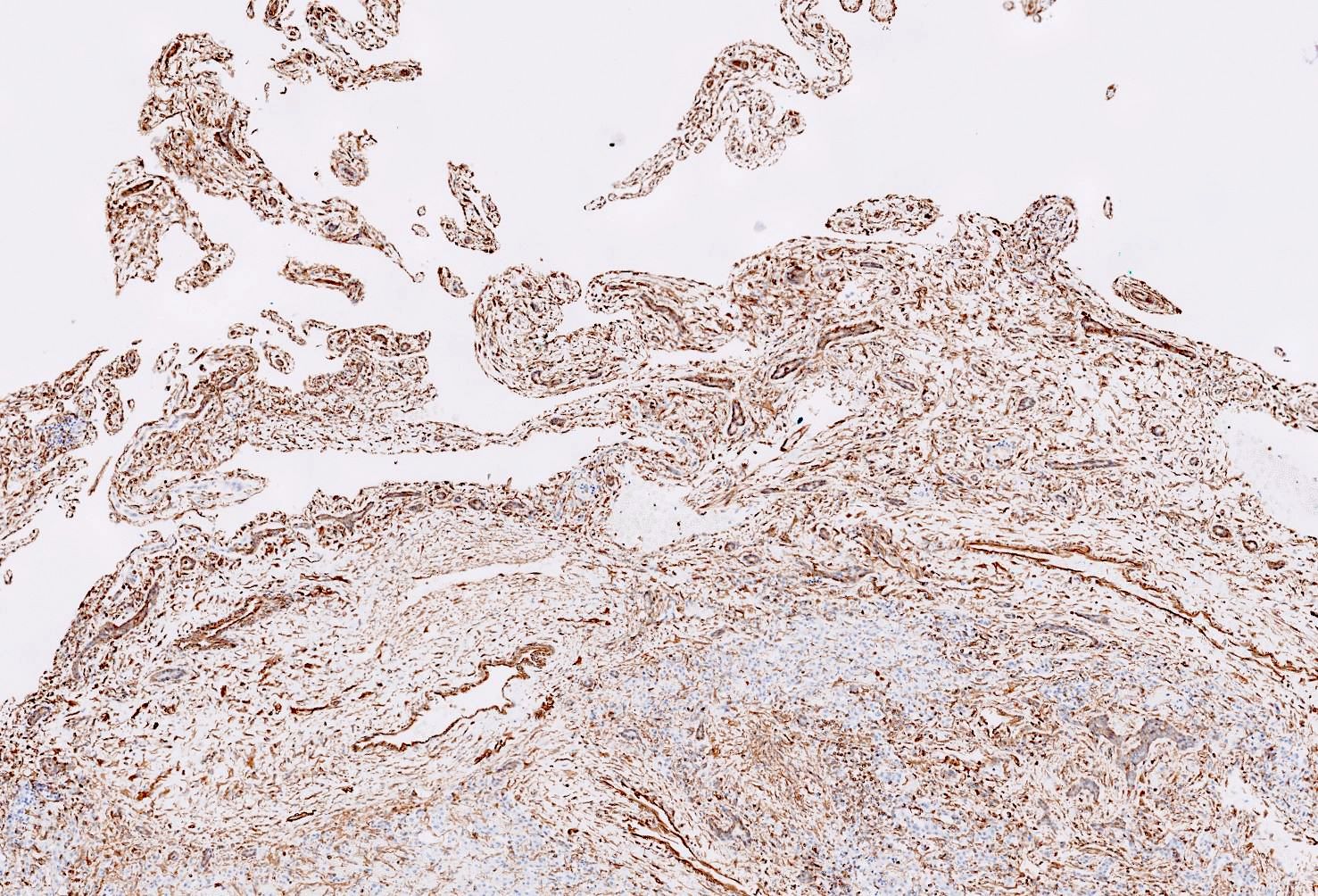
Microscopic (histologic) description
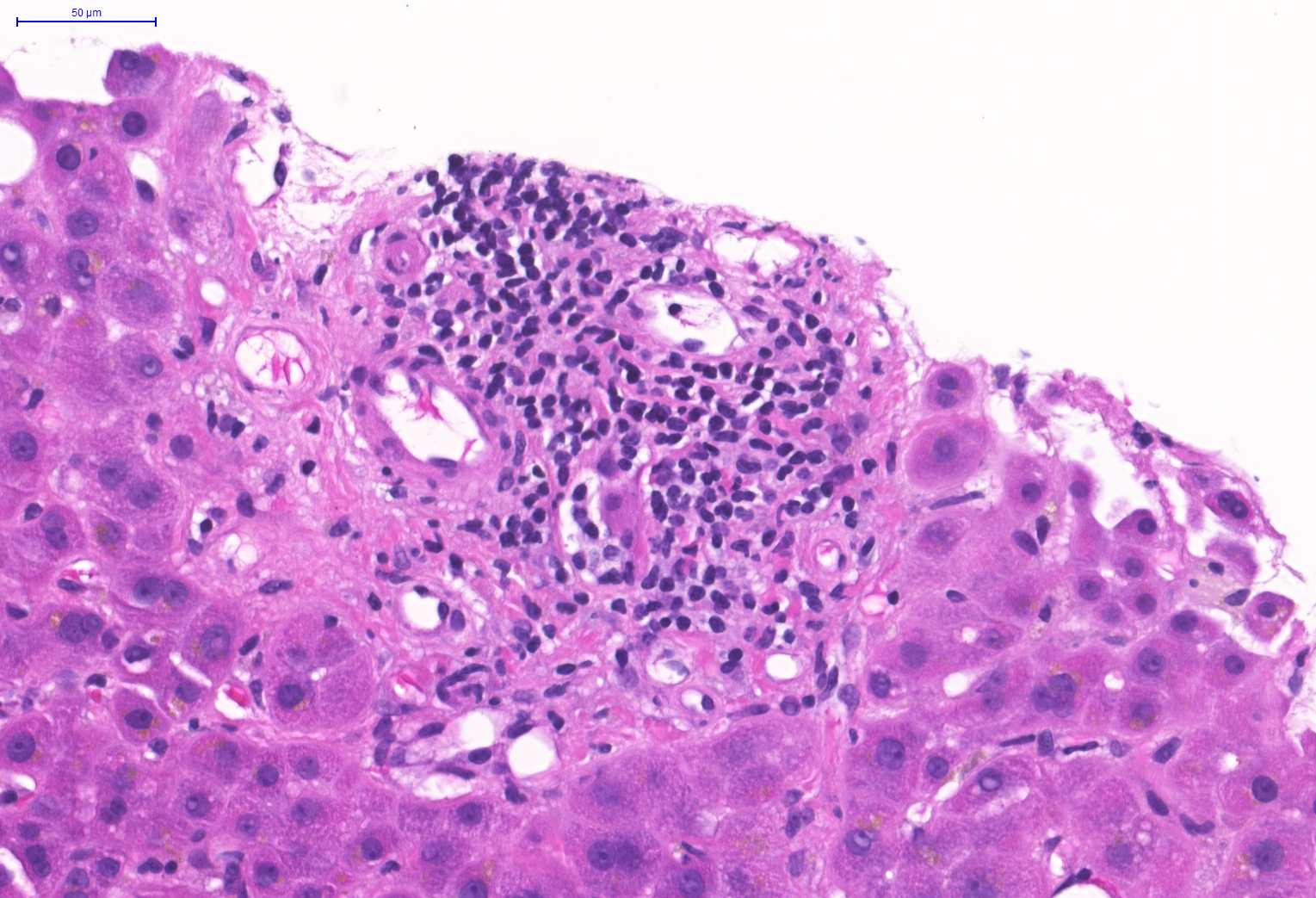
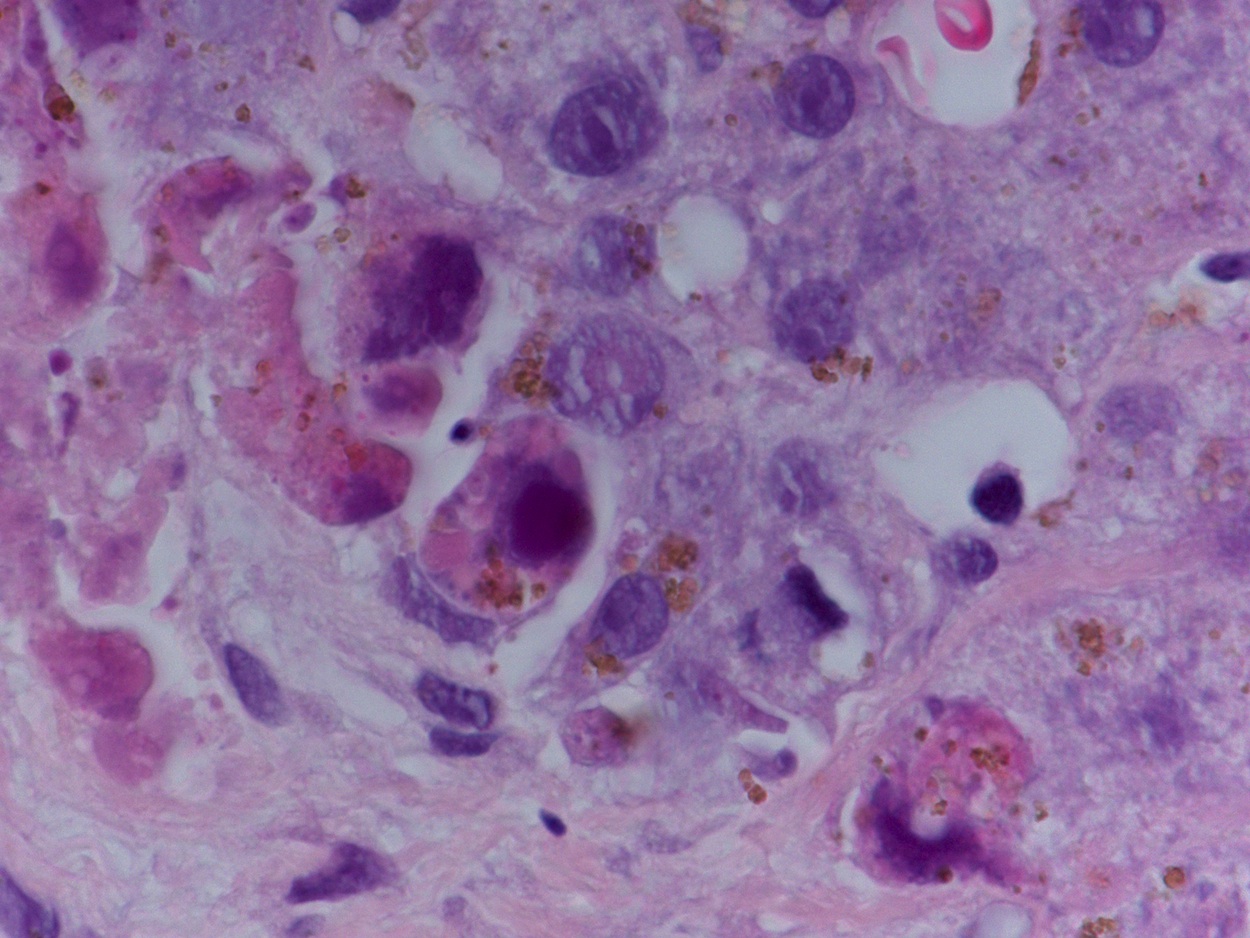
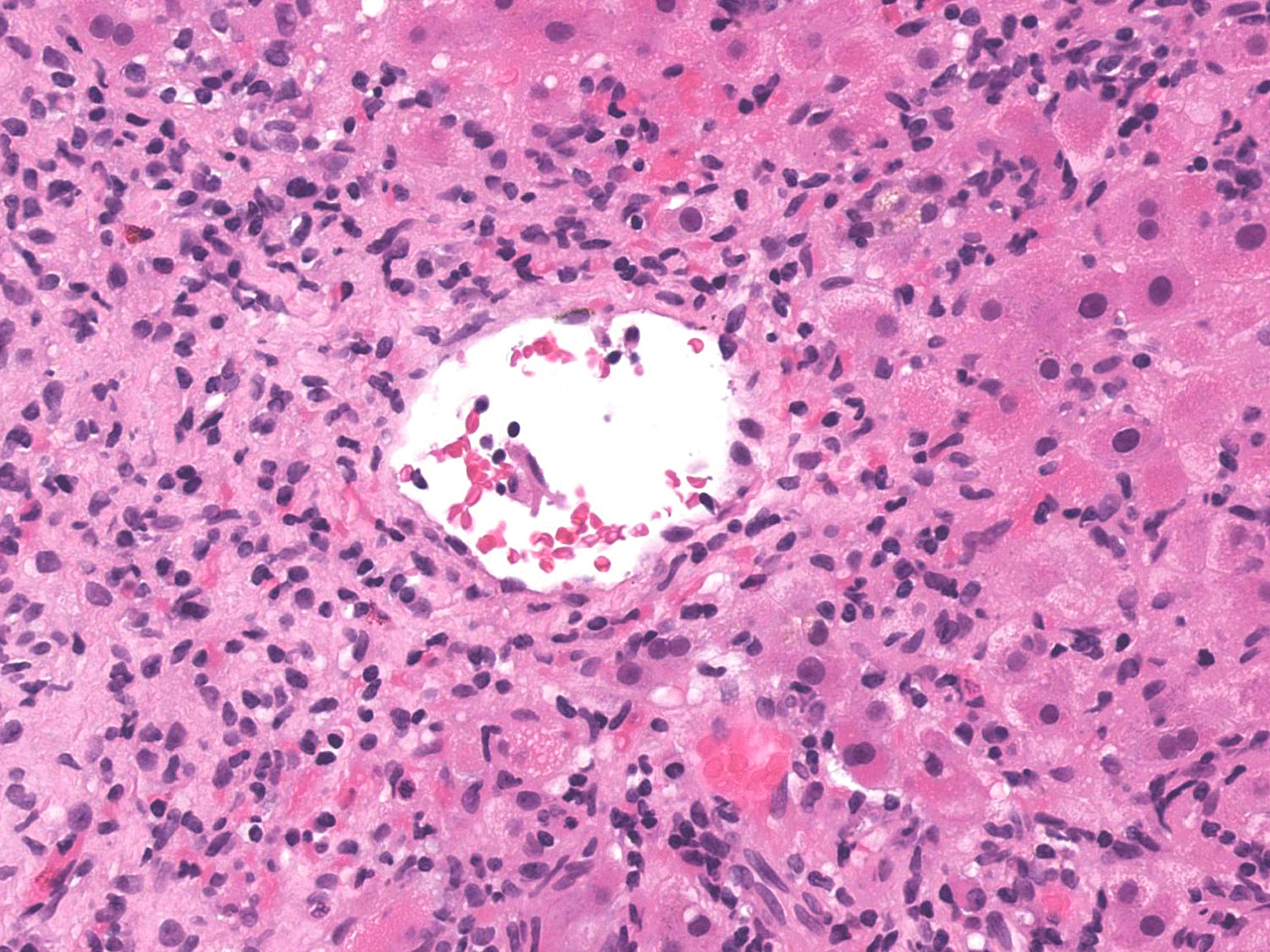
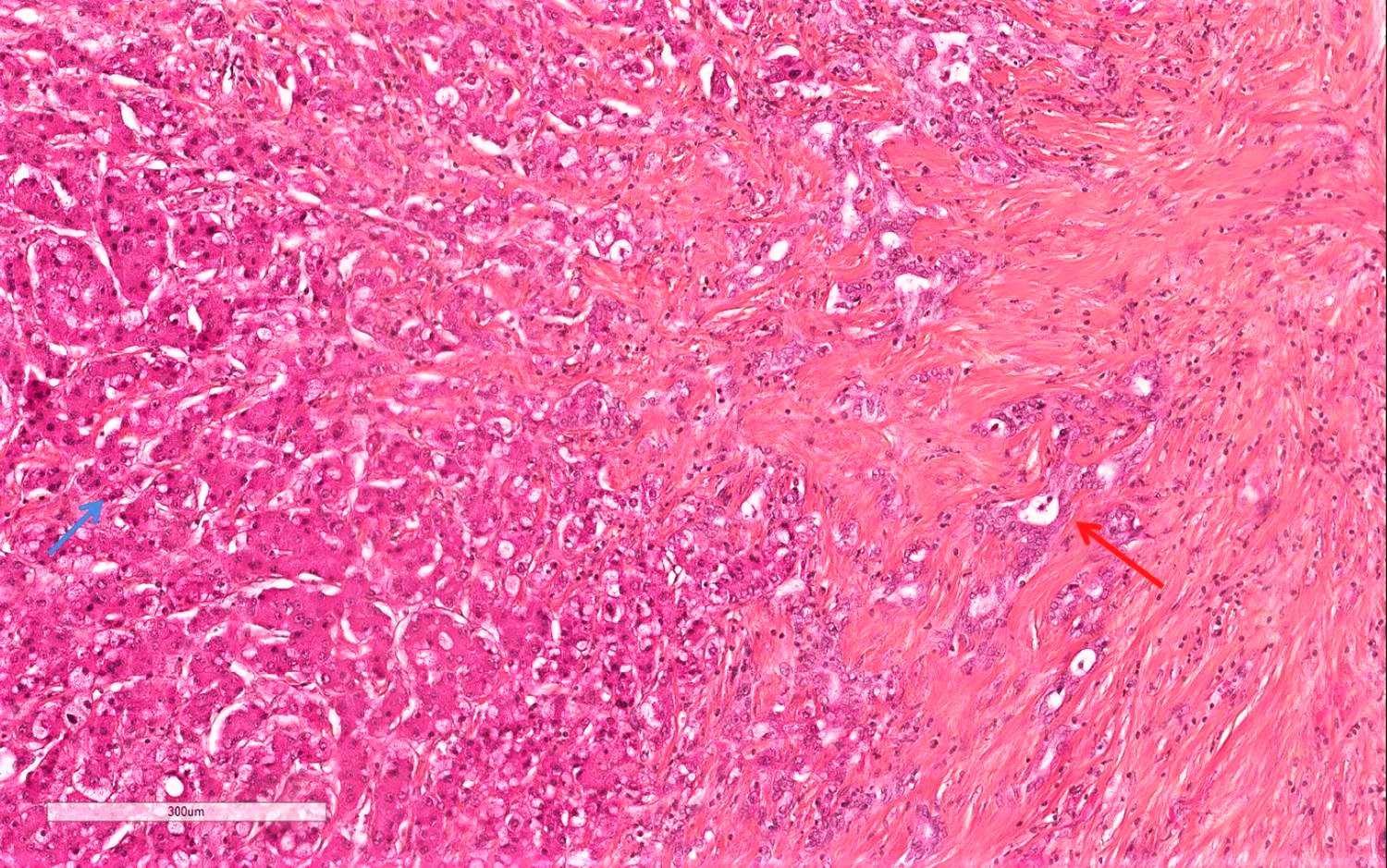
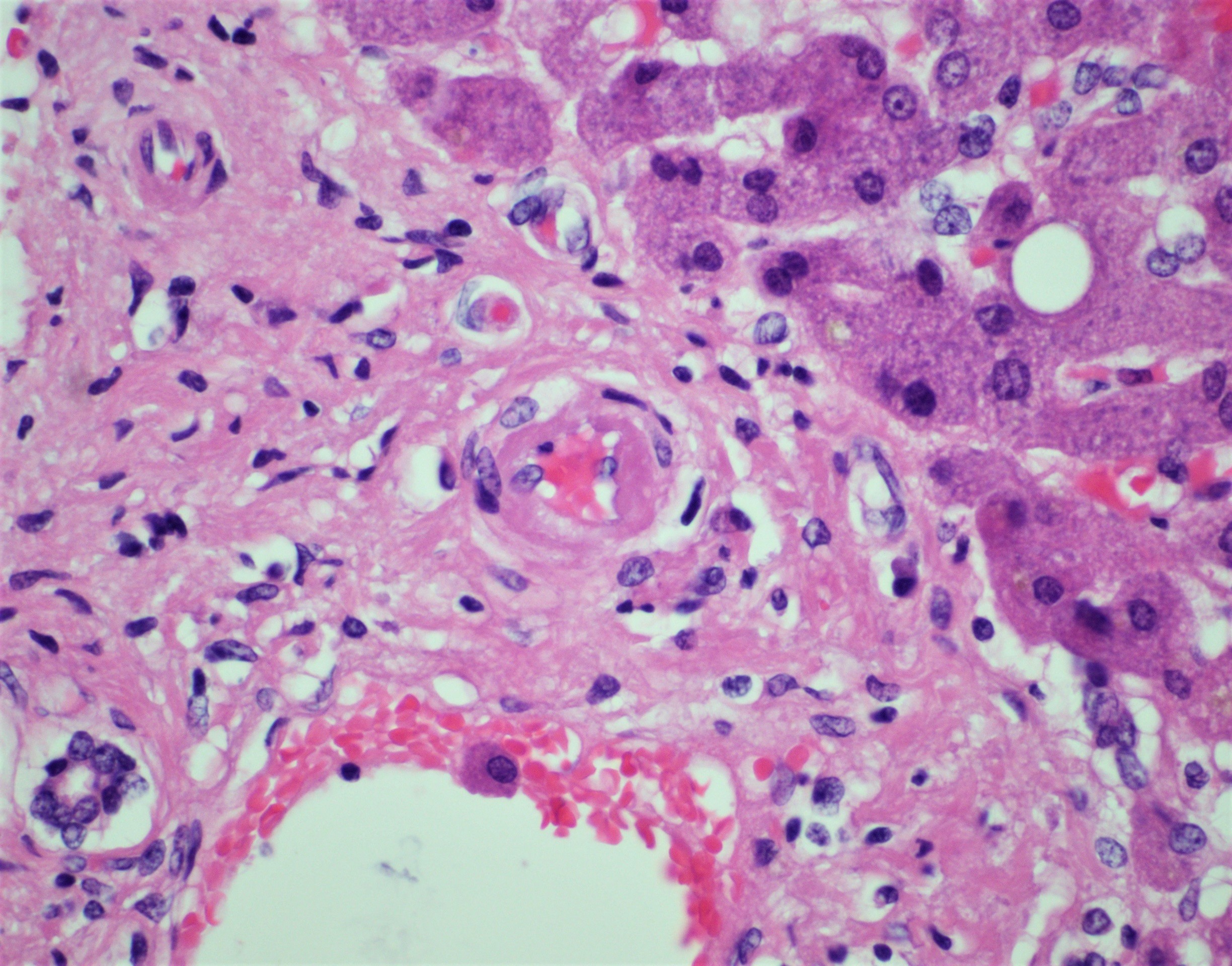
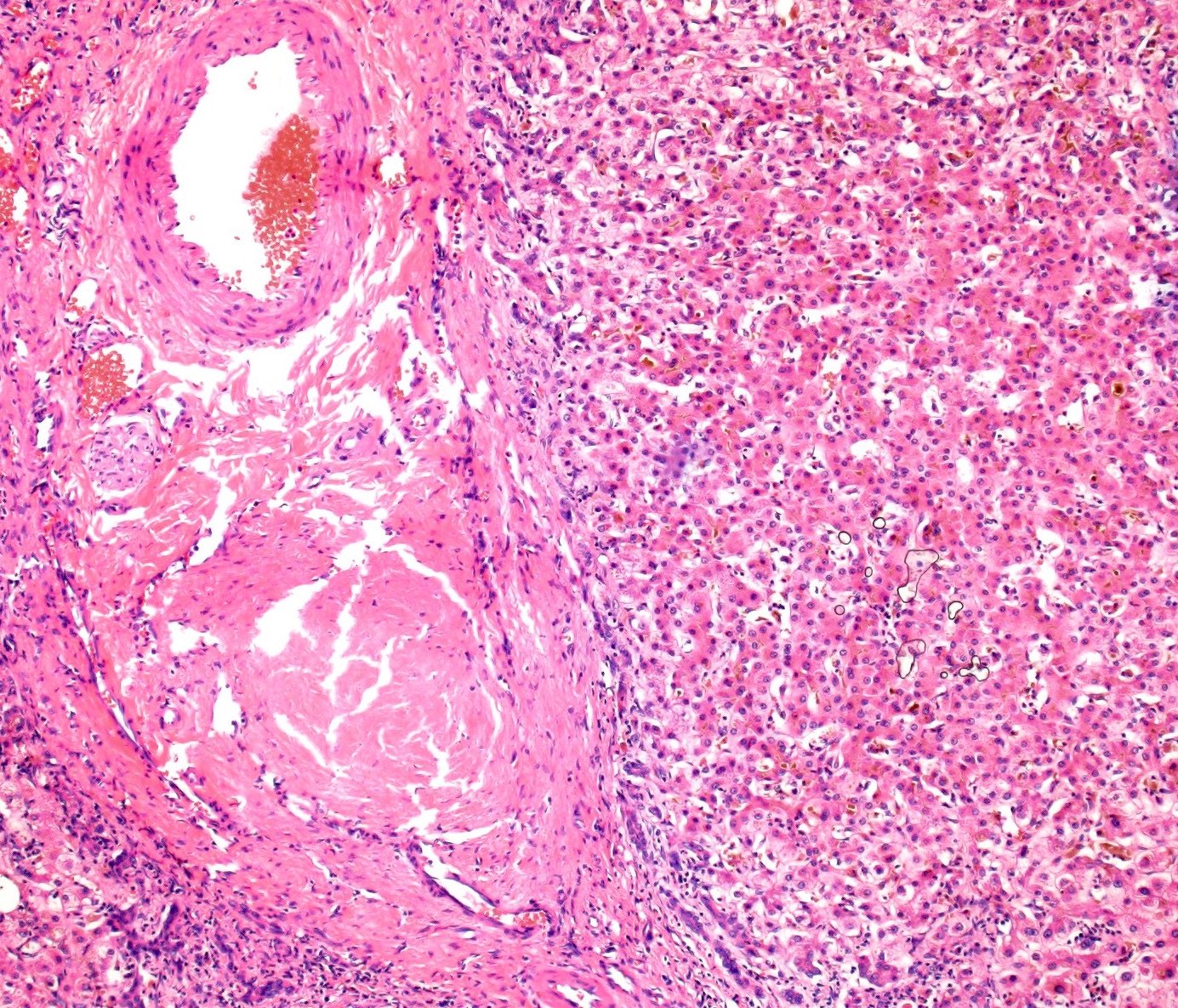
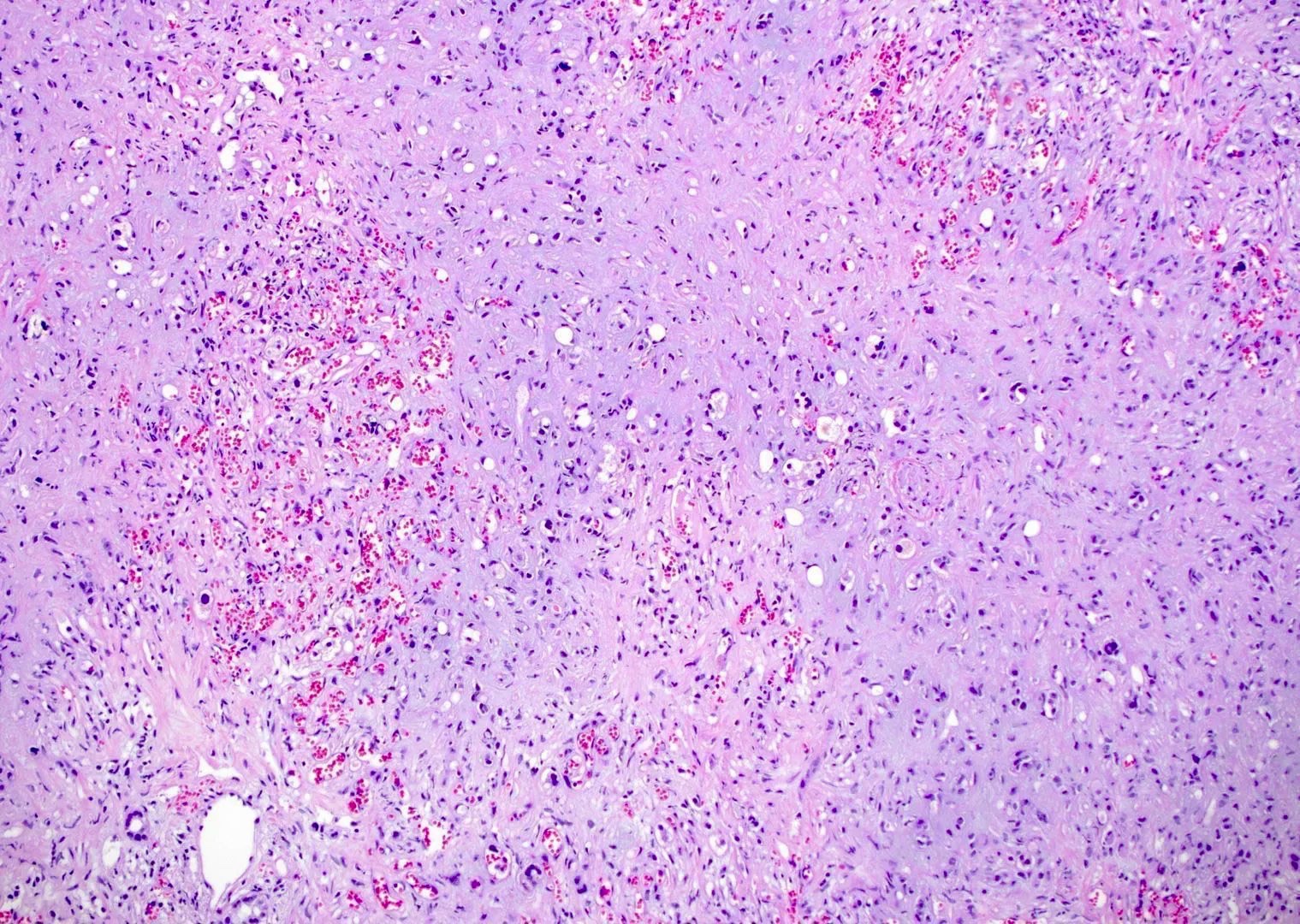
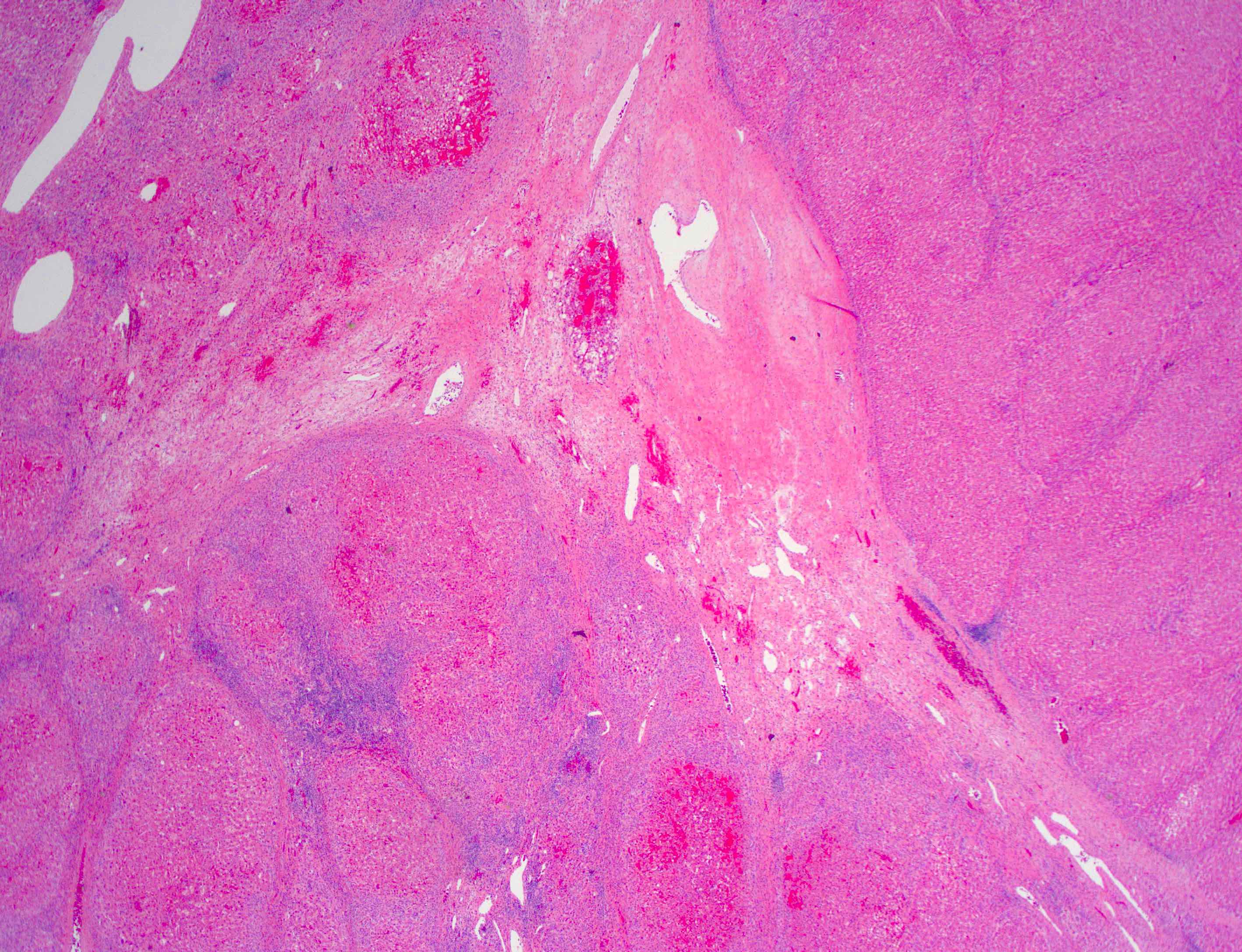
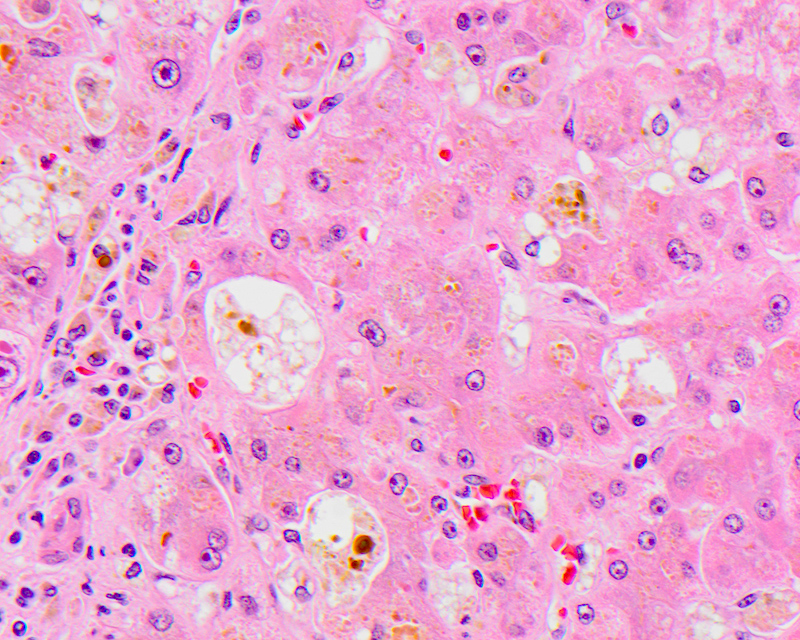
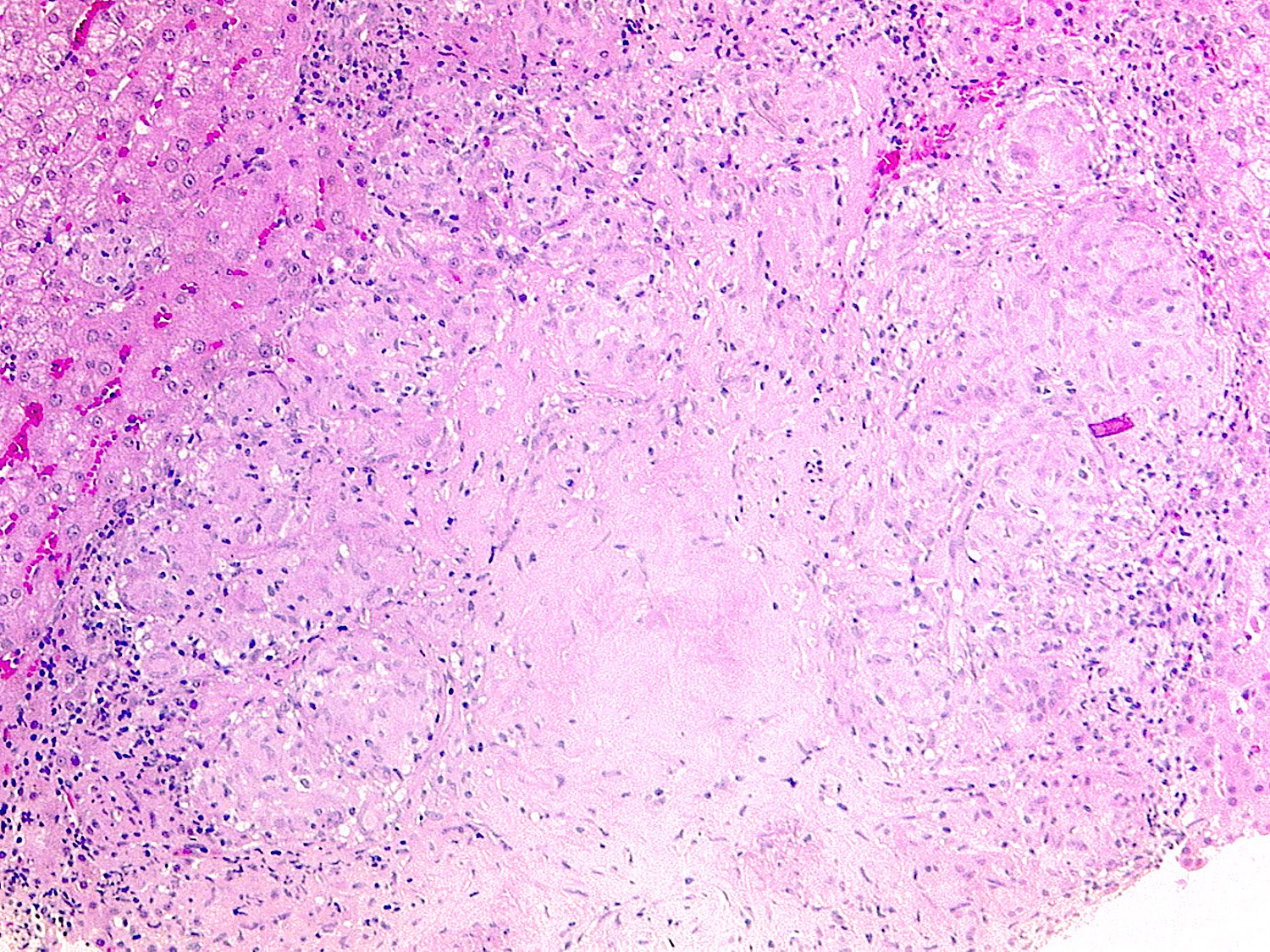
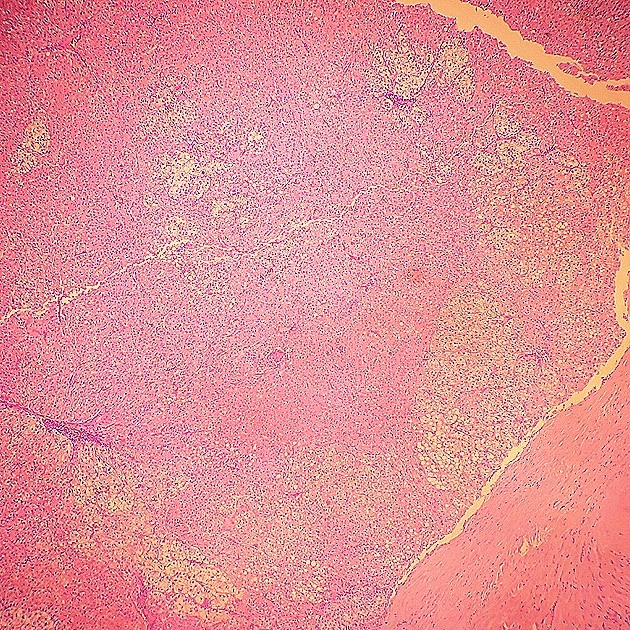
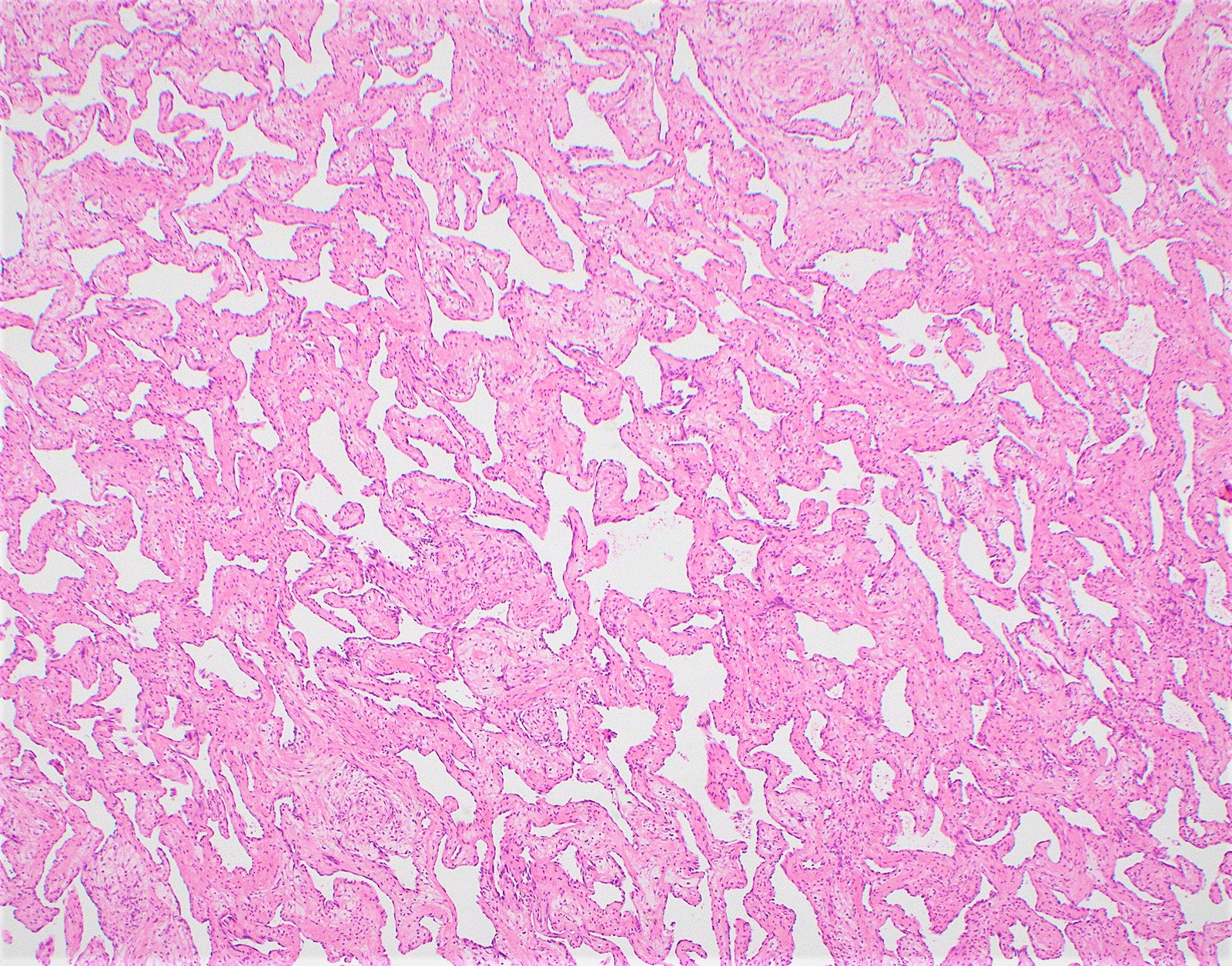
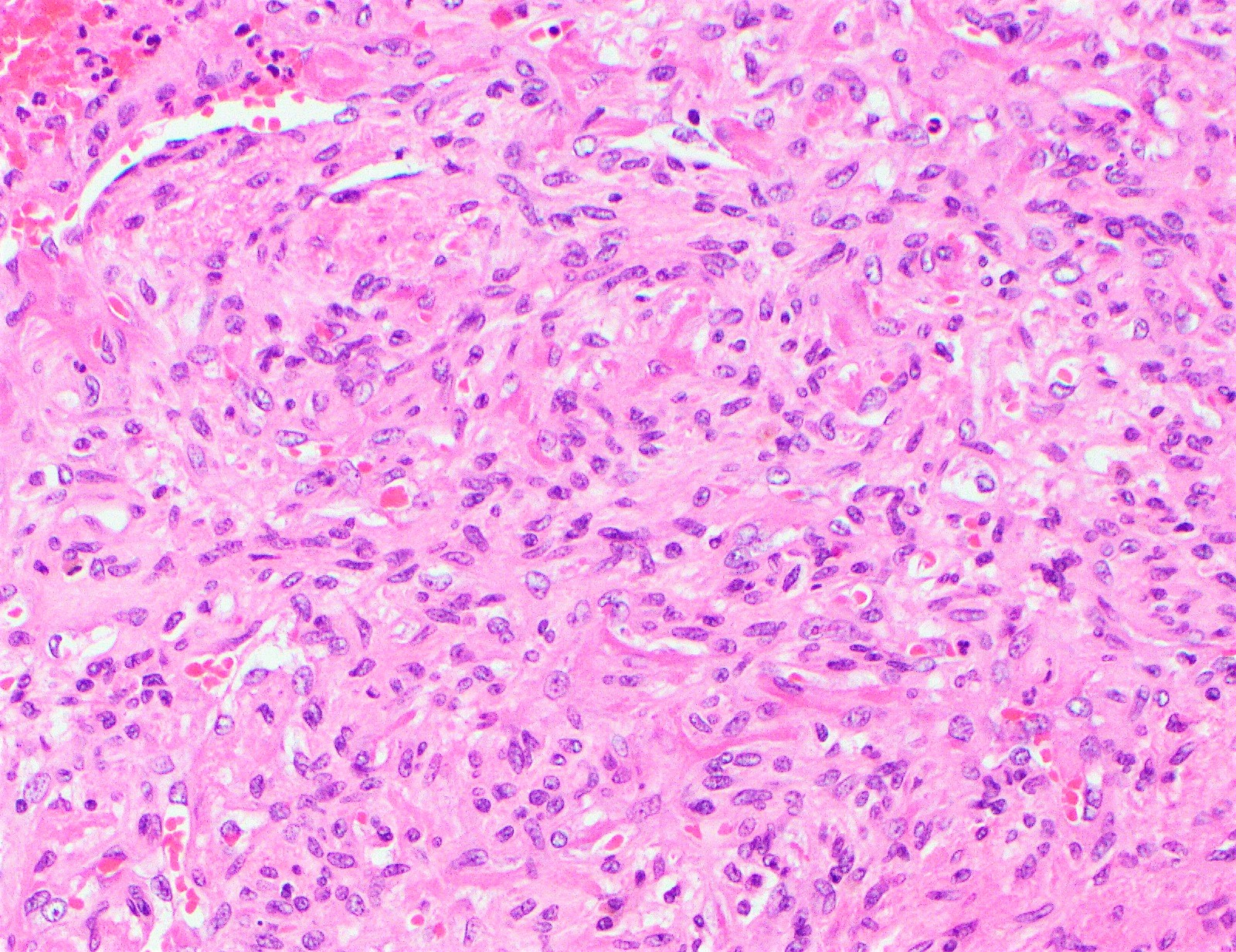
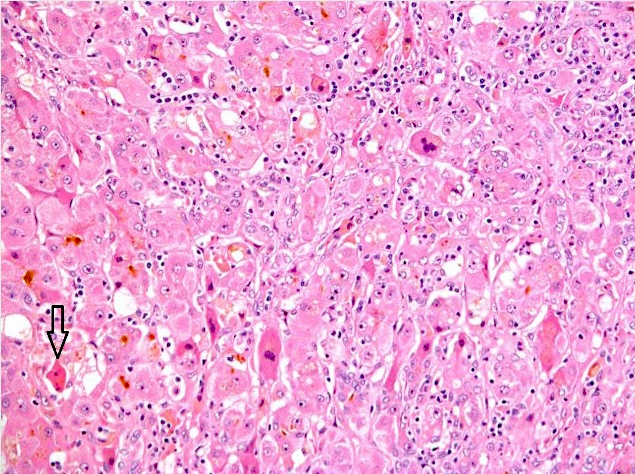
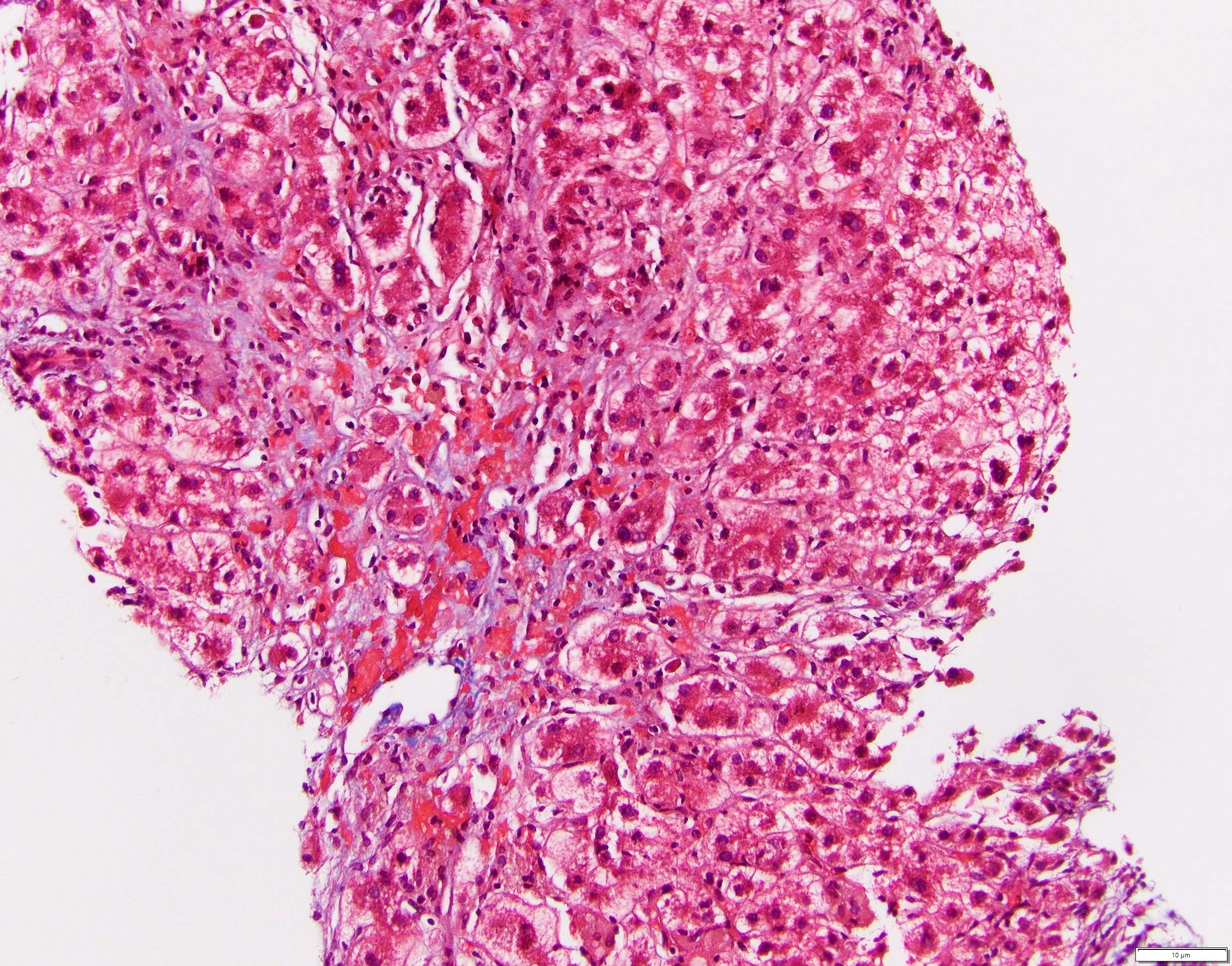
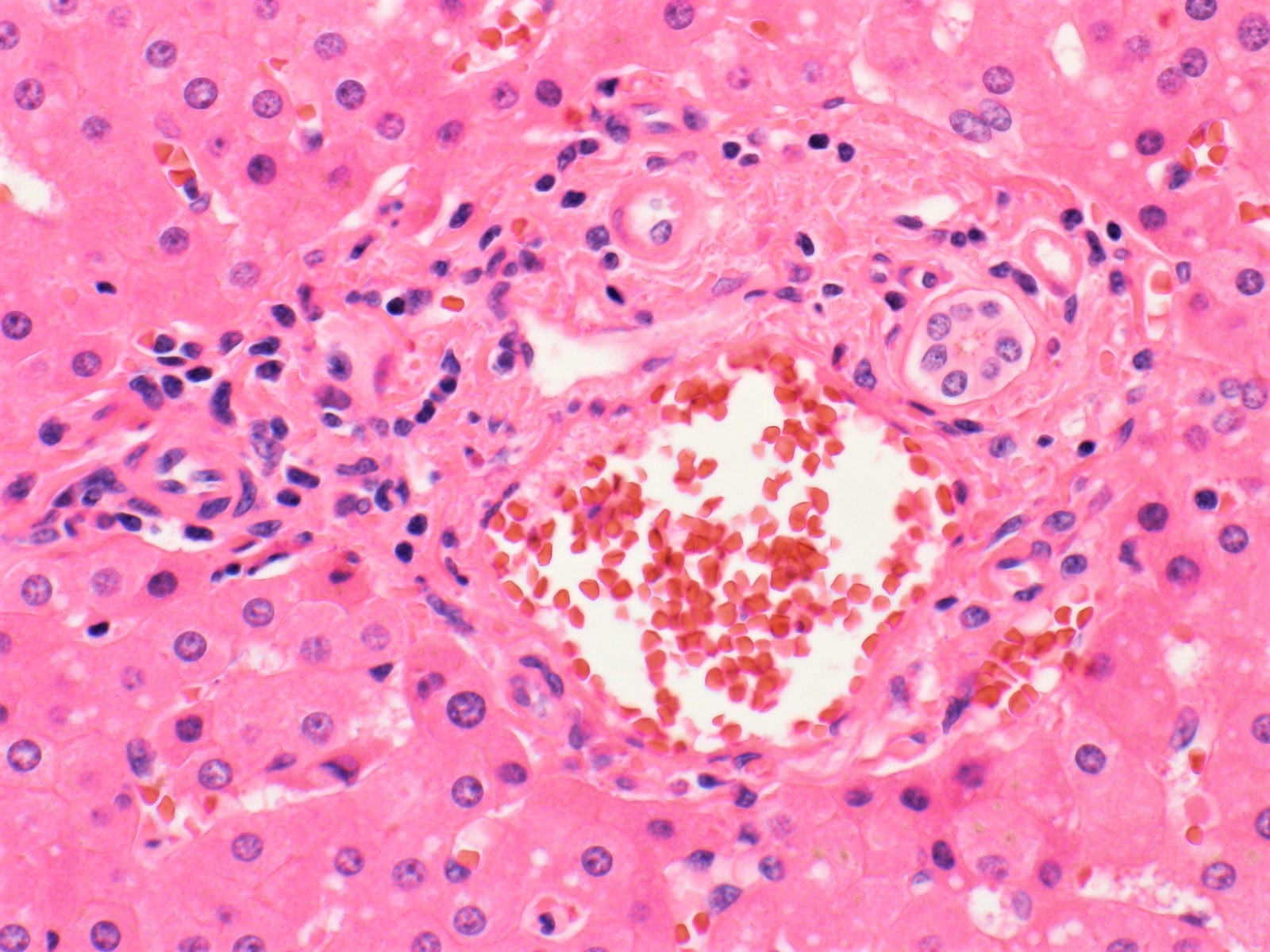
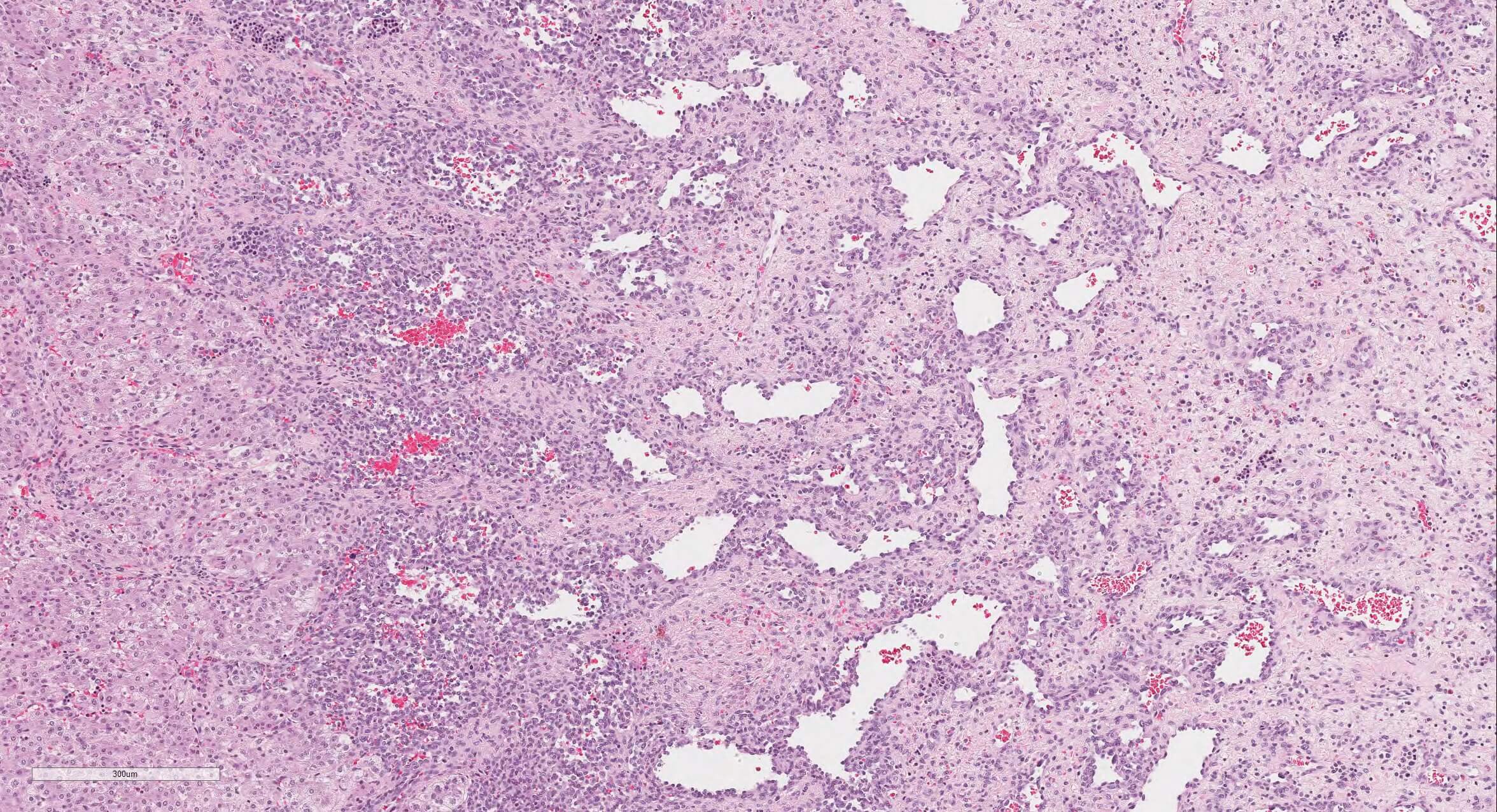
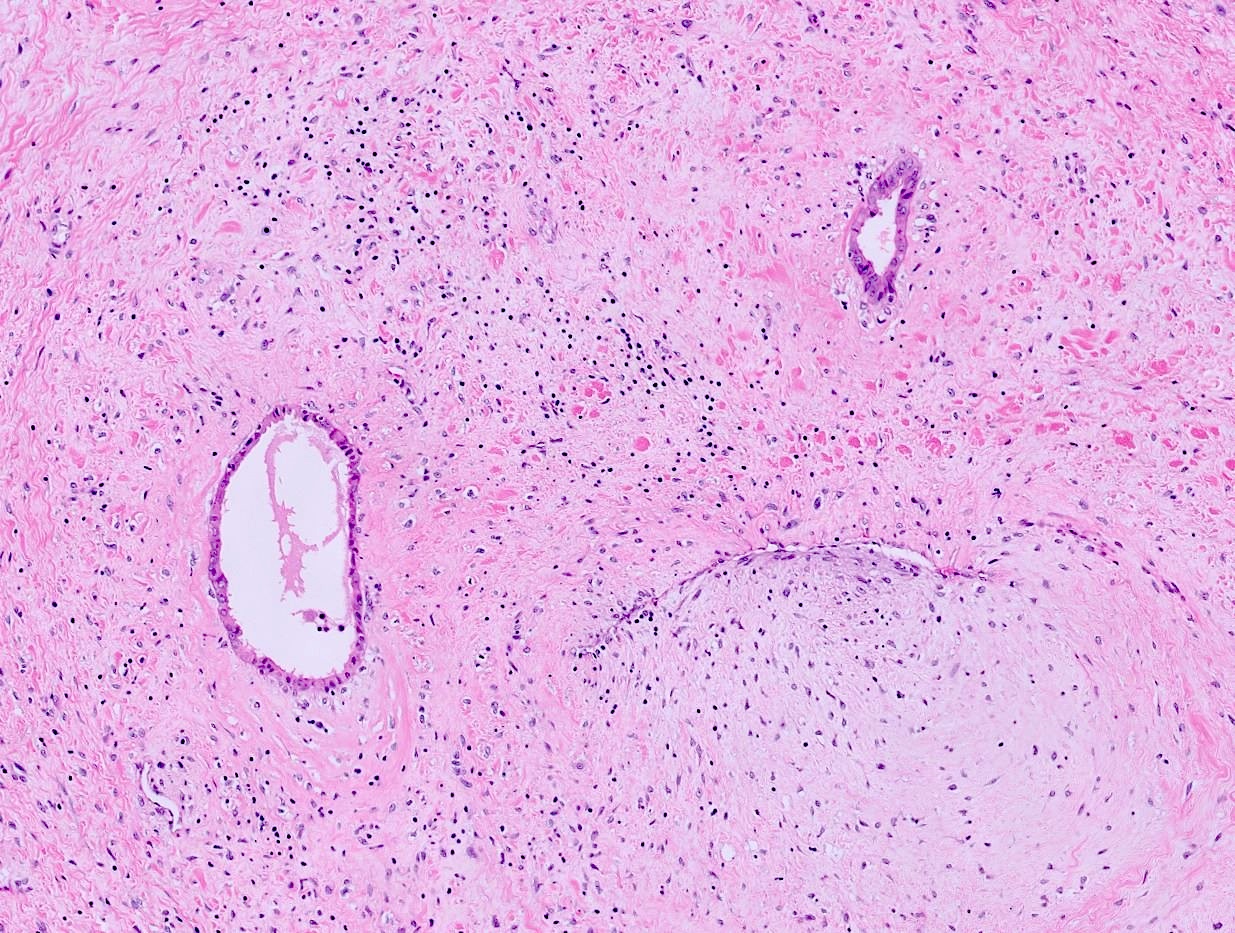
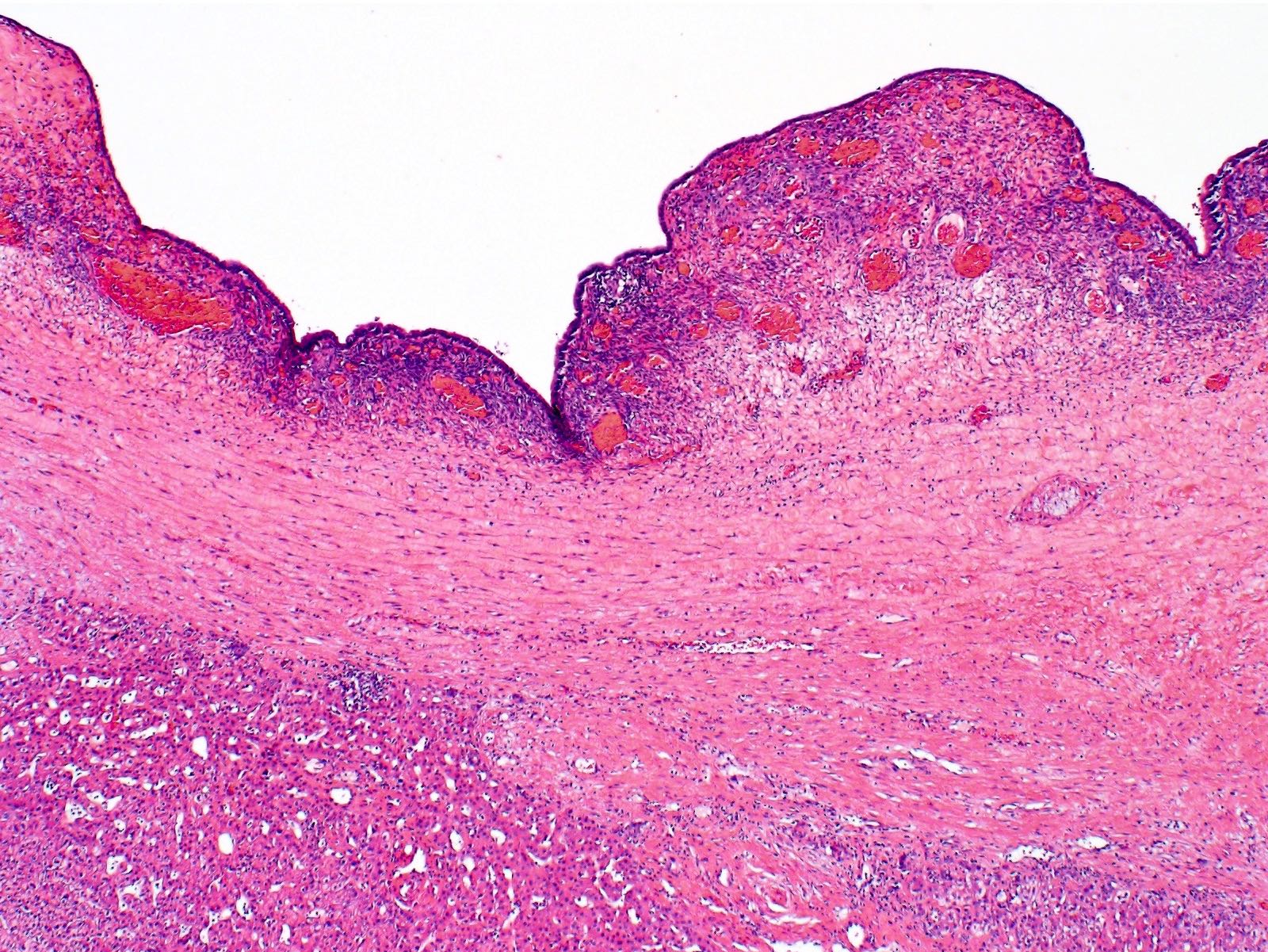
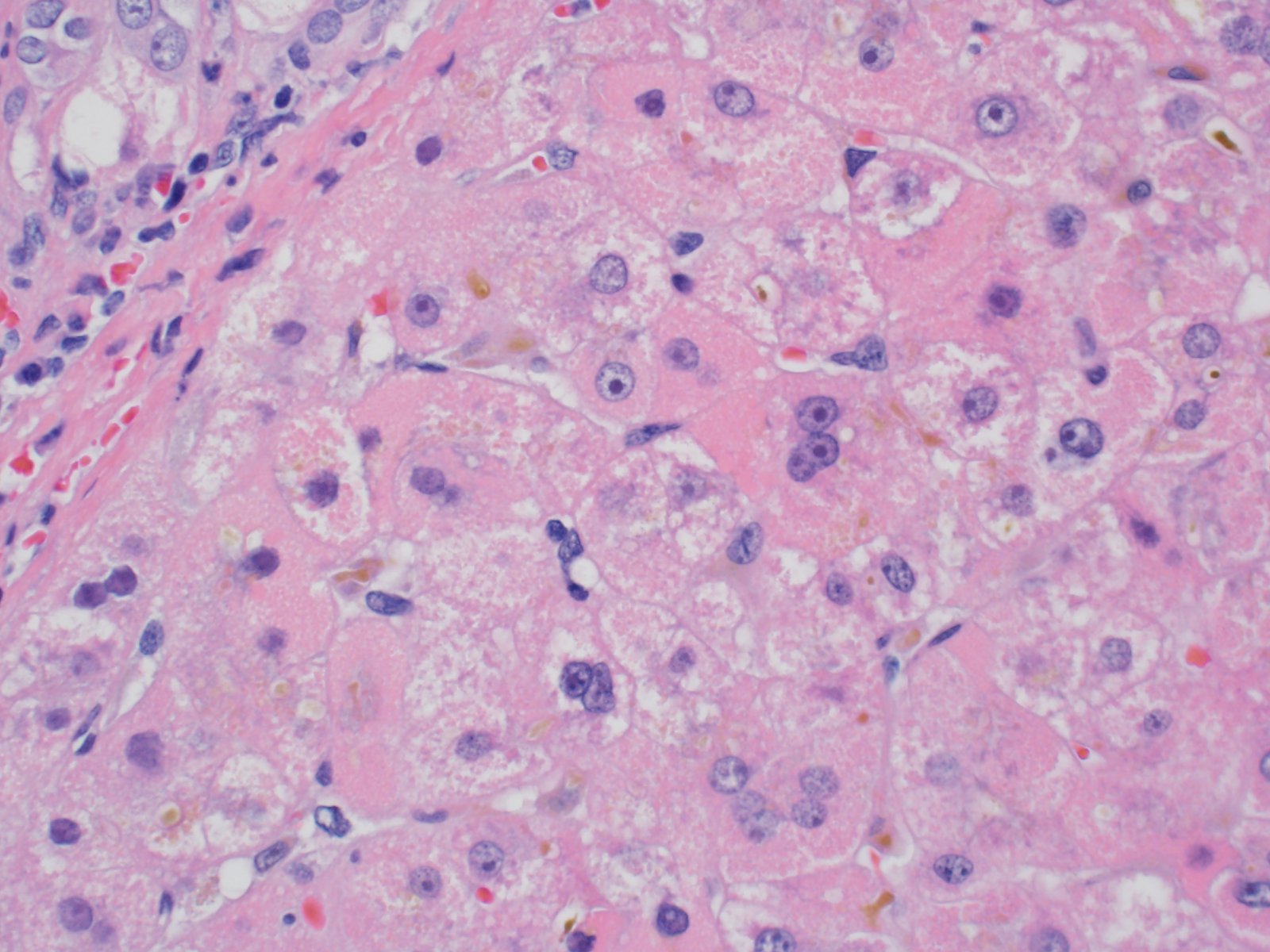
- Hyperacute rejection:
- Portal edema, necrosis, neutrophilic infiltration and ductular reaction
- Platelet fibrin thrombi in sinusoidal spaces, portal veins and central veins
- Hepatocyte necrosis, hemorrhage and (if untreated) confluent necrosis
- Necrotizing arteritis
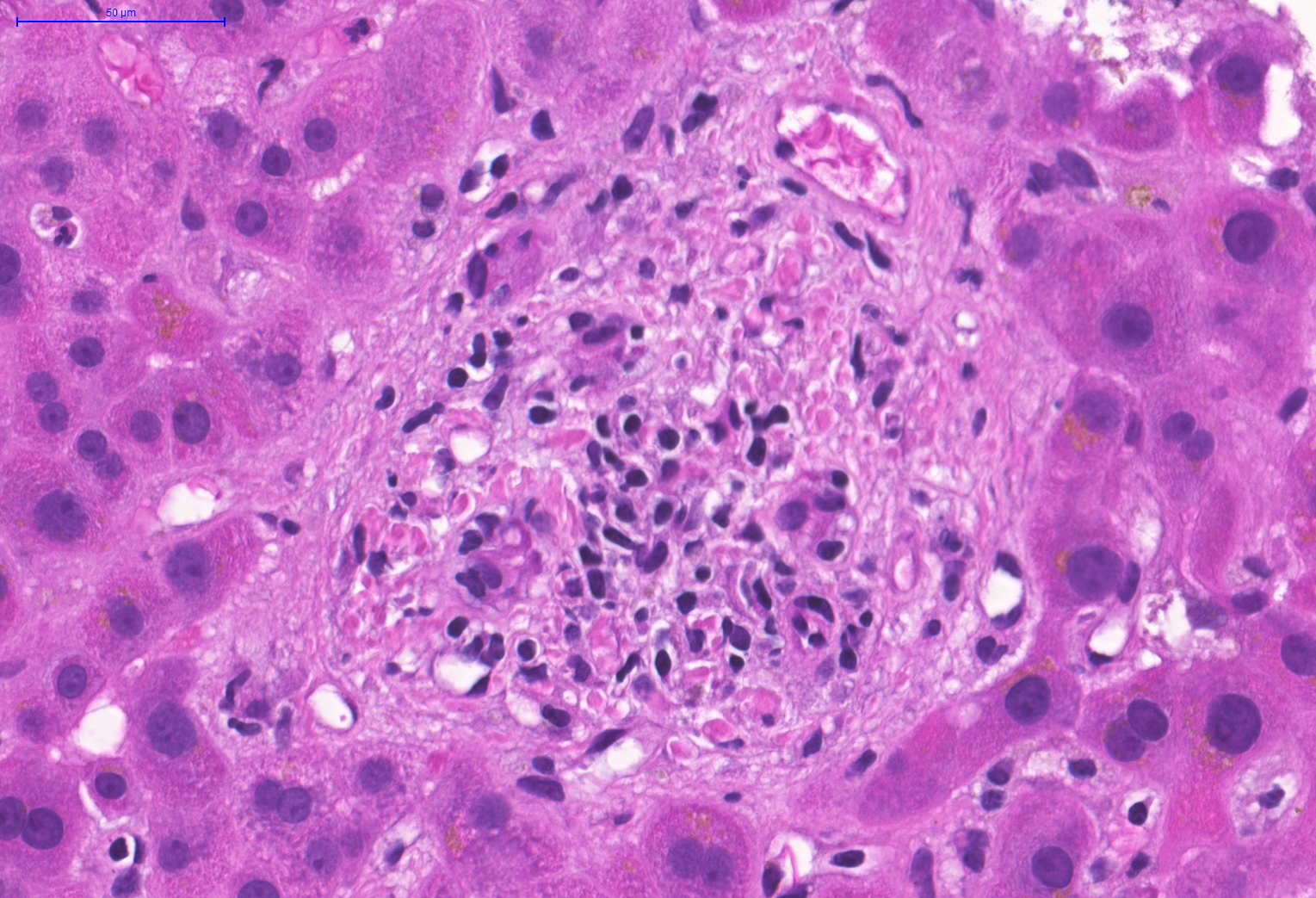
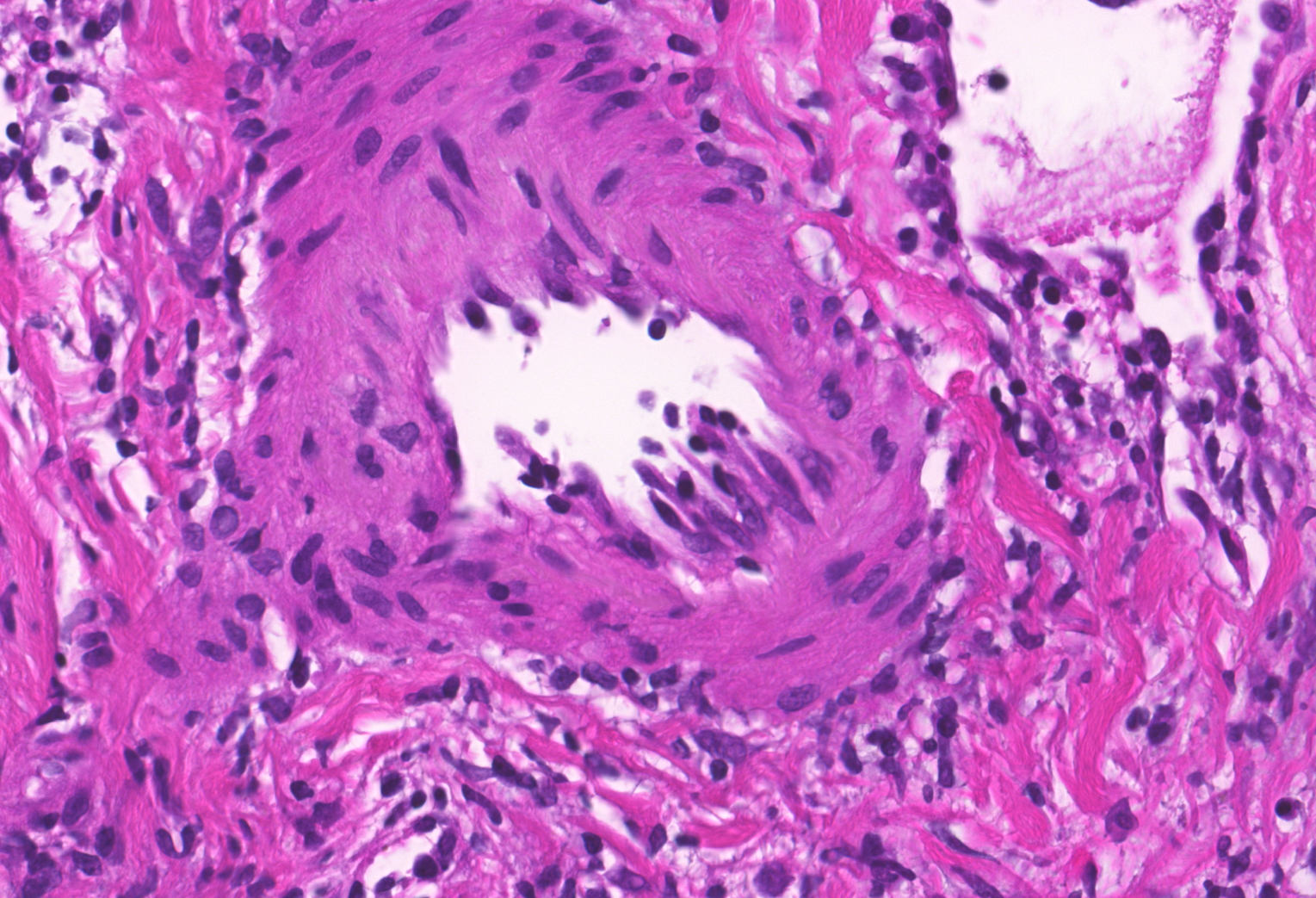
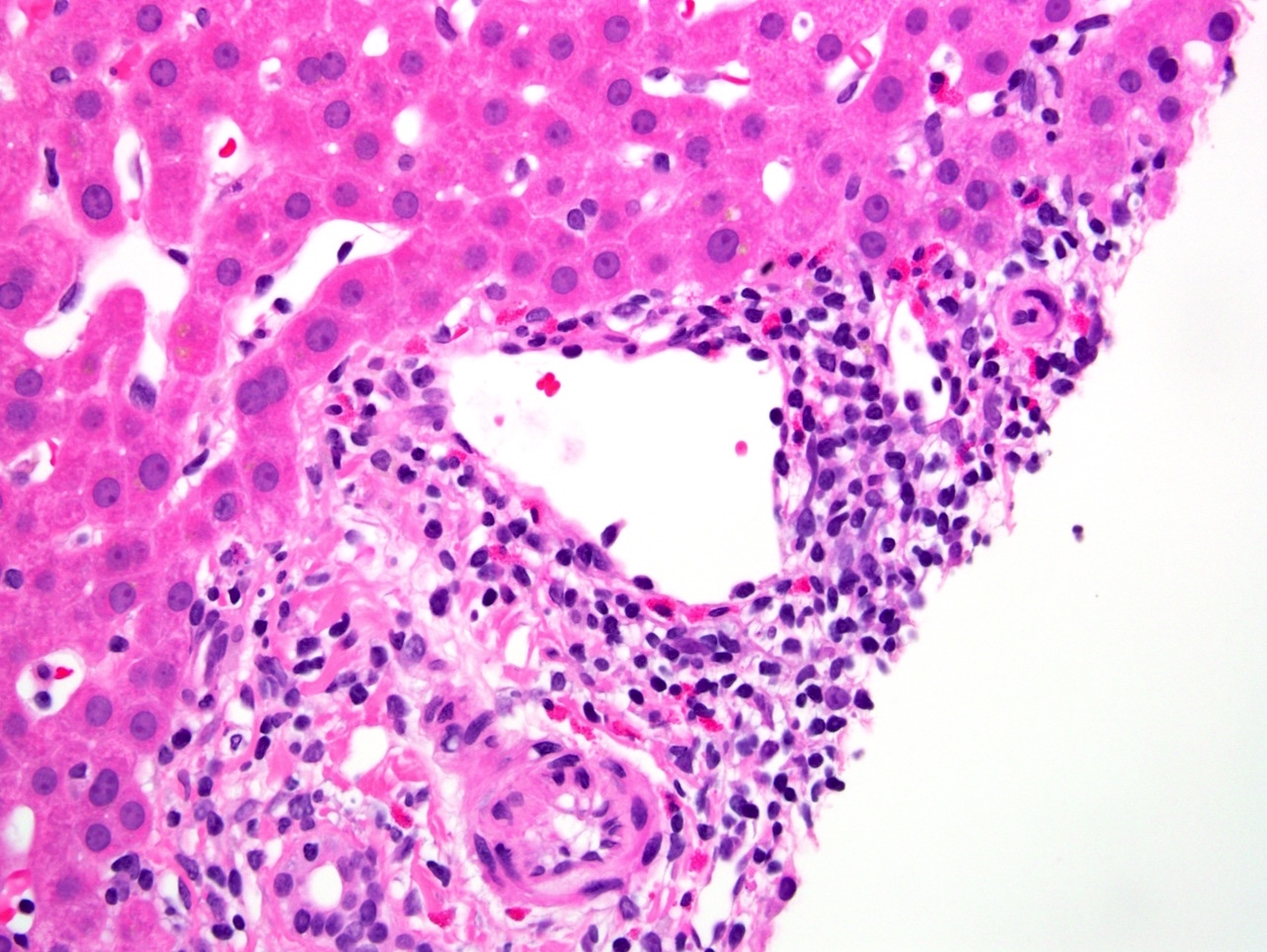
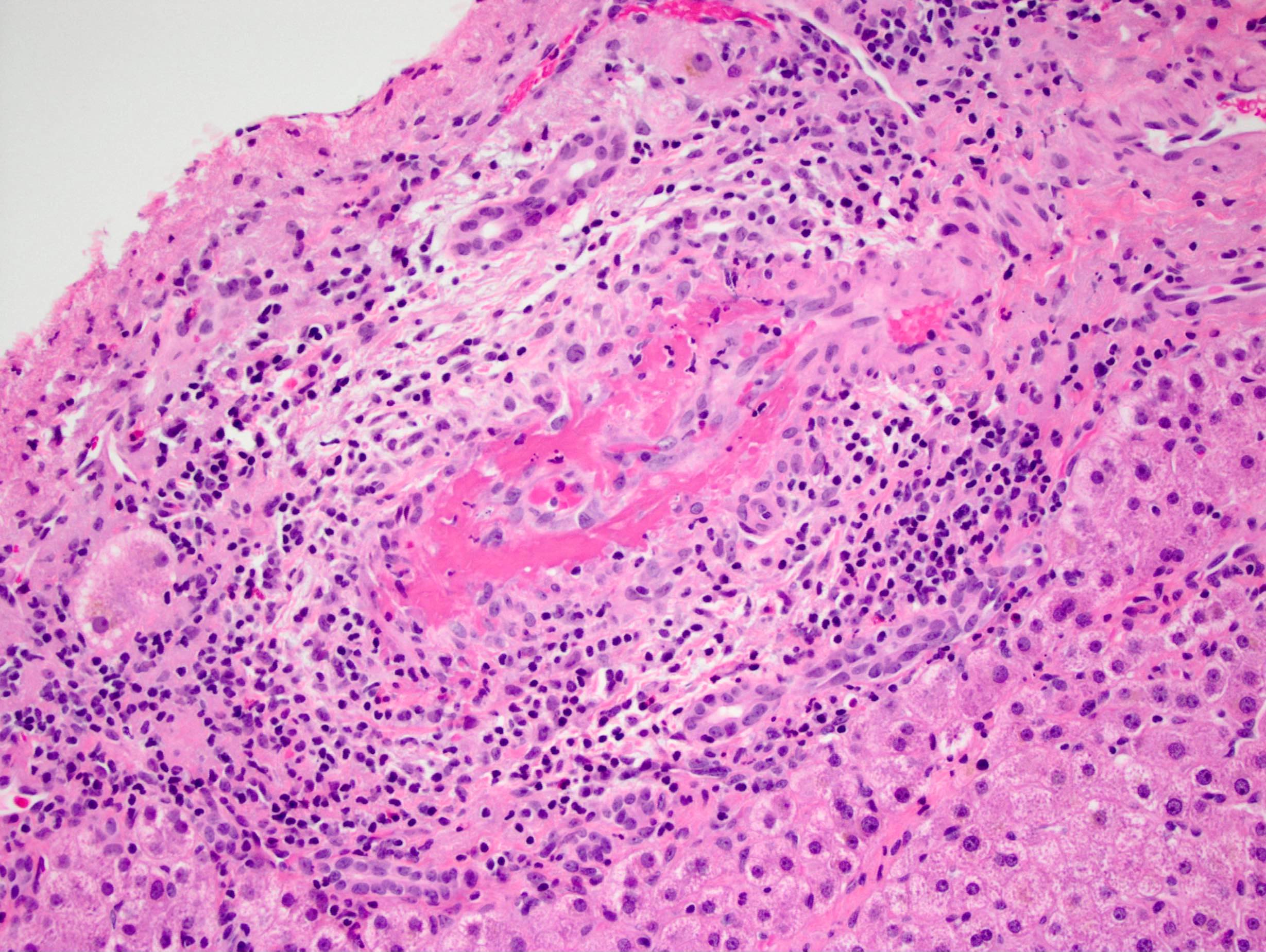
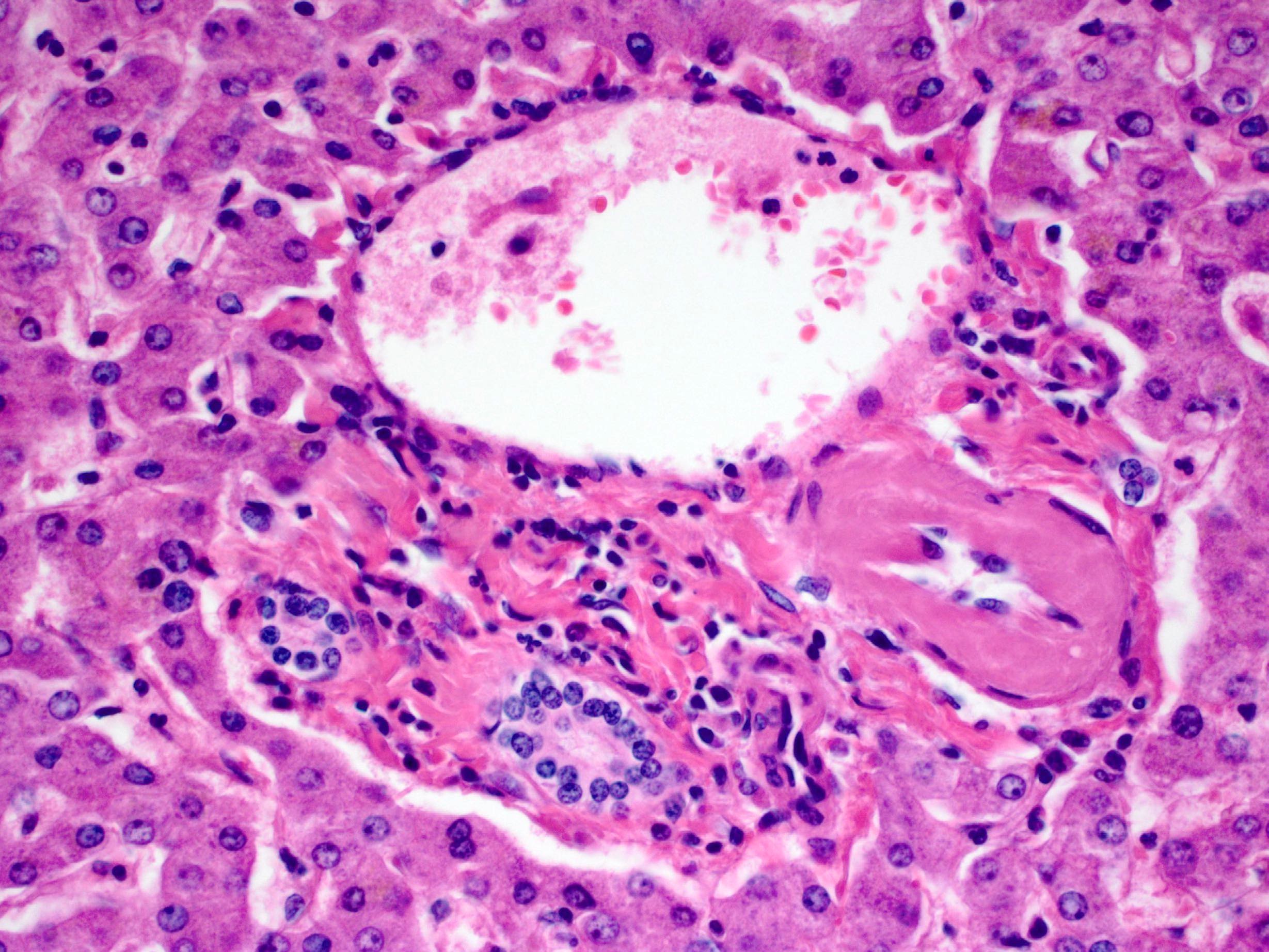
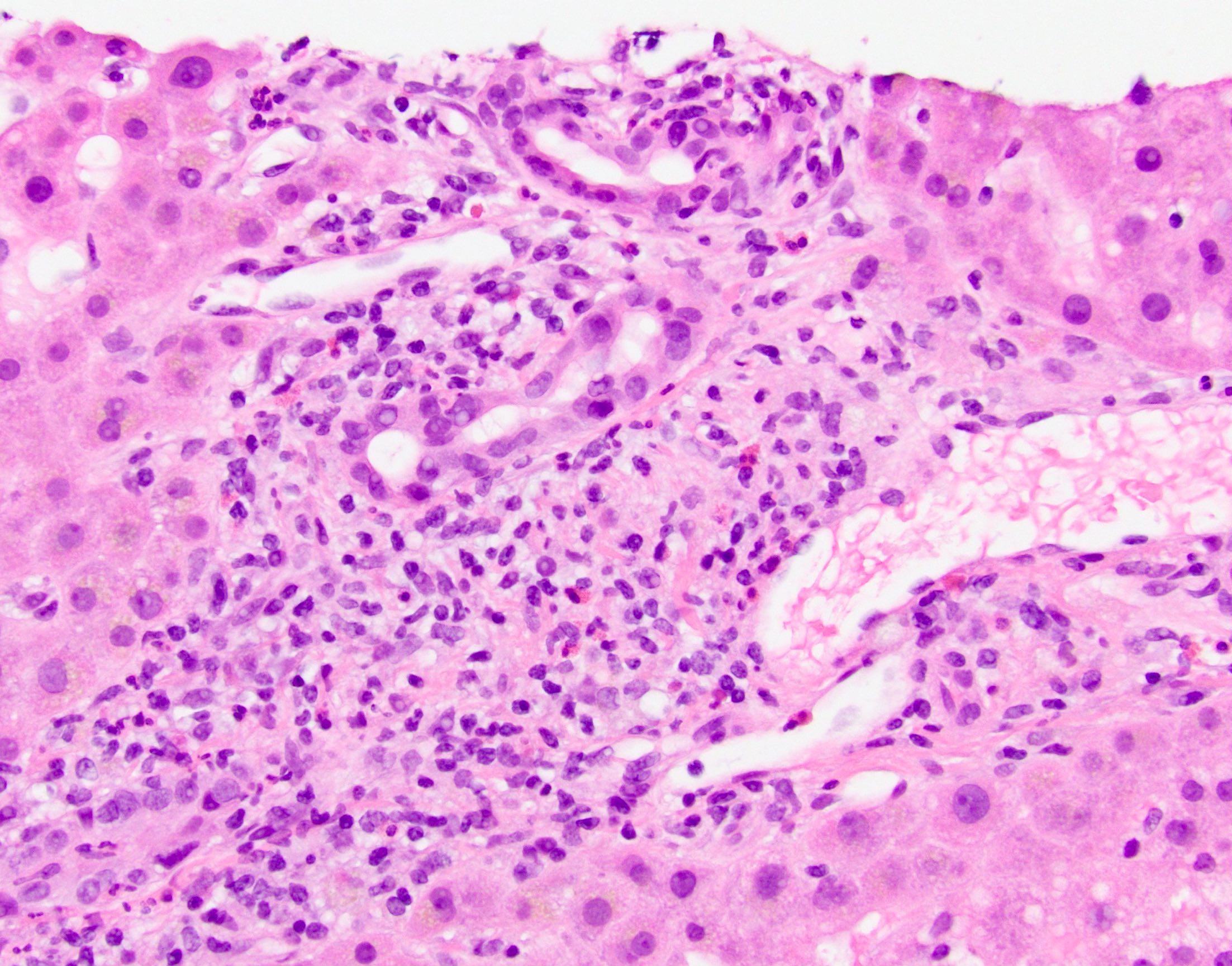
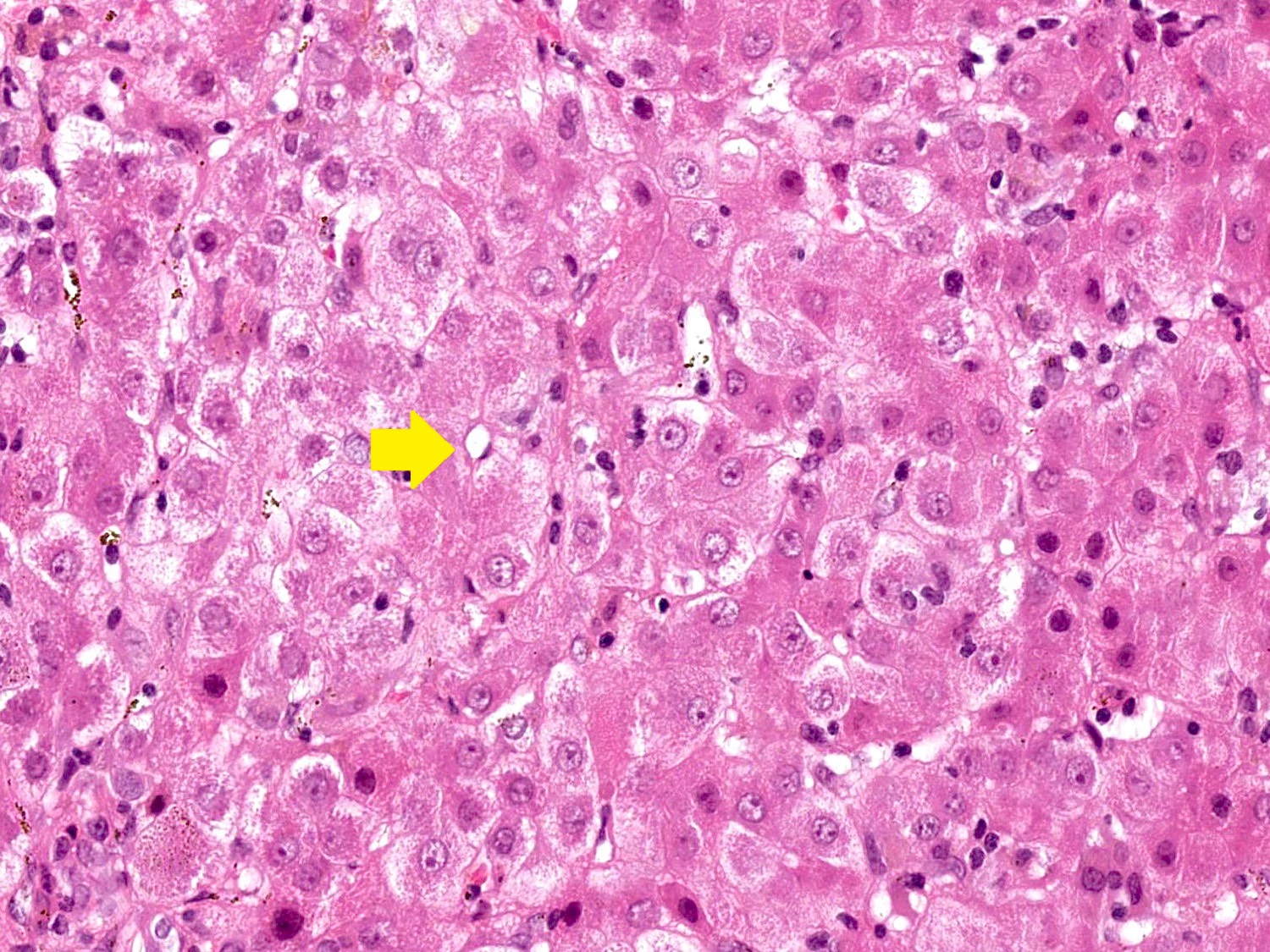
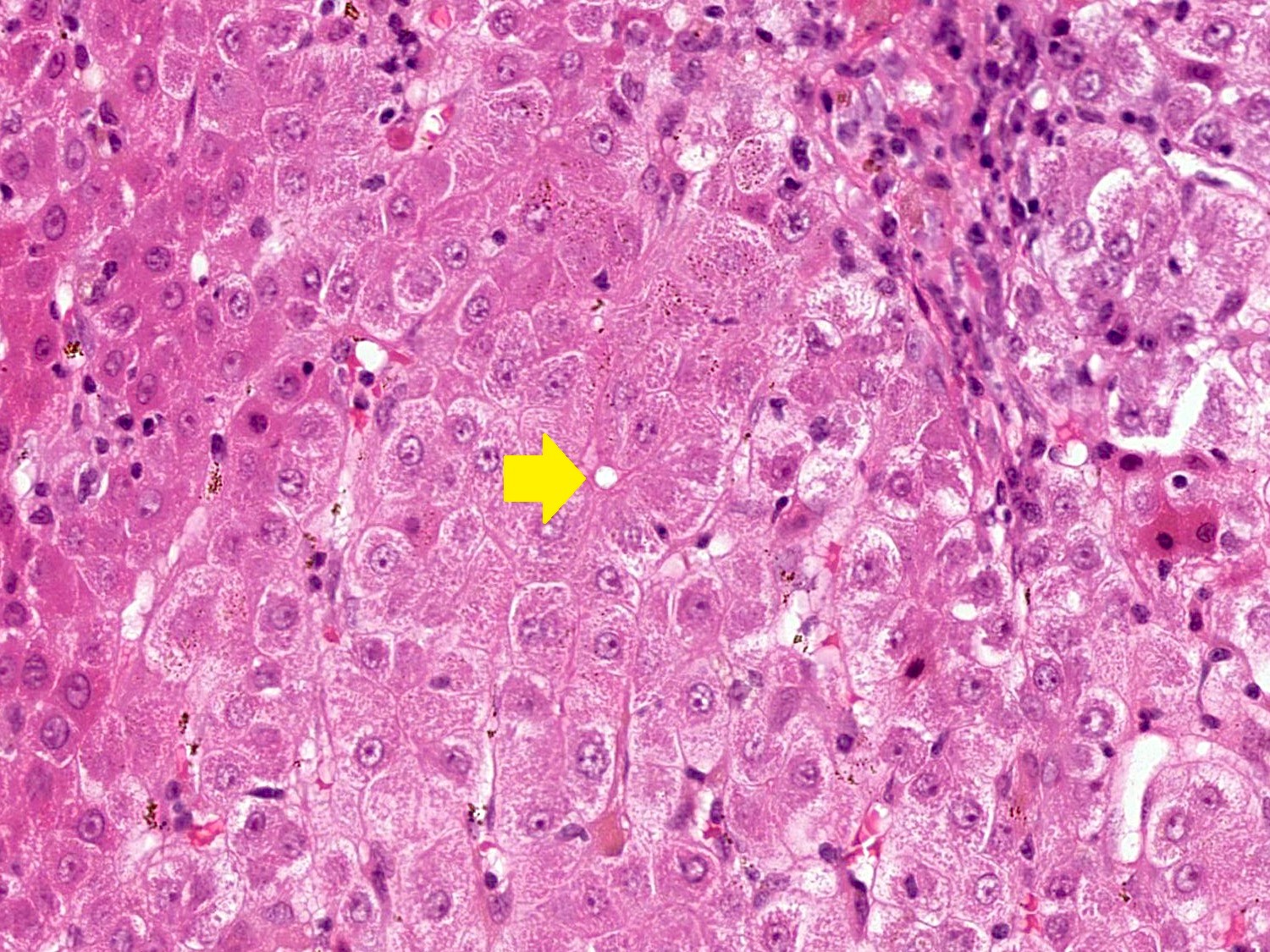
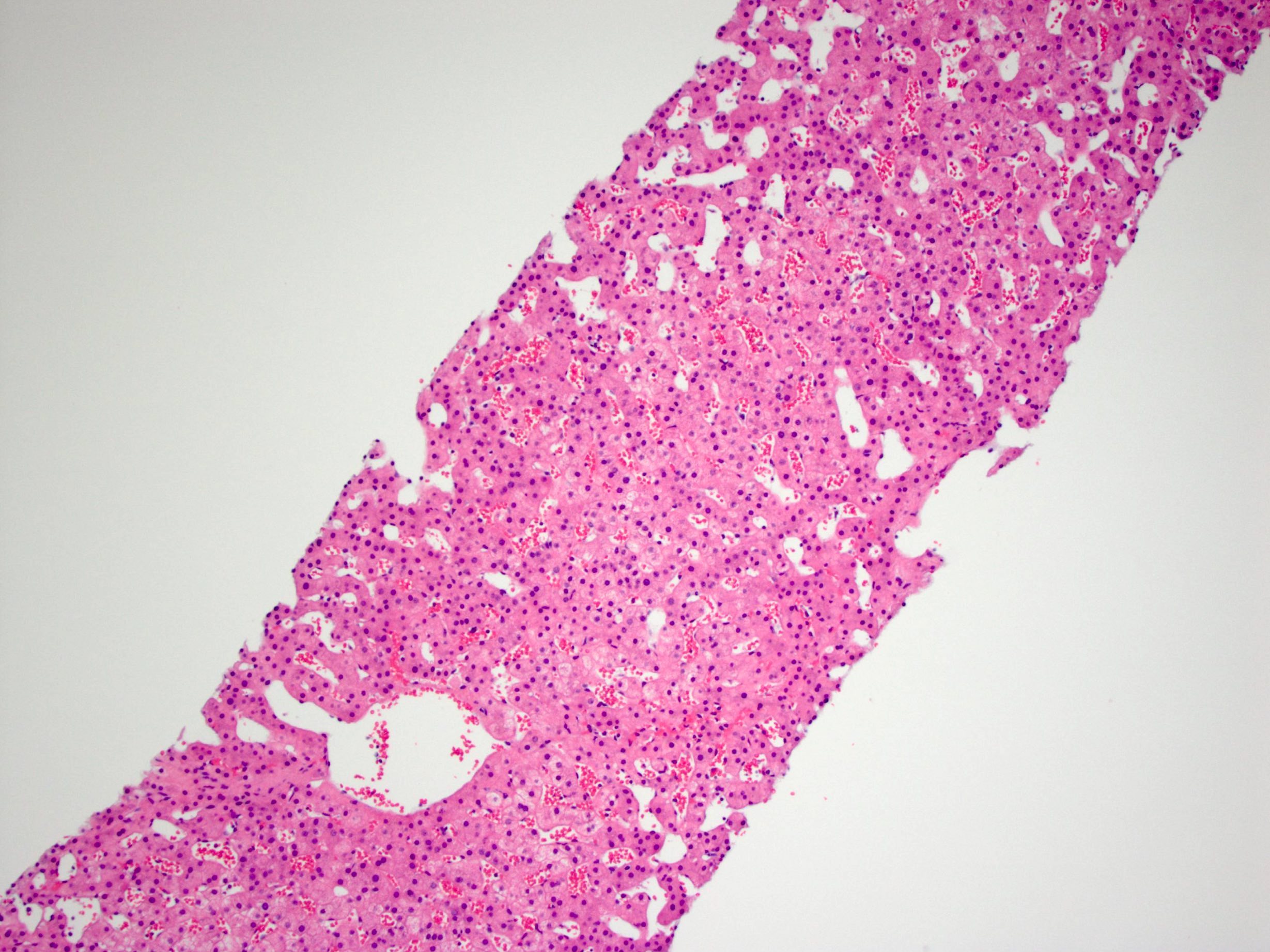
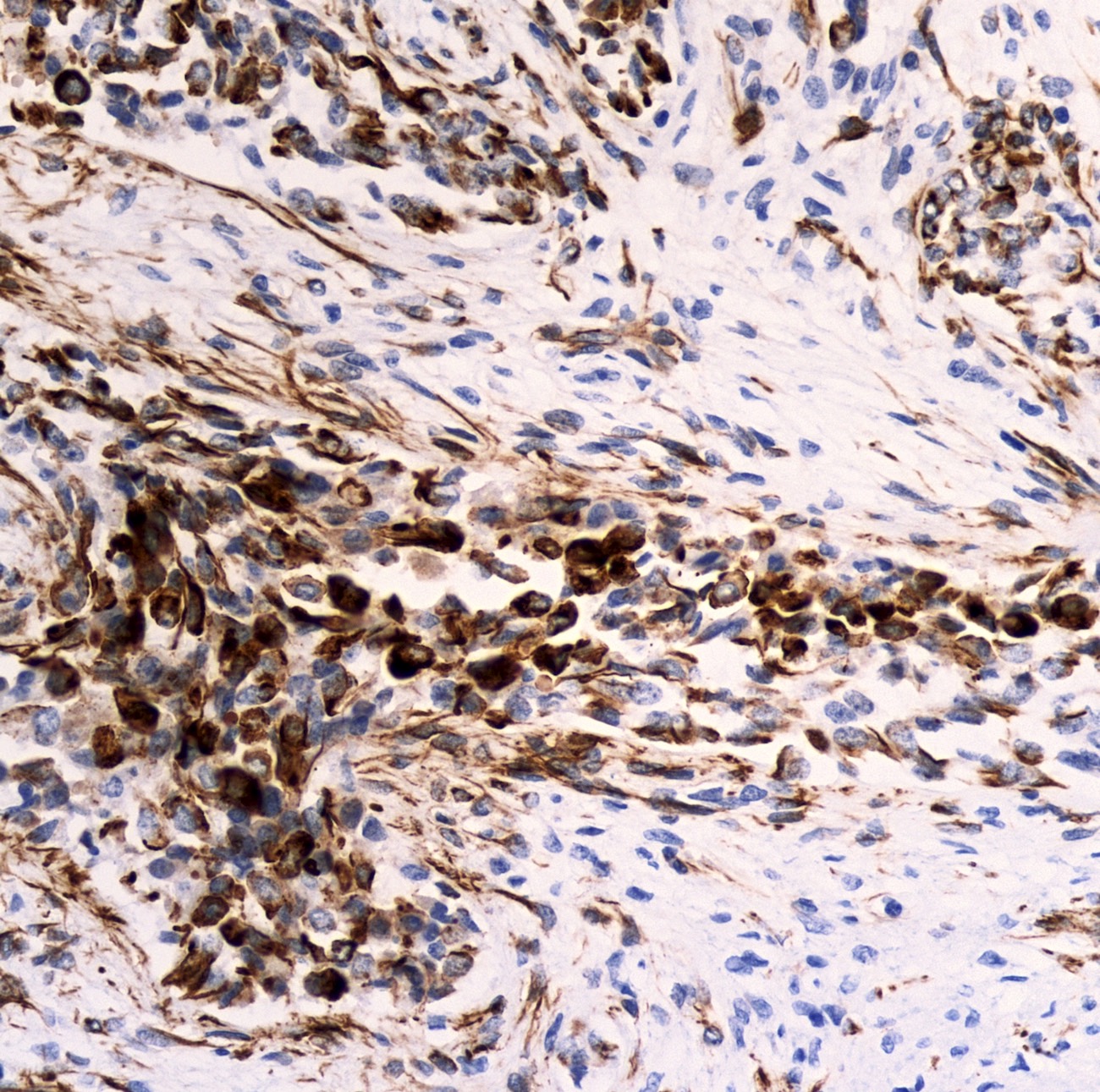
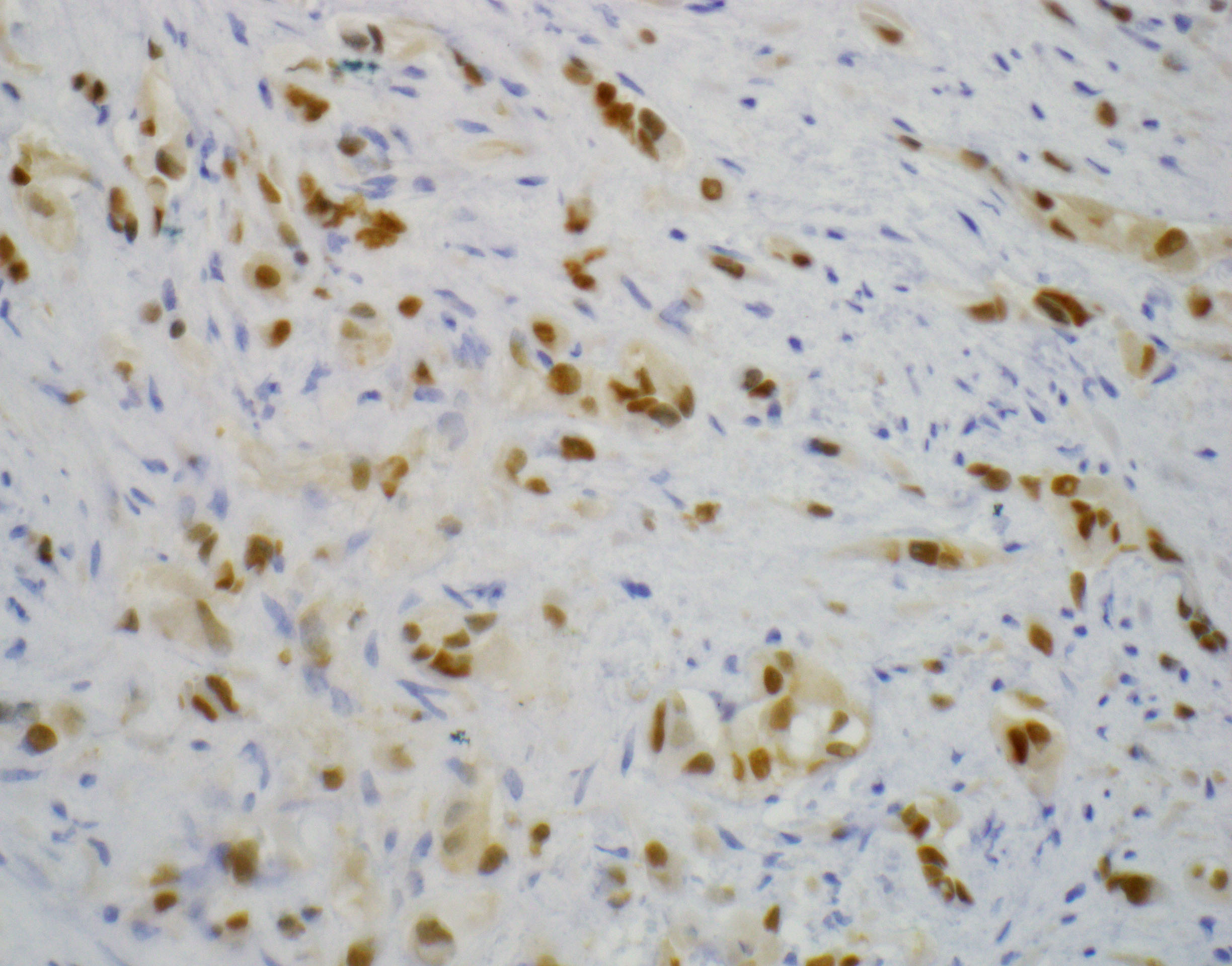
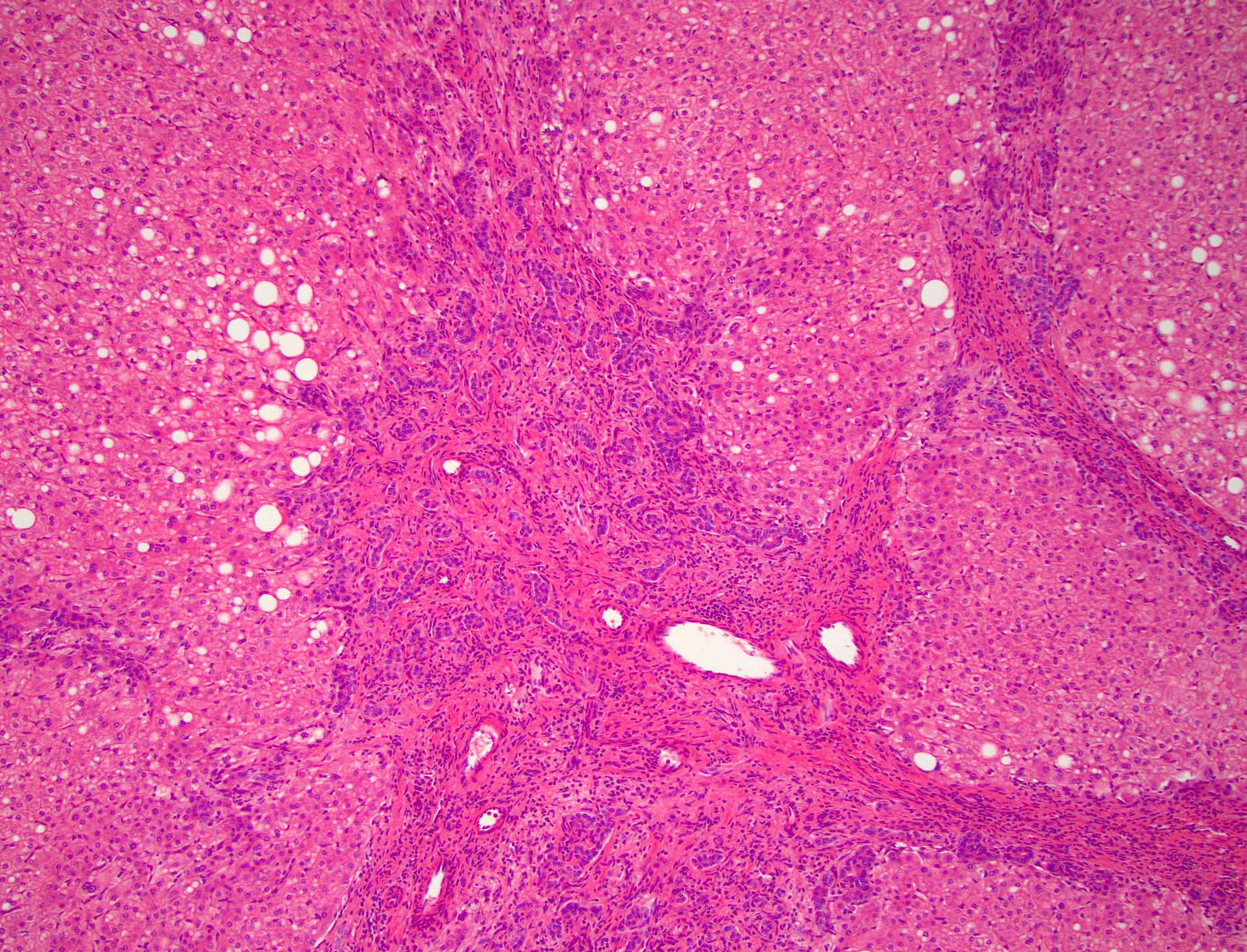
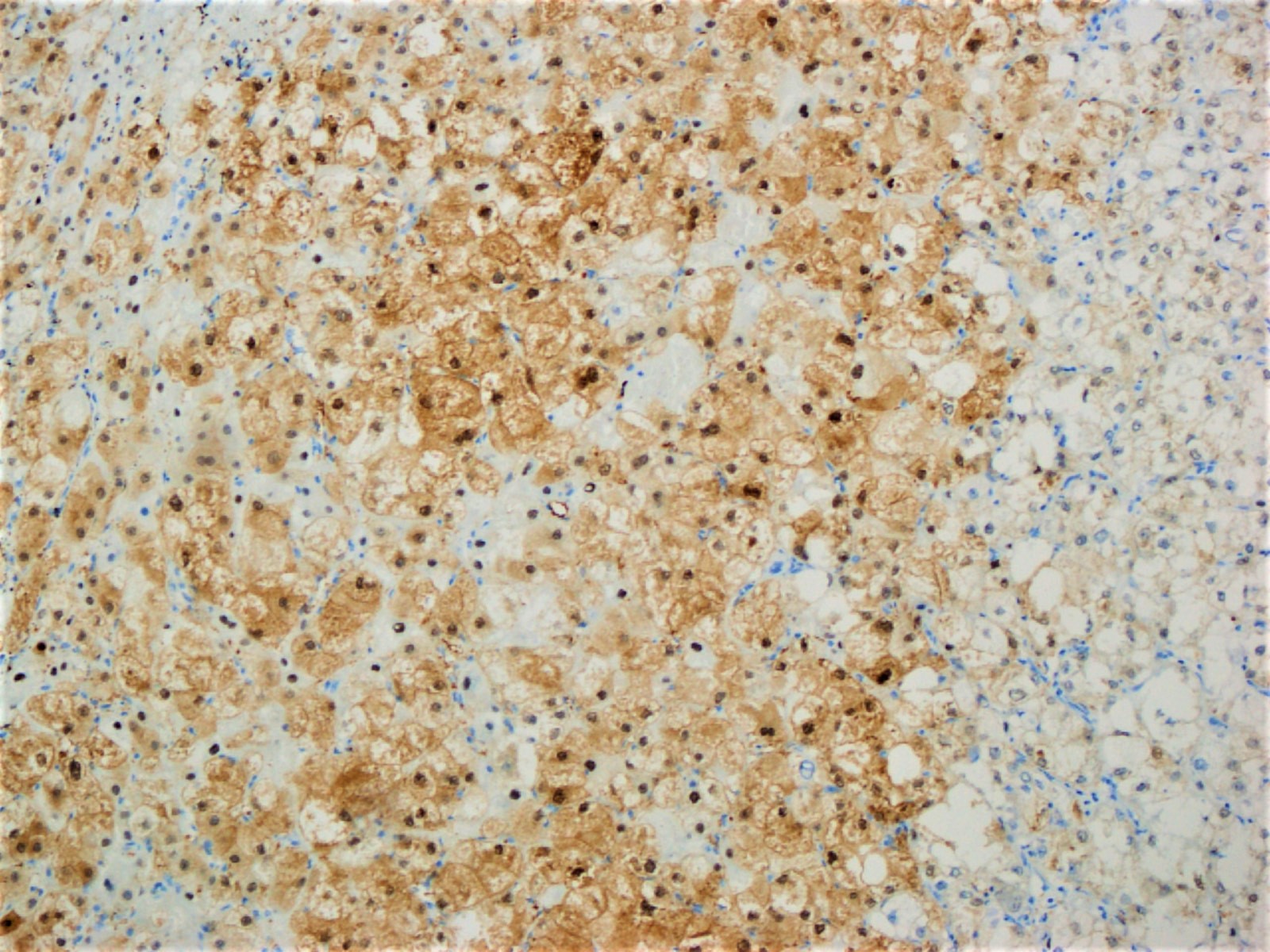
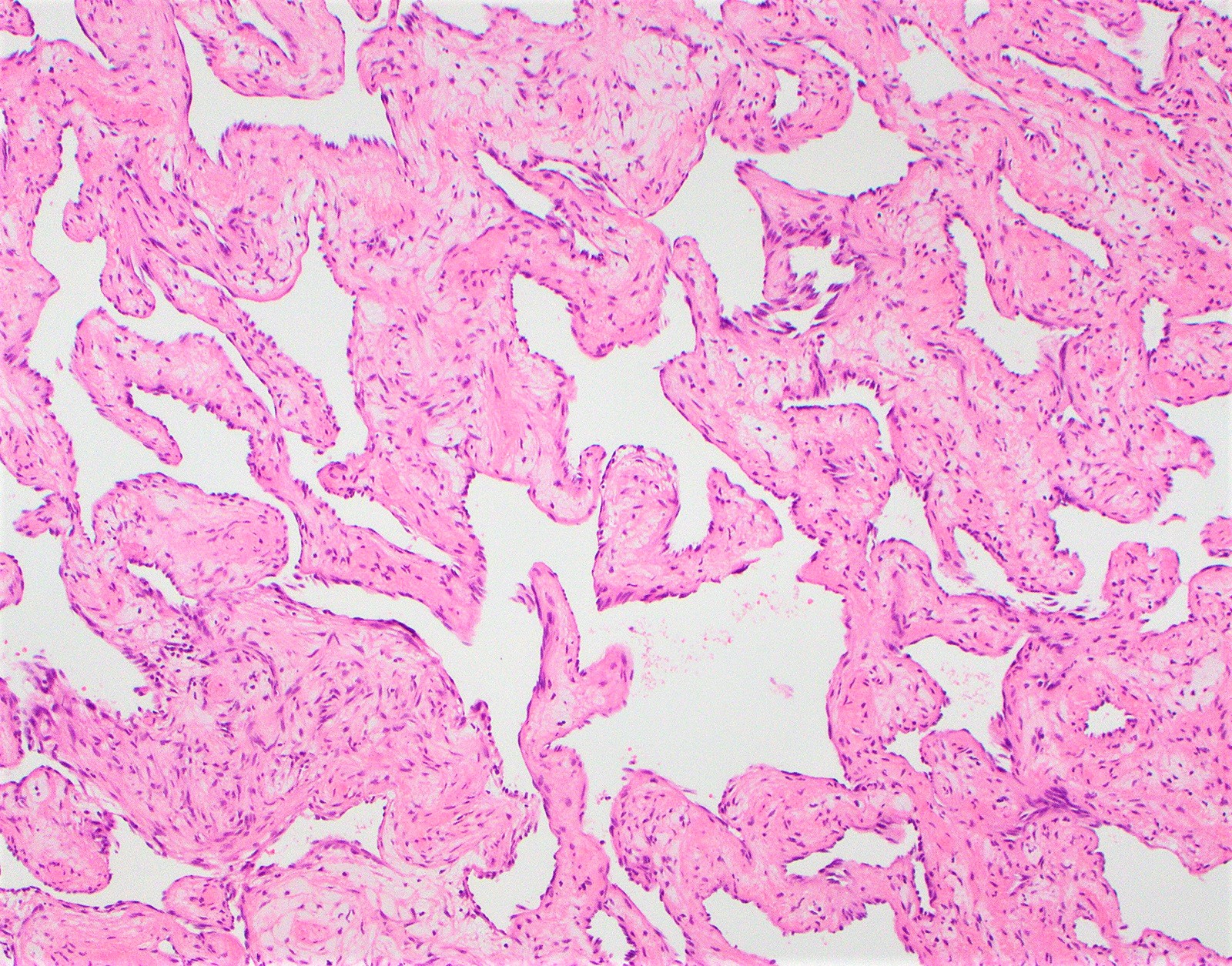
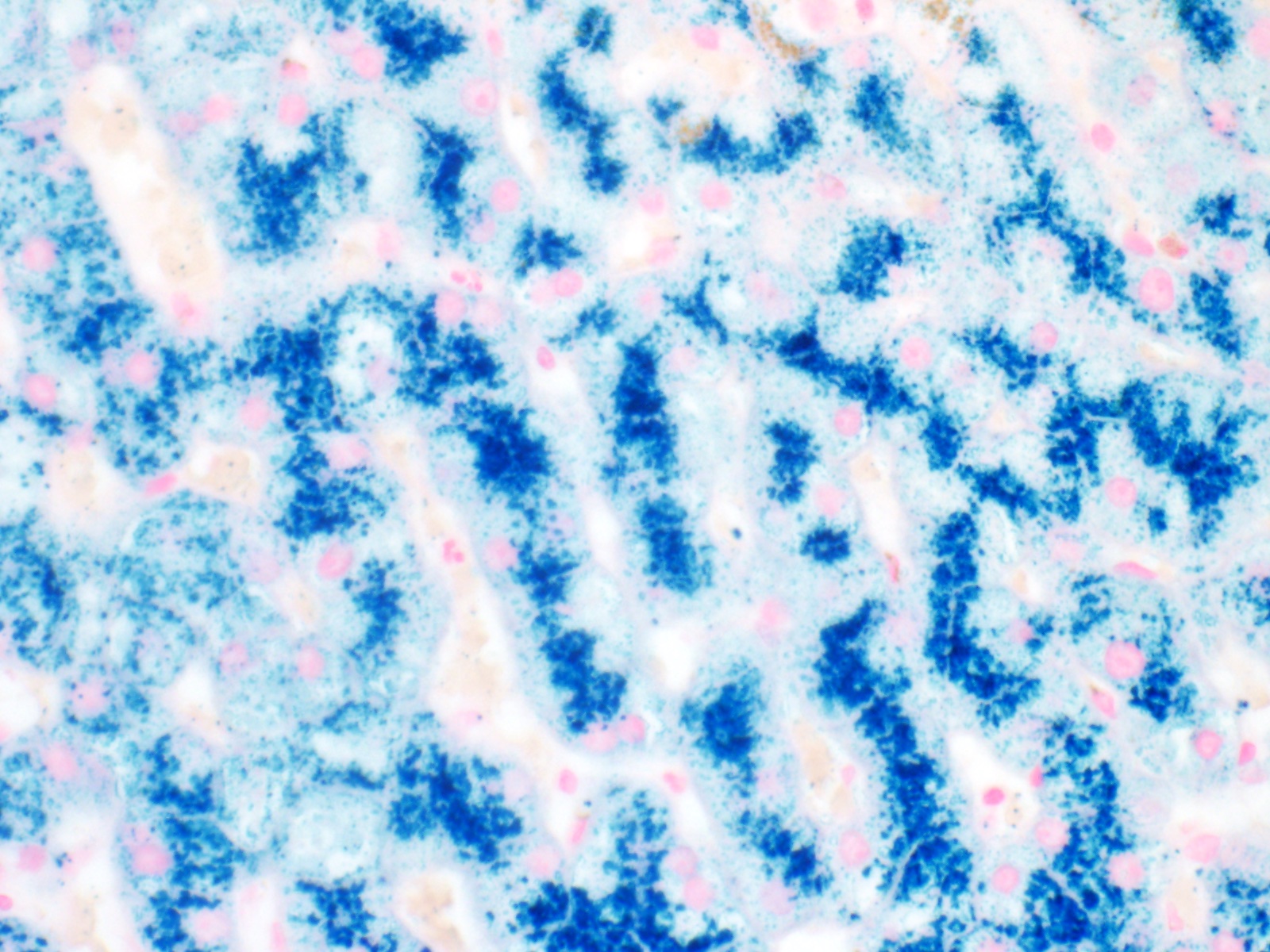
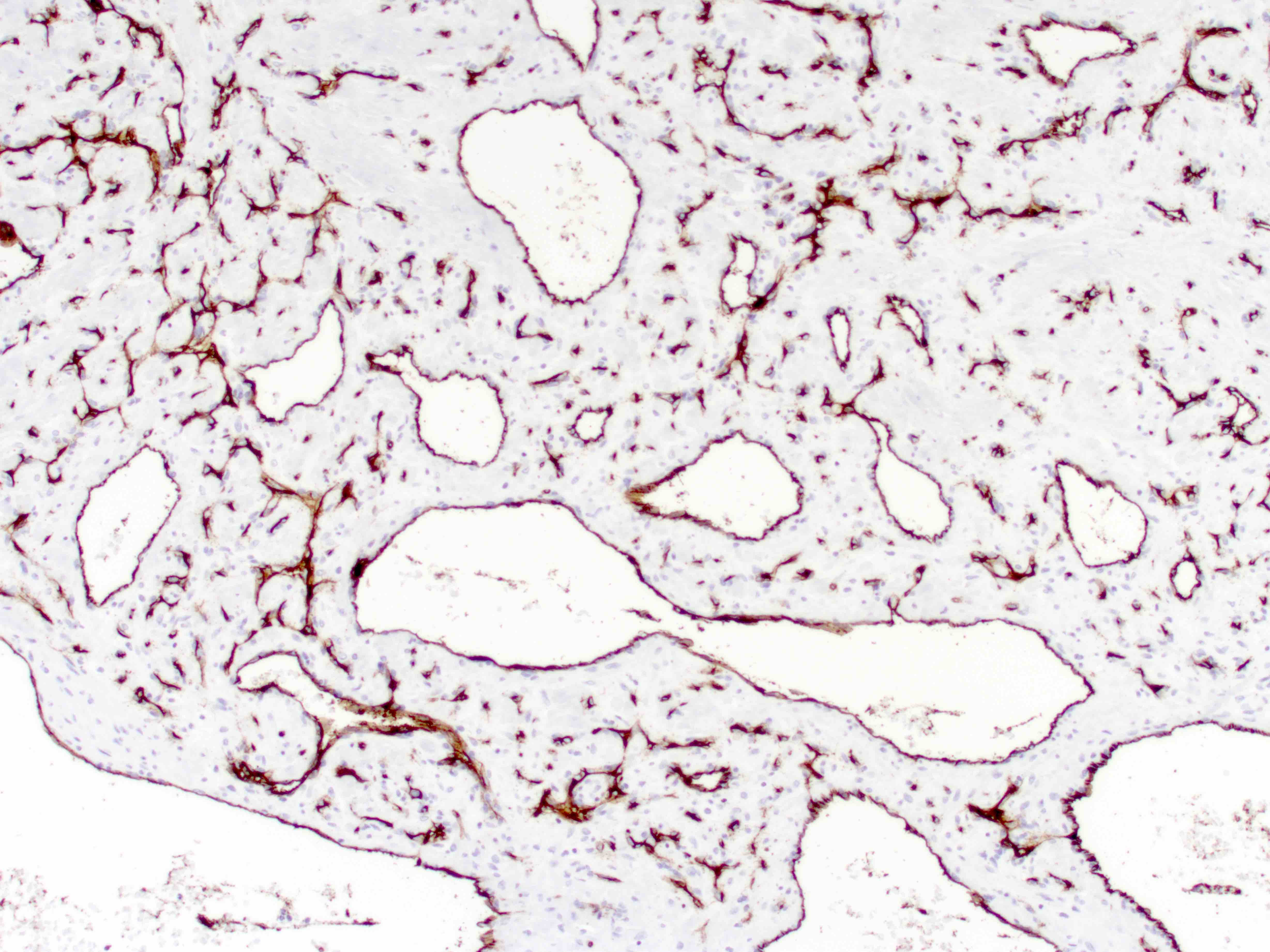
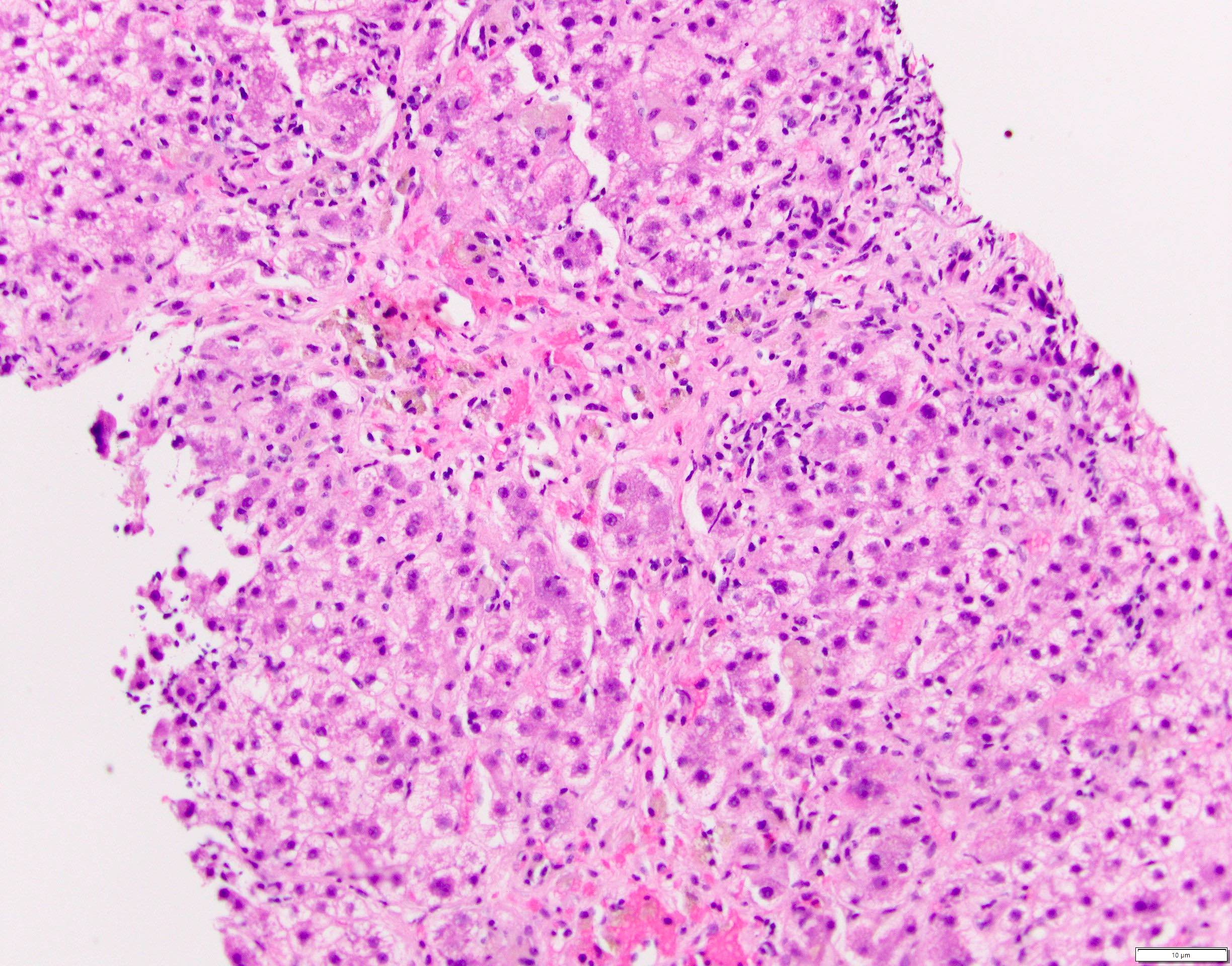
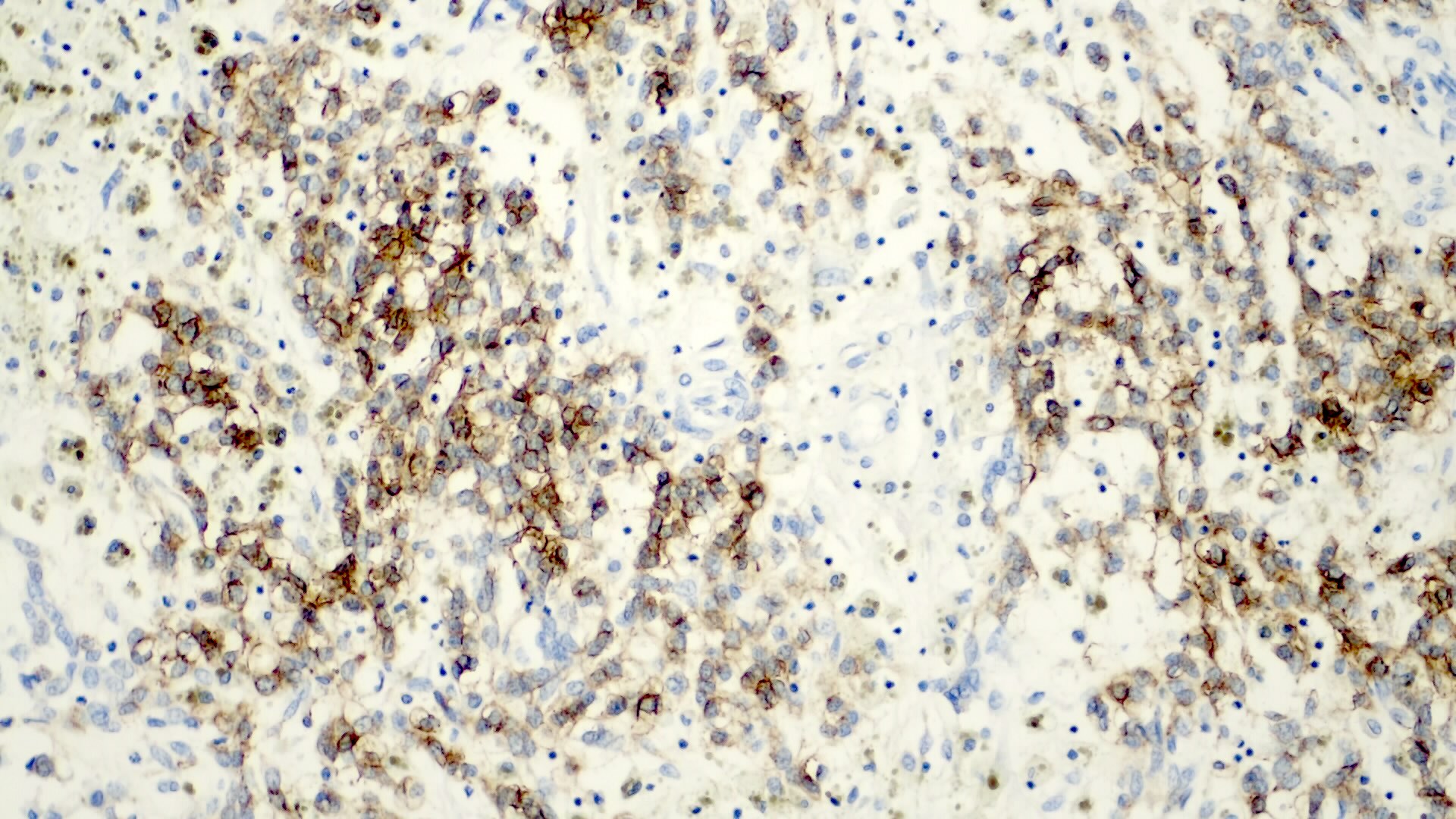
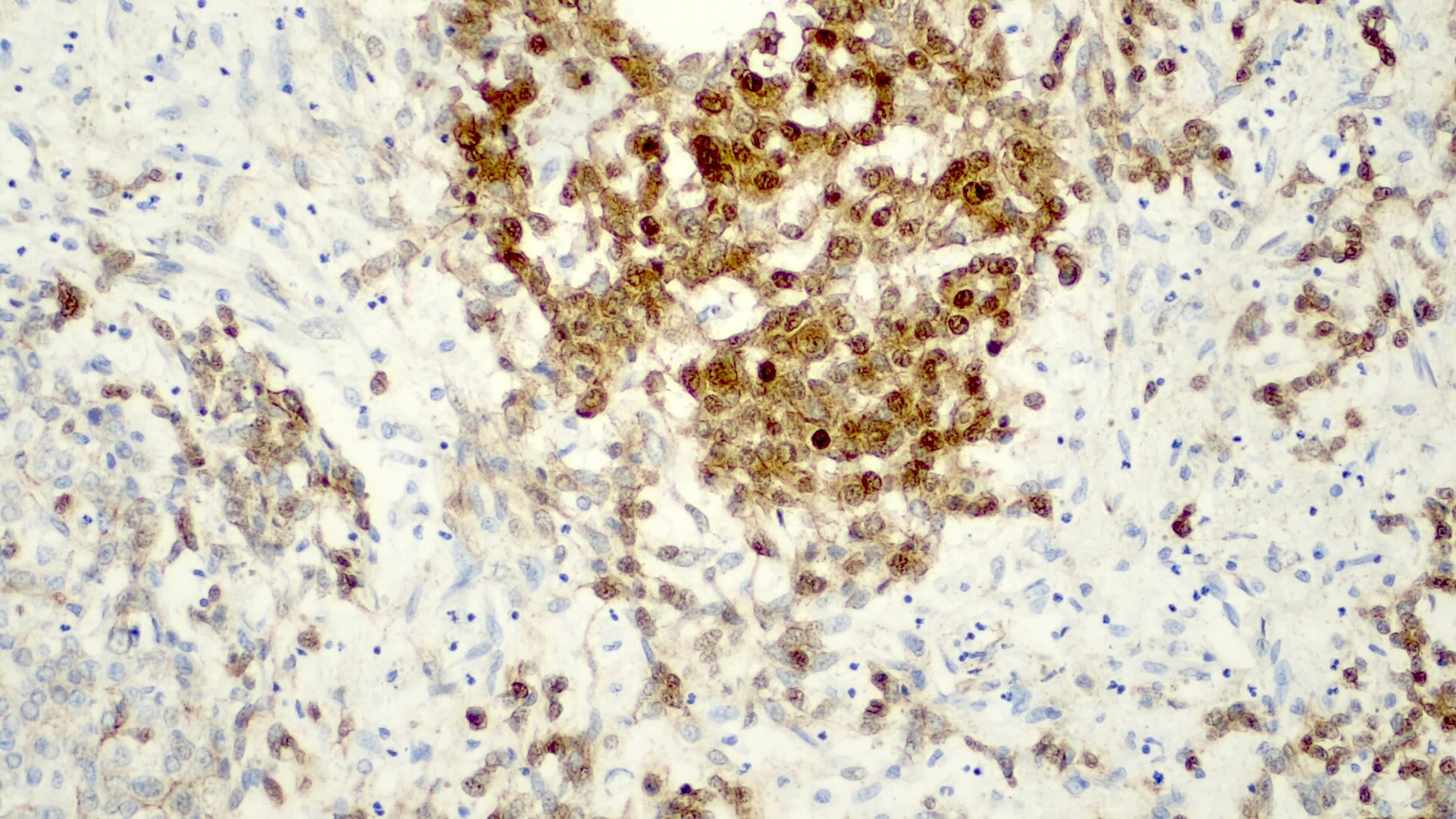
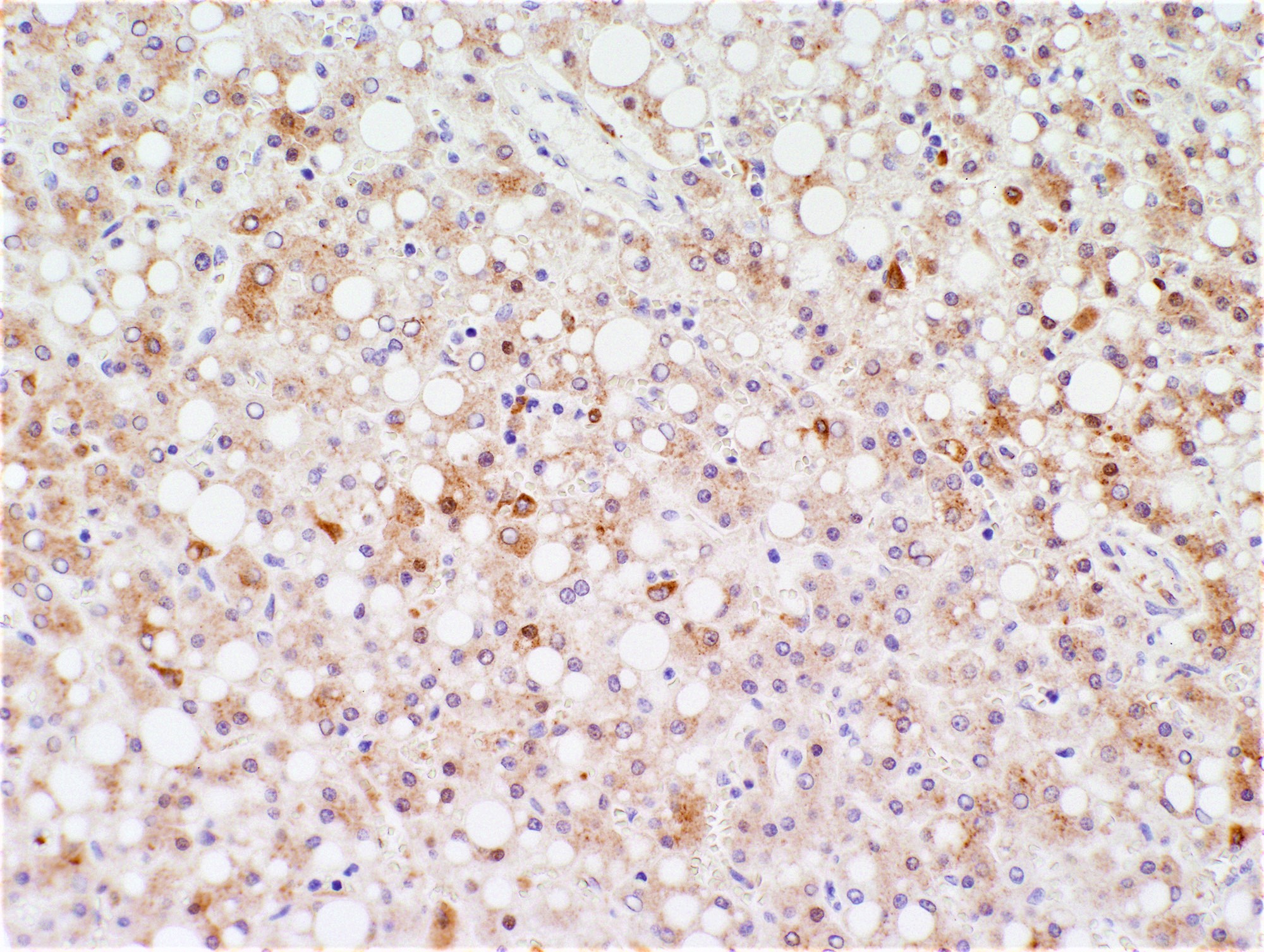
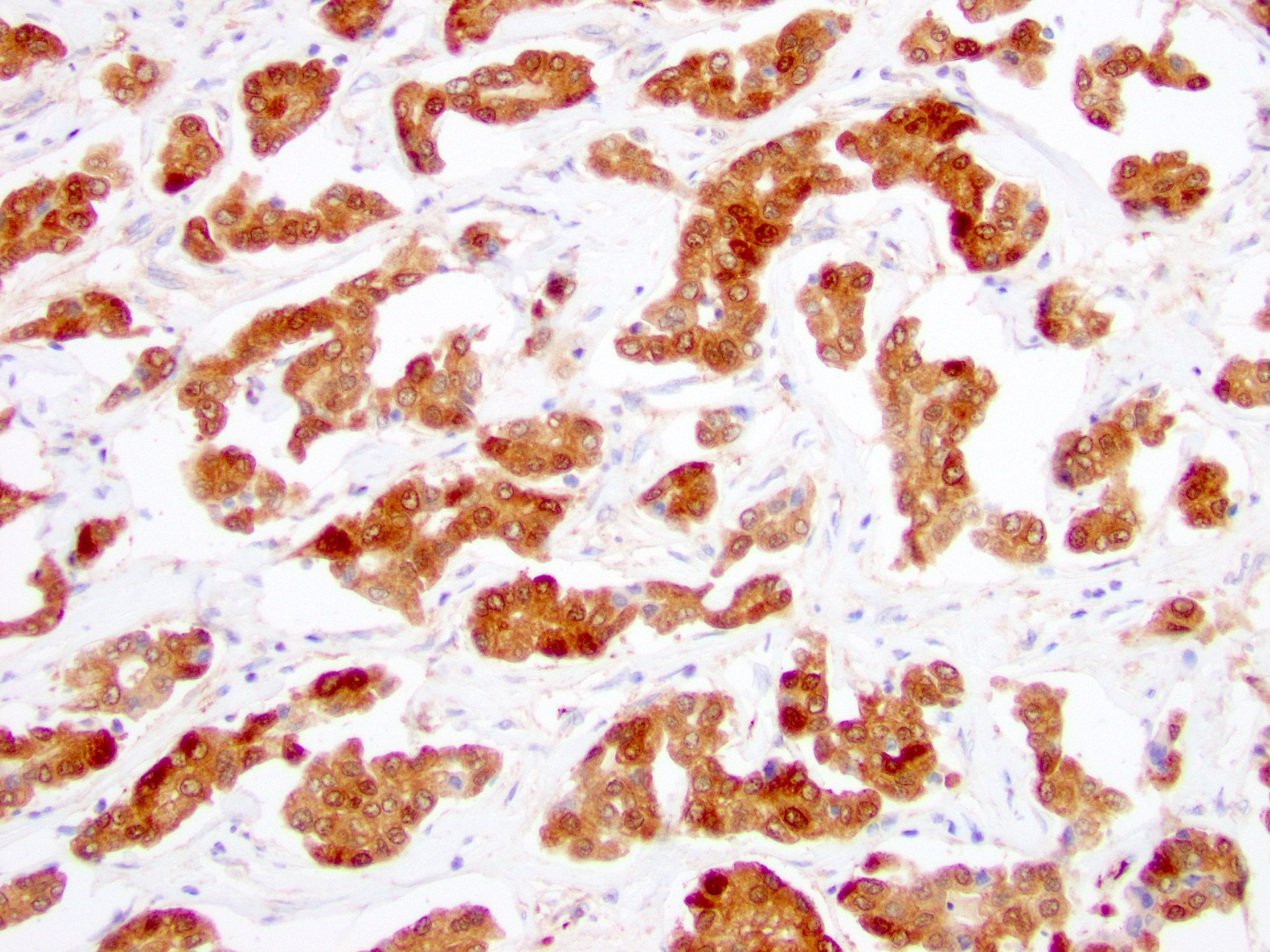
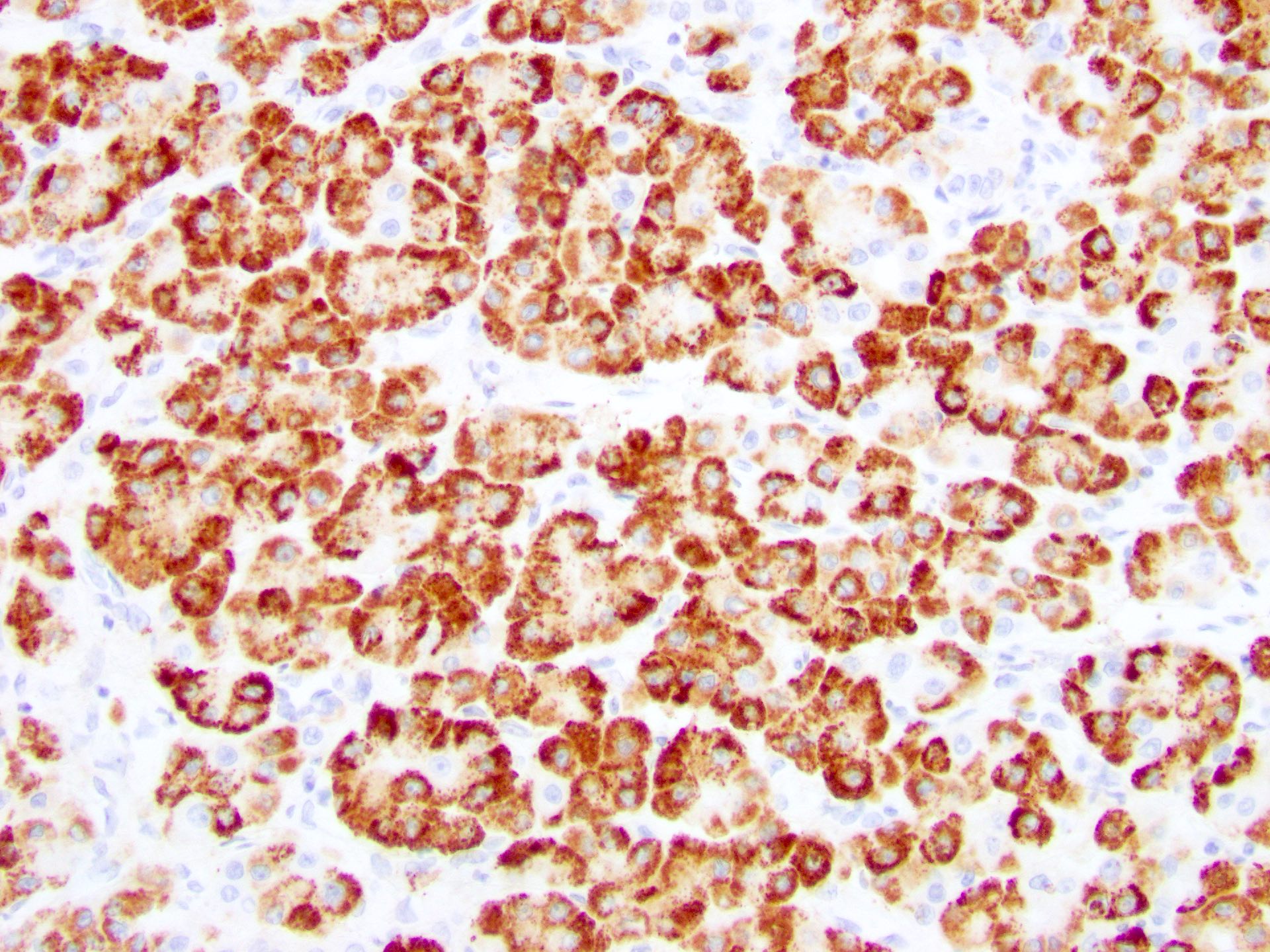
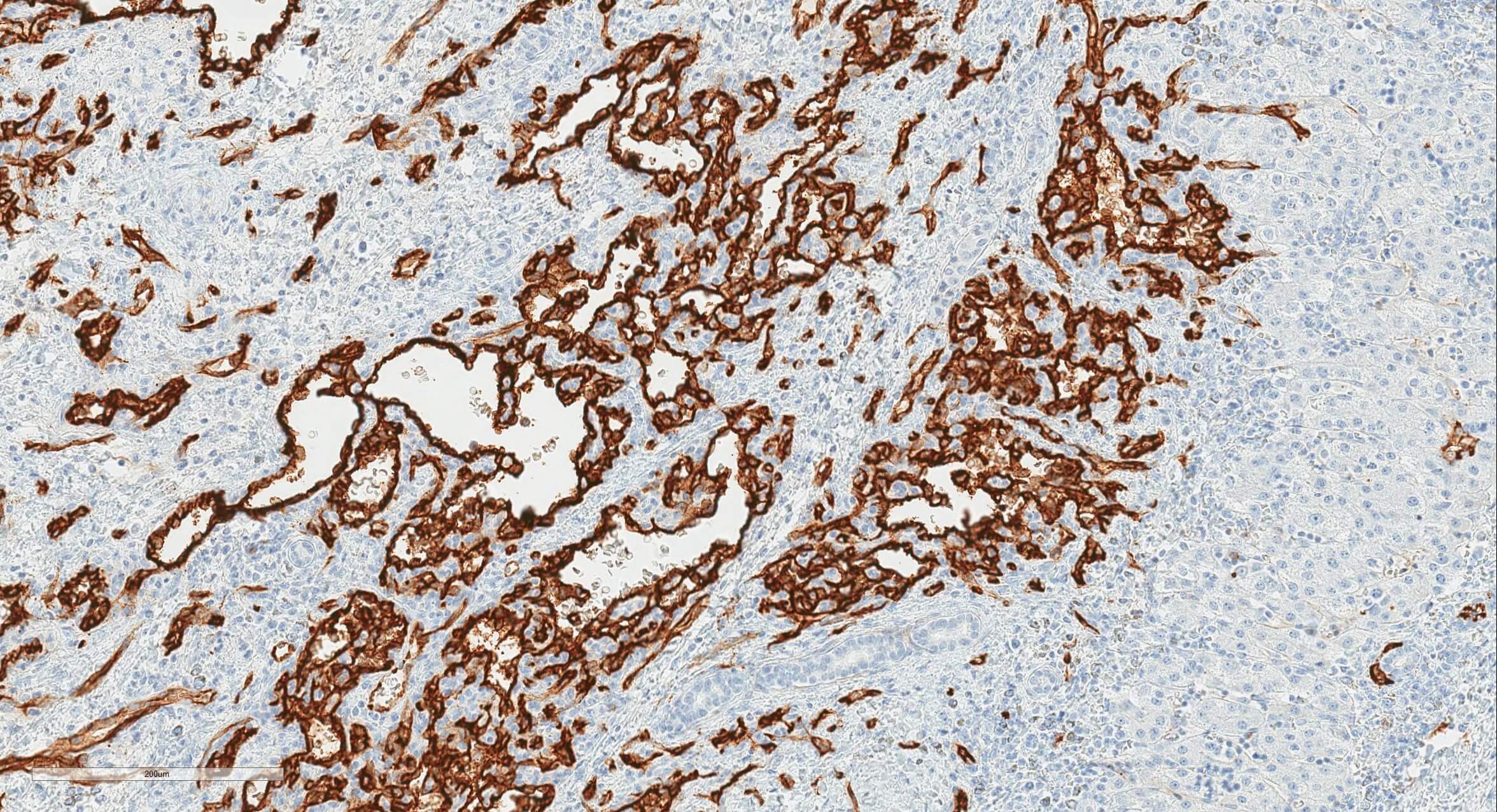
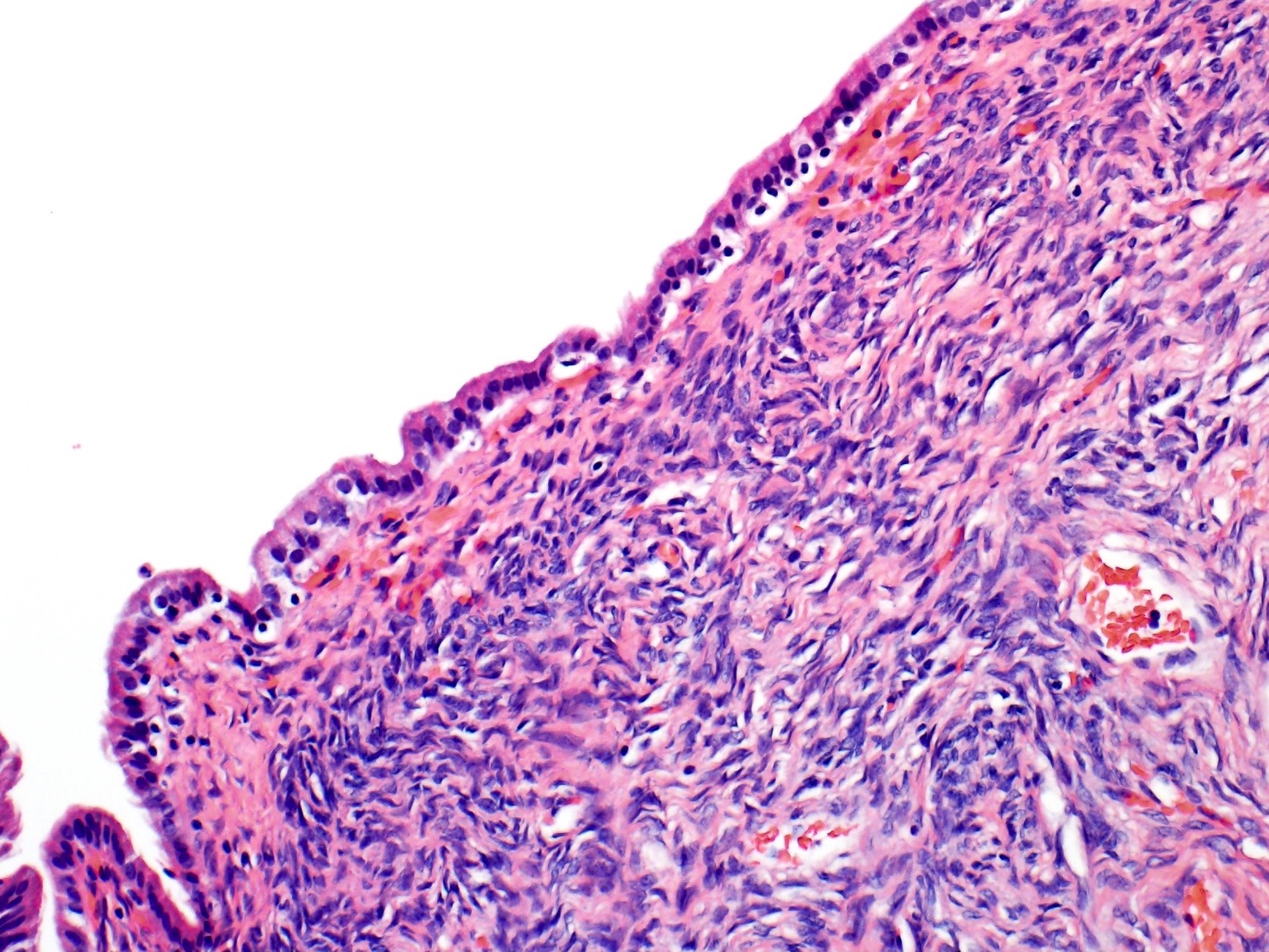
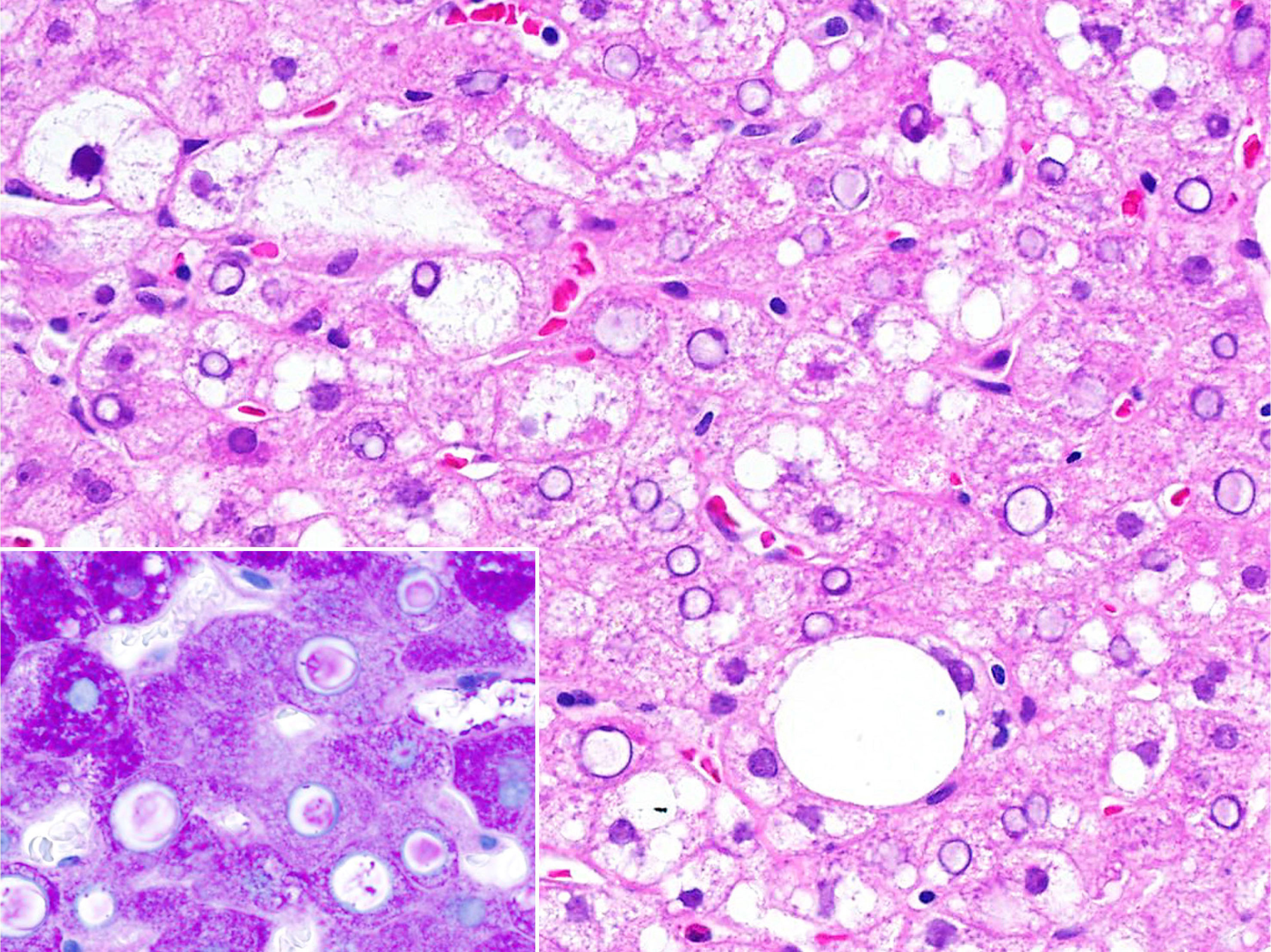
- Acute antibody mediated rejection:
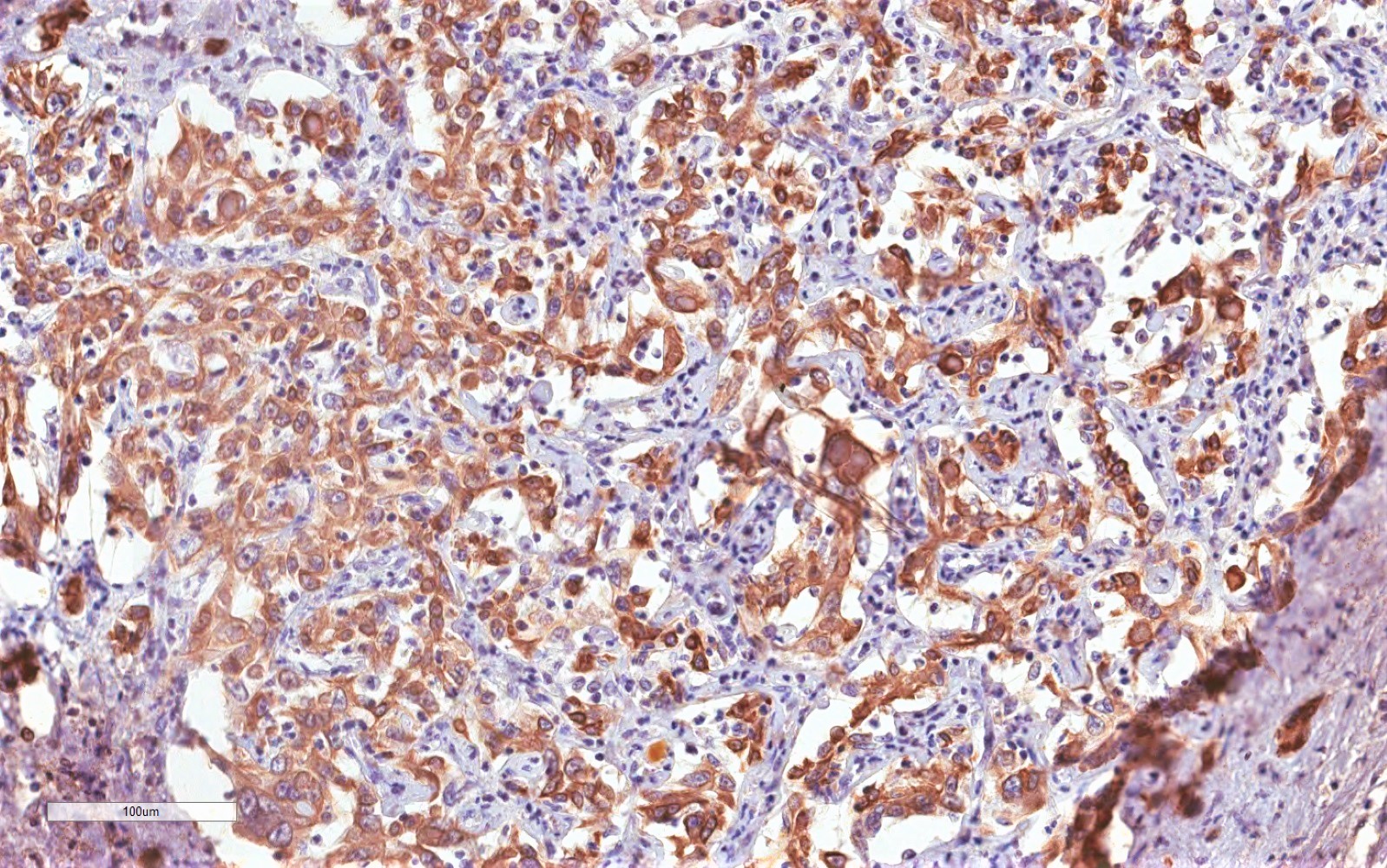
- Microvascular injury with endothelial swelling, dilated capillaries and inlet venules and marginating leukocytes (eosinophils, neutrophils, monocytes, lymphocytes, macrophages)
- Ductular reaction and cholestasis
- Arteritis
- May coexist with TCMR
- Histopathologic lesions are scored based on criteria described by the Banff working group (Am J Transplant 2016;16:2816):
| h score | Histologic criteria |
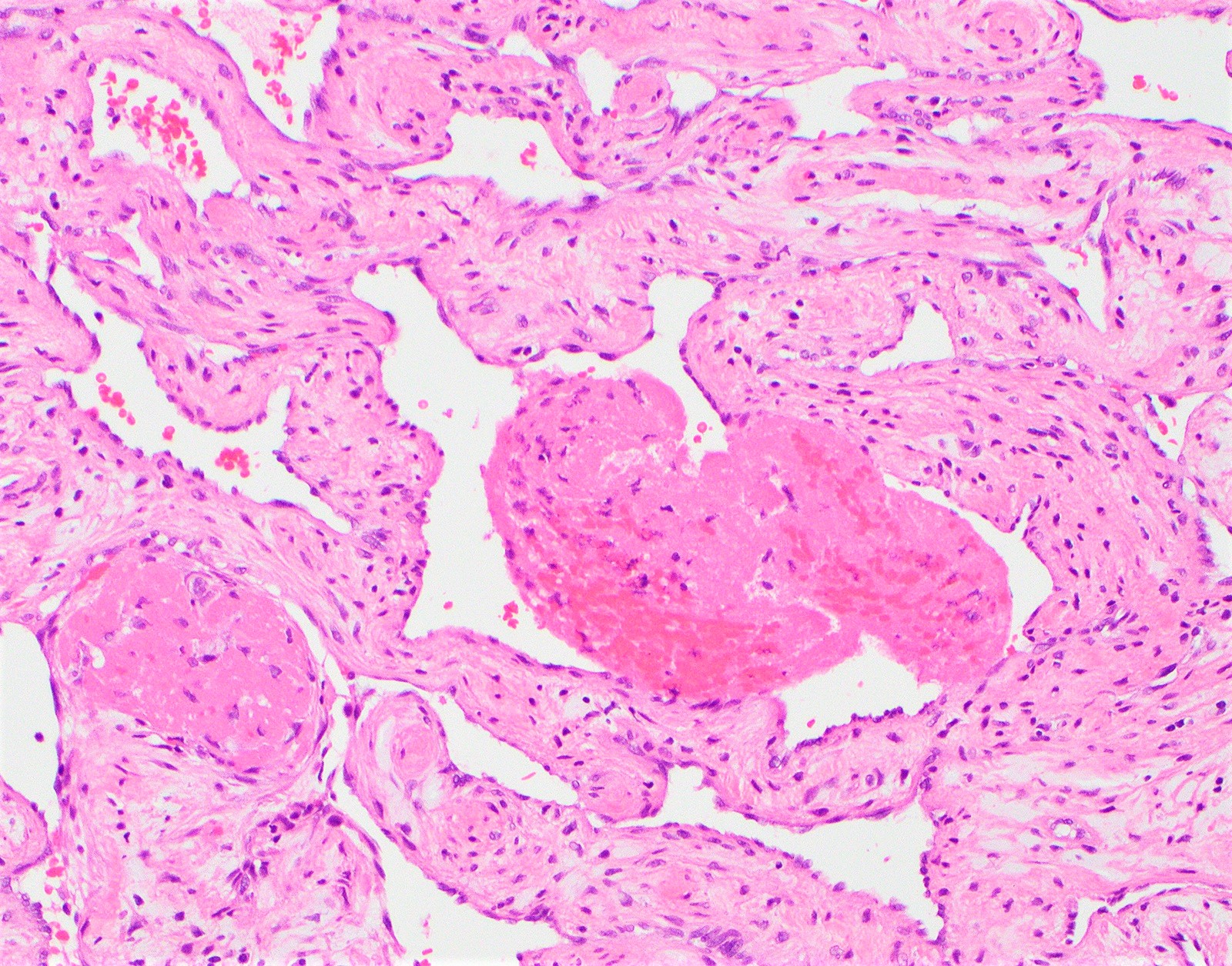
| h score 1 | Portal microvascular endothelial cell enlargement (portal veins, capillaries and inlet venules) involving a majority of portal tracts with sparse microvasculitis defined as 3 - 4 marginated or intraluminal monocytes, neutrophils or eosinophils in the maximally involved capillary with generally mild dilation |
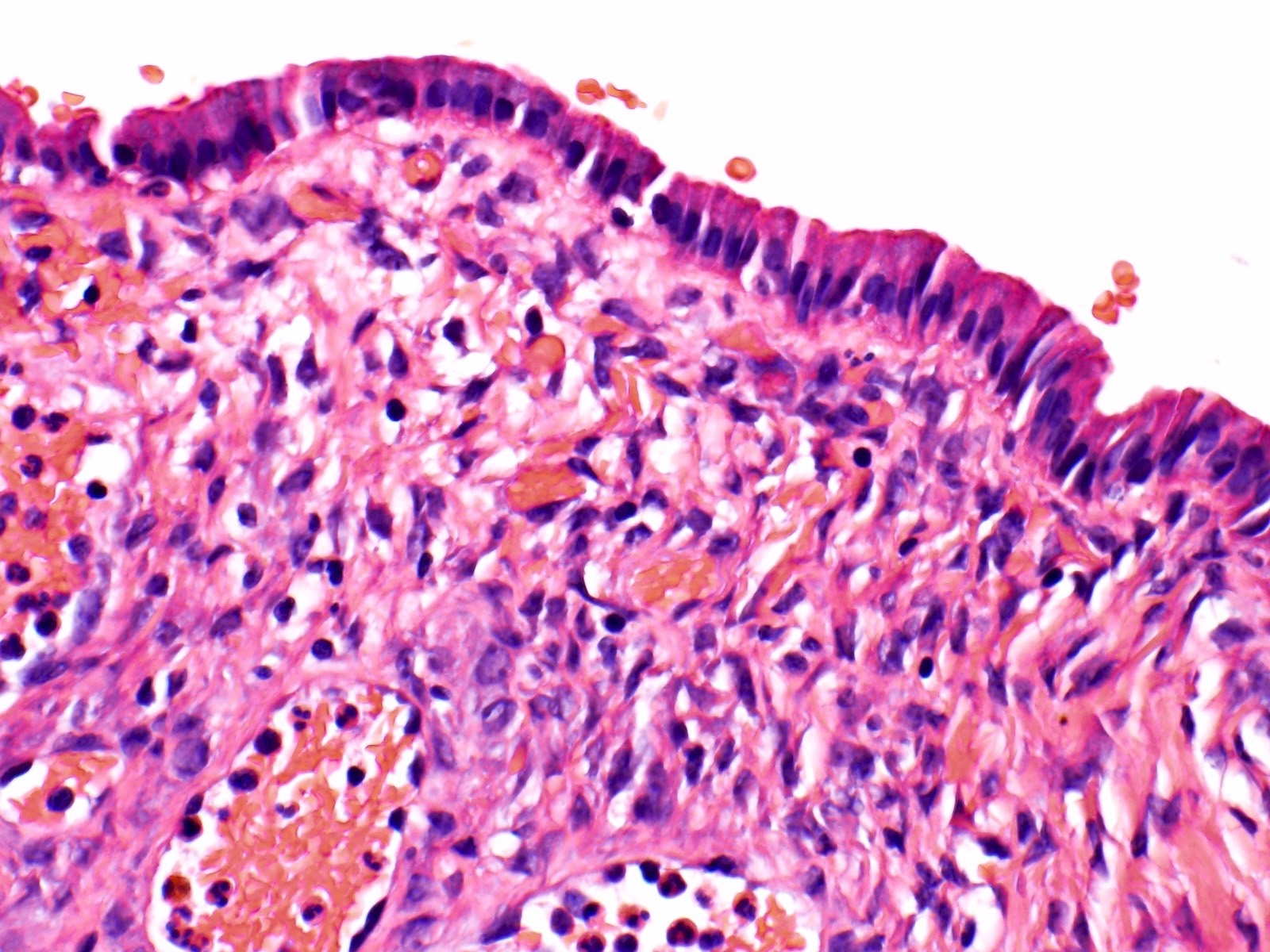
| h score 2 | Monocytic, eosinophilic or neutrophilic microvasculitis / capillaritis, defined as at least 5 - 10 leukocytes marginated or intraluminal in the maximally involved capillary, prominent portal or sinusoidal microvascular endothelial cell enlargement involving a majority of portal tracts or sinusoids, with variable but noticeable portal capillary and inlet venule dilatation and variable portal edema |
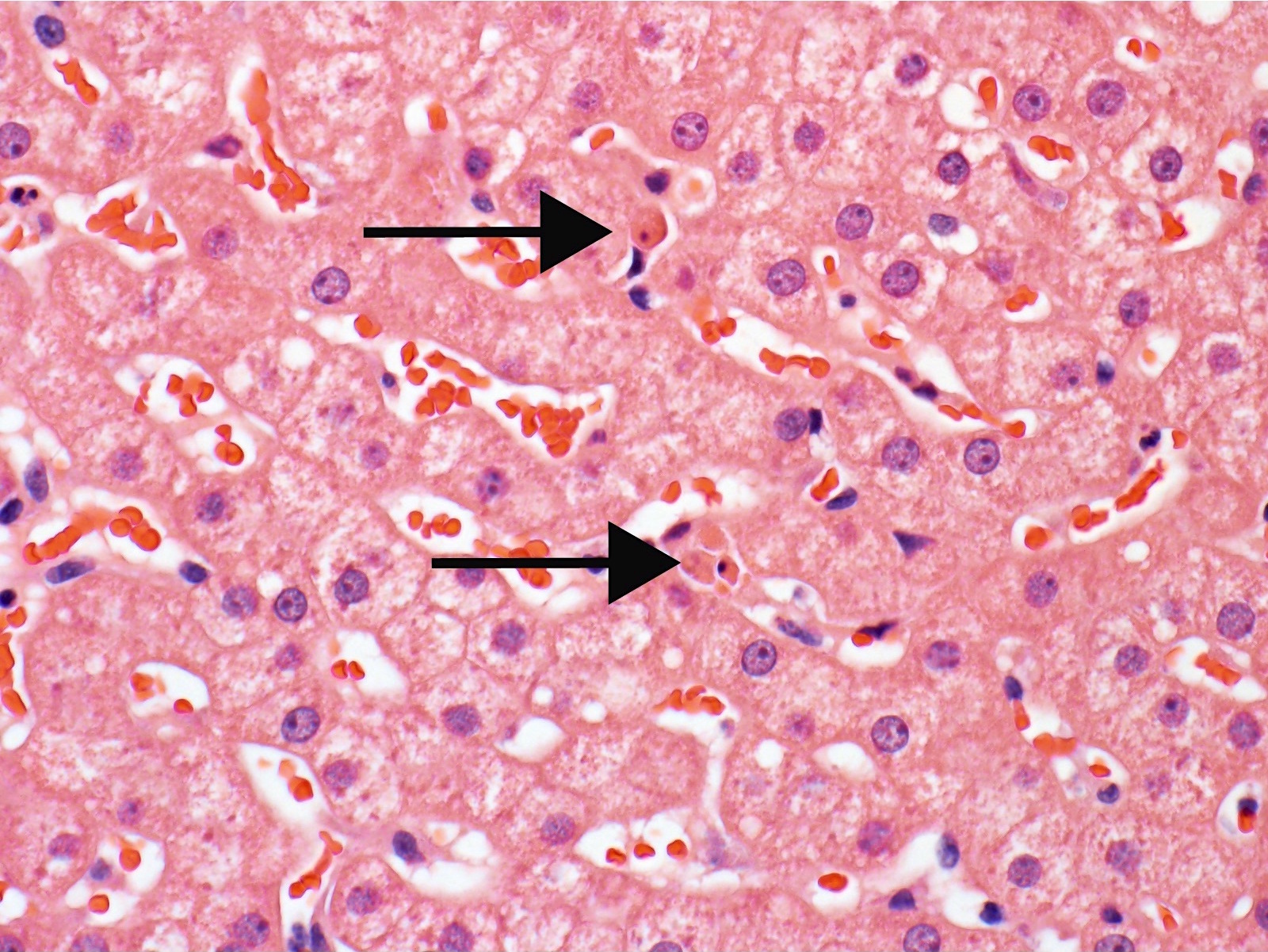
| h score 3 | As above, with marked capillary dilatation, marked microvascular inflammation (10 or more marginated or intraluminal leukocytes in the most severely affected vessels), at least focal microvascular disruption with fibrin deposition and extravasation of red blood cells into the portal stroma or space of Disse (subsinusoidal space) |
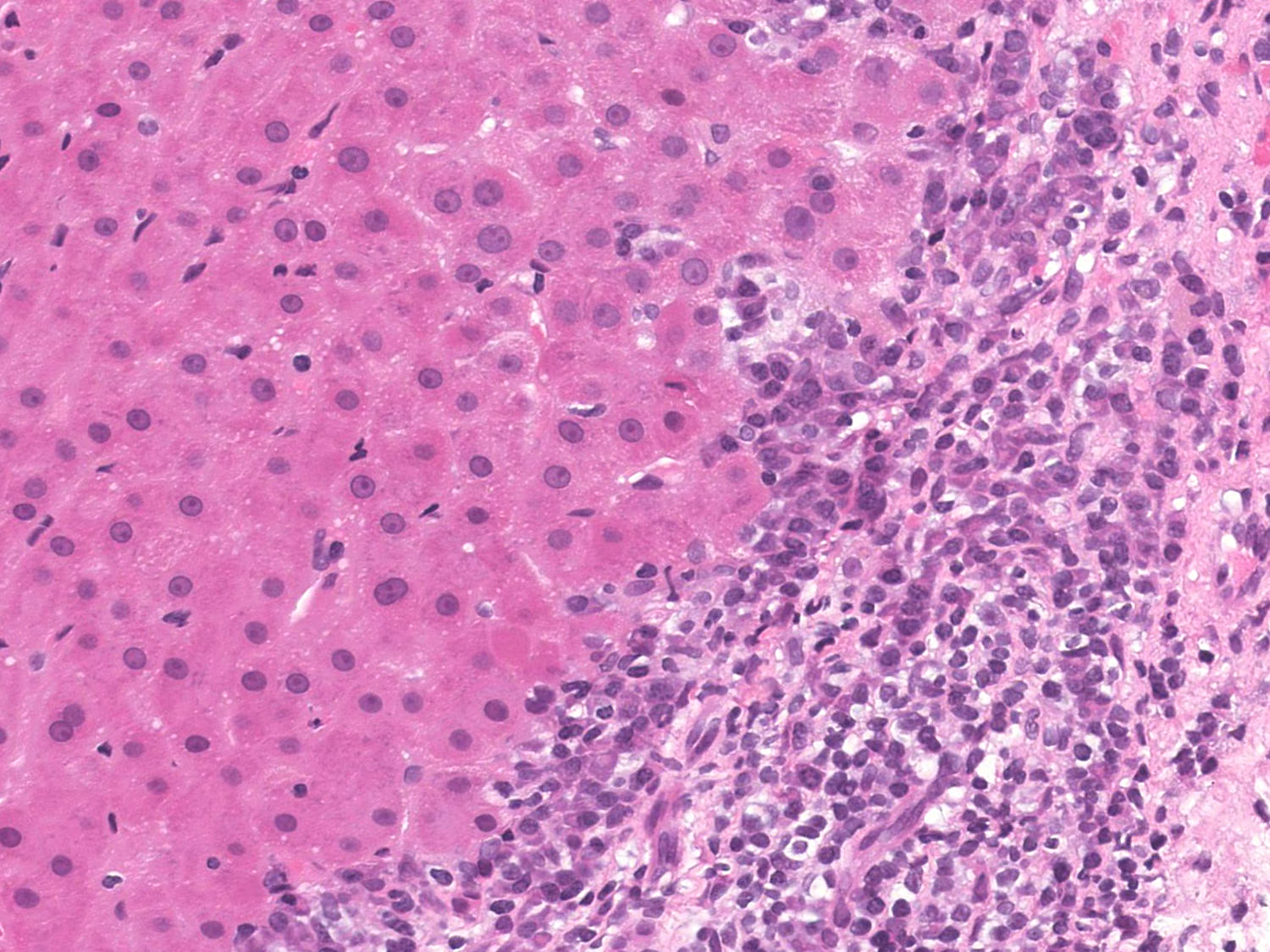
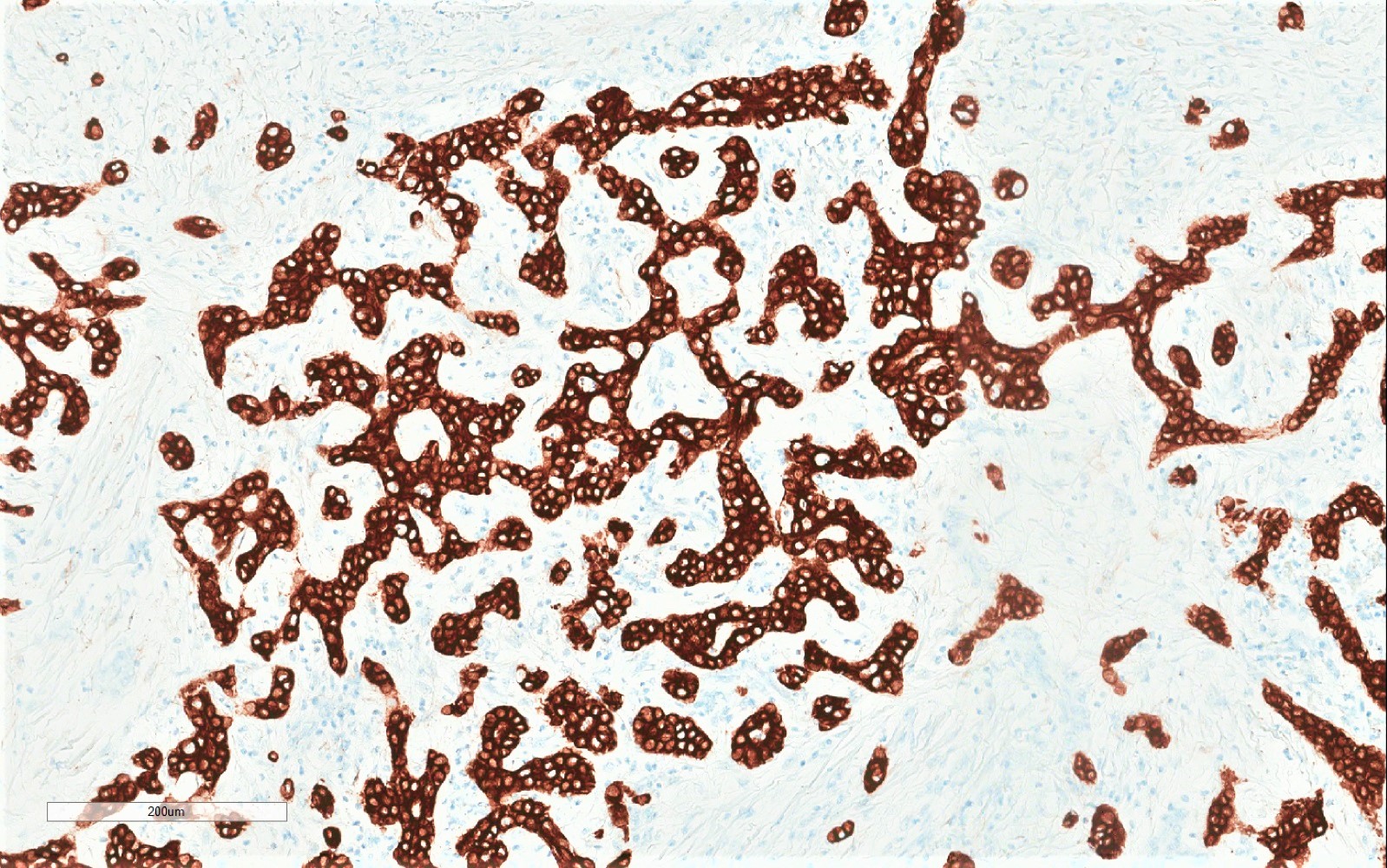
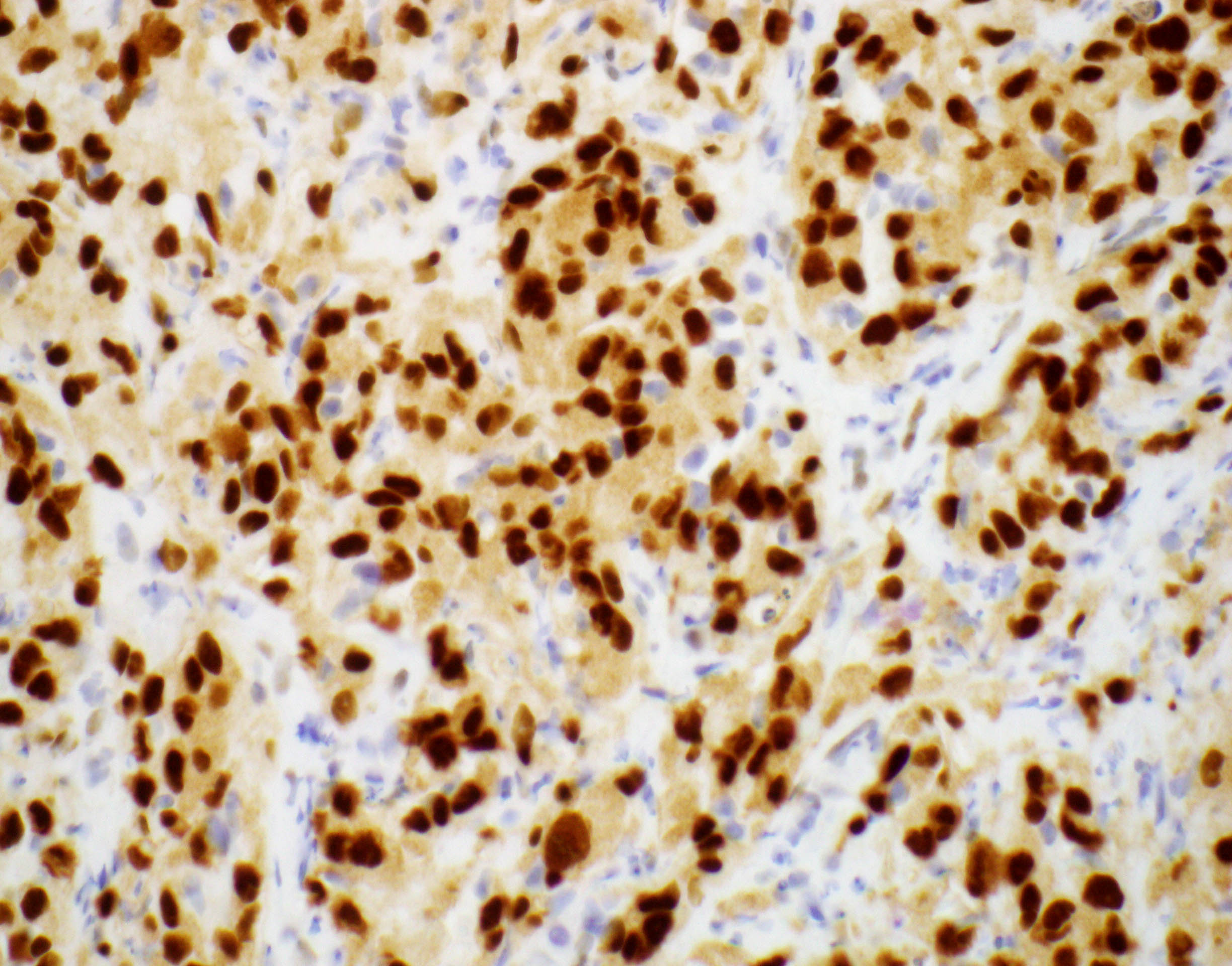
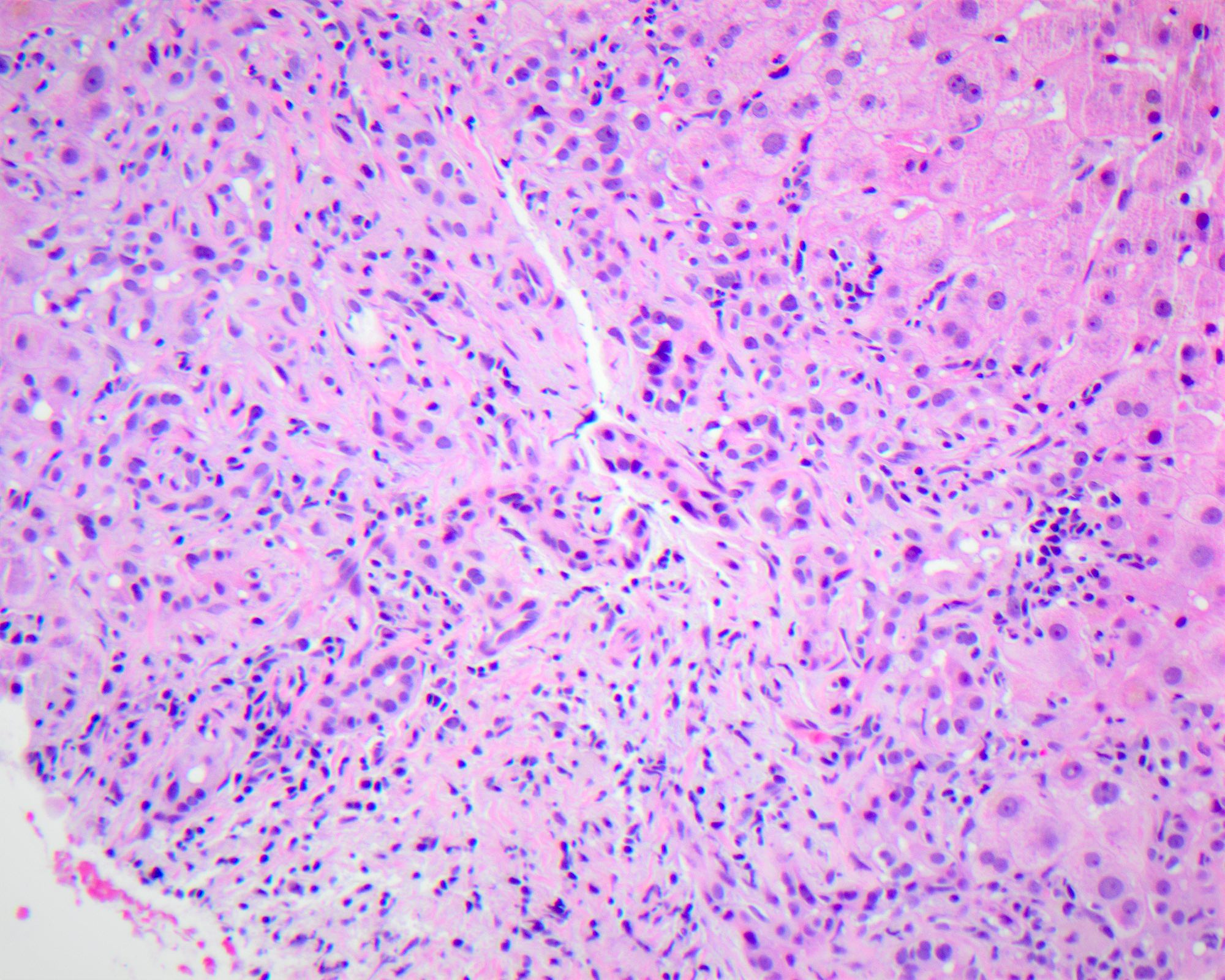
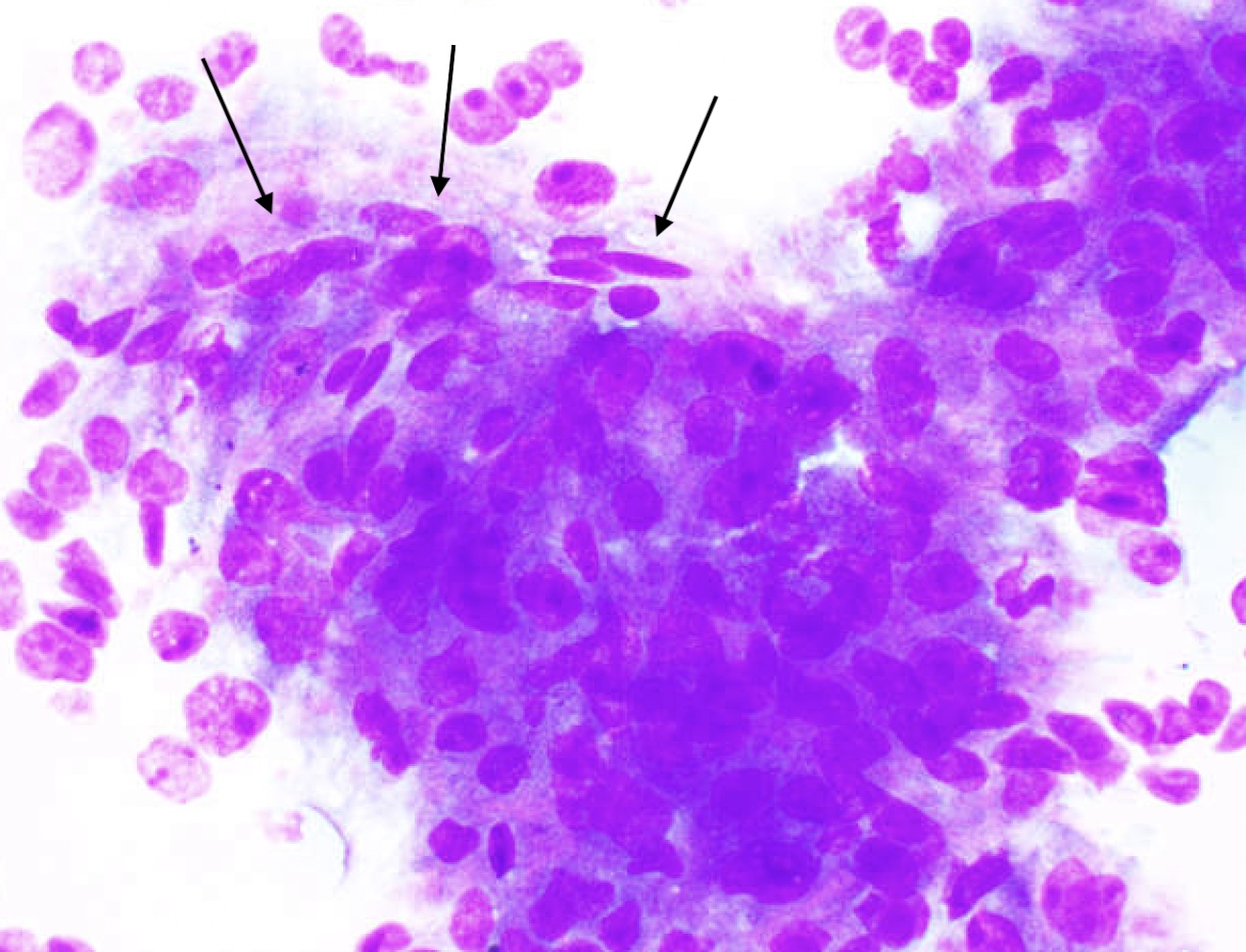
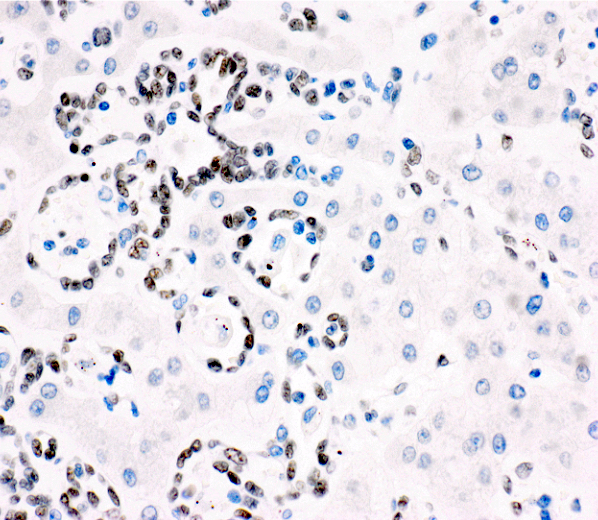
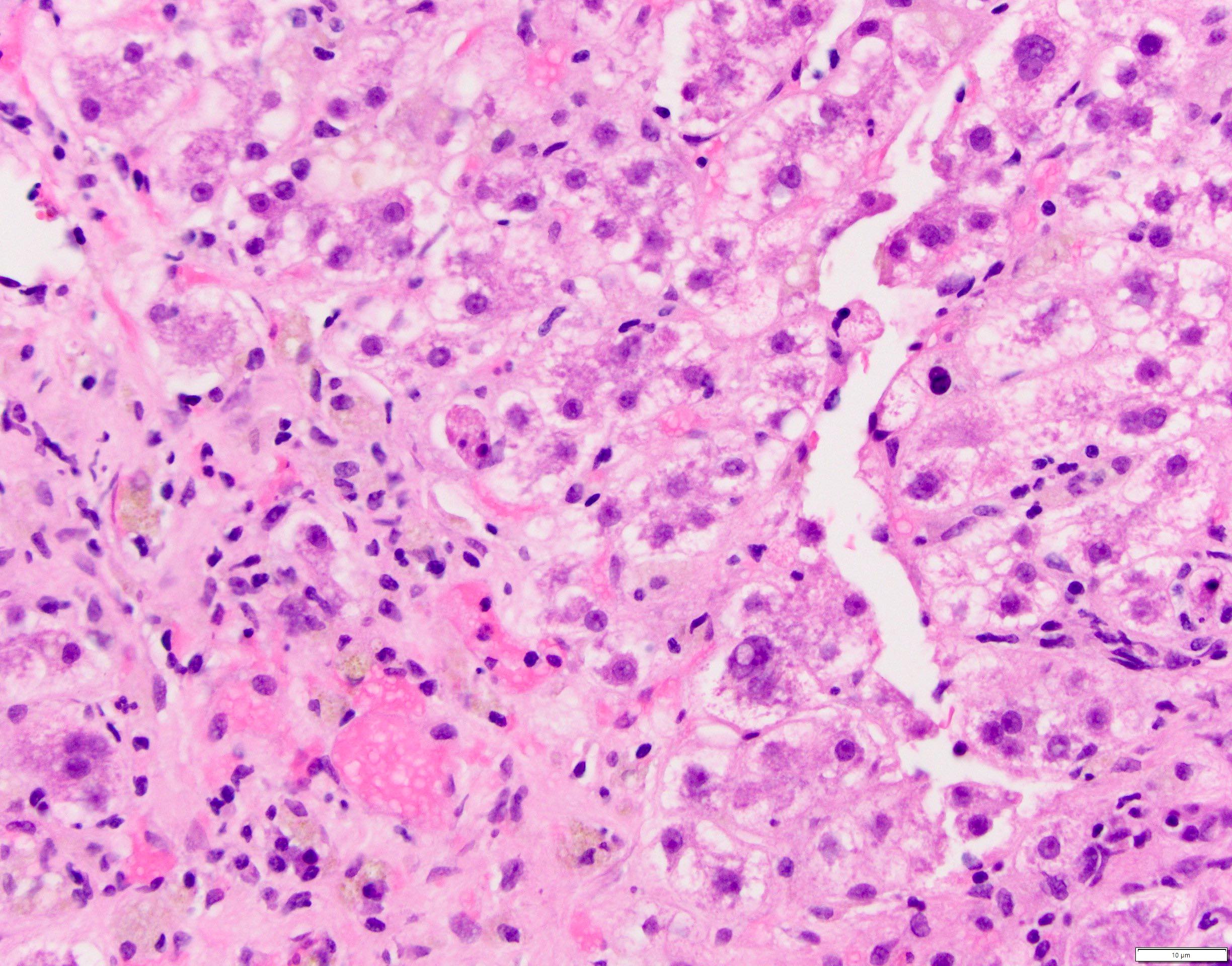
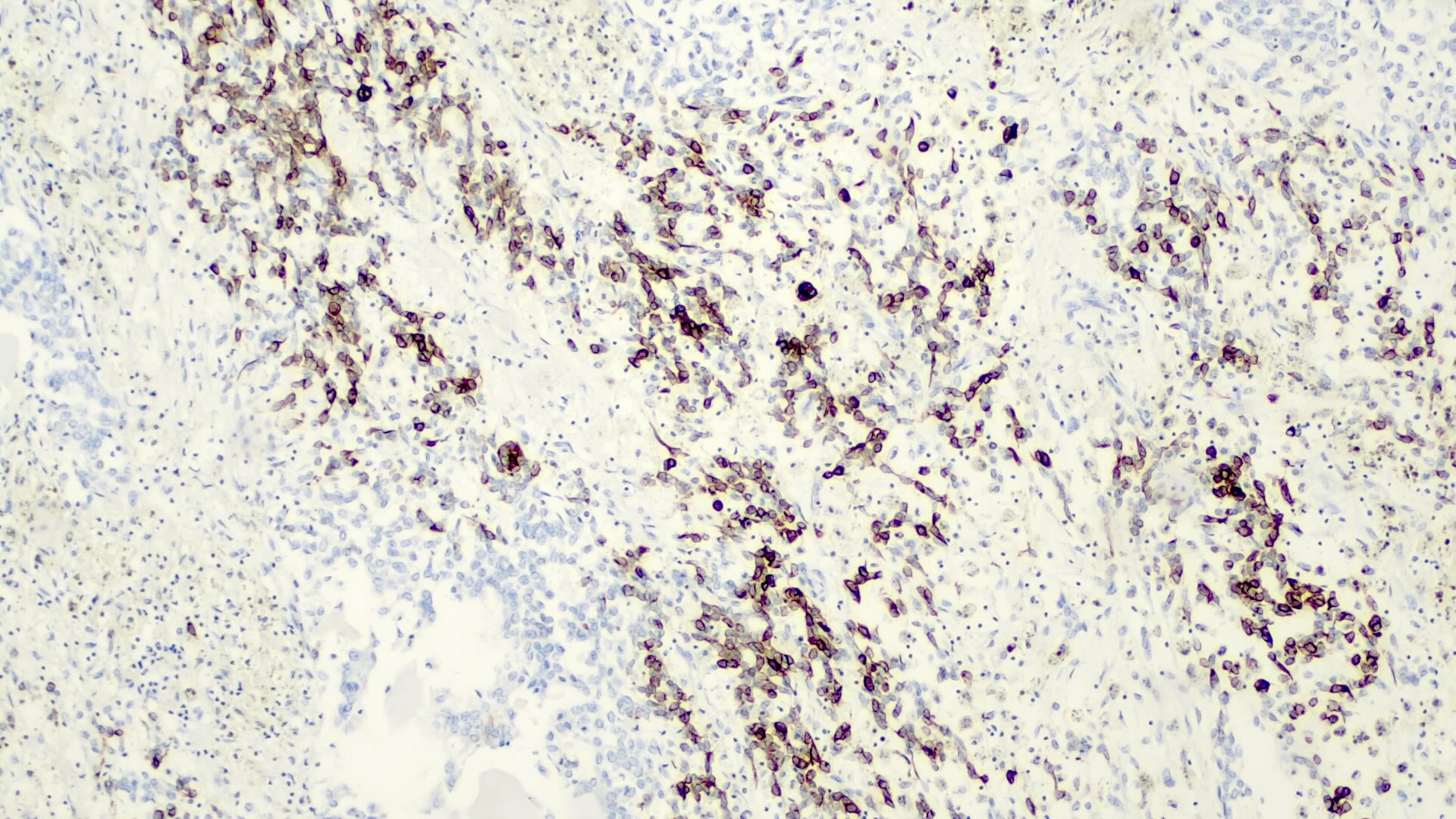
- Plasma cell rich rejection (de novo autoimmune hepatitis / plasma cell hepatitis) must meet criteria 1 and 3, criterion 2 is desirable (Am J Transplant 2016;16:2816):
| Criteria for plasma cell rich rejection | |
| 1 | Plasma cell rich (> 30%) portal or perivenular infiltrates with easily identifiable interface and perivenular necroinflammatory activity; in most cases rejection activity index (RAI) score ≥ 5/9 |
| 2 | Lymphocytic cholangitis is usually present but not required for diagnosis |
| 3 | Original disease other than autoimmune hepatitis |
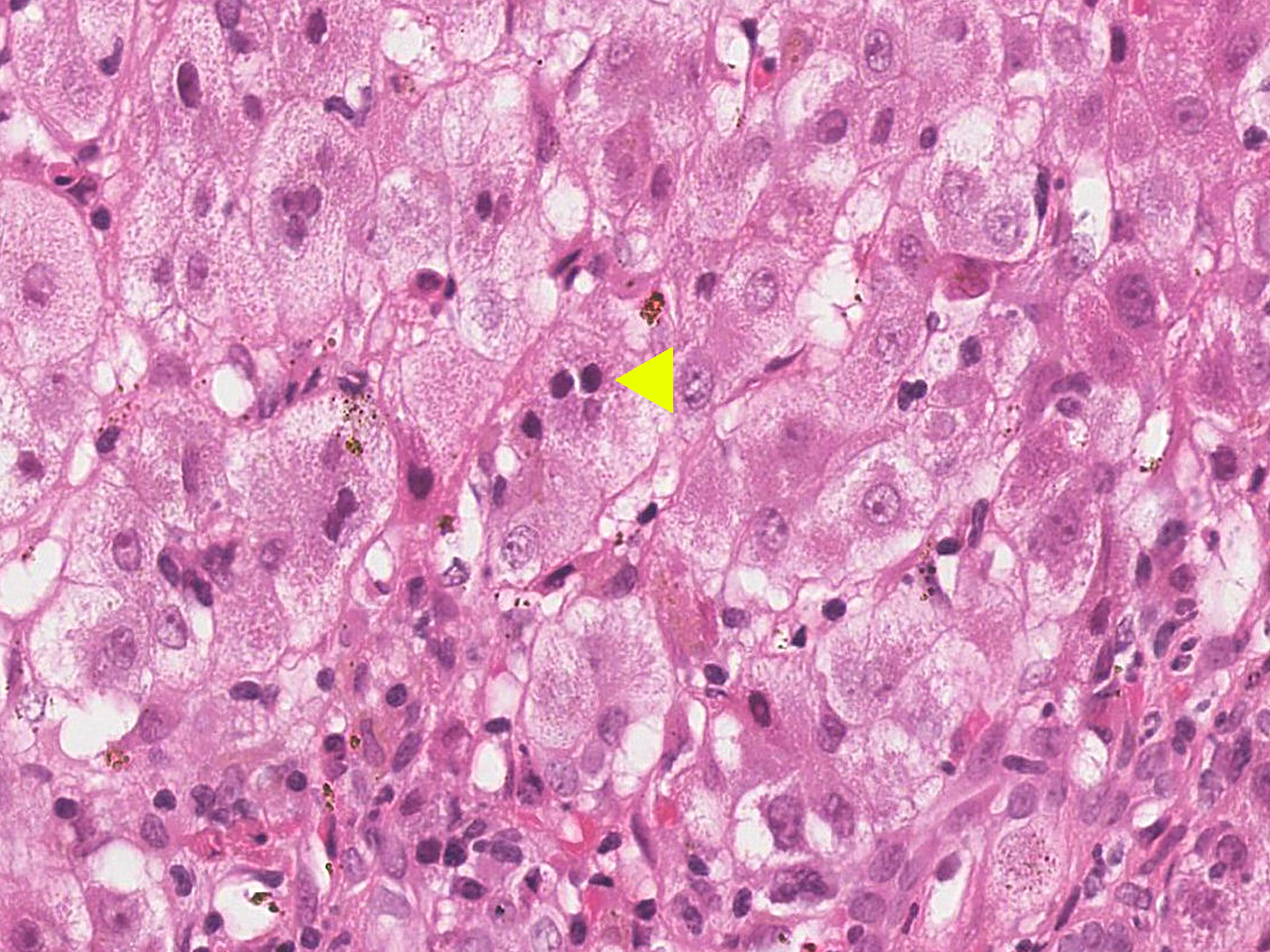
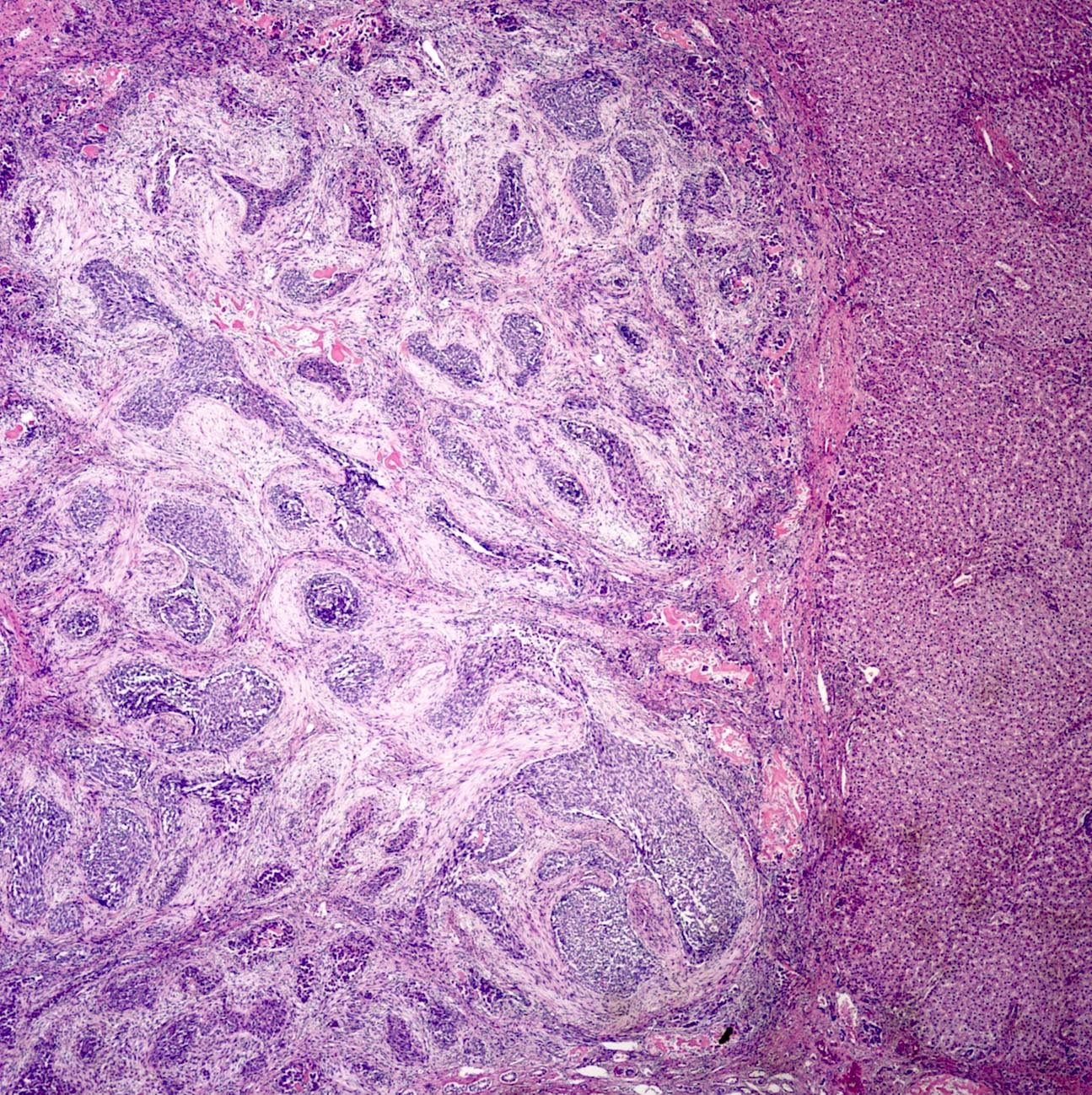
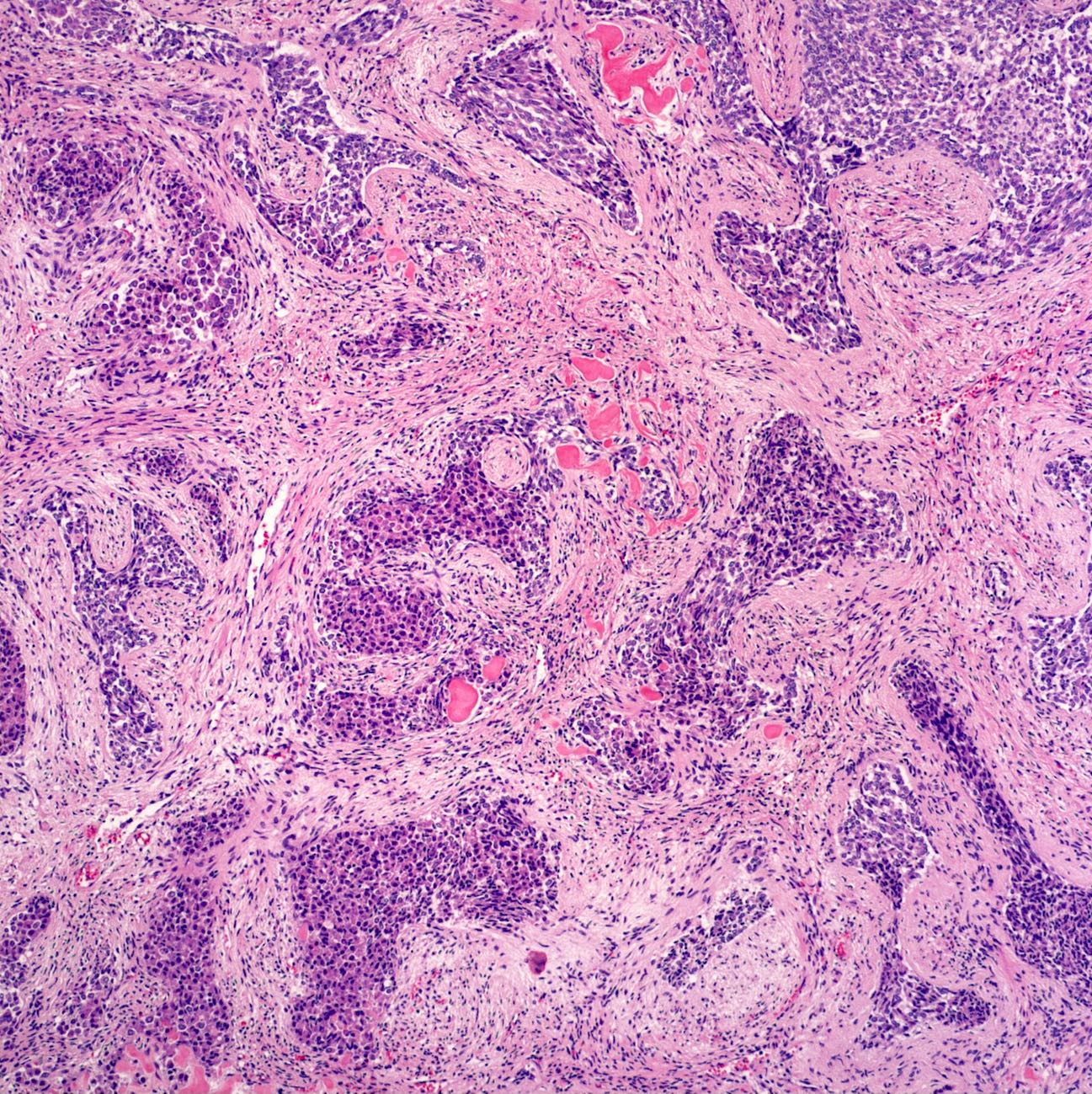
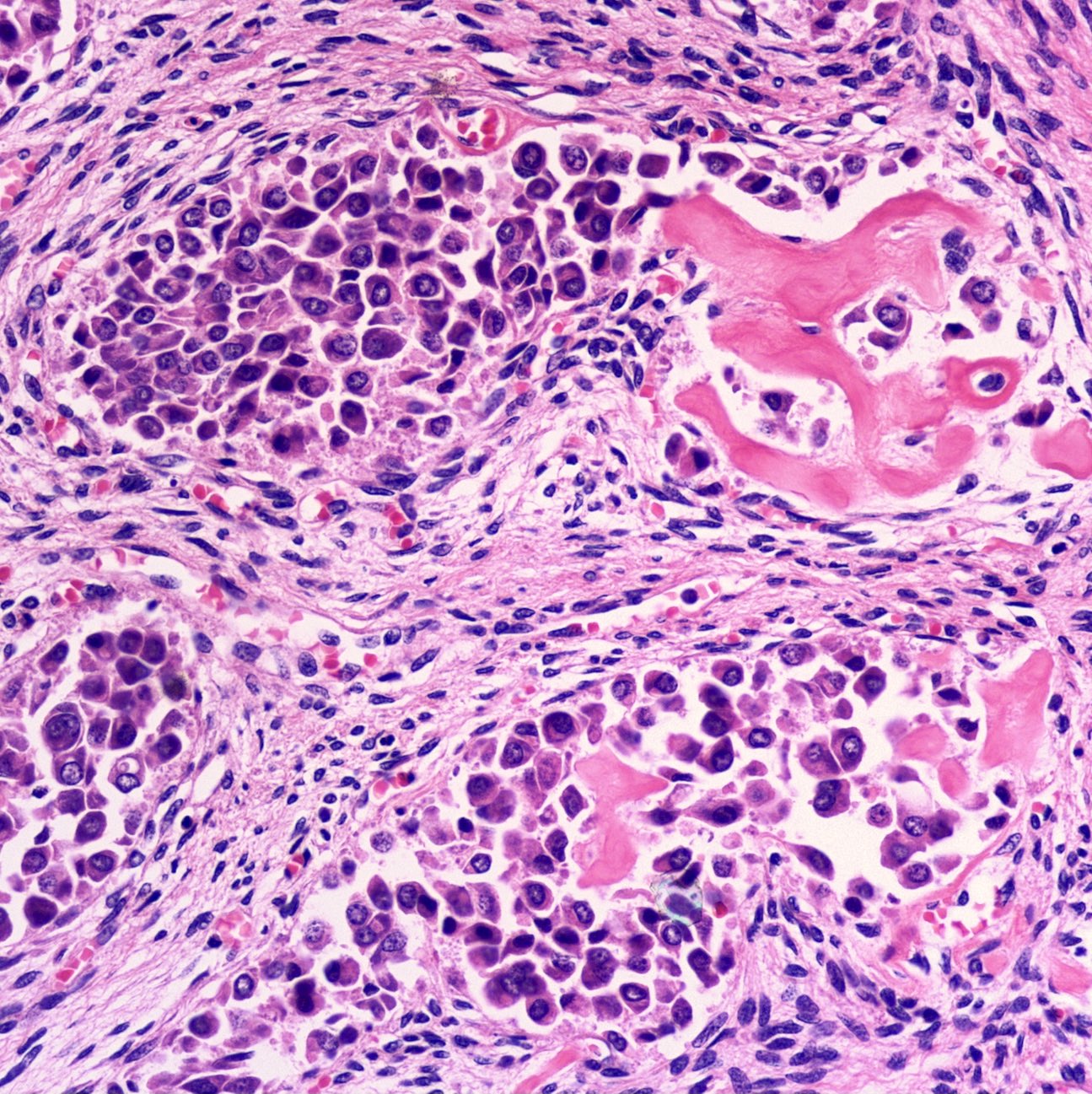
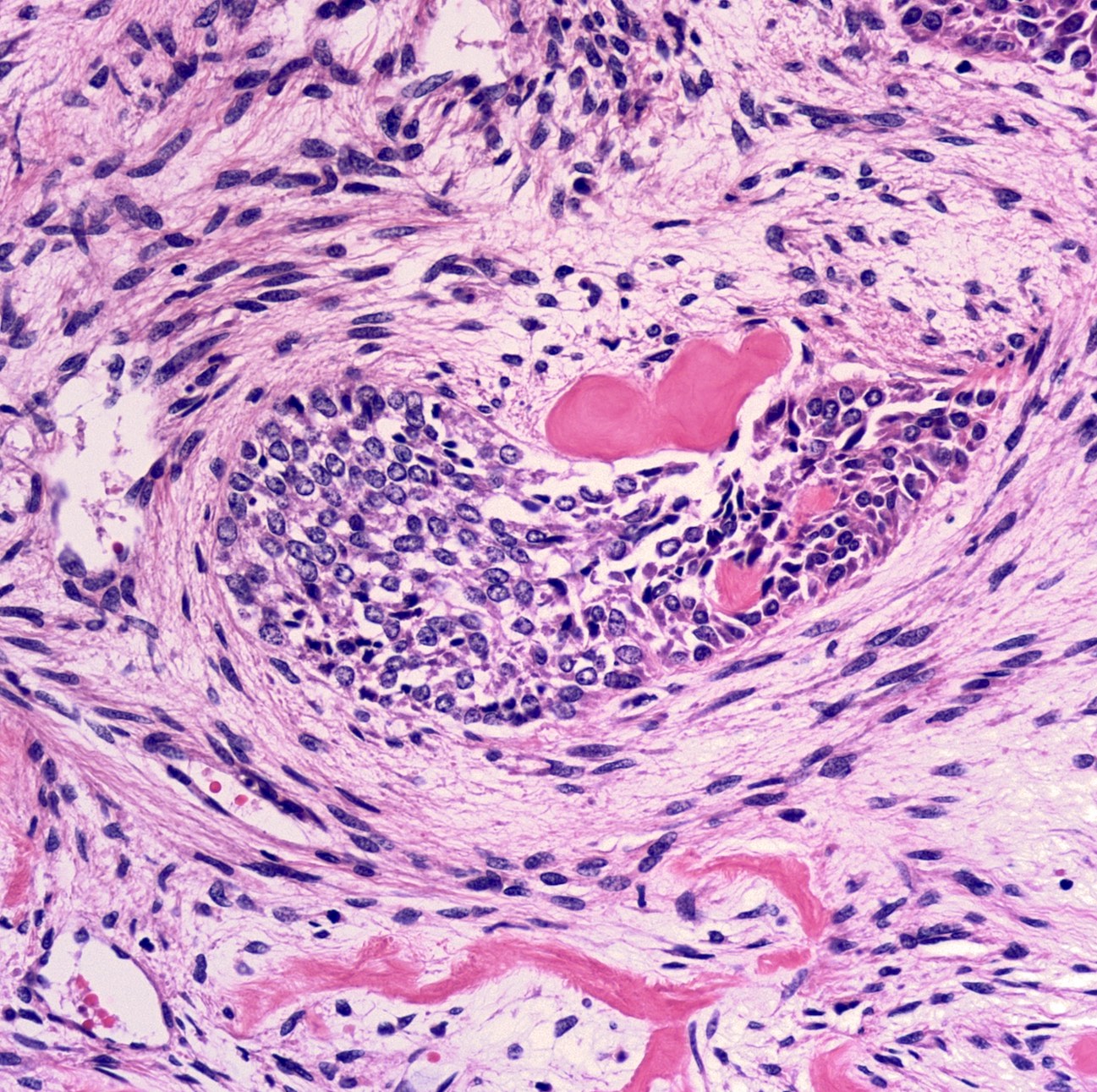
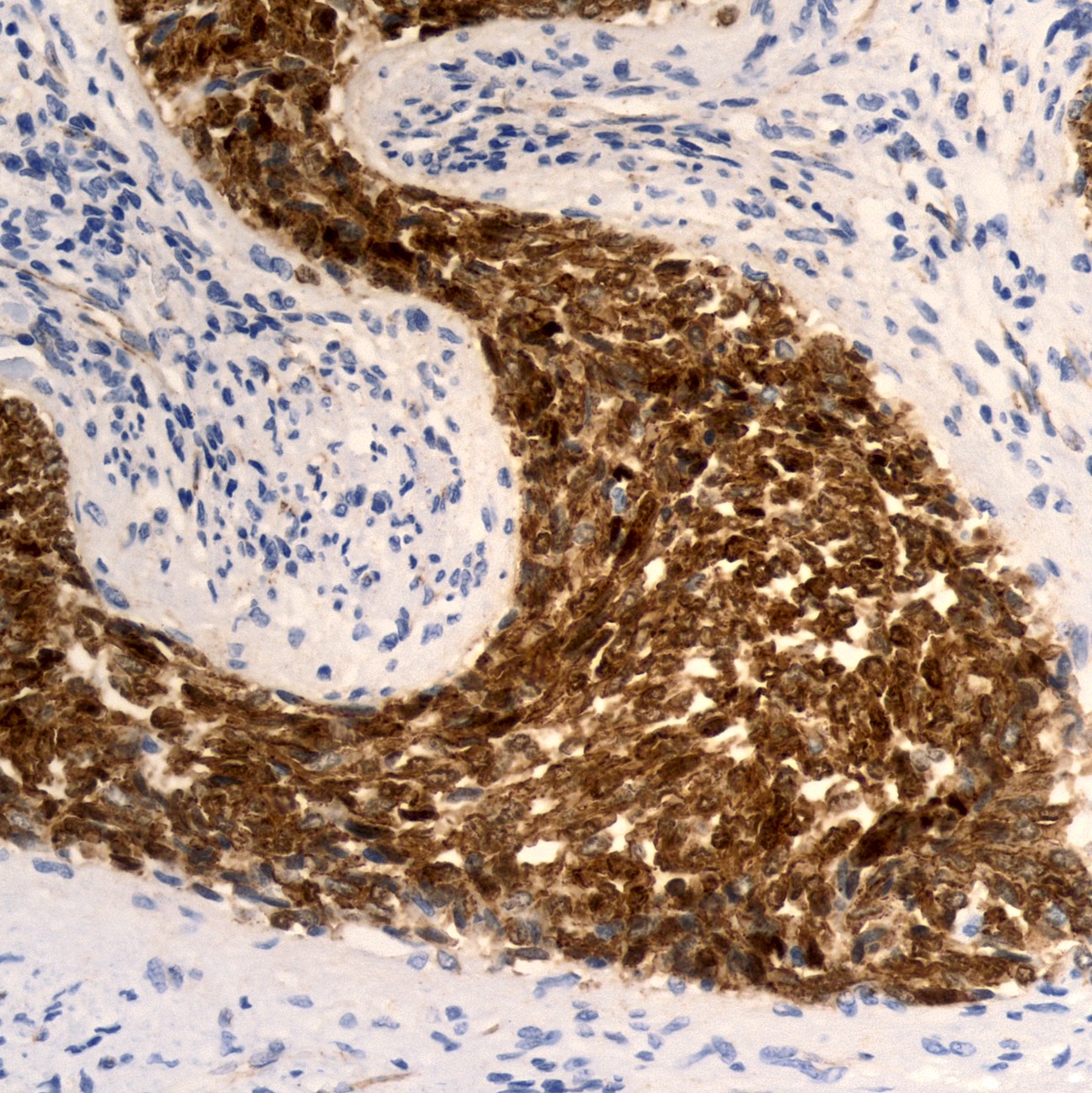
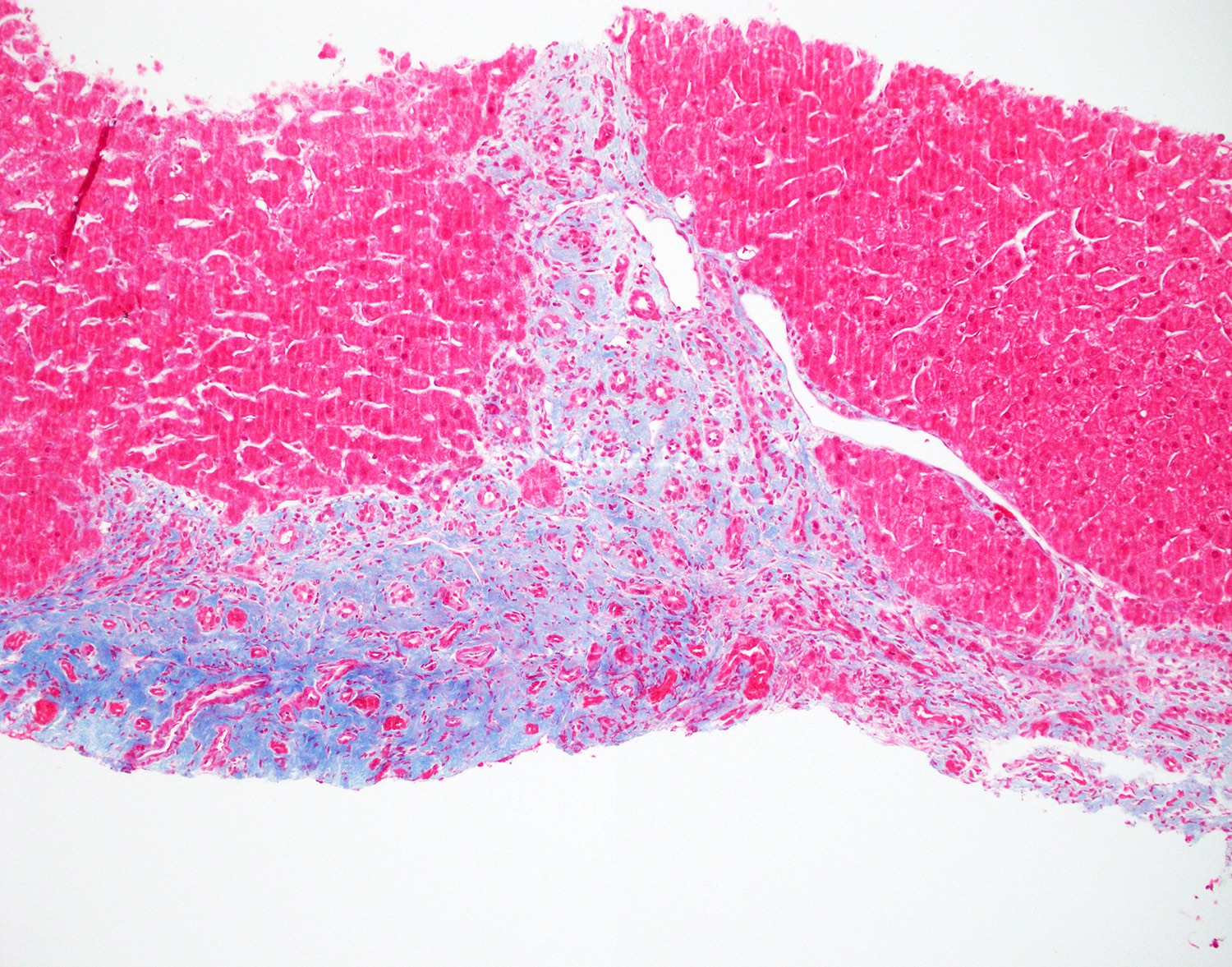
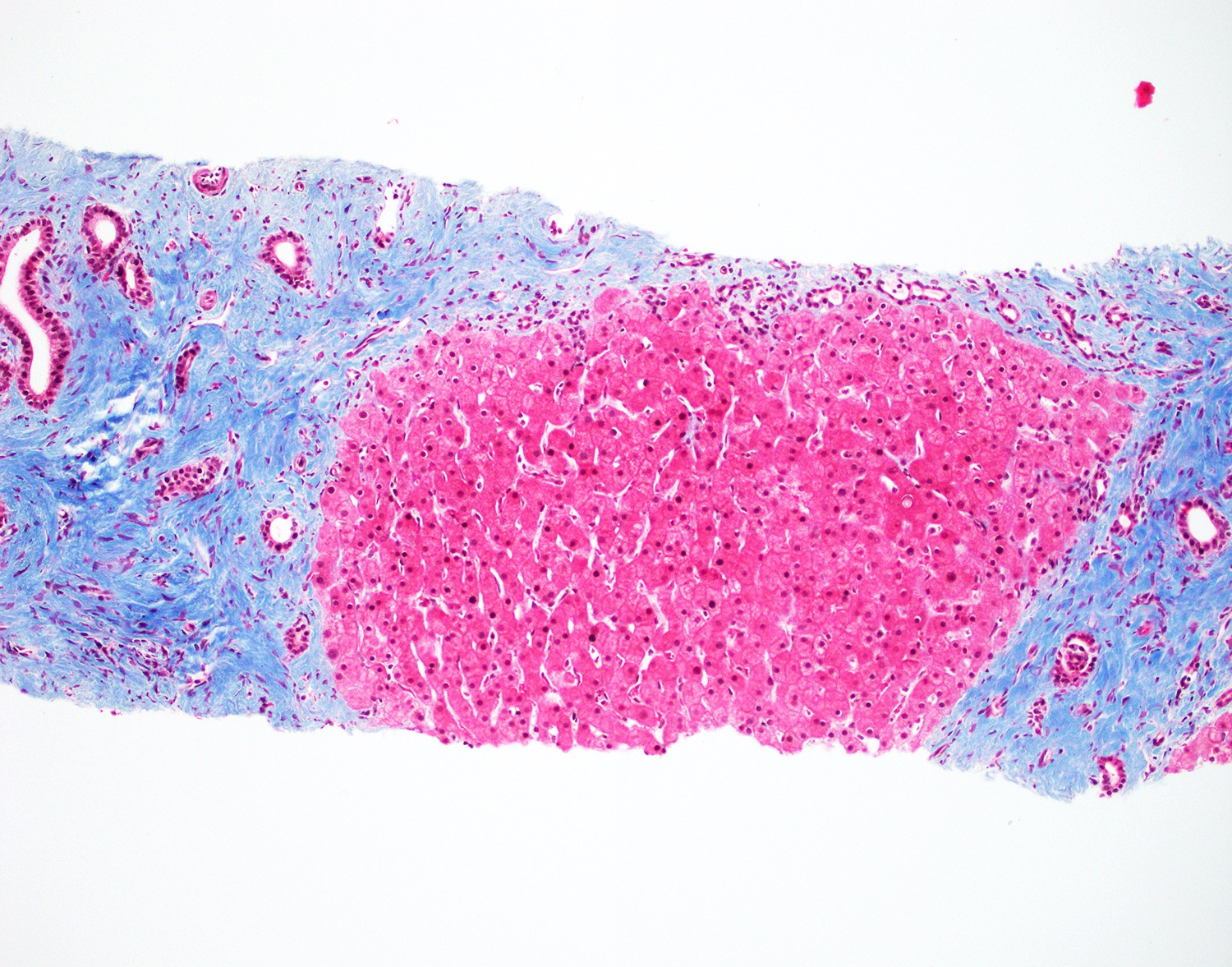
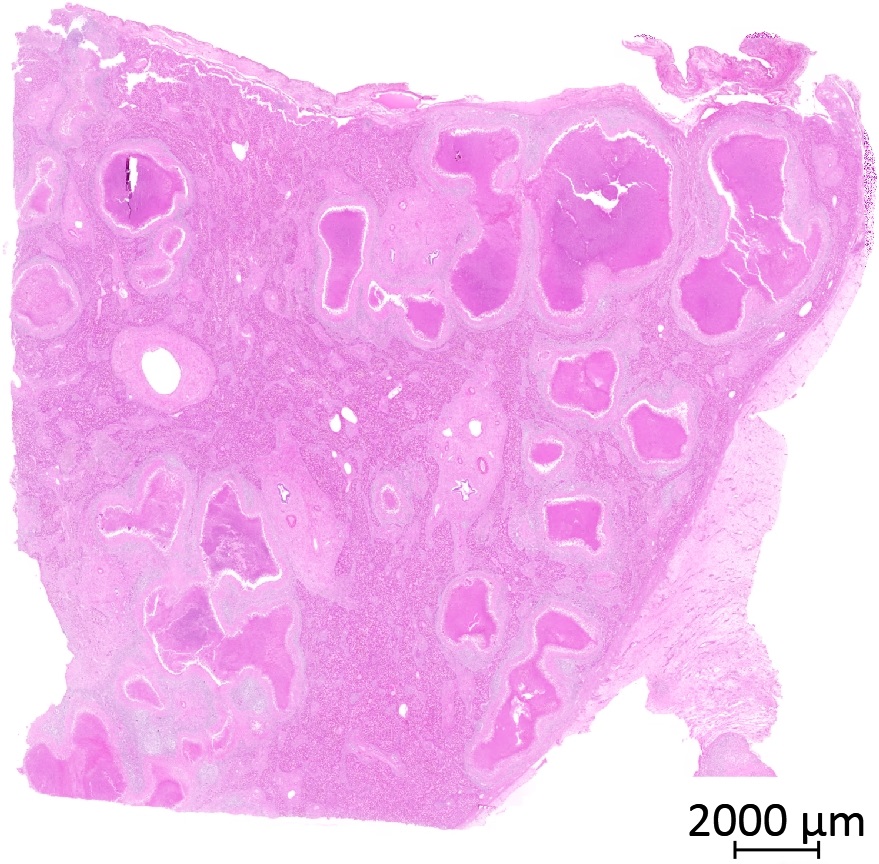
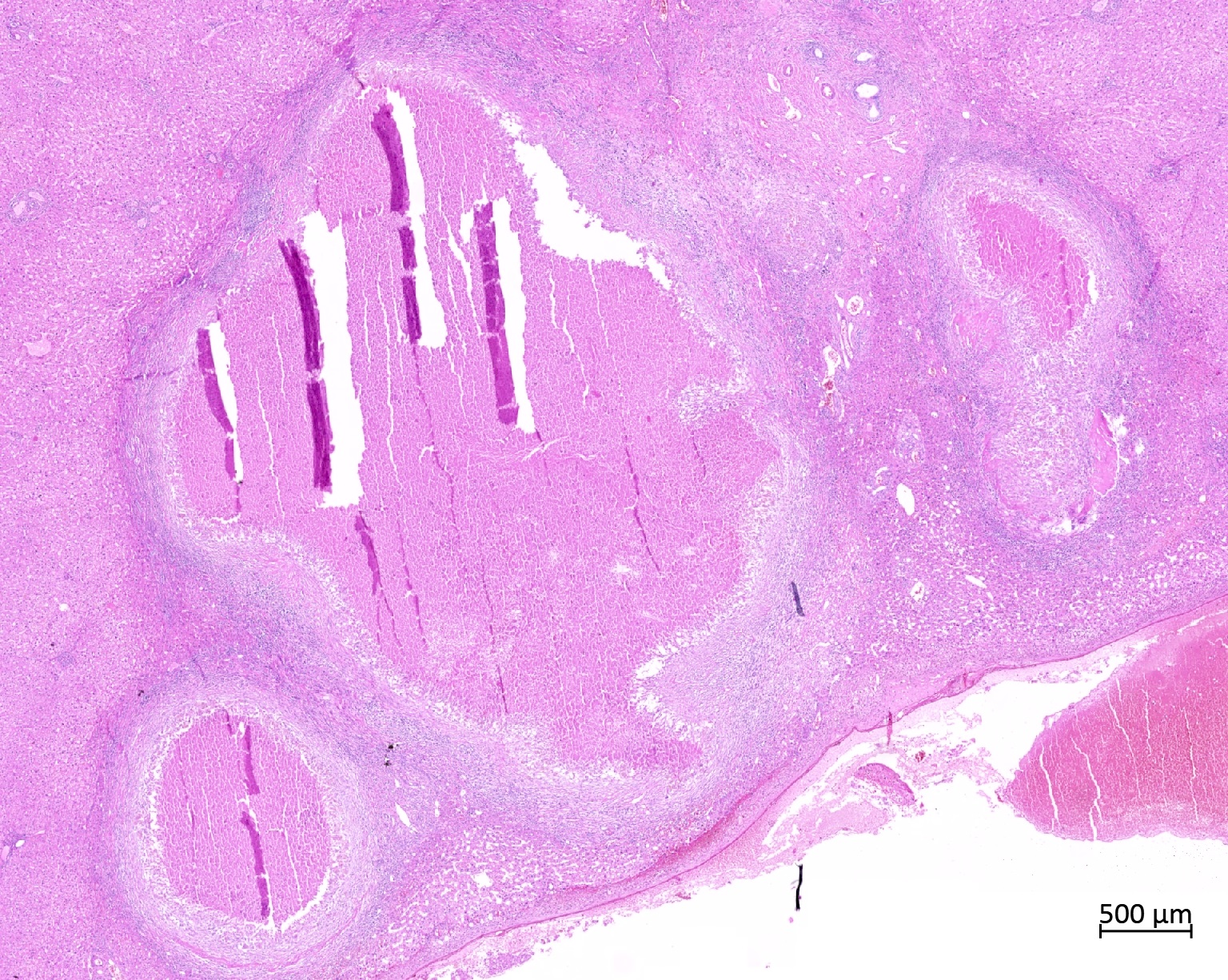
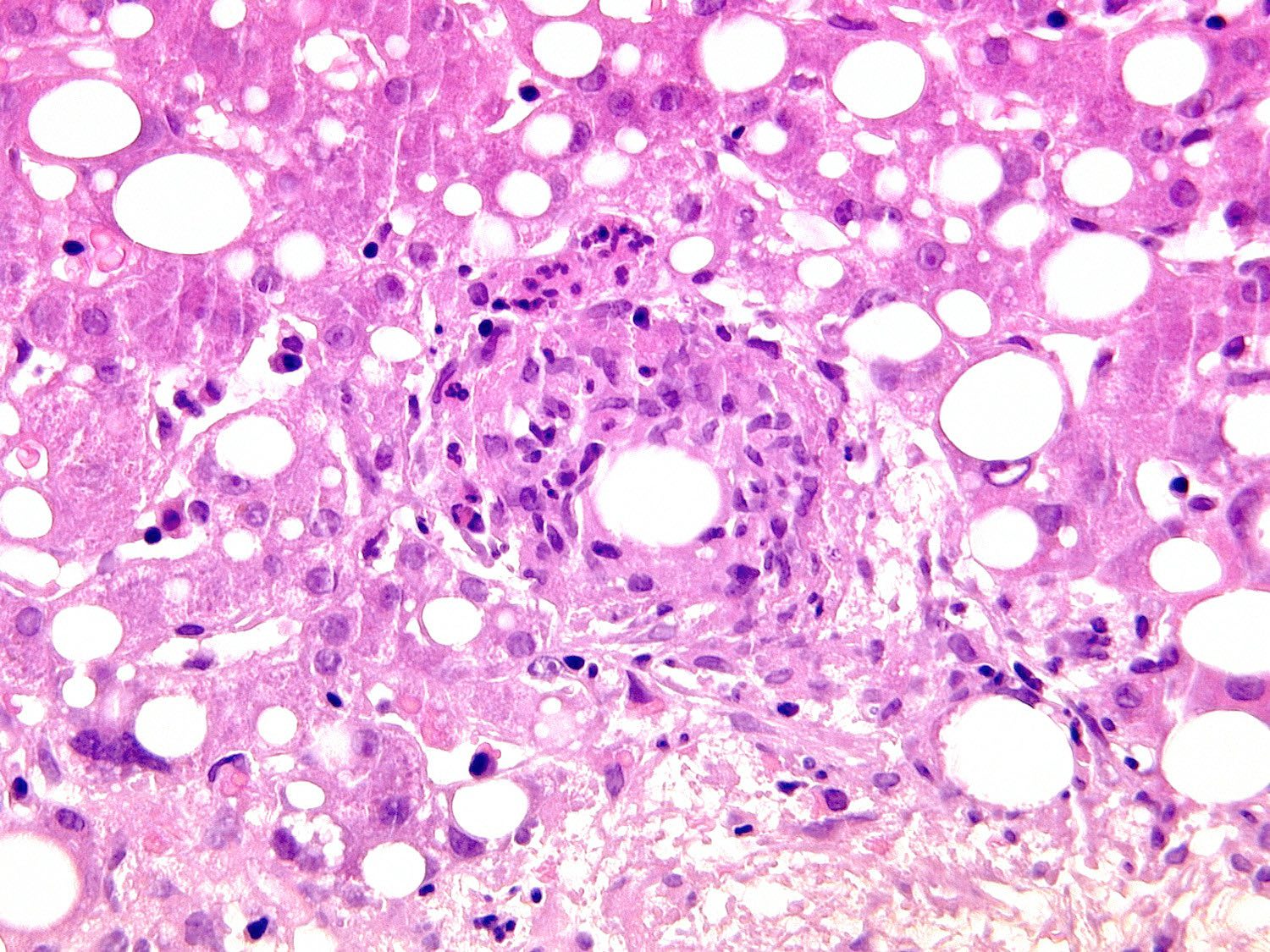
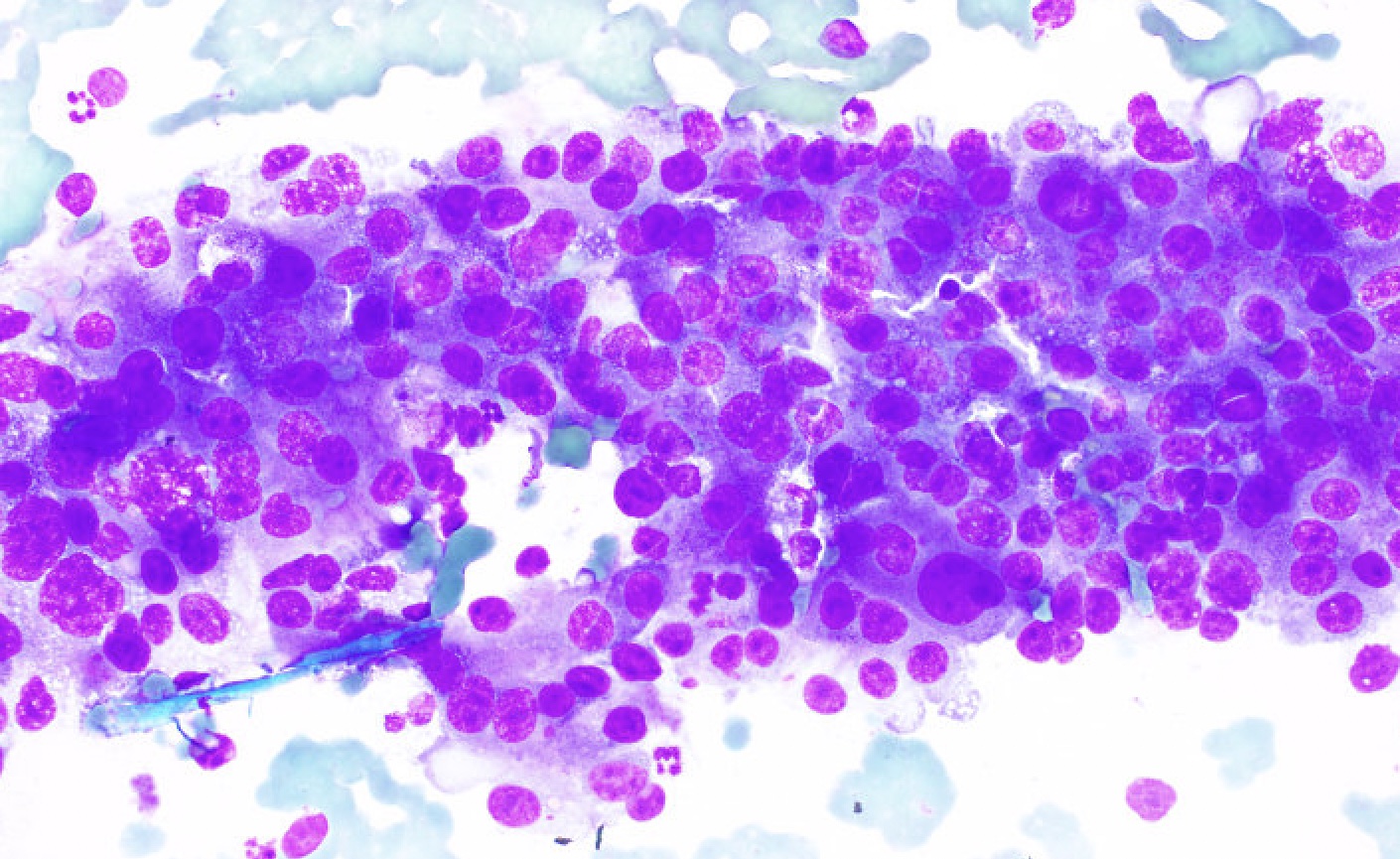
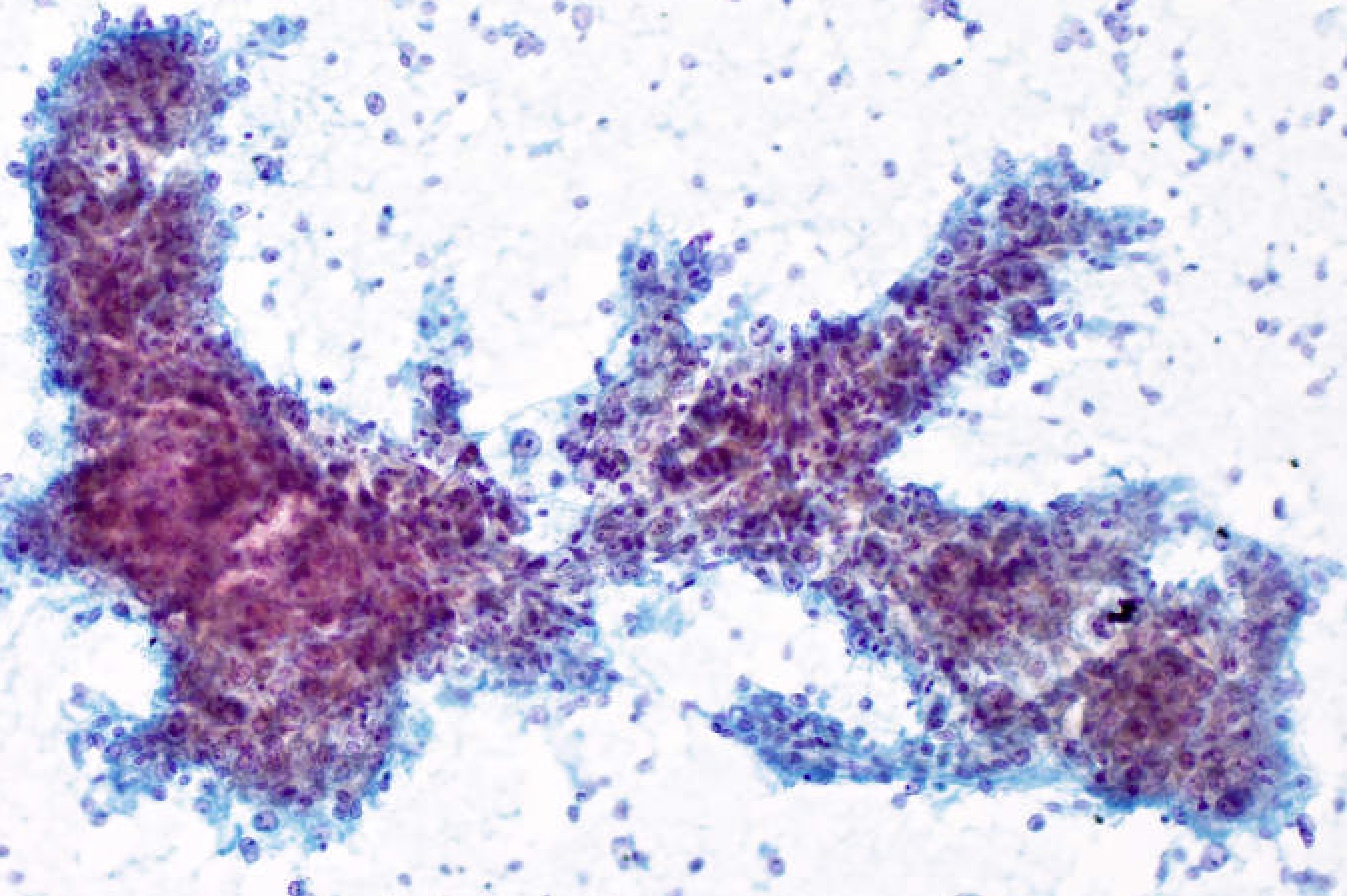
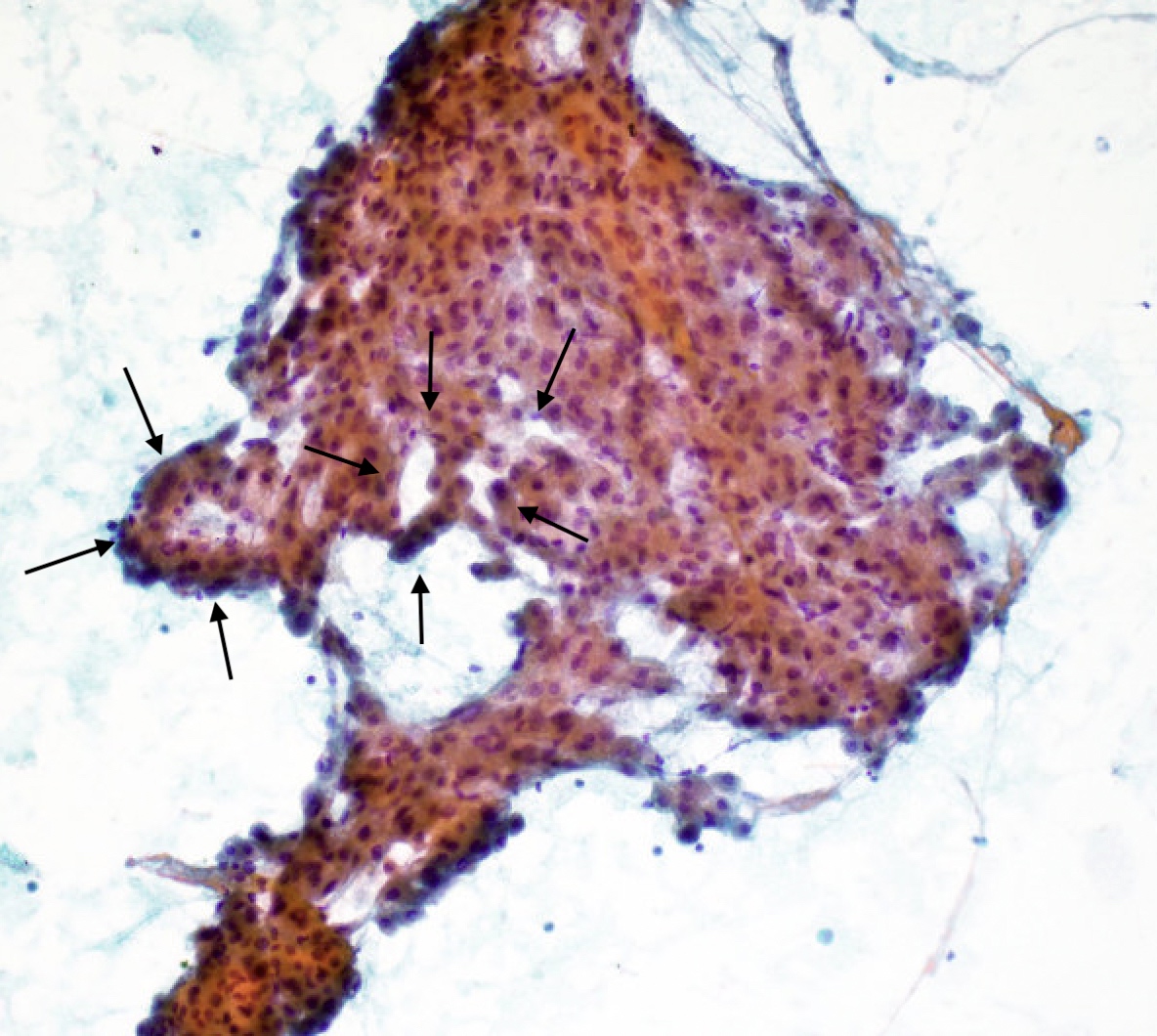
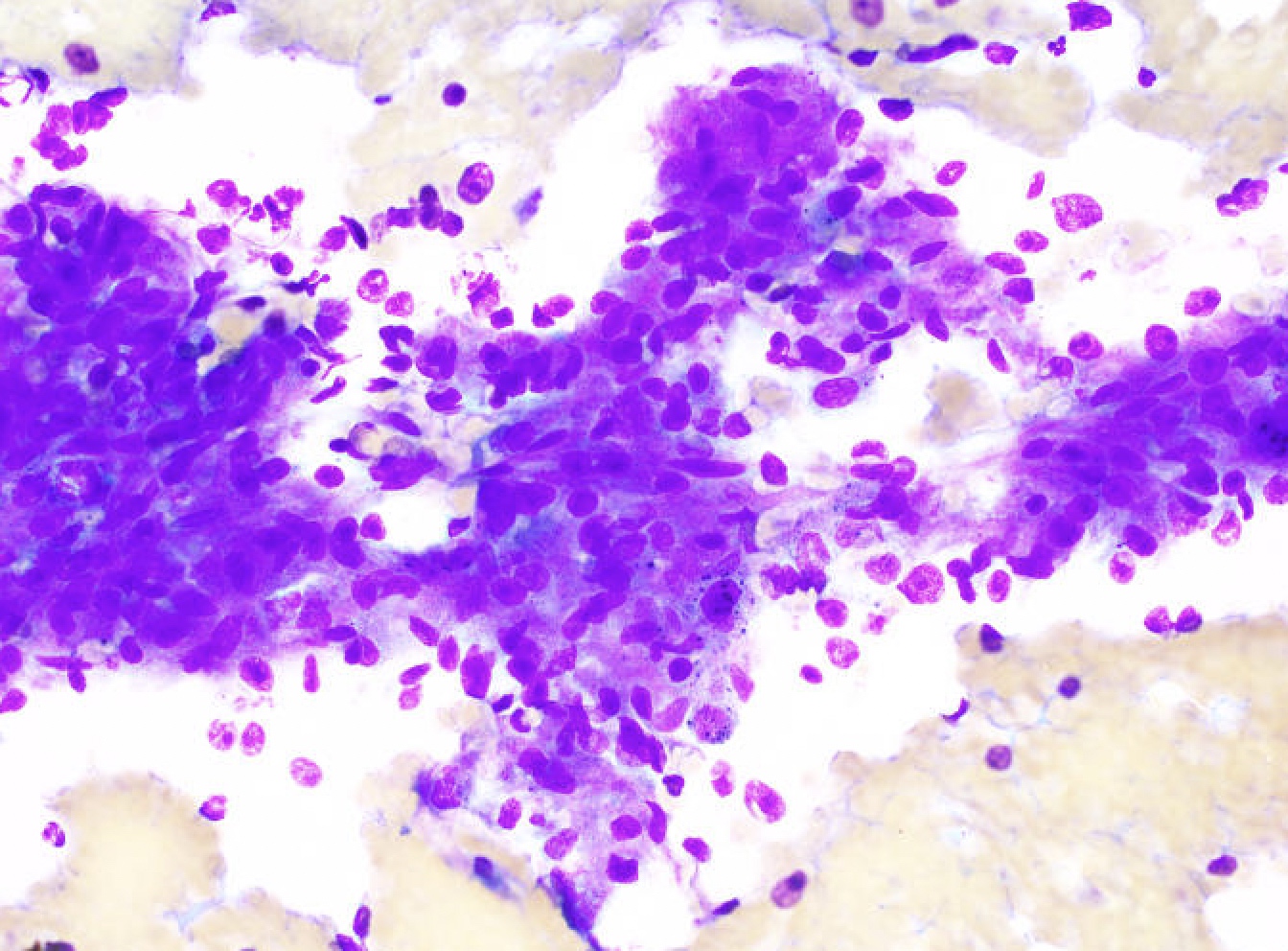
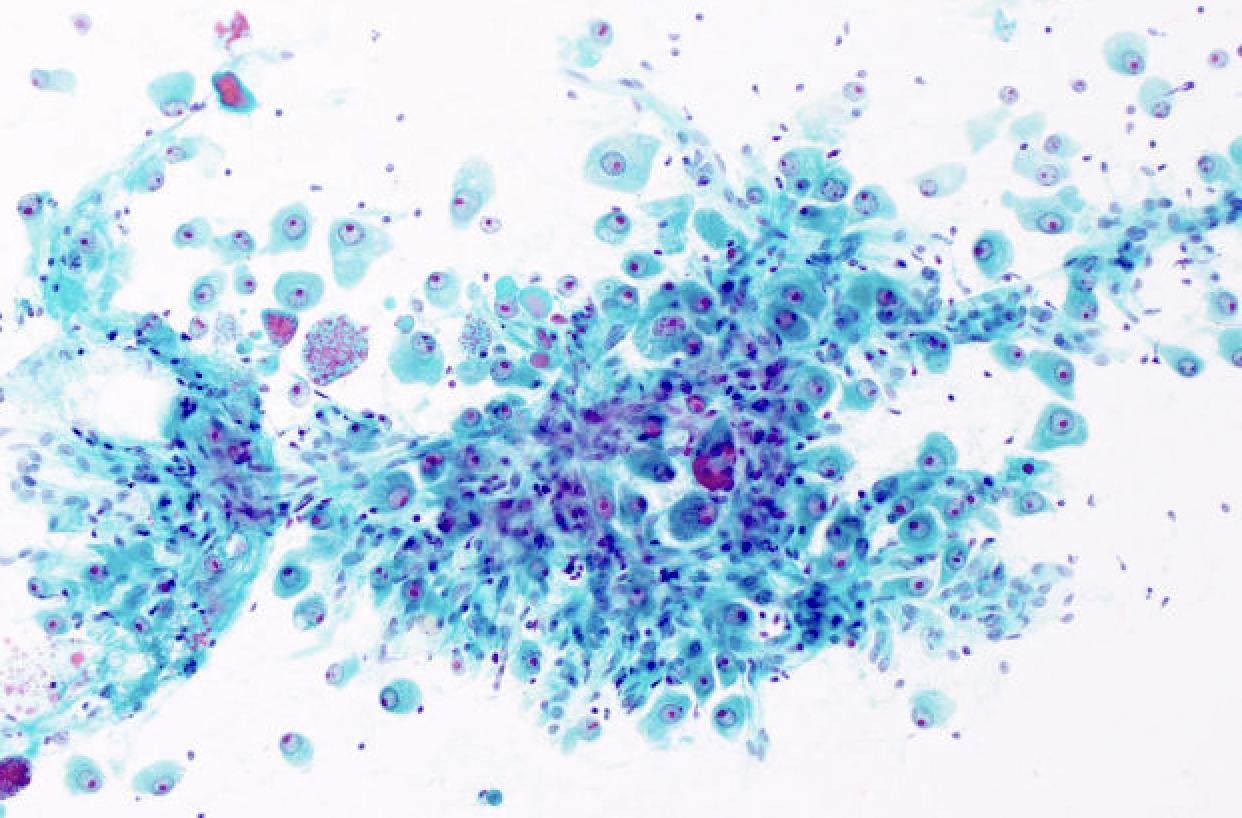
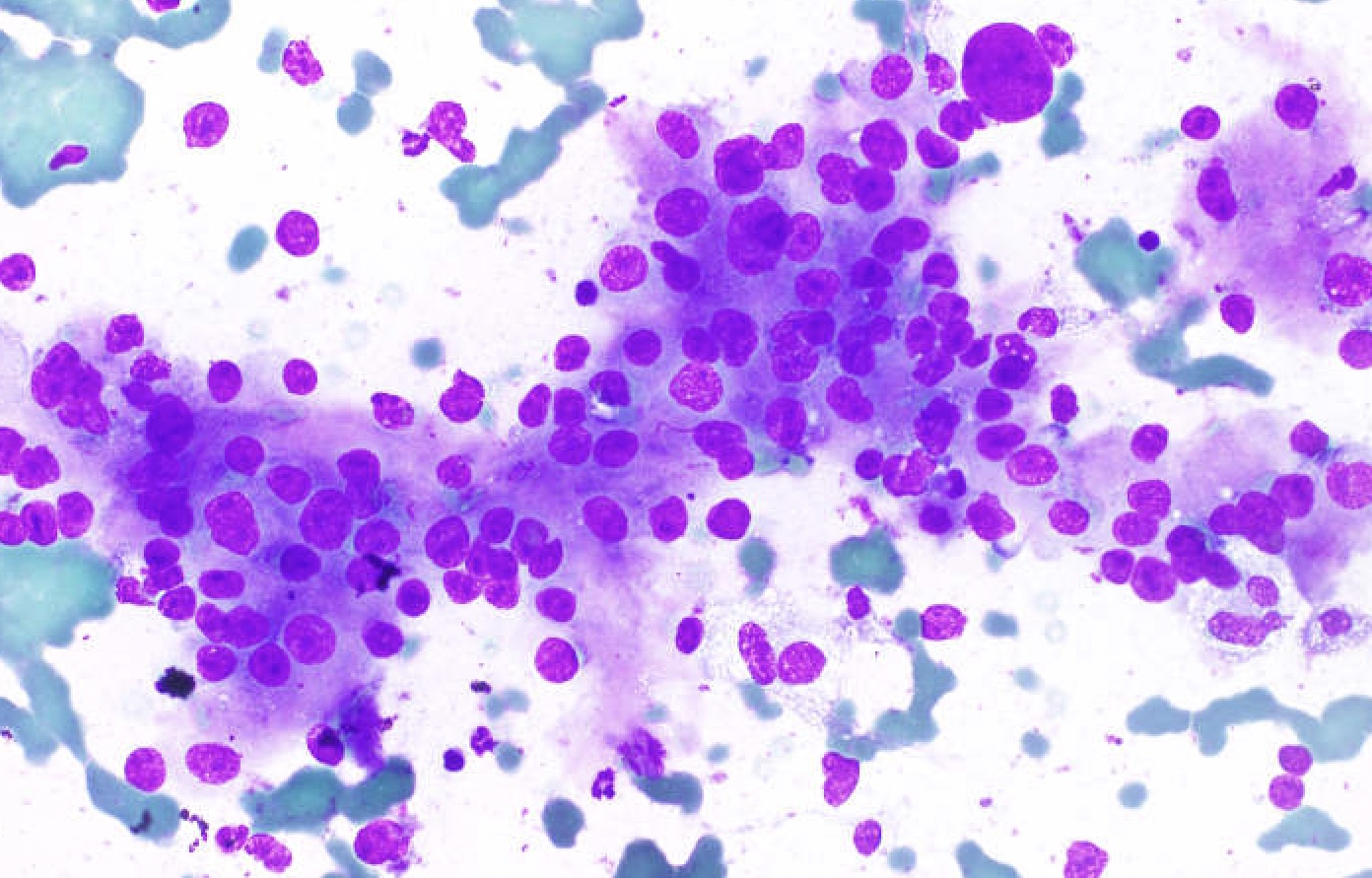
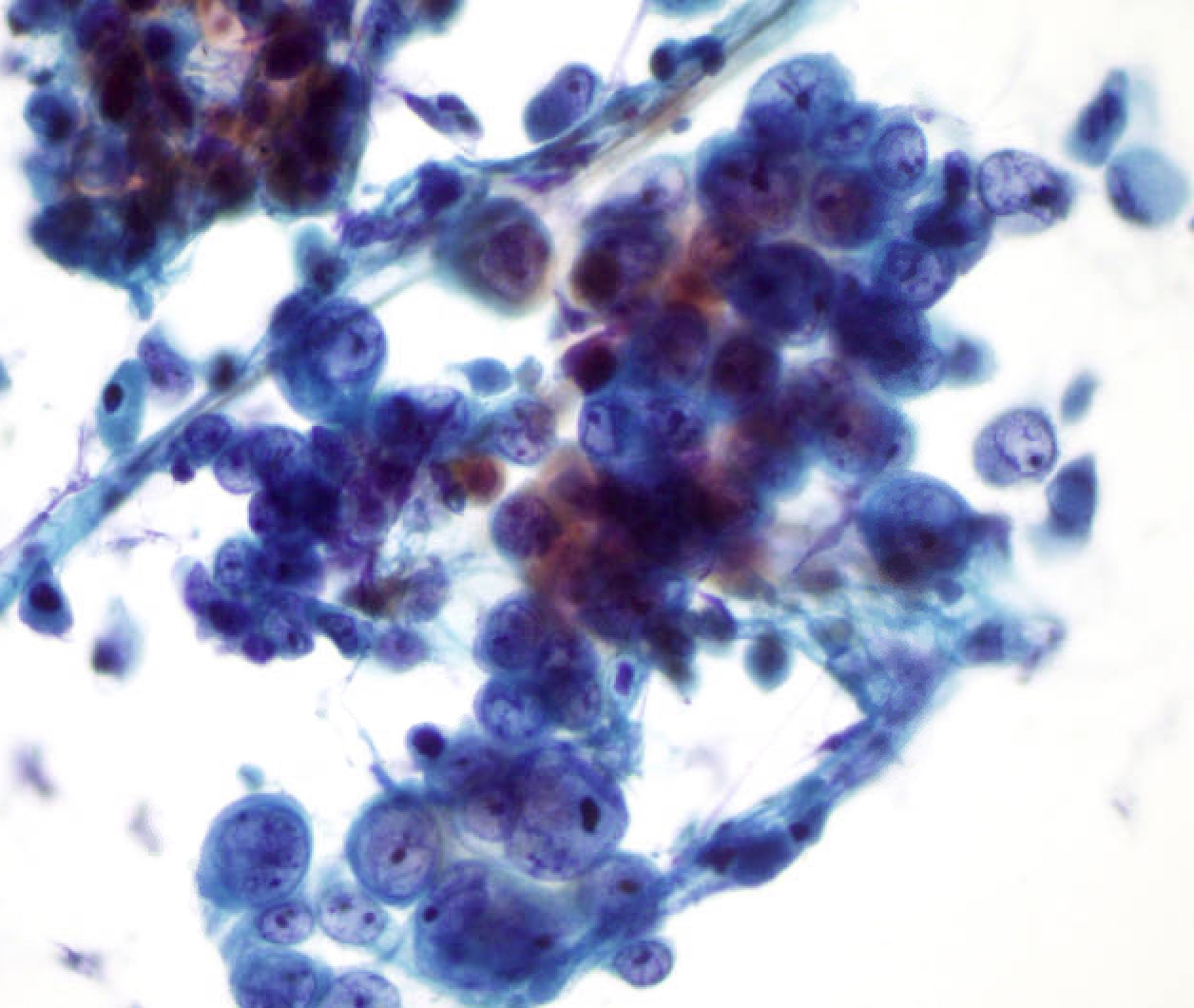
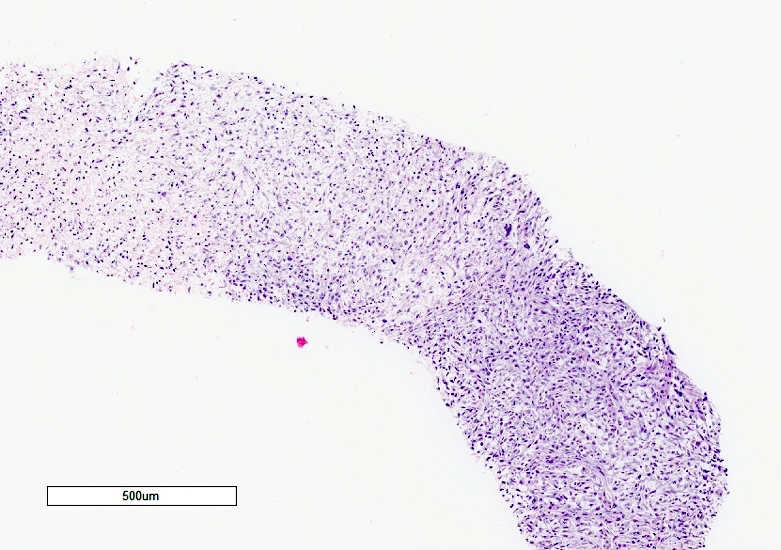
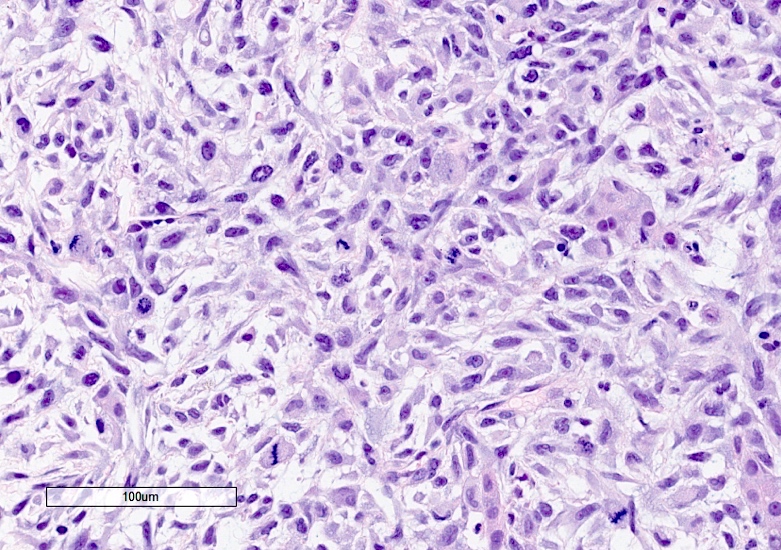
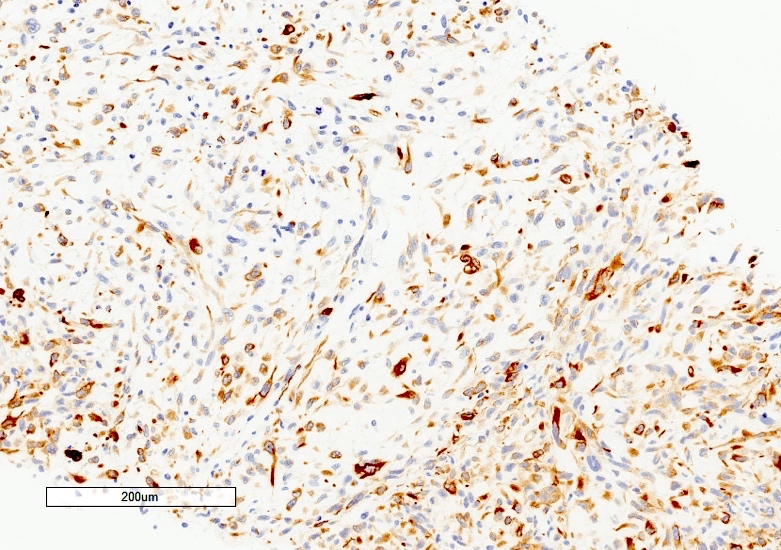
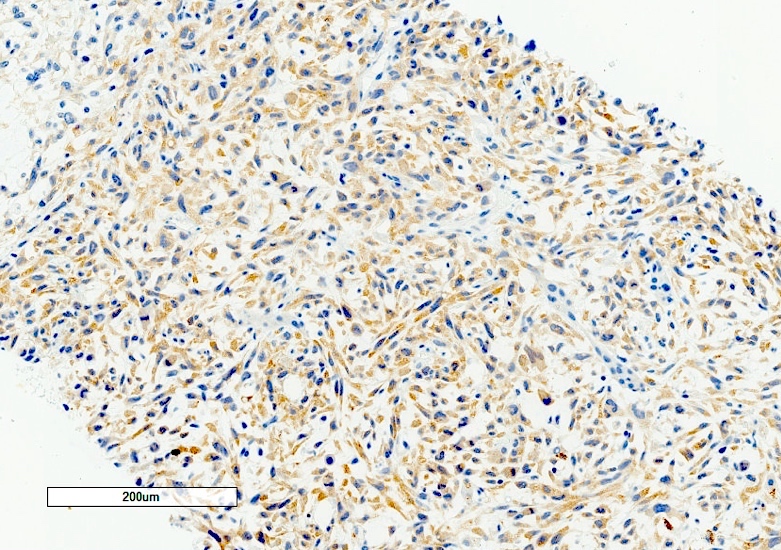
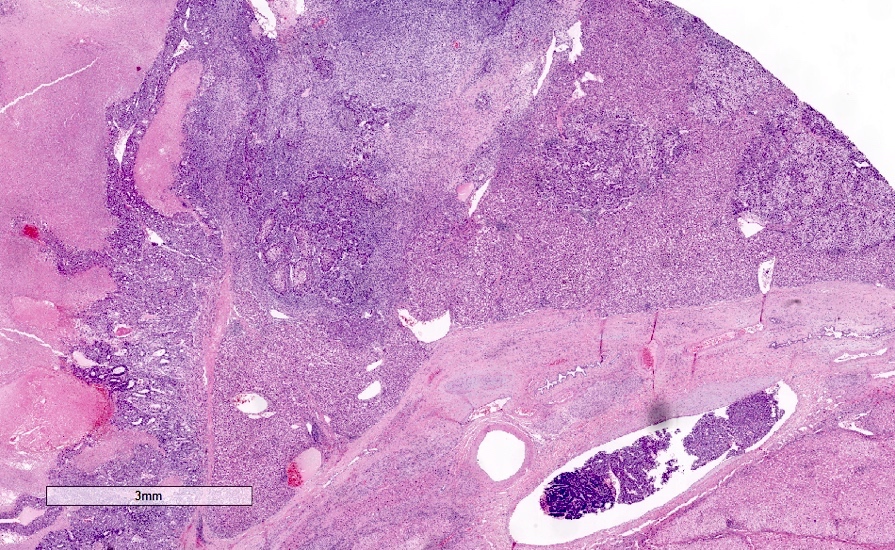
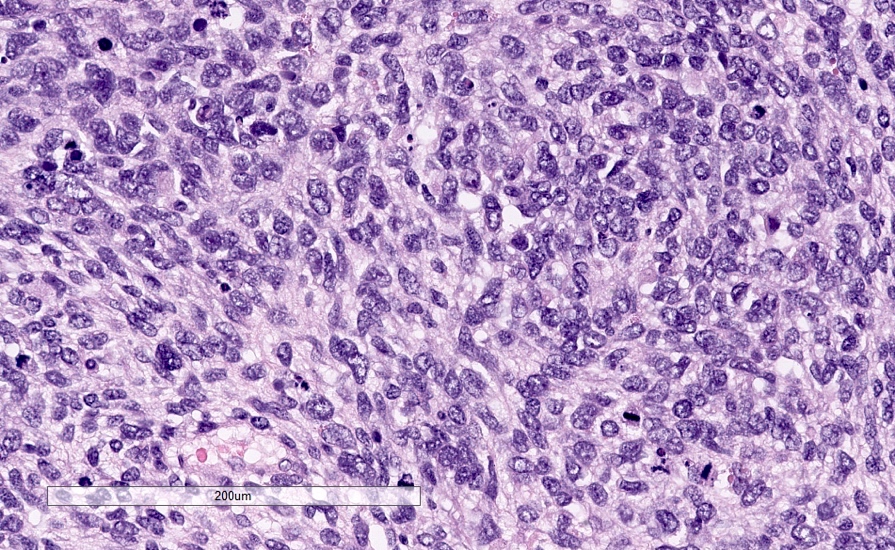
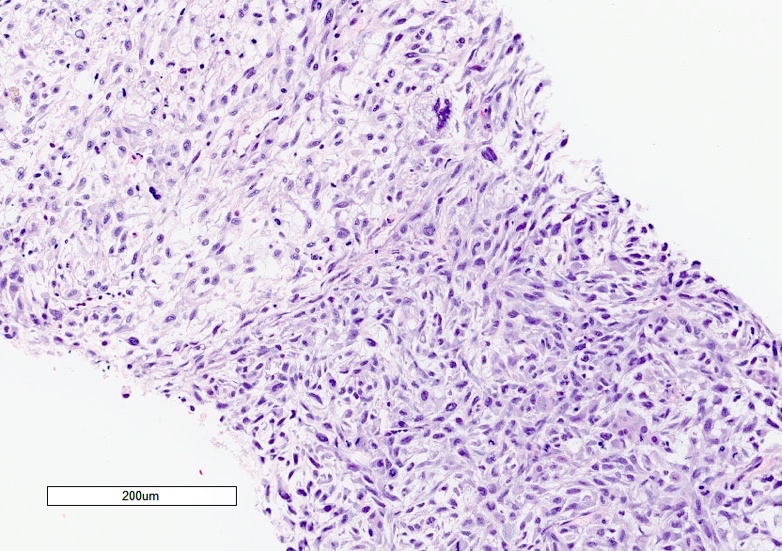
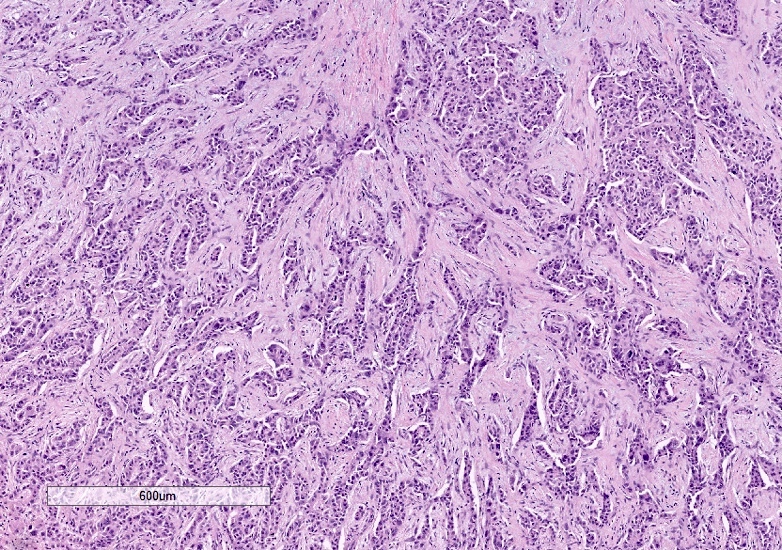
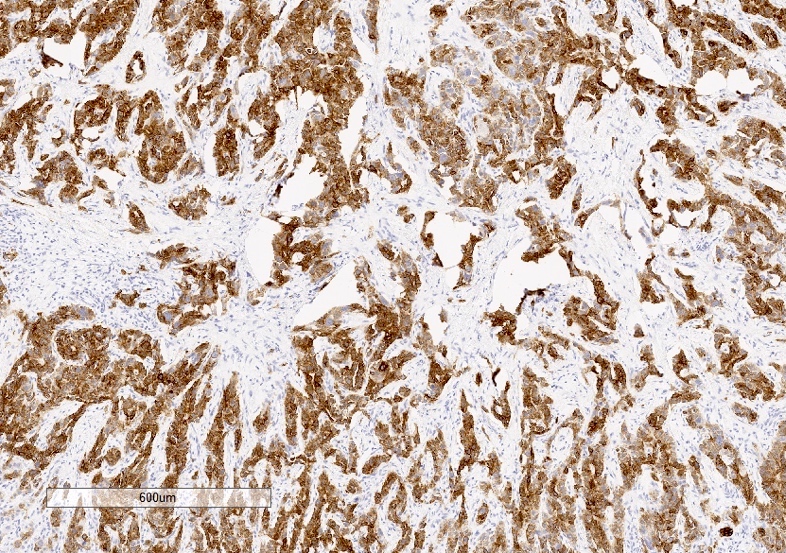
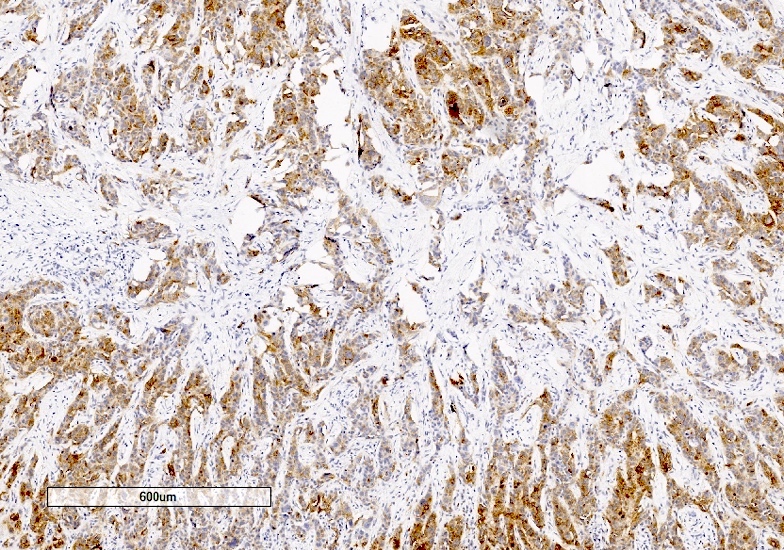
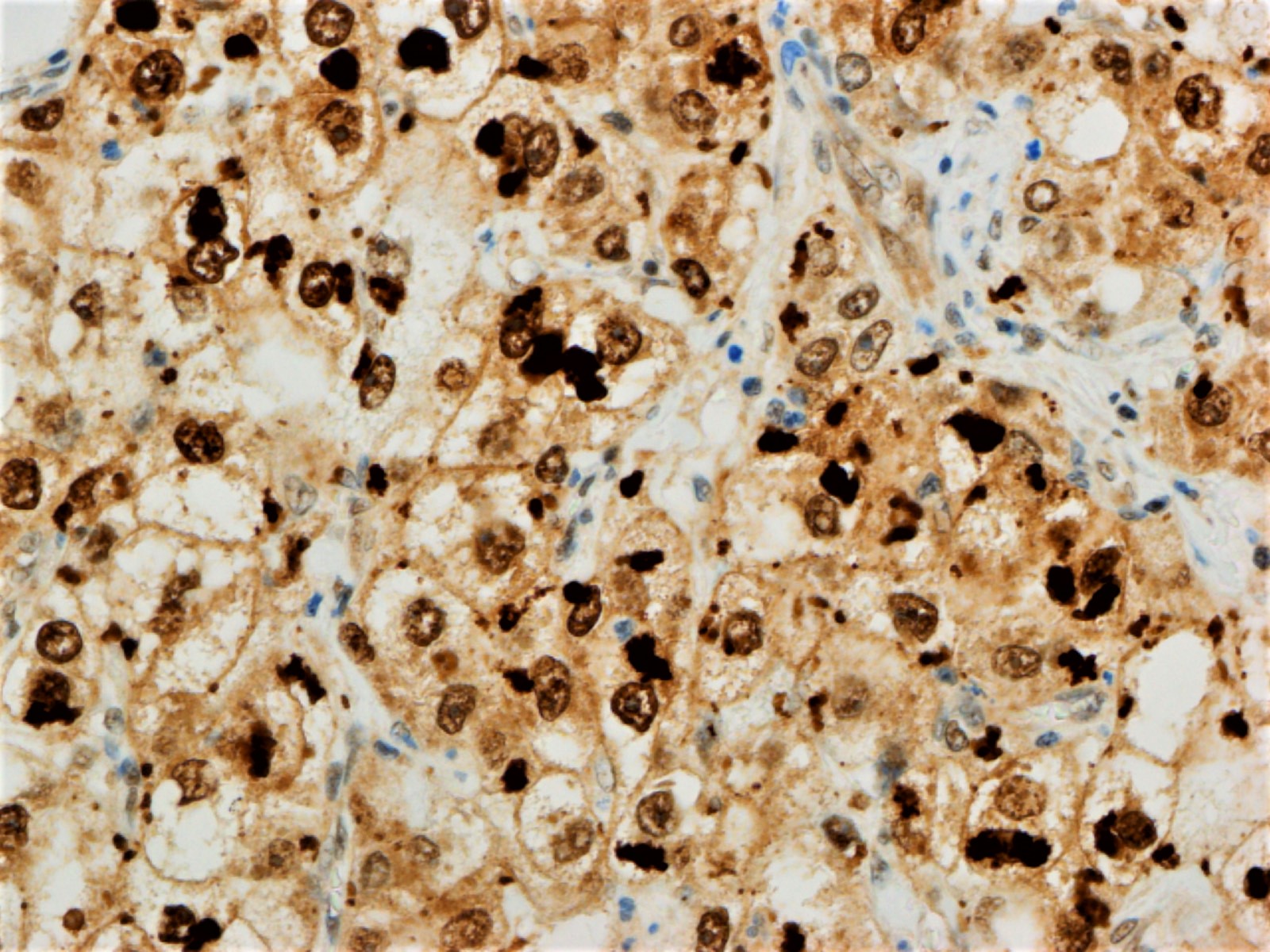
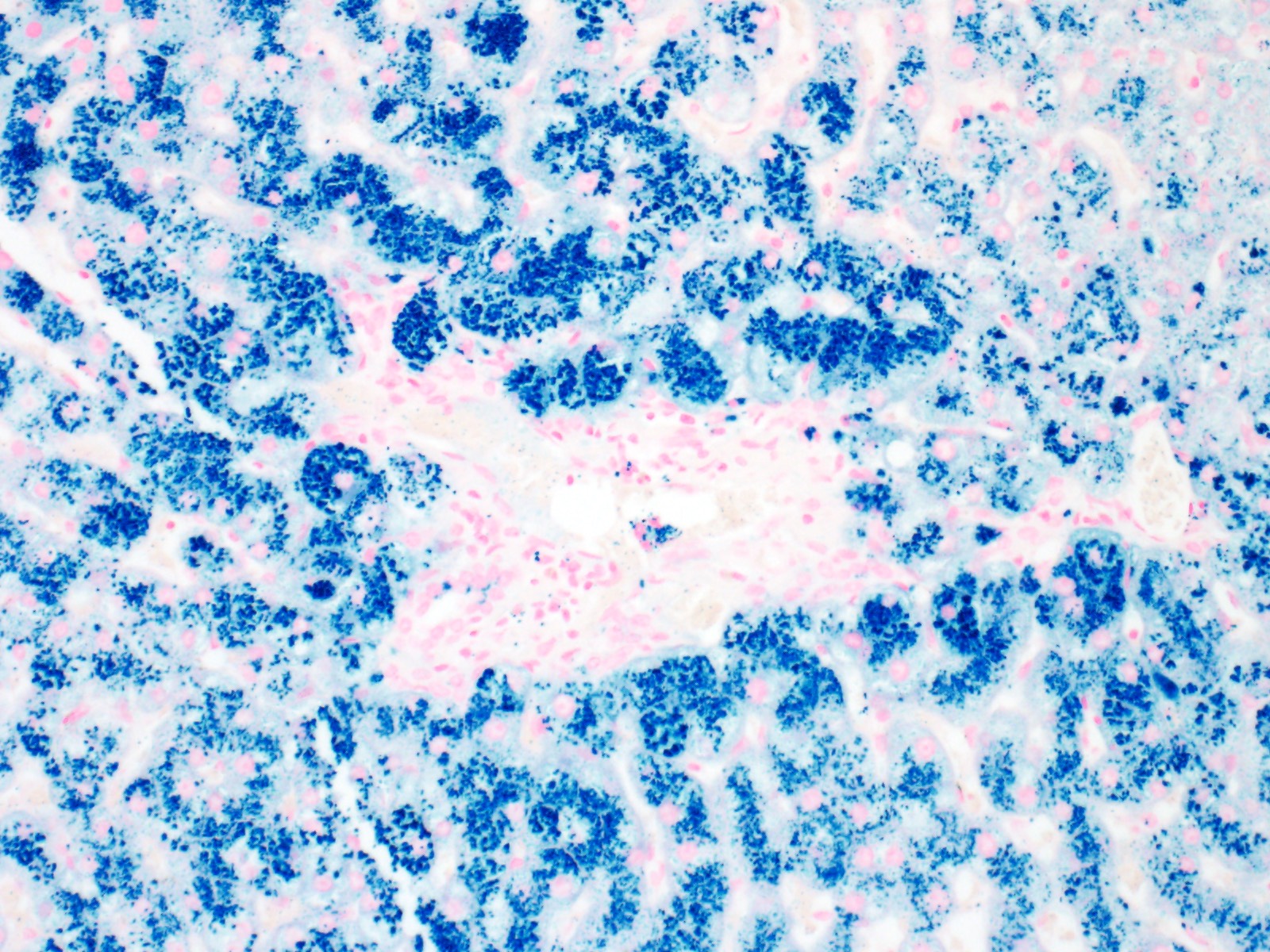
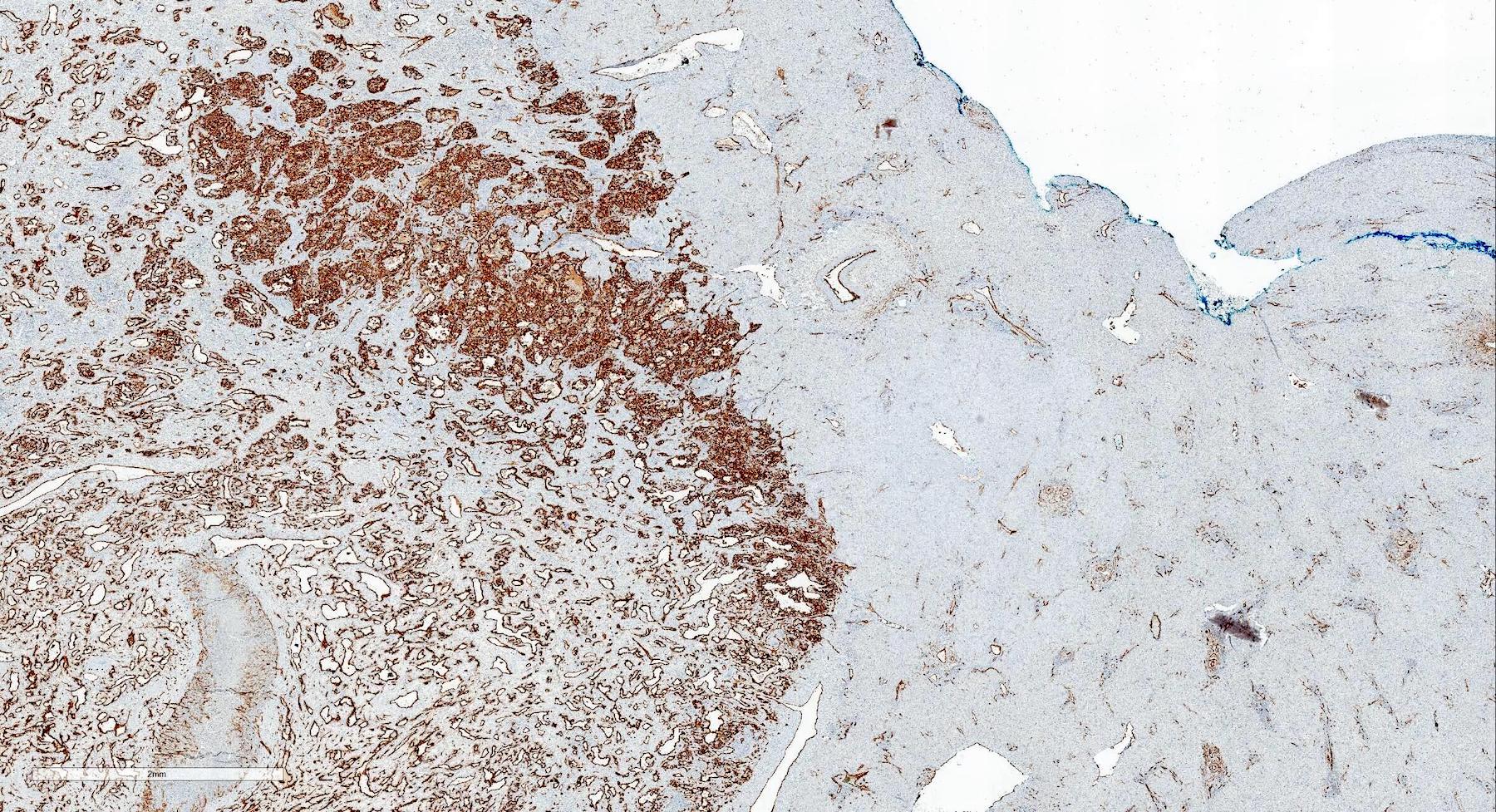
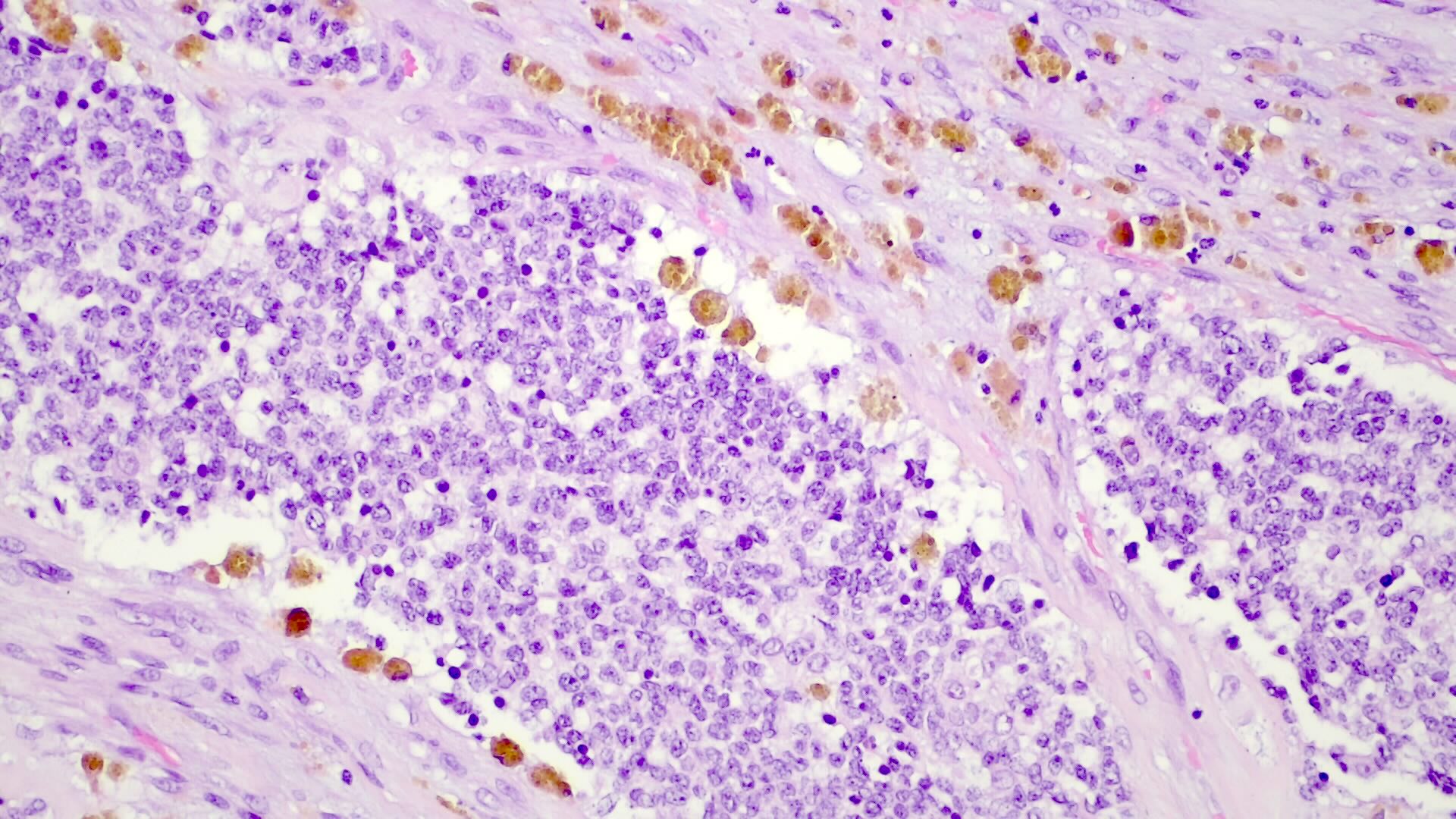
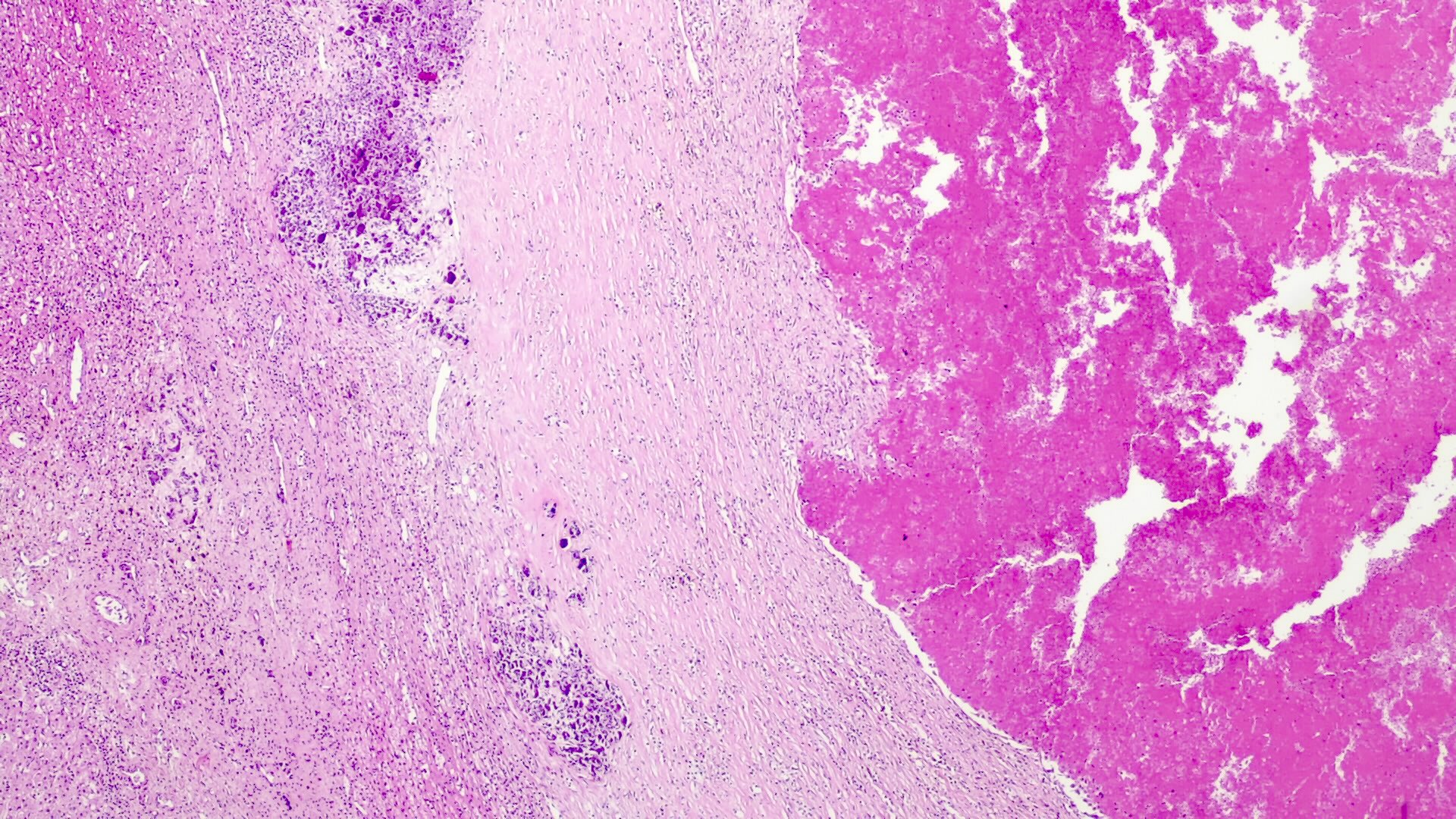
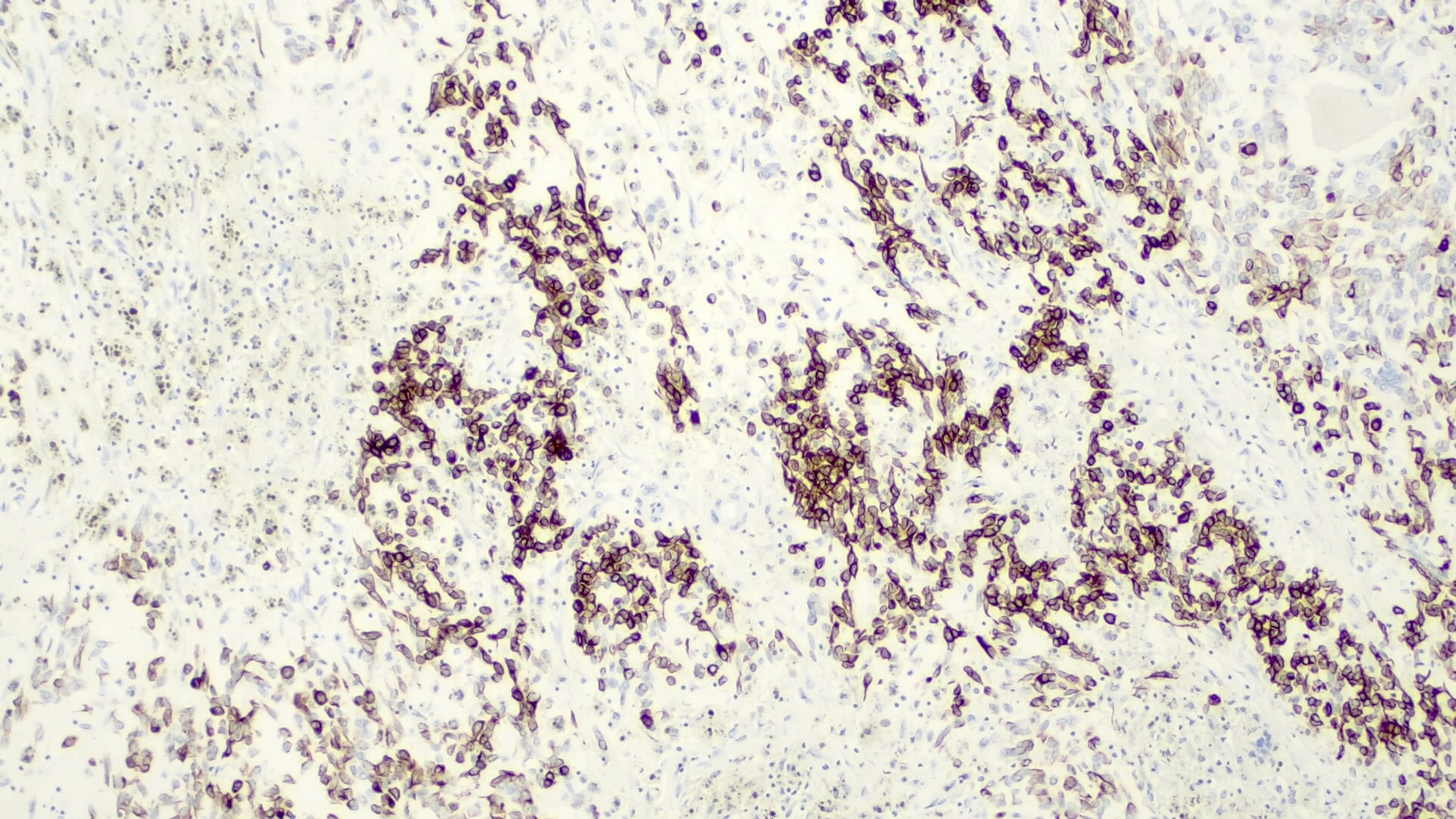
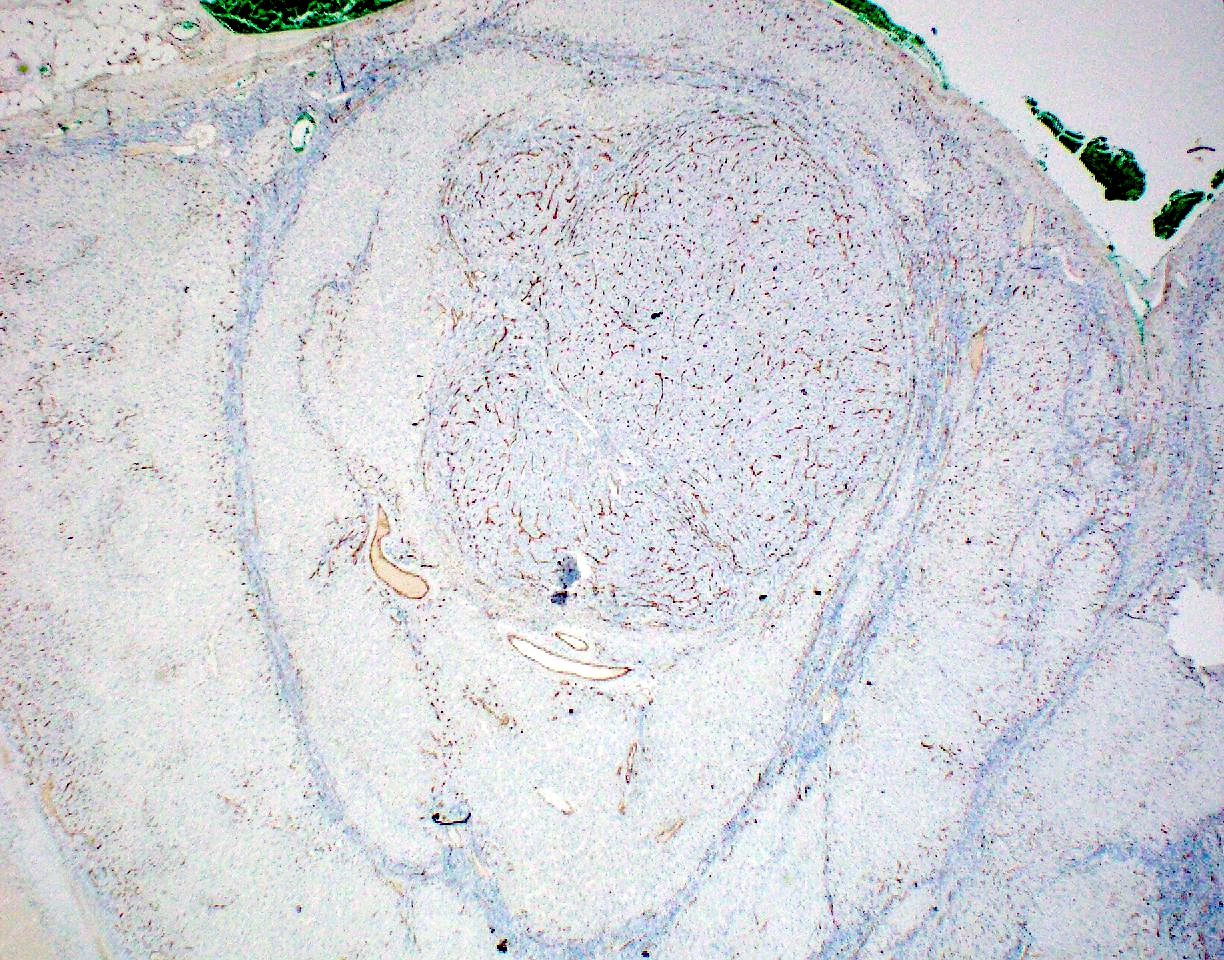
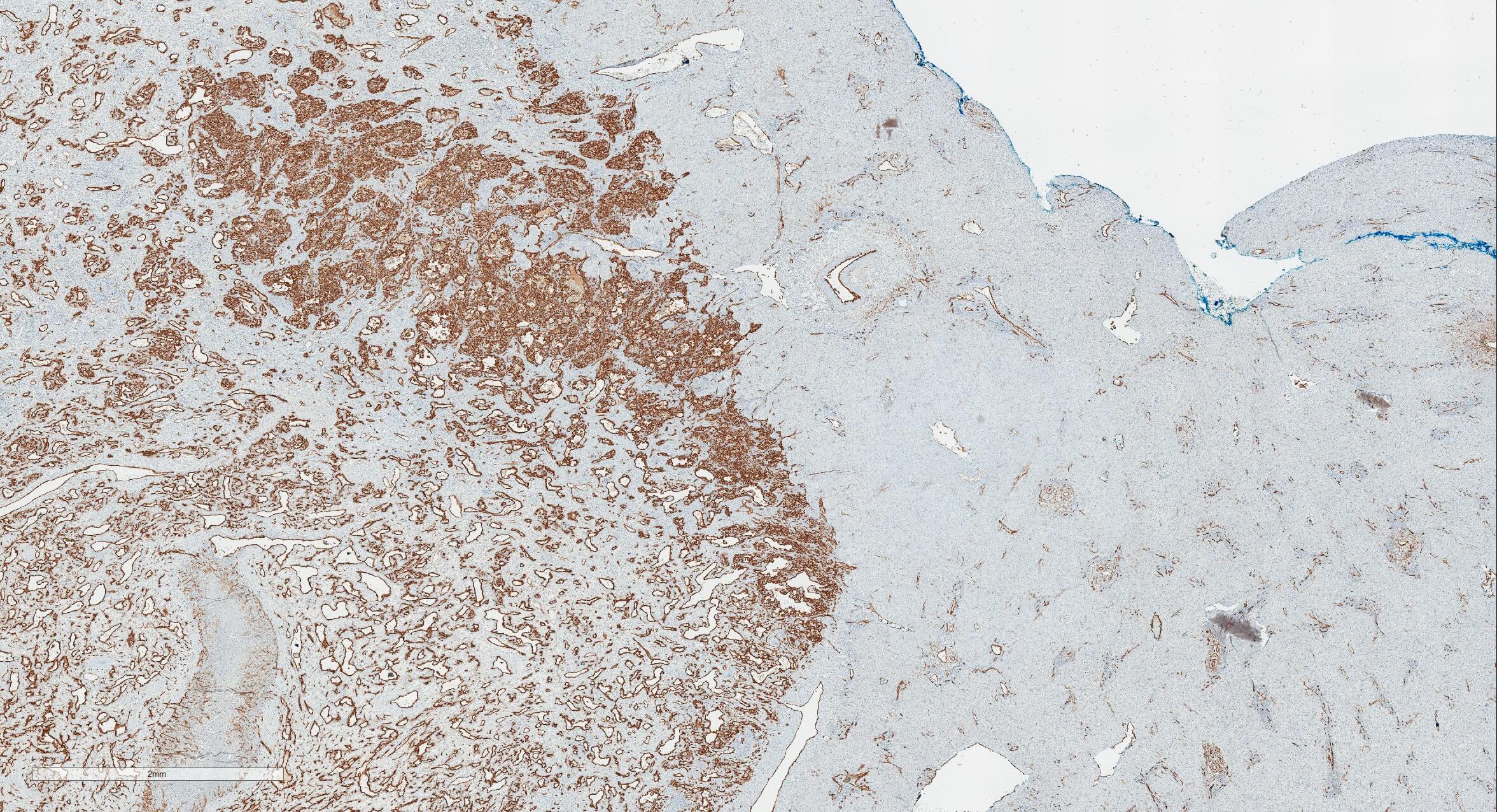
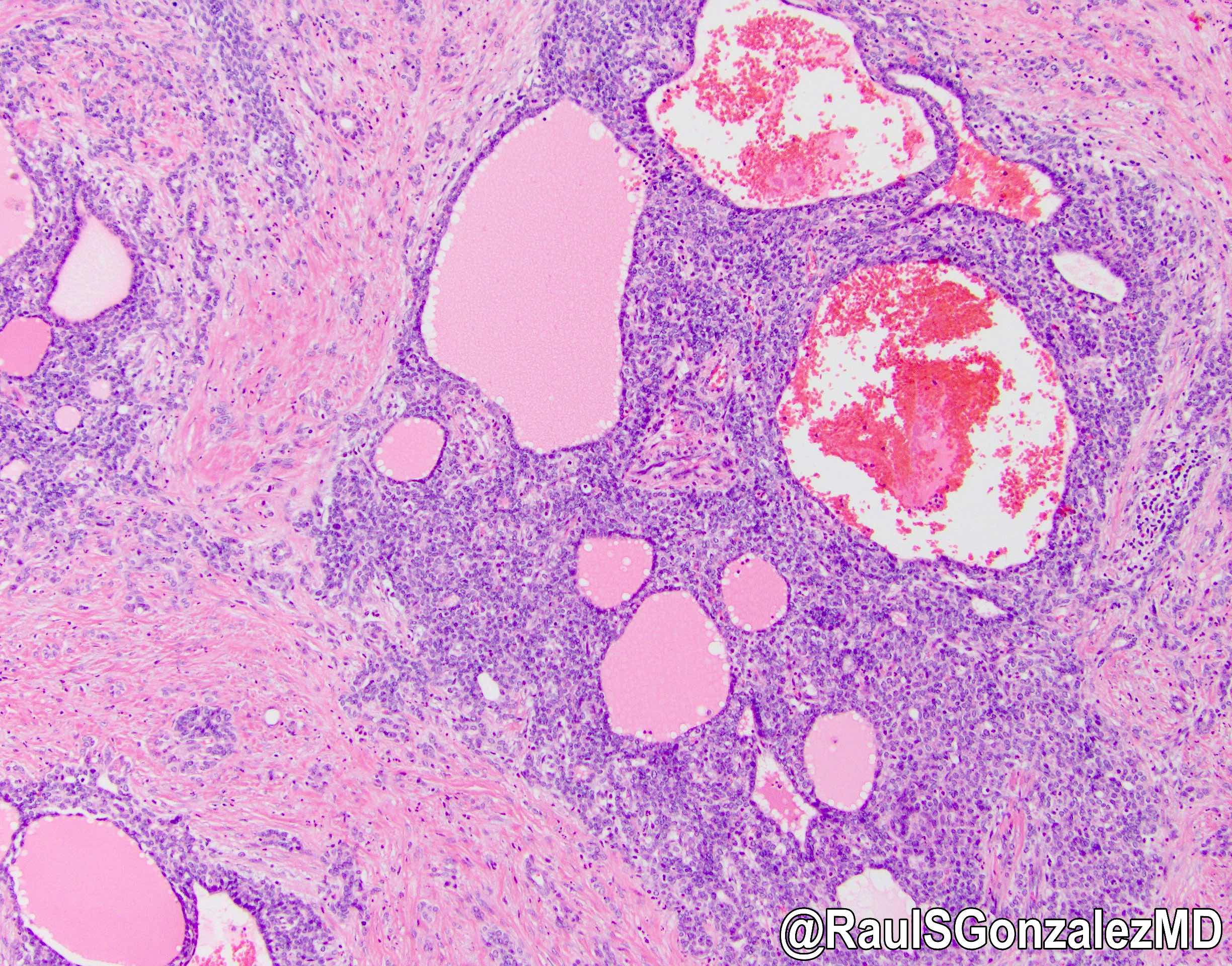
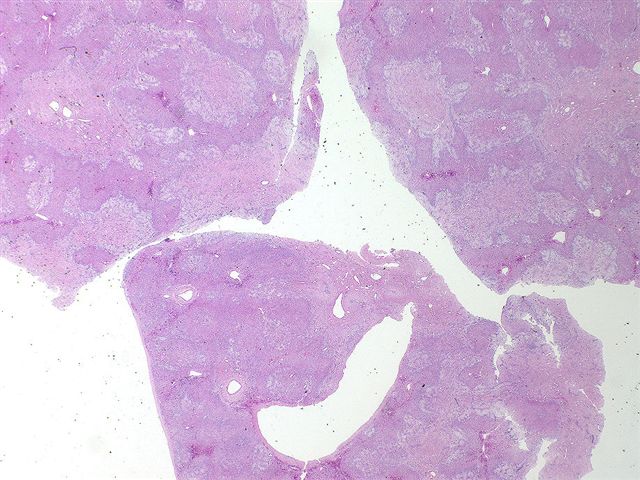
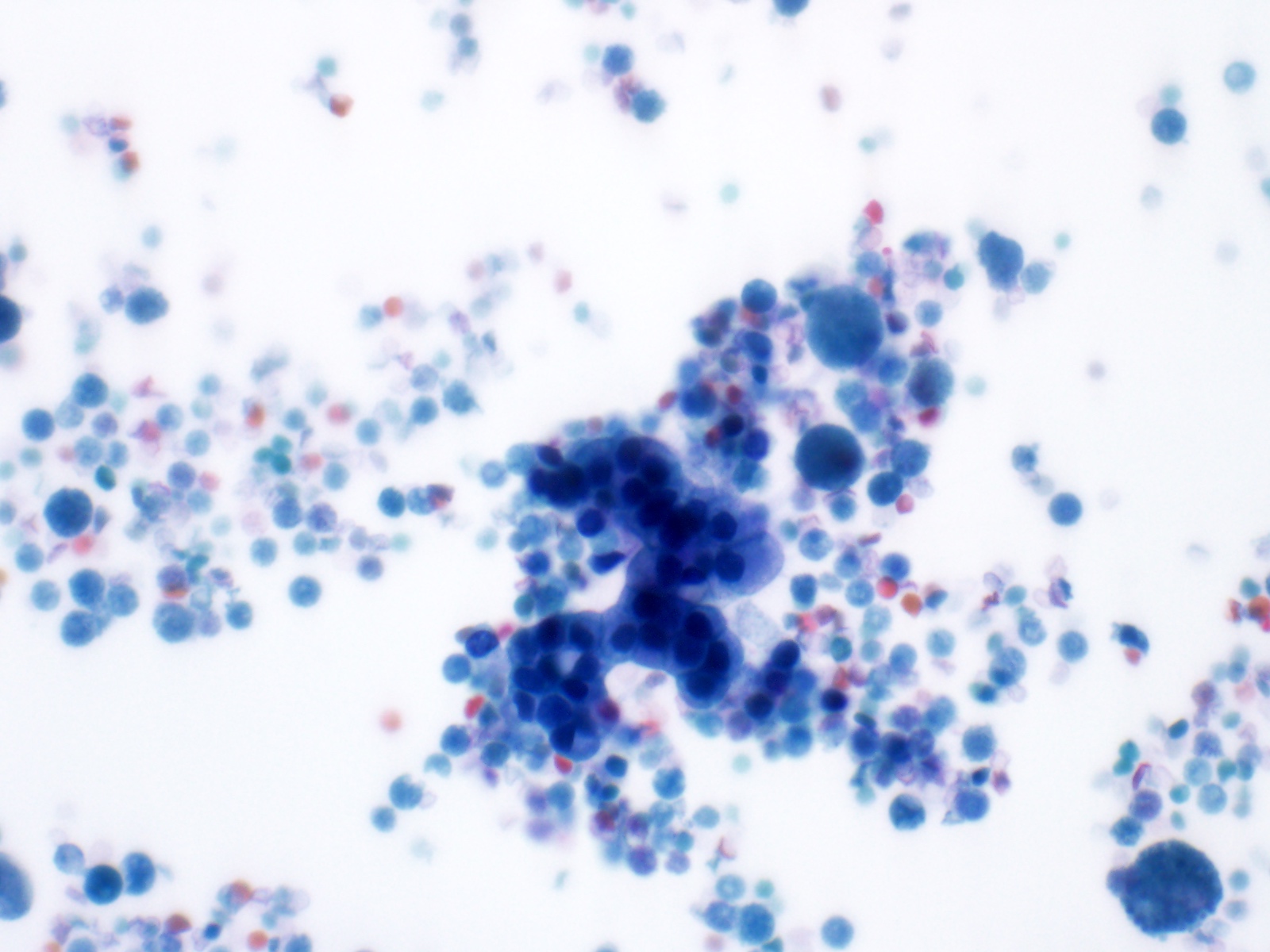
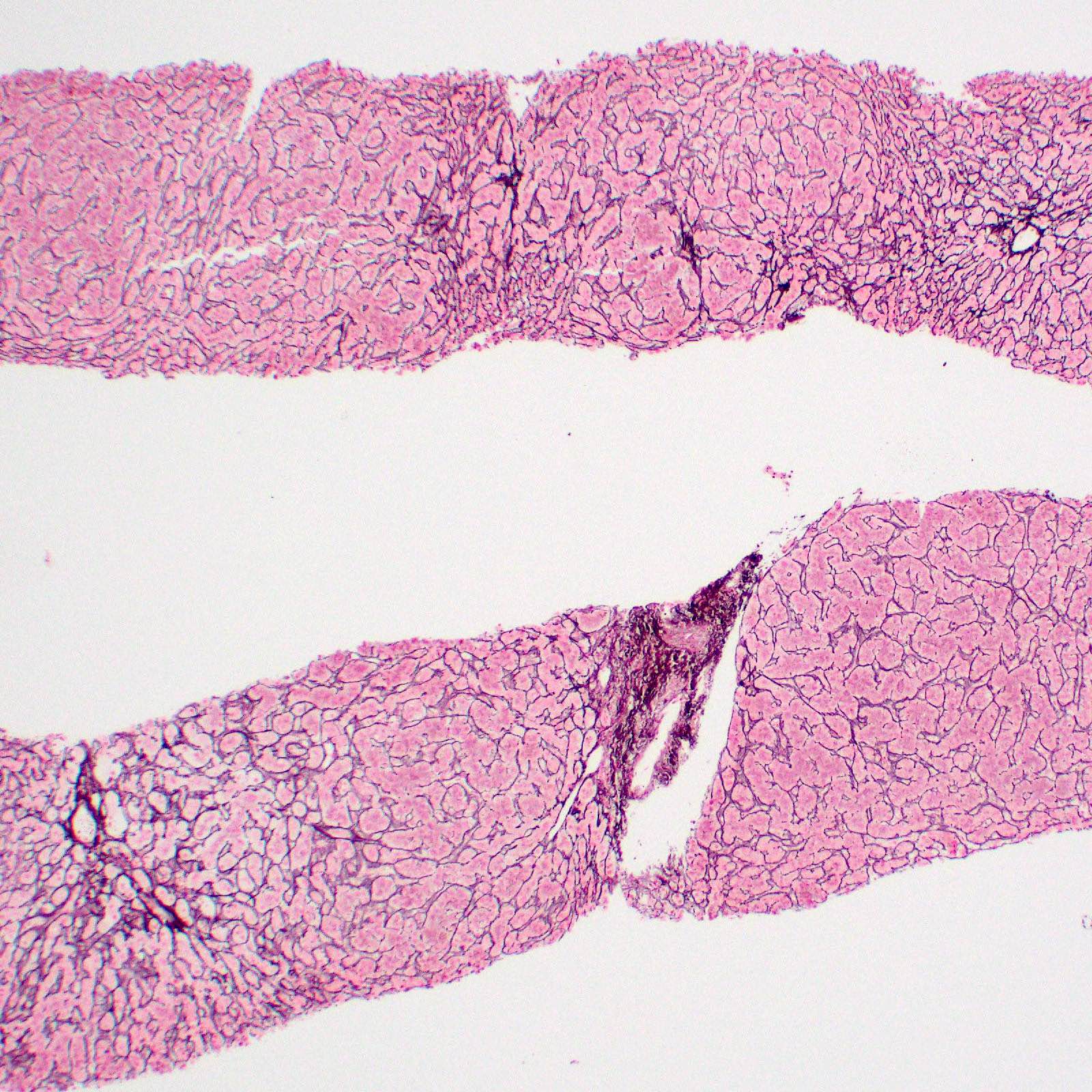
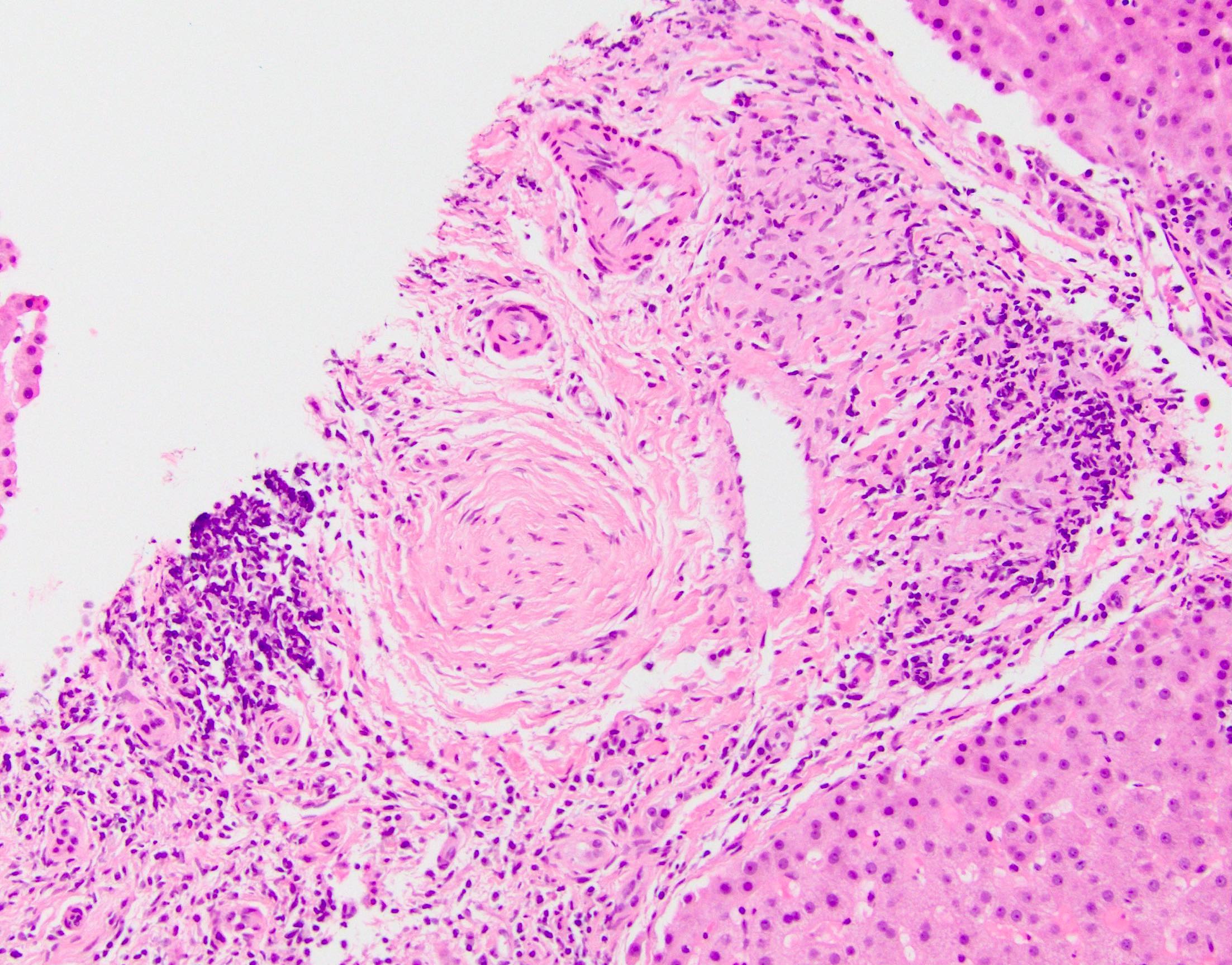
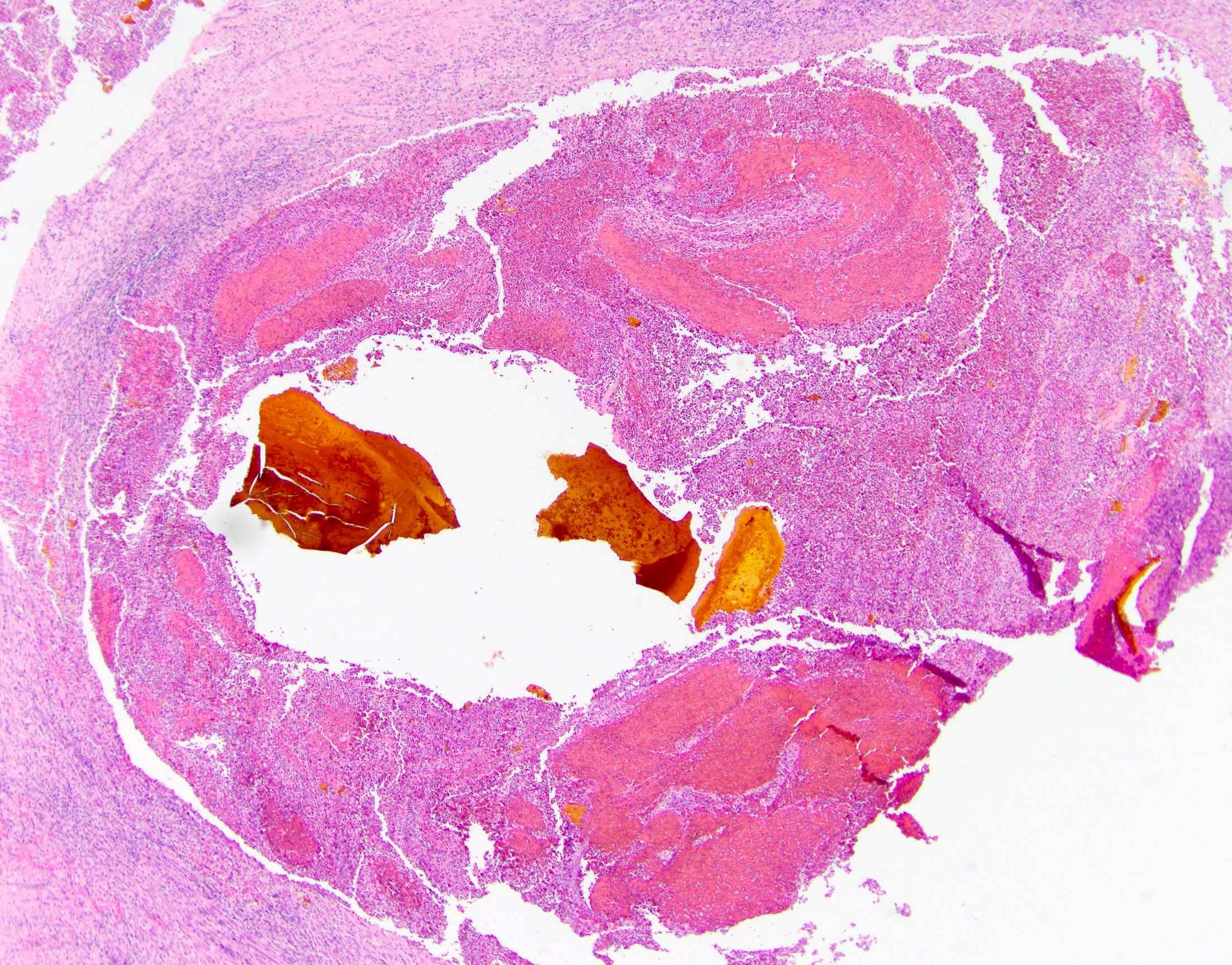
Microscopic (histologic) images
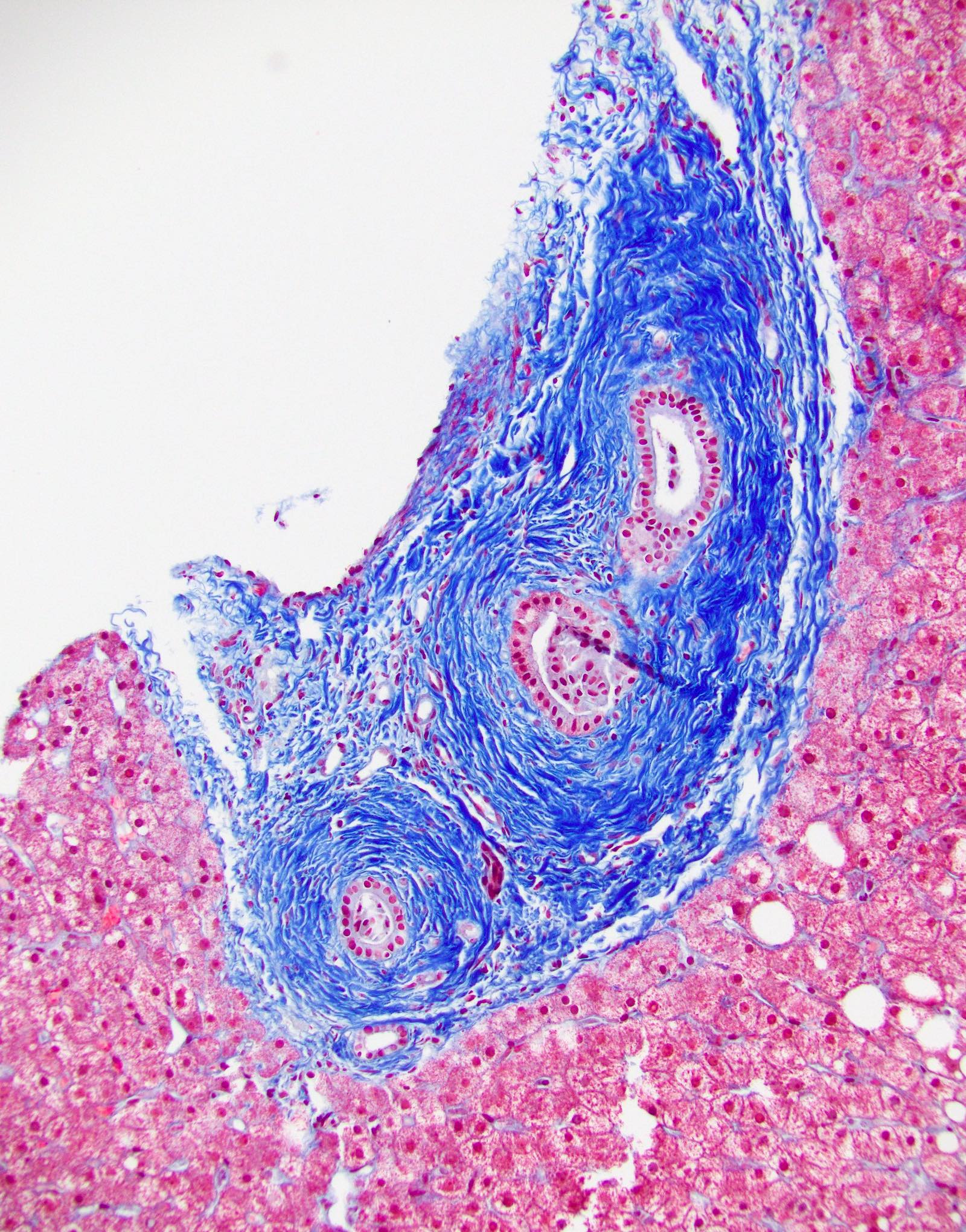
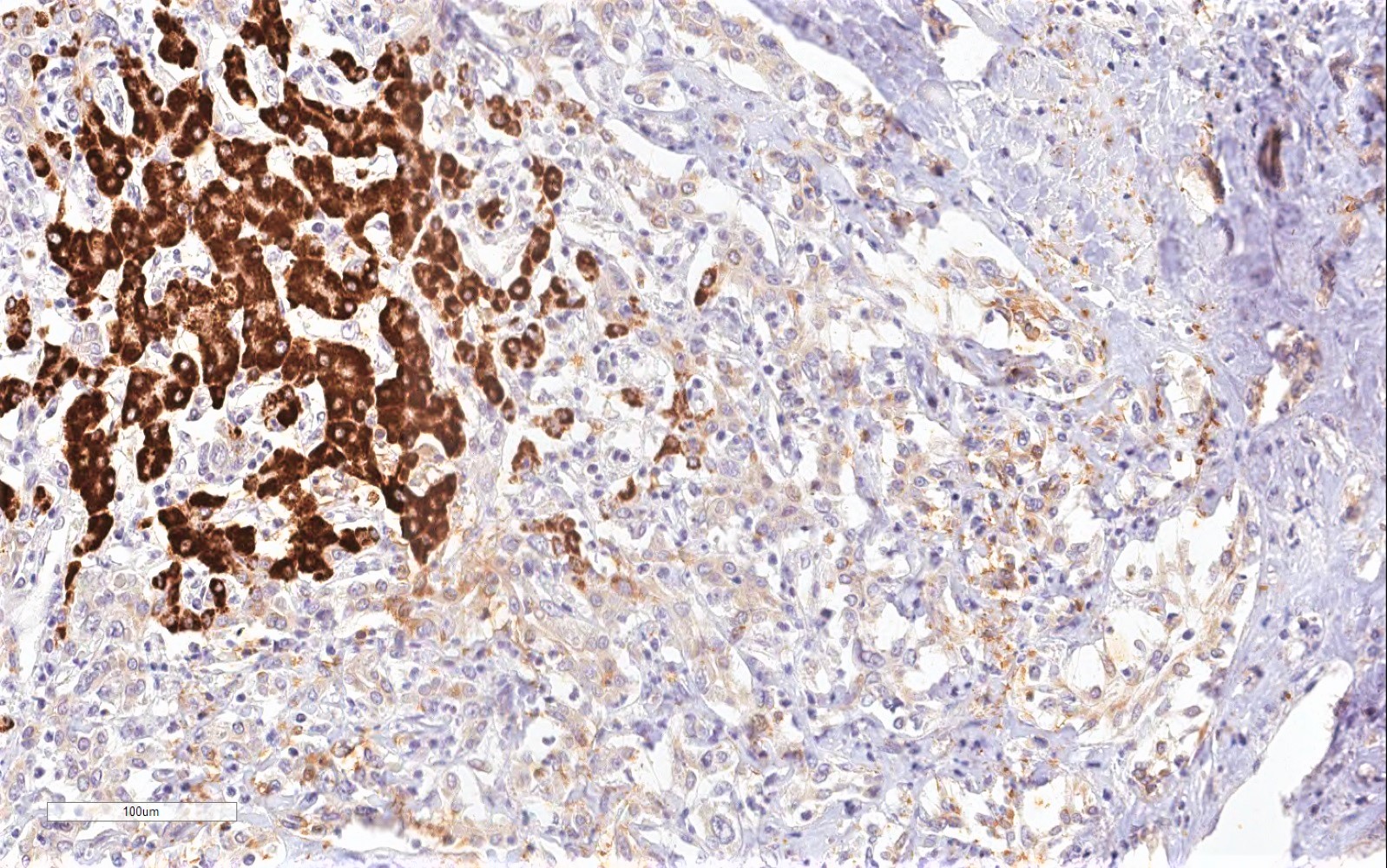
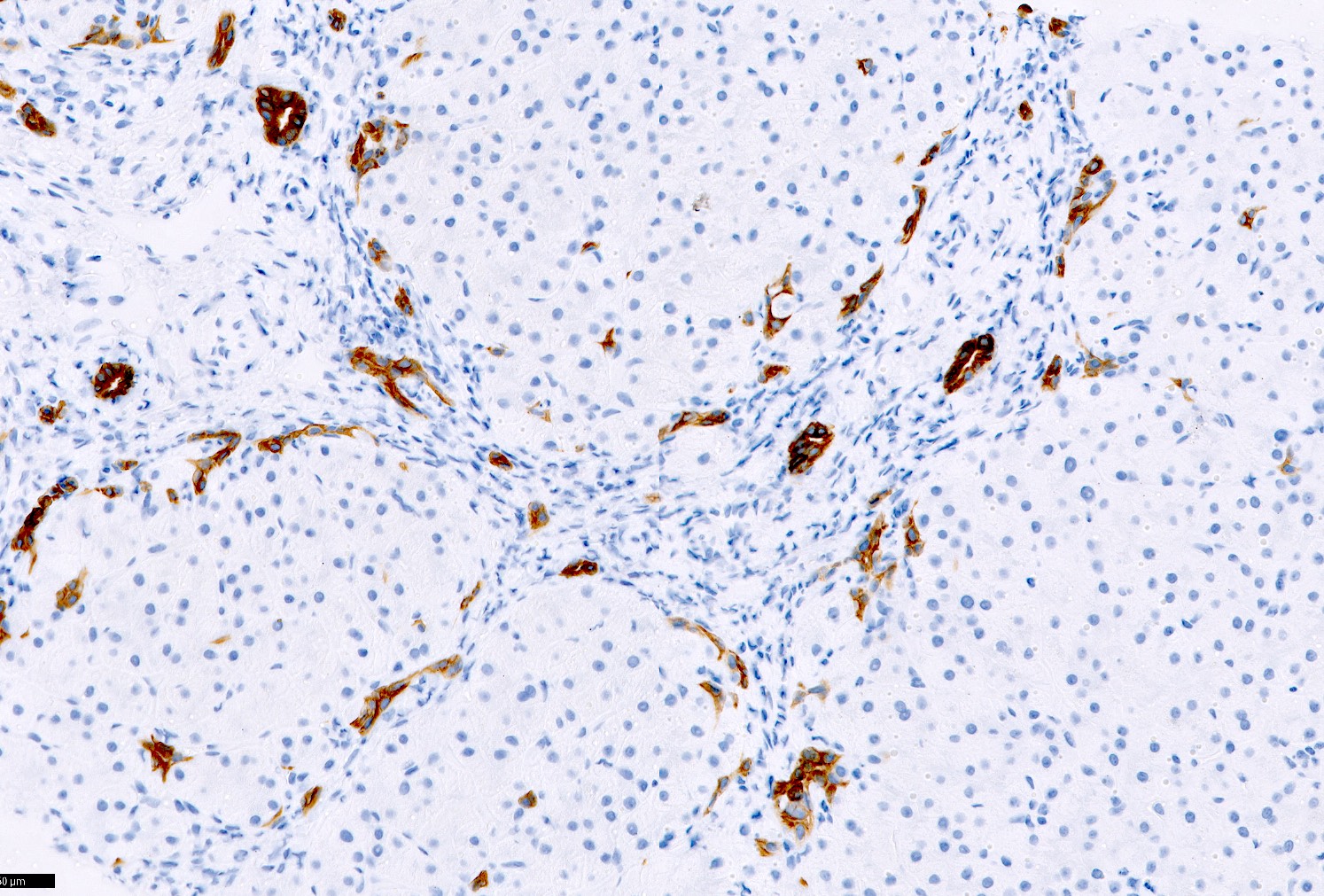
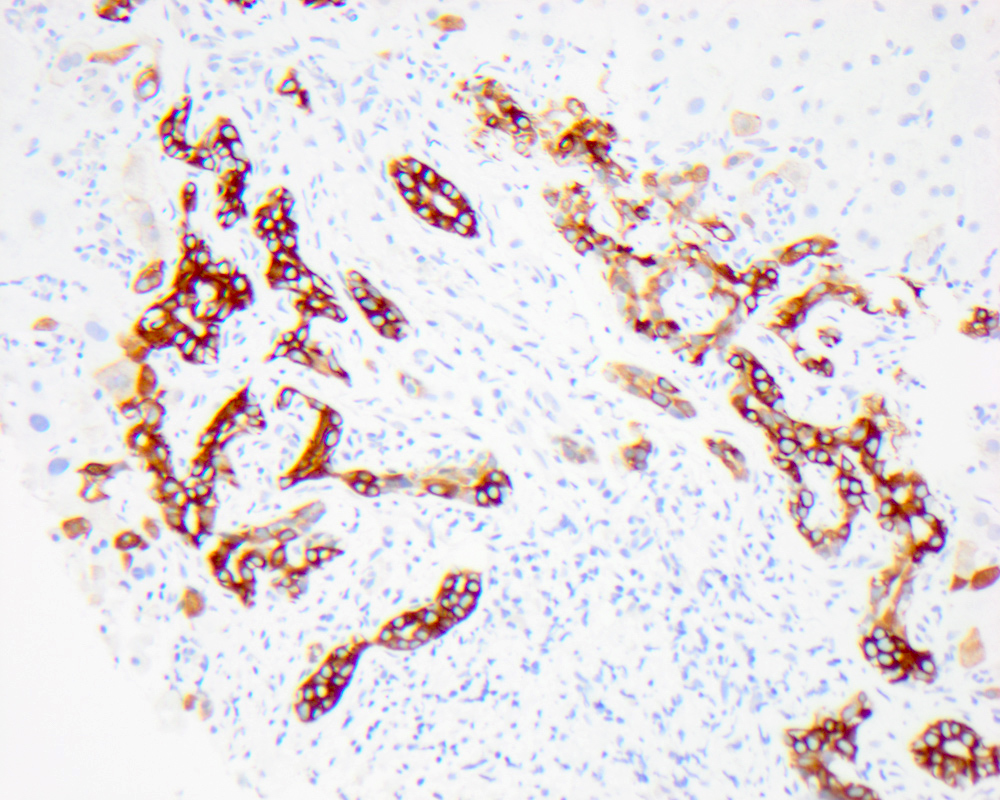
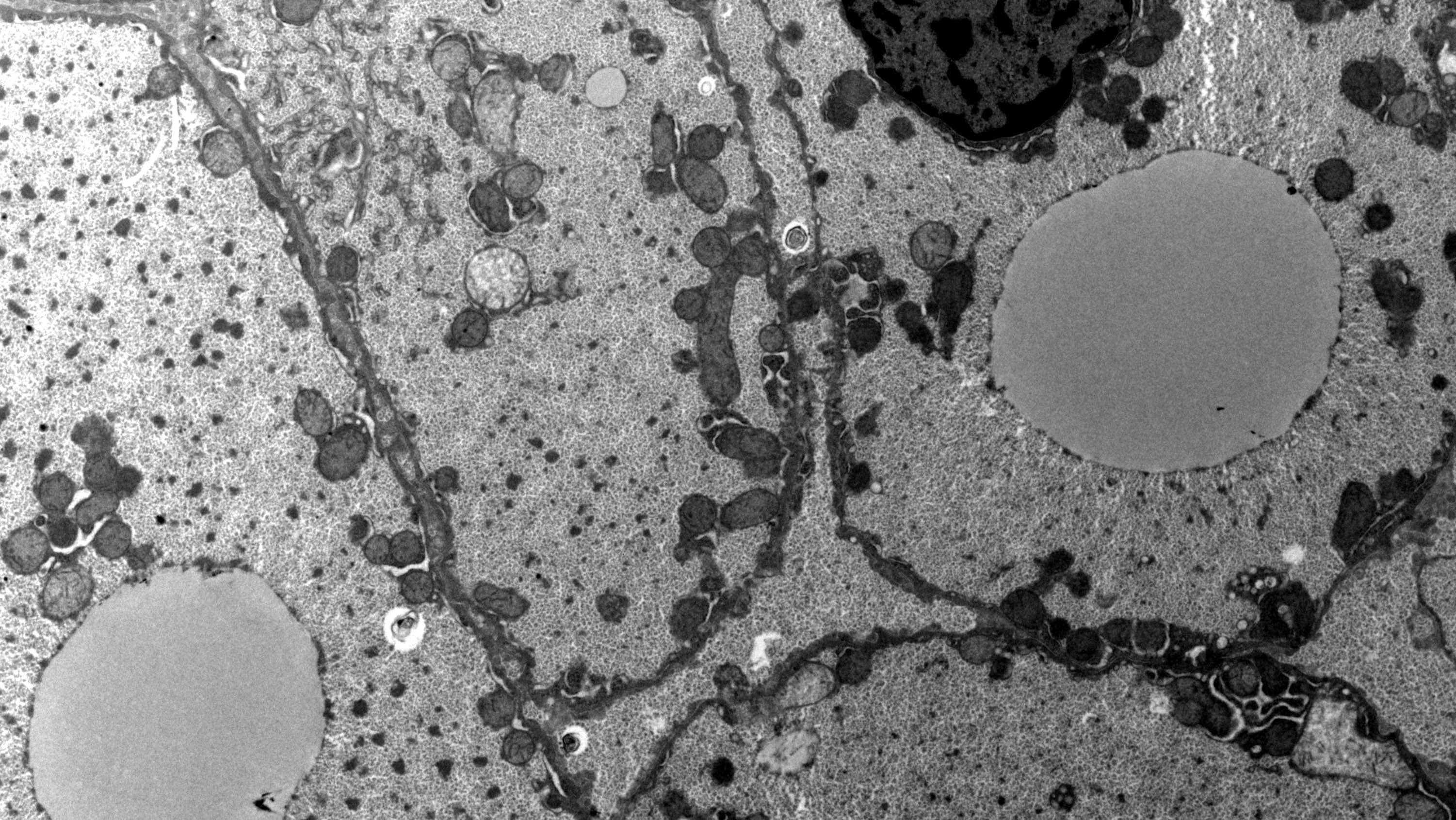
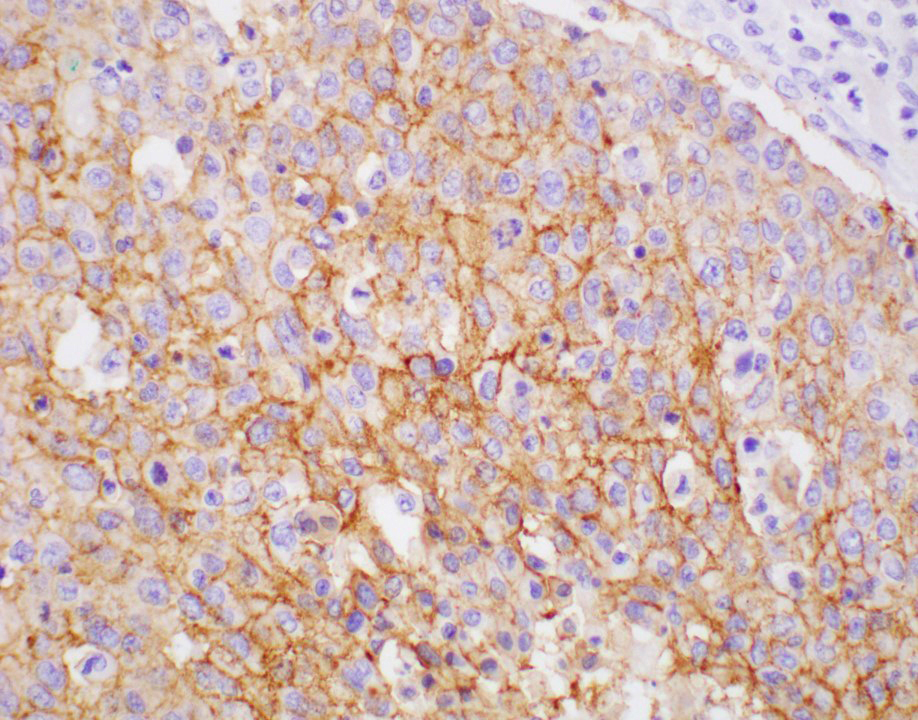
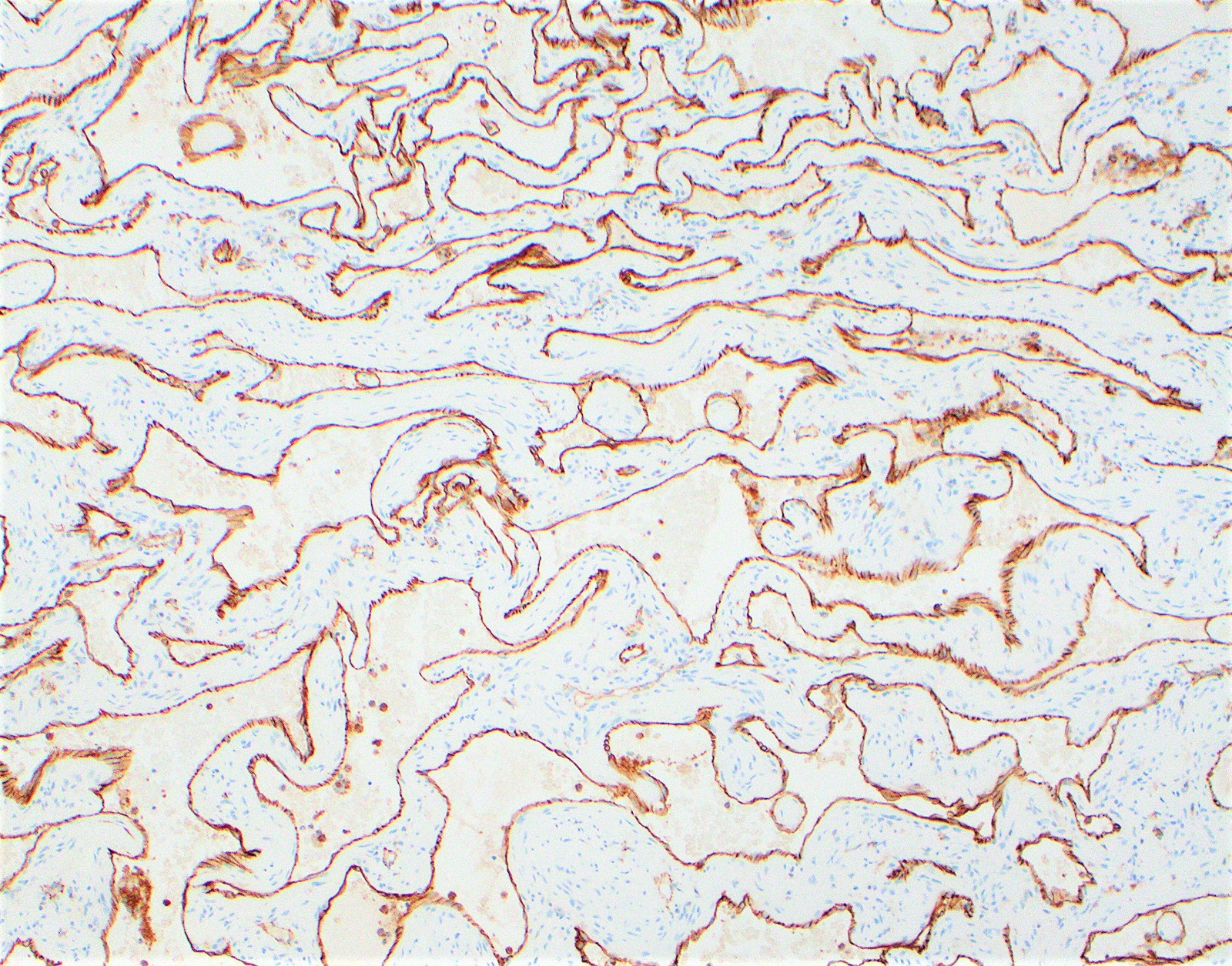
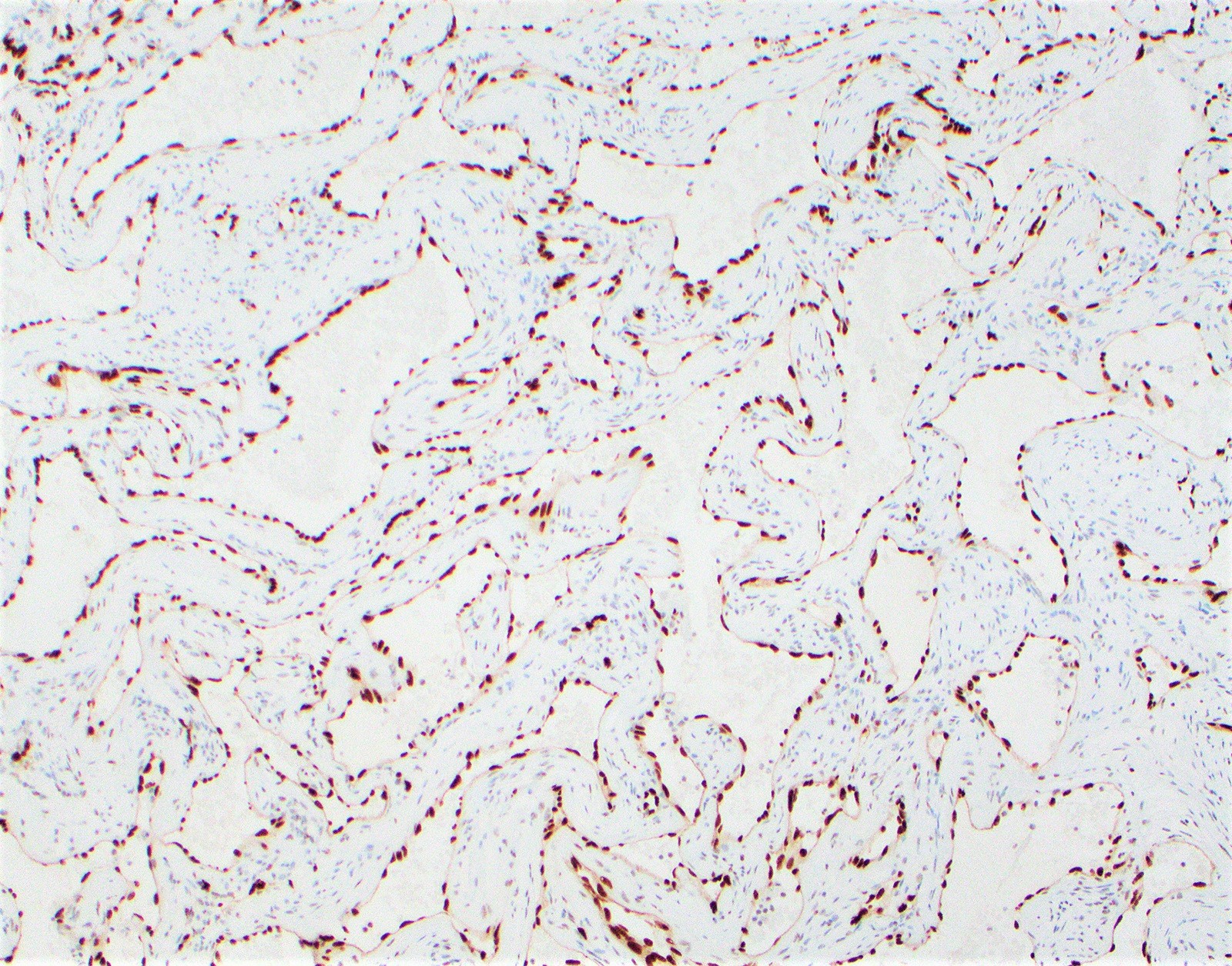
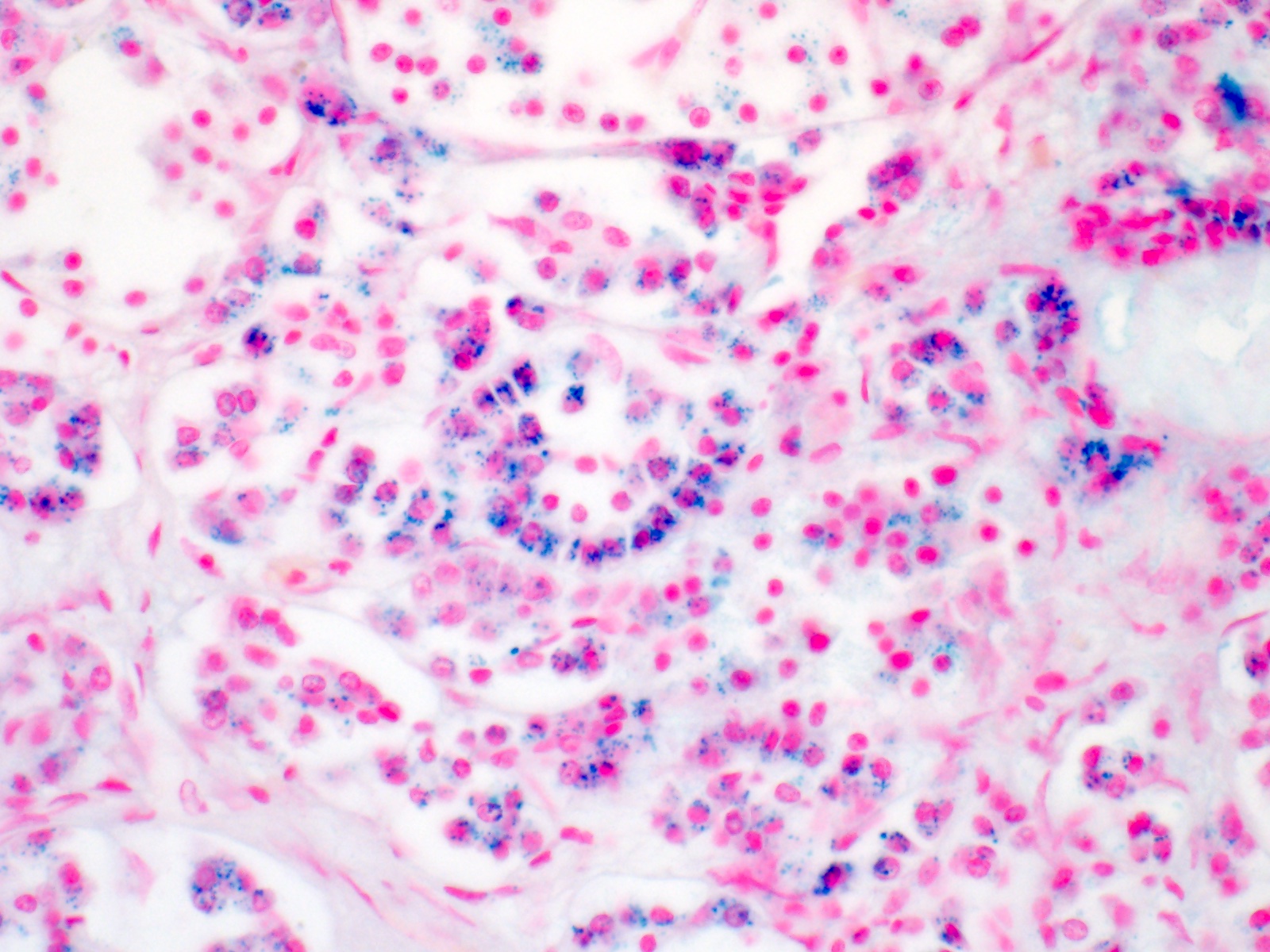
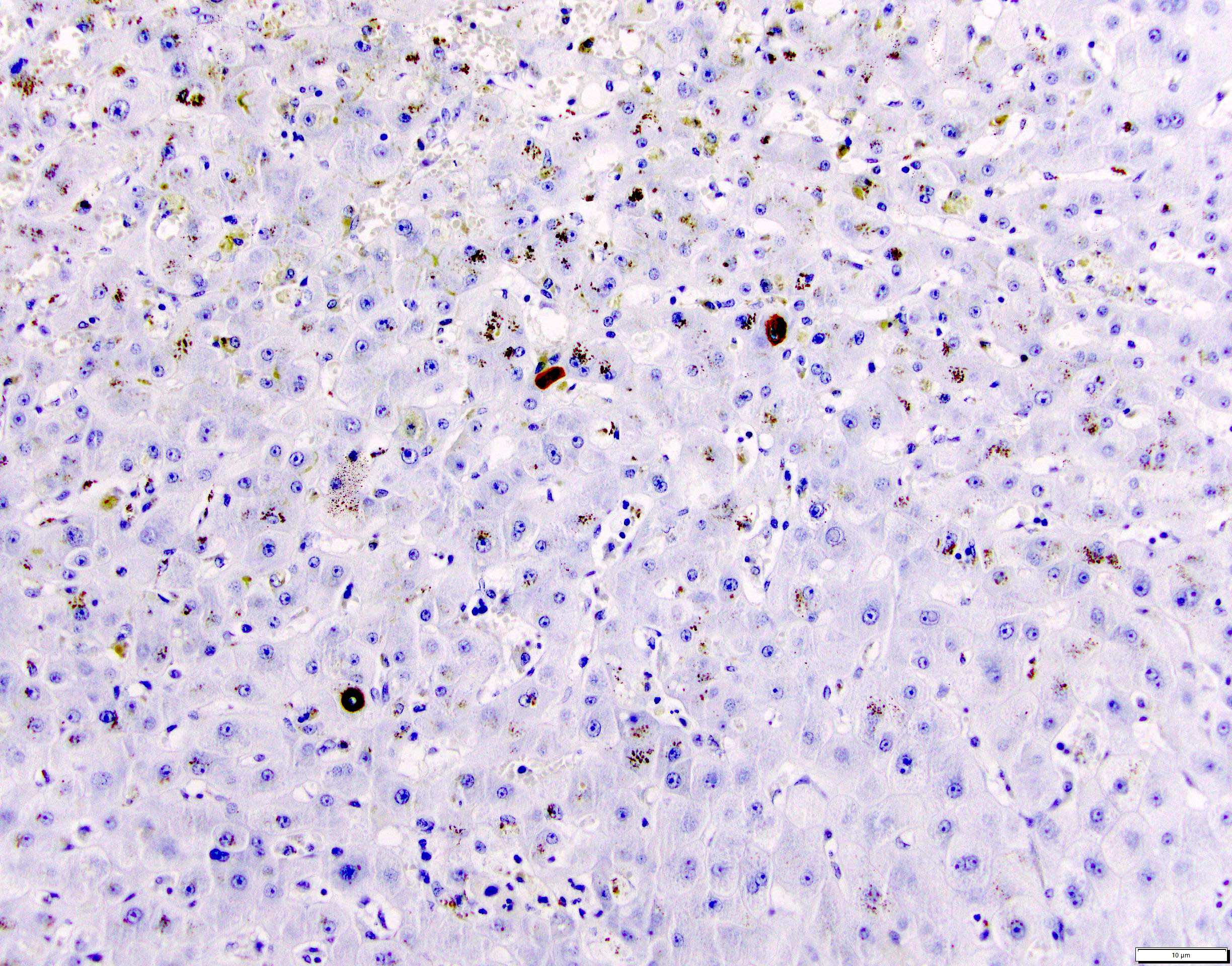
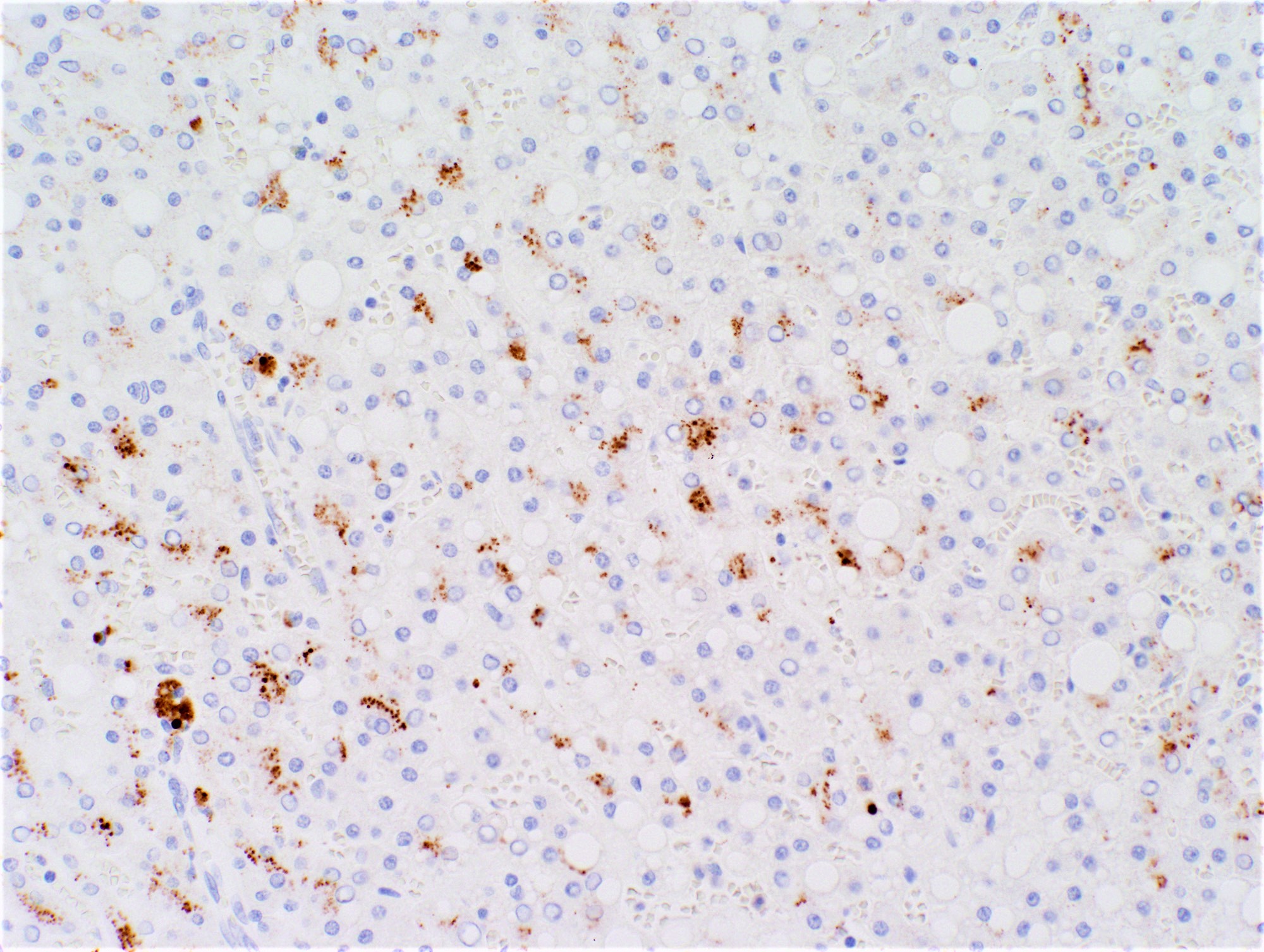
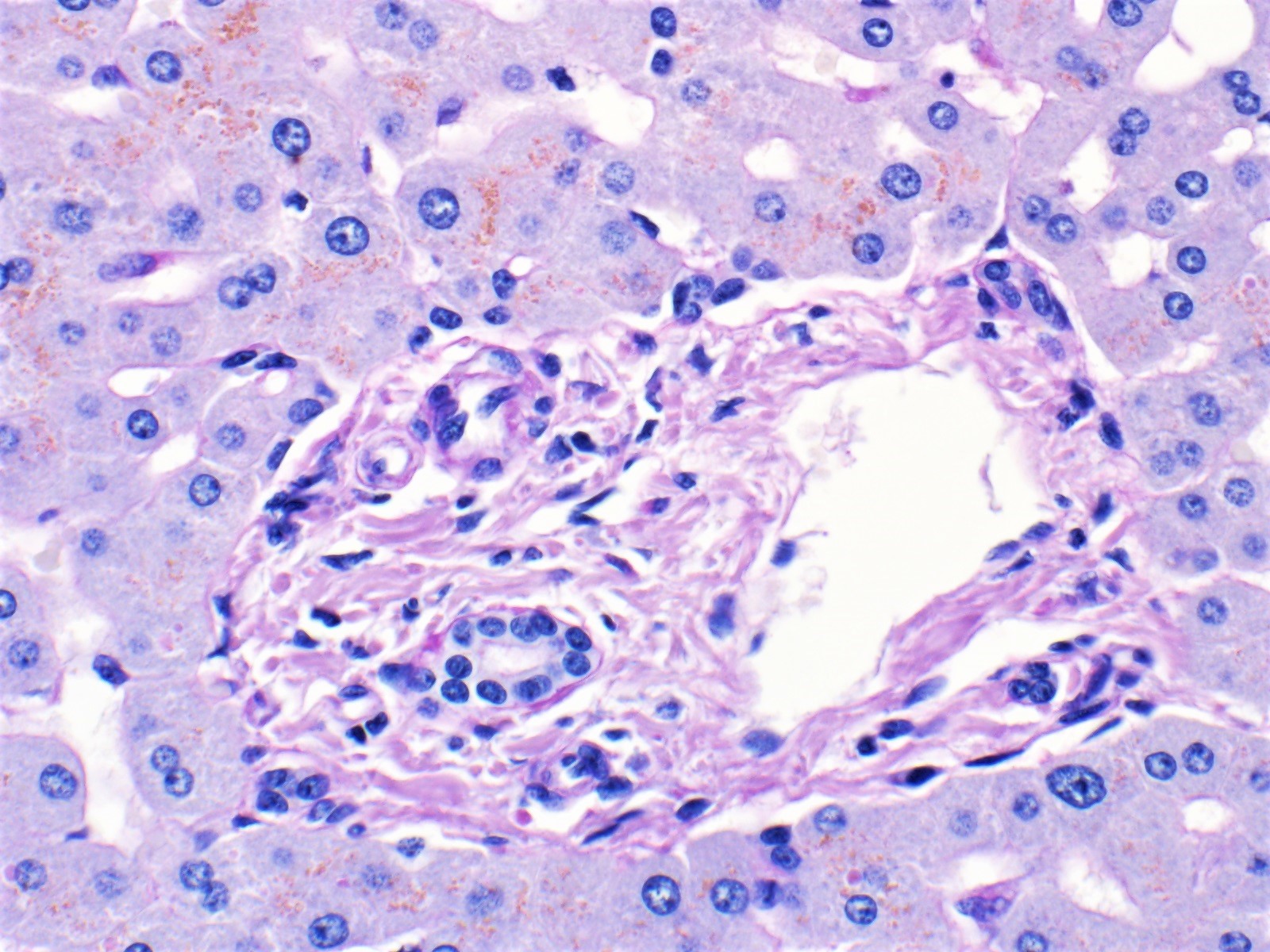
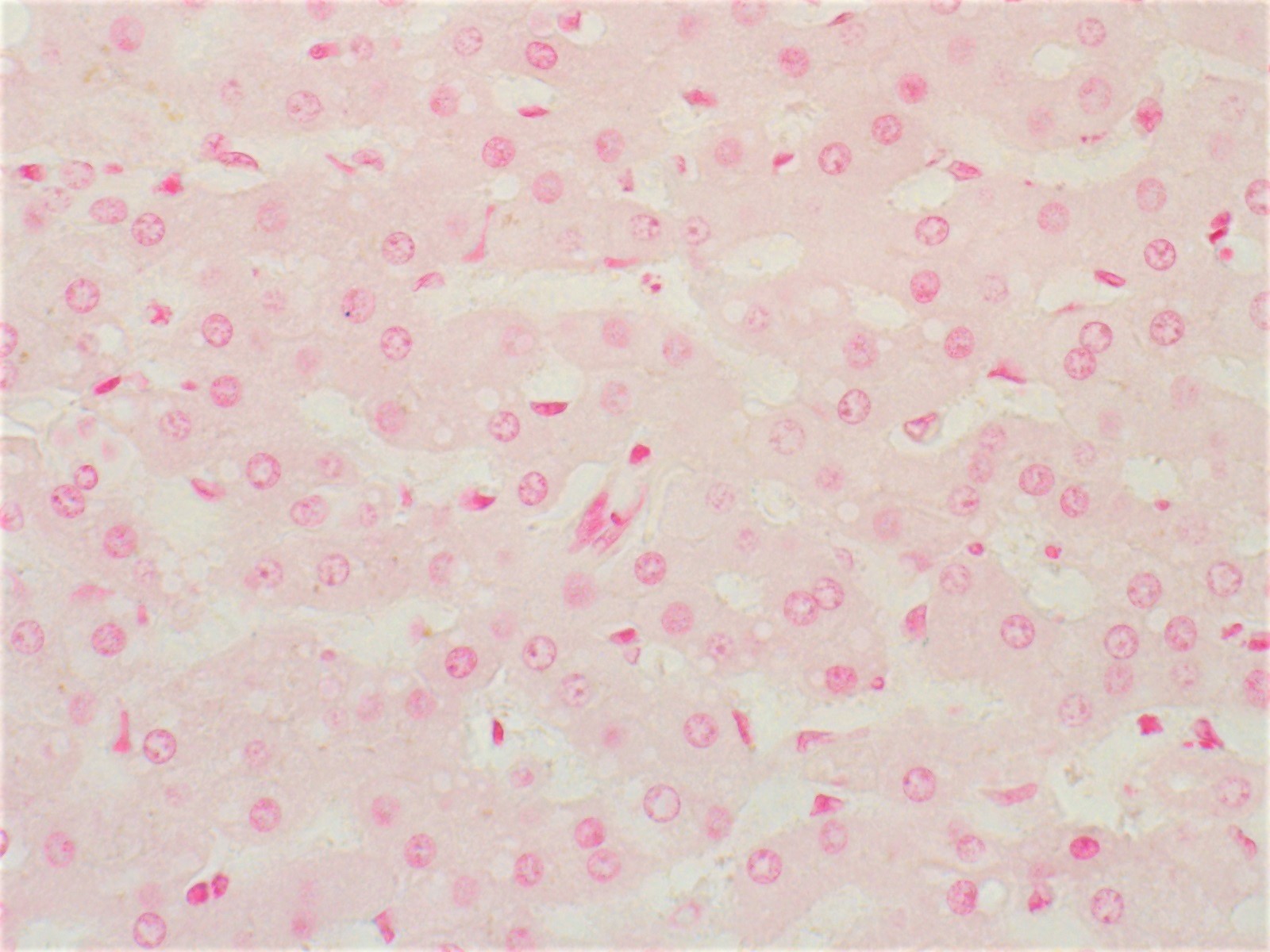
Immunofluorescence description
- C4d on frozen tissue has been used in liver but not very commonly; described as sinusoidal deposits (Liver Transpl 2012;18:641)
- C4d on paraffin tissue is more practical and accessible (see below)
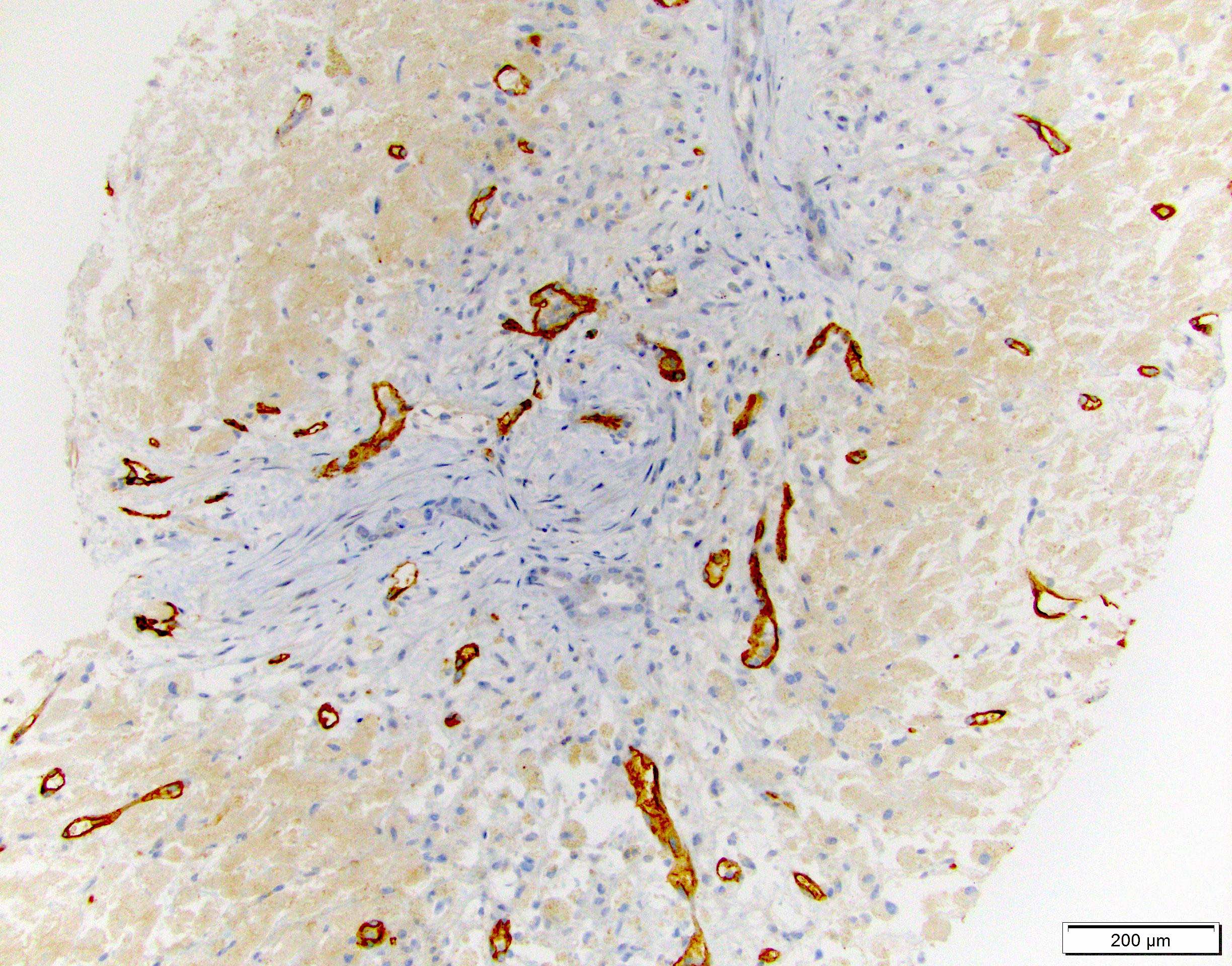
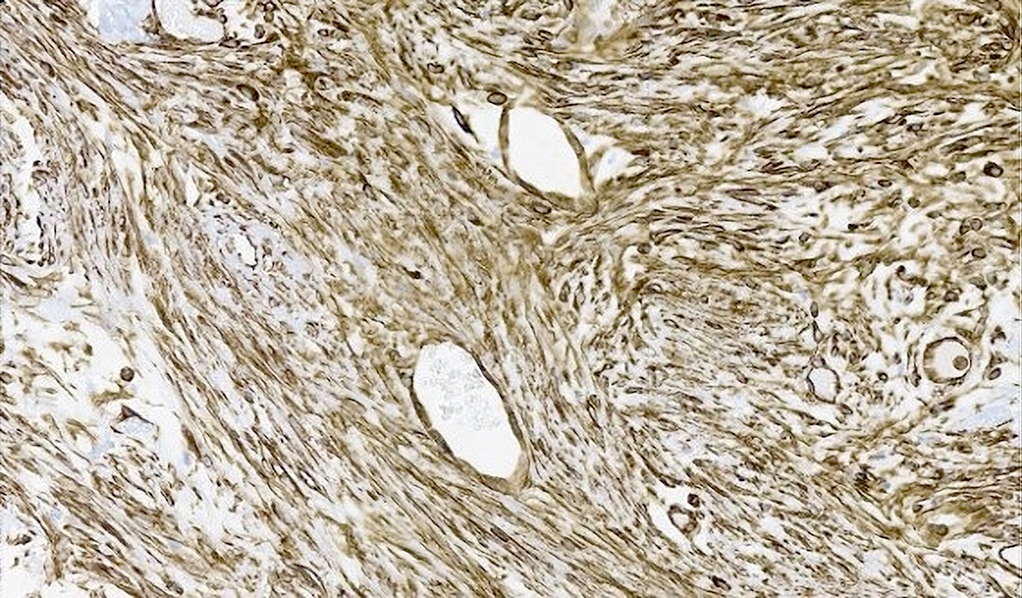
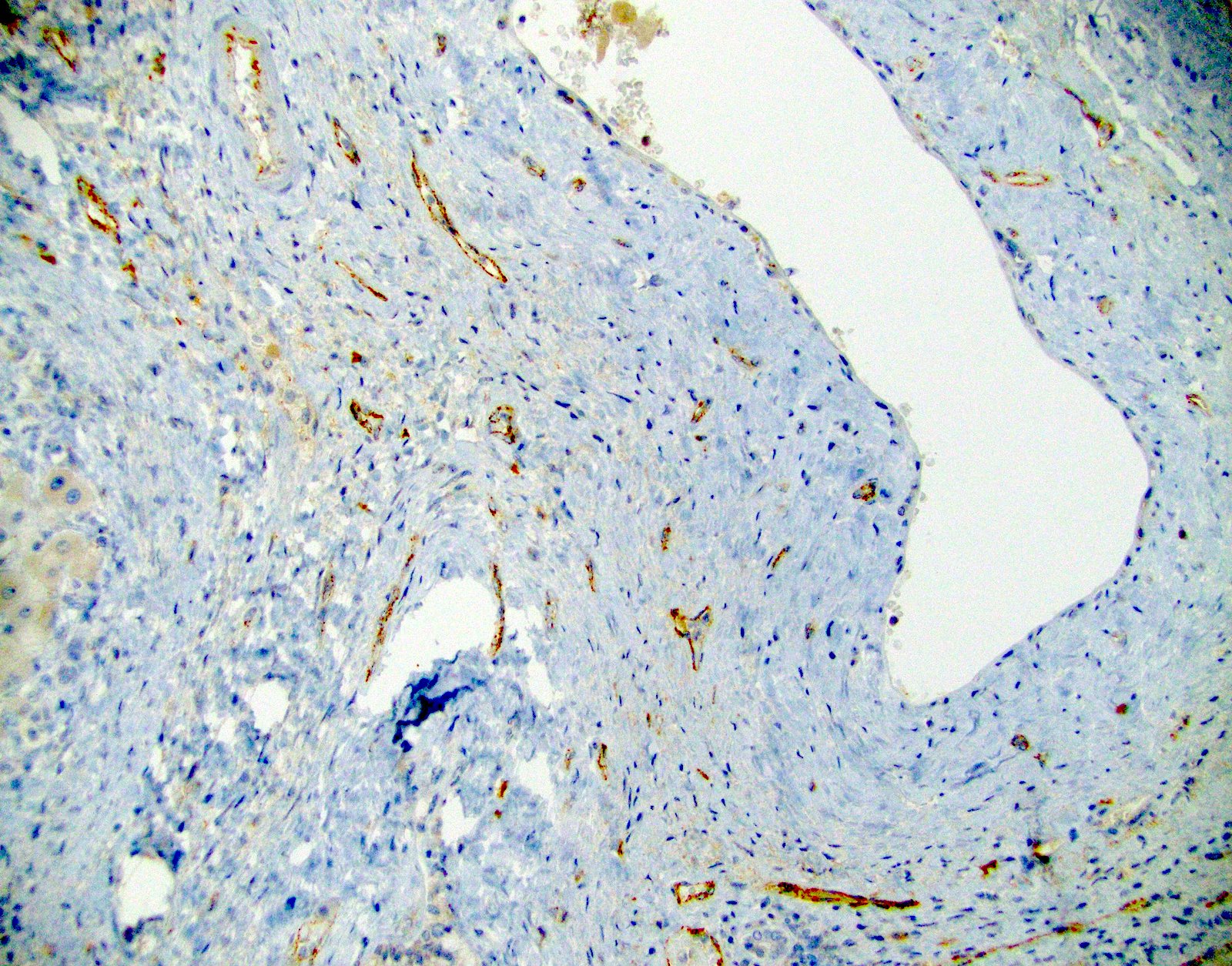
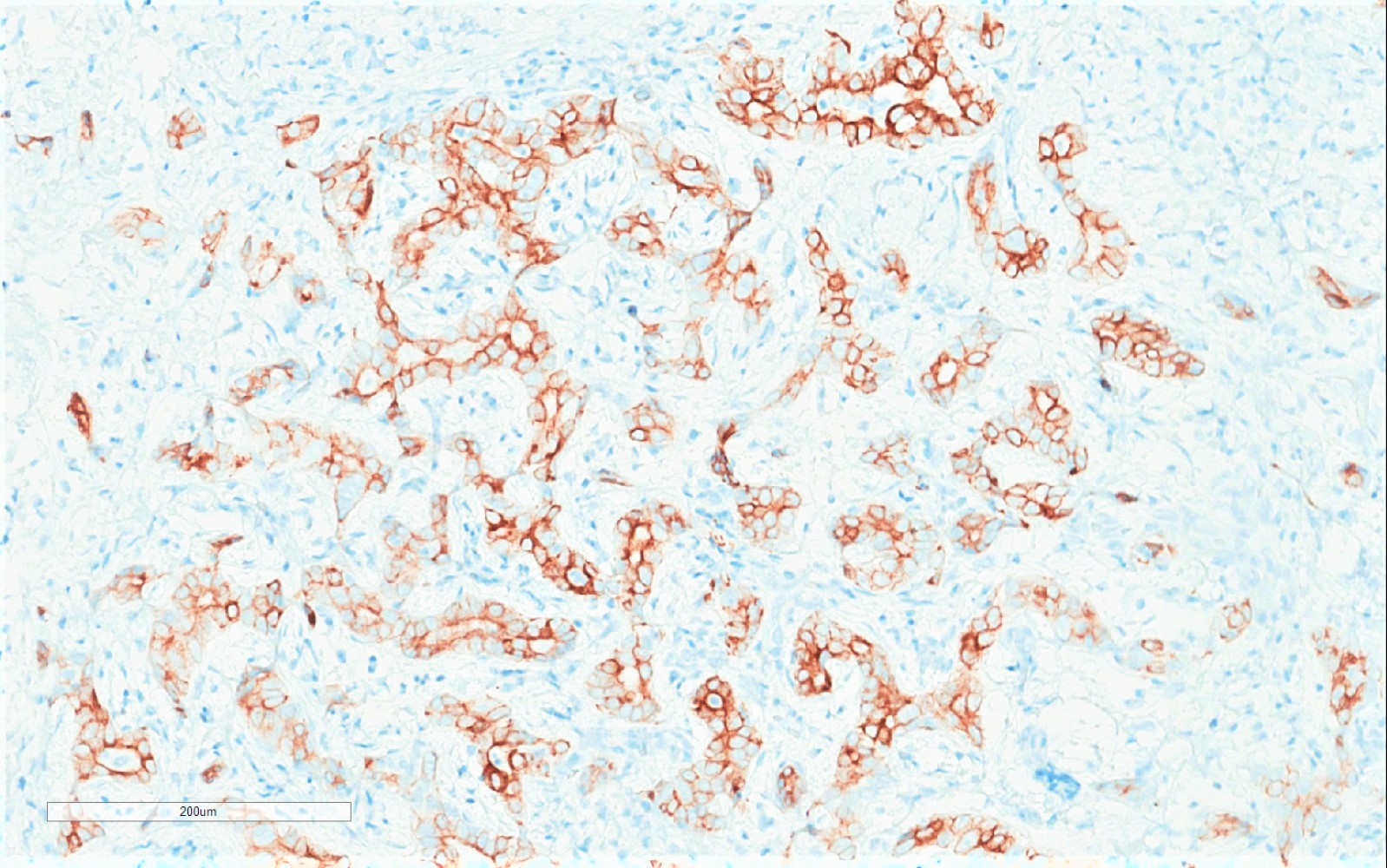
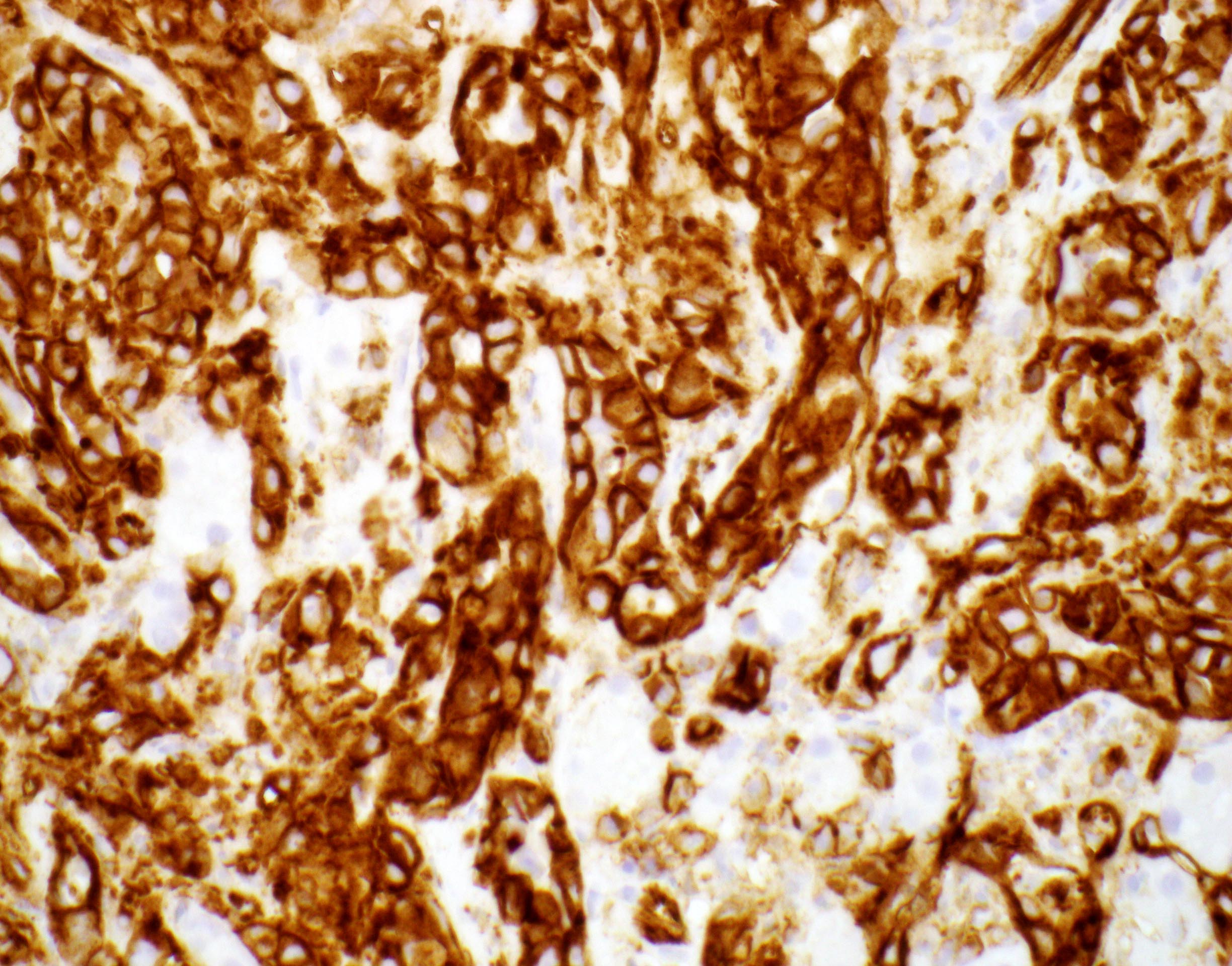
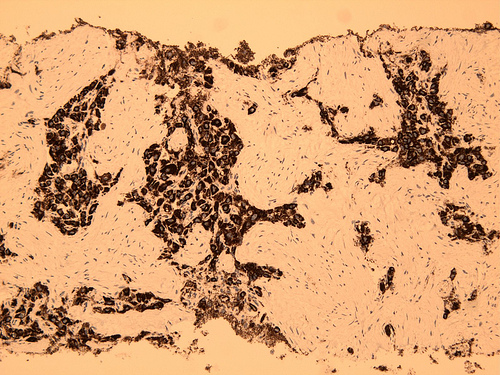
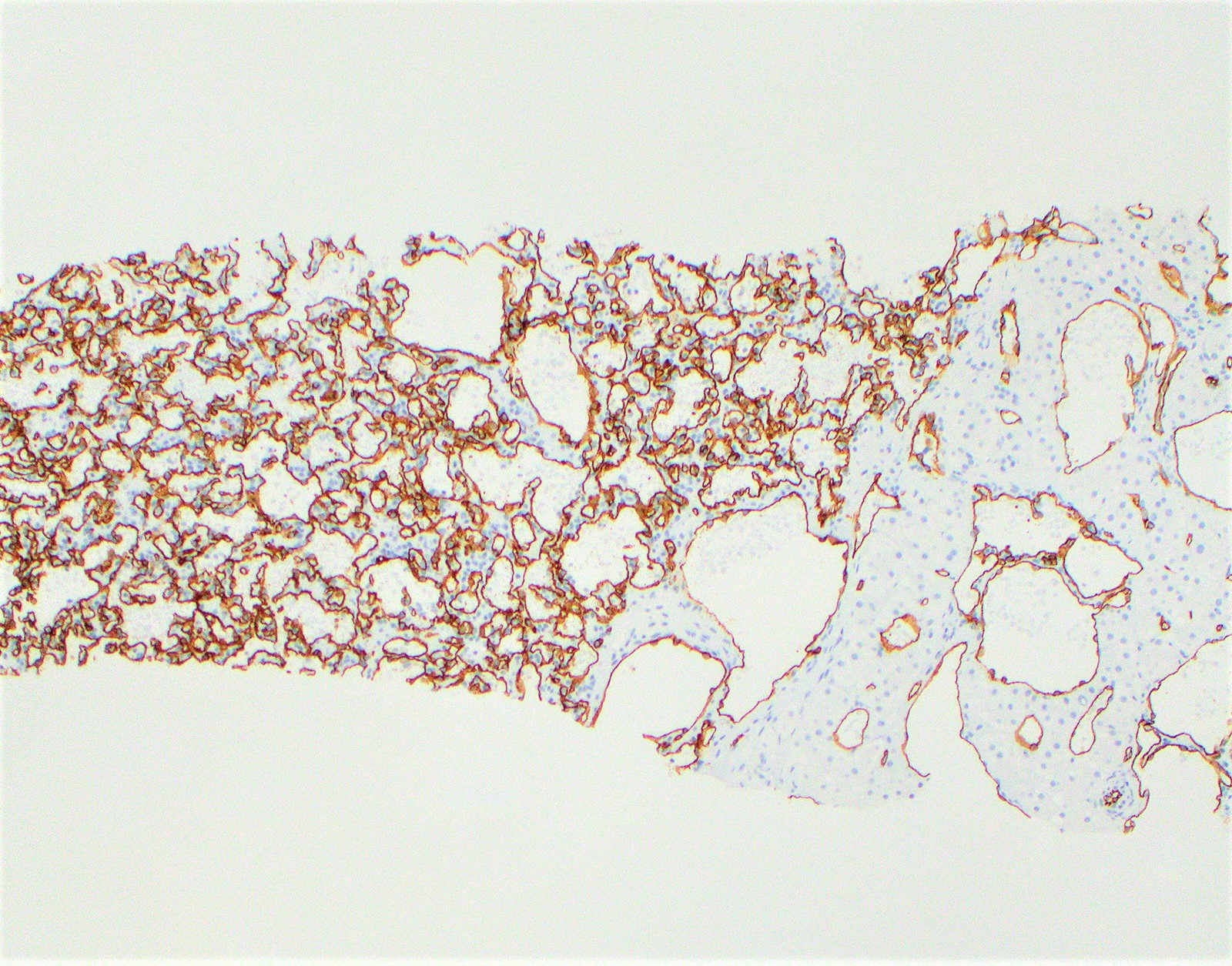
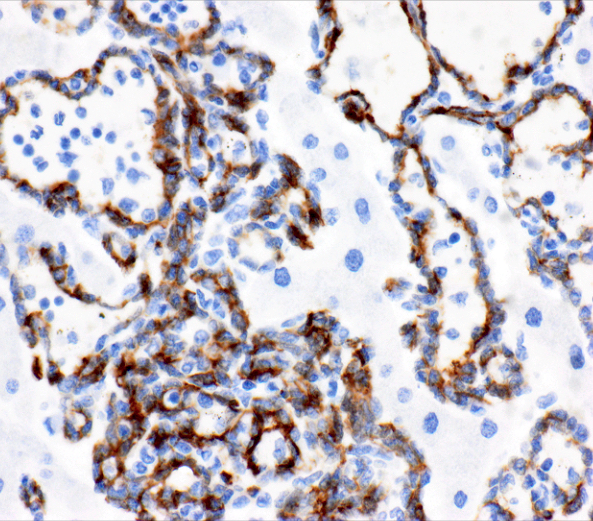
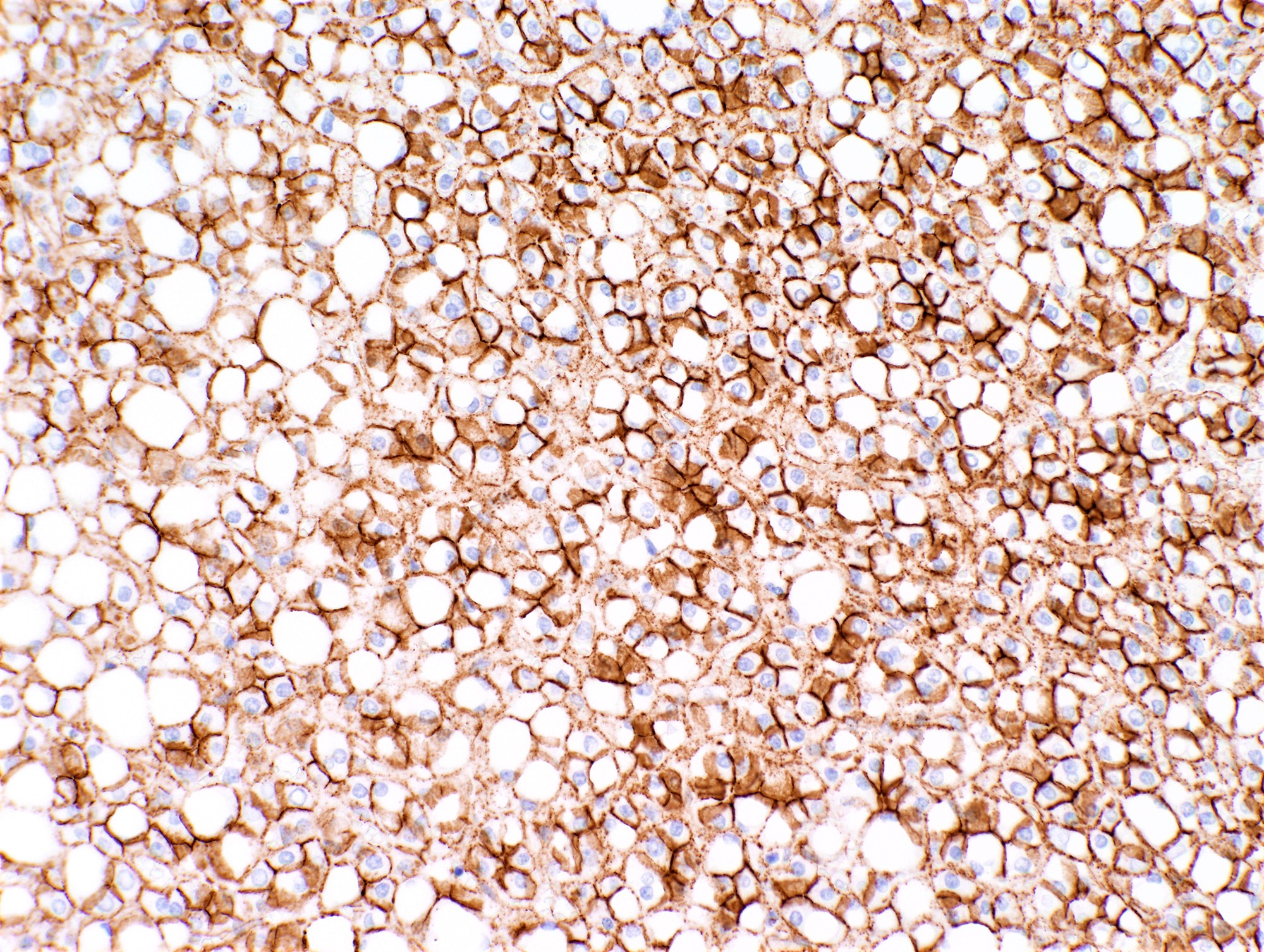
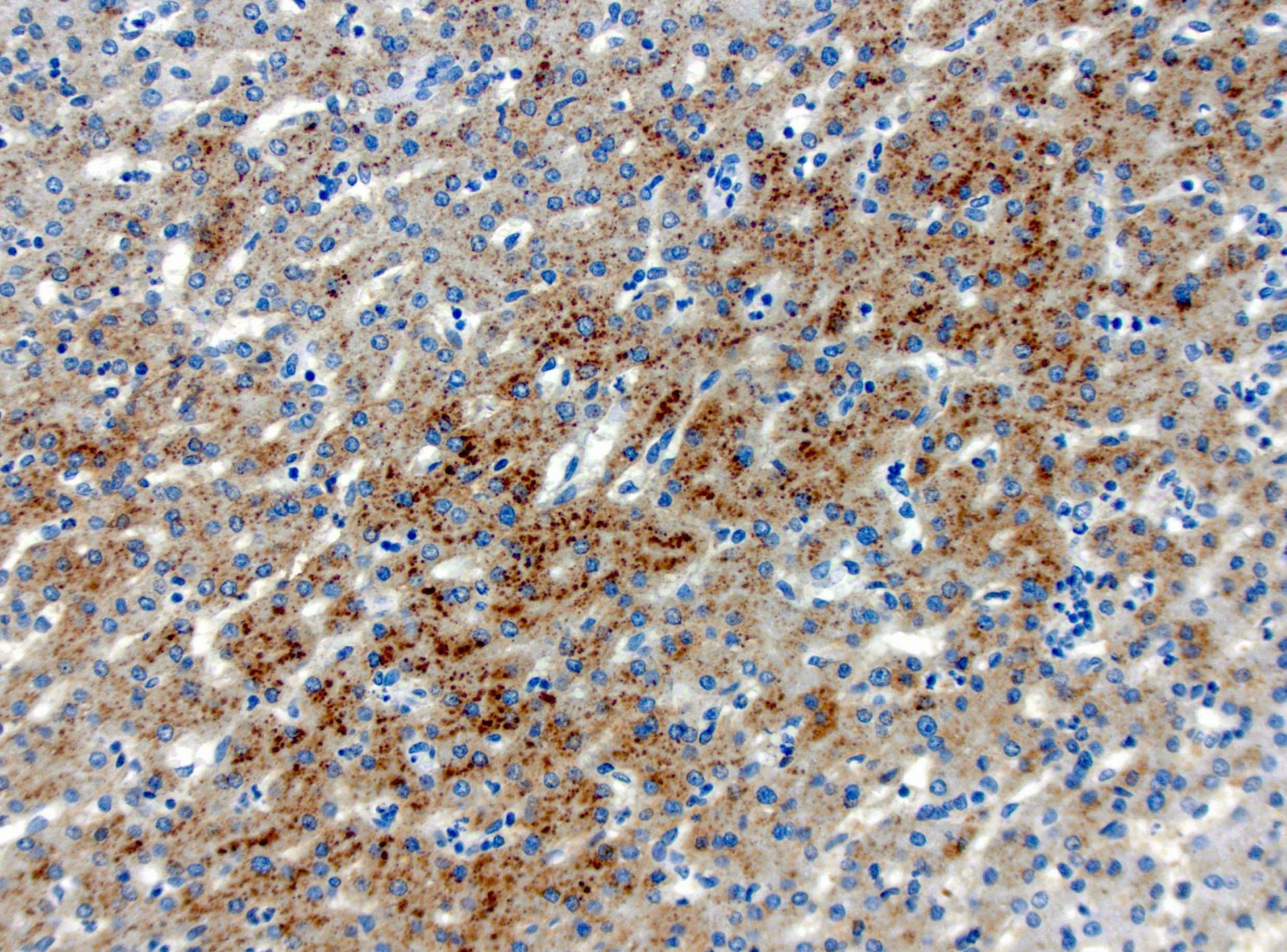
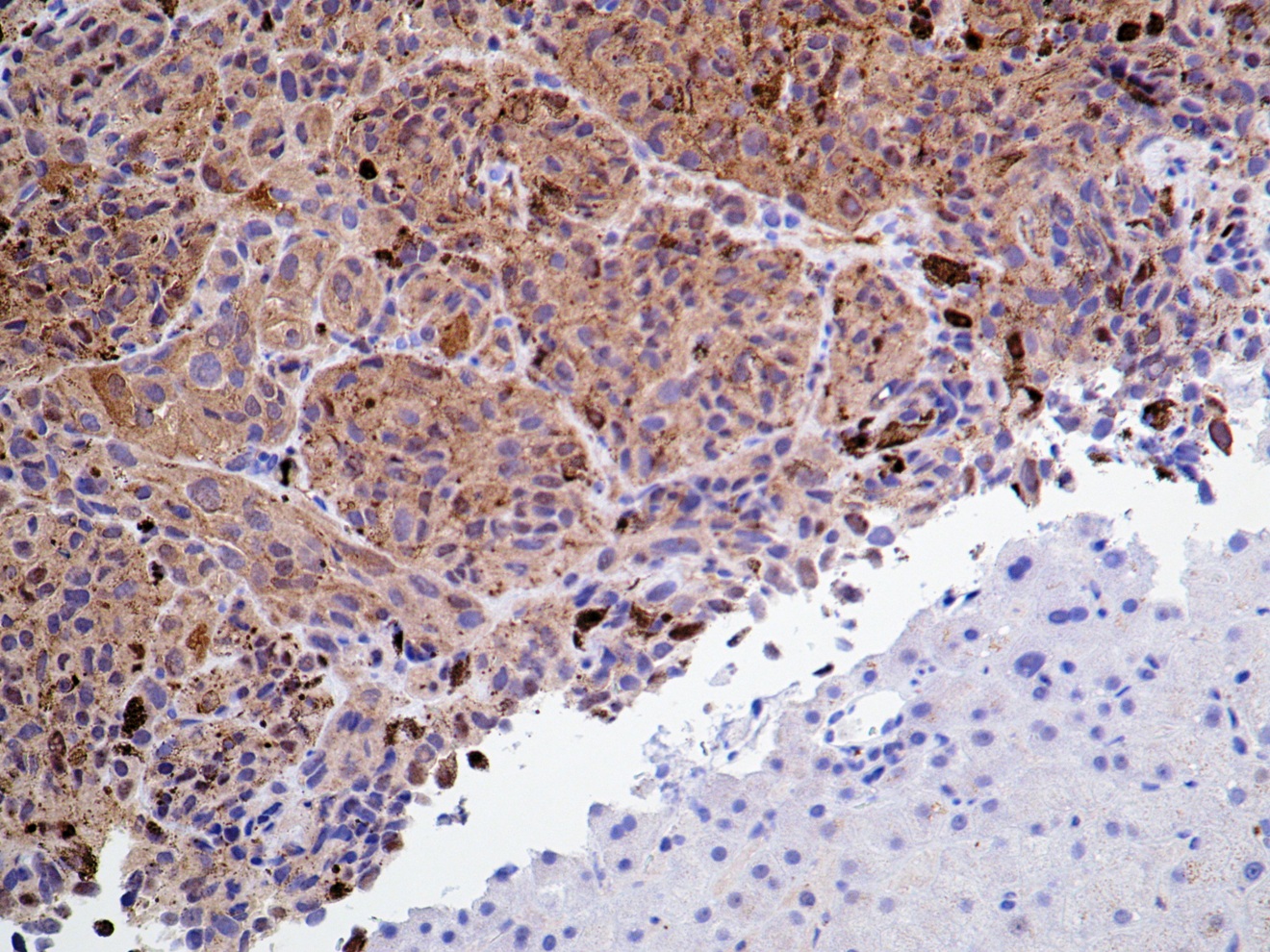
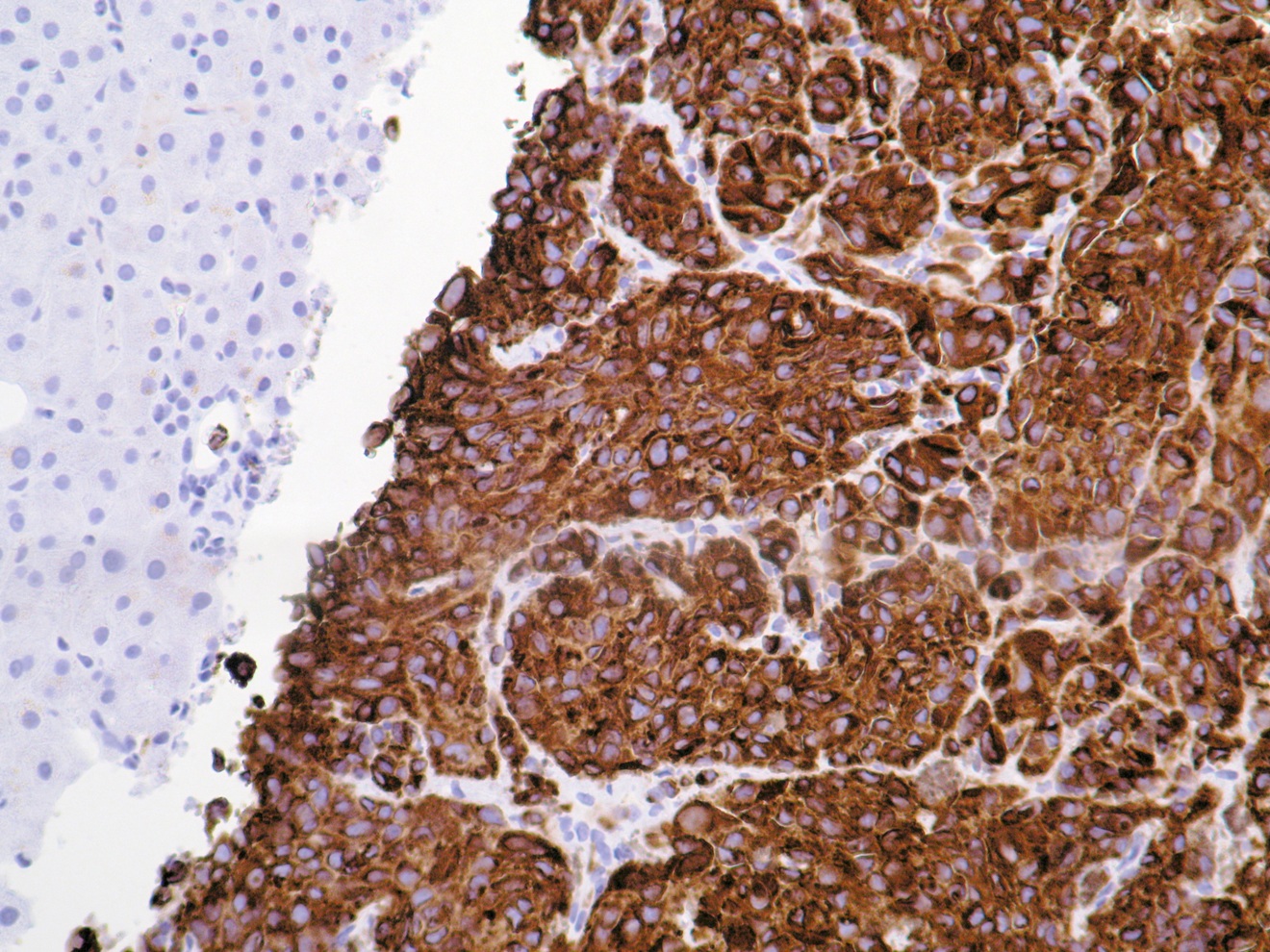
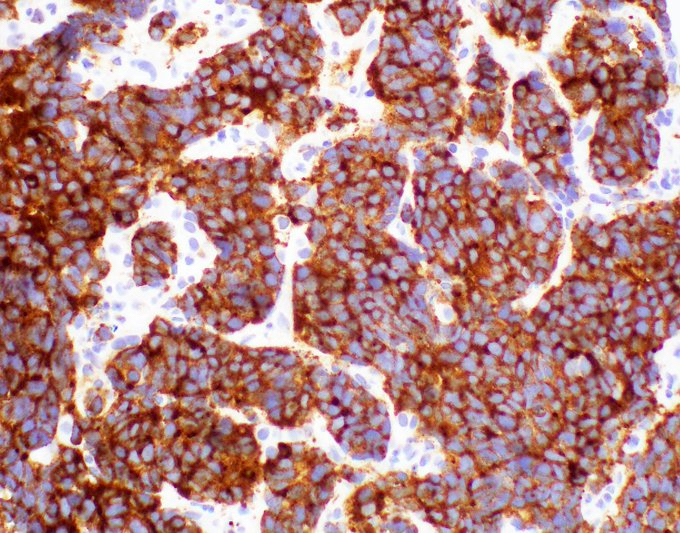
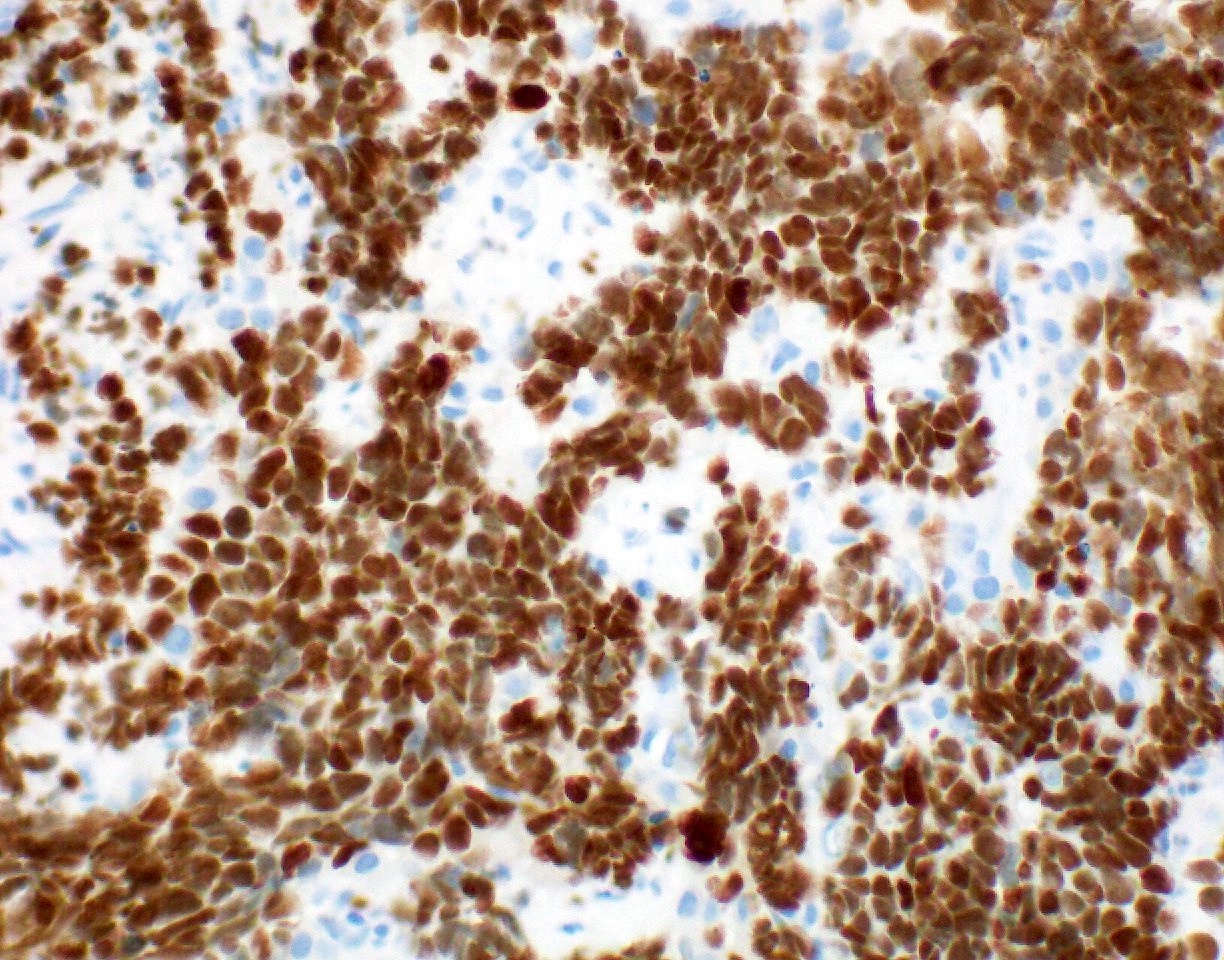
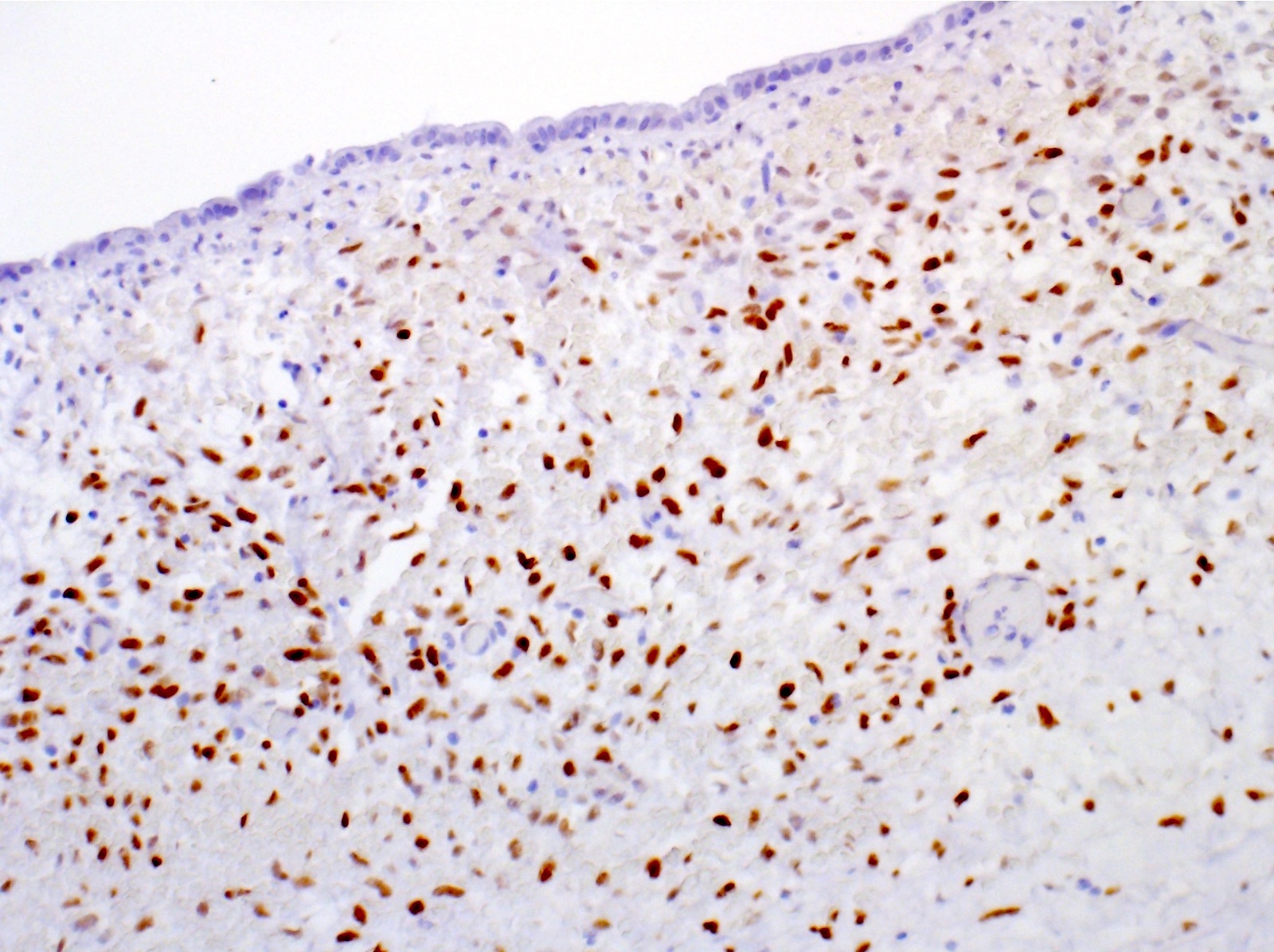
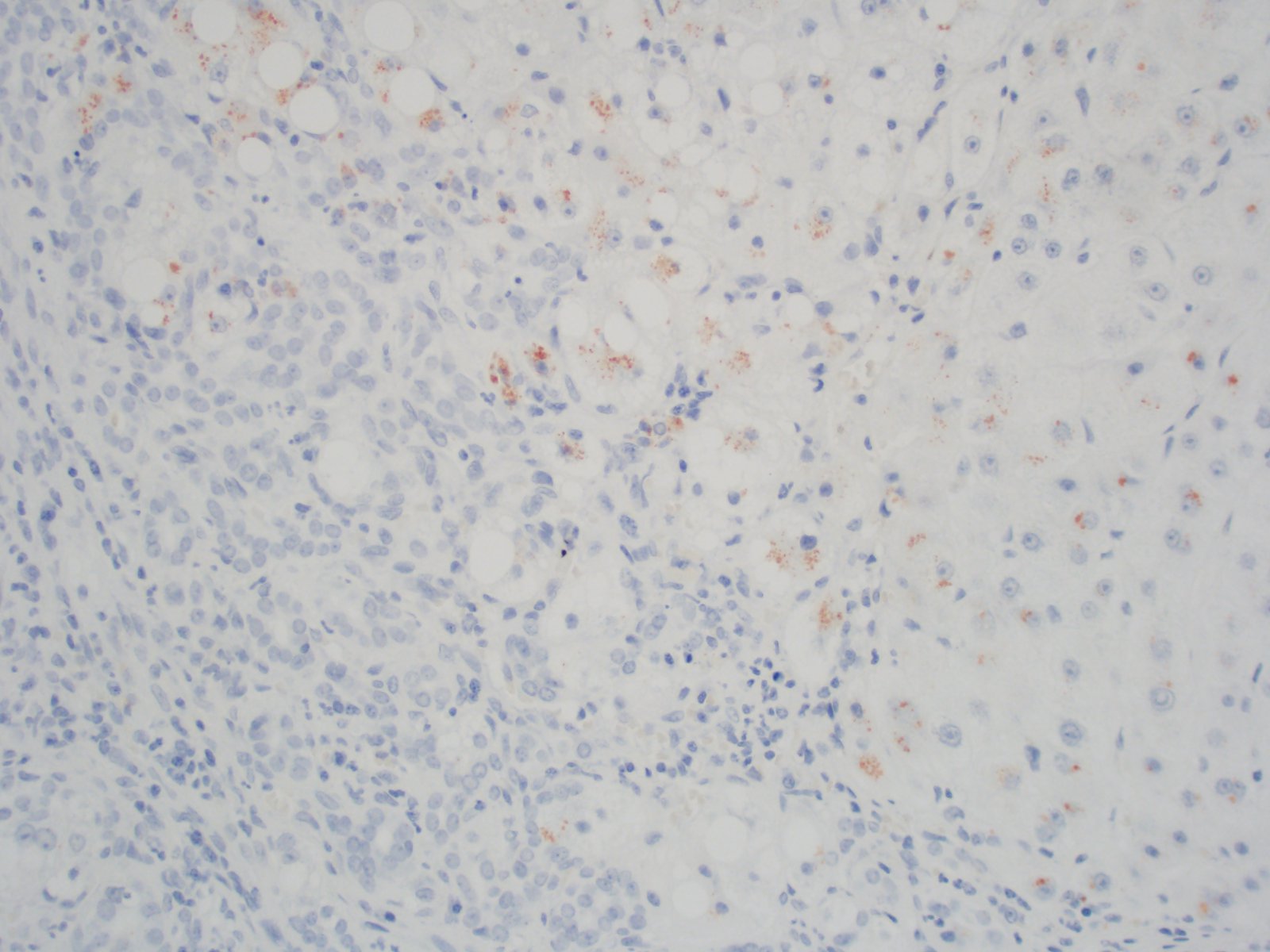
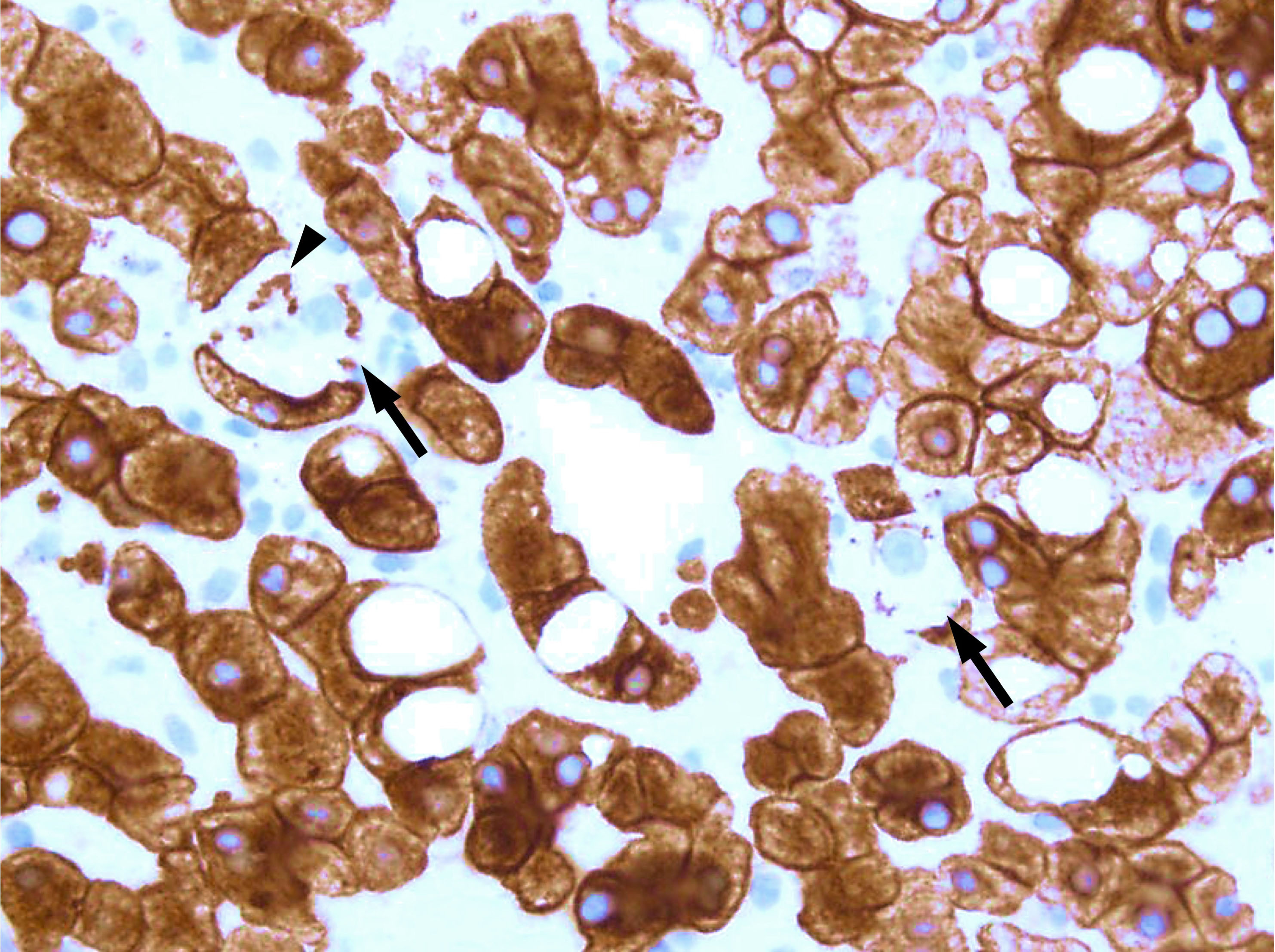
Positive stains
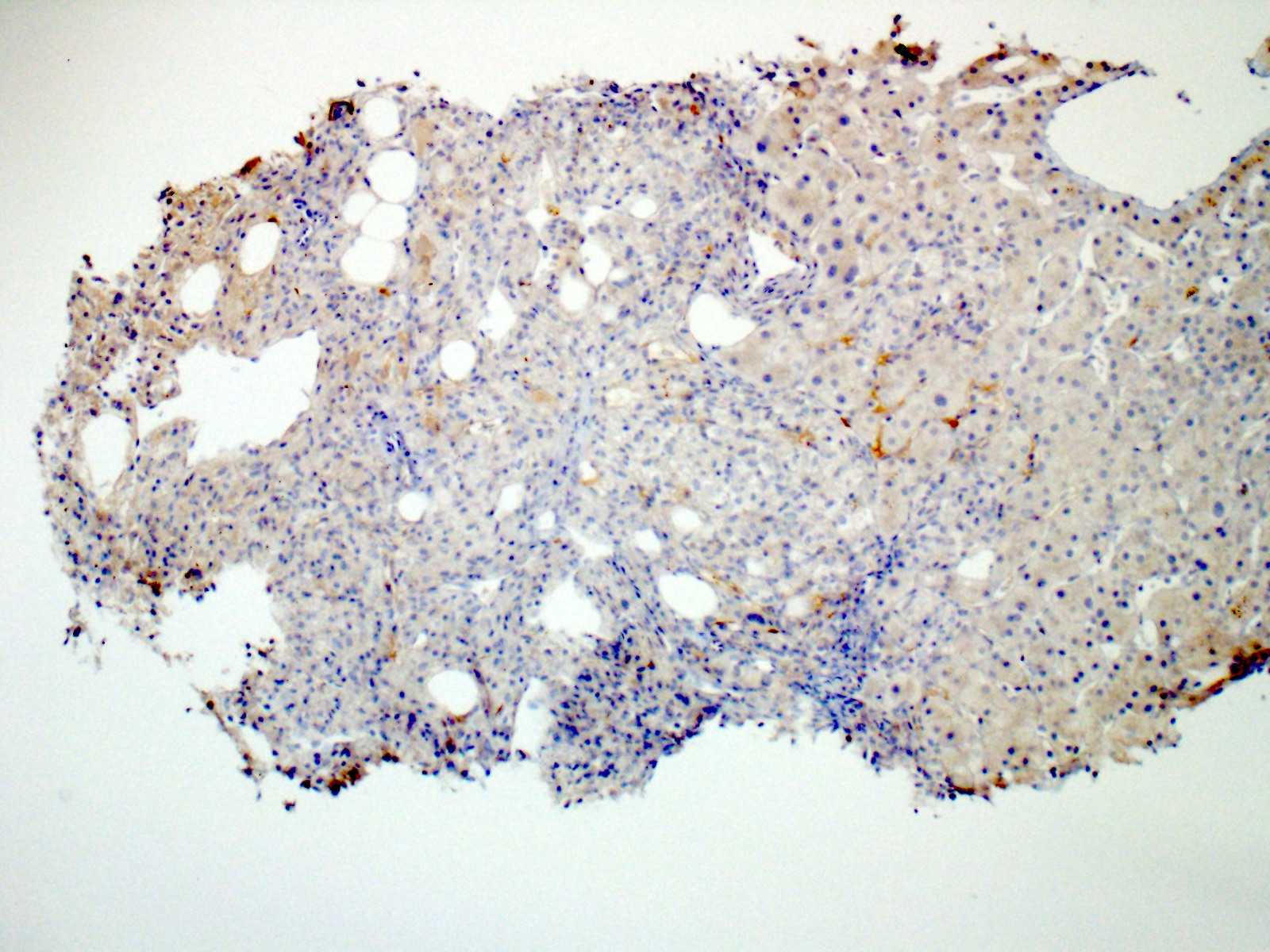
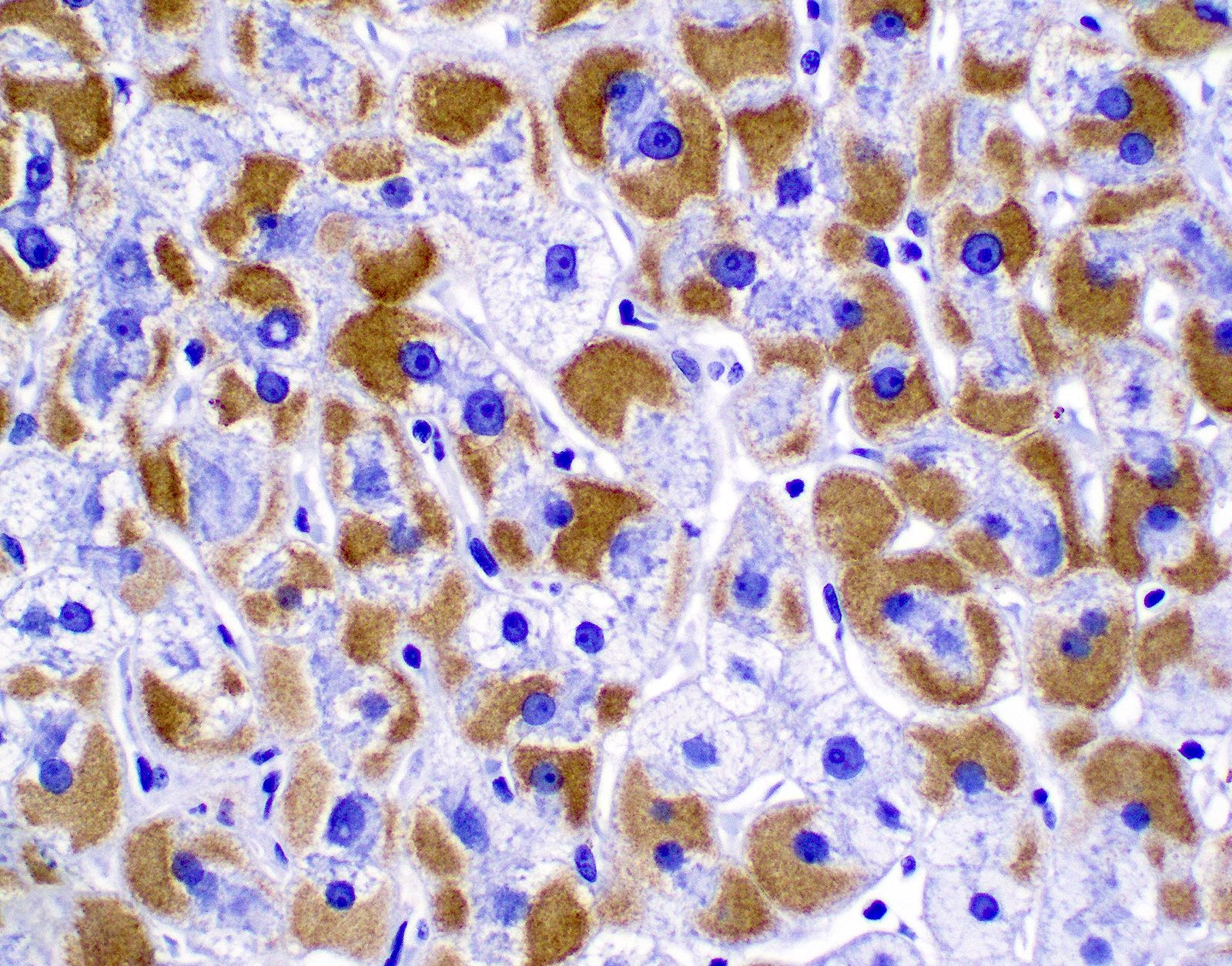
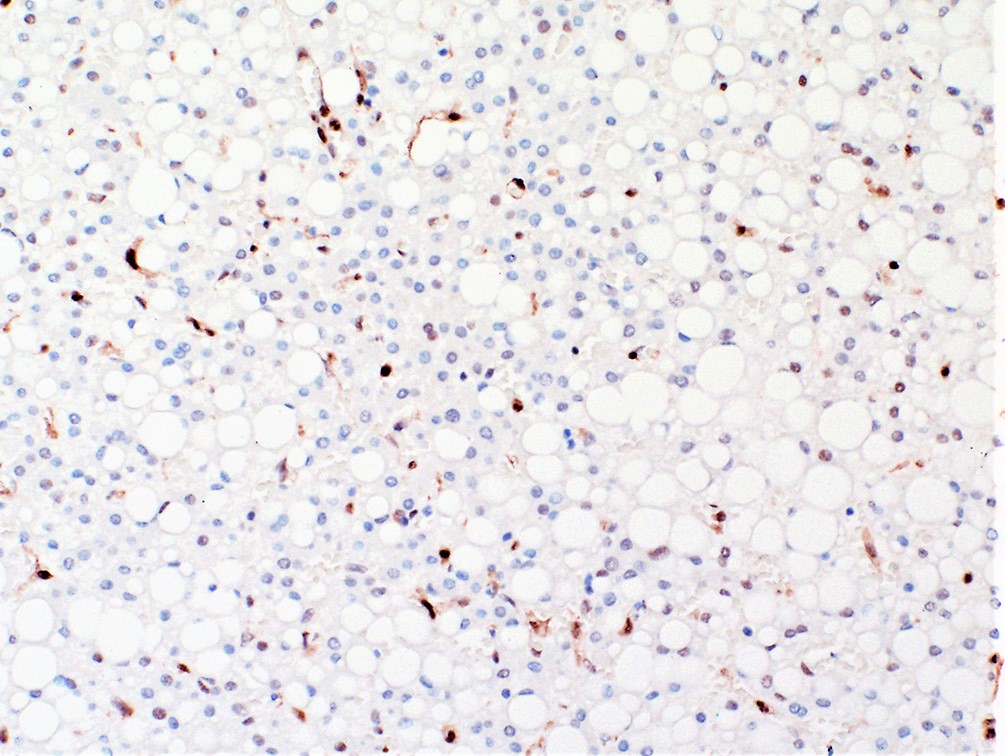
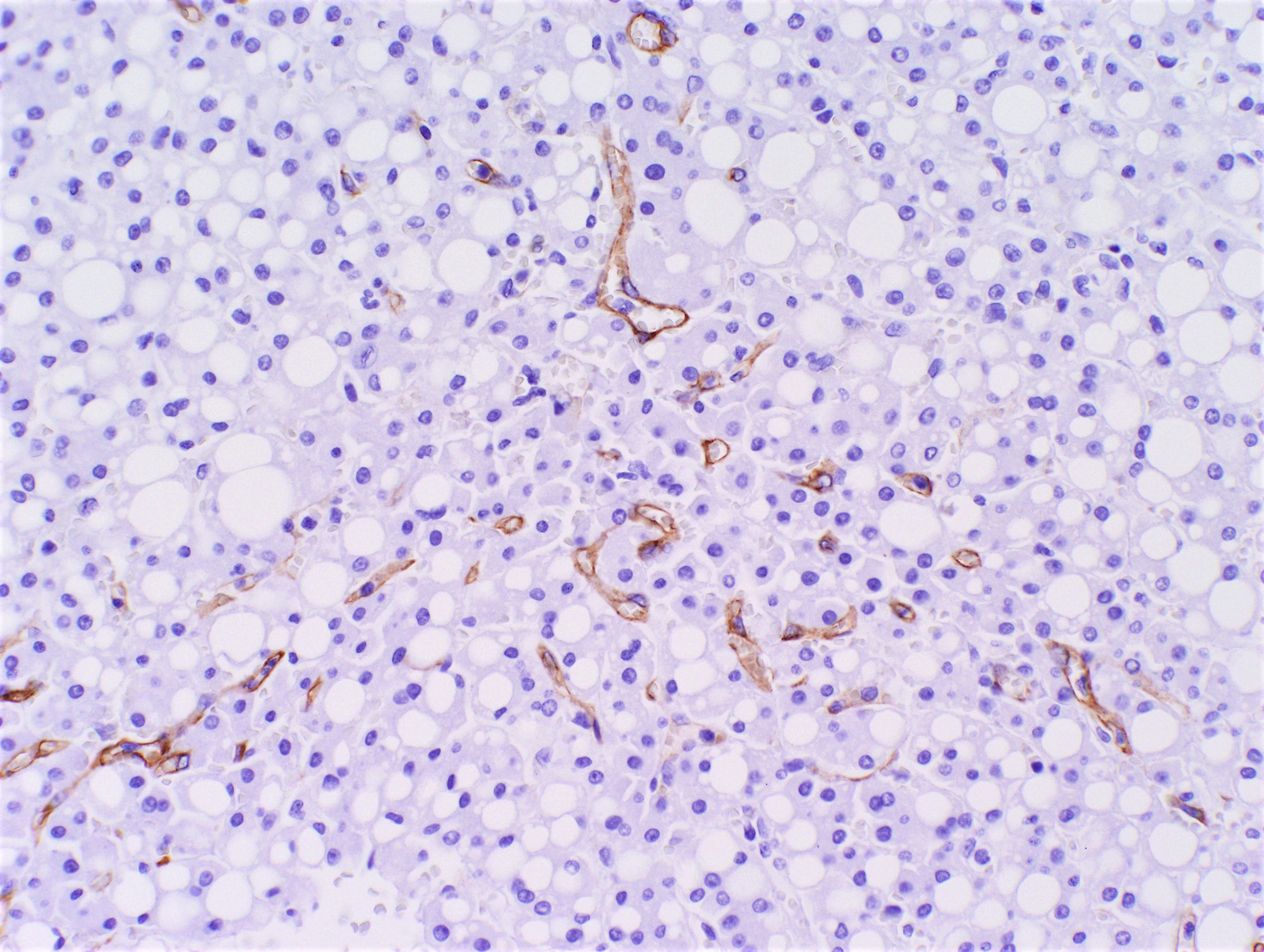
- C4d on paraffin tissue is a successful method for screening and diagnosing AMR in liver allografts (Hum Pathol 2018;73:144)
- To consider a portal tract positive, C4d has to be deposited in > 50% of the circumference of portal microvascular endothelium (portal vein and capillaries)
- C4d immunohistochemistry (performed on paraffin tissue) is scored based on criteria described by the Banff working group (Am J Transplant 2016;16:2816):
C4d score Criteria 0 No C4d deposition in portal microvasculature 1 Minimal: < 10% of portal tracts 2 Focal: 10 - 50% portal tracts 3 Diffuse: > 50% of portal tracts; often with extension; often with extension
into inlet venules and periportal sinusoids
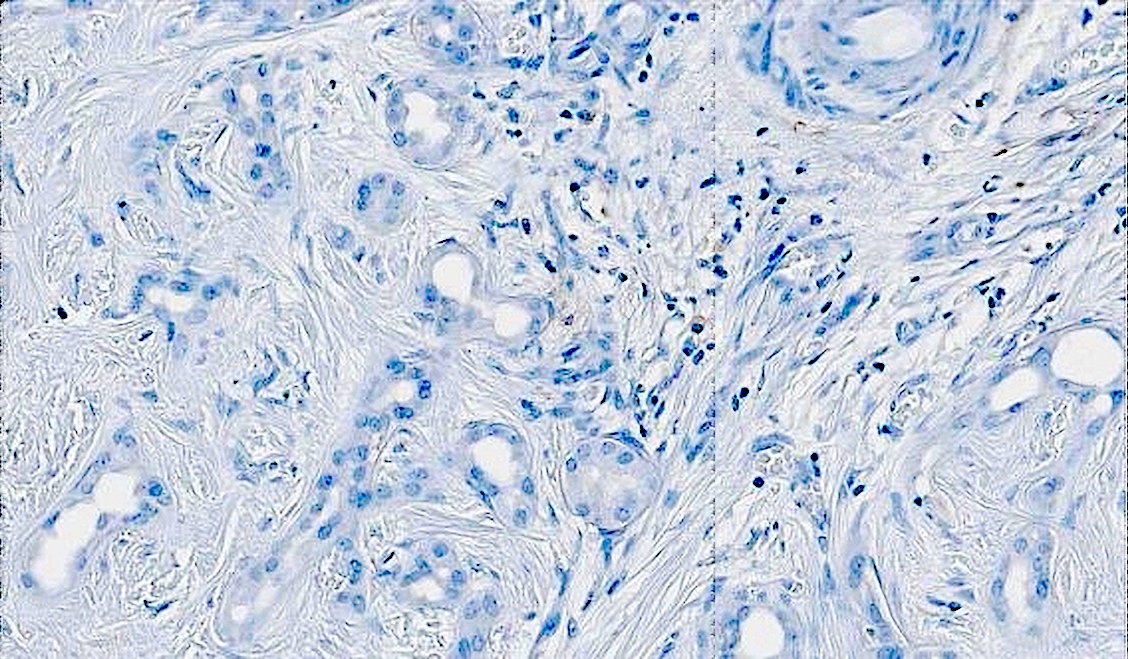
- IgG4 positive plasma cells are increased in plasma cell rich variant
Negative stains
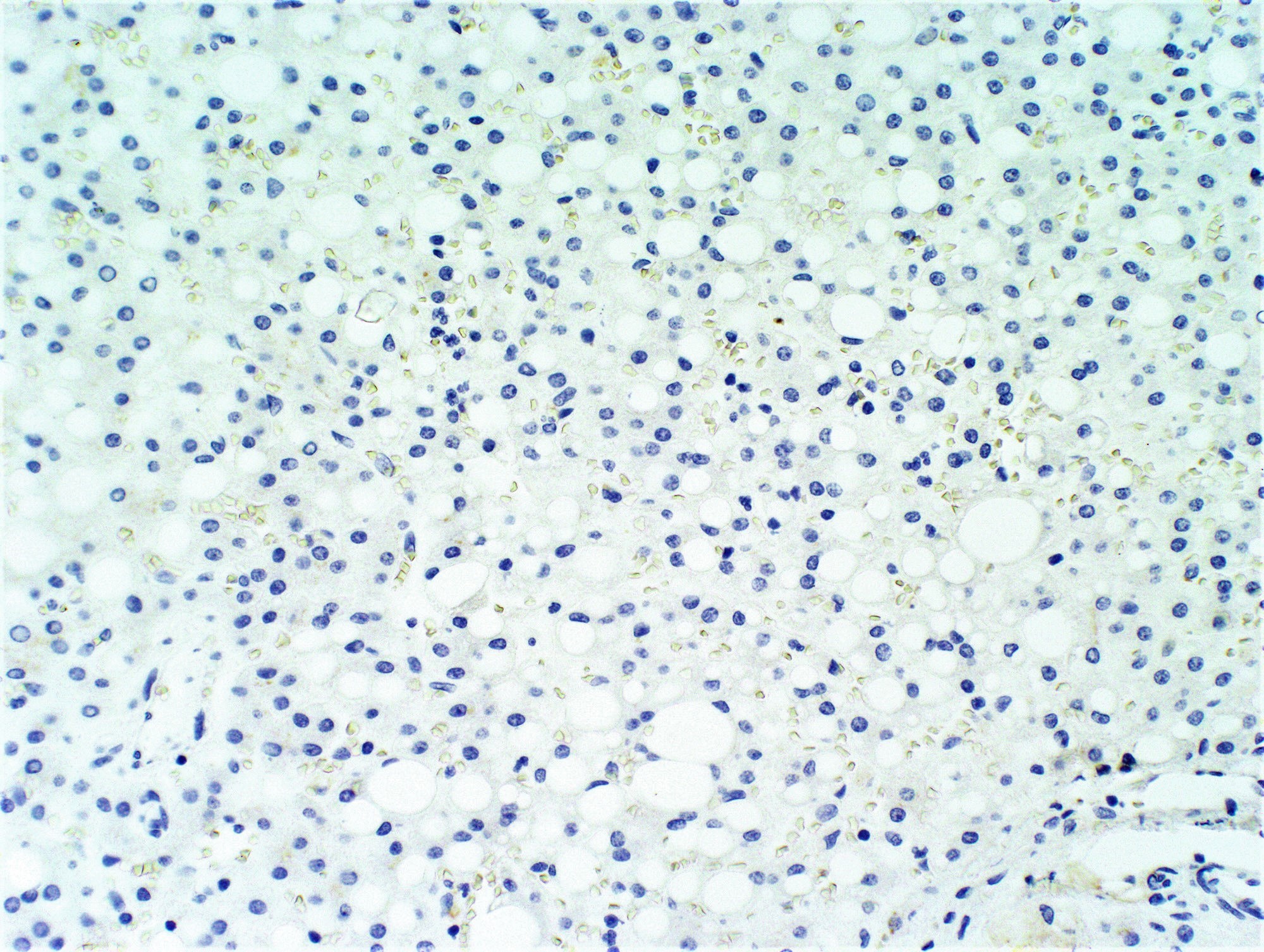
- CK7 and copper stains are generally used to screen and rule out biliary pathology
Sample pathology report
- Liver allograft, needle biopsy:
- Acute antibody mediated rejection with active intimal arteritis
- Portal capillary dilatation, endothelial cell hypertrophy and capillaritis (Banff h score 2/3)
- C4d on paraffin tissue: diffuse uptake by portal microvasculature (Banff C4d score 3/3)
- Liver allograft fibrosis score (Am J Transplant 2012;12:2986):
- Mild portal fibrosis (1/3)
- Moderate subsinusoidal fibrosis (2/3)
- Mild perivenular fibrosis (1/3)
- Acute antibody mediated rejection with active intimal arteritis
Differential diagnosis
- Preservation / reperfusion injury:
- It can be difficult to distinguish early aAMR from reperfusion injury
- aAMR is favored if there is diffuse endothelial cell enlargement, diffuse C4d uptake and portal or perivenular inflammation
- Suboptimal biliary drainage:
- It is occasionally difficult to distinguish aAMR from biliary obstructive changes; both entities can show portal based neutrophilic inflammation, ductular reaction and cholestasis
- aAMR shows endothelial cell hypertrophy and intraluminal leukocyte margination
- Positive C4d, negative CK7 and negative copper stain help rule out imparied biliary drainage
- Recurrent hepatitis C virus infection:
- Small for size syndrome (SFSS):
- Seen in reduced size partial liver allografts (e.g. living donor transplantation / split liver allograft), due to persistent portal vein hypertension and hyperperfusion
- Usually occurs in setting of less than 0.8% graft to recipient body weight ratio
- Occurs early and similarly to early aAMR presents with hyperbilirubinemia and coagulopathy
- Histologically, aAMR shows distinctive capillaritis and C4d uptake distinguishing those two entities
- In aAMR patients are usually sensitized
Additional references
- Am J Transplant 2018;18:1604, Am J Transplant 2015;15:1003, Liver Transpl 2014;20:218, Liver Transpl 2014;20:200, Liver Transpl 2013;19:1001, Liver Transpl 2012;18:984, Curr Opin Organ Transplant 2015;20:314, Curr Opin Organ Transplant 2012;17:280, Transplantation 2017;101:2399, Pediatr Transplant 2017 Feb [Epub ahead of print]
Board review style question #1
- A 60 year old woman, 2 months post living donor liver transplantation from her son presented with jaundice, elevated transaminases and elevated bilirubin. A biopsy showed moderate T cell mediated rejection (TCMR) and the patient received steroids with no significant improvement. Assessment of pretransplant workup showed that the patient is sensitized and had a positive crossmatch. Posttransplant workup showed persistent Donor specific antibodies (multiple specificities, sum MFI 36,928). Imaging studies showed intact biliary tree and normal vascular flow. A repeat biopsy showed capillaritis, portal edema and focal luminal arteritis. According to Banff criteria, what else is needed to establish a definite diagnosis of acute antibody mediated rejection (aAMR)?
- Banff criteria is met, the patient can be diagnosed with acute antibody mediated rejection (aAMR) and no additional requirements are needed
- Diffuse C4d uptake by portal microvasculature (C4d score 3)
- IgG4 staining and quantification of positive plasma cells
- Presence of central perivenulitis and cholestasis
Board review style answer #1
B. Diffuse C4d uptake by portal microvasculature. The patient otherwise met all criteria for a diagnosis of acute antibody mediated rejection (aAMR): 1) Evidence of histopathologic damage (capillaritis), 2) positive donor specific antibody (DSA), 3) reasonable exclusion of other causes by available diagnostic modalities (e.g. imaging) and finally 4) diffuse C4d uptake is needed to complete the criteria and establish the diagnosis. Increased IgG4 positive cells are seen in plasma cell rich rejection and are not part of the criteria in diagnosis of acute antibody mediated rejection (aAMR) or plasma cell rich rejection (Am J Transplant 2013;13:2966). Central perivenulitis and cholestasis can be seen with TCMR, aAMR and cAMR and are not part of the criteria. Central perivenulitis occurs most commonly with portal inflammatory changes but can also occur as an isolated lesion (Histopathology 2020;76:822).
Comment Here
Reference: Acute antibody mediated rejection including hyperacute rejection
Comment Here
Reference: Acute antibody mediated rejection including hyperacute rejection
Board review style question #2
- A 65 year old man underwent liver transplant for Hepatitis C virus (HCV) induced cirrhosis with prior history of interferon treatment. The patient's posttransplant history was complicated by two episodes of early T cell mediated rejection (TCMR). The patient is now 2 years posttransplantation and presents with allograft dysfunction. A biopsy showed portal inflammation with mild cholangitis, interface activity and central perivenulitis. Plasma cells were visibly abundant and constituted about 45% of the inflammation. Hepatitis C virus (HCV) RNA was undetectable. What is the correct diagnosis?
- Idiopathic posttransplantation hepatitis
- Plasma cell rich rejection
- Recurrent autoimmune hepatitis
- Recurrent Hepatitis C virus (HCV)
Board review style answer #2
B. Plasma cell rich rejection. The patient was transplanted for Hepatitis C virus (HCV) and treated with interferon (primary disease other than autoimmune hepatitis). While recurrent Hepatitis C virus (HCV) is a major differential, the central perivenulitis and negative RNA test essentially rule it out. Idiopathic posttransplantation hepatitis is a broad term used to describe chronic hepatitis changes in patients without clinical or serologic evidence of viral hepatitis, autoimmunity or drug induced liver injury (Liver Transpl 2001;7:285). More recently, however, late onset T cell mediated rejection (TCMR) and chronic active acute antibody mediated rejection (aAMR) have been identified as causes of chronic allograft inflammation and fibrosis (Gastroenterology 2018;155:1838, Liver Transpl 2016;22:1593, Liver Transpl 2009;15:S19, Liver Transpl 2018;24:897).
Comment Here
Reference: Acute antibody mediated rejection including hyperacute rejection
Comment Here
Reference: Acute antibody mediated rejection including hyperacute rejection
Acute hepatitis-general
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Acute hepatitis is largely a clinical term used to describe a sudden elevation in liver enzymes that lasts < 6 months in duration
- Can occur de novo or as a flare of various chronic liver diseases
- Acute liver failure is defined as an abrupt onset of severe liver disease that leads to hepatic encephalopathy and coagulopathy shortly after presentation
Essential features
- Acute hepatitis is a clinical term used to describe a sudden elevation in liver enzymes that lasts < 6 months
- Hepatotropic viruses account for the majority of cases, most commonly hepatitis A and B viruses
- Histologic features are fairly nonspecific displaying lobular disarray and can include lobular inflammation, varying degrees of parenchymal necrosis, bile ductular reaction and bland lobular cholestasis
- Features of chronic injury are not present
- Cases of acute hepatitis can resolve spontaneously with supportive therapy, progress to acute liver failure or develop into chronic liver disease
Terminology
- Acute hepatic injury
- Acute liver injury
Epidemiology
- Hepatotropic viruses
- Hepatitis A (HAV)
- Endemic areas include Central and South America, Africa, the Middle East, Asia and the Western Pacific
- Transmission typically occurs through a fecal - oral route; rarely through blood or solid organ transplants
- 1% of cases progress to acute liver failure (CDC: Statistics & Surveillance Viral Hepatitis Surveillance - United States [Accessed 22 April 2022])
- Hepatitis B (HBV)
- Endemic areas include Asia, Africa, South America and the Caribbean
- Routes of transmission include parenterally or through mucosal exposure
- 2% of acute HBV infections can progress to liver failure; HBV accounts for 7% of acute liver failure cases (CDC: Statistics & Surveillance Viral Hepatitis Surveillance - United States [Accessed 22 April 2022])
- Hepatitis C (HCV)
- Acute liver failure remains unknown in HCV infections and acute infection is usually subclinical
- Transmission routes include bloodborne and through sexual activity
- Hepatitis D (HDV)
- Endemic areas include the Mediterranean, Sub-Saharan Africa, the Middle East and Northern South America
- Transmission occurs via a parenteral or mucosal route
- Requires coinfection or superinfection of HBV
- Hepatitis E (HEV)
- Endemic areas include Central and Southeast Asia, North and West Africa and Mexico
- Transmission occurs through a fecal oral route
- 0.1 - 4% of infections progress to acute liver failure (J Gastroenterol Hepatol 2009;24:1484)
- In pregnant women, 30% of infections progress to acute liver failure (Indian J Gastroenterol 2007;26:6)
- Hepatitis A (HAV)
- Drug induced liver injury
- Direct toxins
- Acetaminophen toxicity is the most common cause of acute liver failure in the developed world and accounts for 40 - 50% of cases in the United States, Canada and Europe
- Other offending drugs include antibiotics, neurologic drugs, NSAIDs, statins, immunomodulatory drugs
- Idiosyncratic drug reactions
- Accounts for 10 - 20% of acute liver failure
- Direct toxins
- Rare causes (account for 1% of cases)
- Autoimmune hepatitis
- Most patients are young to middle aged women; however, pediatric, geriatric and male patients may also be affected
- Acute alcoholic hepatitis
- Prevalence is approximately 20% of patients with alcohol use disorder and is associated with a recent period of heavy drinking
- Wilson disease
- Patients typically present between the ages of 5 and 35 years
- Autoimmune hepatitis
Sites
- Acute liver failure can lead to effects on other body systems, including acute renal failure, gastrointestinal bleeding, respiratory failure, cardiovascular collapse, systemic infection and sepsis
Pathophysiology
- Necrosis of minute groups of hepatocytes occurs initially without disturbing the hepatic architecture, usually resulting in complete recovery when the insult resolves
- In severe disease, large groups of hepatocytes die, which leads to necrosis and collapse of the reticulin framework
- Reference: Zakim: Hepatology - A Textbook of Liver Disease, 2nd Edition, 1990
Etiology
- Viral hepatitis
- Hepatotropic viruses (hepatitis A, B, C, D, E)
- Account for 72% of acute hepatitis (N Engl J Med 1993;329:1862)
- Majority of infections are hepatitis A virus (HAV) and hepatitis B virus (HBV)
- Nonhepatotropic viruses
- Herpes simplex virus (HSV), cytomegalovirus (CMV), Epstein-Barr virus (EBV), adenovirus, hemorrhagic fever associated viruses, varicella zoster virus, yellow fever, dengue
- Other infections
- Tick borne diseases, malaria, visceral leishmaniasis, Q fever, leptospirosis
- Drug induced liver injury
- Direct toxins versus idiosyncratic drug reactions
- Rare causes
- Autoimmune hepatitis, acute alcoholic hepatitis, Budd-Chiari, Wilson disease, ischemic hepatitis
- Hepatotropic viruses (hepatitis A, B, C, D, E)
Clinical features
- Most cases range from asymptomatic or subclinical to self limited symptomatic
- Symptomatic cases may present as fatigue, abdominal pain, nausea and vomiting, muscle aches or jaundice
- Severe cases can lead to acute liver failure and may present as (Saxena: Practical Hepatic Pathology, 2nd Edition, 2017):
- Acute onset hepatic encephalopathy (accumulation of toxic substances, cerebral edema and intracranial hypertension)
- Coagulopathy (decreased production of liver coagulation factors [II, V, VII, IX, X], thrombocytopenia and platelet function defects)
- Acute renal failure (prerenal azotemia, acute tubular necrosis, hepatorenal syndrome, drug induced interstitial nephritis)
- Infections (reticuloendothelial system dysfunctions and decreased opsonization of microorganisms)
Diagnosis
- Clinical diagnosis
- Elevated serum alanine aminotransferase and aspartate aminotransferase (ALT, AST) tests
- Viral hepatitis
- Serum antibody tests (IgG, IgM), PCR tests for viral RNA, enzyme linked immunoassay (ELISA) test
- Drug induced hepatitis
- Exclusion of viral hepatitis
- Clinical history is taken to investigate any temporal relationship of drug administration and the presence of abnormal liver tests
- Biopsies typically not performed unless there is a clinical suspicion of a second independent hepatic insult (i.e., underlying chronic liver disease)
- Reference: N Engl J Med 1993;329:1862
Laboratory
- Clinically defined as elevation in aspartate transaminase (AST) and alanine transaminase (ALT) (at least 2x upper normal reference range) for < 6 months (Saxena: Practical Hepatic Pathology, 2nd Edition, 2017)
- Hepatotropic viruses: increase in AST / ALT > 5 times upper limit of normal and alkaline phosphatase (ALP) < 3 times upper limit of normal
- Acute HAV: anti-HAV IgM present for 4 - 6 months
- Acute HBV: anticore IgM, hepatitis B surface antigen (HBsAg)
- Acute HCV: HCV RNA in serum; anti-HCV antibodies may not appear for 6 weeks to 6 months
- Acute HDV: total anti-HDV (IgG and IgM)
- Acute HEV: anti-HEV antibody
- Nonhepatotropic viruses
- CMV: CMV antigenemia
- EBV: monospot test, IgM against EBV viral capsid antigen or EBV viral levels
- Acetaminophen toxicity
- Very high AST and ALT (100x upper limit of normal)
- Acute alcoholic hepatitis
- Marked elevation in bilirubin; slight elevation in transaminases (< 10x upper limit of normal)
- Autoimmune hepatitis
- Increased total IgG, presence of autoantibodies (antinuclear antibody, anti smooth muscle antibody)
- Wilson disease
- Coombs negative hemolytic anemia
- ALP to total bilirubin ratio is low (< 2)
- Hepatotropic viruses: increase in AST / ALT > 5 times upper limit of normal and alkaline phosphatase (ALP) < 3 times upper limit of normal
Prognostic factors
- Cases of acute hepatitis can resolve spontaneously with supportive therapy, progress to acute liver failure or develop into chronic liver disease
- Advanced fibrosis and percentage of necrosis have prognostic significance
- Advanced fibrosis and > 25% necrosis portend a worse prognosis (World J Gastroenterol 2017;23:4303)
Case reports
- 36 year old woman with drug induced liver injury and superimposed acute Epstein-Barr virus hepatitis (Pathology 2019;51:104)
- 51 year old HIV positive man with syphilitic hepatitis presenting as acute cholestatic hepatitis (Hum Pathol 2018;79:184)
- 59 year old woman with cirrhotic primary biliary cholangitis, submassive necrosis and hepatitis E virus (Intern Med 2021;60:1863)
Treatment
- Acute viral hepatitis
- Supportive therapy
- Antiviral therapy for cases of acute hepatitis B
- Drug induced acute hepatitis
- Remove offending medication
- N-acetylcysteine (NAC) for acetaminophen overdose
- Severe acute alcoholic hepatitis
- Supportive therapy combined with or without corticosteroids
- Acute autoimmune hepatitis
- Supportive therapy combined with corticosteroids
- References: Clin Liver Dis 2007;11:525, World J Gastroenterol 2021;27:1691, Lancet Gastroenterol Hepatol 2020;5:494, J Immunol Res 2019;2019:9437043
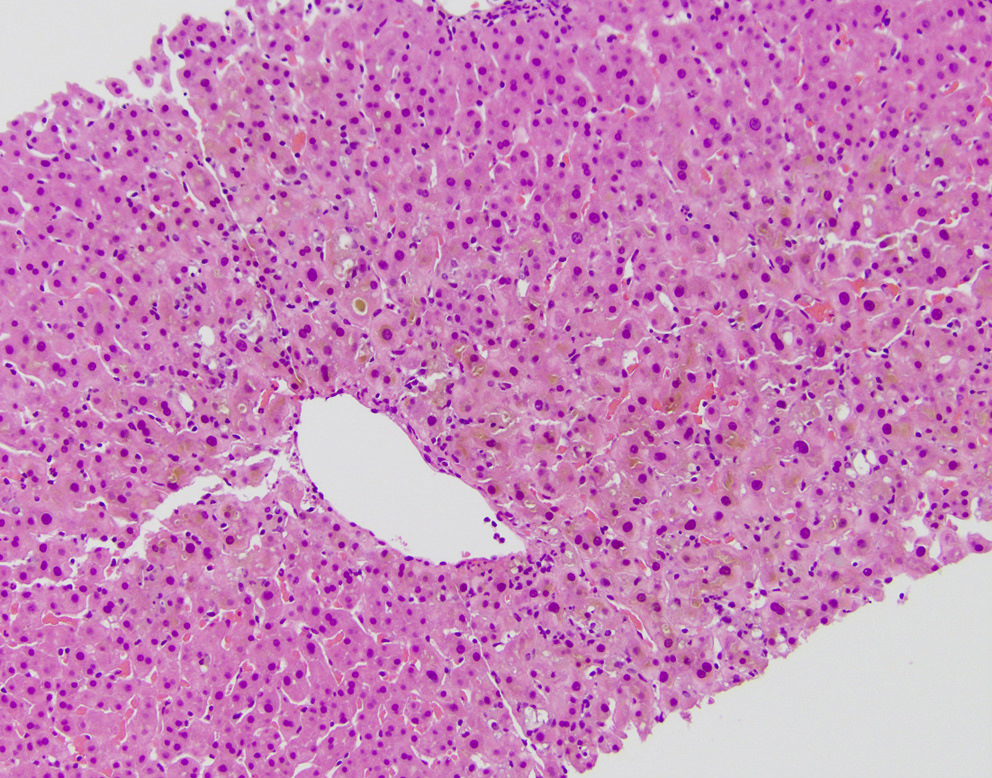
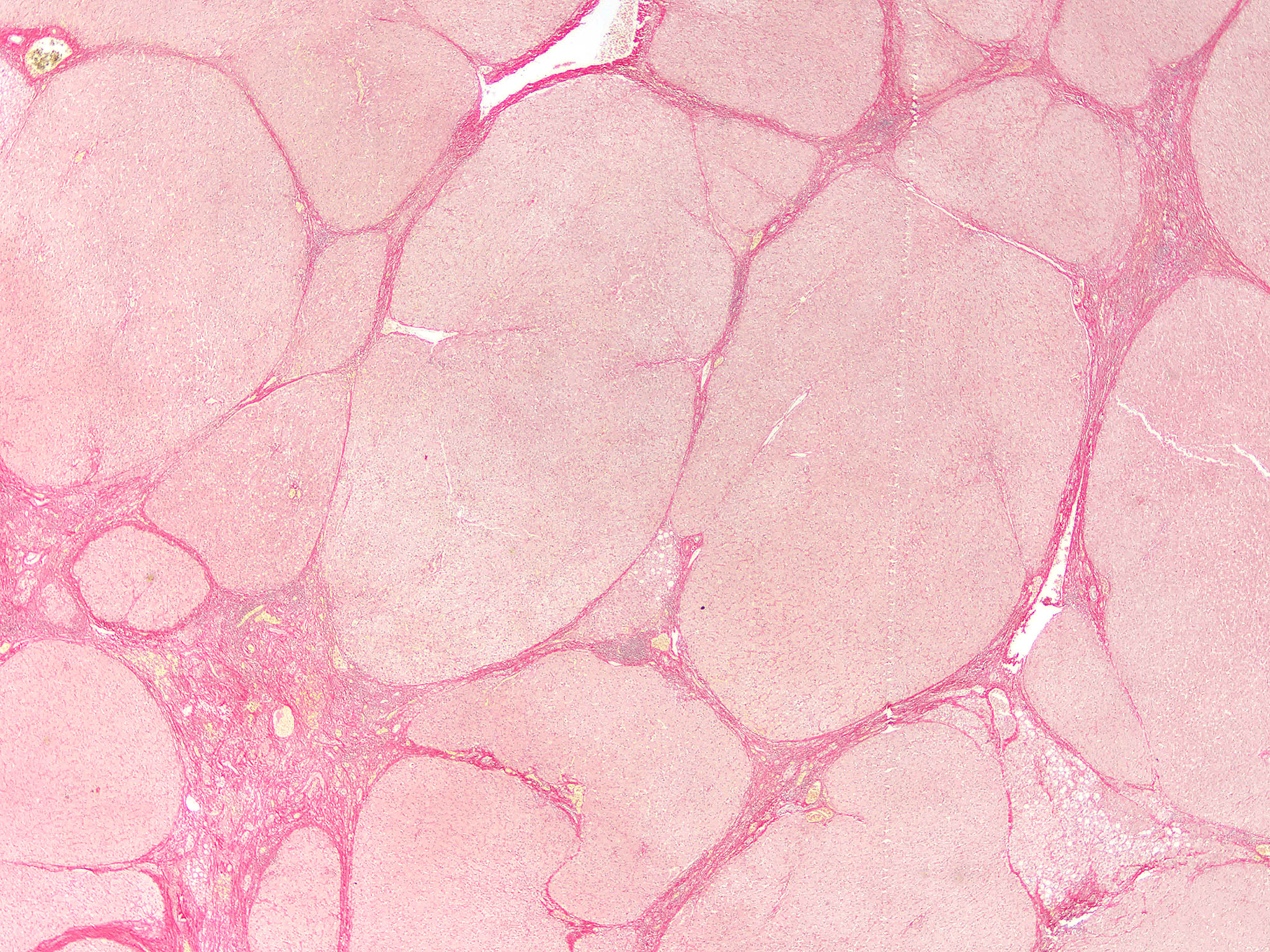
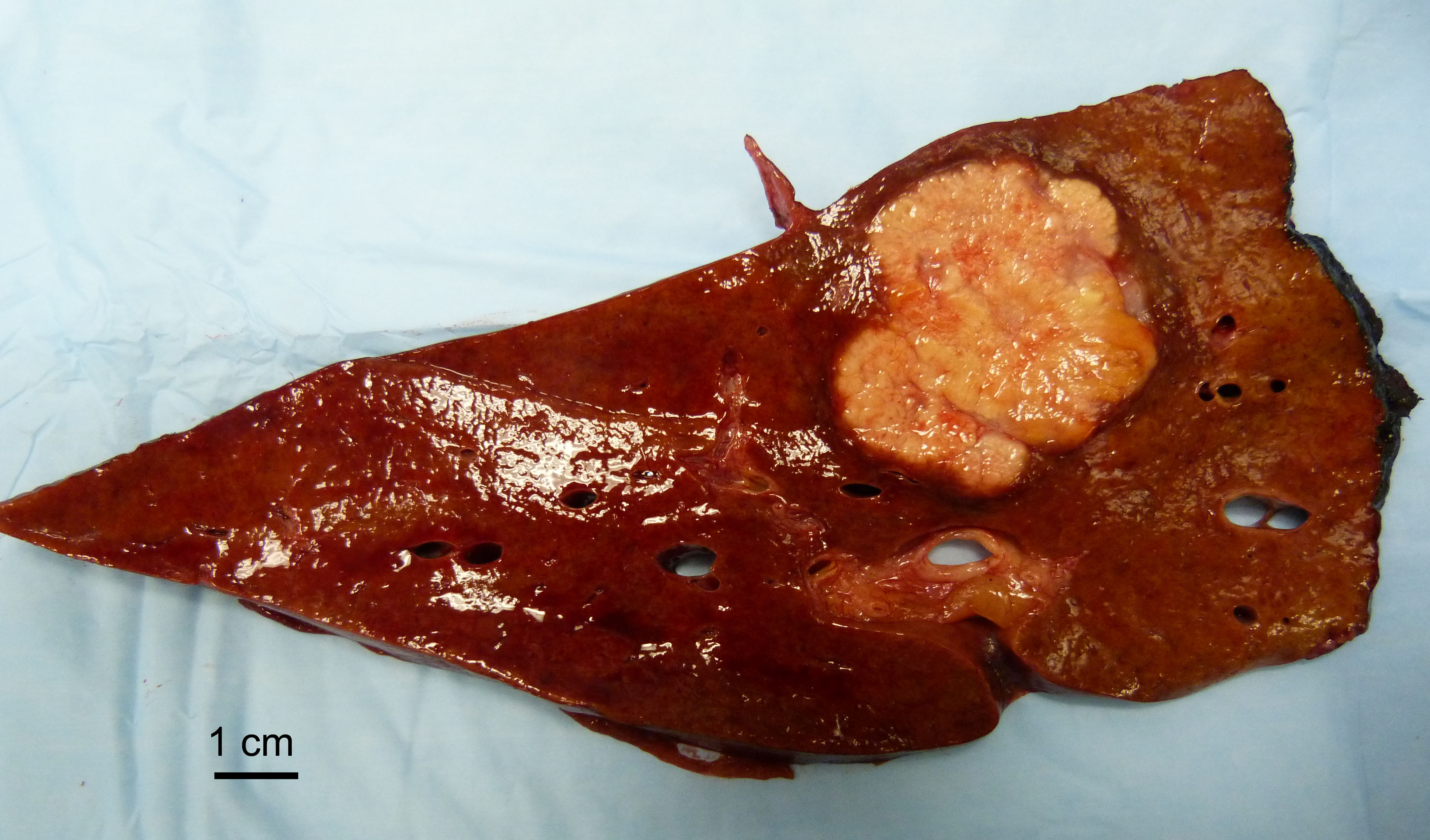
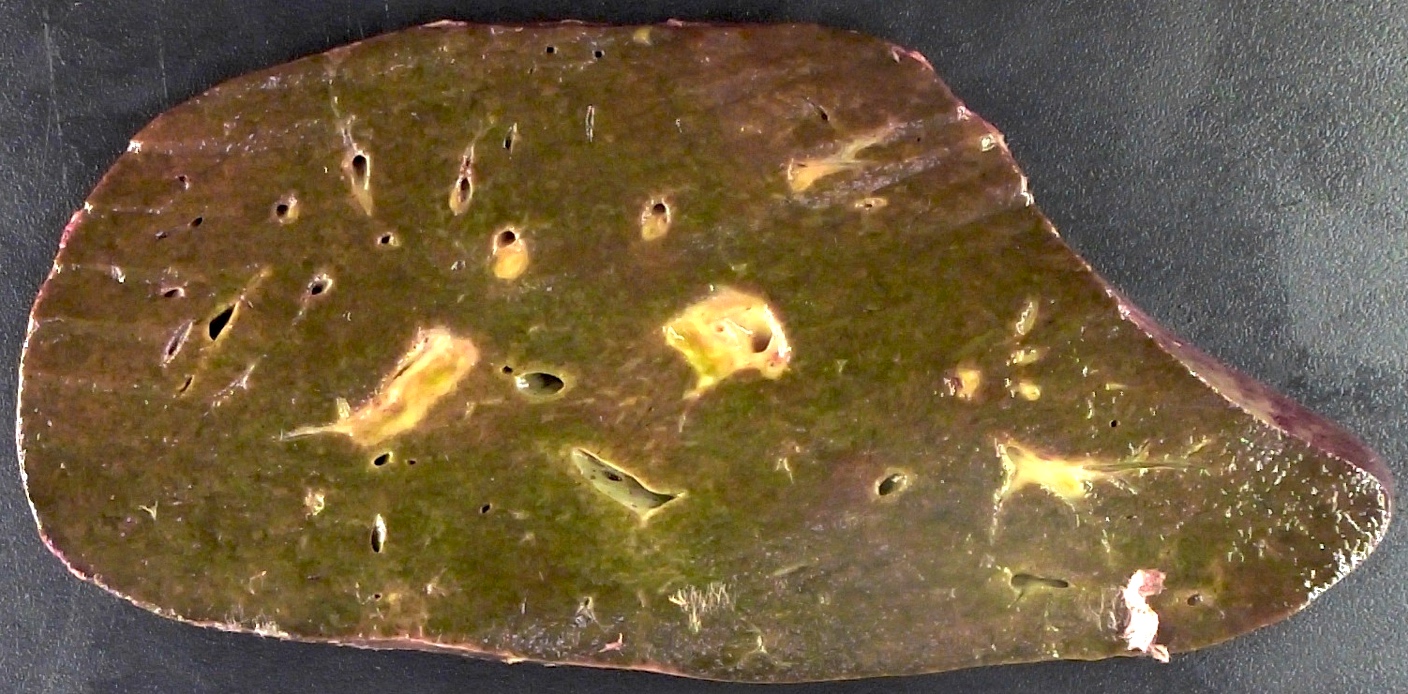
Gross description
- Description of the excised specimen
- Homogenously enlarged and congested, stretching Glisson capsule
- Cut surface is usually reddish brown but can be green-brown in cholestatic cases
- Reference: Saxena: Practical Hepatic Pathology, 2nd Edition, 2017
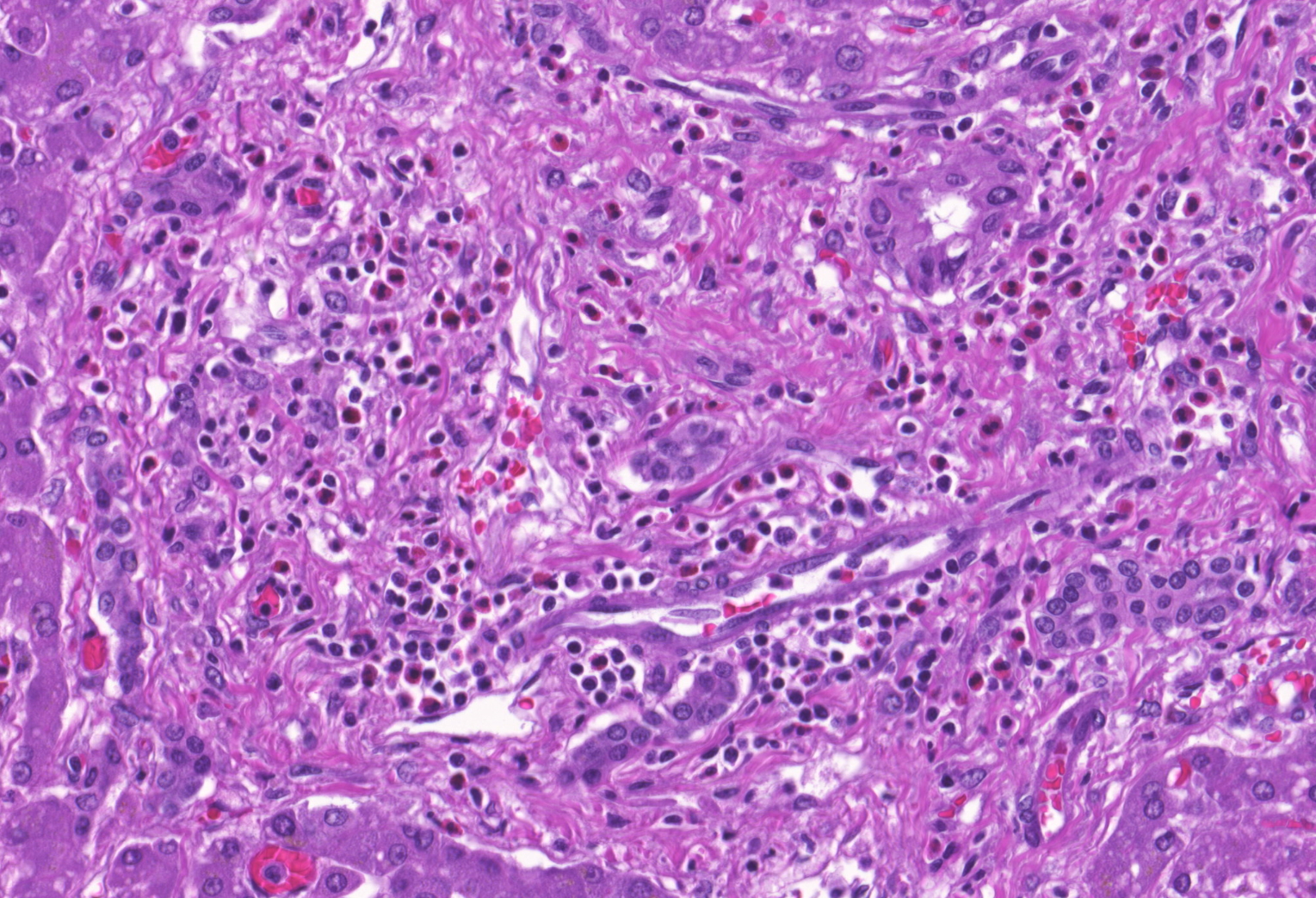
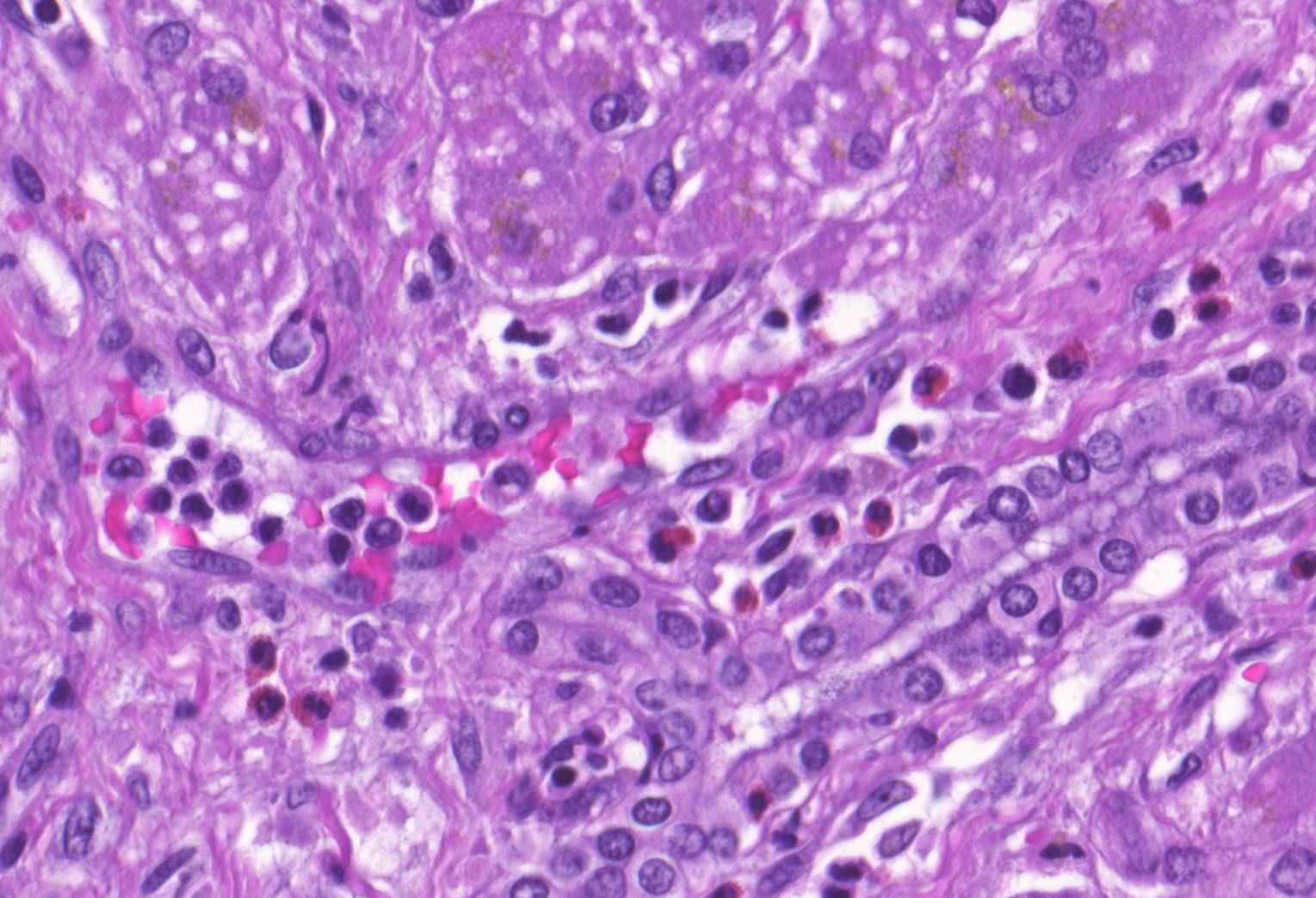
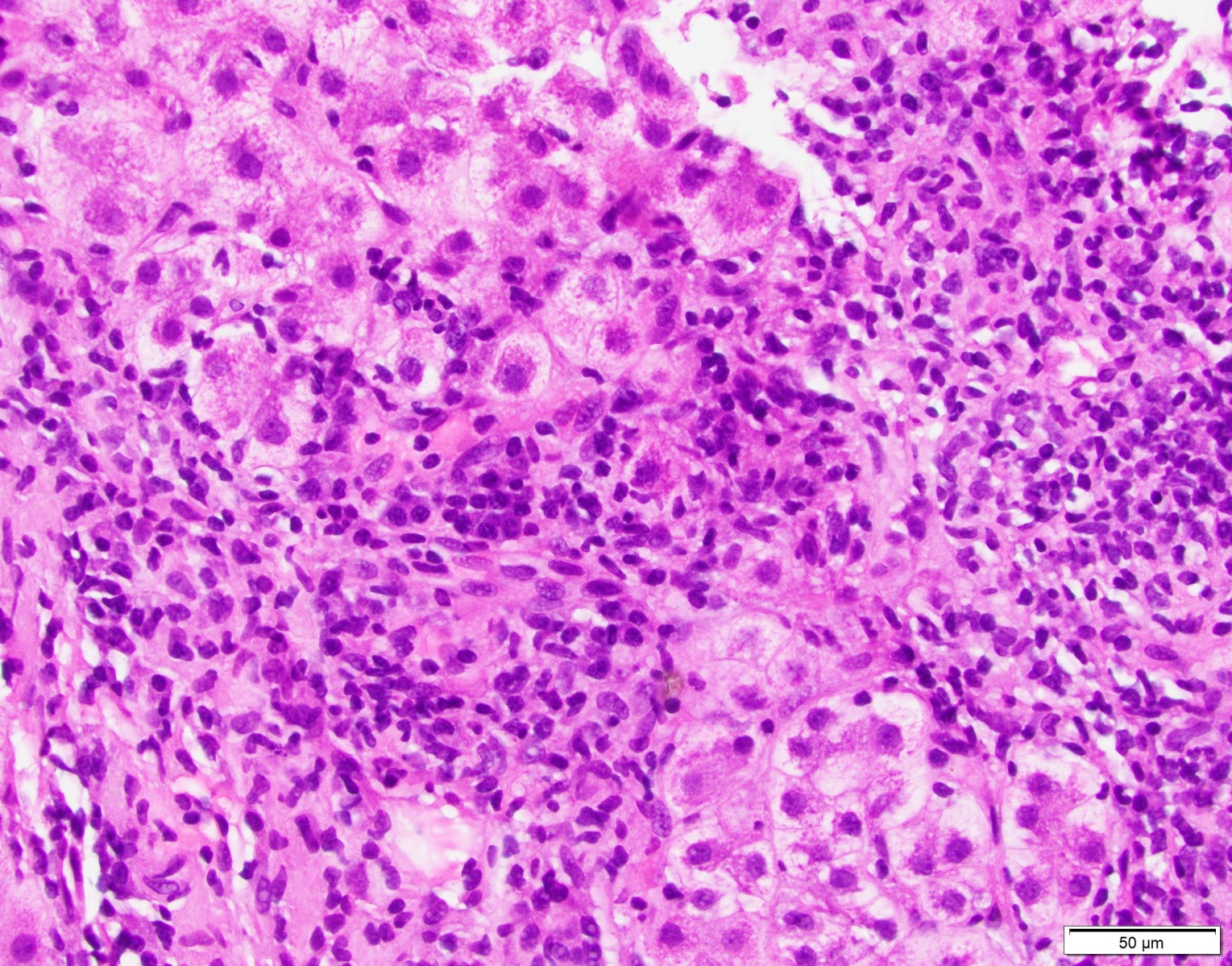
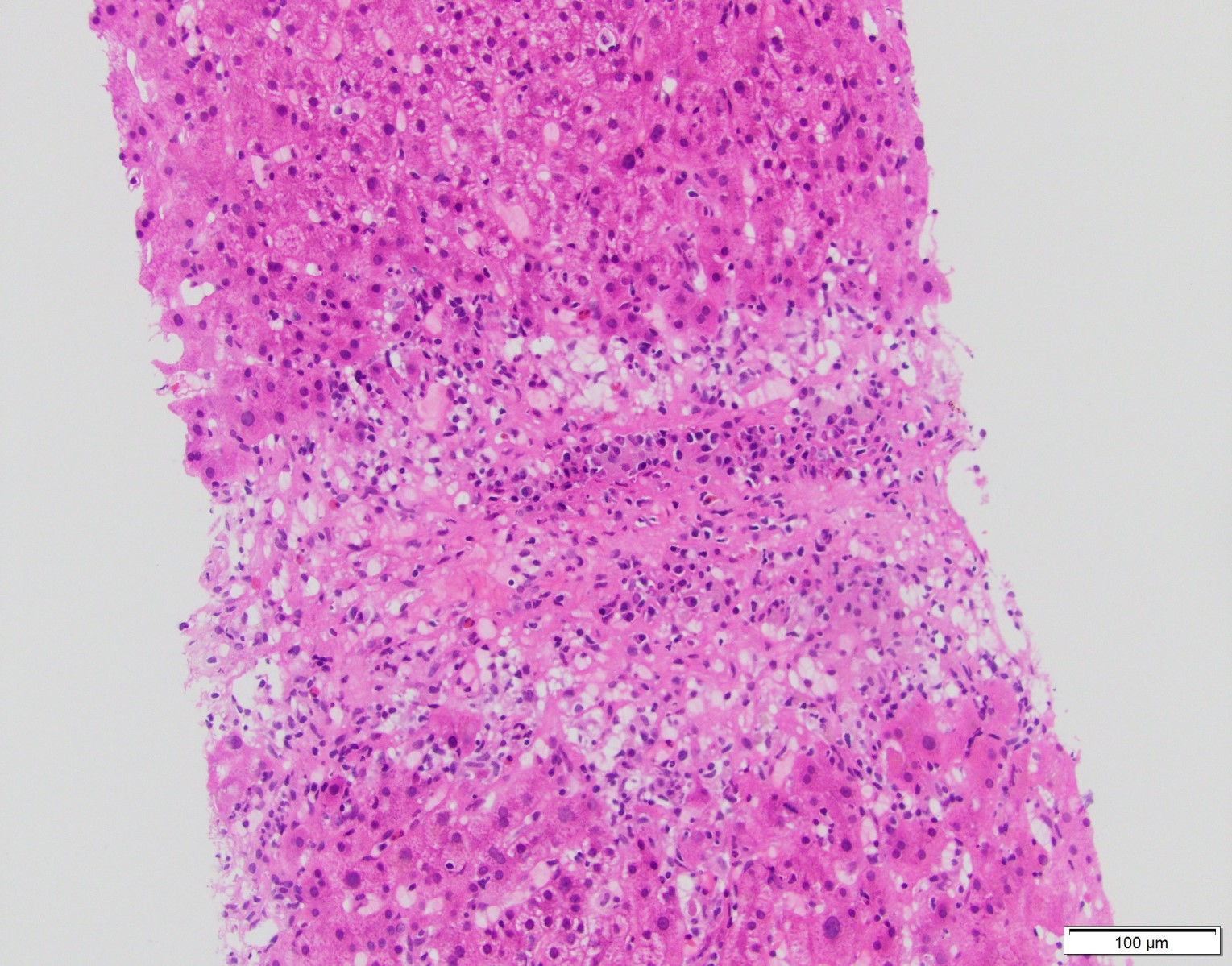
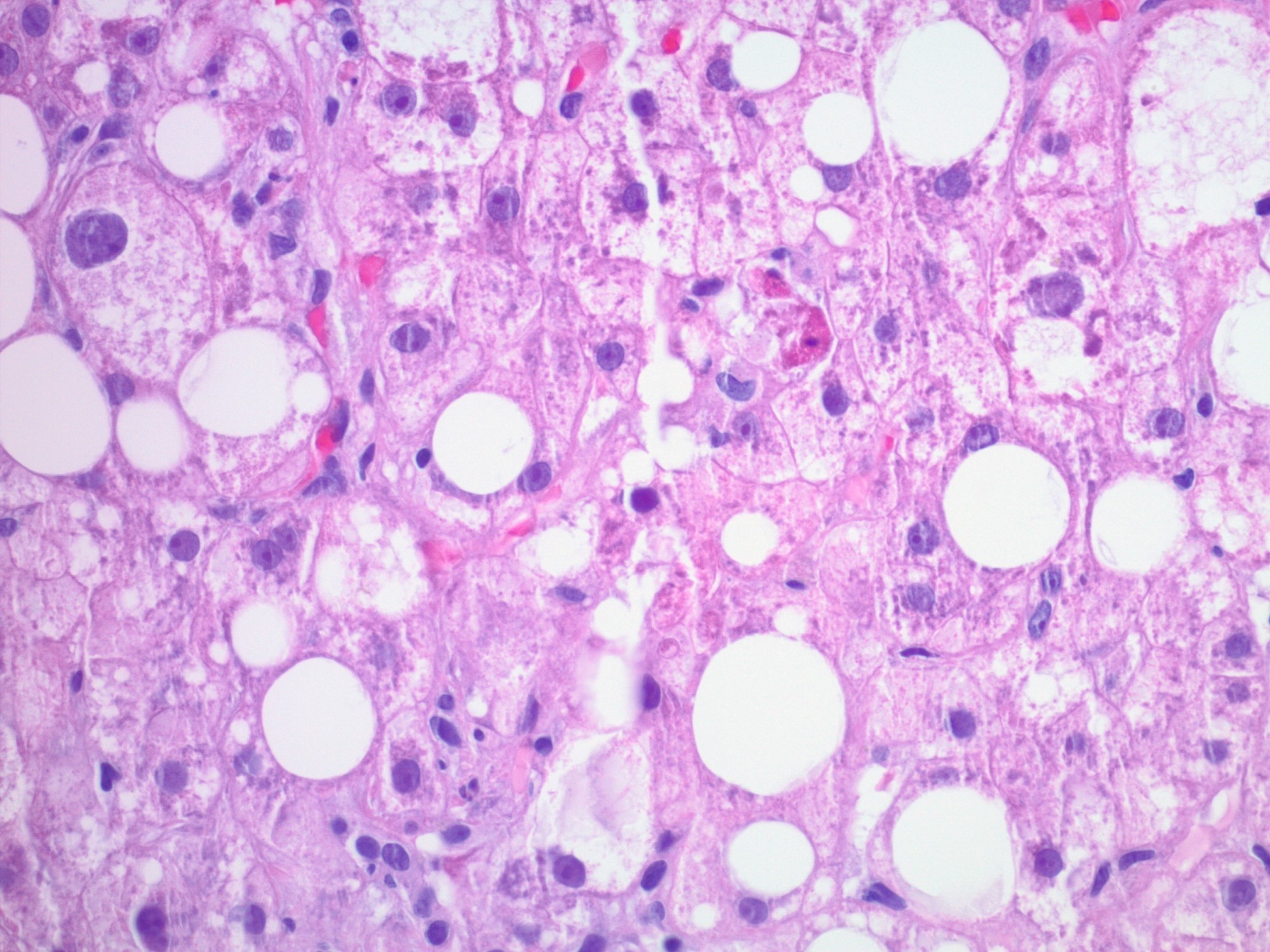
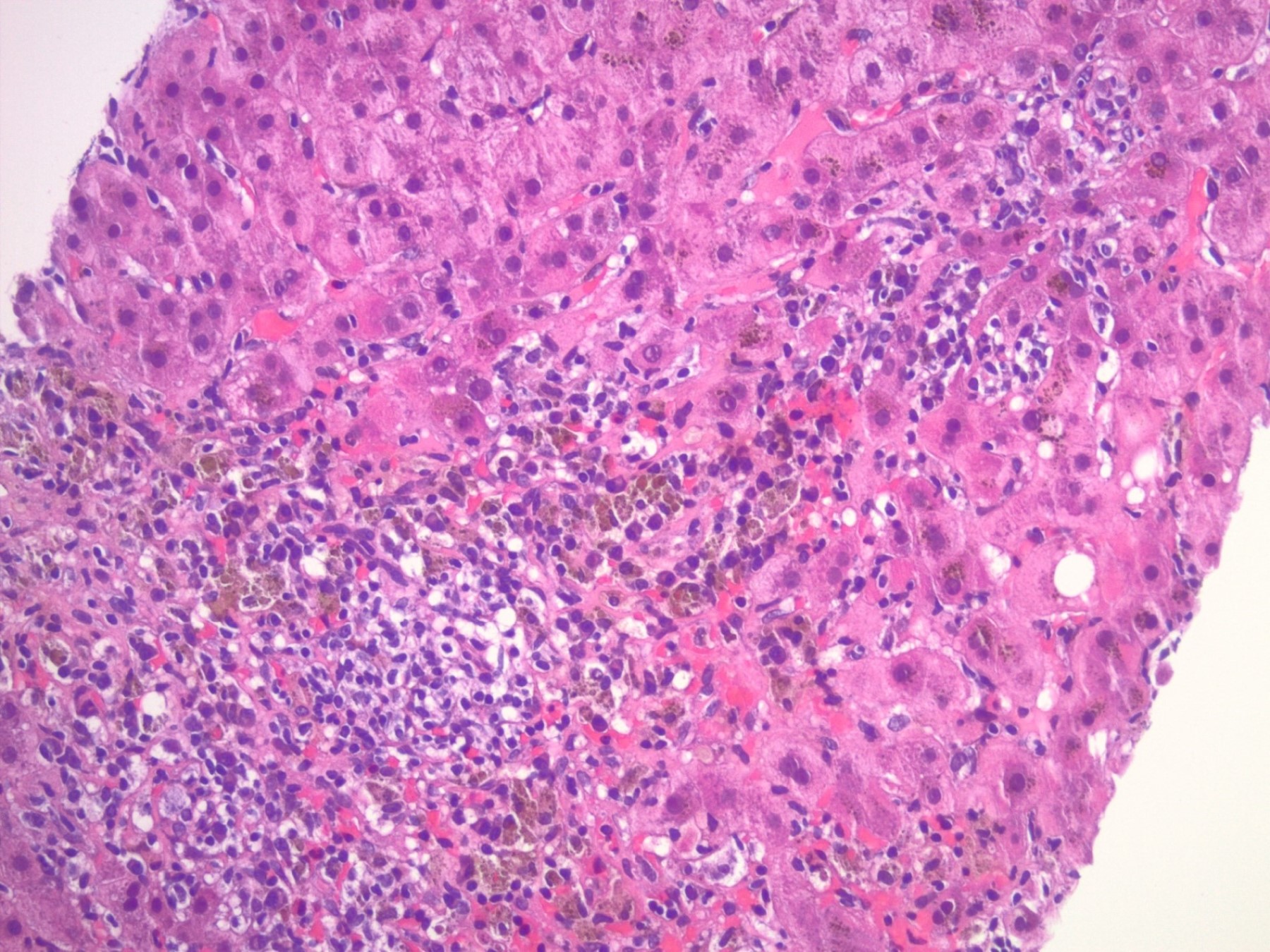
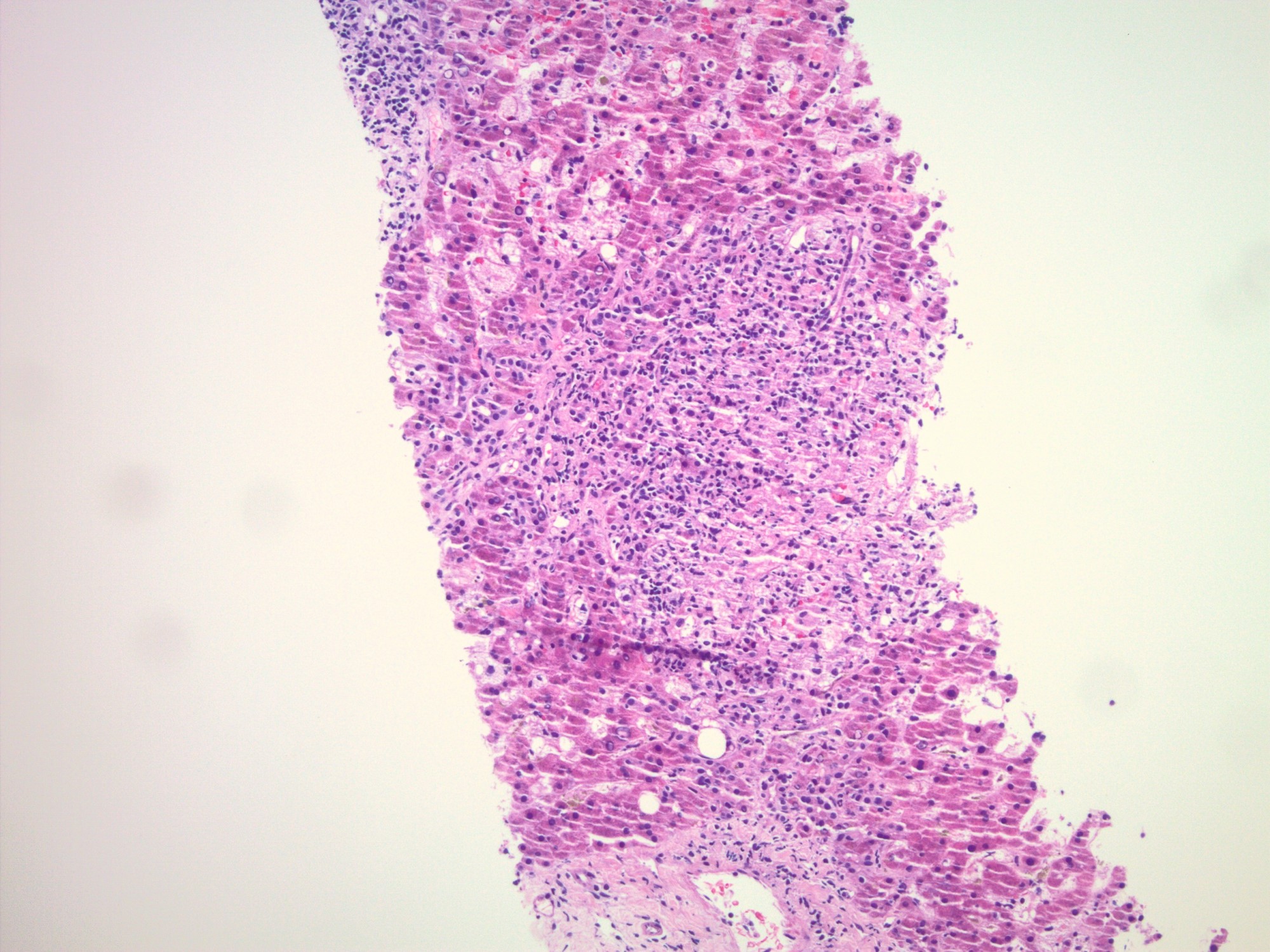
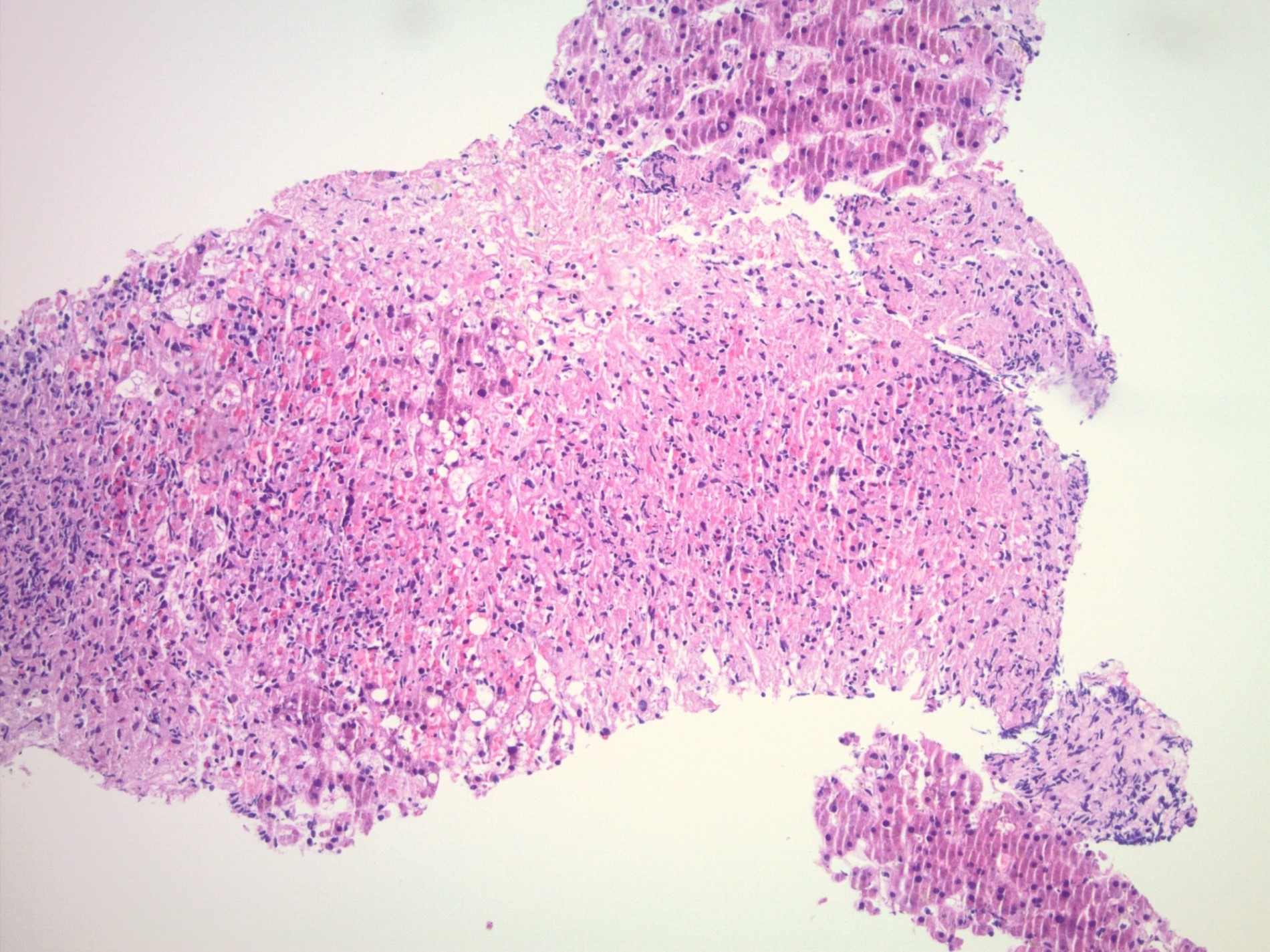
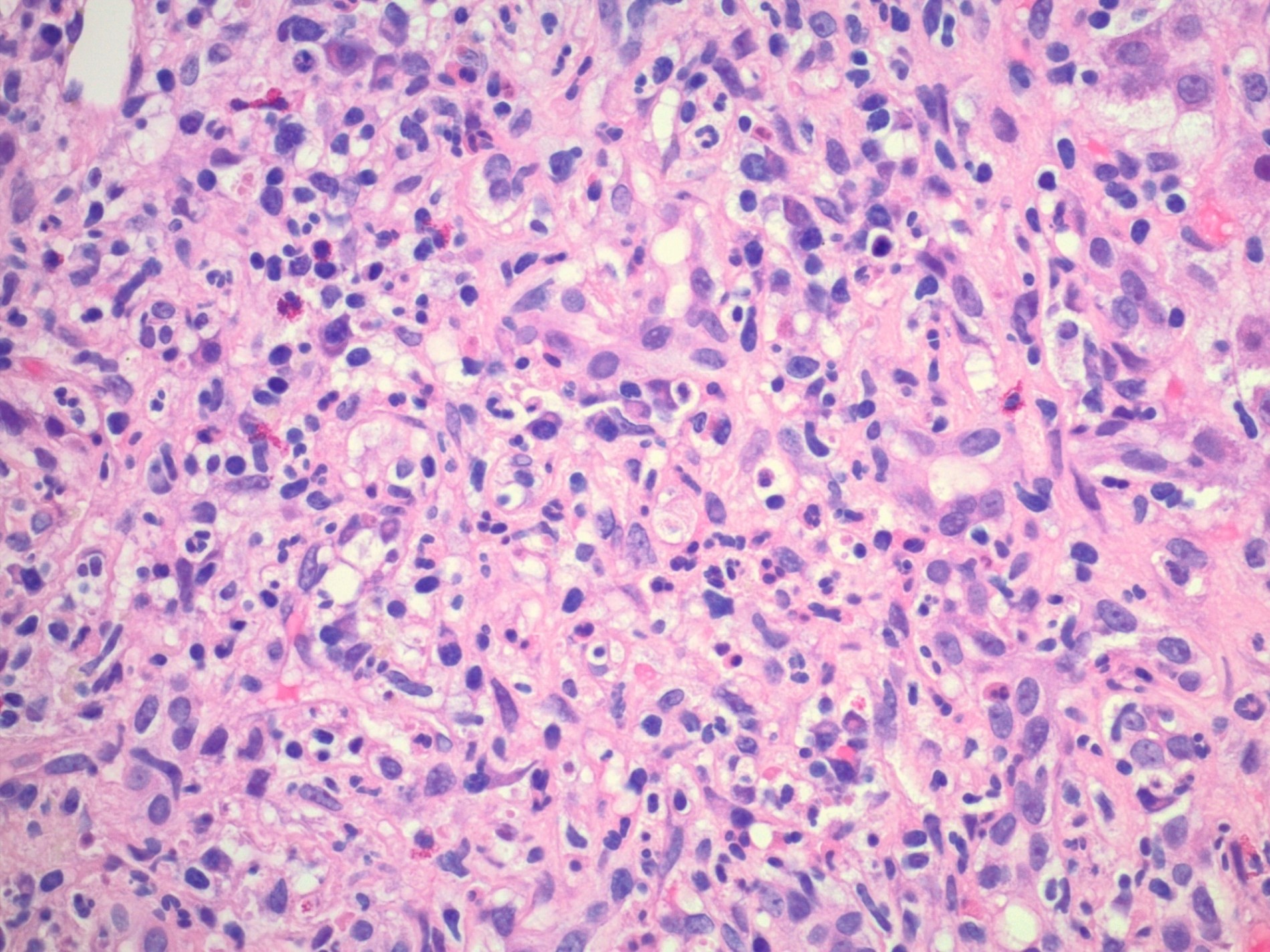
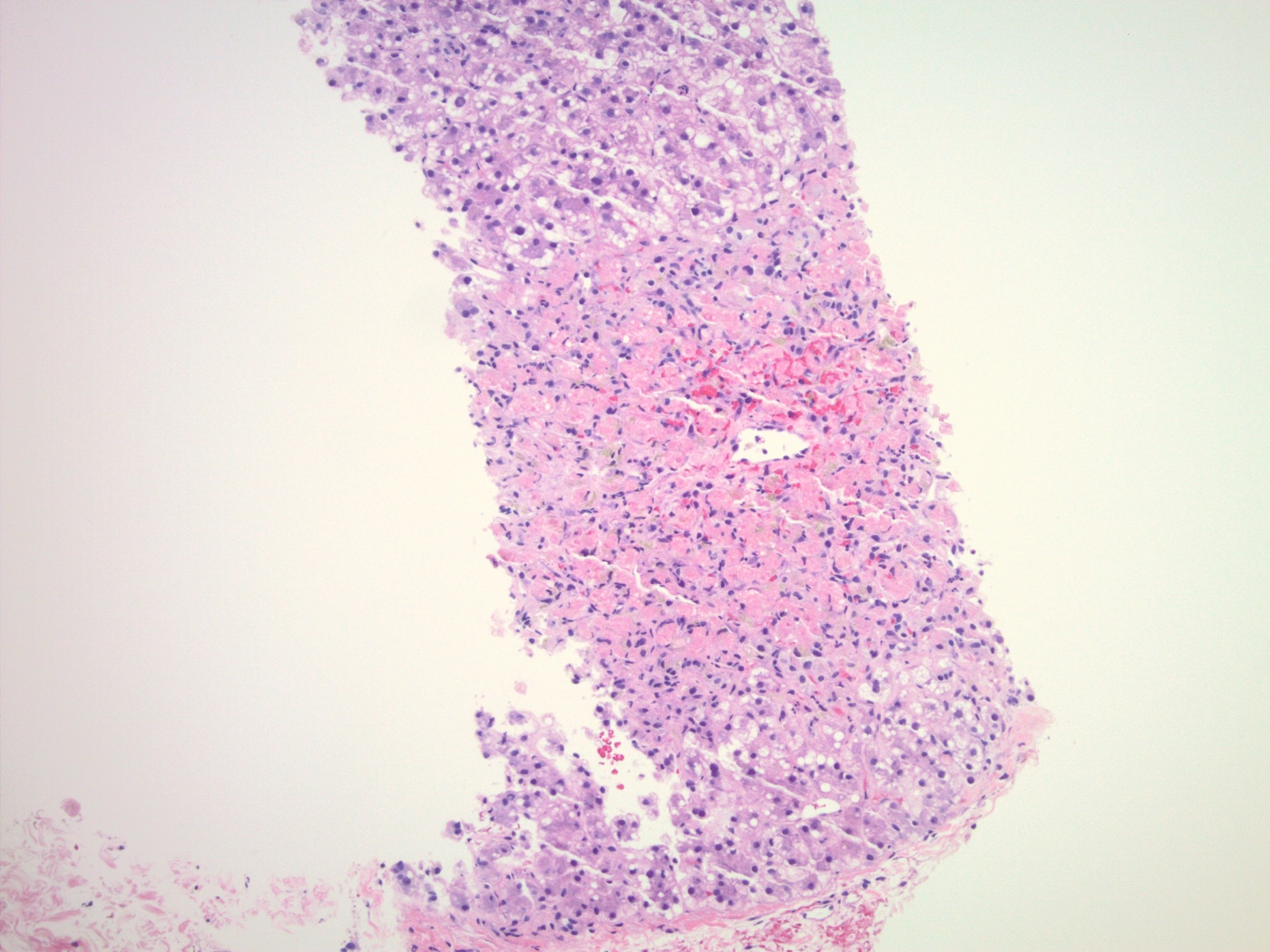
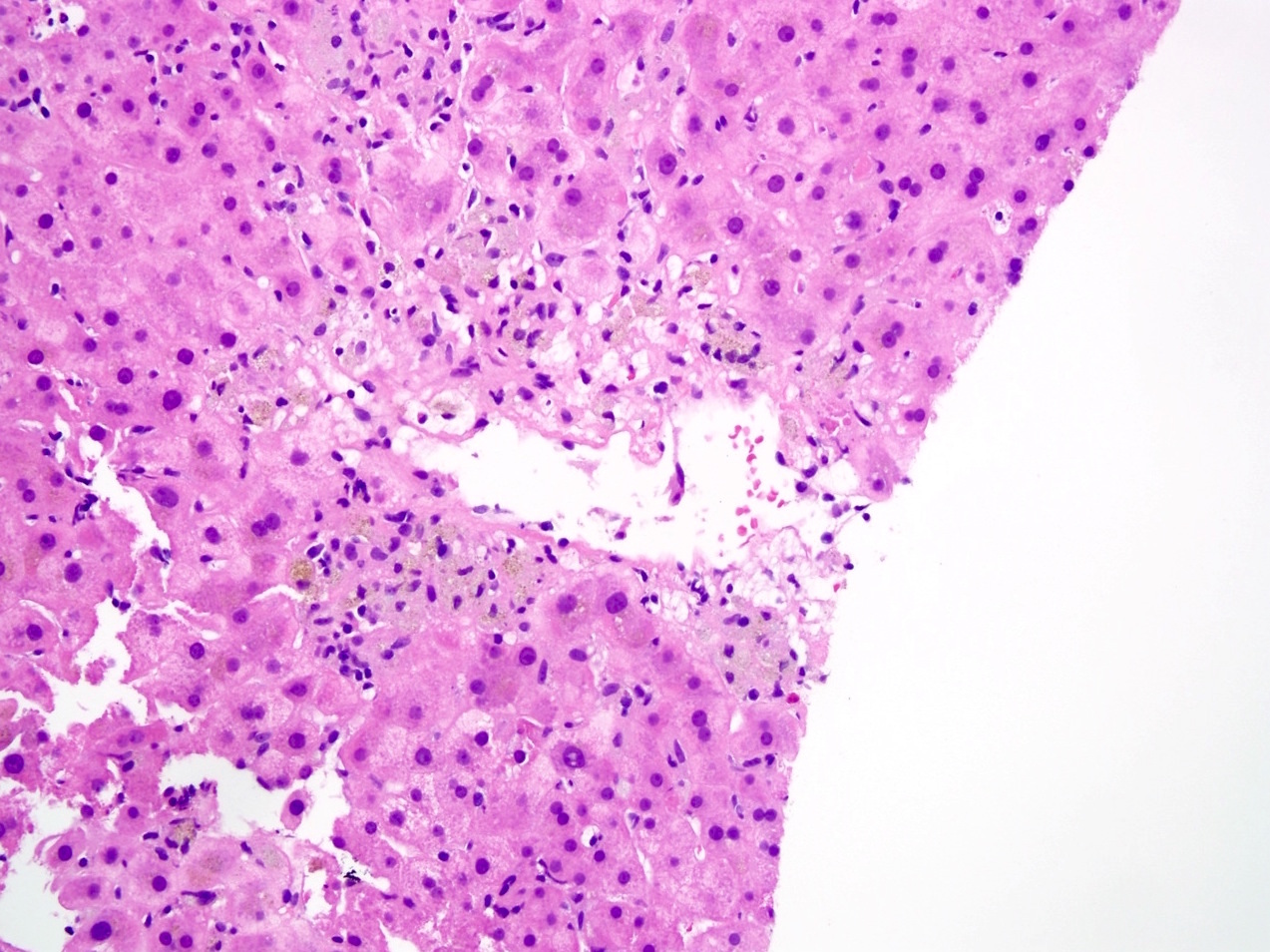
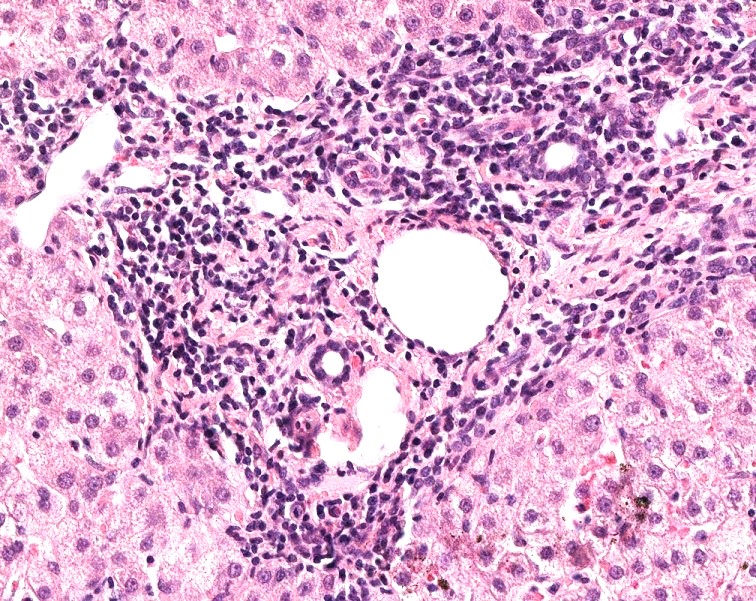
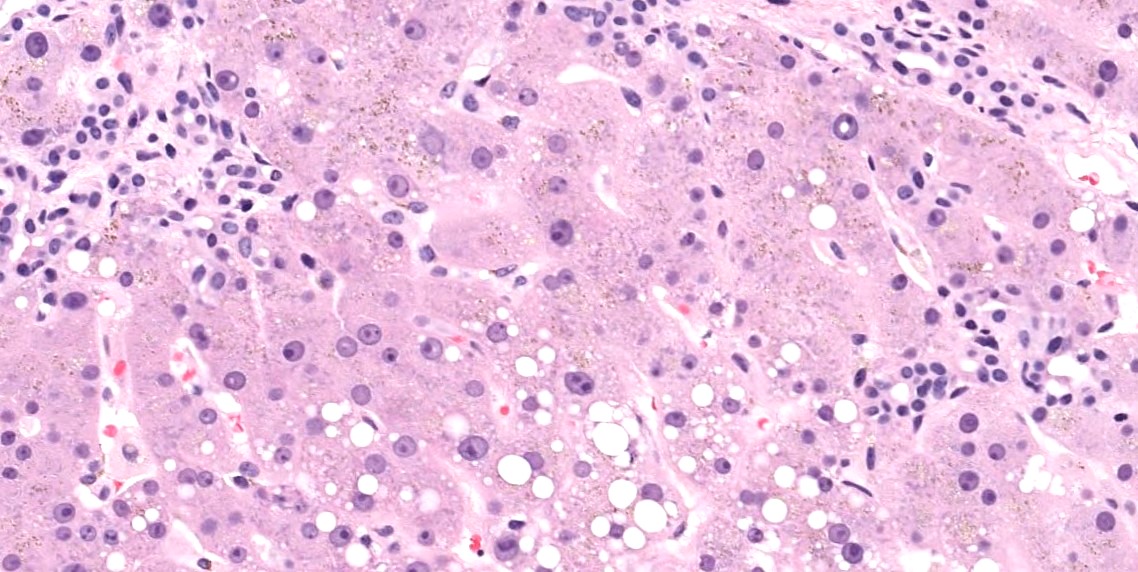
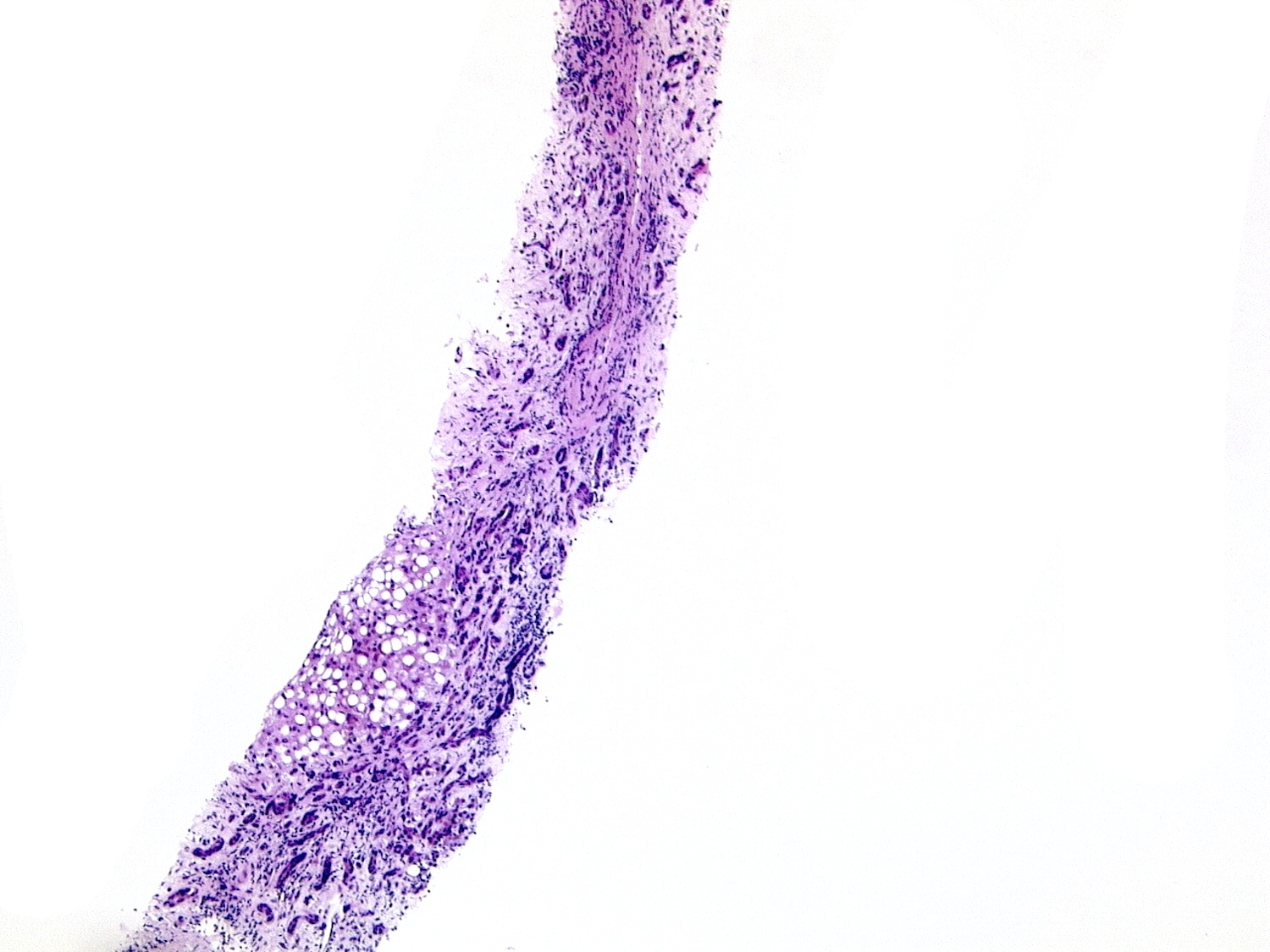
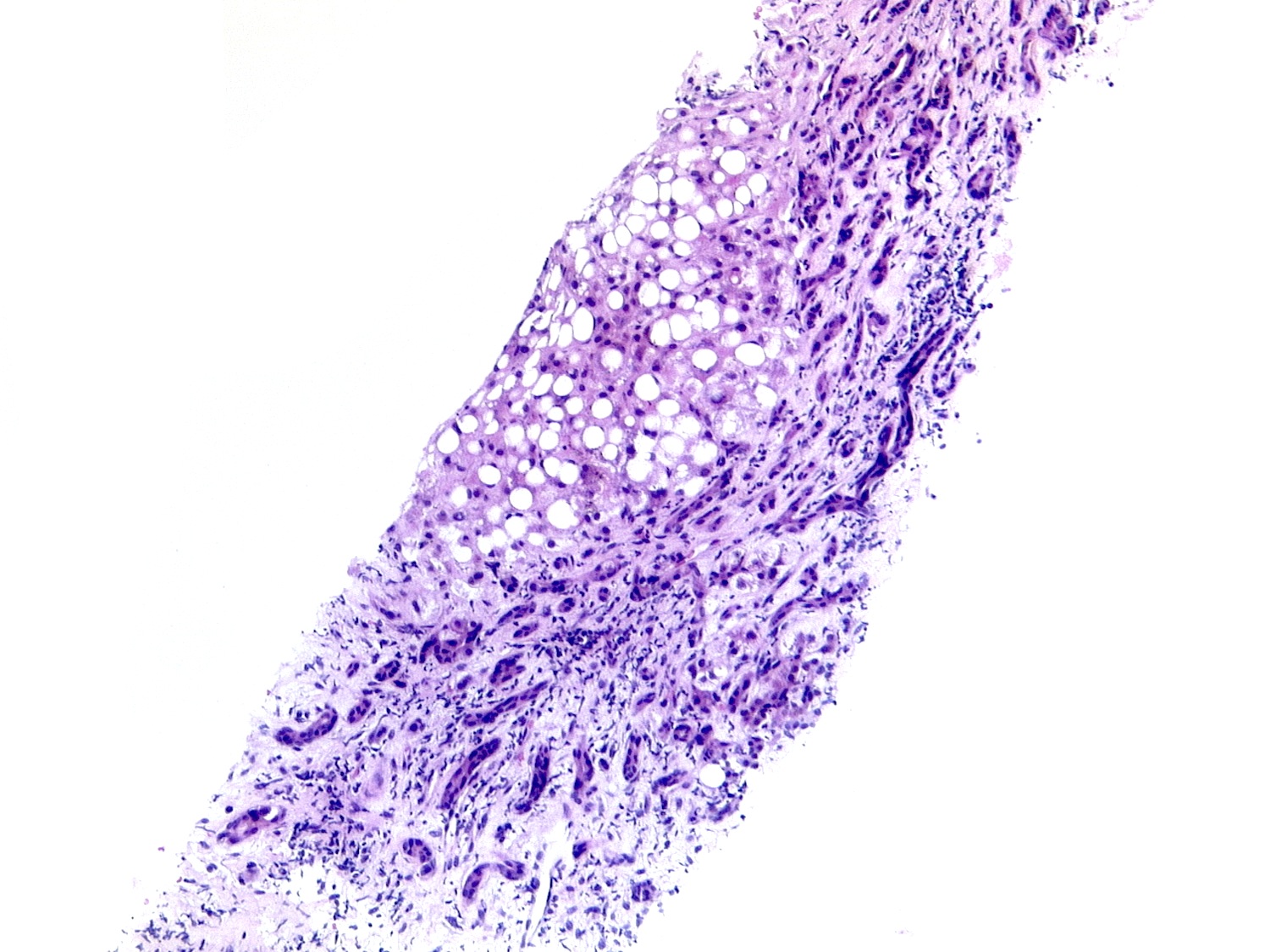
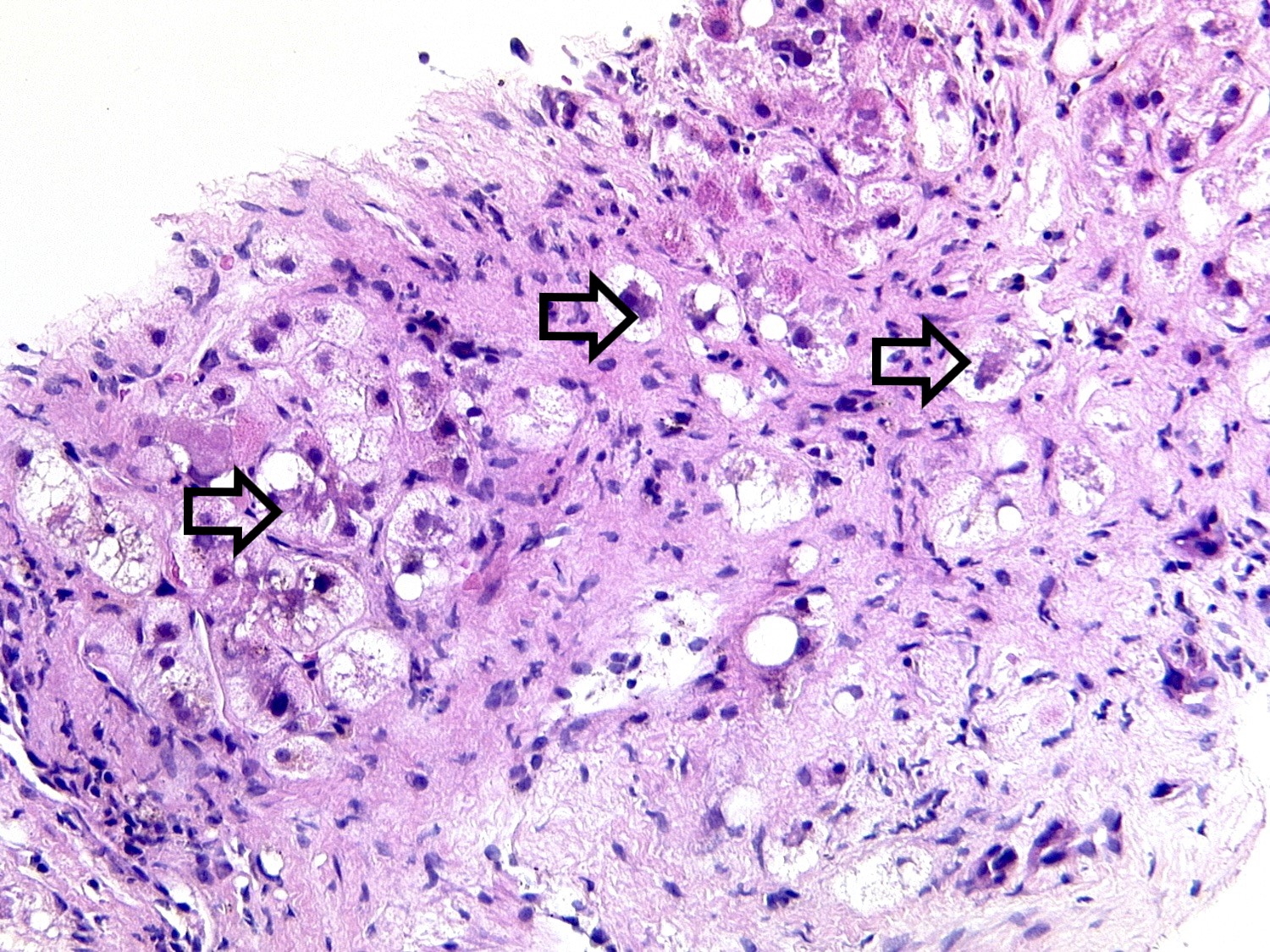
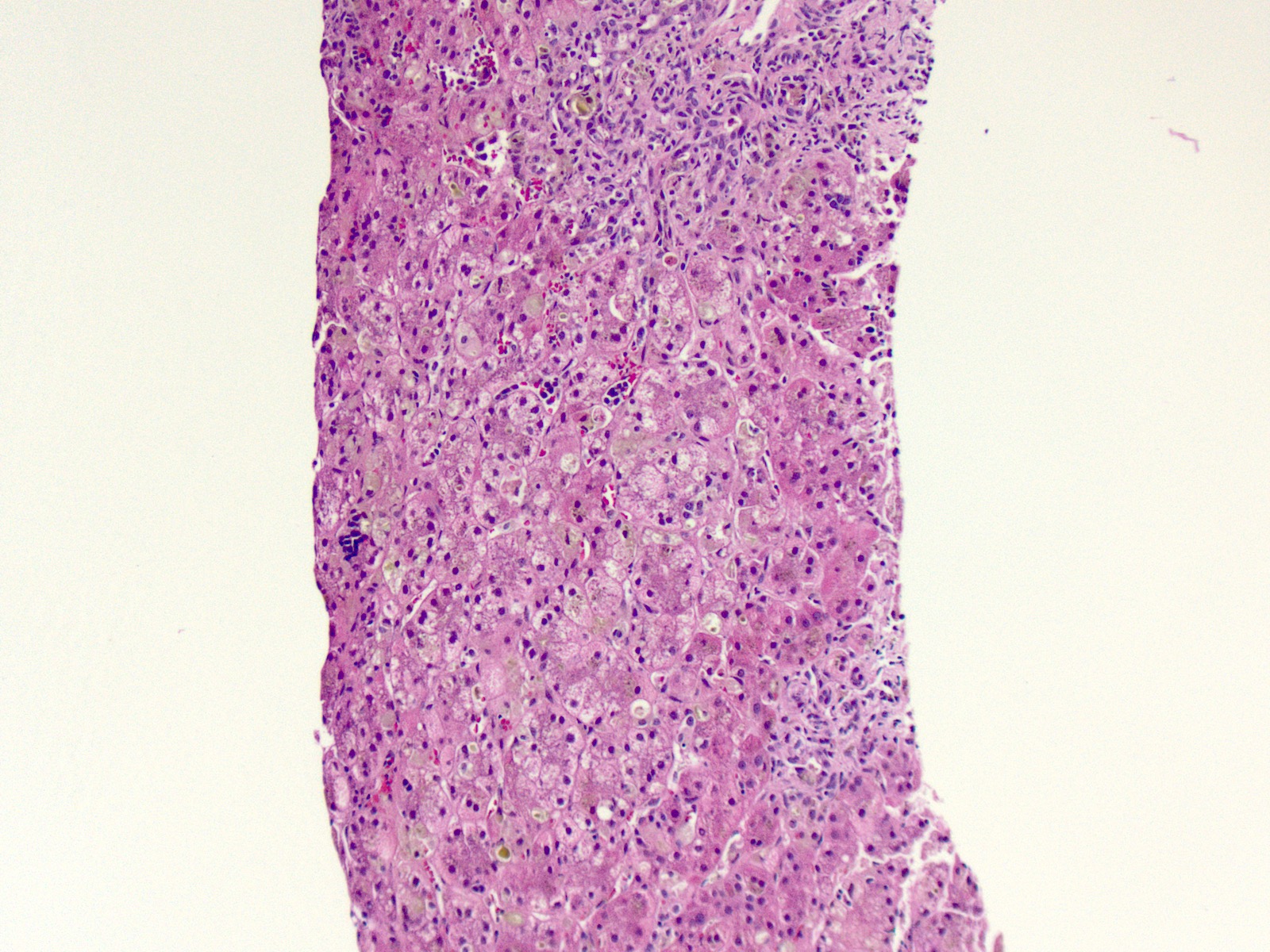
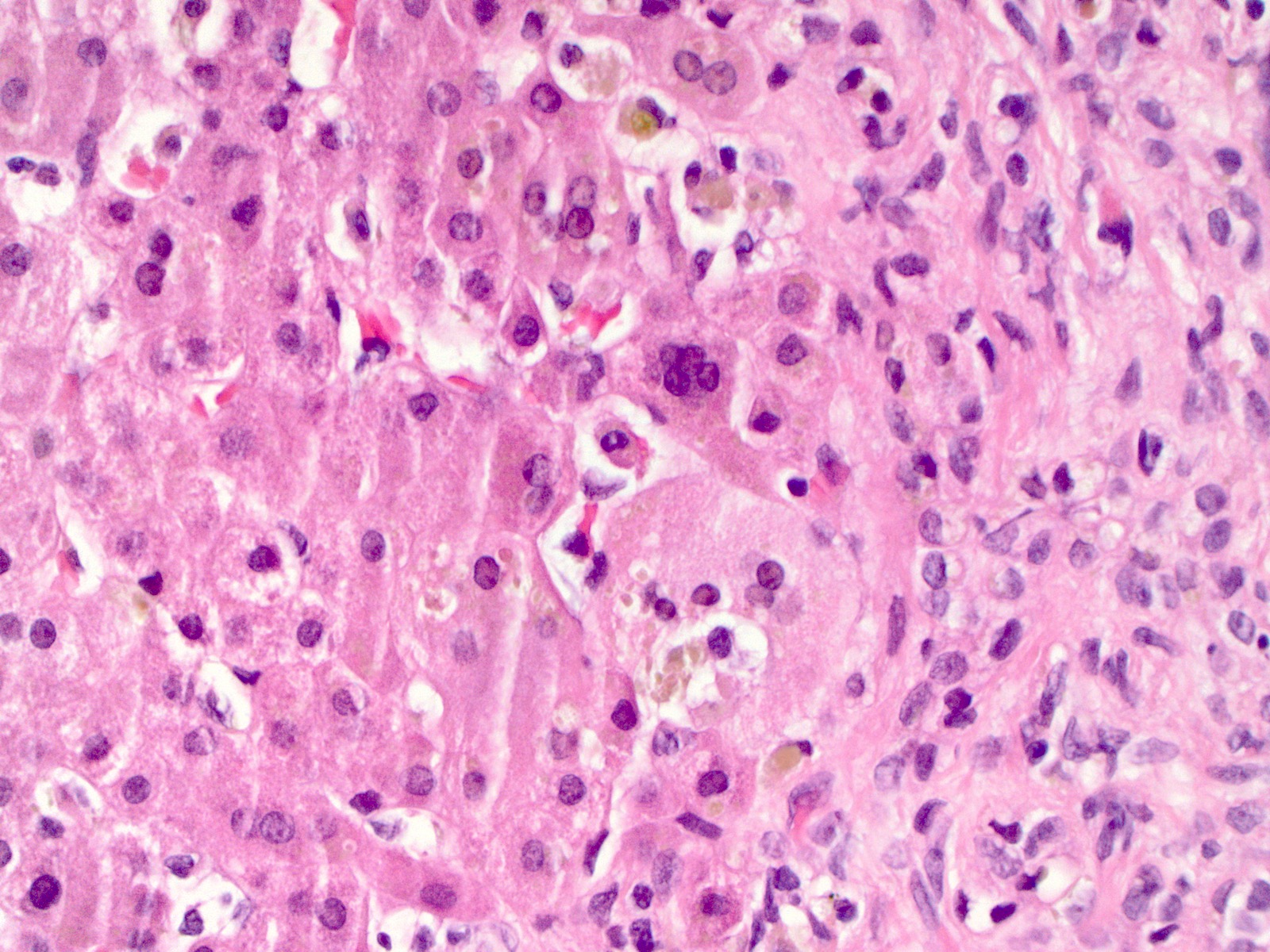
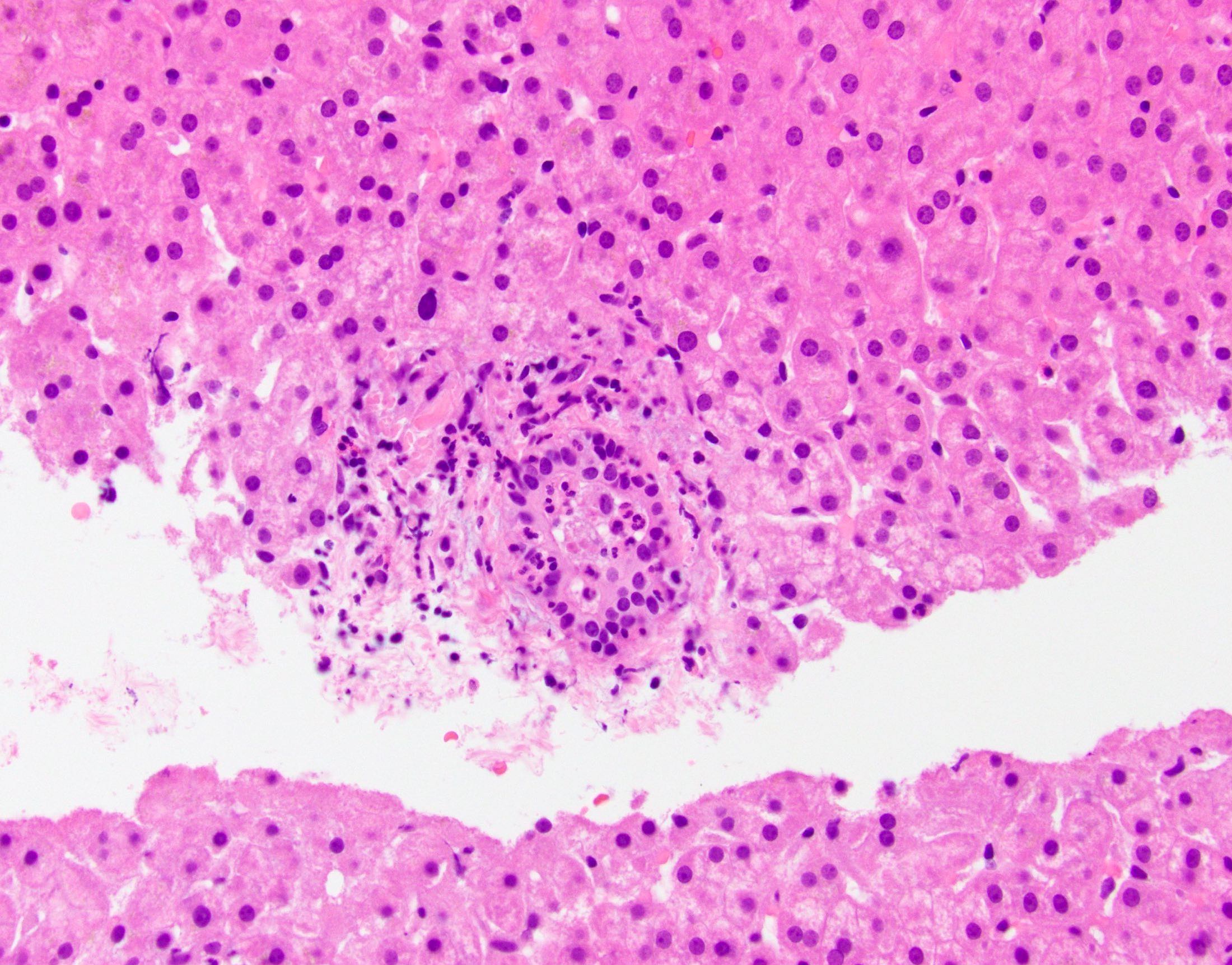
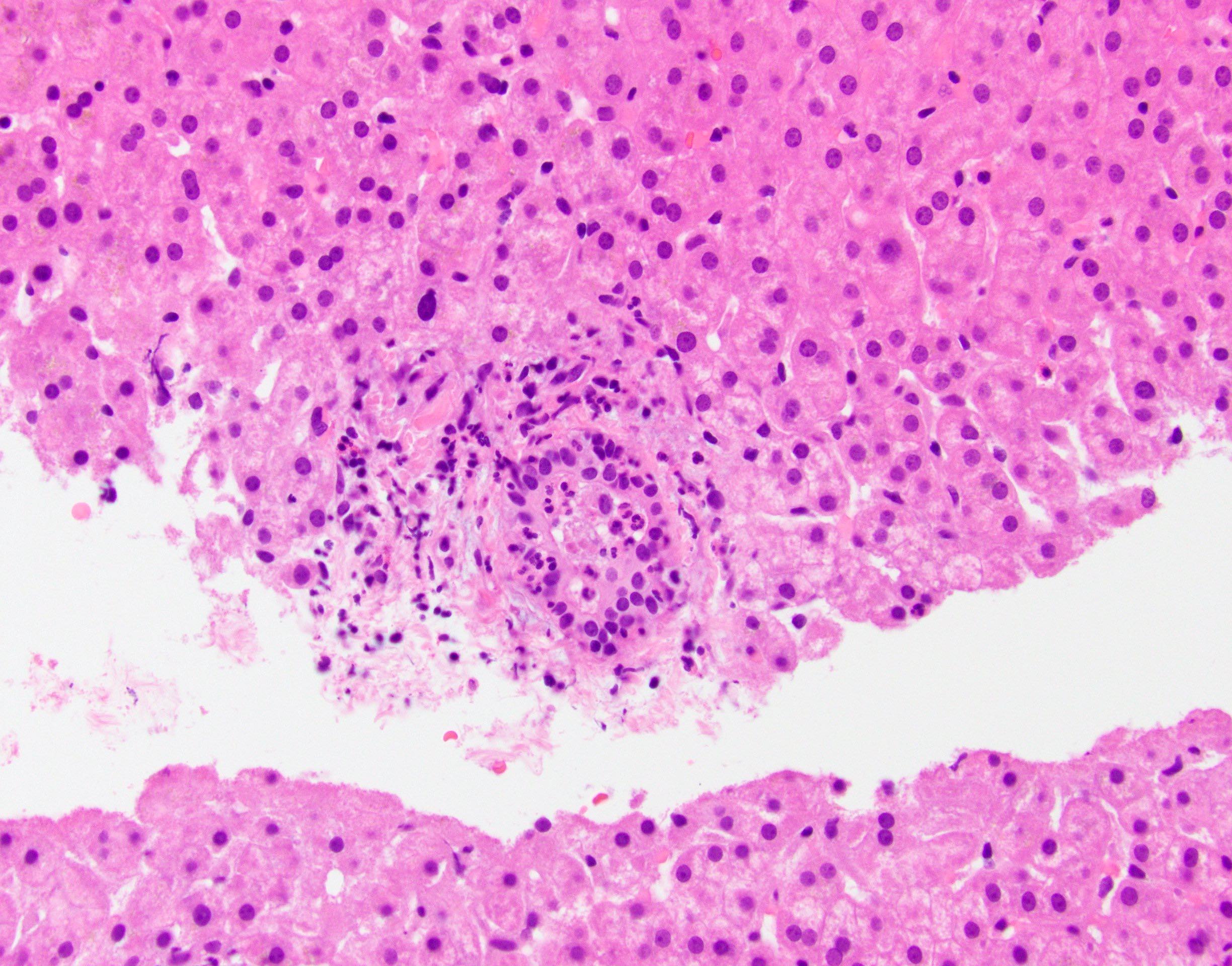
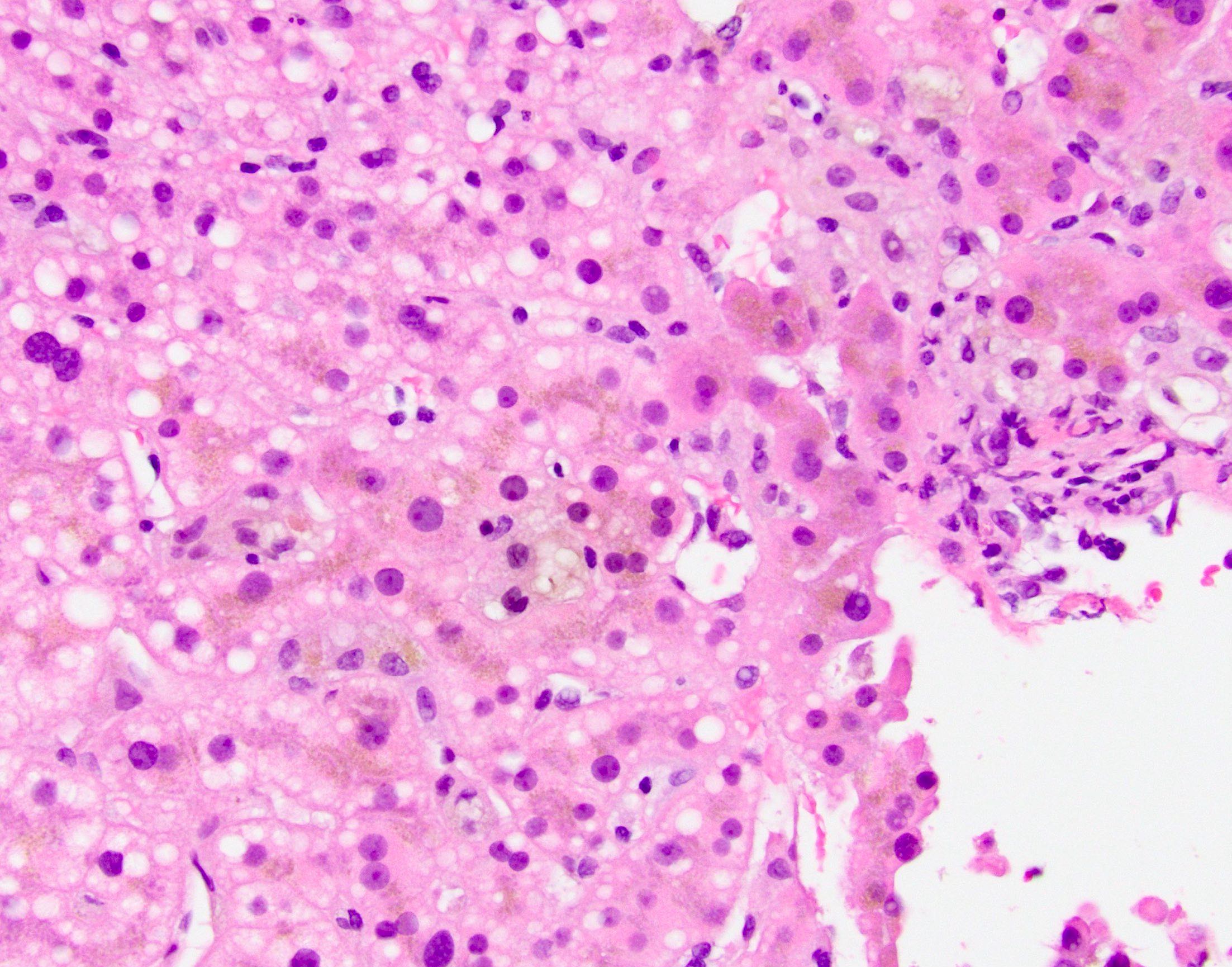
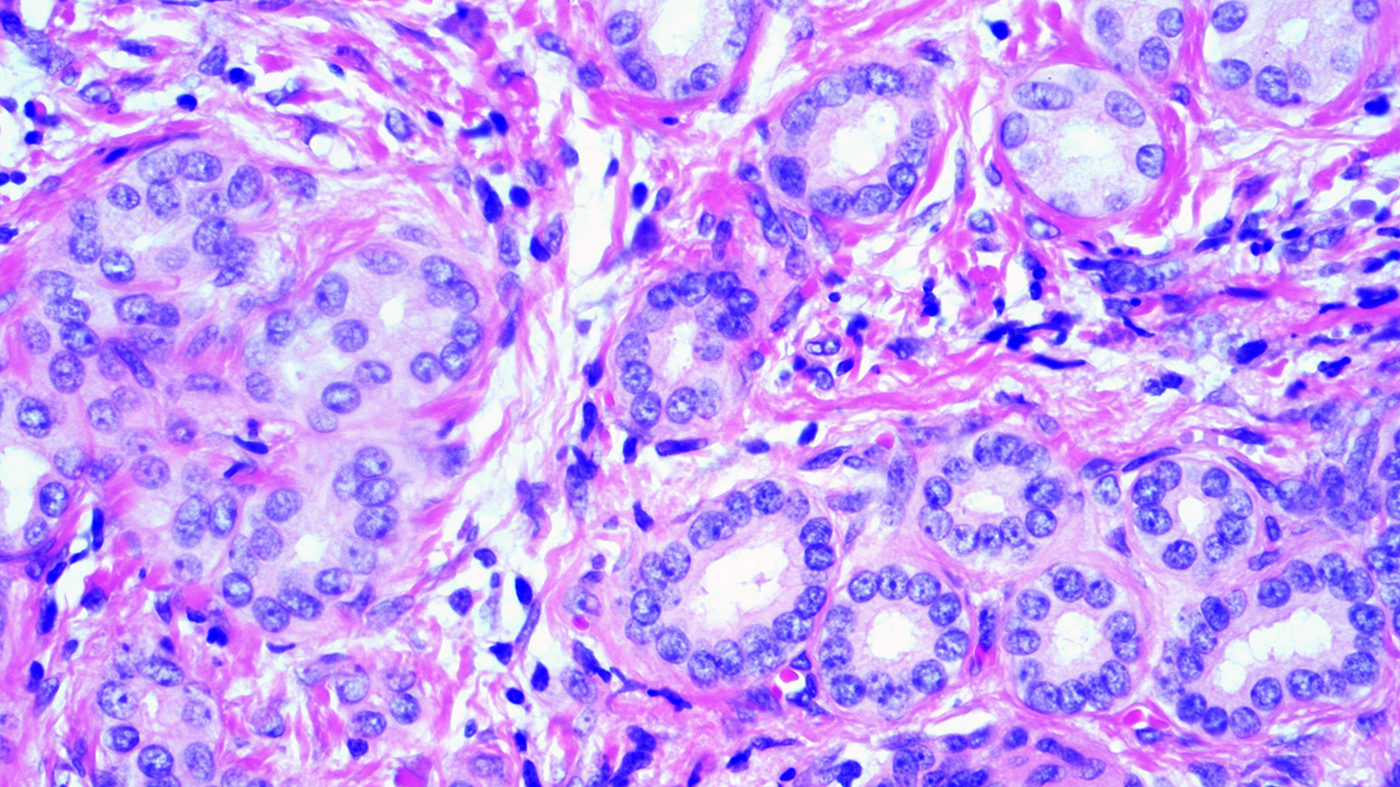
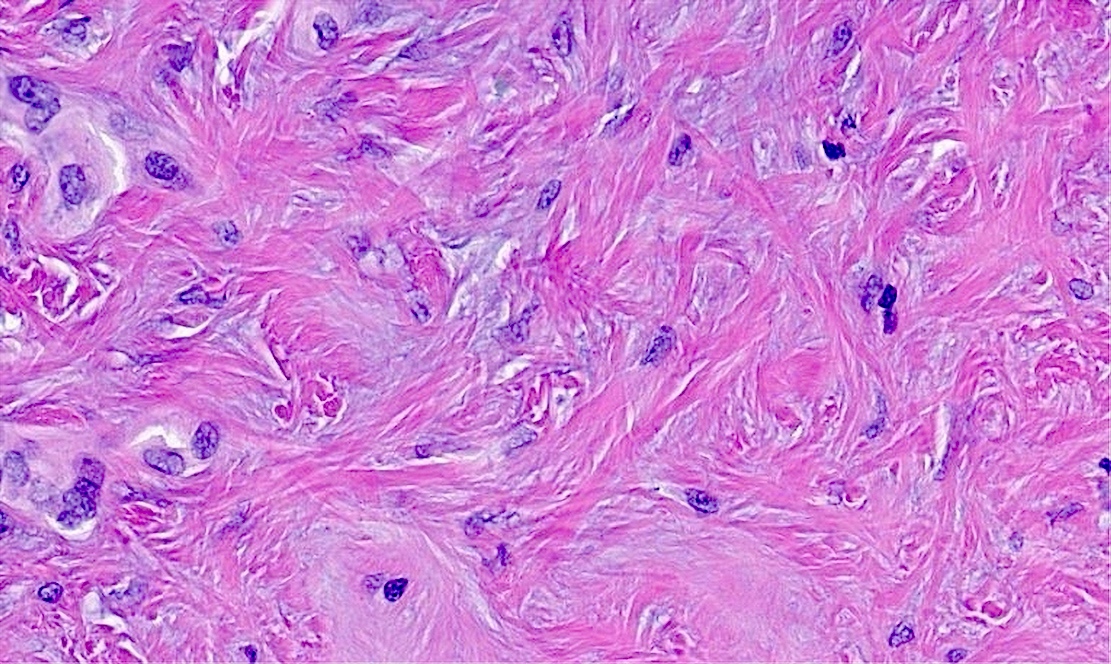
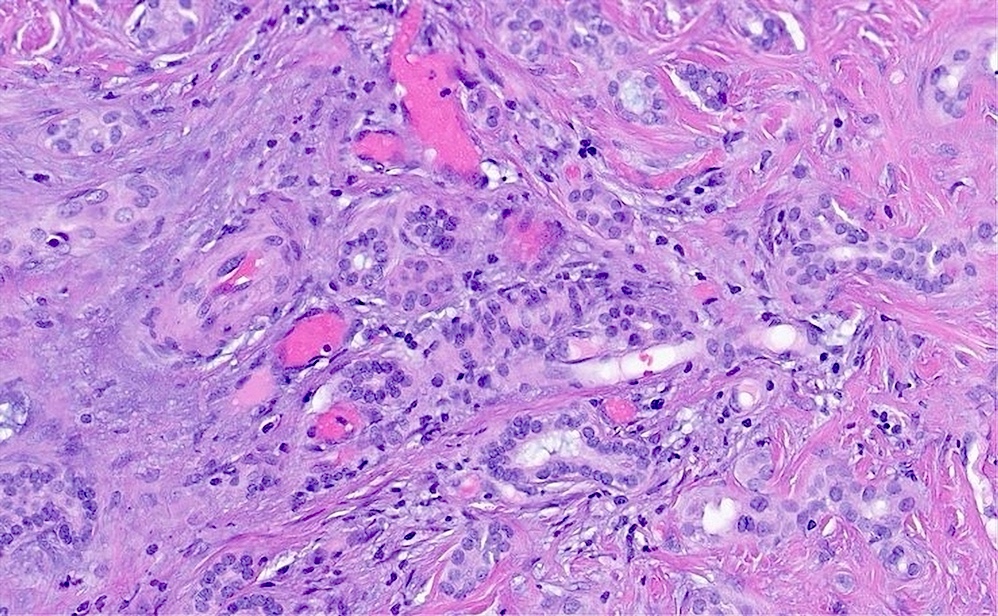
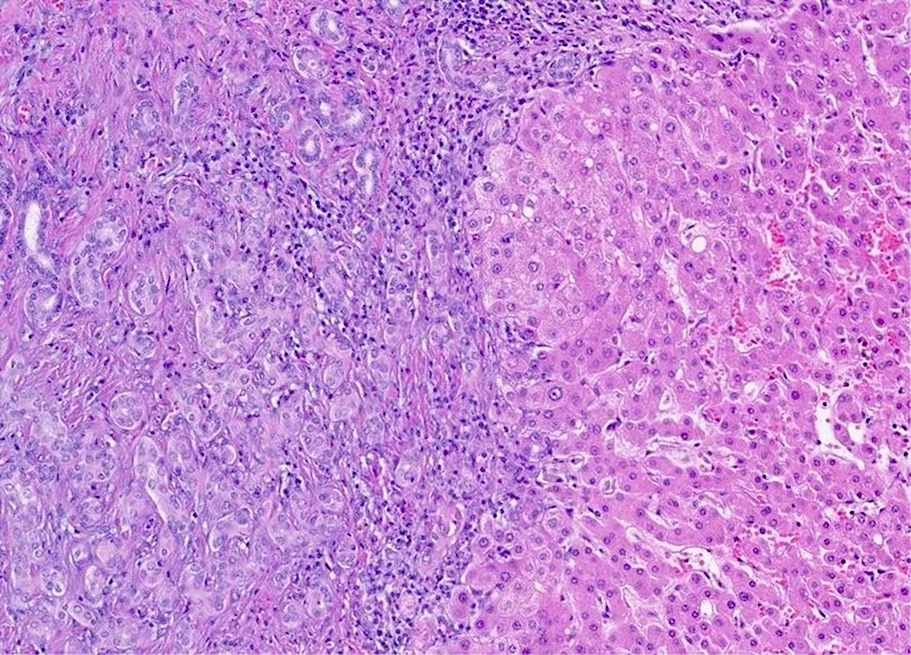
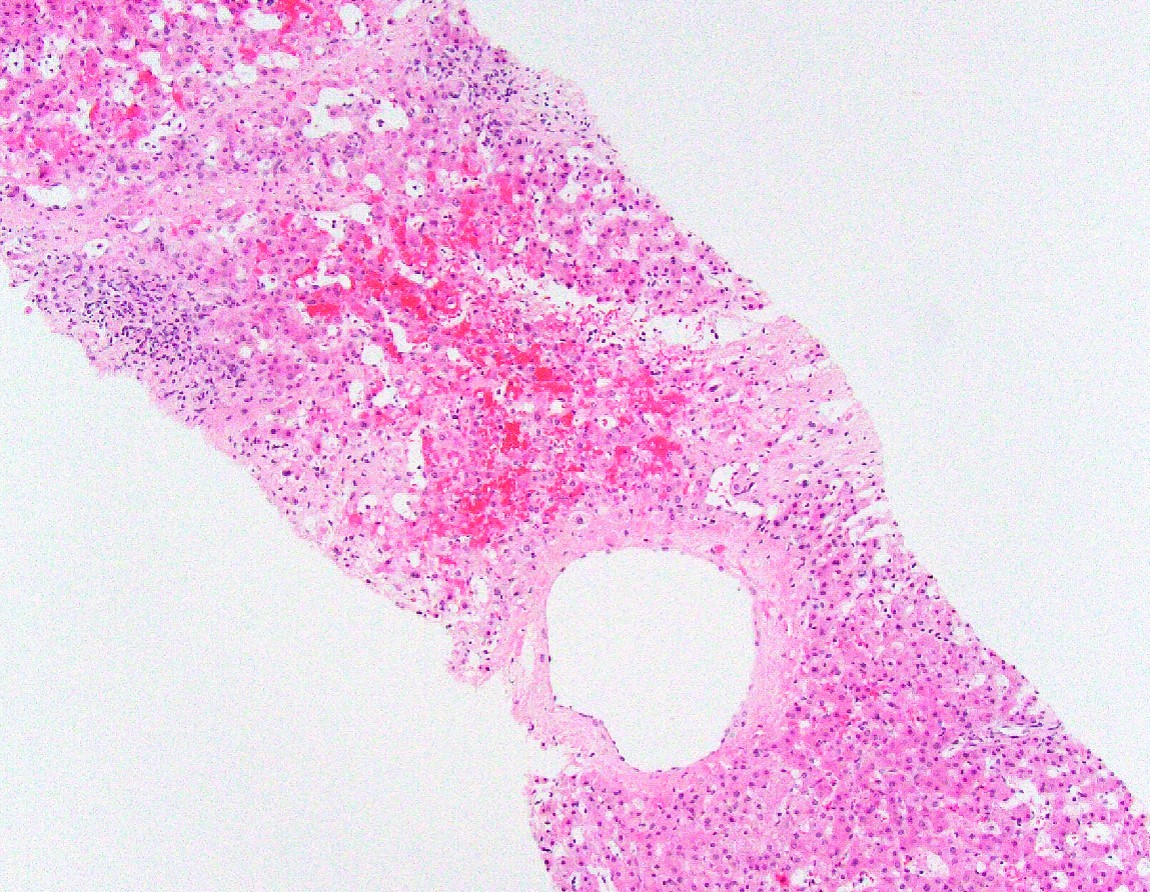
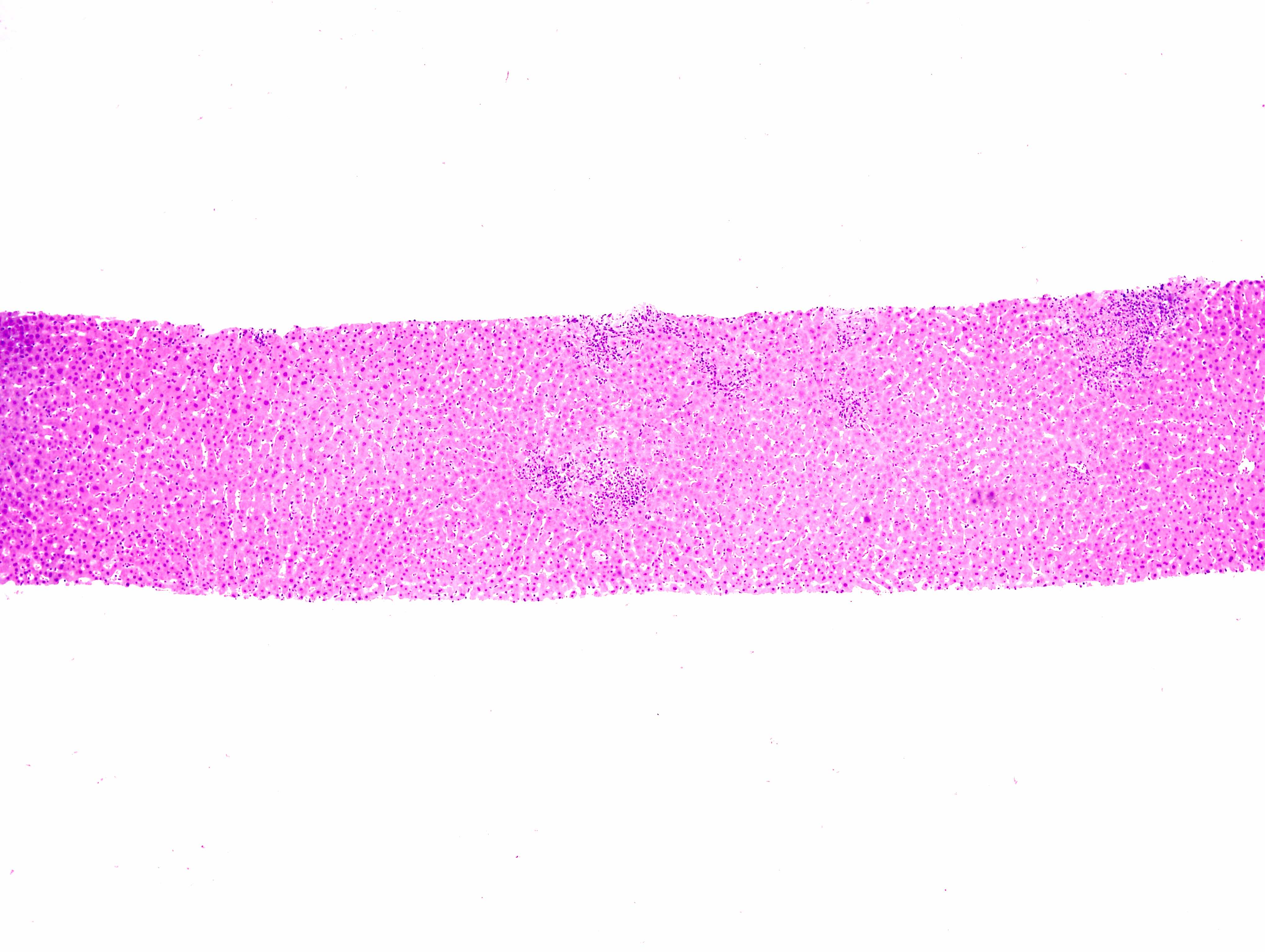
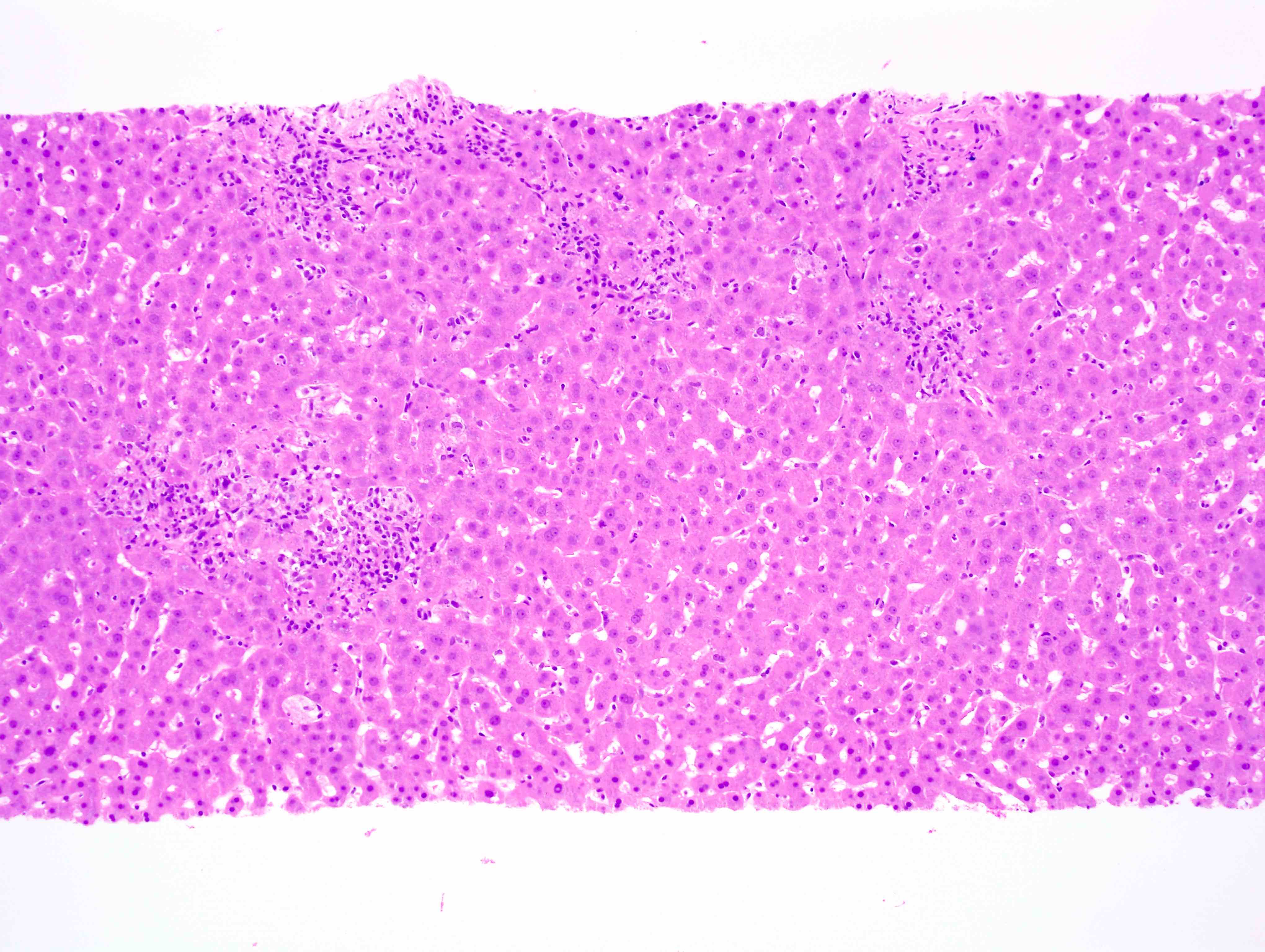
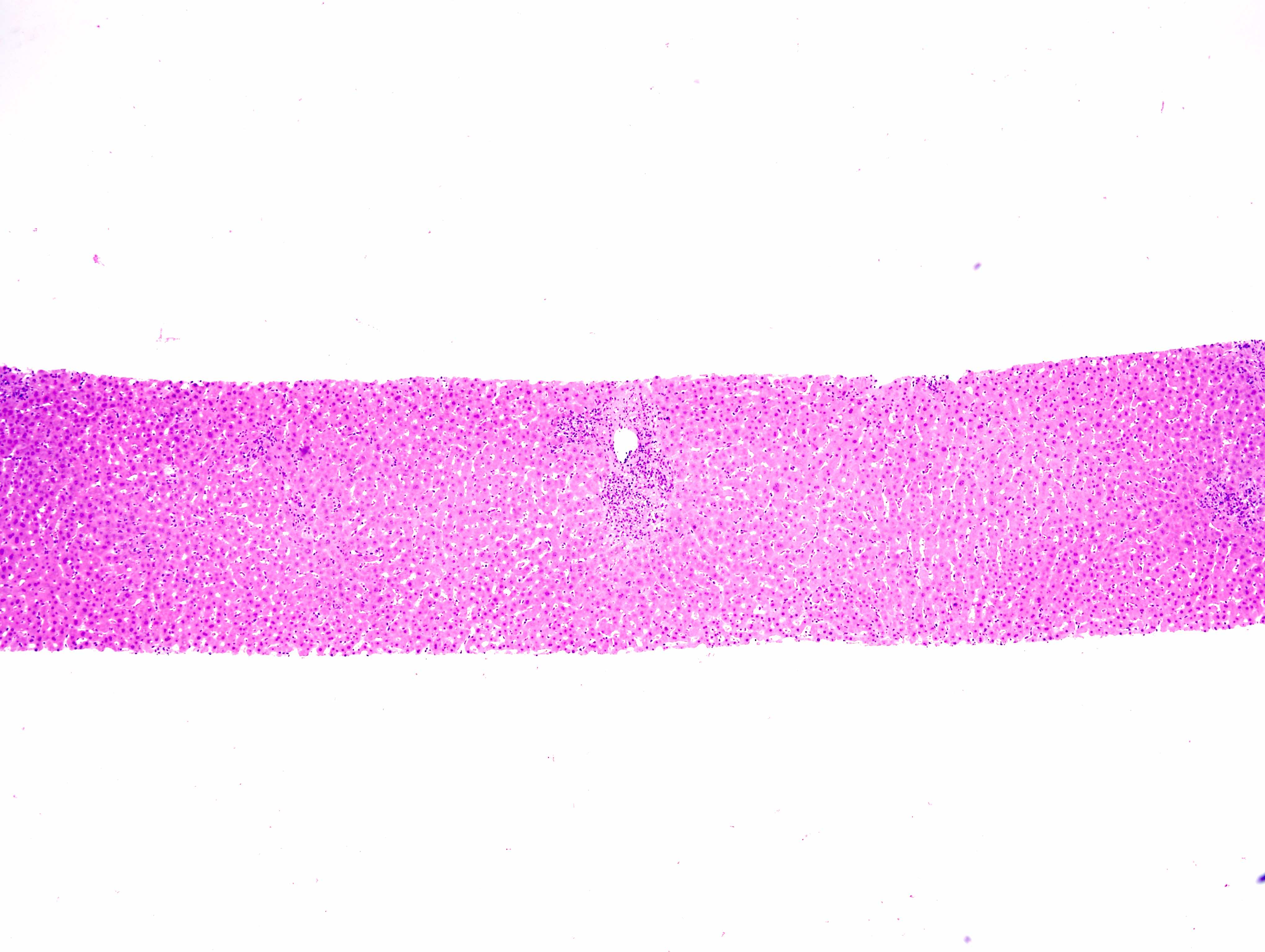
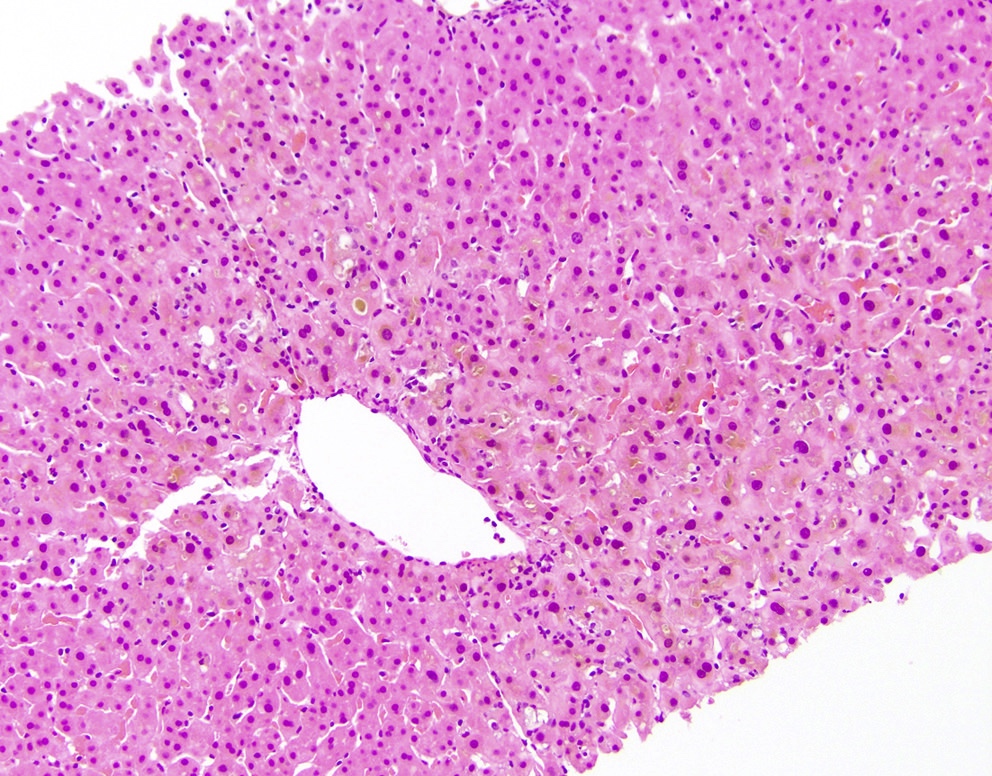
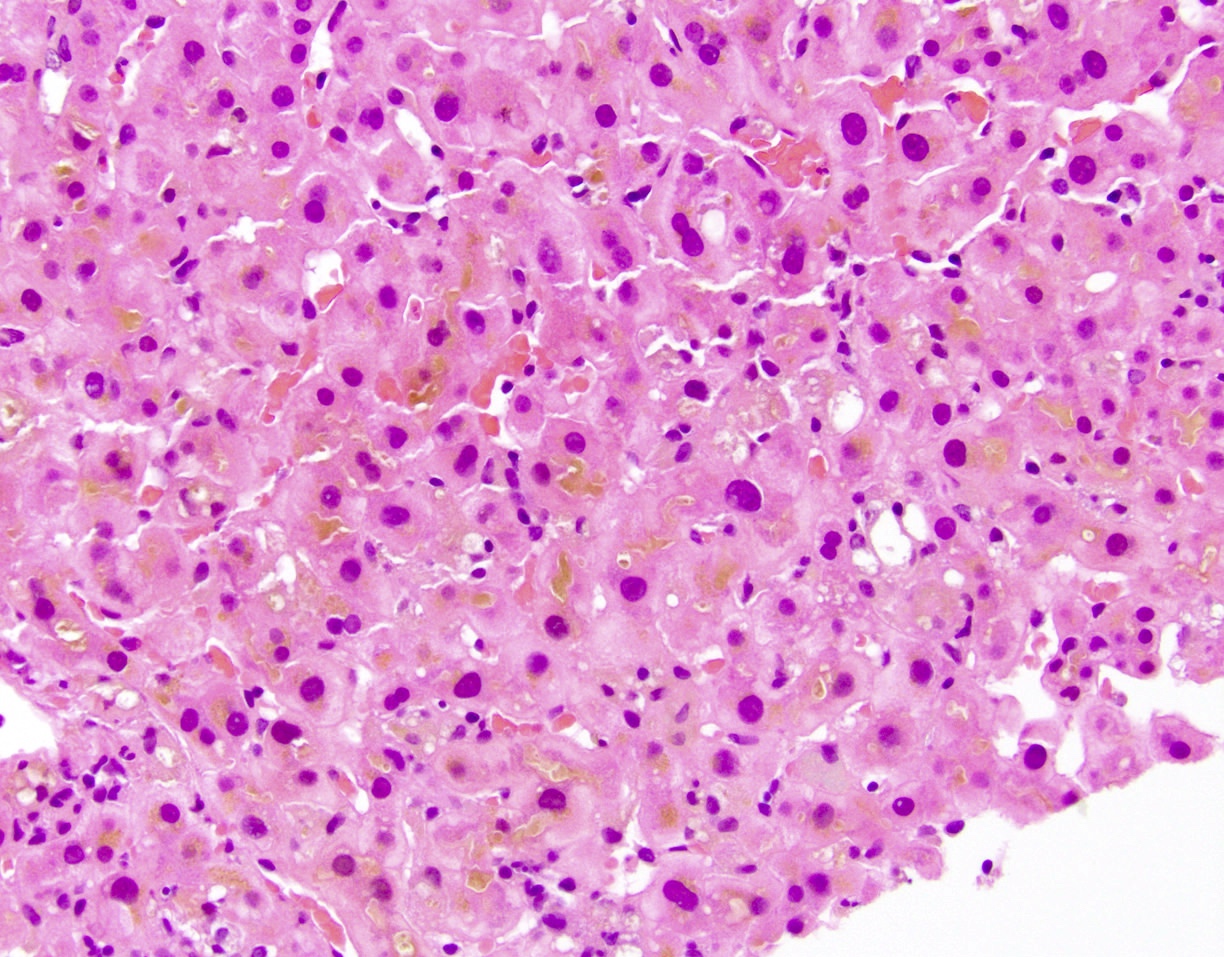
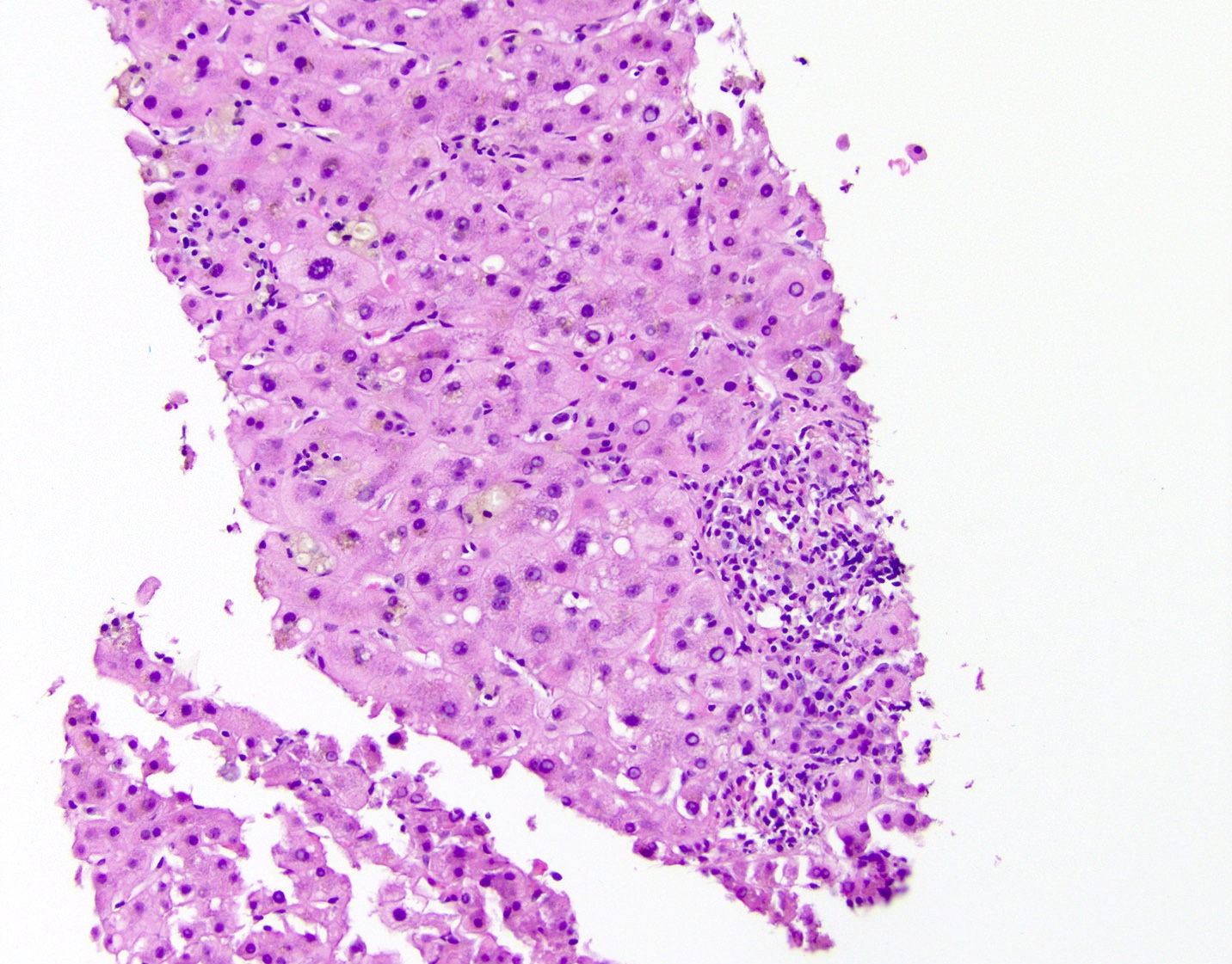
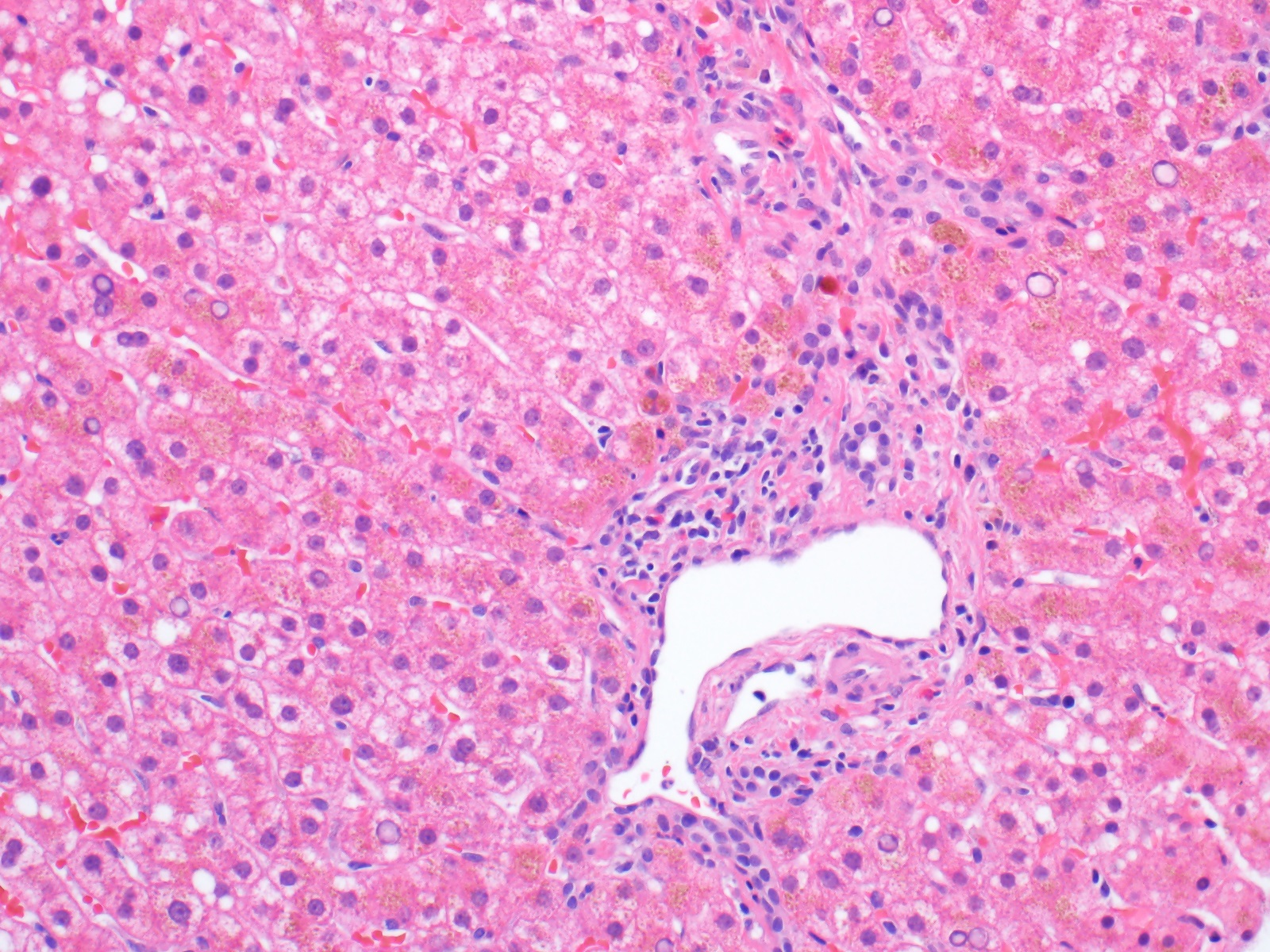
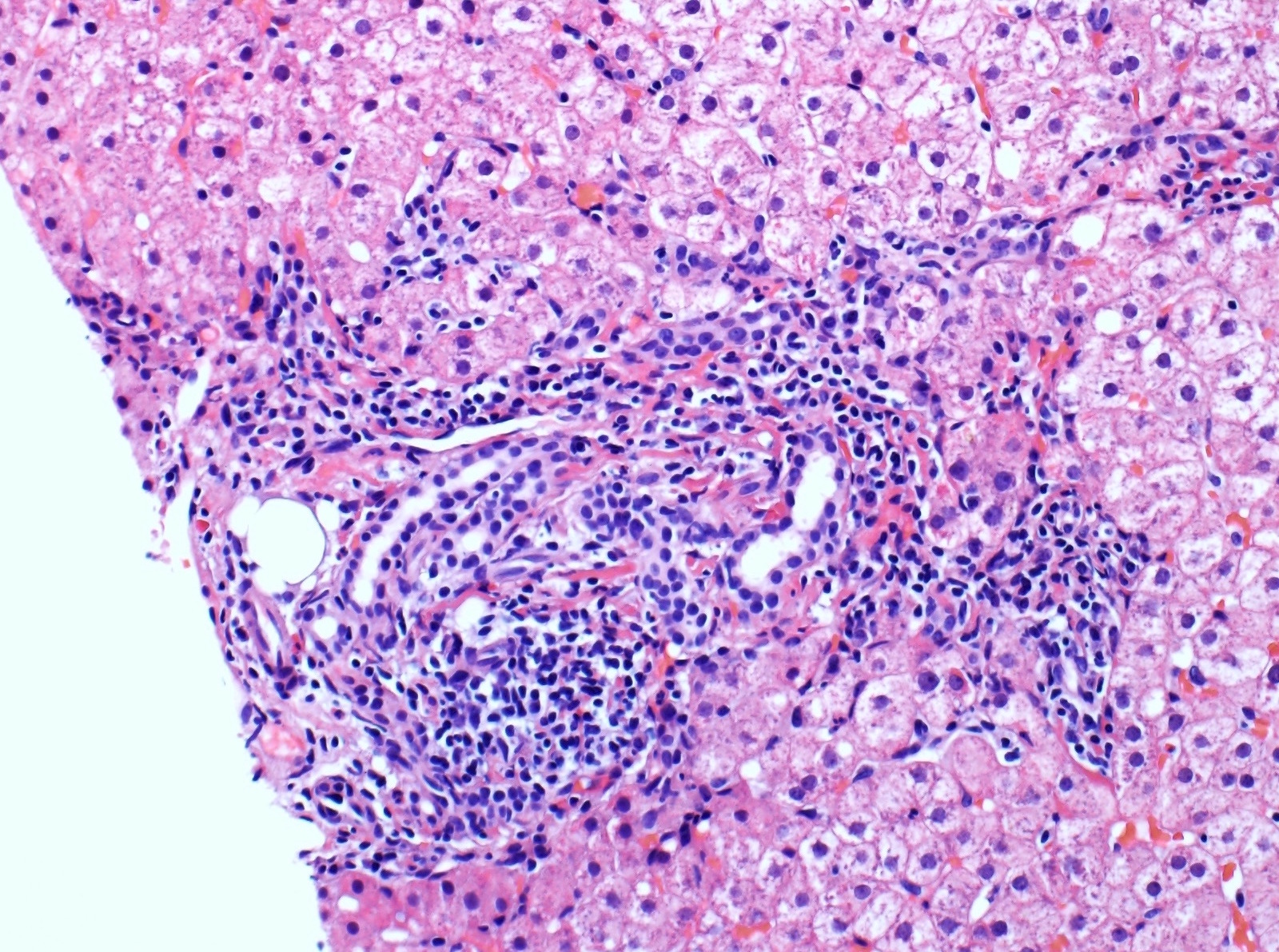
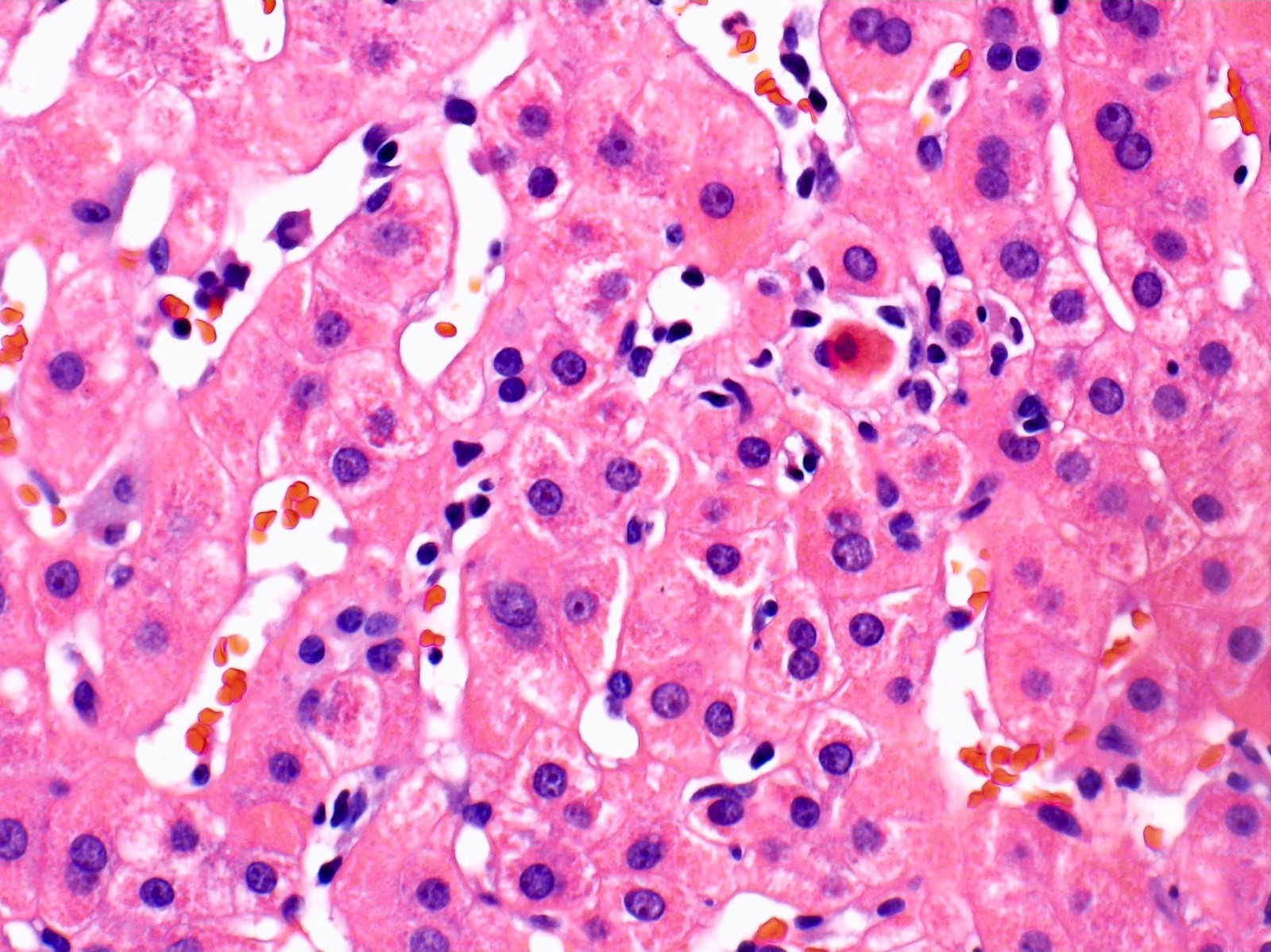
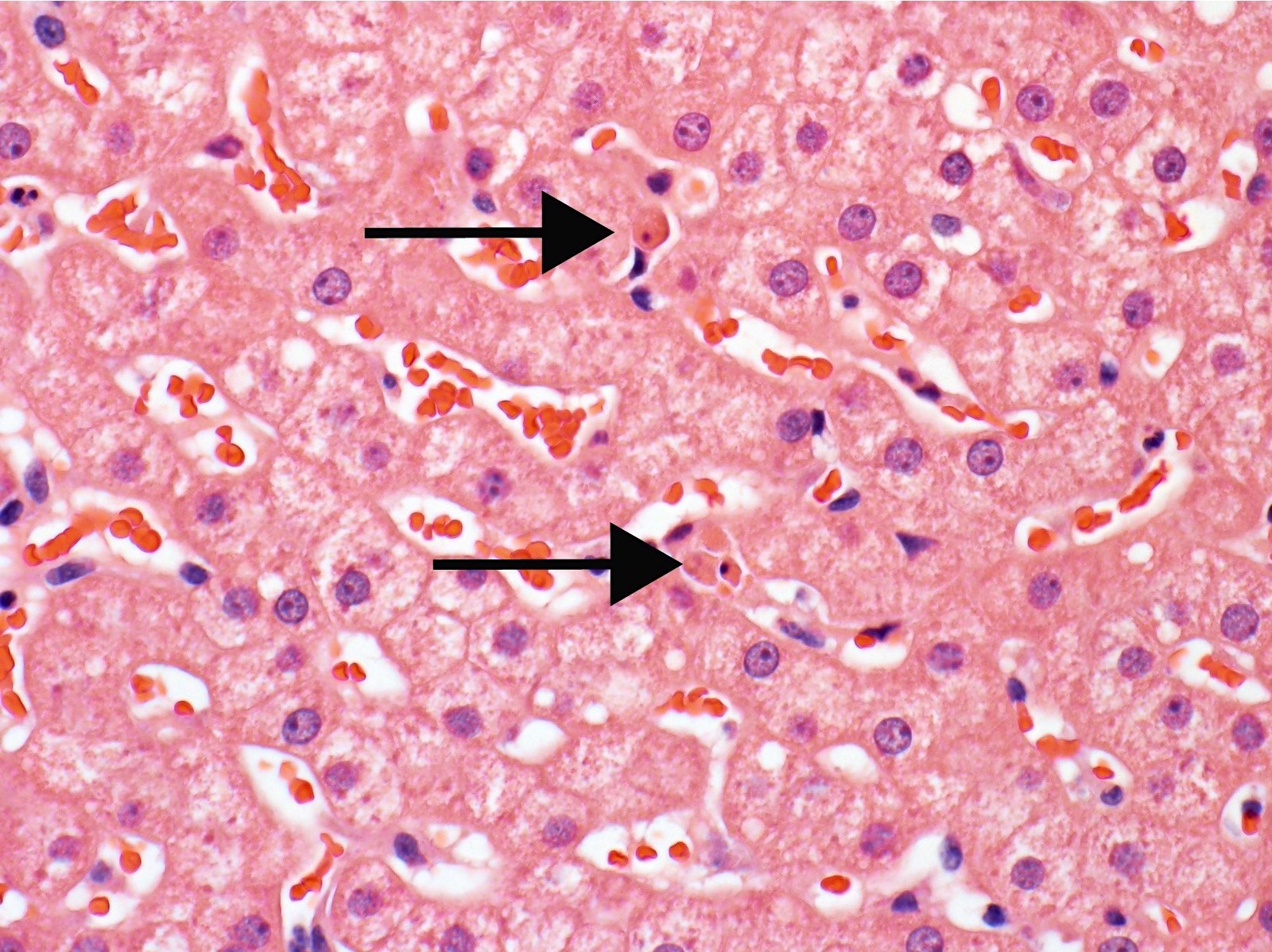
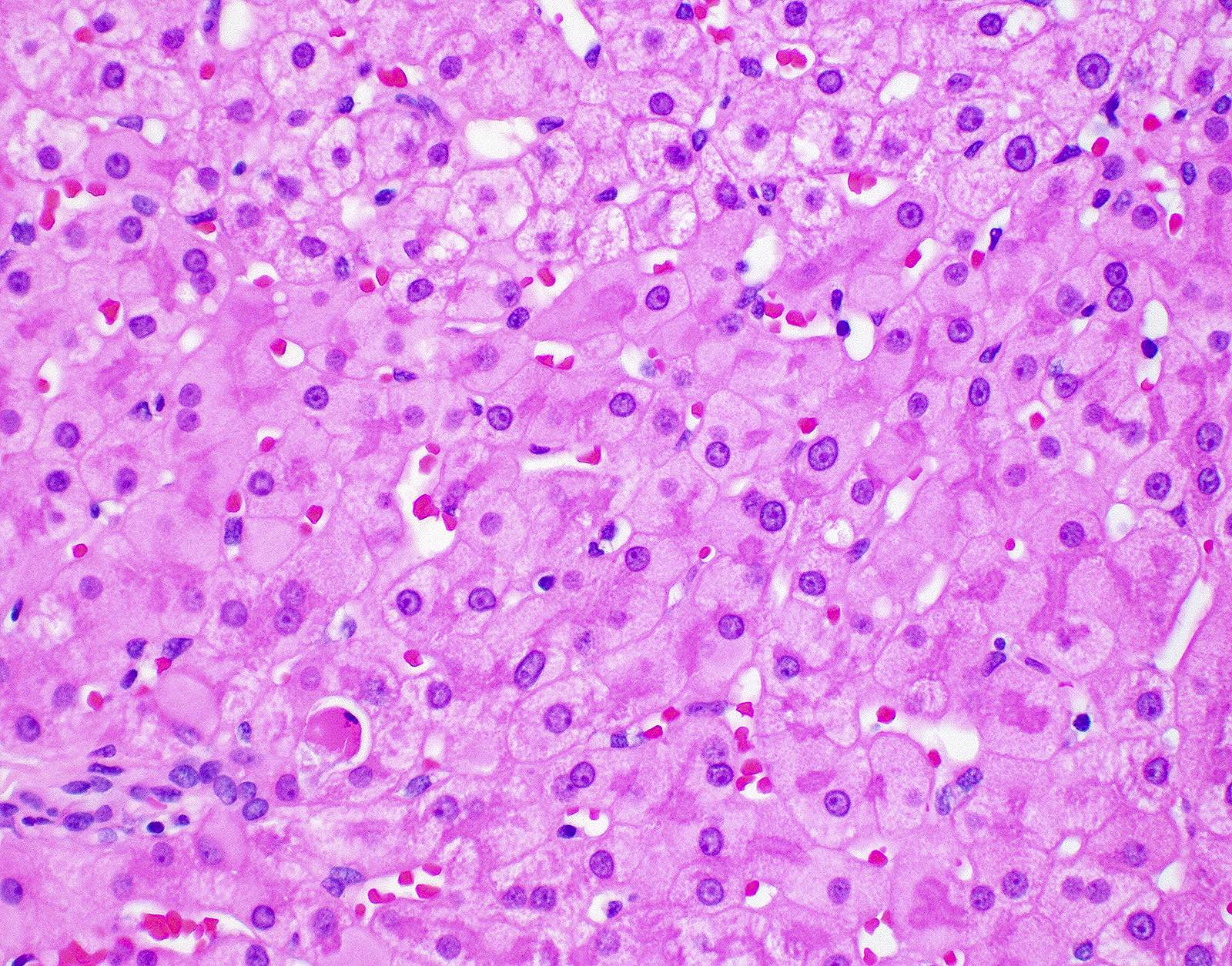
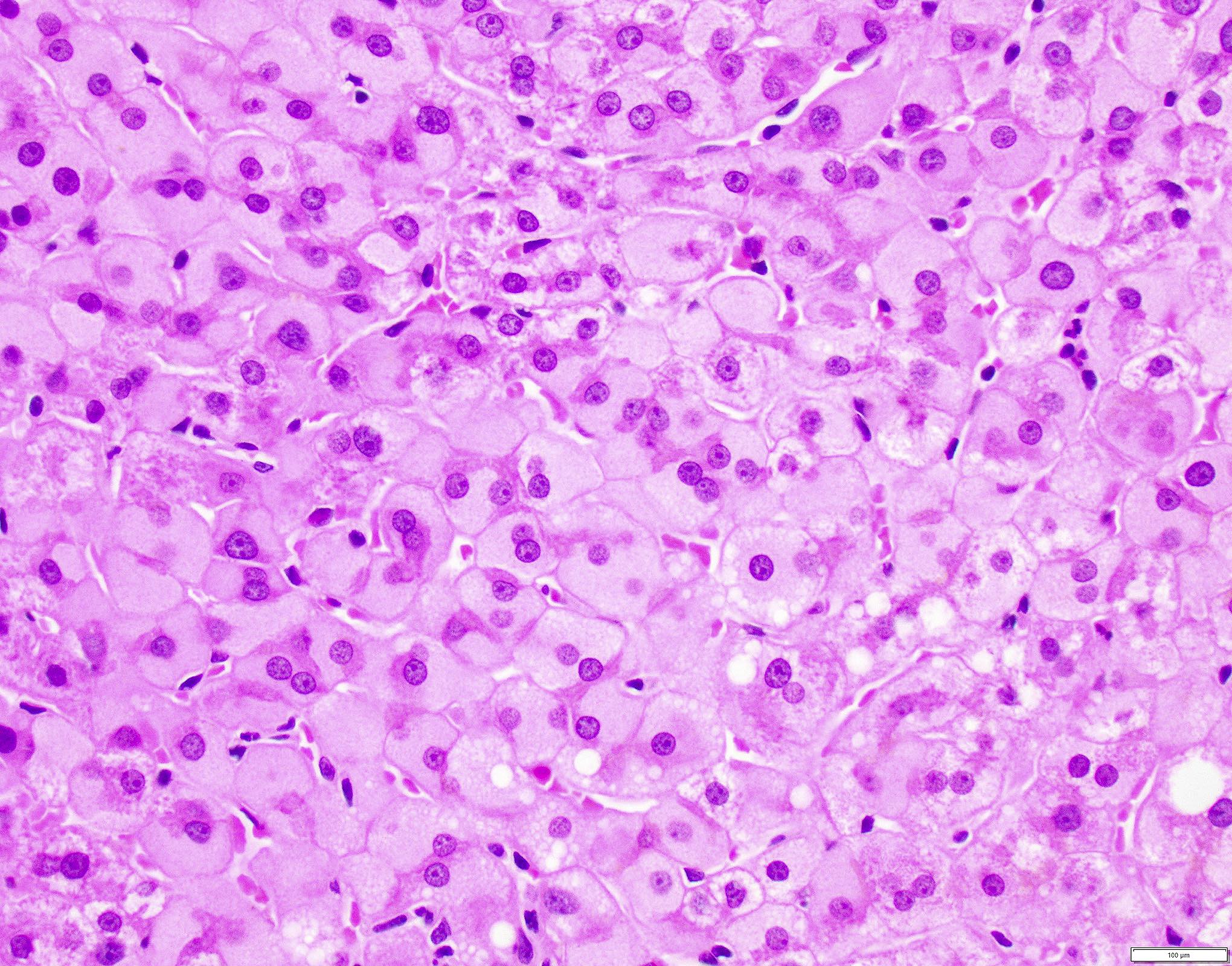
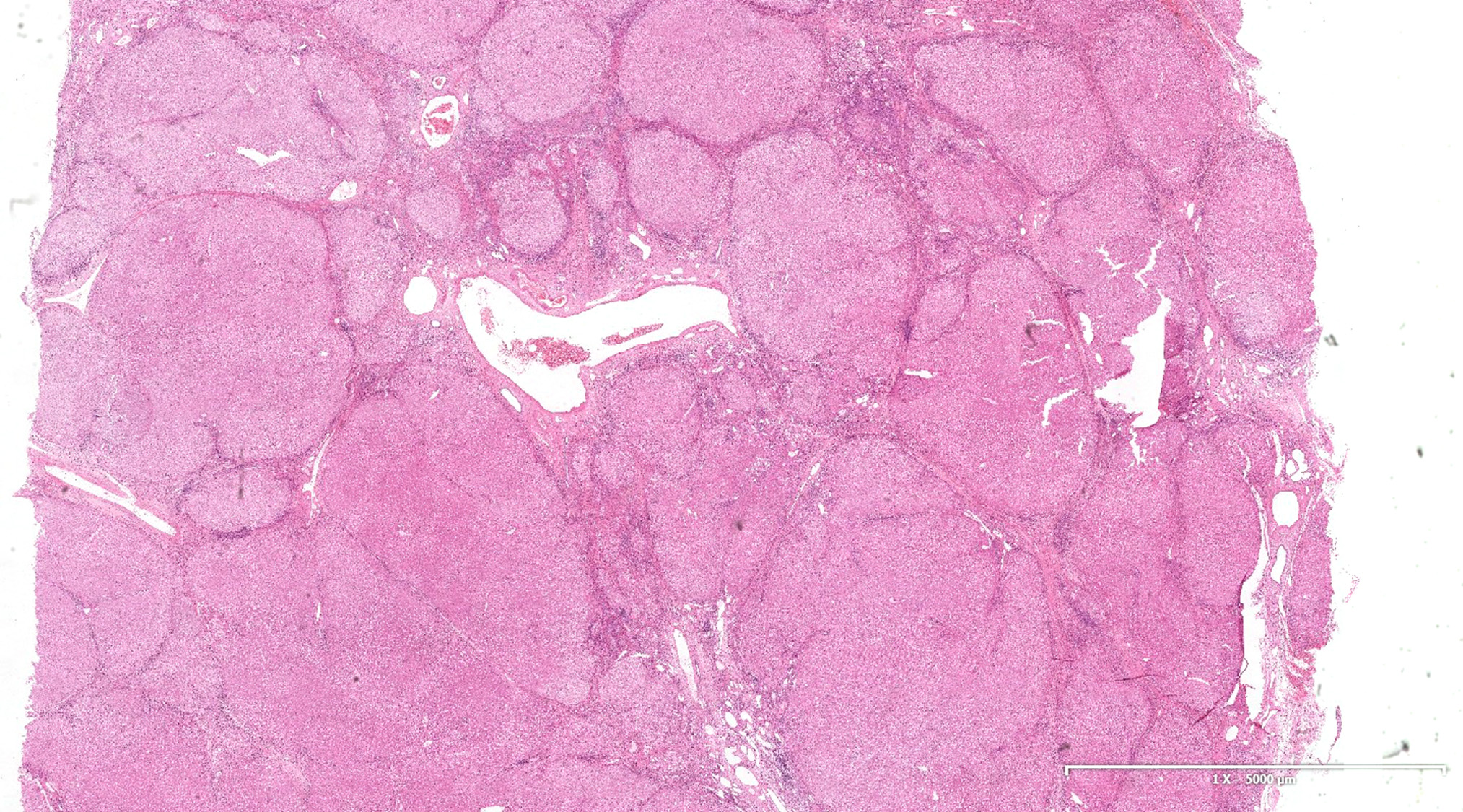
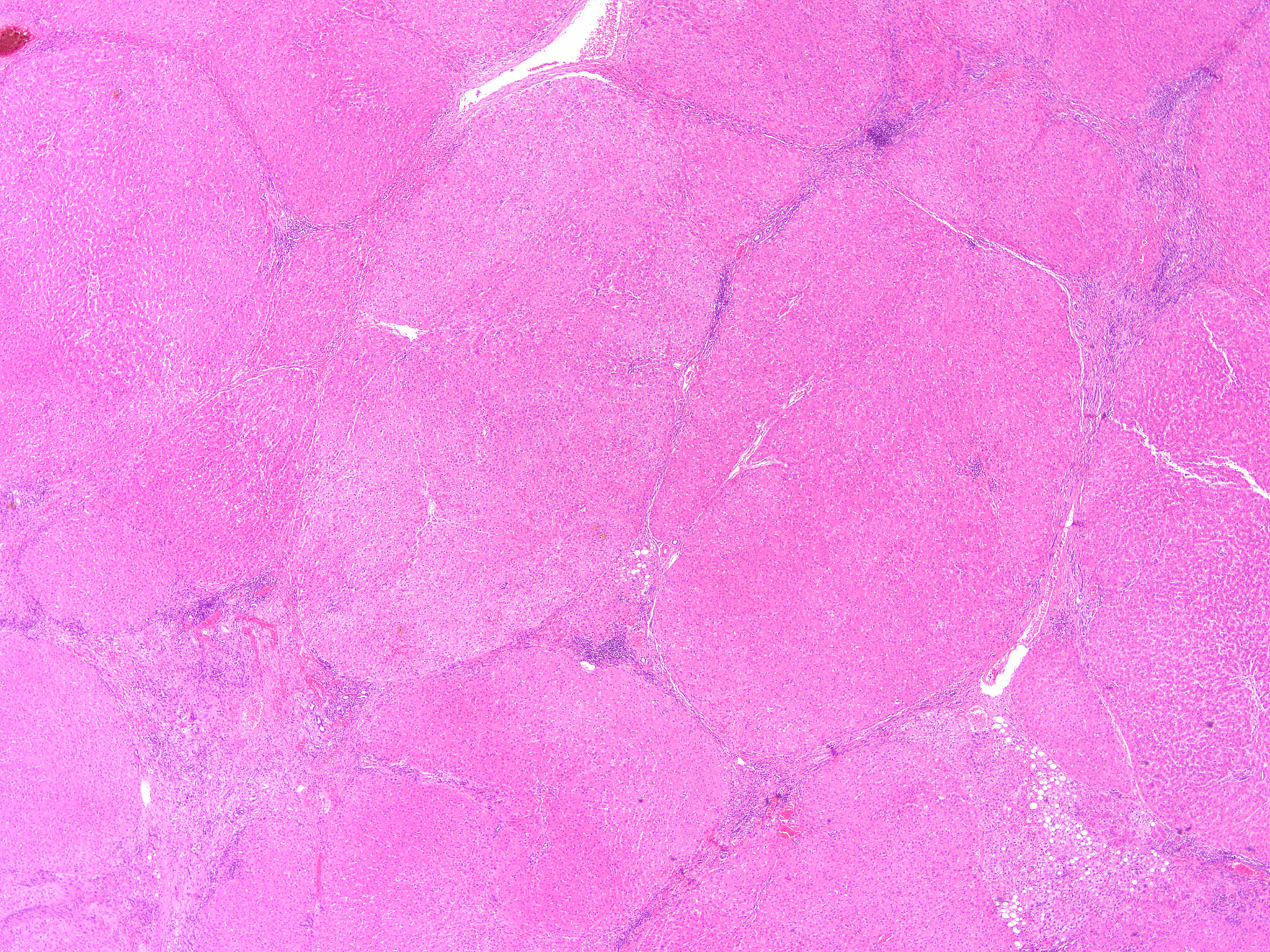
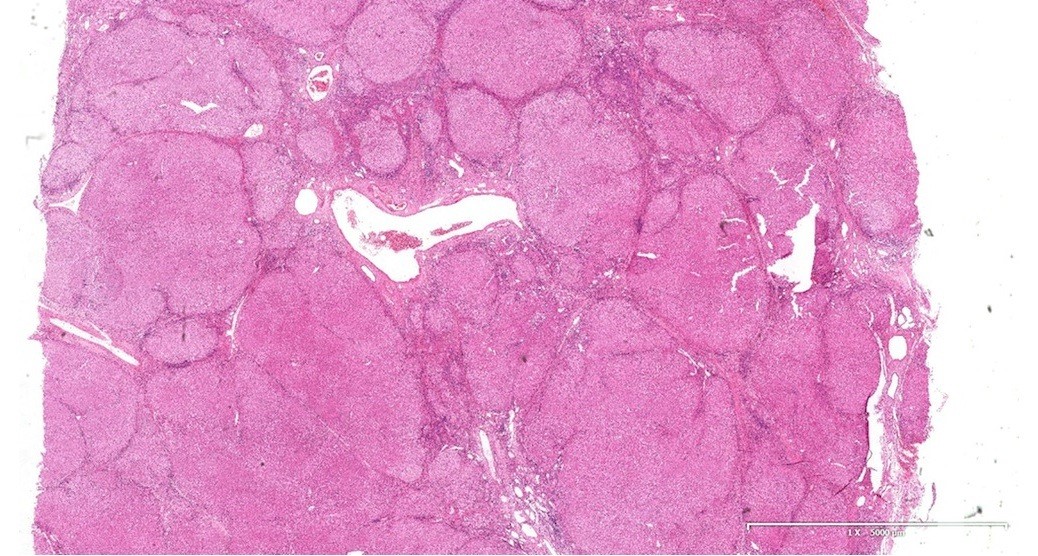
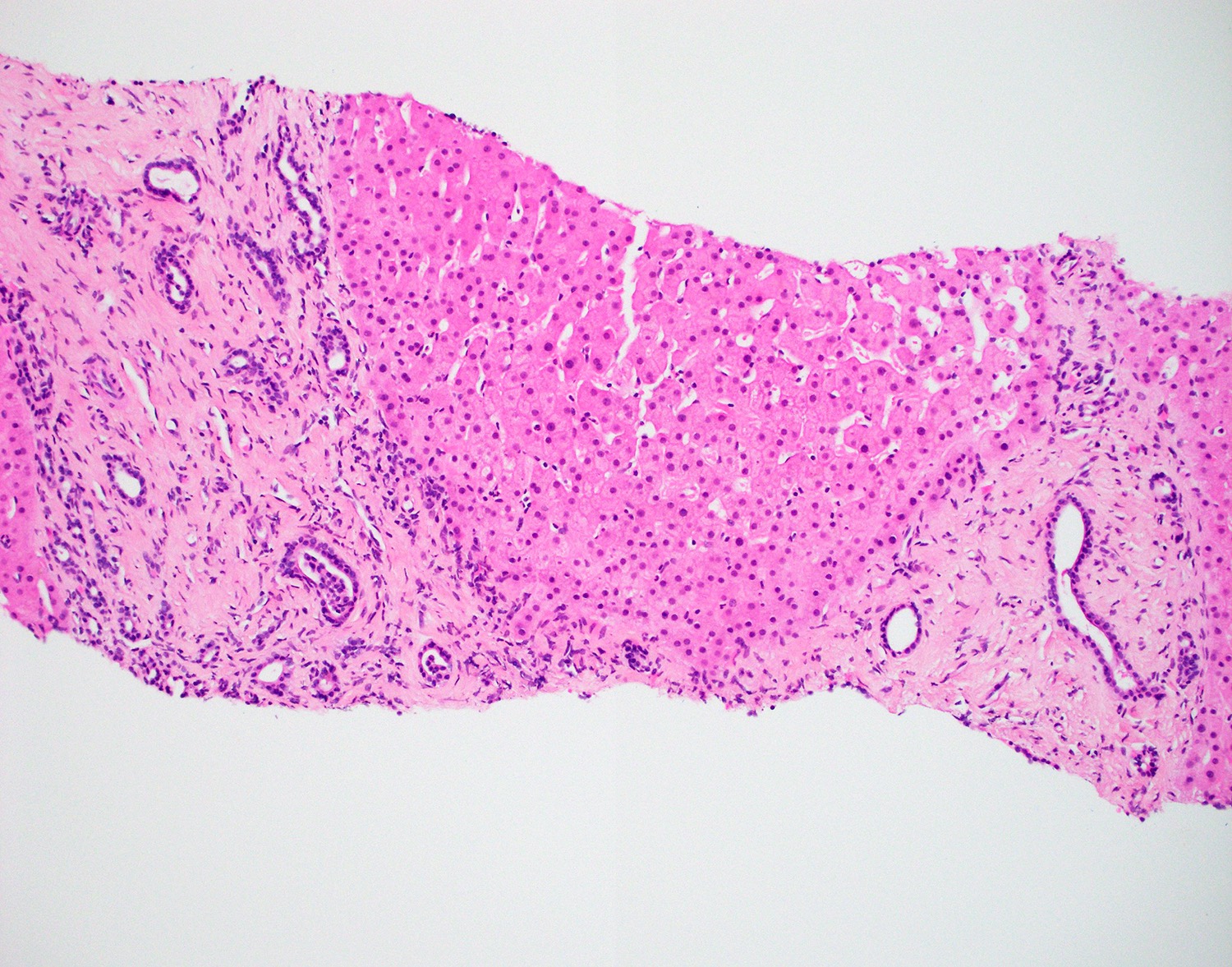
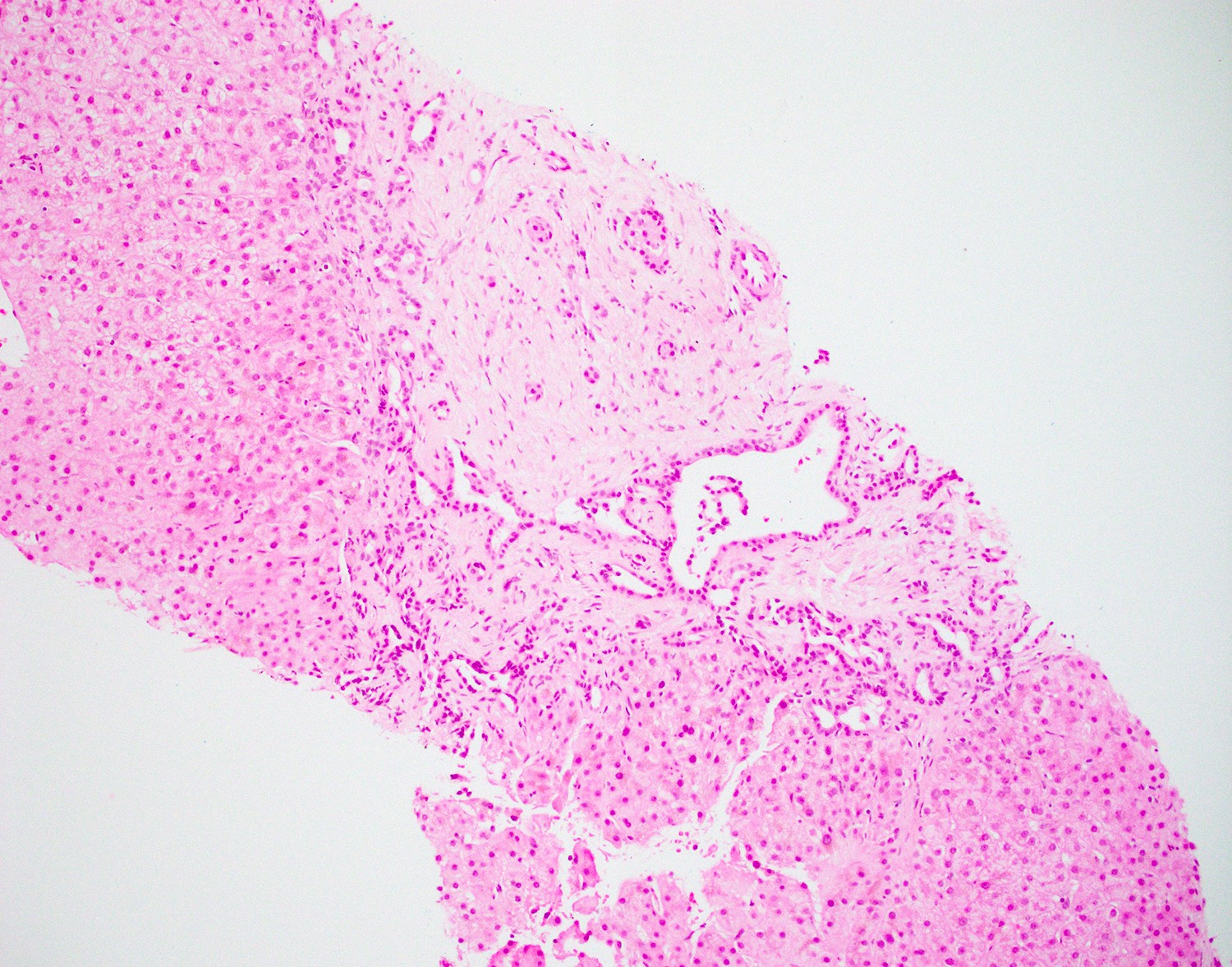
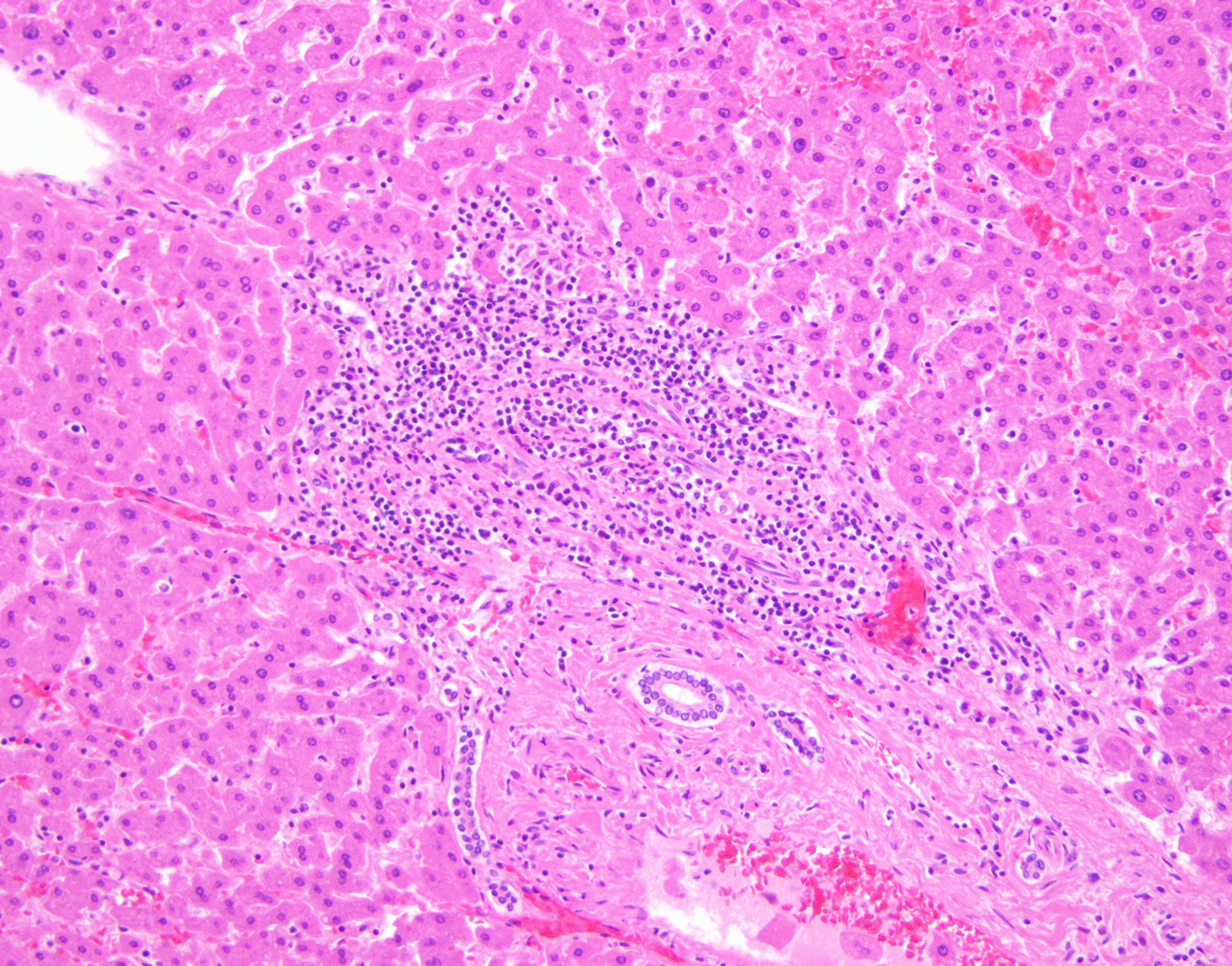
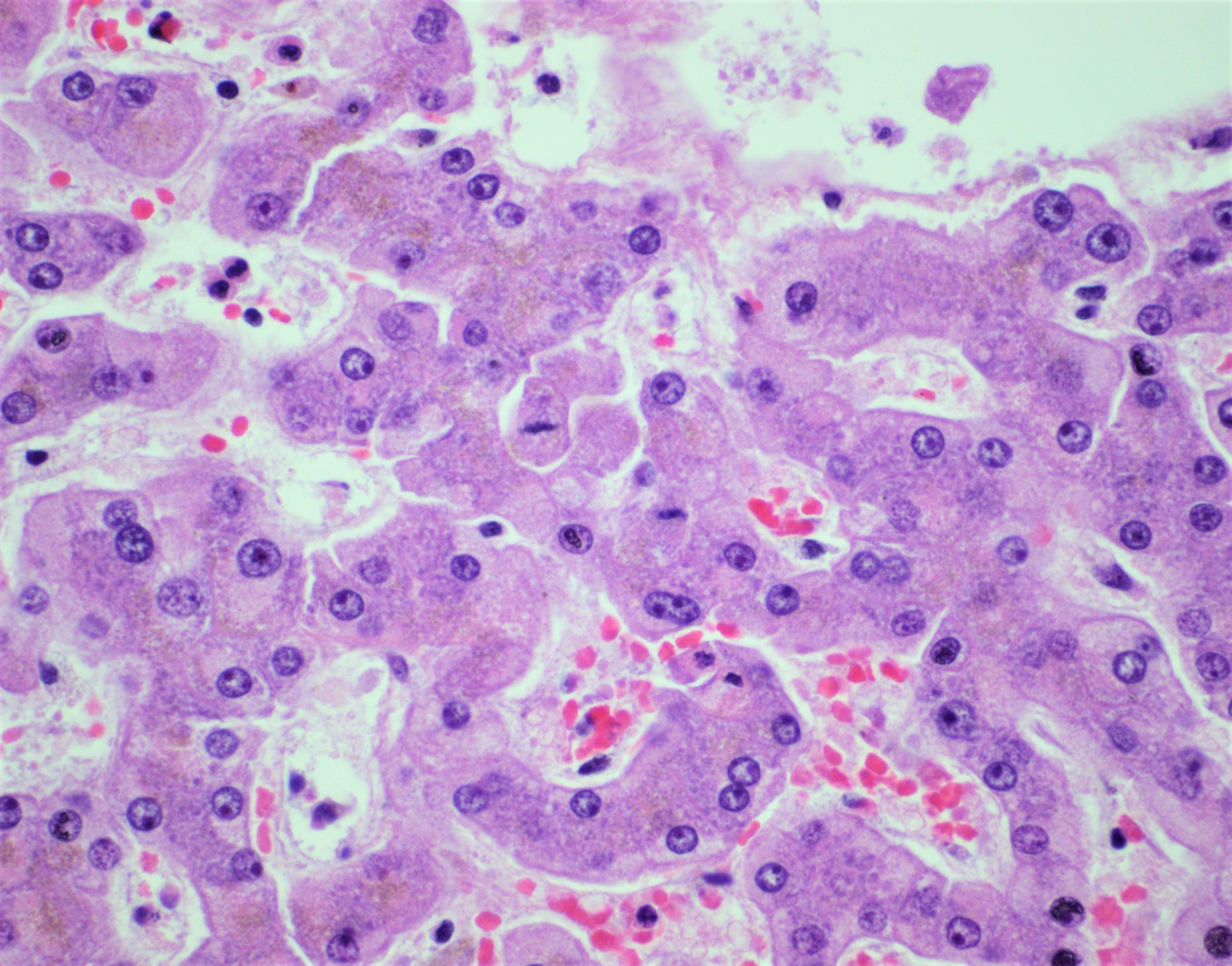
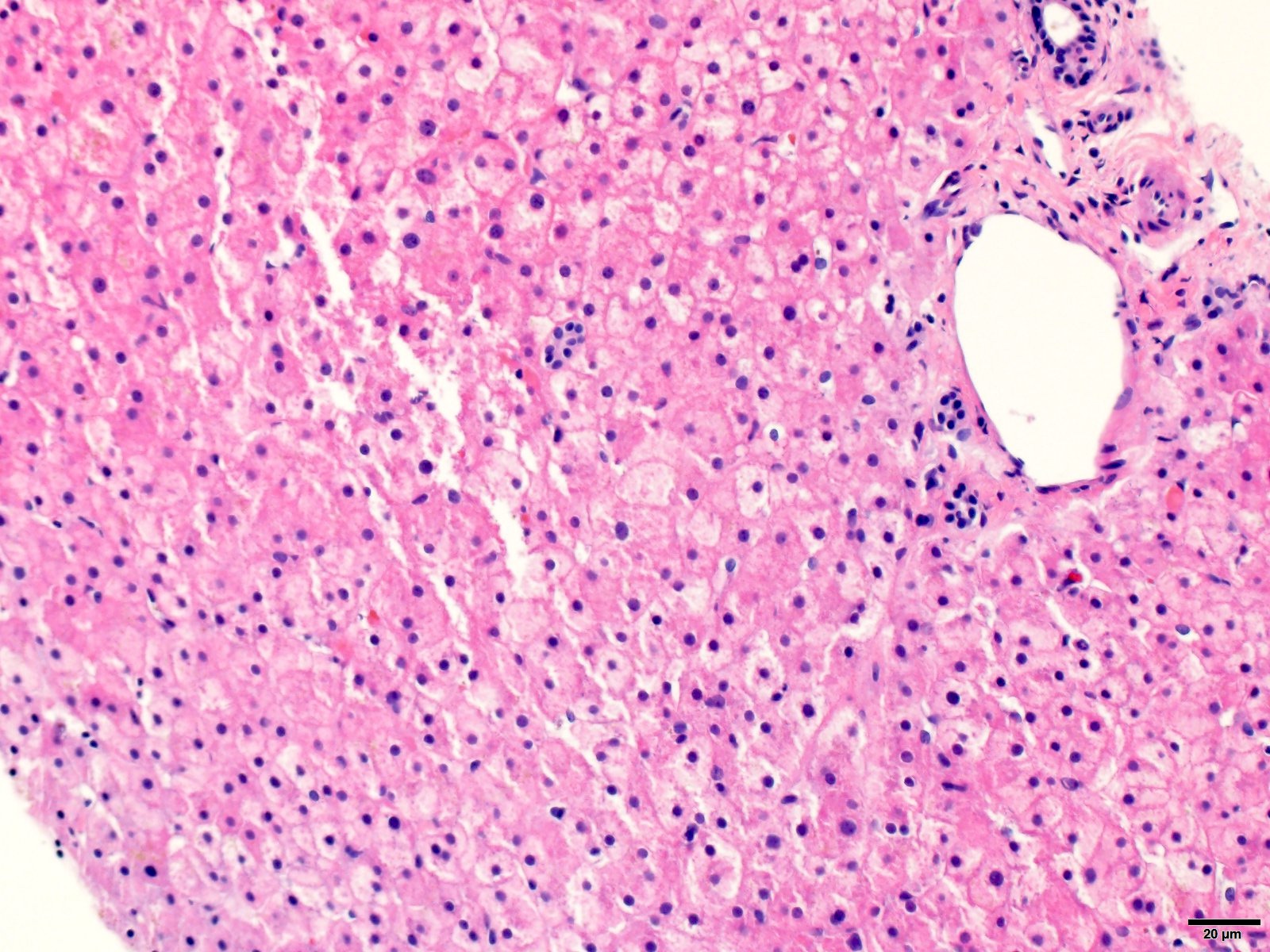
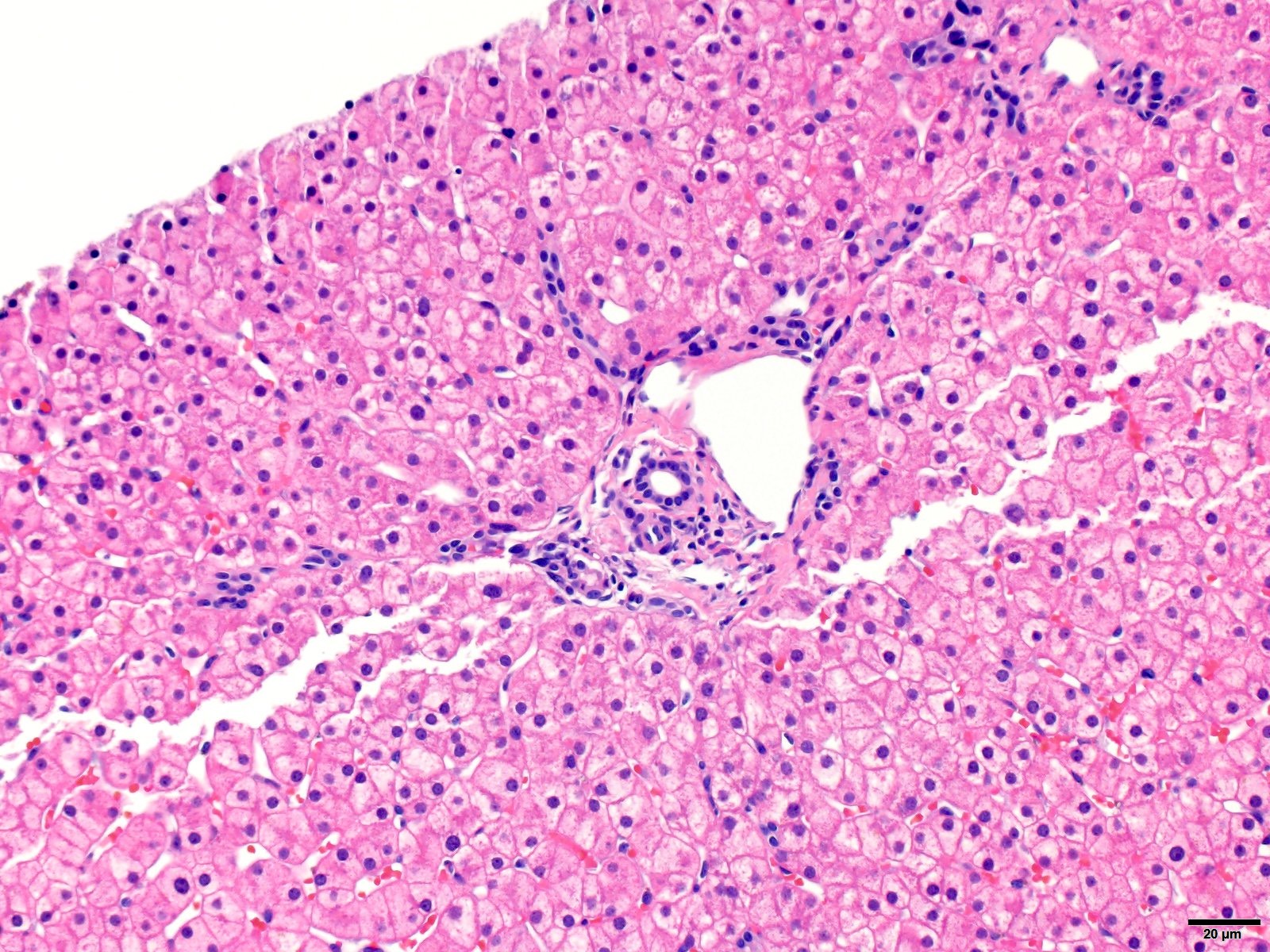
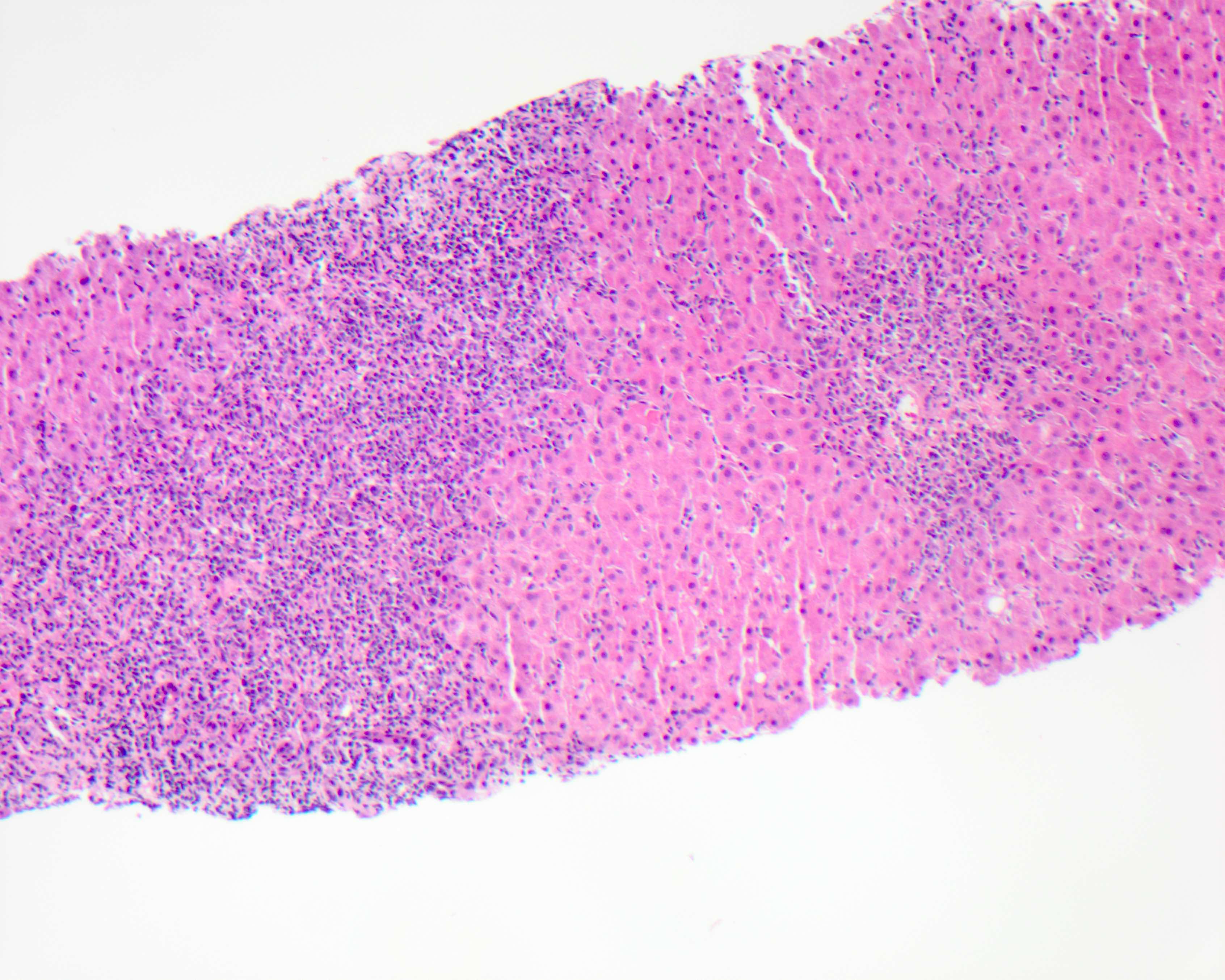
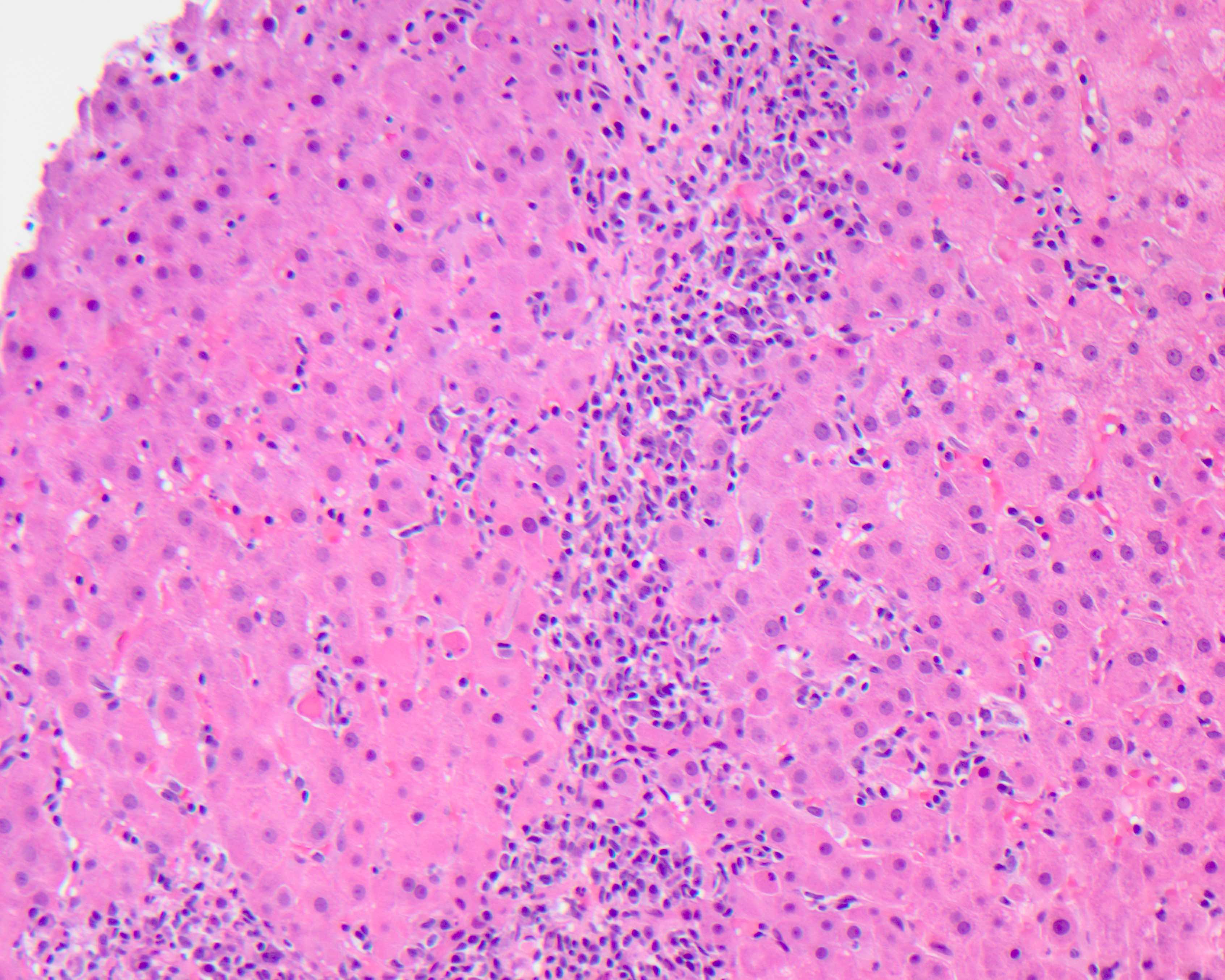
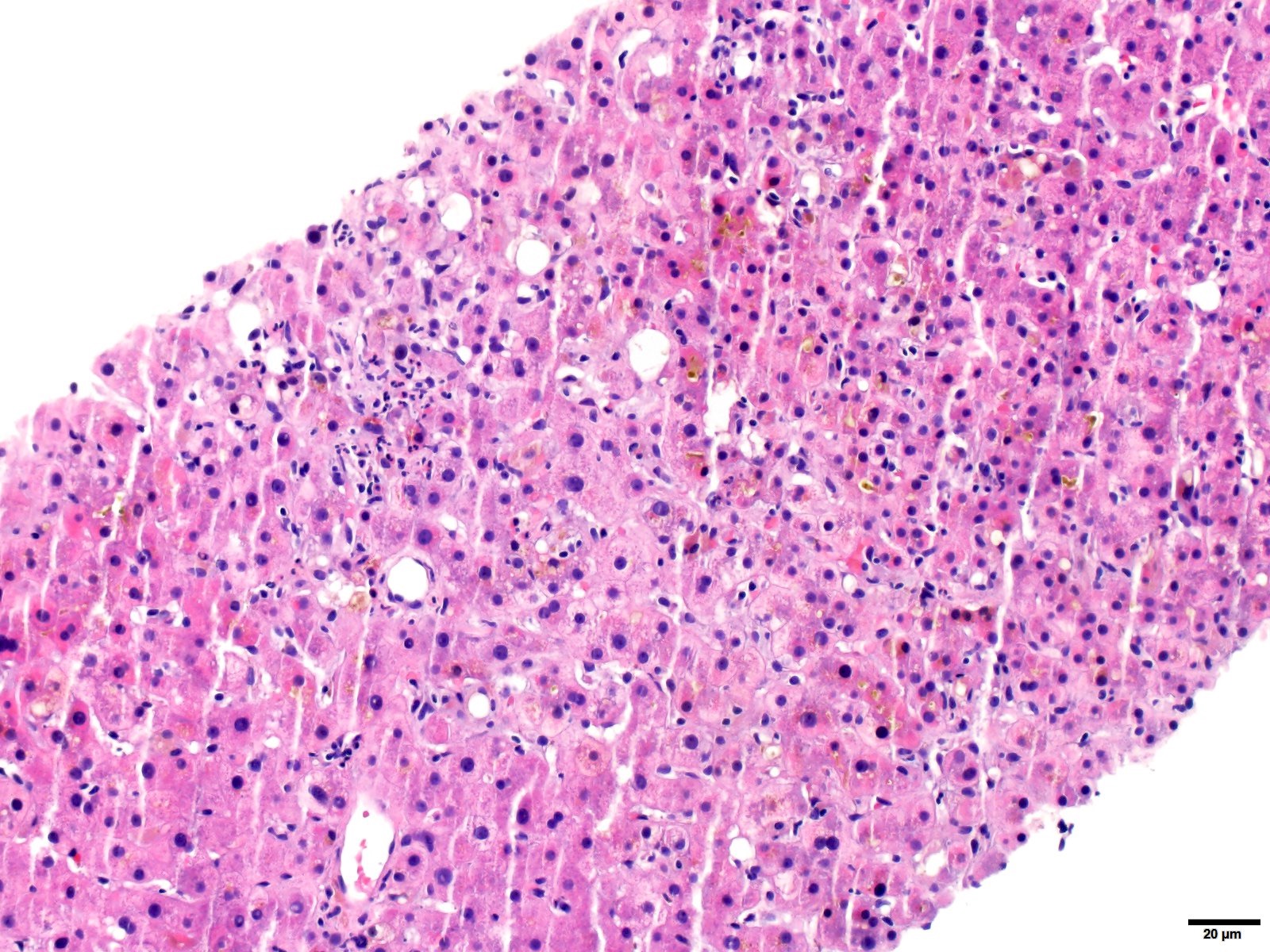
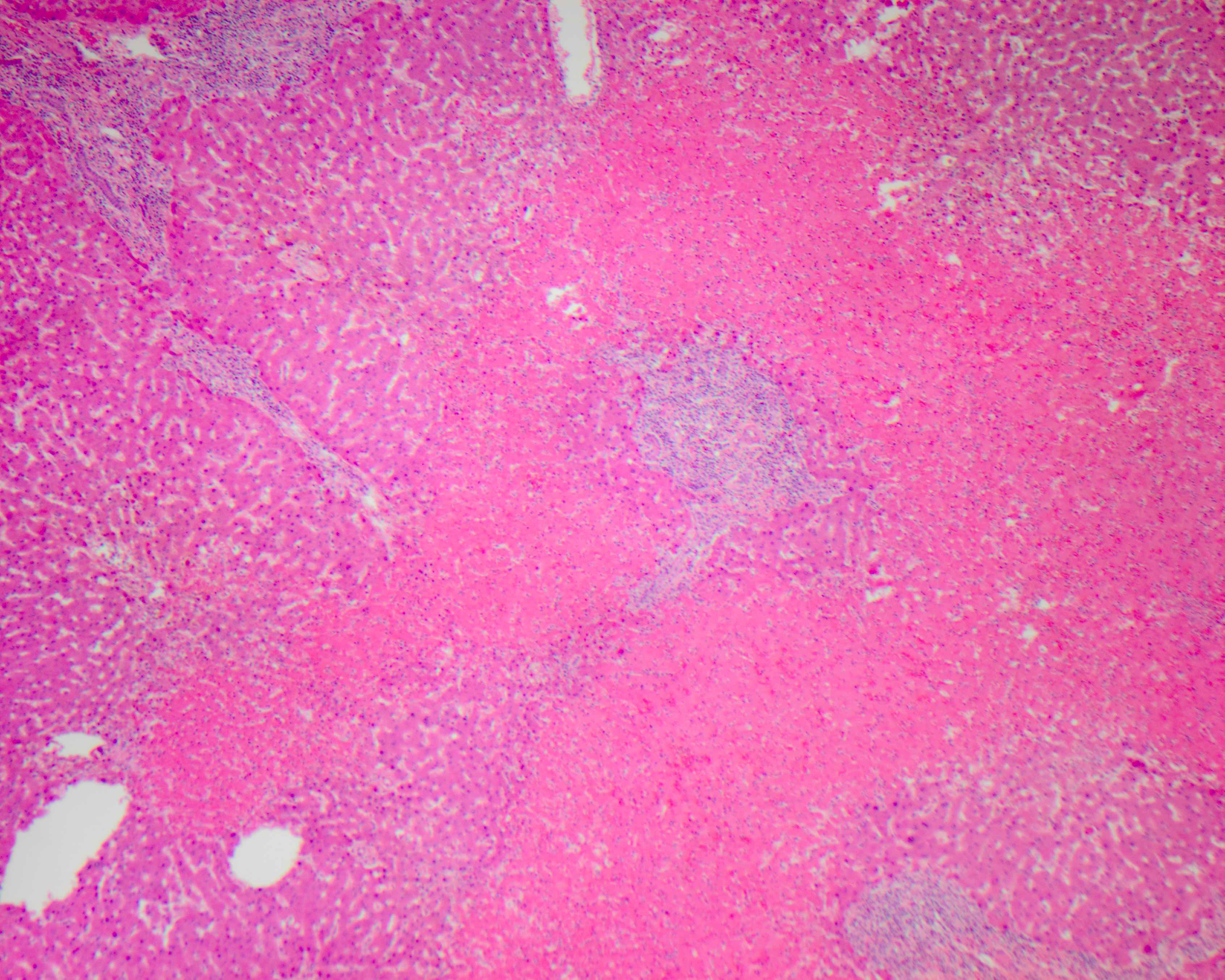
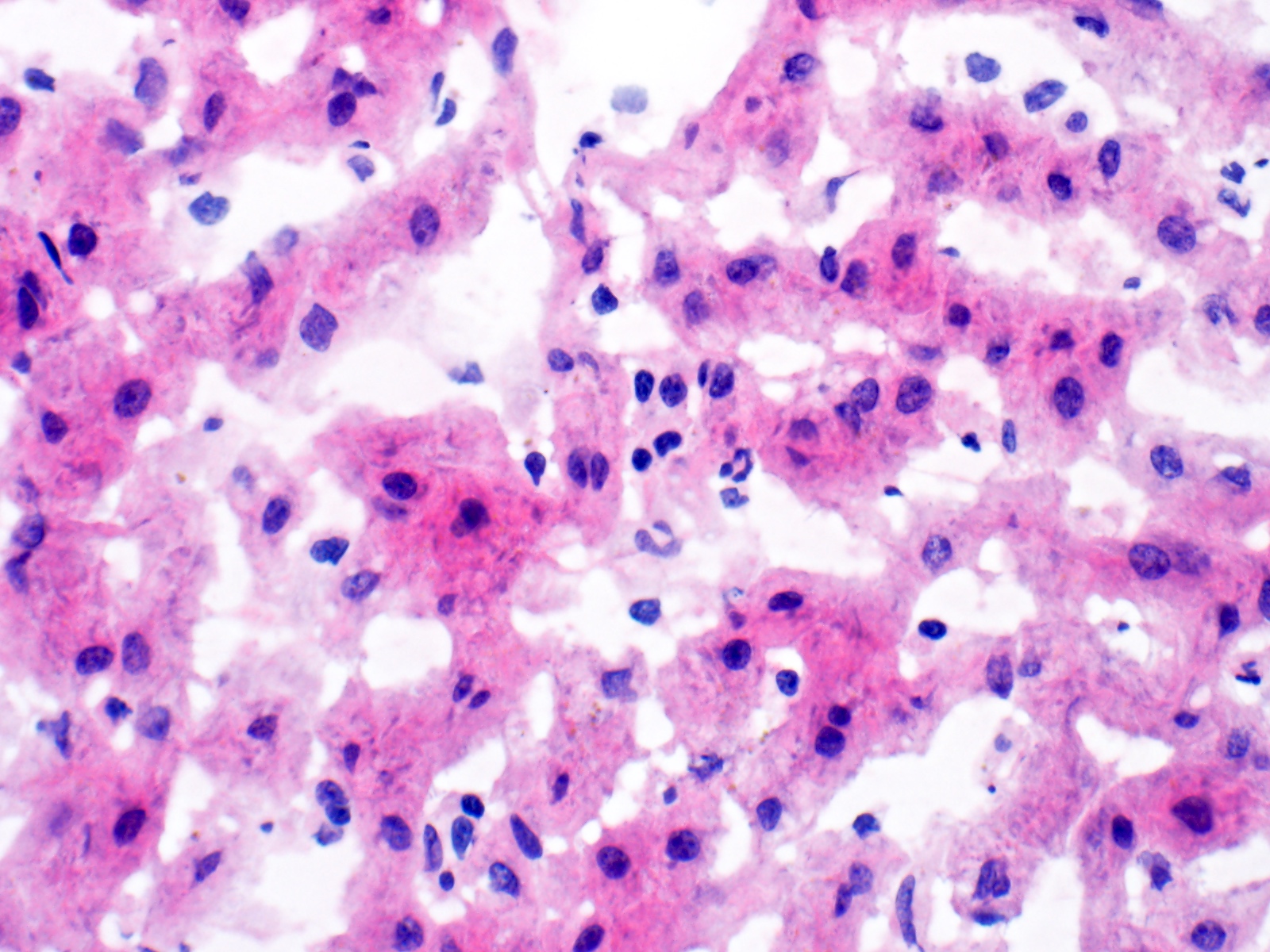
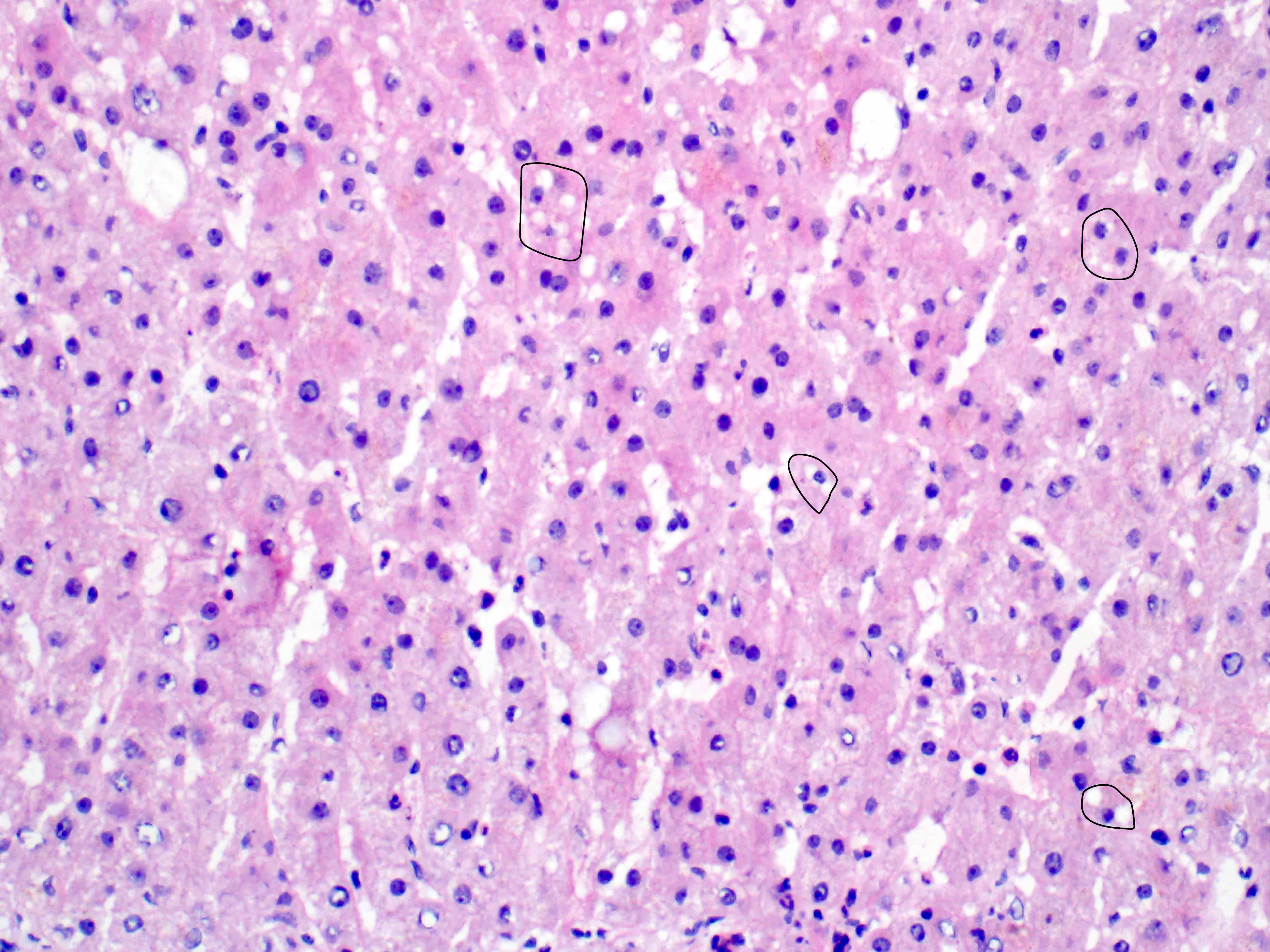
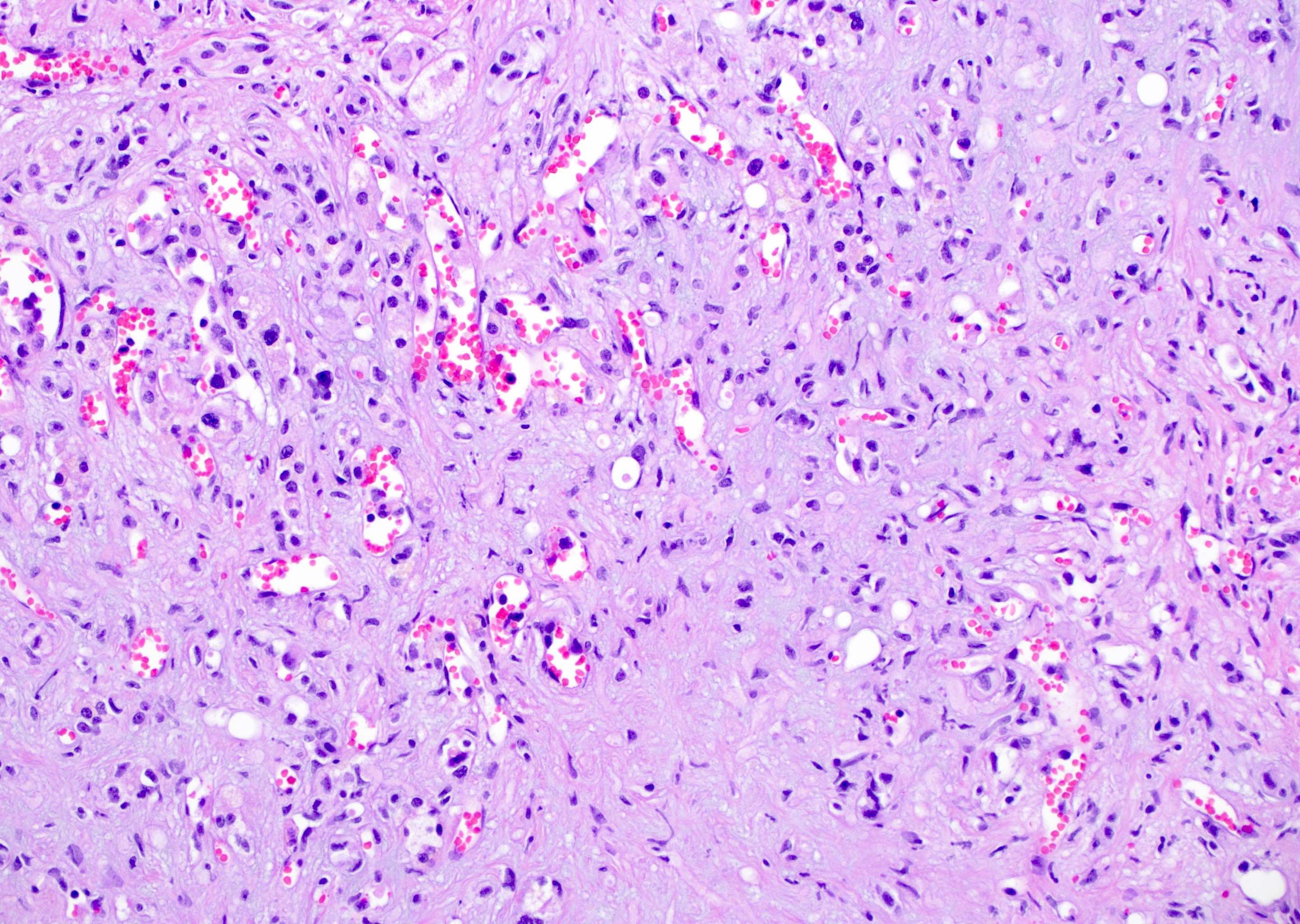
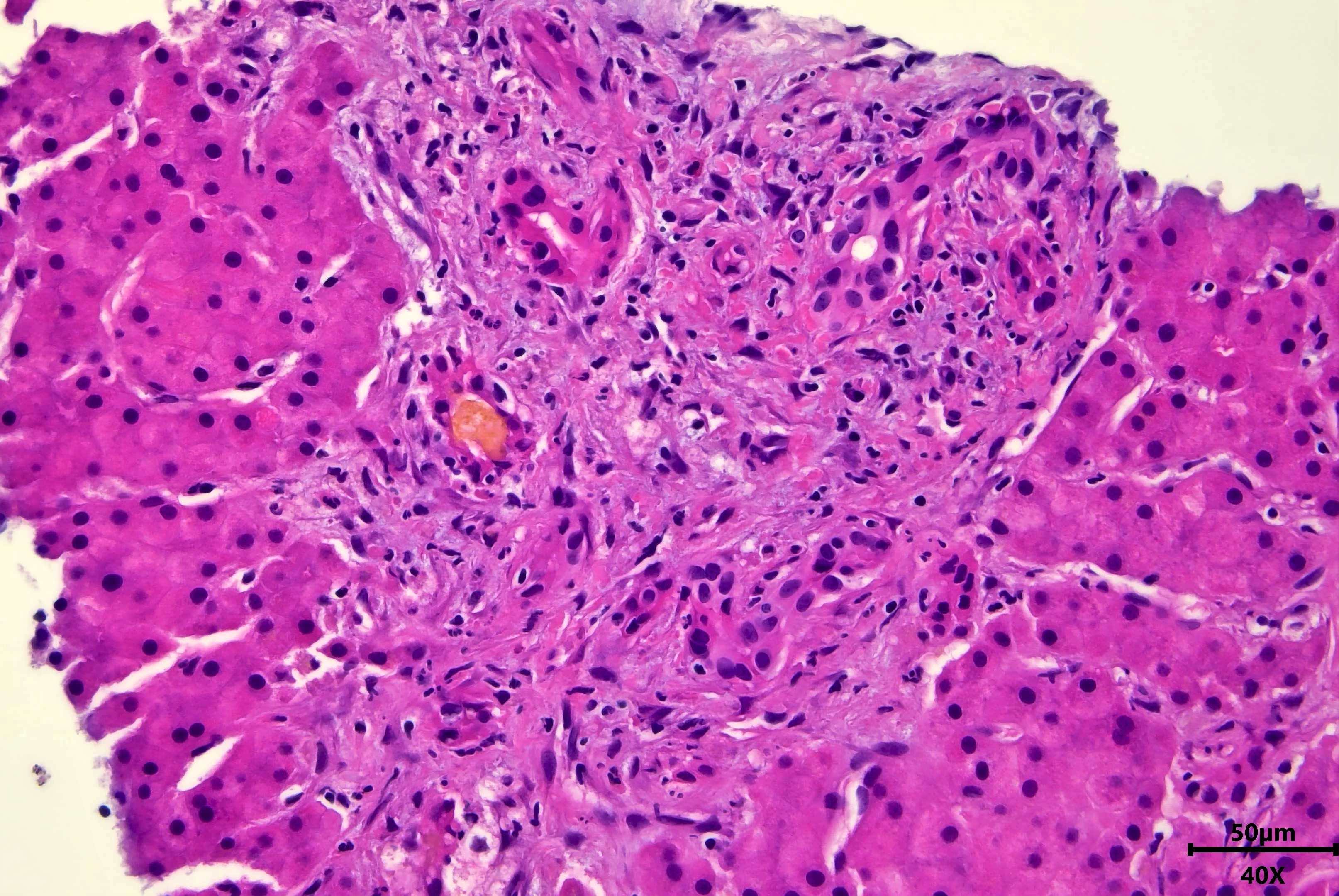
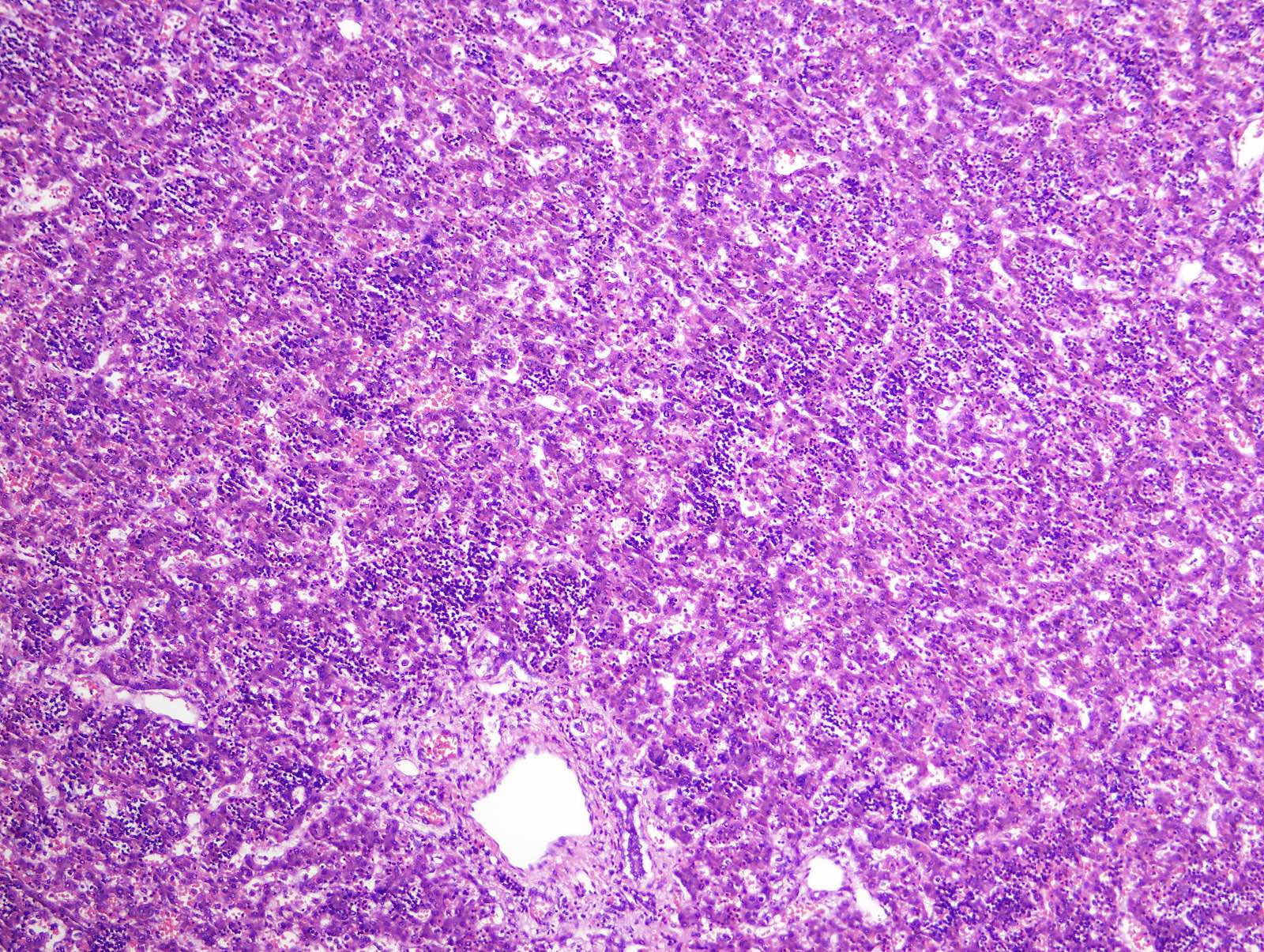
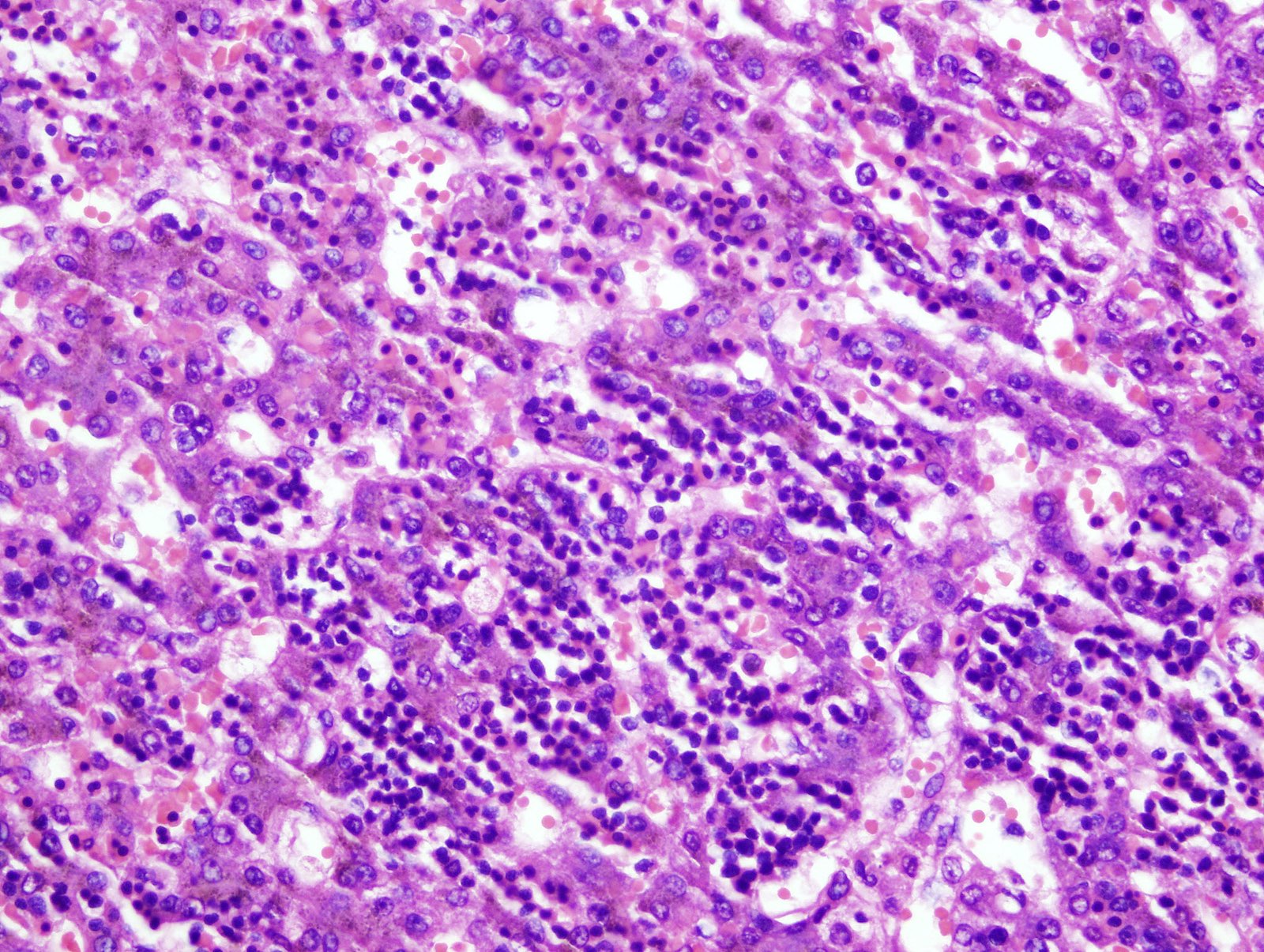
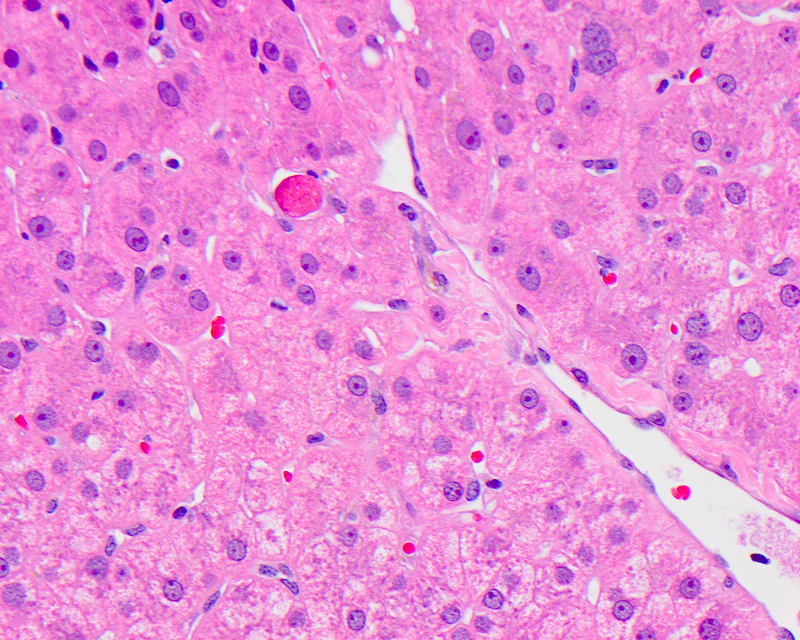
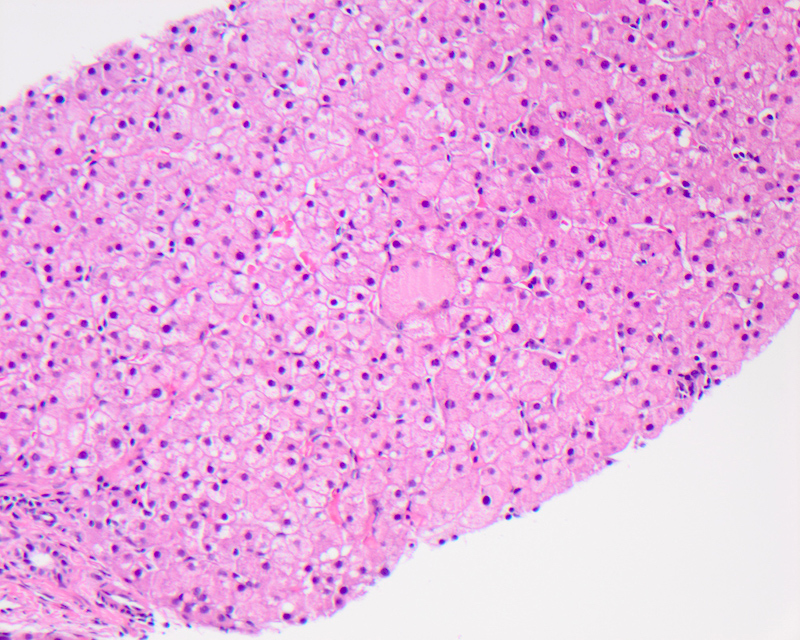
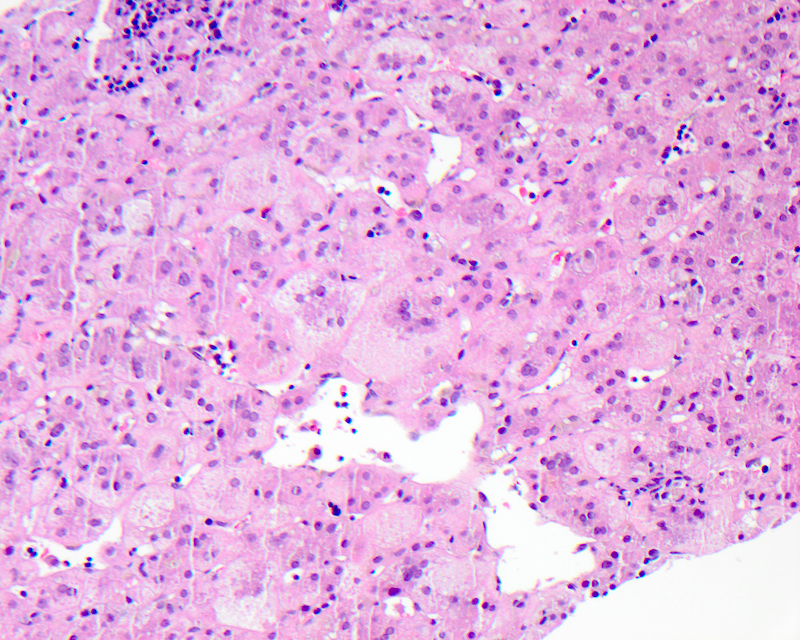
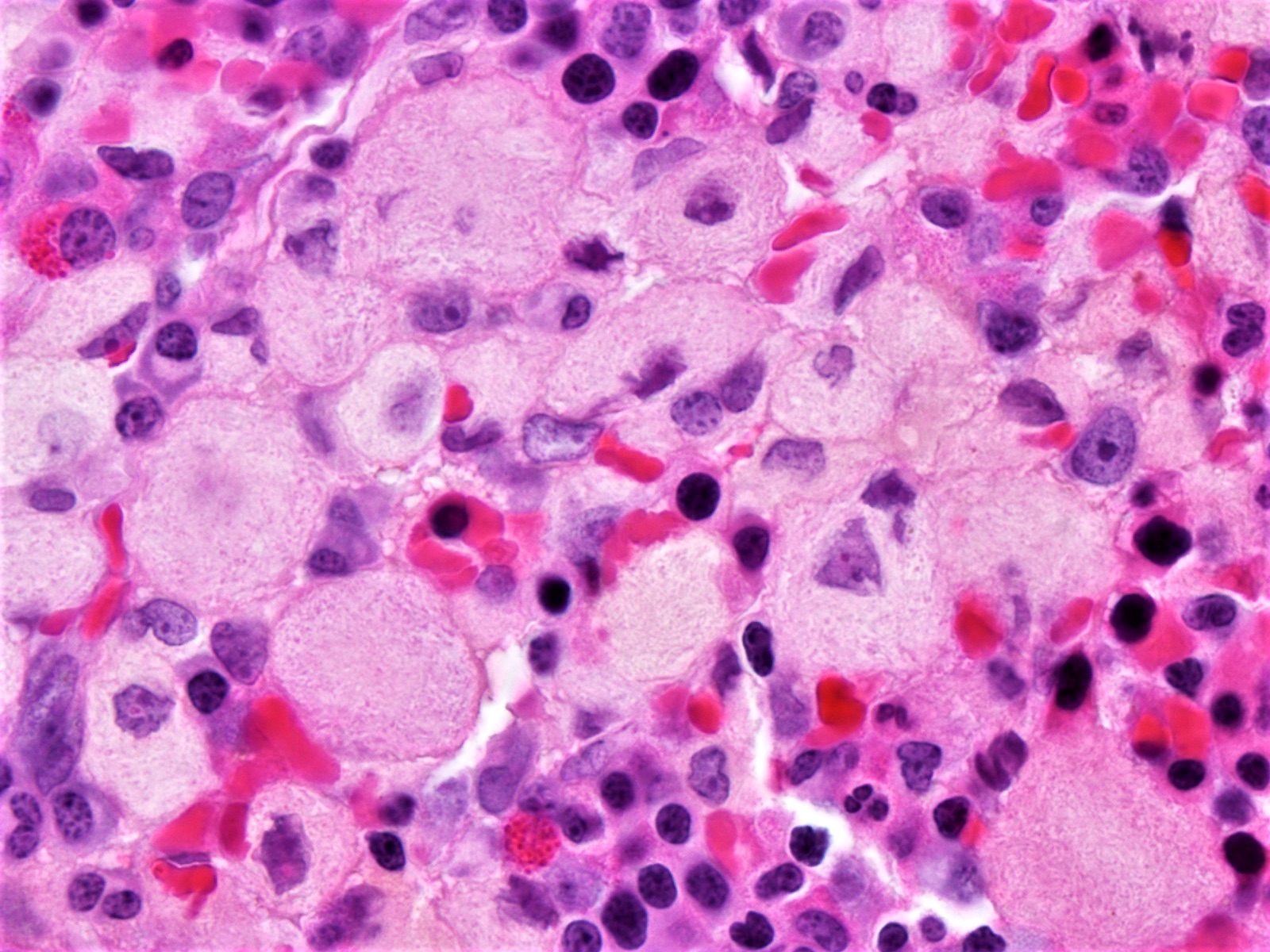
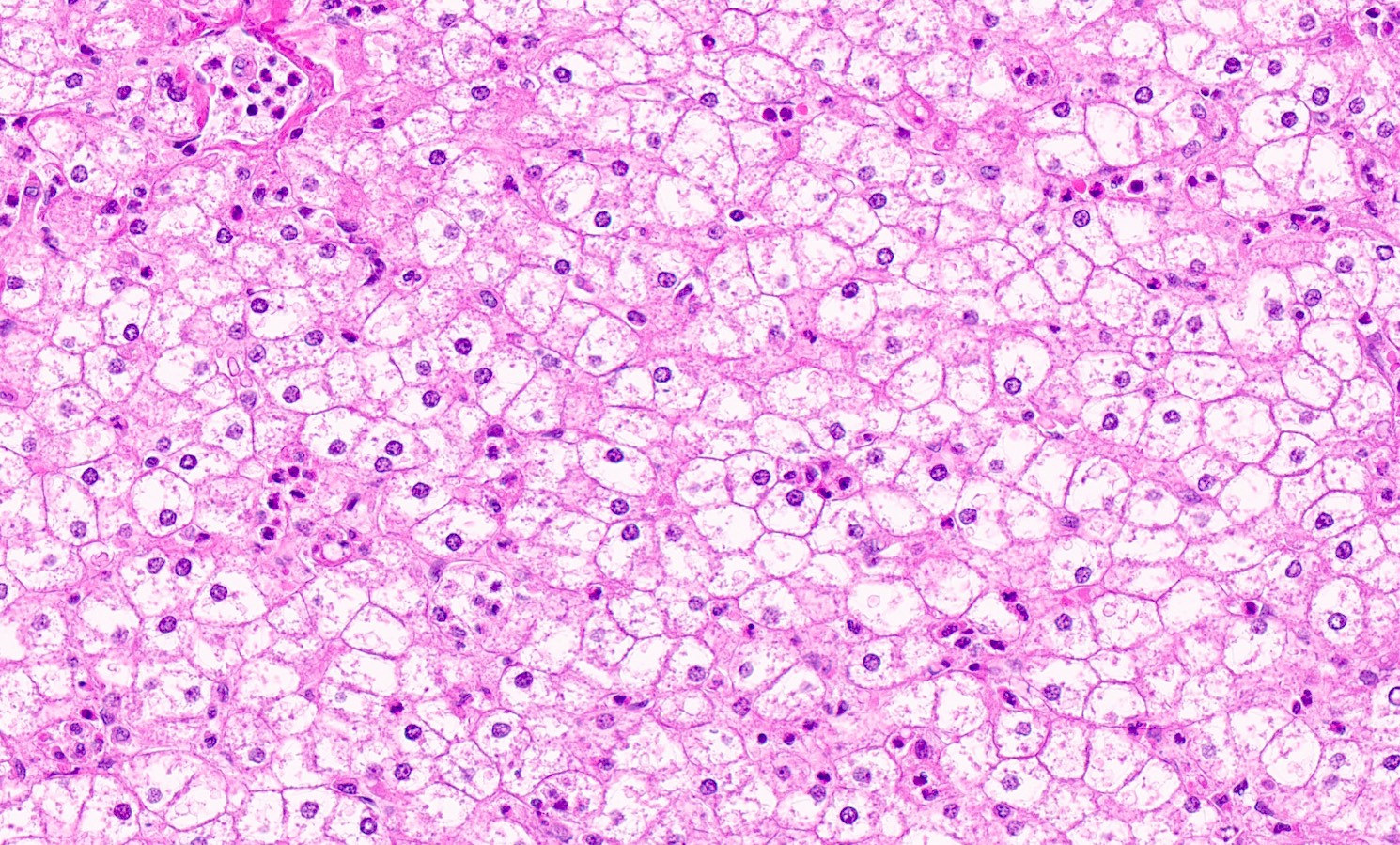
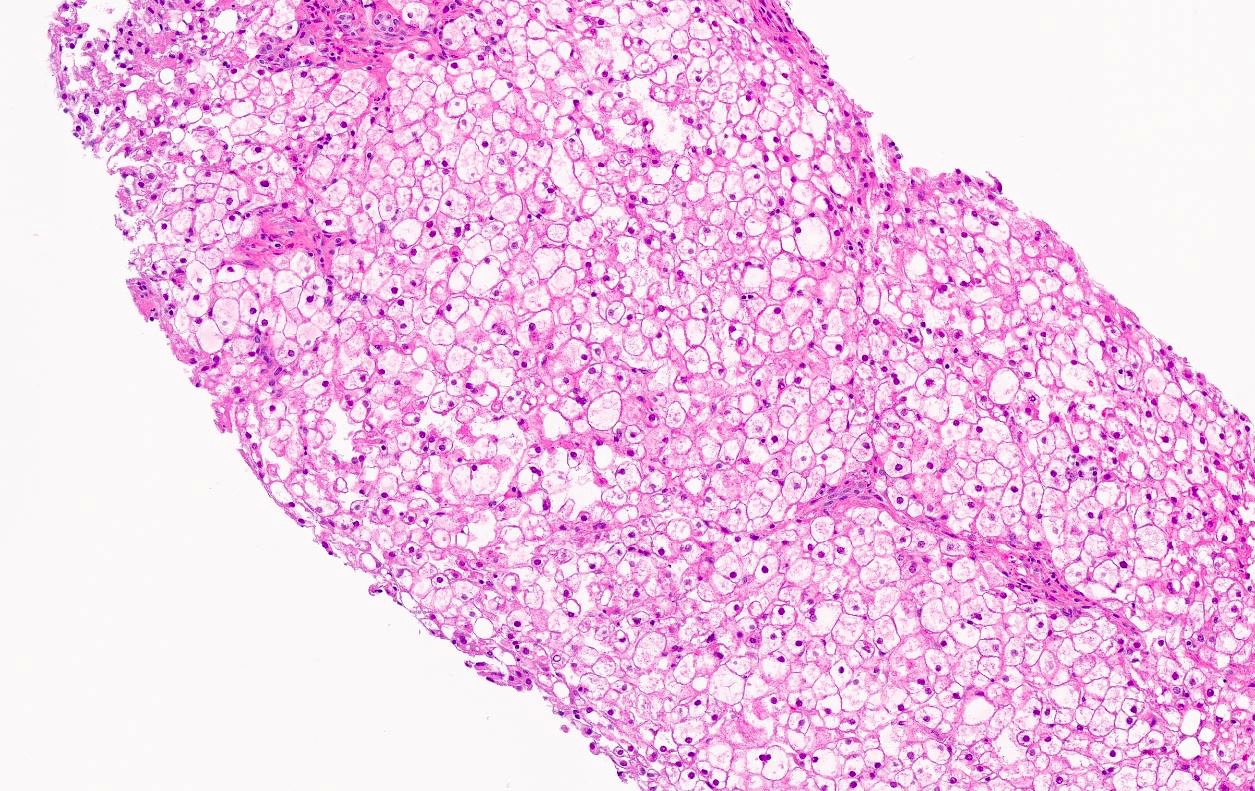
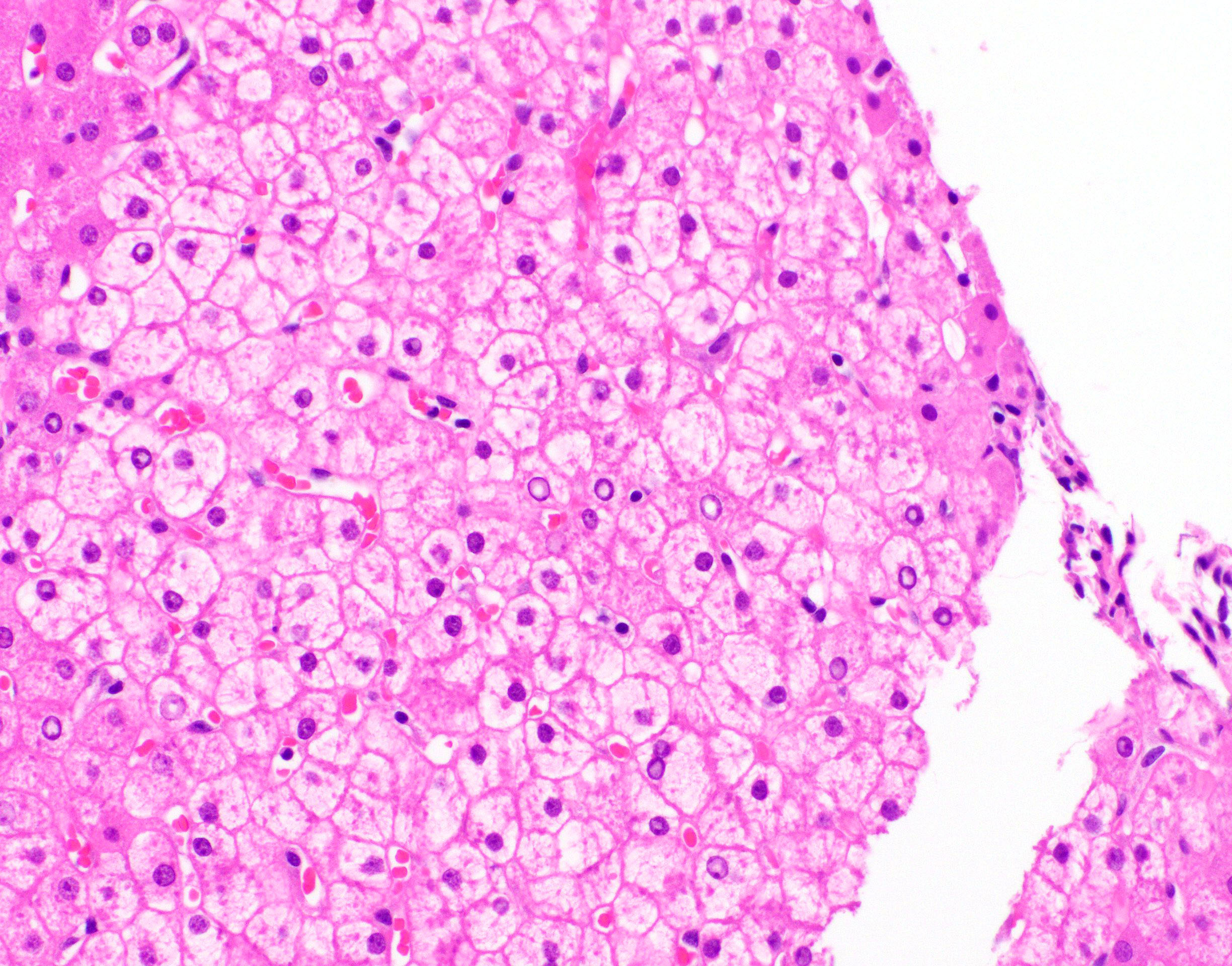
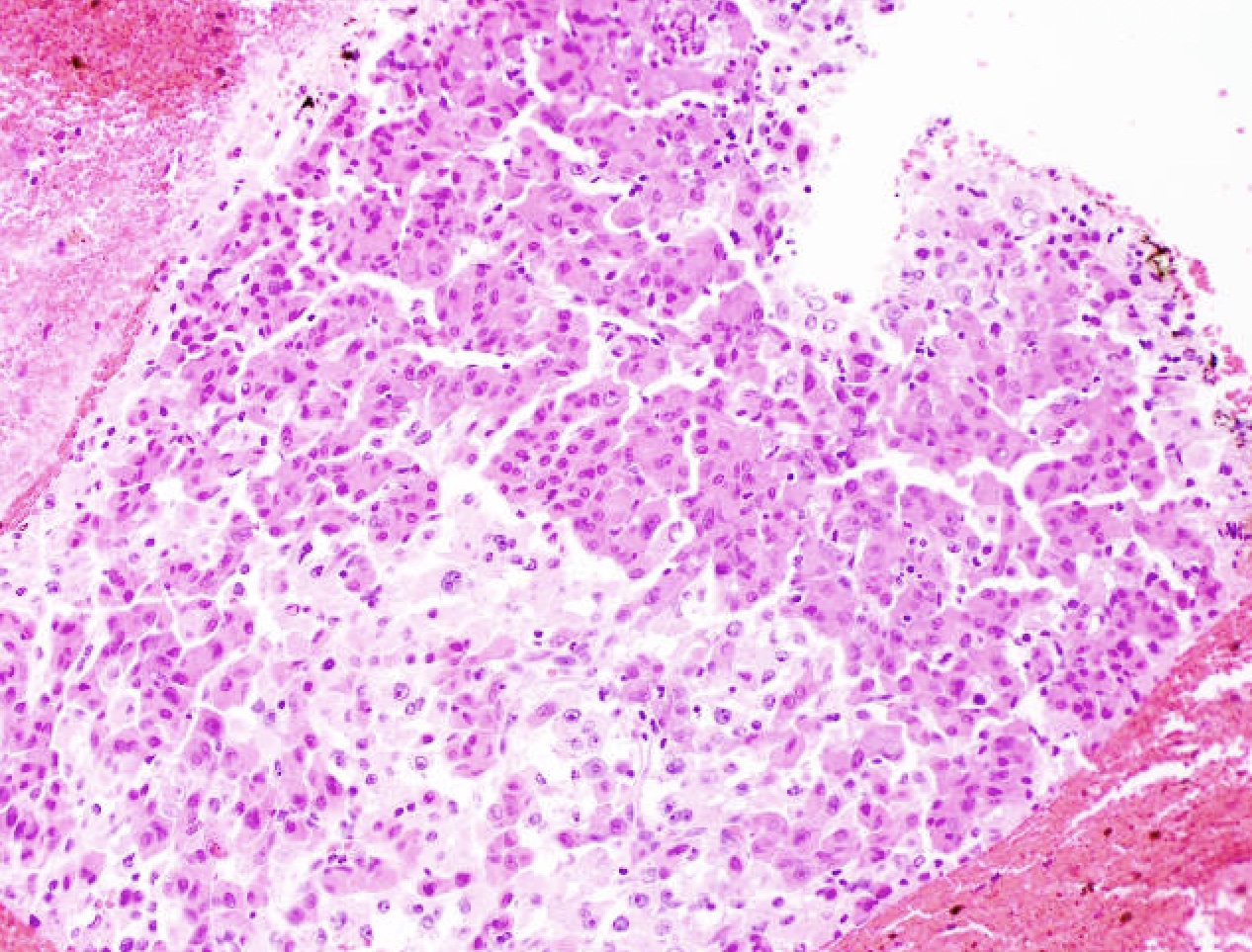
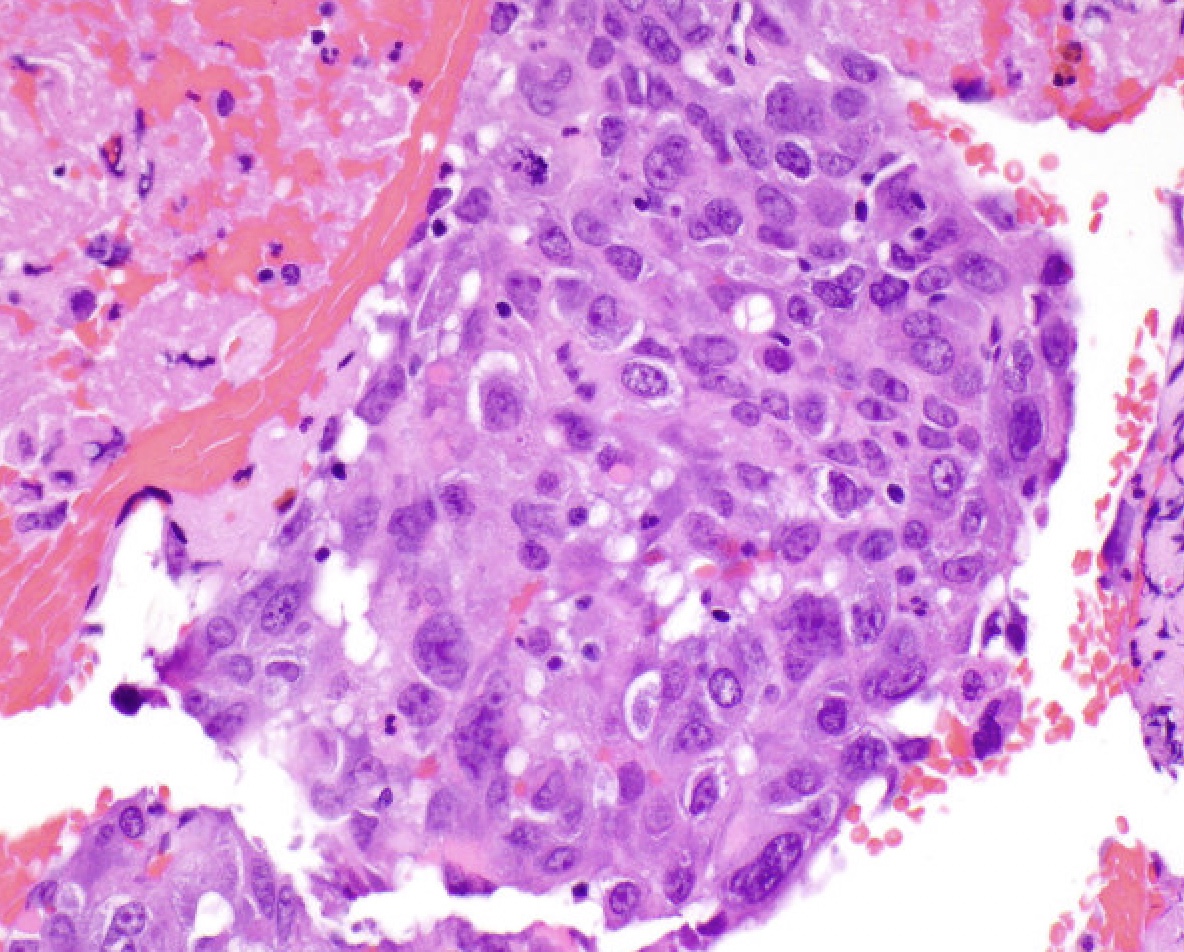
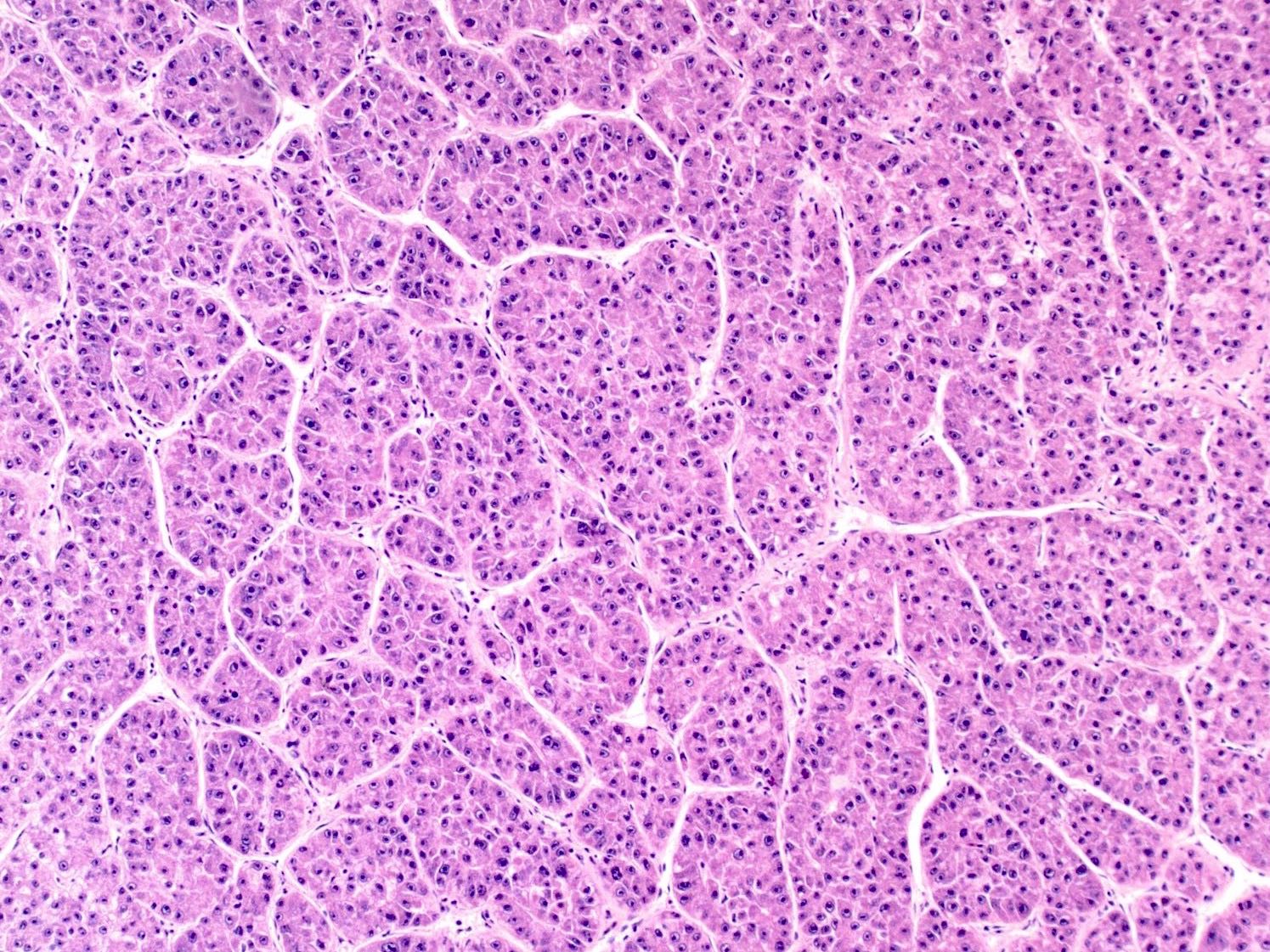
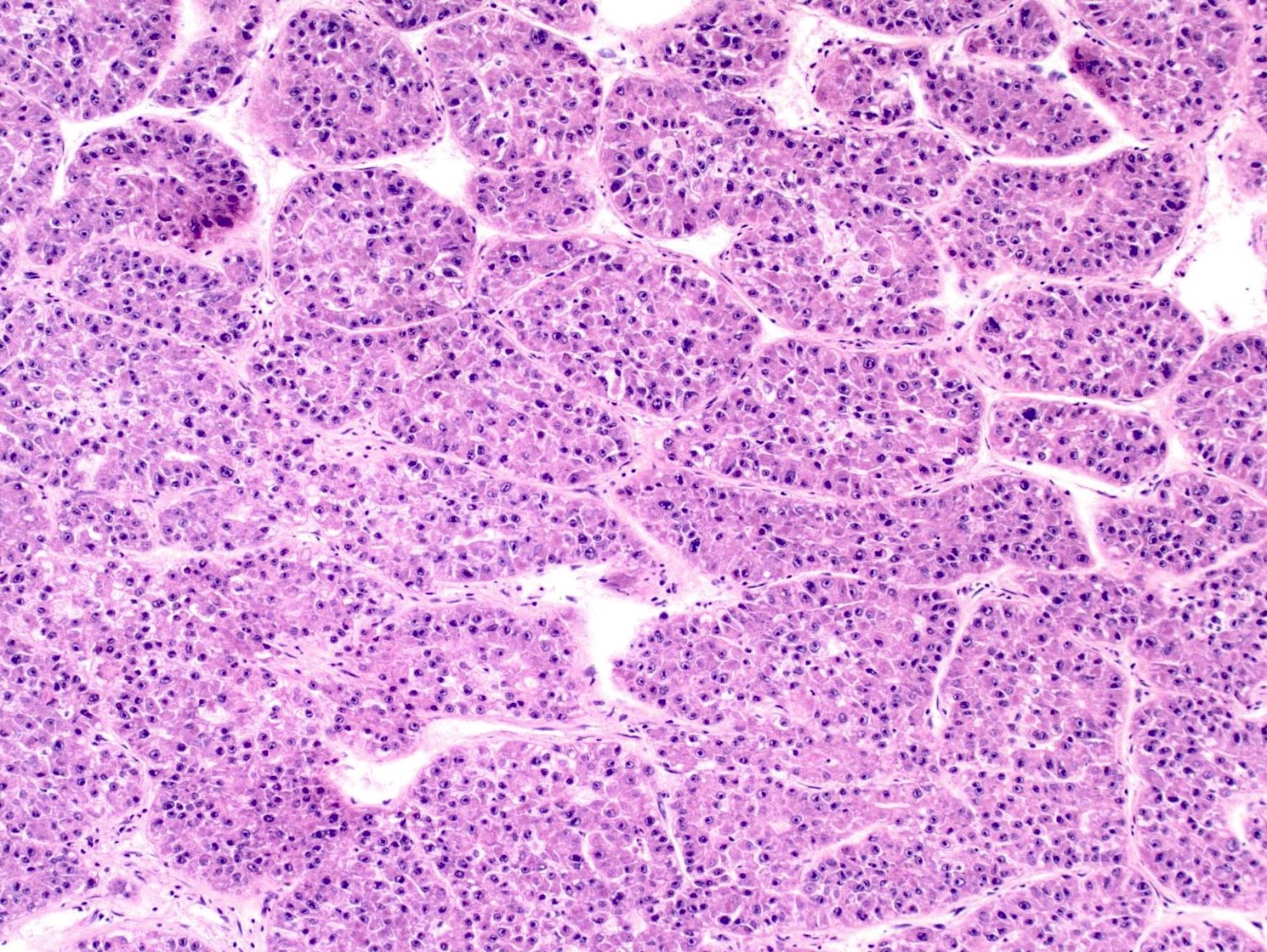
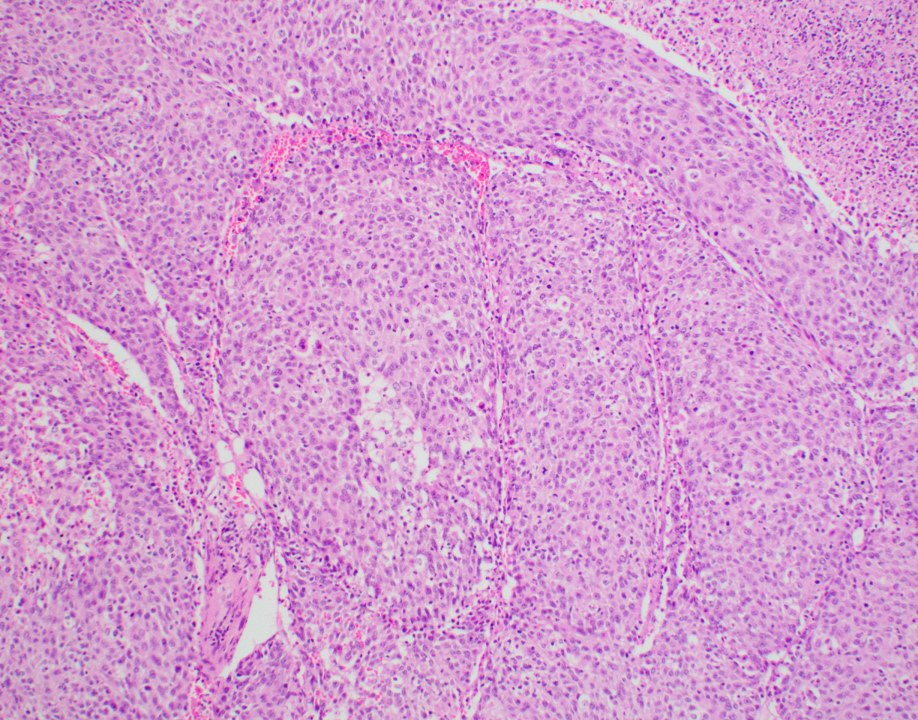
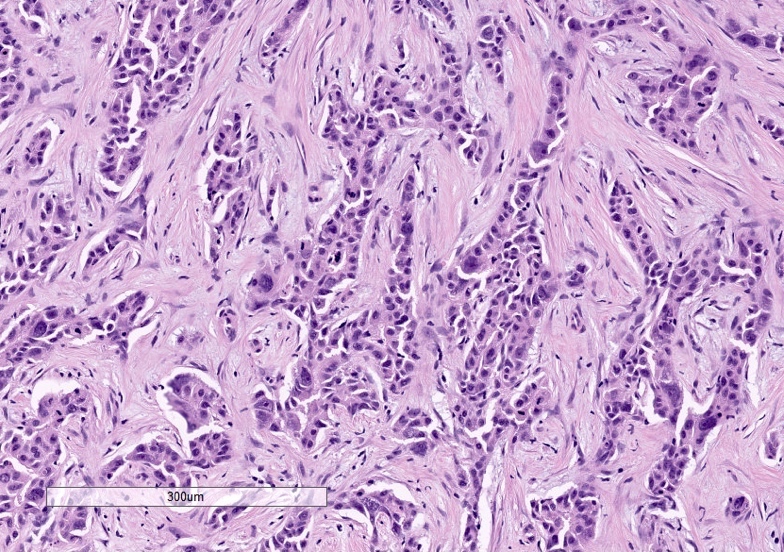
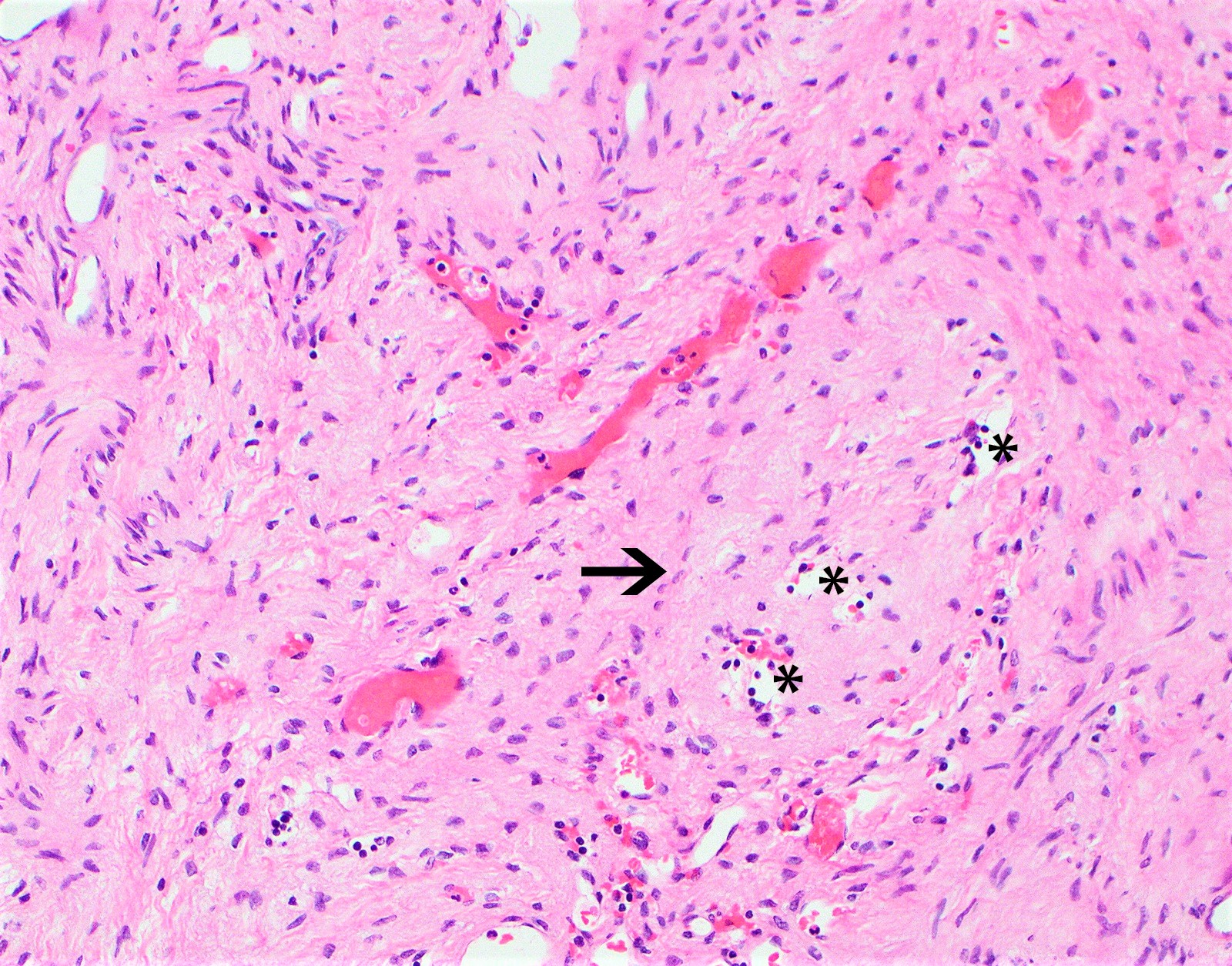
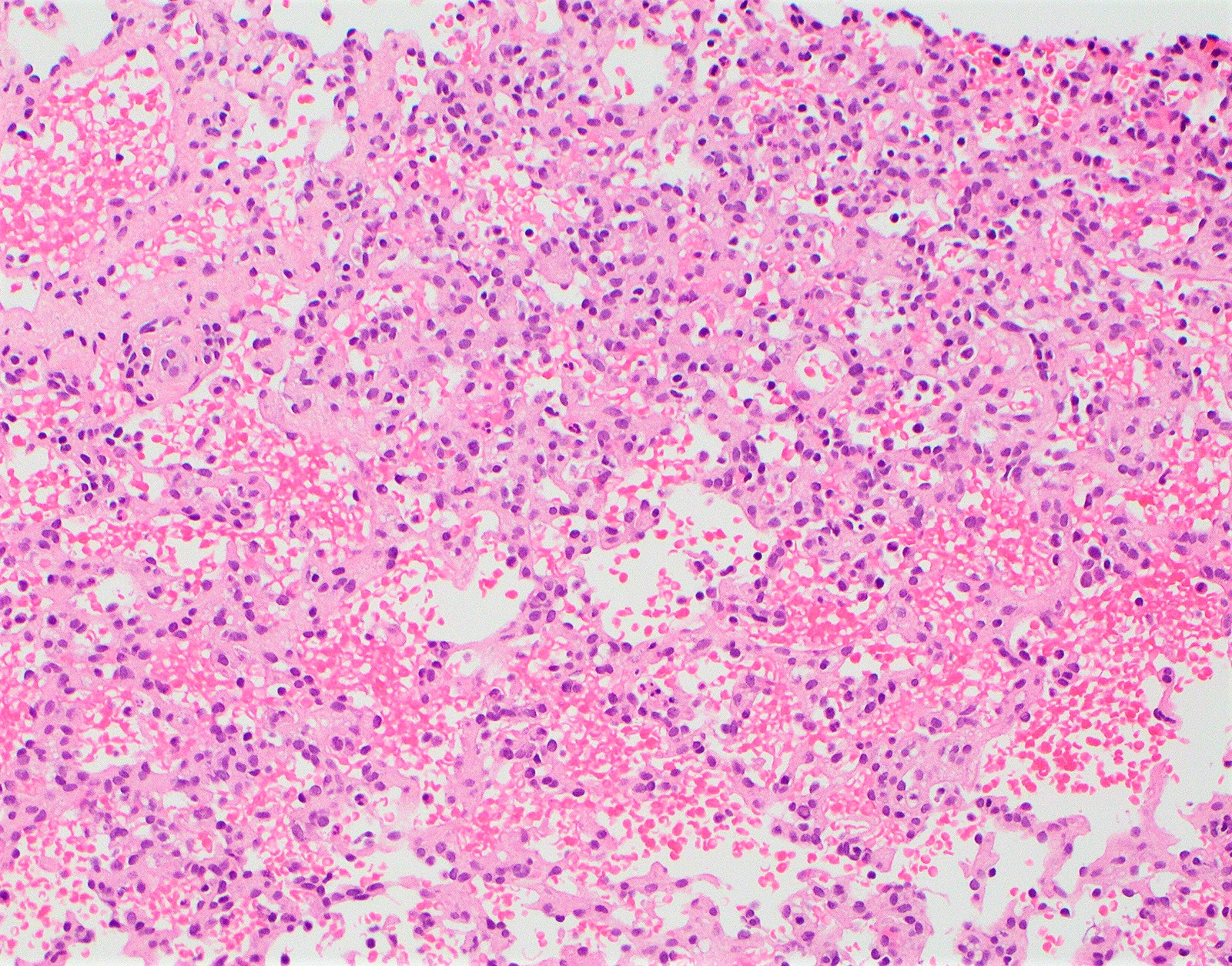
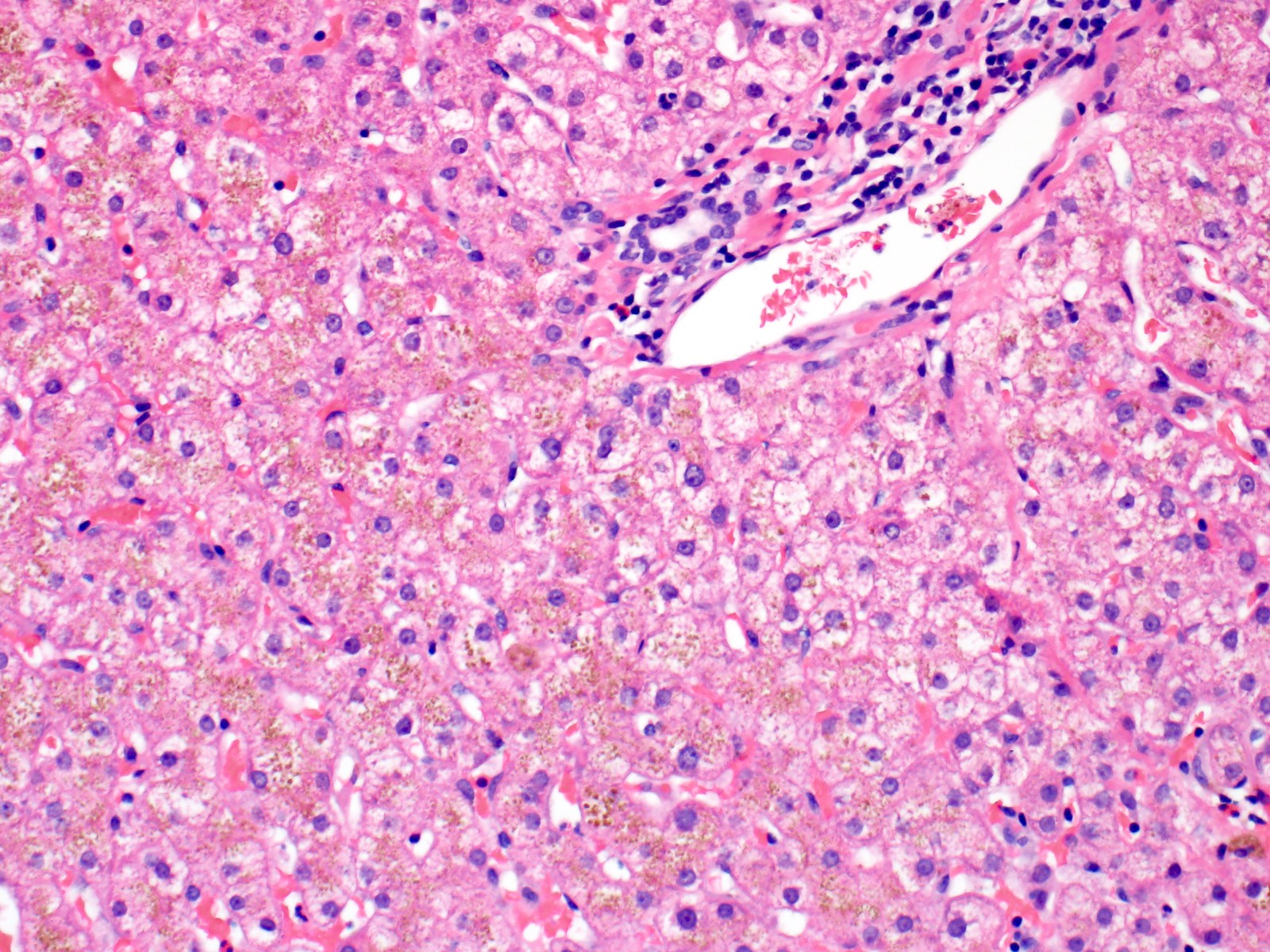
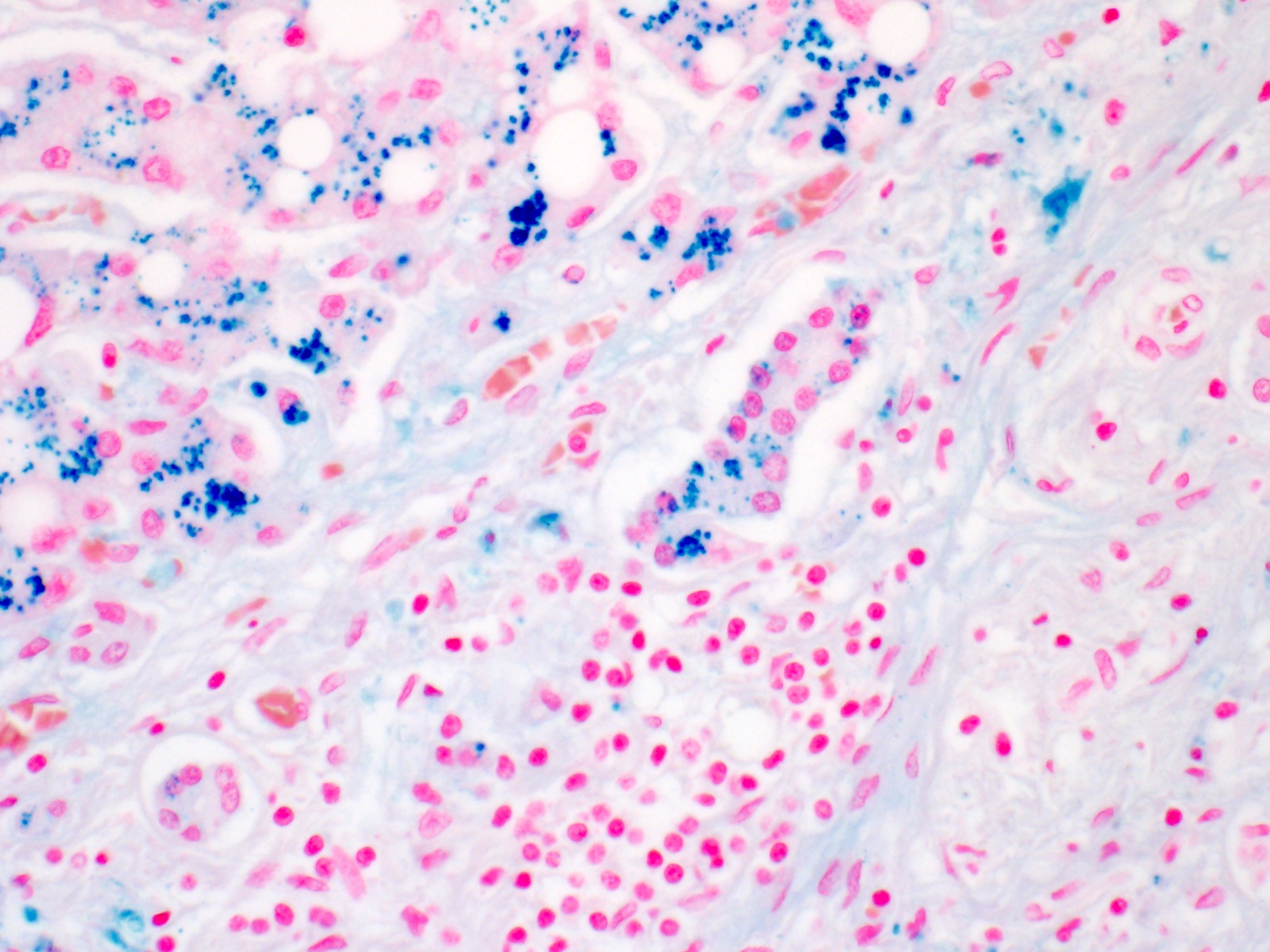
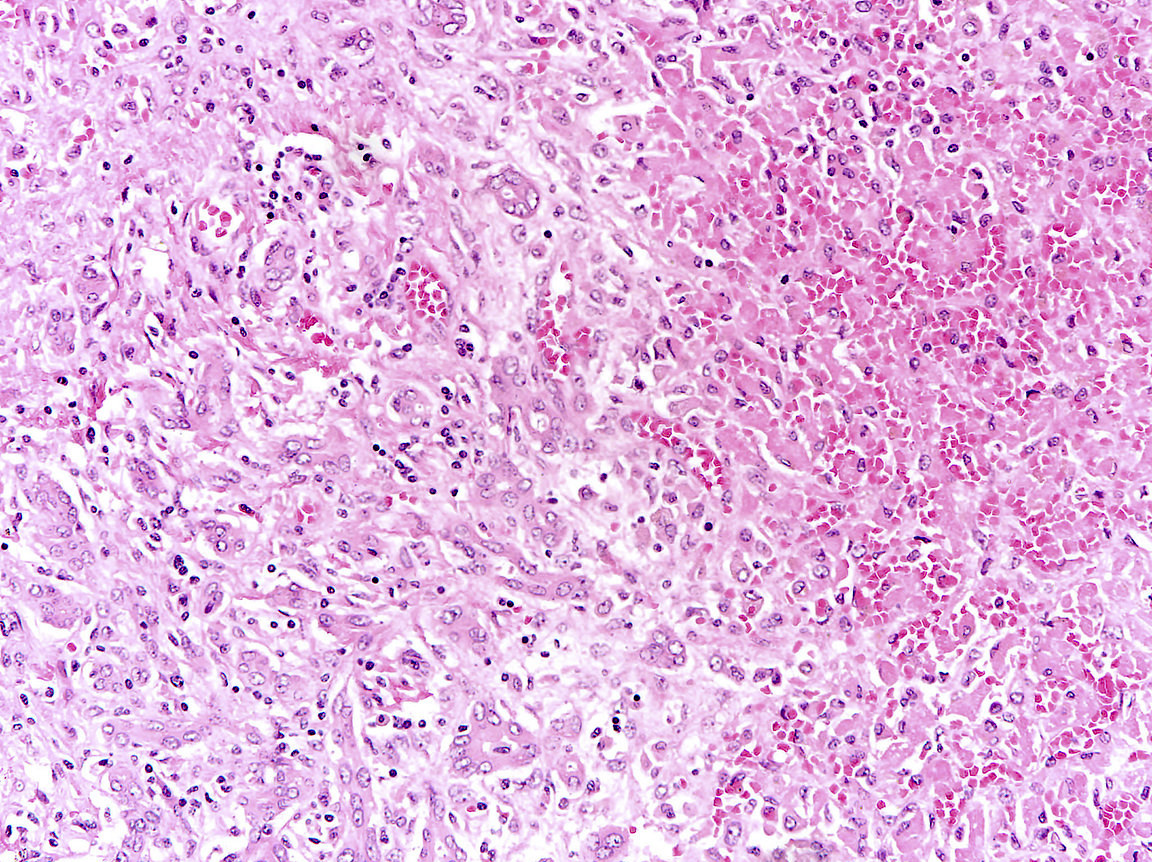
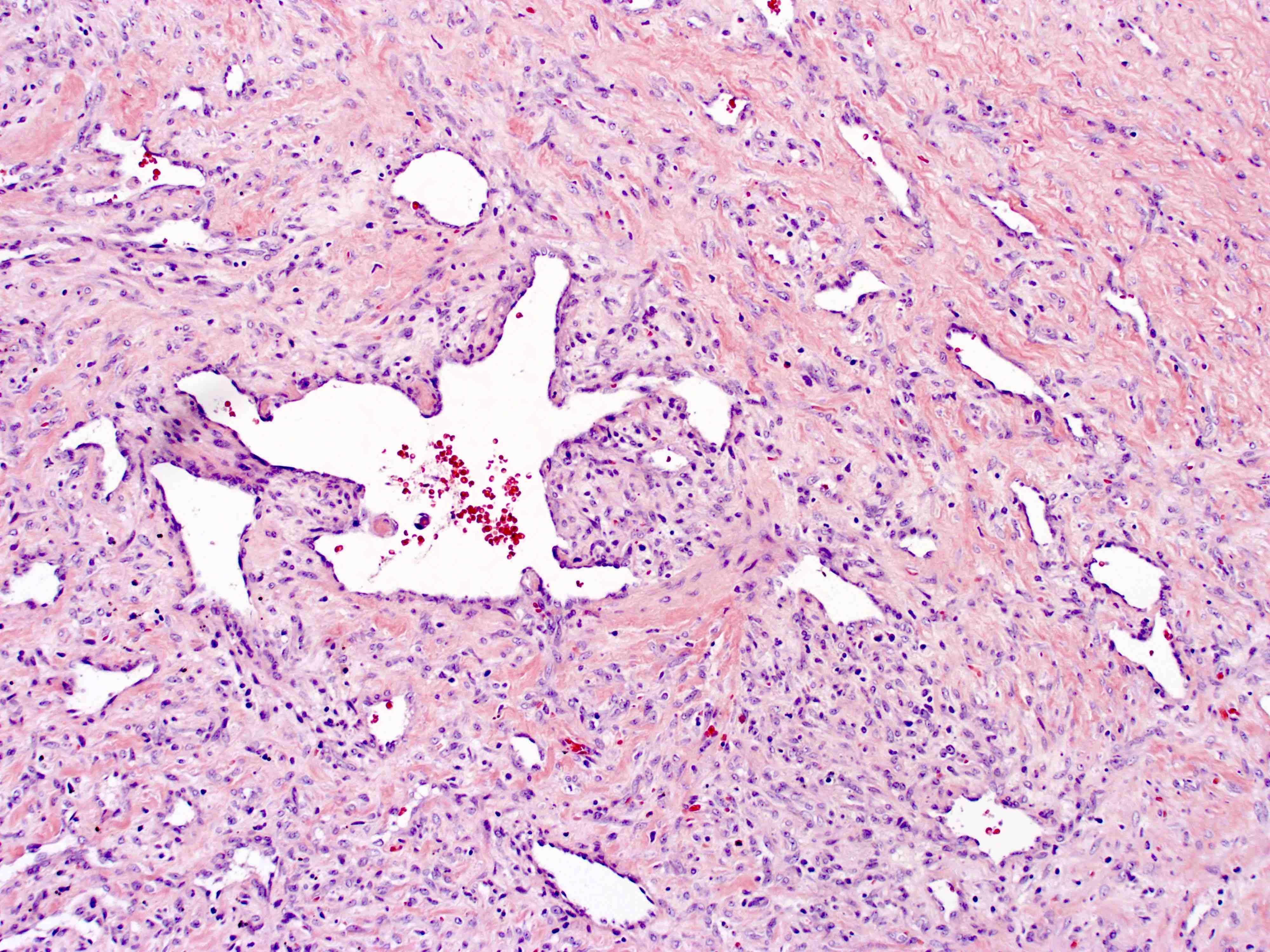
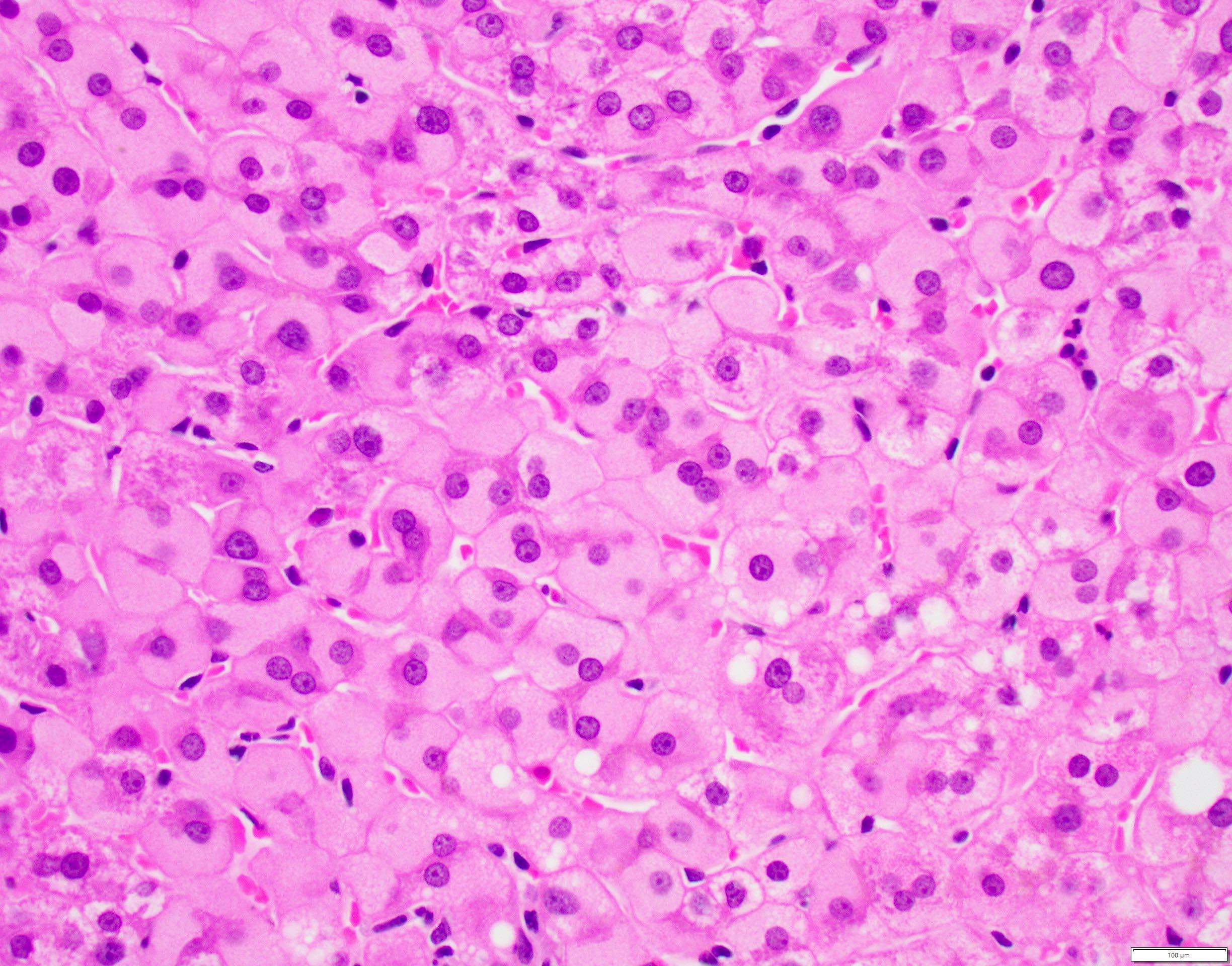
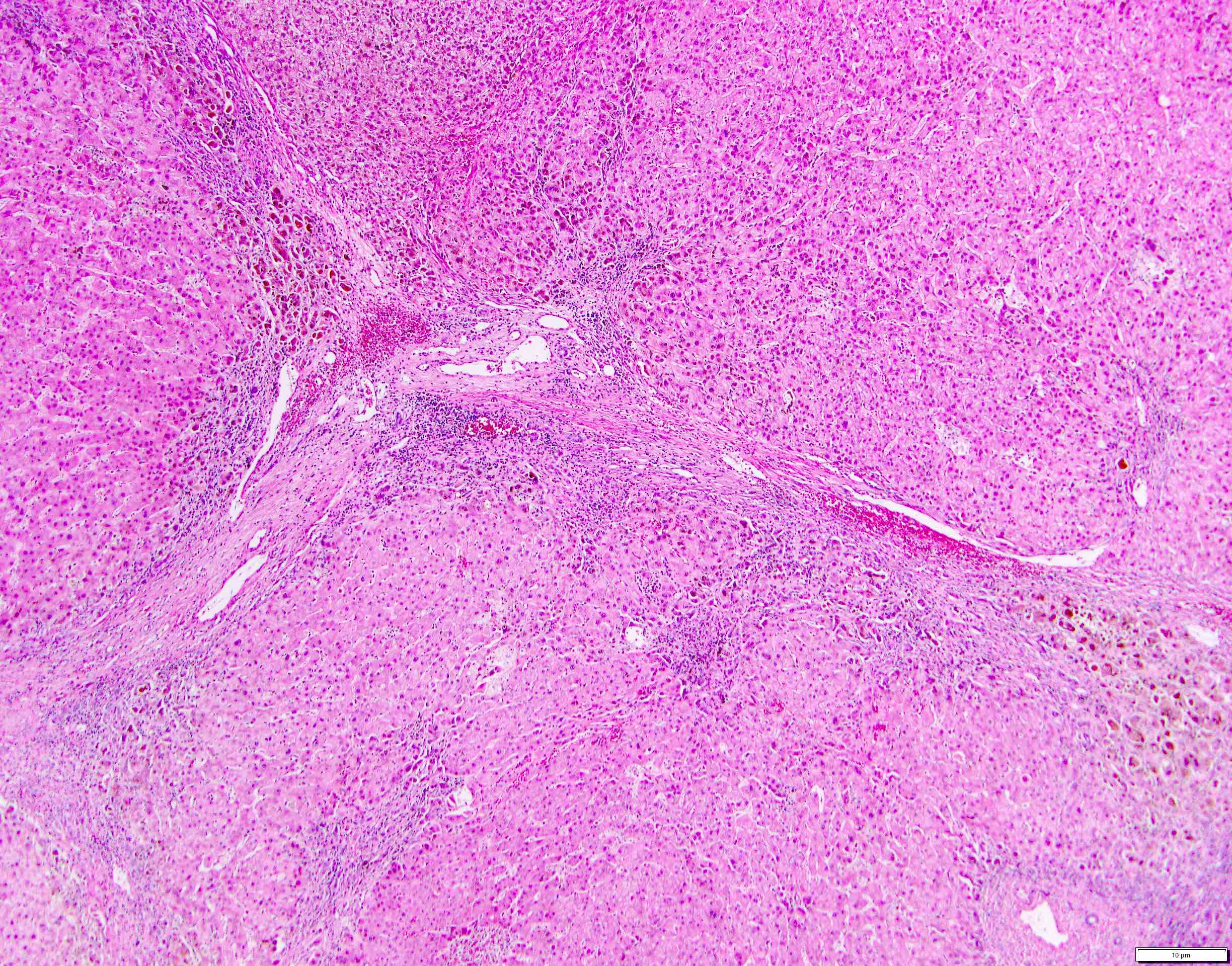
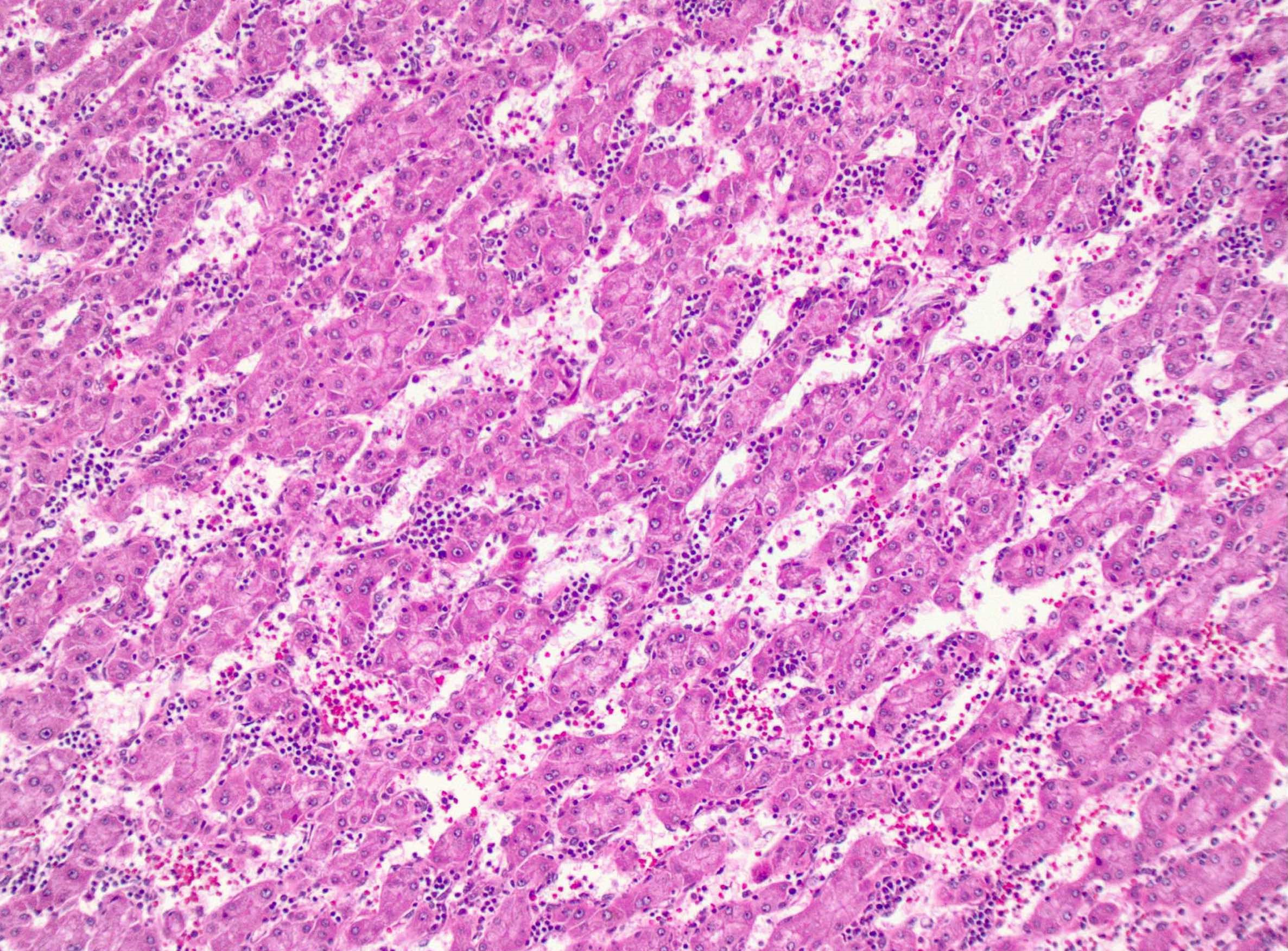
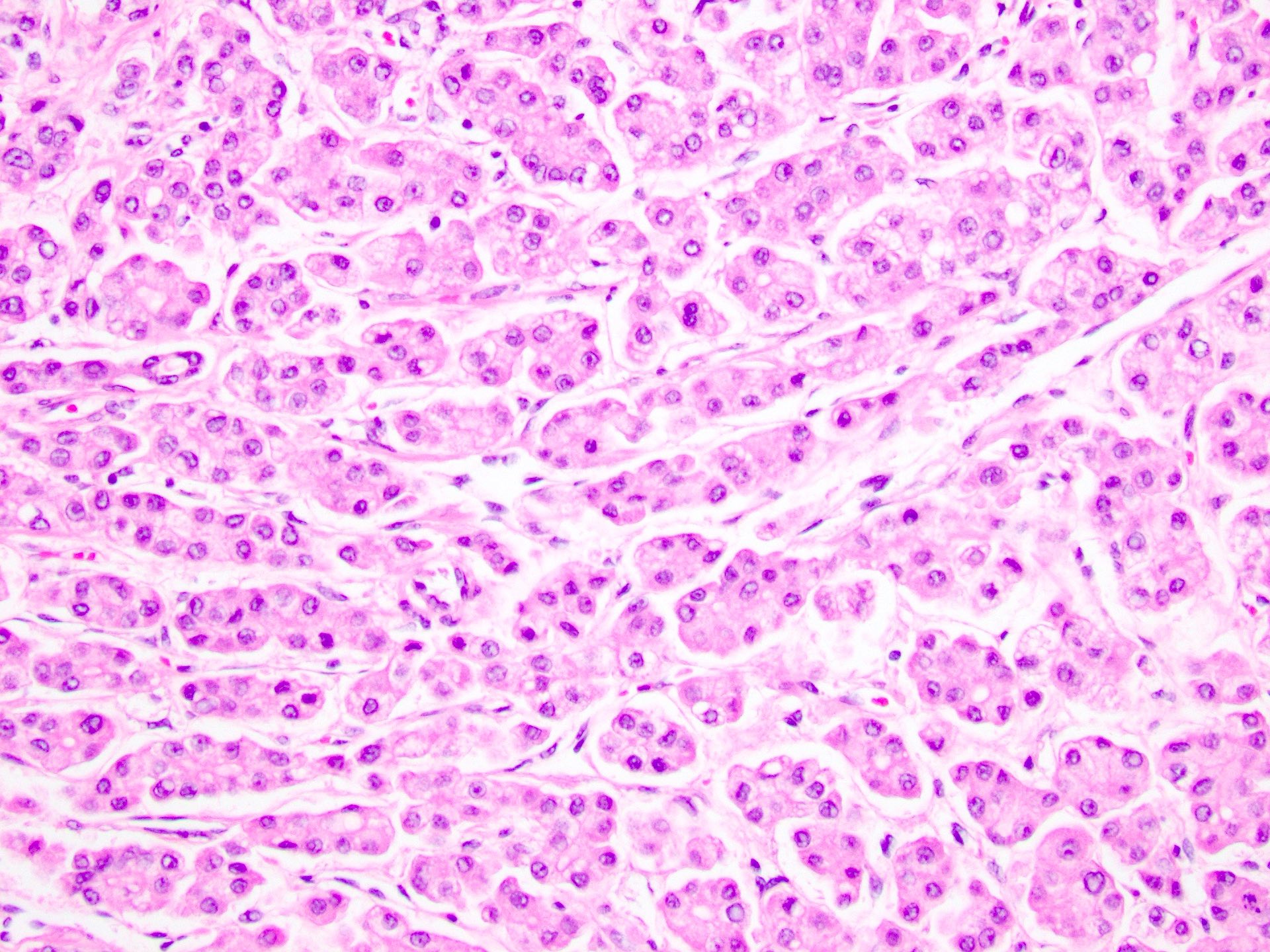
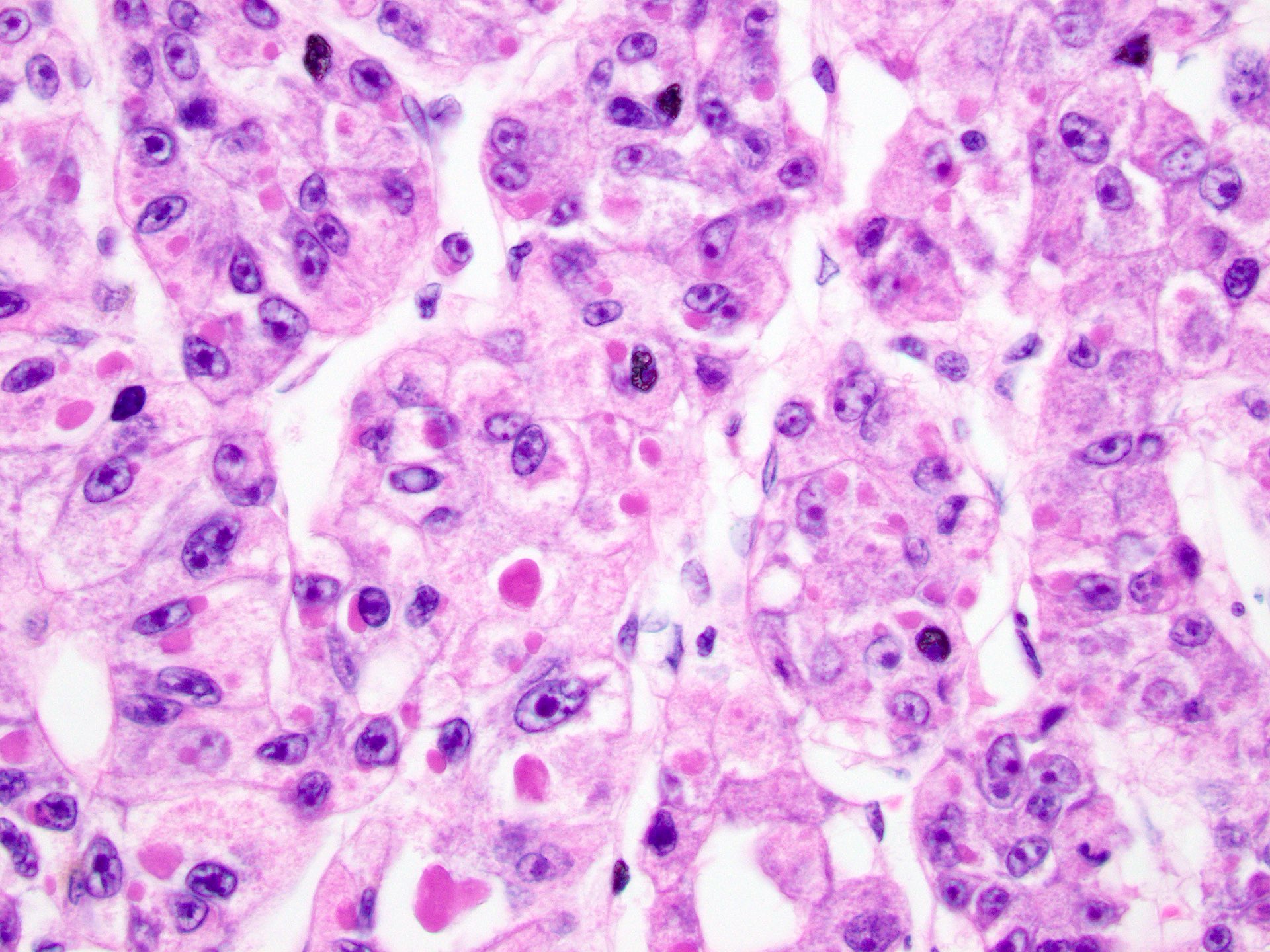
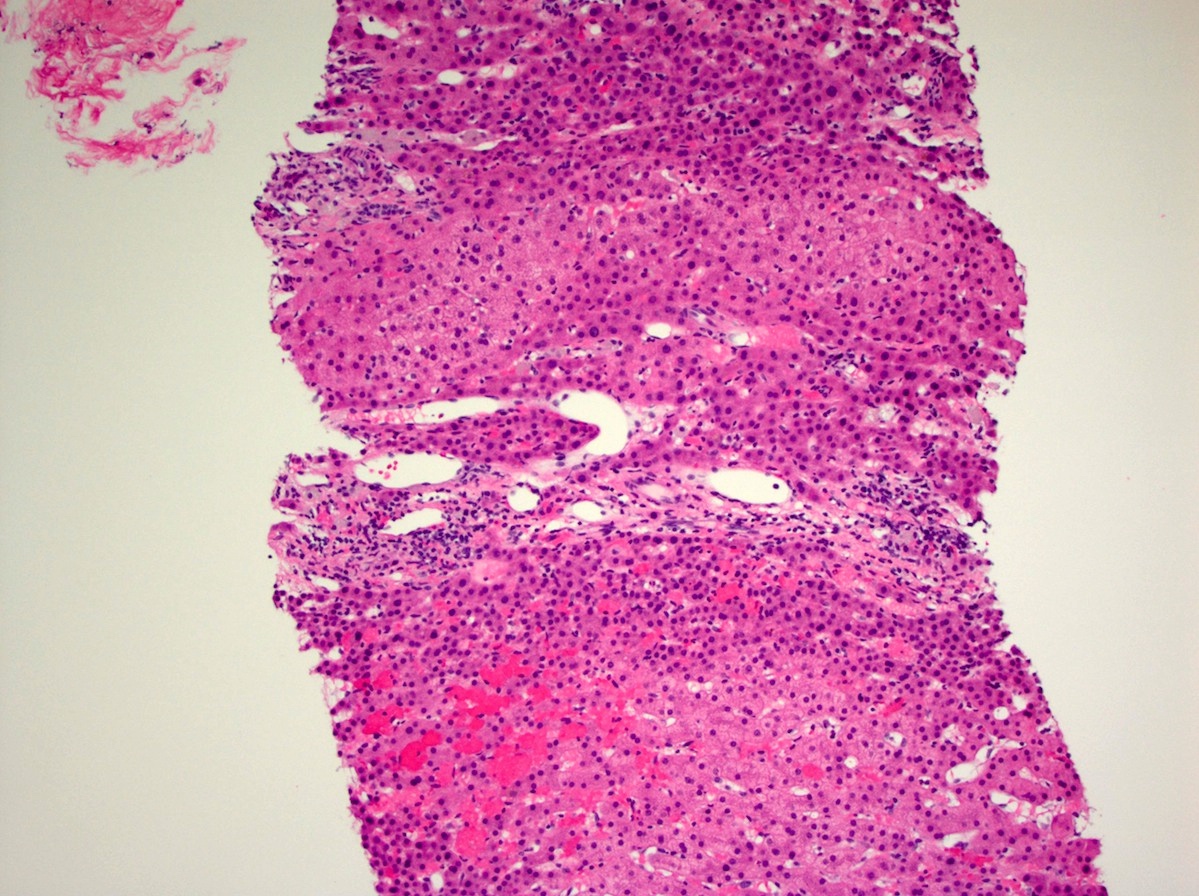
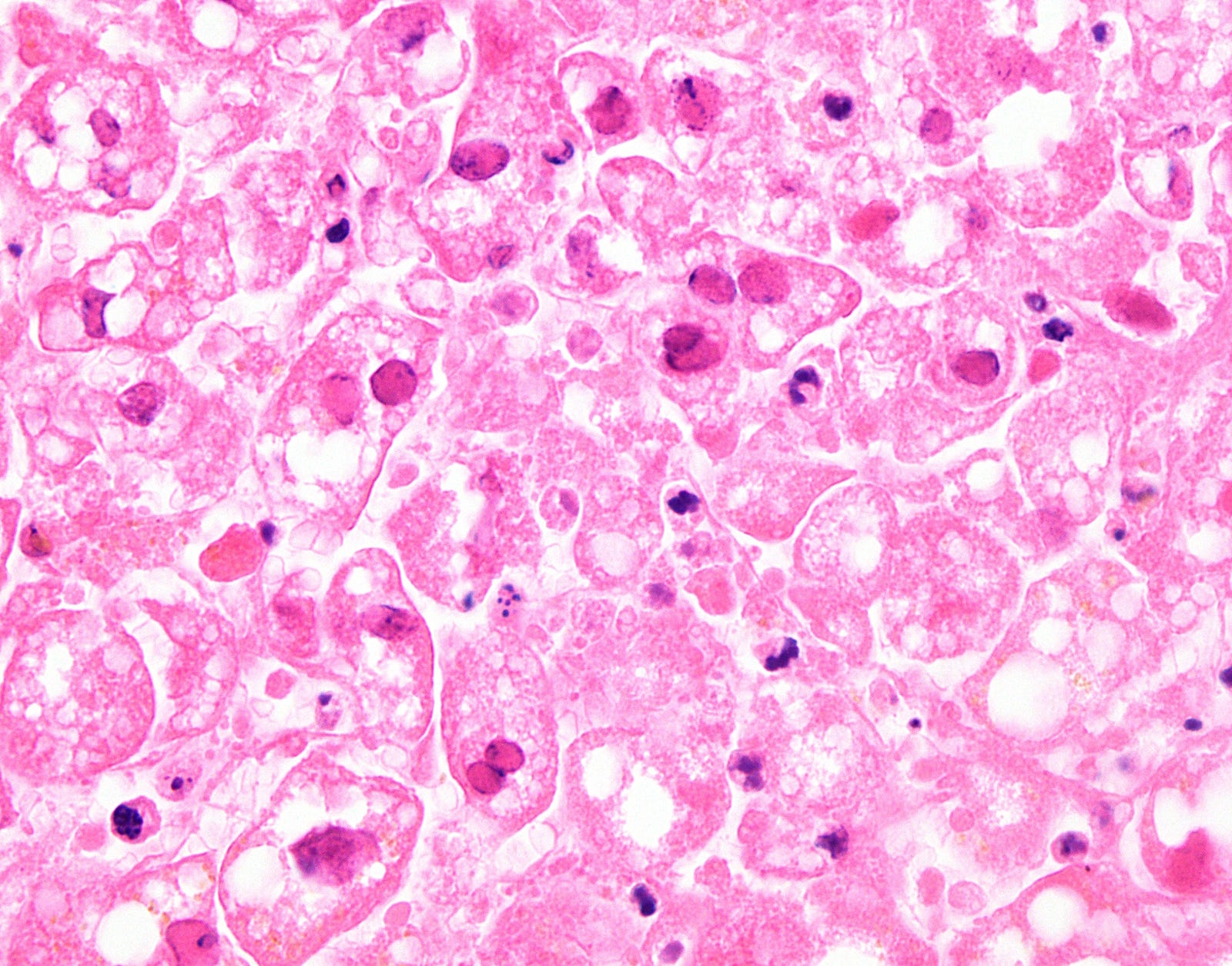
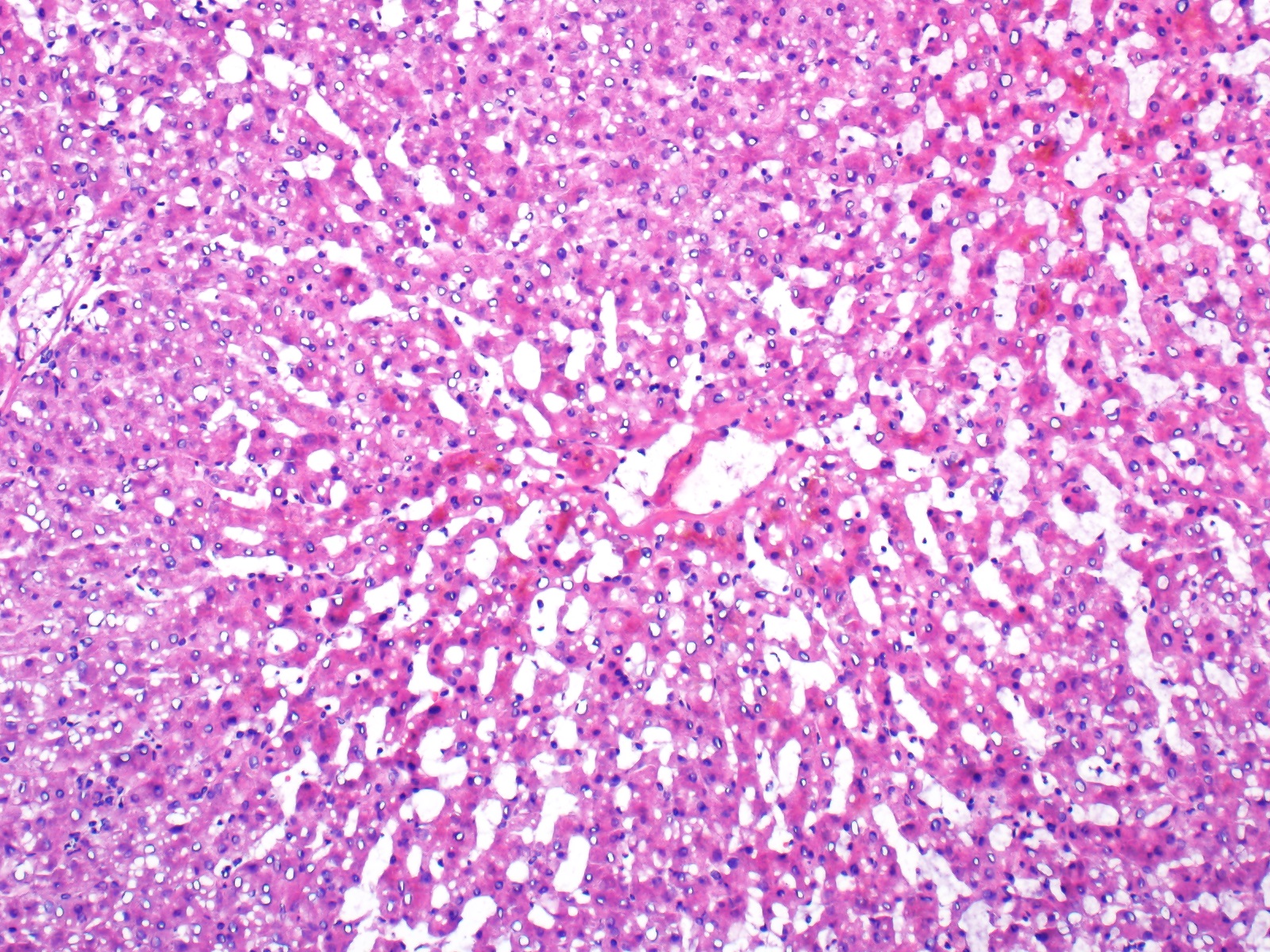
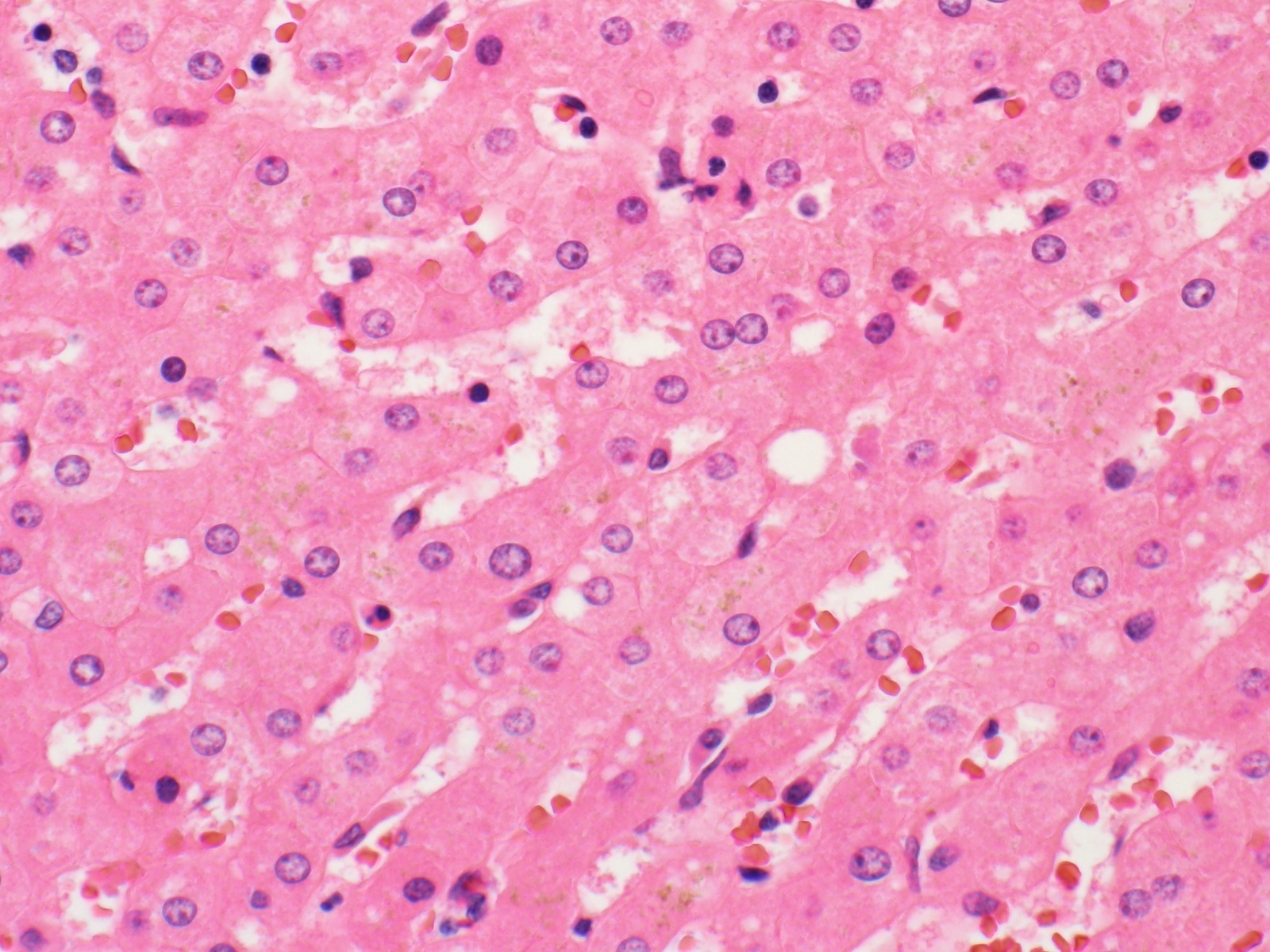
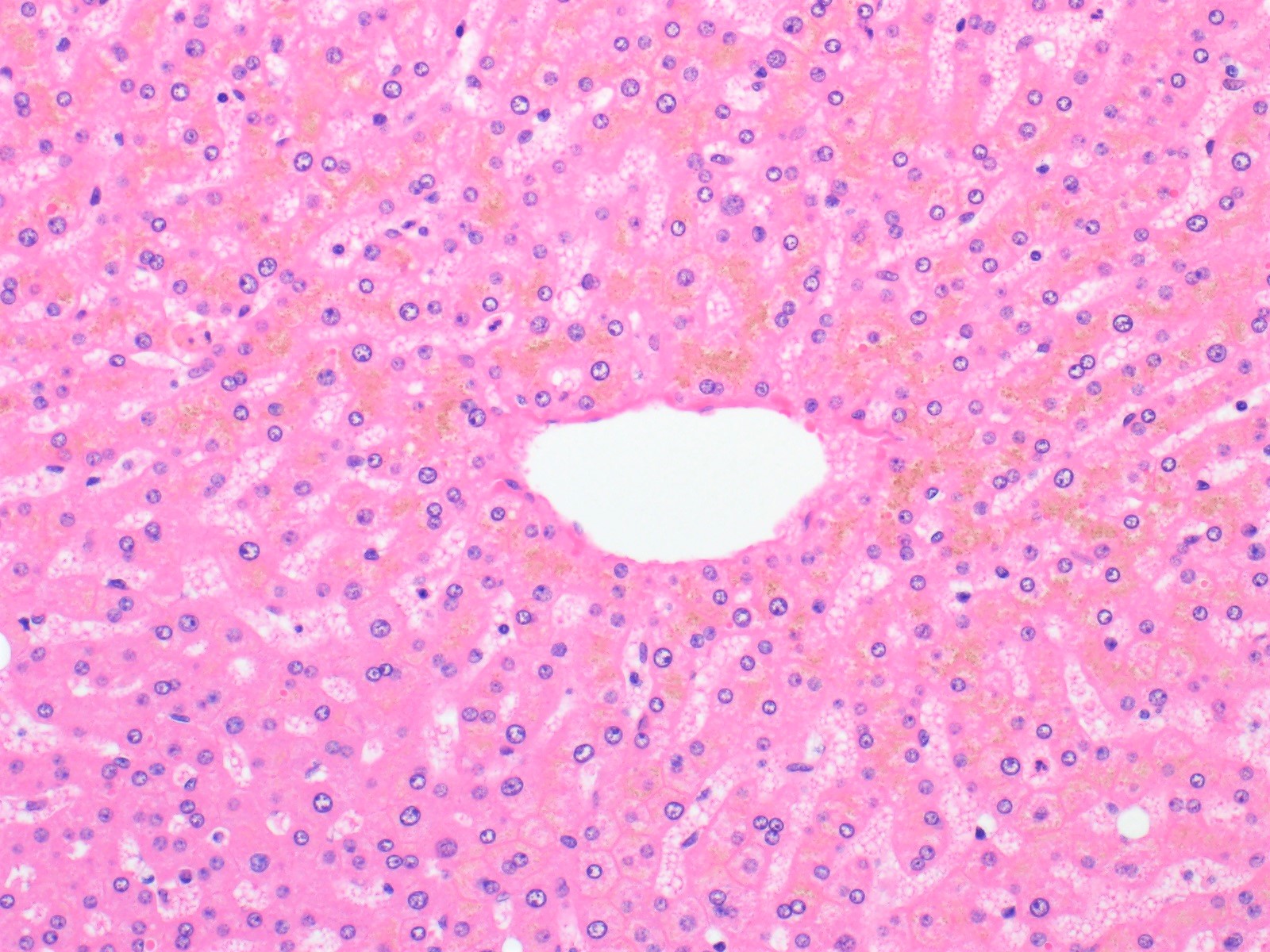
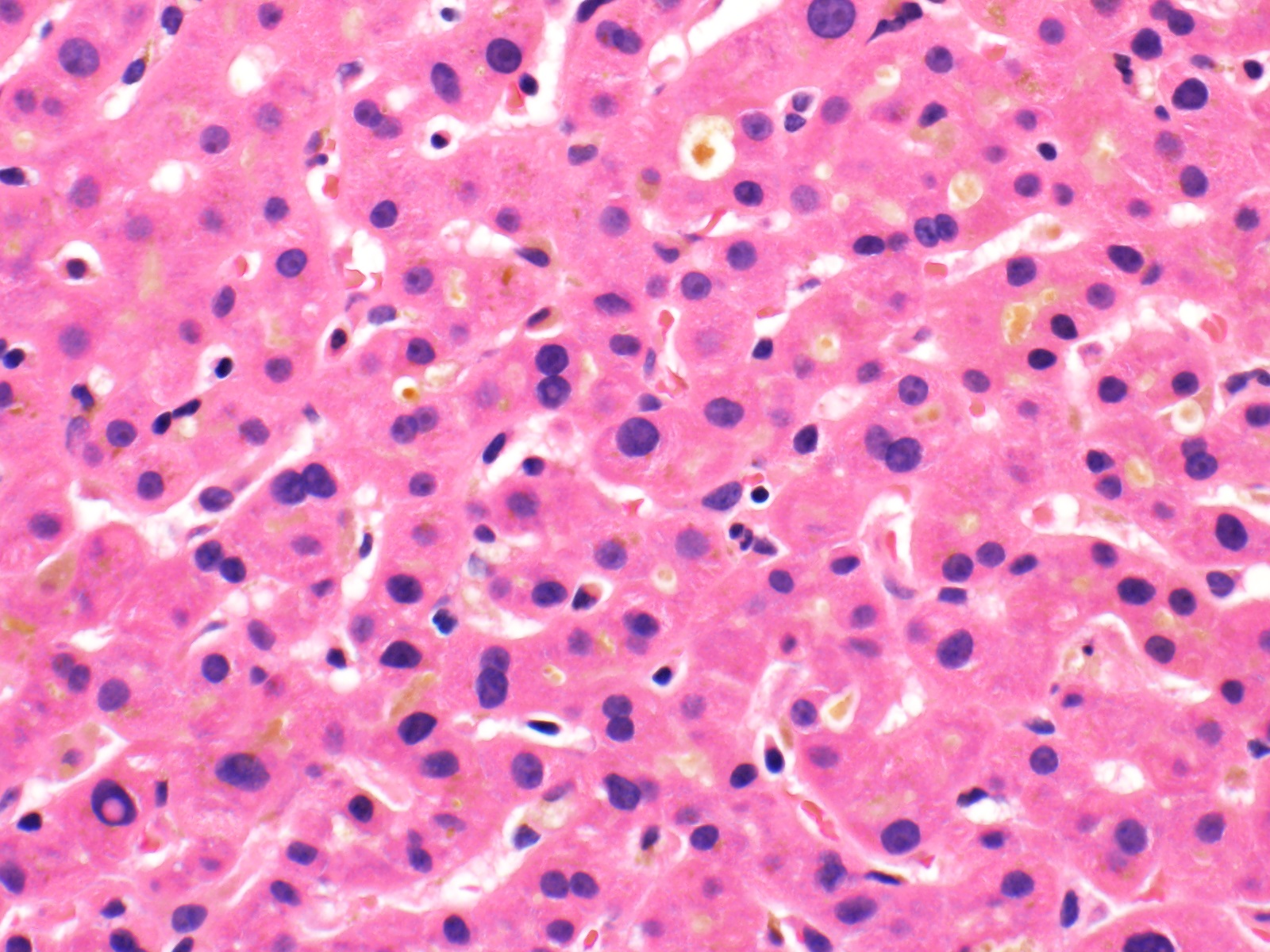
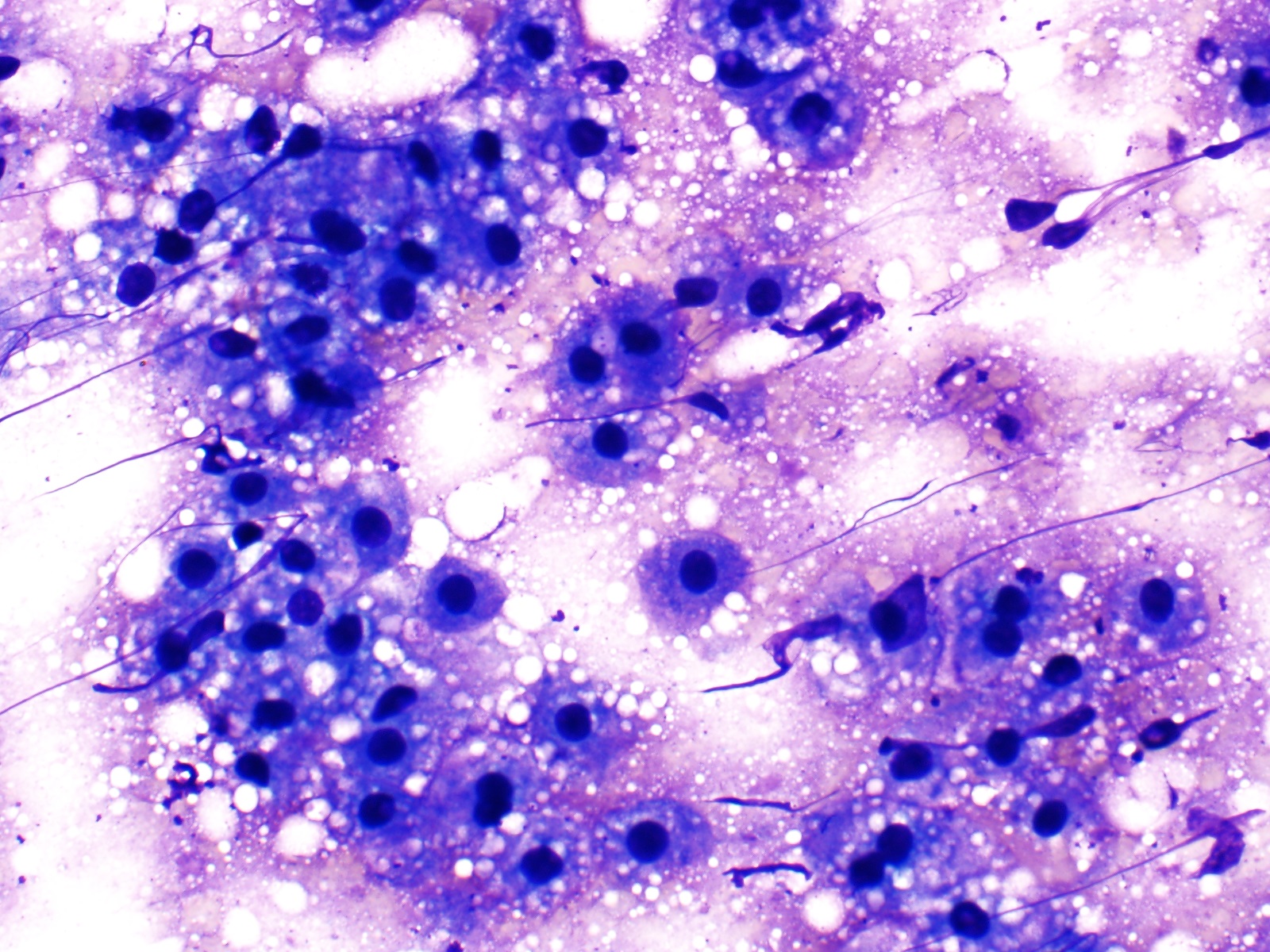
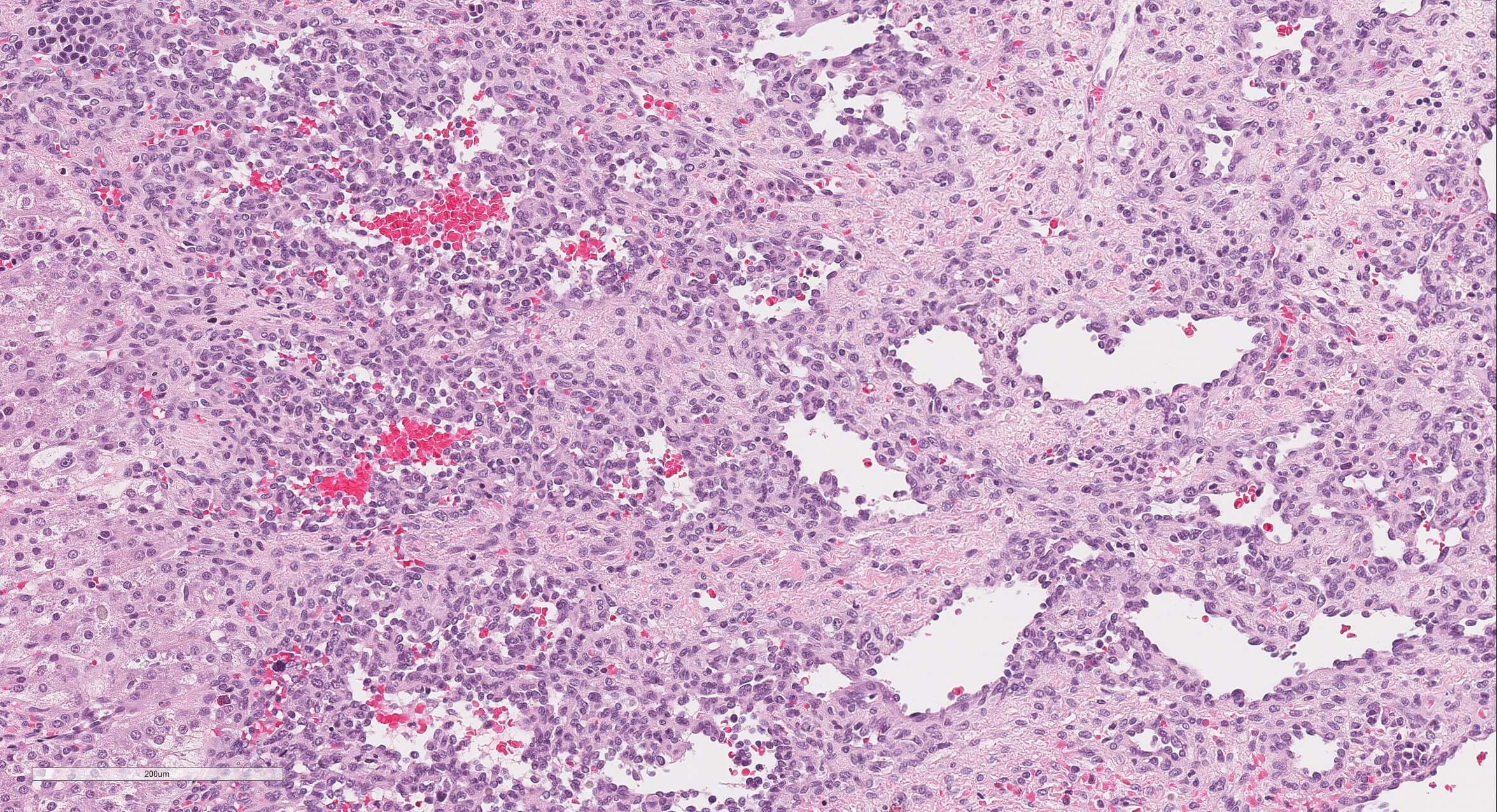
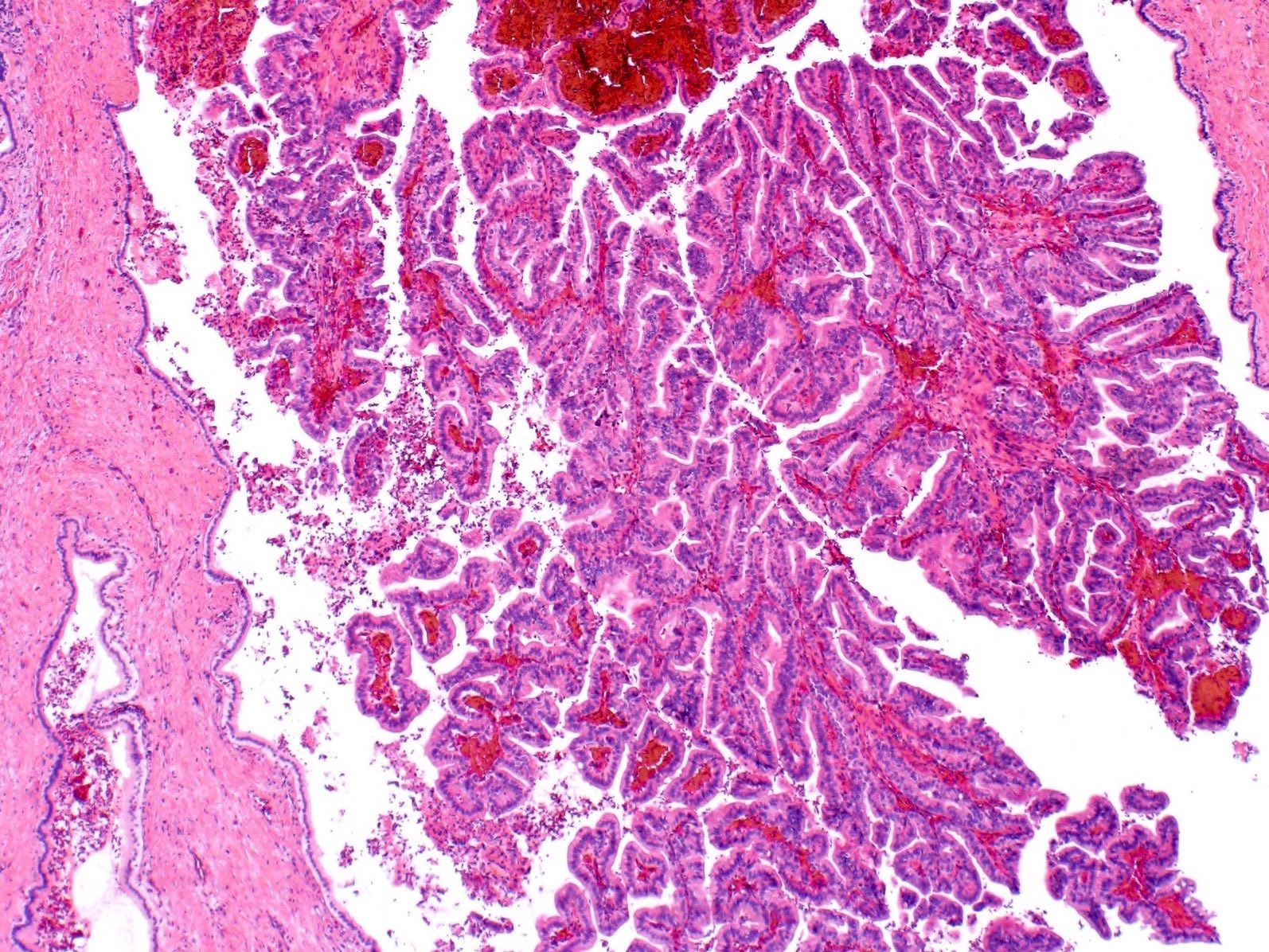
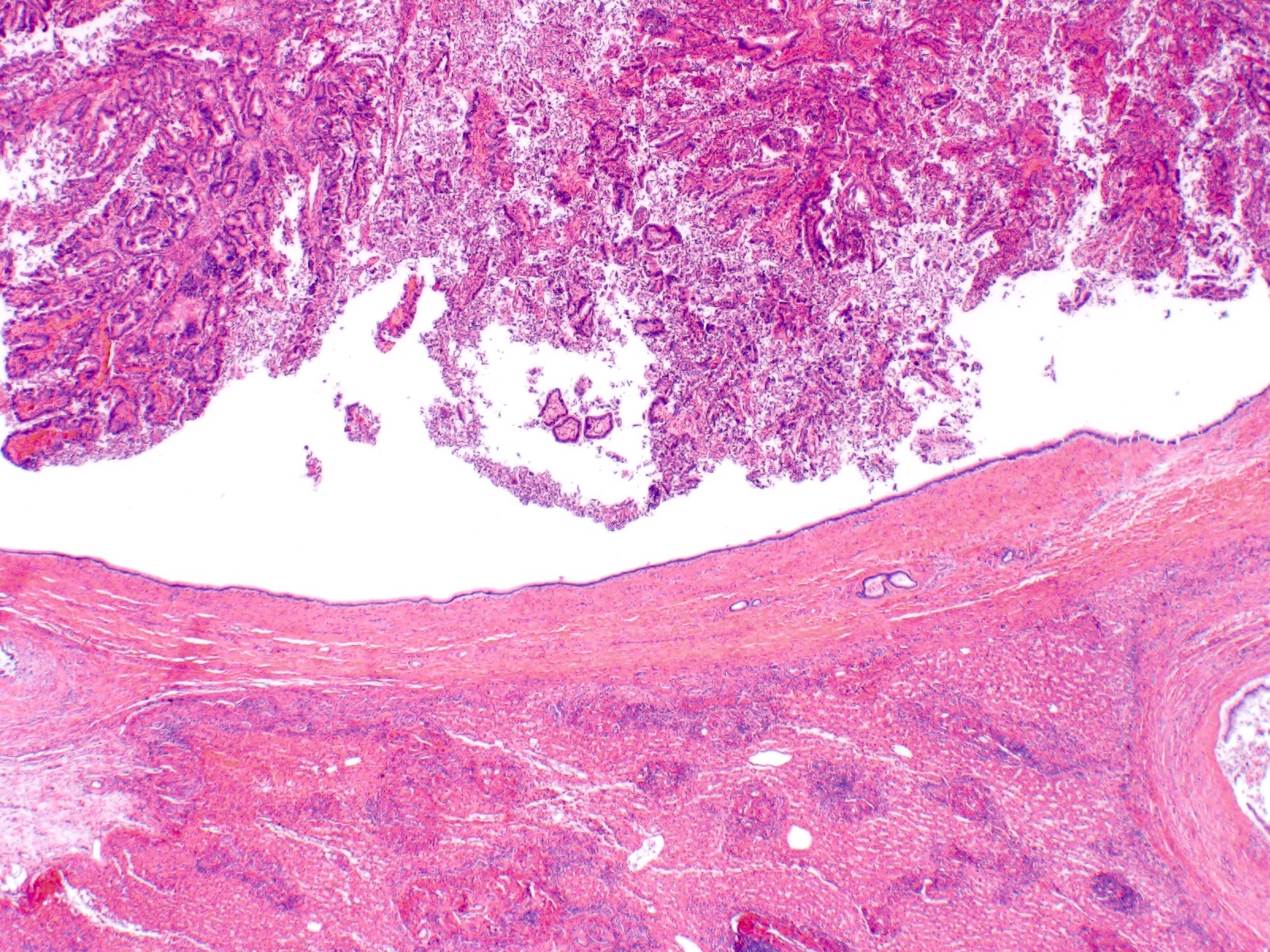
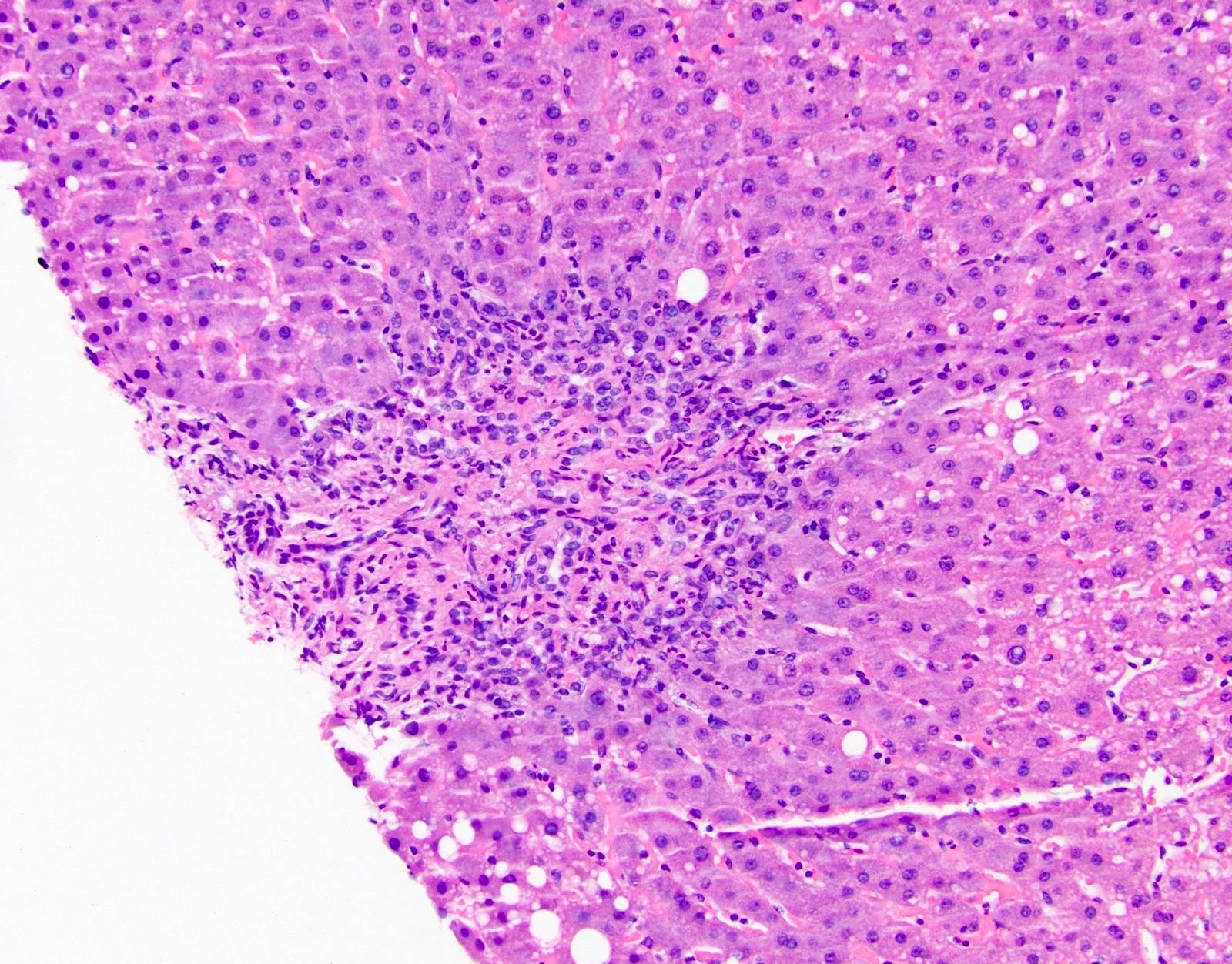
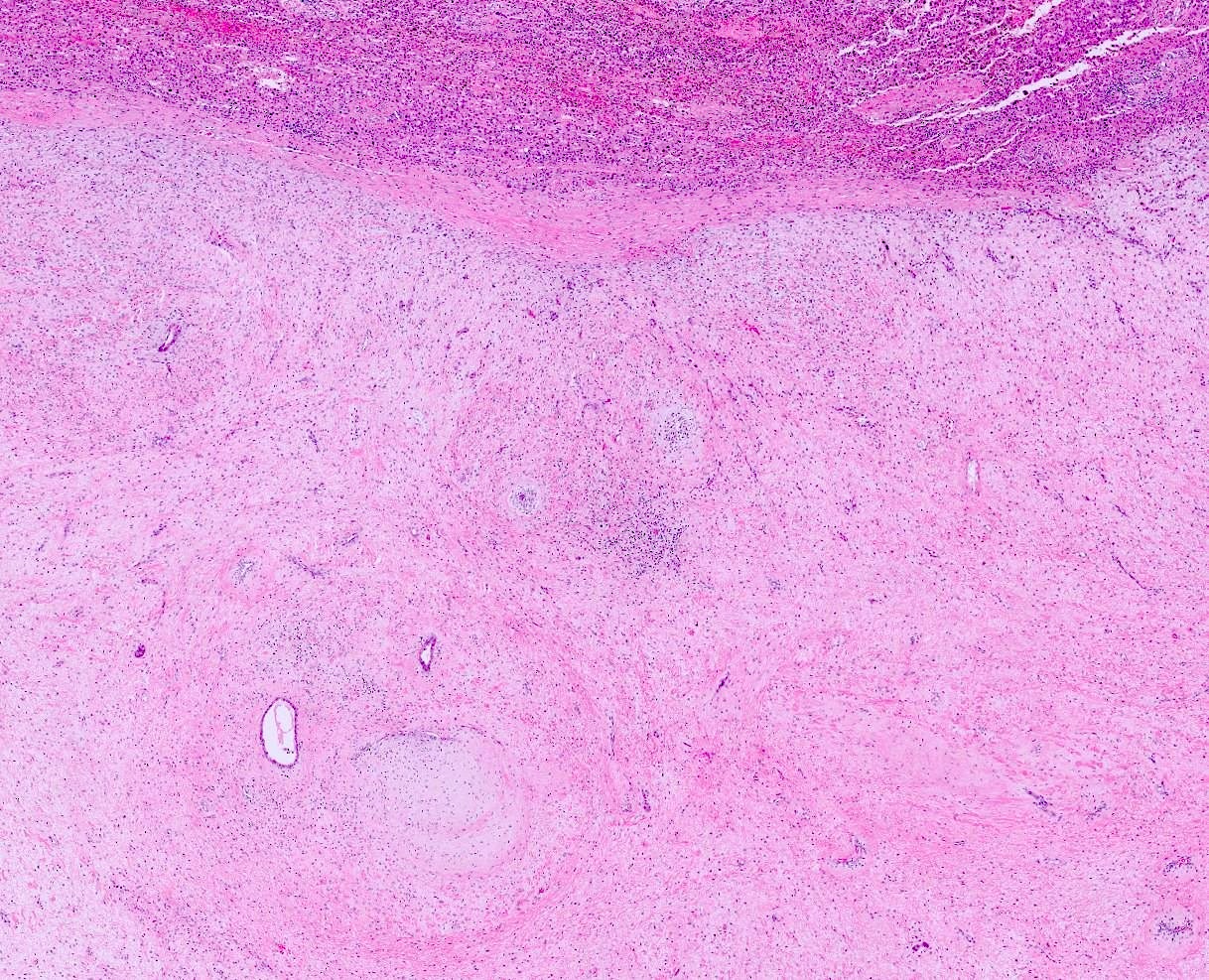
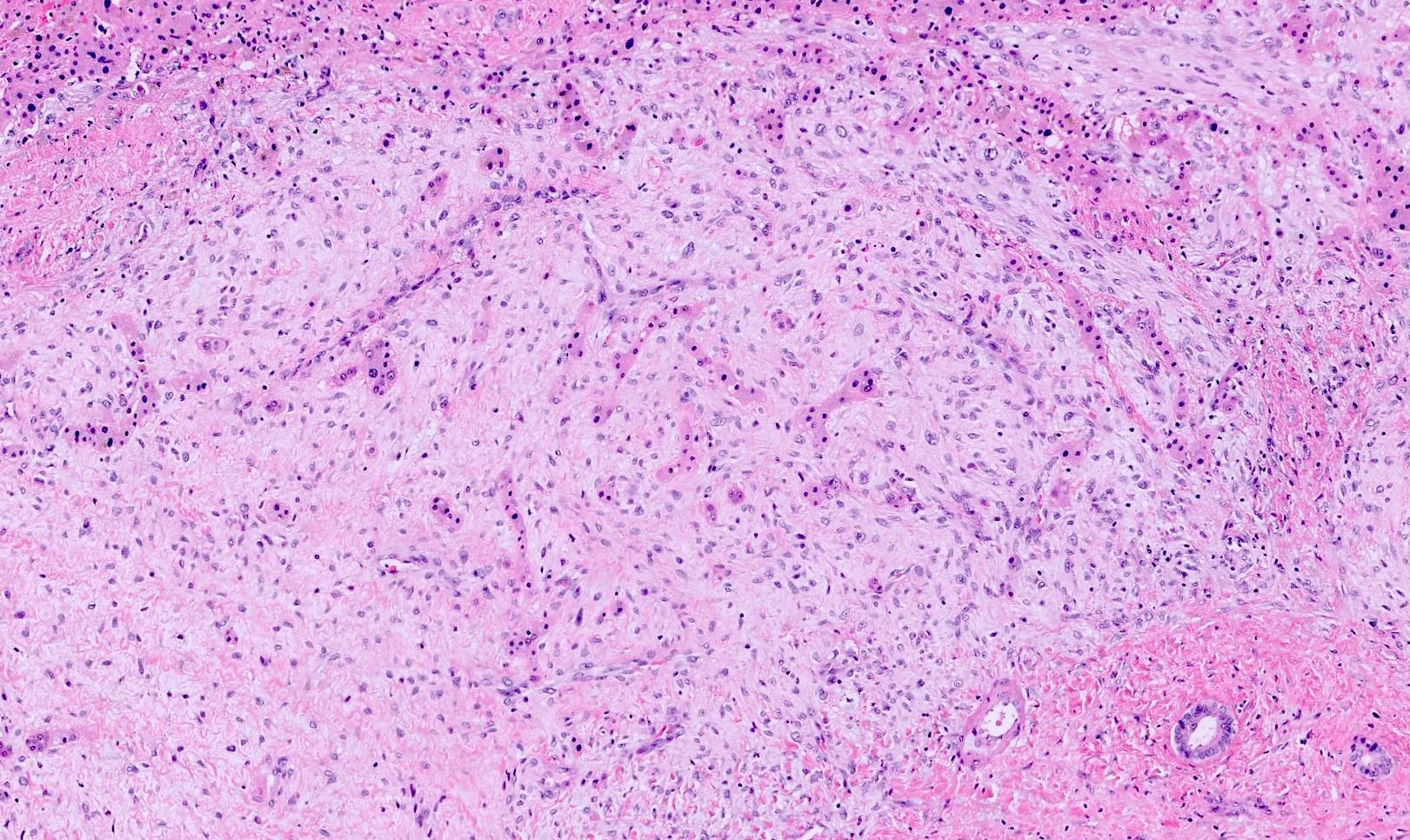
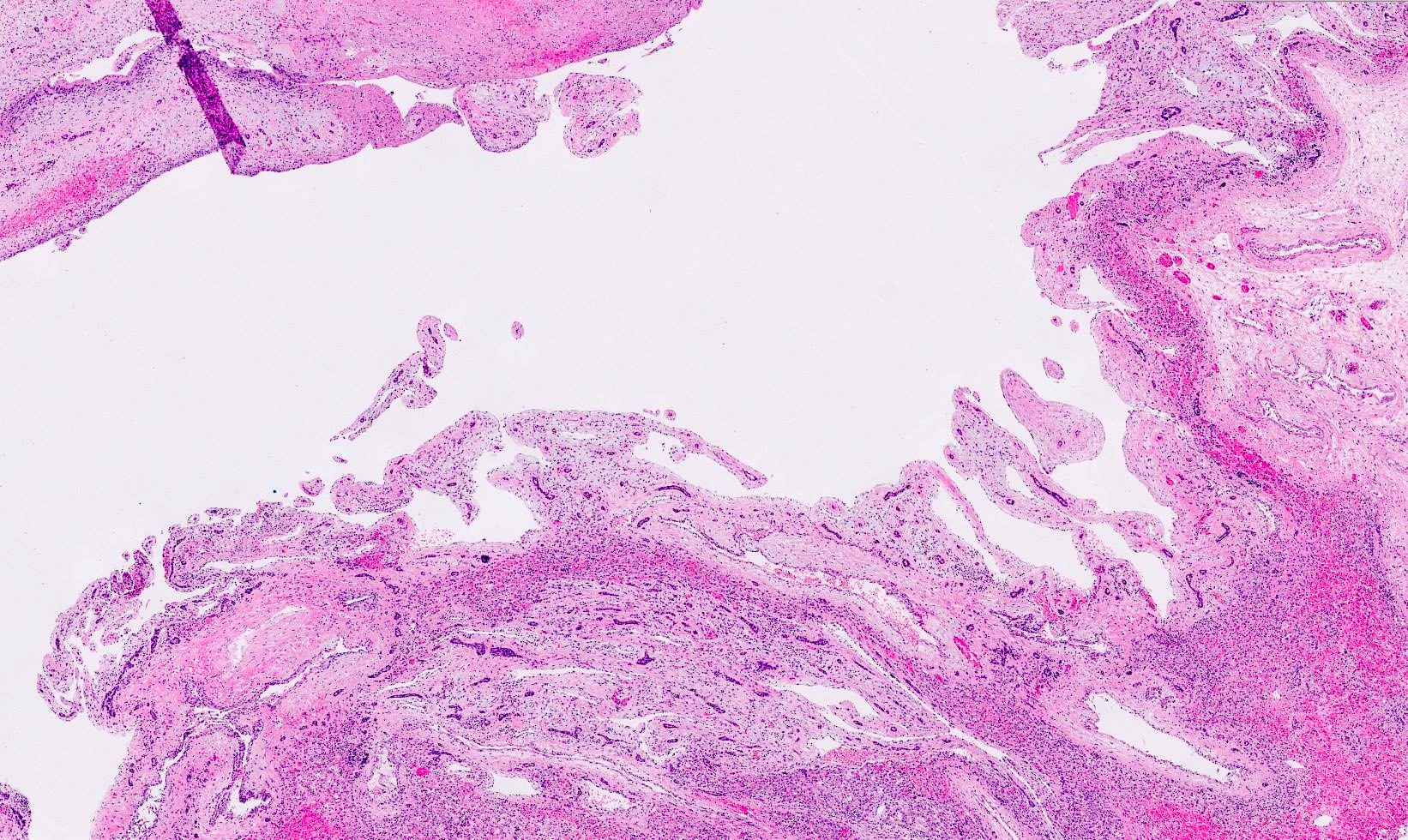
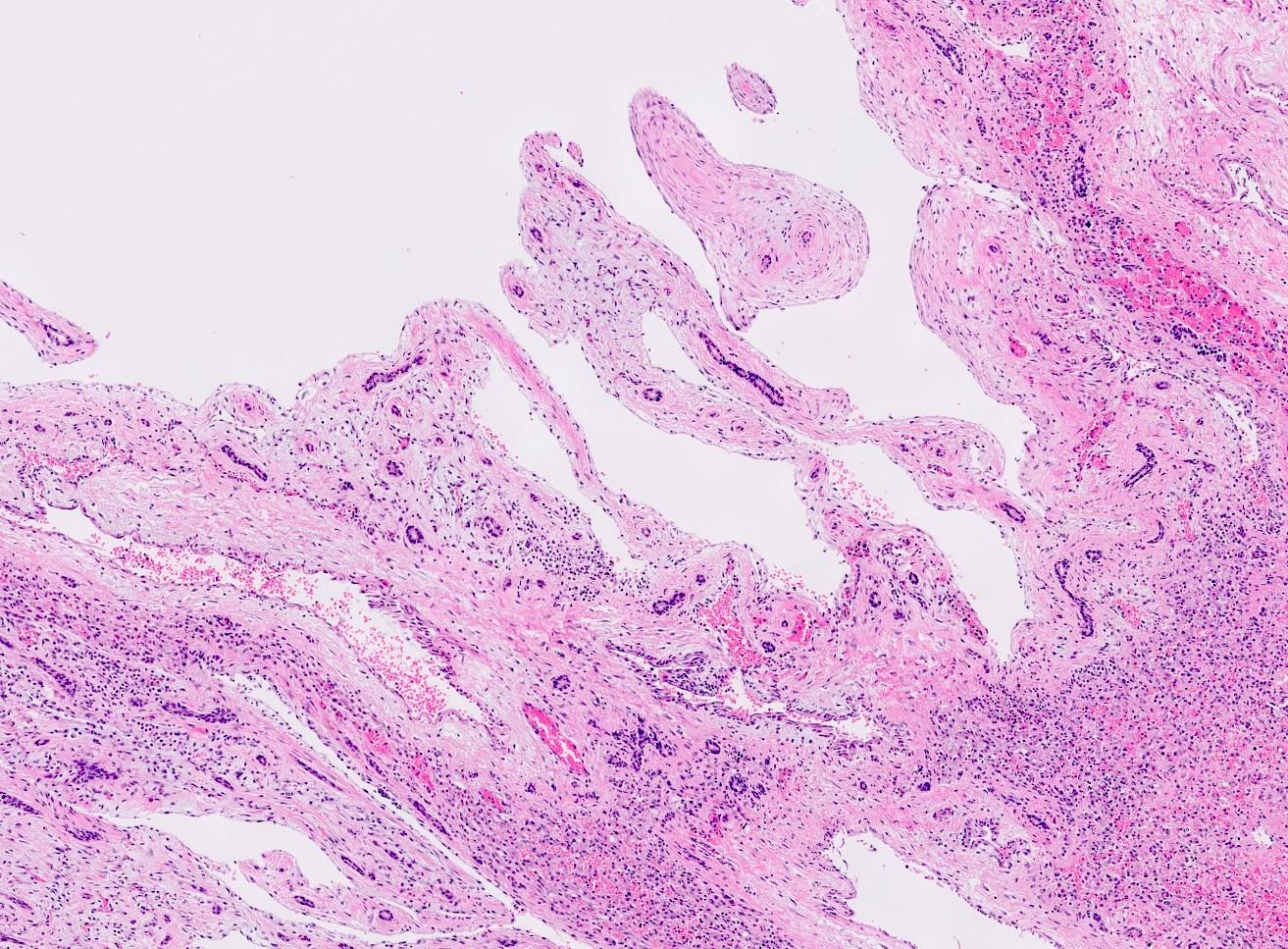
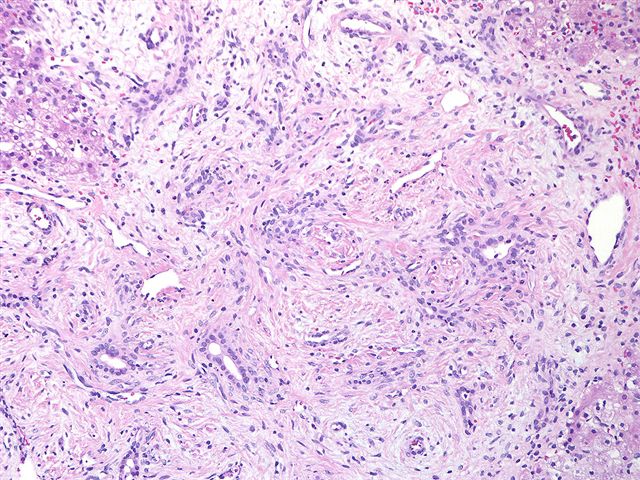
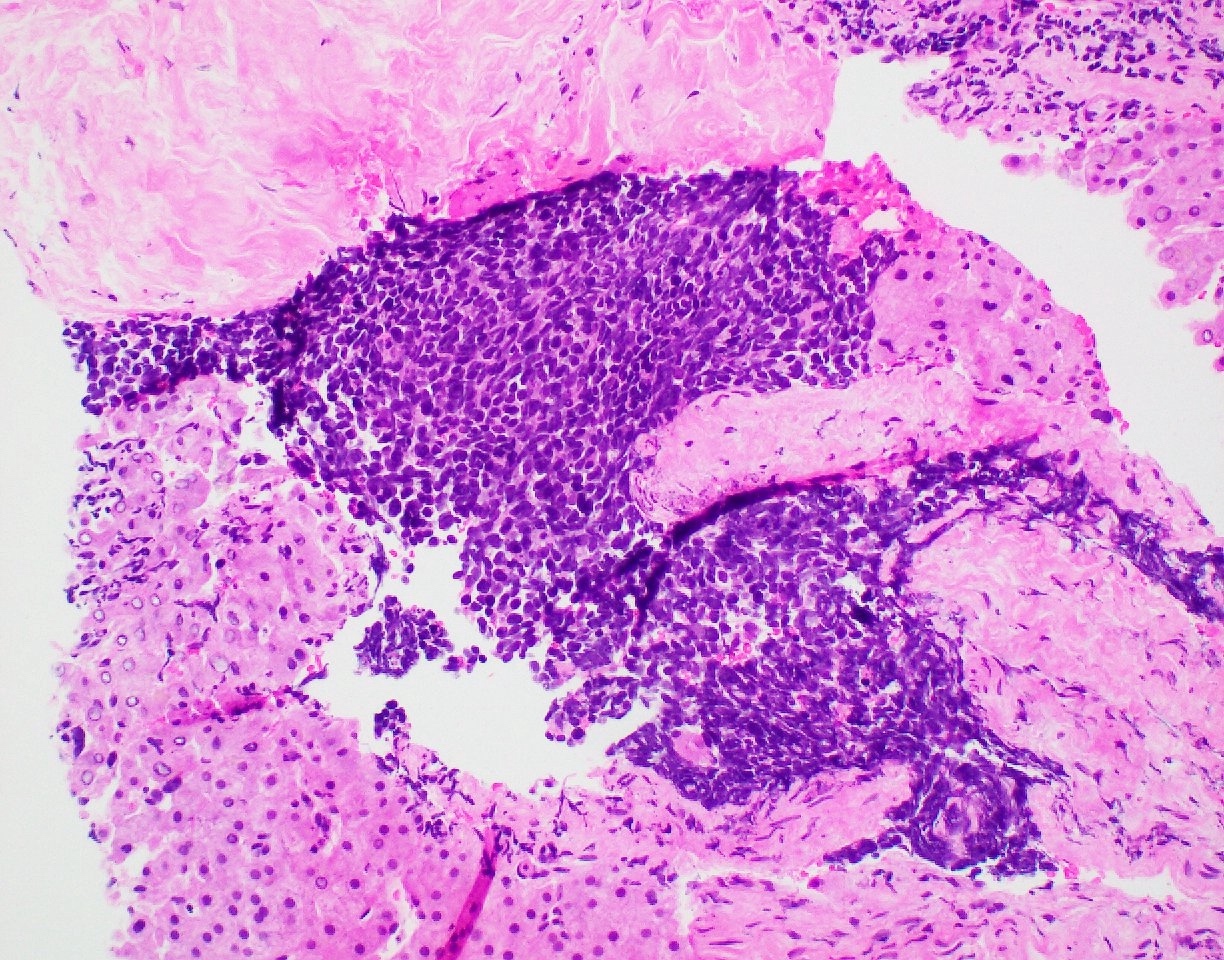
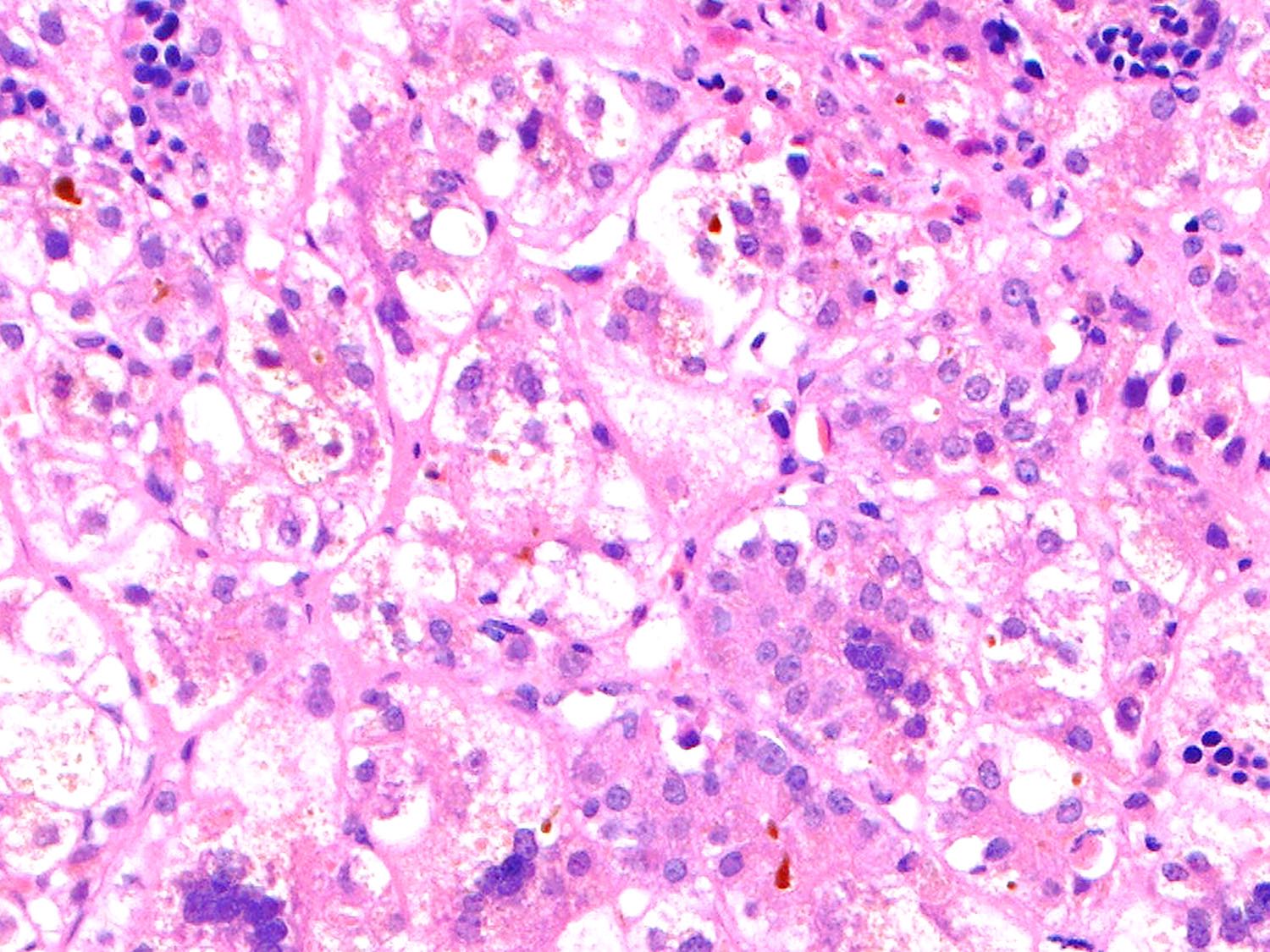
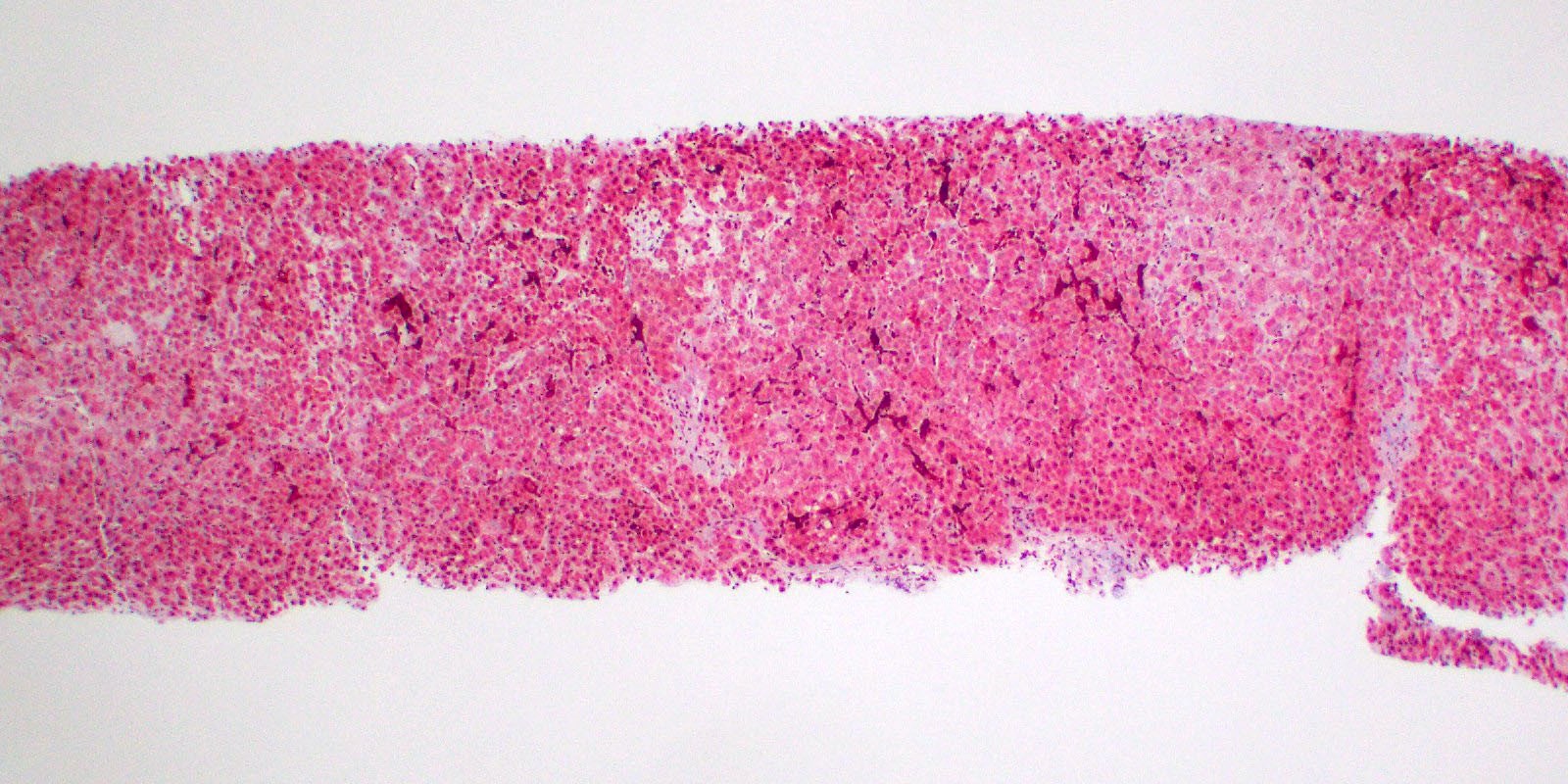
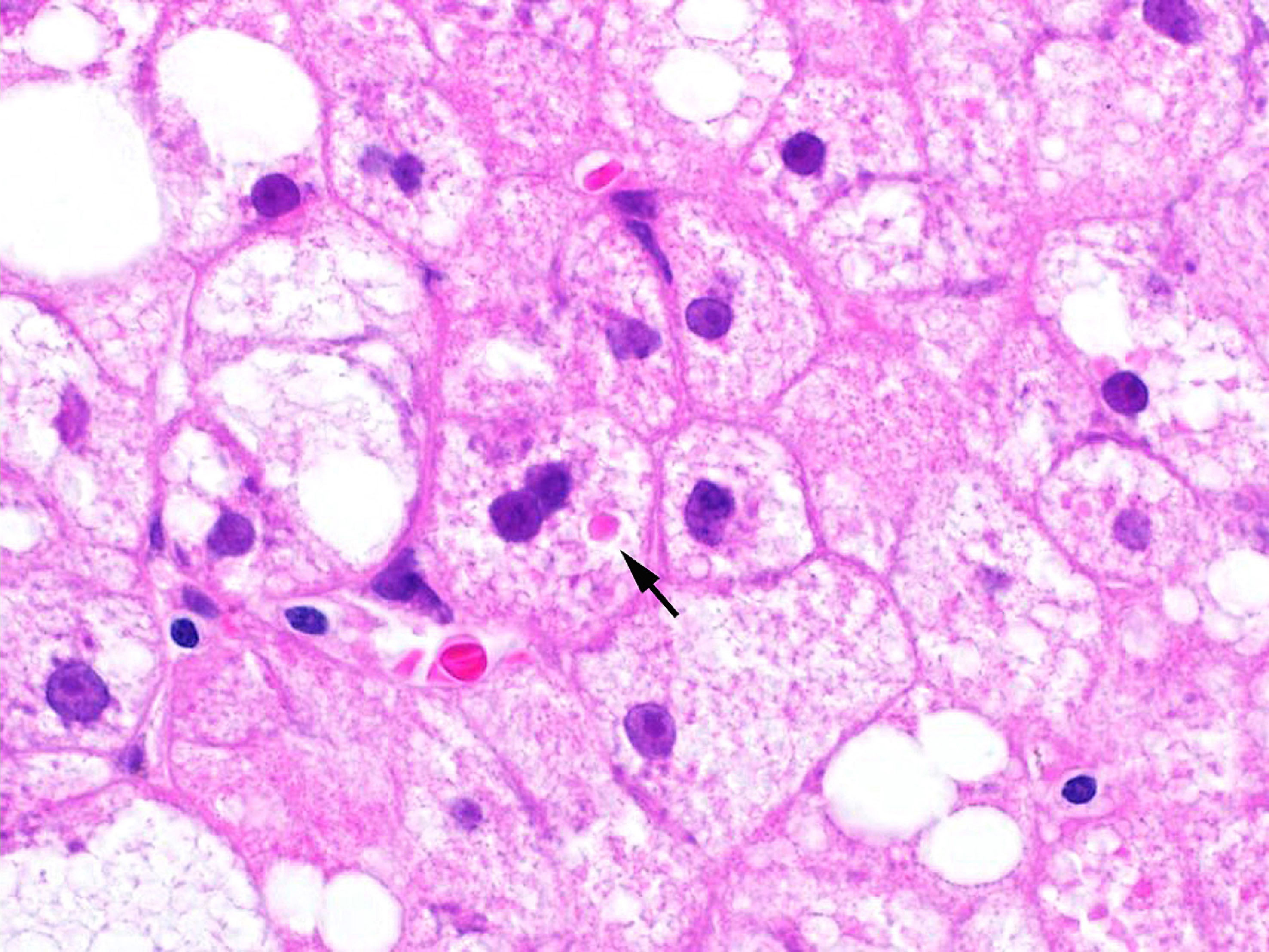
Microscopic (histologic) description
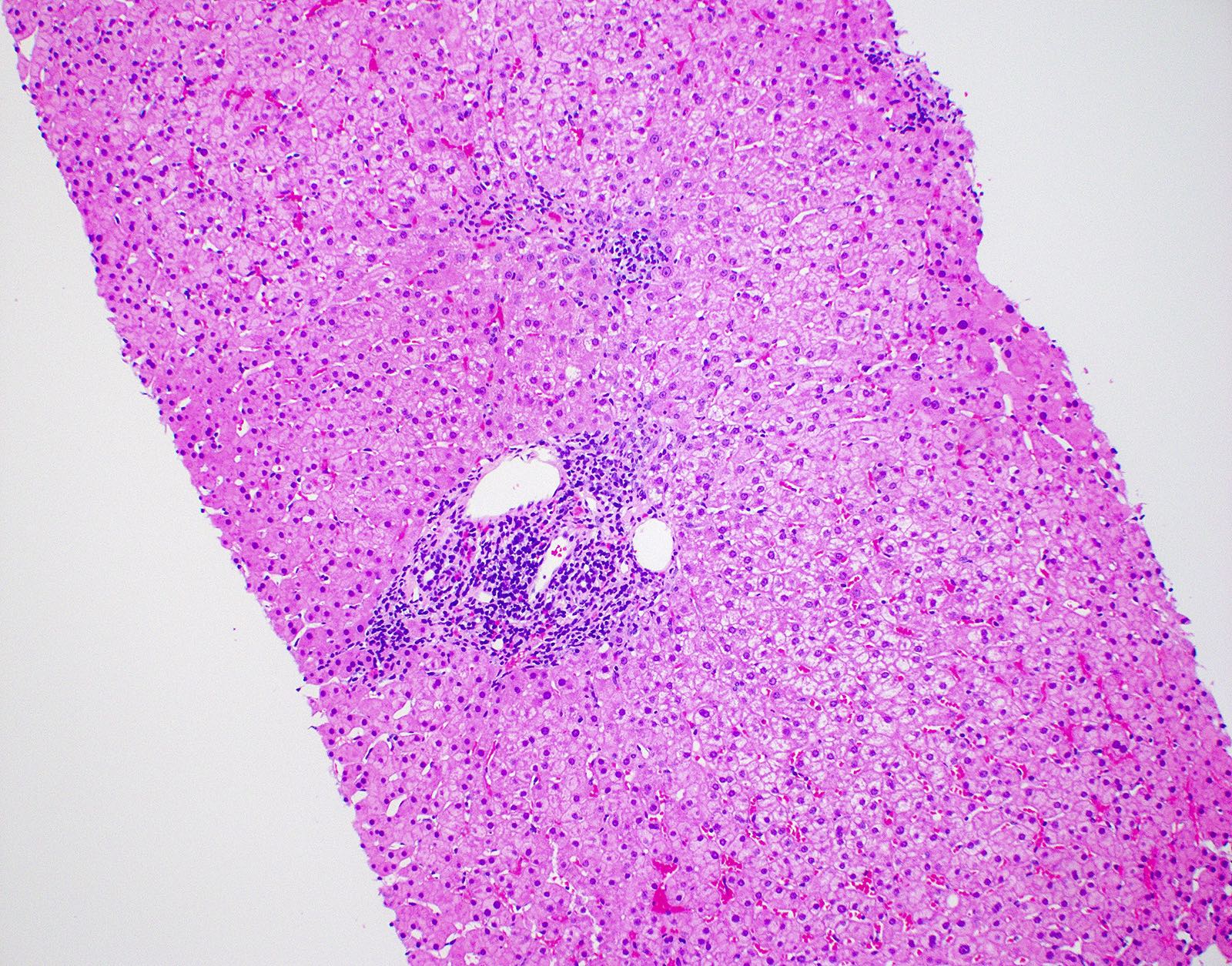
- Lobular disarray
- Disruption of the sinusoidal architecture by cell injury and inflammation
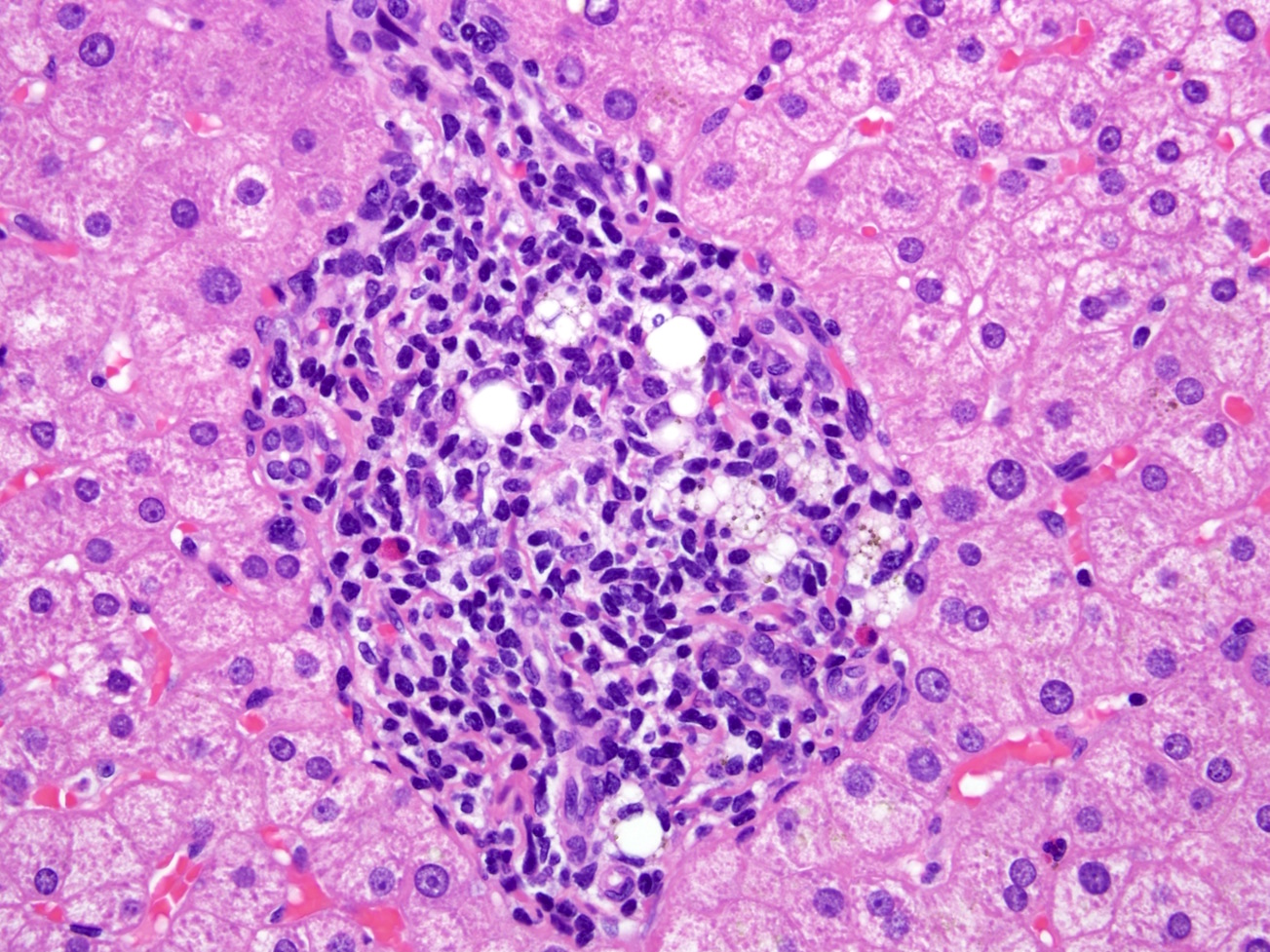
- Lobular inflammation (Saxena: Practical Hepatic Pathology, 2nd Edition, 2017)
- Composed of mainly small T lymphocytes with variable number of macrophages, plasma cells and occasional eosinophils
- Plasma cells may be predominant in acute hepatitis A and B
- Predominantly sinusoidal inflammation with little hepatocyte damage, is characteristic of EBV infection
- Neutrophilic microabscesses or small sinusoidal clusters of neutrophils can sometimes be seen in CMV infection
- Zone 3 accentuation may be seen in some drug induced liver injury
- Granulomas
- Typically seen in infection (tick borne diseases) and drug reactions
- Kupffer cell hyperplasia may be present in more severe cases
- Tick borne diseases, malaria, autoimmune hepatitis
- Resolving cases of acute hepatitis
- Portal tracts have less pronounced inflammation but may be edematous or contain variable amounts of a mononuclear cell infiltrate
- Inflammation from portal tract may spill over, limiting plate mimicking interface activity but hepatocytes are not damaged
- Composed of mainly small T lymphocytes with variable number of macrophages, plasma cells and occasional eosinophils
- Necroinflammation is diffuse but can be heterogenous (Saxena: Practical Hepatic Pathology, 2nd Edition, 2017)
- Lytic or spotty necrosis: foci of inflammation surrounding damaged hepatocytes or minute groups of hepatocytes (Gut 2005;54:1162)
- Confluent necrosis: zonal death of larger groups of hepatocytes, leading to collapse of reticulin framework, typically starts in zone 3 (Gut 2005;54:1162)
- Zone 1 or zone 1 - 2 necrosis can rarely be seen in acute hepatitis A infection
- Punched out necrosis can be seen in nonhepatotropic viral infections (adenovirus, HSV) and can have an azonal pattern
- Central hyaline necrosis can be seen in acute alcoholic liver disease and shows central confluent necrosis with obliteration of the central vein and accompanying neutrophilic inflammation
- Bridging necrosis
- Severe acute hepatitis is characterized by confluent necrosis, linking terminal / central venules to portal tracts
- May mimic septa of chronic liver disease
- Panlobular, panacinar, multilobular, multiacinar, submassive (26 - 75% parenchymal volume), massive necrosis (> 75% parenchymal volume)
- Parenchyma replaced by collapsed stromal inflammatory cells and activated macrophages
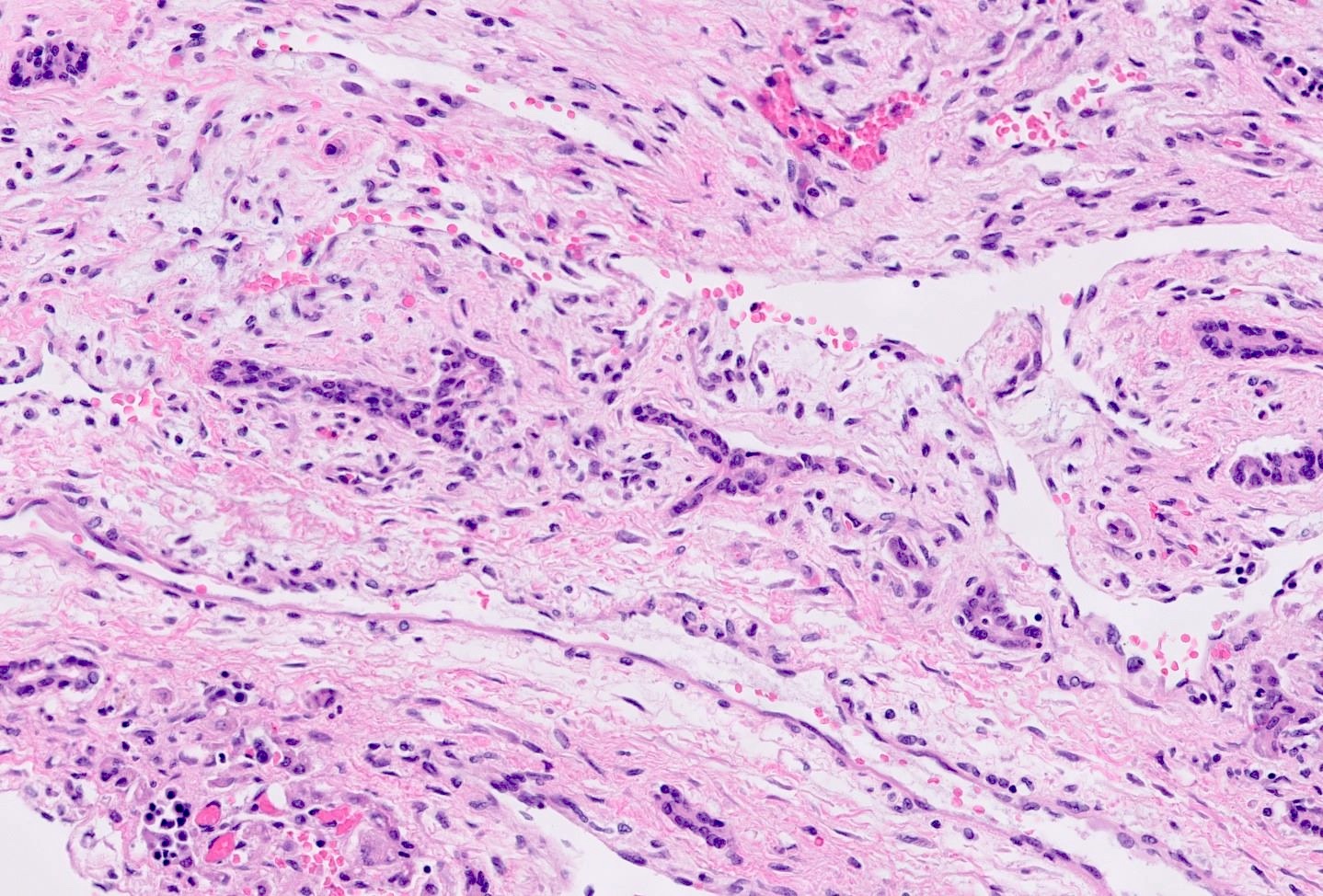
- Hepatocellular damage (Saxena: Practical Hepatic Pathology, 2nd Edition, 2017)
- Apoptotic bodies are degenerated hepatocytes with increased cytoplasmic staining and pyknotic nuclear remnants (Councilman bodies used for yellow fever)
- Minor hepatocyte swelling characterized as rarified, granular or finely vacuolated cytoplasm
- Ballooning degeneration is a more severe swelling characterized by rarified cytoplasm and occasional Mallory hyaline
- Drug reactions, autoimmune hepatitis, acute alcoholic hepatitis, Wilson disease
- Neutrophilic satellitosis: neutrophils surrounding ballooned hepatocytes with Mallory hyaline and is seen in active cases of alcoholic steatohepatitis
- Cholestasis (Saxena: Practical Hepatic Pathology, 2nd Edition, 2017)
- Bland lobular cholestasis may be in canaliculi or (in more severe cases) within the hepatocytes
- Acute hepatitis A, acute hepatitis B
- Drug reactions
- Bland lobular cholestasis may be in canaliculi or (in more severe cases) within the hepatocytes
- Biliary changes
- Bile duct epithelial stratification, cytoplasmic vacuolization, necrosis, altered nuclear polarity, intraepithelial lymphocytosis
- Bile ductular proliferation, which may mimic an obstruction
- Described in some cases symptomatic cases of acute hepatitis C (Am J Surg Pathol 2007;31:1754)
- Drug reactions, Wilson disease
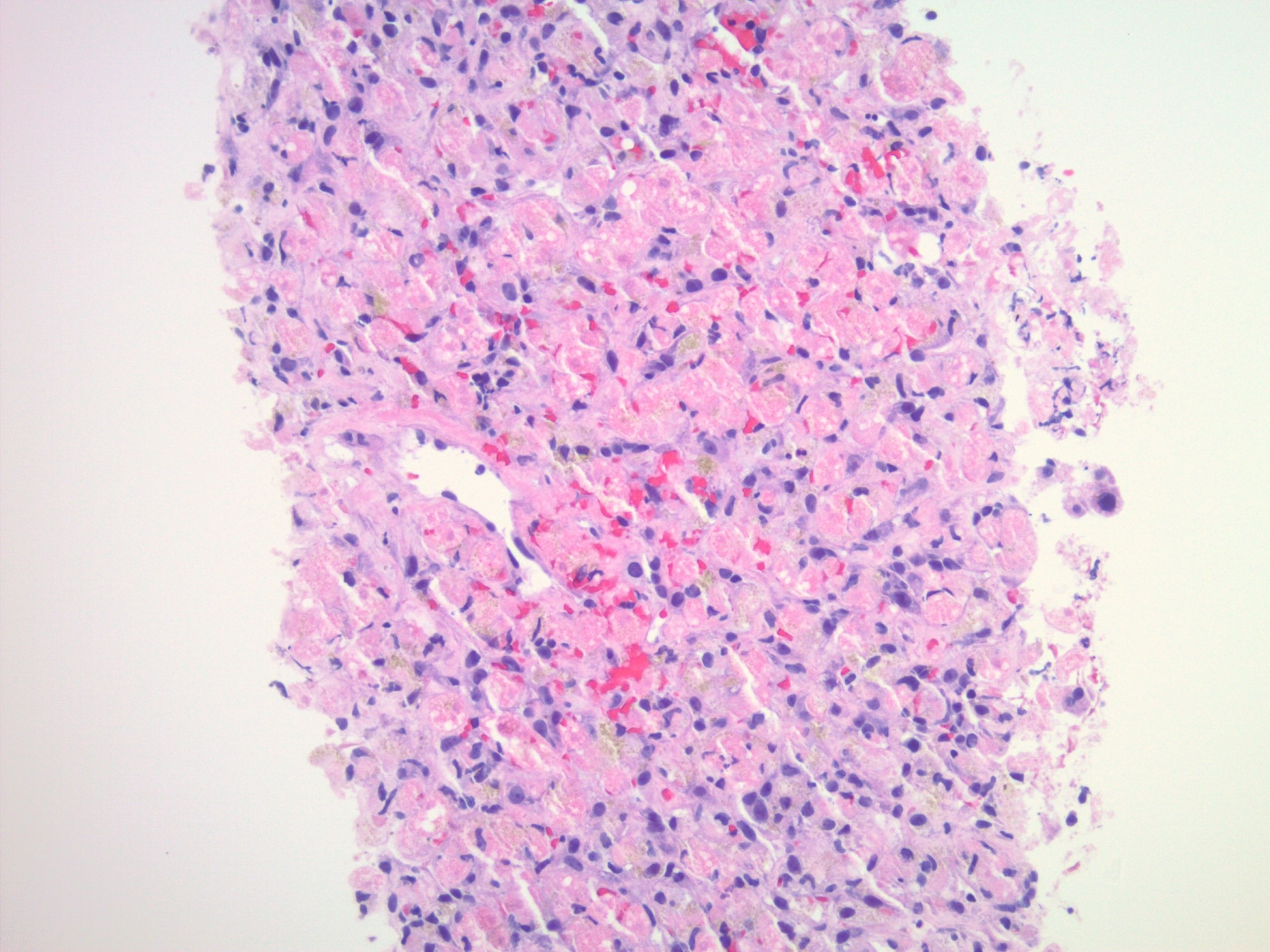
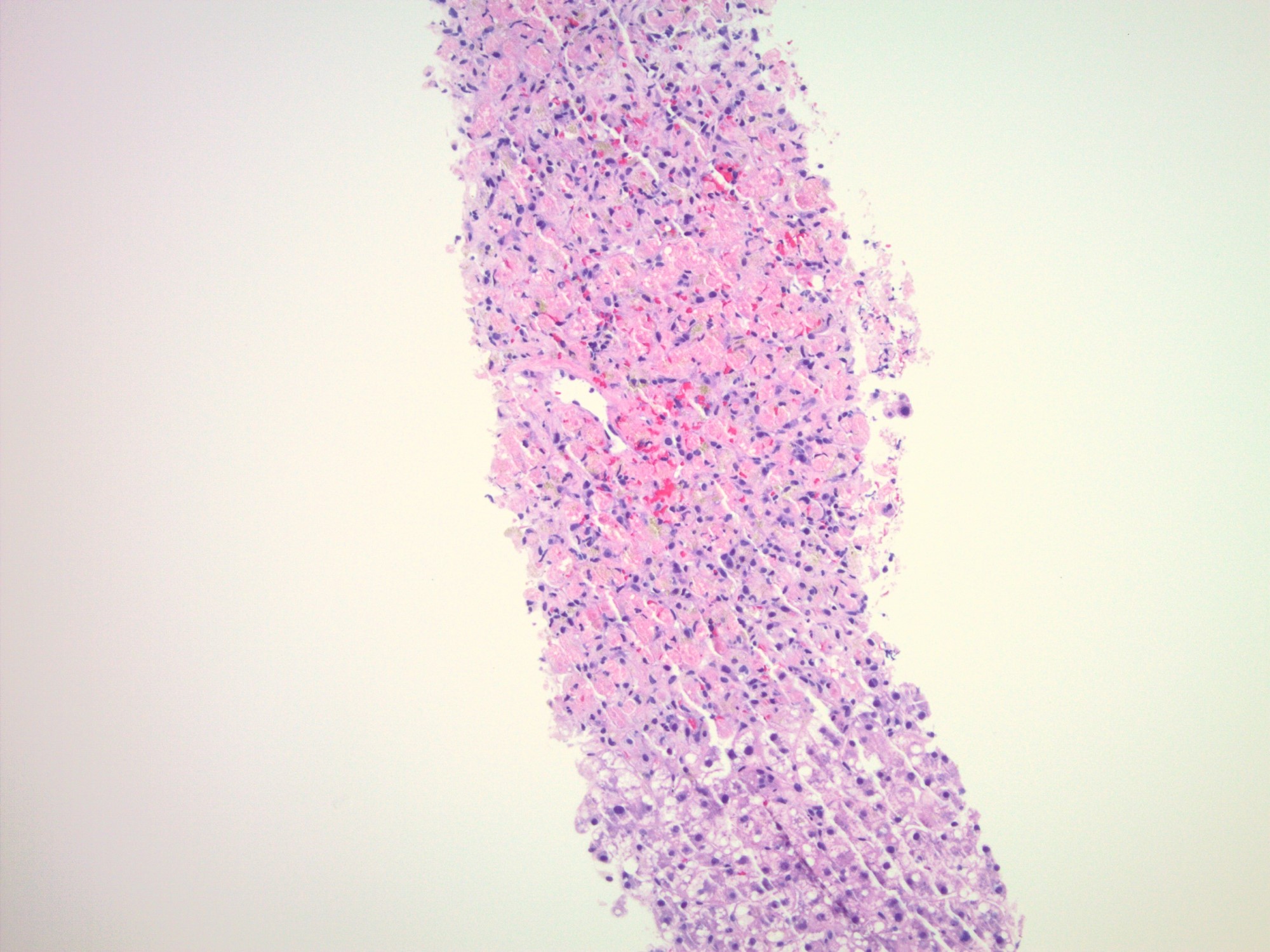
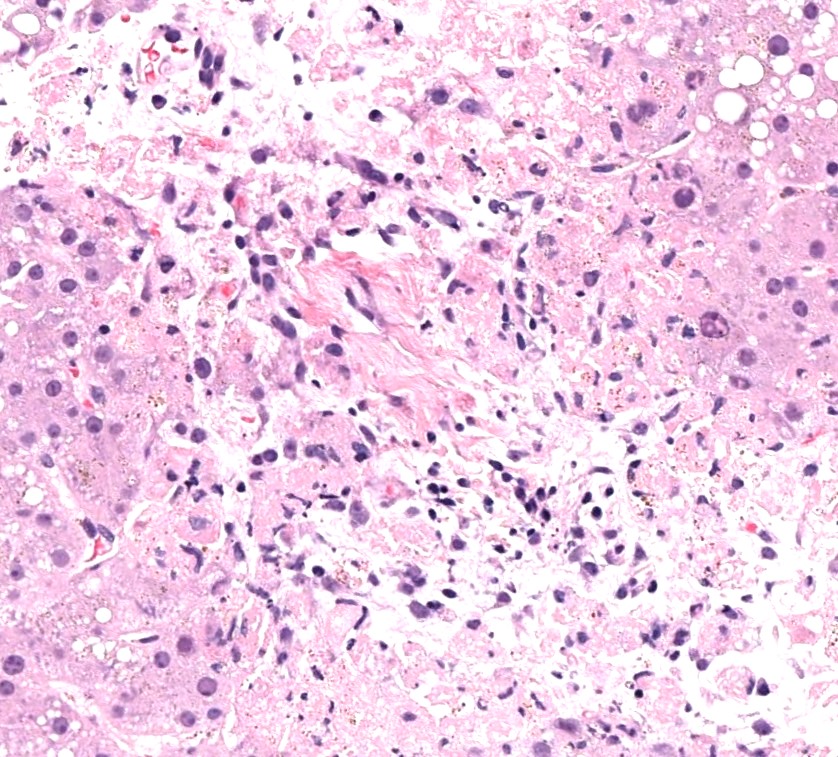
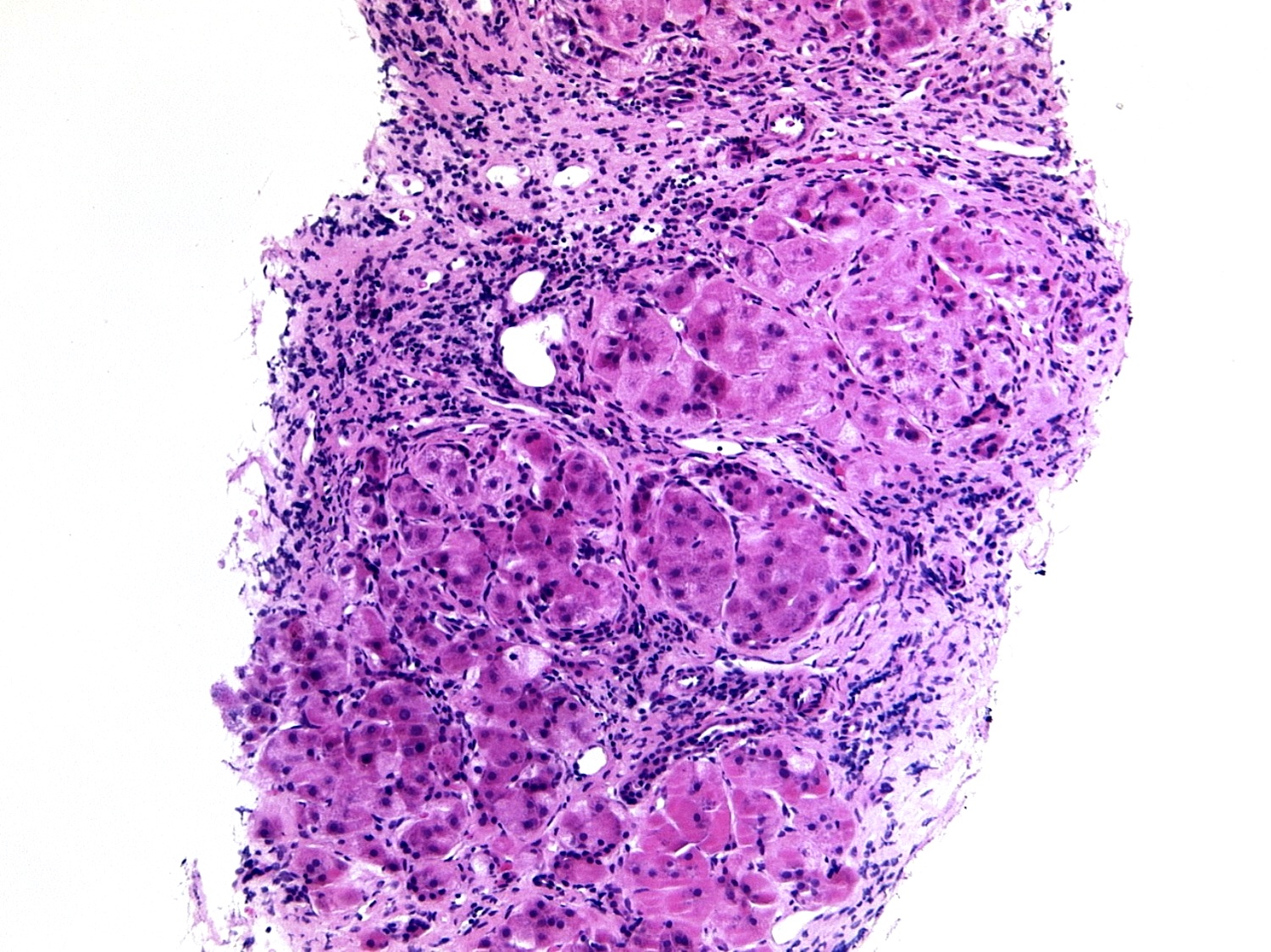
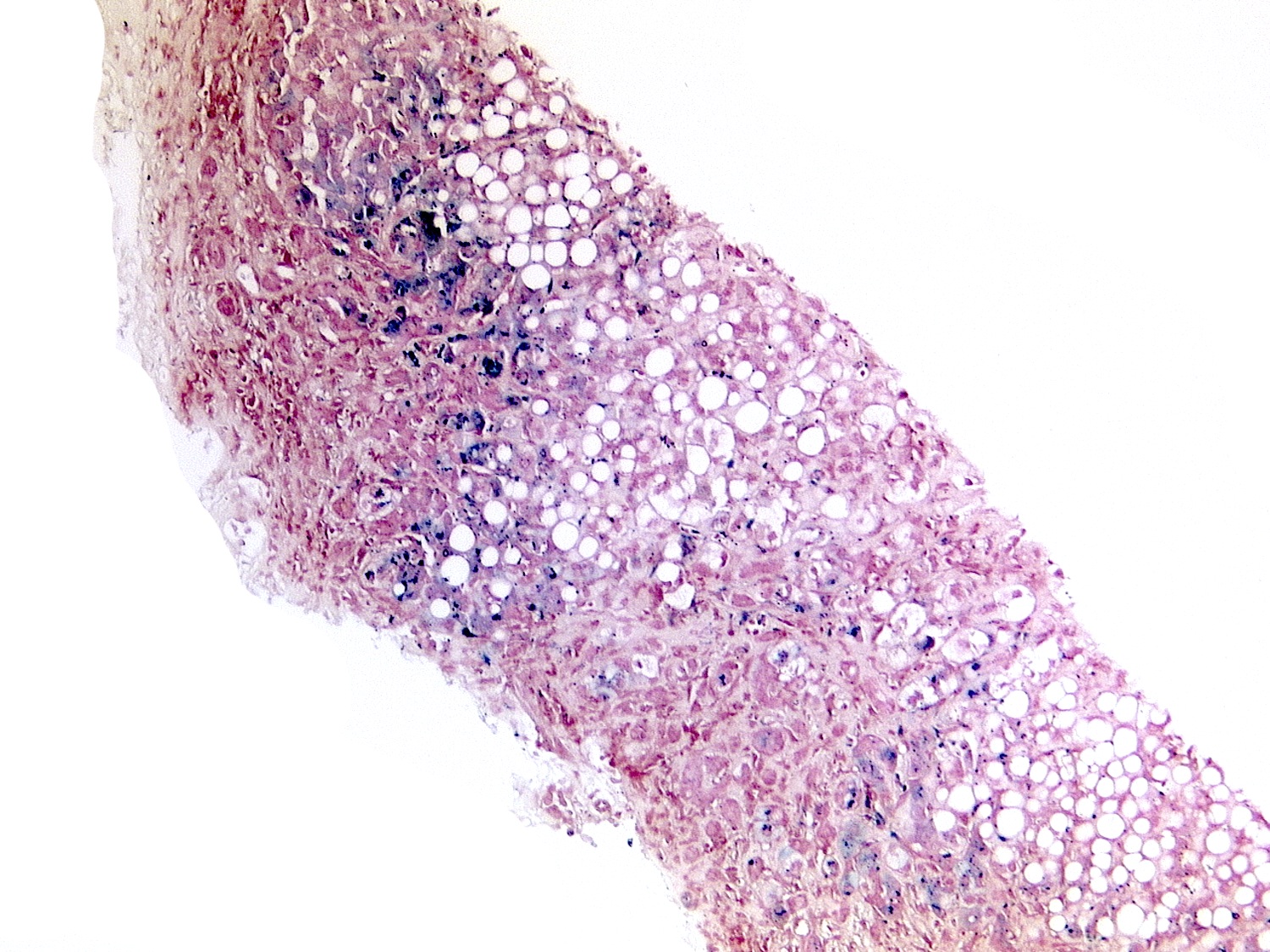
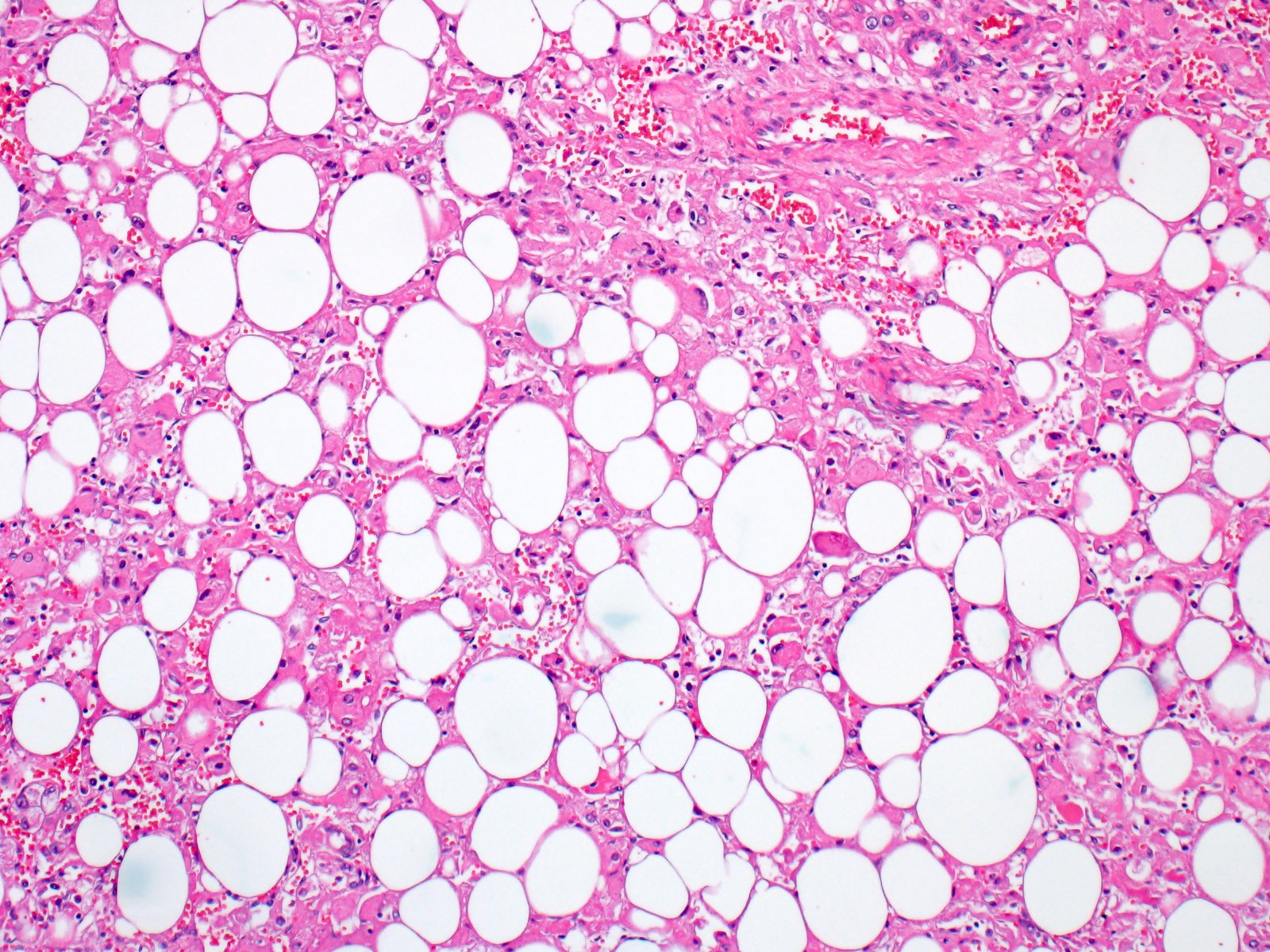
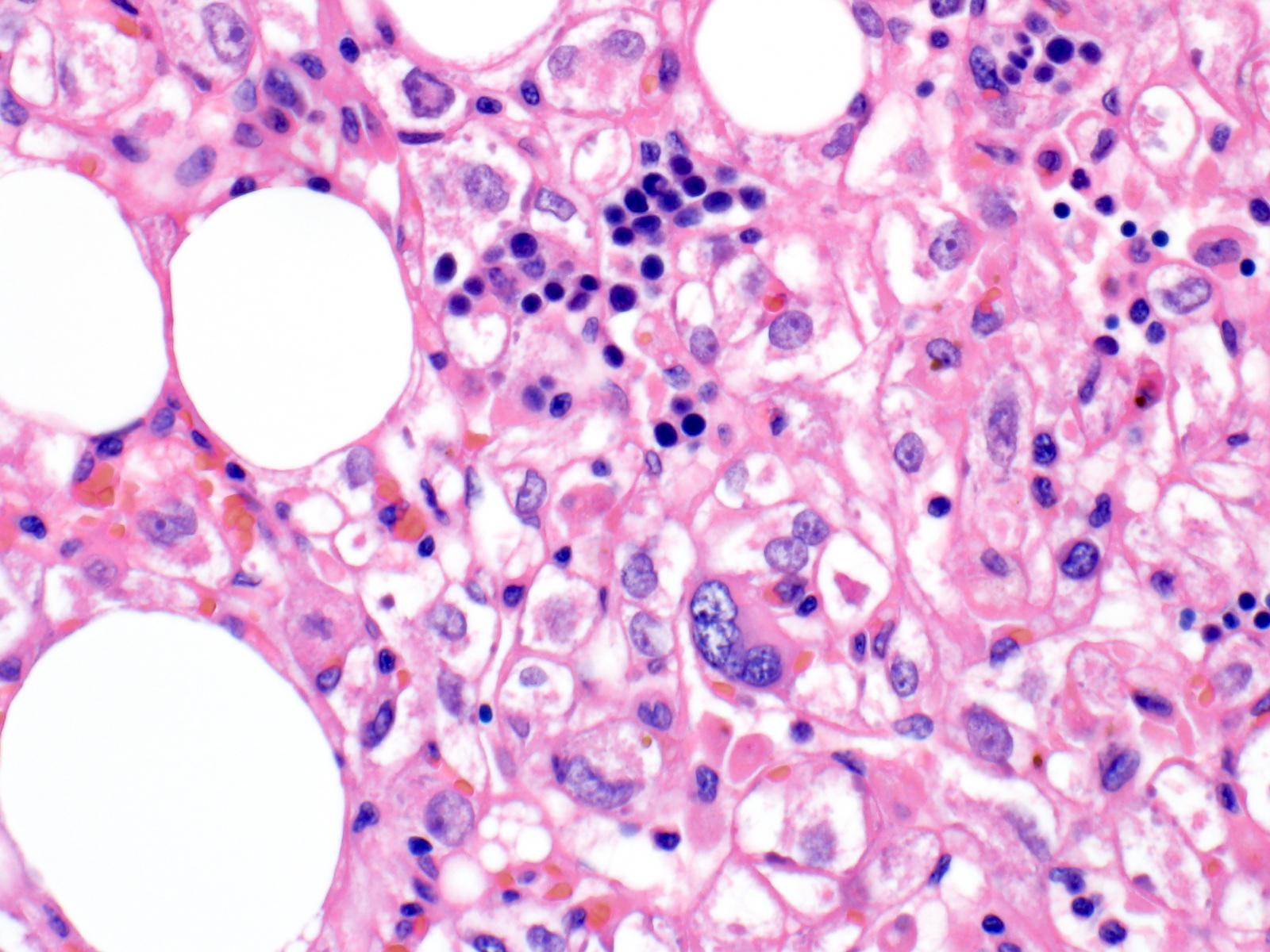
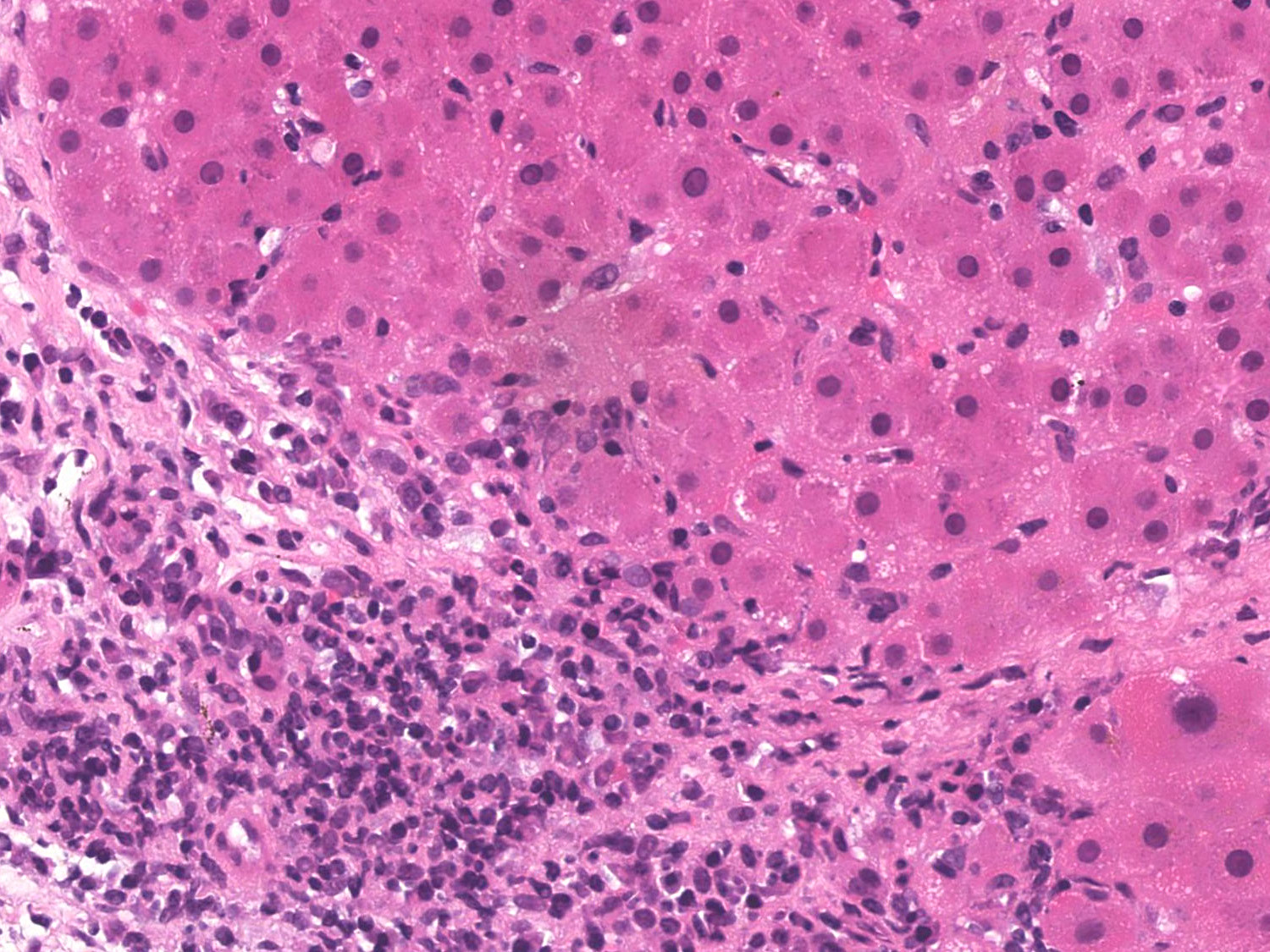
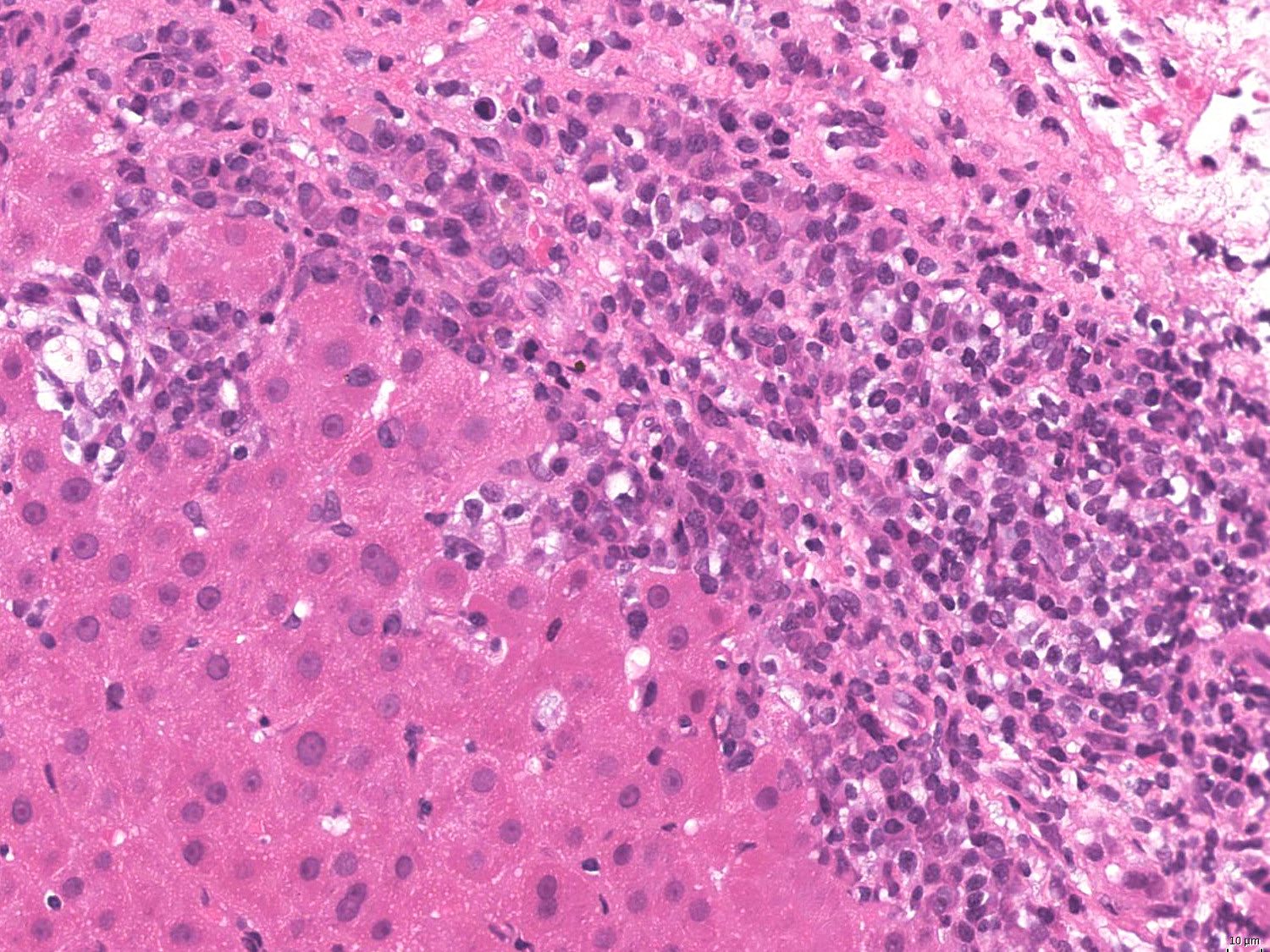
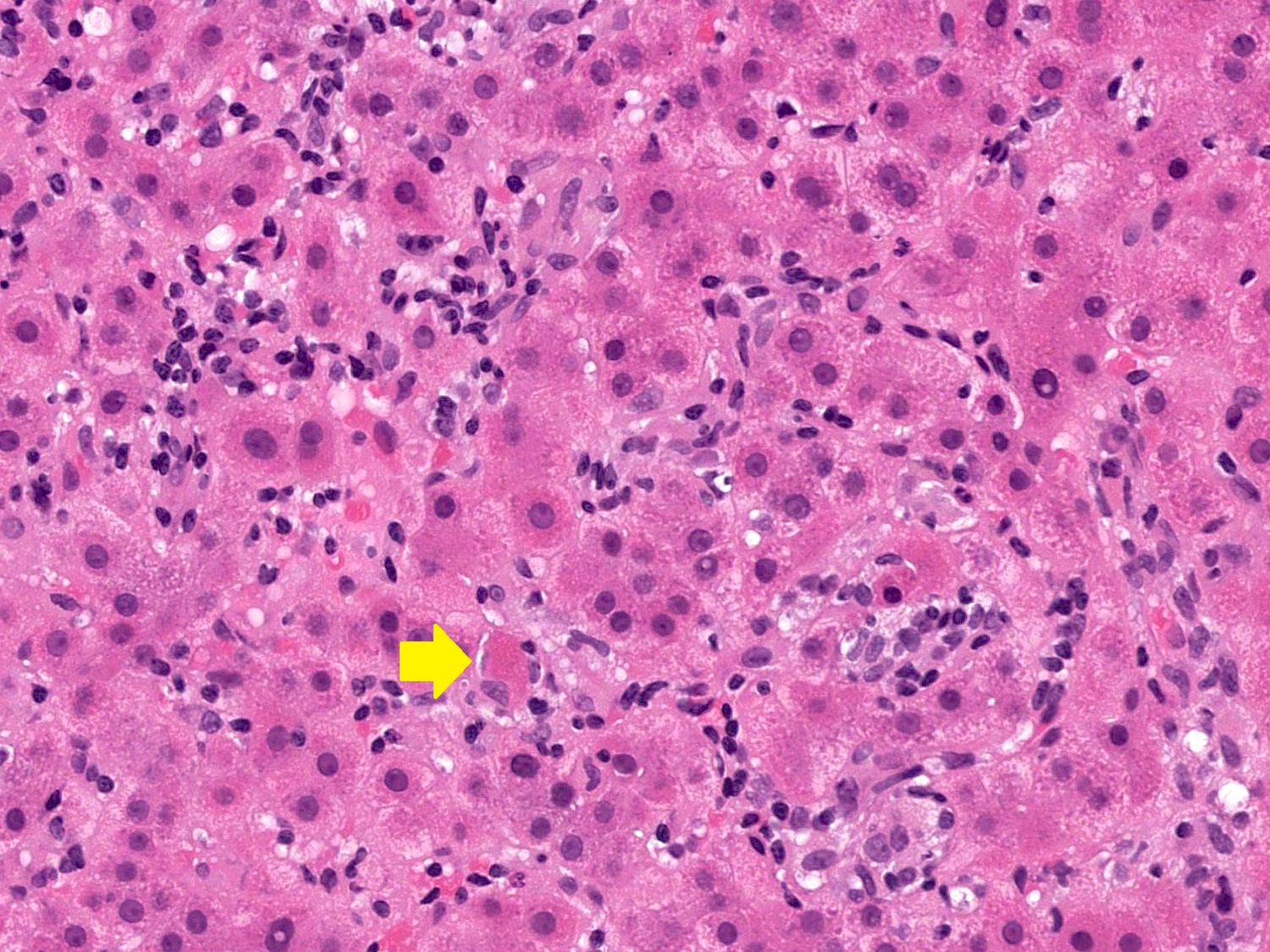
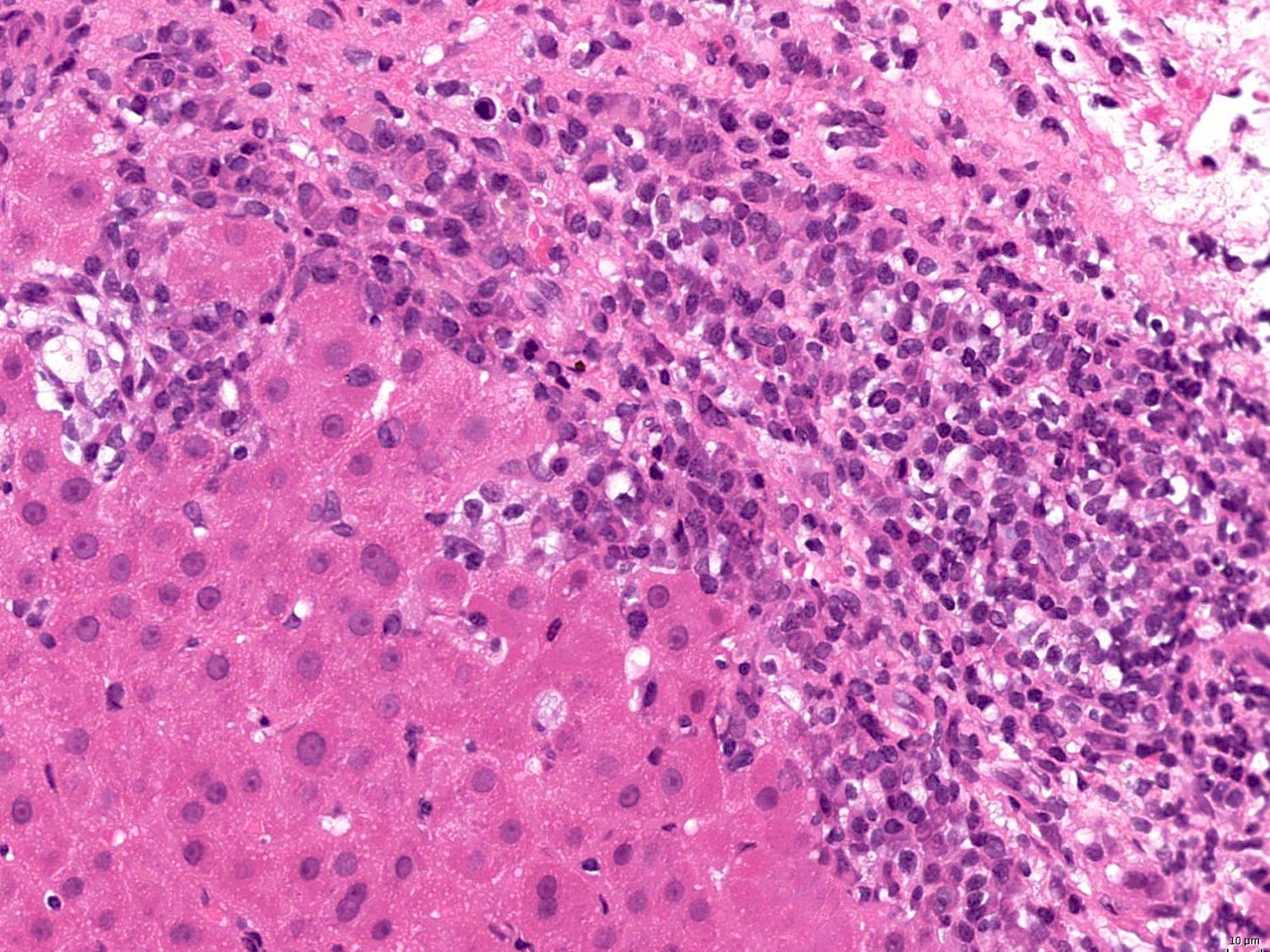
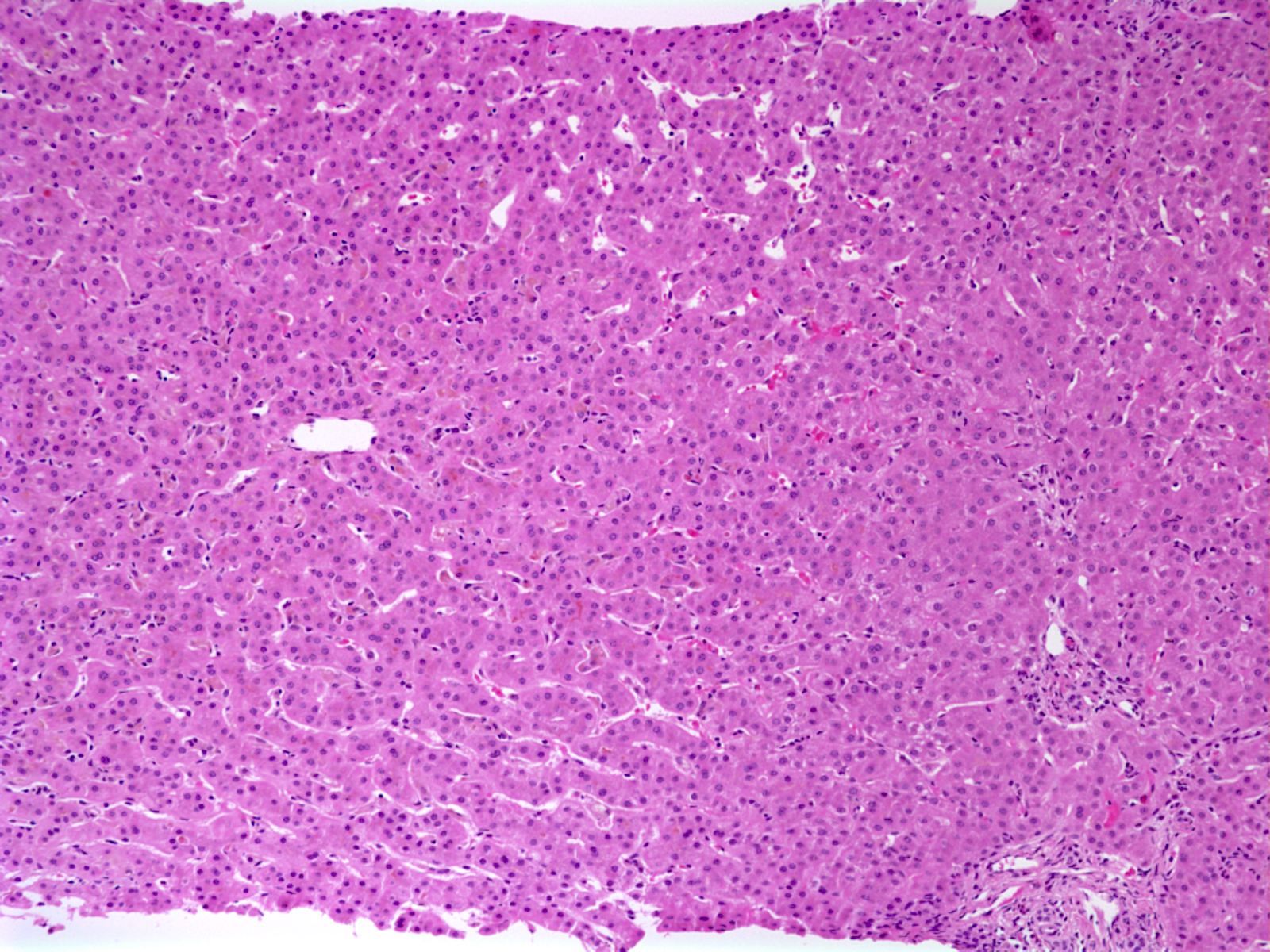
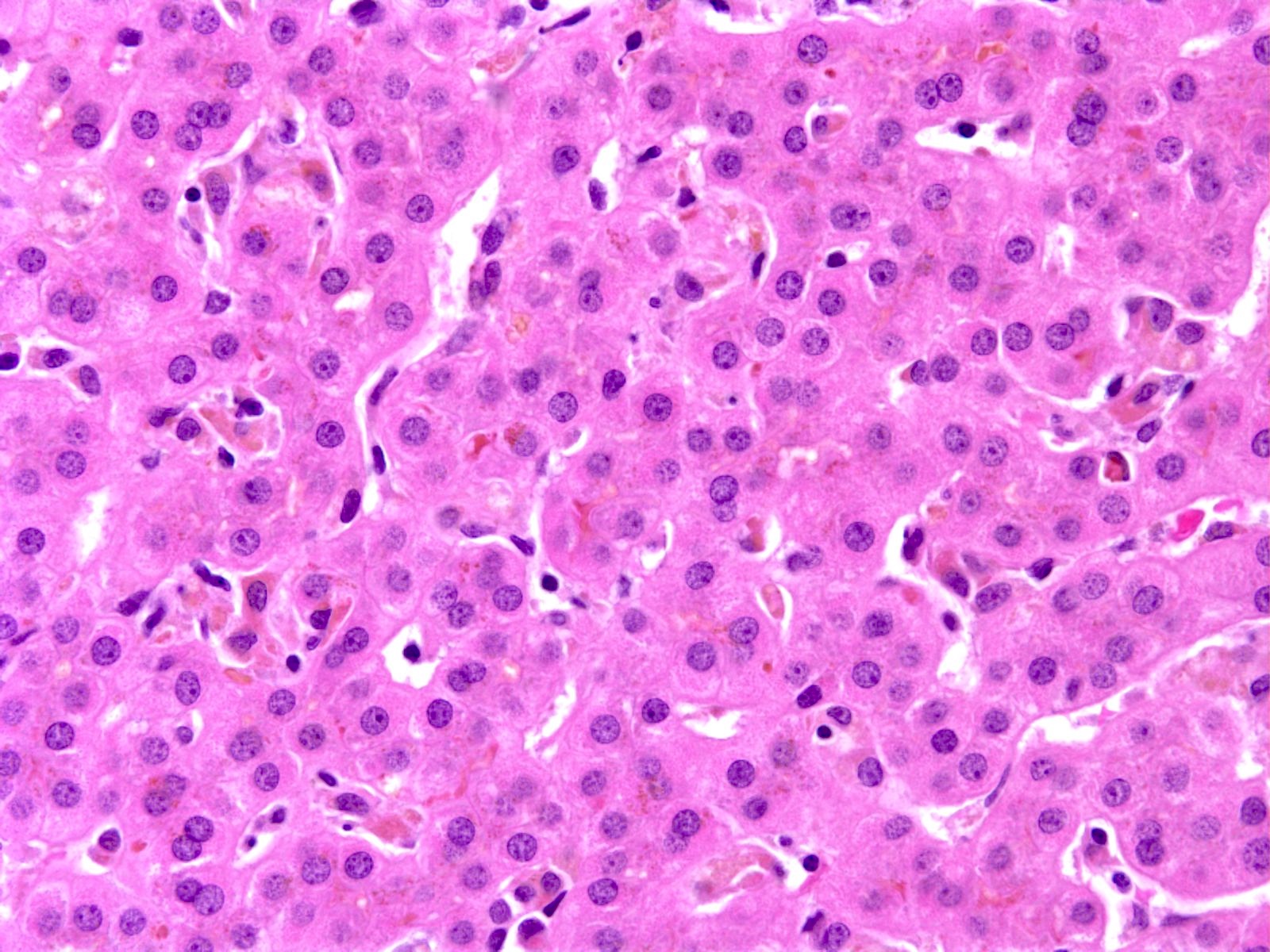
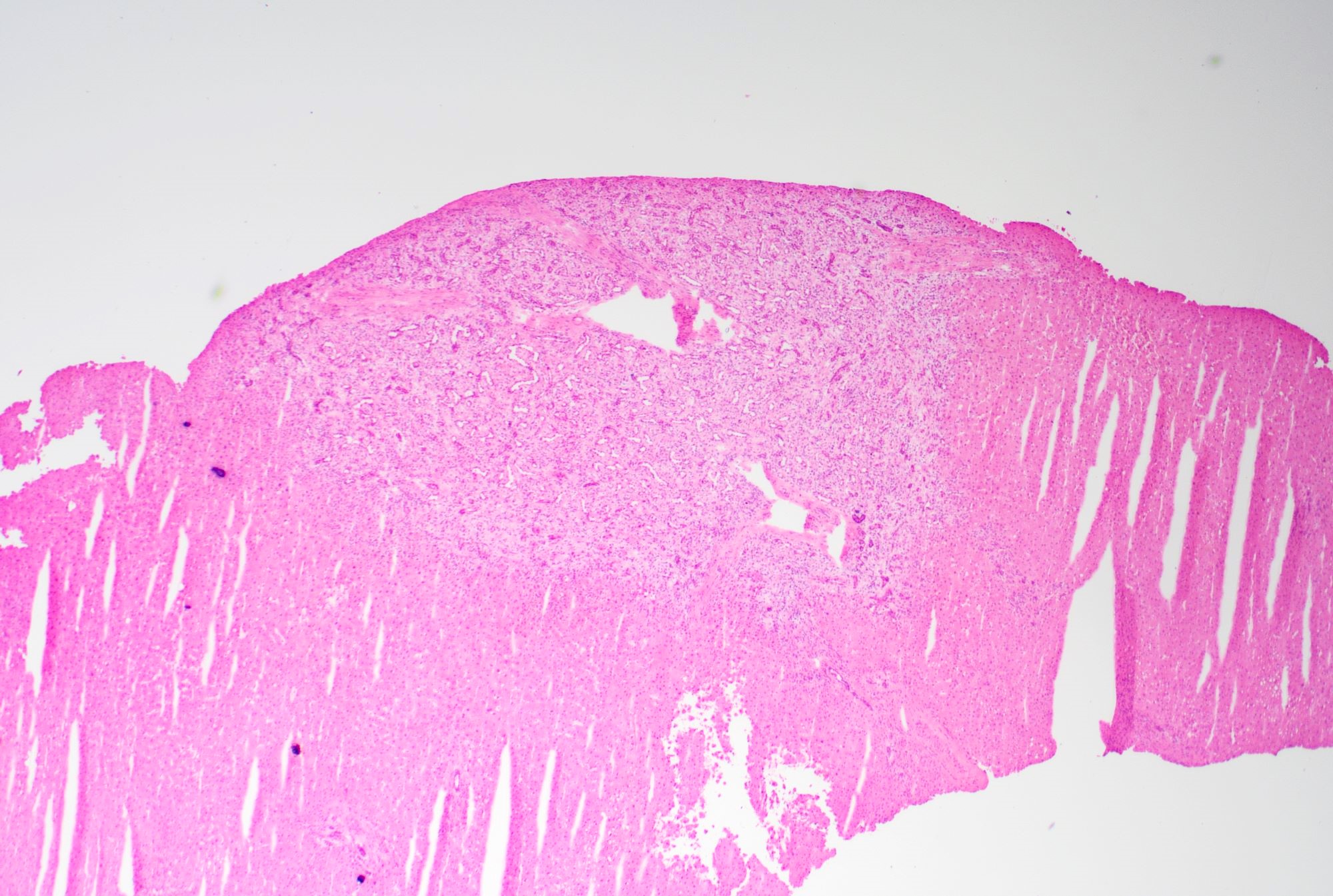
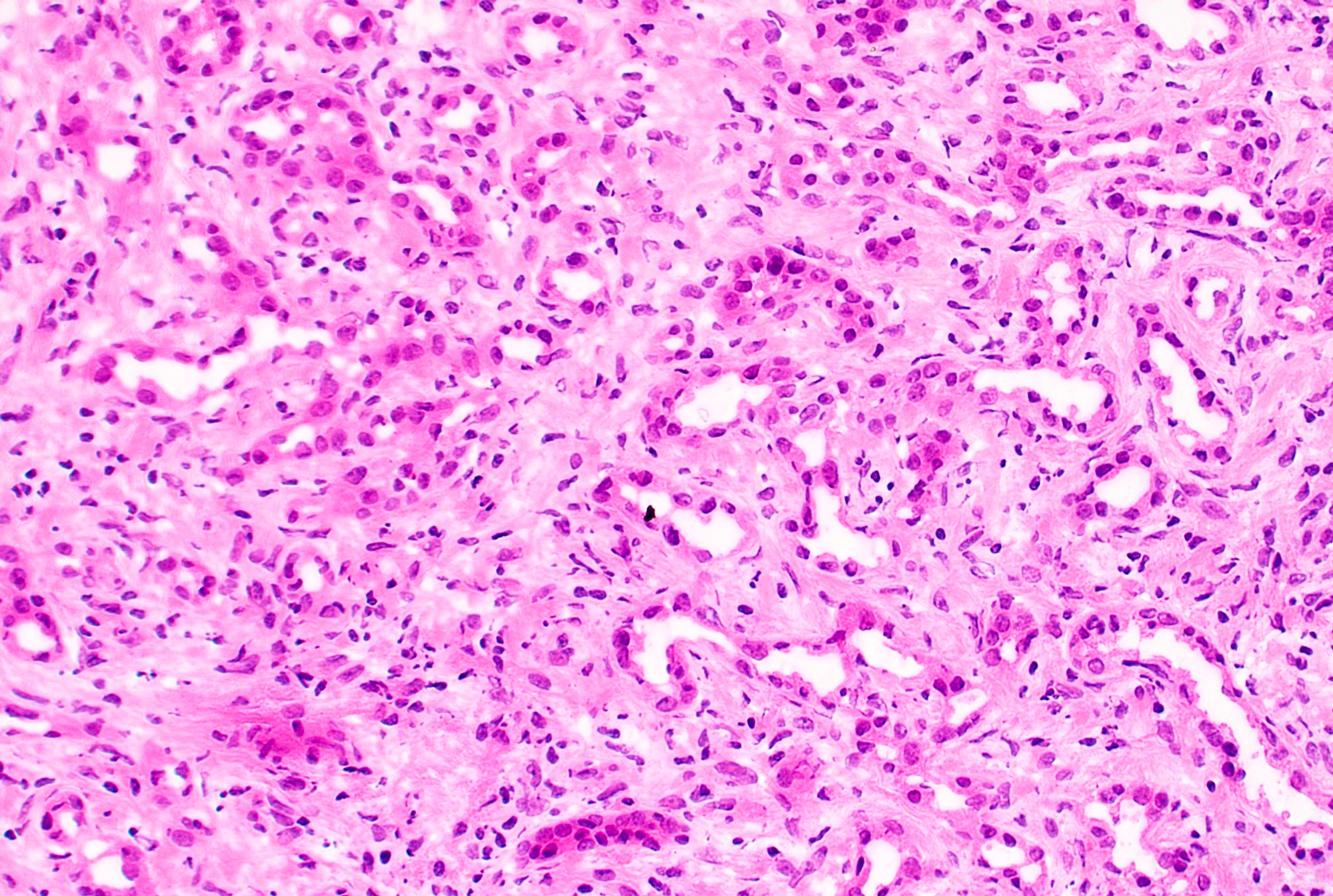
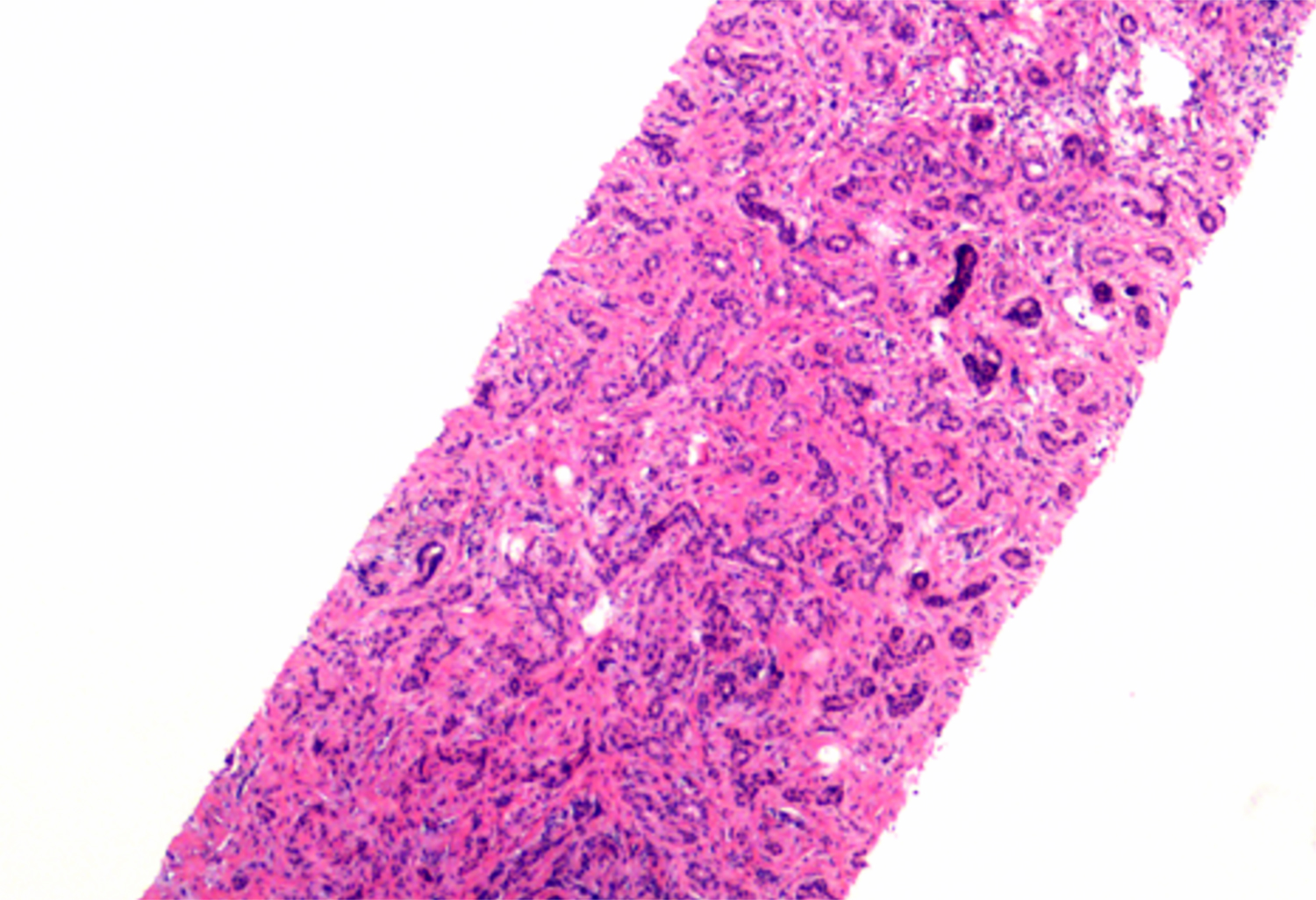
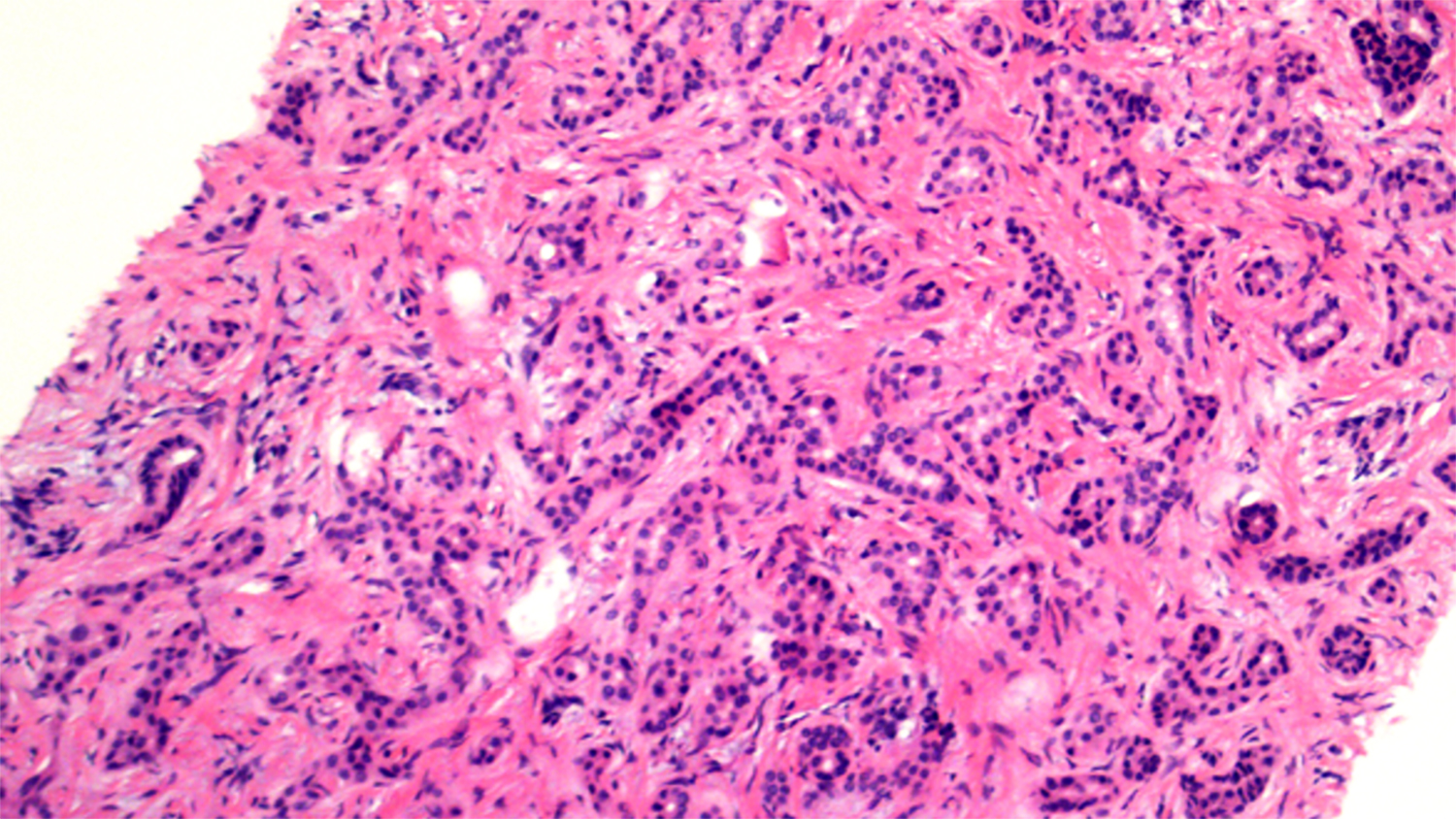
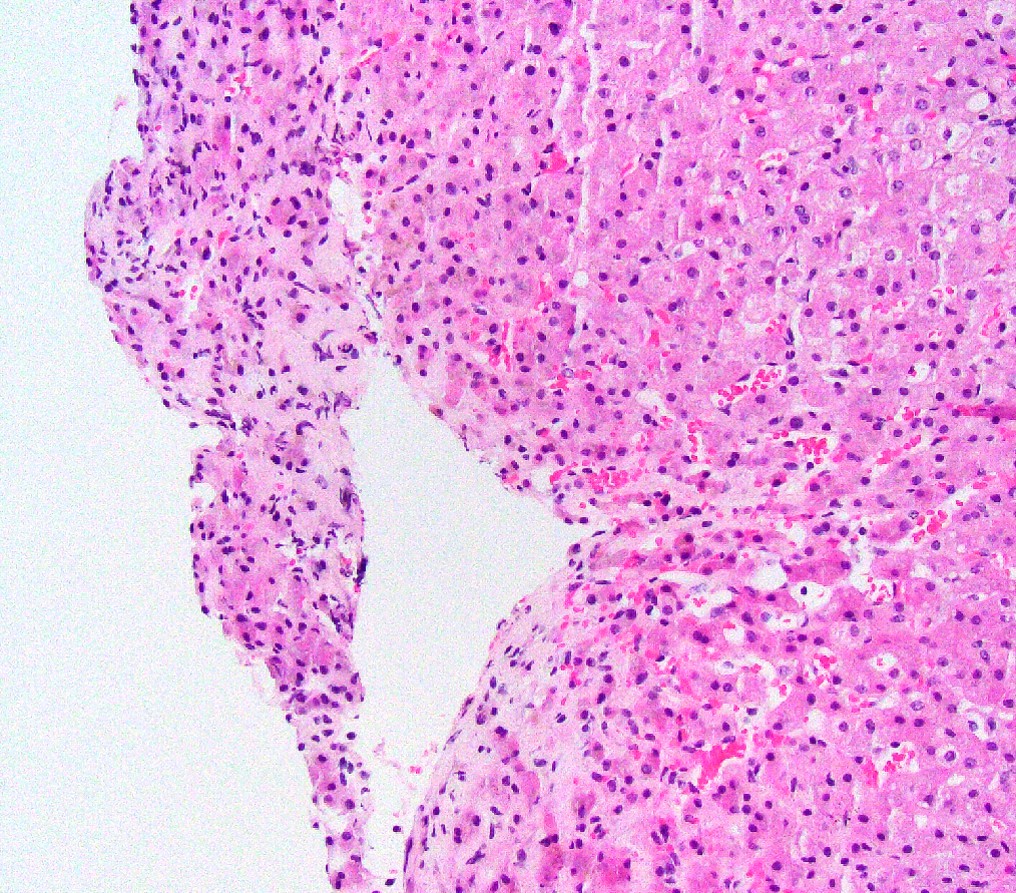
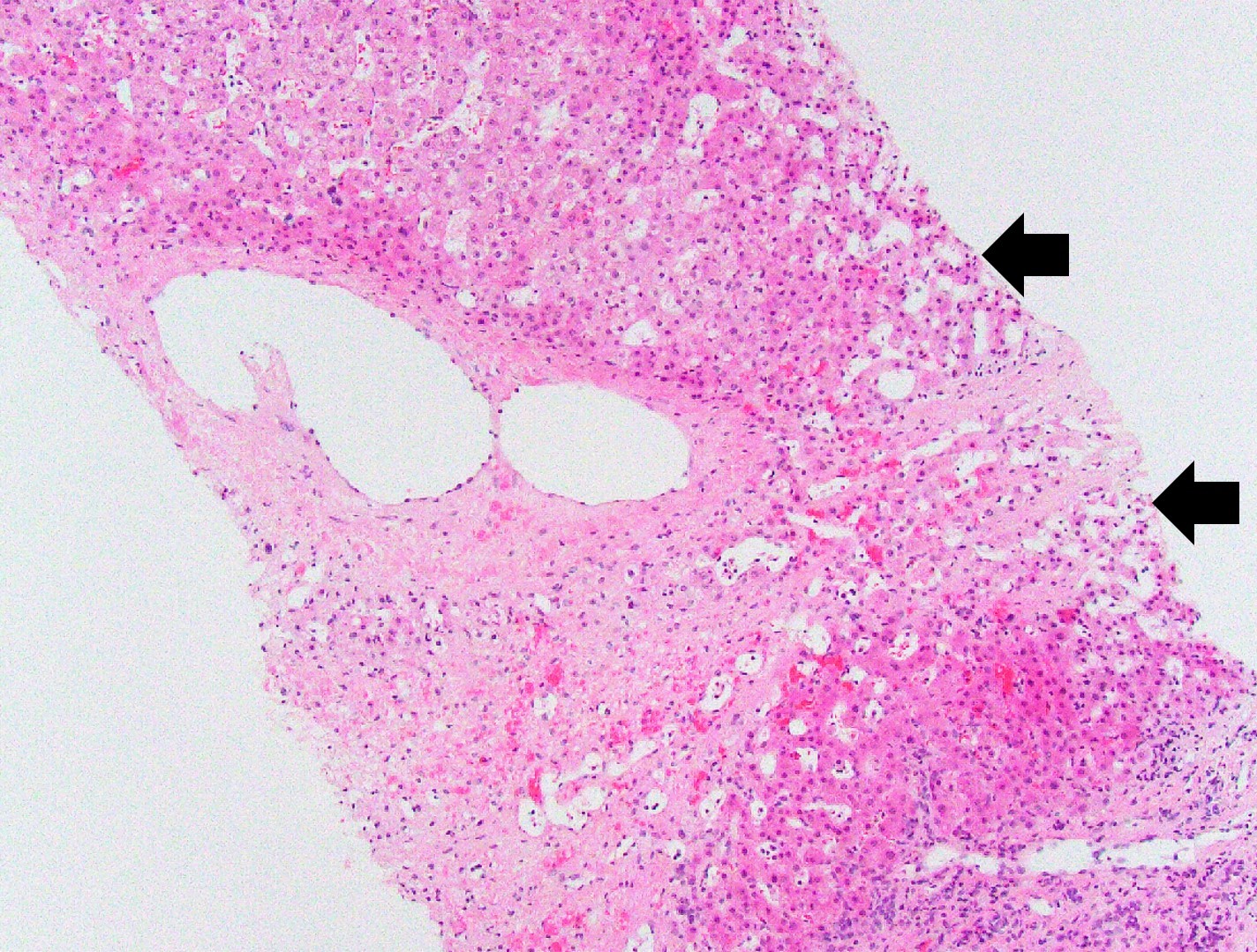
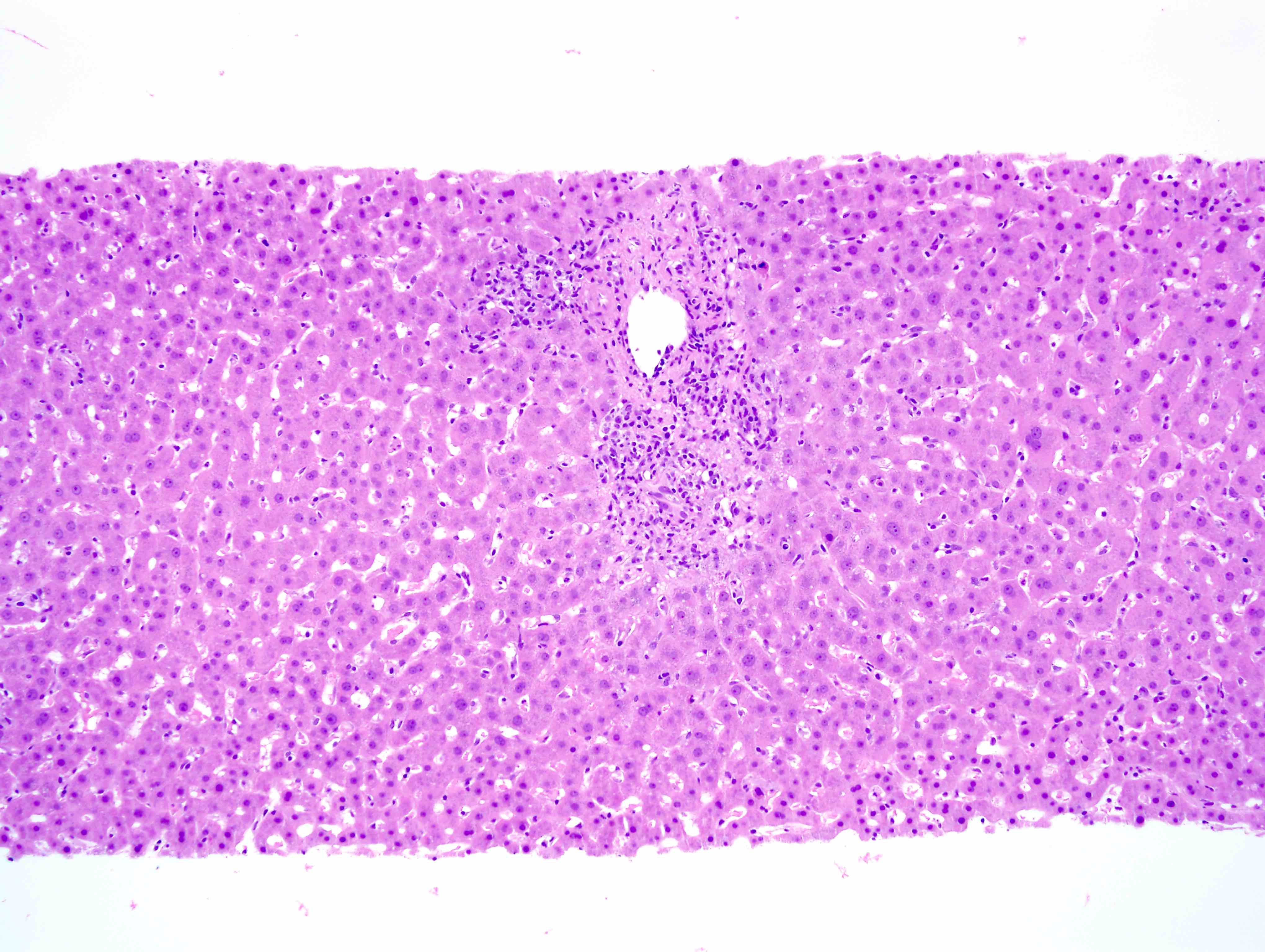
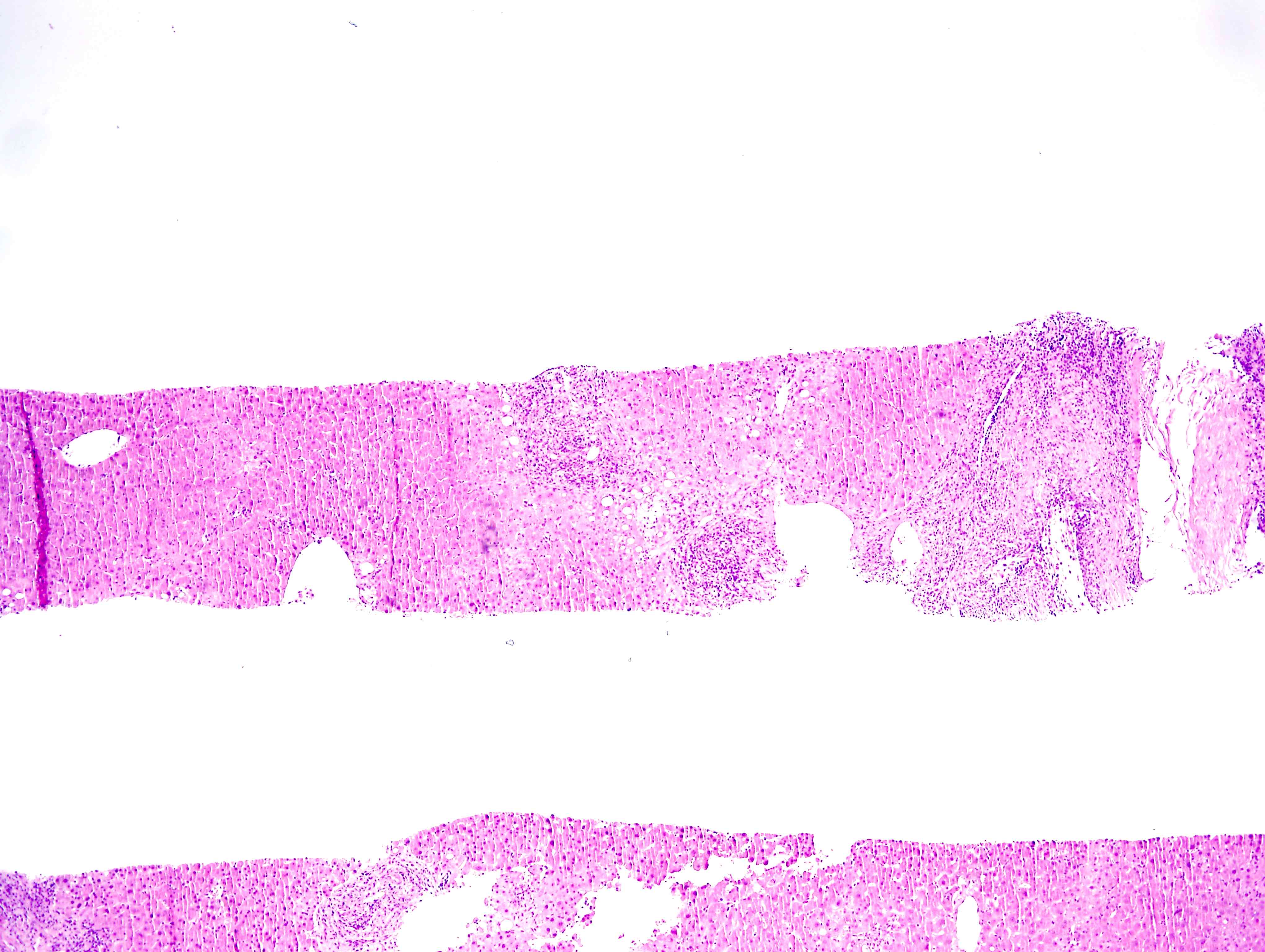
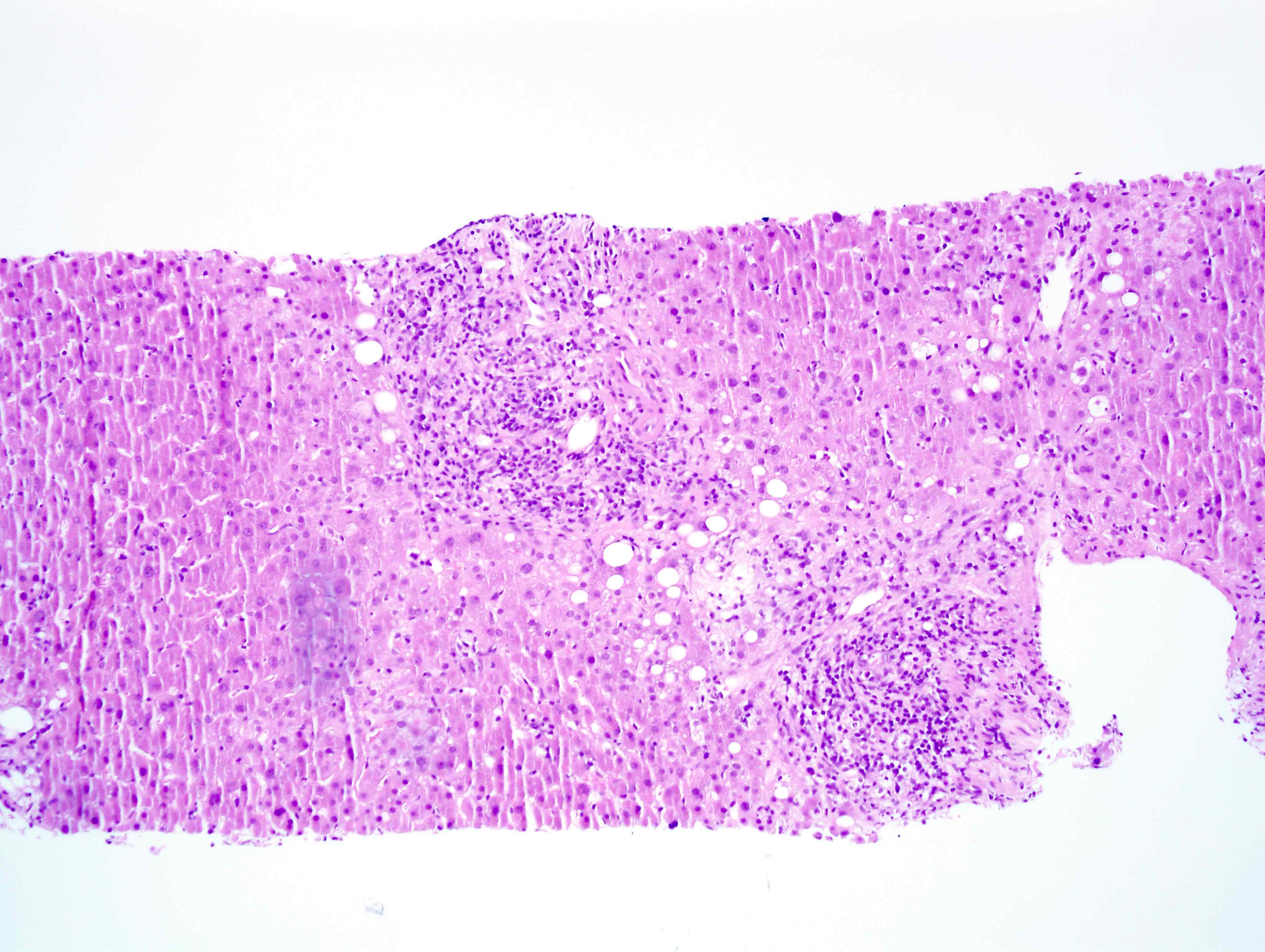
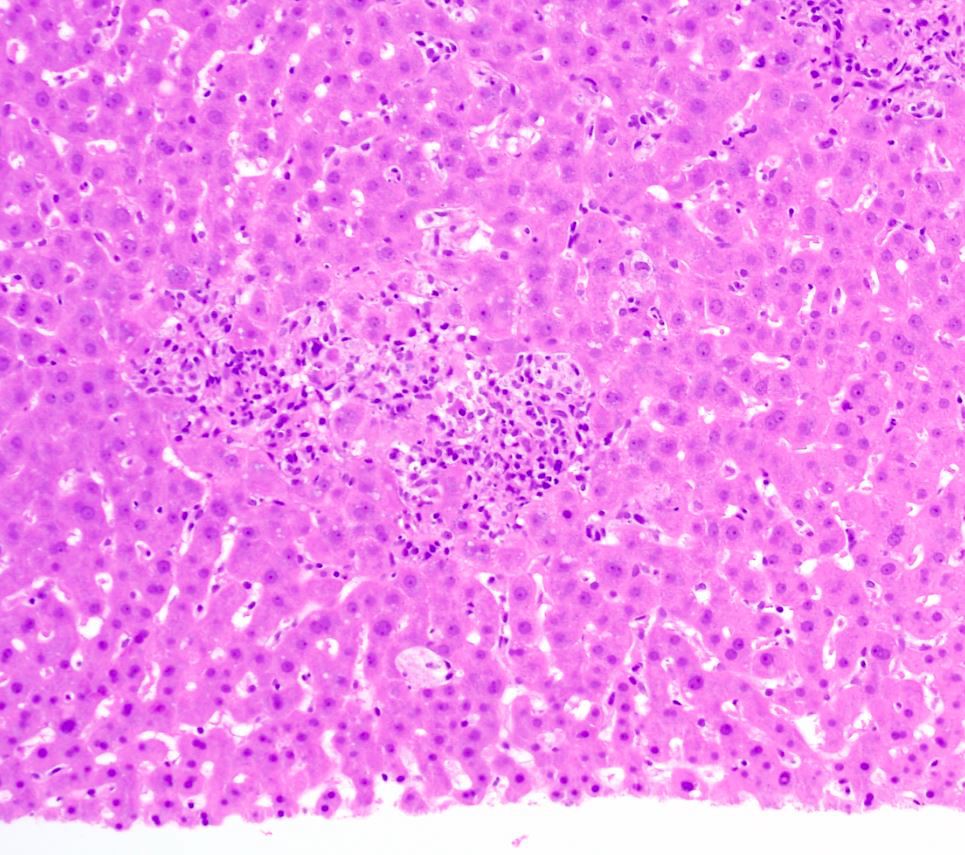
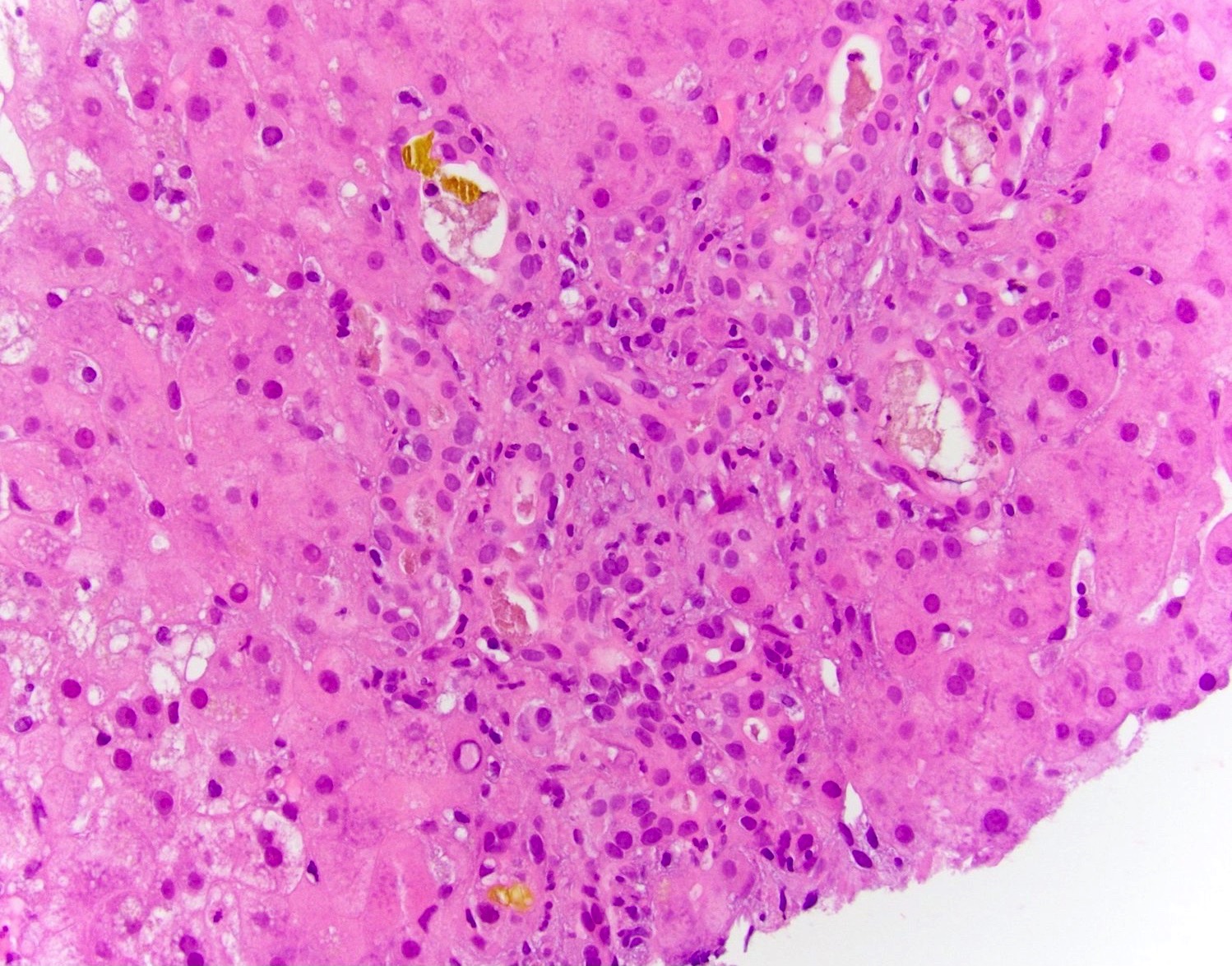
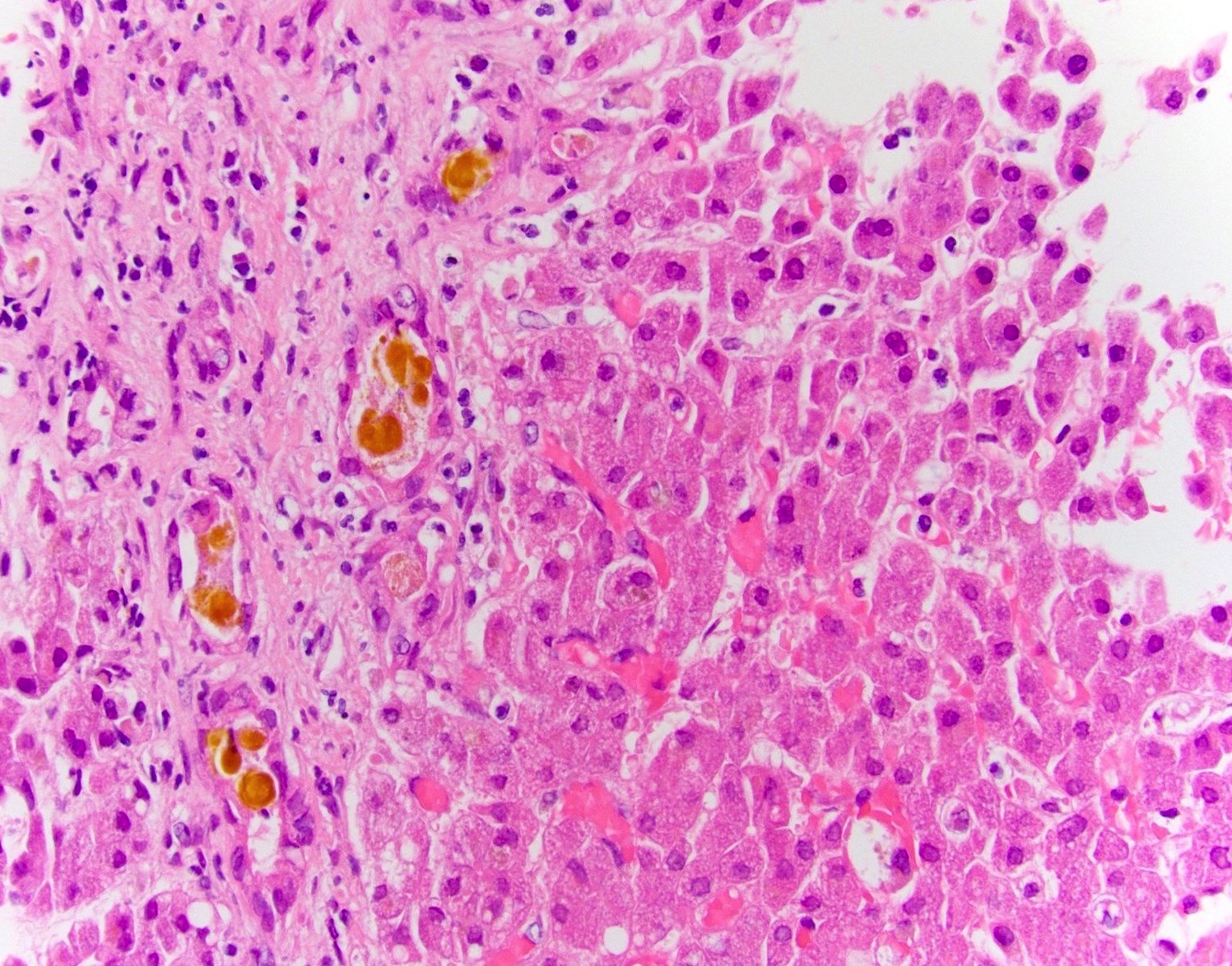
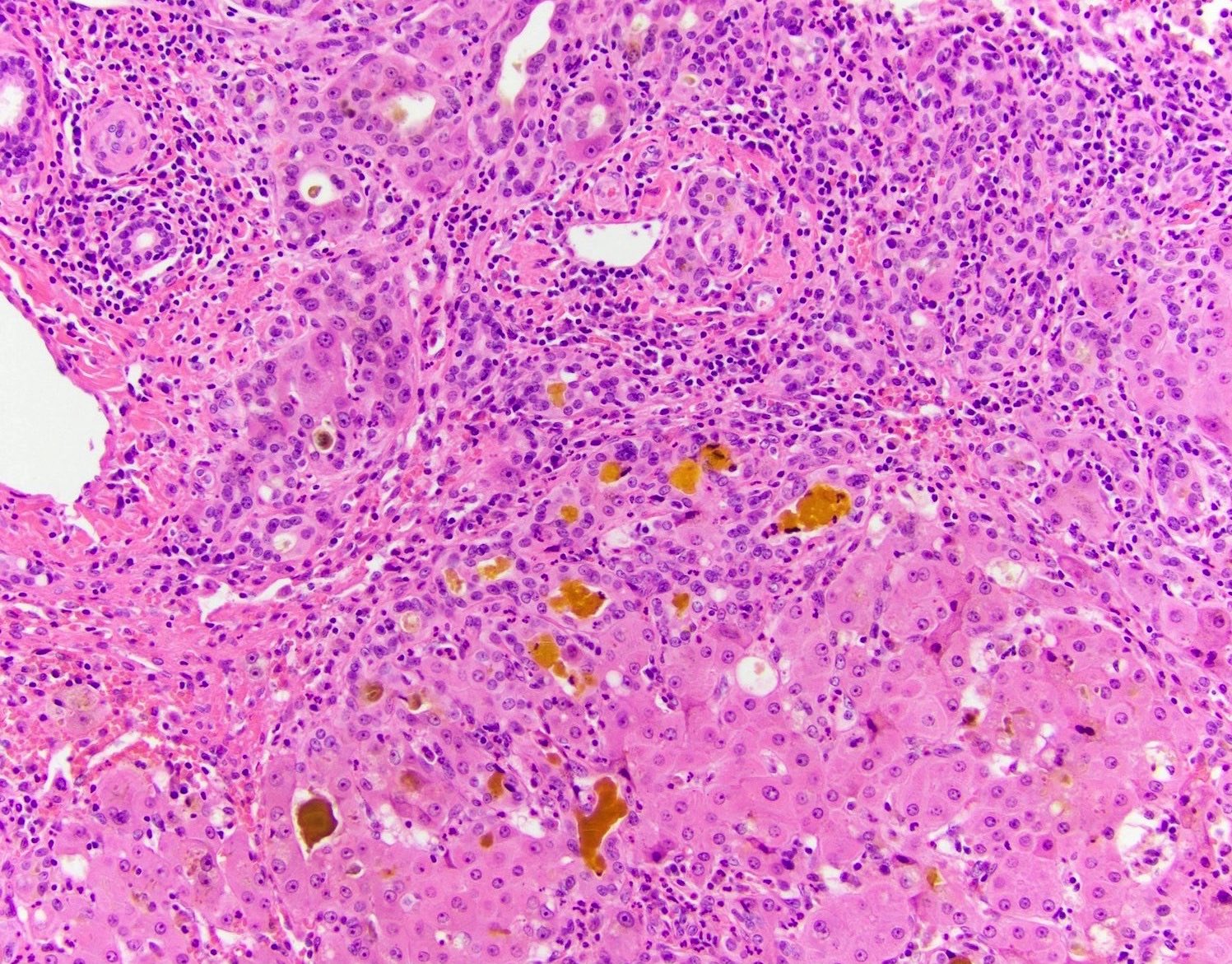
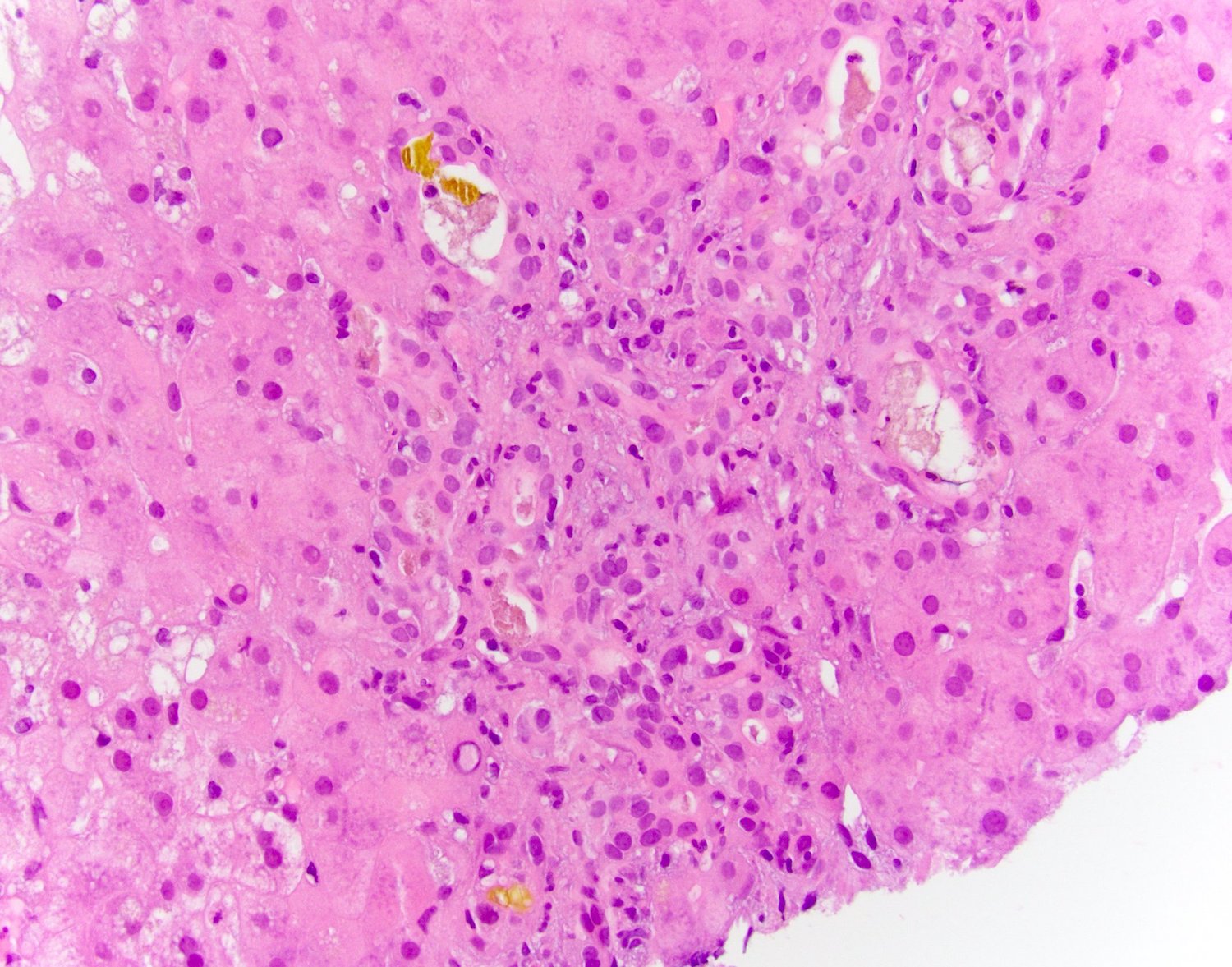
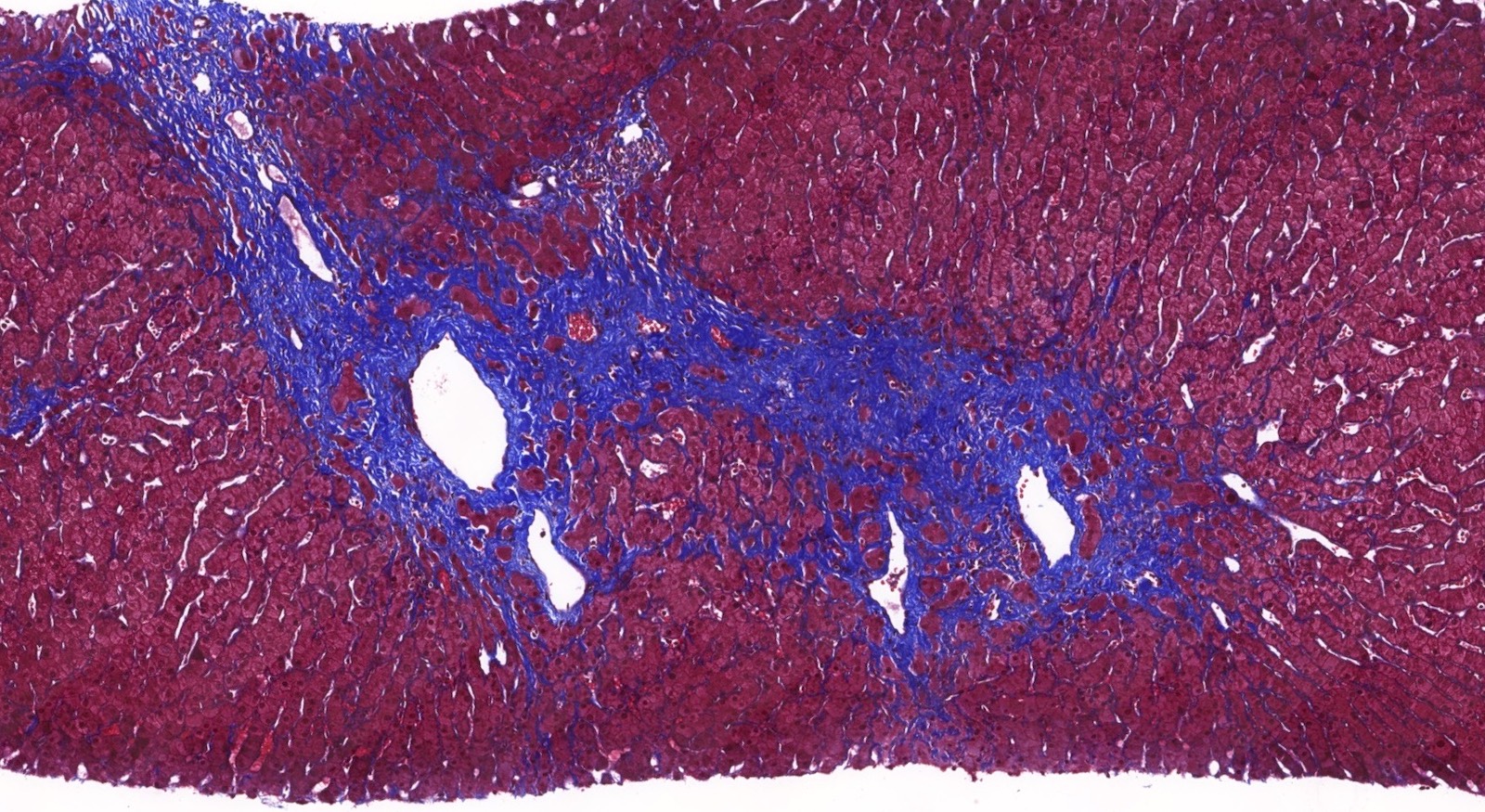
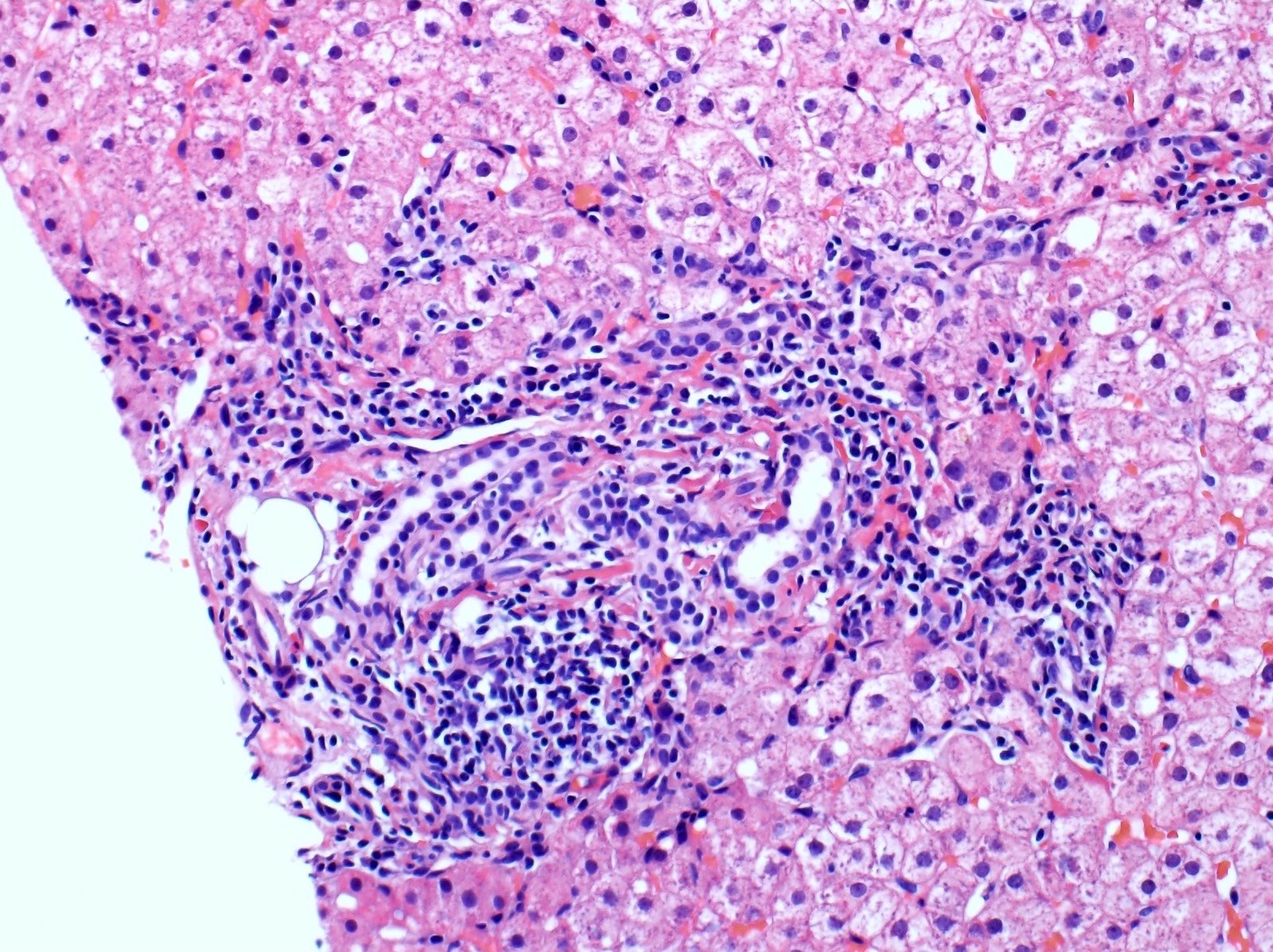
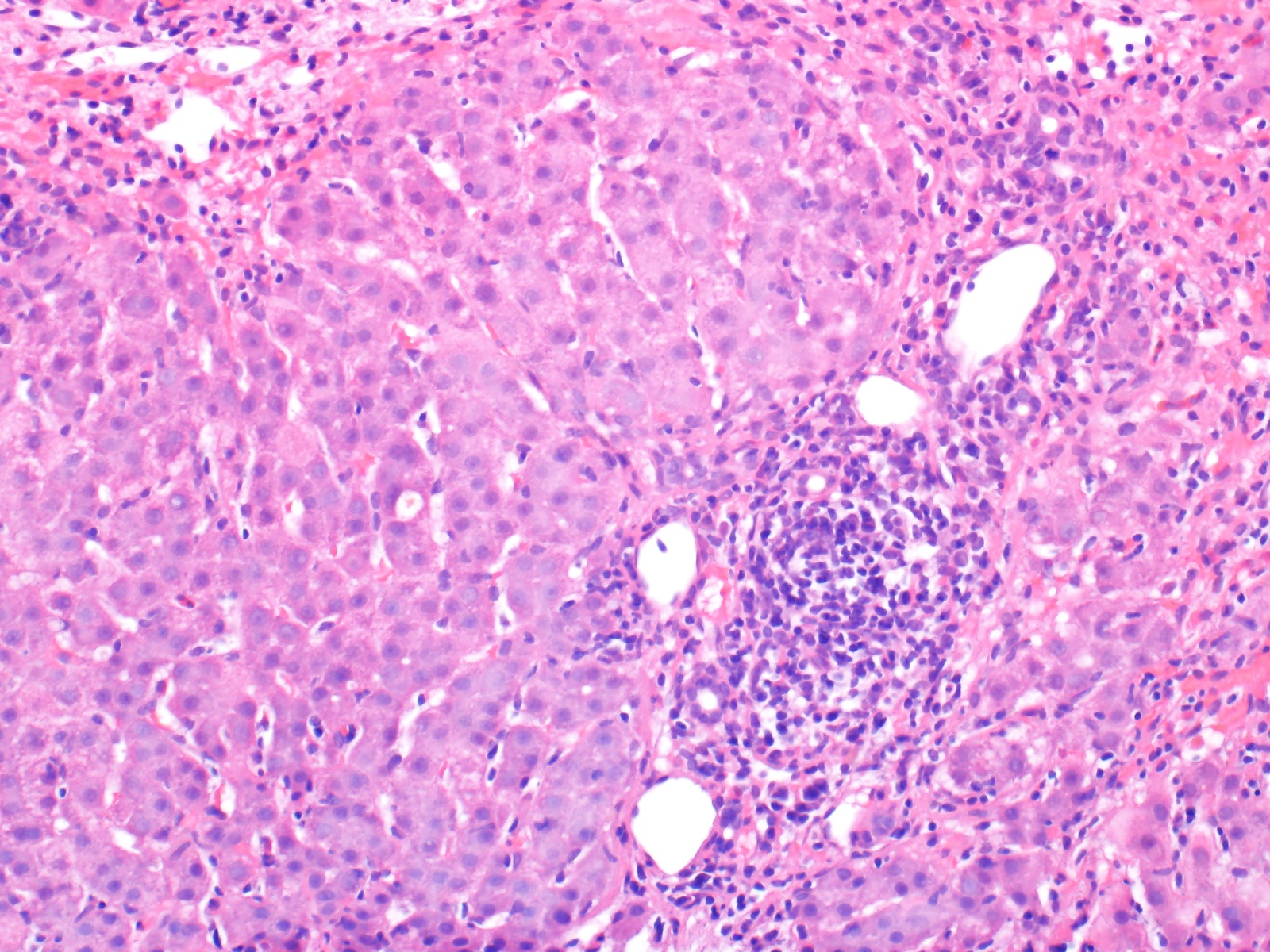
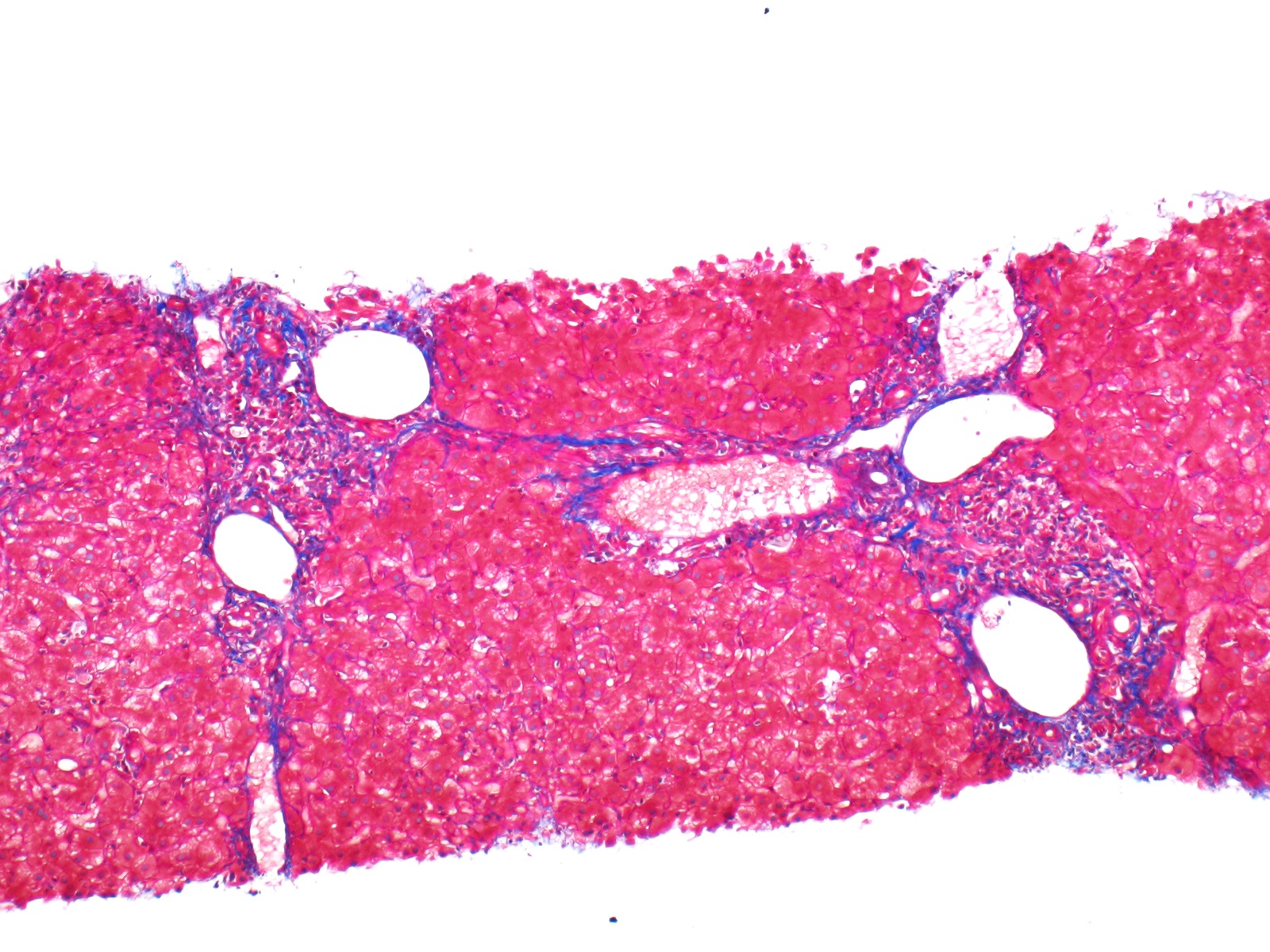
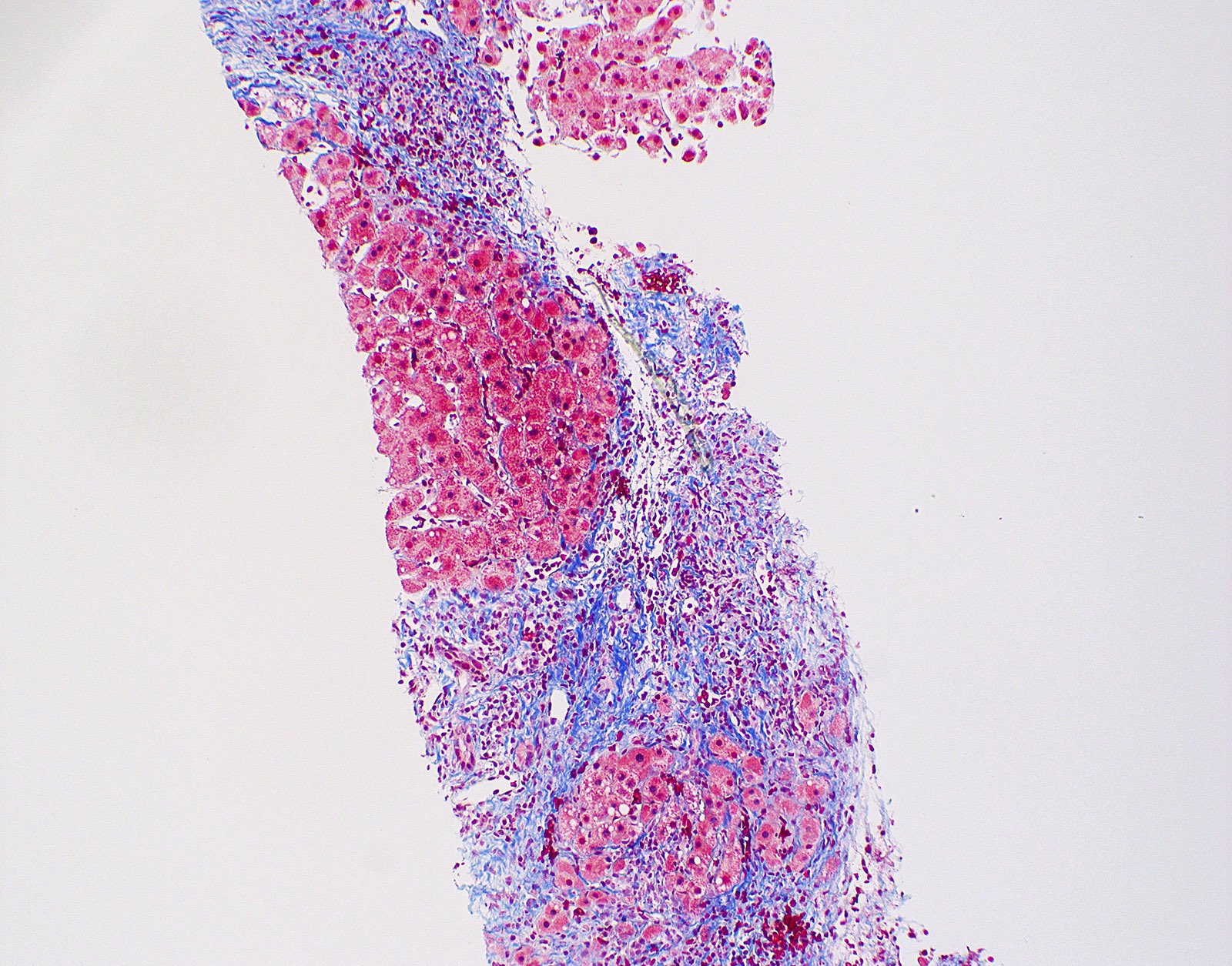
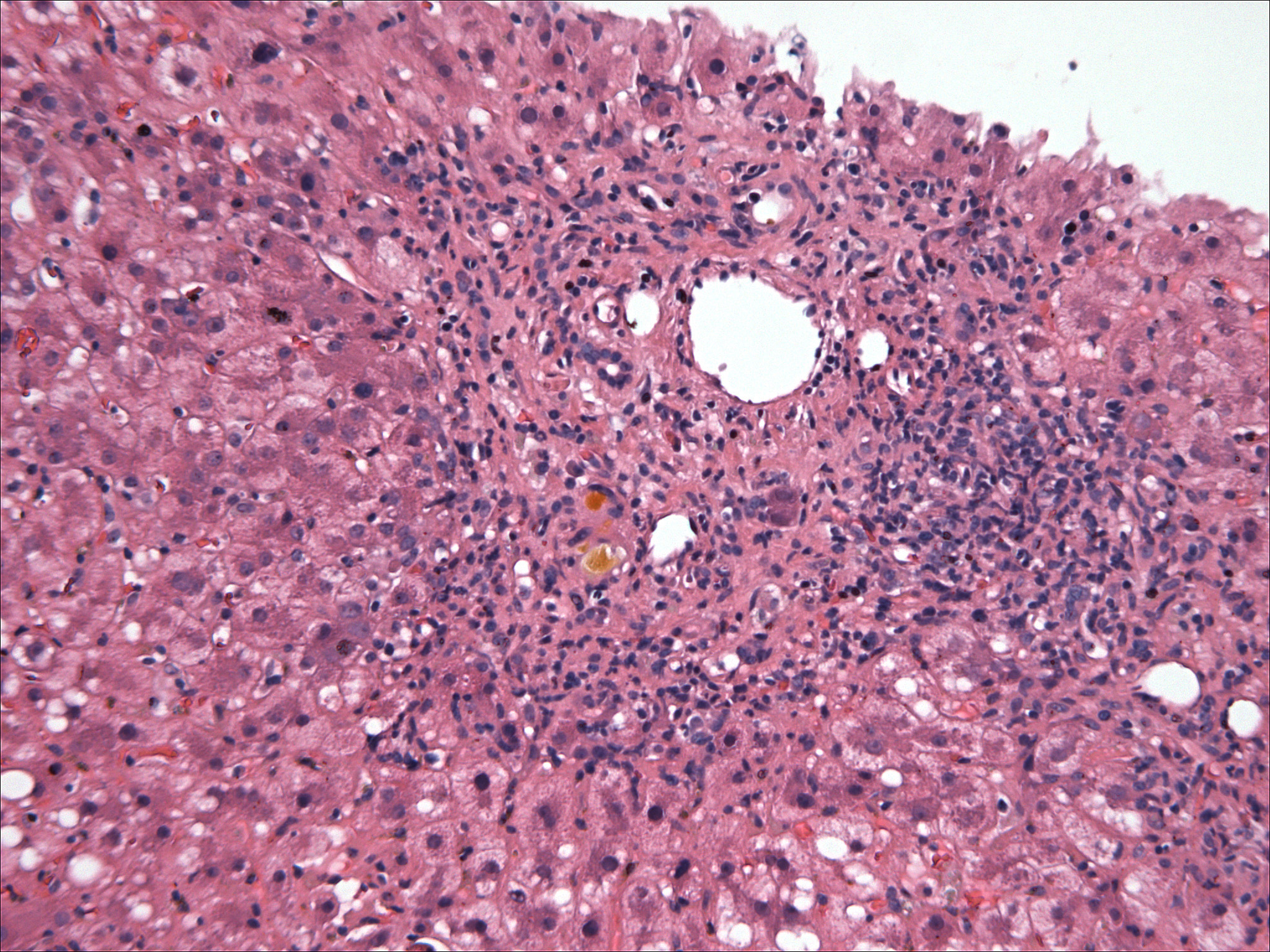
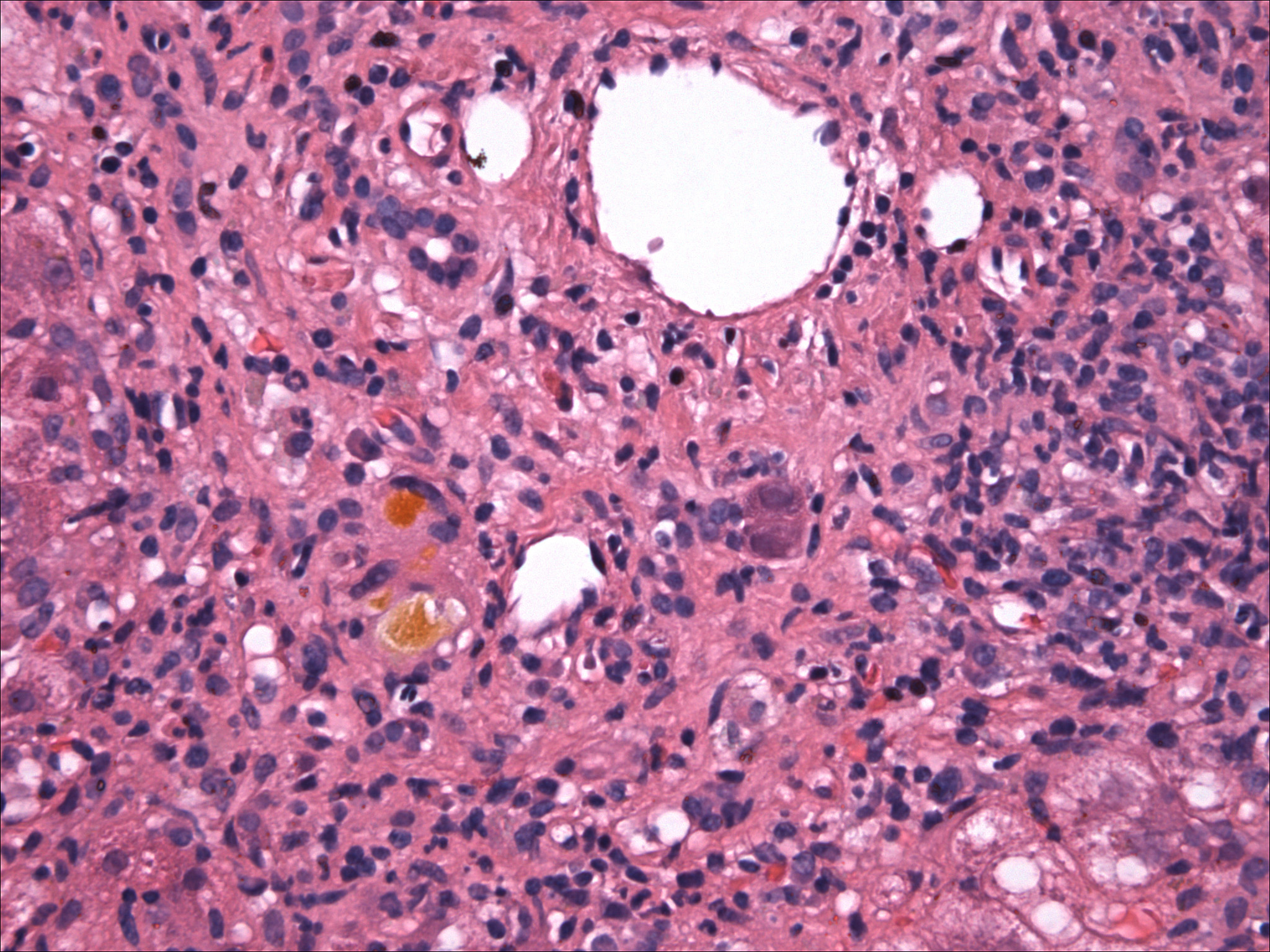
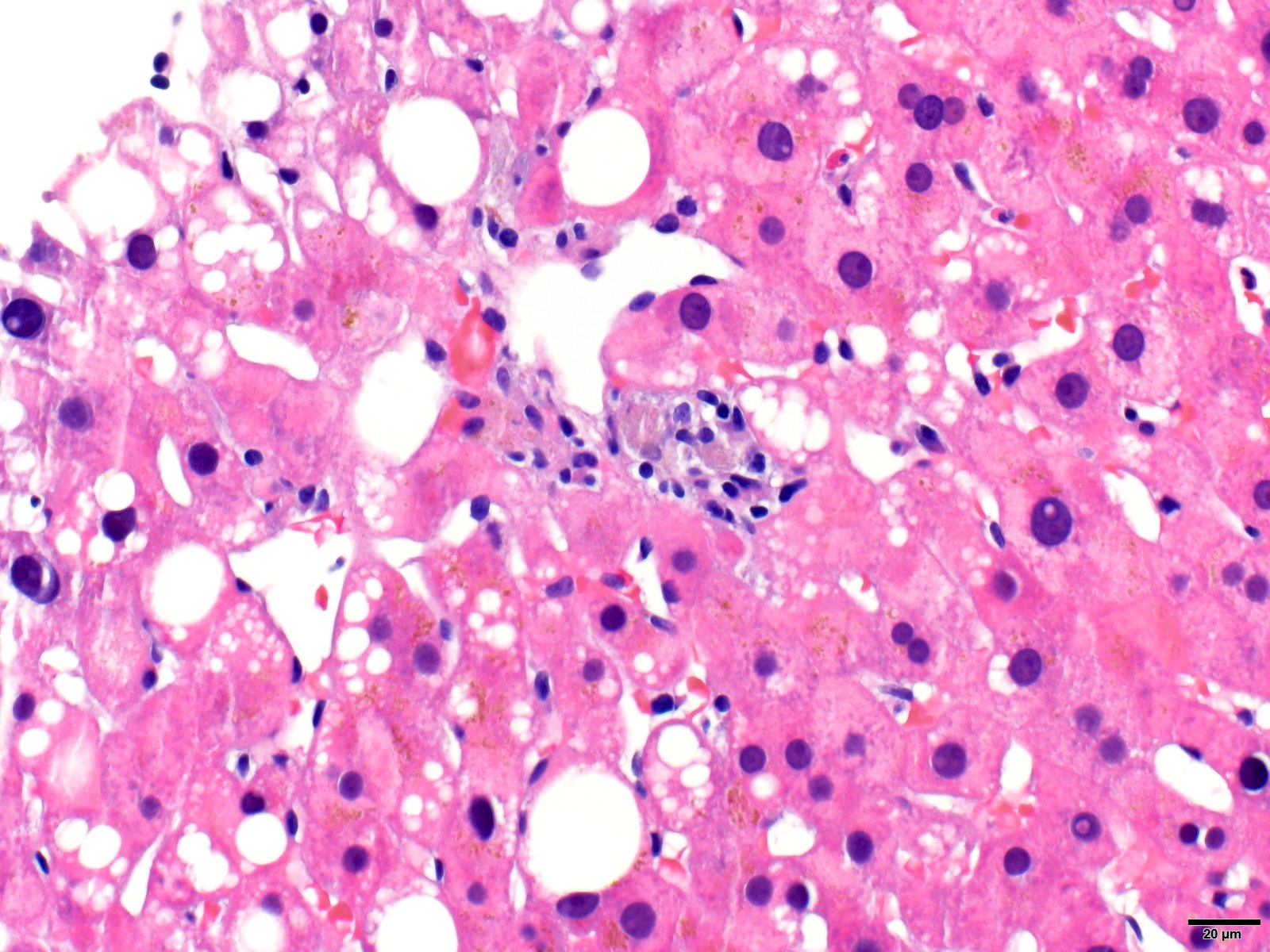
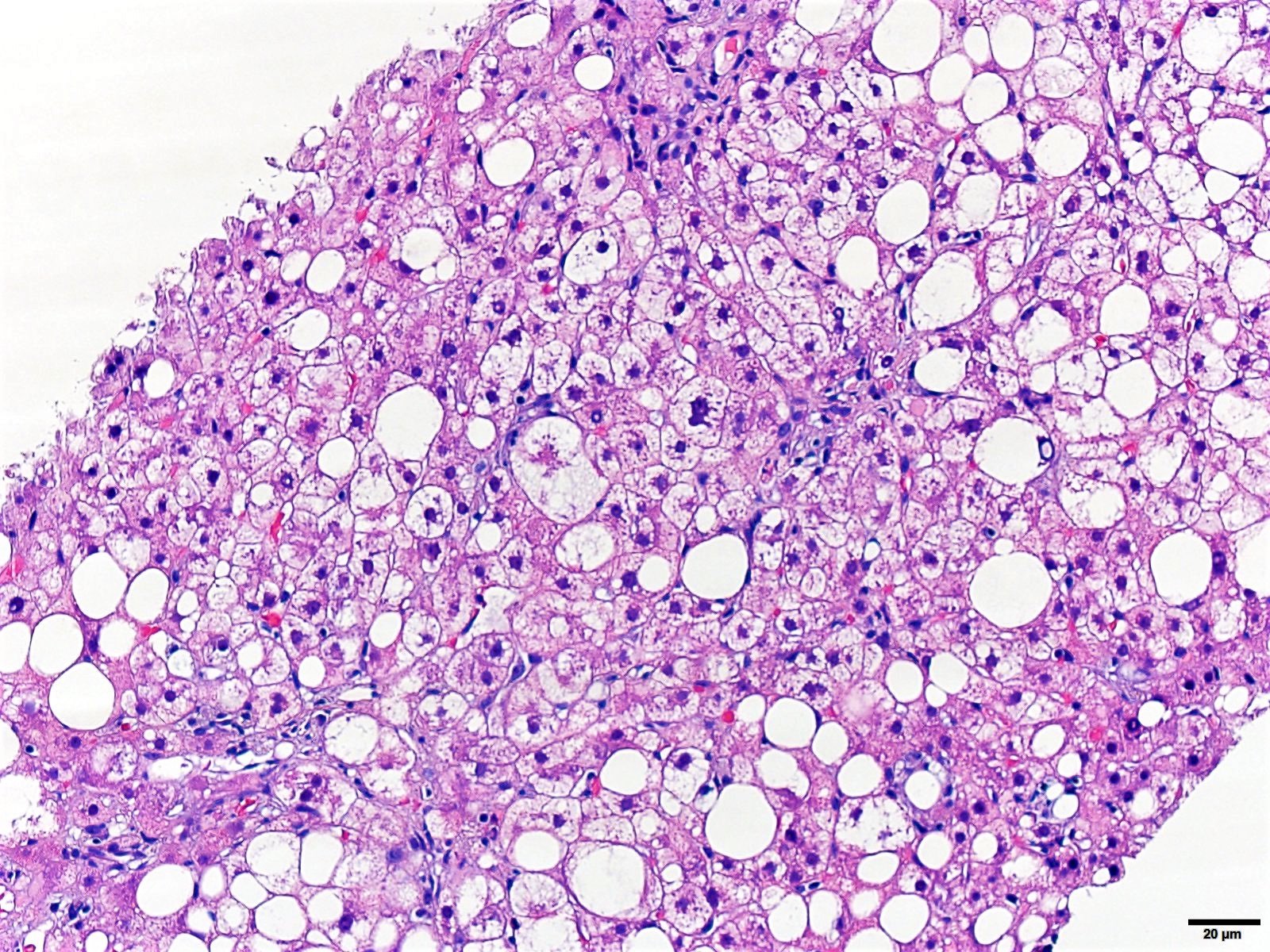
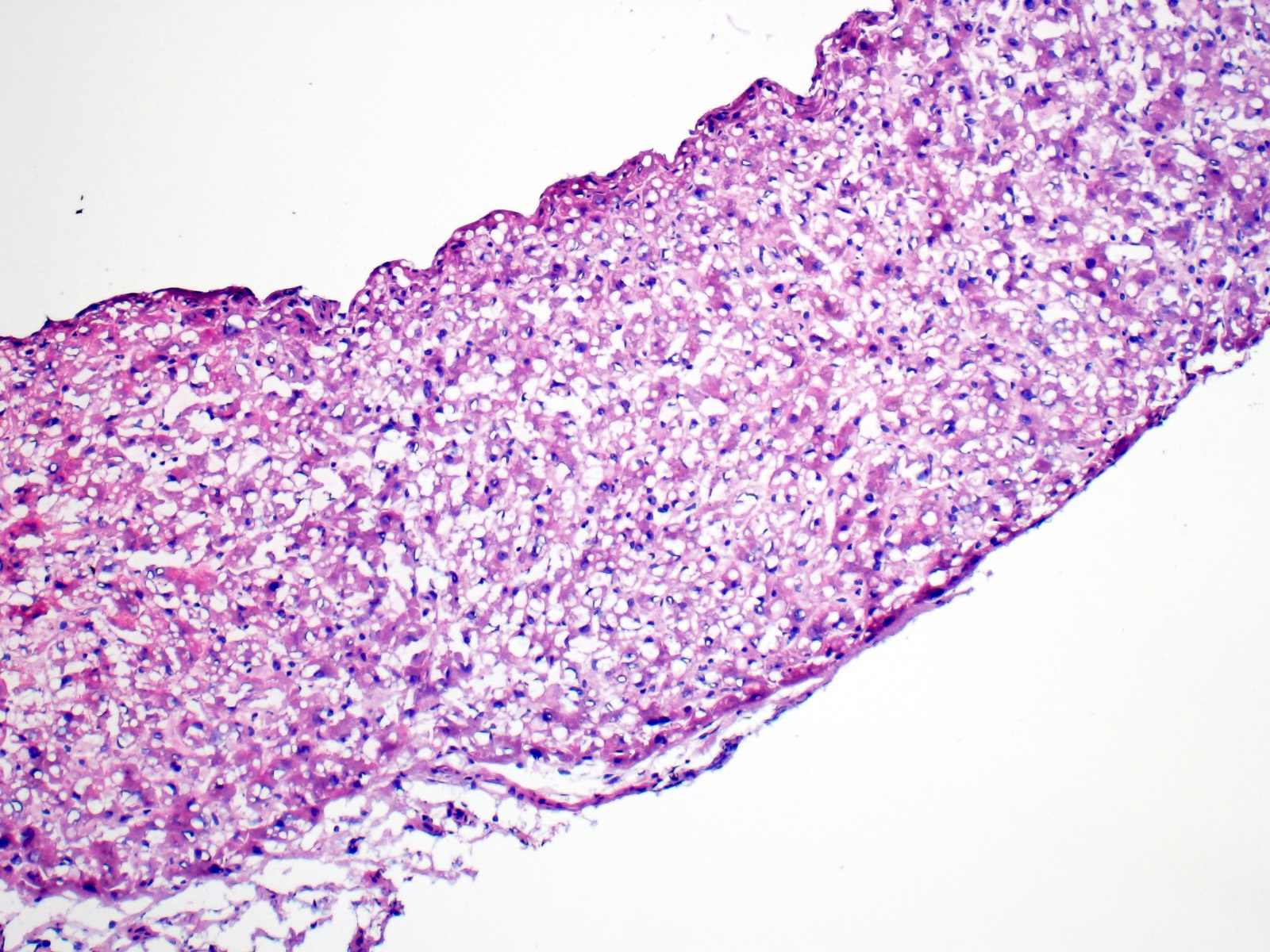
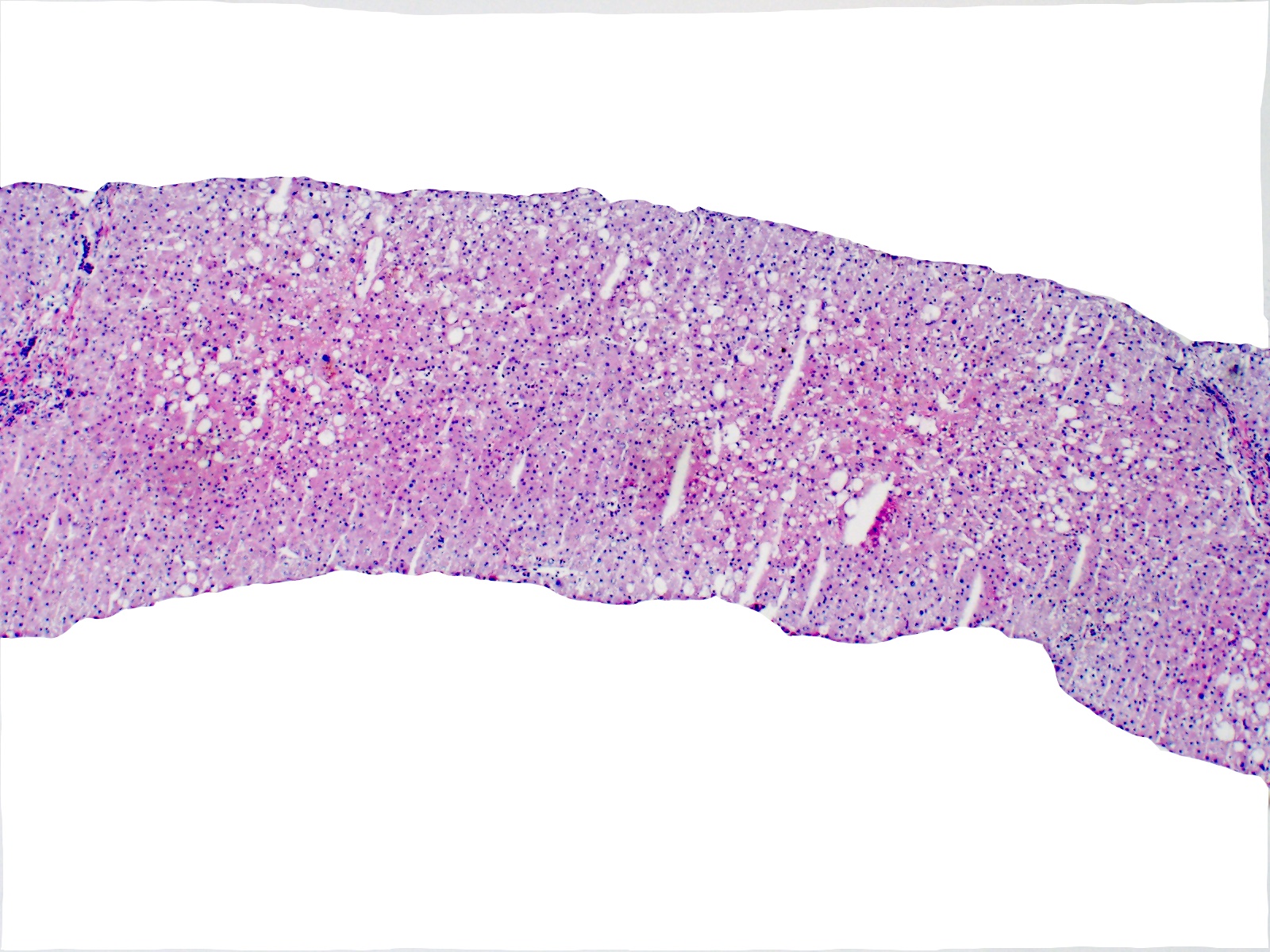
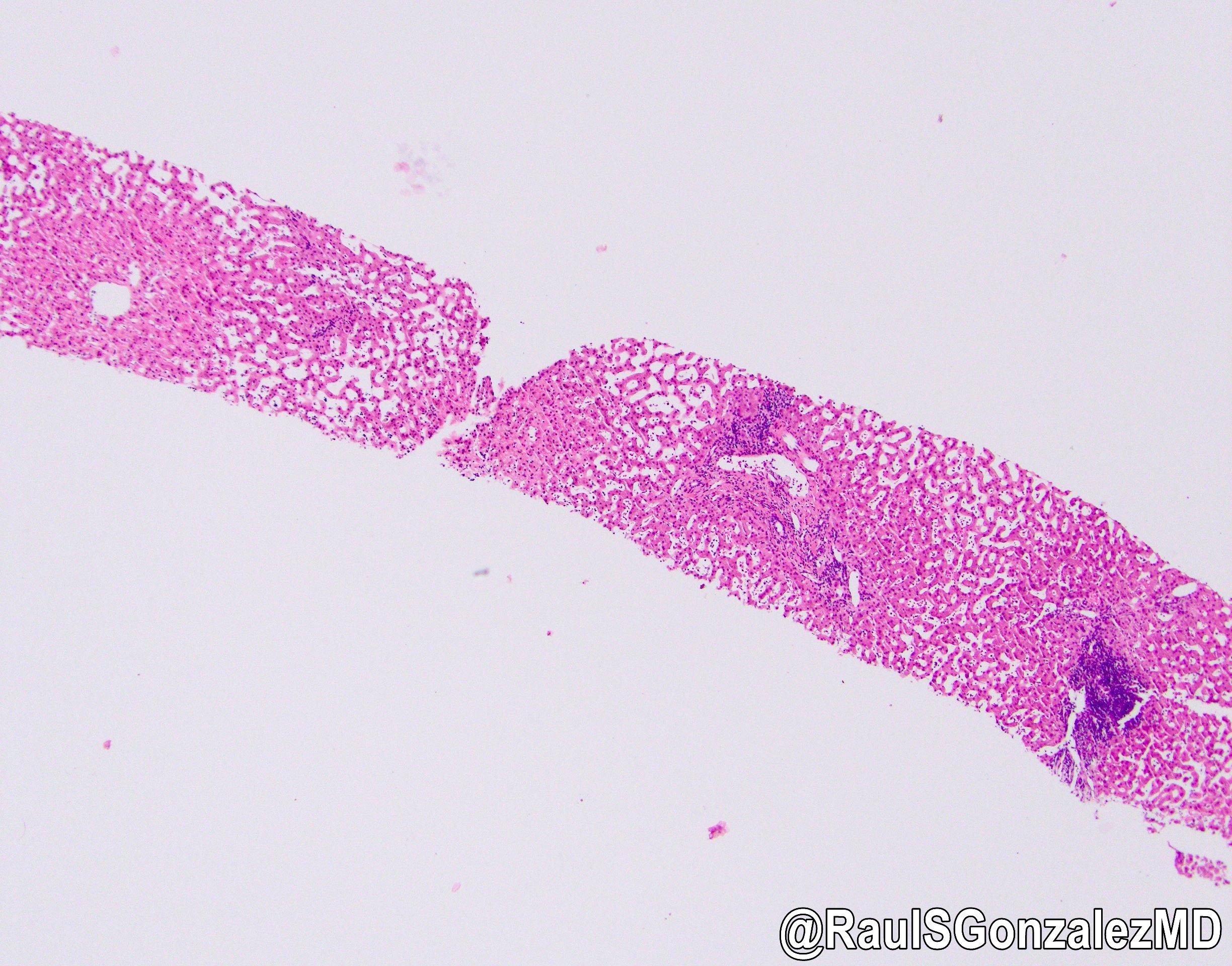
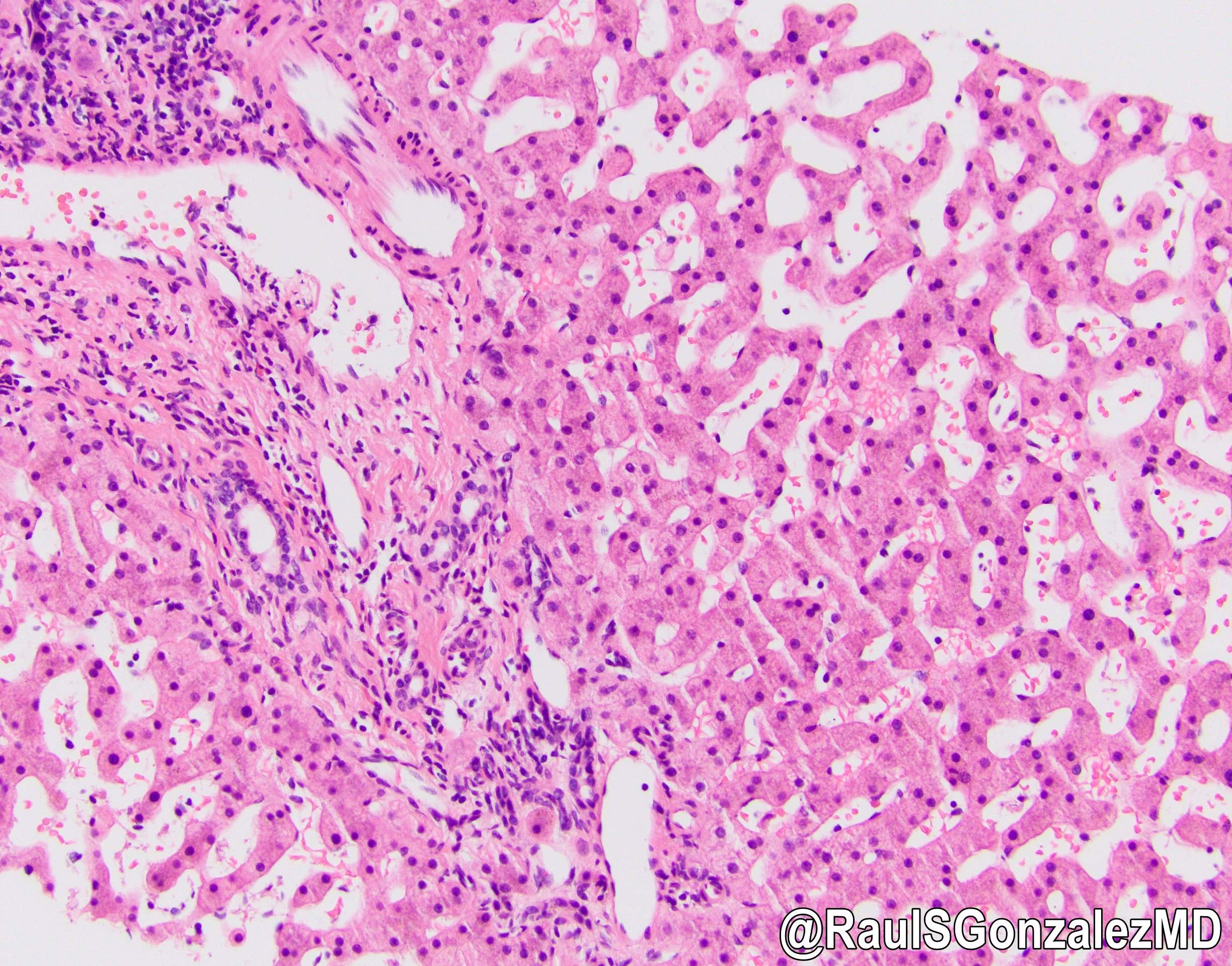
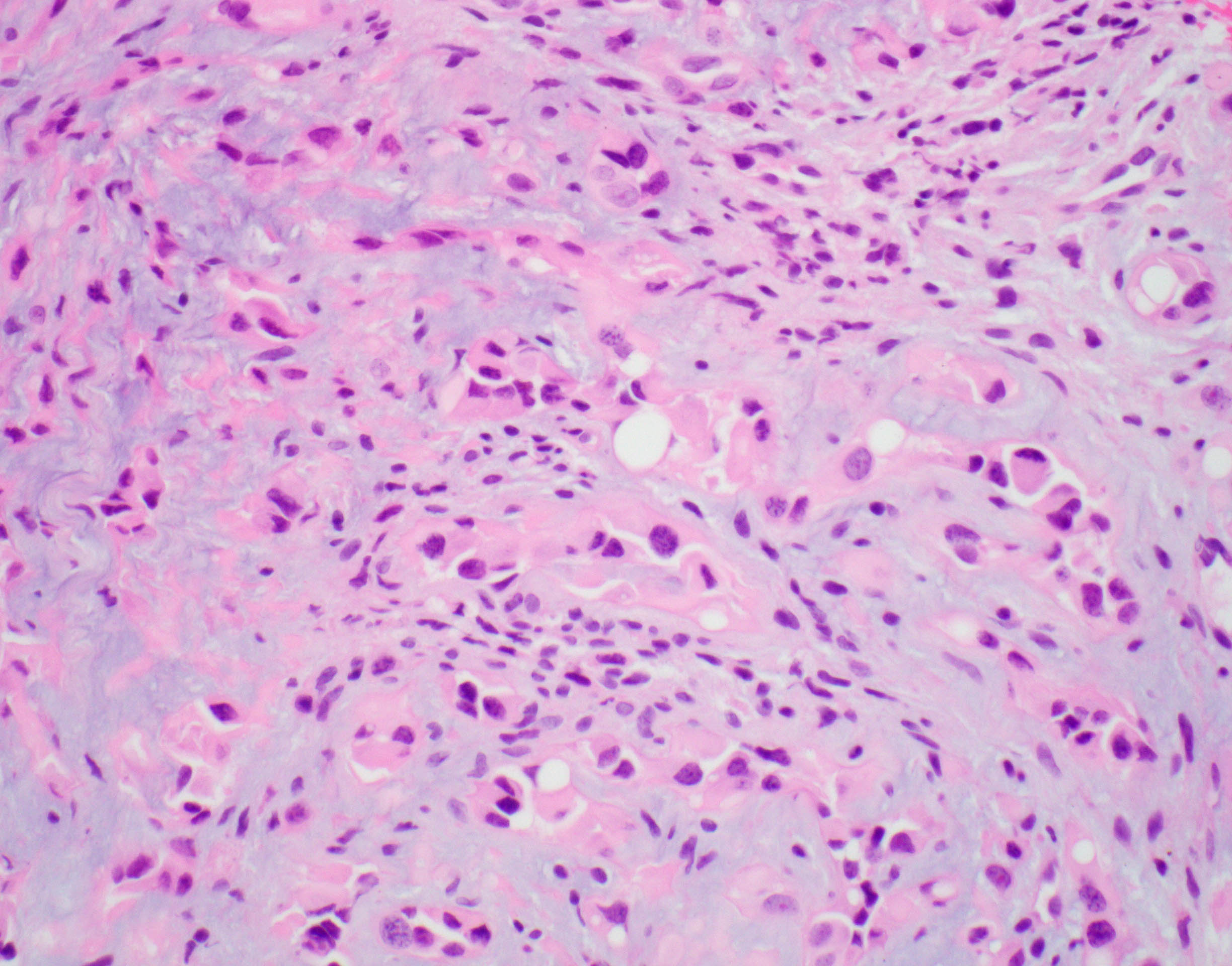
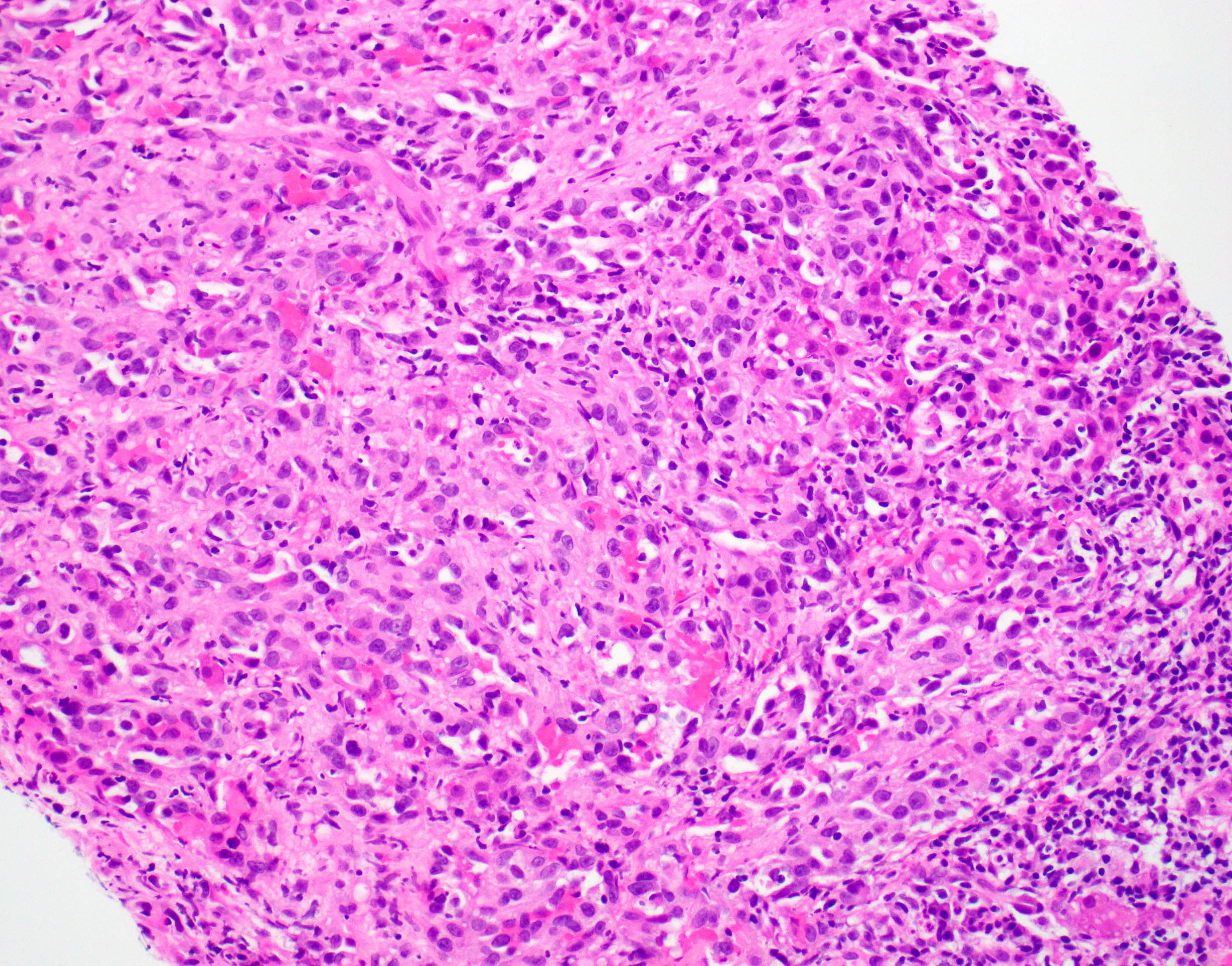
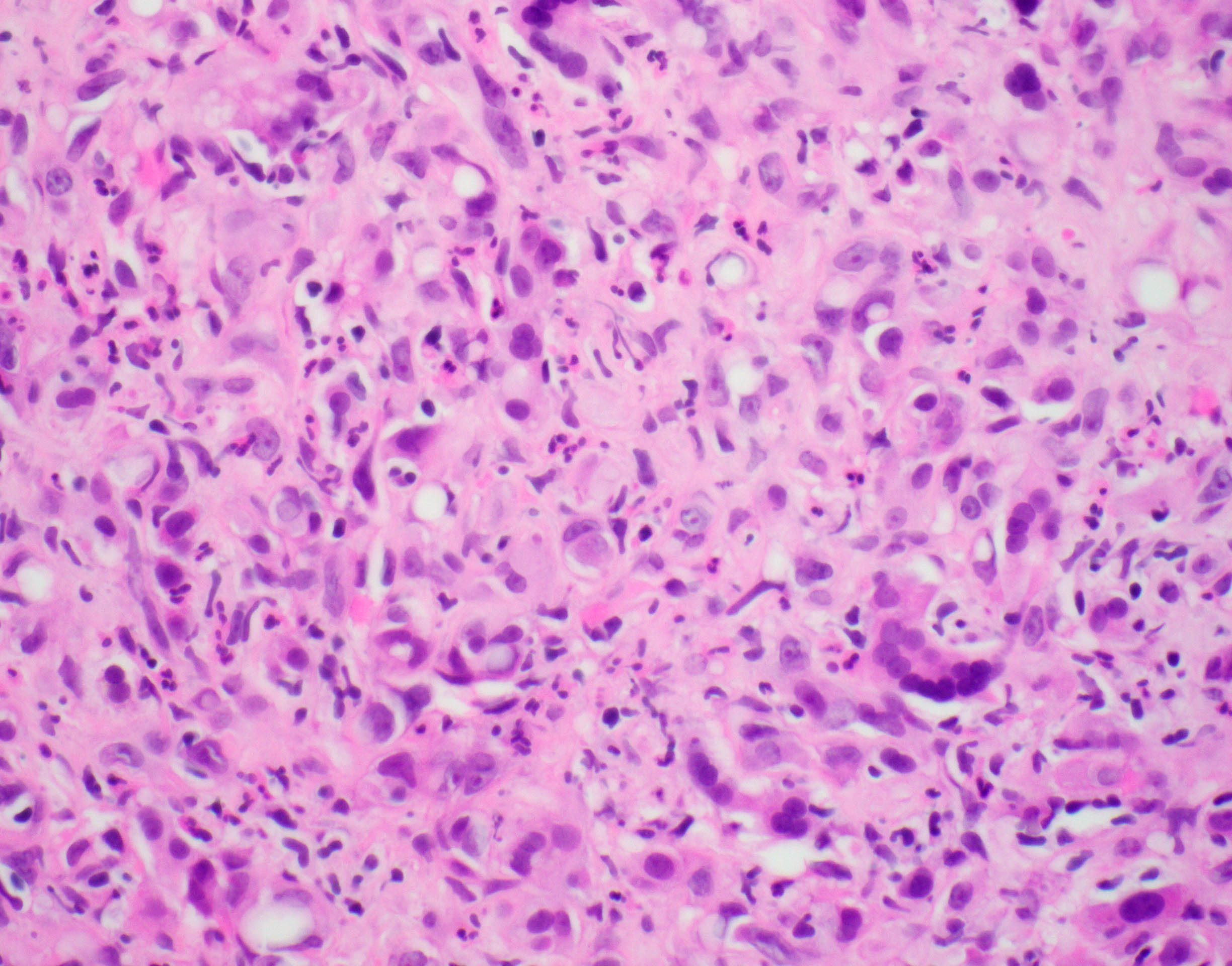
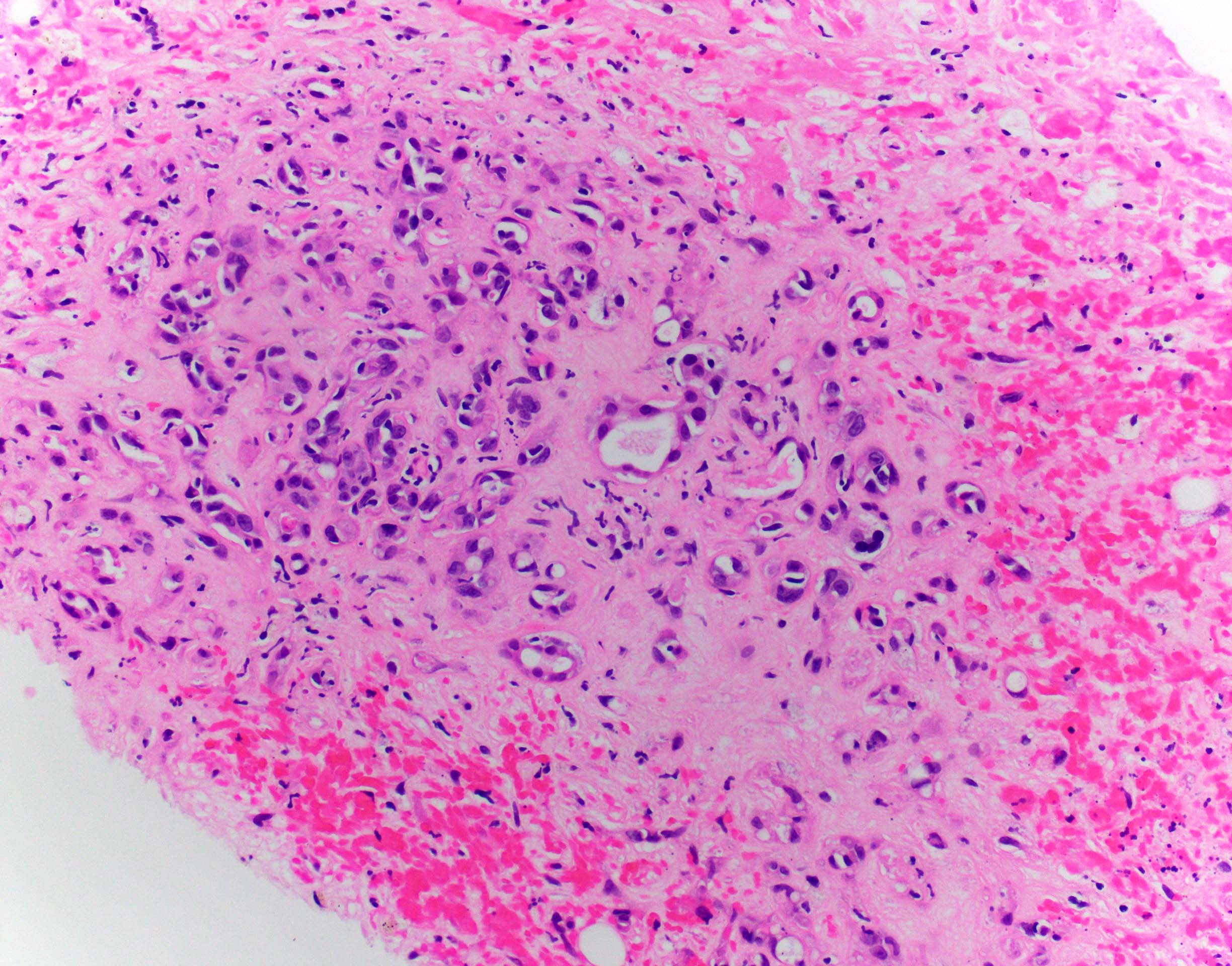
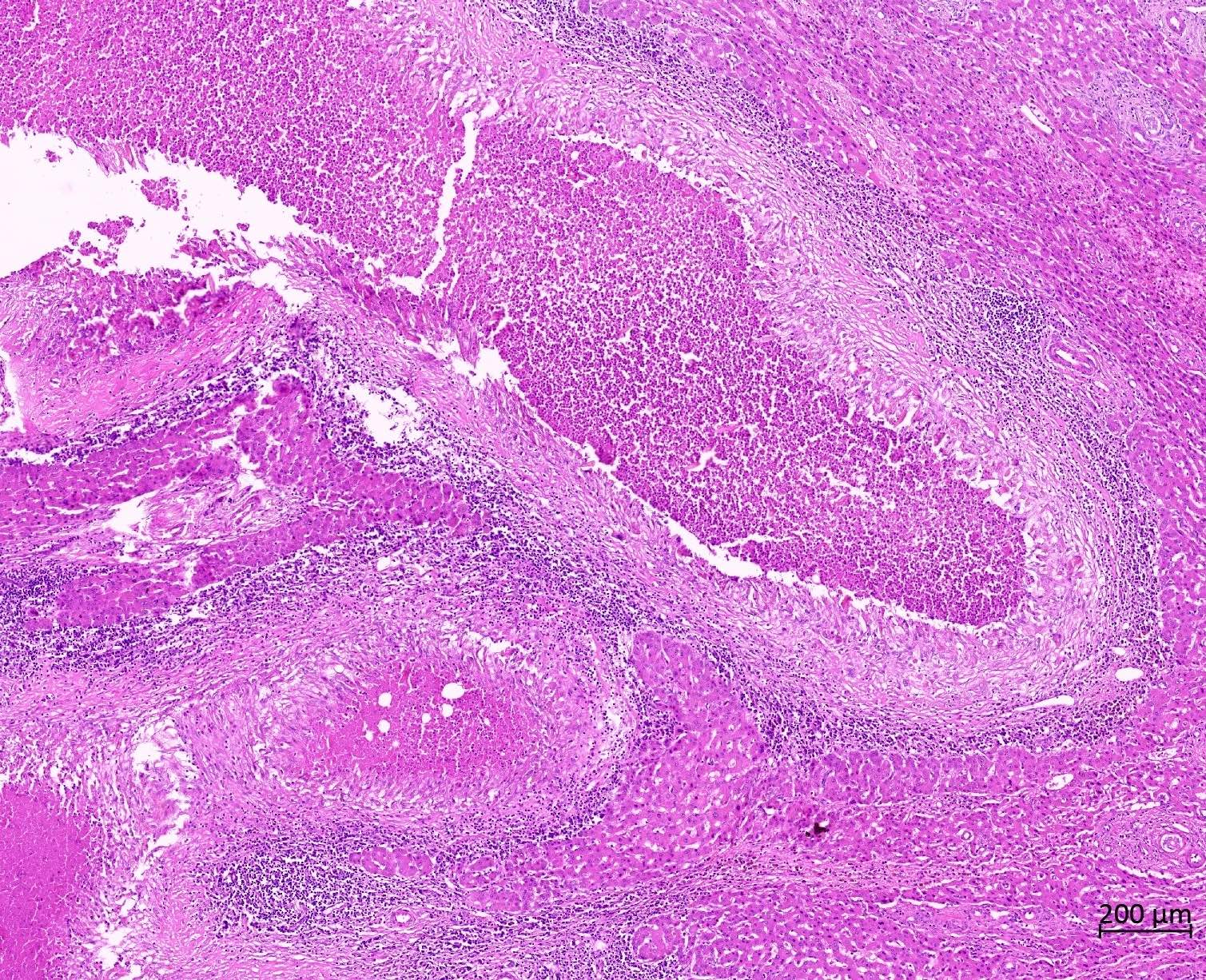
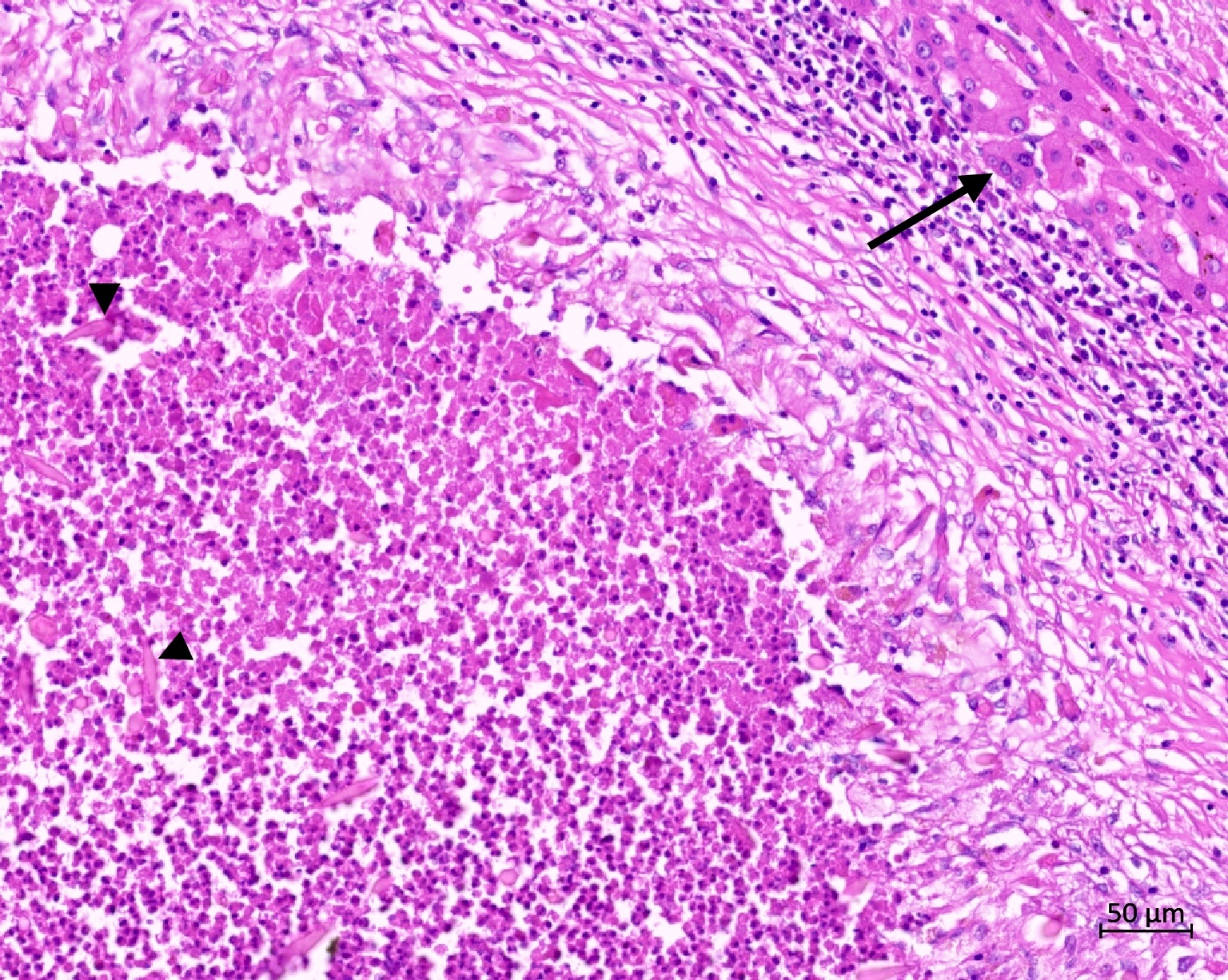
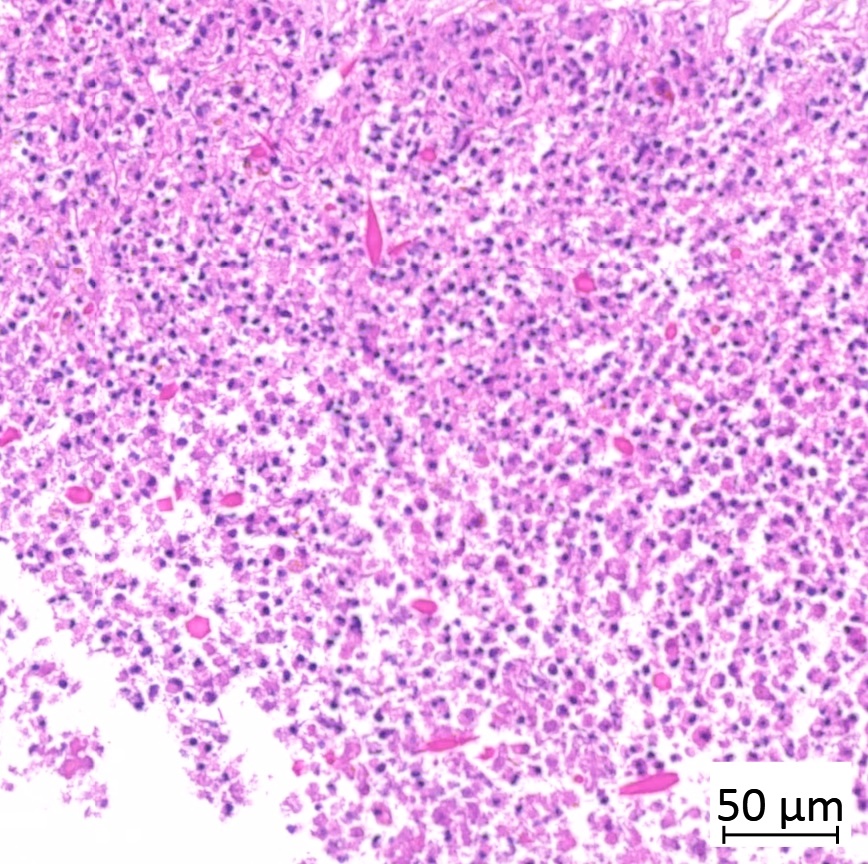
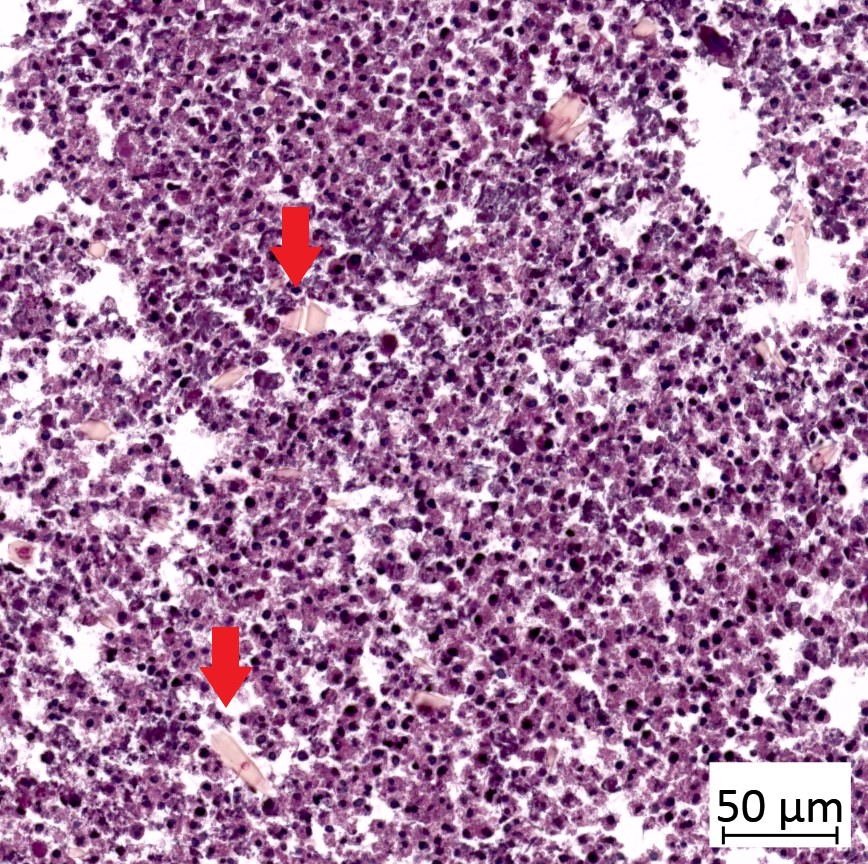
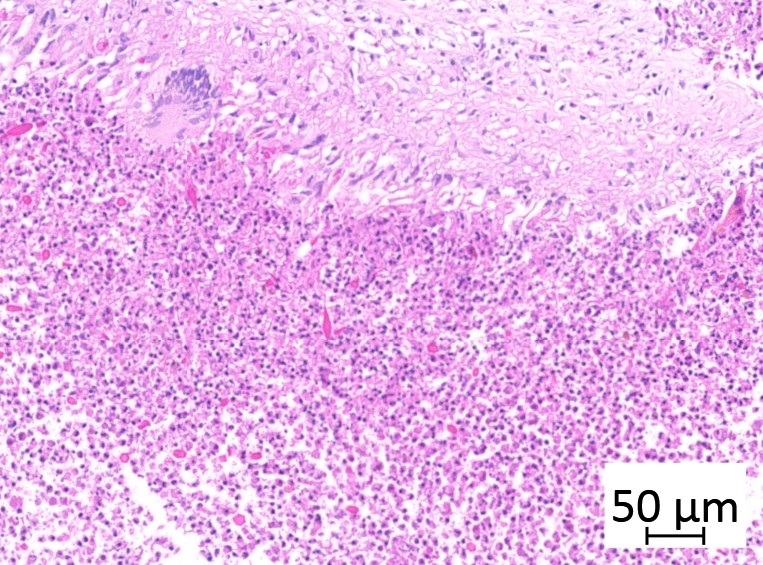
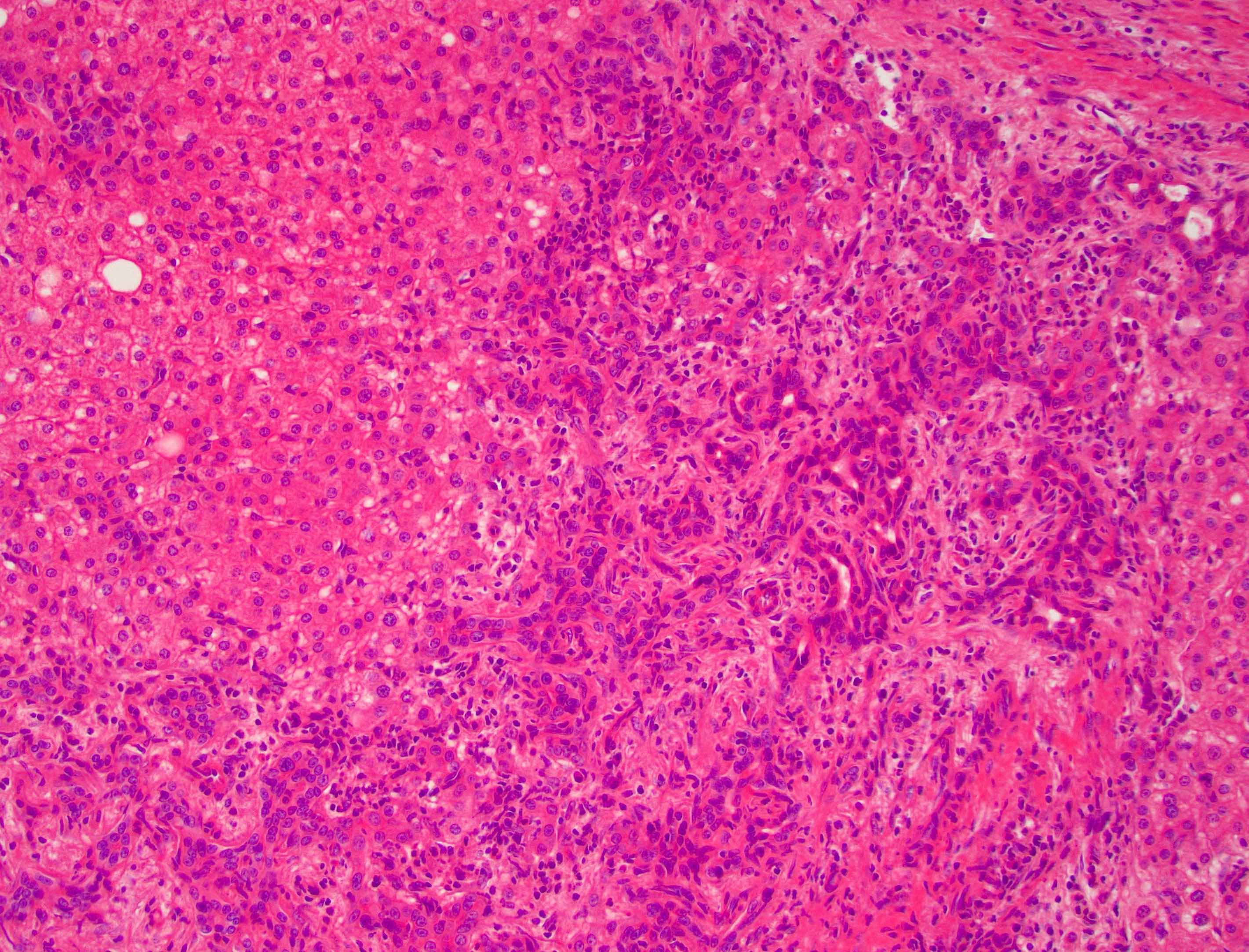
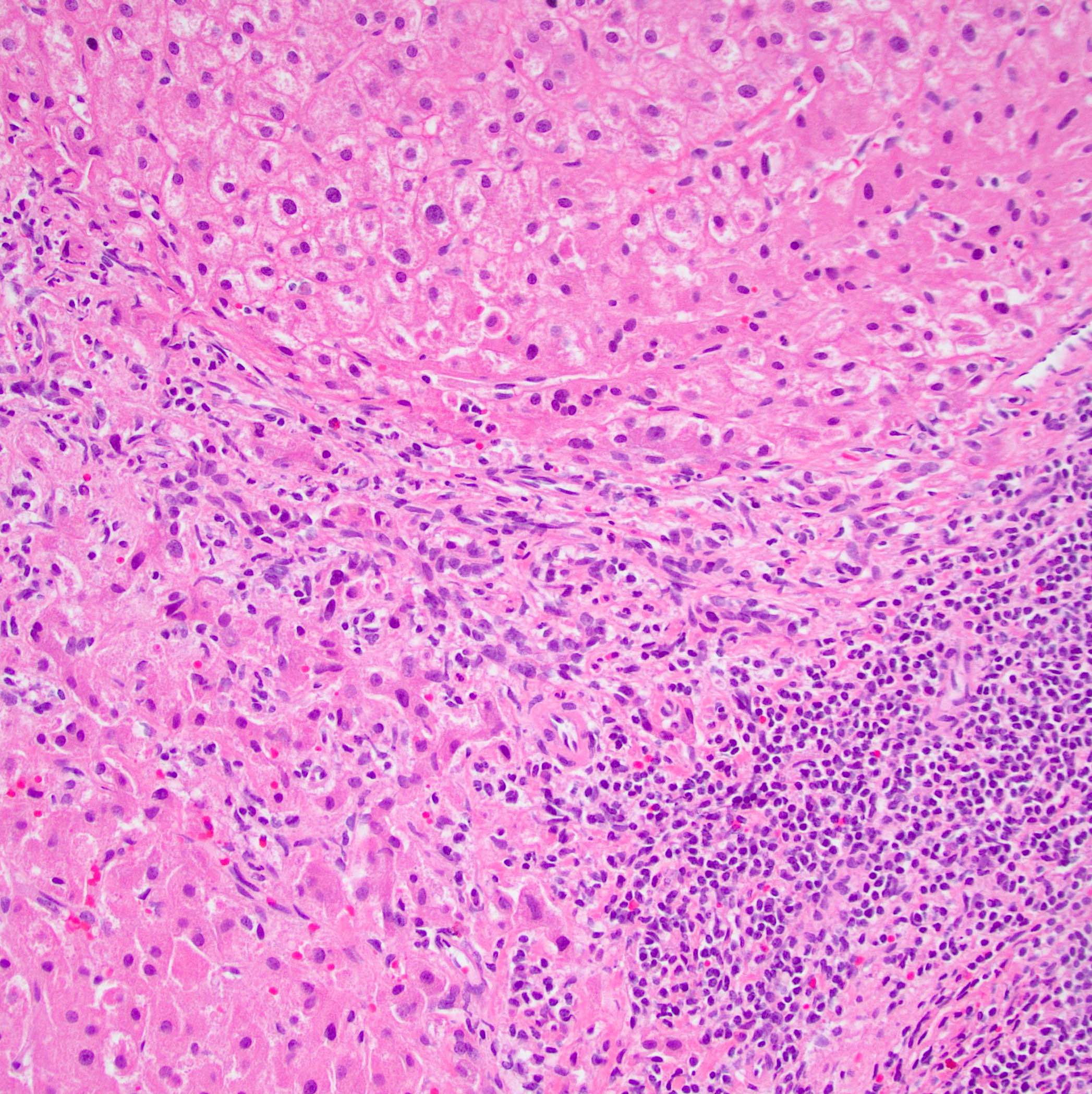
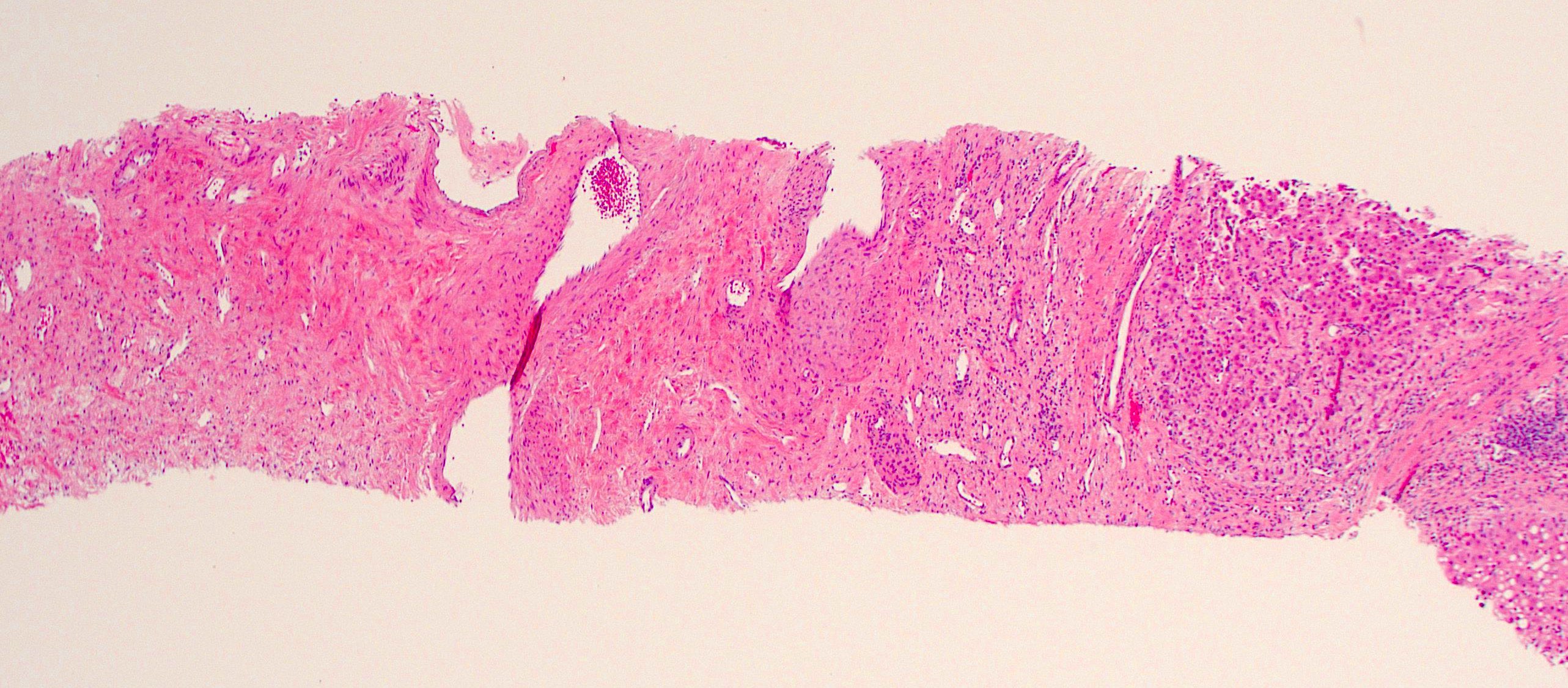
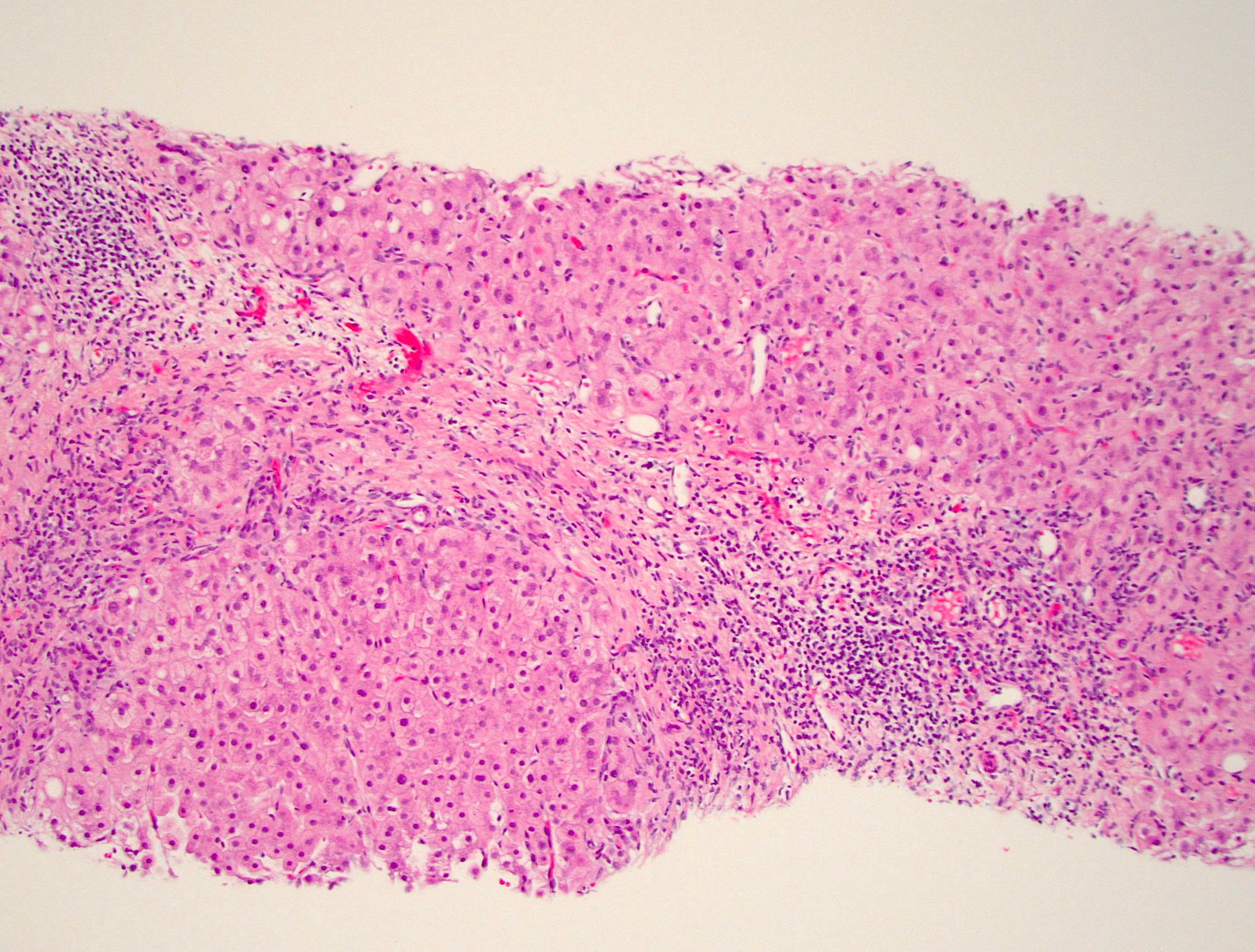
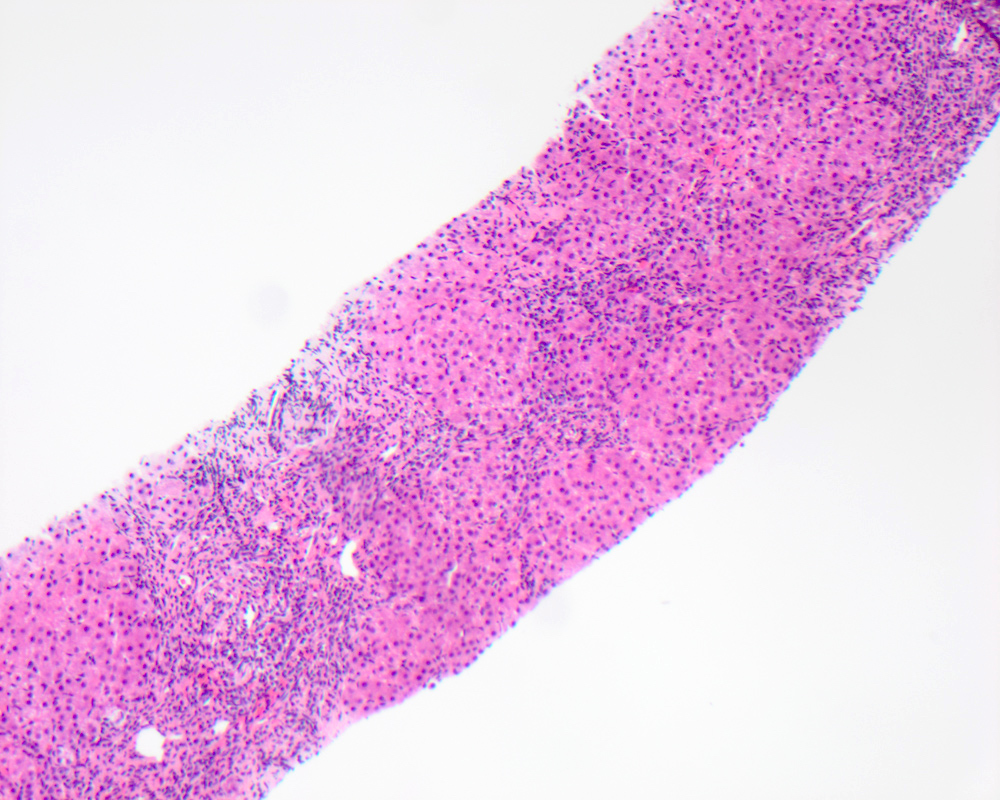
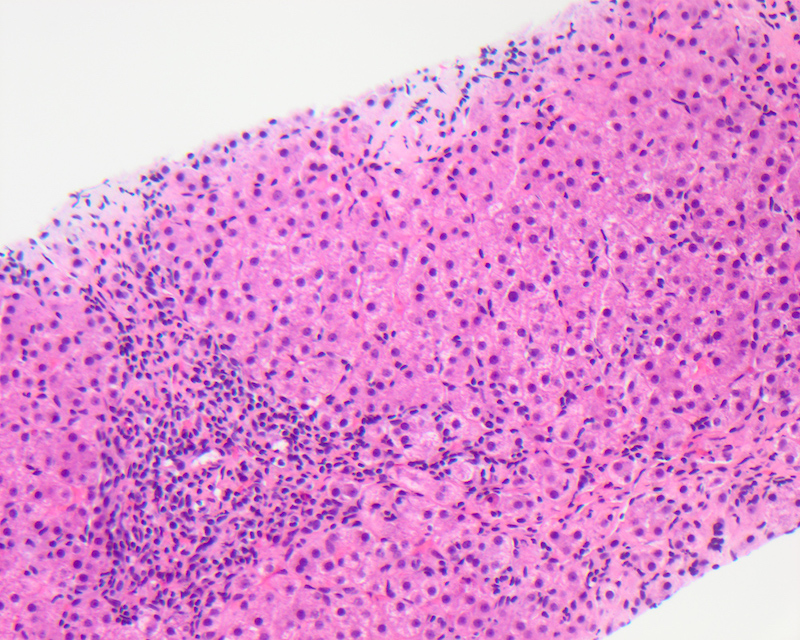
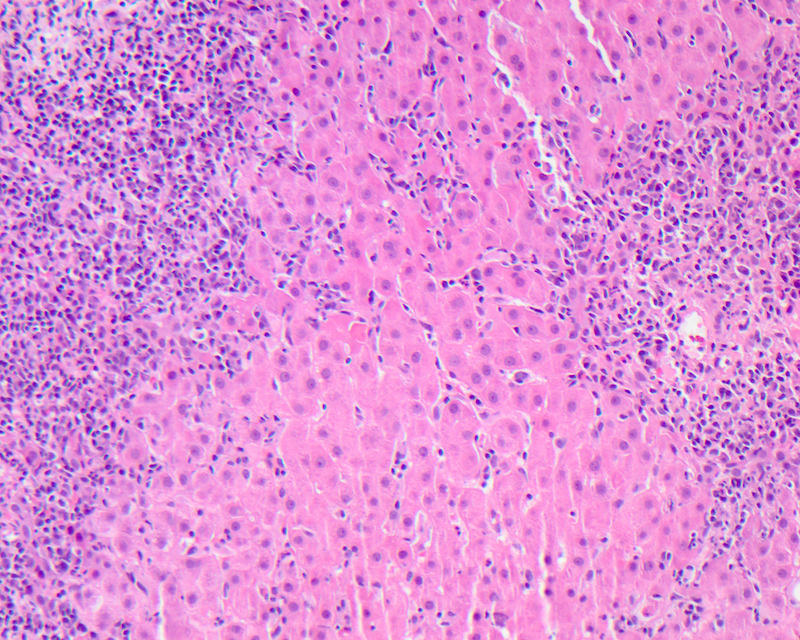
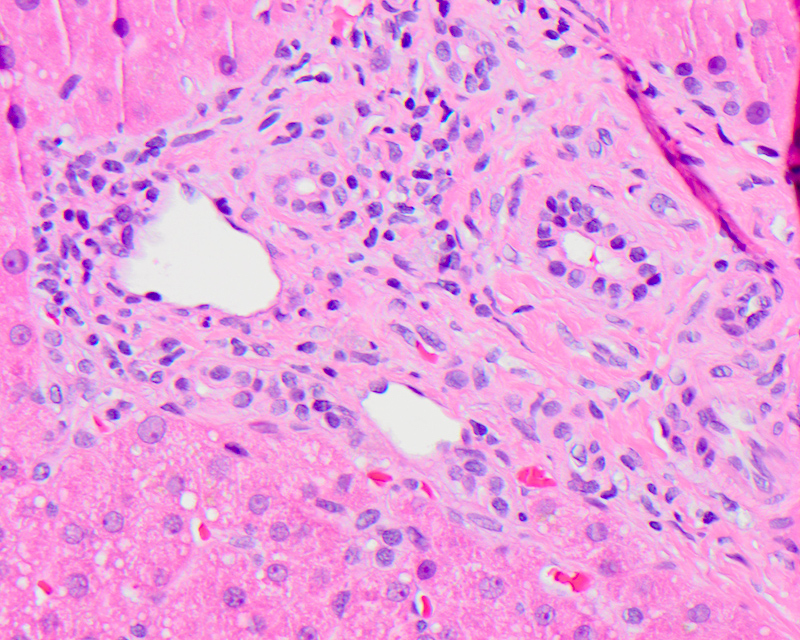
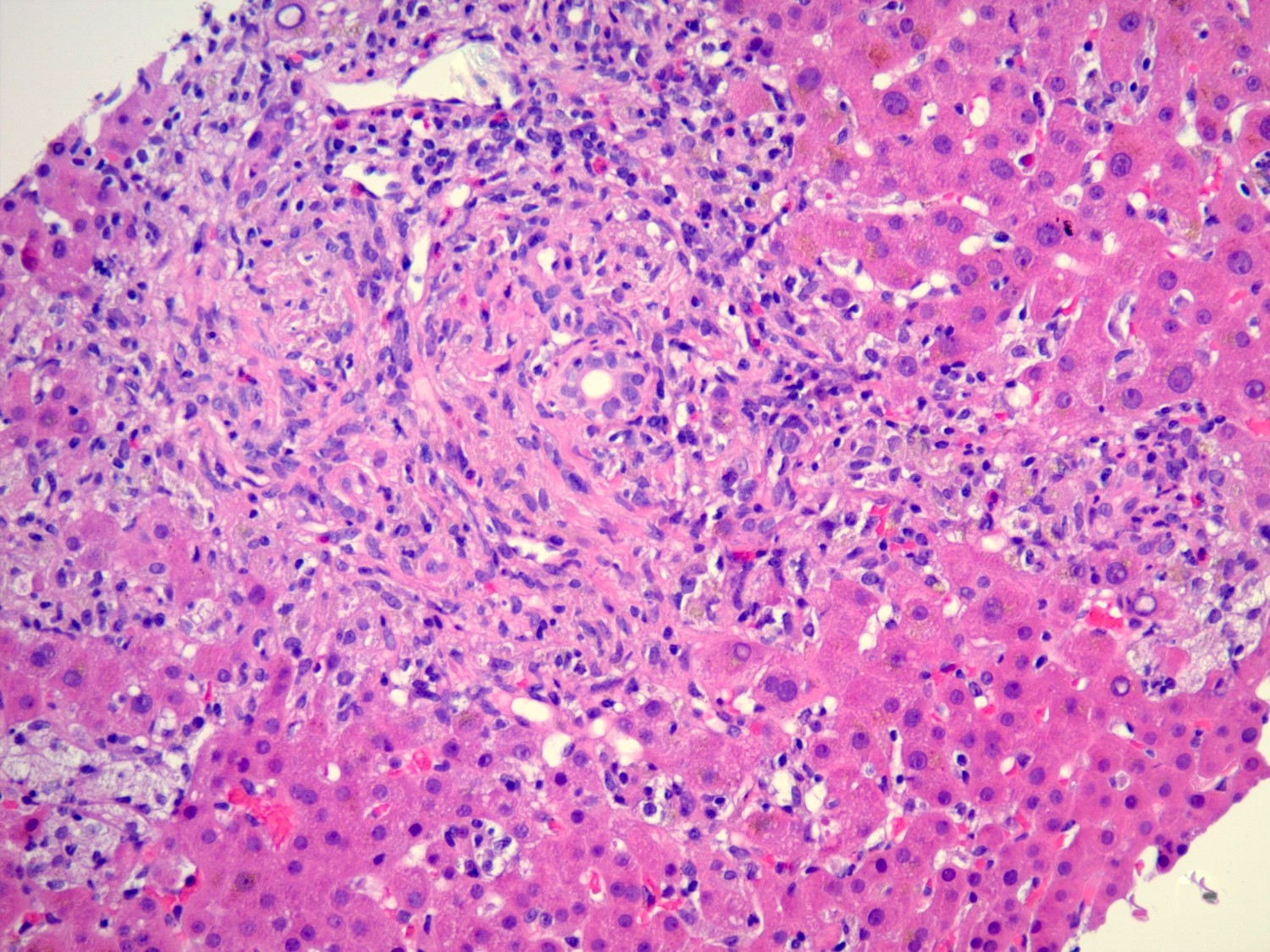
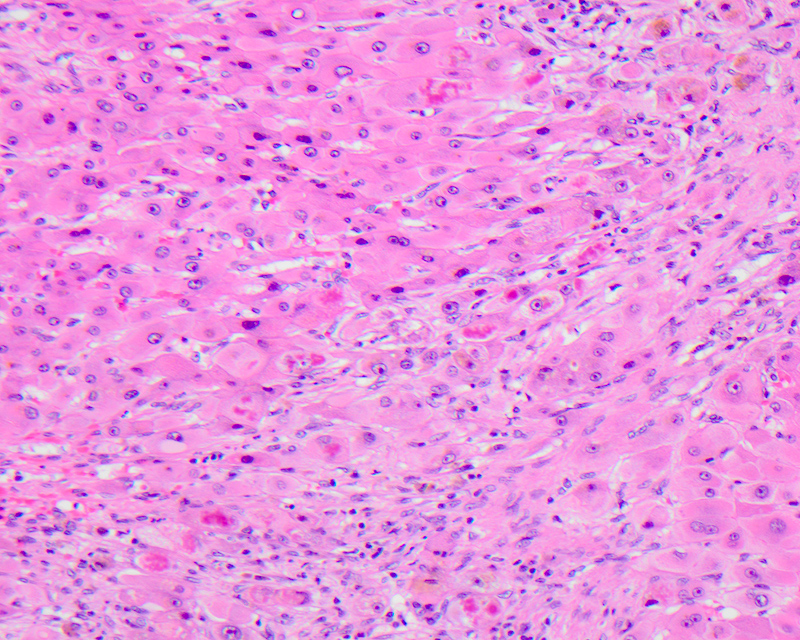
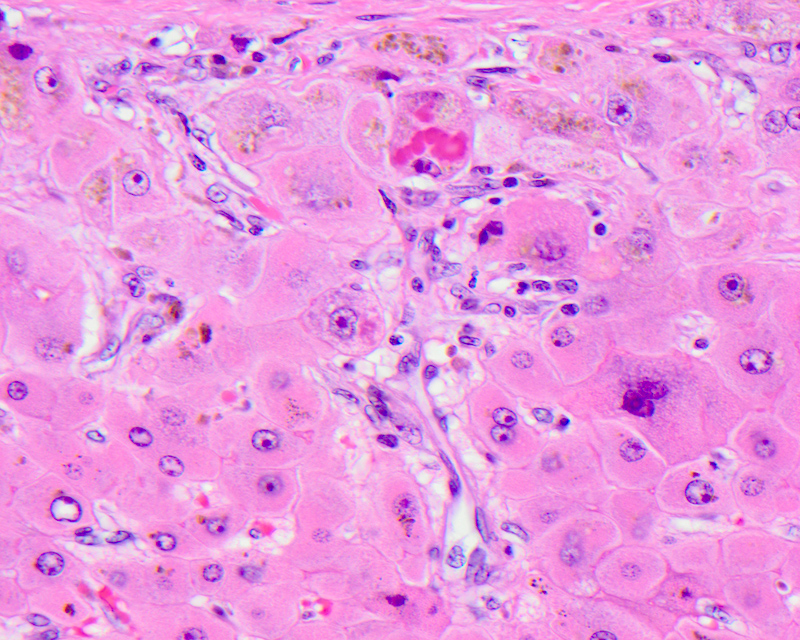
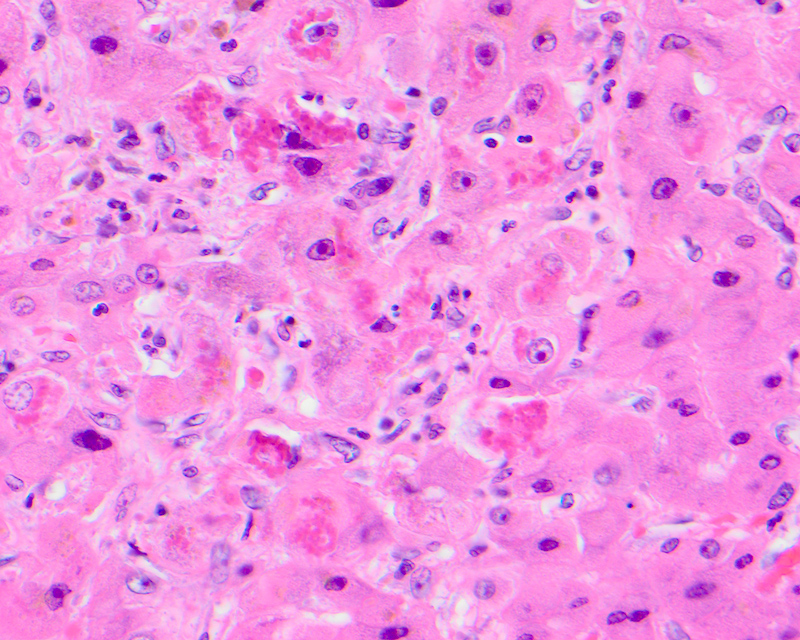
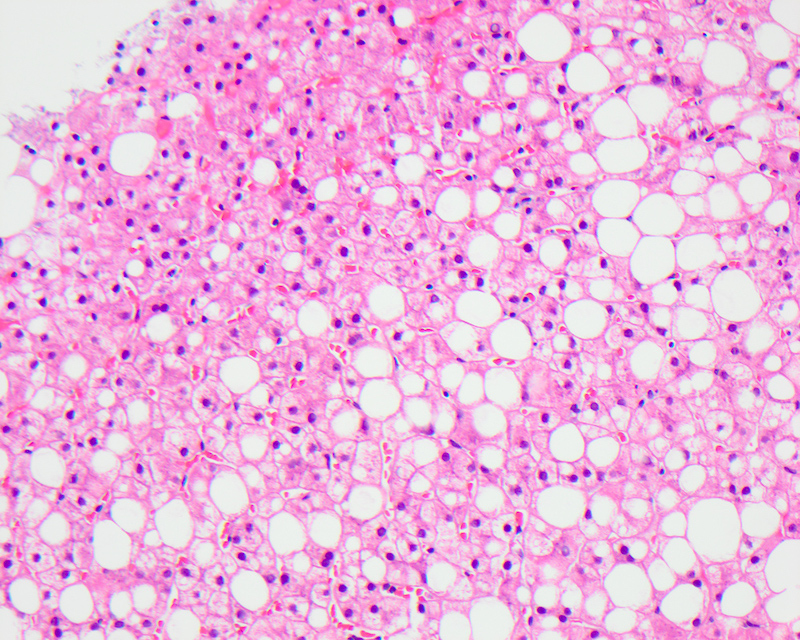
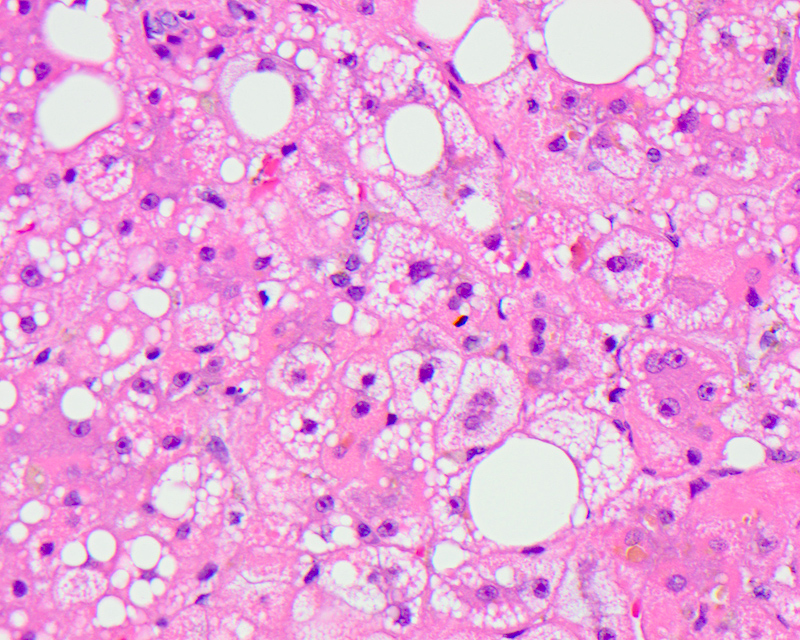
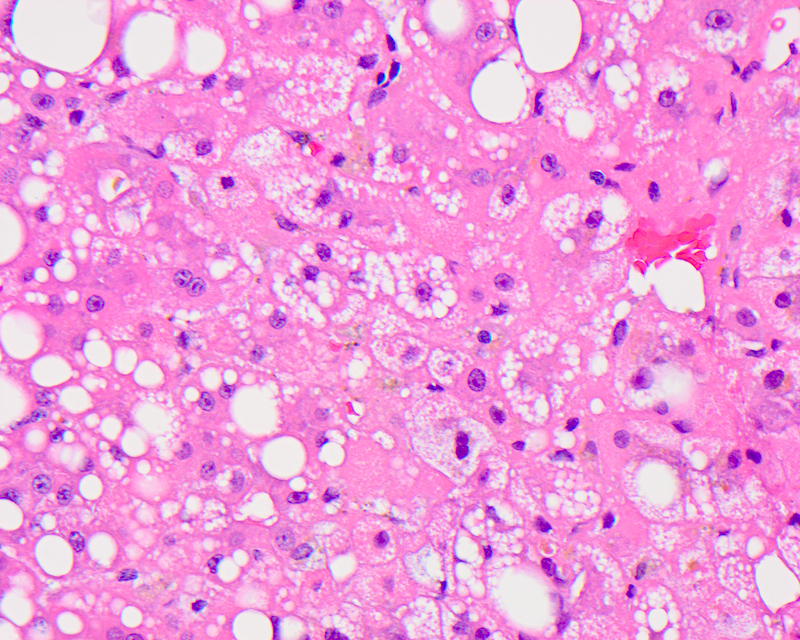
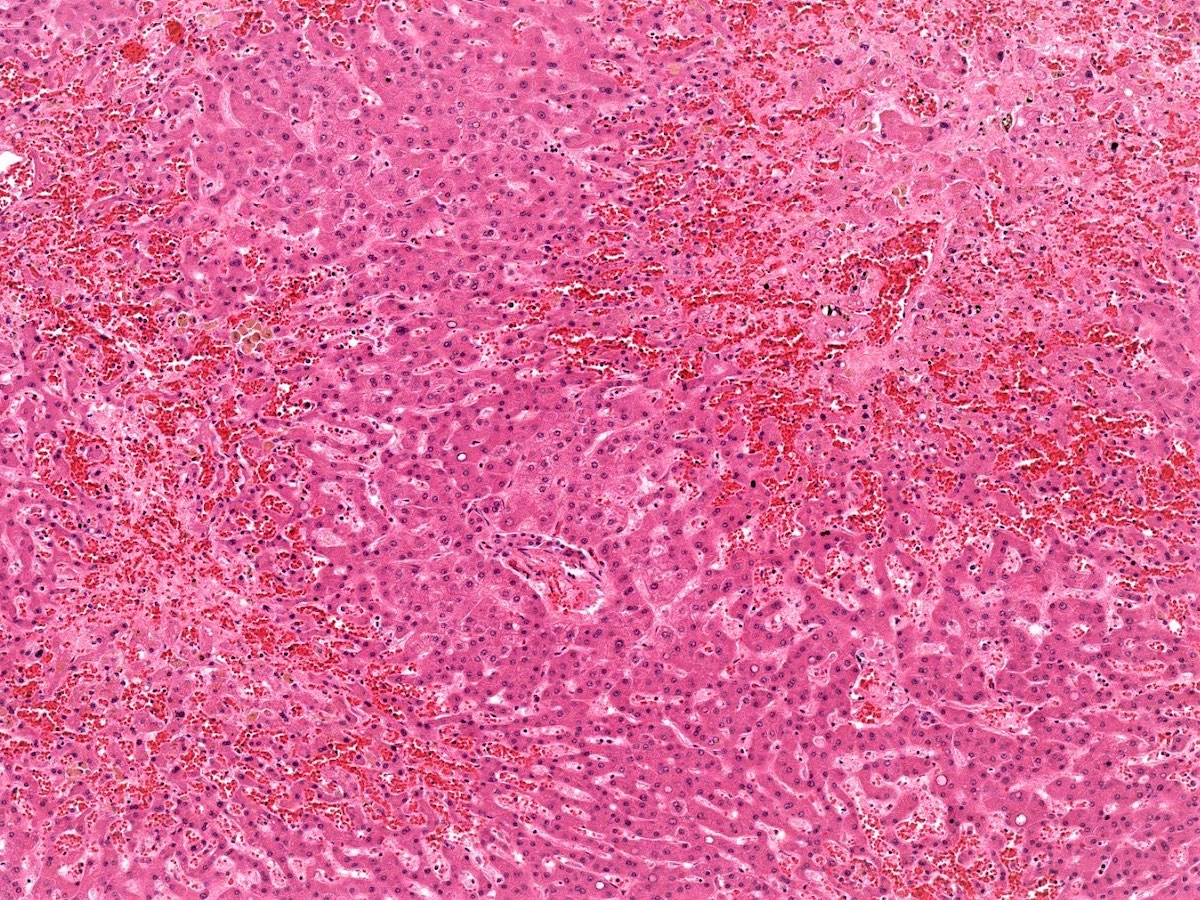
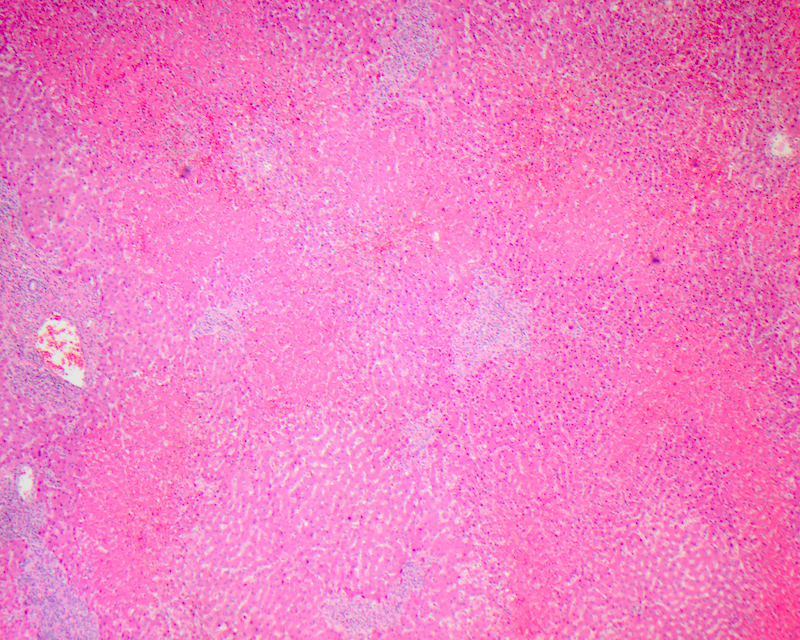
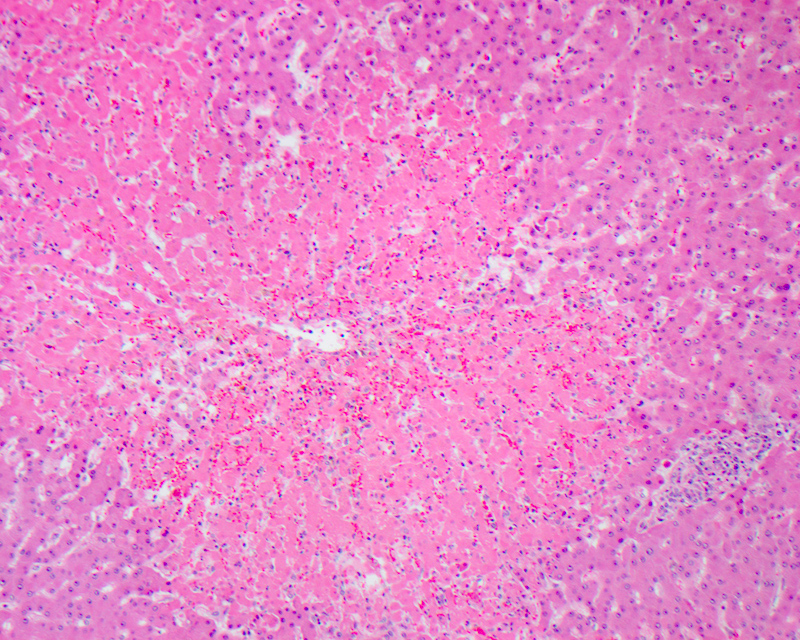
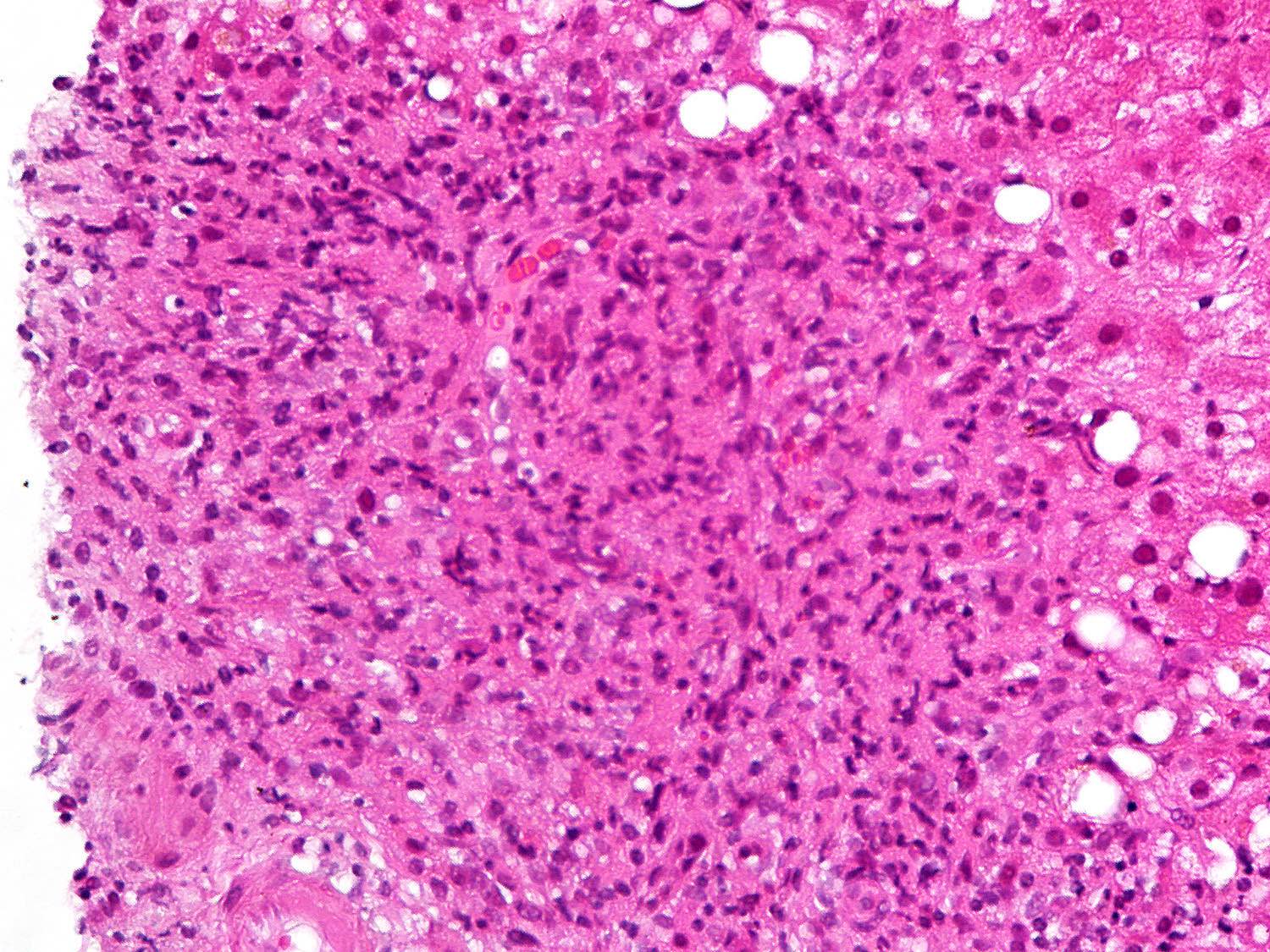
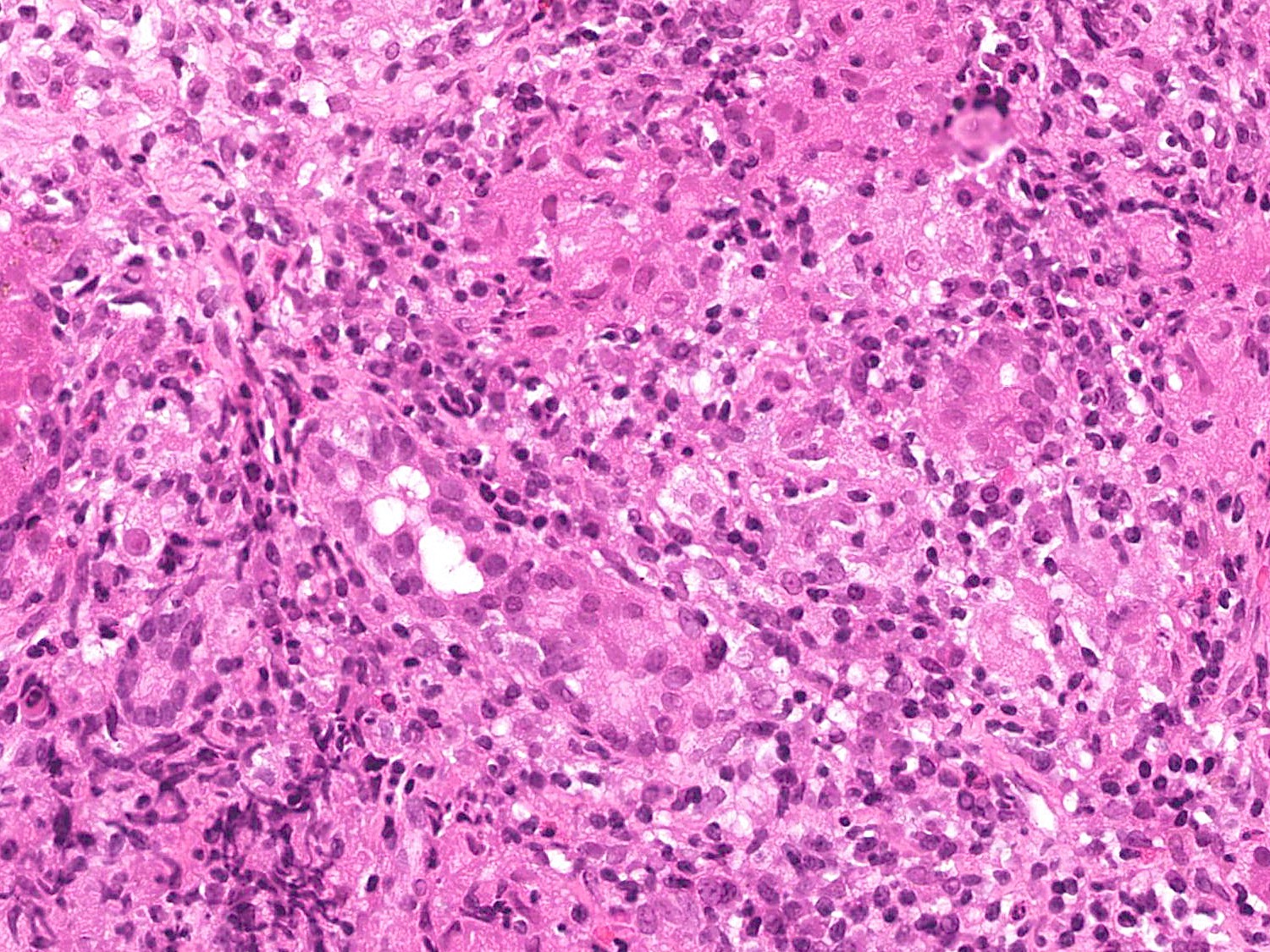
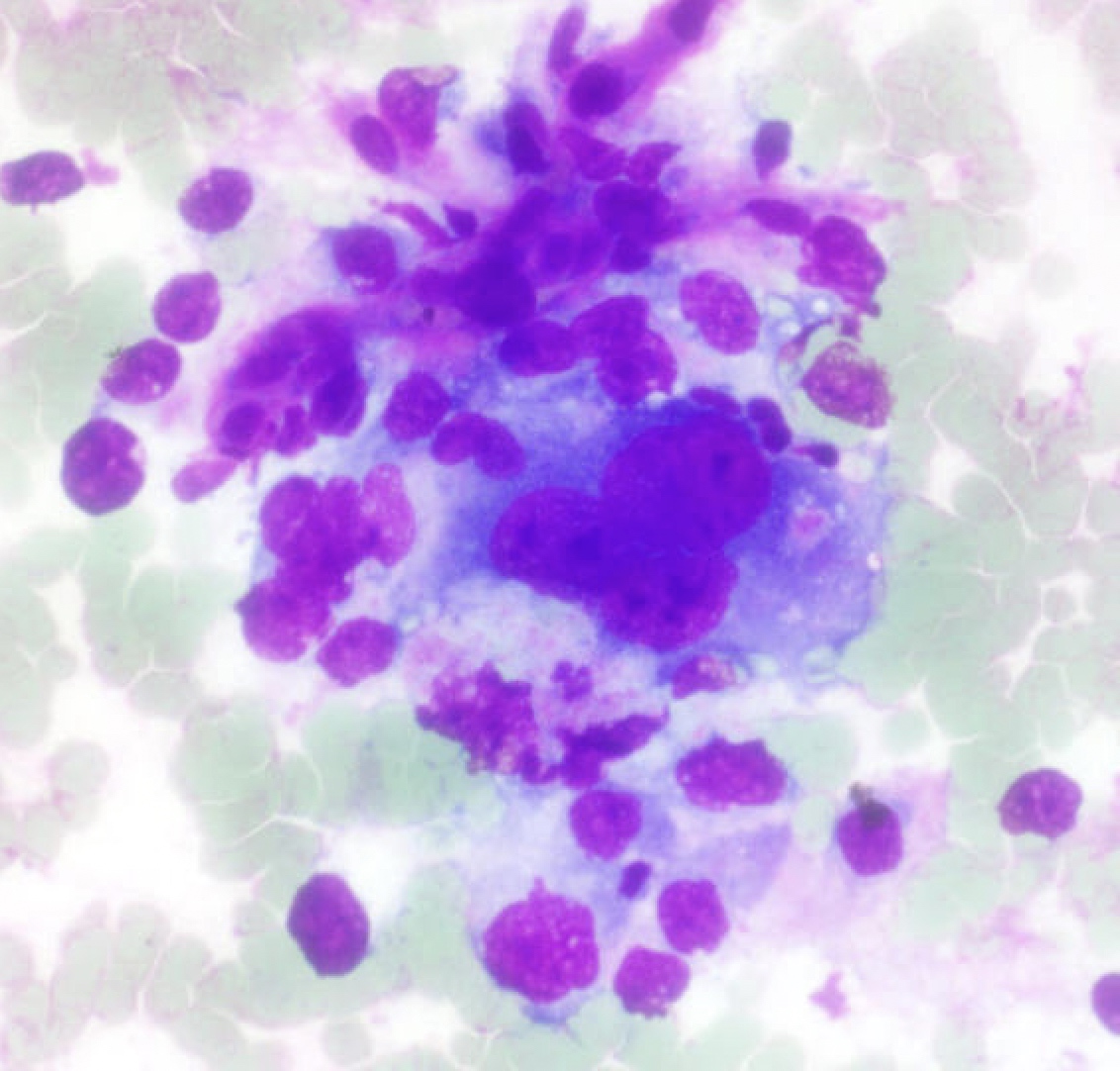
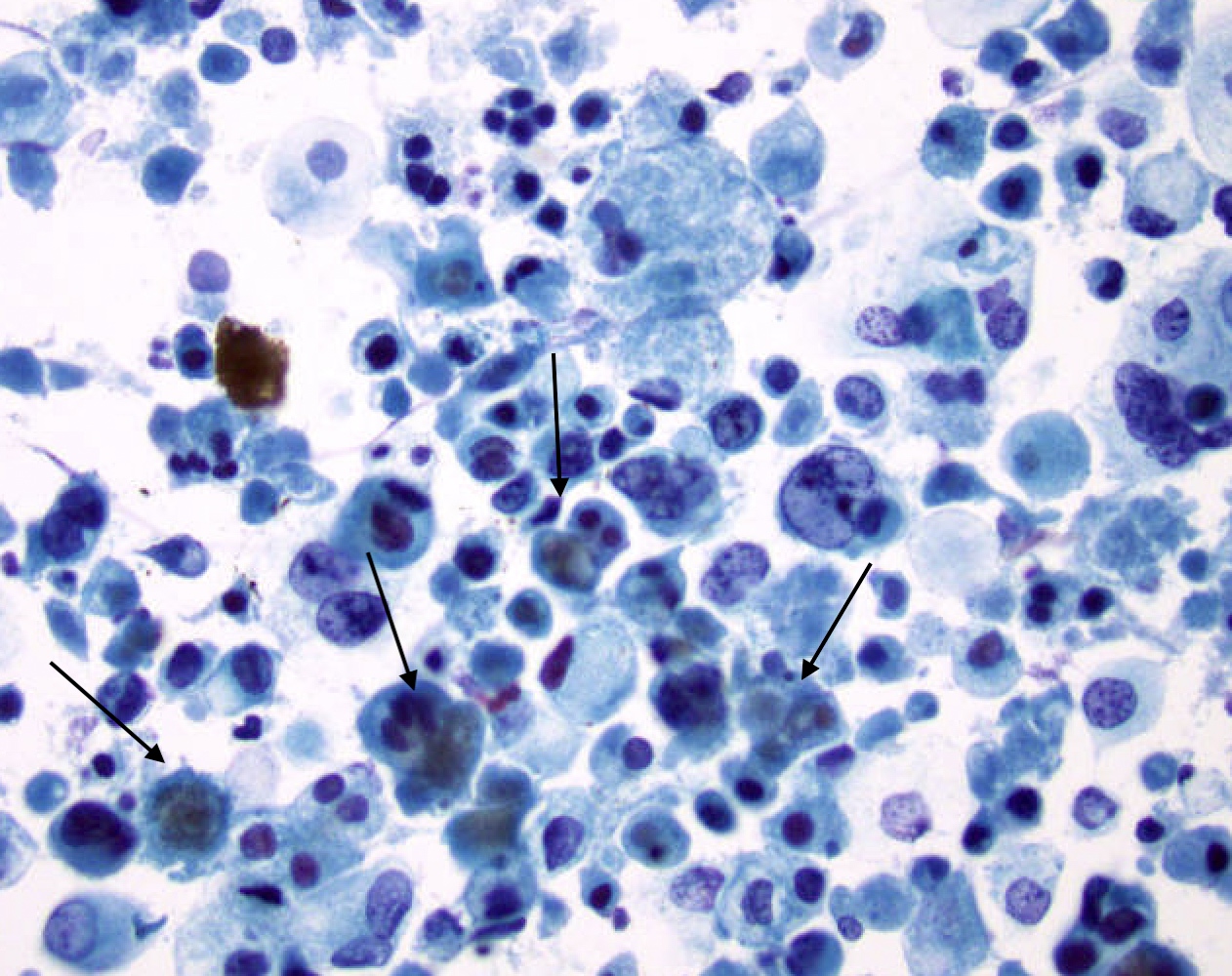
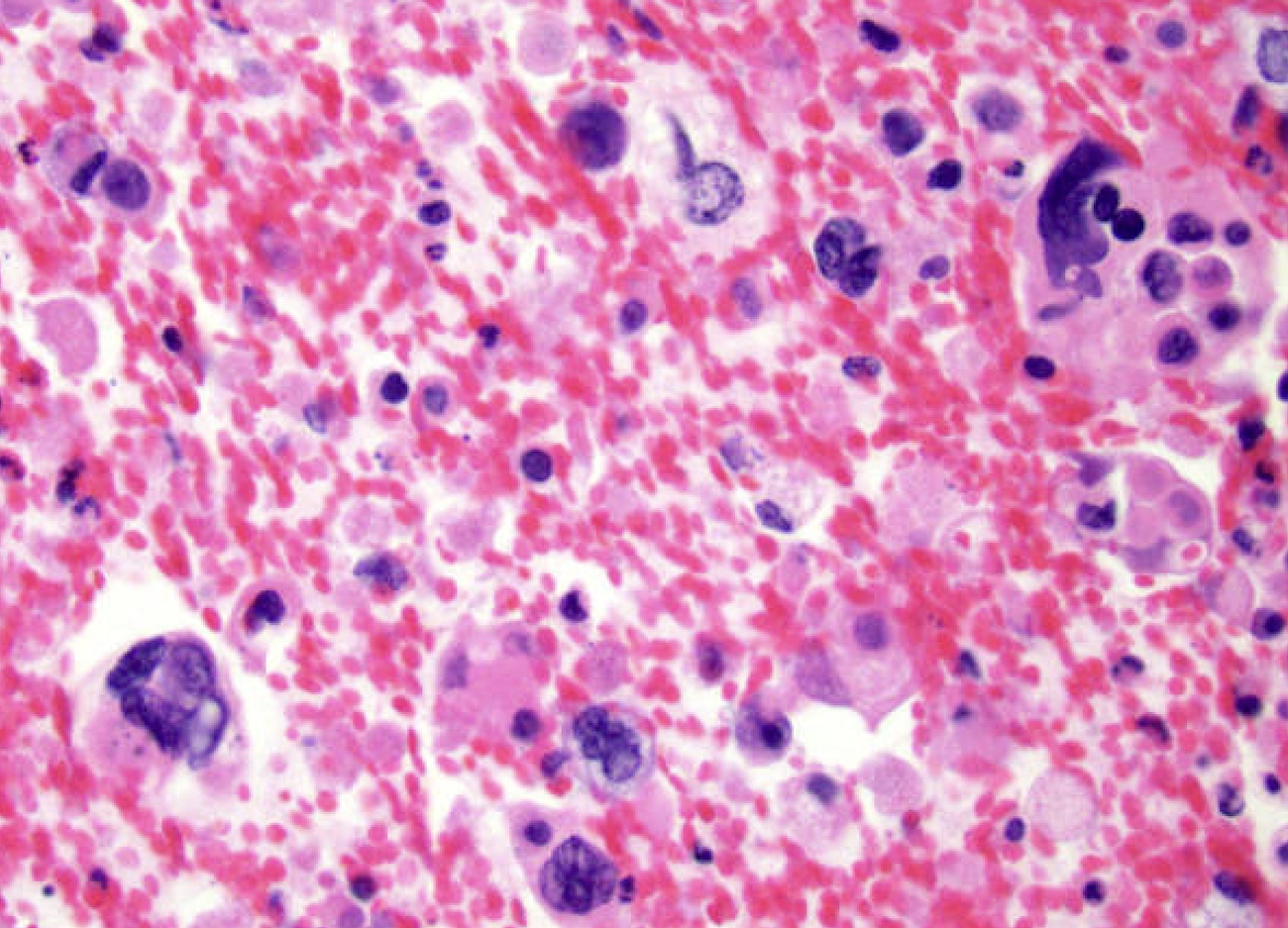
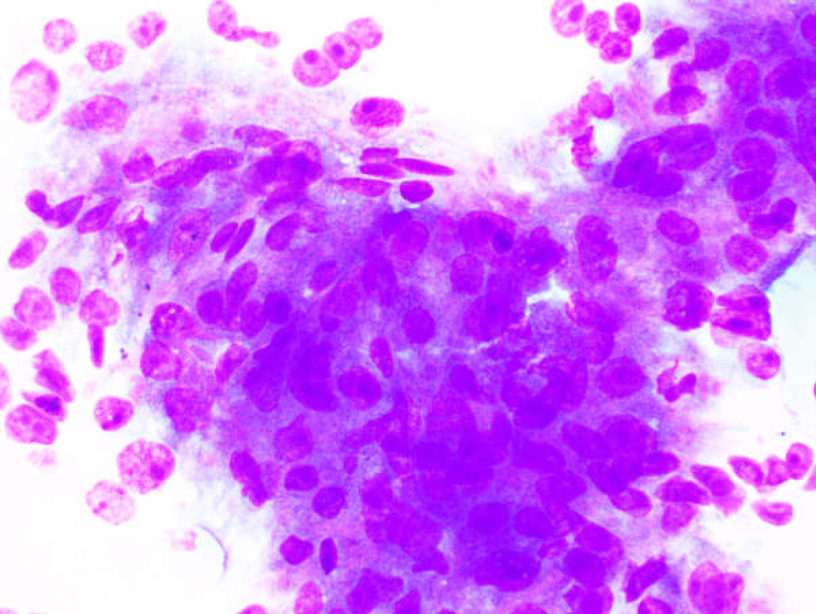
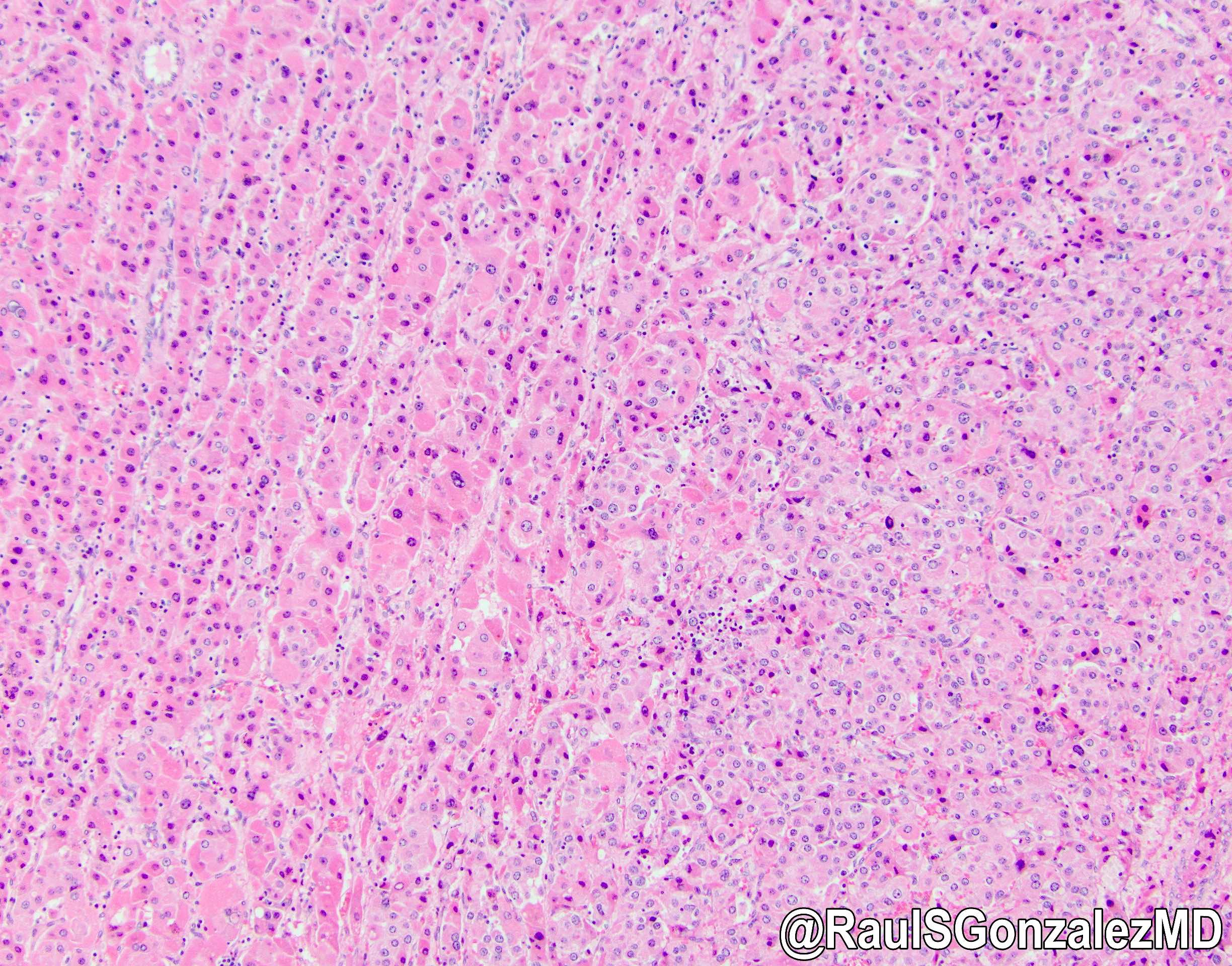
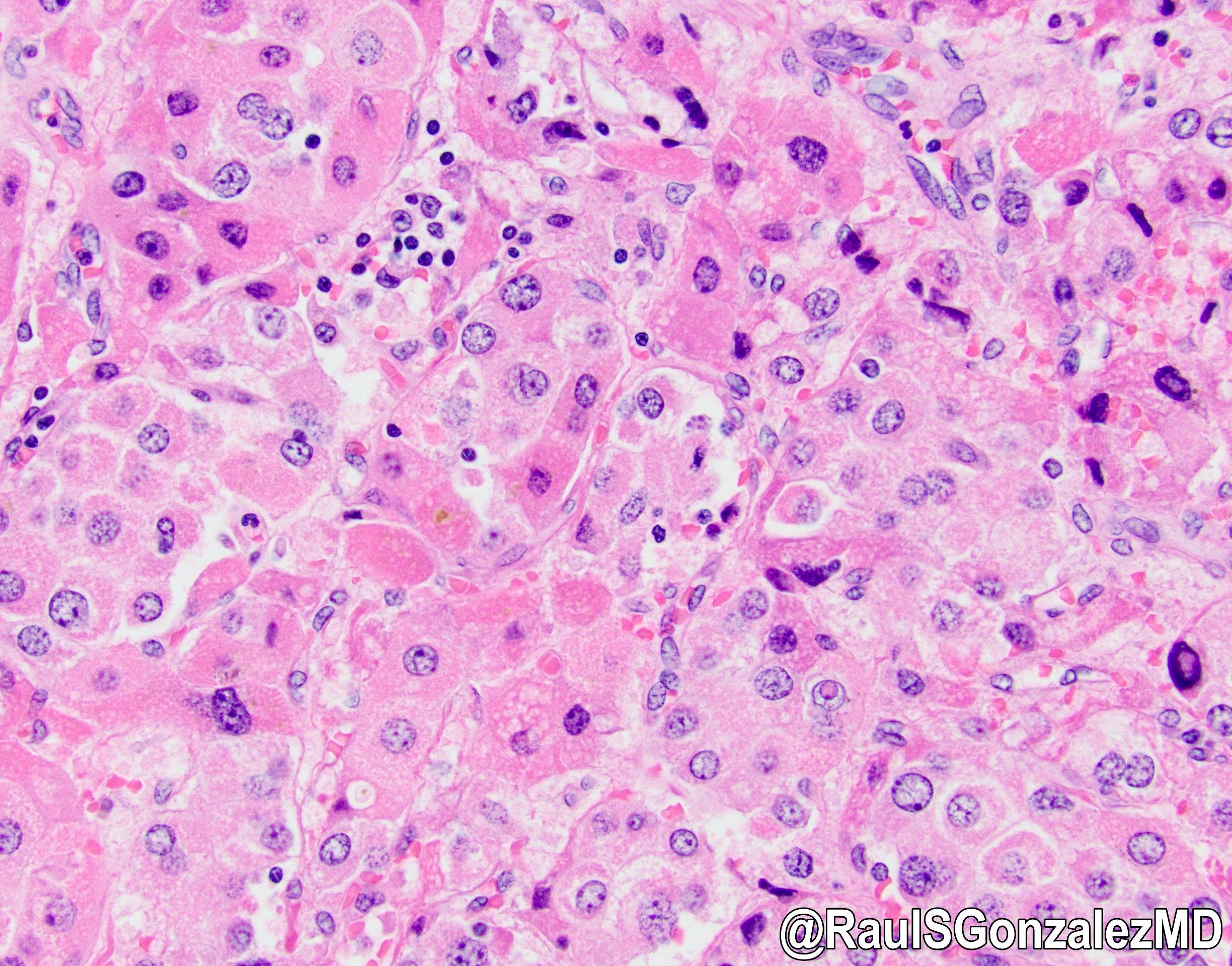
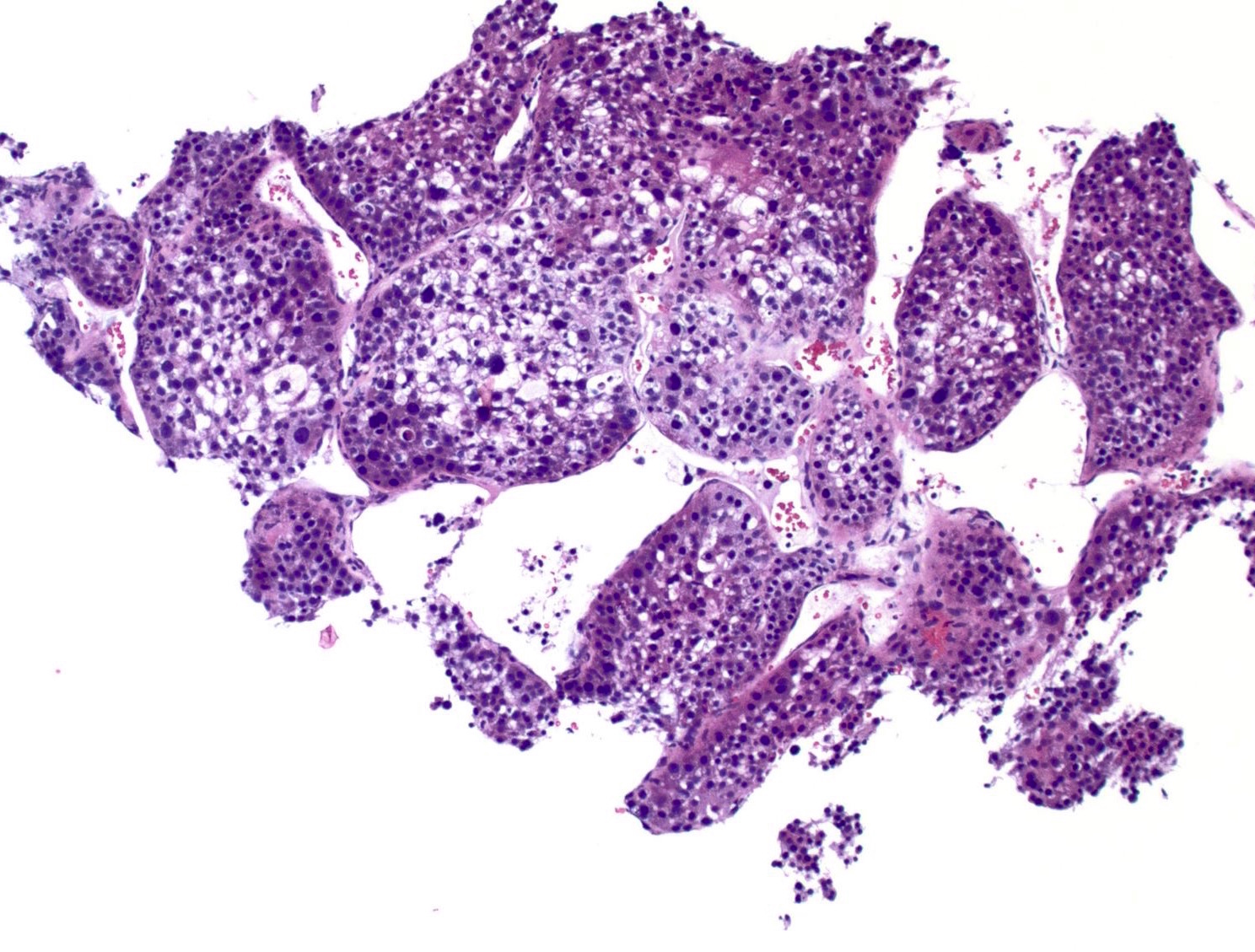
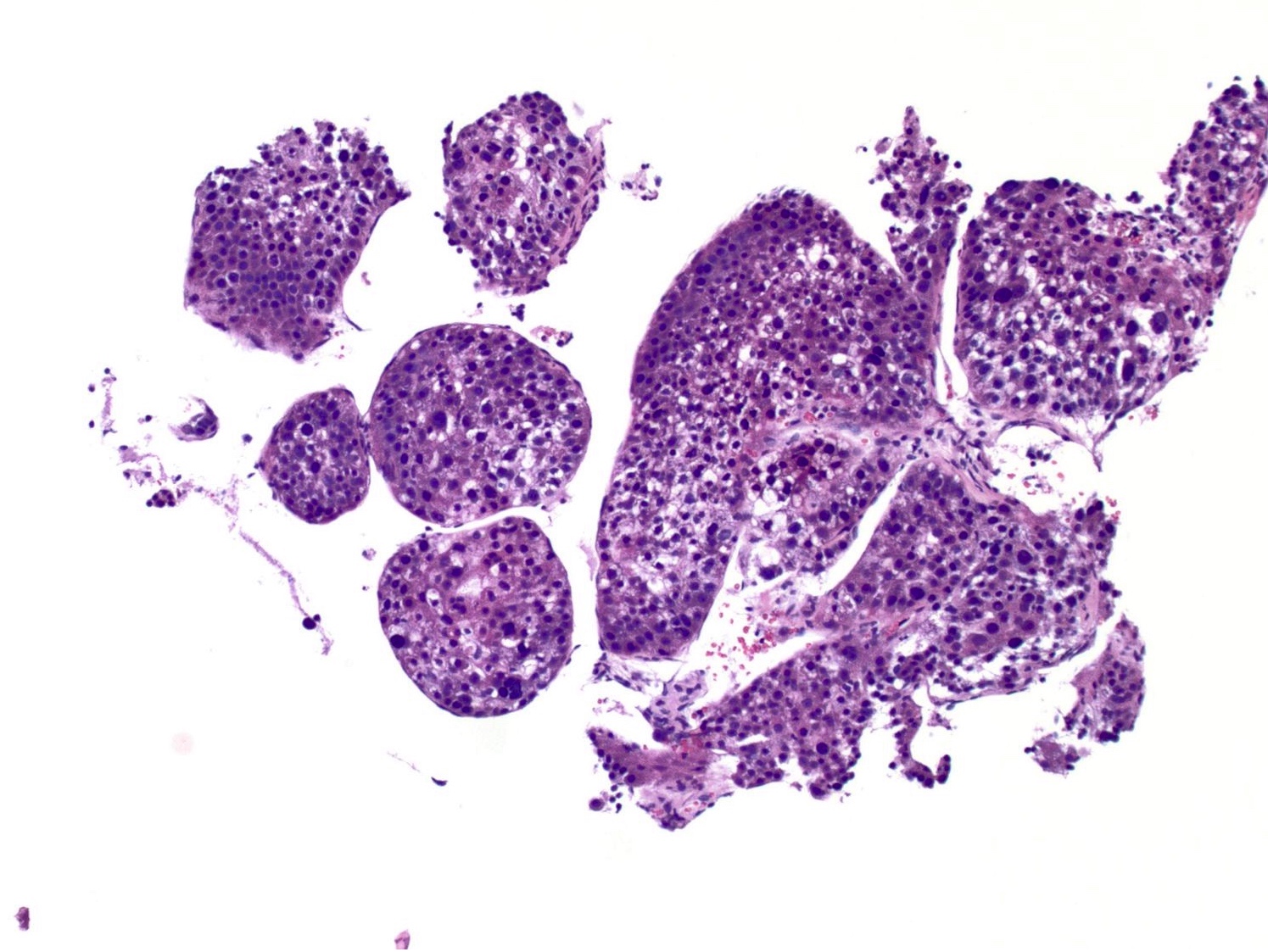
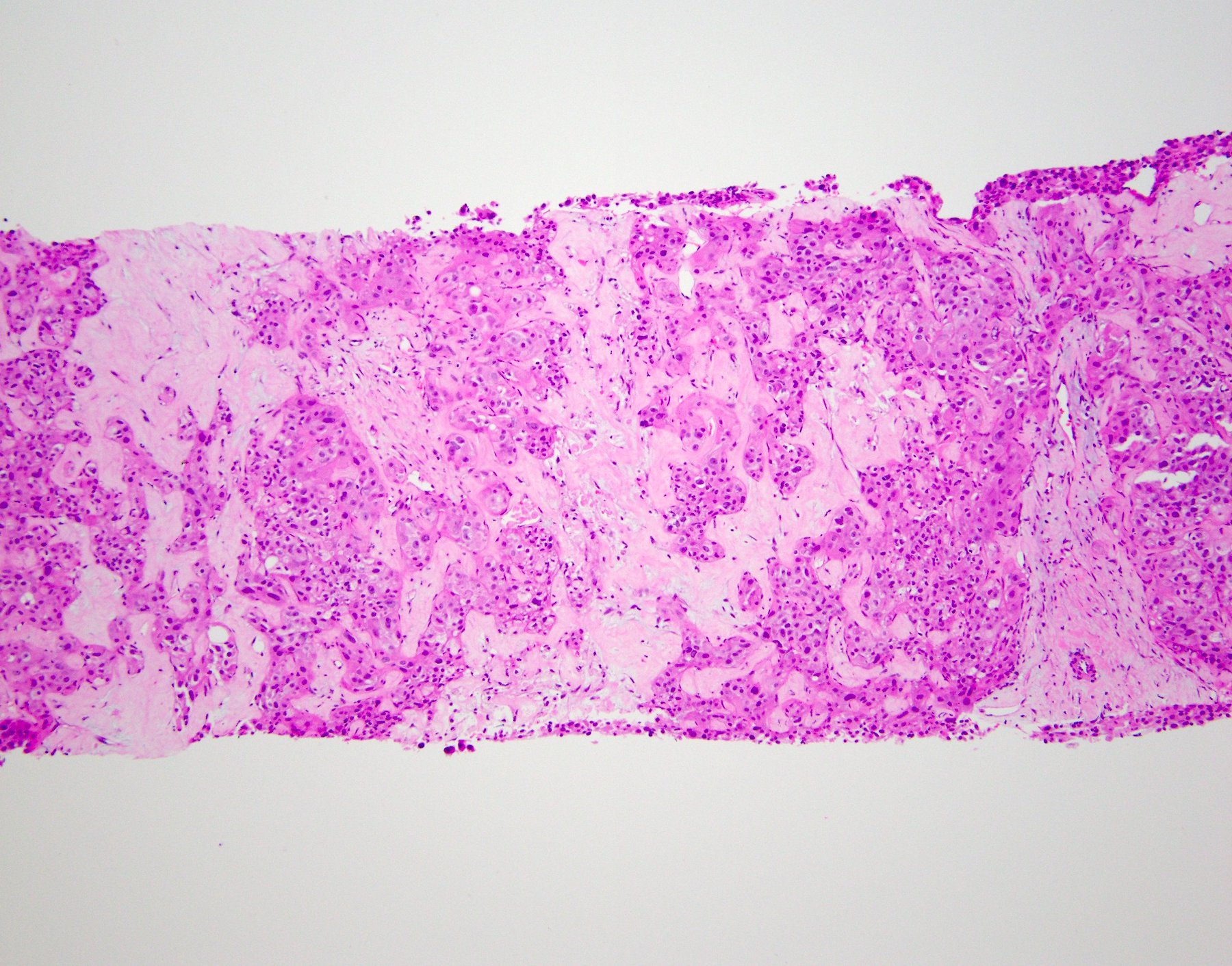
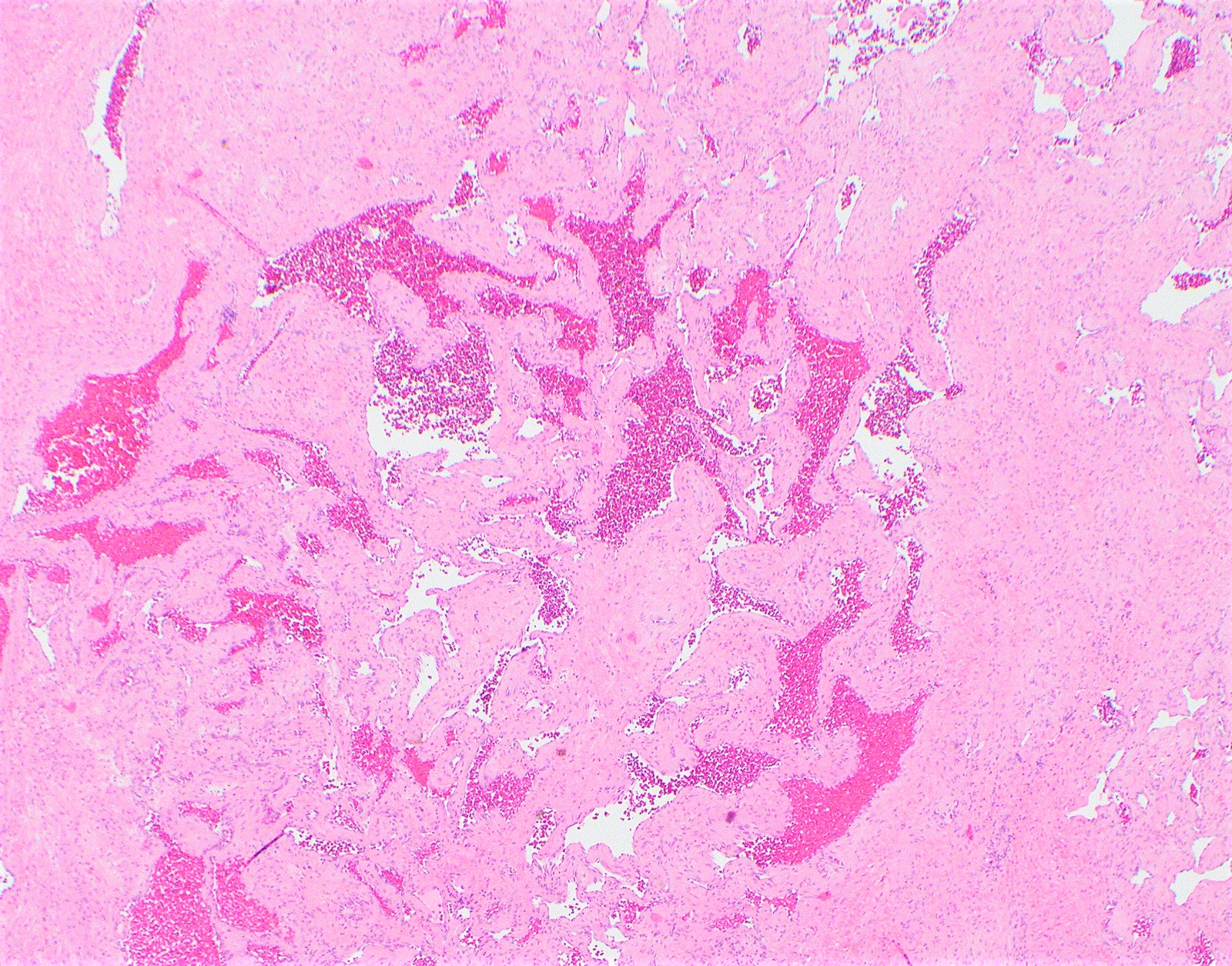
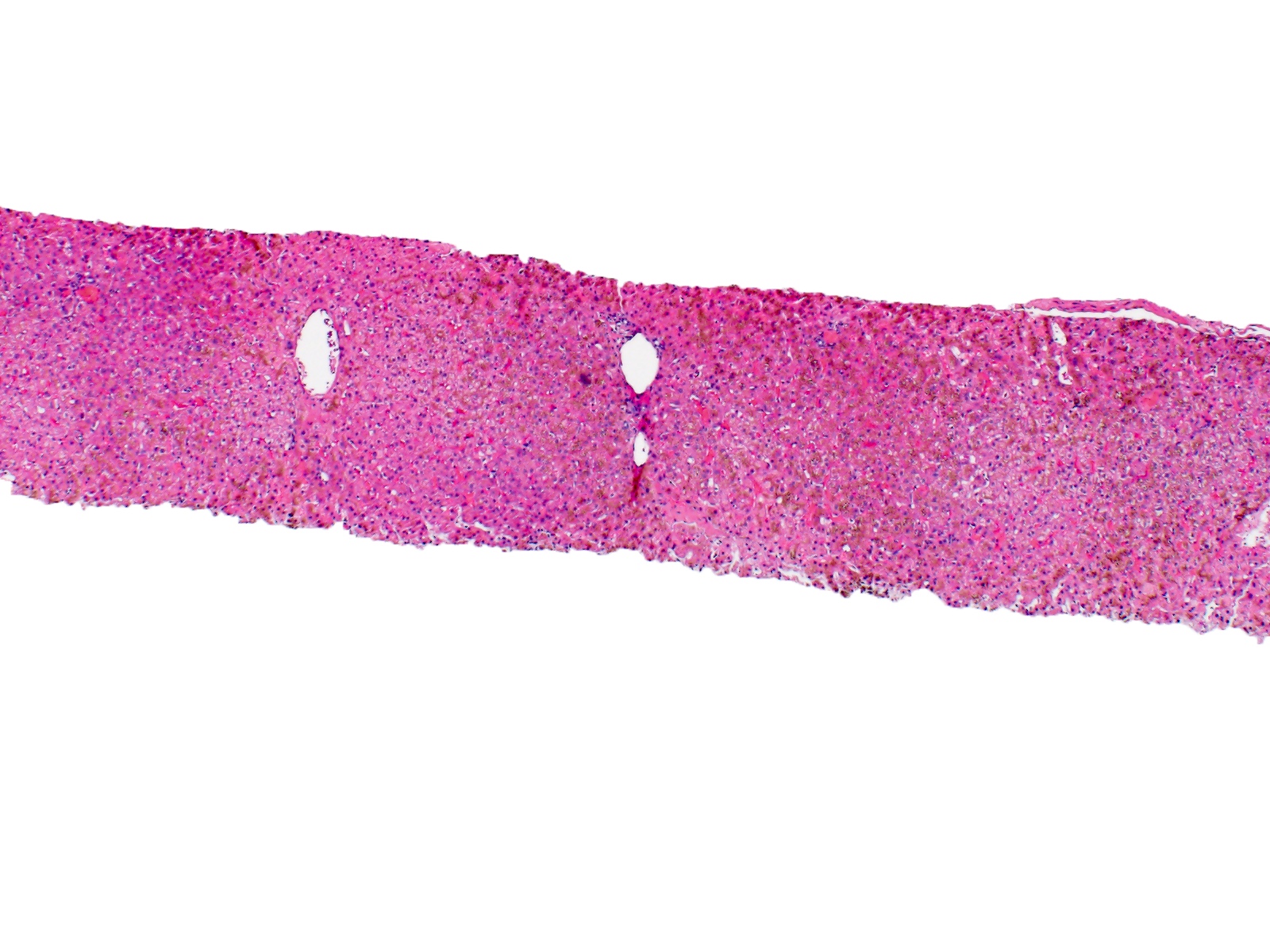
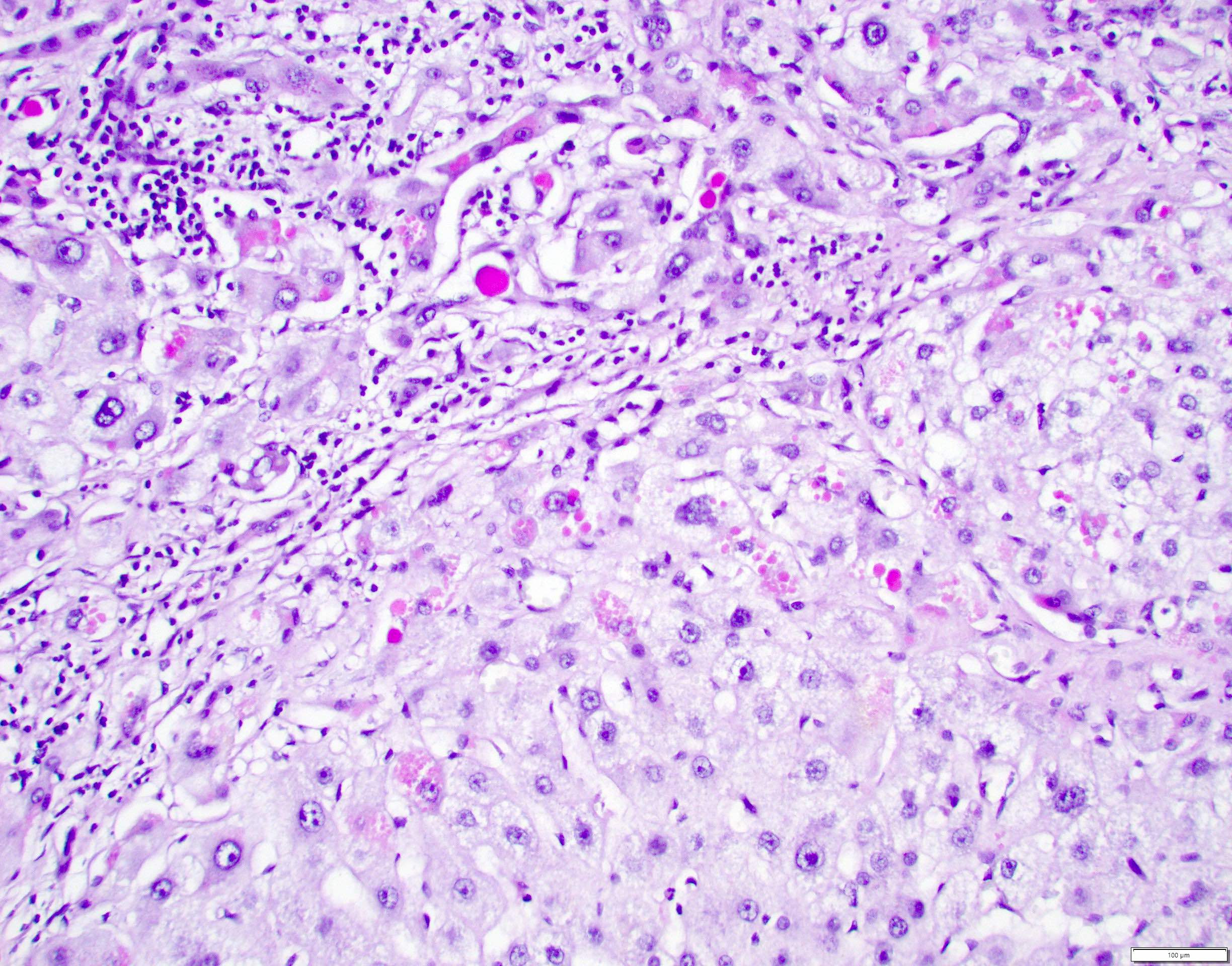
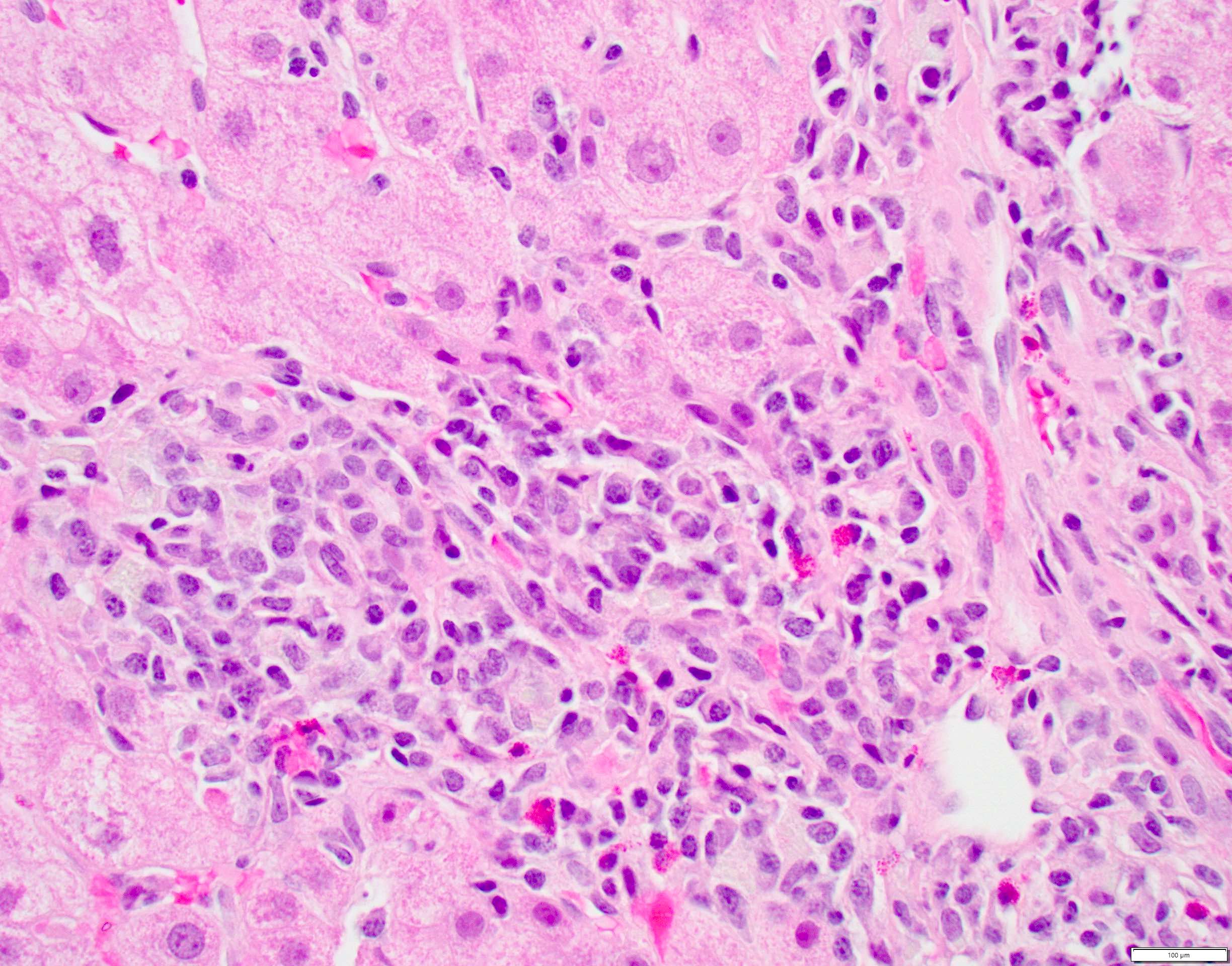
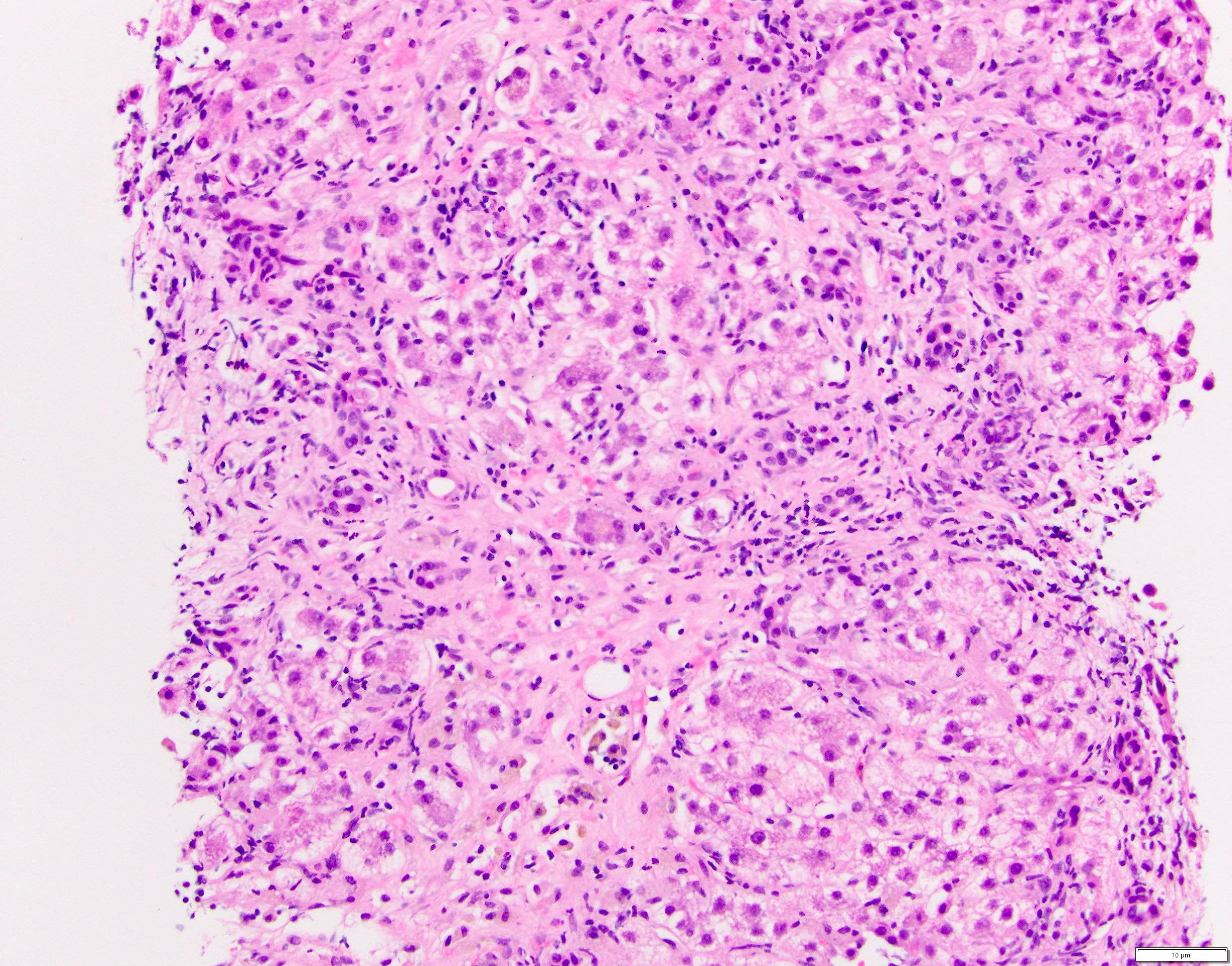
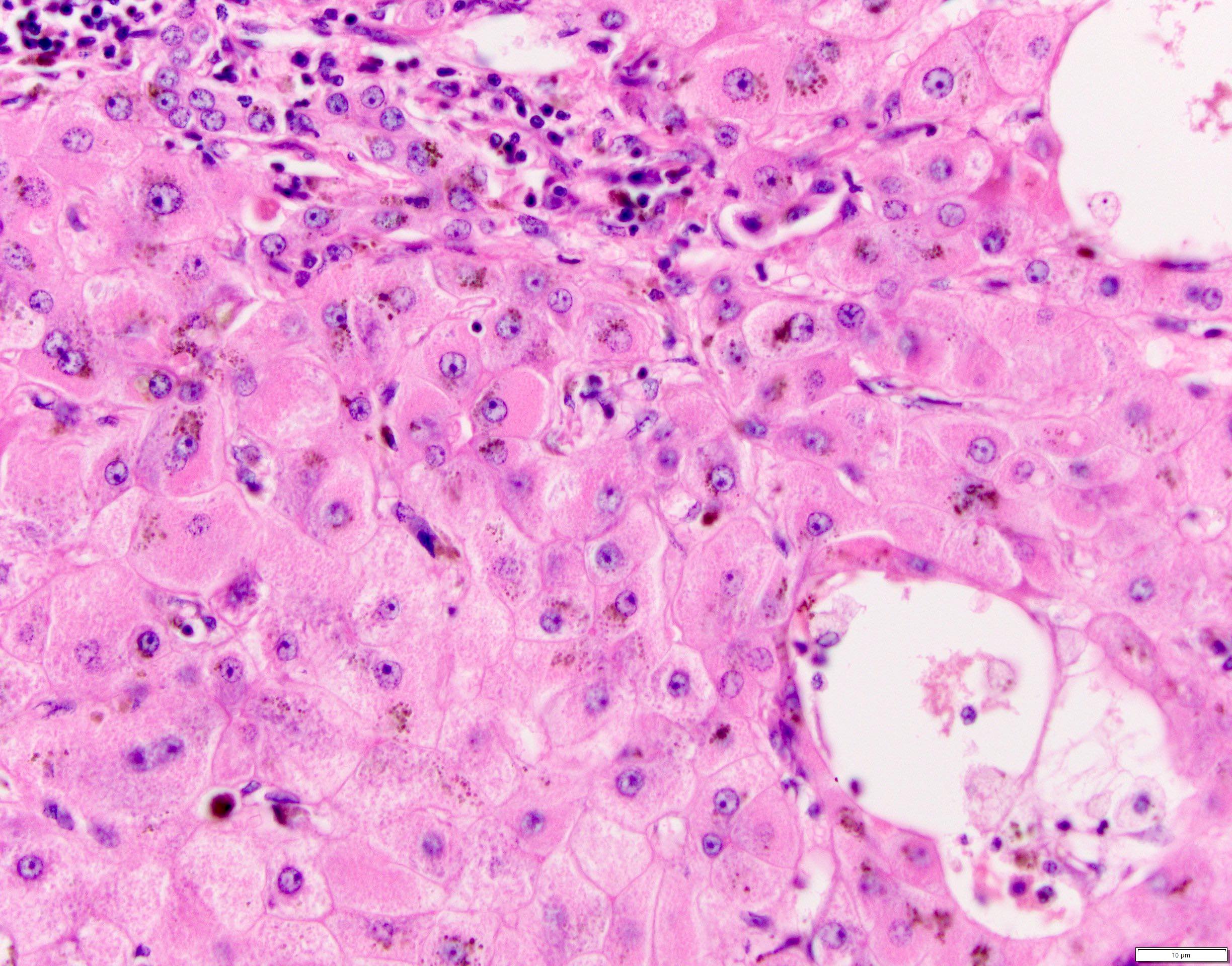
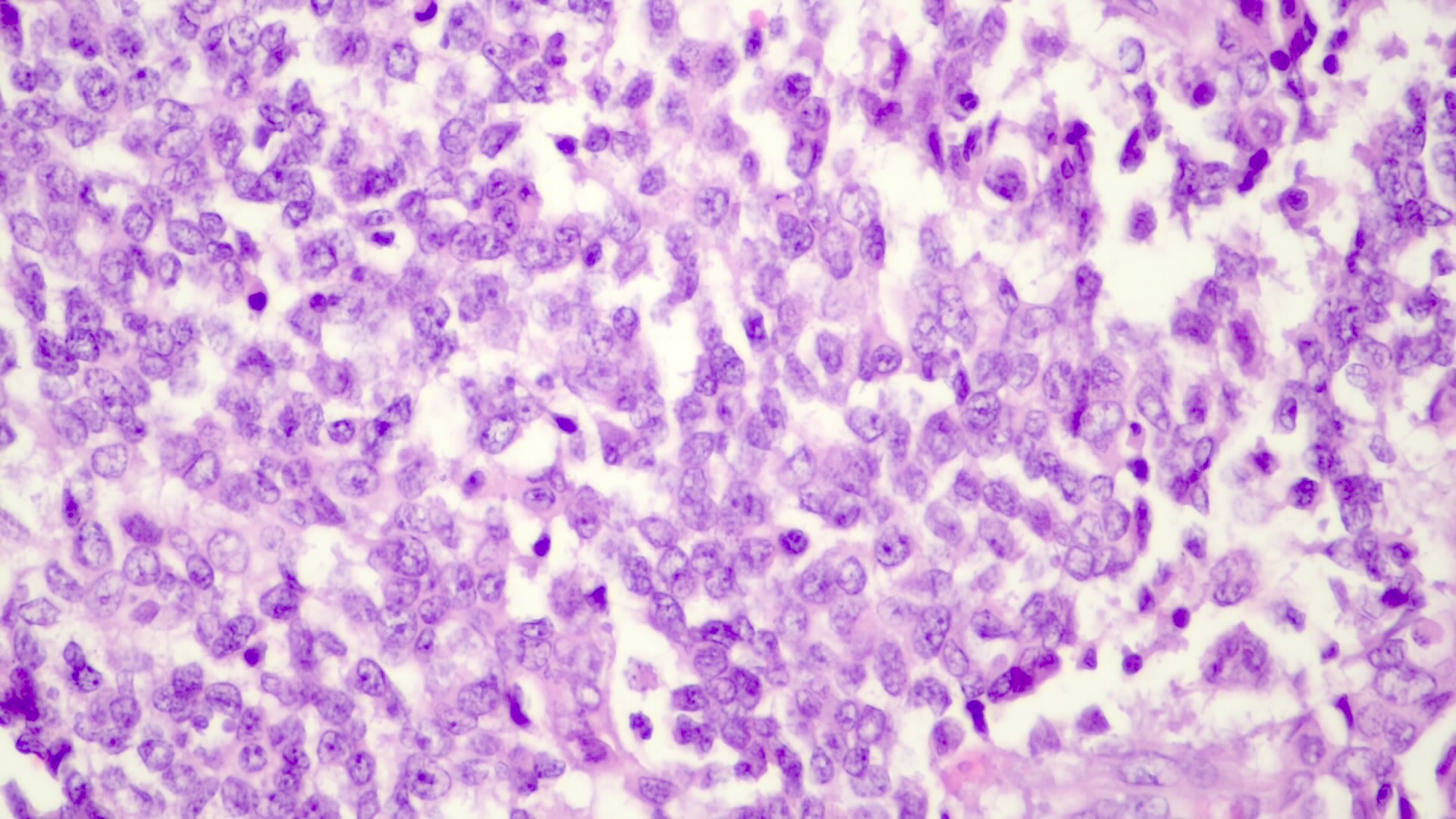
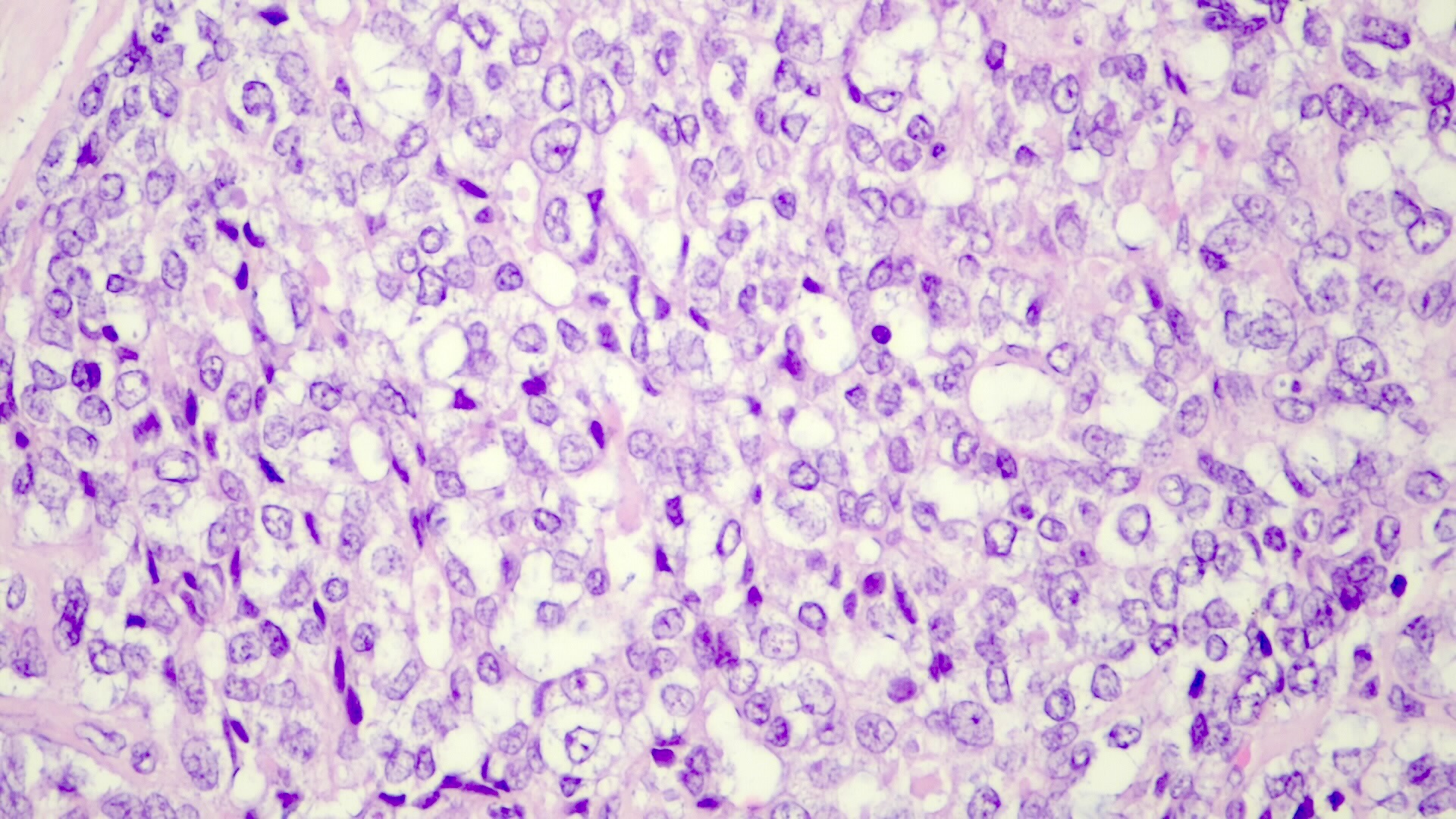
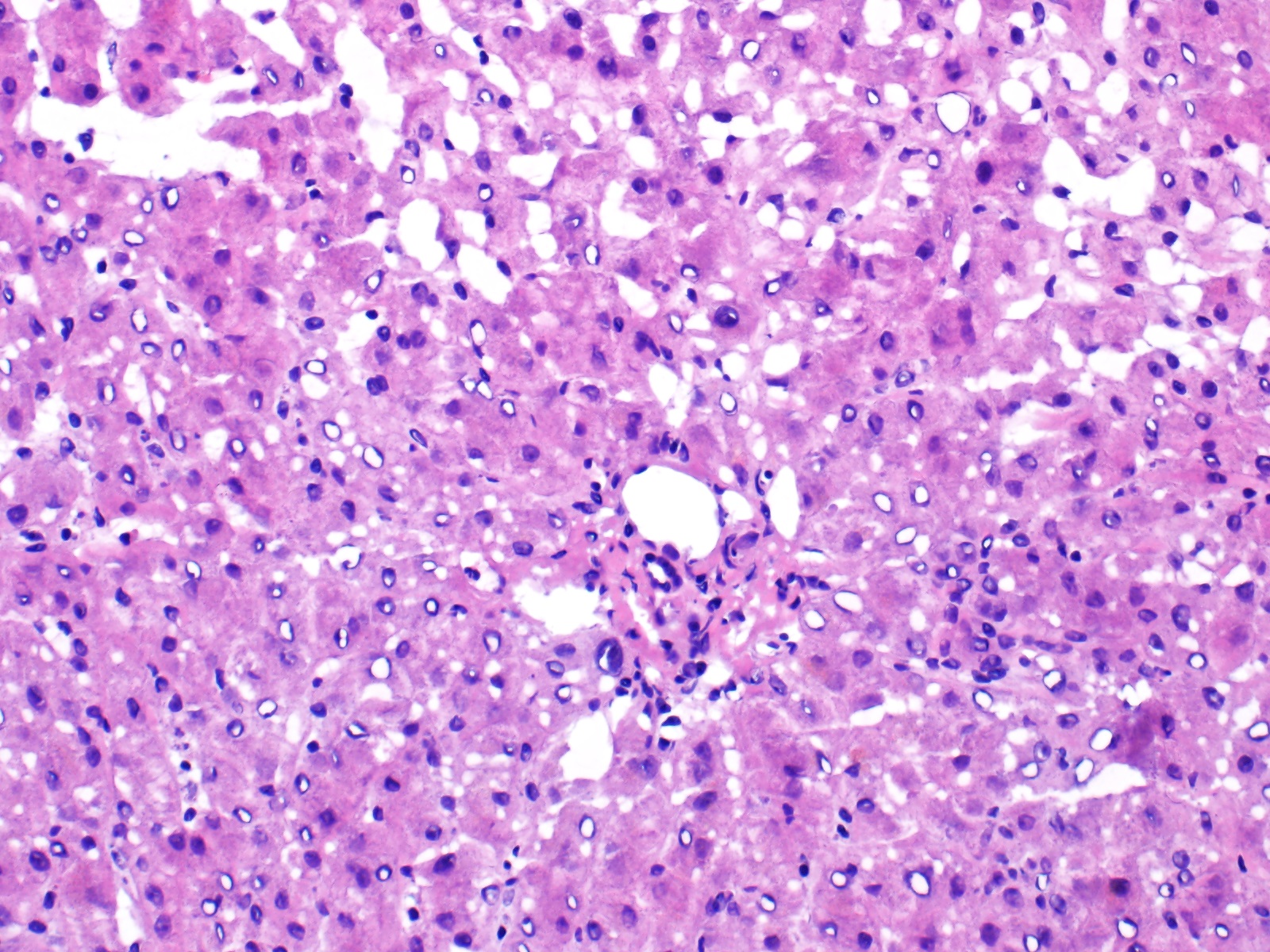
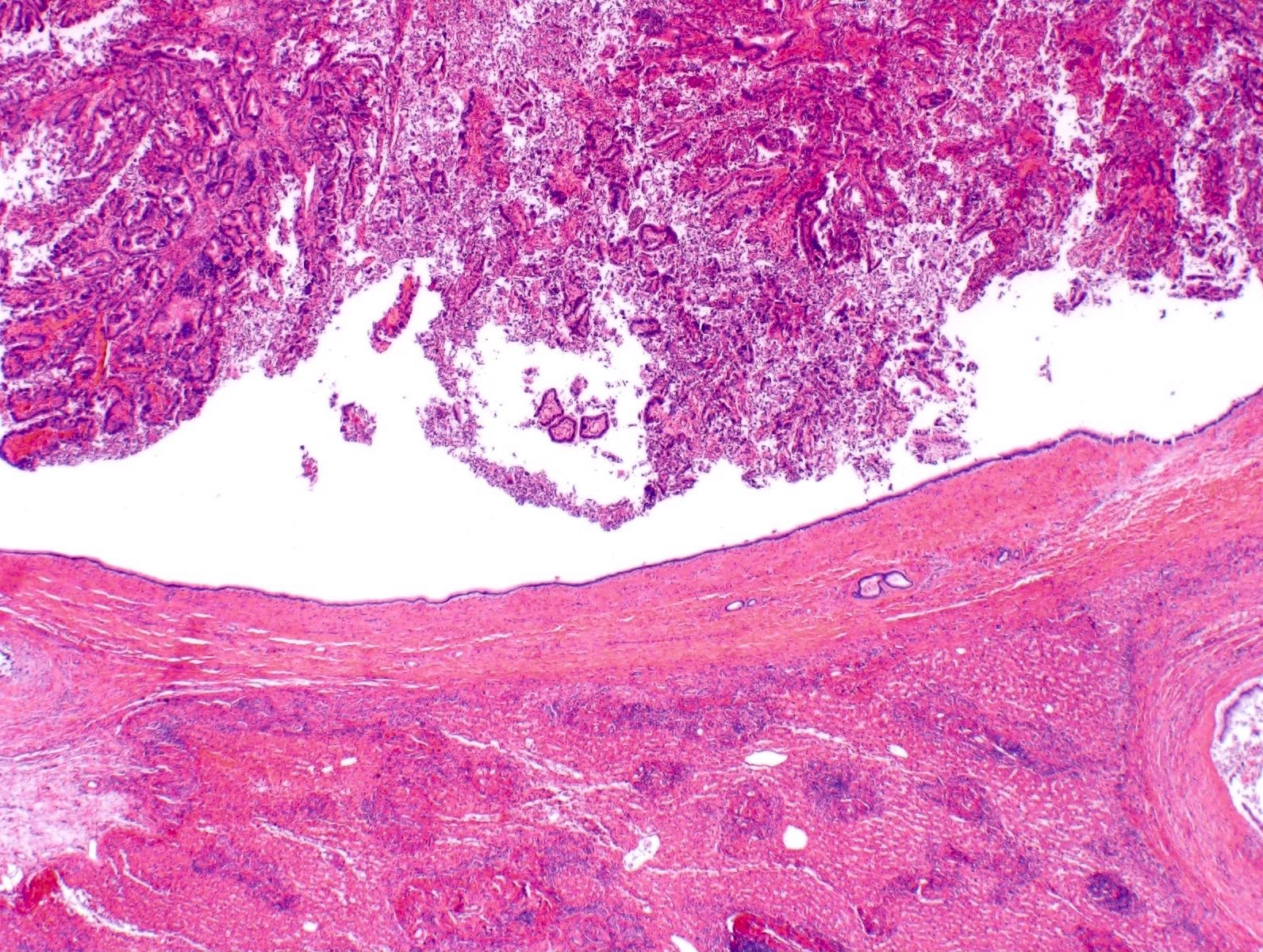
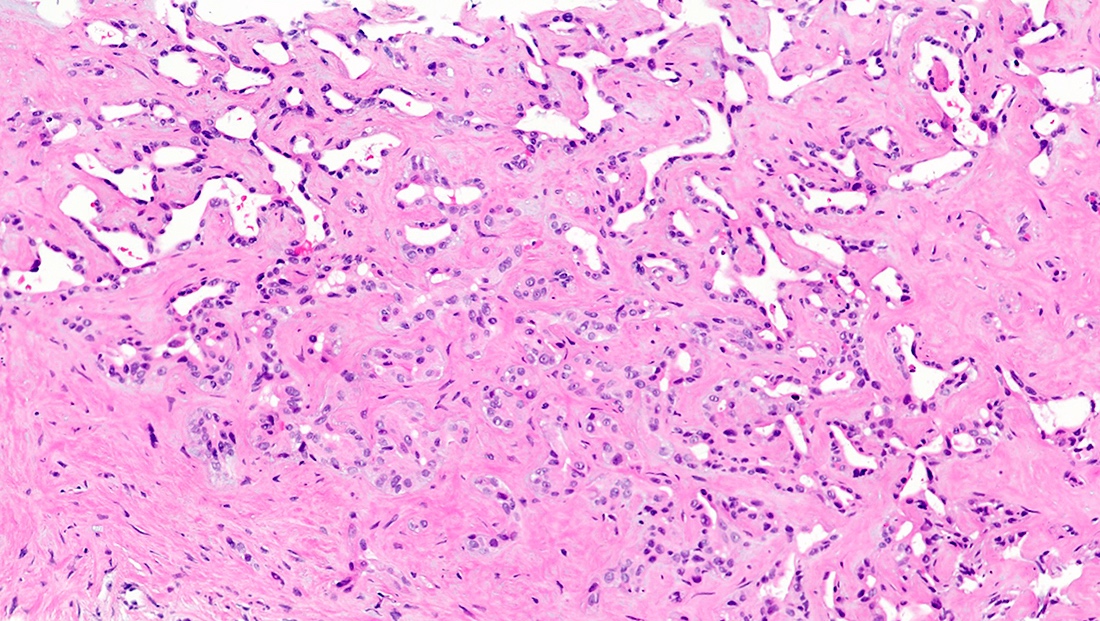
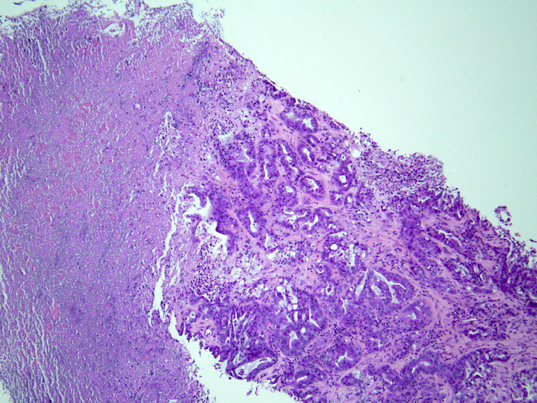
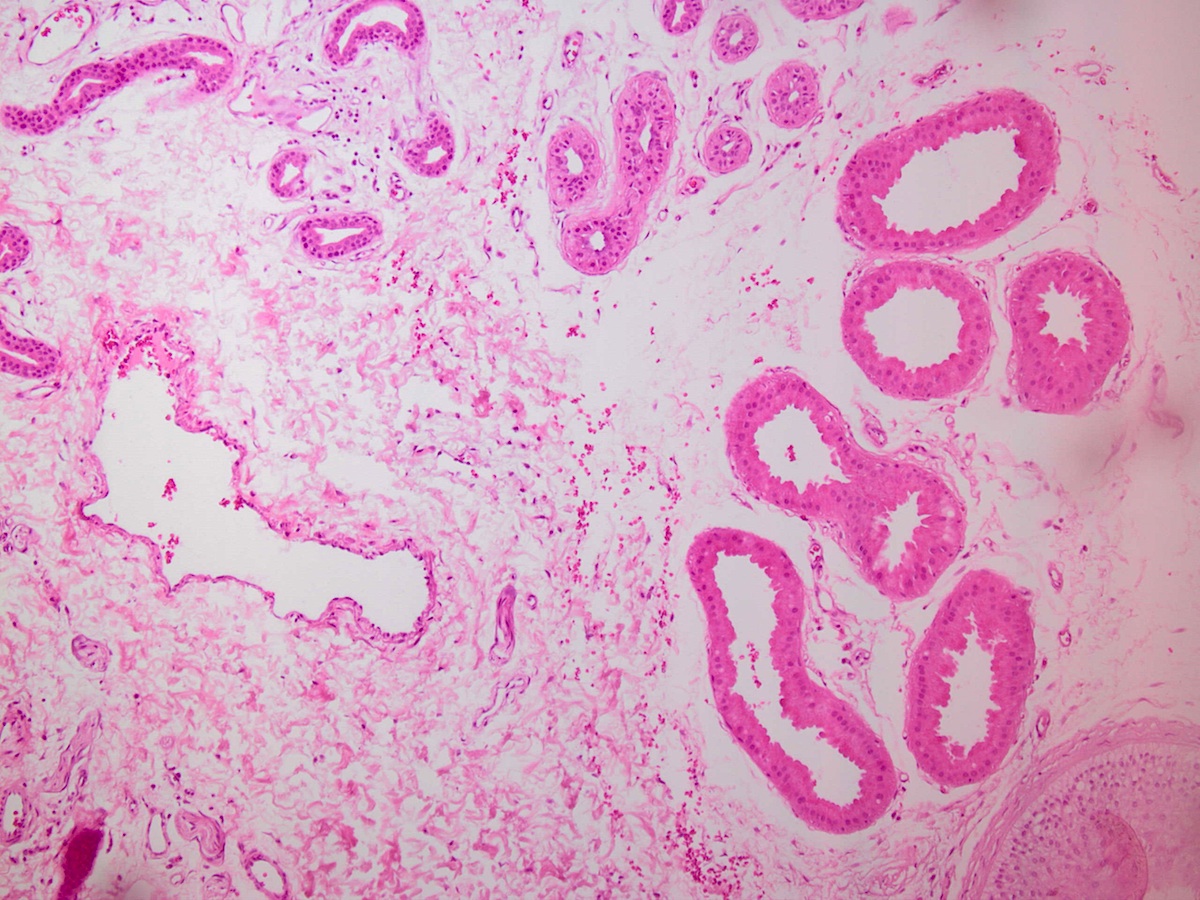
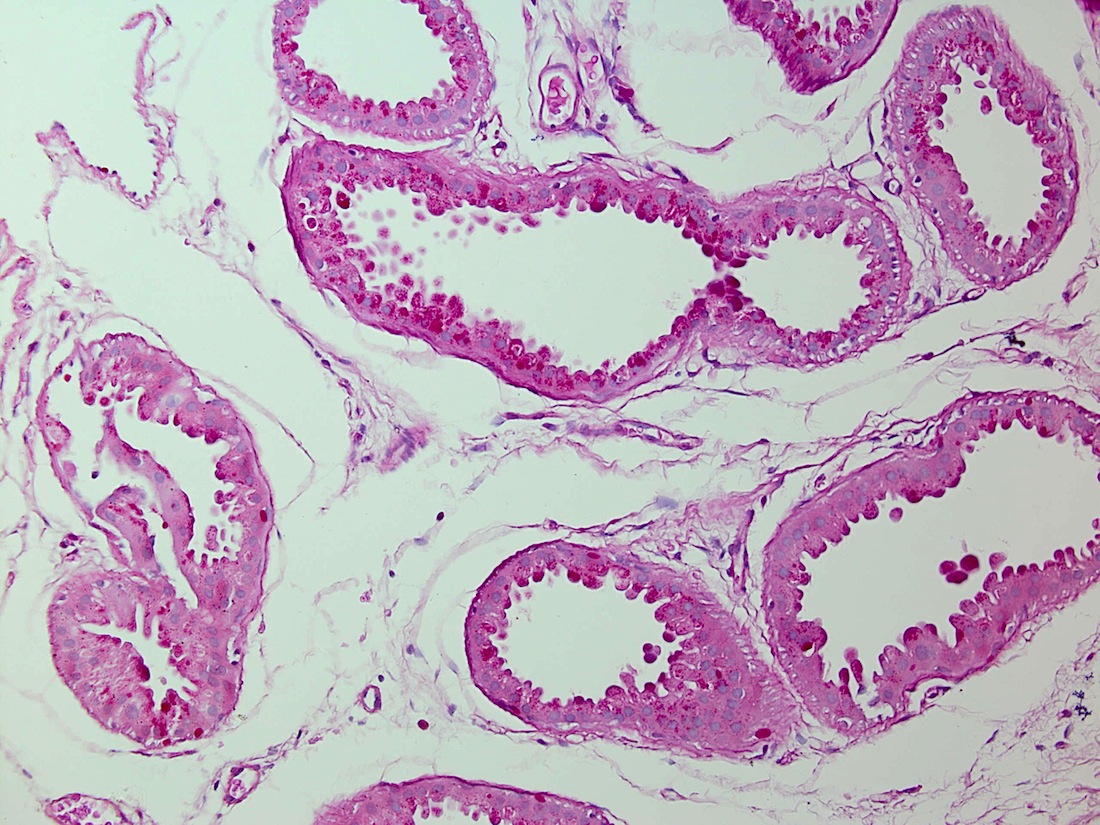
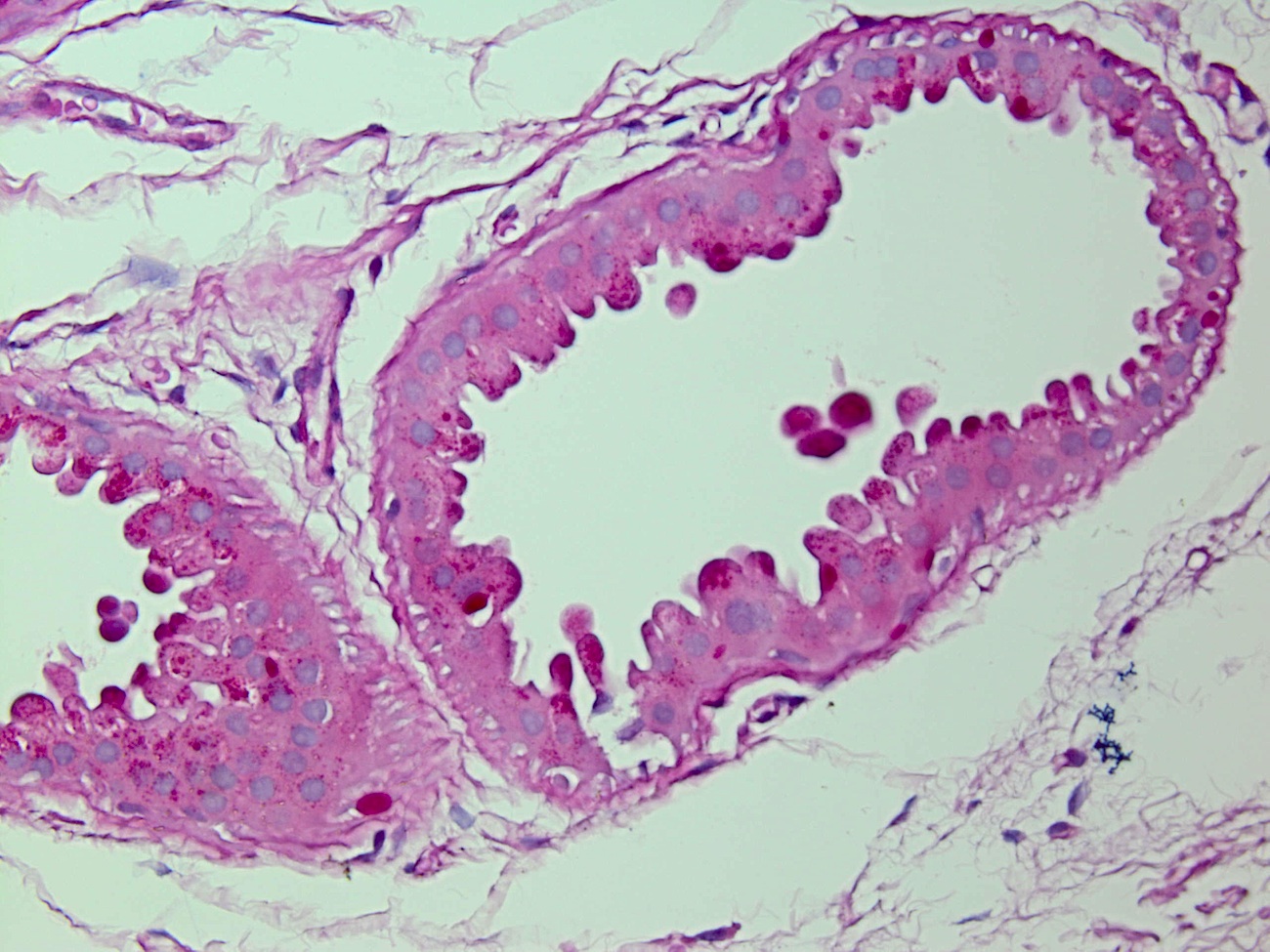
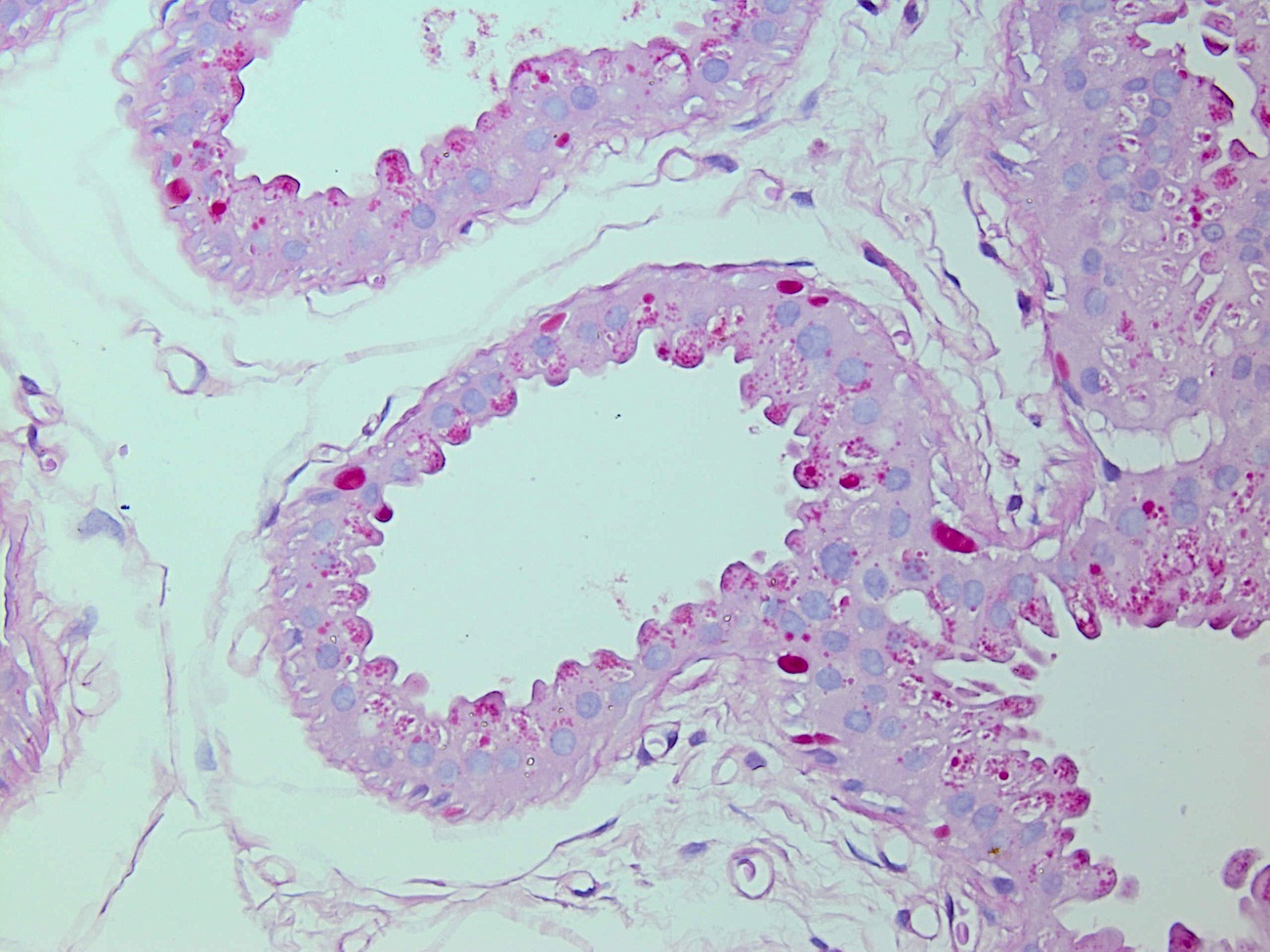
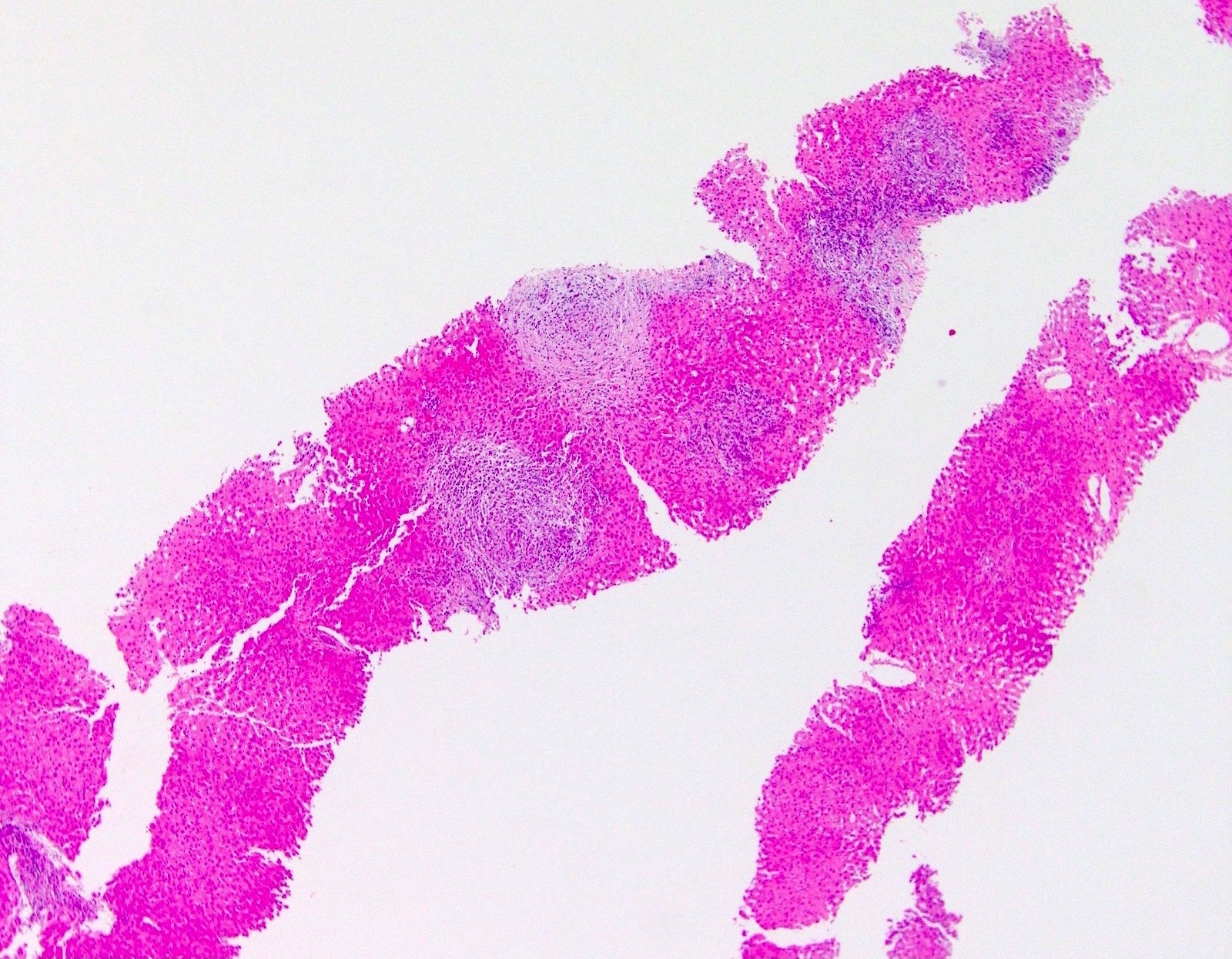
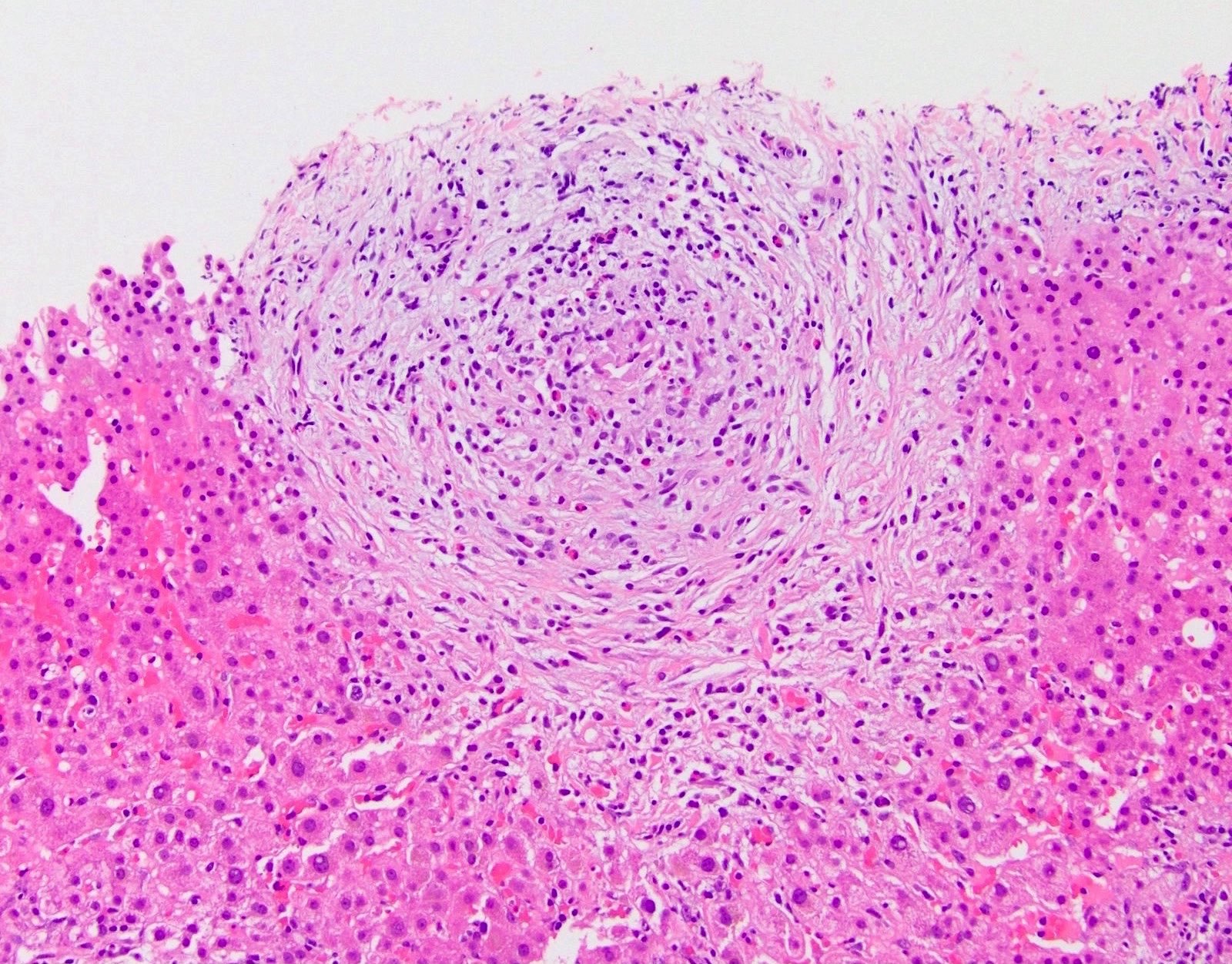
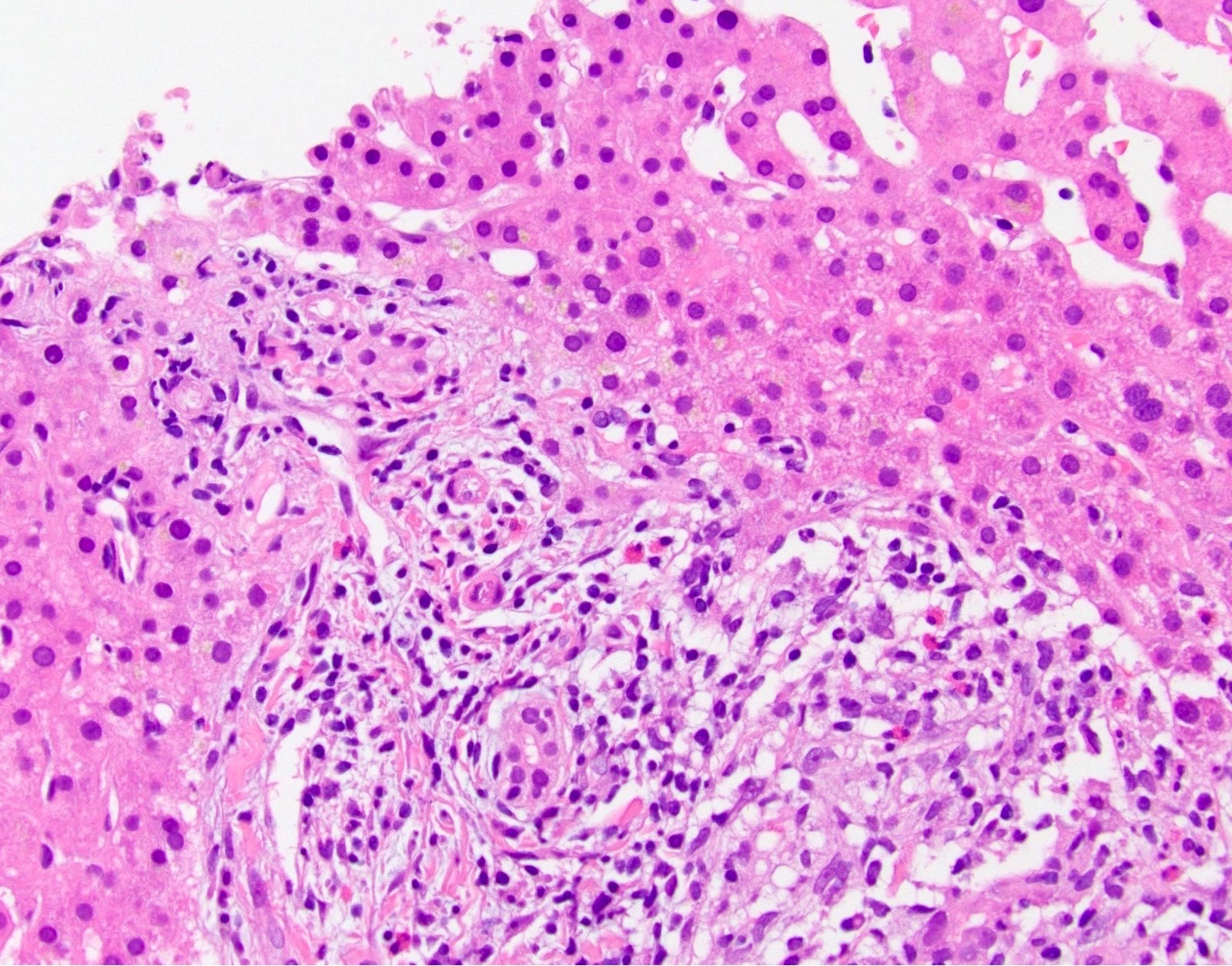
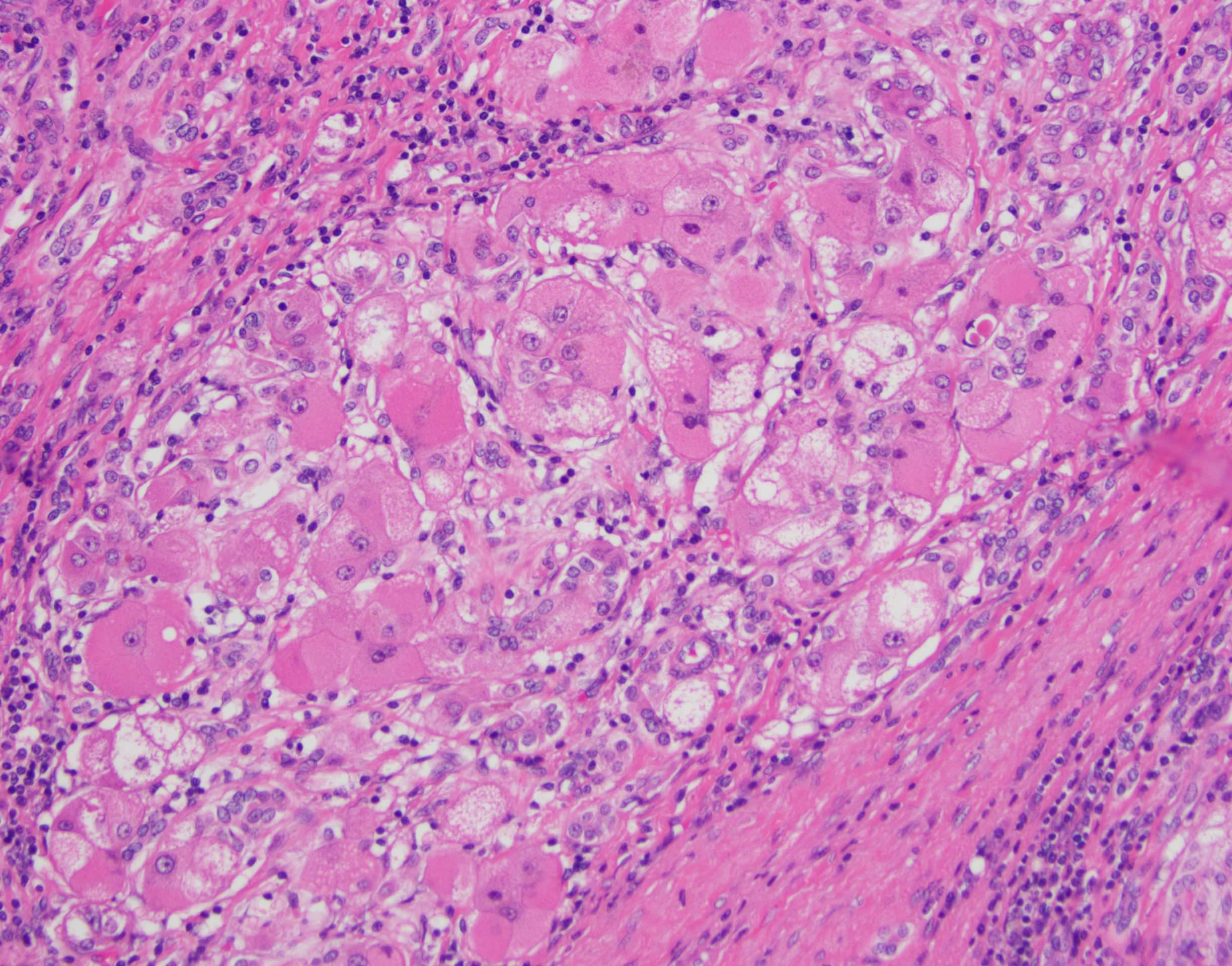
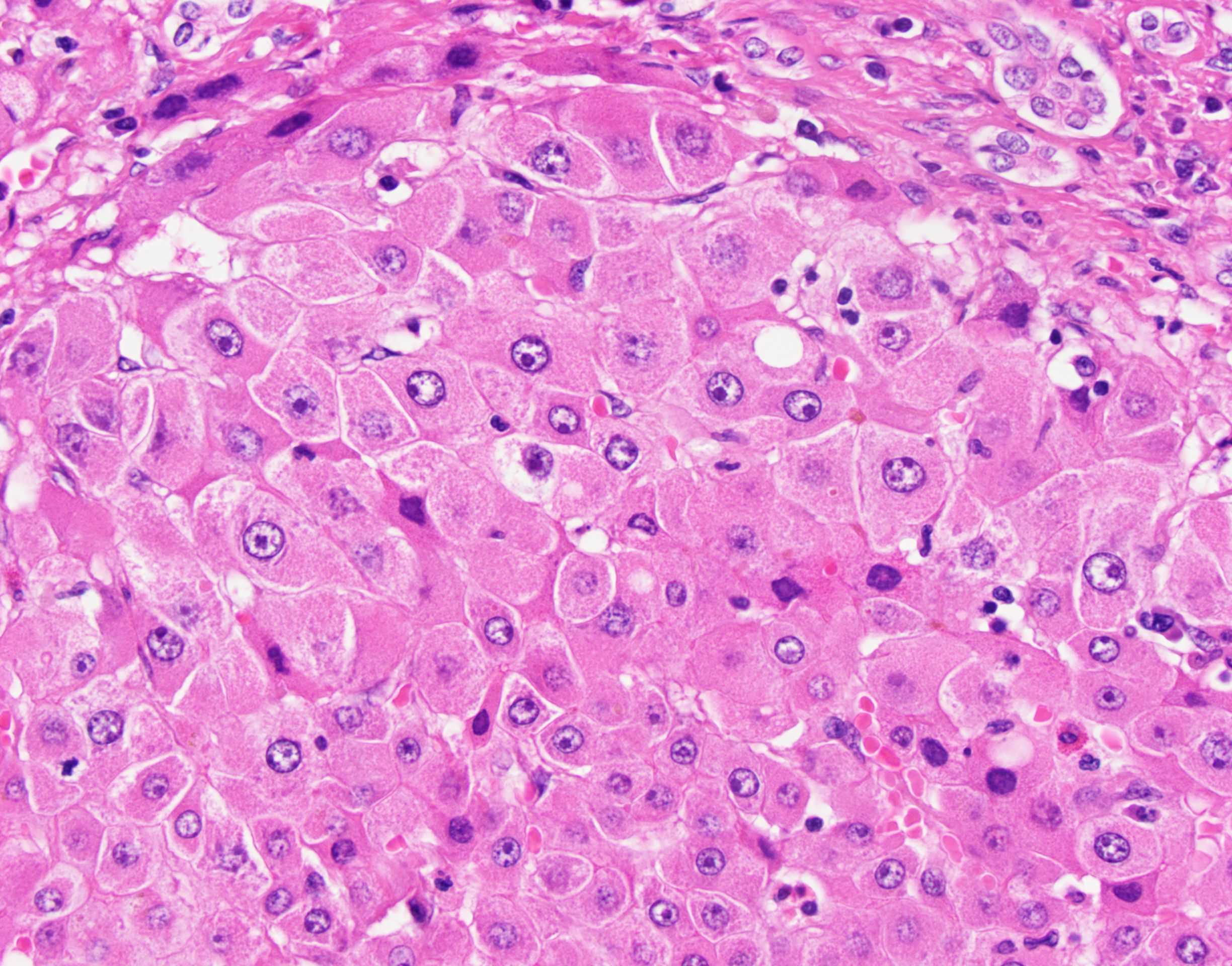
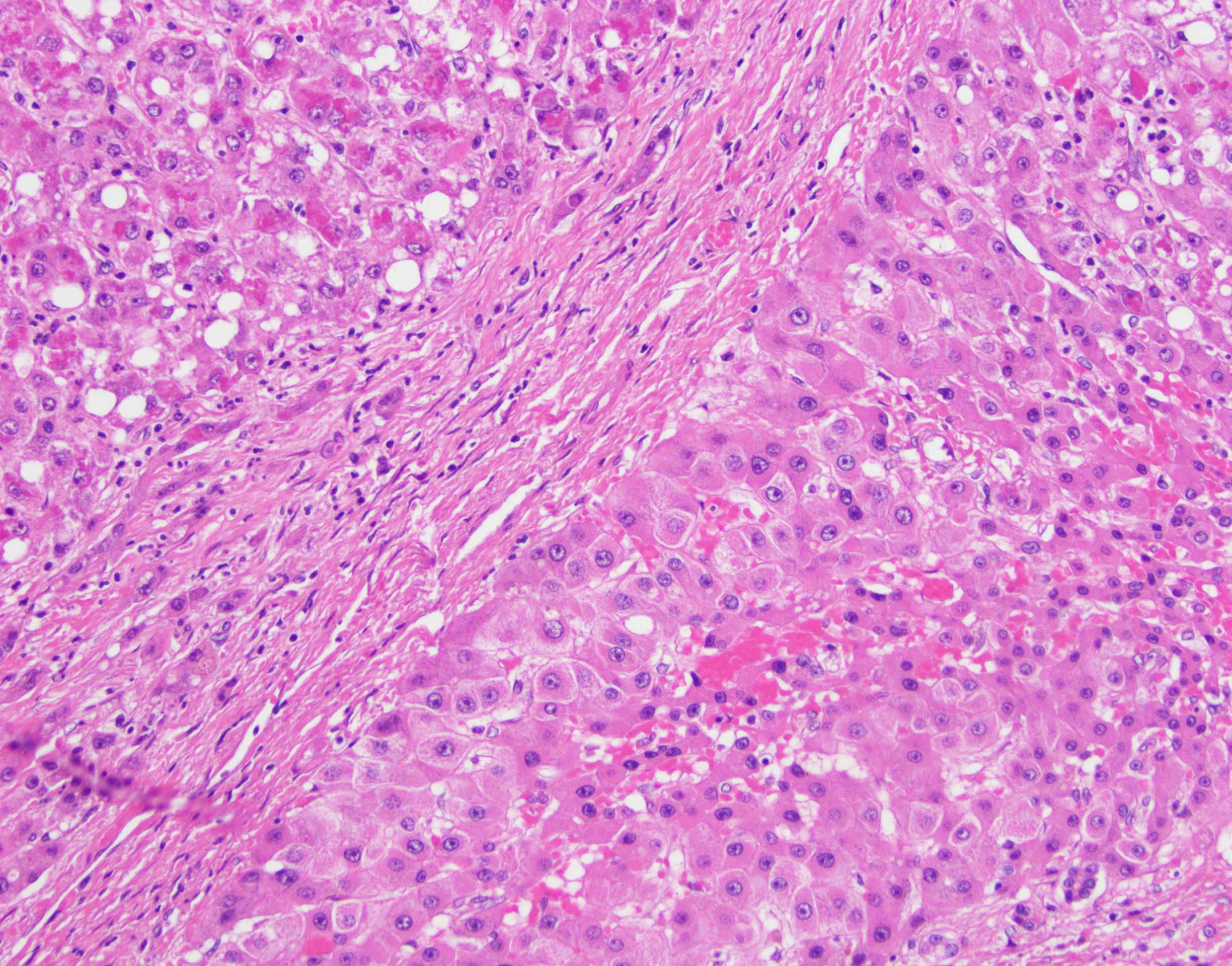
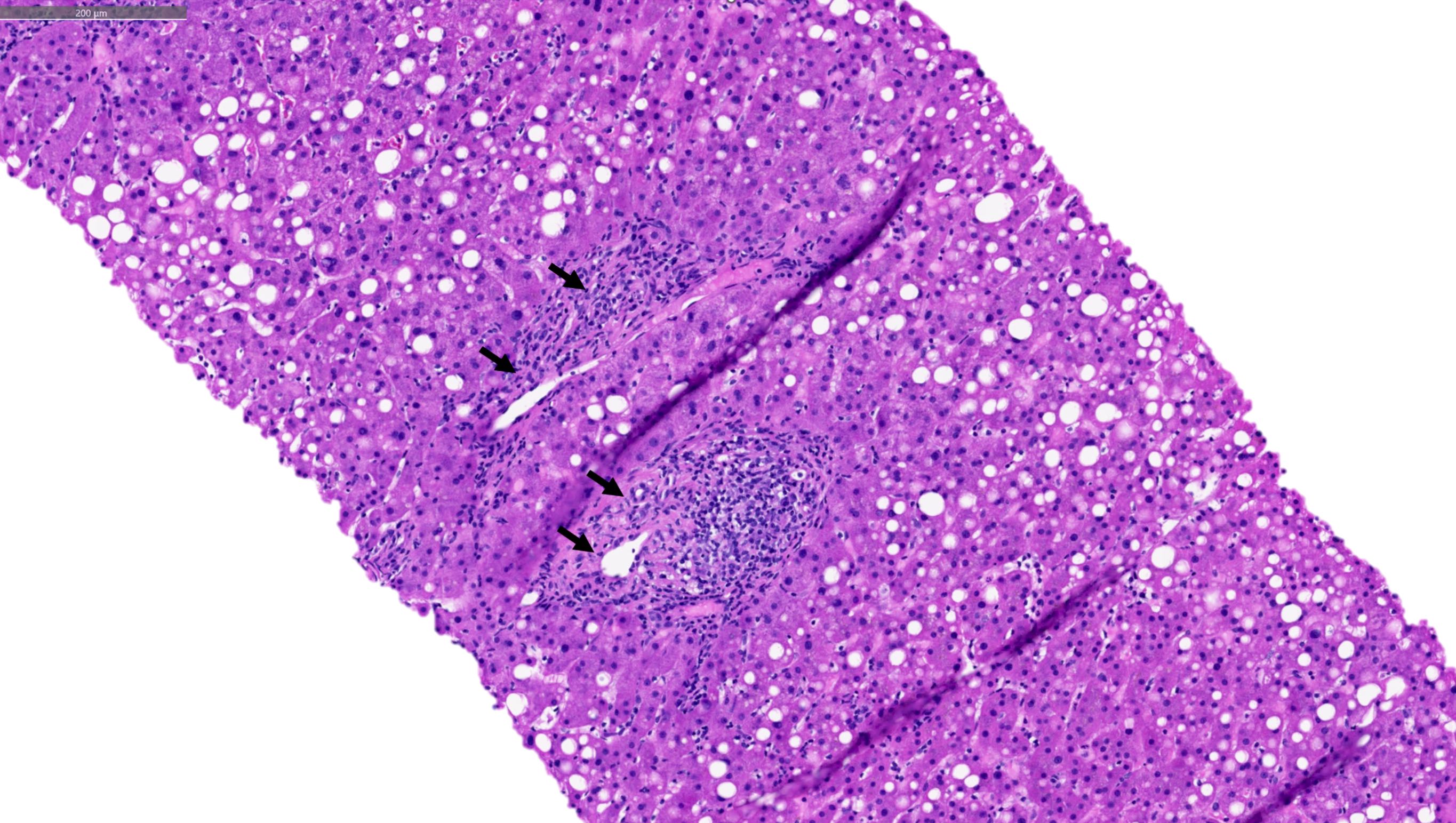
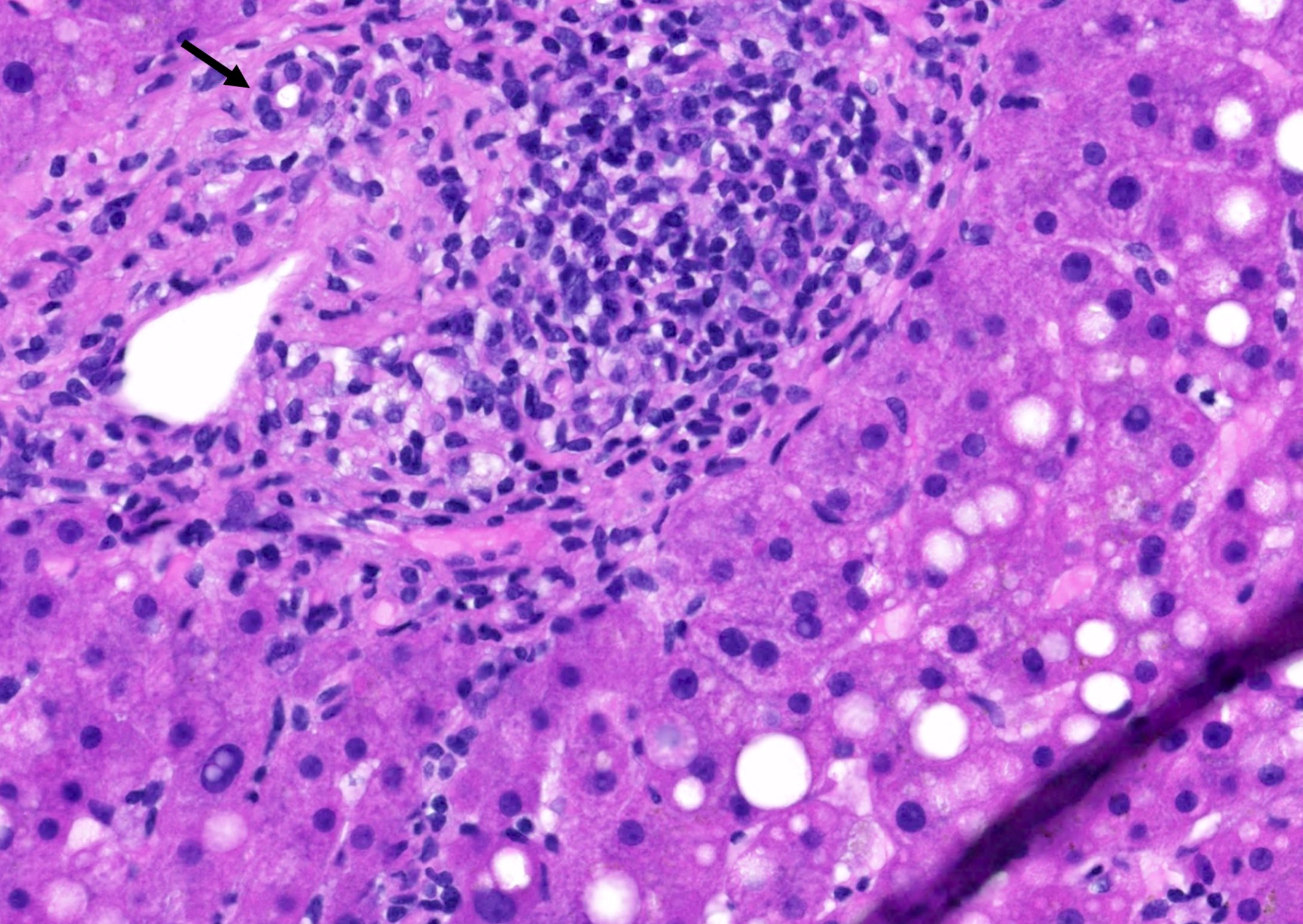
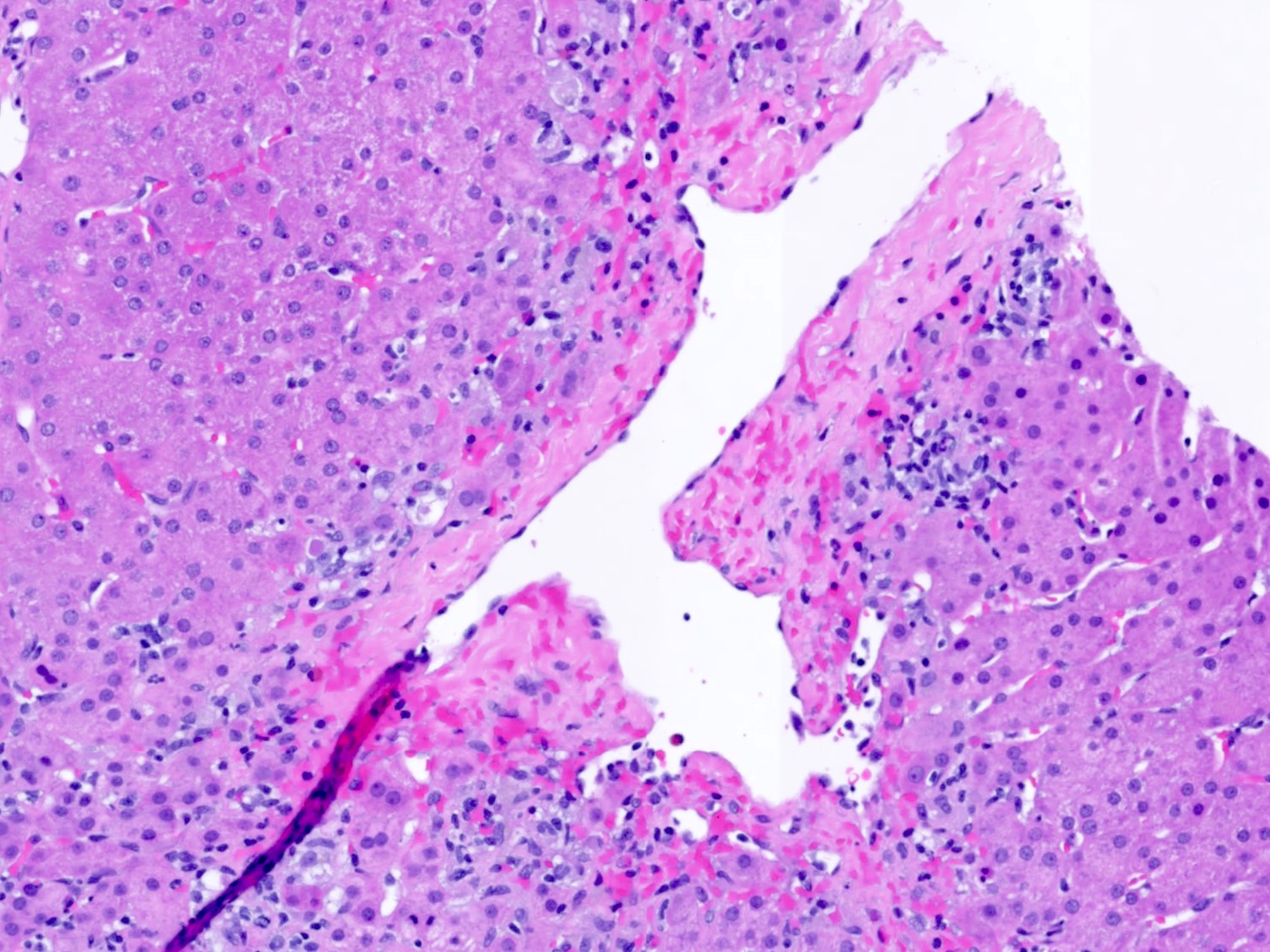
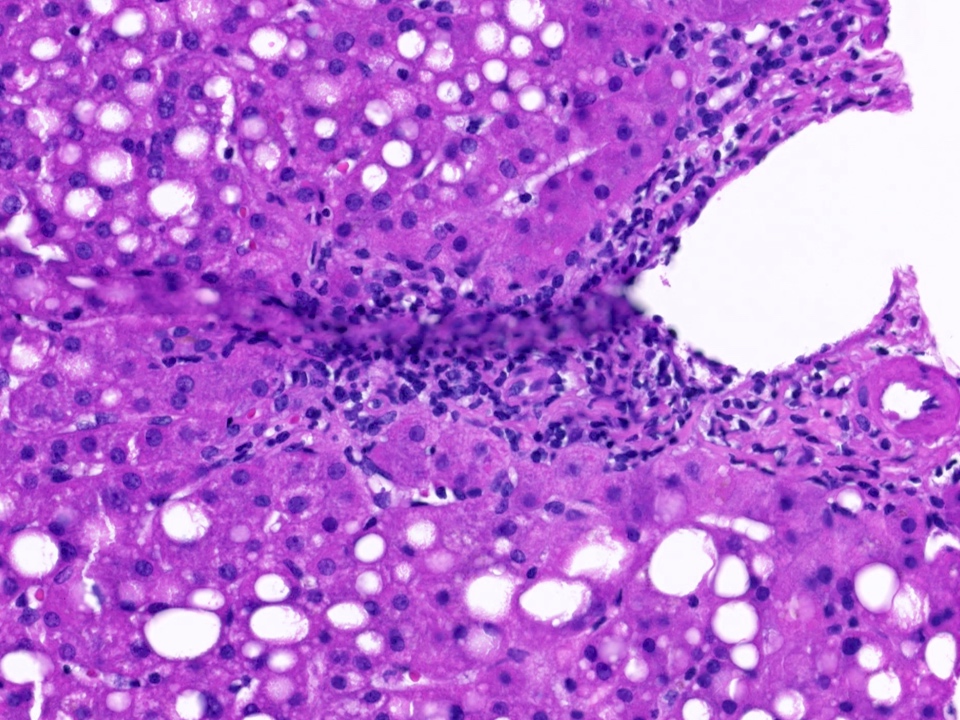
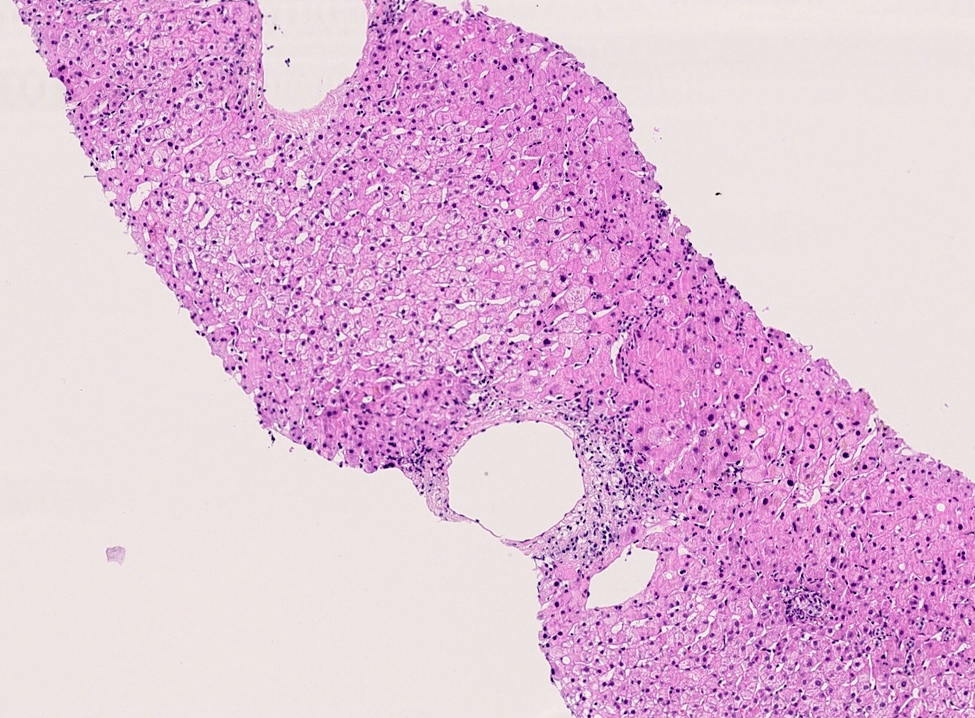
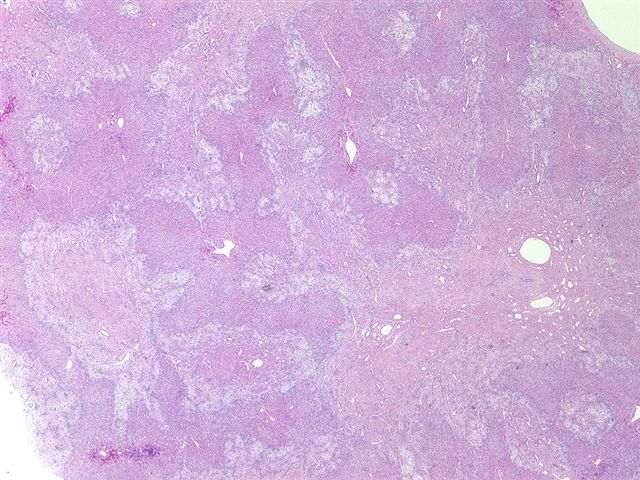
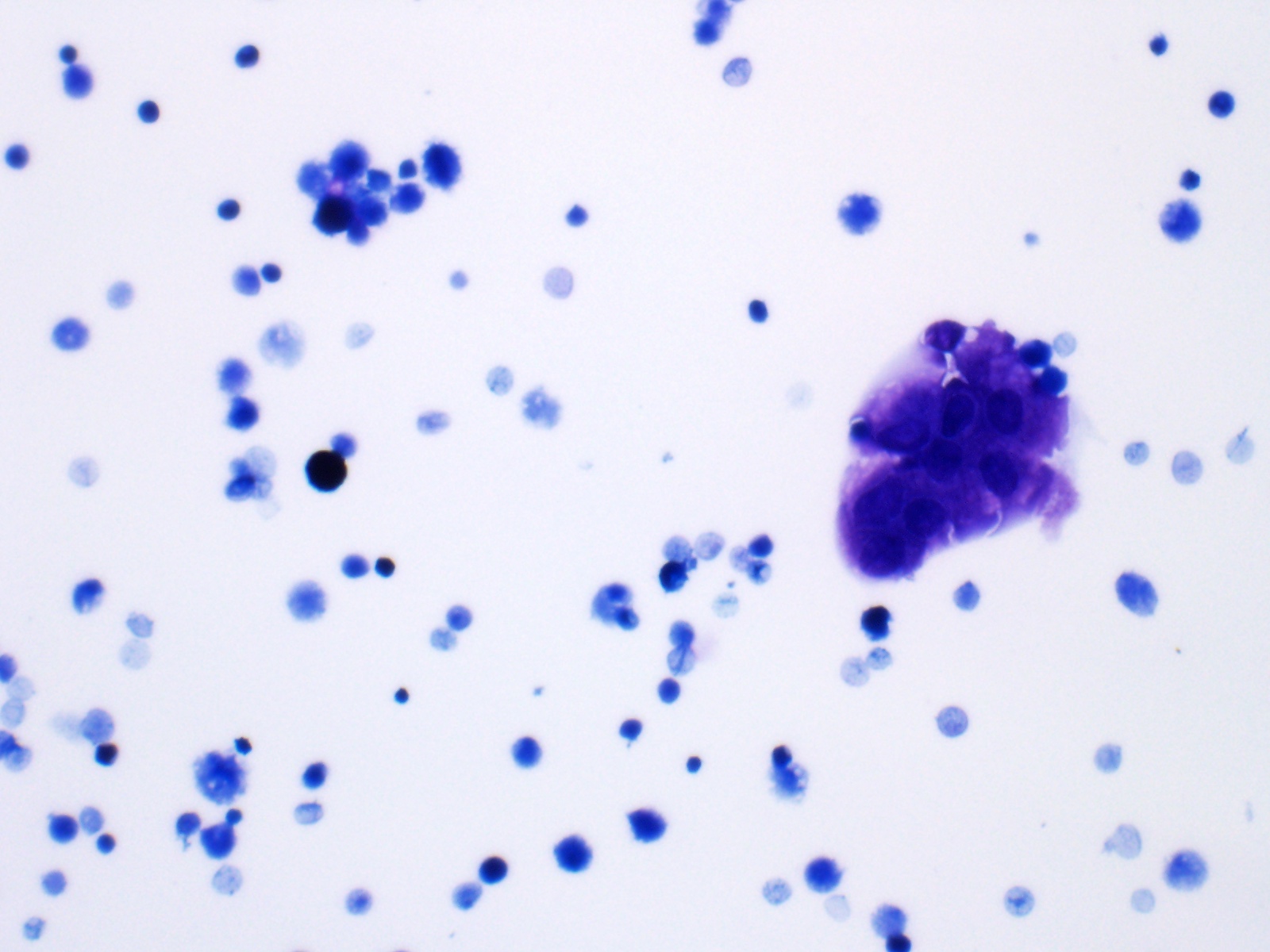
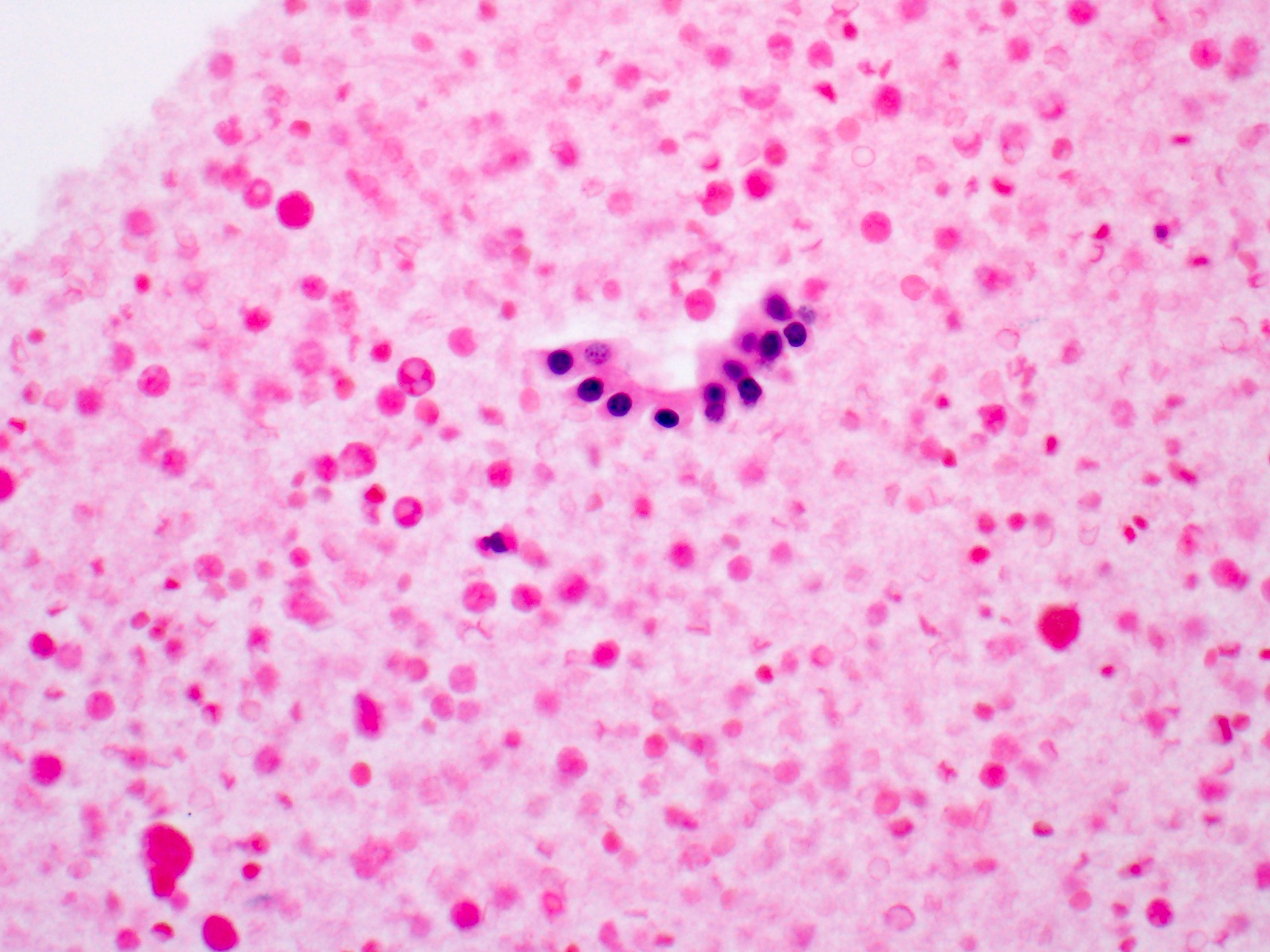
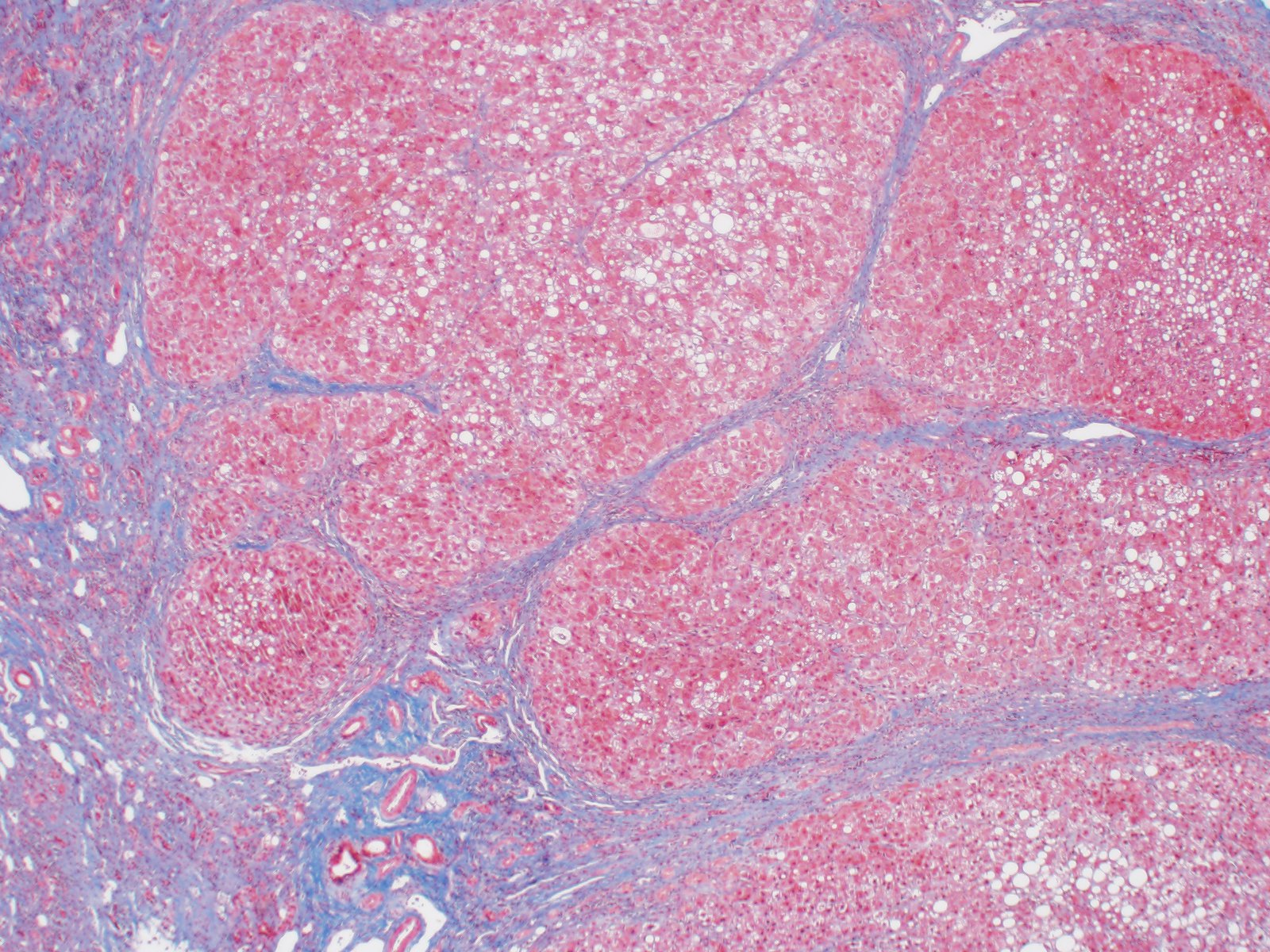
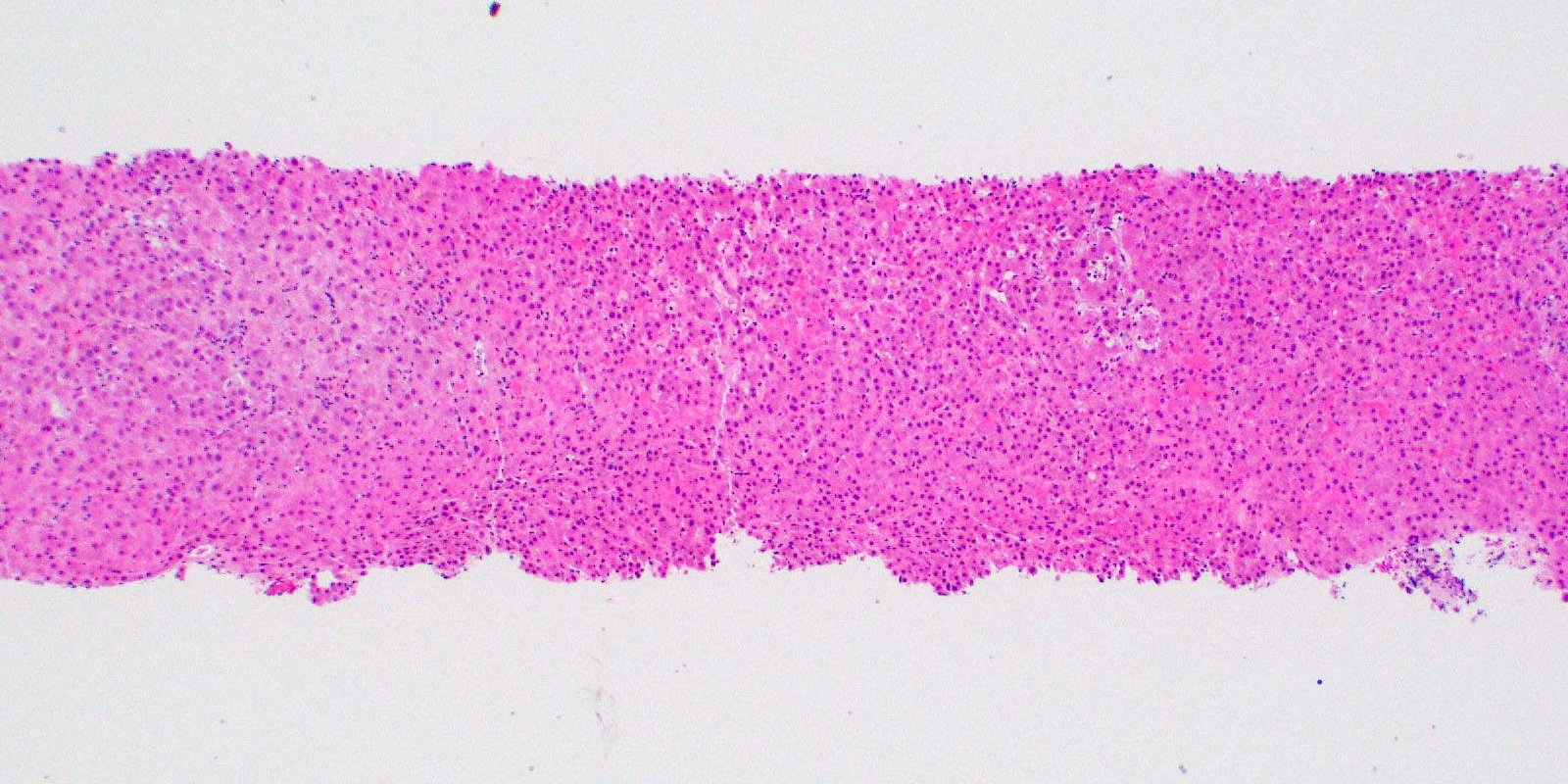
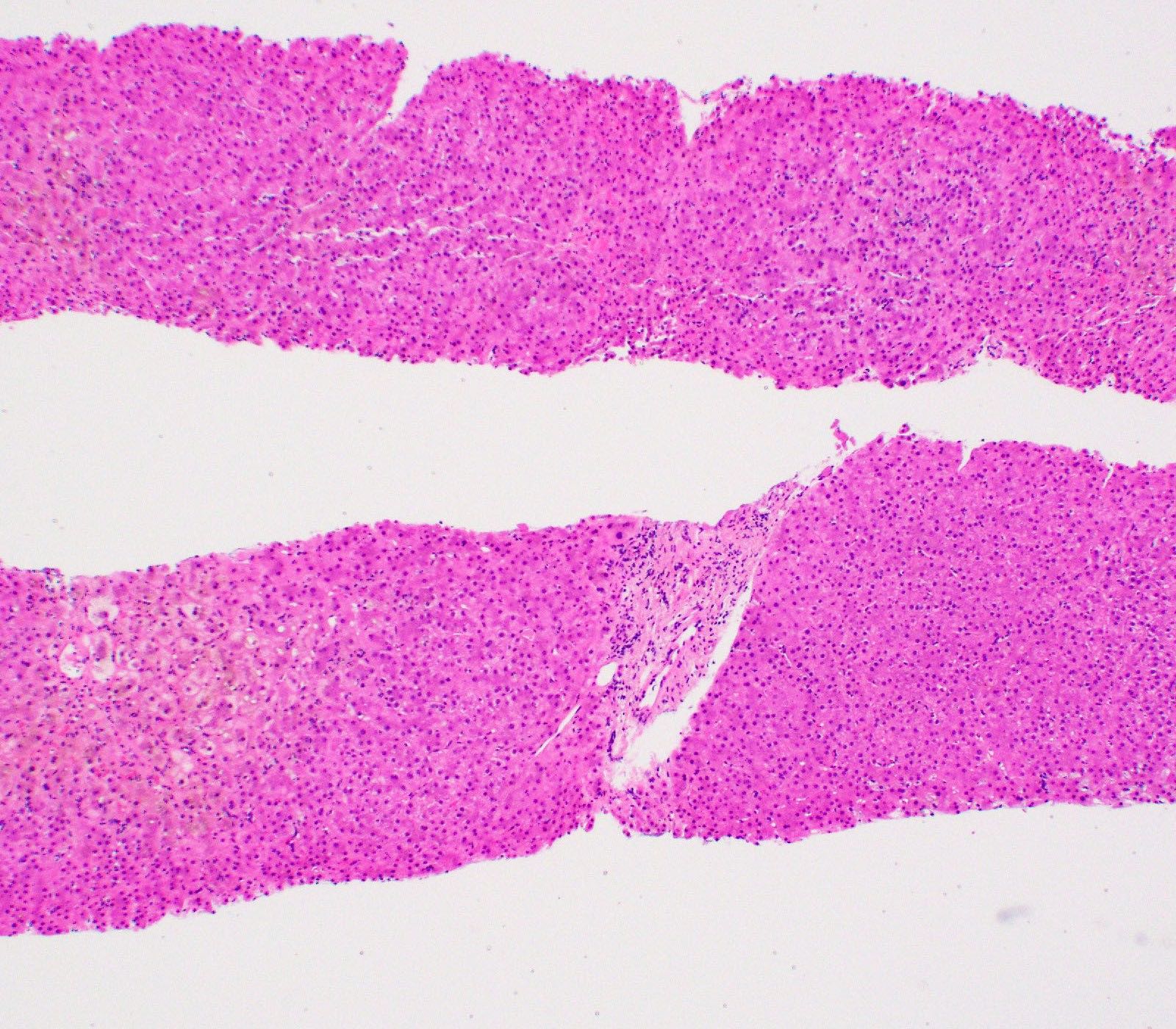
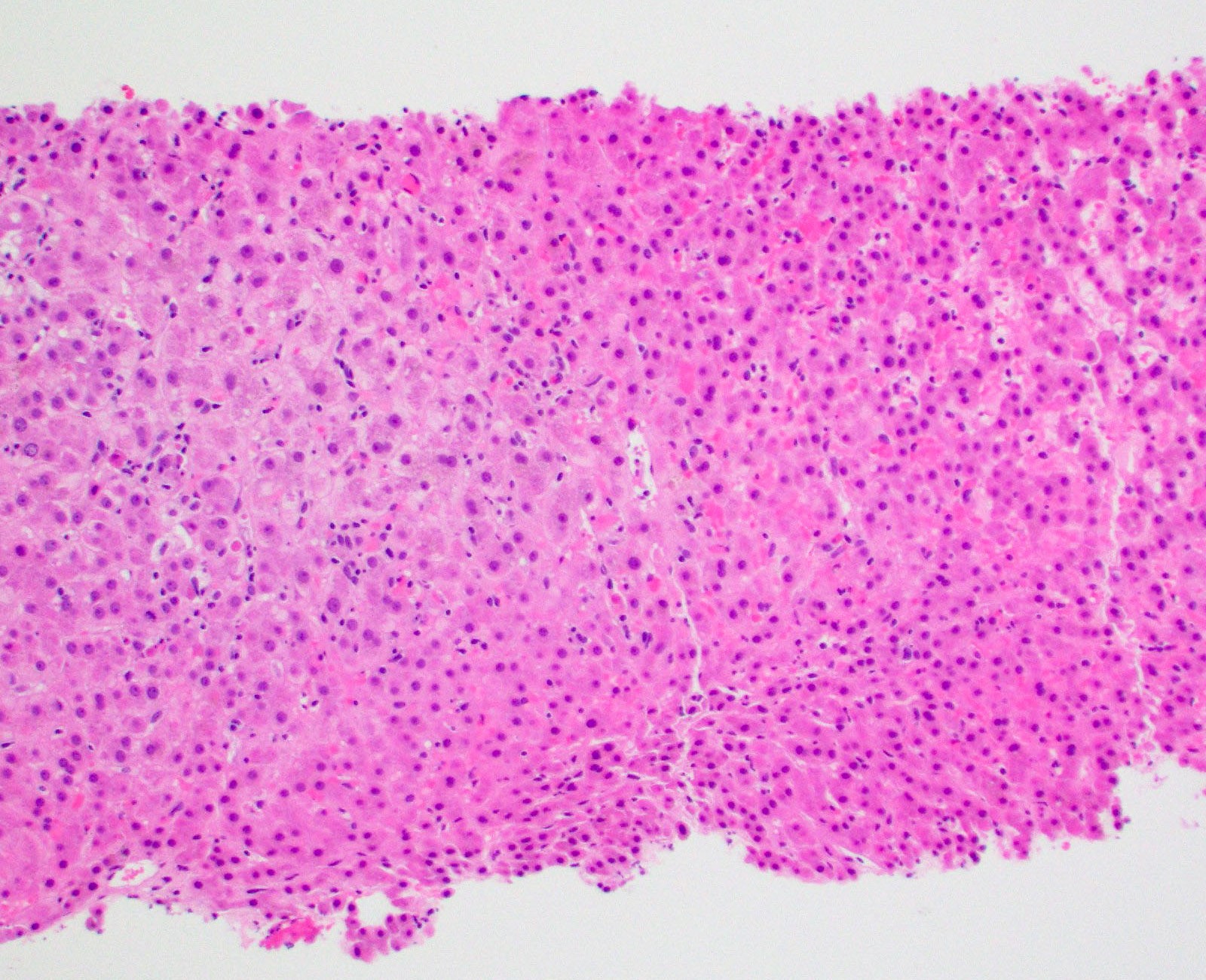
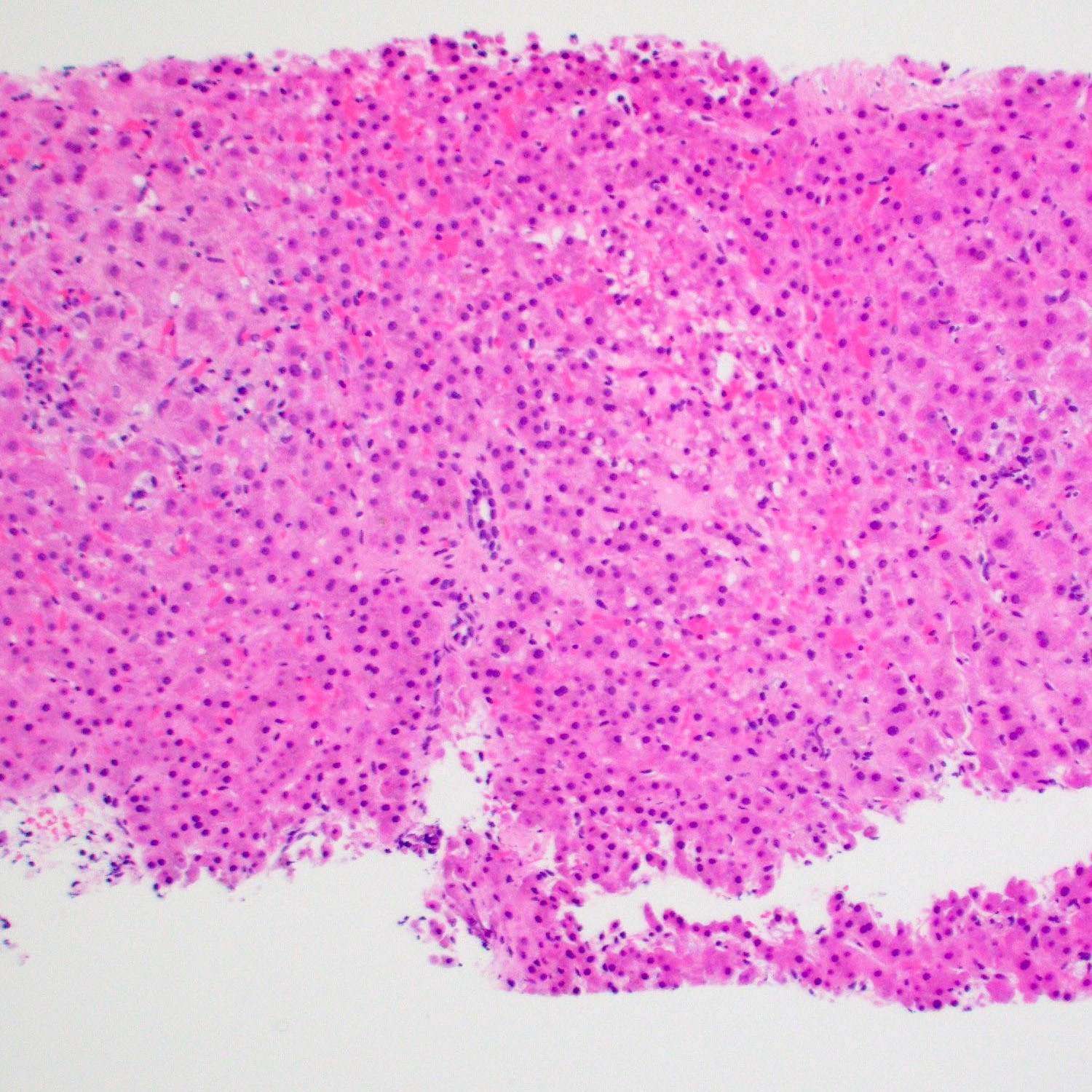
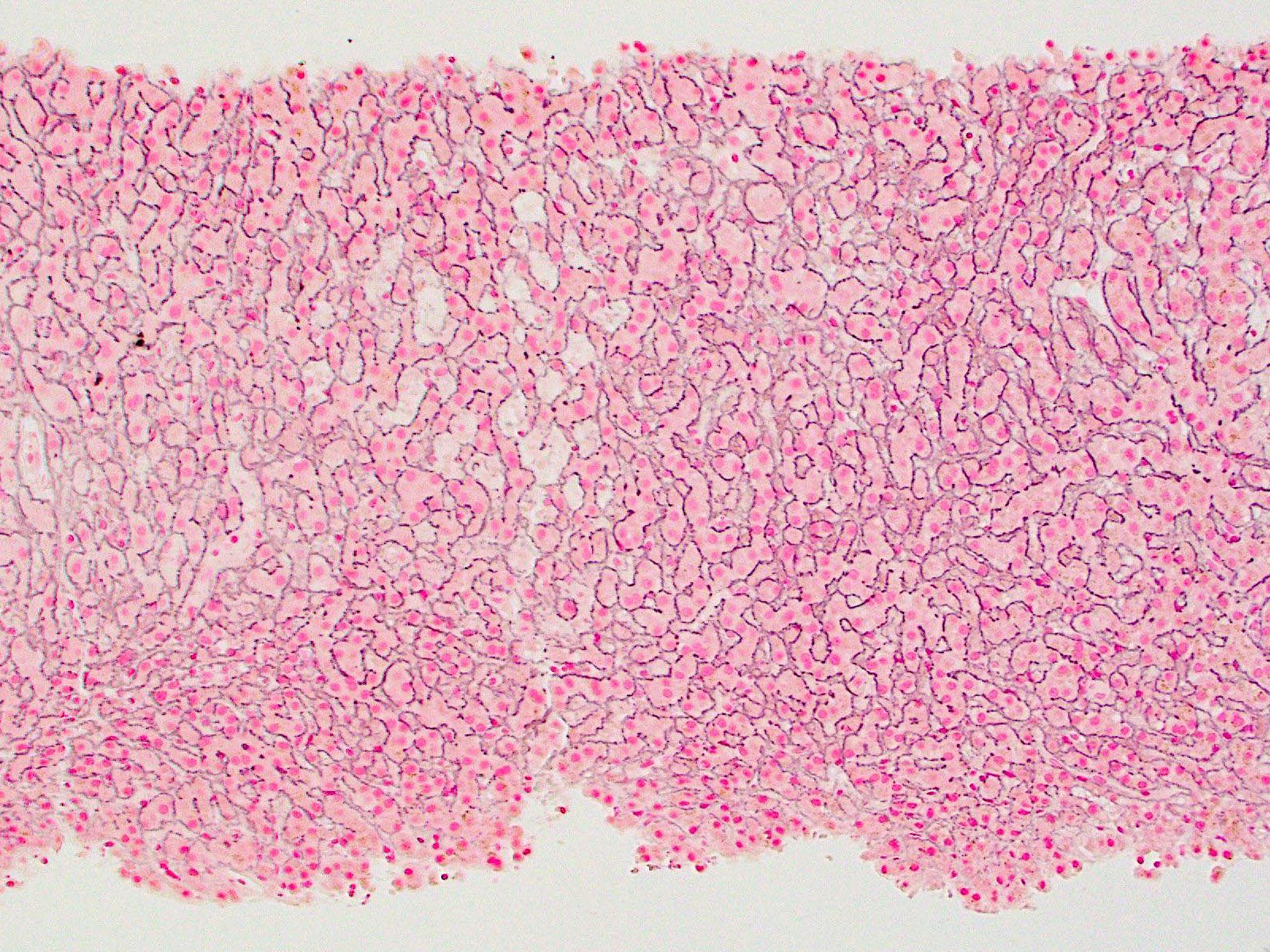
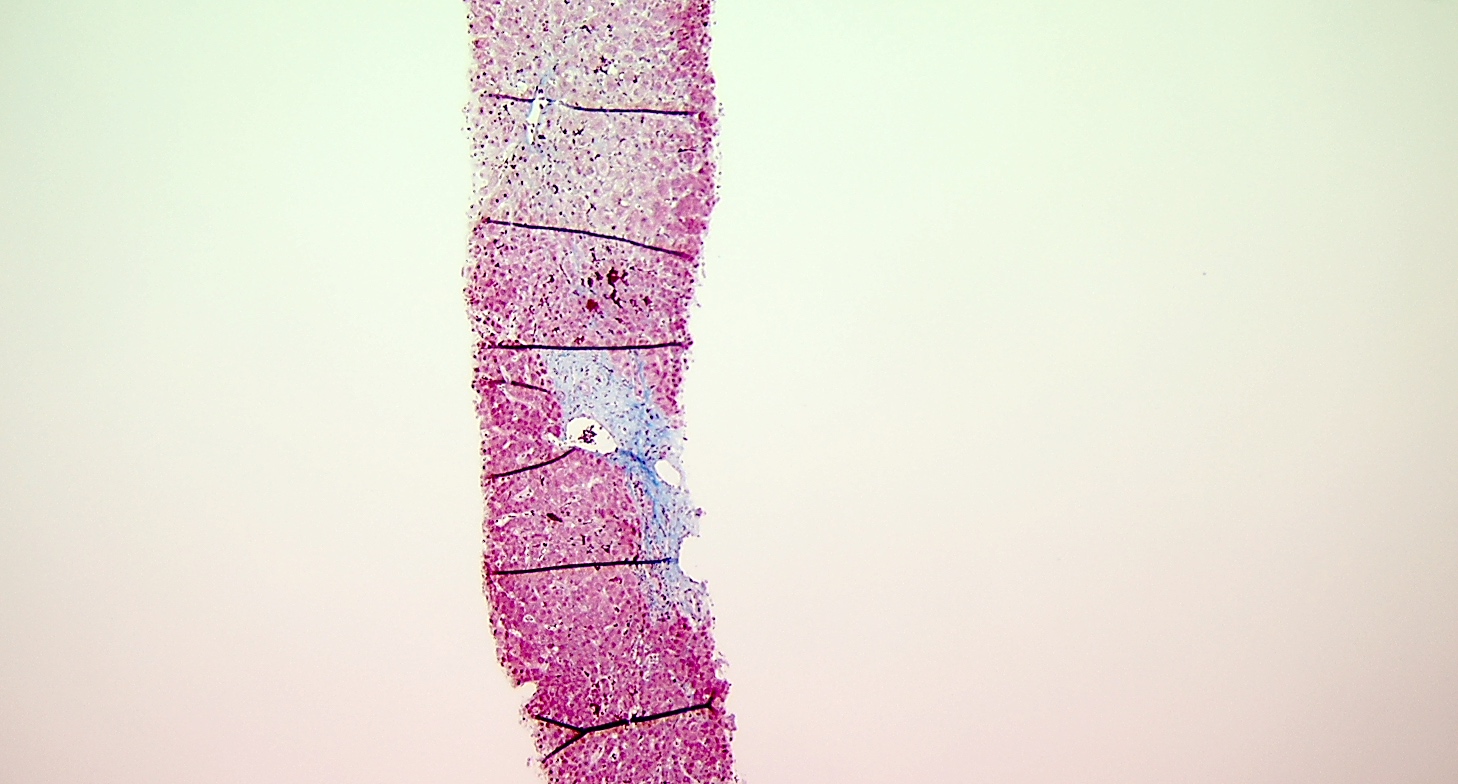
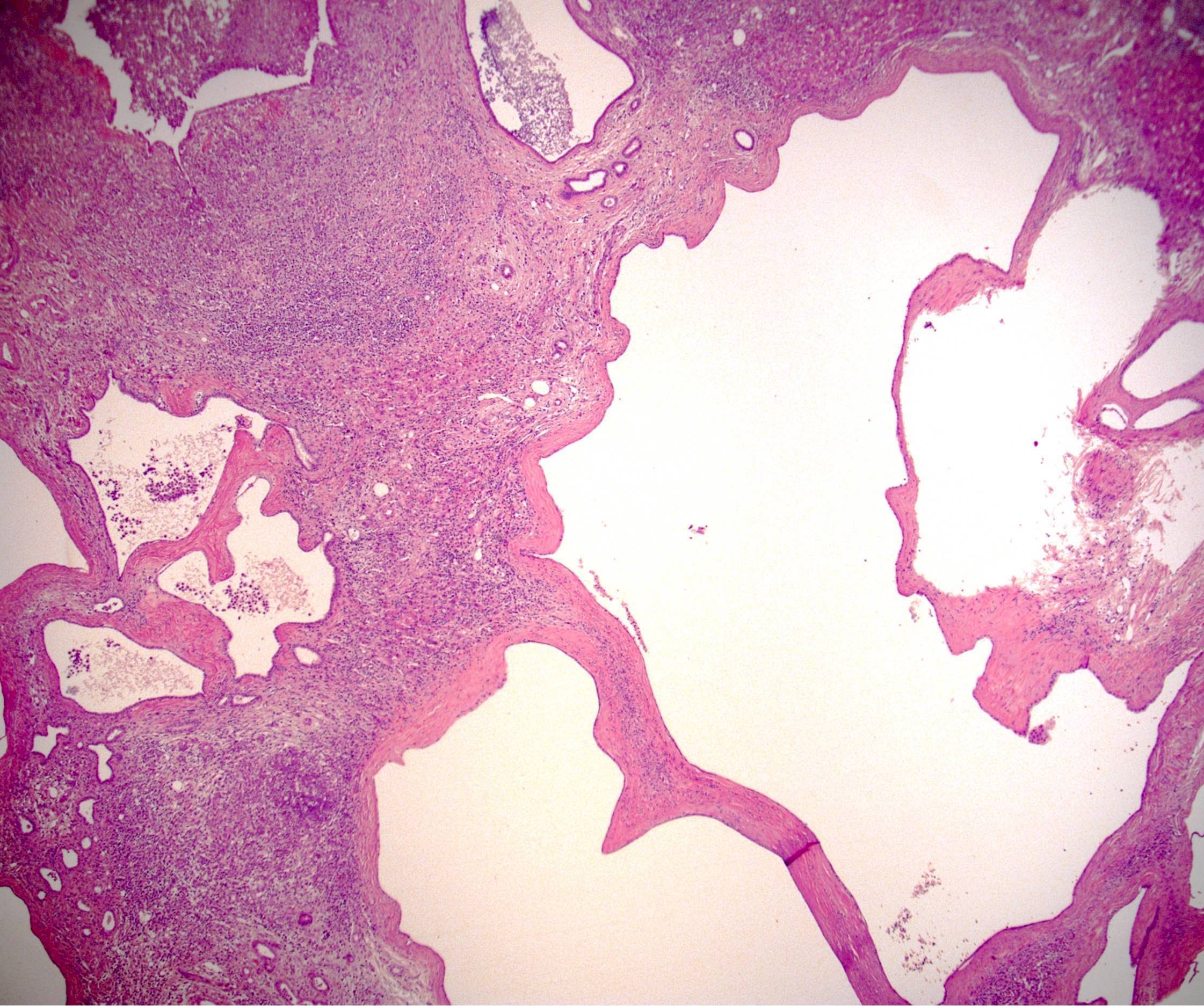
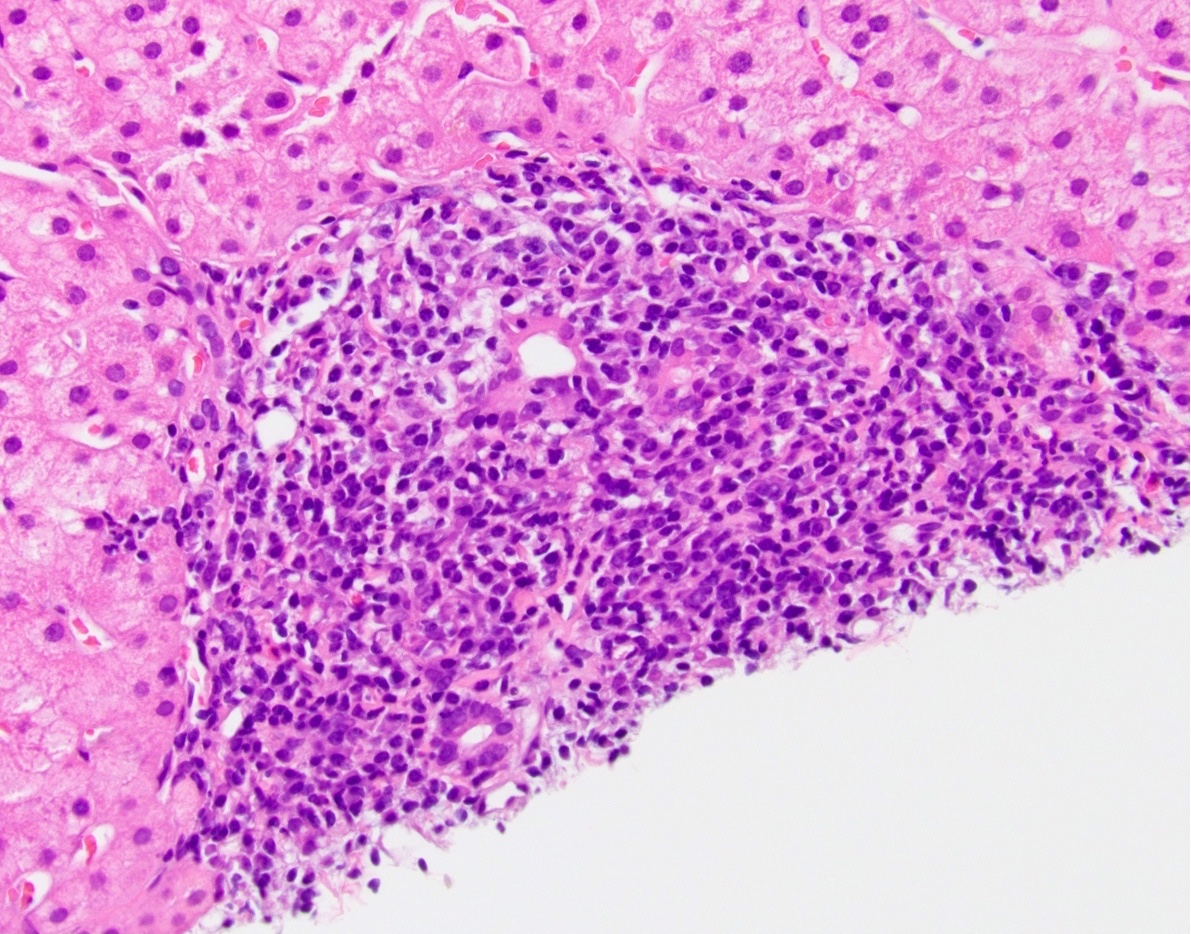
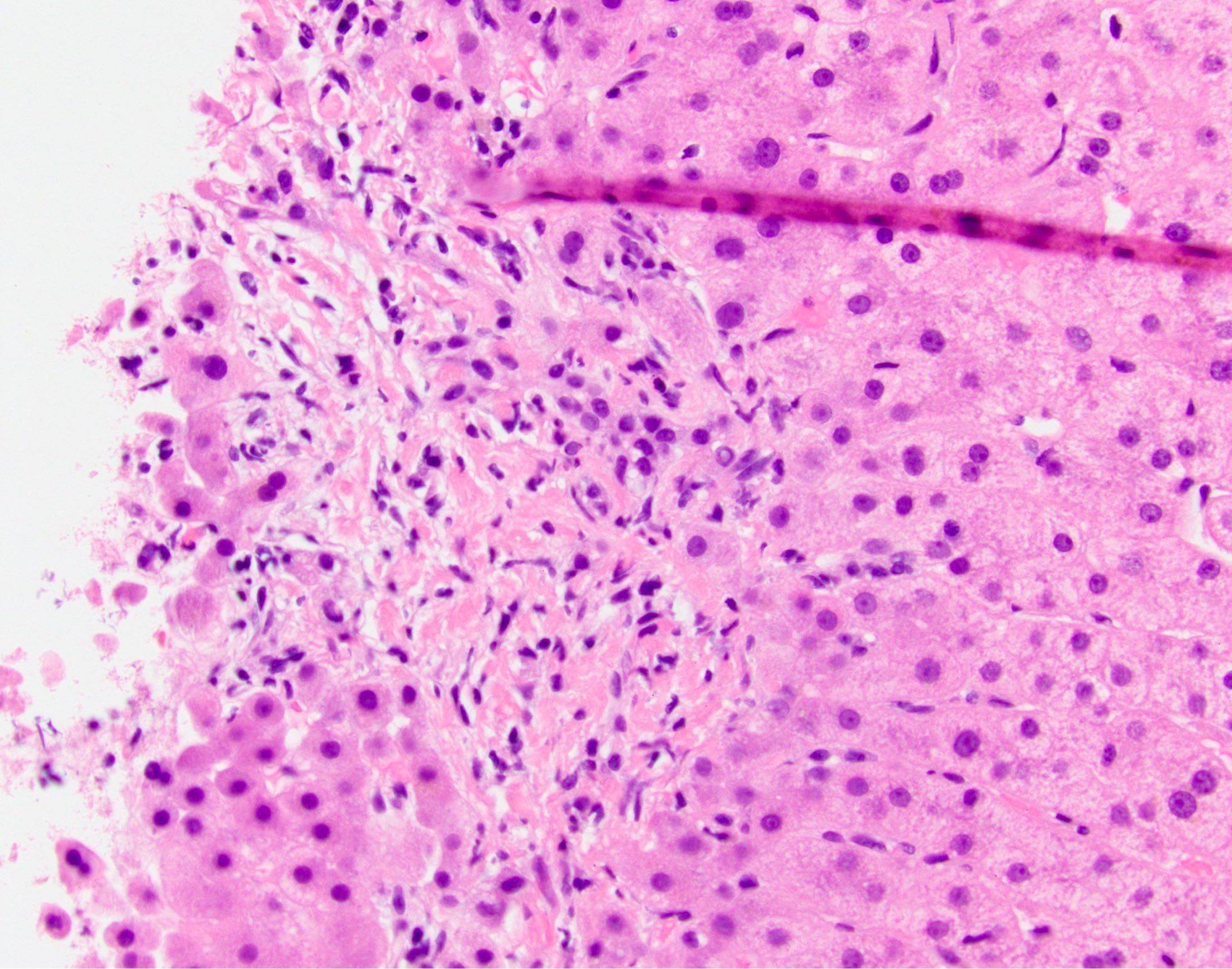
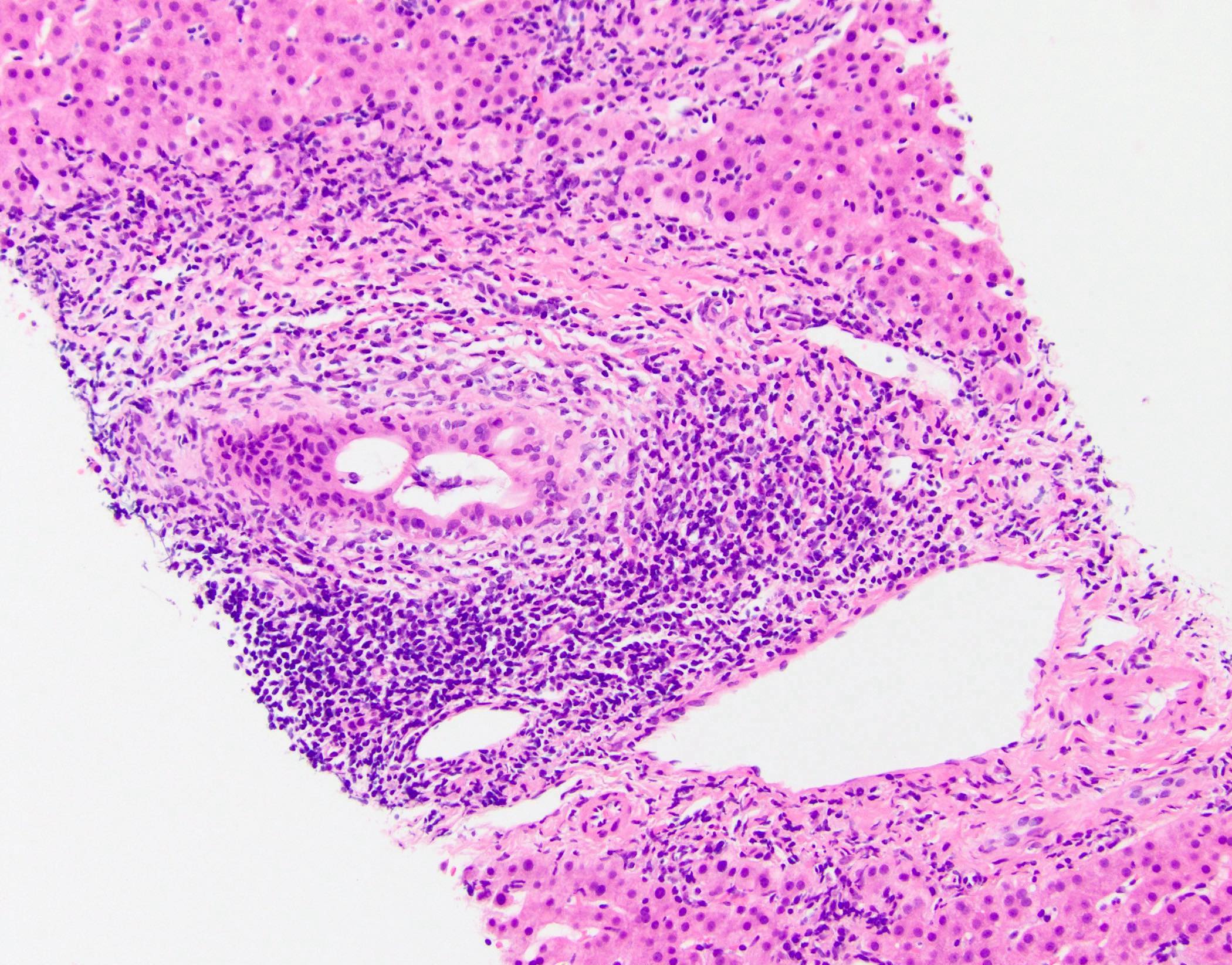
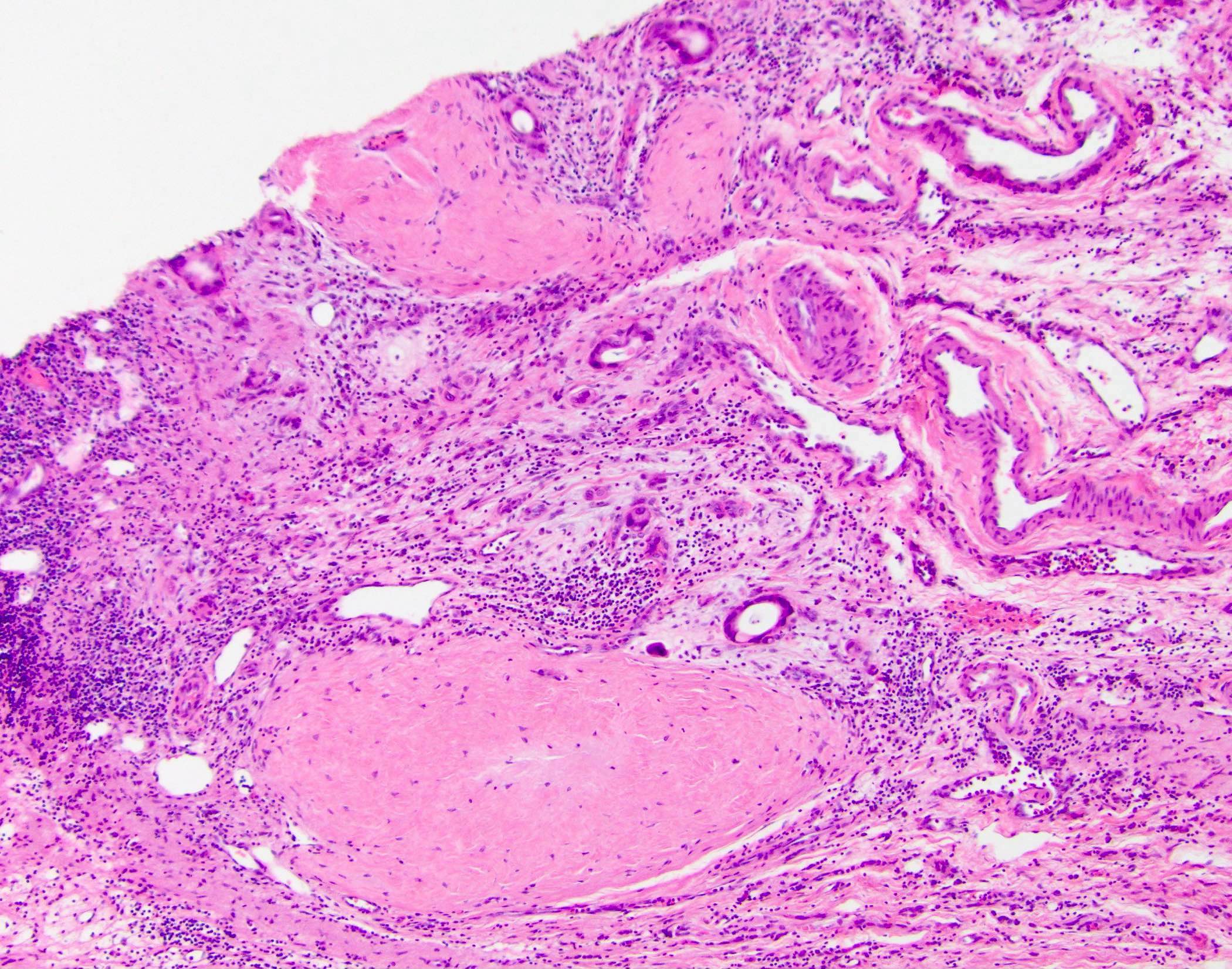
Microscopic (histologic) images
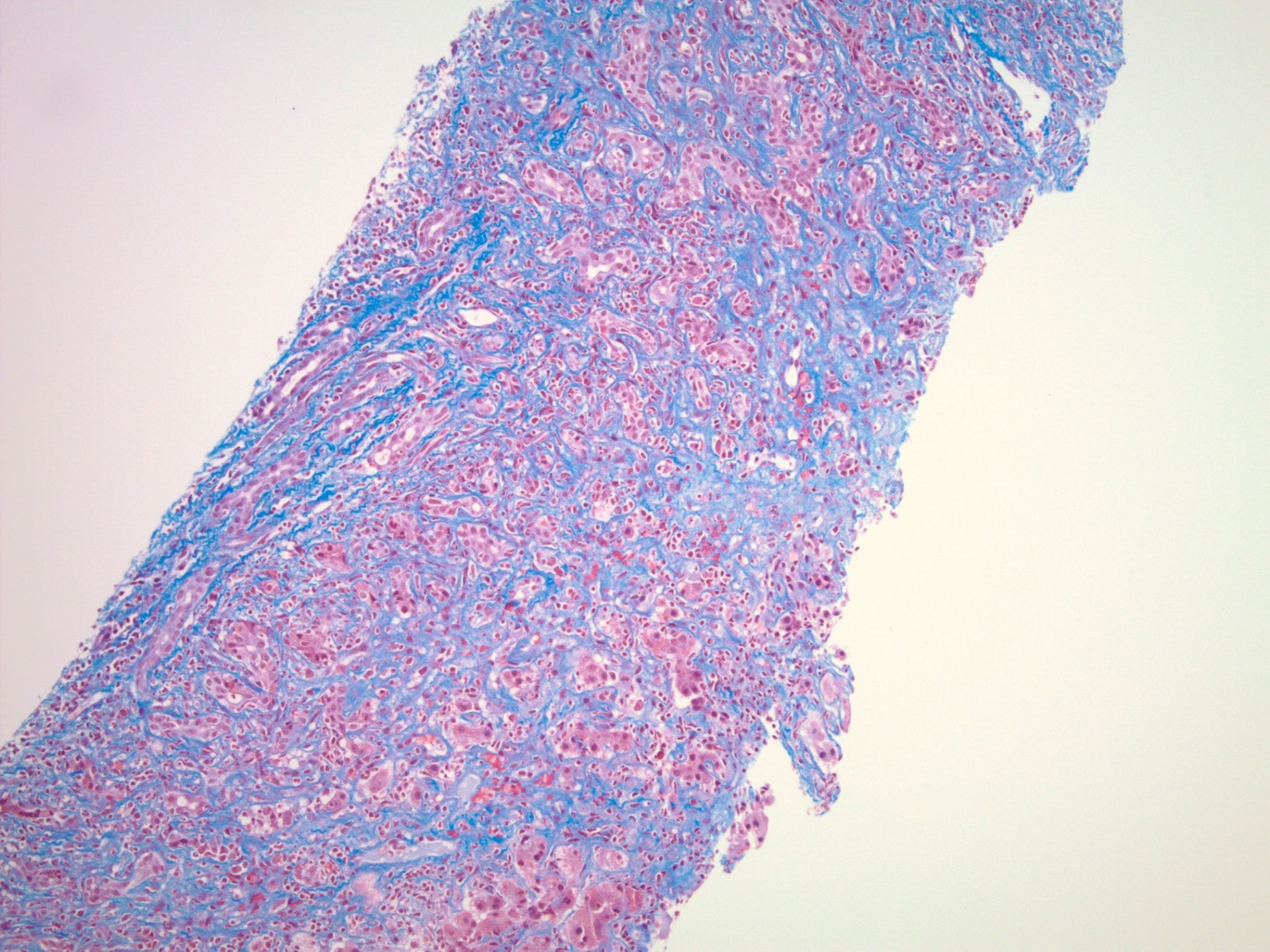
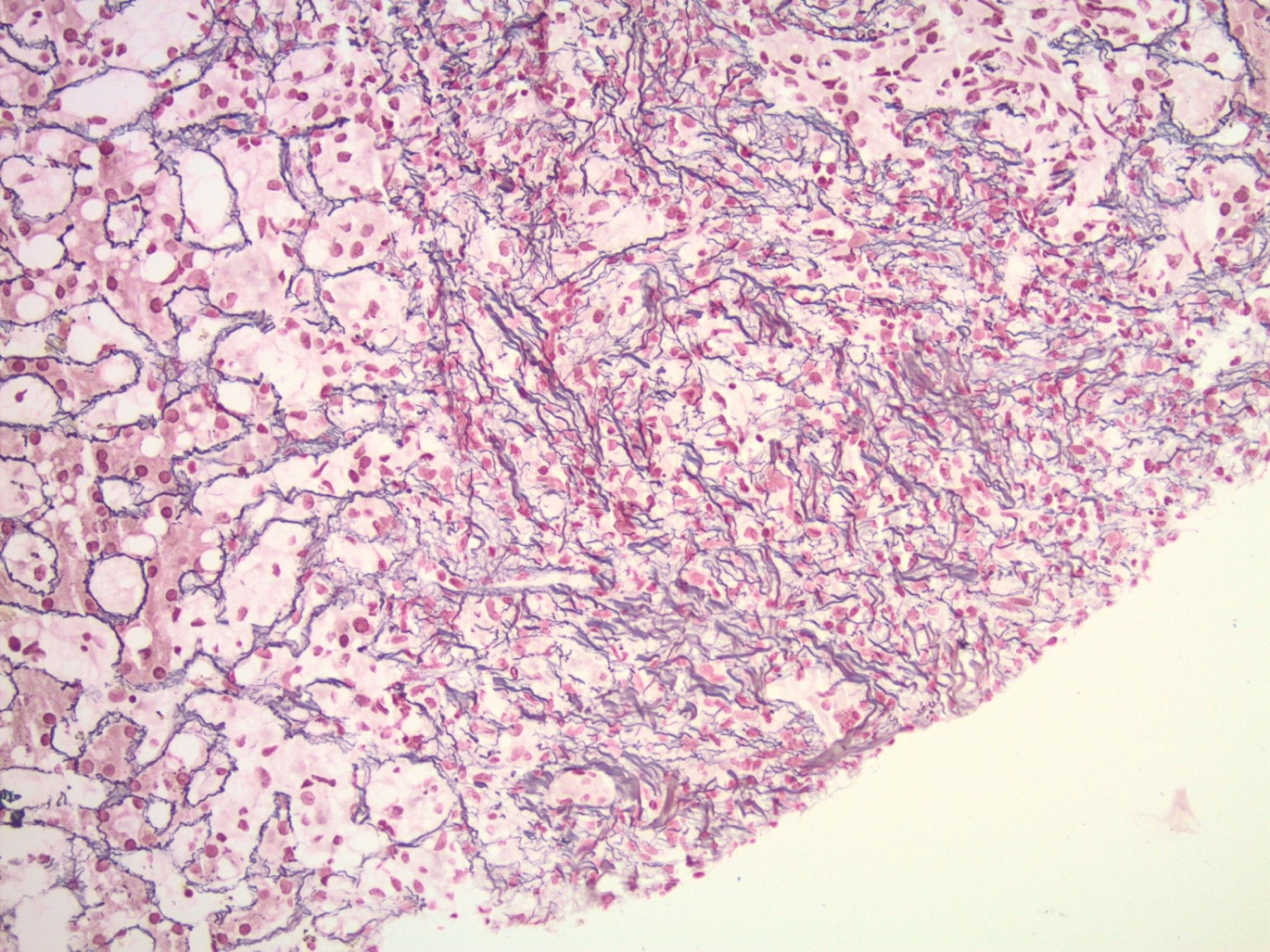
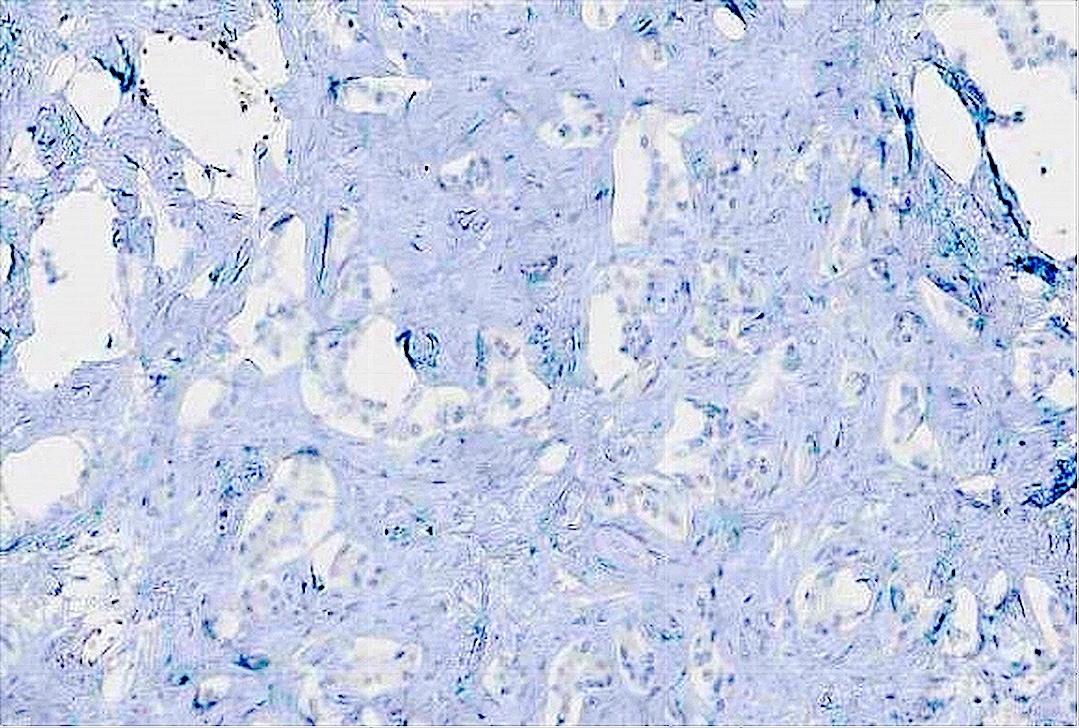
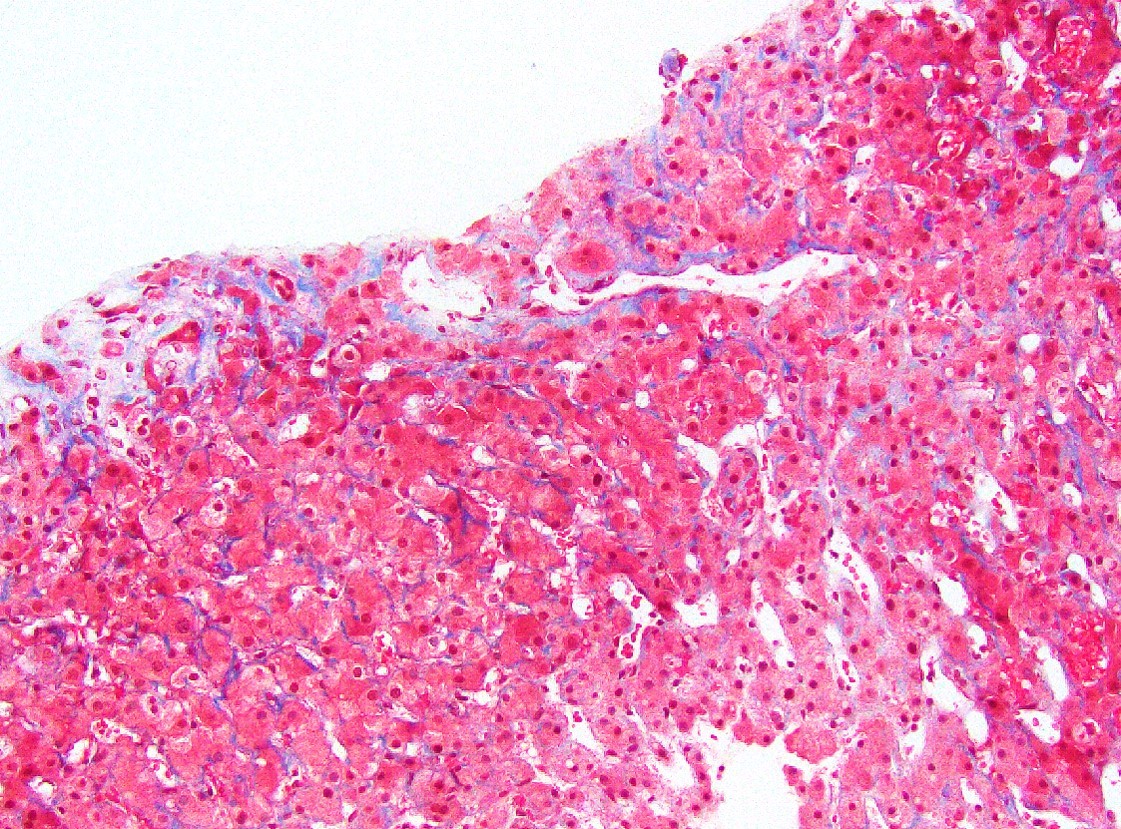
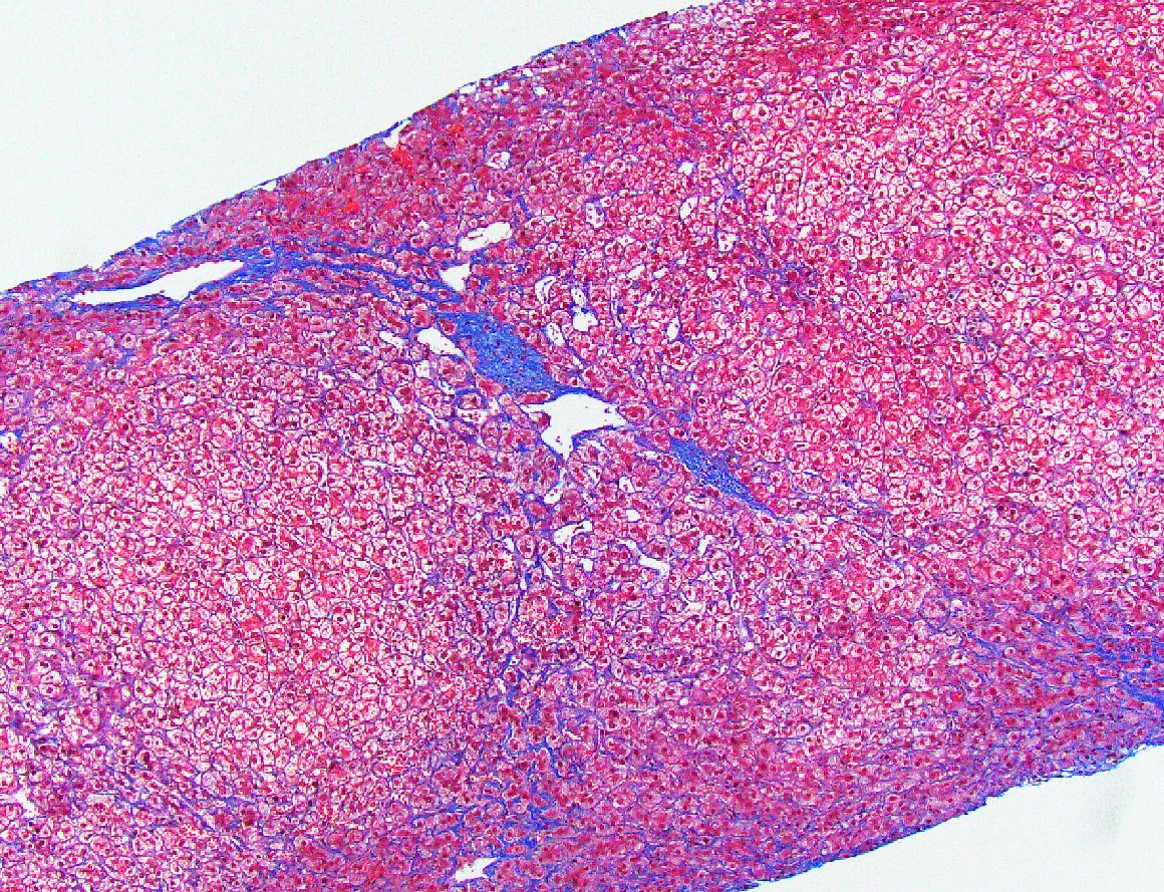
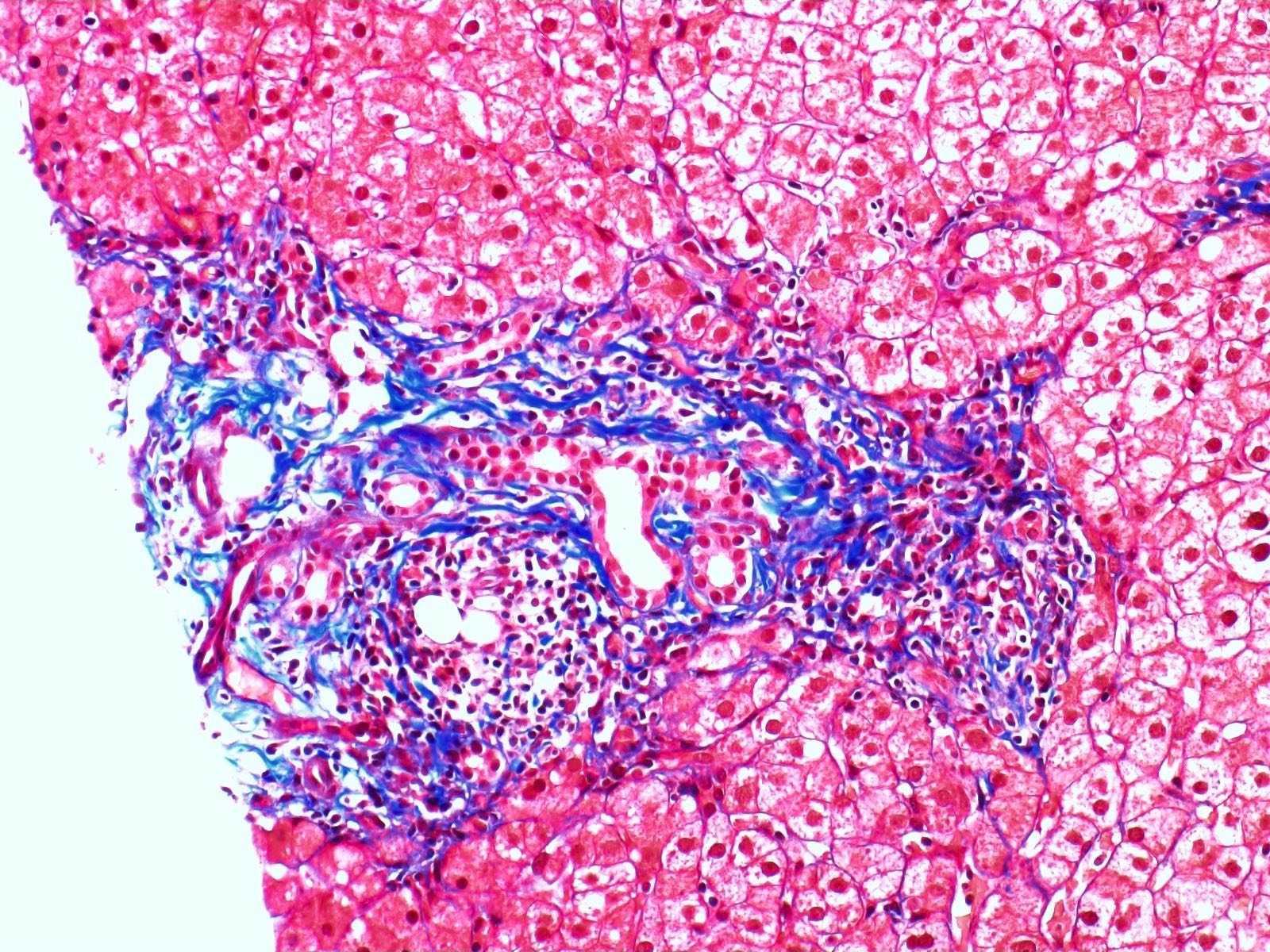
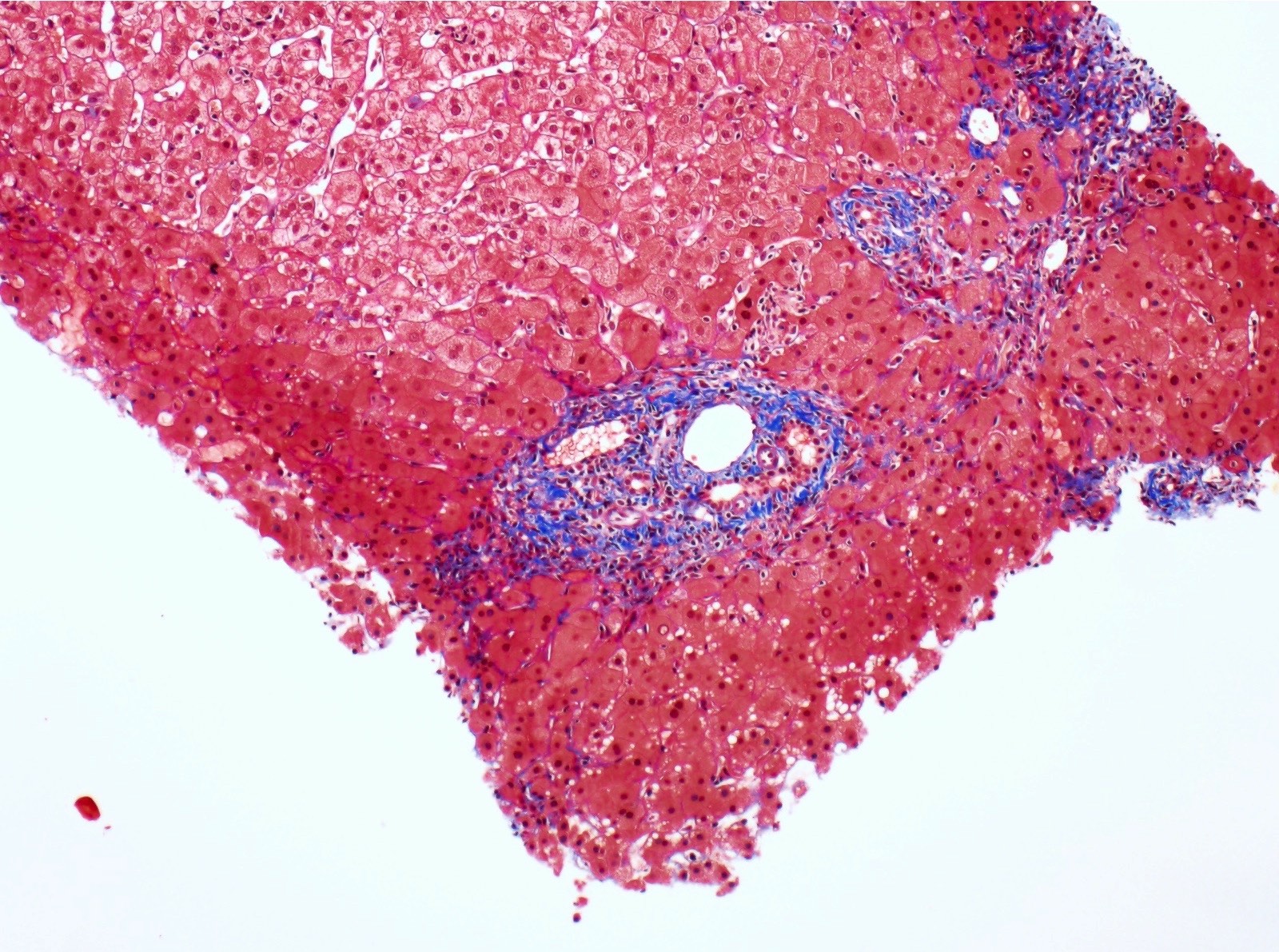
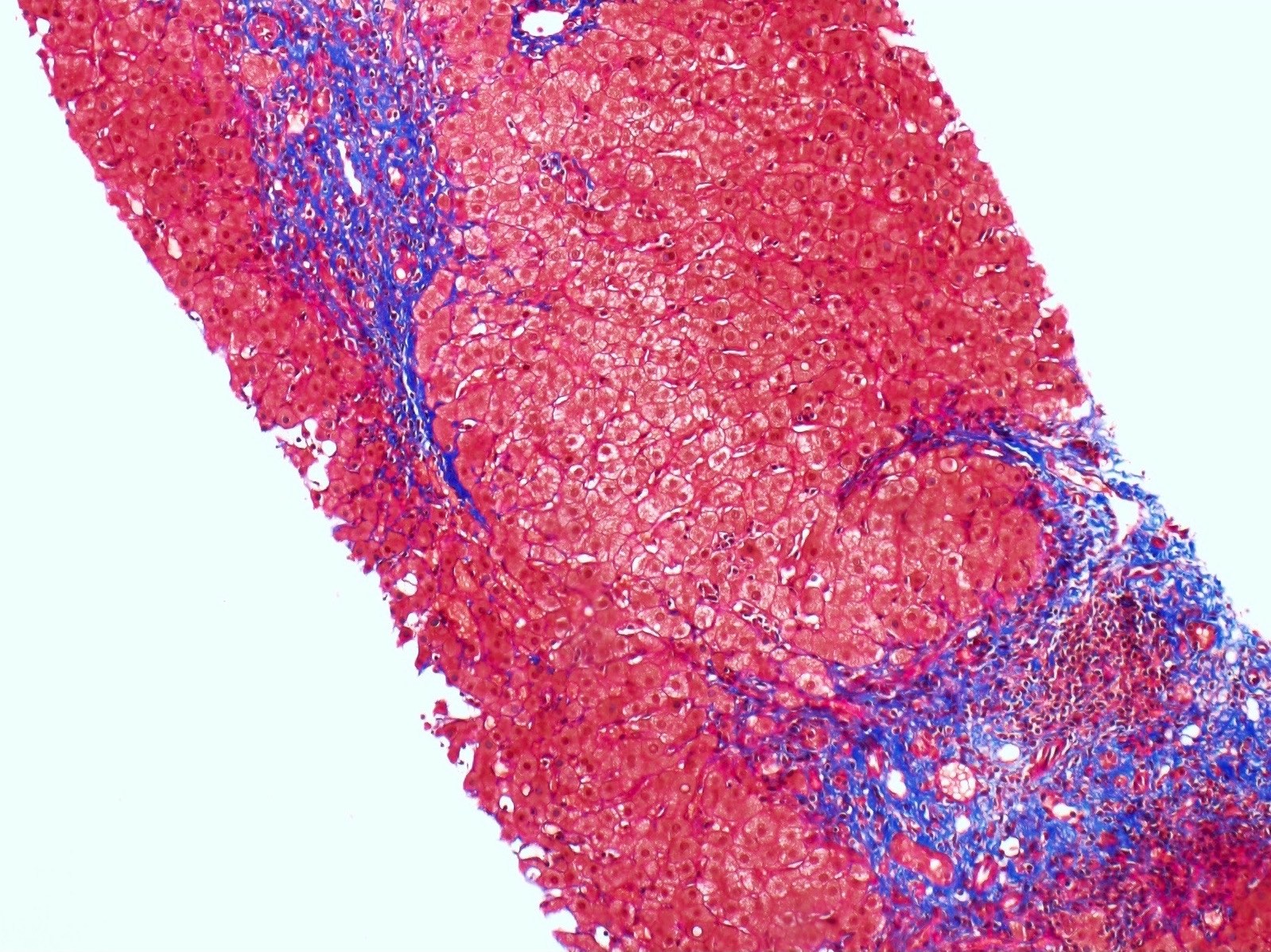
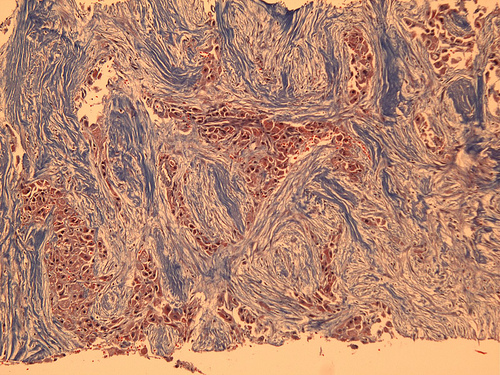
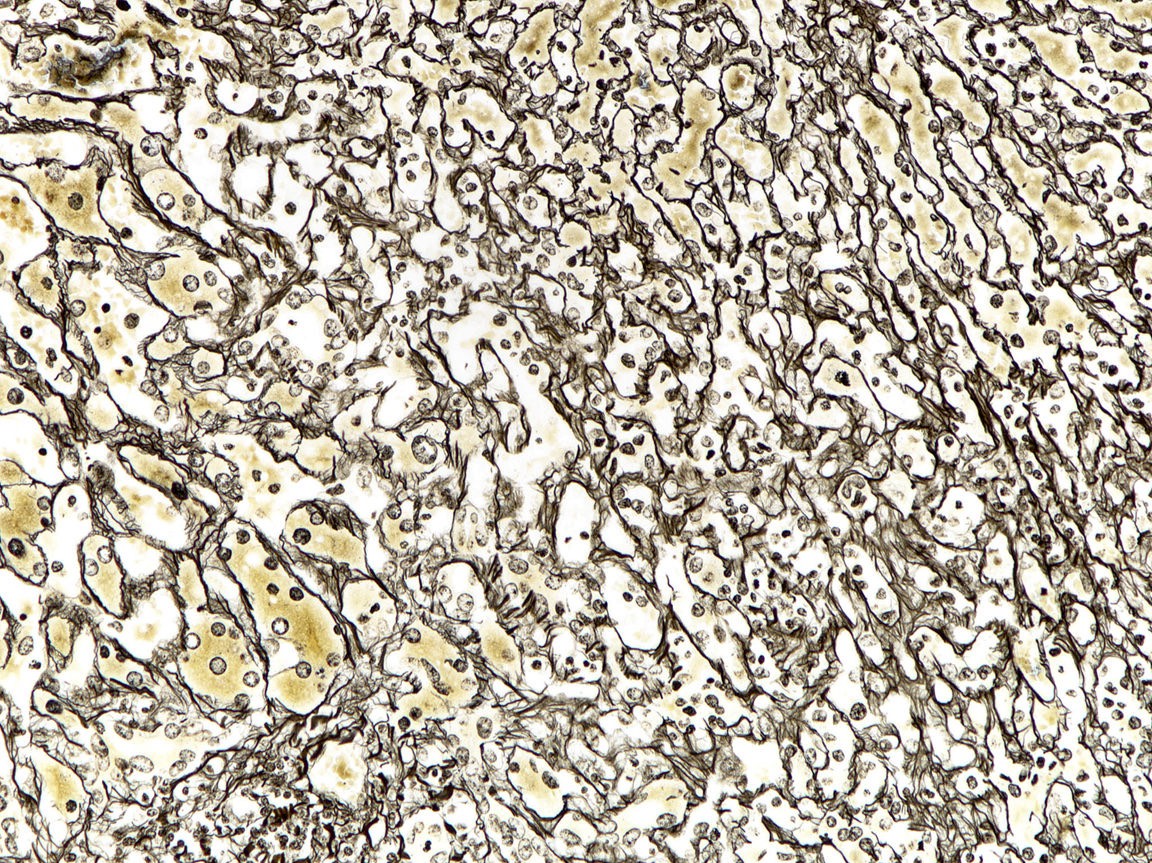
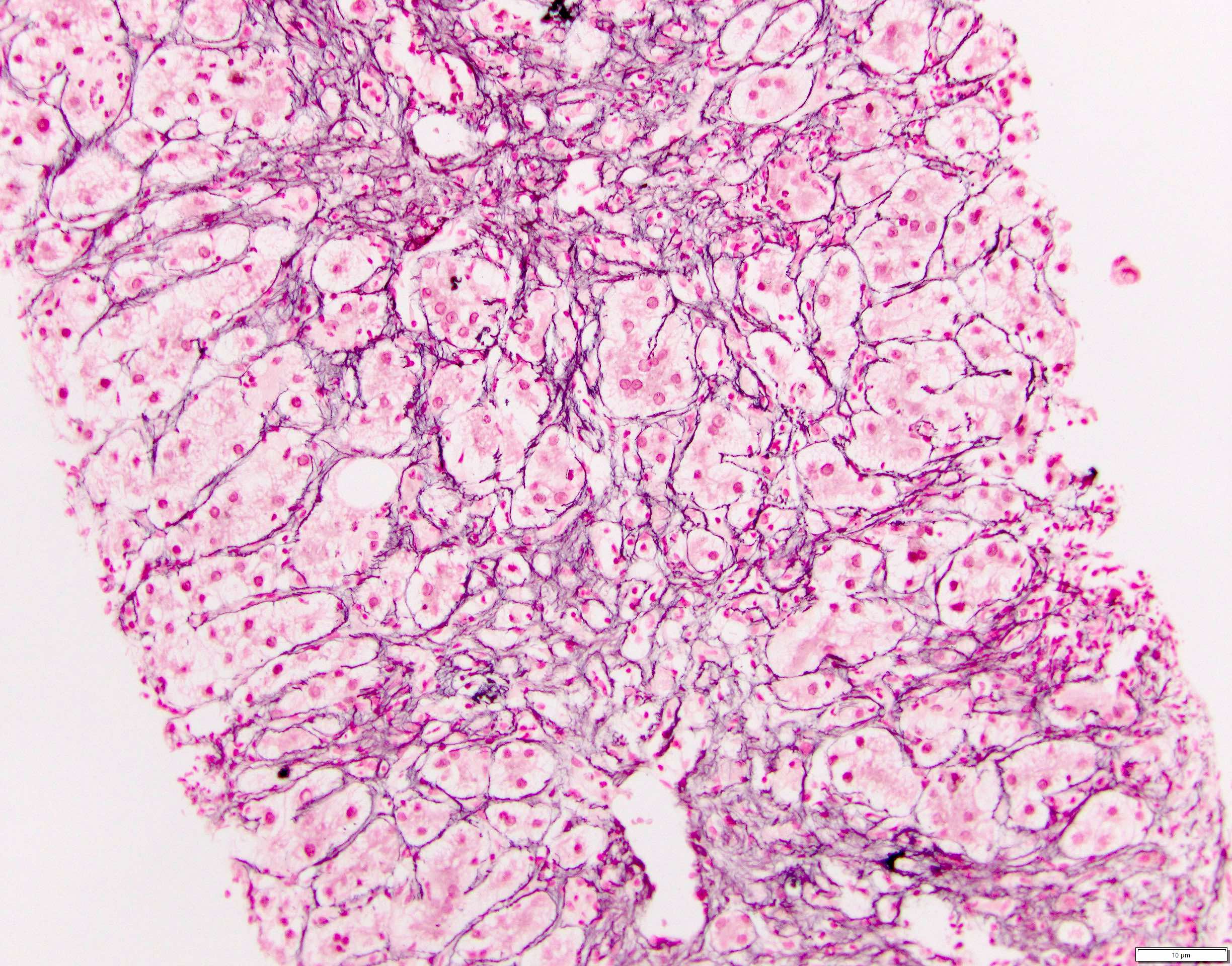
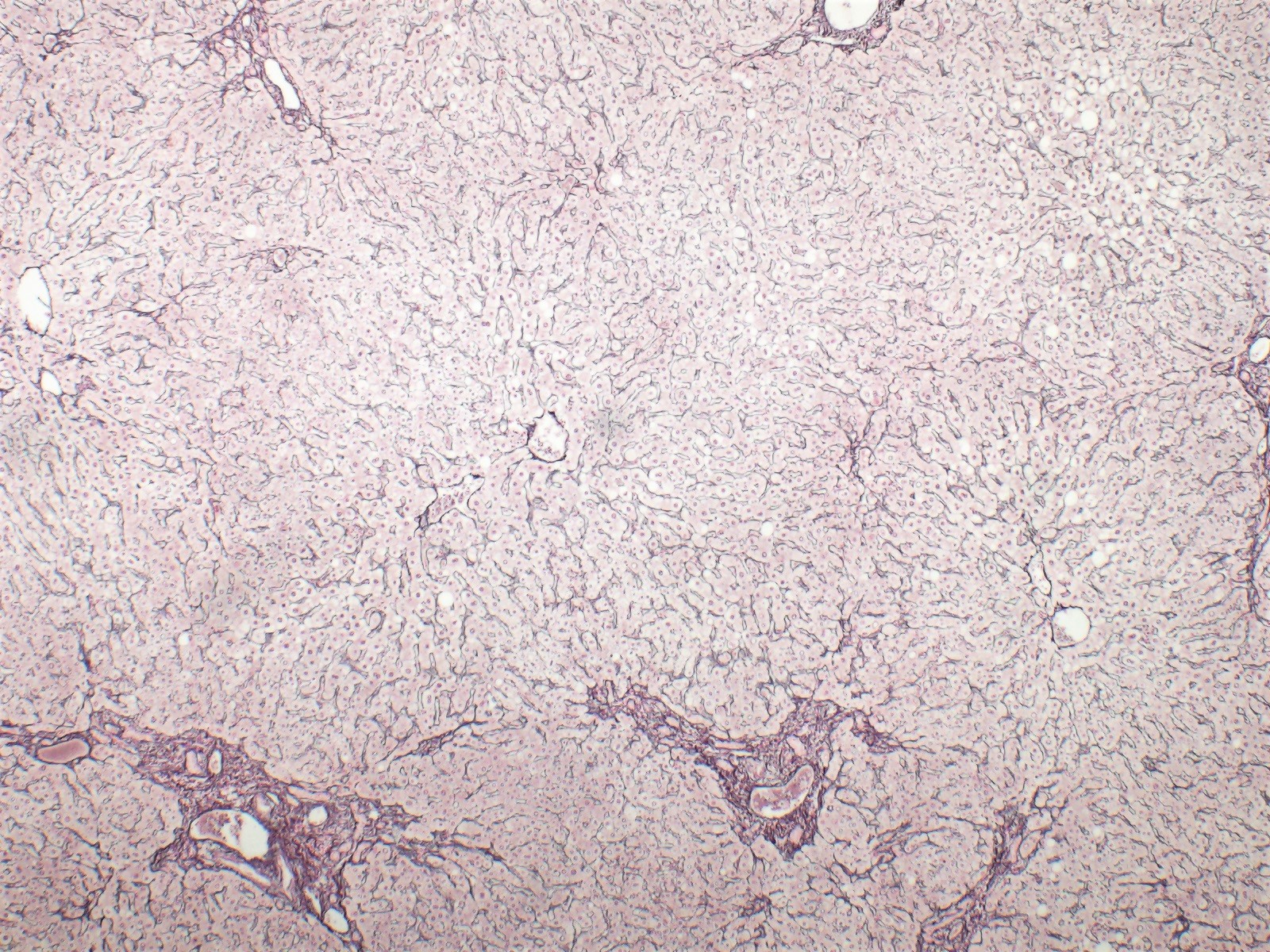
Positive stains
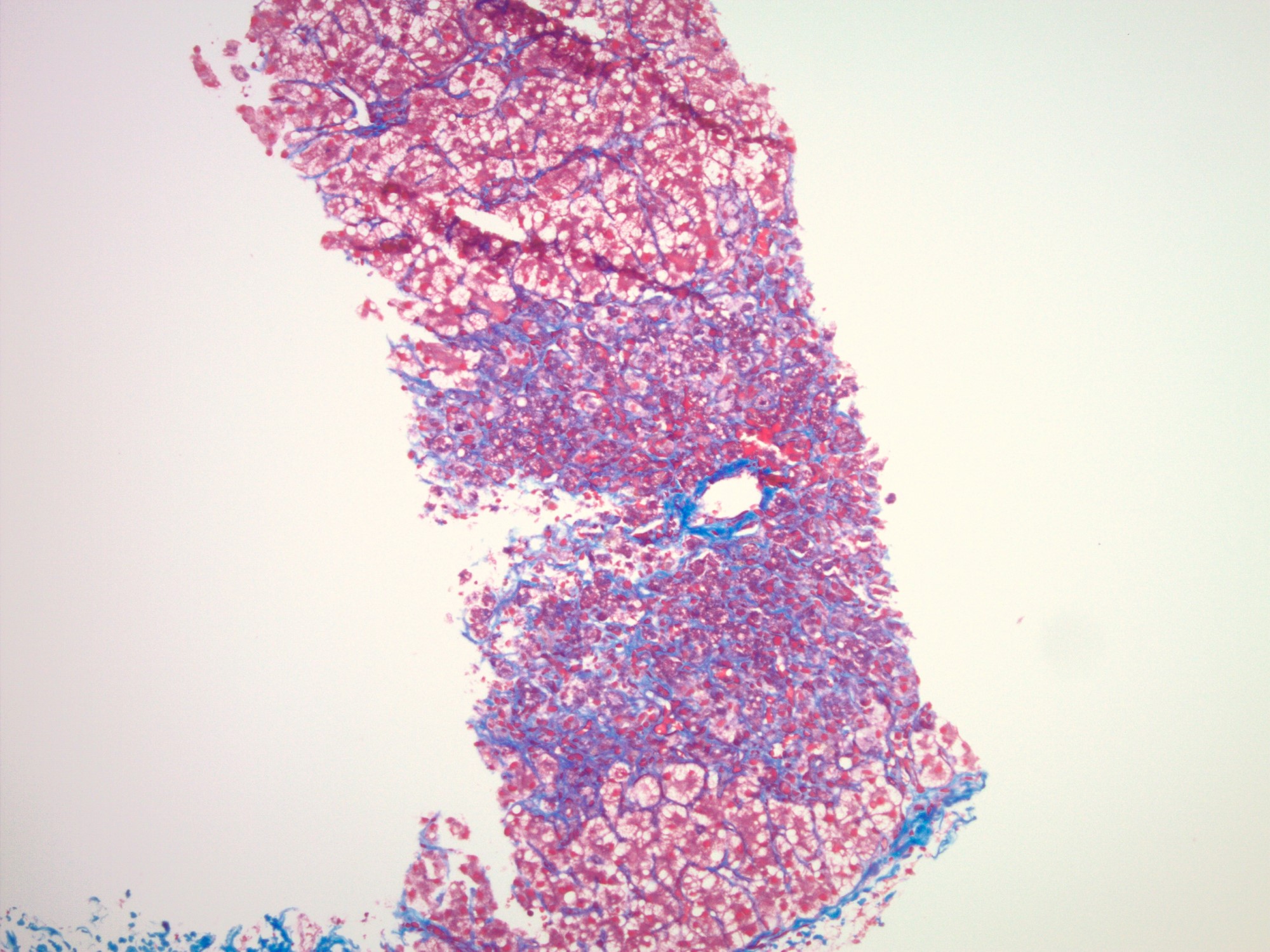
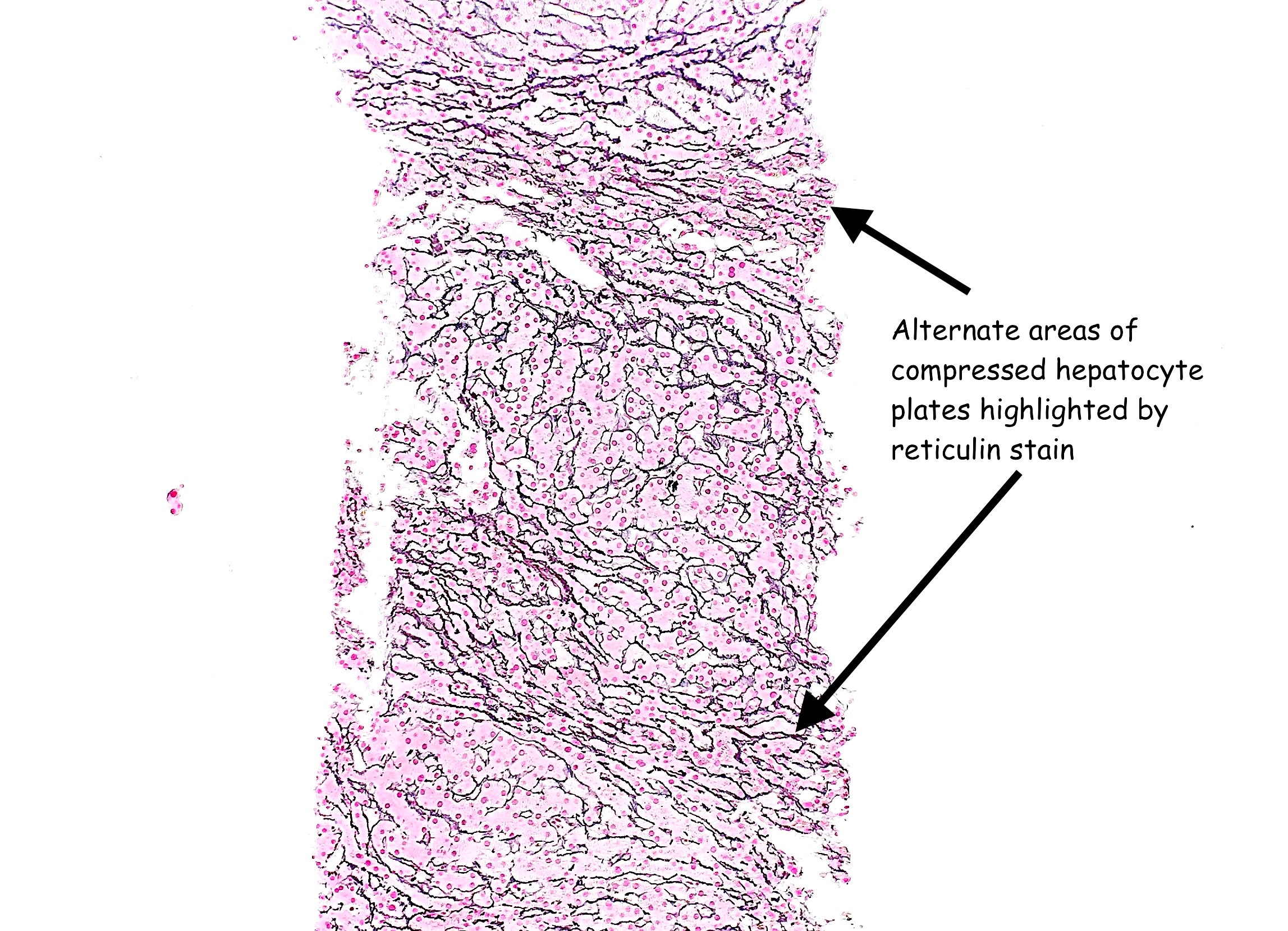
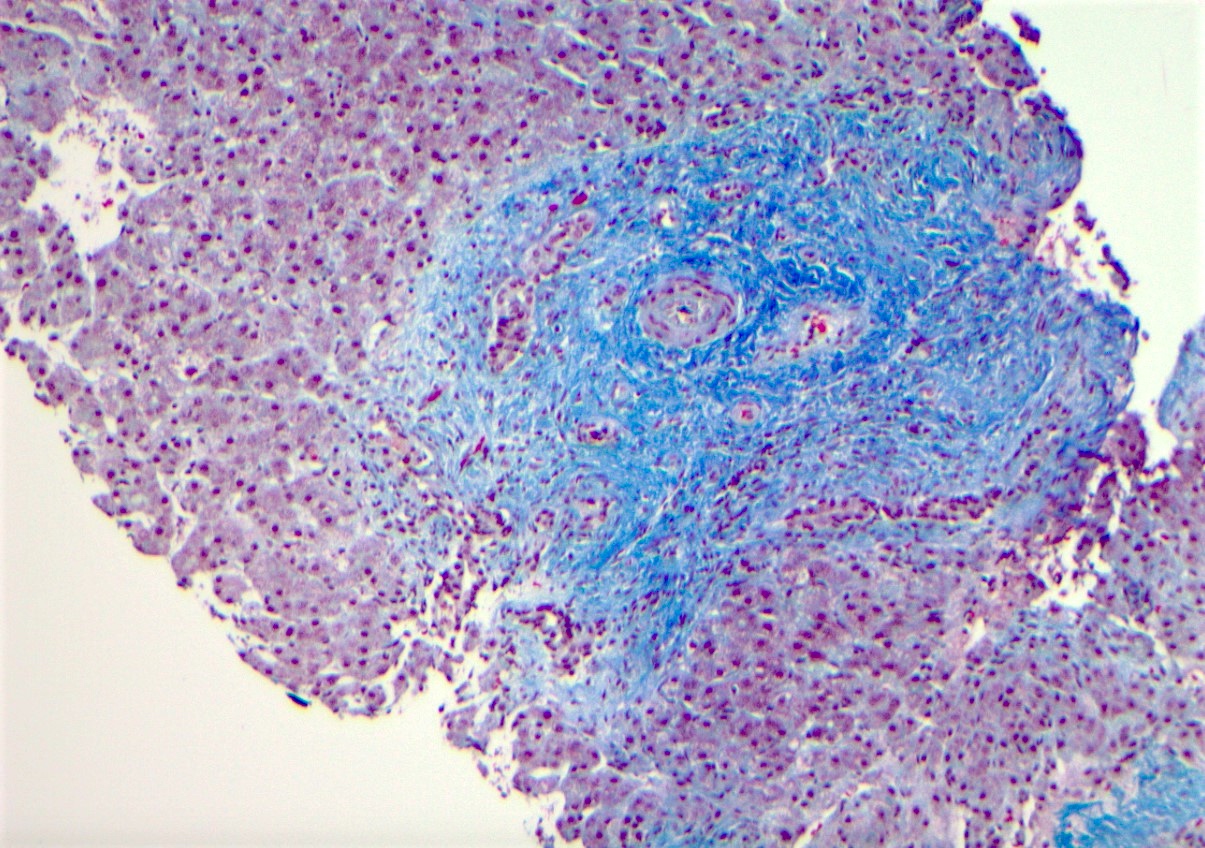
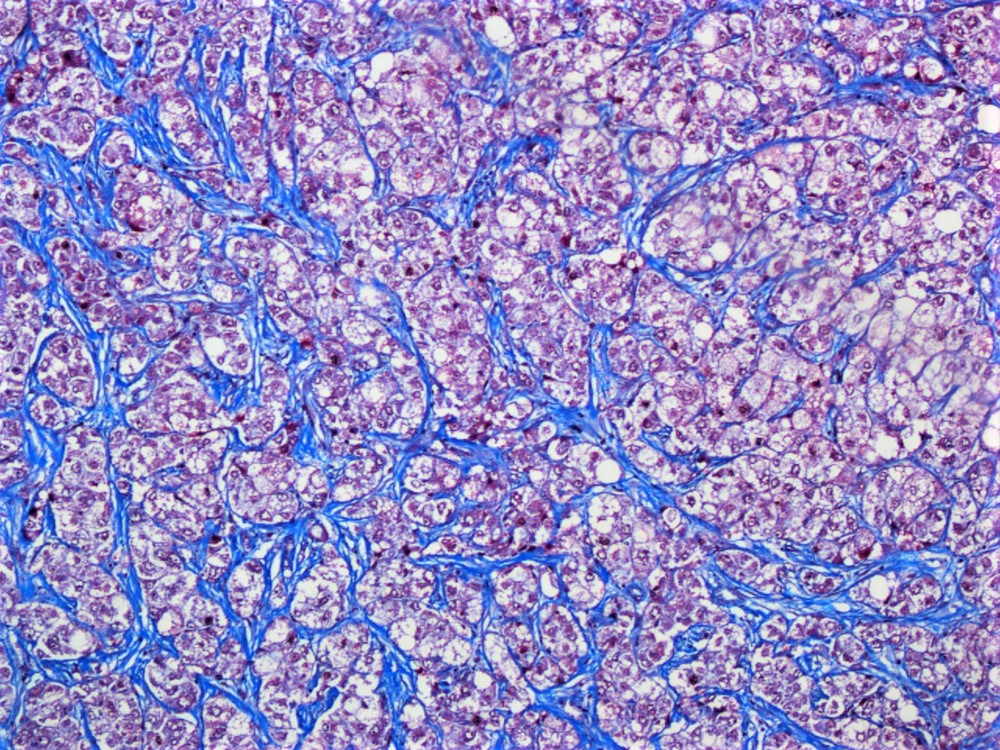
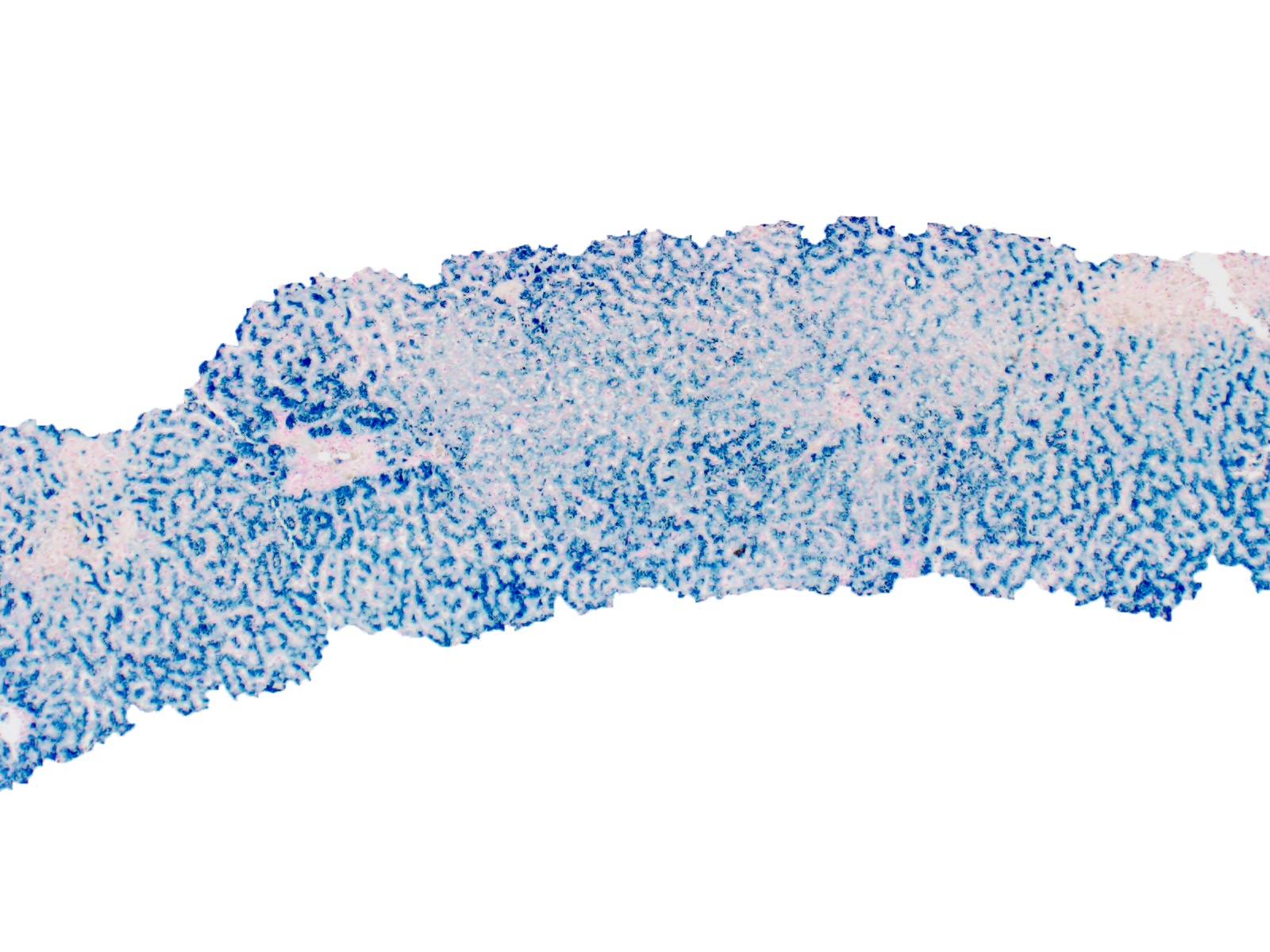
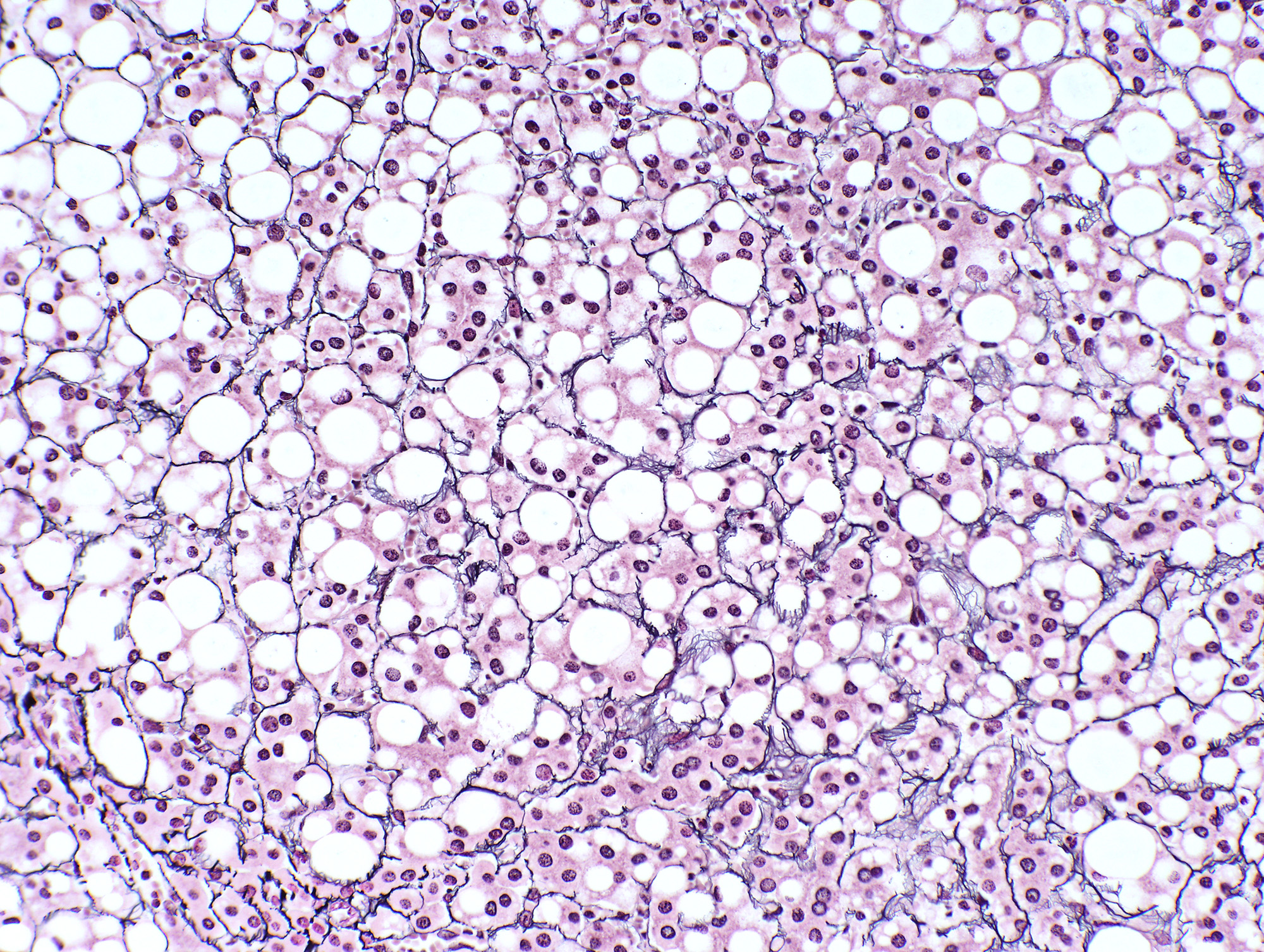
- Reticulin: in areas of parenchymal collapse / necrosis, the reticulin framework will remain and appear condensed as hepatocytes are lost
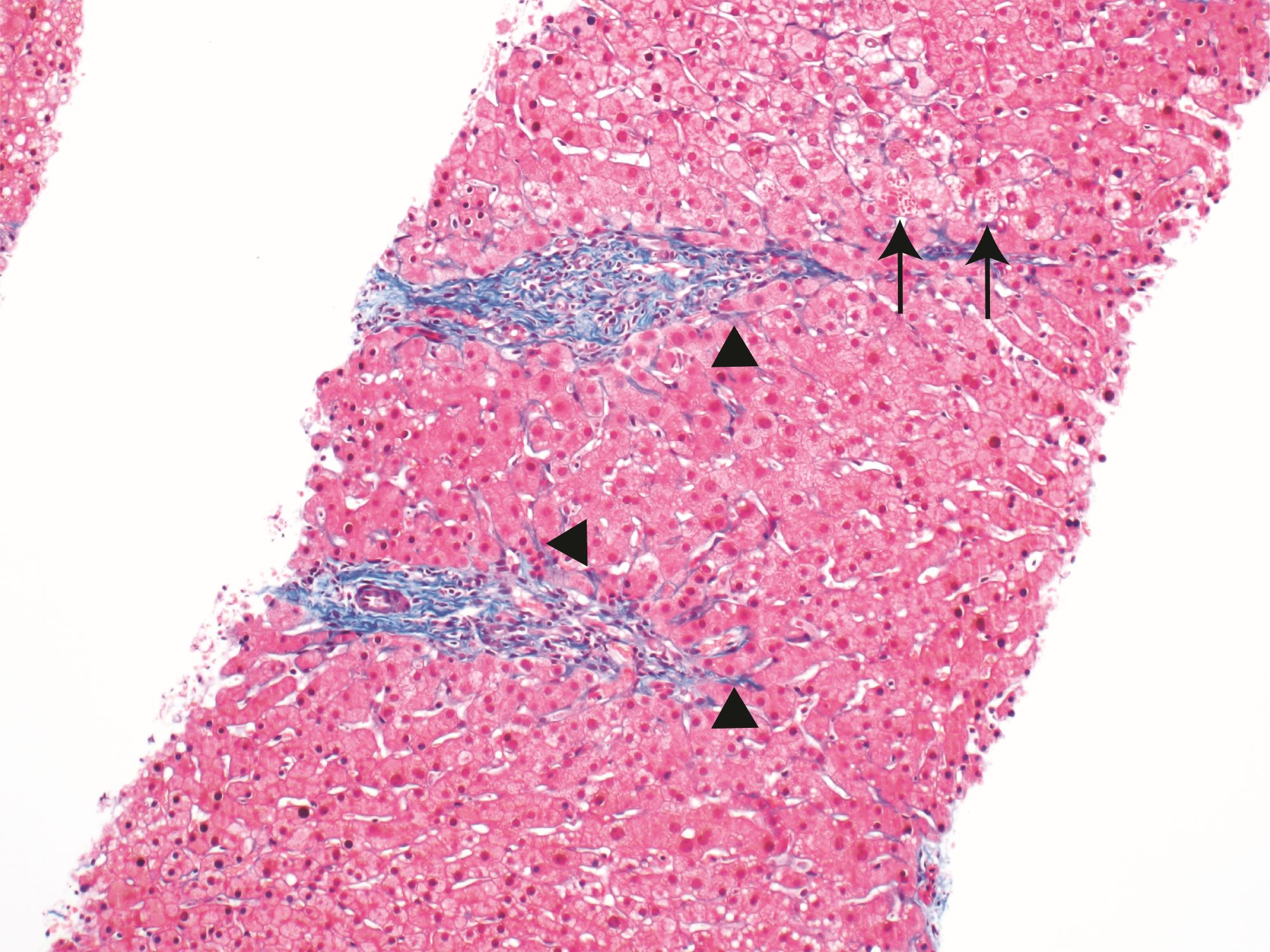
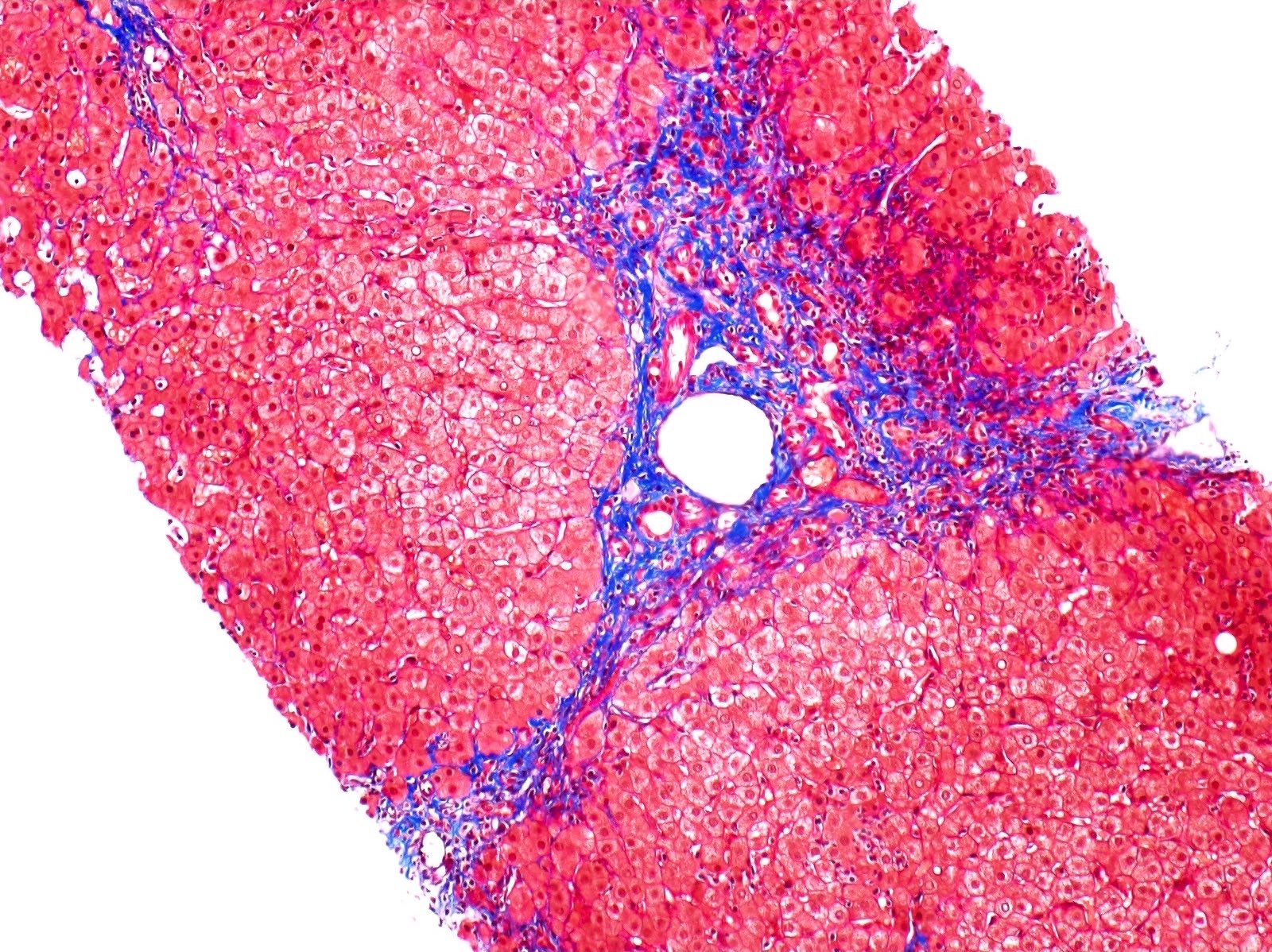
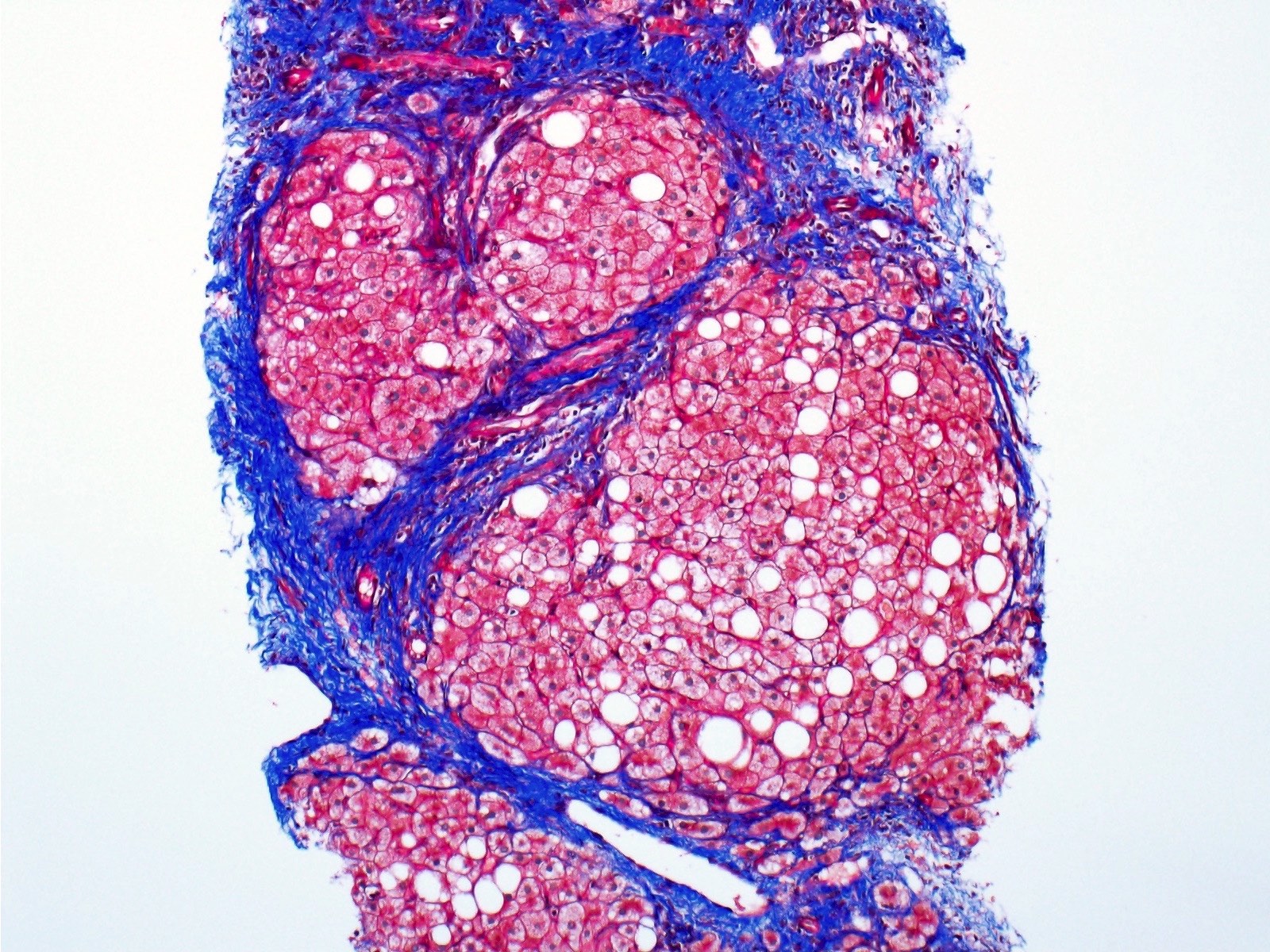
- Trichrome: areas of necrosis and hepatocyte dropout will appear as pale gray-blue staining
- These areas consist of reticulin fibers composed of type 3 collagen and will appear lighter in staining compared to the type 1 collagen fibers
- Reference: Saxena: Practical Hepatic Pathology, 2nd Edition, 2017
Sample pathology report
- Liver, core needle biopsy:
- Zone 3 predominant hepatocyte necrosis with Kupffer cell hyperplasia and early parenchymal collapse (see comment)
- Comment: The biopsy consists of 3 fragments of hepatic parenchyma with zone 3 predominant hepatocyte necrosis, early parenchymal collapse (trichrome stain) and Kupffer cell hyperplasia. Outside of the areas of early parenchymal collapse, there is no significant fibrosis. The lobules contain scattered balloon cells with focal acute inflammation. There is no significant portal inflammation or bile duct injury. The findings are consistent with an acute hepatitis pattern and the differential includes drug induced liver injury. Clinical and serologic correlation is recommended.
Differential diagnosis
- All etiologies listed have similar histologic features with the following subtle differences:
- Viral hepatitis (hepatotropic versus nonhepatotropic):
- Portal infiltrate in hepatitis A may be more robust, contain more plasma cells and there may be spillover across the limiting plate
- Hepatitis E may have a degree of bile pigment accumulation
- Hepatitis C has less ballooning degeneration and fewer apoptotic bodies, compared to other viruses (Liver 1981;1:201)
- EBV infection will show an activated lymphocytic inflammatory infiltrate in sinusoids and portal tracts
- Drug induced liver injury (direct toxins versus idiosyncratic drug reactions):
- Some cases have ductular reaction, neutrophilic inflammation, Kupffer cells, bile duct injury, prominent eosinophils, granulomas, cholestasis
- Autoimmune hepatitis:
- Typically, plasma cell rich inflammation in lobules and portal tracts, occasionally with emperipolesis
- Acute alcoholic hepatitis:
- Numerous ballooned hepatocytes with Mallory hyaline formation, neutrophilic lobular inflammation and occasional lobular cholestasis
- Central hyaline sclerosis
- Nonviral infections (Kupffer cell hyperplasia, cholestasis, steatosis, granulomas)
- Wilson disease:
- Lipofuscin and copper accumulation
- Often shows some degree of liver fibrosis already at the time of acute liver failure
- Viral hepatitis (hepatotropic versus nonhepatotropic):
Additional references
Board review style question #1
Which statement regarding acute hepatitis is true?
- Antibiotics are not considered a drug class that can cause an acute hepatitis
- Hepatitis A and nonhepatotropic viruses do not lead to chronic liver disease
- Hepatitis C can lead to acute liver failure in pregnant women
- Portal fibrosis and neoangiogenesis are features of acute hepatitis
Board review style answer #1
B. Hepatitis A and nonhepatotropic viruses do not lead to chronic liver disease
Chronic viral hepatitis is only caused by hepatotropic viruses (mainly B and C). Portal fibrosis and neoangiogenesis are considered patterns of chronic injury and are not seen in acute hepatitis. Acute hepatitis can be seen in drug induced liver injury. The most common drugs include antibiotics, neurologic drugs, NSAIDs, statins, cardiovascular agents and immunomodulatory drugs. 30% of hepatitis E infections can lead to acute liver failure in pregnant women.
Comment Here
Reference: Acute hepatitis-general
Chronic viral hepatitis is only caused by hepatotropic viruses (mainly B and C). Portal fibrosis and neoangiogenesis are considered patterns of chronic injury and are not seen in acute hepatitis. Acute hepatitis can be seen in drug induced liver injury. The most common drugs include antibiotics, neurologic drugs, NSAIDs, statins, cardiovascular agents and immunomodulatory drugs. 30% of hepatitis E infections can lead to acute liver failure in pregnant women.
Comment Here
Reference: Acute hepatitis-general
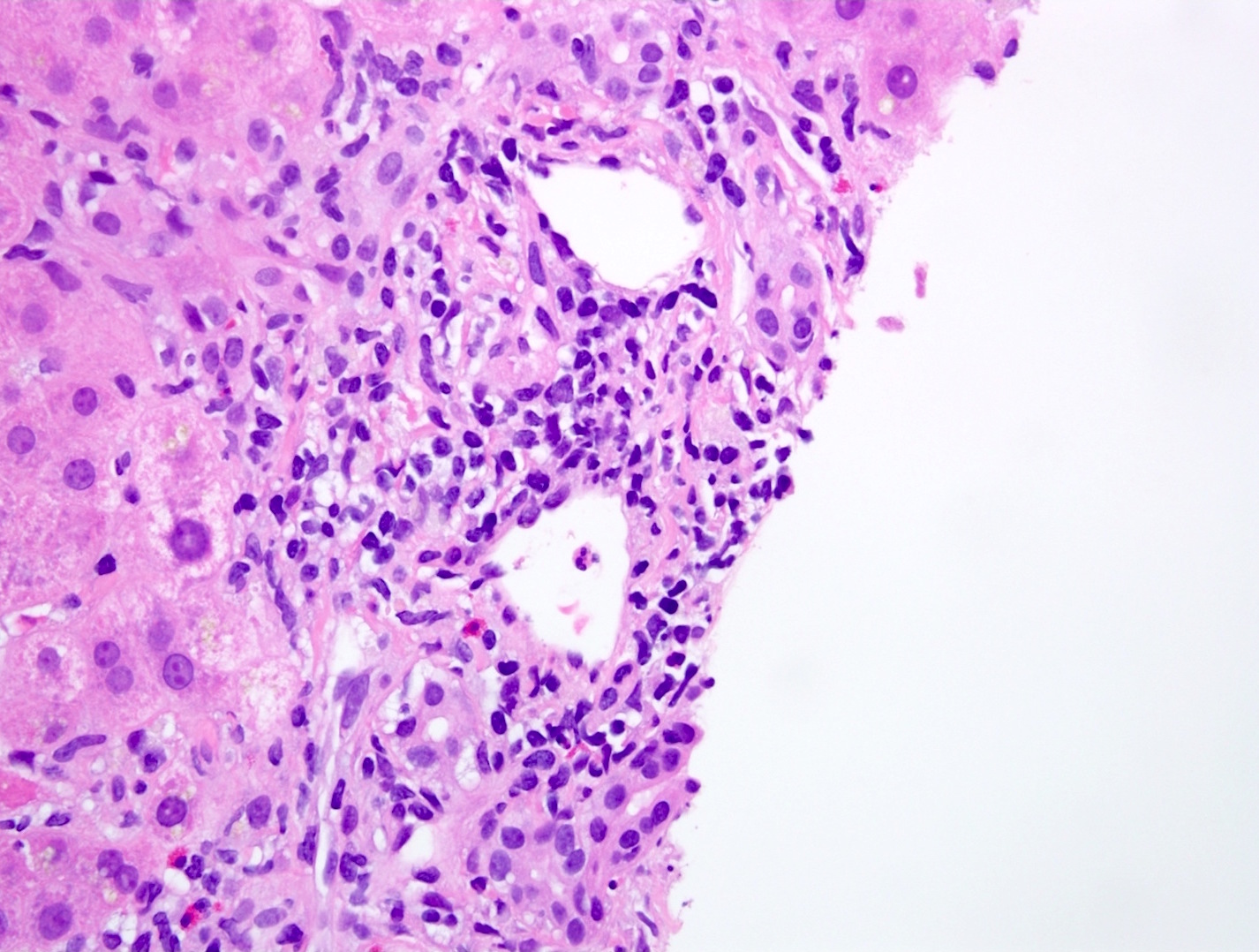
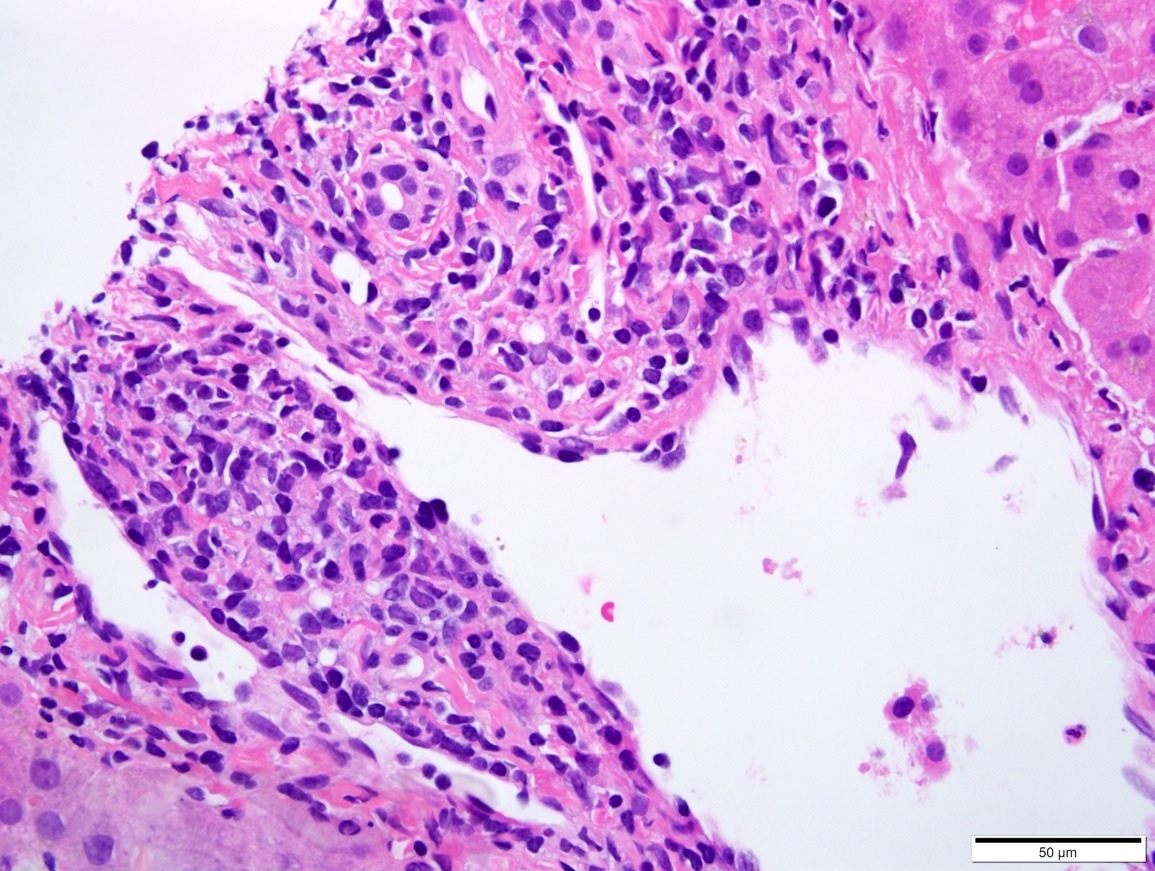
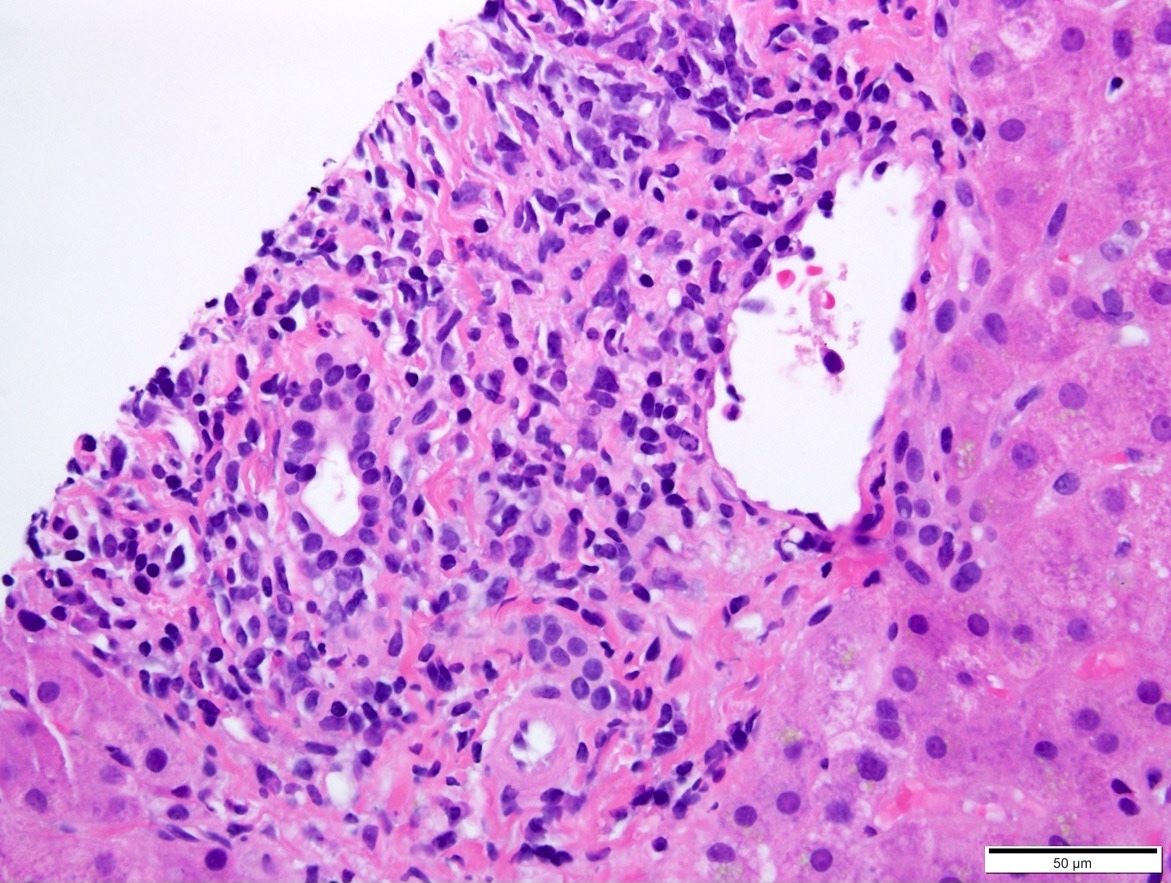
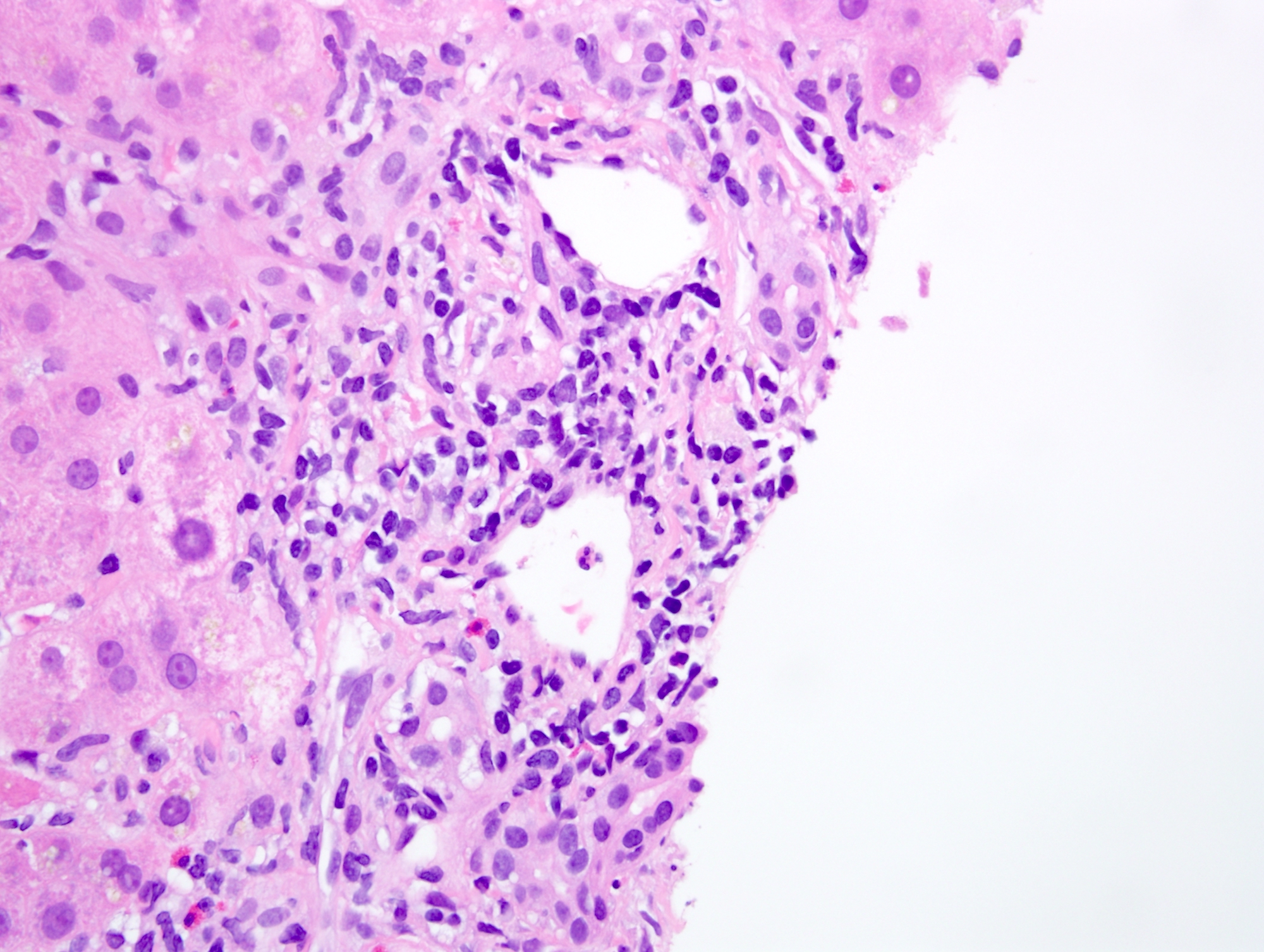
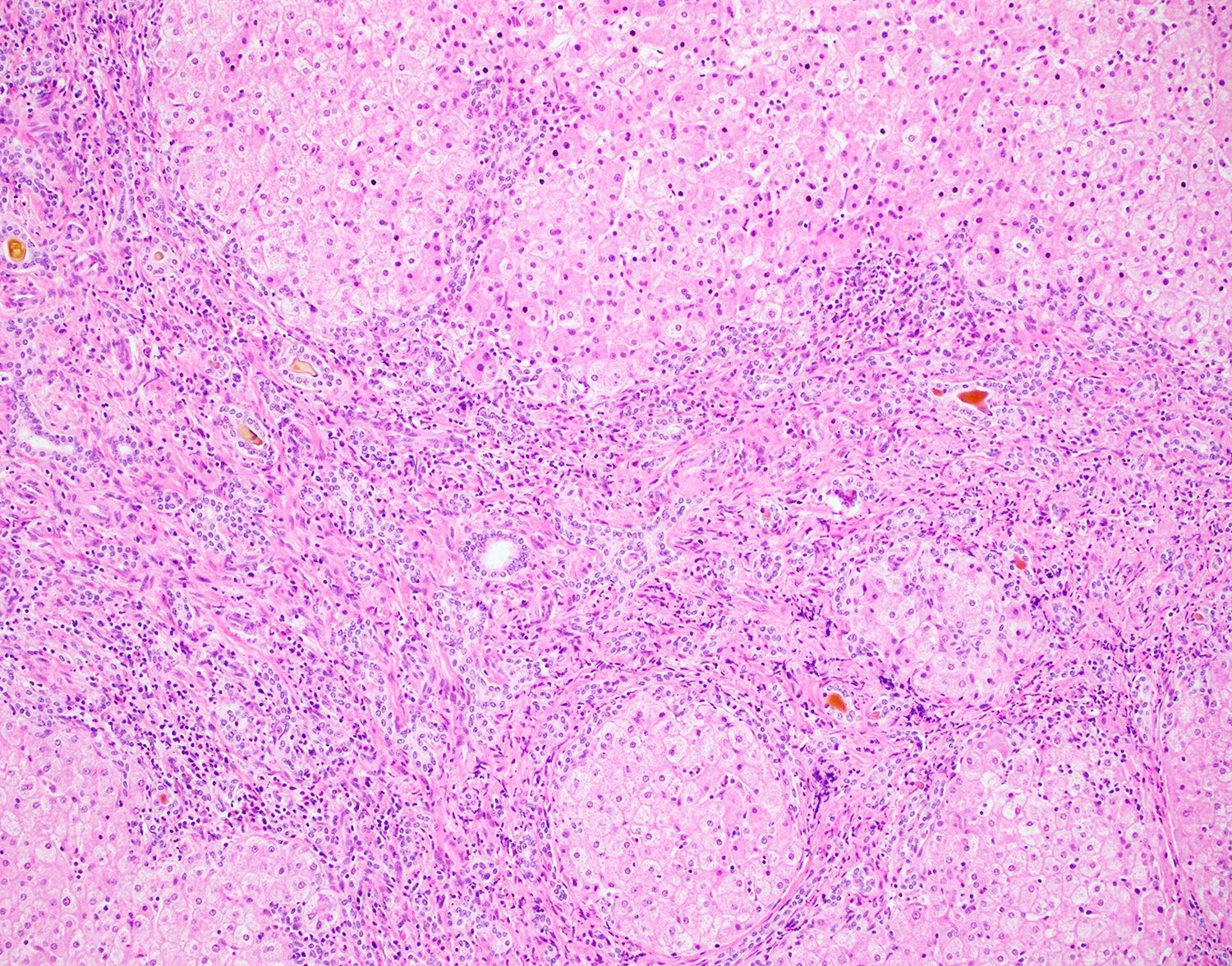
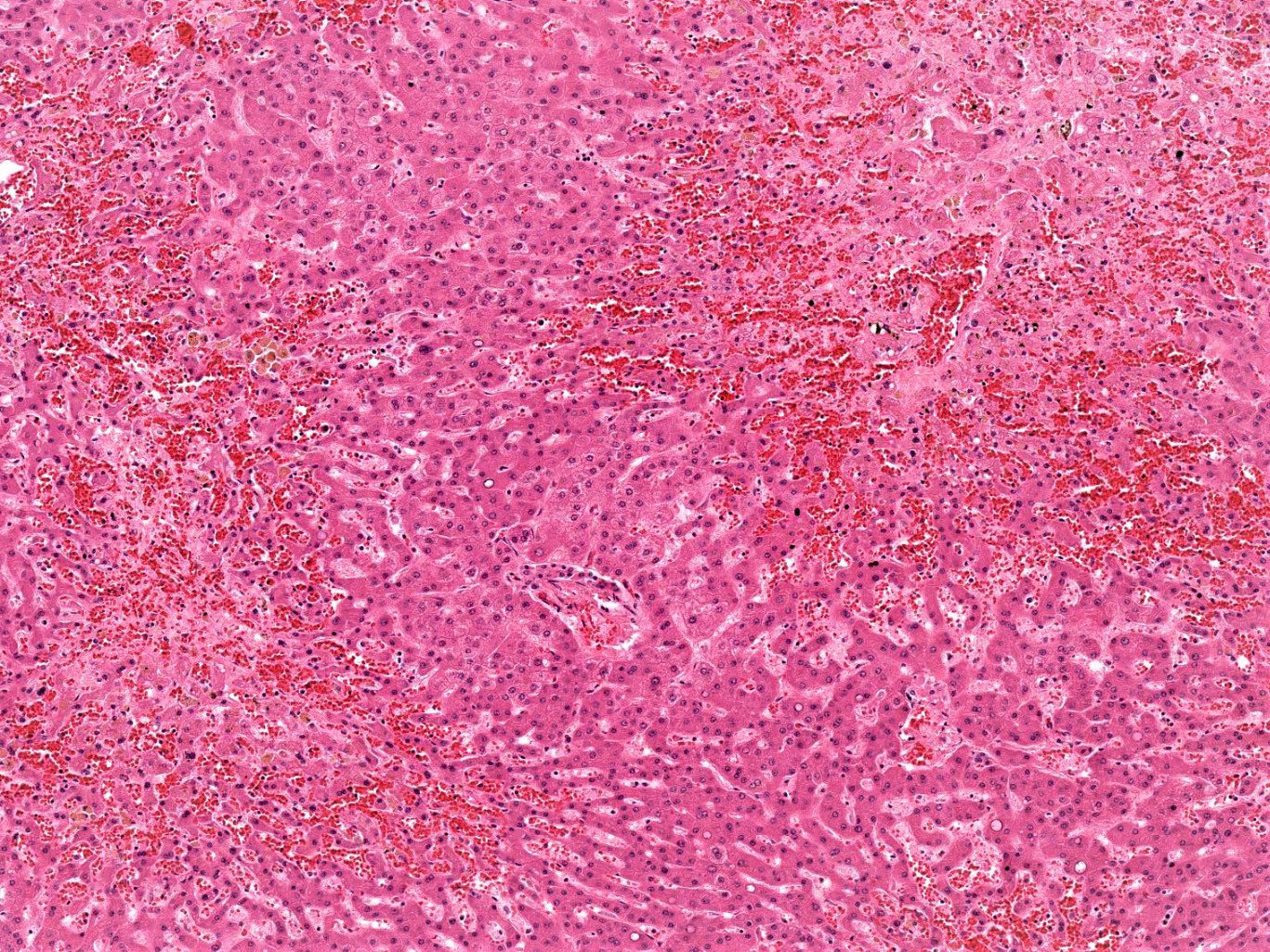
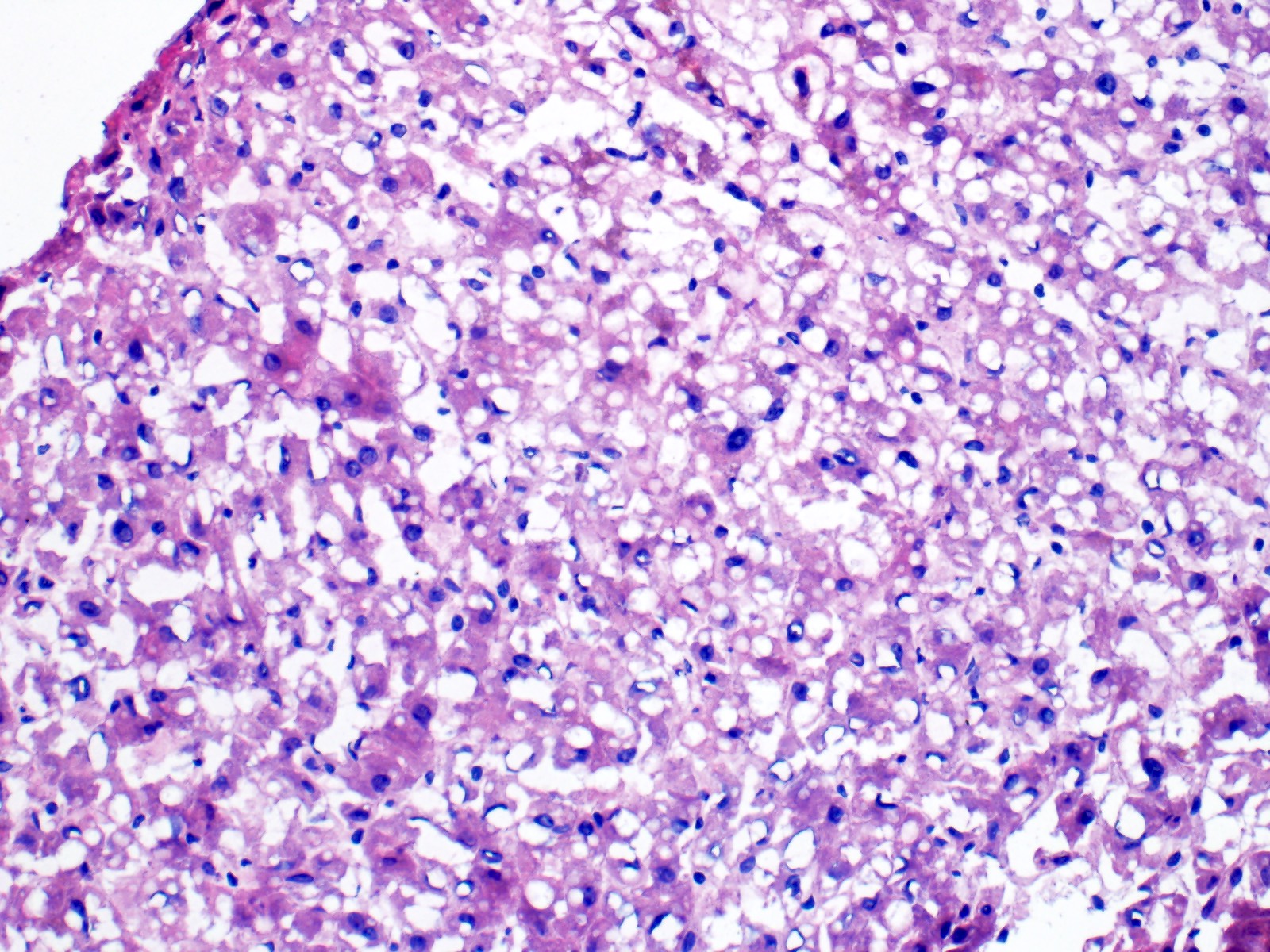
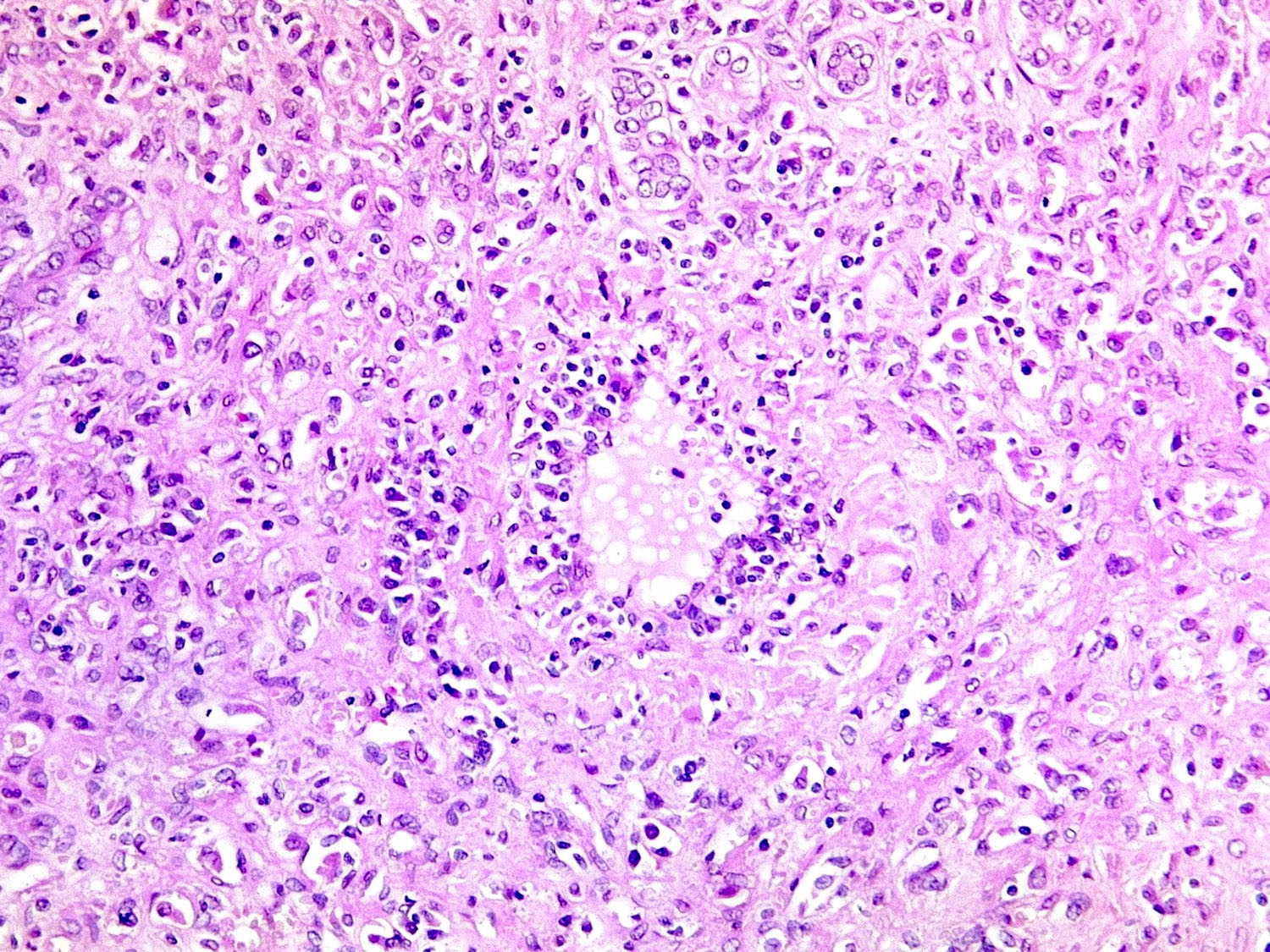
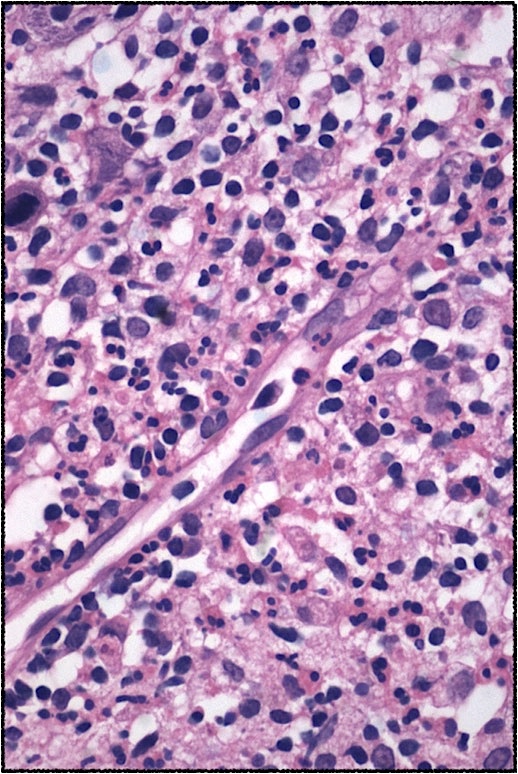
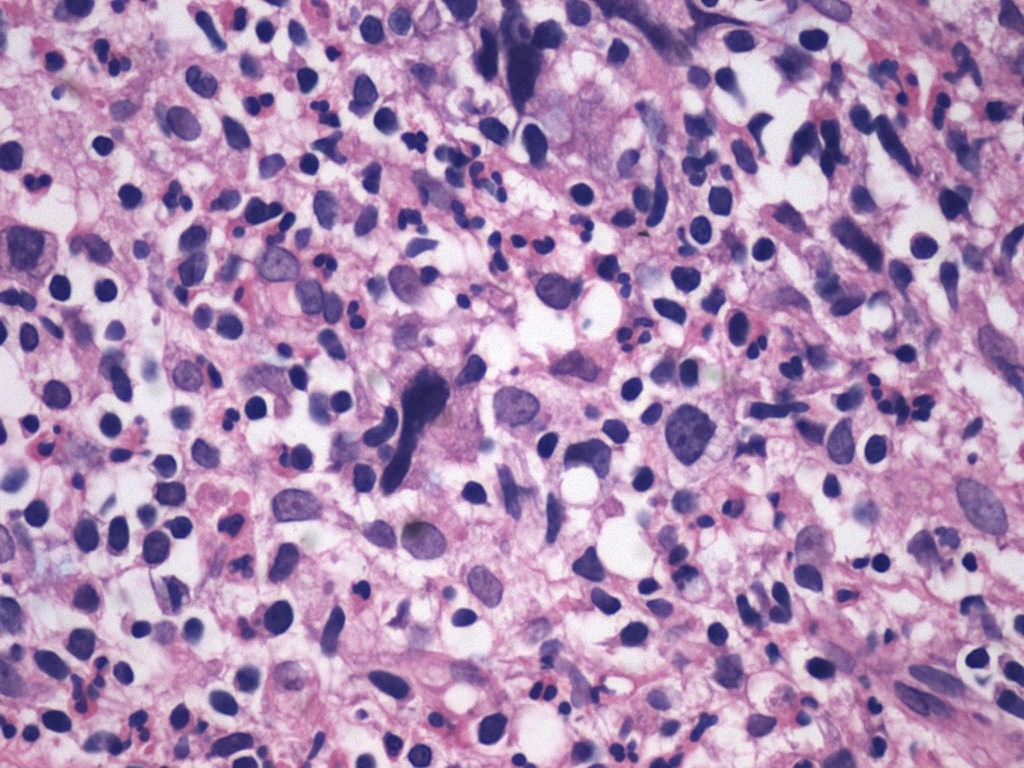
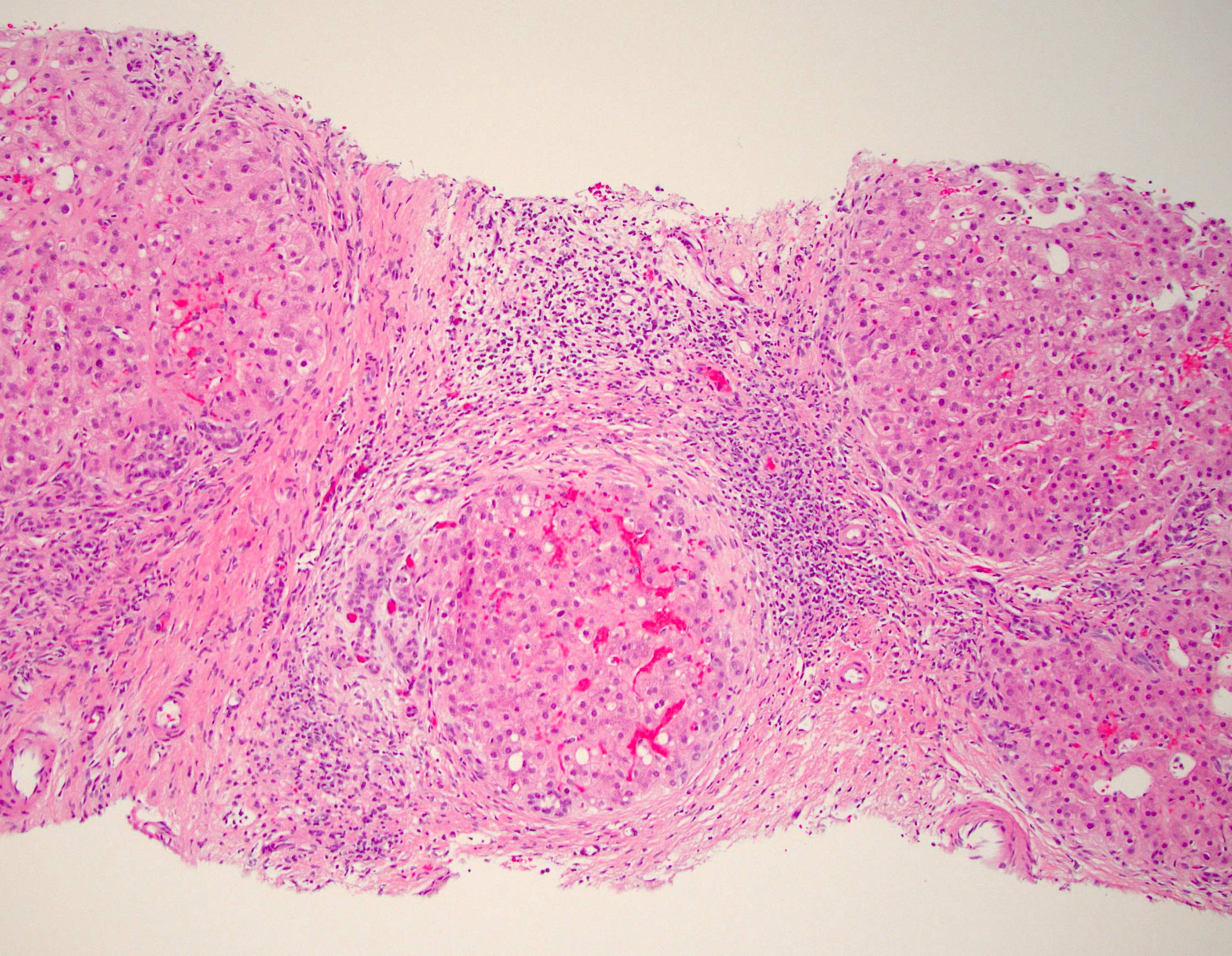
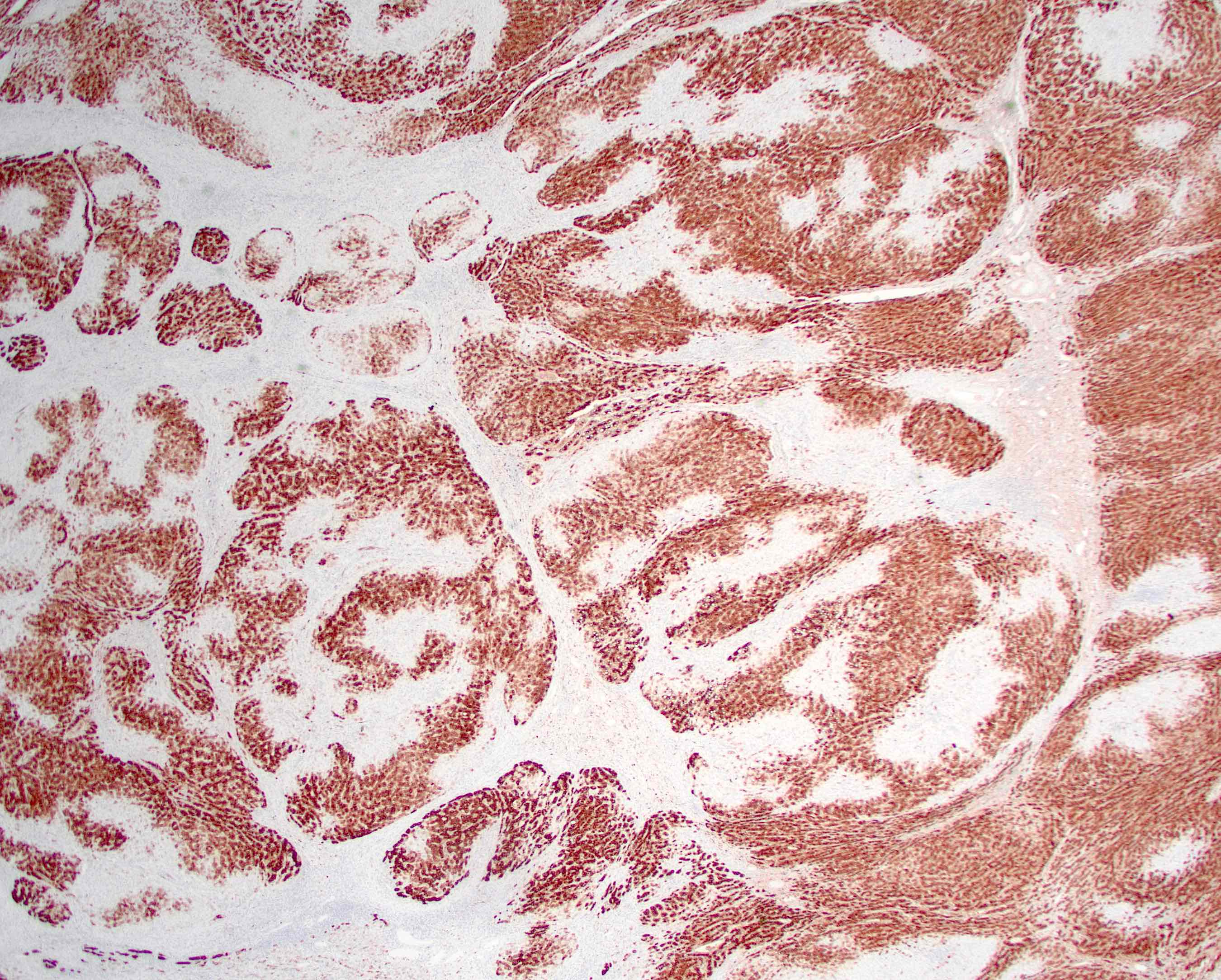
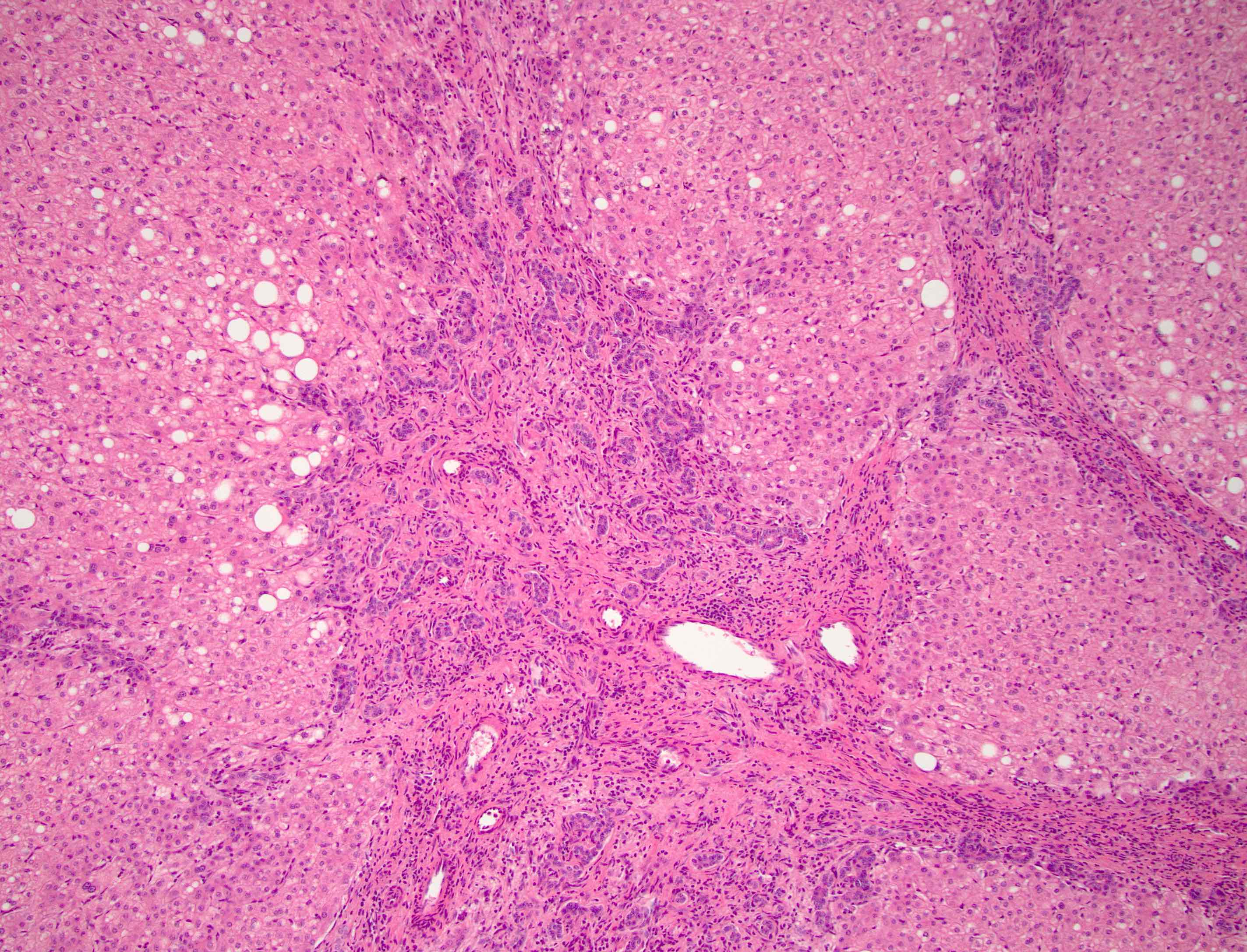
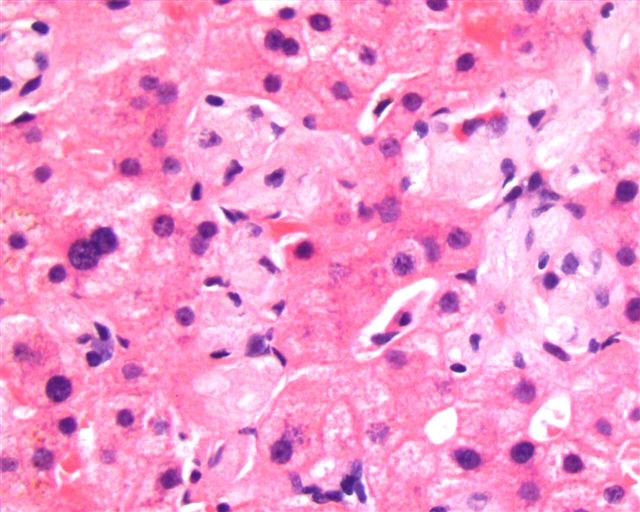
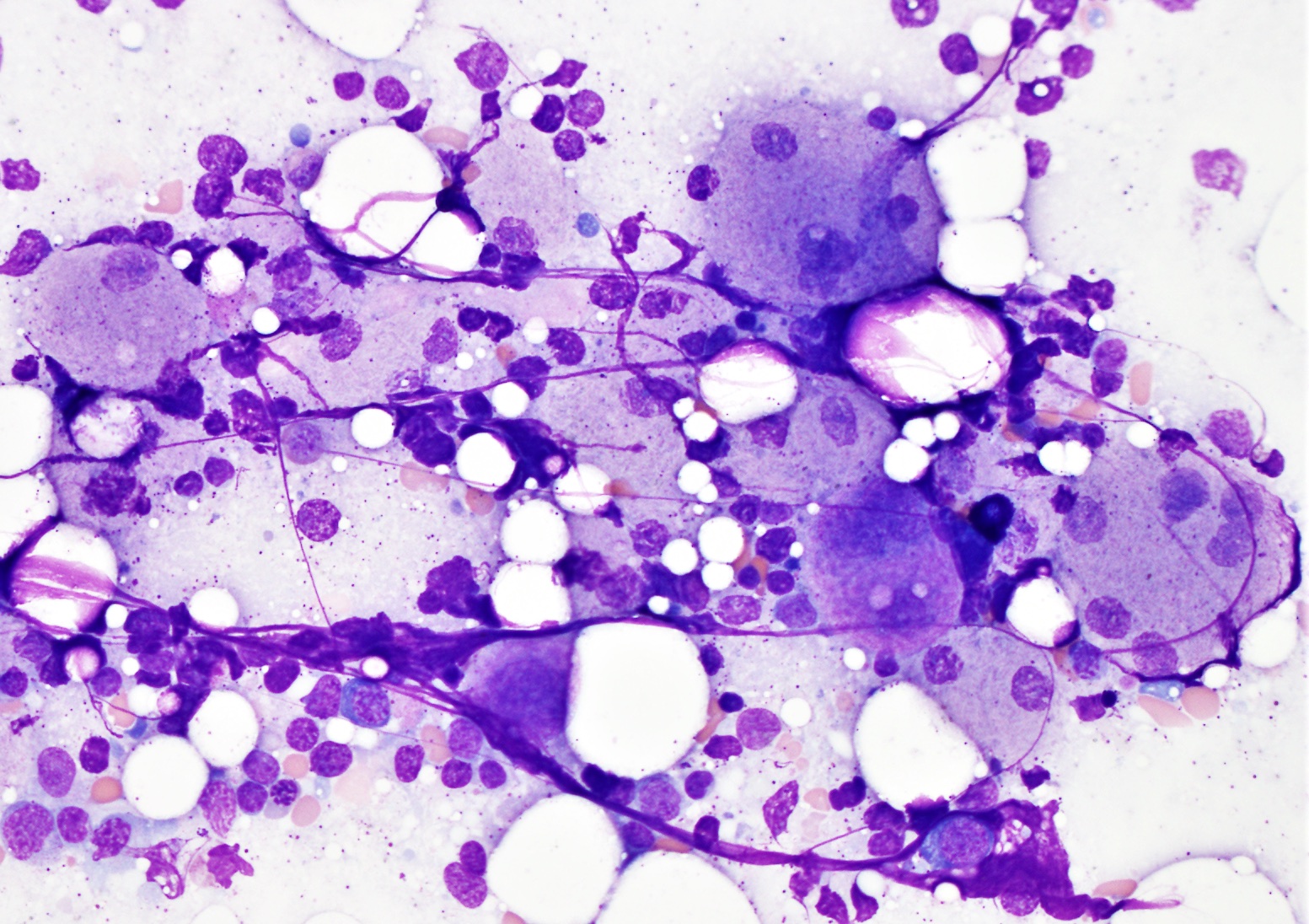
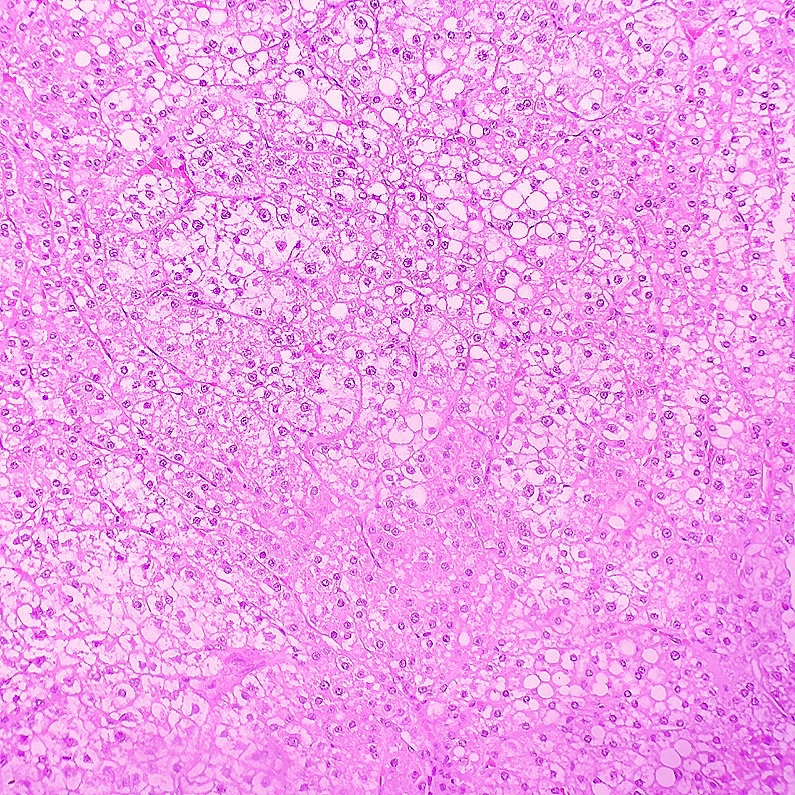
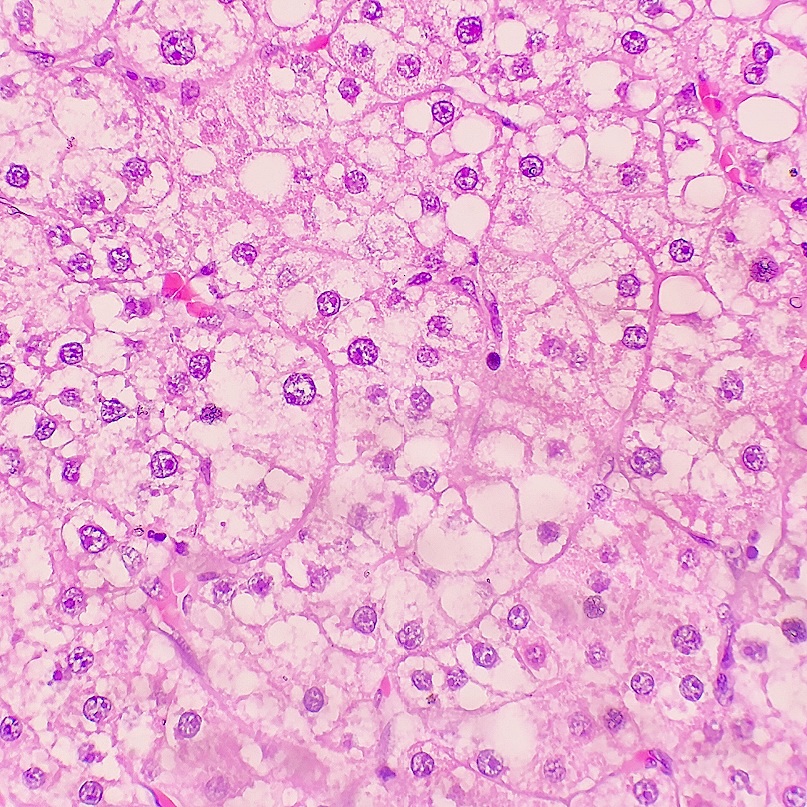
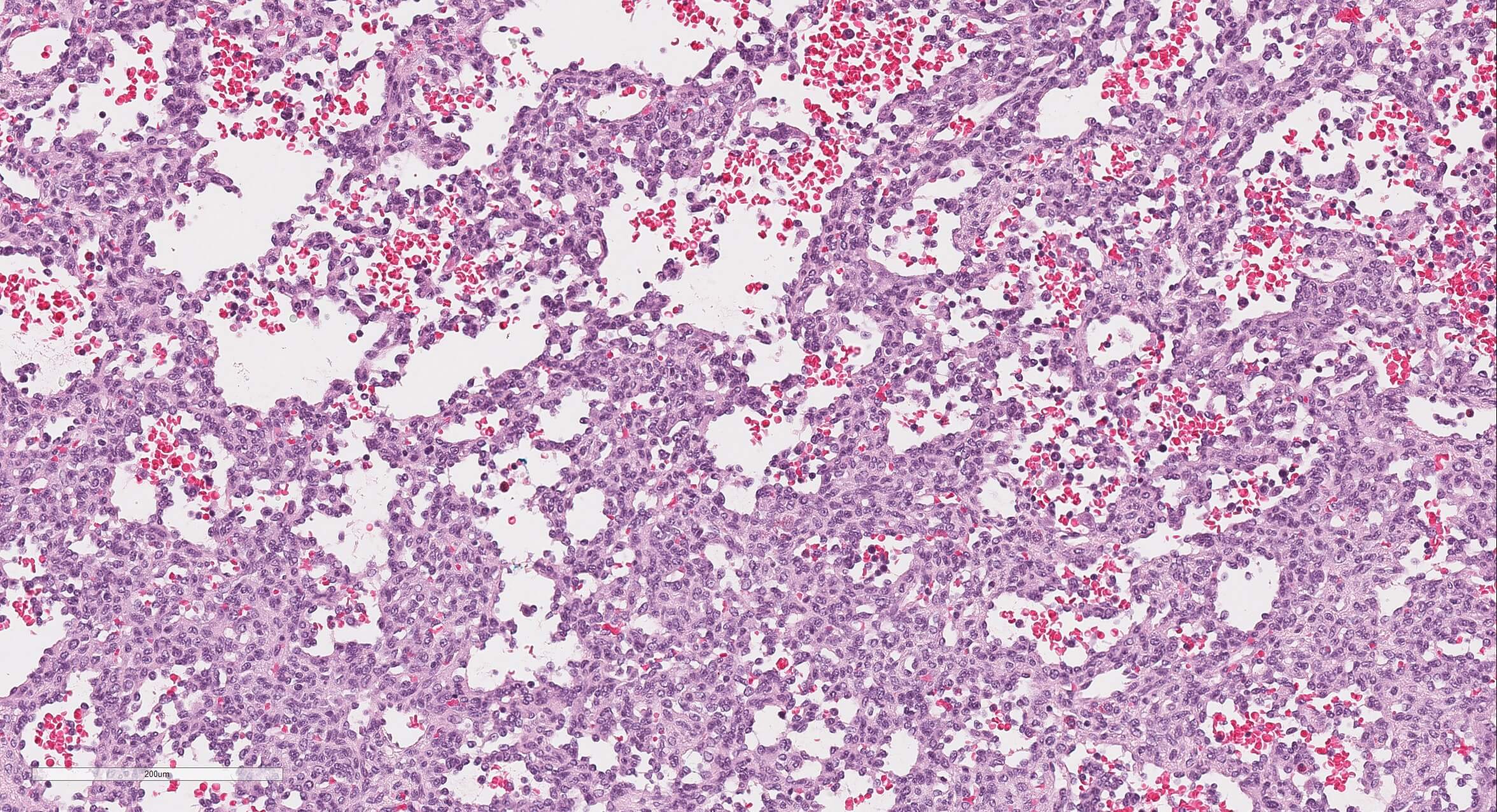
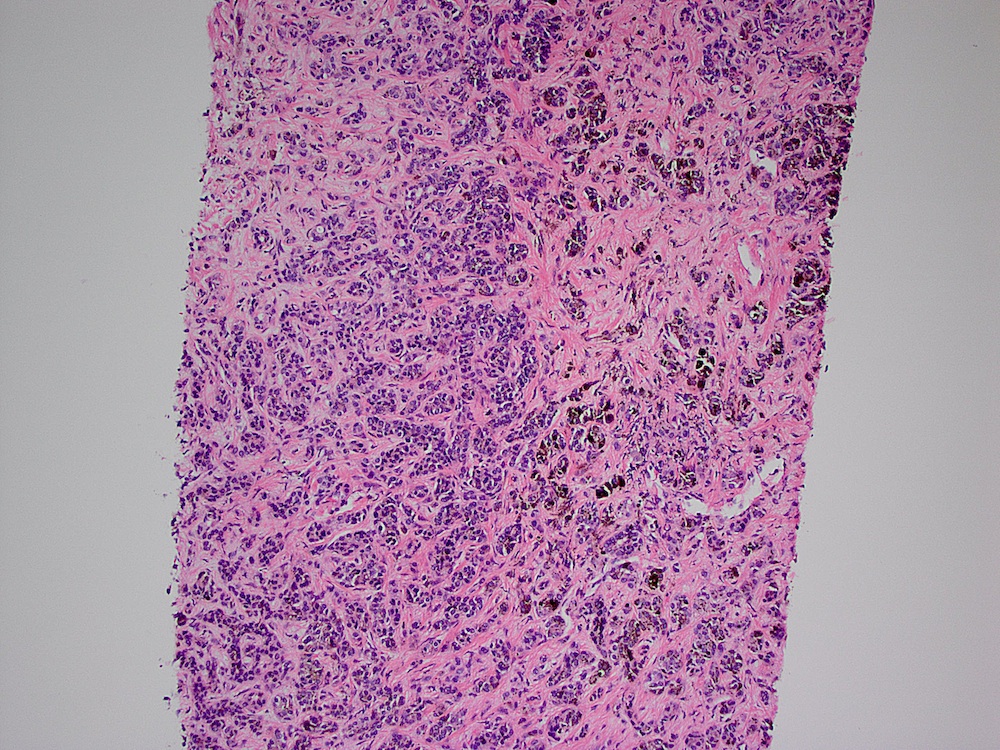
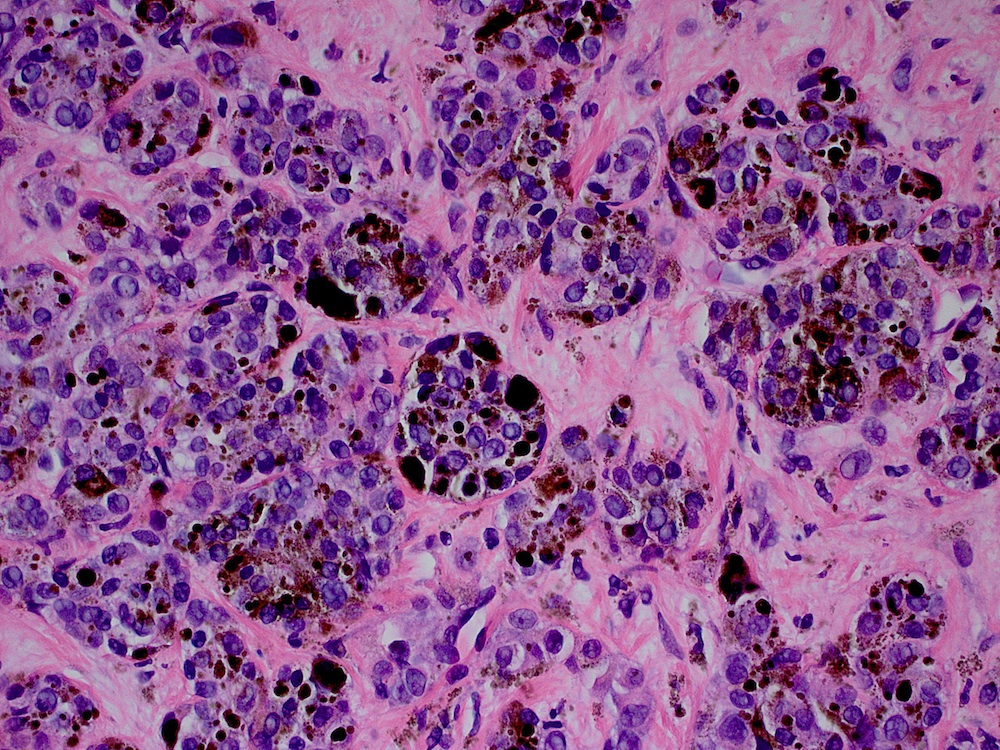
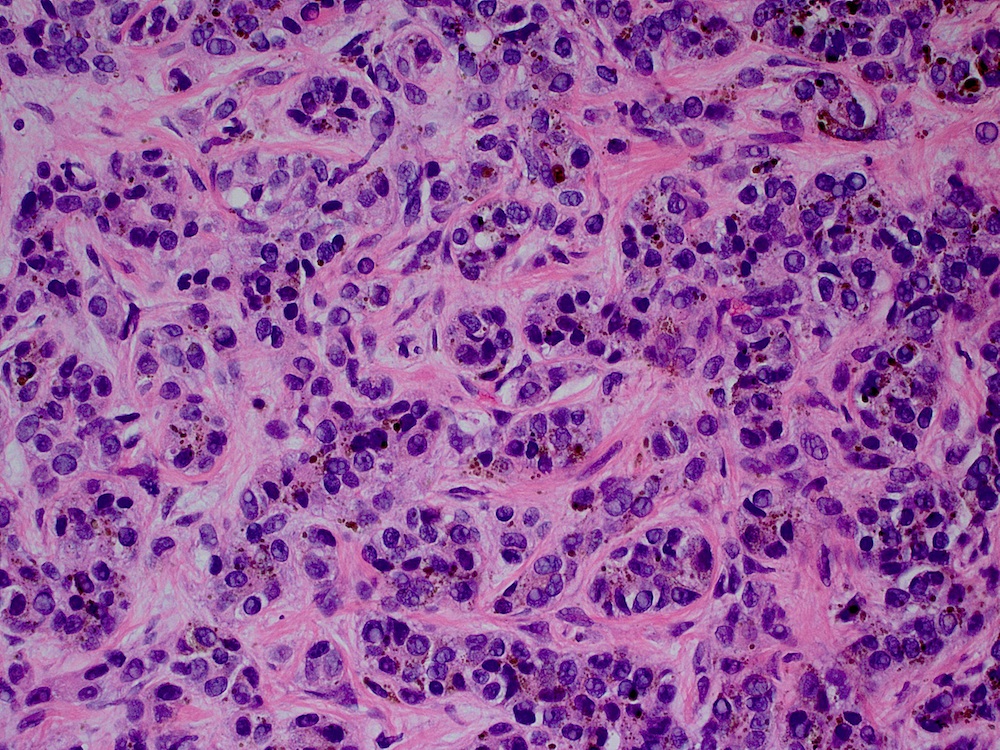
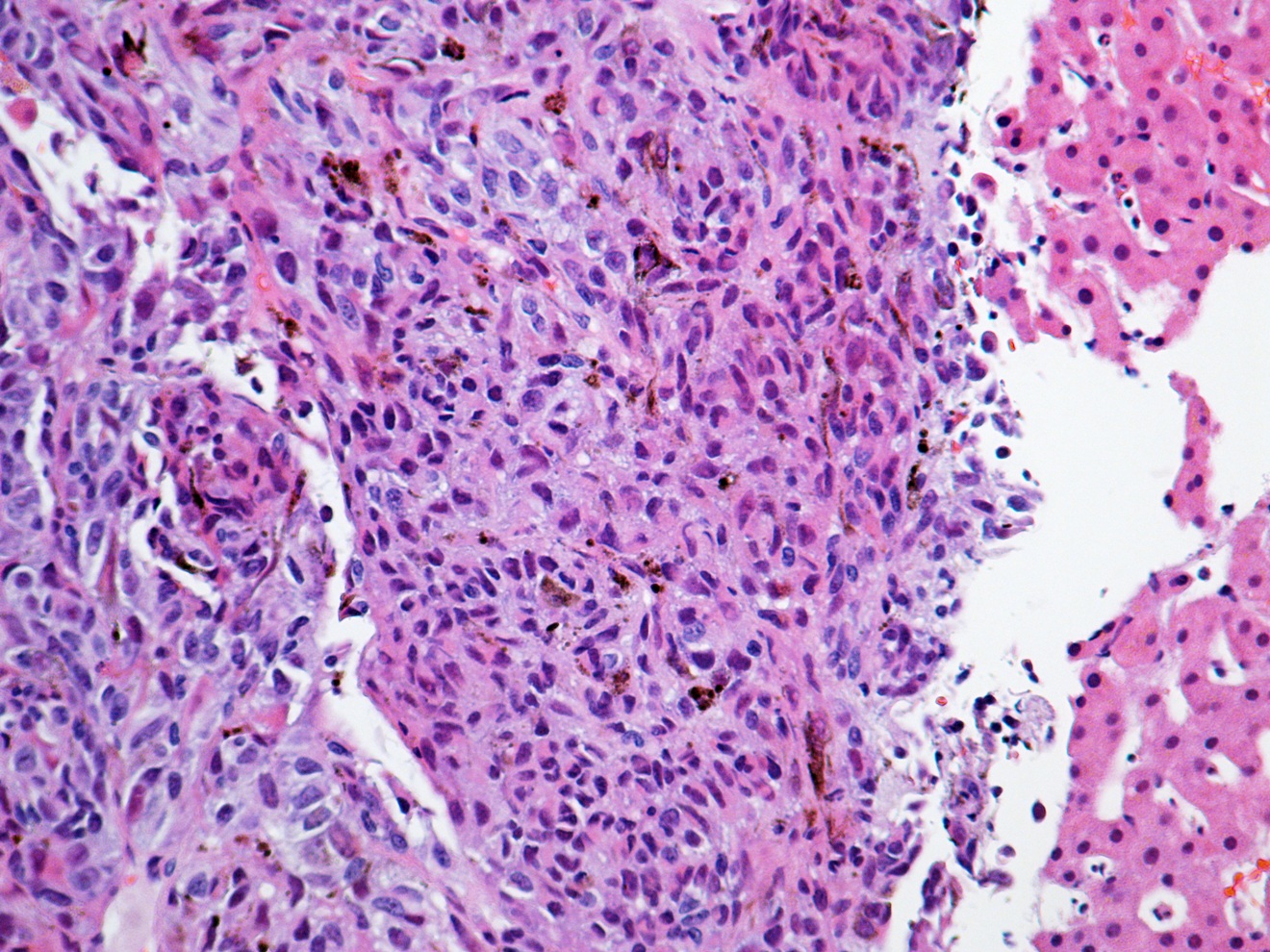
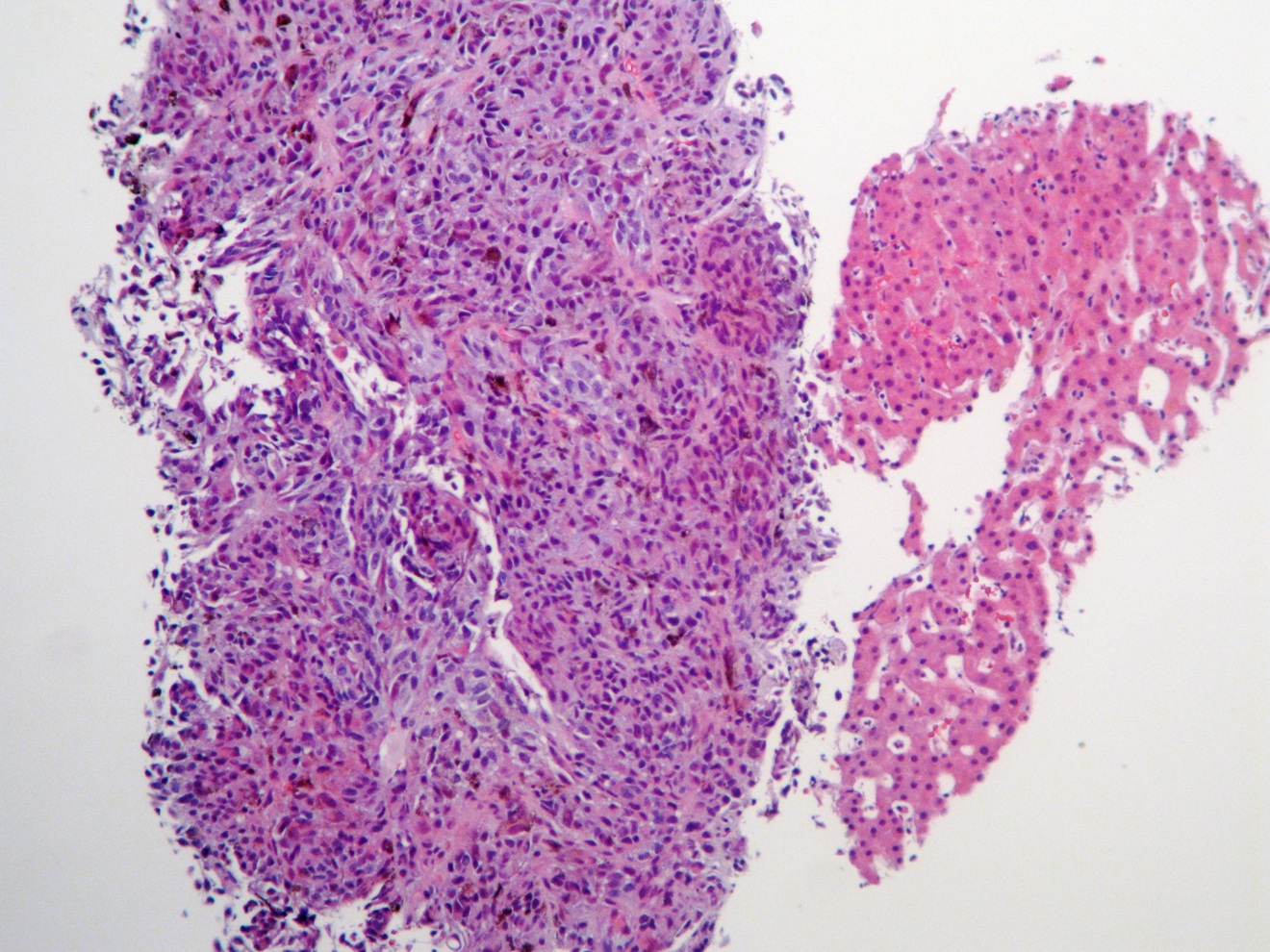
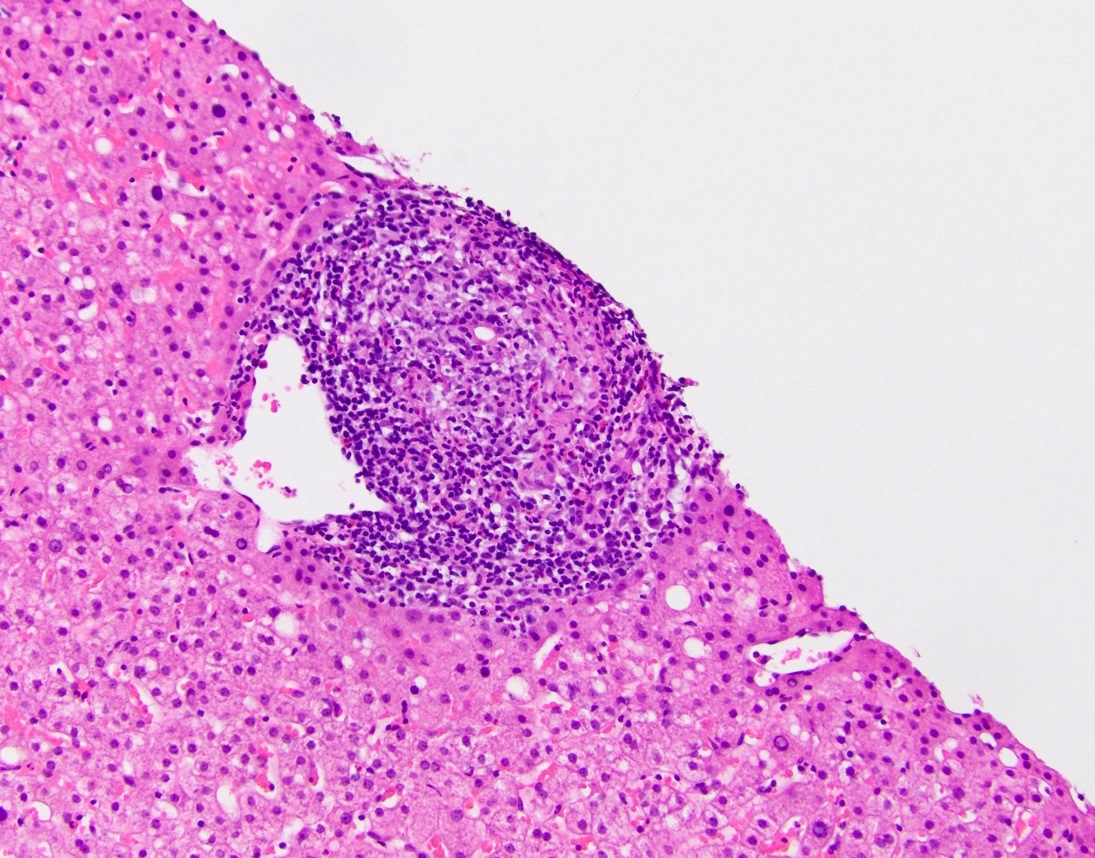
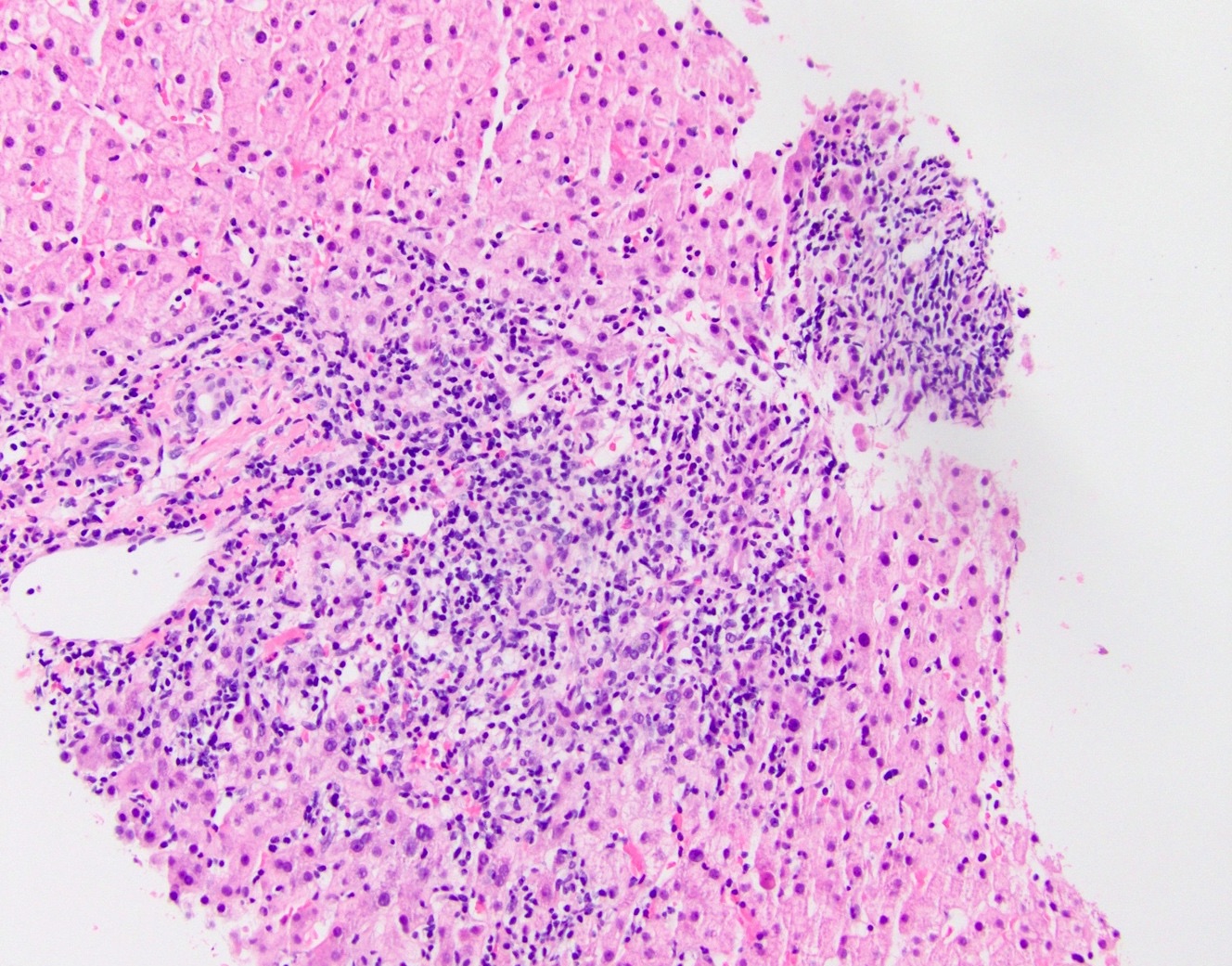
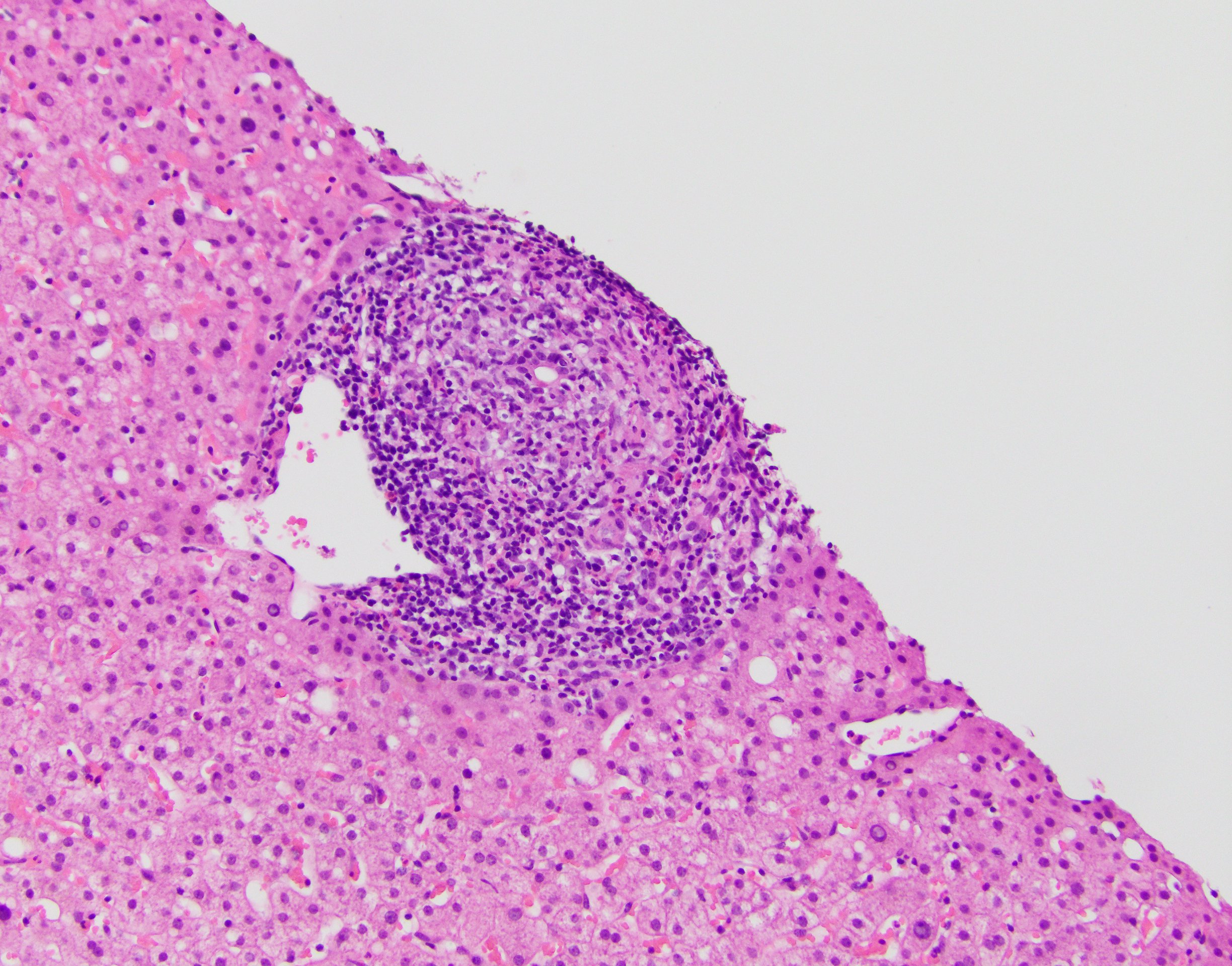
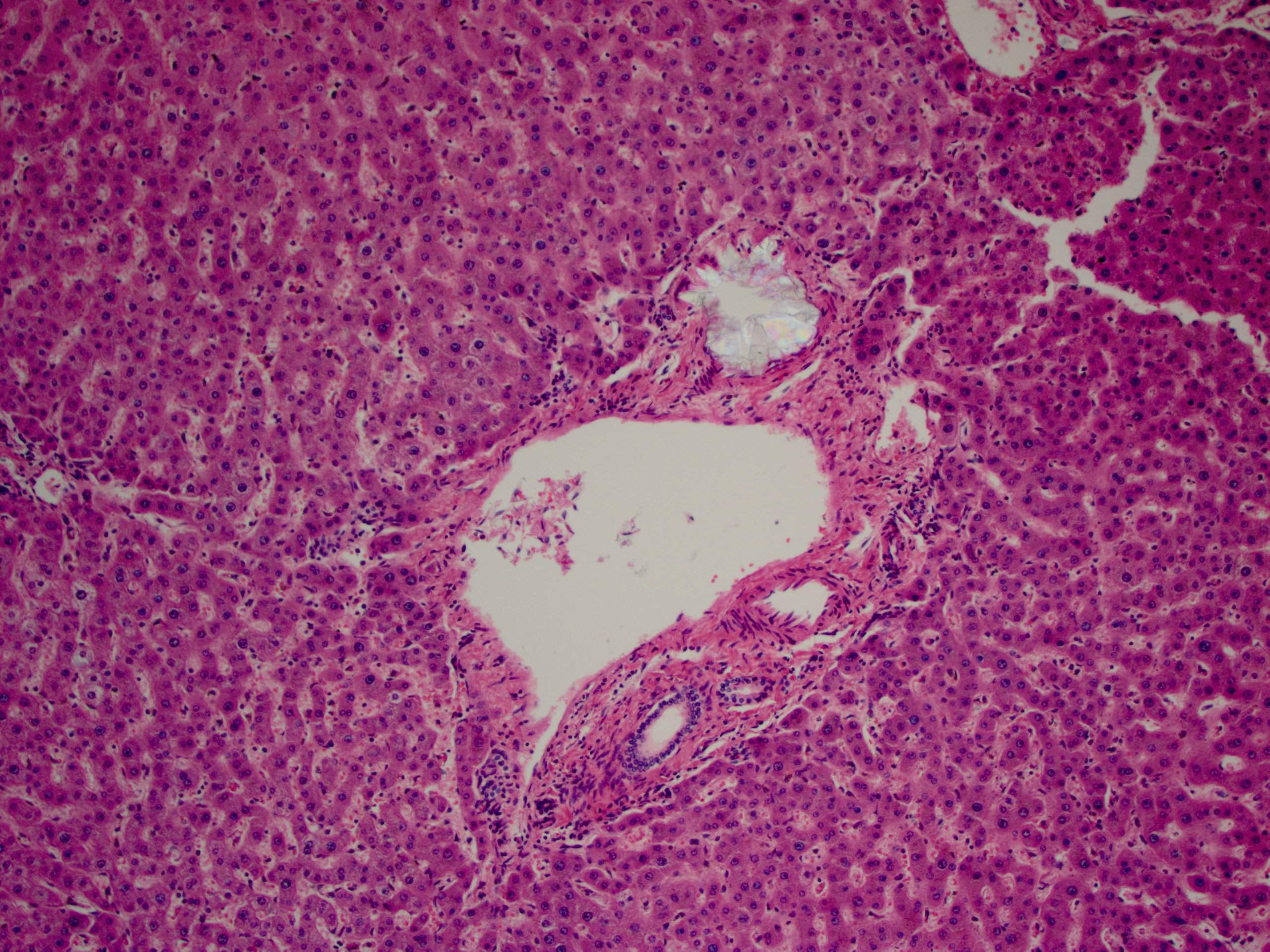
Board review style question #2
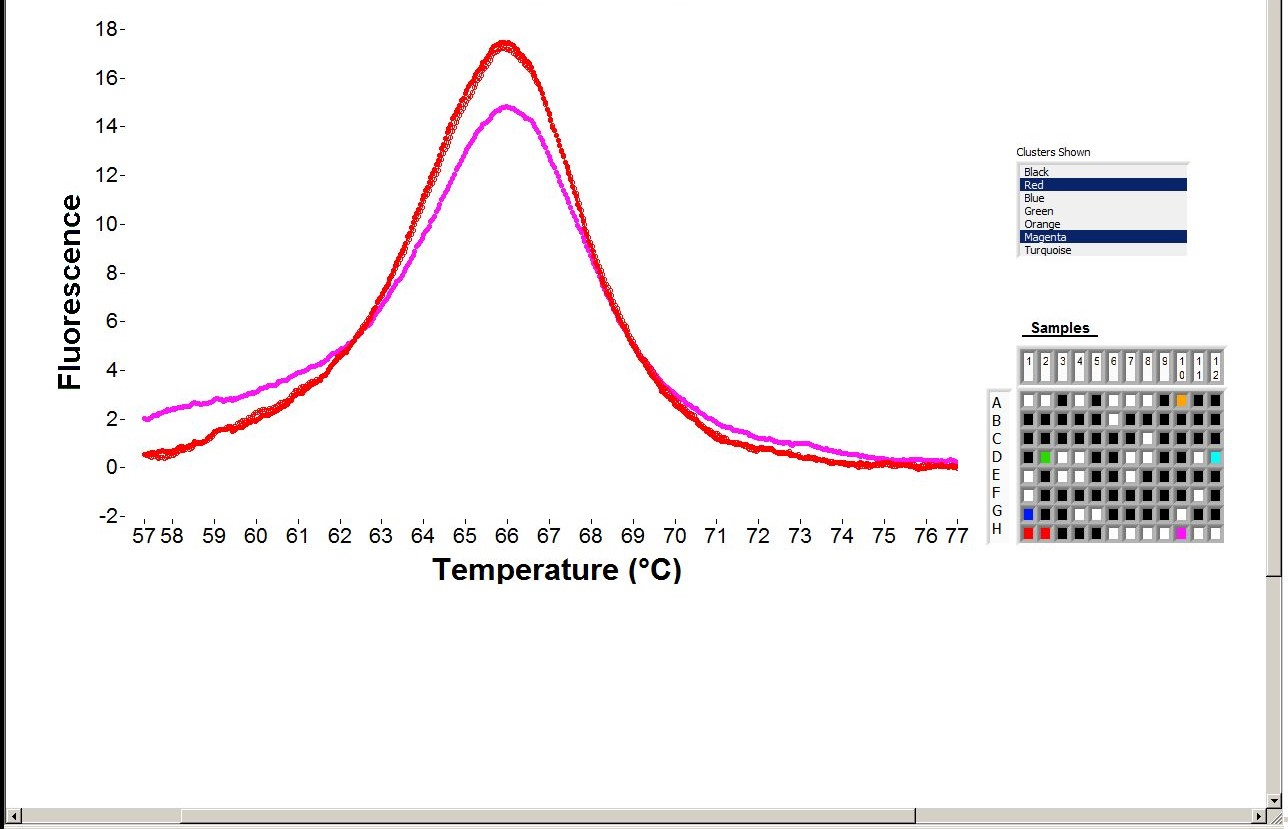
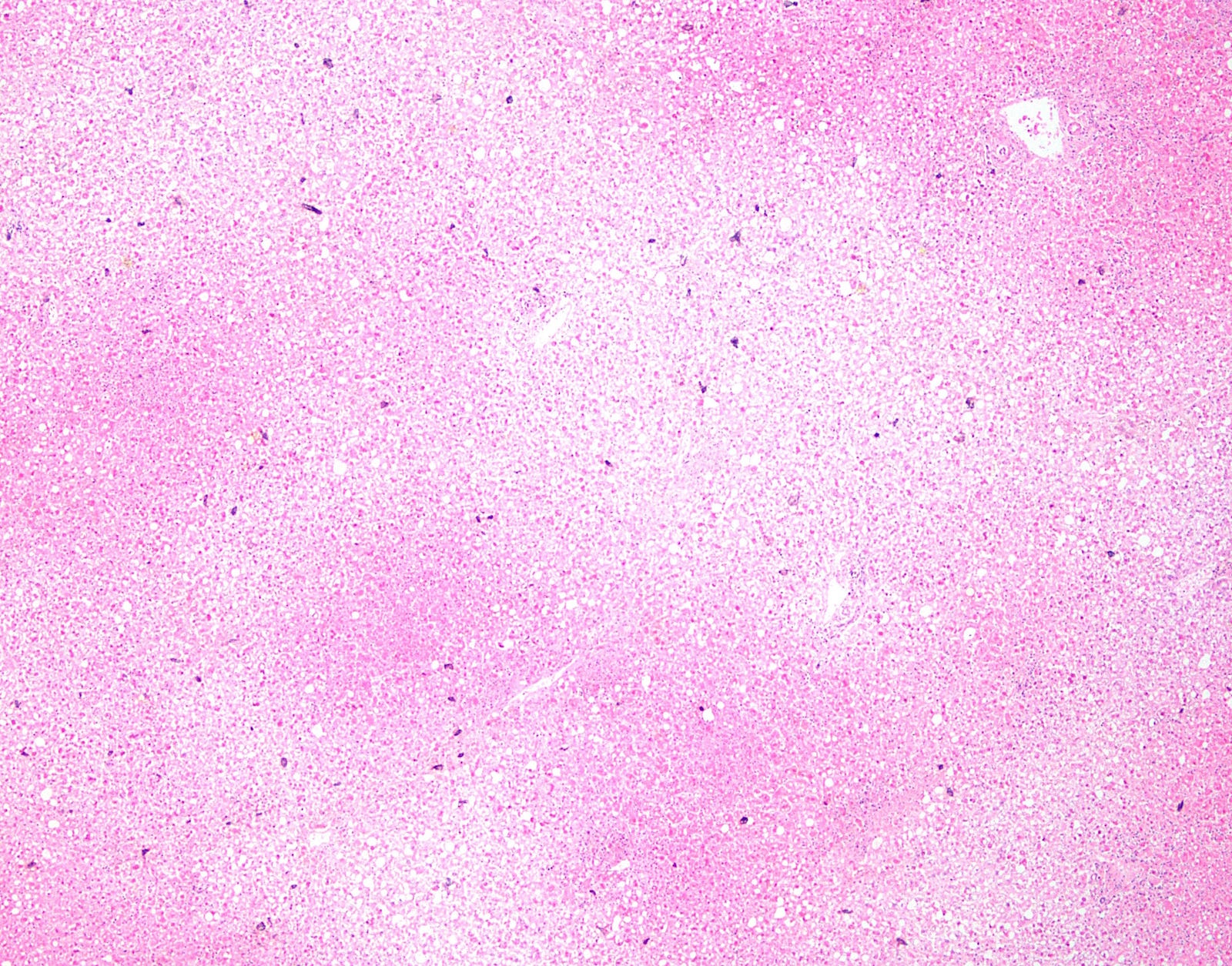
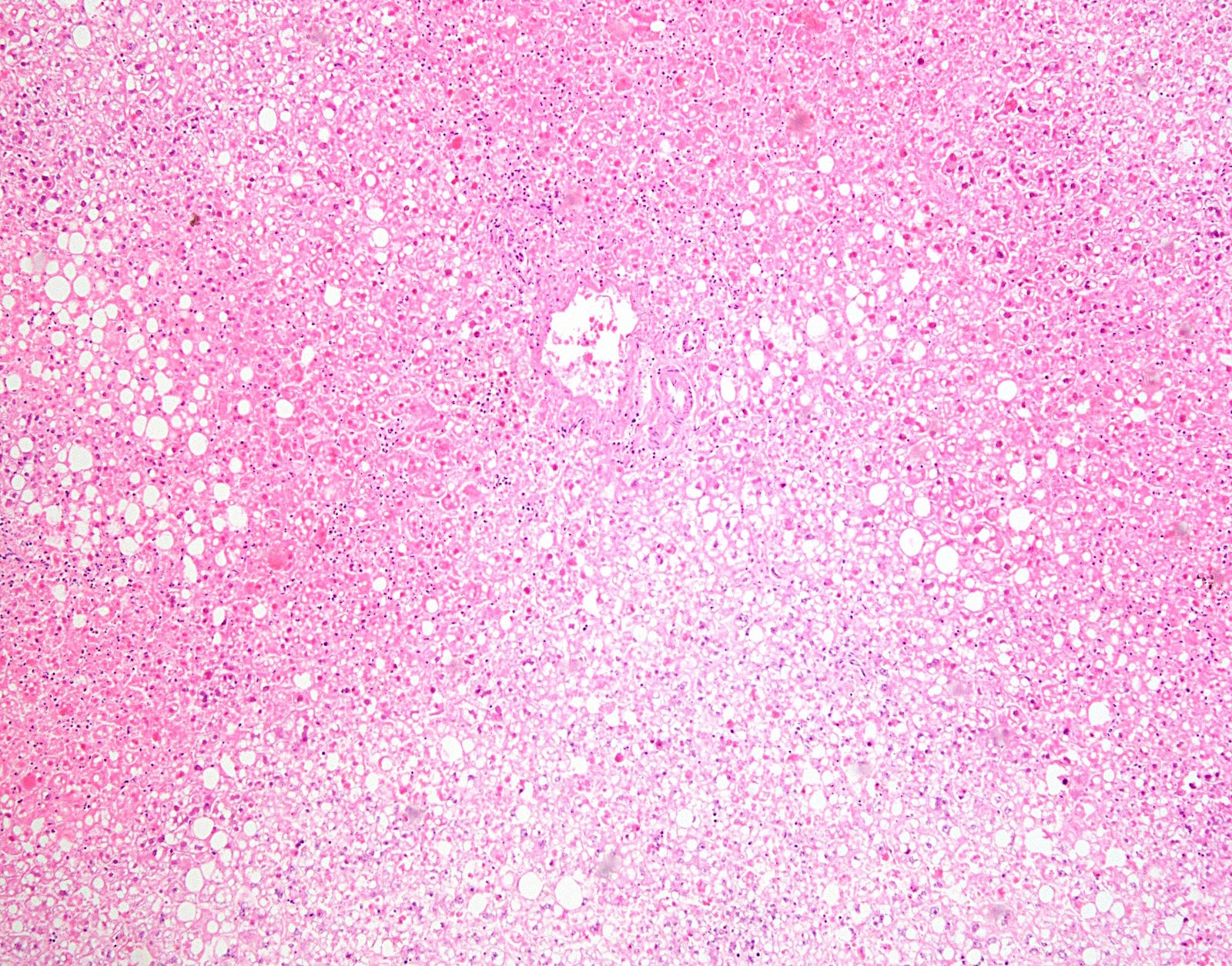
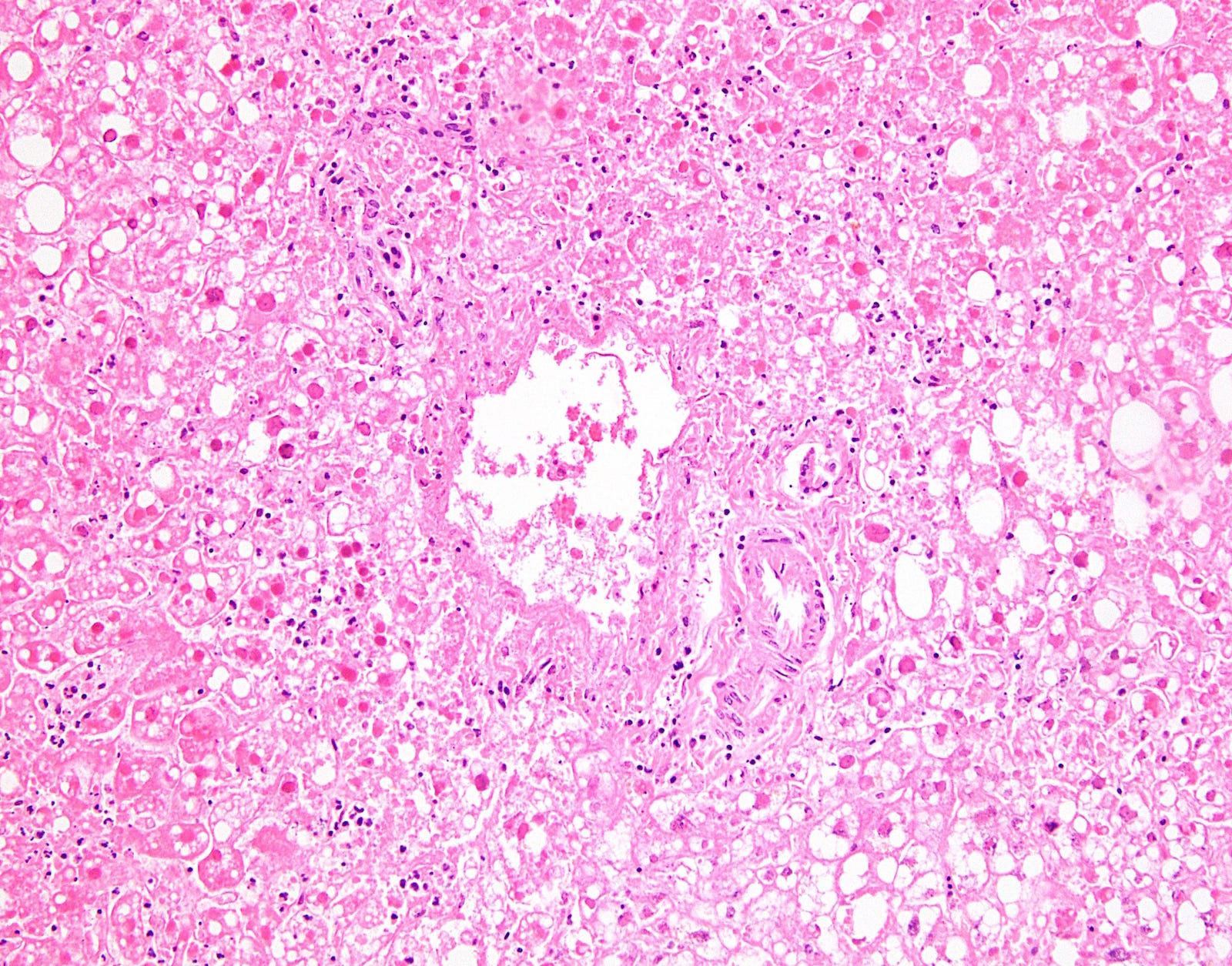
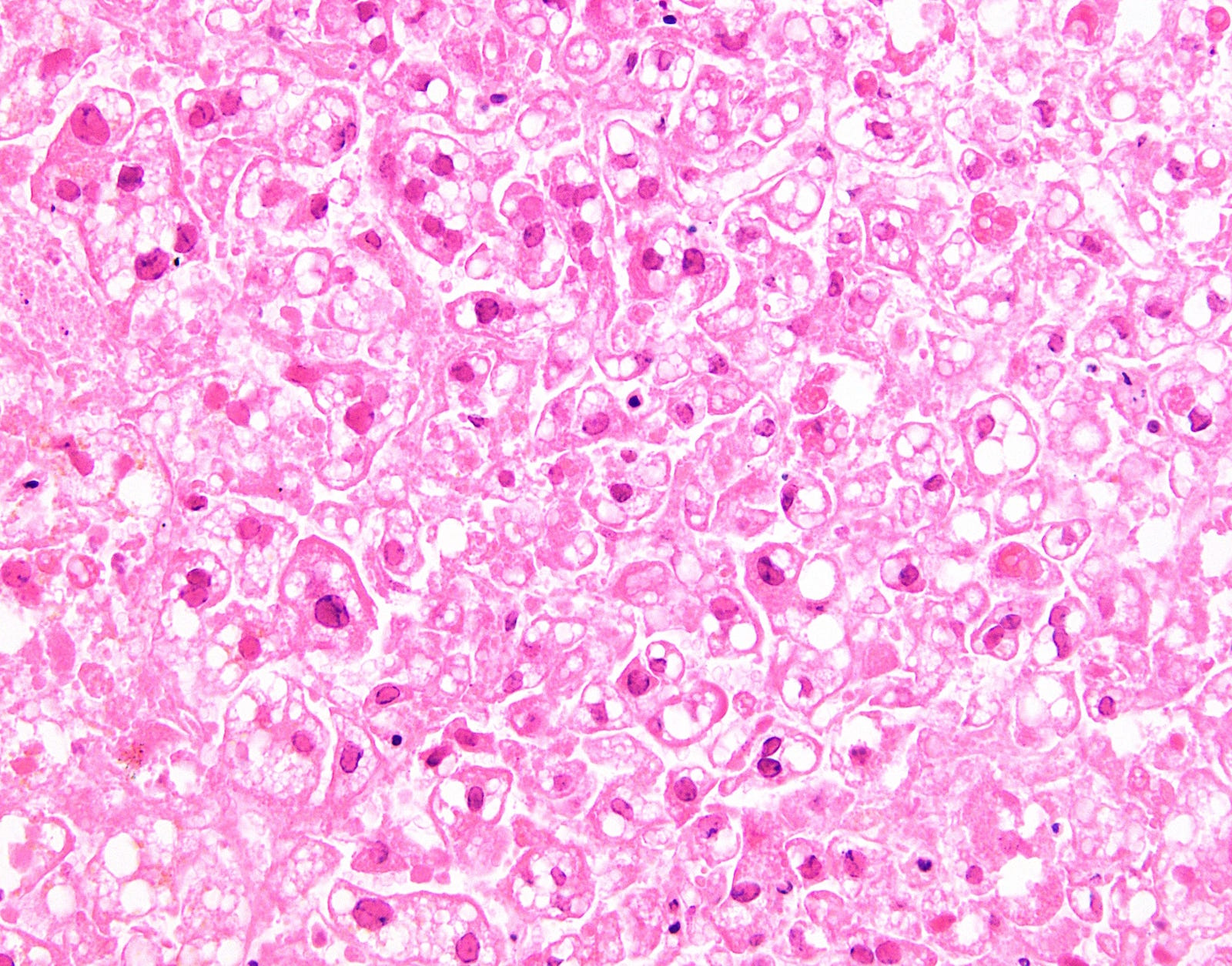
Board review style answer #2
C. Chronic hepatitis C infection
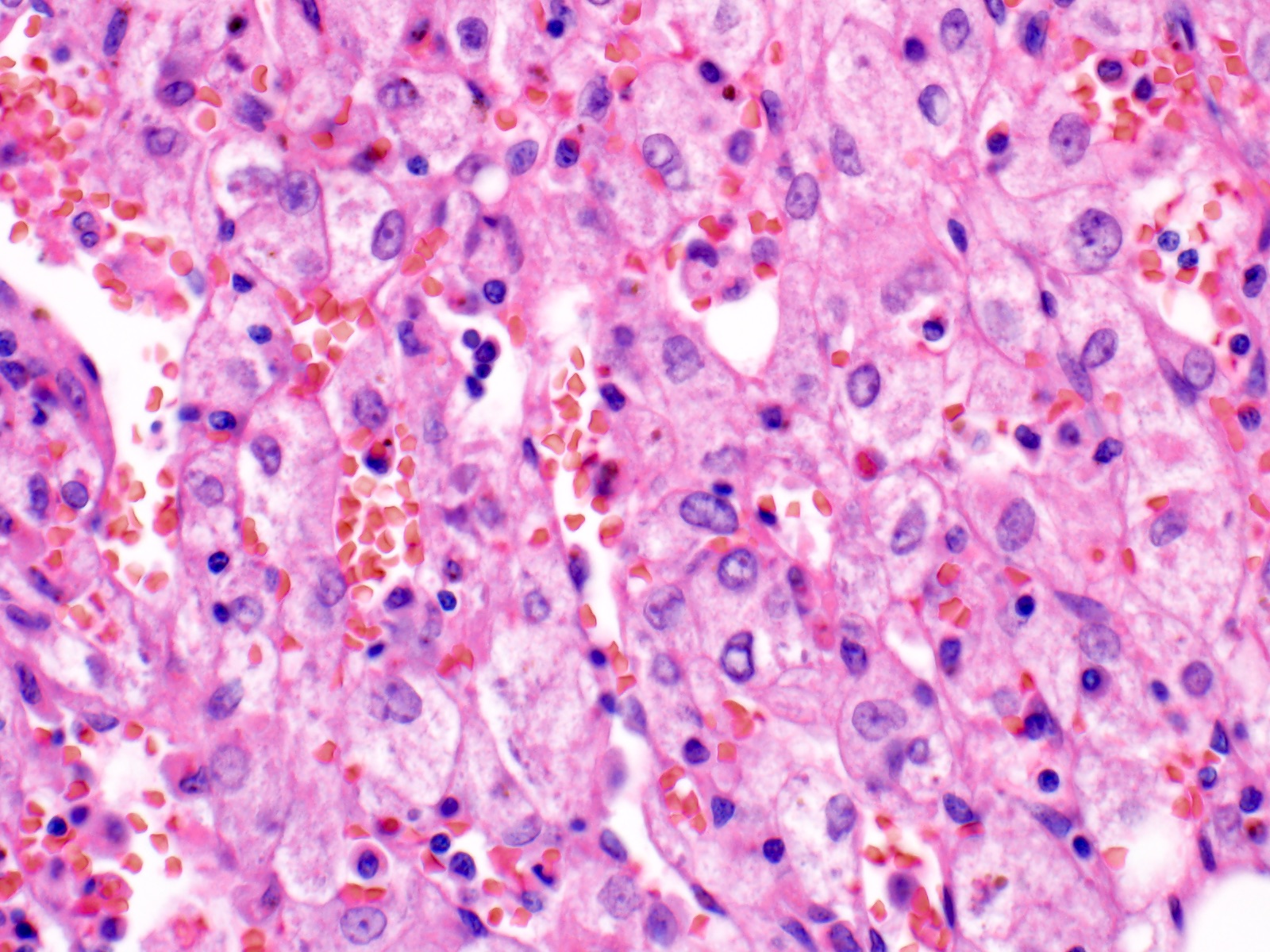
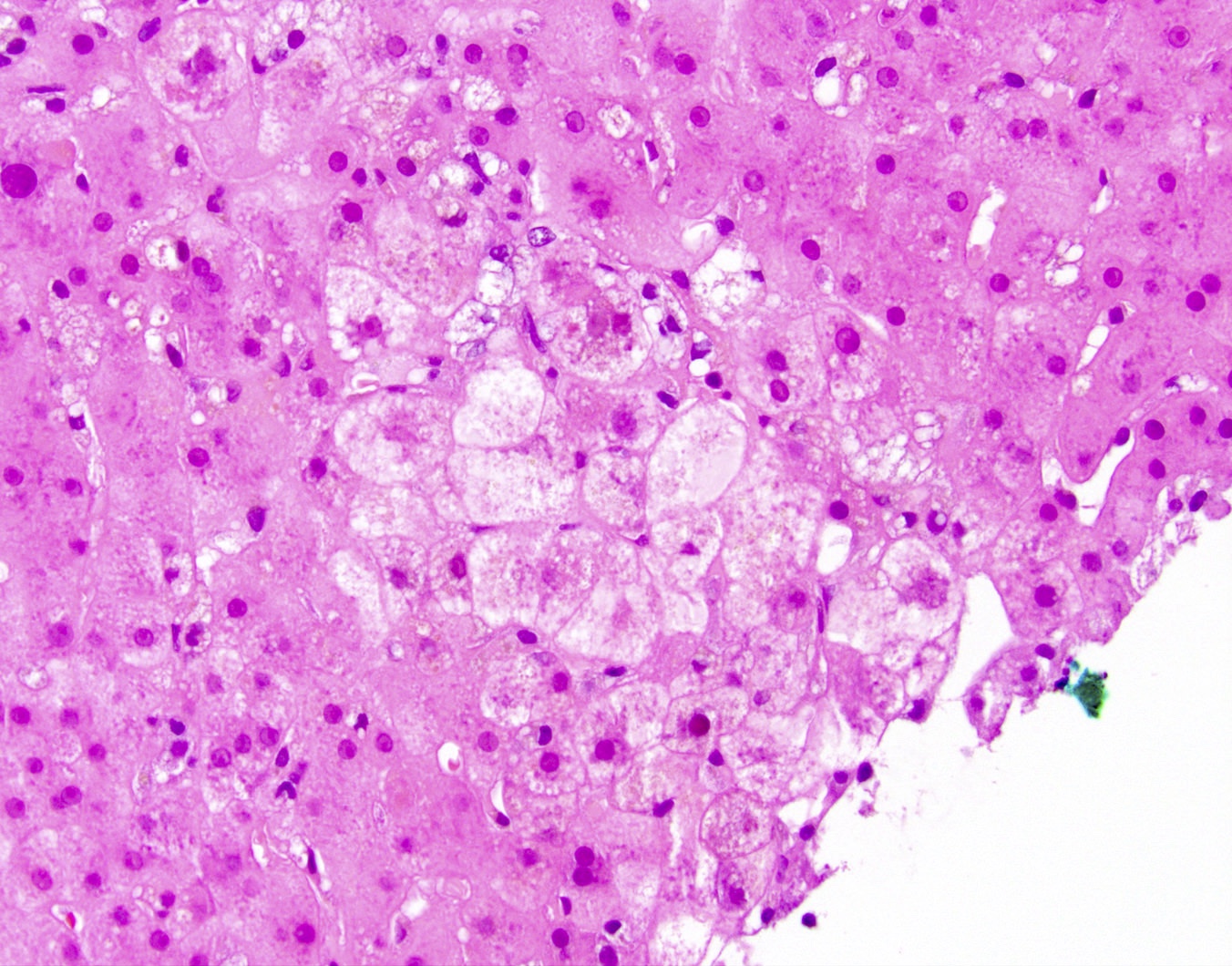
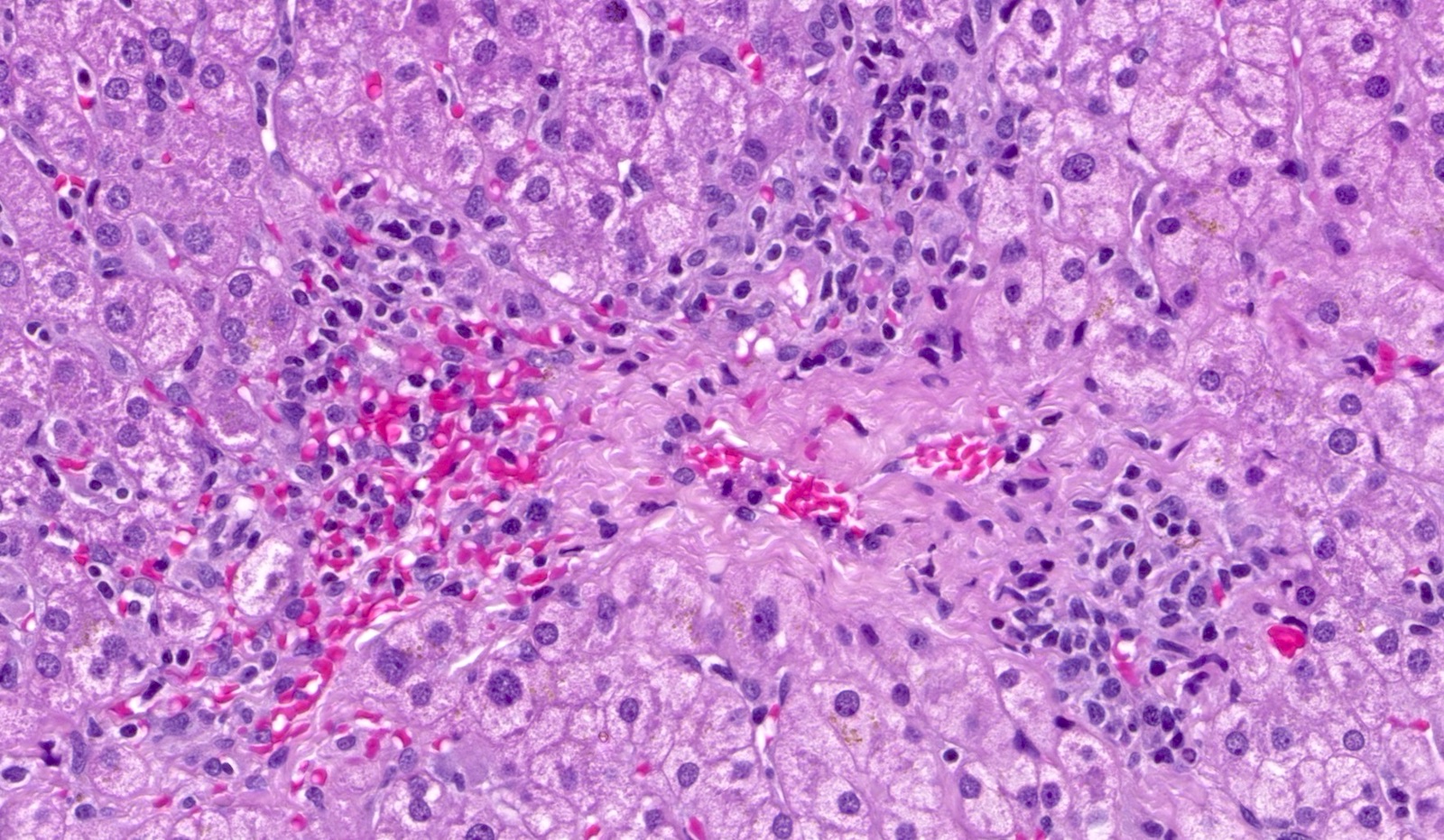
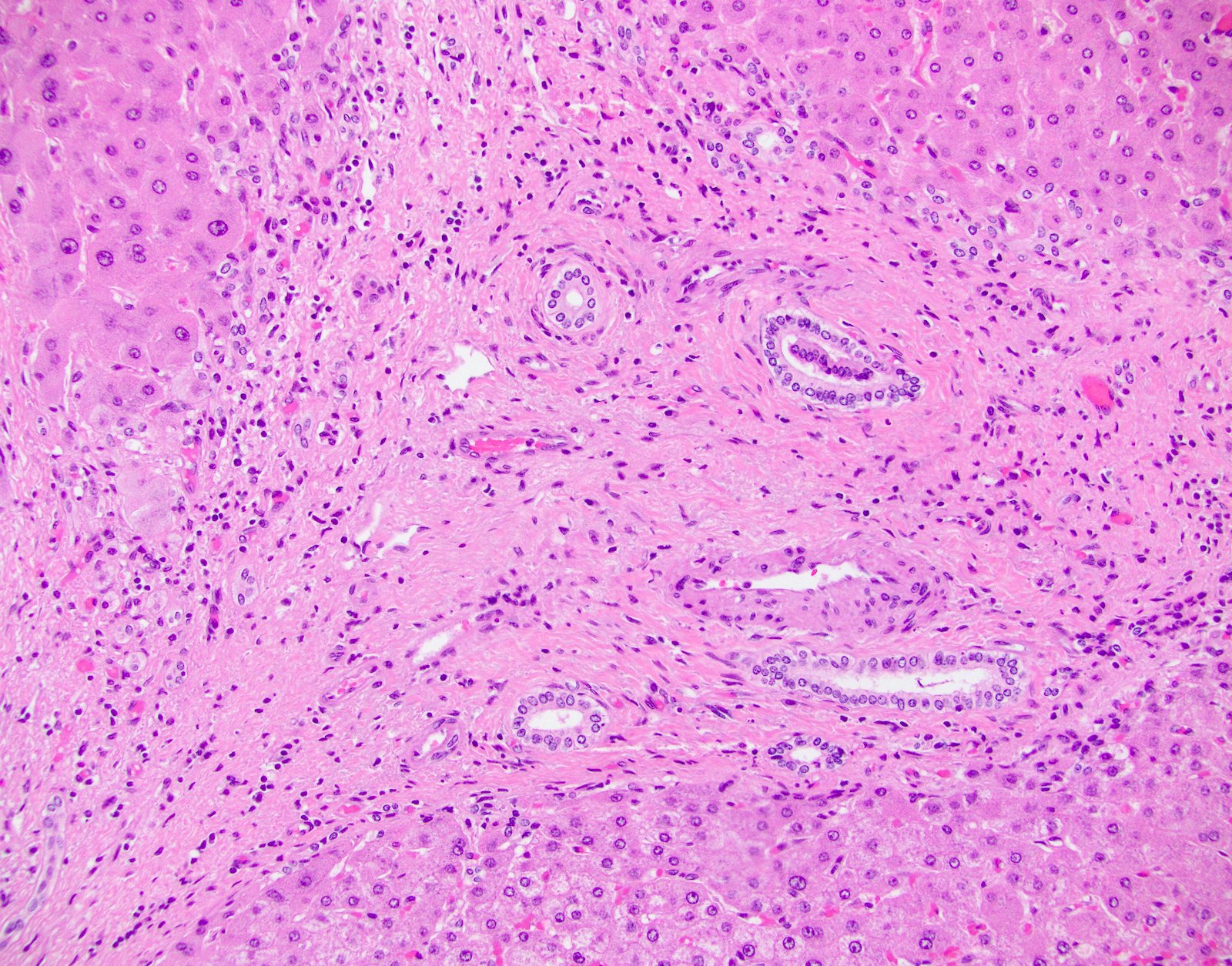
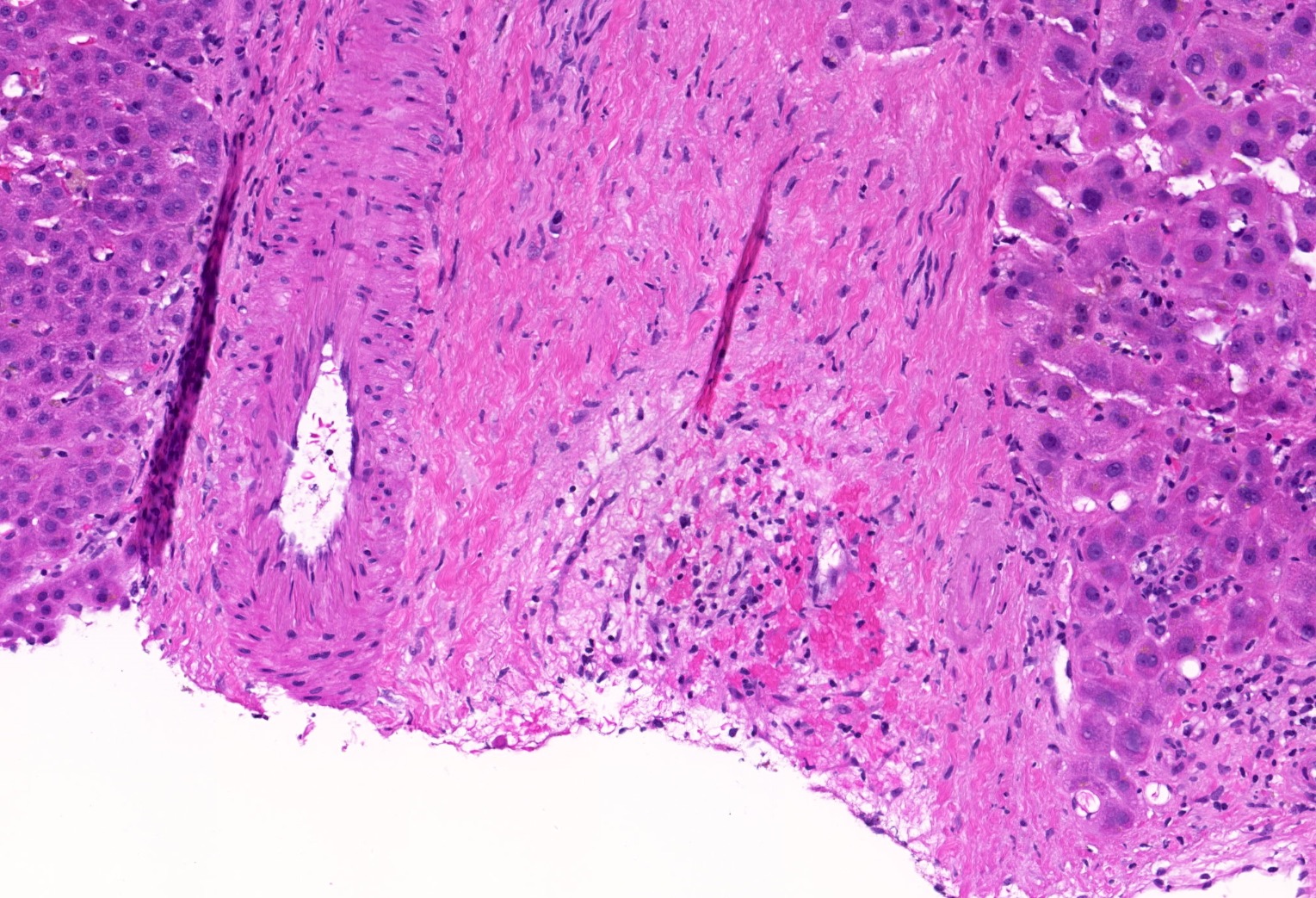
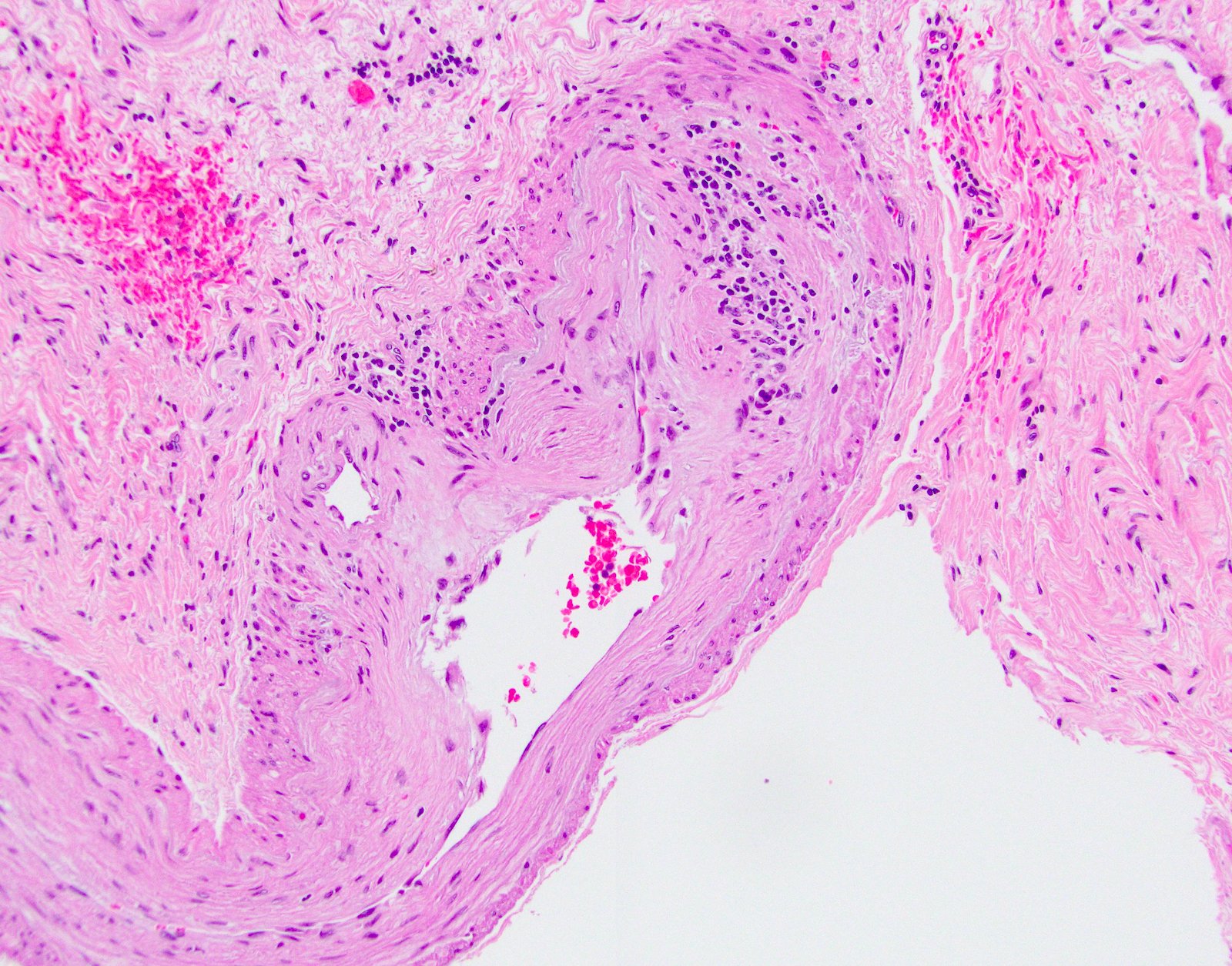
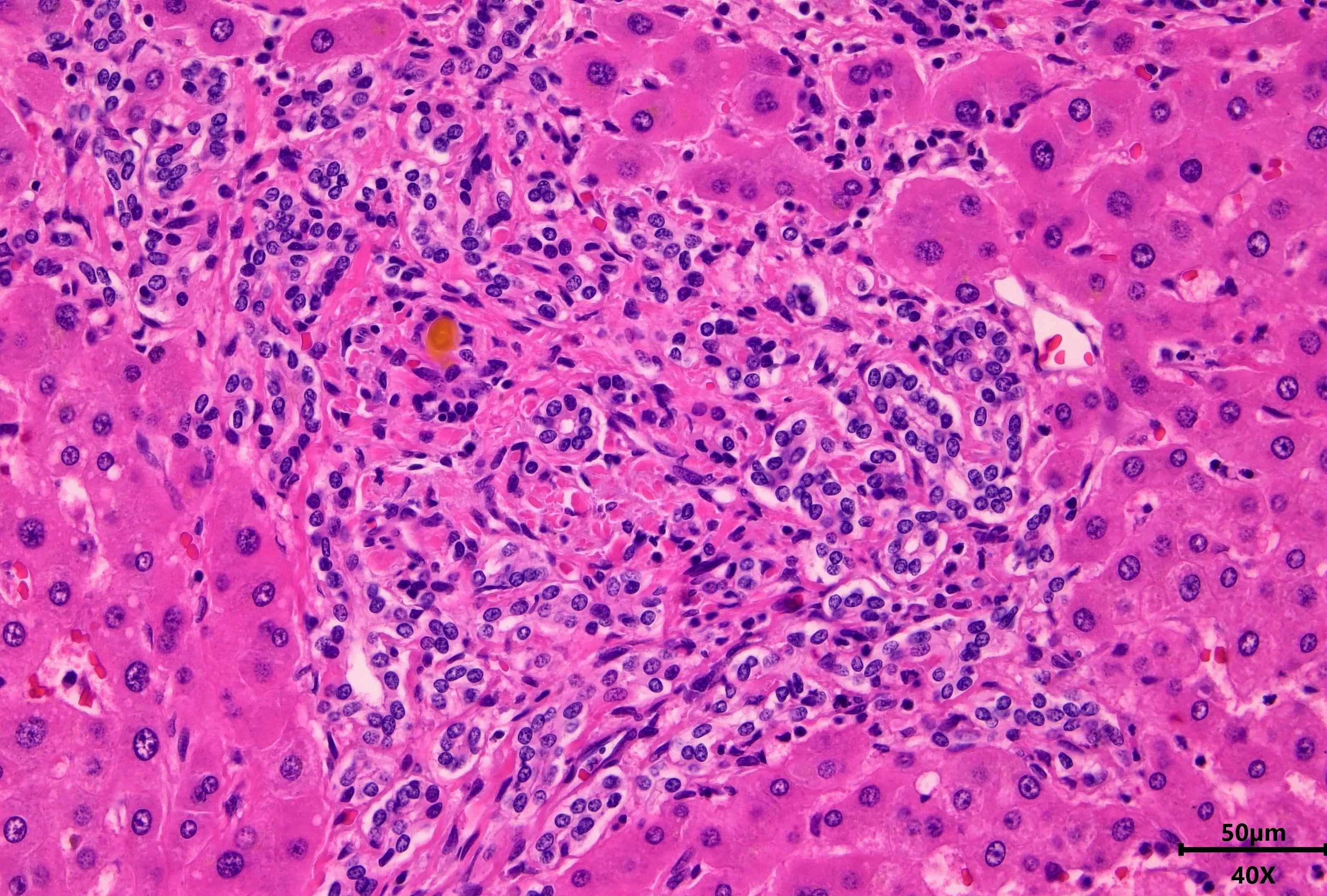
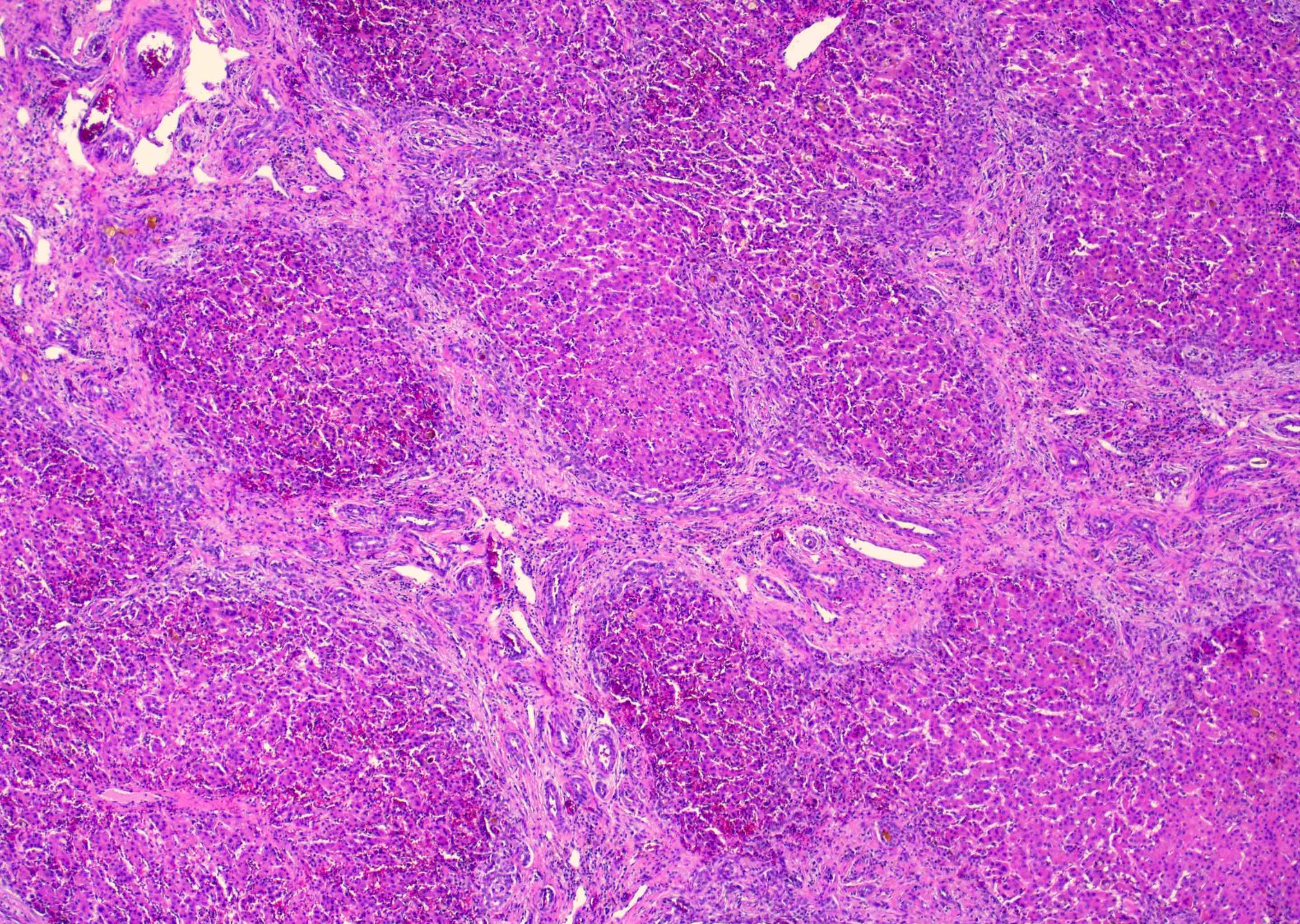
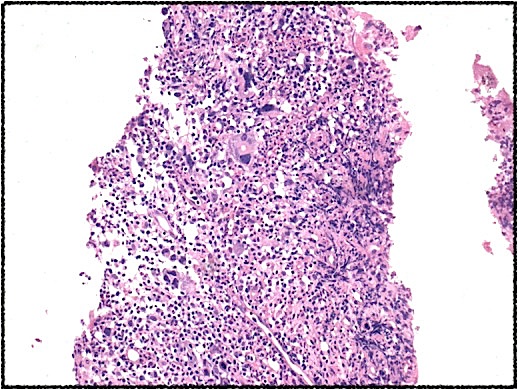
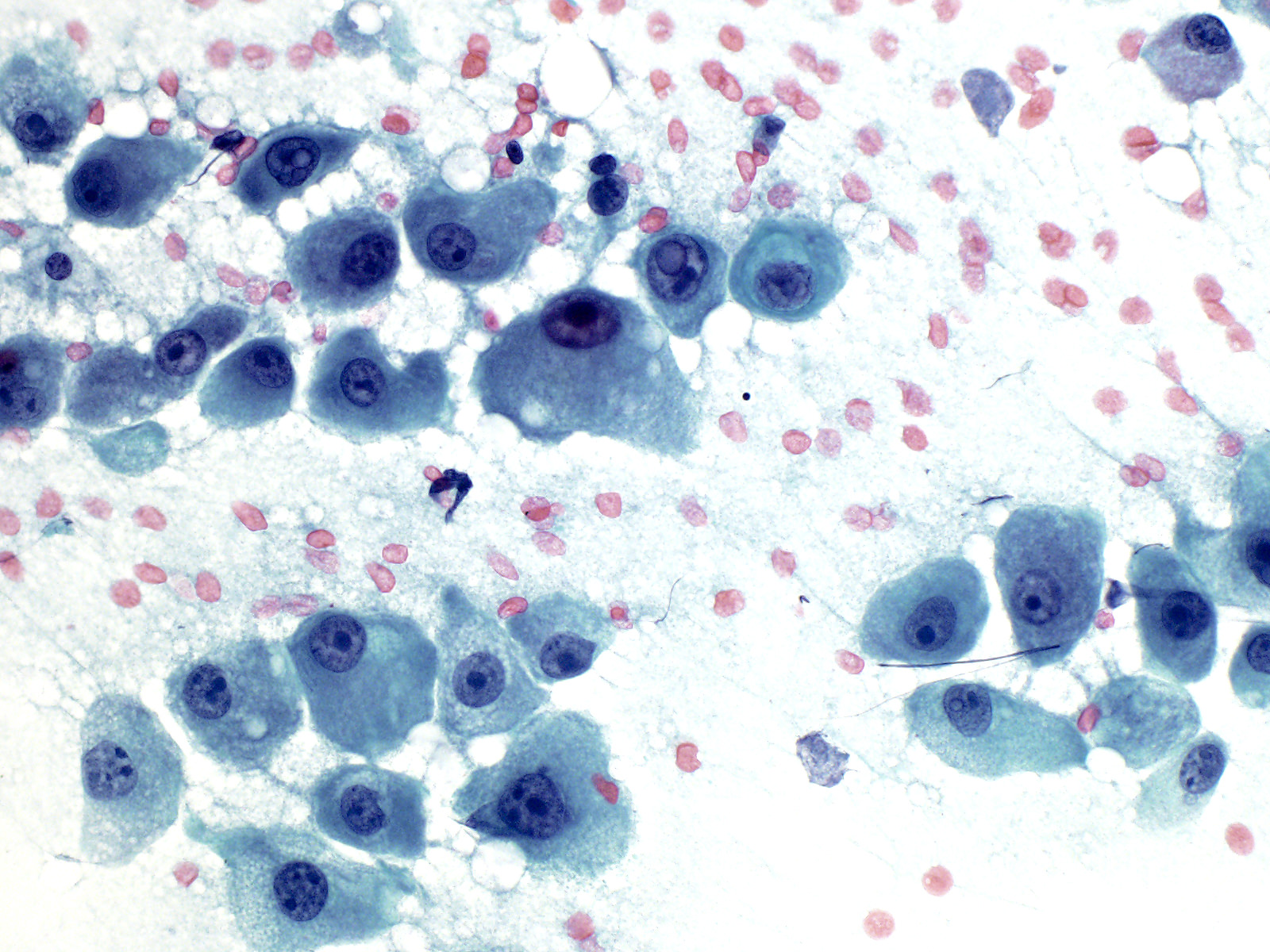
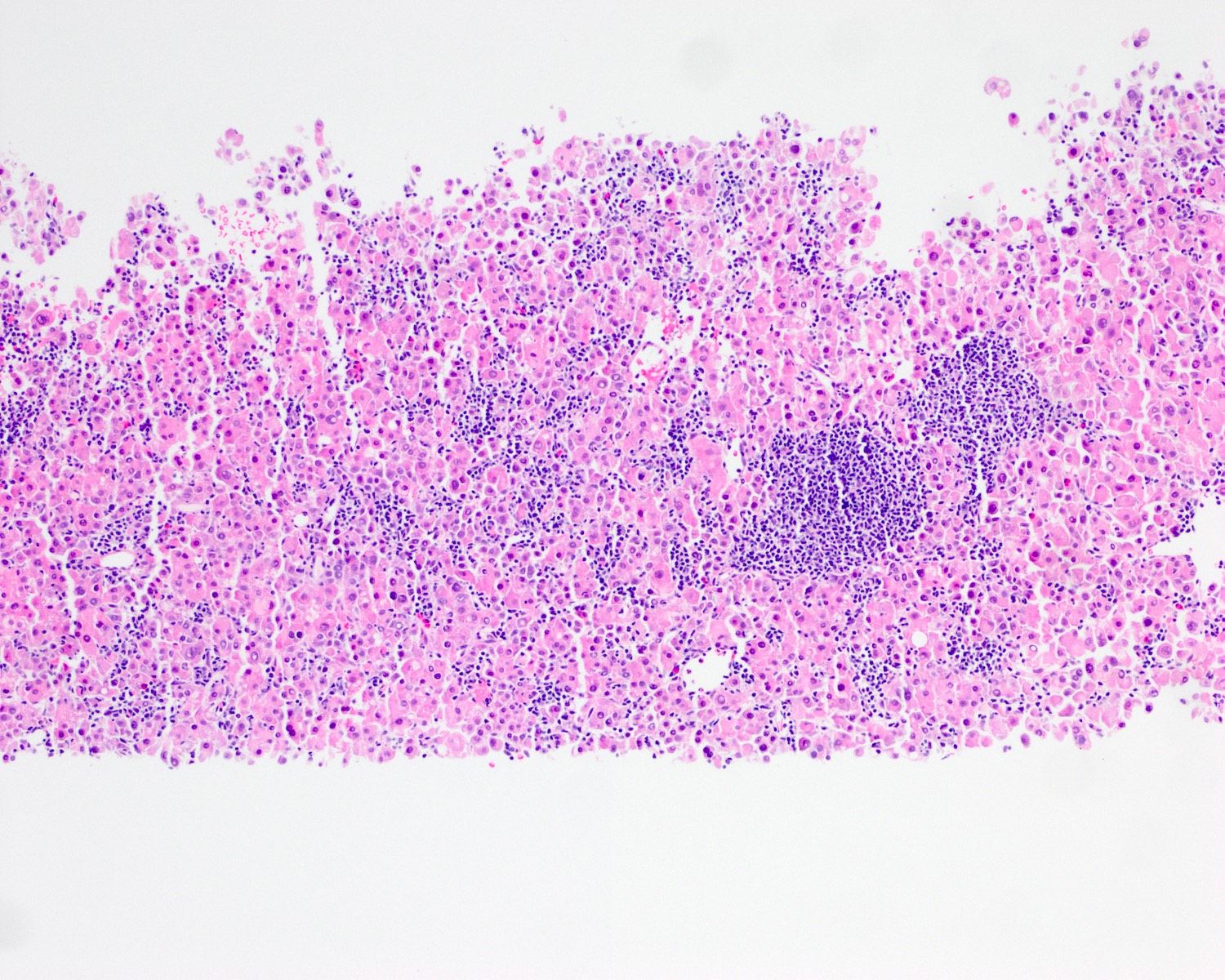
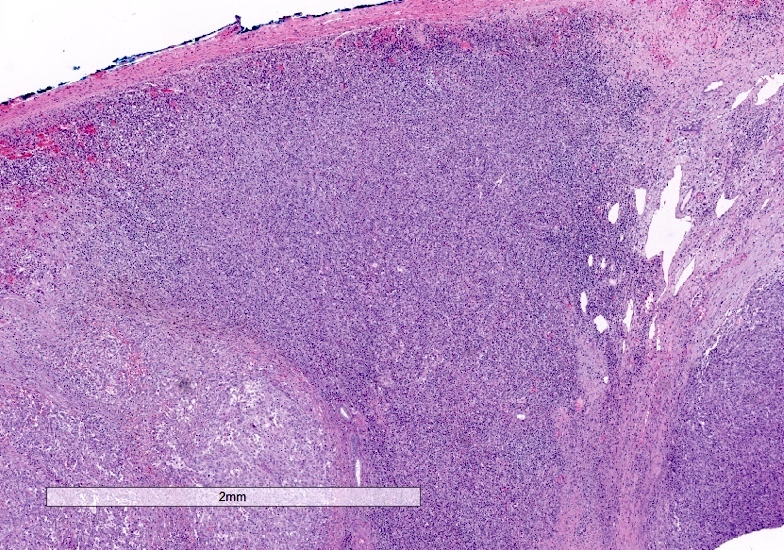
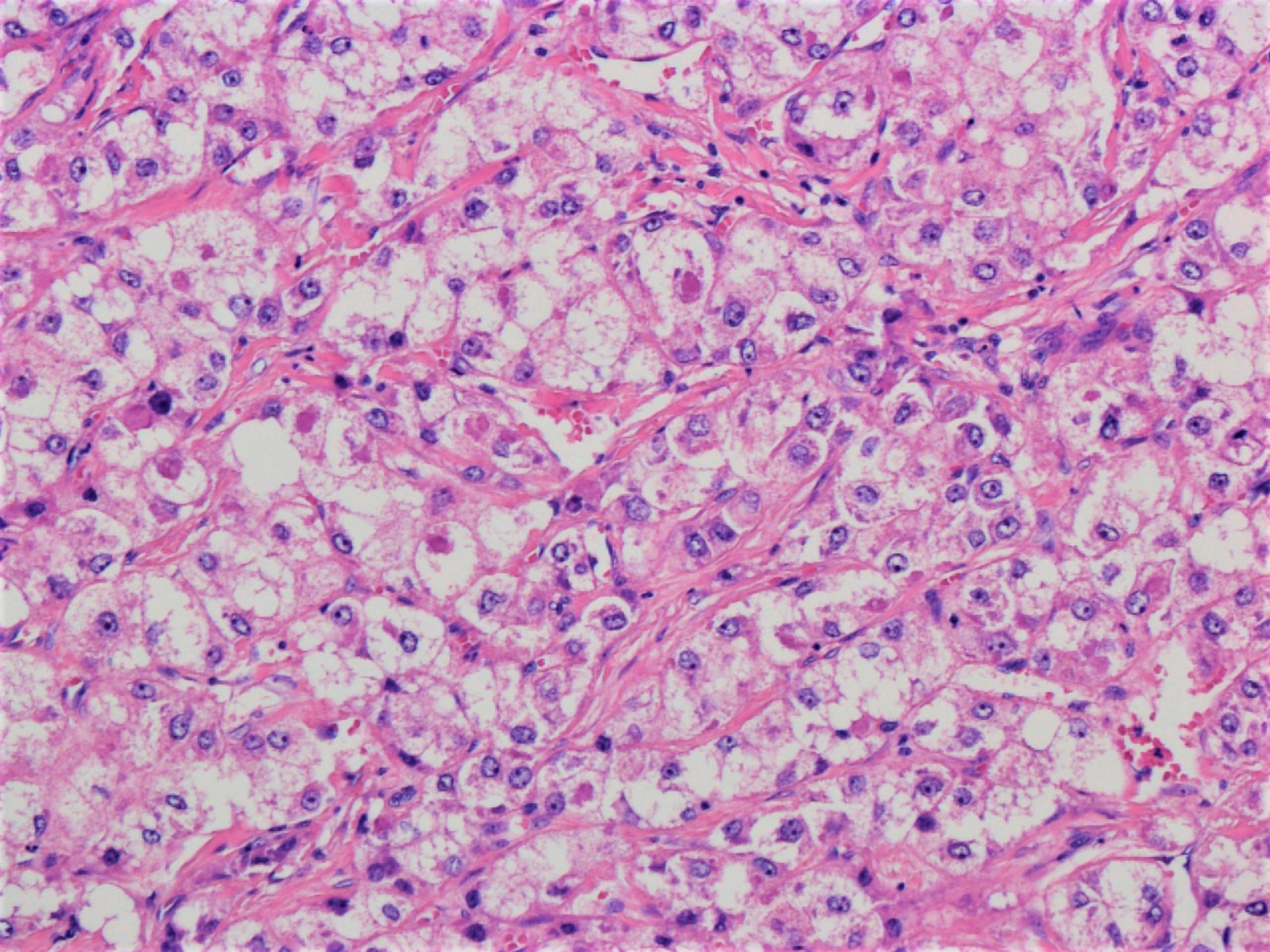
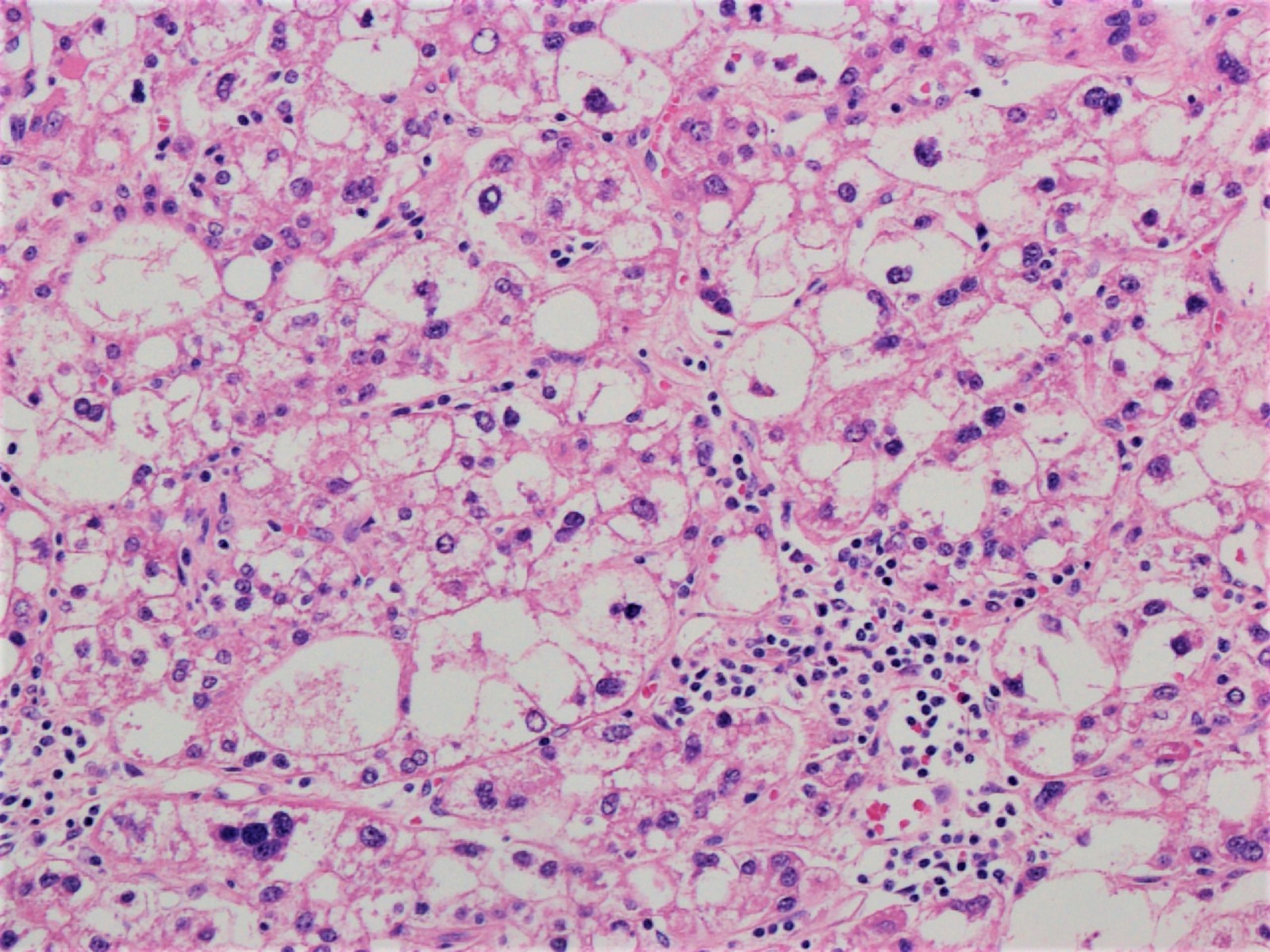
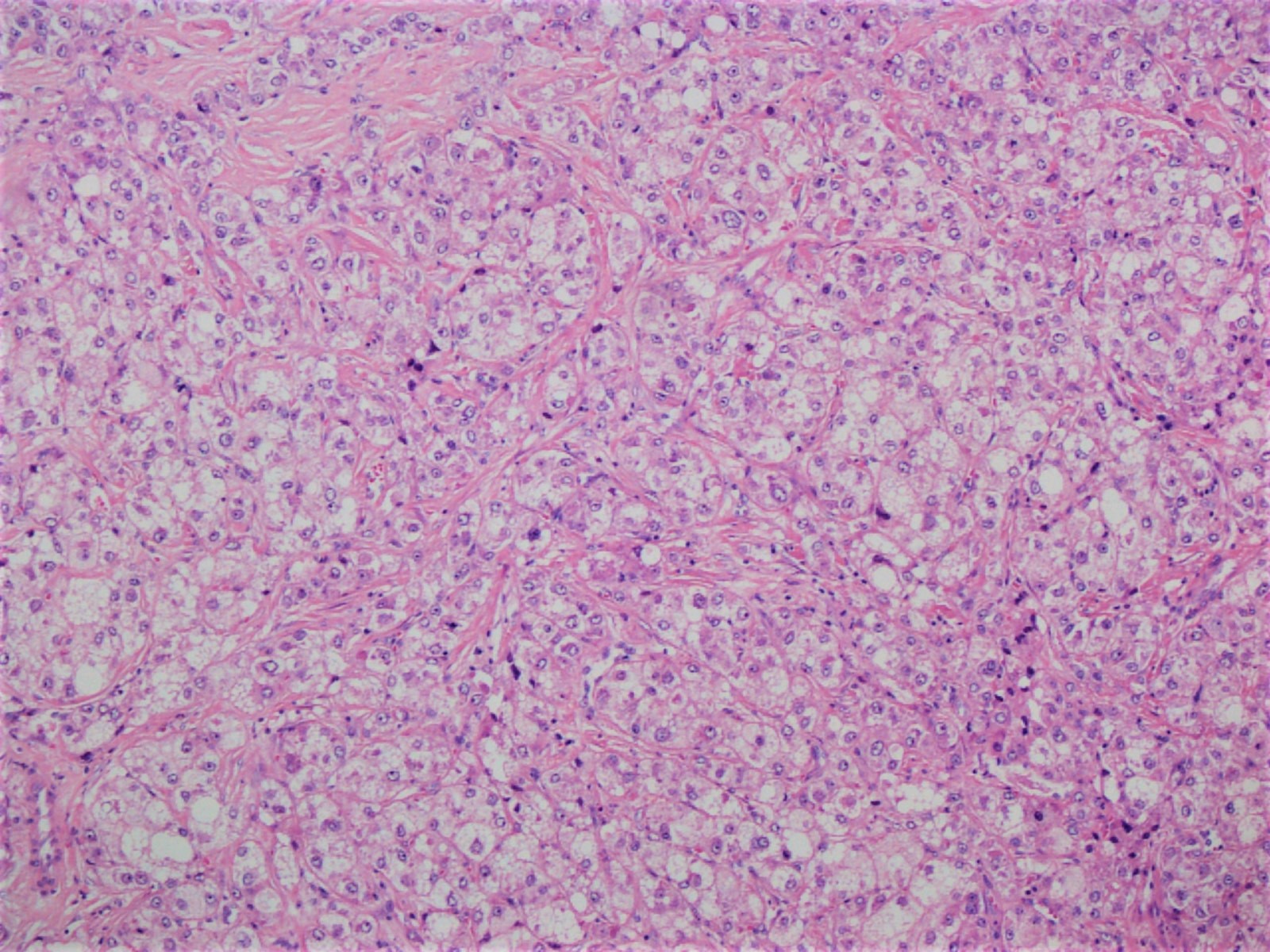
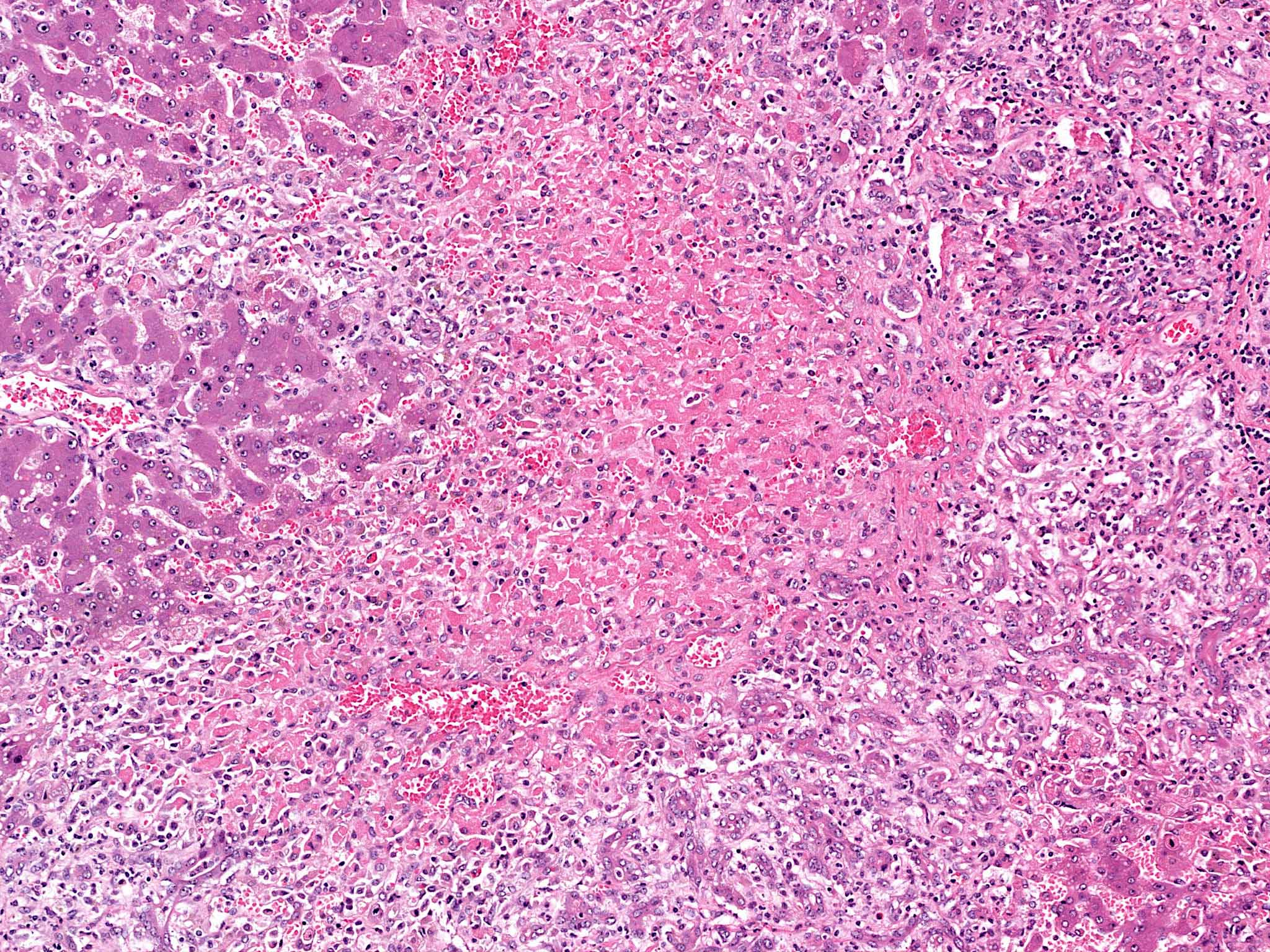
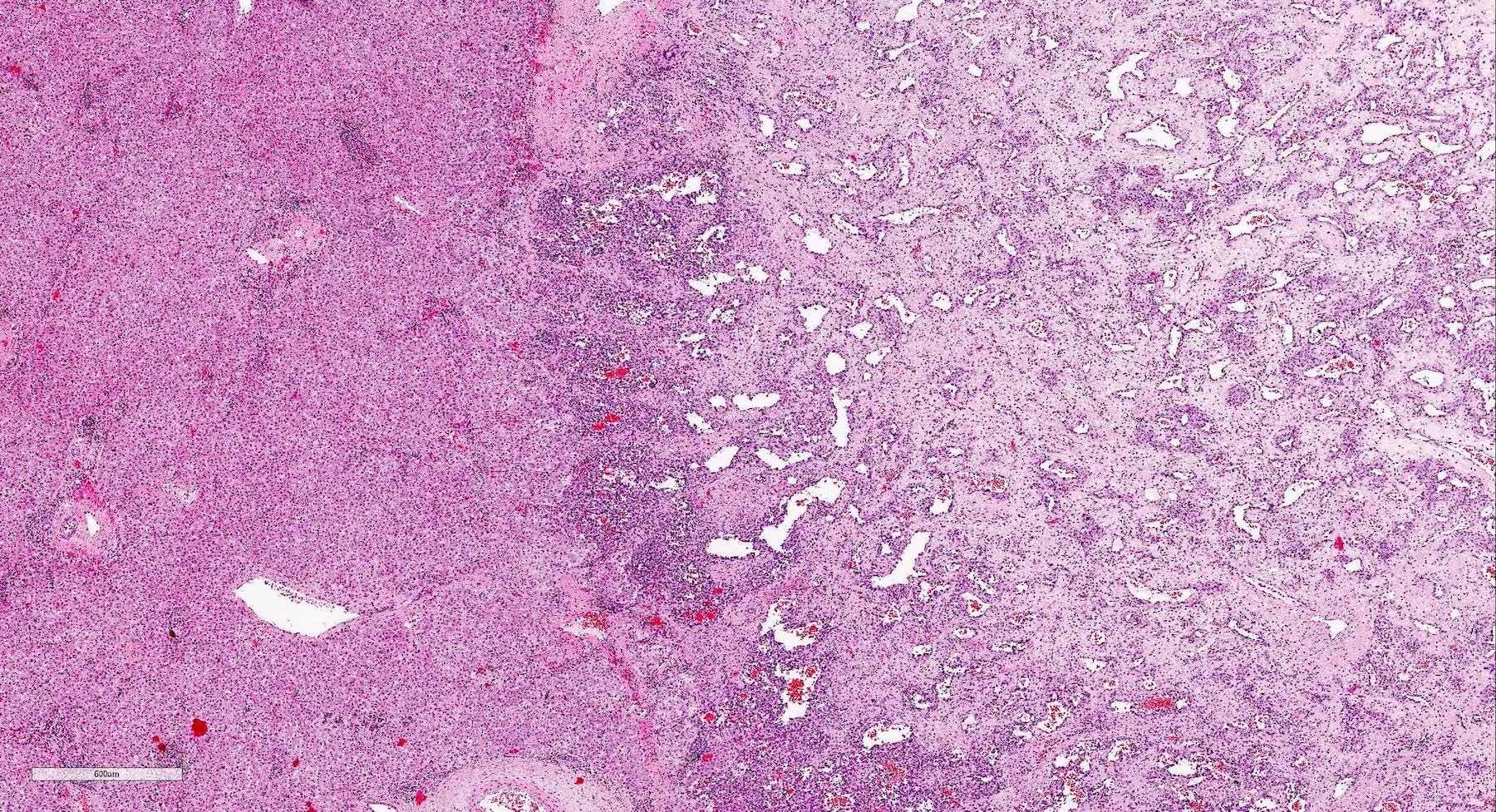
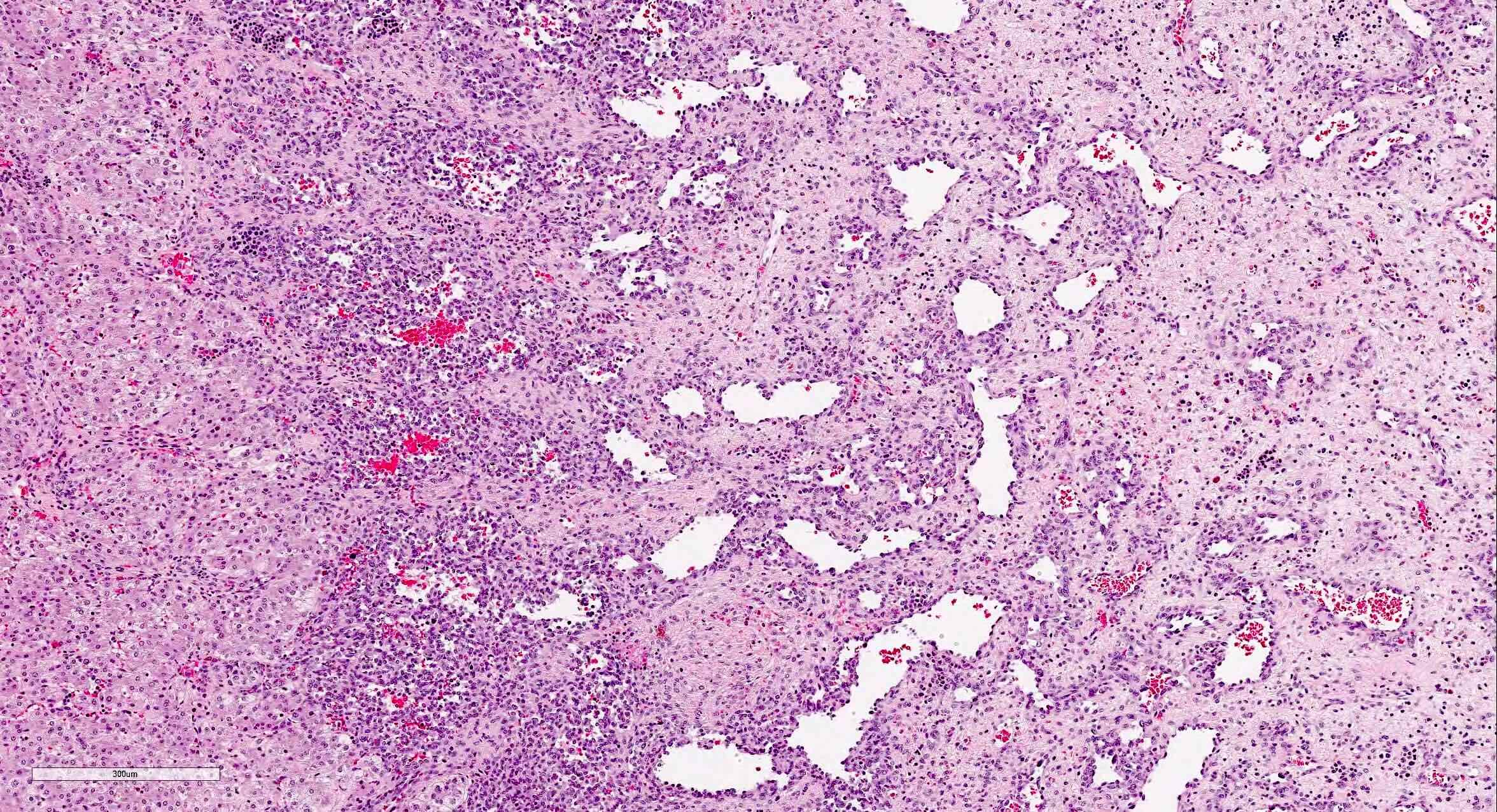
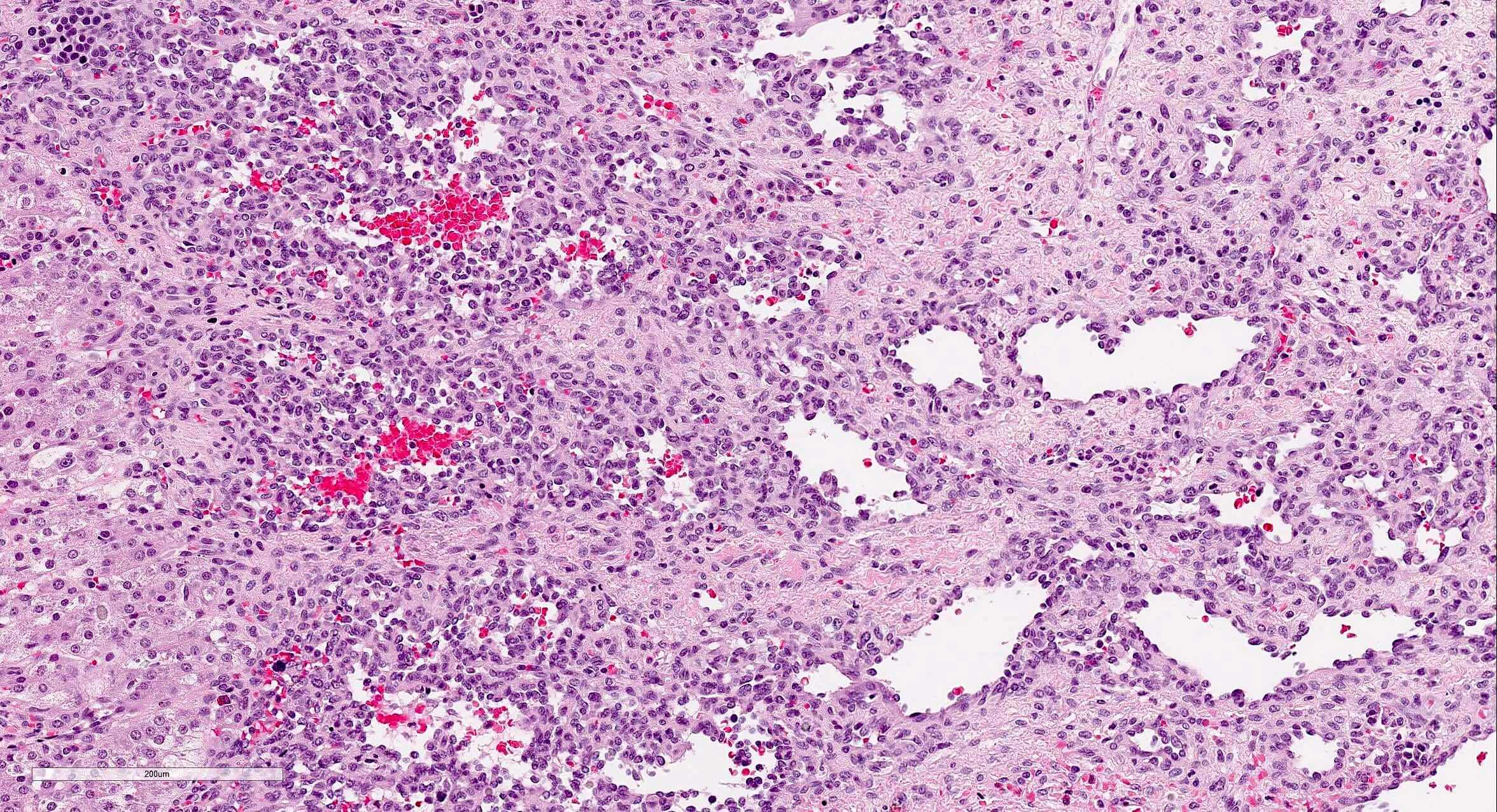
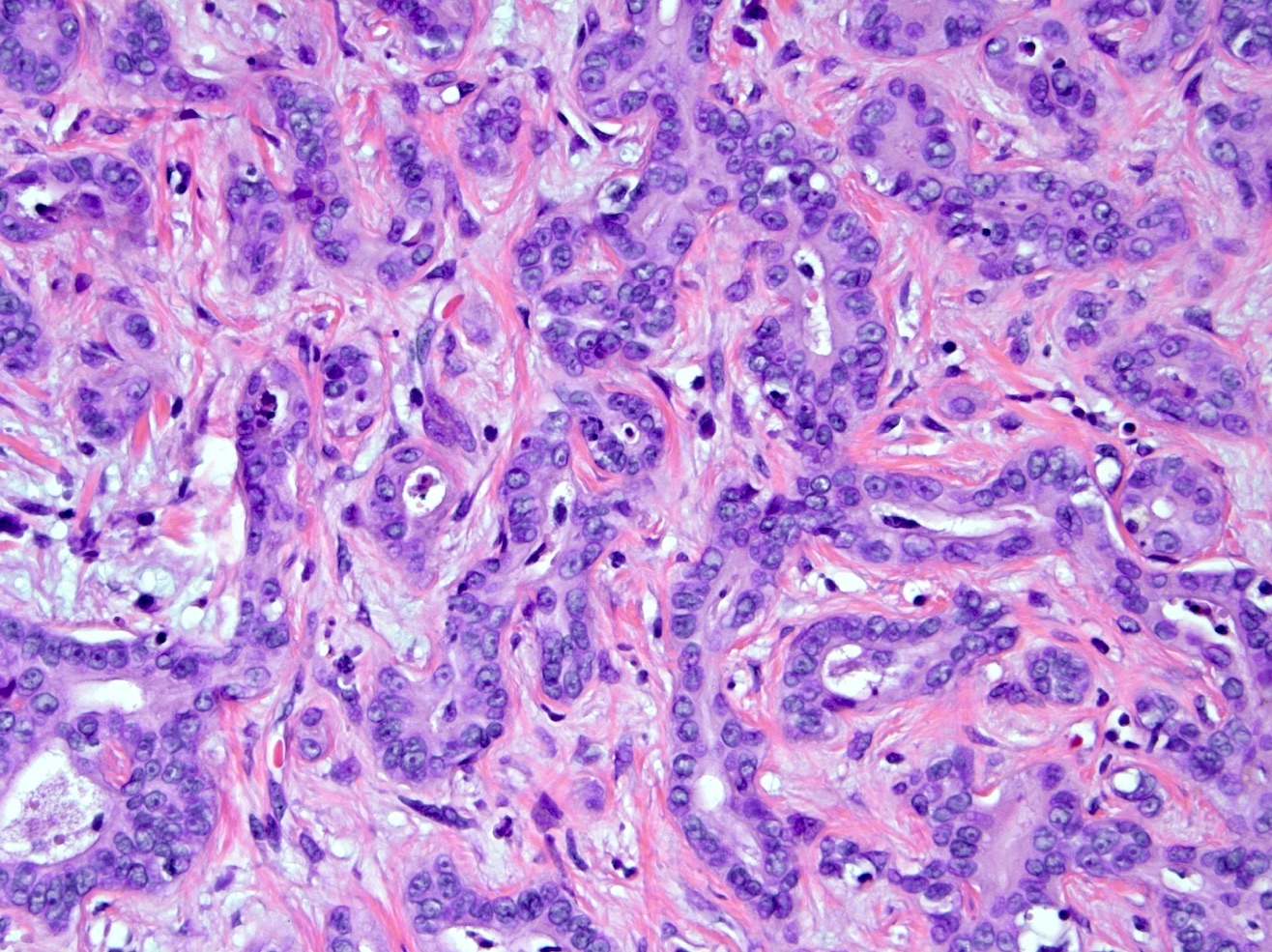
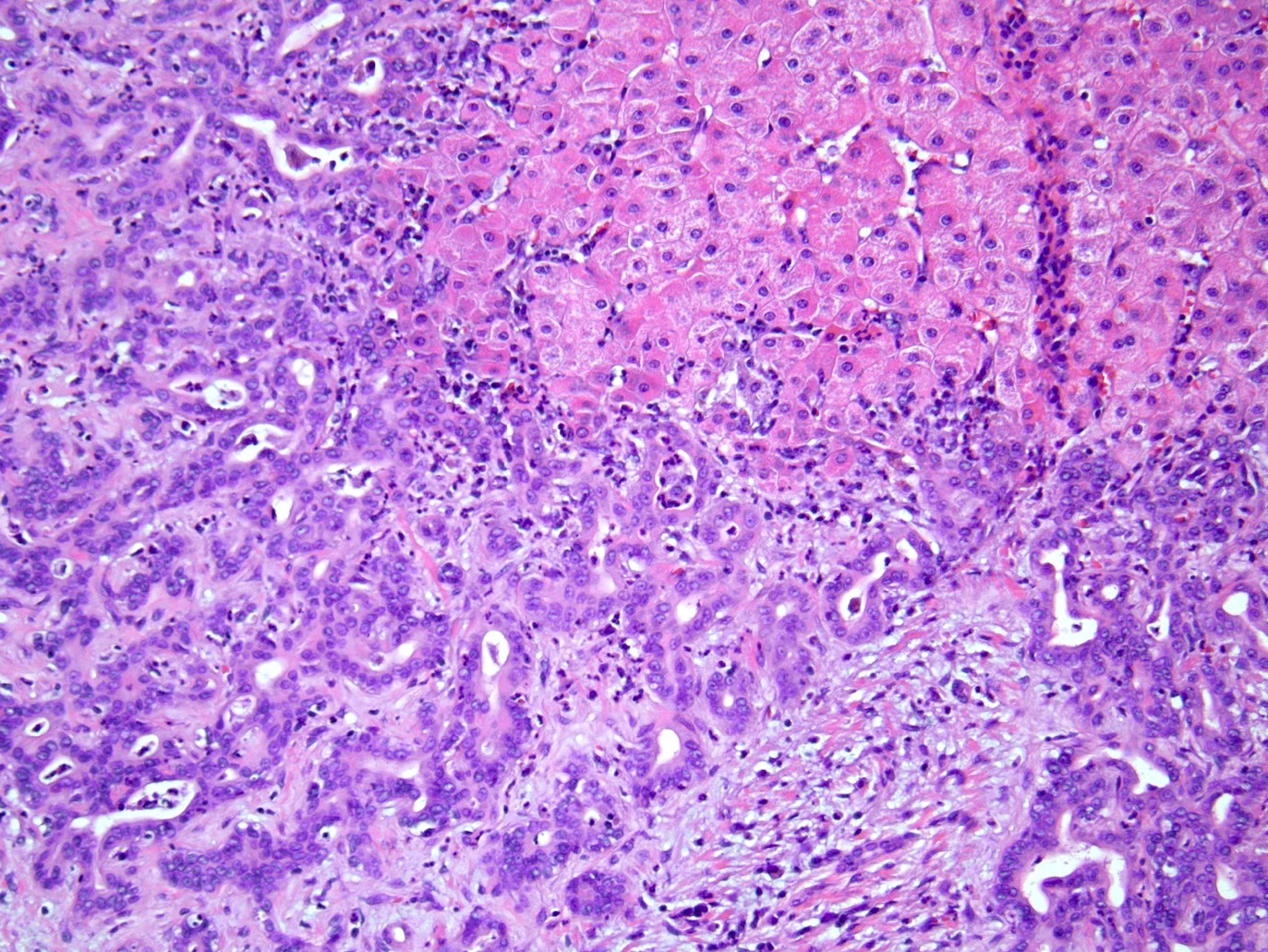
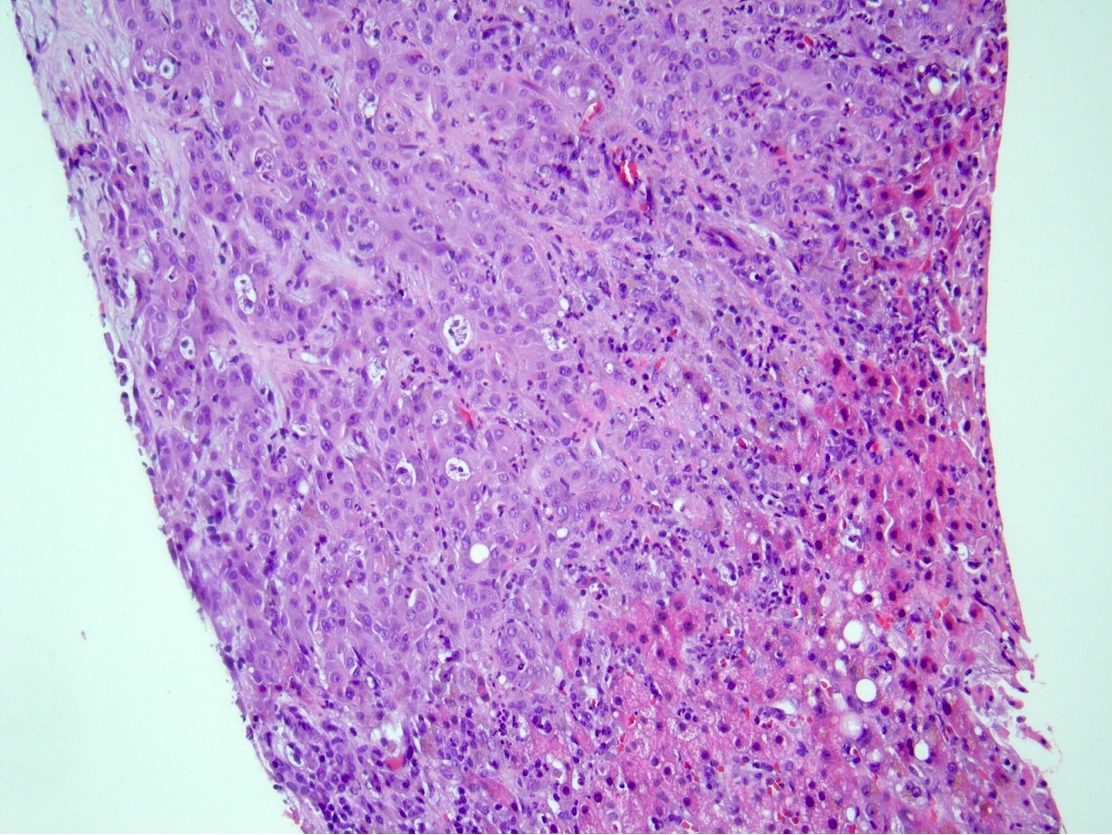
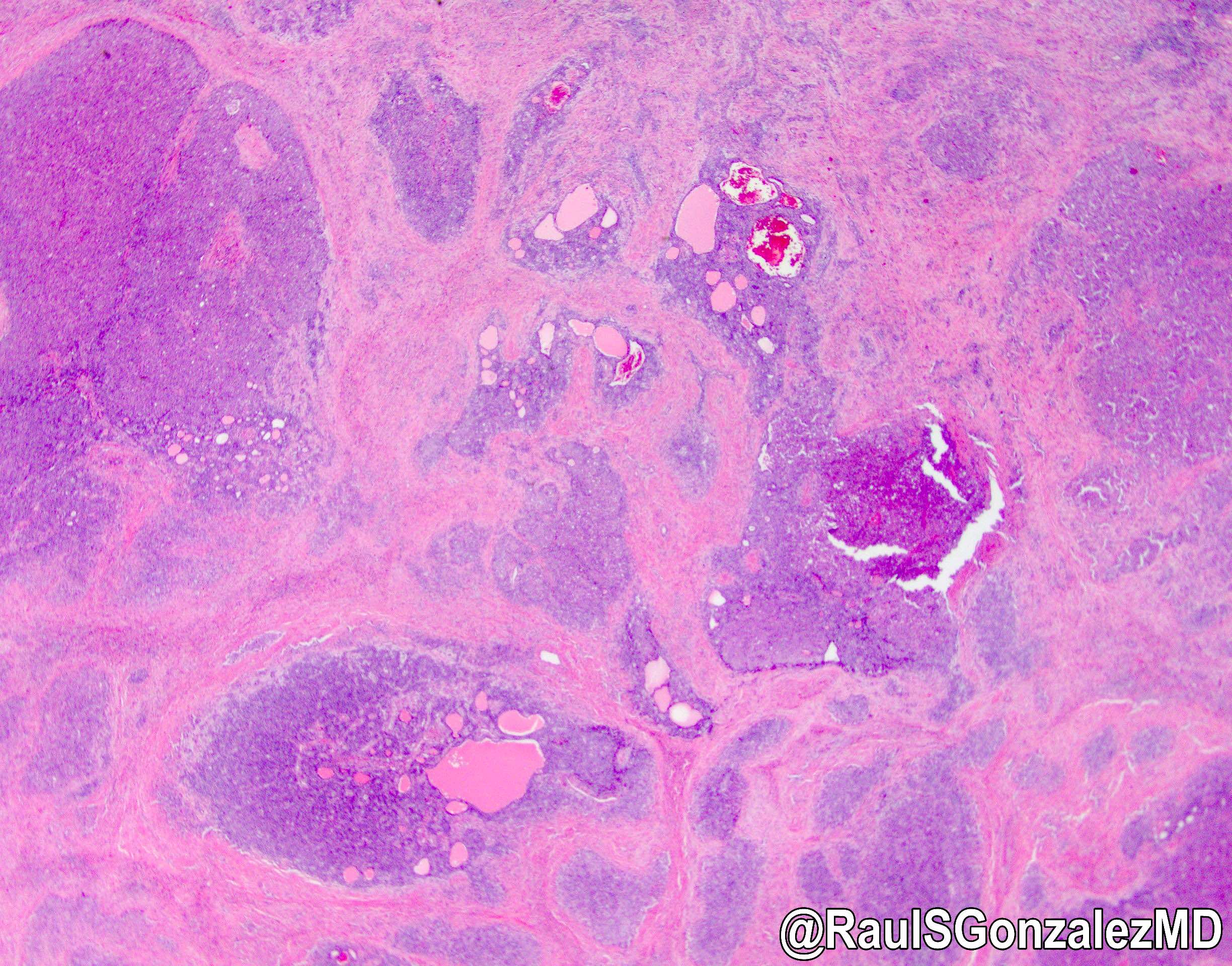
The images depict a zone 3 predominant lobular inflammatory infiltrate with associated confluent necrosis. The findings are consistent with an acute hepatitis pattern of injury. Acute hepatitis C infection is rarely biopsied and most cases of hepatitis C that are biopsied reflect a chronic infection. The histologic features include a mild to moderately dense chronic portal inflammatory infiltrate with focal mild interface activity. Lymphoid aggregates can be present with lymphocytic cholangitis (Poulsen-Christofferson lesion).
Comment Here
Reference: Acute hepatitis-general
The images depict a zone 3 predominant lobular inflammatory infiltrate with associated confluent necrosis. The findings are consistent with an acute hepatitis pattern of injury. Acute hepatitis C infection is rarely biopsied and most cases of hepatitis C that are biopsied reflect a chronic infection. The histologic features include a mild to moderately dense chronic portal inflammatory infiltrate with focal mild interface activity. Lymphoid aggregates can be present with lymphocytic cholangitis (Poulsen-Christofferson lesion).
Comment Here
Reference: Acute hepatitis-general
Acute T cell mediated rejection
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Pathophysiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Immune mediated inflammatory response to the allograft liver by the recipient's immune system
Essential features
- Manifests as sudden elevation in liver enzymes
- Classic histologic findings include mixed portal inflammatory infiltrate, bile duct damage and endothelialitis
- Must be distinguished from recurrent disease and complications of transplant procedure (vascular / biliary damage)
Terminology
- Synonyms include acute cellular rejection, nonductopenic rejection, reversible rejection (Am J Transplant 2016;16:2816, Hepatology 1997;25:658, Liver Transpl 2012;18:1154)
ICD coding
- ICD-10: T86.41 - liver transplant rejection
Epidemiology
- Clinically significant T cell mediated rejection occurs in 20 - 40% of liver transplants with current immunosuppressive regimens
- Usually occurs 5 - 30 days after transplant but can occur months to years later (Am J Transplant 2009;9:301)
Pathophysiology
- Host T cells interact with donor HLA, become activated, then recruit macrophages and granulocytes which mediate tissue destruction (Clin Biochem 2016;49:320)
Clinical features
- Generally mild and nonspecific
- Can be asymptomatic or present with fever, abdominal pain, hepatomegaly or fatigue
Diagnosis
- Requires histologic confirmation on liver biopsy
Laboratory
- In most cases, acute T cell mediated rejection is suspected when there is a relatively abrupt increase in liver enzymes above their baseline (Surg Pathol Clin 2018;11:431)
- Patients may have subtherapeutic levels of antirejection medications (e.g., tacrolimus)
Prognostic factors
- Risk factors and demographics have not been clearly defined, though increased severity of histologic rejection indicates worse outcome for graft if not treated (Am J Med Sci 2018;356:23)
Case reports
- 21 month old girl with nonanastomotic biliary stricture and acute cellular rejection (Exp Clin Transplant 2012;10:176)
- 2 year old girl with HHV 6 infection after liver transplantation with acute graft rejection (Pediatr Transplant 2011;15:E126)
- 48 year old man with acute rejection and novel H1N1 influenza A infection (Hepatobiliary Pancreat Dis Int 2010;9:658)
- 53 year old man with acute graft rejection triggered by interferon treatment for hepatitis C (Transplant Proc 2017;49:1634)
- 67 year old woman with acute liver graft rejection after ipilimumab therapy (Ann Oncol 2017;28:2619)
Treatment
- Most patients with histologically mild rejection do not require additional immunosuppression and show no adverse outcomes
- Moderate and severe rejection are usually treated with additional immunosuppression (Hepatology 1997;25:658)
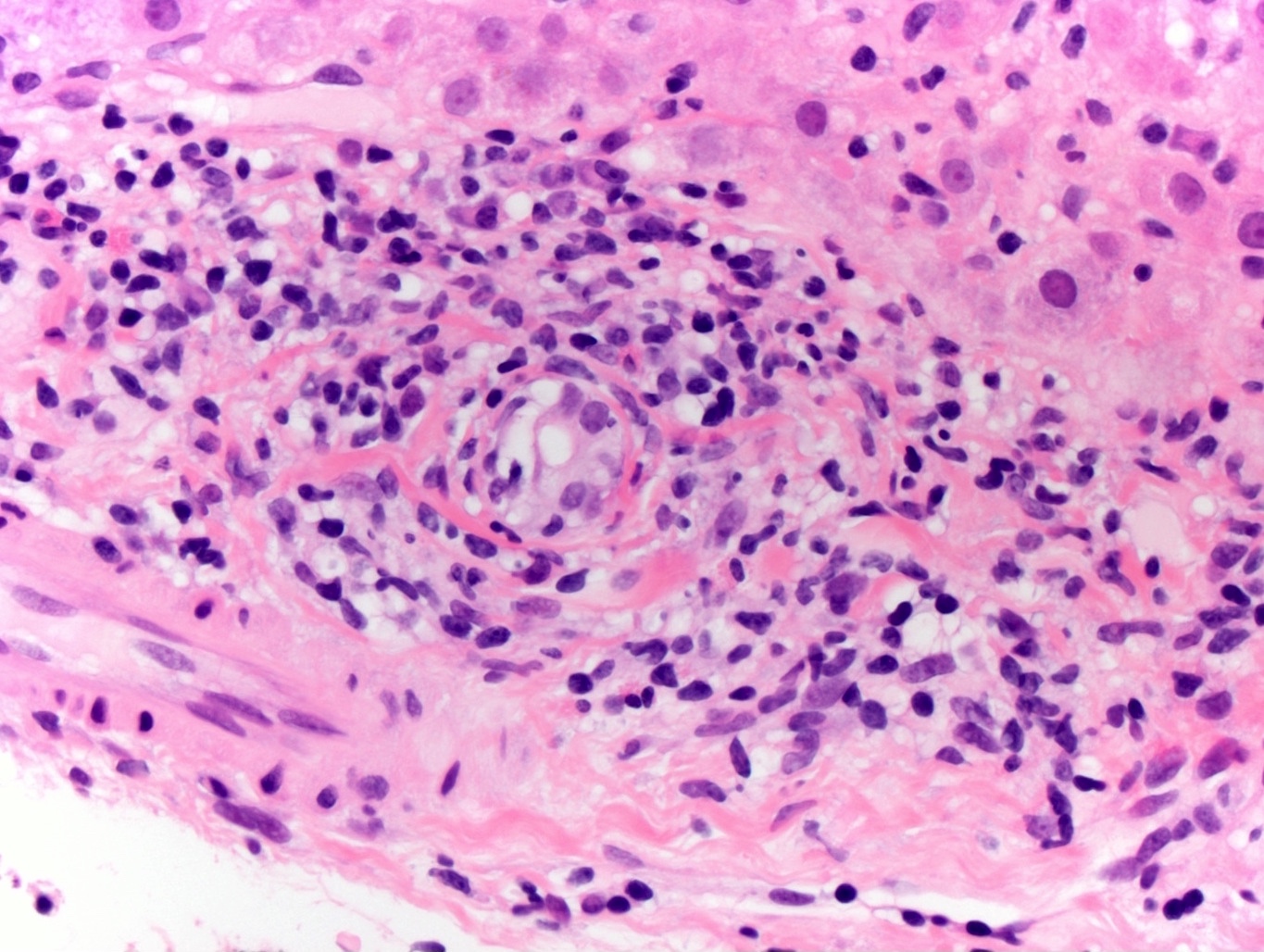
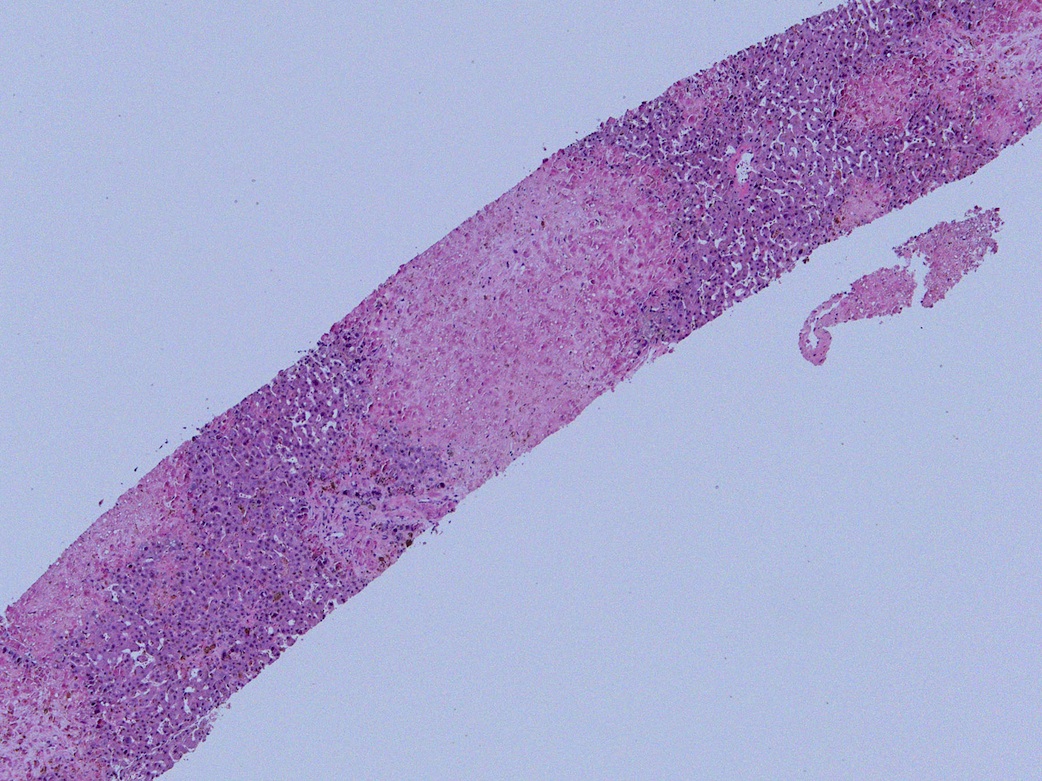
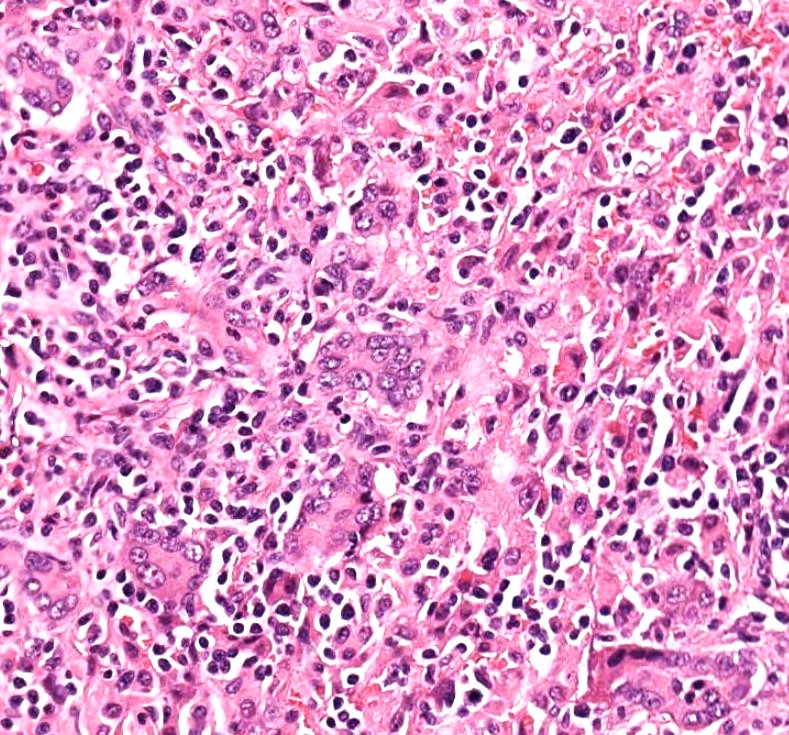
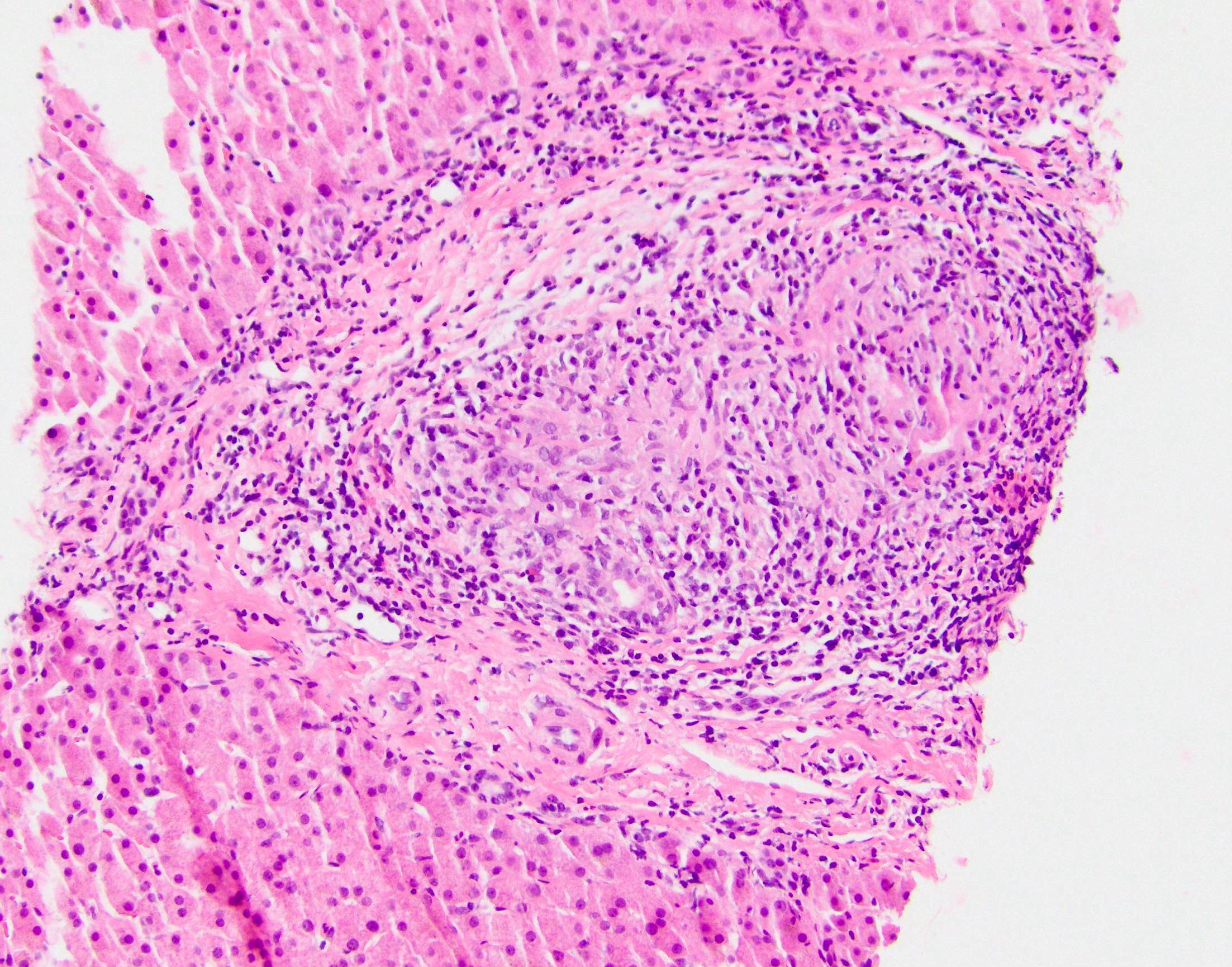
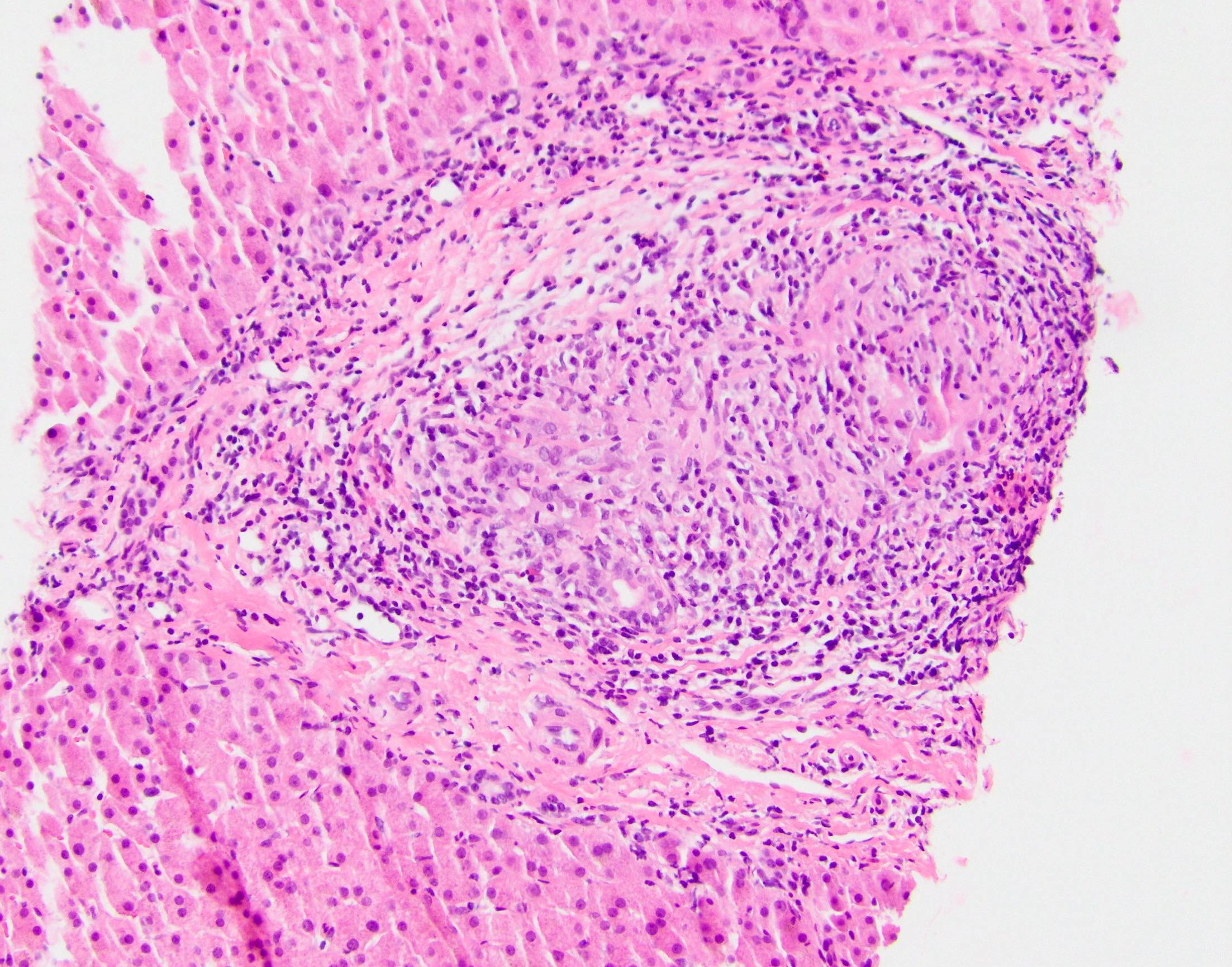
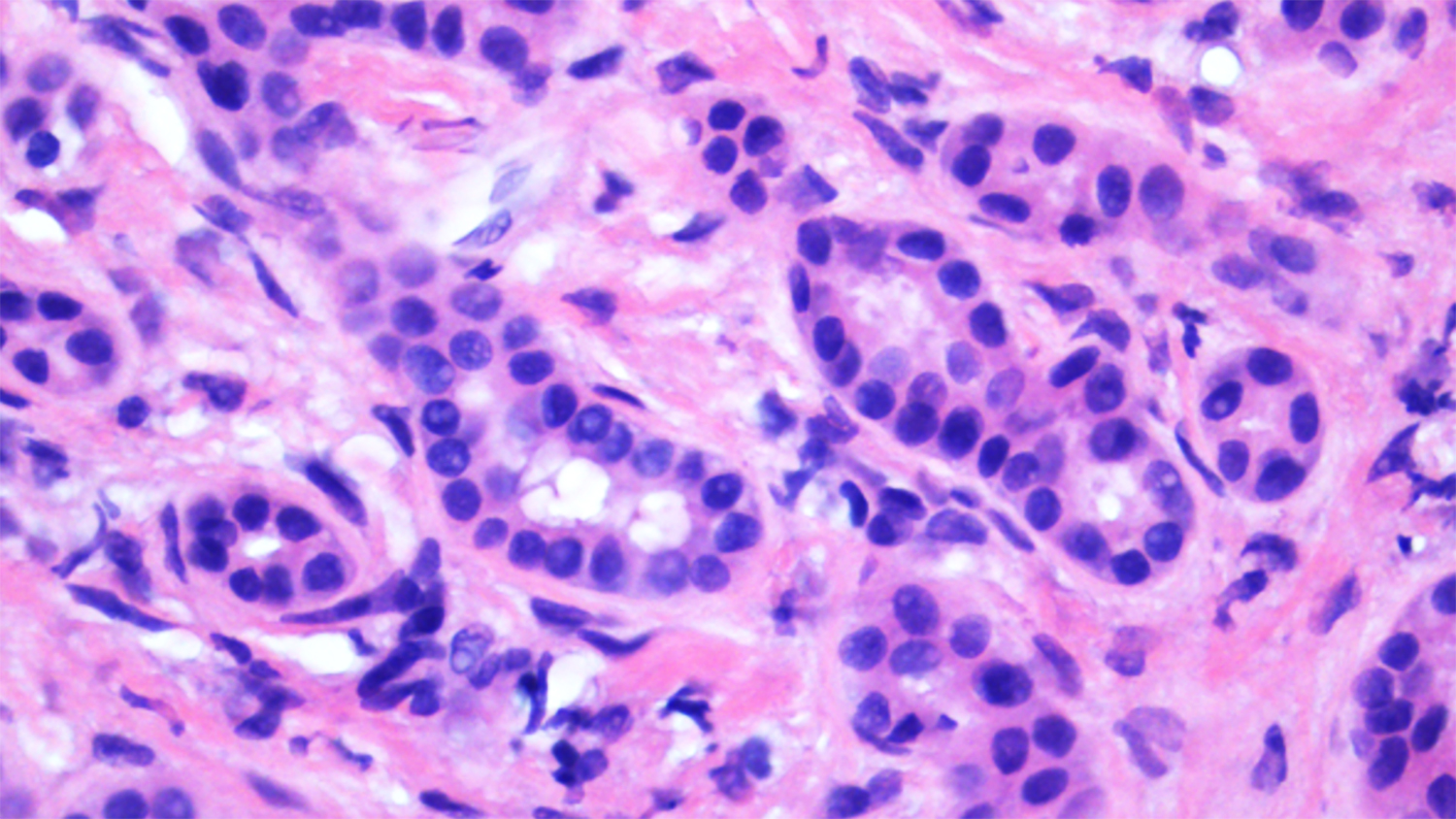
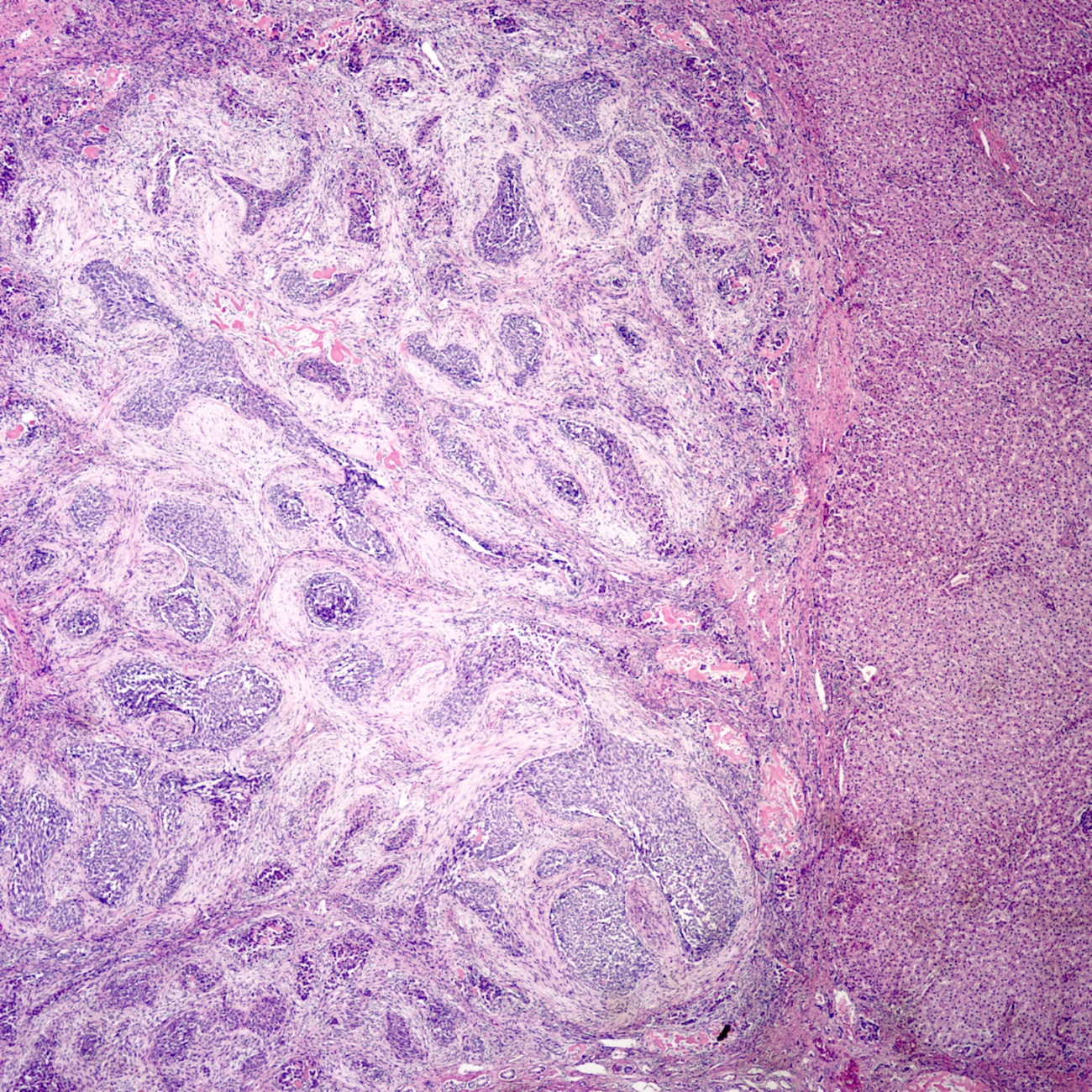
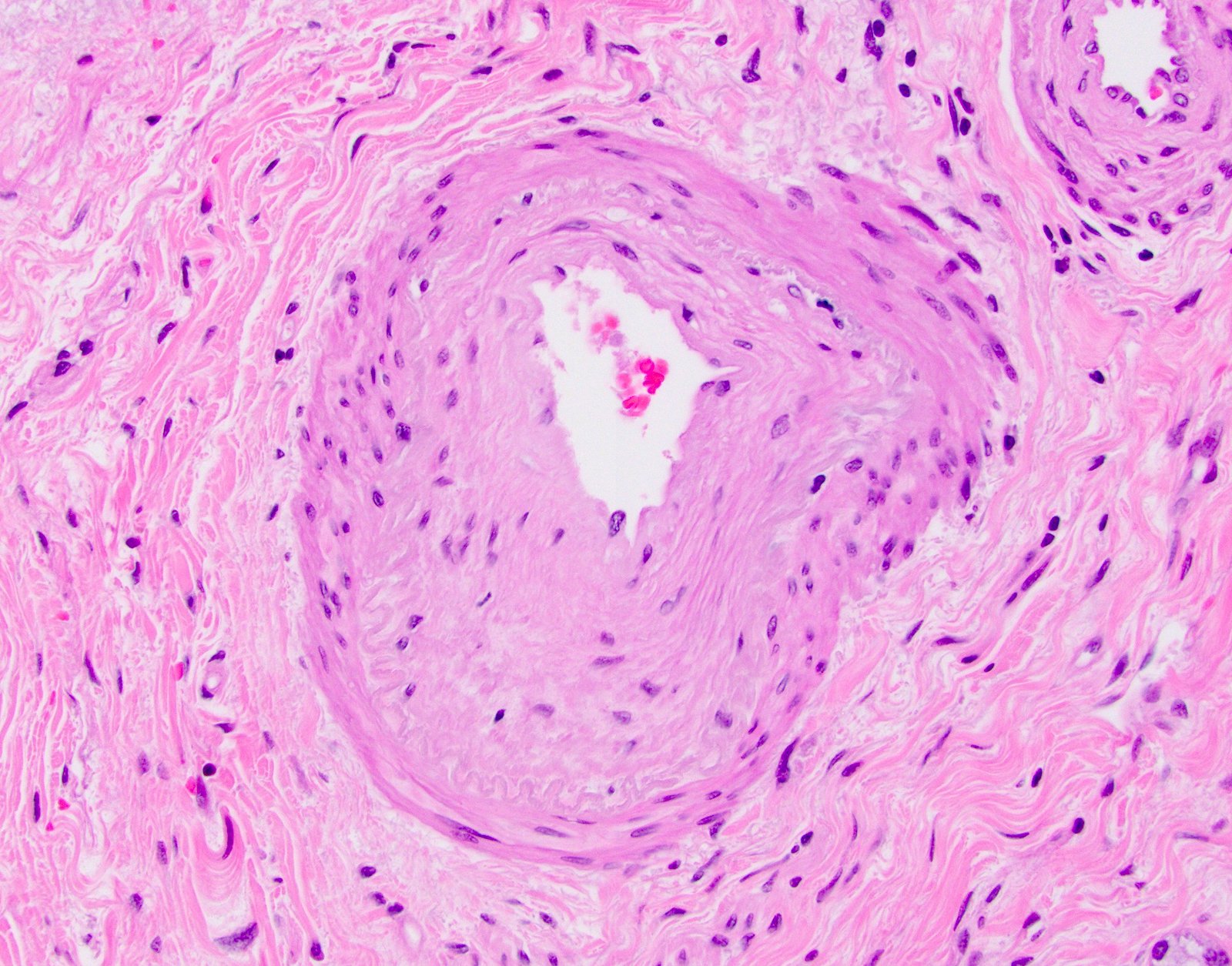
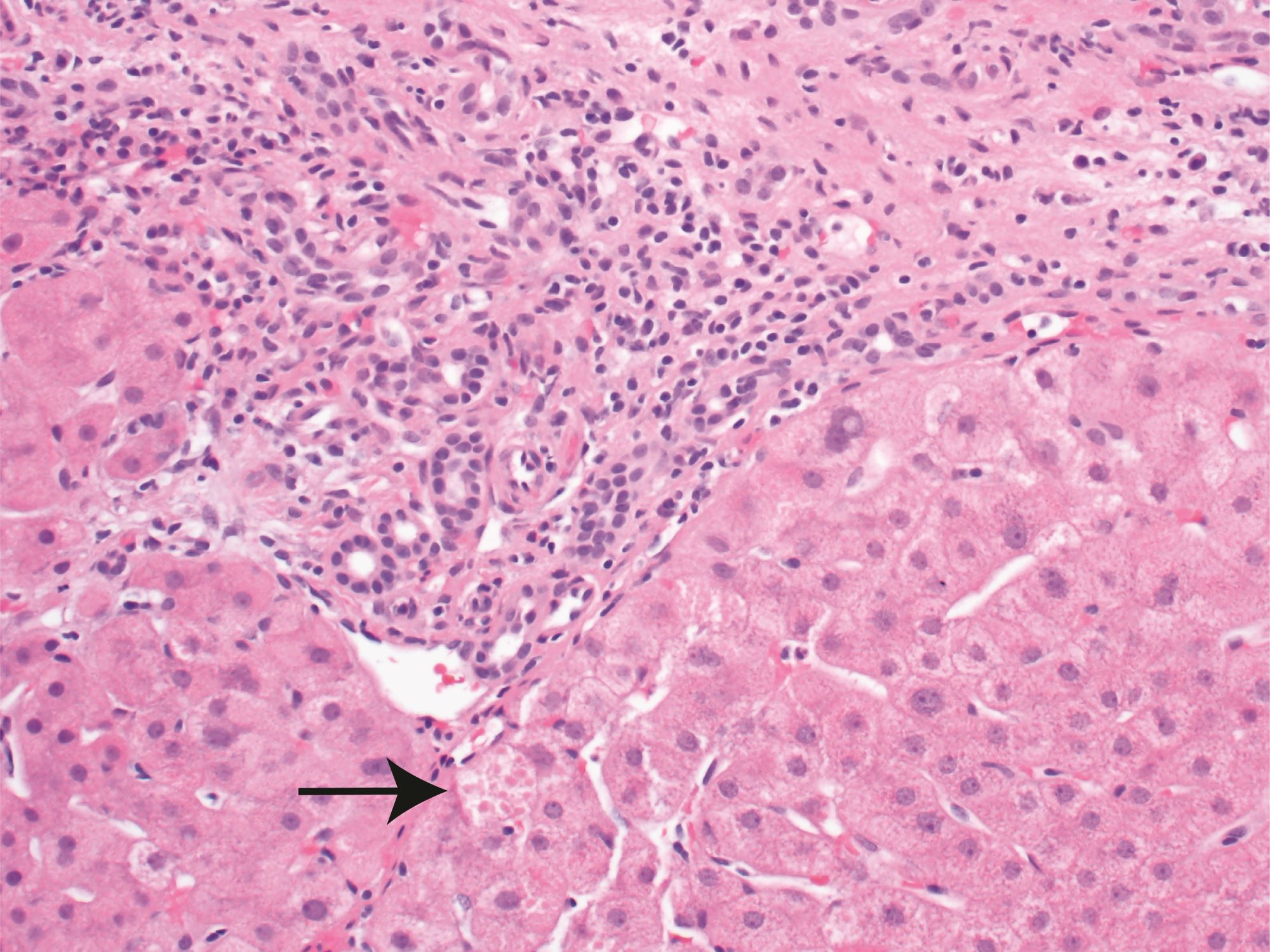
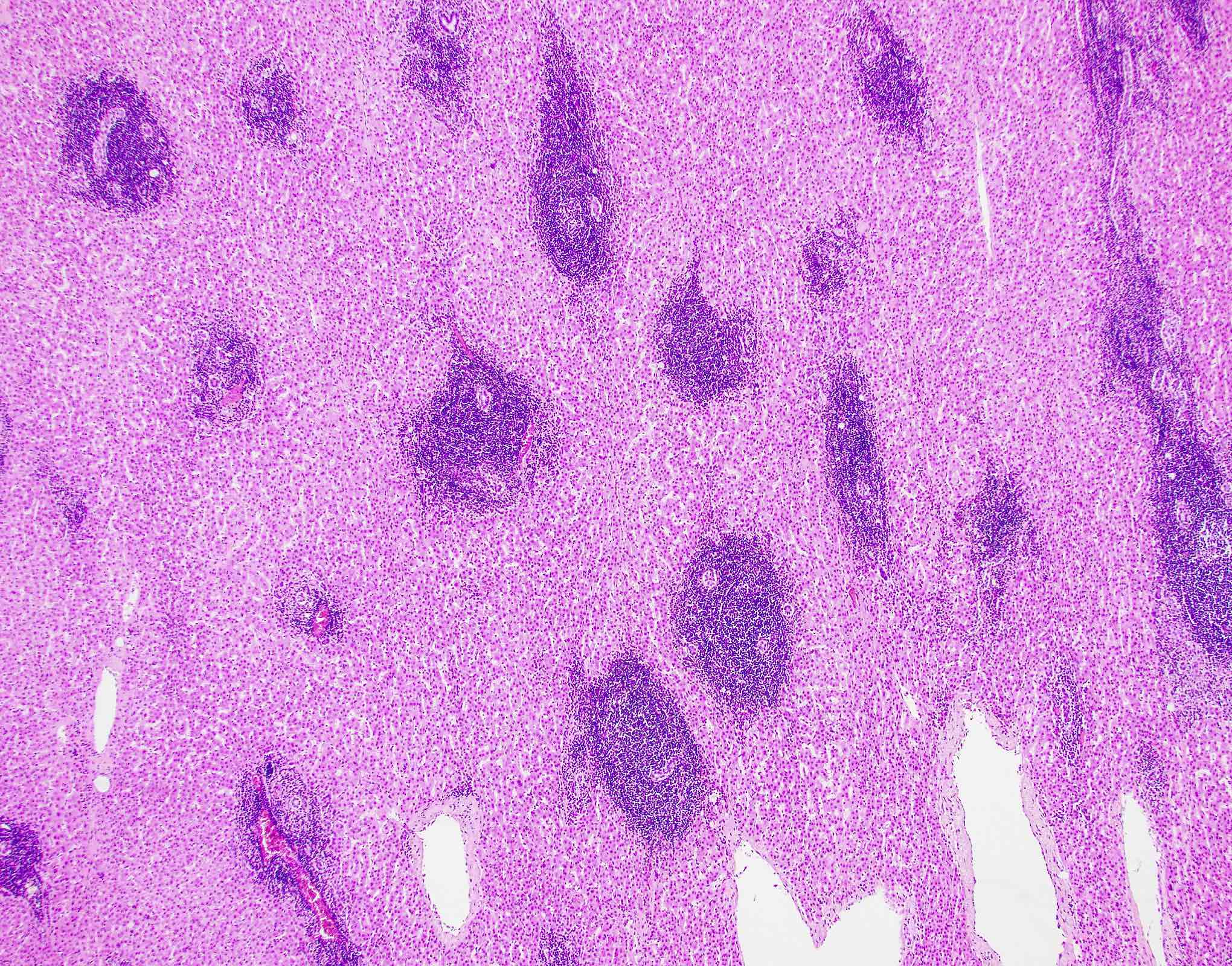
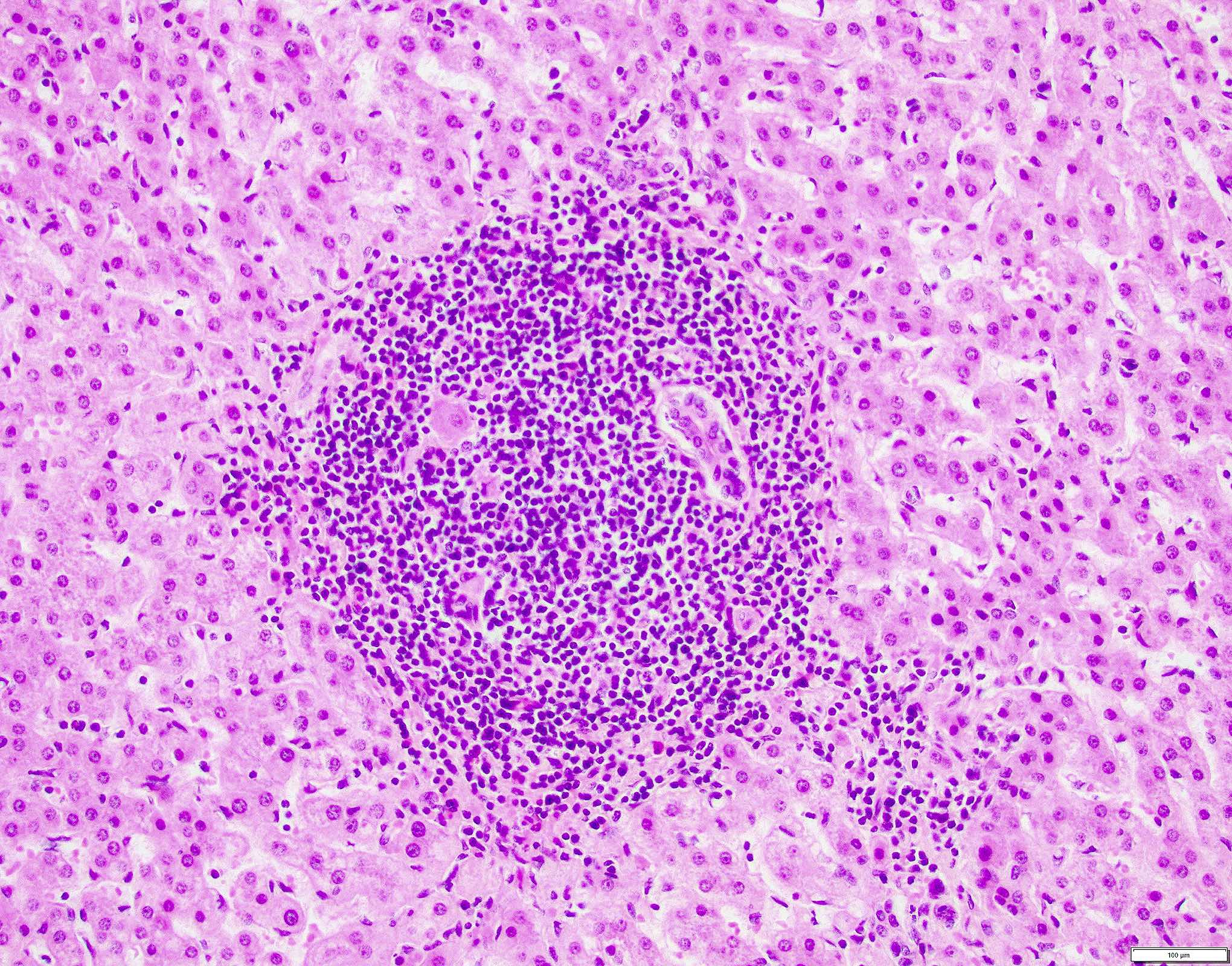
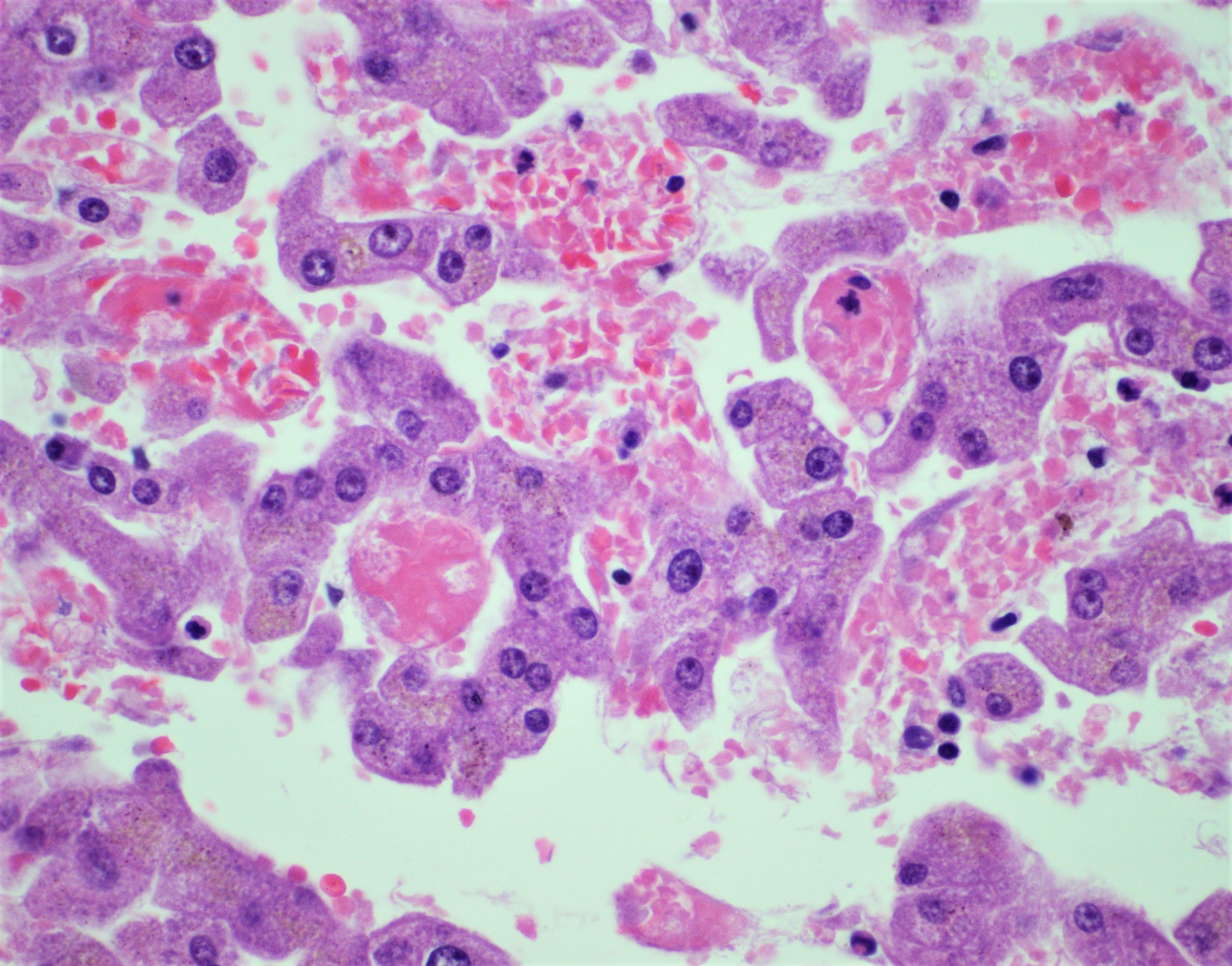
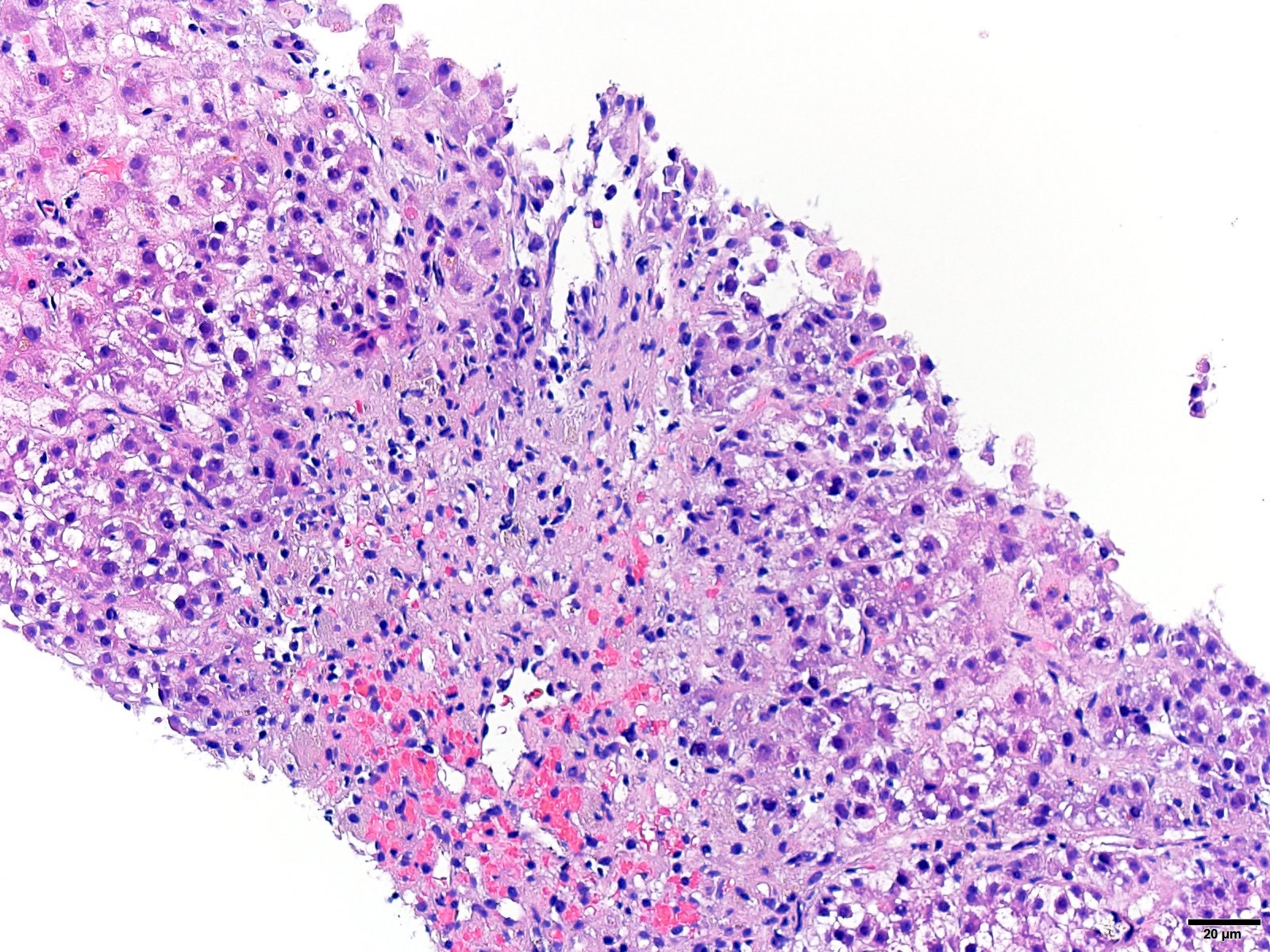
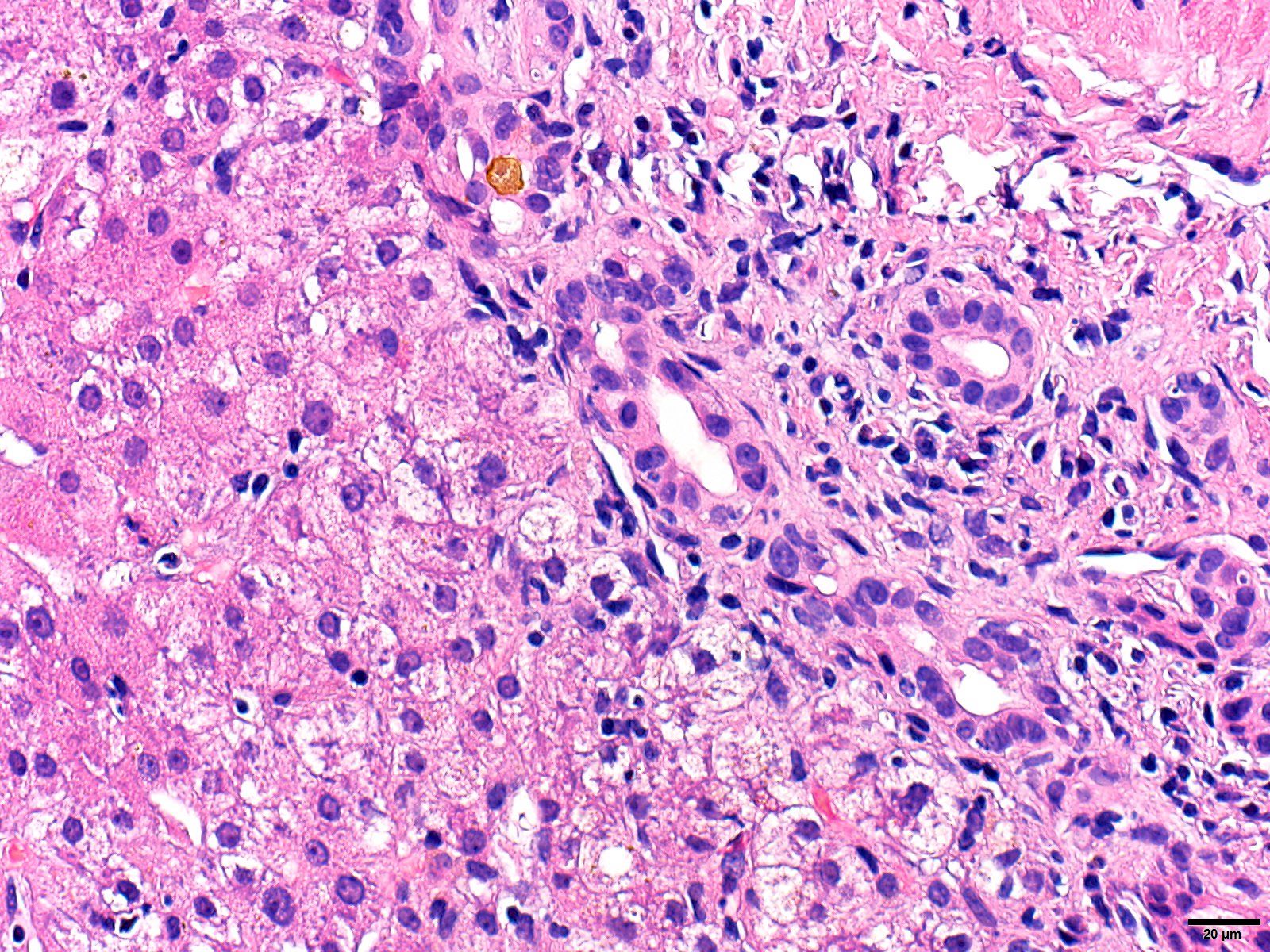
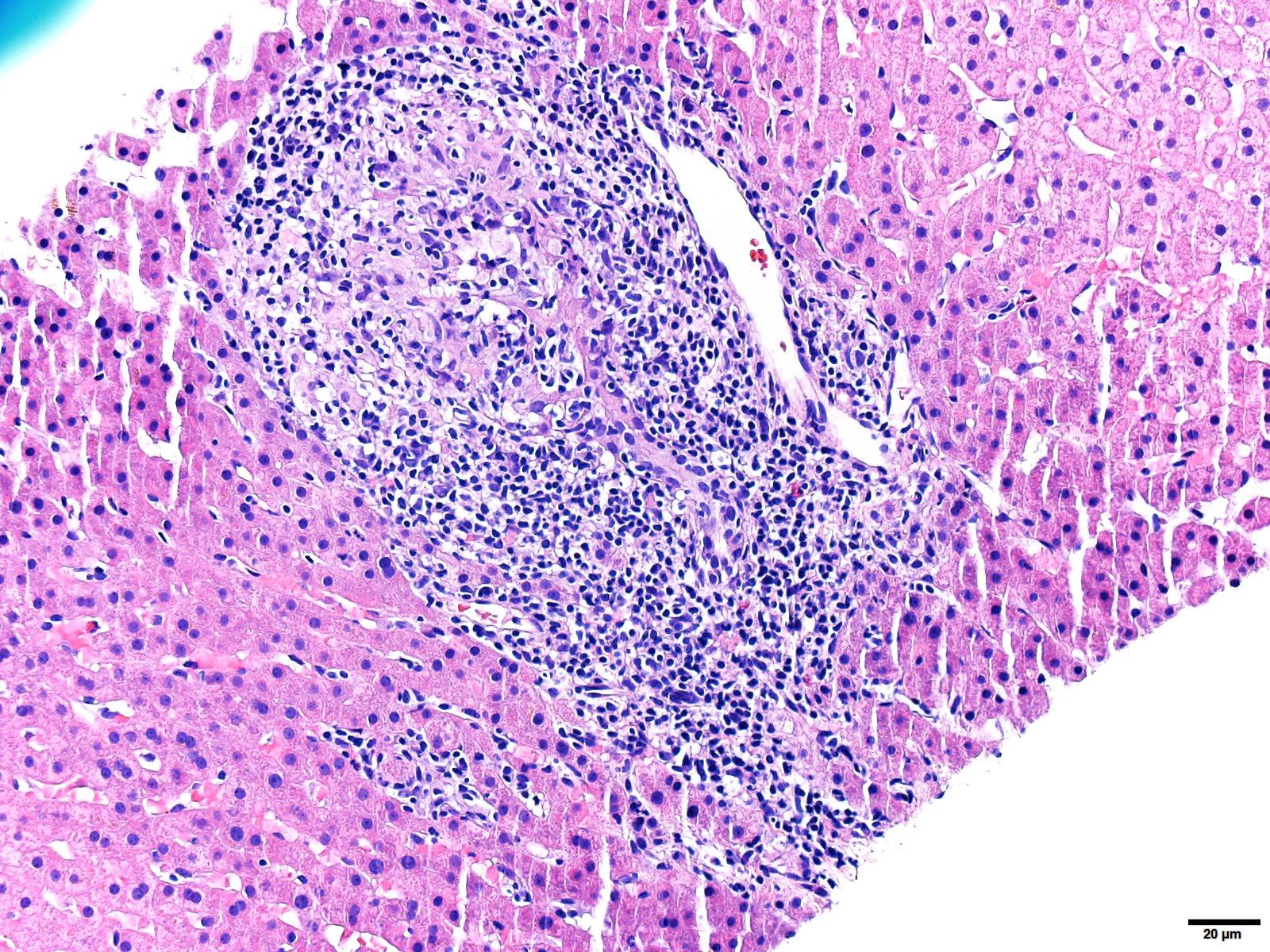
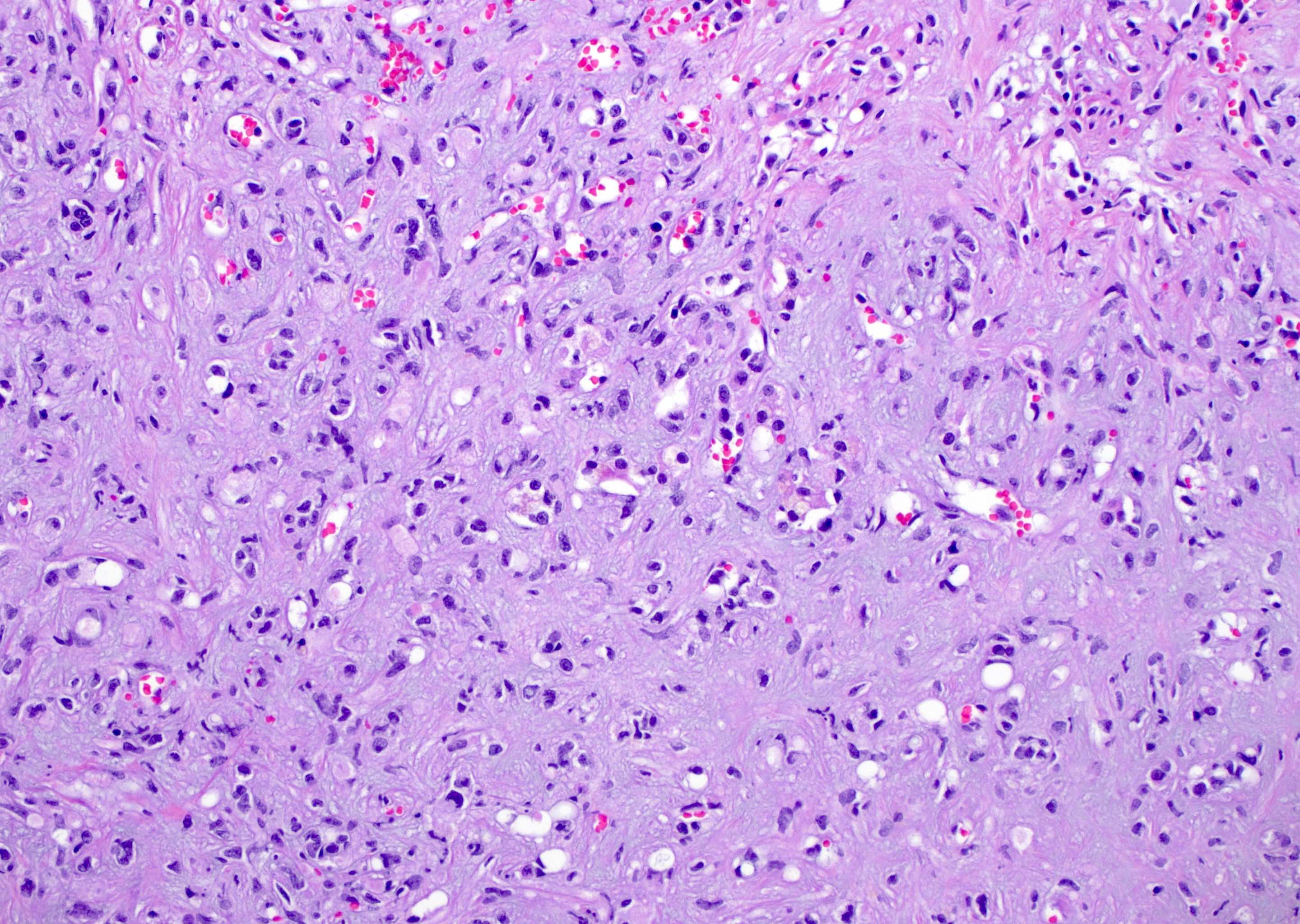
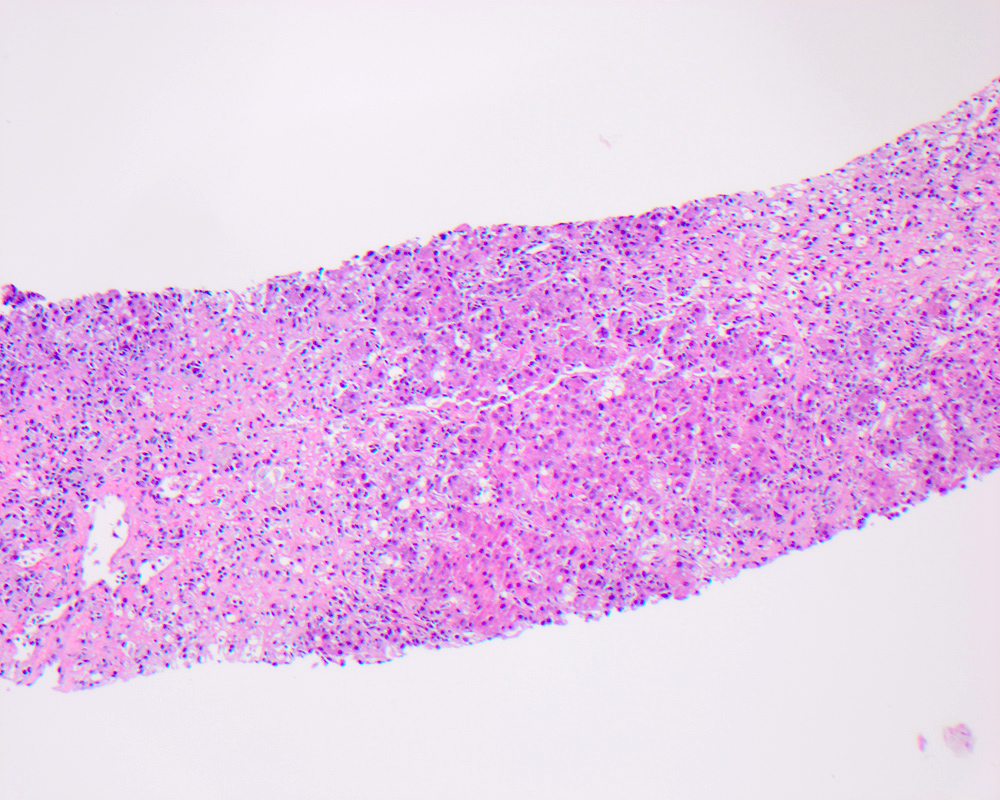
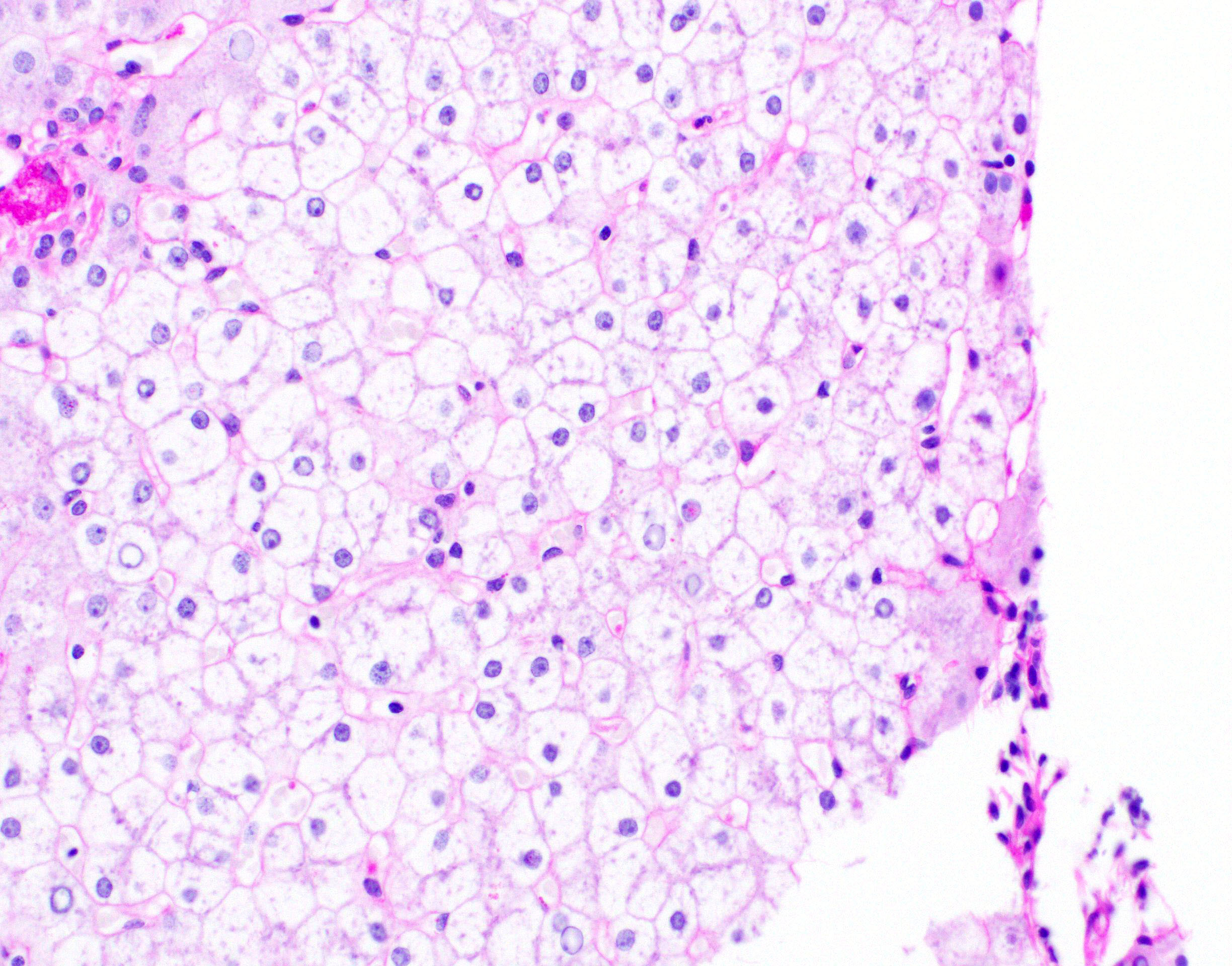
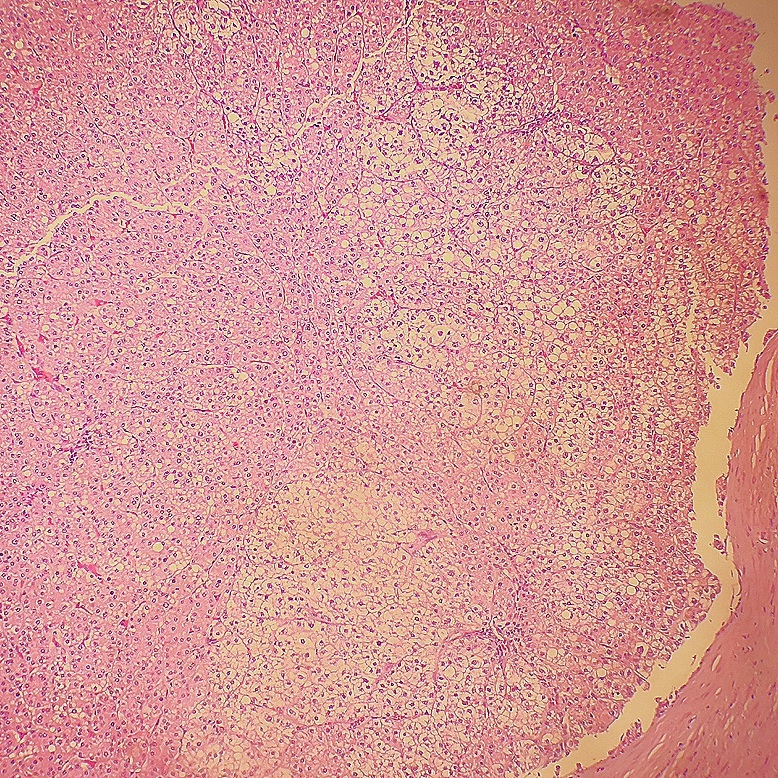
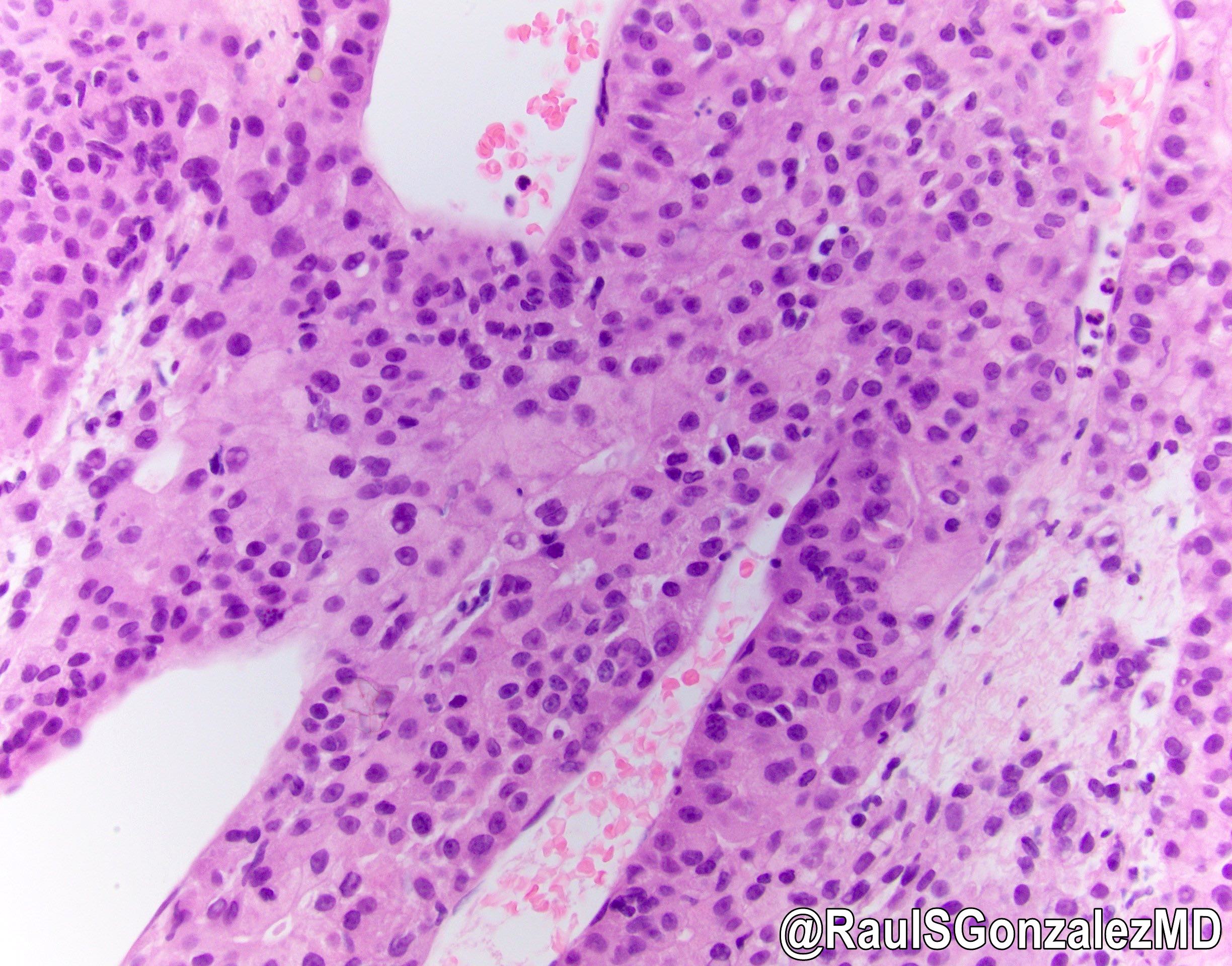
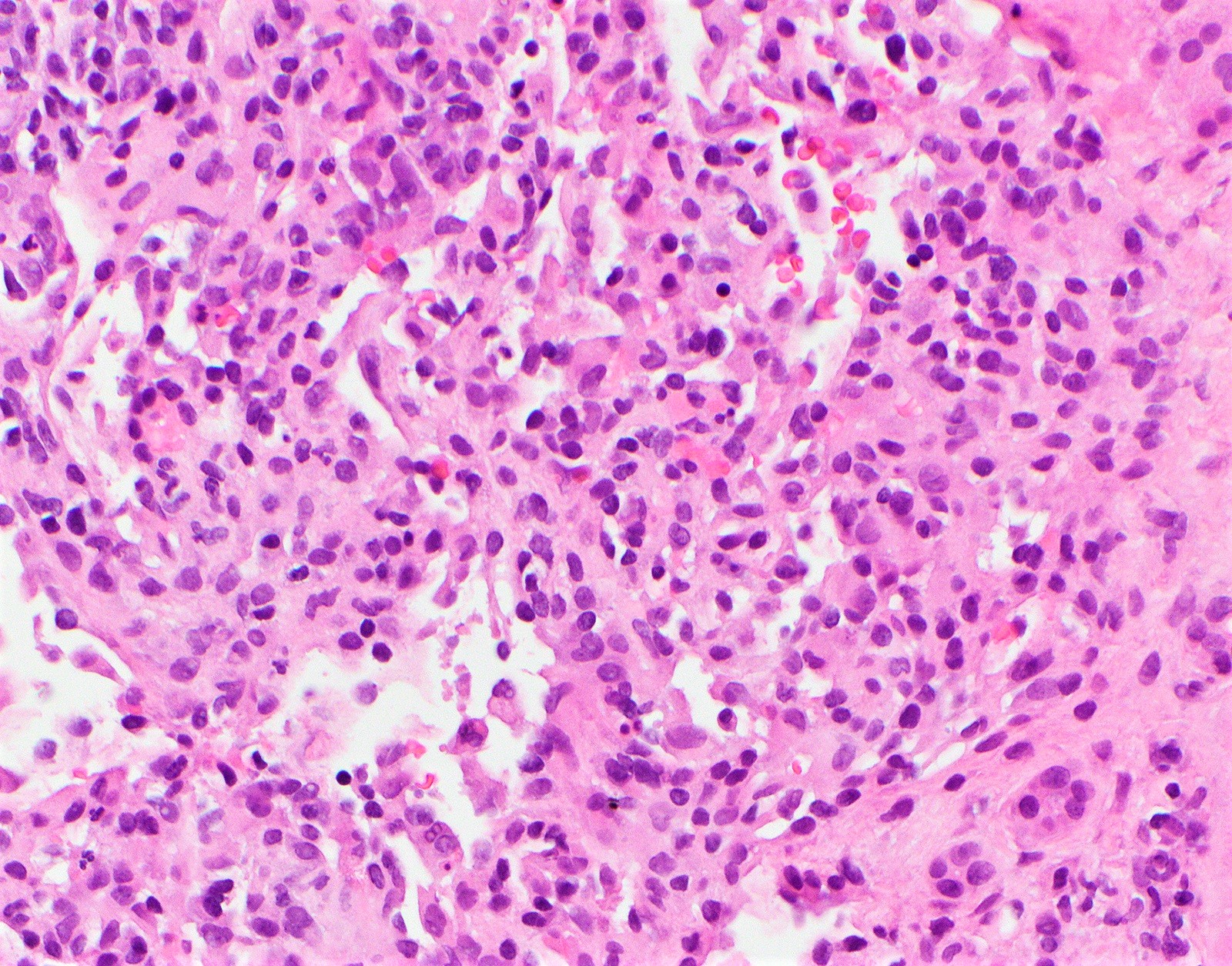
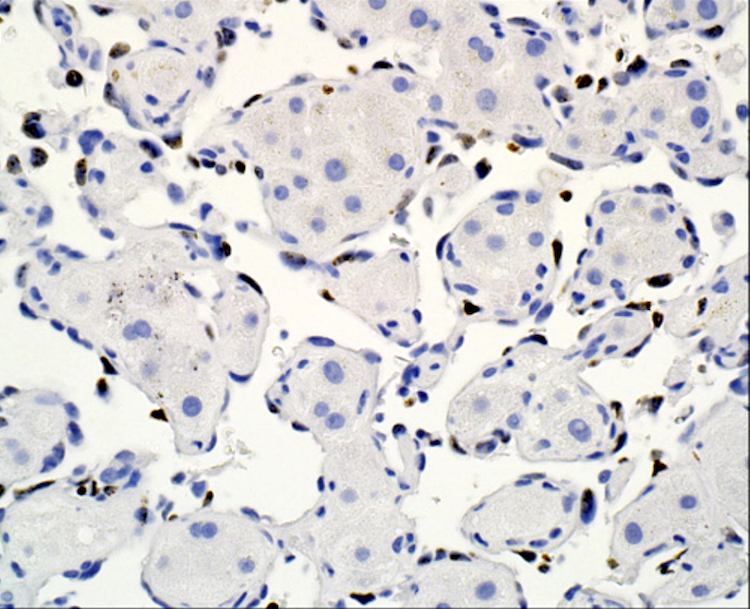
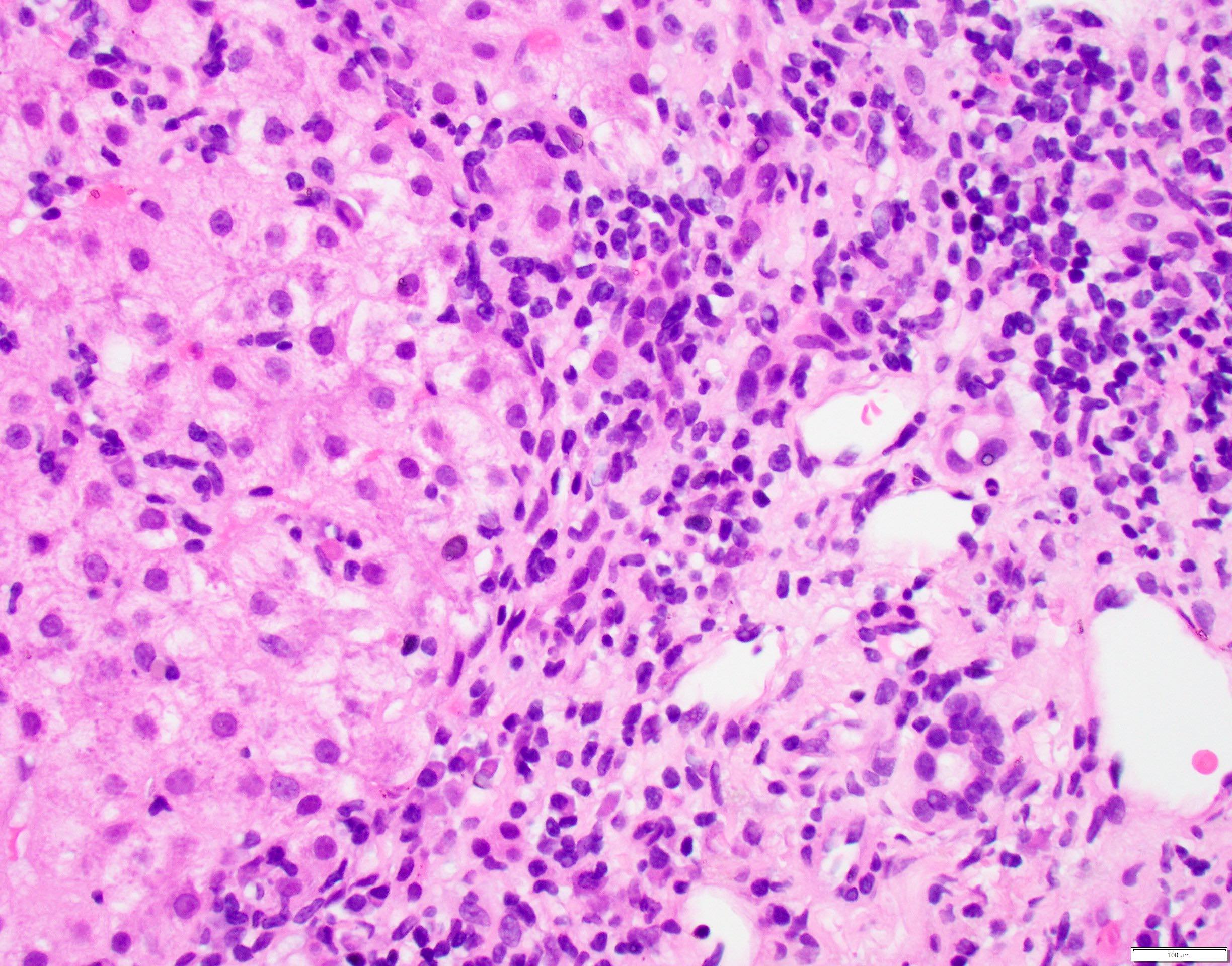
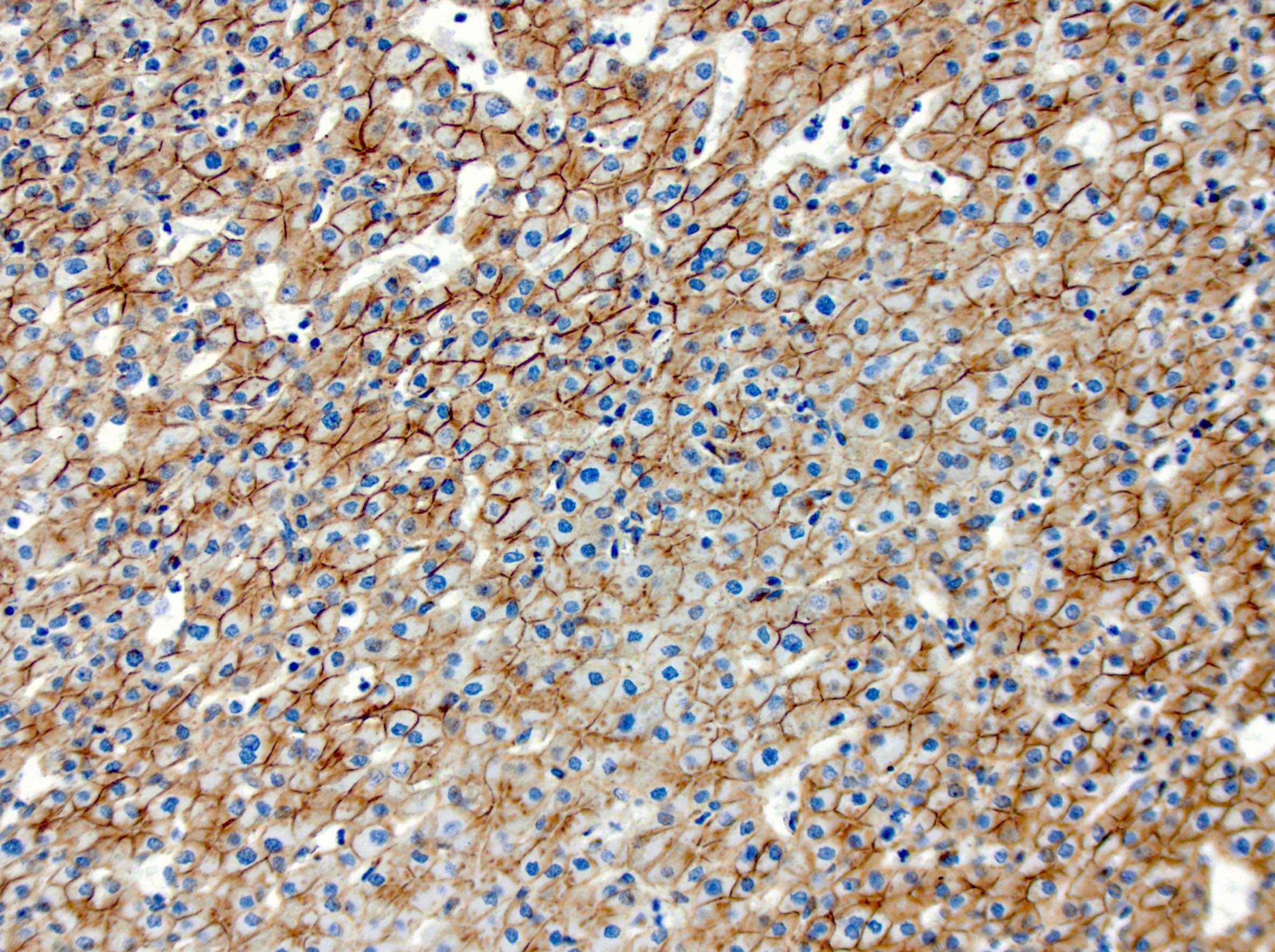
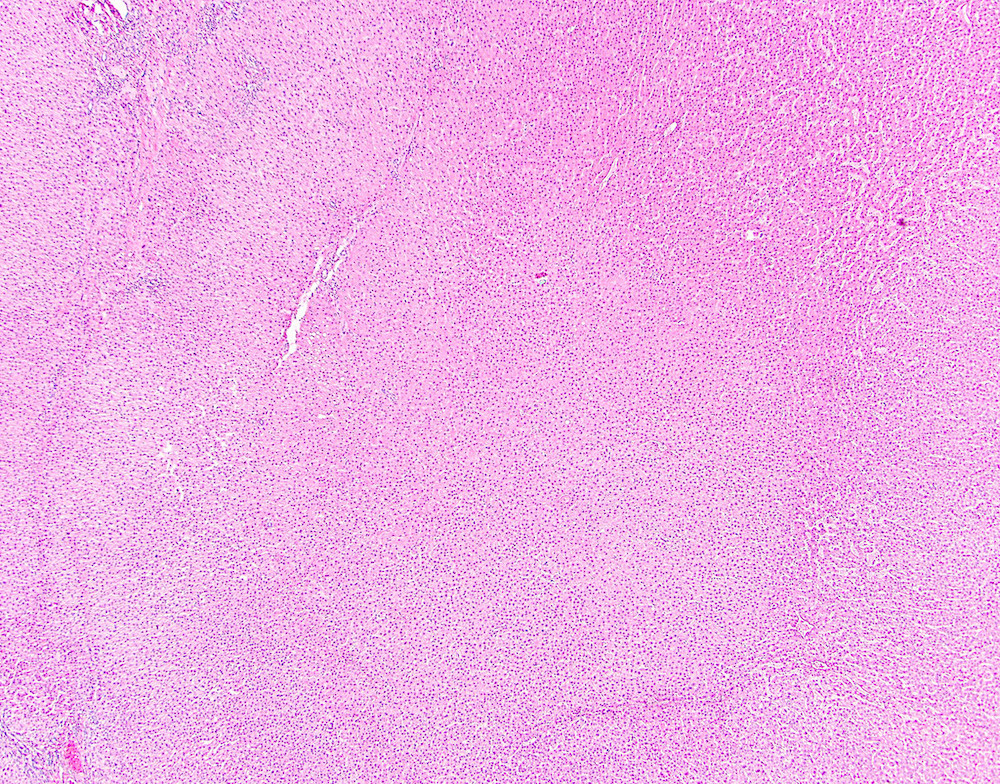
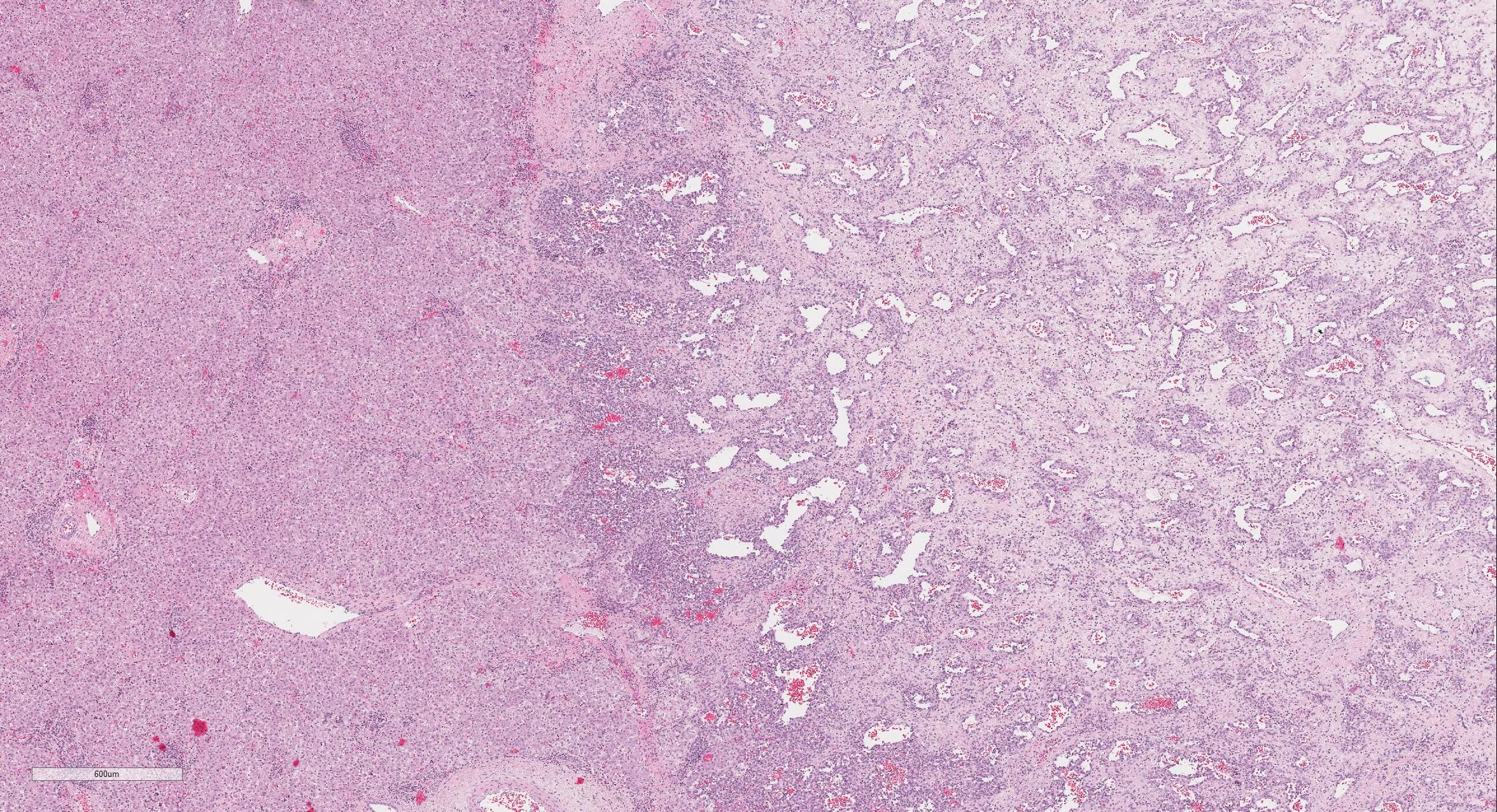
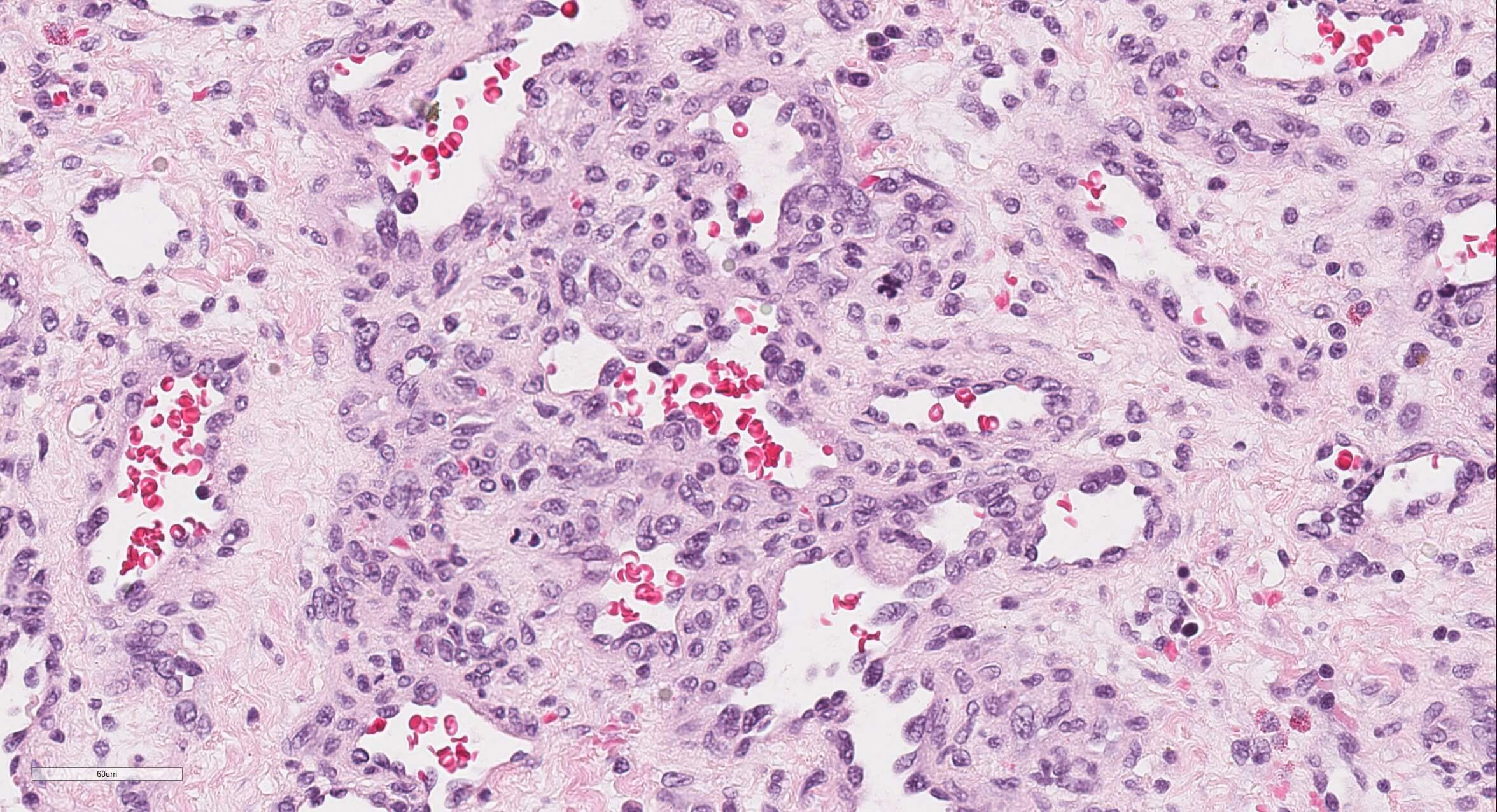
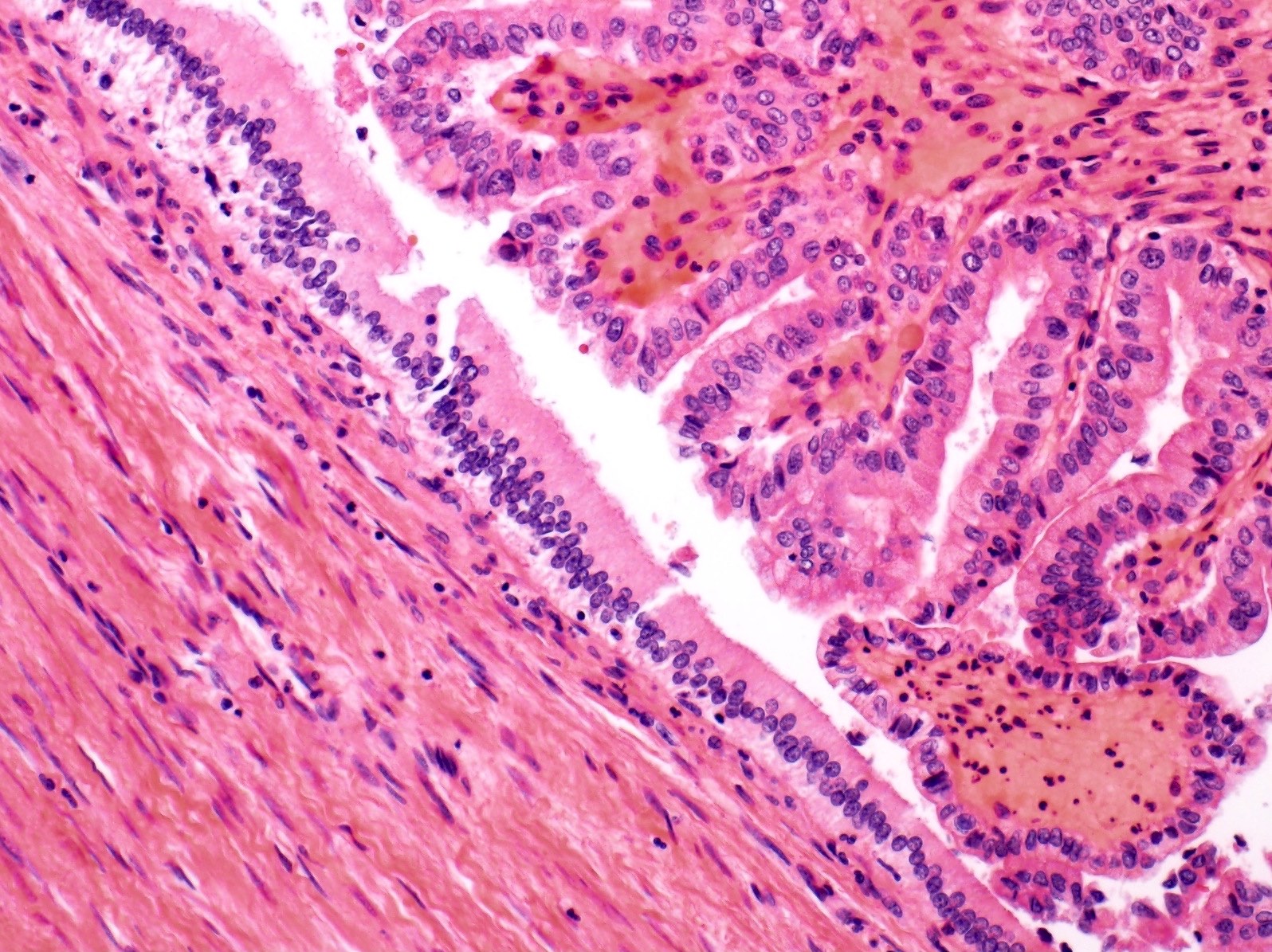
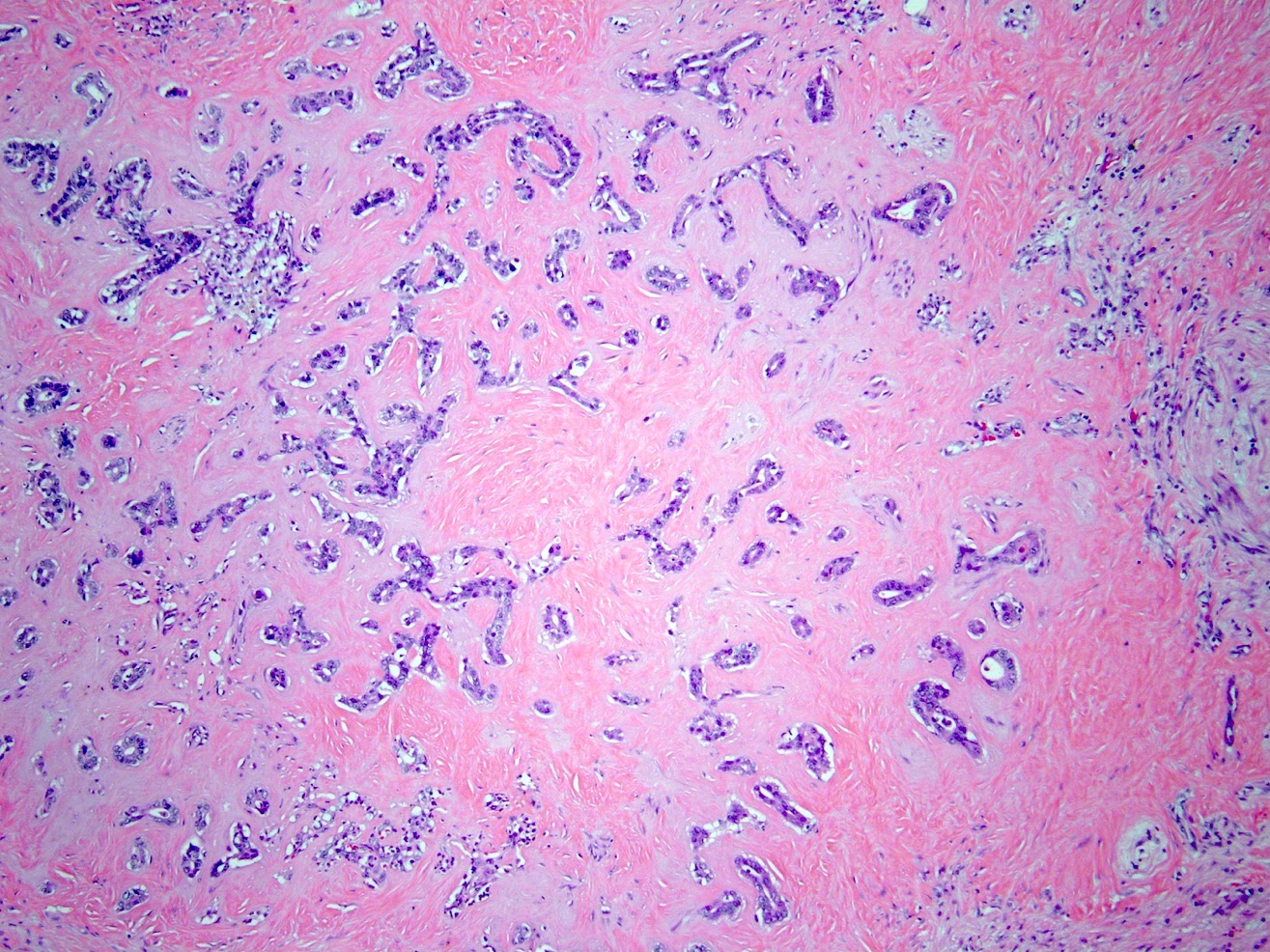
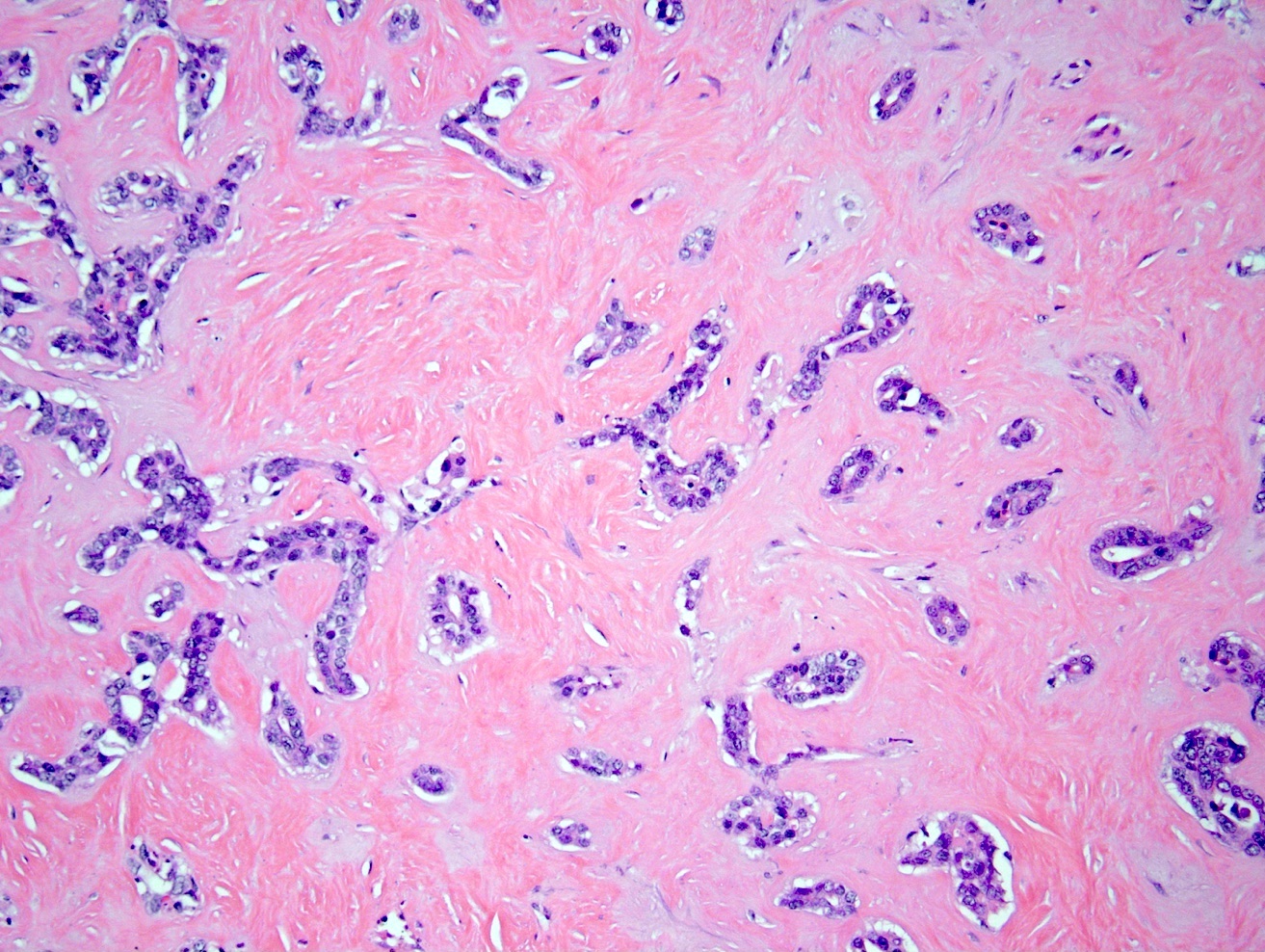
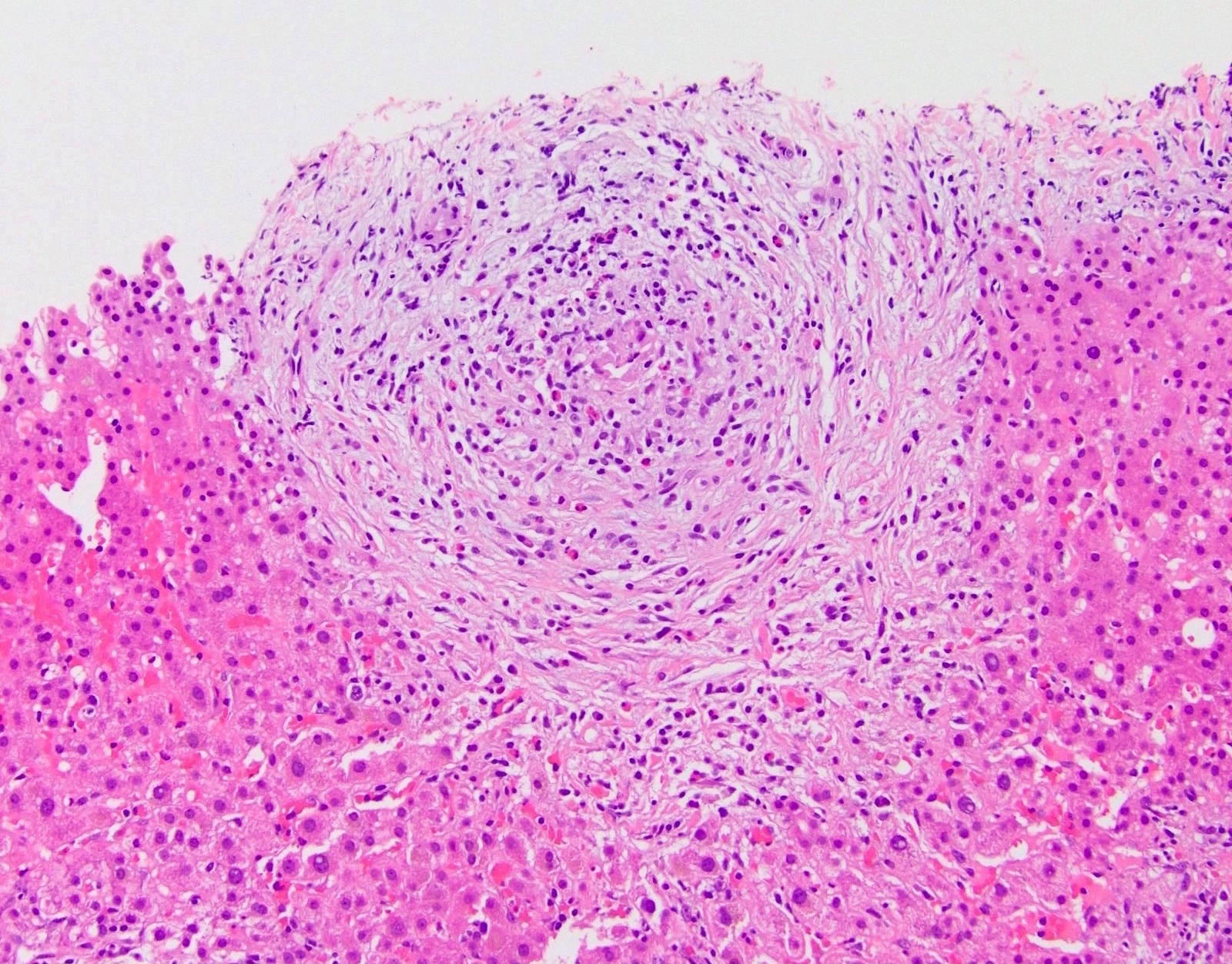
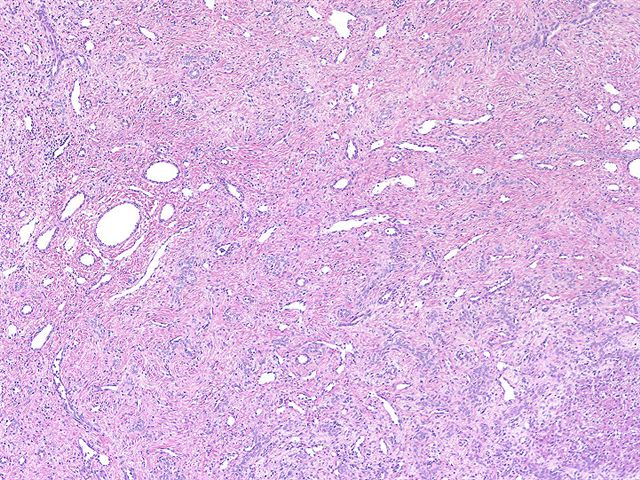
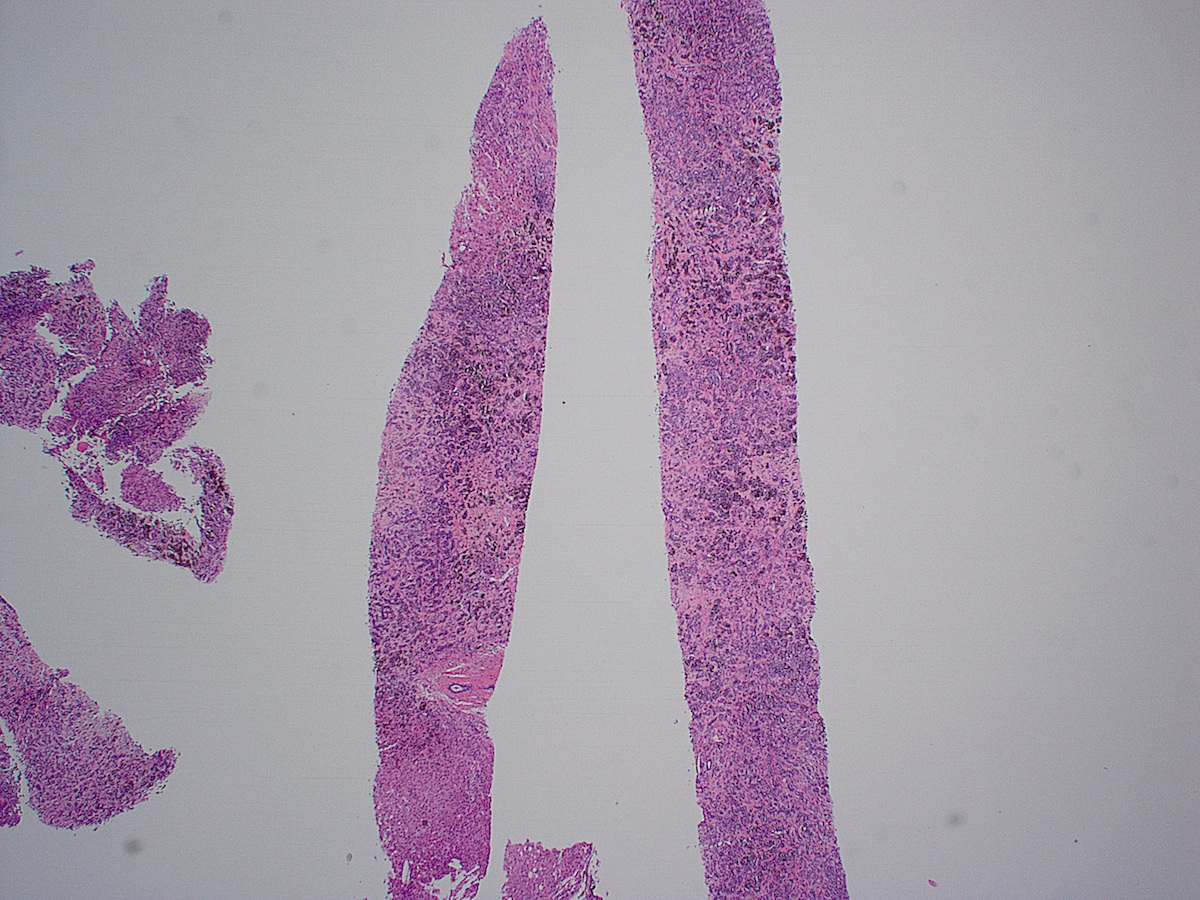
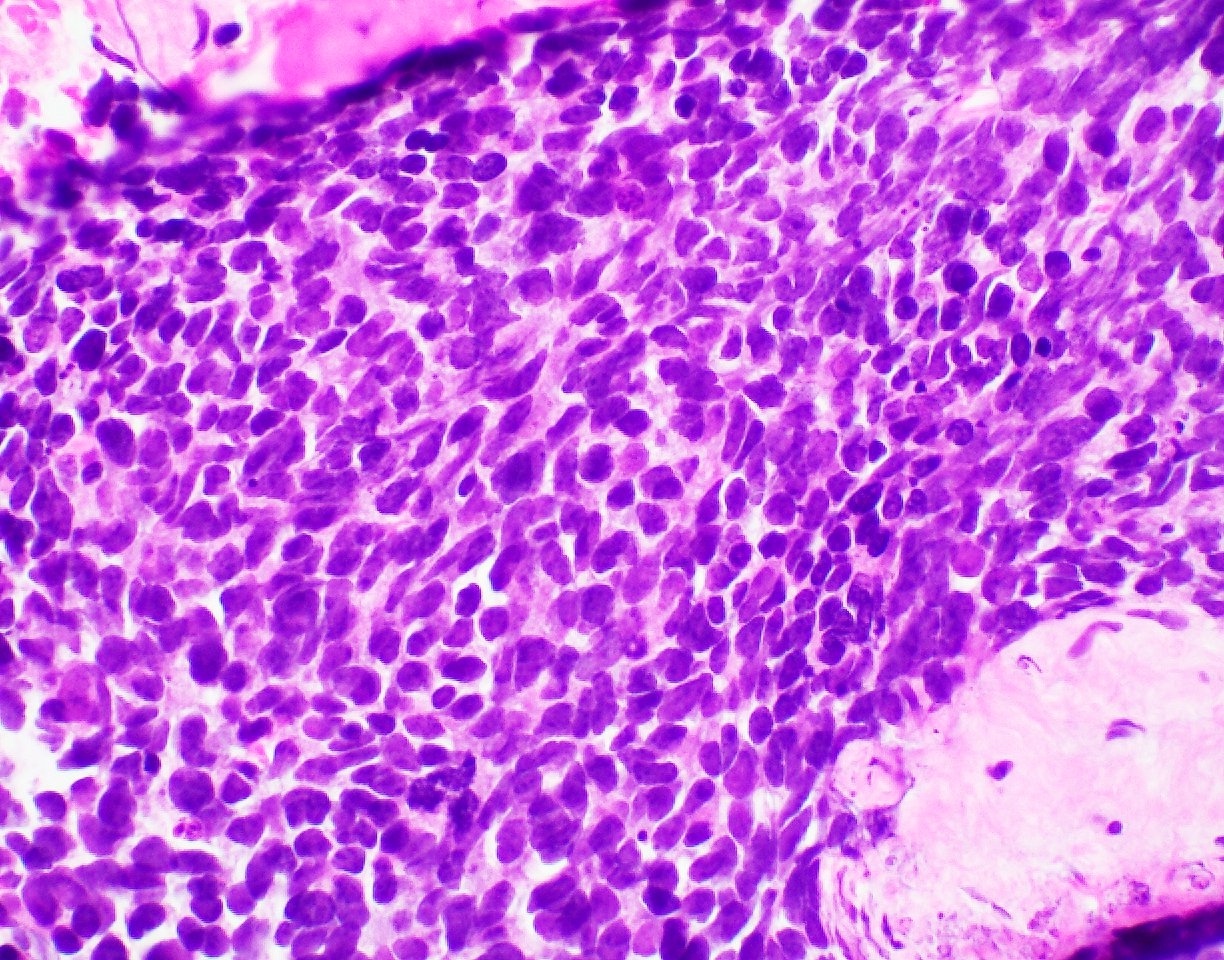
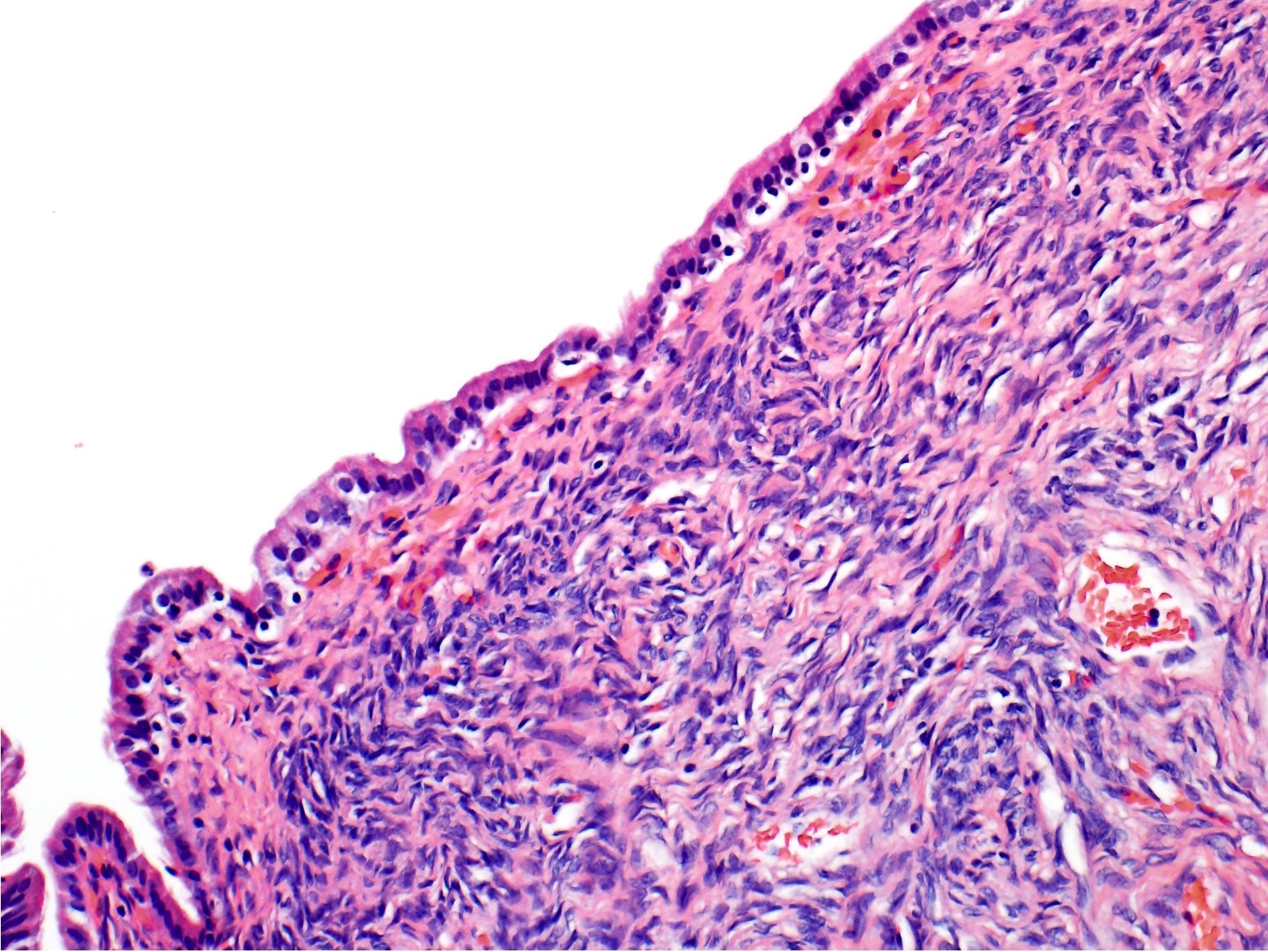
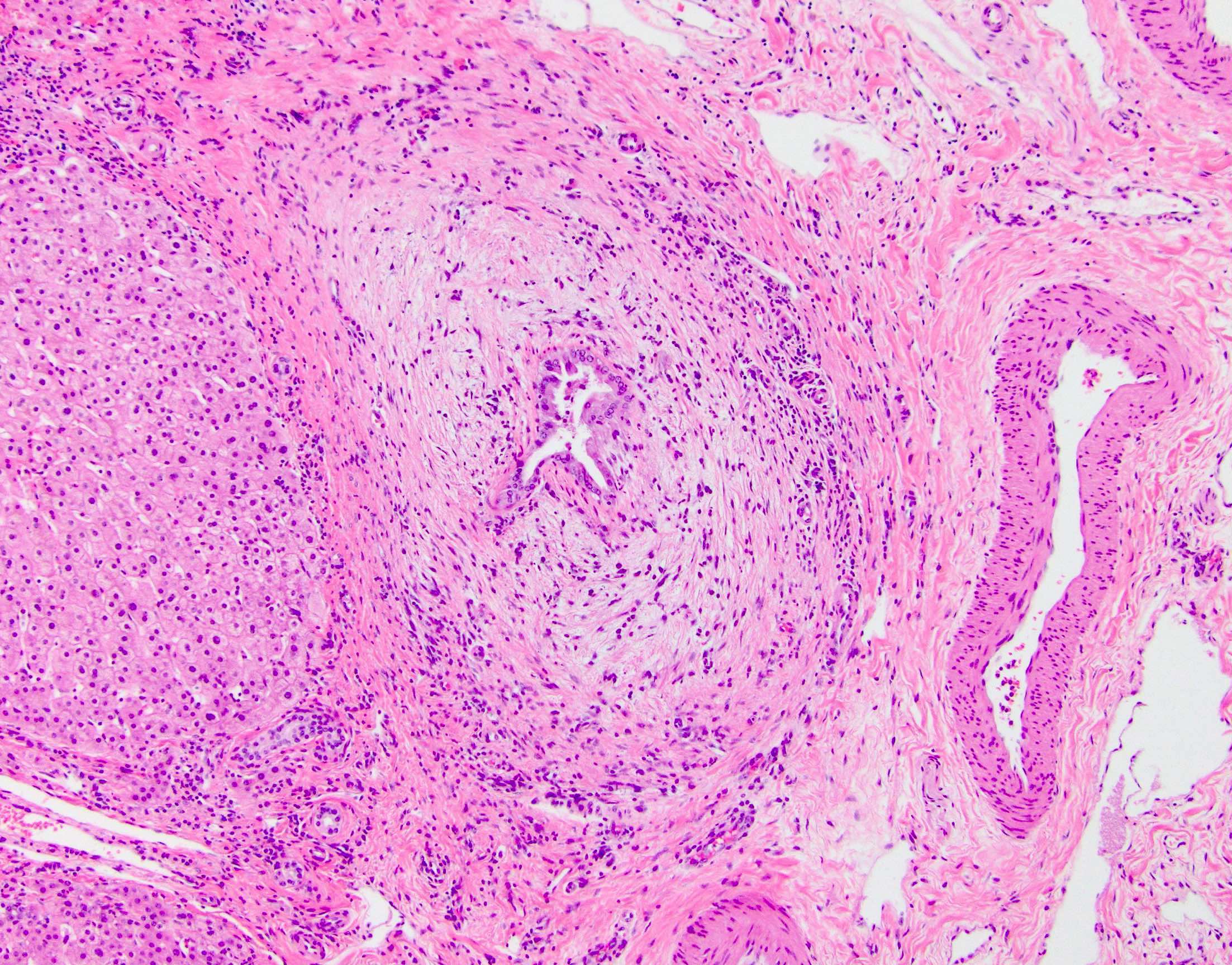
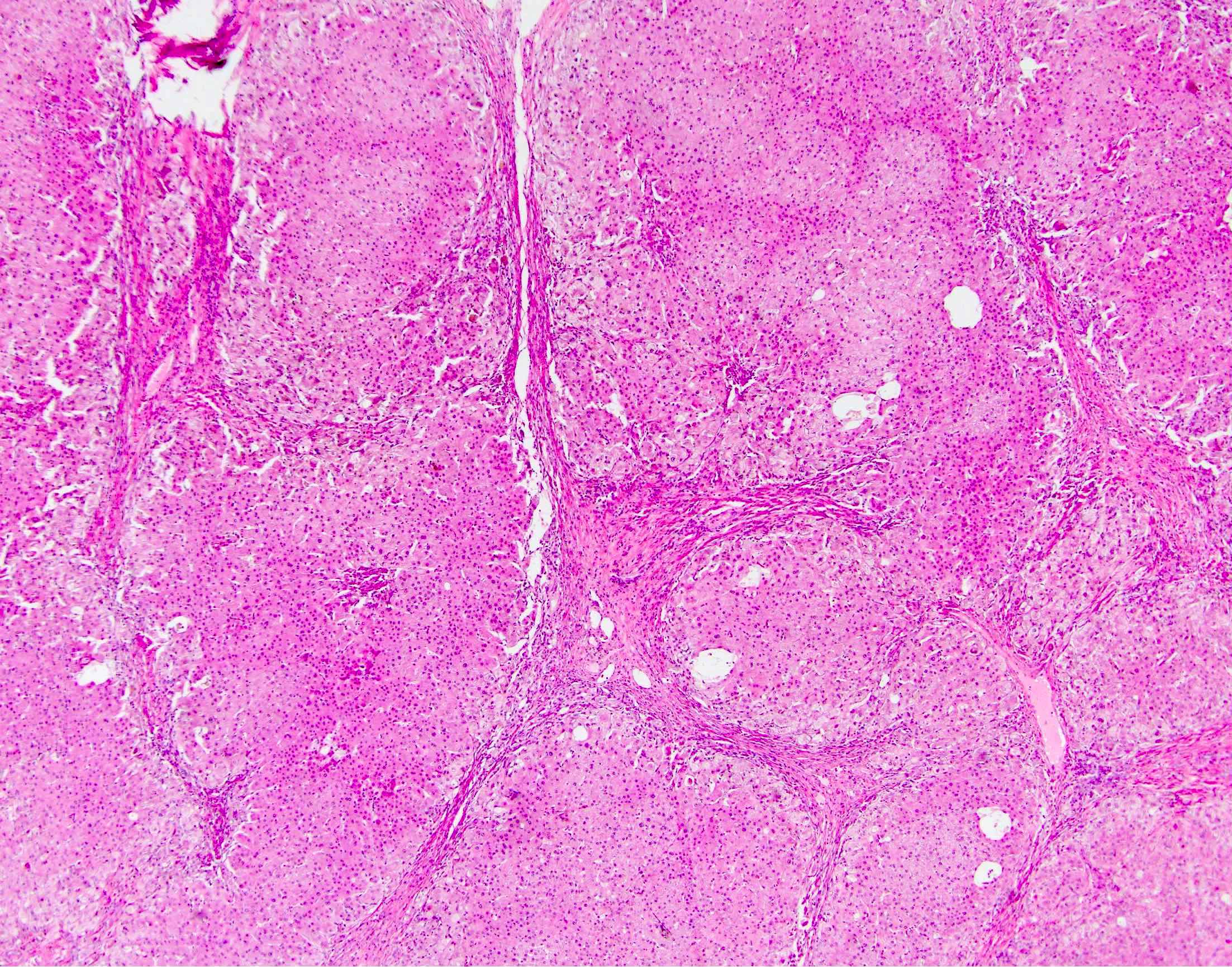
Microscopic (histologic) description
- Typical T cell mediated rejection is characterized by (at least 2 out of 3):
- Mixed portal inflammatory infiltrates: mainly lymphocytes (can appear activated, with larger nuclei and prominent nucleoli) with few eosinophils, plasma cells and possibly neutrophils
- Bile duct injury: intraepithelial lymphocytes in bile duct epithelium with injury such as apoptosis, disordered polarity, vacuolization and increased N:C ratio of the epithelial cells
- Endothelialitis (either in portal veins or central veins): injured / reactive appearing endothelial cells with lymphocytes adjacent and underneath, lifting the endothelial cells from the basement membrane or lymphocytes within the lumen, adherent to endothelial cells
- Other rare patterns of acute T cell mediated rejection include central perivenulitis variant and lobular variant (Transpl Int 2010;23:971, Mod Pathol 2015;28:1275)
- Banff criteria for acute T cell mediate rejection grading (Am J Transplant 2016;16:2816)
- Indeterminate: portal or perivenular inflammatory infiltrate without sufficient tissue damage to meet criteria for a diagnosis of rejection
- Mild: rejection type infiltrate in less than 50% of the portal tracts (often mild and confined to the portal tracts) or less than 50% of the perivenular areas without confluent necrosis / hepatocyte dropout (in cases with isolated perivenular infiltrates)
- Moderate: rejection type infiltrate, expanding more than 50% of portal tracts or perivenular areas with confluent necrosis / hepatocyte dropout limited to a minority of perivenular areas
- Severe: similar to moderate rejection but with spillover into periportal areas or moderate to severe perivenular inflammation extending into the hepatic parenchyma with perivenular hepatocyte necrosis of majority of perivenular areas
- Some centers also report the rejection activity score (Liver Transpl 2006;12:1144):
Portal inflammation Bile duct injury Venous endothelial inflammation Score 1 Mostly lymphocytic inflammation involving minority of portal tracts without expansion A minority of the ducts are cuffed and infiltrated by inflammatory cells with mild reactive changes such as increased N:C ratio of the epithelial cells Subendothelial lymphocytic infiltration involving some but not a majority of the portal or hepatic venules Score 2 Expansion of most or all portal tracts by a mixed infiltrate (containing lymphocytes with occasional blasts, neutrophils and eosinophils)
Consider acute antibody mediated rejection (AMR) if eosinophils are conspicuous and accompanied by edema and microvascular endothelial cellMost or all of the ducts infiltrated by inflammatory cells with less than 50% showing degenerative changes such as nuclear pleomorphism, disordered polarity and cytoplasmic vacuolization of the epithelium Subendothelial infiltration involving most or all of the portal or hepatic venules with or without confluent hepatocyte necrosis / dropout involving a minority of perivenular regions Score 3 Same as score 2 with inflammatory spillover into the periportal parenchyma As above for score 2, with most or all of the ducts showing degenerative changes or focal luminal disruption As above for 2, with moderate or severe perivenular inflammation that extends into the perivenular parenchyma and is associated with perivenular hepatocyte necrosis involving a majority of perivenular regions
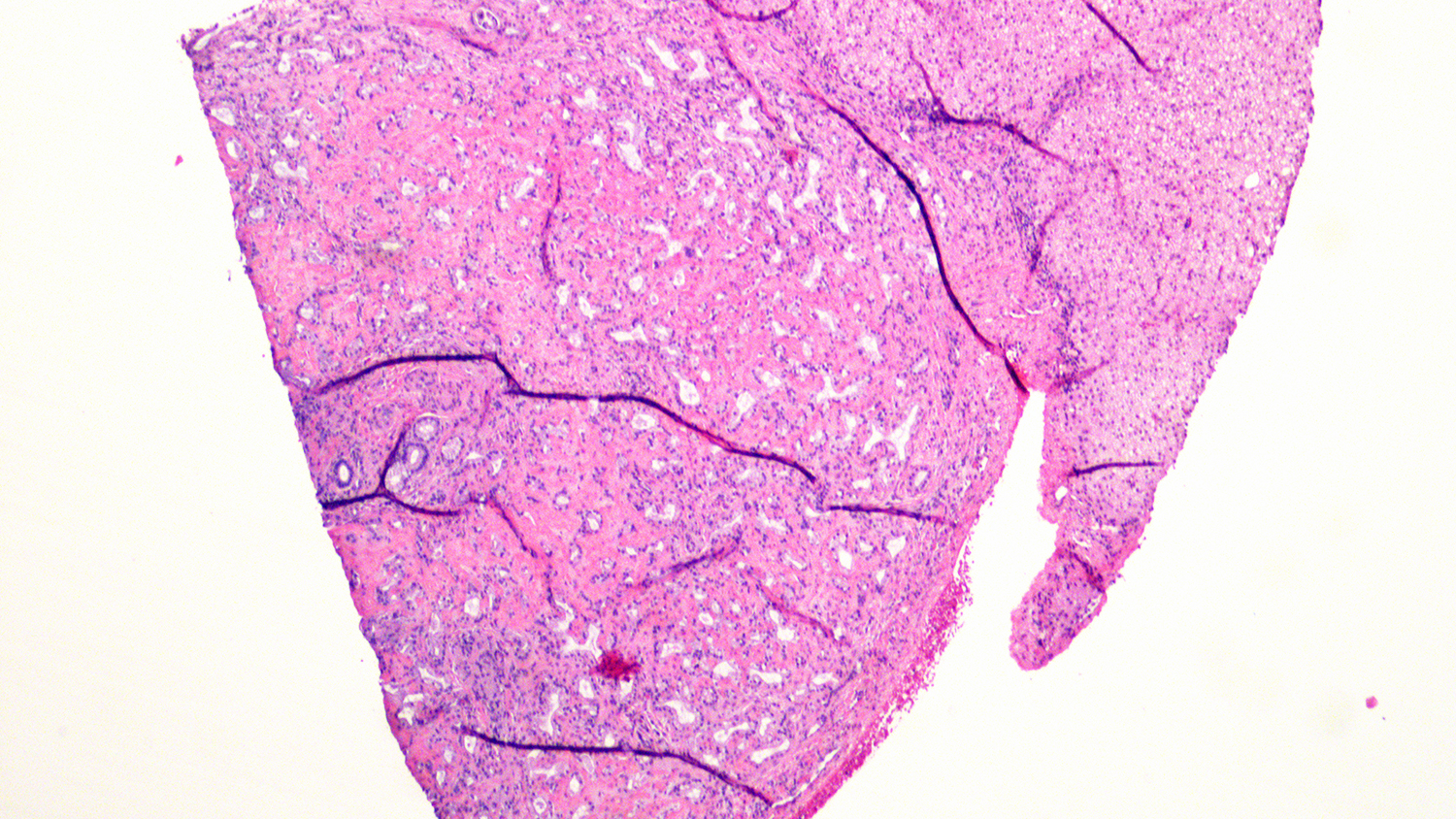
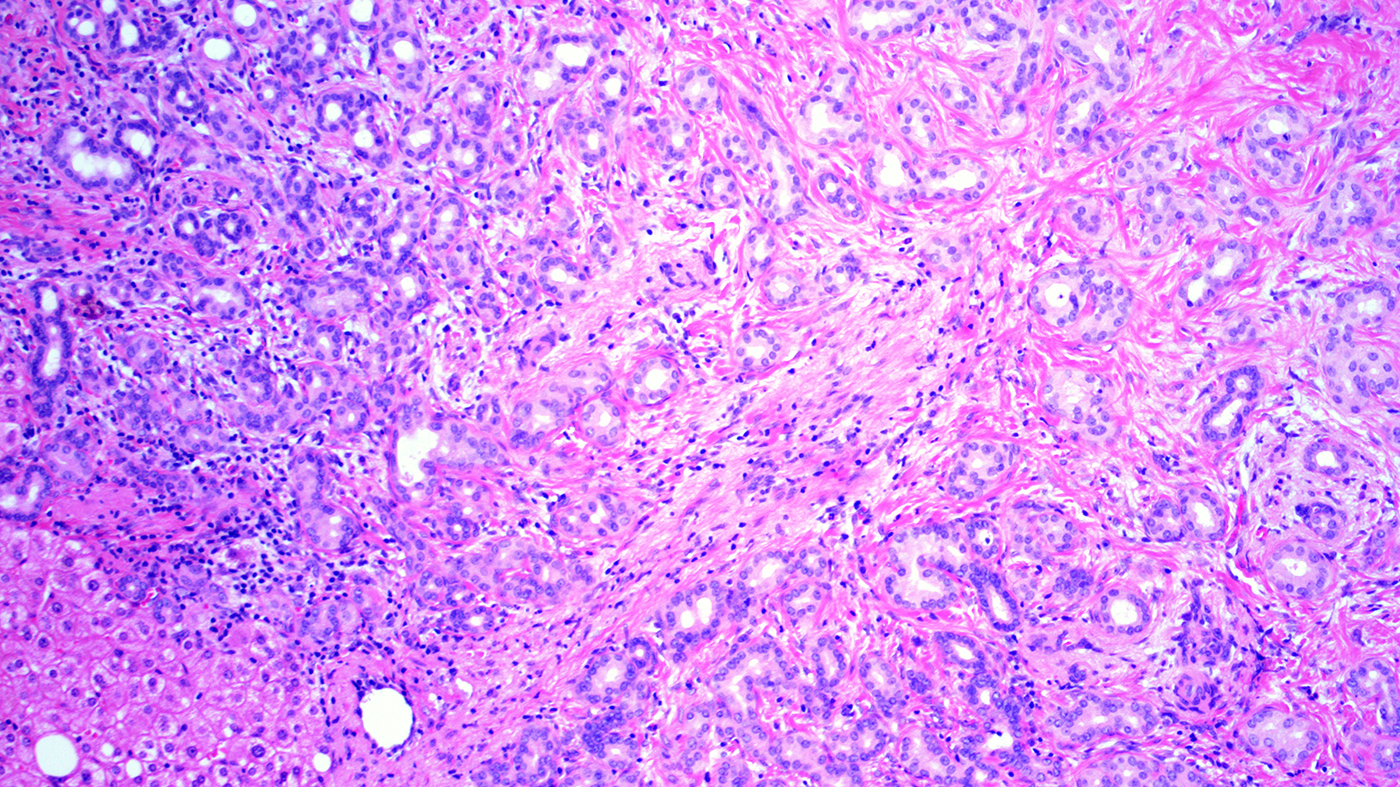
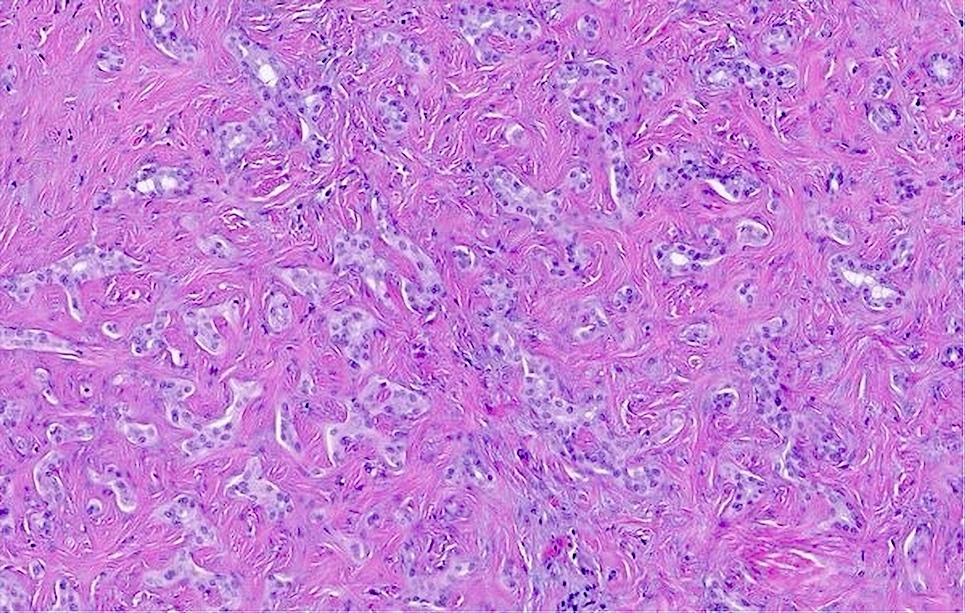
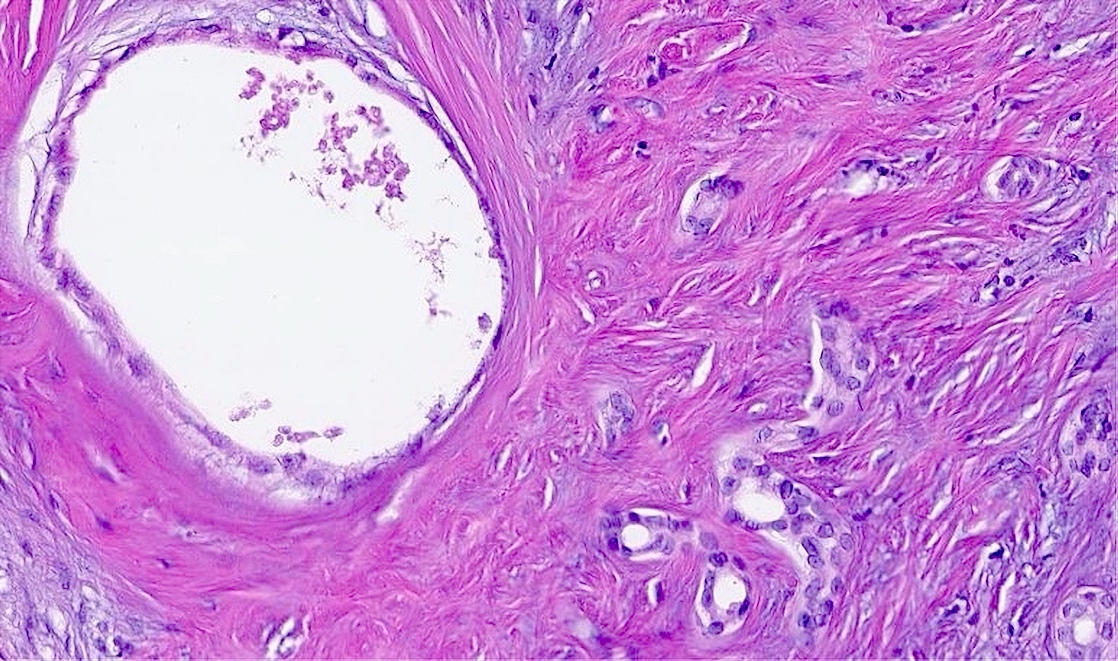
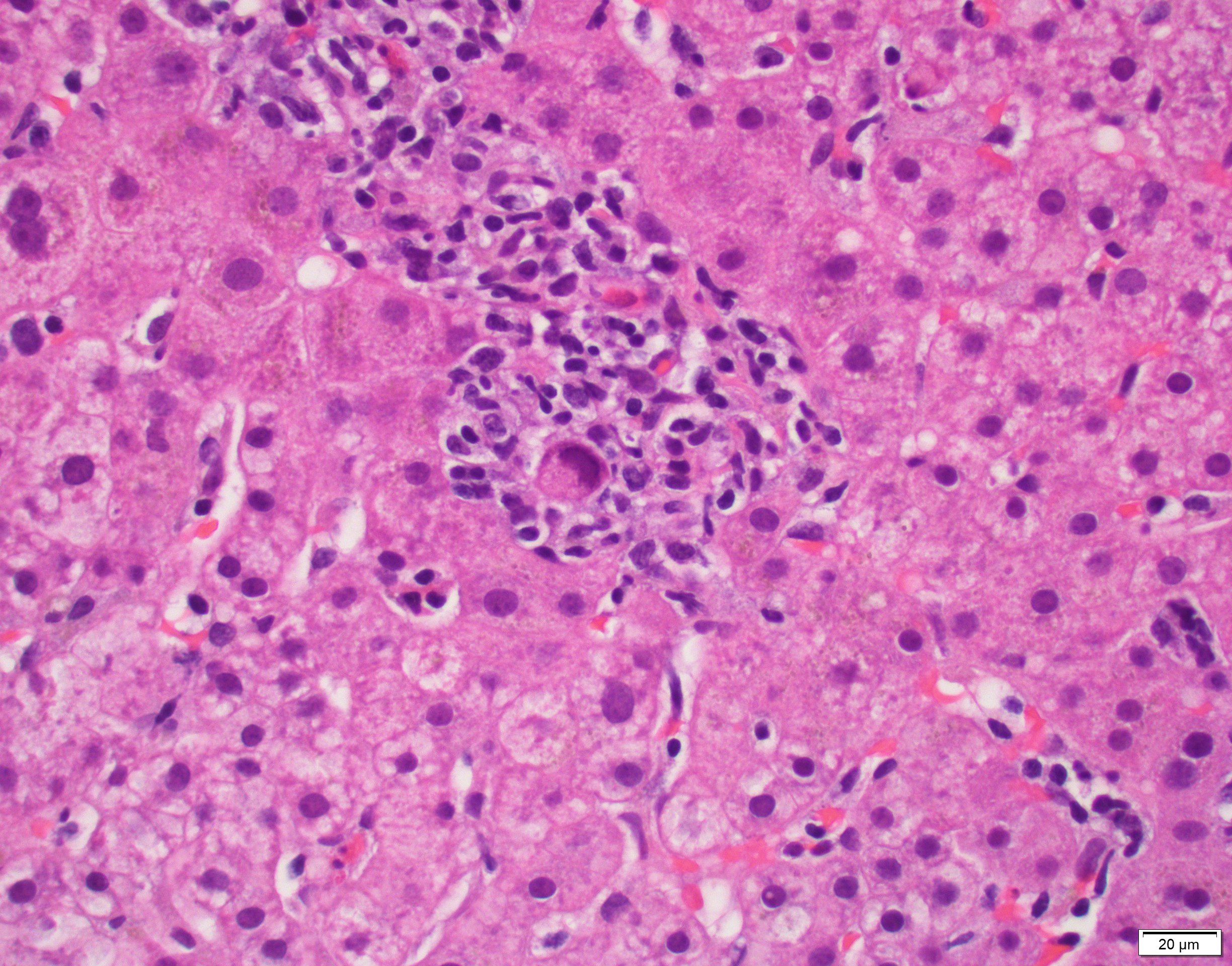
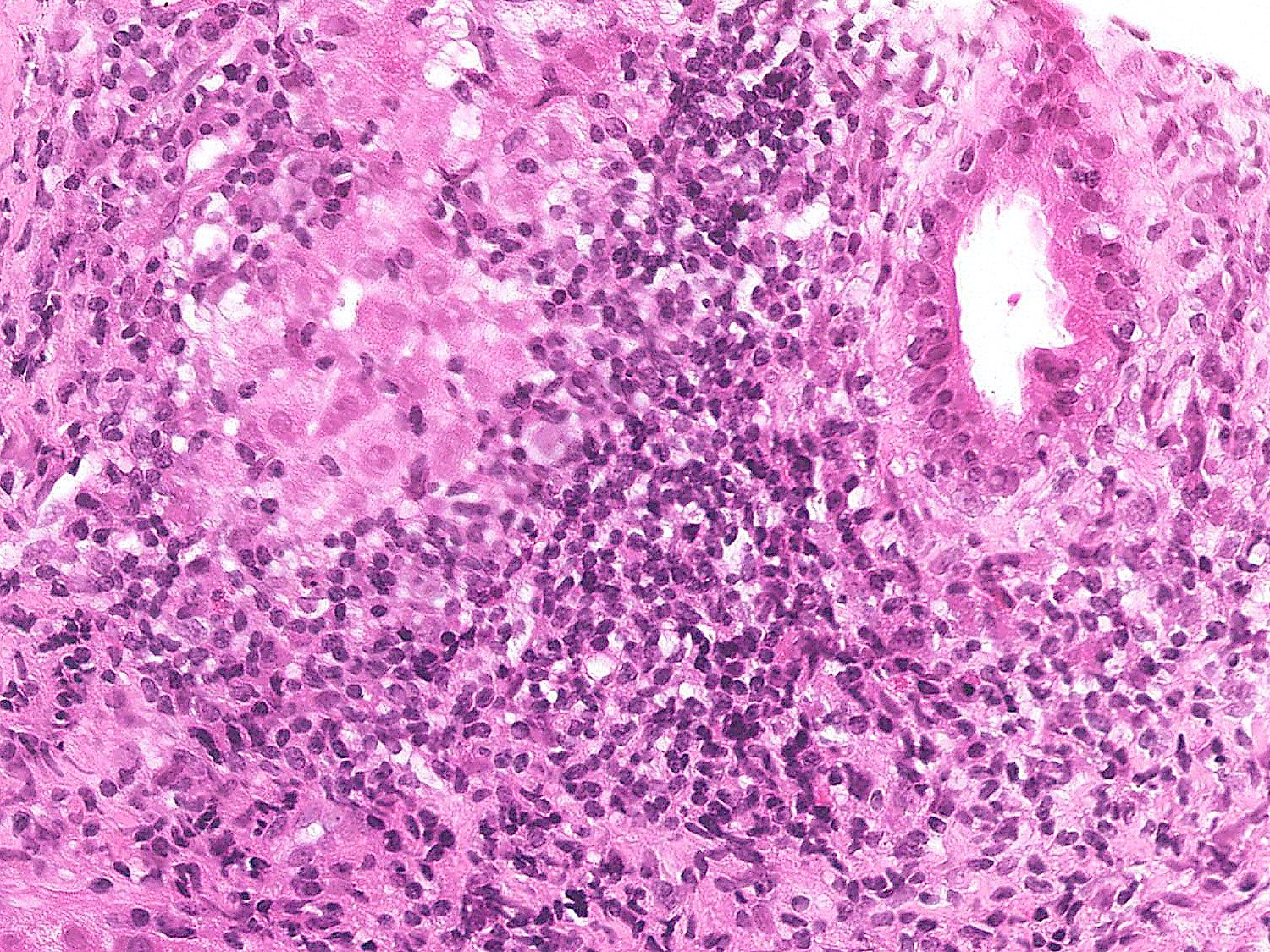
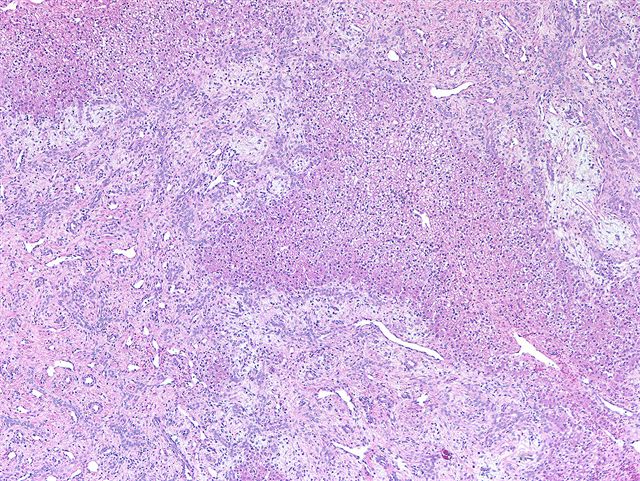
Microscopic (histologic) images
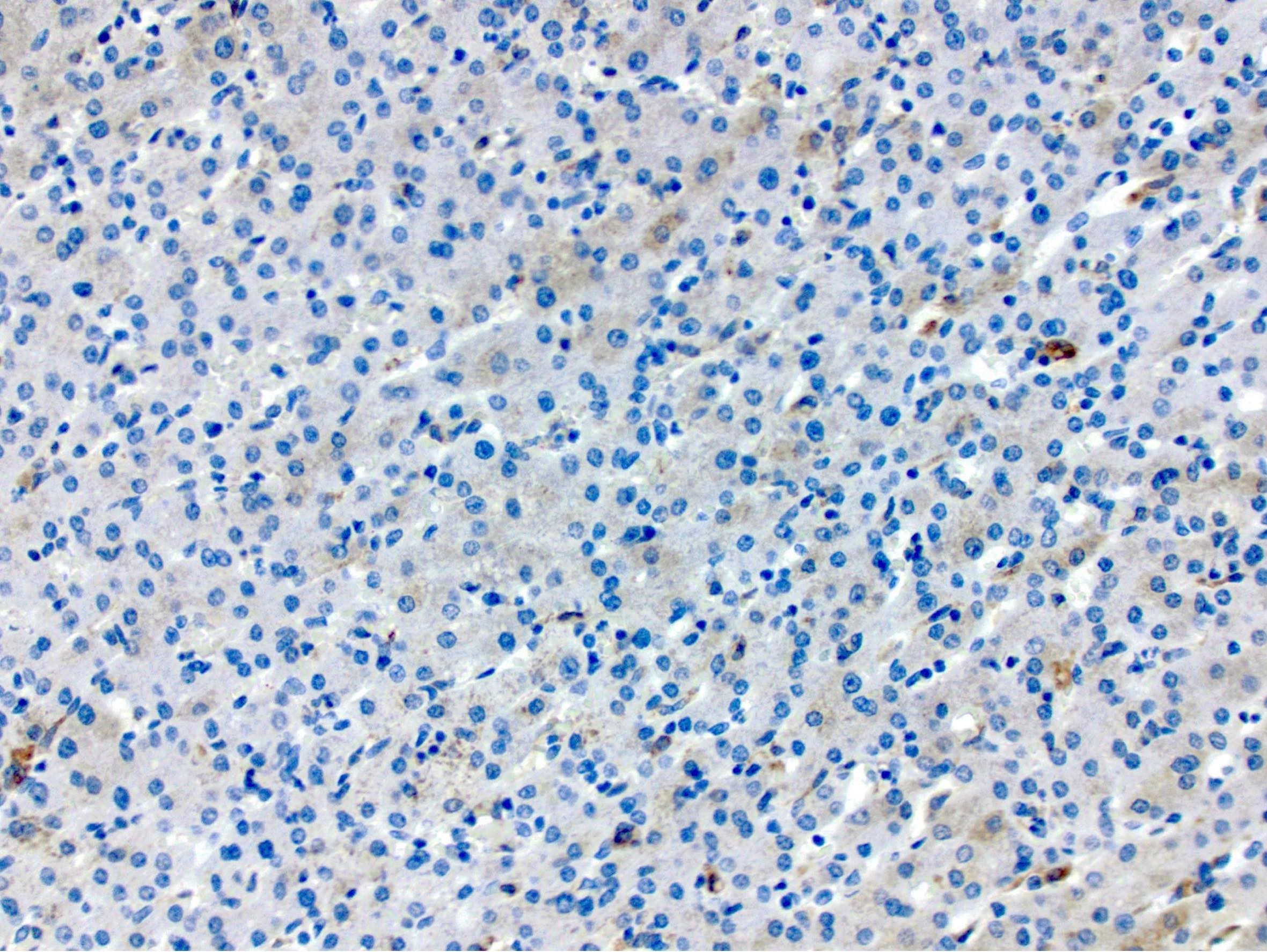
Positive stains
- Immunostains are not necessary and often not useful
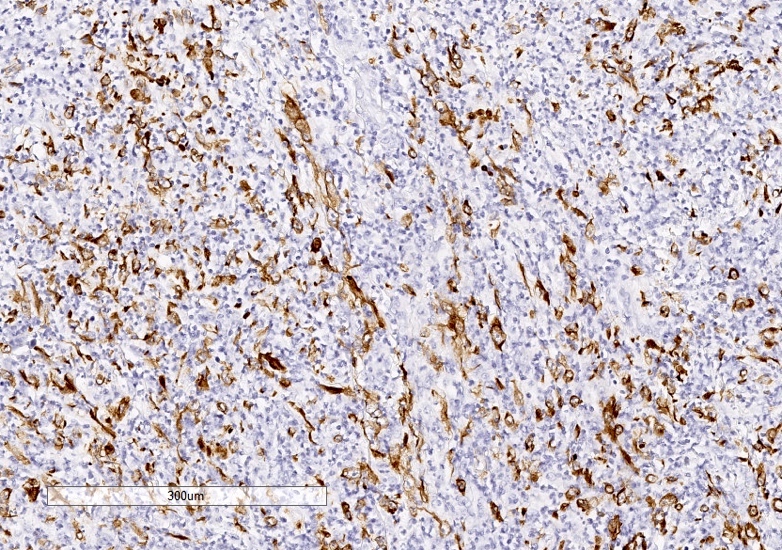
- In cases where the differential includes lymphoproliferative disorders, immunophenotyping the lymphocytes can be helpful: acute cellular rejection is predominantly T cell infiltrate (CD3 positive)
- C4D stain can be considered in cases where an element of antibody mediated rejection is suspected (Am J Transplant 2016;16:2816)
Sample pathology report
- Liver, biopsy, __ days posttransplant:
- Mild mixed portal inflammation with rare ductitis and bile duct injury, favor acute cellular rejection (mild) (see comment)
- Comment: The biopsy is adequate, consisting of 1 core containing up to at least 13 portal tracts for evaluation. There is mixed mild portal inflammation, predominantly composed of lymphocytes with rare eosinophils, plasma cells and neutrophils. Although there is no definitive endothelialitis, rare ductitis and bile duct injury are identified. Native bile ducts are present in the majority of the portal tract. PAS and PASD stains illustrate bile ducts and show no PAS+, diastase resistant globules. Trichrome and reticulin stains are unremarkable. An iron stain is negative. Overall, the findings of portal inflammation, rare ductitis and bile duct injury raise the possibility of acute cellular rejection (favor mild). Clinical correlation is recommended.
Differential diagnosis
- Recurrent hepatitis C:
- Lobular inflammation with hepatocyte injury (single cell apoptosis or spotty necrosis involving groups of hepatocytes)
- In more severe cases, lymphocytic interface hepatitis can be seen (Ann Transplant 2008;13:12)
- Posttransplant lymphoproliferative disorder and Epstein-Barr virus:
- Monomorphic PTLD will have clonal B cell proliferation
- Polymorphic and nondestructive PLTD will show an inflammatory infiltrate consisting of lymphocytes and plasma cells; endothelialitis should not be present
- Immunophenotyping the lymphocytes can be helpful: T cell mediated rejection is predominantly T cell infiltrate (CD3 positive) (Pediatr Transplant 2019;23:e13357)
- Hepatitis E:
- Presentation is variable and can include lobular disarray, lobular and portal inflammation, hepatocyte necrosis / regeneration and potentially severe interface activity; immunohistochemistry or serology may be useful in diagnosis (Adv Anat Pathol 2018;25:273, Clin Res Hepatol Gastroenterol 2018;42:e68)
- Human herpesvirus 6:
- May show mild inflammation and hepatocyte injury; no endothelialitis or bile duct injury (Transpl Infect Dis 2019;21:e13014, Pediatr Transplant 2011;15:E126)
- Drug induced liver injury:
- Portal edema, portal and lobular mixed inflammatory infiltrate with lymphocytes, eosinophils and plasma; may show endothelialitis, bile duct injury, perivenular necrosis, hepatocyte injury
- Can often be difficult to differentiate histologically, requiring clinical correlation
- Late T cell mediated rejection:
- Characterized by loss of native small bile ducts in portal tracts
- Loss of portal arterioles and sinusoidal foam cell accumulation can also be seen (Hepatology 2000;31:792)
- Antibody mediated rejection:
- Evidence of vascular injury such as portal edema, endothelial cell hypertrophy and eosinophilia within portal microvasculature can be seen in addition to more nonspecific findings such as hepatocyte swelling, ductular reaction and cholestasis (J Immunol Res 2017;2017:3234906)
- Large bile duct injury:
- Large bile duct obstruction due to stricture, gallstones and malignancy can lead to cholestasis and bile ductular reaction
- Cholestasis usually more severe than seen in acute T cell mediated rejection (J Clin Pathol 2018;71:72)
Additional references
Board review style question #1
- A 45 year old man with a history of cirrhosis secondary to hepatitis C infection who is status post liver transplantation 3 years ago presents with mildly elevated liver enzymes (AST 78, ALT 75, ALK Phos 100). A liver biopsy is performed. Which of the following findings would support a diagnosis of acute T cell mediated rejection over a recurrent hepatitis C infection?
- Endothelialitis
- Hepatocyte apoptosis
- Interface hepatitis
- Lobular disarray
- Lobular lymphocytic inflammation
Board review style answer #1
A. Endothelialitis. Of the listed choices, endothelialitis is the most useful finding in supporting a diagnosis of acute cellular rejection. The other options can all be seen in hepatitis C infection, and in the absence of endothelialitis and bile duct injury, may suggest reactivation of hepatitis C infect in a posttransplant patient.
Comment Here
Reference: Acute T cell mediated rejection
Comment Here
Reference: Acute T cell mediated rejection
Board review style question #2
- Based on the grading system for acute T cell mediated rejection, which of the following findings would favor a diagnosis of moderate T cell mediated rejection?
- Diffuse portal inflammatory infiltrate consisting of lymphocytes and eosinophils. Over 50% of central veins show venulitis and perivenular hepatocyte necrosis.
- Endothelialitis in less than 50% of portal areas. No central venulitis or bile duct injury is seen, no significant inflammatory infiltrate is identified.
- Less than 50% of central veins show perivenular necrosis. No inflammation seen in portal areas, no endothelialitis, no bile duct injury.
- Less than 50% of portal areas show expansion by an inflammatory infiltrate consisting of lymphocytes and eosinophils. No endothelialitis or bile duct injury.
- More than 50% of portal areas show expansion by an inflammatory infiltrate consisting of lymphocytes and eosinophils with endothelialitis and occasional bile duct injury.
Board review style answer #2
E. Moderate T cell mediated rejection should involve at least 50% of portal areas and well as occasional central veins. Portal inflammatory infiltrates, endothelilaitis and bile duct injury should also be present.
Comment Here
Reference: Acute T cell mediated rejection
Comment Here
Reference: Acute T cell mediated rejection
Adenovirus hepatitis
Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Adenoviruses are widely distributed viruses that usually cause self limited infections; but in an immunocompromised host they can cause severe infections with injuries to multiple organs, including the liver
- While severe acute liver failure due to adenovirus infection is rare, it is characterized by rapid progression and is frequently fatal
- Such cases were reported in patients after allogeneic hematopoietic stem cell transplantation (HSCT), liver transplantation, chemotherapy regimens and from other causes (Transpl Infect Dis 2021;23:e13496, Infection 2014;42:105)
- However, adenovirus hepatitis can also occur in immunocompetent adults (J Investig Med High Impact Case Rep 2022;10:23247096221079192)
Essential features
- Usually immunocompromised transplant recipients
- Grossly characterized by the presence of coagulative necrosis in liver parenchyma
- Diagnosis made on liver biopsy with confirmation by adenovirus immunostaining
ICD coding
- ICD-10: B97.0 - adenovirus as the cause of diseases classified elsewhere
Epidemiology
- Usually occurs in immunocompromised adults and children
- More frequent in the patients from these groups (Infection 2014;42:105):
- Liver transplant recipients
- Bone marrow transplant recipients
- Patients on (or after) oncology related chemotherapy regimens
- Patients with severe combined immunodeficiency
- HIV infected patients
- Heart, kidney and other transplant recipients
Sites
- Liver
Etiology
- Human adenovirus serotypes C1, C2, C5 and other (Transpl Infect Dis 2021;23:e13496)
- It can be either a primary infection or reactivation of latent infection
Clinical features
- In immunocompetent patients, it causes mild illness with respiratory symptoms, keratoconjunctivitis, gastroenteritis, etc.
- Fever is the most common presenting symptom (Am J Surg Pathol 2017;41:810)
- Other nonspecific signs (e.g., abdominal pain, memory and cognitive disorder, convulsions) were reported (Transpl Infect Dis 2021;23:e13496)
- In immunocompromised patients, severe disease may occur, including fulminant hepatitis
Diagnosis
- Diagnosis of adenovirus hepatitis can be made on liver biopsy with confirmation by adenovirus immunostaining (Am J Surg Pathol 2017;41:810)
- Detection of viral DNA by PCR on blood or broncoalveolar lavage (Transpl Infect Dis 2021;23:e13496, BMC Infect Dis 2021;21:152)
Laboratory
- Viral DNA detection by PCR on blood
- Positive viral culture
- Positive serology for adenovirus
- Elevated serum total bilirubin, lactate dehydrogenase (Transpl Infect Dis 2021;23:e13496)
- Elevated serum alanine aminotransferase (ALT), aspartate aminotransferase (AST) (Am J Surg Pathol 2017;41:810)
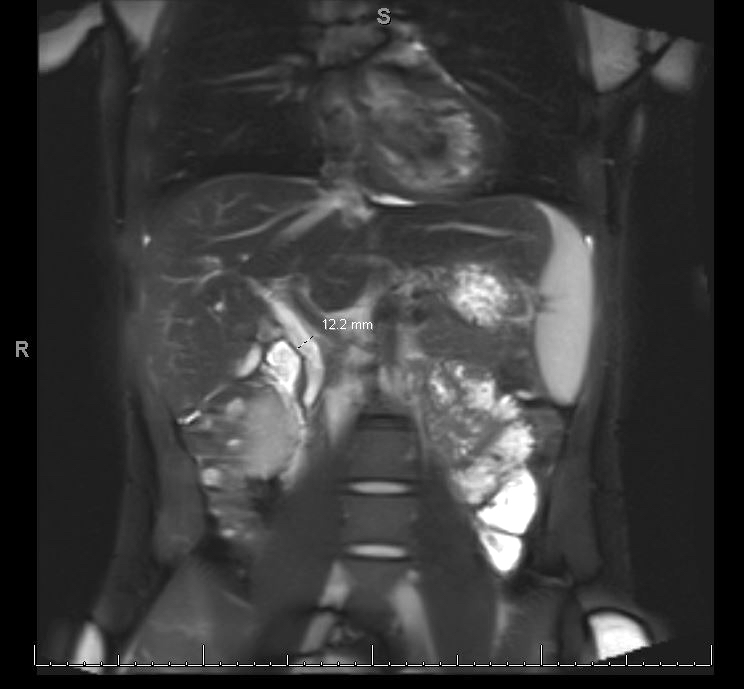
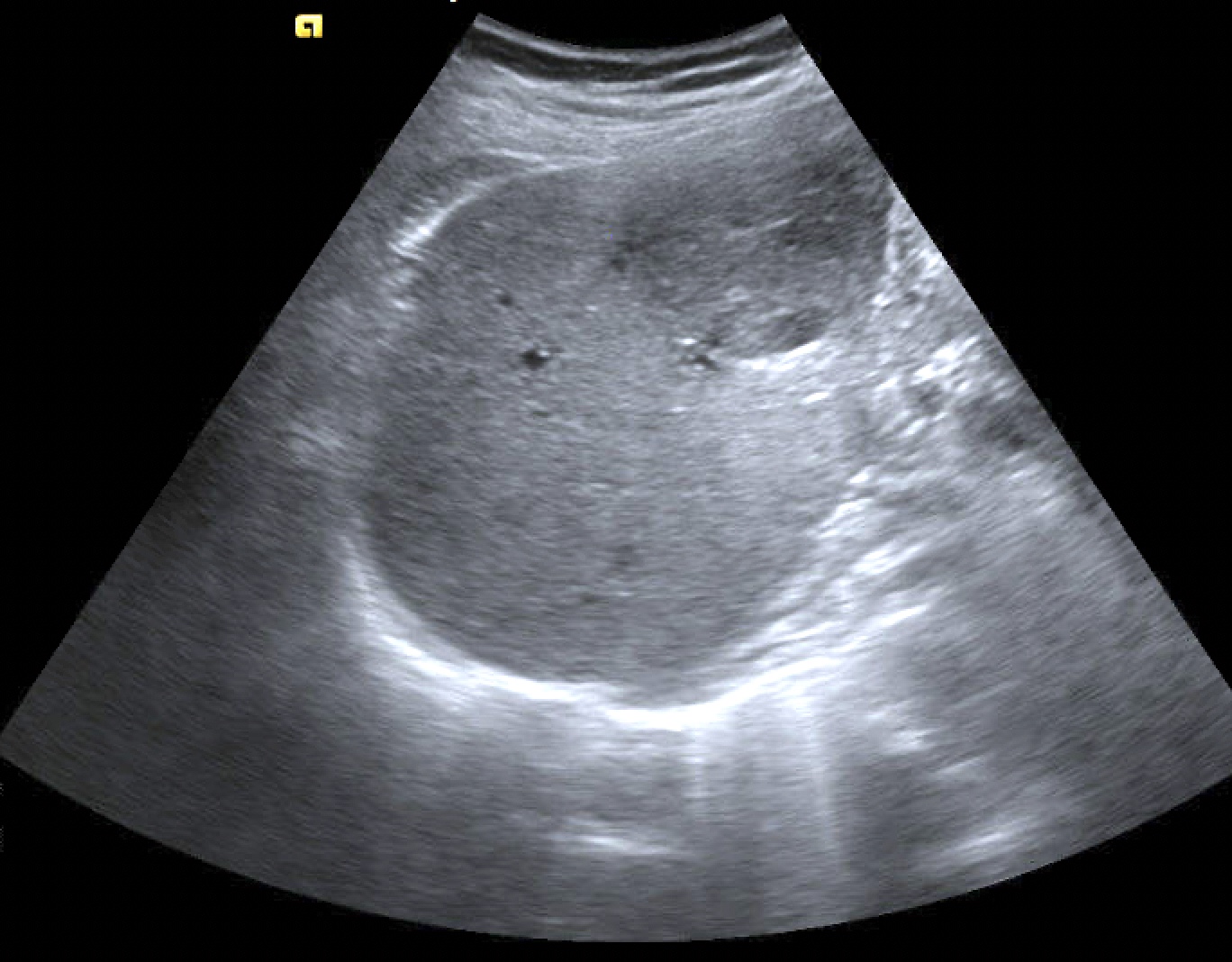
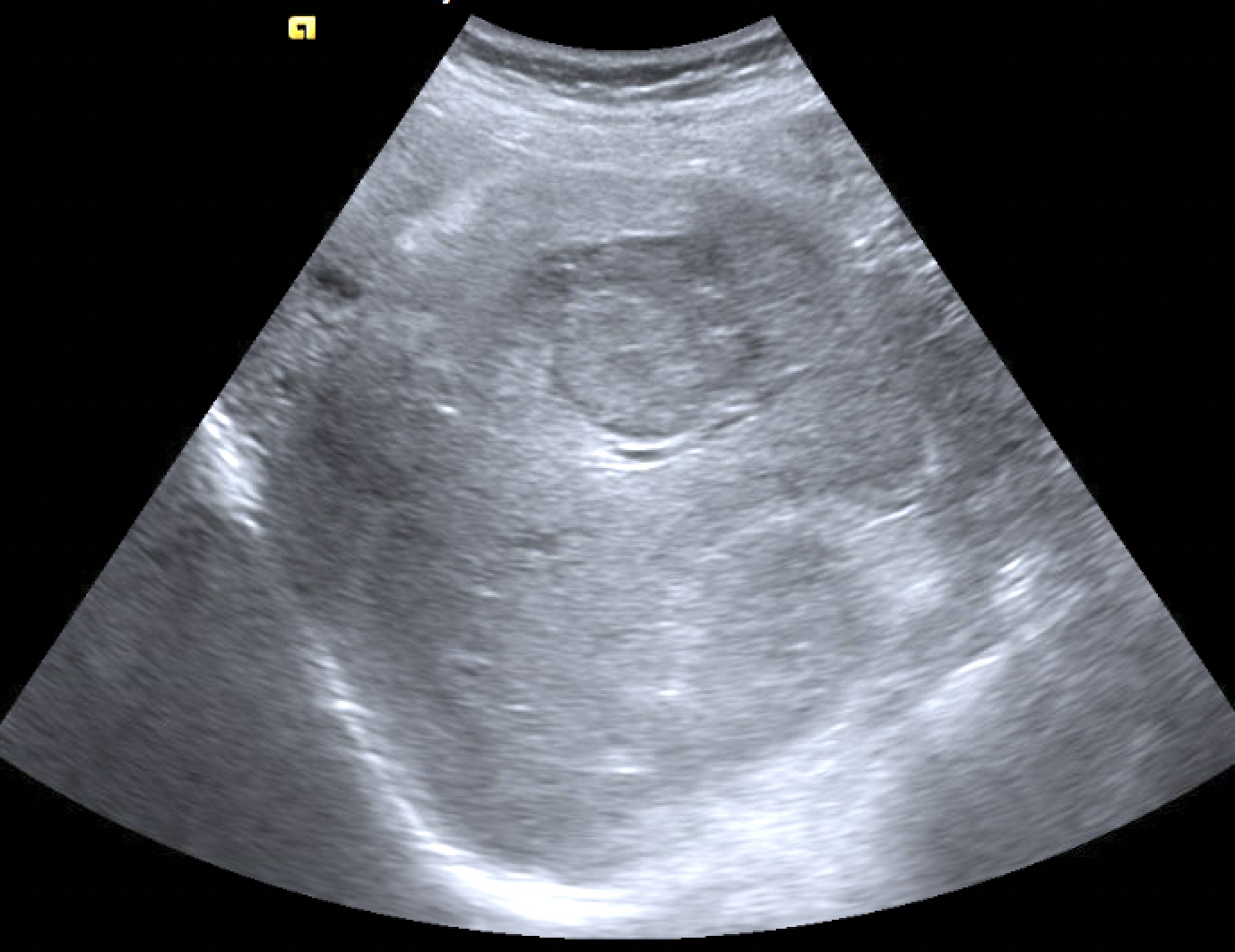
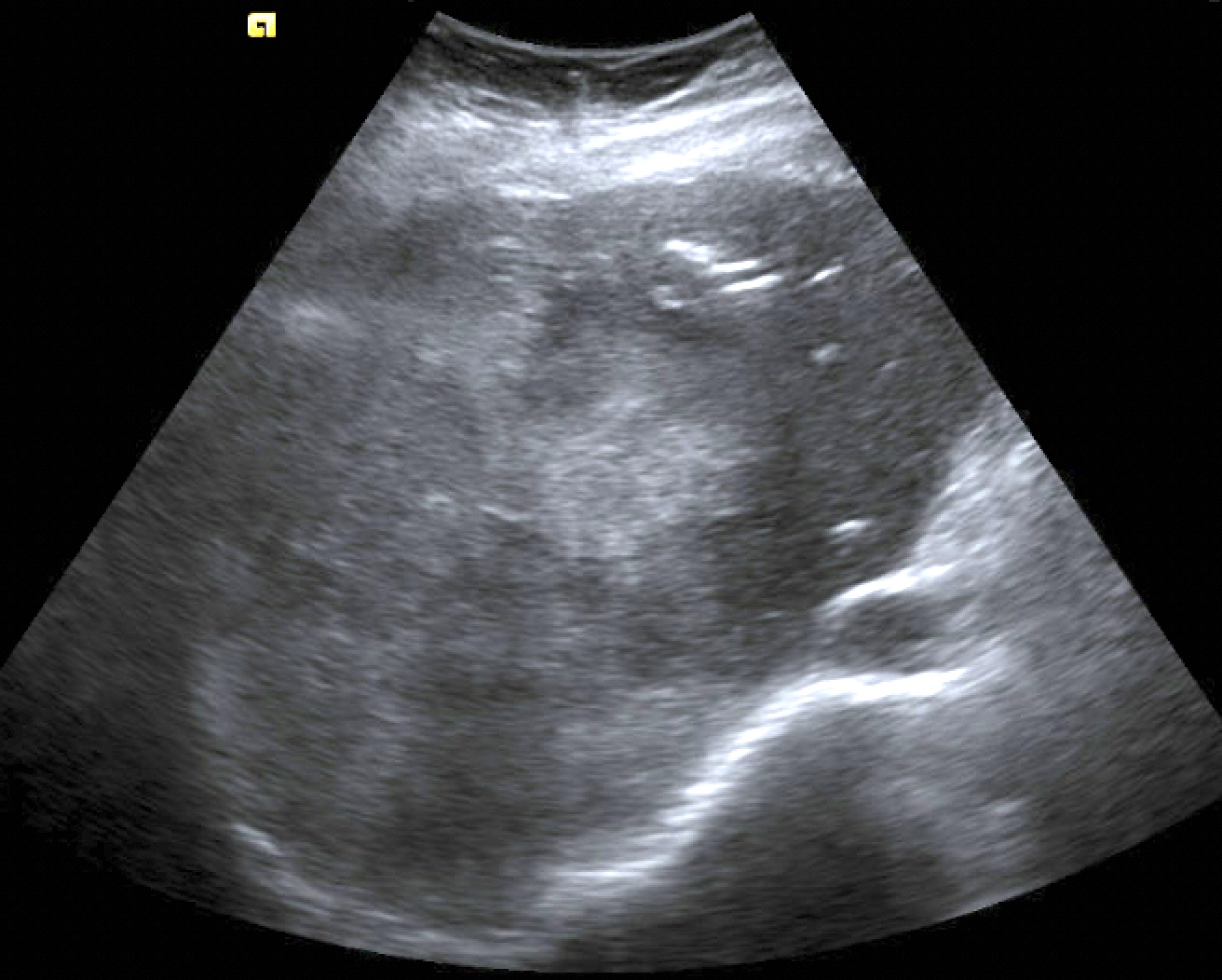
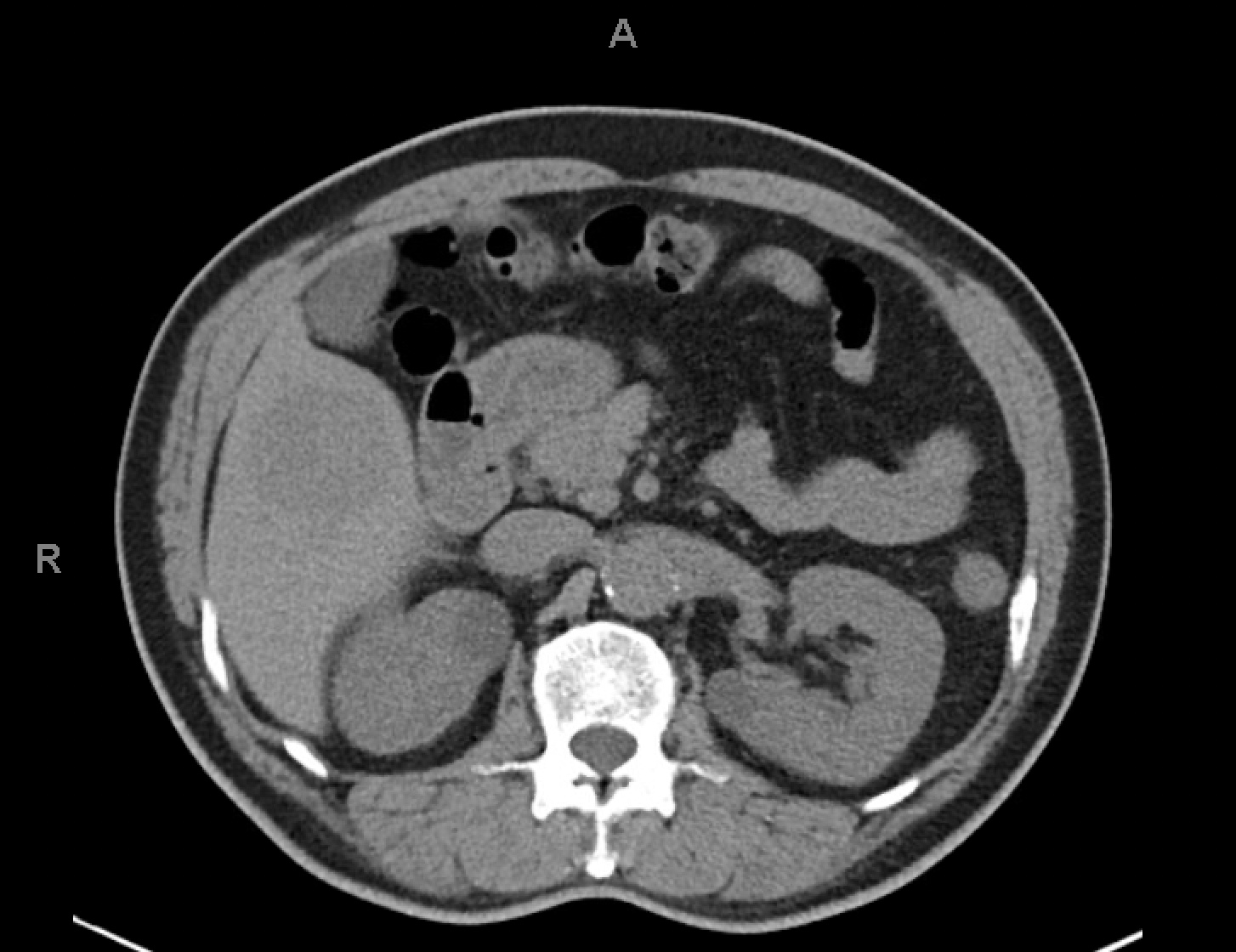
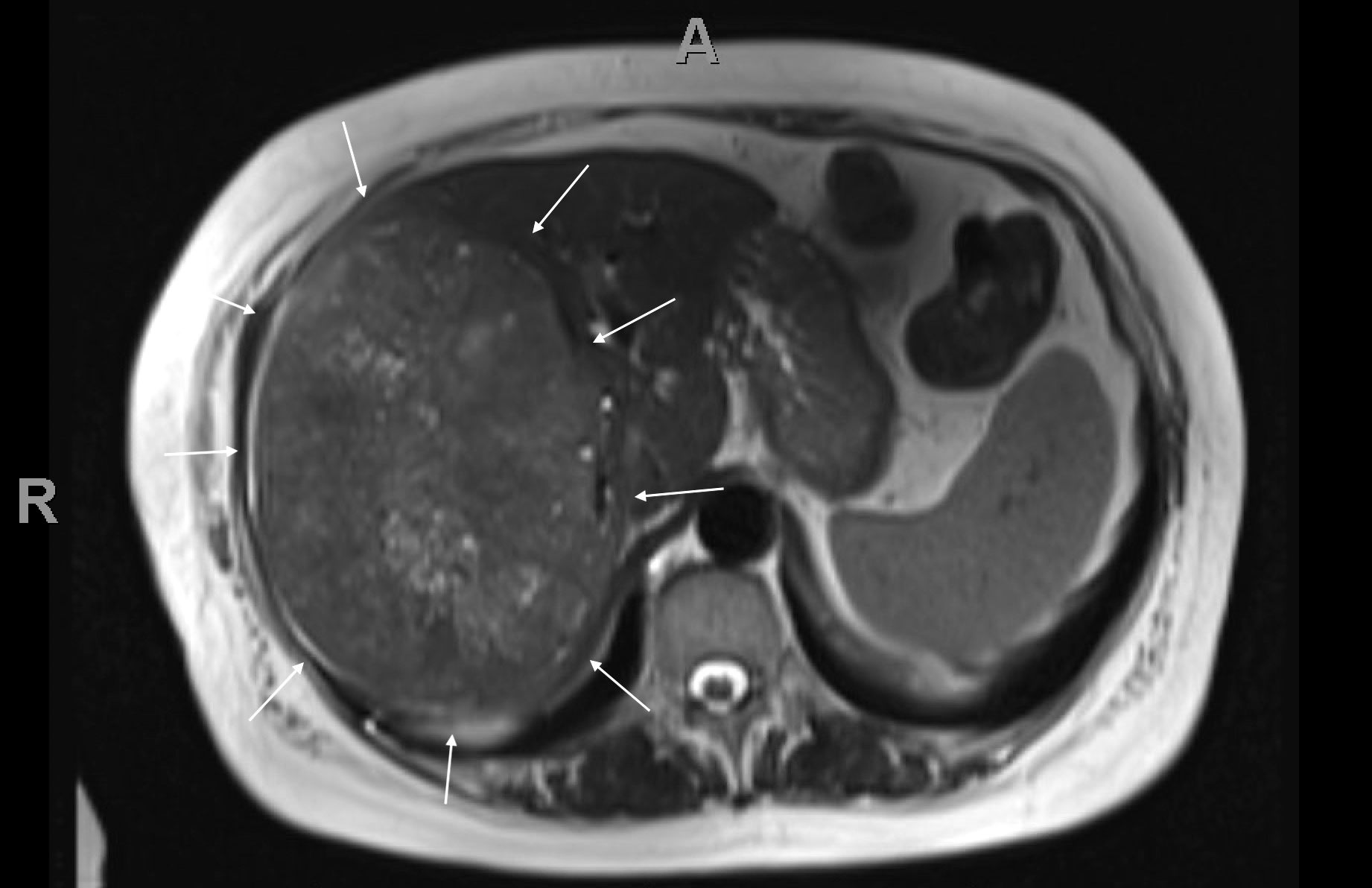
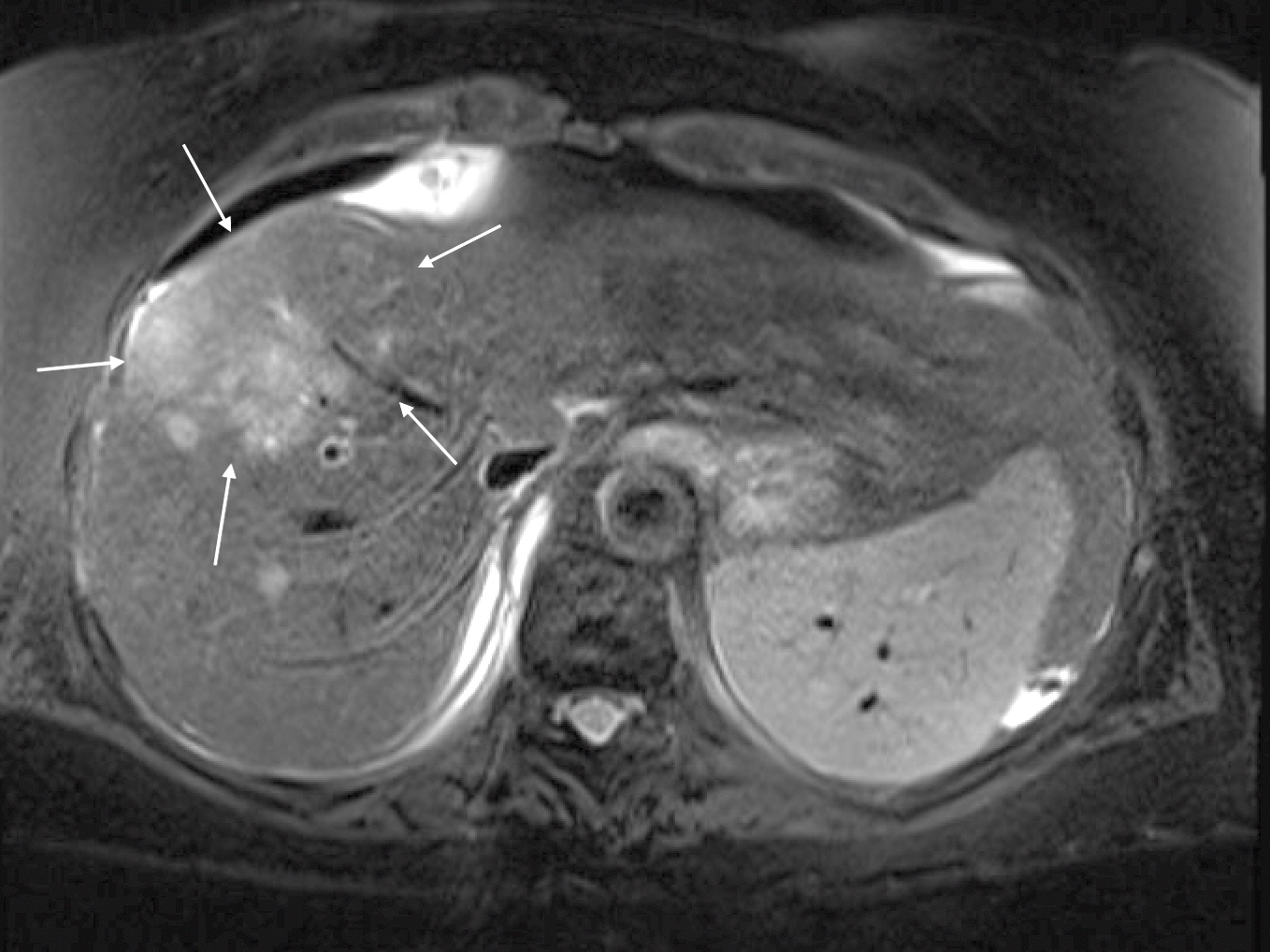
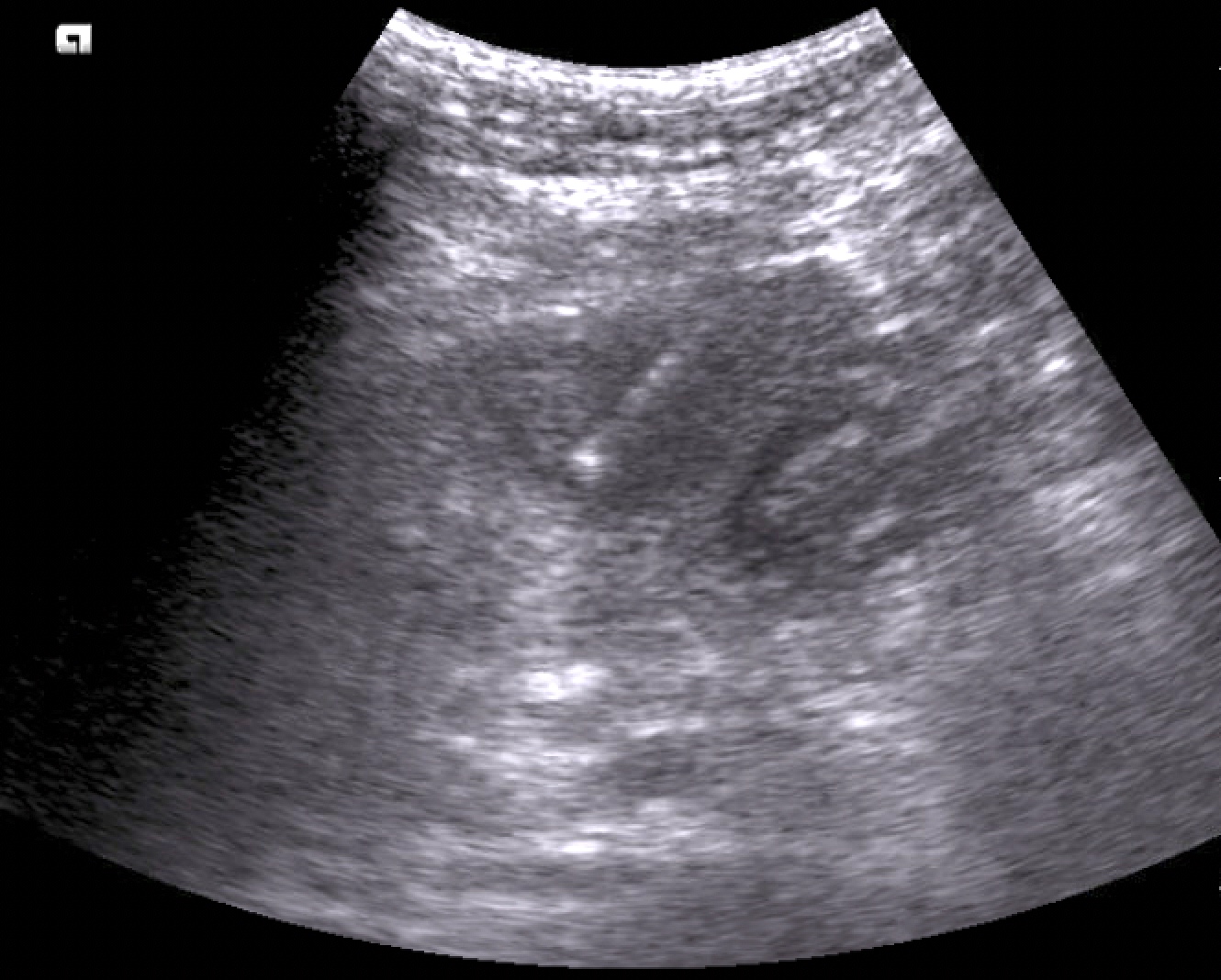
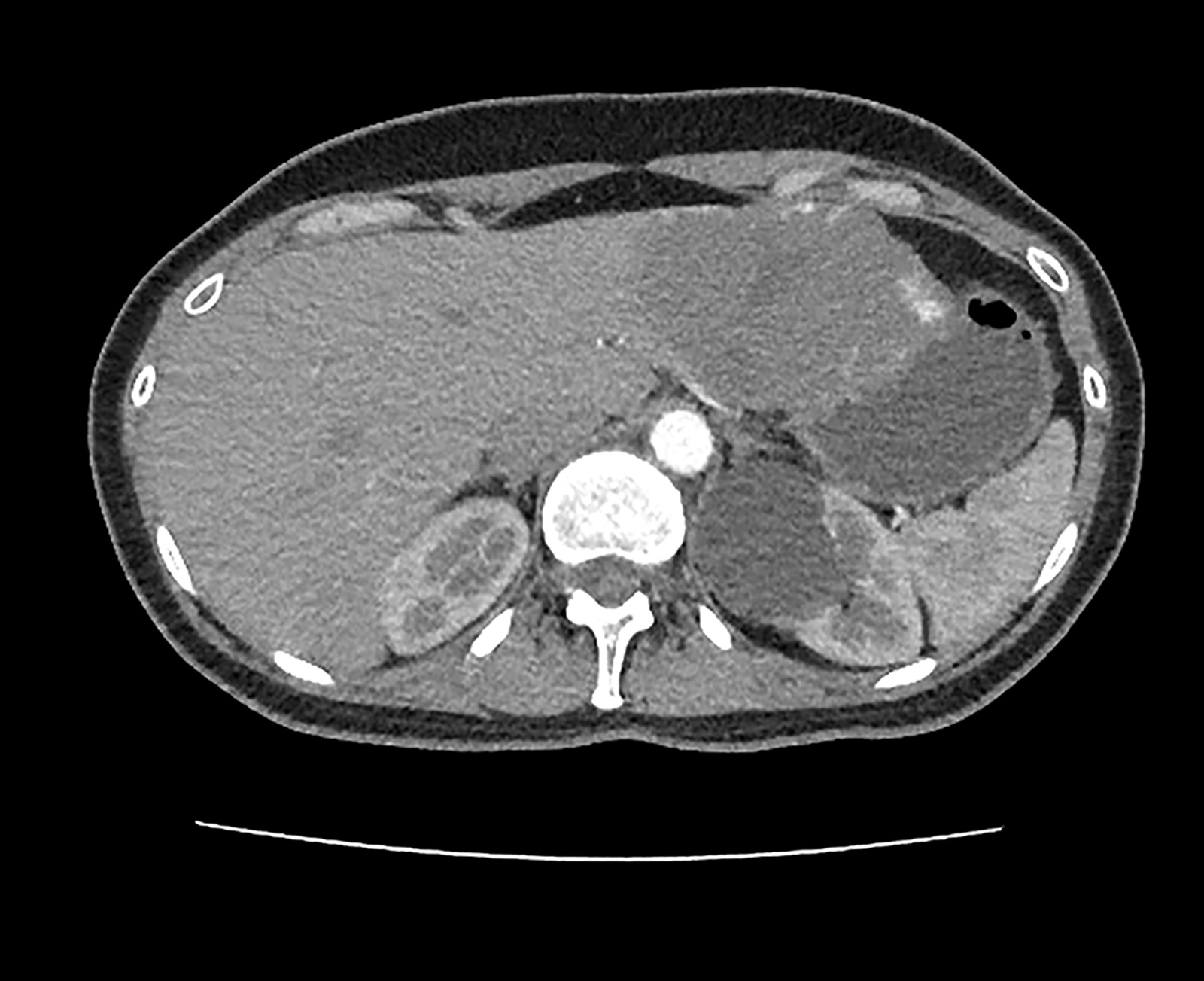
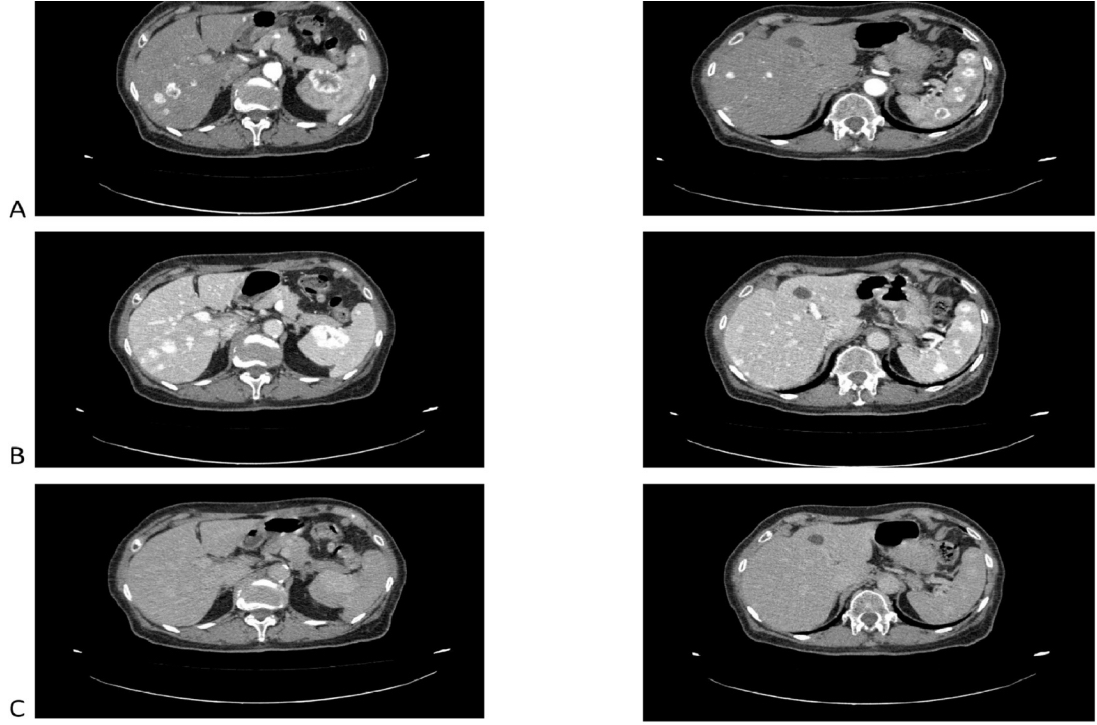
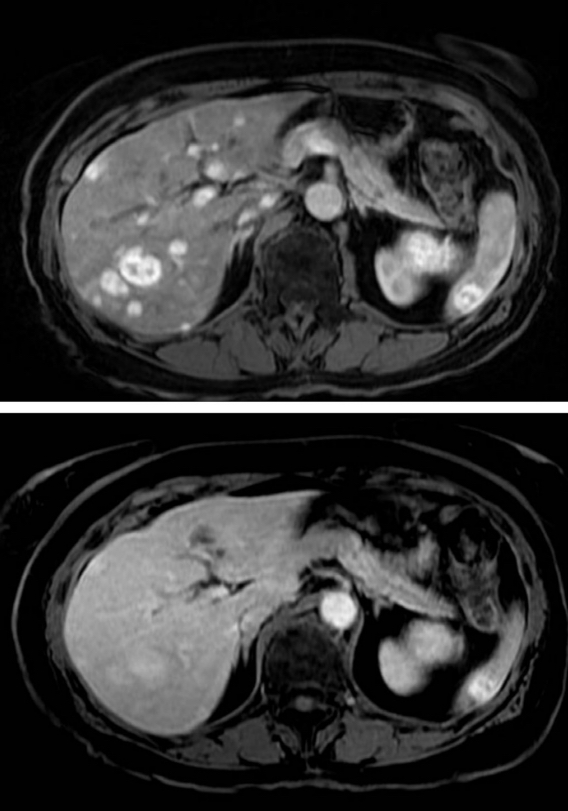
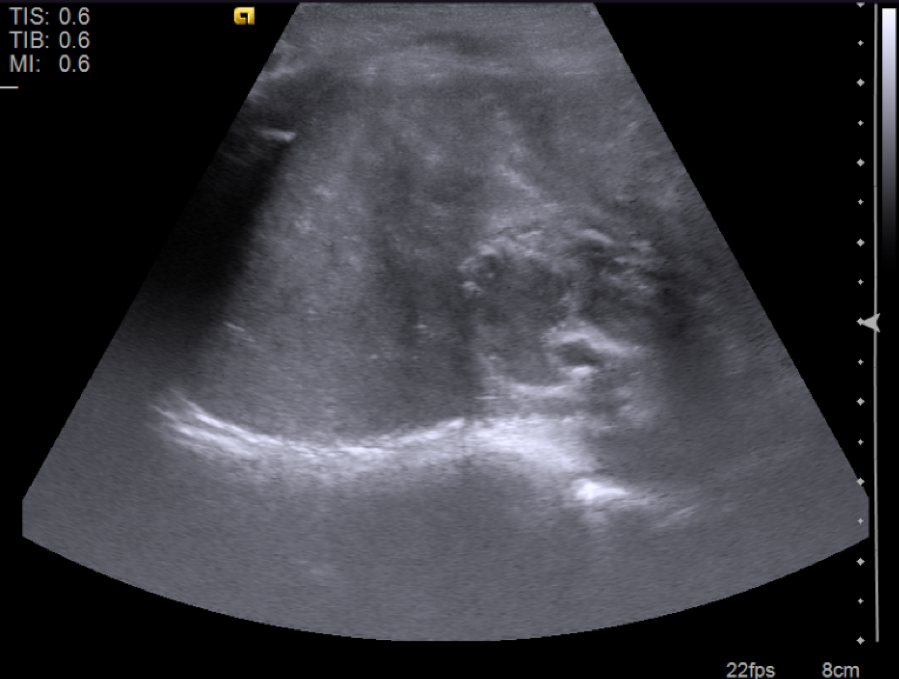
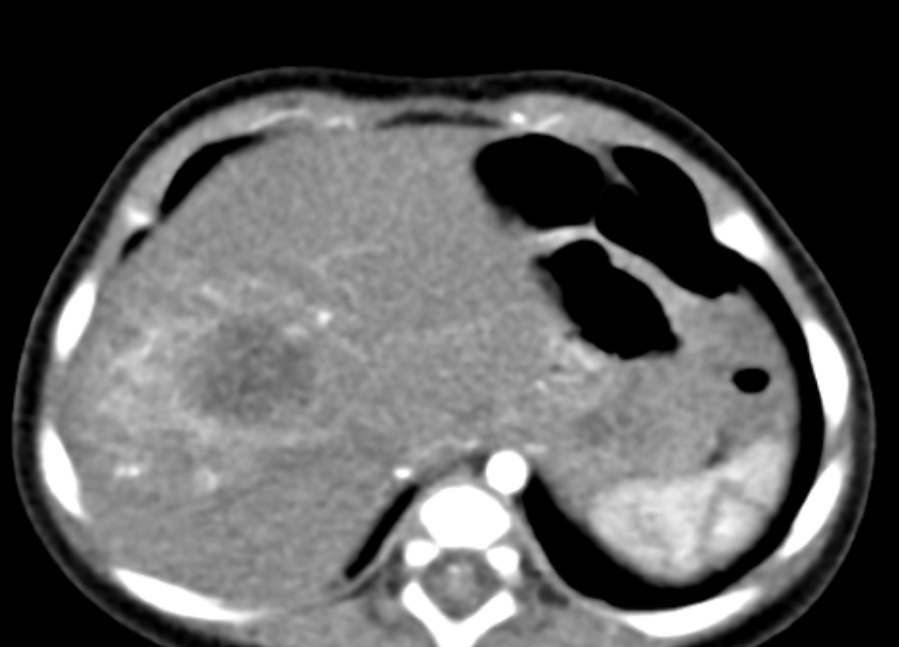
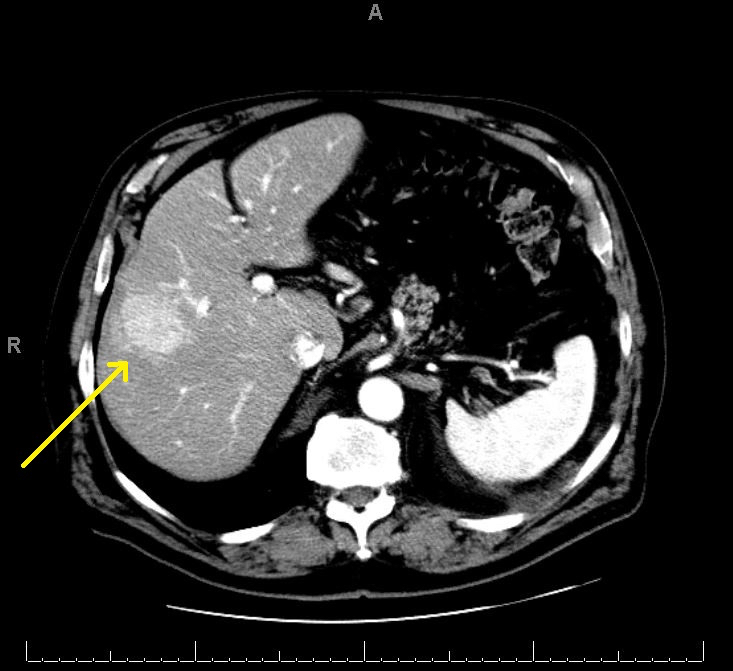
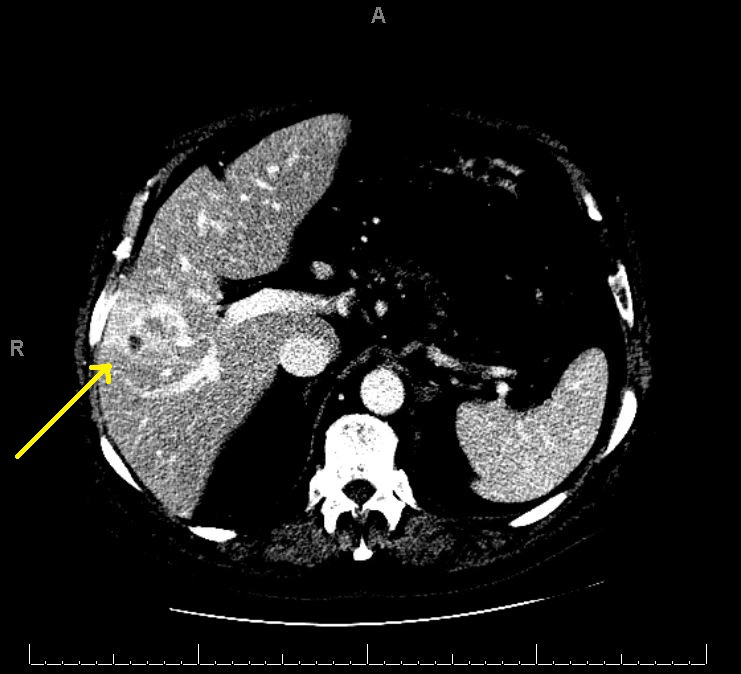
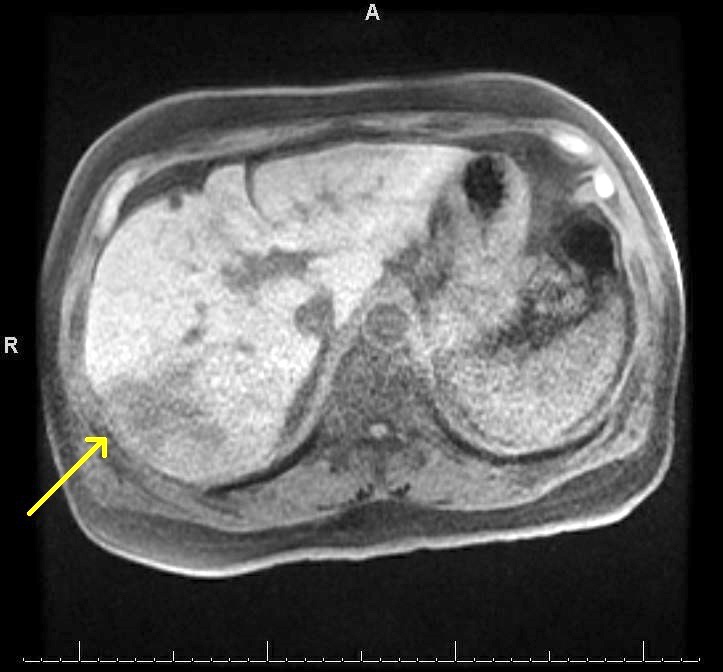
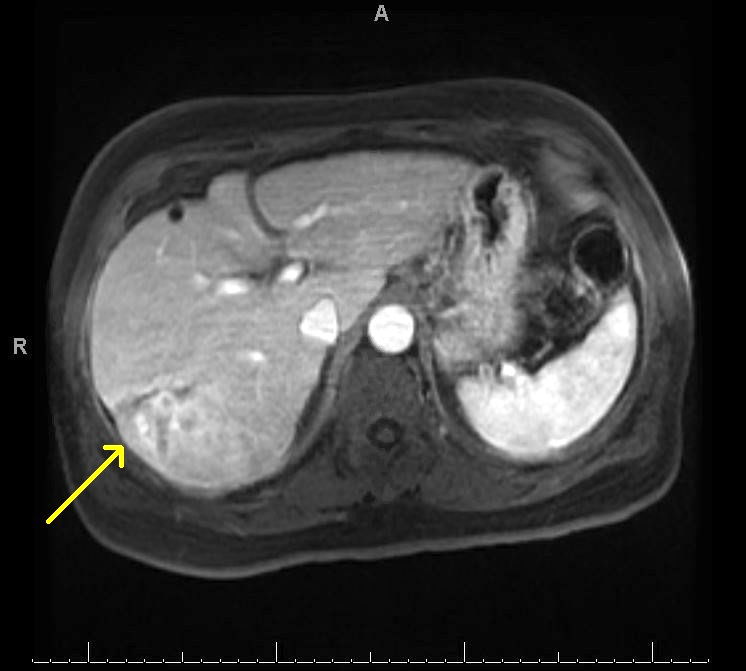
Radiology description
- Abdominal CT may reveal small or large hypodense areas in liver, areas of necrosis (Case Rep Infect Dis 2012;2012:463569)
Prognostic factors
- Rapid progression with massive liver necrosis is usually fatal; patients die secondary to organ failure (Am J Surg Pathol 2017;41:810)
- Surviving patients had limited necrosis at the time of initial diagnosis; these patients also had only relatively mild peak elevations in their serum AST and ALT (mean: 140 and 133, respectively) (Am J Surg Pathol 2017;41:810)
Case reports
- 2 year old boy after a liver transplantation for hepatoblastoma (J Pediatric Infect Dis Soc 2015;4:e1)
- 35 year old immunocompetent woman with fever (J Investig Med High Impact Case Rep 2022;10:23247096221079192)
- 48 year old woman after remission of large B cell lymphoma and autologous HSCT; 51 year old man with acute myeloid leukemia after 4 allogeneic HSCTs (Transpl Infect Dis 2021;23:e13496)
- 59 year old man with T cell prolymphocytic leukemia who had focal liver lesions on abdominal CT with suspicion of metastatic disease (Ann Hepatol 2014;13:827)
- 66 year old man on a chemotherapy regimen for mantle cell lymphoma developed fulminant adenovirus hepatitis (Pathol Int 2018;68:259)
Treatment
- Supportive care (Am J Surg Pathol 2017;41:810)
- Antiviral therapy can be helpful (J Investig Med High Impact Case Rep 2022;10:23247096221079192, Liver Transpl 2022;28:505)
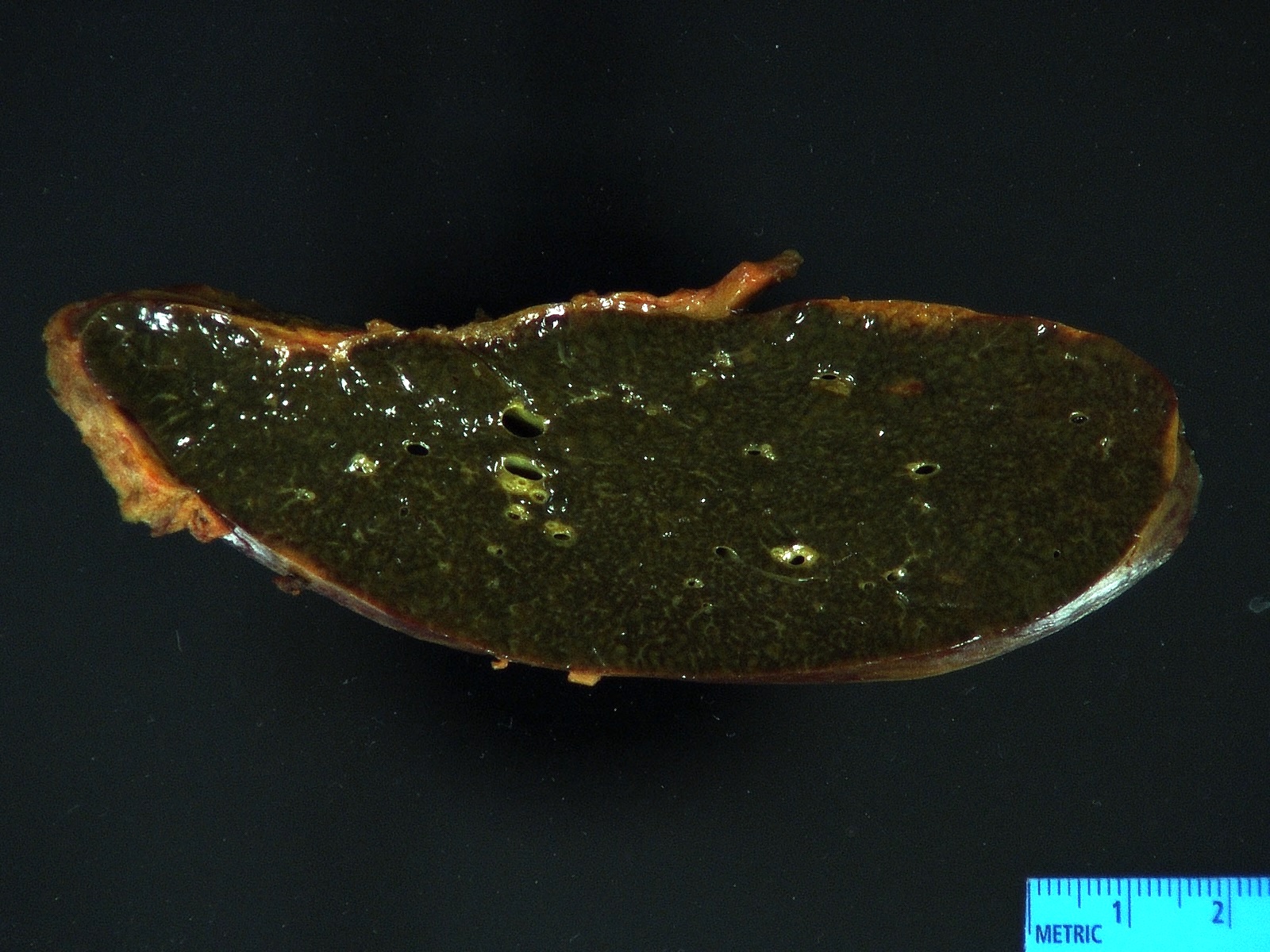
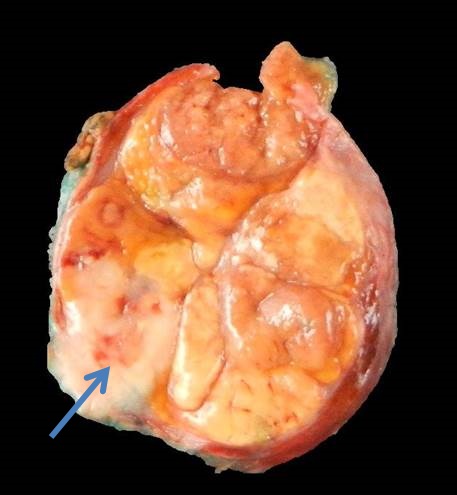
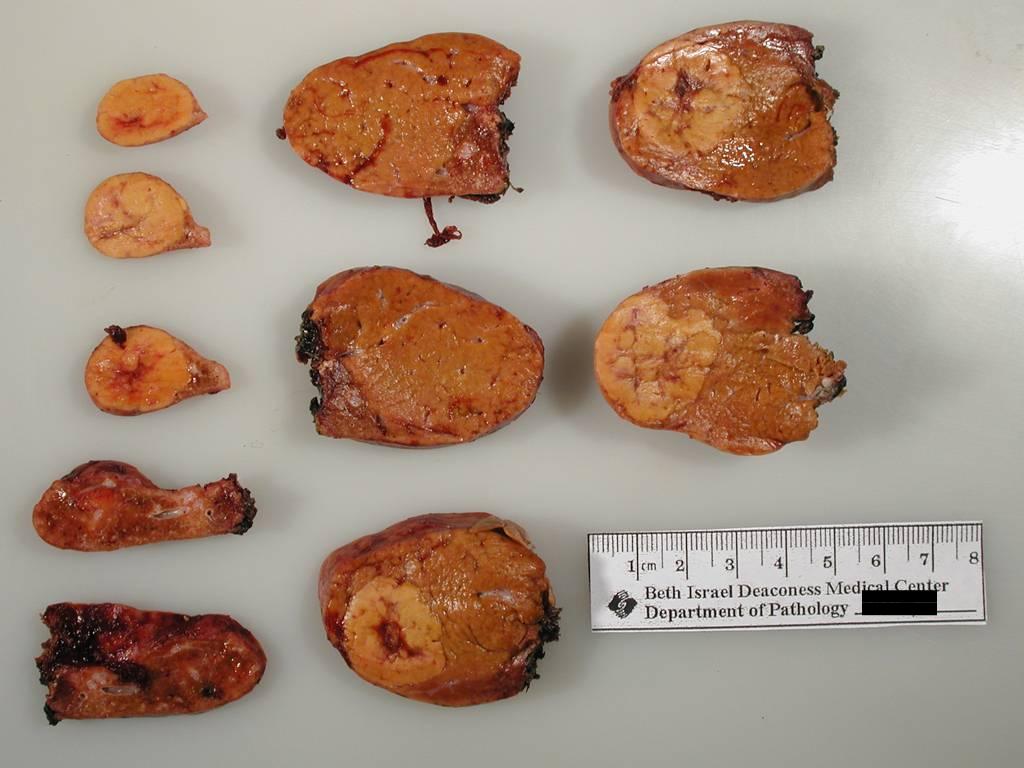
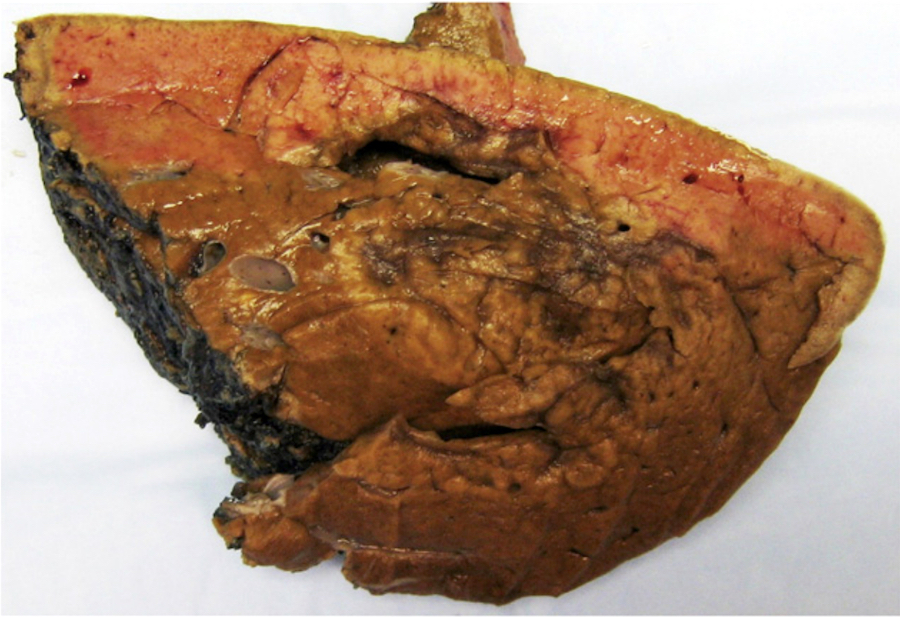
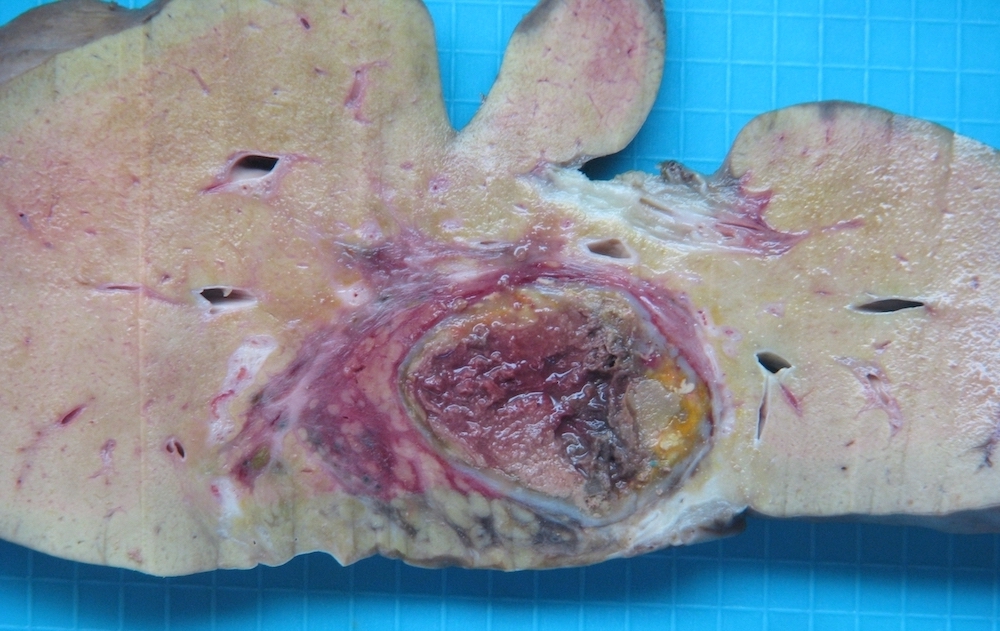
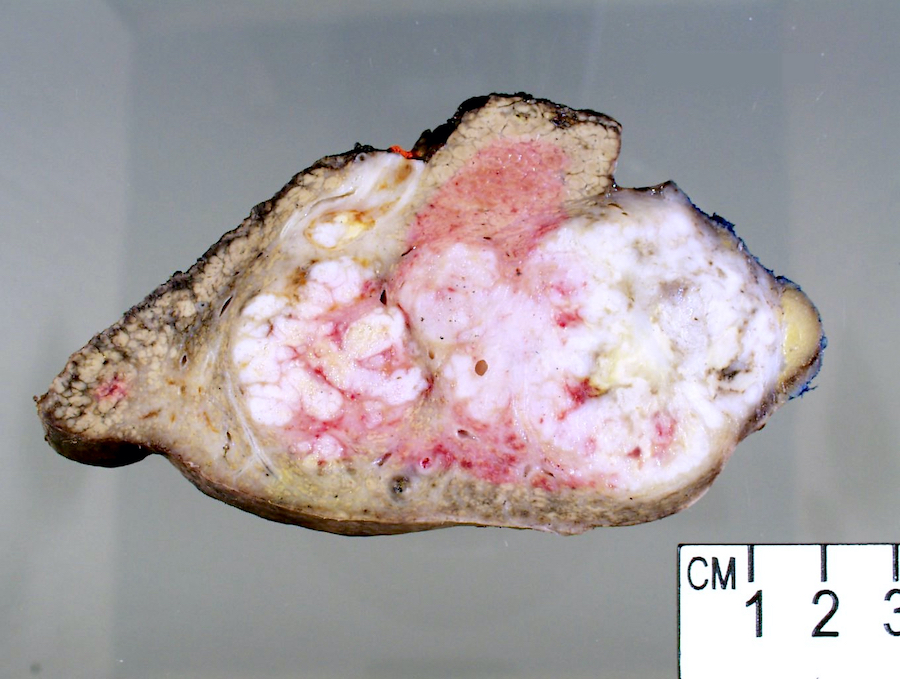
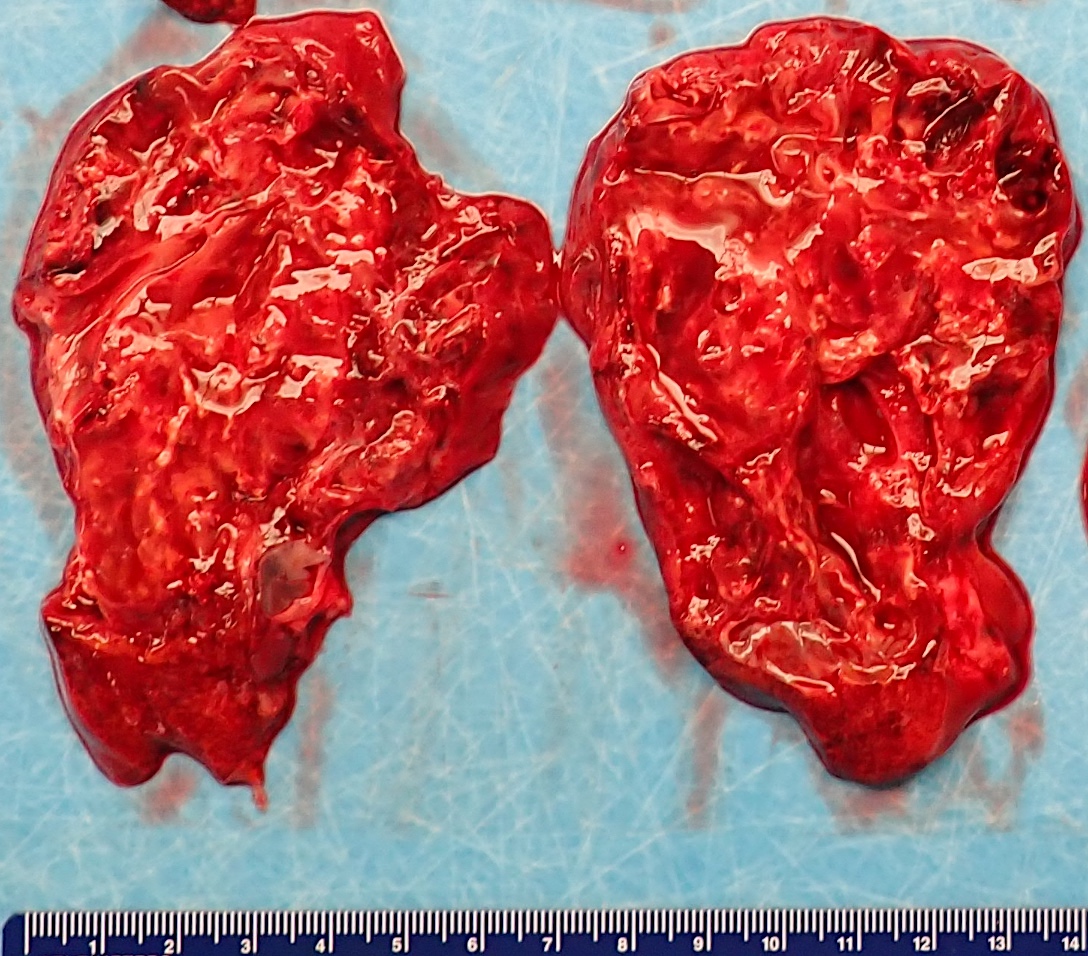
Gross description
- Liver parenchyma demonstrates reddish brown color on the cut surface (Pathol Int 2018;68:259)
- Heterogeneous areas of coagulative necrosis present in liver parenchyma (Am J Surg Pathol 2017;41:810)
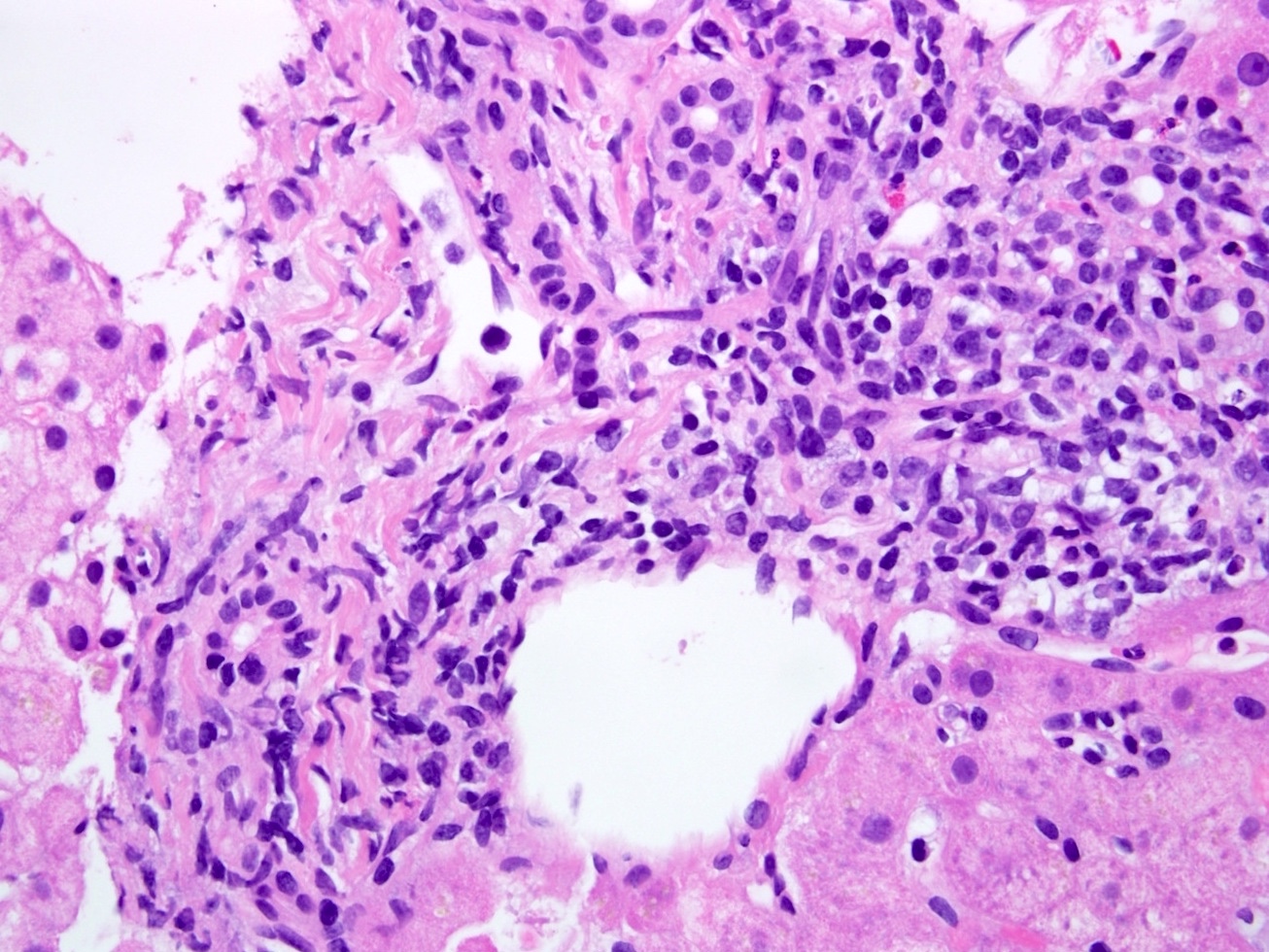
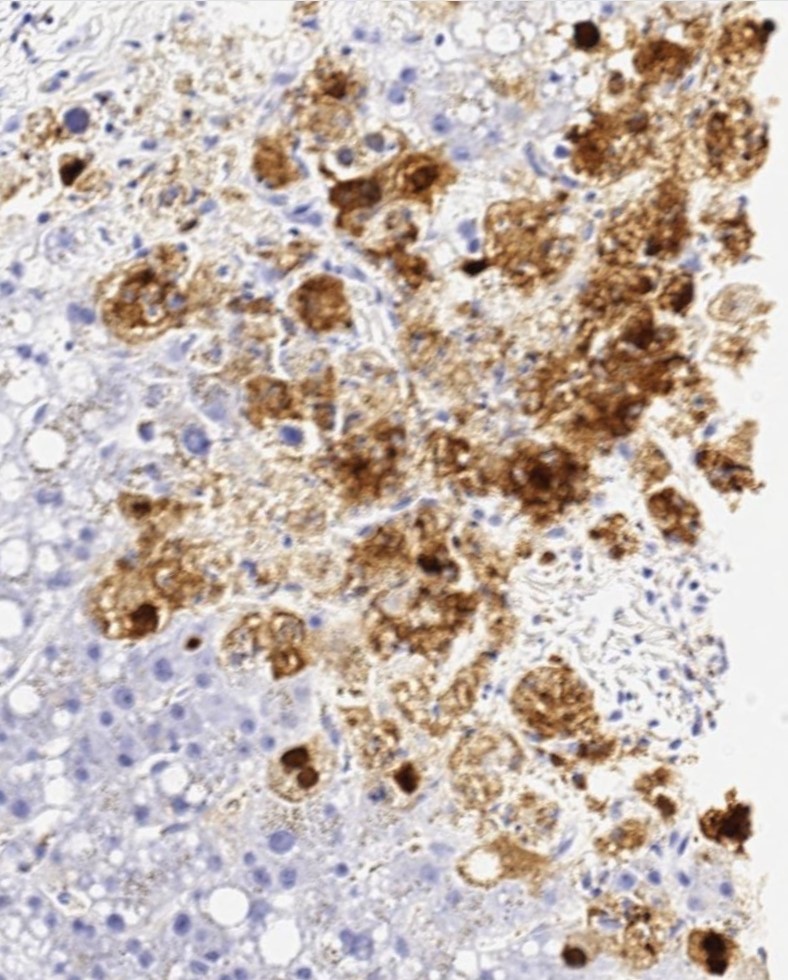
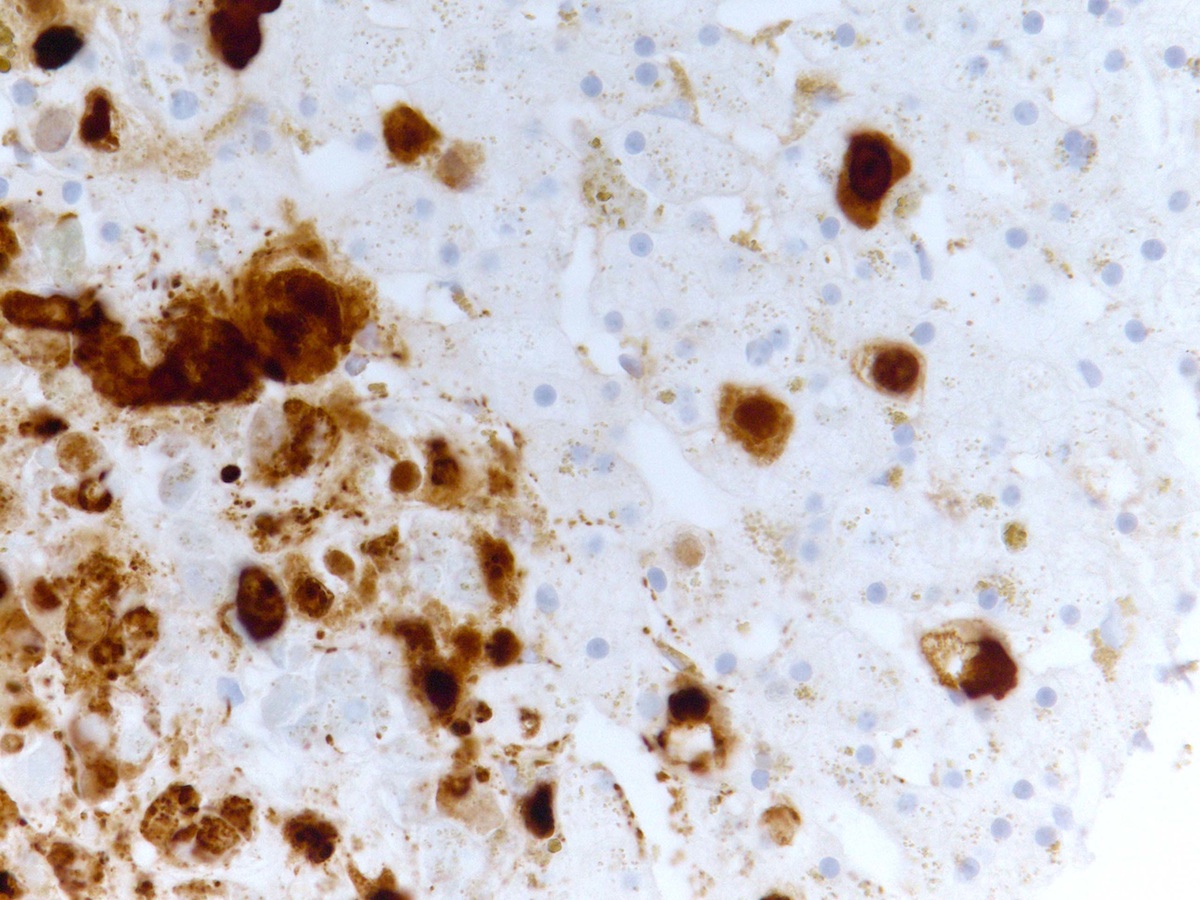
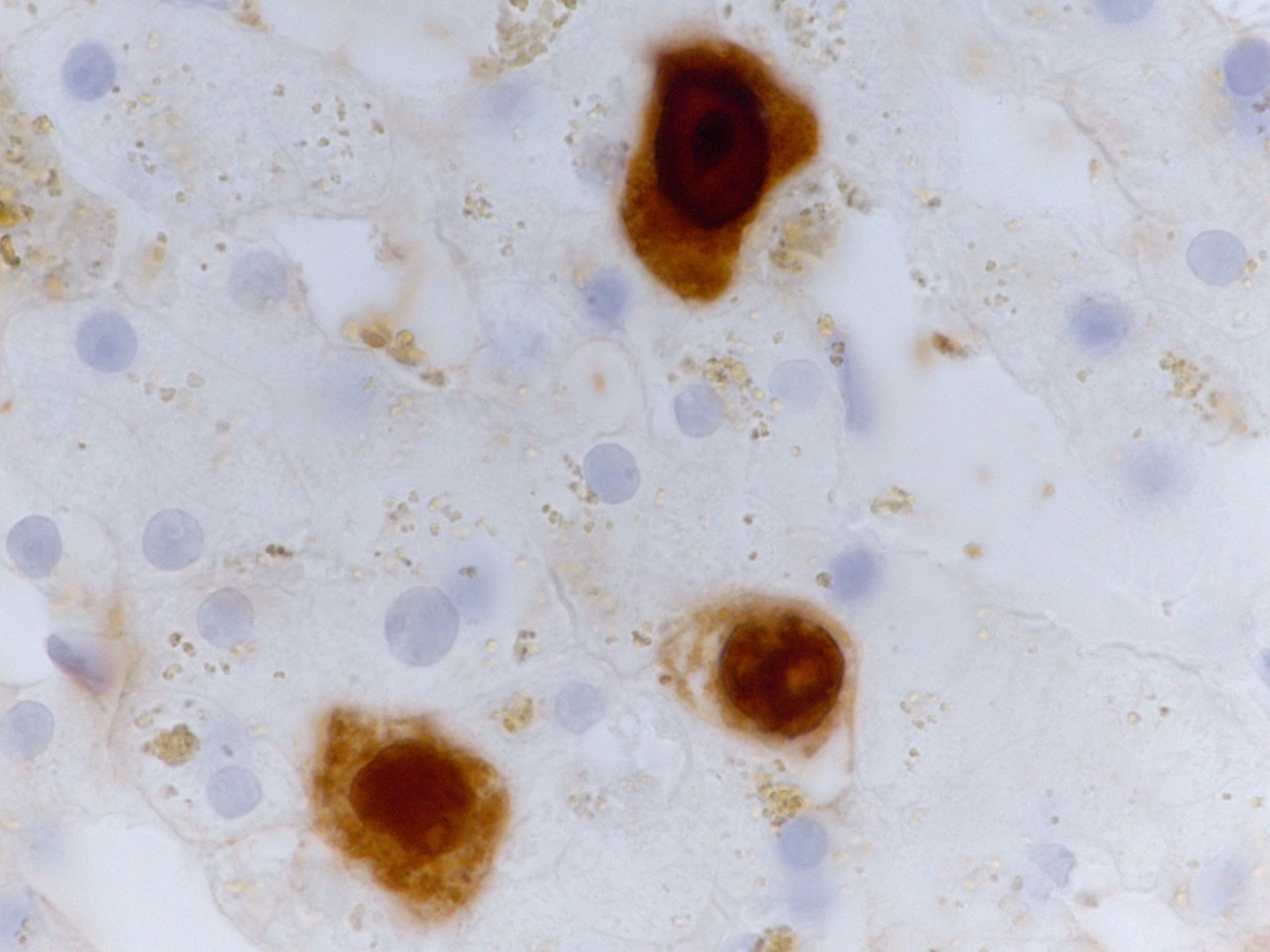
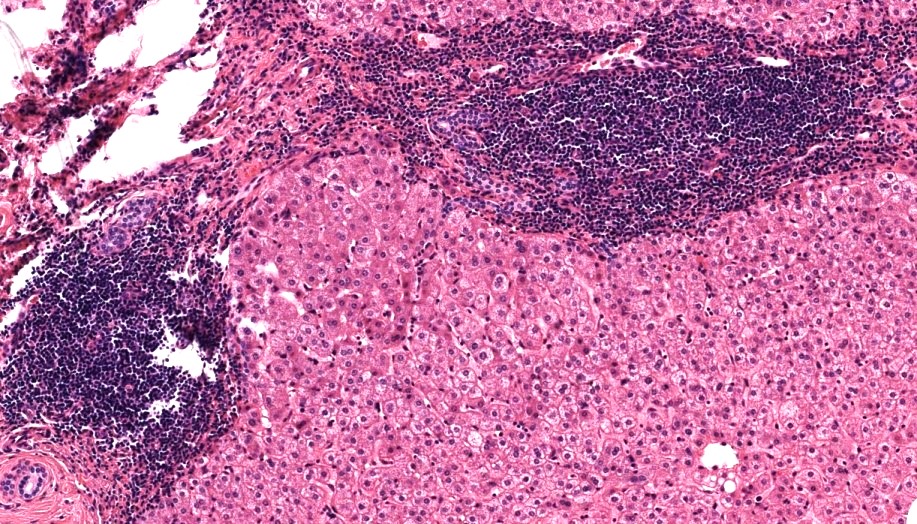
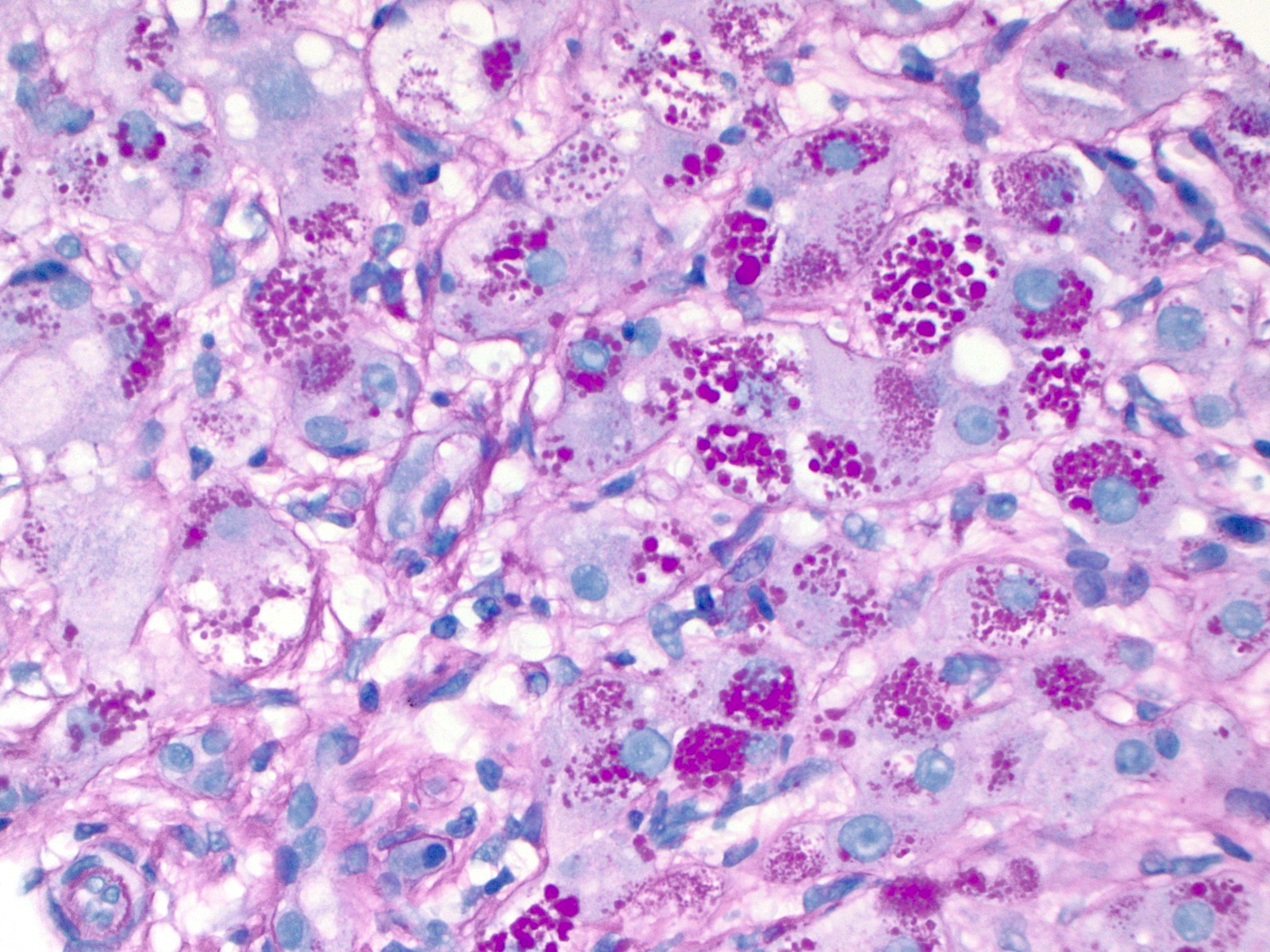
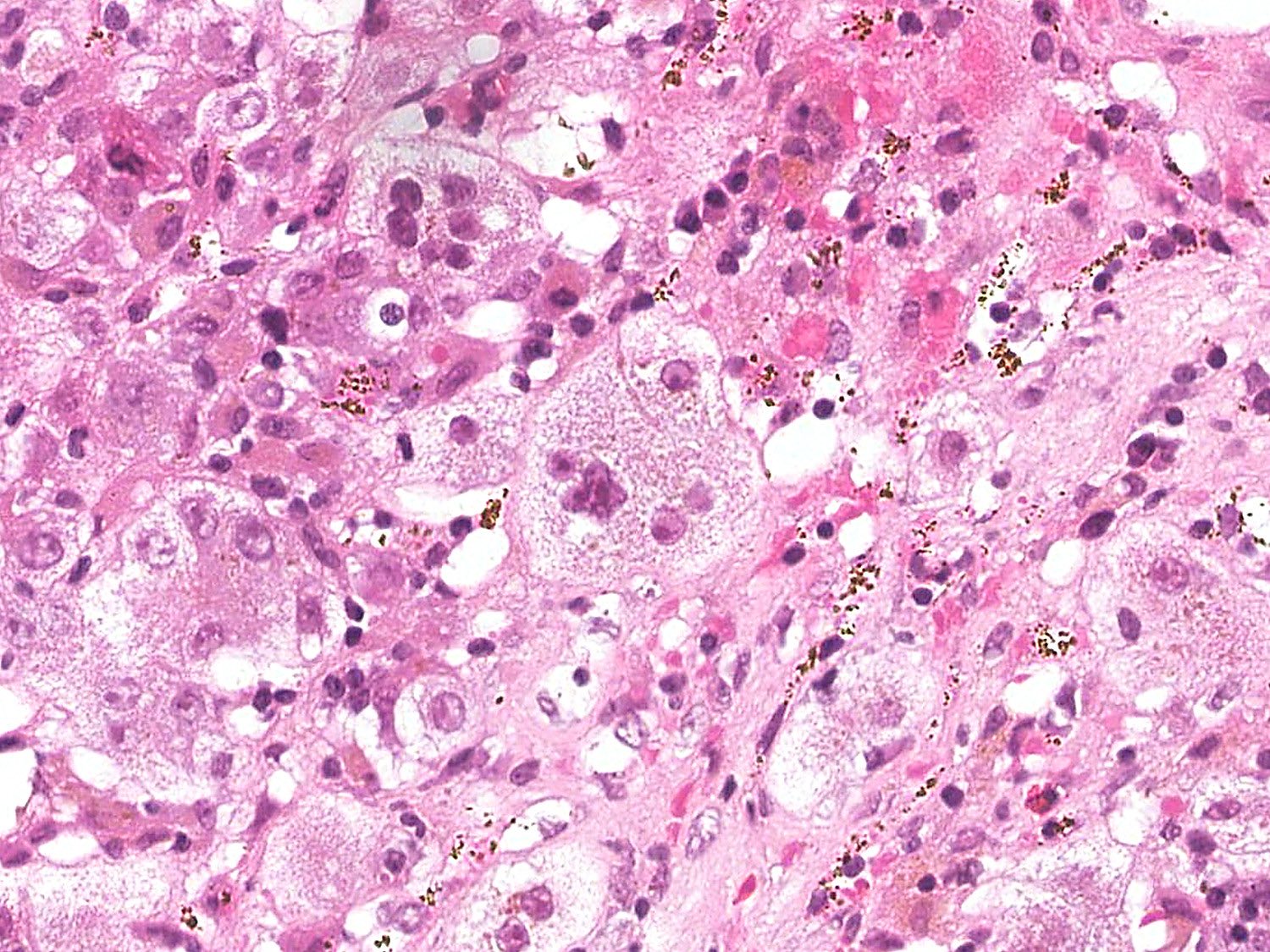
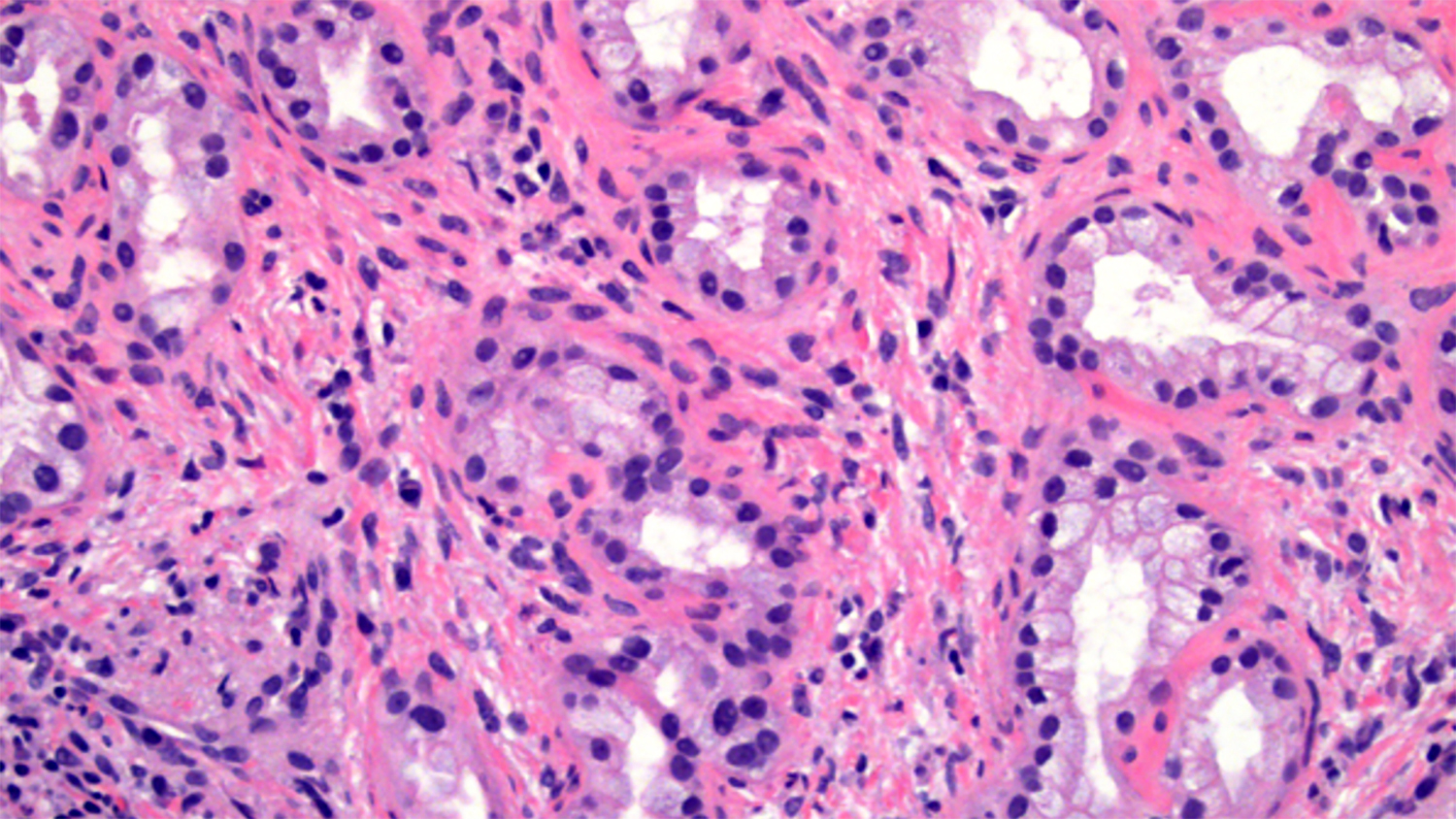
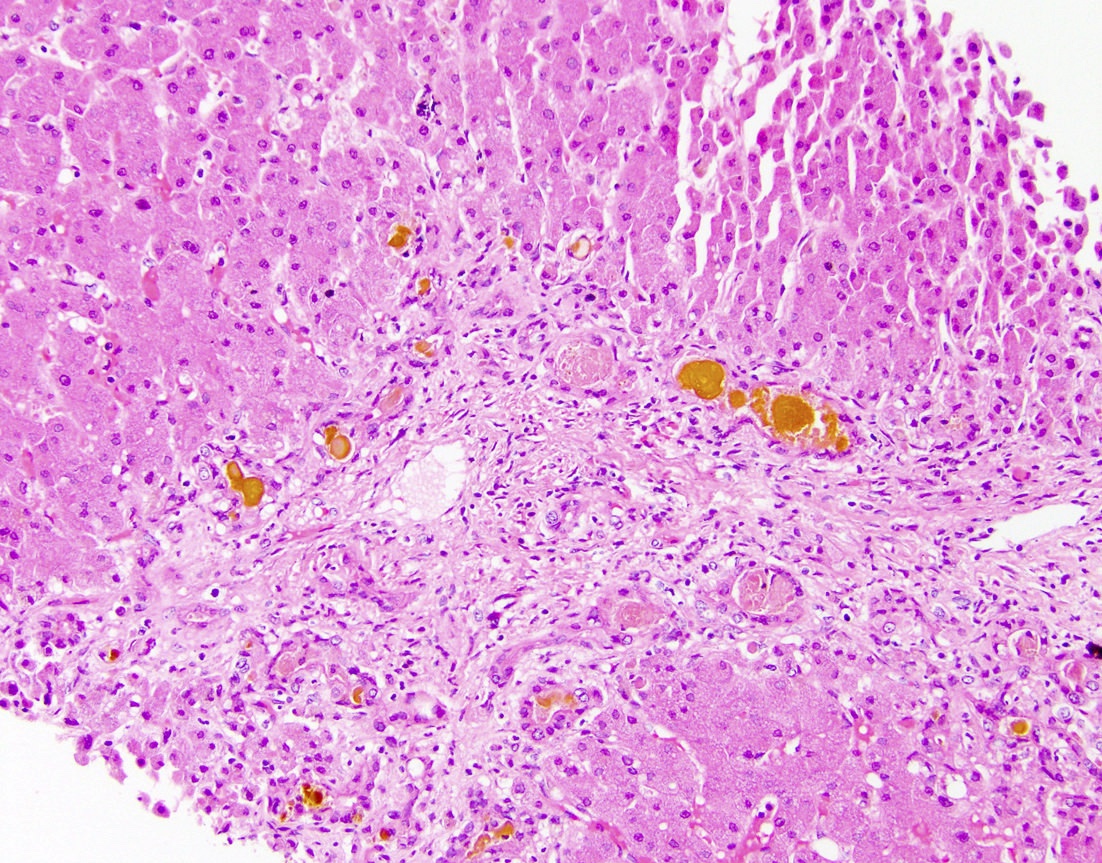
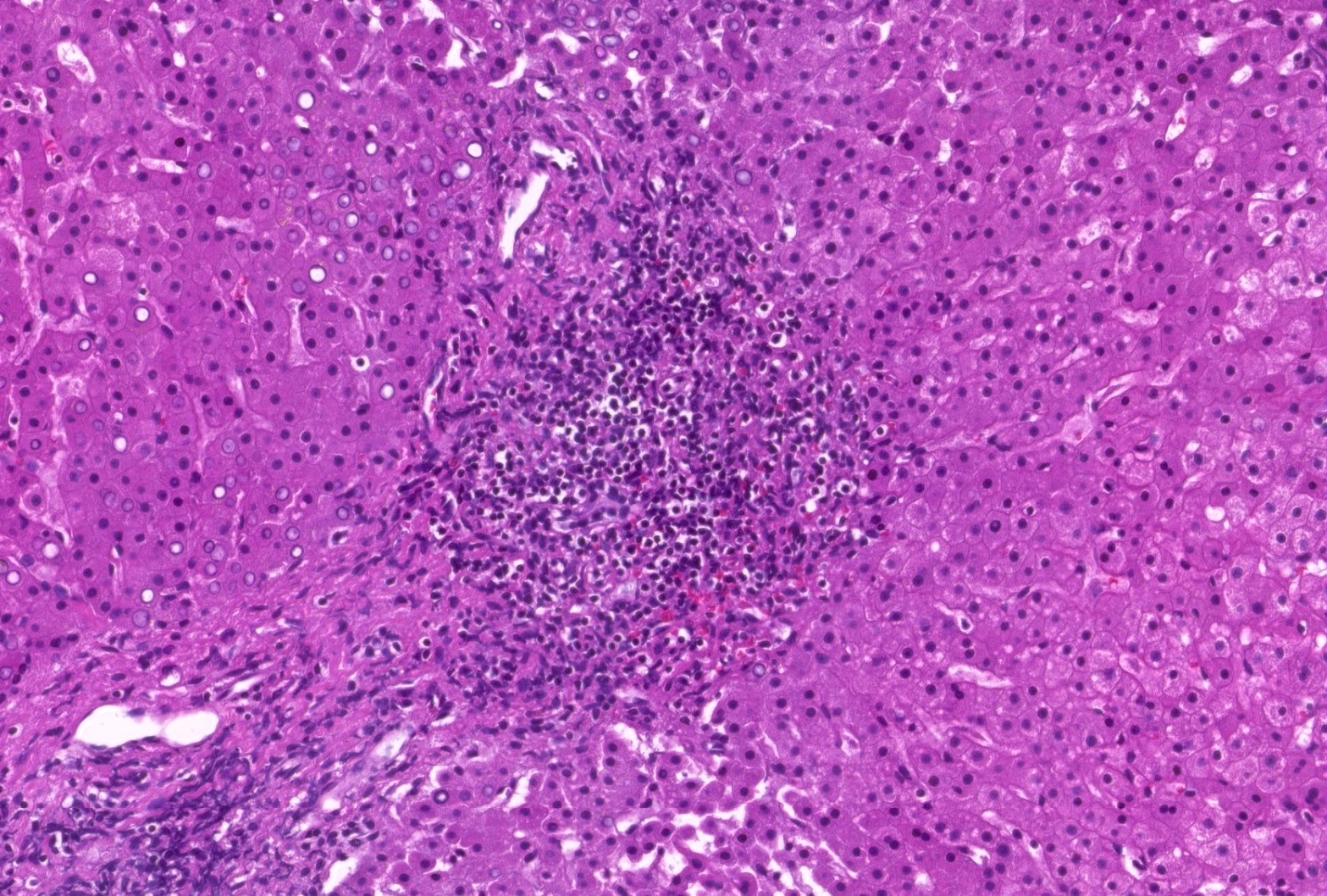
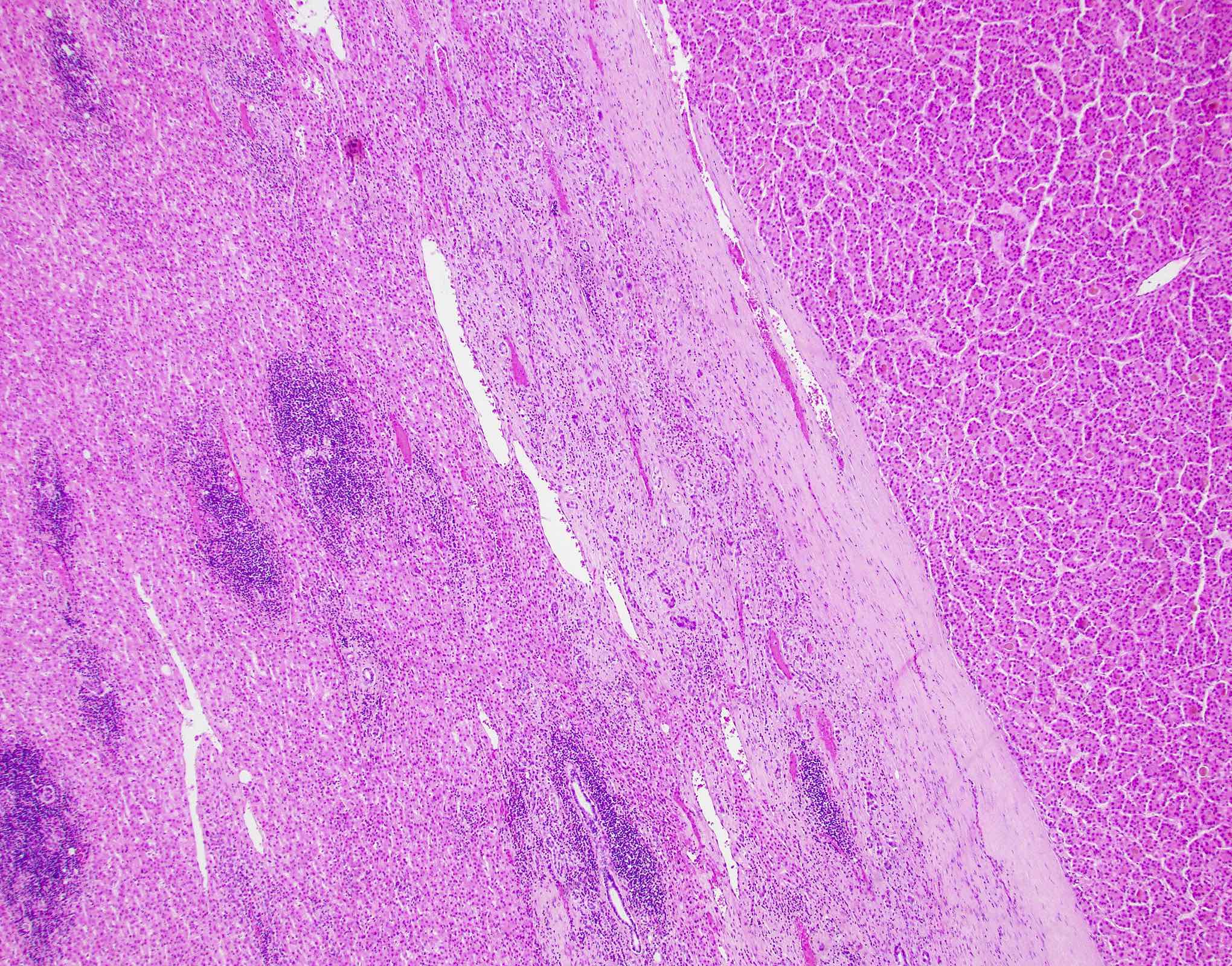
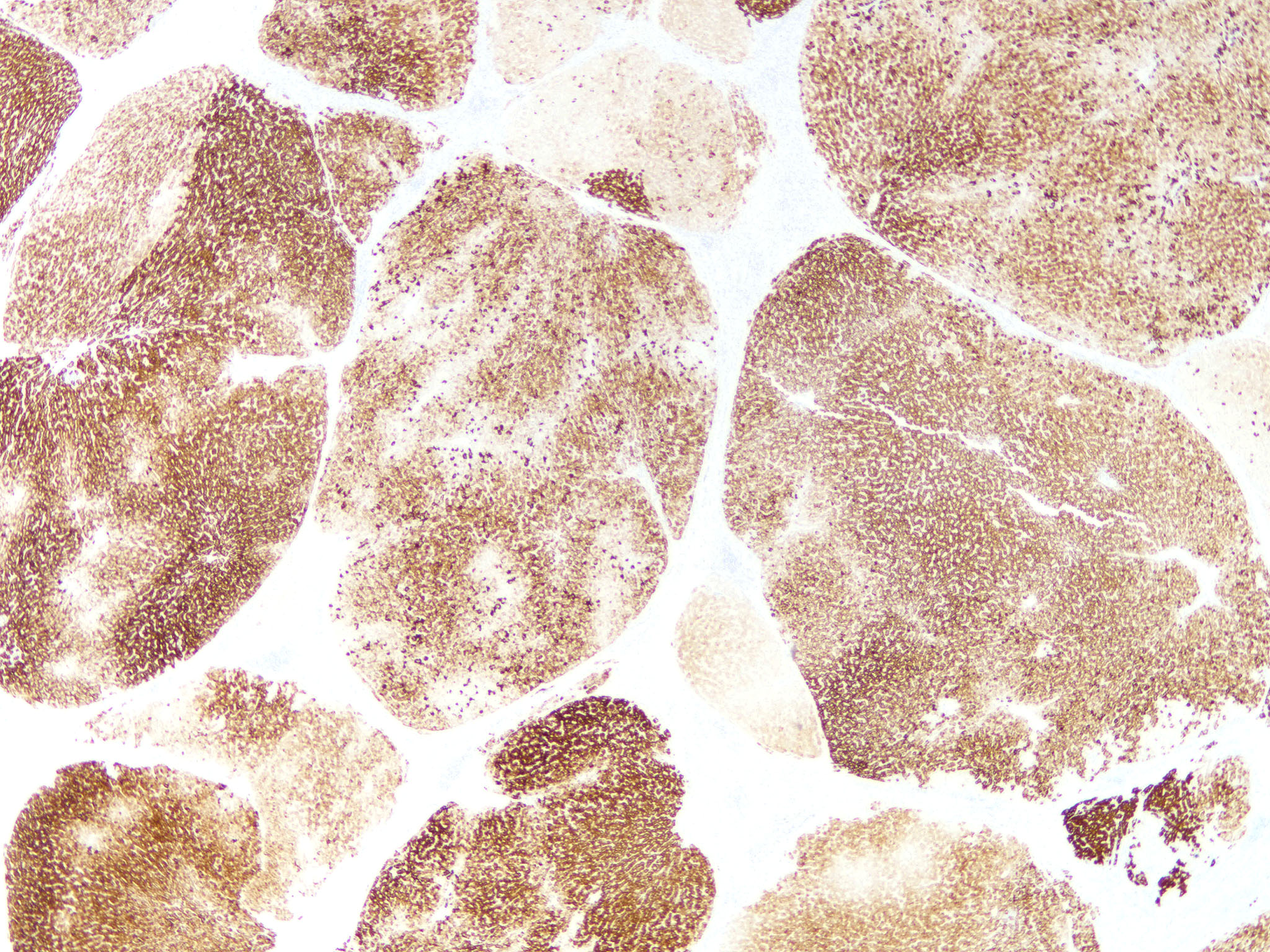
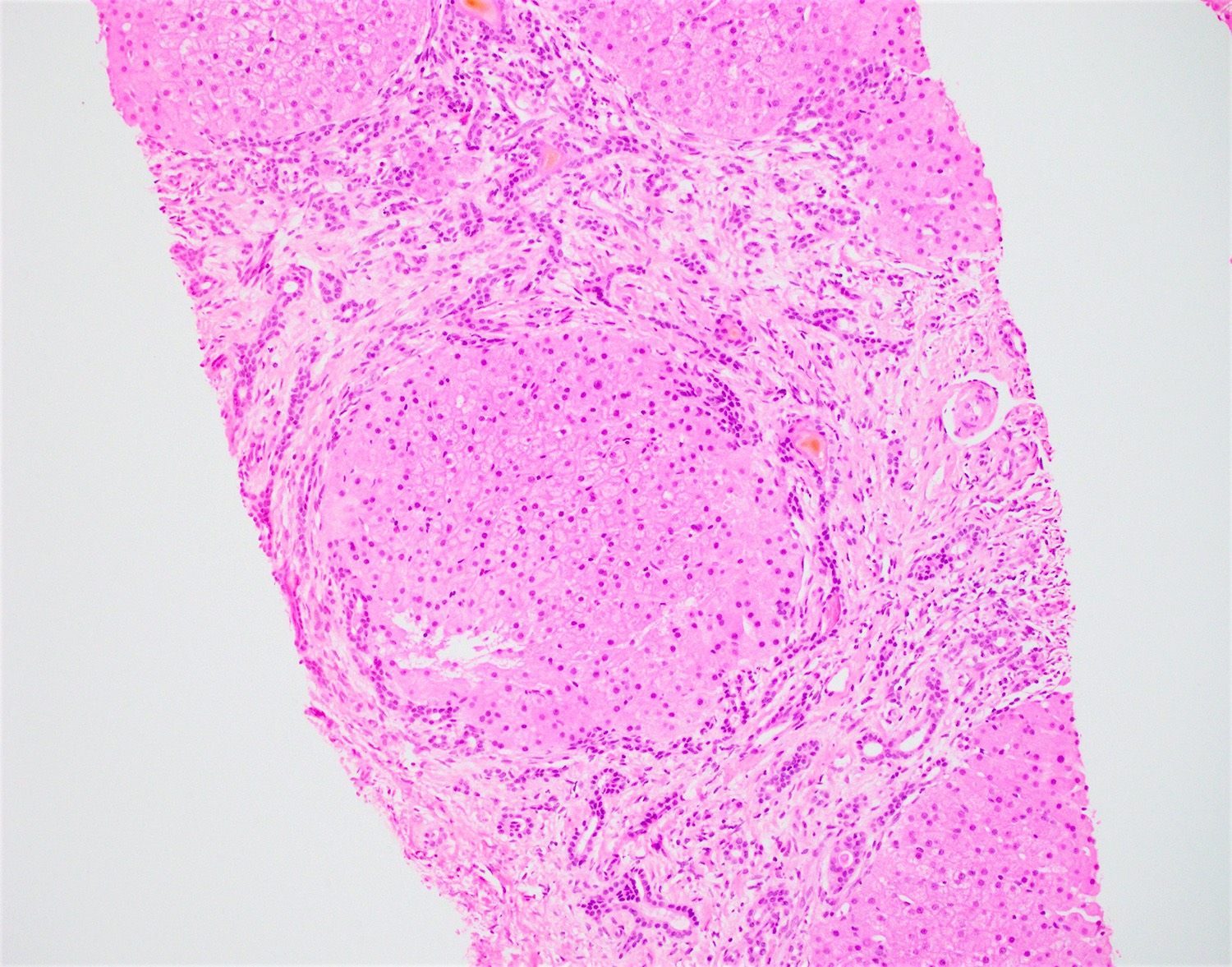
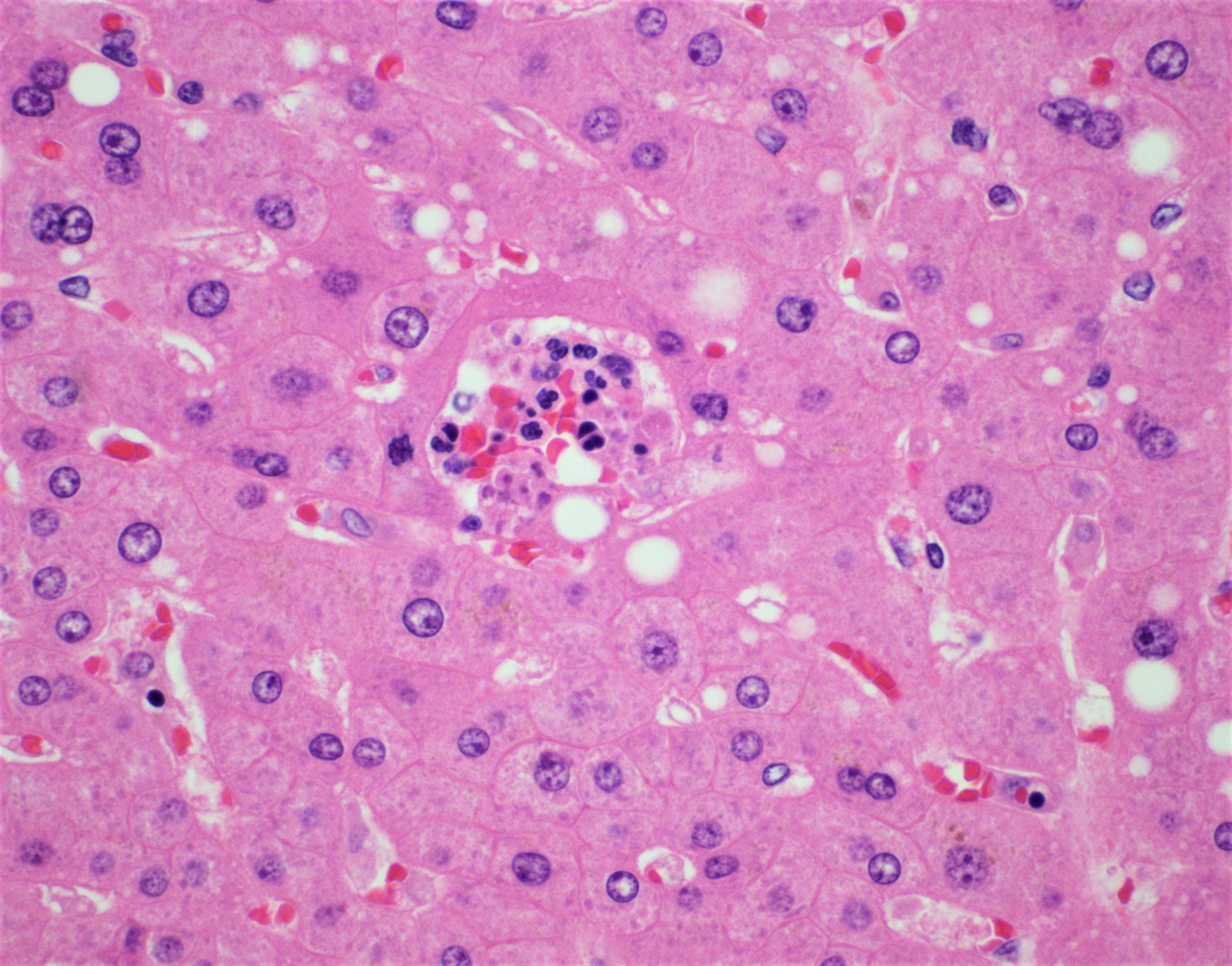
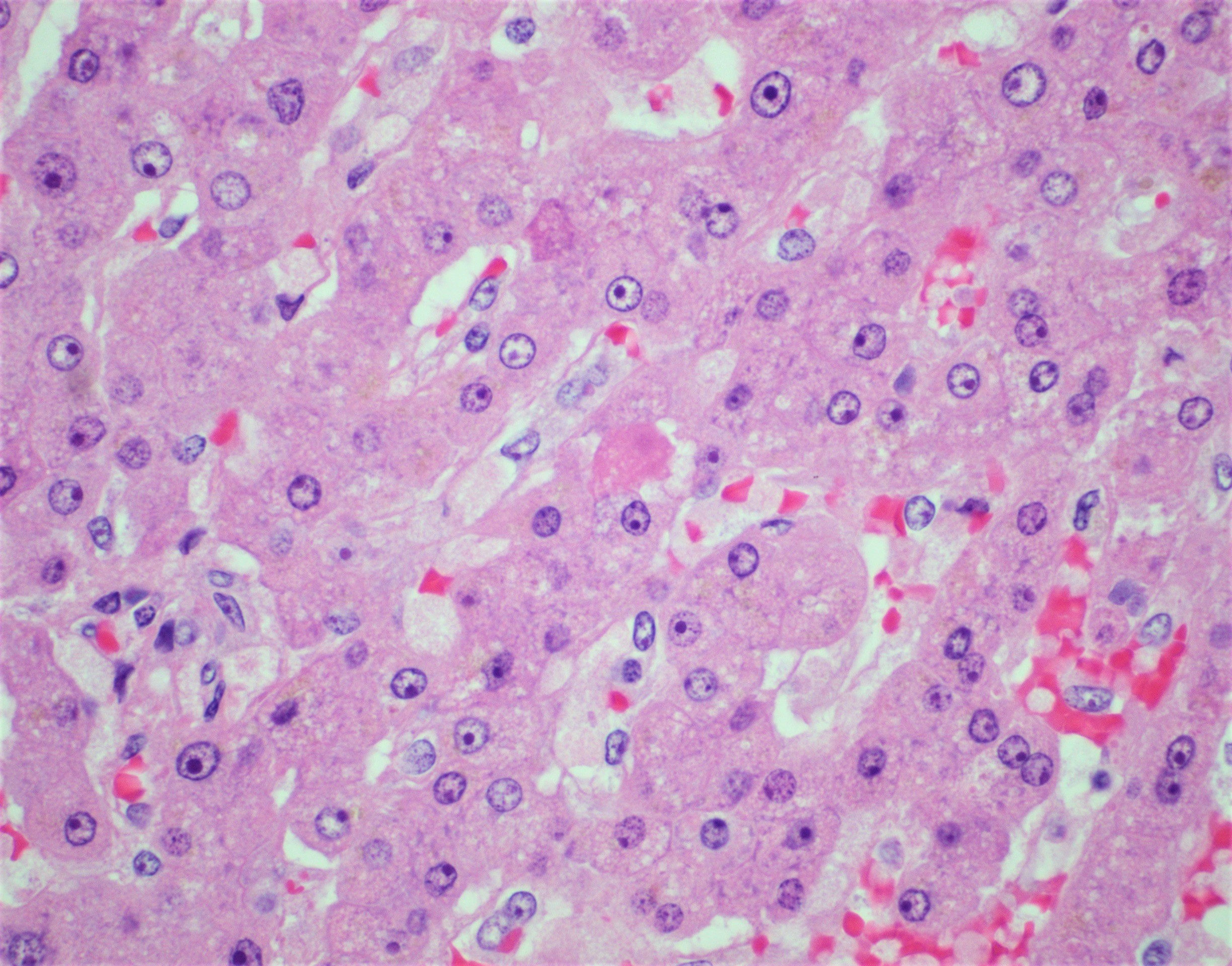
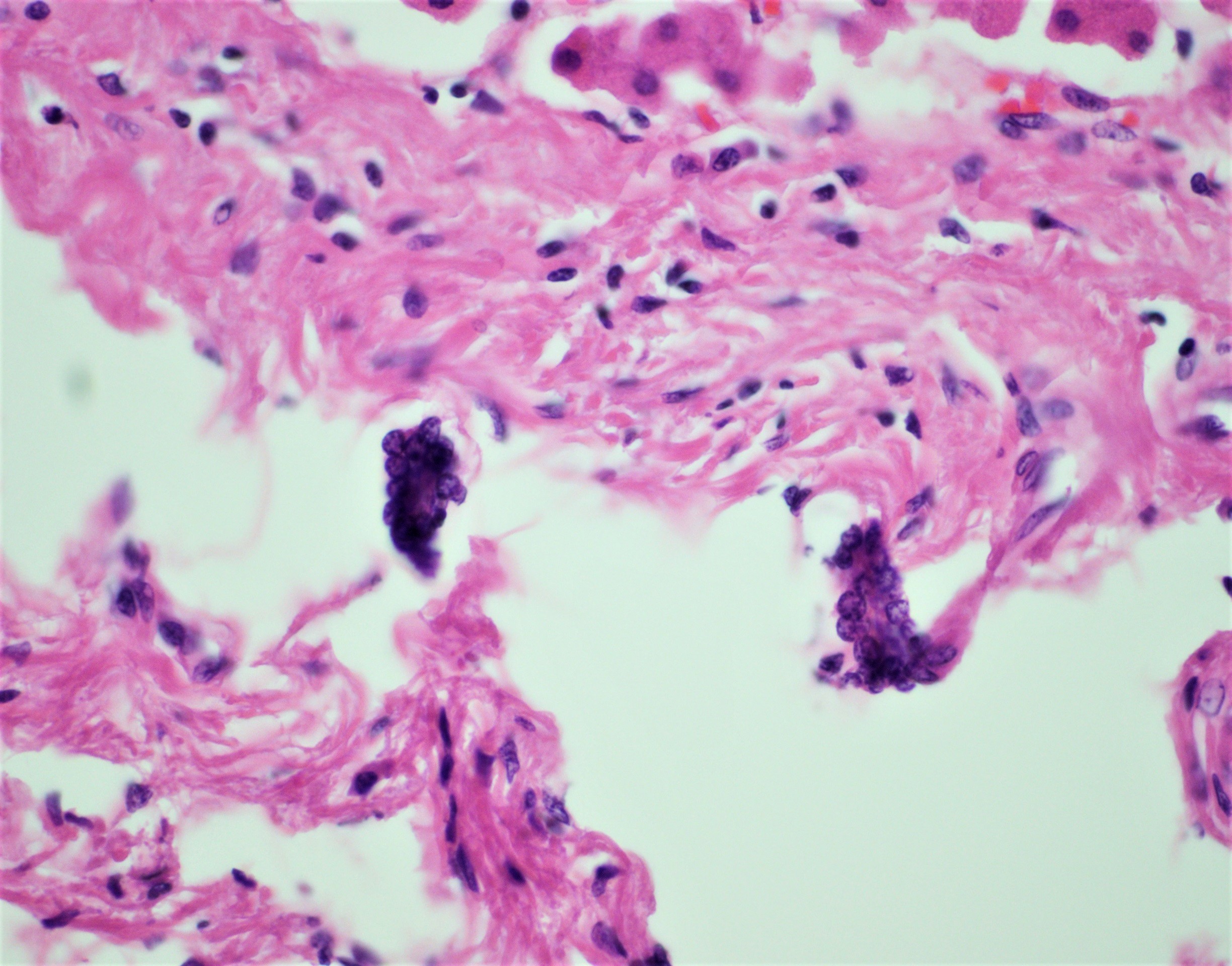
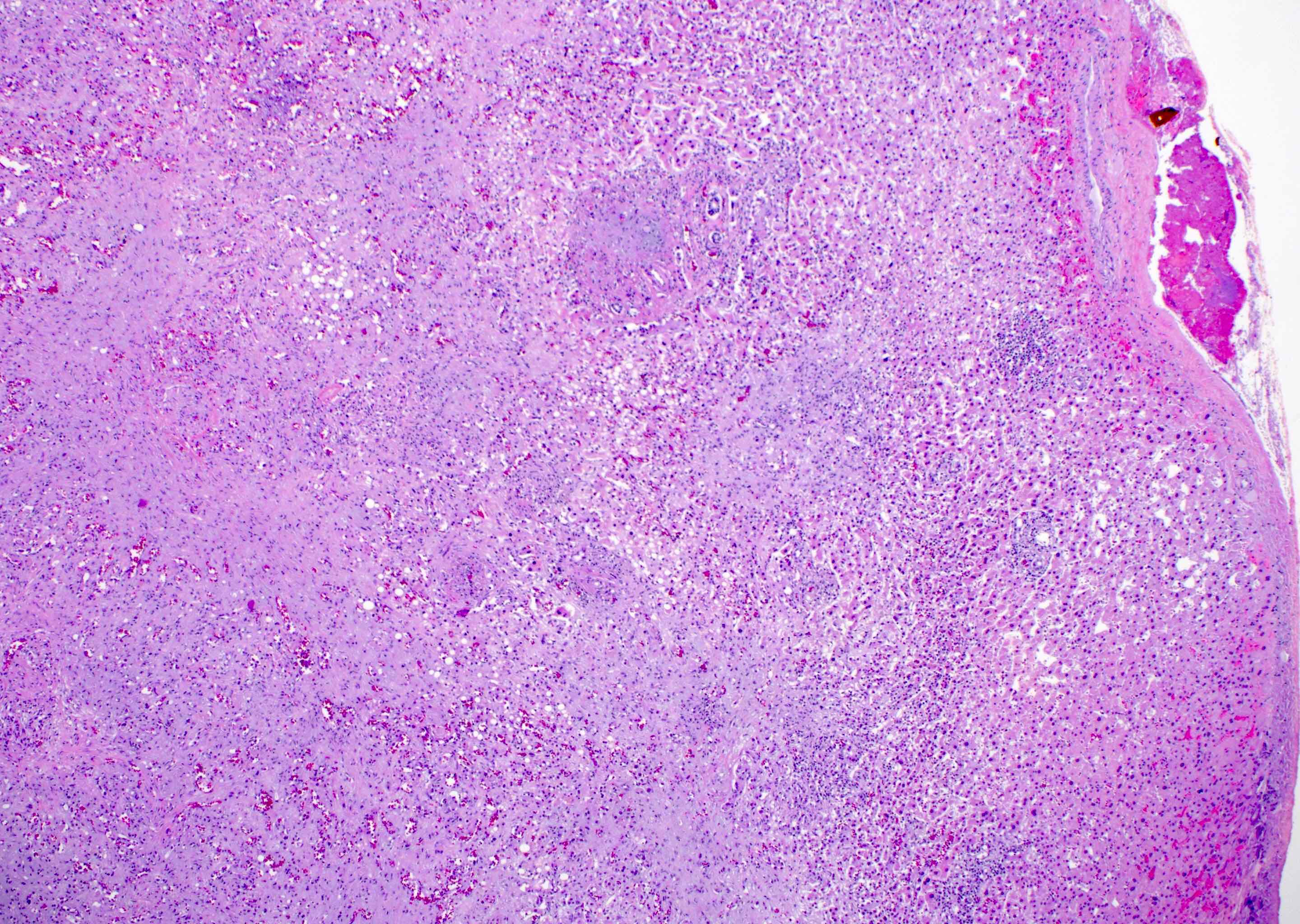
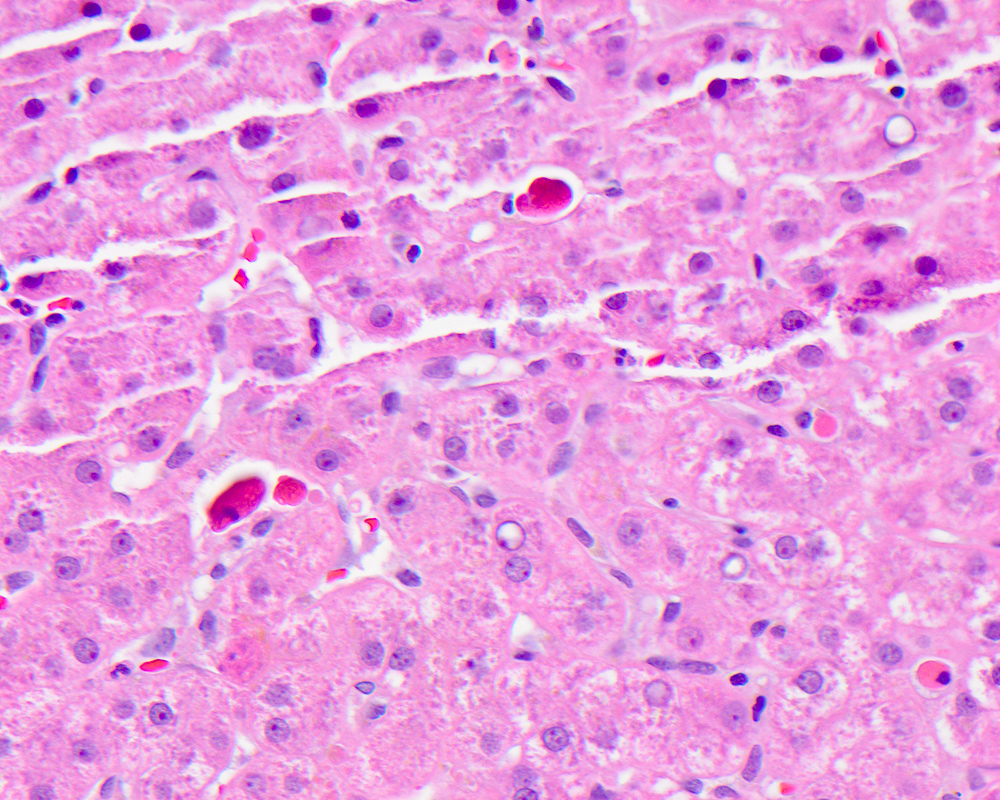
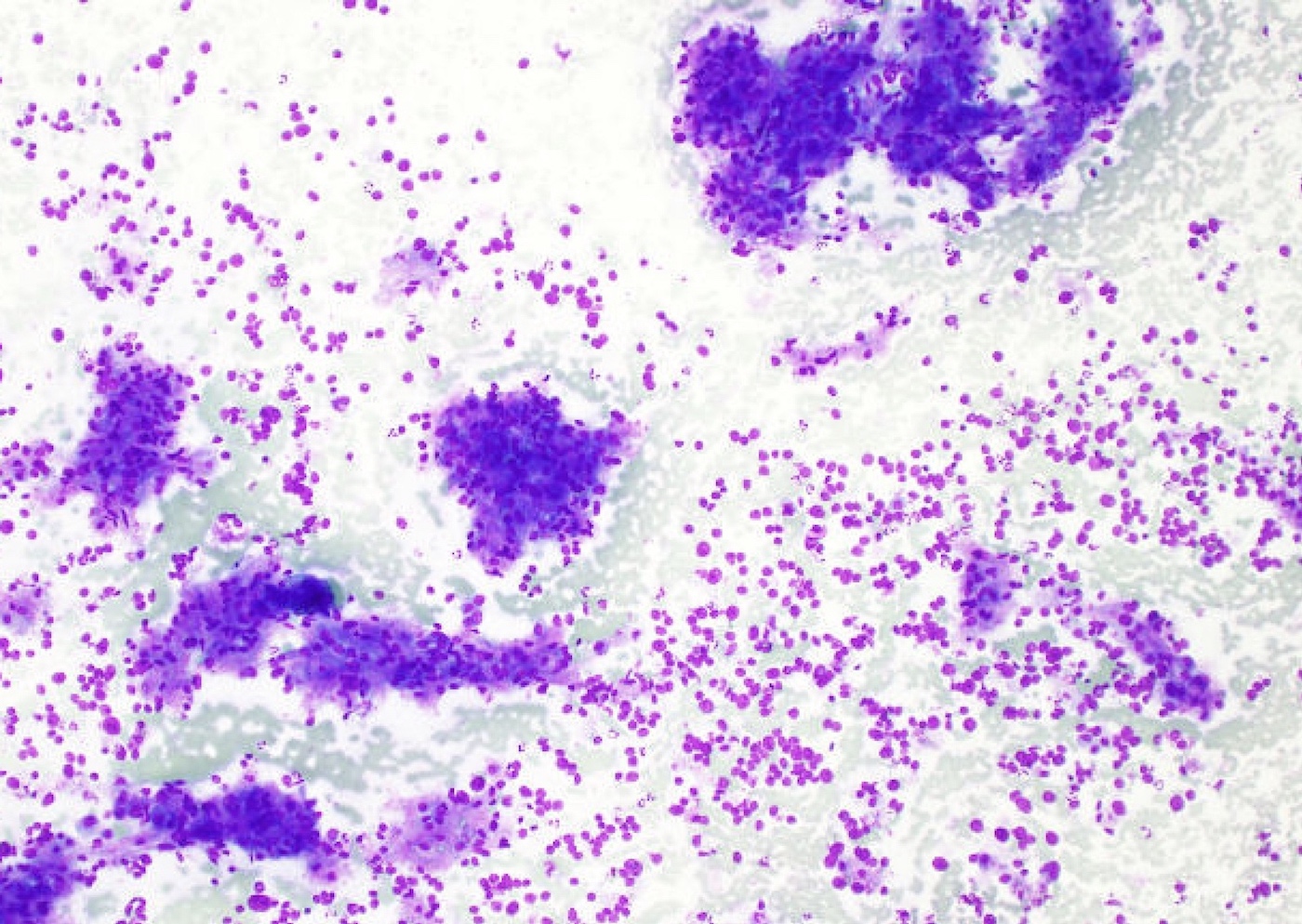
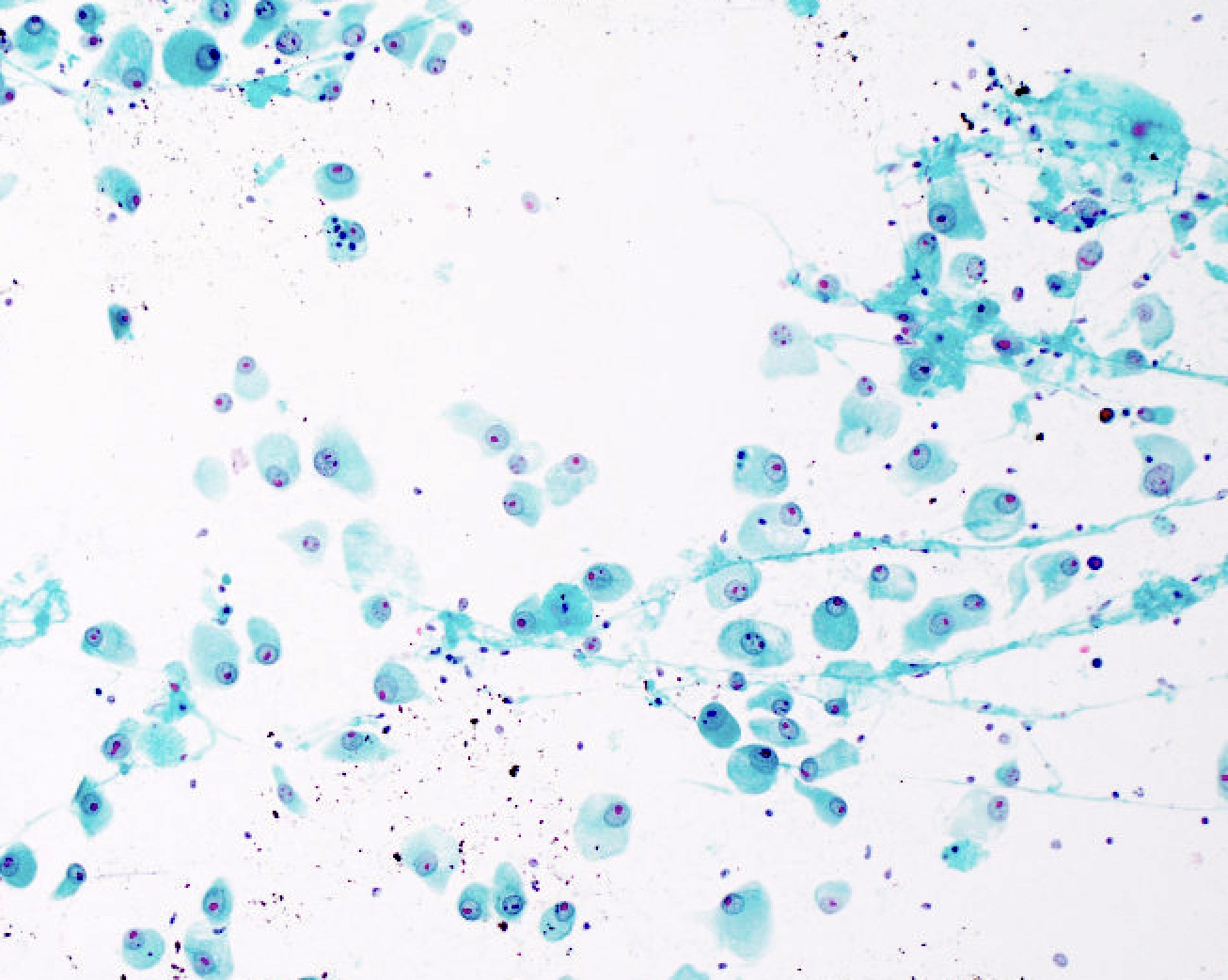
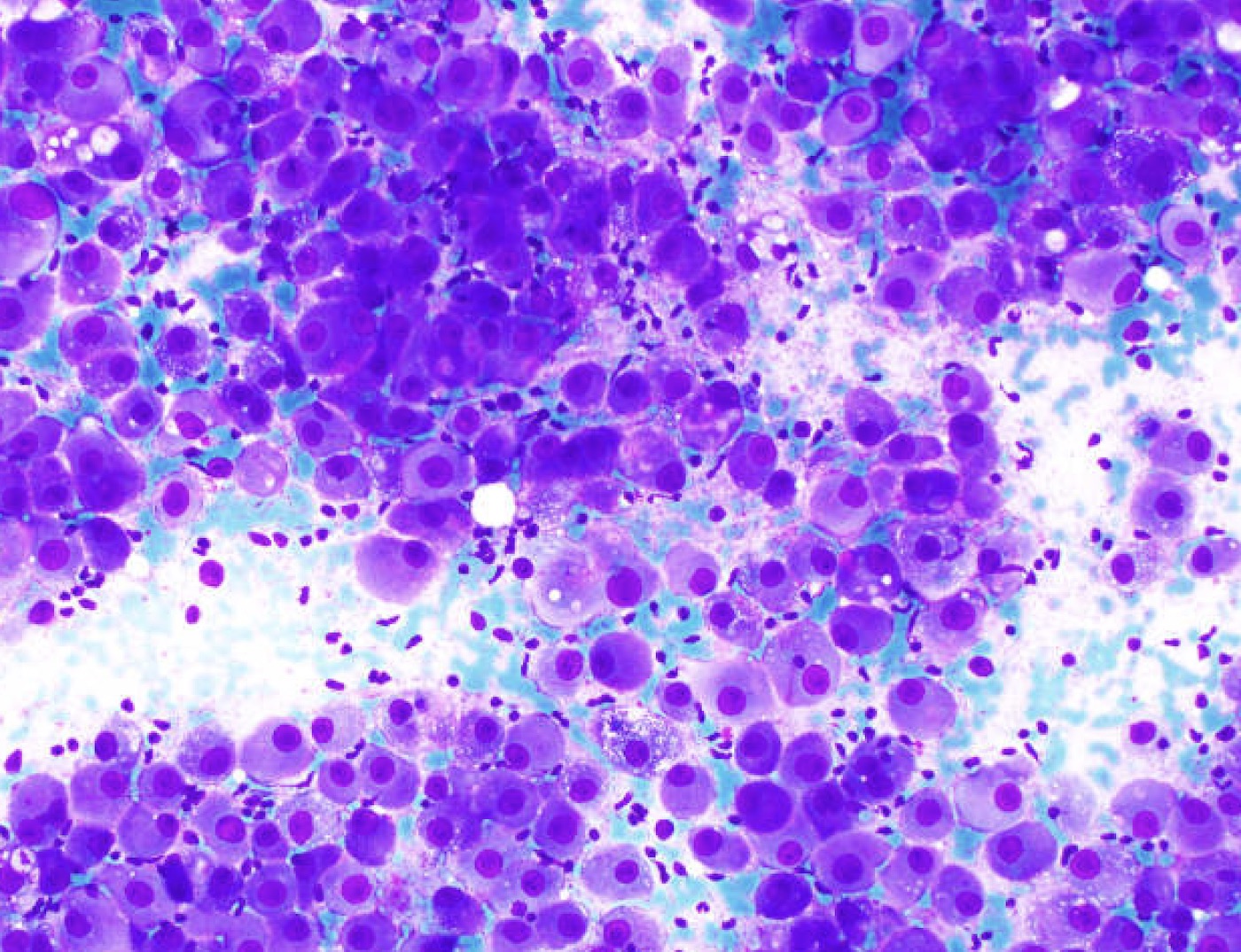
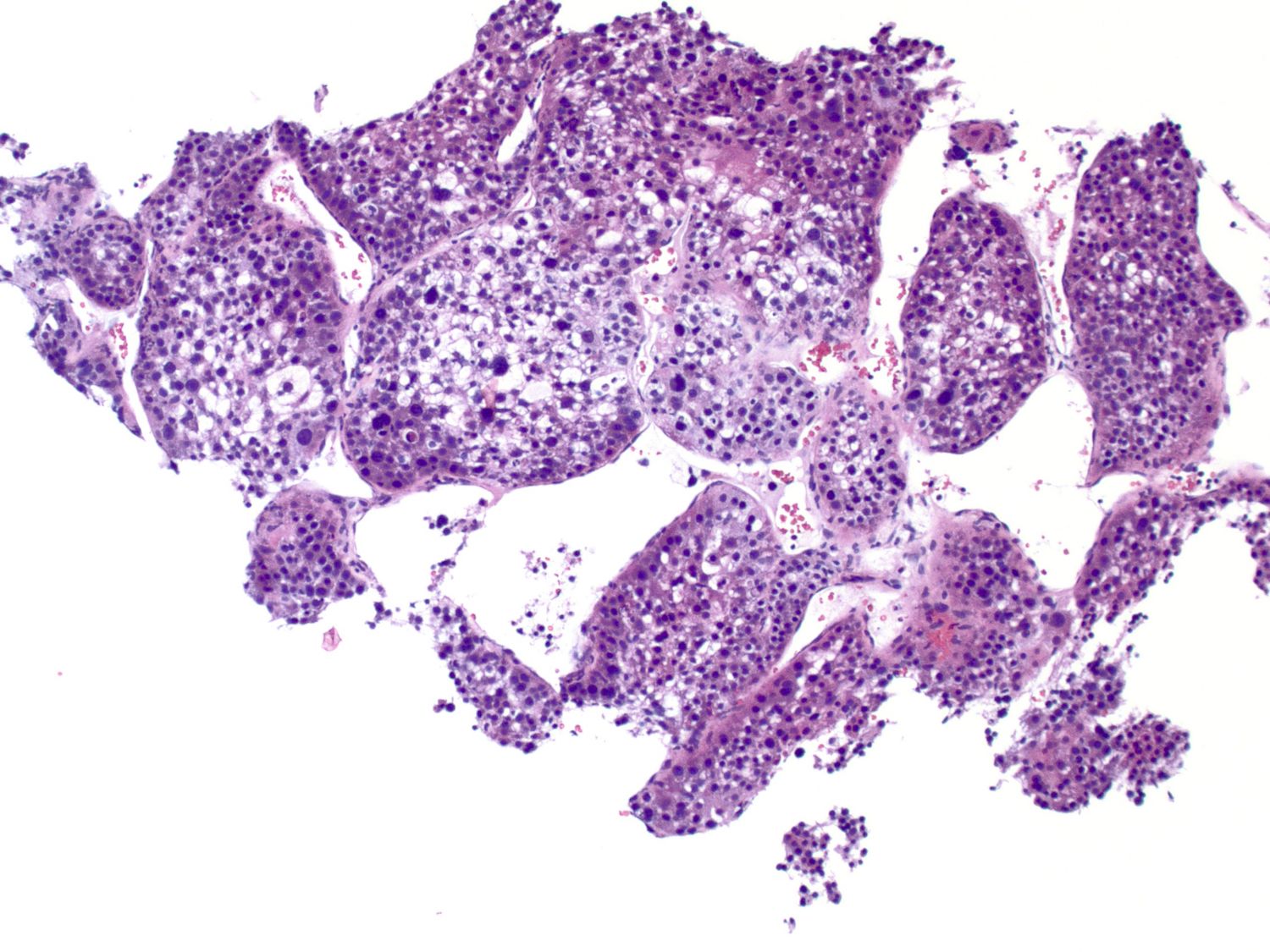
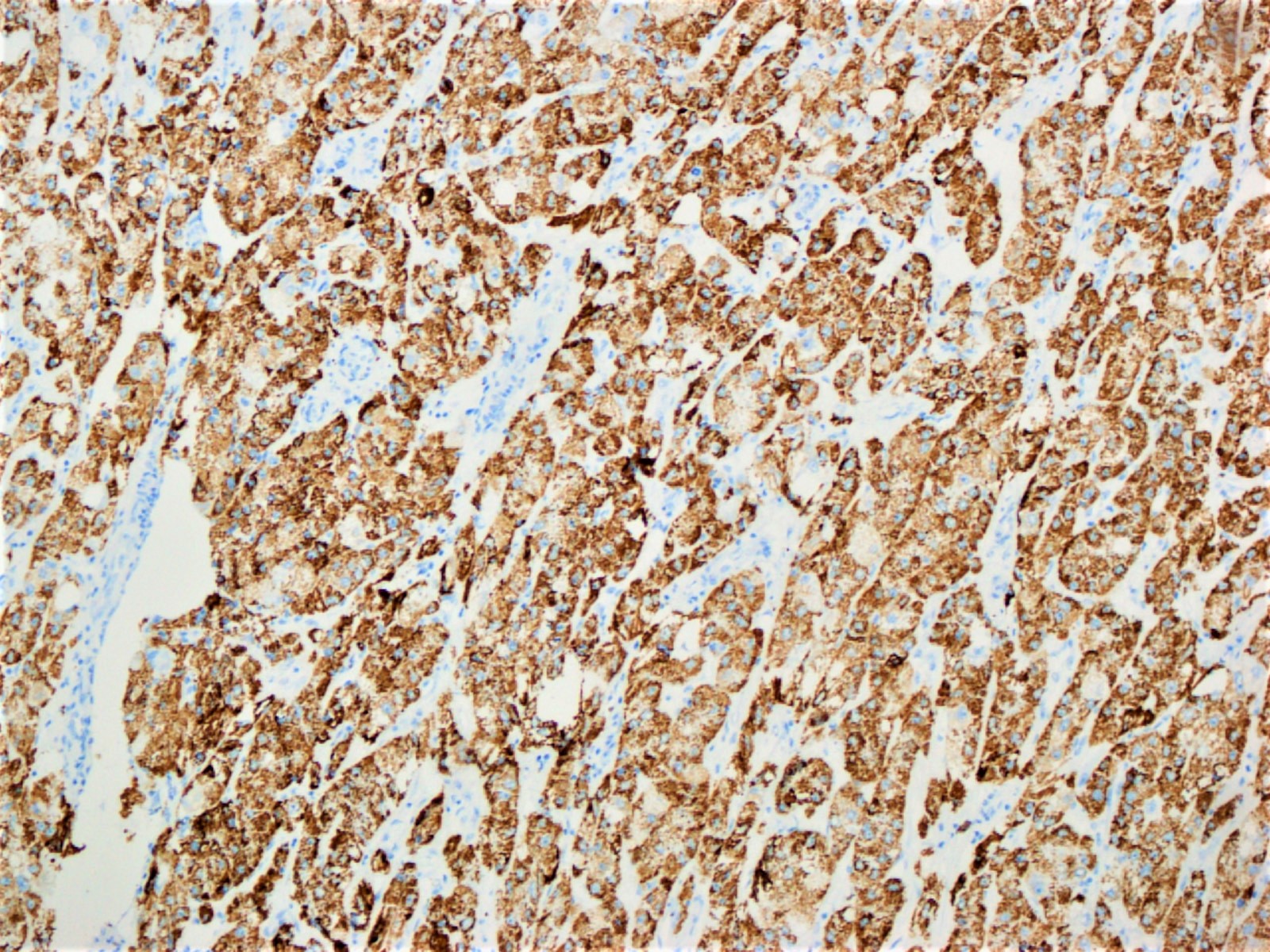
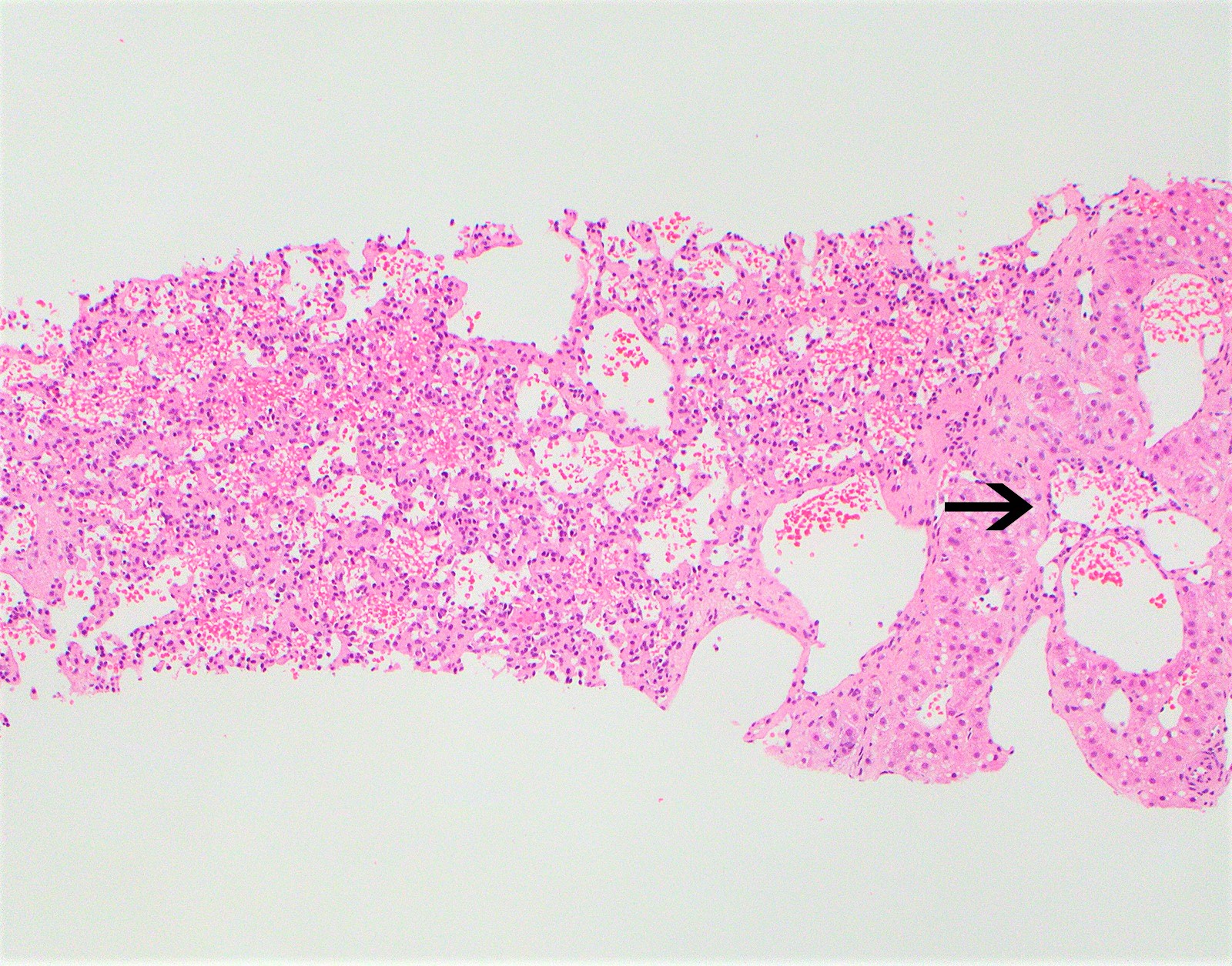
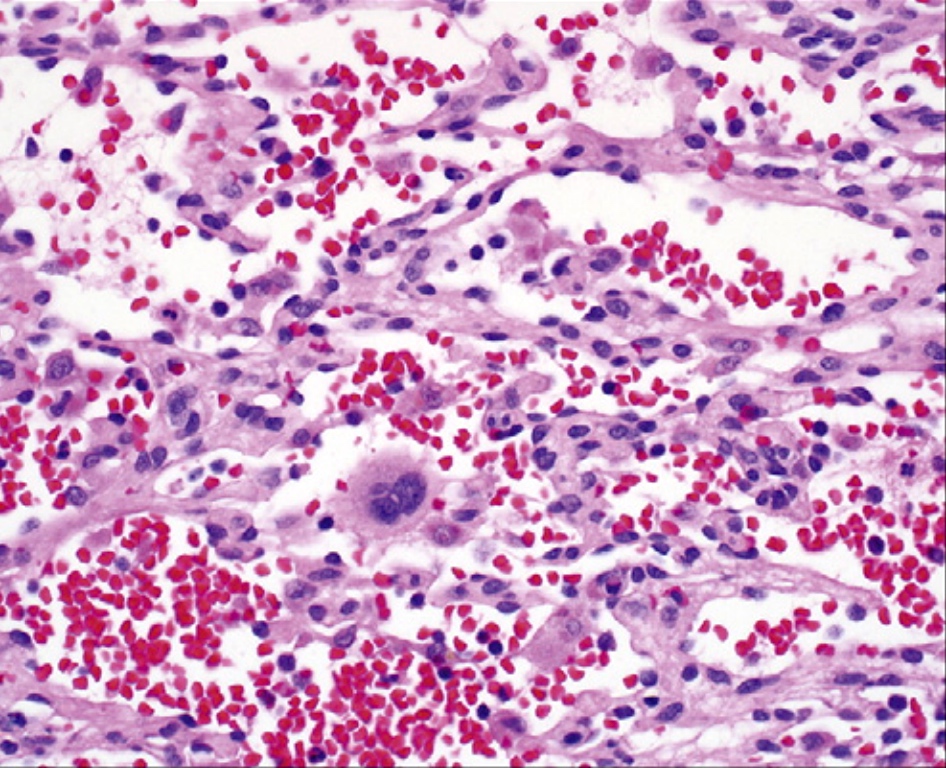
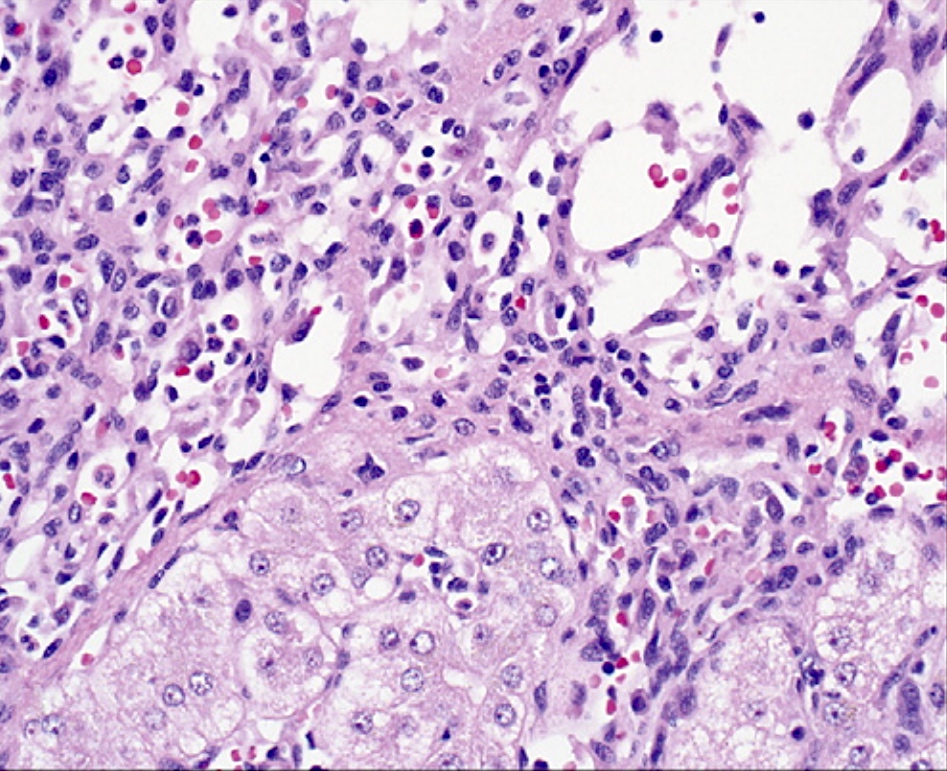
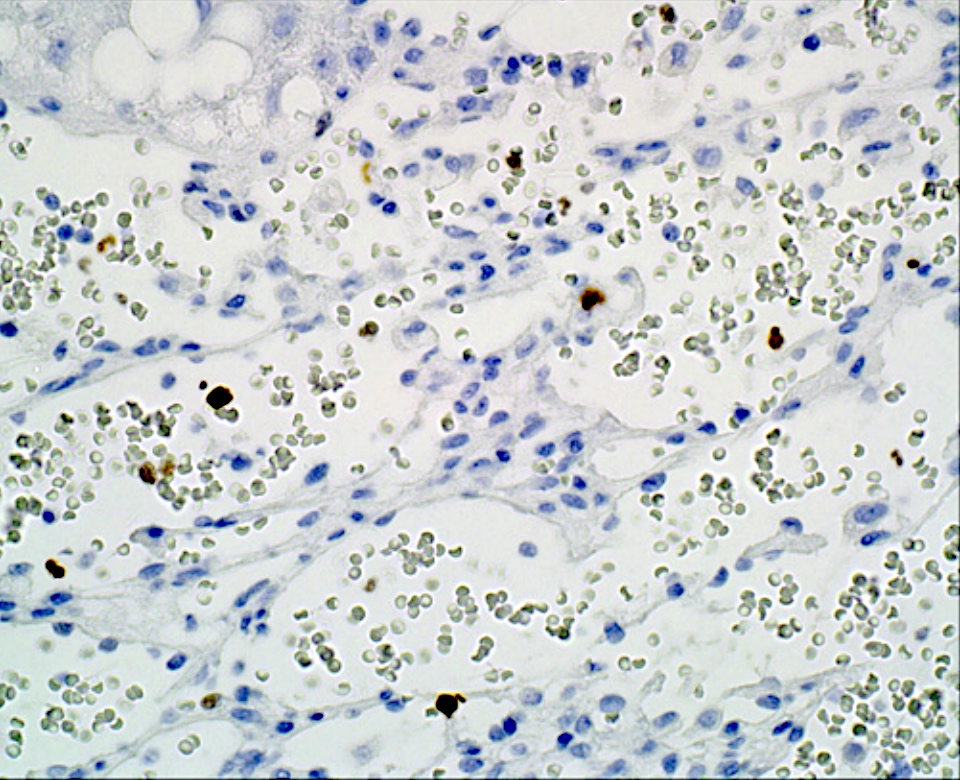
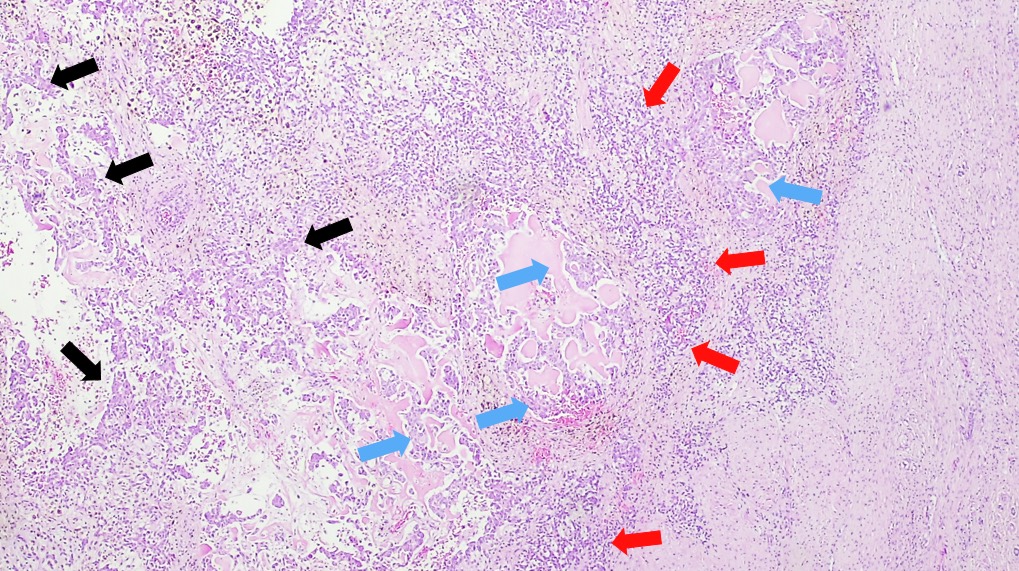
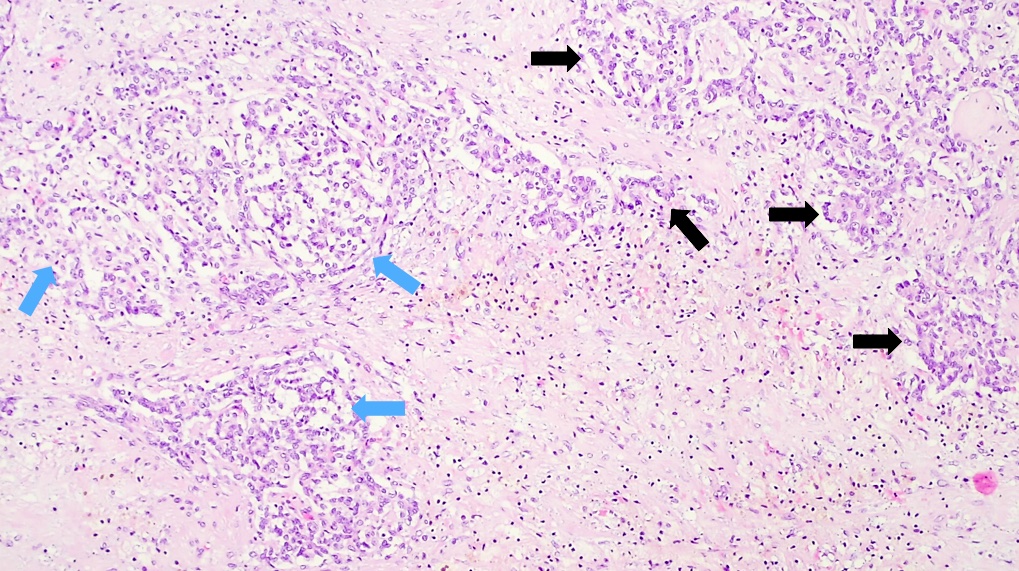
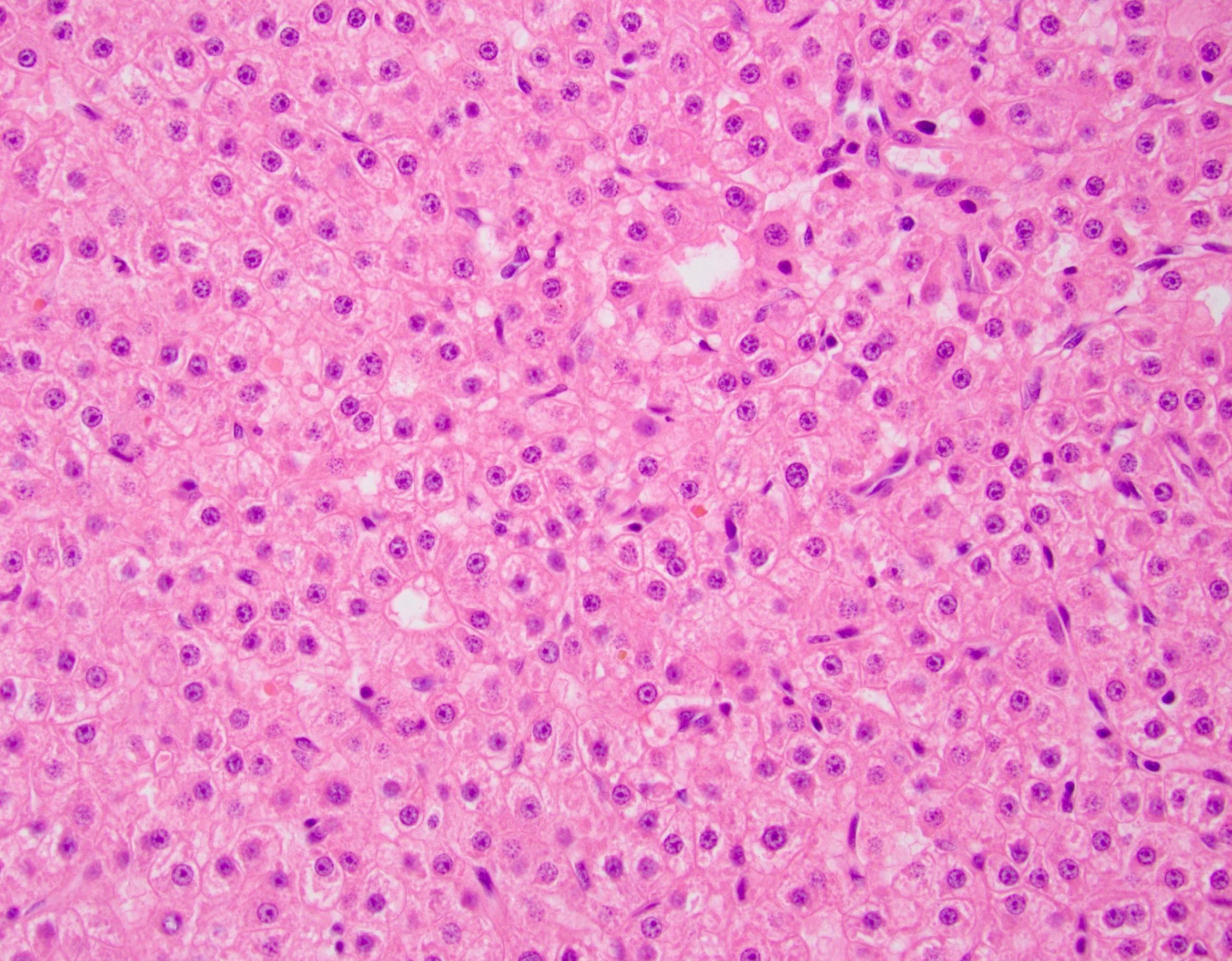
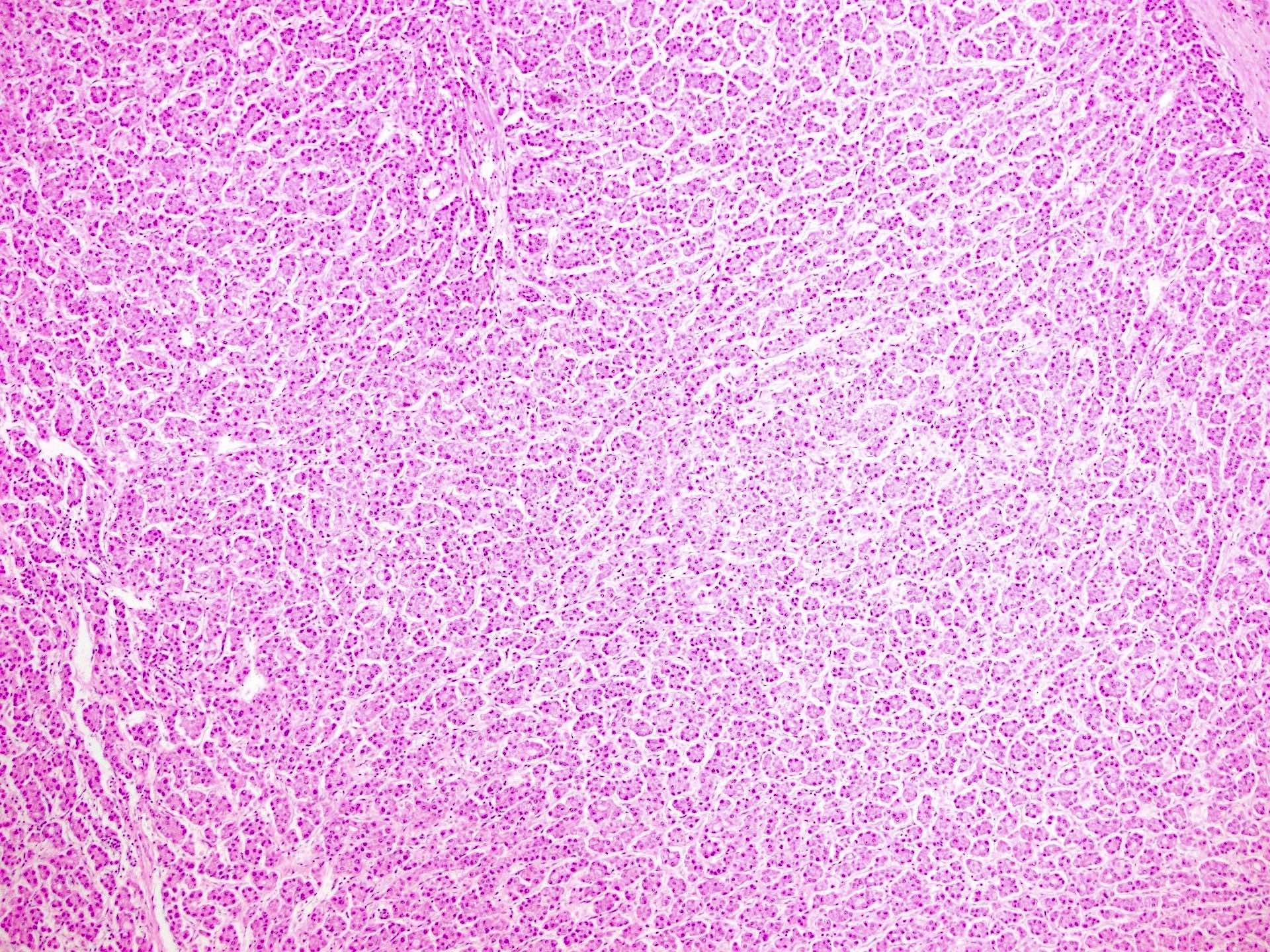
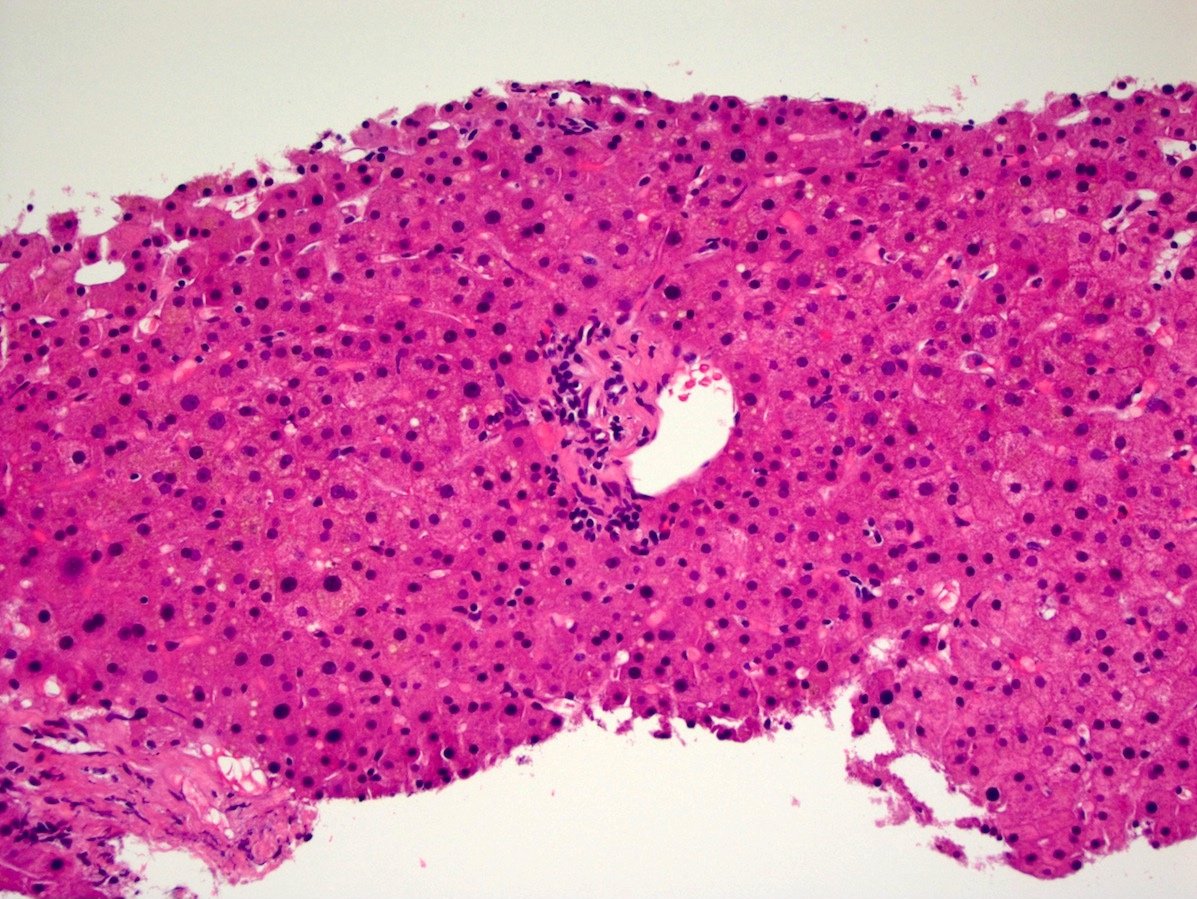
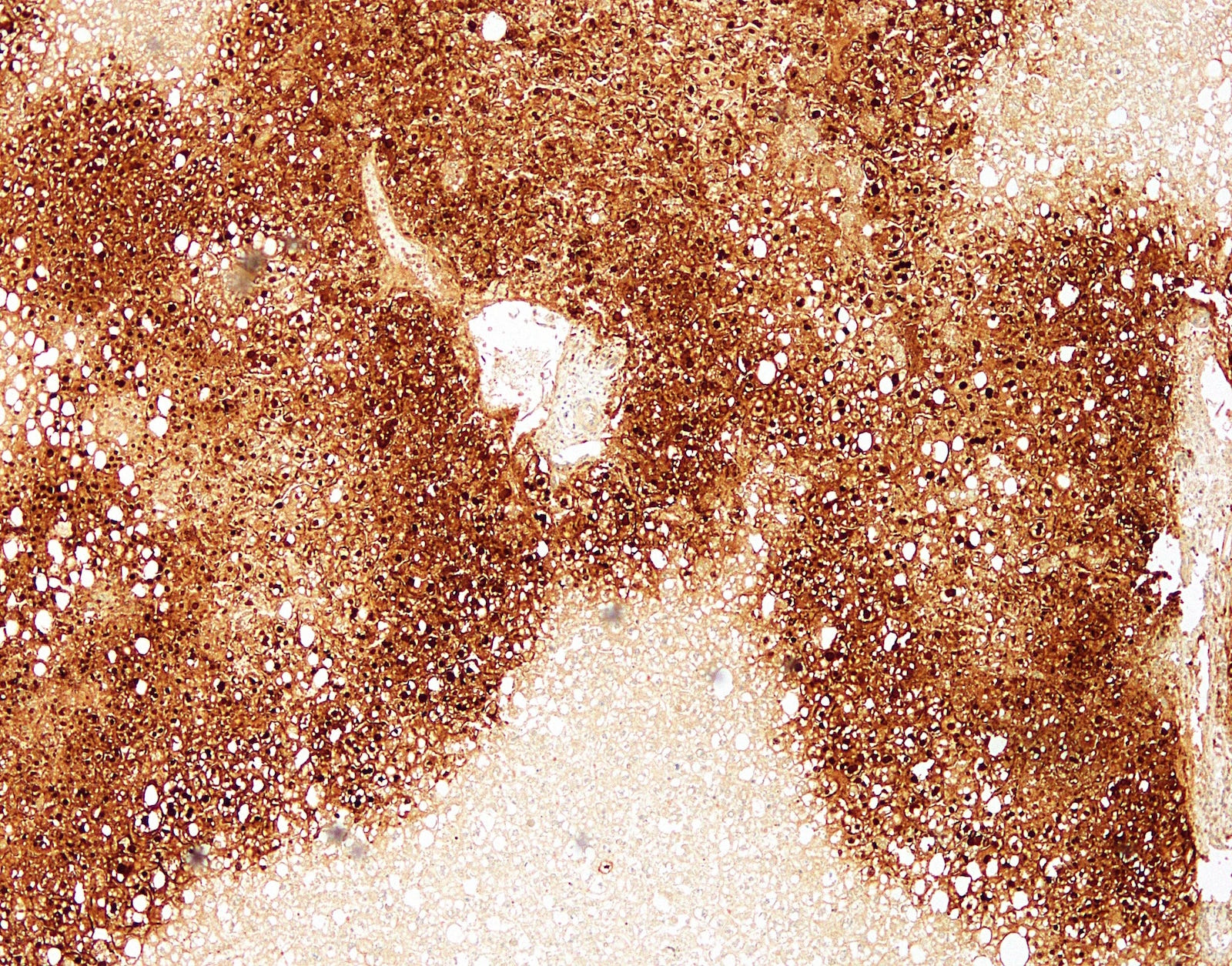
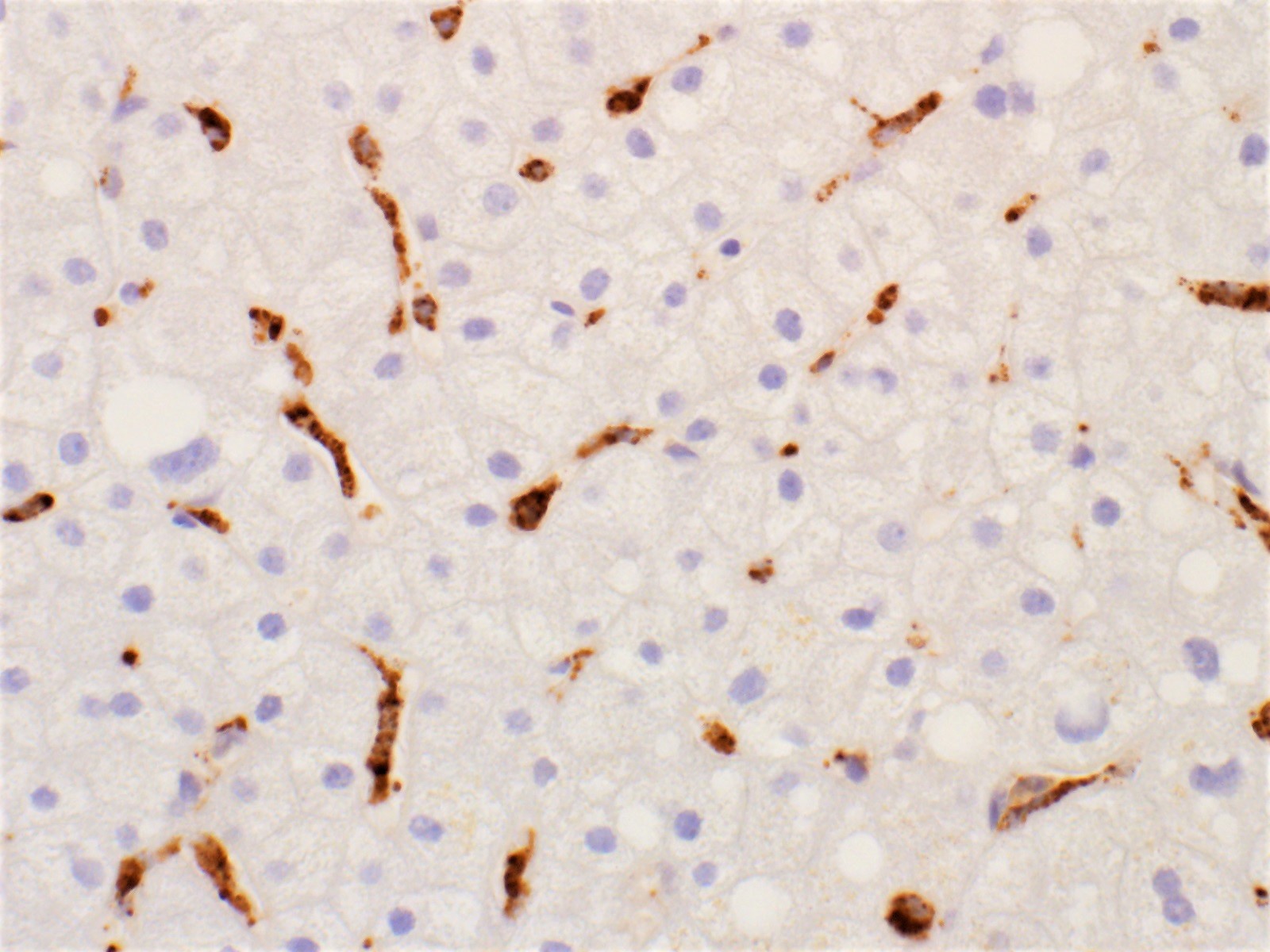
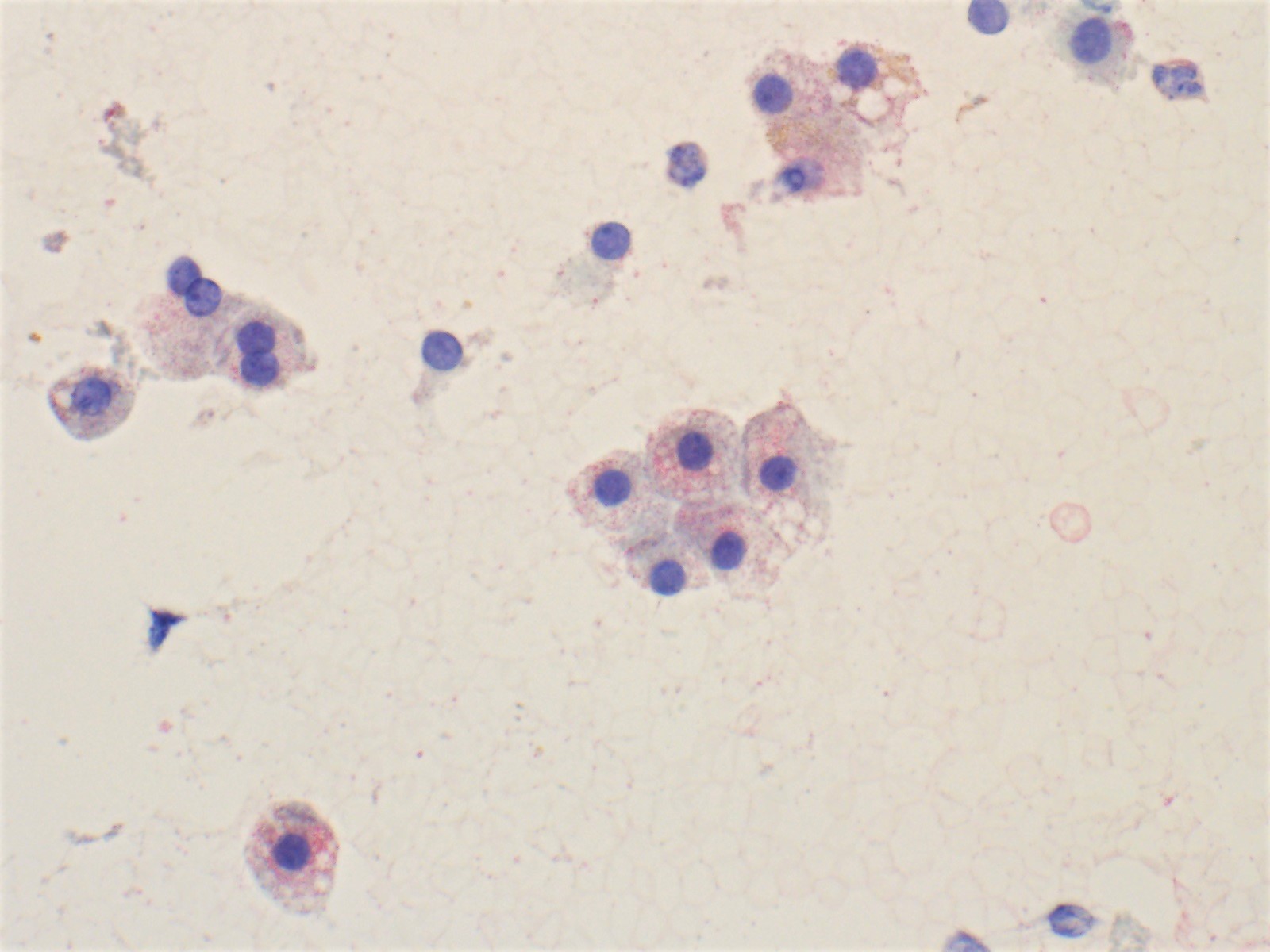
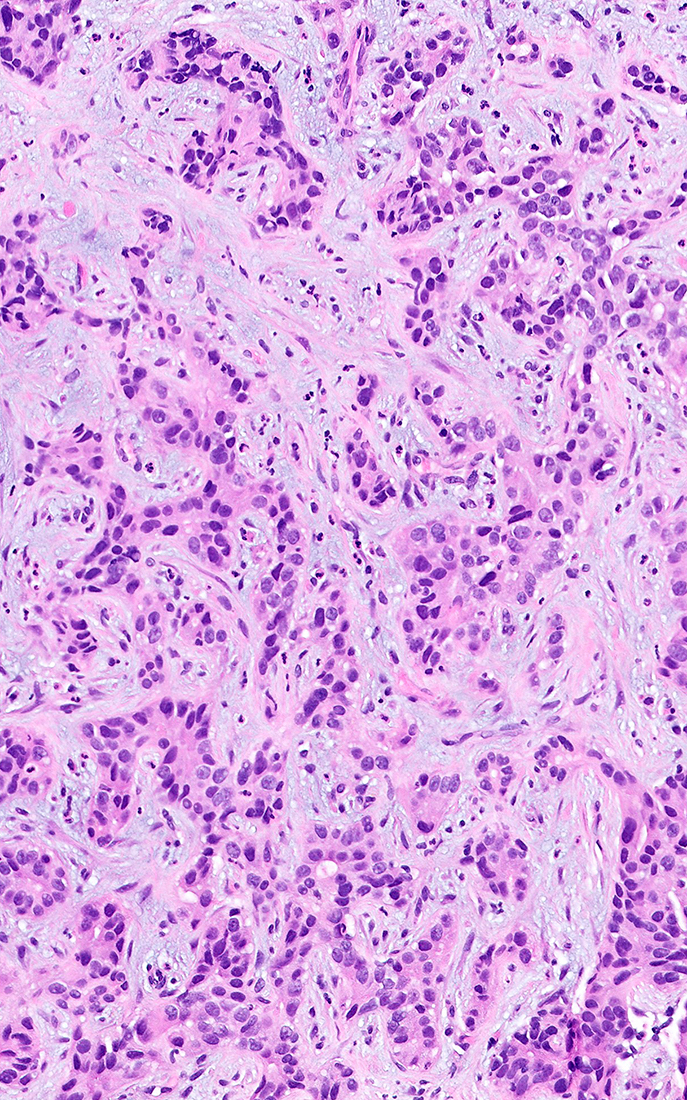
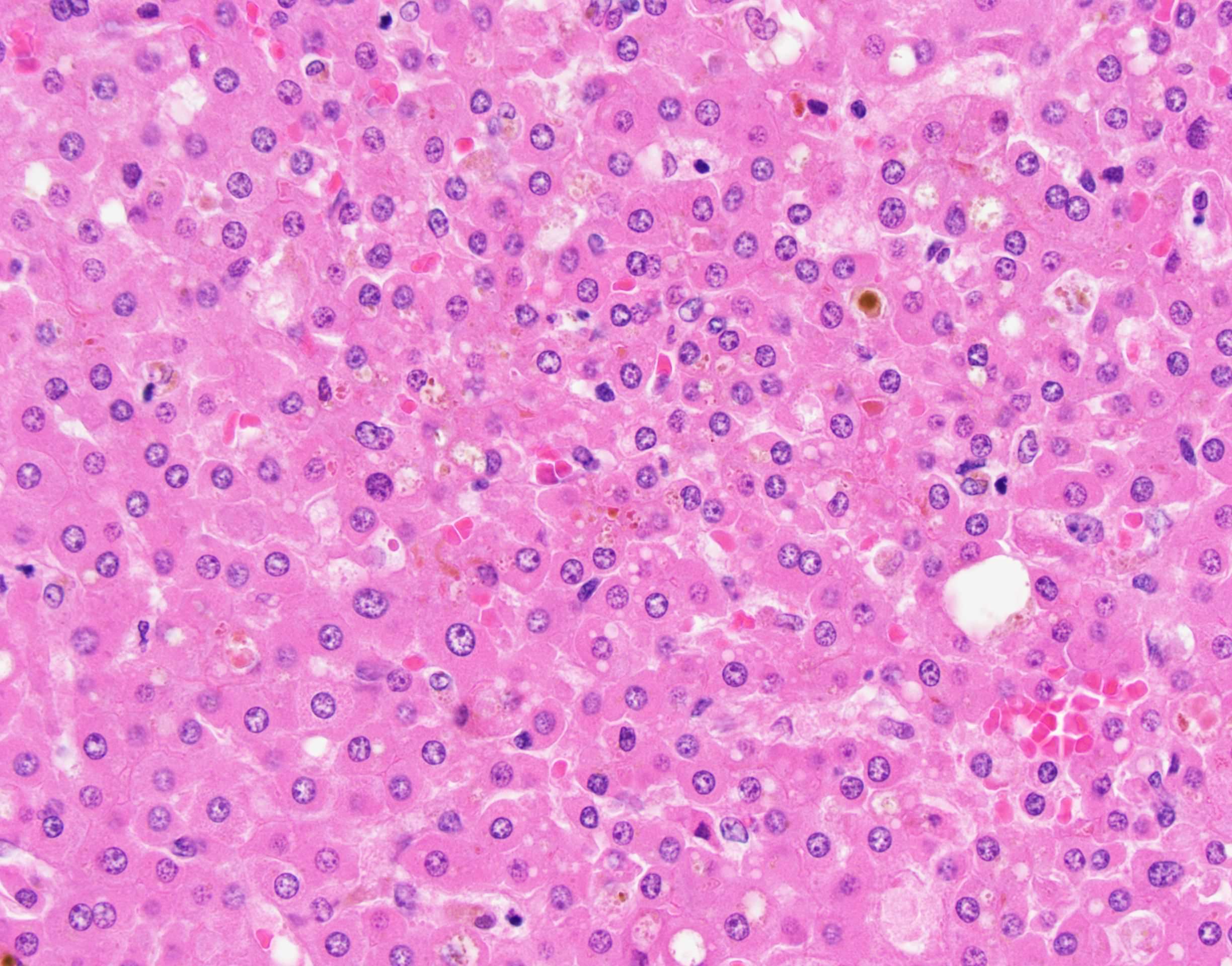
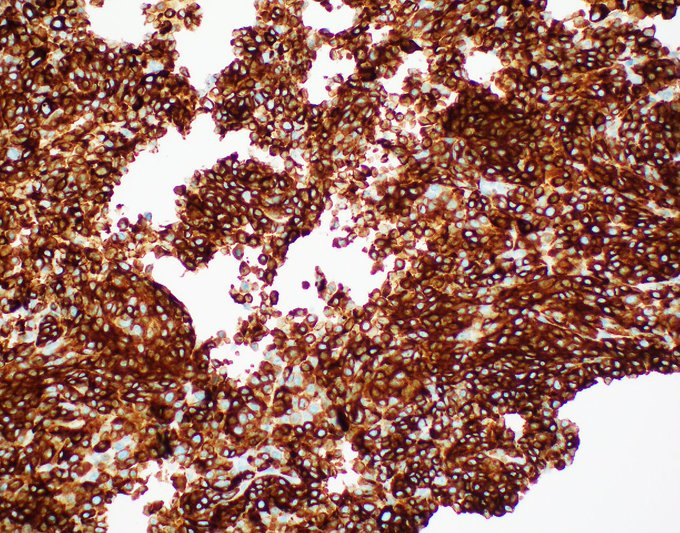
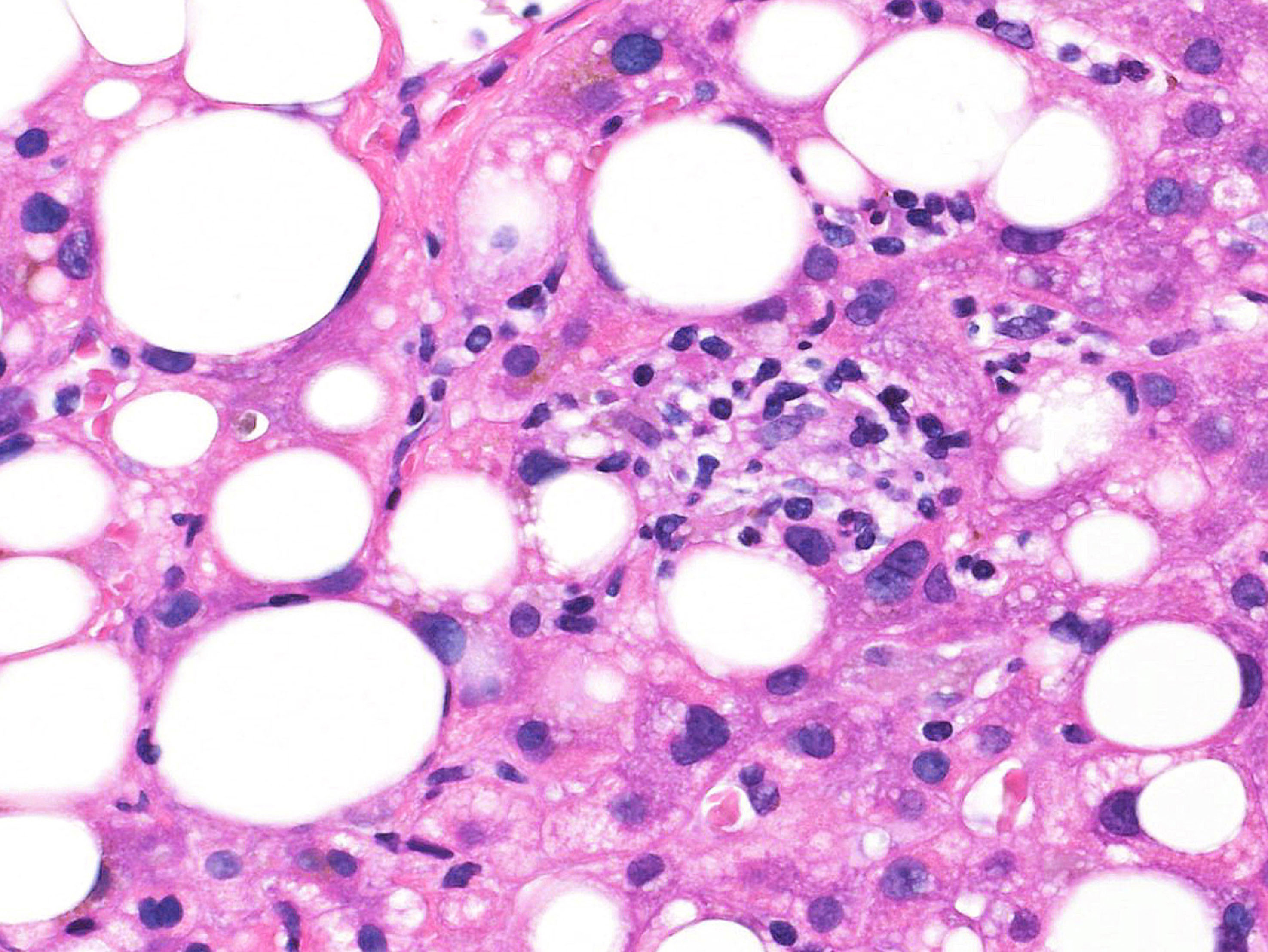
Microscopic (histologic) description
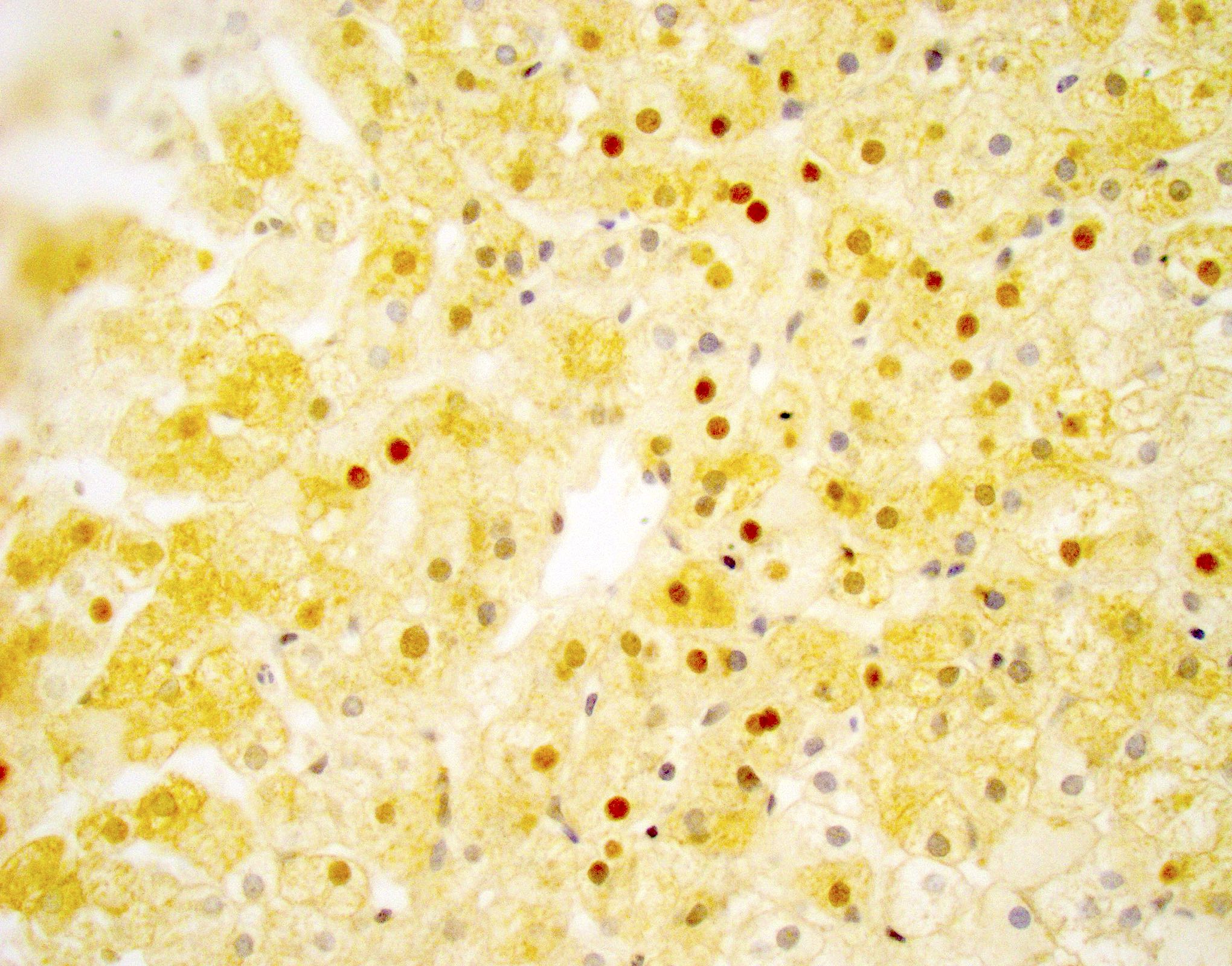
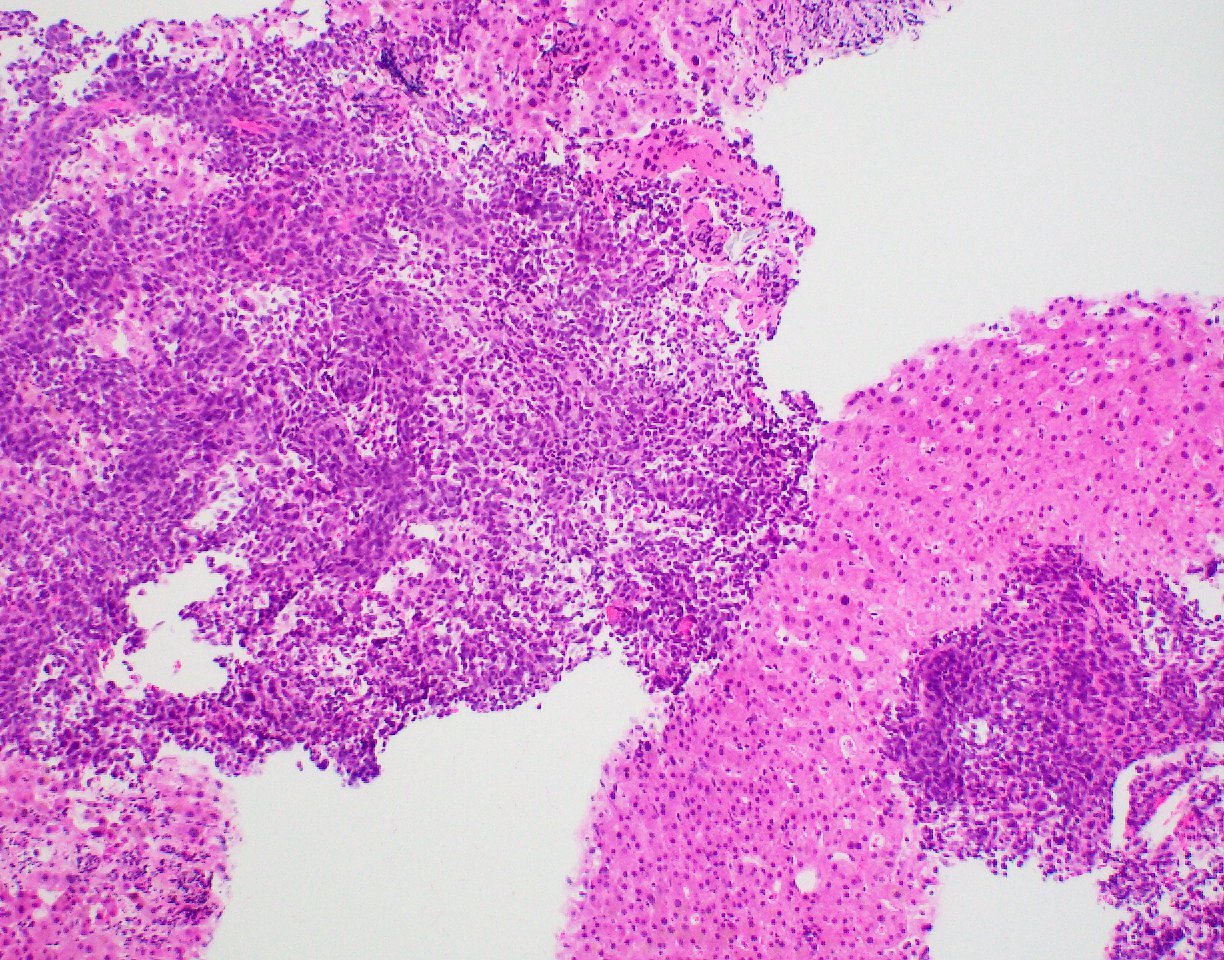
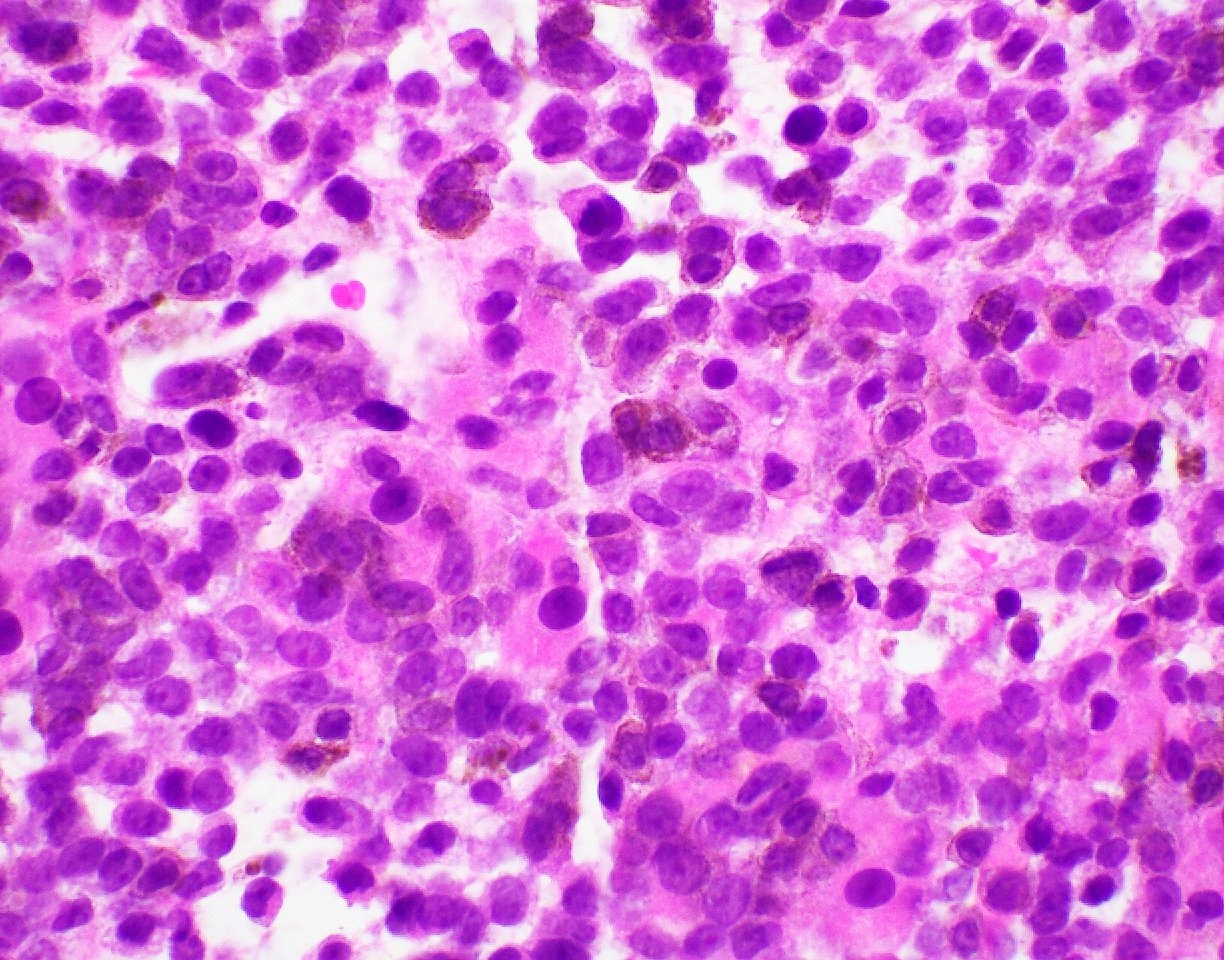
- Focal to massive coagulative necrosis in liver without particular zonal distribution (Am J Surg Pathol 2017;41:810)
- Intranuclear viral inclusions within hepatocytes with smudged or glassy appearance (Am J Surg Pathol 2017;41:810)
- Viral inclusions within the biliary epithelium (Am J Surg Pathol 2017;41:810)
- Mild or absent inflammation, portal tract granulomas may be present (Am J Surg Pathol 2017;41:810)
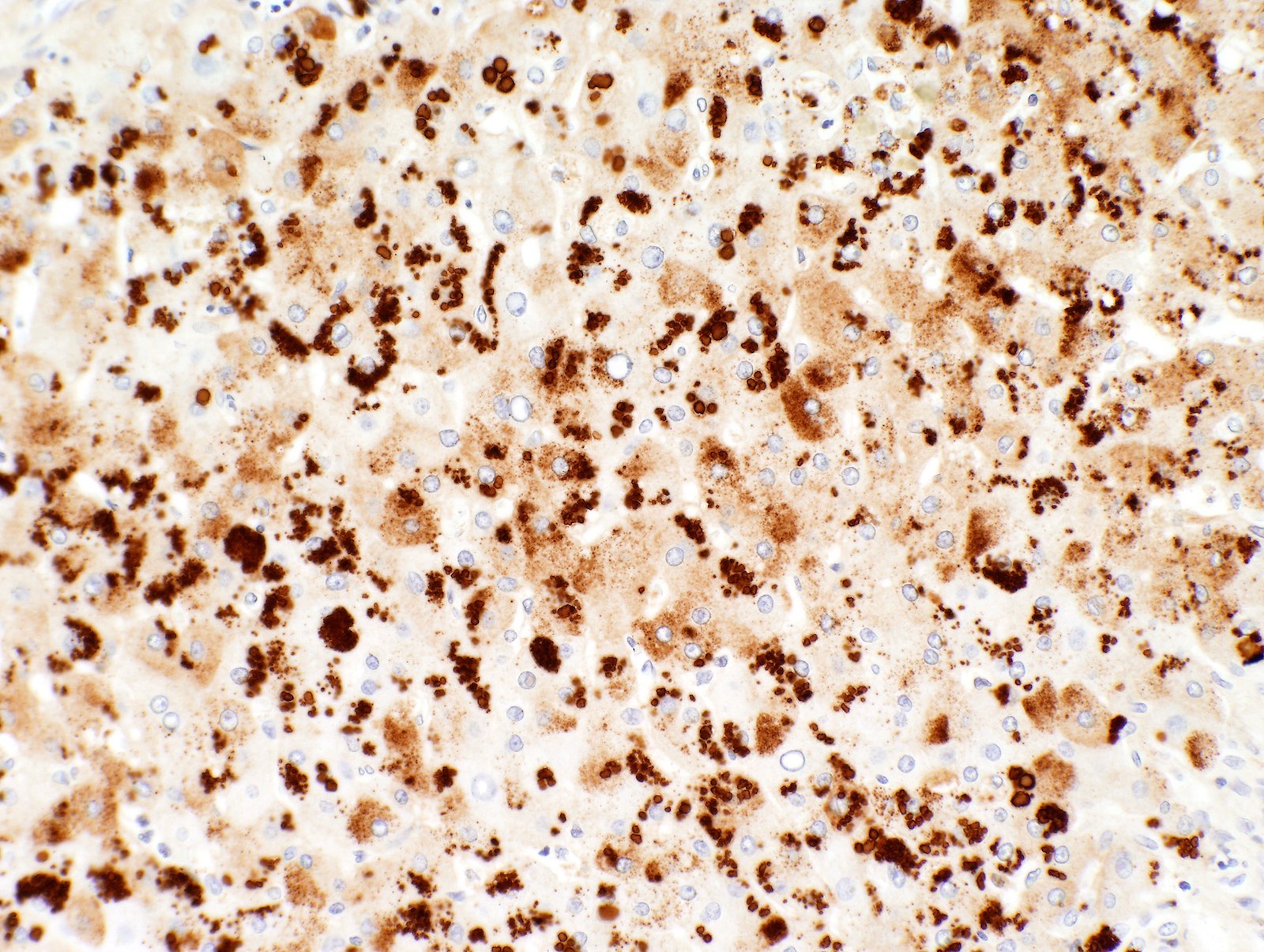
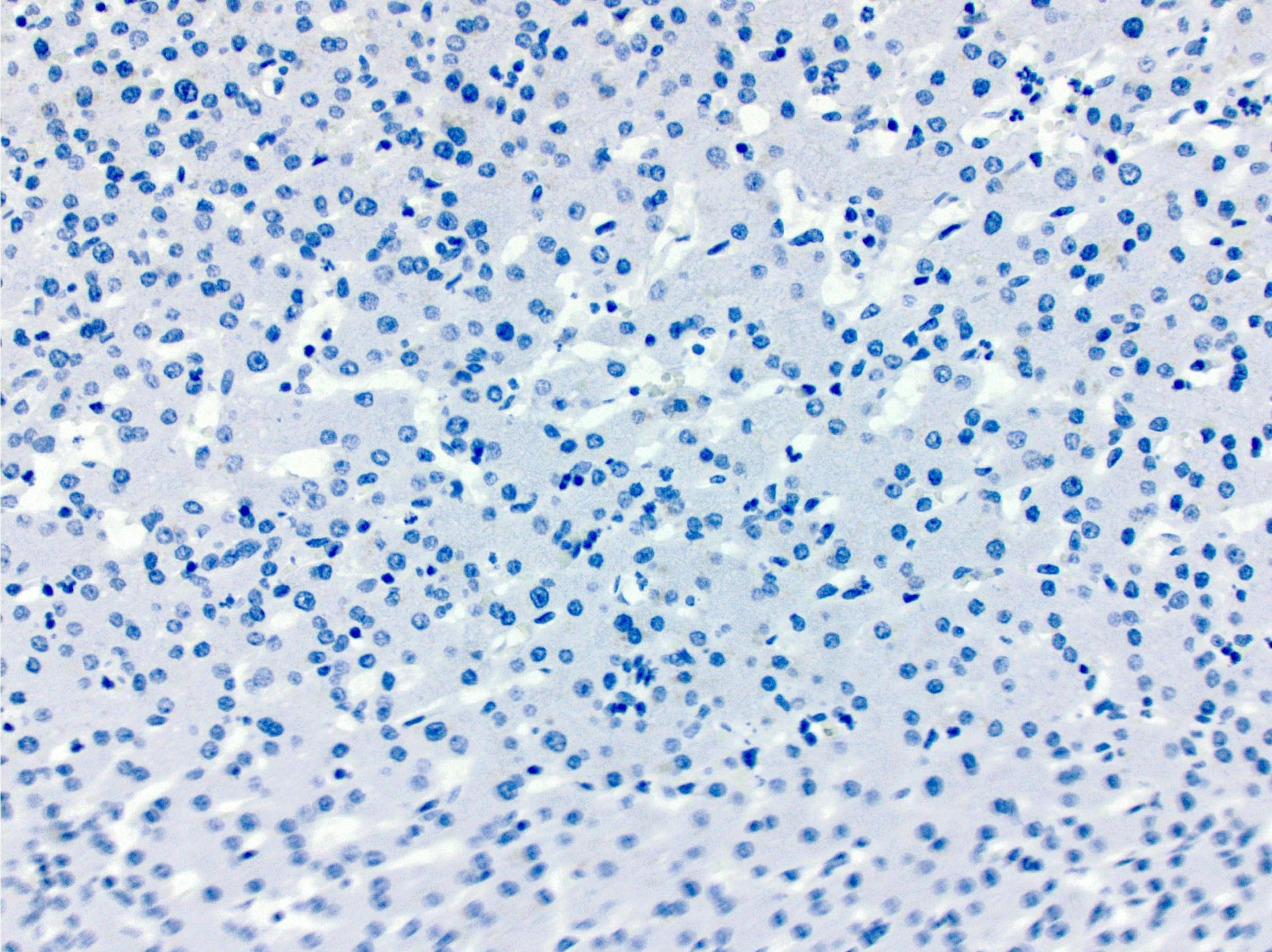
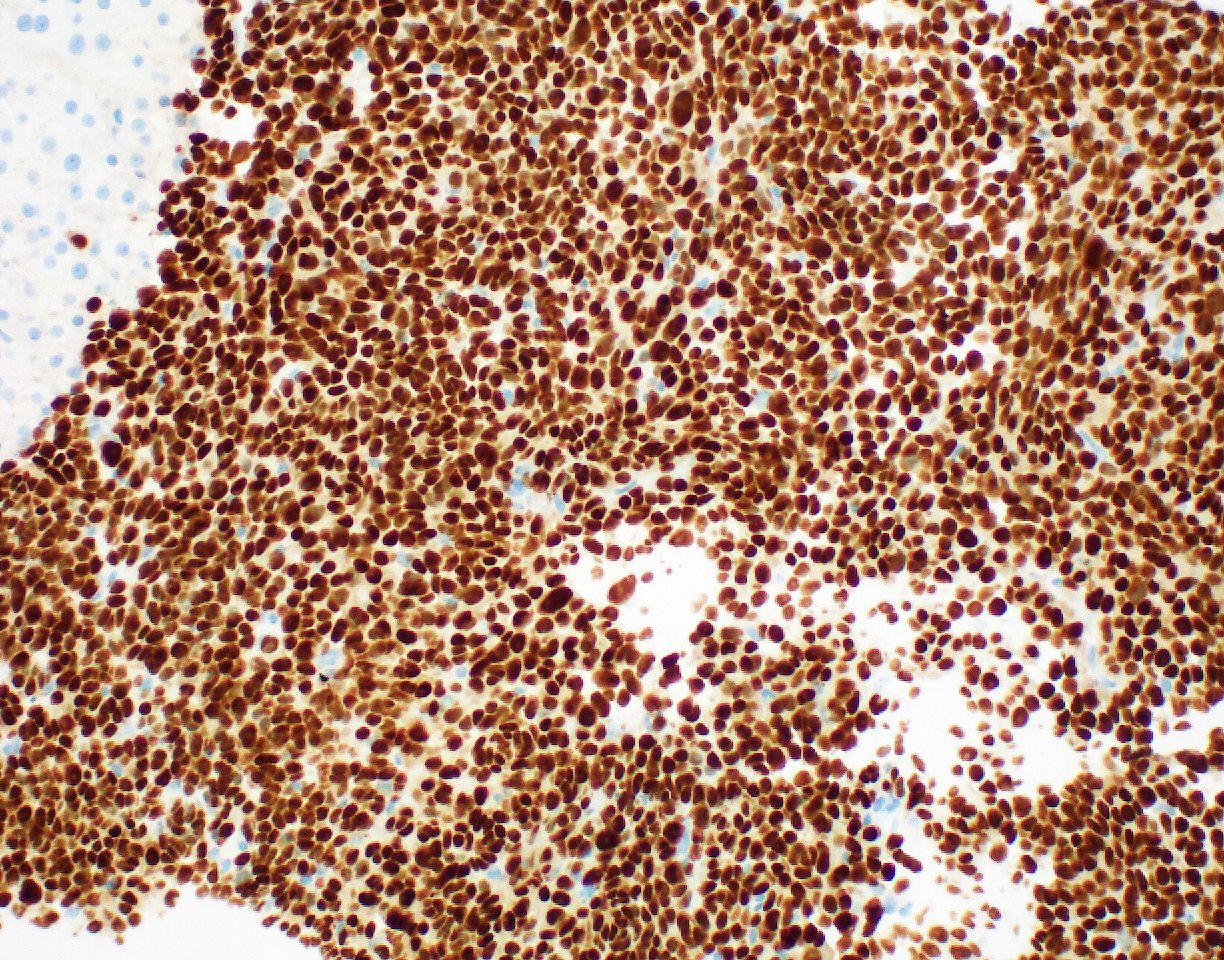
- Immunostaining for adenovirus demonstrates strong nuclear staining and is used for confirmation of the diagnosis because immunocompromised patients can have herpes simplex, cytomegalovirus and other viral infections
Microscopic (histologic) images
Positive stains
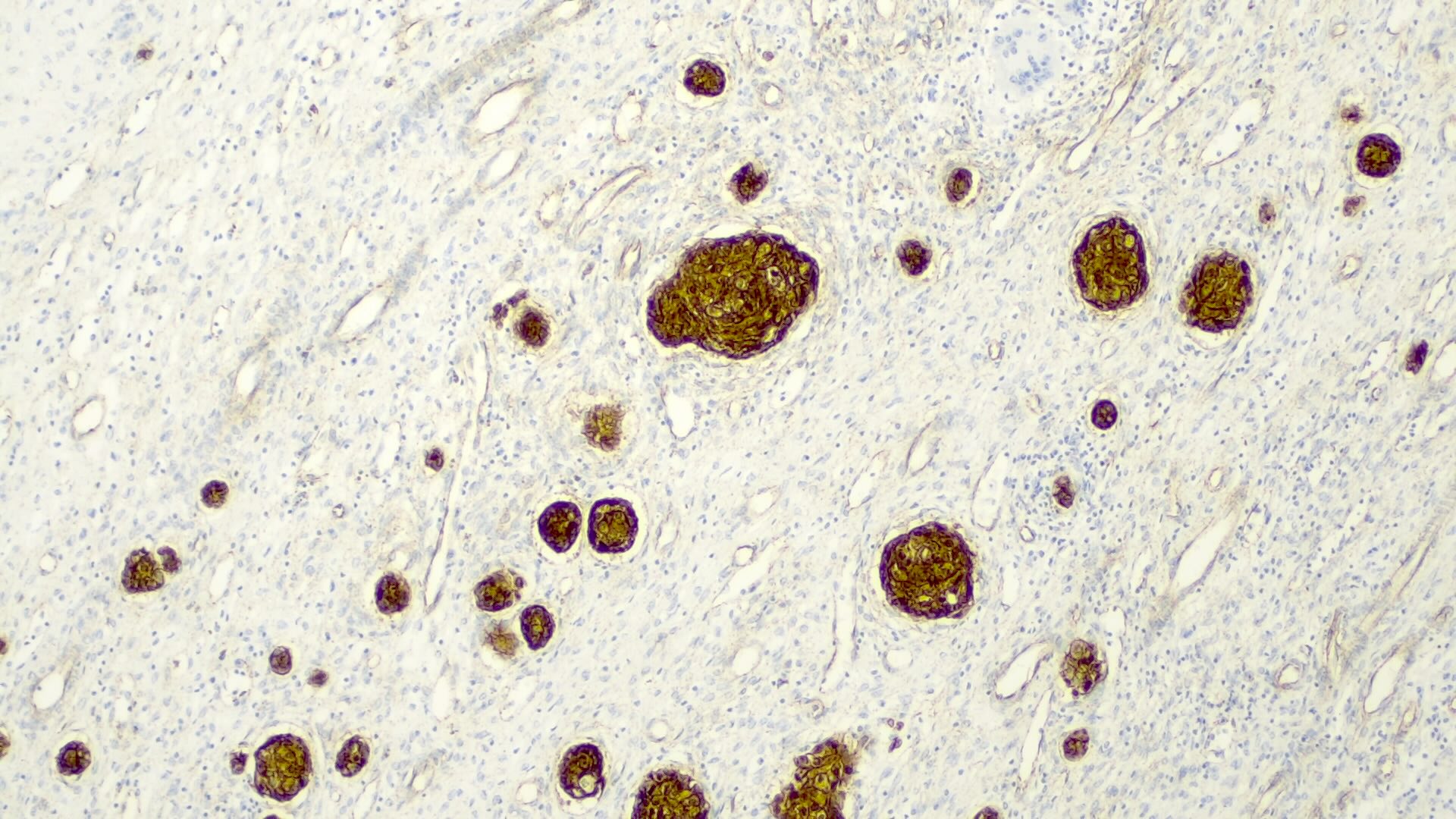
- Adenovirus immunohistochemistry (nuclear staining)
Negative stains
Sample pathology report
- Liver, biopsy:
- Hepatitic injury pattern with focal coagulative necrosis, consistent with adenovirus hepatitis (positive adenovirus immunohistochemistry); negative for portal fibrosis (see comment)
- Comment: The patient's clinical history of stem cell transplantation for acute myeloid leukemia and positive serology for adenovirus is noted.
Differential diagnosis
- Cytomegalovirus hepatitis:
- Neutrophilic microabscesses may be present
- Characteristic intranuclear / cytoplasmic inclusions for CMV
- Positive CMV immunostain, both intranuclear and cytoplasmic
- Herpes simplex virus hepatitis:
- Hemorrhagic necrosis may be present
- Multinucleation of hepatocyte nuclei
- Positive immunostain is helpful
- Varicella zoster virus hepatitis:
- Histologic features are nonspecific
- Immunostain and PCR can be helpful
- Drug induced liver injury:
- May show cholestatic injury pattern
- Lacks viral inclusions
Board review style question #1
Which of the following denotes classical morphological findings in the liver biopsy from a patient with adenovirus hepatitis?
- Hepatocytes with enlarged, smudged nuclei and intranuclear inclusion bodies
- Lymphoid aggregates in portal tracts, epithelial damage of small bile ducts
- Neutrophilic microabscess
- Presence of multinucleated giant cells
- Prominent mononuclear infiltrate within portal tracts and sinusoids
Board review style answer #1
A. Hepatocytes with enlarged, smudged nuclei and intranuclear inclusion bodies
Comment Here
Reference: Adenovirus hepatitis
Comment Here
Reference: Adenovirus hepatitis
Board review style question #2
What immunohistostaining pattern is typical for liver cells in adenovirus hepatitis?
- Cytoplasmic inclusions staining
- Diffuse staining of cytoplasm
- Partial or complete membrane staining
- Strong nuclear staining
Board review style answer #2
Alagille syndrome
Table of Contents
Definition / general | Essential features | Pathophysiology | Clinical features | Microscopic (histologic) description | Microscopic (histologic) imagesDefinition / general
- Also called arteriohepatic dysplasia
- Represents the etiology behind syndromic paucity of bile ducts
Essential features
- Genetic disorder with vascular, biliary and other anomalies
- Absence of intrahepatic bile ducts with clinical severity ranging from severe neonatal cholestasis mimicking biliary atresia to childhood intermittent jaundice
- Progression to cirrhosis is rare
Pathophysiology
- 2 distinct genetic mechanisms:
- Vast majority (ALGS1) are autosomal dominant, due to mutations in Jagged1 gene on chromosome 20p12, which encodes a ligand for NOTCH1 and plays a role in epithelial mesenchymal interactions (Nat Genet 1997;16:235)
- Gene penetrance is high but expression is variable; 50 - 70% patients have new mutations
- Second genetic abnormality (ALGS2) accounting for small proportion of cases, is related to the mutations in the gene encoding NOTCH2 on chromosome 1p13 and has more severe renal disease (Am J Hum Genet 2006;79:169)
- Vast majority (ALGS1) are autosomal dominant, due to mutations in Jagged1 gene on chromosome 20p12, which encodes a ligand for NOTCH1 and plays a role in epithelial mesenchymal interactions (Nat Genet 1997;16:235)
Clinical features
- Reported incidence is 1:30,000 of live births
- Common clinical features: abnormal inverted triangular facies, posterior embryotoxon in the eye (Digital Reference of Ophthalmology: Cornea & External Diseases [Accessed 25 October 2017]), pulmonary stenosis or more severe congenital heart disease, butterfly vertebrae or other vertebral arch anomalies, other skeletal anomalies such as short distal phalanges or clinodactyly
- Several renal abnormalities such as tubulointerstitial nephropathy, membranous nephropathy, mesangiolipidosis, renovascular hypertension, etc. have been reported
- Liver findings are characterized by progressive loss of bile ducts with or without hypoplasia of extrahepatic bile ducts, hypoplasia of gallbladder and cholelithiasis, leading to jaundice and pruritus (Nat Genet 1997;16:235, Nat Genet 1997;16:235)
- It can mimic other causes of high GGT cholestasis, particularly biliary atresia
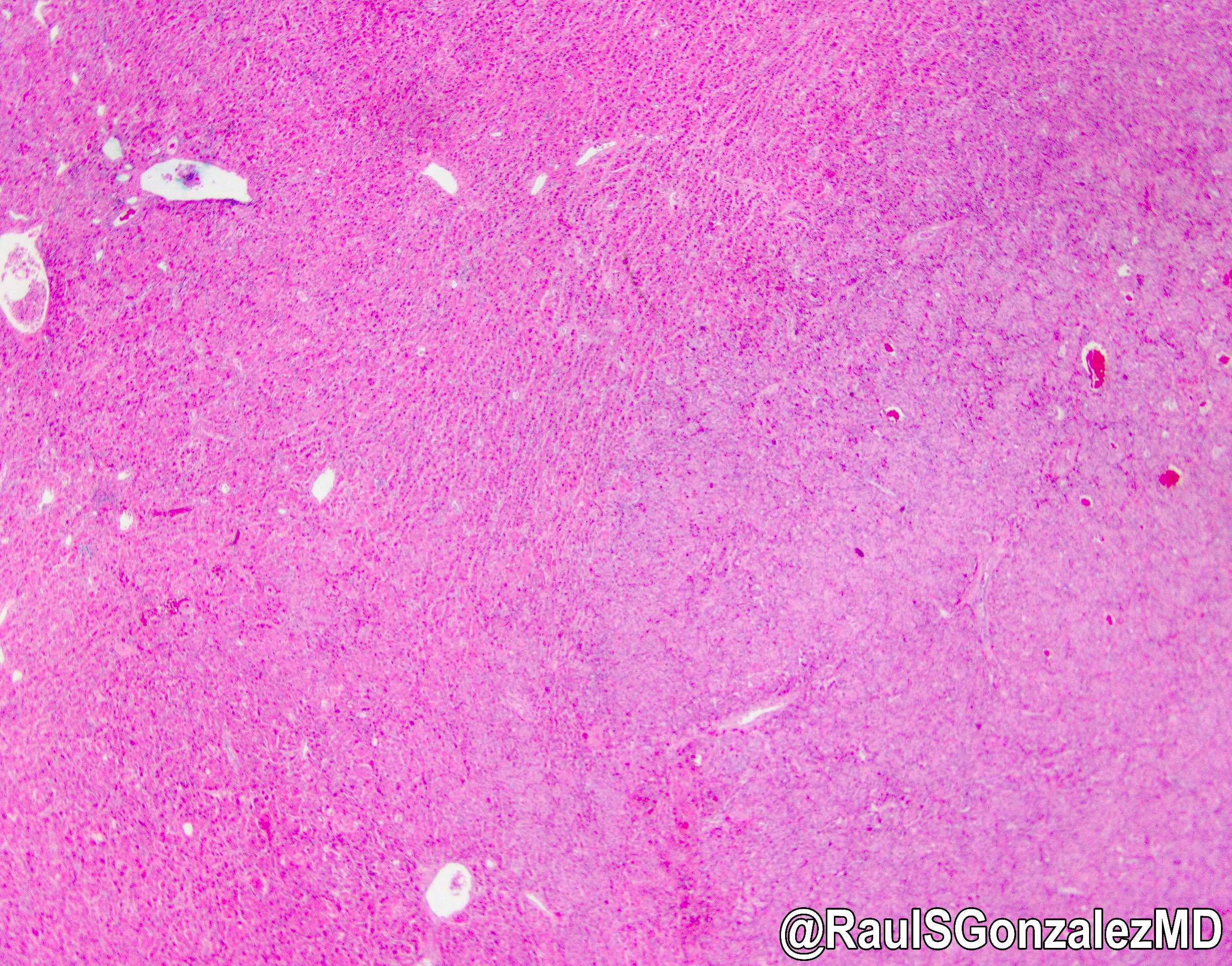
Microscopic (histologic) description
- Portal tracts are devoid of bile ducts; the ratio of bile ducts to portal tracts is 0 to 0.4 (normal 0.9 to 1.8) (Pediatr Pathol 1988;8:1)
- Ductular reaction is typically absent but rare examples present with ductular reaction in early infancy (Nat Genet 1997;16:235)
- Giant cell transformation and periportal copper deposits can be seen
- Progression to cirrhosis is rare
- Liver transplantation is reserved for patients with progressive liver disease or intractable pruritus
- Mortality is related to liver disease, cardiac abnormalities and intracranial bleeding
- Patients may survive into adulthood but with increased risk of hepatic failure and hepatocellular carcinoma
Alcoholic liver disease
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Liver damage caused by excessive alcohol consumption
Essential features
- Liver damage caused by excessive alcohol consumption
- Steatosis, steatohepatitis or perivenular and pericellular fibrosis are typical histological features
Terminology
- Alcoholic liver disease
ICD coding
Epidemiology
- 90 - 95% of heavy drinkers develop steatosis; up to 35% develop advanced alcoholic liver diseases (i.e., alcoholic hepatitis, fibrosis, cirrhosis or hepatocellular carcinoma) (J Hepatol 2012;57:399)
- Proportion of current drinkers among the total population in 2016: 43.0% (world), 59.9% (European region), 54.1% (region of the Americas), 53.8% (Western Pacific region), 33.1% (Southeast Asian region), 32.2% (African region) and 2.9% (Eastern Mediterranean region) (WHO: Global Status Report on Alcohol and Health 2018 [Accessed 6 December 2021])
- Harmful alcohol use is associated with 5.3% of all deaths and 5.1% of disability adjusted life years (DALYs) worldwide in 2016 (WHO: Global Status Report on Alcohol and Health 2018 [Accessed 6 December 2021])
- Cirrhosis accounts for 607,000 and 22.2 million alcohol attributable death and DALYs, respectively (WHO: Global Status Report on Alcohol and Health 2018 [Accessed 6 December 2021])
- Liver cancer accounts for 84,000 alcohol attributable cancer deaths (WHO: Global Status Report on Alcohol and Health 2018 [Accessed 6 December 2021])
Sites
- Liver
Pathophysiology
- Alcohol enhances hepatic lipid biosynthesis
- Excess NADH generation from alcohol dehydrogenase and acetaldehyde dehydrogenase
- Impaired assembly / secretion of lipoproteins
- Increased peripheral fat catabolism
- P450 induction causes other drugs to be transformed to toxic metabolites; free radicals, from microsomal oxidation of alcohol, damage proteins and membranes
- Alcohol directly affects microtubular and mitochondrial function, also induces immunologic attack on hepatic neoantigens
- Acetaldehyde (alcohol metabolite) causes lipid peroxidation and acetaldehyde protein adduct formation
- Collagen deposition by perisinusoidal hepatic stellate (Ito) cells is due to Kupffer cell activation (release of TNFα, IL1 / 6, TGFβ), platelet activating factor, influx of neutrophils into parenchyma
- Alcohol also causes derangements of vascular perfusion
- Alcohol consumption results in translocation of gut bacteria into the portal system along with lipopolysaccharides that interact with toll-like receptors and results in production of inflammatory and immunogenic mediators such as TNFα and interferons (World J Hepatol 2011;3:114)
Etiology
- Excessive regular alcohol consumption (> 20 g/day for females and > 30 g/day for males)
Clinical features
- Nonspecific clinical features for any chronic liver disease
- Odor of alcohol on breath
- Alcohol withdrawal syndrome: fine tremor, psychomotor agitation, transient hallucinations or illusions, tachycardia
- Reference: J Hepatol 2018;69:154
Diagnosis
- Alcoholic liver disease (J Hepatol 2018;69:154):
- Regular alcohol consumption of > 20 g/day for females and > 30 g/day for males
- AND clinical or biological abnormalities suggestive of liver injury
- Alcoholic hepatitis (Hepatology 2020;71:306):
- Recent onset (< 8 weeks) of jaundice
- Heavy alcohol consumption (> 40 g/day for females and > 60 g/day for males for ≥ 6 months or < 60 days of abstinence before the onset of jaundice)
- Serum aspartate transaminase (AST) > 50 IU/L, AST/alanine transaminase (ALT) > 1.5 and both AST & ALT < 400 IU/L
- Serum bilirubin > 50 µmol/L (3 mg/dL)
- In presence of diagnostic uncertainly, liver biopsy is required to confirm histologically alcoholic steatohepatitis and rule out other diagnoses
Laboratory
- Serum AST:ALT > 2
- Elevated serum gamma glutamyltransferase (GGT; sensitivity 42 - 86%; specificity 40 - 84%) (J Hepatol 2018;69:154)
- Elevated mean corpuscular volume (MCV; sensitivity 24 - 75%; specificity 56 - 96%) (J Hepatol 2018;69:154)
- Elevated percentage of carbohydrate deficient transferrin per total transferrin (%CDT; sensitivity 25 - 84%; specificity 70 - 98%) (J Hepatol 2018;69:154)
Prognostic factors
- Increasing the risk of alcohol related liver injury (Hepatology 2020;71:306):
- Drinking pattern: daily drinking, drinking while fasting, binge drinking
- Female
- Genetics: PNPLA3, TM6SF2, MBOAT7, HSD17B13
- Smoking cigarettes
- Increased BMI
- Concurrent liver disease: chronic viral hepatitis, genetic hemochromatosis, nonalcoholic fatty liver disease
- Ameliorating the risk of alcohol related liver injury:
- Coffee consumption
Case reports
- 27 year old man with alcoholic hepatitis presenting with high levels of triglyceride, direct hyperbilirubinemia and elevated ALP without an obvious obstruction cause (Case Rep Gastroenterol 2020;14:448)
- 47 year old woman with alcoholic hepatitis masquerading as tumor infiltration (Clin Case Rep 2019;7:2174)
- 55 year old man with severe alcoholic hepatitis and superimposed Candida esophagitis, who was found to have leukemoid reaction during diagnostic workup (Cureus 2020;12:e9747)
- 67 year old man with acute liver injury and false positive results of enzymatic ethanol assay secondary to lactic acidosis due to intravascular large B cell lymphoma (BMJ Case Rep 2019;12:e229814)
Treatment
- Abstinence is the most important treatment
- Corticosteroid should be considered for patients with severe alcoholic hepatitis without contraindications to the corticosteroid (J Hepatol 2018;69:154, Hepatology 2020;71:306)
- Intravenous N-acetylcysteine may be combined with corticosteroid in patients with severe alcoholic hepatitis (J Hepatol 2018;69:154, Hepatology 2020;71:306)
- Liver transplantation for alcoholic cirrhosis
Gross description
- Early stage: enlarged liver with diffuse yellowish greasy appearance
- Later stage:
- Typical micronodular cirrhosis
- Mixed micronodular and macronodular cirrhosis after abstinence
- Yellowish greasy (due to steatosis) or greenish (due to cholestasis)
- Reference: Clin Liver Dis 2016;20:473
Gross images
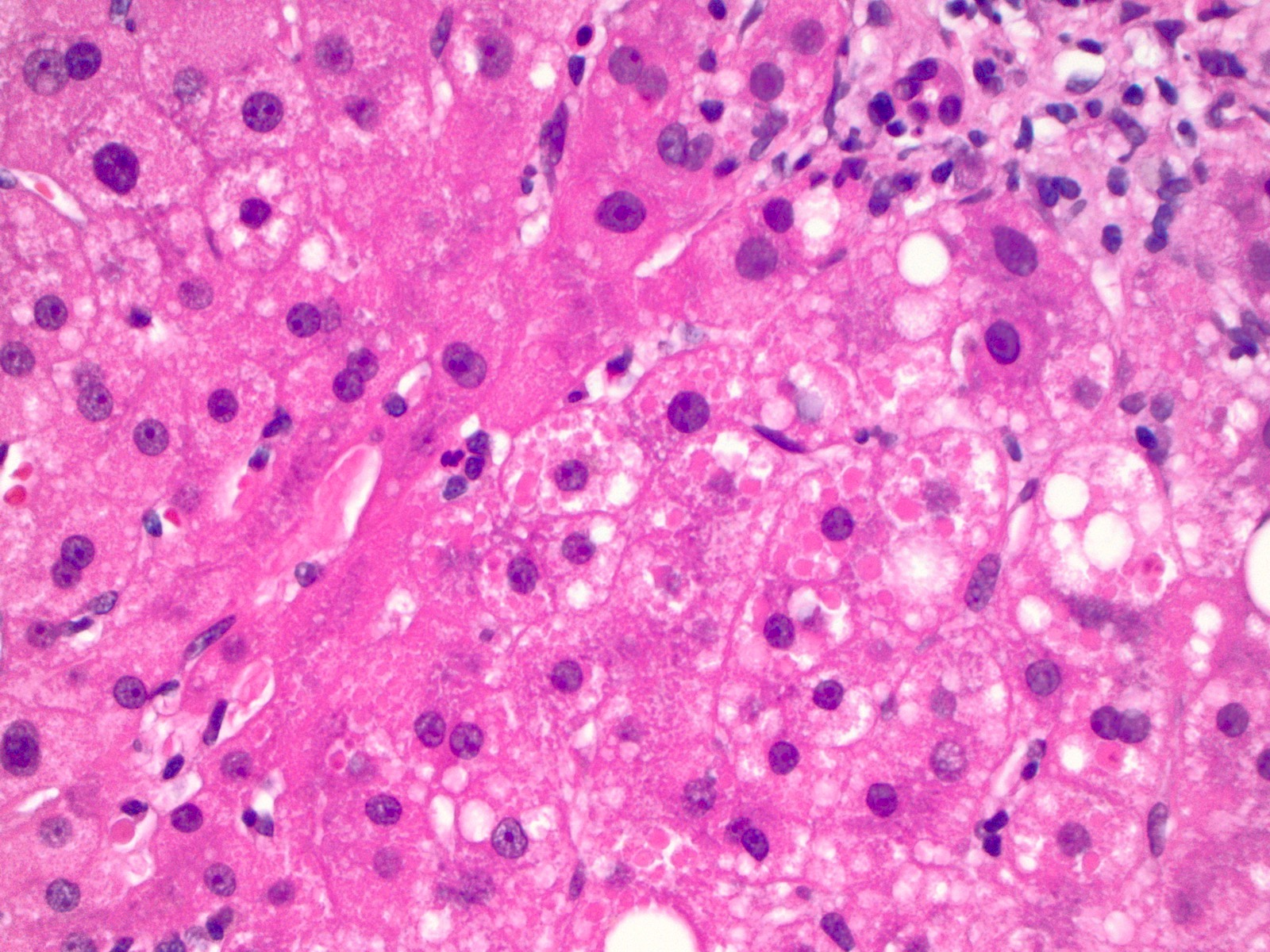
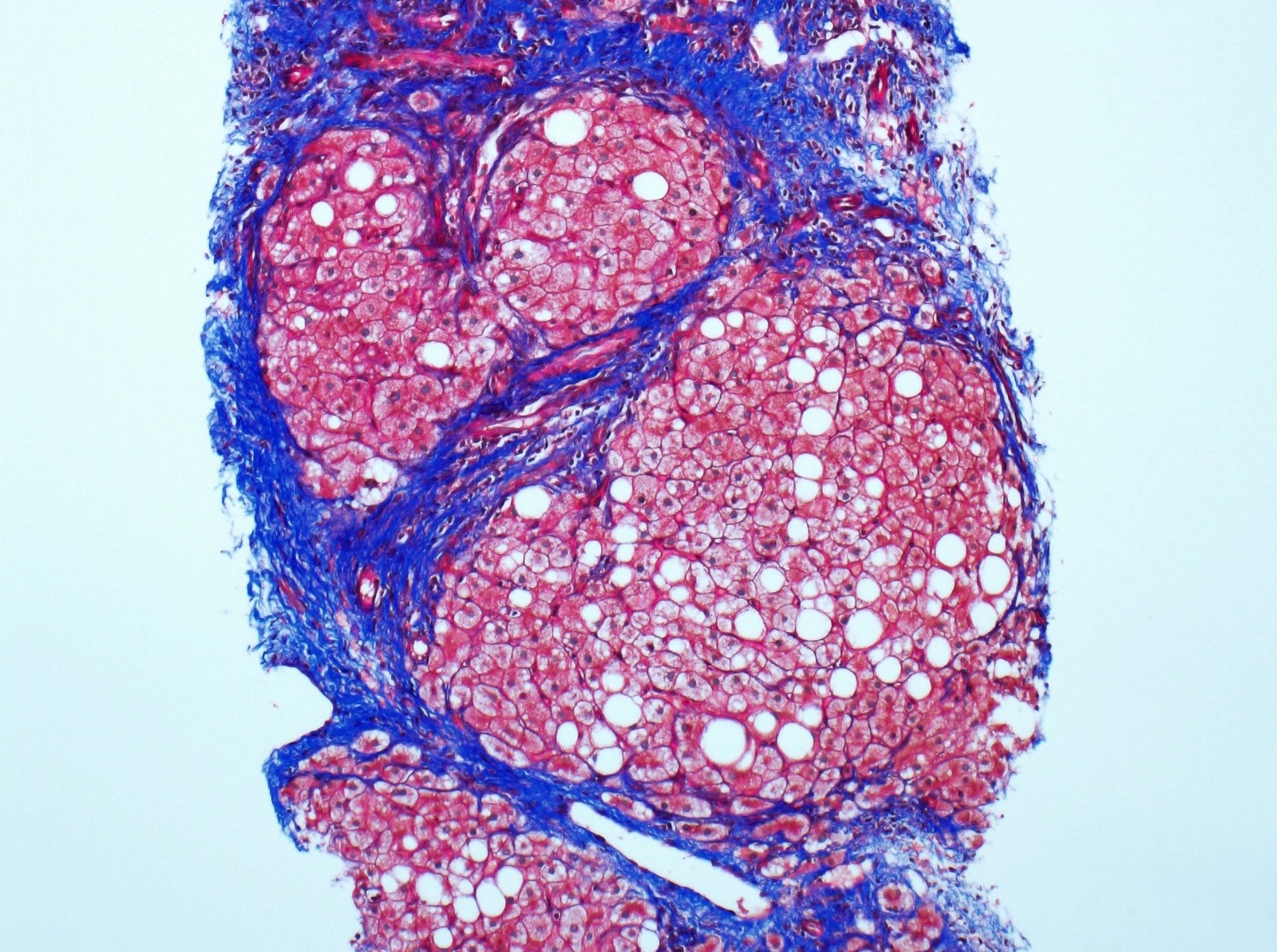
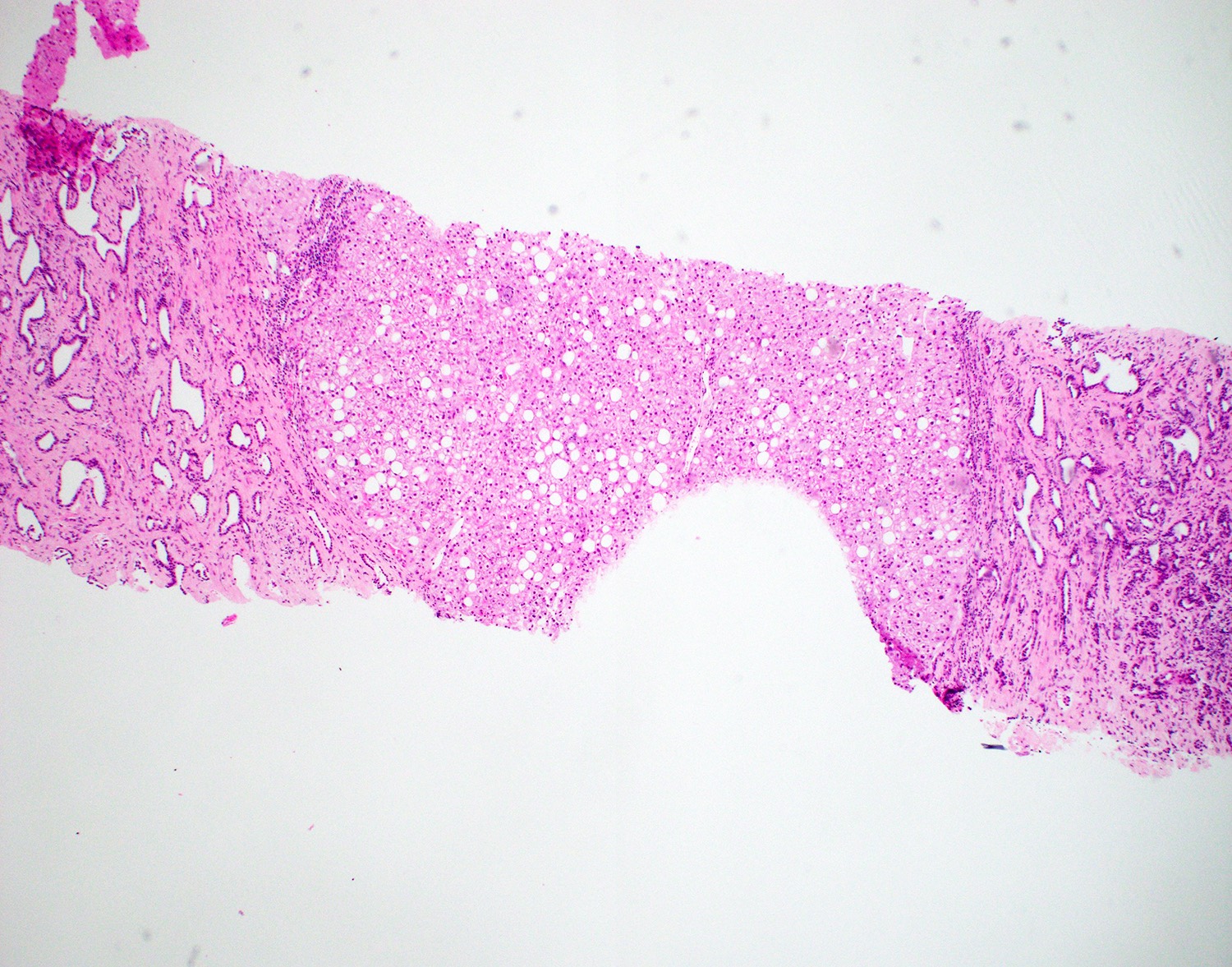
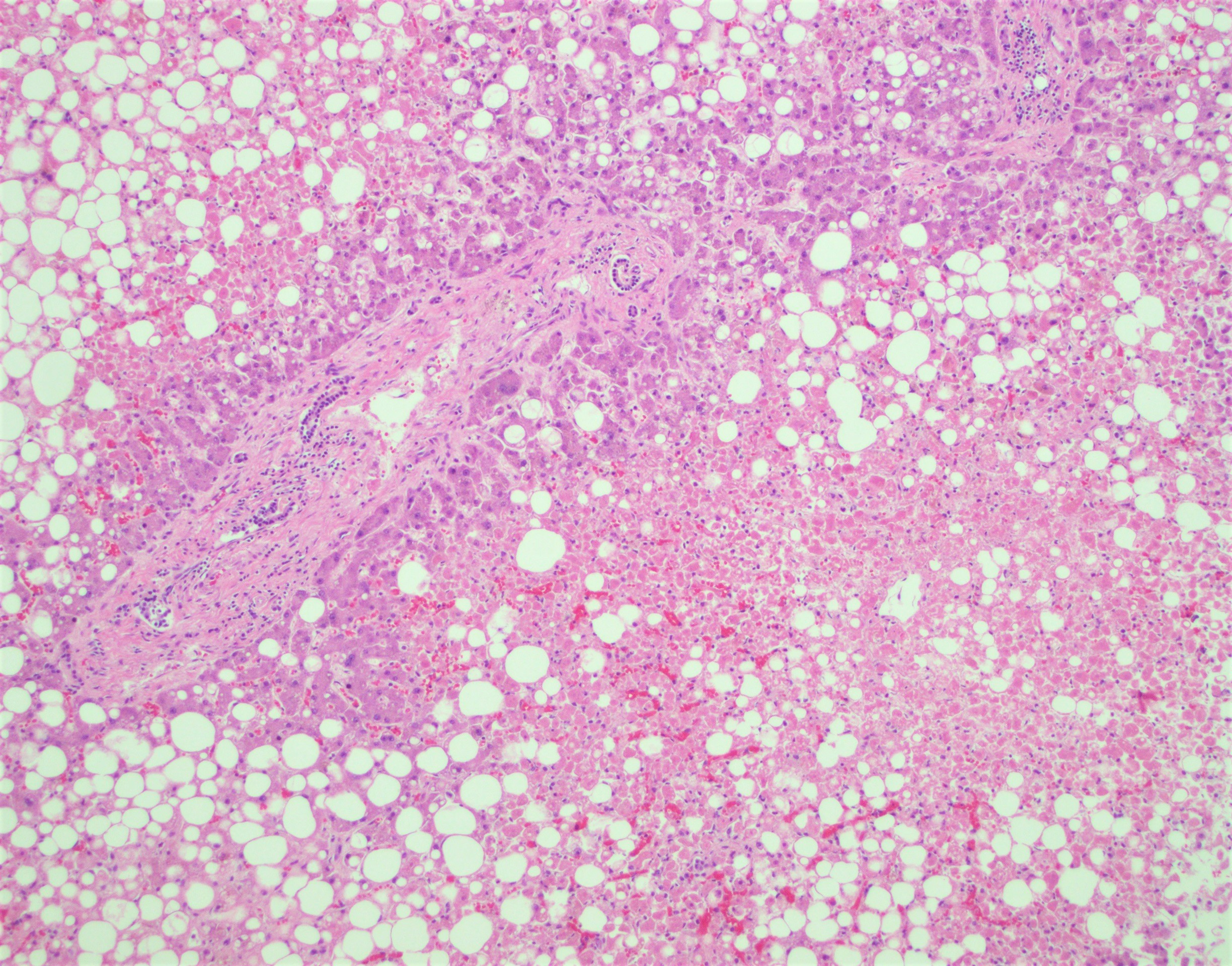
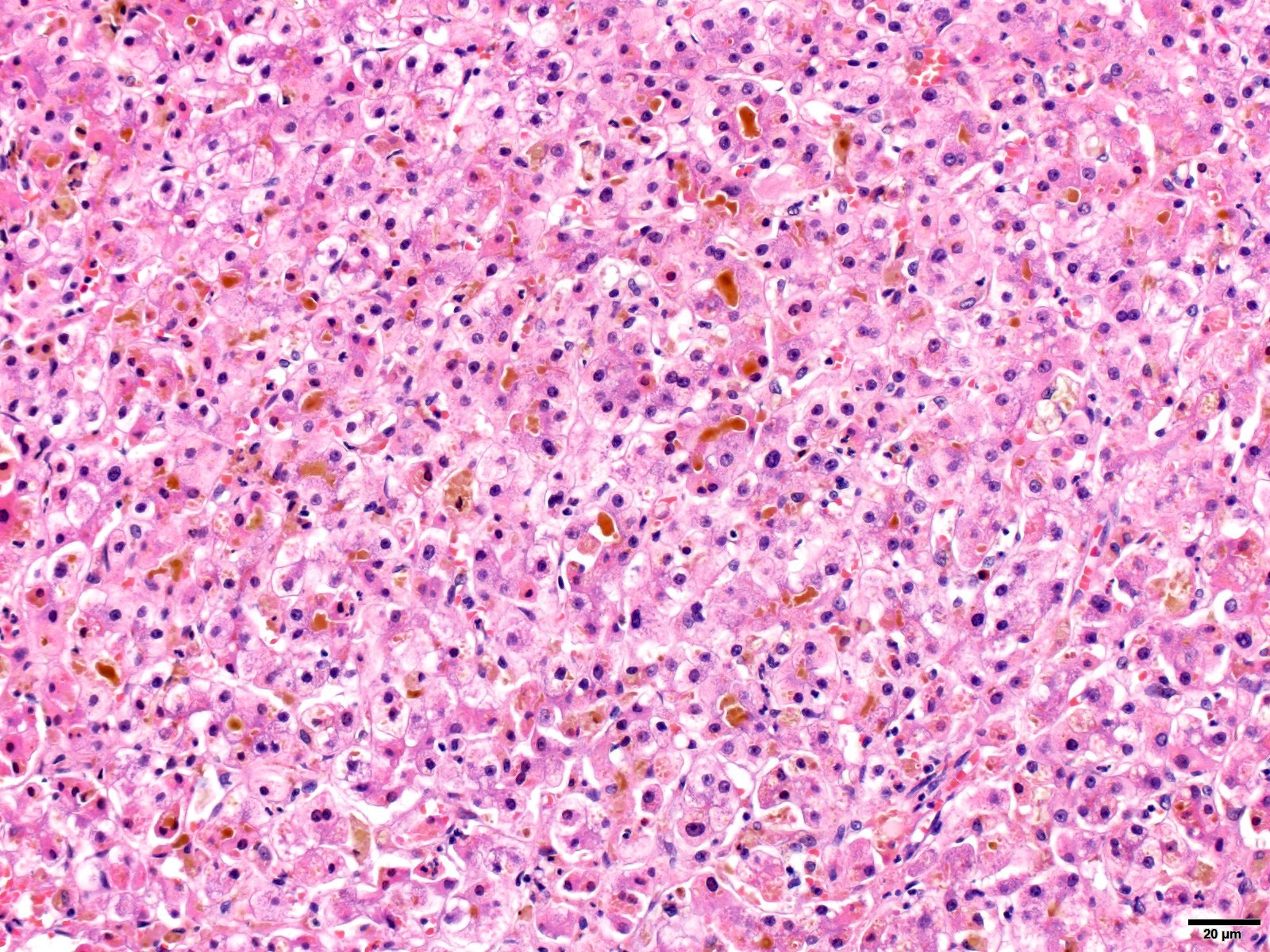
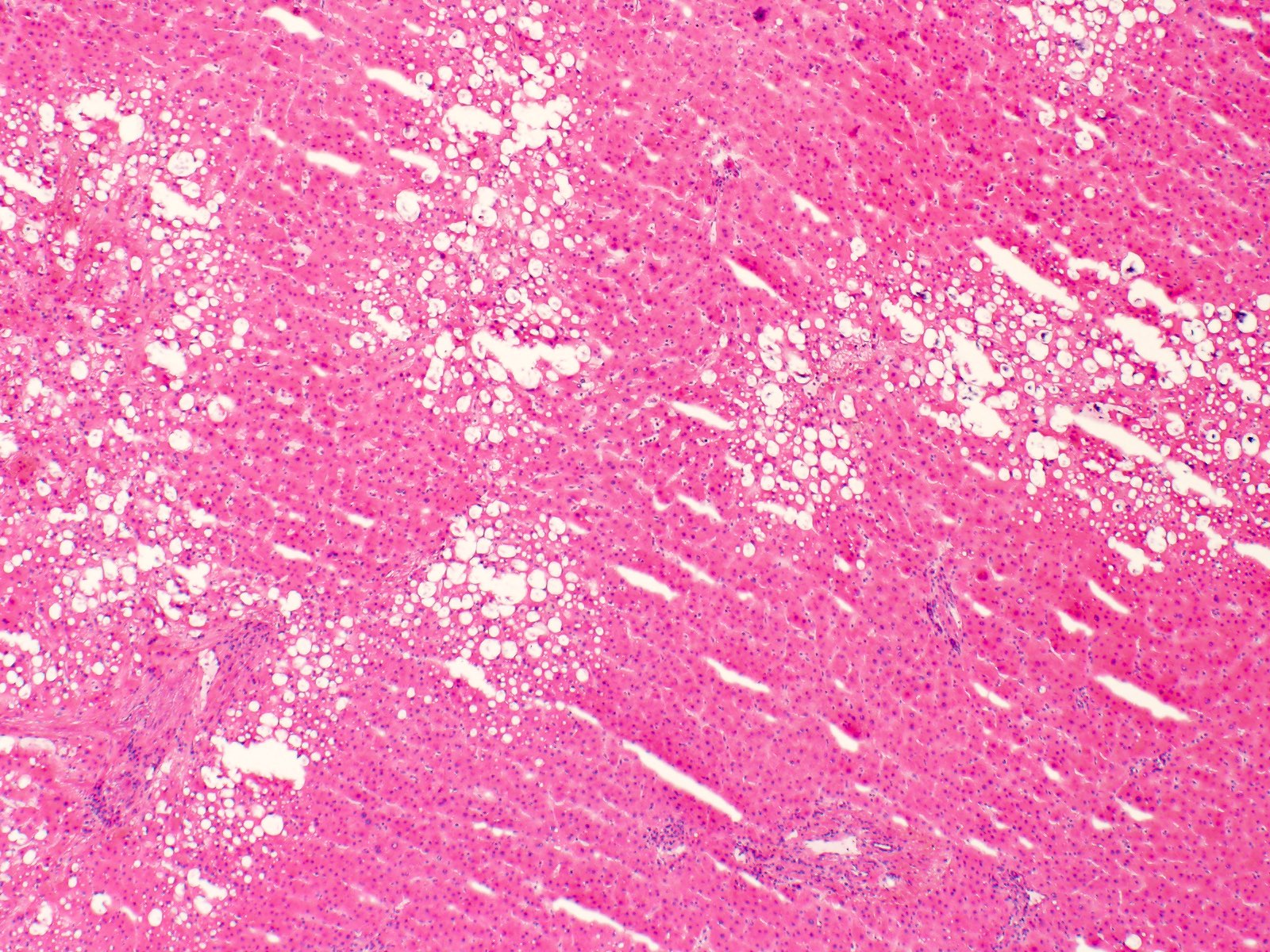
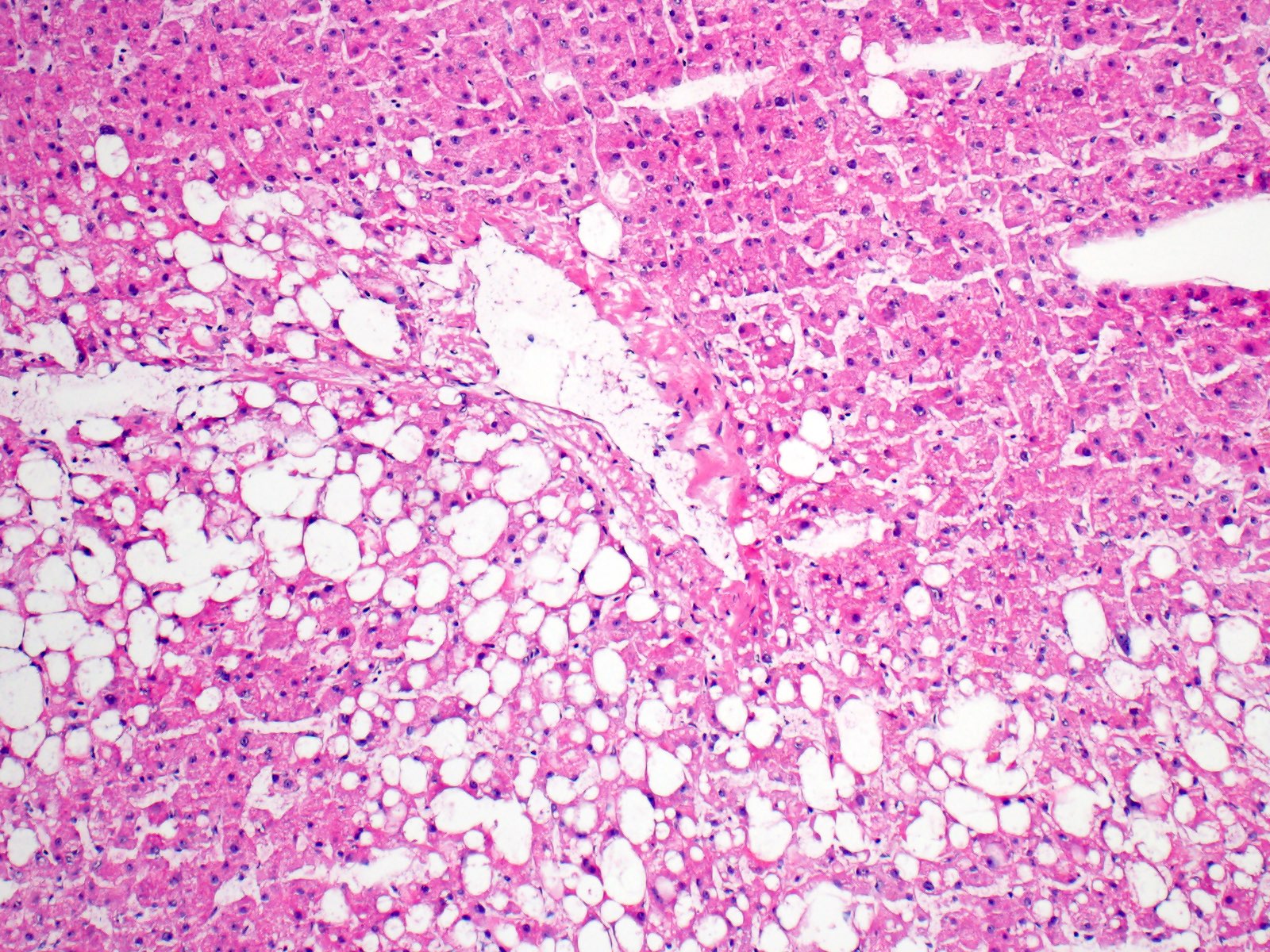
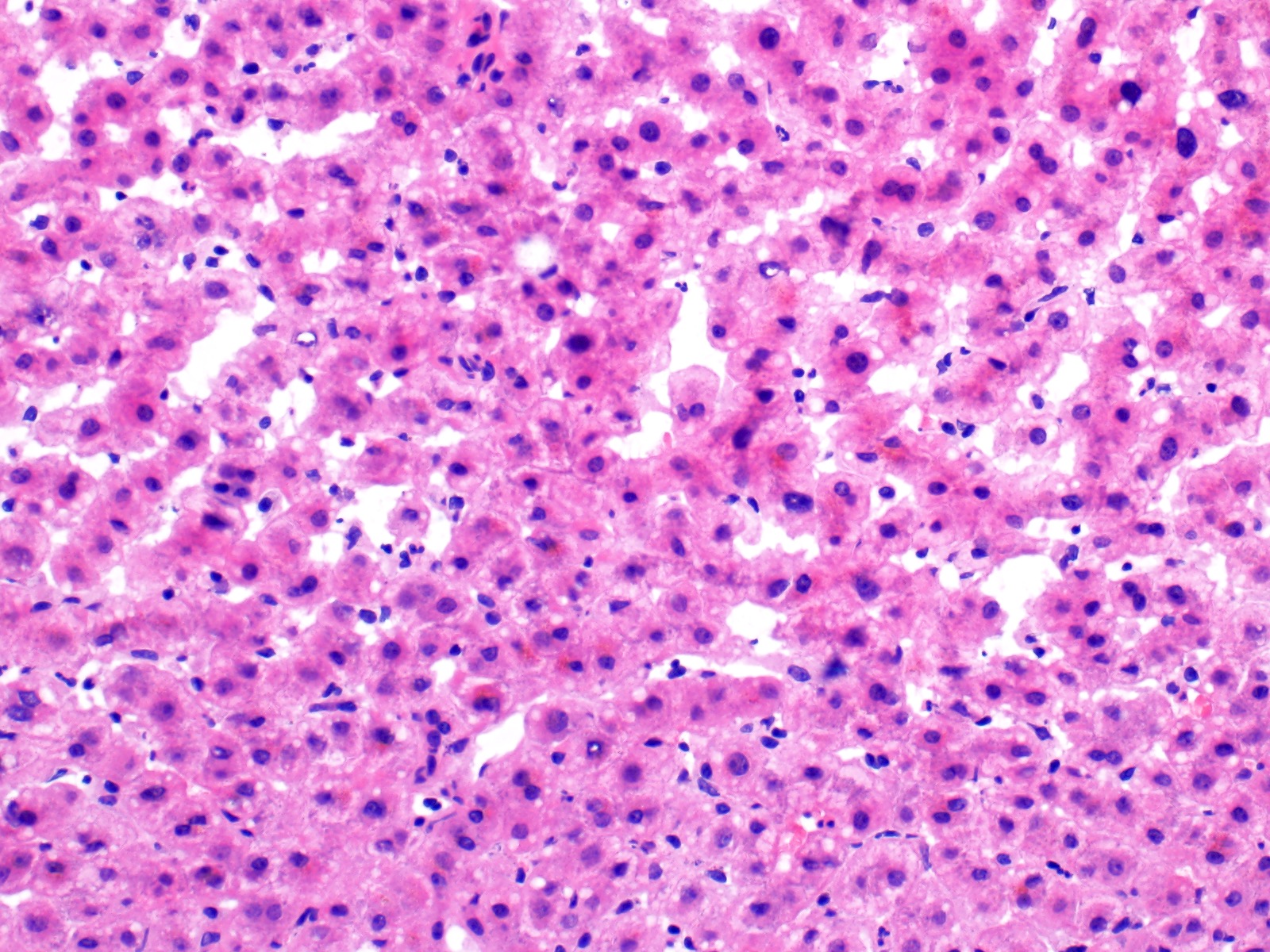
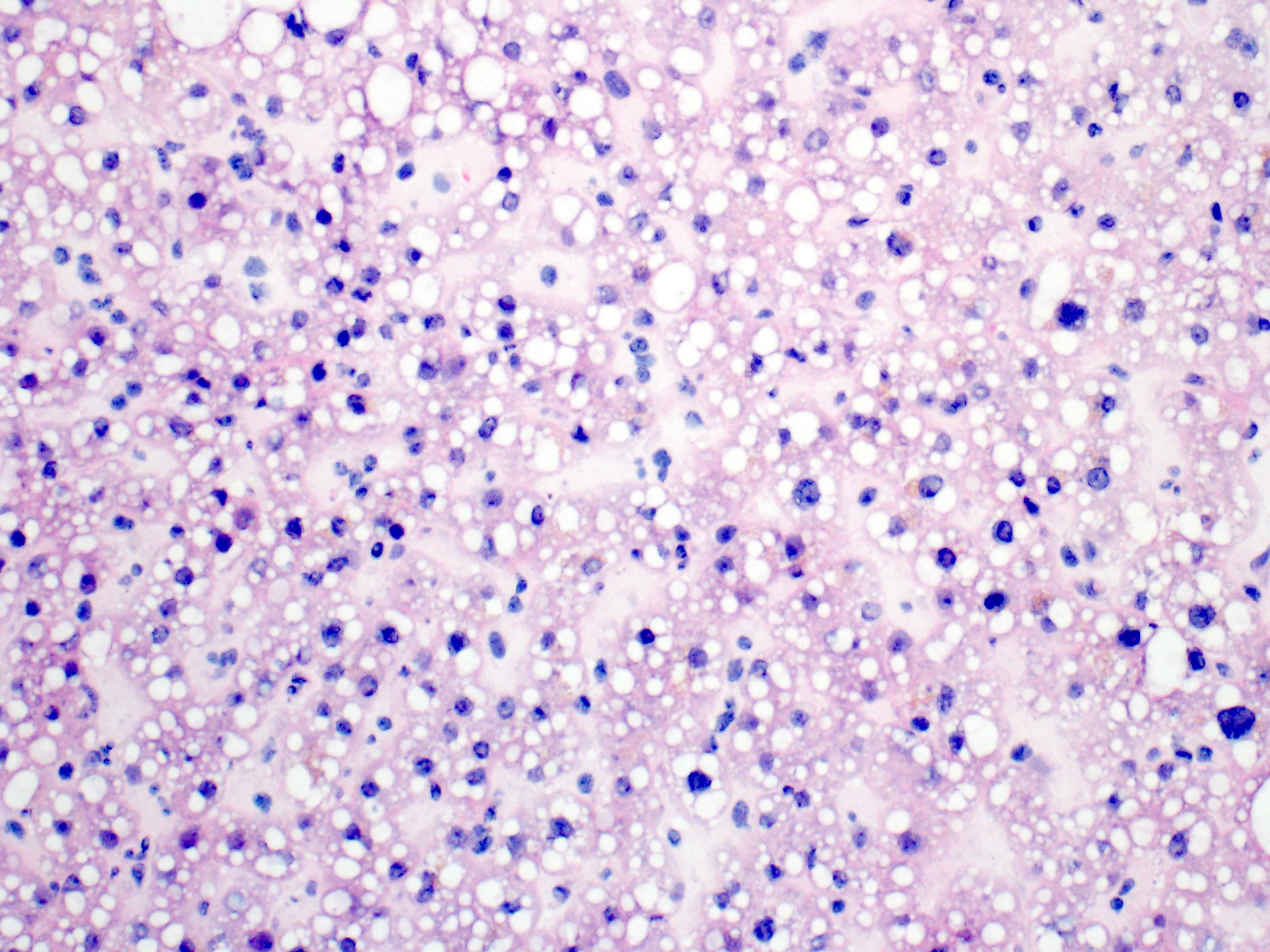
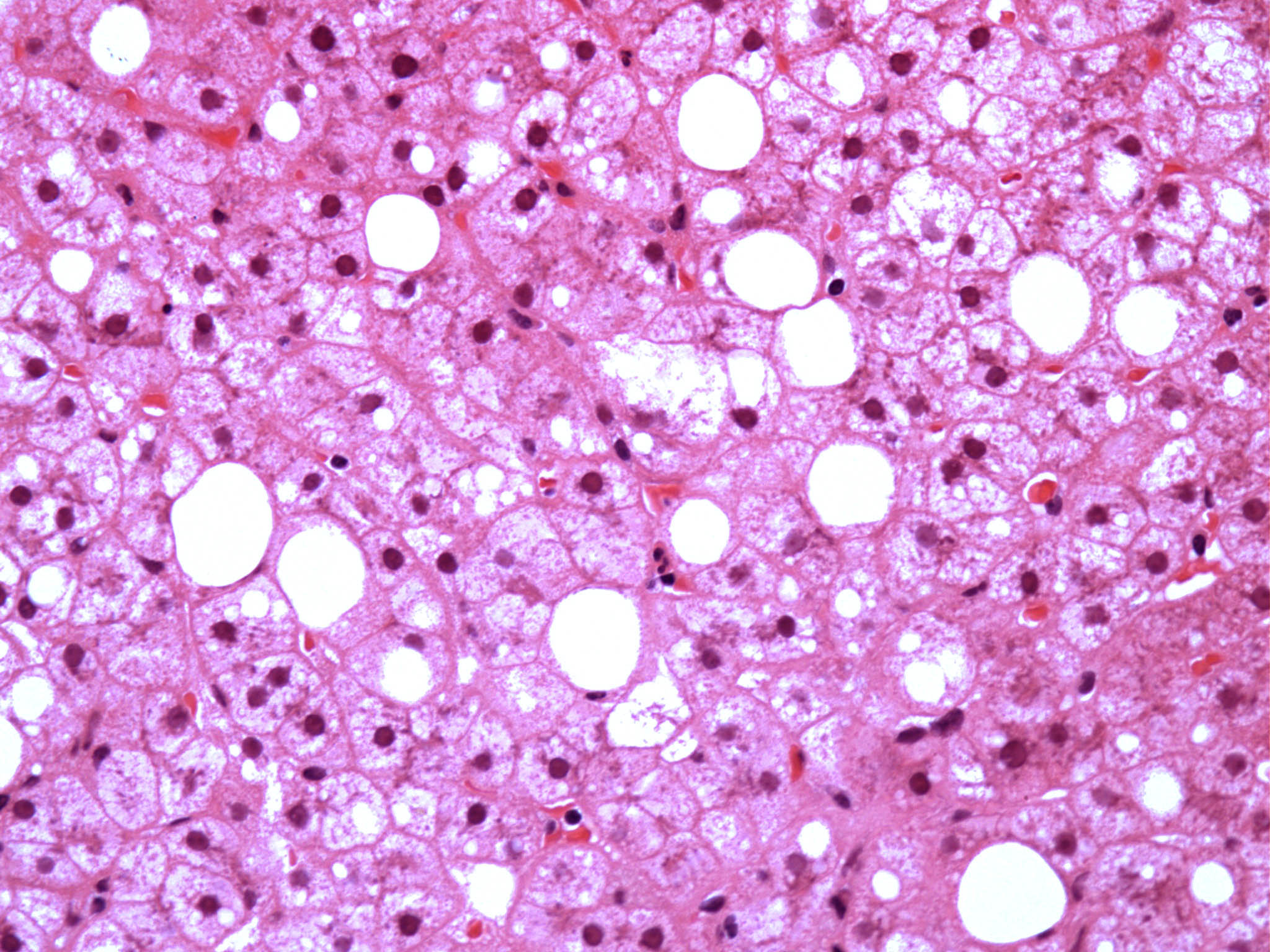
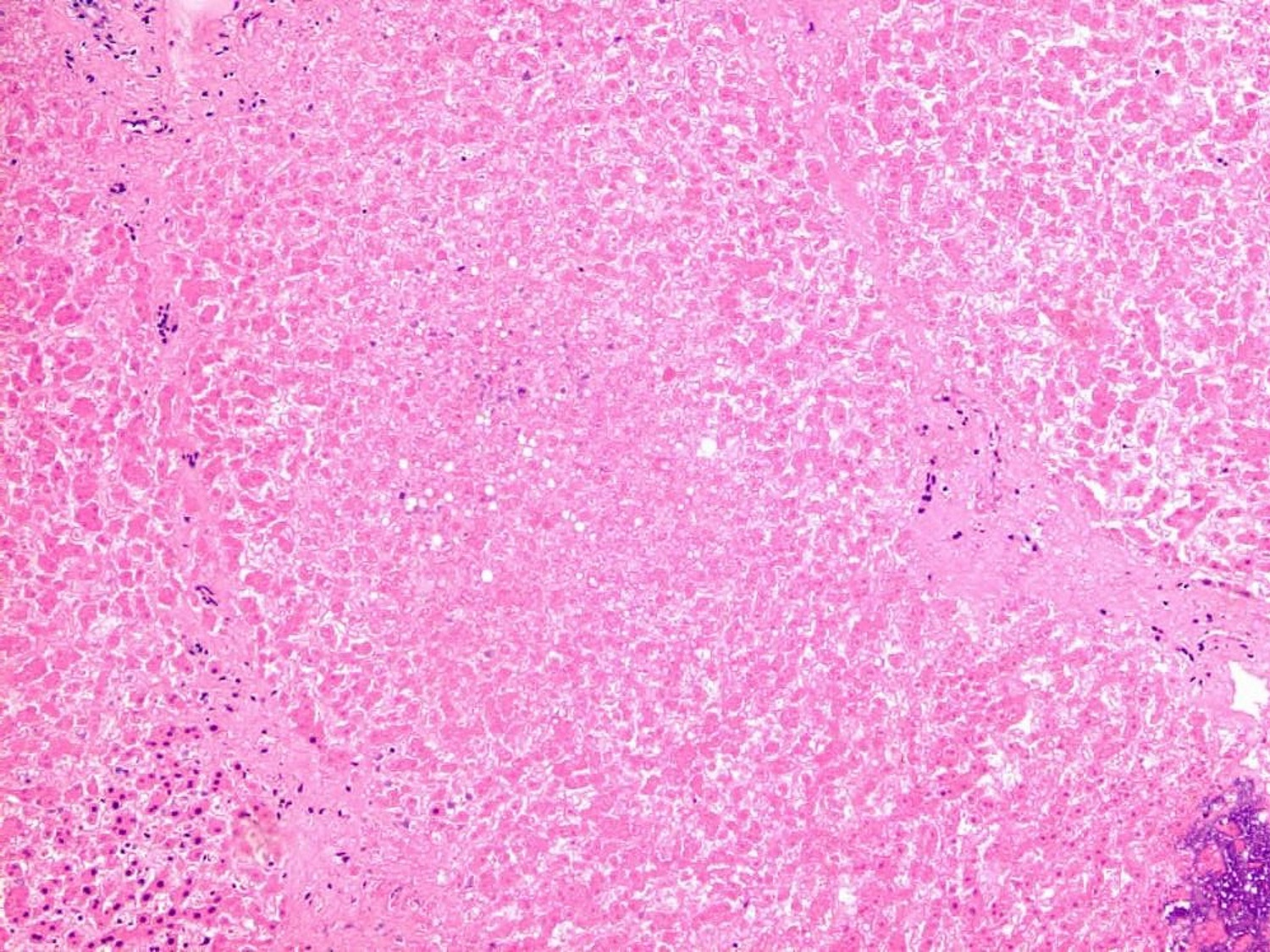
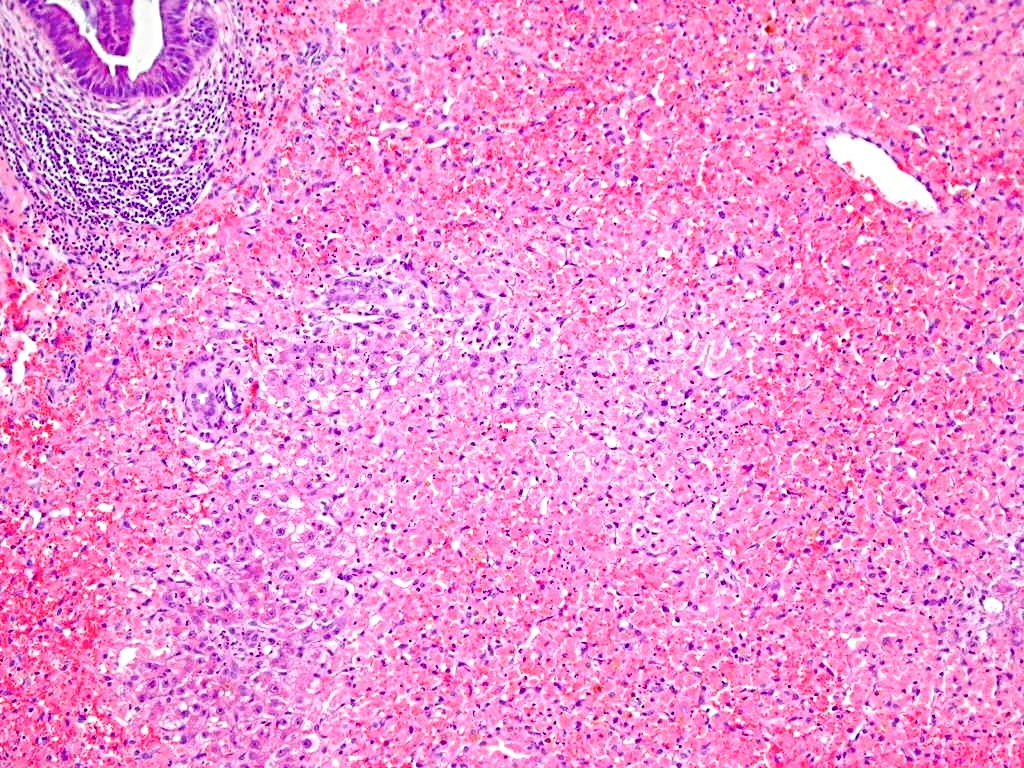
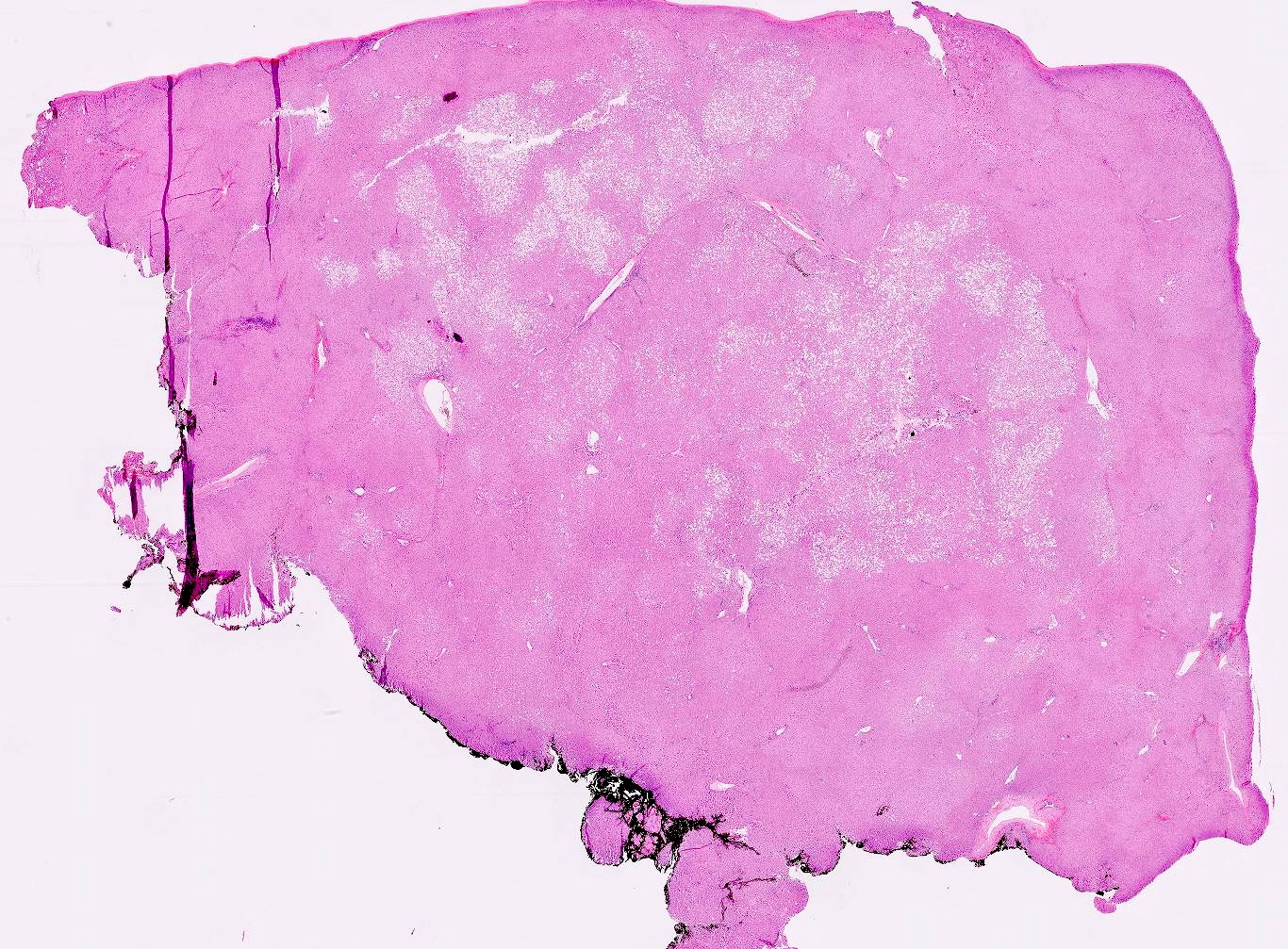
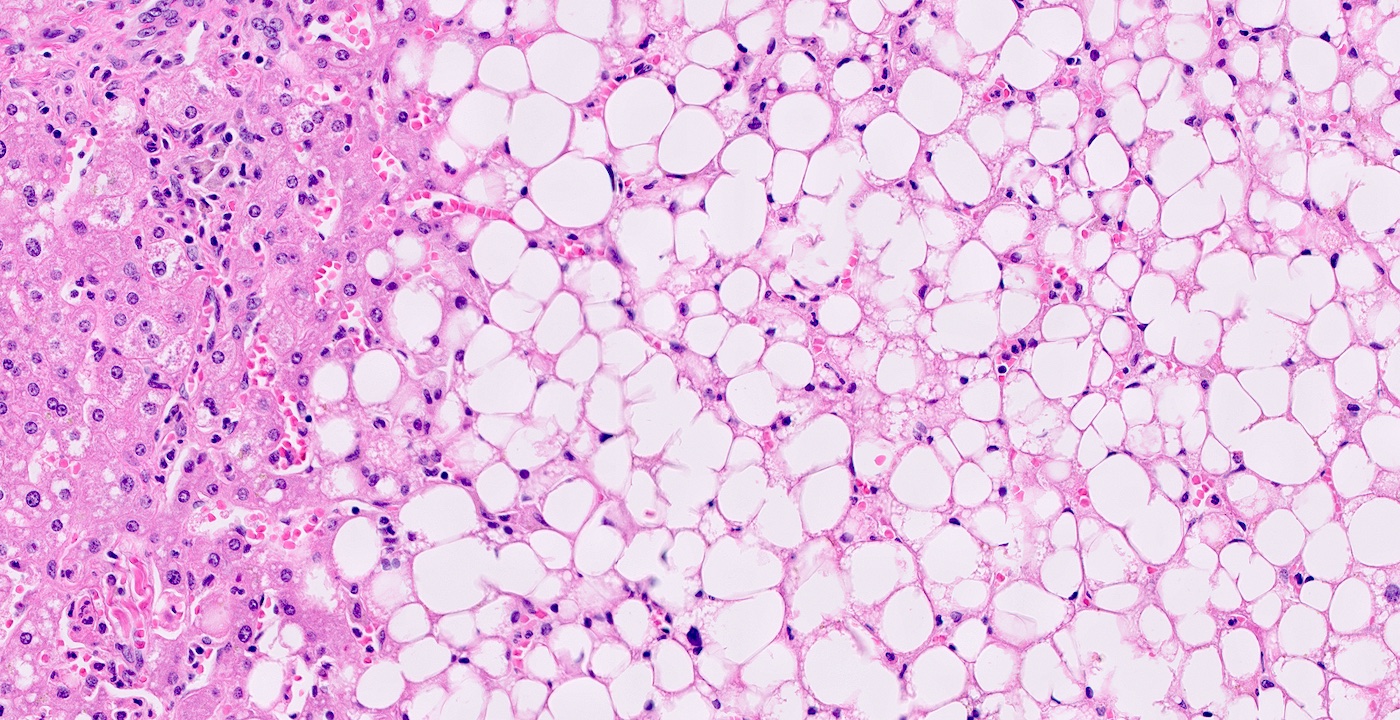
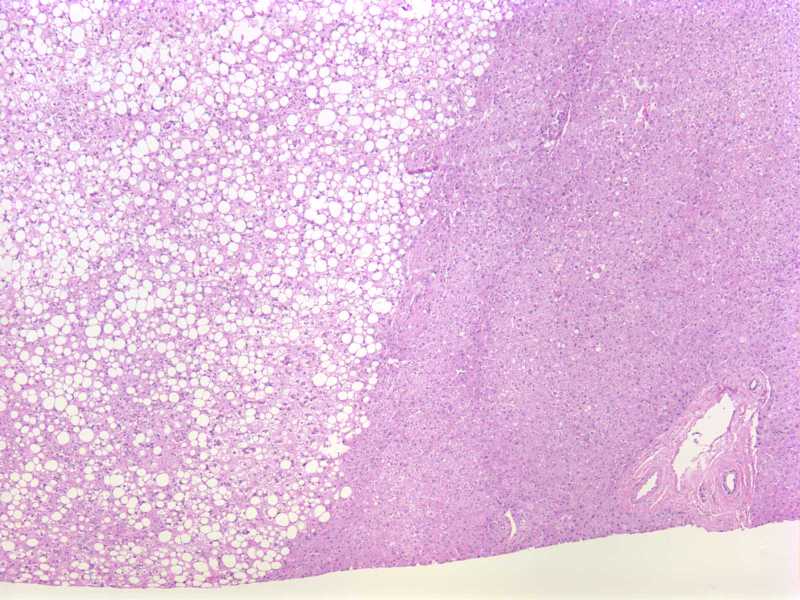
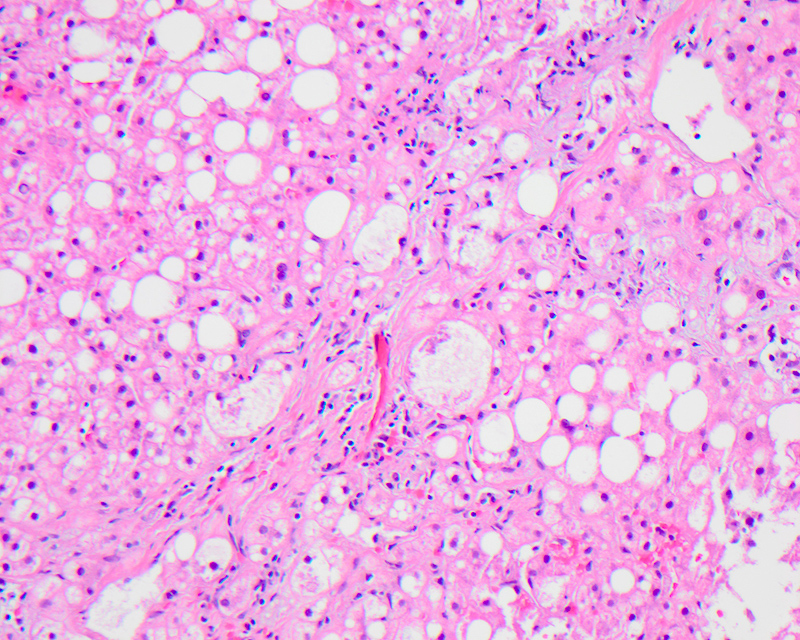
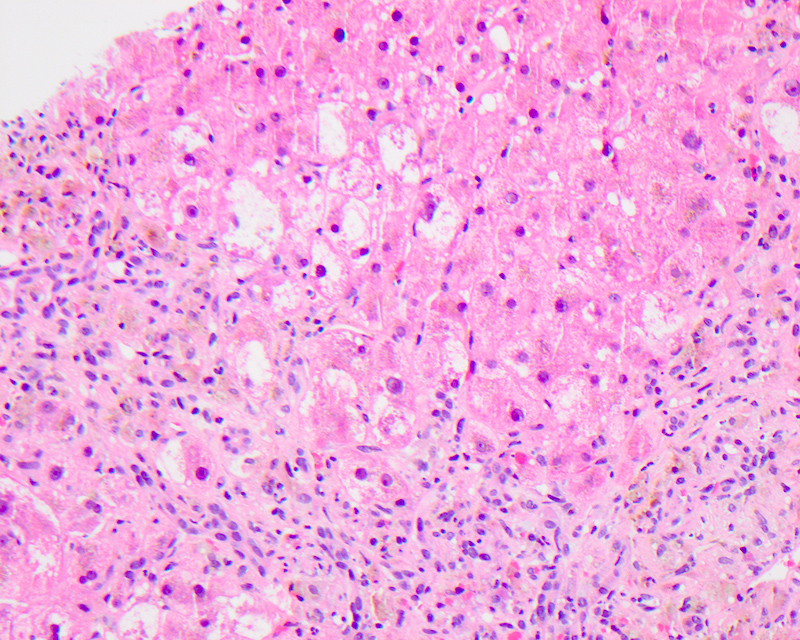
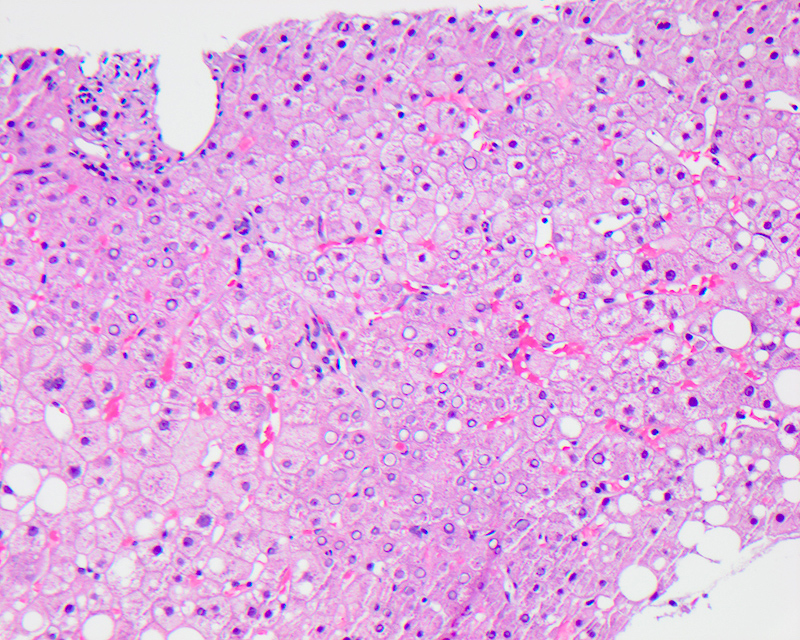
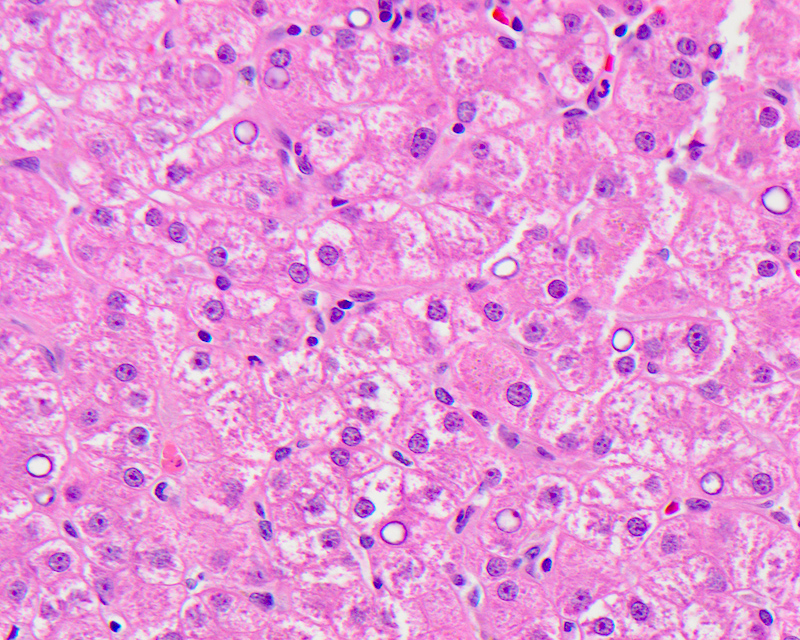
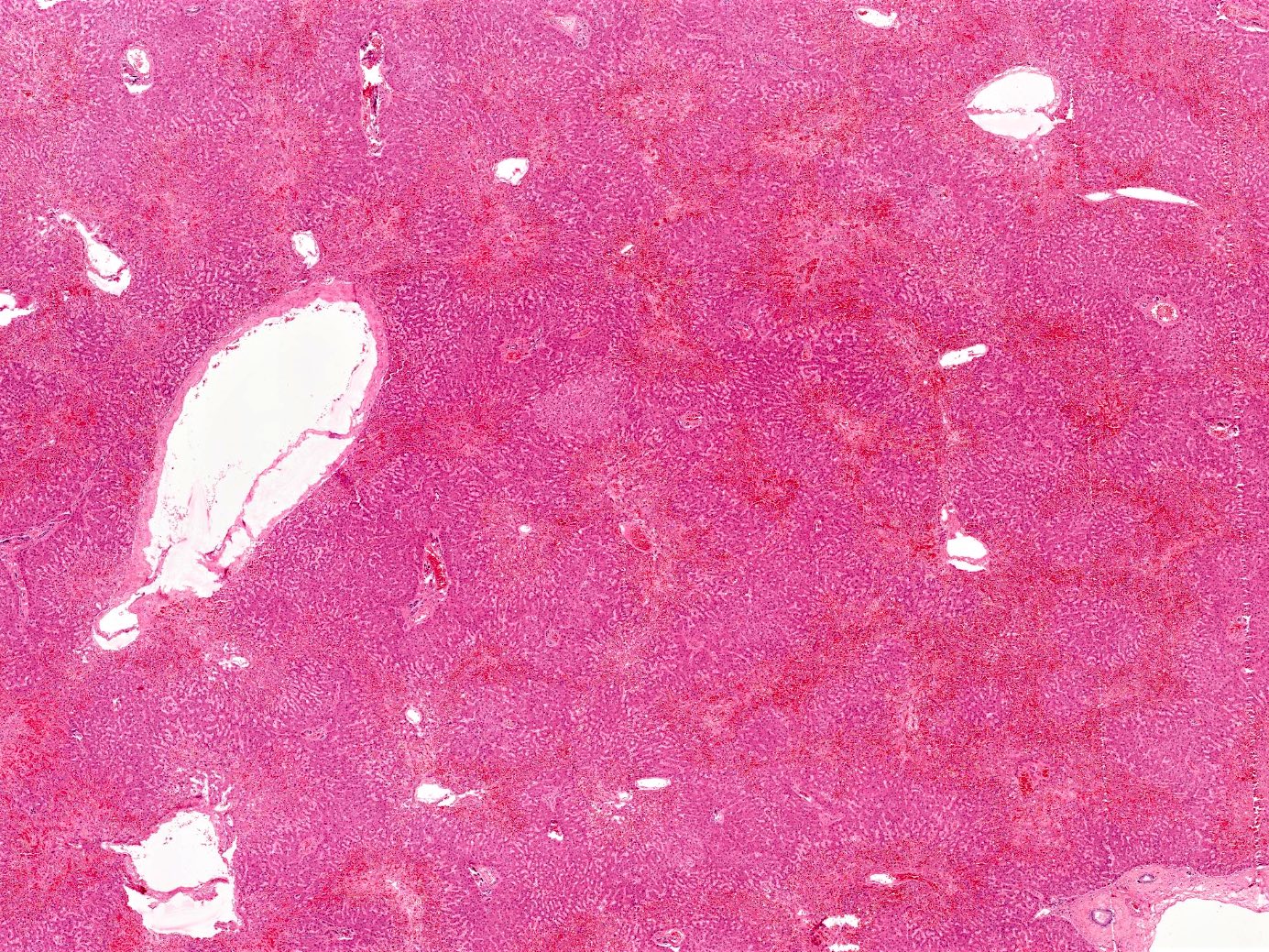
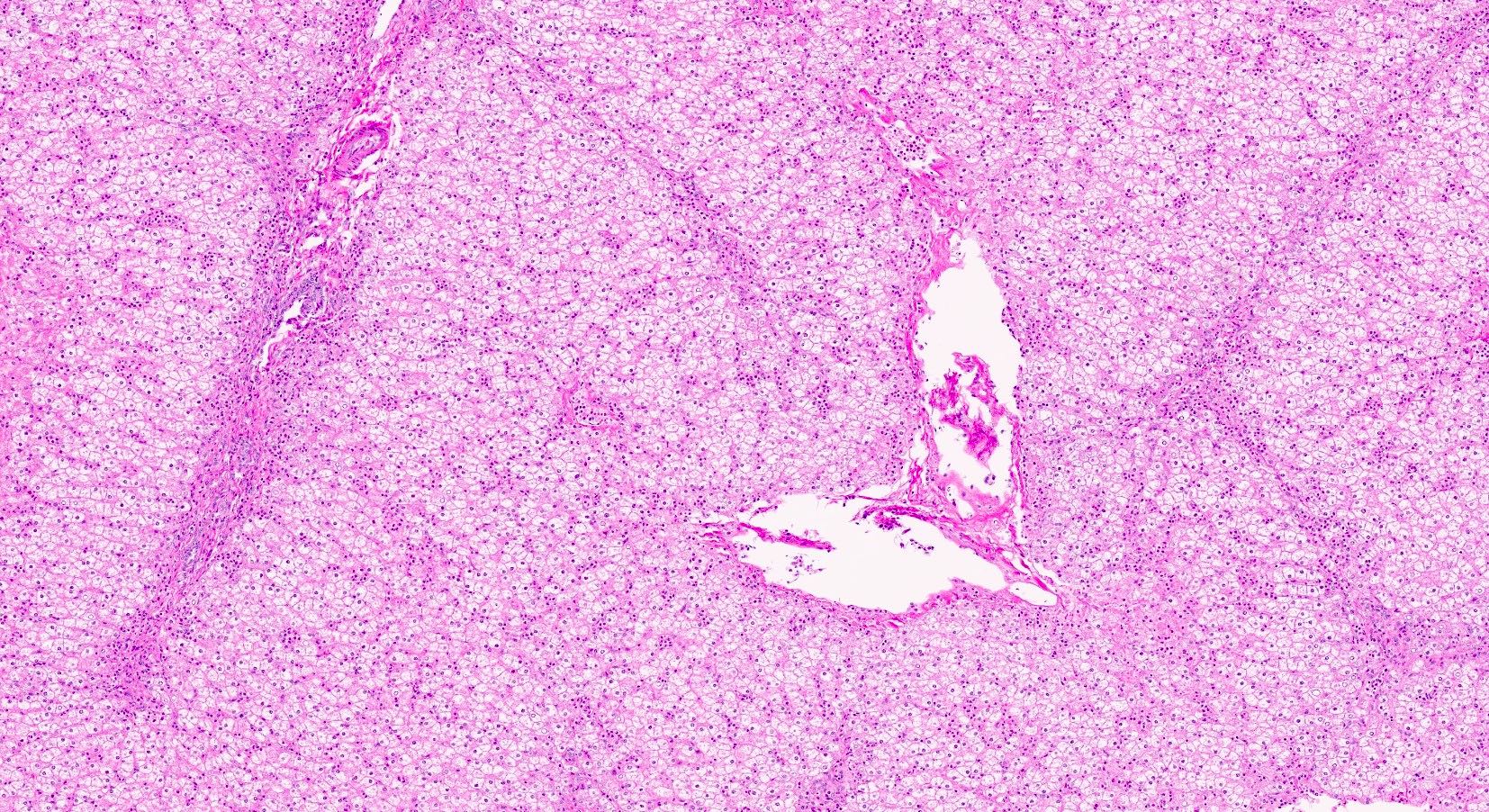
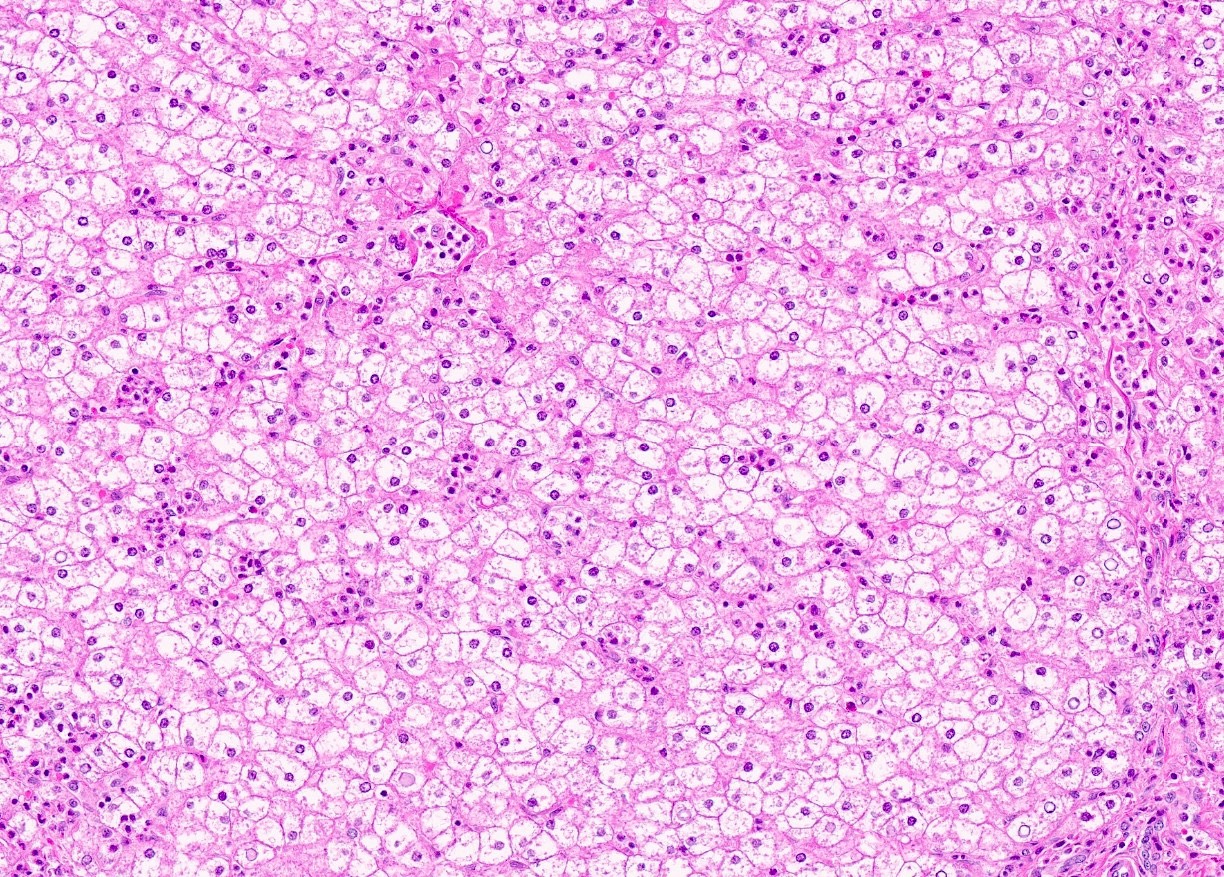
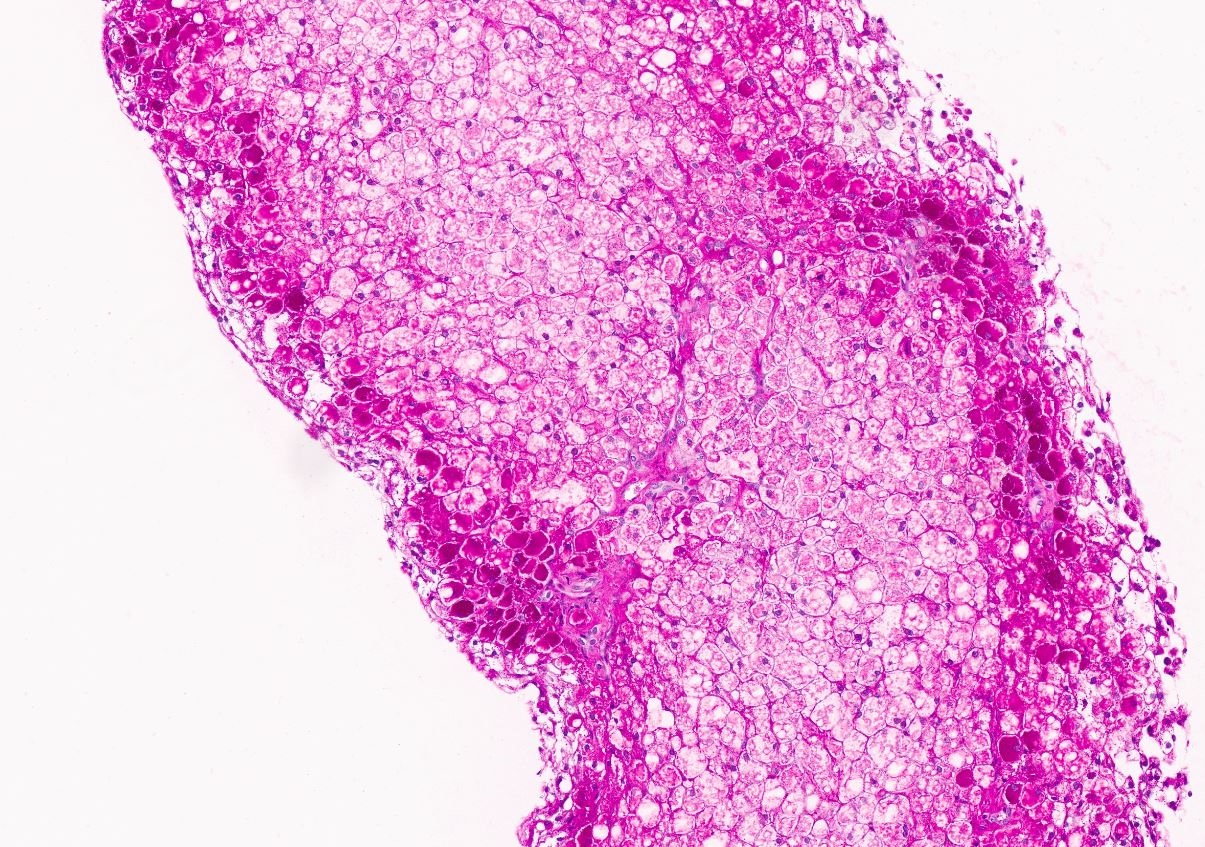
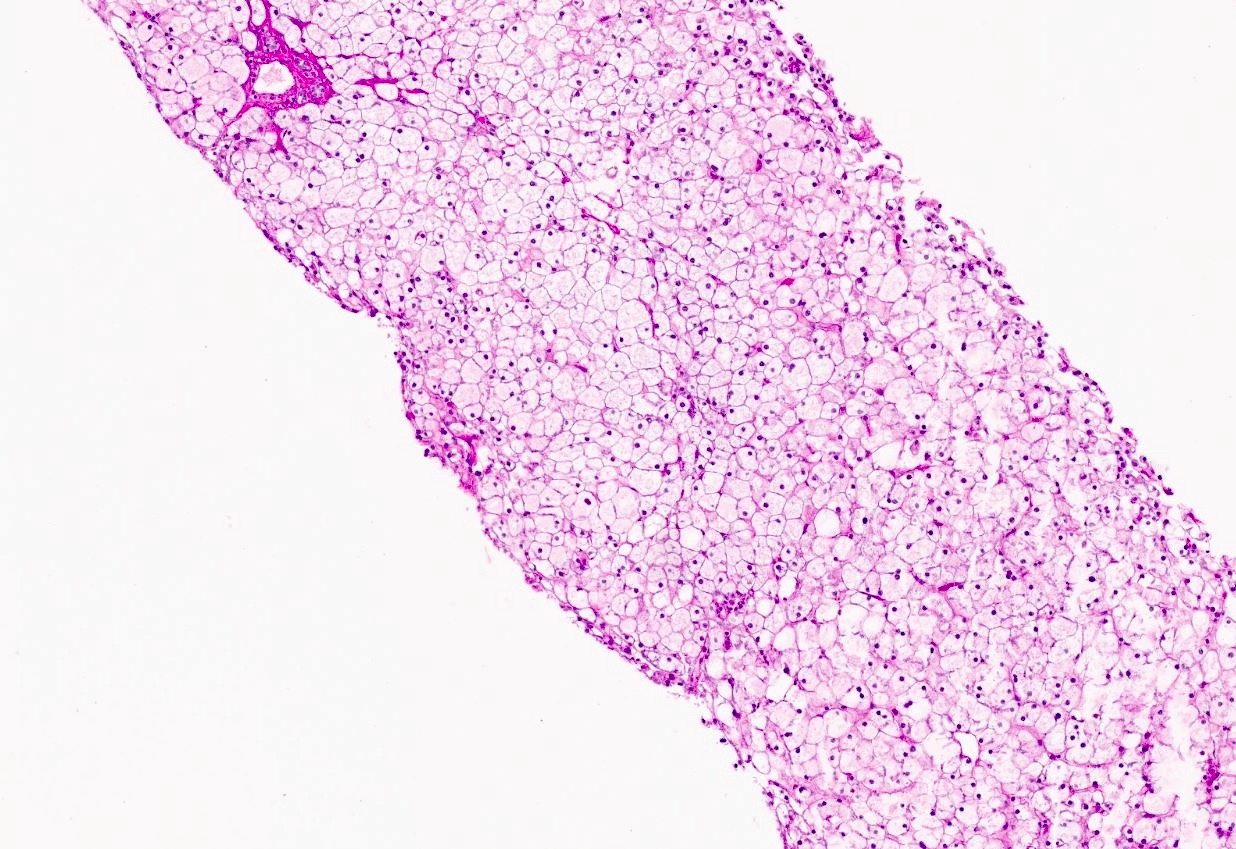
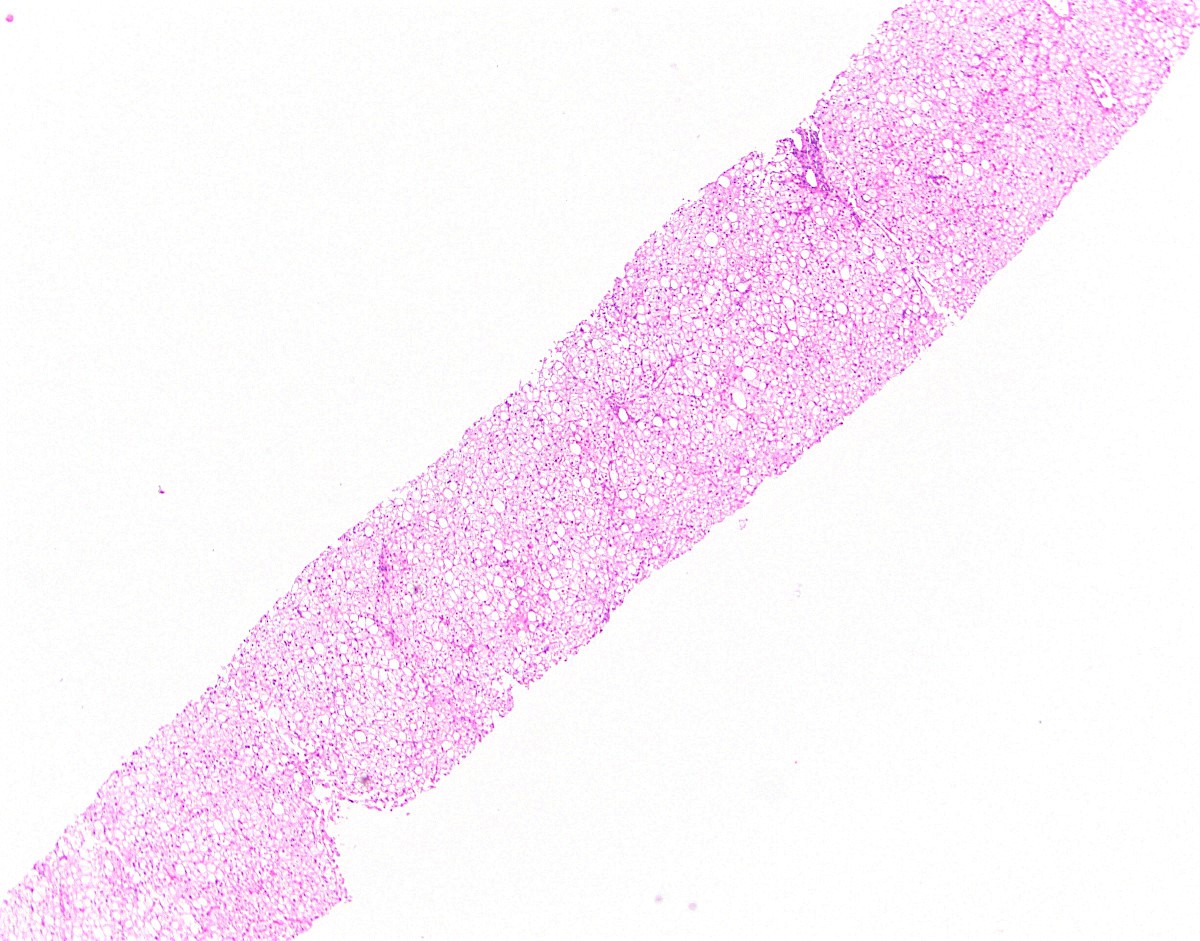
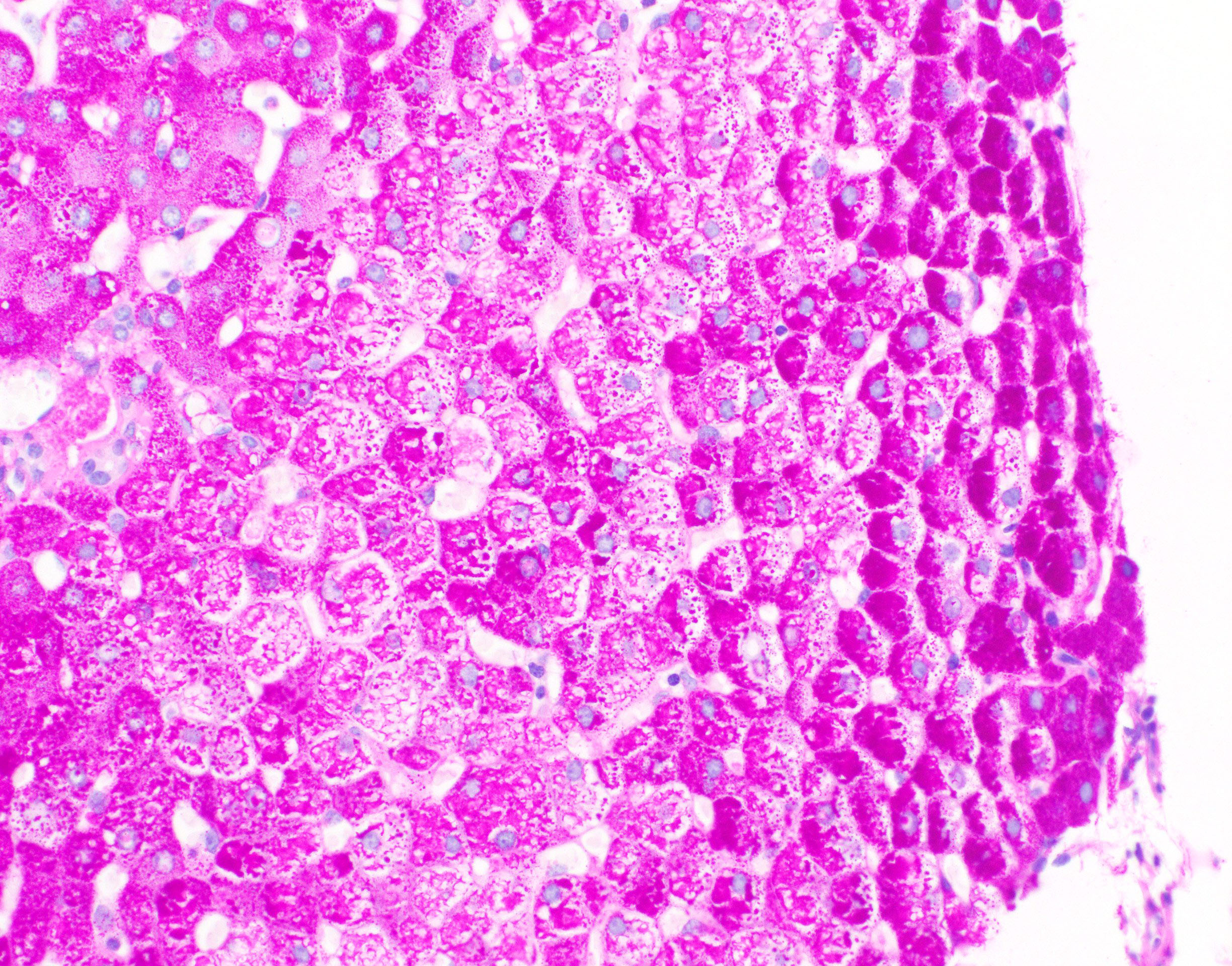
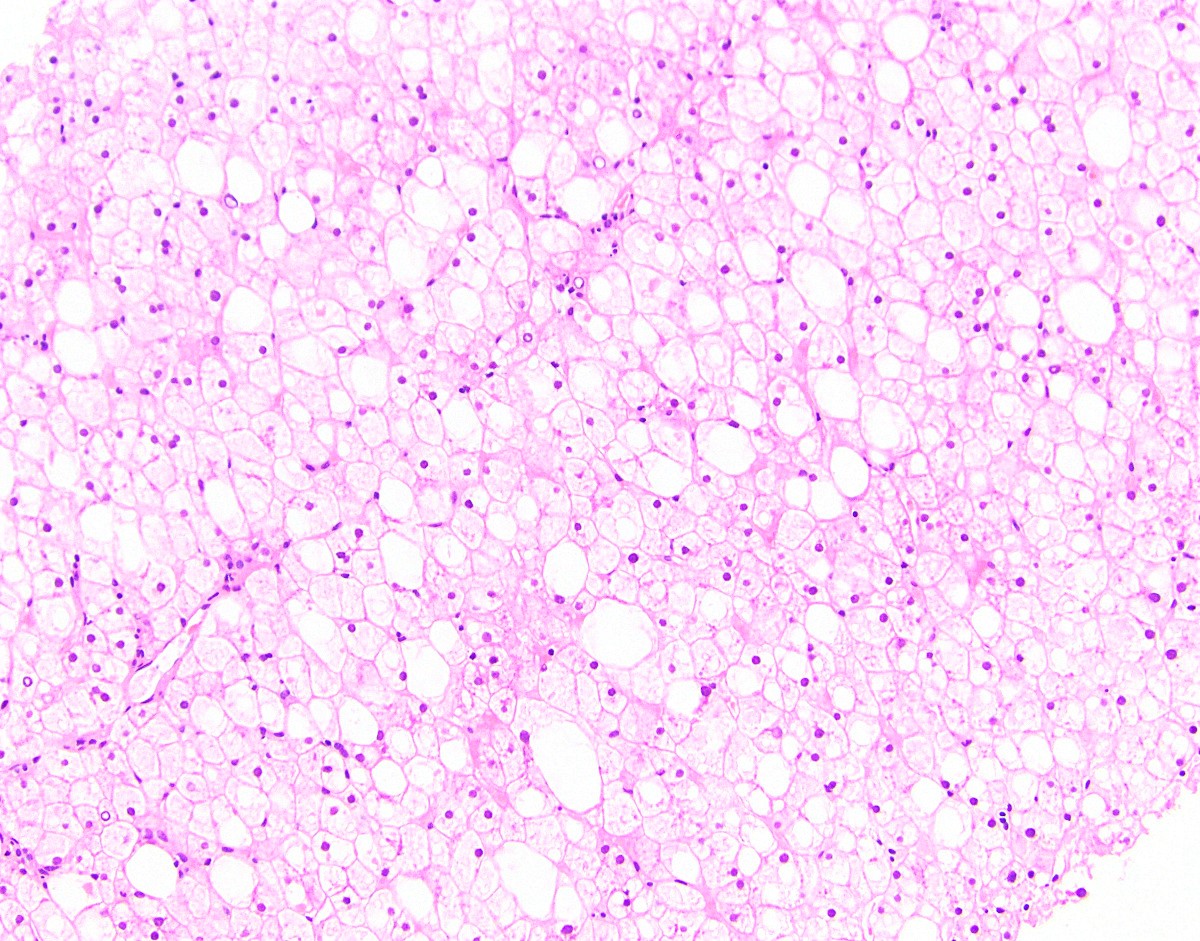
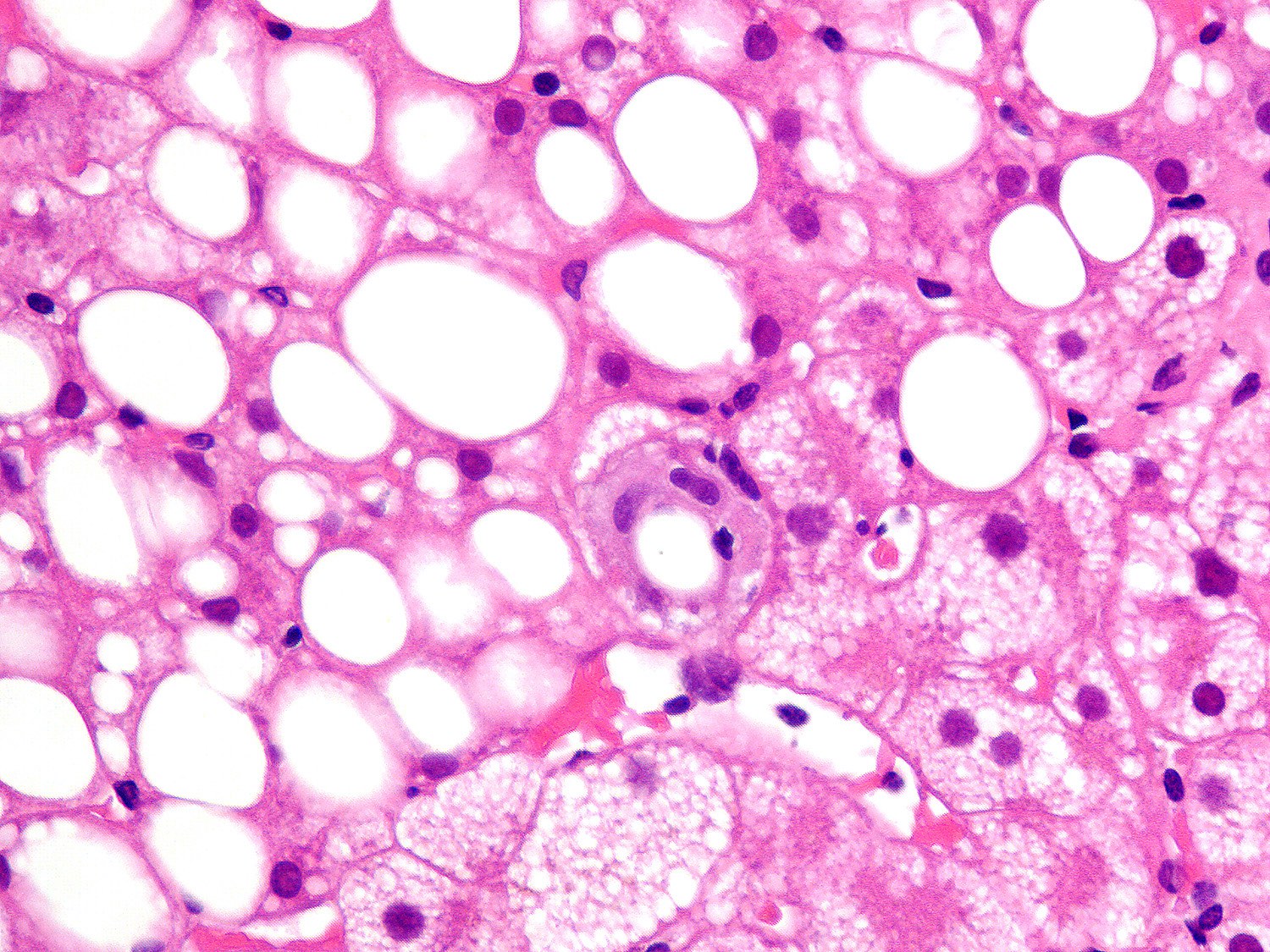
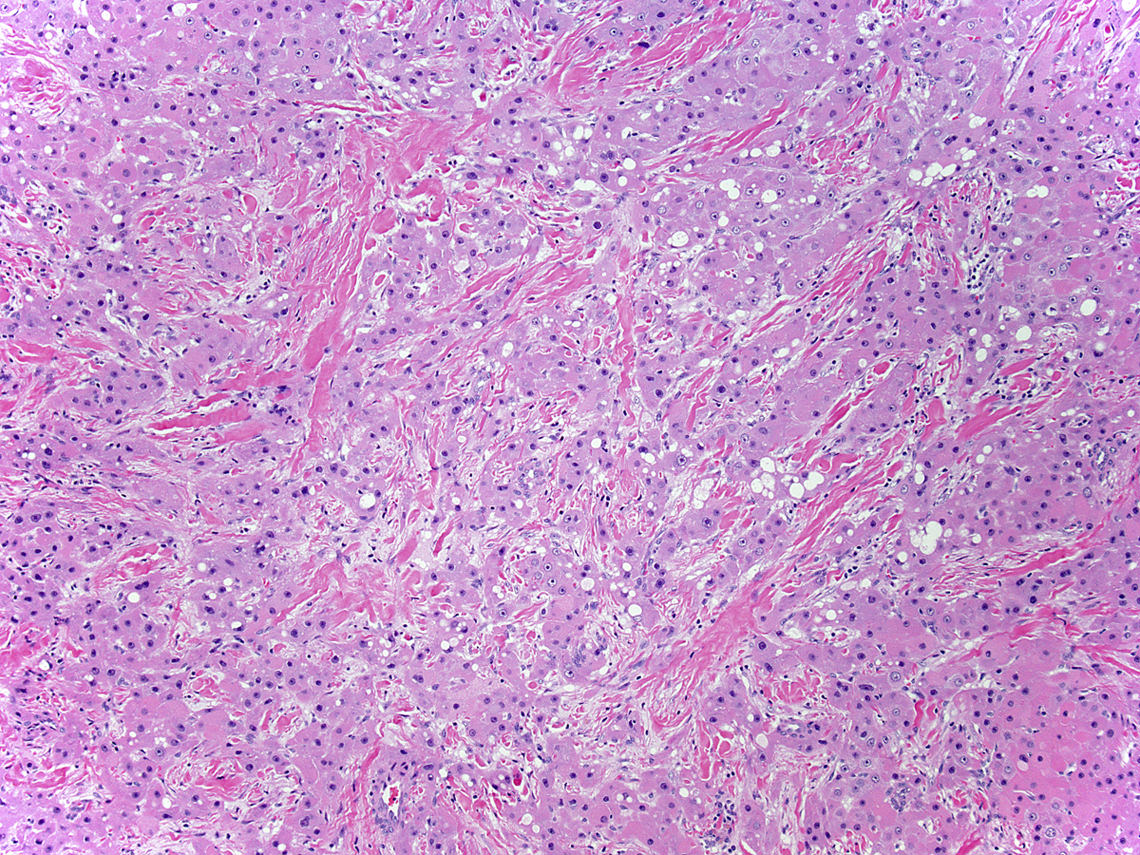
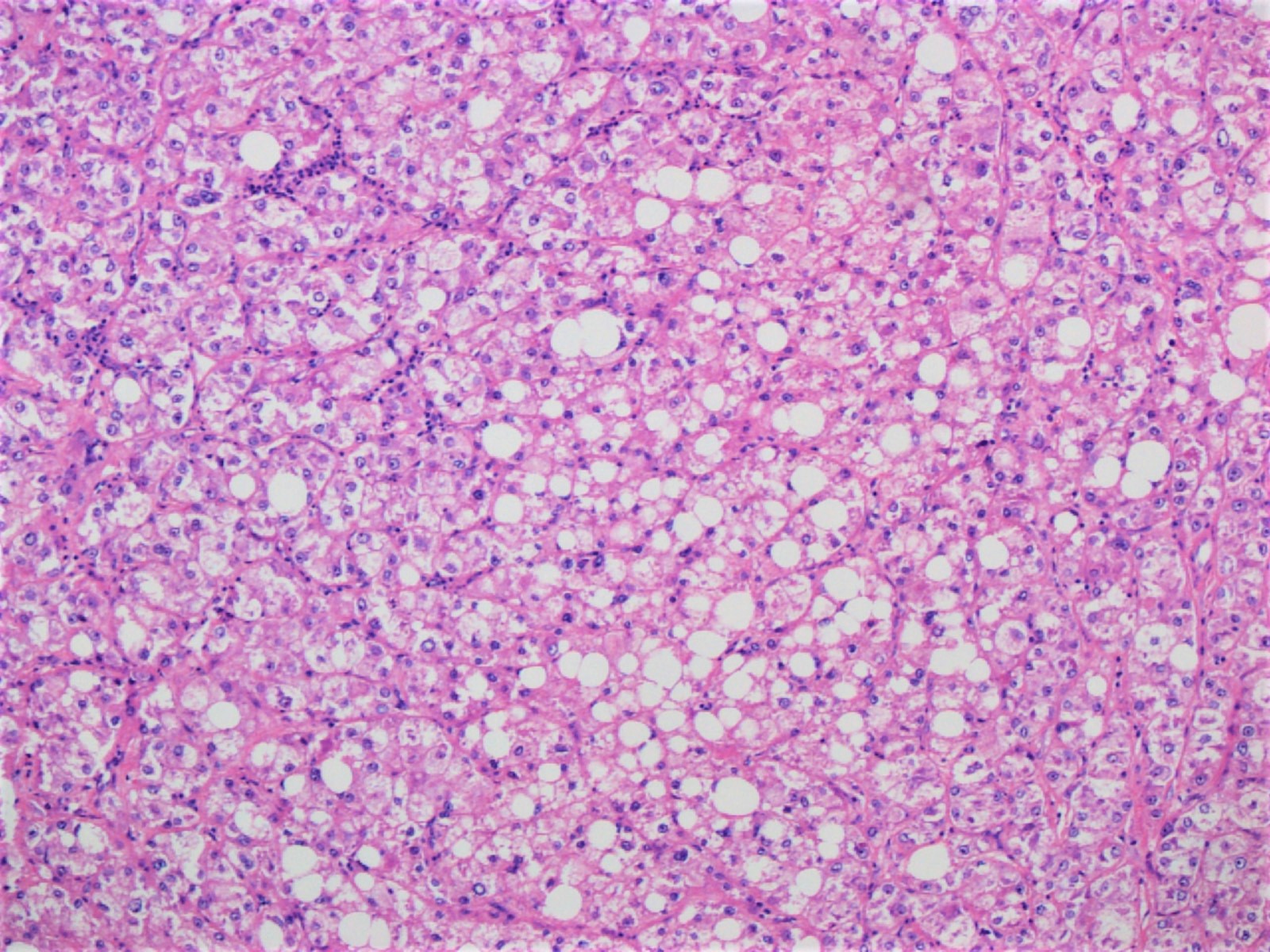
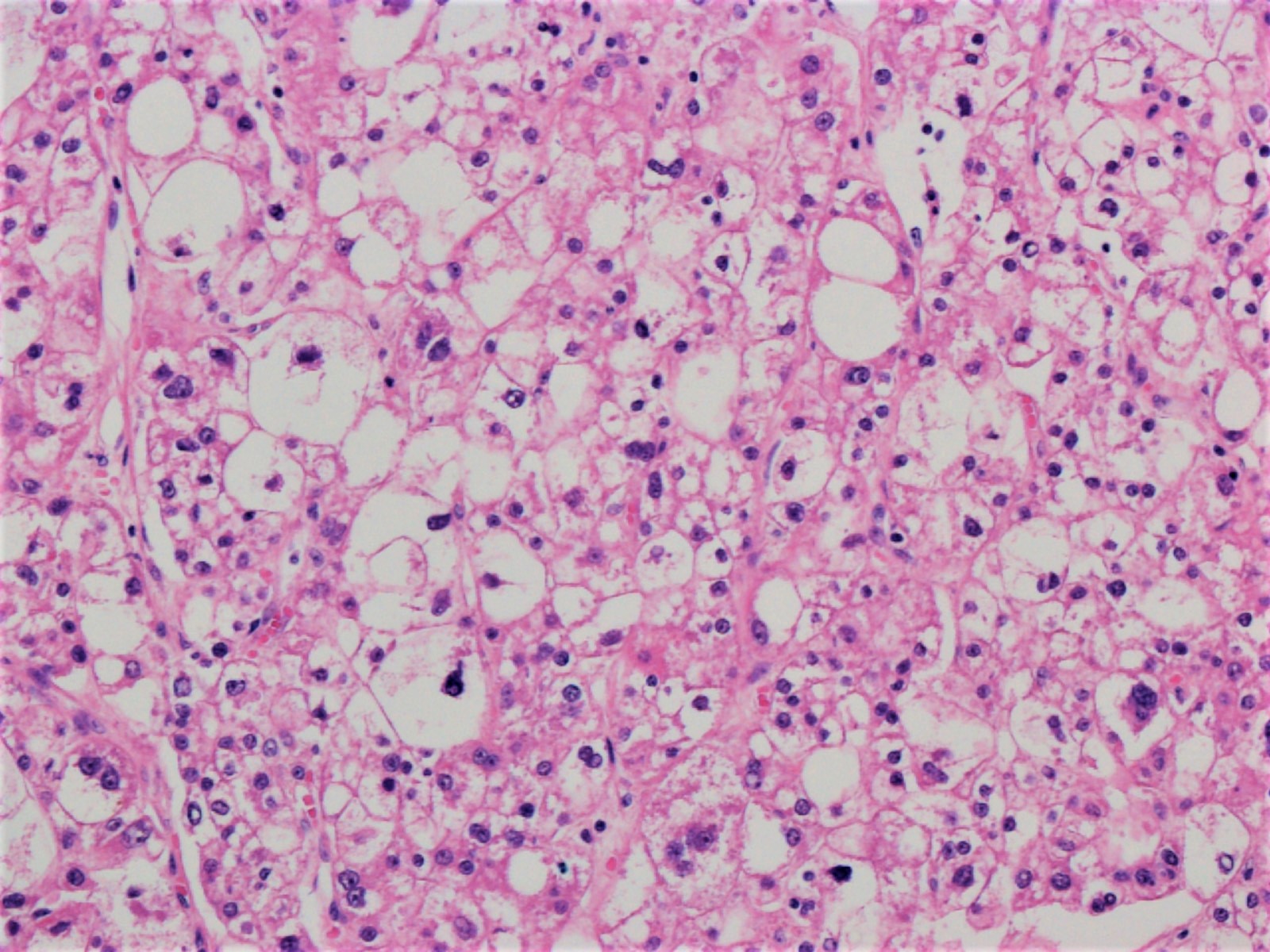
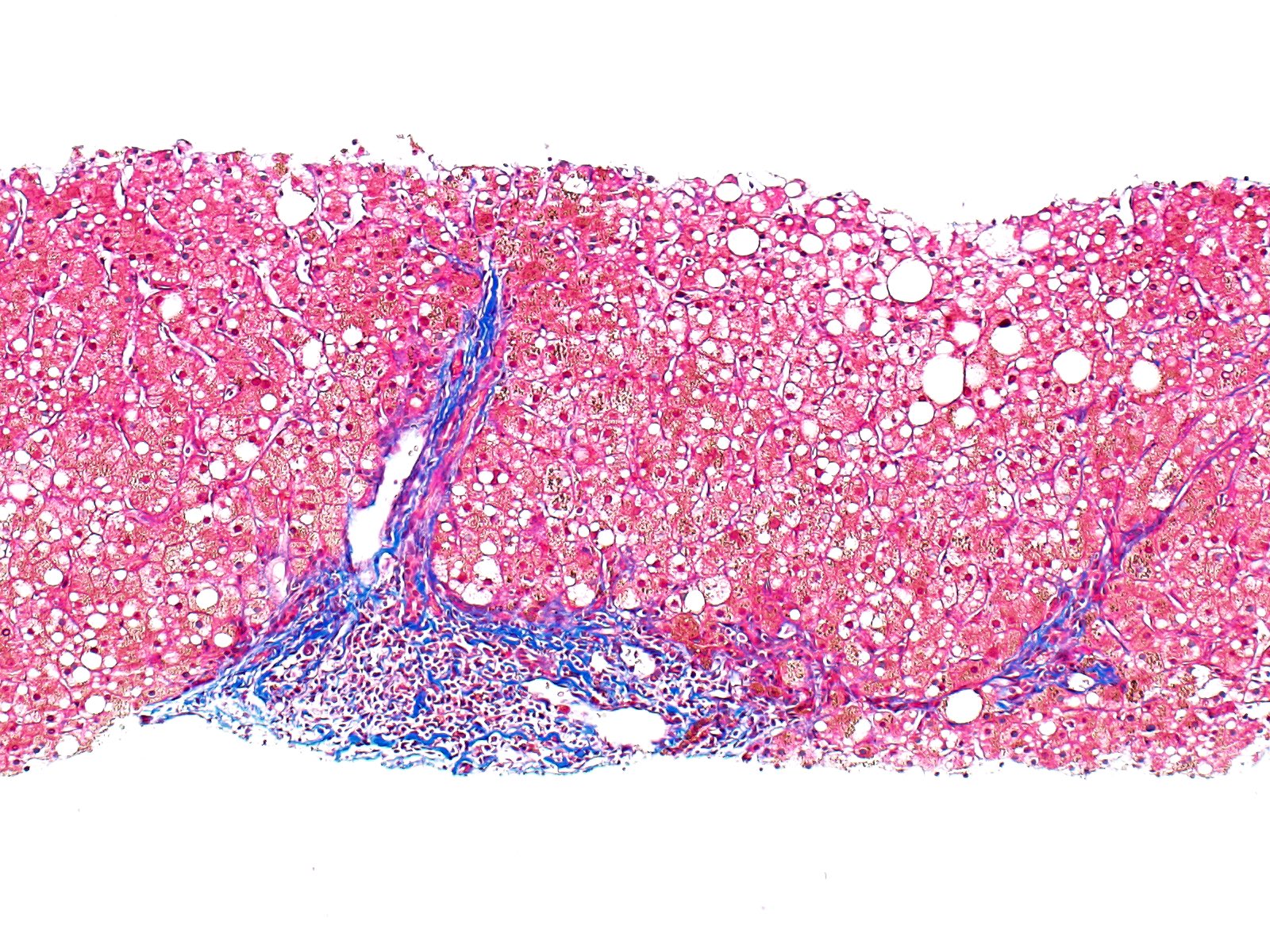
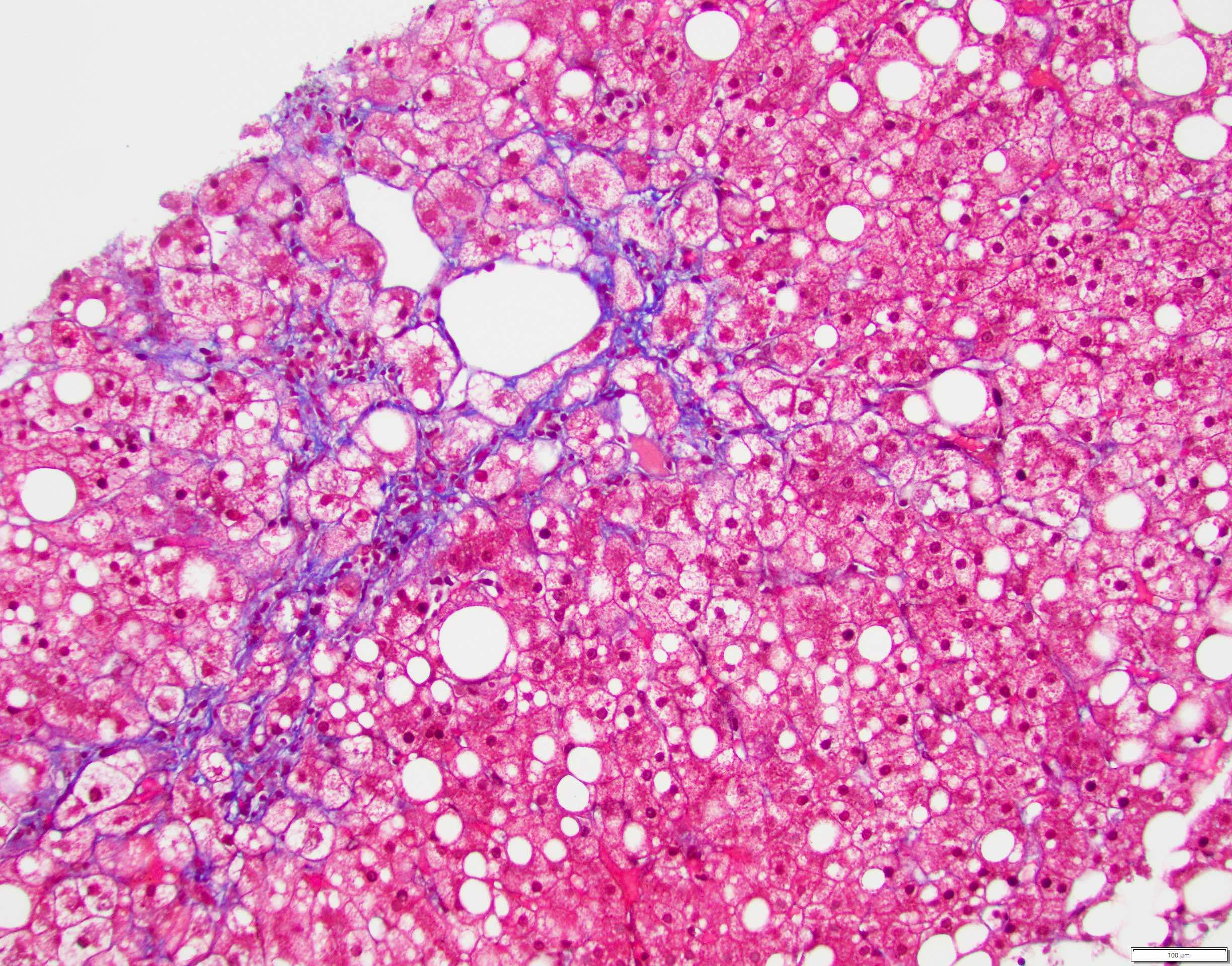
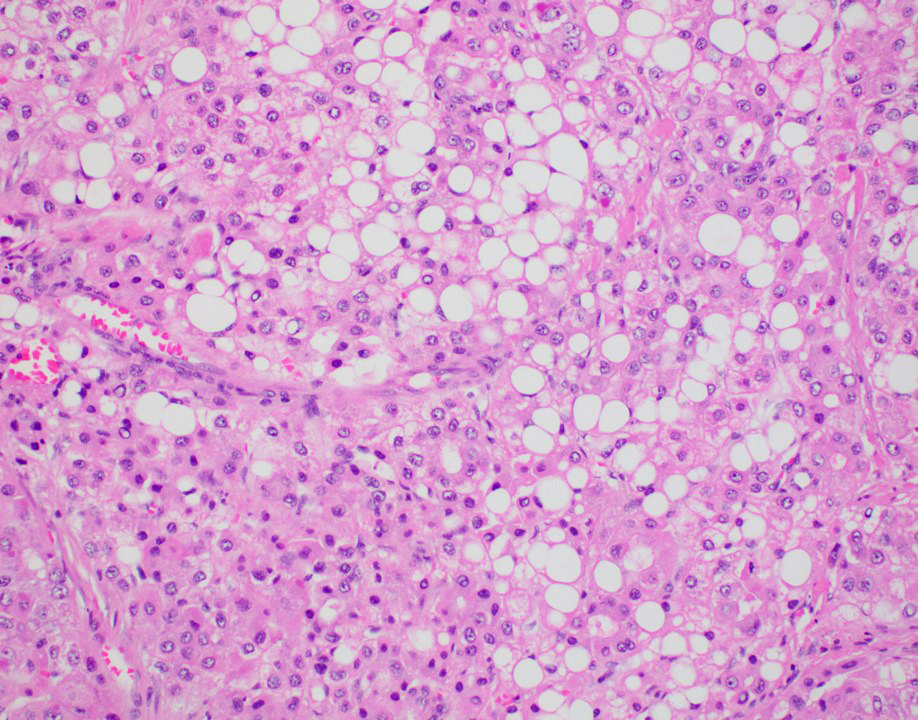
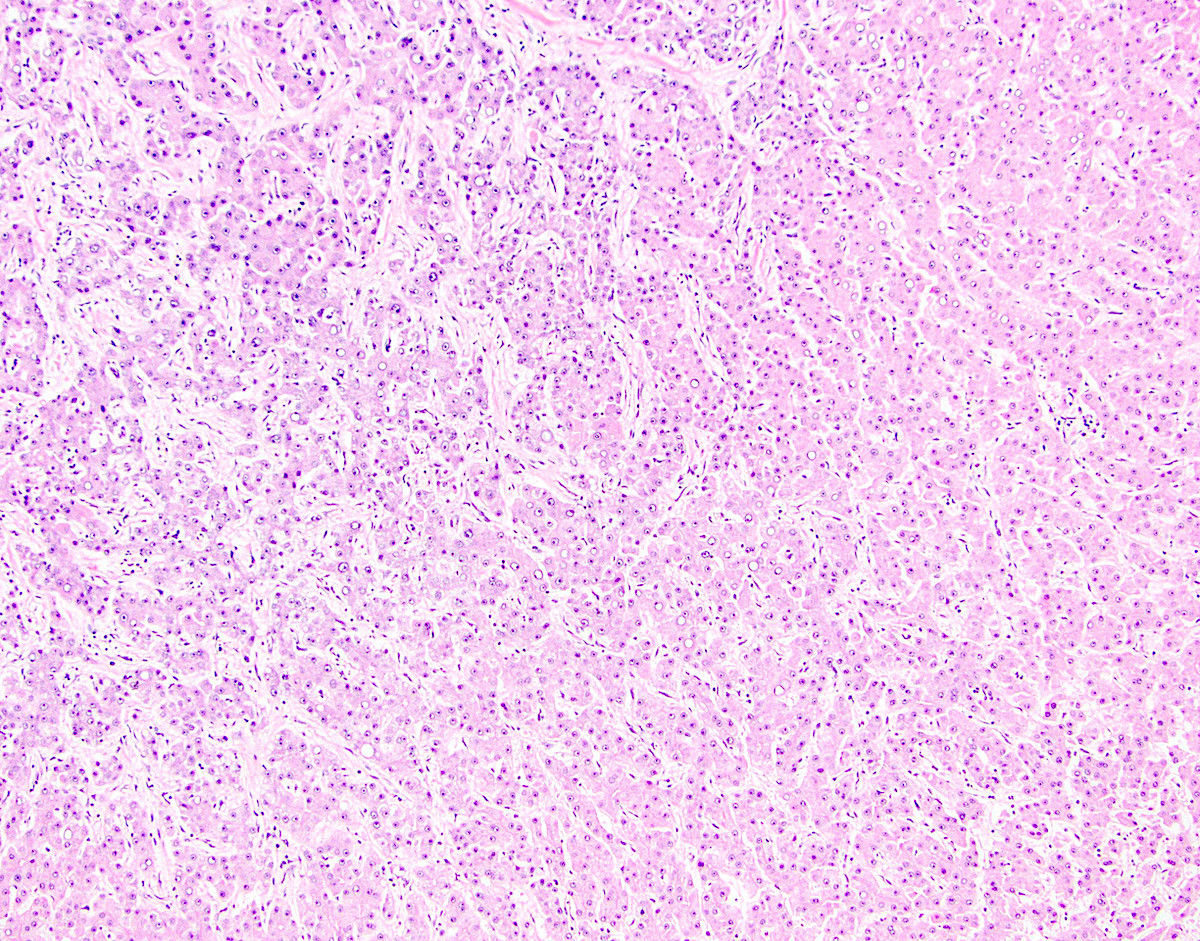
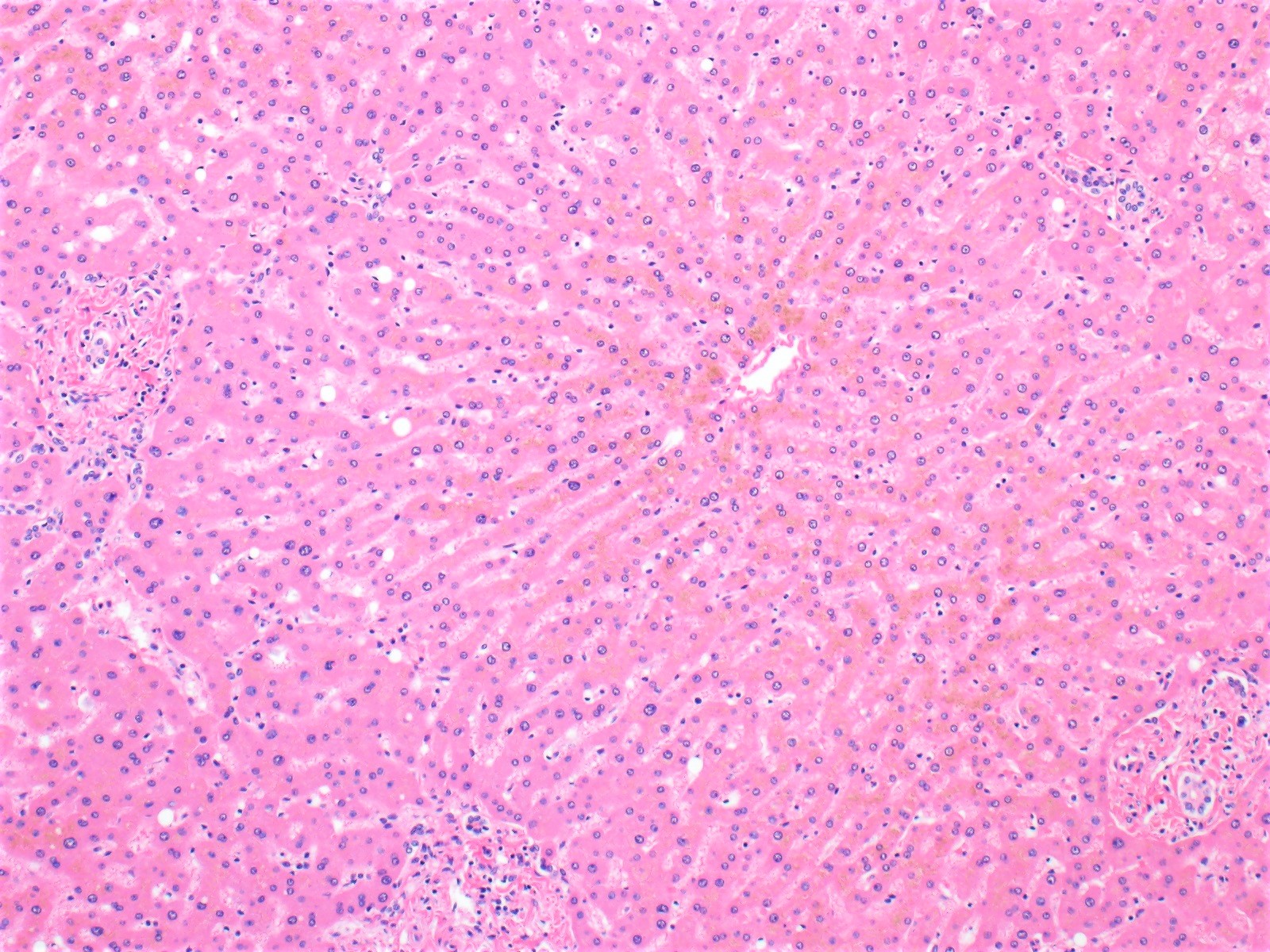
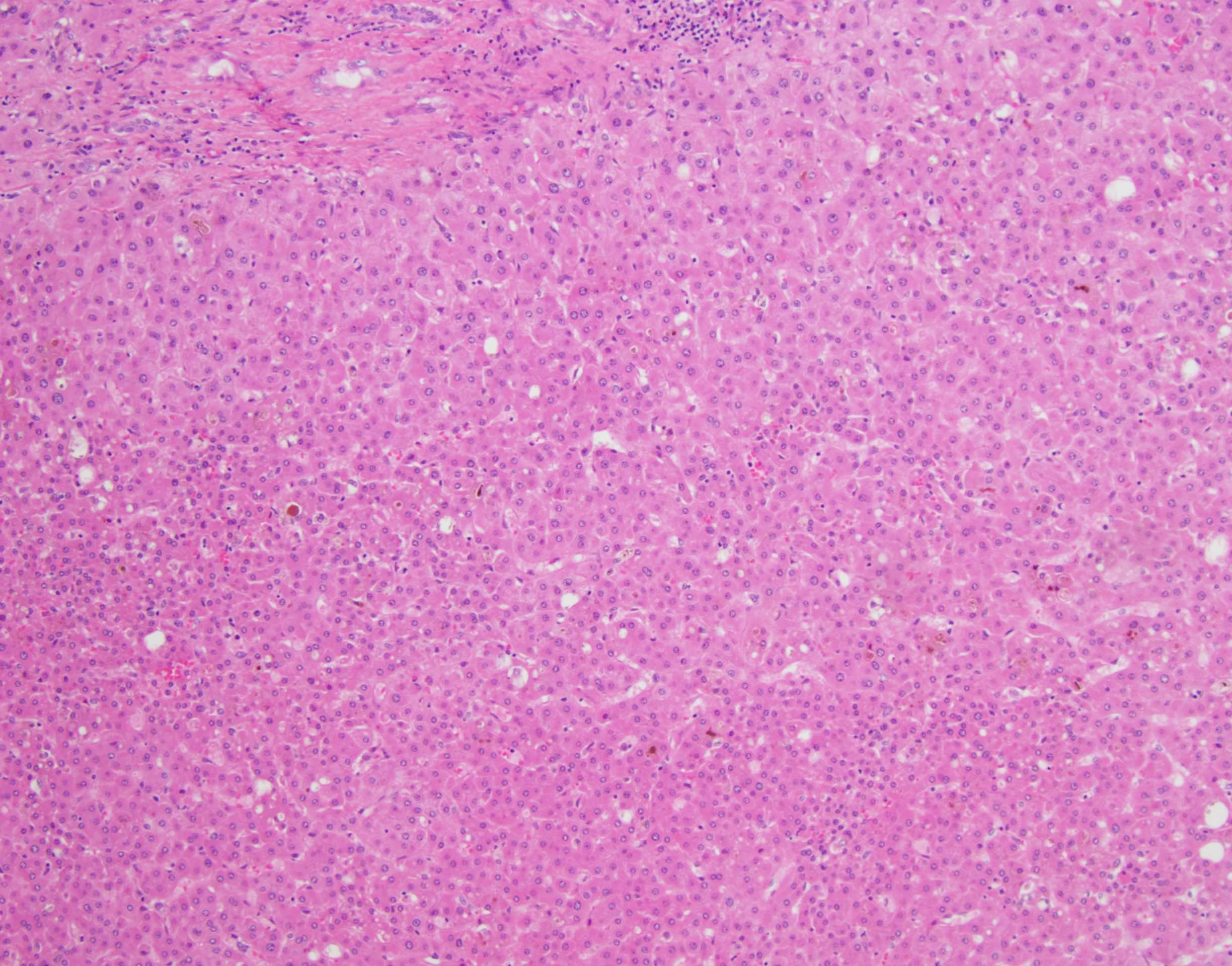
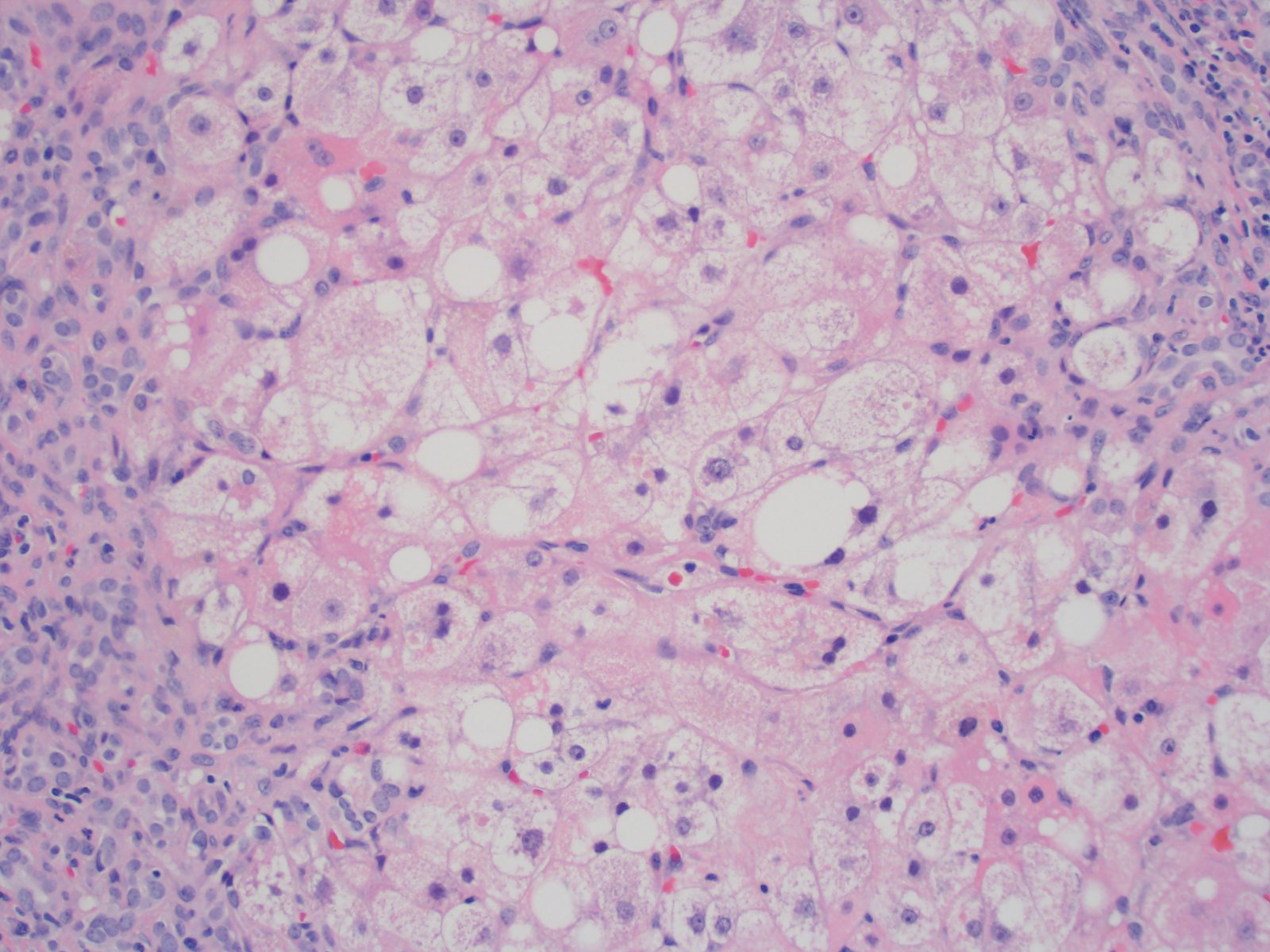
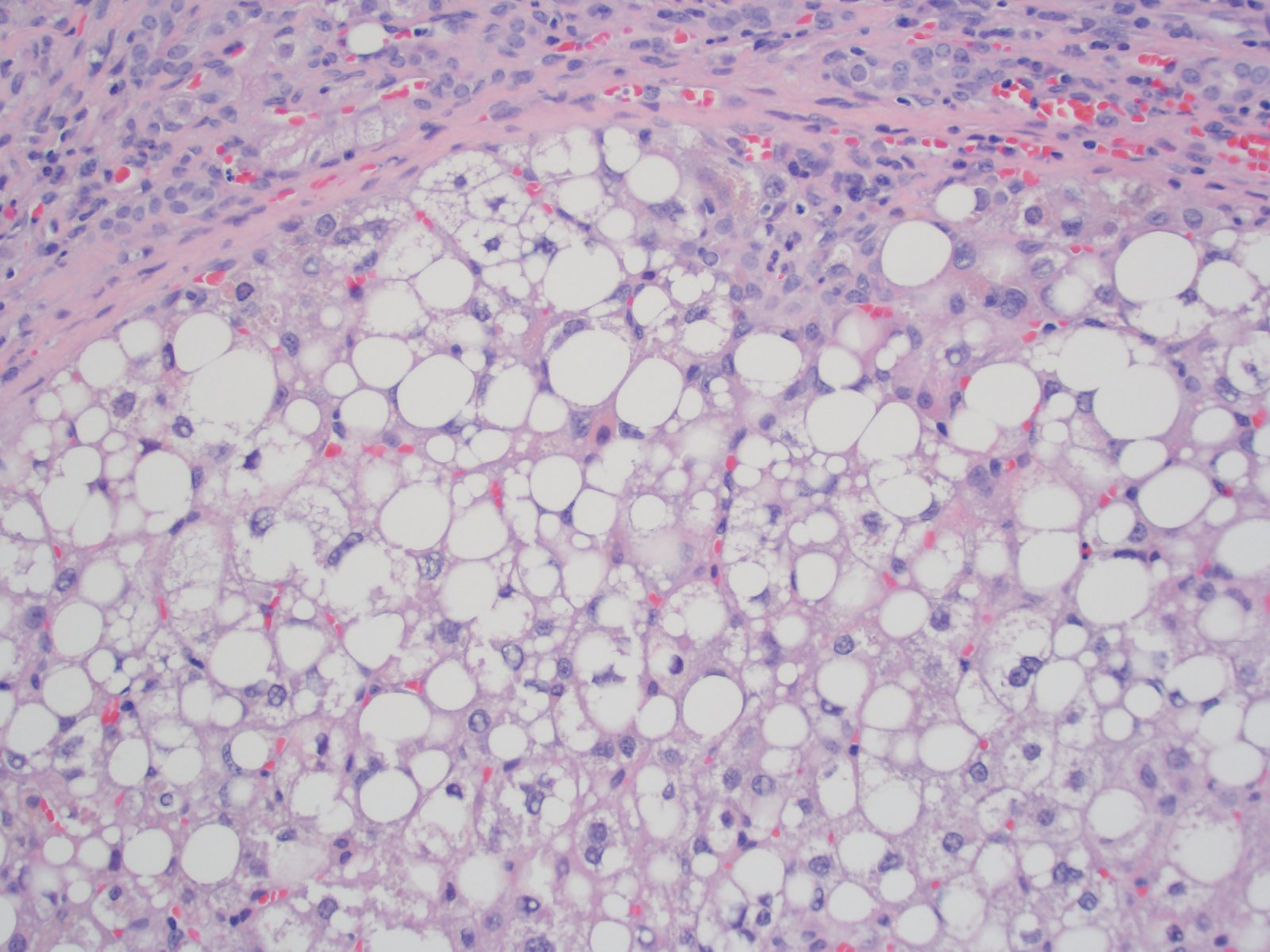
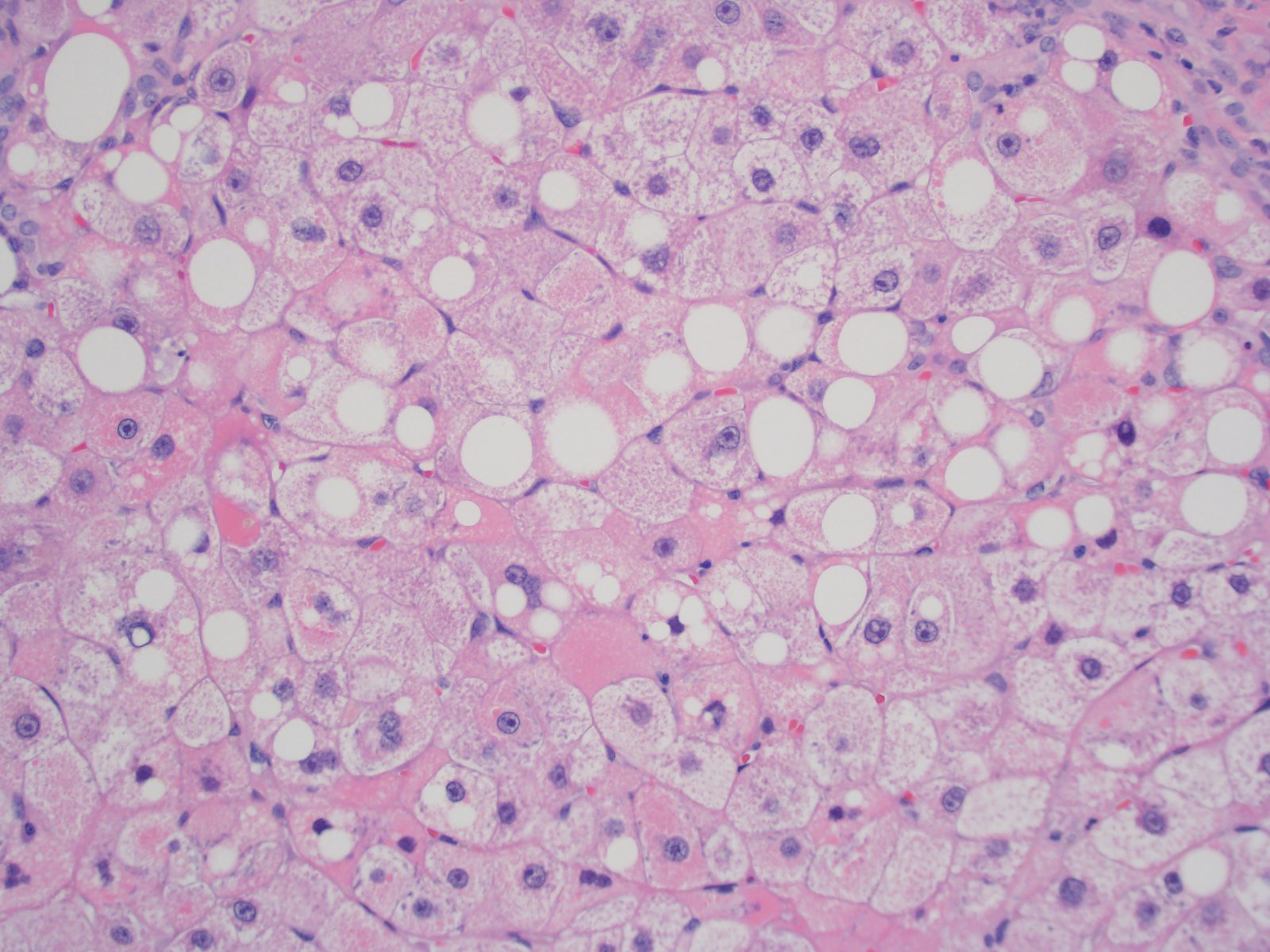
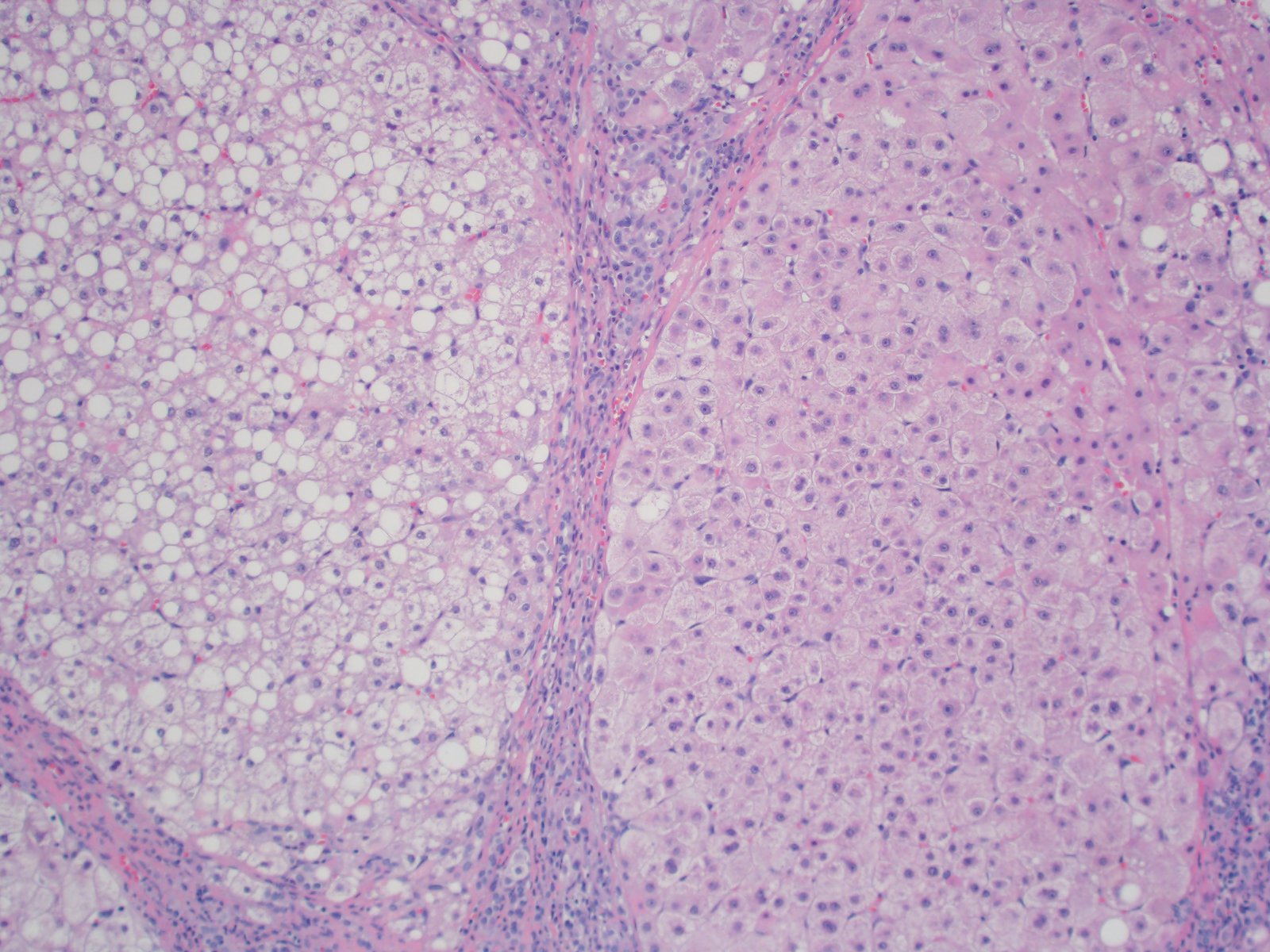
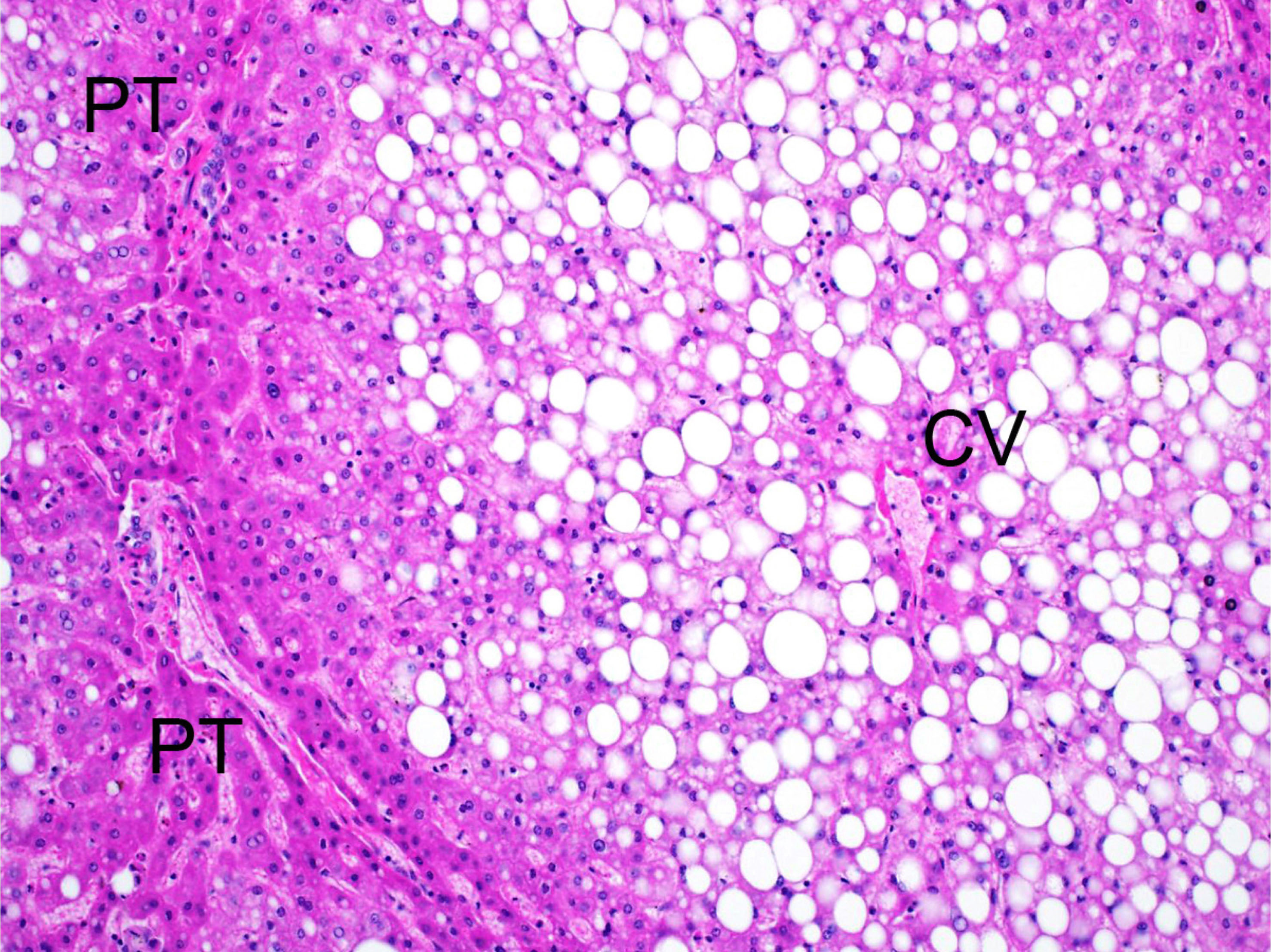
Microscopic (histologic) description
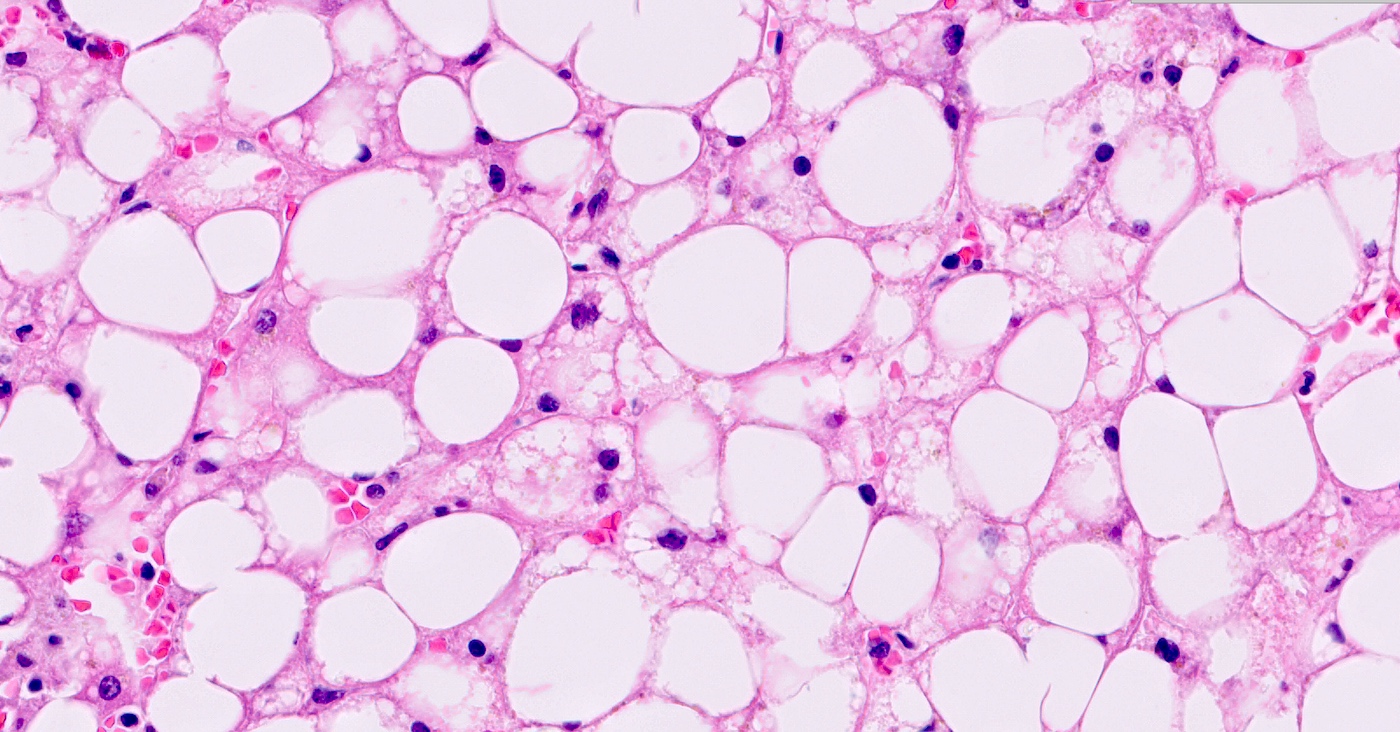
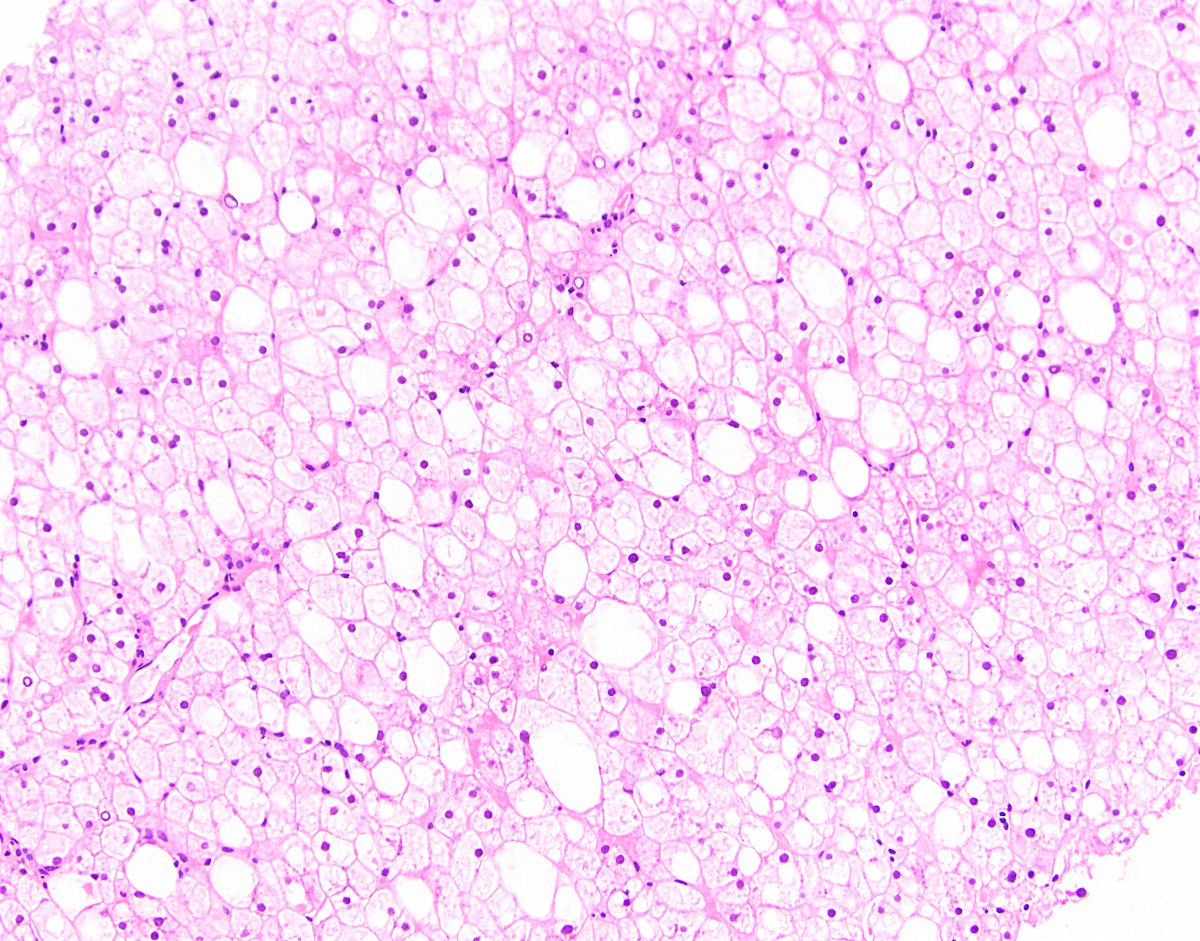
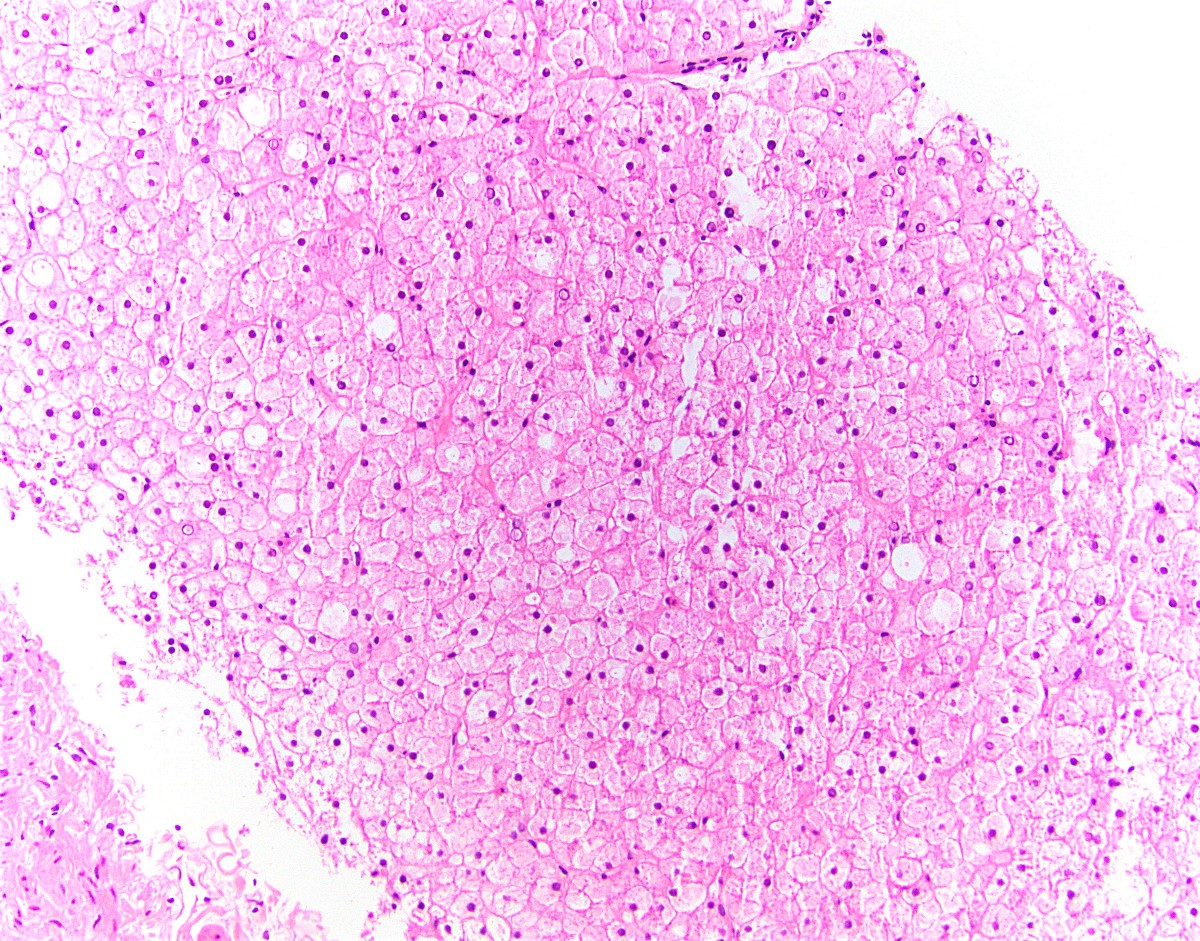
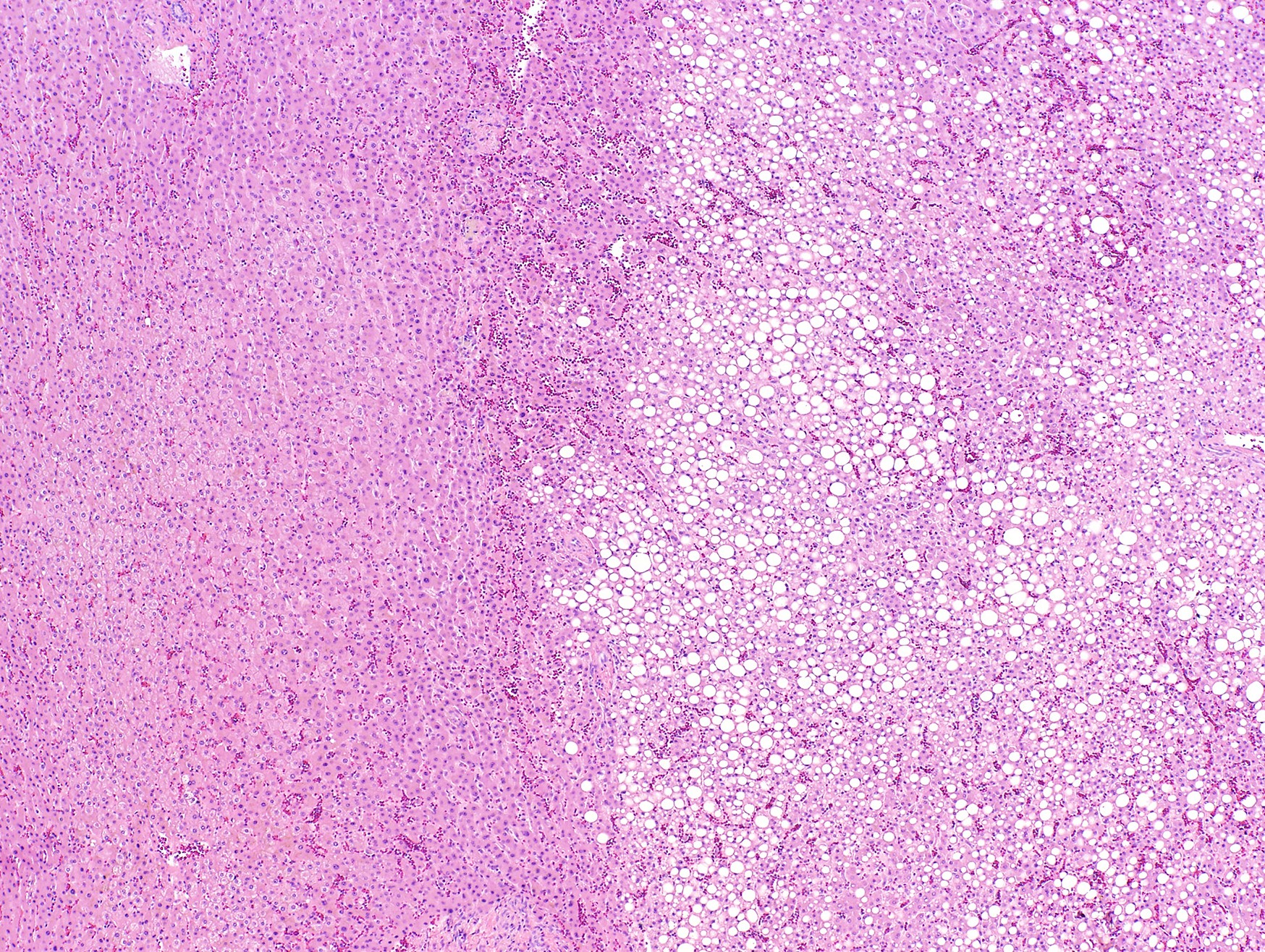
- Steatosis:
- Most common and earliest form of alcoholic liver disease
- Predominantly macrovesicular steatosis: large droplet (classical; a single large fat droplet displacing the nucleus to the periphery) and small / medium droplets
- First appears in perivenular region (zone 3) and spreads to other regions if drinking persists; may disappear within 1 month after alcohol cessation
- Whether it is a benign, nonprogressive lesion is controversial (J Hepatol 2012;57:399)
- Association between degree of steatosis and disease progression is also controversial
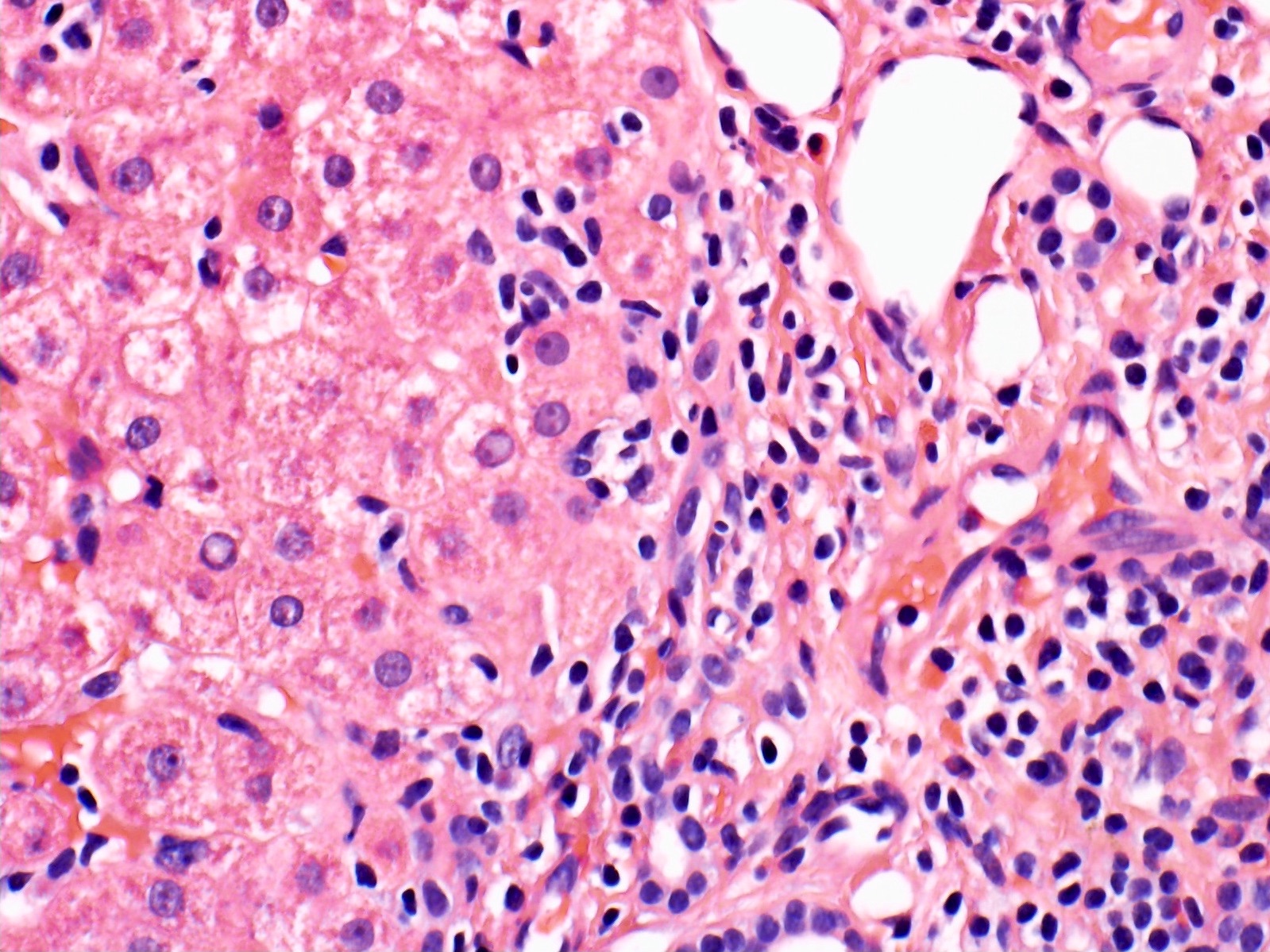
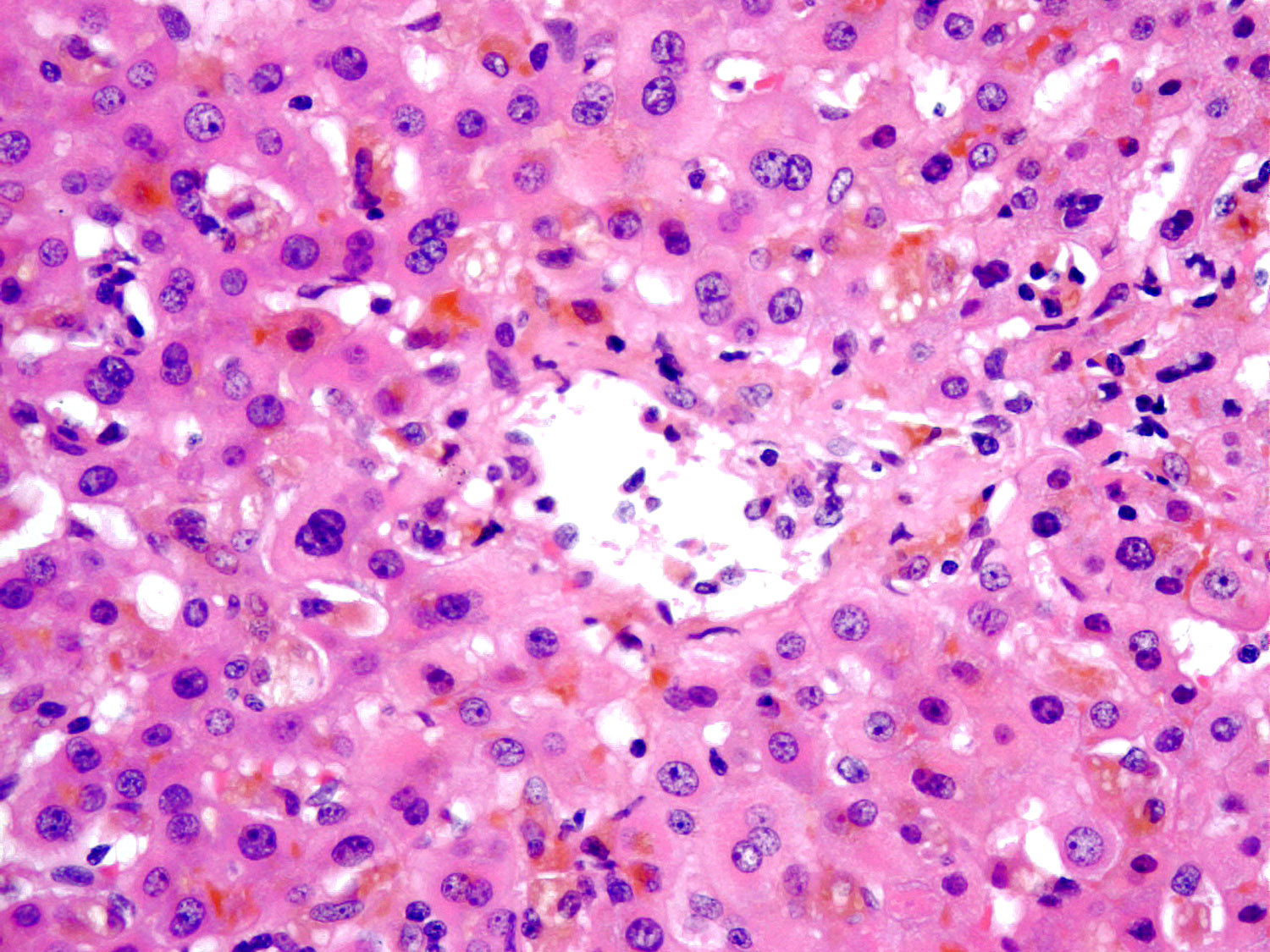
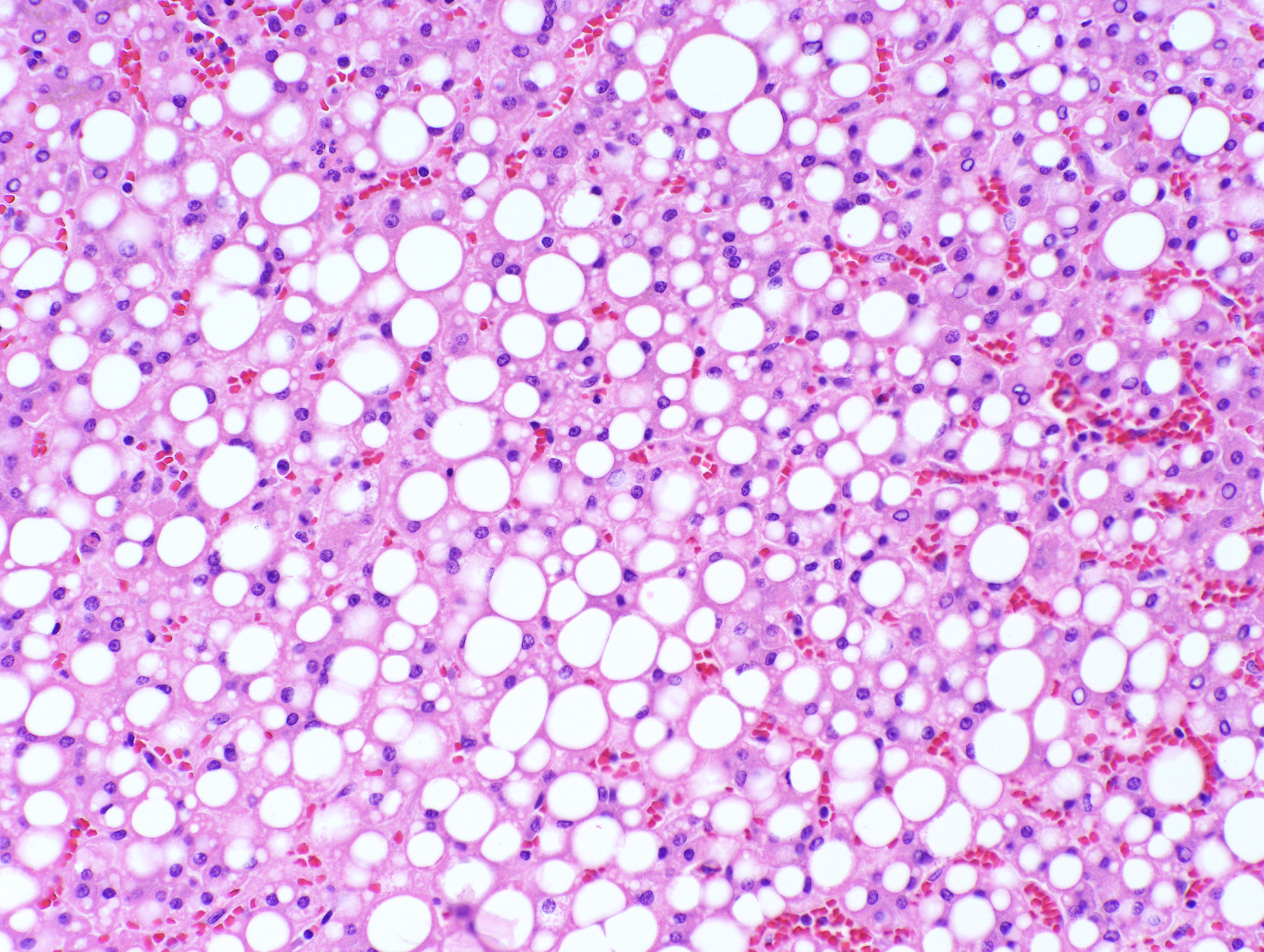
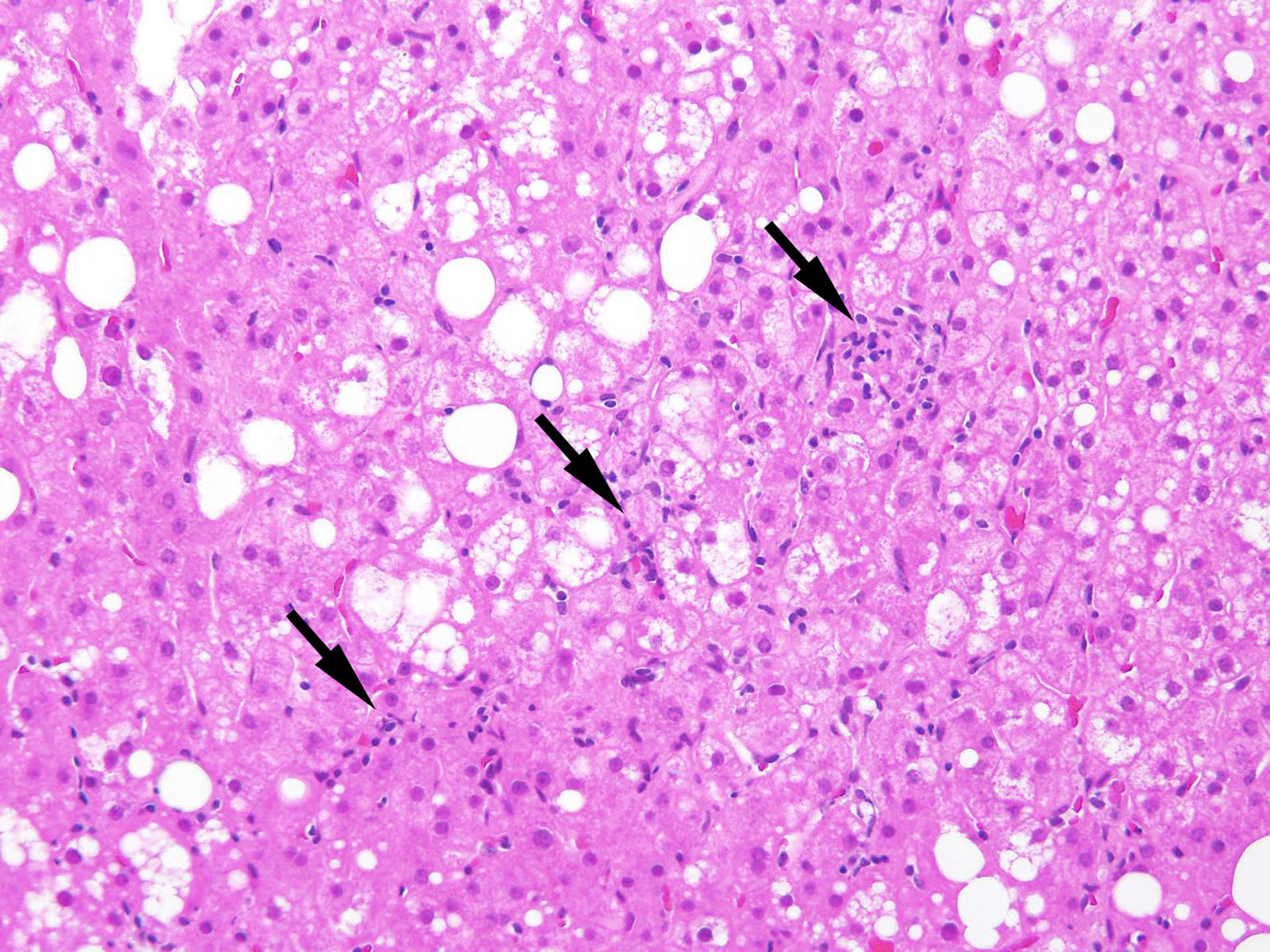
- Alcoholic steatohepatitis:
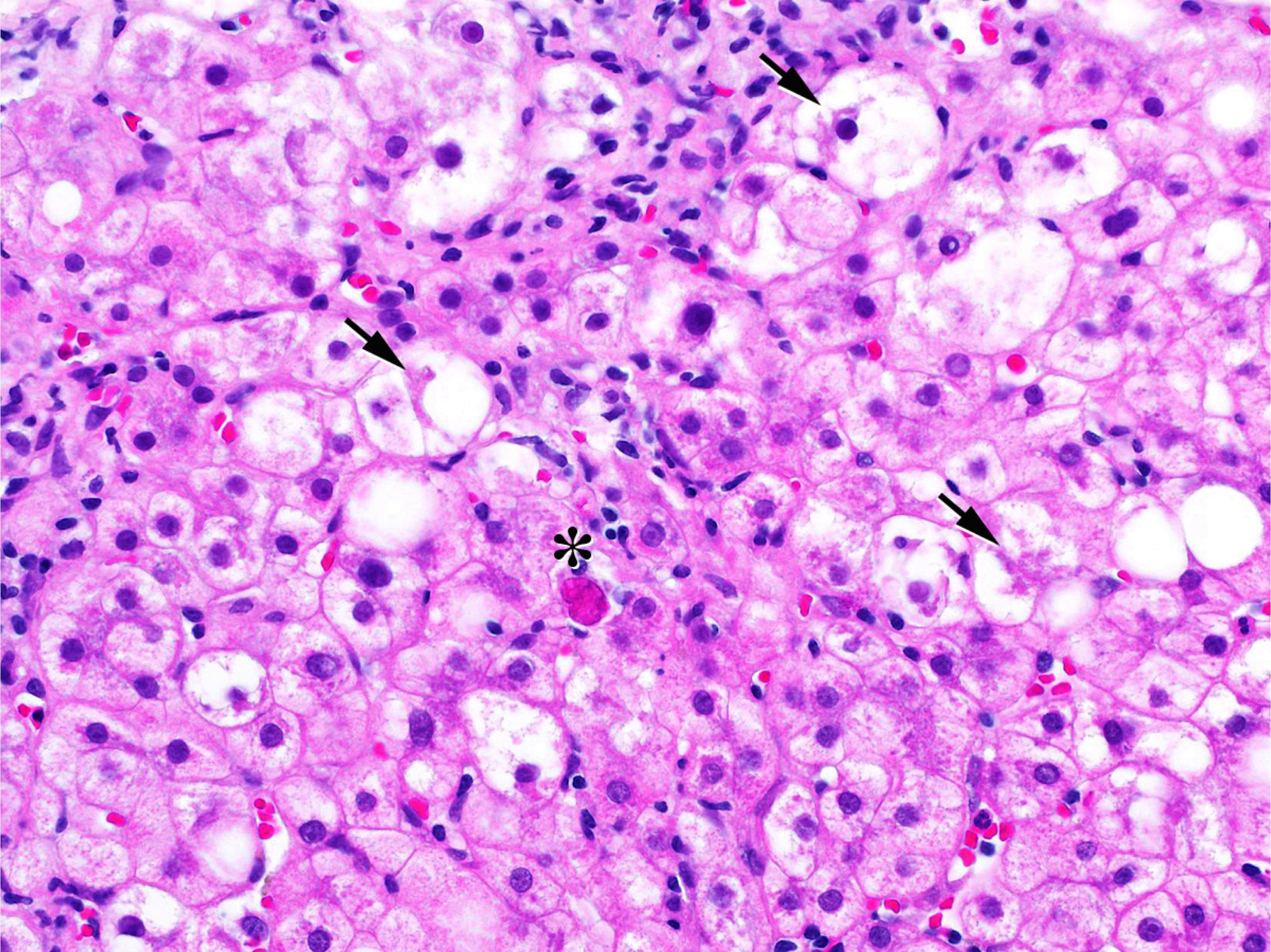
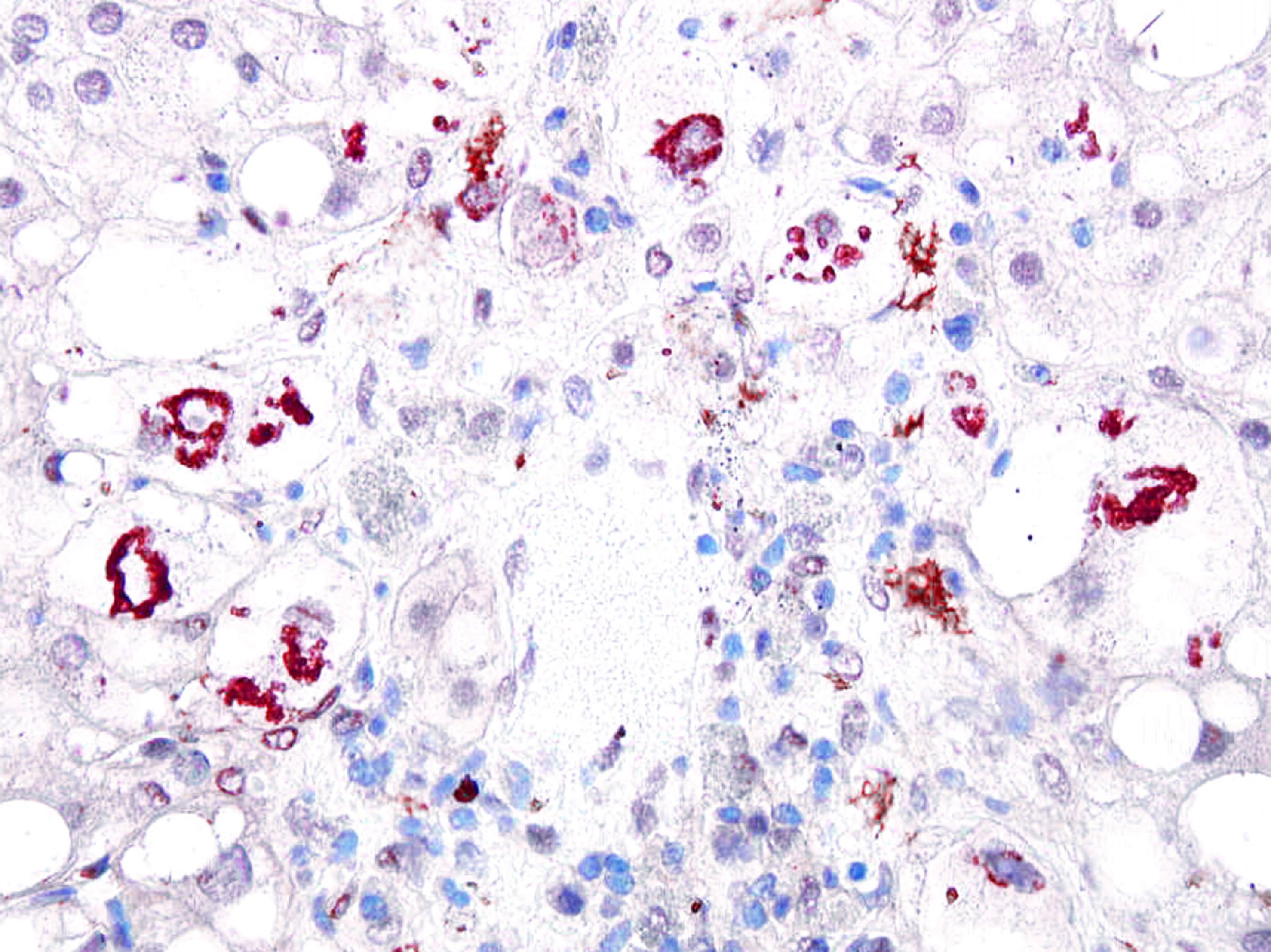
- Steatosis with inflammation and ballooning degeneration, which is the hallmark of hepatocellular injury in steatohepatitis
- Ballooning degeneration is characterized by cellular swelling, rarefaction of the hepatocytic cytoplasm and clumped strands of intermediate filaments
- Satellitosis is featured by ballooned hepatocyte surrounded by neutrophils
- Mallory-Denk body, also known as Mallory body or Mallory hyaline, is a deeply eosinophilic, ropy intracytoplasmic inclusion that represents aggregates of misfolded intermediate filaments with other different classes of proteins, including p62 and ubiquitin
- Often but not necessarily found in ballooned hepatocytes (Exp Cell Res 2007;313:2033)
- Persists for several months after cessation of drinking
- Associated with increased risk of progression to cirrhosis
- Fibrosis is not a necessary diagnostic feature; perivenular and pericellular (perisinusoidal) fibrosis is characteristic for fatty liver disease; as disease progresses, portal / periportal fibrosis, bridging fibrosis and cirrhosis will develop
- Alcoholic hepatitis histologic score is proposed to predict 90 day mortality based on 4 parameters: fibrosis, bilirubinostasis, neutrophilic infiltration and giant mitochondria (Gastroenterology 2014;146:1231)
- Alcoholic cirrhosis:
- Classically micronodular cirrhosis
- Steatosis and ballooned hepatocytes may burn out in advanced fibrosis or cirrhosis
- Other pathological lesions:
- Lipogranuloma
- Giant mitochondria: associated with recent heavy alcohol intake and disease progression (J Clin Pathol 1992;45:412)
- Acute foamy degeneration: rare, extensive microvesicular steatosis with no / minimal inflammatory activity; clinically presents with jaundice, abdominal pain and hepatomegaly (Gastroenterology 1983;84:683)
- Sclerosing hyaline necrosis: fibrous obliteration of terminal hepatic venule (phlebosclerosis) due to perivenular fibrosis; severe form of alcoholic hepatitis associated with noncirrhotic portal hypertension
- Iron deposition: usually mild; mainly in hepatocytes (grade 1 - 2) and occasionally in Kupffer cells
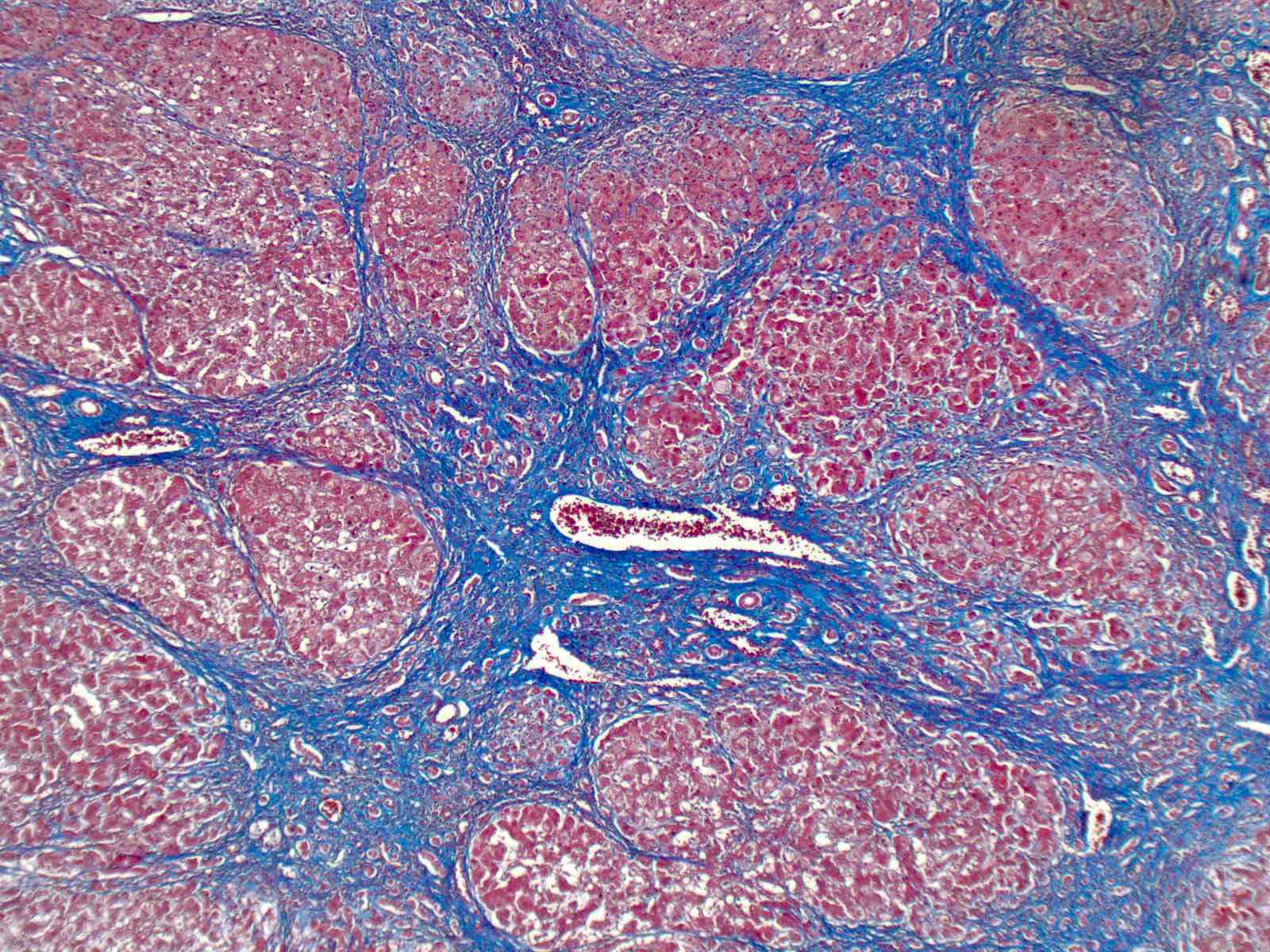
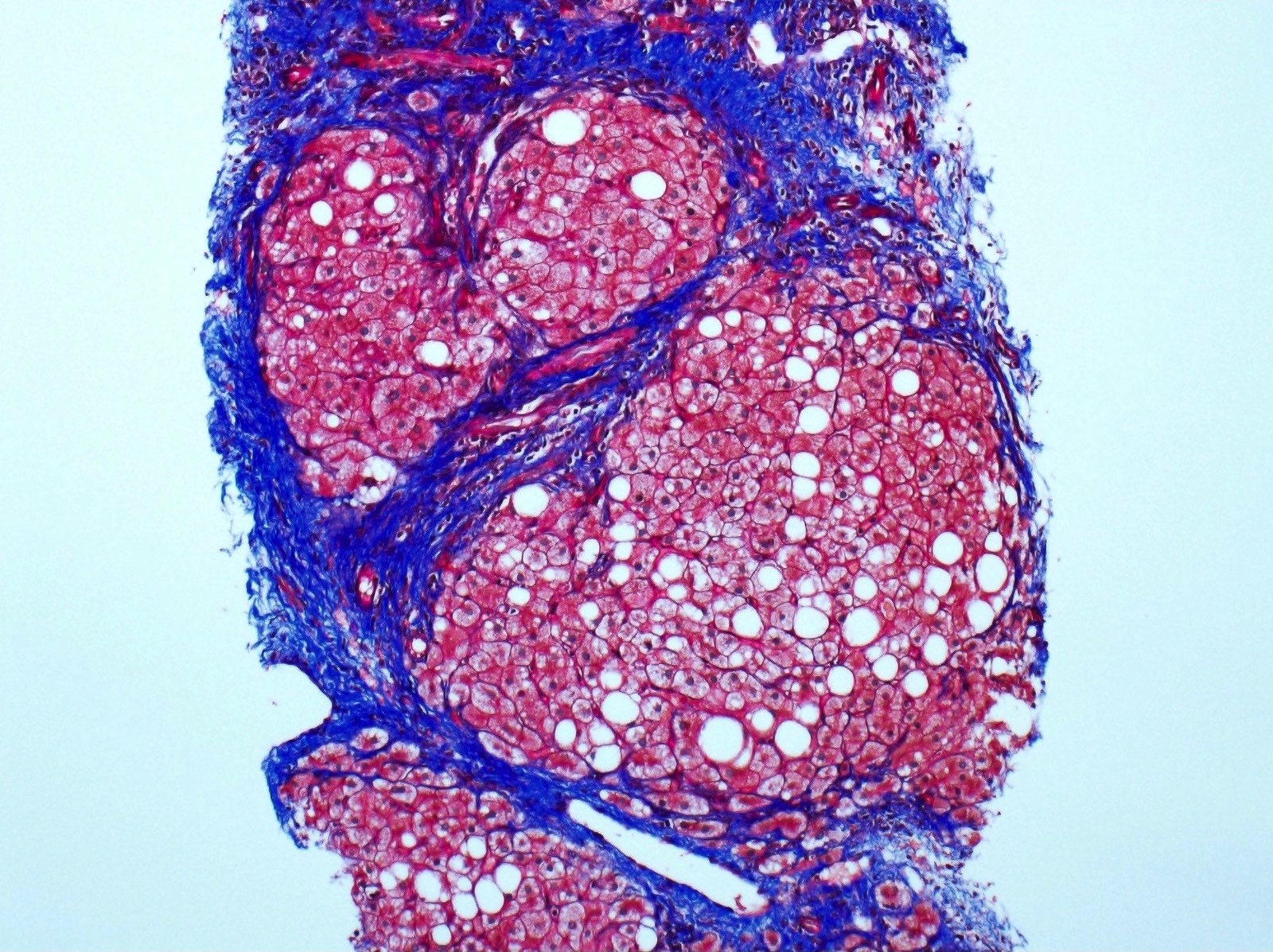
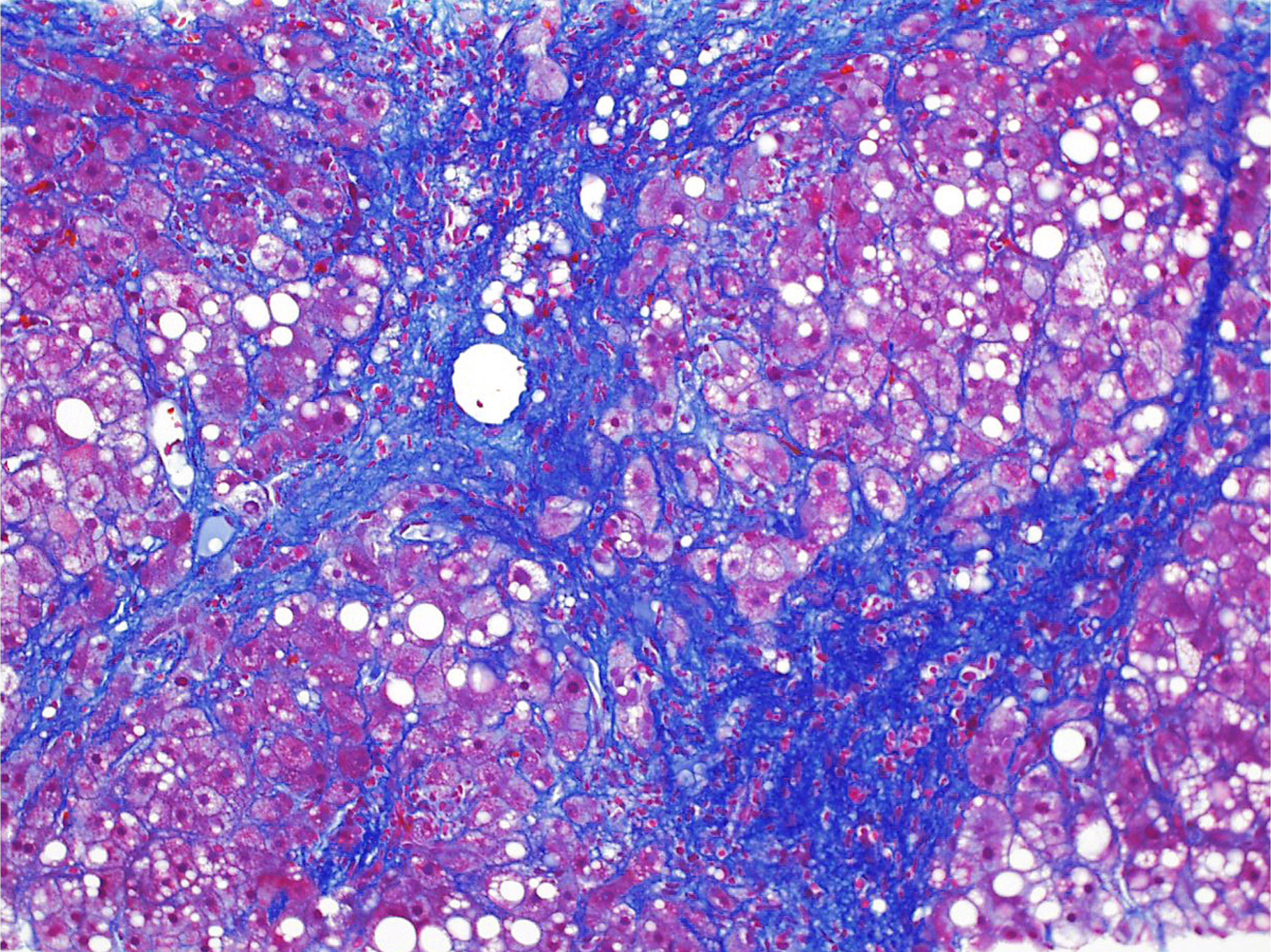
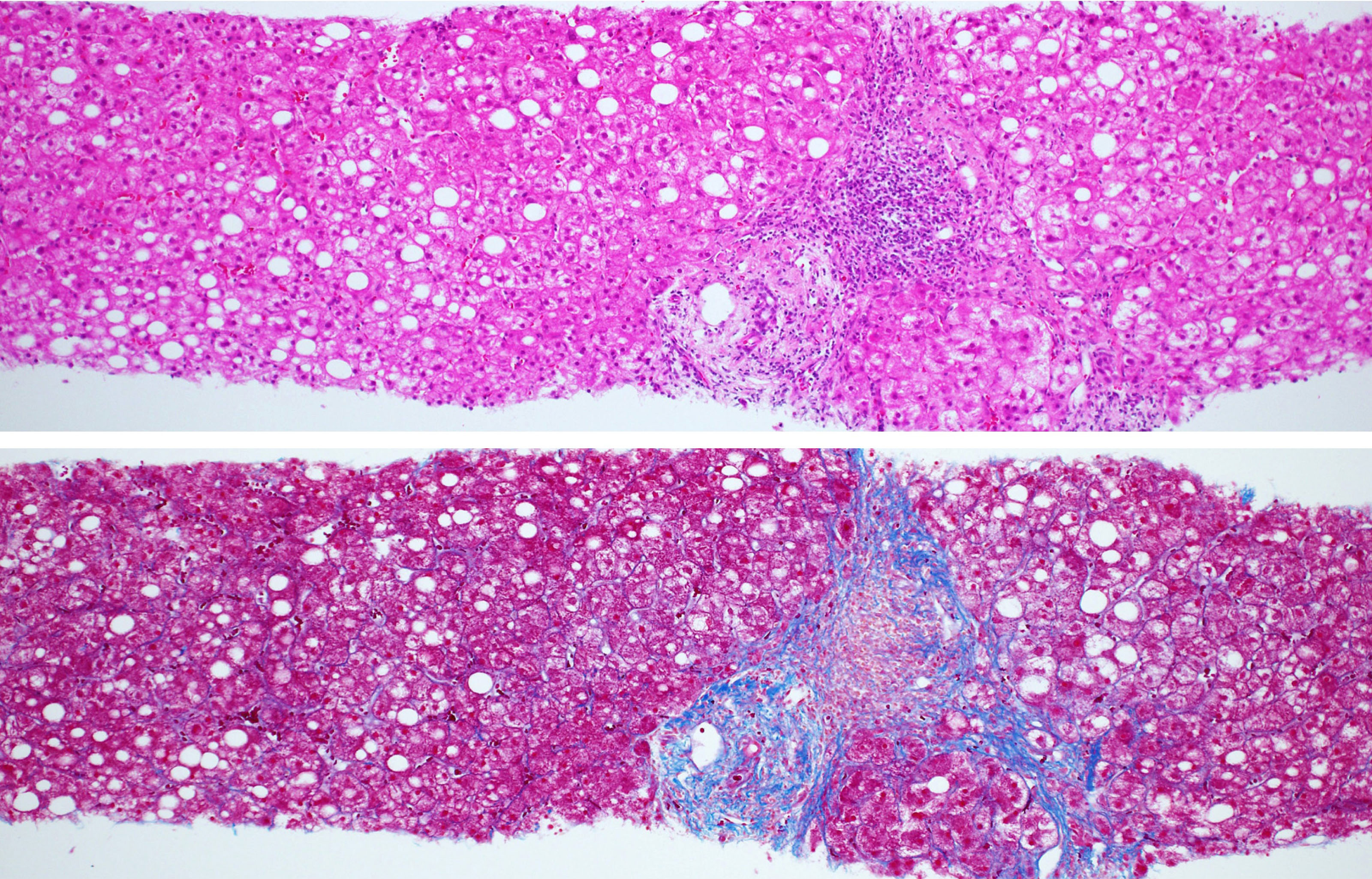
Microscopic (histologic) images
Virtual slides
Positive stains
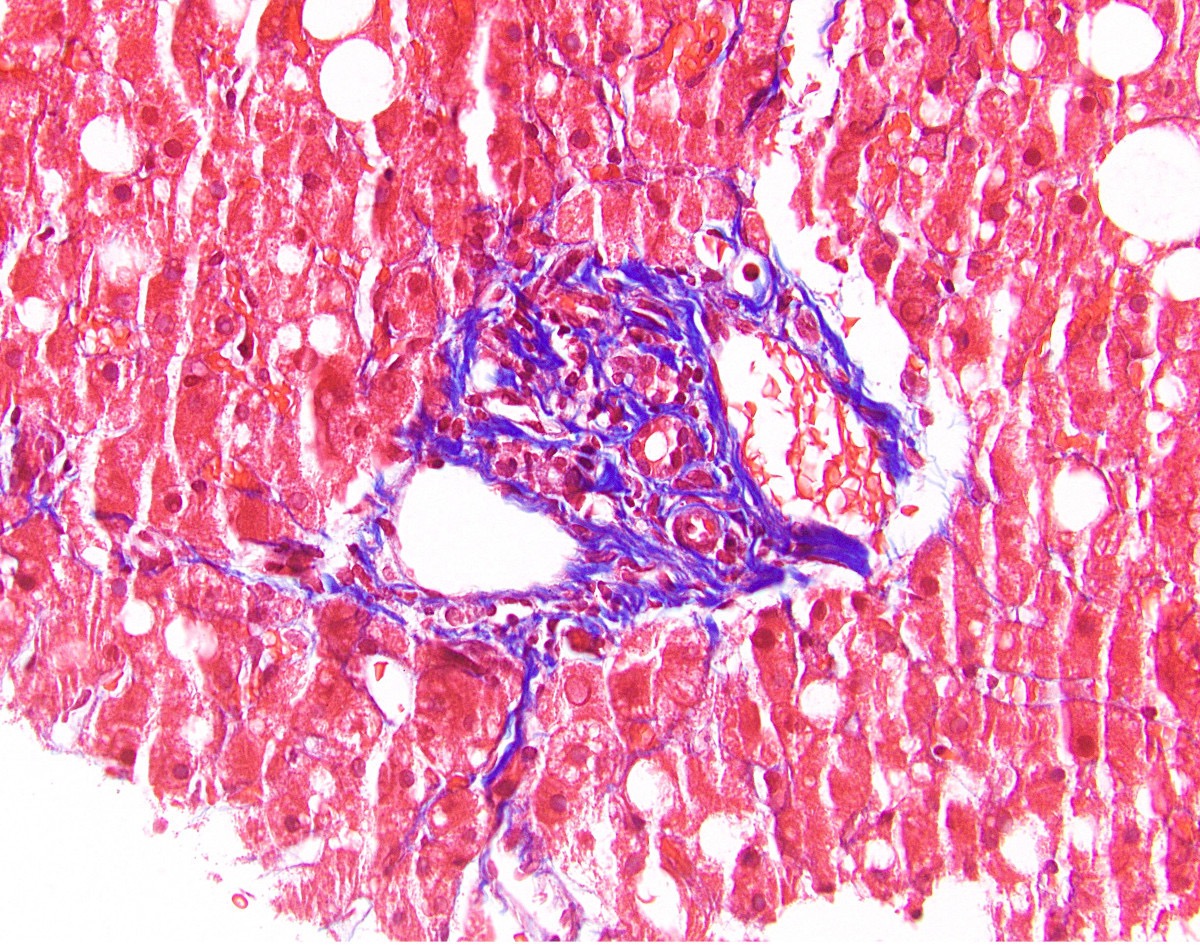
- Stains for collagen (Masson trichrome / Sirius red / reticulin): highlight perivenular and pericellular fibrosis
- Ubiquitin, p62, CK8/18: highlight Mallory-Denk bodies (Exp Cell Res 2007;313:2033)
Sample pathology report
- Liver, right lobe, biopsy:
- Moderate steatosis with perivenular and pericellular fibrosis (see comment)
- Negative for significant lobular necroinflammatory activity
- Negative for bridging fibrosis or cirrhosis
- Negative for malignancy
- Comment: In view of significant alcoholic consumption in absence of metabolic risks, the overall features are consistent with alcoholic steatosis.
- Liver, native, transplantation:
- Cirrhotic liver, clinically alcoholic cirrhosis
- Negative for significant steatosis, ballooning degeneration or Mallory-Denk bodies, consistent with abstinence
- Negative for dysplasia or malignancy
Differential diagnosis
- Chronic viral hepatitis C:
- Steatosis is typically mild at most
- Presence of lymphocyte predominant portal inflammation, portal lymph follicle, bead-like sinusoidal lymphocyte infiltration and mild bile duct injury differentiates hepatitis C from alcoholic liver disease
- Drug induced liver injury (e.g., amiodarone, glucocorticoids, methotrexate, synthetic estrogens, tamoxifen)
- Nonalcoholic fatty liver disease:
- Pathologically almost indistinguishable from alcoholic liver disease
- Alcoholic liver disease has few specific pathological changes and all are rare:
- Acute foamy degeneration
- Sclerosing hyaline sclerosis
- Acute / chronic cholestasis and sinusoidal obstruction syndrome
- Alcoholic liver disease tends to have more Mallory-Denk bodies and giant mitochondria, much less glycogenated nuclei and has satellitosis (ballooned hepatocyte surrounded by neutrophils), although all of these are nonspecific
- Key distinguishing feature is in fact the amount of alcohol consumption obtained from clinical history
- Consumption of 2 standard drinks/day for men and 1 standard drink/day for women is endorsed as the acceptable threshold to define nonalcoholic
- Wilson disease:
- Mild steatosis, glycogenated nuclei and Mallory-Denk bodies
- Deposition of copper associated protein (particularly in hepatocytes out of periportal region) differentiates Wilson disease from alcoholic liver disease
- Other uncommon inherited metabolic diseases
Board review style question #1
Which of the following histological features is useful to differentiate alcoholic liver disease from nonalcoholic fatty liver disease?
- Acute foamy degeneration
- Ballooning degeneration
- Mallory-Denk body
- Satellitosis
- Severe steatosis
Board review style answer #1
A. Acute foamy degeneration. Acute foamy degeneration (diffuse microvesicular steatosis) is a rare presentation of severe acute alcoholic hepatitis presenting with jaundice and hepatomegaly. Rapid recovery occurs on abstinence from alcohol. Diffuse microvesicular steatosis is not a histological feature of nonalcoholic fatty liver disease.
Comment Here
Reference: Alcoholic liver disease
Comment Here
Reference: Alcoholic liver disease
Board review style question #2
Board review style answer #2
E. p62. The highlighted structures are Mallory-Denk bodies, which are misfolded and aggregated intermediate filaments combined with other different classes of proteins, including p62 and ubiquitin. They are immunoreactive to CK8/18, p62 and ubiquitin.
Comment Here
Reference: Alcoholic liver disease
Comment Here
Reference: Alcoholic liver disease
Alpha-1 antitrypsin deficiency
Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Electron microscopy description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Genetic metabolic disorder causing deficiency of alpha-1 antitrypsin deficiency (AAT) and leading to disease in the lungs and liver
Essential features
- Different phenotypes have different clinical presentations
- Should be included in the differential diagnosis for all cases of early onset cirrhosis
- PASD and AAT positive eosinophilic intracytoplasmic globules within hepatocytes
- Absence does not rule out AAT deficiency
ICD coding
- ICD-10: E88.01 - Alpha-1 antitrypsin deficiency
Epidemiology
- Age at diagnosis: 20 - 50 (Methods Mol Biol 2017;1639:9)
- Smoking: younger age at presentation
- Infants (small subset of patients)
- Caucasian / Northern European descent (Methods Mol Biol 2017;1639:9)
- M = F (Methods Mol Biol 2017;1639:9)
- Genetic mutation: codominant inheritance (see Etiology)
Sites
- Liver
- Lungs
Pathophysiology
- AAT is a serine proteinase inhibitor
- From the serpin superfamily
- Secreted by hepatocytes (primary source) and also epithelial cells in the lung and GI tract, neutrophils and macrophages (Trends Mol Med 2014;20:116)
- AAT structure = beta pleated sheets and alpha helices (Methods Mol Biol 2017;1639:9, Mutat Res 2017 Jul;773:14)
- Normal process (Methods Mol Biol 2017;1639:9):
- Folding and glycosylation occur in the endoplasmic reticulum, which allows for export from the cell
- Reactive loop of AAT is cleaved by proteinase binding
- Cleaved reactive loop binds to the beta sheet
- Mutated process (Methods Mol Biol 2017;1639:9, Mutat Res 2017 Jul;773:14, Trends Mol Med 2014;20:116):
- Mutation causes a change in the tertiary structure
- Noncleaved reactive loops from AAT can bind to other beta sheets, resulting in molecular linkage
- Process is called loop sheet polymerization
- Misformed AAT cannot be exported from the cell
- Leads to AAT accumulation and endoplasmic reticulum stress response
Etiology
- AAT encoded by SERPINA1 gene located on chromosome 14 (Methods Mol Biol 2017;1639:9, Trends Mol Med 2014;20:116)
- Multiple genetic variants:
- "M" = wild type allele
- "Z" and "S" = most common mutant alleles (Methods Mol Biol 2017;1639:9)
- "Z" mutant allele accounts for 90% of disease (Methods Mol Biol 2017;1639:9)
- Numerous other rare alleles (J Biol Chem 1995;270:16864)
- Mmalton, etc.
- 4 phenotypes (Methods Mol Biol 2017;1639:9, Orphanet J Rare Dis 2008;3:16):
- Normal = normal function and plasma levels of AAT
- "M" phenotype (PiMM)
- Present in > 99% of world population
- Deficient = abnormal function and low plasma levels of AAT
- Mutant phenotype with "Z" or "S" alleles (PiSZ, PIZZ, etc.)
- Present in < 1% of world population
- Null = no detectable AAT in plasma
- Proteins are truncated or unstable; leads to degradation
- Very rarely causes liver disease and no hepatocyte inclusions will be present
- Does cause lung disease
- Present in < 0.1% of world population
- Dysfunctional = normal plasma levels of AAT
- AAT does not function correctly
- Present in < 0.1% of world population
- Normal = normal function and plasma levels of AAT
Clinical features
- Liver complications are variable (Clin Liver Dis 2018;22:643)
- May be asymptomatic until adulthood (Clin Liver Dis 2017;21:355)
- Adults: cirrhosis, chronic hepatitis, portal hypertension, jaundice, hepatocellular carcinoma, liver failure (rare) (Clin Liver Dis 2018;22:643, Aliment Pharmacol Ther 2018;47:877)
- Neonates: neonatal hepatitis syndrome, cholestasis (Clin Liver Dis 2018;22:643)
- Children: chronic hepatitis, portal hypertension (isolated), hepatomegaly, splenomegaly, jaundice (Clin Liver Dis 2018;22:643, Aliment Pharmacol Ther 2018;47:877)
Diagnosis
- Low serum concentration of AAT (Methods Mol Biol 2017;1639:9, Mutat Res 2017 Jul;773:14)
- < 50% of the normal reference range = no further tests needed (Mutat Res 2017 Jul;773:14)
- Caution: AAT is an acute phase reactant and so may show small elevations with systemic inflammatory states
- Absence of alpha-1 band on serum protein electrophoresis (Methods Mol Biol 2017;1639:9)
- Genotype analysis (Mutat Res 2017 Jul;773:14, Clin Liver Dis 2018;22:643)
- Phenotype of AAT protein (Clin Liver Dis 2018;22:643)
- Either genotype or phenotype analysis can be used as gold standard
Laboratory
- Elevated: bilirubin (conjugated or unconjugated), ALT, AST (Clin Liver Dis 2018;22:643)
- Decreased: albumin, vitamin K (Clin Liver Dis 2018;22:643)
- Advanced disease: decreased platelet count and synthetic function of liver
- See also Diagnosis
Prognostic factors
- Depends on the genetic phenotype (see also Etiology)
Case reports
- Infant girl with jaundice (Pediatr Dev Pathol 2017;20:176)
- 33 and 63 year old men with tuberculosis and AAT deficiency (Int J Mycobacteriol 2017;6:187)
- 39 year old man with ongoing respiratory and abdominal symptoms (Cureus 2018;10:e3494)
- 60 year old man with liver failure following partial hepatectomy (World J Gastroenterol 2016;22:3289)
Treatment
- Liver transplant is the only curative option (Clin Liver Dis 2017;21:355)
- AAT replacement (Mutat Res 2017 Jul;773:14)
- IV purified pooled human AAT
- Inhaled in aerosolized form
Gross description
- Most common specimen: explanted native liver at the time of transplant
- Hepatomegaly (Aliment Pharmacol Ther 2018;47:877)
- Nodular and fibrotic (Aliment Pharmacol Ther 2018;47:877)
Microscopic (histologic) description
- Adults: range of following findings (Aliment Pharmacol Ther 2018;47:877)
- Eosinophilic intracytoplasmic globules in hepatocytes
- Usually in zone 1, near portal triads
- Most suggestive feature of AAT deficiency
- Fibrosis: ranges from minimal periportal fibrosis to cirrhosis
- Mild portal inflammation: predominantly lymphocytic
- Mild steatosis: often in periportal hepatocytes
- Eosinophilic intracytoplasmic globules in hepatocytes
- Neonates (Hepatology 1988;8:307, Am J Surg Pathol 2010;34:1498):
- Intracytoplasmic globules may be absent or difficult to detect in neonates
- Hepatitis
- Extrahepatic biliary atresia like features including:
- Lobular cholestasis
- Bile ductular reaction
- Giant cell transformation of hepatocytes
- Variable fibrosis
Microscopic (histologic) images
Positive stains
- Diastase resistant periodic acid Schiff (PAS) positive globules
- AAT positive globules
- Caution: inflamed and reactive hepatocytes may show background staining in the absence of AAT deficiency
Electron microscopy description
- Enlarged endoplasmic reticulum with moderately electron dense fibrillary inclusions (Ultrastruct Pathol 2020;44:32)
Sample pathology report
- Liver biopsy in an adult with elevated transaminases and total bilirubin:
- Liver, random, ultrasound guided needle core biopsy:
- Hepatocytes with cytoplasmic PAS diastase positive globules compatible with alpha-1 antitrypsin deficiency
- Cholestasis and mild portal chronic inflammation
- Periportal fibrosis noted on trichrome stain
- See comment and microscopic description
- Comment: Immunohistochemistry for AAT is positive in the cytoplasmic globules and supports the diagnosis. Correlation with laboratory findings is recommended.
- Liver, random, ultrasound guided needle core biopsy:
- Hepatectomy at the time of transplant:
- Liver, native, hepatectomy:
- Liver with cirrhosis / stage 4 fibrosis
- PAS positive, diastase resistant hepatocyte cytoplasmic globules present, consistent with patient's history of AAT deficiency
- Negative for malignancy
- Liver, native, hepatectomy:
Differential diagnosis
- Megamitochondria (Hepatology 2004;39:1423):
- Tend to be smaller
- Do not preferentially occur in zone 1 hepatocytes
- Congestive hepatopathy (Am J Clin Pathol 1983;79:697):
- Alpha-1 antichymotrypsin deficiency (Histopathology 1990;16:221, Hum Pathol 2000;31:575):
- Neonatal hepatitis (Am J Surg Pathol 2010;34:1498):
- Wide variety of causes resulting in this injury pattern
- Cirrhosis:
- AAT like globules sometimes seen in end stage liver of any etiology
Board review style question #1
Which of the following is true of alpha-1 antitrypsin (AAT) deficiency in the liver?
- Electron microscopy would show intramitochondrial fibrillary inclusions
- Globules are negative for PASD and positive for AAT immunohistochemistry
- Globules represent misfolded protein within the endoplasmic reticulum
- Intracytoplasmic globules are the diagnostic feature
- Number of globules correlates with disease severity
Board review style answer #1
C. Globules represent misfolded protein within the endoplasmic reticulum. Although the intracytoplasmic globules are highly suggestive of alpha-1 antitrypsin deficiency, they are not diagnostic. In fact, there are no definitive diagnostic criteria for this disease (Answer D). Additionally, the globules are variably present and may be absent in some cases. There is also no correlation between the number of globules and disease severity (Answer E). When present, the globules are positive for both PASD and AAT (Answer B). These globules represent collections of misfolded protein. On electron microscopy the fibrillary inclusions are located within the endoplasmic reticulum, not within the mitochondria (Answer A).
Comment Here
Reference: Alpha-1 antitrypsin deficiency
Comment Here
Reference: Alpha-1 antitrypsin deficiency
Board review style question #2
Which of the following additional findings is most often seen associated with alpha-1 antitrypsin (AAT) deficiency in the liver of adult patients?
- Early onset cirrhosis
- Elevated tissue concentration of AAT
- High AST and low ALT
- Mild steatosis
- No detectable AAT in plasma
Board review style answer #2
A. Early onset cirrhosis. Although AAT does indeed collect in the hepatocytes due to its inability to be released from the ER, tissue levels are not routinely tested (Answer B). Rather, AAT levels are measured in the plasma. An AAT deficient phenotype is most common and would have a low but still detectable plasma level of AAT. This phenotype has the mutant "z" or "s" alleles. A null phenotype is much rarer and no AAT can be detected in the plasma of such patients due to degradation of the protein entirely (Answer E). A dysfunctional phenotype is also rare, but although the protein does not function properly there are normal plasma levels of AAT. Other laboratory abnormalities would be elevations in both AST and ALT (Answer C) indicating hepatocyte stress. A sole elevation in AST would be more consistent with alcoholic liver injury. Histologically, hepatic steatosis may be present but this finding is variable and much less common than fibrosis or cirrhosis (Answer D). In fact, early onset cirrhosis should prompt suspicion and testing for alpha-1 antitrypsin deficiency.
Comment Here
Reference: Alpha-1 antitrypsin deficiency
Comment Here
Reference: Alpha-1 antitrypsin deficiency
Amiodarone
Anatomy
Table of Contents
Definition / general | Embryology | Physiology | Accessory lobe | Diagrams / tables | Clinical images | Microscopic (histologic) images | VideosDefinition / general
- 1,200 - 1,600 g
- Dual blood supply of portal vein (2/3) and hepatic artery (1/3) via porta hepatis (common hepatic bile duct exists in same region)
- Blood exits liver via left and right hepatic veins to inferior vena cava
- Divided into right and left lobes by Cantlie line projecting between gallbladder fossa and vena cava and defined by middle hepatic vein
- Right lobe is divided into anterior and posterior segments by right hepatic vein
- Left lobe is divided into medial and lateral segments by left hepatic vein
- Intrahepatic biliary tree: classified into intrahepatic large bile ducts (grossly visible with fibrous ductal wall and peribiliary glands) and small bile ducts
- Regional lymph nodes: hilar, hepatoduodenal ligament, caval
Embryology
- Arises at embryonic junction (septum transversum): where ectoderm of amnion meets endoderm of yolk sac (externally) and where foregut meets midgut (internally); mesenchymal structure of transverse septum provides support so blood vessels and liver can form in underlying splanchnic mesoderm (UNSW Embryology: Gastrointestinal Tract - Liver Development [Accessed 23 October 2017])
- Hepatic diverticulum buds from ventral foregut at end of third week, grows into primitive septum transversum
- Liver forms from endodermal cells of diverticulum, termed hepatoblasts and mesenchyme
- Blood supply primarily from umbilical vein; also portal vein and hepatic artery
- Placenta clears wastes in bile and absorbs nutrients and umbilical vein blood bypasses liver via ductus venosus
- All elements of the biliary tree are recognizable by week 5, although bile duct system not complete until after birth; derived from endoderm (large ducts) and embryonic ductal plate (smaller intrahepatic ducts) (Dig Surg 2010;27:87)
- Hematopoietic cells are present in embryonic / fetal liver but absent at term
Physiology
Bile:
Bile acids:
Images hosted on other servers:
Bile acid circulation:
Jaundice:
Bilirubin:
- Liver produces about 500 ml/day of bile
- Promotes dietary fat absorption via detergent action of bile salts; eliminates waste products (bilirubin, excess cholesterol, xenobiotics) that are insufficiently water soluble to be excreted into urine
Bile acids:
- Carboxylate steroid molecules, derived from cholesterol, that promote bile flow and secretion of phospholipid and cholesterol
- Primary bile acids are cholic acid and chenodeoxycholic acid, secreted as taurine and glycine conjugates; two secondary ones (deoxycholic and lithocholic acid) are formed in the colon by bacterial action
Images hosted on other servers:
Bile acid circulation:
- All bile acids are reabsorbed via sodium bile acid cotransporter in apical membrane of ileal enterocytes and transported back to liver
- Enterohepatic circulation of bile acids maintains a large endogenous pool of bile acids for digestive and excretory purposes
Jaundice:
- Also called icterus
- Discoloration of skin and sclera due to disruption of bile formation by either retention of pigmented bilirubin or block in bilirubin secretion (cholestasis)
Bilirubin:
- End product of heme degradation
- 200 mg produced daily from old red blood cells broken down via monocyte phagocytic system in spleen, liver, marrow
- Also from turnover of P450 cytochromes and premature destruction of marrow red blood cells (with ineffective erthyropoiesis)
- Red blood cells are broken down and produce hemoglobin
- Globin proteins are removed, leaving heme molecule
- Heme is converted to biliverdin via heme oxygenase
- Biliverdin is converted to bilirubin via biliverdin reductase
- Bilirubin is bound to serum albumin since it is insoluble in blood at physiologic pH; the % unbound increases in severe hemolytic disease or if protein binding drugs displace bilirubin
- Hepatocytes take in bilirubin at sinusoidal membrane, conjugate it with glucuronic acid using bilirubin uridine diphosphate glucuronosyltransferase (UGT) in endoplasmic reticulum, then bilirubin is excreted into bile
- Bacteria have beta glucuronidases which deconjugate and degrade bilirubin to colorless urobilinogens, excreted in feces as stercobilin, a brown pigment that colors stools
- 20% of urobilinogens are reabsorbed in ileum / colon, returned to liver, reexcreted into bile
- Some urobilinogen is reabsorbed and excreted by the kidney, oxidized to urobilin - a pigment that gives amber color to urine
Accessory lobe
- May appear clinically as hepatic mass
- Anterior abdominal wall defects are frequently associated with accessory hepatic lobes
- Can present with torsion (Surg Radiol Anat 2011;33:819)
Diagrams / tables
Microscopic (histologic) images
Videos
Development of foregut related to the peritoneum
Angiomyolipoma
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Benign mesenchymal tumor composed of smooth muscle cells, adipocytes and blood vessels
Essential features
- Hepatic perivascular epithelial cell tumor (PEComa) composed of 3 components, present in variable amounts and growth patterns: smooth muscle, fat and blood vessels
- Usually sporadic but ~ 5 - 10% occur in the setting of tuberous sclerosis
- Generally benign, although rare malignant behavior has been reported and is difficult to predict (Histopathology 2012;61:863)
- Smooth muscle component, which usually predominates, shows positive staining with HMB45, SMA and MelanA
Terminology
- Hepatic epithelioid angiomyolipoma (HEAML)
- PEComa
ICD coding
Epidemiology
- F > M; mean age ~ 56 years old (HPB (Oxford) 2020;22:622)
Sites
- Hepatic parenchyma (right lobe > left lobe > caudate lobe) (Histopathology 2012;61:863)
Pathophysiology
- Sporadic: mutations in TSC2 → upregulation of mTOR signaling + activation of Wnt signaling pathway (Histopathology 2018;73:101, Histopathology 2015;66:695)
- Tuberous sclerosis: germline mutations in TSC1 or TSC2
Clinical features
- ~ 5 - 10% occur in tuberous sclerosis patients, where they are more likely to be multiple and associated with renal angiomyolipoma (Am J Surg Pathol 1999;23:34)
Diagnosis
- Biopsy required for diagnosis as radiologic features are overlapping with other entities, especially hepatocellular carcinoma (HCC)
- Ultrasound, CT or MRI alone result in correct diagnosis in < 33% of patients (Clin Radiol 2020;75:88)
- Ultrasound + CT + MRI with or without angiography result in correct diagnosis in 52% of patients (J Surg Oncol 2011;103:807)
Radiology description
- Ultrasound: heterogeneously echogenic lesion with hypoechoic foci
- CT: hypoattenuating lesion showing arterial and persistent enhancement without washout
- MRI: heterogeneously T2 hyperintense lesion with variable T1 intensity; MRI is best modality for detecting fat component
- Reference: Clin Radiol 2020;75:88
Radiology images
Prognostic factors
- Rarely (< 5%) display malignant behavior (recurrence, metastasis) but this is difficult to predict
- High risk features: size > 5 cm, infiltrative growth pattern, high nuclear grade / nuclear pleomorphism and high cellularity, mitoses > 1/50 high power fields, necrosis and vascular invasion (Sarcoma 2012;2012:541626, Am J Surg Pathol 2005;29:1558)
Case reports
- 31 year old man with ruptured hepatic mass (Clin Mol Hepatol 2017;23:179)
- 45 year old woman with hepatic mass, enlarging from 12 to 20 cm over 5 years (J Surg Case Rep 2020;2020:rjaa353)
- 50 year old woman with abdominal pain and liver mass (In Vivo 2017;31:1169)
- 54 year old woman with right upper quadrant pain and liver mass (Case Reports Hepatol 2019;2019:2362618)
- 65 year old woman with hepatic mass noted on annual health check ultrasound (Korean J Gastroenterol 2018;71:49)
Treatment
- Surgical resection
- Conservative management / watchful waiting with imaging at regular intervals can be employed if diagnosis is confirmed by biopsy
- Reference: HPB (Oxford) 2020;22:622
Gross description
- Well circumscribed, unencapsulated or partially encapsulated, gray to tan to yellow, rubbery, soft liver mass with patchy areas of red-brown hemorrhage (Histopathology 2012;61:863)
- Nonneoplastic background liver usually noncirrhotic
Gross images
Frozen section description
- Because the epithelioid component is often the dominant cell type in these lesions, frozen section can often mimic HCC, showing pleomorphic cells with ample eosinophilic cytoplasm and prominent nucleoli (Korean J Gastroenterol 2018;71:49)
- Unlike HCC, usually arises in noncirrhotic liver
Microscopic (histologic) description
- Composed of 3 components present in variable amounts and growth patterns: smooth muscle (usually predominant), fat and blood vessels
- Smooth muscle component may be spindled, intermediate, epithelioid or pleomorphic (Histopathology 2012;61:863)
- Epithelioid smooth muscle cells typically show ample eosinophilic cytoplasm and round to oval nuclei with prominent small nucleoli
- Nuclear pleomorphism is present at least focally in all tumors and marked cytologic atypia is seen in ~ 25% (Histopathology 2012;61:863)
- Low mitotic rate
- Vascular component includes 4 types of neoplastic blood vessels (cellular, hemangiopericytic, glomeruloid, aneurysmal) as well as nonneoplastic sinusoidal type and collagenous blood vessels; large, dilated vessels may be present at tumor / nontumor interface (Histopathology 2012;61:863)
- May show foci of extramedullary hematopoiesis
- May have an infiltrative border with nonneoplastic liver, which is usually not cirrhotic
- Can be classified based on the relative amounts of the 3 tissue types: mixed (conventional) type (> 20% of each of the 3 tissue types); lipomatous (> 80% fat); angiomatous (> 80% blood vessels); myomatous (> 80% smooth muscle); angiomyomatous, myoangiomatous, myolipomatous, lipomyomatous, lipoangiomatous, angiolipomatous (Histopathology 2012;61:863)
Microscopic (histologic) images
Virtual slides
Cytology description
- Fine needle aspiration has been rarely reported
- Clusters of adipocytes and mesenchymal cells with granular to fibrillary cytoplasm, pleomorphic oval nuclei and occasional prominent nucleoli (Ann Saudi Med 2001;21:324)
- No mitoses or necrosis (Ann Saudi Med 2001;21:324)
Positive stains
- HMB45 (smooth muscle component)
- SMA (smooth muscle component)
- MelanA (smooth muscle component)
- KIT / CD117 (Am J Surg Pathol 2002;26:493)
Negative stains
Molecular / cytogenetics description
- Sporadic: mutations in TSC2 via next generation sequencing (NGS) (Histopathology 2018;73:101)
Sample pathology report
- Liver, partial hepatectomy:
- Angiomyolipoma (see comment)
- Comment: Sections show a tumor composed of epithelioid cells, adipocytes and blood vessels. The epithelioid cells show positive staining for HMB45 and SMA and negative staining for keratin (AE1 / AE3) and hepatocyte markers (arginase and HepPar). The positive HMB45 and SMA stains support melanocytic and smooth muscle differentiation, respectively. The negative keratin stain argues against carcinoma and the negative HepPar and arginase stains argue against hepatocellular adenoma and hepatocellular carcinoma. Overall, the morphologic and immunohistochemical features are those of angiomyolipoma.
Differential diagnosis
- Hepatocellular carcinoma:
- Hepatocellular adenoma:
- Gastrointestinal stromal tumor:
- Metastatic melanoma (J Cutan Pathol 2020;47:824):
- Lacks lipomatous component
- More diffusely S100 positive
- High mitotic rate
- Clinical history of melanoma
- Metastatic carcinoma:
Board review style question #1
The cells in this image of a liver tumor show positive staining for HMB45 and negative staining for arginase. Which of the following is true about this lesion?
- It frequently recurs or metastasizes following resection
- It is a rare variant of hepatocellular carcinoma with good prognosis
- It is associated in about 5 - 10% of cases with tuberous sclerosis
- It is more common in men than in women
Board review style answer #1
C. It is associated in about 5 - 10% of cases with tuberous sclerosis
Comment Here
Reference: Angiomyolipoma
Comment Here
Reference: Angiomyolipoma
Board review style question #2
Board review style answer #2
Angiosarcoma
Table of Contents
Definition / general | Causes | Clinical features | Case reports | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Differential diagnosisDefinition / general
- Rare (10 - 30 annual cases in U.S.) but most common hepatic primary sarcoma in adults (2% of all primary liver tumors)
Causes
- 25 - 42% associated with exposure to androgen steroids, arsenic, Thorotrast (radiocontrast agent thorium dioxide, used through 1950s, detect its α particle emissions via autoradiography), vinyl chloride (Wikipedia: Thorotrast [Accessed 30 November 2017])
- Patients with exposure to Thorotrast or vinyl chloride may have synchronous cholangiocarcinoma or hepatocellular carcinoma
- Rarely associated with chemotherapy, copper sulfate, estrogens, hereditary hemochromatosis, phenelzine, radiotherapy
- Cases with above known causes usually have latent period of 20 - 35 years, are accompanied by fibrosis or cirrhosis, have precursor conditions of hypertrophy and atypia of hepatocytes and sinusoidal lining cells but are histologically similar to idiopathic cases
Clinical features
- 75% men, usually age 50+ years; rare in children
- Nonoperative biopsy may cause severe bleeding and death
- Most patients die within 6 months from hepatic failure or intra-abdominal bleeding
- Metastasizes widely, often to lung (vinyl chloride cases usually don't have distant metastases)
Case reports
- 71 year old man with metastatic hepatic epithelioid angiosarcoma (Arch Pathol Lab Med 2001;125:968)
Gross description
- Multicentric, involves right and left lobes
- Diffusely infiltrative, hemorrhagic and gray white solid nodules with blood filled cavities
- Thorotrast associated tumors have subcapsular hepatic and splenic deposits of yellow chalky material
Microscopic (histologic) description
- Tumor composed of infiltrative, freely anastomosing vascular channels
- Tumor cells grow along sinusoids adjacent to hepatic cords
- Tumor cells have abundant, pale eosinophilic cytoplasm, poorly defined cell borders, are usually pleomorphic with hyperchromatic nuclei but may be only mildly atypical
- Also variably prominent nucleoli, blood filled cavities present are lined by tumor cells that may be papillary
- 75% have vascular invasion of portal or hepatic vein branches; frequent mitotic activity
- Precursor stage has endothelial hypertrophy and hyperplasia
- Also epithelioid cells with abundant cytoplasm and prominent nucleoli, bizarre tumor giant cells, fibrosarcoma-like spindle cells, cholestatic hepatocellular rosettes with bile plugs, tumor cell phagocytic activity and extramedullary hematopoiesis
- Childhood cases: may have kaposiform areas of spindle cells with PAS+ intracytoplasmic globules; no prominent myxoid areas
- Thorotrast exposed patients: have brown gray refractile but not birefringent granules of Thorotrast free or within macrophages
- Also precursor stage with endothelial hypertrophy and hyperplasia
Positive stains
- CD34, CD31, factor VIII related antigen and Ulex europaeus lectin type 1 (may not be present in poorly vasoformative areas)
- Also Prox1 (reflects the lymphatic endothelial phenotype), claudin5
Negative stains
- Keratin (but positive in 12 - 35%)
Electron microscopy description
- Weibel-Palade bodies
Molecular / cytogenetics description
- 50% of vinyl chloride associated cases have A:T to T:A transversion in p53
Differential diagnosis
- Epithelioid hemangioendothelioma:
- Less atypia, less mitotic activity, less necrosis, often prominent fibrous and hyalinized stroma
- Fibrosarcoma:
- Very rare; not particularly vascular; CD31 negative
- Hepatocellular carcinoma:
- Atypical hepatocytes, normal endothelial cells
- Kaposi sarcoma:
- HIV+, have extrahepatic nodules, portal distribution and lack angiosarcomatous foci
- Peliosis hepatis
- Reactive bile ductular proliferation, reactive lymphoid hyperplasia:
- Reactive, lack atypical endothelial lining cells
Arterial disorders
Table of Contents
Definition / general | Essential features | Etiology | Clinical features | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Board review style question #1 | Board review style answer #1Definition / general
- Pathologic insult to the hepatic artery or its intrahepatic branches
- Rare and often difficult to diagnose clinically
Essential features
- Most forms of arterial insult may impact the hepatic artery
- Depending on type of injury, patients may experience no symptoms, as portal vein compensatorily supplies more blood flow to liver
- Hepatic artery thrombosis is rare outside of the transplant setting
Etiology
- Many and varied
- Vasculitides that can affect the hepatic artery include polyarteritis nodosa, giant cell arteritis, Takayasu arteritis and granulomatosis with polyangiitis
Clinical features
- Patients with hepatic artery occlusion (due to thrombosis, neoplasia, vasculitis or trauma) present with severe abdominal pain, high transaminases, variable circulatory shock
- Arterial occlusion may cause infarction, although retrograde arterial flow through accessory vessels and portal supply may sustain liver parenchyma
- Some forms of hepatic arterial damage (atherosclerosis, cryoglobulinemia, amyloidosis) may occur without any clinical manifestations
Microscopic (histologic) description
- Ischemia causes centrilobular (zone 3) or localized (infarct type) coagulative necrosis
- Surviving parenchyma may show acidophil bodies or ballooning degeneration
- Compromise of arterial flow (e.g. hepatic artery thrombosis) can also lead to ischemic cholangiopathy, with necrosis of large bile ducts
- Diabetic patients may develop hyaline arteriolosclerosis (Am J Surg Pathol 2015;39:1000)
- Takayasu arteritis may be associated with hepatic sinusoidal dilatation (Ann Hepatol 2011;10:559)
- Transplanted livers may experience arterial flow abnormalities, causing increased mitoses, apoptosis and increased Ki67 index (Mod Pathol 2012;25:1594)
Microscopic (histologic) images
Sample pathology report
- Liver, allograft, orthotopic transplantation:
- Liver with hepatic artery thrombosis, diffuse zonal necrosis and focal ischemic cholangiopathy
- Margins of resection unremarkable.
Board review style question #1
Which of the following is most likely to cause necrosis of large intrahepatic bile ducts?
- Budd-Chiari syndrome
- Hepatic artery thrombosis
- Portal vein thrombosis
- Primary sclerosing cholangitis
- Viral hemorrhagic fever
Board review style answer #1
Ascending cholangitis
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Etiology | Clinical features | Diagnosis | Laboratory | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Infection of the extrahepatic biliary system, often due to obstruction (Infect Dis Clin North Am 2000;14:521)
Essential features
- Highly morbid infection of large bile ducts
- Histologic correlate is neutrophils within epithelium and lumen of interlobular bile ducts
Terminology
- Also called acute cholangitis, suppurative cholangitis
ICD coding
- ICD-10: K83.09 - other cholangitis
Epidemiology
- Typically a secondary process that occurs in an already diseased bile duct (stricture, etc.) (Postgrad Med J 2007;83:773)
- Can occur following the Kasai procedure to correct extrahepatic biliary atresia (J Pediatr Surg 1989;24:729, J Pediatr Surg 2004;39:1800)
Etiology
- Common infectious causes include E. coli, Klebsiella, enterococci (Postgrad Med J 2007;83:773)
- Rarely due to adenovirus (Pediatr Dev Pathol 2003;6:156)
Clinical features
- Symptoms include Charcot cholangitis triad: jaundice, fever and right upper quadrant abdominal pain (World J Gastrointest Pathophysiol 2018;9:1)
- May lead to a hepatic pyogenic abscess
Diagnosis
- Based on the Tokyo Guidelines, which incorporate systemic inflammation, cholestasis and imaging (J Hepatobiliary Pancreat Sci 2018;25:17, ANZ J Surg 2017;87:554)
Laboratory
- Endoscopic retrograde cholangiopancreatography (ERCP) obtained bile can be cultured to guide antibiotic therapy (Dig Dis 2019;37:155)
- Blood culture may be less successful
Case reports
- 64 year old woman with Ascaris infection (Eur J Intern Med 2016;34:e7)
- 72 year old man with Lactococcus lactis cremoris bacteremia (J Med Case Rep 2009;3:3)
- 73 year old man who has recently done heavy lifting (Case Rep Gastroenterol 2017;11:500)
- 93 year old woman with biliary enteric fistula (ACG Case Rep J 2018;5:e60)
Treatment
- Biliary drainage and antibiotic therapy
Microscopic (histologic) description
- Neutrophils within lumens of interlobular bile ducts and also infiltrating duct (not ductule) epithelium (Lefkowitch: Scheuer's Liver Biopsy Interpretation, 9th Edition, 2015)
- Note: neutrophils sprinkled throughout ductular reaction is a typical component of ductular reaction and should NOT be considered evidence of infection or of ascending cholangitis
- Larger ducts often unaffected
- Findings of other concomitant biliary processes (e.g. large duct obstruction) may also be present
Sample pathology report
- Liver, biopsy:
- Hepatic parenchyma with cholestasis and neutrophils involving bile duct lumens and epithelium (see comment)
- Comment: The findings are concerning for acute (ascending) cholangitis in the proper clinical context.
Differential diagnosis
- Acute cellular rejection of liver transplant:
- Neutrophils within duct lumen may rarely be present
- Clinical correlation necessary, as duct complications / infection can also occur in the posttransplant setting
- Sepsis:
- May occur alongside ascending cholangitis
- Nonspecific cholestasis and acute / chronic inflammation, though ductular cholestasis is highly suggestive of sepsis
Board review style question #1
Neutrophils filling the lumens of native interlobular bile ducts are most suggestive of which diagnosis?
- Ascending cholangitis
- Cholangiocarcinoma
- Primary biliary cholangitis
- Primary sclerosing cholangitis
- Recurrent pyogenic cholangitis
Board review style answer #1
Board review style question #2
A patient presents with fever, jaundice and abdominal pain. Liver enzymes are elevated and a liver biopsy is performed. Findings are visible in the figure above. Based on this, which of the following steps may be included in the patient's therapy?
- Antibiotics
- Bile duct excision
- Platinum based chemotherapy
- Steroids
- Ursodeoxycholic acid
Board review style answer #2
Ascites
Table of Contents
Definition / general | Essential features | Pathophysiology | Laboratory | Treatment | Clinical images | Cytology description | Cytology imagesDefinition / general
- Ascites is abnormal excessive accumulation of fluid in peritoneal cavity
- It is the most common of the 3 major complications of cirrhosis (ascites, hepatic encephalopathy and bleeding varices) (Hepatology 1987;7:122)
- It is also one of 5 parameters of the Child-Pugh score, the most widely used system for liver function assessment (Medicine (Baltimore) 2016;95:e2877)
- Presence of ascites is associated with poorer overall survival in patients with cirrhosis (1 year 85%, 5 year 56%) (Clin Gastroenterol Hepatol 2006;4:1385) and hepatocellular carcinoma (Chin J Cancer 2014;33:481)
Essential features
- Pending
Pathophysiology
Combination of these factors, which reinforce each other:
- Elevated hydrostatic pressure due to portal hypertension
- Reduced osmotic pressure due to hypoalbuminemia
- Renal retention of sodium and water due to activation of renin angiotensin aldosterone system (RAAS)
- Decreased effective circulatory volume due to ascites
Laboratory
- Ascitic fluid cell count and differential
- Polymorphonuclear leukocyte (PMN) count > 250 cells/mm3 in the absence of an intra abdominal, surgically treatable source of infection indicates spontaneous bacterial peritonitis (Hepatology 1982;2:399), which complicates about 12% of cirrhotic patients with ascites (Dig Liver Dis 2001;33:41)
- Serum ascites albumin gradient (SAAG) (Am J Gastroenterol 2009;104:1401)
- > 1.1 g/dL indicates portal hypertension
- < 1.1 g/dL indicates nonportal hypertension causes including malignancies, tuberculous peritonitis and nephrotic syndrome
- Cytology
- Only positive in peritoneal carcinomatosis (sensitivity of 96.7% if 3 samples from different paracentesis procedures) (Hepatology 1988;8:1104)
- Almost always negative in cirrhotic patients, even those known to have hepatocellular carcinoma (Cytojournal 2009;6:16)
Treatment
- First line (Hepatology 2013;57:1651)
- Cessation of alcohol when present
- Sodium restriction
- Dual diuretics (usually spironolactone and furosemide)
- Discontinue nonsteroid anti-inflammatory drugs
- Evaluation for liver transplantation
- Second line
- Discontinue beta blockers, angiotension converting enzyme inhibitors and angiotension receptor blockers
- Serial therapeutic paracentesis
- Transjugular intrahepatic portosystemic stent shunt (TIPSS)
- Evaluation for liver transplantation
- Third line
- Peritoneovenous shunt
Cytology description
- Ascites fluid cytology is almost always negative in patients with cirrhosis, even those known or suspected to have hepatocellular carcinoma (Cytojournal 2009;6:16)
Cytology images
Autoimmune cholangitis
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Essentially regarded as primary biliary cholangitis in patients with no detectable antimitochondrial antibody (Dig Dis Sci 1995;40:1232, Clin Liver Dis 2004;8:177)
- May in reality serve as a "wastebasket" heading for various related biliary diseases, though this remains unclear (Hepatology 2000;31:1231, Adv Anat Pathol 2002;9:244)
Essential features
- Mimics primary biliary cholangitis clinically and histologically, except antimitochondrial antibody is not detected
- Advanced techniques often do uncover antimitochondrial antibody in these patients
Terminology
- Also called antimitochondrial antibody negative primary biliary cholangitis (AMA negative PBC), autoimmune cholangiopathy
ICD coding
- ICD-10: K74.3 - primary biliary cirrhosis
Epidemiology
- Represents 5 - 10% of patients who otherwise fit diagnostic criteria for primary biliary cholangitis
Sites
- Not applicable
Pathophysiology
- Unclear; presumably autoimmune
Etiology
- Autoimmune disease
- Rare cases have been linked to IgG4 systemic disease, though these more likely represent IgG4 related sclerosing cholangitis (Acta Gastroenterol Latinoam 2011;41:55, J Med Case Rep 2011;5:485)
Clinical features
- More common in women; causes pruritus, fatigue
- Patients may be slightly younger on average than those with primary biliary cholangitis (Dig Dis Sci 1995;40:1232)
- May have worse outcome than antimitochondrial antibody positive primary biliary cholangitis patients (Scand J Gastroenterol 2016;51:745)
- Some patients may seroconvert to antimitochondrial antibody positivity (J Hepatol 1996;25:574)
Diagnosis
- Effectively the same as primary biliary cholangitis, except antimitochondrial antibody negative; true stringent criteria have not been defined (Clin Liver Dis 2018;22:589)
Laboratory
- Positive antinuclear antibody and smooth muscle antibody (at higher rates than primary biliary cholangitis patients); negative antimitochondrial antibody
- May have higher aspartate transaminase and bilirubin levels than primary biliary cholangitis patients (Hepatology 2000;31:1231)
- More sophisticated techniques (including primary biliary cholangitis specific antinuclear antibodies, such as Gp210 and sp100) have shown that many antimitochondrial antibody negative primary biliary cholangitis patients are in fact antimitochondrial antibody positive (Clin Res Hepatol Gastroenterol 2016;40:553, Hepatology 2007;45:659)
- Emerging biomarkers for diagnosis have been identified, though they show poor sensitivity (Clin Chem Lab Med 2017;56:25, Gastroenterol Res Pract 2019;2019:8959103)
Case reports
- 31 year old woman with pruritus, fatigue and weight loss (Euroasian J Hepatogastroenterol 2015;5:122)
- 47 year old woman with painless thyroiditis (Intern Med 1999;38:244)
- 59 year old woman with antimitochondrial antibody positive primary biliary cholangitis converted to antimitochondrial antibody negative (J Korean Med Sci 1999;14:102)
Treatment
- Ursodeoxycholic acid, which may be less successful than for antimitochondrial antibody positive patients
Microscopic (histologic) description
- Essentially the same as primary biliary cholangitis, except perhaps with less chronic portal inflammation
- Florid duct lesions (granulomas destroying bile ducts), lobular granulomas, duct injury and disarray, duct inflammation, ductular reaction, lobular cholestasis, ductopenia late
Microscopic (histologic) images
Sample pathology report
- Liver, biopsy:
- Biliary pattern injury with duct injury, ductular reaction and focal florid duct lesions (see comment)
- Comment: The changes are compatible with primary biliary cholangitis. Given the patient's reported negative antimitochondrial antibody, the overall findings may be most consistent with autoimmune cholangitis (antimitochondrial antibody negative primary biliary cholangitis).
Differential diagnosis
- Primary biliary cholangitis:
- Key distinction is antimitochondrial antibody status (positive in primary biliary cholangitis, negative in autoimmune cholangitis)
- Drug induced liver injury:
- Requires clinical correlation to rule out drug cause (Gastroenterology Res 2019;12:211)
- IgG4 related sclerosing cholangitis:
- Findings typically centered around large ducts, with sclerosis and prominent plasmacytic inflammation (Korean J Hepatol 2011;17:76)
Board review style question #1
What is the key distinction between primary biliary cholangitis and autoimmune cholangitis?
- Alkaline phosphatase level
- Antimitochondrial antibody status
- Antineutrophil cytoplasmic antibody status
- Antinuclear antibody status
- Anti-smooth muscle antibody status
Board review style answer #1
Board review style question #2
A 45 year old woman complaining of jaundice is found to have elevated liver enzymes. The figure above shows a liver biopsy. The patient's physician orders serology for antimitochondrial antibodies, which returns as negative. Which of the following is the most likely explanation?
- The liver sample must have actually come from a different patient
- The patient has autoimmune cholangitis
- The patient has sarcoidosis
- The patient has tuberculosis
- The serology testing returned a false negative result
Board review style answer #2
Autoimmune hepatitis
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Immune mediated inflammatory liver disease of uncertain cause (Hepatology 2020;72:671)
Essential features
- Diagnosis is based on combination of clinical, laboratory and histological features
- More common in female patients
- Classic (but not sole) serologic association is with anti smooth muscle antibody
- Typical histological features include interface hepatitis, portal lymphocytic or lymphoplasmacytic infiltrate, hepatocyte rosetting and emperipolesis (though latter 2 falling out of favor)
Terminology
- Previously known as lupoid hepatitis
ICD coding
- ICD-10: K75.4 - autoimmune hepatitis
Epidemiology
- Incidence is highest in North America (42.9/100,000), followed by Europe (10.7 - 23.9/100,000) (J Gastroenterol Hepatol 2015;30:1230)
- M:F = 1:4 - 6
- Usual age of presentation depends on subtype:
- Type 1: bimodal (10 - 25 years and 45 - 70 years)
- Type 2: < 15 years
Sites
- Liver
Etiology
- Unknown; genetic and environmental factors may play roles in pathogenesis (J Hepatol 2015;62:S100)
- Genetic predisposition:
- North America / Europe: HLA-DR3 (DRB1*0301) and HLA-DR4 (DRB1*0401)
- China / Japan: HLA-DR4 (DRB1*0405)
Clinical features
- Most patients have nonspecific symptoms: fatigue (85%), anorexia, nausea, weight loss, jaundice, pruritus, amenorrhea
- 25 - 34% are asymptomatic
- 25 - 75% have episodes of acute / fulminant hepatitis
- 14 - 44% have concurrent extrahepatic autoimmune disorders, including autoimmune thyroiditis, rheumatoid arthritis, Sjögren syndrome, vitiligo or ulcerative colitis (Hepatology 2020;72:671)
- Incidence of cirrhosis at presentation varies widely: North America (59 - 85%), Middle East (22.2 - 45.5%), China (24.8%), Japan (6.4 - 12.8%) (J Gastroenterol Hepatol 2015;30:1230)
- Burnt out autoimmune hepatitis is one of the most common causes of cryptogenic cirrhosis (Scand J Gastroenterol 2010;45:60)
- Hepatocellular carcinoma risk: pooled incidence of 3.06/1,000 patient years; 10.07/1,000 patient years in cirrhotic patients (Clin Gastroenterol Hepatol 2017;15:1207)
Diagnosis
- Diagnosis is based on combination of clinical, laboratory and histological features
- Revised diagnostic International Autoimmune Hepatitis Group (IAIHG) scoring system (J Hepatol 1999;31:929):
- Complex system evaluating 11 clinical, laboratory and histological factors
- For research purposes; not designed for clinical practice
- Simplified diagnostic International Autoimmune Hepatitis Group scoring system (Hepatology 2008;48:169):
- Simple system evaluating 4 laboratory and histological factors: serum autoantibodies, IgG, liver histology and viral hepatitis serology
- Cutoff values for probable and definite autoimmune hepatitis are 6 points (88% sensitivity and 97% specificity) and 7 points (81% sensitivity and 99% specificity), respectively
- American Association for the Study of Liver Diseases (AASLD) guidance statement (Hepatology 2020;72:671):
- Compatible histological findings
- Elevated aspartate aminotransferase / alanine aminotransferase
- Elevated IgG or positive serological marker(s)
- Exclusion of other diseases resembling autoimmune hepatitis
- Subtypes:
- Type 1: positive for antinuclear antibody or anti smooth muscle antibody; 10% have other autoimmune disorders
- Type 2: positive for anti liver kidney microsomal antibody or anti liver cytosol type 1 antibody positive; often presents with acute or fulminant hepatitis; 17% have other autoimmune disorders
- Type 3: controversial subtype. positive for antisoluble liver antigen / liver pancreas; clinical and laboratory features indistinguishable from type 1 (Gut 2001;49:589)
- About 10% of autoimmune hepatitis fits into following scenarios
- Overlap syndrome
- Autoimmune hepatitis / primary biliary cholangitis (PBC)
- Autoimmune hepatitis / primary sclerosing cholangitis (PSC)
- Variant syndromes
- Seronegative autoimmune hepatitis (Gut 2001;49:589)
- Antimitochondrial antibody positive autoimmune hepatitis (Gut 2001;49:589)
- IgG4 associated autoimmune hepatitis (J Gastroenterol Hepatol 2019;34:742)
- Overlap syndrome
Laboratory
- Serum autoantibodies (J Autoimmun 2013;46:17):
- Antinuclear antibody: positive in 75% of type 1 autoimmune hepatitis; not associated with disease course or outcome
- Anti smooth muscle antibody: positive in 95% of type 1 autoimmune hepatitis; not associated with disease course or outcome
- Anti liver kidney microsomal: diagnostic for type 2 autoimmune hepatitis; associated with younger age at presentation, fulminant hepatic failure and partial IgA deficiency
- Anti liver cytosol type 1: diagnostic for type 2 autoimmune hepatitis; associated with more severe inflammation and rapid progression to cirrhosis
- Antisoluble liver antigen / liver pancreas: positive in 20 - 50% of autoimmune hepatitis; associated with more severe disease, treatment dependence, relapse after drug withdrawal and need for transplantation
- Elevated liver enzymes; ALT / AST > ALP
- Serum immunoglobulin G (IgG): marker for diagnosis (> 1.1 x upper limit of normal [ULN]) and monitoring treatment response (Hepatology 2010;51:2193)
Prognostic factors
- Good prognostic factor: IgG4 associated autoimmune hepatitis (J Gastroenterol Hepatol 2019;34:742)
- Poor prognostic factors: extreme age (≤ 20 years or ≥ 60 years), failure to normalize alanine aminotransferase within 6 months of onset of therapy, serum albumin ≤ 35 g/L (J Gastroenterol Hepatol 2015;30:1230)
Case reports
- 32 year old man with concurrent autoimmune hepatitis and advanced AIDS (Case Reports Hepatol 2019;2019:5326428)
- 48 year old woman with autoimmune hepatitis with overlap systemic lupus erythematosus (BMJ Case Rep 2020;13:e237341)
- 65 year old man with IgG4 associated autoimmune hepatitis (BMC Gastroenterol 2020;20:420)
Treatment
- Corticosteroids alone or with azathioprine to achieve normalization of serum transaminases and IgG
- If no response, add other immunosuppressants (e.g. cyclosporine, tacrolimus or mycophenolate mofetil) and consider liver transplantation
- Good long term prognosis with 10 year survival rate of 80 - 100% (J Gastroenterol Hepatol 2015;30:1230, Hepatology 2010;51:2193)
- Treatment outcome
- Biochemical remission: aspartate aminotransferase, alanine aminotransferase and IgG normalization
- Histological remission: absence of inflammation in liver biopsy
Microscopic (histologic) description
- Typical morphological changes:
- Portal plasma cell rich inflammation
- Interface hepatitis, formerly referred to as piecemeal necrosis: portal inflammatory cells eroding through the limiting plate between the portal tract and liver parenchyma
- Emperipolesis: active penetration of lymphocytes into and through a hepatocyte
- Hepatocyte rosettes
- Variable fibrosis (about 10% of autoimmune hepatitis does not show any fibrosis at initial presentation)
- Lobular necroinflammatory activity: usually accompanied by portal and periportal inflammation
- Uncommon morphological changes:
- Perivenular necrosis: up to 17% of autoimmune hepatitis with or without typical portal and periportal changes; associated with more severe disease activity and lower histological stage
- Intrahepatic cholestasis (bilirubinostasis)
- Syncytial multinucleated giant cells: autoimmune hepatitis is the most common cause (30%) of postinfantile giant cell hepatitis, which is rare in adults (0.1 - 0.25% of all hepatitis) (Hepat Res Treat 2013;2013:601290)
- Mild bile duct injury / inflammation: present in up to 24% of classical autoimmune hepatitis (Hepatology 2001;34:659)
- Chronic biliary disease or overlap syndrome only need to be considered in the presence of more extensive bile duct injury, florid duct lesions, ductular reaction, ductopenia, chronic cholestasis, portal granulomas or periductal fibrosis (clinical and laboratory findings must separately be met for both autoimmune hepatitis and primary sclerosing cholangitis / primary biliary cholangitis)
- IgG4 associated autoimmune hepatitis: > 10 IgG4 positive plasma cells/high power field
- Simplified International Autoimmune Hepatitis Group scoring system:
- Typical of autoimmune hepatitis (sensitivity: 40 - 59%; specificity: 55 - 96%) (Mod Pathol 2017;30:773, Hepatology 2008;48:169)
- Interface hepatitis with lymphocytic or lymphoplasmacytic infiltrate
- Hepatocyte rosettes
- Emperipolesis
- Compatible with autoimmune hepatitis
- Chronic hepatitis with lymphocytic infiltrate
- Without all 3 typical features
- Typical of autoimmune hepatitis (sensitivity: 40 - 59%; specificity: 55 - 96%) (Mod Pathol 2017;30:773, Hepatology 2008;48:169)
- Recent studies have suggested hepatocyte rosettes and emperipolesis are not specific features of autoimmune hepatitis (Hum Pathol 2018;82:51, Mod Pathol 2017;30:773)
- Grading and staging is usually performed according to systems developed for viral hepatitis, such as Batts and Ludwig
Microscopic (histologic) images
Negative stains
- CK7 (negative in periportal hepatocytes)
- Copper
- Reference: Mod Pathol 2017;30:773
Sample pathology report
- Liver, biopsy:
- Chronic hepatitis with dense portal lymphoplasmacytic infiltrate, moderate interface hepatitis, mild lobular necroinflammatory activity and moderate periportal fibrosis (see comment)
- Comment: In view of hepatitic liver enzyme derangement, serum antinuclear antibody titer (1:320), seropositivity of smooth muscle antibody and elevated serum IgG (1.2 x ULN), the overall features are consistent with autoimmune hepatitis.
Differential diagnosis
- Clinical presentation, including serology, is very important for resolving the differential diagnosis
- Chronic hepatitis C:
- Portal lymphocytic infiltrate with lymphoid follicles
- Less severe interface hepatitis
- Mild bile duct injury
- Mild steatosis
- Drug / toxin reaction:
- No reliable histological features differentiating autoimmune hepatitis and drug induced liver injury
- Clinical correlation with drug history is essential
- Hepatitis A:
- May resemble acute / early phase of autoimmune hepatitis (prominent plasma cells and interface hepatitis)
- No fibrosis
- Viral serology is crucial
- Overlap syndromes (Ulster Med J 2011;80:15)
- Primary biliary cholangitis:
- Unequivocal bile duct injury with chronic cholatestasis
- Only mild interface hepatitis and lobular necroinflammatory activity
- Cholestatic liver enzyme derangement or seropositivity of antimitochondrial antibody
- Primary sclerosing cholangitis:
- Periductal fibrosis with chronic cholatestasis
- Only mild interface hepatitis and lobular necroinflammatory activity
- Cholestatic liver enzyme derangement or seropositivity of antineutrophil cytoplasmic antibodies
- Classic liver imaging findings helpful to establish this diagnosis
- More common in male patients
Additional references
Board review style question #1
Which of the following features are considered typical for autoimmune hepatitis?
- Florid duct lesion and seropositivity for antimitochondrial antibody
- Interface hepatitis and seropositivity for smooth muscle antibody
- Pericellular fibrosis and seropositivity for antinuclear antibody
- Periductal concentric onion skin fibrosis and seropositivity for antineutrophil cytoplasmic antibodies
Board review style answer #1
B. Interface hepatitis and seropositivity for smooth muscle antibody
Comment Here
Reference: Autoimmune hepatitis
Comment Here
Reference: Autoimmune hepatitis
Board review style question #2
A middle aged woman without significant past medical history presents with acute onset of fatigue and jaundice. Blood tests show markedly elevated aspartate aminotransferase and alanine aminotransferase and high titer antinuclear antibody. Serology for smooth muscle antibody and antimitochondrial antibody are both negative. A liver biopsy demonstrates the above finding. Which of the following laboratory results should be assessed before issuing the diagnosis of consistent with autoimmune hepatitis?
- Elevated serum IgG
- Negative serology for viral hepatitis A
- Normal serum alkaline phosphatase
- Positive serology for liver kidney microsomal
Board review style answer #2
B. Negative serology for viral hepatitis A. Portal plasmacytic infiltration with interface hepatitis may also occur in viral hepatitis A.
Comment Here
Reference: Autoimmune hepatitis
Comment Here
Reference: Autoimmune hepatitis
Benign recurrent intrahepatic cholestasis
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Definition / general
- Benign recurrent intrahepatic cholestasis (BRIC) is a rare autosomal recessive disease of hepatocanalicular protein transporters characterized by recurrent episodes of jaundice and pruritis that resolve spontaneously without subsequent liver damage
- Considered to be a known clinical entity in the spectrum of primary familial intrahepatic cholestasis (PFIC)
- First described by Summerskill and Walshe in 1959 (Z Gastroenterol 1998;36:379)
Essential features
- Cholestasis during attacks but no histologic progression to fibrosis
- Autosomal recessive disease
- Subclassified into 2 types (BRIC1 and BRIC2), which are caused by mutations of ATP8B1 and ABCB11 genes, respectively (the same genes that are mutated in progressive familial intrahepatic cholestasis [PFIC]) (Case Rep Gastroenterol 2022;16:110)
- BRIC and its subtypes can be considered as a mild form of the more severe progressive familial intrahepatic cholestasis (PFIC)
- Mainly affects patients in early life or before their twenties (World J Hepatol 2020;12:64)
- Diagnosis is based on clinical suspicion after excluding other causes of cholestasis and can be confirmed by genetic testing
Terminology
- Formerly known as Summerskill-Walshe-Tygstrup syndrome
- Benign recurrent intrahepatic cholestasis (BRIC)
ICD coding
Epidemiology
- Incidence is ~1 in 50,000 - 100,000 people worldwide (J Clin Exp Hepatol 2014;4:25)
- Age at diagnosis is typically ≤ 20 years of age
- M = F
- Genetic mutation: autosomal recessive inheritance (see Etiology)
Sites
- Liver
Pathophysiology
- Genetic mutations that lead to impaired bile salt excretion, which causes impaired functioning of the canalicular pump, leading to cholestasis (see Etiology and Molecular / cytogenetics description)
Etiology
- Autosomal recessive disorder is associated with mutation of ATP8B1 and ABCB11 genes
- Nonsense and missense mutations in those genes will lead to partial protein expression for bile canalicular protein transport (complete deletion of protein expression will show a severe form of cholestasis, which is known as primary familial intrahepatic cholestasis [types 1 and 2]) (Hepatology 2009;50:1597)
- Defective ATP8B1 gene is located on chromosome 18 and encodes F1C1, which causes impaired bile salt excretion, while defective ABCB11 gene is located on chromosome 2, which causes impaired functioning of the canalicular pump, leading to cholestasis
Clinical features
- Patients will experience spontaneous resolution within a few weeks to some months
- Presents without liver parenchymal involvement toward chronic liver disease
- Episodes are precipitated by stress, infections, medications or oral contraceptives and pregnancy (Front Med (Lausanne) 2022;9:897108)
Diagnosis
- Clinical picture and history after excluding other forms of cholestasis
- Genetic testing can be confirmatory
- Luketic and Shiffman diagnostic criteria includes (J Clin Diagn Res 2016;10:OD01)
- At least 2 episodes of jaundice with free interval of months to years
- Laboratory investigations suggestive of intrahepatic cholestasis
- Cholestasis induced severe pruritus
- Cholangiography showing normal intra and extrahepatic bile ducts
- Liver histology suggests cholestasis with no advanced fibrosis
- Absence of other causes of cholestasis
Laboratory
- Serum alanine aminotransferase (ALT) and aspartate aminotransferase (AST) are usually normal
- Mildly elevated bilirubin concentrations
- Mildly elevated gamma glutamyl transferase (GGT) values
Radiology description
- Unremarkable biliary tree by cholangiography
Prognostic factors
- Favorable; prognosis is good and does not usually lead to fibrosis
Case reports
- 21 year old man presented with pruritis and jaundice (Case Rep Gastrointest Med 2020;2020:2894293)
- 27 year old man presented with complaints of jaundice for 2 weeks (J Clin Diagn Res 2016;10:OD01)
- 27 year old Hispanic woman presented with jaundice, pruritus and weakness for 4 weeks (ACG Case Rep J 2020;7:e00412)
- 29 year old man presented with severe jaundice (World J Hepatol 2020;12:64)
Treatment
- Treatment is symptomatic with antipruritics, ursodiol (ursodeoxycholic acid) and rifampicin (Scand J Gastroenterol 2023;58:512)
Microscopic (histologic) description
- Canalicular and intracellular cholestasis with associated hepatocyte rosettes
- No associated inflammation, bile duct loss or marked ductular reaction
- No advanced fibrosis
- Reference: Case Rep Gastrointest Med 2020;2020:2894293
Microscopic (histologic) images
Molecular / cytogenetics description
- Mutation in ATP8B1 gene that is located on chromosome 18 and encodes F1C1, which causes impaired bile salt excretion due to partial protein expression
- Mutation in ABCB11 gene is located on chromosome 2, which causes impaired functioning of the canalicular pump, leading to cholestasis
- Rare cases have been associated with TJP2 gene mutation (JPGN Rep 2021;2:e087)
Sample pathology report
- Liver, biopsy:
- Liver parenchyma with mild cholestasis (canalicular and intracellular); no fibrosis (see comment)
- Comment: The patient's history of recurrent attacks of jaundice and pruritis are noted. Sections show liver core biopsies with bland cholestasis (both canalicular and intracytoplasmic). No associated inflammation, bile ductular reaction or bile duct loss is seen. No fibrosis is seen.
Differential diagnosis
- Diagnosis is usually by excluding other causes of cholestasis in young patients with disease recurrence
- Progressive familial intrahepatic cholestasis (Clin Res Hepatol Gastroenterol 2019;43:20):
- Severe form of cholestasis that leads to chronic liver disease
- Autosomal recessive disease
- Mutations in the same genes involved in BRIC (genes are either deleted or have frameshift mutations rather than missense mutations leading to complete loss of canalicular protein pump synthesis and manifested in a severe clinical presentation)
- Intrahepatic cholestasis of pregnancy (StatPearls: Pregnancy Intrahepatic Cholestasis [Accessed 26 June 2023]):
- Associated with pregnancy
- Symptoms and enzymes return to normal following delivery and recur with subsequent pregnancies
- Extrahepatic biliary atresia (J Pediatr Surg 1999;34:1706):
- Presents as neonatal cholestasis
- Ultrasound: absence of the gallbladder and the triangular cord sign
- Cholangiography is confirmatory
- Late infancy with pruritus:
- Bile acid synthetic defects:
- Present with cholestasis and normal GGT
- Serum bile acid concentration is low or absent
- Pruritus is mild or absent
- Response to bile acid therapy is good
- Drug induced cholestasis:
- Antimicrobials or acetaminophen may impair bile flow through hepatocellular damage, resulting in episodic cholestasis
Additional references
Board review style question #1
What statement is true regarding benign recurrent intrahepatic cholestasis (BRIC)?
- Biliary tree usually shows severe strictures by radiology
- Frameshift mutation or deletion in ATP8B1 gene or ABCB11 genes
- Liver parenchyma with cirrhosis
- Normal serum alanine aminotransferase (ALT) and aspartate aminotransferase (AST)
- Usually associated with cystic fibrosis
Board review style answer #1
D. Normal serum alanine aminotransferase (ALT) and aspartate aminotransferase (AST). Serum ALT and AST are usually normal in cases of BRIC. Answers A and C are incorrect because BRIC is not usually associated with advanced liver disease / cirrhosis or abnormal biliary tree by imaging. Answer B is incorrect because the mutated genes show missense mutations and not frameshift mutations. Answer E is incorrect because BRIC is not usually associated with cystic fibrosis.
Comment Here
Reference: Benign recurrent intrahepatic cholestasis
Comment Here
Reference: Benign recurrent intrahepatic cholestasis
Bile duct adenoma
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Bile duct adenoma is a benign biliary neoplasm consisting of uniformly distributed small bile ducts in a background of fibrotic stroma
Essential features
- Benign epithelial tumor
- Most commonly a solitary subcapsular nodule (90%)
- Frequently an incidental finding at surgery or autopsy
- Frequently submitted for frozen section to rule out metastatic process
- Can be difficult to distinguish from adenocarcinoma, especially on frozen section
- Uniform distribution of small tubules with no cytological atypia or mitotic figures
- Frequent BRAF V600E mutation supports a neoplastic process
Terminology
- Also known as peribiliary gland hamartoma, cholangioma, cholangioadenoma
ICD coding
- ICD-O: 8160/0 - bile duct adenoma
- ICD-11: 2E92.7 & XH6KR6 - benign neoplasm of liver or intrahepatic bile ducts & bile duct adenoma
Epidemiology
- Usually adults (age > 20), no gender predilection
- Accounts for 1.3% of primary liver tumors and 2.4% in a total of 1,456 resection cases for primary liver tumors and explant for liver cirrhosis (Am J Surg Pathol 1988;12:708, Pathol Int 2014;64:551)
Sites
- Liver, typically subcapsular location
Pathophysiology
- Originally considered to be a reactive ductular proliferation in response to focal injury, a localized biliary healing response equivalent to the function of a peribiliary gland or pyloric gland metaplasia in the foregut or a hamartomatous process (Am J Surg Pathol 1988;12:708, Am J Surg Pathol 2010;34:1312, Am J Surg Pathol 1996;20:858)
- Presence of frequent BRAF V600E mutation supports a neoplastic process (Hepatology 2015;61:403, Histopathology 2015;67:562, Histopathology 2017;70:485)
Etiology
- Unknown; whether focal injury acts as trigger event remains controversial
Clinical features
- Mostly an incidental finding during surgery or autopsy
- Frequently submitted for frozen section to rule out metastatic process
Diagnosis
- Clinical presentation and histopathologic findings
Radiology description
- Hypointense on T1 weighted images, hyperintense on T2 weighted images
- Characteristic arterial phase hyperenhancement that persists into the portal venous and delayed phases on CT and MRI (Diagn Interv Radiol 2018;24:249)
Prognostic factors
- Potential and controversial precursor to intrahepatic cholangiocarcinoma (Histopathology 2021;78:310, Hepatology 2015;61:403, Histopathology 2015;67:562)
Case reports
- 18 month old boy with a large (10 cm) exophytic solid liver tumor (World J Gastrointest Surg 2019;11:414)
- 35 year old woman with resolution of bile duct adenomas after discontinuing oral contraceptive pills (Middle East J Dig Dis 2016;8:327)
- 62, 65 and 76 year old men were identified as having a bile duct adenoma (Endosc Int Open 2018;6:E1312)
- 70 year old man with an incidental finding of intrahepatic bile duct adenoma during laparoscopic distal gastrectomy for gastric cancer (Int Cancer Conf J 2018;8:7)
Gross description
- Usually subcapsular, well circumscribed but nonencapsulated
- Majority are solitary but can be multiple
- Firm, gray-white
- Size ranging from 1 to 20 mm (mean: 5.8 mm) (Am J Surg Pathol 1988;12:708)
Frozen section description
- Usually solitary subcapsular lesion, well circumscribed and nonencapsulated
- Bland small tubular proliferation in a background of fibrotic stroma
- Lack of marked nuclear atypia, mitotic figures, necrosis or intraluminal bile
- Potential diagnostic pitfalls: cellular stroma, back to back compact architecture, mucin production, unusual variant (oncocytic, clear cell, etc.), cytologic atypia enhanced by frozen section artifact
Frozen section images
Microscopic (histologic) description
- Relatively uniform distribution of small tubules with little to no lumen
- Lined by single layer of cuboidal cells with no cytological atypia or mitotic figures
- Well circumscribed with fibrotic stroma
- No intraluminal bile; the ducts do not communicate with the biliary tree
- Rarely, variants with clear cell change, oncocytic features, mucin secreting and alpha-1 antitrypsin droplets (Am J Surg Pathol 2001;25:956, Case Rep Pathol 2014;2014:874826, Case Rep Pathol 2014;2014:282010, Dig Surg 2002;19:324, Int J Surg Pathol 2008;16:218)
Microscopic (histologic) images
Cytology description
- Abundant normal appearing biliary epithelium
- Often admixed with benign hepatocytes
- Cell block may be useful
- Reference: Sidawy: Fine Needle Aspiration Cytology, 1st Edition, 2007
Positive stains
- Typical biliary immunoprofile (positive for CK7 and CK19)
- Expression of foregut antigens (positive for MUC5AC and MUC6) (Am J Surg Pathol 2010;34:1312)
- Ki67 proliferation rate is low (should not be more than 10%)
- BRAF V600E immunoreactivity in 53% of cases (Histopathology 2015;67:562)
- p16INK4a immunoreactivity in 81% of cases (Am J Surg Pathol 2014;38:364)
Negative stains
Molecular / cytogenetics description
- Majority of bile duct adenomas are positive for albumin in situ hybridization, a feature that distinguishes it from metastatic pancreatic adenocarcinoma (Histopathology 2016;69:423)
Sample pathology report
- Liver, wedge biopsy:
- Intrahepatic bile duct adenoma (see comment)
- Comment: The biopsy demonstrates the proliferation of small tubules with no cytological atypia embedded in the fibrous stroma, consistent with bile duct adenoma.
Differential diagnosis
- Cholangiocarcioma or metastatic adenocarcinoma:
- Cytological atypia, mitosis, size may be > 2 cm
- Infiltrative growth pattern
- Extensive expression of EZH2, no or low expression of p16INK4a (Am J Surg Pathol 2014;38:364)
- Ki67 > 10%
- Lymphovascular or perineural invasion
- Von Meyenburg complex (biliary microhamartoma):
- Angulated, branching and irregularly dilated ducts
- Intraluminal bile plugs
Board review style question #1
A 55 year old man with pancreatic adenocarcinoma was admitted for Whipple procedure. A small liver nodule was noted during surgery and sent for intraoperative consultation. A representative photomicrograph of the frozen section is shown. Which of the following is the most likely diagnosis?
- Bile duct adenoma
- Metastatic pancreatic adenocarcinoma
- Reactive ductular proliferation
- Von Meyenburg complex
Board review style answer #1
A. Bile duct adenoma. The diagnosis of a bile duct adenoma is favored during intraoperative consultation, largely attributed to the presence of uniform distribution of small tubules in a background of fibrous stroma. There are no worrisome morphological features, such as infiltrative growth pattern, desmoplastic stromal reaction, marked cytological atypia, frequent mitosis and necrosis.
Comment Here
Reference: Bile duct adenoma
Comment Here
Reference: Bile duct adenoma
Board review style question #2
Which gene is most frequently mutated in bile duct adenoma?
- BRAF
- KRAS
- p53
- SMAD4
Board review style answer #2
A. BRAF mutations are present in about 53% of bile duct adenomas.
Comment Here
Reference: Bile duct adenoma
Comment Here
Reference: Bile duct adenoma
Biliary adenofibroma
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Definition / general
- Premalignant hepatic neoplasm of bile duct origin with epithelial and myofibroblastic stromal components
Essential features
- Benign neoplasm defined histologically by an epithelial component comprised of tubuloacinar and cystically dilated glands and a stromal component comprised of myofibroblast type cells in a background of extensive fibrosis (Patholog Res Int 2010;2010:504584)
- May undergo malignant transformation to cholangiocarcinoma or rarely biliary adenosarcoma (Case Rep Surg 2022;2022:5280884, Hum Pathol 2018;73:108)
- Primary differential includes von Meyenburg complex, bile duct adenoma, simple biliary cysts, biliary cystadenoma, peritoneal inclusion cysts and cholangiocarcinoma (Patholog Res Int 2010;2010:504584, ACG Case Rep J 2018;5:e72)
- Rare: ~35 reported cases
Terminology
- Biliary adenosarcoma may be applicable if the stromal component is malignant (Hum Pathol 2018;73:108)
ICD coding
- ICD-O: 9013/0 - adenofibroma, NOS
- ICD-11: 2E92.7 & XH91Y8 - benign neoplasm of liver or intrahepatic bile ducts & adenofibroma, NOS
Epidemiology
- Rare: ~35 reported cases
- Median age: ~57 years (BMC Med Imaging 2022;22:47)
- No predilection for men or women (Asian J Surg 2023;46:2229)
Sites
- Liver; slight predilection for right lobe
Pathophysiology
- Thought to be a primary epithelial neoplasm with secondarily induced stroma (Am J Surg Pathol 2003;27:693)
- Originates from interlobular or larger bile ducts per D10 and 1F6 staining (Am J Surg Pathol 2003;27:693)
- Stromal component spindle cells are myofibroblastic per immunostains
- May represent neoplastic transformation of von Meyenburg complexes (Am J Surg Pathol 2003;27:693)
- Malignant transformation may be associated with accumulation of oncogenic and tumor suppressor mutations such as TP53, KIT and NRAS (Surg Case Rep 2019;5:104, Case Rep Surg 2022;2022:5280884)
Etiology
- Precise etiology unknown at this time
Clinical features
- Majority of cases present with dull, intermittent epigastric pain
- Rarely presents as a palpable epigastric mass (Case Rep Surg 2022;2022:5280884, AJR Am J Roentgenol 2002;179:280)
- Postprandial nausea / vomiting, weight loss or changes in appetite (Hepatology 2017;65:380, Case Reports Hepatol 2012;2012:793963)
- Other cases are usually asymptomatic and discovered incidentally
- May undergo transformation to intrahepatic cholangiocarcinoma or rarely adenosarcoma (Case Rep Surg 2022;2022:5280884, Hum Pathol 2018;73:108)
- Von Meyenburg complexes may be present in background of tumor (BMC Med Imaging 2022;22:47)
- May rarely present in the background of other primary biliary neoplasms such as mucinous cystic neoplasm (ACG Case Rep J 2018;5:e72)
Diagnosis
- Ultrasound, computed tomography (CT) and magnetic resonance imaging (MRI) used to screen for lesion
- Histology is gold standard
- WHO essential criteria
- Solid microcystic epithelial neoplasm
- Microcystic and tubuloacinar glandular structures lined by nonmucinous biliary epithelium
- Supporting fibroblastic / myofibroblastic stroma
- WHO essential criteria
Laboratory
- Unremarkable liver function tests (LFTs)
- CA 19-9 elevated in a minority of cases (Case Rep Surg 2022;2022:5280884, Taehan Yongsang Uihakhoe Chi 2021;82:721)
Radiology description
- Ultrasound
- Rarely demonstrates a hypoechoic or hyperechoic mass (BMC Med Imaging 2022;22:47)
- Contrast enhanced: early enhancement (World J Clin Cases 2022;10:1366)
- Generally not ideal for complex cystic lesions
- CT
- Solitary, hypodense lobulated solid cystic mass with well defined margins, internal septation and capsular retraction (BMC Med Imaging 2022;22:47)
- MRI (BMC Med Imaging 2022;22:47, Korean J Gastroenterol 2019;74:356)
- Generally considered most reliable screening method
- Solitary, subcapsular, multilocular, solid cystic mass
- T1 weighted: low intensity
- T2 weighted: high intensity; well circumscribed, lobular mass with no intrahepatic bile duct communication
- Contrast enhanced: delayed enhancement
- Features favoring malignancy (BMC Med Imaging 2022;22:47)
- Multiple lesions
- Poorly defined margins
- Unilocular
- Marked enhancement in arterial phase and washout in venous phase
- Peripheral edematous halo
- Diffusion weighted imaging (DWI): restricted diffusion
- Portal venography (BJR Case Rep 2015;1:20150100)
- Portal vein branches moderately displaced with faintly enhancing mass in background
Radiology images
Prognostic factors
- Benign form is associated with favorable prognosis and no risk of recurrence
- Malignant form has risk of local recurrence and distant metastasis
- Recurrence with pulmonary metastasis has been reported (AJR Am J Roentgenol 2002;179:280)
Case reports
- 30 year old woman with an upper abdominal mass between liver and duodenum (Case Rep Gastroenterol 2022;16:535)
- 44 year old asymptomatic woman with a history of chronic hepatitis B and right liver mass (Taehan Yongsang Uihakhoe Chi 2021;82:721)
- 63 year old man with epigastric pain and palpable upper abdominal mass (Case Rep Surg 2022;2022:5280884)
Treatment
- Partial liver resection or hepatectomy is usually curative for benign and malignant forms
- Lobectomy recommended if large or malignant (Pathol Res Pract 2016;212:468)
- Preoperative portal vein embolization (BJR Case Rep 2015;1:20150100)
- Robotic enucleation shows promising results (BMJ Case Rep 2021;14:e242737)
- Value of chemoradiation is not known in a setting of malignancy
Gross description
- Well circumscribed, unencapsulated, solid cystic mass measuring 5 to 16 cm (BMC Med Imaging 2022;22:47, Patholog Res Int 2010;2010:504584)
- White-purple or white-tan, spongy cut surface
Microscopic (histologic) description
- Benign (Patholog Res Int 2010;2010:504584)
- Complex nonmucinous, tubuloacinar glandular structures
- Lining cells are cuboidal to flattened with central round to ovoid nuclei, amphophilic cytoplasm and no significant atypia
- Red blood cells or eosinophilic material may be present in lumina
- Rare papillary projections into lumina
- Cystically dilated glands lined by a single layer of flat epithelial cells
- Moderately cellular fibrous stroma containing bland, myofibroblastic spindle cells
- Mild chronic inflammation characterized by scattered lymphocytes may be present
- Complex nonmucinous, tubuloacinar glandular structures
- Malignant
- Columnar cells with elongated hyperchromatic or vesicular nuclei and atypical mitoses (BMC Med Imaging 2022;22:47)
- Complex papillary, cribriform and back to back architecture (BMC Med Imaging 2022;22:47)
- Eosinophilic cytoplasm with apocrine features including snouts and decapitation secretions (BMC Med Imaging 2022;22:47)
- Fibrous stroma is less prominent or outright absent
- Capsular, lymphovascular or perineural invasion (BMC Med Imaging 2022;22:47)
- Osseous metaplasia has rarely been reported (Hum Pathol 2018;73:108)
Microscopic (histologic) images
Cytology description
- Cytologic features have not been described for this entity
- FNA may be avoided due to possible risk of seeding in setting of malignancy (BJR Case Rep 2015;1:20150100)
Positive stains
- Epithelium
- CK7, CK8/18, CK19
- CA 19-9, CEA, CAM5.2, MUC1 / EMA often positive
- D10 (supports interlobular duct origin) (Am J Surg Pathol 2003;27:693)
- CDH17, CD56 (Surg Case Rep 2019;5:104)
- BAP1 retained if benign
- Stroma
- Ki67 index
- Benign: < 10%, < 1% (in stromal component)
- Malignant: 20 - 30% (BMC Med Imaging 2022;22:47)
Negative stains
- Epithelium
- Stroma
Electron microscopy description
- Electron microscopy findings have not been reported for this entity
Molecular / cytogenetics description
- Monosomy 22 in benign form (Cancer Genet Cytogenet 1997;93:183)
- Associated with benign mesenchymal neoplasms
- PCR / NGS
- CDKN2A loss of function mutation (J Gastrointest Oncol 2016;7:E107)
- TP53 and KIT mutations (Surg Case Rep 2019;5:104)
- NRAS mutation if malignant (Case Rep Surg 2022;2022:5280884)
- Array comparative genomic hybridization
- CCND1 and ERBB2 amplification (Case Rep Surg 2022;2022:5280884)
- Microsatellite stable (MSS) (Surg Case Rep 2019;5:104)
Sample pathology report
- Liver, left lateral segment, segmentectomy:
- Biliary adenofibroma (see comment)
- Comment: Histologic evaluation reveals benign appearing bile ducts without significant cytologic or architecture atypia. Immunohistochemical stains with adequate controls show the lesional cells to be positive for CK7 with low Ki67 and wild type staining pattern with p53. The lesional cells are negative for PAX8, TTF1, CK20, NKX3, HepPar1, arginase and glypican 3. BAP1 immunostain is retained. Overall, based on morphology, low Ki67 and BAP1 retention, a benign biliary lesion is favored. Due to the presence of extensive fibroblastic stroma, this entity may be further classified as biliary adenofibroma.
Differential diagnosis
- Von Meyenburg complex (Patholog Res Int 2010;2010:504584):
- Usually presents as multiple, small (< 0.5 cm) cysts
- Irregular curvilinear ducts lined by cuboidal or flattened cells
- May exhibit dense fibrous stroma similar to adenofibroma
- Bile duct adenoma:
- Small (usually < 1 cm)
- Closely packed tubules with cuboidal lining and narrow lumina
- Cystic dilation is rarely present
- Fibrous stroma is less prominent
- Congenital biliary cyst / simple cyst:
- Usually multiple
- Strong association with autosomal dominant polycystic disease due to PKD1 or PKD2 mutations
- Serous cystadenoma:
- Often large (up to 15 cm)
- Small cysts lined by cuboidal or flattened cells with clear cytoplasm
- Mucinous cystic neoplasm (ACG Case Rep J 2018;5:e72):
- Cholangiocarcinoma:
- Infiltrating glands in fibrous stroma
- Neoplastic cells exhibit at least mild atypia
- May arise in background of chronic schistosomiasis or primary sclerosing cholangitis
- CA 19-9 and CA125 exhibit greater elevation
- Large, homogenous mass with irregular margins by imaging
- Albumin in situ hybridization (ISH) + (80%)
- Benign cystic mesothelioma / peritoneal inclusion cyst (Patholog Res Int 2010;2010:504584):
- Cysts lined by bland cuboidal or flattened mesothelial cells
- Prominent chronic inflammatory infiltrate usually present
- Presents as papillae protruding into cystic lumina
- Calretinin, HBME1, CK5/6, WT1+
- Hepatic endometrial cyst (Eur J Med Res 2015;20:48):
- Exclusively present in women
- Well circumscribed cystic lesion, often with thick overlying fibrous capsule
- Histology is characterized by at least 2 of the following
- Endometrial glands lined by Mullerian epithelium
- Endometrial type stroma
- Hemosiderin laden macrophages
- Epithelial and stroma cells positive for ER, PR and PAX2
- Stromal cells positive for CD10
- Intraductal papillary neoplasm of bile ducts (Proc (Bayl Univ Med Cent) 2019;32:124):
- Histologically characterized by intraductal papillary growth pattern with fibrovascular cores
- May present with pancreatobiliary, intestinal, gastric or oncocytic phenotypes
- Typically multifocal
- Frequently presents with high grade cytologic features
- May undergo malignant transformation into cholangiocarcinoma
- Hepatic foregut cyst (Diagn Pathol 2015;10:81):
- Small (< 4 cm) unilocular cysts
- Typically benign and asymptomatic
- Primarily found in segment 4 of the left lobe
- From deep to superficial, histologically characterized by inner ciliated pseudostratified columnar epithelium, loose lamina propria, smooth muscle band and outer fibrous capsule
- Epithelium may contain goblet cells or gastric metaplasia
Additional references
Board review style question #1
The image above was taken from the right hepatic lobe of a 54 year old woman who presented with dull right upper quadrant (RUQ) pain that began 2 weeks ago. Liver function tests were unremarkable. Per MRI, a large solid cystic mass was identified. Left lateral segmentectomy was pertinent for a single 15.3 cm solid cystic mass with white-purple, spongy cut surface. By immunostaining, a subset of cells were positive for CK7 and CK19 while negative for CK20, CDX2, calretinin and HBME1. The surrounding cells were positive for SMA and vimentin and negative for desmin, ER and PR. The Ki67 index was < 3% while p53 exhibited wild type staining in lesional cells. What is the patient's diagnosis?
- Bile duct adenoma
- Biliary adenofibroma
- Biliary cystadenoma
- Peritoneal inclusion cyst
- Von Meyenburg complex
Board review style answer #1
B. Biliary adenofibroma. The presence of neoplastic glands with biliary type epithelium in an abundantly fibrous stroma (per morphology and immunohistochemistry) in addition to the large size and solid cystic nature of the lesion favors biliary adenofibroma. The large size of this lesion is virtually unheard of among other biliary lesions such as bile duct adenomas and von Meyenburg complexes. Moreover, bile duct adenomas generally lack the overt fibrous stroma of this lesion while von Meyenburg complexes usually present as multiple lesions with irregular curvilinear glands by histology. Though biliary cystadenomas may also present as large cystic masses, the lesion in question does not harbor the clear cytoplasm of serous cystadenoma and lacks the mucin and ER / PR+ ovarian stroma of the mucinous type. Finally, the lesion lacks the papillary luminal infoldings and mesothelial immunohistochemical profile of peritoneal inclusion cysts.
Comment Here
Reference: Biliary adenofibroma
Comment Here
Reference: Biliary adenofibroma
Biopsy
Definition / general
- Core biopsies are 1 - 3 cm by 1 - 2 mm, representing only .002% of total liver mass
- Adequacy important; difficult to diagnosis chronic hepatitis with less than 4 identifiable portal tracts
- Recommended to routinely obtain levels, trichrome stain (highlights type I collagen), possibly reticulin stain (highlights type III collagen framework) and iron stain (to assess iron overload)
- "Clinical history is necessary to render an interpretation rather than a description of the biopsy" - Rosai
- Difficult to differentiate well differentiated hepatocellular carcinoma from benign lesions or poorly differentiated hepatocellular carcinoma as hepatic origin on small biopsy
- Avoid subcapsular hepatic parenchyma in interpretation, as it normally contains delicate fibrous extensions from the capsule; may show scarring out of proportion to the remainder of the biopsy (Curr Gastroenterol Rep 2000;2:27)
Features to examine
- Adequacy of biopsy, site of biopsy (is it from liver?), architecture on low power; portal tracts, lobules, central veins; assess inflammation (degree, type), necrosis, fibrosis, tumor cells
- Portal tracts: presence of vein, artery and bile duct
- Inflammation: type, severity, relationship to bile duct or other structures
- Bile duct changes: inflammation, proliferation or loss, necrosis, cholestasis, atypia
- Vascular changes: inflammation, thrombosis, thickening
- Lobular changes: inflammation, necrosis, sinusoids, cell plates, inclusions, amyloid, fibrosis
- Central veins: size and shape, inflammation and fibrosis
- Final diagnosis should include clinical data, as histologic features are usually insufficient for a nonneoplastic diagnosis
Budd-Chiari syndrome
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Definition / general
- Venous outflow obstruction caused by occlusion of hepatic outflow
- Either acute thrombotic occlusion (usually fatal) or subacute / chronic occlusion with hepatomegaly, ascites, abdominal pain
Essential features
- Thrombotic outflow obstruction developing from various causes
- Patients may experience fatal acute occlusion or may develop symptomatic chronic occlusion leading to cirrhosis
- Sinusoidal dilation and portal tract changes are the most common findings on biopsy
Terminology
- Also called hepatic vein thrombosis
- Historically, Budd-Chiari syndrome technically referred to the triad of painful hepatomegaly, ascites and liver dysfunction
- Membranous obstruction of the vena cava / obliterative hepatocavopathy likely represents recanalized thrombosis, more commonly seen in developing countries
ICD coding
- ICD-10: I82.0 - Budd-Chiari syndrome
Epidemiology
- Occurs in roughly 0.001% of the population
Sites
- Occlusion may occur anywhere from hepatic venules to inferior vena cava
Pathophysiology
- In addition to outflow obstruction, patients often have decreased portal perfusion with eventual compensatory increase in arterial inflow (Hepatology 2003;37:510)
Etiology
- Hepatic vein thrombosis can occur for a variety of reasons (contraceptives, steroids, myeloproliferative disorders, paroxysmal nocturnal hemoglobinuria, pregnancy, postpartum state, hepatocellular carcinoma with inferior vena cava occlusion), though 30% of cases are idiopathic
- Venous obliteration can lead to bridging fibrosis and eventually cirrhosis (Hepatology 1998;27:488)
Clinical features
- Symptoms include painful hepatomegaly, jaundice, ascites and possibly liver failure
- Elevation of transaminases and alkaline phosphatase (Mod Pathol 2004;17:874)
Diagnosis
- Typically diagnosed by radiology, though some cases may be missed
Prognostic factors
- High mortality for acute thrombotic occlusion (especially if all 3 hepatic veins are occluded)
- 5 year survival of 50% for chronic form
Treatment
- Anticoagulation; portosystemic venous shunt (causes reverse flow through portal vein); angiography (to dilate obstruction)
Gross description
- Swollen, congested liver with reddish purple, tense capsule
Microscopic (histologic) description
- Severe centrilobular congestion / necrosis, progressing to centrilobular fibrosis
- Sinusoidal dilation, portal tract expansion / fibrosis and ductular reaction in zones 1 and 3 may be seen (Am J Surg Pathol 2014;38:205)
- Large regenerative nodules, focal nodular hyperplasia and hepatocellular adenomas can develop (Histopathology 2004;44:172)
Microscopic (histologic) images
Sample pathology report
- Liver, biopsy:
- Liver parenchyma with prominent zone 3 sinusoidal dilation (see comment)
- Comment: The findings are most consistent with outflow obstruction (e.g., Budd-Chiari syndrome). Trichrome and iron stains are unremarkable.
Differential diagnosis
- Cardiac / congestive hepatopathy:
- More commonly shows pericellular / sinusoidal fibrosis and fibrosis around central vein (Arch Pathol Lab Med 2017;141:98)
Additional references
Board review style question #1
Which of the following histologic findings is commonly seen in Budd-Chiari syndrome?
- Central vein thrombosis
- Lobular inflammation
- Periportal necrosis
- Sinusoidal dilation
Board review style answer #1
Calcifying nested stromal epithelial tumor
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Rare primary tumor of the liver
- Nonhepatocytic and nonbiliary origin (Arch Pathol Lab Med 2019;143:264)
- Nests of epithelioid and spindle cells with an associated desmoplastic, myofibroblastic stroma and variable calcification or ossification
- Can occur in children of all ages with a female predominance
Essential features
- Often presents as a solitary, well demarcated and lobulated mass with a variable degree of calcification
- Characterized by a nested morphologic growth pattern composed of epithelioid and spindle cells with variable degrees of calcification or ossification
Terminology
- Calcifying nested stromal epithelial tumor (CNSET) of the liver
- Ossifying malignant mixed epithelial and stromal tumor
- Ossifying stromal epithelial tumor
- Desmoplastic nested spindle cell tumor of the liver
ICD coding
Epidemiology
- Age: 2 - 34 years (Arch Pathol Lab Med 2019;143:264)
- M:F = 1:2.5
- Association: Beckwith-Wiedemann syndrome, Cushing type syndrome, Klinefelter syndrome (World J Surg Oncol 2018;16:227, Eur J Med Genet 2017;60:136, Am J Surg Pathol 2005;29:10)
Sites
- Predilection to arise within the right lobe of the liver (Arch Pathol Lab Med 2019;143:264, Mod Pathol 2021;34:1696)
Pathophysiology
- Histogenesis is uncertain
- Several postulations have been raised regarding the origin of the tumor cells (Arch Pathol Lab Med 2019;143:264)
- Epithelial origin with differentiation toward a mesenchymal phenotype
- Mesenchymal origin with the expression of WT1, which reflects a mesenchymal to epithelial phenotype
- Impaired mesenchymal epithelial transition supported by increased expression of mesenchymal epithelial transition factors SNAIL, SLUG, TWIST, c-Met, vimentin and beta catenin
Etiology
- Unknown
- History of oral contraceptive use has been proposed (Int J Surg Pathol 2011;19:268)
Clinical features
- No specific clinical features
- Can present with abdominal pain / distention
- May be associated with Beckwith-Wiedemann syndrome, Cushing type syndrome or Klinefelter syndrome
- Symptoms typically resolve after resection of the liver tumor; however, up to 57% of cases metastasize and recur (Mod Pathol 2021;34:1696)
Diagnosis
- Nests of epithelioid and spindle cells with an associated desmoplastic myofibroblastic stroma
- Variable amount of calcification or ossification
- Expression of cytokeratin, WT1 and beta catenin
Laboratory
- Normal liver function tests and serum tumor markers (AFP and CEA)
Radiology description
- CT:
- Large, well circumscribed, macrolobulated masses, with enhancement and calcification
- Areas of calcification appear hyperdense, whereas cystic or myxoid components within the tumor appear hypodense (Clin Imaging 2016;40:137, Clin Nucl Med 2015;40:131)
- MRI:
- Predominant T1 hypointensity and T2 hyperintensity (Clin Imaging 2016;40:137, Clin Nucl Med 2015;40:131)
- Main differential diagnosis on radiology includes hepatoblastoma, fibrolamellar hepatocellular carcinoma or a calcified hemangioma
Prognostic factors
- Indolent behavior but may recur and metastasize
- Large size, infiltrative growth, vascular invasion, necrosis and increased mitotic activity are risk factors associated with recurrence or metastasis (Am J Surg Pathol 2009;33:976, Mod Pathol 2021;34:1696)
Case reports
- 2 year old girl presented with an incidentally detected calcified liver lesion on a chest radiograph (Radiol Case Rep 2021;16:2337)
- 14 year old girl with Beckwith-Wiedemann syndrome (Eur J Med Genet 2017;60:136)
- 20 year old man with Klinefelter syndrome (World J Surg Oncol 2018;16:227)
- 23 year old woman underwent liver resection for a large hepatic lesion (World J Hepatol 2014;6:155)
- 28 year old woman presented with mild abdominal pain and normal laboratory values (Front Surg 2022;9:875782)
Treatment
- Wedge resections for smaller tumors and partial hepatectomy or liver transplant for larger tumors (Pediatr Transplant 2017;21:e13000)
- Complete resection is curative in more than half of the reported cases
- Uncertain whether chemotherapy holds any benefit with the current available data
Gross description
- Solitary or multiple, mean of 12.6 cm (range 2.1 - 30 cm), well demarcated and lobulated mass with variable calcifications (Arch Pathol Lab Med 2019;143:264)
- Homogenous, tan, granular appearing texture
- May have cystic changes
- May display irregular borders or satellite tumor nodules (Arch Pathol Lab Med 2019;143:264, Mod Pathol 2021;34:1696)
Microscopic (histologic) description
- Well defined nests of relatively bland appearing cells surrounded by variably cellular bands of desmoplastic stroma
- Cells are small, uniformly spindled to large eosinophilic epithelioid cells
- Spindle cells within the nests are arranged in short fascicles at the periphery of the nest, while the epithelioid cells are more apparent in the central portion of the nests
- Stroma surrounding the nests is comprised of spindled cells with long, tapered, cytoplasmic processes, tapered nuclei, bland nuclear chromatin and a small pinpoint nucleolus typical of myofibroblasts
- Foci of psammoma-like calcifications, osteoid material (ossification) and areas of cystic degeneration, necrosis and myxoid change may be present
- In most cases, mitotic activity is < 1 per 10 high power fields (HPFs); increased mitotic activity with up to 22 mitoses per 10 HPFs has been reported (Mod Pathol 2021;34:1696)
- Entrapped, normally formed, mature appearing bile ducts as well as cords of hepatocytes may be seen within the tumor
- Vascular invasion is rare (and is likely related to tumor recurrence or metastasis) (Int J Surg Pathol 2011;19:268, Mod Pathol 2021;34:1696)
Microscopic (histologic) images
Cytology description
- Spindle cells have oval nuclei with stippled chromatin
- Epithelioid cell nuclei are bland and round with finely stippled chromatin and variably conspicuous nucleoli
Positive stains
- AE1 / AE3, vimentin, cytoplasmic and nuclear beta catenin
- Variable CK7, CK8, CK18 and CK19
- Nuclear WT1 with cases of cytoplasmic dot-like paranuclear pattern positivity
- Patchy positivity with CD117, S100, CD99, neuron specific enolase, CD57, CD56 and progesterone receptor
Negative stains
- CK20, synaptophysin, chromogranin A, desmin, CD34, arginase1, INSM1, KIT, HepPar1, polyclonal CEA (canalicular pattern), AFP, HMB45, inhibin A, estrogen receptor, albumin ISH and thyroid transcription factor
Electron microscopy description
- Abundance of rough cytoplasmic reticulum and mitochondria with no evidence of neuroendocrine differentiation (Pediatr Dev Pathol 2008;11:469)
Molecular / cytogenetics description
- Large deletions in exon 3 (155 and 228 base pairs) or other mutations of the beta catenin gene (Hum Pathol 2012;43:1815, Mod Pathol 2021;34:1696)
- TERT promoter alterations (Mod Pathol 2021;34:1696)
Sample pathology report
- Liver, segment 6, partial hepatectomy:
- Calcifying nested stromal epithelial tumor, 11.0 cm (see comment)
- Surgical margins negative for tumor
- Comment: This well demarcated and lobulated mass is present in a background liver without cirrhosis. Microscopically, the tumor is composed of epithelioid and spindle cell nests surrounded by band of desmoplastic stroma. Foci of psammoma-like calcifications and osteoid material (ossification) are present. No mitosis, necrosis or lymphovascular invasion is seen. Immunohistochemically, the tumor cells are positive for cytokeratin AE1 / AE3, vimentin, beta catenin (cytoplasmic and nuclear) and WT1 (nuclear and dot-like perinuclear), whereas negative for HepPar1, CK20, synaptophysin and HMB45. Albumin ISH is negative. The tumor morphology along with immunoprofile is consistent with calcifying nested stromal epithelial tumor. The tumor is completely excised and is 2.2 cm from the closest resection margin.
Differential diagnosis
- Synovial sarcoma:
- SYT::SSX1 and SYT::SSX2 are characteristic translocations
- Hepatoblastoma:
- Desmoplastic small round cell tumor:
- Typically is both positive for WT1 stain and t(11;22) WT1::EWS translocation
- Metastatic gastrointestinal stromal tumor:
Board review style question #1
Which of the following is true about the liver tumor shown above?
- Grossly characterized by large, poorly defined or infiltrative masses, with variable degrees of calcification
- Histopathologically characterized by nests of spindled and epithelioid cells surrounded by a desmoplastic stroma with occasional psammomatous calcification and ossification
- Most commonly seen in adults and with a male predominance
- Positive for AE1 / AE3, vimentin, HepPar1 and AFP
- The tumor is of hepatocellular origin and positive for albumin by in situ hybridization
Board review style answer #1
B. This tumor is histopathologically characterized by nests of spindled and epithelioid cells surrounded by a desmoplastic stroma with occasional psammomatous calcification and ossification
Comment Here
Reference: Calcifying nested stromal epithelial tumor
Comment Here
Reference: Calcifying nested stromal epithelial tumor
Board review style question #2
Which of the following is true about calcifying nested stromal epithelial tumor of the liver?
- Liver function tests (aspartate aminotransferase and alanine aminotransferase) and serum tumor markers (alpha fetoprotein [AFP] and carcinoembryonic antigen) are typically abnormal
- May be associated with cortisol related syndrome or Beckwith-Wiedemann syndrome
- Most commonly seen in adults and with a male predominance
- Regarded to be of hepatocellular origin with nests of epithelioid and spindle cells and variable calcification, even ossification
- Similar to desmoplastic small round cell tumor, typically positive for WT1 and t(11;22) WT1::EWS
Board review style answer #2
B. May be associated with cortisol related syndrome or Beckwith-Wiedemann syndrome
Comment Here
Reference: Calcifying nested stromal epithelial tumor
Comment Here
Reference: Calcifying nested stromal epithelial tumor
Cardiac (congestive) hepatopathy and Fontan associated liver disease
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Manifestations of chronic, passive congestion of the liver in the setting of heart failure or other heart defects (Clin Liver Dis (Hoboken) 2016;8:68)
Essential features
- Congestive hepatopathy can result from various cardiac diseases
- Similar hepatic manifestations following Fontan palliation in congenital heart defects is recognized as Fontan associated liver disease (Int J Mol Sci 2020;21:9420, Semin Thorac Cardiovasc Surg 2022;34:653, Pediatr Radiol 2021;51:2598)
Terminology
- Hepatic venous outflow obstruction
- Chronic passive congestion of the liver
- Congestive hepatopathy
- Cardiac hepatopathy
- Cardiac sclerosis
- Cardiac cirrhosis
ICD coding
Epidemiology
- Any cause of right sided heart failure can lead to congestive hepatopathy
- Widespread use of heart transplantation and major advances in medical and surgical management have significantly altered the profile of patients with congestive hepatopathy (Int J Mol Sci 2020;21:9420)
- Cases due to noncongenital heart failure are declining
- Cases following Fontan surgery (Fontan associated liver disease) are on the rise
Sites
- Liver
Pathophysiology
- Hepatic manifestations result from passive venous congestion / impaired hepatic venous drainage, secondary to chronic right sided heart failure (Int J Mol Sci 2020;21:9420)
- Fontan associated liver disease (FALD) (Int J Mol Sci 2020;21:9420):
- Functional structural alterations in the liver following Fontan creation (total cavopulmonary connection achieved by implanting a surgical shunt to divert blood from the inferior and superior vena cava to the pulmonary arteries) passively carry blood to the functionally single ventricular chamber
- Bypass leads to chronic hepatic venous congestion, secondary to high pressure nonpulsatile flow in the inferior vena cava
- Lack of subpulmonary ventricle also leads to diminished cardiac preload for the systemic ventricle, resulting in chronically low cardiac output
- FALD's natural history is poorly understood; at present, there are no methods to identify or predict patients that will eventually develop clinically significant advanced liver disease
Etiology
- Right sided heart failure or right ventricular failure (RVF), whether primary or secondary
- In the adult population, RVF is usually a result of left ventricular failure (Interact Cardiovasc Thorac Surg 2018;27:921)
- Primary RVF (Card Fail Rev 2019;5:140):
- Chronic conditions leading to pressure overload
- Congenital heart defects (pulmonic stenosis, those with right ventricular outflow obstruction or RV exposed to systemic pressure)
- Chronic conditions leading to volume overload (Card Fail Rev 2019;5:140):
- Valvular insufficiency involving tricuspid or pulmonic valves
- Congenital heart disease with left to right shunt (atrial septal defect, anomalous pulmonary venous return)
- Fontan associated liver disease (Int J Mol Sci 2020;21:9420):
- Recognized consequence of Fontan palliation in patients born with univentricular physiology, congenital heart disease
- Intrinsic RV myocardial disease / injury (Interact Cardiovasc Thorac Surg 2018;27:921):
- Ischemia or infarct
- Infiltrative disease (e.g., sarcoidosis, tumor, amyloidosis)
- Arrhythmogenic right ventricular dysplasia
- Cardiomyopathy
- Microvascular disease
- Impaired RV filling (Interact Cardiovasc Thorac Surg 2018;27:921):
- Constrictive pericarditis
- Tricuspid stenosis
- Systemic vasodilatory shock
- Cardiac tamponade
- Superior vena cava syndrome
- Hypovolemia
Clinical features
- Usually asymptomatic and in such a scenario, passive liver congestion may be incidentally discovered through abnormalities in routine laboratory evaluations (Clin Liver Dis (Hoboken) 2016;8:68)
- When symptomatic, patients may experience
- Dull right upper quadrant pain
- Jaundice
- Clinical stigmata of portal hypertension are generally absent until cirrhosis ensues (Clin Liver Dis 2002;6:947)
- Progressive dyspnea
- Hepatomegaly
- Gastroesophageal varices
- Ascites
- Hepatojugular reflux
- Peripheral edema
Diagnosis
- Diagnosis is often made by abnormal laboratory workup (see Laboratory findings)
- Liver biopsy may be performed if liver tests are persistently abnormal after heart failure treatment or as part of the heart or combined heart / liver transplant workup
Laboratory
- Unconjugated hyperbilirubinemia (total bilirubin < 3 mg/dL [51.31 micromol/L])
- Elevated aminotransferases (< 2 - 3 fold)
- Mild hypoalbuminemia in 30 - 50% of patients (Clin Liver Dis 2002;6:947)
- Prolonged prothrombin time / international normalized ratio (PT / INR)
- Ascitic fluid may show high serum to ascites albumin concentration gradient (JAMA 2016;316:340)
- Gradients ≥ 1.1 g/dL (11 g/L) are specific for ascites due to portal hypertension (the serum albumin concentration minus the ascitic albumin concentration [SAAG]) (JAMA 2016;316:340)
- High ascitic total protein content (typically > 2.5 g/dL [25 g/L]) plus a SAAG ≥ 1.1 g/dL (11 g/L) suggests congestive hepatopathy and differentiates portal hypertension from cirrhosis (typically total protein < 2.5 g/dL [25 g/L] plus a SAAG ≥ 1.1 g/dL [11 g/L])
Radiology description
- Ultrasound (US) may be used to evaluate hemodynamic properties of the liver in patients with congestive hepatopathy (CH)
- Doppler US is the most cost effective and expeditious modality for assessing blood flow direction and velocity in the hepatic vasculature
- Common US findings of CH (Acta Radiol Diagn (Stockh) 1982;23:361, Am J Cardiol 1984;53:579):
- Dilated inferior vena cava
- Dilated hepatic veins
- Degree of dilatation correlates with the severity of heart failure
- CT and MR imaging can show a number of characteristic findings helpful for the diagnosis of CH (Diagn Interv Radiol 2020;26:541)
- Hepatomegaly in acute congestion
- Atrophic nodular liver in patients with chronic congestion and cirrhosis
- As seen on the US, the inferior vena cava and hepatic veins are dilated; in severe cases, venous shunts can be observed between the hepatic veins
- Increased prevalence of hyperenhancing hepatic nodules that appear similar to focal nodular hyperplasia
- Presence of cirrhosis increases the risk for hepatocellular carcinoma in patients with CH; this diagnosis must be taken into consideration
- Reference: Radiographics 2016;36:1024
Prognostic factors
- Clinical outcome generally depends on the severity of underlying cardiac disease; progression to cirrhosis does not necessarily correlate with worse prognosis and reversibility may be achieved by optimization of cardiac function (Clin Liver Dis (Hoboken) 2016;8:68)
Case reports
- 7 year old girl with Fontan associated liver disease and hepatic adenomatosis (Pediatr Cardiol 2010;31:861)
- 36 year old woman with focal nodular hyperplasia in the setting of Fontan associated liver disease (Korean J Intern Med 2022;37:480)
- 40 year old man with Fontan associated liver disease and ruptured hepatocellular carcinoma (SAGE Open Med Case Rep 2020;8:2050313X20922030)
Treatment
- Management of the underlying heart condition with optimization of cardiac output
- Treatment options include diuresis, left ventricular assist device (LVAD) implantation and liver transplantation (Clin Liver Dis (Hoboken) 2016;8:68)
Gross description
- Sinusoidal congestion resulting in a classic nutmeg appearance
- Advanced fibrosis may lead to a firm and nodular cut surface
- Reference: Clin Liver Dis (Hoboken) 2016;8:68
Microscopic (histologic) description
- Sinusoidal dilatation and congestion
- Centrilobular hepatocyte atrophy or dropout
- Centrilobular and perisinusoidal fibrosis (heterogeneous distribution but generally starts in zone 3 hepatocytes)
- Portal fibrosis in up to 75% of cases
- Minimal portal inflammation and ductular reaction
- Nodular regenerative hyperplasia (Rev Esp Cardiol (Engl Ed) 2018;71:192)
- Hepatocellular carcinoma may arise in the setting of cirrhosis (J Thorac Cardiovasc Surg 2005;129:1348, JHEP Rep 2021;3:100249)
- Focal nodular hyperplasia and hepatic adenoma may also occur (JACC Case Rep 2019;1:175, J Thorac Cardiovasc Surg 2005;129:1348, Pediatr Cardiol 2010;31:861)
- Pseudoground glass and eosinophilic cytoplasmic inclusions (Torbenson: Biopsy Interpretation of the Liver, 4th Edition, 2021, Mod Pathol 2000;13:679)
- Congestive hepatic fibrosis score shows a good correlation with the right atrial pressure (Mod Pathol 2014;27:1552):
- Score 0: no fibrosis
- Score 1: central zone fibrosis
- Score 2A: central zone and mild portal fibrosis, with accentuation at central zone
- Score 2B: at least moderate portal fibrosis and central zone fibrosis, with accentuation at portal zone
- Score 3: bridging fibrosis
- Score 4: cirrhosis
Microscopic (histologic) images
Positive stains
- Special stains for fibrosis evaluation: Masson trichrome or Sirius red
- Special stain for nodular regenerative hyperplasia and fibrosis evaluation: reticulin
Sample pathology report
- Liver, biopsy:
- Liver with patchy sinusoidal dilatation and congestion, in keeping with Fontan associated liver disease (congestive hepatopathy)
- Heterogeneous degree of fibrosis with portal, perivenular and perisinusoidal fibrosis with focal portal to central bridging fibrosis (congestive hepatic fibrosis score 2A-3 of 4)
- No significant portal inflammation, lobular activity, steatosis or cholestasis
Differential diagnosis
- Budd-Chiari syndrome:
- Centrilobular hepatocyte necrosis is more common
- Sinusoidal obstruction syndrome:
- Marked centrilobular hemorrhagic necrosis in the early phase and occlusion of the central veins by fibrous tissue in later stages of the disease
- Ischemia:
- Centrilobular coagulative hepatocyte necrosis is more common
Additional references
Board review style question #1
Which of the following histologic features is typical of congestive hepatopathy?
- Bile duct injury
- Feathery degeneration of hepatocytes
- Microvesicular steatosis
- Obliterated portal veins
- Perisinusoidal fibrosis
Board review style answer #1
E. Perisinusoidal fibrosis
Comment Here
Reference: Cardiac (congestive) hepatopathy and Fontan associated liver disease
Comment Here
Reference: Cardiac (congestive) hepatopathy and Fontan associated liver disease
Board review style question #2
Board review style answer #2
C. Constrictive pericarditis
Comment Here
Reference: Cardiac (congestive) hepatopathy and Fontan associated liver disease
Comment Here
Reference: Cardiac (congestive) hepatopathy and Fontan associated liver disease
Caroli disease
Table of Contents
Definition / general | Clinical features | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosisDefinition / general
- Also called communicating cavernous biliary ectasia
- Autosomal recessive disorder, mildly associated with autosomal dominant and autosomal recessive polycystic kidney disease (Wikipedia: Caroli Disease [Accessed 25 October 2017])
- Due to arrest of remodeling of ductal plate of larger intrahepatic bile ducts
- Usually presents during childhood and early adulthood (Curr Gastroenterol Rep 2007;9:151)
- Larger ducts of intrahepatic biliary tree are segmentally dilated and may contain inspissated bile; when progressive, leads to intrahepatic stones, recurrent cholangitis, portal hypertension, cholangiocarcinoma and liver failure
- Usually associated with congenital hepatic fibrosis; 7 - 14% develop dysplasia and cholangiocarcinoma
- Often gallstones, ulcer, hyperplasia
- Poor prognosis, with death due to sepsis or liver failure
- Caroli syndrome: Caroli disease plus congenital hepatic fibrosis
Clinical features
- Jaundice, right upper abdominal pain, fever; due to associated complications of hepatolithiasis or bacterial cholangitis
Gross description
- 1 - 4 cm cysts separated by normal bile ducts
Microscopic (histologic) description
- Dilated ducts lined by cuboidal or columnar epithelium with fibrotic duct wall
Microscopic (histologic) images
Differential diagnosis
- Primary sclerosing cholangitis:
- Autoimmune disorder associated with inflammatory bowel disease; not inherited; fibrosing cholangitis with onion skinning around affected ducts
Checkpoint inhibitor associated hepatitis
Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Pathophysiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Immunohistochemistry & special stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Immune related adverse event secondary to immune checkpoint inhibitors such as anti-PD1 (nivolumab, pembrolizumab), anti-PDL1 (atezolizumab, avelumab, darvalumab) and anti-CTLA4 medications (ipilimumab and tremelimumab)
Essential features
- Incidence varies; CTLA4 inhibitors are slightly more hepatotoxic than PD1 inhibitors; combination therapy increases risk
- Presents as mild acute hepatitis pattern of injury (panlobular hepatitis), perivenular infiltrate with endothelialitis, biliary pattern with bile ductular proliferation, mixed portal inflammation with little lobular necroinflammation
ICD coding
- ICD-10: K71.6 - Toxic liver disease with hepatitis, not elsewhere classified
Epidemiology
- Hepatotoxicity presents as elevations of ALT or AST and can occur at any time but typically presents after 6 - 12 weeks of therapy (J Clin Oncol 2012;30:2691)
- The rate of hepatotoxicity varies between different inhibitors
- With CTLA4 inhibitors, the incidence of all grade hepatotoxicity is 3 - 9% (J Clin Oncol 2012;30:2691)
- With PD1 inhibitors the rate is 1 - 3% (Lancet 2014;384:1109, N Engl J Med 2015;372:320, Int J Cancer 2017;141:1018)
- Combination therapies increase the risk to 11 - 20% (Stem Cell Investig 2017;4:32, N Engl J Med 2015;372:2006, J Clin Oncol 2017;35:3851)
Pathophysiology
- Caused by immune dysregulation secondary to immune therapy
Clinical features
- Mild serum aminotransferase elevations, usually self limited, occur in approximately 10 - 50% of patients (Proc Natl Acad Sci U S A 2003;100:8372, Ann Oncol 2010;21:1712, Melanoma Res 2013;23:47, Invest New Drugs 2013;31:1071)
- ALT elevations > 3 - 5 times normal (approximately 0.5 - 1.5%), usually respond to corticosteroids (N Engl J Med 2010;363:711, N Engl J Med 2012;366:2443, N Engl J Med 2015;372:2521, Nature 2014;515:558, J Clin Oncol 2017;35:2117)
- Severe cases with systemic symptoms and highly increased levels of liver function tests (ALT > 1,000 IU/L) (Invest New Drugs 2013;31:1071)
- Rare cases of fulminant hepatitis and death
Diagnosis
- Elevation of liver function tests with history of immune therapy medication use, along with characteristic biopsy related changes and excluding other causes of liver injury
Laboratory
- Most common finding is asymptomatic elevation of liver function tests (AST / ALT)
Radiology description
- In severe cases with ALT > 1,000 IU/L, imaging findings were characterized by mild hepatomegaly, periportal edema and periportal lymphadenopathy (Invest New Drugs 2013;31:1071)
- Mild cases showed normal imaging findings (Invest New Drugs 2013;31:1071)
Prognostic factors
- Normalization of liver function tests and response to steroids after discontinuation of checkpoint inhibitors; however, disease can still progress histologically even when liver function tests normalize (JHEP Rep 2019;1:66)
Case reports
- 45 year old man with ipilimumab associated cholestatic hepatitis (Melanoma Res 2017;27:380)
- 48 year old man with lung adenocarcinoma and cholestatic liver injury secondary to pembrolizumab (Intern Med 2019;58:3283)
- 52 year old man with lung and liver metastasis of malignant melanoma developed fulminant hepatitis after 34 weeks of nivolumab treatment (Case Rep Oncol 2017;10:368)
- 53 year old woman with refractory immune checkpoint inhibitor hepatitis successfully treated by infliximab (JHEP Rep 2019;1:66)
- 67 year old man with pembrolizumab induced hepatitis (Pathology 2017;49:789)
- 74 year old woman with recurrent renal cell carcinoma developed nivolumab induced hepatitis (J Oncol Pharm Pract 2020;26:459)
Treatment
- Most patients respond to systemic corticosteroids (JHEP Rep 2019;1:66)
- Discontinuation of offending medication (JHEP Rep 2019;1:66)
- Infliximab can be considered as a rescue therapy (JHEP Rep 2019;1:66)
Microscopic (histologic) description
- Histologic features of both anti-CTLA4 or anti-PD1 / PDL1 associated hepatitis:
- Acute hepatitis pattern (panlobular hepatitis): perivenular infiltrate with endothelialitis (Mod Pathol 2018;31:965)
- Biliary pattern: bile ductular proliferation, mild mixed portal inflammation with little lobular necroinflammation
- Other less common features:
- Centrilobular confluent necrosis, plasmacytosis, bile duct injury, microabscesses (Mod Pathol 2018;31:965)
- Specific for anti-CTLA4 associated hepatitis: granulomatous inflammation, severe lobular necroinflammatory activity and central vein endothelialitis (Rheumatology (Oxford) 2019;58:vii17, J Hepatol 2018;68:1181, Invest New Drugs 2013;31:1071)
- Specific for anti-PD1 / PDL1 associated hepatitis: no granulomatous inflammation, infrequent central vein endothelialitis (Rheumatology (Oxford) 2019;58:vii17, J Hepatol 2018;68:1181, Invest New Drugs 2013;31:1071)
Microscopic (histologic) images
Immunohistochemistry & special stains
- Large numbers of CD3+ and CD8+ lymphocytes, whereas CD20+ B cells and CD4+ T cells are fewer in checkpoint inhibitor induced liver injury than in autoimmune hepatitis or drug induced liver injury (Mod Pathol 2018;31:965)
- Anti-PD1 / L1 hepatitis: similar proportions of CD4+ and CD8+ infiltrates in portal tracts, with CD8+ cells dominating lobular infiltrates
- Anti-CTLA4 hepatitis: predominance of CD8+ cells in portal tracts and lobules
Sample pathology report
- Liver, biopsy:
- Liver with moderate portal and lobular lymphocyte infiltrate with mild bile duct injury, most consistent with medication associated injury (see comment)
- Comment: Patient history of advanced melanoma status posttreatment with nivolumab and negative viral and autoimmune serologies are noted. The majority of the portal tracts and lobules are involved by moderate lymphocytes with scattered eosinophils and plasma cells with focal bile duct injury. Overall, the findings are most consistent with immune therapy associated liver injury.
Differential diagnosis
- Other causes of immune mediated hepatitis include:
- Viral hepatitis:
- Acute:
- Lobular disarray with diffuse lobular inflammation, hepatocyte swelling, necrosis and regeneration
- Lobular inflammation generally exceeds portal inflammation
- Chronic:
- Predominantly portal or periportal hepatitis with varying degrees of parenchymal inflammation, hepatocellular injury and fibrosis
- Acute:
- Graft versus host disease:
- Bile duct epithelial cell damage is key distinguishing feature differentiating GVHD from other types of hepatic injury
- Endotheliitis can also be present
- Autoimmune hepatitis:
- Can be treated or untreated
- If treated, the biopsy may be normal or contain mild chronic hepatitis without specific histological features
- If untreated, the biopsy can contain chronic hepatitis with plasma rich inflammation and interface activity
- Can be treated or untreated
- Viral hepatitis:
Additional references
- J Gastrointest Oncol 2018;9:220, LiverTox: Nivolumab [Accessed 11 June 2020], LiverTox: Pembrolizumab [Accessed 11 June 2020], LiverTox: Atezolizumab [Accessed 11 June 2020], LiverTox: Avelumab [Accessed 11 June 2020], LiverTox: Ipilimumab [Accessed 11 June 2020], LiverTox: Durvalumab [Accessed 11 June 2020]
Board review style question #1
Which of the following are typical features of checkpoint inhibitor associated hepatitis?
- Bridging fibrosis with lobular atrophy
- Macrovesicular and microvesicular steatosis
- Mallory-Denk bodies and hepatocyte ballooning
- Mild portal tract inflammation with mild lobular activity
Board review style answer #1
D. Mild portal tract inflammation with mild lobular activity
Comment Here
Reference: Checkpoint inhibitor associated hepatitis
Comment Here
Reference: Checkpoint inhibitor associated hepatitis
Board review style question #2
A 67 year old man with a history of autoimmune hepatitis completed 6 cycles of pembrolizumab therapy for metastatic melanoma. He began developing abdominal pain and jaundice, with ALT > 1,000 IU/L. He underwent a liver biopsy and findings are shown above. Which of the following findings favors checkpoint inhibitor hepatitis over autoimmune hepatitis?
- Dense portal based plasma cell rich inflammatory infiltrates with interface activity
- Hepatocytic swelling, spotty necrosis, multiple lobular granulomata
- Macrovesicular steatosis, zone 3 ballooning, Mallory-Denk bodies
- Mild lobular and portal activity
Board review style answer #2
D. Mild lobular and portal activity
Comment Here
Reference: Checkpoint inhibitor associated hepatitis
Comment Here
Reference: Checkpoint inhibitor associated hepatitis
Cholangitis lenta / sepsis
Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Laboratory | Case reports | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Cholangitis lenta was originally a term referring to a rare clinical form of chronic sepsis (Hum Pathol 1982;13:19)
- Now typically used by pathologists to refer to microscopic bile ductular cholestasis (Am J Surg Pathol 2017;41:1607), often in the context of sepsis
Essential features
- Cholangitis lenta currently functions as a synonym for bile ductular cholestasis
- Ductular reaction with bile ductular cholestasis is concerning (but not specific) for sepsis
Terminology
- Additional terms include cholangiolar cholestasis or subacute nonsuppurative cholangitis (Am J Surg Pathol 2017;41:1607)
- Lenta appears to mean slow
Pathophysiology
- Cause of biliary abnormalities in septic patients is complex, likely multifactorial (Crit Care 2012;16:235)
Laboratory
- Positive microbiology cultures common (Am J Surg Pathol 2017;41:1607)
- Bilirubin levels often high (Lefkowich: Scheuer's Liver Biopsy Interpretation, 9th Edition, 2015)
Case reports
- Child with sepsis and hepatorenal syndrome (Fetal Pediatr Pathol 2018;37:424)
Microscopic (histologic) description
- Dilated, peripherally located bile ductular reaction that contains inspissated bile
- Other common findings include portal tract inflammation, duct injury, hepatocyte ballooning or necrosis and canalicular cholestasis (Am J Surg Pathol 2017;41:1607)
Microscopic (histologic) images
Sample pathology report
- Liver, biopsy:
- Biliary pattern injury with ductular reaction, prominent ductular cholestasis and moderate portal inflammation (see comment)
- Comment: The clinical concern for liver failure is noted. The histologic findings raise the possibility of sepsis, though they are not specific for that diagnosis.
Differential diagnosis
- Ductular cholestasis can be seen in:
- Sepsis:
- Histology not entirely specific, with other biliary pattern injury and inflammation often seen; clinical correlation needed
- Neonatal alpha-1 antitrypsin deficiency:
- PASD positive protein globules in hepatocytes
- Extrahepatic biliary atresia:
- Biliary pattern injury in young patients; clinical correlation needed
- Cirrhosis:
- Cause of cirrhosis not necessarily biliary
- Post transplant liver biopsies:
- Occurs in both adult and pediatric patients (Am J Surg Pathol 2017;41:1607, Transplantation 1998;65:692)
- Clinical correlation needed
- Sepsis:
Board review style question #1
A patient presents with jaundice and general malaise. Workup indicates acute liver failure, along with an elevated white blood cell count. Liver biopsy shows the findings in the image above. What is the most likely diagnosis?
- Acetaminophen toxicity
- Alpha-1 antitrypsin deficiency
- Primary biliary cholangitis
- Sepsis
Board review style answer #1
Board review style question #2
What is the term typically used by pathologists to refer to bile ductular cholestasis?
- Biliary cholangitis
- Cholangitis lenta
- Fibrosing cholestatic hepatitis
- Obstructive cholestasis
Board review style answer #2
Choledochal cyst
Table of Contents
Definition / general | Diagrams / tables | Clinical images | Gross description | Microscopic (histologic) descriptionDefinition / general
- Cystic dilatations of the biliary tree; can involve the extrahepatic biliary radicles, the intrahepatic biliary radicles or both
- Classified into 5 types (Am J Surg 1977;134:263)
- Classically presents with pain, right upper quadrant mass and jaundice, particularly in children
- Cholangitis symptoms may predominate in adults
- Usually women
- 14% develop adenocarcinoma with increasing age
Gross description
- Often huge cysts
Microscopic (histologic) description
- Thick fibrous wall, often inflamed
- Discontinuous columnar epithelium; variable squamous metaplasia (Can J Surg 2009;52:434)
Cholestasis
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Pathophysiology | Etiology | Clinical features | Laboratory | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Decrease in bile flow due to hepatocellular dysfunction or biliary obstruction
Essential features
- Microscopically visible bile, usually in hepatocyte cytoplasm or canaliculi
- Seen in most forms of biliary pattern injury
Terminology
- Bland cholestasis refers to cholestasis as an isolated microscopic finding
- Cholestatic hepatitis refers to microscopic cholestasis alongside inflammatory findings (that is, hepatitis)
- Histologic cholestasis sometimes referred to as bilirubinostasis
ICD coding
- ICD-10: K71.0 - toxic liver disease with cholestasis
Pathophysiology
- Bile is produced in hepatocytes and flows as follows: hepatocyte canaliculi → canals of Hering → bile ductules → interlobular bile ducts → larger bile ducts → duodenum
- Injury or obstruction at any point along biliary flow can lead to cholestasis
Etiology
- Most typically seen in biliary disease (primary sclerosing cholangitis, primary biliary cirrhosis) or drug induced liver injury (Hepatology 2011;53:1377)
- Other causes include pregnancy, benign familial recurrent cholestasis, sepsis (World J Gastroenterol 2009;15:2049)
Clinical features
- Patients with cholestasis may have jaundice, pruritus (due to bile acid deposition in skin), skin xanthomas (due to hyperlipidemia), deficiencies of fat soluble vitamins (A, D, E, K)
- Clinical cholestasis may not correlate with histologic cholestasis
Laboratory
- Elevated serum alkaline phosphatase (present in bile duct epithelium and hepatocyte canalicular membrane), elevated serum bilirubin
Treatment
- Varies depending on etiology
- Ursodeoxycholic acid and obeticholic acid can improve symptoms of cholestatic liver disease (Hepatology 2002;36:525 GR)
Microscopic (histologic) description
- Bile pigment (yellow / green / brown) visible histologically within hepatic parenchyma, usually perivenular
- May be present within hepatocyte cytoplasm, hepatocyte canaliculi, ductule lumens or large duct lumens
- Chronic cholestasis leads to cholate stasis / feathery degeneration of periportal hepatocytes – enlarged, swollen cells with clear / granular cytoplasm
Microscopic (histologic) images
Sample pathology report
- Liver, biopsy:
- Hepatic parenchyma with mild chronic inflammation and lobular cholestasis (see comment)
- Comment: The findings suggest cholestatic hepatitis. Possible etiologies, depending on clinical findings, include primary biliary cirrhosis, drug induced liver injury, viral hepatitis, and primary sclerosing cholangitis.
Differential diagnosis
- Other brownish pigments that can mimic bile histologically include lipofuscin (may be present in cytoplasm but not canaliculi) and hemosiderin (darker, duskier brown)
- Differential for bland cholestasis:
- Drug induced liver injury (e.g., anabolic steroids), early duct obstruction, benign recurrent intrahepatic cholestasis, acute cholestasis of pregnancy
- Differential for cholestatic hepatitis:
- Primary sclerosing cholangitis (inflammation usually minimal), primary biliary cholangitis, viral hepatitis, large duct obstruction, progressive familial intrahepatic cholestasis
- Differential for ductular cholestasis:
- Sepsis, cirrhosis (any cause), dehydration, extrahepatic biliary atresia, ductal plate malformations
Board review style question #1
Board review style answer #1
B. Anabolic steroid injury
Comment here
Reference: Liver and intrahepatic bile ducts - nontumor - Cholestasis
Comment here
Reference: Liver and intrahepatic bile ducts - nontumor - Cholestasis
Board review style question #2
Liver injury with cholestasis typically results in an increase of what laboratory value?
- Alanine aminotransferase
- Albumin
- Alkaline phosphatase
- Aspartate aminotransferase
Board review style answer #2
C. Alkaline phosphatase
Comment here
Reference: Liver and intrahepatic bile ducts - nontumor - Cholestasis
Comment here
Reference: Liver and intrahepatic bile ducts - nontumor - Cholestasis
Chronic antibody mediated rejection
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Laboratory | Radiology description | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Antibody mediated immune injury to liver allografts, resulting in significant fibrosis and persistent inflammation (Am J Transplant 2016;16:2816)
- Consequence of chronic long term immunologic injury (EBioMedicine 2016;9:346)
- Leading cause of retransplantation after 10 years in children (Clin Transplant 2018;32:e13227)
- Second leading cause of retransplantation in adults after disease recurrence (Clin Transplant 2018;32:e13227)
Essential features
- Liver allograft fibrosis
- Unexplained mononuclear, interface or perivenular inflammation / necroinflammatory activity
- Evidence of circulating donor specific antibodies
- C4d deposition
Terminology
- Chronic active antibody mediated rejection (cAMR) (Am J Transplant 2016;16:2816)
- Humoral rejection is considered an old term
ICD coding
- ICD-10: T86.41 - Liver transplant rejection
Epidemiology
- Incidence about 8% at 10 years posttransplantation
- Risk factors:
- Retransplantation (Am J Transplant 2014;14:867)
- Young age (Ann Transplant 2017;22:333)
- Cyclosporine immunosuppression (Am J Transplant 2013;13:1541)
- Low calcineurin inhibitor level (Am J Transplant 2013;13:1541)
Sites
- Liver allografts
- Also occurs in other solid organ allografts such as kidney (Am J Transplant 2017;17:28)
Pathophysiology
- Linked to anti-class II donor specific antibodies (DSA), AT1R and portal inflammation (Transplantation 2017;101:2399, Liver Transpl 2008;14:1582)
- Persistent de novo donor specific antibodies, usually directed at HLA-DQ (Am J Transplant 2013;13:1541, Am J Transplant 2016;16:603)
Clinical features
- Mostly asymptomatic with normal or near normal liver function tests (Liver Transpl 2016;22:1593)
- Mostly detected on protocol biopsies
Diagnosis
- Criteria and categories for the diagnosis of cAMR were defined by the Banff working group (Am J Transplant 2016;16:2816)
| Probable chronic active AMR (all 4 criteria must be met) | |
| 1 | Histopathologic evidence of injury consistent with cAMR (both required):
|
| 2 | Recent evidence of circulating HLA DSA in serum samples |
| 3 | At least focal C4d positive (> 10% portal tract microvascular endothelia); see Acute AMR for C4d scoring |
| 4 | Reasonable exclusion of other insults that might cause a similar pattern of injury |
| Possible chronic active AMR | |
| 1 | As above but C4d staining is negative or minimal (criteria 1, 2 and 4 met) |
- Criteria are intended to be stringent to prevent overdiagnosis and do not include more recently described lesions (see Microscopic description); as more lesions are described, the criteria will likely be updated
- Banff suggests that liver allograft fibrosis scoring be performed in 3 separate compartments (portal, sinusoidal and perivenular) according to Venturi et al. (Am J Transplant 2012;12:2986)
Liver allograft fibrosis semiquantitative scoring system by Venturi et al. (Am J Transplant 2012;12:2986)
| | | | | |
| Portal tracts | No fibrosis | Nonexpanding fibrosis in less than 50% of portal tracts | Fibrosis in more than 50% of portal tracts or expansion into short fibrous septa into periportal parenchyma | Marked expansion of most or all portal tracts with portal to portal or portal to central bridging fibrosis with or without occasional nodules |
| Sinusoids (zones 1 and 2) | No fibrosis | Little fibrosis with thin focal collagen deposits involving less than 50% of sinusoids | Little fibrosis with thin diffuse collagen deposits involving more than 50% of sinusoids or thicker but focal fibrosis in less than 50% of sinusoids | Thick, marked and diffuse sinusoidal fibrosis |
| Centrilobular vein | No fibrosis | Circular perivenular fibrosis involving less than 50% of central veins without invasion into the perivenular parenchyma | Circular perivenular fibrosis in more than 50% of central areas or expansion into short fibrous septa into perivenular parenchyma | Marked centrilobular fibrosis with bridging to other central or portal areas |
- Scores from each compartment are added for a total score out of 9
Laboratory
- Evidence of DSA (HLA or non-HLA); mostly HLA class II DQ
- Negative testing for hepatitis B, C and E (Liver Transpl 2016;22:1593)
- Serum markers of fibrosis have been proposed, including hyaluronic acid and embryonic liver fodrin (Liver Transpl 2016;22:1593)
- No serum markers of inflammation are currently recommended
Radiology description
- Multiple imaging modalities can detect hepatic fibrosis to varying degrees:
- Magnetic resonance elastography (Clin Gastroenterol Hepatol 2015;13:440)
- Acoustic radiation force impulse (J Pediatr Gastroenterol Nutr 2014;58:382, Pediatr Radiol 2013;43:545)
- Transient elastography (J Pediatr Gastroenterol Nutr 2013;56:72, Pediatr Transplant 2013;17:525)
- In general, these modalities are more effective in detecting advanced fibrosis
- Less effective in detecting milder fibrosis when used on split liver allografts and when cholestasis is present
Case reports
- Report of 4 cases with cAMR and obliterative portal venopathy (Pediatr Transplant 2018; 22:e13124)
Treatment
- Retransplantation for failed allografts
Gross description
- Explanted livers show a fibrotic multinodular and rubbery cut surface
- May show a green cholestatic cut surface
Microscopic (histologic) description
- Inflammation (Clin Transplant 2018;32:e13227, Liver Transpl 2016;22:1593, Liver Transpl 2018;24:897):
- Chronic hepatitis pattern of mononuclear inflammation with interface hepatitis or lobular and perivenular inflammation
- Perivenulitis
- Vascular changes (Pediatr Transplant 2018; 22:e13124, Am J Transplant 2018;18:1534):
- Obliterative portal venopathy with nodular regenerative hyperplasia-like changes
- Obliterative arteriopathy or isolated arterial "V" lesions (age inappropriate arterial fibrointimal hyperplasia with no T cell mediated rejection) with or without intimal inflammation arterial lesions are associated with subsequent T cell mediated rejection (TCMR), graft failure and C4d positivity; most C4d positive cases show additional histologic features encountered in cAMR such as portal and perivenular inflammation (rejection activity index / RAI 1 - 2) and at least moderate periportal, perivenular or sinusoidal fibrosis (Am J Transplant 2018;18:1534)
- Bile duct changes (Liver Transpl 2018;24:897):
- Biliary epithelial senescence and duct loss may be seen but at lower rates
- Distinct fibrosis patterns (Am J Transplant 2016;16:603, Transplantation 2017;101:2062, Clin Transplant 2018;32:e13227, Liver Transpl 2016;22:1593, Liver Transpl 2018;24:897):
- Dense acellular portal collagen deposition: portal collagenization
- Distinct subsinusoidal and perivenular fibrosis
- Focal nodular hyperplasia-like changes: usually without the map-like glutamine synthetase staining pattern or dystrophic vasculature usually seen in classic focal nodular hyperplasia lesions
Microscopic (histologic) images
Positive stains
- Focal to diffuse C4d uptake by portal microvasculature (portal veins and capillaries) that may extend to inlet venules
Sample pathology report
- Allograft liver, explant:
- Chronic hepatitis, favoring chronic active antibody mediated rejection
- C4d on paraffin tissue: diffuse uptake by portal microvasculature (portal vein and capillaries) and inlet venules
- Strong DSA present (antidonor DQ)
- Obliterative arteriopathy
- Portal venopathy
- Allograft fibrosis score (Am J Transplant 2012;12:2986):
- Portal: 3/3
- Central: 3/3
- Sinusoidal: 1/3
- Chronic hepatitis, favoring chronic active antibody mediated rejection
Differential diagnosis
- In general, causes of chronic hepatitis and fibrosis fall in the differential diagnosis
- Idiopathic posttransplantation hepatitis:
- Category that describes otherwise unexplained allograft hepatitis
- Evidence points towards late and chronic rejection (TCMR and cAMR) as causes of this pattern (Liver Transpl 2016;22:1593)
- Recurrent hepatitis C:
- Decreasing cause of liver transplantation and posttransplant liver disease
- Can be ruled out by quantitative PCR
- Hepatitis E virus infection:
- Underdiagnosed in liver allografts (occurs in 1 - 28% of liver allografts)
- Can lead to chronic hepatitis and cirrhosis (Gastroenterology 2011;140:1481, J Hepatol 2014;61:1418)
- Can be excluded by laboratory investigations and immunohistochemical and in situ hybridization techniques
Board review style question #1
Board review style answer #1
C. Focal to diffuse C4d uptake. Criteria for the diagnosis of chronic active antibody mediated rejection include presence of at least focal C4d uptake in addition to histologic features (at least mild necroinflammatory activity and moderate fibrosis). While microvasculitis with dilated portal capillaries can be seen with chronic active antibody mediated rejection, it is a feature seen with acute antibody mediated rejection. It is important to keep in mind that acute antibody mediated rejection may overlap with chronic active antibody mediated rejection. Cholangitis and bile duct inflammation are components of T cell mediated rejection rather than antibody mediated rejection. Classic chronic rejection is characterized by ductopenia; however, the concept of chronic rejection is evolving as its pathophysiology is further characterized.
Comment Here
Reference: Liver - Chronic antibody mediated rejection
Comment Here
Reference: Liver - Chronic antibody mediated rejection
Board review style question #2
An isolated arterial "V" lesion is defined as age inappropriate arterial fibrointimal hyperplasia with or without associated inflammation without the presence of T cell mediated rejection. What is its significance in liver allografts?
- Almost all are negative for C4d staining
- It is not associated with T cell mediated rejection
- It is only significant in kidney allografts and has no significance in liver allografts
- It suggests underlying chronic active antibody mediated rejection
Board review style answer #2
D.Isolated arterial lesions are rarely encountered in liver allografts and until recently their clinical significance was not known. A recent series of cases showed that isolated arterial "V" lesions are associated with subsequent T cell mediated rejection, graft failure and C4d positivity. The majority of C4d positive cases also showed additional histologic features encountered in chronic active antibody mediated rejection such as portal and perivenular inflammation (rejection activity index / RAI 1 - 2) and at least moderate periportal, perivenular or sinusoidal fibrosis (Am J Transplant 2018;18:1534).
Comment Here
Reference: Liver - Chronic antibody mediated rejection
Comment Here
Reference: Liver - Chronic antibody mediated rejection
Chronic ductopenic rejection (pending)
Table of Contents
Definition / generalDefinition / general
[Pending]
Chronic hepatitis
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Liver injury occurring for at least 6 months as a result of hepatocyte based injury and inflammation, most commonly due to viral or autoimmune hepatitis (Am J Surg Pathol 1995;19:1409)
Essential features
- Viral infection, deregulated inflammatory cells or other insults leading to chronic hepatocyte injury and hepatic stellate cell activation (Middle East J Dig Dis 2016;8:166, Physiol Rev 2008;88:125)
- Morphologically characterized by fibrosis, which is frequently accompanied by portal inflammation with interface activity or lobular necroinflammatory activity (Am J Surg Pathol 1995;19:1409)
- Progressive portal based fibrosis ultimately leads to liver cirrhosis (end stage liver disease) (Clin Liver Dis (Hoboken) 2021;17:222)
- Distinct etiology and morphology from steatohepatitis and biliary disorders, though all may be associated with chronic liver injury and cirrhosis (Am J Surg Pathol 1995;19:1409)
Terminology
- Chronic active hepatitis
- Chronic persistent hepatitis
- Chronic lobular hepatitis (Am J Surg Pathol 1995;19:1409)
ICD coding
- ICD-10:
- B18.0 - chronic viral hepatitis B with delta agent
- B18.1 - chronic viral hepatitis B without delta agent
- B18.2 - chronic viral hepatitis C
- B18.8 - other chronic viral hepatitis
- B18.9 - chronic viral hepatitis, unspecified
- K73.0 - chronic persistent hepatitis, not elsewhere classified
- K73.1 - chronic lobular hepatitis, not elsewhere classified
- K73.2 - chronic active hepatitis, not elsewhere classified
- K73.8 - other chronic hepatitis, not elsewhere classified
- K73.9 - chronic hepatitis, unspecified
Epidemiology
- Dependent on underlying etiology
Sites
- Liver parenchyma
Pathophysiology
- Hepatocytes are injured by viral infection, drugs, deregulated inflammatory cells or abnormal accumulation of metabolites, leading to activation of hepatic stellate cells, which produce increased extracellular matrix resulting in fibrosis (Middle East J Dig Dis 2016;8:166, Physiol Rev 2008;88:125)
Etiology
- Chronic viral hepatitis
- Hepatitis B virus (HBV)
- Hepatitis C virus (HCV)
- Hepatitis D virus (HDV)
- Autoimmune hepatitis
- Metabolic disease
- Drug induced chronic hepatitis (rare) (J Clin Pathol 2009;62:481)
- Lisinopril
- Sulfonamides
- Trazodone
- Uracil
- Tegafur
- Tamoxifen
- Methotrexate
- Minocycline
- Clometacin
- Methyldopa
- Nitrofurantoin
Clinical features
- May lack symptoms until end stage (cirrhosis)
- Associated signs and symptoms include (World J Gastroenterol 2022;28:5910):
- General: fatigue (most common), malaise, mild discomfort in the right upper quadrant, anorexia
- Impaired biliary tract function: jaundice, pruritus
- Portal hypertension: gastroesophageal varices, ascites, edema, splenomegaly
- Impaired hepatocyte metabolism: spider angiomata, hepatic encephalopathy, easy bleeding / bruising
Diagnosis
- Clinicopathologic diagnosis requires integration of clinical history (including associated signs and symptoms described above), laboratory testing and biopsy results (Am J Surg Pathol 1995;19:1409)
- Ongoing liver injury lasting at least 6 months (Am J Surg Pathol 1995;19:1409)
- Longstanding clinical signs / symptoms or laboratory abnormalities
- Fibrosis represents pathologic correlate of chronic liver injury
- Biopsy is gold standard for determining grade and stage
- Laboratory testing is essential for determining etiology
- Transient elastography (FibroScan) can also be used to estimate stage / extent of fibrosis (World J Gastroenterol 2014;20:11033, World J Gastroenterol 2014;20:2854)
Laboratory
- Serological testing for hepatitis B, C and D and autoantibodies (may be positive, depending on etiology)
- Aminotransferase levels (AST, ALT may be elevated)
- Several serum markers for evaluating liver fibrosis have been proposed but none are widely used (World J Gastroenterol 2014;20:11033, World J Gastroenterol 2014;20:2854)
Radiology description
- MRI and CT findings in cirrhosis
- Surface and parenchymal nodularity
- Hypertrophy of the caudate lobe and lateral segments of the left lobe
- Atrophy of the posterior segments of the right lobe
- Ultrasound findings in cirrhosis
- Surface nodularity
- Course and heterogeneous echotexture
- Segmental hypertrophy / atrophy
- Doppler flow changes indicative of portal hypertension
- Splenomegaly
- Ascites (Radiopaedia: Cirrhosis [Accessed 28 February 2023])
Prognostic factors
- Amount of fibrosis (stage) is a key predictor of progression to end stage liver disease (cirrhosis) and adverse clinical outcomes (i.e., a need for liver transplant or liver related death in patients with hepatitis C) (World J Gastroenterol 2014;20:2854, Hepatology 2010;51:585)
- Amount of inflammation (grade) is associated with fibrosis progression (stage) in patients with hepatitis C (Pathol Int 2002;52:683)
- Rate of progression to end stage liver disease depends on many other factors including age, sex, underlying etiology of liver injury and response to treatment (J Interferon Cytokine Res 2017;37:97, Gut Liver 2016;10:429)
Case reports
- 28 year old man with acute on chronic liver failure and hemolysis (EJIFCC 2019;30:99)
- 46 year old man with HBV cirrhosis and dermatomyositis (World J Clin Cases 2019;7:1206)
- 55 year old man with jaundice (N Engl J Med 2019;380:1955)
- 56 year old man with Guillain-Barré syndrome and chronic active hepatitis C (BMC Infect Dis 2019;19:636)
- 72 year old man successfully treated for HBV, HCV and HEV (J Infect Public Health 2020;13:149)
Treatment
- Dependent on underlying etiology
Gross description
- In cirrhosis, the liver is generally firm and demonstrates a micronodular or macronodular pattern
- Color ranges from beefy red (normal) to dark green (cholestasis) or yellow (steatosis) (World J Gastroenterol 2016;22:1357)
Microscopic (histologic) description
- Fibrosis
- Required for pathologic diagnosis of chronic hepatitis in the absence of clinically confirmed chronic liver disease
- Progressive fibrosis of the limiting plate leads to enlargement of portal tracts and stellate periportal fibrous extension
- May lead to portal - portal or portal - central fibrous bridging, culminating in cirrhosis, which is usually micronodular (nodules < 3 mm in diameter) or mixed micronodular and macronodular type
- Portal inflammation
- Mononuclear infiltration of portal tracts (mostly CD4+ T lymphocytes with some plasma cells)
- Lymphoid aggregates or follicles may be present (most common in hepatitis C infection)
- Interface hepatitis
- Previously called piecemeal necrosis
- Hepatocyte apoptosis and inflammation at the stromal - parenchymal interface (interface of portal tract and lobule)
- Mononuclear infiltrate (mostly CD8+ T lymphocytes)
- Lobular hepatitis
- Mononuclear infiltrate of the hepatic parenchyma (lobules)
- Apoptotic / necrotic hepatocytes (Councilman bodies) in zones 2 and 3
- Reference: Am J Surg Pathol 1995;19:1409
Microscopic (histologic) images
Virtual slides
Positive stains
- Trichrome stain can help with the assessment of the amount of scarring and fibrosis present (stage)
Sample pathology report
- Liver, core biopsy:
- Chronic hepatitis with mild portal and lobular necroinflammatory activity (grade 2, scale 0 - 4, Batts-Ludwig methodology) and periportal fibrosis (stage 2, scale 0 - 4, Batts-Ludwig methodology), consistent with clinical history of chronic hepatitis C
Differential diagnosis
- Primary biliary cholangitis (PBC):
- Can have portal based inflammation with interface activity and lobular activity
- Florid duct lesions not seen in chronic hepatitis
- Clinical history may include elevated alkaline phosphatase, gamma glutamyl transpeptidase, serum IgM and antimitochondrial autoantibodies
- Lymphoma or leukemia infiltrating into the liver:
- Can have portal lymphocytic inflammation
- Lacks interface hepatitis and portal based fibrosis
- May have monomorphism and marked atypia of the infiltrating cells
- Chronic steatohepatitis:
- Can have portal and lobular lymphocytic inflammation
- Has steatosis / fat (may also be seen in chronic hepatitis)
- Centrizonal, pericellular fibrosis not seen in chronic hepatitis
- May be morphologically indistinguishable from chronic hepatitis at late stage (cirrhosis)
- Active hepatitis with bridging necrosis:
- Has portal inflammation with interface activity and lobular inflammation
- Bridging necrosis can cause a nodular appearance from low power, mimicking bridging fibrosis or cirrhosis
- Trichrome staining is paler in zones of dropout / necrosis than in fibrous areas
Additional references
Board review style question #1
- An asymptomatic 35 year old woman has elevated serum aminotransferases (aspartate aminotransferase [AST] and alanine aminotransferase [ALT]). A liver biopsy was performed. What is the most likely underlying etiology of these findings?
- Alcoholic liver disease
- Infection with hepatitis C
- Oxaliplatin induced liver injury
- Tylenol overdose
- Valproic acid associated liver injury
Board review style answer #1
Board review style question #2
Board review style answer #2
Chronic hepatitis-grading / staging
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Sites | Diagrams / tables | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Sample pathology report | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Batts-Ludwig system is the most widely used scale for assessing grade (amount of necroinflammatory activity) and stage (degree of fibrosis) in chronic hepatitis
Essential features
- Chronic hepatitis: liver fibrosis that occurs as a result of hepatocyte based injury and inflammation, most commonly due to viral or autoimmune hepatitis
- Separate scoring systems should be used for steatohepatitis and biliary disorders
- Grade: amount of necroinflammatory activity; indicates rate of disease progression
- Stage: amount of fibrosis; indicates how far disease has progressed
Terminology
- Pathology report should state which grading and staging system (scale) is used for scoring
- Batts-Ludwig system is most common (Am J Surg Pathol 1995;19:1409)
- Other staging systems include Knodell, Ishak, Scheuer and METAVIR (Hepatology 1981;1:431, J Hepatol 1995;22:696, J Hepatol 1991;13:372, Hepatology 1994;20:15)
ICD coding
- ICD-10:
- B18.0 - chronic viral hepatitis B with delta agent
- B18.1 - chronic viral hepatitis B without delta agent
- B18.2 - chronic viral hepatitis C
- B18.8 - other chronic viral hepatitis
- B18.9 - chronic viral hepatitis, unspecified
- K73.0 - chronic persistent hepatitis, not elsewhere classified
- K73.1 - chronic lobular hepatitis, not elsewhere classified
- K73.2 - chronic active hepatitis, not elsewhere classified
- K73.8 - other chronic hepatitis, not elsewhere classified
- K73.9 - chronic hepatitis, unspecified
Sites
- Liver parenchyma
Microscopic (histologic) description
- Batts-Ludwig system is the most common grading and staging system (Am J Surg Pathol 1995;19:1409)
- Scale 0 - 4 for grade and stage
- Grade: amount of portal / periportal and lobular activity (count whichever is greater)
- Portal / periportal activity
- 0: none or confined to portal tracts
- 1: minimal, patchy interface hepatitis
- 2: mild interface hepatitis involving some or all portal tracts
- 3: moderate interface hepatitis involving all portal tracts
- 4: severe interface hepatitis / bridging necrosis
- Lobular activity
- 0: none
- 1: minimal - rare spotty necrosis (can find 1 - 2 dead hepatocytes in biopsy)
- 2: mild - scattered necrotic hepatocytes
- 3: moderate - confluent necrosis (clusters of dead hepatocytes)
- 4: severe - bridging necrosis
- Portal / periportal activity
- Stage: amount of fibrosis
- 0: no increased fibrous tissue
- 1: fibrous portal expansion
- 2: periportal fibrosis with periportal septa
- 3: bridging fibrosis with portal - portal fibrous septa and distorted architecture
- 4: probable or definite cirrhosis with nodule formation
Microscopic (histologic) images
Positive stains
- Trichrome highlights fibrosis (dark blue) and is used to determine stage; do not overstage when edema / pale blue is present
- Sirius red also highlights fibrosis
Sample pathology report
- Liver, biopsy:
- Chronic hepatitis with mild portal and lobular necroinflammatory activity (grade 2, scale 0 - 4, Batts-Ludwig methodology) and bridging fibrosis (stage 3, scale 0 - 4, Batts-Ludwig methodology), consistent with clinical history of chronic hepatitis C
Additional references
Board review style question #1
- Which of the following is true about the finding shown above?
- Indicative of fibrosis and used to determine grade in a patient with chronic hepatitis C
- Indicative of fibrosis and used to determine stage in a patient with chronic hepatitis C
- Indicative of lobular necroinflammatory activity and used to determine grade in a patient with chronic hepatitis C
- Indicative of lobular necroinflammatory activity and used to determine stage in a patient with chronic hepatitis C
Board review style answer #1
C. Indicative of lobular necroinflammatory activity and used to determine grade in a patient with chronic hepatitis C
Comment Here
Reference: Chronic hepatitis - grading / staging
Comment Here
Reference: Chronic hepatitis - grading / staging
Board review style question #2
-
A 55 year old man with chronic hepatitis C undergoes liver biopsy for grading and staging. Sections show portal based inflammation, with mild interface activity. Within the lobules, there are foci of confluent necrosis (clusters of dead hepatocytes) but not bridging necrosis. Trichrome stain shows portal fibrous expansion without definite septae formation or bridging. What would be the most appropriate grade and stage according to the Batts-Ludwig methodology (scale 0 - 4)?
- Grade 1, stage 2
- Grade 1, stage 3
- Grade 2, stage 1
- Grade 2, stage 3
- Grade 3, stage 1
Board review style answer #2
Chronic viral hepatitis
Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Chronic viral hepatitis is defined as inflammation of the liver due to persistent viral replication for at least 6 months
- Inflammatory process results in progressive liver damage and fibrosis
Essential features
- Chronic viral hepatitis is commonly caused by 3 viruses: hepatitis B, hepatitis C and hepatitis D virus; other chronic viral hepatitides are less common
- Long term infection results in chronic inflammation of the liver parenchyma that is characterized by portal inflammation, interface hepatitis and fibrosis
- Progressive fibrosis may result in cirrhosis and increases risk for developing hepatocellular carcinoma
- Reference: Infect Dis Clin North Am 2019;33:1045
ICD coding
Epidemiology
- Chronic viral hepatitis is a major global public health problem that affects hundreds of millions of people
- An estimated 257 million people are living with chronic hepatitis B infection
- 71 million are living with chronic hepatitis C infection (Infect Dis Clin North Am 2019;33:1045)
- Results in long term liver inflammation that may lead to cirrhosis or hepatocellular carcinoma, causing an estimated 1.4 million deaths annually (Curr Opin HIV AIDS 2017;12:302)
- Hepatitis B virus (HBV) (JAMA 2018;319:1802, Infect Dis Clin North Am 2019;33:1045)
- Chronic HBV infection has high endemicity in Central and East Asia, sub-Saharan Africa and the Western Pacific Regions
- Transmitted through sexual contact, blood and vertically from mother to child
- HBV usually causes an acute hepatitis but chronic hepatitis develops in ~90% of infected infants versus ~10% of adult patients
- There are 8 genotypes (A - H) in humans; type A responds favorably to interferon based therapy and type C is associated with more advanced liver fibrosis and increased risk of hepatocellular carcinoma
- Up to 40% of untreated patients may develop cirrhosis
- Hepatitis C virus (HCV)
- Transmission is primarily bloodborne (Infect Dis Clin North Am 2019;33:1045)
- Increased risk of transmission via sexual intercourse is reported in HIV positive men who have sex with men (Infect Dis Clin North Am 2019;33:1045)
- Infection causes acute hepatitis and the virus is cleared in some (Nat Rev Dis Primers 2017;3:17006)
- Acute HCV infection leads to chronic HCV in 75% to 85% of people (Nat Rev Dis Primers 2017;3:17006)
- Percentage of transition to chronic infection is higher for patients coinfected with HIV and ~2.6 million people are estimated to be coinfected (Nat Rev Dis Primers 2017;3:17006)
- 10% to 30% of patients develop cirrhosis over 30 years (N Engl J Med 2011;364:2429)
- People with HCV cirrhosis have a 4% to 5% cumulative annual incidence of hepatocellular carcinoma (Nat Rev Dis Primers 2017;3:17006)
- Hepatitis D virus (HDV)
- HDV infection is higher in areas where HBV is endemic and transmission is similar to HBV (Gut 2021;70:1782)
- High prevalence areas include the Mediterranean region, Middle East, the Indian subcontinent, Japan, Taiwan, Greenland, the Horn of Africa, West Africa, the Amazon and certain areas of the Pacific (Infect Dis Clin North Am 2019;33:1045)
- HDV superinfection in chronic HBV usually results in chronic HDV infection, occurring in 80% of cases (Cold Spring Harb Perspect Med 2014;4:a021550)
- Compared with chronic HBV infection, chronic HBV / HDV coinfection is associated with a higher risk of cirrhosis, occurring in 50% to 70% of cases within 5 to 10 years of diagnosis (Gut 2021;70:1782)
- ~12 million people infected with HBV are coinfected with HDV (Gut 2021;70:1782)
- Hepatitis E virus (HEV) (Infect Dis Clin North Am 2019;33:1045)
- Uncommon cause of chronic viral hepatitis
- 8 HEV genotypes but only HEV1 and HEV2 are human viruses
- Typically causes acute hepatitis and is self limiting
- Chronic infection in the immunocompromised or during pregnancy
- Primarily waterborne, shed in feces
- Outbreaks in Asia, Africa and Latin America
Sites
- Liver parenchyma
Pathophysiology
- Chronic viral hepatitis is associated with chronic inflammation of the hepatocytes as a result of oxidative stress and immune response directed to infected hepatocytes
- Growth factors, chemokines and cytokines produced by infected hepatocytes recruit immune cells, resulting in a local inflammatory response
- Hepatocellular damage and proinflammatory signaling activates hepatic stellate cells to differentiate to myofibroblasts, resulting in fibrinogenesis (Front Cell Infect Microbiol 2020;10:587628)
Etiology
- 3 viruses are known to commonly cause chronic hepatitis (Infect Dis Clin North Am 2019;33:1045)
- Hepatitis B virus (HBV) (JAMA 2018;319:1802)
- Small enveloped, partially double stranded DNA virus
- HBV consists of an inner nucleocapsid composed of hepatitis B core antigen (HBcAg) that is complexed with a polymerase and circular viral DNA ~3.2 kb in size, all contained within an outer envelope embedded with hepatitis B surface antigen (HBsAg)
- Hepatitis B envelope antigen (HBeAg) located between core and lipid membrane, secreted and accumulates in serum
- Hepatitis C virus (HCV)
- HCV is a positive sense, single stranded RNA virus of 9.6 kb (Infect Dis Clin North Am 2019;33:1045)
- Hepatitis D virus (HDV) (Gut 2021;70:1782)
- Negative sense single stranded RNA virus of 1.7 kb and 35 to 36 nm in diameter
- HDV utilizes HBsAg for entry and infection of hepatocytes, with HBsAg incorporated in its viral envelope and thus requires HBV coinfection for transmission and replication
- Hepatitis E virus (HEV) (Infect Dis Clin North Am 2019;33:1045)
- Single stranded, positive sense RNA virus of 7.2 kb
- Shed in feces as a nonenveloped virus but are in lipid enveloped form in blood
- HEV is noncytopathic and clinical presentation is determined by host response
- Typically causes acute infection and is self limiting but can cause chronic infection in immunosuppressed patients (Cold Spring Harb Perspect Med 2019;9:a031872)
Clinical features
- Clinical presentation can vary between individuals
- Some patients can be asymptomatic for several years but a small number can progress rapidly to cirrhosis (Infect Dis Clin North Am 2019;33:1045)
- Characteristic symptoms include anorexia, malaise and fatigue (JAMA 2018;319:1802)
- Some patients develop right upper quadrant pain due to hepatic inflammation
- Jaundice is typically absent in the chronic phase of infection (Nat Rev Dis Primers 2017;3:17006)
- Hepatomegaly, ascites and peripheral edema may be observed in later stages (Infect Dis Clin North Am 2019;33:1045)
- Alanine aminotransferase level may be within reference range in chronic infection but can fluctuate between mild elevation and > 2 times the upper limit of normal (Infect Dis Clin North Am 2019;33:1045)
- Extrahepatic manifestations can occur in multiple organs
- HBV infection may cause rash, fever, arthralgia, glomerulonephritis, acute necrotizing vasculitis (polyarteritis nodosa) (Hepatology 2009;49:S13)
- HCV has been associated with cryoglobulinemia, non-Hodgkin lymphoma, glomerulonephritis, insulin resistance and diabetes (Nat Rev Dis Primers 2017;3:17006)
Diagnosis
- Clinical history and physical exam
- Laboratory evaluation
- Biopsy is the gold standard for staging liver fibrosis
- Liver biopsy for diagnosis is no longer commonly performed due to availability of reliable serological and virological tests (World J Gastroenterol 2015;21:12141)
- Transient elastography (World J Gastroenterol 2014;20:11033)
Laboratory
- Liver function tests
- Aminotransferases typically normal in chronic infection but can be mildly elevated to > 2 times the upper limit of normal (Infect Dis Clin North Am 2019;33:1045)
- Serological testing for HBV, HCV and HDV antibodies
- Viral PCR if serology positive (Infect Dis Clin North Am 2019;33:1045, JAMA 2018;319:1802, Nat Rev Dis Primers 2017;3:17006, Gut 2021;70:1782)
Radiology description
- In the acute phase, imaging features are nonspecific and diagnosis is based on serologic, virologic and clinical findings (Radiographics 2004;24:937)
- Morphologic features of cirrhosis on CT, MRI and ultrasound include (Abdom Radiol (NY) 2017;42:2037)
- Liver surface nodularity
- Atrophic right lobe and segment IV
- Hypertrophy of the caudate and lateral left lobes
- Right hepatic posterior notch
- Expanded gallbladder fossa
- Narrow hepatic veins < 5 mm
- Enlargement of the hilar periportal space > 10 mm
- Additionally, ultrasound may show (Abdom Radiol (NY) 2017;42:2037)
- Heterogeneous or coarsened echotexture
- Color Doppler flow changes that are suggestive of portal hypertension
- Fatty appearance
Prognostic factors
- Fibrosis stage is a key prognostic factor and patients with cirrhosis have greater risk of hepatic decompensation
- Active inflammation drives the development of fibrosis (Hepatology 2009;49:S61)
- Serologic and virologic response to treatment affects rate of progression (JAMA 2018;319:1802)
- In HBV, HBeAg positive chronic hepatitis is characterized by sustained viral replication and may result in significant liver damage (Infect Dis Clin North Am 2019;33:1045)
- HBeAg negative seroconversion is characterized by suppression of viral replication, reduction in liver inflammation and association with a lower risk of disease progression (Infect Dis Clin North Am 2019;33:1045)
Case reports
- 27 year old woman with acalculous cholecystitis secondary to chronic HCV (Cureus 2022;14:e26484)
- 39 year old woman with HEV superinfection leading to reactivation of chronic HBV (BMJ Case Rep 2018;2018:bcr2017223616)
- 48 year old man with chronic HBV and terbinafine induced HBV reactivation (Cureus 2020;12:e11958)
- 50 year old woman with a history of chronic HBV with negative seroconversion of autoantibodies following antiviral treatment (World J Clin Cases 2021;9:1196)
Treatment
- Hepatitis B virus (Infect Dis Clin North Am 2019;33:1045)
- Vaccination is key to prevention
- Nucleoside / nucleotide analogs such as entecavir, tenofovir disoproxil or tenofovir alafenamide in chronic HBV
- Pegylated interferon alpha (treatment of choice in HDV infection)
- Hepatitis C virus
- Direct acting antivirals (DAA) in combination to target specific steps in HCV replication (Infect Dis Clin North Am 2019;33:1045)
- 3 proteins targeted: NS3/4A protease, NS5B polymerase and NS5A protein
- Combination therapy such as elbavir / grazoprevir or sofosbuvir / velpatasvir (Nat Rev Dis Primers 2017;3:17006, Infect Dis Clin North Am 2019;33:1045)
- Addition of ribavirin to DAA regimen depending on viral genotype and if patient has developed cirrhosis (Nat Rev Dis Primers 2017;3:17006)
- Interferon therapy is still the most frequently used treatment in several Asian countries (Nat Rev Dis Primers 2017;3:17006)
Gross description
- Nonspecific changes in early stages
- Enlarged and yellow (fatty change) or green (cholestasis)
- Firm, nodular appearance with a micronodular or macronodular pattern in later stages (World J Gastroenterol 2016;22:1357, StatPearls: Hepatic Cirrhosis [Accessed 15 February 2023])
Microscopic (histologic) description
- Histologic appearance of chronic viral hepatitis includes patterns that are common to all etiologies of chronic hepatitis
- Portal inflammation
- Predominantly consisting of lymphocytes with few admixed plasma cells and histiocytes (Dig Liver Dis 2011;43:S331)
- Interface hepatitis (piecemeal necrosis)
- Lymphocytic infiltrate at the boundary of the portal tract extending into the liver parenchyma with associated hepatocyte damage (Dig Liver Dis 2011;43:S331)
- Lobular changes that include
- Inflammation of the liver parenchyma (variable)
- Focal and confluent necrosis
- Apoptosis (apoptotic / councilman bodies) (Dig Liver Dis 2011;43:S331)
- Fibrosis
- Is seen in varying degrees depending on the stage of the disease and is progressive
- Fibrous portal expansion seen in earlier stages, progressing with the formation of fibrous septa that may lead to bridging fibrosis and ending with cirrhosis (Dig Liver Dis 2011;43:S331)
- Cirrhosis characterized by fibrotic bands with loss of architecture and nodule formation (Hepatology 2009;49:S61)
- Certain morphologic features are characteristic but not diagnostic of a particular viral etiology
- HBV (Dig Liver Dis 2011;43:S331, Hepatology 2009;49:S61)
- Ground glass appearance of hepatocytes due to proliferation of smooth endoplasmic reticulum containing HBsAg
- Lafora disease and fibrinogen storage disease also demonstrate ground glass hepatocytes
- Both will be highlighted by Shikata orcein and Victoria blue stain
- Can be distinguished with immunohistochemical stains for HBsAg or HBcAg
- Sanded nuclei (eosinophilic nuclear inclusions)
- HDV coinfection is associated with relatively high necroinflammation
- HCV (Hepatology 2009;49:S61, Dig Liver Dis 2011;43:S331, World J Gastroenterol 2016;22:1357)
- Nodular lymphoid aggregates
- Bile duct damage (Poulsen-Christofferson lesion) with lymphocytic infiltrate
- Steatosis, macrovesicular or mixed macrovesicular and microvesicular (more common in HCV but may also be seen in HBV)
- Iron deposition
Microscopic (histologic) images
Positive stains
- Trichrome stain is used to evaluate the degree of fibrosis present
- HBsAg immunohistochemical stain shows cytoplasmic staining (diffuse or focal) (Trop Gastroenterol 2002;23:16, Clin Liver Dis (Hoboken) 2013;2:S8)
- HBcAg immunohistochemical stain shows nuclear staining (Trop Gastroenterol 2002;23:16, Clin Liver Dis (Hoboken) 2013;2:S8)
- HBV ground glass hepatocytes can be highlighted with Shikata orcein and Victoria blue stains (Hepatology 2009;49:S61)
Videos
Viral hepatitis
Chronic hepatitis histopathology
Sample pathology report
- Liver, biopsy:
- Chronic hepatitis with mild activity (METAVIR grade A1) and moderate periportal fibrosis with focal bridging (Scheuer stage 2/4) (see comment)
- Comment: The findings are consistent with the patient's history of chronic hepatitis B infection.
Differential diagnosis
- Other nonviral causes of chronic hepatitis
- Autoimmune hepatitis:
- Inflammatory infiltrates in autoimmune hepatitis tend to be plasma cell rich (Hepatology 2009;49:S61)
- Nonalcoholic or alcoholic steatohepatitis (Metabolism 2016;65:1080):
- Steatosis and ballooned hepatocytes are usually present but may be absent in late stage disease
- Centrizonal pattern of injury and fibrosis
- Primary biliary cholangitis (Dig Liver Dis 2011;43:S331, Clin Liver Dis (Hoboken) 2021;17:227):
- Granulomatous destruction of bile ducts, cholate stasis and accumulation of copper associated proteins in periportal hepatocytes are suggestive of primary biliary cirrhosis
- Florid duct lesions, which are not seen in chronic viral hepatitis
- May have positive serology for antimitochondrial antibodies
- Elevated alkaline phosphatase
- Primary sclerosing cholangitis (Dig Liver Dis 2011;43:S331, Clin Liver Dis (Hoboken) 2021;17:227):
- Onion skin fibrosis of medium sized bile ducts
- May be positive for antineutrophil cytoplasmic antibodies
- Elevated alkaline phosphatase
- Alpha-1 antitrypsin deficiency (Hepatology 2009;49:S61, Dig Liver Dis 2011;43:S331):
- Presence of periportal eosinophilic globules with PASD stain
- Hemochromatosis (Mod Pathol 2007;20:S3, Dig Liver Dis 2011;43:S331):
- Hemosiderin accumulation in hepatocytes and Kupffer cells
- Can be highlighted with Prussian blue stain
- Wilson disease (Dig Liver Dis 2011;43:S331, Mo Med 2010;107:113):
- Histopathologic findings are not specific
- Positive copper stain in hepatocytes and Kupffer cells
- A negative stain does not exclude Wilson disease
- Laboratory findings (ceruloplasmin, serum / urine copper) and clinical findings (Kayser-Fleischer rings)
- Drug induced liver injury (Hepatology 2009;49:S61, US Gastroenterol Hepatol Rev
2010;6:73, Dig Liver Dis 2011;43:S331):
- Can show varying histology; histopathologic findings are not specific
- Strong clinical suspicion and chronologic relationship between drug administration and onset of pathology
- Autoimmune hepatitis:
- Acute hepatitis with bridging fibrosis:
- Bridging necrosis seen in acute hepatitis can mimic the appearance of bridging fibrous septa seen in chronic hepatitis
- Trichrome stain can help distinguish
- Lymphoma or leukemic involvement of the liver (Am J Hematol 2017;92:1362, Am J Clin Pathol 2014;141:119):
- Infiltrate consists of atypical lymphocytes; may be monomorphic
- Immunohistochemistry and gene rearrangement studies to identify aberrancy
Board review style question #1
Board review style answer #1
D. Hepatitis B surface antigen. The ground glass appearance is due to the proliferation of smooth endoplasmic reticulum and the accumulation of intracellular HBsAg. While HBcAg expression in HBeAg positive individuals is correlated with increased DNA titer and increased hepatic activity index, the accumulation of HBcAg, HBeAg and HBV DNA does not produce the characteristic ground glass appearance of hepatocytes in chronic HBV.
Comment Here
Reference: Chronic viral hepatitis
Comment Here
Reference: Chronic viral hepatitis
Board review style question #2
In a patient with chronic viral hepatitis, which of the following combinations of findings on a liver biopsy would be most suggestive of a chronic hepatitis C infection?
- Ground glass hepatocytes with sanded nuclei
- Portal based inflammation with interface activity
- Portal expansion with bridging fibrous septa
- Nodular lymphoid aggregates, bile duct damage (Poulsen lesion) and steatosis
Board review style answer #2
D. Nodular lymphoid aggregates, bile duct damage (Poulsen lesion) and steatosis. While not diagnostic, the presence of nodular lymphoid aggregates, bile duct damage (Poulsen lesion) and steatosis are considered characteristic of HCV infection. Ground glass hepatocytes are seen in HBV infection and represent the accumulation of HBsAg. Portal based inflammation with interface activity and fibrosis are general features of chronic viral hepatitis and are not specific to HCV.
Comment Here
Reference: Chronic viral hepatitis
Comment Here
Reference: Chronic viral hepatitis
Cirrhosis
Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Diffuse nodulation of liver due to fibrous bands subdividing liver into regenerative nodules
Essential features
- Diffuse nodulation of liver due to fibrous bands subdividing liver into regenerative nodules
- Viral hepatitis B / C, alcoholic liver disease, nonalcoholic (metabolic associated) fatty liver disease are most common causes
ICD coding
Epidemiology
- Major cause of global health burden, accounting for 1.2% of disability adjusted life years (DALYs) and 2% of deaths worldwide in 2010 (Lancet 2012;380:2197, Lancet 2012;380:2095)
Sites
- Liver
Pathophysiology
- Combination of processes (J Hepatol 2017;66:778)
- Fibrosis: excessive production of collagen type I / III by hepatic stellate cells with or without portal fibroblasts through chronic inflammation (tumor necrosis factor [TNF] alpha), transforming growth factor [TGF] beta, IL1), cytokines from Kupffer cells, endothelial cells, bile duct cells, hepatocytes and disruption of extracellular matrix and toxins
- Regeneration of hepatocytes through proliferation of progenitor cells of the ductular reaction
- Parenchymal extinction due to vascular disruption
- Regression (J Hepatol 2015;63:1038)
- Cirrhosis is potentially reversible after successful treatment of chronic liver disease, e.g. viral hepatitis
- Cessation of chronic damage allows hepatocyte recovery and modulates the microenvironment
- Shifting balance from inflammation to resolution results in phenotypic adjustments of immune cells
- Myofibroblasts are deactivated by senescence, apoptosis and inactivation
- Matrix degradation also occurs
Etiology
- Prevalence of causes varies by geographic location
- Common causes include:
- Chronic viral hepatitis B (with or without D) and C
- Fatty liver disease: alcoholic and nonalcoholic (metabolic associated)
- Metabolic: hereditary hemochromatosis, alpha-1 antitrypsin deficiency, Wilson disease
- Immune mediated: autoimmune hepatitis, primary biliary cholangitis, primary sclerosing cholangitis
- Chronic biliary obstruction
- Drug induced liver injury
- Cryptogenic (idiopathic) cirrhosis: accounts for 8 - 9% of liver transplants in the U.S.; burnt out nonalcoholic fatty liver disease (NAFLD) / nonalcoholic steatohepatitis (NASH) is a common cause of cryptogenic cirrhosis (Hepatology 2000;32:689)
Clinical features
- General (nonspecific): malaise, fatigue, anorexia, weight loss
- Specific (due to impaired liver function):
- Impaired protein synthesis (leukonychia [white nails], ascites, bruising)
- Impaired biliary excretion (jaundice, pruritus)
- Impaired nitrogen metabolism (hepatic encephalopathy)
- Impaired estrogen metabolism (palmar erythema, spider nevus, testicular atrophy, gynecomastia)
- Complications:
- Decompensation: development of jaundice, ascites, variceal hemorrhage or hepatic encephalopathy
- Portal hypertension: ascites (with or without spontaneous bacterial peritonitis), splenomegaly, esophageal / gastric varices
- Liver failure: coagulopathy, hepatic encephalopathy, hepatorenal syndrome, hepatopulmonary syndrome, portopulmonary hypertension
- Hepatocellular carcinoma: cirrhosis is a key risk factor and the annual incidence of HCC among cirrhotic patients is 2 - 8% (Lancet 2014;384:2053, Hepatology 2010;51:1972)
Diagnosis
- Ultrasound, CT or MRI radiologically
- Elastography
- Liver biopsy
Laboratory
- Clinical subclassification of cirrhosis uses blood with or without clinical parameters
- Child-Pugh score / grade (J Hepatol 2005;42:S100)
- 5 parameters: albumin, bilirubin, international normalized ratio (INR) / prothrombin time, ascites and hepatic encephalopathy
- Each parameter is assigned from 1 - 3
- Total score ranges from 5 - 15 and is categorized as grade A (5, 6), B (7 - 9) and C (10 - 15)
- Model for end stage liver disease (MELD) score (J Hepatol 2005;42:S100)
- 3 parameters: bilirubin, creatinine and INR
- Used to prioritize need for liver transplantation
- Albumin bilirubin (ALBI) score / grade (J Clin Oncol 2015;33:550)
- 2 parameters: albumin, bilirubin
- Simple, objective and evidence based alternative of Child-Pugh score / grade
Radiology description
- There are multiple nodular isodense lesions deforming the liver margin on the arterial phase CT
Case reports
- 28 year old woman with cirrhosis secondary to autoimmune hepatitis and alpha-1 antitrypsin ZZ phenotype (Cureus 2021;13:e12606)
- 44 year old man with Wilson disease presenting with muscle stiffness, gait instability and liver cirrhosis (Lancet 2020;396:990)
- 62 year old man with cirrhosis took daily probiotics and developed Lactobacillus associated spontaneous bacterial peritonitis (Cureus 2020;12:e11896)
Treatment
- Treating the underlying cause of cirrhosis
- Treating and preventing complications (ascites, hepatic encephalopathy, variceal hemorrhage, and portal hypertension)
- Avoid additional liver injury (e.g. alcohol)
- Patients with MELD ≥ 15 or decompensation should be referred to a transplant center (Hepatology 2014;59:1144)
- Regular ultrasound surveillance of HCC (Hepatology 2018;68:723)
Gross description
- Multiple regenerative nodules throughout the entire liver, separated by bridging fibrosis
Gross images
Microscopic (histologic) description
- Nonbiliary type cirrhosis:
- Diffuse disruption in architecture of the entire liver (loss of normal central - portal relationship)
- Bridging fibrous septa
- Rounded parenchymal nodules of regenerating hepatocytes
- Biliary type cirrhosis:
- Diffuse disruption in architecture of the entire liver (loss of normal central - portal relationship)
- Bridging fibrous septa
- Irregular, jigsaw puzzle shaped parenchymal nodules of regenerating hepatocytes with peripheral pale halo (peripheral septal edema, loose packed fibrous tissue and chronic cholestasis of periseptal hepatocytes leading to feathery degeneration)
- Alcoholic type cirrhosis:
- Micronodular cirrhosis, Mallory bodies, fatty change
- Perivenular and pericellular fibrosis (highlighted with trichrome stain) with partial / complete obliteration of central vein (identifiable as central vein due to lack of arterioles)
- More prominent bridging from central zone to central zone and central zone to portal zone than in other causes of cirrhosis
- Usually few inflammatory cells, unless superimposed viral or alcoholic hepatitis
- Subclassification: micronodular (< 3 mm) versus macronodular (≥ 3 mm)
- Typically not very clinically significant
- Former is more commonly associated with alcoholic liver disease, genetic hemochromatosis and Wilson disease, whereas the latter is more frequently associated with viral hepatitis
- Micronodular cirrhosis and macronodular cirrhosis may be transformed into each other in either direction, depending on disease activity (Arch Pathol Lab Med 2000;124:1599)
- Difficult to assess in liver biopsy specimen
- Subclassification: Laennec fibrosis scoring system (J Hepatol 2011;55:1004)
- 4A: mild cirrhosis; marked septation with rounded contours or visible nodules; most septa are thin (1 broad septum allowed)
- 4B: moderate cirrhosis with at least 2 broad septa
- 4C: severe cirrhosis with at least 1 very broad septum or many minute nodules
- Excellent interobserver agreement (kappa 0.83)
- Correlate with severity of portal hypertension and Child-Pugh and MELD scores
Microscopic (histologic) images
Positive stains
- Trichrome: highlights fibrous septa
- Sirius red: highlights fibrous septa
- Reticulin: highlights fibrous septa
Sample pathology report
- Liver, biopsy:
- Steatohepatitis with cirrhosis (see comment)
- Comment: In clinical history of diabetes mellitus and hypertension without significant alcoholic consumption, the overall features are consistent with metabolic associated fatty liver disease with cirrhosis.
Differential diagnosis
- Congenital hepatic fibrosis:
- Absence of regenerative nodules
- Dilated irregular ducts embedded in broad fibrous septa
- Focal nodular hyperplasia:
- Localized lesion with absence of diffuse nodulation
- Nodular regenerative hyperplasia:
- Absence of fibrous septa
- Alternating hepatocyte atrophy and hypertrophy highlighted on reticulin stain
Board review style question #1
Board review style answer #1
C. Feathery degeneration
Ballooning degeneration is a hallmark pathological change of steatohepatitis, which is not associated with biliary type cirrhosis (answer A). Bilirubinostasis may be present in late biliary type cirrhosis but is not associated with periseptal halo (answer B). Feathery degeneration is one of the features of chronic cholestasis contributing to the periseptal halo in biliary type cirrhosis (answer C). Florid duct lesion is one of the characteristic features of primary biliary cholangitis, which is not associated with periseptal halo (answer D). Periductal fibrosis is one of the characteristic features of primary sclerosing cholangitis, which is not associated with periseptal halo (answer E).
Comment Here
Reference: Cirrhosis
Ballooning degeneration is a hallmark pathological change of steatohepatitis, which is not associated with biliary type cirrhosis (answer A). Bilirubinostasis may be present in late biliary type cirrhosis but is not associated with periseptal halo (answer B). Feathery degeneration is one of the features of chronic cholestasis contributing to the periseptal halo in biliary type cirrhosis (answer C). Florid duct lesion is one of the characteristic features of primary biliary cholangitis, which is not associated with periseptal halo (answer D). Periductal fibrosis is one of the characteristic features of primary sclerosing cholangitis, which is not associated with periseptal halo (answer E).
Comment Here
Reference: Cirrhosis
Board review style question #2
A 60 year old man was admitted with massive hematemesis and hypovolemic shock. He failed to respond to resuscitation. Postmortem examination revealed a liver shown as above. What is the most likely cause of his massive gastrointestinal bleeding?
- Acute gastritis
- Aortoesophageal fistula
- Esophageal varices
- Hepatocellular carcinoma
- Peptic ulcer
Board review style answer #2
Combined hepatocellular carcinoma-cholangiocarcinoma
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Definition / general
- Combined hepatocellular carcinoma-cholangiocarcinoma (cHCC-CC) is a rare primary liver malignancy
- cHCC-CC exhibits, unequivocally, both hepatocytic and biliary differentiation within the same tumor; collision tumors are excluded
- Primary liver tumor composed of homogenous biphenotypic tumor cells, called intermediate cell carcinoma, is considered a subtype of cHCC-CC
- Cholangiolocellular carcinoma (CLC) is now included in the cholangiocarcinoma classification in the 2019 WHO classification (5th edition); a tumor that exhibits a CLC component associated with a hepatocellular carcinoma component can be classified as cHCC-CC
- Diagnosis of cHCC-CC should be based on routine histopathology with hematoxilin and eosin; immunohistochemistry is used as a supplemental diagnostic tool
- Reference: J Hepatol 2021 Feb 2 [Epub ahead of print]
Essential features
- cHCC-CC is a specific entity within primary liver malignancies
- cHCC-CC is a primary liver carcinoma with unequivocal presence of both hepatocytic and cholangiocytic differentiation
- Diagnosis is based on H&E morphology
- Expression of immunohistochemical markers alone is not sufficient for diagnosis
Terminology
- These terms should no longer be used:
- Mixed HCC-CCA
- Mixed hepatobiliary carcinoma
- Hepatocholangiocarcinoma
- HCC-CC with stem cell features
ICD coding
Epidemiology
- < 1% of liver primary malignancies (Liver Transpl 2014;20:952)
Sites
- cHCC-CC has an intrahepatic localization
Pathophysiology
- 3 different hypotheses have been postulated for the development of cHCC-CC (J Hepatol 2021 Feb 2 [Epub ahead of print]):
- Incidental coexistence of hepatocellular carcinoma (HCC) and intrahepatic cholangiocarcinoma (ICC) within the same tumor
- Malignant transformation of a hepatic progenitor cell
- Dedifferentiation of an HCC or ICC
Etiology
- Classical risk factors of hepatocellular carcinoma or intrahepatic cholangiocarcinoma also seem to predispose towards the development of cHCC-CC (Chin Clin Oncol 2016;5:66)
- Viral hepatitis
- Alcohol intake
- Nonalcoholic steatohepatitis
- Likelihood of liver cirrhosis in patients with cHCC-CC has been reported to be intermediate between the high proportion seen in patients with hepatocellular carcinoma and the lower prevalence in patients with intrahepatic cholangiocarcinoma
- Due to the rarity of the disease, the existence of specific risk factors to the development of cHCC-CC remains unknown
Clinical features
- cHCC-CC is predominantly observed in male patients
- No specific clinical symptoms; fatigue, obstructive jaundice, weight loss or abdominal discomfort may occur
- Reference: BMC Cancer 2016;16:158
Diagnosis
- Preoperative diagnosis of cHCC-CC is very complex since there are no specific noninvasive imaging features; however, the existence of overlapping features between hepatocellular carcinoma and intrahepatic cholangiocarcinoma is highly suggestive
- Gold standard diagnosis is based on histologic analysis of resected specimens after extensive tumor sampling (Hepatobiliary Pancreat Dis Int 2020;19:515)
Laboratory
- Alpha fetoprotein > 400ng/ml in 21.1% of cHCC-CC cases
- CA19-9 > hepatocellular carcinoma but < intrahepatic cholangiocarcinoma
- CEA elevated in 25% of cHCC-CC patients
- Reference: Hepatobiliary Pancreat Dis Int 2020;19:515
Radiology description
- Imaging features of cHCC-CC are heterogeneous and overlap with those of hepatocellular carcinoma and intrahepatic cholangiocarcinoma
- Amount of each component seems to be a key determinant of cHCC-CC radiological features
- If hepatocellular carcinoma predominates, an intense contrast uptake during the arterial phase with a washout in the venous phase is observed on CT
- If intrahepatic cholangiocarcinoma predominates, progressive centripetal enhancement, capsule retraction or peripheral rim enhancement is observed on CT
- Reference: Liver Int 2019;39:2386
Radiology images
Prognostic factors
- Main unfavorable prognostic factors are (J Gastroenterol Hepatol 2019;34:1074):
- Large tumor size (> 5 cm)
- Presence of satellite nodules
- Lymph node metastasis
- Vascular invasion
- Portal vein invasion
- High tumor stage
- Free surgical margin < 2 cm
- Prognosis is worse than hepatocellular carcinoma and similar to that of intrahepatic cholangiocarcinoma
- Recurrence rate after surgery is high (up to 80% at 5 years)
Case reports
- 27 year old Caucasian woman with a past medical history of imperforate anus, tetralogy of Fallot and Abernethy malformation (Hepatology 2016;64:1800)
- 31 year old Caucasian woman with persistent right sided rib pain (Gastrointest Cancer Res 2012;5:199)
- 51 year old man, HBV carrier, found to have high alpha fetoprotein (Int J Clin Exp Pathol 2013;6:737)
- 54 year old Japanese woman with abdominal distension (Pathol Res Pract 2020;216:152908)
- 68 year old man who presented with fluctuant fever, chills and sweating (Cell Biochem Biophys 2014;69:1)
Treatment
- Management of cHCC-CC is not standardized
- Surgical resection with lymph node dissection is the only curative option (Ann Surg Oncol 2009;16:623)
- Liver transplantation is contraindicated (Dig Liver Dis 2017;49:467)
- Locoregional therapies (arterial chemoembolization, radiofrequency) and systemic chemotherapy have been proposed for nonoperated patients
Gross description
- Lobular and firm mass
- Yellowish white pattern
- Well demarcated without capsule
- Reference: J Hepatol 2021 Feb 2 [Epub ahead of print]
Gross images
Microscopic (histologic) description
- Classical cHCC-CC contains areas of both typical hepatocellular carcinoma and typical intrahepatic cholangiocarcinoma, the former having any / all of the possible cytological and architectural features of hepatocellular carcinoma and the latter distinctly an adenocarcinoma with malignant glands, usually lying within a dense stromal background
- The components may be intermixed or lie in separate regions of a tumor, although focal areas of merging can often be discerned
- There are no published consensus guidelines for minimum amounts of hepatocellular carcinoma or intrahepatic cholangiocarcinoma to qualify for the diagnosis
- Intermediate cell carcinoma is composed of a monomorphic tumor with tumor cells smaller than normal hepatocytes but larger than the above described stem progenitor cell phenotype
- They have intermediate features between hepatocytes and cholangiocytes
- Tumor cells may be cuboidal to oval shaped, with pale or pink cytoplasm
- Tumor cells may be arranged in trabeculae or cords, solid nests or strands and set within a background of marked desmoplastic or acellular hyalinized stroma
- Elongated, ill defined gland-like structures may be present, suggestive of tubules but well defined glands are not observed
- Tumor cell atypia and mitoses are uncommon
- Mucin production is absent
- It is a biphenotypic tumor on immunohistochemistry
- Cholangiolocellular carcinoma (CLC) can be part of cHCC-CC if a hepatocellular carcinoma component is present; alone, CLC is now considered a subtype of intrahepatic cholangiocarcinoma
- CLC closely resembles the epithelial component of ductular reaction
- CLC consists of thin, malignant ductular-like structures that may appear to radiate from or surround a portal tract in a tubular, cord-like, anastomosing pattern (antler-like pattern) within dense, hyalinized stroma
- Tumor may show trabecular and replacing growth at its interface with the surrounding nontumorous liver
- CLC is mucin negative
- Reference: Hum Pathol 2020;96:48
Microscopic (histologic) images
Positive stains
- Hepatocellular carcinoma component: HepPar1 (75 - 85%), arginase1 (85 - 95%), glypican 3 (50 - 80%), pCEA canalicular staining (50 - 80%), CD10 canalicular staining (50 - 75%)
- pCEA and CD10 are the most specific markers for confirming a hepatocellular carcinoma
- Intrahepatic cholangiocarcinoma component: CK7 (> 90%), CK19 (> 75%), EpCAM (> 90%)
- Reference: Hum Pathol 2020;96:48
Negative stains
- Hepatocellular carcinoma component: Alpha fetoprotein (AFP) (30%), CK7 (20 - 30%), CK19 (10 - 15%), EpCAM (10 - 20%)
- Intrahepatic cholangiocarcinoma component: HepPar1, arginase1, pCEA, CD10, AFP, glypican 3 (5%)
- Reference: Hum Pathol 2020;96:48
Molecular / cytogenetics description
- Most frequently mutated driver genes in cHCC-CC are TP53, TERT promoter, AXIN1 and KMT2D (Cancer Cell 2019;35:932)
Sample pathology report
- Liver, tumor resection:
- Classical combined hepatocellular carcinoma-cholangiocarcinoma (see comment)
- Comment: This diagnosis is made based on morphological and phenotypical considerations. A tumor proliferation with 2 entangled components is observed: a well differentiated hepatocellular carcinoma component and a well differentiated intrahepatic cholangiocarcinoma component. The hepatocellular carcinoma component is composed of microtrabecular, massive and macrotrabecular architecture. Tumor cells are hepatoid and midsize with eosinophilic cytoplasm. The intrahepatic cholangiocarcinoma component is constituted of glandular, malformed and trabecular structures of small cuboidal cells. These tumor cells are accompanied by desmoplastic stroma. In the periphery of the tumor, we observed vascular and perineural invasion. There were no satellite nodules. Immunohistochemical staining showed cytoplasmic positivity of HepPar1 and glypican 3 in the hepatocellular carcinoma component and cytoplasmic positivity of CK7, CK19 and EpCAM in the intrahepatic cholangiocarcinoma component.
Differential diagnosis
- Hepatocellular carcinoma:
- Only features of hepatocellular carcinoma (no cholangiocarcinoma component)
- Pseudoglands in hepatocellular carcinoma should not be confused with the true glandular formation observed in intrahepatic cholangiocarcinoma
- Identification of bile can be very helpful
- There is no mucosecretion
- Importantly, marked bile ductular reaction with atypia adjacent to hepatocellular carcinoma due to mass effect is not an uncommon finding and one should be cautious not to overinterpret these atypical ductules as the cholangiocarcinoma component of a combined HCC‐CC
- Intrahepatic cholangiocarcinoma:
- Only features of intrahepatic cholangiocarcinoma with or without cholangiolocellular carcinoma component (no hepatocellular component)
- Mucin production
- Abundant desmoplastic stroma
Board review style question #1
Which of the following statements is correct regarding the liver neoplasm shown above?
- It is a cholangiolocellular carcinoma
- It is a hepatocellular carcinoma
- It is a poorly differentiated carcinoma
- It is an intrahepatic cholangiocarcinoma
- It shows unequivocal features of both hepatocytic and cholangiocytic differentiation
Board review style answer #1
E. It shows unequivocal features of both hepatocytic and cholangiocytic differentiation. It is, in fact, a combined hepatocellular carcinoma-cholangiocarcinoma.
Comment Here
Reference: Combined hepatocellular carcinoma-cholangiocarcinoma
Comment Here
Reference: Combined hepatocellular carcinoma-cholangiocarcinoma
Congenital hepatic fibrosis
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Hereditary form of ductal plate malformation affecting interlobular bile ducts, leading to excessive embryonic bile ducts and fibrosis
- Heterogeneous group of genetic disorders predominantly in an autosomal recessive manner
- Associated with hepatorenal ciliopathies caused by disruption of the physiological functions of cilia
- One of the fibrocystic liver diseases, which include Caroli disease, autosomal dominant polycystic kidney disease, autosomal recessive polycystic kidney disease and choledochal cysts
Essential features
- Commonly presents with portal hypertension and hepatosplenomegaly in children or young adults
- Classic histological triad with evolution
- Abnormal bile duct profile
- Small bile ductal structures lining at the limiting plate or embedded at the center of the portal tracts
- Bile ducts are often dilated, ectatic or have entrapped fibrous stroma
- May or may not contain inspissated bile in the lumen
- Hypoplastic portal vein radicles and prominent portal arteries
- Expansile portal fibrosis progresses to bridging with broad septa separating hepatocytes into islands but lacking the nodular regeneration of hepatocytes seen in cirrhosis
- Abnormal bile duct profile
Terminology
- Ductal plate malformation, fibrocystic liver disease
ICD coding
Epidemiology
- Estimated incidence: 1 in 10,000 - 20,000 live births (J Pak Med Assoc 2016;66:984)
- Age (J Pediatr Gastroenterol Nutr 2012;54:580)
- Predominantly affects infants and children, with median age of onset at 2 years
- Age range: birth to 75 years old
- No apparent sex predilection (J Pediatr Gastroenterol Nutr 2012;54:580)
Sites
- Primary location: liver
- Organs involved in syndromic manifestation: kidney, pancreas, lungs and brain (J Med Genet 2003;40:311)
Pathophysiology
- Normal bile duct morphogenesis is a timely regulated process (see Diagrams / tables) (J Med Genet 2003;40:311, Mech Dev 2003;120:81)
- Embryonic day 13.5 - 14.5: precursor cells express biliary specific cytokeratins and migrate closer to the portal mesenchyme
- Embryonic day 15.5: portal vein and the surrounding mesenchyme induce the precursor cells to form a continuous ring called ductal plate
- Embryonic day 16.5: ductal plate becomes partially bilayered
- Embryonic day 17.5: focal dilation between the 2 layers leads to bile duct formation starting from the hilum to the periphery, followed by progressive regression of the remaining ductal plate
- Hereditary / sporadic genetic mutations lead to imbalanced proliferation and apoptosis during ductal plate remodeling, resulting in persistence of embryonic duct profile in ductal plate configuration (J Med Genet 2003;40:311, Hepatology 1992;16:1069, Clin Res Hepatol Gastroenterol 2014;38:407)
- Postnatal pathologic changes
- Variable fibrosis as a consequence of ductal plate malformation or stimulation of the matrix forming cells (Clin Res Hepatol Gastroenterol 2014;38:407)
- Generally, minimal inflammation except when complicated by cholangitis
- Recurrent cholangitis can lead to progressive fibrosis with functional impairment similar to cirrhosis
Etiology
- Genetic disease primarily in autosomal recessive inheritance pattern
- May be associated with Caroli disease (Caroli syndrome) (Cureus 2020;12:e11029)
- Caroli disease
- Rare autosomal recessive disorder
- Prevalence of 1 in 1,000,000 people
- Cystic dilation of large intrahepatic bile ducts
- Caroli syndrome: Caroli disease with congenital hepatic fibrosis
- Caroli disease
- Hepatorenal ciliopathies: mutations in genes encoding proteins on primary cilia (J Med Genet 2003;40:311, Front Pediatr 2018;5:221, Am J Med Genet C Semin Med Genet 2009;151C:296, Mol Cell Pediatr 2015;2:8)
- Autosomal recessive polycystic kidney disease (ARPKD)
- Mutations in fibrocystin / polyductin (PKHD1) on chromosome 6
- Most common ciliopathy of childhood
- Autosomal dominant polycystic kidney disease (ADPKD)
- Mutations in polycystin 1 (PKD1) on chromosome 16
- Mutations in polycystin 2 (PKD2) on chromosome 4
- Nephronophthisis (OMIM: Nephronophthisis 1; NPHP1 [Accessed 23 June 2021])
- Mutations in nephrocystin 1 (NPHP1) on chromosome 2
- Controversial whether the hepatic fibrosis in nephronophthisis is true congenital hepatic fibrosis
- Joubert syndrome (OMIM: Joubert Syndrome 1; JBTS1 [Accessed 23 June 2021])
- Mutations in at least 30 genes
- Heterogeneous disorders characterized by cerebellar dysgenesis
- Meckel-Gruber syndrome (OMIM: Meckel Syndrome, Type 1; MKS1 [Accessed 23 June 2021])
- Lethal mutations in at least 8 genes (MKS)
- Jeune syndrome
- Also known as Jeune asphyxiating thoracic dysplasia
- Mutations in at least 11 genes
- Mutations in dynein 2 (DYNC2H1) and IFT complex B (IFT80) are the most common
- Bardet-Biedl syndrome (OMIM: Bardet-Biedl Syndrome 1; BBS1 [Accessed 23 June 2021])
- Mutations in at least 14 genes (BBS)
- Autosomal recessive polycystic kidney disease (ARPKD)
Clinical features
- Wide range of presentations, depending on age of disease onset and concomitant kidney involvement (J Pak Med Assoc 2016;66:984, Am J Clin Pathol 2020;153:119)
- In children or young adults with early disease onset, disease is progressive and may require liver or kidney transplant
- Portal hypertension and related symptoms
- Hepatosplenomegaly
- Recurrent cholangitis if presents as Caroli syndrome (Cureus 2020;12:e11029)
- Portopulmonary hypertension
- Hepatocellular carcinoma or cholangiocarcinoma, though rare, can be present
- May spontaneously regress or "burn out" in some patients
- Adults may be asymptomatic or with only mild disease
- In children or young adults with early disease onset, disease is progressive and may require liver or kidney transplant
Diagnosis
- Clinical suspicion of concurrent portal hypertension and chronic kidney disease in teenager or young adult
- Imaging: integrated use of ultrasound and abdominal MRI at baseline and follow ups; CT may be helpful (Pediatr Radiol 2009;39:100)
- Diagnostic liver biopsy showing classic histology
Laboratory
- Blood test: normal or elevated liver enzymes
- Thrombocytopenia and leukopenia due to hypersplenism (J Pediatr Gastroenterol Nutr 2012;54:580)
Radiology description
- Ultrasound (Pediatr Radiol 2009;39:100)
- Diffusely increased and coarsened liver echogenicity, splenomegaly and intra and extrahepatic biliary cysts / dilatations
- Periportal thickening
- Macroscopic cystic or fusiform dilatations of the intra and extrahepatic bile ducts
- Magnetic resonance imaging (MRI) (Pediatr Radiol 2009;39:100)
- Enlarged, nodular and misshapen liver with disproportionately hypertrophic left and caudate lobes
- Cystic dilatation of intrahepatic bile ducts; periportal hepatic fibrosis
Radiology images
Prognostic factors
- Variable; depends on age of onset / degree of involvement
- Children often experience much more severe portal hypertension related symptoms than adults (Gastroenterol Res Pract 2020;2020:8284274)
- Disease onset during neonatal period is a good predictor of the need for transplant (J Pediatr Gastroenterol Nutr 2013;57:161)
- Patients with Caroli syndrome often develop end stage renal disease requiring combined liver and kidney transplant (Cureus 2020;12:e11029)
- Excellent outcome in pediatric and adults patients after transplant (Transpl Int 2021 Apr 20 [Epub ahead of print])
- Rarely associated with hepatobiliary cancer, particularly cholangiocarcinoma (J Pediatr Gastroenterol Nutr 2012;54:580)
Case reports
- 2 year old boy with history of autosomal recessive polycystic kidney disease presented with variceal bleeding secondary to portal hypertension (Cureus 2020;12:e11029)
- 2 year old girl with abdominal distension with persistent hypertransaminasemia and cholestasis and 12 year old boy with hepatomegaly and splenomegaly of 2 years duration (Pan Afr Med J 2021;38:188)
- 5 year old boy with congenital hypothyroidism presented with abnormal liver function tests (World J Clin Cases 2021;9:1475)
- 6 year old girl with recurrent gastrointestinal bleed (World J Gastroenterol 2016;22:9865)
- 25 year old woman with hepatosplenomegaly of 3 months duration presented with abdominal pain and fever (Medicine (Baltimore) 2019;98:e15600)
Treatment
- Manage complications related to portal hypertension (J Pak Med Assoc 2016;66:984)
- Varices: medical management followed by sclerotherapy or band ligation
- Transjugular intrahepatic portosystemic shunts
- Antibiotics for cholangitis
- Liver transplant is the only curative treatment
Gross description
- Enlarged and firm liver with variable nodularity
- Cyst formation and duct dilatation is more common in Caroli syndrome
Microscopic (histologic) description
- Classic histological triad
- Abnormal bile duct profile
- Small ductal structure at the periphery of the fibrous septa
- May or may not contain inspissated bile in the lumen
- Hypoplastic portal vein branches
- Progressive fibrosis: bridging fibrosis with broad septa separating hepatocytes into islands
- Lack of nodular regenerative hepatocytes
- Abnormal bile duct profile
- Evolution of the lesion as patients age
- Infant: circumferential arrangement of ectatic and anastamosing ductal structures surrounding the hypoplastic portal veins
- Ductal structures decrease in size and number with increased fibrosis
- Fully evolved lesion is described in classic histological triad
Microscopic (histologic) images
Positive stains
Negative stains
- Iron: lack of intracytoplasmic iron deposition
- PAS / PASD: lack of intracytoplasmic inclusions
- Reticulin: lack of regenerative nodules
Molecular / cytogenetics description
- PKHD1 gene in autosomal recessive polycystic kidney disease
- PKD1 and PKD2 genes in autosomal dominant polycystic kidney disease
- NPHP1 gene in nephronophthisis (OMIM: Nephronophthisis 1; NPHP1 [Accessed 23 June 2021])
- DYNC2H1, IFT80 and 11 additional genes for Jeune syndrome
- See Etiology for more information
Sample pathology report
- Liver, biopsy:
- Ductal plate malformation consistent with congenital hepatic fibrosis (see comment)
- Comment: The biopsy is adequate for evaluation. Portal tracts diffusely demonstrate ductal plate malformations consisting of bile duct structures with irregular contours and regions of mild dilatation. Portal tracts / fibrous septa are without significant inflammation, interface activity or portal edema. Inspissated bile is noted in small ductal structures at the interface of fibrous septa and hepatic parenchyma. No lobular inflammation or steatosis is noted. Portal expansion by fibrosis is highlighted on trichrome stain. There is no evidence of cirrhosis. Iron and PASD stains show no additional pathologic findings.
- Overall, the histology of this biopsy demonstrates diffuse ductal plate malformation, consistent with congenital hepatic fibrosis (fibrous bands account for 50% of the biopsy volume). Ductal plate malformation disease in the liver is often associated with polycystic renal disease or other cystic abnormalities of tubules. In the present case, the overall features are those of congenital hepatic fibrosis but there may be overlap with other fibropolycystic conditions such as Caroli syndrome. A clinical evaluation to assess the presence or absence of portal hypertension in the setting of these liver biopsy changes warrants consideration.
Differential diagnosis
- Von Meyenburg complex:
- Also known as biliary duct hamartoma or bile duct microhamartoma
- Incidental small nodular lesion consists of mildly dilated ductal structures lined by flat epithelium in hyalinized stroma
- Typically small and may present as multiple lesions
- Autosomal dominant polycystic liver disease:
- Often becomes symptomatic in adulthood because liver cysts increase in number and size with age
- Mutations in hepatocystin (PRKCSH) on chromosome 19
- Mutations in SEC63 protein (SEC63) on chromosome 6
- Mutations in low density lipoprotein receptor related protein 5 (LRP5) on chromosome 11
- Solitary bile duct cyst:
- Incidental solitary unilocular cyst containing clear fluid
- Simple cuboidal / columnar epithelium with bland fibrovascular stroma
- No portal hypertension
- Choledochal cysts:
- Triad of abdominal mass, colicky pain and jaundice
- May present with cirrhosis and portal hypertension due to secondary biliary cirrhosis
- May be associated with colonic or duodenal atresia, anomalies of pancreas or congenital heart defects
- Thick wall cyst with variable inflammation and fibrosis
- Epithelium is usually denuded but can demonstrate metaplastic changes
- Cirrhosis:
- Diffuse nodular regeneration of hepatocyte and remodeling of hepatic architecture
- May show prominent bile ductular proliferation
- Varying degree of inflammation
- Compromised liver function
- No association with polycystic kidney disease
- Hepatoportal sclerosis (Hepat Med 2016;8:81):
- Under the term idiopathic noncirrhotic portal hypertension
- Multifactorial (infection, autoimmune, etc.)
- In young patient with portal hypertension and concurrent kidney disease, clinically mimics congenital hepatic fibrosis
- Portal fibrosis and portal vein with medial hypertrophy and venular dilatation
- Liver biopsy may show nodular regenerative hyperplasia and focal bile duct abnormality
- Recurrent pyogenic cholangitis:
- Associated with liver flukes or bile duct stones
- Dilation and fibrosis of bile ducts with acute inflammation and intraductal abscesses
- Other features include secondary sclerosing cholangitis
- Increased risk of developing cholangiocarcinoma
Additional references
Board review style question #1
A 2 year old boy was found to have portal hypertension while being evaluated in the hospital. A liver biopsy was performed. Which of the following findings is true regarding this disease entity?
- Adults experience much more severe symptom than pediatric patients
- Commonly associated with hepatobiliary cancer
- Liver transplant is the only curative treatment
- Symptoms resolve completely with no intervention
Board review style answer #1
C. Liver transplant is the only curative treatment
Comment Here
Reference: Congenital hepatic fibrosis
Comment Here
Reference: Congenital hepatic fibrosis
Board review style question #2
A 59 year woman with a history of diabetes presented with elevated liver enzymes and positive antimitochondrial antibody concerning for primary biliary cholangitis. A liver biopsy was performed. What is the most appropriate diagnosis?
- Bile duct malformation consistent with congenital hepatic fibrosis
- Primary biliary cholangitis
- Primary sclerosing cholangitis
- Steatosis and steatohepatitis with bridging fibrosis
Board review style answer #2
A. Bile duct malformation consistent with congenital hepatic fibrosis. This patient has undiagnosed congenital hepatic fibrosis. Adult onset congenital hepatic fibrosis may be asymptomatic or experience minor symptoms compared with pediatric patients.
Comment Here
Reference: Congenital hepatic fibrosis
Comment Here
Reference: Congenital hepatic fibrosis
COVID-19
Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Pathophysiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Electron microscopy images | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) primarily causes pulmonary disease but has been implicated in hepatic injury
- Coronavirus disease 2019 (COVID-19) viral hepatitis is defined by the clinical, laboratory and histopathological hepatic changes secondary to SARS-CoV-2 infection
Essential features
- Despite being primarily a pulmonary disease, SARS-CoV-2 infection has been shown to affect extrapulmonary sites, including the liver
- COVID-19 viral hepatitis is defined by the clinical, laboratory and histological liver abnormalities in the setting of real time reverse transcription polymerase chain reaction (RT PCR) proven SARS-CoV-2 infection
- Common laboratory findings include mild elevation of liver function tests: aspartate aminotransferase (AST) > alanine aminotransferase (ALT)
- Histologically, nonspecific findings include macrovesicular steatosis, lobular necroinflammation and portal inflammation
- Viral RNA can be detected in liver tissue by qRT PCR in approximately half of patients who die of COVID-19, although mainly at low levels
ICD coding
- ICD-10:
- ICD-11:
Epidemiology
- Liver injury is more common in severe cases (Lancet 2020;395:497)
- Incidence of elevated serum liver enzymes in hospitalized patients with COVID-19 ranges from 14% to 58% (AASLD: Clinical Best Practice Advice for Hepatology and Liver Transplant Providers During the COVID-19 Pandemic [Accessed 25 May 2022])
- Characteristics of U.S. patients with SARS-CoV-2 and liver enzyme elevation (Hepatology 2020;72:807):
- Median age 65 years
- M > F
- Hispanic / Latino > White > Black
- 5% have underlying chronic liver disease
Pathophysiology
- Angiotensin converting enzyme receptor 2 (ACE2) is the main mode of entry for the virus into the cell
- ACE2 is found on cholangiocytes, endothelial cells and rarely in hepatocytes
- Several possible mechanisms of injury seem to be implicated in SARS-CoV-2 liver injury (Liver Int 2020;40:1278)
- Immune mediated damage secondary to the inflammatory / cytokine response to COVID-19 infection
- Direct cytotoxicity as a result of active viral replication in hepatic cells
- Hypoxic hepatitis
- Drug induced liver injury (DILI)
Clinical features
- Most commonly, respiratory symptoms and fever
- Digestive symptoms, including anorexia, nausea, vomiting and diarrhea in a subset of patients
- Liver involvement manifests as rising liver function tests or acute hepatitis or cholestasis in the setting of COVID-19 infection (Lancet Gastroenterol Hepatol 2020;5:776)
- Common comorbidities: hypertension and diabetes (Hepatology 2020;72:807)
Diagnosis
- RT PCR based SARS-CoV-2 RNA detection from respiratory samples
- Quantitative RT PCR of liver tissue can confirm viral presence in the liver
- SARS-CoV-2 RNA has been detected in the stool of patients with COVID-19 (J Chin Med Assoc 2020;83:521)
- Microscopic examination of liver tissue
Laboratory
- Liver injury:
- Primarily mild elevation of AST and ALT (1 - 2 times upper limit of normal) (Hepatology 2020;72:807, Mil Med Res 2020;7:28)
- AST > ALT > bilirubin > alkaline phosphatase (ALP)
- Gamma glutamyl transferase (GGT) has been reported to be elevated in up to 54% of patients with COVID-19 during hospitalization (Lancet Gastroenterol Hepatol 2020;5:428)
- Other markers (Int J Infect Dis 2020;95:304):
- Lymphopenia, thrombocytopenia, hypoalbuminemia
- Inflammatory markers: elevated D dimer, C reactive protein, IL6, lactate dehydrogenase, creatine kinase and ferritin
Radiology description
- Fatty liver by ultrasound in up to 46% of patients (Mil Med Res 2020;7:28)
Prognostic factors
- Overall risks include:
- Older age
- Underlying diseases
- Secondary infection (Intensive Care Med 2020;46:846)
- Liver specific risk associations include:
- Higher AST, ALT, ALP
- Hypoalbuminemia
- Elevated inflammatory markers (Hepatology 2020;72:807)
Case reports
- 6 month old girl with a history of biliary atresia, status post living donor liver allograft from a COVID-19 positive donor (Arch Pathol Lab Med 2020;144:929)
- 25 year old woman with intermittent fever, 34 year old woman with fever, cough and bilateral lung consolidations and 45 year old previously healthy woman with fever (Hepatology 2004;39:302)
- 25 year old man, 38 year old man and 40 year old woman who developed prolonged and severe cholestasis during recovery from critical cardiopulmonary COVID-19 (Am J Gastroenterol 2021;116:1077)
- 53 year old man, 75 year old woman and 87 year old man with preexisting decompensated cirrhosis (Hepatol Int 2020;14:478)
- 59 year old woman with a chief concern of dark urine (Am J Gastroenterol 2020;115:941)
Treatment
- Liver damage is often transient
- Supportive care
- Patients with abnormal liver function should be closely monitored when using off label lopinavir / ritonavir, chloroquine, hydroxychloroquine and tocilizumab (Lancet Gastroenterol Hepatol 2020;5:776)
- According to the FDA, liver biochemistries should be checked in all patients prior to starting and daily while receiving remdesivir
- Liver transplant might be necessary in the setting of progressive biliary injury and liver failure secondary to COVID-19 cholangiopathy (Am J Gastroenterol 2021;116:1414)
Gross description
- No specific gross pathology
- Varying degrees of steatosis
- Congestion and ischemia (likely perimortem pathology in autopsy cases)
Microscopic (histologic) description
- Steatosis (Liver Int 2020;40:2110, Hum Pathol 2021;109:59)
- Common (up to 75% of patients)
- Predominantly macrovesicular
- Usually mild (involving < 33% of the liver parenchyma) and often azonal
- Usually not associated with ballooning and Mallory-Denk bodies
- Acute hepatitis (lobular necroinflammation) (Liver Int 2020;40:2110)
- Present in up to 50% of cases
- Usually mild severity (80% of cases)
- Foci contain apoptotic hepatocytes plus lymphocytes and rare histiocytes without prominent plasma cells
- Lobular mitoses
- Portal inflammation (Liver Int 2020;40:2110)
- Up to half of cases
- Minimal to mildly increased portal mononuclear cells (lymphocytes and macrophages)
- Rarely interface hepatitis
- Biliary findings / COVID-19 cholangiopathy
- Mild and focal lobular cholestasis (up to 38% of cases) (Mod Pathol 2020;33:2147)
- Ductopenia, severe cholangiocyte injury, ductular reaction, variable portal inflammation, variable fibrosis (Am J Gastroenterol 2021;116:1077)
- Acute or chronic large duct obstruction without clear bile duct loss (Am J Gastroenterol 2021;116:1414)
- Vascular pathology
- Focal
- Phlebosclerosis (reminiscent of veno-occlusive disease), more often with involvement of portal venule (rarely of central vein)
- Abnormalities of portal arterioles:
- Arteriolar muscular hyperplasia
- Hyalinosis and rare fibrinoid necrosis with endothelial apoptosis
- Sinusoidal erythrocyte aggregation (up to 44%) and platelet microthrombi (up to 70%) (Hepatol Res 2021;51:1000, Hum Pathol 2021;109:59)
- Uncommon findings
- Thrombotic bodies: pale ovoid sinusoidal platelet rich inclusions seen in sinusoidal spaces (CD61+)
- Large megakaryocytes
- Perimortem pathology
- Congestion
- Centrilobular ischemic necrosis
- Reference: Mod Pathol 2020;33:2147
Microscopic (histologic) images
Positive stains
- IHC and ISH for SARS-CoV-2 can be used to detect virus in lung, particularly during the acute phase of diffuse alveolar damage and occasionally in other organs, such as placenta
- Needs validation in the liver
Electron microscopy images
Molecular / cytogenetics description
- RT PCR of liver autopsy samples positive in up to 55% of COVID-19 deceased (Mod Pathol 2020;33:2147, Clin Gastroenterol Hepatol 2021;19:1726)
- Range from 10 copies to 9,254 copies/μl RNA
Videos
Liver histopathological findings in COVID-19 autopsies
Clinical insights: COVID-19 and the liver
Sample pathology report
- Liver, right lobe, core biopsy:
- Acute hepatitis and macrovesicular steatosis consistent with clinical history of SARS-CoV-2 infection
Differential diagnosis
- Reactivation of preexisting liver diseases:
- Correlate with clinical history
- Chronic hepatitis (commonly hepatitis C virus, hepatitis B virus, autoimmune hepatitis):
- Fibrosis implies chronicity, which would not be present in acute COVID-19; however, it has been described in subacute / chronic post COVID-19 biliary injury (Am J Gastroenterol 2021;116:1077, Am J Gastroenterol 2021;116:1414)
- Lymphoid aggregates are common in chronic hepatitis but are not typically encountered in COVID-19
- Preexisting fatty liver disease:
- Clinical risk factors
- Frank steatohepatitis does not seem to be a feature of COVID-19
- Chronic biliary tract disease:
- Features of primary sclerosing cholangitis / secondary sclerosing cholangitis have been reported in post COVID cholangiopathy (Am J Gastroenterol 2021;116:1414)
- Correlate with clinical history
- Drug induced liver injury (Surg Pathol Clin 2018;11:297):
- Clinical history of exposure to hepatotoxic drug
- May show prominent eosinophilia
- May show features reminiscent of autoimmune hepatitis
- Not always possible to distinguish from COVID-19 injury
Additional references
Board review style question #1
The liver sample shown above is from a patient with COVID-19. The histopathological process depicted in the image above is more often associated with which of the following conditions?
- Acetaminophen toxicity
- Autoimmune hepatitis
- COVID-19 associated hepatitis
- Primary biliary cholangitis
- Primary sclerosing cholangitis
Board review style answer #1
B. Autoimmune hepatitis. The finding of interface hepatitis is more common in autoimmune hepatitis but has been described in patients with COVID-19.
Comment Here
Reference: Viral hepatitis - COVID-19
Comment Here
Reference: Viral hepatitis - COVID-19
Board review style question #2
What is the most common histopathologic hepatic finding in patients dying of COVID-19?
- Apoptotic bodies
- Disseminated microthrombi
- Interface hepatitis
- Lobular necroinflammation
- Macrovesicular steatosis
Board review style answer #2
Cystic fibrosis
Table of Contents
Definition / general | Treatment | Gross description | Microscopic (histologic) description | Electron microscopy description | Additional referencesDefinition / general
- Most common lethal genetic disease in US of whites; affects 1 per 2,000 - 4,500 newborns
- 1 in 20 in the U.S. are carriers; most common mutation is ΔF508 of protein that regulates chloride ion transport on chromosome #7 (seen in 70% with disease)
- Mutations cause reduced chloride ion in secretions, thicker respiratory secretions, upper respiratory infections, late pancreatic insufficiency; also cause defective cilia and infertility, meconium ileus (5 - 10%), intussusception
- Liver disease in 11% (Pediatr Rep 2011;3:e21)
- May present as neonatal cholestasis
- Children with CF liver disease have a more severe CF phenotype than do CF patients without liver disease but a subgroup will not manifest clinically significant liver disease as adults (Am J Gastroenterol 2011;106:104)
Treatment
- Ursodeoxycholic acid (Curr Opin Pulm Med 2007;13:529)
- Liver transplantation (if end stage liver disease, Am J Transplant 2012;12:954)
Gross description
- Lung: emphysema, bronchiectasis, abscess
- Liver: fibrosis
Microscopic (histologic) description
- Macrovesicular steatosis, focal biliary cirrhosis (focal findings of inspissated granular eosinophilic, PAS positive material within portal bile ductules, chronic inflammatory infiltrate in portal tract, bile duct proliferation), cirrhosis (10% by age 25)
Electron microscopy description
- Filamentous material in bile ducts
Additional references
Cytomegalovirus hepatitis
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Immunofluorescence description | Immunofluorescence images | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Infection of the liver caused by cytomegalovirus (CMV), causing liver damage, ranging from asymptomatic to liver inflammation, failure and even death
- Most clinically significant infections are seen in immune compromised hosts, such as in AIDS, organ transplant recipients, hematopoietic stem cell transplantation, pregnancy and congenital infection (Microbiol Spectr 2016;4:1)
Essential features
- Mostly seen in immunocompromised hosts (AIDS, organ transplant recipient, hematopoietic stem cell transplantation)
- Histopathology characterized by cytomegaly, with cytoplasmic and nuclear inclusions
Terminology
- CMV hepatitis
- HHV5 hepatitis
ICD coding
- ICD-10: B25.1 - cytomegaloviral hepatitis
Epidemiology
- Seroprevalence of cytomegalovirus ranges from 45 to 100%, with higher prevalence in South America, Africa and Asia and lowest in Western Europe and the United States
- Seropositivity is independently associated with advancing age, female sex, foreign birthplace, high household crowding and low socioeconomic status (Gastroenterol Clin North Am 2020;49:331)
- Incidence of cytomegalovirus hepatitis in immunocompromised hosts ranges from 2 to 34% due to reactivation or reinfection (Clinics (Sao Paulo) 2015;70:515, Cureus 2020;12:e10745)
- Cytomegalovirus hepatitis is noted in 17% of liver transplant recipients (Clin Infect Dis 1996;22:537)
Sites
- Liver parenchyma (hepatocytes, Kupffer cells, biliary epithelium, endothelial cells)
Pathophysiology
- Can be acquired before birth, at birth or later in life
- Following initial active infection, it may remain latent for years; reactivation usually occurs in the setting of immune compromise
- Hematogenous spread leads to systematic viral dissemination involving the liver as well
- Direct cytopathogenicity: cytolytic process of cytomegalovirus
- Indirect cytopathogenicity
- Host mediated defense against virus
- Cytolytic effect of CD8+ and cytokines (IL17, IFNγ and TNF) mediated damage by CD4+
- Leading to
- Acute hepatitis
- Granulomatous hepatitis
- Necrotizing hepatitis (J Clin Transl Hepatol 2021;9:106)
- Portal vein thrombosis associated hepatitis and Budd-Chiari syndrome (Gastroenterol Clin North Am 2020;49:331)
Etiology
- Cytomegalovirus (CMV or HHV5) - a double stranded DNA virus
- Belongs to the Herpesviridae family
- Transmission through saliva, tears, urine, breast milk, semen and other body fluids
- Primary infection followed by lifelong latency
- Reactivation with visible presentation mostly in an immune compromised state (Pathogens 2019;8:213)
Clinical features
- Immunocompetent hosts can often be clinically silent
- In immunocompromised hosts, mononucleosis-like illness is a common presentation with fever, malaise, myalgia, nausea and abdominal pain
- Jaundice
- Congenital infection is characterized by asymptomatic to severe infection with jaundice, hepatosplenomegaly, encephalitis and chorioamnionitis
- Liver transplant patients can present with the symptoms of acute cellular rejection (Gastroenterol Clin North Am 2020;49:331)
Diagnosis
- Serology: titer of cytomegalovirus specific IgM and IgG (ELISA)
- Antigen detection: by immunofluorescence technique using an antibody against CMV pp65 and immediate / early antigens of cytomegalovirus
- PCR: qualitative and quantitative
- Histopathology (gold standard): H&E and immunohistochemistry
- Viral culture is an obsolete technique due to low sensitivity and longer time for diagnosis (Inflamm Intest Dis 2016;1:15)
Laboratory
- Subclinical elevation of transaminases (alanine transaminase [ALT] > aspartate aminotransferase [AST]) (J Clin Transl Hepatol 2021;9:106)
- Elevation is higher in immunocompetent patients in comparison to immunocompromised patients
- 3 - 9% of patients show an elevation in alkaline phosphatase and total bilirubin (jaundice)
- Serology
- IgM positivity indicates primary infection or viral reactivation
Radiology description
- Nonspecific findings of acute hepatitis (Radiopaedia: Acute Hepatitis [Accessed 21 February 2023])
- Ultrasound findings
- Hepatomegaly with hypoechoic echotexture
- Raised periportal echogenicity
- CT scan: not a first line imaging modality
- Hepatomegaly with possible decreased parenchymal attenuation
- Might show reduced attenuation around the portal system and hepatic hilum suggestive of periportal edema
- Might show lymphadenopathy (periportal and hepatoduodenal)
Radiology images
Prognostic factors
- Determined by underlying immunocompromised conditions and the type of immunosuppressive regimens in use
- Spontaneous resolution in immunocompetent hosts
- Mononucleosis-like pattern usually resolves within a few weeks
- Chronic liver disease is uncommon
- Reference: J Clin Transl Hepatol 2021;9:106
Case reports
- 35 year old obese woman with epigastric pain and vomiting for 2 months (Case Rep Gastroenterol 2016;10:36)
- 35 year old man presented to the emergency department with a 2 week history of low grade fever (Am J Case Rep 2020;21:e925495)
- 59 year old man with complaints of fever for 3 weeks (Cureus 2020;12:e10745)
- 64 year old woman presented with a 1 week history of lethargy and fever (BMJ Case Rep 2020;13:e234811)
- 66 year old woman presented with a 1 month history of yellow coloration of the eyes and skin, abdominal distension, dark colored stool and pale urine (World J Gastroenterol 2015;21:12505)
Treatment
- Immunocompetent patients do not need treatment and can recover without intervention
- In immunocompromised patients, treatment focuses on prevention and involves
- Prophylaxis treatment: after organ transplant with antivirals, prescribed for at least 3 months
- Preemptive treatment: for organ transplant and immunocompromised patients
- Antiviral drugs used are
- Intravenous ganciclovir
- Valganciclovir (J Clin Transl Hepatol 2021;9:106)
Microscopic (histologic) description
- Classic cytomegalovirus specific cytopathic effects are seen in hepatocytes, biliary epithelium, Kupffer cells and endothelial cells (Gastroenterol Clin North Am 2020;49:331)
- Infected cells have both cytoplasmic and nuclear enlargement, with cytoplasmic and nuclear inclusions, respectively (characteristic feature)
- Cytoplasmic inclusions are multiple, smaller, light staining, intracytoplasmic and basophilic / amphophilic granules of various size
- Nuclear inclusion is distinct, single, large, dense, intranuclear and has owl eye morphology: large glassy round to oval masses within the nucleus separated by a clear halo from the thickened nuclear membrane
- Mononucleosis-like pattern is characterized by a prominent mononuclear infiltrate within portal tracts and sinusoids; granulomas may also be present but viral inclusions are usually absent
- Immunocompromised patients have an overall low degree of inflammatory mononuclear infiltrate (J Clin Transl Hepatol 2021;9:106)
- Other nonspecific changes include mild lobular hepatitis, hepatocellular necrosis, patchy portal mononuclear infiltrate and microabscesses
- Immunohistochemistry is used when cytomegalovirus inclusion is not seen in H&E stain
- Cytomegalovirus antibody (DDG9 and CCH2) immunostain is utilized
Microscopic (histologic) images
Virtual slides
Immunofluorescence description
- A pp65 CMV antigenemia assay detects CMV antigens in peripheral blood polymorphonuclear cells
- Indirect immunofluorescence staining using monoclonal antibody
- In solid organ transplantation, a small number of antigen positive cells (10 per 50,000 polymorphonuclear cells) generally indicates asymptomatic infection, whereas a large number (> 50 antigen positive cells per 50,000 polymorphonuclear cells) indicates a 60% likelihood of CMV disease (Clin Infect Dis 1996;22:537)
Positive stains
- CMV immunohistochemistry (nuclear and cytoplasmic staining)
Negative stains
Molecular / cytogenetics description
- Qualitative PCR is used to detect cytomegalovirus in a tissue sample
Videos
Histopathology liver - congenital cytomegalovirus disease
Sample pathology report
- Liver, biopsy:
- Consistent with cytomegalovirus (CMV) hepatitis (positive CMV immunostain) (see comment)
- Comment: The patient's history of liver transplantation and being under the treatment of immunosuppressive drugs, along with positive CMV PCR for cytomegalovirus is noted. CMV immunostain highlights intranuclear and intracytoplasmic inclusions within portal tracts.
Differential diagnosis
- EBV associated hepatitis:
- Mimics mononuclear pattern of CMV hepatitis
- Distinguished by positive EBV in situ hybridization and positive heterophil antibodies
- Herpes simplex virus hepatitis:
- Foci of geographic necrosis
- HSV cytopathic effect characterized by multinucleation, margination of chromatin and ground glass nuclei
- HSV immunostain positive
- Adenovirus hepatitis:
- Focal to massive coagulative necrosis
- Immunostain for adenovirus is positive
- Transplant rejection:
- Pericentral ballooning degeneration and single cell apoptosis
- No viral cytopathic effect
- Mixed inflammatory cell infiltrate, endothelialitis and bile duct damage / injury would be expected in acute cellular rejection
Additional references
Board review style question #1
A 43 year old man with a known case of HIV and type 1 diabetes mellitus, under treatment, presented with complaints of decreased appetite and fatigue for 2 weeks. The abdomen was soft with mild hepatomegaly. Baseline liver profile showed the following: total bilirubin 72 (2 - 21) mg/dL, alanine transaminase (ALT) 54 (0 - 42) U/L, alkaline phosphatase 619 (40 - 129) U/L, gamma glutamyl transferase (GGT) 952 (8 - 61) U/L, lactate dehydrogenase (LDH) 247 (135 - 225) U/L, albumin 26 (35 - 52) g/L and direct bilirubin 95 (0 - 5) µmol/L. The histopathology of ultrasound guided liver biopsy is depicted in the image shown above. What characteristic finding is highlighted in the figure?
- Cytoplasmic and nuclear inclusions
- Diffuse lymphocytic sinusoidal infiltrate
- Foci of geographic necrosis
- Pericentral ballooning degeneration
Board review style answer #1
A. Cytoplasmic and nuclear inclusions. The image shows inclusion bodies visible in the nucleus and the cytoplasm, consistent with cytomegalovirus. Answers B - D are incorrect because the image does not show diffuse lymphocytic sinusoidal infiltrate, foci of geographic necrosis or pericentral ballooning degeneration.
Comment Here
Reference: Cytomegalovirus hepatitis
Comment Here
Reference: Cytomegalovirus hepatitis
Board review style question #2
Board review style answer #2
A. Cytomegalovirus hepatitis. The histology findings described above and the immunocompromised condition of the patient signify cytomegalovirus hepatitis. Answers B - D are incorrect because such inclusions are not observed in drug induced hepatitis, EBV hepatitis or hepatitis A.
Comment Here
Reference: Cytomegalovirus hepatitis
Comment Here
Reference: Cytomegalovirus hepatitis
Diagnostic patterns-differential diagnosis
Table of Contents
Definition / general | Essential features | Acute hepatitis pattern | Almost normal / near normal liver | Hepatitic pattern of injury | Resolving hepatitis pattern | Fatty liver | Cholestatic patterns | Bland lobular cholestasis | Bland ductular cholestasis or cholangitis lenta | Biliary obstruction pattern | Ductopenia | Chronic biliary / cholestatic injury / cholestatic hepatitis pattern | Cytoplasmic changes / abnormal deposition | Bland lobular necrosis | Granulomatous inflammation | Vascular injury pattern | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Identification of histologic features that define different patterns of liver injury to formulate appropriate differential diagnoses
Essential features
- Almost normal / near normal liver: minimal to absent histological findings but must look for changes in portal triad and lobules (cytoplasmic inclusions, steatosis, cholestasis, sinusoidal changes and altered hepatic plate architecture)
- Acute hepatitis pattern: mild to marked lobular inflammation and portal inflammation with hepatocyte necrosis
- Chronic hepatitis pattern: prominent chronic inflammatory infiltrate with occasional germinal centers in portal tracts with variable interface activity and less lobular inflammation than in acute hepatitis
- Resolving hepatitis pattern: scattered clusters of Kupffer cells and pigmented, ceroid laden, portal based macrophages with minimal chronic inflammation and hepatocyte regeneration
- Fatty liver - steatohepatitic pattern: more severe form of steatosis with hepatocyte ballooning, Mallory hyaline, lobular inflammation or fibrosis
- Cholestatic patterns: characterized by intracytoplasmic bile (hepatocanalicular cholestasis) and changes of chronic cholestasis
Acute hepatitis pattern
- Acute liver failure is an abrupt onset of liver disease or worsening liver function, either de novo or superimposed onto chronic liver disease
- Features of acute hepatitis pattern can overlap with other forms of hepatitis (chronic panlobular, cholestatic)
- Clinically, it is divided as hyperacute, acute and subacute liver failure, based on the duration of clinical presentation to development of serious symptoms, such as encephalopathy and coagulopathy
- Histologic pattern of injury can range from mild to marked lobular inflammation and hepatocyte necrosis
- Acute liver failure is associated commonly with drug induced liver injury (acetaminophen toxicity, idiosyncratic drug reactions), acute viral hepatitis, nonhepatotropic viruses (adenovirus, herpes simplex virus [HSV], cytomegalovirus [CMV], Epstein-Barr virus [EBV]), other infections (tick borne diseases, malaria), autoimmune hepatitis and Wilson disease
- Advanced fibrosis and percentage of necrosis in acute hepatitis have prognostic significance, with advanced fibrosis and > 25% necrosis indicating a worse prognosis (World J Gastroenterol 2017;23:4303)
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Almost normal / near normal liver
- Biopsies are usually prompted by unexplained abnormal liver enzymes, abnormal imaging or clinical presentations indicating liver etiology (portal hypertension, ascites)
- This pattern can be very challenging because of a broad differential diagnosis and potential to overlook subtle histologic findings leading to misdiagnosis
- Histologic findings are minimal to absent and there is no significant lobular or portal inflammation, fatty change, cholestasis or fibrosis
- It is still important to look for changes in the portal triad (bile ducts, hepatic arteries, portal veins) and in the lobules (cytoplasmic inclusions, steatosis, cholestasis, sinusoidal changes and altered hepatic plate architecture)
- Differential diagnosis for an almost normal liver biopsy includes systemic conditions (amyloidosis, Crohn's disease, celiac disease, thyroid disease, hypervitaminosis A), vascular disorders (portal venopathy, nodular regenerative hyperplasia and hepatoportal sclerosis, low grade or intermittent ischemic injury), genetic and metabolic conditions, drug effects, infection (sepsis, hepatotropic and nonhepatotropic viruses) and malignancy (leukemia, lymphoma)
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Hepatitic pattern of injury
- Chronic hepatitis pattern is characterized by a prominent chronic inflammatory infiltrate with occasional germinal centers in the portal tracts, with varying amounts of interface activity
- Lobular inflammation is typically not as pronounced as what is seen in acute hepatitis
- Varying degrees of fibrosis might be present, depending on the length and severity of the chronic injury
- Acute and chronic hepatitis are clinical terms defined by the length of time of liver enzyme elevations
- Common diseases with the chronic hepatitic pattern of injury are chronic viral hepatitis (B and C), autoimmune hepatitis, primary biliary cholangitis, drug reactions and acute cellular rejection
- Plasma cell predominant / autoimmune pattern shows dense portal inflammation with increased plasma cells, scattered eosinophils and brisk interface activity
- It is commonly seen in autoimmune hepatitis, primary biliary cholangitis, drug induced liver injury (nitrofurtantoin, minocycline, methyldopa) and occasionally in viral hepatitis A, B and C
- Giant cell predominant pattern is characterized by the presence of large, multinucleated hepatocytes throughout the lobules
- Referred to as postinfantile (adult) type giant cell hepatitis
- Associated conditions include neonatal cholestasis in pediatric patients, autoimmune hepatitis, systemic diseases like systemic lupus erythematosis, immune thrombocytopenic purpura (ITP) and infections with CMV, HHV6, EBV, HIV
- Panacinar / panlobular pattern refers to a moderate lymphocytic or lymphoplasmacytic inflammatory infiltrate involving both portal tracts and hepatic lobules in a diffuse and uniform manner and may represent either an acute process or an acute flare of a chronic disease
- Associated conditions include acute viral hepatitis (nonhepatotropic), acute flare of chronic viral hepatitis (hepatitis B), drug induced liver injury and autoimmune hepatitis
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Resolving hepatitis pattern
- Resolving hepatitis pattern of injury consists of scattered clusters of Kupffer cells and pigmented, ceroid laden, portal based macrophages with minimal chronic inflammation and hepatocyte regeneration
- Common causes include acute self limited viral infection or an idiosyncratic drug reaction, where the drug was stopped before the liver biopsy was performed
- PASD special stain can highlight the clusters of pigmented macrophages in sites of prior mild lobular injury
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Fatty liver
- Fatty liver disease results from the accumulation of fat droplets in the cytoplasm of hepatocytes (steatosis), with varying amounts of associated inflammation, hepatocyte injury and fibrosis (steatohepatitis)
- Steatosis is subdivided into macrovesicular (large and small droplet) and microvesicular patterns
- Steatosis is graded by a semiquantitative approach: minimal (< 5%), mild (5 - 33%), moderate (34 - 66%) and marked (> 67%)
- Steatohepatitic pattern is a more severe form of steatosis and includes additional features of hepatocyte injury (hepatocyte ballooning, Mallory hyaline), lobular inflammation or fibrosis
- Common etiologies of macrovesicular steatosis and steatohepatitis include metabolic syndrome, alcohol use, drug effect (amiodarone toxicity, methotrexate, steroids), Wilson disease and neoplasm (hepatic adenoma, steatohepatitic variant of hepatocellular carcinoma)
- Microvesicular steatosis is rarer and can occur in acute fatty liver of pregnancy, HELLP syndrome, Reye syndrome, medication toxicity (tetracycline, valproic acid), alcoholic foamy degeneration and mitochondrial toxicity / dysfunction
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Cholestatic patterns
- Pattern of injury characterized by intracytoplasmic bile (hepatocanalicular cholestasis) and changes of chronic cholestasis, with or without inflammation and obstructive features
- Cholate stasis refers to hepatocyte injury (periportal hepatocyte swelling / feathery degeneration, with or without Mallory hyaline)
Bland lobular cholestasis
- In this pattern, the major finding is hepatocanalicular / lobular cholestasis, usually in a zone 3 distribution, without significant inflammation or changes of biliary obstruction; typically there is no ductopenia or evidence of advanced fibrosis
- Bile plugs are found in both the hepatocytes and in the bile canaliculi
- This pattern is seen in drug related liver injury, severe systemic illness, sepsis and paraneoplastic syndromes (lymphomas)
Bland ductular cholestasis or cholangitis lenta
Biliary obstruction pattern
- Biliary obstructive pattern is characterized by changes in the portal tracts, including bile ductular proliferation, mild mixed inflammation (neutrophils and lymphocytes) and portal edema
- Degree of changes correlates roughly with the acuity and severity of the obstruction
- Lobular cholestasis can range from absent to marked, depending on the duration and severity of the obstruction, with accompanying minimal to mild lobular inflammation
- Common etiologies of this pattern include downstream biliary obstruction from strictures, stones, tumors, ischemia, infection, vascular outflow disease, severe acute hepatitis and biliary atresia
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Ductopenia
- Ductopenia is defined as the loss of bile ducts in at least 50% of portal tracts in an adequate biopsy
- True ductopenia is usually associated with significantly elevated alkaline phosphatase levels
- Ductopenia is commonly associated with Alagille syndrome, primary sclerosing cholangitis, strictures, stones, tumors, primary biliary cholangitis, chronic liver allograft rejection, graft versus host disease, ischemic cholangiopathy, drug effect and paraneoplastic syndromes (Hodgkin, T cell lymphomas)
- Immunohistochemical stain for cytokeratin 7 is an excellent tool to evaluate for ductopenia; additionally, a copper stain can highlight copper deposition in the periportal hepatocytes, which can be seen in most cases of established ductopenia
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Chronic biliary / cholestatic injury / cholestatic hepatitis pattern
- This is a nonspecific overlapping pattern used when the overall findings are not sufficient for a diagnosis of the biliary obstructive pattern and do not fit for bland lobular cholestasis or ductopenia
- Bile ductular proliferation can range from absent to mild and patchy, with associated mild bile duct lymphocytosis and injury, mild nonspecific portal inflammation, absent to minimal lobular inflammation and lobular cholestasis
- This pattern is seen most commonly in drug reactions and viral infections and may also been seen in early stage primary biliary cholangitis or primary sclerosing cholangitis
- These subtle and equivocal histologic changes are best supported by immunohistochemistry with cytokeratin 7, which helps assess bile duct loss and identification of proliferating intermediate hepatocytes, a feature of chronic cholestasis
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Cytoplasmic changes / abnormal deposition
- Most cytoplasmic changes are classified as either diffuse cytoplasmic clearing or distinct cytoplasmic inclusions
- Diffuse cytoplasmic clearing usually results from glycogen accumulation, seen in poorly controlled diabetes, glycogen storage disease and urea cycle defects
- Ground glass change is characterized as large pale inclusions occupying the majority of the cytoplasm and is commonly seen in chronic hepatitis B or drug effects
- Smaller, more eosinophilic inclusions in zone 1 hepatocytes are seen in alpha-1 antitrypsin deficiency
- Smaller eosinophilic inclusions in zone 3 hepatocytes are seen in chronic passive congestion of the liver
Bland lobular necrosis
- Bland lobular necrosis is the result of direct liver injury that is not immune mediated and has relatively little or no inflammation
- Bland lobular necrosis pattern of injury is associated with larger areas of necrosis and is distinct from spotty necrosis, usually seen in other hepatitic patterns of injury
- Zone 3 hepatocyte necrosis is commonly seen in drug reactions (acetaminophen) toxins and ischemia
- Isolated zone 1 and zone 2 patterns of necrosis are rare and are associated with heavy metal toxicity, industrial chemicals, poisons and hepatitis A
- Punched out necrosis is a pattern of somewhat round, well circumscribed, azonal areas of necrosis, most commonly viral in origin (HSV, varicella zoster virus, adenovirus)
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Granulomatous inflammation
- Single or numerous necrotizing or nonnecrotizing granulomas can be found in the portal tracts or lobules
- Common conditions with granulomatous inflammation include primary biliary cholangitis, sarcoidosis, drug effect, infection (mycobacterial, bacterial, fungal) and paraneoplastic syndrome
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Vascular injury pattern
- Vascular diseases resulting in hepatic injury are classified as hepatic arterial disease, portal vein disease, sinusoidal disease, peliosis hepatitis or hepatic vein disease
- Most common pattern is vascular outflow disease, usually from cardiac disease or thrombosis of the hepatic veins or vena cava, presenting with zone 3 predominant sinusoidal dilatation, congestion and zone 3 fibrosis
- Portal vein disease is more subtle, with findings of varying degrees of herniation, atrophy, loss and fibrosis of the portal veins, with or without associated nodular regenerative hyperplasia of the lobules
- Hepatic arterial disease is very uncommon, with low grade or intermittent arterial obstruction leading to bland lobular spotty necrosis with little or no inflammation
- Peliosis hepatitis refers to irregular blood filled cysts without any endothelial lining and is a histologic finding in debilitating illnesses, like tuberculosis, AIDS, cancer, malnutrition and medications, like estrogens / androgens
- See Nodular regenerative hyperplasia
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Additional references
- Torbenson: Biopsy Interpretation of the Liver, 3rd Edition, 2015, Saxena: Practical Hepatic Pathology - A Diagnostic Approach, 1st Edition, 2011, Torbenson: Atlas of Liver Pathology - A Pattern Based Approach, 1st Edition, 2020, Torbenson: Surgical Pathology of the Liver, 1st Edition, 2018, Burt: MacSween's Pathology of the Liver, 7th Edition, 2018, Lefkowitch: Scheuer's Liver Biopsy Interpretation, 9th Edition, 2016
Board review style question #1
Board review style answer #1
A. Cytokeratin 7. The image shows bile ductular proliferation, usually highlighted by cytokeratin 7 immunohistochemical stain.
Comment Here
Reference: Diagnostic patterns-differential diagnosis
Comment Here
Reference: Diagnostic patterns-differential diagnosis
Board review style question #2
Peliosis hepatis is commonly associated with which condition?
- Estrogen intake
- HSV
- Inborn errors of metabolism
- Obesity
- Reye syndrome
Board review style answer #2
A. Estrogen intake. Peliosis hepatitis refers to irregular blood filled cysts, without any endothelial lining and is a histologic finding in debilitating illnesses, like tuberculosis, AIDS, cancer, malnutrition and medications, like estrogens / androgens.
Comment Here
Reference: Diagnostic patterns-differential diagnosis
Comment Here
Reference: Diagnostic patterns-differential diagnosis
Donor liver frozen section evaluation
Table of Contents
Definition / general | Essential features | Terminology | Sites | Diagrams / tables | Clinical features | Diagnosis | Prognostic factors | Case reports | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Click here for the frozen section procedure topic
- Frozen section evaluation of donor liver biopsies, including assessment of fat, fibrosis, necrosis and inflammation, is a key component in determining if a donor liver is suitable for transplantation
Essential features
- Exclusion of potential donor livers based on frozen section findings of severe steatosis, ischemic necrosis, prominent portal inflammation or fibrosis or malignancy reduces the rate of primary nonfunction of transplanted livers (Transplantation 1993;56:1403)
- Amount of large droplet macrovesicular fat is a key factor in determining suitability of liver for transplantation and should be assessed first (Hepatology 2022;75:1014)
- Other histologic features including amount of small droplet macrovesicular fat and presence of fibrosis, inflammation, necrosis and granulomas should also be reported, as these may affect the transplant surgeon's decision to use the graft
- True microvesicular steatosis is essentially never seen in donor liver frozen sections, though some donor network forms include this feature
Terminology
- Liver allograft biopsy
Sites
- Liver
Diagrams / tables
Clinical features
- Multiple donor related factors are considered when surgeon determines whether to use a donor liver, including (Front Med Technol 2023:5:1079003)
- Age
- Body mass index (BMI)
- Clinical history of alcohol or intravenous (IV) drug use
- Laboratory values
- Warm and cold ischemia time
- Gross appearance of the liver
- Histologic features on frozen section
- Transplant surgeons also consider recipient status
- Healthier recipients may be better able to tolerate marginal organs
- Extended donor criteria may be utilized for select recipients (Clin Liver Dis 2017;21:289)
- Includes donor organs from patients with advanced age, steatosis, viral hepatitis, certain other transmissible infections, cardiac death or prolonged ischemia time
- Intended to increase the number of available donor organs
Diagnosis
- Selection of donor livers for transplantation is entirely at the discretion of the transplant surgeon (see Clinical features)
- Pathologists typically receive very limited information about the donor and no information about the recipient
- Amount of large droplet macrovesicular fat in donor liver is one of the key histologic features that define suitability for transplantation (Hepatology 2022;75:1014)
- < 30% large droplet macrovesicular fat generally does not preclude transplantation
- > 60% large droplet macrovesicular fat generally considered unsuitable for transplantation
- 30 - 60% large droplet macrovesicular fat generally considered borderline and other features including small droplet macrovesicular fat may be considered
- Fibrosis and inflammation are also important, particularly for extended criteria donors
- Organs with advanced fibrosis, bridging or greater, are typically excluded
- Inflammation should be moderate or less (Clin Liver Dis 2017;21:289)
- Other histologic features including amount of small droplet macrovesicular fat and presence of necrosis and granulomas should also be reported, as these may affect the transplant surgeon's decision to use the graft
Prognostic factors
- Exclusion of potential donor livers based on frozen section findings of severe steatosis, ischemic necrosis, prominent portal inflammation or fibrosis or malignancy reduces the rate of primary nonfunction of transplanted livers (Transplantation 1993;56:1403)
- Amount of large droplet macrovesicular fat is key factor in determining suitability of liver for transplantation (Hepatology 2022;75:1014)
- Severe large droplet macrovesicular steatosis (> 60%) in donor liver is associated with adverse outcomes including primary nonfunction, early allograft dysfunction and postreperfusion syndrome (Hepatology 1994;20:829, Transplantation 1989;47:903, Transplantation 1993;56:1403, Transplant Proc 1991;23:1536)
- Moderate to severe small droplet macrovesicular steatosis (> 30%) in graft is associated with increased risk for acute cellular rejection and bile duct loss in recipient (Am J Surg Pathol 2017;41:365)
Case reports
- 16 year old liver donor used for split liver transplant wherein one recipient developed fatty liver disease and one did not (World J Hepatol 2016;8:659)
- 56 and 58 year old men who received steatotic donor livers (Am J Transplant 2019;19:2640)
- 100 year old female liver donor with graft; recipient functioning well 9 months posttransplant (Am J Transplant 2023 Sep 25 [Epub ahead of print])
Frozen section description
- 2.0 cm long core needle biopsy or 1.5 cm² subcapular wedge biopsy from the anterior inferior edge of the liver are recommended for evaluation (Arch Pathol Lab Med 2013;137:270)
- Large droplet fat (Hepatology 2022;75:1014)
- Subtype of macrovesicular steatosis
- Single droplet distending the hepatocyte
- At least slightly larger than nearby hepatocytes lacking fat
- Hepatocyte nucleus, if present, displaced to cell periphery
- Assessed in 3 step process (Hepatology 2022;75:1014)
- At low power, determine % of parenchyma that stands out as white = LP%
- At high power, determine what % of these areas are truly large droplet fat = HP%
- Determine actual large droplet fat amount as percentage of total hepatocyte parenchyma by calculating HP% of LP% = large droplet fat percentage (LDF%)
- Small droplet fat
- Subtype of macrovesicular steatosis
- All fat droplets that do not meet criteria of large droplet fat or microvesicular steatosis (Hepatology 2022;75:1014)
- Assessed at high power after assessment of LDF%
- At high power, determine % of hepatocytes not involved by large droplet fat that contain small droplet fat = sHP%
- Determine actual small droplet fat amount as percentage of total hepatocytes by calculating sHP% of total hepatocytes (estimate total number of hepatocytes as 100% - LDF%)
- Scored based on percent of hepatocytes involved, not on percent of parenchyma
- Small droplet fat plus large droplet fat cannot exceed 100%
- Microvesicular fat
- Tiny fat droplets that impart a foamy appearance to hepatocytes
- Essentially never seen in liver donor biopsies
- Some standardized donor network forms may incorrectly refer to small droplet fat as microvesicular fat
- Fibrosis
- Appears as dense, eosinophilic material that may extend out from central veins or portal tracts entrapping adjacent hepatocytes
- Clues to advanced fibrosis include distortion of normal architecture, including loss of regular spacing of portal tracts and central veins, as well as presence of bridging septa (Surg Pathol Clin 2018;11:453)
- Other abnormalities including inflammation, granulomas and necrosis should also be reported if applicable
Frozen section images
Microscopic (histologic) description
Microscopic (histologic) images
Sample pathology report
- Donor liver, biopsy:
- Mild steatosis (see frozen section diagnosis and comment)
- Frozen section diagnosis
- Specimen type / size / description: liver core
- Fibrosis: none
- Portal infiltrates: mild, some or all portal areas
- Large droplet fat, % of hepatic parenchyma involved: 10%
- Small droplet fat, % of hepatocytes involved: 10%
- Centrilobular necrosis: no
- Evidence of cholestasis: no
- Evidence of lipofuscin: yes
- Evidence of active lobular inflammation: no
- Other pathology: no
- Comment: Frozen sections correlate with permanent sections.
Differential diagnosis
- Mimickers of large droplet fat:
- Dilated sinusoids:
- Elongated, somewhat irregular / wavy appearance
- Not circular
- Medium sized fat droplets:
- Should be counted as small droplet fat
- Smaller than nearby hepatocytes without fat
- Do not distend nucleus
- Dilated sinusoids:
- Mimickers of small droplet fat:
- Frozen section artifact:
- May occur when biopsies are submitted in saline
- May be visible overlying nuclei or sinusoids
- Often diffusely involve entire core or swaths of core
- Often pale pink rather than white
- Frozen section artifact:
- Microvesicular steatosis:
- Outdated terminology for macrovesicular small droplet fat
- Some standardized donor network forms may include this diagnosis
- Essentially never seen in donor liver biopsies
Additional references
Board review style question #1
A 60 year old man with a body mass index (BMI) of 40 suffered severe trauma and his organs are being evaluated for donation. This image is a frozen section from the right lobe of his liver. Assuming this field of view is representative of the entire biopsy, how should the amount of fat be reported?
- 0% large droplet macrovesicular steatosis; 0% small droplet macrovesicular steatosis; frozen section artifact is present
- 5% large droplet macrovesicular steatosis; 90% small droplet macrovesicular steatosis
- 5% macrovesicular steatosis; 90% microvesicular steatosis
- 95% macrovesicular steatosis (medium sized droplets); 0% microvesicular steatosis
Board review style answer #1
B. 5% large droplet macrovesicular steatosis; 90% small droplet macrovesicular steatosis. About 5% of this biopsy is large droplet fat, which comprises large droplets greater than the size of a nonfatty hepatocyte. About 90% of the hepatocytes contain small droplets, which do not significantly distend the hepatocyte cytoplasm or displace the nucleus.
Answer C is incorrect because microvesicular steatosis (tiny droplets that lend a foamy appearance to the hepatocytes) is not seen here. Answer D is incorrect because it is critical to divide macrovesicular steatosis into large and small droplet components, as they have different prognostic implications. Answer A is incorrect because the droplets are white and do not overlap with sinusoids or nuclei, as frozen section artifact droplets typically do.
Comment Here
Reference: Donor liver frozen section evaluation
Comment Here
Reference: Donor liver frozen section evaluation
Board review style question #2
A 30 year old woman with a body mass index (BMI) of 40 suffered severe trauma and her organs are being evaluated for donation. This image is a frozen section from the right lobe of her liver. How should the amount of fat be reported?
- 0% large droplet macrovesicular steatosis; 0% small droplet macrovesicular steatosis; frozen section artifact is present
- 30% large droplet macrovesicular steatosis; 30% small droplet macrovesicular steatosis
- 50% large droplet macrovesicular steatosis; 10% small droplet macrovesicular steatosis; centrizonal fibrosis is present
- 50% macrovesicular steatosis; 10% microvesicular steatosis
- 60% macrovesicular steatosis; 0% microvesicular steatosis
Board review style answer #2
C. 50% large droplet macrovesicular steatosis; 10% small droplet macrovesicular steatosis; centrizonal fibrosis is present. About 50% of this biopsy is large droplet fat, which comprises large droplets greater than the size of a nonfatty hepatocyte. About 90% of the hepatocytes contain small droplets, which do not significantly distend the hepatocyte cytoplasm or displace the nucleus. Fibrosis is seen near the central vein, around 10 o'clock.
Answer B is incorrect because most of the fat in this biopsy is large droplet fat (droplets larger than the size of a nonfatty hepatocyte). Answer D is incorrect because microvesicular steatosis (tiny droplets that lend a foamy appearance to the hepatocytes) is not seen here. Answer E is incorrect because it is critical to divide macrovesicular steatosis into large and small droplet components, as they have different prognostic implications. Answer A is incorrect because the droplets are large, white, round and do not overlap with sinusoids or nuclei, as frozen section artifact droplets typically do.
Comment Here
Reference: Donor liver frozen section evaluation
Answer B is incorrect because most of the fat in this biopsy is large droplet fat (droplets larger than the size of a nonfatty hepatocyte). Answer D is incorrect because microvesicular steatosis (tiny droplets that lend a foamy appearance to the hepatocytes) is not seen here. Answer E is incorrect because it is critical to divide macrovesicular steatosis into large and small droplet components, as they have different prognostic implications. Answer A is incorrect because the droplets are large, white, round and do not overlap with sinusoids or nuclei, as frozen section artifact droplets typically do.
Comment Here
Reference: Donor liver frozen section evaluation
Drug / toxin induced hepatitis (DILI)-general
Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Electron microscopy description | Sample pathology report | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Liver injury associated with exposure to certain drugs or toxins
- Drug / toxin reactions can be intrinsic or predictable when they are dose dependent (e.g., acetaminophen) or idiosyncratic and unpredictable when they are dose independent (e.g., isoniazid)
Essential features
- Diagnosis is based on the likelihood of DILI: time to onset, time to recovery, clinicopathological phenotype, exclusion of other causes, potentially offensive drug / toxin being a known cause of liver injury, and response to re-exposure
- Very wide range of clinical and pathological presentations
ICD coding
- ICD-10: K71.6 - toxic liver disease with hepatitis, not elsewhere classified
Epidemiology
- 10 - 20/100,000 based on prospective population based studies (Hepatology 2002;36:451, Am J Gastroenterol 2012;107:1380, Gastroenterology 2013;144:1419)
- Leading cause of acute liver failure and one of the major reasons for liver transplantation in the U.S. and Europe (Hepatology 2010;52:2065)
- Conventional medications are the most common cause of idiosyncratic DILI in the U.S. and Europe, whereas herbal medicine and dietary supplements are the major cause in Asia (Liver Int 2007;27:465)
Pathophysiology
- Underlying mechanisms include direct / indirect toxicity, aberrant metabolism producing toxic metabolites and immune mediated hypersensitivity
Etiology
- Drug dependent risk factors (J Hepatol 2019;70:1222):
- Dose
- Hepatic drug metabolism
- Lipophilicity
- Special moieties: toxic metabolite, oxidative stress, mitochondrial liability, hepatobiliary transport inhibition
- Concomitant drug / toxin
- Host dependent risk factors (J Hepatol 2019;70:1222):
- Age
- Gender
- Ethnicity
- Alcohol consumption
- Pregnancy
- Underlying liver disease or comorbidity
Clinical features
- Very wide range of clinical and pathological presentations can result; the time of onset after drug exposure varies from hours to months
- Clinical manifestations range from asymptomatic deranged liver function to fulminant hepatic failure and death
- Mimics all forms of acute, chronic, vascular or neoplastic liver diseases caused by other etiologies
- Reference: J Hepatol 2019;70:1222
Diagnosis
- Diagnosis is based on likelihood of DILI
- Time to onset
- Time to recovery
- Clinicopathological phenotype
- Exclusion of other causes
- Potentially offensive drug / toxin being a known cause of liver injury
- Response to re-exposure
- LiverTox, which is produced by NLM (National Library of Medicine) and NIDDK (National Institute of Diabetes and Digestive and Kidney Disease), provides up to date, accurate and easily accessed information on drug induced liver injury
Laboratory
- R value = [serum alanine aminotransferase (ALT) / upper limit of normal (ULN)] / [serum alkaline phosphatase (ALP) / ULN]
- Hepatocellular injury: R value ≥ 5 or ALT elevation ≥ 5 fold above ULN
- Cholestatic injury: R value ≤ 2 or ALP elevation ≥ 2 fold above ULN
- Mixed injury: R value between 2 and 5
- Liver biopsy may be considered in suspected DILI if:
- Elevated serum autoimmune markers
- Disease progresses or fails to resolve on withdrawal of suspected agent
- Reference: J Hepatol 2019;70:1222
Prognostic factors
- 5 - 20% may develop chronic DILI (Hepatology 2006;44:1581, Gastroenterology 2014;147:96, Gastroenterology 2019;156:2230)
- DILI severity grading (U.S. Drug Induced Liver Injury Network) (Hepatology 2010;52:730)
- Score 1 (mild): elevated ALT or ALP but total bilirubin < 2.5 mg/dL and international normalized ratio (INR) < 1.5
- Score 2 (moderate): elevated ALT or ALP and total bilirubin ≥ 2.5 mg/dL or INR ≥ 1.5
- Score 3 (moderate - severe): elevated ALT, ALP, total bilirubin or INR and hospitalization or ongoing hospitalization is prolonged because of a DILI episode
- Score 4 (severe): elevated ALT or ALP and total bilirubin ≥ 2.5 mg/dL and at least 1 of the following:
- Liver failure (INR > 1.5, ascites or encephalopathy)
- Other organ failure due to DILI
- Score 5 (fatal): death or liver transplantation due to DILI
Case reports
- 34 year old woman with acute cholestatic hepatitis after Moderna vaccination (J Hepatol 2022 Apr 18 [Epub ahead of print])
- 39 year old woman with acute cholestatic hepatitis after herbal supplement containing ashwagandha root extract (J R Coll Physicians Edinb 2021;51:363)
- 51 year old man with vanishing bile duct syndrome after infliximab for malignant melanoma (Cureus 2022;14:e21940)
- 61 year old woman with secondary sclerosing cholangitis after apatinib and vinorelbine for metastasis breast cancer (Thorac Cancer 2021;12:1912)
- 80 year old woman with amiodarone induced submassive necrosis in background of cirrhosis (ACG Case Rep J 2015;2:116)
Treatment
- Most patients recover spontaneously after withdrawal of offensive agent
- Specific therapy targeted for specific forms of DILI:
- Steroid for drug induced autoimmune hepatitis or those with marked hypersensitivity features
- Ursodeoxycholic acid for drug induced chronic cholestasis
- N-acetylcysteine for acetaminophen hepatoxicity
- Carnitine for valproate hepatotoxicity
- Reference: J Hepatol 2019;70:1222
Microscopic (histologic) description
- Morphological patterns can be categorized into the following:
- Necroinflammatory injury:
- Acute hepatic necrosis: acetaminophen, carbon tetrachloride
- Drug induced autoimmune hepatitis: diclofenac, halothane, indomethacin, infliximab, methyldopa, minocycline, nitrofurantoin, statins (J Hepatol 2019;70:1222)
- Granulomatous hepatitis: allopurinol, carbamazepine, methyldopa, phenytoin, quinidine, sulphonamides (J Hepatol 2019;70:1222)
- Cholestatic injury:
- Bland cholestasis: oral contraceptives
- Acute cholestatic hepatitis: amoxicillin / clavulanate, phenothiazines (Gut 1992;33:368)
- Chronic cholestatic injury: chlorpromazine, azathioprine, androgens, amoxicillin clavulanate, carbamazepine, chlorpromazine, erythromycin, estradiol, flucloxacillin, phenytoin, terbinafine, cotrimoxazole (Hepatology 1994;20:1437, J Hepatol 2019;70:1222)
- Steatosis and steatohepatitis:
- Microvesicular steatosis: amiodarone, didanosine, stavudine, valproate, zalcitabine, aspirin (Reye syndrome) (J Hepatol 2019;70:1222)
- Macrovesicular steatosis and steatohepatitis: corticosteroids, 5-fluorouracil, irinotecan, methotrexate, tamoxifen (J Hepatol 2019;70:1222)
- Vascular lesion:
- Sinusoidal obstruction syndrome: antineoplastic cytotoxic agents (Paediatr Drugs 2010;12:277)
- Budd-Chiari syndrome: oral contraceptives, dacarbazine (Postgrad Med J 2015;91:692)
- Nodular regenerative hyperplasia: azathioprine, busulphan, bleomycin, cyclophosphamide, chlorambucil, cysteine arabinoside, carmustine, doxorubicin, 6-thioguanine, oxaliplatin (J Hepatol 2019;70:1222)
- Sinusoidal dilatation and peliosis: oral contraceptives (Dig Liver Dis 2015;47:e10)
- Neoplasm and neoplasm-like lesion:
- Focal nodular hyperplasia (FNH): oral contraceptives (not associated with FNH pathogenesis; associated with larger and more symptomatic FNH)
- Hepatocellular adenoma: oral contraceptives, anabolic steroids (J Gastroenterol 2000;35:557)
- Angiosarcoma and cholangiocarcinoma: thorotrast (Hepatology 1995;22:1674, Cancer 1982;49:2161)
- Adaptive change:
- Pseudo ground glass inclusion: barbiturates, diazepam, cyanamide, transplant patients on multiple immunosuppressive drugs (steroids, tacrolimus and mycophenolate mofetil) (J Clin Pathol 2009;62:481)
- Necroinflammatory injury:
Microscopic (histologic) images
Electron microscopy description
- Amiodarone: lamellar lysosomal inclusion bodies representing phospholipidosis (Hum Pathol 1990;21:59)
Sample pathology report
- Liver, biopsy:
- Intrahepatic cholestasis without any significant necroinflammatory activity or fibrosis (see comment)
- Comment: The histological features are those of bland cholestasis. Differential diagnoses include drug induced liver injury, sepsis, shock, paraneoplastic syndrome, intrahepatic cholestasis of pregnancy and familial disorders of bile acid transporter. According to the case note, the patient has used oral contraceptive pills for a few months. Oral contraceptive pills are one of the most common medications associated with drug induced bland cholestasis. Recommend correlation with clinical impression, drug history and disease progress after withdrawal of the oral contraceptive pill.
Board review style question #1
Which medication is associated with microvesicular steatosis?
- Corticosteroid
- Didanosine
- Methotrexate
- Tamoxifen
Board review style answer #1
B. Didanosine. Didanosine is associated with microvesicular steatosis, whereas the other 3 drugs are associated with macrovesicular steatosis.
Comment Here
Reference: Drug / toxin induced hepatitis (DILI) - general
Comment Here
Reference: Drug / toxin induced hepatitis (DILI) - general
Board review style question #2
A patient was found to have an incidental liver tumor during routine checkup. You received the wedge excision of the liver tumor. Microscopic examination revealed a well differentiated hepatocellular neoplasm. The hepatocytes were bland and arranged in trabeculae of up to 2 cells with intact reticulin framework. Unpaired arterioles were noted. Which medication is associated with this hepatic mass lesion?
- Azathioprine
- Ethanol
- Oral contraceptive pill
- Thorotrast
Board review style answer #2
C. Oral contraceptive pill. The description of the tumor is typical for hepatocellular adenoma. Oral contraceptive pills are a risk factor associated with hepatocellular adenoma.
Comment Here
Reference: Drug / toxin induced hepatitis (DILI) - general
Comment Here
Reference: Drug / toxin induced hepatitis (DILI) - general
Drug / toxin induced hepatitis-acetaminophen
Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Intentional or unintentional overdose of acetaminophen, also known as paracetamol and N-acetyl-p-aminophenol, leading to liver injury
Essential features
- Acute hepatic necrosis related to acetaminophen overdose
- Acetaminophen overdose is one of the most common intentional or unintentional drug overdoses
- Acute liver failure associated with acetaminophen overdose is one of the most frequent causes of liver transplantation
ICD coding
- ICD-10
- X40 - accidental poisoning by and exposure to nonopioid analgesics, antipyretics and antirheumatics
- X60 - intentional self poisoning by and exposure to nonopioid analgesics, antipyretics and antirheumatics
- Y10 - poisoning by and exposure to nonopioid analgesics, antipyretics and antirheumatics, undetermined intent
- ICD-11
- PB24 - unintentional exposure to or harmful effects of analgesics, antipyretics or nonsteroidal anti-inflammatory drugs
- PC94 - intentional self harm by exposure to or harmful effects of analgesics, antipyretics or nonsteroidal anti-inflammatory drugs
- PH44 - exposure to or harmful effects of undetermined intent of analgesics, antipyretics or nonsteroidal anti-inflammatory drugs
Epidemiology
- Acetaminophen is one of most used analgesic and antipyretic drugs, either as a standalone medication or combined with other medications (prescription or over the counter)
- In the U.S., 43 million adults take some form of acetaminophen
- 7.5% take over the counter acetaminophen at least weekly (Expert Rev Clin Pharmacol 2014;7:341)
- Acetaminophen overdose may lead to hepatotoxicity and annually accounts for > 80,000 emergency department visits, > 30,000 hospitalizations and 42% of all cases of acute liver failure in the U.S. (Arch Toxicol 2015;89:193)
- 61.8% of overdoses were unintentional but 30.5% were associated with a suicide attempt (J Clin Gastroenterol 2016;50:85)
- For acetaminophen overdoses, 30.3% were with this drug only, 14.1% were with a combination containing diphenhydramine and 56.6% were with a combination containing an opioid (J Clin Gastroenterol 2016;50:85)
Pathophysiology
- Normally, < 10% of acetaminophen is metabolized by the cytochrome p450 system in the liver to generate N-acetyl-p-benzoquinone imine (NAPQI)
- NAPQI is then quickly metabolized to nontoxic metabolites by glutathione
- NAPQI may accumulate, secondary to acetaminophen overdose, due to upregulation of the cytochrome p450 system (through chronic use of alcohol, isoniazid, rifampicin or phenobarbital) or depletion of glutathione (due to malnutrition or chronic liver disease), which leads to hepatotoxicity through mitochondrial dysfunction, cell death and modulation of the innate immune system (Arch Toxicol 2015;89:193)
Etiology
- Intentional or unintentional overdose of acetaminophen
- Maximal recommended dosage is 4 g/day (adult) or 50 - 75 mg/kg/day (children) (Cleve Clin J Med 2010;77:19)
Clinical features
- Most overdose patients are asymptomatic initially but progress to acute liver failure if untreated
- Initial presentation of acute liver failure includes abdominal pain, fatigue, anorexia and fever
- Later presentation includes jaundice, coagulopathy and encephalopathy, which may be complicated by shock, pulmonary edema and acute renal failure (Arch Toxicol 2015;89:193)
- Of those who developed acute liver failure, 7.1% required liver transplantation, 29.3% required hemodialysis and 16.7% died (J Clin Gastroenterol 2016;50:85)
Diagnosis
- Combination of drug history, liver biochemistry and serum acetaminophen
Laboratory
- Liver biochemistry
- Serum acetaminophen
Prognostic factors
- Factors associated with poor clinical outcome include older age, unintentional overdose, repeated supratherapeutic doses, excessive alcohol consumption, chronic liver disease (Arch Toxicol 2015;89:193)
Case reports
- 14 year old girl with acetaminophen induced Stevens-Johnson syndrome and acute liver failure (J Dermatol 2021;48:1423)
- 24 year old woman with acetaminophen associated fulminant hepatorenal syndrome (Clin Case Rep 2021;9:e04037)
- 36 year old woman with acetaminophen associated acute liver failure (Am J Case Rep 2023;24:e938500)
- 43 year old woman with delayed acetaminophen absorption associated acute liver failure (Case Rep Crit Care 2022;2022:3672248)
- 60 year old woman with intravenous acetaminophen associated acute liver failure (BMJ Case Rep 2022;15:e251305)
Treatment
- Activated charcoal minimizes GI absorption of acetaminophen if administered within 4 hours of an acute overdose (Arch Toxicol 2015;89:193)
- N-acetylcysteine minimizes hepatotoxicity by replenishing glutathione stores (Arch Toxicol 2015;89:193)
- Liver transplantation is the last resort for patients progressing to acute liver failure despite N-acetylcysteine
Microscopic (histologic) description
- Acute hepatic necrosis characterized by extensive zone 3 or panacinar necrosis with minimal inflammatory infiltrate
Microscopic (histologic) images
Sample pathology report
- Liver, recipient explant, hepatectomy:
- Acute hepatocellular necrosis (see comment)
- Comment: Extensive panacinar hepatocellular necrosis is accompanied by minimal inflammatory infiltrate and ductular necrosis. Provided by known drug history of acetaminophen overdose, the overall features are consistent with acetaminophen overdose associated liver failure.
Differential diagnosis
- Nonhepatotropic viral hepatitis (e.g., herpes simplex virus and adenovirus):
- Correlate with drug history and viral serology / PCR tests
- Histology shows viral inclusions, which could be highlighted by immunostains
- Other drug / toxin induced liver injury:
- Correlate with drug history and serum acetaminophen level
- Vascular disorders (e.g., shock, acute Budd-Chiari syndrome):
- Correlate with drug history and serum acetaminophen level
- Histology shows sinusoidal congestion and zone 3 / panacinar hemorrhagic necrosis
Additional references
Board review style question #1
Board review style answer #1
D. Zone 3 / panacinar hepatocellular necrosis. Zone 3 / panacinar hepatocellular necrosis is the typical pathological feature of acetaminophen associated liver injury. Answers A - C are incorrect because antibiotics (e.g., amoxicillin / clavulanate), oral contraceptive and iron overdose are typical drugs / toxins leading to acute cholestatic injury, bland cholestasis and zone 1 hepatocellular necrosis, respectively.
Comment Here
Reference: Drug / toxin induced hepatitis-acetaminophen
Comment Here
Reference: Drug / toxin induced hepatitis-acetaminophen
Board review style question #2
Which of the following is associated with a better prognosis in acetaminophen induced liver injury?
- Chronic hepatitis B
- Cirrhosis
- Excessive alcohol consumption
- Younger age
Board review style answer #2
D. Younger age. Answers A - C are incorrect because older age rather than younger age, excessive alcohol consumption and chronic liver disease are associated poorer outcome of acetaminophen induced liver injury.
Comment Here
Reference: Drug / toxin induced hepatitis-acetaminophen
Comment Here
Reference: Drug / toxin induced hepatitis-acetaminophen
Ductular reaction
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Case reports | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Complex, dynamic and nonspecific reaction to liver injury and disease (acute and chronic), characterized by a ductular phenotype, possibly but not necessarily of ductular origin, at the portal - parenchymal interface
- May arise from:
- Proliferation of preexisting cholangiocytes
- Progenitor cells (local or circulating cells probably bone marrow derived)
- Rarely, biliary metaplasia of hepatocytes
Essential features
- Ductular reactions (DRs) are a response to a wide variety of hepatobiliary injuries that aim to restore compromised physiological function after liver injury
- Variable degree of bile duct profiles, portal edema, fibrosis and an inflammatory infiltrate composed mostly (but not always) of neutrophils
- Ductular reactions are predominantly associated with biliary diseases but can be seen secondary to any liver injury as a response in bipotential hepatic progenitor cells to differentiate into either cholangiocytes (bile ductular profiles) or hepatocytes
- Ductular reactions are characterized by simultaneous expression of biliary antigens (CK7, CK19, OV6) and hepatocyte antigens (e.g. HepPar1, albumin, alpha-1 antitrypsin, alpha fetoprotein) and other markers such as NCAM1 / CD56
- Outcomes of ductular reactions are diverse and include hepatic parenchymal regeneration, fibrogenesis and hepatocarcinogenesis, depending on the duration and severity of underlying pathology
Terminology
- Ductular reaction was coined by Popper et al. in 1957 and has subsequently been used in the hepatology literature, sometimes interchangeably with ductular proliferation
ICD coding
Epidemiology
- Predominantly associated with biliary diseases but can be seen secondary to any liver injury
Sites
- Portal - parenchymal interface in liver
Pathophysiology
- Liver or biliary injury → activation of hepatic progenitor cells, induction of self proliferation of cholangiocytes and transdifferentiation of hepatocytes, resulting in proliferation of bile ductules
- Inflammatory cytokines (IL13, IL6, IL8, etc.) induce proliferation of cholangiocytes and recruitment of inflammatory cellular components, as well as edema and hepatic progenitor cells niche that consists of macrophages, myofibroblasts and matrix and is associated with liver fibrogenesis during liver injury (Hepatology 2019;69:420)
- Mechanisms and associated cellular and tissue components may differ, depending on the underlying pathology / etiology
Etiology
- Any injury / insult to liver / biliary tree induces a response in bipotential hepatic progenitor cells to differentiate into either cholangiocytes (bile ductular profiles) or hepatocytes
- Biliary / cholestatic disorders are more common:
- Primary biliary cholangitis (PBC)
- Primary sclerosing cholangitis (PSC)
- Biliary atresia
- Bile duct obstruction (tumor, stone, stricture)
- Alcoholic and nonalcoholic fatty liver disease
- Chronic viral hepatitis (HBV, HCV)
- Autoimmune hepatitis
- Acute liver failure
- Total parenteral nutrition (TPN)
- Focal nodular hyperplasia
- Hepatocellular adenoma - inflammatory type
- Neoplasms - benign and malignant
- Biliary / cholestatic disorders are more common:
- Reference: Hepatology 2011;54:1853
Clinical features
- Depend on the underlying etiology (associations)
Diagnosis
- Liver biopsy
Laboratory
- Nonspecific - could range from normal to abnormal liver function tests
- Cholestatic pattern of liver enzymes - biliary diseases
- Hepatocellular pattern - nonbiliary diseases
Case reports
- 32 week old boy with biliary atresia and total parenteral nutrition associated with ductular reaction (BMC Pediatr 2019;19:72)
- 51 year old man with hepatocellular carcinoma with associated malignant ductular reaction (Int J Clin Exp Pathol 2020;13:1073)
Microscopic (histologic) description
- Traditionally divided into typical and atypical ductular reactions; however, this distinction is subtle, with low reproducibility - no classification with universal consensus
- Typical: ductules have a recognizable lumen lined by cuboidal cells and are the result of proliferation of preexisting ductules
- Atypical: ductules are thin, elongated structures lined by flattened cells that extend irregularly into the lobules, lack easily discernible lumina and are closely related to progenitor cell activation
- Most classifications emphasize on the type of ductules, however the term ductular reaction essentially implies proliferation of cholangiocytes and recruitment of inflammatory cellular components (neutrophils, lymphocytes etc) as well as edema and hepatic progenitor cells niche that consists of macrophages, myofibroblasts and matrix; neutrophils are part of the matrix as a result of chemotactic inflammatory cytokines and do not represent cholangitis / ascending cholangitis - they are mostly confined to the stroma of portal-lobular interface; no bile ductular intraepithelial neutrophils
- Classification systems based on pathobiology and epithelial - mesenchymal differentiation
- Desmet classification (Virchows Arch 2011;458:251)
- DR type 1
- Represents multiplication of preexisting cholangiocytes; immediate rescue mechanism against cholestatic parenchymal damage
- Develops fast, favoring cholehepatic cycling of bile acids
- DR type 2
- Represents activation of hepatic progenitor cells
- Type 2A: develops slowly, creating additional canalicular outlets and a larger cholangiocytic resorbing surface favoring cholehepatic cycling in chronic cholestasis
- Type 2B: creates ductules in hypoxic areas; plays a role in new portal tract induction during liver growth
- DR type 3
- Represents progenitor cell based parenchymal regeneration after liver injury
- DR type 1
- Clerbaux et al. / Jain R et al. classification (Adv Anat Pathol 2021;28:72)
- DR type 1 / noninvasive
- Proliferating ductular profiles are limited to the portal mesenchyme; there is no ductular metaplasia or hepatic progenitor cell proliferation
- Associated with large duct obstruction
- DR type 2 / minimally invasive
- Ductular profiles are largely limited to portal mesenchyme with some extension into lobules; there may be ductular metaplasia
- Nonspecific pattern often seen in chronic cholestatic diseases (PBC, PSC, etc.)
- DR type 3 / invasive
- Extensively proliferating ductules deeply invasive into lobules and accompanied with hepatic progenitor cell proliferation
- Associated with massive hepatic necrosis or parenchymal loss
- DR type 1 / noninvasive
- Desmet classification (Virchows Arch 2011;458:251)
| | ||
| Typical: arising from preexisting ductules and confined to the portal mesenchyme | Type 1: typical ductular reaction | Noninvasive: typical ductular reaction |
| Atypical: characterized by structures extending beyond the portal mesenchyme and associated with progenitor cell activation | Type 2: atypical ductular reaction with ductular metaplasia of hepatocytes | Minimally invasive: ductular reaction that expands 20 - 80 μm beyond portal mesenchyme |
| Type 3: atypical ductular reaction with progenitor cell proliferation | Invasive: ductular reaction that expands > 80 μm beyond portal mesenchyme |
- Reference: Am J Pathol 2019;189:1501
Microscopic (histologic) images
Positive stains
- Simultaneous expression of biliary antigens (CK7, CK19, OV6) and hepatocyte antigens (HepPar1, albumin, alpha-1 antitrypsin, biliary glycoprotein 1 detected by canalicular staining with polyclonal anti-CEA and occasionally alpha fetoprotein) and other markers, such as NCAM1 / CD56
- Turányi et al. immunohistochemical classification of ductular reactions (Histopathology 2010;57:607):
- Type P (primitive):
- Type D (differentiating):
- Type O (obstruction):
Negative stains
Videos
Ductular reaction in liver disease
Sample pathology report
- Liver, needle core biopsy:
- Severe cholestasis with marked ductular reaction and fibrosis, suggestive of extrahepatic biliary atresia
Differential diagnosis
- Ductal plate malformation:
- Anastomosing, angulated and dilated biliary channels in irregular, bland fibrous stroma, continuous with biliary tree
- Bile ducts often contain inspissated bile
- Bile duct hamartoma / adenoma:
- Compact network of simple noncystic tubular ducts or more complex tortuous arrangement, with small or indistinct lumina
- Epithelium has abundant cytoplasm and pale nuclei compared with interlobular bile ducts in adjacent liver
- Often grossly apparent lesion
- Well differentiated intrahepatic cholangiocarcinoma:
- Larger, infiltrative lesion with desmoplastic stroma and nuclear / cytologic atypia
Additional references
Board review style question #1
The ductular profiles in the ductular reaction at the portal - parenchymal interface are highlighted best by which of the following panels of immunohistochemical stains?
- Alpha-1 antitrypsin, CK19, CK7, EMA
- CD56, glypican 3
- CK7, arginase1
- EMA, albumin, GPC3
- HepPar1, alpha fetoprotein, CK20
Board review style answer #1
Board review style question #2
Board review style answer #2
Echinococcal cyst
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Cestode (tapeworm) infection widespread across the world
- Common cause of hepatic cysts; caused by the larval form of Echinococcus tapeworms: Echinococcus granulosus (most common, causes cystic disease), Echinococcus multilocularis (less common, causes alveolar disease), Echinococcus vogeli (polycystic disease) and Echinococcus oligarthus (extremely rare, unicystic form)
Essential features
- Cestode (tapeworm) infection widespread across the world
- Echinococcus granulosus is the most common (classic hydatid cyst)
- E. granulosus cysts consist of inner, middle and outer layers
- Inner layer is a germinal layer with brood capsules and protoscolices (adult tapeworm heads)
- Middle layer consists of hyalinized, laminated and acellular material
- Outer layer consists of granulation tissue and fibrosis
Terminology
- Hydatid disease
ICD coding
- ICD-10: B67. 90 - echinococcosis, unspecified
Epidemiology
- Common cause of hepatic cysts worldwide, particularly in sheep and cattle in farming areas in Middle East, Greece, Australia, North Africa and parts of South America
- In U.S., usually in immigrants from above areas
- Reference: World J Gastroenterol 2012;18:1425
Sites
- 60 - 70% in liver; also brain, lung, other sites
- Frequently communicates with biliary tract (Iran J Med Sci 2013;38:2)
- Rare in breast (0.27% of cases) but should be considered in the differential diagnosis of a breast mass in endemic regions (J Gynecol Obstet Biol Reprod (Paris) 1986;15:187)
Pathophysiology
- Mucosal attachment of tapeworm to small intestine in definitive hosts, such as dogs (CDC: Echinococcosis [Accessed 4 March 2022])
- Ingestion of eggs in contaminated feces can infect humans
- Larval oncospheres are released from eggs and are transported to liver by portal vein
- Oncospheres grow into cysts enlarging at slow pace of about 10 - 15 mm per year
- Cysts are composed of protoscolices and daughter cysts (J Clin Transl Hepatol 2016;4:39)
Etiology
- Liver as primary site of infection:
- E. granulosus
- E. multilocularis
Clinical features
- Often asymptomatic for years due to slow growth but hepatic and pulmonary symptoms are most common
- Symptoms can be secondary to cyst rupture or compression of other structures
- Bacterial infection, bile duct compression, cholangitis, rupture into peritoneal or pleural cavities
- Portal hypertension secondary to portal vein compression
- Breast masses (Folia Med (Plovdiv) 2020;62:23)
- Rupture of cysts in the lung may cause intense cough or vomiting of cystic materials (Curr Opin Pulm Med 2010;16:257)
- Clinically may resemble carcinoma
- Parasitic flatworm (tapeworm) of class Cestoda (i.e., a cestode) (Pritt: Creepy Dreadful Wonderful Parasites Blog - Answer to Case 514 [Accessed 4 March 2022])
- Member of family Taeniidae due to presence of an armed rostellum (i.e., 2 rows of hooklets) (Pritt: Creepy Dreadful Wonderful Parasites Blog - Answer to Case 514 [Accessed 4 March 2022])
- Echinococcus granulosus is a complex of closely related organisms (Pritt: Creepy Dreadful Wonderful Parasites Blog - Answer to Case 514 [Accessed 4 March 2022])
- E. granulosus sensu stricto is most common species causing human disease worldwide
- E. canadensis and E. ortleppi also cause human disease
- Species are differentiated via molecular means
- Alveolar echinococcosis is caused by infection with larval stage of E. multilocularis, a 1 - 4 millimeter long tapeworm found in foxes, coyotes, dogs (definitive hosts)
- E. multilocularis human infection is less common but has more aggressive and invasive growth that resembles a tumor and is not contained within a large parent cyst (Pritt: Creepy Dreadful Wonderful Parasites Blog - Answer to Case 514 [Accessed 4 March 2022])
- E. oligarthra and E. vogeli are rare causes of human echinococcosis in South and Central America (Pritt: Creepy Dreadful Wonderful Parasites Blog - Answer to Case 514 [Accessed 4 March 2022])
- Breast: slow growing lesion, may mimic fibroadenoma, phylloides or rarely intracystic carcinoma; may become infected and be indistinguishable radiologically from an abscess
Diagnosis
- Usually made by ultrasound or CT scan supported by positive hydatid serology
Laboratory
- Monoclonal antibodies to hydatid antigens detection by immunoelectrophoresis, enzyme linked immunosorbent assay (ELISA) and immunoblots
- Immunoblots have the highest sensitivity, followed by ELISA and immunoelectrophoresis
- Antigen assays have more specificity but lower sensitivity than antibody assays
- Unruptured cysts may not produce antibody response (J Clin Transl Hepatol 2016;4:39)
Radiology description
- Ultrasound / CT scan reveal cysts with septations
- Breast: on mammography, lesions may be well circumscribed, oval or spherical densities with smooth lobulated margins; peripheral calcification may be present
- Breast: on ultrasound, may see double wall sign (cyst wall as 2 echogenic layers), snowstorm sign (due to movement of scolices within the cyst), waterlily sign (floating membranes due to detached endocyst / daughter cyst), scroll sign (due to folding of the detached endocyst) (J Clin Ultrasound 2014;42:502, Singapore Med J 2010;51:e72)
Radiology images
Prognostic factors
- Although mortality is uncommon, fatalities have been reported in rare cases of anaphylactic shock or cardiac tamponade (Acta Cardiol 2005;60:39)
- Ruptured cystic disease may require lifelong antiparasitic therapy to prevent recurrence
- Most common complications are mechanical and superinfection (Am J Trop Med Hyg 2019;101:628)
Case reports
- 8 year old girl with cystic echinococcosis involving left ventricle (Medicine (Baltimore) 2019;98:e15267)
- 25 year old man with abdominal pain, syncope and hypotension (N Engl J Med 2015;372:265)
- 31 year old year old woman with painless breast lump for 1 year (Int J Surg Case Rep 2015;7C:115)
- 32 year old man with an Echinococcus cyst in liver and pancreas (BMC Infect Dis 2019;19:661)
- 62 year old woman with a huge Echinococcus cyst in liver resembling malignancy (J Med Case Rep 2017;11:113)
- Echinococcus found in a single liver cyst (Pritt: Creepy Dreadful Wonderful Parasites Blog - Case of the Week 514 [Accessed 4 March 2022])
- Objects seen in liver cyst aspirate (Pritt: Creepy Dreadful Wonderful Parasites Blog - Case of the Week 537 [Accessed 4 March 2022])
Treatment
- Surgical resection
- Cyst rupture during surgery may cause urticaria, anaphylaxis or recurrence of infection
- Puncture, aspiration, infusion of protoscolicidal agent, reaspiration
- Preferred technique due to lower risk of anaphylaxis or recurrence (BMC Surg 2019;19:95)
Gross description
- Echinococcus granulosus: typical cyst is spherical, up to 30 cm or more in diameter, has a fibrous rim and frequently contains several daughter cysts
- Echinococcus multilocularis: multilocular, necrotic, cystic cavities containing thick pasty material; fibrous rim is absent
- Reference: Zhonghua Bing Li Xue Za Zhi 2021;50:650
Gross images
Microscopic (histologic) description
- E. granulosus
- Cyst wall has 3 structural components:
- Outer acellular laminated membrane (1 mm thick)
- Germinal membrane (a transparent nucleated lining)
- Protoscolices, attached to the membrane and budding from it
- Protoscolices are ovoid and contain hooklets (birefringent under polarized light) and a sucker
- Outer fibrotic layer with granulation tissue with increased eosinophils also exists
- Cyst wall has 3 structural components:
- E. multilocularis
- Irregular cysts with laminated membrane without germinal membrane or protoscolices
- Invasion of liver parenchyma can create inflammatory / granulomatous reaction or extensive peripheral necrosis and fibrosis
- Reference: Zhonghua Bing Li Xue Za Zhi 2021;50:650
Microscopic (histologic) images
Positive stains
- Hooklets are acid fast positive on Ziehl-Neelsen stain; also stain with GMS (J Cytol Histol 2016;7:1000422)
Videos
Bird's eye view of Echinococcus
Sample pathology report
- Liver, excision:
- Echinococcal cyst
- Comment: There are degenerated echinococcal cysts that contain abundant debris with protoscolices fragments.
Differential diagnosis
- Other tapeworm infections: cysticercosis (Taenia solium)
- Fibropolycystic liver disease:
- Lacks 3 layered cyst, protoscolices
- Numerous cystic lesions similar to solitary cysts, covered by cuboidal to flat biliary epithelium
- Amoebic or pyogenic abscess:
- Lacks 3 layered cyst, protoscolices
- Nuclear fragments with inflammatory cells
- Organisms with foamy cytoplasm and eccentric round nucleus
- Ingested red blood cells pathognomonic of Entamoeba histolytica
- Trophozoites look like macrophages
Additional references
Board review style question #1
A 45 year old man presented with weakness, weight loss and abdominal pain for a month. An ultrasound showed a cystic lesion in liver. The cystic lesion was resected and revealed cysts consisting of inner, middle and outer layers. Which of the following is the best diagnosis?
- Cystic hepatocellular carcinoma
- Echinococcus granulosus cysts
- Hemorrhagic cysts
- Polycystic liver disease
Board review style answer #1
Board review style question #2
A 65 year old woman presented with fever, jaundice, weight loss and abdominal discomfort. She lives in the countryside with her 2 dogs. CT scan of liver revealed large cystic mass, suspected to represent an echinococcal cyst. Which of the following is the most likely microscopic feature?
- Cystic lesion with inner, middle and outer layers and protoscolices
- Ingested red blood cells
- Numerous cystic lesions similar to solitary cysts, covered by cuboidal epithelium
- Organisms with foamy cytoplasm and eccentric round nucleus
Board review style answer #2
A. Cystic lesion with inner, middle and outer layers and protoscolices
Comment Here
Reference: Echinococcal cyst
Comment Here
Reference: Echinococcal cyst
Entamoeba histolytica abscess
Table of Contents
Definition / general | Diagrams / tables | Radiology images | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Differential diagnosisDefinition / general
- Also called amebic abscess; more common than pyogenic abscess worldwide but not in US (Med Clin North Am 1989;73:847)
- Common in developing world (Exp Parasitol 2010;126:366)
- Usually fecal oral spread; may also be sexually transmitted (Clin Infect Dis 2009;49:346)
- Complication of 3 - 9% of amebiasis cases
- Trophozoite:
- Active stage that exists only in host and in fresh loose feces; 10 - 60 microns with small, single, round nucleus with distinctive karyosome
- Thick, beaded nuclear membrane
- Bubbly cytoplasm with ingested red blood cells
- Complications: bacterial superinfection, extension or perforation into other structures; death in < 1% of cases
- Diagnosis: serology is 90% sensitive
Treatment
- Metronidazole, surgery only if complications
Gross description
- Well circumscribed, firm cavities, usually right sided near liver dome
- Initially yellow, later odorless, orange brown, pasty, necrotic material resembles anchovy sauce
Microscopic (histologic) description
- Shaggy necrotic fibrinous zone, granulation tissue, no / rare neutrophils (not actually an "abscess"), peripheral trophozoites up to 60 microns with small eccentric nucleus and cytoplasmic vacuoles that may contain red blood cells
- Resemble histiocytes
- Adjacent liver has fibrosis, chronic inflammation and reactive hepatocytes
Cytology description
- Use saline wet mounts and stained material
- 50% positive if material obtained from periphery; very rarely positive if from center of cyst
Differential diagnosis
- Macrophages:
- Bean shaped nuclei, fine chromatin, delicate nuclear membrane, small nucleoli
Epithelioid hemangioendothelioma
Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Epithelioid hemangioendothelioma (EHE) is a malignant vascular tumor composed of epithelioid cells within a distinctive myxohyaline stroma
Essential features
- Rare malignant vascular neoplasm composed of epithelioid endothelial cells in a background of myxohyaline stroma
- Often presents as multifocal disease in the liver; may be confused for metastatic disease
- Most cases characterized by presence of WWTR1-CAMTA1 gene fusion, subset of cases characterized by YAP1-TFE3 fusion
ICD coding
- ICD-O: 9133/3 - epithelioid hemangioendothelioma, malignant
- ICD-11: 2B5Y & XH9GF8 - other specified malignant mesenchymal neoplasms; epithelioid hemangioendothelioma, NOS
Epidemiology
- Mostly affects middle aged adults (30 - 50 years); rare in children
- Incidence slightly F > M (Cancer 1999;85:562)
Sites
- Soft tissue, visceral organs (liver and lung), bone
- Often presents as multifocal disease in liver
- Some patients present with both liver and lung or spleen involvement
Etiology
- Sporadic
Clinical features
- Often discovered incidentally in the liver
- Most cases asymptomatic
- May present with abdominal discomfort, weight loss
- Rare cases may present with hemoperitoneum and may cause noncirrhotic portal hypertension
- Multifocal involvement of both left and right hepatic lobes seen in up to 87% of patients (Transplantation 2017;101:555)
- Extrahepatic disease seen in 37% of patients (Transplantation 2017;101:555)
Diagnosis
- Made on biopsy (preferable) or cytology specimen
Radiology description
- Radiological findings variable
- Ultrasound: hypoechoic nodules
- CT: hypodense nodules
- MRI: in 30% of cases, the nodules have targetoid appearance with low signal intensity on T1; high signal intensity on T2 called bright dark sign
- References: Case Rep Gastroenterol 2020;14:56, Case Rep Gastrointest Med 2019;2019:7530845
Prognostic factors
- Variable clinical course (ranges from stable / indolent disease to progressive with metastasis)
- Distant metastatic rate is 20 - 30%
- Better prognosis than angiosarcoma of the liver
- Histological features do not reliably predict outcome but increased cellularity and necrosis may be poor prognostic factors (Cancer 1999;85:562)
Case reports
- 25 year old man with multifocal EHE treated successfully with liver transplant (Clin Case Rep 2019;8:108)
- 30 year old man with Crohn's disease presenting with multifocal EHE (Case Rep Gastroenterol 2020;14:56)
- 33 and 62 year old men with metastatic hepatic EHE treated with doxorubicin & olaratumab (Ther Clin Risk Manag 2020;16:141)
- 65 year old woman with YAP1-TFE3 rearranged hepatic EHE (Case Rep Gastrointest Med 2019;2019:7530845)
- 74 year old man with solitary hepatic EHE treated with hepatic resection (Case Rep Gastroenterol 2018;12:402)
Treatment
- Solitary disease: resection (curative)
- Multifocal disease: observation, liver transplantation, chemotherapy
- References: Dig Liver Dis 2020;52:1039, Cancer 2006;107:2108
Gross description
- Can range in size from subcentimeter nodules to large, coalescing masses > 10 cm
- Cut surface is white and firm and can have infiltrative pattern with prominent myxohyaline or fibrous stroma
- Background liver appears normal
- References: Case Rep Gastroenterol 2020;14:56, Case Rep Gastroenterol 2018;12:402
Frozen section description
- Epithelioid, stellate and spindle cells with fine chromatin with occasional intracytoplasmic vacuoles in myxohyaline stroma
Microscopic (histologic) description
- EHE with WWTR1-CAMTA1 gene fusion
- Cords, nests, solid sheets and single cells with infiltrative growth pattern in myxohyaline / fibrous stroma with increased cellularity at tumor edge
- Invasion of sinusoids, portal and hepatic veins
- No vascular channel formation
- Cells can be epithelioid, stellate, spindle with fine chromatin
- Eosinophilic cytoplasm with occasional intracytoplasmic vacuoles ("blister cells")
- < 10% can have atypical histological features like nuclear pleomorphism, increased mitotic activity, solid sheet pattern and necrosis
- EHE with YAP1-TFE3 gene fusion (rare in liver)
- Well formed vascular channels and areas of solid growth
- Epithelioid cells with bright eosinophilic cytoplasm
- Lacks the characteristic stromal component seen in classic EHE
- References: Cancer 1982;50:970, Am J Surg Pathol 1997;21:363
Microscopic (histologic) images
Cytology description
- Round to polygonal plasmacytoid cells with minimal pleomorphism and few mitoses
- Frequent nuclear grooves and psuedoinclusions
- Dense cytoplasm with occasional intracytoplasmic lumina
- Hyaline stroma
- Reference: Am J Clin Pathol 2011;136:739
Positive stains
- Vascular markers: CD31, CD34 and ERG
- Keratins: especially CK8 and CK18
- WWTR1-CAMTA1 gene fusion tumors: positive for CAMTA1 (Am J Surg Pathol 2016;40:94)
- YAP1-TFE3 fusion tumors: nuclear expression of TFE3
- AE1 / AE3, CK7: usually negative, though a few cases can be positive (Ann Diagn Pathol 2020;49:151589
Negative stains
- EMA
- Desmin
- HepPar1
- Reference: Am J Surg Pathol 1997;21:363
Electron microscopy description
- Weibel-Palade bodies, prominent intracytoplasmic vacuoles, endothelial cells with elaborate intercellular contacts and desmosomes (Cancer 1982;50:970)
Electron microscopy images
Molecular / cytogenetics description
- Multifocal hepatic disease is monoclonal
- t(1;3)(p36.3;q25) WWTR1-CAMTA1 gene fusion is characteristic, found in up to 90% of cases
- Fusion of WWTR1 to CAMTA1 results in dysregulation of the Hippo pathway, driving oncogenic transformation
- YAP1-TFE3 fusion found in small subset of tumors
- Similar to WWTR1, YAP1 is a downstream transcriptional regulator of the Hippo pathway
- References: Sci Transl Med 2011;3:98ra82, Genes Chromosomes Cancer 2011;50:644, Genes Chromosomes Cancer 2013;52:775
Molecular / cytogenetics images
Videos
Laparoscopic segment 6 liver resection for hepatic EHE
Overview of vascular tumors of the skin (by Dr. Jerad Gardner)
Sample pathology report
- Liver, core biopsy:
- Epithelioid hemangioendothelioma (see comment)
- Comment: FISH testing for CAMTA1 / WWTR1 fusion is positive. IHC for CAMTA1 shows nuclear positivity.
Differential diagnosis
- Angiosarcoma:
- Angiosarcomas have greater atypia and more mitoses and tend to be hemorrhagic with destructive growth pattern
- No nuclear staining for CAMTA1
- Adenocarcinoma (including cholangiocarcinoma):
- Sclerotic hepatocellular carcinoma:
- Abundant fibrous stroma separating nests or trabeculae of tumor cells
- Positive for arginase1, CK7 and glypican 3
- Negative for vascular markers
- Epithelioid hemangioma:
- Most commonly cutaneous and soft tissue lesions in head and neck, followed by distal extremities and trunk; visceral organs rare with lung being the only reported organ
- Histology shows proliferation of well formed small blood vessels lined by plump and epithelioid endothelial cells with mild cytological atypia; no myxohyaline stroma seen as in epithelioid hemangioendothelioma
- Marked lymphoplasmacytic infiltrates, prominent lymphoid follicles and abundant eosinophils are present, a feature not seen in epithelioid hemangioendothelioma
- Tumor cells express endothelial markers CD31, ERG and CD34 and can be EMA and keratin positive
- FOSB can be positive
- Immunostain for CAMTA1 negative
- Anastomosing hemangioma:
- Anastomosing sinusoidal capillary sized vessels with scattered hobnail endothelial cells
- Mild cytologic atypia and no multilayering of cells seen
- Mitoses are absent or rare (Am J Surg Pathol 2013;37:1761)
- No myxohyaline stroma seen
- Frequent GNAQ and GNA14 activating hotspot mutation seen, similar to those described in hepatic small vessel neoplasm (Am J Surg Pathol 2018;42:1201)
- Immunostain for CAMTA1 negative
Additional references
Board review style question #1
A liver biopsy of a 45 year old woman with multiple liver lesions is shown. Regarding this entity, which of the following is true?
- AE1 / AE3, CK7 and CDX2 are usually positive
- Arginase1, glypican 3 and albumin ISH are usually positive
- CD31, ERG and CAMTA1 are usually positive
- GNAQ mutations are common
Board review style answer #1
C. CD31, ERG and CAMTA1 are usually positive. This photo shows a tumor with poorly vasoformative epithelioid and spindle shaped cells growing in small nests and cords. Other scattered single cells are seen in a background of myxohyaline stroma. These histologic findings as well as multifocal presentation are consistent with an epithelioid hemangioendothelioma. EHE is a low grade malignant vascular neoplasm that commonly occurs in younger patients (30 - 50 year old), has a slight female predominance and may arise in multiple areas in the body (soft tissue and visceral organs, liver, lung). Epithelioid hemangioendothelioma is usually defined by a WWTR1-CAMTA1 fusion (~ 90% of cases), with a subset defined by a YAP1-TFE3 fusion. Epithelioid hemangioendothelioma is negative for arginase1, glypican 3, albumin ISH, CK7 and CDX2. They are usually negative for AE1 / AE3. GNAQ mutations are seen in a vast majority of cases of anastomosing hemangioma but not EHE.
Comment Here
Reference: Epithelioid hemangioendothelioma
Comment Here
Reference: Epithelioid hemangioendothelioma
Board review style question #2
The presence of a WWTR1-CAMTA1 fusion transcript, resulting in t(1;3) translocation can be used as a molecular test to confirm diagnosis of which vascular tumor?
- Epithelioid angiosarcoma
- Epithelioid hemangioma
- Epithelioid hemangioendothelioma
- Pseudomyogenic hemangioendothelioma
Board review style answer #2
C. Epithelioid hemangioendothelioma. Epithelioid hemangioendothelioma are low grade malignant vascular neoplasms and may arise in multiple areas in the body (soft tissue and visceral organs, liver, lung). They usually have a WWTR1-CAMTA1 fusion (~ 90% of cases). The WWTR1-CAMTA1 translocation is present in EHE across all anatomical sites and fusion of WWTR1 to CAMTA1 results in dysregulation of the Hippo pathway, driving oncogenic transformation. A separate translocation YAP1-TFE3 has been identified in a subset of tumors and YAP1, similarly to WWTR1, is a downstream transcriptional regulator of Hippo pathway. Epithelioid hemangiomas are characterized by recurrent fusion genes involving FOS or FOSB in as many as half the cases. Psuedomyogenic hemangioendothelioma is caused by a balanced translocation t(7;19)(q22;q13) resulting of fusion of SERPINE1 to FOSB and ACTB-FOSB. No recurrent gene fusions have been described in angiosarcoma, though MYC amplification can be seen, primarily in the setting of irradiation or lymphedema associated angiosarcoma.
Comment Here
Reference: Epithelioid hemangioendothelioma
Comment Here
Reference: Epithelioid hemangioendothelioma
Epstein-Barr virus hepatitis
Table of Contents
Definition / general | Laboratory | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Differential diagnosis | Additional referencesDefinition / general
- Affects immunocompetent and immunocompromised
- Usually acute self limited disease resembling infectious mononucleosis; rarely causes hepatic failure and death in patients with immunodeficiency syndromes
Laboratory
- Elevated transaminase levels (80%), high EBV serum viral load; elevated bilirubin in only 7%
- In some cases, infiltrating CD8+ T cells but not hepatocytes, are infected with EBV (Hum Pathol 2001;32:757)
- May cause polymorphic B cell hyperplasia or lymphoma in immunocompromised
Microscopic (histologic) description
- Predominantly sinusoidal infiltrate of atypical T lymphocytes with minimal necrosis
- Presence of atypical lymphocytes may coincide with Downey cells in peripheral blood
- Associated with viral associated hemophagocytic syndrome, with prominent erythrophagocytosis by sinusoidal Kupffer cells and portal histiocytes
- Variable mitotic figures and small epithelioid granulomas
- No bile duct injury or venulitis
Microscopic (histologic) images
Differential diagnosis
- CMV
- Diphenylhydantoin drug reaction
- Hepatitis C
- Sinus histiocytosis with massive lymphadenopathy:
- Nodular, portal areas uninvolved
Additional references
Erythropoietic protoporphyria
Table of Contents
Definition / general | Diagrams / tables | Gross images | Microscopic (histologic) description | Electron microscopy descriptionDefinition / general
- Excess production of free protoporphyrin from the bone marrow, most commonly due to deficiency of the enzyme ferrochelatase; causes characteristic cutaneous photosensitivity and in a minority of patients leads to end stage liver disease necessitating liver transplantation (J Inherit Metab Dis 2011;34:539, World J Gastroenterol 2010;16:4526)
- Paracrystalin protoporphyrin deposition in hepatocytes and precipitation in the biliary canaliculi
- Prognosis depends on extent of liver disease (Orphanet J Rare Dis 2009;4:19)
Microscopic (histologic) description
- Deep brown colored bile in canaliculi, bile ducts and Kupffer cells with red Maltese cross under polarized light
Electron microscopy description
- Starburst crystalline array
Extrahepatic biliary atresia
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Biliary atresia or obliterative cholangiopathy is a multifactorial fibrosing and destructive disease that involves both extrahepatic and intrahepatic bile ducts
- Common cause of pathologic infant jaundice that presents in the initial few weeks of life
Essential features
- Clinically presents as cholestatic jaundice of infants with normal gestational age
- Radiologic evidence of absent or atretic gallbladder
- Obstructive pattern of injury featuring extensive bile ductular reaction, portal edema, mixed portal inflammation, bile plugs in ductules, portal fibrosis and lobular cholestasis
Terminology
- Extrahepatic biliary atresia
ICD coding
- ICD-10: Q44.2 - atresia of bile ducts
Epidemiology
- More frequently seen in Asian countries; incidence ranges from 1 in 5,000 - 10,000 (Taiwan and Japan) (J Autoimmun 2016;73:1)
- 1 in 15,000 - 20,000 in Europe and North America (J Pediatr 2017;187:253)
- Most are term infants with normal birth weight
Sites
- Both extra and intrahepatic bile ducts are affected
- Based on the level of injury, it is further divided into 3 types (Ann Surg 2011;254:577)
- Type 1 (~5% of cases)
- Atretic common bile duct
- Patent right and left hepatic ducts and common hepatic duct
- Gallbladder often has bile
- Type 2 (~2% of cases)
- Atresia within common hepatic duct
- Gallbladder is empty
- Type 3 (> 90% of cases)
- Atresia of porta hepatis area (proximal portions of extrahepatic biliary tract)
- Gallbladder atretic
- Type 1 (~5% of cases)
Pathophysiology
- Inflammatory destruction of extrahepatic biliary system in genetically susceptible individuals
Etiology
- Exact etiology is not known
- Suggested mechanisms include (Pediatr Transplant 2005;9:646)
- Genetic defects in morphogenesis and development
- Associated anomalies seen in 20% of cases
- Most common is polysplenia or asplenia (biliary atresia splenic malformation syndrome)
- Other associated malformations include absent inferior vena cava, cardiac anomalies, situs inversus, intestinal malrotation, duodenal atresia and anomaly of the portal vein
- Cystic biliary atresia
- Comprises 5 - 10% of patients and is identified on antenatal ultrasound in ~50% of cases
- Defective prenatal hepatic circulation
- Viral infections
- Cytomegalovirus (CMV)
- Rubella
- Rotavirus
- Intrauterine or perinatal toxin exposure
- Immunologic dysfunction
- Genetic defects in morphogenesis and development
Clinical features
- Persistent neonatal jaundice (Lancet 2009;374:1704)
- Dark urine, pale stools and failure to thrive
- Clinical phenotypes include
- Fetal / embryonal or prenatal form
- 10 - 35% of cases
- Symptoms start shortly after birth
- Associated with extrahepatic developmental anomalies
- Perinatal or acquired form
- 65 - 80% of cases
- Jaundiced after a few weeks of birth
- No associated congenital anomalies
- Fetal / embryonal or prenatal form
Diagnosis
- Ultrasound
- Hepatobiliary iminodiacetic acid (HIDA) scan (Trop Gastroenterol 2012;33:62)
- Percutaneous liver biopsy
- Shows histologic evidence of biliary obstruction
- Intraoperative cholangiography (Pediatr Surg Int 2006;22:140)
- Confirmatory procedure before surgical intervention
- Limited diagnostic role for endoscopic retrograde cholangiopancreatography
Laboratory
- Serum conjugated hyperbilirubinemia (J Pediatr Gastroenterol Nutr 2016;62:799)
- Elevated alkaline phosphatase
- Elevated ϒ glutamyl transferase (GGT)
Radiology description
- Absent or atretic gallbladder on ultrasound
- HIDA scan findings include good hepatic intake with reduced / failure to excrete into intestine
- Specificity of this finding is low as absent excretion can be seen in other pediatric cholestatic liver disease
- Reference: Trop Gastroenterol 2012;33:62
Prognostic factors
- With Kasai portoenterostomy (KPE), ~35% of patients with a native liver survive > 10 years (J Pediatr Gastroenterol Nutr 2019;69:416)
- Recurrent episodes of ascending cholangitis and sepsis in those who do not respond to Kasai portoenterostomy
- Progression to cirrhosis with portal hypertension and required orthotopic liver transplantation
- Patient survival after transplantation is ~85% at 10 years
Case reports
- 2 day old girl with biliary and duodenal atresia (Nucl Med Mol Imaging 2019;53:356)
- 2 month old girl with icterus and positive COVID-19 (Int J Surg Case Rep 2022;90:106705)
- 81 day old girl with cystic biliary atresia (BMC Pediatr 2018;18:158)
- 4 month old girl with jaundice, acholic stools and high colored urine since day 5 of life (Indian J Radiol Imaging 2021;31:689)
Treatment
- Kasai portoenterostomy
- Liver transplantation
Gross description
- Dark green and nodular explanted liver
Gross images
Microscopic (histologic) description
- Histologic findings vary in the course of disease
- Nonspecific findings in early biopsies
- Variable cholestasis
- Extramedullary hematopoiesis
- Little bile ductular proliferation
- Nonspecific findings in early biopsies
- Portal tracts (Am J Surg Pathol 2016;40:1601, Clin Gastroenterol Hepatol 2011;9:357)
- Portal edema
- Bile ductular proliferation
- Bile plugs / ductular cholestasis
- Mixed portal inflammation
- Prominent hepatic arteriole
- Portal and periportal fibrosis
- Progress to bridging and cirrhosis in later stages of disease
- Hepatic lobules
- Cholestasis
- Minimal inflammation
- With or without hepatocyte giant cell transformation
- With or without extramedullary hematopoiesis
- Hilar plate
- Fibrosis
- Small sized or obstructed bile ducts
- Variable periductal inflammation
Microscopic (histologic) images
Positive stains
- CK7, CK19: positive expression in bile ductular proliferation
- CD56 / NCAM: proliferating ductules in most cases of extrahepatic biliary atresia are positive
Molecular / cytogenetics description
- Mutations leading to laterality defects like CFIC and ZIC3 are identified in ~10% of biliary atresia patients (J Hepatobiliary Pancreat Sci 2013;20:459)
- JAG1 gene has also been associated with the pathogenesis of biliary atresia
Sample pathology report
- Liver, needle core biopsy:
- Bile ductular reaction with lobular cholestasis (see comment)
- Comment: Portal tracts expanded with edema, extensive bile ductular reaction and rare ductules with bile plugs. The lobules show cholestasis with minimal inflammation and rare hepatocyte giant cell transformation. The findings are compatible with biliary atresia. Other possibilities include large duct obstruction, total parenteral nutrition associated cholestasis and alpha-1 antitrypsin deficiency.
Differential diagnosis
- Choledochal cyst:
- Thick fibrous wall without much inflammation
- Minimal bile ductular reaction
- Imaging findings are helpful
- No area of atresia
- Normal appearing gallbladder
- Alpha-1 antitrypsin deficiency:
- Decreased serum alpha-1 antitrypsin level
- PASD positive cytoplasmic globules may not be seen in infants < 3 months old
- Total parenteral nutrition associated cholestasis:
- Clinical history of total parenteral nutrition
- Neonatal hepatitis:
- Notable giant cell transformation with mild cholestasis
- Focal or mild bile ductular reaction
- Alagille syndrome:
- Ductular reaction is typically absent but rare examples present with ductular reaction in early infancy
- Paucity of intrahepatic bile ducts
- Characteristic clinical manifestations of Alagille syndrome
- CMV infection:
- Presence of viral inclusions
- Serum PCR for CMV viremia
- Progressive familial intrahepatic cholestasis type 3 (PFIC3):
- Age at onset varies from infancy to 20 years
- Elevated gamma glutamyl transferase, unlike PFIC1 and PFIC2
- Histologic findings are similar to biliary atresia including expanded portal tracts with extensive bile ductular reaction
- Mutations in ABCB4 gene which codes for MDR3
Board review style question #1
A 6 week old term female infant presented with jaundice and dark urine. Liver function tests revealed conjugated hyperbilirubinemia and elevated gamma glutamyl transferase levels. No gallbladder was visualized on ultrasound abdomen examination. Liver biopsy image is shown above. What is the diagnosis?
- Biliary atresia
- Choledochal cyst
- Neonatal hepatitis
- Paucity of bile ducts
Board review style answer #1
A. Biliary atresia. The patient is presenting with jaundice, cholestatic pattern of liver function test, nonvisualization of gallbladder by imaging and biopsy finding of bile ductular reaction with bile plug. This is likely due to biliary atresia. Answer B is incorrect because in a choledochal cyst, usually the gallbladder appears normal by imaging. Bile ductular reaction in choledochal cysts is usually mild. Answer C is incorrect because of the absence of prominent giant cell transformation and bile ductular reaction is usually mild. Answer D is incorrect because ductular reaction is typically absent in paucity of bile ducts.
Comment Here
Reference: Extrahepatic biliary atresia
Comment Here
Reference: Extrahepatic biliary atresia
Board review style question #2
Which of the following therapies is offered first for infants diagnosed with biliary atresia?
- Kasai portoenterostomy
- Liver transplant
- Steroids
- Ursodeoxycholic acid
Board review style answer #2
A. Kasai portoenterostomy establishes bile flow in the majority of infants. Kasai portoenterostomy is not curative but establishes bile flow in the majority of infants and is an important bridge to liver transplantation. Answer B is incorrect because a liver transplant is not the first therapy option offered; it is done as an initial option in those not responsive or who fail Kasai portoenterostomy. Answer C is incorrect because medical management with steroids is not a standard treatment option for biliary atresia. Answer D is incorrect because medical management with ursodeoxycholic acid is not a standard treatment option for biliary atresia.
Comment Here
Reference: Extrahepatic biliary atresia
Comment Here
Reference: Extrahepatic biliary atresia
Extramedullary hematopoiesis
Table of Contents
Definition / general | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosisDefinition / general
- Usually discovered incidentally or associated with anemia
- Rarely presents as liver mass
- Only very few liver nodules of EMH have been described in the literature (Diagn Cytopathol 1997;16:51)
Case reports
- 52 year old woman with 2.5 cm, 5 cm and 7 cm liver masses and normal serum AFP (Arch Pathol Lab Med 2003;127:631)
Treatment
- Radiation or hydroxyurea if symptomatic
Microscopic (histologic) description
- Erythroid precursors in sinusoids (resemble lymphocytes), myeloid precursors in portal tracts (resemble mixed portal infiltrate or eosinophils in neonates)
- Also megakaryocytes within sinuses
Microscopic (histologic) images
Differential diagnosis
- Abscess / infections
- Lymphoproliferative disorder
- Prominent megakaryocytic component may suggest atypical or malignant diagnosis
Fasciola hepatica
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Parasitic infection of liver and biliary tract; parasitic flatworm included in the trematode group; infects hepatobiliary system of various mammals, including humans (Mahmud: Medical Parasitology, 1st Edition, 2017)
Essential features
- Presentation with tumor-like masses
- Tract shaped granulomas contain necrotic material in their lumens with increased eosinophils
- Numerous Charcot-Leyden crystals may be seen in necrosis
Terminology
- Liver fluke or sheep liver fluke
ICD coding
- ICD-10: B66.3 - fascioliasis
Epidemiology
- Human infections are distributed globally, mainly in sheep rearing countries
Sites
- Mostly liver, bile ducts and gallbladder
Pathophysiology
- Parasite penetrates liver capsule, migrates into bile ducts, to large bile ducts and gallbladder (Burt: MacSween's Pathology of the Liver, 7th Edition, 2017)
Etiology
- Transmitted to humans from watercress or other freshwater plants containing metacercariae (Mahmud: Medical Parasitology, 1st Edition, 2017, Burt: MacSween's Pathology of the Liver, 7th Edition, 2017)
Clinical features
- Presentation changes according to phase of illness
- Invasion phase: fever, hepatomegaly, upper abdominal pain, ascending bacterial cholangitis, obstructive jaundice, blood eosinophilia
- Biliary phase: hepatomegaly, right upper quadrant pain, fever and blood eosinophilia, biliary colic, epigastric pain, fatty food intolerance, nausea, jaundice and pruritus (Burt: MacSween's Pathology of the Liver, 7th Edition, 2017)
- Mass may present incidentally at radiologic imaging
- Rare signs / symptoms include acute pancreatitis and involvement of the pancreas or kidney; anaphylaxis has not been described (Turk J Gastroenterol 2010;21:183, BMC Gastroenterol 2004;4:15)
Diagnosis
- Demonstration of eggs in feces or aspirated bile (Mahmud: Medical Parasitology, 1st Edition, 2017)
- Histologically, the organism can be seen in the bile ducts in the mass removed due to the tumor (Turk Patoloji Derg 2019;35:58)
Laboratory
- Eosinophilia reaching 30% or more of the total white blood cell (WBC) count (Burt: MacSween's Pathology of the Liver, 7th Edition, 2017)
Radiology description
- Ultrasound: hepatic parenchymal heterogeneity, dilatation of the bile duct with wall thickening, peripheral hypoechoic nodular lesions (Clin Microbiol Infect 2005;11:859)
- CT / MRI: multiple, small, hypodense lesions 2 - 10 mm in diameter and microabscesses arranged in a tunnel-like branching pattern (tortuous tracts), with frequent subcapsular locations of the lesions
- In rare instances, abscess-like lesions 7 - 10 cm in diameter can be seen and may be mistakenly considered a tumor
- Liver capsular thickening and subcapsular hemorrhage can also be detected (Clin Imaging 2016;40:251)
Prognostic factors
- Capsular invasion can cause subcapsular hematomas
- Choledochal obstruction can cause cholangitis (Res Rep Trop Med 2020;11:149)
- Resection is mostly curative
Case reports
- 9 year old girl with liver abscess (APSP J Case Rep 2015;6:27)
- 26 and 52 year old women with fascioliasis cases mimicking liver tumors (Turk Patoloji Derg 2019;35:58)
- 48 year old woman with abdominal distension (Am J Trop Med Hyg 2013;89:1212)
- 48 year old woman with Fasciola hepatica mimicking sepsis without eosinophilia (Turkiye Parazitol Derg 2014;38:131)
- 63 year old man with Fasciola hepatica in FNA of a liver mass (Cytopathology 2015;26:259)
- 65 year old woman with right upper quadrant discomfort (J Radiol Case Rep 2010;4:13)
- 87 year old man with Fasciola hepatica infection mimicking cholangiocarcinoma (Korean J Parasitol 2014;52:193)
- 4 fascioliasis cases occurring in the same family (Korean J Parasitol 2017;55:55)
Treatment
- Triclabendazole is the treatment of choice; bithionol is an alternative drug (Mahmud: Medical Parasitology, 1st Edition, 2017)
Gross description
- Solitary or multiple solid to cystic nodules with necrosis that may resemble metastases
Microscopic (histologic) description
- Dilated intrahepatic bile ducts may contain adult flukes
- Tract shaped necrotic debris
- Eosinophils
- Charcot-Leyden crystals (Turk Patoloji Derg 2019;35:58)
- Eosinophilic granulomas: center of dense inflammatory cells composed predominantly of eosinophils with scattered Charcot-Leyden crystals surrounded by a palisade of granulomatous (histiocytic) response (Am J Surg Pathol 2001;25:1316)
- Histiocytes
- Rarely, eggs (Burt: MacSween's Pathology of the Liver, 7th Edition, 2017)
Microscopic (histologic) images
Cytology description
- Cohesive clusters of epithelioid histiocytes representing granulomas
- Eosinophils
- Charcot-Leyden crystals (Cytopathology 2015;26:259)
Videos
Fascioliasis caused by Fasciola hepatica
Sample pathology report
- Liver, right hepatectomy:
- Fascioliasis / massive necrosis (see comment)
- Comment: When clinical, histopathological and laboratory findings are evaluated together, the case can be accepted as fascioliasis. Clinicopathological correlation is recommended.
Differential diagnosis
- Any tumor:
- Necrosis can be seen but eosinophils and Charcot-Leyden crystals are typically absent
- Histologic identification of neoplastic cells
- Echinococcus granulosus:
- PASD / PAS positive acellular lamellar membrane and scolices
- Echinococcus alveolaris / multilocularis:
- Macroscopically seems more invasive, PASD / PAS positive membranes
- Can be invasive or metastatic
- Toxocara species:
- Similar clinical, radiologic and histologic findings
- Presence of pets in the history may be meaningful for Toxocara
- Antigen tests can differentiate
- Granulomatous infections, such as M. tuberculosis:
- Inflammation does not contain eosinophils
Board review style question #1
Which of the following findings of Fasciola hepatica is a common presenting symptom?
- Abdominal pain
- Acute pancreatitis
- Anaphylactic reaction
- Splenomegaly
Board review style answer #1
A. Abdominal pain and fever are common findings. Acute pancreatitis and other organ involvement are uncommon and anaphylaxis has not been described.
Comment Here
Reference: Fasciola hepatica
Comment Here
Reference: Fasciola hepatica
Board review style question #2
A 25 year old man presents with a liver mass, which is suspicious for malignancy on imaging. PET scan shows little uptake. There is no history of malignancy and the patient denies taking any medication. A trucut biopsy is done (shown above) and shows necrosis, which includes eosinophils and Charcot-Leyden crystals. There are a few hepatocytes in the biopsy, which show mostly reactive changes. What is the most likely diagnosis and appropriate next step?
- Drug reaction, recommend discontinuation of drugs
- Parasite, consistent with Fasciola hepatica
- Tumor, biopsy must be done again to see tumor cells
- Echinococcus granulosus
Board review style answer #2
B. Parasite, consistent with Fasciola hepatica. Charcot-Leyden crystals and eosinophils suggest Fasciola hepatica and not a drug reaction. No tumor cells are identified. There is no suggestion of an acellular lamellar membrane or scolices associated with Echinococcus.
Comment Here
Reference: Fasciola hepatica
Comment Here
Reference: Fasciola hepatica
Focal fatty change
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Steatosis is normally a diffuse process; however, a more localized form called focal fatty change (FFC) was first described in 1980 (Gastroenterology 1980;78:247)
Essential features
- Benign, asymptomatic and incidental finding in 10 - 20% of livers
- Uncommon in infants and young children
- Major clinical importance lies in its differentiation from other lipomatous liver lesions
Terminology
- Focal fatty change, focal steatosis, focal fatty infiltration
ICD coding
- ICD-10: K76.0 - fatty (change of) liver, not elsewhere classified
Epidemiology
- Incidental finding found in approximately 10 - 20% of livers
- Prevalence increases with advancing age:
- 0% for 1 month - 4 years
- 7.3% for 5 - 9 years
- 10.2% for 10 - 14 years
- 25.6% for 15 - 19 years (AJR Am J Roentgenol 2001;177:1035)
Sites
- Typical areas include the gallbladder fossa, subcapsular, left lobe medial segment near the fissure for the ligamentum teres, anterior to the porta hepatis and around the inferior vena cava
Pathophysiology
- May be caused by relative ischemia due to decreased portal venous blood flow or decreased delivery of substances via the portal vein
- Aberrant vascular supply to the liver other than the portal vein or hepatic artery
- Aberrant localized (endogenous or exogenous) insulin effects: injection or intraperitoneal administration of insulin in patients with peritoneal hemodialysis has led to unusual patterns of focal liver steatosis in the subcapsular region (AJR Am J Roentgenol 2003;180:1601)
Clinical features
- Causes no mass effect or symptoms
Diagnosis
- Contrast enhanced ultrasound (CEUS)
- Abdominal CT with or without contrast
- MRI with fat suppression
- Radionuclide liver scan (Clin Nucl Med 1986;11:503)
- Definitive diagnosis with biopsy can be established in clinically challenging cases where it is difficult to distinguish from metastatic disease
Laboratory
- Liver function tests are usually within normal limits
Radiology description
- Hypodense appearance on CT scan makes it difficult to differentiate fatty infiltration from metastatic disease, particularly when multiple lesions are present
- In focal fatty infiltration, the normal hepatic vessels traverse the area of decreased attenuation, a finding not usually present in malignancy
- Persistent isoenhancement on contrast enhanced ultrasound compared with liver parenchyma
- MRI with fat suppression is more sensitive than T1 and T2 weighted imaging for fatty infiltration, with fatty infiltration having decreased signal intensity compared with normal liver
- Decreased signal on opposed phase T1 weighted imaging
- Reference: Medicine (Baltimore) 2019;98:e15431
Case reports
- 30 year old man with a history of chronic hepatitis C (World J Radiol 2014;6:932)
- 49 year old woman with multifocal lesions of the liver, interpreted as angiomyolipomas (Ann Ital Chir 2003;74:217)
- 60 year old woman who had undergone subtotal gastrectomy for gastric cancer (Br J Radiol 1998;71:888)
Treatment
- Directed against underlying disorder
Gross description
- May be solitary or multifocal
- Well demarcated, unencapsulated nodule(s) with a yellow greasy cut surface
- Measures up to 4.0 cm
- Predominantly subcapsular in location
- Reference: Gastroenterology 1980;78:247
Gross images
Microscopic (histologic) description
- Well demarcated, unencapsulated areas of severe and typically, macrovesicular steatosis, surrounded by hepatic parenchyma that contains little or no steatosis
- Portal tracts and terminal hepatic veins are present throughout the lesion in a normal architectural pattern
- Adjacent nonsteatotic liver parenchyma may be congested without fibrosis or cirrhosis
- Reference: Gastroenterol Hepatol (N Y) 2007;3:199
Microscopic (histologic) images
Cytology description
- Aspirates are cellular with numerous benign hepatocytes in a background of blood
- Hepatocytes are isolated or organized in sheets
- Characterized by large, intracytoplasmic, clear vacuoles that displace nuclei to the periphery of the cells, sometimes flattening them against the cytoplasmic membrane
- Displaced nuclei by intracytoplasmic, clear vacuoles give these cells a signet ring appearance, resembling signet ring carcinoma
- Special stains:
- PASD stain will give negative results, confirming that intracytoplasmic vacuoles are not constituted of mucus
- Reference: Acta Cytol 2002;46:567
Positive stains
- Oil Red O
- Sudan Black B
- Reference: Cytojournal 2005;2:7
Negative stains
- PASD
- Mucicarmine
- Reference: Cytojournal 2005;2:7
Sample pathology report
- Liver lesion, needle biopsy specimen:
- Focal fatty change (see comment)
- Comment: Within some of the cores are areas of benign liver tissue that show relatively more extensive steatosis, portal tracts that are quite distant from each other and liver cell plates that are slightly thickened (reticulin stain). Based on the given information of a hypodense mass having been biopsied, these findings are consistent with focal fatty change (also known as focal steatosis).
Differential diagnosis
- HNF1α inactivated hepatocellular adenoma:
- Yellow / pale cut surface due to diffuse fatty change
- Markedly steatotic hepatocytes intermingled with clear hepatocytes
- Has other typical features of HCA: unpaired arteries, lack of portal tracts
- Negative LFABP is a surrogate marker for HNF1α inactivation
- Hepatocellular carcinoma, steatohepatitic variant:
- Most occur in background of cirrhosis
- Neoplastic hepatocytes in trabeculae of more than 3 cells thickness
- High nuclear to cytoplasmic ratio, mitoses, unpaired arteries, lack of portal tracts
- Trabecular pattern or pseudoglandular architecture is typically seen
- Angiomyolipoma:
- Focal nodular hyperplasia:
- Nodular but lacks the lipomatous component
- Unencapsulated, well circumscribed lesion with central stellate scar
- Fibrous septa contain thick walled arteries with peripheral ductular reaction but no true bile ducts
- Myelolipoma:
- Variable proportion of hematopoietic precursor cells scattered throughout mature fat
- Lipoma:
Additional references
Board review style question #1
Which of the following liver lesions contains portal tracts and central veins throughout the lesion?
- Focal fatty change
- Focal nodular hyperplasia
- Hepatocellular carcinoma
- HNF1α inactivated hepatocellular adenoma
- Lipoma
Board review style answer #1
Board review style question #2
A 60 year old woman with poorly controlled diabetes mellitus and remote history of gastric cancer was found to have multifocal hypodense lesions in the liver, detected incidentally on an abdominal CT scan. A representative core needle biopsy of the lesion is shown above. What is your diagnosis?
- Focal fatty change
- Focal nodular hyperplasia
- Hepatocellular carcinoma
- Lipoma
- Metastatic gastric adenocarcinoma
Board review style answer #2
Focal nodular hyperplasia
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Common, benign, nonneoplastic mass forming lesion of the liver
- Widely accepted to be a hyperplastic and regenerative response of hepatocytes to local vascular abnormalities (Visc Med 2020;36:292)
Essential features
- Benign, nonneoplastic hepatocellular mass lesion predominantly affecting women
- Majority are solitary and have a central scar on imaging and gross examination
- Classic histologic features include fibrous septa, nodules of hepatocytes, abnormal thick walled vessels, bile ductular reaction and chronic inflammation
- Glutamine synthetase demonstrates characteristic map-like staining by immunohistochemistry
Terminology
- Focal nodular hyperplasia (FNH)
- Has also been known as focal cirrhosis, pedunculated adenoma, solitary hyperplastic nodule, mixed adenoma, hamartoma and hamartomatous cholangiohepatoma (Autops Case Rep 2014;4:5)
ICD coding
- ICD-10: K76.89 - other specified diseases of liver
Epidemiology
- Second most common benign liver tumor, with the incidence being between 0.3 and 3%
- Female predominance (F:M = 9:1)
- Most commonly occurs in adults between 30 and 40 years of age but has also been reported in children and older adults
- Reference: Visc Med 2020;36:292
Pathophysiology
- Not fully understood but accepted as a hyperplastic and regenerative response of hepatocytes due to abnormal perfusion by local vascular malformations (Autops Case Rep 2014;4:5, Visc Med 2020;36:292)
Etiology
- Local vascular malformations that have been associated with FNH include hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu disease), Budd-Chiari syndrome and hepatic hemangiomas (Visc Med 2020;36:292, Autops Case Rep 2014;4:5)
- Increased estrogen (oral contraceptive use and pregnancy) is not required for lesion development (Autops Case Rep 2014;4:5)
Clinical features
- Patients are typically asymptomatic and many lesions are diagnosed incidentally on imaging or at autopsy (Visc Med 2020;36:292, Autops Case Rep 2014;4:5)
- Patients with large lesions can experience vague symptoms, including abdominal discomfort or pain (Visc Med 2020;36:292)
- Enlargement of the lesion can occur with oral contraceptive use and pregnancy (Visc Med 2020;36:292, Autops Case Rep 2014;4:5)
Diagnosis
- Diagnosis is typically made on imaging
- Biopsy may be needed to rule out malignancy with noncharacteristic imaging
Laboratory
- Patients may have mild elevations in liver transaminases along with alkaline phosphatase and gamma glutamyl transpeptidase (GGT) but these are not diagnostic (Visc Med 2020;36:292, Autops Case Rep 2014;4:5)
Radiology description
- Solitary, well circumscribed, unencapsulated and lobulated mass (Radiographics 2022;42:1043)
- Has variable echogenicity on ultrasound, so computed tomography (CT) and magnetic resonance imaging (MRI) may be preferred (Cureus 2020;12:e6813)
- Color and power Doppler ultrasound improve visualization by demonstrating the central feeding artery and characteristic spoke wheel pattern of branching vessels in the radiating septa (Radiographics 2022;42:1043)
Prognostic factors
- Overall excellent prognosis
- No evidence for malignant transformation (Visc Med 2020;36:292)
- Rupture, bleeding or necrosis is rare (Visc Med 2020;36:292)
- Larger and more symptomatic lesions have been observed among patients taking oral contraceptives (Autops Case Rep 2014;4:5)
Case reports
- 3 year old girl with a right sided abdominal mass (Proc (Bayl Univ Med Cent) 2018;31:97)
- 30 year old man with liver lesion concerning for hepatocellular carcinoma (Diagnostics (Basel) 2021;12:44)
- 33 year old woman with a liver lesion within an accessory lobe (Medicine (Baltimore) 2020;99:e21357)
- 43 year old man with acute abdominal pain due to hepatic tumor rupture (Front Oncol 2022;12:873338)
- 44 year old woman using oral contraceptives with liver mass (Am J Case Rep 2019;20:1124)
- 89 year old man with past medical history of kidney cancer and growing liver lesion (Clin J Gastroenterol 2020;13:413)
Treatment
- If a definitive diagnosis of FNH is made through imaging or biopsy, no long term follow up is necessary
- Patients can be reimaged after 6 months to confirm stability of the lesion
- Surgery should be reserved for symptomatic patients or highly suspicious lesions where malignancy cannot be excluded
- Transcatheter arterial embolization (TAE) has been successful in patients with large FNH where surgery would be high risk
- Reference: Visc Med 2020;36:292
Gross description
- Well defined, nonencapsulated, lobulated and firm lesion, slightly lighter in color than the surrounding parenchyma (Visc Med 2020;36:292)
- Most commonly a solitary lesion (~66% of cases) (Liver Int 2009;29:459, Clin Liver Dis (Hoboken) 2021;17:244)
- Characteristic central, stellate fibrovascular zone (also described as a central scar, fibrous scar or scar-like fibrosis), which occurs in up to ~60% of lesions (Autops Case Rep 2014;4:5, Clin Liver Dis (Hoboken) 2021;17:244)
- Lesions typically measure between 4 and 8 cm but can measure up to 20 cm in greatest dimension (Autops Case Rep 2014;4:5)
- Can be associated with other lesions, including hemangiomas and hepatocellular adenomas (Visc Med 2020;36:292)
- Pedunculated forms are very rare (J Clin Med 2023;12:6034)
Gross images
Frozen section description
- Occasionally seen during frozen sections for transplant evaluation, often as a small subcapsular nodule
- It is important to distinguish the presence of FNH from cirrhosis in these cases since the fibrous bands surrounding benign hepatocytes will be focal and not diffuse
- Reference: UPMC: Donor Allograft Frozen Sections [Accessed 24 January 2024]
Frozen section images
Microscopic (histologic) description
- Classically described as focal cirrhosis since FNH has fibrous bands separating the liver into nodules but is only focal, limited to the mass lesion and not diffuse (Visc Med 2020;36:292)
- Nodules of hepatocytes are formed by fibrous septa, which may coalesce into a central scar that characteristically contains abnormally thick walled vessels, which may demonstrate fibromuscular hyperplasia, myxomatous change or myointimal hyperplasia (Visc Med 2020;36:292, Autops Case Rep 2014;4:5)
- Fibrous septa also contain a bile ductular reaction and an inflammatory cell infiltrate (Visc Med 2020;36:292, Autops Case Rep 2014;4:5)
- Features of cholestasis, including feathery degeneration of hepatocytes and Mallory-Denk bodies, may be present
- Hepatocytes are cytologically bland and are arranged in plates 1 - 2 cells thick (Autops Case Rep 2014;4:5)
- Clues to the diagnosis on biopsy material include proliferating ductules at the junction of the fibrous bands and hepatocellular nodules, fibrous septa (thick or thin bands), large abnormal arteries and cholate stasis (Hum Pathol 2005;36:1210)
Microscopic (histologic) images
Cytology description
- Bland appearing hepatocytes, arranged as single cells to trabeculae of 2 - 3 cells thick
- Bile duct epithelium of cuboidal to columnar cells with nuclear palisading can be present
- Stromal elements may also be present
- It is important that only the lesion (and not the surrounding parenchyma) is sampled in order to make an accurate diagnosis
- Reference: World J Surg Oncol 2004;2:5
Positive stains
- Glutamine synthetase: strong, patchy, map-like pattern is highly specific (J Clin Med 2023;12:6034, Histopathology 2021;79:791, Liver Int 2009;29:459)
- Trichrome: fibrous bands surrounding nodules of hepatocytes (World J Hepatol 2014;6:580, Hum Pathol 2005;36:1210)
- CK7 and CK19: positive in the ductular reaction
- CK7 will also highlight periportal cholestatic hepatocytes (Hum Pathol 2005;36:1210)
- HepPar1 and arginase1: benign hepatocyte nodules (Lab Invest 2008;88:78, Am J Surg Pathol 2010;34:1147)
- Reticulin: retained framework without loss or thickened cell plates (Visc Med 2020;36:292)
- CD34: vascular structures and spaces, expression decreases further away from the septa (Hum Pathol 2005;36:1210)
Molecular / cytogenetics description
- Increased expression levels of ANGPT1 and ANGPT2 mRNA, which are associated with angiogenesis (Clin Mol Hepatol 2016;22:199)
- Beta catenin pathway is activated, including the downstream target, glutamine synthetase; however, no mutations in beta catenin have been described (Insights Imaging 2015;6:347)
Sample pathology report
- Liver, lesion, wedge resection:
- Focal nodular hyperplasia (see comment)
- Comment: This liver specimen shows a benign hepatocellular lesion with fibrous septa containing thick walled vessels, bile ductular reaction and mild chronic inflammation. CK7 highlights a ductular reaction in the fibrous bands. Glutamine synthetase demonstrates map-like staining. Beta catenin shows membranous staining without abnormal nuclear expression. The morphology and immunoprofile are compatible with a diagnosis of focal nodular hyperplasia.
Differential diagnosis
- Hepatocellular adenoma (Hepatology 2006;43:515, Ann Diagn Pathol 2019;38:126, Clin Liver Dis (Hoboken) 2021;17:244):
- Benign hepatocellular neoplasm
- Occurs in women of childbearing age
- Associated with oral contraceptive use
- By definition, occurs in noncirrhotic liver
- May progress to malignancy, unlike FNH, depending on subtype
- Histologically does not contain portal structures, is composed of benign hepatocytes with cell plates of normal thickness and has so called naked arteries scattered throughout the tumor
- Glutamine synthetase will not show the characteristic map-like positivity
- Fibrolamellar hepatocellular carcinoma (Surg Pathol Clin 2018;11:377):
- Malignant hepatocellular neoplasm with distinct clinicopathologic features
- Occurs in young people with no background liver disease
- Similar to FNH, fibrolamellar hepatocellular carcinoma may have a central scar on imaging and gross examination
- Histologically, fibrolamellar hepatocellular carcinoma is composed of nests or trabeculae of large oncocytic cells with abundant cytoplasm and nuclei with open chromatin and prominent nucleoli set within a collagenous background arranged in parallel bands
- CK7 and CD68 positive
- Glutamine synthetase will not show the characteristic map-like positivity
- Lastly, fibrolamellar hepatocellular carcinoma demonstrates a consistent DNAJB1::PRKACA fusion in 95% of cases, which is not seen in FNH
- Focal nodular hyperplasia-like (FNH-like) nodules (Comp Hepatol 2003;2:7, Radiol Clin North Am 2022;60:795, J Hepatol 2008;49:61, Hum Pathol 2023;142:20):
- FNH-like lesions or nodules have the histologic features of FNH but occur in the cirrhotic liver or in association with other diseases particularly Budd-Chiari syndrome
- FNH does not occur in the cirrhotic liver
- FNH-like changes next to another mass lesion (HPB (Oxford) 2002;4:135, Lamps: Diagnostic Pathology - Hepatobiliary and Pancreas, 2nd Edition, 2017):
- Can see fibrosis, ductular reaction, inflammation or cholestasis next to any mass lesion including malignancy
- Typically changes are focal, involving portion(s) of biopsy core(s)
- Glutamine synthetase staining is not map-like
- Hepatic hemangioma (Visc Med 2020;36:292):
- Most common benign liver tumor with an incidence up to 20%
- Occurs more commonly in women
- Typically, an incidental finding on imaging studies
- Most commonly solitary
- Composed entirely of vascular channels and may be of cavernous (most common), capillary or anastomosing types
- Lacks the bile ductular reaction, inflammation and hepatocyte nodules seen in FNH
- Will be most problematic on small biopsies that only sample the central scar of FNH; look carefully for the bile ductular reaction, inflammatory infiltrate and hepatocyte nodules
- Cirrhosis (Med Clin North Am 2022;106:437):
- Diffuse process that causes hepatic fibrosis leading to the formation of fibrous bands that separate the liver into nodules
- Histologic evidence or clinical history of liver disease
- No abnormal thick walled vessels and is not a focal lesion
- Glutamine synthetase will not show characteristic map-like positivity; however, be aware that inflammatory type hepatocellular adenomas can show a pseudo map-like pattern (about 10 - 15% of cases), which is challenging to interpret and a potential diagnostic pitfall
- Attention to morphology and serum amyloid A immunohistochemistry (which should be positive in adenoma and not in FNH) can help favor one over the other in such cases
- Some lesions may be indeterminate and a multidisciplinary approach may be needed to determine treatment strategy (Mod Pathol 2014;27:62)
Additional references
Board review style question #1
Board review style answer #1
D. Vascular malformations. The liver tumor shown in the picture depicts focal nodular hyperplasia (FNH). While the pathogenesis is unknown, it is generally accepted to be a hyperplastic reaction due to a vascular malformation, which makes answer D correct. Answers A and B are incorrect because there is no link between alcohol or hepatitis C and FNH, even though they can be tied to multiple other liver lesions. Answer C is incorrect because estrogen (typically through oral contraceptives or pregnancy) is not necessary for the development of FNH but has been found to influence the growth of the lesion.
Comment Here
Reference: Focal nodular hyperplasia
Comment Here
Reference: Focal nodular hyperplasia
Board review style question #2
Which of the following findings would be most diagnostic of focal nodular hyperplasia (FNH)?
- Arginase positivity
- CK7 positivity
- Glutamate synthetase strong map-like positivity
- Mutated beta catenin
Board review style answer #2
C. Glutamate synthetase strong map-like positivity. Strong map-like positivity of glutamate synthetase is highly specific for FNH. Answer A is incorrect because arginase positivity in FNH is not specific due to generally staining hepatocytes. Answer B is incorrect because the ductular reaction would be highlighted by CK7 but this is also not specific to FNH. Answer D is incorrect because beta catenin is only activated in FNH, not mutated.
Comment Here
Reference: Focal nodular hyperplasia
Comment Here
Reference: Focal nodular hyperplasia
Foregut cyst
Table of Contents
Definition / general | Case reports | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Additional referencesDefinition / general
- Rare, < 100 cases reported
- Intrahepatic ileal and duodenal duplications and ciliated foregut cysts have been described
- 4 cm or smaller, have smooth muscle bundles in cyst wall
- Slightly more common in men and in medial segment of left hepatic lobe
- Resemble bronchiolar epithelium
Case reports
- 51 year old man with ciliated foregut cyst with squamous cell carcinoma (Arch Pathol Lab Med 1999;123:1115)
Gross description
- Solitary, rarely multilocular, 1 - 4 cm
Microscopic (histologic) description
- Ciliated pseudostratified columnar epithelium with goblet cells, subepithelial connective tissue, 1 - 3 smooth muscle layers, outer fibrous capsule
Additional references
Forms of hepatic injury
Table of Contents
Definition / general | Acidophil body | Ballooning (feathery) degeneration | Bile ductules | Bridging necrosis | Centrilobular necrosis | Giant cell transformation | Glycogen nuclei | Interface hepatitis | Interlobular bile duct | Mallory hyaline | Macrovesicular steatosis | Microvesicular steatosis | Passive congestion | Submassive necrosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- This broad topic highlights the pathophysiology, microscopic findings and associated hepatic diseases with commonly encountered structural changes, patterns of cell damage and necrosis, intracellular hepatic changes and common patterns of biliary reaction to injury in hepatology
Acidophil body
- Active form of programmed cell death, resulting in hepatocyte shrinkage, nuclear chromatin condensation (pyknosis) and fragmentation (karyorrhexis)
- Also called Councilman body, single cell death, apoptotic body
- Councilman bodies are essentially synonymous with acidophil bodies and were described as hepatocyte necrosis in the pathology of yellow fever; some pathologists prefer to restrict this term to the context of yellow fever
- Pathophysiologically and biochemically, cells undergoing apoptosis exhibit externalization of phosphatidylserine on the outer leaflet of plasma membrane, increased mitochondrial membrane permeability and release of proteins from the intermembrane space with activation of caspases and endonucleases, resulting in cleavage of structural proteins and DNA
- Usually a nonspecific finding to describe a dead hepatocyte, most commonly seen in major inflammatory hepatic diseases: viral hepatitis, autoimmune hepatitis, alcoholic and nonalcoholic steatohepatitis, drug induced liver injury and low grade / transient ischemia
- Microscopically identified as smaller, shrunken, more eosinophilic round body generally lacking a nucleus or with a small shriveled nucleus, with or without accompanying inflammation
- Spotty necrosis is used to describe necrosis of minute clusters of hepatocytes with scattered acidophil bodies, usually in association with lymphocytic inflammation
- Focal necrosis refers to necrosis involving larger groups of hepatocytes within a lobule, usually associated with scattered acidophil bodies
- References: Liver Int 2004;24:85, Hepatology 2004;39:273, Histopathology 1983;7:195
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Ballooning (feathery) degeneration
- Term used to describe swelling and rounding up of injured hepatocytes in the setting of marked hepatitis or cholestasis; considered a sign of progression to hepatocyte apoptosis and cell death
- Also called feathery degeneration in the setting of chronic cholestasis
- Pathophysiologically, ballooning is a result of severe cell injury, depletion of adenosine triphosphate (ATP) and rise in intracellular calcium, leading to loss of plasma membrane volume control and disruption of the hepatocyte intermediate filament network
- Commonly seen in alcoholic and nonalcoholic steatohepatitis and cholestatic liver disease but can also be seen in viral hepatitis and certain drug induced liver injury
- Grossly, liver may be transformed into swollen and turgid organ, exhibiting pallor
- Microscopically:
- Can be identified at low power as hepatocytes 2 - 3 times the size of normal adjacent hepatocytes
- Ballooned cells lose their usual polygonal shape and become rounded with watery edematous wispy rarified cytoplasm that is less eosinophilic than the neighboring cells with vacuolization and lacking fat accumulation
- These cells demonstrate clumping of intermediate filaments, characterized as strands of eosinophilic, ropey cytoplasmic material (see Mallory hyaline below)
- Feathery degeneration specifically refers to pale, swollen, injured hepatocytes in a periportal or periseptal (edge of cirrhotic nodule) distribution in livers with chronic cholestasis due to retention of bile salts
- Cholate stasis is synonymous with feathery degeneration
- Negative immunohistochemical stains: absent or decreased cytoplasmic immunostaining for intermediate filament by cytokeratin 8 and cytokeratin 18
- Reference: J Hepatol 2008;48:821
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Bile ductules
- Bile ductules are small epithelial tubular structures at the periphery of the portal tracts, lined by 4 to 5 small cuboidal cholangiocytes and usually traversing the portal tract mesenchyme between terminal bile ducts and canals of Hering
- Also referred to as cholangioles
- Cells of origin for bile ductules are postulated to be hepatic progenitor stem cells and metaplastic hepatocytes
- Microscopically, bile ductules are distinctly different from bile ducts, which are tubular structures located in the central region of the portal tract, usually accompanied by a similarly sized hepatic artery
- Bile ductular proliferation is the proliferation of small bile ductules at the periphery of the portal tract and can represent biliary obstruction when accompanied by neutrophils and portal edema or a pattern of liver injury (as ductules are a source of liver progenitor cells)
- Bile ductular reaction is used when the proliferating bile ductules are accompanied by neutrophils present in the stroma adjacent to the ductules (though many pathologists consider ductular proliferation and ductular reaction synonymous)
- Bile ductular reaction can be associated with biliary obstruction (type I), active hepatitis (type II) and massive liver necrosis (type III)
- Positive immunohistochemical stains: cytokeratin 7, cytokeratin 19
- References: Hepatology 2019;69:420, Semin Diagn Pathol 1998;15:259, Virchows Arch 2011;458:271, Mod Pathol 2004;17:874, Histopathology 2010;56:415
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Bridging necrosis
- Necrosis is the predominant mode of death with onset of irreversible injury, in states of extreme ATP depletion (as during ischemia or hypoxic cell injury), toxic injury (as from acetaminophen) and oxidative stress with reactive oxygen species formation
- Pathophysiologically, necrosis is accompanied by extensive damage to all cellular membranes, swelling of lysosomes, vacuolization of mitochondria and extensive catabolism of cellular membranes, proteins, ATP and nucleic acid, with karyolysis and release of cellular contents
- Necrosis is a common denominator in acute and chronic liver diseases and it is usually followed by progressive fibrosis, with persistence of the underlying cause
- Multiple commonly identified patterns of necrosis: apoptosis / acidophil body (individual cell necrosis), spotty and focal necrosis, zonal necrosis, bridging necrosis, piecemeal necrosis (interface hepatitis), confluent necrosis (submassive and massive necrosis)
- Although the patterns of necrosis are not entirely specific, they can be important clues towards determining or confirming the underlying cause and severity of liver disease
- Bridging necrosis refers to septa of confluent necrosis (large area of hepatocyte necrosis with inflammation) bridging adjacent central veins of hepatic lobules and portal triads
- 3 main types: central - central (linking perivenular areas), central - portal (linking terminal hepatic venules to portal tracts) and portal - portal (linking portal tracts)
- Usually associated with severe acute viral hepatitis, autoimmune hepatitis, drug induced hepatitis (acetaminophen toxicity) or other toxin exposure
- Portal - portal bridging necrosis is common in conditions in which portal tracts are widened (e.g. chronic hepatitis or biliary tract disease)
- Central - central bridging necrosis is seen in parenchymal hypoperfusion and venous outflow obstruction
- Central - portal bridging necrosis is a fairly common feature of viral acute hepatitis and also seen in exacerbations of chronic hepatitis
- Connective tissue stains like Masson trichrome, elastin and reticulin are helpful in differentiating between bridging necrosis and bridging fibrosis; elastin fibers are found only in established septa but not in areas of recent parenchymal collapse and necrosis; trichrome stain shows some dull blue staining in the necrotic zones, representative of collapsing residual parenchymal framework; reticulin stain shows compression of the parenchymal framework in the necrotic zones
- References: Am J Dig Dis 1978;23:1076, N Engl J Med 1970;283:1063, Clin Liver Dis (Hoboken) 2017;10:53, Acad Forensic Pathol 2018;8:256
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Centrilobular necrosis
- Refers to a distribution of necrosis within the centrilobular tissue of the hepatic lobule around the central vein (acinar zone 3), most prone to ischemia and metabolic toxin injury
- Centrilobular zone (acinar zone 3) is especially vulnerable to ischemic injury due to anatomic location at the distal end of afferent blood flow
- Microscopically shows ischemic necrosis characterized by coagulative hepatocyte necrosis, pyknotic or karyorrhectic nuclei, sharply demarcated with apoptotic bodies at the interface of healthy and necrotic hepatocytes; sinusoidal dilation and congestion can be prominent if a component of right sided heart failure is present
- Usually associated with ischemia, drugs, venous outflow impairment, preservation / reperfusion injury, alcoholic hepatitis
- Another important cause is ischemia and static liver injury associated with circulatory failure or shock, severe venous outflow impairment, commonly seen at autopsy
- Needs to be distinguished from coagulative necrosis, where hepatocyte necrosis is away from the central vein
- Reference: Clin Liver Dis 2017;21:89, J Gastroenterol Hepatol 1993;8:530
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Giant cell transformation
- Defined as the coalescence of hepatocytes with 3 or more nuclei, with or without free floating canalicular or intracellular pigmented inclusions
- Can be nonspecific or a part of various neonatal and adult conditions
- Pathophysiologically, in adults it is thought to be due to the detergent action of retained bile salts, leading to dissolution of plasma membranes and coalescence of adjacent hepatocytes
- Seen as a part of adult giant cell hepatitis, also referred to as postinfantile giant cell hepatitis or syncytial giant cell hepatitis
- Commonly caused by a viral infectious etiology, like HHV6A, CMV, HEV and EBV; can be seen in autoimmune hepatitis, drugs, chronic cholestatic conditions, including primary biliary cholangitis, hepatitis C
- In neonates, it is postulated that giant cells result from mitotic inhibition of the growing liver by an injurious agent
- Seen in neonatal giant cell hepatitis and associated with neonatal cholestatic syndromes, alpha-1 antitrypsin deficiency, Niemann-Pick disease type C, bile salt export pump (BSEP) deficiency
- References: Ann Hepatol 2009;8:68, Hepat Res Treat 2013;2013:601290, J Clin Exp Hepatol 2016;6:244, Am J Surg Pathol 2010;34:1498
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Glycogen nuclei
- Glycogenated nuclei are clear vacuoles that typically fill up most of the nuclei, leaving only a small rim of chromatin at the nuclear edges
- Found anywhere in the lobule but more common in zone 1 periportal hepatocytes
- Usually tend to cluster in small discrete patches but can be seen as single scattered hepatocytes
- Pathophysiologically the significance is unclear; some studies suggest they are indicative of hepatocyte senescence
- Commonly seen in diabetes, steatosis, pediatric liver disease, Wilson disease, some drugs, glycogenic hepatopathy
- References: World J Diabetes 2015;6:321, J Clin Pathol 2012;65:557
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Interface hepatitis
- Defined as damage and progressive loss of hepatocytes at the interface of the lobular parenchyma and connective tissue / stroma of the portal zone, accompanied by a variable degree of inflammation and fibrosis
- Inflammatory infiltrate is composed mainly of lymphocytes, with or without plasma cells and can be accompanied by fibrosis of the affected areas with new formation of collagen and other extracellular matrix components
- Progressive interface hepatitis usually results in more severe fibrosis
- Also called as piecemeal necrosis, periportal hepatitis, interface activity, periportal activity
- Sometimes also referred to as classical or lymphocytic piecemeal necrosis in order to distinguish it from biliary, ductular and fibrotic piecemeal necrosis, which are found in chronic biliary tract disease
- Pathophysiologically, when liver injury occurs at the interface involving destruction of hepatocytes with an influx of inflammatory cells, the limiting plate (row of hepatocytes surround the portal tract) is compromised or destroyed, leading to proliferation of the canals of Hering and ductular compartment, giving rise to ductular reaction
- Formerly the defining feature of chronic active hepatitis due to viral causes; however, can be seen in acute and chronic hepatitis from other causes including autoimmune hepatitis
- Spillover is a term used for presence of an inflammatory infiltrate at the interface that does not damage the limiting plate
- References: Liver Transpl 2008;14:946, Exp Mol Pathol 2001;71:137
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Interlobular bile duct
- Also called interlobular ductule
- Carries bile produced by hepatocytes which travels through an intralobular network of bile canaliculi, draining into the canal of Hering and then into bile ductules
- Usually a part of the interlobular portal triad, microscopically localized by looking for the larger portal tracts; however, they are inconsistently sampled in needle biopsy specimens
- Cells of the ducts are cuboidal epithelium, resting on a basement membrane, with increasing amount of connective tissue
- Common degenerative changes include cytoplasmic vacuolization, eosinophilic change, nuclear pleomorphism and hyperchromasia
- Biliary epithelial swelling and atrophy, disordered nuclear polarity and sloughing can be seen in both inflammatory and neoplastic conditions
- Nuclear pyknosis, apoptosis, fading and uneven spacing usually anticipate duct loss and are seen in injured ducts as variably distorted ducts with irregularly shaped lumens
- Injury of the bile ducts is commonly seen with bile duct obstruction, chronic biliary disease or as a nonspecific reaction in any chronic liver disease
- Reference: Kaplowitz: Drug-Induced Liver Disease, 1st Edition, 2002
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Mallory hyaline
- Misfolded, aggregated and clumped intracellular cytoskeletal filaments due to alterations in the hepatocellular cytokeratin assembly, usually seen in ballooned hepatocytes and an indication of cellular injury
- Also referred to as Mallory-Denk body, alcoholic hyaline, intracytoplasmic hyaline
- Pathophysiologically, Mallory hyaline is formed due to the aberrant crosslinking, increased phosphorylation, partial proteolytic degradation and inadequate functioning of the normal ubiquitination of cytoskeletal proteins
- Commonly accumulate in alcoholic and nonalcoholic steatohepatitis, Wilson disease, cholestatic conditions (e.g. primary biliary cholangitis), following exposure to certain drugs like amiodarone, focal nodular hyperplasia and hepatocellular carcinoma
- On light microscopy, seen as irregular aggregates of clumped or ropy amorphous dense eosinophilic material in the cytoplasm most commonly in ballooned hepatocytes, sometimes forming a ring around the nucleus or surrounded by neutrophils
- Positive immunohistochemical and special stains: cytokeratin 8 / 18, ubiquitin, p62, stain blue with chromotrope aniline blue (CAB) special stain
- References: Med Mol Morphol 2010;43:13, Exp Cell Res 2007;313:2033, Hepatology 2007;46:851, J Pathol 1988;155:9, Virchows Arch 1998;432:143
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Macrovesicular steatosis
- Lipid filled hepatocytes with large fat droplets
- Radiographic modalities, including ultrasonography, magnetic resonance spectroscopy and magnetic resonance imaging, can detect fat in liver with high sensitivity and specificity; increased echogenicity of the liver, blurring of vascular margins and increased acoustic attenuation are features seen on ultrasound
- On gross examination, liver has a pale yellow appearance with greasy consistency; the color is due to retained carotenes
- Microscopically, usually large fat droplets are seen in hepatocytes (exceeding 20 micrometers), typically 1 per cell, pushing the nucleus to the periphery and giving an appearance of a signet ring / adipocyte; macrovesicular steatosis can be of the small droplet or large droplet type
- Seen in alcoholic or nonalcoholic liver disease and steatohepatitis, obesity, diabetes, chronic hepatitis C, protein calorie malnutrition, total parenteral nutrition, drugs effect (methotrexate or corticosteroids), Wilson disease
- More common than microvesicular steatosis
- Distribution of macrovesicular fat can be variable and seen in perivenular (centrilobular or acinar zone 3) zones in alcoholic steatosis and periportal areas or acinar zone 1 in wasting diseases like HIV / AIDS, severe protein calorie malnutrition and after corticosteroid therapy
- Grade of steatosis is usually reported based on the percentage of hepatocytes that contain lipid vacuoles:
- Minimal < 5% (essentially normal)
- Mild 6 - 33%
- Moderate 34 - 66%
- Severe > 67%
- Grading of steatosis has a major significance in evaluating liver transplant suitability of the donor and large droplet steatosis affecting > 30% of the liver graft hepatocytes is a poor prognostic indicator for graft survival in the recipient
- References: Radiology 2013;267:422, Biomed Res Int 2015;2015:168905, Nat Rev Gastroenterol Hepatol 2013;10:686, Front Physiol 2019;10:429, StatPearls: Nonalcoholic Fatty Liver [Accessed 15 April 2021]
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Microvesicular steatosis
- Lipid filled hepatocytes with innumerable small fat droplets around a centrally placed nucleus
- Diffuse microvesicular steatosis is considered a serious condition with hepatic dysfunction and coma
- Pathophysiologically, the development of microvesicular steatosis is thought to be secondary to impairment of beta oxidation due to inherited or acquired mitochondrial DNA mutations or deletions or direct inhibition of beta oxidation by drug metabolites in drug induced microvascular steatosis
- Microscopically seen as multiple tiny droplets (1 - 2 micrometers in diameter), imparting a foamy appearance to the cytoplasm that do not displace but can sometimes indent the nucleus; these numerous small droplets are sometimes barely visible at the resolution of light microscopy
- Seen in acute fatty liver of pregnancy, drug reactions like valproic acid, amiodarone and nucleoside analog toxicity, fatty acid β oxidation defects, Reye syndrome, mitochondrial DNA depletion and deletion syndromes, total parenteral nutrition, alcoholic foamy degeneration, inborn errors of metabolism disorders
- Pathologists sometimes disagree on interpretation of microvesicular steatosis vs. small droplet macrovesicular steatosis
- References: J Hepatol 2011;55:654, Acta Clin Belg 1990;45:311, Toxicol Pathol 2004;32:19
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Passive congestion
- Acute liver injury to due to sudden, profound reduction in systemic blood flow
- Also referred to as acute hepatic ischemic necrosis, ischemic hepatitis, shock liver, hypoxic hepatitis, congestive hepatopathy, congested liver in cardiac disease
- Clinical findings are those of right sided heart failure, mild right upper quadrant abdominal pain (due to hepatomegaly and stretching of the hepatic Glisson capsule)
- Improvement of the hemodynamic status may result in rapid, dramatic hepatic response with normalization of serum transaminases within several days and complete recovery
- Pathophysiologically, stasis of blood in the hepatic parenchyma, due to impaired hepatic venous drainage, leads to the dilation of central hepatic veins and hepatomegaly; elevated hepatic venous pressure and decrease in hepatic venous flow causes hypoxic injury to hepatocytes and eventual diffuse hepatocyte death and fibrosis
- Most common causes of passive hepatic congestion are congestive heart failure, restrictive cardiomyopathy, constrictive pericarditis, right sided valvular disease involving the tricuspid or pulmonary valves, severe hypovolemia, septic shock, massive pulmonary embolism, hyperpyrexia, heat stroke
- 2 major commonly recognized histologic patterns of ischemic liver disease include centrilobular ischemic necrosis and hepatic infarction; these have the same basic pathophysiological process but differ in extent and distribution of hepatic damage
- On gross examination, the liver appears enlarged, firm and tender, with characteristic nutmeg appearance and darker zones representing the ischemic congested centrilobular areas alternating with pale areas
- Microscopic examination reveals perivenular sinusoidal congestion and increased pigment in the hepatocytes; prolonged cardiac failure can lead to liver cell necrosis and focal inflammatory infiltrates, as well as perivenular fibrosis extending to the portal tracts
- References: Clin Liver Dis (Hoboken) 2017;10:49, Int J Angiol 2011;20:135
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Images hosted on other servers:
Submassive necrosis
- Refers to necrosis that affects a larger substantial area of hepatocytes rather than single cell programmed cell death
- Also referred to as confluent necrosis
- Most commonly seen in severe hepatitis, either due to viral, autoimmune or drug induced cases; in these conditions, necrosis is accompanied by an inflammatory reaction, usually associated with hepatic failure
- Less commonly, when submassive necrosis is seen in conditions leading to hypoperfusion of hepatic parenchyma, like shock, left ventricular failure, heatstroke or acetaminophen toxicity, it is accompanied by little or no inflammation
- May be zonal, involving a certain zone of the acini / lobule or nonzonal and random
- Confluent necrosis may bridge adjacent structures (bridging necrosis), extend over multiple lobules or acini (panlobular or panacinar necrosis) or extend over multiple lobules or acini (multilobular or multiacinar necrosis)
- In cases with submassive necrosis in which viable tissue remains, there is a striking proliferation of neocholangioles (bile ductules) as a reactive process, which over time, is followed by fibrous scarring
- References: Clin Liver Dis (Hoboken) 2017;10:53, Acad Forensic Pathol 2018;8:256
Contributed by Krutika S. Patel, M.B.B.S., M.D. and Annika L. Windon, M.D.
Additional references
- Torbenson: Biopsy Interpretation of the Liver, 3rd Edition, 2014, Saxena: Practical Hepatic Pathology - A Diagnostic Approach, 1st Edition, 2011, Torbenson: Surgical Pathology of the Liver, 1st Edition, 2017, Burt: MacSween’s Pathology of the Liver, 7th Edition, 2017, Lefkowitch: Scheuer’s Liver Biopsy Interpretation, 9th Edition, 2015
Board review style question #1
Board review style answer #1
E. Ubiquitin. The image shows Mallory hyaline, seen as irregular aggregates of clumped dense eosinophilic material in the cytoplasm and representing misfolded, aggregated and clumped intracellular inclusions of intermediate cytokeratin due to alterations in the hepatocellular cytokeratin assembly, usually seen in ballooned hepatocytes. Mallory hyaline shows positive immunohistochemical staining for cytokeratin 8 / 18, ubiquitin and p62.
Comment Here
Reference: Forms of hepatic injury
Comment Here
Reference: Forms of hepatic injury
Board review style question #2
A predominant microvesicular pattern of steatosis is associated with
- Alcoholic steatohepatitis
- Corticosteroid therapy
- Diabetes
- Obesity
- Reye syndrome
Board review style answer #2
E. Reye syndrome. Microvesicular steatosis is commonly seen in acute fatty liver of pregnancy, toxicity of drugs like valproic acid and nucleoside analogs, fatty acid beta oxidation defects, Reye syndrome, mitochondrial DNA depletion and deletion syndromes, total parenteral nutrition, alcoholic foamy degeneration and inborn errors of metabolism. Macrovesicular steatosis is commonly seen in alcoholic or nonalcoholic liver disease and steatohepatitis, obesity, diabetes, hepatitis C, protein calorie malnutrition, total parenteral nutrition and drugs like corticosteroids.
Comment Here
Reference: Forms of hepatic injury
Comment Here
Reference: Forms of hepatic injury
Gaucher disease
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Gaucher disease (GD) is an autosomal recessive lysosomal storage disorder caused by mutation of the GBA1 gene that codes for glucocerebrosidase (GCase)
- Impaired activity of GCase causes its substrate, glucocerebroside, to accumulate in lysosomes of reticuloendothelial system (liver, spleen, bone marrow)
- Macrophages (Gaucher cells) become laden with lipid and dysfunctional
Essential features
- One of the most common lysosomal storage disorders with a predisposition among those of Ashkenazi Jewish descent
- Caused by mutation in GBA1 gene on chromosome 1q that codes for GCase enzyme
- Impaired enzymatic activity leads to accumulation of Gaucher cells in reticuloendothelial system (liver, spleen, bone marrow), which leads to hepatosplenomegaly and bone marrow infiltration with cytopenia and bone pain
- Diagnosis is made by assessing GCase activity
- Treatment includes enzyme replacement therapy (GCase infusions) and substrate reduction therapy
Terminology
- Gaucher disease (pronounced as GO-SHEY)
ICD coding
- ICD-10: E75.22 - Gaucher disease
Epidemiology
- First described in 1882 in a patient with massive splenomegaly (Int J Mol Sci 2017;18:441)
- Prevalence is highest among the Ashkenazi Jewish population (Eastern European) with a frequency of 6% compared to 0.7 - 0.8% of all other ethnic groups (Hematology 2017;22:65)
Sites
- Liver
- Hepatomegaly with or without elevated liver enzymes (alkaline phosphatase, aminotransferase) due to intracellular accumulation of Gaucher cells and secondary inflammatory response
- Concurrent chronic liver diseases such as chronic viral hepatitis, steatohepatitis and vascular diseases are often seen
- Liver fibrosis (20 - 50% of cases) and cirrhosis with portal hypertension due to accumulation of Gaucher cells inciting an inflammatory response with fibrosis causing ischemia, infarction and progression of liver fibrosis (Mol Genet Metab Rep 2020;22:100564)
- Focal liver lesions also known as Gaucheroma (benign cluster of Gaucher cells associated with inflammation, fibrosis and iron accumulation)
- Increased risk of chronic liver disease and hepatocellular carcinoma due to cirrhosis
- Hypergammaglobulinemia and hyperferritinemia with probable underlying factor include chronic inflammation, impaired macrophage function and dysregulation in hepcidin - ferroportin axis
- Spleen
- Splenomegaly with focal splenic lesions characterized by clusters of Gaucher cells involving mostly the splenic cords in the red pulp
- Extramedullary hematopoiesis
- Bone marrow
- Infiltration of bone marrow by Gaucher cells causes reduced hematopoiesis and cytopenia
- Reduced proportion of marrow fat
- Bone
- Skeletal remodeling is also affected by replacement of marrow adipocytes with Gaucher cells; this causes fractures, remodeling defects, loss of bone mineral density and bone infarction
- Renal involvement is rare but proteinuria with or without renal insufficiency can occur
- Reference: Am J Hematol 2015;90:S6
Pathophysiology
- Mutation in GBA1 gene causes decrease in GCase activity with accumulation of glucocerebroside within activated macrophages (Gaucher cells) that infiltrate liver, spleen, bone marrow and other organs, leading to organomegaly
- Gaucher cells release cytokines and chemokines (IL1 beta, IL6, TNF alpha, IL10, IL18 and CCL18)
- Accumulated glucocerebroside is metabolized into sphingosine that can cause direct damage to hepatocytes, hematopoietic cells and the CNS
- GGase deficiency causes reduced osteoblast differentiation and function, reduced bone mineral deposition, defective bone remodeling caused by decreased bone formation leading to bone weakening, cortical thinning and trabecular resorption
- Infiltration of marrow by Gaucher cells leads to change in medullary microenvironment and compression of intraosseous blood vessels with potential bone infarction and necrosis
- References: Int J Mol Sci 2017;18:441, Am J Hematol 2015;90:S6
Etiology
- Autosomal recessive disease caused by mutation in gene GBA1 that codes for GCase causing impaired function and excessive accumulation of glucocerebroside in the reticuloendothelial system (liver, spleen, bone marrow)
- GD patients inherit 2 copies of mutated GBA1 (homozygous) from parents who are carriers
- Reference: Am J Hematol 2015;90:S6
Clinical features
- Splenomegaly is often the initial presentation
- Primary hypersplenism with anemia and thrombocytopenia, leukopenia also occurs frequently
- Hepatomegaly occurs late in the disease course with an increase in liver enzymes
- Bone marrow involvement / infiltration leading to anemia, thrombocytopenia, plasma cell dyscrasia
- Skeletal involvement in the form of osteopenia, osteoporosis, defective bone remodeling, osteonecrosis
- Pulmonary involvement in the form of interstitial lung disease
- Central nervous system (CNS) involvement
- Impaired cognition (type I GD)
- Convulsions, intellectual disability, apnea (type II GD)
- Myoclonus, seizures, dementia (type III GD)
- Categorized into 3 main types
- Type I: nonneuronopathic; most common type (90 - 95% of GD); variable presentation from asymptomatic patients discovered incidentally to early childhood presentation (OMIM: Gaucher Disease, Type I; GD1 [Accessed 1 May 2023])
- Type II: acute and severe neuronopathic type; affects CNS in infants, usually death before third year of life (OMIM: Gaucher Disease, Type II; GD2 [Accessed 1 May 2023])
- Can cause hydrops fetalis
- Perinatal lethal / collodion type: most severe form of type II with clinical manifestations presenting before birth and causing neonatal death
- Type III: subacute or juvenile neuronopathic, with systemic and CNS involvement, including oculomotor symptoms (OMIM: Gaucher Disease, Type III; GD3 [Accessed 1 May 2023])
- Intermediate in severity
- Associated with increased risk of multiple myeloma (relative risk: 5.9) (Blood 2005;105:4569)
- References: Expert Rev Endocrinol Metab 2018;13:107, Hematology 2017;22:65, J Bone Miner Res 2019;34:996
Diagnosis
- Diagnosis is made by assessing GCase activity in circulating lymphocytes or fibroblast culture; < 10 - 15% of mean normal activity is diagnostic
- Disease activity or response to therapy is evaluated by measuring biochemical markers in activated macrophages (e.g., chitotriosidase, angiotensin converting enzyme, ferritin, chemokine CCL18 / PARC)
- Genotype testing in Ashkenazi Jewish patients for the most common alleles (L444P, N370S, IVS2+1g>a, V394L and R496H)
- References: Int J Mol Sci 2017;18:441, Am J Hematol 2015;90:S6
Laboratory
- Anemia
- Thrombocytopenia due to hypersplenism
- Hyperferritinemia
- Hypergammaglobulinemia
- GCase enzyme activity assay
- Serum protein electrophoresis
- Bone marrow
- Large (30 - 100 micron) macrophages with fibrillary pale blue to grey cytoplasm
- Liver biopsy
- Performed for hepatomegaly and shows clusters of Gaucher cells (macrophages with amphophilic cytoplasm resembling wrinkled tissue paper)
- Reference: Mol Genet Metab Rep 2020;22:100564
Radiology description
- Radiographic / Xray findings
- Erlenmeyer flask deformity (enlargement of metaphysis and absence of the typical concave diametaphyseal curve) in distal femur
- Osteonecrosis, proximal femur
- Osteopenia
- Lytic lesions
- MRI performed to assess skeletal involvement
- Osteonecrosis
- Gaucher cell infiltration produce low signal on T1 - T2 weighted images
- Degree of bone marrow infiltration by Gaucher cells
- CT / ultrasound findings
- Hepatosplenomegaly
- Bone scan
- Decreased uptake
- EEG and swallowing studies for neuronopathic GD
- Reference: J Bone Miner Res 2019;34:996
Prognostic factors
- Variable prognosis depending on clinical type of disease, ranging from asymptomatic to fatal outcome
- Type I: normal life span
- Type II: patients die within first 3 years of life
- Type III: intermediate between type I and type II
- Early diagnosis and treatment can have a good outcome
- Reference: Mol Genet Metab 2021;132:49
Case reports
- 4 year old Albanian boy diagnosed with GD type 1 through newborn screening presented with multiple osteonecrosis in femur on follow up (JIMD Rep 2022;63:414)
- 15 year old boy who presented with fever, pulmonary interstitial fibrosis and hepatomegaly and was ultimately diagnosed with GD (J Med Case Rep 2018;12:306)
- 18 year old man diagnosed with neuroblastoma, also found to have GD (Blood Cells Mol Dis 2018;68:106)
- 24 year old woman diagnosed as carrier of GD when she presented with gestational thrombocytopenia and anemia that did not respond to any medications (J Med Case Rep 2022;16:203)
- 38 year old man who presented with solitary swelling of proximal tibia, mimicking a musculoskeletal tumor (J Orthop Case Rep 2022;12:64)
Treatment
- Enzyme replacement therapy, which includes glucocerebrosidase IV infusions
- FDA approved Cerezyme (imiglucerase), VPRIV (velaglucerase alfa) and Elelyso (taliglucerase alfa) effective against hematologic, visceral and bone symptoms
- Not known to be effective against neurologic symptoms
- Substrate reduction therapy (oral medication) to reduce the accumulation of toxic substrate
- Cerdelga (eliglustat), a glucosylceramide synthase inhibitor, is indicated only for type 1 GD
- Zavesca (miglustat) for type 1 GD; not known to be effective against neurological symptoms (Ann Neurol 2008;64:514)
- Symptomatic treatment
- Bone remodeling: targeted treatments and vitamin D
- Splenectomy for hypersplenism
- Analgesics for bone pain and joint pain
- Bone marrow transplant only in cases of neuronopathic GD
- Somatic cell gene therapy under investigation
- References: Expert Rev Endocrinol Metab 2018;13:107, Mol Genet Metab 2021;132:49, Eur J Pharmacol 2022;926:175023
Gross description
- Bone
- Mass-like lesions that are soft, hemorrhagic and irregular, resulting in extensive localized bone loss
- Osteonecrosis of bone appears as pale yellow zones
- Spleen
- Splenomegaly with pale homogenous cut surface with reddish yellow nodules of infarction
- References: Am J Hematol 2016;91:736, J Orthop Case Rep 2022;12:64
Microscopic (histologic) description
- Bone marrow, liver, spleen
- Infiltration by Gaucher cells containing abundant cytoplasm with fine, fibrillary, amphophilic characteristics resembling wrinkled tissue paper
- May have increased reticulin fibers and reduced fat in bone marrow biopsy
- Liver often demonstrates infiltration in the zone 3 region by Gaucher cells
- Small focal accumulations (Gaucheroma) or diffuse replacement by large, ovoid histiocytes (30 - 100 microns) with abundant, fibrillary eosinophilic granular cytoplasm resembling wrinkled tissue paper
- Small, bland nucleus that may be centrally or eccentrically located
- Cytoplasm has periodic acid Schiff diastase (PASD) resistant granules
- Reference: Mol Genet Metab Rep 2020;22:100564
Microscopic (histologic) images
Cytology description
- Wright-Giemsa stained bone marrow aspirate shows Gaucher cell containing abundant granular or fibrillary, blue-gray cytoplasm with wrinkled tissue paper-like appearance
Positive stains
- PAS and PASD are positive in Gaucher cells (diastase resistant)
- Iron
- CD68
- Reference: Arch Pathol Lab Med 2008;132:851
Negative stains
- Phospholipid stains, acid fast stains, CD11b, CD40
Electron microscopy description
- Elongated / rod shaped lysosomes filled with tubular structures
Molecular / cytogenetics description
- Gene encoding glucocerebrosidase (Gcase) GBA1 is located on the long arm of chromosome 1 (1q21) and genetic testing is performed using saliva or blood samples
- DNA result is obtained by whole gene sequencing or selective sequencing within families
- More than 400 different mutations have been described in GBA1 gene; most prevalent are N370s, L444P
- c.1226A>G (N370S) mutation is common in the Ashkenazi Jewish population and most of these patients are asymptomatic
- L444P mutation seen in GD is at high risk for developing CNS complications
- Homozygous (D409H) mutation presents with cardiac complications
- References: Int J Mol Sci 2017;18:441, Mol Genet Metab 2021;132:49
Videos
Gaucher disease involving bone
Sample pathology report
- Liver, right lobe, needle core biopsy:
- Gaucher disease involving liver (see comment)
- Comment: Sections of the liver biopsy show clusters of Gaucher cells (pale staining histiocytes with striated cytoplasm, PASD positive) involving mainly the perivenular zone with atrophy of hepatocyte plates.
Differential diagnosis
- Pseudo-Gaucher cells:
- Mimic Gaucher cells on light microscopy but iron stain negative and lack the typical electron microscopy findings seen in GD (Turk J Haematol 2014;31:428)
- Seen in conditions that cause rapid cell turnover (e.g., myeloproliferative and myelodysplastic neoplasms, myeloma)
- Mycobacterial infection (AFB stain+)
- Sea blue histiocytosis (Arch Pathol Lab Med 2008;132:851):
- Seen in various conditions with increased marrow cell turnover (e.g., myeloproliferative or myelodysplastic neoplasms)
- Macrophage contains ceroid (insoluble lipid pigment); inclusions are globular (not fibrillary)
- Stains more intensely blue with Wright-Giemsa than Gaucher cells
- Niemann-Pick disease (Humpath.com: Niemann-Pick Diseases [Accessed 6 June 2023]):
- Lipid storage disorder caused by sphingomyelinase deficiency, which leads to accumulation of lipids in histiocytes that appear foamy
- Electron microscopy shows lamellar inclusions in lysosomes
Board review style question #1
A 5 year old boy presents to the clinic for evaluation of peripheral pancytopenia. His parents are of Ashkenazi Jewish descent. On physical examination, he has hepatosplenomegaly. Bone marrow aspirate smears show large cells with fibrillary cytoplasm that are positive for periodic acid Schiff (PASD) stain. Which of the following lysosomal enzymes are most likely deficient?
- Alpha galactosidase
- Glucocerebrosidase
- Hexosaminidase A
- Sphingomyelinase
Board review style answer #1
B. Glucocerebrosidase. Gaucher disease is caused by deficiency of glucocerebrosidase due to mutation of the GBA1 gene. Glucocerebrosidase deficiency causes abnormal accumulation of its substrate, glucocerebroside, in the macrophages of liver, spleen, bone marrow, etc. Patients can present with pancytopenia, hepatosplenomegaly and bone pain with fractures. Diagnosis can be made on finding a low glucocerebrosidase enzyme level in peripheral blood leukocytes. Answer D is incorrect because sphingomyelinase A deficiency is seen in Niemann-Pick Disease. The clinical presentation may overlap with Gaucher disease; however, there is an accumulation of foamy vacuolated macrophages in Niemann-Pick disease. Answer A is incorrect because alpha galactosidase deficiency is seen in Fabry disease, which typically presents with neurological manifestations. Answer C is incorrect because hexosaminidase deficiency is seen in Tay-Sachs disease.
Comment Here
Reference: Gaucher disease
Comment Here
Reference: Gaucher disease
Board review style question #2
Which of the following clinical characteristics is associated with type I Gaucher disease?
- Gastric ulcers
- Hydrops fetalis
- Normal expected life span
- Oculomotor symptoms
Board review style answer #2
C. Normal expected life span. Type 1 Gaucher disease is nonneuronopathic and associated with a normal life span. Answer A is incorrect because Gaucher disease is not typically associated with gastric symptoms. Answers B and D are incorrect because hydrops fetalis is associated with type 2 Gaucher disease and oculomotor symptoms are associated with type 3.
Comment Here
Reference: Gaucher disease
Comment Here
Reference: Gaucher disease
Glycogen storage diseases
Table of Contents
Definition / general | Essential features | ICD coding | Type 0 | Type I | Type Ia | Type Ib | Type Ic and Id | Type III | Type IV | Type VI | Type IX | Type XI | Sample pathology report | Board review style question #1 | Board review style answer #1Definition / general
- Called GSD, also glycogenosis and dextrinosis
- Groups of diseases caused by various enzyme deficiencies that result in abnormal glycogen synthesis or glycolysis, typically within the muscles or liver cells (EXCLI J 2019;18:30, Genet Med 2013;15:106)
- Overall GSD incidence is estimated to be 1 case per 20,000 - 43,000 live births (World J Gastroenterol 2007;13:2541)
- 23 types of GSD have been recognized, involving different organs (Genet Med 2016;18:1037)
- Liver, skeletal muscle, heart and the central nervous system are the most common organs involved (Genet Med 2016;18:1037)
- Classified by the organ affected and the enzyme deficiency involved
- GSD types I, III, 0, XI, IX, VI and IV affect the liver (with 80% of hepatic GSD being type I, III or IX) (Ultrastruct Pathol 2011;35:183)
- Some GSD types can affect both the liver and muscles (III and IXb) (Ultrastruct Pathol 2011;35:183)
- Associated with hypoglycemia and hepatomegaly (Genet Med 2013;15:106)
Essential features
- Rare disorder
- Group of rare inborn disorders of glycogen metabolism
- Variable expressivity and most patients present with hepatomegaly and hypoglycemia
- Increased incidence of hepatic adenoma and hepatocellular carcinoma
ICD coding
Type 0
Definition / general
Diagnosis
Treatment
Microscopic (histologic) description
- Also called aglycogenosis
- Rare, autosomal recessive
- Deficiency in glycogen synthase (chromosome 12p12.2)
- Clinically, hyperglycemia, glycosuria, hyperlactic acidemia, which alternate with hypoglycemia and hyperketonemia during fasting
- Due to the hyperglycemia and hyperuricemia, the child may be thought to have an early stage of diabetes, especially considering that the liver is not enlarged
- Symptoms of GSD type 0 are those associated with hypoglycemia
- Developmental delay may be seen in some children
Diagnosis
- Liver biopsy
- Enzymatic evaluation of the liver tissue reveals low to absent glycogen synthase activity
- Genetic / molecular testing can be performed with either liver or muscle tissue to further confirm that there is mutation of the glycogen synthase gene (chromosome 12p12.2)
- Currently, gene mutational analysis is performed to provide a definitive diagnosis (World J Gastroenterol 2007;13:2541)
Treatment
- Symptoms ameliorate with protein rich meals and bedtime feeding of uncooked cornstarch in low fat or skim milk
Microscopic (histologic) description
- Small amounts of glycogen and moderate steatosis
Type I
Definition / general
Microscopic (histologic) description
Microscopic (histologic) images
Contributed by Nigar Anjuman Khurram, M.D.
Electron microscopy description
- Also known as von Gierke disease or hepatorenal glycogenosis
- Occurs in an autosomal recessive pattern
- Type Ia: glucose-6-phosphatase (G6Pase) deficiency
- Type Ib: translocase T1 deficiency
- Type Ic: translocase T2 deficiency (carries inorganic phosphates from microsomes into cytosol and pyrophosphates from cytosol into microsomes)
- Type Id: deficiency in transporter that translocates free glucose molecules from microsomes
- Incidence of GSD type Ia is 1 per 100,000 - 400,000 births per year in the White population
- GSD types Ib and Ic are even less frequent
- Incidence of 1 in 20,000 in the Ashkenazi Jewish population (Ultrastruct Pathol 2011;35:183)
- May present as severe hypoglycemia and increased lactic acid, triglycerides and uric acid shortly after birth
- Older children have short stature and may develop eruptive xanthomas, rickets, anemia, chronic renal disease due to hyperuricemia and renal stones
- Tissue type affected is different with the GSD type I subtypes: type Ia - liver, kidney, intestine; type Ib - liver; and type Ic - liver
- Diagnosis of GSDI established in a proband by identification of biallelic pathogenic variants in either G6PC1 (GSDIa) or SLC37A4 (GSDIb)
- If molecular genetic testing is inconclusive, hepatic enzyme activity analysis is only available for glucose-6-phosphatase catalytic activity (GSDIa) (GeneReviews: Glycogen Storage Disease Type I [Accessed 14 July 2023])
Microscopic (histologic) description
- Distended liver cells with a uniform distribution of glycogen
- Liver cells arranged in mosaic pattern with plant like appearance
- Steatosis with hyper glycogenated nuclei
- Fibrosis may also be present
Microscopic (histologic) images
Contributed by Nigar Anjuman Khurram, M.D.
Electron microscopy description
- Abundant and uniform distribution of glycogen within enlarged hepatocytes
- Increased cytoplasmic glycogen, enlarged organelles, lipid droplets, glycogenated nuclei
Type Ia
Definition / general
Diagnosis
Case reports
Treatment
Gross description
Microscopic (histologic) description
- Rare
- Caused by the deficiency of glucose-6-phosphatase (G6Pase) catalytic activity
- Laboratory findings include hypoglycemia, deranged liver function tests (LFTs), lactic acidosis, hyperuricemia and hyperlipidemia
- Clinical presentation: hypoglycemia and marked hepatomegaly in first year of life; later in life, short stature, chronic lactic acidosis, focal segmental glomerulosclerosis, hepatic adenomas, iron deficiency, enterocolitis, gout, osteoporosis
Diagnosis
- Biallelic pathogenic variants in G6PC1 (GSDIa) or SLC37A4 (GSDIb) on molecular genetic testing
- Deficient hepatic enzyme activity (glucose-6-phosphatase catalytic activity [GSDIa]) from a liver biopsy specimen
Case reports
- 17 year old woman with hepatocellular carcinoma with glycogen storage disease type 1a (Pediatr Int 2020;62:744)
- 28 year old woman with multiple hepatic adenomas (Arch Pathol Lab Med 2003;127:e402)
Treatment
- Continuous dietary nasogastric infusion of glucose or frequent oral uncooked cornstarch at 3 - 6 hour intervals during the day and at night
- Liver transplantation may be necessary if not compliant with dietary restrictions or with refractory hyperglycemia or hepatocellular carcinoma (World J Gastroenterol 2007;13:2541)
- Gene therapy using adenovirus vectors has been evaluated in murine models of GSD type I (World J Gastroenterol 2007;13:2541)
Gross description
- Massive hepatomegaly
- May have variable sized tumor nodules
Microscopic (histologic) description
- Large hepatocytes with prominent cell membrane and glycogenated nuclei
- PAS+ accumulated glycogen
- Rarely contains Mallory hyaline and steatosis in hepatic adenomas
Type Ib
Definition / general
- Caused by a defect in glucose-6-phosphate exchanger SLC37A4 (transporter)
- Normal G6Pase activity in frozen tissue and lowered activity in fresh specimens
- Recurrent infections, neutropenia and neutrophil dysfunction are recognized as distinctive features (J Pediatr 2000;137:187)
- Another distinctive feature of GSD-Ib is the observation of inflammatory bowel disease (Crohn's)-like colitis (J Pediatr 1986;109:55, Turk J Pediatr 2005;47:180)
- Clinical presentation: young children may have frequent otitis, gingivitis, boils, intermittent diarrhea; although it is rare, terminal kidney disease may develop and kidney transplantation may be necessary
- Treatment includes dietary therapy, granulocyte colony stimulating factor (G-CSF) therapy may restore myeloid functions and liver transplantation to prevent malignant transformation of hepatic adenomas and for refractory hypoglycemia
Type Ic and Id
Definition / general
- Liver microsomal transport of phosphate and glucose is deficient in GSD-Ic and GSD-Id
Type III
Definition / general
Diagnosis
Case reports
Treatment
Gross description
Microscopic (histologic) description
Electron microscopy description
- Also called Cori disease
- Autosomal recessive
- Rare disease of variable clinical severity affecting primarily the liver, heart and skeletal muscle
- Deficiency of debrancher enzyme amylo-1,6-glucosidase due to various mutations causes hypoglycemia (Hum Mol Genet 2009;18:2045)
- Most individuals with GSD III survive into adulthood
- GSD IIIa: most common subtype (85%), liver and muscle involvement
- GSD IIIb: 15%; liver involvement only
Diagnosis
- Demonstration of excessive and structurally abnormal glycogen accumulation with shorter outer branches and deficient debranching enzyme activity in frozen liver or muscle biopsy samples
- Deficient identification of pathogenic mutations in the AGL gene on both alleles
Case reports
- 56 year old woman known to be affected by GSD III and liver cirrhosis complicated by hepatocellular carcinoma (J Clin Gastroenterol 2000;31:80)
Treatment
- Individuals with GSD III and advanced liver disease should be considered for liver transplant
Gross description
- Hepatomegaly
Microscopic (histologic) description
- Liver or muscle biopsy demonstrate a vacuolar accumulation of nonmembrane bound glycogen primarily in the cytoplasm
- Lipid vacuoles are less frequent in GSD III (compared to GSD I)
- Steatosis, hepatocyte ballooning
- Presence of fibrosis, ranging from minimal periportal fibrosis to micronodular cirrhosis, is noted in GSD III (not in GSD I)
- Stored material in GSD III is periodic acid-Schiff positive and diastase sensitive within the cytoplasm
Electron microscopy description
- Increased cytoplasmic glycogen, lipid droplets, glycogenated nuclei
Type IV
Definition / general
Diagnosis
Case reports
Treatment
Microscopic (histologic) description
Electron microscopy description
Differential diagnosis
- Also called Andersen disease, Brancher deficiency, amylopectinosis, glycogen branching enzyme deficiency
- Rare, autosomal recessive, caused by deficiency of glycogen branching enzyme on 3p14, leading to excessive deposition of structurally abnormal, amylopectin-like glycogen in affected tissues, causing irreversible tissue and organ damage
- Clinically, extremely heterogeneous, owing in part to variation in tissue involvement
- Fatal perinatal neuromuscular subtype: in utero with fetal akinesia, polyhydramnios and fetal hydrops; death usually in the neonatal period
- Congenital neuromuscular subtype: newborn period with profound hypotonia, respiratory distress and dilated cardiomyopathy; death usually in early infancy
- Classic (progressive) hepatic subtype: may appear normal at birth but rapidly develop failure to thrive
- Hepatomegaly, liver dysfunction and progressive liver cirrhosis, hypotonia and cardiomyopathy
- Without liver transplantation, death from liver failure usually occurs by age 5
- Nonprogressive hepatic subtype: hepatomegaly, liver dysfunction, myopathy and hypotonia; likely to survive without progression of the liver disease and may not show cardiac, skeletal muscle or neurologic involvement
- Childhood neuromuscular subtype: rare, variable course, ranging from onset in the second decade with a mild disease course to a more severe, progressive course resulting in death in the third decade
Diagnosis
- Demonstration of glycogen branching enzyme (GBE) deficiency in liver, muscle or skin fibroblasts
- Identification of biallelic pathogenic variants in GBE1 on molecular genetic testing (GeneReviews: Glycogen Storage Disease Type IV [Accessed 19 July 2023])
Case reports
- 10 month old boy with massive hepatomegaly (Arch Pathol Lab Med 2002;126:630)
Treatment
- Liver transplantation
- Liver transplantation is helpful also for muscular involvement due to systemic microchimerism after liver allotransplantation and amelioration of pancellular enzyme deficiencies (Eur J Pediatr 1999;158:S43, N Engl J Med 1991;324:39)
Microscopic (histologic) description
- Hepatocellular periodic-acid Schiff positive, diastase resistant inclusions of the abnormal glycogen deposits
Electron microscopy description
- Filamentous nonbranching cytoplasmic aggregates
Differential diagnosis
- Lafora disease:
- Similar inclusions but not coarsely clumped, older age with epilepsy, myoclonus, dementia
Type VI
Definition / general
Diagnosis
Treatment
Microscopic (histologic) description
Microscopic (histologic) images
Contributed by Miguel Reyes-Mugica, M.D. and Nigar Anjuman Khurram, M.D.
Electron microscopy description
Electron microscopy images
Contributed by Miguel Reyes-Mugica, M.D. and Nigar Anjuman Khurram, M.D.
Additional references
- Also called Hers disease; liver glycogen phosphorylase deficiency
- Rare, autosomal recessive
- Most commonly affected group is the Mennonite community
- Clinically, asymptomatic hepatomegaly and growth retardation
- Usually has a benign course with mild to moderate hypoglycemia
Diagnosis
- Enzyme assay using liver, leukocytes and erythrocytes
- Gene mutation analysis can also be performed
Treatment
- Avoiding prolonged fasting and ingestion of a bedtime snack to avoid early morning hypoglycemia
Microscopic (histologic) description
- Small mosaic pattern and irregular distension of the hepatocytes due to glycogen deposition
- Microsteatosis, mild periportal fibrosis and septal formation may be present
Microscopic (histologic) images
Contributed by Miguel Reyes-Mugica, M.D. and Nigar Anjuman Khurram, M.D.
Electron microscopy description
- Large pools of monoparticulate glycogen interspersed with glycogen rosettes and lipid vacuoles with glycogen embedded
- Hepatocytes have irregularly shaped aggregates of low density granular material scattered within the glycogen, giving a starry sky appearance
Electron microscopy images
Contributed by Miguel Reyes-Mugica, M.D. and Nigar Anjuman Khurram, M.D.
Additional references
Type IX
Definition / general
Diagnosis
Treatment
Microscopic (histologic) description
Microscopic (histologic) images
Contributed by @RaulSGonzalezMD on Twitter
Electron microscopy description
Additional references
- Deficiency in phosphorylase kinase (PhK)
- Types involving the liver are mainly classified into 2 forms: the X linked liver form (there are 2 subtypes; XLG-I and XLG-II) and autosomal recessive form
- X linked liver phosphorylase kinase (alpha subunit) deficiency (PHKA2 related GSD type IX)
- Mildest GSD with low phosphorylase activity in the absence of adenosine monophosphate
- Most common signs and symptoms present between 1 and 5 years and include hepatomegaly, growth retardation (68%), hypotonia, deranged liver function tests, fasting hyperketosis, hypoglycemia
- Hepatomegaly and growth retardation usually resolve during puberty
- Splenomegaly and cirrhosis are very rare
- Autosomal liver and muscle phosphorylase kinase (beta subunit) deficiency (PHKB related GSD type IX)
- Autosomal recessive
- Deficiency in the beta subunit of phosphorylase kinase
- Hepatomegaly with abdominal distension, mild growth retardation and lipidemia
- When symptoms are present, the liver is primarily affected with the potential for cirrhosis
- Autosomal liver phosphorylase kinase (gamma subunit) deficiency (PHKG2 related GSD type IX)
- Autosomal recessive
- Deficiency in the gamma subunit of liver phosphorylase
- Associated with liver cirrhosis, renal tubular acidosis or neurologic disorders
Diagnosis
- Diagnosis can be made with enzyme analysis of liver tissue and by gene mutation analysis
Treatment
- Symptoms ameliorate with protein rich meals and bedtime feeding of uncooked cornstarch in low fat or skim milk
Microscopic (histologic) description
- X linked liver phosphorylase kinase (alpha subunit) deficiency (PHKA2 related GSD type IX)
- Biopsy shows irregular distension of hepatocytes with glycogen
- Hepatocytes are organized into a mosaic pattern
- Microsteatosis may be seen
- Autosomal liver and muscle phosphorylase kinase (beta subunit) deficiency (PHKB related GSD type IX): both liver and muscle biopsies show glycogen accumulation by light and electron microscopy
Microscopic (histologic) images
Contributed by @RaulSGonzalezMD on Twitter
Contributed by @RaulSGonzalezMD on Twitter (see original post here)">
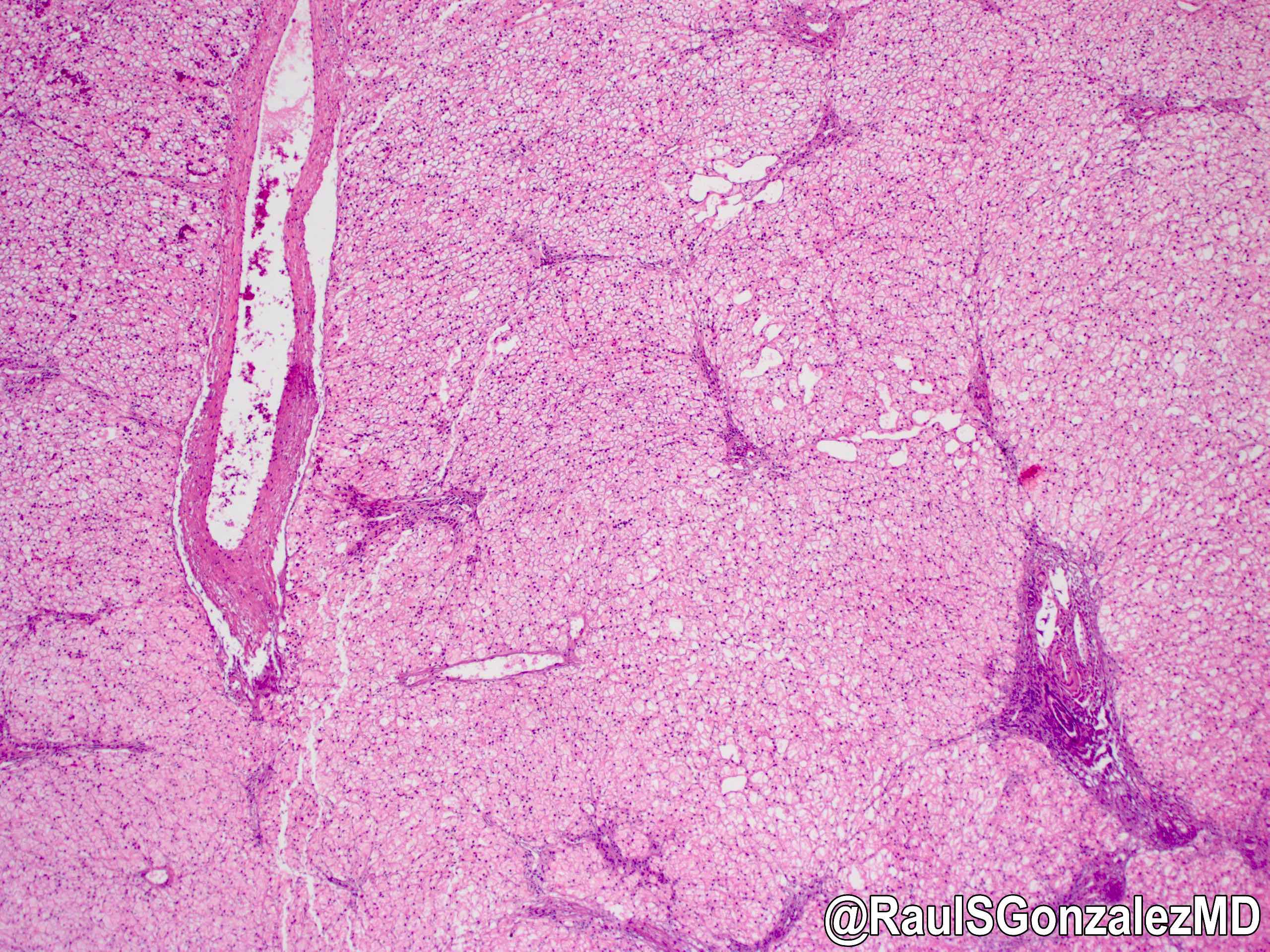 Contributed by @RaulSGonzalezMD on Twitter (see original post here)">
Contributed by @RaulSGonzalezMD on Twitter (see original post here)">
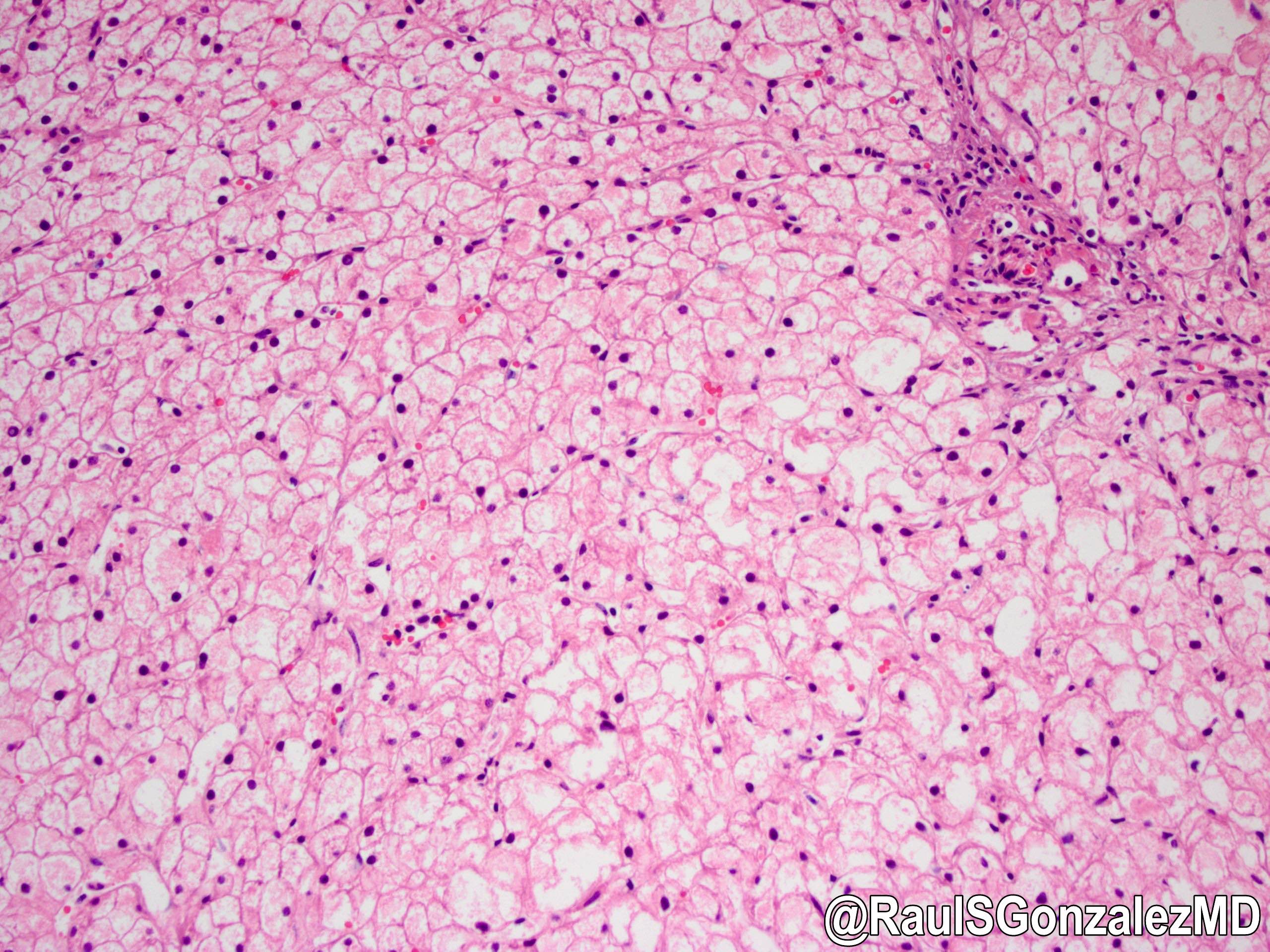
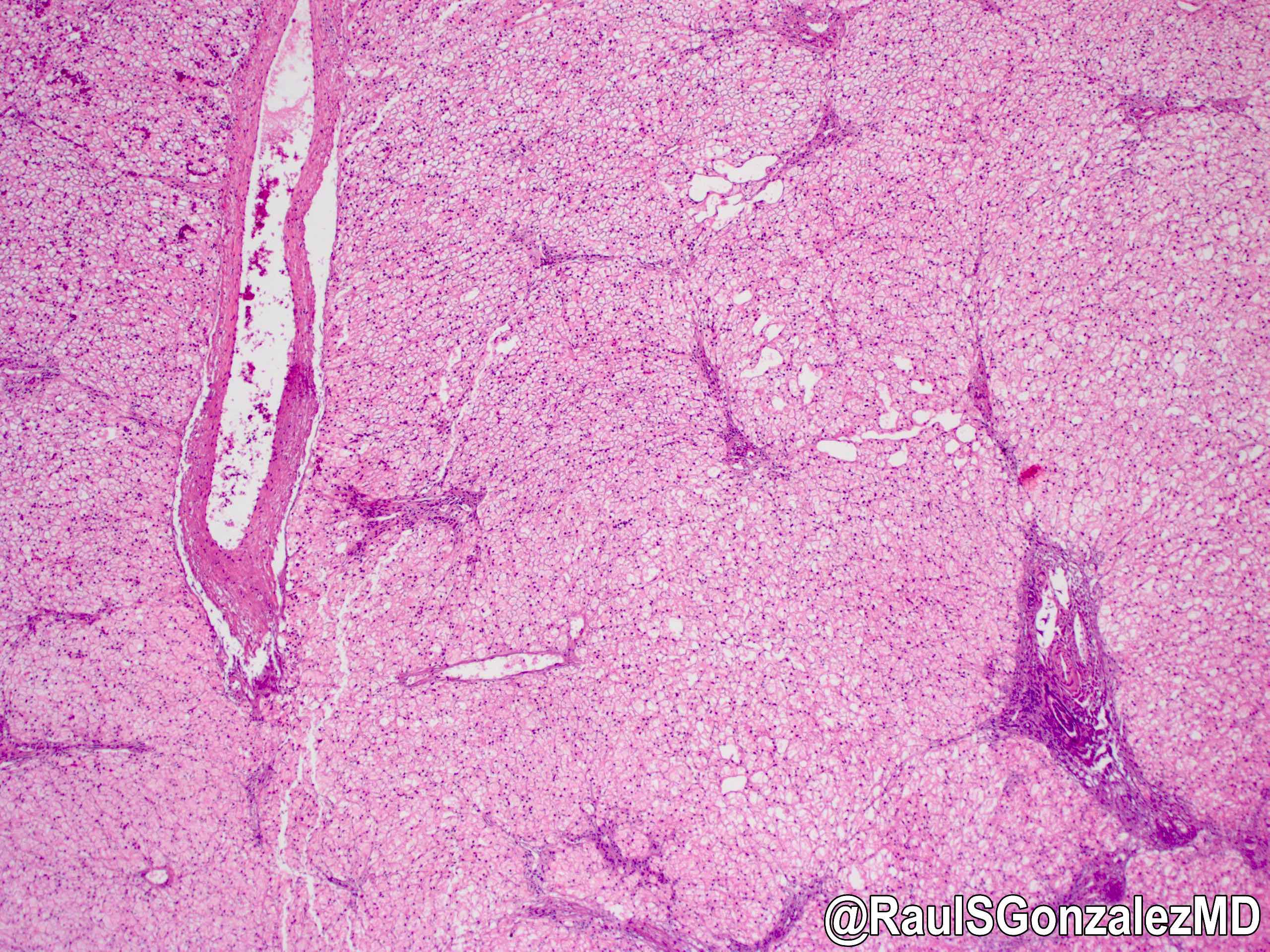 Contributed by @RaulSGonzalezMD on Twitter (see original post here)">
Contributed by @RaulSGonzalezMD on Twitter (see original post here)">
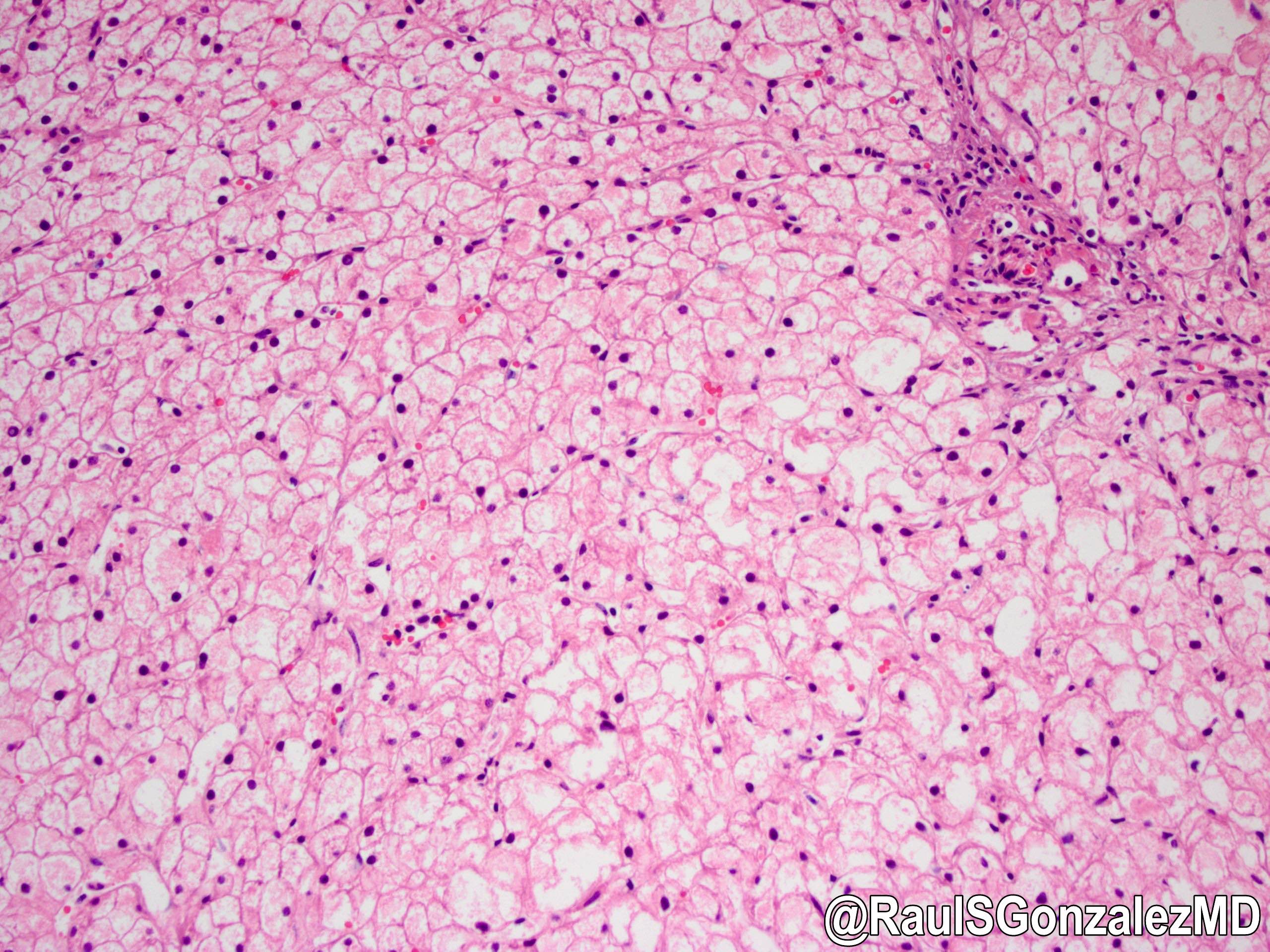
Glycogen storage disease
Electron microscopy description
- X linked liver phosphorylase kinase (alpha subunit) deficiency (PHKA2 related GSD type)
- Extensive monoparticulate glycogen, glycogen rosettes and frequent lipid vacuoles containing glycogen particles
- Starry sky pattern attributed to scattered areas with finely granular organelle free clear zones alternating with densely packed glycogen particles
- Mitochondria tend to be decreased in size and numbers; skeletal muscle is normal
Additional references
Type XI
Definition / general
Diagnosis
Case reports
Treatment
Microscopic (histologic) description
- Also called Fanconi-Bickel syndrome
- Rare, autosomal recessive
- Responsible gene is glucose transport 2 gene (GLUT2), localized to 3q26.1-q26
- Defective transport of monosaccharide across the membranes
- Clinically, hepatorenal glycogen accumulation, fasting hypoglycemia, postprandial hyperglycemia and hypergalactosemia, proximal renal tubular dysfunction, marked stunted growth, dwarfism in older patients, hypercholesterolemia, hyperlipidemia, pancreatitis, generalized osteopenia
Diagnosis
- Detected by neonatal screening for galactose
Case reports
- 2 siblings with familial Fanconi syndrome with malabsorption and galactose intolerance, normal kinase and transferase activity (Acta Paediatr Scand 1981;70:527)
Treatment
- Liver transplantation
- Liver transplantation helpful also for muscular involvement due to systemic microchimerism after liver allotransplantation and amelioration of pancellular enzyme deficiencies (Eur J Pediatr 1999;158:S43, N Engl J Med 1991;324:39)
Microscopic (histologic) description
- Excessive glycogen accumulation with steatosis
Sample pathology report
- Liver, needle biopsy:
- Hepatic parenchyma with features suggestive of glycogen storage disease (see comment)
- Comment: The morphologic features are classic for glycogen storage disease (GSD), with a plant cell-like morphology, intracytoplasmic glycogen on PAS staining, which disappears after digestion with diastase. There is also mild steatosis and no significant nuclear glycosylation. The electron microscopic analysis also shows massive amounts of intracytoplasmic free glycogen. The main variants of GSD with features of this appearance are I, III, VI and IX. However, these diseases have overlapping histopathologic features and therefore are best distinguished enzymatically and genetically. Given the lack of significant hypoglycemia, types VI and IX are favored. Further genetic / enzymatic analysis is required to definitively establish the specific subtype of GSD. Glycogen storage disease enzyme assay is pending and will be reported in an addendum.
Board review style question #1
Deficiency of amylo-1,6-glucosidase debranching enzyme results in which of the following glycogen storage disease (GSD) types?
- GSD type 0, aglycogenosis
- GSD type I, hepatorenal glycogenosis / von Gierke disease
- GSD type III, Cori disease
- GSD type IV, Andersen disease
- GSD type XI, Fanconi-Bickel syndrome
Board review style answer #1
C. GSD type III, Cori disease.
In GSD type III / Cori disease, deficiency of debrancher enzyme amylo-1,6-glucosidase due to various mutations causes hypoglycemia. Answer A is incorrect because GSD type 0 / aglycogenosis is caused by deficiency of glycogen synthase. Answer B is incorrect because GSD type 1, hepatorenal glycogenosis / von Gierke disease is caused by glucose-6 phosphatase deficiency. Answer D is incorrect because GSD type IV / Andersen disease is caused by a deficiency of glycogen branching enzyme on 3p14. Answer E is incorrect because GSD type XI / Fanconi-Bickel syndrome is caused by glucose transport 2 gene.
Comment Here
Reference: Glycogen storage diseases
Comment Here
Reference: Glycogen storage diseases
Glycogenic hepatopathy
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Hepatomegaly, raised liver enzymes and abundant glycogen in hepatocytes related to uncontrolled diabetes mellitus
Essential features
- Mauriac syndrome: rare phenomenon in type 1 diabetics characterized by excessive hepatic glycogen deposition, elevated liver enzymes, hepatomegaly, obesity, cushingoid features and late puberty
- Presents with abdominal pain, hepatomegaly, nausea, vomiting and ketoacidosis
- Histologic correlate is glycogenic hepatopathy: diffuse pale appearance of hepatocyte cytoplasm and glycogenated hepatocyte nuclei
Terminology
- Hepatic / liver glycogenosis
- Diabetes mellitus associated glycogen storage hepatomegaly
- Mauriac syndrome: rare phenomenon in type 1 diabetics characterized by excessive hepatic glycogen deposition, elevated liver enzymes, hepatomegaly, obesity, cushingoid features and late puberty (Arch Dis Child 2014;99:354)
ICD coding
- ICD-10: E74.00 - glycogen storage disease, unspecified
Epidemiology
- Higher prevalence in diabetic patients, particularly type 1 diabetics (BMC Pediatr 2012;12:160)
- Mostly in children and young adults
- Slightly higher incidence in women (World J Hepatol 2018;10:172)
Sites
- Liver
Etiology
- Prolonged hyperglycemia due to uncontrolled diabetes mellitus leads to accumulation of glycogen in hepatocytes, resulting in hepatomegaly and elevation of liver enzymes (World J Hepatol 2018;10:172)
Clinical features
- Abdominal pain, hepatomegaly, nausea and vomiting, history of ketoacidosis
Diagnosis
- Clinical and pathological association is required for diagnosis
Laboratory
- Hyperglycemia
- Elevated transaminases or alkaline phosphatase
- Elevated hemoglobin A1C, which shows poor glycemic control (Clin Gastroenterol Hepatol 2017;15:927)
Radiology description
- Hyperdense liver on CT without contrast
Prognostic factors
- Good prognosis with medical treatment (World J Hepatol 2018;10:172)
- Blood sugar control helps to adjust liver enzymes and microscopic features (Saudi Med J 2017;38:89)
Case reports
- 15 year old boy with glycogenic hepatopathy (Case Reports Hepatol 2018;2018:6037530)
- 18 year old woman with diabetes and Mauriac syndrome (Case Rep Crit Care 2016;2016:6072909)
- 19 year old woman with diabetes and glycogenic hepatopathy (BMJ Case Rep 2019;12:e228524)
- 25 year old man with diabetes and suicide by high dose insulin presented with glycogenic hepatopathy (J Am Coll Emerg Physicians Open 2020;1:1097)
- 44 year old woman with diabetes and glycogenic hepatopathy (ACG Case Rep J 2018;5:e31)
Treatment
- Blood sugar control by adjusting insulin and diet (Saudi Med J 2017;38:89)
- Improvement of glycogenic hepatopathy observed after pancreatic transplantation in diabetic patients (Ann Hepatol 2012;11:554)
Gross description
- Not applicable, as liver transplantation is not indicated for this diagnosis
Microscopic (histologic) description
- Hepatocytes are enlarged / swollen with pale cytoplasm, glycogenated nuclei, giant mitochondria and accentuated cytoplasmic membranes (Am J Surg Pathol 2006;30:508)
- Mosaic appearance of parenchyma due to compression of sinusoids, resulting in a sheet-like appearance of the hepatocyte architecture
- Macrovesicular steatosis may be present
- No or minimal inflammation or fibrosis
Microscopic (histologic) images
Positive stains
- PAS stain shows glycogen in hepatocytes
Negative stains
- PASD stain is unremarkable (glycogen is digested by diastase)
Electron microscopy description
- Excessive glycogen in hepatocyte cytoplasm and nuclei
Sample pathology report
- Liver, biopsy:
- Glycogenic hepatopathy (see comment)
- Comment: Sections show diffuse hepatocyte enlargement with pale cytoplasm and prominent cytoplasmic membranes. A PAS stain shows glycogen accumulation in hepatocytes. The findings are consistent with the reported history of poorly controlled type 1 diabetes. The differential diagnosis includes glycogen storage diseases.
Differential diagnosis
- Normal liver:
- Pale or enlarged hepatocytes can be confused with normal or fixation artifact
- Fatty liver disease:
- Predominant finding is macrovesicular steatosis; background hepatocytes may be ballooned or have giant mitochondria but this should not be diffuse
- Fatty liver disease also shows Mallory hyaline and zone 3 pericellular fibrosis
- Glycogen storage diseases:
- Inherited disease in children without diabetes history
- Liver enzyme deficiency (glucose 6-phosphatase catalytic activity)
- Mutations in G6PC or G6PT1 genes (EXCLI J 2019;18:30)
- Electron microscopy shows cytoplasmic inclusions consisting of fibrillar glycogen
Board review style question #1
A 15 year old boy with diabetes presented with nausea, vomiting and hepatomegaly. Lab testing reveals HbA1C = 11, aspartate aminotransferase (AST) = 130, alanine aminotransferase (ALT) = 146. Liver biopsy shows excessive glycogen accumulation in hepatocytes. Which of the following is the best initial management?
- Blood sugar control
- Interferon
- Liver transplant
- Pancreas transplant
Board review style answer #1
Board review style question #2
A 21 year old woman with insulin dependent diabetes mellitus presented with abdominal pain, ketoacidosis and hepatomegaly. Her liver biopsy demonstrated pale, enlarged hepatocytes that were strikingly positive on PAS stain. Which of the following is the most likely diagnosis?
- Alcoholic fatty liver disease
- Glycogen storage disease
- Glycogenic hepatopathy
- Hepatitis A
Board review style answer #2
Granulomatous hepatitis
Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Etiology | Clinical features | Diagnosis | Case reports | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Liver disease characterized by the presence of granulomas in the liver
Essential features
- Liver disease characterized by the presence of granulomas in the liver
- There are different etiologies, which may be associated with different subtypes of granulomas
ICD coding
- ICD-10: K75.3 - granulomatous hepatitis, not elsewhere classified
Epidemiology
- Hepatic granulomas are present in 2 - 15% of all liver biopsy and excision specimens (Pathol Res Pract 2011;207:359)
Etiology
- Found in a wide range of infectious and noninfectious conditions (Nat Rev Gastroenterol Hepatol 2011;8:455)
- Immune mediated: primary biliary cholangitis (PBC), autoimmune hepatitis
- Fatty liver disease with lipogranuloma (see alcoholic and nonalcoholic fatty liver disease [NAFLD])
- Drug induced liver injury
- Foreign material: periportal talc or other material from intravenous drug abusers, beryllium, mineral oil, thorotrast
- Neoplastic disorder: lymphoma (Hodgkin and non-Hodgkin), hepatocellular carcinoma, cholangiocarcinoma, inflammatory pseudotumor-like follicular dendritic cell sarcoma
- Systemic disease (e.g., chronic granulomatous disease, Crohn's disease, sarcoidosis, systemic lupus erythematosus, IgG4 disease and other connective tissue disorders)
- Idiopathic: 10 - 15% of all hepatic granulomas
- Diagnosis of exclusion; excellent prognosis (J Clin Pathol 2003;56:850)
Clinical features
- Clinical manifestations depend on the underlying etiology
Diagnosis
- Identification of the presence of granulomas in the liver histologically
- Clinical, radiological and microbiological correlations are required to reveal the underlying etiology
Case reports
- 12 year old boy with IL2RA defect presented with granulomatous hepatitis (Ther Adv Chronic Dis 2022;13:20406223221116798)
- 37 year old man with primary hepatic sarcoidosis mimicking primary biliary cholangitis (J Yeungnam Med Sci 2022;39:256)
- 52 year old woman developed granulomatous hepatitis after immune checkpoint blockade for metastatic melanoma (J Immunother 2021;44:71)
- 58 year old woman with Augmentin induced granulomatous hepatitis (J Clin Transl Hepatol 2021;7:280)
- 68 year old woman developed granulomatous hepatitis in Richter transformation of chronic lymphocytic lymphoma to Hodgkin lymphoma (Am J Case Rep 2021;22:e932904)
Microscopic (histologic) description
- Morphology (epithelioid, suppurative, fibrin ring or lipogranuloma) may suggest underlying etiology
- Epithelioid granuloma (aggregates of epithelioid histiocytes with or without multinucleated giant cells): infectious and noninfectious (e.g., primary biliary cholangitis, drug induced liver injury, foreign body reaction, sarcoidosis, Crohn's disease, chronic granulomatous disease, lymphoma)
- Caseating epithelioid granuloma (necrotic debris at the center surrounded by aggregates of epithelioid histiocytes with or without multinucleated giant cells): typically associated with infections, most notably tuberculosis
- Suppurative granuloma (granulomatous inflammation with stellate abscess formation or suppurative inflammation): bartonellosis, yersinosis, tularemia, listerosis, melioidosis, actinomycosis and fungal infection
- Fibrin ring granuloma (also known as doughnut granuloma; central fat globule surrounded by a circumferential rim of fibrin and histiocytes): originally pathognomonic for Q fever (Coxiella burnetii); now considered as nonspecific and could be associated with mycobacterial infection, staphylococcal bacteremia, leishmaniasis, toxoplasmosis, cytomegalovirus, Epstein-Barr virus, acute hepatitis A, systemic lupus erythematosus, allopurinol toxicity and lymphoma
- Lipogranuloma (central fat globule surrounded by histiocytes without a fibrin ring): alcoholic and nonalcoholic fatty liver disease, mineral oil
Microscopic (histologic) images
Sample pathology report
- Liver, right lobe, biopsy:
- Granulomatous hepatitis without significant fibrosis (see comment)
- Comment: The biopsy shows lobular necroinflammatory activity and scattered noncaseating epithelioid granulomas. Infectious and noninfectious causes need to be considered. From the clinical history, the patient received a course of Augmentin for his upper respiratory tract infection before he was admitted for jaundice. Augmentin is one of several offensive agents associated with drug induced granulomatous hepatitis. Clinical follow up and monitoring of his liver function are recommended. Although histochemical stains for infectious agents (Gram, Grocott, PAS, PASD and Ziehl-Neelsen) do not reveal any specific organism, correlation with microbiological investigation is still recommended to exclude any infection.
Board review style question #1
Which disease is classically associated with fibrin ring granulomas in the liver?
- Familial Mediterranean fever
- Q fever
- Scarlet fever
- Viral hemorrhagic fever
Board review style answer #1
B. Q fever. Fibrin ring granuloma (also known as doughnut granuloma; central fat globule surrounded by a circumferential rim of fibrin and histiocytes) is originally pathognomonic for Q fever (Coxiella burnetii) but now considered as nonspecific features. Answers A, C and D are incorrect because familial Mediterranean fever, scarlet fever and viral hemorrhagic fever are not associated with granulomatous disease in the liver.
Comment Here
Reference: Granulomatous hepatitis
Comment Here
Reference: Granulomatous hepatitis
Board review style question #2
Board review style answer #2
C. Phosphotungstic acid hematoxylin (PTAH) is useful to highlight a thin rim of fibrin surrounding the central fat globule of the fibrin ring granuloma. Answers A, B and D are incorrect because mucicarcimine, PASD and ZN do not stain the fibrin in the fibrin ring granuloma although they are useful to identify microorganisms associated with granulomatous inflammation.
Comment Here
Reference: Granulomatous hepatitis
Comment Here
Reference: Granulomatous hepatitis
Grossing, frozen section & features to report
Table of Contents
Grossing | Frozen section | Features to report - gross | Features to report - microscopic description | Features to report - organizations | Fat in donor liver biopsiesGrossing
- At least one section per 2 cm of tumor for large tumors, including tumor center and periphery
- Submit entire tumor, if can do so in 5 sections or less
- Adjacent and distant uninvolved liver
- Resection margins
- Portal and hepatic veins
- Porta hepatis
- Lymph nodes
- Gallbladder, if present
- Other tissues or organs
- Save intervening levels on biopsies for special stains
Frozen section
- Click here for the frozen section procedure topic
- Accurate and reliable for intraoperative diagnosis of suspected liver lesions - biliary hamartoma is most common entity confused with a malignant tumor (J Clin Pathol 2006;59:352)
- Pretransplant frozen section also used to evaluate donor livers for macrovesicular steatosis, although discrepancies exist with permanent sections in 7% (J Clin Med Res 2011;3:191)
- Optimally, should have clinical data and serum AFP levels available
- Should know if specimen is from a mass
Features to report - gross
- Tumor location (left, right or both lobes), tumor margin as circumscribed or infiltrative
- Presence of hemorrhage, necrosis, central scar and bile
- Extension to adjacent structures
- Other unusual features: unusually large cirrhotic nodules
- References: Arch Pathol Lab Med 2000;124:41, CAP: Protocol for the Examination of Specimens from Patients with Hepatocellular Carcinoma [Accessed 6 December 2017]
Features to report - microscopic description
- Tumor histologic type, tumor grade (specify grading system) and pattern
- Number and size (3 dimensions) of tumor nodules
- Status of resection margins (ask surgeon which margins are important to evaluate)
- Severity of fibrosis (none, mild, moderate, severe, cirrhosis)
- Angiolymphatic invasion
- Mitotic rate
- Findings in nonmalignant liver, including cirrhosis, iron deposition, other tumors, portal vein thrombosis, hepatocyte dysplasia and hepatitis
- Regional lymph nodes: number examined, number and location with metastatic tumor
Features to report - organizations
Fat in donor liver biopsies
HCC - clear cell variant
Table of Contents
Definition / general | Clinical features | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Differential diagnosisDefinition / general
- Predominant appearance of neoplastic hepatocytes with abundant clear cytoplasm
- Predominant in 5 - 16% of cases but some clear cells present in 20 - 40% of cases
- Clear cytoplasm is due to cytoplasmic fat or glycogen
- May need to hunt for typical hepatocellular carcinoma to rule out metastatic tumor
Clinical features
- Elevated serum AFP (92%), may have hypoglycemia or hypercholesterolemia
- Similar prognosis as classic hepatocellular carcinoma (World J Gastroenterol 2010;16:764)
Microscopic (histologic) description
- Trabecular, pseudoacinar, solid or mixed patterns of large number of neoplastic hepatocytes with abundant clear cytoplasm (glycogen or lipid) and round nuclei
- May have bland nuclear features
- May have intracytoplasmic bile (5 - 33%)
- Usually no intratumoral fibrosis except in areas of hemorrhage and necrosis
- Must distinguish from HCC variant with foamy histiocytes (Case Rep Gastroenterol 2010;4:286)
Microscopic (histologic) images
Positive stains
- Polyclonal CEA (canalicular pattern, 63%), HepPar1 (82 - 97%, Mod Pathol 2000;13:874)
- ISH for albumin mRNA (93%, Am J Surg Pathol 2000;24:177)
- Ubiquitin (for Mallory bodies)
Differential diagnosis
- Balloon cell melanoma:
- Clear cell neuroendocrine tumors:
- Epithelioid angiomyolipoma:
- Metastatic renal (PAX2+, EMA+), adrenal (inhibin+, MelanA+, calretinin+) or ovarian carcinoma:
- No classic hepatocellular carcinoma present
HCC - cytology
Table of Contents
Definition / general | Essential features | CTP coding | Sites | Laboratory | Radiology description | Radiology images | Case reports | Cytology description | Cytology images | Sample pathology report | Differential diagnosis of well and moderately differentiated HCC | Differential diagnosis of poorly differentiated HCC | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Most common primary malignancy of the liver
- Hepatocytic differentiation
- Fine needle aspiration is a useful tool in the diagnosis of hepatocellular carcinoma (HCC)
Essential features
- 70 - 90% arise in cirrhotic patients
- Elevated alpha fetoprotein (AFP)
- Accuracy of cytopathologic diagnosis of HCC is high (> 90%) (J Surg Oncol 1991;48:246, Diagn Cytopathol 2002;26:283, Acta Cytol 2013;57:332)
- Common pitfalls:
- False negative: well differentiated HCC mistaken as benign lesion or nonneoplastic liver (false nondiagnostic)
- False positive: dysplastic nodules and benign hepatic tumors mistaken for well differentiated HCC
- Misdiagnosis: poorly differentiated HCC mistaken for metastatic carcinoma
- Cell blocks are useful to confirm hepatocellular differentiation with immunohistochemical stains (arginase1, HepPar1, glypican 3)
CTP coding
Sites
- Liver
- Common metastatic sites: lymph nodes and lungs
- Less common metastatic sites: adrenal glands, bone, kidney, spleen and ovary
Laboratory
- Elevated alpha fetoprotein (AFP)
Radiology description
- Ultrasound typically shows a distinct hepatic nodule; when a nodule is detected through ultrasound, diagnosis is complemented by CT and MRI (Eur J Radiol 2018;101:72)
- Dynamic CT or MRI (contrast enhanced imaging) shows a typical pattern of intense enhancement during arterial phase when compared to surrounding parenchyma and progressive decrease during venous phases (wash out) (Eur J Radiol 2018;101:72)
- When the typical findings are present, a biopsy is not always mandatory for the diagnosis of HCC (Eur J Radiol 2018;101:72)
- Liver Imaging Reporting and Data System (LI-RADS) classifies liver nodules detected on dynamic CT / MRI into categories depending on the risk of malignancy (Eur J Radiol 2018;101:72, Radiology 2018;289:816):
- LI-RAD 1: definitely benign
- LI-RAD 2: probably benign
- LI-RAD 3: intermediate probability of malignancy
- LI-RAD 4: probably HCC
- LI-RAD 5: definitely HCC
Radiology images
Contributed by Lawrence Hsu Lin, M.D., Ph.D. and Tamar C. Brandler, M.D., M.S.
Case reports
- 20 year old woman with lung mass (Int J Clin Exp Pathol 2013;6:1942)
- 32 year old woman with mediastinal lymphadenopathy (Cytojournal 2011;8:2)
- 36 year old man with neck mass (Int J Surg Case Rep 2013;4:76)
- 56 year old man with breast mass (Cytojournal 2012;9:21)
- 64 year old man with hilar lymphadenopathy (Respirol Case Rep 2021;9:e00792)
Cytology description
- Highly cellular smears
- Cytologic features of the neoplastic cells depend on the level of differentiation of HCC
- Well and moderately differentiated show resemblance to normal hepatocytes with:
- Polygonal monotonous cells
- Granular cytoplasm
- Enlarged nuclei
- Increased nuclear to cytoplasmic ratio
- Nuclear membrane irregularity
- Coarse chromatin
- Prominent macronucleoli
- Bile may be present in cytoplasm
- Cytoplasmic inclusions (Mallory-Denk bodies, hyaline inclusions, ground glass) may be present
- Nuclear pseudoinclusions
- Poorly differentiated HCC shows no resemblance to hepatocytes:
- Marked nuclear pleomorphism
- Multinucleated tumor cells
- Spindle cells
- Atypical mitosis
- Necrosis
- Well and moderately differentiated show resemblance to normal hepatocytes with:
- Numerous isolated cells and large naked nuclei
- Nuclear crowding and overlapping cells
- Thickened cell cords (trabeculae) with endothelial wrapping, sometimes better appreciated on cell block
- Pseudoglandular structures (pseudoacinar pattern), sometimes better appreciated on cell block
- Peripheral endothelial cells (endothelial wrapping around neoplastic cells)
- Transgressing vessels (vessels transversing neoplastic tissue)
- Cytologic features of fibrolamellar subtype of HCC
- Larger neoplastic cells than in ordinary HCC
- Lower nuclear to cytoplasmic ratio than in ordinary HCC
- Fibrous stroma fragments
- Specific cytologic features may suggest subtypes of HCC
- Clear cells: clear cell HCC (Diagn Cytopathol 1997;17:306, Acta Cytol 1991;35:671)
- Spindle cells: sarcomatoid HCC
- Immunohistochemistry and special stains
- Reticulin: highlights the thickened trabeculae (> 3 cells) (Mod Pathol 1997;10:1258)
- Arginase1 (ARG1): cytoplasmic and nuclear; highly sensitive and specific (Cancer Cytopathol 2012;120:230, Cancer Cytopathol 2012;120:223)
- HepPar1 (hepatocyte paraffin 1): cytoplasmic and granular; highly sensitive, expressed in 50% of poorly differentiated HCC (Am J Surg Pathol 2002;26:978, Pathol Oncol Res 2015;21:379, Diagn Cytopathol 2004;30:1)
- Glypican 3 (GPC3): cytoplasmic; high sensitivity in poorly differentiated and scirrhous hepatocellular carcinoma, low sensitivity in well differentiated hepatocellular carcinoma, negative in benign and nonneoplastic liver (Diagn Cytopathol 2009;37:629, Pathol Oncol Res 2015;21:379)
- Alpha fetoprotein (AFP): cytoplasmic; highly specific but low sensitivity (Am J Surg Pathol 2002;26:978)
- Polyclonal CEA: canalicular pattern; limited sensitivity in poorly differentiated HCC (Acta Cytol 1997;41:1147, Diagn Cytopathol 2004;30:1)
- TTF1: cytoplasmic; positivity is highly variable and clone dependent (Am J Clin Pathol 2006;125:519, Am J Clin Pathol 2004;121:343)
- CD34: highlights endothelial cells wrapping around thickened trabeculae (Diagn Cytopathol 2004;30:1)
- CAM5.2: positive (Hum Pathol 2002;33:1175, Am J Clin Pathol 1993;99:551)
- CK7, CK19, CK20: usually negative but can be positive in a few cases (Hum Pathol 2002;33:1175)
Cytology images
Contributed by Lawrence Hsu Lin, M.D., Ph.D. and Tamar C. Brandler, M.D., M.S.
Images hosted on other servers:
Sample pathology report
- Liver, mass, ultrasound guided aspiration biopsy (smears and cell block):
- Moderately differentiated hepatocellular carcinoma, positive for malignancy (see comment)
- Comment: Cellular sample showing atypical monotonous cells with enlarged nuclei, abundant granular cytoplasm arranged in trabecular and pseudoglandular patterns with transgressing vessels. Single bare nuclei are present in the background. Immunohistochemical stains show that the neoplastic cells are reactive for HepPar1, arginase1, glypican 3. Polyclonal CEA stain shows a canalicular pattern. Immunohistochemical stains for CK7 and CK20 are nonreactive. The morphologic and immunohistochemical profile supports the diagnosis of moderately differentiated hepatocellular carcinoma.
Differential diagnosis of well and moderately differentiated HCC
- Normal liver:
- Presence of normal appearing hepatocytes may represent a sampling error, hepatic adenoma, focal nodular hyperplasia or regenerative nodule; therefore, correlation with imaging is needed to establish if there was a sampling issue
- Features of normal appearing hepatocytes:
- Low nuclear to cytoplasmic ratio
- No nuclear atypia
- No prominent nucleoli
- Hepatic adenoma:
- Normal appearing hepatocytes
- Normal trabeculae (1 - 3 cells thick)
- No transgressing vessels
- Intact reticulin and glypican 3 negative
- Focal nodular hyperplasia:
- Normal appearing hepatocytes
- Normal trabeculae (1 - 3 cells thick)
- No transgressing vessels
- Bile duct cells
- Fragments of fibrous stroma
- Intact reticulin and glypican 3 negative
- Regenerative nodule:
- Normal appearing hepatocytes
- Normal trabeculae (1 - 3 cells thick)
- Intact reticulin
- Dysplastic nodule:
- Cytologic atypia
- Normal trabeculae (1 - 3 cells thick)
- Intact reticulin
- Well differentiated neuroendocrine tumor:
- Salt and pepper chromatin, rosette formation
- Synaptophysin+, chromogranin+, CD56+, INSM1+
- Angiomyolipoma:
Differential diagnosis of poorly differentiated HCC
- Intrahepatic cholangiocarcinoma:
- Intracytoplasmic mucin
- Glandular architecture
- Positive for mucicarmine
- Immunohistochemistry: positive for CK7, CK19, MOC31; negative for hepatocytic markers
- Combined hepatocellular / cholangiocarcinoma:
- Challenging diagnosis
- Dual population with HCC features and adenocarcinoma morphologic and immunohistochemical profile (Acta Cytol 1997;41:1269)
- Diagnostic pitfall if one of the components is not sampled
- Metastatic neoplasms:
- Metastatic neoplasms are the most common malignancy in the liver
- History of other primary neoplasm
- Often no evidence of cirrhosis in background liver
- Negative for hepatocytic immunohistochemical stains
- Specific morphologic and immunohistochemical features can indicate primary site
- Gastric adenocarcinoma:
- Intracellular mucin, glandular architecture, signet ring cell morphology
- Colon adenocarcinoma:
- Gastrointestinal stromal tumor:
- Spindle morphology
- c-KIT / CD117+, DOG1+
- Breast carcinoma:
- Ductal carcinomas show larger cluster of neoplastic cells, whereas lobular carcinoma can have bland appearance with discohesive pattern and signet ring cell morphology
- GATA3+, mammaglobin+, ER / PR variable, p40-, CK7+, CK20-
- Lung adenocarcinoma:
- Thyroid carcinoma:
- Renal cell carcinoma (clear cell):
- Urothelial carcinoma:
- Prostate adenocarcinoma:
- Neuroendocrine neoplasms:
- Salt and pepper chromatin, rosette formation
- Synaptophysin+, chromogranin+, CD56+, INSM1+
- Small cell carcinoma:
- Small cells with hyperchromatic nuclei and nuclear molding
- Synaptophysin+, chromogranin+, CD56+, INSM1+
- Squamous cell carcinoma:
- Melanoma:
- Sarcomas:
- Spindled, round or pleomorphic cells
- Gastric adenocarcinoma:
Additional references
Board review style question #1
Board review style answer #1
Board review style question #2
Which of the following is the most common neoplasm in the liver?
- Cholangiocarcinoma
- Hepatocellular adenoma
- Hepatocellular carcinoma
- Lymphoma
- Metastatic carcinoma
Board review style answer #2
HCC - fibrolamellar variant
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Definition / general
- Uncommon yet distinctive primary hepatocellular malignancy
- Typically affects young individuals from teens to 40 years
- Large oncocytic neoplastic cells forming tumor tongues separated by collagen bundles
- Characteristically no underlying chronic liver disease
- > 95% of cases harbor the oncogenic DNAJB1-PRKACA fusion gene formed by intrachromosomal deletion on chromosome 19 (Mod Pathol 2018;31:141)
- Rare cases related to biallelic PRKAR1A loss (Hepatology 2018;68:1441)
- Likely a distinct entity due to unique distinctive clinical, histologic and molecular biologic features
Essential features
- Primary hepatocellular neoplasm
- Eosinophilic tumor cells characterized by ample granular cytoplasm
- Intratumoral fibrosis
- Recurrent protein kinase A oncogenic driver abnormalities
Terminology
- Fibrolamellar carcinoma
ICD coding
- ICD-10: C22.0 - liver cell carcinoma
Epidemiology
- Predilection for teenage to 40 years old
- ~99% of cases diagnosed under the age of 50 years at presentation (Mod Pathol 2018;31:141)
- Propensity for late recurrence
Sites
- Liver
Etiology
- Almost all are characterized by DNAJB1-PRKACA oncogenic driver fusion gene (for other mutations, refer to Molecular / cytogenetics description below) (Science 2014;343:1010)
- No chronic liver disease
Clinical features
- Rare over 50 years old
- No gender preference
- Symptoms related to hepatic mass (Semin Diagn Pathol 2017;34:146)
- Rarely associated with gynecomastia or other paraneoplastic phenomena (Lancet 1984;1:538)
- Not associated with viral hepatitis, inborn errors of metabolism or cirrhosis
- Metastasizes to abdominal lymph nodes and peritoneum with greater propensity than conventional hepatocellular carcinoma (Eur J Pediatr Surg 2014;24:461)
Diagnosis
- Combination of
- Compatible histomorphology
- Appropriate immunophenotype (CK7, CD68 positive) or detection of key genomic events (DNAJB1-PRKACA, PRKACA rearrangement, PRKACA amplification, PRKAR1A loss)
Laboratory
- Serum alpha fetoprotein is classically not elevated
- No other routinely used serum or plasma markers
- Circulating tumor DNA assay has yet to be made commercially available
Radiology description
- CT scan and MRI: nonspecific findings; central scar (similar to focal nodular hyperplasia) may be identified; often calcified
Prognostic factors
- Perhaps the most controversial aspect of fibrolamellar carcinoma - not adequately stratified by current AJCC staging scheme
- Features associated with adverse outcome: vascular invasion, number of tumors, surgical resectability (Cancer 2006;106:1331, J Gastrointest Surg 2016;20:1725, Oncology 2013;85:197)
Case reports
- Carney complex
- 9 year old boy (J Pediatr Endocrinol Metab 2007;20:247)
- 14 year old girl 5 years after hepatocellular adenoma (Arch Pathol Lab Med 2004;128:222)
- 53 year old woman with synchronous auricular myxoma (Case Rep Pathol 2015;2015:241708)
- Peritoneal spread
- 23 year old woman with ovarian metastasis (Rom J Morphol Embryol 2017;58:187)
- 26 year old woman (Eur J Radiol 1999;32:119)
Treatment
- Surgery is the only curative option (Am J Gastroenterol 2009;104:2617)
- Early detection of relapse with multimodality therapy improves survival (Eur J Surg Oncol 2009;35:617)
Gross description
- Single (75%), large (frequently > 10 cm), hard, well circumscribed, bulging, tan tumor with fibrous bands
- Central stellate scar is noted in approximately 70%
- Variable bile staining, hemorrhage and necrosis
Microscopic (histologic) description
- Trabecula, sheets or cords of neoplastic cells with abundant oncocytic cytoplasm cells in background of dense collagen bundles frequently arranged in parallel lamellae
- Cells are large and polygonal with well defined cell borders
- Abundant granular and eosinophilic cytoplasm due to abundant mitochondria
- Pale or pink bodies are frequently noted but not necessary for diagnosis
- Typical nuclear features include open chromatin and prominent macronucleoli (Adv Anat Pathol 2007;14:217)
- Vascular invasion may be seen
- Histologically, fibrous bands coalesce into central scar
- Nonneoplastic liver is within normal histologic limits
- Radiologic calcification corresponds to stromal calcification
- Calcified individual cells may be identified as well
- Variable: focal nuclear anisonucleosis, sheet-like growth without intervening fibrous bands, pseudoglandular or pelioid patterns
Microscopic (histologic) images
Contributed by Rondell P. Graham, M.B.B.S. and @RaulSGonzalezMD on Twitter
Case #161
Images hosted on other servers:
Cytology description
- Individual cells with ample cytoplasm, open nuclear chromatin and prominent nucleoli; may contain bile
Cytology images
Positive stains
- HepPar1 and CK7 (Mod Pathol 2010;23:1180, Histopathology 1990;17:101)
- CD68 (Mod Pathol 2011;24:390)
- CK19
- Also fibrinogen (pale bodies), alpha-1 antitrypsin, polyclonal CEA and CAM 5.2 (CK8 / 18)
Negative stains
- Liver fatty acid binding protein (LFABP)
- In rare cases PRKAR1A; often individuals with the Carney complex
Electron microscopy description
- Numerous mitochondria
- Abundant endoplasmic reticulum membranes with concentric whorls
- Internalized canaliculi lined by microvilli (Mod Pathol 2017;30:892)
Molecular / cytogenetics description
- > 95% of cases are characterized by DNAJB1-PRKACA fusion gene; diagnostic tests exist
- Rare cases characterized by biallelic PRKAR1A loss (mostly in patients with the Carney complex) instead of the above fusion gene (Hepatology 2018;68:1441)
- Single case characterized by PRKACA amplification without the above genomic changes has been identified (Surg Pathol Clin 2018;11:377)
- Transcriptome has been published and revealed multiple insights (Proc Natl Acad Sci U S A 2015;112:E5916)
- Overall fewer chromosomal abnormalities than classic hepatocellular carcinoma (Mod Pathol 2009;22:134)
Sample pathology report
- Liver, segment 3, resection:
- Fibrolamellar hepatocellular carcinoma (see synoptic report and comment)
- Comment: A trichrome stain shows no significant fibrosis. An iron stain is unremarkable.
Differential diagnosis
- Cholangiocarcinoma:
- Truly glandular, often conspicuous pleomorphism
- Focal nodular hyperplasia:
- Ductular reaction around central scar
- Lesional cells are not characteristically oncocytic
- Does not have the nuclear features of fibrolamellar carcinoma
- Hepatocellular carcinoma, sclerosing variant:
- No oncocytes, smaller tumor cells, pseudoglandular pattern common
- Metastatic carcinoma with sclerotic stroma:
- Conspicuous pleomorphism
- Neuroendocrine tumors:
- Only oncocytic examples
- Nuclear features are often not typical of fibrolamellar carcinoma
- Positive for neuroendocrine markers
- Paraganglioma:
- May have abundant oncocytic cytoplasm
- Round nuclei without the typical features of fibrolamellar carcinoma, vascular stroma without dense fibrosis
- Positive for neuroendocrine markers and negative for cytokeratins (Am J Surg Pathol 2002;26:945)
Board review style question #1
What is the characteristic status of the nonneoplastic liver in patients with fibrolamellar carcinoma?
- Chronic viral hepatitis C without advanced fibrosis
- Cirrhosis due to chronic viral hepatitis B
- Glycogen storage disease
- Normal
- Steatohepatitis
Board review style answer #1
HCC - lymphocyte rich
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Rare subtype of hepatocellular carcinoma (HCC) designated by the WHO; characterized by a dense lymphoid infiltrate with more lymphocytes than tumor cells
Essential features
- Striking lymphocytic infiltrate is a defining feature
- Not associated with Epstein-Barr virus (EBV) or microsatellite instability
Terminology
- May be called lymphoepithelioma-like HCC when the tumor is poorly differentiated (Gastroenterol Clin North Am 2017;46:365)
ICD coding
- ICD-10: C22.7 - other specified carcinomas of liver
Epidemiology
- Incidence ≤ 1% of HCC
- Based on a review of 42 cases reported in the literature, there appears to be a male predominance (M:F = 2.8:1), with mean age of 58 years (range: 39 - 81 years) (Am J Surg Pathol 2015;39:304, Hepatology 1998;27:407, Histopathology 2000;37:523)
Sites
- Liver
Etiology
- Approximately half of cases have underlying cirrhosis or chronic infection with hepatitis B / C (Am J Surg Pathol 2015;39:304)
Clinical features
- Very rare tumor with limited clinical and outcome data
Diagnosis
- Imaging modalities for diagnosis of HCC: multiphasic computed tomography (CT) or magnetic resonance imaging (MRI)
- Tissue biopsy is indicated if imaging is not diagnostic of HCC
Laboratory
- Elevation in serum alpha fetoprotein (AFP)
Radiology description
- Dynamic perfusion pattern of arterial hyperenhancement and venous or delayed phase washout is characteristic of HCC
Prognostic factors
- May have better prognosis in comparison to classic HCC (Am J Pathol 2017;187:1438, Am J Surg Pathol 2015;39:304)
- Majority of patients present with low stage disease, a single lesion, and without vascular invasion (Am J Surg Pathol 2015;39:304)
- Prognostic factors for HCC: stage (TNM), single lesion (versus multifocal), size, vascular invasion, portal vein thrombosis, severity of underlying liver disease (Liver Int 2009;29:502, J Surg Oncol 2018;117:644)
Case reports
- 37 year old woman with chronic hepatitis B and C infection (Medicine (Baltimore) 2017;96:e9416)
- 58 year old man with elevated serum AFP (Int J Clin Exp Pathol 2017;10:7893)
- 78 year old woman with a liver mass (J Liver Cancer 2021;21:69)
- 79 year old man with a liver mass (World J Surg Oncol 2013;11:97)
- 81 year old woman with chronic hepatitis C infection (World J Gastroenterol 2015;21:10468)
Treatment
- Surgical resection
- Radiofrequency ablation
- Transarterial chemoembolization (TACE)
- Transplantation (e.g., Milan criteria, modified by some institutions) (Nat Rev Gastroenterol Hepatol 2017;14:203)
Gross description
- Majority present as a solitary lesion (Am J Surg Pathol 2015;39:304)
Microscopic (histologic) description
- Cords and trabeculae of tumor cells in a dense lymphoid stroma (lymphocytes outnumber tumor cells in most fields)
- Lymphoid infiltrate predominantly T cells with scattered B cells and germinal centers
- May show piecemeal necrosis
- Histologic grade usually well to moderately differentiated
- If poorly differentiated, the term lymphoepithelioma-like HCC may be used (Gastroenterol Clin North Am 2017;46:365)
- May have focal syncytial growth
Microscopic (histologic) images
Positive stains
- Cytokeratin
- Hepatocellular markers (arginase1, glypican 3, HepPar1) variably positive
- Majority of lymphocytes are CD3+ / CD8+ cytotoxic T cells (Am J Surg Pathol 2015;39:304)
Negative stains
Molecular / cytogenetics description
- Most cases negative for EBV in situ hybridization (ISH); EBV positivity reported in one study (Diagn Mol Pathol 2004;13:183)
- Tumor infiltrating lymphocytes not associated with microsatellite instability (Am J Surg Pathol 2015;39:304)
- Lymphocyte rich hepatocellular carcinoma has been shown to have focal amplification of chromosome 11q13.3, which is considered to be an immune checkpoint signature, making them a promising target for immunotherapy (J Pathol 2019;249:166)
Sample pathology report
- Liver, mass, core biopsy:
- Lymphocyte rich hepatocellular carcinoma (see comment)
- Comment: The tumor shows histologic features of lymphocyte rich hepatocellular carcinoma with nests and cords of hepatoid cells within a dense lymphoid stroma. The tumor cells are positive for pancytokeratin, HepPar1 and glypican 3, and negative for CK7, CK19 and mucicarmine. EBV in situ hybridization is negative.
Differential diagnosis
- Lymphoepithelioma-like cholangiocarcinoma:
- Classic HCC with increased lymphocytes:
- Tumors with only mild to moderate increase in lymphocytes should be classified as conventional HCC
- Lymphoma (primary hepatic lymphoma or secondary involvement by systemic disease):
- Dense infiltrate of atypical B or T cells
- No intermixed neoplastic hepatocytes
- Positive hematolymphoid markers (depends on the entity), negative cytokeratin and hepatocellular markers
- Inflammatory myofibroblastic tumor:
- Tumor of myofibroblasts with plasma cells, lymphocytes and eosinophils
- ALK+ spindle cells (subset)
- IgG4 related disease:
- Abundant IgG4+ plasma cells, systemic disease, elevated serum IgG4
- Inflammatory variant of angiomyolipoma:
- Inflammatory pseudotumor-like follicular / fibroblastic dendritic cell sarcoma:
- Inflammatory pseudotumor (nonneoplastic):
- Mixed inflammation, granulomas, necrosis / abscess, rule out AFB, T. pallidum, parasites
- No intermixed neoplastic hepatocytes
Additional references
Board review style question #1
Board review style answer #1
Board review style question #2
Which of the following features is characteristic of lymphocyte rich hepatocellular carcinoma (HCC)?
- Cytokeratin is usually negative
- Has a worse prognosis in comparison to classic HCC
- It is one of the more common variants of HCC
- Lymphocytes outnumber tumor cells in most fields
- Most cases are positive for Epstein-Barr virus in situ hybridization
Board review style answer #2
D. Lymphocytes outnumber tumor cells in most fields
Comment Here
Reference: Lymphocyte rich hepatocellular carcinoma
Comment Here
Reference: Lymphocyte rich hepatocellular carcinoma
HCC - macrotrabecular massive
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Diagnosis | Laboratory | Prognostic factors | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Subtype of hepatocellular carcinoma with macrotrabecular pattern (≥ 6 - 10 cells thick) (Am J Surg Pathol 2019;43:943, Hepatology 2018;68:103, J Hepatocell Carcinoma 2022;9:661)
- Macrotrabecular pattern in > 50% of the tumor
Essential features
- Hepatocellular carcinoma with > 50% growth having a macrotrabecular pattern (≥ 6 - 10 cells thick) (Am J Surg Pathol 2019;43:943, Hepatology 2018;68:103, J Hepatocell Carcinoma 2022;9:661)
- Presents with higher grade and stage compared to conventional hepatocellular carcinoma (Am J Surg Pathol 2019;43:943)
- Associated with high serum alpha fetoprotein (AFP) (Am J Surg Pathol 2019;43:943, Hepatology 2018;68:103)
- Poor prognosis with early recurrence and poor overall survival (Hepatology 2018;68:103, J Hepatol 2017;67:727)
- Vascular invasion is common (J Hepatol 2017;67:727)
- Associated with TP53 mutations and FGF19 amplification (J Hepatol 2017;67:727)
Terminology
- Macrotrabecular massive hepatocellular carcinoma (MTM HCC)
- Macrotrabecular hepatocellular carcinoma (MT HCC)
ICD coding
- ICD-O: 8170/3 - hepatocellular carcinoma
- ICD-11: 2C12 & H00048 - malignant neoplasms of liver or intrahepatic bile ducts & hepatocellular carcinoma
Epidemiology
- Relative frequency: 10 - 15% (Am J Surg Pathol 2019;43:943, Hepatology 2018;68:103, J Hepatocell Carcinoma 2022;9:661)
- Male predominant (71 - 79%)
Sites
- Liver
Etiology
- HBV infection, HCV infection, alcohol intake, nonalcoholic steatohepatitis (NASH) or other / undetermined etiologies (Am J Surg Pathol 2019;43:943, Hepatology 2018;68:103)
Diagnosis
- Based on light microscopic examination of tissue with compatible histomorphology findings (hepatocellular carcinoma with > 50% growth having a macrotrabecular pattern [≥ 6 - 10 cells thick])
Laboratory
- Serum AFP level (> 100 ng/mL) is elevated in 40 - 73% patients (Am J Surg Pathol 2019;43:943, Hepatology 2018;68:103)
Prognostic factors
- Worse prognosis with larger tumor size, macrovascular invasion, microvascular invasion, poor differentiation; these are frequent findings (Hepatology 2018;68:103, J Hepatol 2017;67:727)
- High tumor stage compared to conventional hepatocellular carcinoma
- High early and overall recurrence; low recurrence free and overall survival (Hepatology 2018;68:103, Am J Surg Pathol 2019;43:943, J Hepatol 2017;67:727)
Treatment
- Surgical resection
- Radiofrequency ablation
- Transarterial chemoembolization (TACE)
- Transplantation
Gross description
- Large tumor size (66% > 50 mm) with satellite nodules or macrovascular invasion (Hepatology 2018;68:103, J Hepatol 2017;67:727)
- Background liver with or without cirrhosis
Microscopic (histologic) description
- Hepatocellular carcinoma with > 50% growth having a macrotrabecular pattern (≥ 6 - 10 cells thick) (Am J Surg Pathol 2019;43:943, Hepatology 2018;68:103)
- Trabeculae observed in cross sections are bordered by a complete rim of CD34 positive endothelial cells in more than half of the tumor area (vessels encapsulating tumor clusters [VETC]) (Hepatology 2020;71:183)
- Associated with micro and macrovascular invasion (> 60%) (Am J Surg Pathol 2019;43:943, J Hepatol 2017;67:727)
- Associated with higher tumor cell grade and presence of anaplastic tumor cells (Am J Surg Pathol 2019;43:943)
Microscopic (histologic) images
Contributed by Xuchen Zhang, M.D., Ph.D.
Positive stains
- Same as markers for conventional hepatocellular carcinoma (variably positive): hepatocytic differentiation markers (HepPar1, arginase1, polyclonal CEA and CD10 in canalicular pattern, AFP and albumin mRNA ISH), cytokeratin CAM 5.2 and malignant markers (glypican 3, glutamine synthetase and p53)
- Endothelial specific molecule 1 (ESM1) stains the sinusoidal stromal cells forming nearly a continuous positive surrounding of macrotrabeculae (Clin Cancer Res 2019;25:5859)
Negative stains
- CK7, CK19, mucin (mucicarmine), MOC31 and BerEP4
Molecular / cytogenetics description
- Often harbor TP53 mutations or FGF19 amplifications (J Hepatol 2017;67:727)
- Positive for albumin mRNA ISH
Sample pathology report
- Liver, segment 5, mass, biopsy:
- Hepatocellular carcinoma, poorly differentiated, with macrotrabecular pattern (see comment)
- Comment: Histologic sections show thickened cords that are composed of polygonal tumor cells with distinct cell membranes, eosinophilic cytoplasm, high N:C ratio, prominent nucleoli, conspicuous mitoses and necrosis. The thickened cords contain more than 6 - 10 cells thick tumor cells, consistent with macrotrabecular pattern. This pattern of hepatocellular carcinoma has been recently categorized as macrotrabecular massive subtype.
- Liver, right lobe, right hepatectomy:
- Poorly differentiated hepatocellular carcinoma, macrotrabecular massive subtype (see comment and synoptic report)
- Nonneoplastic background liver with chronic hepatitis B and portal fibrosis (grade 1 of 4, stage 1 of 4)
- Comment: The current hepatocellular carcinoma shows mixed acinar, trabecular and macrotrabecular histologic patterns. The macrotrabecular pattern component accounts for 70% of the entire tumor. The tumor cells in the macrotrabeculae (≥ 6 - 10 cells thick) show marked nuclear pleomorphism with numerous mitoses and prominent nucleoli. Anaplastic giant tumor cells are present. Immunohistochemical stains show that the tumor cells are positive for arginase1, HepPar1 and focally positive for glypican 3. Peritumoral microvascular invasion is present. Also noted grossly is that there is a tumor thrombus in one of the portal vein branches; this is confirmed microscopically.
Differential diagnosis
- Trabecular hepatocellular carcinoma:
- Hepatocellular carcinoma with trabecular growth pattern of < 6 cells thick
Additional references
Board review style question #1
Which of the following hepatocellular carcinoma subtypes is associated with worse prognosis and frequent vascular invasion?
- Clear cell subtype
- Fibrolamellar
- Lymphocyte rich
- Macrotrabecular massive
- Steatohepatitic
Board review style answer #1
Board review style question #2
Board review style answer #2
HCC - sarcomatoid variant
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Hepatocellular carcinoma (HCC) variant, partially or entirely composed of malignant spindle cells
Essential features
- Component of spindle cell morphology
- Area of conventional HCC usually present to support the diagnosis
- Worse prognosis than classic HCC
- Sarcomatoid transformation associated with repeated chemotherapy / chemoembolization
Terminology
- Also called spindle cell HCC, pseudosarcomatous HCC
- May be called carcinosarcoma when heterologous elements are present (Gastroenterol Clin North Am 2017;46:365, J Clin Oncol 2014;32:e63)
ICD coding
- ICD-10: C22.7 - other specified carcinomas of liver
Epidemiology
- Incidence ranges from 0.3% of HCC in resected specimens to 9.4% in autopsy series (Cancer Med 2021;10:6227, Cancer 1987;59:310, Cancer Chemother Pharmacol 1989;23:S4)
- Patients tend to be older and predominantly male (Hepatology 2019;69:209, J Cancer Res Clin Oncol 2022;148:1685)
Sites
- Liver
Pathophysiology
- Associated with expression of genes related to epithelial mesenchymal transition (EMT) and inflammation (Int J Cancer 2021;149:546)
- Higher expression of PDL1 in tumor cells and infiltration by immune cells compared to conventional HCC (Int J Cancer 2021;149:546, Aging (Albany NY) 2021;13:15126)
Etiology
- Similar etiologic factors to classic HCC (J Cancer Res Clin Oncol 2022;148:1685)
- Sarcomatoid change is more frequent in patients undergoing repeated chemotherapy or transarterial chemoembolization (Cancer Chemother Pharmacol 1989;23:S4)
Clinical features
- Larger tumor size, advanced stage and higher incidence of extrahepatic disease (e.g., lymph nodes, lungs, bone) compared to classic HCC (Cancer Med 2021;10:6227, World J Gastroenterol 2020;26:4327, J Cancer Res Clin Oncol 2022;148:1685)
Diagnosis
- Imaging modalities for diagnosis of HCC: multiphasic computed tomography (CT) or magnetic resonance imaging (MRI)
- Tissue biopsy is indicated if imaging is not diagnostic of HCC
Laboratory
- Lower serum alpha fetoprotein (AFP) compared to classic HCC (Surg Pathol Clin 2013;6:367, World J Gastroenterol 2020;26:4327)
Radiology description
- Large hepatic mass with central necrosis and peripheral rim enhancement (may mimic hepatic abscess or cholangiocarcinoma) (J Comput Assist Tomogr 2008;32:745)
Radiology images
Prognostic factors
- Worse prognosis compared to classic HCC (Hepatology 2019;69:209, Ann Surg Oncol 2015;22:S1048, Cancer Med 2021;10:6227, Int J Cancer 2021;149:546, World J Gastroenterol 2020;26:4327, J Cancer Res Clin Oncol 2022;148:1685)
- Prognostic factors for HCC: stage (TNM), single lesion versus multifocal, size, vascular invasion, portal vein thrombosis, severity of underlying liver disease (Liver Int 2009;29:502, J Surg Oncol 2018;117:644)
Case reports
- 56 year old man with abdominal pain and suspected hepatic abscess (Medicine (Baltimore) 2020;99:e22489)
- 62 year old man with a history of hepatitis B (J Cancer Res Ther 2015;11:665)
- 68 year old woman with abdominal distension (World J Surg Oncol 2017;15:219)
- 68 year old man with a right liver mass (Diagn Pathol 2015;10:40)
- 70 year old man with right upper quadrant pain (J Clin Oncol 2014;32:e63)
Treatment
- Surgical resection (Int J Surg 2018;55:145, Ann Surg Oncol 2015;22:S1048)
- Radiofrequency ablation
- Transarterial chemoembolization (TACE)
- Transplantation (e.g., Milan criteria, modified by some institutions, Nat Rev Gastroenterol Hepatol 2017;14:203)
Gross description
- Poorly circumscribed, lobulated mass; may contain areas of necrosis and possibly heterologous elements
Gross images
Microscopic (histologic) description
- Partially or entirely composed of malignant spindle cells
- Component of classic HCC is often present to help confirm the diagnosis
- Spindle component may have variable cellularity, nuclear pleomorphism, frequent mitoses
- If heterologous elements are present, the term carcinosarcoma may be used
- Various types of heterologous elements have been reported, including rhabdoid, osteoid and chondroid differentiation; may have pleomorphic and osteoclast-like giant cells (Virchows Arch 1999;434:511, Am J Surg Pathol 2007;31:817, Pathol Int 2000;50:919, Clin Mol Hepatol 2014;20:313, Diagn Pathol 2015;10:40)
Microscopic (histologic) images
Positive stains
- Cytokeratin variably positive (20 - 60%) (Cancer 1987;59:310, Cancer 1996;77:51)
Negative stains
- Hepatocellular markers (HepPar1, arginase1, glypican 3) typically negative in the sarcomatoid component
- Sarcomatoid markers (e.g., vimentin, actin): typically negative in the carcinomatous component
Molecular / cytogenetics description
- Negative albumin mRNA by ISH in the sarcomatoid component (Pathol Res Pract 2013;209:249)
- Molecular alterations: CDKN2A, EPHA5, FANCM, MAP3K1 mutations (Cancer Med 2021;10:6227)
- Common cell of origin of epithelial and sarcomatoid components (same TP53 mutation), with clonal evolution (J Clin Oncol 2014;32:e63)
Sample pathology report
- Liver, mass, core biopsy:
- Hepatocellular carcinoma, sarcomatoid variant (see comment)
- Comment: This tumor shows two distinct morphologies. One component shows features of classic hepatocellular carcinoma, while the second component shows sarcomatoid features, including pleomorphic spindle cells. Cytokeratin is variably positive and hepatocellular markers (HepPar1, arginase1 and glypican 3) are negative in the sarcomatoid component, as is typical for this variant.
Differential diagnosis
- Sarcoma (undifferentiated pleomorphic sarcoma and fibrosarcoma):
- Clinical history of sarcoma
- Will not have area of classic HCC
- Immunohistochemistry (entirely negative for pancytokeratin) and potentially molecular testing (e.g., next generation sequencing cancer gene panel) are necessary for diagnosis
- Undifferentiated primary liver carcinoma:
- Shows no specific differentiation except epithelial based on morphology and immunohistochemistry (pancytokeratin+)
- No evidence of differentiation towards HCC or cholangiocarcinoma
- May be albumin ISH+
- Metastatic sarcomatoid carcinoma:
- Will not have area of classic HCC
- Clinical history of carcinoma
- Usually multiple nodules
- Immunohistochemistry (pancytokeratin+) and potentially molecular testing (e.g., next generation sequencing cancer gene panel) are necessary for diagnosis
- Negative for hepatocellular markers, positive keratin staining (usually patchy, perhaps only for high molecular weight keratins, e.g., as detected on MNF116)
Board review style question #1
Which of the following histologic features is characteristic of the sarcomatoid variant of hepatocellular carcinoma?
- Contains components of conventional HCC and spindle cell morphology
- Cytokeratin is always negative in the sarcomatoid component
- Hepatocellular markers are usually positive in the sarcomatoid component
- Must be entirely composed of malignant spindle cells
- Necrosis is not a common feature
Board review style answer #1
A. Contains components of conventional HCC and spindle cell morphology
Comment Here
Reference: Sarcomatoid hepatocellular carcinoma
Comment Here
Reference: Sarcomatoid hepatocellular carcinoma
Board review style question #2
Which of the following is true regarding the sarcomatoid variant of hepatocellular carcinoma (HCC)?
- Associated with a better prognosis than classic HCC
- Higher serum AFP in comparison to classic HCC
- More common in patients undergoing repeated chemotherapy or transarterial chemoembolization
- Patients are predominantly female
- There is a lower incidence of extrahepatic spread in comparison to classic HCC
Board review style answer #2
C. More common in patients undergoing repeated chemotherapy or transarterial chemoembolization
Comment Here
Reference: Sarcomatoid hepatocellular carcinoma
Comment Here
Reference: Sarcomatoid hepatocellular carcinoma
HCC - scirrhous type
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Subtype of hepatocellular carcinoma (HCC) designated by the WHO, with abundant fibrous stroma separating nests and trabecula of tumor cells
Essential features
- Unencapsulated, often subcapsular location, may have satellite lesions
- Abundant fibrous stroma (> 50% of tumor) but lacks central scar or radiating fibrous bands
- May mimic intrahepatic cholangiocarcinoma on imaging and gross evaluation
Terminology
- Also called sclerosing variant of HCC
ICD coding
- ICD-10: C22.7 - other specified carcinomas of liver
Epidemiology
- Incidence ranges from 0.2 - 4.6% of all HCC (J Gastroenterol Hepatol 2006;21:1470)
Sites
- Liver, often subcapsular
Pathophysiology
- Molecular alterations: TSC1 / TSC2 mutations (J Hepatol 2017;67:727)
- Associated with expression of transforming growth factor beta (TGFβ), epithelial - mesenchymal transition (EMT) and stem cell / progenitor related genes (J Hepatol 2017;67:727, Hepatology 2012;55:1776)
Etiology
- Similar etiologic factors to classic HCC
- May arise in cirrhotic and noncirrhotic liver (Dig Dis Sci 2012;57:1698)
Clinical features
- No differences in patient demographics, presence of cirrhosis or serum alpha fetoprotein (AFP) levels, in comparison with classic HCC (Surg Pathol Clin 2013;6:367)
- Association with hypercalcemia and hypophosphatemia has been described (Liver 1981;1:33)
Diagnosis
- Imaging modalities for diagnosis of HCC: multiphasic computed tomography (CT) or magnetic resonance imaging (MRI)
- Tissue biopsy is indicated if imaging not diagnostic of HCC
Laboratory
- Elevation in serum alpha fetoprotein (AFP)
Radiology description
- Radiographic appearance may be similar to intrahepatic cholangiocarcinoma
- Contrast enhanced CT scan shows peripheral ring enhancement in arterial phase and delayed central enhancement in venous phase (Eur J Radiol 2009;69:123)
Prognostic factors
- Comparison of prognosis with classic HCC shows conflicting results (Surg Pathol Clin 2013;6:367)
- Prognostic factors for HCC: stage (TNM), single lesion versus multifocal, size, vascular invasion, portal vein thrombosis, severity of underlying liver disease (Liver Int 2009;29:502, J Surg Oncol 2018;117:644)
Case reports
- 60 year old man with cirrhosis and a 1.5 cm liver nodule (World J Gastroenterol 2009;15:2296)
- 67 year old woman with epigastric pain (Clin Gastroenterol Hepatol 2009;7:A28)
- 68 year old man with hereditary hemochromatosis (Semin Diagn Pathol 2017;34:126)
Treatment
- Surgical resection
- Radiofrequency ablation
- Transarterial chemoembolization (TACE)
- Transplantation (e.g., Milan criteria, modified by some institutions) (Nat Rev Gastroenterol Hepatol 2017;14:203)
Gross description
- Unencapsulated, gray-white, firm, lobulated mass, often with serrated border
- Often subcapsular, may have satellite nodules
- More extensive fibrosis than fibrolamellar variant; no radiating fibrous bands, no central scar
- Gross appearance may be similar to intrahepatic cholangiocarcinoma
- Reference: Surg Pathol Clin 2013;6:367
Microscopic (histologic) description
- Abundant fibrous stroma separating nests / trabeculae of tumor cells
- Criteria for amount of intratumoral fibrosis is > 50% (Gastroenterol Clin North Am 2017;46:365)
- Absence of fibrous capsule, no necrosis or hemorrhage, may contain intratumoral portal tracts and prominent tumor infiltrating lymphocytes (Pathol Int 2005;55:724, Hepatogastroenterology 2009;56:1086)
- Clear cell change, steatotic change and hyaline bodies may be present (J Gastroenterol Hepatol 2006;21:1470, Hum Pathol 2019;86:222)
- Less frequently poorly differentiated and more likely to have steatosis than nonscirrhous HCC (Hum Pathol 2019;86:222)
Microscopic (histologic) images
Cytology description
- Cells are polygonal with distinct cell membranes, high N:C ratio and round nuclei and may have prominent nucleoli (similar to moderately differentiated HCC)
Positive stains
- Glypican 3 and arginase1 in 90% of cases (Mod Pathol 2013;26:782)
- CK7, CK19 and EpCAM in majority of cases (Histopathology 2005;47:382)
Negative stains
- HepPar1 and polyclonal CEA in > 50% (Surg Pathol Clin 2013;6:367)
- Mucin (e.g., mucicarmine)
Molecular / cytogenetics description
- Associated with TSC1 / TSC2 mutations (J Hepatol 2017;67:727)
Sample pathology report
- Liver, mass, partial hepatectomy:
- Scirrhous hepatocellular carcinoma (see comment)
- Comment: This tumor shows histologic features of scirrhous hepatocellular carcinoma with nests and trabecula of hepatoid cells within a dense fibrous stroma. The tumor cells show positive staining for glypican 3, arginase1 and CK7, as is typical for this variant.
Differential diagnosis
- Fibrolamellar variant:
- Intrahepatic cholangiocarcinoma:
- Metastatic carcinoma of pancreas:
- May form glands / tubules with cytoplasmic or intraluminal mucin
- Glypican 3-, arginase1-, albumin ISH-
- Epithelioid hemangioendothelioma:
- Myxoid stroma, blister cells with red blood cells in lumens or vacuoles
- CD34+, ERG+, CD31+, FLI1+, mucicarmine-, variable pankeratin, CAMTA1+, TFE3+ (subset) (Arch Pathol Lab Med 2009;133:967)
- Hepatocellular carcinoma with therapy induced fibrosis:
- May be difficult or impossible to distinguish from scirrhous HCC
- Check treatment history; look for other evidence of injury (e.g., necrosis, embolization beads)
Additional references
Board review style question #1
Board review style answer #1
Board review style question #2
Which of the following is true regarding the scirrhous variant of hepatocellular carcinoma?
- Association with hypocalcemia has been described
- CK7 and CK19 are often negative
- It is associated with TSC1 / TSC2 mutations
- There is often necrosis or hemorrhage
Board review style answer #2
HCC - steatohepatitic
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- WHO recognized histological variant of hepatocellular carcinoma (HCC) in which the tumor cells show histologic features resembling nonneoplastic steatohepatitis
- This variant usually arises in the setting of steatohepatitis (Am J Surg Pathol 2010;34:1630)
Essential features
- Variant of hepatocellular carcinoma with histologic features resembling nonneoplastic steatohepatitis (Am J Surg Pathol 2010;34:1630)
- Arises in the setting of nonalcoholic steatohepatitis as well as alcoholic steatohepatitis (Am J Surg Pathol 2010;34:1630, Am J Surg Pathol 2020;44:1406)
- May have yellow appearance on cut surface of tumor
- Ubiquitin immunohistochemical stain can be used to highlight Mallory-Denk bodies
- Associated with S1 molecular subclass (TGFβ pathway activation) (Liver Int 2016;36:108)
Terminology
- Steatohepatic variant of hepatocellular carcinoma
ICD coding
- No specific code for steatohepatitic HCC
Epidemiology
- Age sixth to seventh decade (similar to conventional HCC) (Am J Surg Pathol 2010;34:1630)
- M > F (similar to conventional HCC) (Am J Surg Pathol 2010;34:1630)
- Represents 5 - 20% of HCC
Sites
- Liver
Pathophysiology
- Similar to HCC
Etiology
- Nonalcoholic steatohepatitis (Am J Surg Pathol 2010;34:1630)
- Obesity
- Diabetes
- Hypertension
- Dyslipidemia
- Alcoholic steatohepatitis (Am J Surg Pathol 2020;44:1406)
- May arise in absence of fatty liver disease or metabolic syndrome (Hum Pathol 2015;46:1769)
Clinical features
- See Etiology
Diagnosis
- Similar to HCC
Laboratory
- Similar to HCC
Radiology description
- Prominent fatty deposits on MRI (Clin Radiol 2021;76:160.e15)
Prognostic factors
- Similar prognosis to conventional HCC
Case reports
- 49 year old woman with hepatitis C related chronic liver disease (Trop Gastroenterol 2014;35:49)
- 65 year old man with history of diabetes and hypertension with 4.8 cm liver mass (Indian J Surg Oncol 2014;5:161)
Treatment
- Similar to HCC
Gross description
- May show yellow cut surface
Microscopic (histologic) description
- Hepatocellular carcinoma with ≥ 50% of tumor showing 3 or more of the following steatohepatitis-like features (Am J Surg Pathol 2010;34:1630):
- Steatosis
- Hepatocyte ballooning
- Mallory-Denk bodies
- Inflammation
- Pericellular fibrosis
Microscopic (histologic) images
Cytology description
- Trabecular fragments of atypical hepatocytes with steatotic vacuoles (Indian J Surg Oncol 2014;5:161)
Positive stains
- Similar to conventional hepatocellular carcinoma (arginase1, HepPar1, glypican 3, canalicular staining pattern with CD10 and polyclonal CEA, albumin in situ hybridization, reticulin can highlight thickened trabeculae)
- Ubiquitin stain highlights Mallory-Denk bodies
- C reactive protein (J Hepatol 2017;67:727)
- Trichrome stain highlights pericellular fibrosis
- Oil red O or Sudan Black stains can highlight fat content but must be performed on frozen tissue section
Molecular / cytogenetics description
- Associated with S1 molecular subclass (TGFβ pathway activation) (Liver Int 2016;36:108)
- Associated with G4 subgroup (JAK / STAT pathway activation, lack of mutations in CTNNB1, TP53 and TERT promoter) (J Hepatol 2017;67:727)
Sample pathology report
- Liver mass, needle biopsy:
- Moderately differentiated hepatocellular carcinoma, steatohepatitic variant
Differential diagnosis
- Clear cell variant of hepatocellular carcinoma:
- Tumor cells contain glycogen, may contain some fat
- Will not show inflammatory features, such as ballooning degeneration of hepatocytes or Mallory-Denk bodies
- Benign liver with steatohepatitis:
- Lacks features of malignancy, such as increased N/C ratio, thickened trabeculae, unpaired arteries
Additional references
Board review style question #1
Board review style answer #1
E. Steatohepatitis. Steatohepatitic hepatocellular carcinoma most commonly arises in the setting of steatohepatitis, either alcoholic or nonalcoholic.
Comment Here
Reference: HCC - steatohepatitic
Comment Here
Reference: HCC - steatohepatitic
Board review style question #2
Which of the following is true regarding staining of steatohepatitic hepatocellular carcinoma?
- Oil red O stain must be performed on formalin fixed paraffin embedded tissue
- PAS stain will show that the clear droplets contain dense glycogen
- Trichrome stain generally shows a thick fibrous capsule with minimal intratumoral fibrosis
- Ubiquitin stain can be used to highlight Mallory-Denk bodies
Board review style answer #2
D. Ubiquitin stain can be used to highlight Mallory-Denk bodies. Mallory-Denk bodies may not be present in all cases of steatohepatitic hepatocellular carcinoma but immunohistochemical stain for ubiquitin can be used to confirm or highlight their presence. The cytoplasmic vacuoles in steatohepatitic hepatocellular carcinoma contain predominantly lipid, not glycogen, so they would not be expected to stain with PAS. Oil red O and Sudan Black stains must be performed on frozen tissue (most fat is removed during tissue processing for paraffin embedding). Steatohepatitic hepatocellular carcinoma classically shows a pericellular fibrosis pattern.
Comment Here
Reference: HCC - steatohepatitic
Comment Here
Reference: HCC - steatohepatitic
HCC - undifferentiated variant
Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Clinical features | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Primary liver tumor that can be diagnosed as carcinoma based on immunohistochemistry but cannot be further classified (Surg Pathol Clin 2013;6:367)
- May show molecular abnormalities supporting a diagnosis of hepatocellular carcinoma (HCC)
Essential features
- Primary liver tumor that can be diagnosed as carcinoma based on immunohistochemistry (e.g. cytokeratin+) but hepatocellular immunostains are negative (e.g. arginase1- and HepPar1-)
- Solid or trabecular growth pattern with high N/C ratios and nuclear pleomorphism
- May be albumin in situ hybridization (ISH)+
ICD coding
- ICD-10: C22.7 - Other specified carcinomas of liver
Epidemiology
- Rare, accounting for < 2% of all epithelial liver tumors (Torbenson: Tumors of the Liver, Series 4, 2018)
- Male preponderance
Clinical features
- May present with abdominal pain and fever (Intern Med 2011;50:519)
Prognostic factors
- May have worse prognosis in comparison to classic HCC (Torbenson: Tumors of the Liver, Series 4, 2018)
- Prognostic factors for HCC: stage (TNM), single lesion versus multifocal, size, vascular invasion, portal vein thrombosis, severity of underlying liver disease (Liver Int 2009;29:502, J Surg Oncol 2018;117:644)
Case reports
- 54 year old man with multiple liver tumors (Jpn J Clin Oncol 1998;28:401)
- 56 year old man with intraabdominal hemorrhage (Surg Case Rep 2017;3:12)
- 57 year old man with fever and right upper quadrant pain (Intern Med 2011;50:519)
Treatment
- Surgical resection
- Radiofrequency ablation
- Transarterial chemoembolization (TACE)
- Transplantation (e.g. Milan criteria, modified by some institutions, Nat Rev Gastroenterol Hepatol 2017;14:203)
Microscopic (histologic) description
- Solid or trabecular growth pattern
- High N/C ratio
- Pleomorphism
- No histologic features of classic HCC
Microscopic (histologic) images
Positive stains
Negative stains
- Hepatocellular markers (arginase1, glypican 3, HepPar1)
Molecular / cytogenetics description
- May be albumin ISH+
Sample pathology report
- Liver, mass, core biopsy:
- Poorly differentiated carcinoma; see comment
- Comment: This tumor shows a poorly differentiated carcinoma with tumor cells positive for pancytokeratin and negative for CK7, CK19, mucicarmine and hepatocellular markers (HepPar1, arginase1 and glypican 3). Albumin in situ hybridization is positive in tumor cells. We favor consideration as an undifferentiated hepatocellular carcinoma; correlation with molecular testing can be helpful (e.g. next generation sequencing cancer gene panel).
Differential diagnosis
- Poorly differentiated HCC: similar histologic appearance but positive for hepatocellular markers (HepPar1, arginase1 and glypican 3)
- Poorly differentiated intrahepatic cholangiocarcinoma: similar histologic appearance but evidence of mucin production or molecular abnormalities characteristic of cholangiocarcinoma (e.g. IDH1 / 2 mutations)
- Metastatic undifferentiated carcinoma: similar histologic appearance, requires clinical / imaging correlation; albumin ISH-
Board review style question #1
Which of the following features is true regarding the undifferentiated variant of hepatocellular carcinoma (HCC)?
- Albumin ISH is always negative
- Arginase1 is usually positive
- Cytokeratin is usually negative
- Has a better prognosis in comparison to classic HCC
- May show solid or trabecular growth pattern
Board review style answer #1
E. May show solid or trabecular growth pattern
Comment Here
Reference: Undifferentiated hepatocellular carcinoma
Comment Here
Reference: Undifferentiated hepatocellular carcinoma
Board review style question #2
Which variant of hepatocellular carcinoma is characterized by positive cytokeratin but albumin ISH and all hepatocellular markers are negative?
- Fibrolamellar
- Lymphoepithelioma-like
- Sarcomatoid
- Scirrhous
- Undifferentiated
Board review style answer #2
Hemangioma
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Benign vascular tumors further classified based on characteristic morphologic findings
- Predominately asymptomatic with no reported malignant transformation
Essential features
- Hepatic hemangiomas are the most common benign tumor of the liver
- Classification is based on characteristic histologic features; there should be no significant cytologic atypia or mitotic activity
- Vast majority of hemangiomas are asymptomatic and require no intervention; larger lesions (> 5 cm) are more likely to be symptomatic and susceptible to complications such as hemorrhage, rupture and Kasabach-Merritt syndrome
- No cases of malignant transformation have been documented
Terminology
- Cavernous hemangioma
- Most common subtype of hepatic hemangioma
- Capillary hemangioma
- Extremely rare
- Anastomosing hemangioma
- Rare, newly described variant
- More frequently occurs in genitourinary tract
- Sclerosing / sclerosed hemangioma
- Hepatic small vessel neoplasm
- Rare, with mild atypical features
- Benign or low grade entity in adults
- No cases of recurrences or metastasis reported
ICD coding
Epidemiology
- Most common benign hepatic tumor (Visc Med 2020;36:292)
- Prevalence as high as 20% in general population (Visc Med 2020;36:292)
- Occurs at any age but the third to fifth decade is most common
- Female predominance, F:M = 5:1 (Visc Med 2020;36:292)
Sites
- Most often found in right lobe of liver, particularly segment IV, subcapsular location (J Med Life 2015;8 Spec Issue:4)
Etiology
- Precise pathogenesis unknown
- Arises from vascular malformation (Visc Med 2020;36:292)
- Vascular endothelial growth factor (VEGF) may contribute to development of hepatic hemangiomas (Visc Med 2020;36:292)
- Hormone replacement, oral contraceptives and pregnancy may contribute to growth of hepatic hemangiomas; however, the lesions are negative for estrogen and progesterone receptors (Visc Med 2020;36:292, World J Gastroenterol 2020;26:11)
Clinical features
- Vast majority are asymptomatic and incidental findings on imaging studies
- Large tumors (> 5 cm) are more likely to be symptomatic
- Spontaneous hemorrhage is uncommon; 1 literature review shows only 46 cases between 1898 and 2010 (Visc Med 2020;36:292, J Hepatobiliary Pancreat Sci 2011;18:797)
- Kasabach-Merritt syndrome is a rare, potentially life threatening consumptive coagulopathy leading to intravascular coagulation and thrombocytopenia (Visc Med 2020;36:292, StatPearls: Kasabach Merritt Syndrome [Accessed 11 December 2020])
- Occurs in 26% of hemangiomas > 15 cm
- Reversible with resection of hemangioma
Diagnosis
- Predominantly based on imaging studies
- Core needle biopsy contraindicated due to risk of hemorrhage and low diagnostic yield (J Med Life 2015;8 Spec Issue:4)
Laboratory
- Alkaline phosphatase (ALP) and gamma glutamyl transferase (GGT) usually within normal limits (Visc Med 2020;36:292)
- Alpha fetoprotein (AFP), carcinogenic antigen 19-9 (CA 19-9) and carcinogenic antigen (CEA) within normal limits (J Med Life 2015;8 Spec Issue:4)
Radiology description
- Multiple modalities available (J Med Life 2015;8 Spec Issue:4)
- Overall stable findings on serial exam are a reliable indicator of benignity
- Contrast enhancing ultrasonographic and technetium-99m scintigraphy are most specific
- Ultrasound (US)
- Conventional: well circumscribed homogenous nodule; hyperechoic in smaller lesions, mixed echogenicity in larger lesions
- Contrast enhancing: more specific; peripheral nodular enhancement in arterial phase, centripetal filling in late phase
- Computer tomography (CT)
- Well circumscribed hypodense lesion
- Contrast demonstrates peripheral nodular enhancement with progressive centripetal filling
- Magnetic resonance imaging (MRI)
- Well circumscribed homogenous lesion
- Hypointense on T1, hyperintense with "cotton wool" appearance on T2
- Technetium-99m scintigraphy
- Perfusion / blood pool mismatch
- Cold lesion in early phase, intensive activity in late phase
Prognostic factors
- Most patients remain asymptomatic and without complication
- No malignant transformation has been reported (Visc Med 2020;36:292)
- < 40% may grow over time and the clinical significance of growth rate is uncertain (World J Gastroenterol 2020;26:11)
Case reports
- 56 year old man with history of gastrointestinal stromal tumor, now with incidental right hepatic lobe mass (J Radiol Case Rep 2019;13:32)
- 57 year old man with lateral hepatic mass (Radiol Case Rep 2018;13:1025)
- 70 year old woman with liver mass and abdominal pain (Rom J Morphol Embryol 2018;59:557)
- 78 year old man with abdominal pain and hypotension (Rev Esp Enferm Dig 2016;108:431)
- 83 year old woman with jaundice, hypofibrinogenemia and thrombocytopenia (Surg Case Rep 2015;1:93)
Treatment
- If small and asymptomatic, surveillance via serial imaging is sufficient (Visc Med 2020;36:292, World J Gastroenterol 2020;26:11)
- If large, symptomatic or malignancy cannot be excluded, surgical management is indicated (Visc Med 2020;36:292, World J Gastroenterol 2020;26:11)
- Surgical management includes: enucleation, segmental resection, lobectomy and rarely transplant
- Nonsurgical management includes angiographic embolization, portal vein embolization, radiofrequency ablation and irradiation (Visc Med 2020;36:292, World J Gastroenterol 2020;26:11)
Gross description
- Most often solitary lesions
- Usually < 4 cm but range from a few millimeters to > 30 cm in size
- If > 10 cm, referred to as giant hemangioma
- Well circumscribed with red-brown, spongy / honeycombed cut surface
Microscopic (histologic) description
- Cavernous hemangioma
- Circumscribed proliferation of variably sized, dilated and thin walled vessels lined by a single layer of flat endothelial cells
- No cytologic atypia or mitosis
- Vascular spaces separated by fibrous septa containing small vessels
- Focal thrombi, calcification, hyalinization, extramedullary hematopoiesis and stromal edema may be present
- May have irregular interface with surrounding hepatic parenchyma
- Sclerosing / sclerosed hemangioma
- Abundant fibrotic stroma that compresses and replaces lesional vessels
- Only vague outline of residual vessels may be present; elastin or trichrome may aid in highlighting such vessels
- Capillary hemangioma
- Lobular proliferation of small, thin walled vessels lined by a single layer of bland endothelial cells
- Anastomosing hemangioma
- Overall well circumscribed; anastomosing, small, capillary-like vessels lined by endothelium with mild cytologic atypia and focal hobnailing
- Thrombi are frequent
- Hyaline globules and extramedullary hematopoiesis may be present
- May resemble angiosarcoma but lacks infiltrative growth, severe cytologic atypia or mitotic activity
- Hepatic small vessel neoplasm
- Similar to anastomosing hemangioma but with infiltrative proliferation of small, thin walled vessels around portal tracts and into adjacent liver parenchyma
- Lined by flattened to plumped or hobnailed endothelial cells
- Extramedullary hematopoiesis may be present
- Lack of multilayering, papillary architecture, significant cytologic atypia, mitotic activity and necrosis
- Ki67 proliferation index most helpful tool in distinguishing from angiosarcoma (Hum Pathol 2016;54:143)
Microscopic (histologic) images
Positive stains
- Endothelial markers: CD31, CD34, ERG, FLI1, Factor VIII are strongly and uniformly positive
- Elastin and trichrome useful in highlighting lesional vessels in sclerosing hemangioma
- Ki67 proliferation index is most helpful tool in distinguishing hepatic small vessel neoplasm from angiosarcoma
- Mean nuclear labeling 3.7% and 42.8% respectively
Negative stains
Molecular / cytogenetics description
- Most hemangiomas have no recurrent genetic abnormalities
- 70 - 90% of anastomosing hemangiomas or hepatic small vessel neoplasms have GNAQ, GNA14 or GNA11 alterations (Am J Surg Pathol 2018;42:1201, Virchows Arch 2020;476:475)
Sample pathology report
- Liver, segment IV, segmentectomy:
- Cavernous hemangioma (3.5 cm in greatest dimension)
Differential diagnosis
- Angiosarcoma:
- Infiltrative with ill defined borders
- Severe cytologic atypia, increased mitotic activity and necrosis
- High Ki67 proliferation index
- No GNAQ, GNA14 or GNA11 alterations
- Juvenile hemangioendothelioma:
- Proliferation of capillary-like vessels with central fibrous scar
- Vessels lined by plump endothelial cells
- Epithelioid hemangioendothelioma:
- Multinodular with ill defined borders
- No vascular channel formation or poorly defined vascular spaces lined by atypical epithelioid cells
- > 90% with recurrent fusion gene WWTR1-CAMTA1 (Genes Chromosomes Cancer 2011;50:644)
- Peliosis hepatis:
- Predominately lakes of blood, no endothelial cell lining
- Hereditary hemorrhagic telangiectasia:
- Dilated vascular channels within portal tracts and surrounding areas
- Aberrant portal vessels present
- Segmental atrophy or nodular elastosis:
- May mimic sclerosing / sclerosed hemangioma
- Variable amount of elastosis and fibrosis with islands of residual hepatocytes, cystic dilated bile ducts and abnormally thick walled vessels (Am J Surg Pathol 2011;35:364)
- No vascular channel formation or residual outlines of vascular channel
Additional references
Board review style question #1
What subtype of hepatic hemangioma is most common?
- Anastomosing
- Capillary
- Cavernous
- Hepatic small cell neoplasm
- Sclerosing / sclerosed
Board review style answer #1
Board review style question #2
A 35 year old woman presents with an incidental 2.5 cm hepatic mass. A representative field from the resection specimen is shown above. The lesional cells are positive for FLI1 and CD34. Which stain would be most useful in distinguishing hepatic small vessel neoplasm from angiosarcoma?
- Cytokeratin
- ER / PR
- Glypican 3
- Ki67
- Podoplanin
Board review style answer #2
Hemochromatosis
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Most common autosomal recessive disorder in Caucasians, caused by decreased hepcidin activity due to mutations in iron metabolism genes such as HFE (Nat Rev Dis Primers 2018;4:18016)
- Characterized by increased iron absorption, toxic iron accumulation and end organ damage
Essential features
- Caused by mutations in iron metabolism genes, such as HFE, resulting in hepcidin deficiency and increased iron absorption, toxic iron accumulation and end organ damage (Nat Rev Dis Primers 2018;4:18016)
- Diagnosis can be confirmed with HFE genetic testing but liver biopsy may still be necessary to assess fibrosis
- Excess iron accumulates predominantly in hepatocytes, in a periportal (early) to panlobular (advanced) distribution
- Hemochromatosis patients with cirrhosis have up to 100 times the chance of developing hepatocellular carcinoma than the general population (J Hepatol 2010;53:3)
- Distinct from secondary hemochromatosis (secondary iron overload), which occurs in the setting of inherited or acquired disorders of erythropoiesis or frequent blood transfusions (Dtsch Arztebl Int 2009;106:499)
Terminology
- Type 1 hemochromatosis (specifically refers to HFE associated hemochromatosis)
- Primary or inherited iron overload
- Bronze diabetes
- Hereditary hemochromatosis
ICD coding
Epidemiology
- M:F = 2:1
- Men typically develop symptoms at 40 - 60 years old
- Women typically develop symptoms after menopause
- Predominantly seen in people of northern European descent
- Estimated prevalence: 1 in 300 - 500 (StatPearls: Hemochromatosis [Accessed 16 July 2021])
- Due to relatively high prevalence of HFE mutations (Semin Liver Dis 2005;25:411)
- Non HFE hemochromatosis is seen worldwide (StatPearls: Hemochromatosis [Accessed 16 July 2021])
Sites
- Liver, heart, pancreas, skin, gonads, joints
Pathophysiology
- Iron is absorbed by duodenal enterocytes via divalent metal transporter 1 (DMT1) (Semin Liver Dis 2005;25:411)
- Can be transported into plasma by ferroportin (FPN1) or can be stored as ferritin and excreted in feces when enterocyte is sloughed
- Iron in plasma is bound to transferrin (Semin Liver Dis 2005;25:411)
- Cannot be excreted
- Hepatocytes take up transferrin bound iron via transferrin receptor 1 (TFR1) or TFR2 (Semin Liver Dis 2005;25:411)
- Can also take up nontransferrin bound iron if transferrin highly saturated
- Kupffer cells take up iron mainly by phagocytosing senescent erythrocytes (Semin Liver Dis 2005;25:411)
- Can be transported into plasma via ferroportin
- Hepcidin (HAMP) is master regulator of iron homeostasis (Semin Liver Dis 2005;25:411, StatPearls: Hemochromatosis [Accessed 16 July 2021], Nat Rev Dis Primers 2018;4:18016)
- Peptide hormone produced in the liver in the presence of sufficient transferrin bound iron
- Inhibits dietary iron absorption in gut and release of iron from macrophages by inhibiting ferroportin
- Hemojuvelin (HJV) binds bone morphogenetic protein receptor (BMPR) (Nat Rev Dis Primers 2018;4:18016)
- BMP6 production increases with increased cellular iron stores
- Signaling through BMP6-BMPR-HJV promotes hepcidin transcription
- Hereditary hemochromatosis protein (HFE) normally promotes hepcidin transcription (Nat Rev Dis Primers 2018;4:18016)
- Interacts with TFR1
- Loss of function mutations in HFE → decreased hepcidin → increased ferroportin activity → increased iron absorption (hemochromatosis type 1) (Semin Liver Dis 2005;25:411, StatPearls: Hemochromatosis [Accessed 16 July 2021], Nat Rev Dis Primers 2018;4:18016)
- Loss of function mutations in HAMP (gene encoding hepcidin)→ increased ferroportin activity → increased iron absorption (hemochromatosis type 2b) (Nat Rev Dis Primers 2018;4:18016)
- Loss of function mutations in HJV → decreased hepcidin → increased ferroportin activity → increased iron absorption (hemochromatosis type 2a) (Nat Rev Dis Primers 2018;4:18016)
- Loss of function mutations in TFR2→ decreased hepcidin → increased ferroportin activity → increased iron absorption (hemochromatosis type 3) (Nat Rev Dis Primers 2018;4:18016)
- Gain of function mutations in FPN1 (gene encoding ferroportin) → increased iron absorption (hemochromatosis type 4) (Nat Rev Dis Primers 2018;4:18016)
- Excess iron accumulation in organs and tissues leads to increased oxidative stress, cell death and organ damage (StatPearls: Hemochromatosis [Accessed 16 July 2021])
- Liver
- Fibrosis and cirrhosis
- Increased risk of hepatocellular carcinoma by up to 100 times (J Hepatol 2010;53:3)
- Pancreas
- Diabetes
- Other affected organs include:
- Heart
- Arrhythmias, dilated cardiomyopathy, congestive heart failure
- Joints
- Arthropathy (pain)
- Pituitary gland
- Hypogonadotropic hypogonadism
- Skin
- Hyperpigmentation, bronzing of skin
- Heart
- End organ damage is exacerbated by alcohol use and viral hepatitis
- Liver
Etiology
- Usually caused by loss of function point mutations in HFE gene (Nat Rev Dis Primers 2018;4:18016, Semin Liver Dis 2005;25:411)
- Autosomal recessive
- Most common mutation is C282Y
- Iron overload develops clinically in 25 - 60% of homozygotes
- Other mutations include H63D and S65C
- More rare and generally less severe disease
- Can also be caused by mutations in other iron related genes, including HAMP, HJV and TFR2 (Nat Rev Dis Primers 2018;4:18016)
Diagrams / tables
Clinical features
- Classic triad: liver cirrhosis, diabetes mellitus, bronzing of skin (Am J Hematol 2006;81:202)
- May also have joint pain, fatigue, abdominal pain
Diagnosis
- Laboratory testing (Nat Rev Dis Primers 2018;4:18016)
- If iron overload is suspected, screen with transferrin saturation and serum ferritin
- If transferrin saturation is ≥ 45% and ferritin is elevated, perform genetic testing
- PCR testing targeted for C282Y variable H63D and S65C
- Screening asymptomatic patients without family history of hemochromatosis with genetic testing is not recommended, due to high frequency of HFE mutations and variable penetrance (J Hepatol 2010;53:3)
- First degree relatives of patients with hemochromatosis should undergo genetic testing
- Liver biopsy:
- Was the gold standard but is no longer required for diagnosis in the presence of genetic testing
- Tissue can be used to determine hepatic iron concentration (HIC) via mass spectrometry
- Useful to confirm diagnosis of hepatic iron overload when genetic testing for common HFE mutations is negative (Clin Liver Dis (Hoboken) 2021;17:232)
- Hepatic iron index (HII) = hepatic iron concentration / patient’s age in years (Clin Liver Dis (Hoboken) 2021;17:232)
- HII values < 1.0 are normal
- HII values 1.0 to 1.9 indicate mild iron accumulation
- Heterozygous for HFE or other hemochromatosis associated mutation
- Alcoholic liver disease
- HII values > 1.9 indicate iron overload
- Homozygous HFE or other hemochromatosis associated mutation
- Cirrhosis
- Recommended to assess fibrosis when serum ferritin > 1,000 ug/L (J Hepatol 2010;53:3)
- Imaging:
- MRI can be used to quantify iron and determine distribution of iron in the liver
- Transient elastography may help assess fibrosis and cirrhosis
Laboratory
- Transferrin saturation ≥ 45% (J Hepatol 2010;53:3)
- Elevated ferritin
- May have elevated liver enzymes (AST, ALT) with disease progression
Radiology description
- MRI can be used to determine distribution of iron deposition and quantify the iron (Insights Imaging 2012;3:173)
- Increased iron leads to accelerated T2 relaxation and reduced signal intensity
- Dual energy CT can also be used to quantitate iron (Radiology 2015;277:95)
Radiology images
Prognostic factors
- Life expectancy is normal if diagnosed and managed before end organ damage develops
- Prognosis is poor after development of cirrhosis, hepatocellular carcinoma, diabetes or cardiomyopathy
- Patients with cirrhosis have up to a 100 times greater chance of developing hepatocellular carcinoma than the general population (J Hepatol 2010;53:3)
Case reports
- 28 year old Chinese man with abnormal liver function tests (Front Genet 2020;11:77)
- 45 year old man with recurrent intermittent skin changes (ACG Case Rep J 2019;6:e00247)
- 48 year old man with atrial fibrillation (Eur Heart J Case Rep 2020;4:1)
- 65 year old man with disseminated Cryptococcus (Autops Case Rep 2020;10:e2020180)
Treatment
- Therapeutic phlebotomy / venesection
- Frequency based on hemoglobin, serum ferritin and transferrin saturation (Br J Haematol 2018;181:293)
- Chelation therapy may be considered if therapeutic phlebotomy is not available or contraindicated or as an adjunct to phlebotomy in severe cases
Gross description
- Dark brown discoloration of liver and other involved organs
- Hepatomegaly (StatPearls: Hemochromatosis [Accessed 16 July 2021])
Gross images
Frozen section description
- Granular brown-black pigment within periportal (milder) or panlobular (more severe) hepatocytes (Arch Pathol Lab Med 2013;137:270)
- Potential donor livers with severe hepatocellular iron overload are generally not accepted for transplantation (Arch Pathol Lab Med 2013;137:270)
Microscopic (histologic) description
- Liver:
- Iron appears as dark brown granular pigment, predominantly within hepatocytes
- Pericanalicular pattern (Clin Liver Dis (Hoboken) 2021;17:232)
- Periportal deposition initially, extending towards zones 2 and 3 with disease progression
- Iron pigment may also be seen in cholangiocytes and Kupffer cells, especially at later stages
- Fibrosis develops over time
- Amount of iron can be graded semi quantitatively (Mod Pathol 2007;20:S31)
- Scheuer methodology (scale 0 - 4) based on ease of observation of iron granules at various magnifications (World J Gastroenterol 2007;13:4755, J Pathol Bacteriol 1962;84:53)
- Iron appears as dark brown granular pigment, predominantly within hepatocytes
- Heart:
- Iron within cardiomyocytes (Int Heart J 2018;59:427)
- Pancreas:
- Iron within acinar cells (Diabetes Care 2014;37:e137)
- Interstitial fibrosis
- Joints:
- Acute synovitis
- Calcium pyrophosphate deposition (pseudogout) (N Engl J Med 2016;374:2575)
- Skin:
- Iron in dermal macrophages and fibroblasts (Transl Sci Rare Dis 2017;2:101)
- Increased melanin production
- Testes:
- Atrophy (hypogonadism), most likely due to iron deposition in anterior pituitary gonadotropin producing cells (Basic Clin Androl 2017;27:13)
Microscopic (histologic) images
Positive stains
Negative stains
- Rhodanine (copper) stain (Semin Diagn Pathol 2018;35:381)
- Hall’s (bilirubin) stain (Am J Clin Pathol 1960;34:313)
Molecular / cytogenetics description
- Type 1 (HFE hemochromatosis)
- Hemochromatosis (HFE) mutation
- Most common mutation is C282Y
- Compound heterozygosity with H63D, S65C and mutations at other loci have been reported (J Hepatol 2010;53:3)
- Non HFE hemochromatosis (StatPearls: Hemochromatosis [Accessed 16 July 2021])
- Type 2 (juvenile hemochromatosis)
- Hepcidin (HAMP) or hemojuvelin (HJV) mutation
- Often have hypogonadism at presentation
- Cardiac iron deposition typically results in heart failure, usually before the age of 30 (Am J Hematol 2006;81:202)
- Type 3
- Transferrin receptor 2 (TFR2) mutation
- Type 4
- Ferroportin 1 (FPN1, SLC40A1) mutation
- Autosomal dominant
- Type 2 (juvenile hemochromatosis)
Molecular / cytogenetics images
Sample pathology report
- Liver, biopsy:
- Extensive hepatocellular siderosis consistent with hereditary hemochromatosis (see comment)
- Comment: An iron stain shows extensive iron accumulation in hepatocytes with periportal accentuation. There is no evidence of fatty liver disease or chronic hepatitis, the other entities that can have siderosis. The pattern of intracellular iron deposition in hepatocytes in the clinical setting of homozygous HFE C282Y mutation is consistent with hereditary hemochromatosis.
Differential diagnosis
- Secondary hemochromatosis (StatPearls: Hemochromatosis [Accessed 16 July 2021]):
- Excess hepatic iron is usually predominantly sinusoidal, within Kupffer cells
- Iron overload due to transfusions, chronic liver disease, congenital atransferrinemia, oral intake of iron, ineffective erythropoiesis
- Hepatitis C:
- Positive HCV antibody screen
- Presence of portal inflammation with lymphoid aggregates
- Fatty liver disease:
- Steatosis, ballooned hepatocytes, centrizonal fibrosis
- Cholestasis:
- Bile is canalicular (extracellular) as well as intracellular
- Lipofuscin pigment:
- Lipofuscin pigment has a centrizonal distribution and is usually light brown
- Neonatal hemochromatosis (Hepatology 2006;43:654):
- Hepatic iron overload presenting soon after birth
- Thought to be a consequence of intrauterine liver failure (J Hepatol 2012;56:1226)
Board review style question #1
Board review style answer #1
Board review style question #2
Which of the following patterns of iron deposition is most consistent with hemochromatosis?
- Centrilobular, intracellular deposition within hepatocytes
- No specific pattern of deposition
- Panlobular, intracellular deposition within Kupffer cells
- Periportal, intracellular deposition within hepatocytes
- Periportal, intracellular deposition within Kupffer cells
Board review style answer #2
Hepatic failure
Table of Contents
Definition / general | Terminology | Epidemiology | Etiology | Clinical features | Fuliminant hepatic failure | Case reports | Treatment | Gross images | Microscopic (histologic) description | Microscopic (histologic) imagesDefinition / general
- Characterized by acute and severe hepatic abnormalities with a high short term mortality (Gut 2017;66:541)
- May occur with or without preexisting chronic liver disease
- Various clinical definitions exist:
- Acute hepatic failure
- North America (AASLD): coagulopathy (INR ≥ 1.5) and hepatic encephalopathy without preexisting cirrhosis and with an illness of < 26 weeks duration
- Europe (EASL): liver damage (elevated serum transaminases) and impaired liver function (jaundice and INR > 1.5) with an onset of encephalopathy within 24 weeks in absence of chronic liver disease (J Hepatol 2017;66:1047)
- Acute on chronic hepatic failure
- Europe (EASL CLIF): acute liver decompensation (ascites, encephalopathy, gastrointestinal bleeding or bacterial infection) in preexisting chronic liver disease defined by the chronic liver failure sequential organ failure assessment [CLIF-SOFA] score and 28 day mortality > 15% (Gastroenterology 2013;144:1426)
- Asia Pacific (APASL): jaundice (serum bilirubin level of ≥ 5 mg/dL) and coagulopathy (INR ≥ 1.5 or prothrombin activity of > 40%), which are complicated within 4 weeks by clinical ascites or encephalopathy in patients with previously diagnosed or undiagnosed chronic liver disease (including cirrhosis) (Gut 2017;66:541)
- Acute hepatic failure
Terminology
- Acute hepatic failure may also refer to fulminant hepatic failure, fulminant hepatitis or massive hepatic necrosis
Epidemiology
- Acute hepatic failure: 2,000 cases per year in the U.S.
- Acute on chronic hepatic failure: 24% - 40% of hospitalized patients with cirrhosis (Gut 2017;66:541)
Etiology
- Acute hepatic failure (J Hepatol 2017;66:1047)
- Acetaminophen (up to 43%)
- Nonacetaminophen drug induced liver injury (up to 32%)
- Acute hepatotropic virus hepatitis (up to 68%)
- Others (up to 27%)
- Unknown (up to 27%)
- Acute on chronic hepatic failure (Gut 2017;66:541)
- Chronic viral hepatitis (12 - 81%)
- Alcoholic liver disease (7 - 75%)
- Others (3 - 22%)
- Unknown (4 - 20%)
Clinical features
- Jaundice
- Coagulopathy
- Hepatic encephalopathy
- In patients with acute on chronic hepatic failure, clinical features of cirrhosis may also be present
Fuliminant hepatic failure
- Uncommon (< 1%) complication of acute viral hepatitis
- Progresses from onset of symptoms to hepatic encephalopathy in 2 - 3 weeks in previously healthy patient
- Orderly regeneration due to massive destruction of confluent lobules
- Liver can regenerate after massive necrosis if connective tissue framework is intact
- Regeneration: portal ductules increase in size and number and become dilated
- Individual hepatocytes with clear cytoplasm appear from ductules
- Ductules are transformed into hepatocytes and form round cell clusters, which organize into trabeculae with fibrosis
- Lobular architecture is established
- May become normal at 14 months (Mod Pathol 2000;13:152)
- Causes: viruses (hepatitis B, C), drugs (acetaminophen, carbon tetrachloride, halothane, isoniazid, rifampin), acute fatty liver of pregnancy, hepatic vein obstruction, hyperthermia, ischemia, tumor, Wilson disease
- Subfulminant hepatitis: less rapid, up to 3 months to hepatic encephalopathy
Case reports
- 15 year old boy with autoimmune hepatitis / primary sclerosing cholangitis overlapping syndrome who developed acute on chronic liver failure (Clin Exp Hepatol 2017;3:28)
- 42 year old woman with massive hepatic necrosis following ingestion of acetic acid (concentrated) (Arch Pathol Lab Med 2000;124:127)
- 51 year old woman with acute hepatic failure due to massive sinusoidal infiltration of liver by breast cancer cells (BMC Gastroenterol 2017;17:166)
- 60 year old man with acute hepatic failure due to pembrolizumab for metastatic liver cancer (Medicine (Baltimore) 2017;96:e9431)
- 60 year old woman with massive hepatic necrosis following exposure to phenytoin and trimethoprim / sulfamethoxasole (Arch Pathol Lab Med 2000;124:1800)
- 63 year old woman with subacute hepatic failure after administration of troglitazone (Hum Pathol 2000;31:250)
- 63 year old woman with acute on chronic hepatic failure due to sorafenib for hepatitis B related hepatocellular carcinoma (Mol Clin Oncol 2017;7:693)
- Two people from the same family with acute hepatic failure due to acute hepatitis A (Medicine (Baltimore) 2017;96:e7847)
Treatment
- Liver transplant, auxiliary partial orthotopic liver transplant
- Mortality without liver transplant is 25 - 90% (Semin Liver Dis 2008;28:175)
Gross images
Microscopic (histologic) description
- Panacinar hepatic necrosis with collapse of reticulin framework
- Variable inflammatory infiltrate, depending on etiology
- Variable ductular reaction
- Microscopic features of cirrhosis in patients with acute on chronic hepatic failure
Microscopic (histologic) images
Hepatic failure
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Immunofluorescence description | Immunofluorescence images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Hepatic failure is acute and severe hepatic abnormalities with a high short term mortality (Gut 2017;66:541)
- Acute hepatic failure is hepatic failure in patients without pre-existing chronic liver diseases
- Acute on chronic hepatic failure is hepatic failure in patients with pre-existing chronic liver diseases
Essential features
- Hepatic failure is acute and severe hepatic abnormalities with a high short term mortality (Gut 2017;66:541)
- Hepatic failure is a clinical, not pathological, diagnosis with varied definitions according to different professional organizations
- Depending on whether the patients have preexisting chronic liver diseases, hepatic failure is stratified into acute hepatic failure and acute on chronic hepatic failure
Terminology
- Fulminant hepatic failure may also refer to fulminant hepatitis or massive hepatic necrosis
ICD coding
Epidemiology
- Acute hepatic failure: 2,000 cases per year in the U.S. (Hepatology 2012;55:965)
- Acute on chronic hepatic failure: 24 - 40% of hospitalized patients with cirrhosis (Gut 2017;66:541)
Pathophysiology
N/A
Etiology
- Acute hepatic failure (J Hepatol 2017;66:1047)
- Acetaminophen (up to 43%)
- Nonacetaminophen drug induced liver injury (up to 32%)
- Acute hepatotropic virus hepatitis (up to 68%)
- Others (up to 27%)
- Unknown (up to 27%)
- Acute on chronic hepatic failure (Gut 2017;66:541)
- Chronic viral hepatitis (12 - 81%)
- Alcoholic liver disease (7 - 75%)
- Others (3 - 22%)
- Unknown (4 - 20%)
Diagrams / tables
N/A
Clinical features
- Jaundice
- Coagulopathy
- Hepatic encephalopathy
- In patients with acute on chronic hepatic failure, clinical features of cirrhosis may also be present
Diagnosis
- Hepatic failure is a clinical, not a pathological, diagnosis with varied definitions according to different professional organizations
- Acute hepatic failure
- North America (AASLD): coagulopathy (international normalized ratio [INR] ≥ 1.5) and hepatic encephalopathy without pre-existing cirrhosis and with an illness of < 26 weeks duration (Hepatology 2012;55:965)
- Europe (EASL): liver damage (elevated serum transaminases) and impaired liver function (jaundice and INR > 1.5) with an onset of encephalopathy within 24 weeks in the absence of chronic liver disease (J Hepatol 2017;66:1047)
- Fulminant hepatic failure
- Severe and rapid onset (within 8 weeks) form of acute hepatic failure
- Acute on chronic hepatic failure
- North America (AASLD): liver failure (jaundice and coagulopathy) and ≥ 1 of the 4 major extrahepatic organ failures (kidney, brain, circulation, and respiration) in patients with chronic liver disease with or without cirrhosis (Hepatology 2023 Nov 9 [Epub ahead of print])
- North America (NACSELD): ≥ 2 of the 4 major extrahepatic organ failures (kidney, brain, circulation and respiration) in patients with acutely decompensated cirrhosis (Hepatology 2018;67:2367)
- Europe (EASL CLIF): ≥ 1 of the 6 major organ failures (liver, coagulation, kidney, brain, circulation and respiration) in patients with acutely decompensated cirrhosis (Gastroenterology 2013;144:1426)
- Asia Pacific (APASL): jaundice (serum bilirubin level of ≥ 5 mg/dL) and coagulopathy (INR ≥ 1.5 or prothrombin activity of > 40%), which are complicated within 4 weeks by clinical ascites or encephalopathy in patients with chronic liver disease with or without cirrhosis (Hepatol Int 2019;13:353)
Laboratory
- Deranged liver function: elevated bilirubin and transaminase
- Coagulopathy: elevated INR
- Deranged renal function (in the presence of renal failure): elevated creatinine
- Liver biopsy plays no role in establishing the diagnosis but may be helpful in looking for the underlying etiology
Radiology description
N/A
Radiology images
N/A
Prognostic factors
- Acute on chronic liver failure (ACLF) grade for the short term mortality prediction of patients with acute on chronic liver failure (Gastroenterology 2013;144:1426)
- Chronic Liver Failure Consortium (CLIF-C) ACLF score for the short and intermediate term mortality prediction of patients with acute on chronic liver failure (J Hepatol 2014;60:275)
- Age
- White cell count
- CLIF-SOFA (sequential organ failure assessment): bilirubin, INR, creatinine, mean arterial pressure, PaO2 / SpO2, FiO2, hepatic encephalopathy grade
- Has better predictive accuracy than MELD, MELD-Na and Child-Pugh grade
Case reports
- 15 year old boy with autoimmune hepatitis / primary sclerosing cholangitis overlapping syndrome who developed acute on chronic liver failure (Clin Exp Hepatol 2017;3:28)
- 51 year old woman with acute hepatic failure due to massive sinusoidal infiltration of the liver by breast cancer cells (BMC Gastroenterol 2017;17:166)
- 59 and 63 year old men from the same family with acute hepatic failure due to acute hepatitis A (Medicine (Baltimore) 2017;96:e7847)
- 60 year old man with acute hepatic failure due to pembrolizumab for metastatic liver cancer (Medicine (Baltimore) 2017;96:e9431)
- 62 year old man with COVID-19 triggered acute hepatic failure and rhabdomyosis (Viruses 2023;15:1445)
- 63 year old woman with acute on chronic hepatic failure due to sorafenib for hepatitis B related hepatocellular carcinoma (Mol Clin Oncol 2017;7:693)
- 64 year old man with acute liver failure following immune checkpoint inhibitors for his laryngeal squamous cell carcinoma (Clin Res Hepatol Gastroenterol 2023;47:102203)
Treatment
- Specific treatment if the exact etiology is known
- Supportive and preventive care and management of complications (coagulopathy, renal failure, encephalopathy, sepsis, metabolic disorders)
- Liver support (extracorporeal liver assist device) and liver transplant
- Mortality without liver transplant is 25 - 90% (Semin Liver Dis 2008;28:175)
Clinical images
N/A
Gross description
N/A
Gross images
Frozen section description
N/A
Frozen section images
N/A
Microscopic (histologic) description
- Zonal or panacinar hepatic necrosis with collapse of reticulin framework
- Variable inflammatory infiltrate, depending on etiology
- Variable ductular reaction
- Fibrosis and cirrhosis in patients with acute on chronic hepatic failure
- Reference: Adv Anat Pathol 2016;23:144
Microscopic (histologic) images
Cytology description
N/A
Cytology images
N/A
Immunofluorescence description
N/A
Immunofluorescence images
N/A
Positive stains
N/A
Negative stains
N/A
Electron microscopy description
N/A
Electron microscopy images
N/A
Molecular / cytogenetics description
N/A
Molecular / cytogenetics images
N/A
Videos
N/A
Sample pathology report
- Liver, recipient explant:
- Acute hepatocellular necrosis (see comment)
- Comment: Extensive panacinar hepatocellular necrosis is accompanied by minimal inflammatory infiltrate and ductular necrosis. No significant fibrosis is present in the residual liver parenchyma. Provided by known drug history of acetaminophen overdose, the overall features are consistent with acetaminophen overdose associated acute hepatic failure.
Differential diagnosis
- Severe acute hepatitis:
- Does not fulfill the clinical diagnostic criteria of acute hepatic failure (e.g., absence of coagulopathy and hepatic encephalopathy)
- Requires clinical correlation and investigations
- Chronic liver disease with extrahepatic organ failure:
- There is no clinical feature of acute hepatic decompensation
- Requires clinical correlation and investigations
- Chronic liver disease with nonhepatic encephalopathy / encephalitis (e.g., drug / toxin, uremic encephalopathy):
- There is no clinical feature of acute hepatic decompensation apart from altered mental status
- Requires clinical correlation and investigations
Additional references
Board review style question #1
Board review style answer #1
B. Severe fibrosis or cirrhosis. Acute on chronic hepatic failure occurs in patients with underlying chronic liver disease or cirrhosis; hence, the chronicity feature (fibrosis or cirrhosis) should be present. Answers A, C and D are incorrect because degrees of necroinflammatory activity (necrosis of hepatocytes and inflammatory infiltrate) and regenerative activity (ductular reaction) vary and depend on the underlying etiology and precipitating factors.
Comment Here
Reference: Hepatic failure
Comment Here
Reference: Hepatic failure
Board review style question #2
Which of the following features is associated with acute on chronic hepatic failure?
- Elevated APTT
- Elevated urea
- Hypoalbuminemia
- Shock
Board review style answer #2
D. Shock. Circulatory failure is one of extrahepatic organ failures associated with acute on chronic hepatic failure. Answers A - C are incorrect because elevated PT / INR (rather than APTT), elevated creatinine (rather than urea) and elevated bilirubin (rather than hypoalbuminemia) are also associated with acute on chronic hepatic failure.
Comment Here
Reference: Hepatic failure
Comment Here
Reference: Hepatic failure
Hepatic infantile hemangioma
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Immunofluorescence description | Immunofluorescence images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- A benign vascular tumor with features similar to those of infantile hemangioma of the skin or superficial soft tissue in children
Essential features
- Numerous small and capillary-like vascular channels, especially the periphery region, lined by plump endothelial cells usually in a single layer
- Large cavernous vessels lined by flattened endothelial cells with fibrosis of the surrounding stroma in the center of large lesions
- Entrapment of hepatocytes and small bile ducts at the advancing edges of the lesion
Terminology
- Preferred: hepatic infantile hemangioma (HIH)
- Subtype(s): single / focal HIH (SHIH), multifocal HIH (MHIH) and diffuse HIH (DHIH)
- Not recommended: hemangioendothelioma type 1 or type 2 (type 2 is currently classified as angiosarcoma), infantile hemangioendothelioma; juvenile hemangioma, hepatic small vessel neoplasm
ICD coding
Epidemiology
- Most common hepatic mesenchymal tumor in infants and children (Diagnostics (Basel) 2021;11:333, Pediatr Gastroenterol Hepatol Nutr 2020;23:72)
- F > M, up to 2:1 (J Pediatr Surg 2012;47:165)
- 90% are diagnosed at < 6 months of age (Pediatr Int 2014;56:304)
- Rarely can develop prenatally
- 10 - 15% have coexisting cutaneous or other sites infantile hemangiomas
- Higher risk in patients with multiple cutaneous infantile hemangiomas (J Am Acad Dermatol 2021;84:1378)
- 50% is incidental finding at autopsy
- Association with hepatoblastoma, mesenchymal hamartoma and Beckwith-Wiedemann syndrome
Sites
- Liver
Pathophysiology
- Pathophysiology of HIH is still unknown
- Aberrant response of pluripotent stem cells to stimuli, including hypoxia and the renin angiotensin system have been proposed (Arterioscler Thromb Vasc Biol 2007;27:2664, J Hematol Oncol 2014;7:13, Precis Clin Med 2022;5:pbac006, Clin Cancer Res 2013;19:3360)
Etiology
- No specific proven etiology
- Earlier considered to be associated with multigestational pregnancy, low birth weight and prematurity
Clinical features
- Most cases are asymptomatic and diagnosed incidentally
- Only 9.7% patients detected by regular screening are symptomatic (J Am Acad Dermatol 2021;84:1378)
- May grow progressively and then involute, especially SHIH
- Common symptoms: hepatomegaly, abdominal distension, failure to thrive
- Consumptive hypothyroidism: overexpression of type 3 iodothyronine deiodinase in tumor cells, inactivates thyroid hormone
- Congestive heart failure due to macrovascular (arteriovenous, arterioportal or portovenous) shunting (J Emerg Med 2021;60:107, BMC Cardiovasc Disord 2019;19:216)
- Abdominal compartment syndrome with compromised ventilation and poor inferior vena caval blood return to the heart
- Thrombocytopenia and coagulopathy
- DHIH is associated with more serious manifestations than MHIH (J Pediatr Surg 2012;47:165)
Diagnosis
- Imaging studies
- Histologic examination
- Tumor cells express endothelial cell markers (factor VIII related antigen, ERG, CD31 and CD34) and GLUT1 (except SHIH)
Laboratory
- Usually normal alpha fetoprotein (AFP), rarely elevated due to secretion from entrapped or uninvolved hepatocytes (Hum Pathol 2010;41:763)
Radiology description
- Generally not visualized on ultrasound beyond 18 - 24 months of age
- Ultrasound
- Well defined hypo or hyperechoic
- Multifocal or diffuse
- Hyperenhancement in arterial phase (AJR Am J Roentgenol 2020;214:658)
- MRI
- Homogeneously enhanced
- Hypointense relative to the liver on T1 weighted images
- Hyperintense on T2 weighted images (Eur J Radiol 2010;76:e24)
Prognostic factors
- Mortality as high as 16%, with up to 38% in DHIH (J Pediatr Surg 2015;50:837)
- Proliferative phase for > 2 years of age or new lesion after 1 year of age has worse outcome
- Poor prognostic factors: heart failure, diffuse HIH, abdominal compartment syndrome
Case reports
- Female neonate with hepatic mass diagnosed in utero by ultrasonography (Cureus 2022;14:e25240)
- 10 day old girl presented with high output failure (J Emerg Med 2021;60:107)
- 11 day old boy with giant hepatic infantile hemangioma causing postnatal respiratory arrest (Sisli Etfal Hastan Tip Bul 2020;54:108)
- 18 day old girl presented with jaundice and abdominal mass (Medicine (Baltimore) 2018;97:e12863)
- 2 month old girl with hepatomegaly and diffuse intrahepatic lesions (Front Oncol 2024;14:1336742)
Treatment
- Treatment strategies range from simple observation to a series of medical, surgical and radiological interventions
- Spontaneous involution in 5 - 10% by 6 - 8 months; resection if solitary, otherwise steroids, interferon, propranolol, radiation therapy, embolization or transplantation (World J Surg 2009;33:597, Pediatr Surg Int 2021;37:791, Pediatrics 2019;143:e20183475)
- Regular screening in patients with ≥ 5 cutaneous hemangiomas
- Routine thyroid hormone level monitoring and echocardiography (Semin Pediatr Surg 2020;29:150970)
Clinical images
Not available
Gross description
- Tumors can be single (~55%), multiple or diffuse (~45%) with mean size of 4 cm (range: 0.1 - 15 cm)
- Multifocal lesions usually progress to coalescent nodules diffusely replacing normal hepatic parenchyma (World J Hepatol 2021;13:1316)
- Individual lesions are well defined, noncapsulated, often with fibrotic scarring in the center and red-brown vascularized areas in the periphery; small lesions often appear spongy and red-brown on sectioning
- Hemorrhagic, infarcted and calcified areas can be seen
Frozen section description
Not applicable
Frozen section images
Not applicable
Microscopic (histologic) description
- Noncapsulated and irregular margins extending into surrounding hepatic tissue
- Small, capillary-like vascular channels lined by flattened or plump endothelial cells
- Vascular proliferation is more prominent in the periphery and in the proliferation stage
- Tumor cells have small, bland, hyperchromatic nuclei without marked atypia and may have very rare mitosis
- Rare foci of pseudopapillary proliferation
- Intervening stroma is loosely fibrotic and generally scant
- Stroma undergoes further expansion and becomes more fibrotic towards the center of the tumor
- Entrapped bile ducts and hepatocytes can be seen at the advancing edges of the tumor
- Extramedullary hematopoiesis can be seen
Microscopic (histologic) images
Virtual slides
N/A
Cytology description
- Oval to spindle shaped cells with scant cytoplasm and wavy, kinked and indented nuclear outlines (Cytopathology 2010;21:398, Acta Cytol 2010;54:807)
Immunofluorescence description
N/A
Immunofluorescence images
N/A
Positive stains
- Factor VIII related antigen, CD31, CD34, ERG, GLUT1 (except SHIH)
Negative stains
Electron microscopy description
Not applicable
Electron microscopy images
Not applicable
Molecular / cytogenetics description
Not applicable
Molecular / cytogenetics images
Not applicable
Videos
Not available
Sample pathology report
- Liver, excision:
- Infantile hemangioma (see comment)
- Comment: The resection reveals multiple noncapsulated vascular lesions comprised of numerous small and capillary-like vascular channels lined by plump endothelial cells in a single layer. The lesional cells show strong, diffuse CD31, CD34 and GLUT1 positivity. Ki67 proliferative index is < 1%. The findings are consistent with infantile hepatic hemangioma (multifocal).
- Liver, biopsy:
- Benign vascular neoplasm, consistent with infantile hepatic hemangioma (see comment)
- Comment: Imaging study with multiple liver lesions was noted. The biopsy reveals a benign vascular neoplasm characterized by numerous small and capillary-like vascular channels lined by plump endothelial cells. There are no cytologic atypia, necrosis or other high grade morphologic features. The tumor cells show diffuse, strong CD34, CD31 and GLUT1 positivity. The findings are consistent with infantile hepatic hemangioma.
Differential diagnosis
- Hepatic angiosarcoma:
- Solid spindle areas with marked atypia
- Ki67 proliferation index > 10% (Pediatr Blood Cancer 2017;64:e26627)
- Irregular margins infiltrating into adjacent liver parenchyma
- Variable GLUT1 immunopositivity
- Mesenchymal hamartoma:
- Hypocellular fibromyxoid stroma with bland spindle cells
- Malformed bile duct in duct plate configuration
- Occasionally can have prominent vascular proliferation
- GLUT1 negative
- Cavernous hemangioma:
- Usually well circumscribed
- Variably sized, dilated and thin walled vessels lined by a single layer of flat endothelial cells
- No cytologic atypia or mitosis
- GLUT1 negative
- Hepatic small vessel neoplasm:
- Average patient age 54 years, more common in men (Hum Pathol 2016;54:143)
- Infiltration into adjacent liver parenchyma
- Anastomosing, closely packed vascular spaces lined by flat endothelial cells with occasional hobnailing
- GLUT1 negative
- Recurrent hotspot mutations of GNAQ, GNA11, GNA14 and PIK3CA
Additional references
Board review style question #1
A 5.5 x 3.5 cm lesion in the liver (first image) is identified in the autopsy of a 10 month old girl. External examination reveals multiple cutaneous hemangiomas on the trunk and upper extremities. Microscopic examination of the liver lesion reveals a vascular neoplasm composed of numerous small and capillary-like vascular channels lined by plump endothelial cells with no cytologic atypia in the periphery region (second image). The tumor exhibits an irregular interface with the adjacent liver parenchyma. In the central region of the tumor, there are a few large, cavernous vessels lined by flattened endothelial cells, accompanied by fibrosis of the surrounding stroma (third image). The tumor cells are positive for CD31, CD34 and GLUT1 by immunohistochemistry. Which is the best diagnosis of this lesion?
- Angiosarcoma
- Cavernous hemangioma
- Hepatic infantile hemangioma
- Mesenchymal hamartoma
Board review style answer #1
C. Hepatic infantile hemangioma. The gross photograph and microscopic description identify the lesion as a benign vascular neoplasm. Micrograph shows a vascular neoplasm with numerous small and capillary-like vascular channels lined by plump endothelial cells with no cytologic atypia. In the center of the lesion shows stromal fibrosis and few large, cavernous vessels lined by flattened endothelial cells. CD31, CD34 and GLUT1 are positive in the lesional endothelial cells, confirming diagnosis of hepatic infantile hemangioma. Answer A (angiosarcoma) is incorrect because it should show marked nuclear atypia, abundant atypical mitotic figures and solid spindled areas. Answer B (cavernous hemangioma) is incorrect because it is a common subtype of hepatic hemangioma in adults showing circumscribed proliferation of variably sized, dilated and thin walled vessels lined by a single layer of flat endothelial cells. Answer D (mesenchymal hamartoma, the second most common benign pediatric hepatic tumor after hepatic infantile hemangioma), is incorrect because it is comprised of variable proportions of disorganized arrangements of primitive mesenchyme with benign dilated or branching bile ducts and clusters of normal appearing hepatocytes.
Comment Here
Reference: Hepatic infantile hemangioma
Comment Here
Reference: Hepatic infantile hemangioma
Board review style question #2
Multiple liver lesions (ranging from 0.5 to 3.5 cm) were incidentally identified on ultrasound of a 6 month old girl. A core biopsy was performed which revealed a vascular neoplasm as illustrated in the micrograph (first image). The tumor cells are positive for CD34 (second image) and GLUT1 (third image) by immunohistochemistry. Which immunohistochemical stain is most characteristic for diagnosing this lesion?
- CD31
- CD34
- GLUT1
- HepPar1
Board review style answer #2
C. GLUT1. The microscopy shows a benign appearing vascular neoplasm. GLUT1 is strongly and diffusely positive in infantile hemangiomas and helps to exclude nonneoplastic vessels, vascular malformation, as well as most of the other benign vascular neoplasms that do not express GLUT1. Answers A and B (CD31 and CD34) are incorrect because they are vascular markers that will be positive in all neoplastic or nonneoplastic vessels. Answer D (HepPar1, a hepatocytic marker) is incorrect because it is not helpful in characterizing a vascular lesion.
Comment Here
Reference: Hepatic infantile hemangioma
Comment Here
Reference: Hepatic infantile hemangioma
Hepatic small vessel neoplasm
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Definition / general
- Rare, recently described vascular hepatic neoplasm of uncertain malignant potential that is composed of anastomosing, densely packed, small, thin vessels with infiltrative borders, minimal cytologic atypia and a low proliferative rate
Essential features
- Hepatic small vessel neoplasm that shares similar morphologic and molecular qualities to and is thought to represent anastomosing hemangioma of the liver
- Histologically described as benign, low grade hepatic vascular neoplasm with a mottled, unencapsulated gross appearance with poorly circumscribed borders
- Positive for vascular markers with frequent GNAQ mutations
Terminology
- Hepatic small vessel neoplasm (HSVN)
- Anastomosing hemangioma (AH)
ICD coding
- ICD-10: D37.6 - neoplasm of uncertain behavior of liver, gallbladder and bile ducts
Epidemiology
- Average patient age: 54 years old (24 - 83 years) and more common in males (Hum Pathol 2016;54:143)
Sites
- Hepatic parenchyma (Hum Pathol 2016;54:143)
- Radiographic evidence of concurrent spleen involvement but not histologically proven (BMJ Case Rep 2022;15:e248785)
Pathophysiology
- Shares GNAQ mutations with anastomosing hemangiomas (Mod Pathol 2017;30:722, Hum Pathol 2016;54:143)
Etiology
- Has morphologic and molecular similarities to and may represent anastomosing hemangioma of the liver
Clinical features
- Usually, an asymptomatic solitary liver lesion that is discovered incidentally (Hum Pathol 2016;54:143)
- Rarely, if large enough, may cause epigastric fullness or back pain (Hum Pathol 2018;78:159)
Diagnosis
- Histopathologic diagnosis: infiltrative small vessel vascular neoplasm with mild nuclear atypia and low proliferative index
- Diagnosis can be supported by immunohistochemistry and molecular testing
Laboratory
- Normal complete blood count (CBC), serum chemistry, aspartate aminotransferase (AST), alanine aminotransferase (ALT), alpha fetoprotein (AFP), carcinoembryonic antigen (CEA) and CA19-9 (BMJ Case Rep 2022;15:e248785)
Radiology description
- CT with contrast: hypodense lesions with contrast enhancement in the arterial and portal phase and wash out in the tardive phase
- PET / CT: no evidence of abnormal 18F fluorodeoxyglucose (18F FDG) uptake
- MRI with contrast: atypical vascular tumor with strong and early rim enhancement in arterial phase, with central irregular morphology and gradual enhancement (BMJ Case Rep 2022;15:e248785)
Prognostic factors
- Unknown prognosis and prognostic factors due to scant follow up studies
- Likely low malignant potential (Hum Pathol 2016;54:143)
- Single case report with possible malignant transformation and metastasis (Hum Pathol 2022;29:300671)
Case reports
- 60 year old woman with liver dysfunction and innumerable, diffuse liver nodules (Hum Pathol 2022;29:300671)
- 62 year old man with vague epigastric fullness, 17 cm hepatic lesion (Hum Pathol 2018;78:159)
- Woman in her 70s with concurrent hepatic and splenic lesions (BMJ Case Rep 2022;15:e248785)
Treatment
- Complete resection and close clinical follow up is recommended due to the unknown longterm behavior of this neoplasm (Hum Pathol 2016;54:143)
Gross description
- Poorly circumscribed, unencapsulated, pale tan to brown hemorrhagic lesions with ill defined borders
- Size ranges from < 1 cm to > 15 cm
- No grossly apparent cystic spaces or vessels (Hum Pathol 2016;54:143)
Microscopic (histologic) description
- Anastomosing, closely packed, small thin vascular channels lined by flat to plump endothelial cells with occasional hobnailing
- Infiltrative border with extension between hepatic plates and around portal tracts
- Minimal cytologic atypia
- Absence of necrosis, mitotic activity, prominent nucleoli, nuclear pleomorphism
- Occasional extramedullary hematopoiesis, hyaline globules and vascular thrombi
- Reference: Hum Pathol 2016;54:143
Microscopic (histologic) images
Positive stains
Negative stains
- Pankeratin, HepPar1, p53 (wild type), CD117, S100, c-Myc, GLUT1 (Hum Pathol 2016;54:143)
Molecular / cytogenetics description
- Recurrent activating hotspot mutations of GNAQ, GNA11 and GNA14
- Not found in angiosarcoma
- Recorded in several other vascular lesions: capillary hemangioma, angioma variants, hemangioendothelioma
- Activating hotspot mutation in PIK3CA
- Also found in angiosarcoma
- Reference: Hum Pathol 2016;54:143
Sample pathology report
- Liver, excision:
- Hepatic small vessel neoplasm, 2.5 cm (see comment)
- Comment: The Ki67 proliferative index is approximately 6%. Surgical margins are negative for tumor.
- Liver, biopsy:
- Vascular neoplasm with nuclear atypia (see comment)
- Comment: A neoplastic process consisting of back to back small vessels with mild nuclear atypia is identified. Ki67 immunohistochemical stain highlights ~5% of the endothelial nuclei. Although definitive infiltrative architecture is not present in this sample, these findings are most consistent with the recently described entity hepatic small vessel neoplasm.
Differential diagnosis
- Hepatic angiosarcoma, vasoformative type (more common):
- Marked nuclear pleomorphism, prominent nucleoli, frequent mitoses
- Ki67 proliferative index > 10% (Hum Pathol 2016;54:143)
- Strong and diffuse p53 and c-Myc
- Lacks GNAQ, GNA11, GNA14 mutations
- Epithelioid hemangioendothelioma:
- Lacks zonation pattern, epithelioid morphology, fibromyxoid stroma and intracytoplasmic lumina (Diagn Pathol 2014;9:131)
- Cavernous hemangioma:
- Lacks infiltrative borders
- Large vascular spaces, flat uniform endothelial cells
- Ki67 proliferative index < 1%
Additional references
Board review style question #1
A 2.5 cm liver lesion was incidentally identified on a CT scan of a 55 year old man with no significant medical history. No other lesions are identified radiographically. A core biopsy is performed revealing an infiltrative neoplasm pictured above. ERG is positive while HepPar1 and HHV8 are negative and p53 shows wild type staining. What molecular abnormality would most likely be identified in this neoplasm?
- GNAQ hotspot mutation
- KDR mutation
- MYC amplification
- RAS mutation
- TP53 mutation
Board review style answer #1
A. GNAQ hotspot mutation. The H&E photomicrograph shows a neoplasm consisting of small vessels with unremarkable endothelial cells, infiltrating between hepatic plates, consistent with a hepatic small vessel neoplasm (HSVN). HSVNs (and benign vascular neoplasms such as hemangiomas) are associated with hotpot mutations in the GNAQ family of genes. The other answer choices are mutations commonly identified in hepatic angiosarcoma (Hum Pathol 2022;29:300671).
Comment Here
Reference: Hepatic small vessel neoplasm
Comment Here
Reference: Hepatic small vessel neoplasm
Hepatitis (acute and chronic)-general
Table of Contents
Definition / general | Essential features | ICD coding | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Acute hepatitis:
- Active hepatocellular damage and necrosis caused most often due to viral infection, autoimmune disease or adverse drug reaction
- Histologically characterized by lobular disarray and variable hepatocyte necrosis
- Usually self limited duration of < 6 months
- Chronic hepatitis:
- Persistent and progressive inflammation and injury of hepatocytes
- Histologically characterized by portal based chronic inflammation
- Elevated liver enzymes for > 6 months' duration
Essential features
- Hepatitis can be acute or chronic
- Variable etiology
- Morphologically characterized by lobular inflammation and necrosis, portal inflammation, interface hepatitis and fibrosis / cirrhosis
ICD coding
Sites
- Liver parenchyma
Pathophysiology
- Inflammation of hepatocytes is caused by many factors, such as viruses, autoimmune disorders, drugs and alcohol
- Inflammatory cells along with proinflammatory cytokines can cause hepatocyte degeneration and necrosis; can induce stellate cell activation resulting in fibrosis and even progressing to cirrhosis overtime (Alcohol Alcohol 2019;54:408, Cold Spring Harb Perspect Med 2018;8:a031708)
Etiology
- Viral hepatitis: A, B, C, D, E (World J Gastroenterol 2021;27:1691)
- Less often caused by CMV, EBV, HSV, adenovirus
- Autoimmune hepatitis (J Immunol Res 2019;2019:9437043)
- Drug induced hepatitis (J Clin Pathol 2009;62:481)
- Alcoholic hepatitis (Alcohol Alcohol 2019;54:408)
- Nonalcoholic steatohepatitis
- Metabolic causes:
- Wilson disease
- Alpha-1 antitrypsin deficiency
- Hemochromatosis
Clinical features
- Acute hepatitis:
- Nonspecific constitutional symptoms: fever, fatigue, malaise (World J Gastroenterol 2021;27:1691)
- Jaundice
- Nausea, vomiting, weight loss, abdominal pain
- May present with signs and symptoms of liver failure
- Nonspecific constitutional symptoms: fever, fatigue, malaise (World J Gastroenterol 2021;27:1691)
- Chronic hepatitis:
- Asymptomatic or nonspecific constitutional symptoms
- Often diagnosed on laboratory evaluation (World J Gastroenterol 2021;27:1691)
- May present with features of portal hypertension and cirrhosis in later stages
- Asymptomatic or nonspecific constitutional symptoms
Diagnosis
- Clinical history and physical examination for specific signs and symptoms
- Laboratory evaluation
- Biopsy for grade and stage in chronic hepatitis
Laboratory
- Elevated transaminases (Alcohol Alcohol 2019;54:408)
- Alkaline phosphatase is slightly elevated
- Viral hepatitis: viral serologies will be positive (World J Gastroenterol 2021;27:1691)
- Autoimmune hepatitis: autoimmune serologies will be positive (J Immunol Res 2019;2019:9437043)
- Disease specific tests: urinary copper, ceruloplasmin, alpha-1 antitrypsin levels are helpful
Radiology description
- Acute hepatitis (Radiopaedia: Acute hepatitis [Accessed 20 June 2022]):
- Ultrasound features:
- Hepatomegaly is the most sensitive sign
- Gallbladder wall thickening (most often seen in hepatitis A)
- Periportal edema
- Accentuated brightness of portal vein radicle walls
- Overall echotexture is decreased
- Color / spectral doppler is normal
- CT - not a first line imaging modality:
- Hepatomegaly
- Decreased attenuation around portal system and hepatic hilum
- Diffusely decreased parenchymal attenuation on noncontrast CT
- Periportal or hepatoduodenal lymphadenopathy
- MRI findings are nonspecific and often used to exclude other etiologies of abnormal liver function studies
- Ultrasound features:
- Chronic hepatitis (Radiopaedia: Cirrhosis [Accessed 20 June 2022]):
- Ultrasound:
- Surface nodularity
- Overall coarse and heterogenous echotexture
- Segmental hypertrophy / atrophy
- Signs of portal hypertension
- Splenomegaly
- Fatty change
- Ascites
- CT / MRI - insensitive in early cirrhosis:
- Surface and parenchymal nodularity
- Fatty change
- In advanced cirrhosis, nodular margin and lobar hypertrophy / atrophy may be seen
- Signs of portal hypertension
- Upper abdominal lymphadenopathy in advanced disease
- Ultrasound:
Radiology images
Case reports
- 28 year old woman with abdominal pain, fever and rash (J Family Med Prim Care 2020;9:3749)
- 30 year old man with generalized weakness (Case Rep Gastrointest Med 2018;2018:2139607)
- 45 year old woman with icterus, headache and confusion (ACG Case Rep J 2020;7:e00441)
- 50 year old woman with abnormal liver enzymes on routine labs (ACG Case Rep J 2020;7:e00440)
- 59 year old woman with right upper quadrant (RUQ) pain and intermittent fever (Ann Gastroenterol 2018;31:123)
Treatment
- Based on the underlying etiology
Gross description
- Acute hepatitis:
- Liver is homogenously enlarged and congested, stretching Glisson capsule
- Necrosis and collapse of the liver lobules maybe seen
- Surface is usually reddish brown
- In cholestatic cases, a spectrum of brown to green may be seen
- Chronic hepatitis:
- Nonspecific in early stages
- Can be enlarged with yellow (fatty change in steatosis) to green (in cholestasis)
- In advanced stages the liver is cirrhotic with a firm, nodular appearance; they can have a micronodular or macronodular pattern (World J Gastroenterol 2016;22:1357)
Gross images
Microscopic (histologic) description
- Histological features are broad ranging and can vary based on etiology
- Acute hepatitis:
- Predominantly lobular injury pattern
- Chronic hepatitis:
- Predominantly portal / periportal inflammation, with varying degrees of fibrosis (World J Gastroenterol 2016;22:1357)
- Lobular inflammation and necrosis:
- Necrosis may be spotty, confluent or bridging
- Apoptotic bodies (acidophilic bodies / Councilman bodies)
- Ballooned hepatocytes (Alcohol Alcohol 2019;54:408)
- Canalicular cholestasis
- Portal inflammation (World J Gastroenterol 2016;22:1357):
- Viral hepatitis: primarily composed of lymphocytes, admixed plasma cells, histiocytes; lymphoid follicles are common in hepatitis C
- Autoimmune hepatitis: prominent plasma cell infiltrate with interface activity
- Drug induced: variable histology, mixed inflammatory cells, often rich in eosinophils
- Interface hepatitis (piecemeal necrosis) (Gut Liver 2020;14:430):
- Destruction of hepatocytes in the interface with inflammation extending into the adjacent liver parenchyma
- Fibrosis / cirrhosis (varying degrees, depending on stage of the disease)
Microscopic (histologic) images
Contributed by Rifat Mannan, M.B.B.S., M.D., Alexander Boyd, M.B.Ch.B., Owen Cain, M.B.Ch.B.,
Abhishek Chauhan, Ph.D. and Gwilym J. Webb, M.B.Ch.B., M.A.
Positive stains
- Trichrome stain / reticulin stain: highlights fibrosis / cirrhosis
- PASD: highlights cytoplasmic globules in alpha-1 antitrypsin deficiency
- Hepatitis B surface antigen (HBsAg) immunohistochemistry
- Other viral stains: CMV, adenovirus, HSV, EBER
Videos
Histopathology of liver in viral hepatitis
Histopathology of liver in chronic hepatitis
Sample pathology report
- Liver, needle biopsy:
- Chronic hepatitis B, with mild portal fibrosis (see comment)
- Histologic grade: A1 (METAVIR system)
- Histologic stage: 1/4 (Scheuer system)
- Comment: The patient's clinical history of hepatitis B virus infection (HBV DNA positive by report) is noted.
Differential diagnosis
- Primary biliary cholangitis, primary sclerosing cholangitis:
- Cholestasis with bile duct damage or loss
- Portal inflammation without interface hepatitis
- Alkaline phosphatase is elevated more than transaminases
- Lymphoma / leukemia:
- Portal tract inflammation with severe interface activity
- Infiltrates comprised of atypical lymphocytes
- Gene rearrangement studies and immunohistochemistry can help with diagnosis
- Graft rejection:
- Liver transplant patients
- Portal inflammation with mixed inflammatory cells, including eosinophils
- Lymphocytic cholangitis with duct damage, endothelialitis
Board review style question #1
An asymptomatic 50 year old woman presented with elevated transaminases (aspartate aminotransferase and alanine aminotransferase) on routine laboratory tests. The image above is a micrograph of the liver biopsy. What are the predominant inflammatory cells seen and what could be the underlying etiology?
- Lymphocytic predominance seen in viral hepatitis
- Lymphoid follicles seen in chronic hepatitis C infection
- Mixed inflammatory cells with eosinophils seen in drug induced hepatitis
- Plasma cell predominance seen in autoimmune hepatitis
Board review style answer #1
D. Plasma cell predominance seen in autoimmune hepatitis
Comment Here
Reference: Hepatitis (acute and chronic)-general
Comment Here
Reference: Hepatitis (acute and chronic)-general
Board review style question #2
A 45 year old woman presented with jaundice, vomiting and abdominal pain. Elevated transaminases were found on laboratory testing. Patient is diagnosed with acute viral hepatitis. What would be the microscopic findings in this patient?
- Bile duct proliferation with extensive fibrosis and brown, green plugs
- Lobular disarray with interface hepatitis and plasma cell rich portal inflammation
- Lobular inflammation with confluent necrosis and balloon degeneration
- Necrosis of hepatocytes with atypical lymphocytic infiltration
Board review style answer #2
C. Lobular inflammation with confluent necrosis and balloon degeneration
Comment Here
Reference: Hepatitis (acute and chronic)-general
Comment Here
Reference: Hepatitis (acute and chronic)-general
Hepatitis A virus (HAV)
Table of Contents
Definition / general | Virology | Diagrams / tables | Laboratory | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosis | Additional referencesDefinition / general
- Fecal - oral transmission via contaminated food or water
- Associated with overcrowding or poor sanitation
- Usually children (asymptomatic or symptomatic without jaundice)
- In adults, infection more severe with malaise and jaundice for 7 - 10 days
- Rarely causes massive hepatic necrosis and acute liver failure; fatal in < 0.5% of cases
- May cause acute cholestatic hepatitis with bile ductular proliferation, neutrophils around ducts, cholestasis, hepatocyte ballooning, pseudoglands around bile plugs
- Does not produce chronic disease or carrier state in immunocompetent patients
- Causes 50% of hepatitis cases in US; effective vaccine available
Virology
- Due to picornavirus, 27 nm virion with single stranded RNA
Laboratory
- Serum IgM anti-HAV is more reliable than immunostains
Microscopic (histologic) description
- Periportal inflammation and necrosis, ballooning degeneration, apoptosis
- Cholestasis and increased portal and periportal plasma cells are relatively specific for hepatitis A
- Acidophil bodies or cytolysis are present (collapse of reticulin network where cells have disappeared with appearance of macrophage aggregates)
- Bridging necrosis if severe hepatitis
- Also interface hepatitis (inflammatory infiltrate spills over into adjacent parenchyma to cause necrosis of periportal hepatocytes)
- Relative sparing of centrilobular hepatocytes
Microscopic (histologic) images
Differential diagnosis
- Chronic hepatitis with moderate / severe activity (fibrosis present)
Additional references
Hepatitis B virus (HBV)
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Virology | Etiology | Diagrams / tables | Clinical features | Screening | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Immunofluorescence description | Immunofluorescence images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Hepatitis B is a vaccine preventable disease that causes acute and chronic liver inflammation and is caused by the hepatitis B virus (HBV)
- Hepatitis B has several serological markers
- HBsAg and anti-HBs
- HBeAg and anti-HBe
- Anti-HBc IgM and IgG
Essential features
- Hepatitis B is a virus induced disease that causes acute hepatitis, chronic hepatitis and is associated with an increase in risk for hepatocellular carcinoma
- Hepatitis B is caused by HBV, a partly double stranded DNA virus
- Constitutes a major global health problem that can be prevented by vaccination
- Diagnosis is based on the detection of hepatitis B surface antigen (HBsAg) and IgM hepatitis B core antibody; HBV DNA is present in the initial phase of the infection (MMWR Recomm Rep 2023;72:1)
Terminology
Not relevant
ICD coding
- ICD-10
- ICD-11
Epidemiology
- HBV infection is a major public health problem in most countries with ~2 billion people worldwide showing exposure to the virus and nearly 300 million people carrying an HBV chronic infection (J Clin Virol 2005;34:S1)
- According to estimates by the World Health Organization (WHO), HBV caused 257,000 chronic infections and 887,000 deaths in 2015
- The Centers for Disease Control and Prevention (CDC) estimates there were 2,157 new cases of acute hepatitis B and 5 new cases reported of chronic hepatitis B per 100,000 people during 2020 in the United States
- Virus induced hepatitis is one of the most common causes of liver cirrhosis and liver cancer (J Hepatol 2013;58:593)
Sites
- Liver
- Acute hepatitis
- Chronic hepatitis
- Asymptomatic to chronic liver disease stigmata (jaundice, splenomegaly, ascites, peripheral edema, encephalopathy)
- Extrahepatic manifestations (complications of chronic hepatitis B)
- Polyarteritis nodosa (Medicine (Baltimore) 1995;74:238)
- Glomerular disease (N Engl J Med 1979;300:814)
Pathophysiology
- Immune mediated and direct cytopathic liver injury
- Innate and adaptive immune responses contribute to immune control of HBV infection (World J Gastroenterol 2022;28:881, Front Immunol 2022:13:970938, Annu Rev Pathol 2006:1:23)
- The host's immune response to the virus mediates the hepatocellular damage observed in acute and chronic infections (Annu Rev Immunol 1995:13:29, Front Cell Infect Microbiol 2023:13:1206720)
- Cytotoxic T cell mediated lysis of infected hepatocytes is thought to cause HBV related liver disease (Med Microbiol Immunol 2015;204:11)
- Viral variants
- Mutations in HBV have been identified and can potentially modulate the severity of the liver disease, affecting the level of HBV replication or the expression of immunogenic epitopes; for example, lack of detectable HbsAg in the serum has been correlated to deletions of the pre-S region, allowing viral persistence by eliminating HHLA restricted B cell and T cell epitopes (World J Gastroenterol 2016;22:126)
- Development of chronic infection
- Patients with weak immune systems or who are immunocompromised have an increased risk of progressing to chronic HBV infection (J Hepatol 2003;39:115)
Virology
- HBV is a partly double stranded DNA virus belonging to the family hepadnaviridae (World J Gastroenterol 2009;15:5761)
- Infectious virion (the envelope of the Dane particle) is made of a cell originated membrane containing HbsAg
- Core contains the viral DNA genome, viral polymerase / reverse transcriptase (originating from infected cells), hepatitis B core antigen (HBcAg) and hepatitis B e antigen (HBeAg)
Etiology
Not relevant
Diagrams / tables
Clinical features
- Acute hepatitis B infection
- Variable course ranging from asymptomatic to fulminant hepatitis
- 70% of patients have subclinical course / 30% develop icteric hepatitis (J Infect Dis 1985;151:599)
- Variable course ranging from asymptomatic to fulminant hepatitis
- Chronic hepatitis B infection
- Asymptomatic, fatigue, hepatic failure, cirrhosis, decompensated cirrhosis, hepatocellular carcinoma, extrahepatic manifestations (Hepatology 1988;8:493, Gastroenterology 1992;103:1630, Hepatology 1995;21:77)
Screening
- Presence of hepatitis B surface antigen (HBsAg), hepatitis B surface antibody (anti-HBs) and total hepatitis B core antibody (anti-HBc) (MMWR Recomm Rep 2023;72:1)
Diagnosis
- Acute HBV infection diagnosis
- HBsAg and IgM to HbcAg
- Markers of HBV replication: HBeAg and HBV DNA are present (MMWR Recomm Rep 2023;72:1)
- Chronic hepatitis B is defined as the persistence of HBsAg for greater than 6 months
- HBcAg can be detected throughout the course of the infection and stays in the blood after recovery
- Detection of anti-HBc indicates current or past infection (Hepatology 2018;67:1560)
- Other tests for HBV replication, HBeAg and alanine transaminase (ALT) should be performed to determine if the patient should start antiviral therapy
Laboratory
- See Diagnosis
Radiology description
Not relevant
Radiology images
Not relevant
Prognostic factors
- Per the CDC, the lifetime risk for hepatocellular carcinoma is 40% for men and 15% for women
- Risk of chronic infection is related to age at infection; ~90% of infants with hepatitis B will develop chronic infection, whereas < 5% of immunocompetent adult patients with acute hepatitis B progress to chronic infection (Hepatology 1989;9:452, CDC: Hepatitis B [Accessed 5 February 2024])
- Chronic HBV infection has been associated with increased risk for hepatocellular carcinoma (IARC Monogr Eval Carcinog Risks Hum 2012;100:1)
- CDC reported that 25% of chronic hepatitis B infections progress to liver cancer
- Prognosis is worse in HBV infected patients from endemic areas and patients with chronic hepatitis B (Hepatology 1995;21:77)
- Reduction in inflammation (biopsy determined) is associated with less fibrosis progression (Am J Gastroenterol 2012;107:1388)
Case reports
- 25 year old woman with end stage renal disease of unknown cause received a living donor kidney transplant 6 years previously (Exp Clin Transplant 2019;17:408)
- 41 year old previously healthy woman presenting with asthenia, jaundice and upper abdominal pain at palpation (BMJ Case Rep 2017;2017:bcr2017221763)
- 63 year old Vietnamese woman with IgG kappa myeloma and positive for anti-HBcAb (Leuk Lymphoma 2021;62:1271)
Treatment
- Treatment for most of patients with acute hepatitis B is mainly supportive; for patients who require treatment, tenofovir or entecavir are preferred as a monotherapy (Hepatology 2016;63:261)
- Therapeutic agents approved for the treatment of adults with chronic hepatitis B in the US are Peg-INF-2a, nucleos(t)ide analogs, lamivudine, telbivudine, entecavir and adefovir (Hepatology 2016;63:261)
- HBeAg positive children (ages 2 to 18) with elevated ALT and measurable HBV DNA levels should be in antiviral therapy to achieve sustained HBeAg seroconversion (Hepatology 2016;63:261)
- Pregnant women with HBV DNA > 2 x 105 IU/mL treatment should be based on recommendations for nonpregnant women (Hepatology 2016;63:261)
- Combination of antiviral therapy targeting multiple steps in the HBV lifecycle can be used to restore immune response to HBV (J Clin Med 2020;9:3187)
Clinical images
Not relevant
Gross description
Not relevant
Gross images
Not relevant
Frozen section description
Not relevant
Frozen section images
Not relevant
Microscopic (histologic) description
- Acute phase of hepatitis B
- Inflammatory cell infiltration
- Predominantly lymphocytic infiltrate within the parenchyma and portal tracts (usually perivenular distribution)
- Involvement of portal inflammation is variable
- Plasma cells may also be prominent and few neutrophils and eosinophils may be present (Liver 1985;5:84)
- Compared to acute hepatitis C, acute hepatitis B has periportal inflammation (J Gastroenterol Hepatol 2001;16:209)
- Occult infection and mild portal inflammation, focal necrosis, apoptosis and fibrosis may persist following clinical recovery of acute hepatitis B (Hepatology 2003;37:1172)
- Predominantly lymphocytic infiltrate within the parenchyma and portal tracts (usually perivenular distribution)
- Hepatocellular damage
- Hepatocyte nuclei show prominent nucleoli and a moderate degree of pleomorphism; may show multiple nucleoli
- Changes ranging from a minor degree of cell swelling to cell death, most severe in perivenular areas
- Ballooning degeneration is seen as more severe degrees of cell swelling
- Acidophil bodies or Councilman bodies
- Eosinophilic globule or fragments of apoptotic hepatocytes where deposits of HbsAg are found (Leber Magen Darm 1982;12:146)
- Granular or vacuolated cytoplasm might be present
- Other features: cholestasis, Kupffer cell activation, endotheliitis, bile duct damage, ductular reaction and mild hepatocellular siderosis (Am J Clin Pathol 1984;81:162)
- Inflammatory cell infiltration
- Chronic hepatitis B
- Inflammatory cell infiltration
- Mononuclear infiltration of portal tracts
- Both interface hepatitis and lobular hepatitis can be seen
- Mononuclear infiltration of portal tracts
- Hepatocellular changes
- Hallmark of chronic hepatitis B virus infection
- Ground glass appearance (of the central part of the cytoplasm) of hepatocytes when HBsAg is elevated or in active viral replication (Viruses 2019;11:386)
- Active viral replication can also be demonstrated by hepatocyte nuclei or cytoplasmic stain of HBcAg
- Nuclei of hepatocytes may contain large amounts of core protein and have a pale, homogenous appearance on H&E sections, described as sanded
- Marked variation in size and appearance of hepatocyte nuclei and close contact between hepatocytes and lymphocytes might be seen
- Enlargement of portal tracts due to infiltration of mononuclear cells (J R Soc Med 1985;78:391)
- Lobular spotty necrosis (J R Soc Med 1985;78:391)
- Hepatocyte death, atrophy, regeneration and fibrosis
- Hallmark of chronic hepatitis B virus infection
- Inflammatory cell infiltration
Microscopic (histologic) images
Virtual slides
Not relevant
Cytology description
Not relevant
Cytology images
Not relevant
Immunofluorescence description
Not relevant
Immunofluorescence images
Not relevant
Positive stains
- Reticulin stain is useful in the early stage to evaluate for parenchymal loss (J Clin Chem Clin Biochem 1989;27:345)
- HBsAG / HBcAG: double staining technology staining infected cells showing colocalization of the 2 antibodies
- Macrophages contain diastase periodic acid Schiff (PAS) positive material (J Clin Chem Clin Biochem 1989;27:345)
- Iron stain highlighting iron deposits within hepatocytes or macrophages
- Masson trichrome stain: stains increased collagen accumulation and is an indicator of fibrosis (Semin Diagn Pathol 2006;23:190, Coll Relat Res 1982;2:151)
Negative stains
Not relevant
Electron microscopy description
Not relevant
Electron microscopy images
Not relevant
Molecular / cytogenetics description
Not relevant
Molecular / cytogenetics images
Not relevant
Videos
Not relevant
Sample pathology report
- Liver, nontargeted, core needle biopsy:
- Moderate portal and lobular mononuclear inflammation comprised predominantly of lymphocytes and plasma cells (grade 2) compatible with hepatitis B infection (see comment)
- No steatosis, ballooning degeneration or intracytoplasmic hyaline seen
- Iron stain shows minimal iron deposition in hepatocytes
- Trichrome stain shows no fibrosis
- Reticulin stain highlights unremarkable hepatic cell plates
- Comment: The findings are consistent with the patient’s known viral (hepatitis B) infection with grade 2 inflammatory activity and stage 0 fibrosis.
Differential diagnosis
- Hepatitis C:
- Dense portal lymphocytic infiltrate, including lymphoid follicles with germinal centers (Hepatology 1992;15:572)
- Lobular inflammation is seen in chronic infection
- Steatosis (predominantly macrovesicular with patchy pattern) and bile duct damage (Hepatology 1992;15:572)
- Autoimmune hepatitis:
- Plasma cells in clusters at limiting plate and in areas of interface hepatitis (nonspecific but suggestive) (Clin Gastroenterol Hepatol 2007;5:255)
- Piecemeal necrosis (Hepatology 1992;15:572)
- Hepatocellular rosettes (nonspecific) (Histopathology 2015;66:351)
- Syncytial multinucleated hepatocyte giant cells (Ann Hepatol 2009;8:68)
- Drug induced hepatotoxicity:
- Hepatotoxicity can mimic almost every other type of liver disease
- Dense interface / lobular lymphoplasmacytic infiltrate and hepatocellular injury
- Prominent eosinophilic infiltrate
- Centrizonal necrosis is highly suggestive of drug induced liver injury
- Wilson disease:
- Steatosis and periportal glycogenated nuclei (Am J Clin Pathol 1994;102:443)
- Perinuclear and intracytoplasmic Mallory-Denk bodies in periportal liver cells (Lancet 1979;1:1205)
- Copper storage within periportal hepatocytes
- Alpha-1 antitrypsin deficiency:
- Predominantly lymphocytic portal inflammation
- Eosinophilic ground glass globules, negative / weakly positive on D-PAS (Hum Pathol 2000;31:575)
- Cirrhosis is usually present at diagnosis
- Steatosis and mild cholestasis may be present
Additional references
Board review style question #1
Hepatitis B has the strongest association with development of which of the following malignancies?
- Angiosarcoma of the liver
- Hepatoblastoma
- Hepatocellular carcinoma
- Intrahepatic cholangiocarcinoma
Board review style answer #1
C. Hepatocellular carcinoma. Chronic infection with hepatitis B virus has been established as a major risk factor for hepatocellular carcinoma and there is a strong correlation between the occurrence of hepatocellular carcinoma and endemic hepatitis B virus infection worldwide (Proc Natl Acad Sci U S A 1986;83:8338, J Hepatol 2012;57:69, J Clin Gastroenterol 2013;47:S2, J Natl Cancer Inst 2005;97:265).
Answer D is incorrect because although recent studies suggest that hepatitis B virus infection plays an important etiological role in intrahepatic cholangiocarcinoma (ICC) development, ICC is much less common than hepatocellular carcinoma (World J Gastroenterol 2014;20:5721, J Hepatol 2020;72:95). Answer A is incorrect because angiosarcoma of the liver is a rare type of liver cancer predominantly associated with arsenic and vinyl chloride monomer as causal agents (BMC Gastroenterol 2011;11:142). Answer B is incorrect because although hepatoblastoma should be considered among the differential diagnoses in young patients presenting with HBV infection without cirrhosis, HBV is not a risk factor for hepatoblastoma (World J Gastroenterol 2018;24:3980, Asian Pac J Cancer Prev 2005;6:213).
Comment Here
Reference: Focal nodular hyperplasia
Answer D is incorrect because although recent studies suggest that hepatitis B virus infection plays an important etiological role in intrahepatic cholangiocarcinoma (ICC) development, ICC is much less common than hepatocellular carcinoma (World J Gastroenterol 2014;20:5721, J Hepatol 2020;72:95). Answer A is incorrect because angiosarcoma of the liver is a rare type of liver cancer predominantly associated with arsenic and vinyl chloride monomer as causal agents (BMC Gastroenterol 2011;11:142). Answer B is incorrect because although hepatoblastoma should be considered among the differential diagnoses in young patients presenting with HBV infection without cirrhosis, HBV is not a risk factor for hepatoblastoma (World J Gastroenterol 2018;24:3980, Asian Pac J Cancer Prev 2005;6:213).
Comment Here
Reference: Focal nodular hyperplasia
Board review style question #2
A 63 year old man with a longstanding history of hepatitis B presents with FibroScan results consistent with moderate liver fibrosis. A liver biopsy is performed and is shown above. Which of the following is true regarding this patient’s histologic evaluation for hepatitis B infected hepatocytes?
- Diffuse nuclear expression of HbsAg suggests active viral replication
- Finely granular intranuclear eosinophilic inclusions known as sanded nuclei correspond to HbsAg accumulation in hepatitis B infected hepatocytes
- Ground glass hepatocytes in chronic hepatitis B infection consist of endoplasmic reticulum hyperplasia HbsAg in chronic carriers
- Variation in size and cytology of hepatocyte nuclei can be present and the chronic intralobular inflammatory infiltrate associated with chronic hepatitis B consists of CD4+ lymphocytes
Board review style answer #2
C. Ground glass hepatocytes in chronic hepatitis B infection consist of endoplasmic reticulum hyperplasia HbsAg in chronic carriers, which can be highlighted with Victoria blue special stain (Hepatology 2009;49:S61, Jpn J Exp Med 1974;44:25).
Answer B is incorrect because sanded nucleus in a persistent hepatitis B virus infection indicates excessive core formation and it can be seen on H&E stain (Lab Invest 1976;35:1). Answer A is incorrect because while HbsAg expression can be membranous or cytoplasmic, HbcAg expression may be nuclear or cytoplasmic (Hepatology 2009;49:S61). Extensive nuclear membranous expression of HbcAg is associated with active viral replication and viral load (J Clin Gastroenterol 2003;36:269). Answer D is incorrect because the portal inflammatory infiltrate seen in hepatitis B is usually composed of CD4+ lymphocytes, B lymphocytes and dendritic cells. The intralobular inflammatory infiltrate is usually CD8+ (J Viral Hepat 2019;26:727).
Comment Here
Reference: Focal nodular hyperplasia
Answer B is incorrect because sanded nucleus in a persistent hepatitis B virus infection indicates excessive core formation and it can be seen on H&E stain (Lab Invest 1976;35:1). Answer A is incorrect because while HbsAg expression can be membranous or cytoplasmic, HbcAg expression may be nuclear or cytoplasmic (Hepatology 2009;49:S61). Extensive nuclear membranous expression of HbcAg is associated with active viral replication and viral load (J Clin Gastroenterol 2003;36:269). Answer D is incorrect because the portal inflammatory infiltrate seen in hepatitis B is usually composed of CD4+ lymphocytes, B lymphocytes and dendritic cells. The intralobular inflammatory infiltrate is usually CD8+ (J Viral Hepat 2019;26:727).
Comment Here
Reference: Focal nodular hyperplasia
Hepatitis B virus (HBV)
Table of Contents
Definition / general | Virology | Diagrams / tables | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Additional referencesDefinition / general
- Usually subclinical disease but may lead to fulminant hepatic failure, chronic liver disease and cirrhosis
- Lifetime risk for hepatocellular carcinoma is 40% for men and 15% for women
- Spread by acutely infected patients or chronic viral carriers through intimate / sexual contact, intravenous drug abuse, contaminated blood or infected instruments, maternal to infant via delivery
- Causes 40% of hepatitis cases in US
- Carrier: antigenemia > 6 months, normal ALT and AST, no symptoms; occurs in 10%
- Immunostains may be helpful for chronic disease
- Fibrosing cholestatic hepatitis: unusual presentation of hepatitis B virus in liver allograph recipients
Virology
- Due to hepadnavirus
- Intact virus is known as Dane particle
- Has 28 nm central nucleocapsid core enclosed by outer surface envelope; core contains DNA genome with DNA polymerase, hepatitis B core antigen and hepatitis B e antigen
- Viral envelope contains hepatitis B surface antigen
- Hepatitis B surface antigen (HBsAg): carries no particularly useful clinical information but is first serum marker of active infection
- Hepatitis B core antigen (HBcAg): present in hepatocyte nuclei, not serum; indicates active replication of virus, patient is infective
Microscopic (histologic) description
- Acute: ground glass hepatocytes (finely granular eosinophilic cytoplasm consisting of spherules and tubules of HBsAg) with central ballooning degeneration
Microscopic (histologic) images
Images hosted on other servers:
Positive stains
- Immunostains for HBsAg or HBcAg or orcein stain (highlights HBsAg)
Additional references
Hepatitis C virus (HCV)
Table of Contents
Definition / general | Causes and complications | Virology | Poor prognostic factors | Treatment | Post liver transplant | Case reports | Microscopic (histologic) description | Microscopic (histologic) images | Additional referencesDefinition / general
- 0.2% incidence in US, 170 million people infected worldwide
- 90% of non-A, non-B hepatitis cases, 75 - 95% of transfusion associated hepatitis cases are due to hepatitis C
Causes and complications
- 35% IV drug abuse, 15% household contact or heterosexual exposure, 5% blood transfusion, 45% unknown
- 50 - 80% develop chronic liver disease, 20% of these develop cirrhosis
- High risk for hepatocellular carcinoma, particularly with alcoholic cirrhosis (57% at 10 years)
- Acute liver failure is rare
- CD34+ sinusoidal endothelial cells are a risk factor for hepatocellular carcinoma in HCV associated chronic liver disease (Hum Pathol 2001;32:1363)
- In HIV+ patients, cirrhosis more common if CD4 < 200 cells/microL (Hum Pathol 2000;31:69)
- Complications: deterioration of liver status with cirrhosis in 20% and improvement in 10% with chronic hepatitis C; also hepatocellular carcinoma
Virology
- Flavivirus, enveloped RNA virus
Poor prognostic factors
- Necroinflammatory activity is associated with fibrosis progression (Hum Pathol 2001;32:904)
- Also alcohol consumption, advanced age at the time of infection and immunocompromise
Treatment
- Longterm interferon alpha causes regression of cirrhosis in 5 - 10% (Hum Pathol 2004;35:107)
- Interferon used in combination with ribavirin; orthotopic liver transplantation
- 10% have stainable iron; some hepatologists use iron content and location in patient management
- Occasionally may be due to mutation in gene for hereditary hemochromatosis (Arch Pathol Lab Med 2000;124:1632)
Post liver transplant
- Recurrence of hepatitis C (as opposed to reinfection, which is almost universal) associated with more single cell hepatocyte necrosis (acidophil bodies), bile duct damage, lymphoid aggregates, cholestasis, fibrous septum, viral load (HCV RNA) > 1.25 million viral equivalents/ml
- Recurrence may resemble cellular rejection
- Serial biopsies may be necessary (Hum Pathol 2002;33:277, Arch Pathol Lab Med 2000;124:1623, Mod Pathol 2002;15:897)
- HCV RNA levels are highest at time of active hepatocellular destruction (Mod Pathol 1999;12:1043)
Case reports
- 55 year old man with coexisting hepatocellular carcinoma and diffuse large B cell lymphoma (Arch Pathol Lab Med 2000;124:1532)
- With coexisting diffuse large B cell lymphoma (Am J Surg Pathol 1999;23:1124)
Microscopic (histologic) description
- Predominantly sinusoidal lymphocytic infiltrate, often with lymphoid follicles that surround damaged bile ducts, often involvement of portal tracts
- Mallory hyaline, mild and focal macrovesicular steatosis, minimal necrosis
- Usually no / minimal plasma cells or eosinophils; may have irregular acidophil bodies
- Lymphoid aggregates are specific for hepatitis C but only 50% sensitive
Microscopic (histologic) images
Additional references
Hepatoblastoma
Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Epithelial type | Mixed epithelial mesenchymal type | Diagnosis | Laboratory | Radiology description | Radiology images | Staging | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Malignant primary hepatic blastomatous tumor that reiterates the hepatic development
- Variable combination of epithelial and mesenchymal components
Essential features
- Most frequent liver tumor in children
- Tumor cells recapitulating the embryological stages of hepatic development
- Epithelioid pattern or mixed epithelioid and mesenchymal pattern
- Mainly staged using the PRETEXT (PRE-Treatment EXTent of tumor) system
Epidemiology
- Most frequent liver tumor in children
- 1 - 1.5 cases per million
- Majority of cases (80 - 90%) between 5 months to 6 years old
- Remaining cases in prenatal / neonatal and older children
- Adult tumors are very rare (Surg Oncol 2016;25:339)
- Slight male predominance
Sites
- Liver; some authors refer a preference to the right lobe or state that the tumor starts at the right hepatic lobe (J Hepatol 2012;56:1392)
Pathophysiology
- Current hypothesis is that hepatoblastoma arises from primary hepatoblasts or multipotent hepatic progenitor cells
Etiology
- Majority of cases are sporadic
- Some cases are associated with familial adenomatous polyposis (APC mutations), Beckwith-Wiedemann syndrome and trisomy 18 (Pediatr Blood Cancer 2018;65:e26892)
- Strong association with low birth weight, especially if < 1,000 g and parental smoking
Clinical features
- Usually presents with abdominal enlargement, mass or pain
- Anorexia and weight loss may be reported
- Jaundice is an uncommon feature
Epithelial type
- 56% of hepatoblastomas are epithelial type
Fetal pattern (31%)
- Tumor cells in trabeculae 2 - 3 cells thick (resembling fetal liver), separated by sinusoids lined by CD34+ endothelial cells
- Tumor cells are same size or smaller than in nonneoplastic liver
- Distinct cell membranes, uniform, polyhedral, slightly higher nuclear/cytoplasmic ratio, inconspicuous nucleoli and may contain bile
- Minimal pleomorphism, no / rare mitotic figures
- Have dark and light foci related to amount of glycogen and fat
- Extramedullary hematopoiesis common; no portal tracts, bile ducts or ductules at the periphery
- Reduced reticulin, rare mitosis
- Cholangoblastic if ductular differentiation (CK7 / 19 positive) prominent
- Crowded fetal type: crowded cells and 2+ mitotic figures/10 HPF
Embryonal pattern (19%)
- Sheets, ribbons, rosettes, papillary patterns or trabeculae of variable thickness with immature appearance, discohesive small cells with poorly defined cell borders, basophilic cytoplasm, high N:C ratio, prominent nucleoli, coarse chromatin and increased mitotic figures
- Extramedullary hematopoiesis, necrosis and vascular lakes are common; no fat, glycogen or bile
Macrotrabecular pattern (3%)
- Frequent trabeculae > 10 cells thick throughout the tumor, variable cytologic features
Small cell undifferentiated / anaplastic pattern (3%)
- Most primitive form
- Definition: 70%+ small cell areas; however, even small foci should be reported because associated with poor prognosis
- Discohesive sheets of small uniform keratin+ cells with minimal cytoplasm, indistinct cell borders, oval hyperchromatic nuclei, variable prominent nucleoli and increased mitotic figures (Mod Pathol 2003;16:930)
- Resembles small cell carcinoma at other sites
- May have mucoid stroma, hyalinized septae; bile
- Loss of INI1 associated with rhabdoid phenotype
Mixed epithelial mesenchymal type
Definition / general
Positive stains
Negative stains
Electron microscopy description
Molecular / cytogenetics description
Differential diagnosis
- 44% of hepatoblastomas are mixed epithelial mesenchymal type
- Mixture of fetal / epithelial and mesenchymal cell types
- Teratoid (34%) or not (10%)
- Mesenchymal component has spindle oval cells with minimal cytoplasm, frequent osteoid, fibrous septa, myxoid zones, hemorrhage and necrosis
- Teratoid features are keratinized squamous epithelium, intestinal epithelial, skeletal muscle, mature bone and cartilage, melanin and neuroectodermal structures
Positive stains
- Alpha fetoprotein (negative in small cell type), chromogranin (fetal, epithelial subtypes, usually focal), CK8 / 18 (fetal, epithelial subtypes), CK19 (embryonal subtypes)
- Also EMA, HepPar1 (negative in small cell type), polyclonal CEA (canalicular pattern), vimentin
- Variable hCG, occasional HMB45 and melanin
- Beta catenin (nuclear) in small cell and embryonal types, delta-like protein (DLK), glypican 3 (negative in small cell type), glutamine synthetase
Negative stains
Electron microscopy description
- Immature hepatocytes
Molecular / cytogenetics description
- Gain of Xq in 60%, gain of Xp in 43%, also trisomy 2q (2q+) and trisomy 20, 1p-, 2q-, 4q-, 4q+
- Fetal type usually diploid, embryonal often aneuploid (Hum Pathol 2003;34:864)
- Deletion or translocation of 22q in small cell type (Front Biosci (Elite Ed) 2012;4:1287)
- Also FOXG1 overexpression (Hum Pathol 2007;38:400)
- Yin Yang 1 (YY1) protein (Virchows Arch 2011;458:453)
- SERPINB3 overexpression (Eur J Cancer 2012;48:1219)
Differential diagnosis
- Hepatocellular carcinoma:
- Resembles macrotrabecular variant of hepatoblastoma
- Uncommon in children
- Larger, more pleomorphic tumor cells
- No extramedullary hematopoiesis
- Metastatic tumors:
- More common than hepatoblastoma, primary tumor cells should not resemble hepatocytes
- Lymphoma
- Neuroblastoma
- Rhabdomyosarcoma
- Teratoma
- Undifferentiated sarcoma
- Wilms tumor
- Yolk sac tumor:
- Rare yolk sac cells may be present in hepatoblastoma
Diagnosis
- Usually by a combination of clinical, laboratory and radiology findings (Clin Liver Dis 2018;22:753)
- Biopsy / FNA may be necessary in some cases
Laboratory
- Serum AFP is significantly elevated in the majority of patients (about 90%)
Radiology description
- Ultrasound
- Solid masses that are hyperechoic relative to the adjacent liver, although hypoechoic fibrotic septa can also be seen
- Epithelial hepatoblastomas may appear homogeneous
- Mixed epithelial / mesenchymal tumors exhibit heterogeneous imaging (due to osteoid, cartilaginous and fibrous tissue) and frequently have echogenic calcifications with acoustic shadowing and anechoic foci representing hemorrhage / necrosis (Radiol Bras 2017;50:68)
- Computed tomography
- Well defined mass with regular borders that is hypoattenuating in comparison with the adjacent hepatic parenchyma
- Common diffuse heterogeneous contrast enhancement
- Half of all hepatoblastomas appear lobulated or septated, especially on contrast enhanced images (Radiol Bras 2017;50:68)
Radiology images
Staging
- PRETEXT (PRE-Treatment EXTent of tumor) staging system is the recommended by the Pediatric Hepatic International Tumor Trial (PHITT) (Cancer Imaging 2016;16:21)
- Composed by:
- PRETEXT group describes the extent of tumor in the liver and therefore the amount that must be surgically removed
- Liver is divided into 4 sections: left lateral section (Couinaud segments 2 and 3), left medial section (Couinaud segments 4a and 4b), right anterior section (Couinaud segments 5 and 6) and right posterior section (Couinaud segments 6 and 7)
- PRETEXT I: 1 section is involved and the adjoining are free
- PRETEXT II: 1 or 2 sections are involved and 2 adjoining are free
- PRETEXT III: 2 or 3 sections are involved and no 2 adjoining sections are free
- PRETEXT IV: all sections are involved
- Annotation factors that describe additional risk factors
- Hepatic venous / inferior vena cava involvement
- Portal venous involvement
- Extrahepatic spread of disease
- Multifocal tumor
- Tumor rupture
- Caudate lobe involvement
- Lymph node metastases
- Distant metastases
Prognostic factors
- PRETEXT stages I and II are associated with good prognosis and PRETEXT stage IV is a predictor of bad prognosis
- Multifocal disease, extrahepatic and unresectable vascular involvement, tumor rupture and metastasis at diagnosis are factors of bad prognosis (in the pretreatment evaluation)
- After treatment, poor response to chemotherapy, disease progression under chemotherapy, positive surgical margins and tumor relapse are associated with unfavorable prognosis
- Age < 1 year (good prognosis) versus age > 6 years (worse prognosis) (Pediatr Blood Cancer 2020;67:e28350)
- Normal or low levels of alpha fetoprotein (AFP) are associated with aggressive course and small cell undifferentiated histological subtype
- Serum AFP reduction during treatment is a good prognosis and indicator of response to treatment (BMC Pediatr 2019;19:485)
- Histological evaluation has impact: pure fetal pattern with low mitotic activity is related to good prognosis and small cell undifferentiated pattern is associated with bad prognosis
- Based on staging system, metastases and AFP levels, 5 prognostic groups have been established, with group 1 exhibiting the best prognosis and group 5 the worst (Lancet Oncol 2017;18:122)
Group |
|||
Case reports
- 8 day old girl underwent resection of a large hepatoblastoma (Jpn J Surg 1990;20:331)
- 20 month old boy underwent a biopsy which revealed hepatoblastoma, mixed epithelial and embryonal type without mesenchymal elements (Semin Diagn Pathol 2017;34:192)
- 11 year old boy with stage IV hepatoblastoma with lung and omental metastases at diagnosis (Medicine (Baltimore) 2017;96:e5858)
- 22 year old man with a rapidly expanding right hypochondrial mass (Int J Surg Case Rep 2013;4:204)
Treatment
- Chemotherapy and surgical intervention (Curr Opin Pediatr 2014;26:362)
- Complete surgical resection is essential
- Liver transplantation may be necessary (Transl Gastroenterol Hepatol 2016;1:44)
Gross description
- Single or multinodular tumor
- Well defined boundaries
- Tumors usually exhibit a tan-brown cut surface, especially in the fetal subtype (Medicine (Baltimore) 2018;97:e9647)
- Small cell undifferentiated subtypes have a variegated appearance
- Necrosis and hemorrhage are present in posttreatment specimens
- If osteoid is present, the texture is firm and gritty
Gross images
Microscopic (histologic) description
- Classified by the International Pediatric Liver Tumor Consensus Classification as epithelial or mixed epithelial and mesenchymal
- Epithelial hepatoblastoma may exhibit several patterns (alone or in combination): fetal, embryonal, small cell undifferentiated (SCUD), cholangioblastic and macrotrabecular (J Gastrointest Oncol 2018;9:326)
- Fetal pattern (Pediatr Dev Pathol 2020;23:79)
- Thin trabeculae or nests of small to medium sized cells resembling hepatocytes of the developing fetal liver
- Clear or finely granular cytoplasm with variable amount of glycogen and lipids
- Small round nucleus with indistinct nucleolus
- Foci of extramedullary hematopoiesis are usually present
- Typically has low mitotic activity, referred to as well differentiated hepatoblastoma
- A subset has increased mitotic activity, with decreased cytoplasmatic glycogen and pleomorphic nuclei, referred to as mitotically active hepatoblastoma
- Embryonal pattern (Pediatr Dev Pathol 2020;23:79)
- Resembles the developing liver at 6 - 8 weeks of gestation
- Solid nests or glandular / acinar morphology, with papillae and pseudorosettes
- Dark and granular cytoplasm without glycogen or lipids
- Enlarged nuclei with coarse chromatin, resembling blastemal cells
- Extramedullary hematopoiesis is usually absent
- Increased mitotic activity
- Small cell undifferentiated pattern (Pediatr Dev Pathol 2020;23:79)
- Solid sheets of discohesive small cells (small, round blue tumor)
- Abundant mitoses, apoptosis and necrosis
- Macrotrabecular pattern
- Thick trabeculae (5 - 12 cells thick)
- Trabeculae may be composed of fetal, embryonal, pleomorphic or hepatocellular carcinoma-like cells
- Cholangioblastic pattern
- Small ducts within or around hepatocellular components
- Mesenchymal pattern (Pediatr Dev Pathol 2020;23:79)
- Mature and immature fibrous tissue
- Osteoid or osteoid-like tissue (more abundant after chemotherapy)
- Hyaline cartilage
- Small subset may exhibit teratoid features: endodermal, neuroectodermal (neuronal cells, glial tissue, melanin producing cells) and complex tissue (striated muscle)
Microscopic (histologic) images
Cytology description
- Relies on clinical correlation of a hepatic mass in children, with elevated serum AFP
- Supported by immunohistochemistry
- High grade elements and a mesenchymal component can be identified (Acta Cytol 2005;49:355, Indian J Pathol Microbiol 2005;48:331)
- Necrosis, mitoses and apoptosis may indicate the diagnosis of embryonal and small cell undifferentiated pattern (Acta Cytol 2005;49:355)
Positive stains
- Frequent beta catenin and glutamine synthetase in the epithelial fetal (except the well differentiated and low mitotic subtype) and mesenchymal patterns (Pediatr Dev Pathol 2020;23:79, Biosci Rep 2019;39:BSR20192466)
- AFP in the less differentiated epithelial components
- HepPar1 in the fetal pattern
- Polyclonal CEA
- Glypican 3 in the fetal and embryonal pattern
- Pancytokeratins have variable expression (J Gastrointest Oncol 2018;9:326)
- CK7 and CK19 in the cholangioblastic pattern (J Gastrointest Oncol 2018;9:326)
- INI1 / SMARCB1 usually retained
Negative stains
- INI1 / SMARCB1 is lost in a subset of small cell undifferentiated pattern, which has worse prognosis; some authors believe that this represents a malignant rhabdoid tumor rather than hepatoblastoma (Genes Chromosomes Cancer 2016;55:925)
Molecular / cytogenetics description
- Gene expression profile may be helpful in stratifying patients:
- High risk tumors have upregulation of NFE2L2 activity, high LIN28B, HMGA2, SALL4 and AFP expression and high coordinated expression of oncofetal proteins and stem cell markers
- Low risk tumors have LIN28B and let-7 expression and high HNF1A activity (Hepatology 2017;65:104)
Sample pathology report
- Liver, hepatectomy:
- Hepatoblastoma (see comment)
- Comment: There is a neoplasia with well defined boundaries, composed of small to medium sized cells resembling hepatocytes of the developing fetal liver, arranged in trabeculae and with foci of extramedullary hematopoiesis. The tumor exhibits mostly a fetal pattern, with some areas with a cholangioblastic pattern and a small cell undifferentiated pattern in the periphery of the lesion. There is fibrosis, hemosiderin pigment and osteoid-like tissue in the center, with probable association with neoadjuvant chemotherapy, comprising circa 30% of the lesion volume. No vascular invasion was seen. Nontumoral parenchyma without changes.
Differential diagnosis
- Rhabdoid tumor:
- Positive for desmin
- Rhabdoid morphology, without the diversity of patterns
- Well differentiated hepatocellular carcinoma:
- Positive only for hepatocellular markers
- Usually in a cirrhotic liver background
- No mesenchymal or fetal components
Additional references
Board review style question #1
Regarding evaluation of hepatoblastoma, which staging system has the best prognostic value?
- AJCC
- LI-RADS
- PRETEXT
- TNM
Board review style answer #1
Board review style question #2
Board review style answer #2
Hepatocellular adenoma
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Benign neoplasm of hepatocellular origin arising in the noncirrhotic liver
- Majority are solitary; adenomatosis when > 10 lesions
- Rare cases associated with glycogen storage disease (type 1a), maturity onset diabetes of the young type 3 and Fanconi anemia
- 5 main subtypes based on gene mutations
Essential features
- Arises in noncirrhotic liver
- Female > male, strong association with oral contraceptive exposure
- Unpaired arteries with absence of interlobular bile ducts
Terminology
- Also known as hepatic adenoma and liver cell adenoma
- 5 main subtypes:
- HNF1A mutated hepatocellular adenoma (HA-H, ~35%)
- Beta catenin mutated hepatocellular adenoma (HA-B, ~10%)
- Inflammatory hepatocellular adenoma (HA-I, ~35%)
- Sonic hedgehog (SHH) hepatocellular adenoma (HA-sh, ~5%)
- Hepatocellular adenoma, not otherwise specified (HA-U, ~7%)
ICD coding
- ICD-10: D13.4 - benign neoplasm of liver
Epidemiology
- F > M
- Annual incidence: 1 - 1.5 cases per million population with significantly higher incidence in women taking oral contraceptive pills, approximately 3 per 100,000 (N Engl J Med 1976;294:470)
- Additional risk factors include anabolic steroids, noncontraceptive estrogen supplements, obesity and metabolic syndrome
- Mean age = 37 - 41 years
- Rare in pediatric patients
Sites
- Liver
Pathophysiology
- Based on specific subtypes:
- HNF1A mutated hepatocellular adenoma (HA-H): somatic mutations of TCF1 (HNF1A) gene and rare (< 5%) heterozygous germline mutations of CYP1B1 gene; resultant increase in lipogenesis by promotion of fatty acid synthesis and by downregulation of liver type fatty acid binding protein (LFABP) (Nat Genet 2002;32:312)
- Beta catenin mutated hepatocellular adenoma (HA-B): beta catenin gene activating mutations (exon 7 - 8 and exon 3), resultant stabilization of beta catenin protein and increased or nontransient activation of Wnt / beta catenin signaling pathway (Hepatology 2006;43:515)
- Inflammatory hepatocellular adenoma (HA-I): gain of function mutations of the IL6ST gene, activation of STAT3 signaling pathway and acute phase inflammatory response (Nature 2009;457:200)
- Sonic hedgehog (SHH) hepatocellular adenoma (HA-sh): activation of sonic hedgehog pathway via fusion of promoter of INHBE with GLI1; also upregulation of argininosuccinate synthase 1, which may indicate increased risk of hemorrhage (Gastroenterology 2017;152:880, Hepatology 2017;66:2016, Hepatology 2018;68:964)
Clinical features
- May be asymptomatic and incidentally diagnosed due to imaging performed for an unrelated indication
- Symptomatic lesions present with abdominal pain or hemorrhage
- Risk of hemorrhage increases with size
Diagnosis
- Unpaired arteries are characteristic; interlobular bile ducts are absent
- Cytologic atypia is unusual
- Thin or mildly thickened hepatocyte cell plates
Laboratory
- Liver function tests tend to be normal
- Mild elevation in alpha fetoprotein in some cases
Radiology description
- MRI is the most optimal imaging modality
- Features characteristic of a hepatocellular adenoma over focal nodular hyperplasia include strong hyperintensity on T2 weighting, hyperintensity on T1 weighting, cystic areas, hemorrhagic areas and diffuse intralesional steatosis (Diagn Interv Radiol 2014;20:193)
- Specific features for some subtypes:
- HNF1A mutated hepatocellular adenoma (HA-H): homogeneous dropout of signal on T1 weighted out of phase sequence
- Inflammatory hepatocellular adenoma (HA-I): marked hyperintensity on T2 weighted sequences, hyperintense rim on T2 weighted sequence which corresponds to sinusoidal dilatation, also known as atoll sign
Prognostic factors
- Risk of malignant transformation is higher in
- Men
- Beta catenin mutated hepatocellular adenoma (HA-B)
- Larger tumors
- Reference: Hepatology 2006;43:515
Case reports
- 6 day old boy with multiple adenomas and microvillus inclusion disease (Dig Dis Sci 2013;58:2784)
- 20 year old man with malignant transformation of beta catenin mutated adenoma (Oncology 2017;92:16)
- 23 year old woman with diabetes and malignant transformation of HNF1A mutated adenoma (Semin Liver Dis 2015;35:444)
- 31 year old woman with recurrent adenoma requiring liver transplant (Rev Esp Enferm Dig 2014;106:494)
- 36 year old woman with hematoma following remote trauma (World J Gastroenterol 2013;19:4422)
- 11 cases of malignant transformation of adenoma (Mod Pathol 2014;27:1499)
Treatment
- Male patients: surgical excision irrespective of size
- Female patients: surgical excision if > 5 cm in size and with beta catenin activating mutations (Therap Adv Gastroenterol 2016;9:898)
- Nonsurgical cases: suspension of oral contraceptive pills (if applicable) and imaging follow up
Gross description
- Majority are solitary and well circumscribed
- Uncapsulated or develop ill defined pseudocapsule
- Lighter in color compared with surrounding liver
- Foci of necrosis, hemorrhage and bile staining
- Usually lack significant fibrosis (including central scar) and nodularity
- Reference: Burt: MacSween's Pathology of the Liver, 7th Edition, 2017
Gross images
Microscopic (histologic) description
- Well defined border between the lesion and background liver
- Composed of hepatocytes with no significant cytologic atypia
- Arranged as thin or only mildly thickened cell plates, 1 - 2 cells thick
- May have pseudoacinar arrangement and steatotic foci
- Characterized by unpaired arteries; interlobular bile ducts are absent, some cases show bile ductules
- Foci of hemorrhage, ischemic changes and necrosis
- No cytologic atypia, atypical mitoses and portal / parenchymal invasion
- Reticulin stain helpful to establish near normal hepatocyte plate thickness with only focal loss, particularly in the steatotic areas
- Microscopic features of specific subtypes include:
- HNF1A mutated hepatocellular adenoma (HA-H): characterized by steatosis (fat accumulation in lesional hepatocytes), reticulin staining is mostly intact, some cases / areas show "packeting" (i.e. prominent pericellular staining or almost complete circling of small groups of hepatocytes by reticulin fibers)
- Beta catenin mutated hepatocellular adenoma (HA-B): pseudoacinar arrangement; cytologic abnormalities including nuclear pleomorphism and atypia, multinucleation, prominent nucleoli; steatosis is rare, no significant inflammation
- Inflammatory hepatocellular adenoma (HA-I): may have irregular, poorly circumscribed borders; inflammatory infiltrates and sinusoidal dilatation; may have pseudoportal tracts, which are islands of thick walled arteries with no definite bile ducts but associated ductular reaction
- Hepatocellular adenoma, not otherwise specified (HA-U): morphology characteristic of adenoma but no specific characteristics of the individual subtypes; lesions with extensive hemorrhage and necrosis are currently grouped into this subtype
- References: Burt: MacSween's Pathology of the Liver, 7th Edition, 2017, Diagn Pathol 2016;11:27, Clin Mol Hepatol 2016;22:199, Hepatology 2006;43:515, Arch Pathol Lab Med 2014;138:1090, Front Med (Lausanne) 2017;4:10
Microscopic (histologic) images
Contributed by Monica Abdelmalak, M.D., Avani Pendse, M.D., Ph.D. and Raul S. Gonzalez, M.D.
Cytology description
- Cytologically bland hepatocytes on smears; uniform, regular nuclei with low N/C ratios and rare mitoses (Cibas: Cytology - Diagnostic Principles and Clinical Correlates, 4th Edition, 2014)
- Diagnosis is difficult by cytology alone given that a well differentiated hepatocellular carcinoma is in the differential diagnosis and presence or lack of invasion cannot be evaluated on smears alone
Positive stains
- HepPar1
- Reticulin: intact staining pattern with focal loss in steatotic areas (Arch Pathol Lab Med 2015;139:537)
- Characteristic staining for individual subtypes:
- Beta catenin mutated hepatocellular adenoma (HA-B): beta catenin nuclear (often focal), glutamine synthetase (strong and diffuse)
- Inflammatory hepatocellular adenoma (HA-I): SAA, CRP
Negative stains
- Glypican 3: majority negative (Am J Surg Pathol 2008;32:433)
- CD34: negative or incomplete positive (rare complete positive) (Am J Surg Pathol 2008;32:433)
- HSP70: negative (can be useful to differentiate from hepatocellular carcinoma which shows positive nuclear staining) (Health Educ Q 1989;16:397)
- Characteristic staining for individual subtypes:
- HNF1A mutated hepatocellular adenoma (HA-H): LFABP (positive in background liver)
Sample pathology report
- Liver, partial hepatectomy:
- Hepatic adenoma, HNF1A mutated subtype
- Tumor is __ cm in greatest dimension
- Closest approach to the parenchymal resection margin is __ mm
- Background liver with no specific pathologic diagnosis
- Microscopic description: The tumor is a well differentiated hepatocellular neoplasm morphologically compatible with hepatic adenoma. The tumor is characterized by well circumscribed borders and many of the lesional hepatocytes are steatotic. Bile ducts are absent and scattered unpaired arterioles are present. No significant cytologic atypia, widening of hepatocyte plates or infiltrative features are noted. The tumor also contains foci of hemorrhage, necrosis and rare calcifications. Based on the steatotic morphology and immunohistochemistry profile, the tumor is best classified as HNF1A mutated subtype.
- Hepatic adenoma, HNF1A mutated subtype
- Liver, right lobe, resection:
- Hepatic adenoma, inflammatory subtype, __ cm, __ cm from parenchymal margin
- Hepatic adenoma, HNF1A mutated subtype, __ cm, __ cm from parenchymal margin
- Background liver with no specific pathologic change
Differential diagnosis
- Focal nodular hyperplasia (Clin Mol Hepatol 2016;22:199):
- Prominent central scar detected by imaging or gross evaluation
- Radiating fibrous septa with inflammatory infiltrate and prominent thick walled, abnormal vessels and associated ductular reaction
- Map-like glutamine synthetase positive staining pattern
- Well differentiated hepatocellular carcinoma:
- Mass effect adjacent to mass lesion:
- Sinusoidal dilation may mimic HA-I, especially on biopsy (Hum Pathol 2017;61:105)
- Unpaired arteries and CD34 positivity help confirm HA-I
Board review style question #1

A representative section of a well differentiated hepatocellular lesion shows strong and diffuse positive staining for glutamine synthetase. Which entity should be considered in the differential diagnosis?
- Beta catenin mutated hepatocellular adenoma
- Focal nodular hyperplasia
- Inflammatory type hepatocellular adenoma
- Poorly differentiated hepatocellular carcinoma
Board review style answer #1
A. Beta catenin mutated hepatocellular adenoma (Gastroenterol Hepatol (N Y) 2017;13:740)
Comment Here
Reference: Hepatocellular adenoma
Comment Here
Reference: Hepatocellular adenoma
Board review style question #2
Which of the following is most strongly associated with hepatocellular adenoma?
- Alcohol
- Cigarette smoking
- Nulliparity
- Oral contraceptives
Board review style answer #2
Hepatocellular carcinoma overview
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Primary malignancy of liver with hepatocellular differentiation
Essential features
- Most common (> 80%) primary liver malignancy worldwide
- ~ 80% of hepatocellular carcinoma cases arise in cirrhosis
- Specific subtypes have associated molecular / cytogenetic abnormalities:
- Scirrhous subtype: TSC1 / TSC2 mutations
- Steatohepatitic subtype: frequent IL6 / JAK / STAT activation
- Macrotrabecular massive subtype: TP53 mutation and FGF19 amplification
- Fibrolamellar subtype: DNAJB1-PRKACA fusion gene
Terminology
- "Hepatoma" is old term for hepatocellular carcinoma
ICD coding
Epidemiology
- Most common (> 80%) primary liver malignancy worldwide (Nat Rev Gastroenterol Hepatol 2019;16:589)
- Sixth most common malignancy and fourth most common cause of cancer mortality worldwide (Global Cancer Observatory: Liver Fact Sheet [Accessed 18 January 2021])
- Incidence and age of onset vary geographically
- Asia (72.5%) has the highest incidence worldwide, followed by Europe (9.8%), Africa (7.7%), North America (5%), Latin America and the Caribbean (4.6%) and Oceania (0.4%) (Global Cancer Observatory: Liver Fact Sheet [Accessed 18 January 2021])
- Median age of onset is older than sixth decade in North America and Europe; median age of onset in Asia and Africa is between third and sixth decades (Nat Rev Gastroenterol Hepatol 2019;16:589)
- Gender
- Risk factors:
- Chronic liver disease leading to cirrhosis; most common etiologies leading to this include chronic viral hepatitides (HBV and HCV), heavy alcohol consumption, nonalcoholic fatty liver disease (Nat Rev Gastroenterol Hepatol 2019;16:589, Hepatology 2018;68:723)
- Chronic viral hepatitis is the leading cause of hepatocellular carcinoma worldwide (Philos Trans R Soc Lond B Biol Sci 2017;372:20160274)
- In the United States, chronic hepatitis C is a critical risk factor for hepatocellular carcinoma (Hepatology 2018;68:723)
Sites
- Primary location: liver
- Most common metastatic sites (in decreasing order of frequency): lung, portal vein, portal lymph node, intra-abdominal lymph node, bone (Case Rep Oncol Med 2020;2020:7526042)
Pathophysiology
- Stepwise process (low grade dysplastic nodule → high grade dysplastic nodule → early hepatocellular carcinoma → progressed hepatocellular carcinoma) accompanied by accumulation of molecular alterations (Hepatology 2014;60:1983)
- Molecular alterations include: telomere shortening, TERT activation, cell cycle checkpoint inhibitor inactivation (Nat Genet 2015;47:505)
- TERT promoter mutation is a salient event to hepatocellular carcinoma progression (Hepatology 2014;60:1983)
Etiology
- Cirrhosis
- ~ 80% of hepatocellular carcinoma cases arise in cirrhosis (Hepatology 2018;68:723)
- Patients with cirrhosis from any etiology are at risk for developing hepatocellular carcinoma
- Infectious
- Hepatitis B virus (HBV)
- Direct oncogenic effect by integration of the HBV DNA into the host genome, which subsequently induces genomic instability and mutagenesis of cancer related genes, including p53 and WNT / β catenin pathway; can cause hepatocellular carcinoma without antecedent cirrhosis (J Hepatol 2016;64:S84, N Engl J Med 2019;380:1450)
- HBV vaccination reduces the incidence of hepatocellular carcinoma
- Hepatitis C virus (HCV)
- Lacks direct oncogenic effect; occurs almost exclusively in HCV patients with advanced cirrhosis (N Engl J Med 2019;380:1450)
- Core HCV proteins (NS5A and NS3) induce oxidative stress, which eventually results in activation of NFκB and MAPK pathway, leading to cell proliferation and alteration of apoptotic pathway (Medicina (Kaunas) 2019;55:526)
- Direct acting antiviral therapy and interferon based therapy lowers the risk of hepatocellular carcinoma (Gastroenterology 2017;153:996, Gastroenterology 2017;152:142)
- Hepatitis B virus (HBV)
- Metabolic
- Nonalcoholic fatty liver disease (NAFLD)
- Increased prevalence due to metabolic syndrome, obesity and type 2 diabetes; insulin resistance leads to increased insulin-like growth factor 1 (IGF1), which eventually activates PI3K and MAPK pathways, leading to cell proliferation and inhibition of apoptosis (Medicina (Kaunas) 2019;55:526, PLoS One 2014;9:e97136)
- Limited treatment options available
- Others: hemochromatosis, alpha-1 antitrypsin deficiency, hypercitrullinemia, fructosemia
- Nonalcoholic fatty liver disease (NAFLD)
- Environmental exposures
- Aflatoxins:
- Mycotoxins produced by Aspergillus flavus (aflatoxin B1) and Aspergillus parasiticus
- Contaminates grain, corns and peanuts in tropical and subtropical regions, particularly in Asia and Africa
- Aflatoxin B1 reacts with DNA to form mutagenic adducts, leading to codon 249 mutation of TP53 (Liver Cancer International 2020;1:41)
- Alcohol: major risk factor in the Western countries (J Hepatol 2018;69:1274)
- Others: anabolic steroids, Thorotrast, oral contraceptives, tobacco
- Aflatoxins:
- Developmental / congenital
- Abernethy malformation: congenital vascular malformation, which causes splanchnic venous blood to bypass the liver and drain directly into the systemic circulation; also known as congenital extrahepatic portosystemic shunt (CEPS) (Hepatology 2020;71:658)
- Alagille syndrome: autosomal dominant disorder caused by loss of function in JAG1 (85%) or NOTCH2 (15%), resulting in bile duct paucity (World J Gastroenterol 2018;24:3980)
- Ataxia telangiectasia: autosomal recessive disorder caused by defect in the ATM gene, resulting in increased oxidative stress (World J Gastroenterol 2018;24:3980, Front Pediatr 2019;7:458)
- Bile salt export protein deficiency: mutation in ABCB11 causes poor excretion of bile salt, resulting in chronic inflammation and carcinogenesis (World J Gastroenterol 2018;24:3980, Hepatology 2006;44:478)
- Tyrosinemia type I: mutation in FAH (15q23-q25) leads to deficiency of fumaryl acetoacetate hydrolase in the tyrosine degradation pathway, resulting in accumulation of toxic metabolites including maleylacetoacetate and fumarylacetoacetate (World J Gastroenterol 2018;24:3980)
- Progression of benign entity
- ~ 5% of hepatocellular adenomas undergo malignant transformation (Hepat Oncol 2014;1:421)
Diagrams / tables
Clinical features
- Signs and symptoms: abdominal pain, weight loss, hepatomegaly and splenomegaly, jaundice, ascites
Diagnosis
- Imaging: ultrasound, contrast enhanced CT / MRI with or without diagnostic tissue biopsy (see also figure 1 under diagrams)
- Tissue confirmation not always necessary to establish diagnosis (unlike for most malignancies)
- See radiology description for more details
Laboratory
- Laboratory tests: α fetoprotein is elevated in 70 - 90% of cases and has sensitivity of 60% and specificity of 90% in hepatocellular carcinoma detection; elevated liver function tests (LFTs) Gastroenterology 2009;137:110
Radiology description
- Liver nodule in cirrhosis (N Engl J Med 2019;380:1450) (see also figure 1 under diagrams)
- If < 1cm: ultrasound surveillance every 3 - 4 months
- If > 1cm: contrast enhanced CT / MRI
- Diagnostic features for hepatocellular carcinoma include hyperenhancement during arterial phase and washout in the venous or delayed phase (due to alteration in blood supply during malignant transformation, as benign hepatocytes receive blood supply from portal vein, whereas malignant hepatocyte receive blood supply from hepatic artery)
- If diagnostic features are not identified, evaluate radiologic features from other imaging techniques and consider liver biopsy for histologic diagnosis
- Liver Imaging Reporting and Data System (LI-RADS) contains 5 diagnostic categories:
- LR-1: definitely benign
- LR-2: probably benign
- LR-3: intermediate probability of malignancy
- LR-4: probably hepatocellular carcinoma
- LR-5: definitely hepatocellular carcinoma
Radiology images
Prognostic factors
- 5 year overall survival is 24 - 70% (Ann Surg 2007;245:909)
- 5 year overall survival after transplant for hepatocellular carcinoma = 64% (J Am Coll Surg 2007;204:1016)
- 5 year recurrence free survival after transplant for hepatocellular carcinoma = 61% (J Am Coll Surg 2007;204:1016)
- Prognosis dependent on TNM stage (Amin: AJCC Cancer Staging Manual, 8th Edition, 2017)
- Presence of lymphovascular invasion and poorly differentiated histology are associated with a worse prognosis in solitary hepatocellular carcinoma > 2 cm (World J Gastroenterol 2018;24:4000, Am J Surg Pathol 2002;26:25, Ann Surg Oncol 2013;20:1223)
- Presence of cirrhosis, background liver damage, multifocality, hepatocellular carcinoma diameter > 2 cm and portal vein thrombosis associated with worse prognosis (Ann Surg 2007;245:909, Liver Int 2009;29:502)
- Immunohistochemical expression of CK19, CD90, EpCAM and CD133 are associated with unfavorable prognosis (World J Gastroenterol 2014;20:2098, Histopathology 2006;49:138, Cancer Sci 2003;94:851)
- Subtypes associated with worse prognosis compared with conventional hepatocellular carcinoma: (Gastroenterol Clin North Am 2017;46:365)
- Cirrhotomimetic
- Sarcomatoid carcinoma: epithelial HCC element and mesenchymal spindle cell element; spindle cells without specific lineage; positive for cytokeratins and vimentin
- Carcinosarcoma: epithelial HCC element and mesenchymal spindle cell element; spindle cells of a specific lineage; positive for vimentin, negative for cytokeratins
- Macrotrabecular massive
- Neutrophil rich
- Subtypes associated with a similar to better prognosis compared with conventional hepatocellular carcinoma: (Gastroenterol Clin North Am 2017;46:365)
- Steatohepatitic
- Clear cell
- Chromophobe
- Fibrolamellar
- Lymphocyte rich
- Subtype with variable/unknown prognosis compared with conventional hepatocellular carcinoma:
- Scirrhous
Case reports
- 30 year old man with unintentional weight loss (BMJ Case Rep 2019;12:e230530)
- 38 year old man with Alagille syndrome presented with acute right upper quadrant pain (Radiol Case Rep 2020;16:90)
- 41 year old otherwise healthy Sri Lankan man with progressive abdominal distension (J Med Case Rep 2017;11:34)
- 53 year old man presented with left forehead nodule associated with ipsilateral vision loss (Case Rep Oncol Med 2020;2020:7526042)
- 62 year old man with 10 year history of hepatitis B presented with fever, fatigue and weight loss (Cancer Res Ther 2015;11:665)
Treatment
- Surgical intervention
- Tumor resection for patients with solitary tumor and patients with preserved liver function
- Liver transplant for patients meeting Milan criteria of solitary tumor < 5 cm or up to 3 tumors < 3 cm (Liver Transpl 2004;10:S115)
- Ablation therapy
- Through radiofrequency, microwave, cryoablation and ethanol injection (Liver Transpl 2004;10:S115)
- Transarterial embolization (TEA) and transarterial chemoembolization (TACE) (Liver Transpl 2004;10:S115)
- Systemic therapy
- Sorafenib is a tyrosine kinase that prolongs median survival (N Engl J Med 2008;359:378)
- Barcelona Clinic Liver Cancer (BCLC) algorithm is the most widely applied hepatocellular carcinoma management system, which classifies patients into five stages (see also figure 2 under diagrams) (Liver Transpl 2004;10:S115)
Gross description
- Well circumscribed mass that appears tan-yellow to green (color variation depends on proportion of fat and bile content)
- Areas of hemorrhage and necrosis are common
- Solitary or dominant nodule with multiple satellite nodules or multiple discrete nodules or multiple distinct nodules
- Background liver is usually cirrhotic
- Rarely, hepatocellular carcinoma can have exophytic growth, also known as pedunculated hepatocellular carcinoma (World J Surg 2002;26:1133)
Gross images
Microscopic (histologic) description
- Architectural patterns:
- 4 principal growth patterns, including trabecular, pseudoglandular, solid and macrotrabecular (in decreasing order of frequency)
- 50% of cases have mixed patterns; macrotrabecular pattern is associated with worse prognosis
- Other features include lack of portal triad in the tumor, reduction of normal reticulin framework, expansion of the hepatocyte plates and increased arterialization with unpaired arteries or arterioles
- Cytologic features:
- Polygonal cells with nuclear atypia, including high N/C ratio, irregular nuclear membrane, multinucleation and prominent nuclei
- Cytoplasm varies from clear to eosinophilic, depending on the fat and glycogen content
- Cytoplasmic alterations include Mallory-Denk bodies, hyaline bodies, pale bodies
- Bile production (usually extracellular) may be seen
- Histologic grading (3 tiered system):
- WHO grading system (3 tiered system)
- Well differentiated: tumor cells resemble mature hepatocytes; minimal to mild nuclear atypia
- Moderately differentiated: tumor cells appear malignant on H&E and morphology suggests hepatocellular differentiation; moderate nuclear atypia
- Poorly differentiated: tumor cells appear malignant on H&E and often cannot be distinguished from other poorly differentiated neoplasms; marked nuclear atypia
- Modified Edmondson-Steiner grading system (4 tiered system) (Cancer 1954;7:462)
- Grade I: tumor cells are difficult to differentiated from hyperplastic liver cells
- Grade II: tumor cells resemble mature hepatocytes with slightly larger and more hyperchromatic nuclei; sharp and clear cut cell borders; frequent acini formation
- Grade III: tumor cells are larger and have more hyperchromatic nuclei with less acidophilic cytoplasms; trabecular distortion; numerous tumor giant cells
- Grade IV: tumor cells are intensely hyperchromatic, with scant and less granular cytoplasm; tumor cells appear less cohesive and can appear giant, spindled or short and plump; medullary growth pattern with loss of trabeculation; less acini
- WHO grading system (3 tiered system)
Microscopic (histologic) images
Cytology description
- See also separate cytology topic at HCC-Cytology
- Hypercellular broad clusters of malignant hepatocytes with peripheral endothelial wrapping (Patholog Res Int 2011;2011:587936)
Cytology images
Positive stains
- Arginase1: cytoplasmic or nuclear; useful in confirming hepatocellular differentiation; highly sensitive and specific, thus more useful than HepPar1 for poorly differentiated hepatocellular carcinoma (Am J Surg Pathol 2010;34:1147)
- HepPar1: cytoplasmic and granular; overall highly sensitive but 50% of poorly differentiated hepatocellular carcinoma lose expression (Am J Surg Pathol 2002;26:978)
- Glypican 3: cytoplasmic; high sensitivity in poorly differentiated and scirrhous hepatocellular carcinoma but low sensitivity in well differentiated hepatocellular carcinoma (nonneoplastic liver is negative)
- AFP: cytoplasmic; highly specific but low sensitivity; frequently negative in well differentiated hepatocellular carcinoma
- Polyclonal CEA, villin and CD10 reveal canalicular pattern; limited sensitivity in poorly differentiated hepatocellular carcinoma
- Albumin ISH: high sensitivity for primary liver carcinoma, although this can also be positive in other adenocarcinomas not of biliary origin (Am J Clin Pathol 2019;152:190)
- Pancytokeratins (MNF116 or OSCAR) and CAM5.2 (CK8 / CK18) are positive
- Reticulin: highlights the thickened hepatocyte plates (> 3 cell thick); see also negative stains below
Negative stains
Molecular / cytogenetics description
- Diagnosis of hepatocellular carcinoma often does not require molecular or cytogenetic testing but these ancillary studies can aid in diagnosing difficult cases and identifying a specific subtype of hepatocellular carcinoma (J Hepatol 2017;67:727):
- Scirrhous subtype: TSC1 / TSC2 mutations
- Steatohepatitic subtype: frequent IL6 / JAK / STAT activation
- Macrotrabecular massive subtype: TP53 mutation and FGF19 amplification
- Fibrolamellar subtype: DNAJB1-PRKACA fusion gene
Sample pathology report
- Liver and gallbladder, native, hepatectomy for transplantation:
- Hepatocellular carcinoma, multiple (see comment)
- Comment: Tumor 1 is located in the right lobe and 3 cm in size with no necrosis. Tumor 2 is located in the right lobe and 2.5 cm in size with incomplete necrosis (viable tumor present). Percentage of tumor necrosis for tumor 2 is 75%. Tumor 3 is located in the left lobe and 1.5 cm in size with no necrosis. Tumor 4 is located in the right lobe and 2.5 cm in size with incomplete necrosis (viable tumor present). Percentage of tumor necrosis for tumor 4 is 10%. Tumor 5 is located in the left lobe and 1.5 cm in size with no necrosis. Histologic type is hepatocellular carcinoma with grade G2 - G3: moderately to poorly differentiated. The tumor is confined to the liver and biliary and vascular margins are free of tumor. Vascular invasion present. No lymph nodes submitted or found. AJCC 8th edition pathologic stage is ypT2NX (combined stage II) and UNOS stage is T4a. The background liver shows cirrhosis.
Differential diagnosis
- Hepatocellular adenoma:
- Neoplastic hepatocytes are not expanded on reticulin stain (no loss)
- Noncirrhotic background
- Intrahepatic cholangiocarcinoma:
- Discrete gland formation surrounded by desmoplastic stroma
- Negative for hepatocellular markers; positive for CK7
- Dysplastic nodule in cirrhosis:
- ~ 1 cm lesion in cirrhotic livers seen macroscopically or on imaging
- Intact reticulin network (focal loss may be seen) with preserved portal tracts (although typically reduced in number)
- Cytologic alterations seen may include small cell changes, large cell changes and iron free foci
- Metastatic neuroendocrine neoplasms:
- Positive staining for neuroendocrine markers while negative for hepatocellular markers
- Metastatic carcinomas, such as clear cell renal cell carcinoma (CCRCC):
- Possible clinical history of prior malignancy
- Differing immunohistochemical profile (e.g. clear cell renal cell carcinoma positive for PAX8 while negative for hepatocellular markers)
Additional references
Board review style question #1
Which of the following is true about this liver neoplasm?
- Diffuse CK7 immunohistochemical expression would be expected in this neoplasm
- Hepatitis B is not a risk factor to develop this neoplasm
- Molecular analyses are required to define this neoplasm
- This neoplasm commonly arises in the setting of cirrhosis
Board review style answer #1
D. This neoplasm commonly arises in the setting of cirrhosis. The image demonstrates a hepatocellular carcinoma.
Comment Here
Reference: Hepatocellular carcinoma overview
Comment Here
Reference: Hepatocellular carcinoma overview
Board review style question #2
Which of the following subtypes of hepatocellular carcinoma is associated with a worse prognosis compared with conventional hepatocellular carcinoma?
- Chromophobe hepatocellular carcinoma
- Clear cell hepatocellular carcinoma
- Lymphocyte rich hepatocellular carcinoma
- Sarcomatoid hepatocellular carcinoma
Board review style answer #2
D. Sarcomatoid hepatocellular carcinoma. All of the other answer choices are associated with a similar or better prognosis than conventional hepatocellular carcinoma.
Comment Here
Reference: Hepatocellular carcinoma overview
Comment Here
Reference: Hepatocellular carcinoma overview
Hepatoportal sclerosis
Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Etiology | Clinical features | Diagnosis | Radiology description | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Board review style question #1 | Board review style answer #1Definition / general
- Portal vein abnormalities and bridging fibrosis, causing portal hypertension
Essential features
- Portal hypertension without overt liver failure
- Variety of portal vein changes may be seen histologically
Terminology
- Also called obliterative portal venopathy, noncirrhotic portal fibrosis (Semin Liver Dis 2002;22:59)
- It has recently been suggested that the term hepatoportal sclerosis be retired and replaced with portal vein stenosis and herniated portal vein depending on the particular histologic findings (Histopathology 2019;74:219)
- Sometimes considered synonymous with incomplete septal cirrhosis, although overall this finding is more favored to indicate regressed cirrhosis
Epidemiology
- Relatively uncommon in U.S. but more common in India (Hepatology 2011;54:1071)
Etiology
- Can be idiopathic
- Many cases likely due to extrahepatic or intrahepatic portal venous obstruction, mainly portal vein thrombosis
- Also linked to exposure to arsenic or vinyl chloride, didanosine in AIDS patients (Curr Opin Infect Dis 2011;24:12) and other medications
Clinical features
- Main finding is portal hypertension, without cirrhosis or liver dysfunction
- May occur in children (J Korean Med Sci 2013;28:1507)
Diagnosis
- Tissue generally required for diagnosis; on biopsy, findings are usually only suggestive of or consistent with the diagnosis, due to patchy nature of disease
Radiology description
- Caudate lobe hypertrophy and right hepatic lobe atrophy; advanced cases may show nodularity resembling cirrhosis (AJR Am J Roentgenol 2012;198:370)
Case reports
- 23 year old man with Crohn’s disease and mercaptopurine induced hepatoportal sclerosis (J Crohns Colitis 2013;7:590)
Treatment
- Patients may require anticoagulation if disease is secondary to portal vein thrombosis
Microscopic (histologic) description
- Portal vein abnormalities, including fibrous intimal thickening, vein loss, herniation beyond portal tract borders into hepatic parenchyma and replacement by numerous small vein radicles
- Collagen deposition into space of Disse and periportal areas
- Bridging fibrosis between portal areas without background cirrhosis, although hepatocyte regeneration (nodular regenerative hyperplasia) may be present, as may parenchymal atrophy secondary to portal malperfusion
- Obliteration of portal veins has been specifically linked to didanosine (AIDS 2010;24:1171)
Microscopic (histologic) images
Sample pathology report
- Liver, biopsy:
- Liver parenchyma with herniated portal veins (see comment)
- Comment: The findings are indicative of so called hepatoportal sclerosis, which can cause noncirrhotic portal hypertension. Trichrome and iron stains are unremarkable.
Board review style question #1
- A 60 year old man in the United States with no known history of liver disease develops ascites and is discovered to have portal hypertension. He undergoes biopsy, which shows portal tract abnormalities but no cirrhosis. Additional workup determines he has Factor V Leiden. What is the most likely cause of the patient’s portal hypertension?
- Cirrhosis missed on biopsy
- Granulomatous hepatitis
- Hepatoportal sclerosis
- Schistosomiasis
- Sinusoidal obstruction syndrome
Board review style answer #1
Hereditary hemorrhagic telangiectasia
Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Pathophysiology | Clinical features | Diagnosis | Radiology description | Radiology images | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Molecular / cytogenetics description | Sample pathology report | Board review style question #1 | Board review style answer #1Definition / general
- Hereditary disease causing systemic telangiectasias, including in the liver
Essential features
- Syndrome that can cause telangiectasias or proliferative portal vessels within the liver
- Patients with liver involvement can develop cardiac failure
Terminology
- Also called Osler-Weber-Rendu disease
Epidemiology
- Up to 30% of patients with the syndrome develop liver disease, though not all will be symptomatic (N Engl J Med 2000;343:931)
Pathophysiology
- Vascular abnormalities can cause liver hyperperfusion, resulting in heart failure
Clinical features
- Patients may develop heart failure, portal hypertension and biliary disease from liver involvement (N Engl J Med 2000;343:931)
Diagnosis
- Typically confirmed radiologically
Radiology description
- Tortuous / twisted / enlarged arteries within the liver (Clin Imaging Sci 2012;2:26)
- No correlation between radiologic findings and clinical severity (AJR Am J Roentgenol 2006;187:W399)
Radiology images
Treatment
- Bevacizumab can improve high cardiac output (JAMA 2012;307:948)
- May require liver transplant (Ann Surg 2006;244:854)
Microscopic (histologic) description
- Thin walled portal vessels may proliferate, extend into parenchyma and become associated with fibrosis (periportal telangiectasia) and sinusoidal dilation
- Common hepatic artery is enlarged
- Vascular shunts may be arterioportal, arteriovenous or portovenous (Semin Liver Dis 2008;28:247)
- Background focal nodular hyperplasia or nodular regenerative hyperplasia may be seen (Ultrasound Med Biol 2004;30:1089)
- May rarely cause hepatic necrosis with bile extravasaion (Histopathology 2003;42:265)
Microscopic (histologic) images
Molecular / cytogenetics description
- Patients with liver disease more likely to have ALK1 (ACVRL1) mutation (HHT type 2) than ENG mutation (HHT type 1) (Hum Mutat 2005;25:320)
Sample pathology report
- Liver, biopsy:
- Liver parenchyma with numerous vascular channels within portal tracts and sinusoidal dilation (see comment)
- Comment: The findings are consistent with the patient’s reported history of hereditary hemorrhagic telangiectasia. Trichrome and iron stains are unremarkable.
Board review style question #1
- A patient develops high output cardiac failure with refractory epistaxis and dies. Autopsy shows numerous arteriovenous shunts throughout the liver, accompanied by sinusoidal dilation. Molecular testing on this patient would most likely show a germline mutation in which of the following genes?
A. ALK1 (ACVRL1)
B. FLT4
C. SMAD4
D. TEK
E. VHL
Board review style answer #1
Herpes simplex virus hepatitis
Table of Contents
Definition / general | Essential features | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Laboratory | Radiology images | Prognostic factors | Case reports | Treatment | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Definition / general
- Rare complication of herpes infection resulting in geographic (nonzonal) hemorrhagic necrosis that is usually fatal
- 1% of acute liver failure (Clin Transplant 2009;23:37)
Essential features
- Geographic (nonzonal) hemorrhagic necrosis
- Usually pregnant women or immunocompromised patients
- Often clinically unsuspected (Liver Transpl 2007;13:1428)
- Often not diagnosed until autopsy due to nonspecific clinical features
Epidemiology
- Immunocompromised patients are most susceptible
- Immunocompetent patients can be affected (Am J Clin Pathol 1986;85:694)
- Risk factors include malignancy and pregnancy (mean 31 weeks) (Hum Pathol 1992;23:183)
- Neonates can also acquire herpes congenitally (as it is one of the TORCH infections), with roughly a quarter of them at risk for developing fulminant hepatitis
Sites
- Liver
Etiology
- HSV1 or HSV2
Clinical features
- Uncommon cause of liver failure in adults (Liver Transpl 2008;14:1498)
- Anicteric (not accompanied by jaundice)
- Fever (98%), coagulopathy (84%) and encephalopathy (80%) (Liver Transpl 2008;14:1498)
- Clinical presentation in adults is typically that of shock
Diagnosis
- HSV DNA can be detected in the blood
- 58% diagnosed at autopsy via histologic and immunohistochemical analysis of liver tissue (Liver Transpl 2007;13:1428)
Laboratory
- Marked elevation of liver serum markers (AST, ALT, bilirubin, alkaline phosphatase, GGT)
- Leukopenia
- HSV DNA identified via PCR
Prognostic factors
- Rapid downhill course with acute liver failure, usually fatal (up to 81% of adults) due to massive hepatic necrosis (Clin Transplant 2009;23:37), even with rapid antiviral therapy or liver transplantation (Liver Transpl 2008;14:1498)
- Better survival after transplantation in children (69%) than adults (38%) (J Hepatol 2011;55:1222)
- Worse prognosis (Liver Transpl 2008;14:1498): male gender
- Age > 40 years
- Immunocompromised
- ALT > 5,000 U/L
- Platelet count < 75 x 103/L
- Coagulopathy
- Encephalopathy
- Absence of antiviral therapy
Case reports
- 11 day old boy successfully treated without transplantation (ACG Case Rep J 2017;4:e23)
- 18 year old women with fever and pharyngodynia (Case Reports Hepatol 2017;2017:4630621)
- 41 year old women at 31 weeks of pregnancy with fatal course (Intractable Rare Dis Res 2017;6:124)
- 44 year old woman with nausea and vomiting (Case of the Month #481)
- 67 year old man with lesions mimicking abscess (Case Reports Hepatol 2016;2016:8348172)
- 89 year old man with sepsis secondary to urinary tract infection and fatal course (Eur J Case Rep Intern Med 2018;5:000982)
Treatment
- Empiric antiviral therapy (acyclovir)
- Liver transplantation with lifelong acyclovir prophylaxis
Microscopic (histologic) description
- Geographic (nonzonal) hemorrhagic necrosis
- Viable and nonviable areas distributed in a patchy, seemingly random fashion, sometimes with a clean separating border
- Classic nuclear features of herpes infection (margination, multinucleation, molding) are seen in hepatocytes, though multinucleation is not always observed
Positive stains
- HSV
Sample pathology report
- Autopsy:
- Widespread liver necrosis consistent with herpetic hepatitis (see comment)
- Comment: Geographic (nonzonal) hemorrhagic necrosis of the liver is present, along with viral cytopathic effect in surviving hepatocytes. Immunohistochemistry for HSV1 is positive, confirming the diagnosis.
Differential diagnosis
- The differential diagnosis includes other causes of hepatic necrosis and other causes of viral cytopathic effect:
- Hypoperfusion (e.g., due to hypovolemic shock)
- Can cause zone 3 necrosis
- Medications that cause hepatic necrosis
- Acetaminophen causes zone 3 necrosis
- Unusual substances may primarily induce necrosis in other zones
- Viral hemorrhagic fever (e.g., yellow fever)
- Can cause zone 2 necrosis, possibly also with zone 2 necrosis
- Disseminated intravascular coagulation and eclampsia
- May cause zone 1 necrosis
- Cytomegalovirus
- Can cause prominent "owl's-eye" inclusions in hepatocytes, endothelial cells and biliary epithelium
- Easier to detect in immunocompromised patients
- Fulminant hepatic failure is not the typical presentation but can occur
- Adenovirus
- Close histologic mimicker of hepatic hepatitis
- Causes random zones of necrosis and viral cytopathic effect
- Involved hepatocytes have a basophilic, smudgy nucleus without any multinucleation
- Immunohistochemistry for adenovirus can distinguish adenovirus from herpes
- Herpes zoster virus
- Can cause same histologic picture in liver
- Generally only occurs in immunocompromised patients
- HSV immunostain is negative, but VZV staining is positive
- Measles
- May cause multinucleation without margination or molding
- Eosinophilic cytoplasmic inclusions may be detected
- Necrosis would be spotty
- Hypoperfusion (e.g., due to hypovolemic shock)
Board review style question #1
- Herpes simplex hepatitis causes necrosis of hepatocytes in what pattern?
- Nonzonal necrosis
- Zone 1 necrosis
- Zone 2 necrosis
- Zone 3 necrosis
Board review style answer #1
High grade dysplastic nodule
Table of Contents
Definition / general | Essential features | Terminology | Clinical features | Radiology description | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Definition / general
- Discrete nodules in cirrhotic livers, containing high grade architectural and cytologic changes insufficient for a diagnosis of carcinoma (Hepatology 2009;49:658)
Essential features
- Dysplastic nodules (both low grade and high grade) are associated with higher risk of development of hepatocellular carcinoma
- High grade dysplastic nodules have a higher risk of transformation into hepatocellular carcinoma than low grade nodules and themselves show molecular changes similar to carcinoma (J Hepatol 2003;39:208)
Terminology
- Also called borderline nodule, macroregenerative nodule type II, atypical macroregenerative nodule, atypical adenomatous hyperplasia
Clinical features
- Considered a precursor to hepatocellular carcinoma
- Usually increase in size over time and do not regress
Radiology description
- Reduced portal blood flow in the nodule on computed tomography is an important predictor for development of hepatocellular carcinoma (Cancer 2006;106:636)
- Usually isovascular or hypovascular compared to surrounding parenchyma, whereas hepatocellular carcinoma appears hypervascular
Treatment
- Ablation or resection should be strongly considered
Gross description
- Often vaguely nodular; can be a distinct nodule often in the background of cirrhosis
- Lack a true capsule
- Typically about 1 cm; can be single or multiple
Microscopic (histologic) description
- Increased cellularity (more than 2 times higher than the adjacent nontumoral liver), often with an irregular trabecular pattern
- Cytologic atypia is usually small cell change; large cell change may or may not be seen (Arch Pathol Lab Med 2011;135:704)
- Portal tracts can be present within the nodules
- Unpaired arteries can be present but not in great numbers (Dig Liver Dis 2011;43:S361)
- "Nodule in nodule" appearance may be seen, where the larger nodule is a high grade dysplastic nodule and the inside subnodule is usually a well differentiated hepatocellular carcinoma
Microscopic (histologic) images
Images hosted on other servers:
Molecular / cytogenetics description
- Telomere shortening, increased telomerase activity and strong expression of hTERT mRNA at levels similar to hepatocellular carcinoma (Hepatology 2014;60:1983)
- Inactivation of p21 in contrast to cirrhotic nodules, which show activation (Mod Pathol 2009;22:1121)
Sample pathology report
- Liver, native, orthotopic transplantation:
- Cirrhosis with mild chronic inflammation and two high grade dysplastic nodules (see comment)
- Negative for malignancy.
- Margins of resection unremarkable.
- Comment: The findings are consistent with the patient’s reported history of chronic hepatitis B infection. A trichrome stain confirms cirrhosis. An iron stain is unremarkable.
Differential diagnosis
- Dysplastic focus:
- Typically less than 0.1 cm and not nodular
- Hepatocellular carcinoma:
- Distinction can be difficult
- Carcinoma can be positive for glypican 3, heat shock protein 70 or glutamine synthetase and lacks ductular reaction (Hepatology 2007;45:725)
- Low grade dysplastic nodule:
- Less likely to be nodular
- Atypia and cellular are less severe
Board review style question #1
Board review style answer #1
Histology
Table of Contents
Definition / general | Essential features | Terminology | Physiology | Diagrams / tables | Clinical features | Laboratory | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Liver is the largest solid organ and is located in the right upper quadrant of the abdomen
Essential features
- Functional unit is the hepatic lobule, composed of hepatocyte plates surrounding a central vein with portal tracts at the periphery
- Main cell type is the hepatocyte, which is critical for producing bile and for metabolizing drugs, proteins, fats, carbohydrates and vitamins
- Biliary epithelial cells (cholangiocytes) line bile ducts, which transport and modify bile
- Hepatic stellate cells, located in the space of Disse, store vitamin A and become activated and fibrogenic in response to injury
- Dual blood flow from hepatic artery and portal vein passes through sinusoids and exits the liver via hepatic vein branches
Terminology
- Hepatic: of or relating to the liver
Physiology
- Drug metabolism
- Phase 1 reactions increase polarity and water solubility of compounds through oxidation, reduction and hydrolysis through the cytochrome p450 system
- Phase 2 reactions create less toxic byproducts through transferase reactions and conjugations
- Lipid metabolism
- During prolonged fasting states, free fatty acids (FFAs) produced by lipolysis in adipose tissue are transported to the liver
- FFAs are beta-oxidized in liver to release ketone bodies to fuel the brain or formed into triglycerides for storage or transportation
- Carbohydrate metabolism
- In the fed state, carbohydrates are stored as glycogen in the liver
- In the fasting state, this glycogen can be broken down for systemic use (glycogenolysis)
- Lactate, amino acids and glycerol can be converted into glucose (gluconeogenesis)
- Protein metabolism
- Ingested proteins are broken down into amino acids to be used throughout the body
- Excess amino acids are oxidized for energy or converted into glucose, ketone bodies or fat
- Nitrogen waste products are converted to urea to be excreted in the urine
- Various proteins are synthesized, including albumin, coagulation factors and fibrinolytic components
- Bile production (Compr Physiol 2013;3:1035)
- Bile salts are produced by hepatocytes from cholesterol and conjugated with glycine or taurine, secreted into canaliculi, modified by cholangiocytes and stored and further concentrated in the gallbladder
- Bile salts returning from the GI tract via the portal vein are actively transported into hepatocytes to be recycled
- Free bilirubin is taken up by hepatocytes, conjugated to glucuronic acid and secreted with bile
- Vitamin metabolism
- Vitamin A storage (hepatic stellate cells)
- Vitamin D 25-hydroxylation
- Vitamins A, D, E and K absorption from intestine, which requires bile salts
- B vitamin uptake, storage and metabolism / conversion
Diagrams / tables
Clinical features
- Metabolic differences among the zones of hepatic lobules influence hepatocytes’ susceptibility to viral infection, drug injury, nonalcoholic fatty liver disease and other insults (Exp Biol Med (Maywood) 2017;242:1605)
Laboratory
- Aspartate transaminase (AST) and alanine transaminase (ALT) to evaluate potential hepatocyte damage
- Albumin, coagulation factors, prothrombin time (PT) and partial thromboplastin time (PTT) to evaluate synthetic function
- Alkaline phosphatase and bilirubin to evaluate the biliary system and excretion
- Reference: CMAJ 2005;172:367
Gross description
- Normal weight in adults is 1,400 - 1,600 grams (Am J Surg Pathol 1987;11:709)
- Can be divided into 4 lobes: right, left, caudate and quadrate
- Gallbladder (if present) is located on posterior surface of right lobe
- Dual blood supply (hepatic artery and portal vein) enters at the hilum / porta hepatis on the inferior aspect
- Peritoneum covers the superior, anterior and lateral surfaces
- External surface is smooth and red-brown
- Cut surface is firm and red-brown, with branches of portal vein, hepatic artery, bile ducts and hepatic vein seen throughout
Frozen section description
- Frozen section may be done to evaluate potential donor livers
- Assess for large and small droplet steatosis, fibrosis and inflammation
- Sinusoids may appear prominent and mimic steatosis
- Submitting tissue sample in saline may introduce water artifact mimicking steatosis
- Reference: J Clin Med Res 2011;3:191
Frozen section images
Microscopic (histologic) description
- Main liver cell types
- Hepatocytes
- Arranged in plates 1 - 2 cells thick
- Polygonal cells with round, centrally located nuclei and abundant eosinophilic cytoplasm with fine basophilic granules; can be pleomorphic and multinucleated
- May contain fat vacuoles, glycogen or lipofuscin pigment
- Cholangiocytes (bile duct epithelial cells)
- Line bile ductules and bile ducts
- Cuboidal epithelial cells with round, centrally located nuclei
- Kupffer cells
- Located in the sinusoids
- Mononuclear, phagocytic cells (macrophages) that respond to cell injury
- Bean shaped nucleus with abundant cytoplasm and star shaped cytoplasmic extensions
- Stellate cells
- Located in the space of Disse (not normally seen on H&E)
- Become activated in response to cell injury and differentiate into myofibroblasts
- Store fat and vitamin A (Physiol Rev 2008;88:125)
- Endothelial cells
- Line sinusoids as well as blood vessels
- Indistinct cytoplasm and small, elongated nuclei
- Hepatocytes
- Important microscopic features
- Limiting plate: formed by hepatocytes joining together to form a distinct row around portal tracts
- Bile canaliculi: intercellular space formed by adjacent hepatocytes (often not well visualized in normal liver unless distended)
- Sinusoids
- These separate cords of hepatocytes
- Lined by endothelial cells and Kupffer cells
- Space of Disse: space between endothelial cells and hepatocytes (not well visualized on H&E)
- Central hepatic veins: lined by endothelium; lack valves
- Portal triad / portal tract:
- Hepatic artery: lined by endothelium and a thin muscular layer, approximately the same diameter as a bile duct
- Portal vein: lined by endothelium
- Bile duct: lined by cuboidal epithelium, approximately the same diameter as a hepatic artery
- Not every normal portal tract will always show an artery, vein and bile duct; some will show multiple artery or duct faces (Hepatology 1998;28:323)
- Lymphatics: not normally seen on H&E
- May contain few lymphocytes, macrophages, mast cells and eosinophils
- Tend to be more fibrotic in subcapsular zone
- 2 concepts for describing microscopic architecture
- Acinus: functional unit centered around portal triad to include surrounding central veins
- Lobule: functional unit centered around central vein to include surrounding portal triads
- Periportal zone / zone 1
- Higher content of oxygen and nutrients
- Highest metabolic activity
- Least susceptible to ischemia and toxic injury
- Midlobular zone / zone 2
- Centrilobular zone / zone 3
- Most susceptible to ischemia and toxic injury
- Periportal zone / zone 1
Microscopic (histologic) images
Cytology description
- Hepatocytes
- Polygonal to round cells with abundant dense granular to vacuolated cytoplasm and round, centrally located nuclei with prominent nucleoli
- Arranged singly in 2 dimensional clusters or trabeculae 2 - 3 cell layers thick
- Cholangiocytes (bile duct epithelial cells)
- Cuboidal to columnar cells with scant pale cytoplasm and small, round nuclei with inconspicuous nucleoli
- Arranged in picket fences with nuclear palisading or monolayered honeycomb sheets
- Endothelial cells: rarely seen
- Kupffer cells: rarely seen
- Reference: Cytojournal 2005;2:7
Cytology images
Positive stains
- Hepatocytes: HepPar1, CAM5.2, CD10 (bile canaliculi), polyclonal CEA (bile canaliculi) (Manual of Surgical Pathology 2006;71)
- Cholangiocytes: CK7, CK19, AE1 / AE3
- Kupffer cells: CD68
- Routine stains:
- Trichrome: highlights collagen fibers to assess and stage fibrosis
- Reticulin: highlights reticulin fibers to assess hepatic plates for expansion or collapse
- Periodic acid-Schiff (PAS): highlights glycogen
- Periodic acid-Schiff with diastase (PASD):
- Highlights the basement membrane of bile ducts and ductules
- Stains abnormal alpha-1 antitrypsin globules in hepatocytes in the setting of alpha-1 antitrypsin deficiency
- Iron: aids in evaluating iron deposits in hepatocytes and Kupffer cells
Negative stains
- Hepatocytes: CK7, CK19
- Cholangiocytes: HepPar1 (J Hepatobiliary Pancreat Sci 2012;19:289)
Electron microscopy description
- Kupffer cells, endothelial cells, hepatic stellate cells, sinusoids, bile canaliculi, the space of Disse and intracellular components like mitochondria may be visualized with electron microscopy
- Limited use diagnostically except in the evaluation of some metabolic disorders
- References: World J Gastroenterol 2010;16:2851, Compr Physiol 2013;3:1035
Electron microscopy images
Additional references
Board review style question #1
Board review style answer #1
Board review style question #2
Which of the following tests can be used to evaluate synthetic function of the liver?
- Albumin
- Alkaline phosphatase
- Aspartate transaminase
- Bilirubin
Board review style answer #2
Infantile hemangioendothelioma / hemangioma
Table of Contents
Definition / general | Clinical features | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Differential diagnosisDefinition / general
- Most common hepatic mesenchymal tumor in childhood (20% of all pediatric hepatic tumors)
Clinical features
- 90% are < 6 months old at diagnosis, slight female predominance
- 10 - 40% have coexisting cutaneous cavernous hemangiomas
- 50% are incidental findings at autopsy
- Symptoms: hepatic mass (48%), high output cardiac failure due to shunting through tumor (15%); also Kasabach-Merritt syndrome (bleeding diathesis due to platelet sequestration and severe thrombocytopenia); may be asymptomatic
- Associations: chromosomal abnormalities, developmental abnormalities, hemangiomas, mesenchymal hamartoma, Wilms tumor (Virchows Arch A Pathol Anat Histopathol 1988;413:463)
Laboratory
- Normal AFP (usually), rarely elevated due to secretion from entrapped or nearby hepatocytes (Hum Pathol 2010;41:763)
Radiology description
- Xray: multiple small nodules
Prognostic factors
- Poor prognostic factors: congestive heart failure, jaundice, multiple nodules, lack of cavernous differentiation
- 70% survival (almost always have benign behavior)
- Deaths (when they occur) are usually within 1 month of diagnosis and due to congestive heart failure or platelet consumption leading to bleeding diathesis or massive hemoperitoneum
Case reports
- Newborn with 5.6 cm hepatic mass (Case of the Week #432)
- 56 year old woman with breast DCIS and liver mass (Arch Pathol Lab Med 2001;125:931)
- With pulmonary metastases (J Pediatr Surg 2006;41:e49)
Treatment
- Spontaneous involution in 5 - 10% at 6 - 8 months; resection if solitary, otherwise steroids, interferon, radiation therapy, embolization or transplantation (World J Surg 2009;33:597)
Gross description
- Solitary or multiple, mean 4 cm (range 0.1 to 15 cm) and circumscribed but not encapsulated
- White red tan, soft and spongy
- Larger nodules may have hemorrhagic, fibrotic or calcified central areas
Microscopic (histologic) description
- Well demarcated or infiltrative (35%)
- Pure type 1 change: 80%, orderly proliferation of small, capillary-like vascular spaces, relatively bloodless, may be dilated (particularly centrally) and slightly irregular; lined by bland or plump endothelial cells that may occlude the lumen; vascular channels separated by variable connective tissue; may have interspersed small bile ducts; extramedullary hematopoiesis in 60%, often in vascular lumina; often trapped hepatocytes at periphery; large lesions show thrombosis, fibrosis, myxoid change and calcification; no / rare mitotic figures and no malignant spindle cell component
- Type 2 change: equivalent to angiosarcoma (with aggressive behavior) with irregular branching vascular structures lined by pleomorphic, hyperchromatic endothelial cells, frequent mitotic activity
Positive stains
Differential diagnosis
- Angiosarcoma:
- Adequate sampling is important; has solid sarcomatous areas, vascular and sinusoidal permeation, marked pleomorphism
- May have history of exposure to toxins
- Cavernous hemangioma:
- Less common in children
- Lacks peripheral small vascular proliferation
- Epithelioid hemangioendothelioma:
- Intracellular vascular lumina containing RBCs
- Hepatic vascular malformation with capillary proliferation:
- Typically single large mass, malformed, irregular large vessels and GLUT1-
- Mesenchymal hamartoma:
- Primitive mesenchymal stroma, not a vascular tumor
Intraductal papillary neoplasm of the bile ducts
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Papillary neoplasm consisting of fibrovascular stalks within cystically dilated intrahepatic bile ducts
Essential features
- Papillary neoplasm within dilated intrahepatic bile duct(s)
- Lacks ovarian stroma
- High rate of associated invasive carcinoma (up to 74%) (Hepatology 2012;56:1352)
- WHO classification
- Premalignant: intraductal papillary neoplasm with low grade, intermediate grade or high grade intraepithelial neoplasia
- Malignant: intraductal papillary neoplasm with associated invasive carcinoma
Terminology
- Biliary papillomatosis
- Biliary papilloma
ICD coding
- ICD-O:
- ICD-11: 2E92.7 - benign neoplasm of liver or intrahepatic bile ducts
Epidemiology
- M > F; age: 50 - 70 years (Proc Bayl Univ Med Cent 2019;32:124)
- Most common in Far East (Taiwan, Japan, Korea) (World J Gastroenterol 2013;19:8595)
Sites
- Intrahepatic bile ducts
- Similar lesions can involve extrahepatic bile ducts, pancreas or gallbladder
- Often multifocal
Pathophysiology
- Stepwise progression from low grade dysplasia to high grade dysplasia to invasive carcinoma involving inactivation of TP53 and p16 (early), activating mutations in KRAS (early) and loss of SMAD4 / DPC4 (late) (Mod Pathol 2014;27:73)
Etiology
- May be related to hepatolithiasis and clonorchiasis (liver fluke infection) (Proc Bayl Univ Med Cent 2019;32:124)
Clinical features
- Symptoms resulting from biliary obstruction: jaundice, abdominal pain
Diagnosis
- Imaging (CT, MRI, ultrasound)
- Surgical resection: extensive histologic sampling required to exclude invasive component
Laboratory
- May have elevated bilirubin and alkaline phosphatase due to biliary obstruction
Radiology description
- Bile duct dilatation and intraductal masses can be seen on ultrasound, CT or MRI (Proc Bayl Univ Med Cent 2019;32:124)
Prognostic factors
- Presence of an invasive component is associated with shorter survival, related to depth and percentage of invasion (Mod Pathol 2014;27:73, World J Gastroenterol 2015;21:12498, Hepatology 2012;56:1352)
- Multiple / widespread lesions are difficult to treat and have a poorer prognosis
Case reports
- 38 year old woman with 1 week of acholic stools, jaundice, pruritus and dark colored urine (World J Gastroenterol 2015;21:12498)
- 58 year old man with mild prominence of the left hepatic biliary duct on MRI (Proc Bayl Univ Med Cent 2019;32:124)
- 59 year old woman with multiple episodes of abdominal pain and fever (Endosc Ultrasound 2016;5:274)
- 61 year old Asian man presented with severe right upper quadrant pain (BMJ Case Rep 2017;2017:bcr2016218139)
- 72 year old previously healthy man with right upper abdominal pain (Int J Surg Case Rep 2018;51:102)
Treatment
- Surgical resection is first line treatment
- Palliative approaches include chemotherapy and laser ablation
Gross description
- Soft, friable, villiform mass(es)
- May be pedunculated, sessile or polypoid
Microscopic (histologic) description
- Papillary neoplasm with complex tubulovillous or micropapillary architecture
- Grows within dilated bile ducts
- Lacks ovarian stroma
- May form large, multilocular cysts with thin fibrous septations
- Epithelium may be pancreaticobiliary (most common in European and North American patients), intestinal (more common in Asian patients), gastric (more common in Asian patients) or oncocytic
- Can be classified into type 1 (pancreatic type) and type 2 (nonpancreatic type) intraductal papillary neoplasms of the bile ducts (IPNBs) (Histol Histopathol 2017;32:1001, J Hepatobiliary Pancreat Sci 2018;25:181)
- Type 1 is similar to intraductal papillary mucinous neoplasms (IPMNs) of the pancreas
- Type 1 is more frequently intrahepatic or hilar, while type 2 is more frequently extrahepatic
- Type 2 is more aggressive, with more frequent associated invasive carcinoma
- Reference: Am J Gastroenterol 2012;107:118
Microscopic (histologic) images
Cytology description
- Hypercellular, with broad and double layered sheets of columnar epithelial cells, fine stroma and complex, 3 dimensional branching papillary configurations
Positive stains
- Various mucins, depending on differentiation (Semin Diagn Pathol 2017;34:167)
- MUC5AC and MUC6: gastric type epithelium
- MUC2: intestinal type epithelium
- MUC1 (EMA): pancreatobiliary type epithelium
Negative stains
- ER / PR staining is negative in stroma cells (unlike mucinous cystic neoplasm)
- SMAD4 / DPC4 staining may be lost in invasive component
Sample pathology report
- Liver, left lobe, lobectomy:
- Intraductal papillary neoplasm with low and high grade dysplasia, involving left hepatic duct
- No invasive carcinoma
Differential diagnosis
- Mucinous cystic neoplasm:
- Also is a cystic hepatic lesion that may be lined by biliary type epithelium
- Has ovarian type stroma and does not communicate with biliary lumen
- Cholangiocarcinoma:
- May show areas of cystic degeneration
- Does not communicate with biliary lumen (Pathol Int 2005;55:206)
- Metastatic carcinoma, especially metastatic colorectal adenocarcinoma:
- May show areas of cystic degeneration
- Does not communicate with biliary lumen
- Biliary intraepithelial neoplasia (BilIN):
- Also is located within lumen of large intrahepatic bile ducts
- Typically is < 3 mm in height (not mass forming)
- Simple cyst, simple hepatic cyst, simple biliary cyst, bile duct cyst:
- Lacks papillary projections
- Intraductal tubulopapillary neoplasm of the bile duct (Mod Pathol 2015;28:1249):
- Predominantly comprised of densely packed, nonmucinous tubules
- < 30% papillary growth pattern
Additional references
Board review style question #1
A 72 year old man presented with jaundice. CT scan showed dilatation of the left bile duct, which contained a papillary lesion. An image from the resection specimen is shown. Which of the following is true about this entity?
- It is almost always unifocal
- It lacks ovarian type stroma
- The epithelium is most commonly oncocytic
- There is a strong male predominance
- There is a very low risk of associated invasive carcinoma
Board review style answer #1
B. It lacks type ovarian stroma. This is an intraductal papillary neoplasm, which has a relatively high risk of associated invasive carcinoma (up to 74%). Sex preponderance varies by geographic region but the lesion is more common in men than women in Western countries. The epithelium is most commonly pancreatobiliary in European and North American patients. Intestinal and gastric epithelium are common in Asian patients. Oncocytic epithelium is relatively uncommon. The differential diagnosis of cystic hepatic lesions includes mucinous cystic neoplasms, which do have ovarian type stroma.
Comment Here
Reference: Intraductal papillary neoplasm of the bile ducts
Comment Here
Reference: Intraductal papillary neoplasm of the bile ducts
Board review style question #2
Intraductal papillary neoplasms of the bile ducts in North American and European patients most often have which type of epithelium?
- Gastric
- Intestinal
- Oncocytic
- Ovarian
- Pancreaticobiliary
Board review style answer #2
E. Pancreaticobiliary. Intraductal papillary neoplasms of the bile ducts are most commonly lined by pancreatobiliary epithelium in North American and European patients. Intestinal and gastric epithelium are common in Asian patients. Oncocytic epithelium is relatively uncommon. Ovarian type stroma is associated with mucinous cystic neoplasms, a different type of cystic hepatic lesion.
Comment Here
Reference: Intraductal papillary neoplasm of the bile ducts
Comment Here
Reference: Intraductal papillary neoplasm of the bile ducts
Intrahepatic biliary atresia
Table of Contents
Definition / general | Microscopic (histologic) description | Microscopic (histologic) imagesDefinition / general
- Also called paucity of intrahepatic bile ducts in neonates
- Occurs in syndromic form (Alagille syndrome) or nonsyndromic form (Eur J Hum Genet 2012;20:251)
- In nonsyndromic form, bile duct loss is present from birth
- May actually represent cystic fibrosis, alpha-1-antitrypsin deficiency, trihydroxycoprostanic acidemia
- Bile duct recovery depends on etiology
Microscopic (histologic) description
- Loss of interlobular bile ducts (0.5 ducts/portal tract versus normal 0.9 - 1.8 ducts/portal tract)
- Count only bile ducts accompanying hepatic arterioles in center of portal tracts, keratin staining may be helpful
- Usually minimal ductular proliferation
- No / minimal fibrosis, no / minimal inflammation
Intrahepatic cholangiocarcinoma (small and large duct types)
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Intrahepatic cholangiocarcinoma (iCCA) is a malignant intrahepatic epithelial neoplasm with biliary differentiation, arising in the liver periphery / proximal to the left and right hepatic ducts (WHO 2019)
- iCCA classification systems (Surg Pathol Clin 2018;11:403, Nat Rev Gastroenterol Hepatol 2020;17:557):
- Histologic features
- Small duct type versus large duct type (2 types have morphologic and molecular but not prognostic differences) (Am J Surg Pathol 2018;42:1334)
- Macroscopic growth pattern
- Mass forming
- Periductal infiltrating
- Intraductal
- Mixed growth patterns
- Cell of origin
- Stem cells residing in the canals of Hering
- Stem cells within peribiliary glands
- Histologic features
Essential features
- Nonencapsulated, white-tan and firm intrahepatic mass
- Glandular malignancy with various degrees of atypia and differentiation, infiltrating a dense fibrous stroma
- Exclusion of metastatic adenocarcinoma by review of the patient's clinical history and application of an appropriate immunohistochemistry panel
- Large duct type iCCA: often hilar masses, obstructive cholestasis; share risk factors with extrahepatic bile duct adenocarcinomas (primary sclerosing cholangitis [PSC], liver fluke infection)
- Small duct type iCCA: peripheral, larger liver masses; shares risk factors with hepatocellular carcinomas (viral hepatitis, nonbiliary cirrhosis)
Terminology
- Also known as peripheral cholangiocarcinoma and intrahepatic bile duct carcinoma
ICD coding
- ICD-10: C22.1 - intrahepatic bile duct carcinoma
Epidemiology
- In the United States, the average annual incidence is 1.6 per 100,000/year (Cancer Control 2017;24:1073274817729245)
- 15% of primary liver malignancies worldwide
- Second most common malignancy arising from the liver
- 3% of all cases of gastrointestinal cancer
- ~10% of all bile duct carcinomas
- More common in East Asia, due to endemic liver fluke infection
- Most patients are aged between 55 and 75 years (Cancer Lett 2016;379:198)
- M > F (Cancer Lett 2016;379:198)
Pathophysiology
- Chronic inflammation of the intrahepatic bile ducts with sustained IL6-STAT3 signaling (Nat Rev Gastroenterol Hepatol 2020;17:557)
- IDH, EPHA2 and BAP1 mutations and FGFR2 fusions in iCCA; in contrast to PRKACA and PRKACB fusions, ELF3 and ARID1B mutations in extrahepatic tumors (Nat Genet 2015;47:1003)
- TP53 and SMAD4 mutations
- CpG island hypermethylation are more frequent in liver fluke associated cholangiocarcinoma
Etiology
- Common underlying risk factor: chronic inflammation of the biliary epithelium and bile stasis (Liver Int 2019;39:19)
- Small duct type iCCA:
- Nonbiliary cirrhosis: independent risk factor (Cancer Control 2017;24:1073274817729245)
- Alcoholic steatohepatitis / nonalcoholic steatohepatitis (NASH)
- Hepatitis B / hepatitis C (Cancer Control 2017;24:1073274817729245)
- Large duct type iCCA:
- Primary sclerosing cholangitis: 5 - 20% lifetime risk of developing cholangiocarcinoma (Cancer Control 2017;24:1073274817729245)
- Hepatobiliary parasites: Opisthorchis viverrini, Clonorchis sinensis
- Hepatolithiasis: more common in Southeast Asia and associated with an increased risk of 6 - 50 times
- Caroli disease: a congenital disorder characterized by multifocal, segmental dilatation of large intrahepatic bile ducts
- Choledochal cysts (types I and IV)
- Multiple bile duct hamartomas (von Meyenburg complexes) (Eur J Gastroenterol Hepatol 2009;21:580)
- Thorotrast: a colloidal suspension of thorium dioxide that was used as an intravascular contrast agent until the 1950s, with an increased risk of 300 times (Jarnagin: Blumgart's Surgery of the Liver, Biliary Tract and Pancreas, Volume 1, 6th Edition, 2016)
Clinical features
- Asymptomatic in early stages (Nat Rev Clin Oncol 2018;15:95)
- Nonspecific symptoms in late stages, such as abdominal pain, malaise, fever, night sweats and weight loss / cachexia
- Jaundice / biliary obstruction are uncommon in iCCA, compared with extrahepatic cholangiocarcinoma
Diagnosis
- Clinicopathologic diagnosis by correlation of radiological, laboratory and surgical pathology findings
- Broad investigation of hepatic pathology and other malignancies should be conducted
- Colon cancer risk / screening history
- Alcohol consumption history
- Travel history (liver flukes)
- Viral hepatitis risk and serologies
- Autoimmune hepatitis serologies
- Iron studies (hemochromatosis), copper studies (Wilson disease)
- BMI (NASH)
- Exposure to hepatotoxins (thorotrast, aflatoxin)
- Labs
- CA 19-9, CEA, AFP
- In patients with PSC with or without ulcerative colitis, development of CCA can be predicted with CA 19-9 (a proposed cutoff level of 130 U/mL carries a sensitivity and specificity of 78.6% and 98.5% respectively
- Reference: Surg Oncol Clin N Am 2019;28:587, Surg Pathol Clin 2018;11:403
Laboratory
- Elevated serum CA 19-9
- Elevated serum CA 125
- Variably elevated serum alkaline phosphatase and bilirubin
- Reference: J Coll Physicians Surg Pak 2019;29:962
Radiology description
- Usually single, large, homogeneous mass with irregular margins on CT scan
- No pathognomonic CT / MRI features: may show progressive delayed enhancement, peripheral rim enhancement, subcapsular retraction
- Reference: Radiology 2018;288:7
Prognostic factors
- Serum CEA, CA 19-9, tumor diameter and number, lymph node metastasis, vascular invasion and direct invasion and local extrahepatic metastasis are important prognostic factors (J Clin Oncol 2013;31:1188)
- Periductal infiltration and AJCC 8th edition pT stage (Am J Surg Pathol 2018;42:1334)
Case reports
- 38 year old pregnant woman with 1 week history of headache, nausea, vomiting and right upper abdominal pain (Case Reports Hepatol 2018;2018:6939747)
- 45 year old Thai man with 3 month history of right upper abdominal pain (Case Rep Surg 2018;2018:3862575)
- 58 year old woman with abdominal pain and jaundice (Medicine (Baltimore) 2018;97:e11015)
- 67 year old woman with chest pain and a lung nodule (Am J Case Rep 2018;19:35)
- 70 year old man with mass forming tumor with portal vein and bile duct thrombus (Int J Surg Case Rep 2017;40:13)
Treatment
- Surgical resection of the tumor is the potential curative therapy
- Frequently inoperable, often recur after surgery
- First line treatment for locally advanced or metastatic disease is gemcitabine / cisplatin
- Molecular testing recommended by National Comprehensive Cancer Network (NCCN) for unresectable and metastatic tumors (> 50% of NGS tested subjects have potentially actionable mutations)
- Ongoing clinical trials of targeted therapy: immune checkpoint inhibitors (anti-PD1, anti-PDL1, anti-CTLA4 antibodies), IDH1 inhibitors, AKT / PI3K / mTOR inhibitors, FGFR inhibitors and anti-EGFR and MEK inhibitors
- Reference: Surg Oncol Clin N Am 2019;28:587
Gross description
- Usually large, nonencapsulated, well demarcated, firm (due to desmoplastic reaction), white-tan to gray and nodular intrahepatic mass
- More frequent in the right lobe of the liver
- Satellite nodules are present in 30%
- Calcification is common
- Noncirrhotic background liver in most cases
- Grossly classified into 3 growth patterns (J Gastroenterol 2013;48:647):
- Mass forming: hepatic parenchymal solid mass
- Periductal infiltrating: infiltrates along the portal tracts, causing bile duct strictures
- Intraductal growth: papillary or polypoid growth inside a dilated bile duct
Frozen section description
- Margin status may be assessed via frozen section
- Invasive foci of cholangiocarcinoma are infiltrating glands found as direct stromal invasion, vessel invasion or perineural invasion
Microscopic (histologic) description
- iCCA consists of infiltrating well formed or cribriform glands in an abundant fibrous stroma (Liver Int 2019;39:7, Surg Pathol Clin 2018;11:403)
- Malignant glands are lined by cells with varying degrees of atypia and pleomorphism (Liver Int 2019;39:7)
- Usually well differentiated adenocarcinoma with mild atypia, intracytoplasmic lumina and intraluminal cellular debris; however, focal atypia with marked pleomorphism can also be present (Liver Int 2019;39:7)
- Commonly infiltrates between hepatic parenchymal cords at the periphery of the tumor
- Multicentricity and perineural invasion are common
- Histologic variants include mucinous, signet ring cell, clear cell, lymphoepithelioma-like, thyroid follicular-like, adenosquamous and sarcomatoid
- Small duct type iCCA (Liver Int 2019;39:7)
- Peripheral hepatic parenchyma
- Mass forming
- Cuboidal cells forming small tubular or anastomosing glands
- Variable lymphovascular / perineural invasion
- CD56, N-cadherin, CRP positive
- Subtypes include cholangiolocarcinoma, iCCA with ductal plate malformation-like pattern
- Large duct type iCCA (Liver Int 2019;39:7)
- Proximal to liver hilum
- Periductal infiltrating or mass forming
- Tall columnar cells that form large glands within open lumina; usually contain mucin
- BilIN, IPNB, ITPN are precursors
- Positive lymphovascular / perineural invasion
- MUC5AC, MUC6, S100P and TFF1 positive
Microscopic (histologic) images
Cytology description
- Isolated clusters and sheets of cuboidal or columnar cells with various degrees of nuclear enlargement and pleomorphism
- Wide range of glandular differentiation on cell block; > 10 proliferating ductules on FNA is helpful to differentiate cholangiocarcinoma from metastatic adenocarcinomas (Diagn Cytopathol 2000;22:359)
Positive stains
- CK7 (~90%), CK19 (80 - 90%), CK17, CAM 5.2, MOC31, EMA, monoclonal CEA, polyclonal CEA (diffuse cytoplasmic pattern), claudin4, pVHL (Indian J Pathol Microbiol 2018;61:2)
- Albumin RNA ISH (~80%) but does not differentiate iCCA from hepatocellular carcinoma (Ann Surg Oncol 2015;22:S1609, Am J Surg Pathol 2018;42:1334)
- Glypican 3 and HepPar1 occasionally positive in peripherally located iCCA
Negative stains
- CK20, TTF1, napsin A, ER (Indian J Pathol Microbiol 2018;61:2, Arch Pathol Lab Med 2003;127:1591)
- Progesterone receptor (PR) can be positive in cholangiocarcinoma (31%) (Arch Pathol Lab Med 2003;127:1591)
- GATA3 rarely positive (3%), seen in poorly differentiated iCCA (Appl Immunohistochem Mol Morphol 2020;28:460)
Molecular / cytogenetics description
- Mutations in KRAS (22%), BRAF (7%), EGFR (2%), IDH1 / IDH2 (14%), MET, activation of mTOR, overexpression of cyclin D1, overexpression of p21, inactivating mutations of DPC4 / SMAD4 (13 - 15%) and TP53 (15%) (BMC Cancer 2019;19:185)
- Chromosomal gains of 1q, 5p, 7p, 8q, 17q and 20q and losses of 1p, 4q, 8p, 9p, 17p and 18q (BMC Cancer 2019;19:185)
Sample pathology report
- Right lobe of liver, partial hepatectomy:
- Moderately differentiated adenocarcinoma, 6.5 cm, consistent with intrahepatic cholangiocarcinoma, small duct type
- Resection margins are negative for carcinoma
- Lymphovascular invasion present
- Metastatic adenocarcinoma involving 1 of 3 lymph nodes
- Pathologic TNM stage (AJCC 8th edition): pT2N1
- Background liver with mild steatosis and steatohepatitis; no advanced fibrosis
Differential diagnosis
- Metastatic adenocarcinoma:
- Immunohistochemistry and clinical history are helpful to rule out metastasis
- Hepatocellular carcinoma:
- Combined hepatocellular cholangiocarcinoma:
- Histologic evidence of both hepatocellular and biliary differentiation by H&E morphology and supported by immunohistochemistry (WHO 2019)
- Benign bile ductular reactions:
- Uniform growth pattern with lack of cytologic and architectural atypia and perineural invasion
- Epithelioid hemangioendothelioma:
- Bile duct adenoma:
- Small and well circumscribed, no or minimal cytologic atypia, lack of lymphovascular or perineural invasion
Additional references
- AJR Am J Roentgenol 2000;175:721, J Hepatobiliary Pancreat Sci 2015;22:101, Gut Liver 2017;11:13, Hepatobiliary Surg Nutr 2017;6:22, Hepatobiliary Pancreat Dis Int 2012;11:349, Onco Targets Ther 2017;10:1131, World J Gastrointest Oncol 2011;3:49, WHO Classification of Tumours Editorial Board: Digestive System Tumours, 5th Edition, 2019
Board review style question #1
Board review style answer #1
B. Cuboidal cells forming small tubular or anastomosing glands
Comment Here
Reference: Intrahepatic cholangiocarcinoma (small and large duct types)
Comment Here
Reference: Intrahepatic cholangiocarcinoma (small and large duct types)
Board review style question #2
Which of the following regarding intrahepatic cholangiocarcinoma (iCCA) risk factors is true?
- Alcoholic steatohepatitis / nonalcoholic steatohepatitis are risk factors for large duct type iCCA
- Biliary type cirrhosis is an independent risk factor for small duct type iCCA
- Chronic inflammation of the biliary epithelium is a common risk factor
- Primary sclerosing cholangitis is a risk factor for small duct type iCCA
Board review style answer #2
C. Chronic inflammation of the biliary epithelium is a common risk factor
Comment Here
Reference: Intrahepatic cholangiocarcinoma (small and large duct types)
Comment Here
Reference: Intrahepatic cholangiocarcinoma (small and large duct types)
Lafora disease
Table of Contents
Definition / general | Case reports | Microscopic (histologic) description | Microscopic (histologic) imagesDefinition / general
- Autosomal recessive progressive myoclonus epilepsy due to mutations in the EPM2A (laforin) and EPM2B (malin) genes, with no substantial genotype / phenotype differences between the two (Epileptic Disord 2016;18:38)
Case reports
- 17 year old girl with generalized myoclonus epilepsy following a seizure (Case #361)
Microscopic (histologic) description
- Distinctive polyglucosans (abnormal glycogen), also called Lafora bodies, typically found in brain, periportal hepatocytes, skeletal and cardiac myocytes, eccrine duct and apocrine myoepithelial cells of sweat glands (Epileptic Disord 2016;18:38)
Microscopic (histologic) images
Large duct obstruction
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Obstruction of the large extrahepatic bile ducts, leading to liver injury
Essential features
- May be caused by stricture, gallstones or malignancy
- Typically a clinical diagnosis; uncommonly biopsied
- Histology shows biliary-pattern injury (cholestasis, ductular reaction), often with prominent portal tract edema
Terminology
- May be acute or chronic
- May be termed "mechanical bile duct obstruction"
ICD coding
- ICD10: K83.1 - obstruction of bile duct
Pathophysiology
- Obstruction of bile outflow leads to cholestasis, ductular reaction and liver injury
Etiology
- Usually due to gallstones in common bile duct; other causes include stricture (such as from primary sclerosing cholangitis), malignancy, bile plugs and surgical ligation
Clinical features
- Symptoms include jaundice, nausea, vomiting, abdominal pain, fever
- Biopsies have decreased due to improved imaging
- Without treatment, may progress to fibrosis / cirrhosis with duct loss
Diagnosis
- Typically made by clinical presentation (including rapid onset in acute disease) and radiologic findings
Laboratory
- Increased alkaline phosphatase and conjugated bilirubinemia (J Clin Pathol 1994;47:457)
- Normal prothrombin time
- May demonstrate transient increase in ALT and AST
Radiology description
- Etiology may be visible on imaging; also, ducts proximal to obstruction may be dilated
Case reports
- 40 year old woman with hepatic fascioliasis (Pan Afr Med J 2017;28:44)
- 67 year old man with abdominal aortic aneurysm (BMJ Case Rep 2017;2017:220539)
- 77 year old woman with large enterolith (Korean J Gastroenterol 2016;67:150)
- 84 year old man with gastric adenocarcinoma (Med Case Rep 2019;13:72)
Treatment
- Endoscopic retrograde cholangiopancreatography (ERCP) can remove gallstones and stent stricture
- Antibiotics if secondarily infected
- Surgical intervention may be necessary
Microscopic (histologic) description
- Acute / early changes: centrilobular canalicular cholestasis, followed shortly by portal tract edema, ductular reaction and mild chronic inflammation
- Chronic / late changes: portal tract fibrosis, feathery degeneration of hepatocytes adjacent to cholestasis, bile in Kupffer cells; may develop bridging fibrosis and ultimately cirrhosis
- Lobules minimally affected since injury occurs via portal tracts
- Bile may leak into parenchyma, with adjacent foreign body giant cell reaction
- Cholestasis may be severe (J Clin Pathol 2018;71:72)
Microscopic (histologic) images
Positive stains
- CK7 highlights ductular reaction (as in all biliary pattern injury)
Sample pathology report
- Liver, biopsy:
- Hepatic parenchyma with prominent portal tract edema, ductular reaction and canalicular cholestasis (see comment)
- Comment: The patient’s history of acute-onset nausea and vomiting is noted, along with increased alkaline phosphatase. The findings are most consistent with acute large duct obstruction. The etiology of the obstruction is not evident in this sample; possibilities include primary sclerosing cholangitis, gallstones, duct structure and malignancy.
- Hepatic parenchyma with prominent portal tract edema, ductular reaction and canalicular cholestasis (see comment)
Differential diagnosis
- Primary sclerosing cholangitis:
- Onion skinning fibrosis must be distinguished from portal tract edema
- Primary biliary cholangitis:
- Lobular inflammation often present
- Drug reaction:
- Unlikely, but can mimic duct obstruction; clinical correlation necessary
- Hyperalimentation toxicity:
- Can sometimes mimic duct obstruction; clinical correlation necessary
Board review style question #1
- Which of the following is the first finding chronologically in acute obstruction of large bile ducts?
- Canalicular cholestasis
- Ductitis
- Ductular reaction
- Florid duct lesions
- Portal tract edema
Board review style answer #1
Board review style question #2
Board review style answer #2
Large regenerative nodule
Table of Contents
Definition / general | Essential features | Terminology | Clinical features | Radiology description | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Definition / general
- Benign liver lesion frequently seen in Budd-Chiari syndrome and less commonly in other vascular disorders of the liver or systemic conditions such as autoimmune disease, myeloproliferative disorders and lymphoproliferative disorders (Radiographics 2002;22:847)
Essential features
- Low grade regenerative hepatocellular nodule that often arises in the setting of flow abnormalities
- Low malignant potential
Terminology
- Also known as benign regenerative nodule
Clinical features
- Low malignant potential (Hepatology 1990;12:592, Hepatol Int 2015;9:330)
- Often stabilize or disappear over time
Radiology description
- Predominantly isointense or hypointense relative to background liver on T2 weighted images
Gross description
- Multiple, well circumscribed, round lesions
- Typically 0.5 - 4.0 cm
Microscopic (histologic) description
- Nodules of hyperplastic hepatocytes arranged in thickened hepatic plates
- No distinctive cytoarchitectural features (J Hepatol 2003;39:208)
- Entrapped portal tracts often present
- Surrounding parenchyma shows atrophy and congestion and may undergo fibrosis
Microscopic (histologic) images
Sample pathology report
- Liver, native, orthotopic transplantation:
- Liver parenchyma with bridging fibrosis, prominent sinusoidal dilation and focal large regenerative nodules (see comment)
- Negative for malignancy.
- Margins of resection unremarkable.
- Comment: The findings are consistent with the patient’s reported history of congestive heart failure. The simultaneously explanted heart will be reported separately. A trichrome stain shows bridging fibrosis, focally approaching early cirrhosis. An iron stain is unremarkable.
Differential diagnosis
- Low grade dysplastic nodule:
- Mild increase in cellularity, with occasional large cell change
- Similar to slightly higher malignant potential
- Macroregenerative nodule:
- Similar malignant potential
- Generally occurs in cirrhosis
- Similar if not identical by morphology
Board review style question #1
Large regenerative nodules of the liver often arise in the setting of
- Biliary injury
- Chronic viral hepatitis
- Cirrhosis
- Vascular flow abnormalities
Board review style answer #1
Late T cell mediated (cellular) rejection
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Immunofluorescence description | Immunofluorescence images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Alloimmune injury to the allograft driven primarily by effector T cells (with varying accompaniment by monocytes and macrophages), usually occurring > 3 - 6 months posttransplantation with the potential to produce clinically significant, progressive and chronic structural changes that include vascular, biliary, fibrotic and parenchymal remodeling transformation of the liver architecture (Banff Foundation: Banff Liver Group 2022 [Accessed 3 January 2024])
- Leads to worse patient and graft survival after liver transplantation (Arq Bras Cir Dig 2015;28:212)
Essential features
- Late onset T cell mediated rejection is a form of T cell mediated rejection (TCMR) usually occurring > 1, 3 or 6 months after transplantation (no uniform definition of the time point for late rejections), however, mostly believed to present after 6 weeks of transplantation (Liver Transpl 2019;25:425, Arq Bras Cir Dig 2015;28:212)
- Interface activity and centrilobular necroinflammatory lesions falling within the spectrum of central perivenulitis (with or without portal inflammation) are common features
- Perivenular fibrosis in severe cases
- Evidence of circulating donor specific antibodies
- Frequently in patients noncompliant with immunosuppression (Transplant Direct 2022;8:e1076)
Terminology
- Late onset T cell mediated rejection (Liver Transpl 2019;25:425)
- Idiopathic posttransplantation hepatitis (J Hepatol 2011;55:702)
ICD coding
- ICD-10: T86.41 - liver transplant rejection
Epidemiology
- Incidence rate ranges from 7 to 23% (World J Gastroenterol 2006;12:6674, Transplantation 2013;95:955)
- Young adults (10 - 24 years old) have a significantly higher incidence of late TCMR than controls (Transplant Direct 2022;8:e1076)
- Other risk factors
- Patients with preserved renal function at the time of transplantation (Transplant Direct 2022;8:e1076)
- Documented medication noncompliance
- Young age
- Early moderate to severe or steroid resistant TCMR remains a significant variable for late onset TCMR (Liver Transpl 2019;25:425)
- de novo donor specific antibody (DSA) development (Am J Transplant 2016;16:2816)
Sites
- Liver allografts
- Also occurs in other solid organ allografts, such as the kidney
Pathophysiology
- Indirect antigen recognition (Am J Transplant 2016;16:2816)
- Linked to de novo donor specific antibodies (DSA) development (Transplant Direct 2022;8:e1076)
- Diagnostic designation as TCMR does not exclude a contribution from DSA or innate effector mechanisms but is a practical synoptic recognition of the dominant tissue appearance and associated RNA signature (Banff Foundation: Banff Liver Group 2022 [Accessed 3 January 2024])
Etiology
N/A
Diagrams / tables
Grading descriptors of late onset T cell mediated rejection presenting as isolated central perivenulitis (Hepatology 2006;44:489)
| Description | Biopsy findings |
| Minimal or indeterminate | Perivenular inflammation involving a minority of terminal hepatic veins, with patchy perivenular hepatocyte loss but without confluent perivenular necrosis |
| Mild | As above but involving most terminal hepatic veins |
| Moderate | As above, with focal confluent perivenular hepatocyte dropout and mild or moderate inflammation but without bridging necrosis |
| Severe | As above, with confluent perivenular hepatocyte dropout and inflammation involving most hepatic venules and with central to central bridging necrosis |
Banff working group proposed scoring of late TCMR for further development (Banff Foundation: Banff Liver Group 2022 [Accessed 3 January 2024])
| Subscore | Component | Contribution | Criteria |
| Alloimmune activity grade | Portal inflammation | 0 - 3 | Existing Banff criteria |
| Bile duct damage | 0 - 3 | Existing Banff criteria | |
| More severe lesion: subendothelial inflammation or central perivenulitis | 0 - 4 | Banff rejection activity index (RAI) "v" score or Banff 2006 isolated CP score | |
| Interface hepatitis | 0 - 4 | Proposed criteria (see below) | |
| Fibrosis stage | Periportal | 0 - 3 | Venturi: LAFS |
| Subsinusoidal | 0 - 3 | ||
| Perivenular | 0 - 3 |
Images hosted on other servers:
Clinical features
- May be asymptomatic and detected on surveillance / protocol biopsies
- Some patients present with fever, malaise, abdominal pain, hepatosplenomegaly and rarely, increasing ascites; because most patients are asymptomatic, TCMR is suspected primarily by an increase in values on liver biochemical tests
- Biochemical tests measuring liver function may show a rise in transaminase levels in cases with more prominent lobular changes contrasting with the cholestatic profile that is more typically seen in early portal based acute TCMR
- Presence of cholestasis may signify a more severe form of late onset TCMR, which is less likely to be steroid responsive
- Associated increased risk of developing a number of adverse outcomes including further episodes of TCMR and progression to chronic rejection or allograft failure
- References: Clin Transplant 2008;22:316, Transplant Proc 2001;33:1525
Diagnosis
- Criteria and categories for the diagnosis of TCMR were defined by the Banff working group (see Diagrams / tables) (Am J Transplant 2016;16:2816)
- Portal based inflammation may contain plasma cells and eosinophils with interface activity, portal subendothelitis and to a lesser extent bile duct involvement (less prominent compared with early TCMR)
- Lobular and central vein lesions are common, characterized by central perivenulitis, hemorrhage and hepatocellular dropout
- Isolated arterial "v" lesions have been described, with or without associated inflammatory component (Am J Transplant 2018;18:1534)
- “v” lesions are defined as intimal inflammation, age inappropriate fibrointimal hyperplasia or both, without the presence of associated interstitial T cell mediated rejection (TCMR)
- Arteritis and foamy arteriopathy may be seen when larger arteries are sampled
- Plasma cell rich variant: an atypical variant of rejection with mixed cellular and antibody components (see chronic antibody mediated rejection)
- Plasma cell component exceeding 30% of inflammatory cells
- Primary disease not antibody mediated rejection (AMR)
- Cholangitis can be seen but not a required feature
- Atypical features associated with late TCMR include features seen in chronic viral hepatitis or autoimmune hepatitis (AIH)
Laboratory
- Deranged liver function tests; higher levels of aspartate aminotransferase and alanine aminotransferase, and in severe forms, alkaline phosphatase and gamma glutamyl transferase
- Negative testing for hepatitis B, C and E (Liver Transpl 2016;22:1593)
- Presence of donor specific anti-HLA antibodies (DSA)
- No serum markers of inflammation are currently recommended
Radiology description
- Imaging studies are generally performed to exclude other causes of elevated liver biochemical tests and allograft dysfunction
- Imaging findings in patients with acute TCMR (e.g., liver allograft enlargement) are not specific
Radiology images
N/A
Prognostic factors
N/A
Case reports
- 20 year old woman who underwent liver replacement because of biliary type fibrosis / cirrhosis secondary to Alagille syndrome (Transplant Direct 2022;8:e1076)
Treatment
- For all patients with histologic evidence of acute TCMR of the liver allograft, the baseline maintenance immunosuppressive regimen is assessed and optimized, while the specific approach depends on the patient's drug regimen and baseline liver function
- For patients with rejection activity index (RAI) < 5, treatment usually depends on optimizing immunosuppression; options for immunosuppression include tacrolimus and mycophenolate
- For patients with severe TCMR (i.e., RAI ≥ 5), initial therapy consists of high dose glucocorticoids (e.g., methylprednisolone) followed by a glucocorticoid taper, in addition to optimizing the maintenance immunosuppression regimen (Transplantation 2018;102:727)
- For nonresponders, therapeutic options such as antithymocyte globulin have been used to treat patients with glucocorticoid refractory rejection
- Retransplantation for failed allografts (very rare)
Clinical images
N/A
Gross description
- Rare specimens
- Explanted livers may show necrosis, discoloration or rupture if rejection is severe
Gross images
N/A
Frozen section description
N/A
Frozen section images
N/A
Microscopic (histologic) description
- Portal tract changes
- Portal inflammation: mononuclear portal inflammatory infiltrate (contrasting with the mixed population of cells [lymphocytes, plasma cells, eosinophils, macrophages] seen in biopsies taken during early TCMR < 6 weeks) (Hepatology 2006;44:489)
- Bile duct inflammation damage
- Venous endothelial inflammation
- Interface hepatitis: extension of portal inflammation beyond the limiting plate into the adjacent lobule with damage and progressive loss of hepatocytes at the portal lobular interface
- Lobular parenchyma
- Prominent central perivenular inflammation and hepatocyte dropout with minimal or no portal tract changes (i.e., isolated central perivenulitis) (Histopathology 2020;76:822, Hepatology 2006;44:489)
- Subendothelial inflammation of the portal or central veins is not a required finding
- More prominent interface hepatitis
- Overall appearances may thus come to resemble those seen in chronic viral hepatitis or AIH
- Centrilobular necroinflammatory lesions falling within the spectrum of central perivenulitis (CP), either with or without portal inflammation, are a common feature of late TCMR
- Fibrosis
- Extensive and severe perivenular fibrosis resembling Budd-Chiari syndrome or a sinusoidal obstruction type syndrome can develop as a consequence of severe or persistent central perivenulitis
Microscopic (histologic) images
Virtual slides
N/A
Cytology description
N/A
Cytology images
N/A
Immunofluorescence description
N/A
Immunofluorescence images
N/A
Positive stains
N/A
Negative stains
N/A
Electron microscopy description
N/A
Electron microscopy images
N/A
Molecular / cytogenetics description
N/A
Molecular / cytogenetics images
N/A
Videos
N/A
Sample pathology report
- Liver allograft, needle biopsy:
- Mild perivenular lymphoplasmacytic inflammation with perivenular hepatocyte dropout and fibrosis, favors T cell mediated rejection manifesting primarily as central perivenulitis (rejection activity index: 3/8) (see comment)
- Mild lymphoplasmacytic portal inflammation with ongoing interface activity and capillaritis and focally prominent shunt type vessels
- C4d negative for convincing portal microvascular endothelial cell positivity
- Mild to moderate portal / periportal and severe perivenular fibrosis with focal bridging
- No previous biopsy available for comparison
- Comment: The main histopathological findings include mild lymphoplasmacytic and histiocytic perivenular inflammation, hepatocyte dropout and fibrosis, accompanied by mild patchy lymphoplasmacytic portal inflammation with mild ongoing interface activity but without significant lymphocytic cholangitis or ductopenia. This pattern of injury is most often seen with late onset T cell mediated rejection. However, the differential diagnosis would also include so called de novo autoimmune hepatitis, which some refer to as late onset plasma cell rich T cell mediated rejection, suboptimal hepatic arterial flow or suboptimal venous drainage and drug induced liver injury (DILI).
- T cell mediated rejection is favored because of the combination of portal inflammation with interface activity combined with prevalent and prominent central perivenulitis and the patient's age. Vascular abnormalities are felt to be less likely because of the noticeable lymphoplasmacytic portal and perivenular inflammation but should be reasonably excluded. However, the other possibilities mentioned above cannot be absolutely excluded. Additional serologic studies, such as quantitative serum immunoglobulins and liver directed autoantibodies (ANA, ASMA, LKM, etc.) might provide additional useful information. Correlation with baseline immunosuppression is also suggested as nontacrolimus regimens are more frequently associated with late onset rejection and serum DSA development.
Differential diagnosis
Modified from Banff working group (Hepatology 2006;44:489)
| Histopathological features | Early T cell mediated rejection (TCMR) | Chronic rejection | Autoimmune hepatitis (AIH) † | Hepatitis B / hepatitis C | Primary biliary cirrhosis (PBC) | Primary sclerosing cholangitis (PSC) / bile duct (BD) strictures |
| Portal inflammation | Mononuclear with mild rejection; mixed rejection type infiltrate in moderate to severe | Patchy, mostly lymphoplasmacytic | More prominent mixed infiltrate with often predominant plasma cell component | Patchy, nodular aggregates, predominantly mononuclear | Patchy, with nodular aggregates and granulomas, with bile duct damage, florid duct lesions and lymphocytic cholangitis | Usually mixed inflammation; can be with neutrophilic component, patchy to diffuse depending on stage |
| Interface activity | Occasionally present; severity marks higher grade of rejection | Absent | Defining feature and usually plasma cell rich with necro inflammation | Variable, usually not prominent: necroinflammatory and (ductular type) | Ductular reaction with cholangiolar metaplasia with copper deposition later in disease development | Ductular reaction with portal and periportal edema |
| Bile duct inflammation / damage | Present and usually involves a majority of bile ducts | Focal ongoing lymphocytic bile duct damage; inflammation wanes with duct loss | Variable | Variable; involves minority of ducts | Granulomatous or focally severe lymphocytic cholangitis is diagnostic in proper setting | Periductal lamellar edema, fibrous cholangitis, acute cholangitis, multiple intraportal ductal profiles |
| Bile duct senescence changes / ductopenia | Absent most cases | Senescence / atrophy / atypia involve a majority of remaining ducts | Mostly absent | Absent in most cases | Ductopenia with associated with ductular reaction | Ductopenia associated with ductular reaction |
| Perivenular mononuclear inflammation or hepatocyte dropout | Variable, if defining feature should involve a majority of perivenular regions; may also show subendothelial inflammation of vein | Usually present but mostly mild | Variable, can involve a majority of perivenular regions, similar to rejection; sometimes is plasma cell rich | Variable, involves minority in most cases | Variable but generally mild, if present involves a minority of perivenular regions | Absent |
| Lobular necroinflammatory activity and features | Variable, if present, more around the perivenular regions | Variable, if present, more around the perivenular regions | Disarray variable; variable severity; necroinflammatory activity | Disarray variable; variable severity; necroinflammatory activity | Mild disarray, parenchymal granulomas; periportal copper deposition and cholestasis are late features | Disarray unusual; neutrophils clusters; with or without cholestasis |
| Pattern of fibrosis during progression toward cirrhosis | Rare | Uncommon, if present usually a venocentric pattern; may evolve to biliary pattern over time | Usually macronodular, posthepatitic pattern | Mostly macronodular, hepatitic pattern | Biliary pattern | Biliary pattern |
- ∗ The histopathological findings in this table should be combined with clinical, serological, radiographic and important exclusionary criteria listed to arrive at a final diagnosis
- † The same findings apply to recurrent and de novo AIH
Additional references
N/A
Board review style question #1
What is late onset T cell mediated rejection usually associated with?
- Excessive immunosuppression
- Focal to diffuse C4d uptake
- Immunosuppression noncompliance
- No fibrosis of the allograft
- Old age
Board review style answer #1
C. Immunosuppression noncompliance. Late onset TCMR often presents in patients > 1, 3 or 6 months after transplantation, however, is mostly believed to present after 6 months of transplantation often as a result of noncompliance with immunosuppressive medications. Answer E is incorrect because late onset TCMR has no negative association with age of the recipient. Answer A is incorrect because excessive immunosuppression would lower immune cell counts, decreasing the risk for T cell mediated rejection but would cause other side effects. Answer B is incorrect because C4d deposition is more commonly seen in vascular walls of portal areas and hepatic sinusoidal walls in cases with antibody mediated rejection. Answer D is incorrect because late onset TCMR is associated with atrophy and fibrosis.
Comment Here
Reference: Late T cell mediated (cellular) rejection
Comment Here
Reference: Late T cell mediated (cellular) rejection
Board review style question #2
Per Banff rules, what would perivenular inflammation involving a minority of terminal hepatic veins, with patchy perivenular hepatocyte loss but without confluent perivenular necrosis be regarded as?
- Mild late T cell mediated rejection
- Minimal late T cell mediated rejection
- No rejection
- Severe late T cell mediated rejection
Board review style answer #2
B. Minimal late T cell mediated rejection. Answer C is incorrect because late onset TCMR can involve minority of terminal hepatic veins and that is considered rejection. Answer A is incorrect because mild late T cell mediated rejection involves most terminal hepatic veins. Answer D is incorrect because severe late T cell rejection shows confluent perivenular hepatocyte dropout with inflammation involving most hepatic venules along with central to central bridging necrosis.
Comment Here
Reference: Late T cell mediated (cellular) rejection
Comment Here
Reference: Late T cell mediated (cellular) rejection
Late T cell mediated (cellular) rejection (pending)
Table of Contents
Definition / generalDefinition / general
[Pending]
Liver cell dysplasia
Table of Contents
Definition / general | Essential features | Terminology | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Board review style question #1 | Board review style answer #1Definition / general
- Premalignant foci in liver characterized by morphologic alterations of hepatocytes and sometimes by architectural changes
- Challenging category that encompasses macroscopic and microscopic patterns of change (see also low grade dysplastic nodule and high grade dysplastic nodule) (Hepatology 2009;49:658)
Essential features
- Dysplastic features in hepatocytes that can progress to malignancy as part of a multistep sequence
- May be incidentally discovered or seen in a discrete nodule
Terminology
- Dysplastic foci are incidental submillimeter microscopic lesions in cirrhotic livers containing dysplastic hepatocytes (Arch Pathol Lab Med 2011;135:704)
- Large cell change and small cell change refer to morphologic changes in hepatocytes; these were formerly called large cell dysplasia and small cell dysplasia
- Iron free foci are areas of hepatocytes lacking iron in a liver otherwise suffering significant iron overload; they appear to be preneoplastic (Hepatology 1993;18:1363)
- Terms adenomatous hyperplasia and atypical adenomatous hyperplasia are no longer in use
Gross description
- Dysplastic foci cannot be identified grossly
Microscopic (histologic) description
- Large cell change is defined as an increase in both nuclear and cytoplasmic size, preserving nuclear to cytoplasmic ratio; nuclei are hyperchromatic, pleomorphic and frequently multinucleated
- Small cell change is defined as hepatocytes showing decreased cell volume, increased nuclear to cytoplasmic ratio, mild nuclear pleomorphism, hyperchromasia and cytoplasmic basophilia, giving the impression of nuclear crowding; this pattern is typical of high grade dysplastic nodules
Microscopic (histologic) images
Sample pathology report
- Liver, native, orthotopic transplantation:
- Cirrhosis with mild chronic inflammation and patchy low grade dysplasia (see comment)
- Negative for high grade dysplasia malignancy.
- Margins of resection unremarkable.
- Comment: The findings are consistent with the patient’s reported history of nonalcoholic hepatitis. A trichrome stain confirms cirrhosis. An iron stain is unremarkable.
Board review style question #1
Which of the following is true about hepatocellular dysplasia?
- Dysplastic foci can be identified grossly
- It acts as the precursor to cholangiocarcinoma
- Large cell change has an increased nuclear to cytoplasmic ratio
- Small cell change has mild nuclear pleomorphism and cytoplasmic basophilia
Board review style answer #1
D. Small cell change has mild nuclear pleomorphism and cytoplasmic basophilia
Comment Here
Reference: Liver cell dysplasia
Comment Here
Reference: Liver cell dysplasia
Liver transplantation overview
Definition / general
- 3 year overall survival rate is 70%
- Biopsy necessary to document allograft rejection
- Common reasons for transplant: congenital biliary atresia (children), hepatitis C (adults), cholangiocarcinoma (Clin Liver Dis 2011;15:699)
- Explanted livers from patients with familial amyloidotic polyneuropathy but not apolipoprotein AI amyloidosis with Arg26 mutation can be used for other patients (domino style transplantation) (Hum Pathol 2000;31:40, Mod Pathol 2001;14:577)
- Primary EBV infection reported in 60% of EBV seronegative patients; reactivation in 20% of seropositive patients
- Monitor posttransplant lymphoproliferative disease (polyclonal B cell proliferation, B cell lymphoma) with allograft liver biopsy to detect acute rejection when the immunosuppression is reduced
- May also have surgical complications such as Budd-Chiari syndrome, portal vein thrombosis, arterial thrombosis, biliary tract complications
- Hepatitis B and C usually recur post-transplant (Hum Pathol 2000;31:101)
- Are major causes of cirrhosis (Hum Pathol 1999;30:39)
- Steatosis: microsteatosis in donor liver biopsies has no effect on graft function; ischemic injury with development of steatosis in early posttransplantation period is uncommon, may be associated with hepatitis C and poor clinical outcome (Hum Pathol 2000;31:1209)
- Preservation injury: injury to liver during period from final phase of donor's life to implantation into recipient (Transplantation 2001;71:1566)
Prognostic factors
- Combinations of centrilobular hepatocyte ballooning, dropout and cholestasis are associated with ischemic / perfusion damage early posttransplant (due to harvesting, transporting, reperfusion issues, usually reversible)
- Presence of all three is associated with poor outcome
- Central venulitis is not a prognostic factor (Hum Pathol 2002;33:270)
Case reports
- 57 year old man who accumulated Thorotrast in liver allograft 10 years after transplant (Mod Pathol 2004;17:117)
- 2 cases of extranodal MALT lymphoma posttransplant (Am J Surg Pathol 2000;24:100)
Additional references
Low grade dysplastic nodule
Table of Contents
Definition / general | Essential features | Terminology | Clinical features | Radiology description | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Definition / general
- Discrete nodules in cirrhotic livers containing mild architectural changes
Essential features
- Dysplastic nodules (both low grade and high grade) are associated with higher risk of development of hepatocellular carcinoma
- Low grade dysplastic nodules have a significantly lower risk to transform into carcinoma than high grade nodules (J Hepatol 2003;39:208)
Terminology
- Also called macroregenerative nodule type I, adenomatous hyperplasia, hepatocellular pseudotumor
Clinical features
- Usually ages 40 and older; 67% arise in males
- May progress to hepatocellular carcinoma but usually stabilize or disappear over time instead
Radiology description
- Usually isovascular or hypovascular compared to surrounding parenchyma, whereas hepatocellular carcinoma appears hypervascular
Treatment
- Follow by imaging
Gross description
- Often distinct nodules (can be vague), separated from the surrounding liver by a rim of thin fibrous scar (not a true capsule)
- Usually multiple, 0.5 to 1.5 cm, occasionally up to 5 cm
- Similar in color and texture to surrounding liver; may be pale or bile stained
- Usually found in cirrhotic livers, rarely in acute liver injury or precirrhotic livers
Microscopic (histologic) description
- Monotonous cell population lacking architectural atypia, with mild increase in cellularity compared to surrounding cirrhotic liver (Hepatology 2009;49:658, Dig Liver Dis 2011;43:S361)
- Portal tracts can be identified within the nodules
- Liver cell plates 1 - 2 cells thick (highlighted on reticulin stain)
- Features of hepatocellular carcinoma (pseudoglands or markedly thickened trabeculae) absent
- May have large cell changes in hepatocytes
- Unpaired arteries, which have no accompanying bile ducts, can be prominent in number and size (unlike cirrhotic nodules)
- May have diffuse iron or copper retention (Arch Pathol Lab Med 2011;135:704)
Microscopic (histologic) images
Molecular / cytogenetics description
- May be clonal
- Inactivation of p21 checkpoint in contrast to cirrhotic nodules, which show activation
Sample pathology report
- Liver, native, orthotopic transplantation:
- Cirrhosis with mild chronic inflammation and three low grade dysplastic nodules (see comment)
- Negative for high grade dysplasia or malignancy.
- Margins of resection unremarkable.
- Comment: The findings are consistent with the patient’s reported history of chronic hepatitis C infection. A trichrome stain confirms cirrhosis. An iron stain is unremarkable.
Differential diagnosis
- High grade dysplastic nodule:
- Increased hepatocyte density with moderate cytologic or architectural atypia
- Macroregenerative nodule:
- Similar malignant potential
- Distinction by morphology alone can be difficult
- Distinguishing molecular findings include overexpression of semaphorin E, IGFBP3 and caveolin 1 and increased expression of collagen IV
- References: Lab Invest 2002;82:547, Am J Pathol 2003;162:991
Board review style question #1
Which of the following is true about low grade dysplastic nodules in the liver?
- If unresected, they will always progress to hepatocellular carcinoma
- They are grossly distinct from background cirrhotic nodules
- They are hypervascular radiologically
- They have prominent architectural atypia histologically
Board review style answer #1
B. They are grossly distinct from background cirrhotic nodules
Comment Here
Reference: Low grade dysplastic nodule
Comment Here
Reference: Low grade dysplastic nodule
Macroregenerative nodule
Table of Contents
Definition / general | Essential features | Terminology | Clinical features | Radiology description | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Definition / general
- Discrete regenerative hepatocellular nodule that often arises in the background of cirrhosis
Essential features
- May represent a precursor of hepatocellular carcinoma (Hepatology 1992;16:949)
- Classified into type I and type II, based on cytological and architectural atypia (Cancer 1998;61:99)
- Macroregenerative nodule (MRN) II shows atypical cytologic or architectural features that are insufficient for a diagnosis of malignancy
Terminology
- Also called hepatocellular pseudotumor, adenomatous hyperplasia, adenomatous hyperplastic nodule or adenomatous regeneration
Clinical features
- Most MRNs are seen in cirrhotic livers
- Occurs in about 10% of cirrhotic livers at autopsy or at time of transplantation
- Role of MRN in hepatocarcinogenesis varies in different studies and the true biologic nature of these nodules is uncertain (Int J Hepatol 2016;2016:4390434)
Radiology description
- Well defined isointense nodules relative to the background liver
Gross description
- Usually multiple, large, discrete, tumor-like hepatocellular masses > 1 cm in diameter (rarely > 5 cm)
- Often differ from surrounding nodular parenchyma in color, texture or degree to which they bulge beyond the cut liver surface
Gross images
Microscopic (histologic) description
- Liver cell plates 1 - 2 cells thick, reduced and scattered portal tracts with variable structural distortion (prominent bile ductules, absent interlobular bile ducts)
- Hepatocytes resemble those in adjacent liver and may reflect any disease process there
- MRN type II may have architectural and cytologic atypia
Microscopic (histologic) images
Sample pathology report
- Liver, native, orthotopic transplantation:
- Cirrhosis with mild to moderate chronic inflammation and occasional macroregenerative nodules (see comment)
- Negative for dysplasia or malignancy.
- Margins of resection unremarkable.
- Comment: The findings are consistent with the patient’s reported history of autoimmune hepatitis. A trichrome stain confirms cirrhosis. An iron stain is unremarkable.
Differential diagnosis
- Early hepatocellular carcinoma:
- Can be difficult or impossible to distinguish from MRN type II with cytological atypia
- Large regenerative nodule:
- Low malignant potential
- Less commonly arises in cirrhosis
- Similar if not identical by morphology
Board review style question #1
- Which of these liver lesions is the least likely to arise in the background of cirrhosis?
- High grade dysplastic nodule
- Large regenerative nodule
- Low grade dysplastic nodule
- Macroregenerative nodule
Board review style answer #1
Malnutrition (total parenteral nutrition)
Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Pathophysiology | Clinical features | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Parenteral nutrition provides nutritional support for those patients with prematurity, malabsorption, severe inflammatory bowel disease, necrotizing enterocolitis, congenital gastrointestinal disorders and extensive gastrointestinal surgery, by intravenous infusion of macronutrients (glucose, lipid and amino acids), micronutrients (vitamins and minerals), electrolytes and water
- Hyperalimentation (typically from long-term total parenteral nutrition [TPN]) can cause liver dysfunction that may require combined liver and small bowel transplantation (Dig Dis 1994;12:191, Hepatology 2006;43:9, Gastroenterology 2006;130:S70)
Essential features
- Total parenteral nutrition leads to clinical and pathologic liver injury in 40 - 60% of infants and 15 - 40% of adults (Gastroenterology 2006;130:S70)
- Histology usually shows cholestasis and macrovesicular steatosis
ICD coding
- ICD-10: K71.0 - toxic liver disease with cholestasis
Epidemiology
- More likely to occur in long term, rather than short term, total parenteral nutrition
Pathophysiology
- Poorly understood but likely multifactorial (underlying disease, components and duration of TPN, lack of enteral feeding, recurrent sepsis) (Hepatology 2006;43:9, Aliment Pharmacol Ther 2000;2:54)
Clinical features
- Typically asymptomatic initially
- Usually manifests as mild, reversible liver or biliary injury (Gastroenterol Clin North Am 1989;18:645)
- Infants on total parenteral nutrition may have liver disease progress more rapidly than older patients with jaundice and splenomegaly (Hum Pathol 2012;43:826)
- Clinical severity may not correlate with histologic severity (Hum Pathol 2012;43:826)
- May be fatal (J Pediatr Surg 1982;17:463)
Laboratory
- Elevated conjugated bilirubin is common in children, particularly during sepsis and is usually accompanied by elevation of ALT, ALP and GGT
- Hypoalbuminemia and prolonged PT / INR are late signs
- Thrombocytopenia occurs with splenomegaly secondary to significant liver fibrosis and cirrhosis (Early Hum Dev 2010;86:683)
Prognostic factors
- Total parenteral nutrition may cause more injury in infants small for gestational age or with bronchopulmonary dysplasia (Pediatr Dev Pathol 2004;7:425)
- Fibrosis progresses with increased length of TPN use
Case reports
- 32 week old male on total parenteral nutrition with concern for biliary atresia (BMC Pediatr 2019;19:72)
- 3 year old boy with hepatic encephalopathy (J Neuroimaging 2013;23:248)
- 38 year old man with total parenteral nutrition related cirrhosis (J Gastrointest Surg 2009;13:1717)
- 49 year old man with abnormal liver function (Nutrition 2000;16:1090)
Treatment
- Severe cases may require intestine / liver transplant (Hepatology 2006;43:9)
Microscopic (histologic) description
- Variable histology, most often including canalicular cholestasis and periportal macrovesicular steatosis; also ductular reaction, ductopenia, perivenular fibrosis, microvesicular steatosis (Hum Pathol 2012;43:826)
- Cholestasis is more common in neonates than older children / adults
- Steatosis is more common in older children / adults than neonates
- Significant fibrosis may be seen if total parenteral nutrition administered for more than 6 weeks (Pediatr Dev Pathol 2004;7:425)
- Lipofuscin-like pigment and hemosiderin can be seen
- Prominent eosinophilia in portal tract extramedullary hematopoiesis can be seen in pediatric patients (Arch Pathol Lab Med 1981;105:152)
- Phospholipidosis may occur (Gastroenterology 1988;95:183)
Microscopic (histologic) images
Sample pathology report
- Liver, biopsy:
- Mild macrovesicular steatosis and focal canalicular cholestasis (see comment)
- Comment: The findings may be secondary to the patient’s reported long term use of total parenteral nutrition. Other possibilities include fatty liver disease (potentially alcoholic).
Differential diagnosis
- Must rule out other potential causes of liver injury, including sepsis and pre-existing liver disease (Arch Surg 1988;123:1084, Orthop Clin North Am 1983;14:413, Gastroenterology 1993;104:286)
- Alcoholic liver disease:
- May show steatohepatitis and cholestasis
- Should be considered in adult patients not on total parenteral nutrition
- Steatosis more likely perivenular, not periportal
- Bile duct obstruction:
- Portal edema rarely caused by total parenteral nutrition
- May require clinical correlation (Histopathology 1982;6:787)
- Extrahepatic biliary atresia:
- Clinical correlation often necessary for distinction
- Neonatal hepatitis:
- Giant cell transformation and inflammatory infiltrate more common
Board review style question #1
- What are the 2 most classic histologic findings in the liver from patients on long term total parenteral nutrition?
- Ballooning and necrosis
- Cholestasis and iron deposition
- Cholestasis and steatosis
- Necrosis and steatosis
Board review style answer #1
Board review style question #2
Board review style answer #2
Mesenchymal hamartoma
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Rare, benign hepatic lesion of young children
- Primitive myxoid mesenchyme with benign dilated or branching bile ducts and clusters of normal appearing hepatocytes
Essential features
- Second most common benign pediatric hepatic tumor after infantile hemangioma (Arch Pathol Lab Med 2006;130:1567)
- 80% are diagnosed in infants and children < 2 years old (Arch Pathol Lab Med 2006;130:1567)
- Excellent prognosis with complete resection; rare malignant transformation to embryonal sarcoma has been described
- Variable proportions of mixed solid and cystic areas with disorganized arrangement of primitive mesenchyme, benign bile ducts and normal appearing hepatocytes (Hepat Oncol 2020;7:HEP19)
- Associated with recurrent genetic alterations resulting in activation of chromosome 19 microRNA cluster (C19MC)
Terminology
- Hepatic or giant lymphangiomas, bile cell fibroadenomas, cavernous lympangiomatoid tumors, hepatic cystic hamartoma (SA J Radiol 2020;24:1891)
ICD coding
- ICD-10: D13.4 - benign neoplasm of liver
Epidemiology
- Second most common benign liver tumor in pediatric population
- Incidence: 0.7 cases per million population per year (J Radiol Case Rep 2013;7:35)
- 80% are diagnosed in patients < 2 years old with a slight male predominance (60 - 70% male) (Arch Pathol Lab Med 2006;130:1567)
- Adults rarely affected, with slight female predominance (Hum Pathol 2002;33:893)
Sites
- Pediatric patients: right liver lobe predilection
- Adults: similar involvement of both liver lobes (Hum Pathol 2002;33:893)
Pathophysiology
- Still debated
- Associated with activation of chromosome 19q13.4 microRNA cluster (C19MC) (Pediatr Dev Pathol 2014;17:75)
Clinical features
- Usually sporadic; associations with Beckwith-Wiedemann syndrome and placental mesenchymal dysplasia have been described (Pediatr Dev Pathol 2014;17:75)
- Typically present as an enlarging abdominal mass
- Small lesions are usually asymptomatic
- Large lesions may be associated with abdominal pain, abdominal distention, vomiting, poor weight gain, respiratory distress, cardiac failure and ascites (J Clin Neonatol 2012;1:211)
- Rarely, may undergo malignant transformation to undifferentiated embryonal sarcoma (Hepat Oncol 2020;7:HEP19)
Diagnosis
- Histologic examination
Laboratory
- AFP usually normal or mildly elevated (SA J Radiol 2020;24:1891)
- Occasionally markedly elevated (J Cytol 2015;32:197)
Radiology description
- Complex cystic mass with internal septations on ultrasound
- Complex cystic mass with septal and solid stromal enhancement on CT or MRI
Case reports
- 5 month old girl with Beckwith-Wiedemann syndrome with diarrhea and abdominal mass (ACG Case Rep J 2015;2:258)
- 15 month old asymptomatic boy with large hepatic mass (Case #61)
- 34 month old girl with abdominal distention, respiratory distress and bowel obstruction (J Surg Case Rep 2018;2018:rjx260)
- 46 year old woman with abdominal pain and distension (Transplant Proc 2022;54:1636)
Treatment
- Complete surgical excision: best treatment
- Unresectable cases may require liver transplantation (Transplant Proc 2022;54:1636)
Gross description
- Usually solitary; rarely with intrahepatic satellite nodules
- Well circumscribed mass with mixed solid and cystic areas
- Cysts contain clear, yellow or gelatinous fluid separated by white, yellow or tan firm tissue (Burt: MacSween's Pathology of the Liver, 7th Edition, 2017)
- Size ranging from a few centimeters to 30 cm
- Usually no necrosis, hemorrhage or calcification
- Becomes fibrotic with age
Gross images
Microscopic (histologic) description
- Variable proportions of solid and cystic components with disorganized arrangements of:
- Primitive mesenchyme, with mixture of bland spindled cells and collagen in a loose, myxoid stroma (Burt: MacSween's Pathology of the Liver, 7th Edition, 2017)
- Epithelial components, including benign dilated or branching bile ducts and normal appearing peripherally located hepatocytes
- Loss of normal lobular architecture; no portal tracts (Burt: MacSween's Pathology of the Liver, 7th Edition, 2017)
- Cystic degeneration is frequently seen, giving rise to lymphangioma-like areas (Burt: MacSween's Pathology of the Liver, 7th Edition, 2017)
- No significant cytologic atypia or increased mitoses (Arch Pathol Lab Med 2006;130:1567)
- May resemble breast fibroadenoma at low power
- Frequent extramedullary hematopoiesis is present (Ishak: Tumors of the Liver and Intrahepatic Bile Ducts, 3rd Series, Volume 31, 2001)
- Tends to have more hyalinized fibrous tissue, fewer ductal structures and show more vascularity in adult patients (J Pediatr Surg 2005;40:1681)
Microscopic (histologic) images
Cytology description
- Clusters of bland cuboidal epithelial cells, spindle stromal cells, hepatocytes, myxoid tissue (Burt: MacSween's Pathology of the Liver, 7th Edition, 2017)
- Limited value
Positive stains
- CK7: biliary epithelium
- Vimentin, smooth muscle actin, desmin, alpha-1 antitrypsin: mesenchymal cells
- Glypican 3: entrapped hepatocytes (44%, canalicular and cytoplasmic staining pattern) and mesenchymal component (22%) (Hum Pathol 2012;43:695)
Electron microscopy description
- Myofibroblastic features
Molecular / cytogenetics description
- Activation of chromosome 19q13.4 microRNA cluster (C19MC), either by rearrangement of 19q13 or androgenetic biparental mosaicism (Pediatr Dev Pathol 2015;18:218, Pediatr Dev Pathol 2014;17:75)
Sample pathology report
- Liver mass, resection specimen:
- Hepatic mesenchymal hamartoma (16 cm) (see comment)
- Comment: The neoplasm consists of scattered dilated and angulated ducts lined by cuboidal epithelium in a background of loose myxoid tissue with scattered bland spindle cells. Small islands of entrapped benign hepatic parenchyma are noted. No necrosis or mitotic figures are identified. The tumor is located 0.5 cm from the nearest surgical resection margin. Hilar structures are free of tumor. The adjacent hepatic parenchyma shows congestion and mild portal fibrosis, portal inflammation and proliferation of bile ductules consistent with adjacent mass effect.
- Liver, needle biopsy specimen:
- Hepatic mesenchymal hamartoma (see comment)
- Comment: Lesion is characterized by loose myxomatous stroma with scattered bland stellate shaped mesenchymal cells, branching bile ducts and scattered hepatocytes. The findings are consistent with hepatic mesenchymal hamartoma.
Differential diagnosis
- Myxomatous infantile hemangioma / hemangioendothelioma:
- Most common hepatic mesenchymal tumor in childhood
- Majority affects infants < 6 months old, with slight female predominance
- Can be well circumscribed or infiltrative (35%)
- Type 1 with proliferation of capillary-like vascular spaces lined by bland endothelial cells with no / rare mitotic figures and no malignant spindle cell component
- Type 2 with irregular branching vascular structures lined by pleomorphic, hyperchromatic endothelial cells with frequent mitotic activity
- Positive for GLUT1, CD31, CD34 and factor VIII related antigen
- Undifferentiated embryonal sarcoma:
- Third most common pediatric hepatic tumor, mainly affecting children 6 - 10 years old
- Anaplastic, bizarre tumor cells with prominent eosinophilic cytoplasm and PAS+ diastase resistant hyaline globules
- Mixed epithelial mesenchymal hepatoblastoma:
- Epithelial component with embryonal and fetal hepatocytes with high N:C ratios and marked cellular atypia
- Mesenchymal component has spindle cells, osteoid, cartilage
Board review style question #1
A 9 month old boy with abdominal distention was found to have a 7.3 x 6.5 x 3.4 cm complex cystic mass in the right liver. Histologic examination of the cyst wall revealed the findings shown above. What is the diagnosis?
- Angiomyolipoma
- Bile duct hamartoma
- Hepatic mesenchymal hamartoma
- Myxomatous infantile hemangioma / hemangioendothelioma
- Undifferentiated embryonal sarcoma
Board review style answer #1
Board review style question #2
Which of the following statements regarding hepatic mesenchymal hamartoma is true?
- Associated with recurrent genetic alteration resulting in activation of chromosome 19 microRNA cluster (C19MC)
- Has variable proportions of cystic and solid components and is commonly associated with necrosis with frequent mitotic figures and cytological atypia
- It is the second most common benign hepatic tumor, mainly affecting adults between 20 - 50 years old
- Positive for GLUT1 in the epithelial components
- Radiation therapy is the best treatment method
Board review style answer #2
A. Associated with recurrent genetic alteration resulting in activation of chromosome 19 microRNA cluster (C19MC)
Comment Here
Reference: Mesenchymal hamartoma
Comment Here
Reference: Mesenchymal hamartoma
Metastases
Table of Contents
Definition / general | Case reports | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stainsDefinition / general
- In U.S., only 2% of hepatic malignancies in noncirrhotic liver are hepatic primaries (i.e. 98% are metastases) vs. 77% are hepatic primaries in cirrhotic liver
- Direct extension is common from tumors of extrahepatic bile ducts, gallbladder, pancreas and stomach
- Metastases in adults often from breast, colon, lung, pancreas; in children from neuroblastoma, rhabdomyosarcoma, Wilms tumor
- Unknown primary is often determined to be from lung, pancreas, stomach
- Metastatic nodules tend to outgrow their blood supply and produce central necrosis and umbilication
- Symptoms often of abdominal pain, ascites and jaundice; portal hypertension less common
- Survival usually less than 1 year, longer if primary is neuroendocrine carcinoma or neuroblastoma; also some cases of colon carcinoma with resection of hepatic metastases
- Should compare metastatic tumor to prior malignancies
- Metastatic carcinomatous cirrhosis: metastatic carcinoma to liver, often from breast, that incites an extensive fibrotic reaction simulating cirrhosis
- Breast carcinoma metastatic to liver:
- Posttreatment metastases produce coarsely lobulated appearance known as hepar lobatum, associated with syphilis
- Estrogen receptor 35% sensitive and highly specific; progesterone receptor neither sensitive nor specific (Arch Pathol Lab Med 2003;127:1591)
- Mammoglobin+ and GCDFP15+
- Colon carcinoma metastatic to liver: resection of metastases may improve long term survival
- Hepatoid adenocarcinoma metastatic to liver: may arise in lung or stomach
Case reports
- 38 year old woman with infiltrating ductal carcinoma of breast with associated florid fibrosis (Arch Pathol Lab Med 2001;125:1084)
- 60 year old woman with female adnexal tumor of probable Wolffian origin metastatic to liver (Arch Pathol Lab Med 2000;124:431)
- 62 year old man with rectal polyp with bone and liver metastases (Am J Surg Pathol 1999;23:838)
- 76 year old man with primary tumor in large intestine (Arch Pathol Lab Med 2001;125:1251)
Gross description
- 90% are multiple, variable size, may replace entire liver and locally elevate the capsule or not be visible on external surface
- Often hemorrhage and necrosis; extensive hemorrhage suggests choriocarcinoma, angiosarcoma or thyroid carcinoma
- Cannot determine malignancy based on gross appearance only
- Colon carcinoma metastatic to liver: large umbilicated nodules with extensive necrosis and fibrosis, variable calcification
- Squamous cell carcinoma metastatic to liver: soft nodules due to necrosis and keratinization
Microscopic (histologic) description
- Sinusoidal dilation, cholestasis, portal lymphocytic infiltrate or tumor
- Colon carcinoma metastatic to liver: tubular, papillary or cribriform patterns of columnar cells with basophilic cytoplasm and elongated nuclei, extensive necrosis
- Gastrointestinal stromal tumor (GIST) metastatic to liver: polygonal, spindle to epithelioid cells
- Melanoma metastatic to liver: may replace hepatic cords and grow in trabecular pattern with endothelial lining
- Pancreaticobiliary metastases to liver: atypical angulated glands with desmoplasia
Microscopic (histologic) images
Contributed by Raul S. Gonzalez, M.D. and Semir Vranic, M.D., Ph.D.
Contributed by @liverwei on Twitter
Images hosted on other servers:
Positive stains
Negative stains
- Gastrointestinal stromal tumor (GIST) metastatic to liver: HepPar1, glypican 3
- Hepatoid adenocarcinoma metastatic to liver: CK7, HepPar1, glypican 3
Methotrexate
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Methotrexate in liver can cause reactive changes, steatosis or fibrosis and rarely lymphoma
- Duration and dosage of methotrexate impact the risk of liver damage
- Methotrexate is an immunosuppressant medication, mainly used for treatment of cancer and autoimmune diseases
Essential features
- Methotrexate is an antimetabolite and antifolate
- Mild elevation in liver enzymes, fibrosis and cirrhosis may be observed due to extended usage of methotrexate
- Roenigk classification is used to grade liver biopsies
Terminology
- Methotrexate induced liver fibrosis
ICD coding
- ICD-10: K71.9 - Toxic liver disease, unspecified
Epidemiology
- Methotrexate is the first line therapy for treatment of rheumatoid arthritis worldwide
- Incidence rate of liver enzymes elevation in patients with low dose methotrexate therapy is 13 per 100 patient years
- 20% of patients with low dose methotrexate therapy have elevation in liver enzymes during average of 4.6 years of therapy (PLoS One 2018;13:e0203084)
Sites
- Liver
Pathophysiology
- Methotrexate is an antimetabolite and antifolate (World J Hepatol 2017;9:1092)
- Prevents synthesis of tetrahydrofolate in cells by inhibiting dihydrofolate reductase enzyme
- Presence of folic acid is essential for synthesis of nucleosides
- Therefore, methotrexate hinders synthesis of DNA and RNA, resulting in cell cycle arrest in liver
- Methotrexate inhibits an enzyme causing an increase in extracellular adenosine, which promotes liver fibrosis (Psoriasis (Auckl) 2018;8:21)
- In rheumatoid arthritis, methotrexate causes adenosine accumulation by changing purine metabolism (Joint Bone Spine 2019;86:301)
Clinical features
- Clinically, patients may be asymptomatic or present with jaundice, hepatomegaly or constitutional symptoms including weight change and fever
- Symptoms may present after months to years of using methotrexate
- Elevation in liver enzymes may occur due to high dosage of intravenous methotrexate
- Mild elevation in liver enzymes, fibrosis and cirrhosis may be observed due to extended usage of methotrexate (LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Accessed 8 December 2020])
Diagnosis
- Clinical and pathological association is required for diagnosis of liver injuries caused by toxin or drug (LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Accessed 8 December 2020])
Laboratory
- Normal or elevated aspartate aminotransferase (AST) and alanine aminotransferase (ALT) in patients with methotrexate therapy
Radiology description
- Imaging usually reveals a diffuse hepatic steatosis (Br J Radiol 2018;91:20170959)
Prognostic factors
- Risk of liver damage is associated with the dosage and duration of methotrexate therapy
- Risk of liver damage is intensified by obesity or alcohol usage
- Roenigk classification is used to grade liver biopsies (World J Hepatol 2017;9:1092)
- Patients are advised to stop the medication if their liver shows Roenigk stage IIIB (advanced fibrosis) or Roenigk stage IV (cirrhosis) disease; for Roenigk stage IIIA, repeat of biopsy is advised in 6 months (PLoS One 2018;13:e0203084)
Case reports
- 56 year old woman with rheumatoid arthritis and methotrexate treatment developed primary hepatic lymphoma (Intern Med 2015;54:401)
- 64 year old man with rheumatoid arthritis and methotrexate treatment developed primary hepatic lymphoma (Biomark Res 2015;3:10)
- 82 year old man with rheumatoid arthritis and methotrexate treatment developed lymphoproliferative disorders in liver, spleen and lung (J Med Case Rep 2019;13:196)
- 88 year old woman with rheumatoid arthritis under methotrexate therapy for 6 years developed hepatosplenic Hodgkin lymphoma after methotrexate withdrawal (Mod Rheumatol 2017;27:372)
Treatment
- Folic acid supplement of 1 mg per day lowers the risk of liver enzymes abnormality, mouth ulcers and gastrointestinal issues such as nausea and vomiting
- Periodic monitoring of liver enzymes levels is recommended
- Liver biopsy is suggested for monitoring after 1, 3 and 8 grams cumulative methotrexate (PLoS One 2018;13:e0203084)
- Other disease modifying antirheumatic drugs (DMARDs), such as hydroxychloroquine or etanercept, do not show concurrent adverse effect on liver with methotrexate (LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Accessed 8 December 2020])
Microscopic (histologic) description
- Mainly macrovesicular steatosis but sometimes microvesicular
- Reactive changes, such as hyperchromasia and anisocytosis of hepatocyte nuclei or patchy hepatocyte necrosis
- Portal inflammation
- Periportal fibrosis to central bridging or pericellular fibrosis
- Roenigk classification has 4 grades: grade I (normal to mild fatty changes), grade II (moderate to severe fatty changes), grade IIIA - B (mild to severe periportal fibrosis) and grade IV (cirrhosis) (Arch Dermatol 2007;143:1515)
- Rarely, lymphoproliferative disorders such as primary hepatic lymphoma has been reported after using methotrexate in autoimmune disease patients (Biomark Res 2015;3:10)
Microscopic (histologic) images
Positive stains
- Trichrome stain shows an increase in portal, periportal or bridging fibrosis in methotrexate toxicity
Sample pathology report
- Liver, biopsy:
- Macrovesicular steatosis with periportal and bridging fibrosis (see comment)
- Comment: Macrovesicular steatosis involves approximately 50% of the hepatocytes. A trichrome stain demonstrates periportal and bridging fibrosis. The differential diagnosis includes alcoholic hepatitis, nonalcoholic steatohepatitis or drug induced liver injury (the patient's history of methotrexate use is noted).
Differential diagnosis
- Alcoholic hepatitis:
- History of alcohol use is present
- Often more prominent ballooning degeneration and Mallory hyaline
- Nonalcoholic steatohepatitis:
- Metabolic syndrome is usually a risk factor
- Histologic appearance is generally similar
- Liver injury caused by other drugs:
- Amiodarone can cause steatosis with prominent Mallory hyaline
- Clinical correlation necessary
Board review style question #1
Methotrexate injury in the liver is graded using the Roenigk classification. Which of the following grades indicates methotrexate use should be stopped?
- Stage I
- Stage II
- Stage IIIA
- Stage IIIB
Board review style answer #1
Board review style question #2
Board review style answer #2
Mucinous cystic neoplasm
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Cystic hepatic neoplasm with ovarian type stroma and mucinous epithelium that does not communicate with bile ducts
Essential features
- Multiloculated cystic neoplasm lined by biliary type or mucinous epithelial cells overlying ovarian type stroma
- Usually benign (90%) but may be associated with invasive carcinoma (Mod Pathol 2011;24:1079)
- Complete surgical excision with extensive sampling for histology is required to reduce risk of recurrence and determine if associated invasive carcinoma is present
Terminology
- Hepatobiliary cystadenoma
- Hepatobiliary cystadenocarcinoma (if associated invasive carcinoma)
- Biliary cystadenoma
- Cystadenoma with mesenchymal stroma
ICD coding
- ICD-O:
- ICD-11:
- 2E92.6 - benign neoplasm of gallbladder, extrahepatic bile ducts or ampulla of Vater
- XH6NK7 - mucinous cystic neoplasm with low grade intraepithelial neoplasia
- 2E61.Y - carcinoma in situ of other specified digestive organs
- XH81P3 - mucinous cystic tumor with high grade dysplasia
- 2C15.1 - mucinous cystic neoplasm with associated invasive carcinoma of distal bile duct
- 2C18.1 - mucinous cystic neoplasm with associated invasive carcinoma of perihilar bile duct
- 2C17.1 - mucinous cystic neoplasm with associated invasive carcinoma of other or unspecified parts of biliary tract
Epidemiology
- F > M
- Mean age: 45 years (noninvasive) to 59 years (with invasive component) (Am J Surg Pathol 1994;18:1078)
Sites
- Liver parenchyma
- May rarely involve extrahepatic bile ducts or gallbladder
Pathophysiology
- Ovarian type stroma may originate from developing gonads due to their close proximity to the liver during embryologic development (Dig Surg 2010;27:19)
Etiology
- Unknown at this time
Clinical features
- Typically present with abdominal pain and swelling
- May have symptoms of biliary obstruction (jaundice)
Diagnosis
- Fine needle aspiration and imaging studies cannot reliably distinguish mucinous cystic neoplasms (MCN) from other types of liver cysts
- Definitive diagnosis requires histopathologic confirmation of the ovarian type stroma, usually after surgical excision (Am J Surg Pathol 2018;42:95)
Laboratory
- Serum CA19-9 may be elevated, especially if invasive carcinoma is present
Radiology description
- Large, multilocular cyst with internal septations (World J Gastroenterol 2006;12:6062)
- May show calcifications, mural nodules or papillary projections
- Distinction of benign from malignant is usually not possible on imaging studies (Am J Surg Pathol 2018;42:95)
Radiology images
Prognostic factors
- Complete surgical excision confers a favorable prognosis
- Prognostic significance of invasive component is difficult to determine, as many reported cases with invasive carcinoma lack ovarian type stroma, occur in men and thus may represent intraductal papillary neoplasm rather than mucinous cystic neoplasm (Am J Surg Pathol 1994;18:1078)
Case reports
- 33 year old woman with a rapid progression of a cystic tumor of the liver (Ann Hepatol 2018;17:519)
- 37 year old Tunisian woman who presented with subacute right upper quadrant pain (BMC Gastroenterol 2019;19:103)
- 39 year old woman with complaints of vague abdominal pain and increasing abdominal girth (World J Gastroenterol 2006;12:6062)
- 43 year old woman with an unremarkable previous medical history presented with progressive obstructive jaundice (World J Gastroenterol 2006;12:5735)
- 56 year old woman with a growing solitary unilocular hepatic cyst (Acta Cytol 1993;37:966)
- 60 year old asymptomatic woman with history of echinococcal cyst in the liver (J Surg Case Rep 2012;2012:5)
Treatment
- Complete surgical excision
- Incomplete excision is associated with local recurrence and risk of malignant transformation (World J Surg 2006;30:1560)
Gross description
- Cystic with multiple communicating lobules of varying sizes and a smooth and glistening lining (J Surg Case Rep 2012;2012:5)
- Cystic fluid is usually clear and thin
- Sampling should focus on areas of wall thickening / nodules, potentially submitting the entire lesion
Gross images
Microscopic (histologic) description
- Multiloculated cysts lined by columnar, cuboidal or flattened biliary type, or mucinous epithelial cells overlying ovarian type stroma (Am J Surg Pathol 2018;42:95)
- Ovarian type stroma consists of densely packed, spindle shaped to oval cells that may be focally luteinized
- Should be sampled extensively to rule out high grade dysplasia (frequent mitotic figures, nuclear pleomorphism, complex tubulopapillary projections, etc.) and invasive carcinoma (usually ductal adenocarcinoma)
- Epithelium of larger lesions can become traumatized, showing ulceration, inflammation with xanthogranulomatous reaction, extravasation of cyst fluid into the wall / stroma or scarring and calcifications
Microscopic (histologic) images
Cytology description
- Few groups of bland, degenerated, columnar or cuboidal epithelial cells (Cancer 2002;96:37)
- Inflammatory background (neutrophils, lymphocytes, macrophages) (Cancer 2002;96:37)
- Stromal components (including ovarian type stroma) are usually absent
- Cyst fluid can be assayed for carcinoembryonic antigen and CA19-9 to help distinguish mucinous neoplasms from nonneoplastic lesions
Cytology images
Positive stains
- Ovarian stroma: ER, PR and inhibin A (Hum Pathol 2014;45:761)
- Epithelium: CK7, CK19, CK8 and CK18 (biliary type) or mucicarmine (mucinous areas)
Sample pathology report
- Liver, left lobe, lobectomy:
- Mucinous cystic neoplasm
- No high grade dysplasia or invasive carcinoma present
Differential diagnosis
- Endometriosis (Hum Pathol 2014;45:761):
- Also may have cystically dilated spaces lined by columnar to cuboidal epithelium and surrounded by spindled cellular stroma
- ER+ in both epithelium and stroma, whereas MCNs are ER+ only in stroma
- Typically has stromal iron laden macrophages and CD10 positivity, whereas the stroma in MCNs is CD10-, inhibin+ and often more cellular
- Intraductal papillary neoplasm (IPN):
- Has dilated bile ducts that may resemble cystic space(s) of MCN
- May be lined by biliary type epithelium, like MCN
- Typically communicates with bile duct, unlike MCN
- Lacks ovarian type stroma
- Simple cyst, simple hepatic cyst, simple biliary cyst, bile duct cyst:
- Lined by biliary type epithelium, like MCN
- Lacks ovarian type stroma
Additional references
Board review style question #1
Board review style answer #1
D. There is a strong female predominance (this is a mucinous cystic neoplasm)
Comment Here
Reference: Mucinous cystic neoplasm
Comment Here
Reference: Mucinous cystic neoplasm
Board review style question #2
Which of the following describes the conditions under which mucinous cystic neoplasms of the liver most often occur?
- After the sixth decade of life without sex predominance
- In association with invasive carcinoma
- In males before the third decade of life
- Multifocally and associated with bile ducts
- With abdominal pain as the most common presenting symptom
Board review style answer #2
E. With abdominal pain as the most common presenting symptom
Comment Here
Reference: Mucinous cystic neoplasm
Comment Here
Reference: Mucinous cystic neoplasm
Navajo hepatopathy
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- A rare hepatocerebral mitochondrial DNA (mtDNA) depletion syndrome (MDS) with nonspecific clinical and pathologic features aside from Navajo ancestry (Acta Gastroenterol Belg 2016;79:463)
Essential features
- mtDNA depletion syndrome caused by MPV17 missense mutation (Am J Hum Genet 2006;79:544)
- Nonspecific cirrhotic findings in a patient with Navajo ancestry
- Megamitochondria within hepatocytes
- Mixed macrovesicular and microvesicular steatosis
Terminology
- Navajo neurohepatopathy
- MPV17 related hepatocerebral mitochondrial DNA depletion syndrome
ICD coding
- ICD-10: K74.60 - liver cirrhosis NOS
Epidemiology
- 1 in 1,600 live births of Navajo persons; Southwestern United States predominance (Am J Hum Genet 2006;79:544)
- Presents in infancy / early childhood (Am J Hum Genet 2006;79:544)
- M:F ratio of 1.1:1 (Hum Mutat 2018;39:461)
- There are other MPV17 missense mutations reported, causing similar mtDNA depletion syndrome (Am J Hum Genet 2006;79:544); see Molecular / cytogenetics description section for more details
Sites
- Affects sites that need abundant source of adenosine triphosphate (ATP):
- Liver (Acta Gastroenterol Belg 2016;79:463)
- Cardiac and skeletal muscle (Acta Gastroenterol Belg 2016;79:463)
- Nerves
- ATP is needed for maintenance of myelin
- Lack of ATP leads to degradation of myelin by reactive oxygen species and eventual axonal injury (Acta Neuropathol Commun 2019;7:86)
Pathophysiology
- Autosomal recessive inheritance pattern (Am J Hum Genet 2006;79:544)
- MPV17 encodes channel forming protein of inner mitochondrial membrane and is thought to be involved in deoxynucleotide homeostasis (Am J Hum Genet 2006;79:544)
- Exact pathophysiology is still unclear (Am J Hum Genet 2006;79:544)
- The mutation results in:
- Depletion of mtDNA
- Quantitative decreased synthesis of respiratory chain complexes I, III and IV (Hepatology 2001;34:776)
- Decreased ATP synthesis from electron transport chain (Hepatology 2001;34:776)
- Deformation of mitochondrial cristae (folds within inner membrane to increase surface area for electron transport chain to occur) (Hepatology 2001;34:776)
- Creating megamitochondria
- Decreased ATP causes cascade of effects:
- Increased reliance on glycolysis for ATP production, leading to hypoglycemia and increased lactate production
- Compensatory decrease in CO2
- Affects sites most reliant on ATP; see Sites for more details
- Depletion of mtDNA
Etiology
- Autosomal recessive germline MPV17 missense mutation (Am J Hum Genet 2006;79:544)
- See Molecular / cytogenetics description section for more details
Clinical features
- General features:
- Failure to thrive, with hypoglycemic incidents (J Pediatr 1999;135:482)
- Non anion gap metabolic acidosis (Acta Gastroenterol Belg 2016;79:463)
- Nonspecific elevated liver enzymes, though aspartate transaminase (AST) > alanine aminotransferase (ALT), as in other forms of hepatocyte mitochondrial injury (Acta Gastroenterol Belg 2016;79:463)
- Jaundice and ascites with eventual progression to cirrhosis and liver failure (J Pediatr 1999;135:482)
- Neurologic degradation of myelin and eventually axonal injury (J Pediatr 1999;135:482)
- Muscle weakness due to neuronal degradation and lack of adenosine triphosphate production
- Hepatocerebral presentation is associated with R50Q mutation; see Molecular / cytogenetics description section for more details (Neurotherapeutics 2013;10:186)
- 3 different presentation phenotypes:
- Infantile: presents before 6 months of age with jaundice, failure to thrive and death by 2 years of age (Am J Hum Genet 2006;79:544)
- Childhood: presents between 1 - 5 years old with liver failure and death within 6 months (Am J Hum Genet 2006;79:544)
- Classical: variable onset age of liver disease but with progressive neurological deterioration (Am J Hum Genet 2006;79:544)
- All 3 have peripheral and CNS demyelination
Diagnosis
- Screening: flash frozen tissue sent for quantitative mtDNA analysis
- Liver or muscle biopsy can be used; liver is preferred (Acta Gastroenterol Belg 2016;79:463)
- Flash frozen to -80°C with liquid nitrogen (Acta Gastroenterol Belg 2016;79:463)
- Decreased quantitative mtDNA is a positive screen (< 20% of age matched controls) (Acta Gastroenterol Belg 2016;79:463)
- Diagnosis: whole blood genetic sequencing to show MPV17 homozygous R50Q missense mutation (Am J Hum Genet 2006;79:544)
Laboratory
- Hypoglycemia (Acta Gastroenterol Belg 2016;79:463)
- Elevated lactate (Acta Gastroenterol Belg 2016;79:463)
- Non anion gap metabolic acidosis
- Decreased carbon dioxide (Acta Gastroenterol Belg 2016;79:463)
- Nonspecific findings:
- Elevated liver enzymes: alkaline phosphatase, AST, ALT and gamma glutamyl transferase (GGT)
- AST elevated more than ALT
- AST is a cytoplasmic and mitochondrial enzyme while ALT is cytoplasmic only (Acta Gastroenterol Belg 2016;79:463)
- Prolonged PT / INR and partial thromboplastin time (PTT) (Acta Gastroenterol Belg 2016;79:463)
- Hypofibrinogenemia (Acta Gastroenterol Belg 2016;79:463)
- Hypoalbuminemia (Acta Gastroenterol Belg 2016;79:463)
Radiology description
- Liver ultrasound: nodular and echogenic liver consistent with cirrhosis (Acta Gastroenterol Belg 2016;79:463)
Prognostic factors
- Overall poor prognosis (Acta Gastroenterol Belg 2016;79:463)
- Mortality rates (Hum Mutat 2018;39:461):
- 66% die during infancy
- 13% die in early childhood (1 - 5 years old)
- 2% die in adolescence
- 1% die in early adulthood
- 18% reported alive in 2018 across all age groups
- Oldest reported case at 25 years old
Case reports
- 3 year old boy with nonpainful abdominal swelling (Acta Gastroenterol Belg 2016;79:463)
- 3 children with hepatocerebral mtDNA depletion syndrome (BMC Med Genet 2019;20:167)
- 4 Navajo children with mutilating neuropathy with severe motor involvement (Arch Neurol 1976;33:733)
- 5 families with MPV17 mutations (Am J Hum Genet 2006;79:544)
- 6 children with liver dysfunction (J Pediatr 1999;135:482)
Treatment
- No curative treatment
- Liver transplant
- Roughly 20% of affected children have a liver transplant; this is controversial and considered palliative (Acta Gastroenterol Belg 2016;79:463)
- Transplant can alleviate hepatic dysfunction in the short term; patient will still progress to neurologic dysfunction (Acta Gastroenterol Belg 2016;79:463)
- Roughly 60% of transplanted individuals die during posttransplant period secondary to sepsis, respiratory failure or multi organ failure (Hum Mutat 2018;39:461)
- Nutritional modulation and cofactor supplementation may be beneficial (Neurotherapeutics 2013;10:186)
- Selenium may be beneficial (eNeurologicalSci 2016;2:8)
- Formulas enriched with medium chain triglycerides, uncooked corn starch and frequent feedings are required to prevent hypoglycemia (Hum Mutat 2018;39:461)
- Nucleoside supplementation has been a suggested potential therapy (Hum Mutat 2018;39:461)
Microscopic (histologic) description
- The following features are characteristic but not pathognomonic:
- Mixed macrovesicular and microvesicular steatosis with hepatocanalicular cholestasis (J Pediatr 1999;135:482)
- Ballooning hepatocellular degeneration indistinguishable from typical steatohepatitis
- Red granular hepatocytes containing abnormal megamitochondria (Acta Gastroenterol Belg 2016;79:463)
- Scattered acidophil bodies (Acta Gastroenterol Belg 2016;79:463)
- Bridging fibrosis and cirrhosis with nonspecific portal / septal ductular reaction (J Pediatr 1999;135:482)
- Juxtaposed cirrhotic nodules appear fatty and oncocytic due to variable accumulations of fat and megamitochondria
Microscopic (histologic) images
Positive stains
- Trichrome: effaced nodular architecture with dense bands of bridging fibrosis (Acta Gastroenterol Belg 2016;79:463)
- Copper IHC: positive staining in cirrhotic nodules (nonspecific finding in cirrhosis), so do not use as a positive finding to suggest Wilson disease (Acta Gastroenterol Belg 2016;79:463)
Negative stains
- Iron stain (Acta Gastroenterol Belg 2016;79:463)
- PASD may stain few scattered small intracytoplasmic granules but not the large globules seen in alpha-1 antitrypsin deficiency (Acta Gastroenterol Belg 2016;79:463)
Electron microscopy description
- Enlarged pleomorphic mitochondria with dilated cristae
- Lack of dense mitochondrial matrix granules
- Numerous minute lipid droplets within hepatocytes (Hepatology 2007;46:1218)
Molecular / cytogenetics description
- Autosomal recessive germline MPV17 missense mutation; gene is located on short arm of chromosome 2 (2p23.3)
- Homozygous R50Q: glutamine (Q) replaces arginine (R) at position 50 on both alleles (Am J Hum Genet 2006;79:544)
- Diagnosis is done by sequencing
- There are 22 other reported missense mutations of MPV17 protein that cause similar pathology, i.e. R50W, P64R, etc. (Hum Mutat 2018;39:461)
- However, Navajo ancestry has exclusively been reported with the R50Q mutation (Am J Hum Genet 2006;79:544)
- R50Q mutation has also been reported in patients of Italian, Moroccan and other Arabic ancestries (Am J Hum Genet 2006;79:544)
- Other mutations that cause mtDNA depletion syndrome:
- Mutations in mitochondrial nucleotide synthesis genes includingTK2, SUCLA2, SUCLG1, RRM2B, DGUOK and TYMP (Neurotherapeutics 2013;10:186)
- Mutations in mtDNA replication genes including POLG and C10orf2 (Neurotherapeutics 2013;10:186)
Sample pathology report
- Liver, biopsy:
- Cirrhotic liver with steatohepatitis, hepatocanalicular cholestasis and intracytoplasmic megamitochondria (see comment)
- Comment: A trichrome stain demonstrates an effaced nodular architecture with dense bands of bridging fibrosis (cirrhosis). There is mild portal / septal chronic inflammation consisting predominantly of lymphocytes with rare plasma cells. The inflammation is confined to the fibrous areas and the native bile ducts are not preferentially involved. There is no evidence of ductopenia. There is mixed macrovesicular and microvesicular steatosis with areas of ballooning hepatocellular degeneration indicative of steatohepatitis. There is canalicular and hepatocellular cholestasis. Acidophil bodies are seen and many hepatocytes contain course pink granules, consistent with megamitochondria. These findings in a pediatric patient with cirrhosis and Navajo ancestry would be compatible with Navajo neurohepatopathy in the proper clinical setting. This diagnosis would, however, need to be supported by additional testing (quantitative mtDNA analysis on fresh frozen tissue or genetic testing).
Differential diagnosis
- Other metabolic liver disease such as tyrosinemia, glycogen storage disease, fatty acid oxidation defects and urea cycle disorders:
- Often identified on newborn screen
- Wilson disease:
- Usually presents at an older age
- Hepatic quantitative copper in Wilson disease is much higher compared to the mildly elevated levels seen in Navajo neurohepatopathy
- Drug / toxin mediated injury, especially Reye syndrome and valproate toxicity:
- Both cause mitochondrial dysfunction and subsequent microvesicular steatosis
- Clinical evaluation for offending drugs is indicated
Board review style question #1
Board review style answer #1
Board review style question #2
- Which of the following ancillary studies supports a diagnosis of Wilson disease as opposed to Navajo hepatopathy?
- Markedly elevated liver copper concentration
- Positive copper immunohistochemistry
- Positive MPV17 germline testing
- Reduced hepatic mtDNA content
Board review style answer #2
Neonatal hepatitis
Table of Contents
Definition / general | Terminology | Epidemiology | Etiology | Clinical features | Diagnosis | Case reports | Microscopic (histologic) description | Microscopic (histologic) images | Negative stains | Differential diagnosisDefinition / general
- Neonatal cholestasis is prolonged jaundice beyond 2 weeks of age; it can be simply classified into extrahepatic and intrahepatic causes (Clin Res Hepatol Gastroenterol 2014;38:263)
- Extrahepatic biliary atresia is the most common cause of extrahepatic cholestasis
- Neonatal hepatitis is a nonspecific collective term for intrahepatic cholestasis due to all various etiologies
Terminology
- Also known as neonatal giant cell hepatitis because of frequent syncytial giant cell formation
Epidemiology
- Neonatal cholestasis happens in about 1 in 2,500 - 5,000 term infants (Clin Res Hepatol Gastroenterol 2014;38:263)
Etiology
- Intrahepatic neonatal cholestasis accounts for 60 - 70% of all neonatal cholestasis
- Usual causes include (Front Pediatr 2015;3:43):
- 9 - 17%: metabolic disorders - alpha-1-antrypsin deficiency, cystic fibrosis and hypopituitarism are common (Am J Surg Pathol 2010;34:1498)
- 10%: progressive familial intrahepatic cholestasis (PFIC) (J Clin Exp Hepatol 2014;4:25)
- 10%: preterm (increased incidence of 100 - 200x in infants born before 28 weeks of gestation compared to term infants)
- 1 - 9%: congenital / neonatal infection - cytomegalovirus, enterovirus, hepatitis B, herpes simplex, human herpesvirus 6, rubella, sepsis, syphilis, toxoplasmosis, varicella
- 2 - 6%: Alagille syndrome
- 2%: chromosomal abnormalities - trisomy 18 and Down syndrome (incidence 100x normal term infants)
- 13 - 30%: idiopathic neonatal hepatitis
Clinical features
- Prolonged jaundice beyond 2 weeks of age
- Other clinical features depend on underlying etiology
Diagnosis
- Based on clinical, laboratory, radiological and histological features
Case reports
- Newborn boy with idiopathic neonatal giant cell hepatitis presenting with acute hepatic failure (J Perinatol 2002;22:249)
- 7 week old girl with fatal spontaneous subdural bleeding due to neonatal giant cell hepatitis (Forensic Sci Med Pathol 2011;7:294)
Microscopic (histologic) description
- General nonspecific changes:
- Lobular changes: giant cell transformation (hepatocytes containing 4 - 10 nuclei), variable lobular inflammatory infiltrate and necrosis (spotty, confluent to bridging), canalicular ± hepatocellular bilirubinostasis, extramedullary hematopoiesis
- Portal tract changes: variable portal mononuclear inflammatory infiltrate
- Specific changes depend on underlying etiology
Negative stains
Differential diagnosis
- Extrahepatic biliary atresia:
- Diagnostic accuracy of different methods distinguishing extrahepatic biliary atresia from idiopathic neonatal hepatitis: liver biopsy (97.1%), magnetic resonance cholangiography (MRCP; 70.0%), hepatobiliary scintigraphy (66.7%), ultrasound (65.2%) (Clin Imaging 2009;33:439)
- Ductular reaction and portal fibrosis are essential discriminatory histological features suggestive of extrahepatic biliary atresia (Eur J Gastroenterol Hepatol 2014;26:1300)
- Presence of CD56 / NCAM+ bile duct and ductules favor extrahepatic biliary atresia (Am J Surg Pathol 2003;27:1454)
Neuroendocrine carcinoma
Table of Contents
Definition / general | Case reports | Gross description | Microscopic (histologic) description | Positive stains | Electron microscopy description | Differential diagnosisDefinition / general
- < 100 cases reported; mean age > 40 years, more common in women (Arch Pathol Lab Med 2003;127:1200)
- Normal serum AFP but high serum NSE, chromogranin and synaptophysin levels
- Not associated with chronic liver disease / cirrhosis
- Presents with diarrhea and abdominal pain
- Amphicrine carcinoma: glandular (signet ring morphology, mucicarmine, PASD+, villin+, CDX2+) and neuroendocrine differentiation in same cells (Ann Diagn Pathol 2011;15:355)
Case reports
- 50 year old man with collision tumor of HCC and high grade neuroendocrine carcinoma (Virchows Arch 2006;449:376)
Gross description
- Typically solitary, may be cystic
Microscopic (histologic) description
- Resembles poorly differentiated carcinomas with cellular pleomorphism, nuclear atypia, hyperchromasia and frequent mitotic figures
- May have signet ring morphology with intracytoplasmic vacuoles negative for mucin but positive for neuroendocrine markers (Semin Liver Dis 2010;30:422)
Positive stains
Electron microscopy description
- Dense core granules
Differential diagnosis
- Carcinoid tumor:
- Low (< 2/10 HPF) mitotic activity, minimal nuclear polymorphism
Niemann-Pick disease
Table of Contents
Definition / general | Microscopic (histologic) description | Microscopic (histologic) images | Electron microscopy description | Additional referencesDefinition / general
- Autosomal recessive lysosomal storage disease clinically characterized by neurodegeneration and liver disease (Wikipedia: Niemann-Pick Disease [Accessed 29 January 2024])
- Mutations in the NPC1 and NPC2 genes cause impaired egress of free cholesterol from lysosomes, leading to accumulation of cholesterol and glycosphingolipids
Microscopic (histologic) description
- Foamy Kupffer cells and hepatocytes
Electron microscopy description
- Intralysosomal myelin-like inclusions
Additional references
Nodular regenerative hyperplasia
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Nodular regenerative hyperplasia (NRH) is a nonspecific pattern of liver injury that causes formation of liver nodules separated by regions of atrophy in the absence of fibrous septa
- It is a cause of idiopathic noncirrhotic portal hypertension and can mimic cirrhosis both clinically and radiologically
Essential features
- Diffuse transformation of hepatic parenchyma into regenerative, small (1 - 3 mm) nodules with no advanced fibrosis
- Associated with a variety of underlying hematologic, rheumatic and vascular disorders, as well as use of antineoplastic and immunosuppressive drugs
- Nodules are ill defined and separated by regions of atrophy (best seen on reticulin stain)
- Can lead to portal hypertension if underlying cause is not treated
- NRH and hepatoportal sclerosis / obliterative portal venopathy may coexist (Semin Diagn Pathol 2019;36:395)
Terminology
- Nodular regenerative hyperplasia
ICD coding
Epidemiology
- More prevalent in the elderly population but can be seen in children
- Associated with a variety of vascular diseases, rheumatologic diseases, hematological diseases and use of antineoplastic and immunosuppressive drugs
- Oftentimes an incidental finding on autopsies
- A cohort study of 2,500 autopsies in Canada by Dr. Ian Wanless in 1990 showed NRH present in 64 patients (2.6%) (J Investig Med High Impact Case Rep 2021;9:23247096211044617)
Sites
- Liver
Pathophysiology
- Obliteration of small portal vein radicles causes changes in hepatic blood flow
- Obliterative changes lead to decreased blood flow and atrophy and secondary nodular hyperplasia in areas with increased blood flow
- Above changes can lead to noncirrhotic portal hypertension
- Reference: Lamps: Diagnostic Pathology - Hepatobiliary & Pancreas, 1st Edition, 2011
Etiology
- There is no specific cause of the lesion, however, there are many clinical settings in which NRH can occur, including
- Vascular: portal vein agenesis, cardiac abnormalities, congestive heart failure, portal vein thrombosis, Budd-Chiari syndrome
- Autoimmune: inflammatory bowel disease, myasthenia gravis, celiac disease, primary biliary cirrhosis, scleroderma, sarcoidosis, rheumatoid arthritis, systemic lupus erythematous, polyarteritis nodosa, Beçhet disease
- Malignancy: metastatic breast cancer via portal vein metastasis, carcinoid syndrome, lymphoproliferative and myeloproliferative disorders, Castleman disease
- Other: common variable immunodeficiency, sickle cell anemia, tuberculosis
- Poisoning: arsenic, toxic oil syndrome
- Immunosuppressive agents: azathioprine, mercaptopurine, thioguanine
- Antiretroviral agents: didanosine, stavudine
- Antineoplastic agents: oxaliplatin, isoplatin, busulfan, cytosine arabinoside, chlorambucil, cyclophosphamide, bleomycin, carmustine, doxorubicin, phenytoin, gold and penicillamine
- Other agents: interleukin 2 therapy, thorotrast, methotrexate, oral contraceptives, oxymetholone, trastuzumab
- Reference: Semin Liver Dis 2014;34:240
Diagrams / tables
Clinical features
- Underlying disease is typically evident before NRH becomes symptomatic
- NRH will typically manifest clinically as portal hypertension and its associated sequelae, including variceal bleeding, ascites, splenomegaly and gastrointestinal bleeding
- Reference: J Investig Med High Impact Case Rep 2021;9:23247096211044617
Diagnosis
- Definitive diagnosis is made on liver biopsy but there must be a high index of suspicion and cirrhosis must be ruled out before diagnosis of NRH is made
- Interobserver agreement is low even with diagnostic criteria set forth by Jharap et al. (PLoS One 2015;10:e0120299)
- Imaging modalities like magnetic resonance imaging (MRI), computed tomography (CT) and ultrasound are often employed but their sensitivities and specificities are typically low (World J Gastroenterol 2011;17:1400)
Laboratory
- Liver transaminases and serum bilirubin are usually normal, however, alkaline phosphatase can be elevated in 25% of cases (Lamps: Diagnostic Pathology - Hepatobiliary & Pancreas, 1st Edition, 2011)
Radiology description
- CT: hypodense nodules on unenhanced CT typically measuring ~1 mm (Clin Radiol 2009;64:1190)
- Ultrasound: small, round isoechoic lesions with a thin hyperechoic rim resembling a ring shaped coral reef configuration referred to as an atoll (Br J Radiol 2011;84:e129)
Radiology images
Prognostic factors
- Long term prognosis is uncertain, however, it is usually dependent on the level of the underlying disease causing NRH and the age of patient at diagnosis (Eur J Gastroenterol Hepatol 2010;22:1001)
Case reports
- 46 year old woman with recurrent variceal bleeding (Cureus 2022;14:e28740)
- 56 year old woman with polyarteritis nodosa (J Investig Med High Impact Case Rep 2021;9:23247096211044617)
- 58 year old man with Raynaud phenomenon (J Investig Med High Impact Case Rep 2021;9:23247096211044617)
Treatment
- Mainstay of treatment is treating the underlying etiology causing NRH
- If portal hypertension is present, then portosystemic shunts can be used
- Liver transplantation is rarely necessary and only used in cases of hepatic failure
- Reference: World J Gastroenterol 2011;17:1400
Gross description
- Vaguely nodular cut surface with the nodules having a pale appearance and the borders being darker in color (Semin Diagn Pathol 2019;36:395)
Microscopic (histologic) description
- Vague, ill defined, diffuse parenchymal nodules without fibrous septa between the nodules
- Sinusoidal dilation in areas of hepatocellular atrophy
- Inflammation is absent
- 2 morphologically distinct populations: hypertrophied hepatocytes centrally with atrophic hepatocytes on the periphery
- Atrophic hepatocytes can show feathery degeneration of the cytoplasm
- Hypertrophic cells can compress terminal hepatic venules that can appear shrunken or even be undetectable
- Hypertrophic cells can show regenerative changes (variation in nuclear size, mitotic figures and frequent binucleation)
- Within the center of nodules, there can be portal tracts known as reversed lobulation
- References: World J Gastroenterol 2011;17:1400, Semin Diagn Pathol 2019;36:395
Microscopic (histologic) images
Positive stains
- Reticulin stain will highlight the nodules and the reticulin network will be compressed in between the nodules
Negative stains
- Trichrome stain will show no advanced fibrosis; patchy sinusoidal fibrosis may be seen
Molecular / cytogenetics description
- Methylated RASSF1A, a proapoptotic gene, has been shown to be methylated in hyperplastic hepatocytes in genetic studies (World J Gastroenterol 2011;17:1400)
Sample pathology report
- Liver, core biopsy:
- Nodular regenerative hyperplasia (NRH) (see comment)
- Comment: No significant fibrosis (trichrome stain). The patient's history of elevated alkaline phosphatase is noted. Imaging findings demonstrate diffuse nodularity. The biopsy is adequate for evaluation containing 12 portal tracts. The most striking feature corresponds to the alternating areas of hepatocyte atrophy and hyperplasia (best highlighted in reticulin stain). The portal tracts appear unremarkable with no portal inflammation or bile duct damage. There is no interface activity and the lobules demonstrate regenerative changes within the hyperplastic areas. There is no significant fibrosis on the trichrome stain. PASD stain is negative for diagnostic cytoplasmic inclusions. The overall findings, along with the patient's history of portal hypertension, are in keeping with nodular regenerative hyperplasia.
Differential diagnosis
- Cirrhosis:
- Fibrous septa around nodules are present in cirrhosis but not NRH
- Focal nodular hyperplasia:
- Solitary lesion with central scar and fibrous septa
- Aberrant arterioles and ductular reaction present
- Adenomatosis:
- Lesions are generally larger than in NRH
- Lesions generally do not involve the liver uniformly or diffusely
- Partial nodular transformation:
- Single nodule or multiple nodules at or near the hepatic hilum
- Nodules are generally larger than in NRH
- Venous outflow tract obstruction:
- Hepatocyte atrophy and necrosis can be seen but usually accompanied by sinusoidal dilatation in zone 3 of the hepatic parenchyma
- Red blood cell extravasation in space of Disse can be seen as can elongation and crowding of bile ducts with dilatation of distal bile duct radicles
- Reference: Lamps: Diagnostic Pathology - Hepatobiliary & Pancreas, 1st Edition, 2011
Board review style question #1
Board review style answer #1
D. Nodular regenerative hyperplasia. The ill defined nodules have hypertrophic hepatocytes with atrophic hepatocytes. The small nodules are further highlighted on the reticulin stain and the trichrome stain shows the lack of fibrosis. Answer C is incorrect because no fibrosis is seen on trichrome stain. Answer B is incorrect because no distinct clonal population, nuclear atypia or architectural features typical of hepatocellular carcinoma are present. Answer A is incorrect because the nodules in focal nodular hyperplasia are separated by a fibrous septum. No fibrous septae are seen in the trichrome stain.
Comment Here
Reference: Nodular regenerative hyperplasia
Comment Here
Reference: Nodular regenerative hyperplasia
Board review style question #2
Nodular regenerative hyperplasia is associated with the development of which of the following?
- Cholangiocarcinoma
- Hepatocellular adenoma
- Hepatocellular carcinoma
- Hepatoportal sclerosis / obliterative portal venopathy
Board review style answer #2
D. Hepatoportal sclerosis / obliterative portal venopathy. Hepatoportal sclerosis / obliterative portal venopathy is a possible sequelae of nodular regenerative hyperplasia. Answer B is incorrect because hepatocellular adenoma has not been shown to develop from NRH. Answer A is incorrect because cholangiocarcinoma has not been shown to develop from NRH. Answer C is incorrect because hepatocellular carcinoma has not been shown to develop from NRH.
Comment Here
Reference: Nodular regenerative hyperplasia
Comment Here
Reference: Nodular regenerative hyperplasia
Nonalcoholic fatty liver disease / nonalcoholic steatohepatitis (NASH)
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Nonalcoholic fatty liver disease (NAFLD) is hepatic steatosis generated in association with overweight / obesity, type 2 diabetes mellitus or other metabolic dysregulations
- Morphologically, NAFLD covers all forms of hepatic steatosis with or without inflammation / fibrosis
Essential features
- Macrovesicular hepatosteatosis accentuated on zone 3, potentially accompanying fibroinflammatory changes in metabolic patients
- Presence of concomitant liver disease does not become a reason for excluding metabolic (dysfunction) associated fatty liver disease (MAFLD) (NAFLD/NASH) (Gastroenterology 2020 May;158:1999)
- Steatohepatitis is not the sole progressive form of NAFLD (J Hepatol 2015;62:1148)
- Histologic grade is assessed using a scoring system including steatosis, lobular inflammation and ballooning degeneration (Hepatology 2005;41:1313)
- Patients are at risk for fibrosis, cirrhosis and hepatocellular carcinoma
Terminology
- Nonalcoholic fatty liver disease (NAFLD) refers to any fatty liver disease caused by metabolic dysregulation, as above
- Nonalcoholic steatohepatitis refers to an aggressive form of the disease characterized by inflammation and ballooning in addition to steatosis
- Metabolic (dysfunction) associated fatty liver disease (MAFLD) has been proposed as a new, more accurate term for NAFLD (J Hepatol 2020 Apr 8 [Epub ahead of print])
- Cytoplasmic inclusions known as Mallory-Denk bodies (see microscopic images) are also termed Mallory’s hyaline and intracytoplasmic hyaline
ICD coding
- ICD-10: K76.0 - fatty (change of) liver, not elsewhere classified
Epidemiology
- One of the most important causes of liver disease worldwide in adults and children (Nat Rev Gastroenterol Hepatol 2018;15:11)
- Global prevalence is ~24% (Nat Rev Gastroenterol Hepatol 2018;15:11)
- It largely affects patients with unhealthy metabolic conditions but can occur even in lean individuals (Medicine (Baltimore) 2012;91:319)
Pathophysiology
- Hepatic manifestation of metabolic disorders
- Oxidative stress and lipotoxicity are considered key factors in disease progression (Hepatology 2006;43:506, J Atheroscler Thromb 2009;16:893)
- Genetic variants in patatin-like phospholipase domain containing protein 3 (PNPLA3), transmembrane 6 superfamily 2 (TM6SF2), membrane bound O-acyltransferase domain containing 7 (MBOA7) and hydroxysteroid 17-beta dehydrogenase 13 (HSD17B13) are known modifiers of NAFLD (Clin Med (Lond) 2018;18:s54, J Hepatol 2018;68:268)
Etiology
- Overweight / obesity and type 2 diabetes mellitus (J Hepatol 2020 Apr 8 [Epub ahead of print])
- Other metabolic disorders (dyslipidemia, insulin resistance, hypertension, etc.) (J Hepatol 2020 Apr 8 [Epub ahead of print])
Clinical features
- Most patients with MAFLD (NAFLD) are asymptomatic and diagnosed incidentally (Clin Liver Dis 2016;20:277)
- The prevalence of MAFLD (NAFLD) is high in people of Asian and Hispanic origin (Clin Liver Dis 2018;22:39)
- Fatty livers induced by alternative causes (medications, starvation, inherited disorders of lipid metabolism, etc.) are not metabolic (dysfunction) associated fatty liver disease (J Hepatol 2020 Apr 8 [Epub ahead of print])
Diagnosis
- Clinically or histologically detected hepatic steatosis in patients with metabolic disorders (see diagram)
- Presence of other concomitant liver diseases, including alcoholic liver disease, is not an exclusion criterion (J Hepatol 2020 Apr 8 [Epub ahead of print])
- Disease severity is evaluated semiquantitatively with the NASH Clinical Research Network criteria (Hepatology 2005;41:1313)
- Distinction between simple steatosis and steatohepatitis is unnecessary (J Hepatol 2020 Apr 8 [Epub ahead of print])
- Fatty livers induced by alternative causes (medications, starvation, inherited disorders of lipid metabolism, etc.) are not considered NAFLD (J Hepatol 2020 Apr 8 [Epub ahead of print])
Radiology description
- Bright liver and increased hepatorenal contrast on ultrasound (US) (Tohoku J Exp Med 1983;139:43)
- Liver / spleen attenuation ratio < 1.1 on computed tomography (CT) (Hepatol Commun 2019;3:1347)
- High signal intensity on T1 weighted magnetic resonance images (MRI)
- Whole hepatic lipid volume is quantifiable by using a special MRI technique (Hepatol Res 2019;49:1374)
Radiology images
Prognostic factors
- Presence of fibrosis is a sole prognostic factor in NAFLD (Gastroenterology 2015;149:389, Hepatology 2015;61:1547)
Case reports
- 14.5 year old boy diagnosed histologically as having nonalcoholic fatty liver disease (Cold Spring Harb Mol Case Stud 2018;4: a003087)
- 52 year old man urgently hospitalized because of intraabdominal hemorrhage (J Diabetes 2017;9:311)
- 56 year old woman with nonalcoholic steatohepatitis and Graves disease (Intern Med 2016;55:2019)
- 67 year old obese woman who received methotrexate for rheumatoid arthritis (Int J Clin Exp Pathol 2015;8:1961)
Treatment
- Currently, there is no approved specific therapy
Gross description
- Swollen soft liver with yellowish brown color
- Surface of affected liver becomes irregular with progression of fibrosis
- Some cases show cirrhosis or hepatocellular carcinoma
Frozen section description
- Lipid stain methods (Oil Red O, Sudan black B, filipin, etc.) to detect liver fat can be performed on frozen sections
Microscopic (histologic) description
- Predominantly macrovesicular steatosis in ≥ 5% hepatocytes under low magnification (4x or lower) observation is a sole histologic requirement for diagnosis of NAFLD
- Disease severity is evaluated separately by grade of activity and stage of fibrosis
- Activity grade is assessed according to nonalcoholic fatty liver disease activity score (NAS) using the sum of 3 components (total 0 - 8 points) (Hepatology 2005;41:1313)
- Steatosis (0: < 5%; 1: 5 - 33%; 2: 34 - 66%; 3: > 66%)
- Lobular inflammation (0: none; 1: < 2 foci/20x field; 2: 2 - 4 foci/20x field; 3: > 4 foci/20x field)
- Ballooning degeneration (0: none; 1: few; 2: many)
- Fibrosis stage is assessed into 5 levels; stage 0, none; stage 1, perivenular (zone 3) fibrosis; stage 2, perivenular + portal fibrosis; stage 3, bridging fibrosis; stage 4, cirrhosis (Hepatology 2005;41:1313)
- Other characteristic findings are Mallory-Denk bodies, glycogenated nuclei, giant mitochondria (megamitochondria) and lipogranuloma
- Histologic changes of concomitant liver conditions may be seen
- In NAFLD associated cirrhosis, steatotic hepatocytes may be burnt out, resulting in a loss of visible steatosis, but the term "cryptogenic cirrhosis" should not be used for this condition (J Hepatol 2020 Apr 8 [Epub ahead of print])
Positive stains
- Special stains for collagen (Masson trichrome, Sirius red, Azan-Mallory, etc.) mandatory: faint fibrosis cannot be detected on hematoxylin eosin tissue slides
- Ubiquitin, p62, CK18: Mallory-Denk bodies are stained
- References: Histochem Cell Biol 2008;129:735, Exp Mol Pathol 2011;90:252
Negative stains
- CK18: ballooned hepatocytes are characteristically negative (J Hepatol 2010;53:719)
Sample pathology report
- Liver, needle biopsy:
- Fatty liver, consistent with nonalcoholic fatty liver disease
- NAS 6 points = steatosis 2 + inflammation 2 + ballooning 2
- Stage 2 (perivenular + portal fibrosis)
Differential diagnosis
- Can coexist with any type of liver diseases including alcoholic damage (J Hepatol 2020 Apr 8 [Epub ahead of print])
- Histologic mimics of NAFLD include some genetic conditions (Wilson disease, lysosomal acid lipase deficiency, etc.) and some forms of drug induced liver injury (methotrexate, etc.) (Cold Spring Harb Mol Case Stud 2018;4: a003087, Med Clin North Am 2019;103:991, Int J Clin Exp Pathol 2015;8:1961)
- Differential diagnosis of fatty liver diseases should be made clinically
Board review style question #1
A 78 year old woman with a > 10 year treatment history of rheumatoid arthritis shows elevated serum levels of liver enzymes (AST, 120 IU; ALT, 136 IU; GGT, 129 IU). She is an occasional drinker and does not have metabolic disorders. She is taking methotrexate (MTX). Hepatitis virus B and C are negative and antinuclear antibody is ×160. Liver biopsy, shown above, shows steatosis and inflammation. What should be done next in the diagnostic workup?
- Administration of steroids
- ATP7B gene testing
- Cessation of MTX
- Drug induced lymphocyte stimulation test
- Serum AMA
Board review style answer #1
C. Cessation of MTX. MTX is a first line therapy for rheumatoid arthritis and can cause steatohepatitis that mimics NAFLD.
Comment Here
Reference: Nonalcoholic fatty liver disease (NAFLD) / nonalcoholic steatohepatitis (NASH)
Comment Here
Reference: Nonalcoholic fatty liver disease (NAFLD) / nonalcoholic steatohepatitis (NASH)
Board review style question #2
Board review style answer #2
E. Ubiquitin positive. The inclusion shown is a Mallory-Denk body. It is a ubiquitinated aggregate of keratin filament that occurs in ballooned hepatocytes.
Comment Here
Reference: Nonalcoholic fatty liver disease (NAFLD) / nonalcoholic steatohepatitis (NASH)
Comment Here
Reference: Nonalcoholic fatty liver disease (NAFLD) / nonalcoholic steatohepatitis (NASH)
Other flukes (Clonorchis / Opisthorchis) (pending)
[Pending]
Peliosis hepatis
Table of Contents
Definition / general | Essential features | Terminology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Definition / general
- Multiple blood filled cysts in liver, with several potential causes
Essential features
- Blood filled hepatic spaces of various sizes, usually discovered by radiology or at autopsy
- Several possible etiologies, including Bartonella henselae or B. quintana infection, which also cause spindle cell / vascular proliferation
Terminology
- Two types:
- Peliosis hepatis refers to bland blood filled spaces of various etiologies
- Bacillary peliosis refers to hepatic spindle cell proliferation with small blood vessels and blood filled spaces secondary to Bartonella infection
- Peliosis should not be confused with lipopeliosis
Sites
- Peliosis may occur in liver or spleen
Etiology
- Associated with steroids (anabolic, contraceptive), danazol, azathioprine, vinyl chloride, Bartonella infection in HIV+ patients (Forensic Sci Int 2005;149:25, N Engl J Med 1997;337:1876)
- May be due to hepatocellular necrosis or veno-occlusive disease
Clinical features
- May be asymptomatic or manifest as jaundice, portal hypertension, liver failure, liver rupture or hepatomegaly
- Patients may also have liver or renal transplant, Castleman disease, nodular regenerative hyperplasia, leukemia / lymphoma (Arch Pathol Lab Med 2004;128:1283)
Diagnosis
- Usually incidental finding at autopsy
Radiology description
- Blood filled spaces visible on imaging
Treatment
- Withdrawal of causative drug, if applicable
- Erythromycin or doxycycline for Bartonella infections
Gross description
- Honeycomb liver with multiple round, red purple, blood filled spaces of varying sizes
Microscopic (histologic) description
- Blood lakes of various sizes within the liver, which may be continuous
- In phlebectatic subtype, spaces are lined by endothelium and central veins are dilated
- In parenchymal subtype, spaces are not lined and parenchyma has variable hemorrhagic necrosis (Arch Pathol 1964;77:159)
- May have calcifications (J Ultrasound Med 1996;15:257)
- Background liver may show sinusoidal dilation
- Bacillary peliosis may show angiomatosis, with spindle cell process accompanied by blood vessel proliferation
Microscopic (histologic) images
Contributed by @RaulSGonzalezMD on Twitter
Contributed by @RaulSGonzalezMD on Twitter (see original post here)">
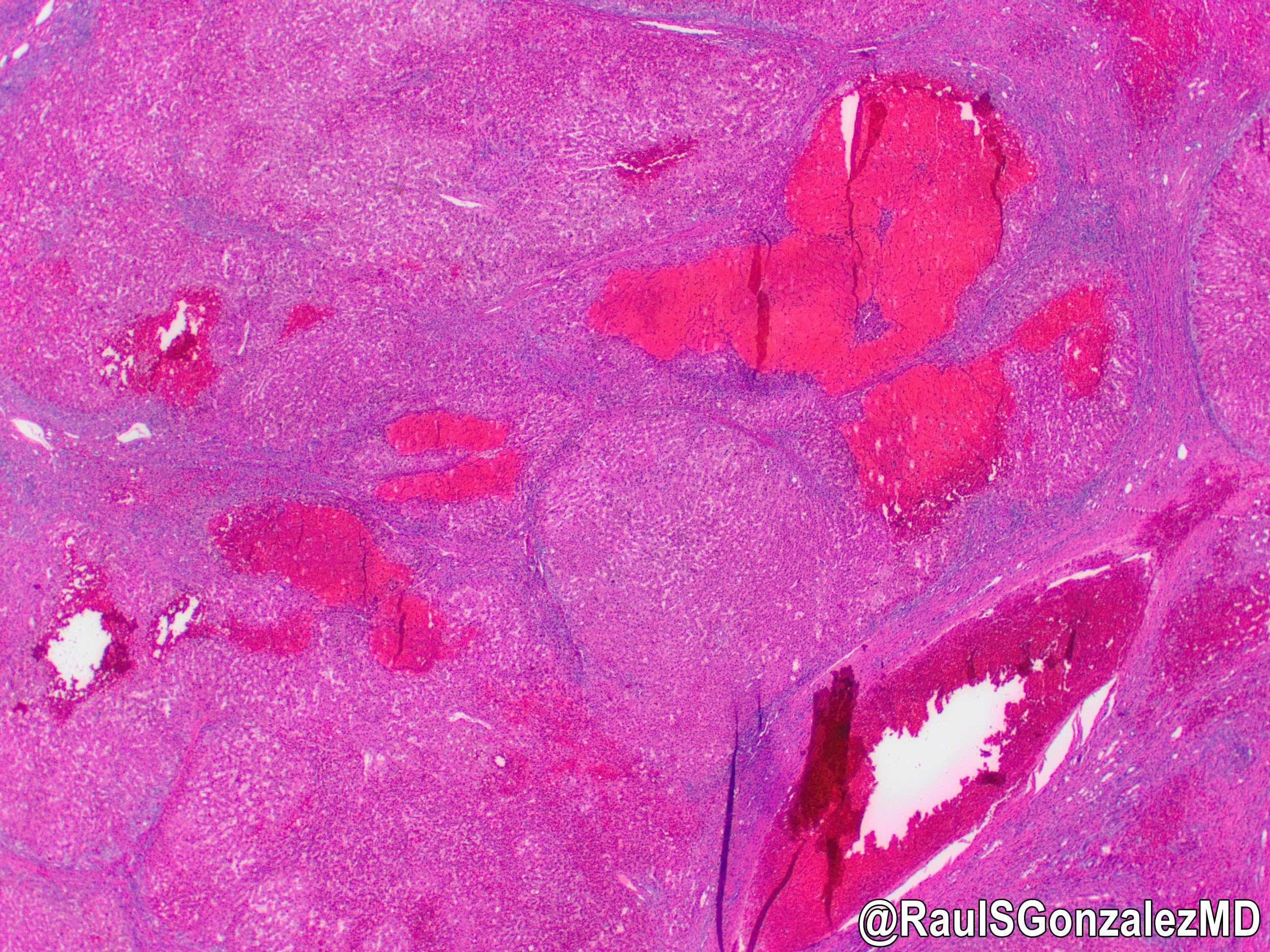 Contributed by @RaulSGonzalezMD on Twitter (see original post here)">
Contributed by @RaulSGonzalezMD on Twitter (see original post here)">
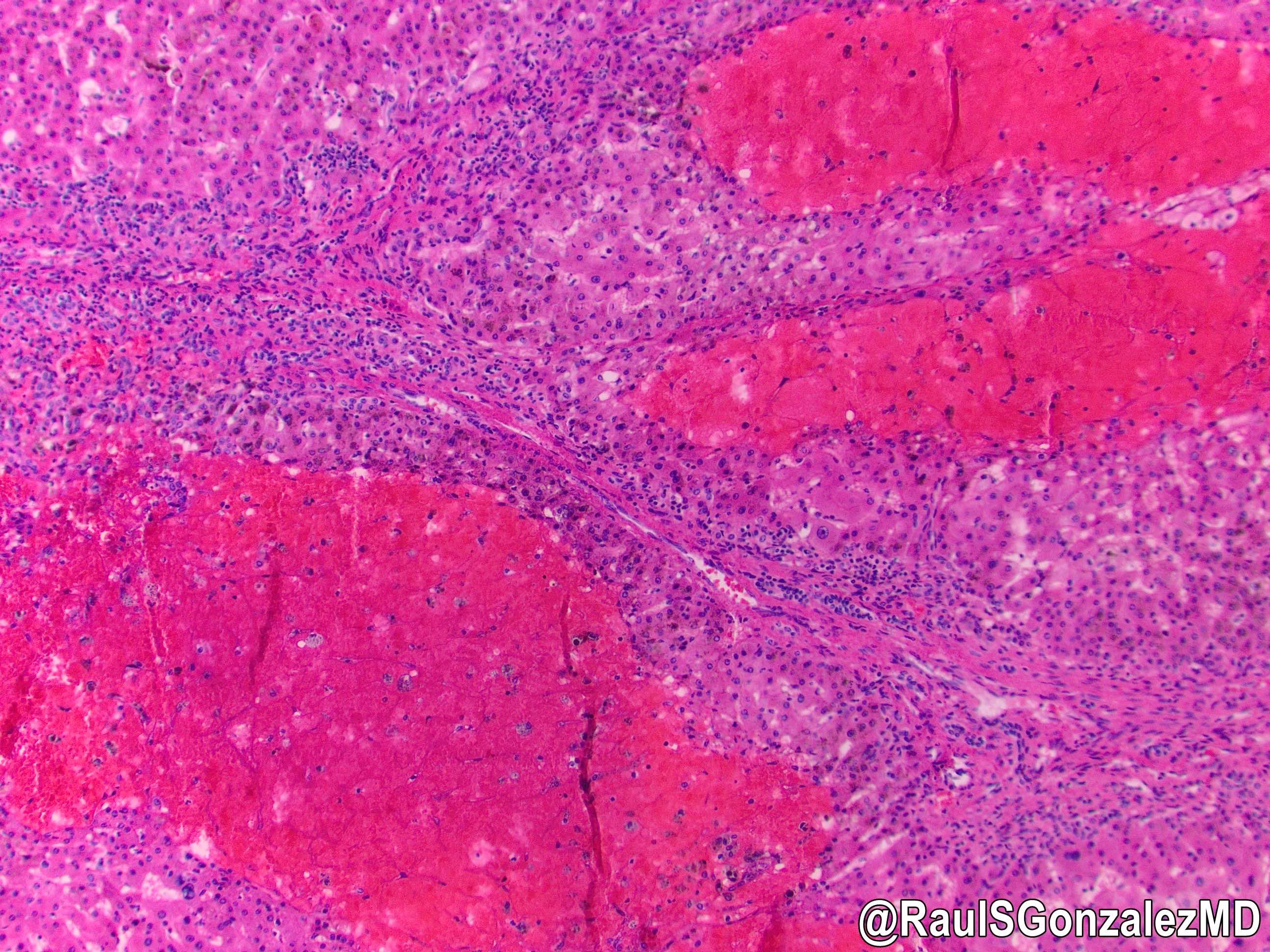
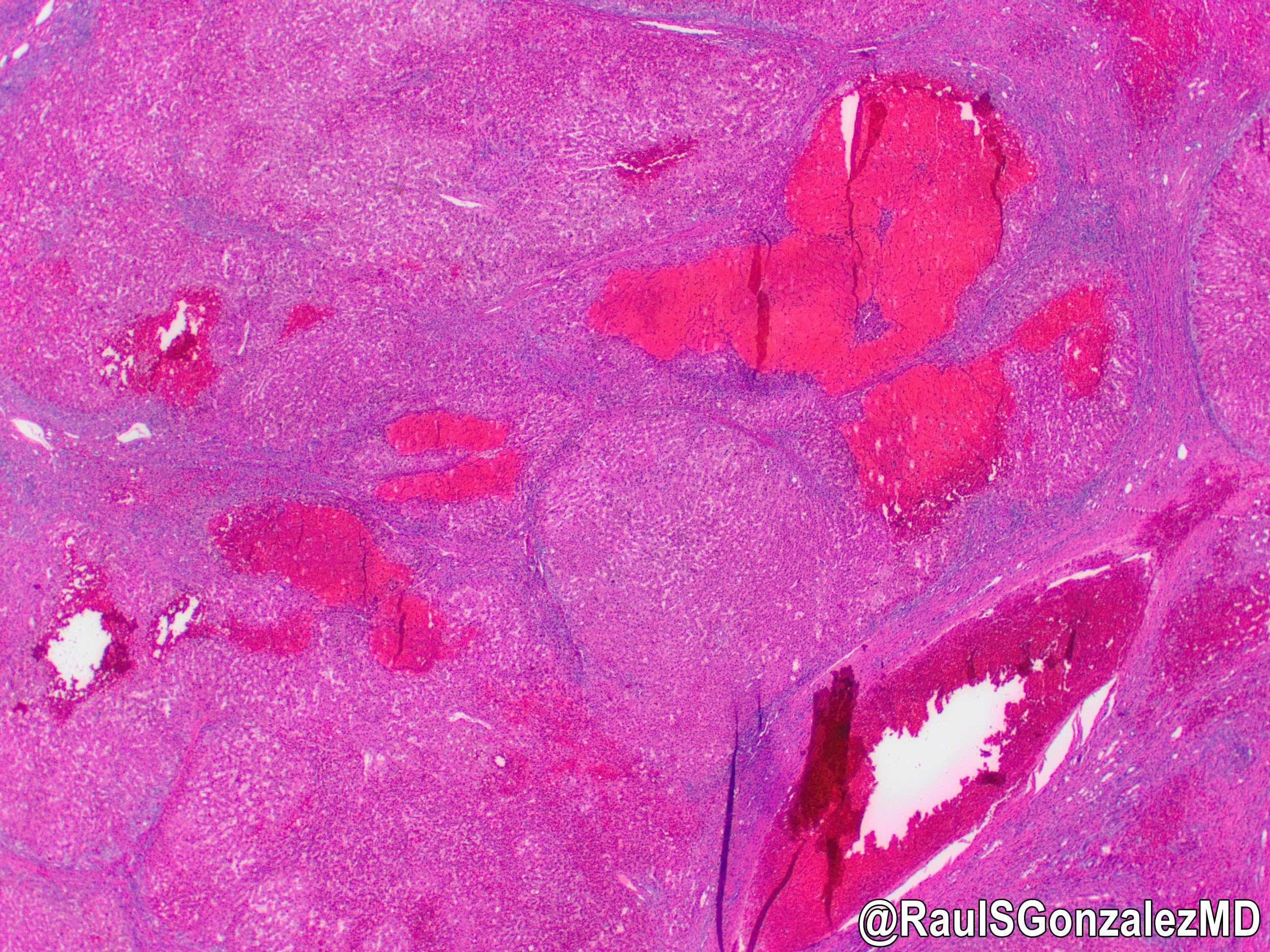 Contributed by @RaulSGonzalezMD on Twitter (see original post here)">
Contributed by @RaulSGonzalezMD on Twitter (see original post here)">
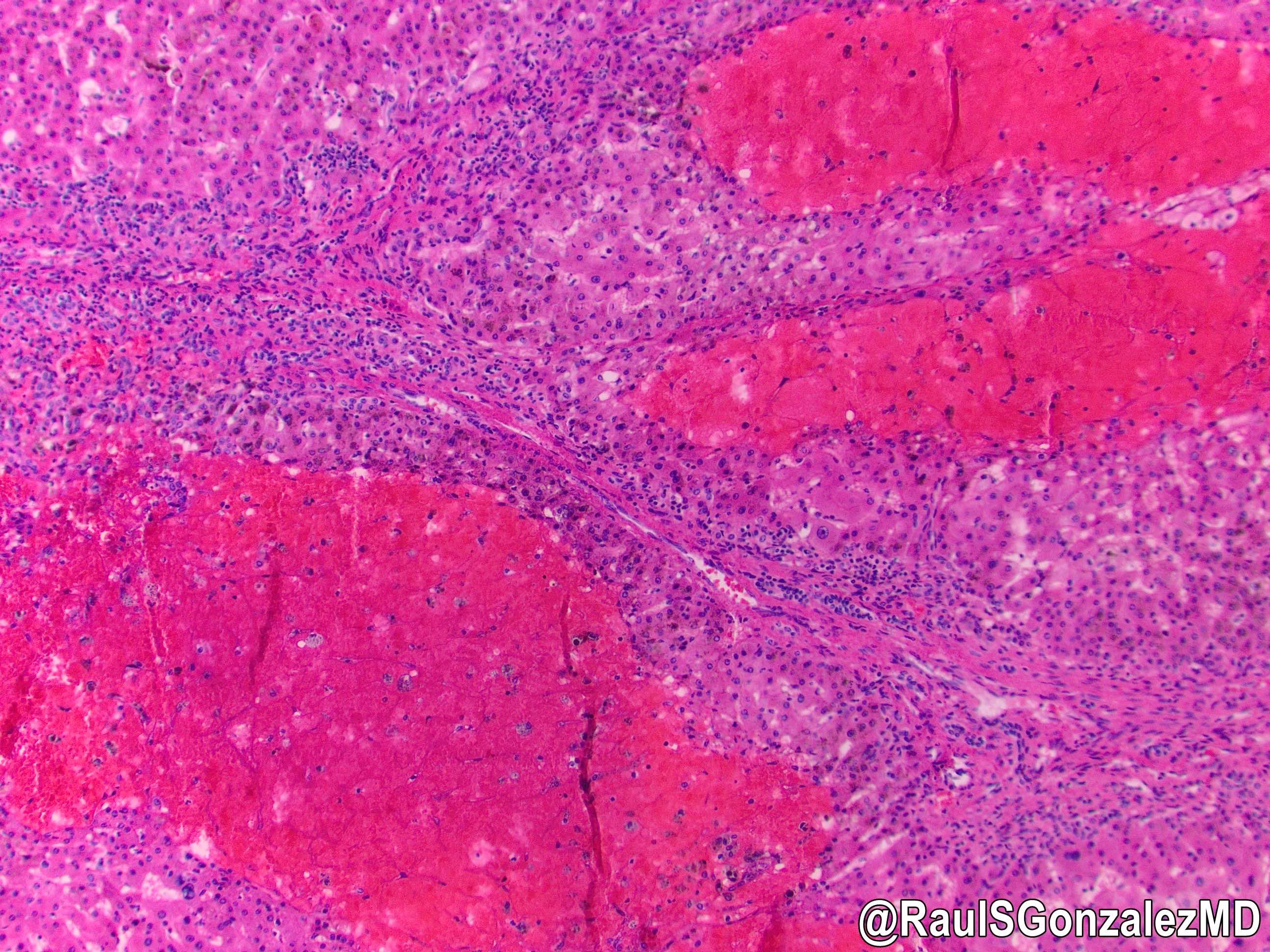
Peliosis hepatis
Images hosted on other servers:
Positive stains
- Warthin-Starry in cases due to Bartonella infection
Sample pathology report
- Liver, biopsy:
- Liver parenchyma with large blood filled cystic spaces and background sinusoidal dilation (see comment)
- Comment: The findings are compatible with peliosis hepatic, which has many potential etiologies. Trichrome and iron stains are unremarkable.
Differential diagnosis
- Hemangioma:
- Discrete lesion with fibrous tissue in background, linking the engorged spaces
- Kaposi sarcoma:
- Can mimic bacillary peliosis but vessels are less well formed
- HHV8 positive
- Peliotic change in hepatocellular carcinoma: background parenchyma clearly malignant (Oncol Lett 2010;1:17)
Board review style question #1
- A 45 year old man presents to the emergency department complaining of abdominal pain but collapses and dies before receiving care. Autopsy shows several findings, including a liver studded with numerous blood filled lakes. Microscopically, these spaces are associated with a vascular / spindle cell proliferation. Which of the following other conditions did the patient likely have?
- Blue rubber bleb nevus syndrome
- Congestive heart failure
- Ganglioneuromatosis
- Hereditary hemorrhagic telangiectasia
- HIV infection
Board review style answer #1
Polycystic liver disease / duct plate malformation
Table of Contents
Definition / general | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Additional referencesDefinition / general
- Autosomal dominant, associated with autosomal dominant (but not autosomal recessive) polycystic kidney disease (71 - 93%) and defect in ADPKD1 gene on #16
- Cysts don't communicate with biliary tree
- 80% occur in females
- Associated with abdominal tenderness, pain with stooping; may present during pregnancy
- Cysts more common with increased age (75% at age 70+ versus < 5% in teenagers)
- 1 - 7% risk of adenocarcinoma if coexisting Caroli disease; otherwise extremely rare
- Complications: infection, cholangiocarcinoma, squamous cell carcinoma
Gross description
- Multiple variably sized unilocular cysts, liver rarely is massively enlarged
Microscopic (histologic) description
- Multiple diffuse cystic lesions resembling solitary cysts, lined by cuboidal to flat biliary epithelium, containing straw colored fluid
- 40% have identifiable von Meyenburg complexes
- Don't contain pigmented material
Microscopic (histologic) images
Additional references
Portal hypertension
Table of Contents
Definition / general | Essential features | Terminology | Etiology | Clinical features | Diagnosis | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Board review style question #1 | Board review style answer #1Definition / general
- Increased blood pressure within portal venous system
Essential features
- Causes are numerous and can be divided into prehepatic, intrahepatic and posthepatic
- Cirrhosis is most common cause
Terminology
- Patients without cirrhosis typically are labeled with "noncirrhotic portal hypertension"
Etiology
- Prehepatic causes include obstructive thrombosis / narrowing of portal vein and shunting of blood into splenic vein via splenomegaly
- Intrahepatic causes include cirrhosis, schistosomiasis (most common noncirrhotic cause in the world), nodular regenerative hyperplasia, granulomatous disease, congenital hepatic fibrosis, hepatoportal sclerosis, severe fatty liver disease including NASH
- Posthepatic causes include congestive heart failure, constrictive pericarditis, hepatic vein outflow obstruction (e.g., Budd-Chiari syndrome), myeloproliferative disorders
- Some cases may be idiopathic (Orphanet J Rare Dis 2015;10:67)
Clinical features
- Clinical complications include ascites, portosystemic venous shunts (hemorrhoidal veins, esophageal varices, etc.), congestive splenomegaly, hepatic encephalopathy
Diagnosis
- Gold standard is measurement of hepatic venous pressure gradient via portal vein catheterization
- Ultrasound is noninvasive and can detect signs of portal hypertension
Microscopic (histologic) description
- Findings vary depending on causative disease; changes may be those of cirrhosis, schistosomiasis, nodular regenerative hyperplasia, hepatoportal sclerosis, granulomatous disease, outflow obstruction or others
- Collapsed portal vein radicles may be seen in pediatric patients (Pediatr Dev Pathol 2003;6:421)
Microscopic (histologic) images
Sample pathology report
- Liver, biopsy:
- Liver with prominent nodular regenerative hyperplasia (see comment)
- Comment: The finding likely explains the patient’s reported portal hypertension. A reticulin stain confirms nodular regenerative hyperplasia. Trichrome and iron stains are unremarkable.
Board review style question #1
- A patient is found to have portal hypertension in the absence of cirrhosis. Considering the most common overall cause of noncirrhotic portal hypertension, which of the following is most likely to be seen on liver biopsy?
- Herniated portal veins
- Mastocytosis
- Nodular hepatocyte parenchyma
- Parasite eggs
- Sinusoidal fibrosis
Board review style answer #1
D. Parasite eggs: schistosomiasis is the most common cause of noncirrhotic portal hypertension in the world
Comment Here
Reference: Portal hypertension
Comment Here
Reference: Portal hypertension
Portal vein obstruction
Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Pathophysiology | Etiology | Clinical features | Radiology description | Radiology images | Case reports | Treatment | Gross images | Microscopic (histologic) description | Sample pathology report | Additional references | Board review style question #1 | Board review style answer #1Definition / general
- Blockage of blood flow through the portal vein into the liver
Essential features
- Malignant and nonmalignant processes may cause portal vein obstruction
- Portal hypertension commonly results
- Biliary abnormalities may also occur
Terminology
- Portal vein obstruction leading to splenomegaly and anemia is termed "Banti syndrome"
- Portal vein obstruction may cause a sclerosing cholangitis-like clinical picture termed "portal biliopathy" (World J Gastroenterol 2012;18:6177, Gut 1992;33:272
Epidemiology
- Relatively rare
Pathophysiology
- Hepatic artery buffer response allows for increased arterial flow to liver when portal vein is obstructed
Etiology
- Prothrombotic disorders, tumor thrombus, cirrhosis, pancreatitis, various infections (e.g. schistosomiasis) (BMC Gastroenterol 2007;7:34)
- Intraabdominal infection and appendicitis are common causes in children
- May be idiopathic
Clinical features
- Signs / symptoms:
- Abdominal pain
- Ascites (massive, intractable)
- Portal hypertension
- Bowel infarction
Radiology description
- Dynamic contrast enhanced CT may show filling defect if secondary to thrombus (Abdom Imaging 2008;33:72)
Case reports
- 28 year old man with portal vein thrombosis (J Am Board Fam Med 2008;21:237)
- 34 year old man with cytomegalovirus infection and portal vein thrombosis (Clin Infect Dis 2007;44:e13)
- 43 year old woman with portal vein thrombosis (Oncol Lett 2015;9:2495)
Treatment
- Anticoagulation if caused by acute portal vein thrombosis (Neth J Med 2009;67:46)
Microscopic (histologic) description
- Sinusoidal dilation, increased portal tract vessels and hepatocyte atrophy may be seen (Virchows Arch A Pathol Anat Histopathol 1989;415:61)
Sample pathology report
- Liver, native, orthotopic transplantation:
- Liver with portal vein thrombosis and patchy sinusoidal dilation and zone 3 necrosis (see comment)
- Comment: The parenchymal findings are mild, as is often the case with portal vein obstruction. Trichrome and iron stains are unremarkable.
Additional references
Board review style question #1
A patient develops portal vein thrombosis secondary to appendicitis.
Based on this information, which of the following is most likely true regarding the patient?
- Has an allograft liver
- Has situs inversus
- Has von Willebrand disease
- Is a child
- Is a woman
Board review style answer #1
Pregnancy
Table of Contents
Acute fatty liver of pregnancy | Intrahepatic cholestasis of pregnancy | Preeclampsia and eclampsia | Viral hepatitisAcute fatty liver of pregnancy
Definition / general
Treatment
Gross description
Microscopic (histologic) description
Positive stains (frozen tissue)
Differential diagnosis
Additional references
- Minimal to modest hepatic dysfunction due to defect in mitochondrial fatty acid oxidation that may progress to hepatic failure
- Usually presents in third trimester of primiparas with bleeding, nausea, vomiting, jaundice, coma
- Incidence of 1 case per 15,000 pregnancies
- 20% have coexisting preeclampsia
- Usually mild but may cause death
Treatment
- Terminate pregnancy
Gross description
- Pale, yellow, small liver
Microscopic (histologic) description
- Microvesicular steatosis in zones 2 or 3 (vacuoles may be very small)
- Also marked ballooning of hepatocytes and macrovesicular fat
- In severe cases, hepatocyte dropout, reticulin collapse, portal tract inflammation
Positive stains (frozen tissue)
- Fat stains (Oil red O, Sudan black)
Differential diagnosis
- Carnitine deficiency
- Jamaican vomiting sickness
- Lábrea hepatitis
- Reye syndrome
- Salicylate intoxication
- Yellow fever
Additional references
Intrahepatic cholestasis of pregnancy
Definition / general
Laboratory
Microscopic (histologic) description
- Second leading cause of gestational jaundice (after viral hepatitis)
- Usually occurs late in pregnancy
- Estrogenic hormones may inhibit hepatocellular bile secretory activity
- Mother at risk for gallstones, malabsorption
- Associated with higher incidence of fetal distress, stillbirths, prematurity
- Symptoms: pruritis in third trimester, dark urine, light stools, jaundice
Laboratory
- Elevated serum bilirubin (< 5 mg/dl), usually conjugated; mildly elevated alkaline phosphatase
Microscopic (histologic) description
- Mild cholestasis without cirrhosis
Preeclampsia and eclampsia
Definition / general
Laboratory
Case reports
Treatment
Gross description
Gross images
Images hosted on other servers:
Microscopic (histologic) description
Microscopic (histologic) images
Images hosted on other servers:
Differential diagnosis
Additional references
- Preeclampsia: complication of pregnancy in third trimester, usually primiparas, with maternal hypertension, proteinuria, peripheral edema, coagulation abnormalities, DIC
- Ecclampsia: preeclampsia, seizures and hyperreflexia; leading cause of maternal death, often due to delay in diagnosis
- Liver disease as part of HELLP syndrome: hemolysis, elevated liver enzymes, low platelets; associated with 4 - 12% of cases of preeclampsia; microangiopathic hemolysis with thrombocytopenia; 10 - 60% infant mortality due to placental abruption, intrauterine ischemia or prematurity
Laboratory
- Early mild increase in liver enzymes, late coagulopathy
Case reports
- Woman in mid 30s with preeclampsia and subcapsular liver hematoma at 23 weeks gestation (Arch Pathol Lab Med 2003;127:1639)
Treatment
- Termination of pregnancy in severe cases
Gross description
- Pale, firm liver with small red hemorrhagic patches (hematoma dissecting under Glisson capsule and causing hepatic rupture)
Gross images
Images hosted on other servers:
Microscopic (histologic) description
- Periportal fibrin deposits with hemorrhage into space of Disse, causing periportal hepatocellular necrosis
- Less commonly bile inspissation in canaliculi and ductules, steatosis, portal lymphoplasmacytic infiltrate
Microscopic (histologic) images
Images hosted on other servers:
Differential diagnosis
Additional references
Viral hepatitis
Primary biliary cholangitis
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Primary biliary cholangitis (PBC) is a chronic, progressive cholestatic liver disease with granulomatous destruction of interlobular bile ducts, leading to fibrosis and ultimately cirrhosis
Essential features
- Typically occurs in middle aged women; extremely rare in children
- Labs include elevated alkaline phosphatase, elevated IgM and the classic antimitochondrial antibody (AMA)
- Histologic changes, including the pathognomonic florid duct lesions, can be patchy
Terminology
- Previously called primary biliary cirrhosis; renamed because not all patients progress to cirrhosis (Clin Res Hepatol Gastroenterol 2015;39:e57)
ICD coding
- ICD-10: K74.3 - primary biliary cirrhosis
Epidemiology
- Reported prevalence of 65.4 women per 100,000 in U.S.; incidence appears to be increasing (Clin Liver Dis 2003;7:795)
Sites
- Involves the most proximal portion of biliary tree, namely the interlobular bile ducts and canals of Hering; larger bile ducts are not typically affected (Hum Pathol 2002;33:983)
Etiology
- Likely autoimmune; associated with Sjögren syndrome, scleroderma, thyroiditis, rheumatoid arthritis, Raynaud phenomenon, membranous glomerulonephritis, systemic lupus erythematosus, celiac disease
Clinical features
- 85% are women, usually ages 40 - 60
- Symptoms include insidious onset of pruritis, malaise, dark urine, light stools, hepatomegaly, xanthomas, and xanthelasma
- Can develop cirrhosis and die from liver failure
- Some patients have overlap disease with autoimmune hepatitis; much more rarely, patients may have overlap with primary sclerosing cholangitis (PSC); in overlap, strict criteria for both diseases must be met (ACG Case Rep J 2018;5:e54)
- Increased risk of hepatocellular carcinoma once cirrhotic but there does not appear to be significant increased risk of cholangiocarcinoma (unlike in primary sclerosing cholangitis)
Diagnosis
- 2 out of 3 of the following criteria are required:
- Serum alkaline phosphatase > 1.5 times the upper limit of normal, antimitochondrial antibody, liver sample showing nonsuppurative destructive cholangitis and destruction of interlobular bile ducts (Autoimmun Rev 2014;13:441)
- Other characteristic clinical features include disease-specific antinuclear antibodies (sp100 and gp210), elevated serum IgM, hypercholesterolemia, xanthomas, Sicca syndrome, pruritus, and fatigue (Autoimmun Rev 2014;13:441)
- Patients who appear to have primary biliary cholangitis except for negative antimitochondrial antibody are said to have AMA-negative primary biliary cholangitis, also called autoimmune cholangitis
Laboratory
- Elevated serum alkaline phosphatase and IgM, AMA in 95%, elevated conjugated bilirubin (late)
- M2 form of AMA, present in 90%, is against E2 subunit of pyruvate dehydrogenase complex
Radiology description
- Parenchymal lace-like fibrosis and periportal halo sign on T2-weighted MRI in some patients (Eur J Radiol 2009;69:523)
Case reports
- 32 year old woman with hypokalemia (Medicine (Baltimore) 2018;97:e13172)
- 51 year old woman treated with sulfasalazine and abatacept (BMJ Case Rep 2018)
- 56 year old woman with rheumatoid arthritis (Cureus 2017;9:e1562)
- 62 year old man with dermatitis herpetiformis (Cureus 2017;9:e1247)
- 74 year old woman with multiple hepatic malignancies (World J Hepatol 2017;9:1378)
Treatment
- Ursodeoxycholic acid and obeticholic acid improve liver function and symptoms but may not halt progression of disease
- Liver transplant for advanced / cirrhotic cases; may eventually recur in the graft
Gross description
- Hepatomegaly early; cirrhosis late
Microscopic (histologic) description
- Dense lymphocytic infiltrate in portal tracts with granulomatous destruction and loss of medium sized interlobular bile ducts, focal and variable within the liver
- May involve sinusoids early
- Periportal Mallory hyaline late, usually minimal neutrophils, variable portal eosinophils; resembles graft versus host disease and graft rejection; ductules derived from periportal hepatocytes are still present; prominent Ito cells with fat vacuoles
- Key finding is the florid duct lesion: interlobular bile ducts (within small portal tracts) are destroyed by poorly formed portal epithelioid granulomas
- Dense lymphocytic infiltrate in portal tracts can also be seen, mimicking hepatitis
- Ductular reaction and duct injury early; duct loss and lobular cholestasis with feathery degeneration late
- Lobules may show macrophage aggregates / small granulomas but typically not much of an inflammatory infiltrate
- The above changes are patchy and may not be present in a given biopsy
- Nodular regenerative hyperplasia may be seen in early disease (Gastroenterology 1992;102:1319)
- Staging:
- Florid duct lesions or portal hepatitis
- Ductular reaction or periportal hepatitis
- Bridging/septal fibrosis or bridging necrosis
- Cirrhosis
Microscopic (histologic) images
Positive stains
- Note: None of these stains are routinely used for diagnosis
- S100: highlights dendritic cells in the basement membrane in early stage disease (Am J Pathol 1989;134:741)
- CD1a: highlights Langerhans cells in biliary epithelium (Am J Surg Pathol 2012;36:732)
- Copper stains: positive within hepatocytes in all chronic cholestatic conditions, including PBC
Sample pathology report
- Liver, biopsy:
- Biliary pattern injury with mild chronic portal inflammation, ductular reaction, and focal changes suggestive of florid duct lesion (see comment)
- Comment: The histologic findings, in addition to the patient’s reported history of antimitochondrial antibody, are consistent with primary biliary cholangitis. A trichrome stain shows minimal periportal fibrosis.
Differential diagnosis
- Autoimmune cholangitis:
- Essentially the same diagnosis, except AMA is negative
- Autoimmune hepatitis:
- More normal alkaline phosphatase, antismooth muscle antibody positive and AMA negative, elevated IgG rather than IgM, lobular inflammation
- Secondary biliary cirrhosis:
- Cirrhotic liver in the setting of longstanding large duct injury
- No AMA or florid duct lesions
- Primary sclerosing cholangitis:
- Minimal inflammation, classic imaging findings
- Large duct obstruction:
- Clinical presentation often acute
- Cholestasis early in the disease process, rather than late
- Drug induced liver injury:
- Can mimic; clinical correlation necessary
Additional references
Board review style question #1
- Which of the 2 following features are considered pathognomonic for primary biliary cholangitis?
- Antimitochondrial antibody and florid duct lesions
- Antineutrophil cytoplasmic antibody and onion skin fibrosis
- Antinuclear antibody and ductular reaction
- Antismooth muscle antibody and interface hepatitis
Board review style answer #1
A. Antimitochondrial antibody and florid duct lesions
Comment Here
Reference: Primary biliary cholangitis
Comment Here
Reference: Primary biliary cholangitis
Board review style question #2
Board review style answer #2
D. Ursodeoxycholic acid. This is primary biliary cholangitis.
Comment Here
Reference: Primary biliary cholangitis
Comment Here
Reference: Primary biliary cholangitis
Primary hyperoxaluria
Table of Contents
Definition / general | Essential features | Epidemiology | Pathophysiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology images | Prognostic factors | Case reports | Treatment | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Molecular / cytogenetics description | Molecular / cytogenetics images | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Primary hyperoxaluria is a rare genetic disorder in which defective glyoxylate metabolism results in excessive oxalate production
- Excess oxalate is deposited as insoluble calcium oxalate salts in the kidneys and systemically (systemic oxalosis), including in the retina (diminished visual acuity), myocardium (conduction defects), blood vessel walls (vascular occlusion and gangrene), skin (livedo reticularis, calcinosis cutis metastatica, gangrene), bone (pain, joint immobility, anemia, fractures) and central nervous system (Curr Rheumatol Rep 2013;15:340, N Eng J Med 2013;369)
Essential features
- Birefringent oxalate crystals are noted in vessel walls and connective tissues of the portal areas of explanted livers, the kidneys (Arch Pathol Lab Med 2002;126:1250) and other affected organs
- Three most common subtypes are caused by mutations in the AGXT (type 1), GRHPR (type 2) and HOGA1 (type 3) genes
Epidemiology
- Primary hyperoxaluria is estimated to affect 1 in 58,000 individuals worldwide and accounts for 1 - 2% of children with end stage renal disease (Clin J Am Soc Nephrol 2012;7:458)
- Type 1 is the most common form, accounting for approximately 80% of cases
- Types 2 and 3 each account for about 10% of cases
- Type 1 likely remains underdiagnosed because of the wide variability in its clinical presentation and age of onset (GeneReviews: Primary Hyperoxaluria Type 1 [Accessed 8 November 2018])
- Prevalence of type 1 in Europe ranges from 1/333,000 - 1/1,000,000 (Nephrol Dial Transplant 2003;18:273, N Engl J Med 2013;369:649)
- Prevalence is higher in certain populations in Tunisia and Kuwait, in Arabs and Druze families of Israel and in Iran due to consanguinity but no common founder variant identified (Pediatr Nephrol 1996;10:479, Transplant Proc 2004;36:1788, Pediatr Nephrol 2006;21:1075, J Am Soc Nephrol 1999;10:2352, Pediatr Nephrol 2001;16:140, Am J Nephrol 2005;25:264, Am J Nephrol 2005;25:269)
Pathophysiology
- Glyoxylate metabolism, which almost exclusively occurs in hepatocytes, is defective and results in excessive oxalate production
- Oxalate excretion is almost entirely via the kidneys, predominantly as highly insoluble calcium salts
- Oversaturation of the renal tubular filtrate leads to crystallization in the renal tubules, nephrocalcinosis and urolithiasis, often with superimposed infection
- Combination of direct renal tubular toxicity and obstruction results in renal injury with subsequent end stage renal failure in the more severe subtypes
- Type 1 is typically the most severely affected of the 3 types (Kidney Int 2014;86:1197, Ann Clin Lab Sci 2013;43:328)
Clinical features
- Typically manifests in infancy or childhood with recurring kidney and bladder stones and other symptoms of systemic oxalosis but some patients are diagnosed in adulthood (Ann Clin Lab Sci 2013;43:328, Pediatr Nephrol 2015;30:1781)
Diagnosis
- Diagnosis is suspected on clinical (recurrent urolithiasis or nephrocalcinosis) and biochemical grounds and can be confirmed with genetic testing for the most common gene mutations (AGXT, GRHPR and HOGA1)
- Antenatal and preimplantation diagnosis is possible in affected families
- Prior to the availability of genetic testing, liver biopsy was required to demonstrate AGT deficiency in type 1
- Immunoblot assays allow analysis of the protein and immunoelectron examination illustrates the near absence of AGT in peroxisomes
Laboratory
- Markedly increased urinary oxalate excretion (> 1 mmol/1.73 m² per day [90 mg/1.73 m² per day])
- As long as glomerular filtration rates are within normal limits, plasma oxalate concentration remains normal
- Calcium oxalate renal and bladder stones
Radiology images
Prognostic factors
- Most type 1 and 2 patients require ongoing medical treatment
- Type 3 becomes clinically silent by age 6 years and does not typically progress beyond mild renal impairment
Case reports
- 10 month old girl with primary hyperoxaluria type 2 and urolithiasis (BMC Med Gene 2017;18:59)
- 21 year old man with primary hyperoxaluria type 1 and partial orthotopic liver transplant (Medicine (Baltimore) 2015;94:e1267)
- 33 year old woman with primary hyperoxaluria type 1 and systemic calcium oxalate deposition (Ann Clin Lab Sci 2013;43:328)
- 54 year old woman with end stage renal disease and primary hyperoxaluria diagnosed based on bone marrow biopsy (Case Rep Hematol 2015;2015:402947)
- 78 year old man with late diagnosis of hyperoxaluria type 3 (Ann Clin Biochem 2017;54:406)
Treatment
- In the most severely affected patients, liver transplantation is currently the only cure as this addresses the underlying causative enzyme deficiency, although the organ is otherwise functionally normal
- Combined liver and renal transplantation is often necessary due to end stage renal disease in types 1 and 2
- Renal transplantation without concomitant liver transplantation is associated with a higher rate of transplant failure due to recurrent oxalate induced renal injury (N Engl J Med 2013;369, Int J Nephrol 2011;2011:864580, Curr Rheumatol Rep 2013;15:340)
Microscopic (histologic) description
- Birefringent oxalate crystals in vessel walls and connective tissues of the portal areas of explanted livers and other affected organs (Arch Pathol Lab Med 2002;126:1250)
Molecular / cytogenetics description
- Type 1 demonstrates mutations in the AGXT gene, which encodes for the hepatic peroxismal enzyme alanine: glyoxylate aminotransferase (AGT)
- Type 2 has defects in the GRHPR gene, which encodes for GRHPR enzyme
- Type 3 demonstrates defects in the HOGA1 gene which encodes for the mitochondrial 4-hydroxy-2-oxoglutarate (HOG) aldolase enzyme
- A small subset of patients (~5%) do not have demonstrable mutations in any of these three genes (N Engl J Med 2013;369, Int J Nephrol 2011;2011:864580)
Differential diagnosis
- Causes of secondary hyperoxaluria (Kidney Int 2009;75:1264, World J Nephrol 2015;4:235)
- Chronic inflammatory bowel disease: short bowel syndrome, cystic fibrosis, post bariatric surgery; enhanced oxalate absorption from the GI tract
- Dietary hyperoxaluria: excessive ingestion of foods high in oxalate, megadose vitamin C ingestion (World J Nephrol 2015;4:235)
- Ethylene glycol poisoning (World J Nephrol 2015;4:235)
- Methoxyflurane anesthesia: discontinued from use in North America in late 1970s, still in use in pediatric and trauma settings in Australia (Emerg Med Australas 2009;21:4)
Board review style question #1
- The type of kidney and bladder stones most often encountered in primary hyperoxaluria are
- Calcium stones
- Mixed stones
- Pyruvate stones
- Struvite stones
Board review style answer #1
A. Calcium stones. Oxalate excretion is almost entirely via the kidneys, predominantly as highly insoluble calcium salts.
Comment Here
Reference: Primary hyperoxaluria
Comment Here
Reference: Primary hyperoxaluria
Board review style question #2
- What is the most common genetic mutation and associated abnormal enzyme affecting 80% of patients with primary hyperoxaluria?
- AGXT gene and AGT enzyme
- GRHPR gene and GRHPR enzyme
- HOGA1 gene and HOG aldolase enzyme
Board review style answer #2
A. AGXT gene and AGT (hepatic peroxismal enzyme alanine: glyoxylate aminotransferase)
Comment Here
Reference: Primary hyperoxaluria
Comment Here
Reference: Primary hyperoxaluria
Primary sclerosing cholangitis
Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Primary sclerosing cholangitis (PSC) is a biliary disease causing progressive stricturing of the biliary tree, leading to cirrhosis and possibly cholangiocarcinoma
Essential features
- Etiology unclear
- Patients are at increased risk of developing ulcerative colitis and cholangiocarcinoma
- Liver biopsy rarely samples the classic "onion skin" periductal fibrosis, meaning typical imaging findings are more reliable for establishing the diagnosis
ICD coding
- ICD-10: K83.01 - primary sclerosing cholangitis
Epidemiology
- Incidence of roughly 1 per 100,000 person years (Hepatology 2011;53:1590)
- Rates may be lower in developing countries, though reliable data are lacking
Sites
- Large intrahepatic and extrahepatic biliary tree affected, including gallbladder (J Hepatol 2008;48:598)
Etiology
- Possibly autoimmune, though etiology uncertain overall
- Gut microbiome has been suggested to play a role (Ann Transl Med 2016;4:512, World J Gastroenterol 2020;26:2768)
- Siblings of primary sclerosing cholangitis patients more likely to develop primary sclerosing cholangitis, suggesting a genetic component (Clin Gastroenterol Hepatol 2008;6:939)
Clinical features
- M:F = 2:1
- Usually age 30 - 50; can occur in children (Hepatology 2017;66:518)
- Half asymptomatic at diagnosis
- Symptoms: fatigue, pruritus, jaundice, right upper quadrant pain / tenderness
- Increased risk for bacterial cholangitis and cholangiocarcinoma (Clin Liver Dis 2016;20:67)
- Up to 70% also have inflammatory bowel disease (particularly ulcerative colitis, although fewer than 10% with ulcerative colitis have primary sclerosing cholangitis) (Gut Liver 2018;12:17)
- Patients may also have an overlap syndrome with autoimmune hepatitis (J Hepatol 2011;54:374)
Diagnosis
- Firm diagnostic criteria do not exist
- British Society of Gastroenterology recently offered extensive PSC diagnosis guidelines (Gut 2019;68:1356)
- Diagnosis generally established by cholestatic lab findings combined with bile duct stricturing on imaging (Lancet 2018;391:2547)
- Liver biopsy useful to rule out other possibilities but generally cannot establish the diagnosis
Laboratory
- Elevated alkaline phosphatase; variable bilirubin
- Many patients are pANCA positive, though this is nonspecific and serology is not helpful in general (World J Gastroenterol 2008;14:3781)
- Usually negative antimitochondrial antibody
Radiology description
- Multifocal bile duct strictures causing a "beads on a string" appearance on magnetic resonance cholangiography and endoscopic retrograde cholangiopancreatography (J Hepatol 2017;66:1265)
- Patients without such imaging findings who otherwise appear to have primary sclerosing cholangitis may have small duct primary sclerosing cholangitis (Gastroenterology 2008;134:975)
Radiology images
Prognostic factors
- Small duct primary sclerosing cholangitis has a better outcome than typical primary sclerosing cholangitis (Gut 2002;51:731)
- Anti-GP2 IgA autoantibodies reportedly indicate poor prognosis (Gut 2017;66:137)
Case reports
- 26 year old man with primary sclerosing cholangitis and ulcerative colitis with low grade dysplasia (J Crohns Colitis 2013;7:e61)
- 33 year old man with primary sclerosing cholangitis and Crohn's disease (Intern Med 2012;51:2077)
- 84 year old woman with primary sclerosing cholangitis and CREST syndrome (J Med Case Rep 2015;9:272)
- 2 patients with overlap between primary sclerosing cholangitis and primary biliary cholangitis (Dig Liver Dis 2015;47:432)
Treatment
- Ursodeoxycholic acid can improve lab values but does not halt disease progression (Lancet Gastroenterol Hepatol 2016;1:68)
- Obeticholic acid also emerging as a treatment (J Hepatol 2020;73:94)
- Only truly effective treatment is liver transplantation, though disease recurs in 33% of patients (Hum Pathol 2003;34:1127)
Gross description
- Alternating fibrosis / stenosis and ectasia of bile ducts, with bile sludge and calculi
- Liver may be distorted or cirrhotic
Microscopic (histologic) description
- Classic finding is "onion skin" fibrosis around affected medium sized bile ducts; smaller ducts rarely affected (except in small duct primary sclerosing cholangitis), meaning biopsy sampling rarely demonstrates this finding
- Progressive atrophy of bile duct epithelium and obliteration of the lumen, leaving a fibrous scar
- Ductular reaction and cholestasis may occur
- Inflammatory infiltrate is typically mild and limited to biliary epithelium and portal tracts, though largest ducts may show increased infiltrate
- Extravasated bile may elicit xanthomatous or granulomatous response
- Portal edema and fibrosis may be seen secondary to obstruction of larger ducts
- Primary sclerosing cholangitis cirrhosis shows the typical biliary jigsaw pattern
- Cholangiocarcinoma may occur in primary sclerosing cholangitis, preceded by intestinal metaplasia and biliary intraepithelial neoplasia (Am J Surg Pathol 2010;34:27)
- Several staging systems exist, with the Ludwig system the most commonly used (Hepatology 2017;65:907):
- Cholangitis / portal hepatitis
- Periportal fibrosis or periportal hepatitis
- Bridging fibrosis or necrosis
- Cirrhosis
Microscopic (histologic) images
Sample pathology report
- Liver, biopsy:
- Liver parenchyma with ductular reaction, bile duct distortion with focal inflammation and minimal portal chronic inflammation (see comment)
- Comment: The reported finding of bile duct stricturing on magnetic resonance cholangiopancreatography is noted. While the histologic findings are not specific, they are compatible with primary sclerosing cholangitis. A trichrome stain shows no significant fibrosis.
Differential diagnosis
- Cholangiocarcinoma:
- May have similar radiologic findings
- Primary biliary cholangitis:
- Florid duct lesions, more prominent inflammation
- Secondary sclerosing cholangitis:
- Due to stones, prior surgery
- "Onion skin" fibrosis and inflammation often more diffuse
- Duct obstruction:
- May occur due to primary sclerosing cholangitis or other causes
- Pure duct obstruction often has early cholestasis
- IgG4 related sclerosing cholangitis:
- More prominent inflammation, with numerous