- T3: mucosal disease
- T4a: moderately advanced local disease - tumor involving deep soft tissue, cartilage, bone or overlying skin
- T4b: very advanced local disease - tumor involving brain, dura, skull base, lower cranial nerves (IX, X, XI, XII), masticator space, carotid artery, prevertebral space or mediastinal structures
Superpage
Superpage Topics
Acinic cell carcinoma
Actinic cheilitis
Adenoid cystic carcinoma
Adenomatoid hyperplasia of minor glands
Adult type rhabdomyoma
Amalgam tattoo
Anatomy & histology
Aphthous ulcers
Caliber persistent artery (pending)
Carcinoma cuniculatum (pending)
Choristoma
Chronic ulcerative stomatitis (pending)
Congenital epulis of newborn
Dermoid / epidermoid cyst
Duplication cyst
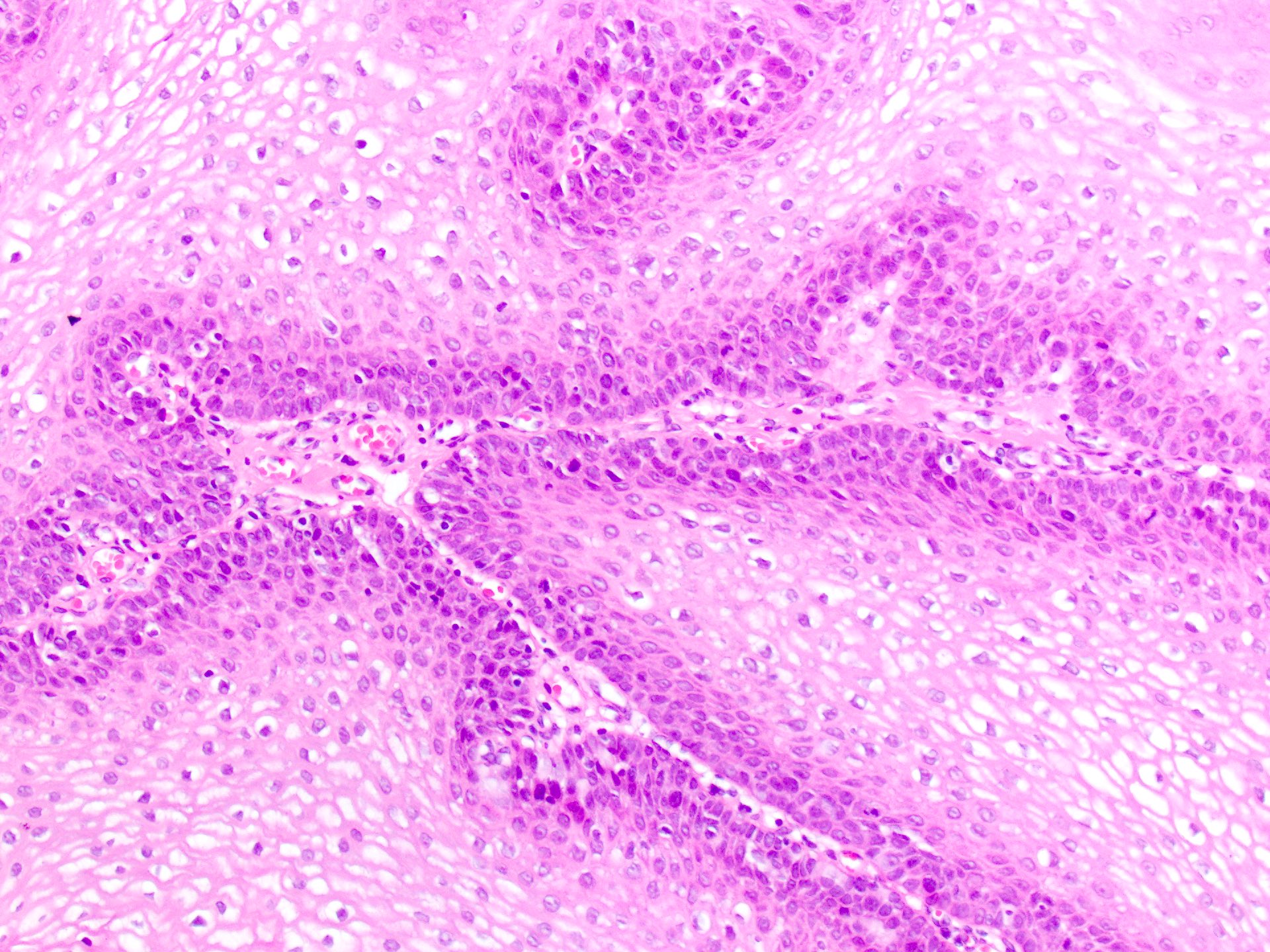
Dysplasia
Ectomesenchymal chondromyxoid tumor
Ephelis
Erythema multiforme
Fordyce granules
Frictional keratosis (pending)
Geographic tongue
Giant cell fibroma
Gingival hyperplasia
Granulomatous inflammation
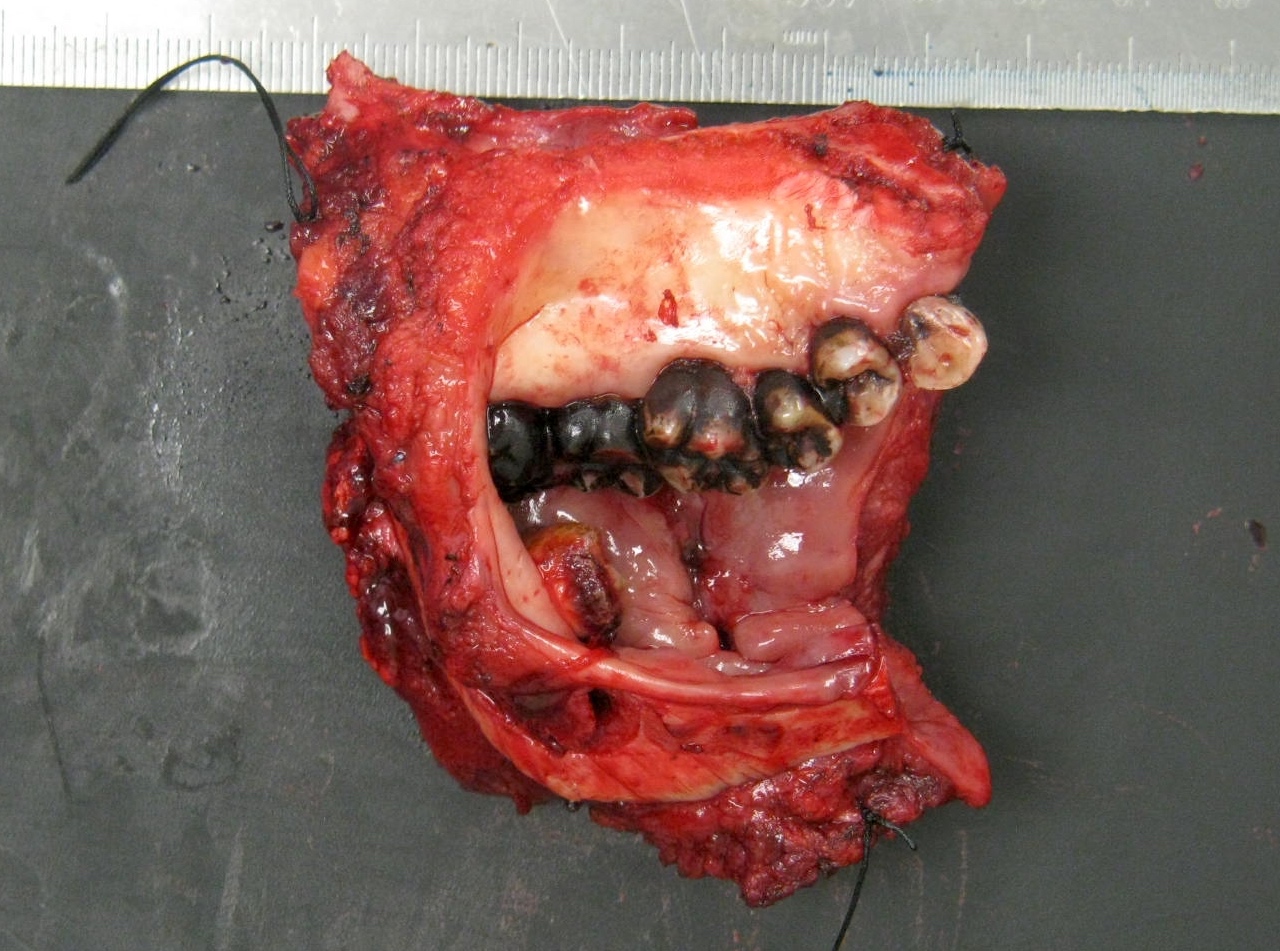
Grossing & features to report
Hairy tongue
Hereditary benign intraepithelial dyskeratosis (pending)
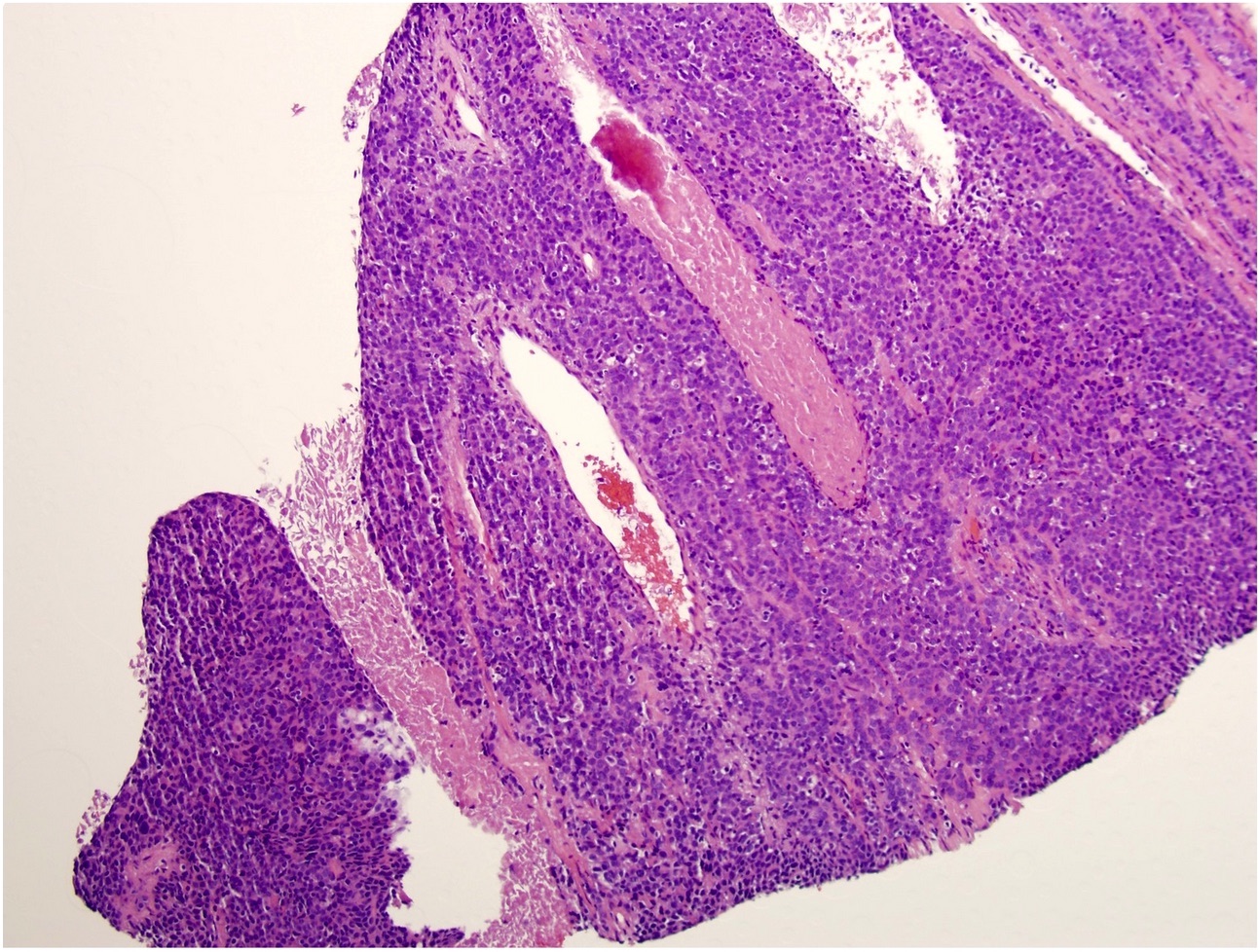
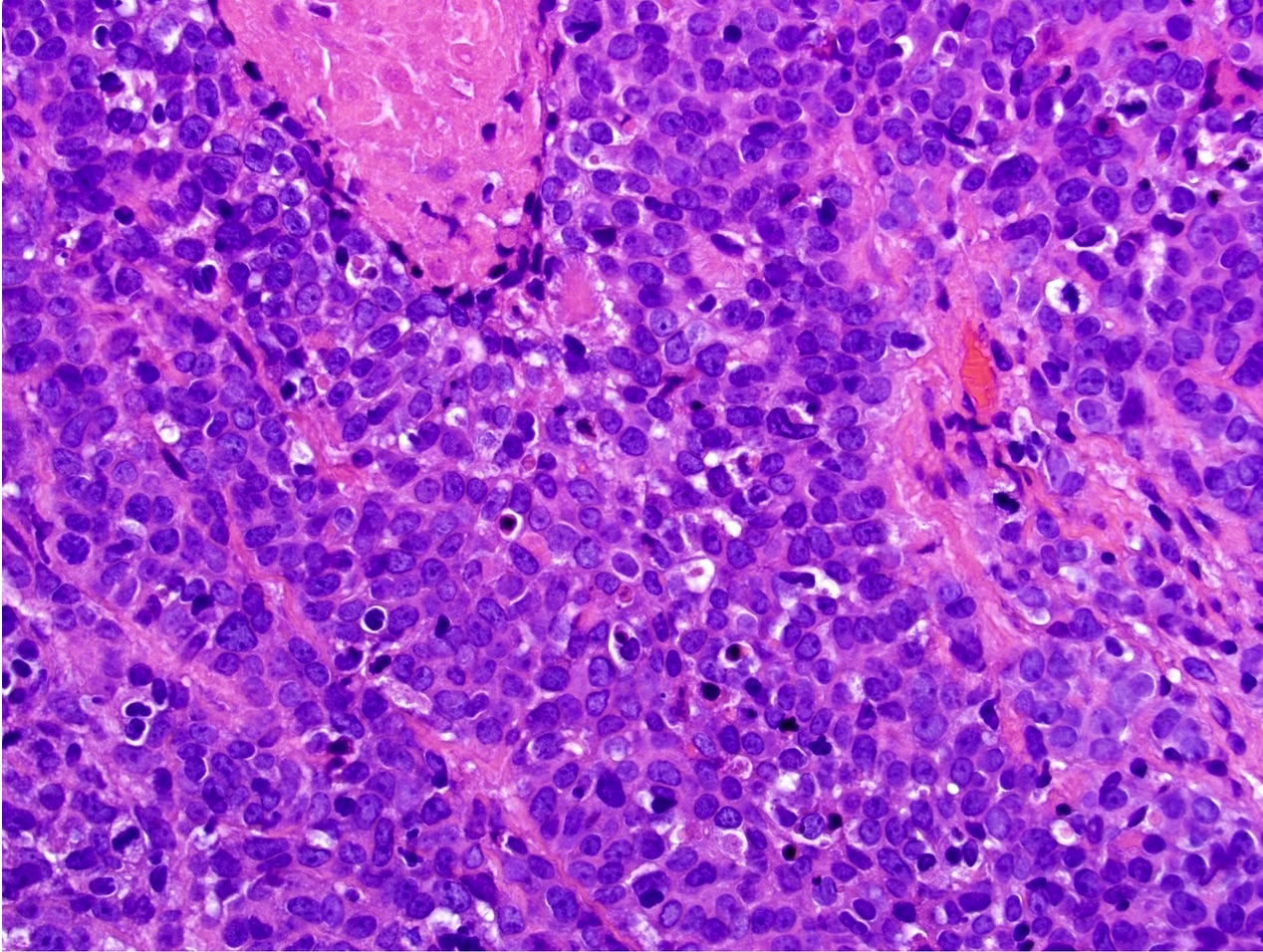
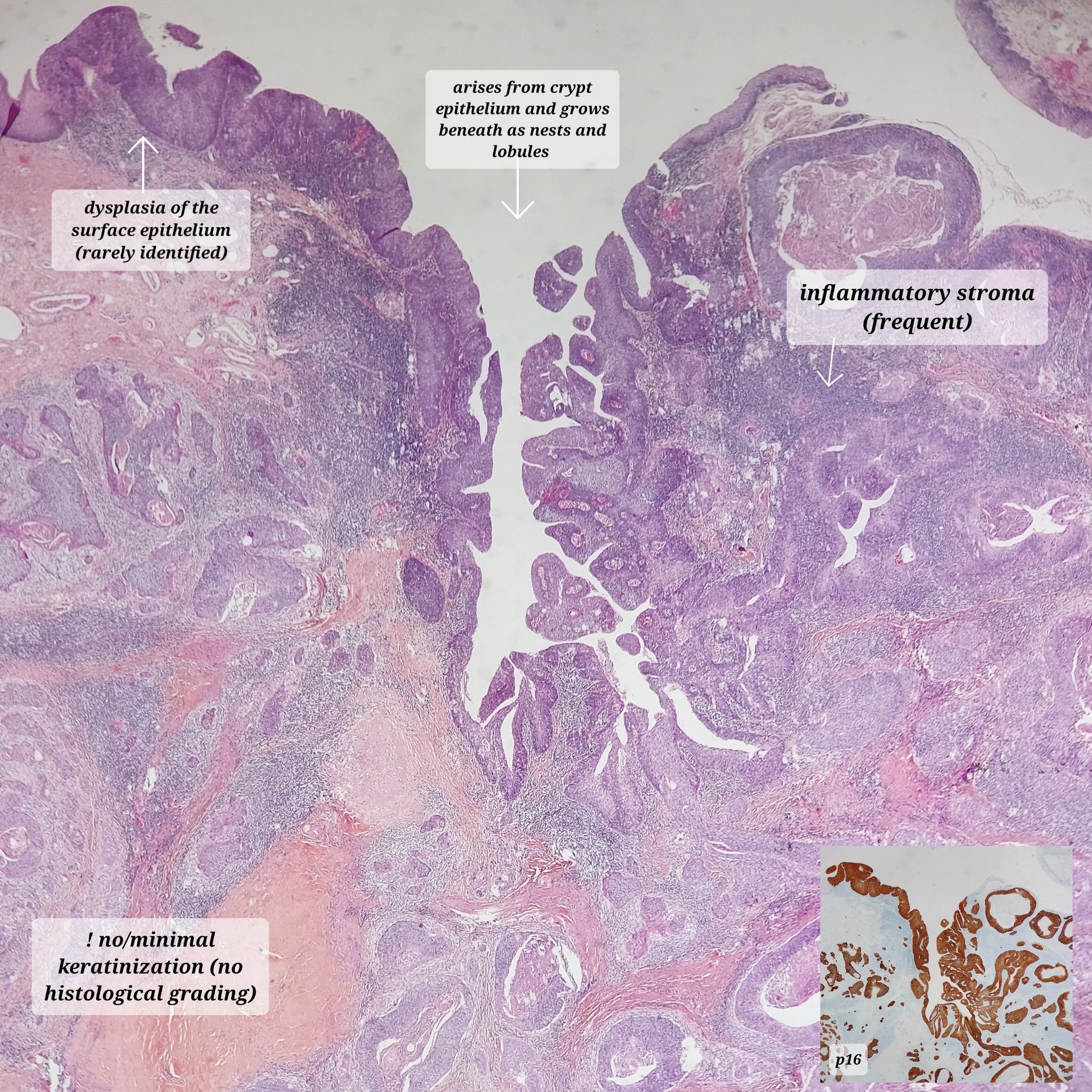
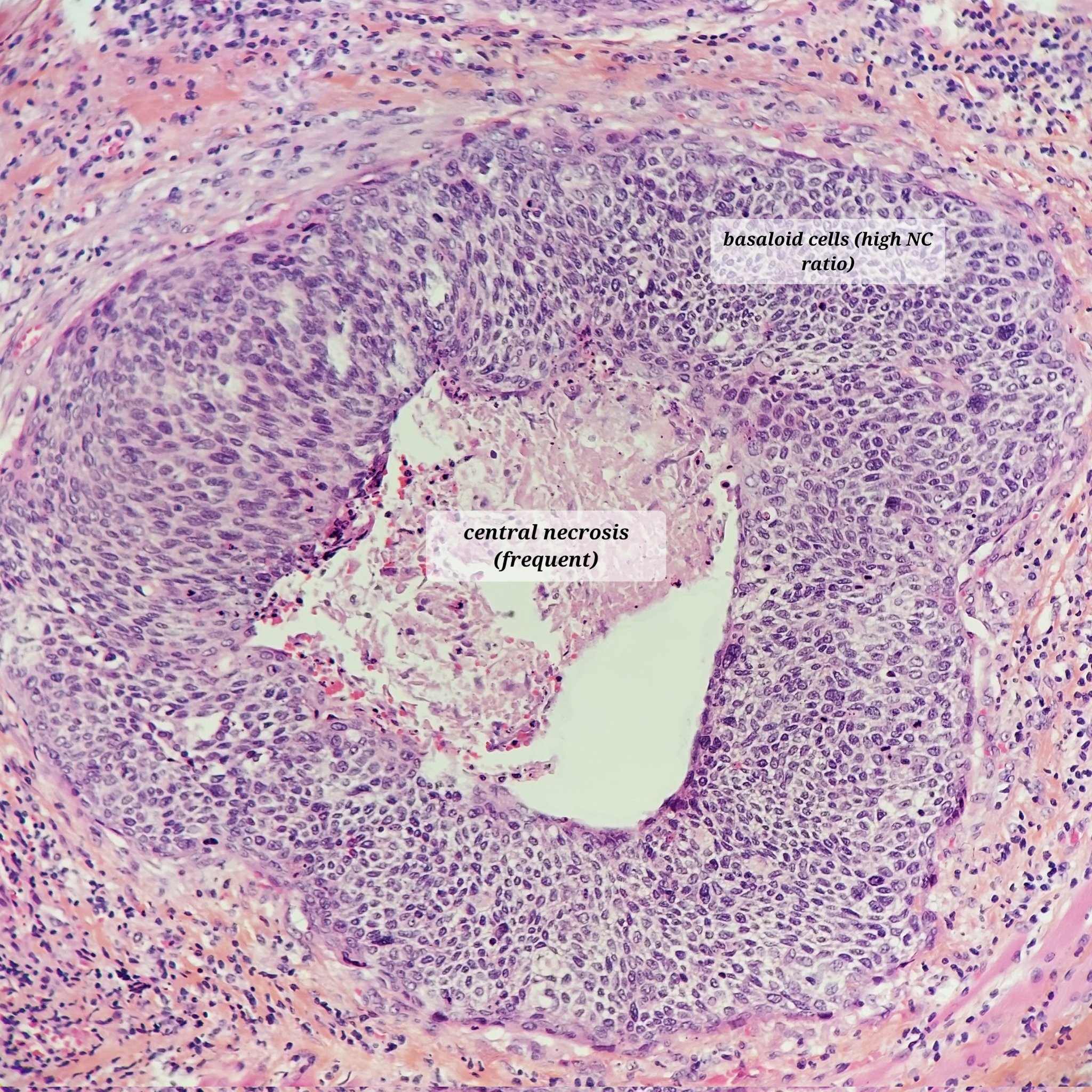
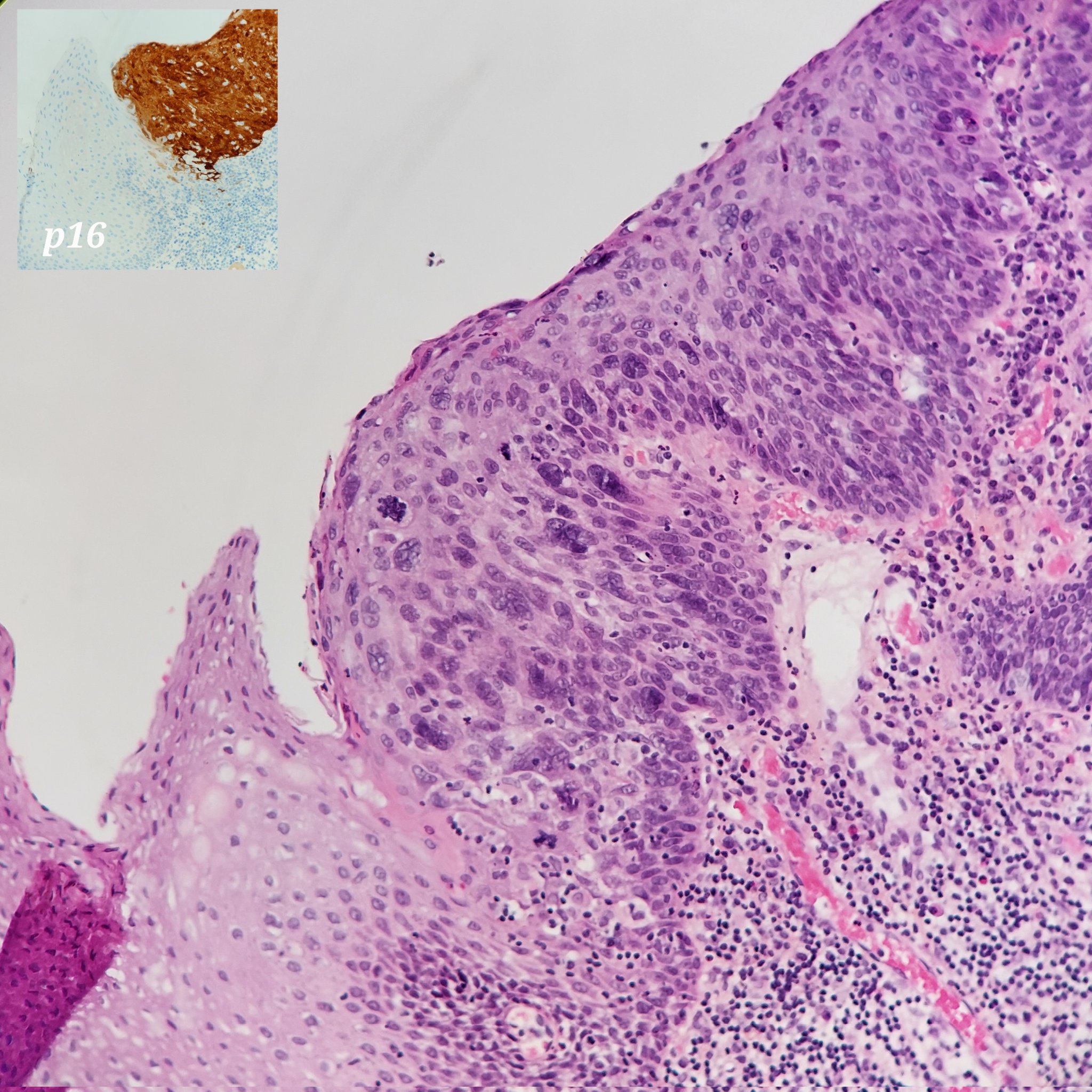
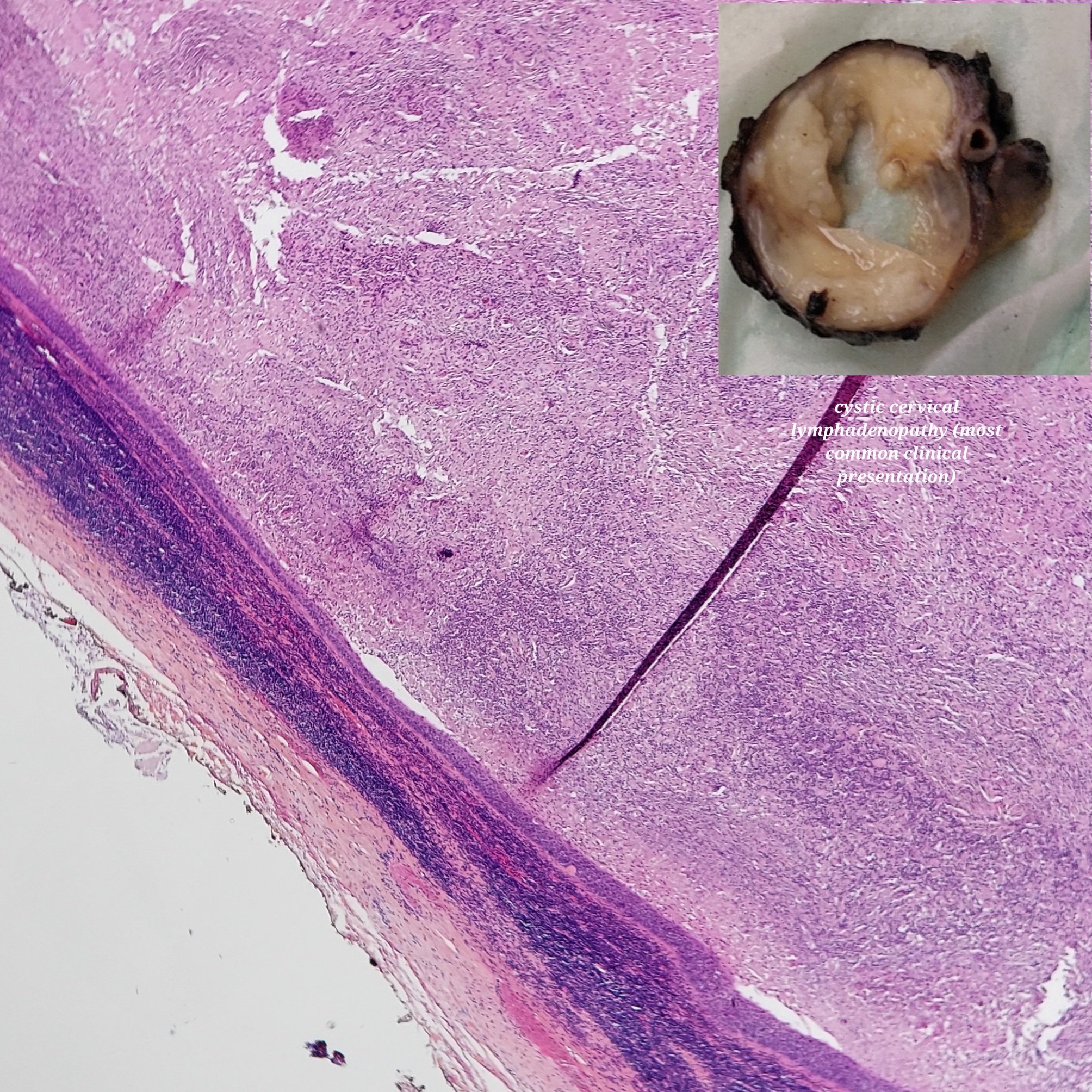
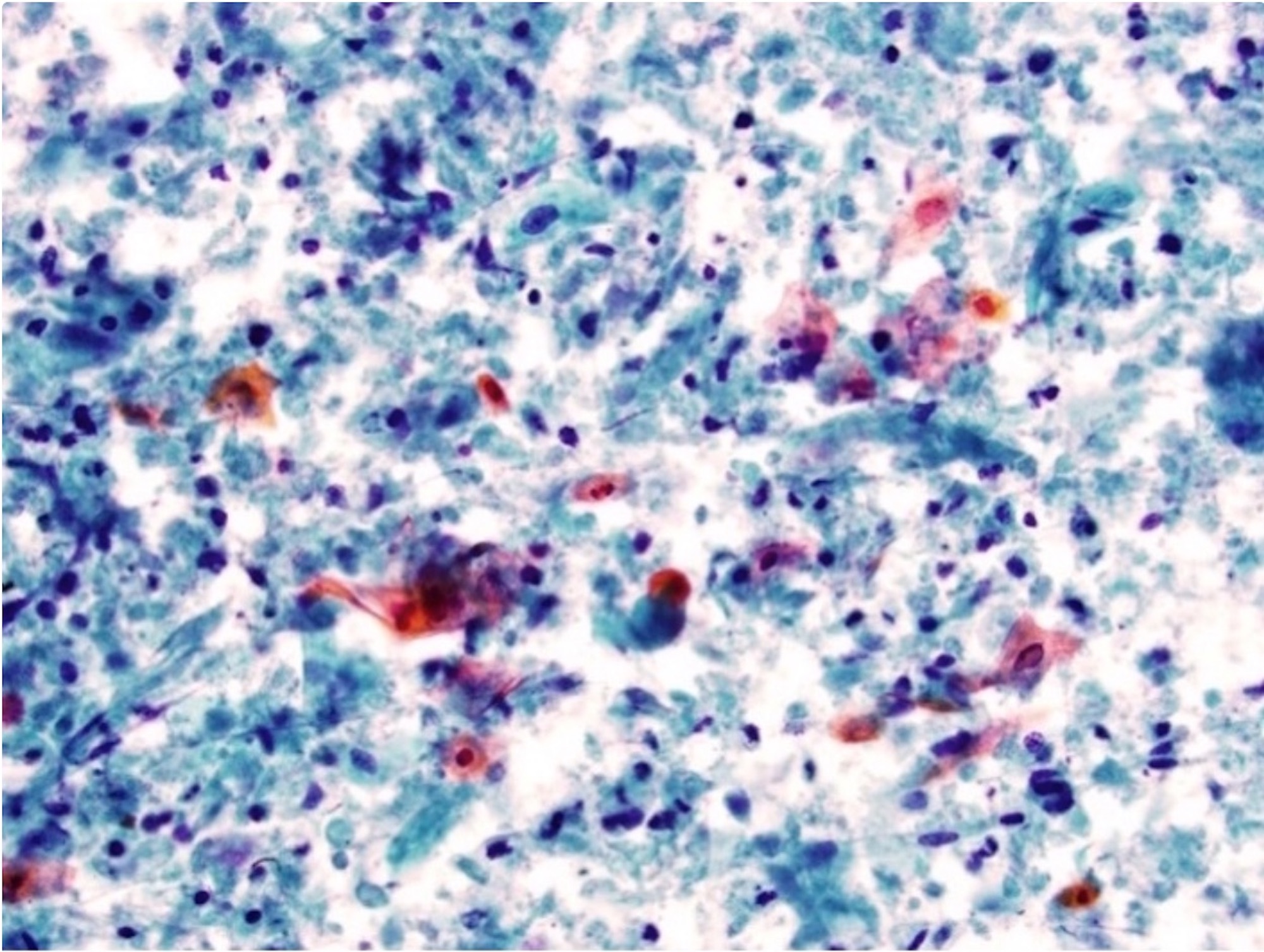
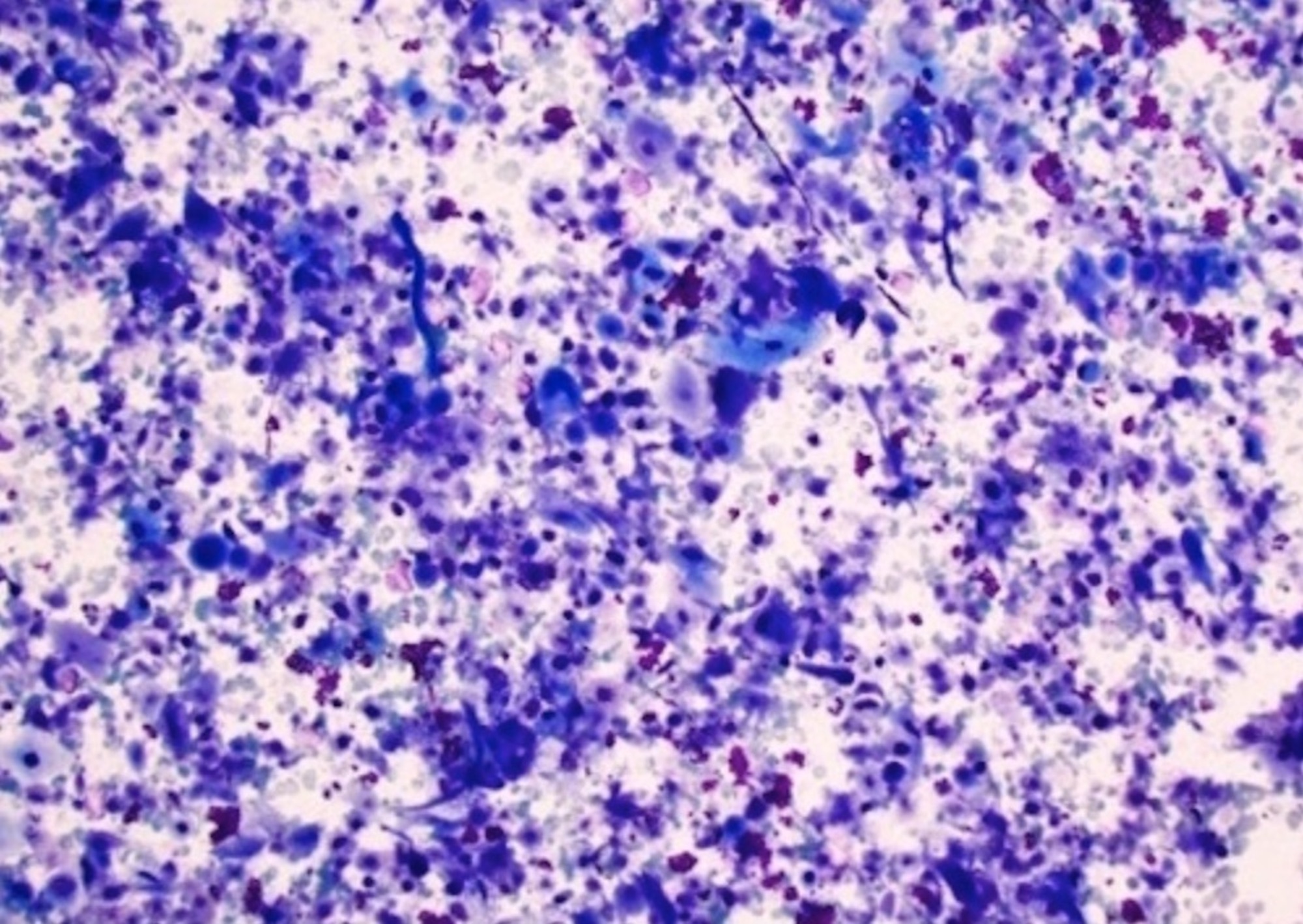
HPV associated
HPV independent
Infections-general
Inflammatory fibrous hyperplasia (pending)
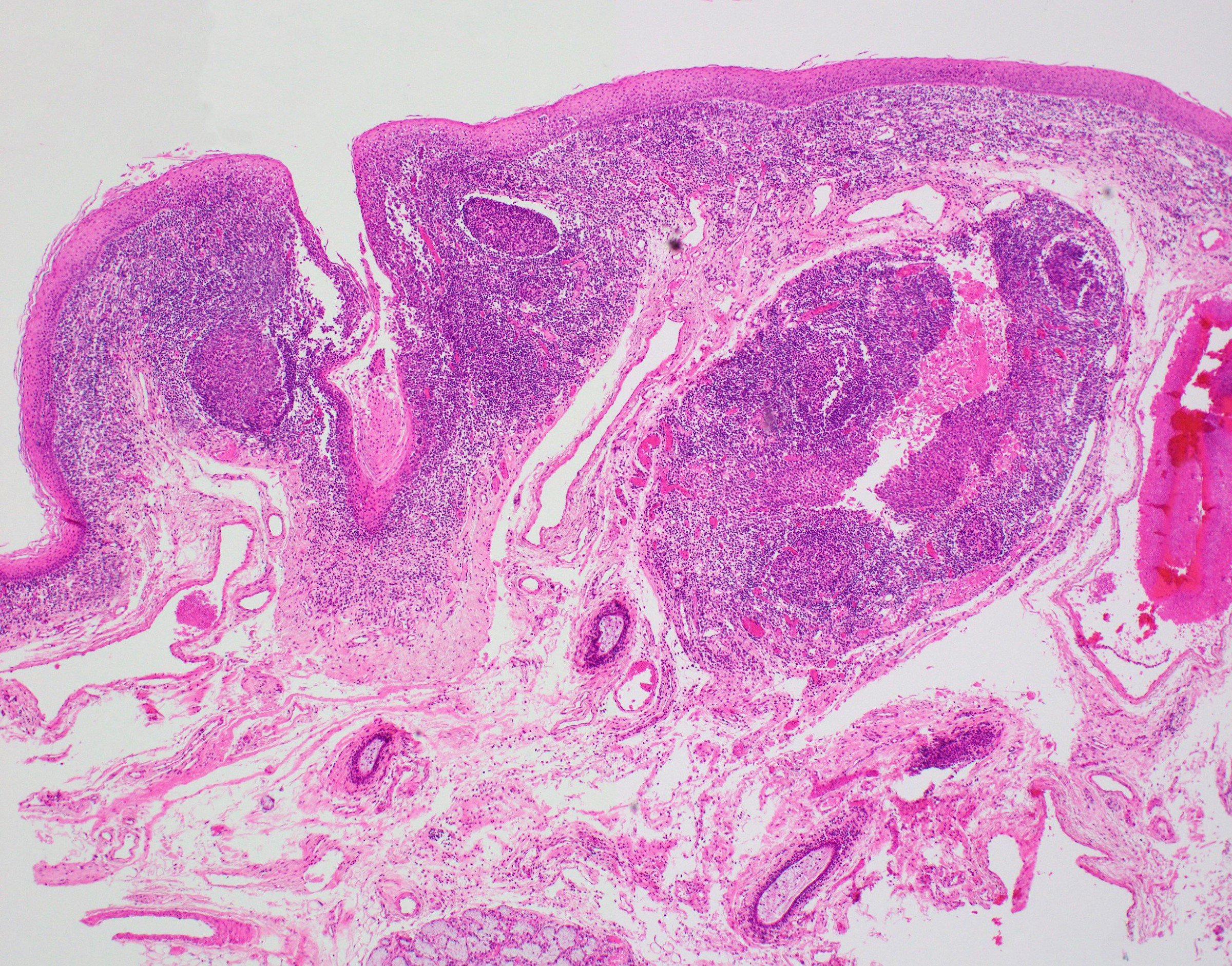
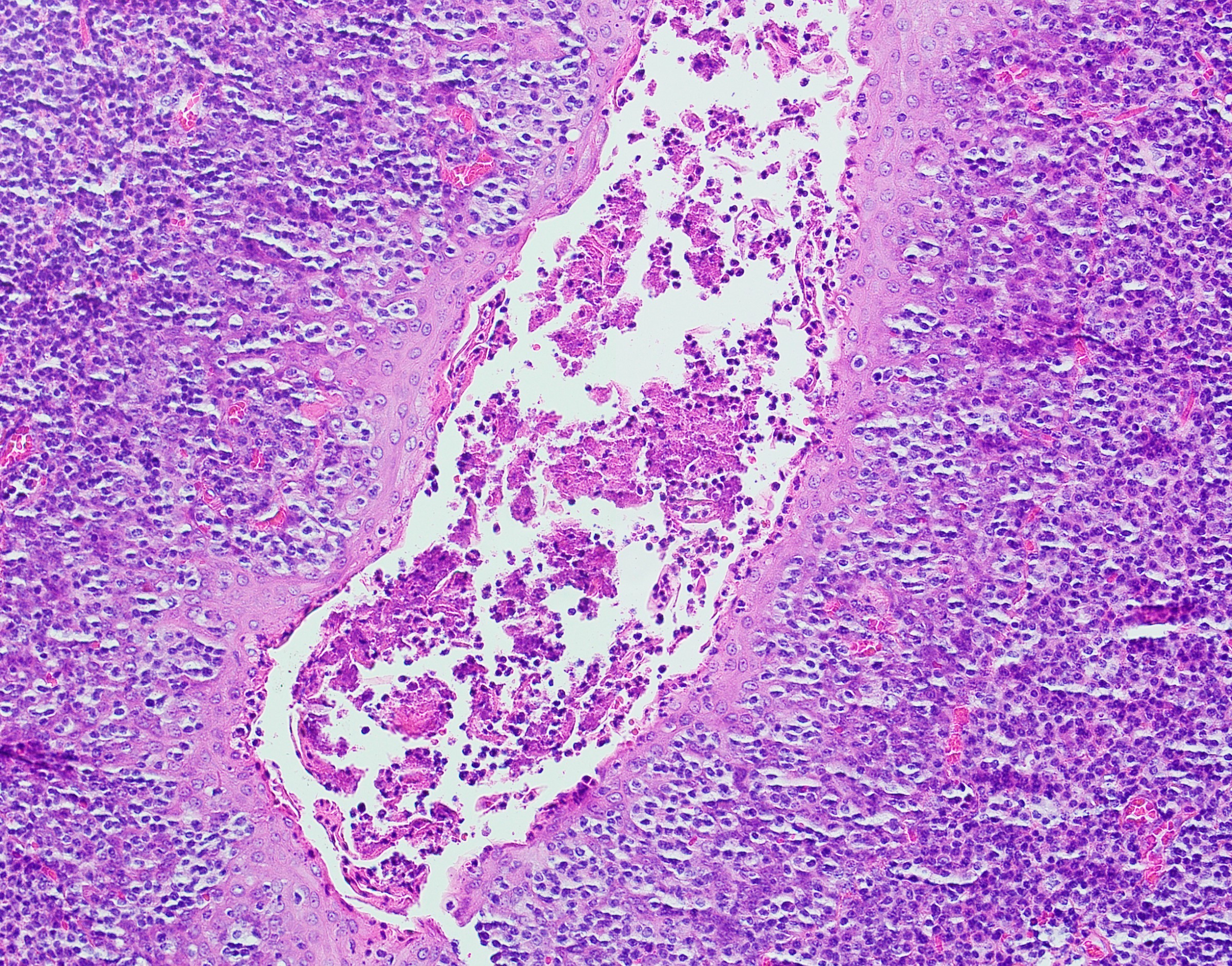
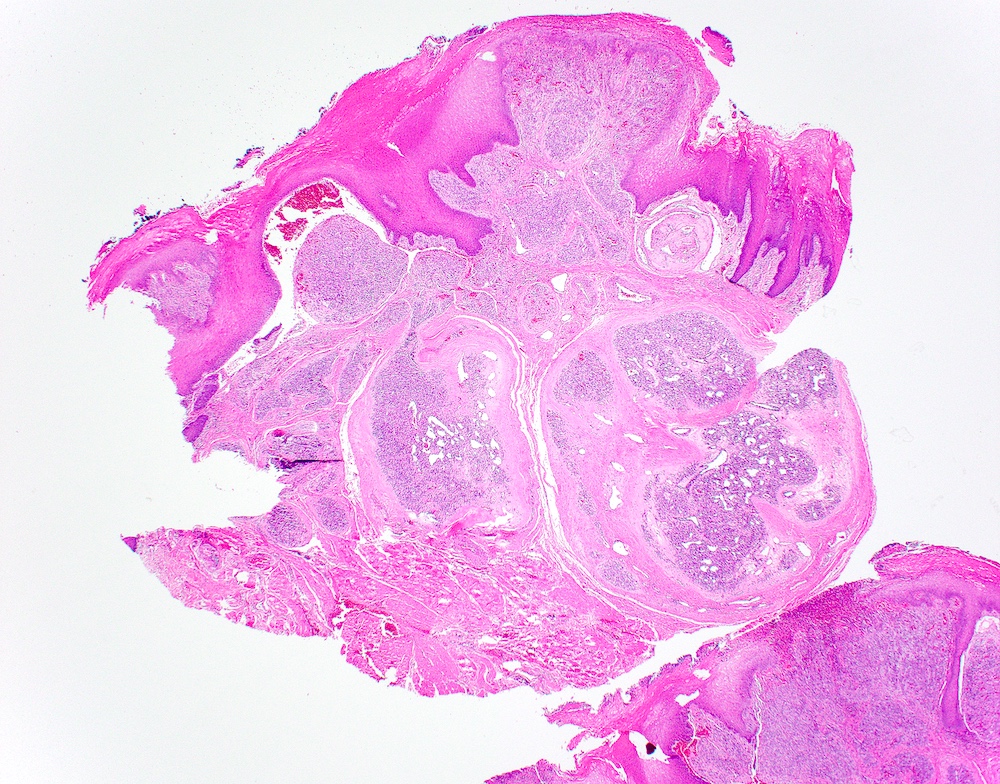
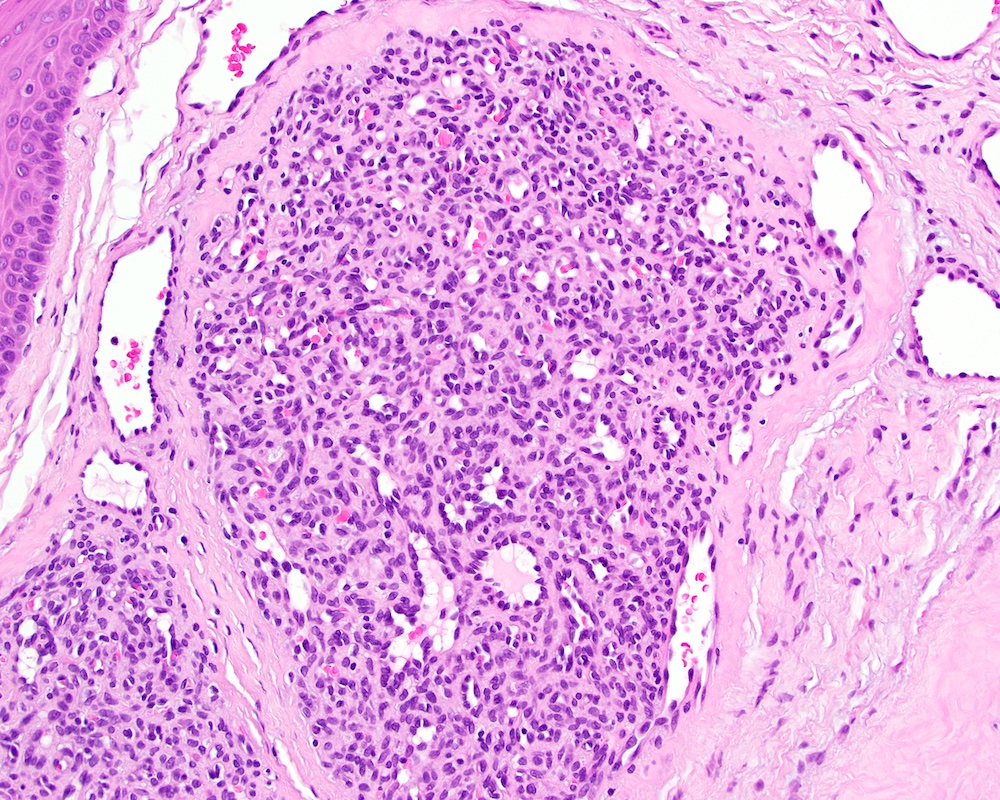
Inflammatory papillary hyperplasia
Irritation fibroma
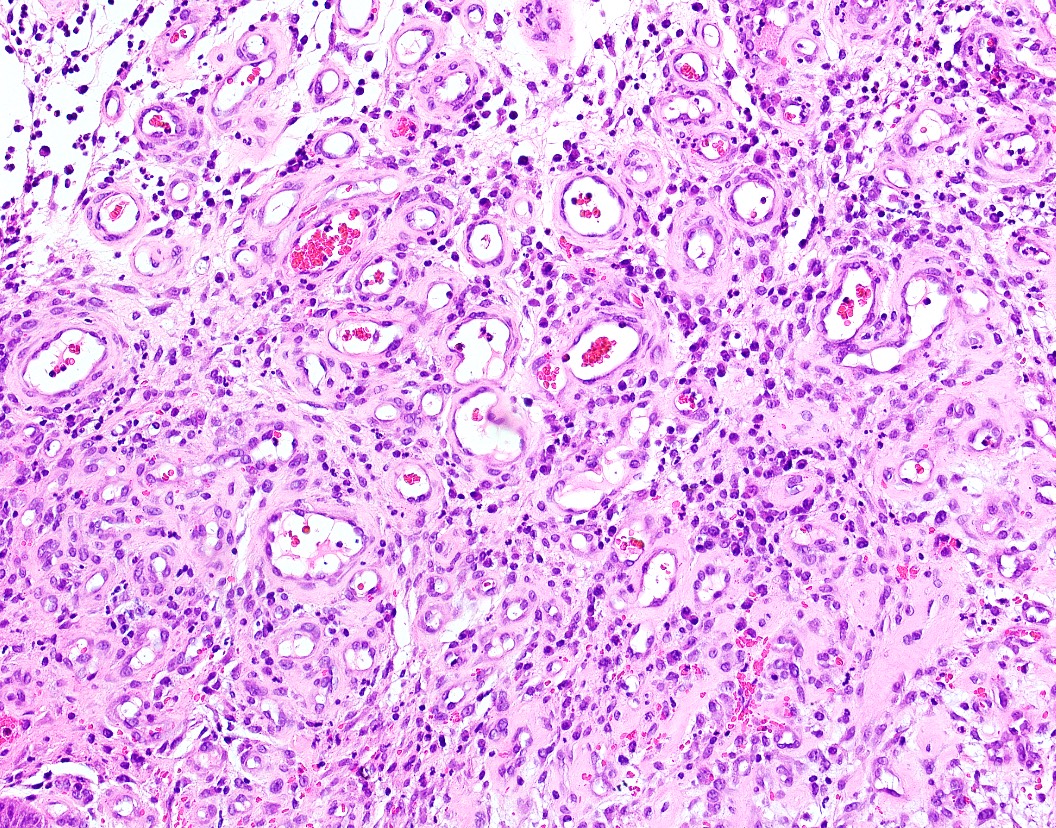
Kaposi sarcoma
Leukoedema (pending)
Leukoplakia
Lichen planus
Lingual thyroid
Lingual tonsil
Low grade myofibroblastic sarcoma
Lymphoepithelial cyst
Median rhomboid glossitis
Melanotic neuroectodermal tumor of infancy (pending)
Melanotic pigmentation
Melkersson-Rosenthal syndrome
Mucocele
Mucoepidermoid carcinoma
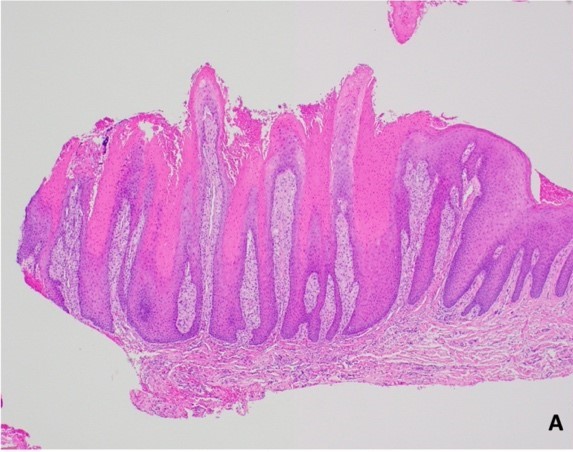
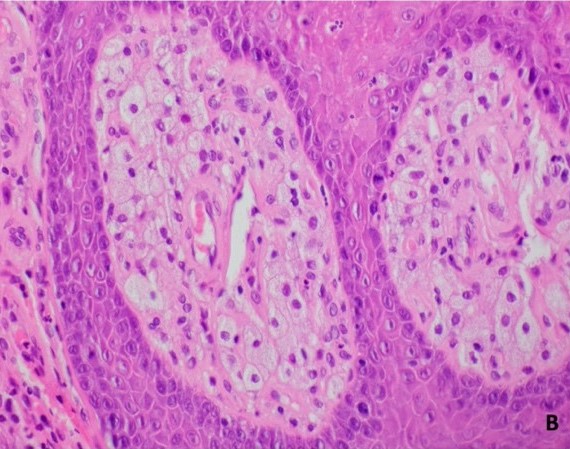
Multifocal epithelial hyperplasia
Nasolabial cyst
Necrotizing sialometaplasia
Nicotine stomatitis (pending)
Oral focal mucinosis (pending)
Oral hairy leukoplakia
Oral mucosal melanoma
Oral mucosal neuroma (pending)
Oral submucosal fibrosis
Oropharnygeal neuroendocrine carcinoma (pending)
Paraneoplastic pemphigus (pending)
Parulis
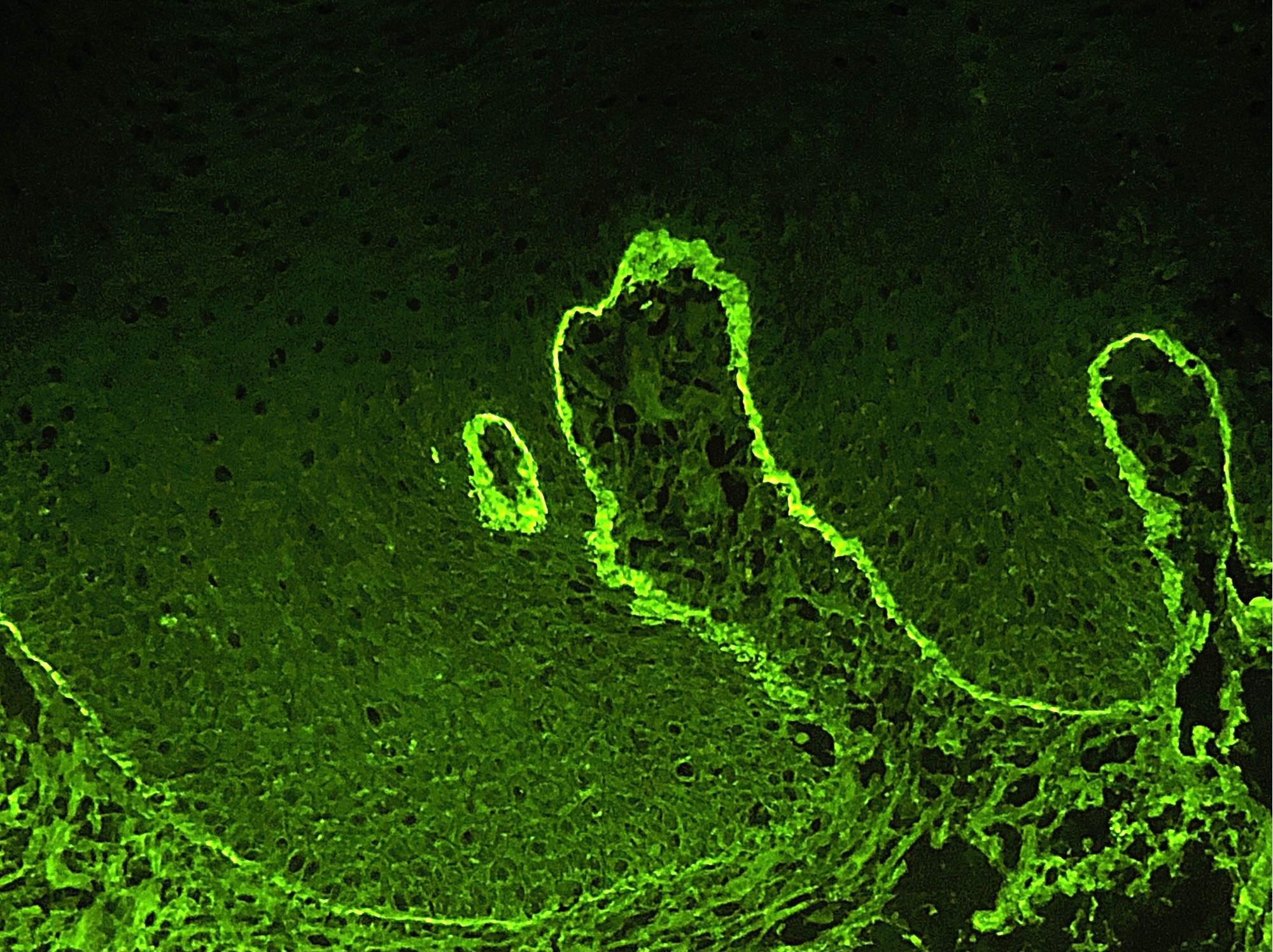
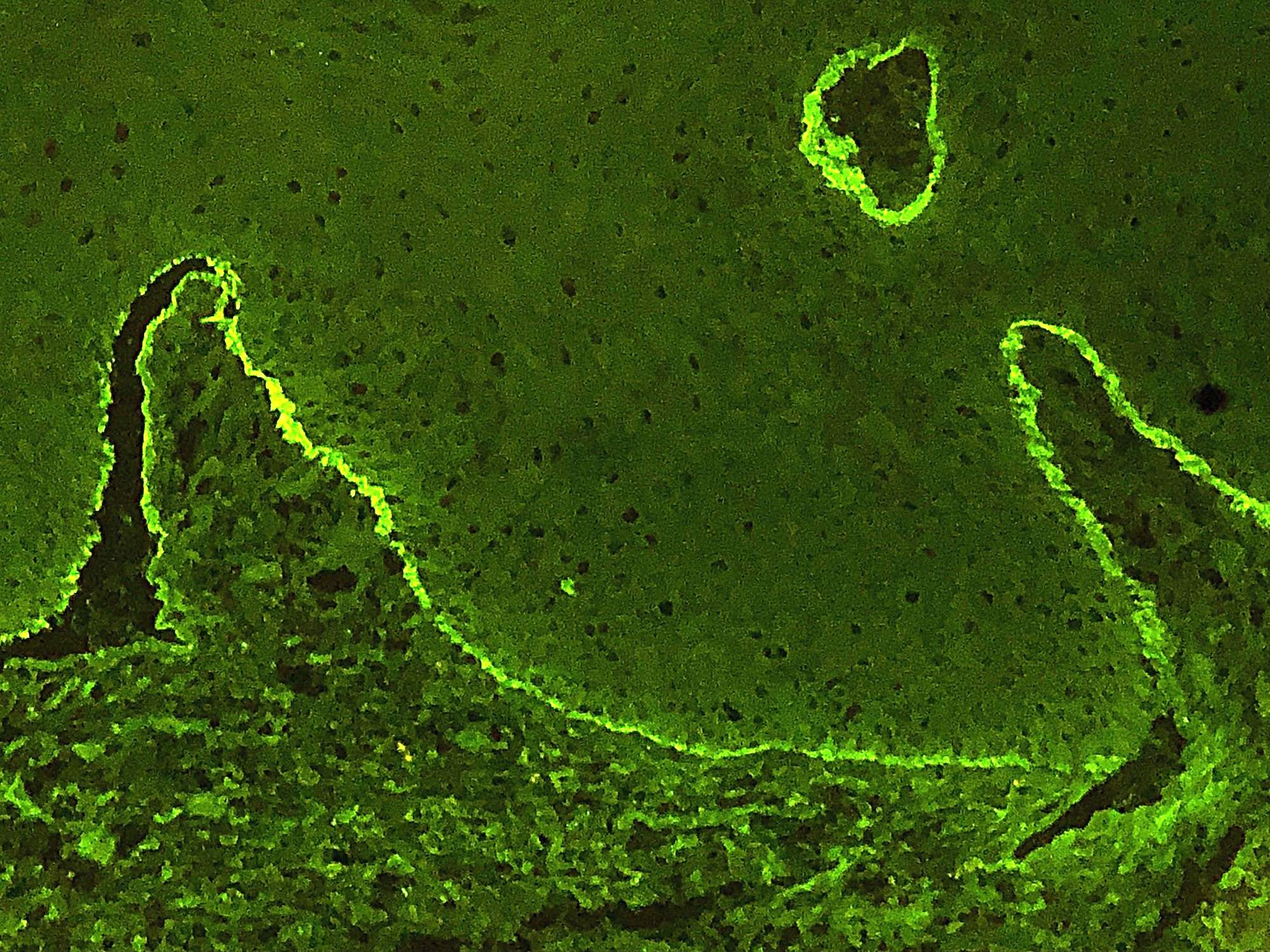
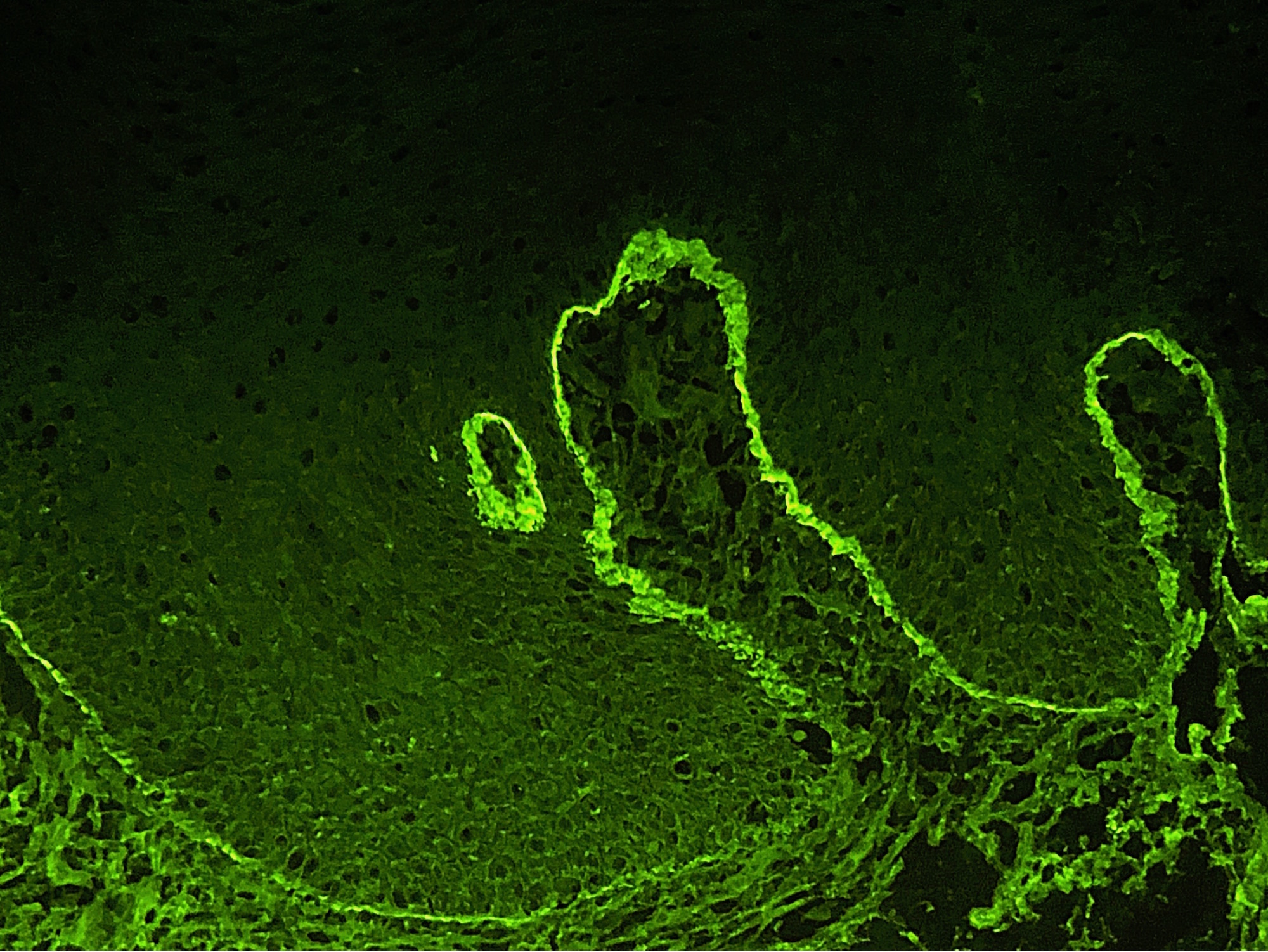
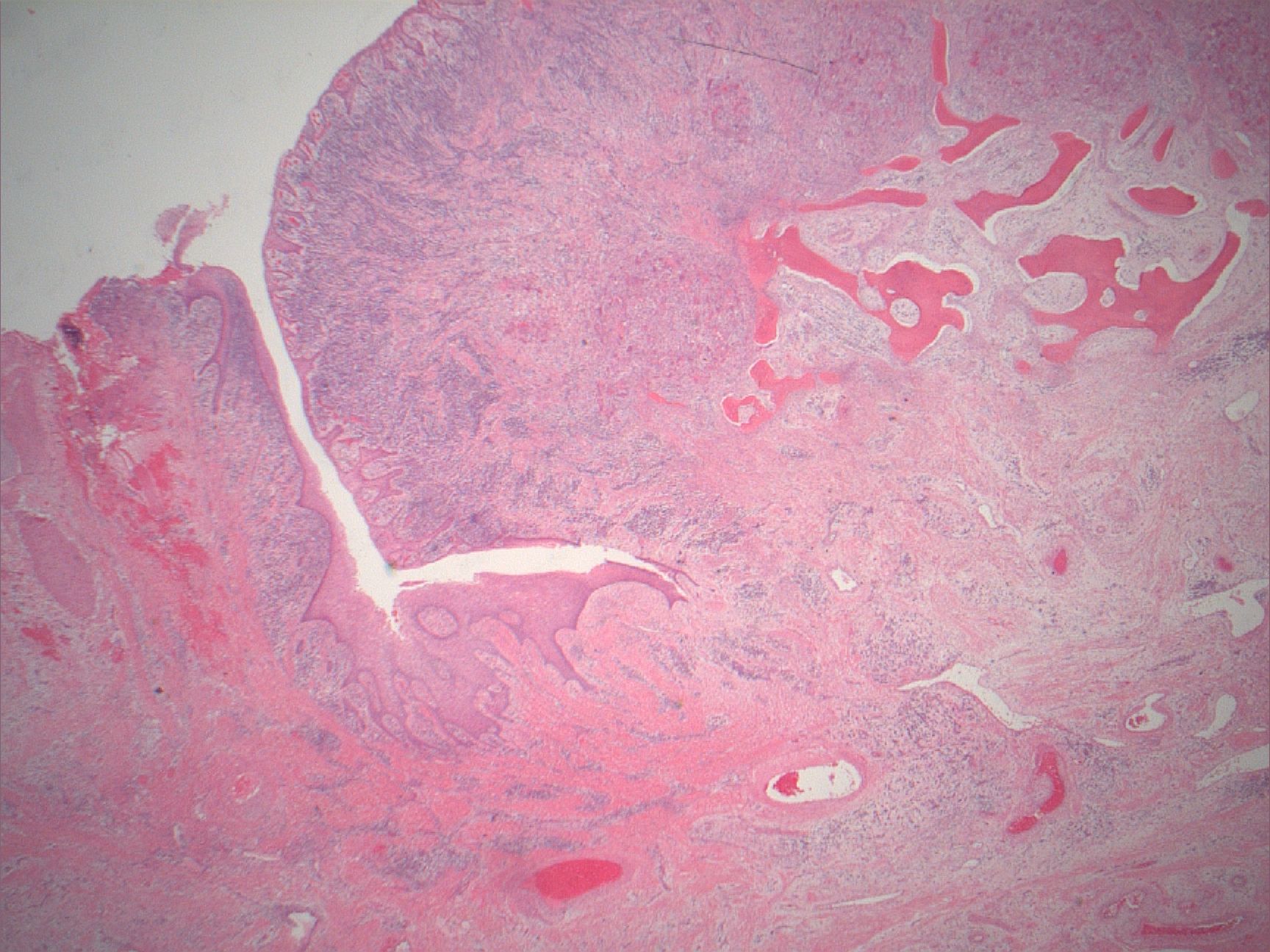
Pemphigoid
Pemphigus vulgaris
Peripheral giant cell granuloma
Peripheral ossifying fibroma
Plasma cell gingivitis
Plasma cell gingivitis (pending)
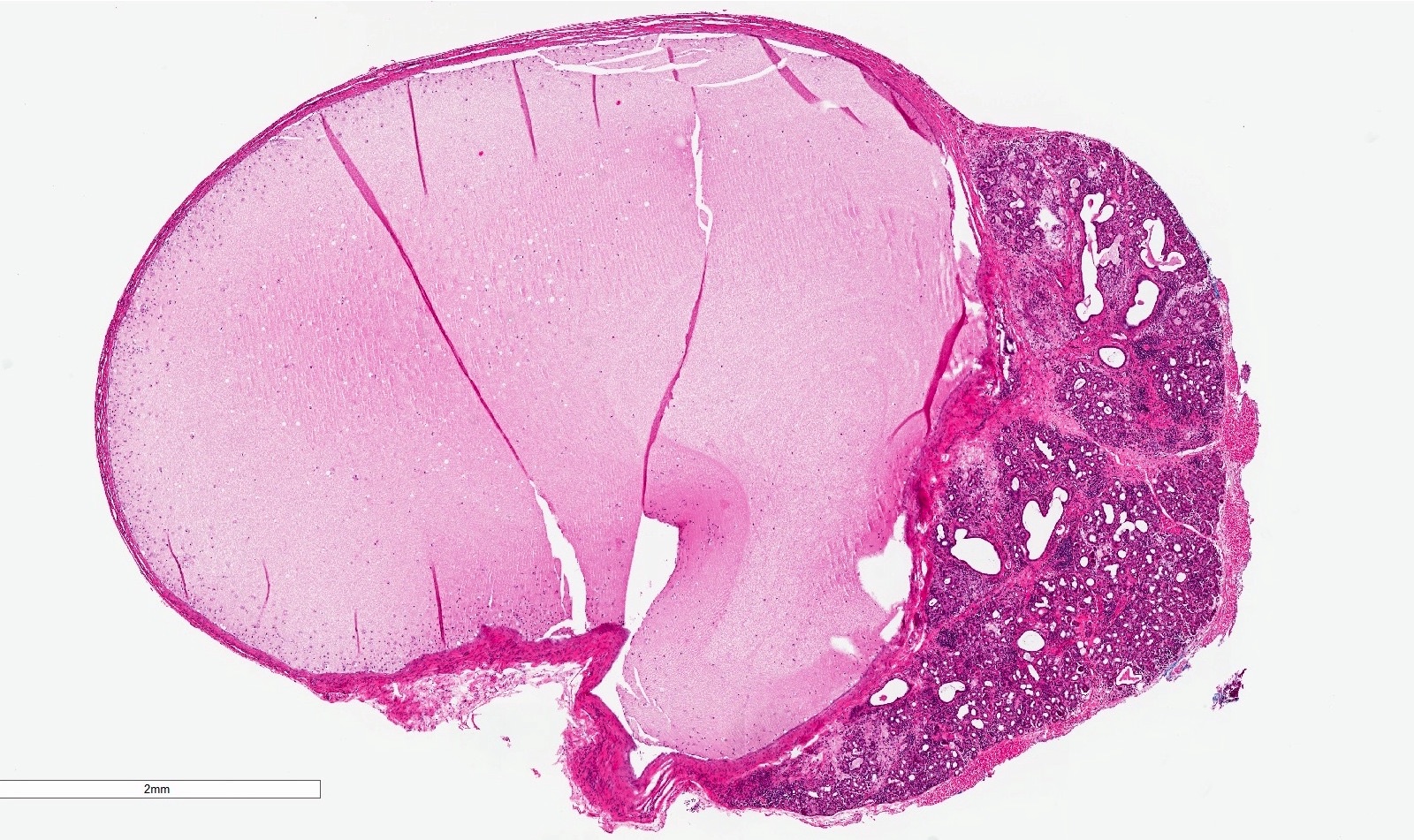
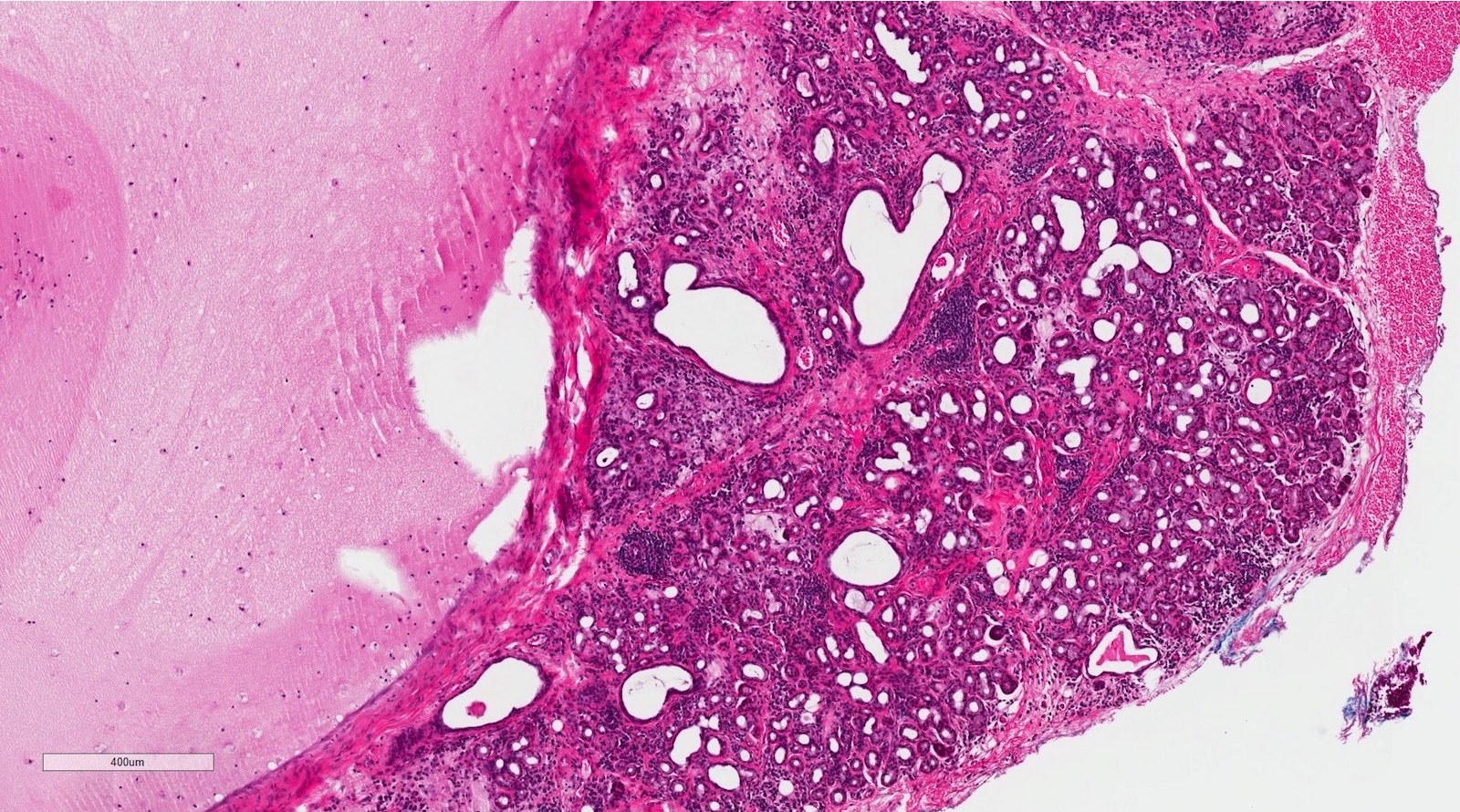
Pleomorphic adenoma
Polymorphous adenocarcinoma
Primary mucosal CD30 positive T cell lymphoproliferative disorder (pending)
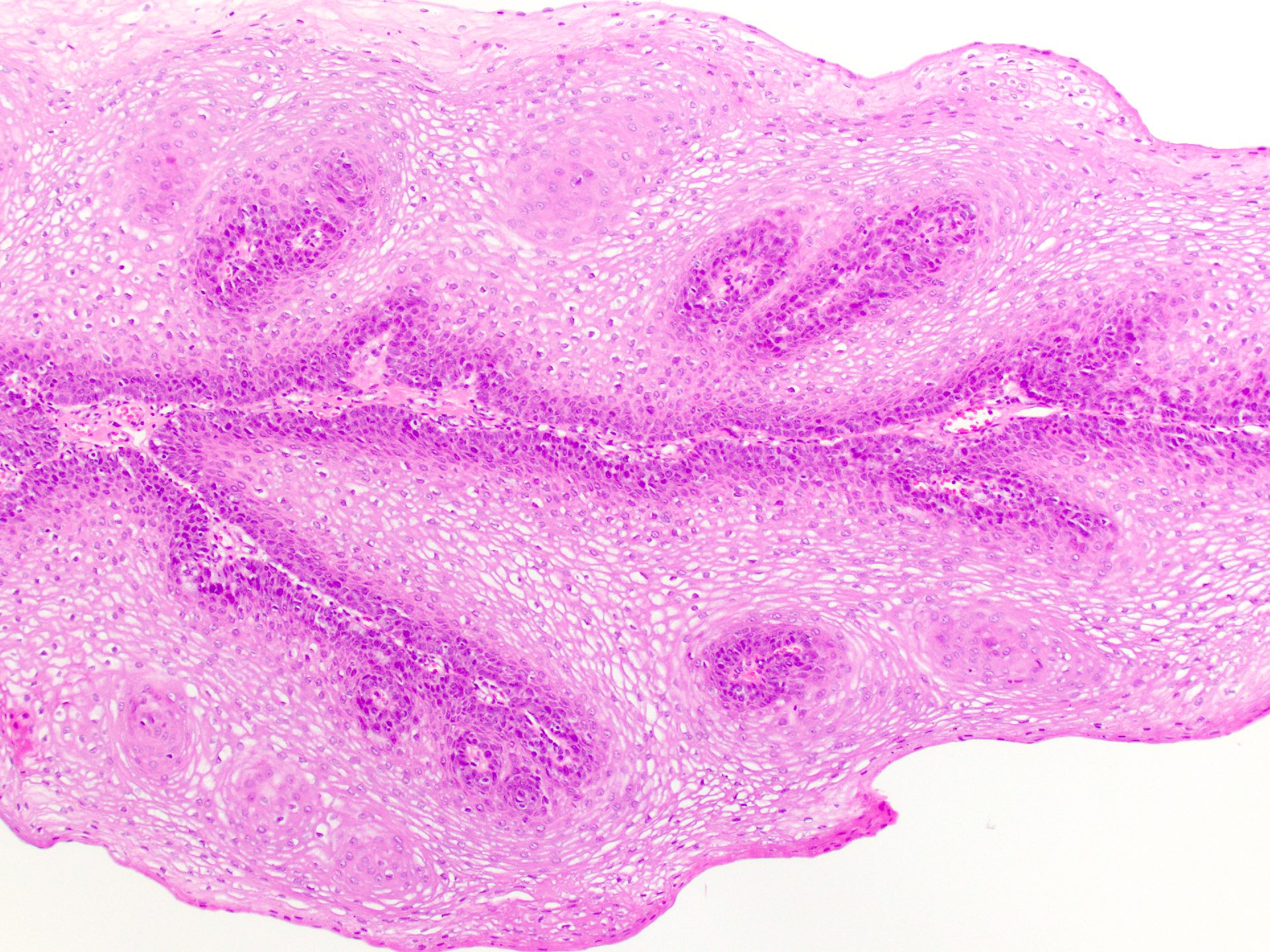
Proliferative verrucous leukoplakia (PVL)
Pseudoepitheliomatous hyperplasia
Pyogenic granuloma
Pyostomatitis vegetans (pending)
Salivary duct cyst
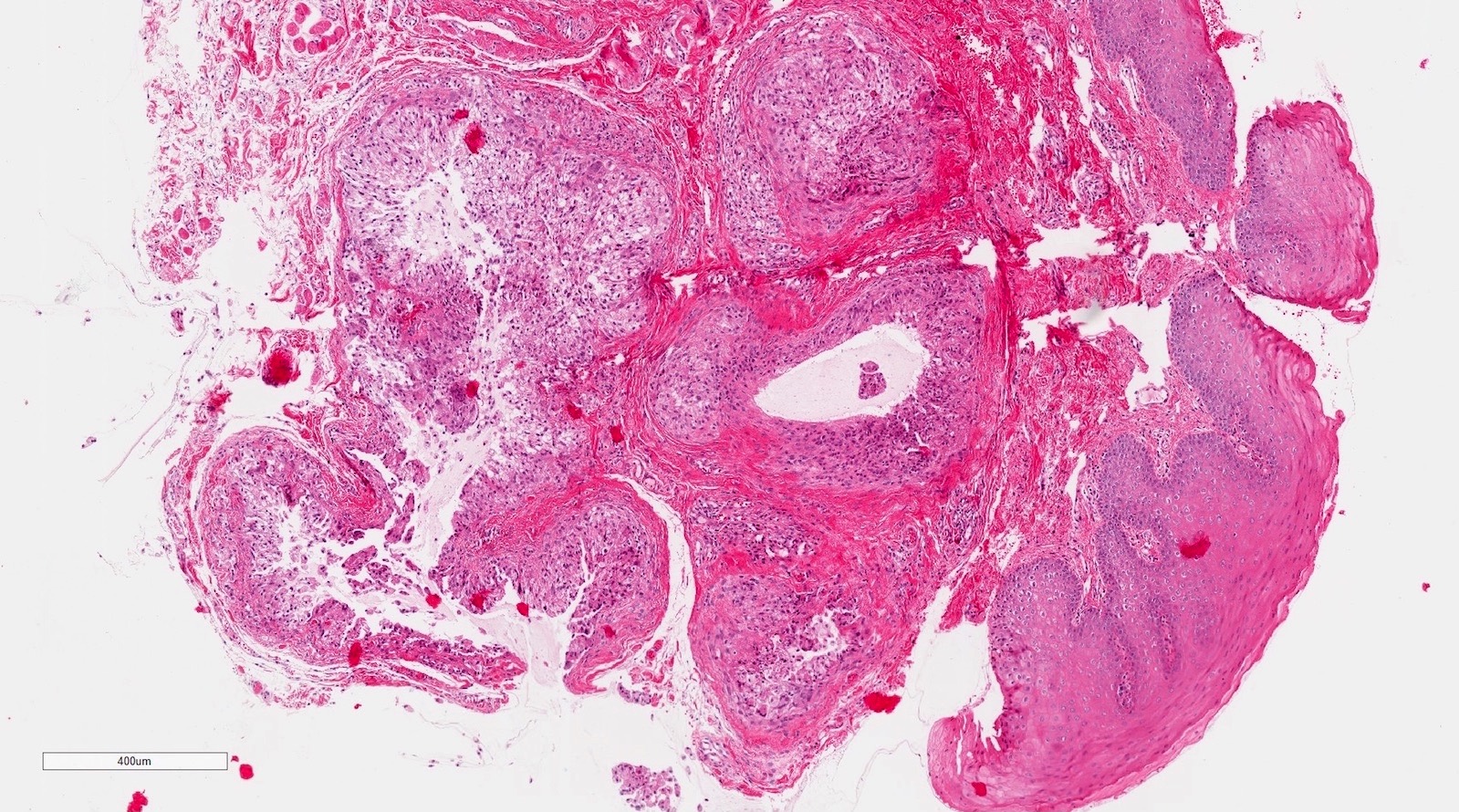
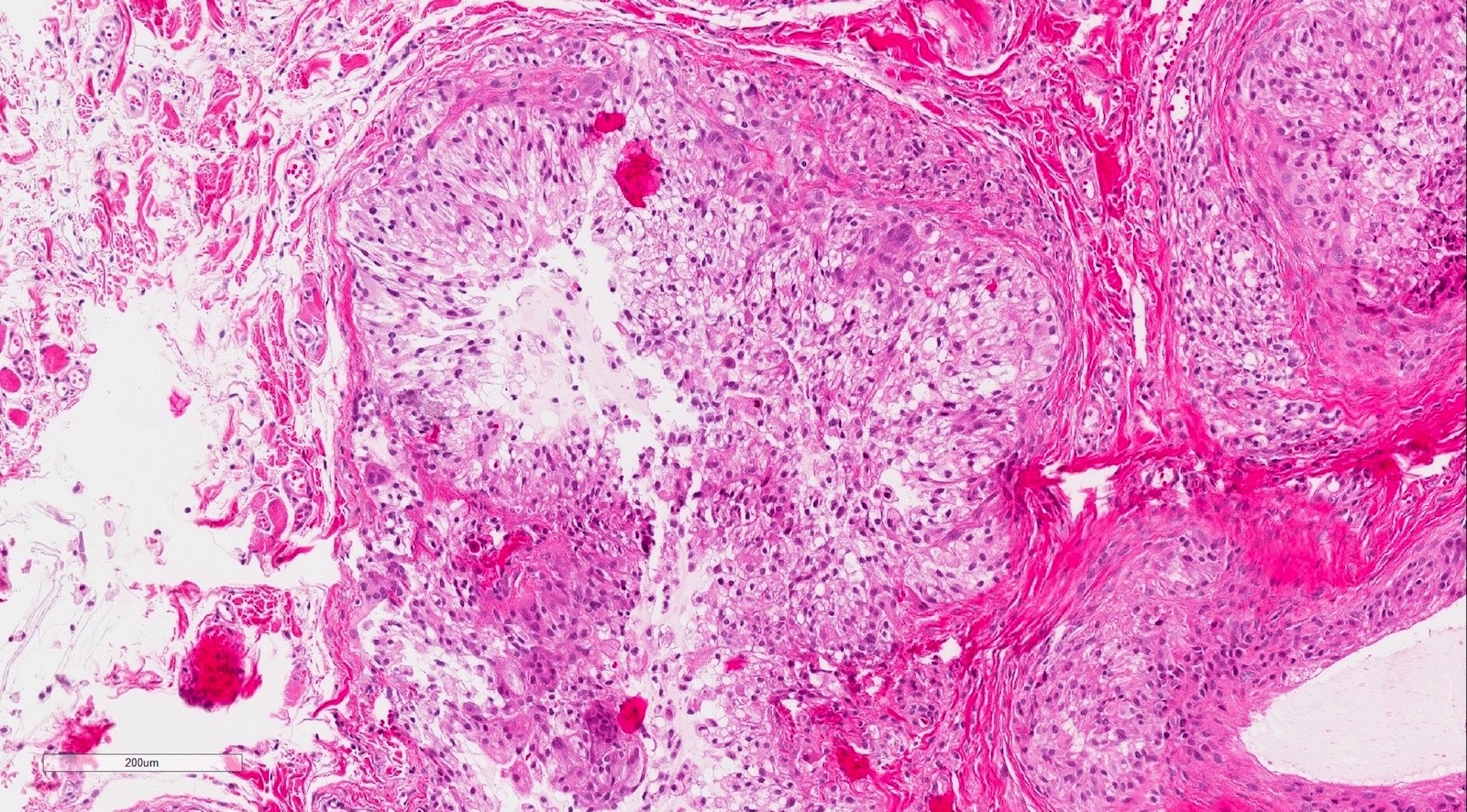
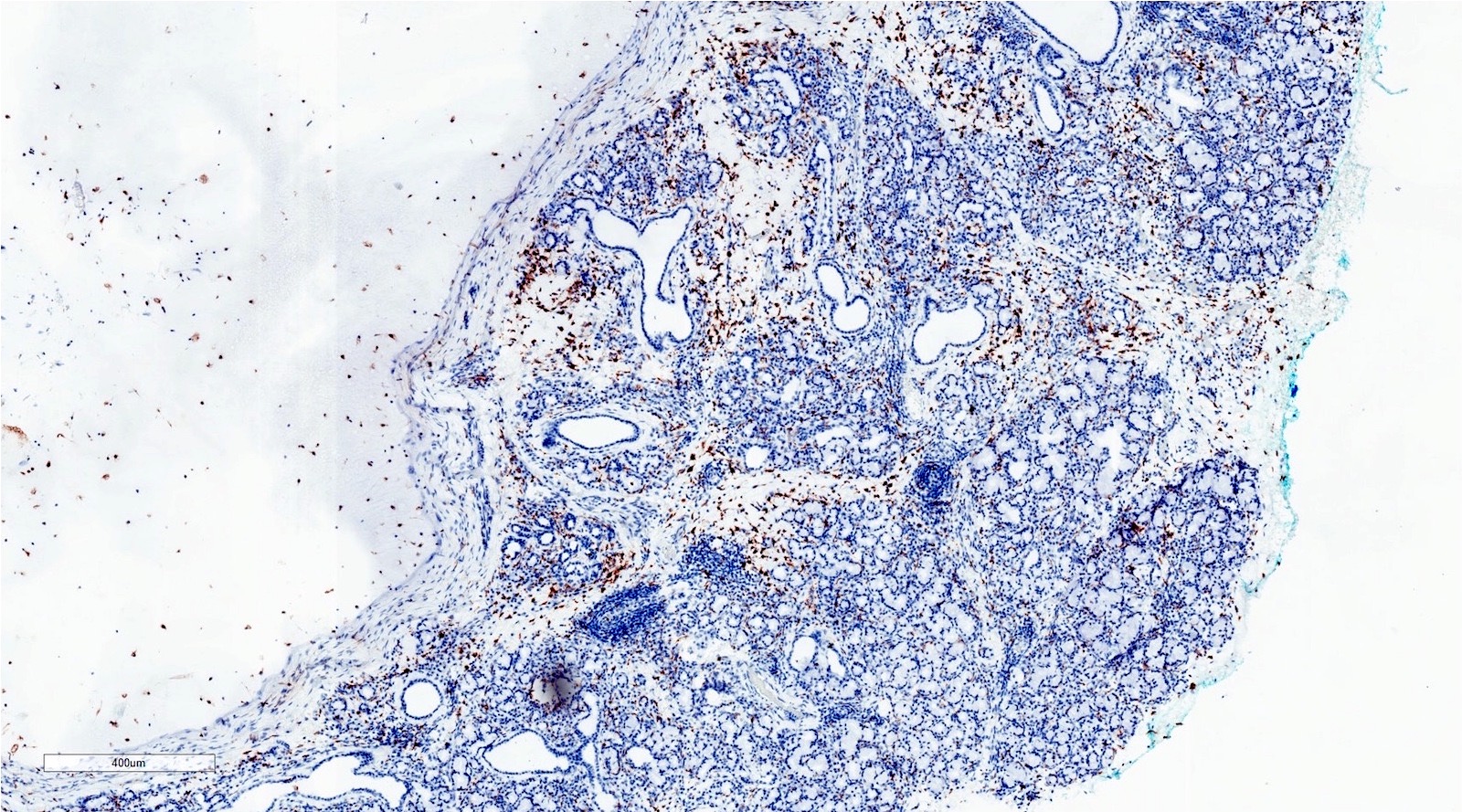
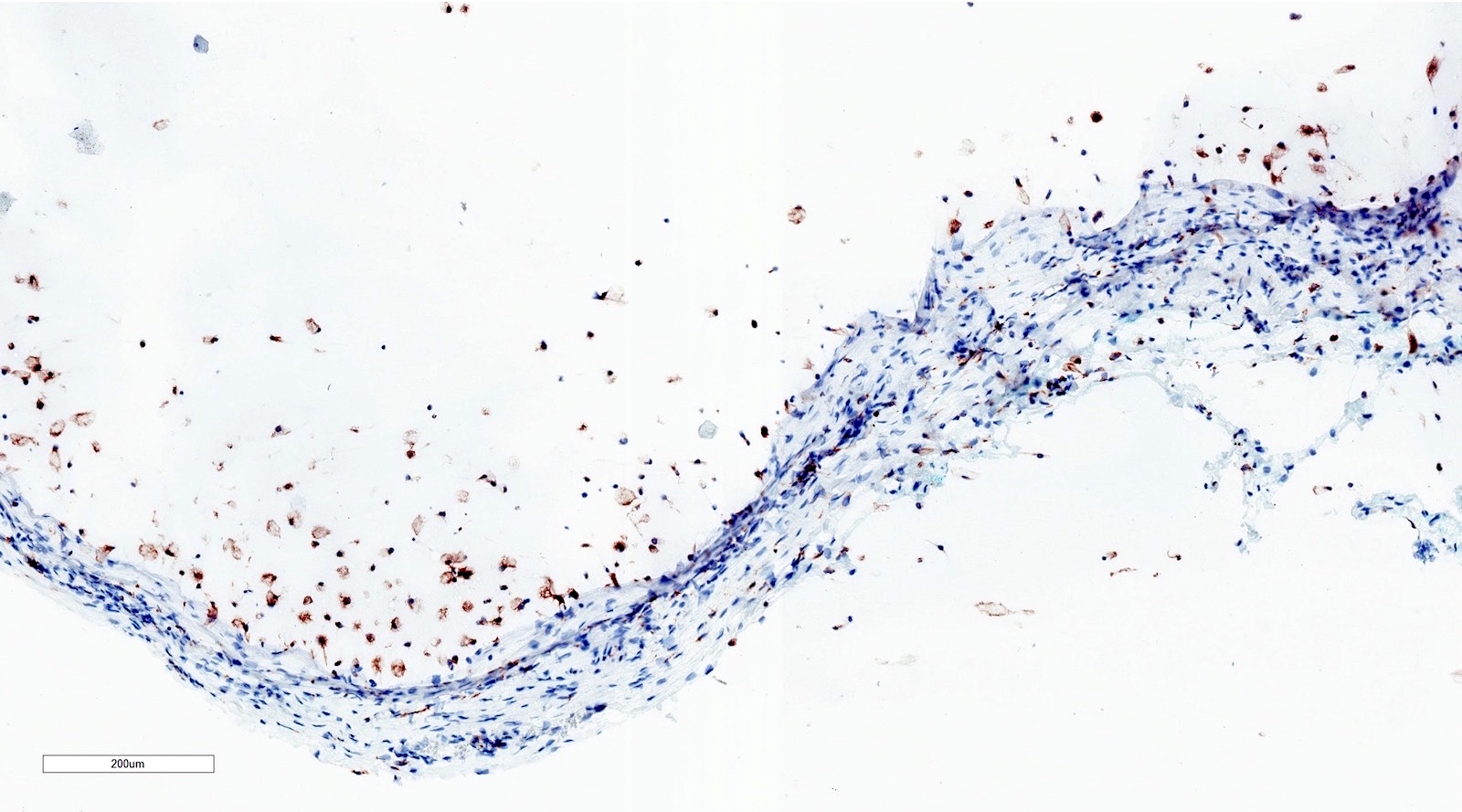
SCC-general
Schwannoma
Smokeless tobacco keratosis
Spongiotic gingival hyperplasia (pending)
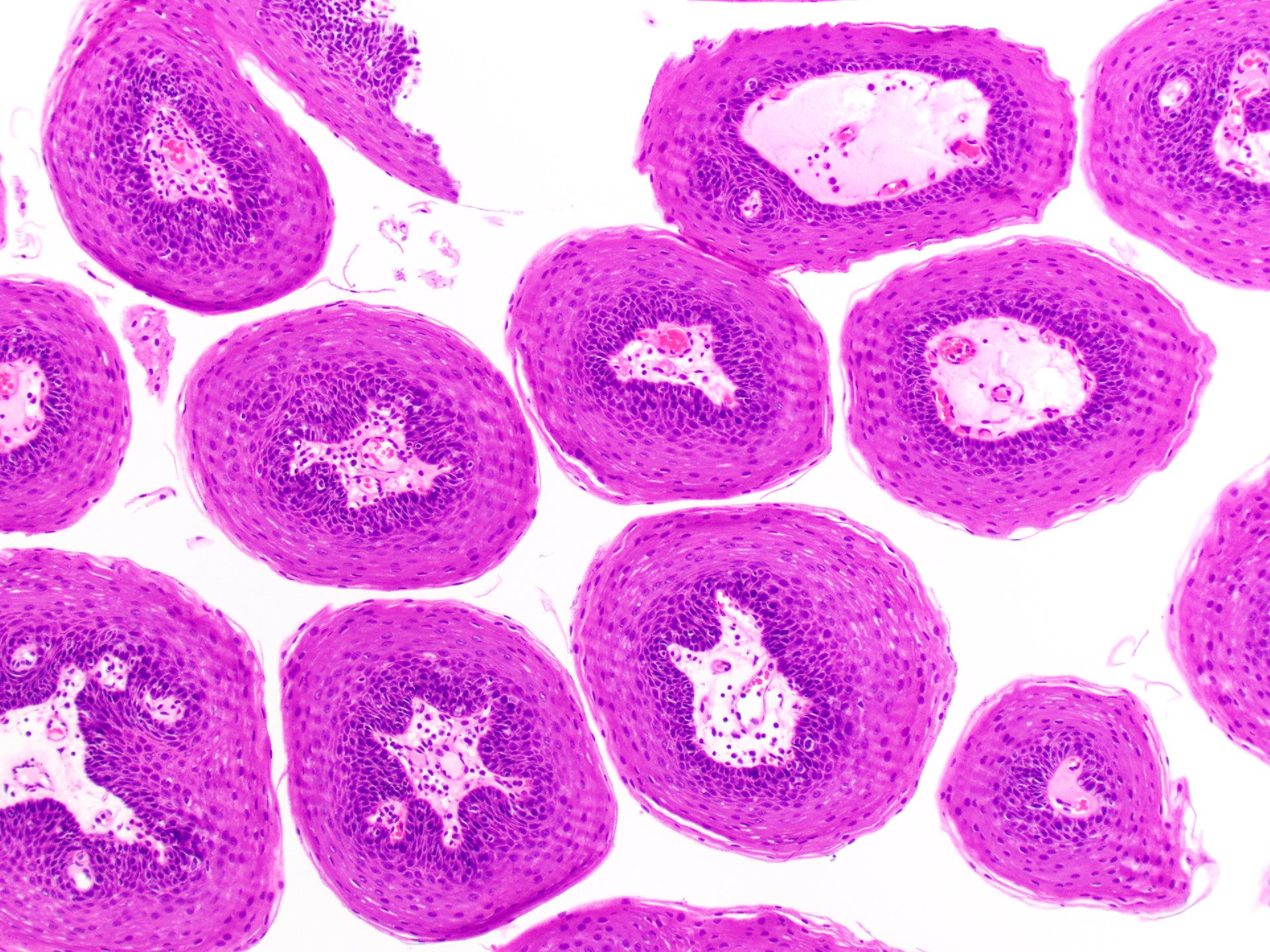
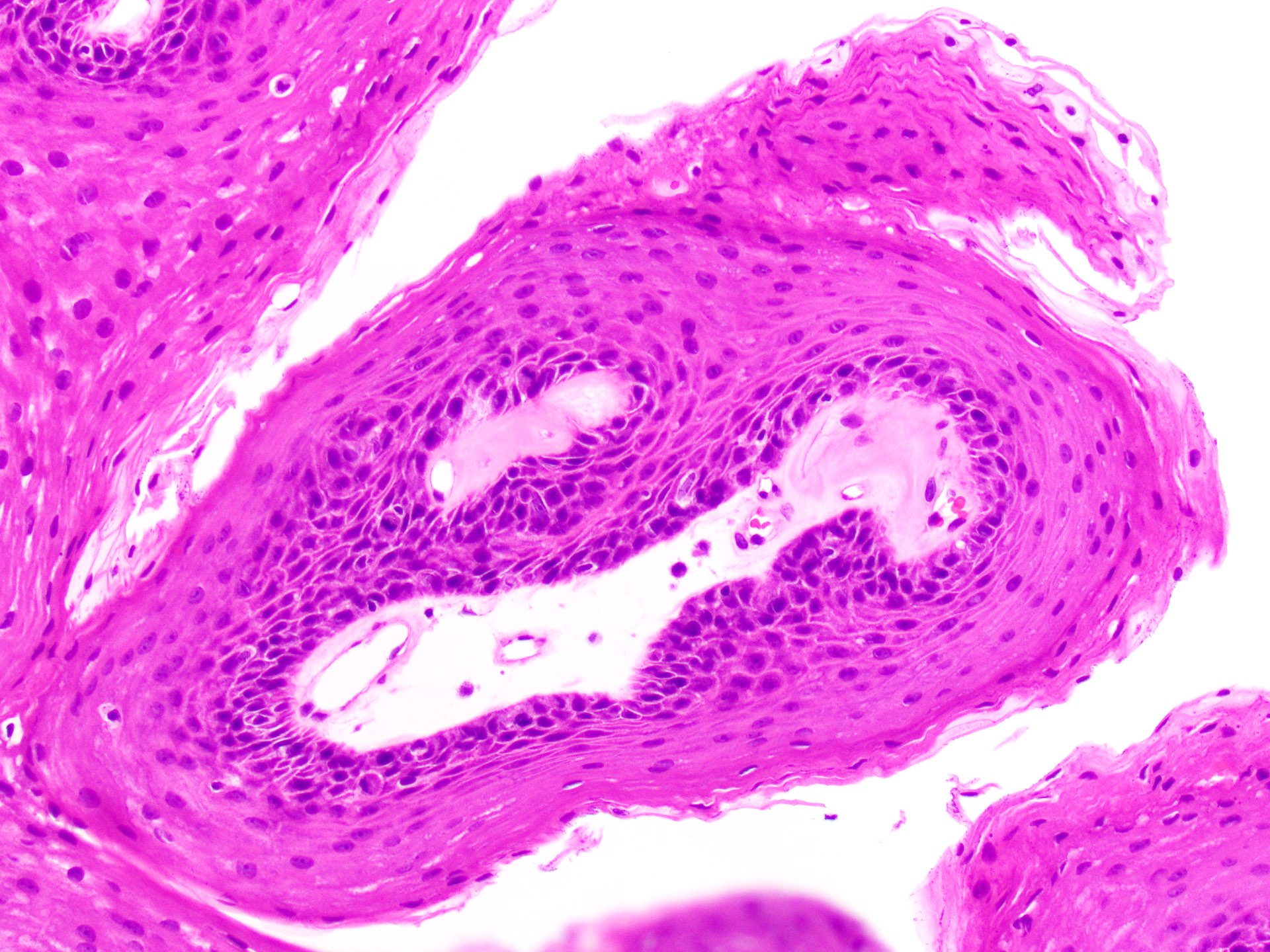
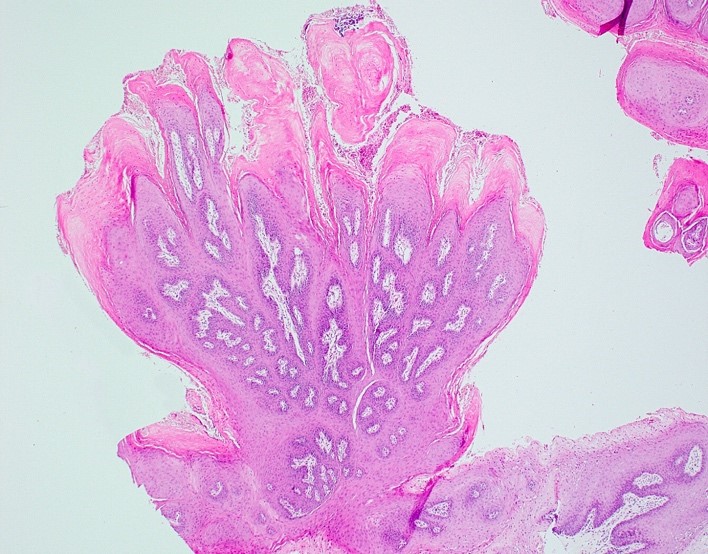
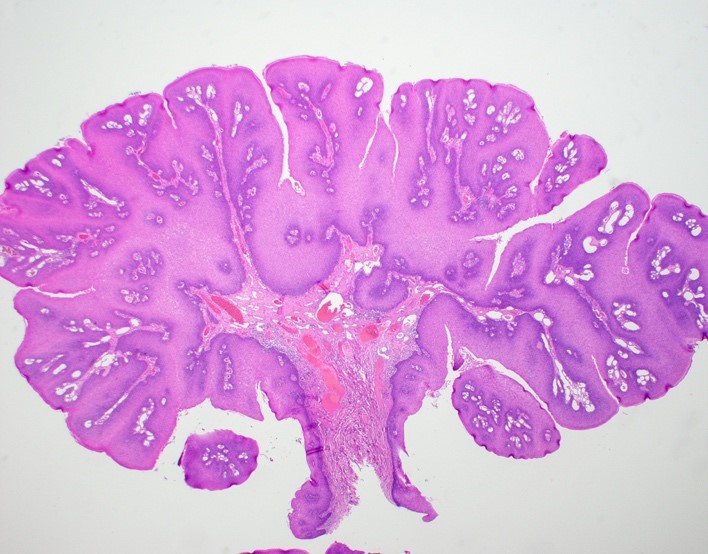
Squamous papilloma
Stafne defect (pending)
Staging features
Staging-mucosal melanoma
Staging-oral cavity
Staging-oropharynx & hypopharynx
Subgemmal neurogenous plaque
Tonsillitis (pending)
Transient lingual papillitis (pending)
Traumatic ulceration with stroma eosinophilia (TUGSE)
Varix / varicosities / varices
Verruca vulgaris
Verruciform xanthoma
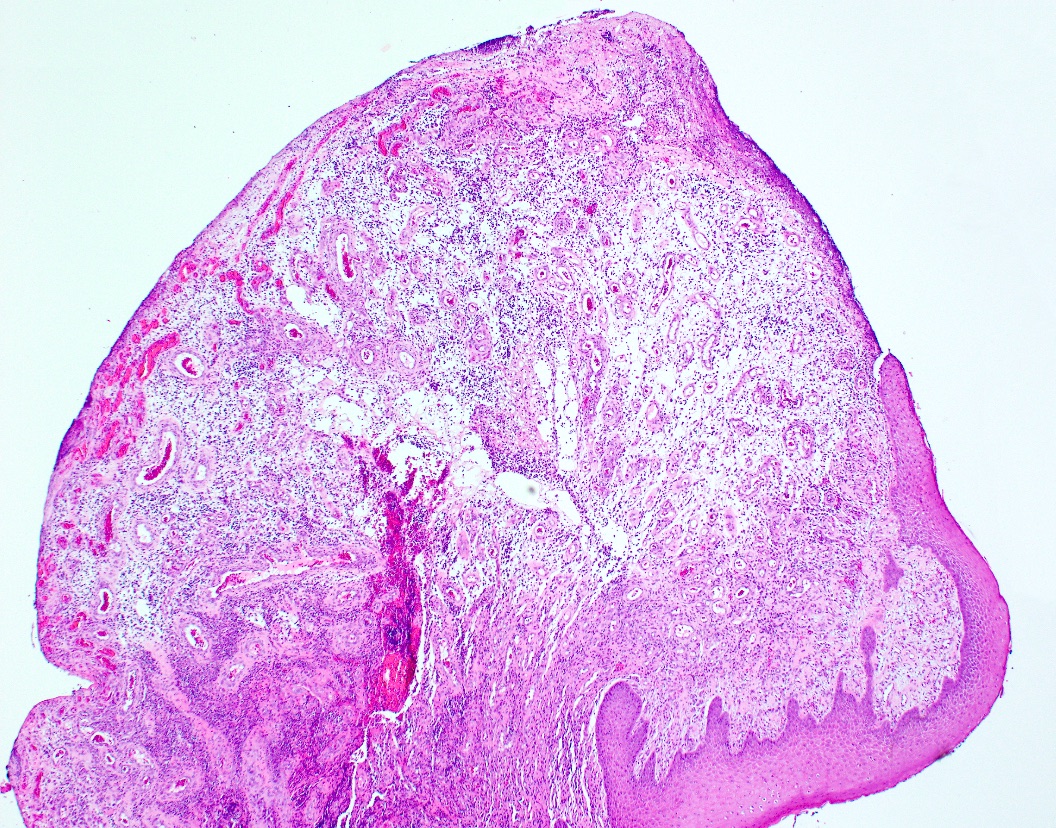
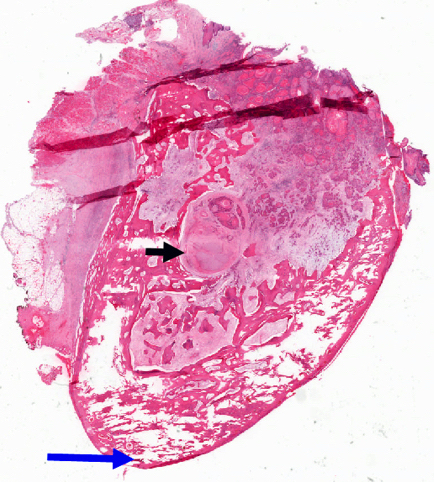
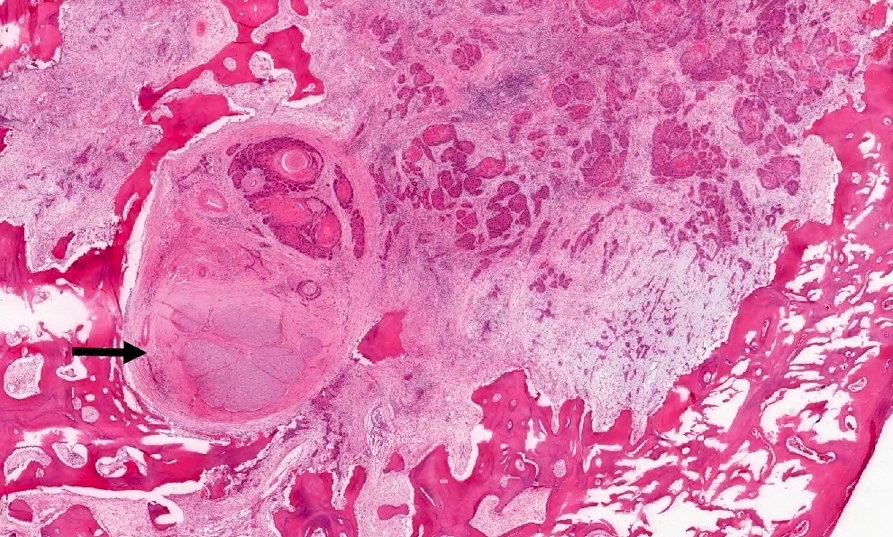
Verrucous carcinoma
White sponge nevus (pending)
WHO classification-oral cavity & oropharynx
WHO classification-oral cavity & oropharynxAcinic cell carcinoma
Actinic cheilitis
Table of Contents
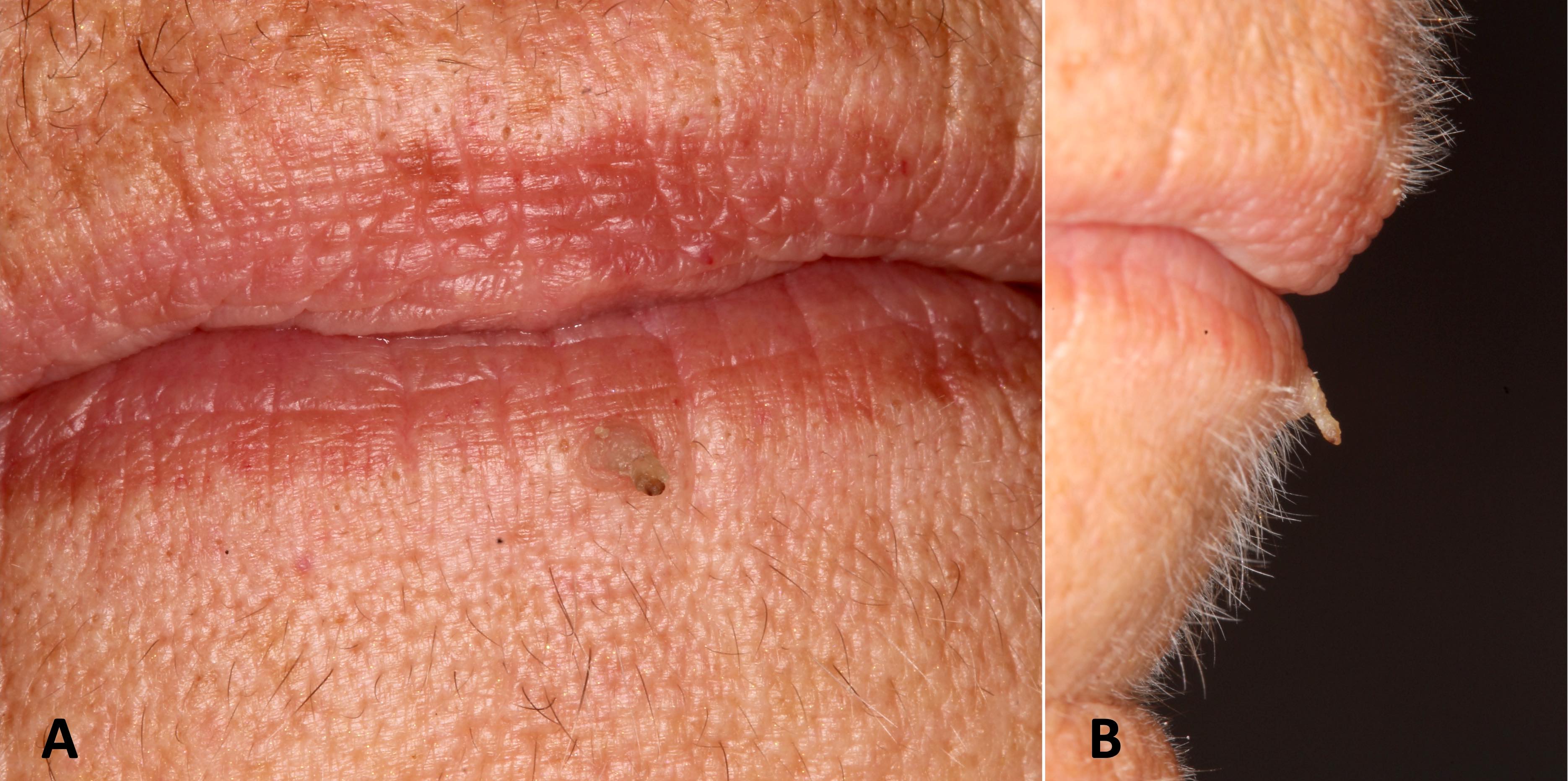
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
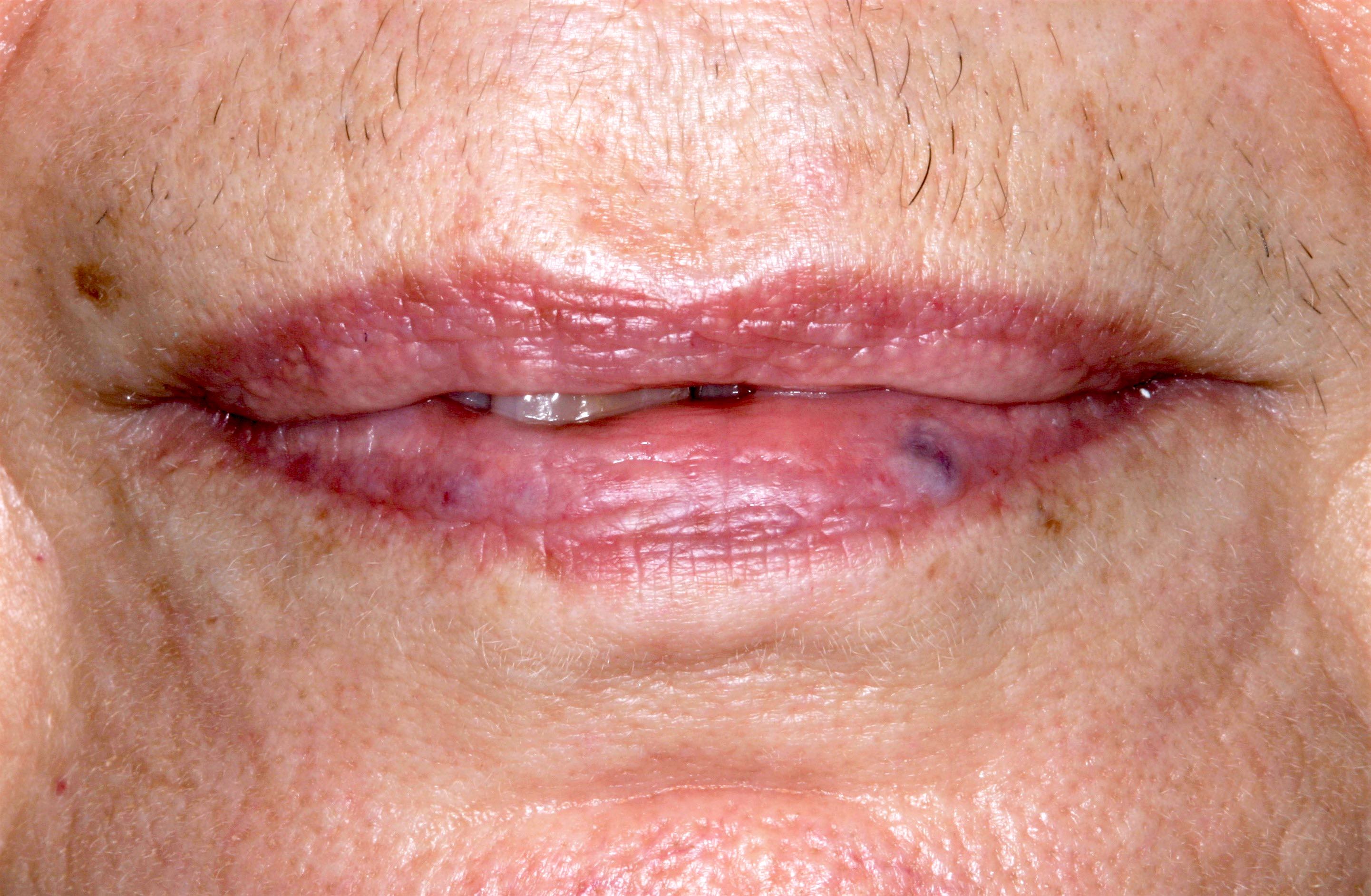
- Common premalignant alteration, usually of the lower lip vermilion, that results from chronic ultraviolet light exposure
Essential features
- Clinically, this manifests as blurring of the demarcation between the vermilion and lip mucosa (Head Neck Pathol 2020;14:899)
- Actinic cheilitis has a strong predilection for fair skinned (> 87%) men (> 70%) over the age of 55; colloquially known as farmer's lip or sailor's lip due to its association with such outdoor occupations (Head Neck Pathol 2020;14:899, AOCD: Actinic Cheilitis [Accessed 4 March 2024])
- Surface epithelium is variably dysplastic and is low risk for malignant transformation (J Investig Clin Dent 2018;9:e12343, StatPearls: Actinic Cheilitis [Accessed 4 April 2024], J Dent Res Dent Clin Dent Prospects 2021;15:285)
- Hyperkeratosis, acanthosis and atrophy of the epithelium may also be present
- Underlying connective tissue exhibits solar elastosis, which appears as a band of amorphous, acellular, basophilic change due to ultraviolet light induced degeneration of collagen and elastin fibers (Head Neck Pathol 2021;15:566)
Terminology
- First described as "scurfy, scaly lip of the outdoor worker" by Montgomery and Culver in 1920, who attributed this to effects of wind and weather; Ayres coined the term chronic actinic cheilitis in 1923 to describe a chronic inflammatory disorder of the lips as a result of actinic or chemically active rays of sunlight (JAMA 1923;81:1183)
- In 1997, Manganaro, Will and Poulos designated actinic cheilitis as a premalignant, irreversible pathosis that most often affects the lower lip vermilion (Gen Dent 1997;45:492)
ICD coding
Epidemiology
- Actinic cheilitis has a strong predilection for fair skinned (> 87%) men (> 70%) over the age of 55 (Head Neck Pathol 2020;14:899)
Sites
- Actinic cheilitis affects the vermilion of the lower lips in 95% of cases (Head Neck Pathol 2020;14:899)
Pathophysiology
- Ultraviolet B (UVB) rays (290 - 320 nm) are the primary cause of actinic damage as 70% is absorbed by the skin (J Oral Med Oral Surg 2023;29:30)
- This form of radiation drives thymine and uracil dimer formation in DNA and RNA, respectively; additionally, UVB rays create 6 - 4 pyrimidine photoproducts and substitutions of cytosine thymine in DNA, which particularly results in mutations to the p53 protein (Photochem Photobiol 2008;84:422)
Etiology
- Ultraviolet radiation from long term sun exposure
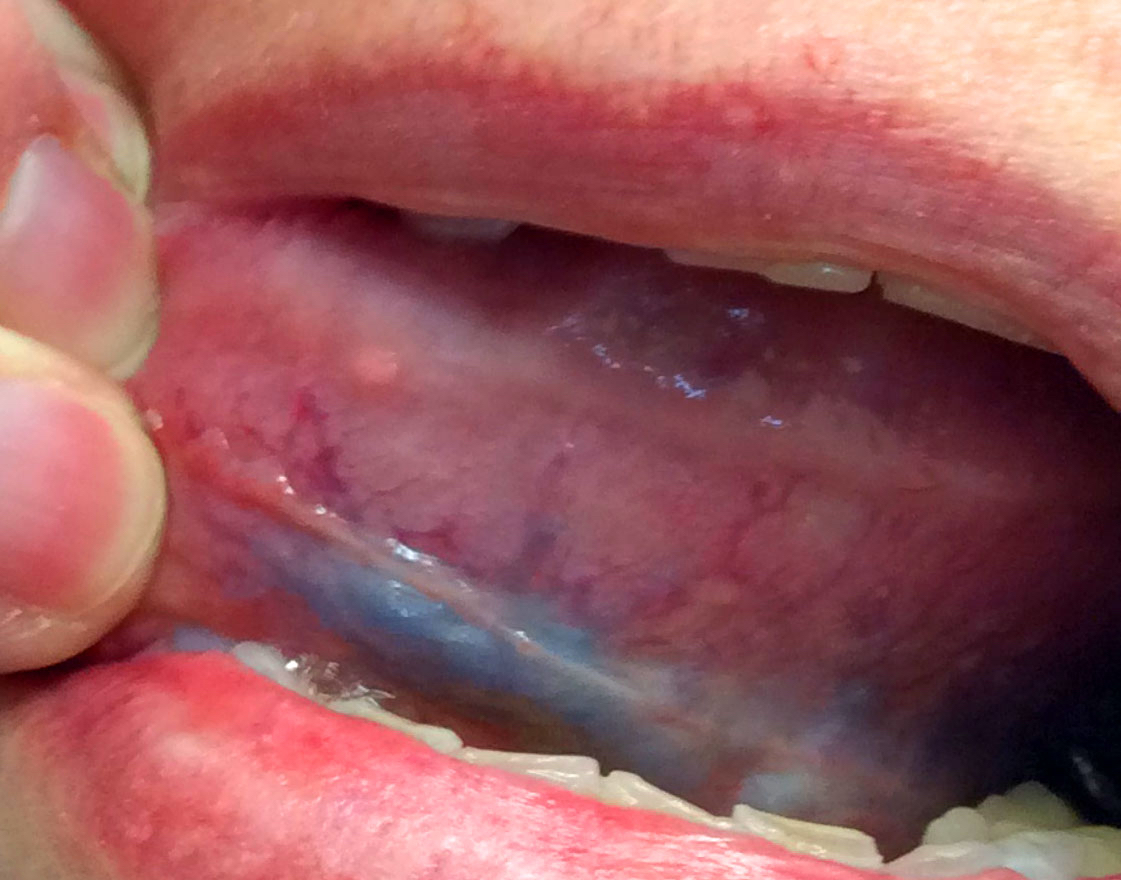
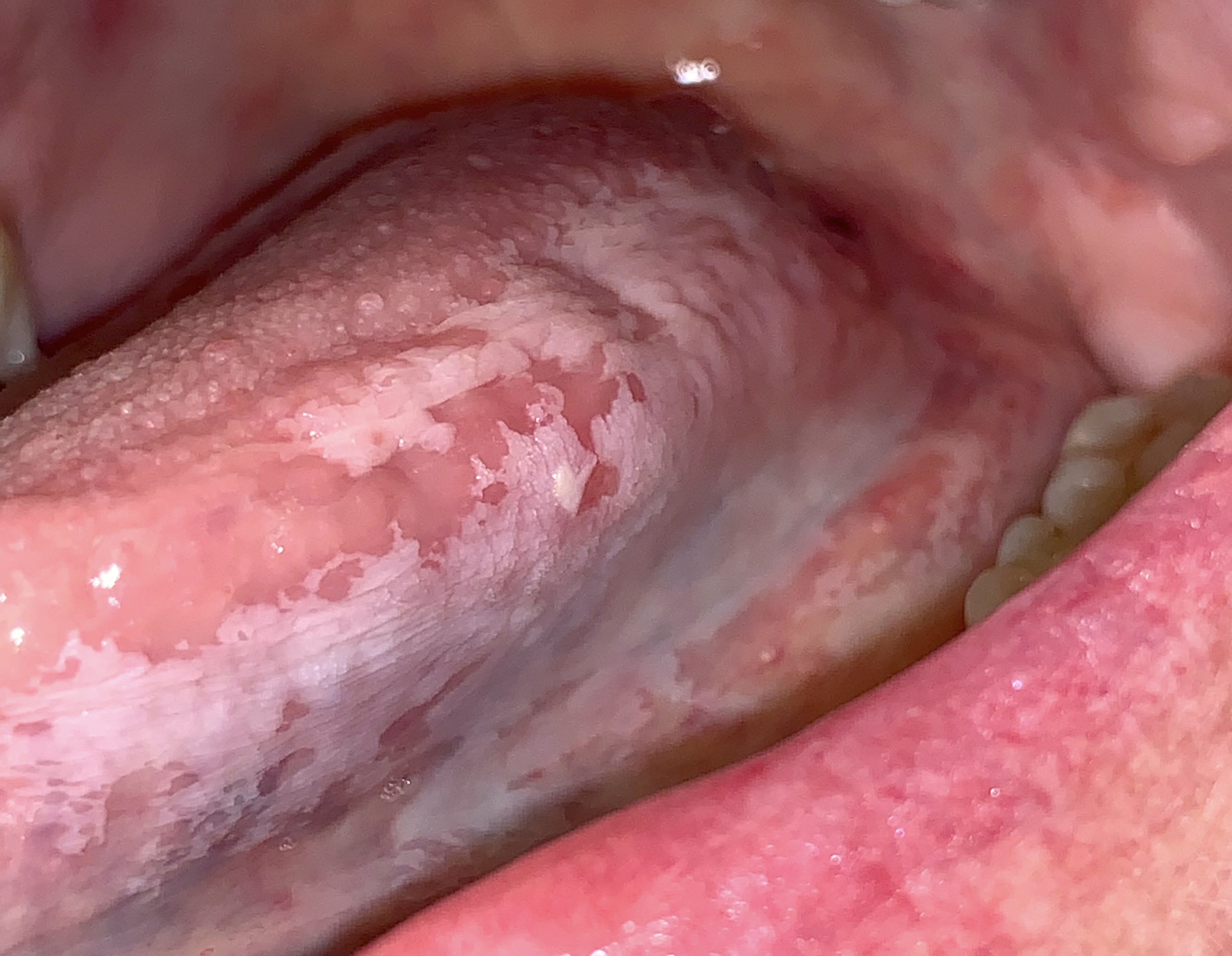
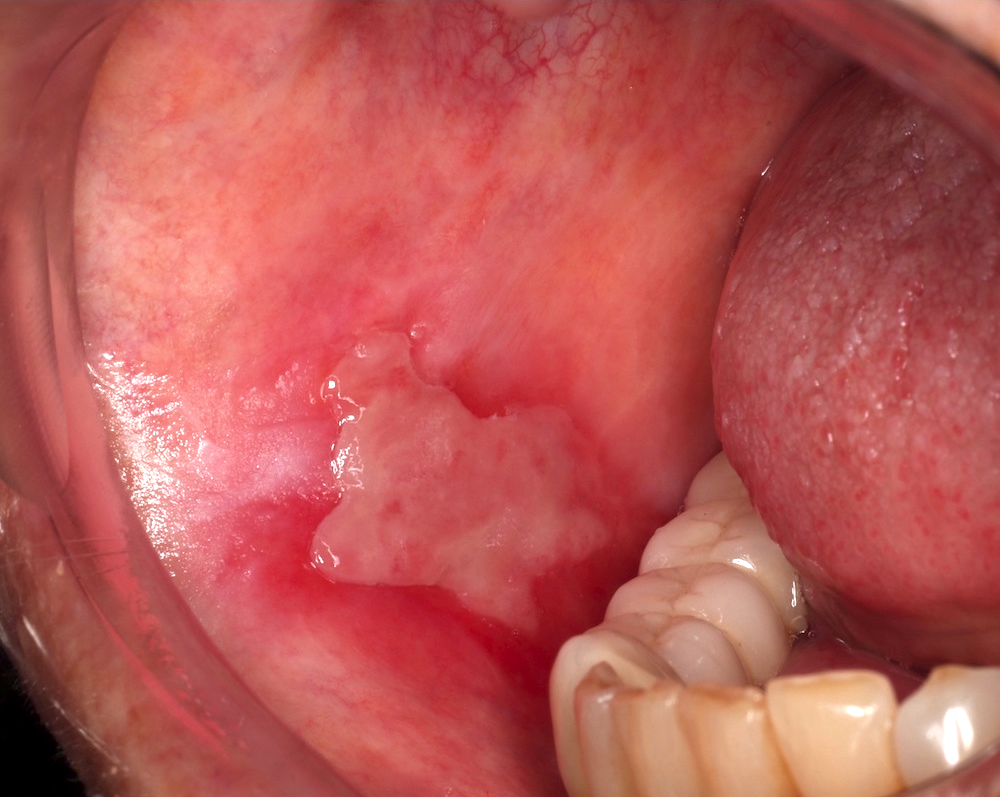
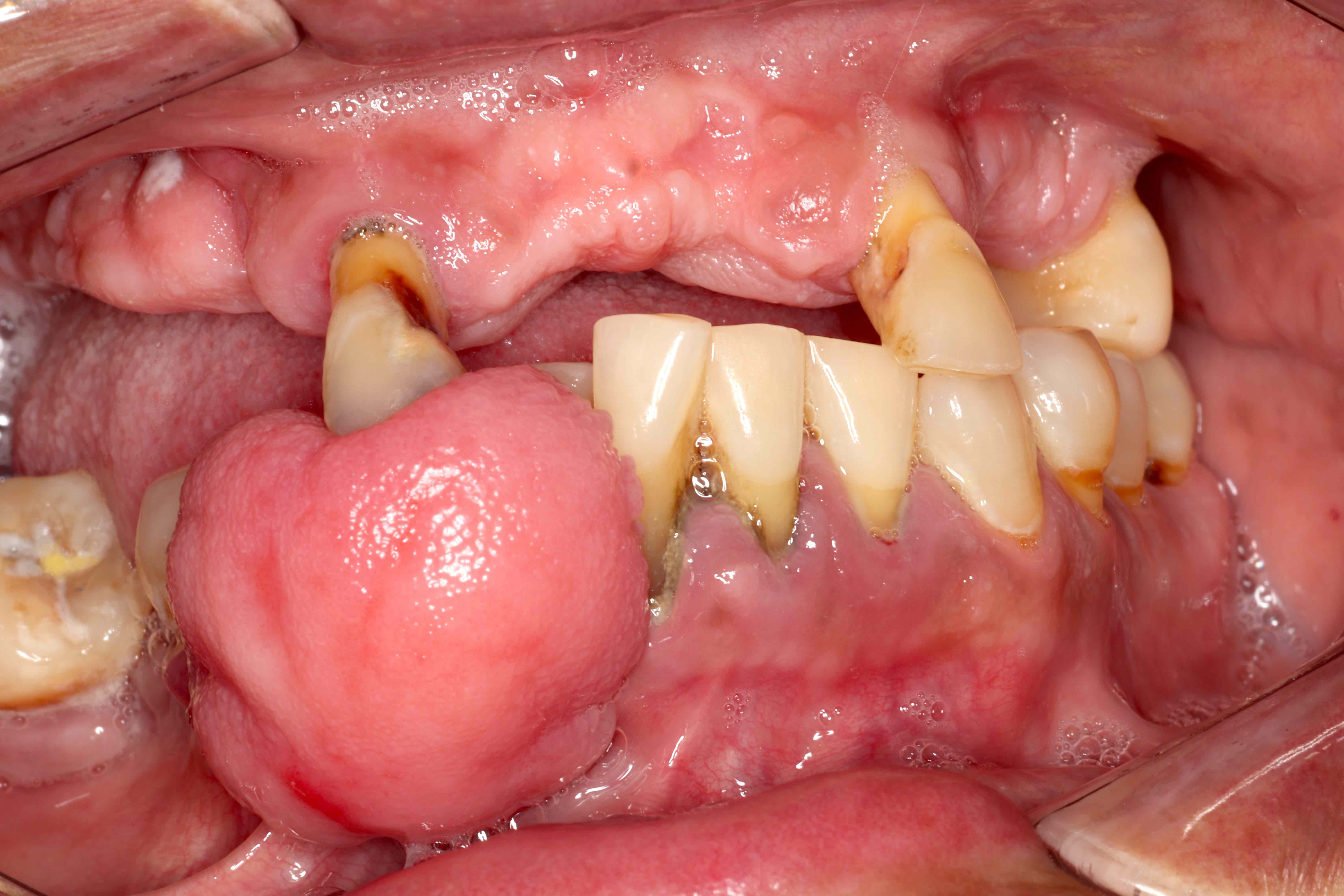
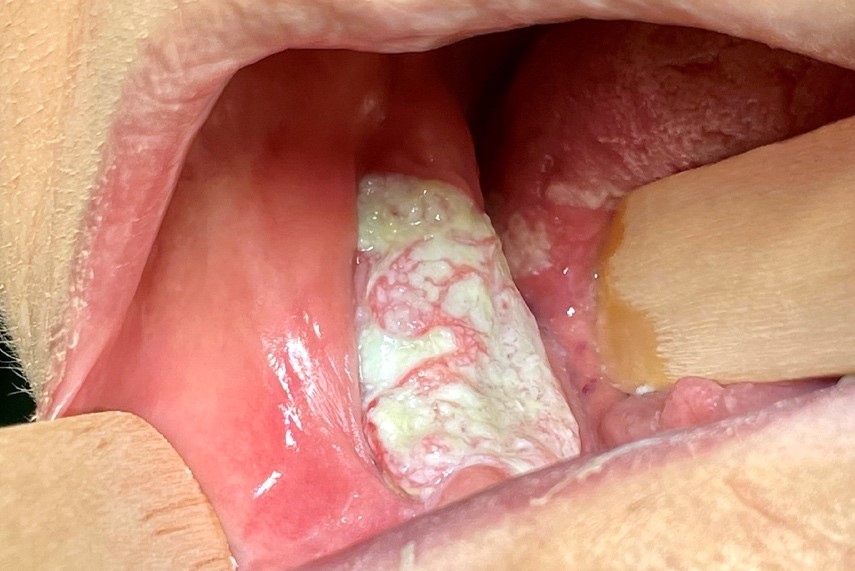
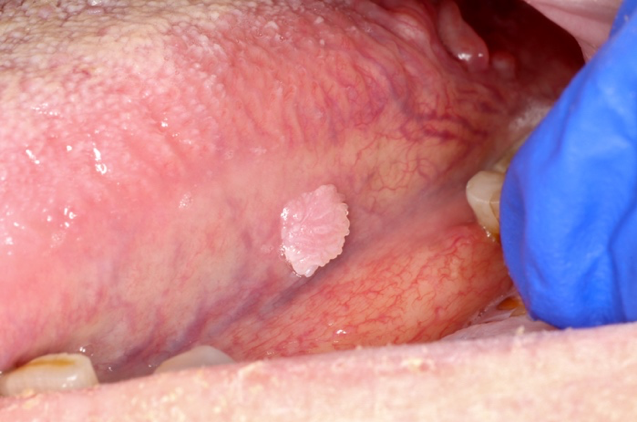
Clinical features
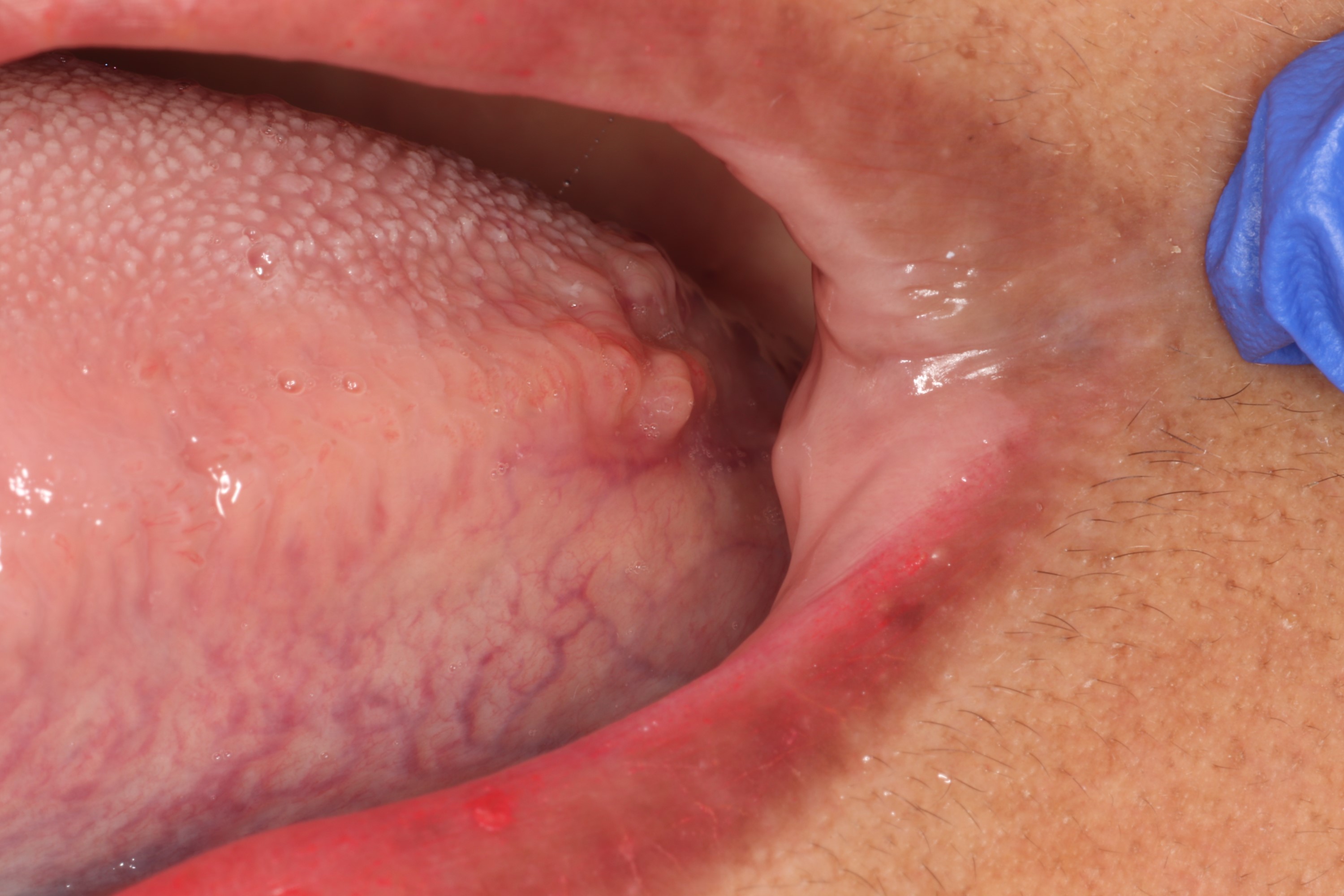
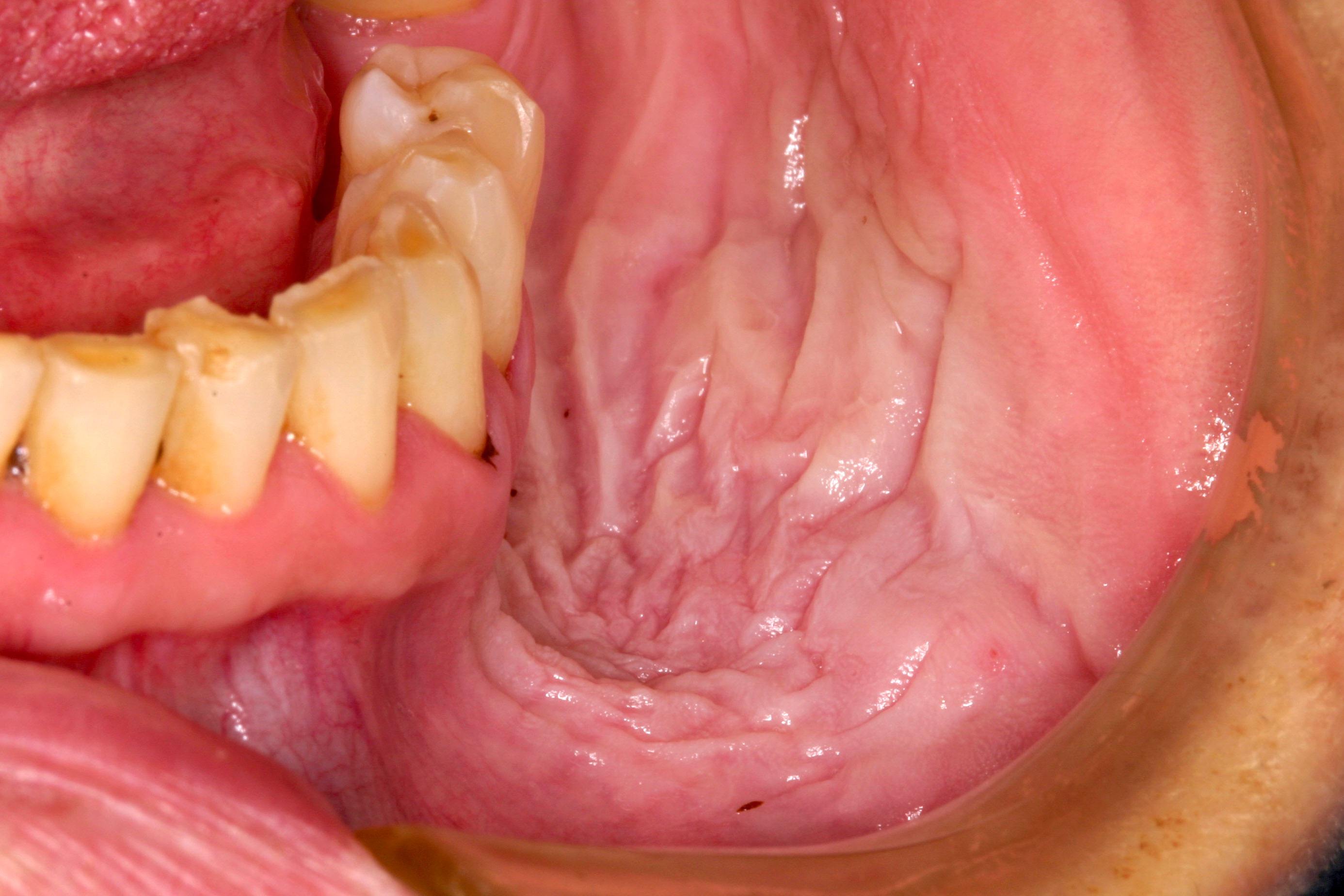
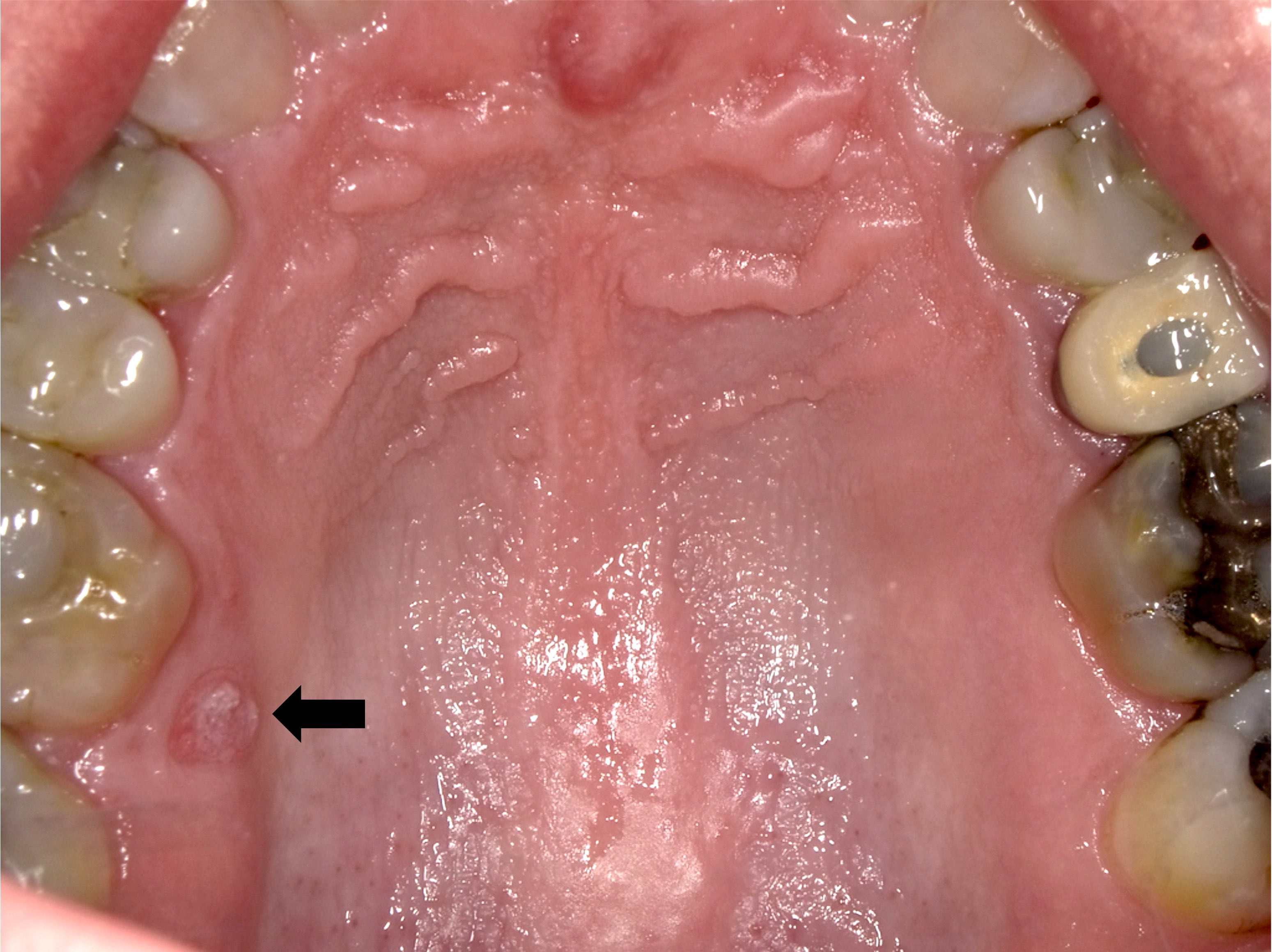
- Actinic cheilitis manifests as a blurred demarcation between the vermilion and the mucosal lip, erythema and edema with subsequent dry scaling / a persistent, nonmigrating crust and in some cases, leukoplakia (BDJ Open 2017;3:17016, J Drugs Dermatol 2011;10:1240)
- Patients typically have a chief concern of persistent chapped lips or lip tightness (AOCD: Actinic Cheilitis [Accessed 4 March 2024])
Diagnosis
- May be detected clinically as blurring between the vermilion and lip mucosa as an incidental finding
- Lip may also be erythematous, swollen or present with white patching
- Biopsy is indicated
Prognostic factors
- Chronic sun exposure without protective measures increases risk for malignant transformation
- Weighted remission rate following surgical treatment (92.8%) is greater than nonsurgical treatment (65.9%)
- Additionally, the recurrence following surgery (8.4%) is lower in comparison to nonsurgical treatment (19.2%) (Oral Dis 2019;25:972)
Case reports
- 51 year old man with a chief concern of a lip lesion that was diagnosed by his dentist (Oral Surg Oral Med Oral Pathol Oral Radiol 2020;130:e203)
- 64 year old, fair skinned man with multiple crusted areas of the lower lip vermilion (Oral Surg Oral Med Oral Pathol Oral Radiol 1980;50:21)
- 67 year old woman with a 2 year history of dryness, thickening and scaling of the entire lower lip that was treated with photodynamic therapy (Phtodermatol Photoimmunol Photomed 2007;23:209)
- 76 year old man presented with a white, hyperkeratotic lesion of the lower lip (Dermatology 2016;232:1)
Treatment
- Surgical treatments, particularly carbon dioxide laser ablation and vermilionectomy, are associated with the most favorable outcomes and the fewest recurrences (J Eur Acad Dermatol Venereol 2021;35:815)
- Nonsurgical treatments for actinic cheilitis consist of a variety of topical therapies, including
- 5-fluorouracil
- Imiquimod
- Trichloroacetic acid
- Ingenol mebutate
- Diclofenac
- Reference: Photodermatol Photoimmunol Photomed 2019;35:11
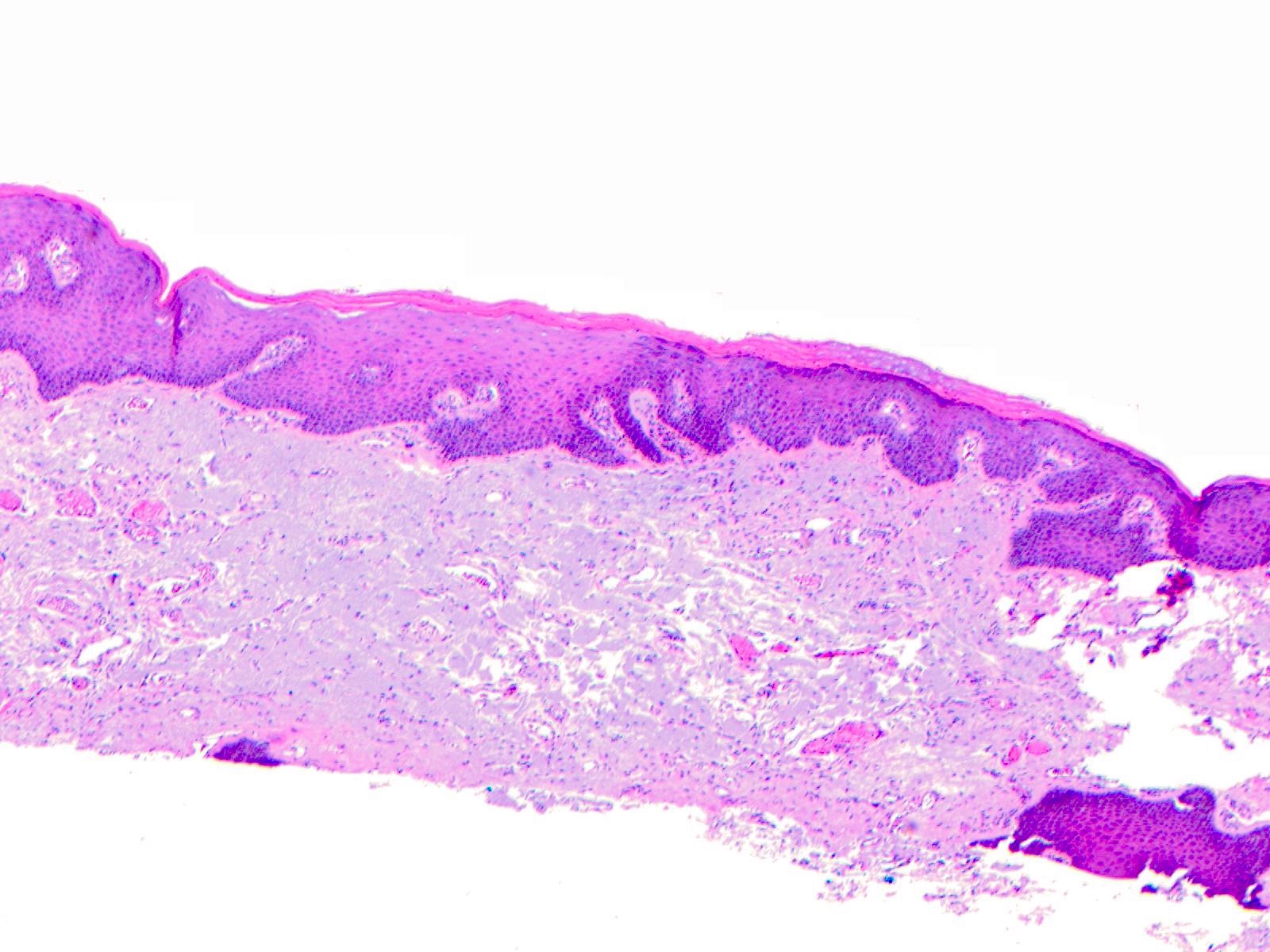
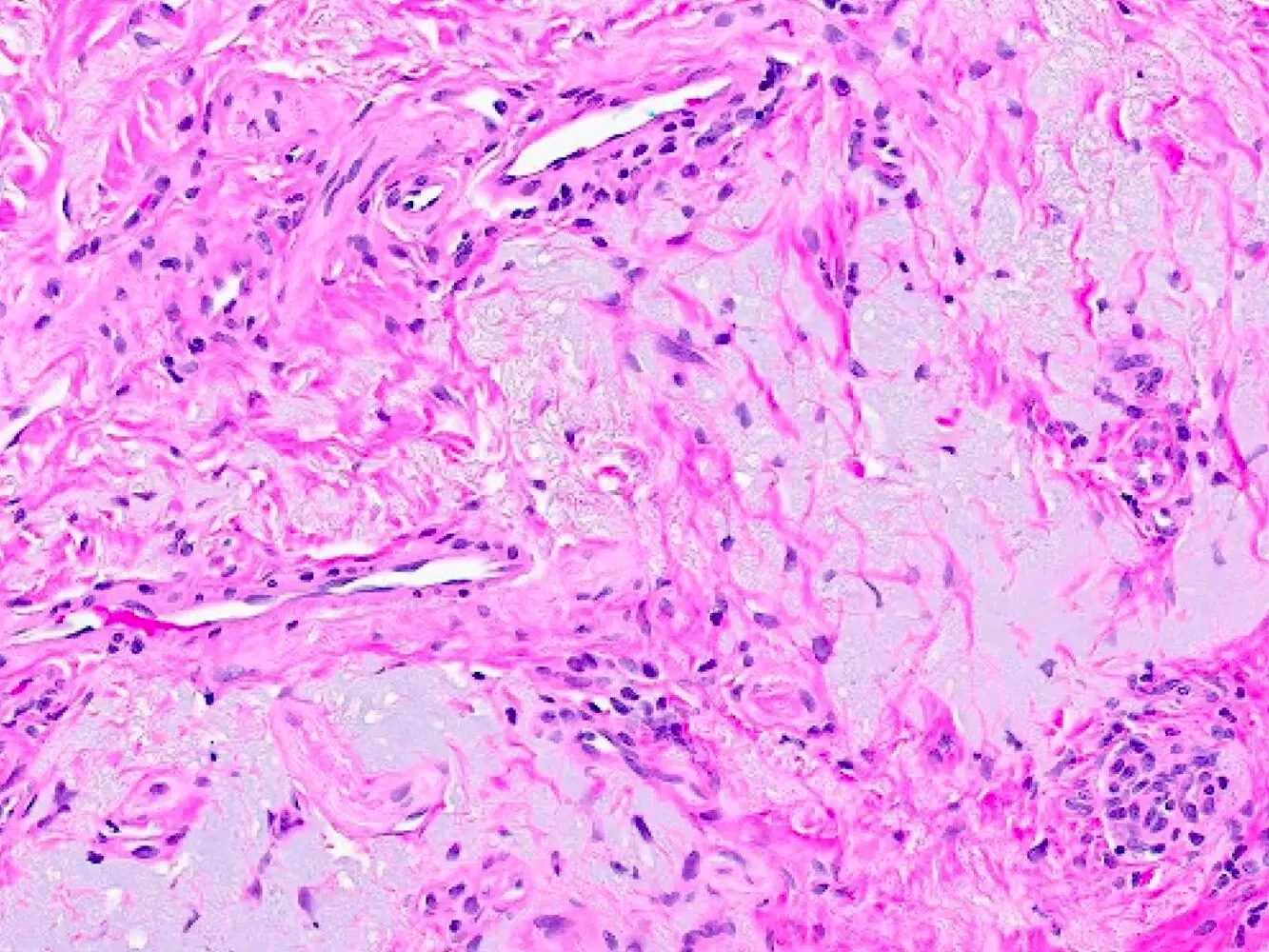
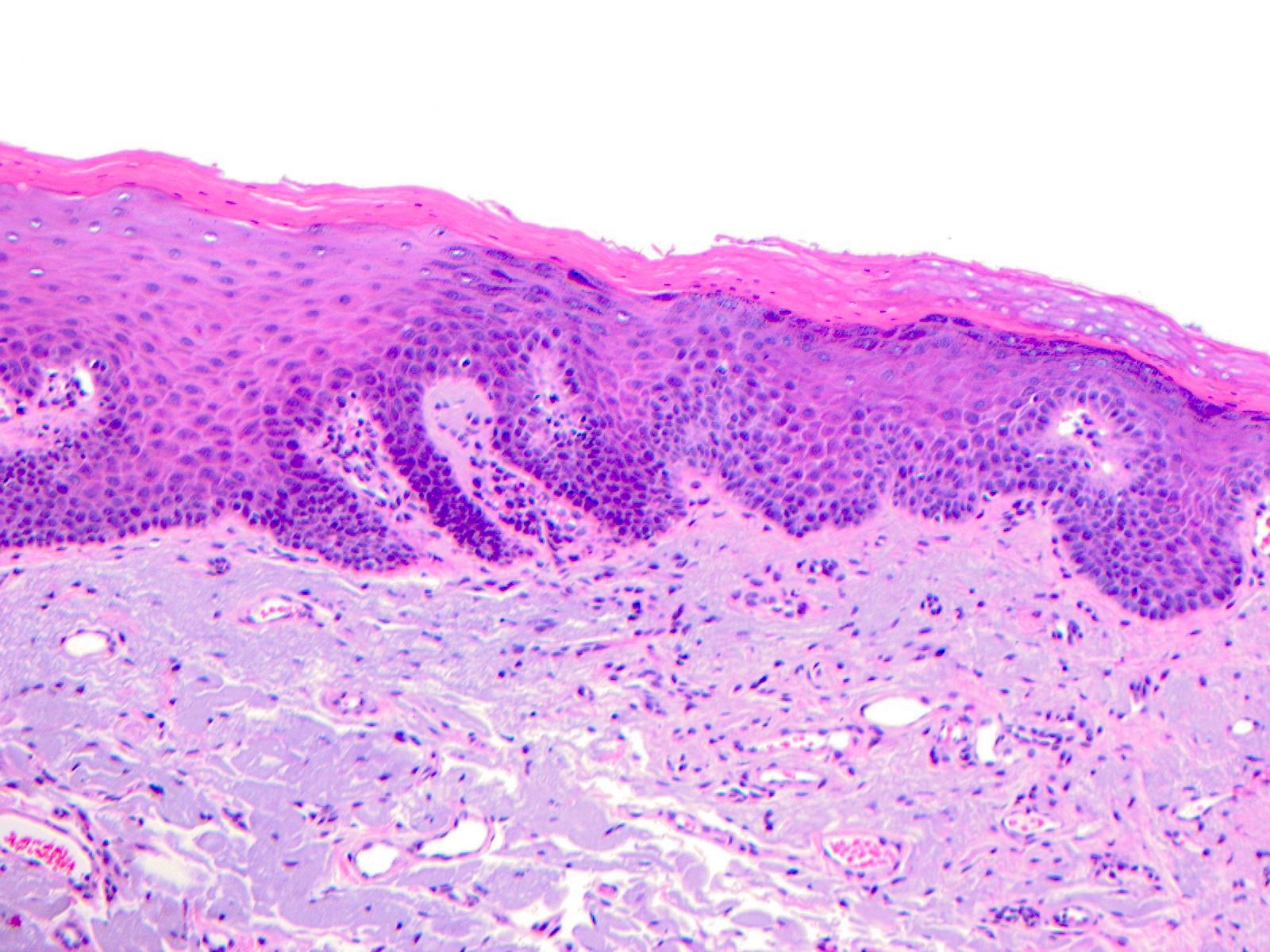
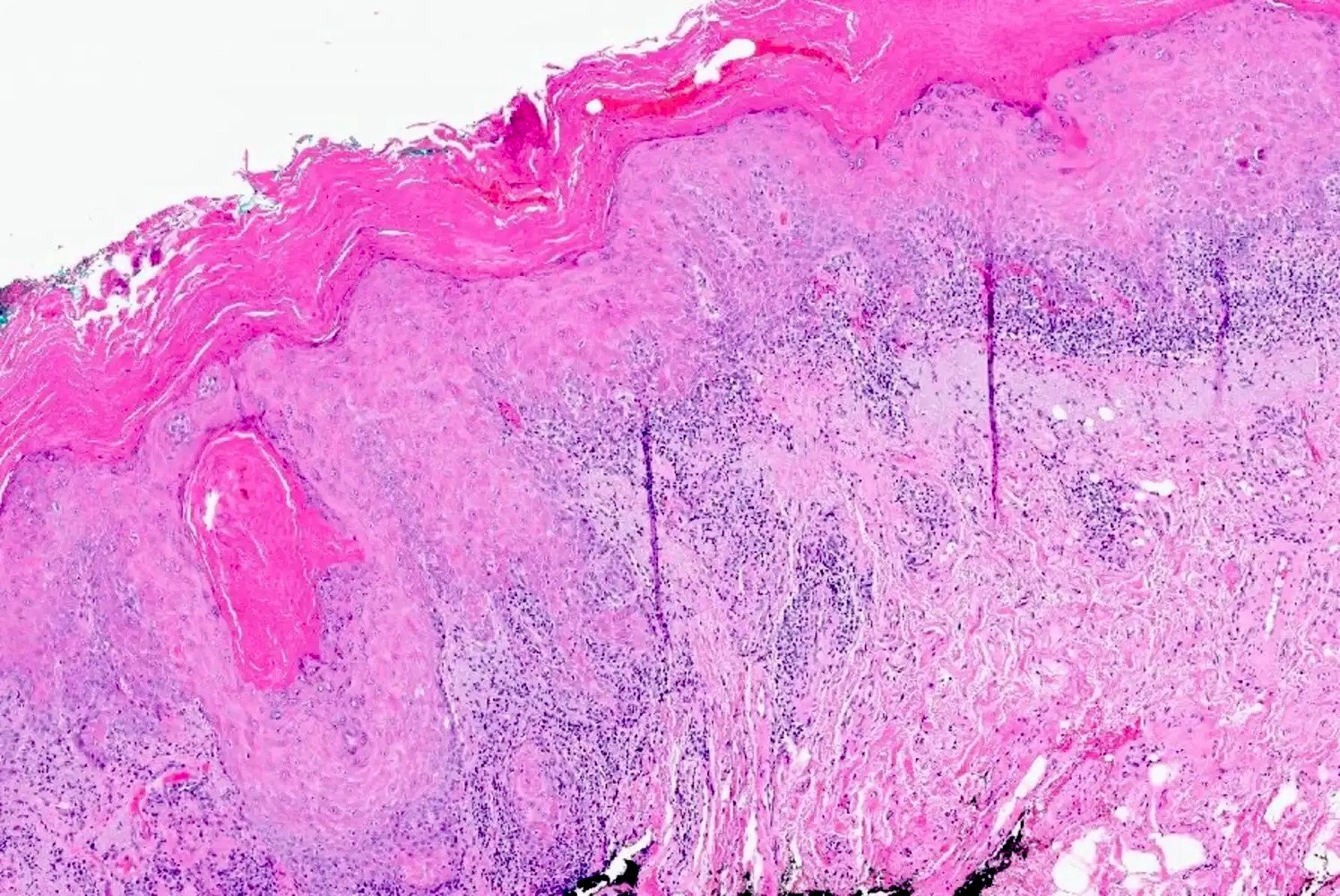
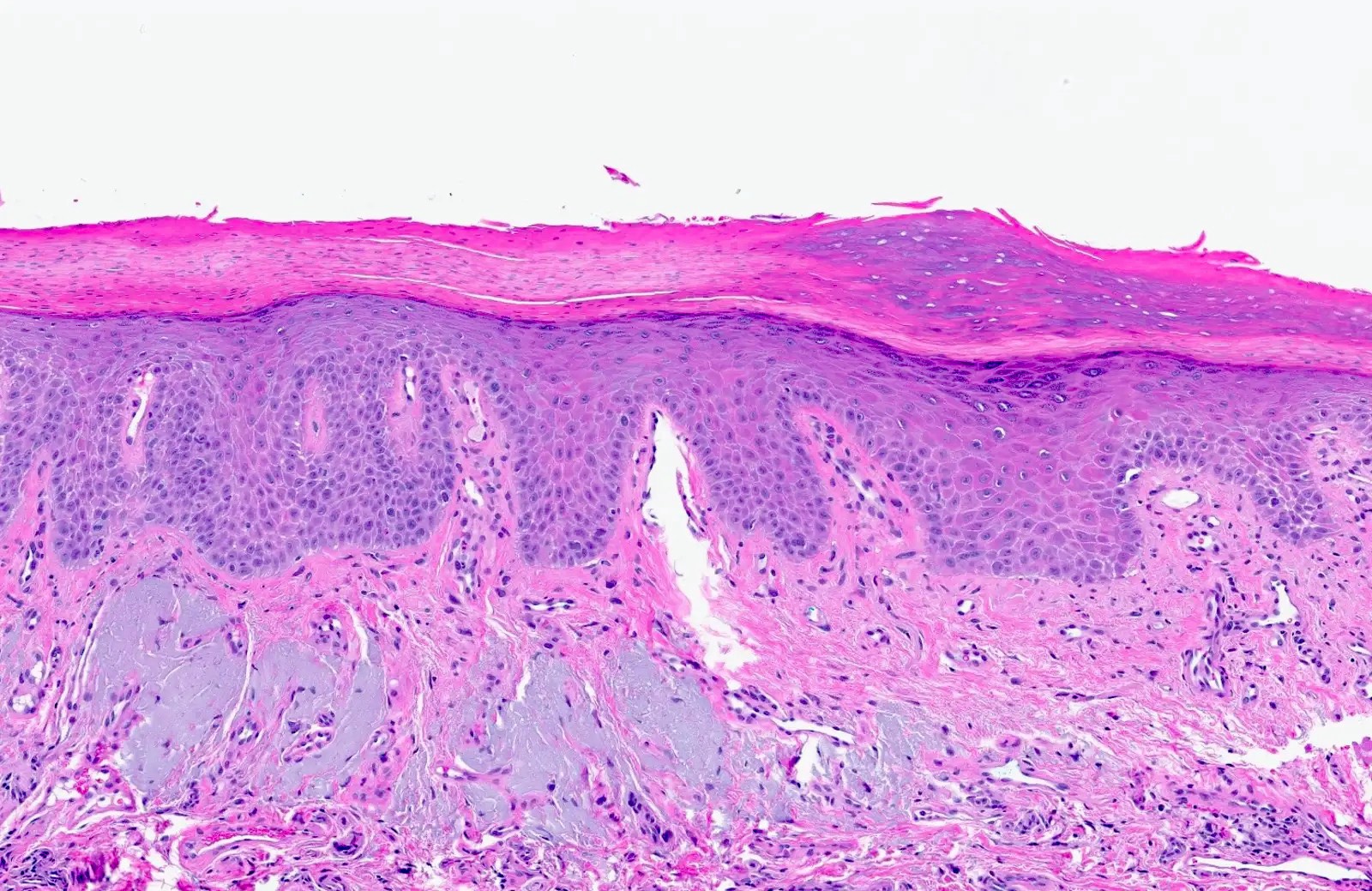
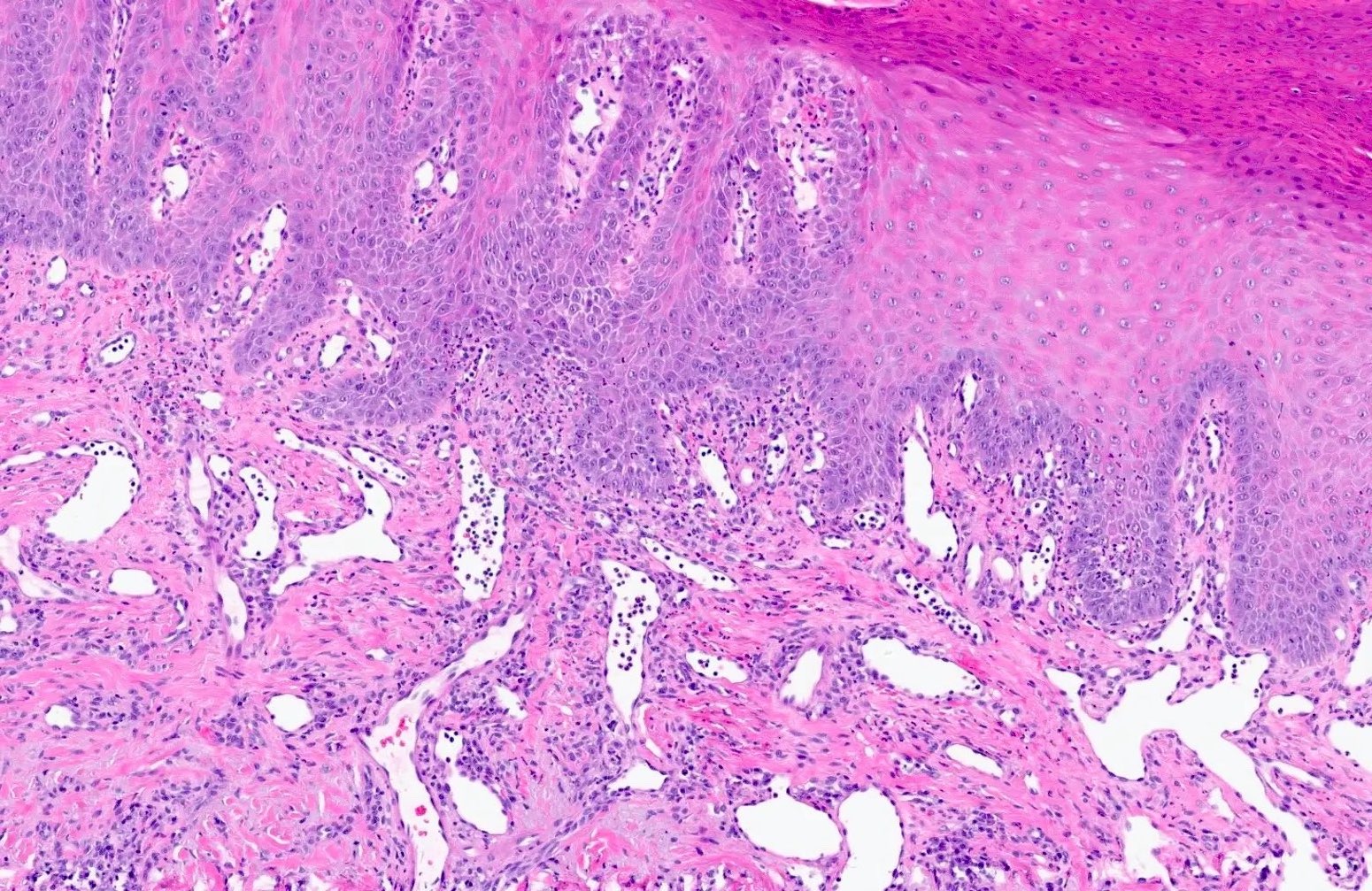
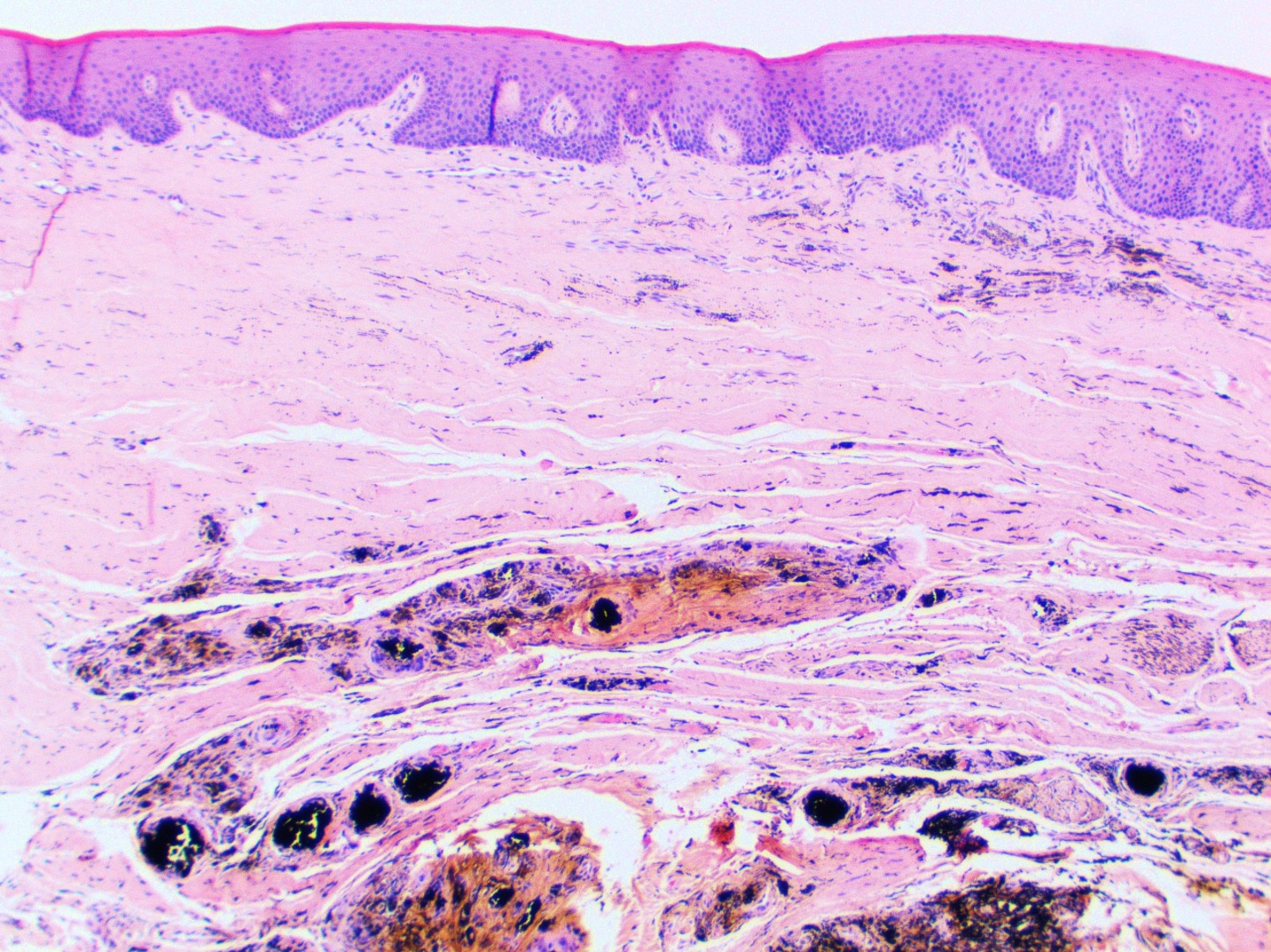
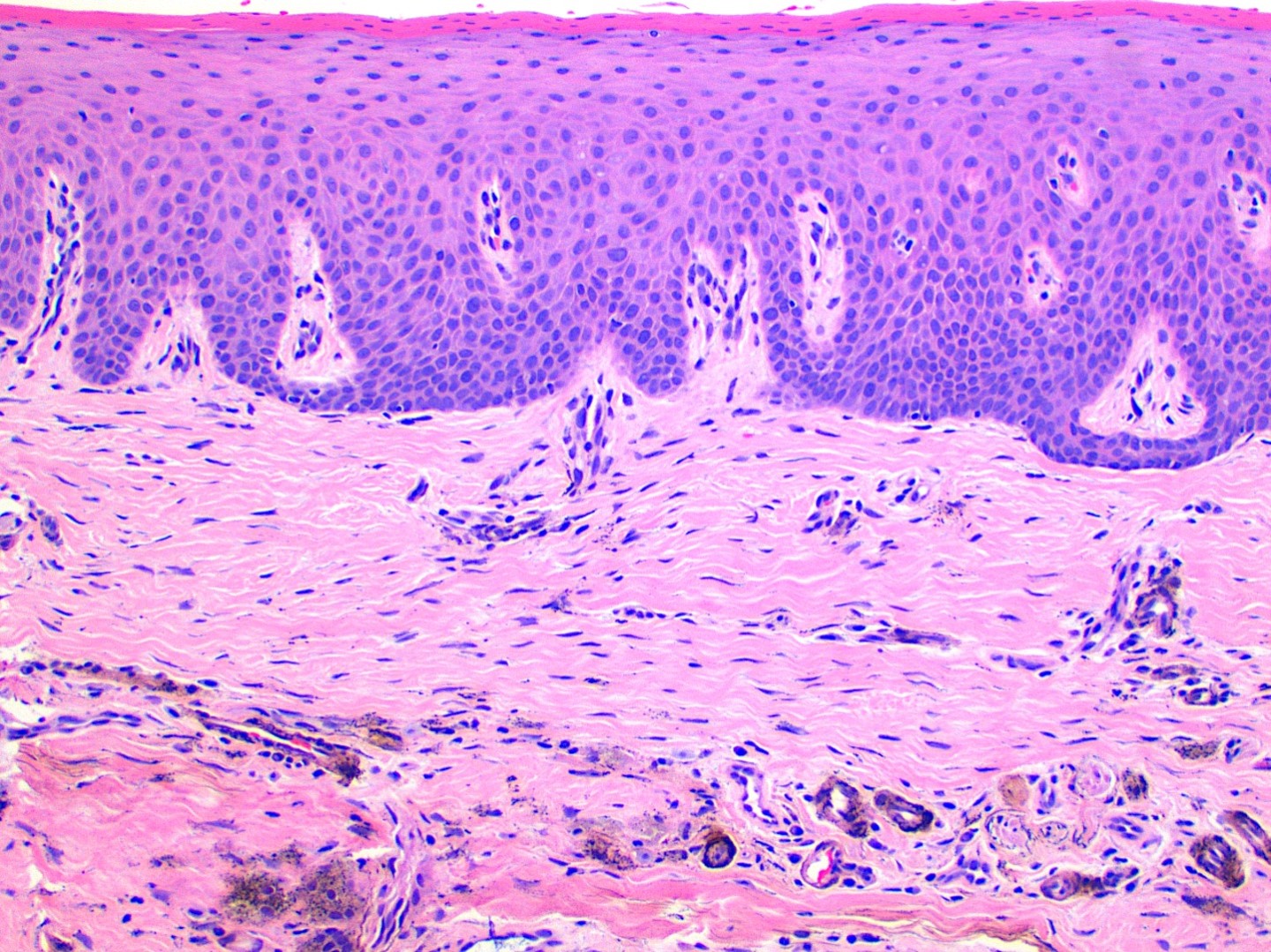
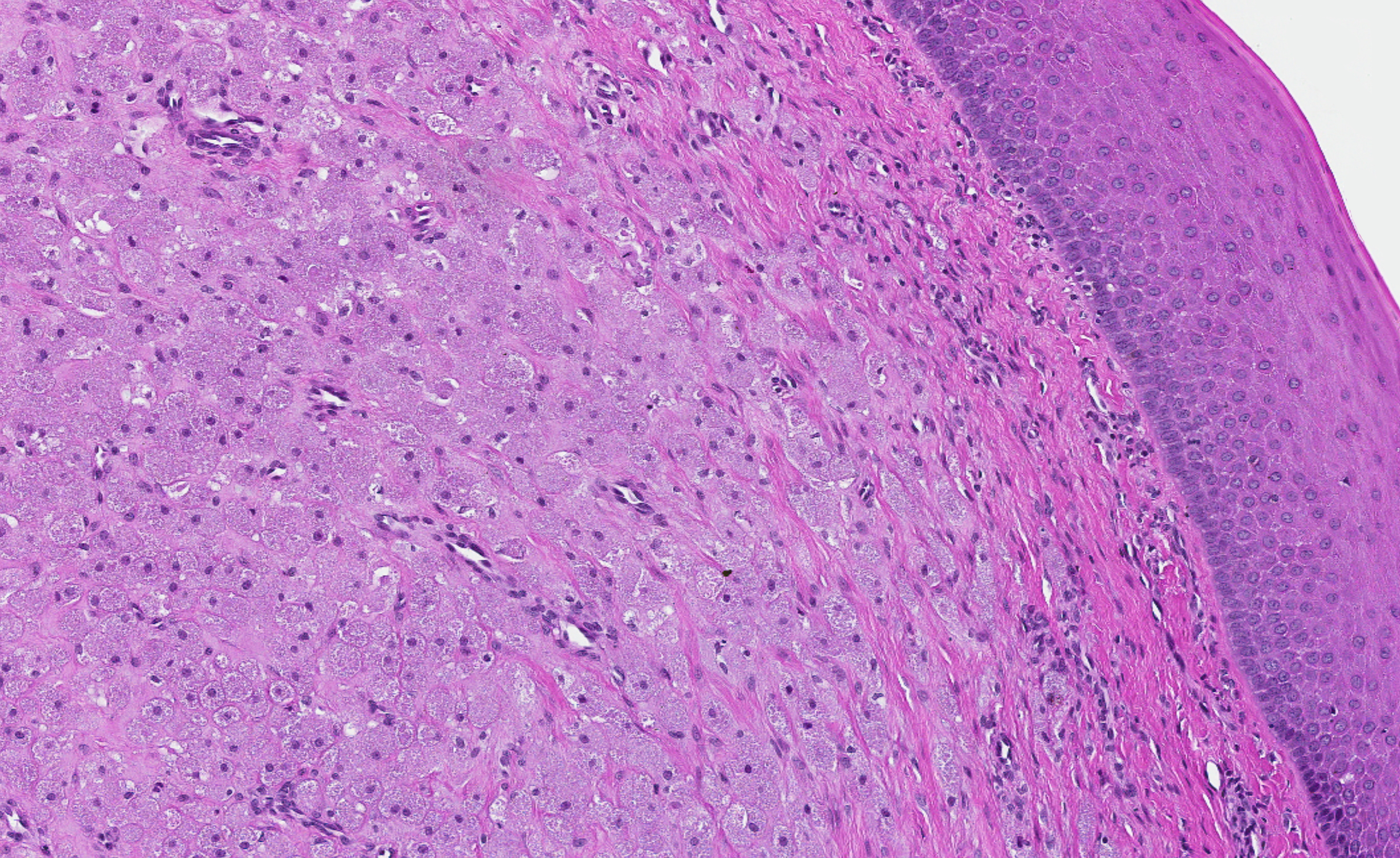
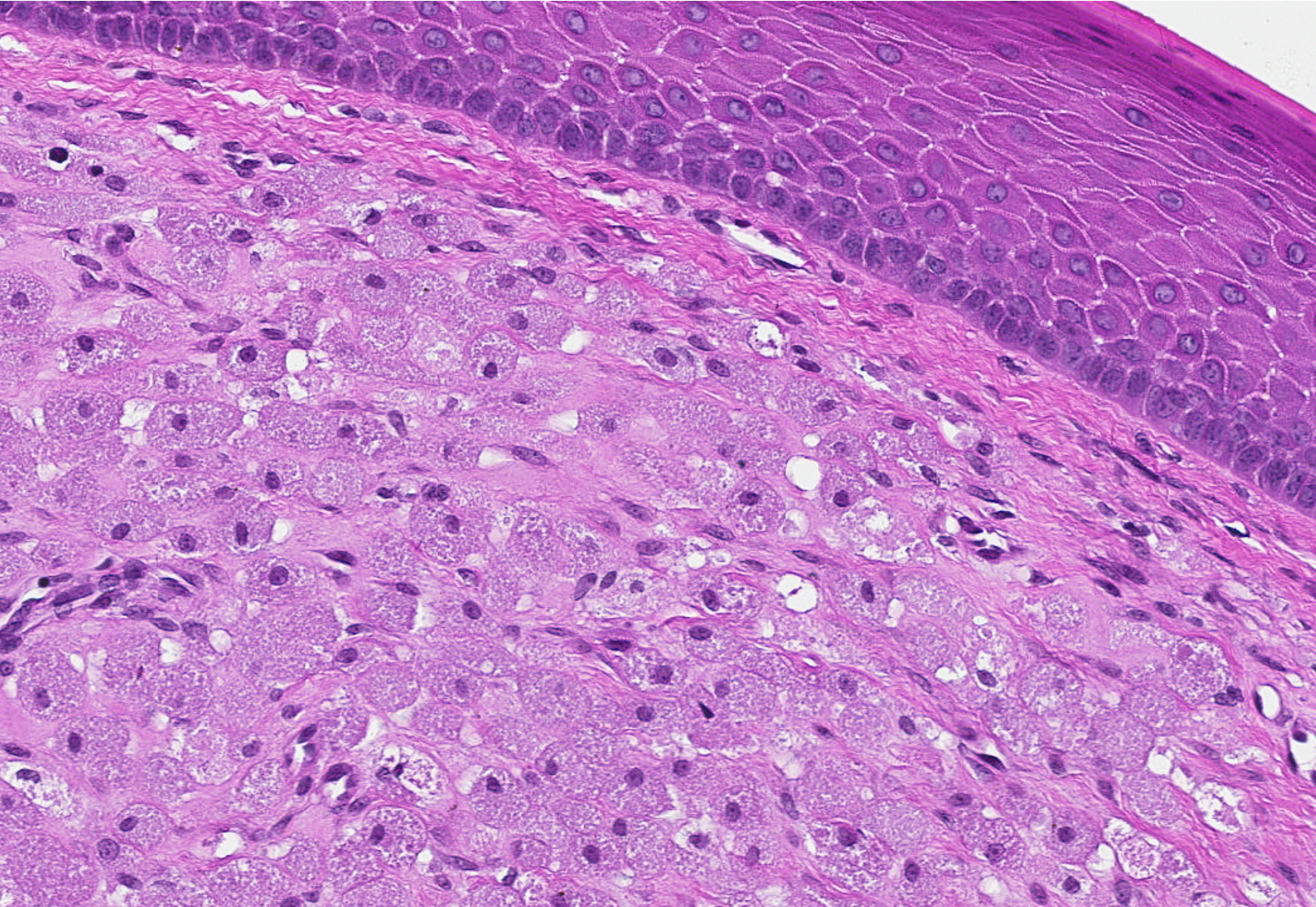
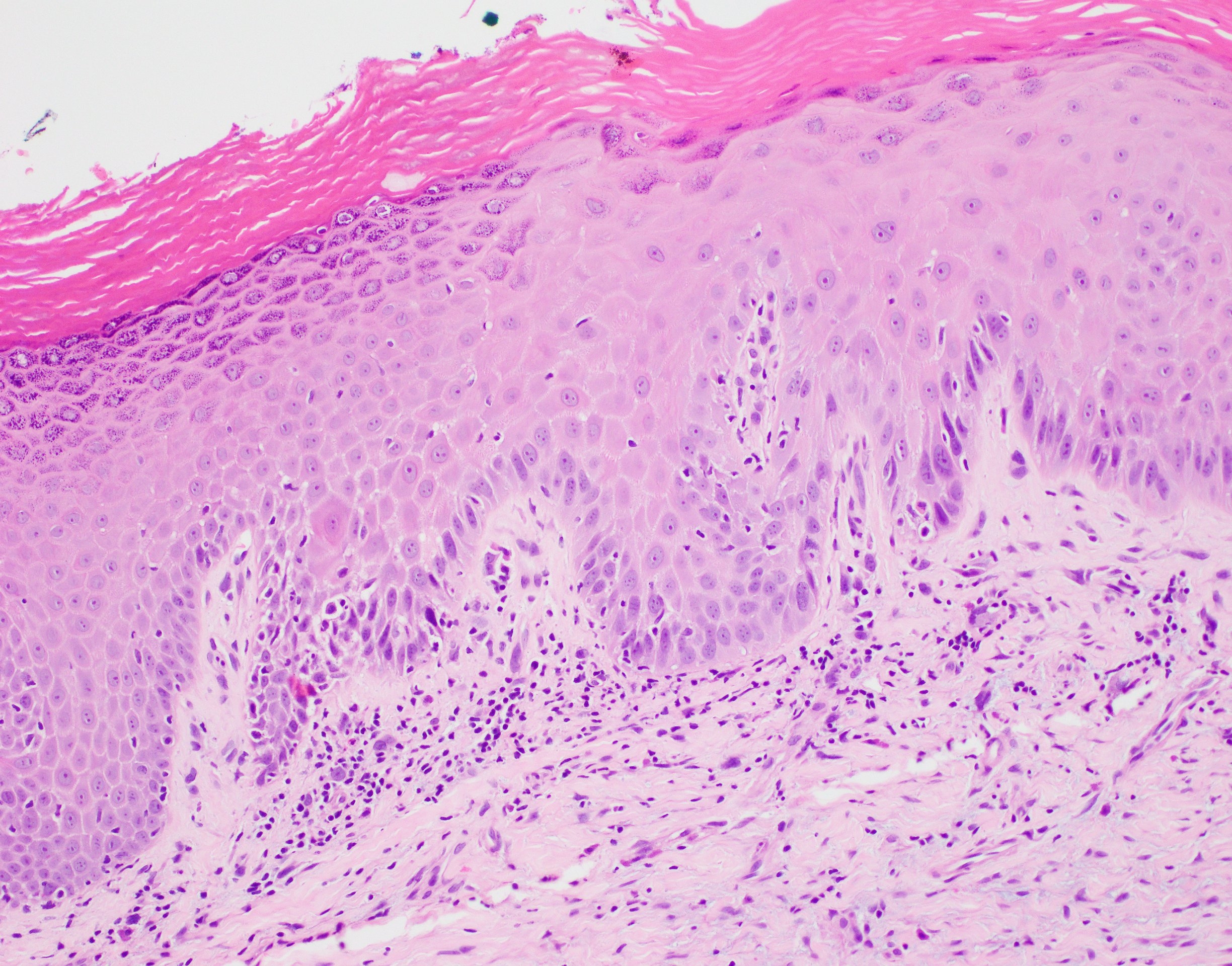
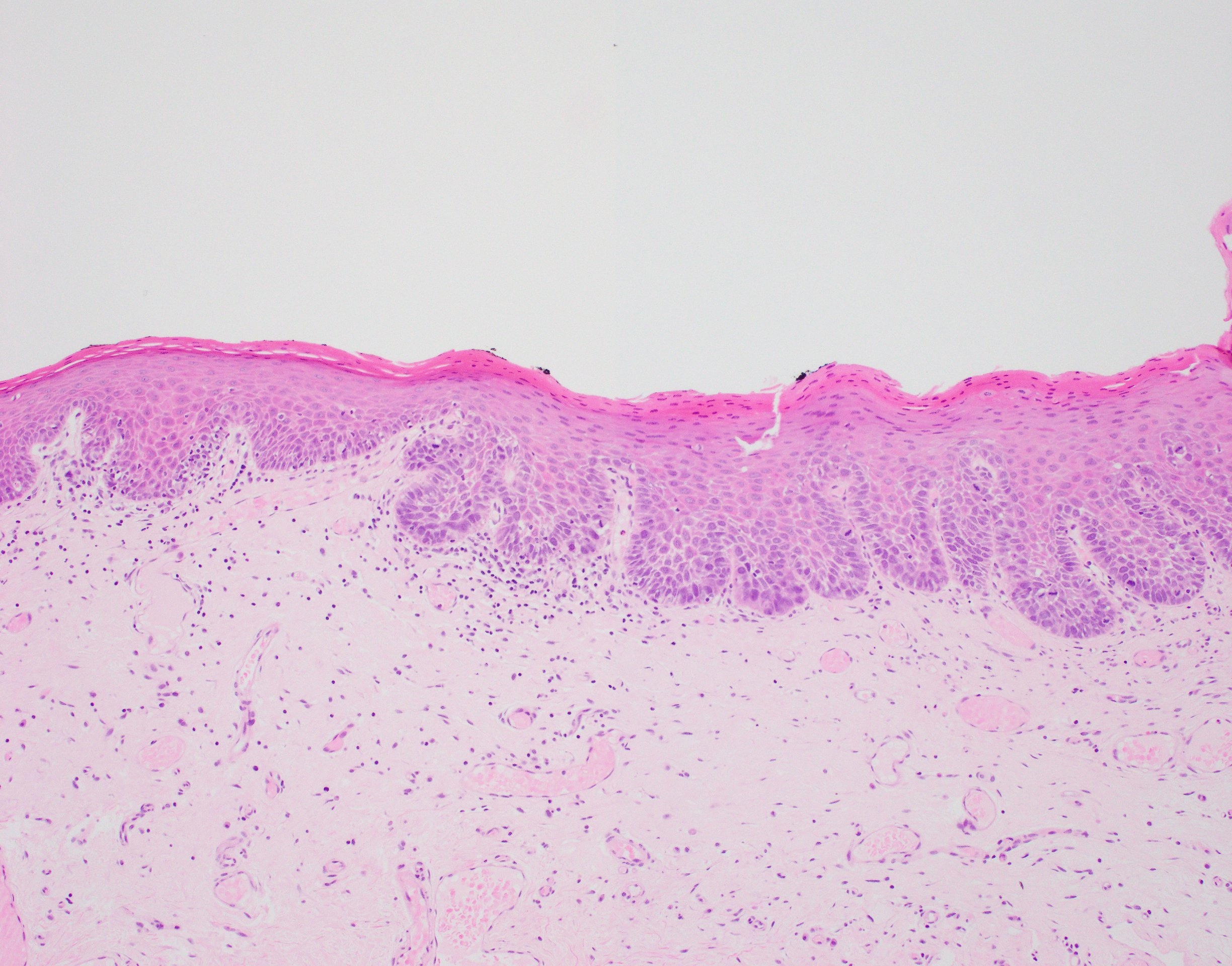
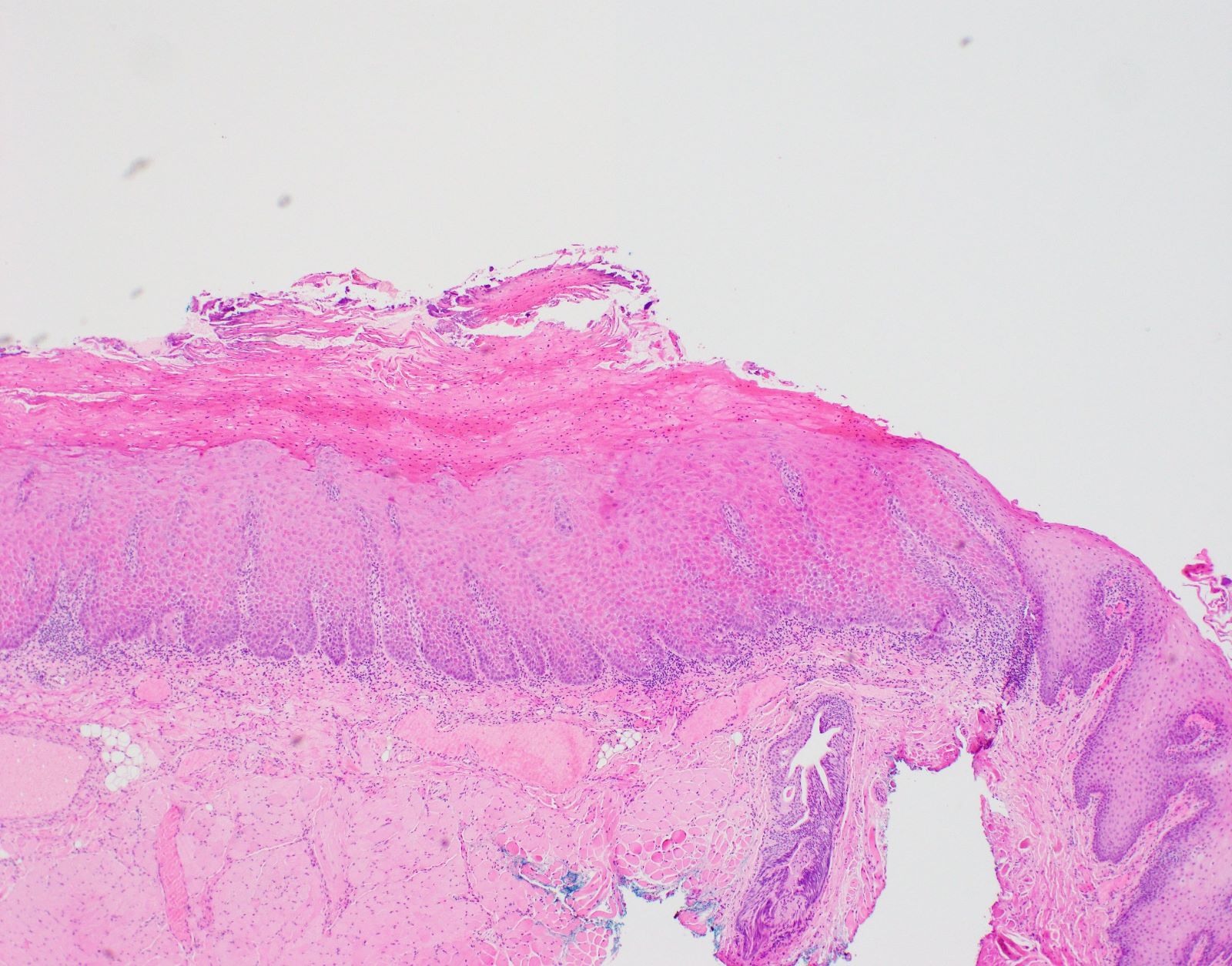
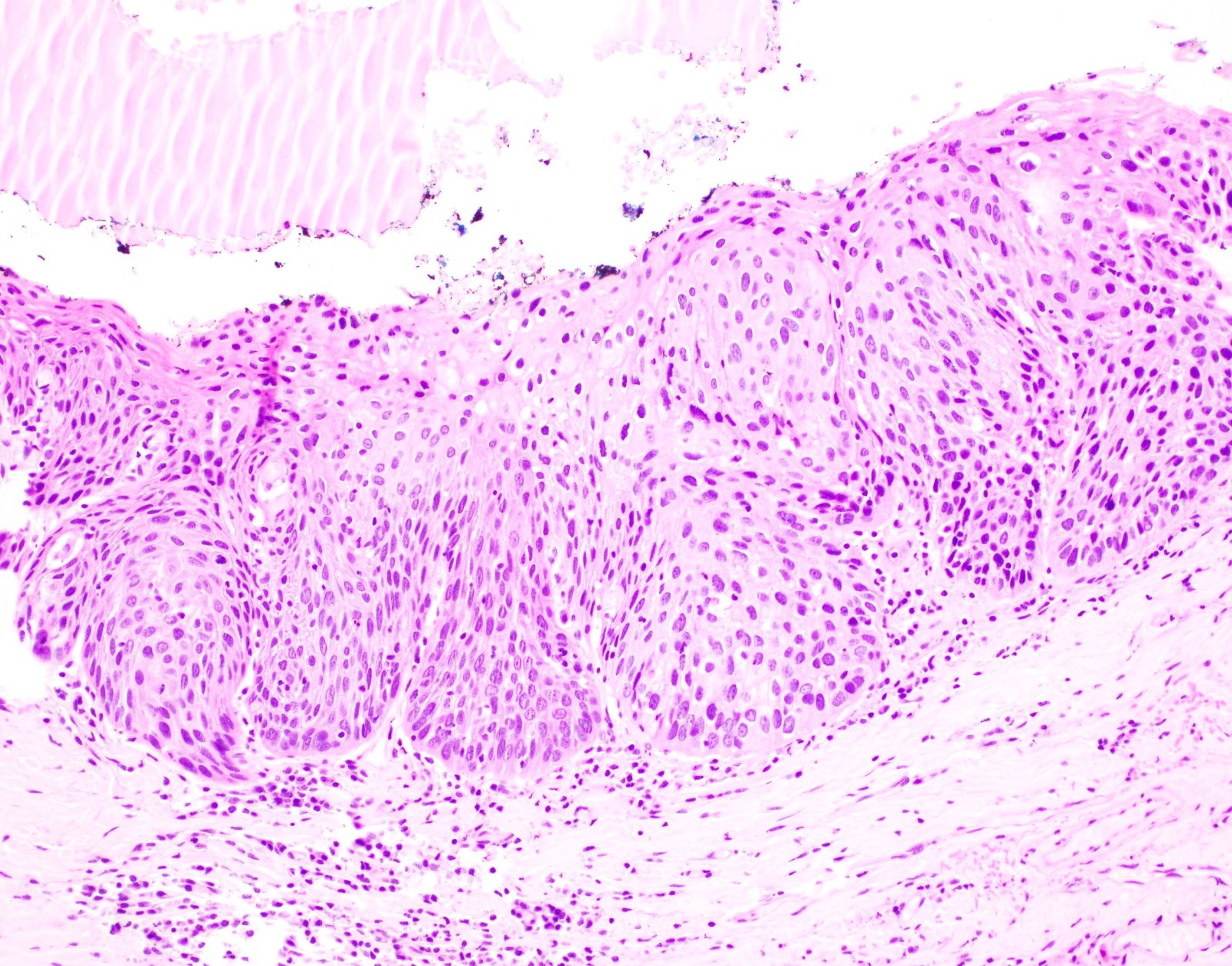
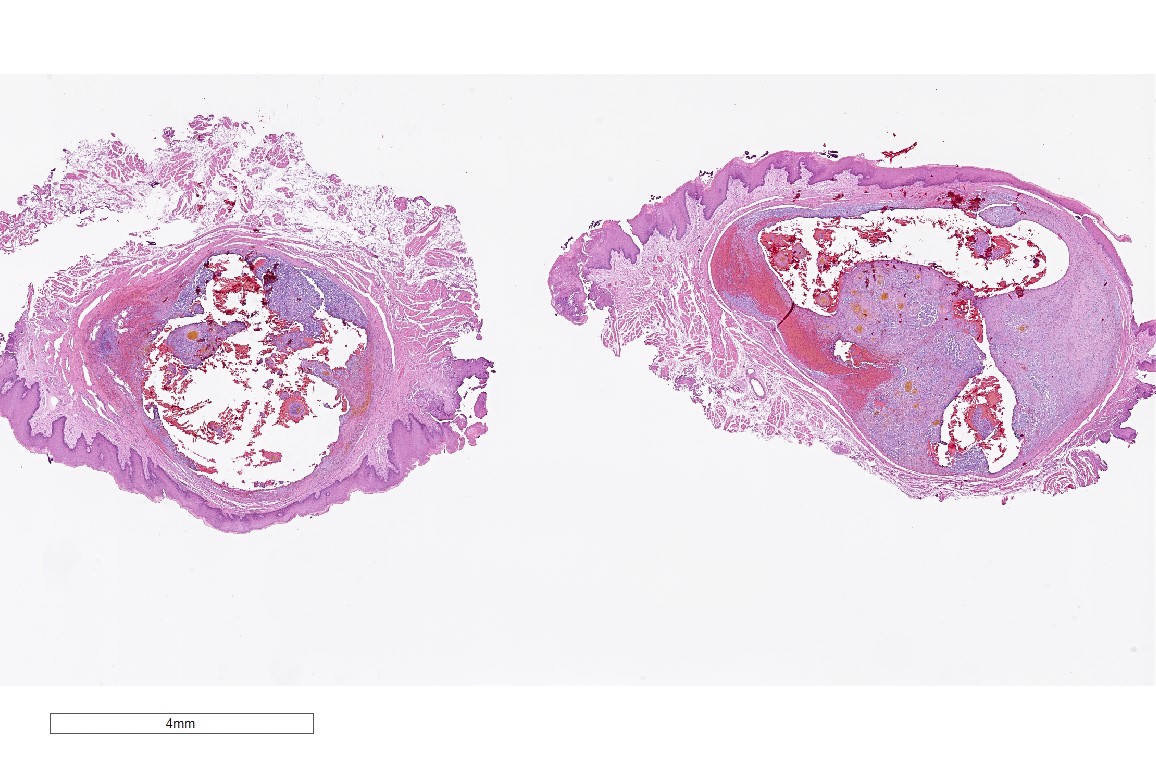
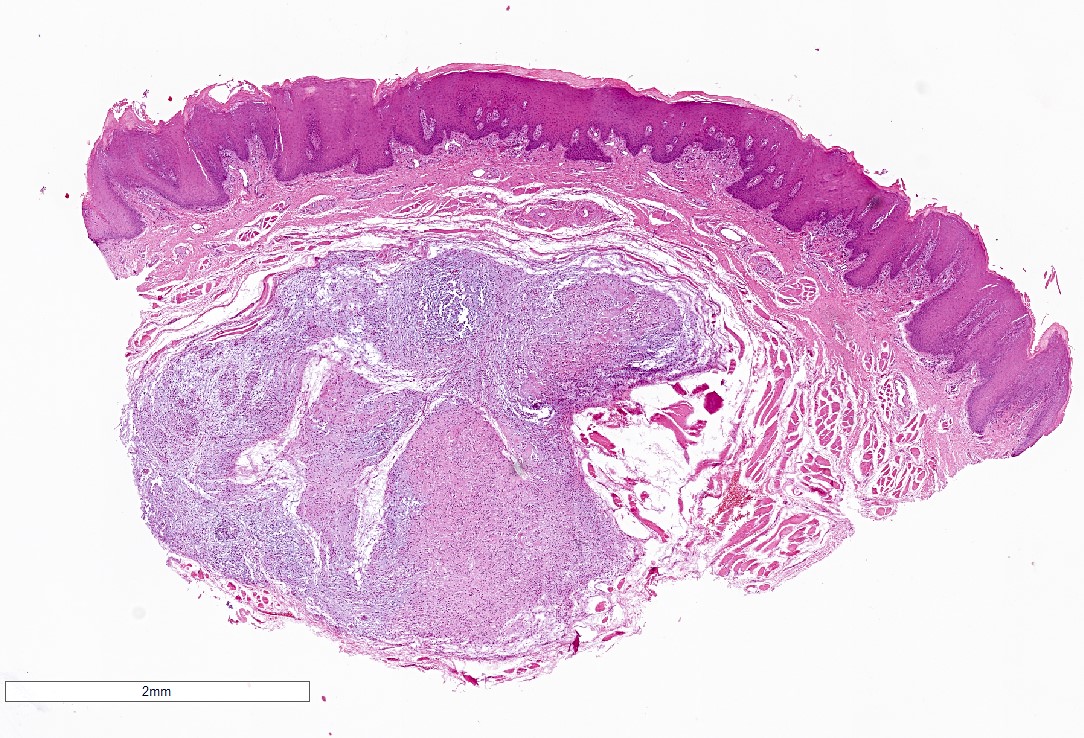
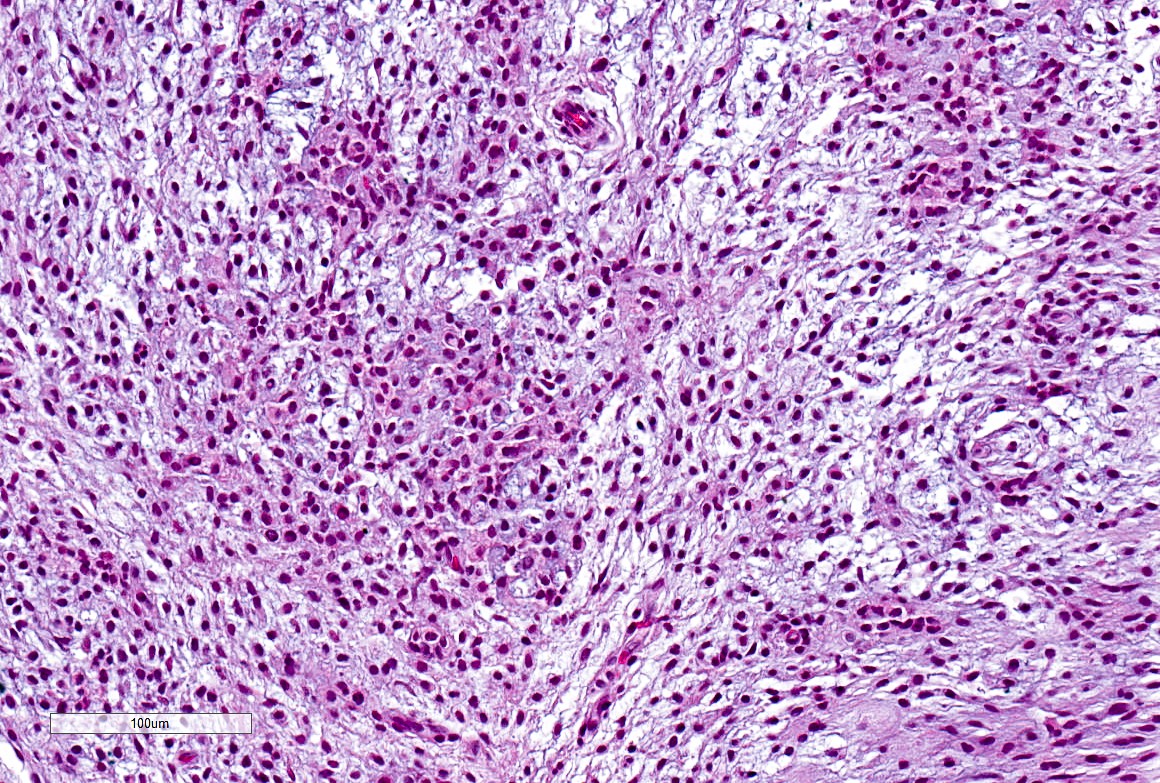
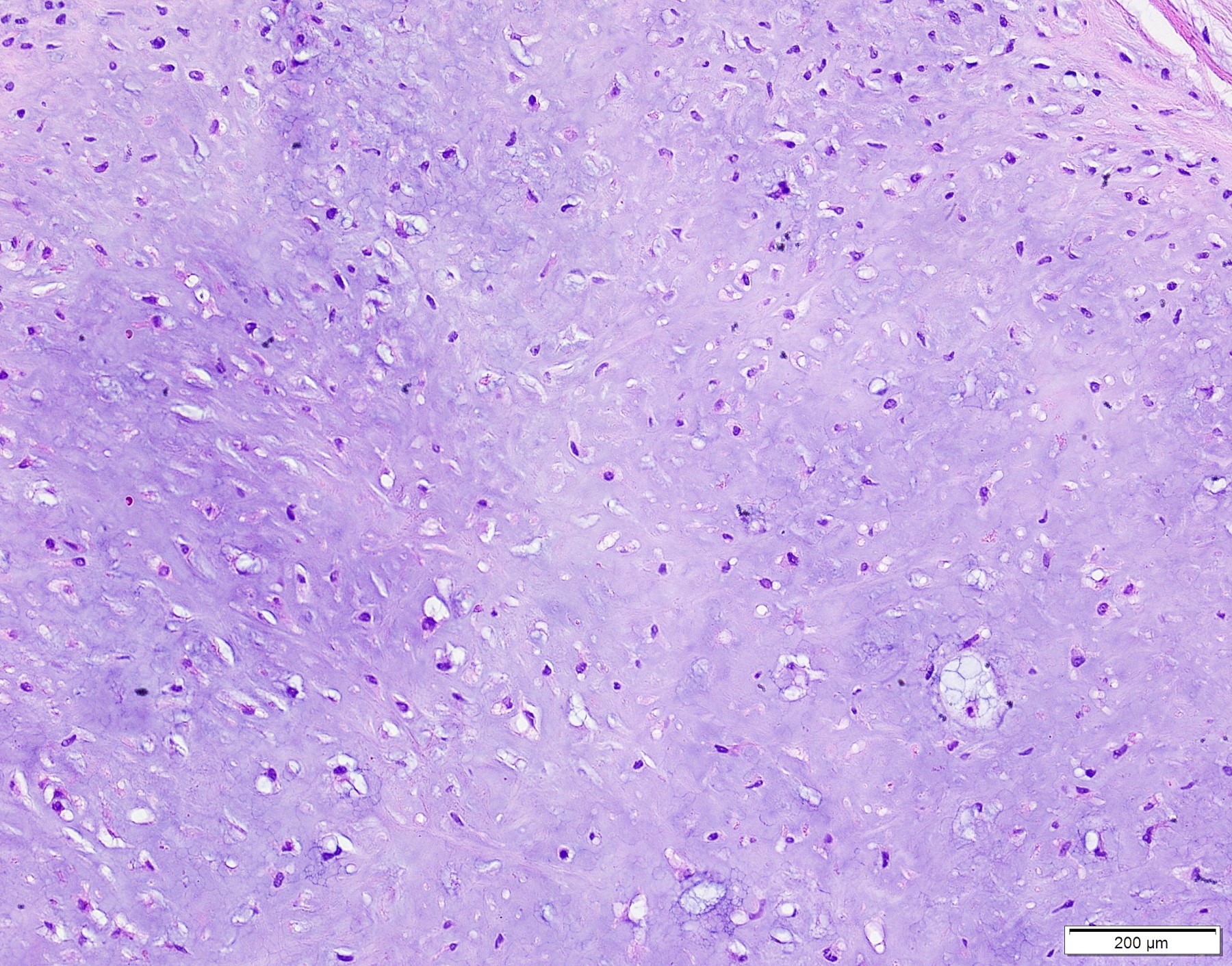
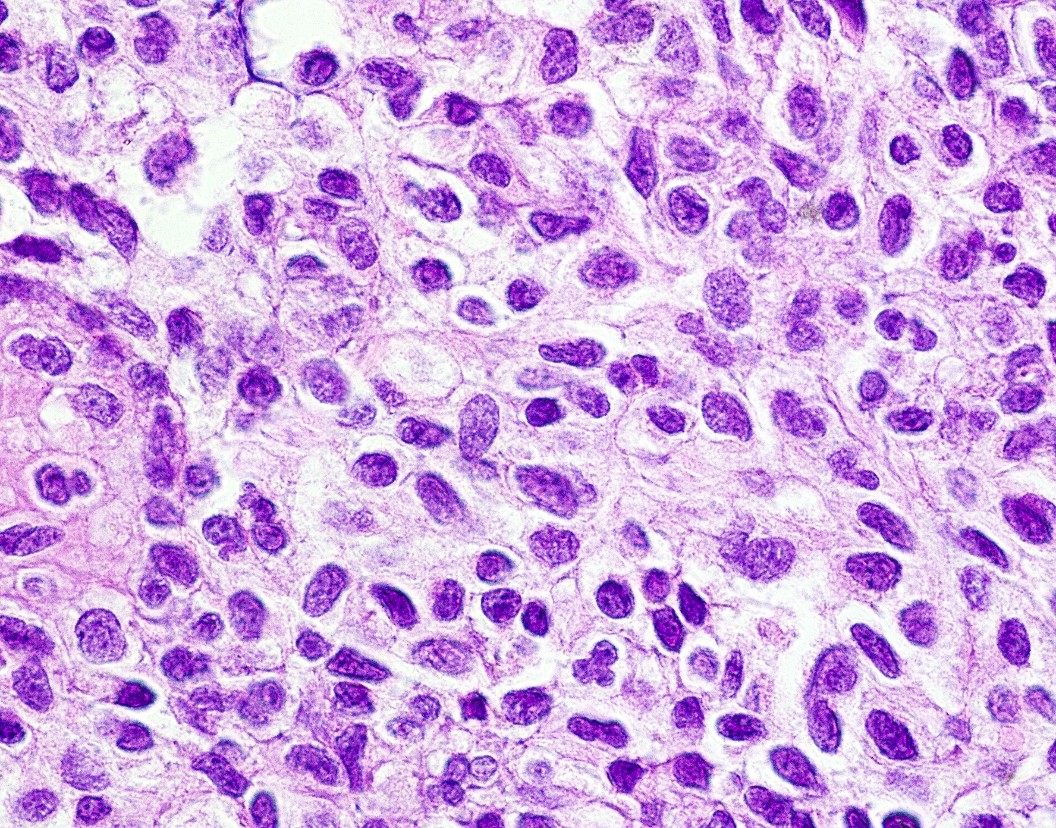
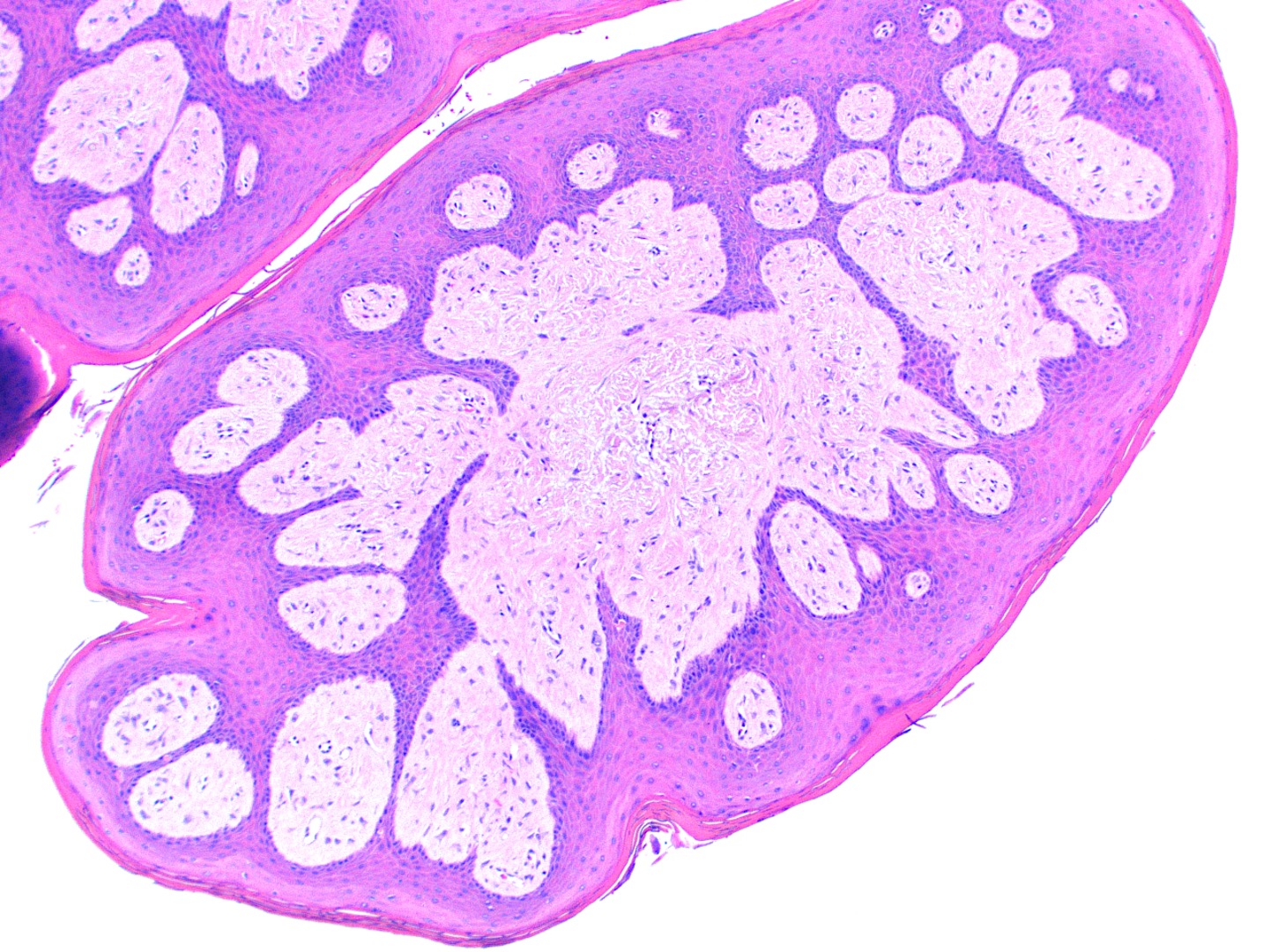
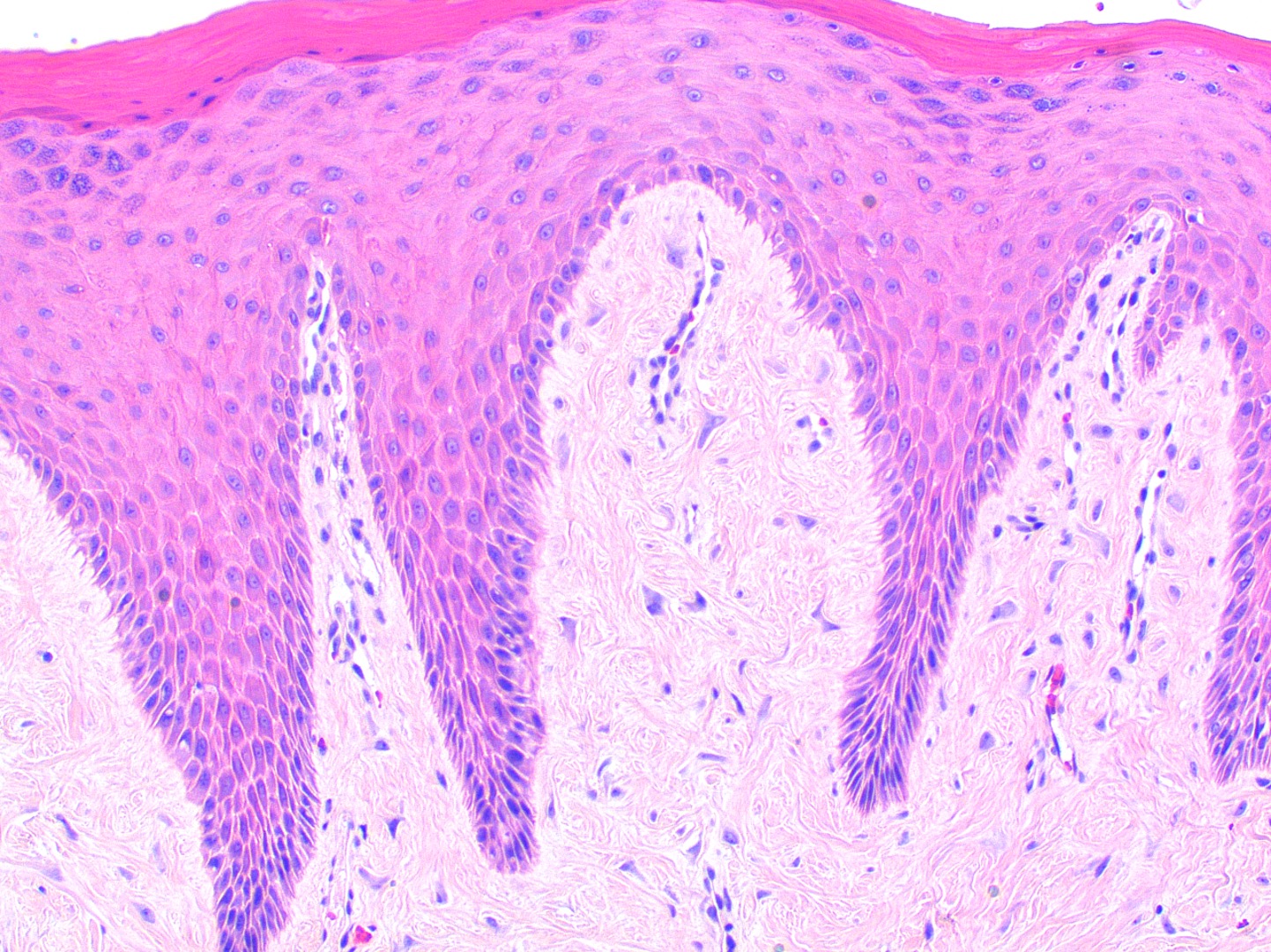
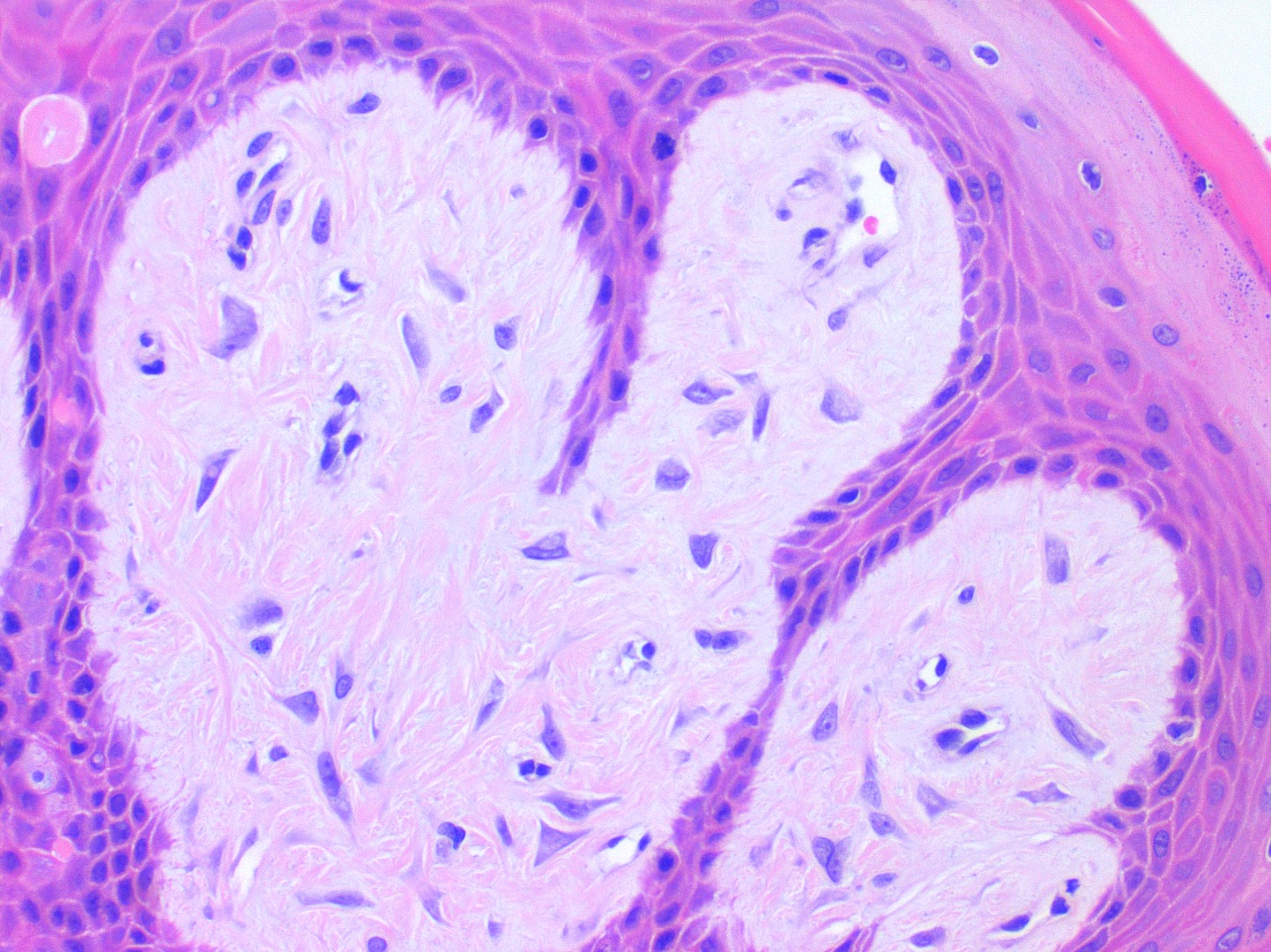
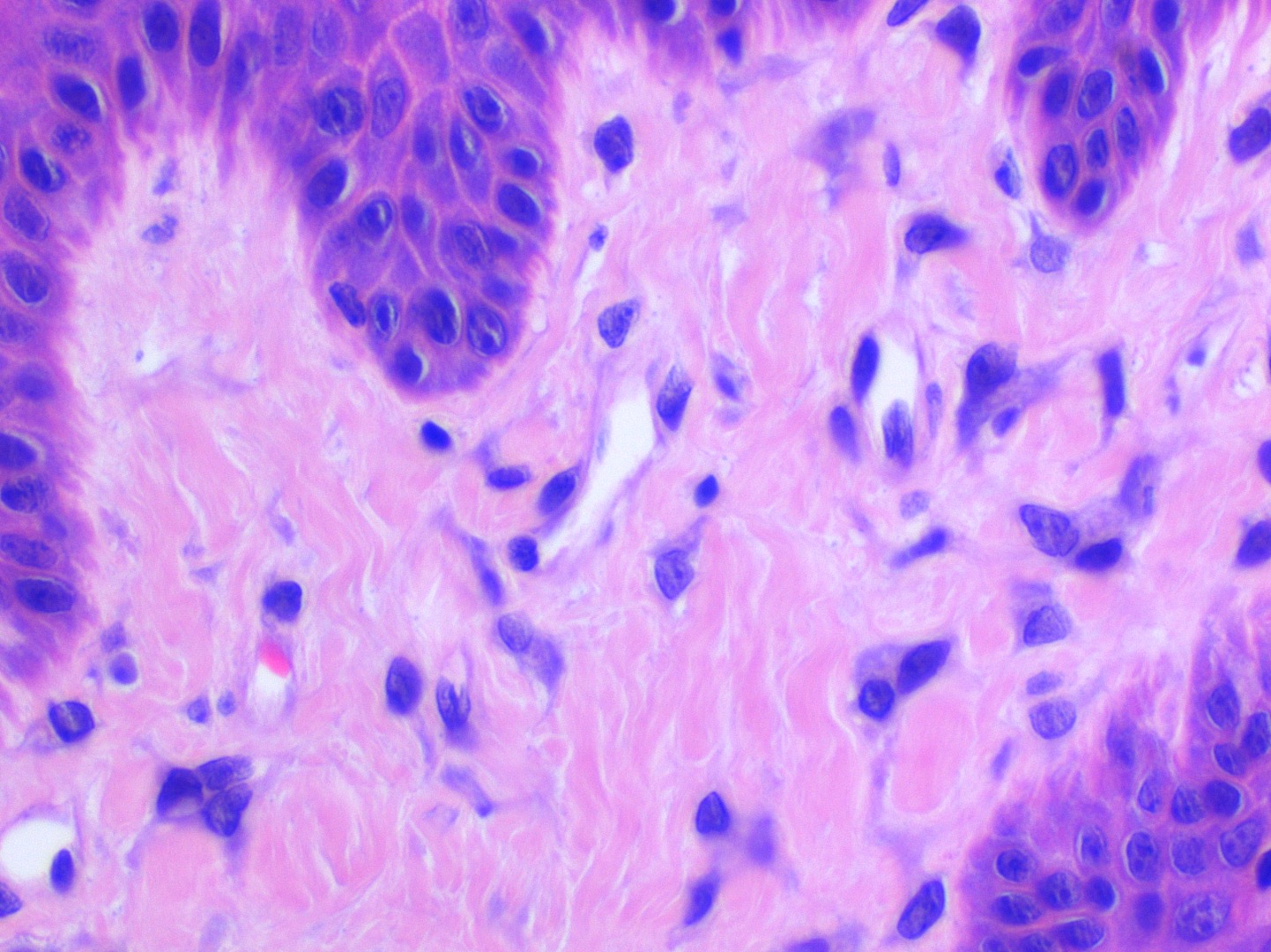
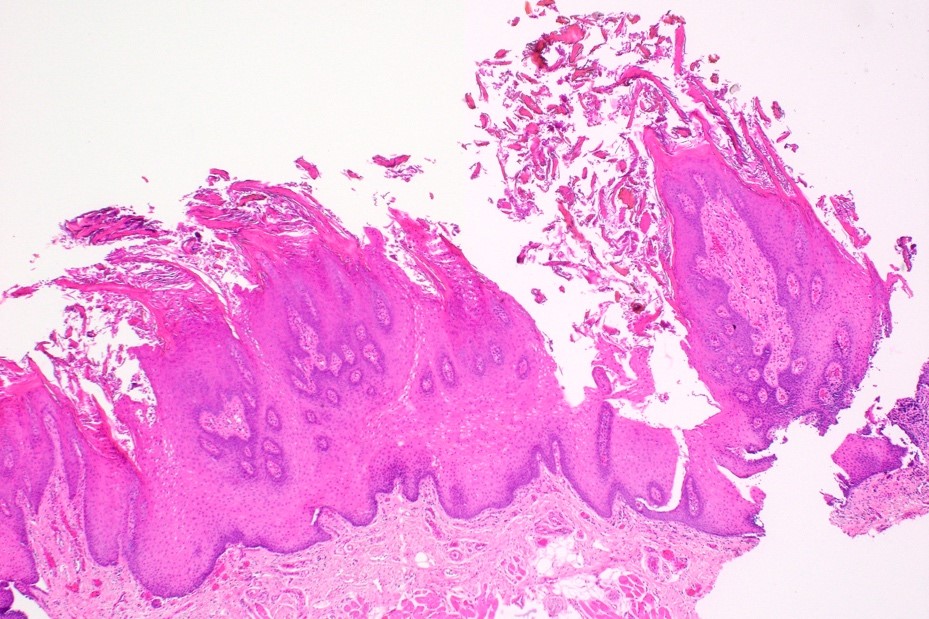
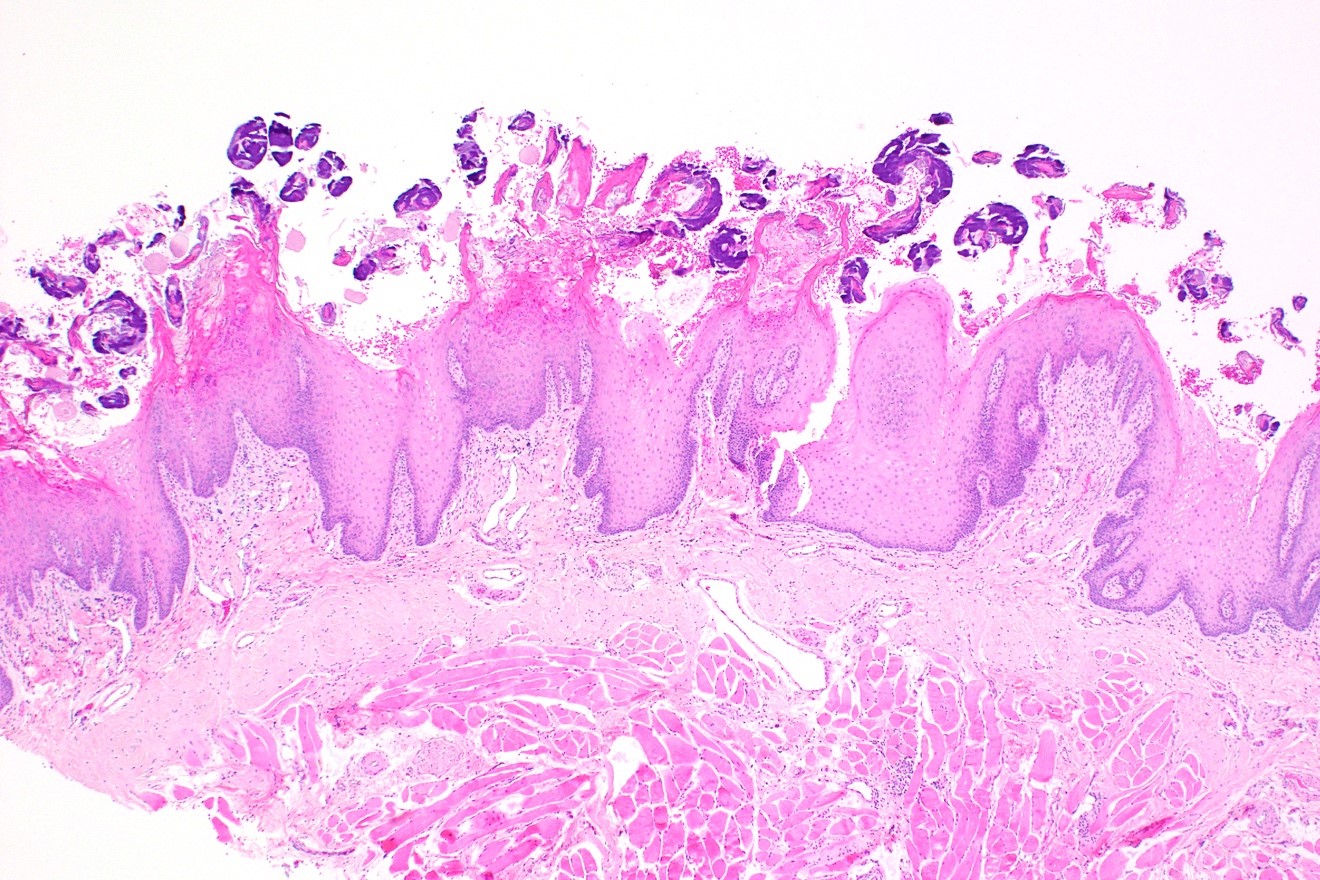
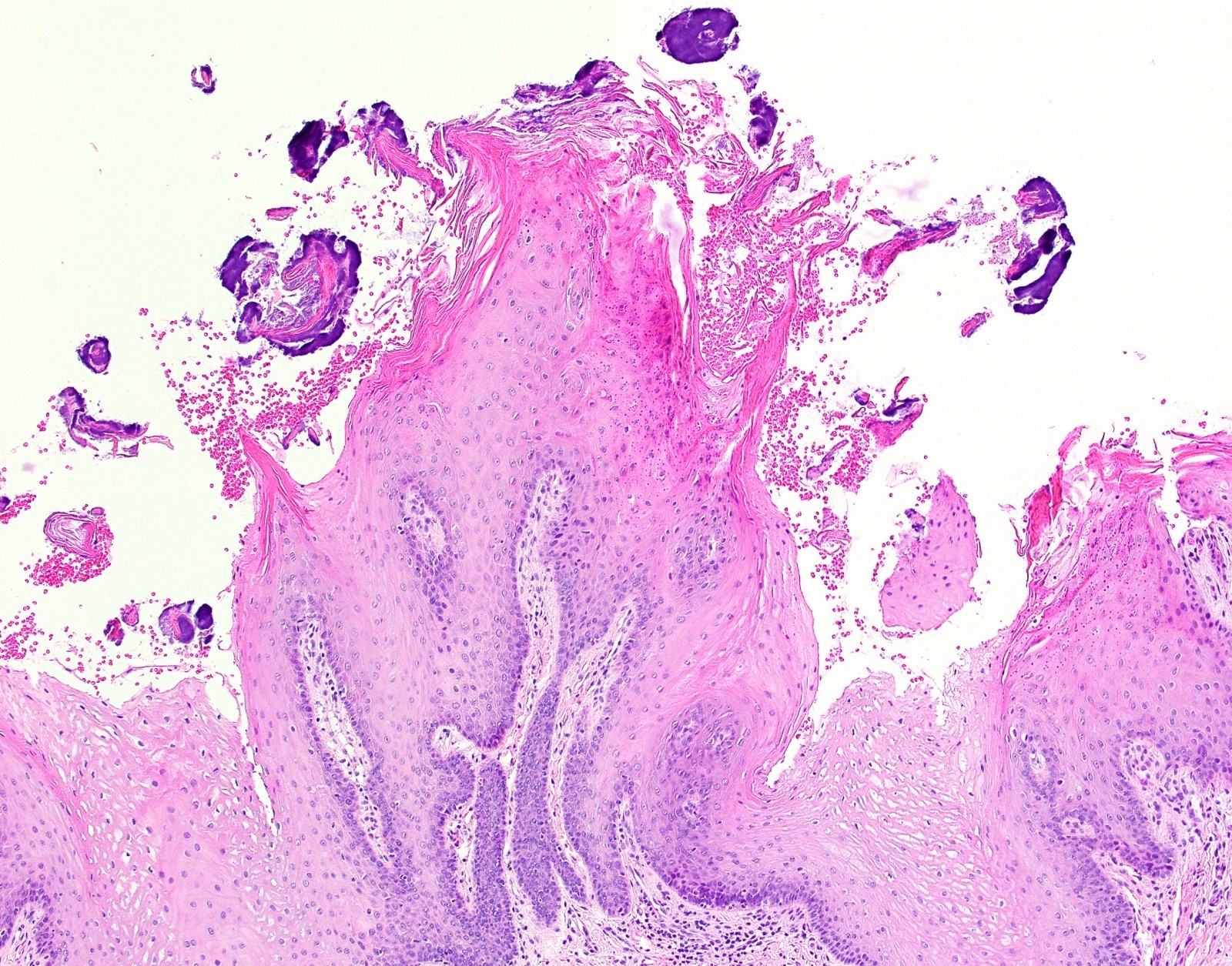
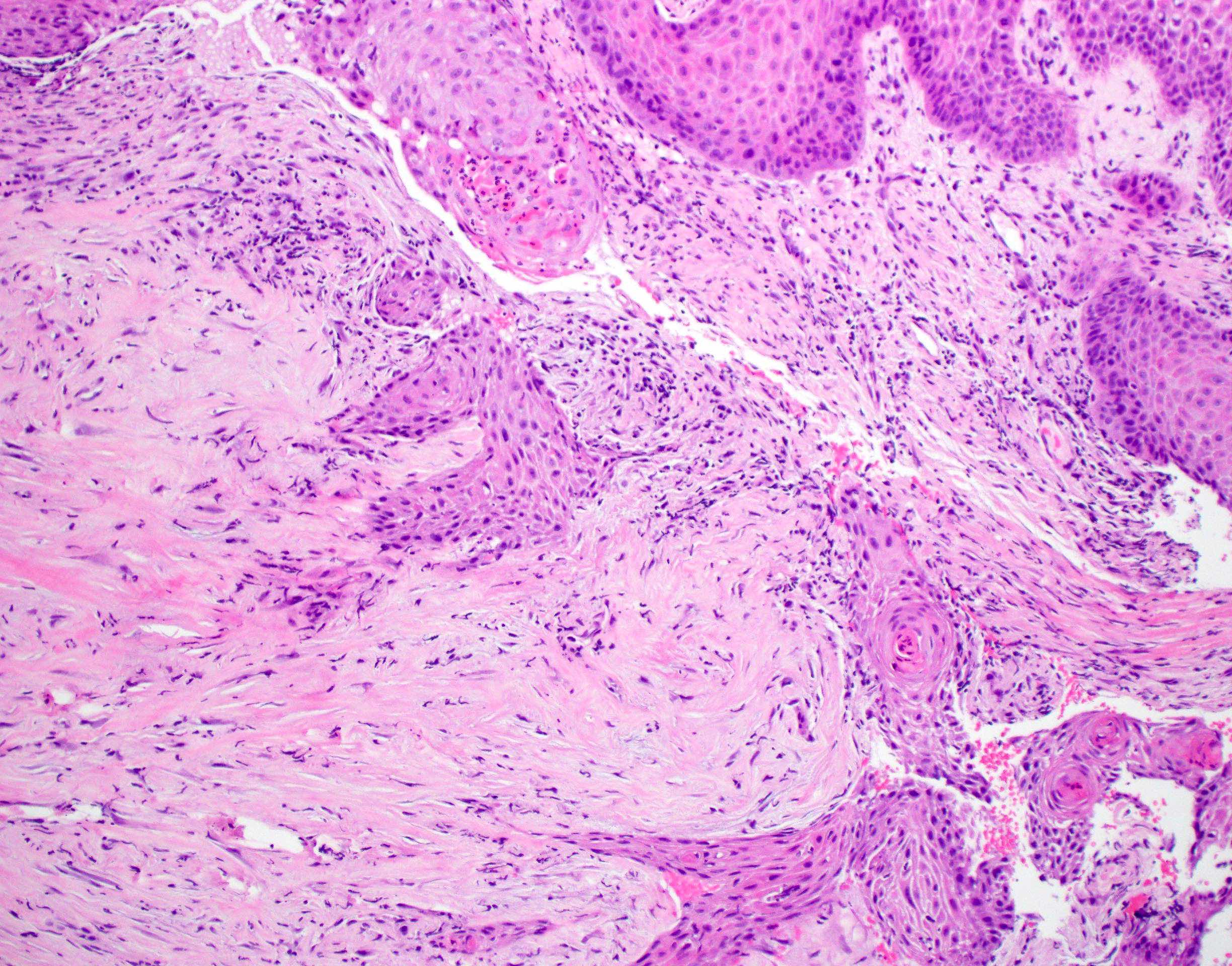
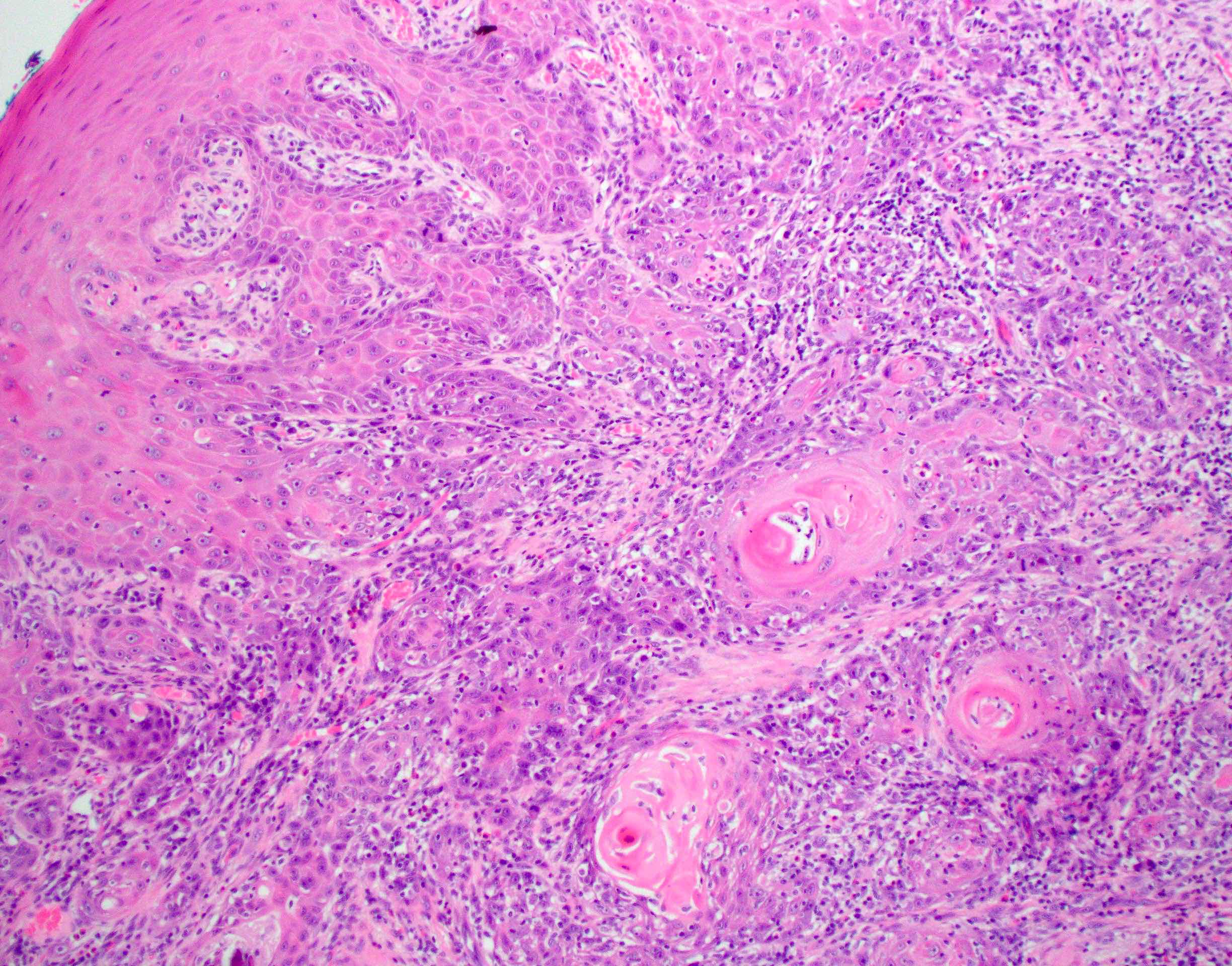
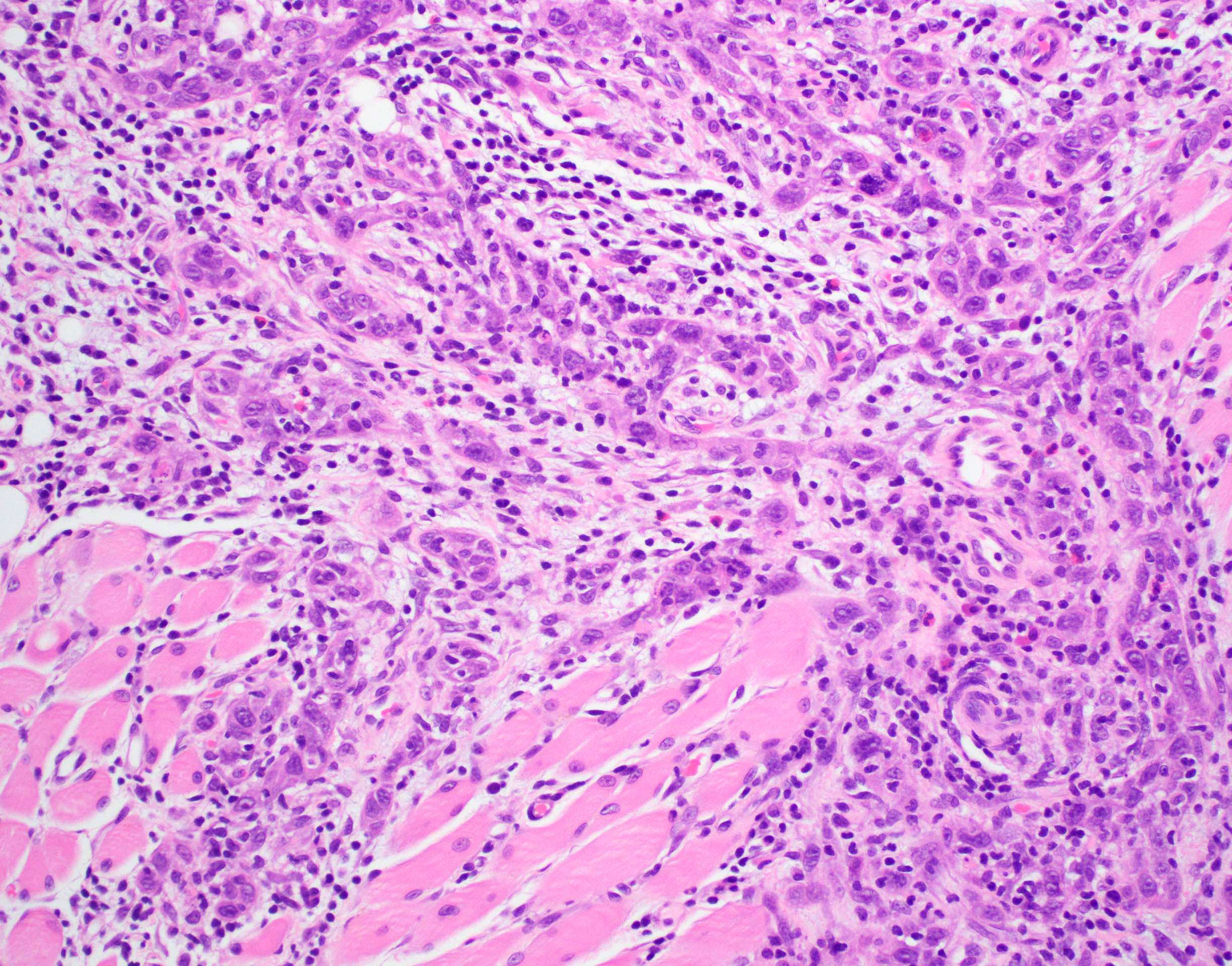
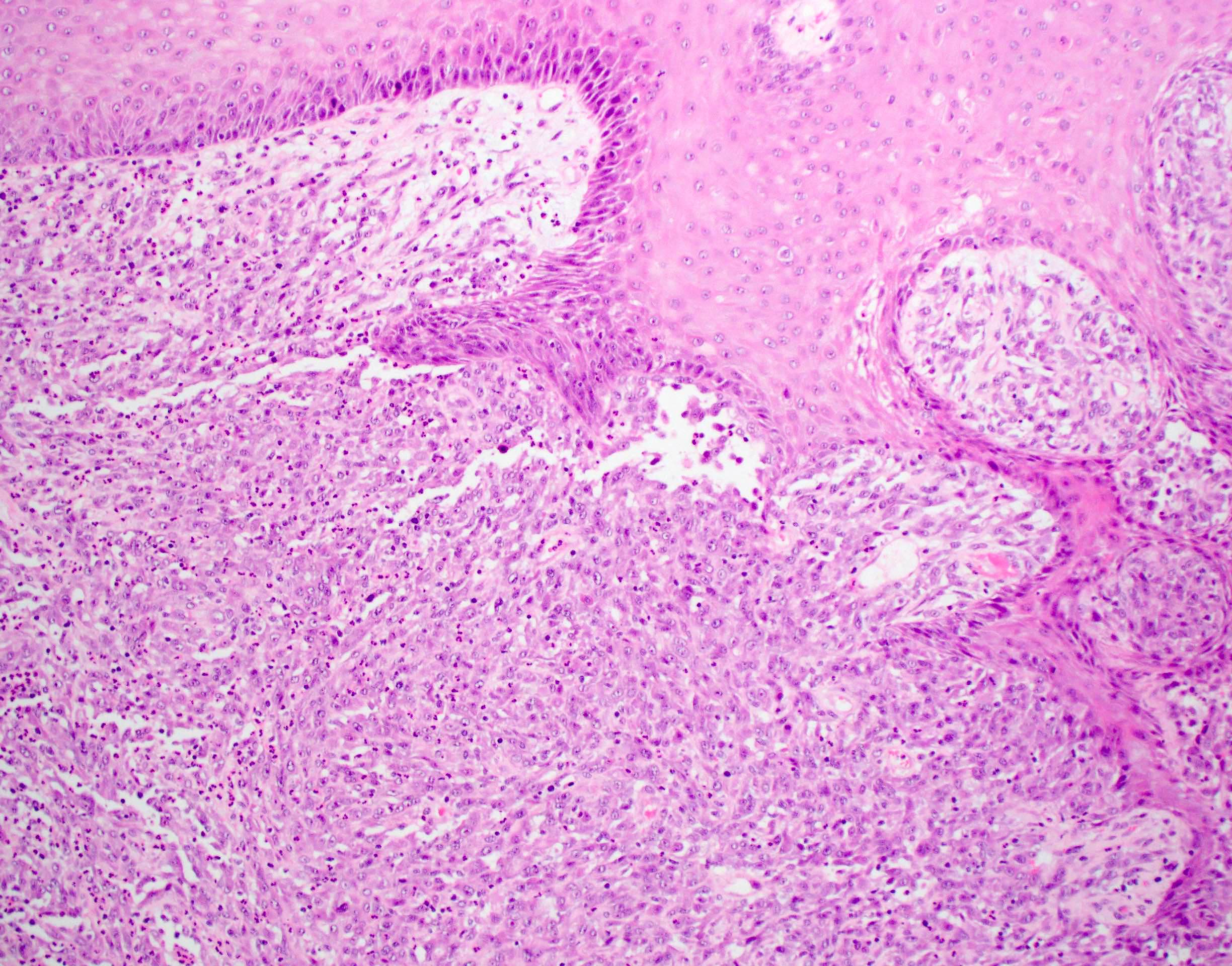
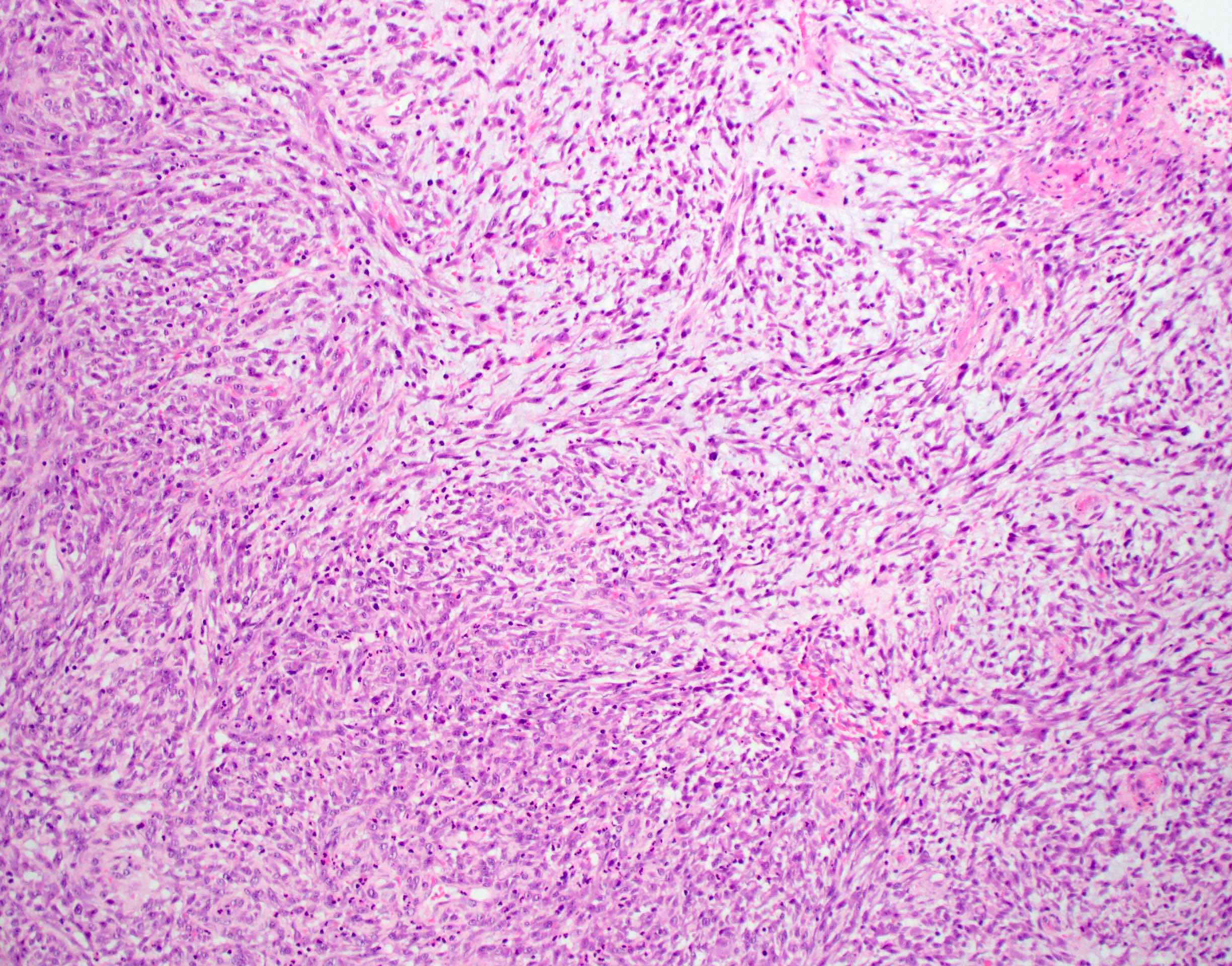
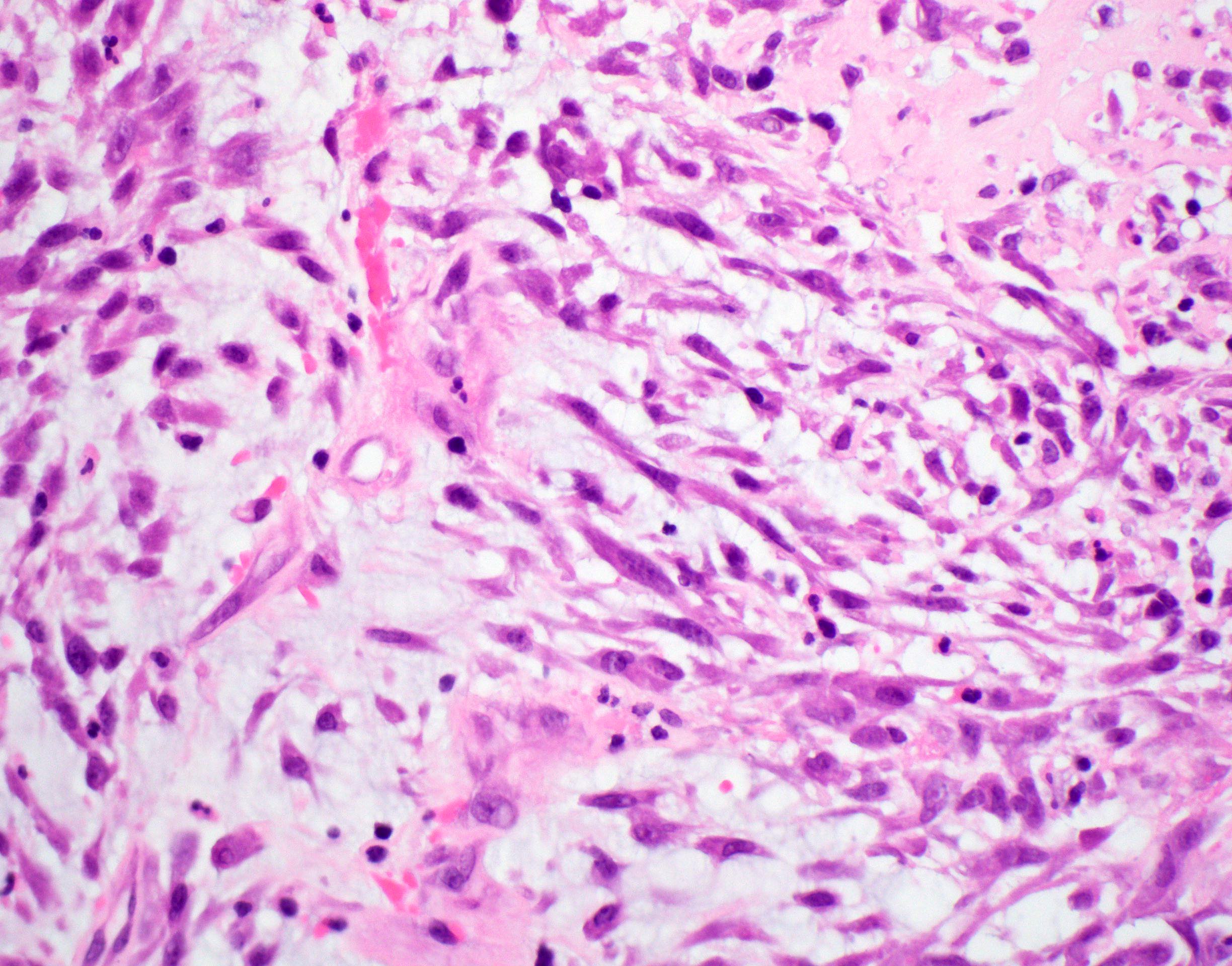
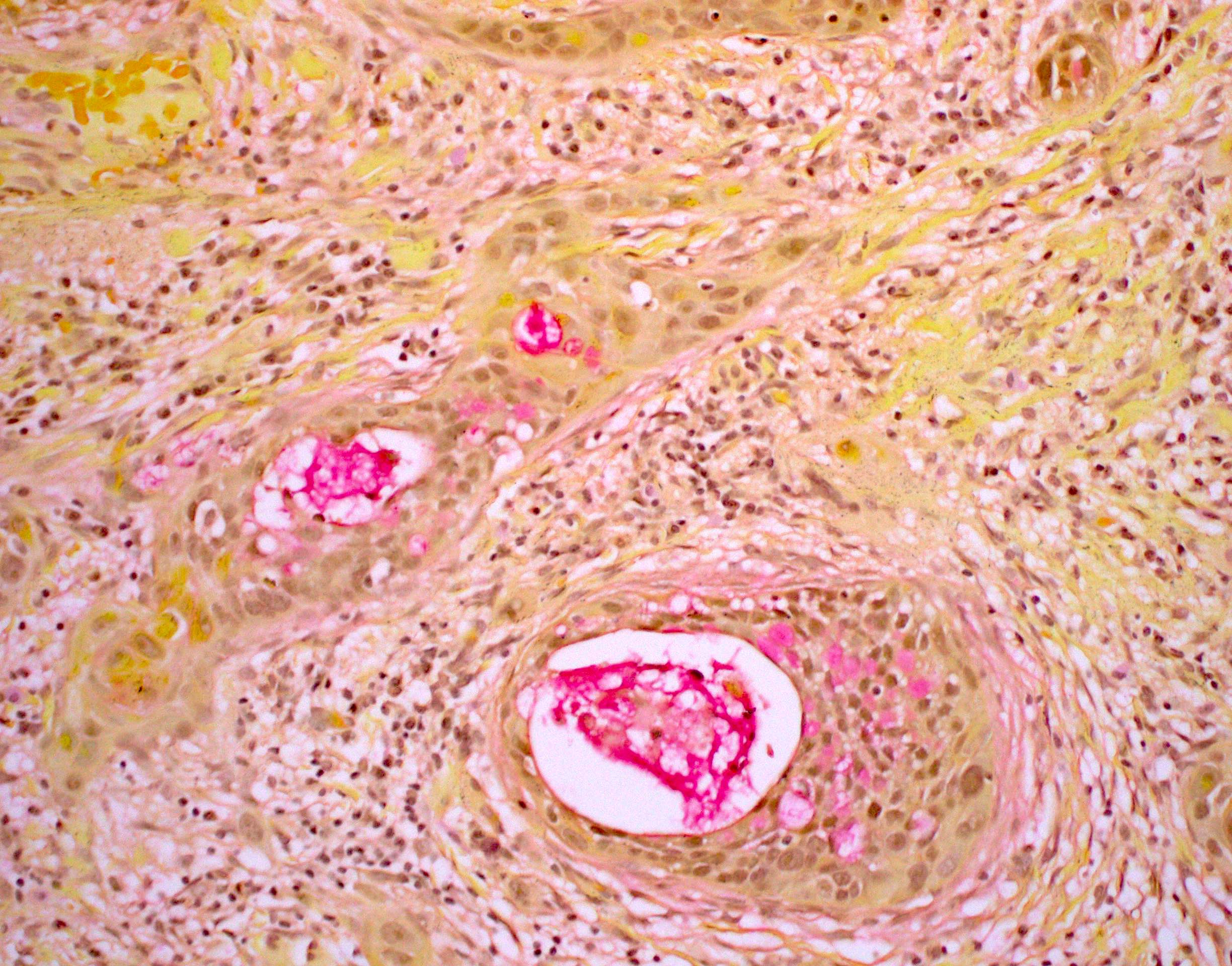
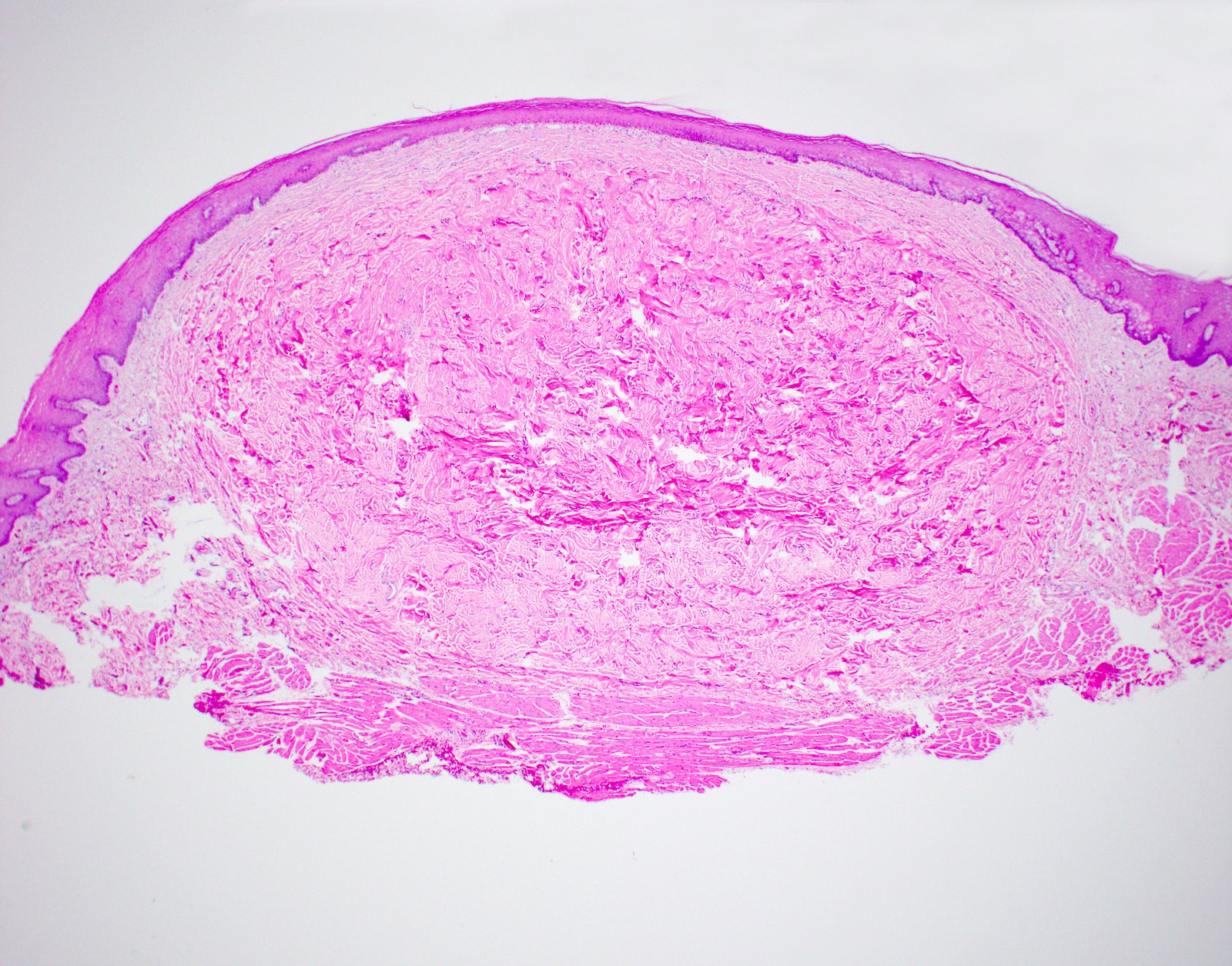
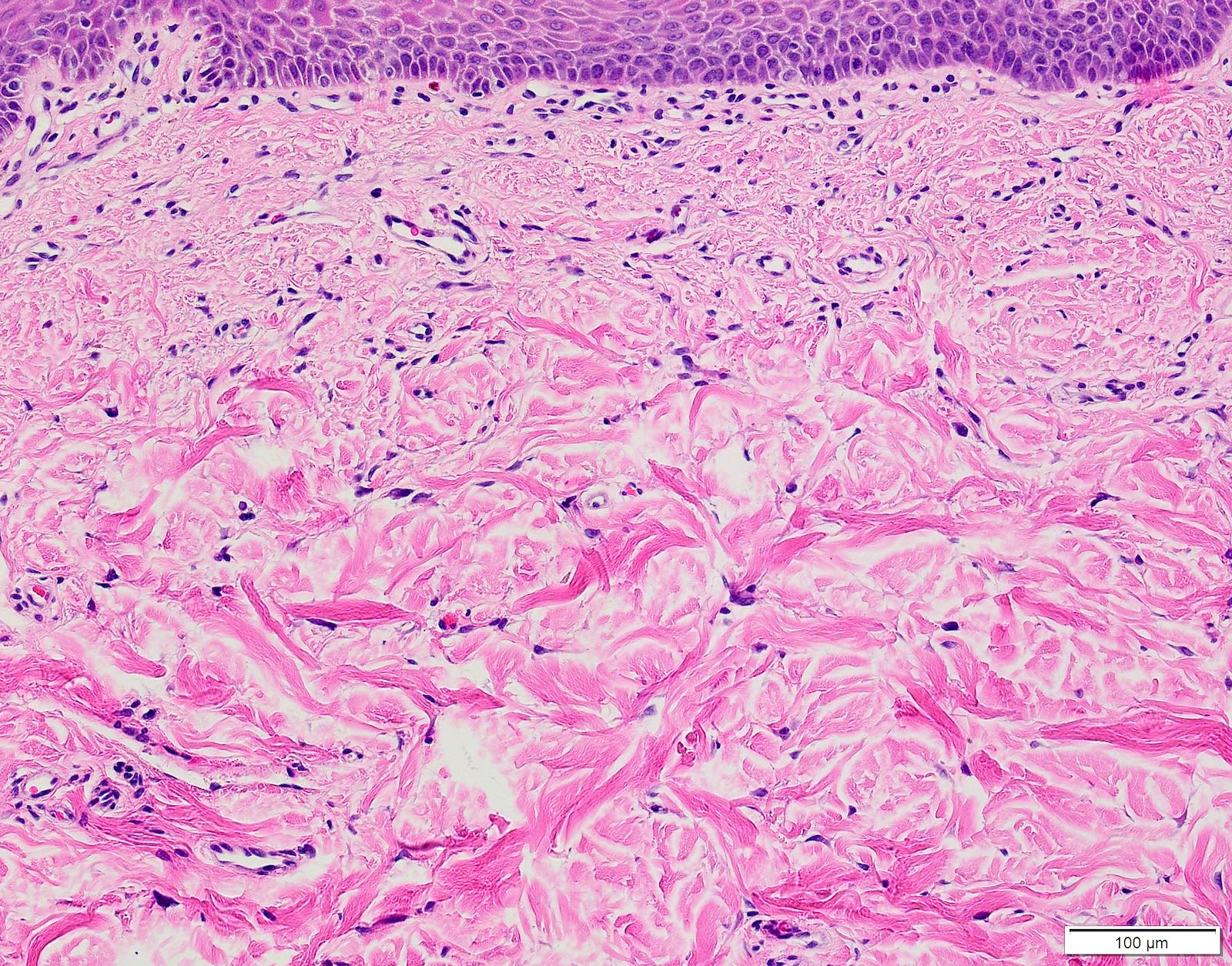
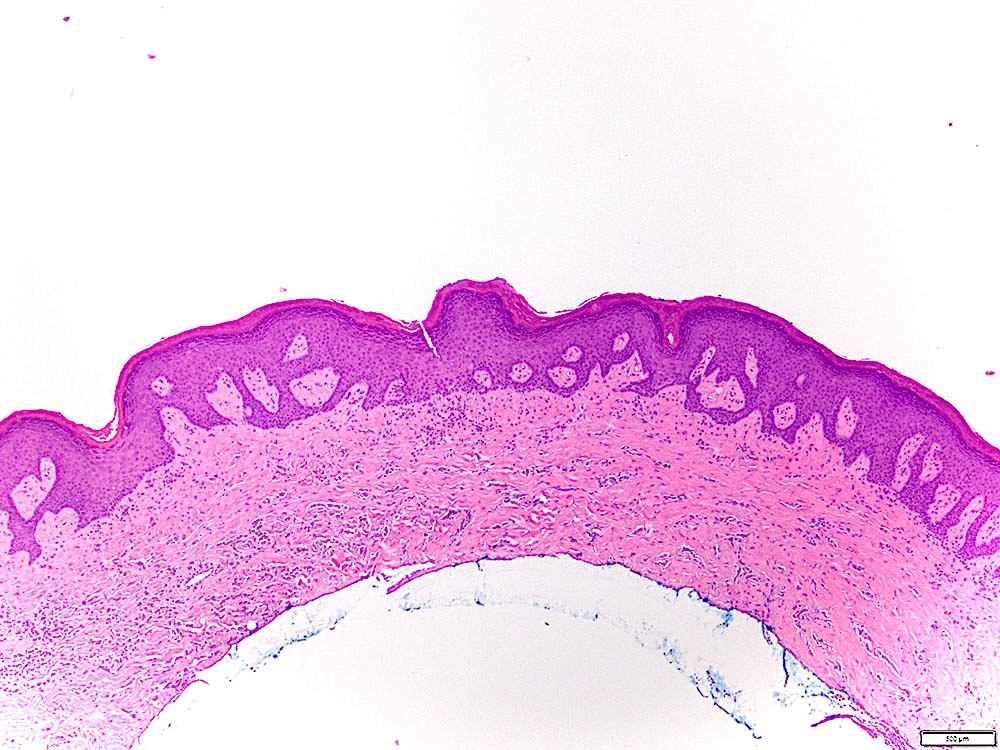
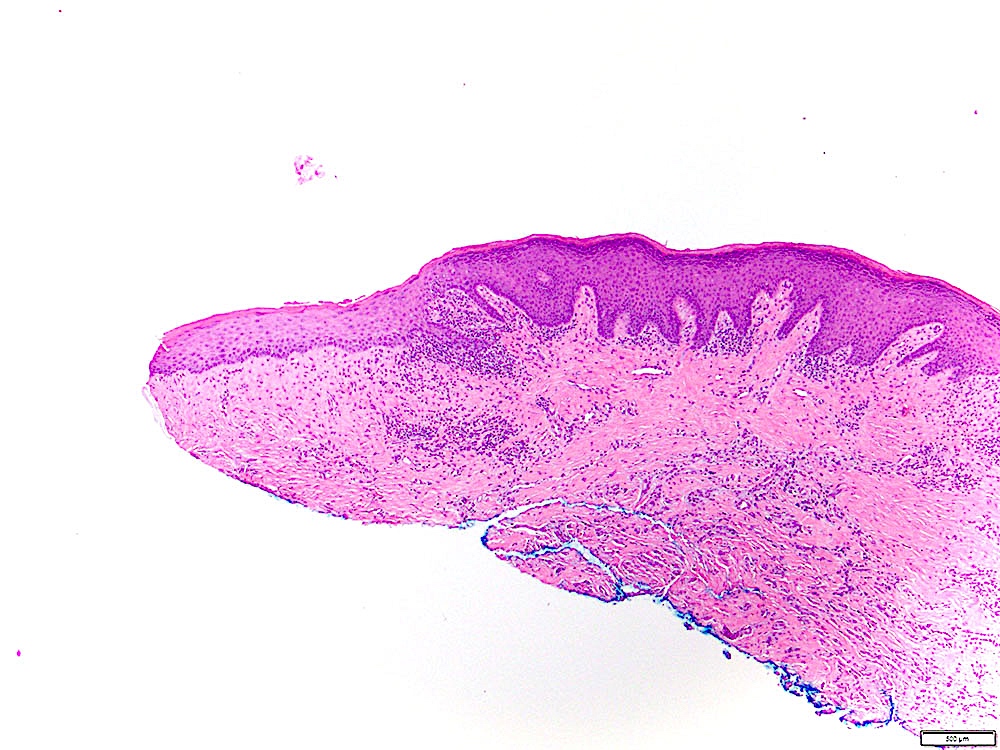
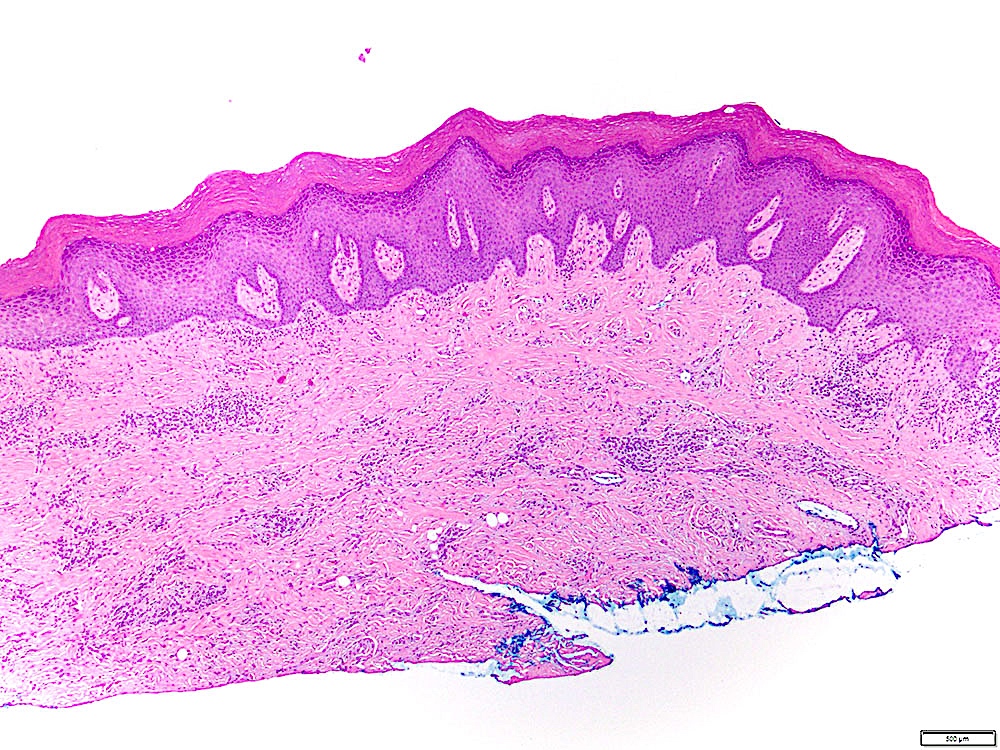
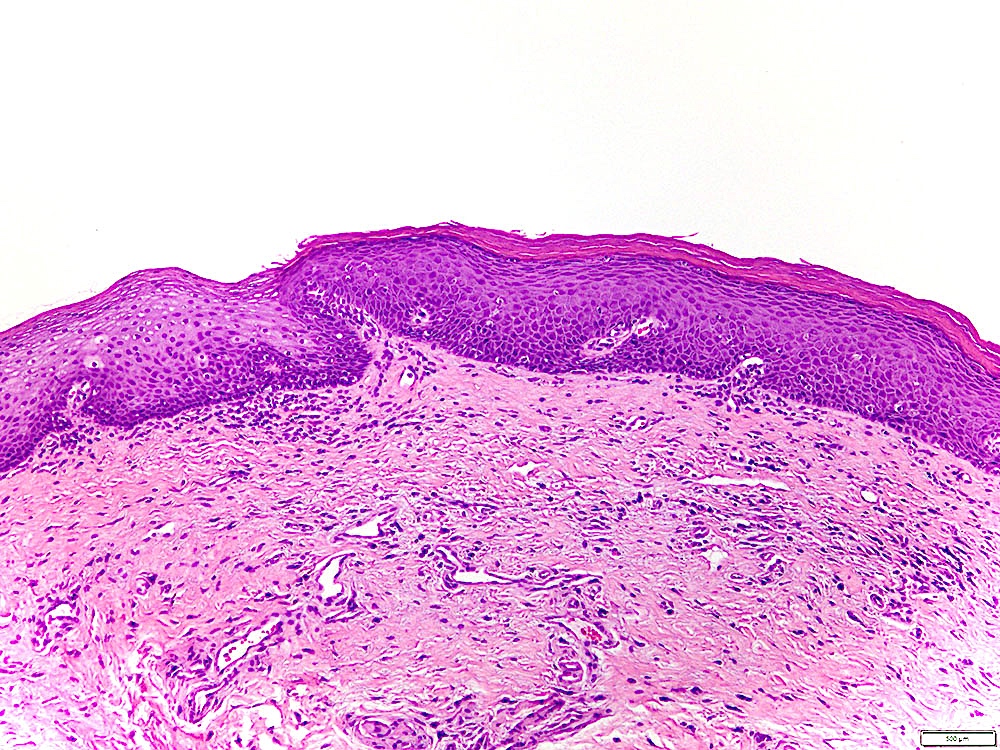
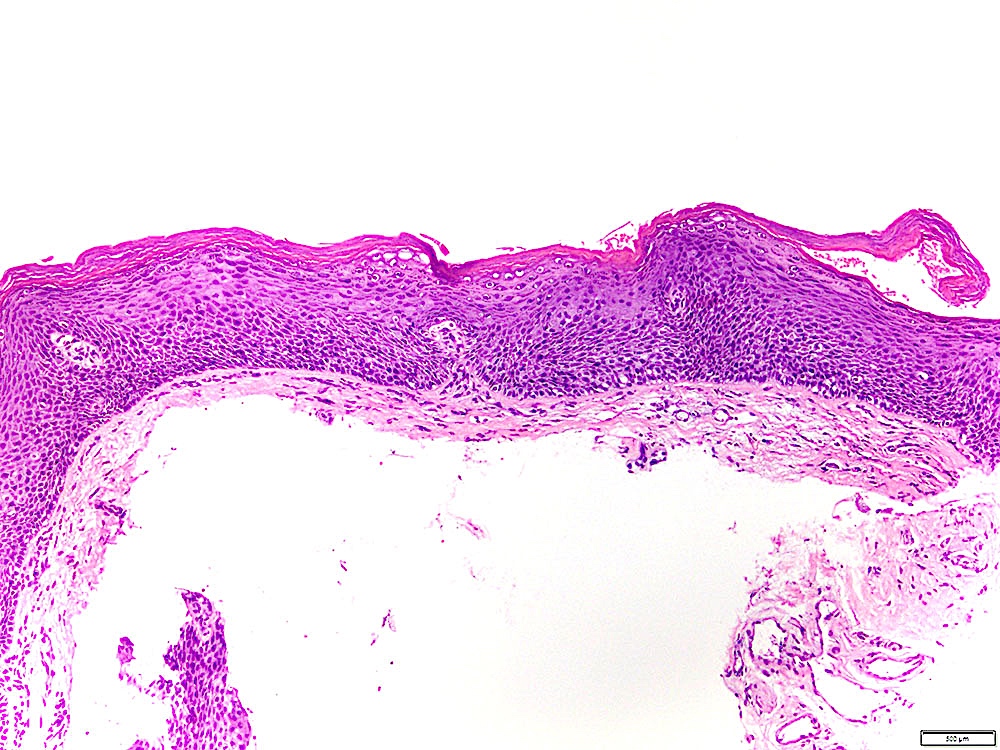
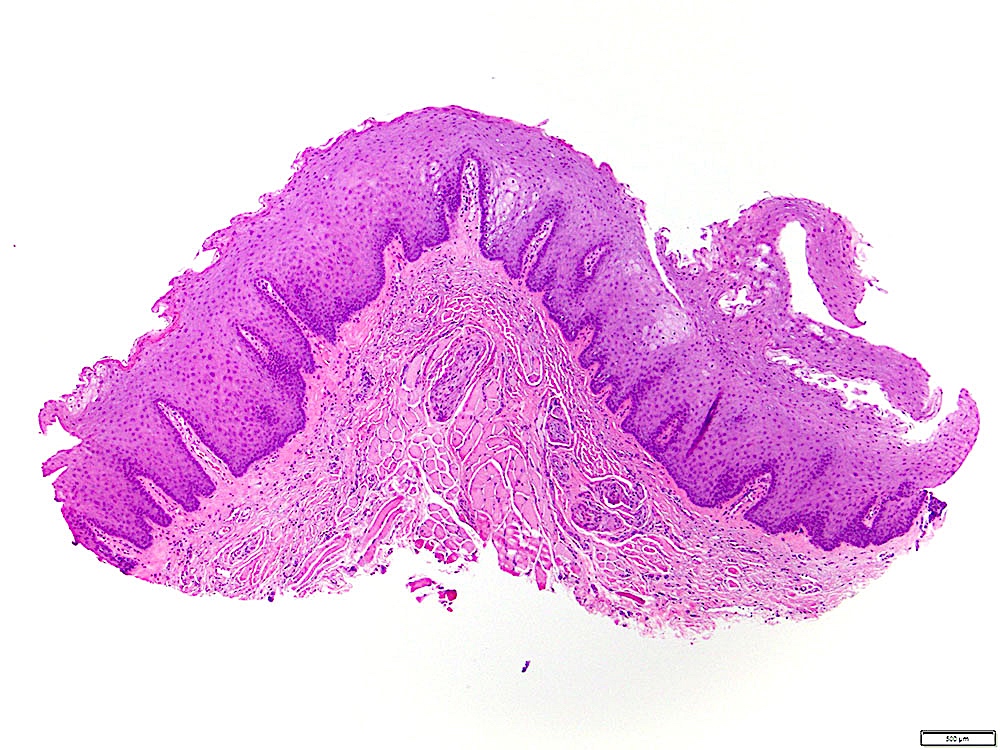
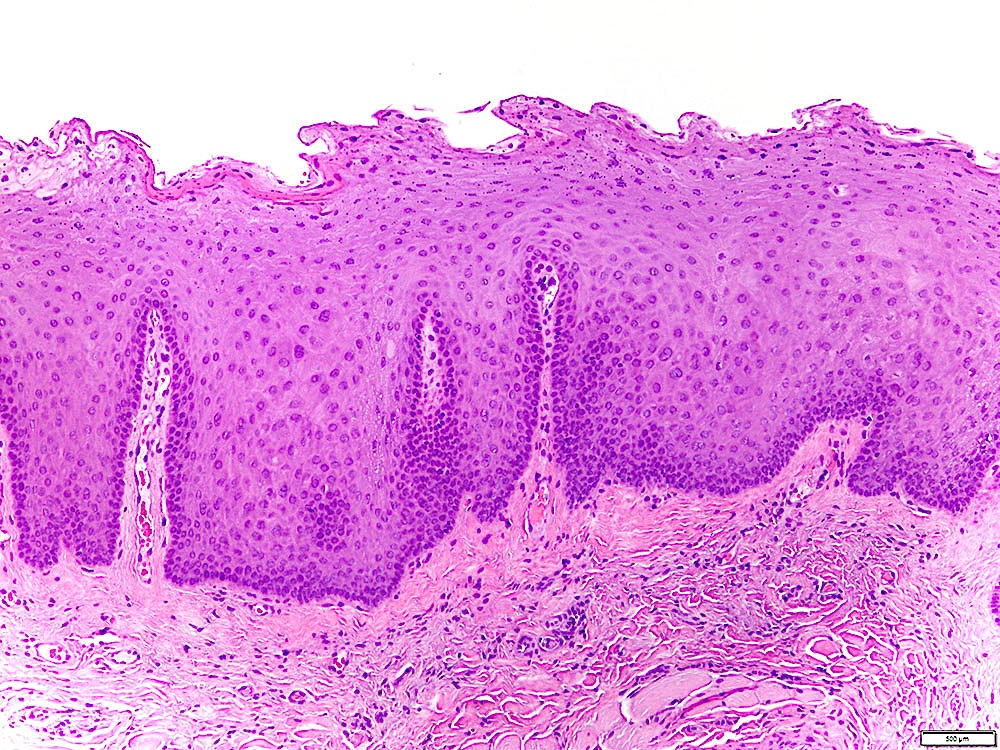
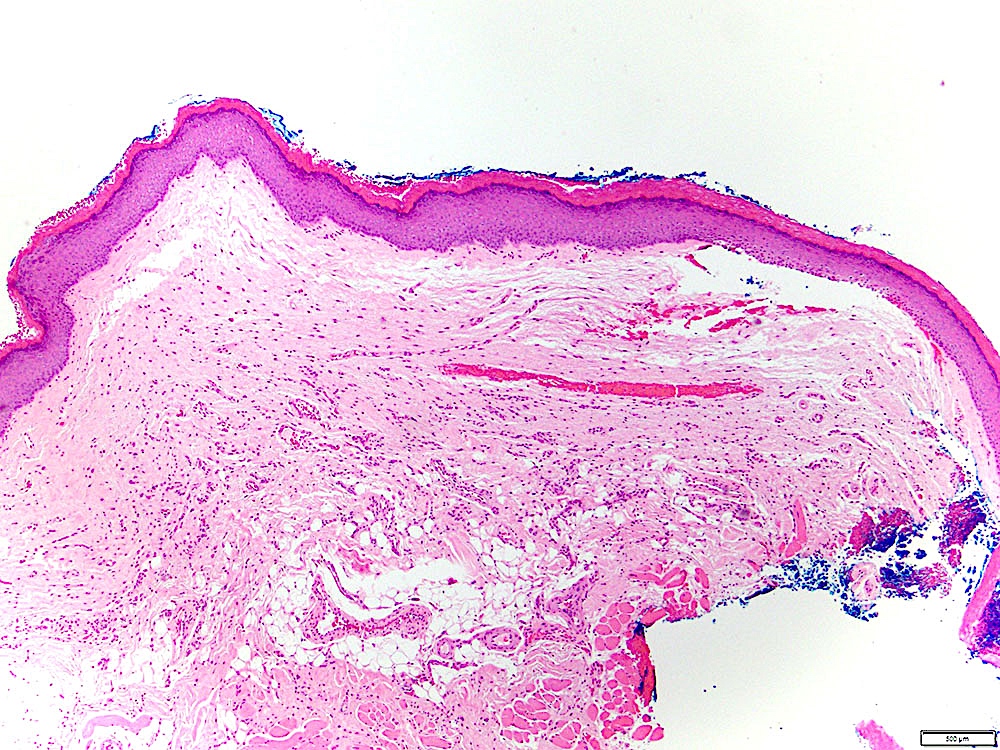
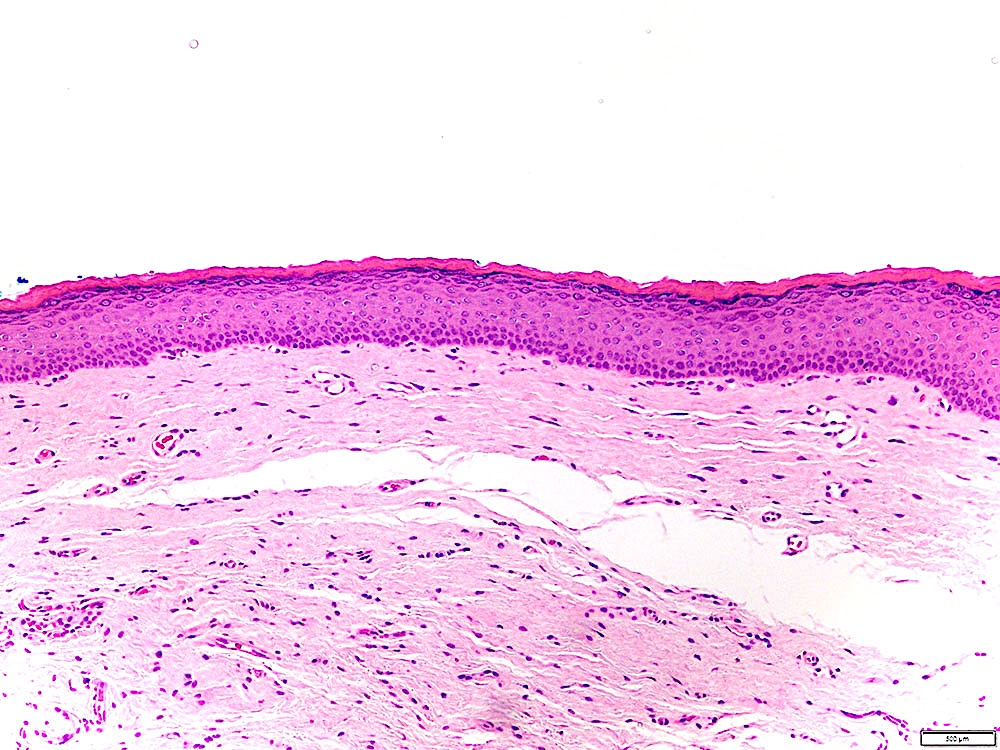
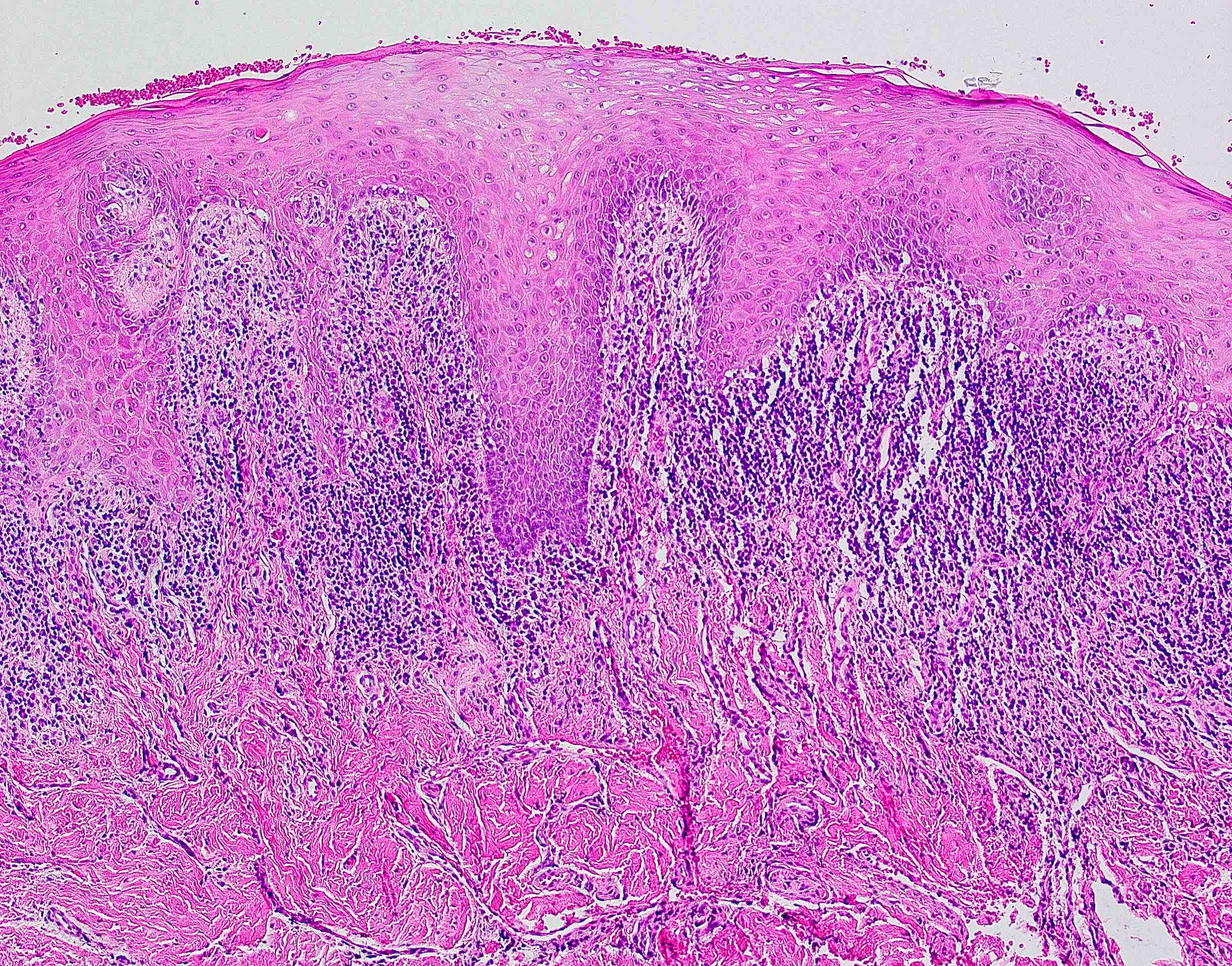
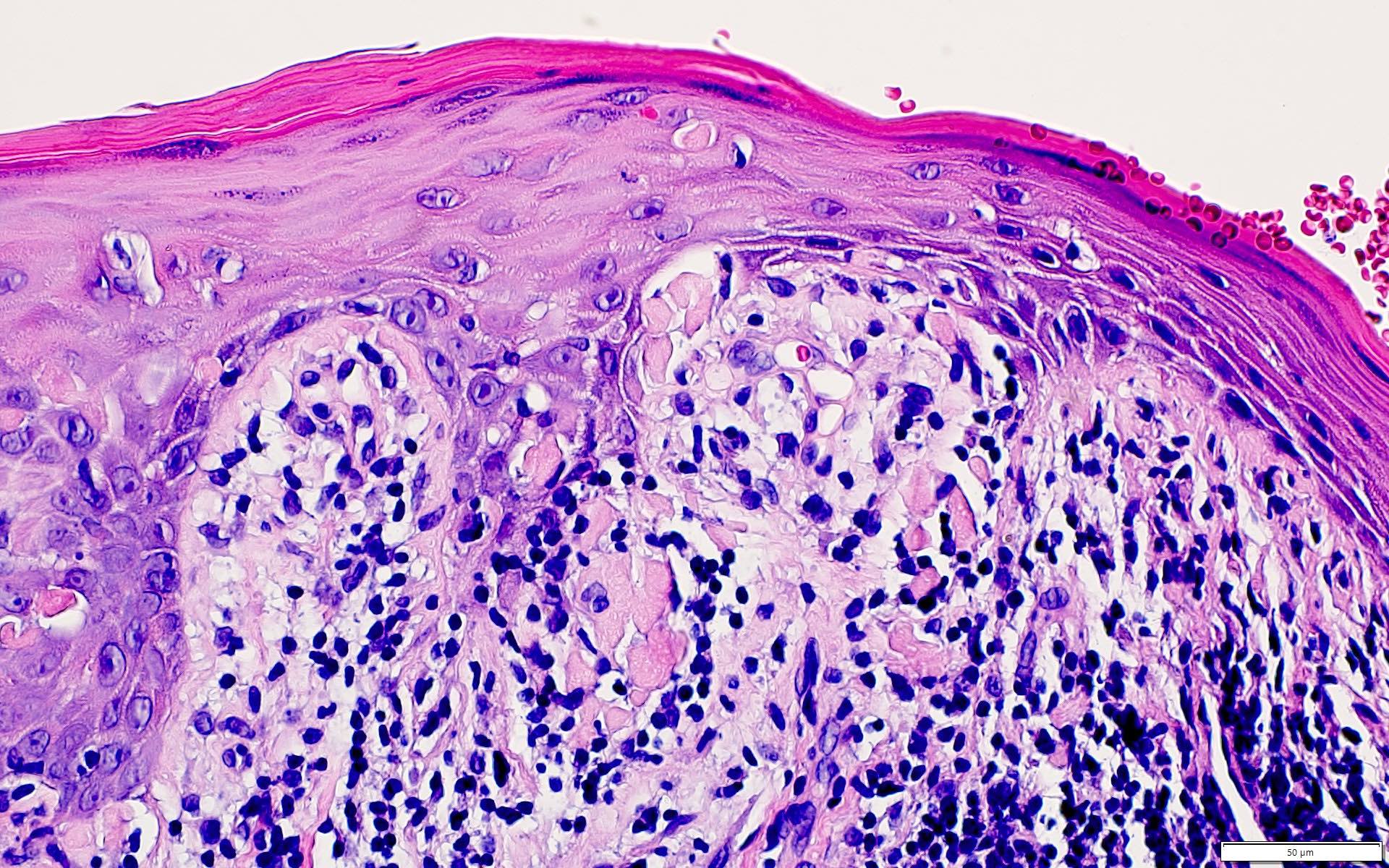
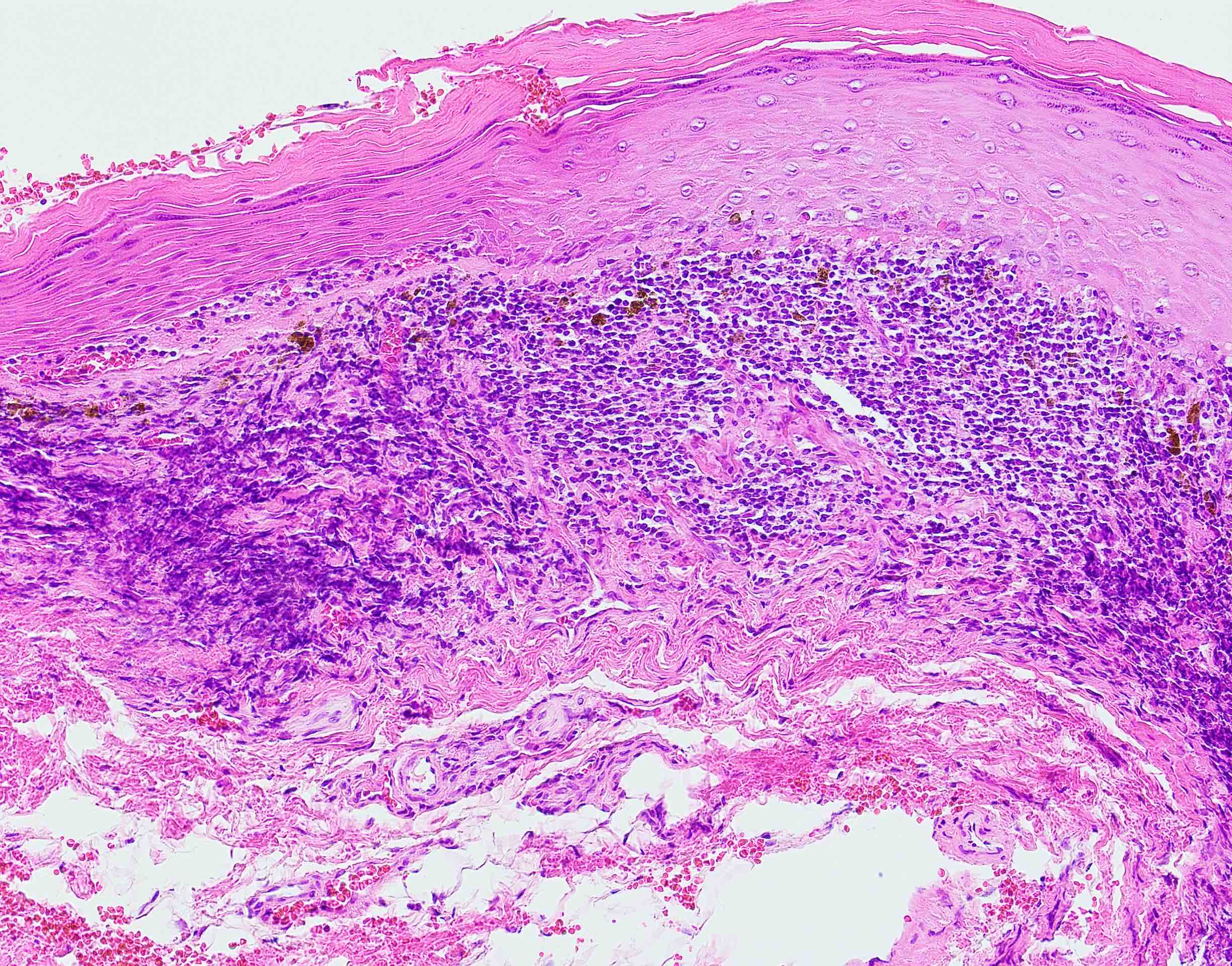
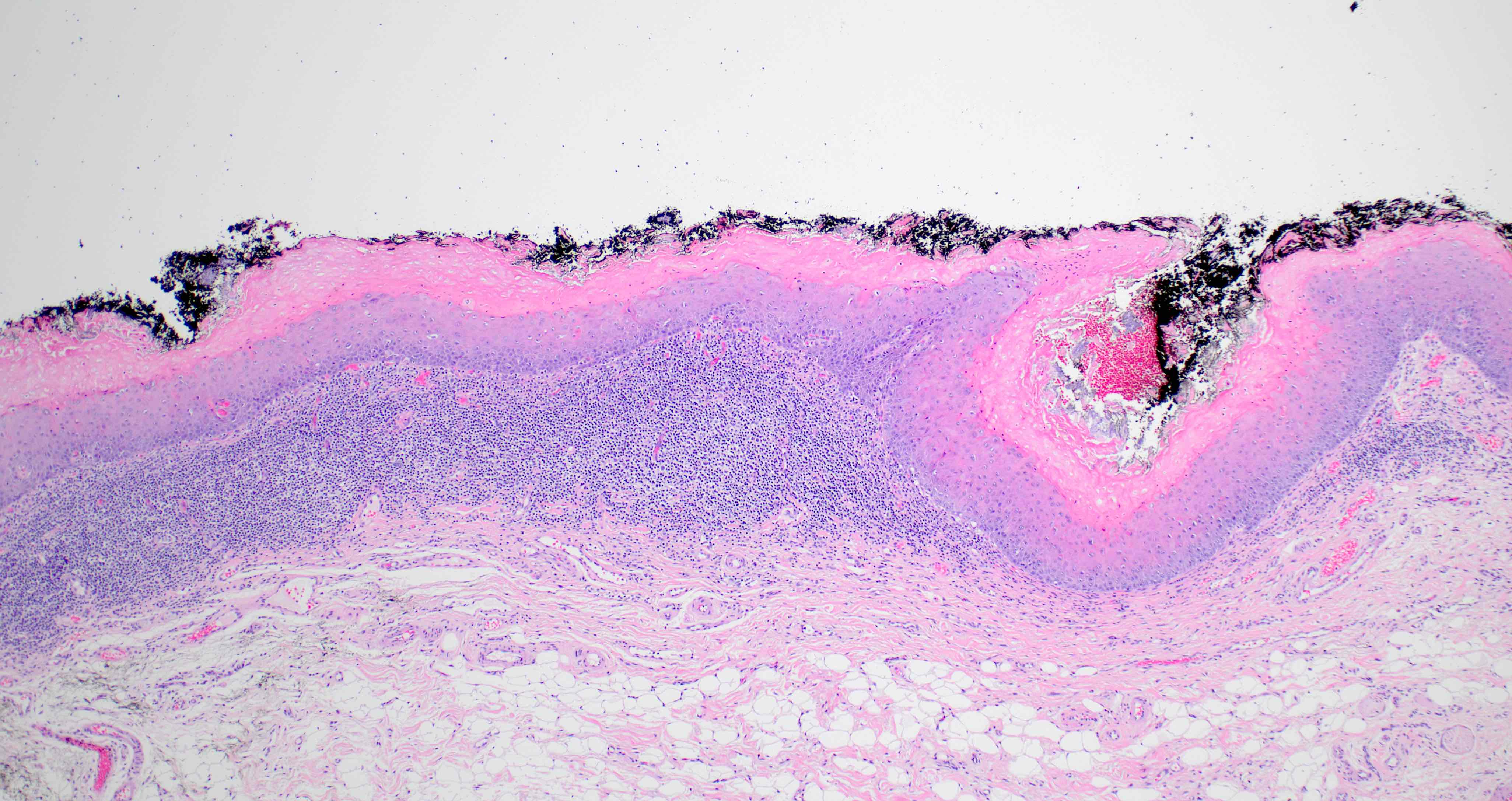
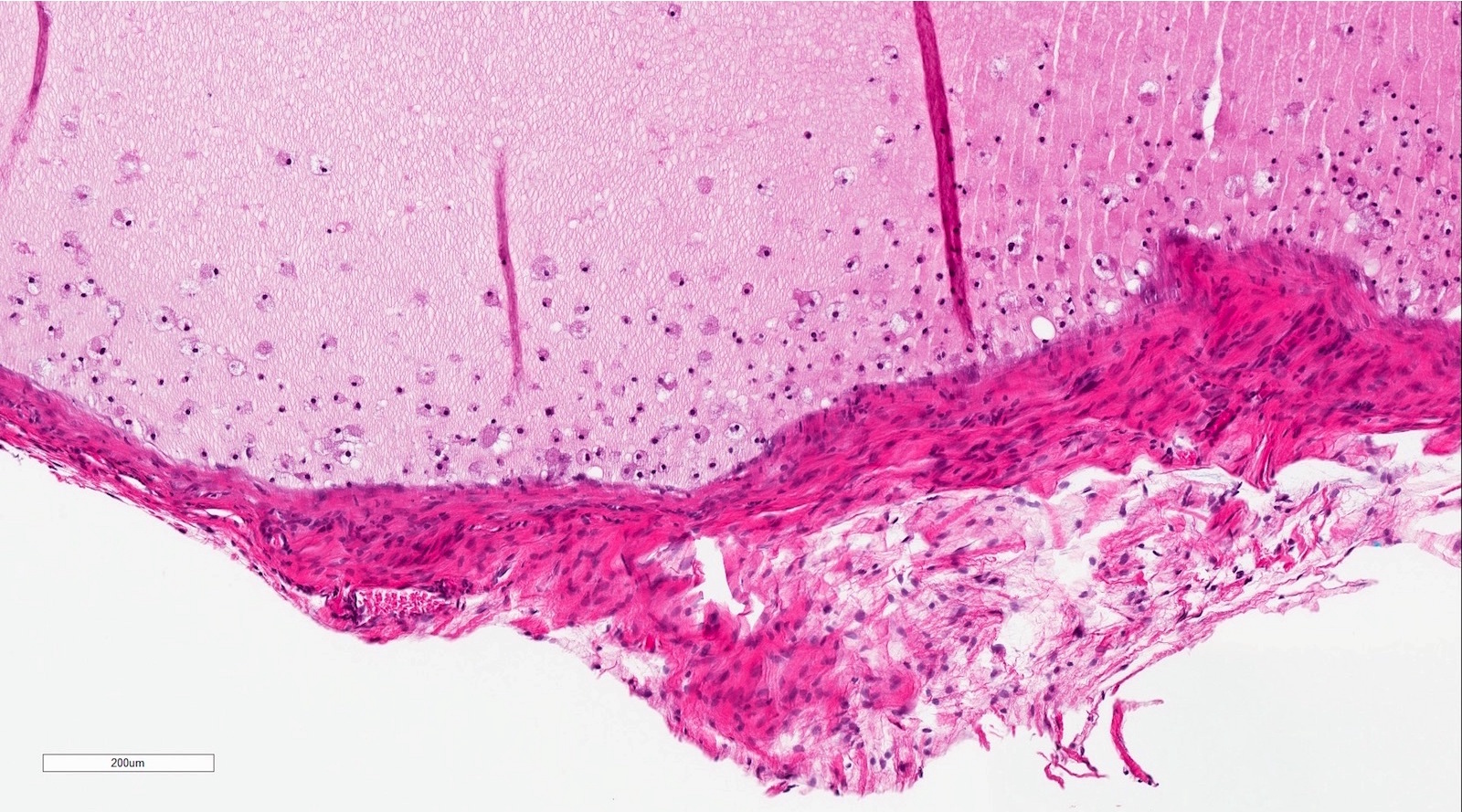
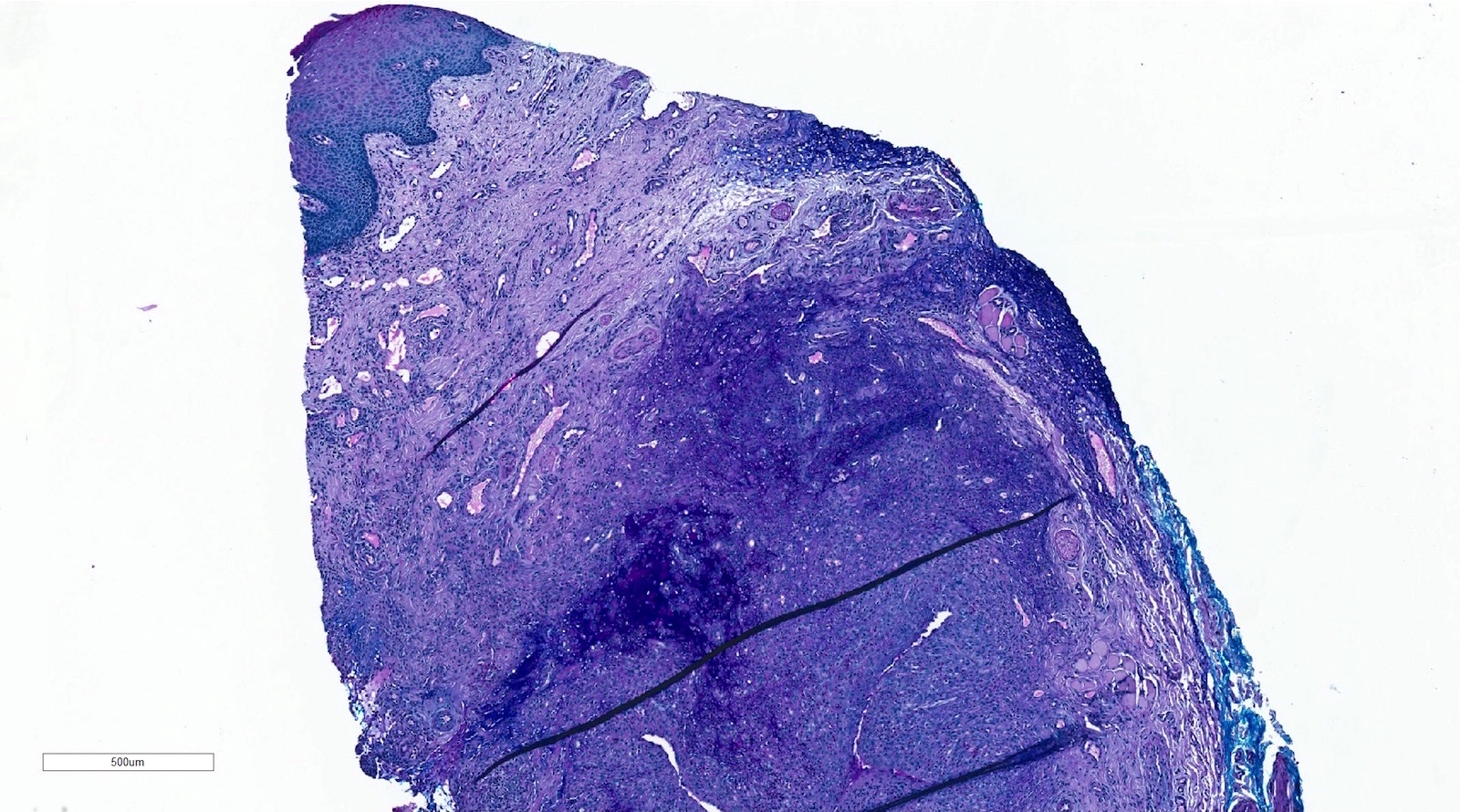
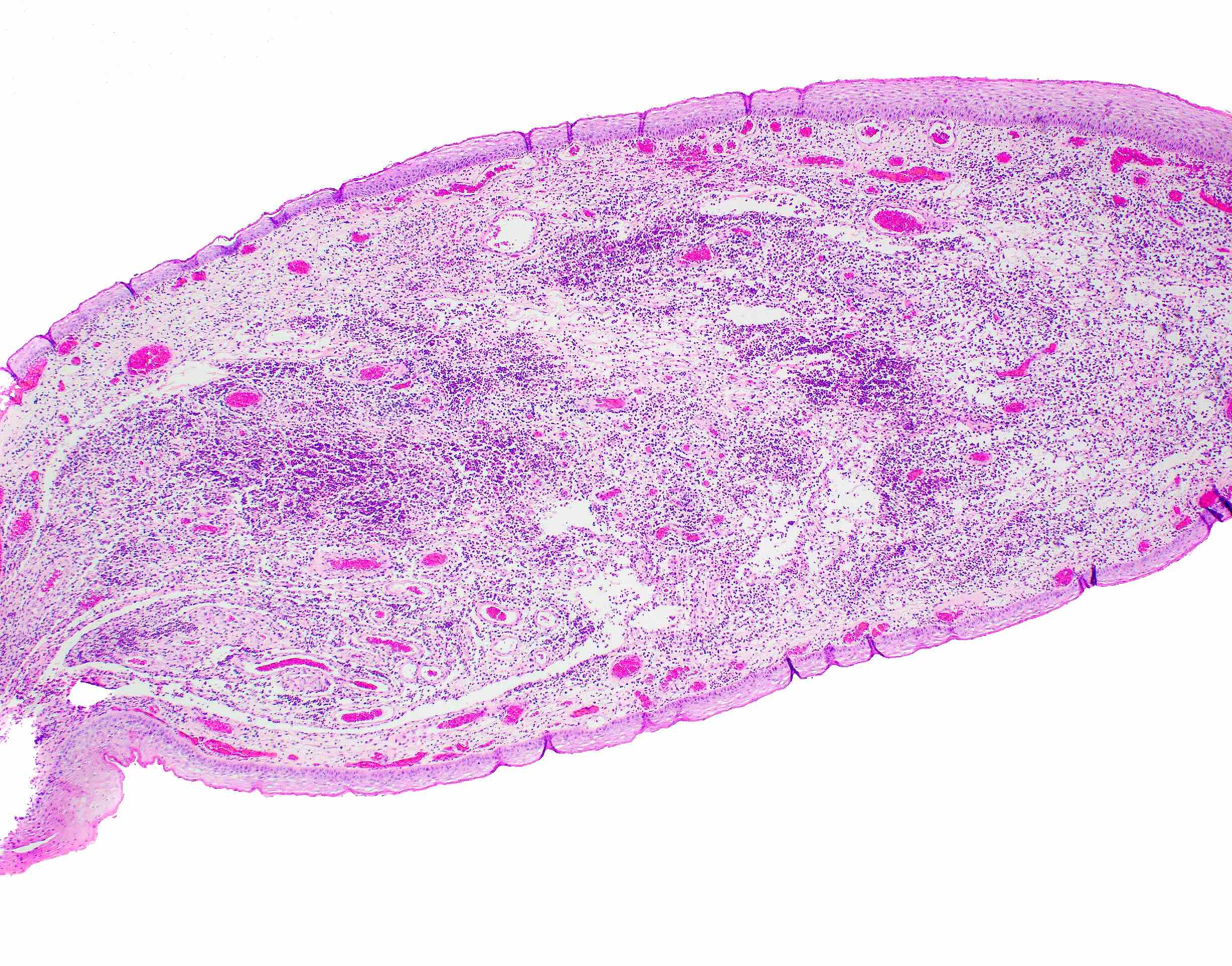
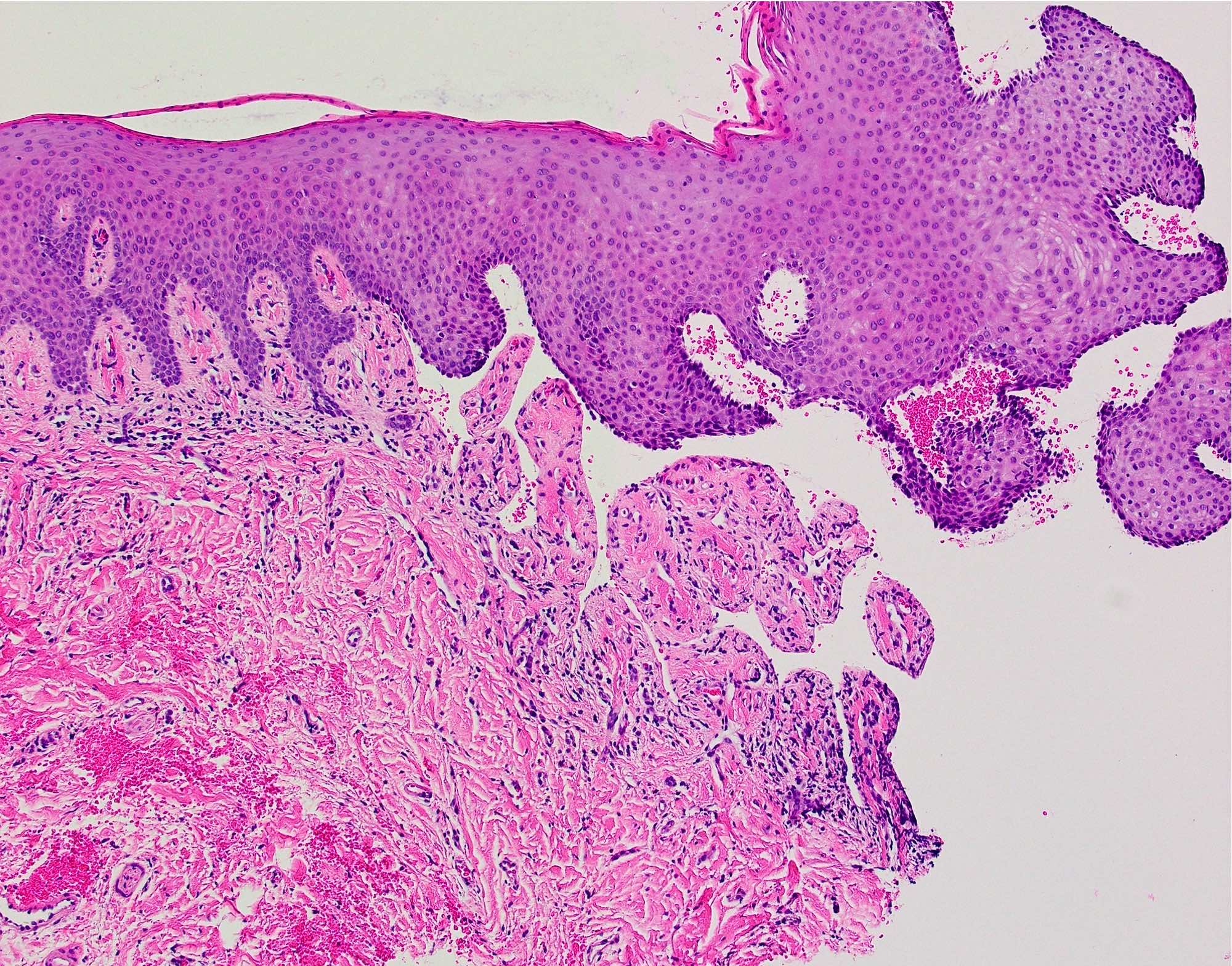
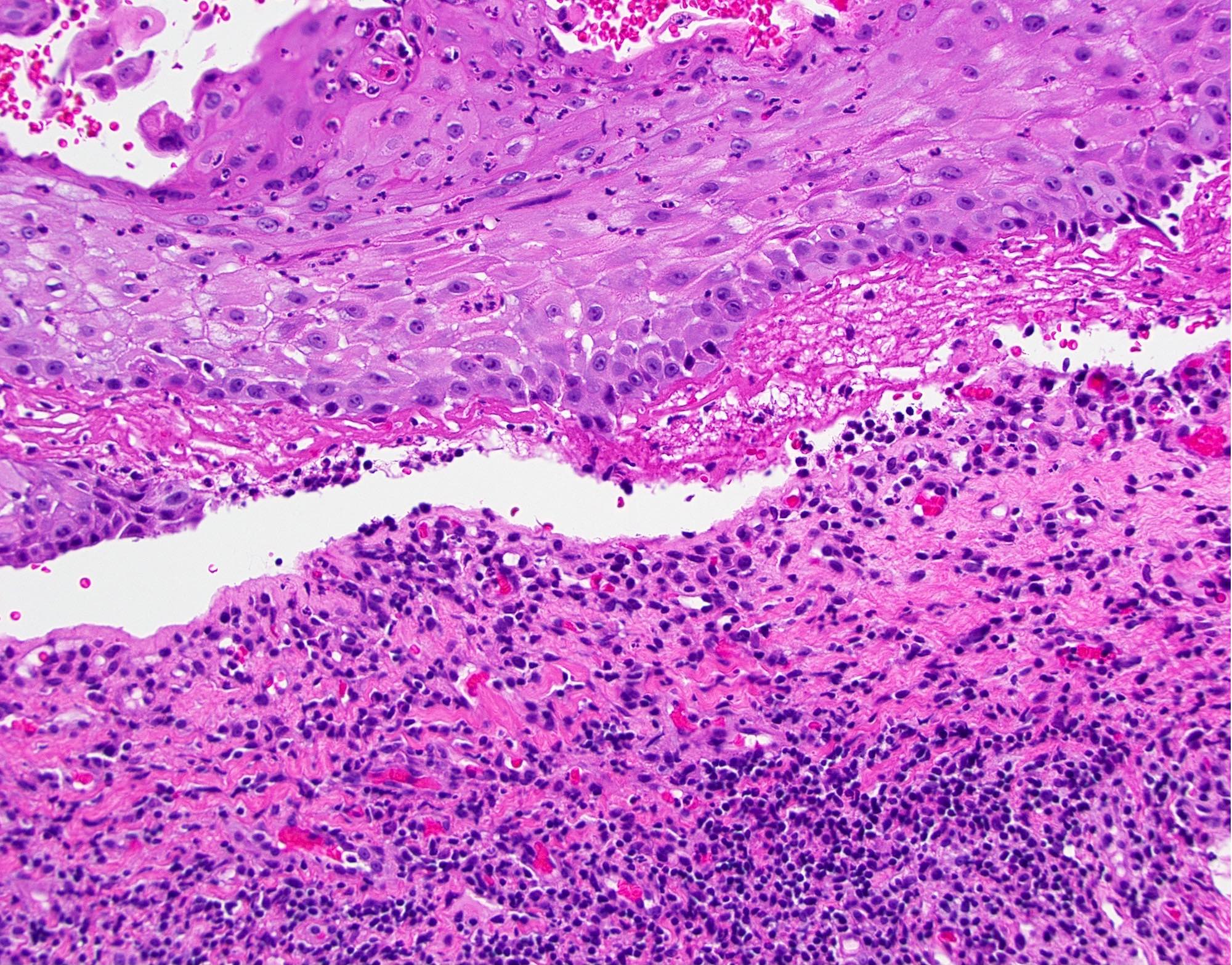
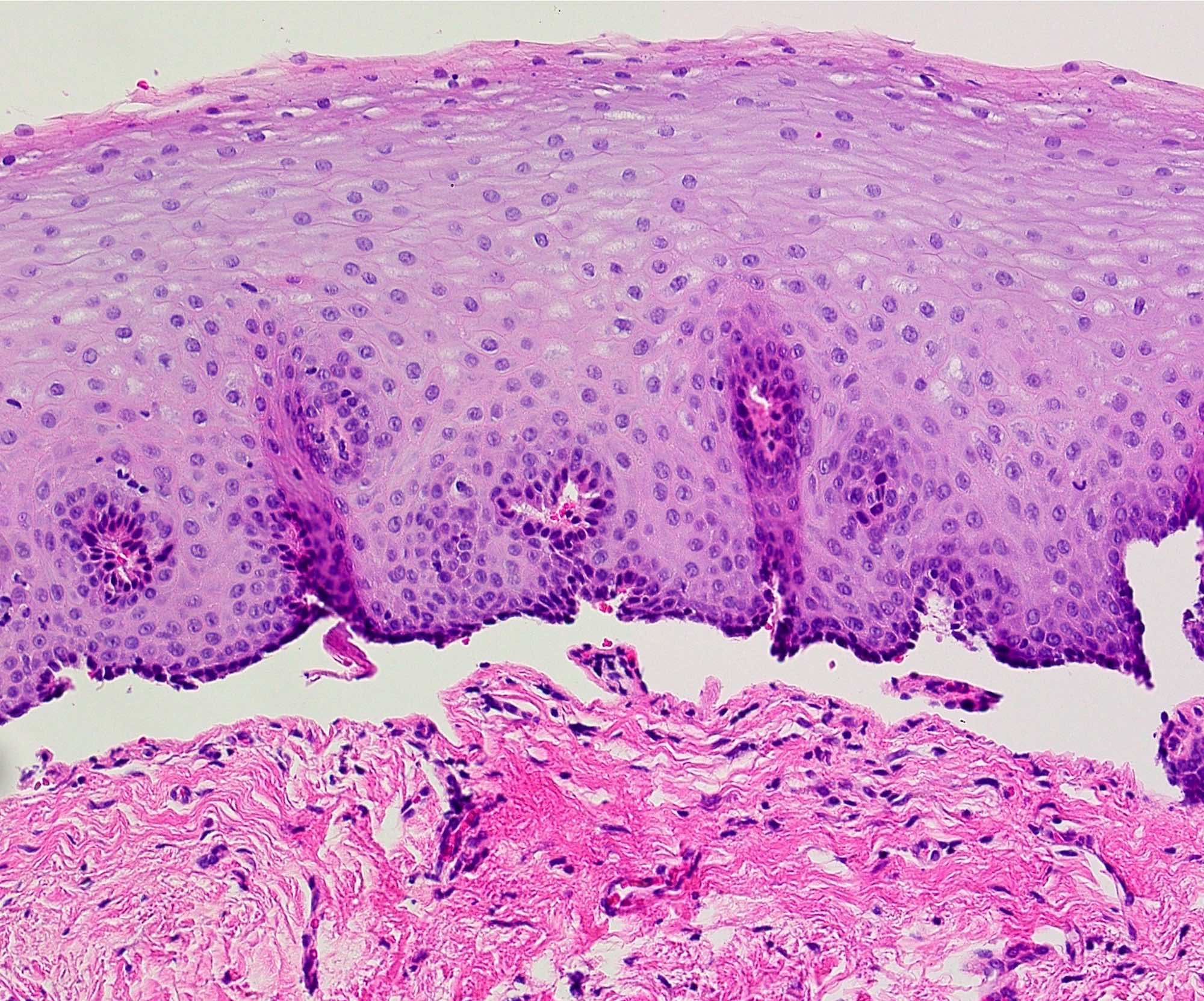
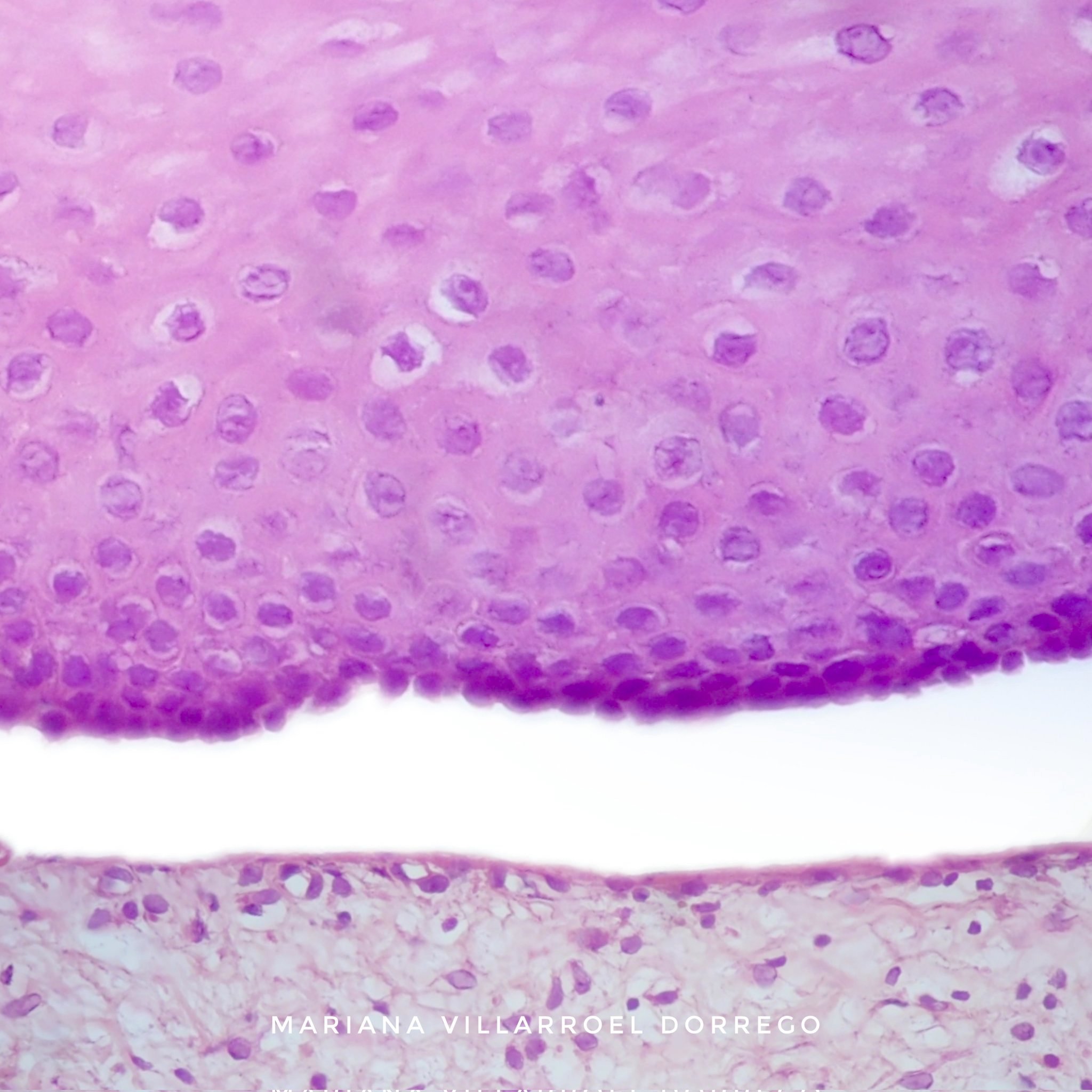
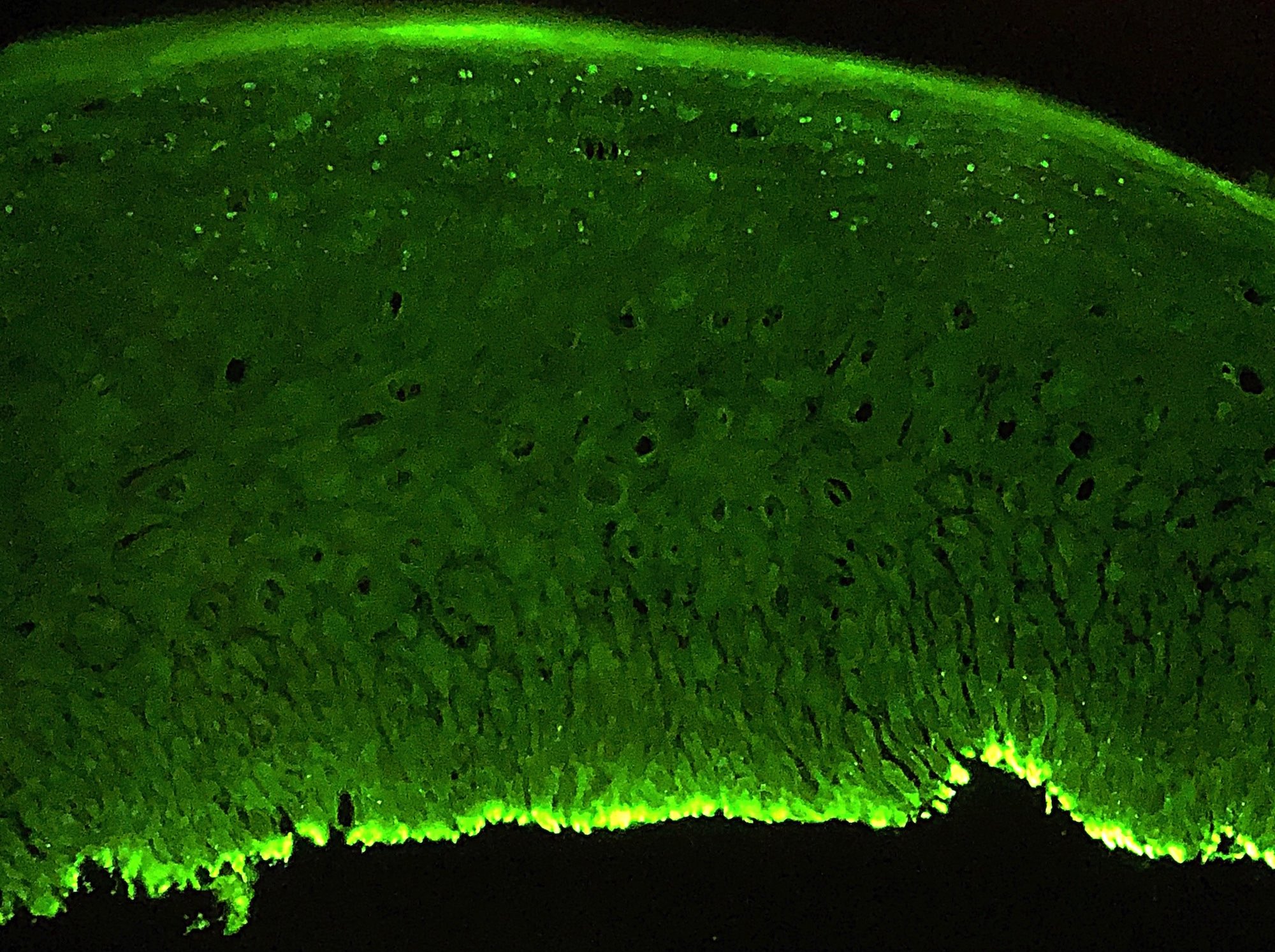
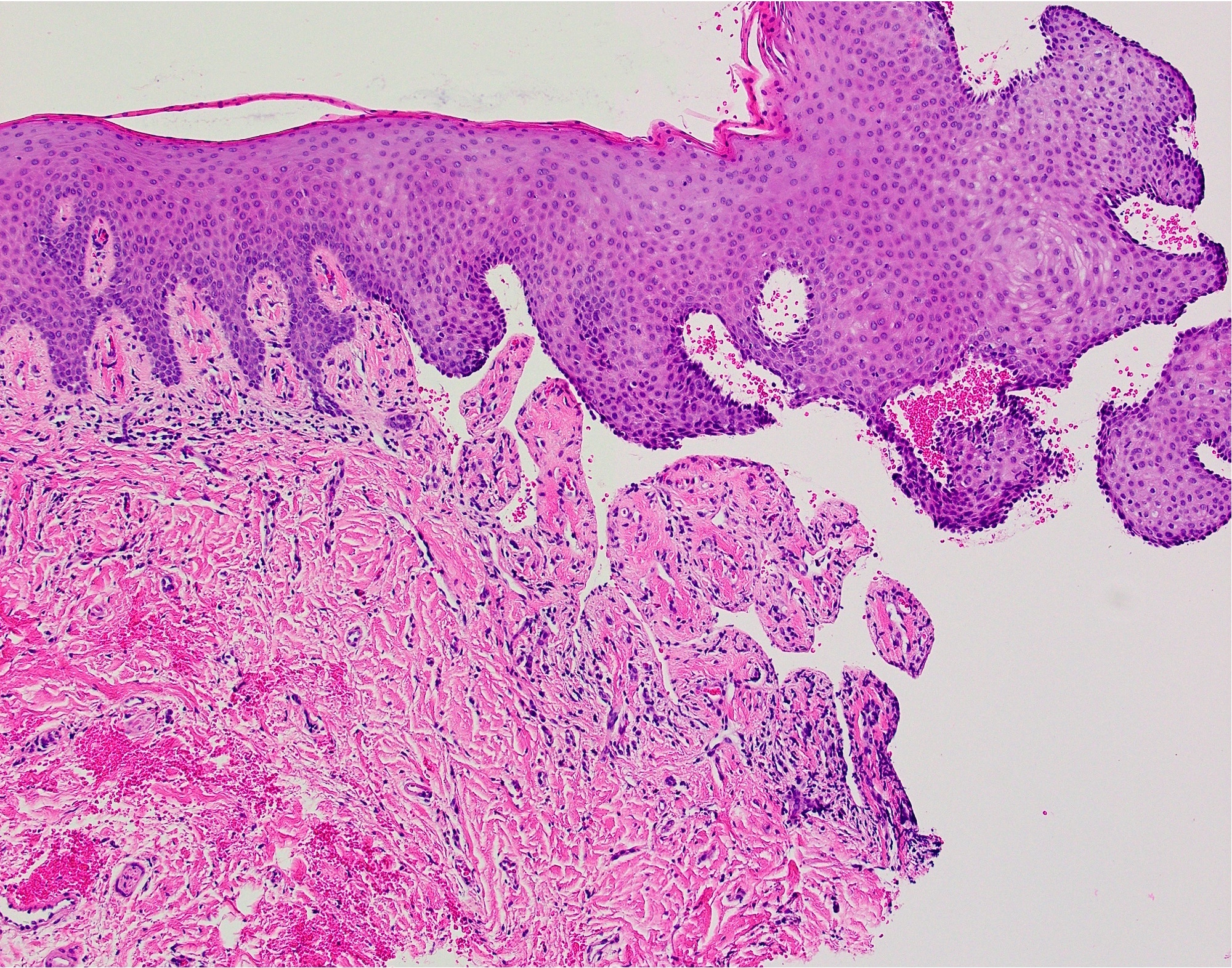
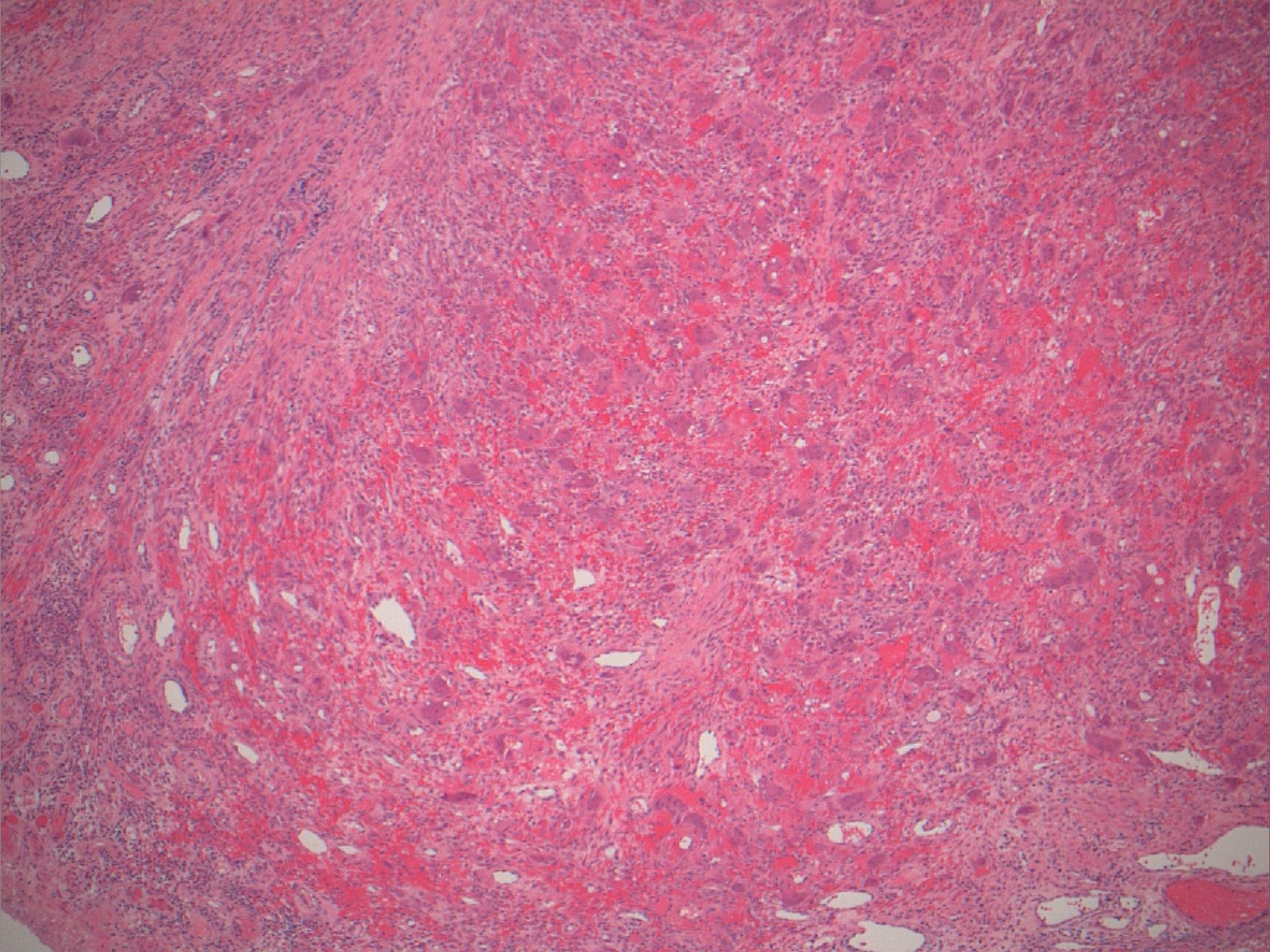
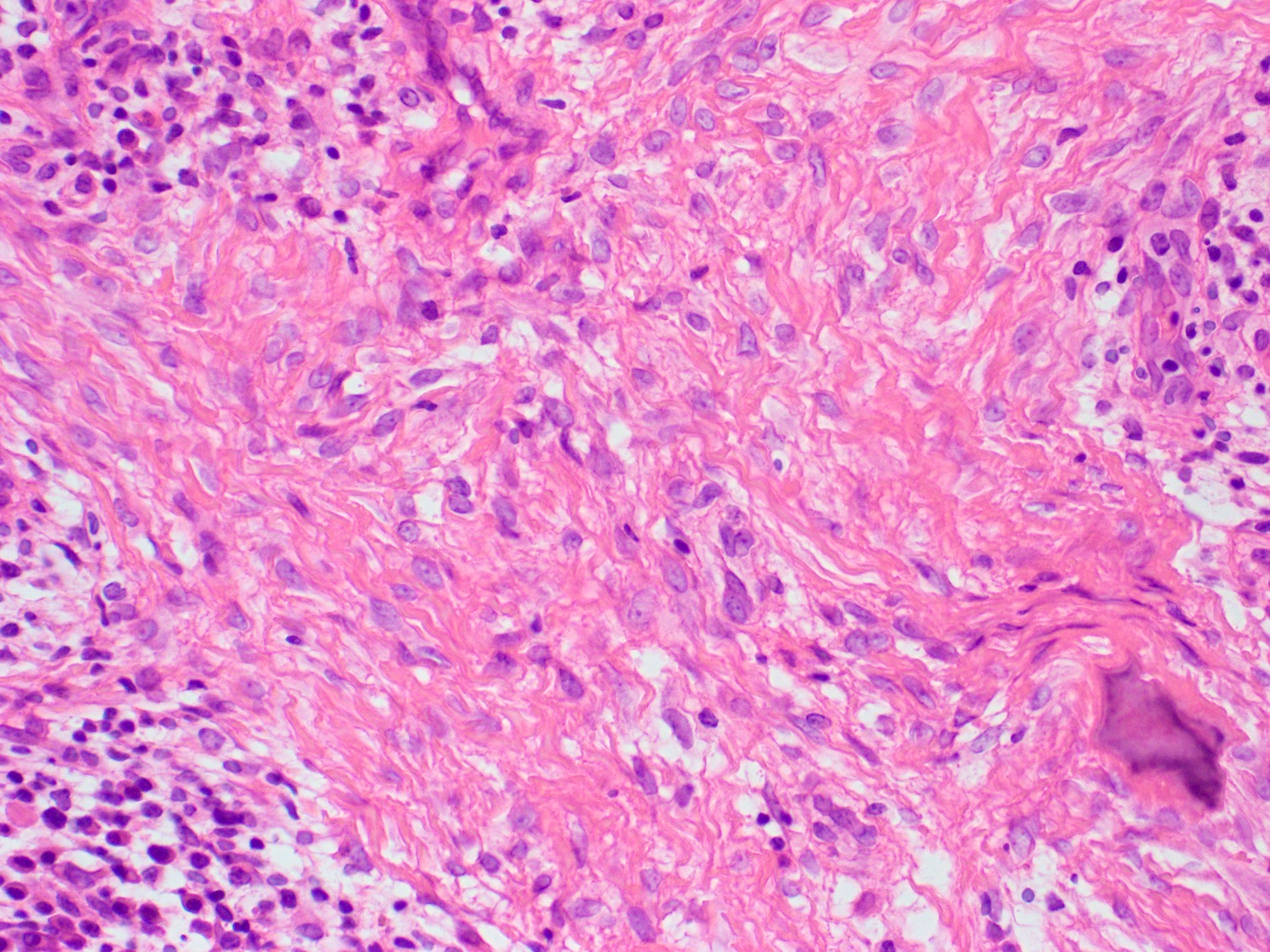
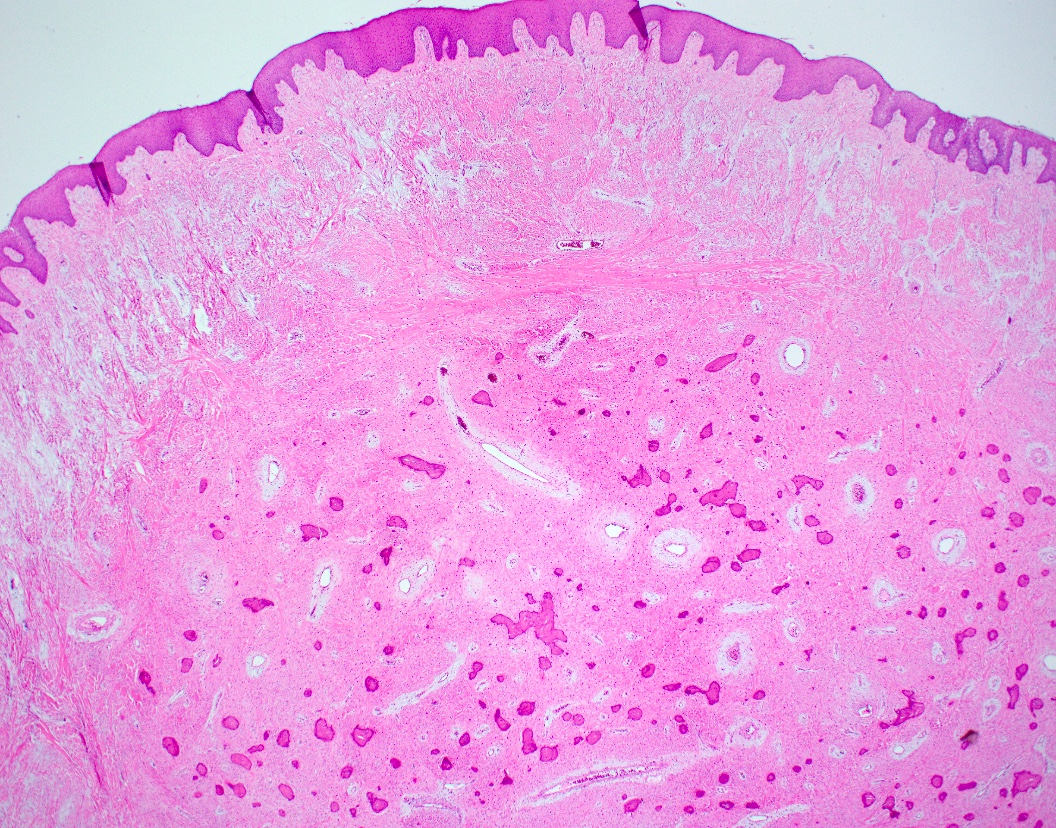
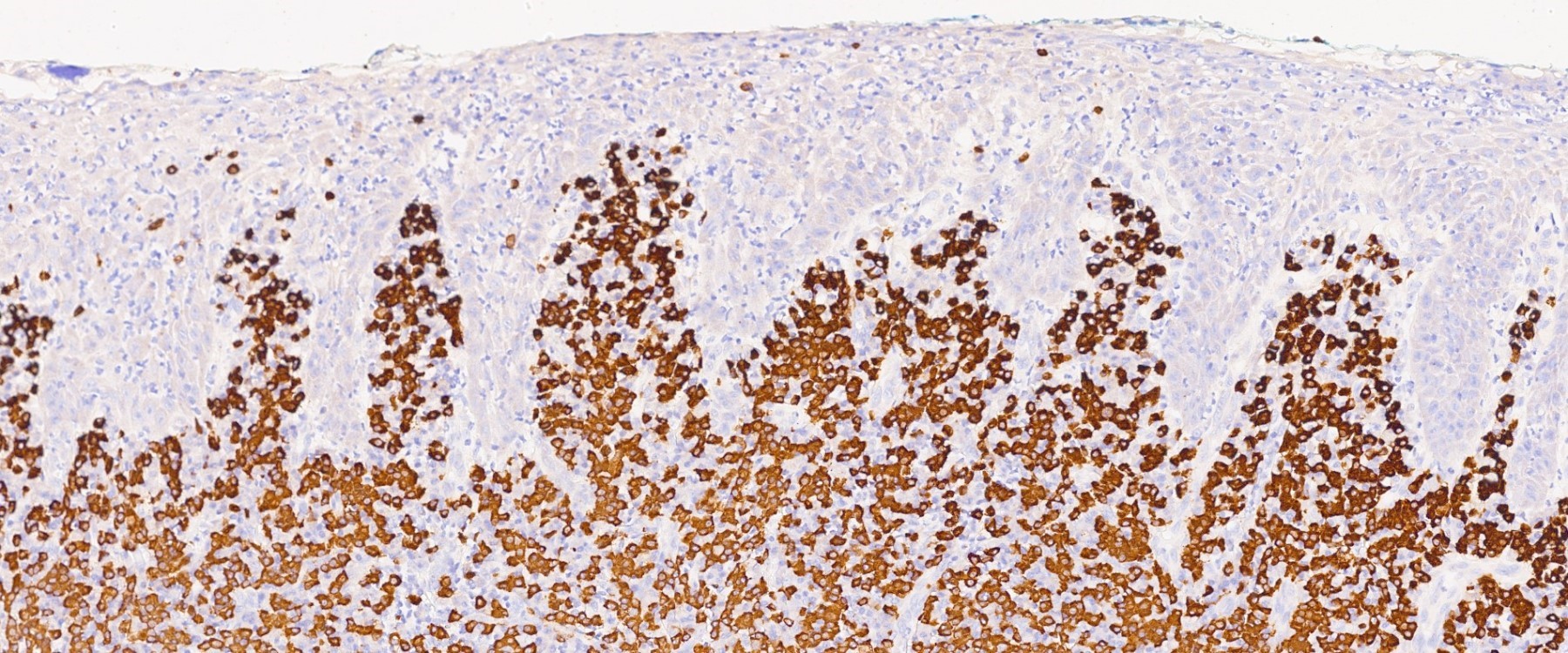
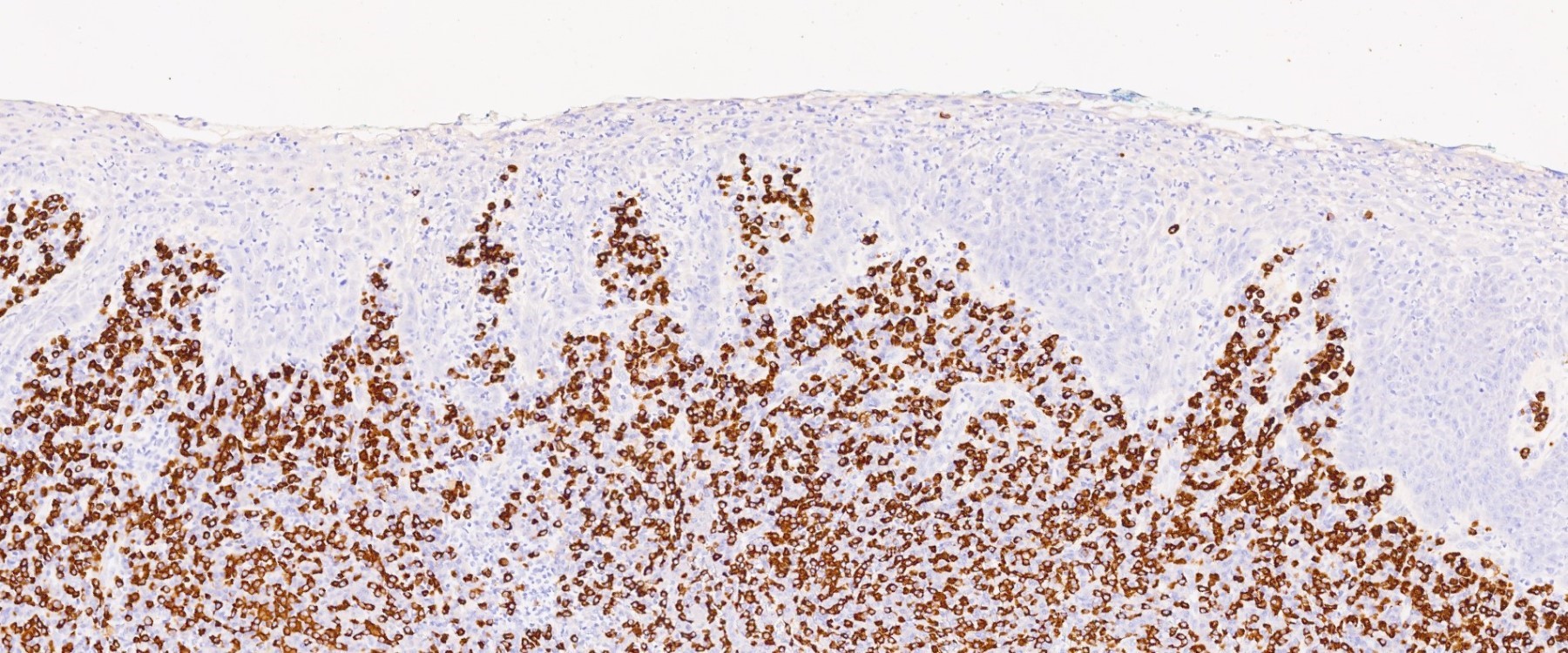
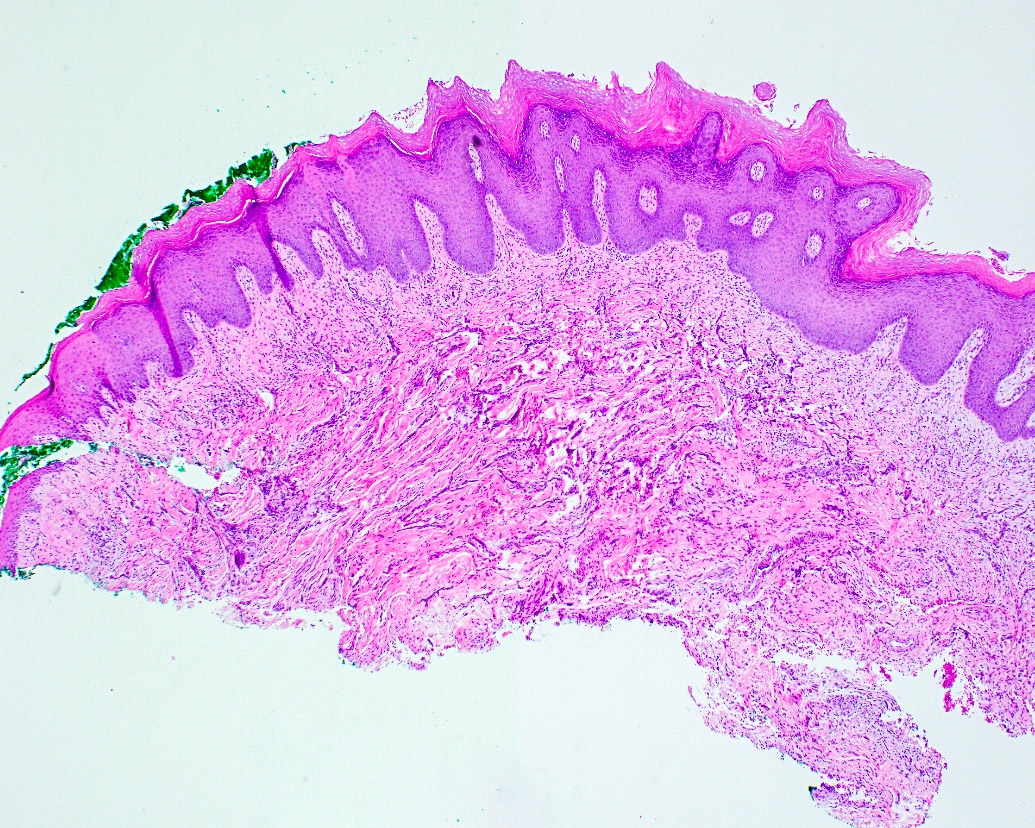
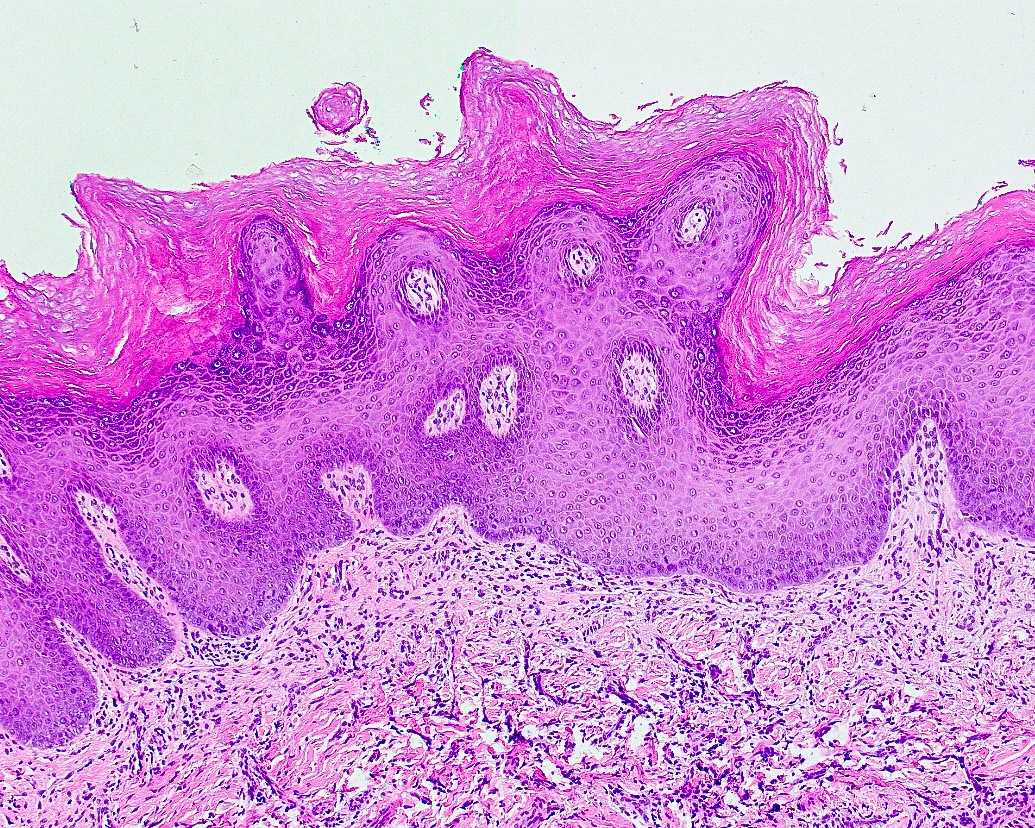
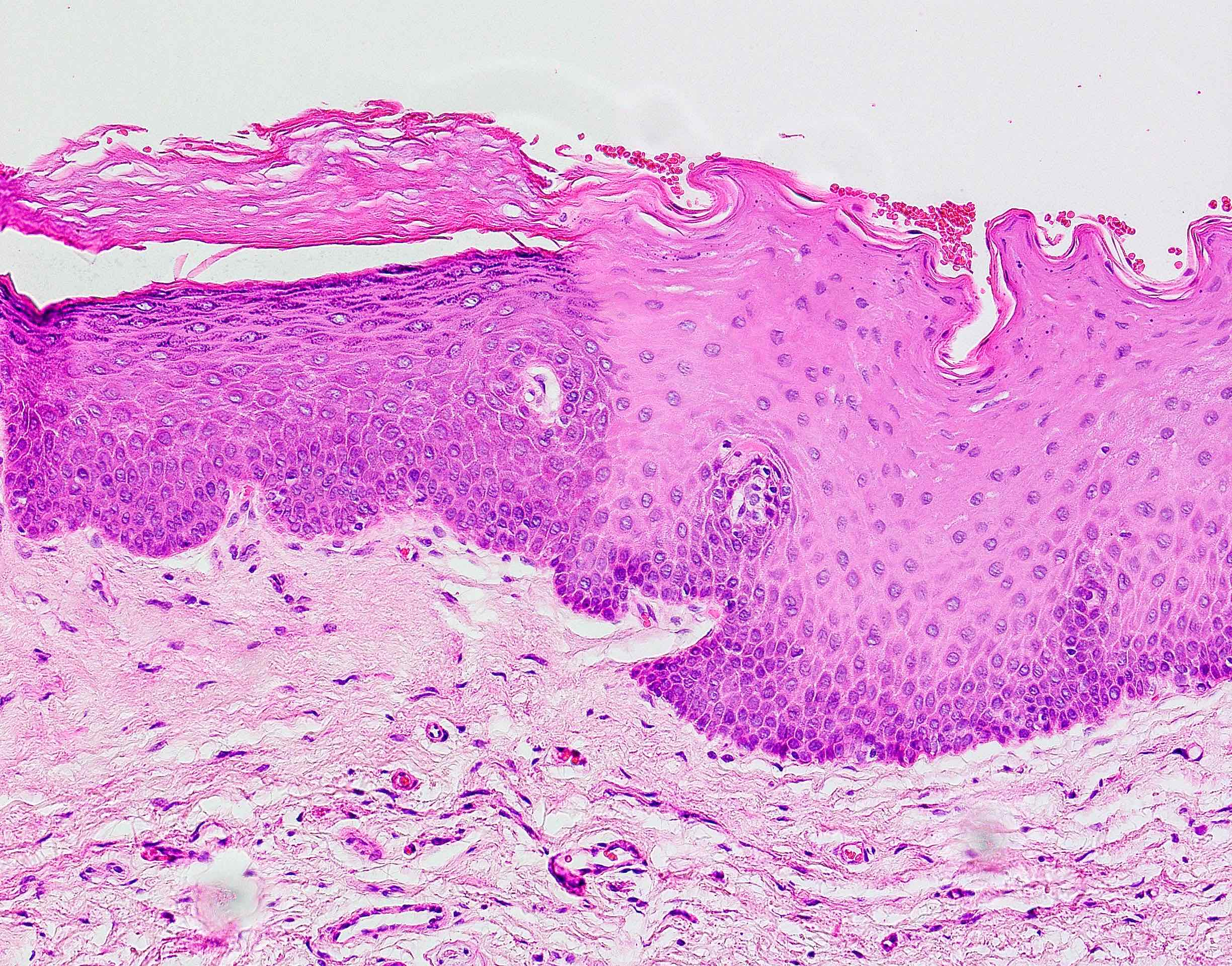
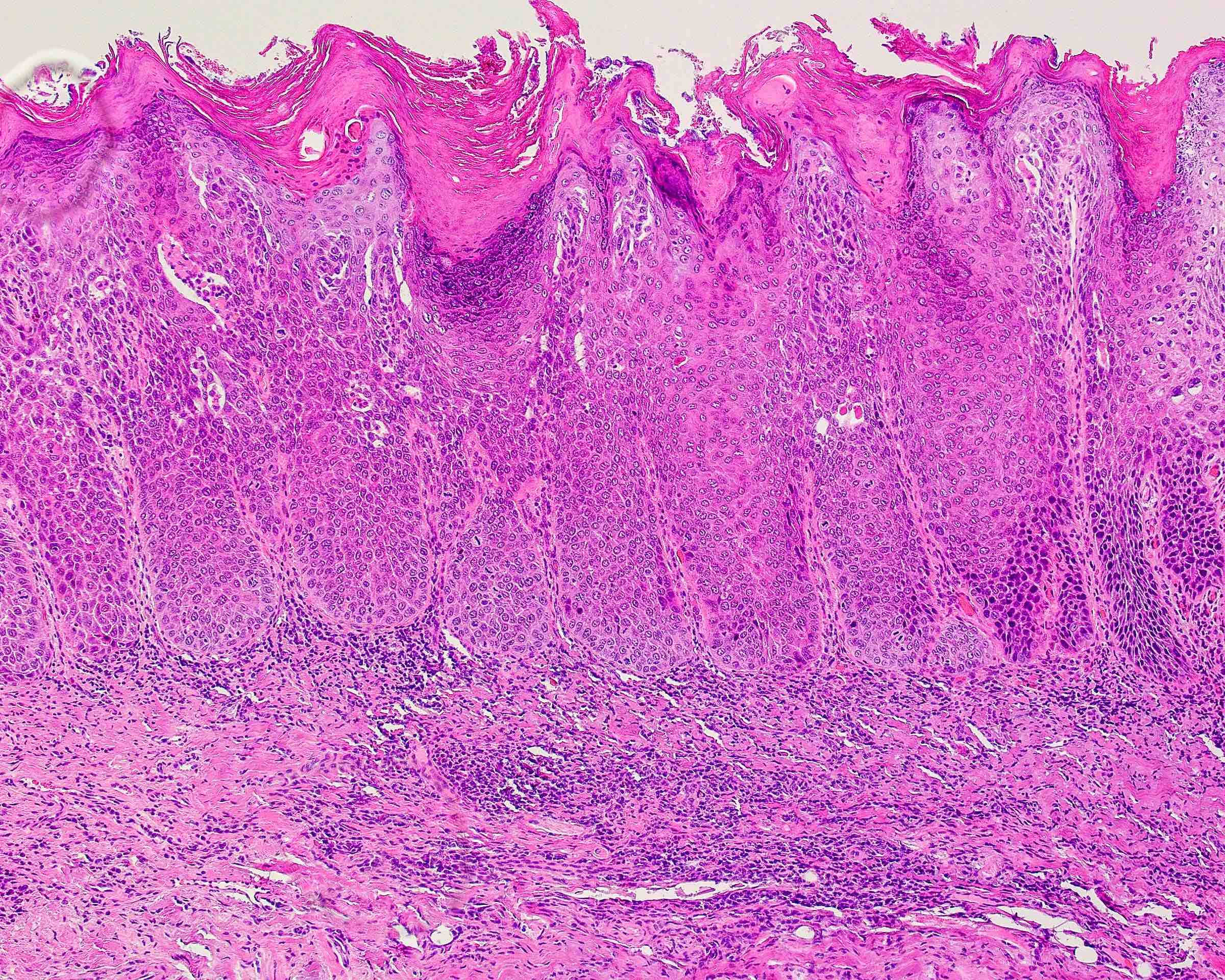
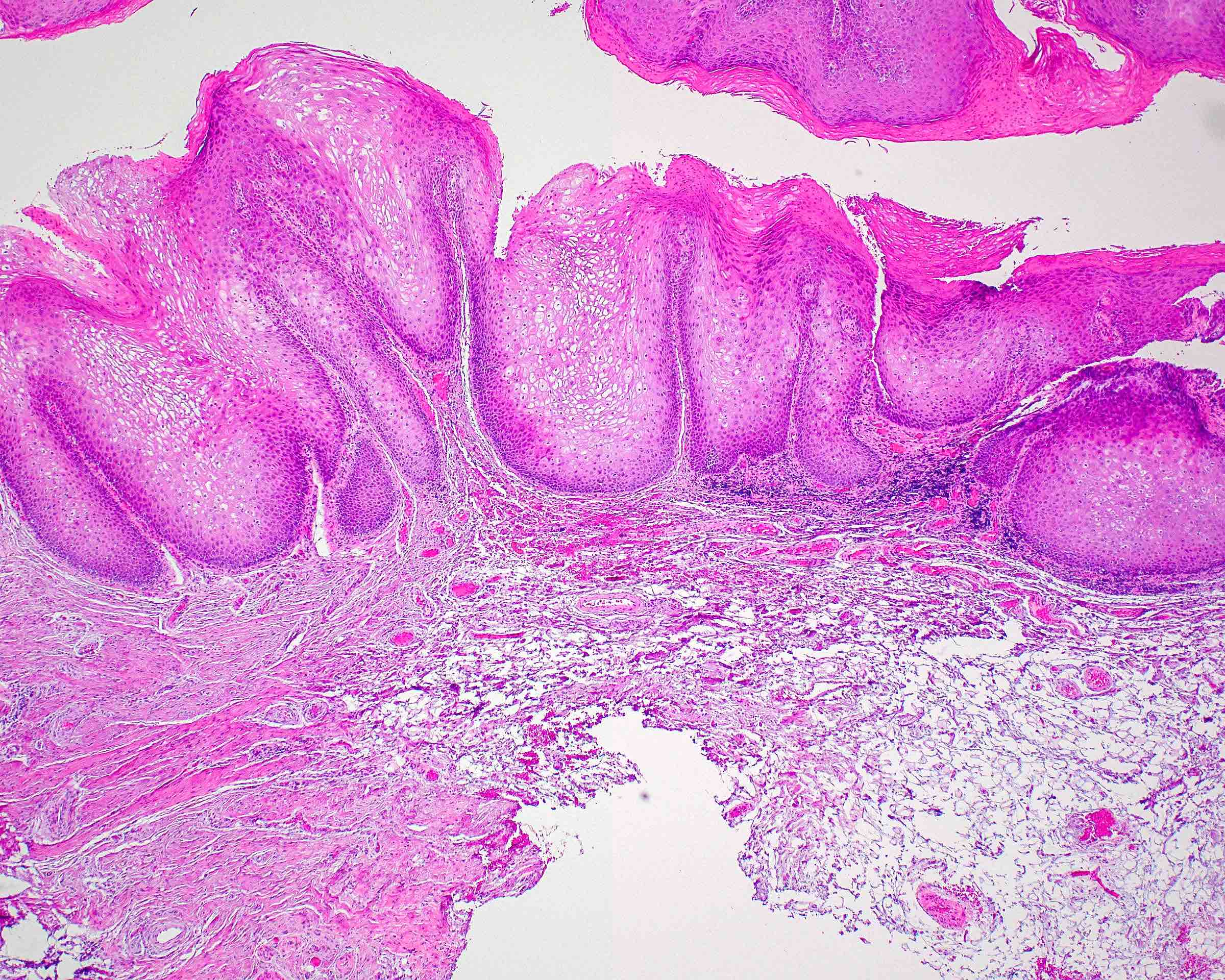
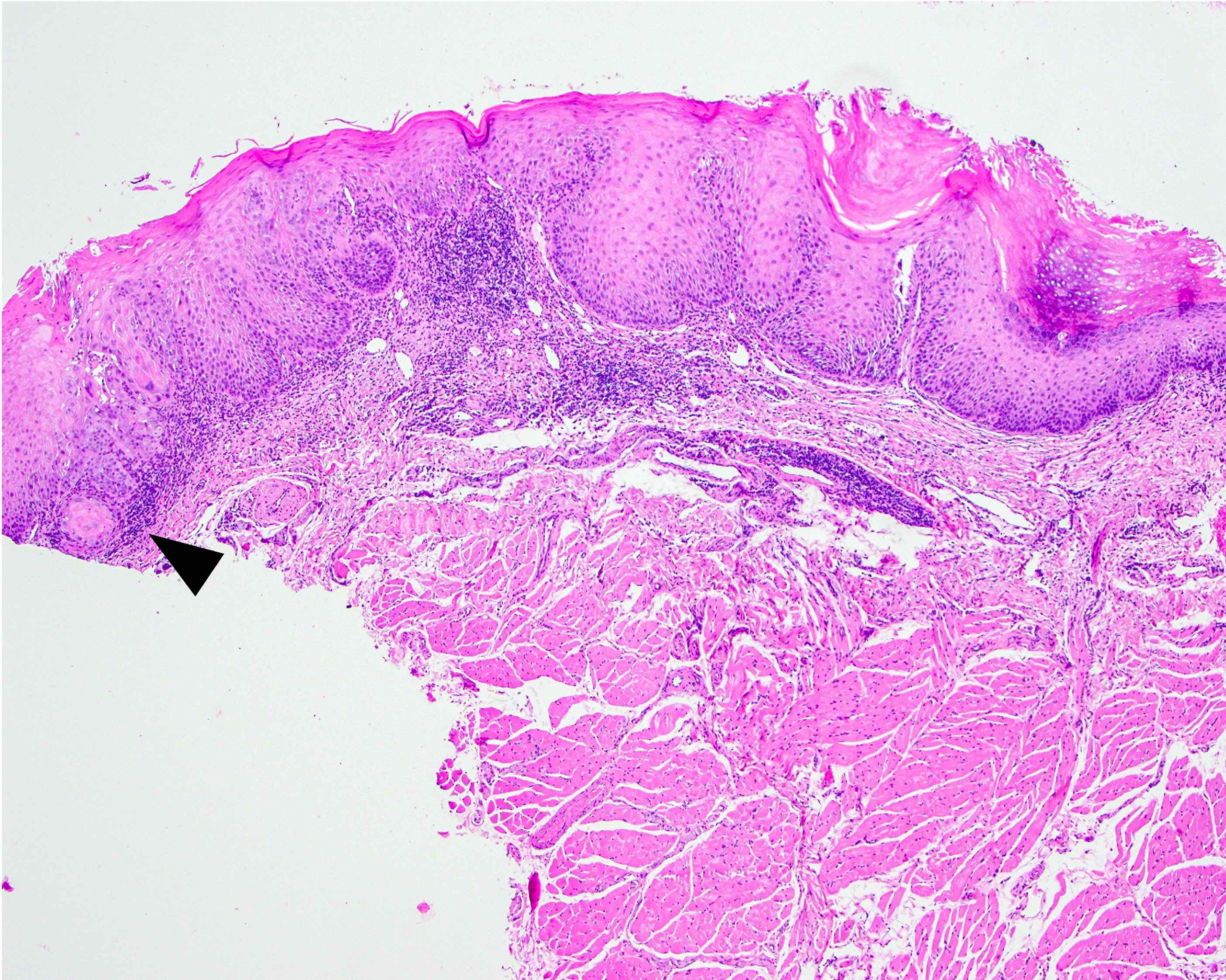
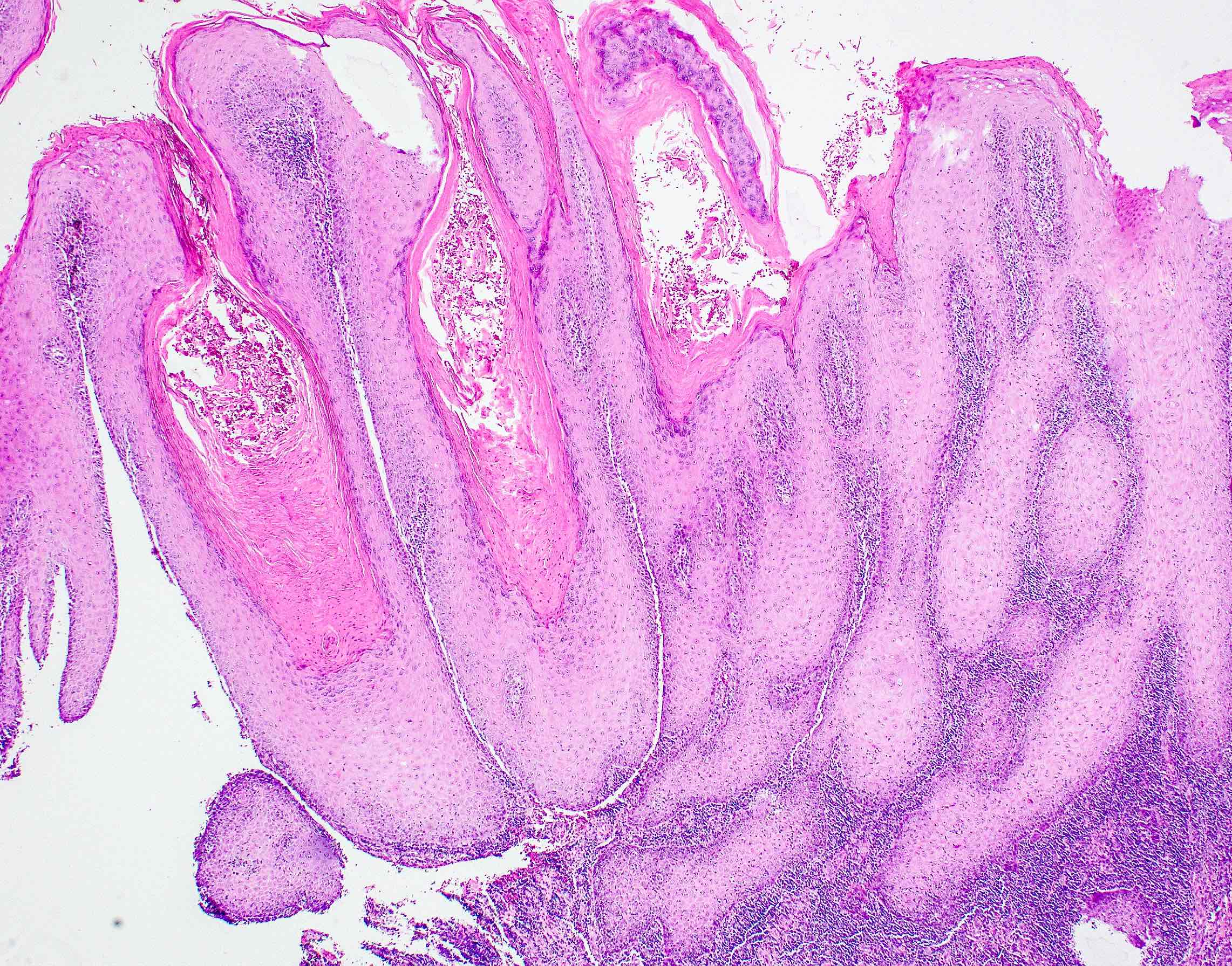
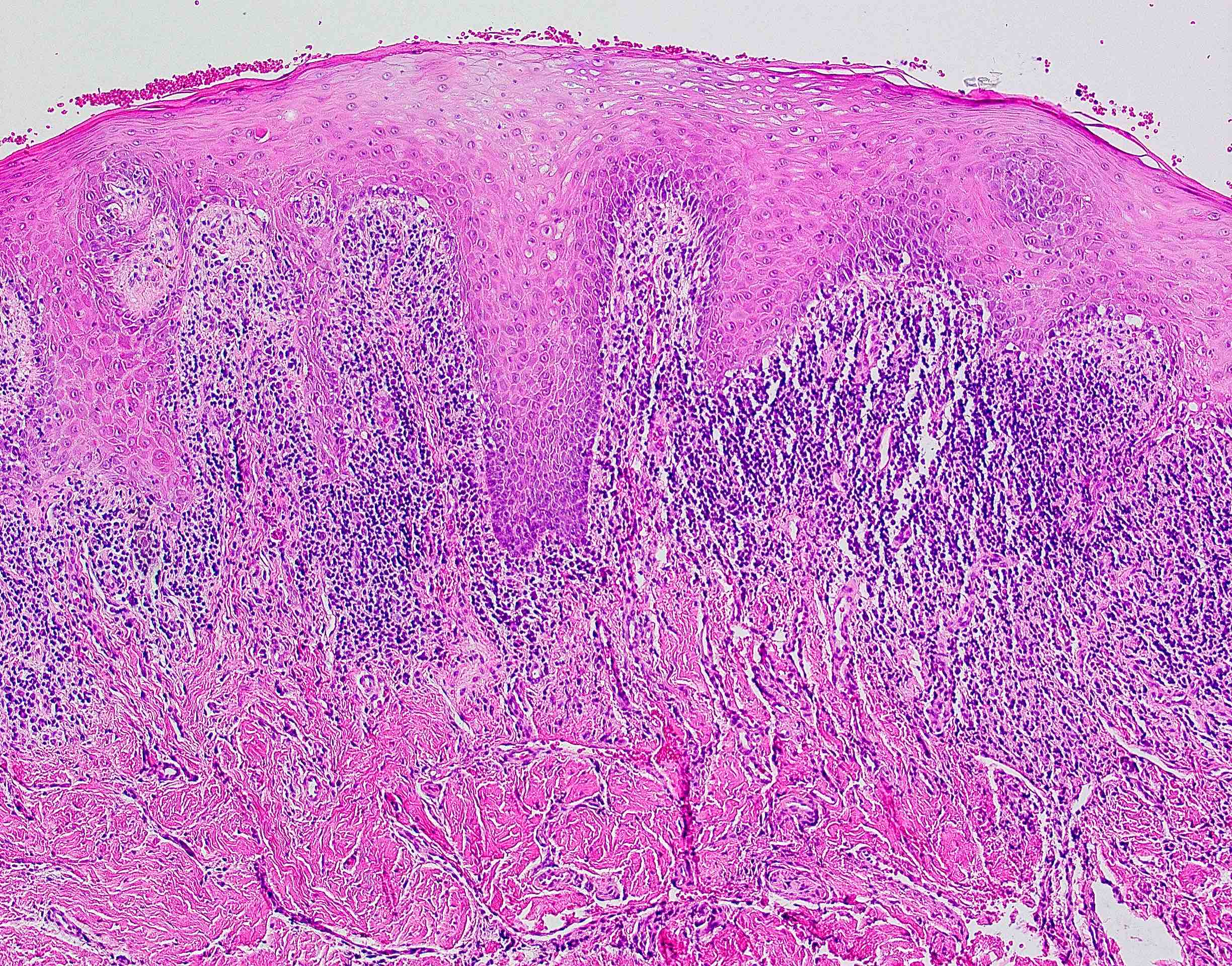
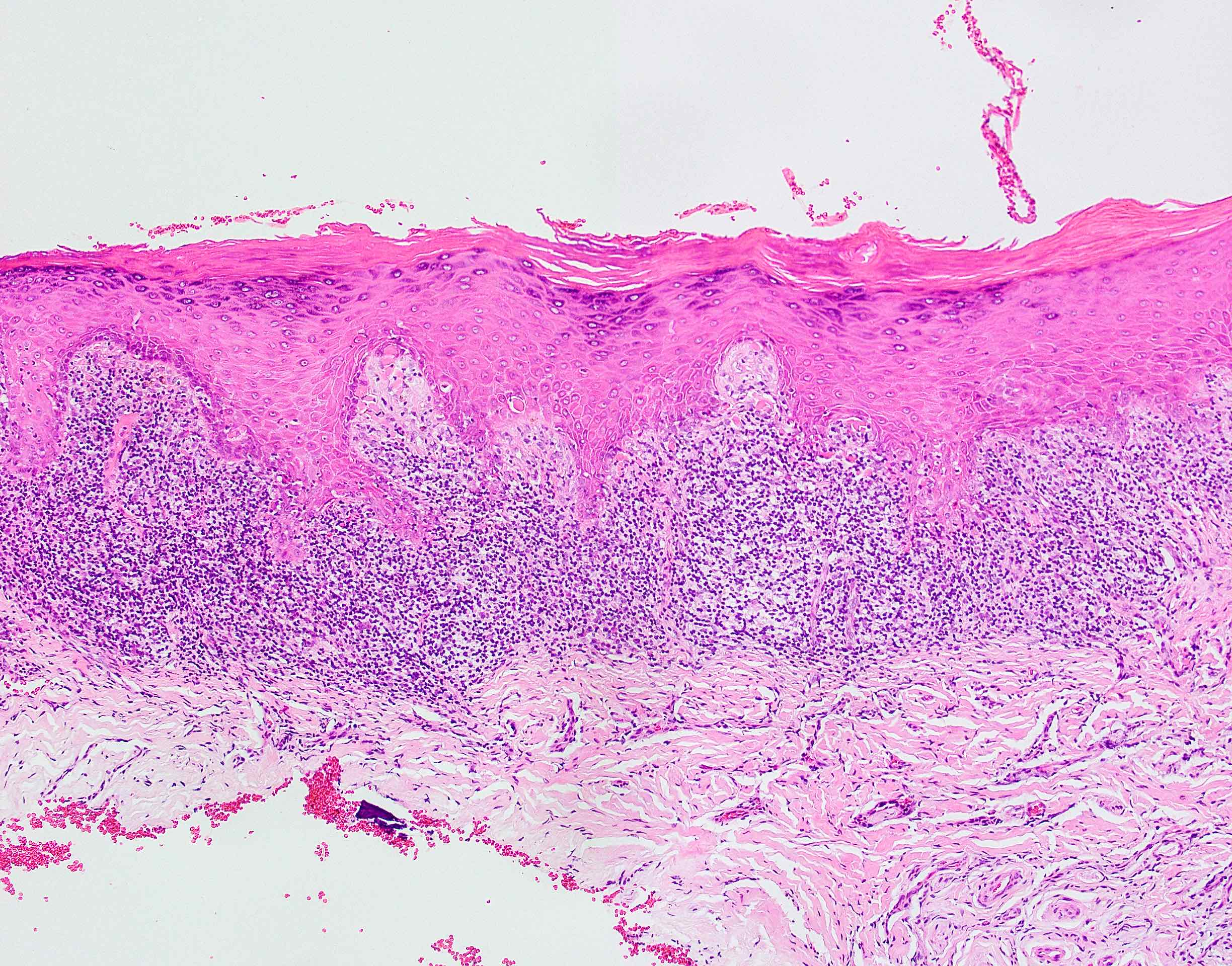
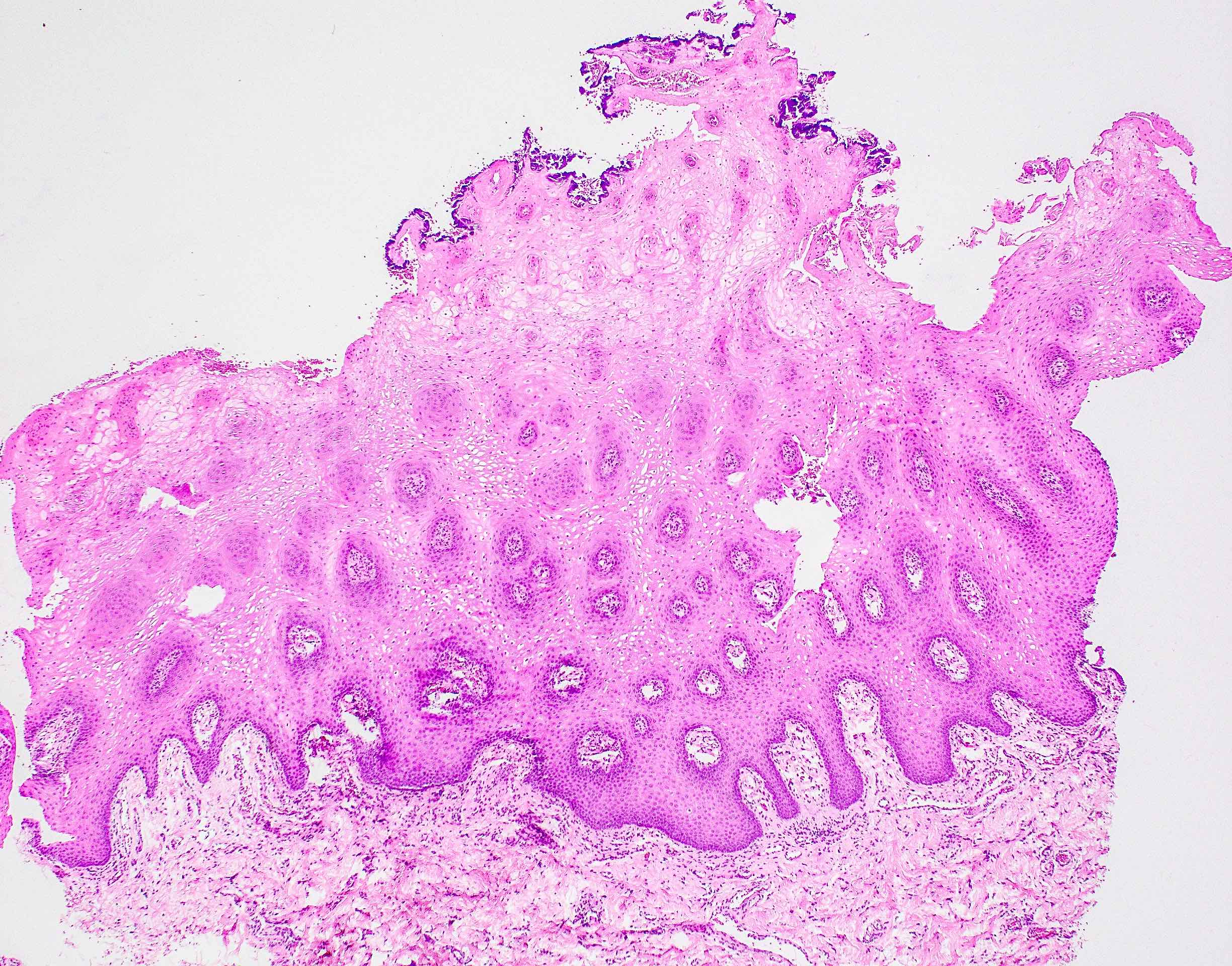
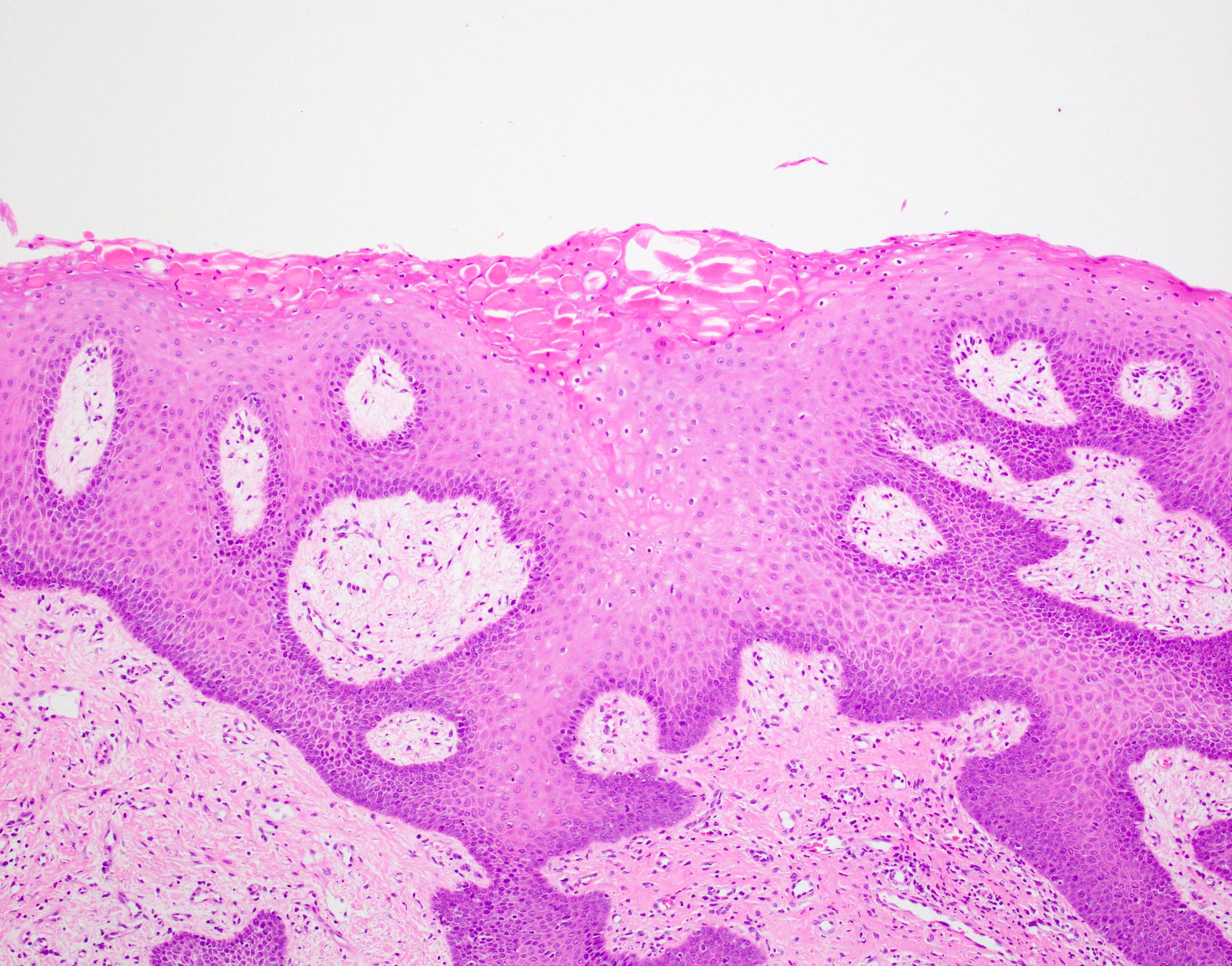
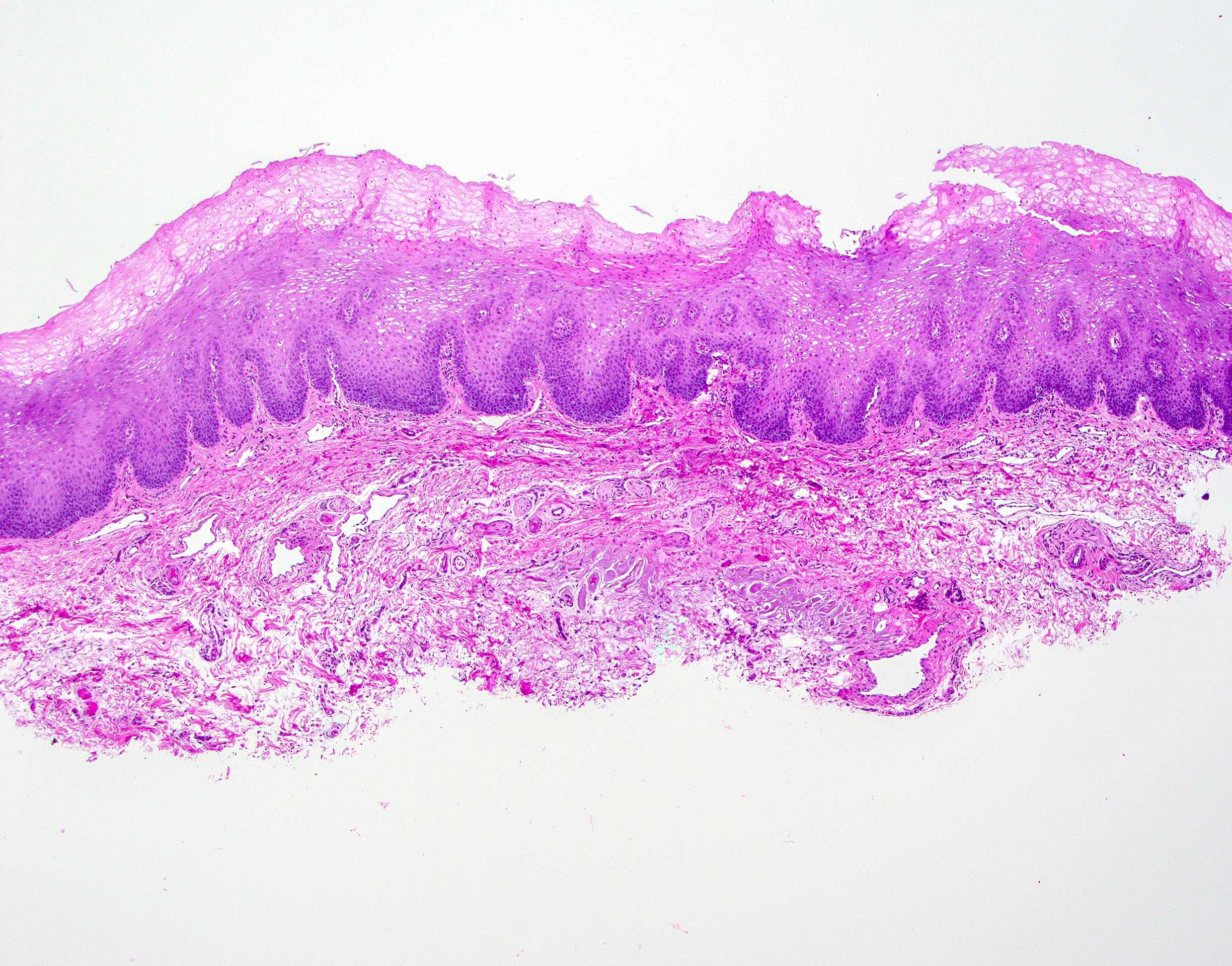
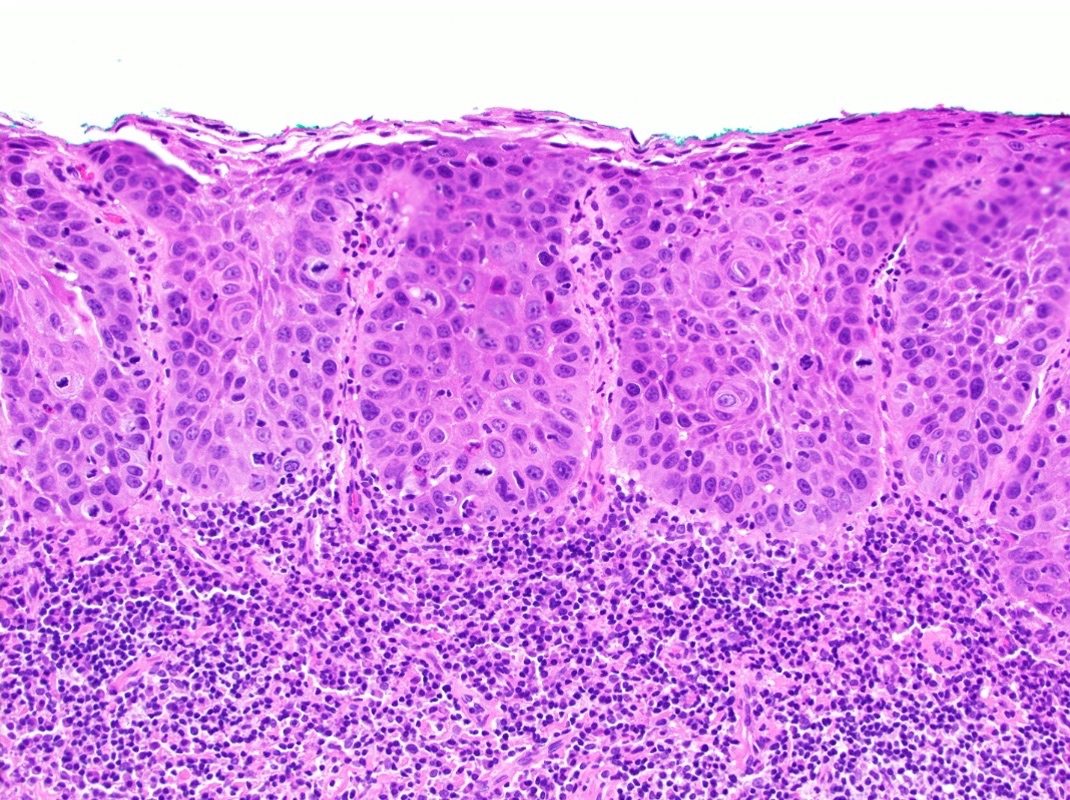
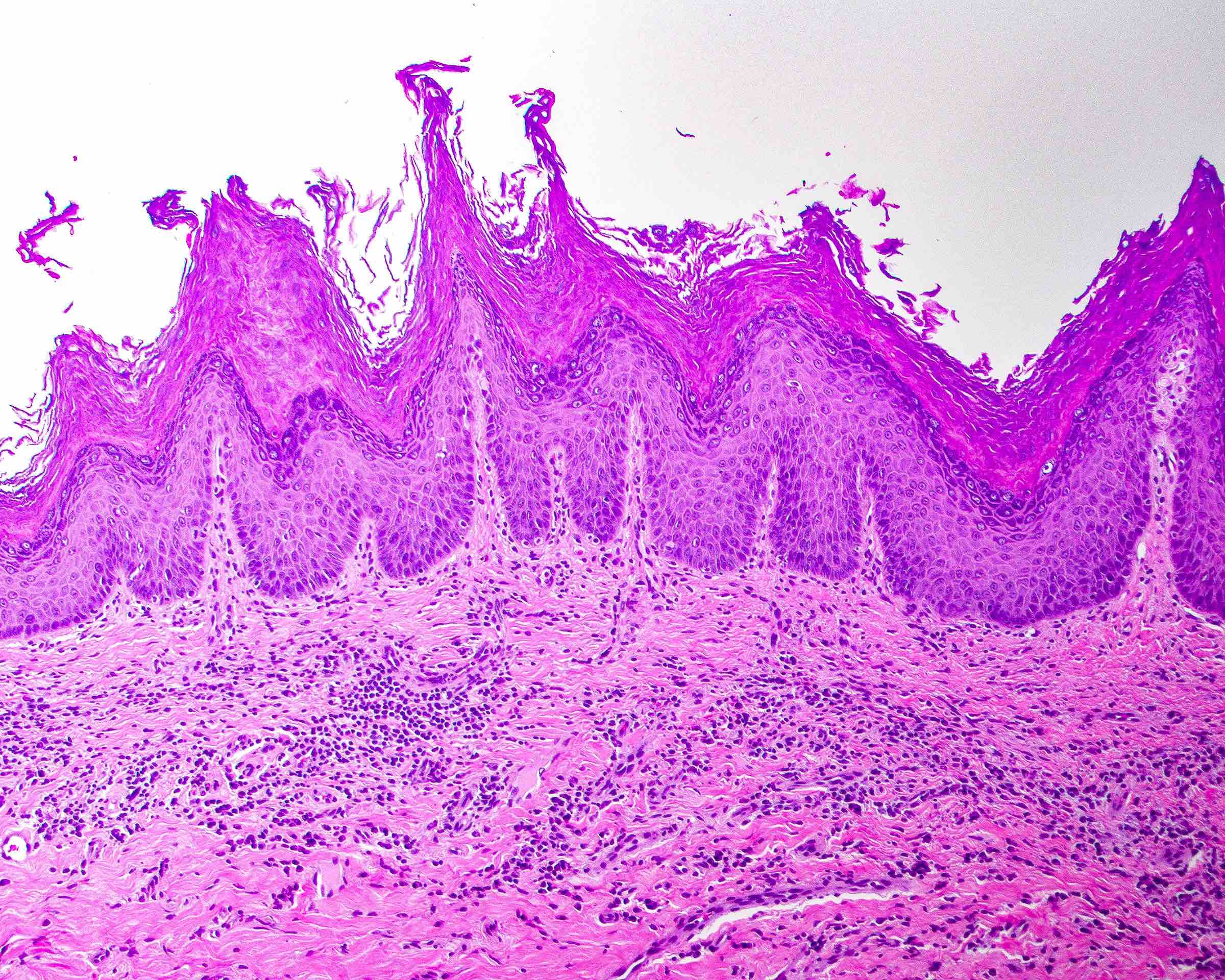
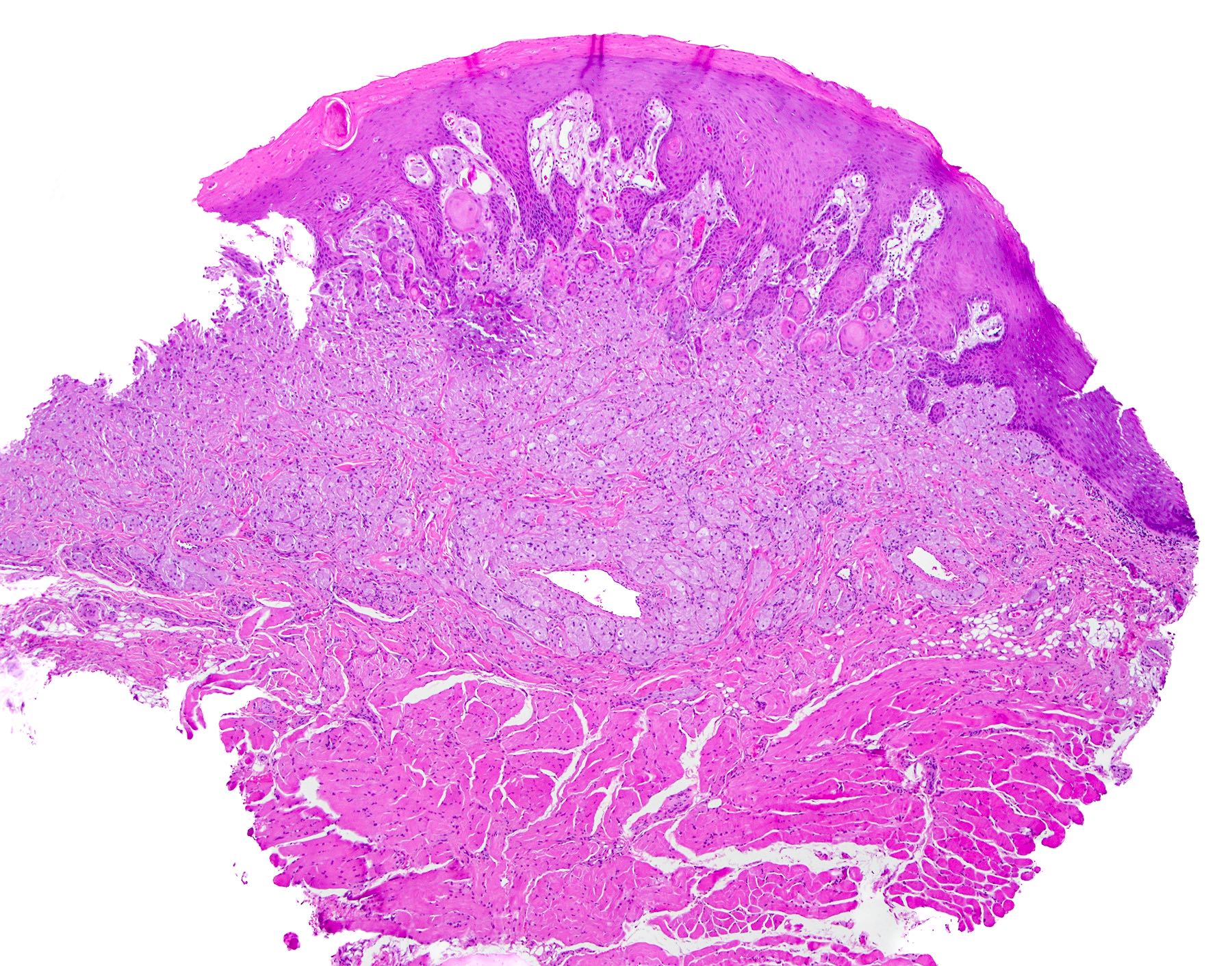
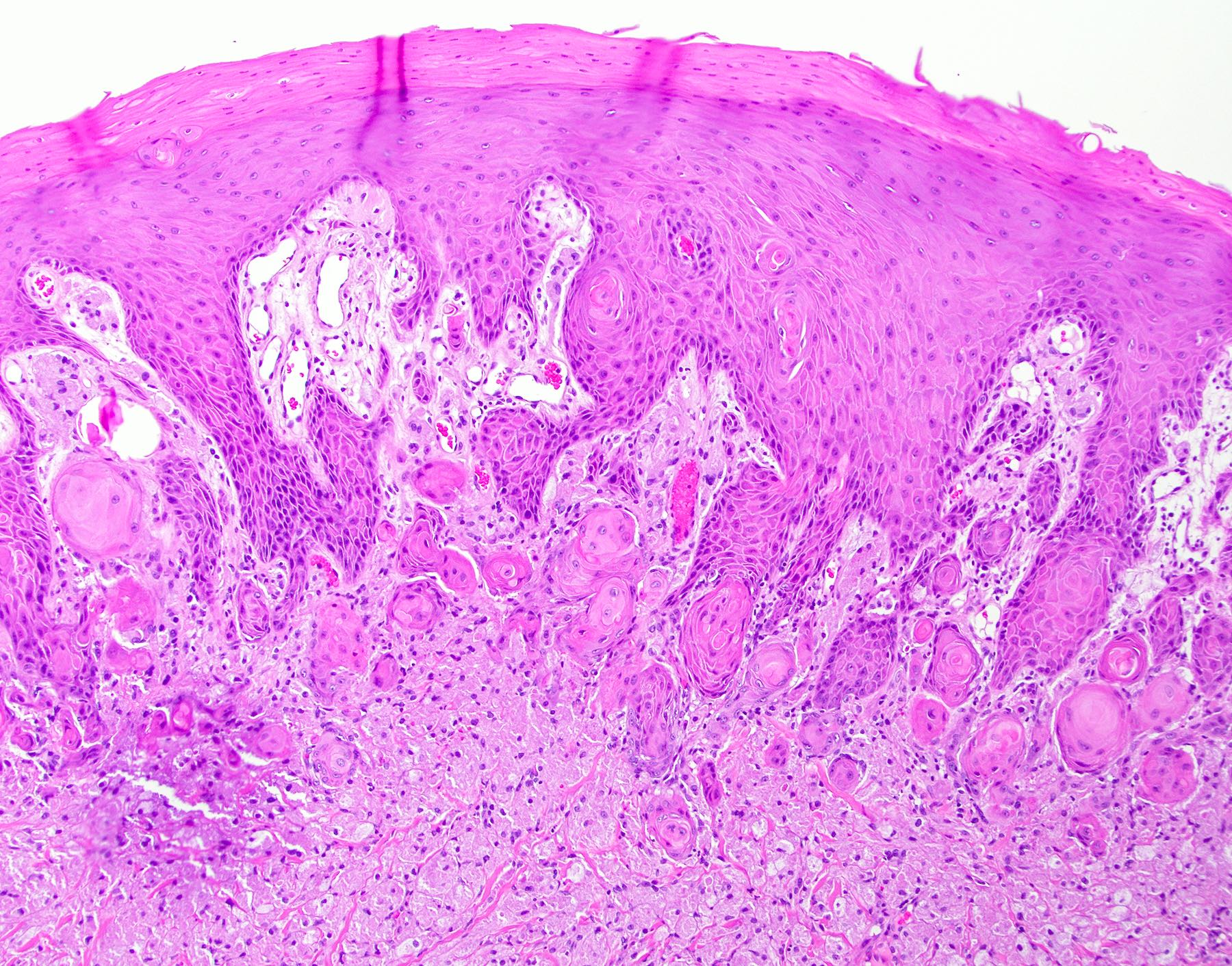
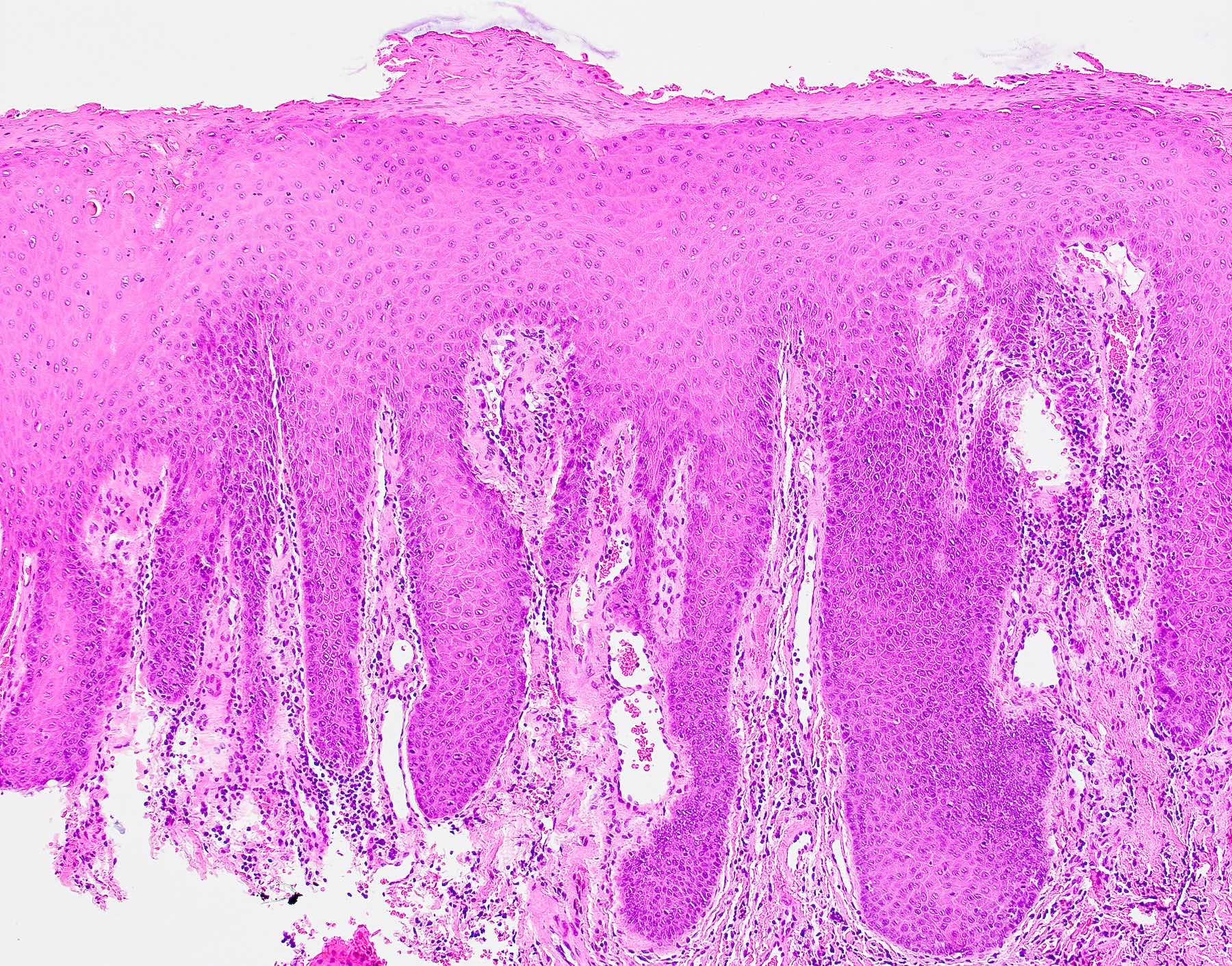
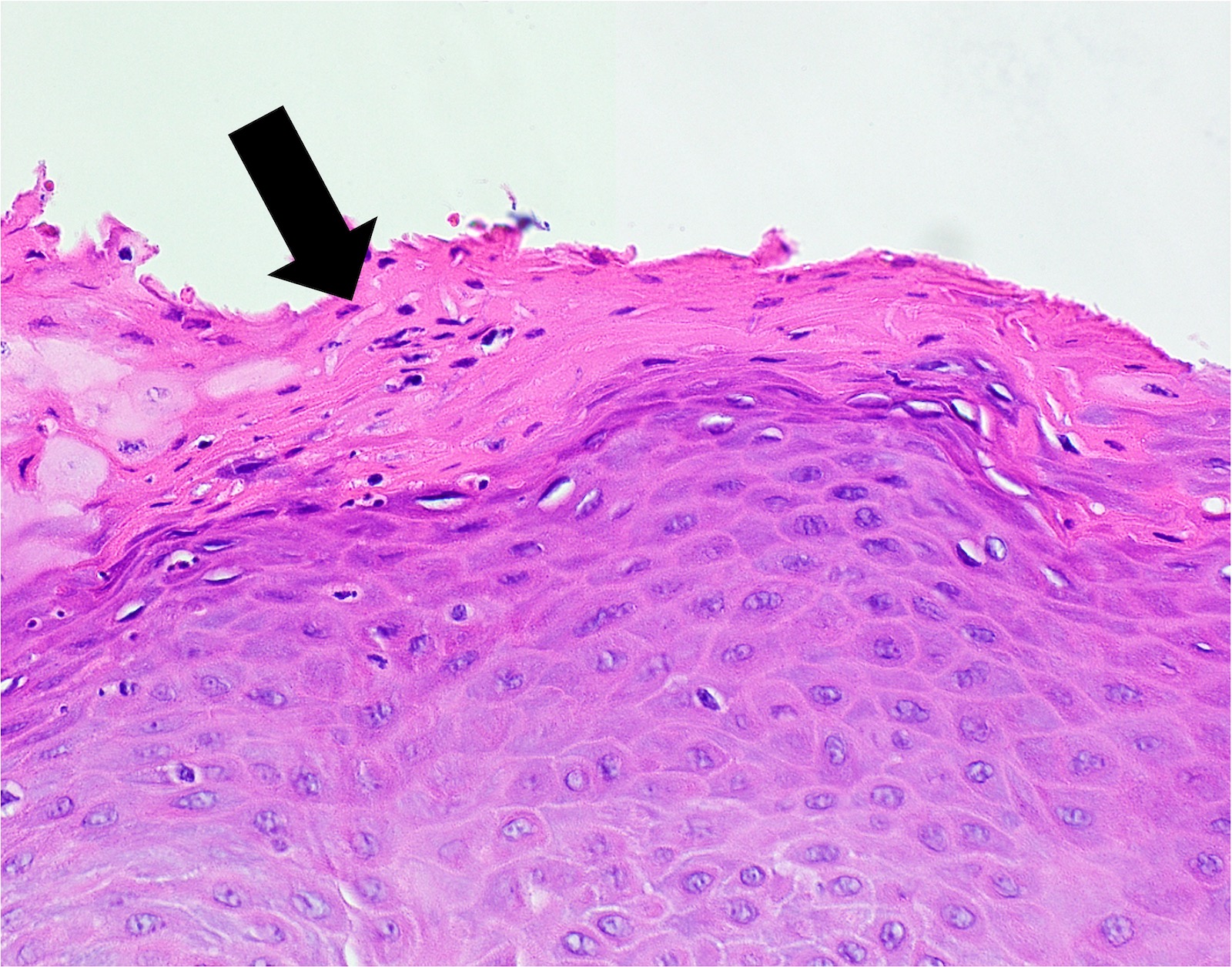
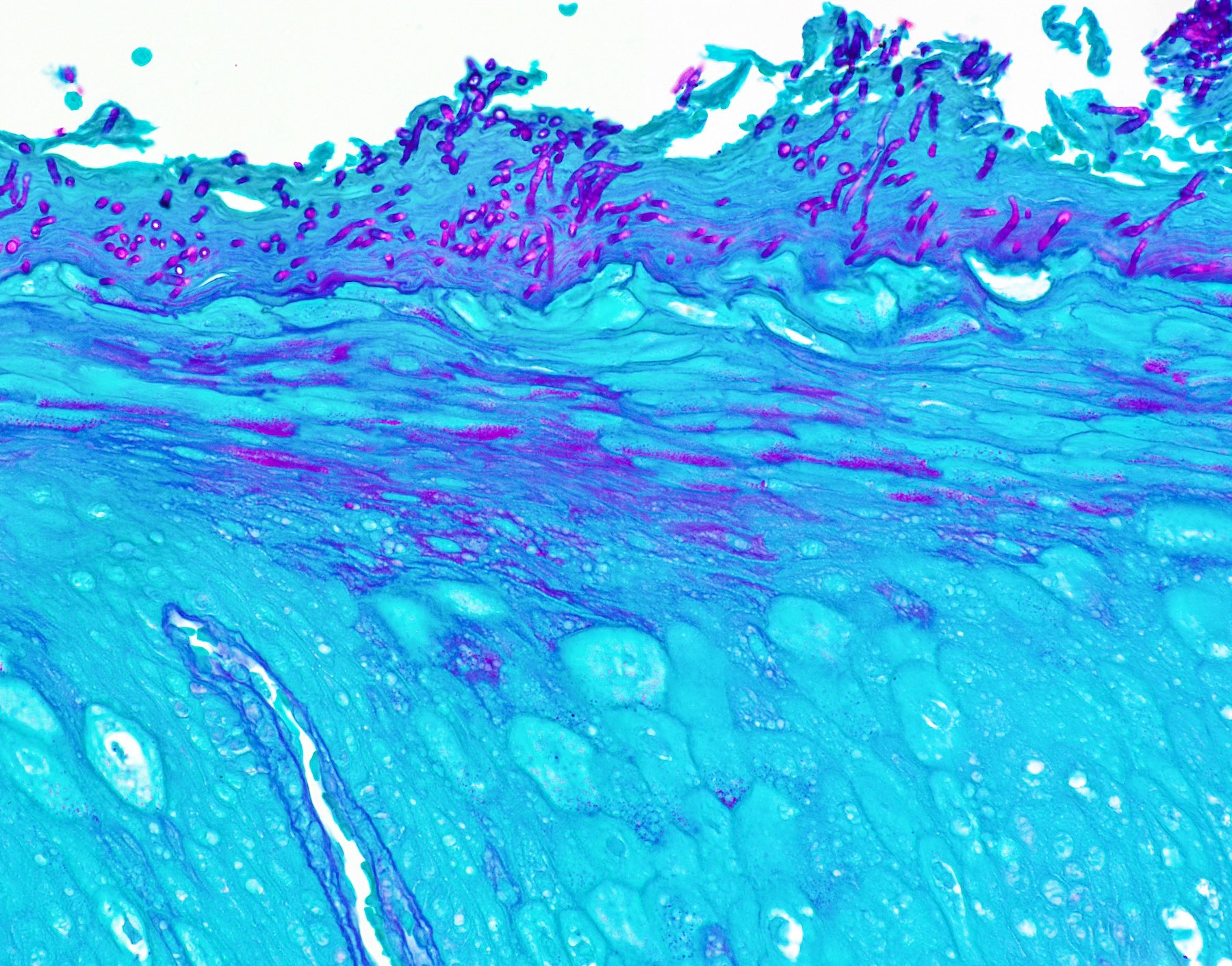
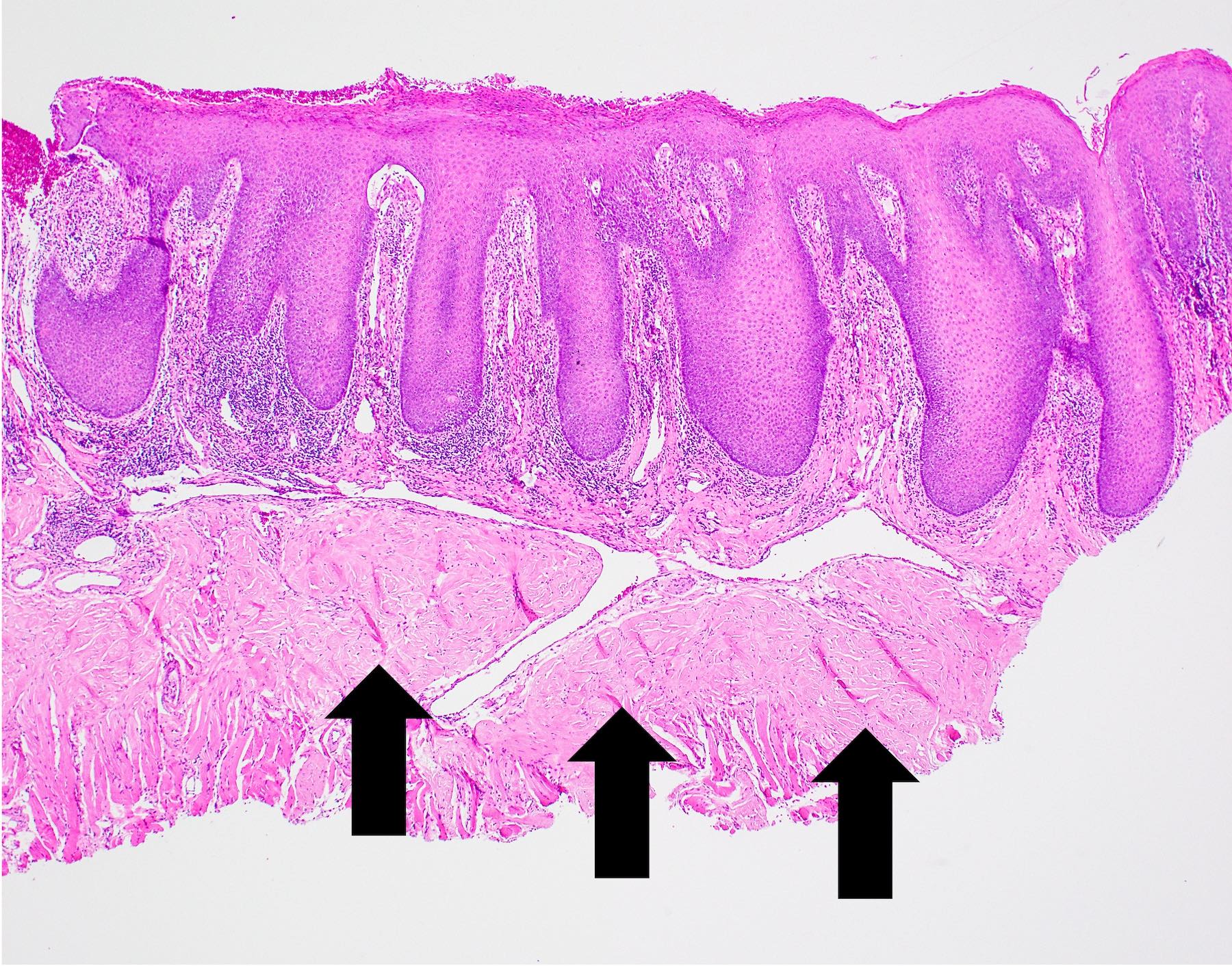
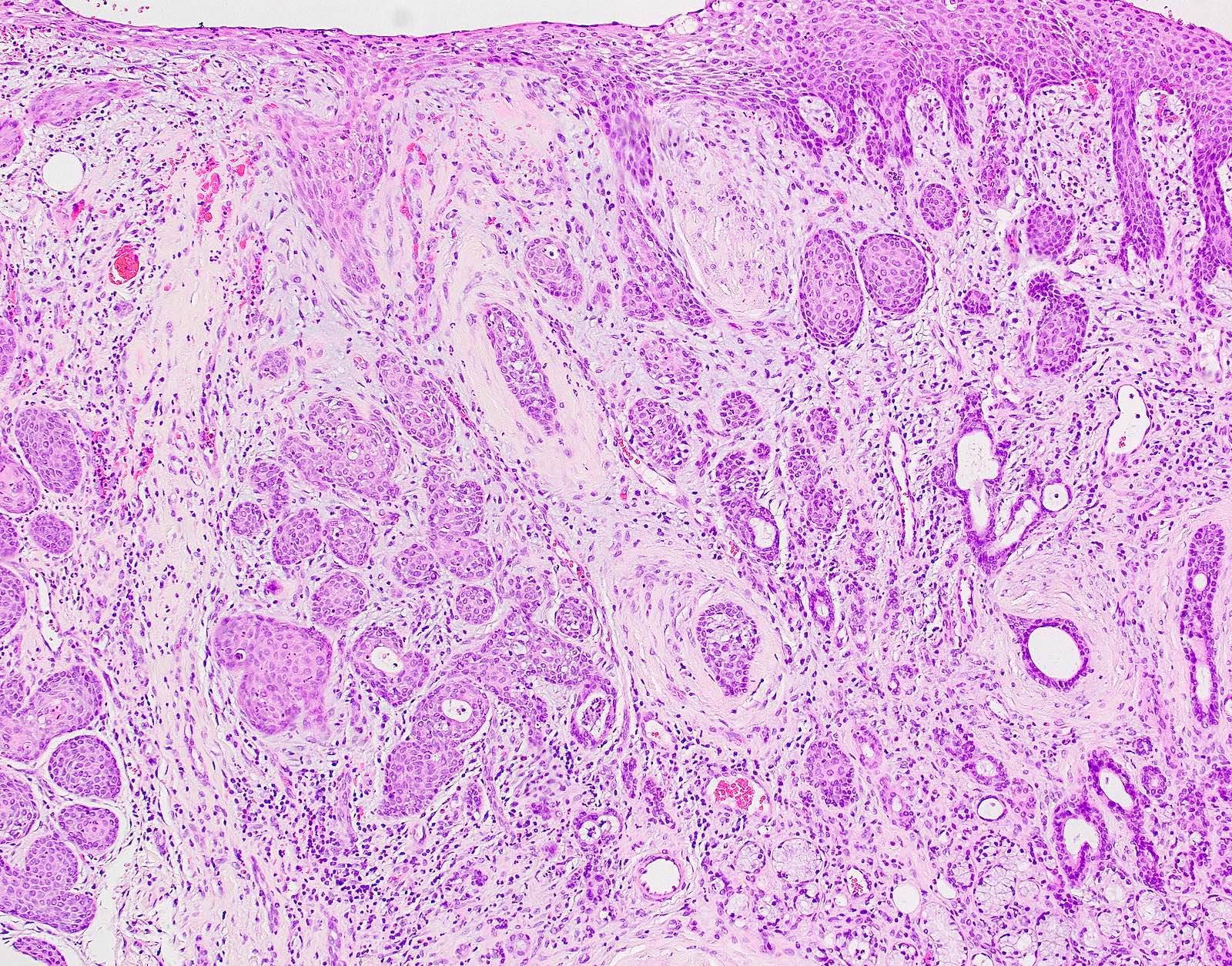
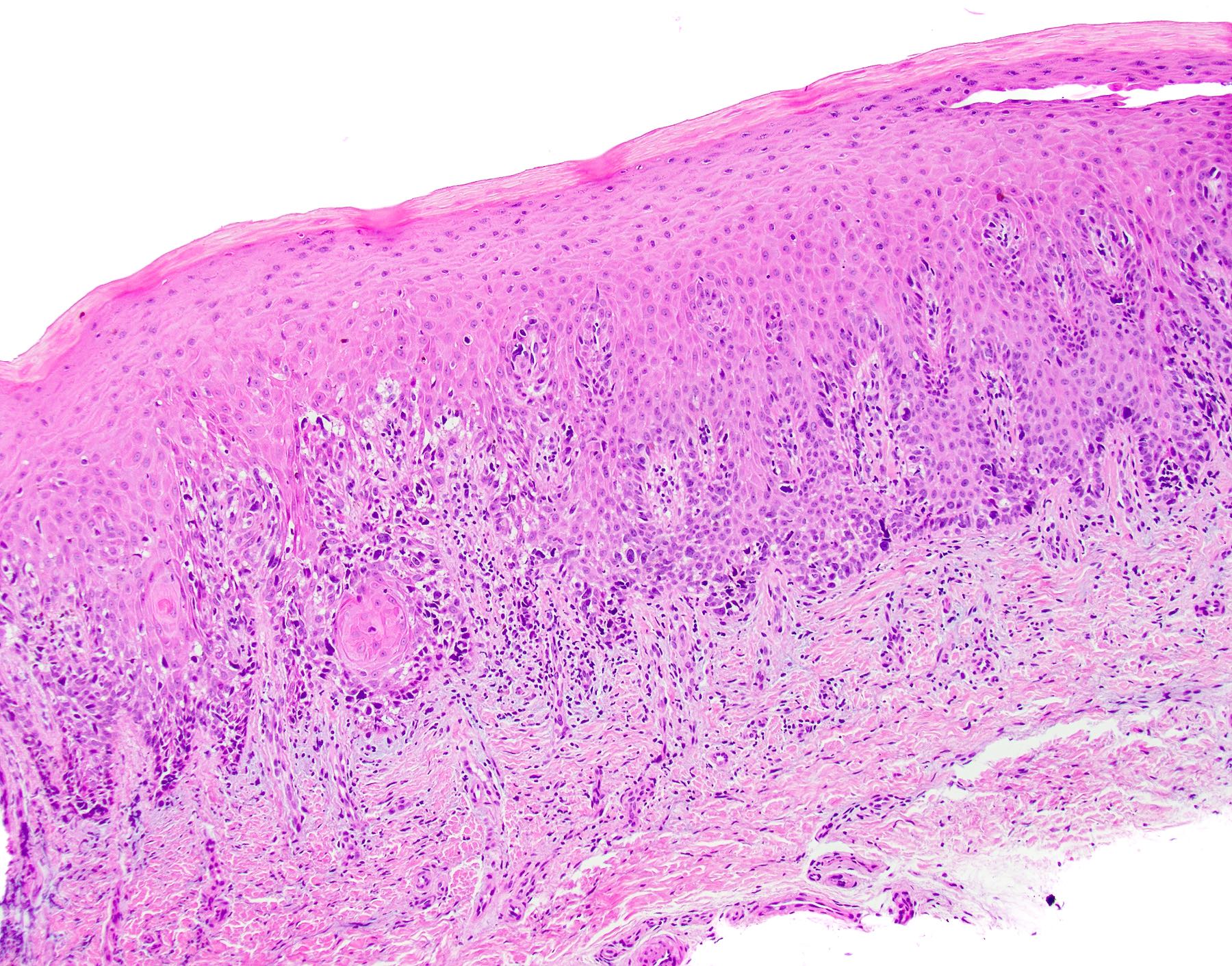
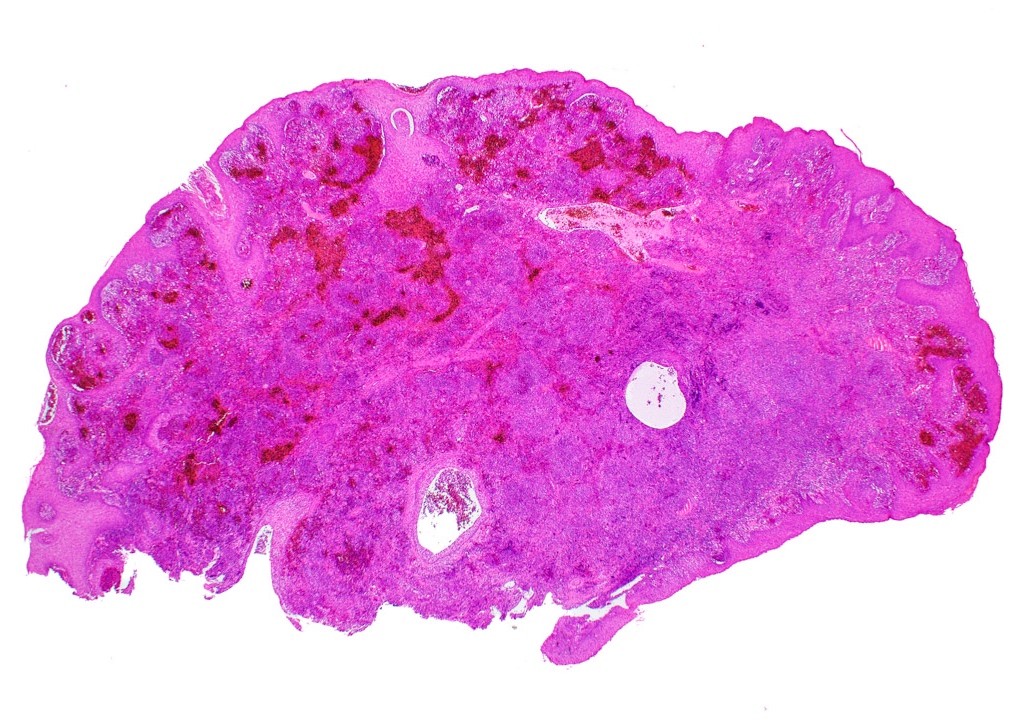
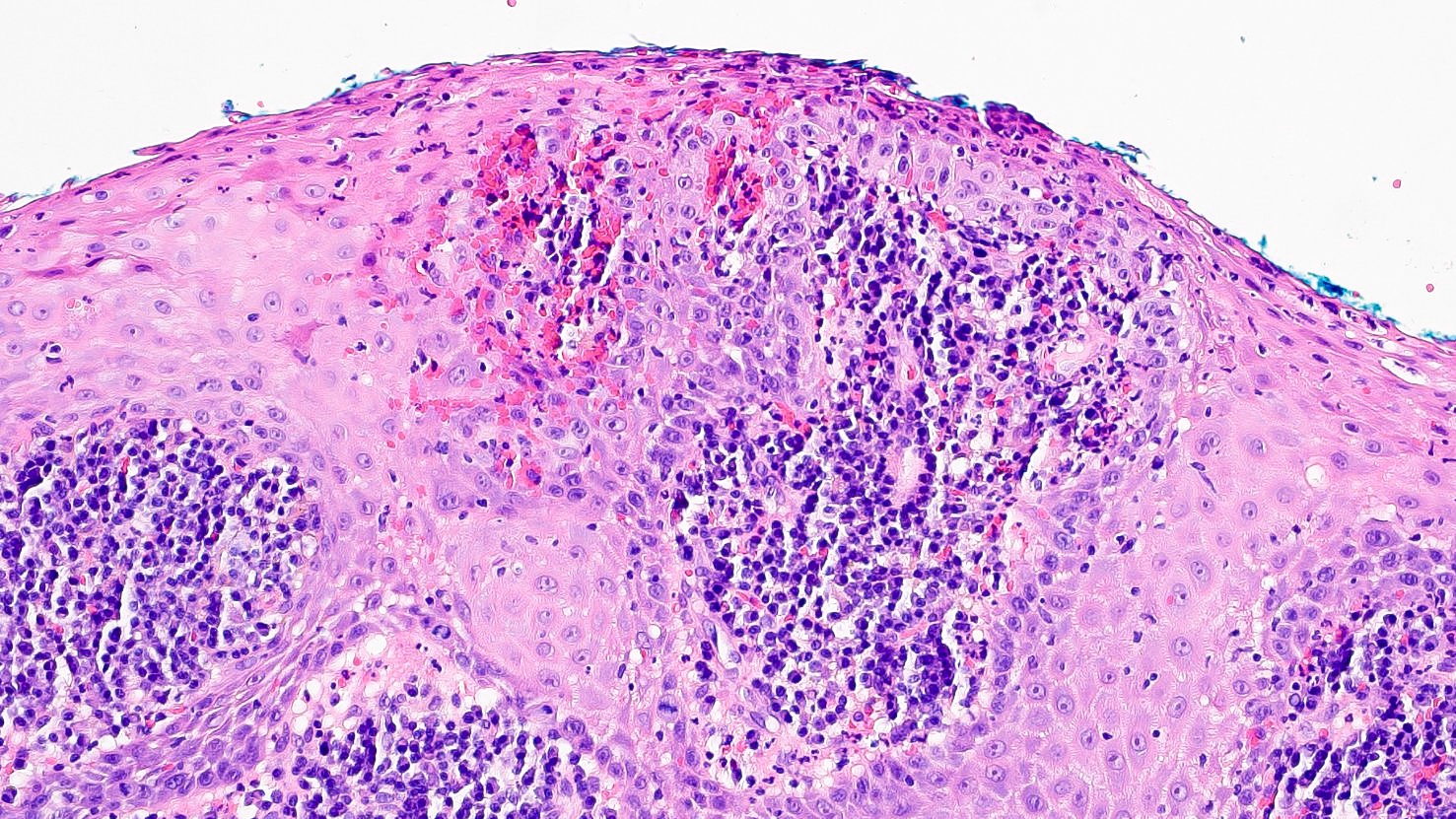
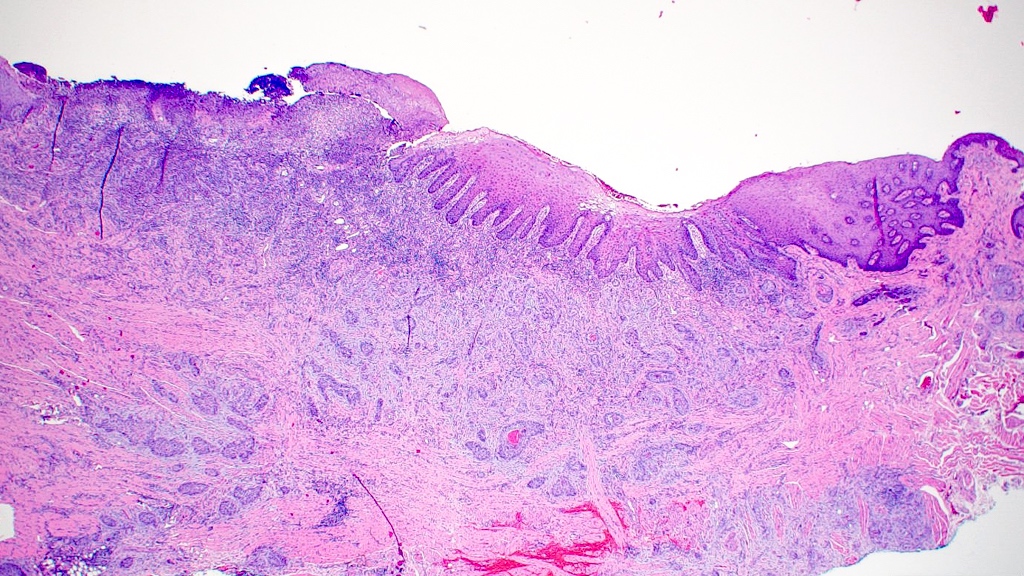
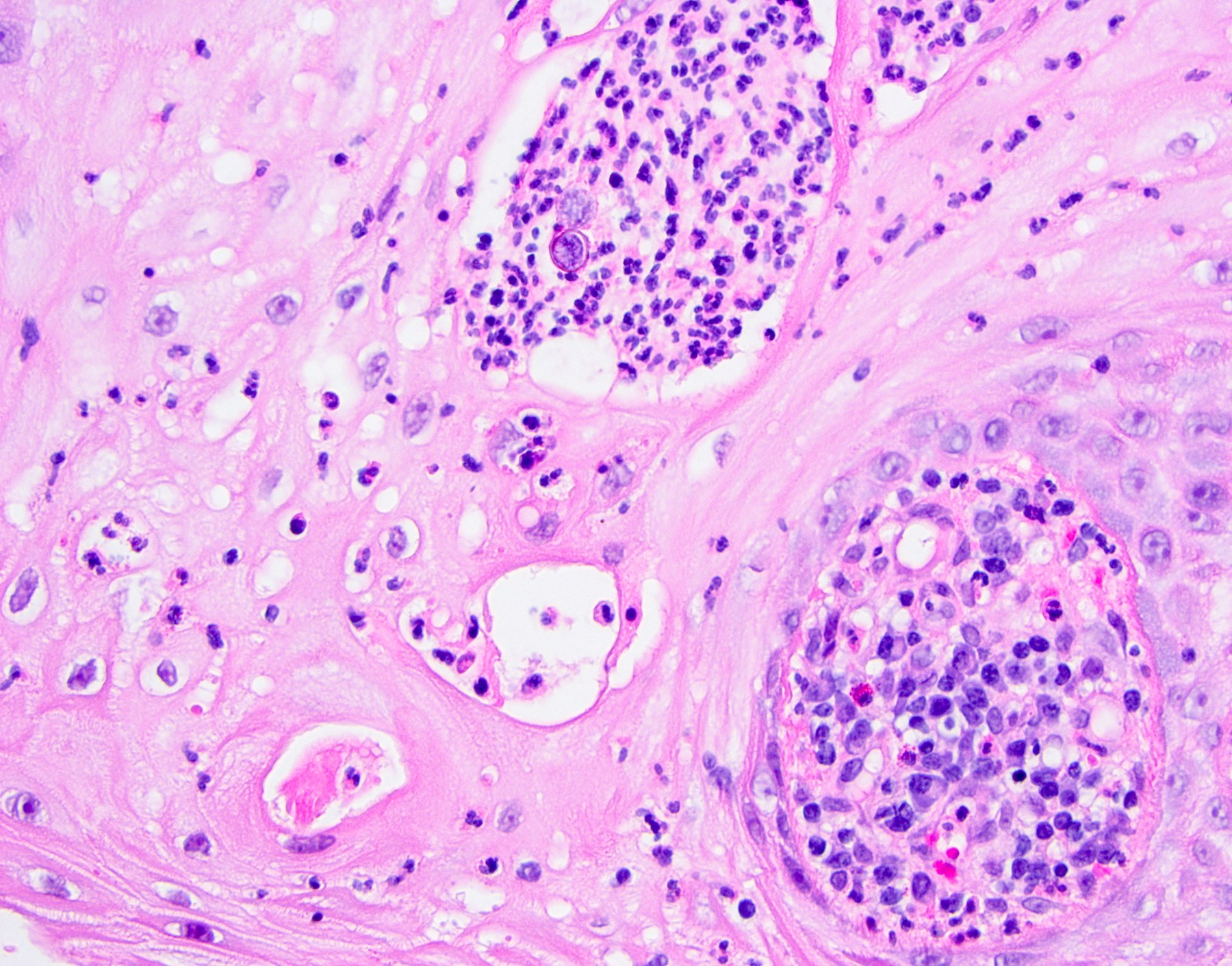
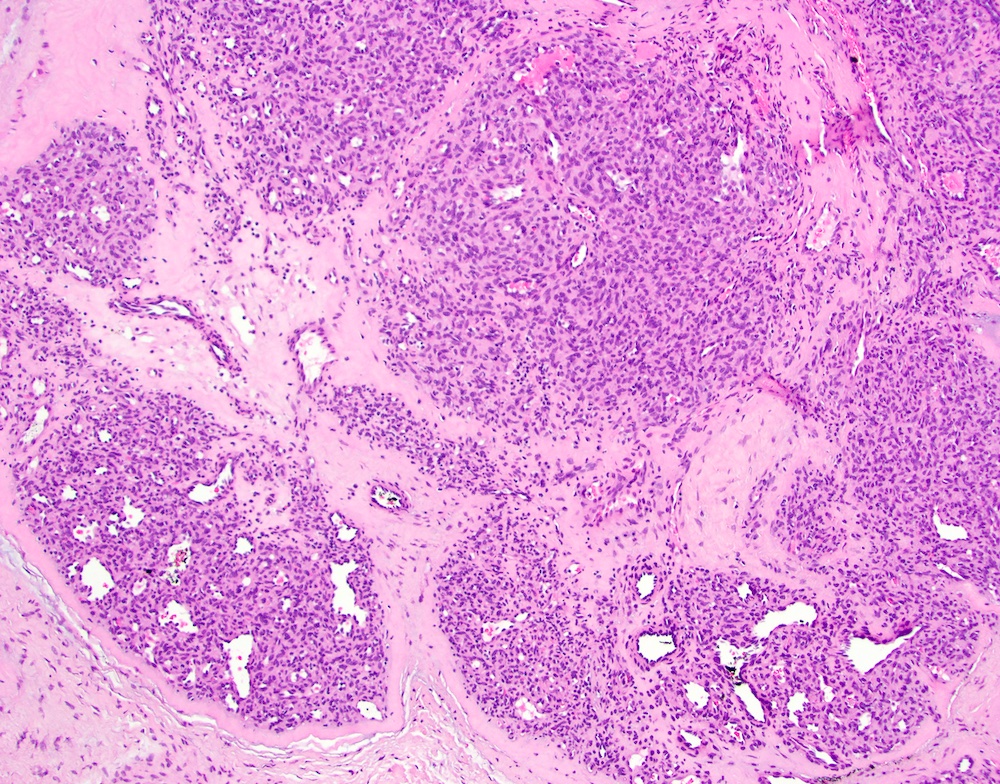
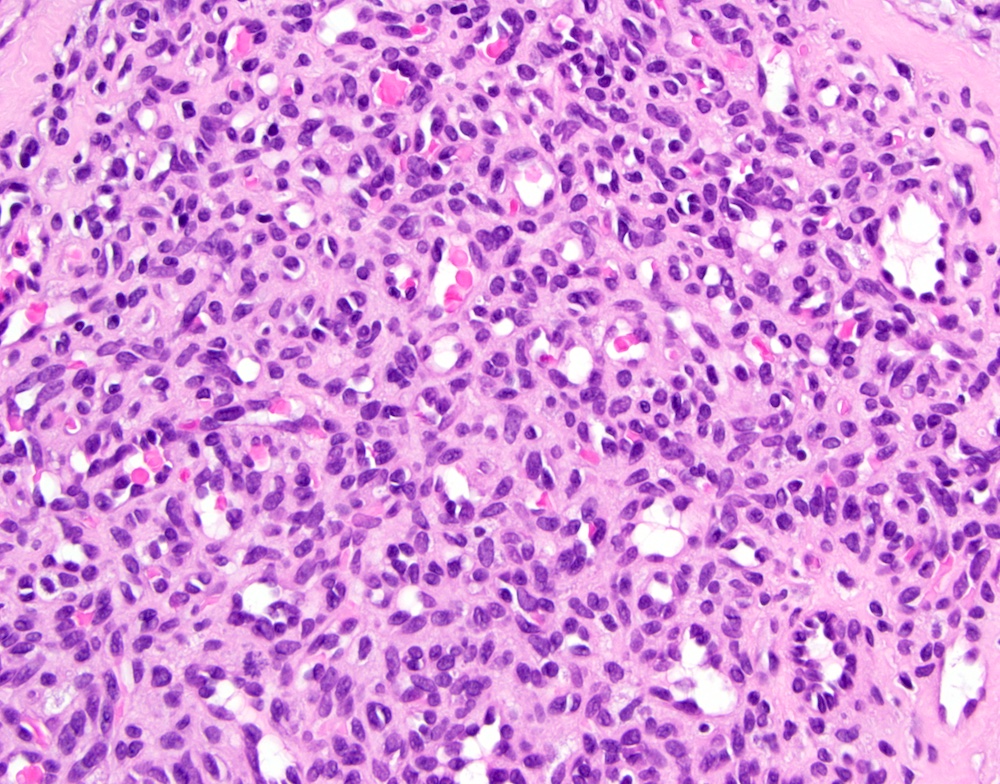
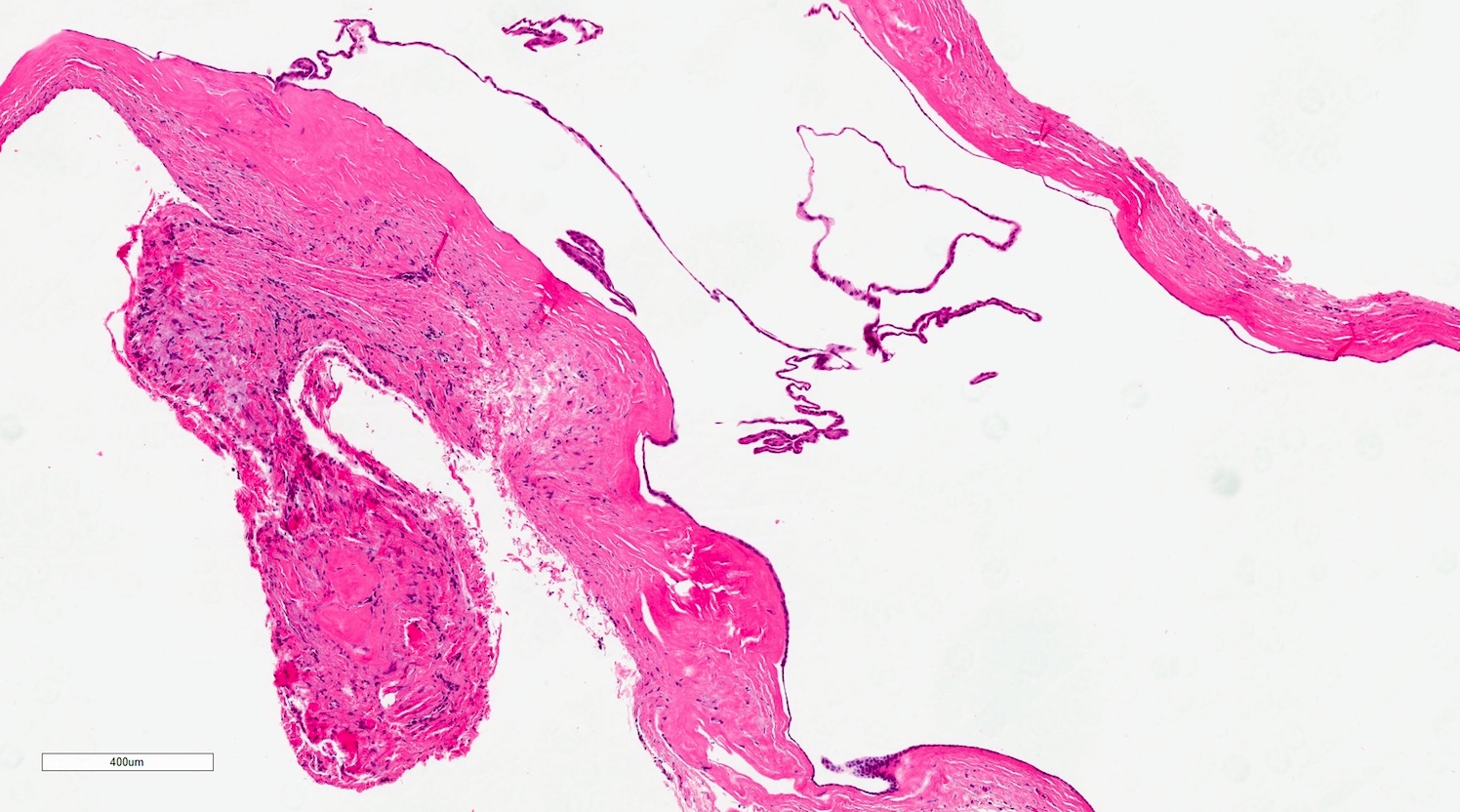
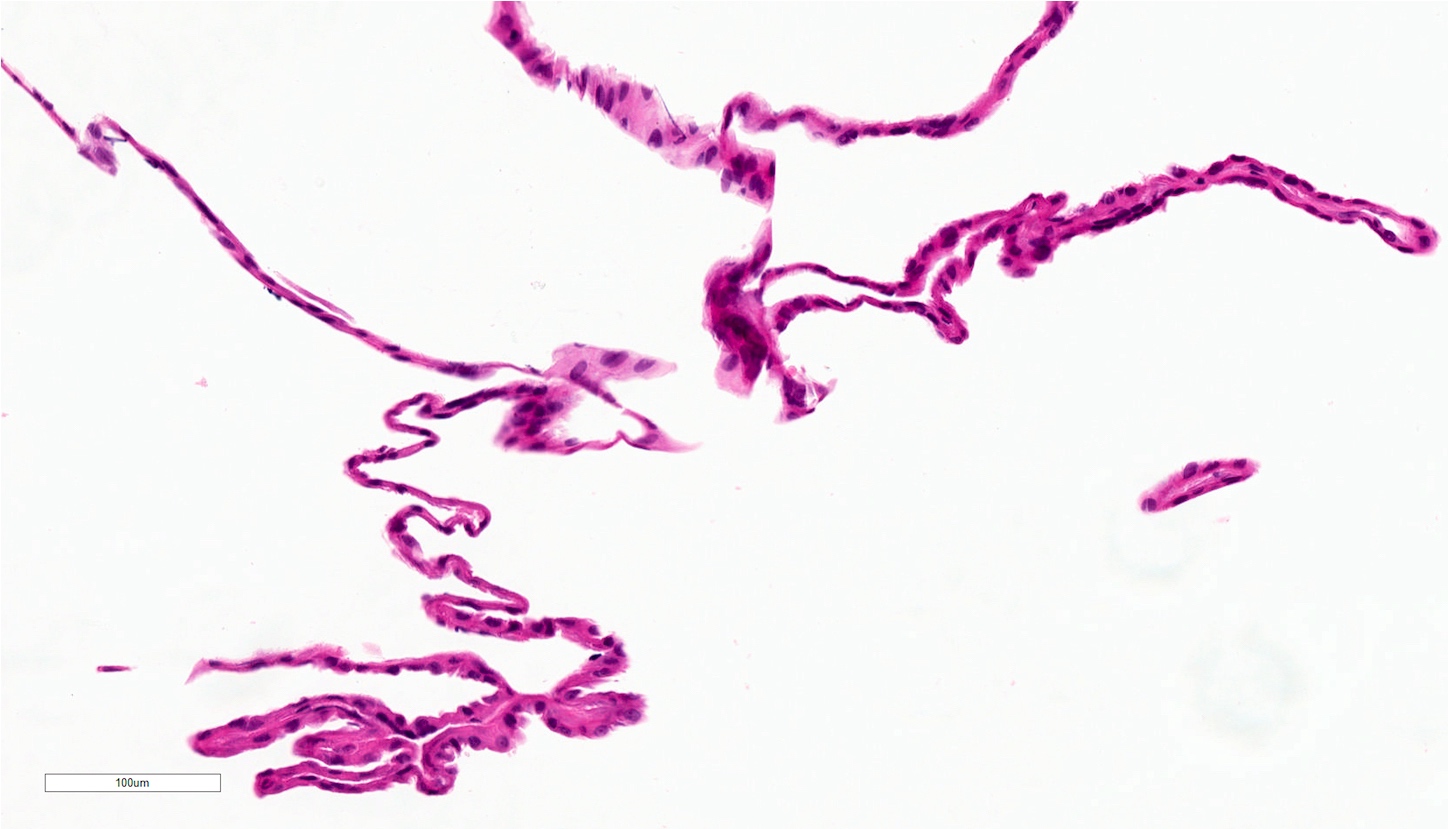
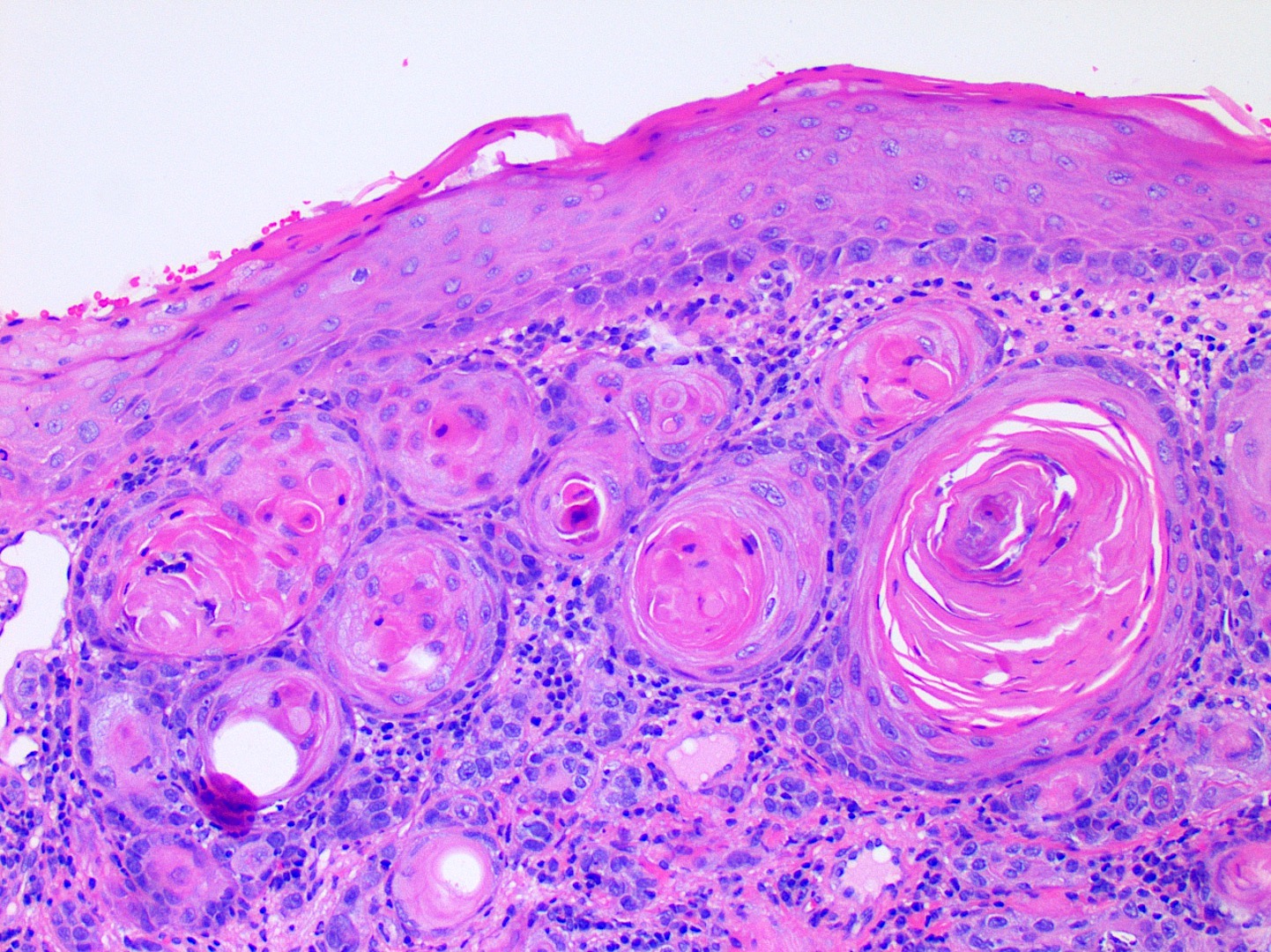
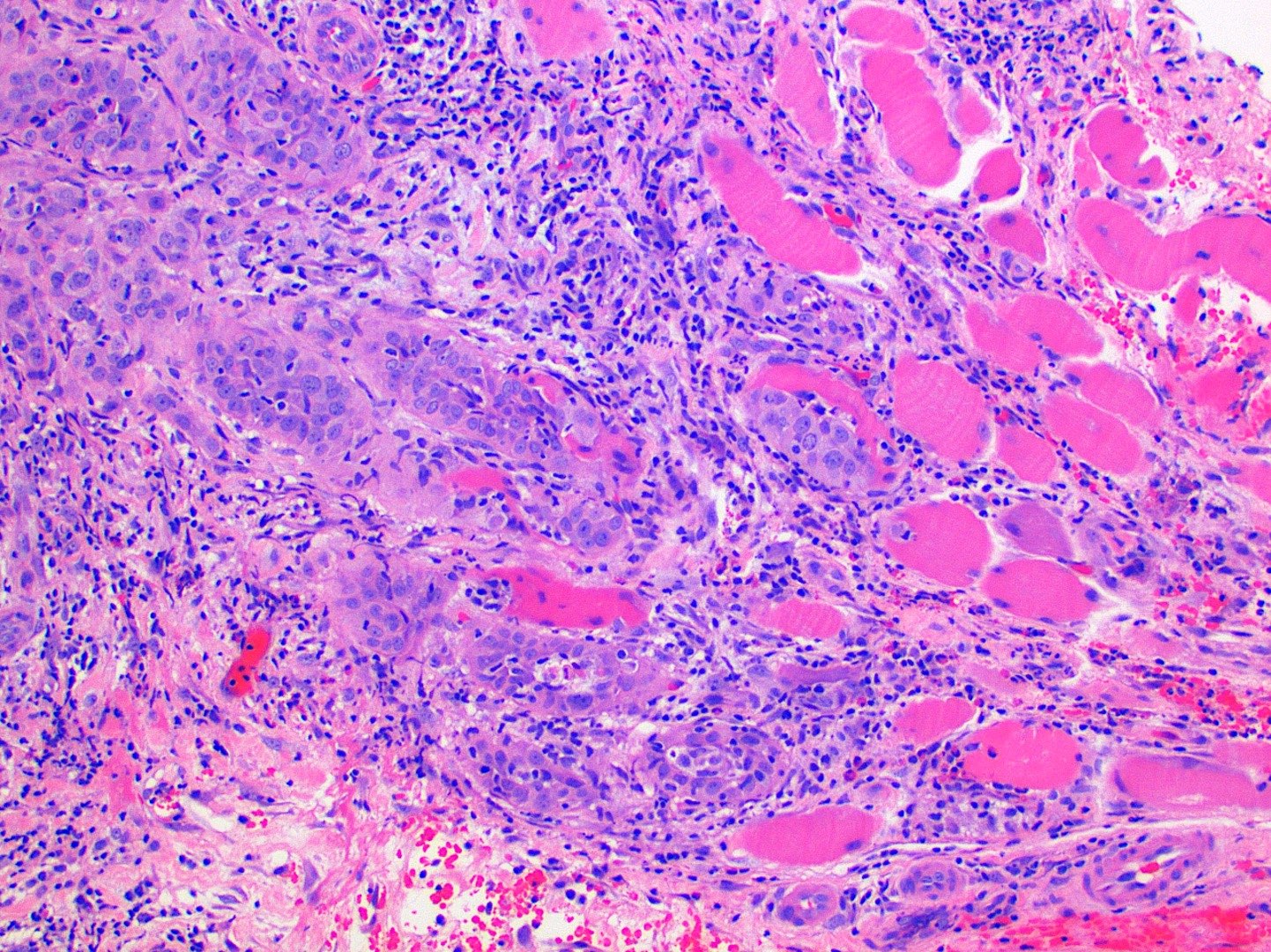
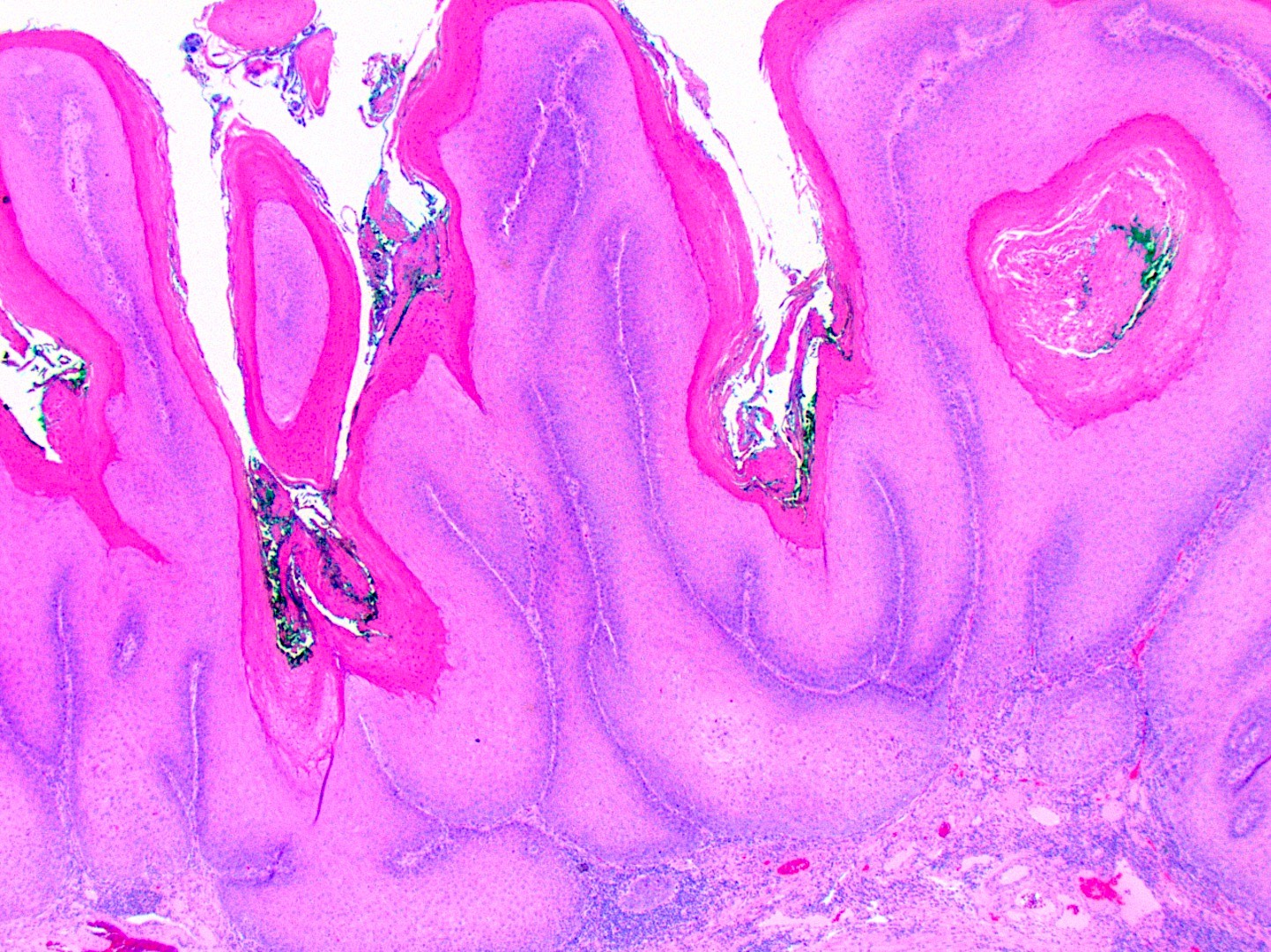
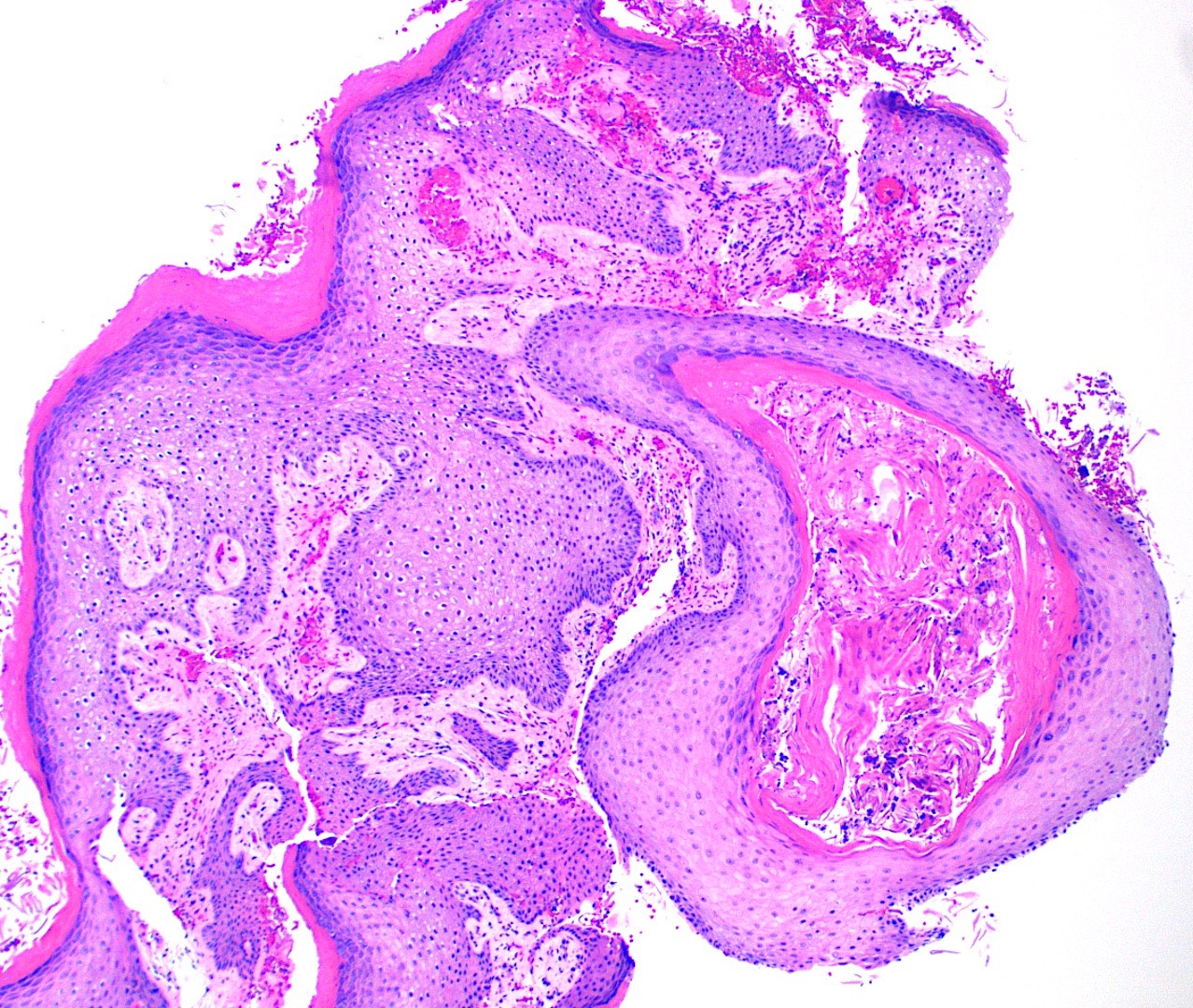
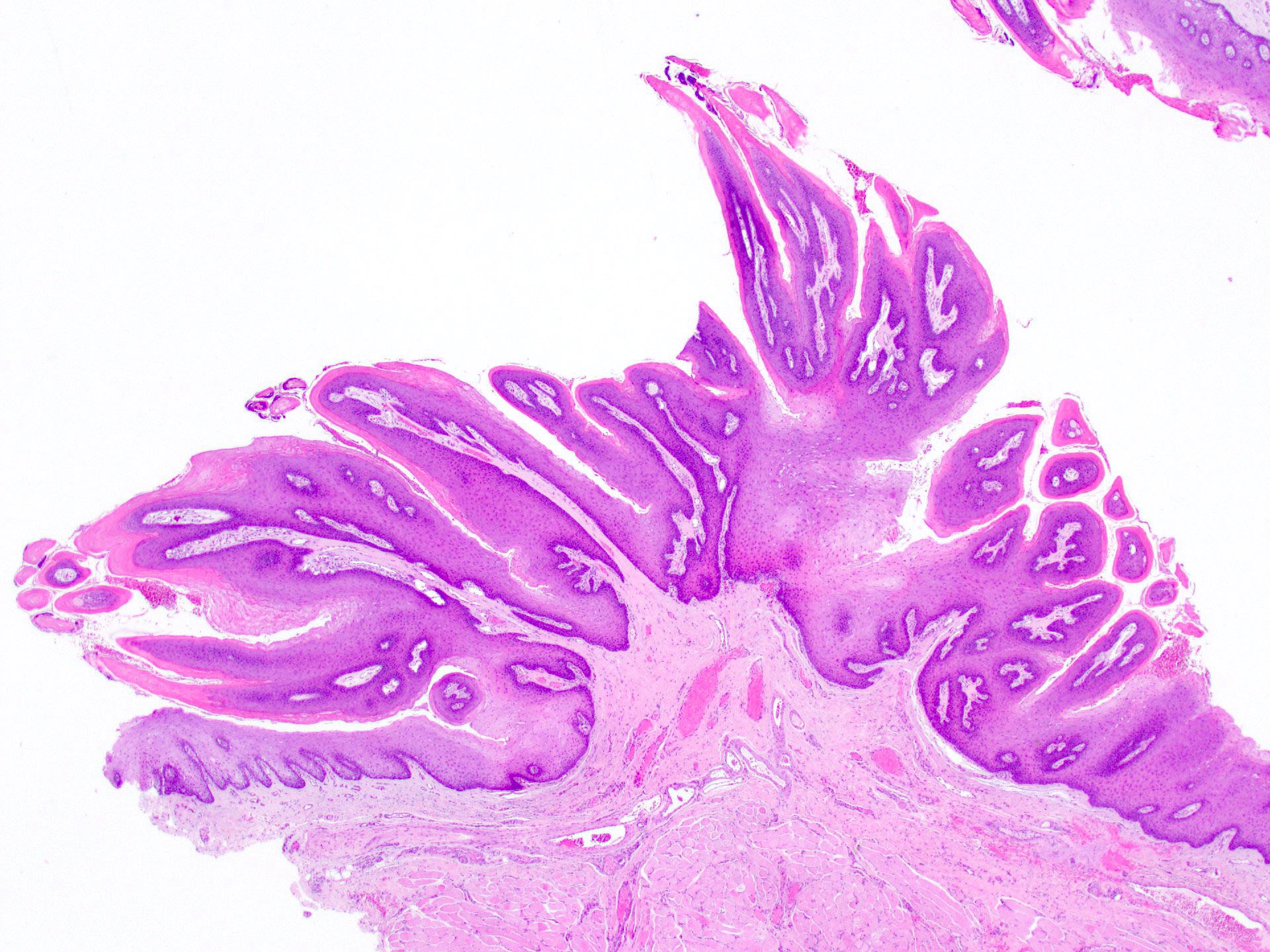
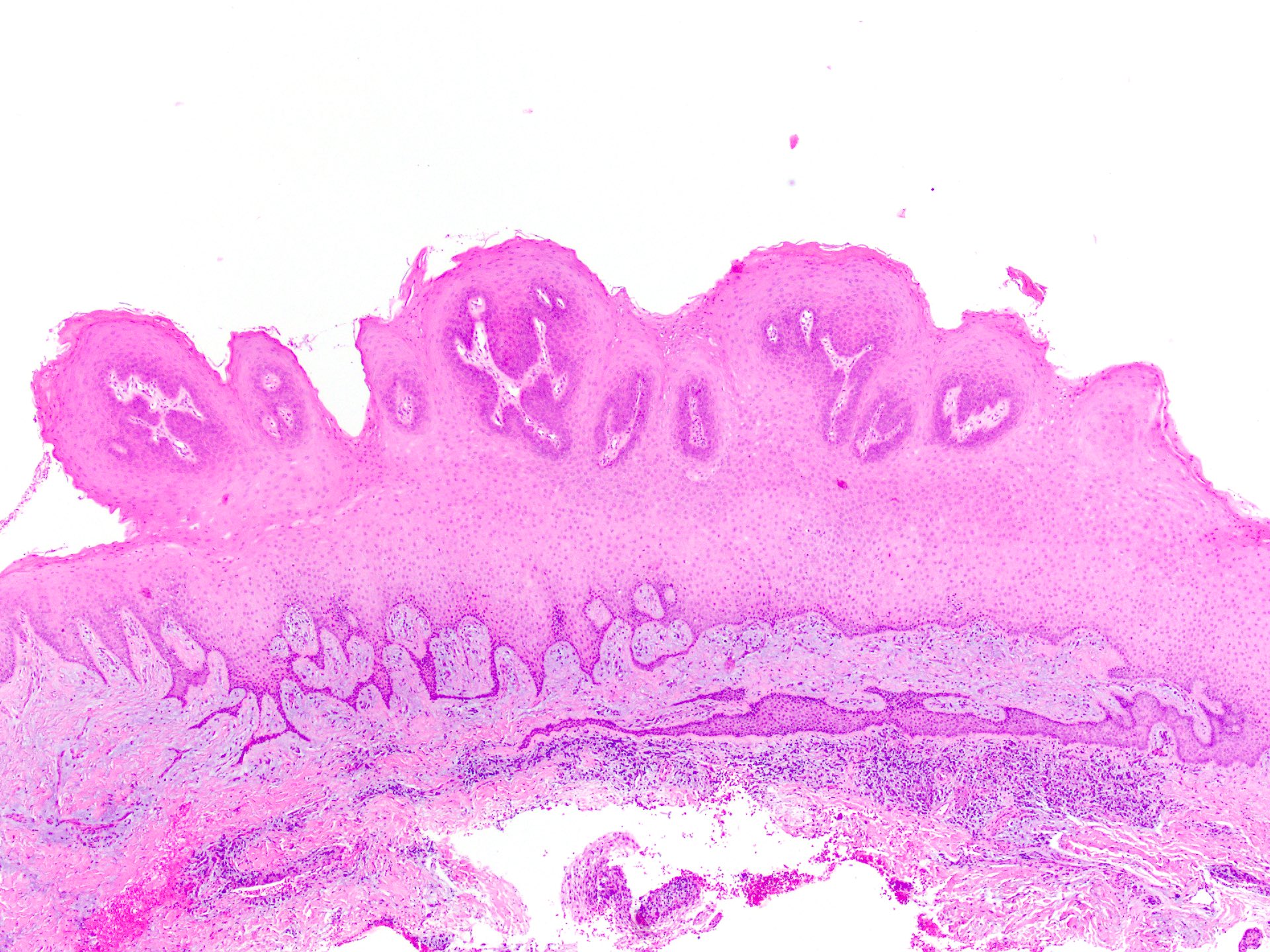
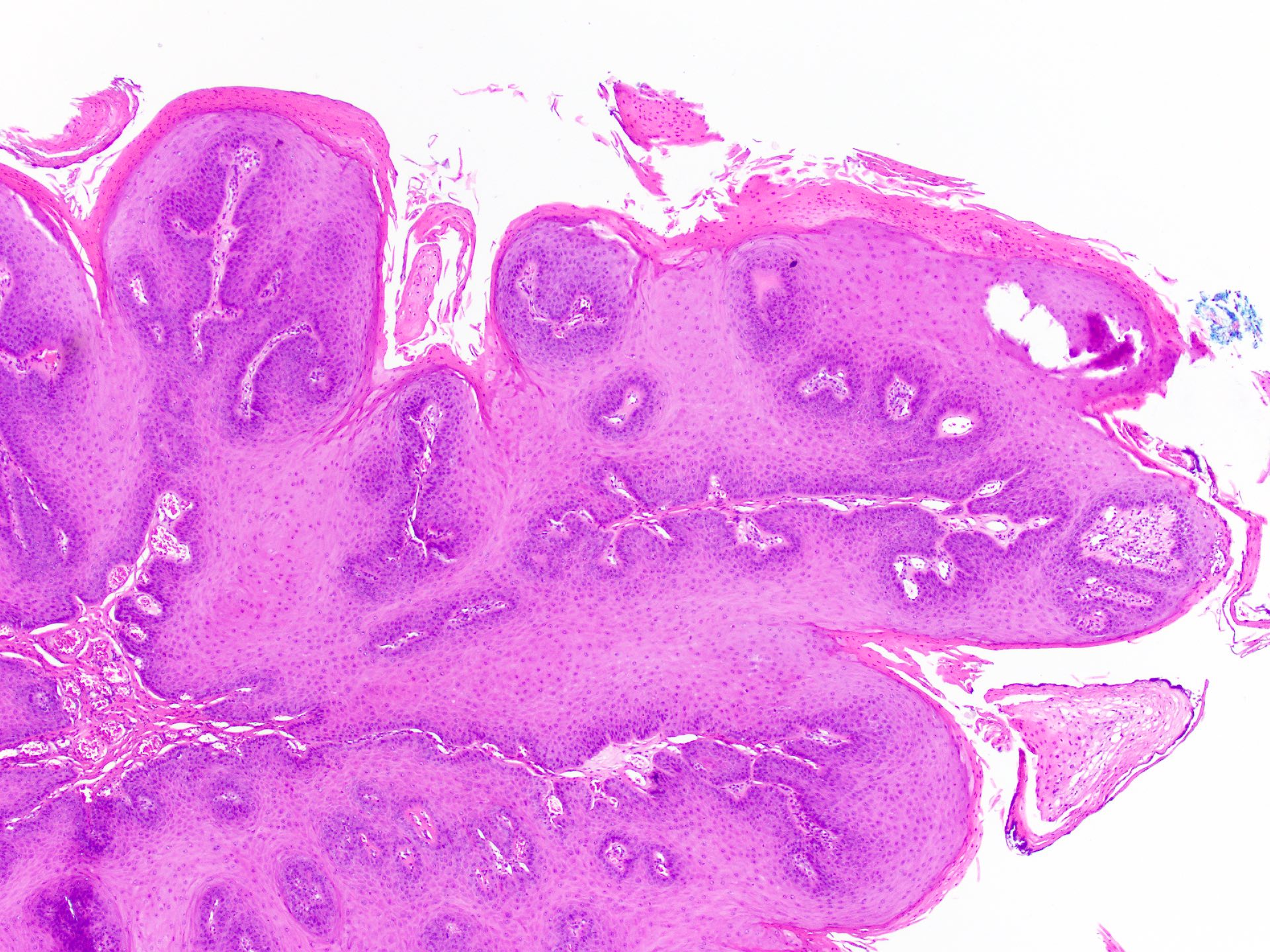
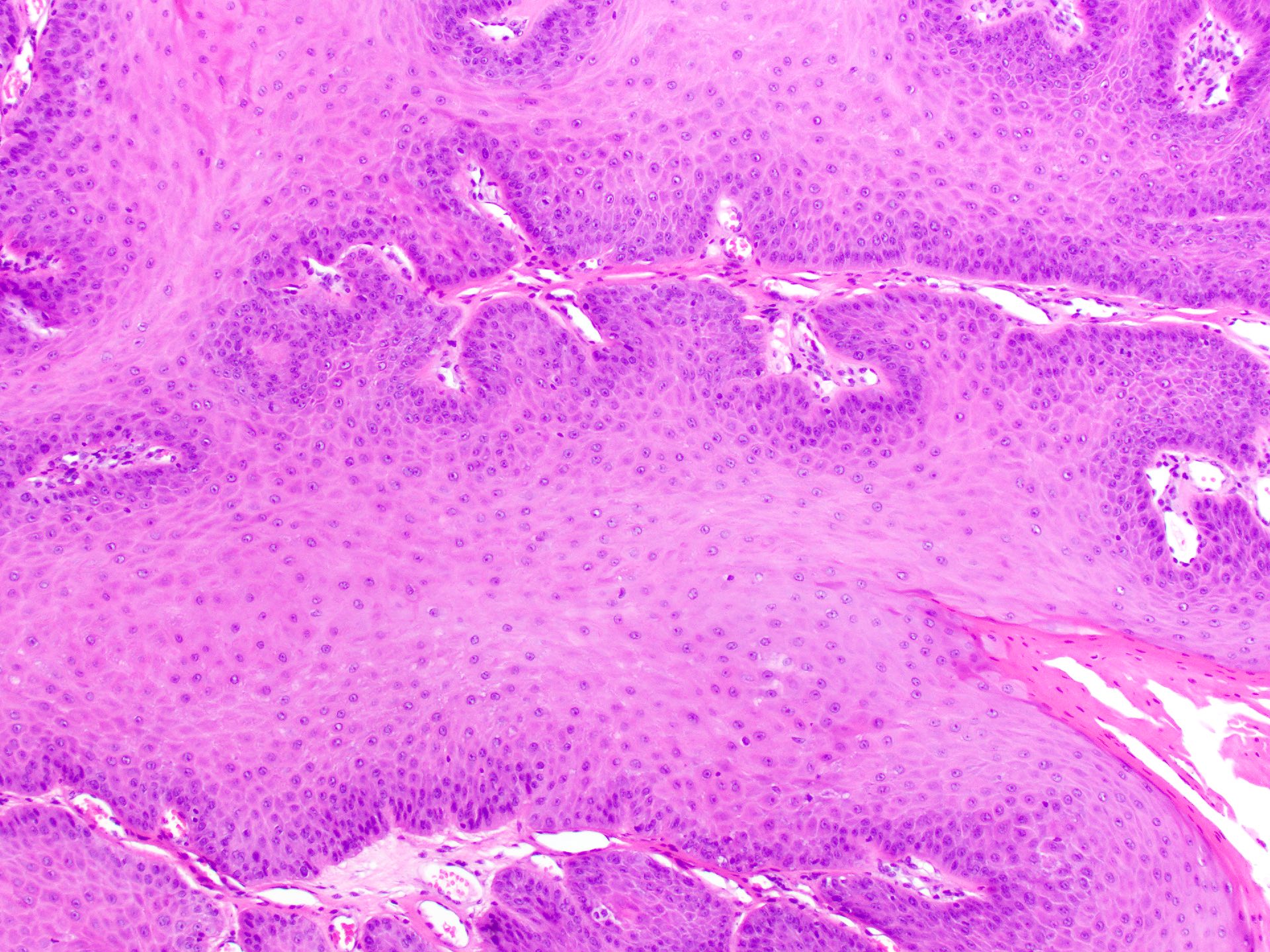
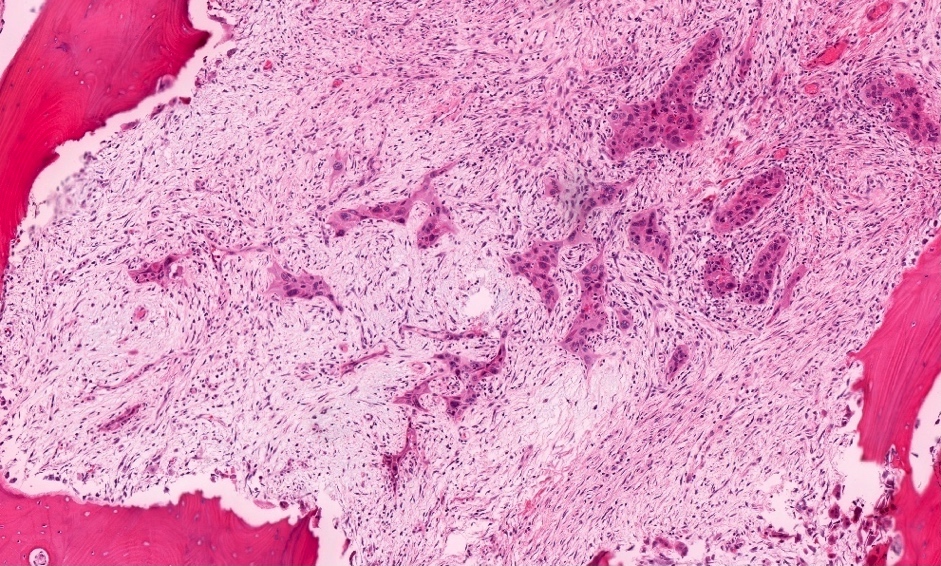
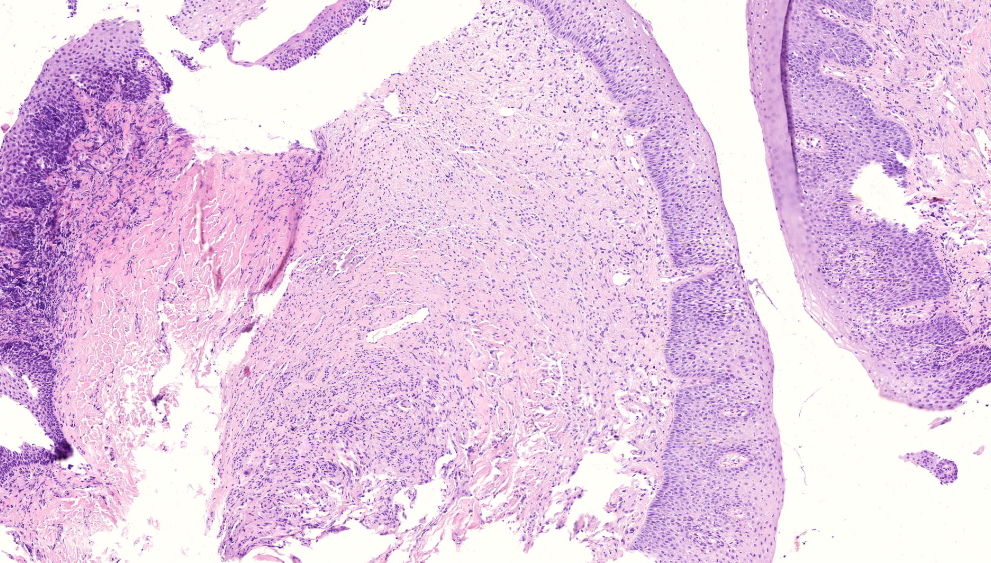
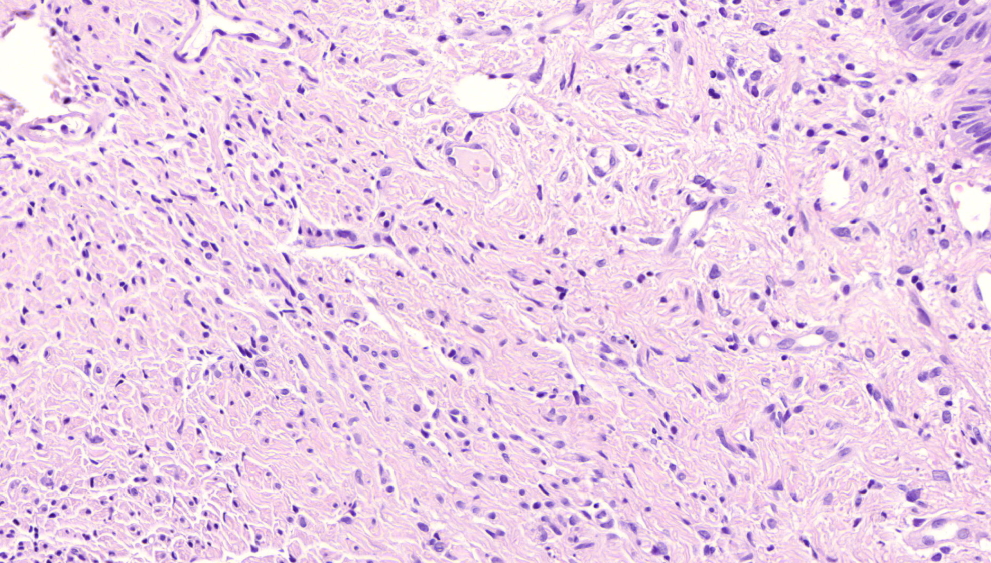
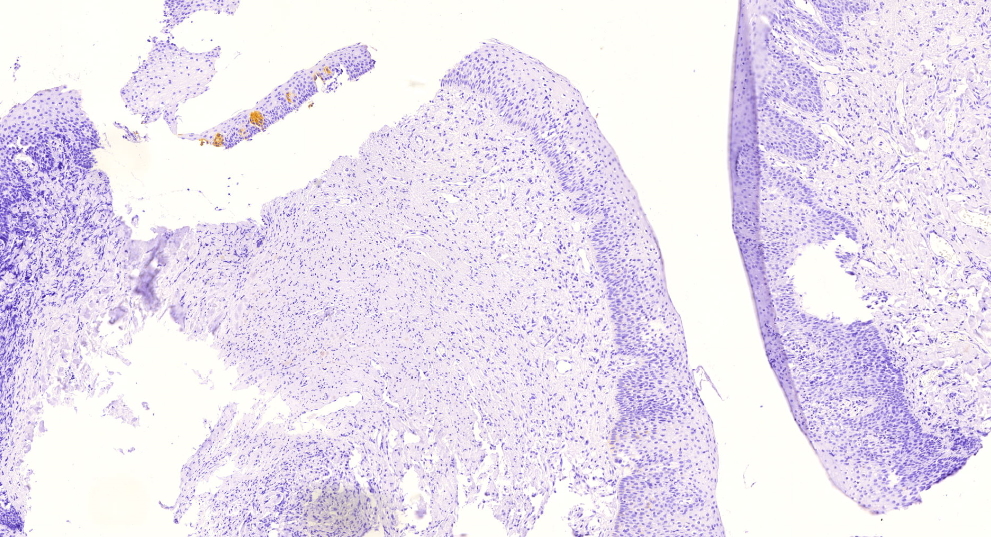
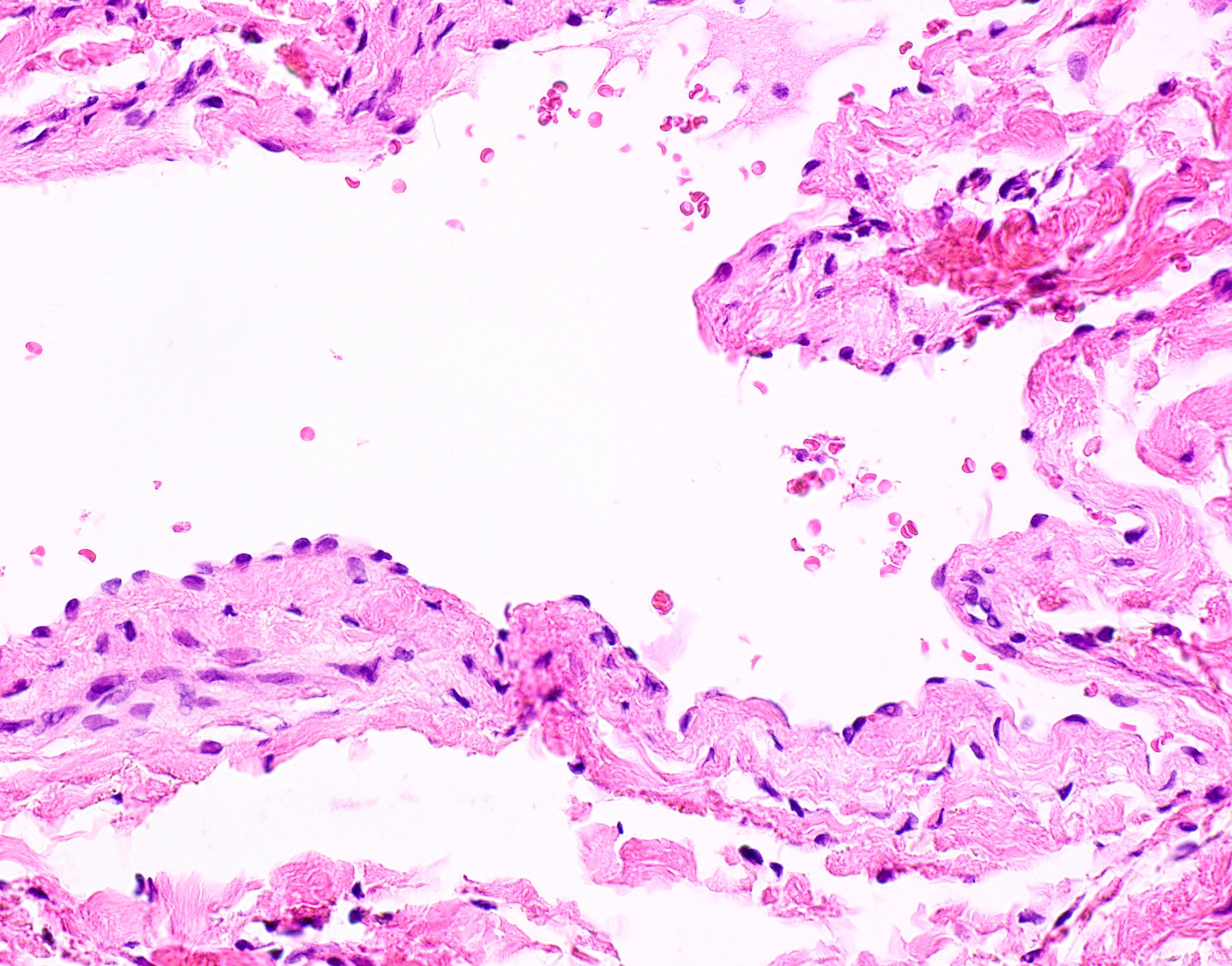
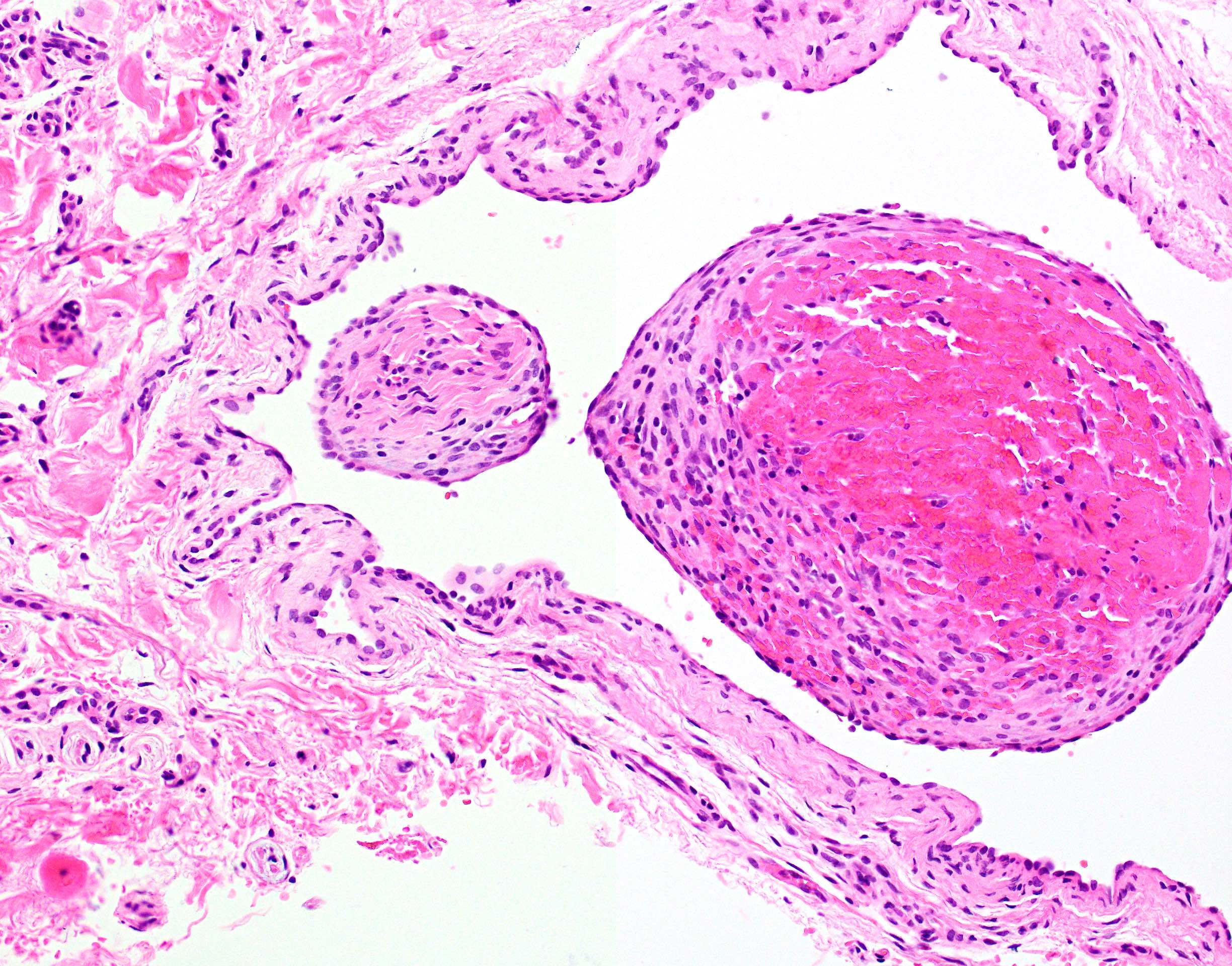
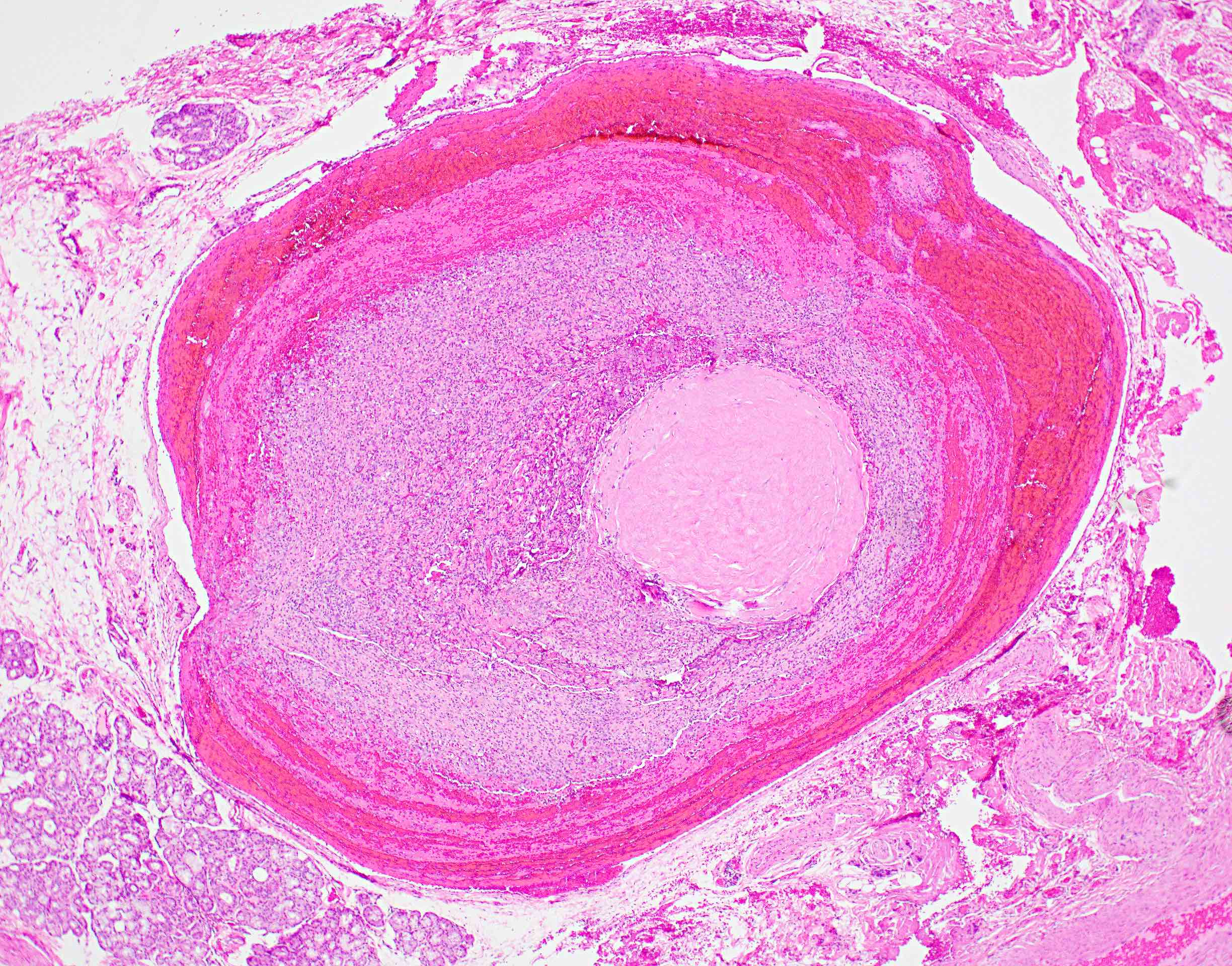
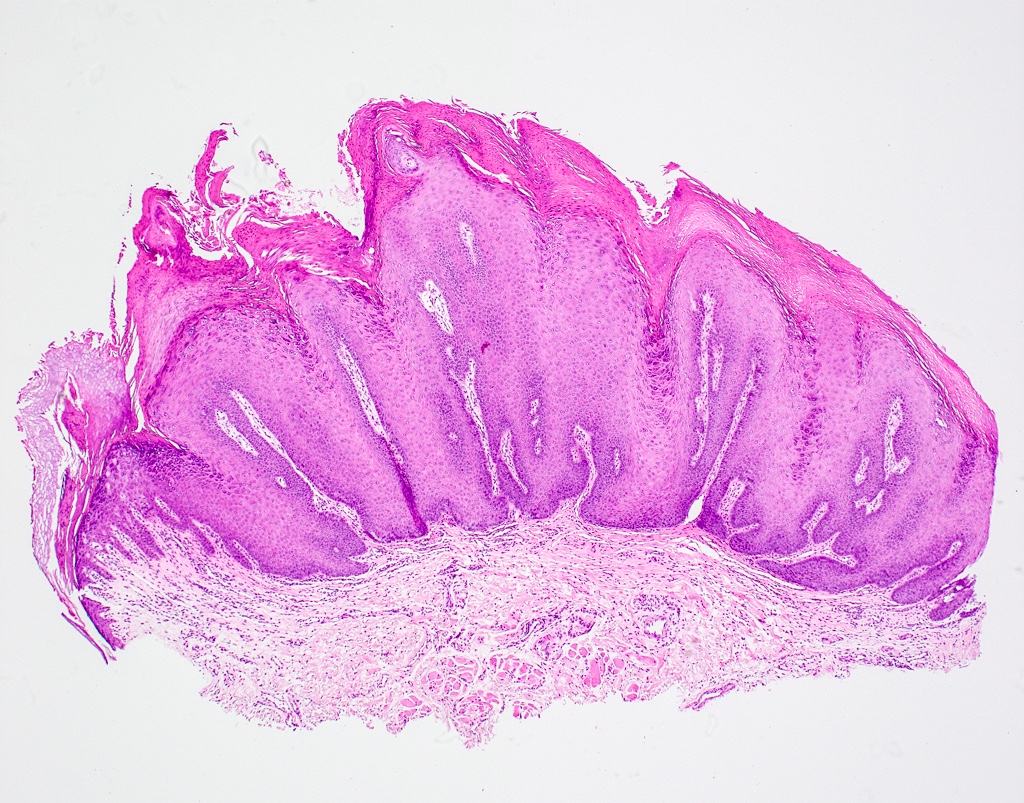
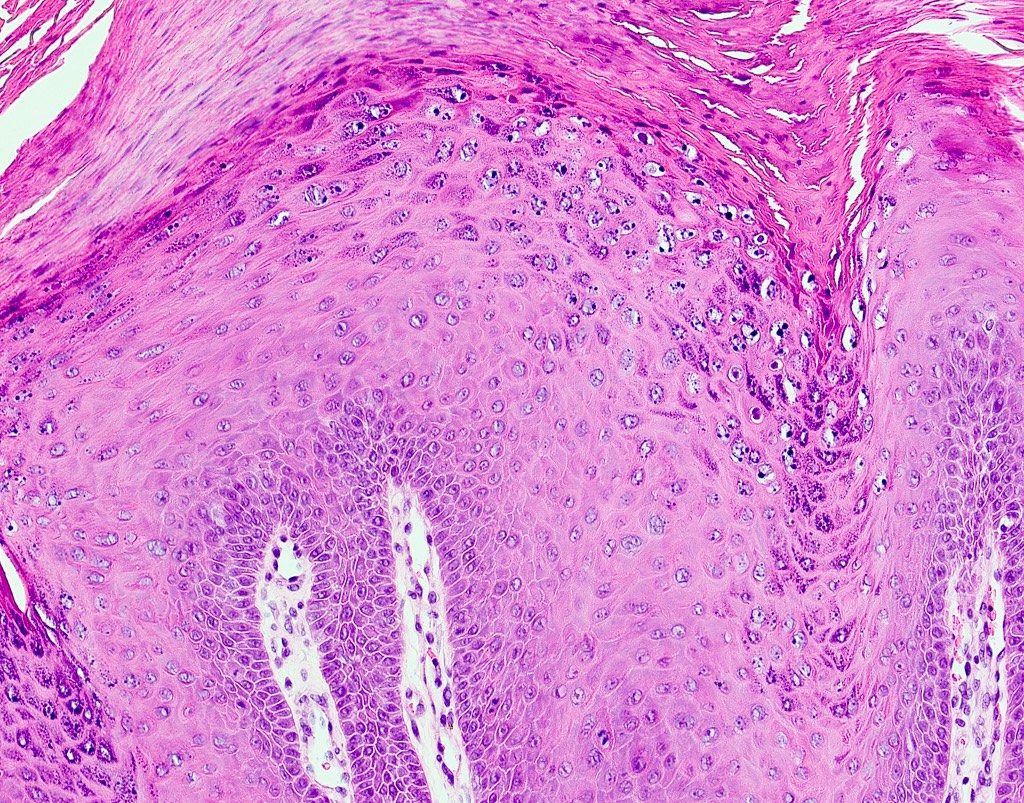
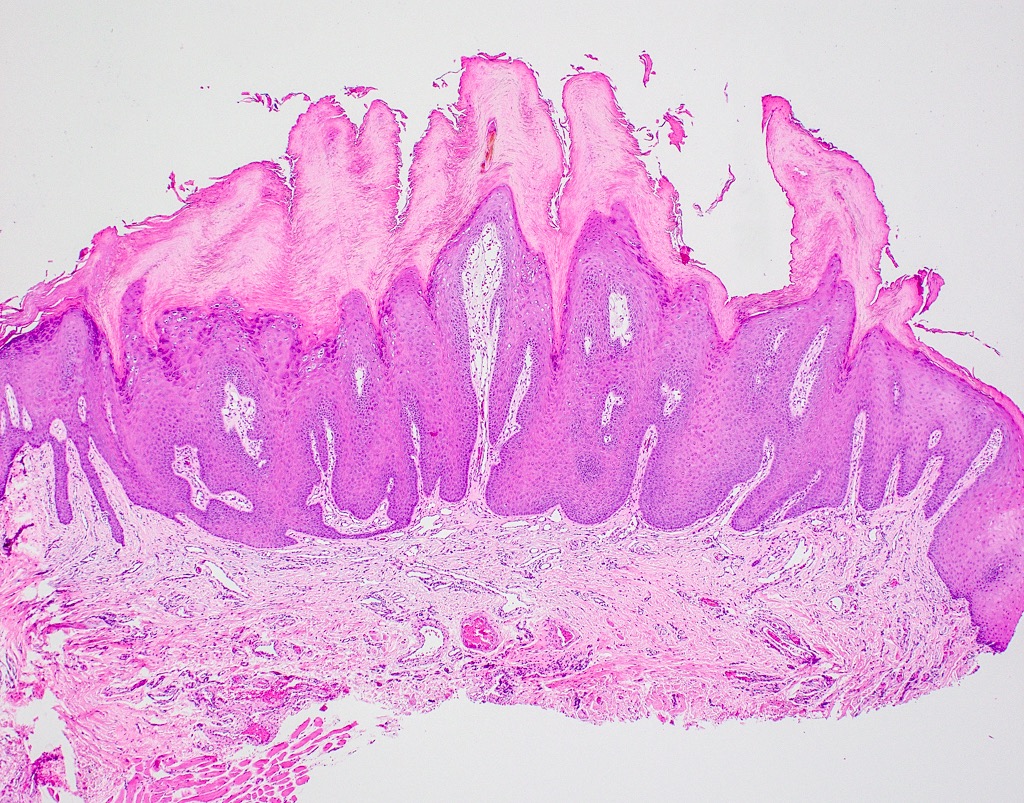
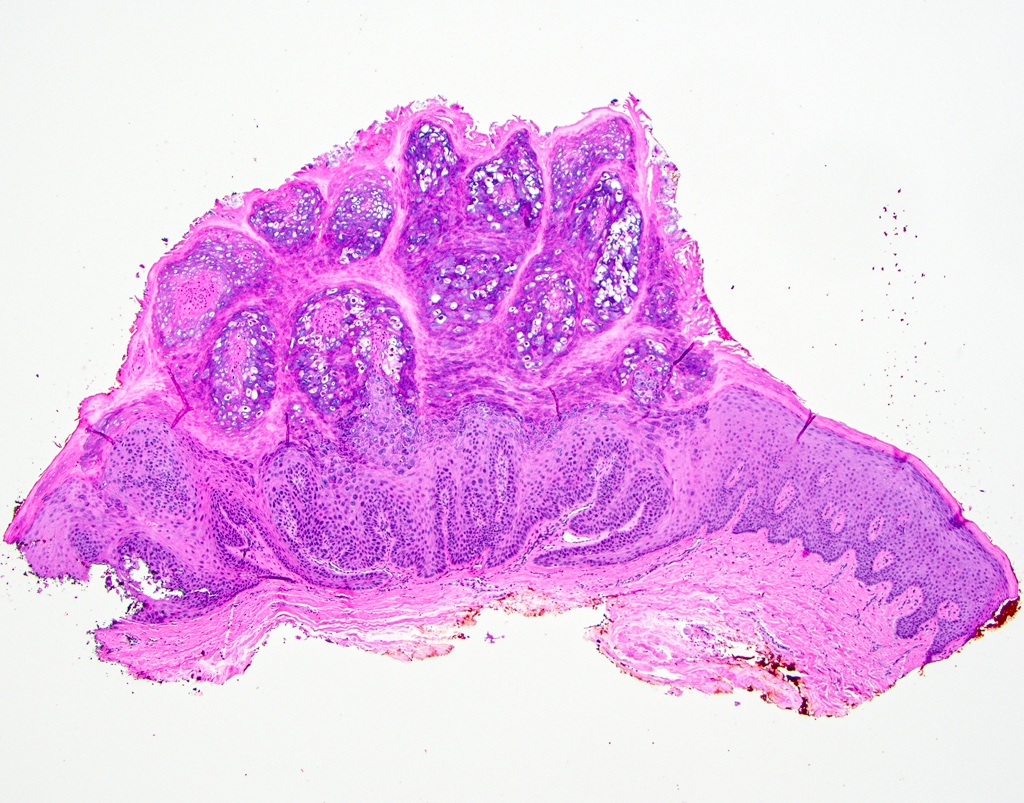
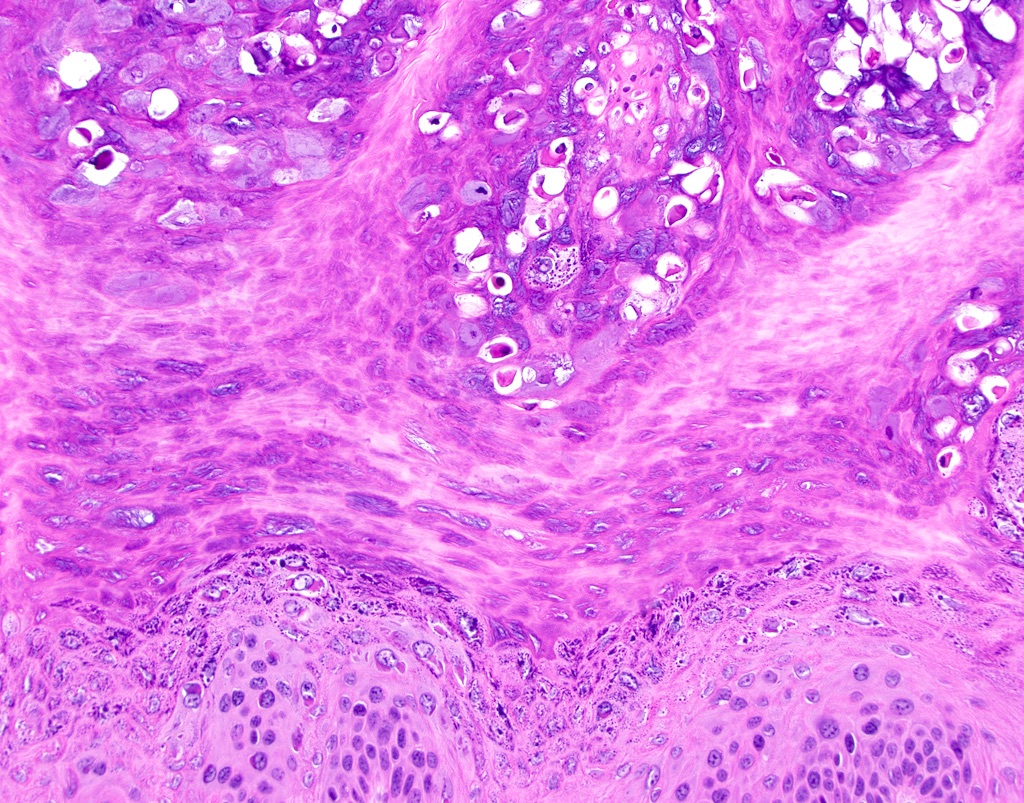
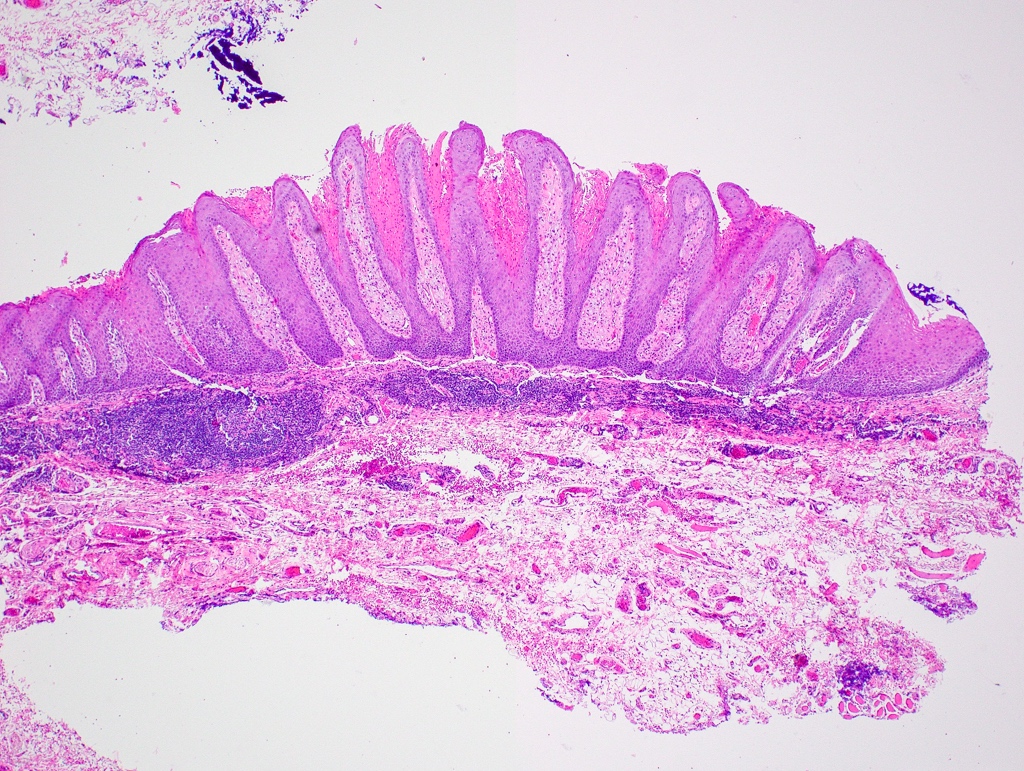
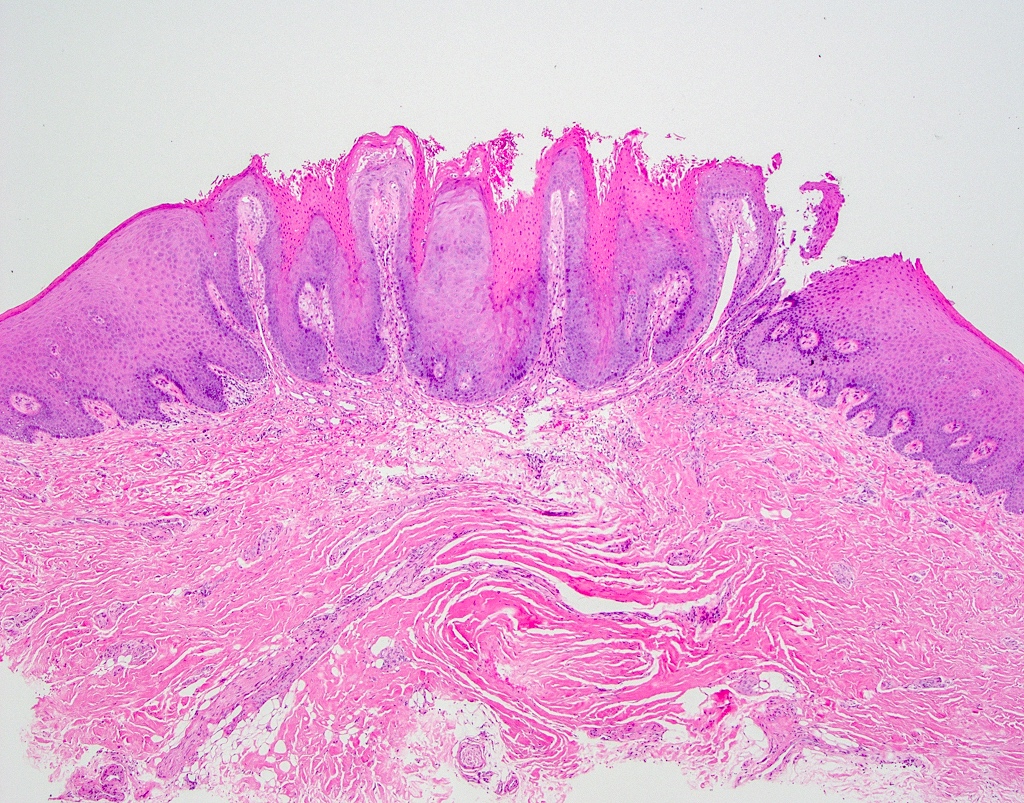
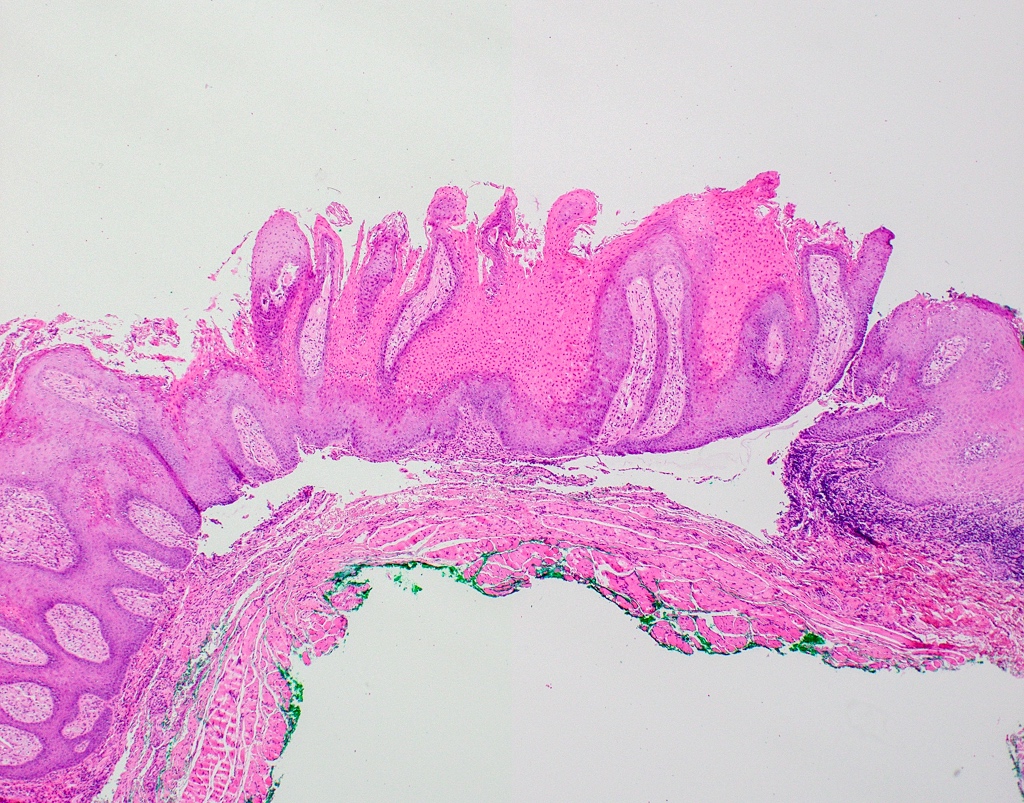
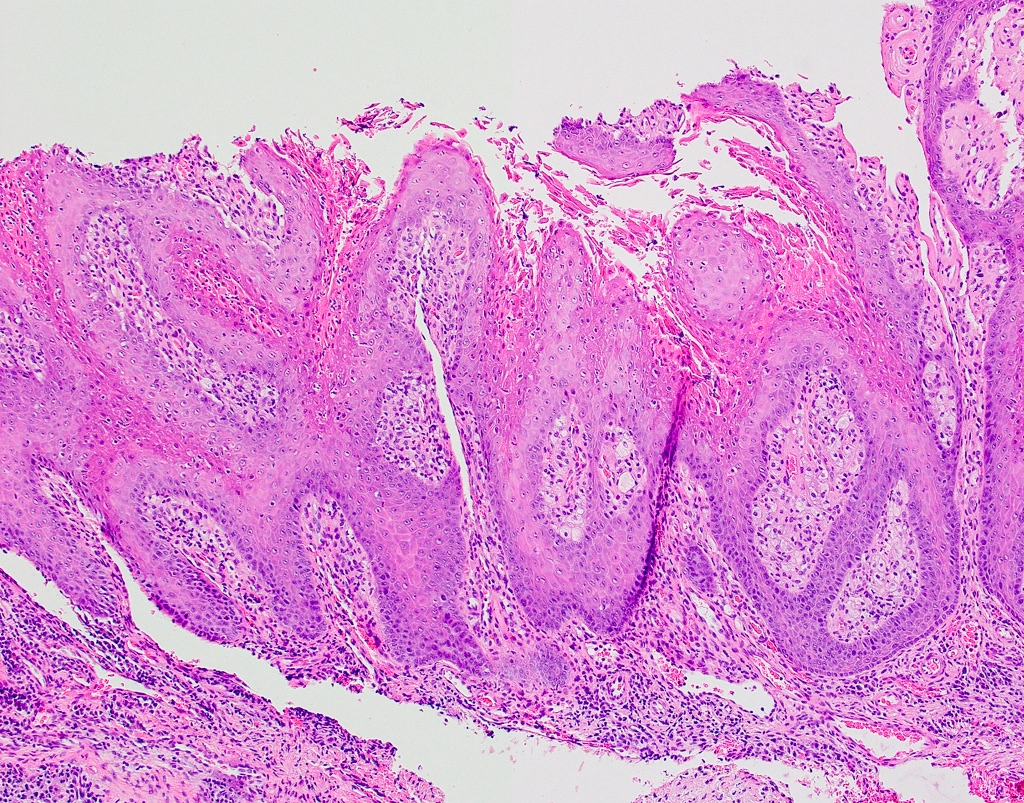
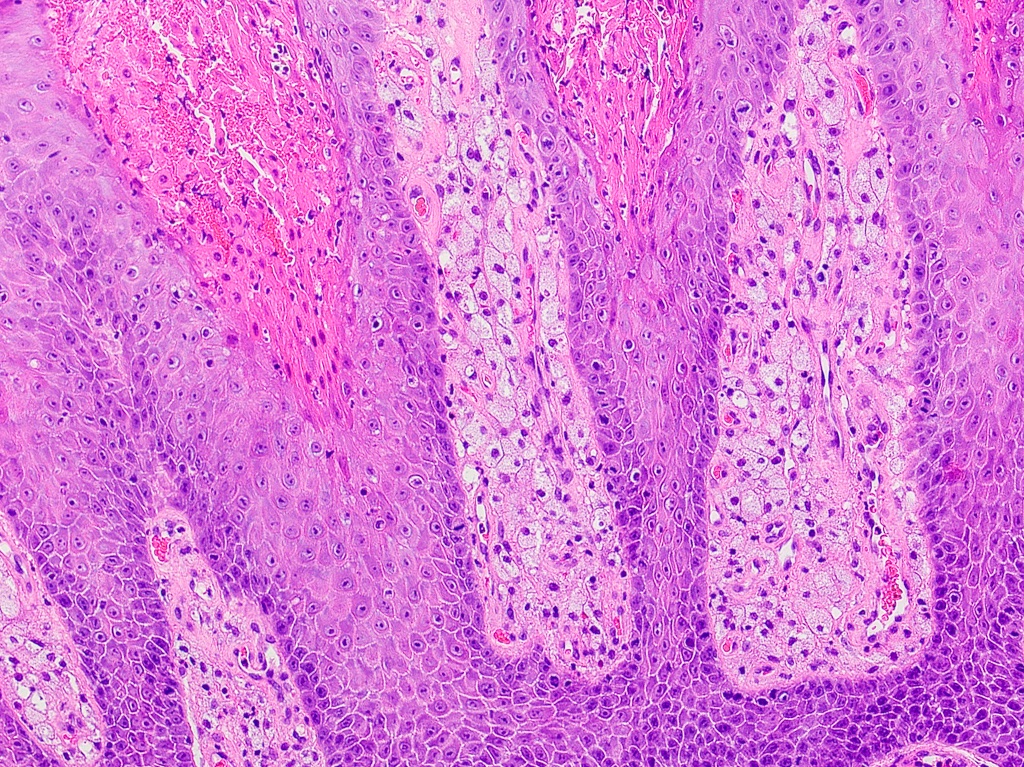
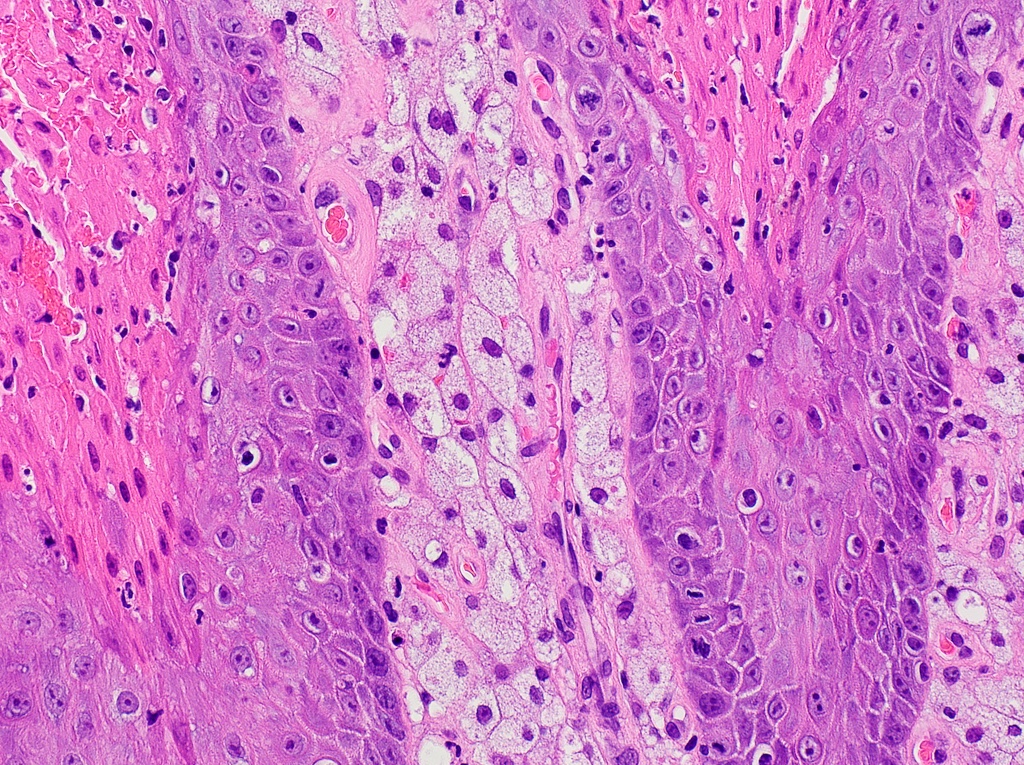
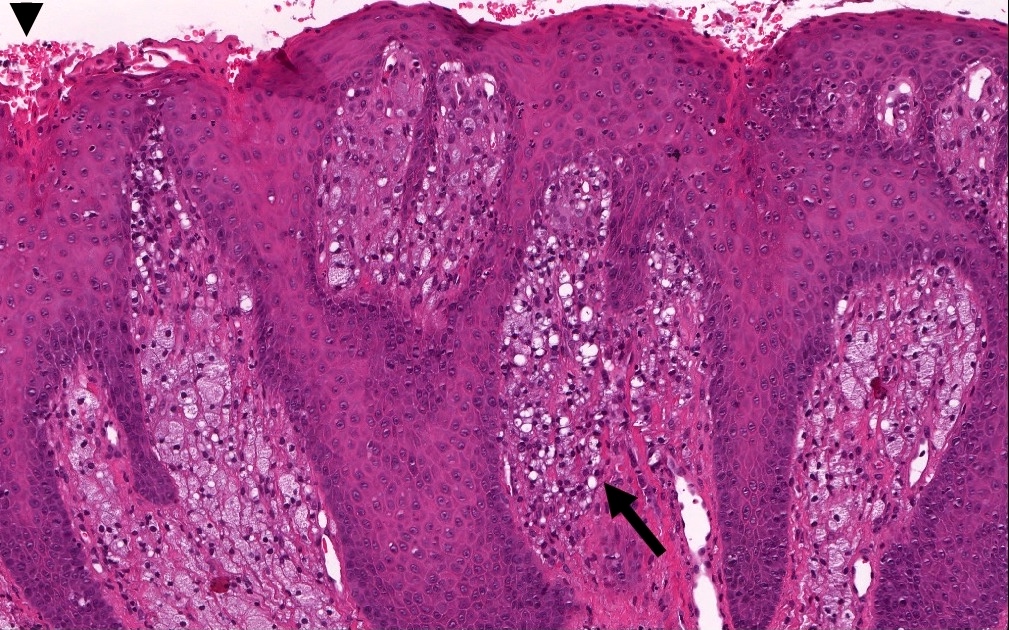
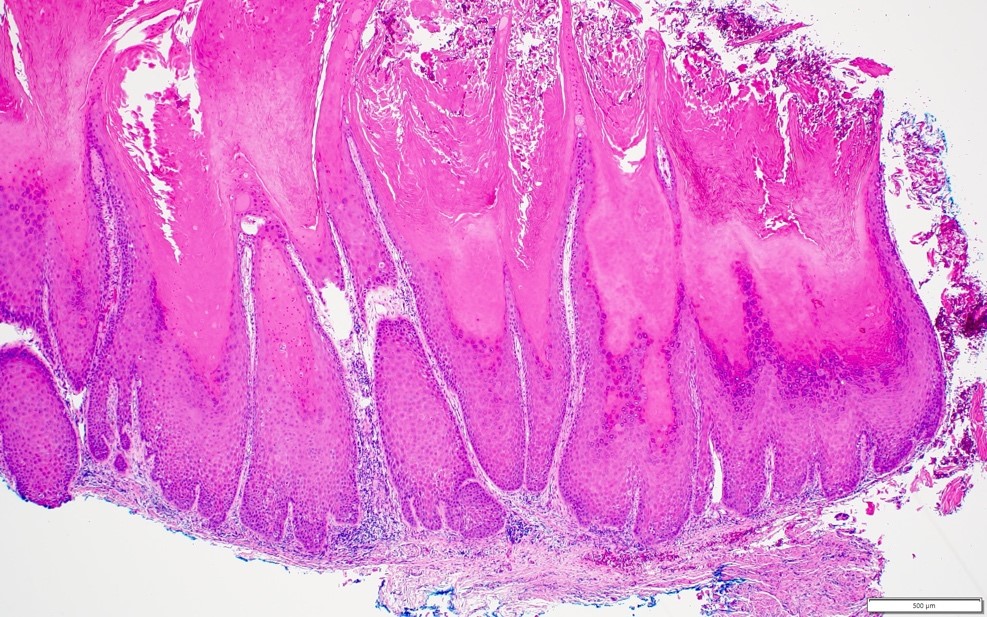
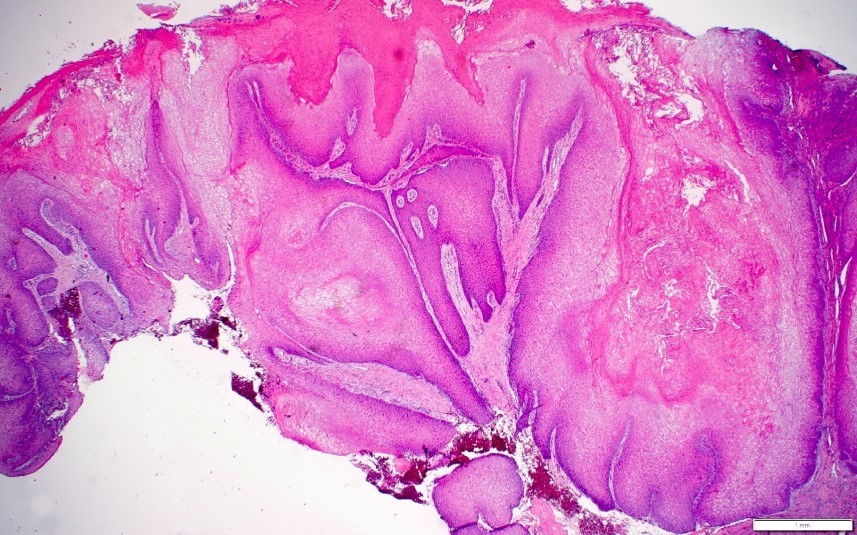
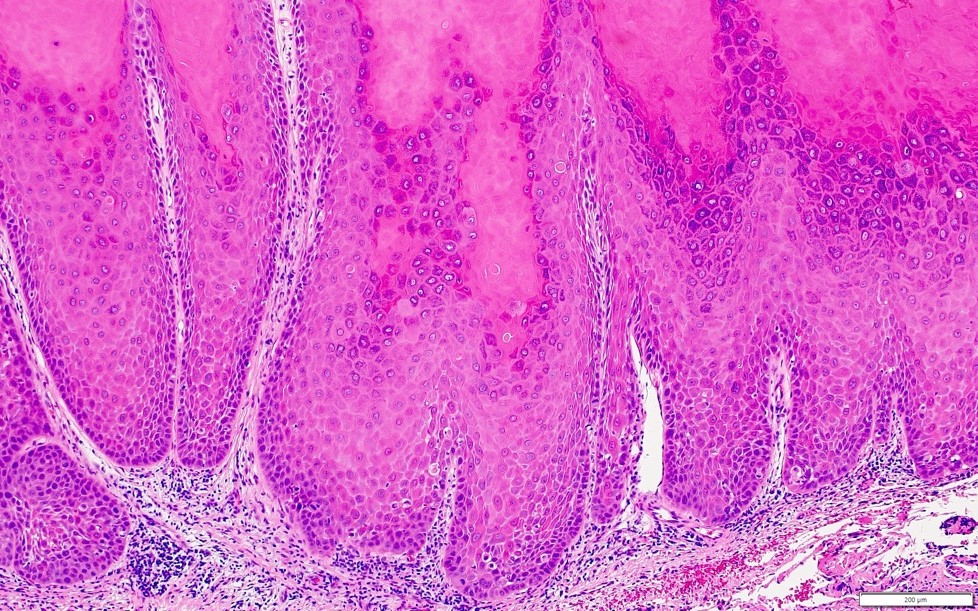
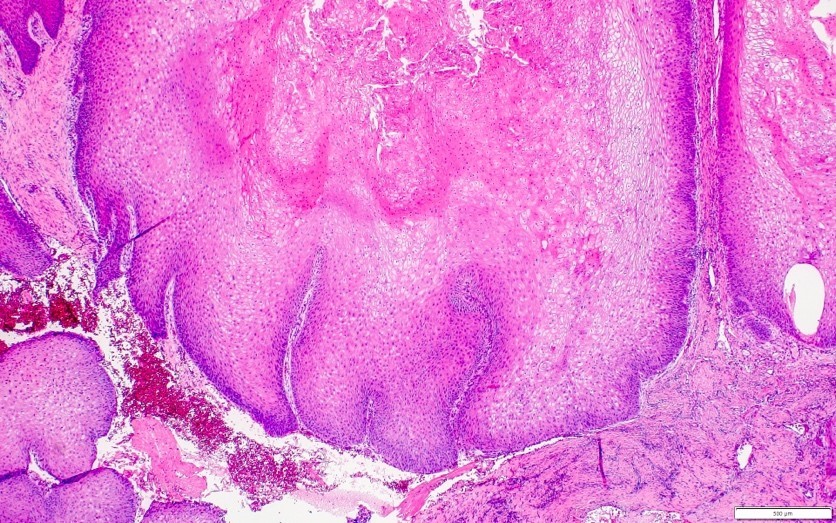
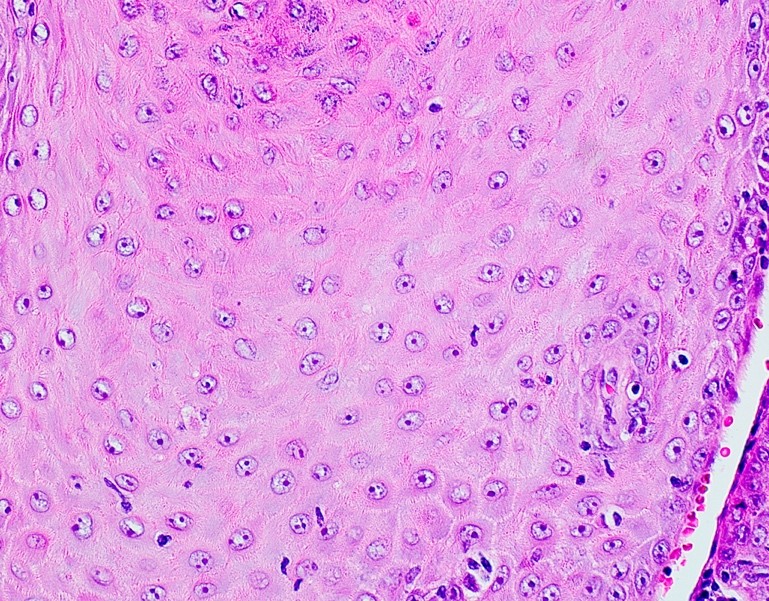
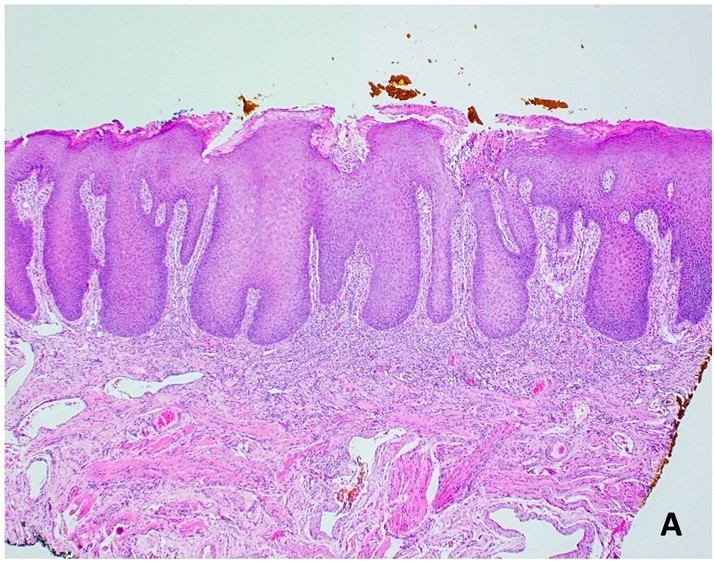
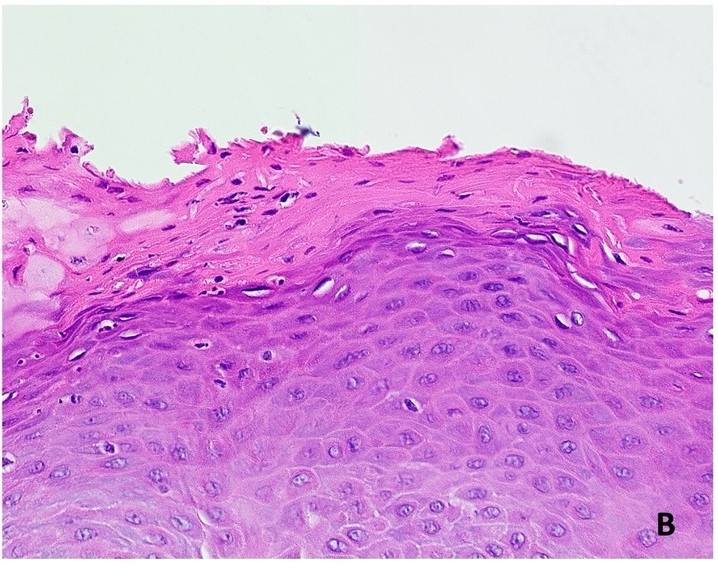
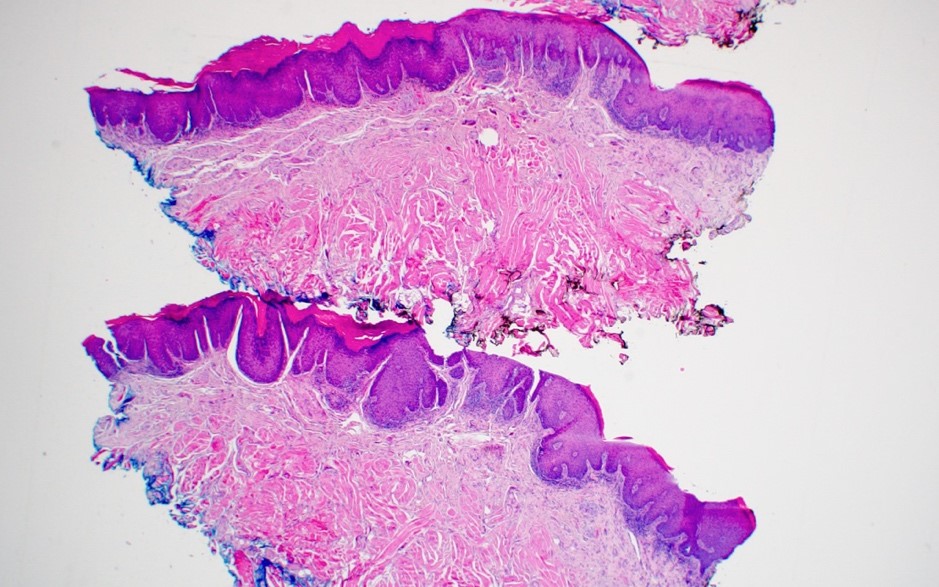
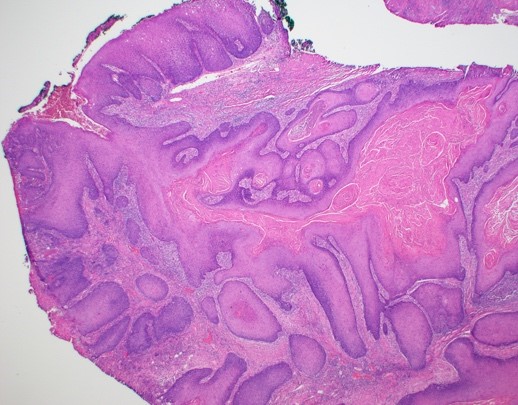
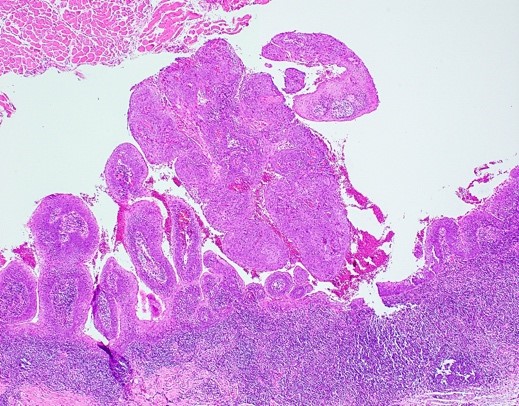
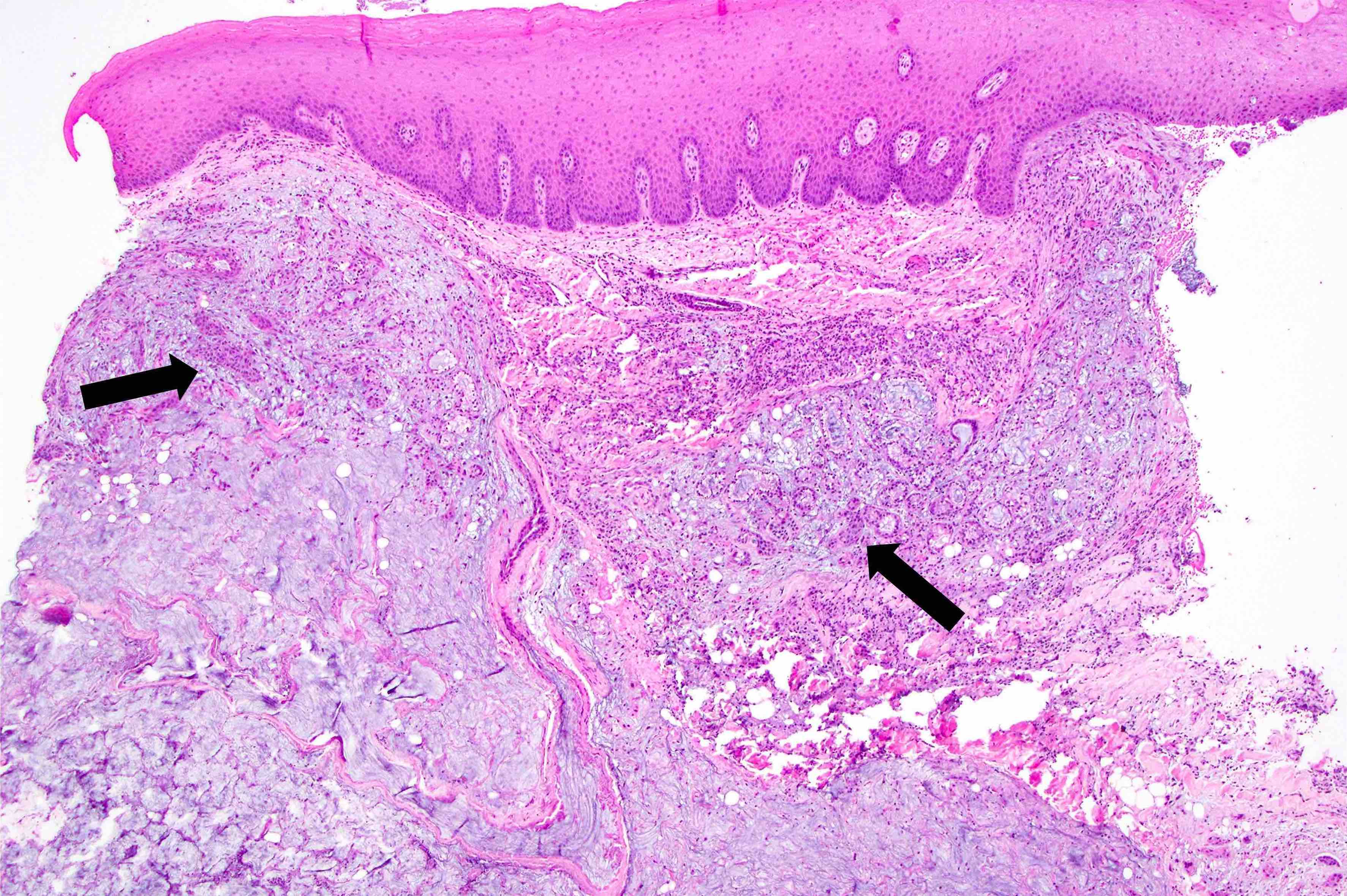
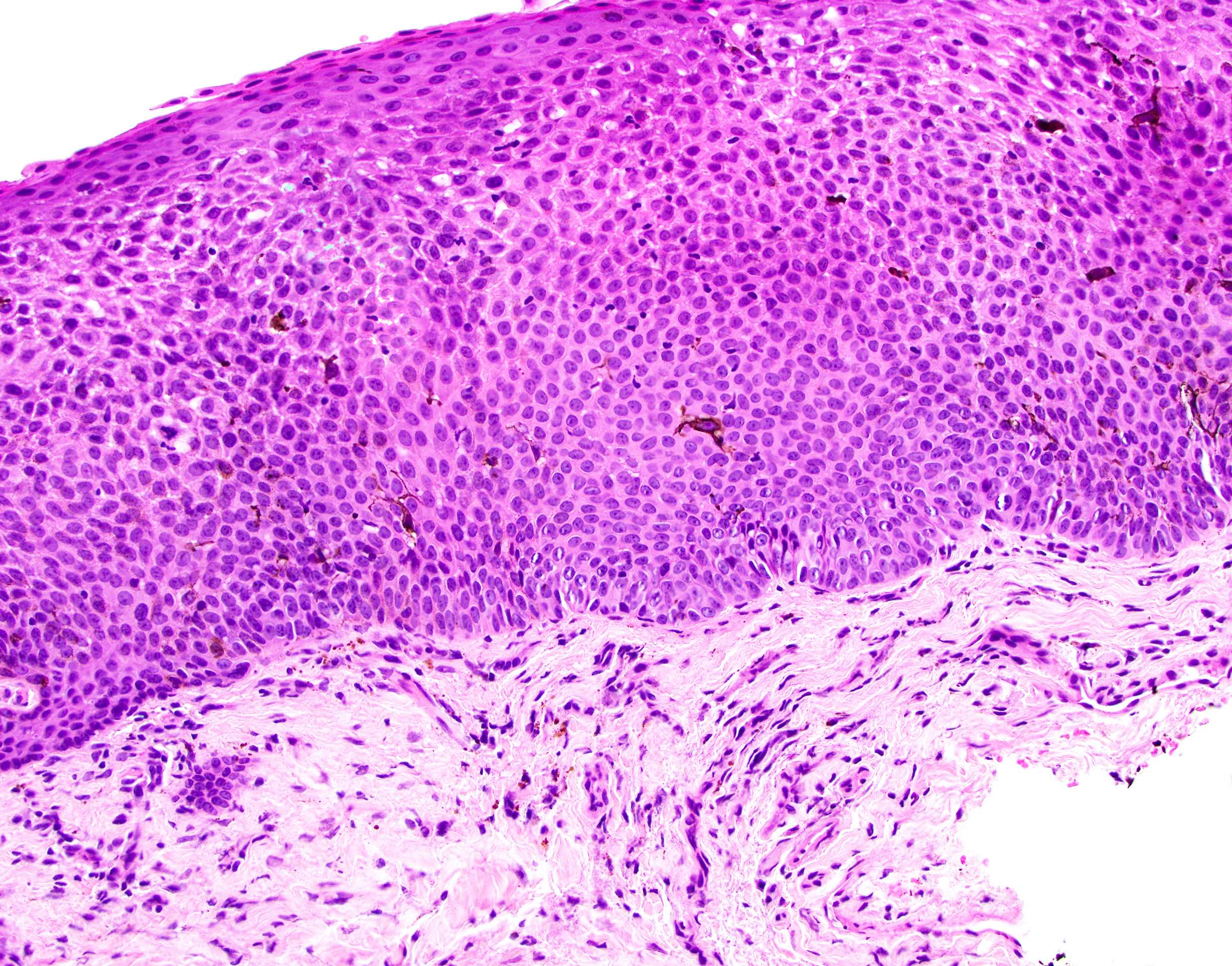
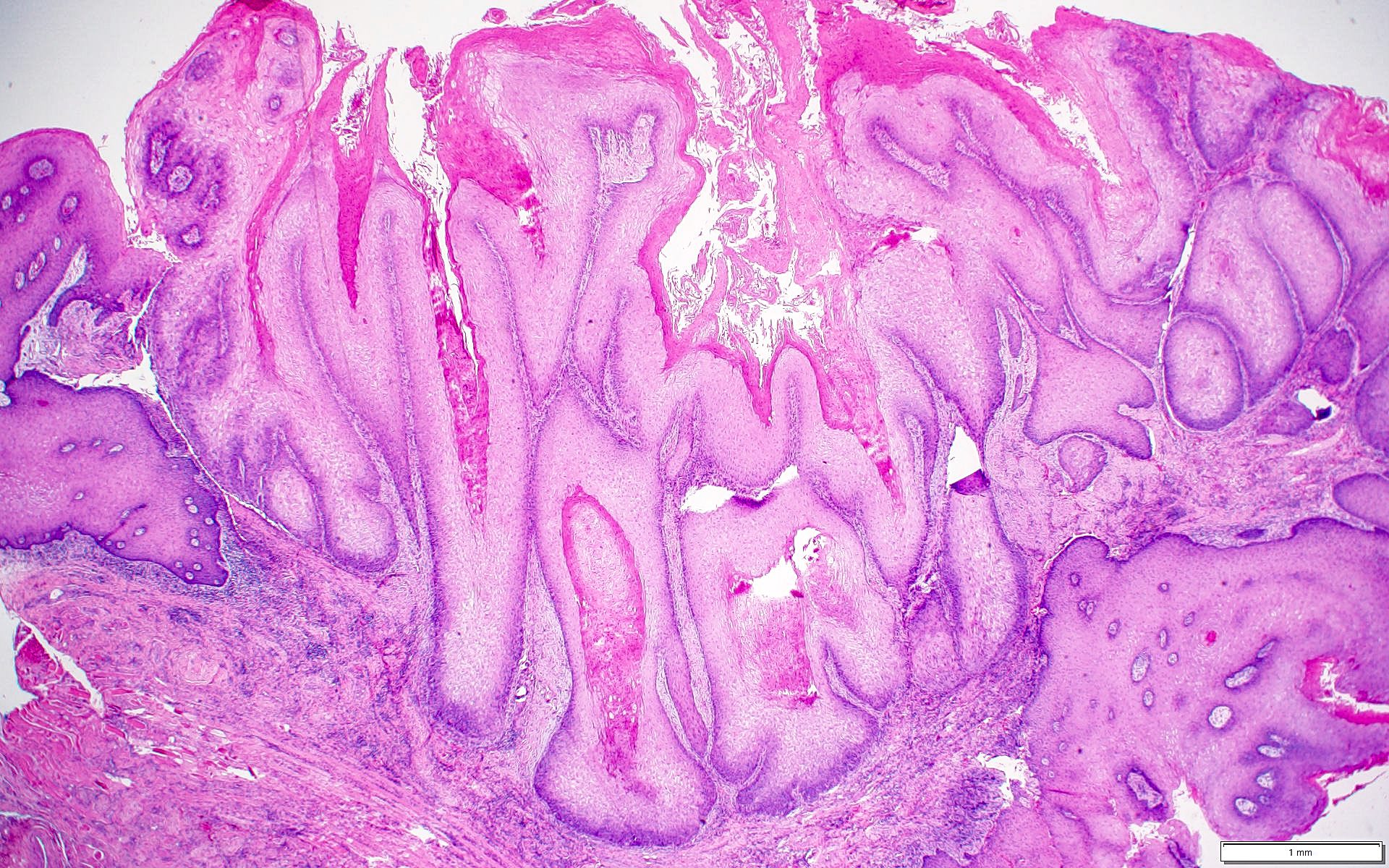
Microscopic (histologic) description
- Surface epithelium is variably dysplastic
- Hyperkeratosis, acanthosis and epithelial atrophy may be noted
- Underlying connective tissue exhibits solar elastosis, which appears as a band of amorphous, acellular, basophilic change due to ultraviolet light induced degeneration of collagen and elastin fibers (Head Neck Pathol 2021;15:566)
- Chronic inflammatory cell infiltrate and dilated blood vessels are often present
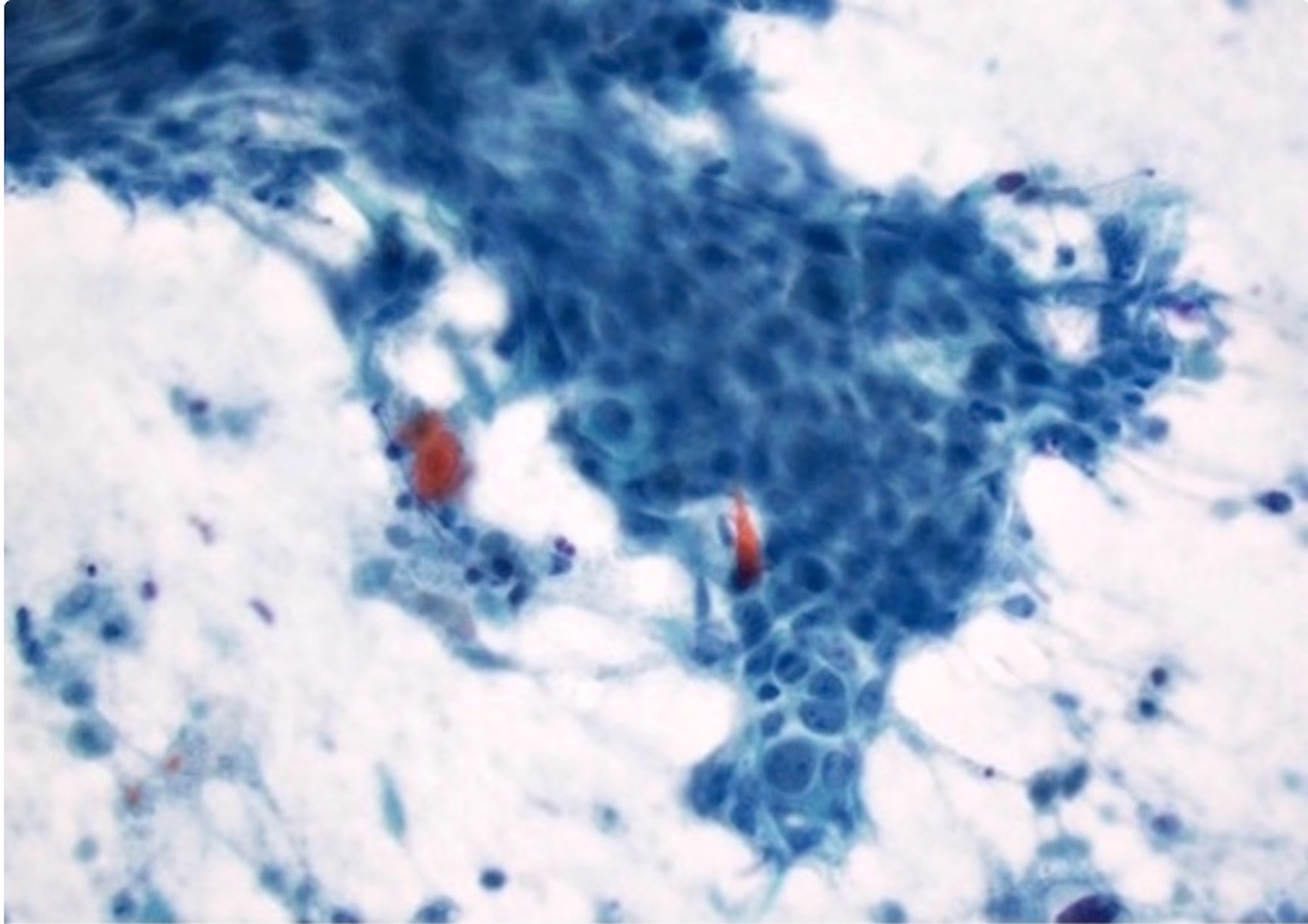
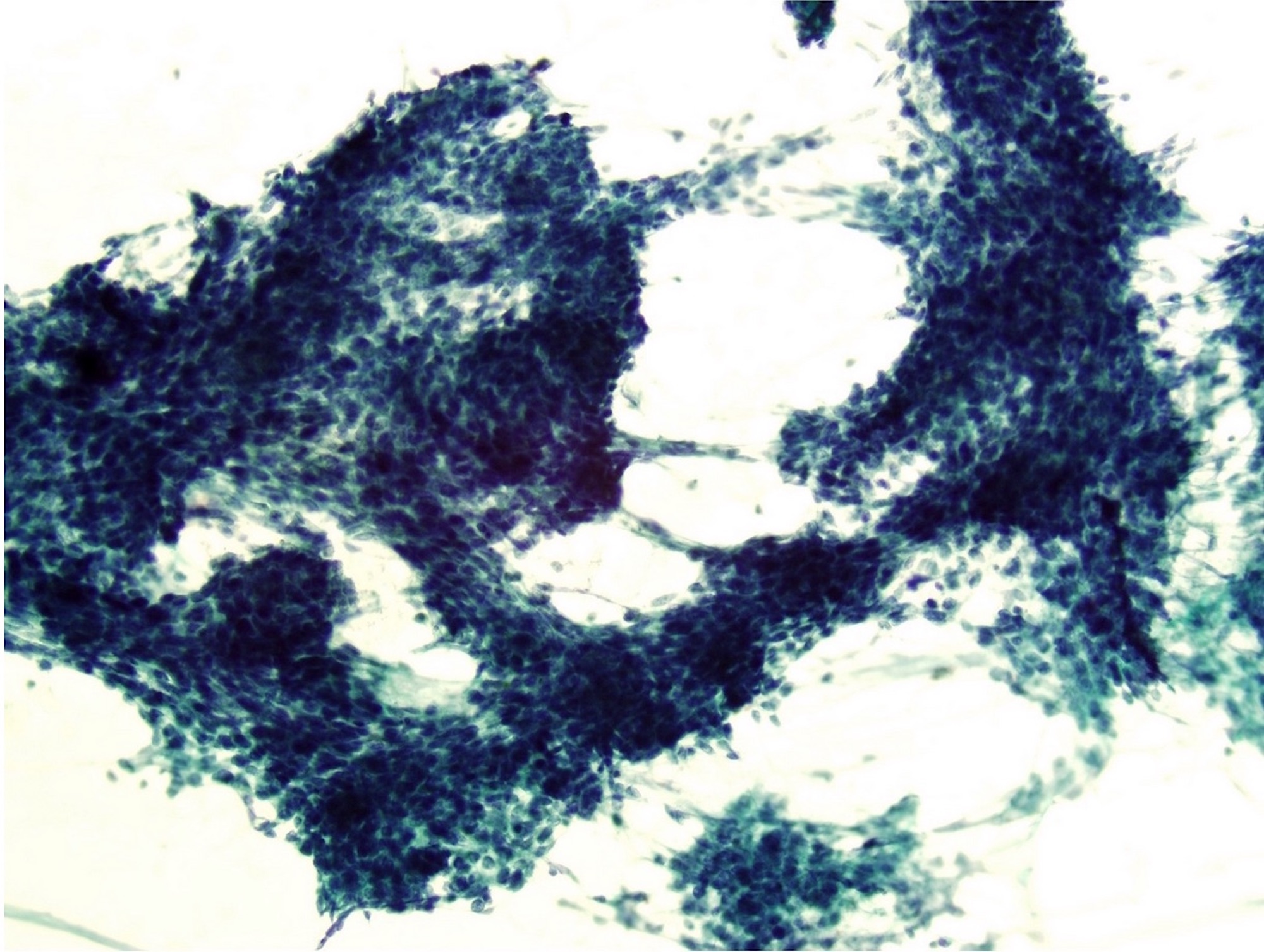
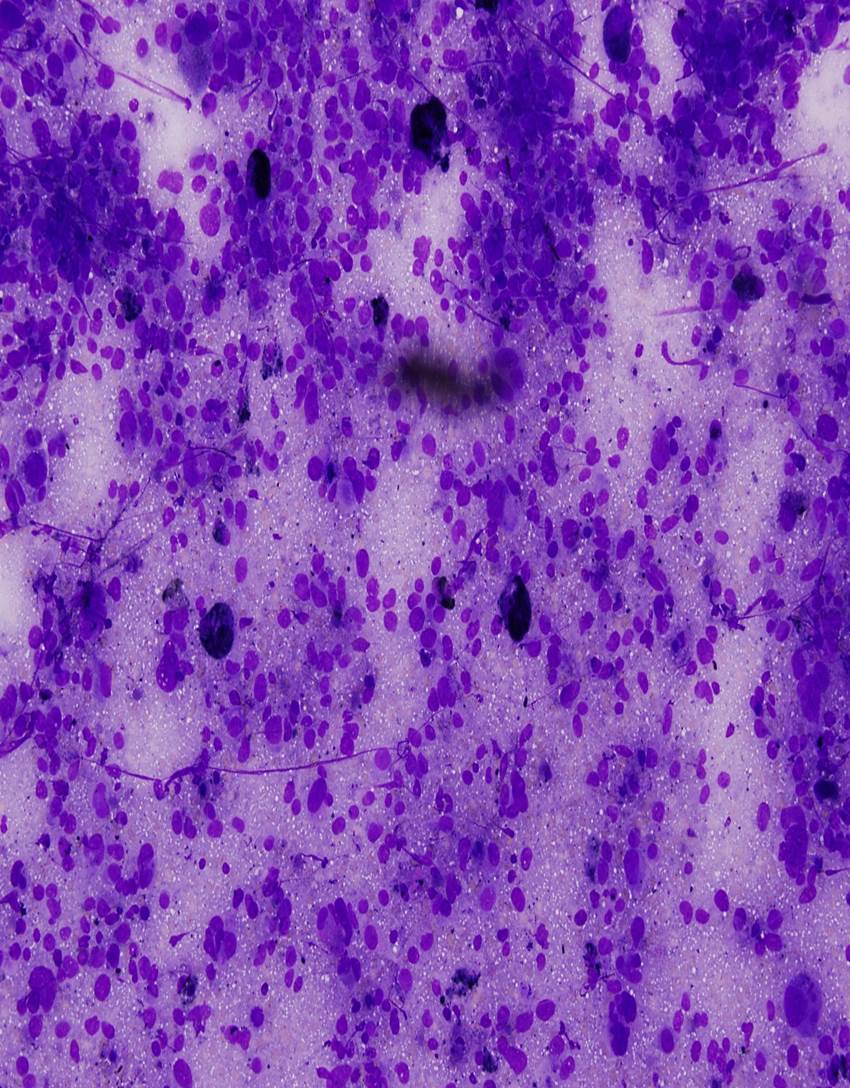
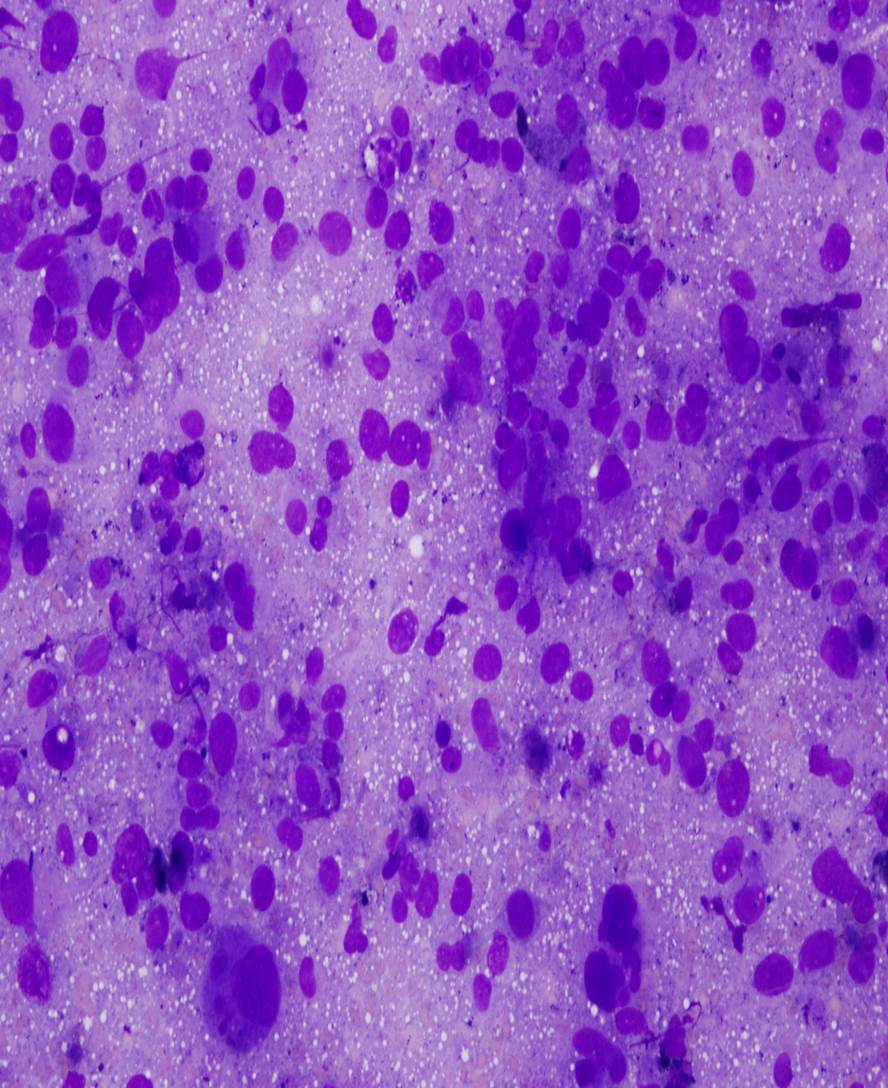
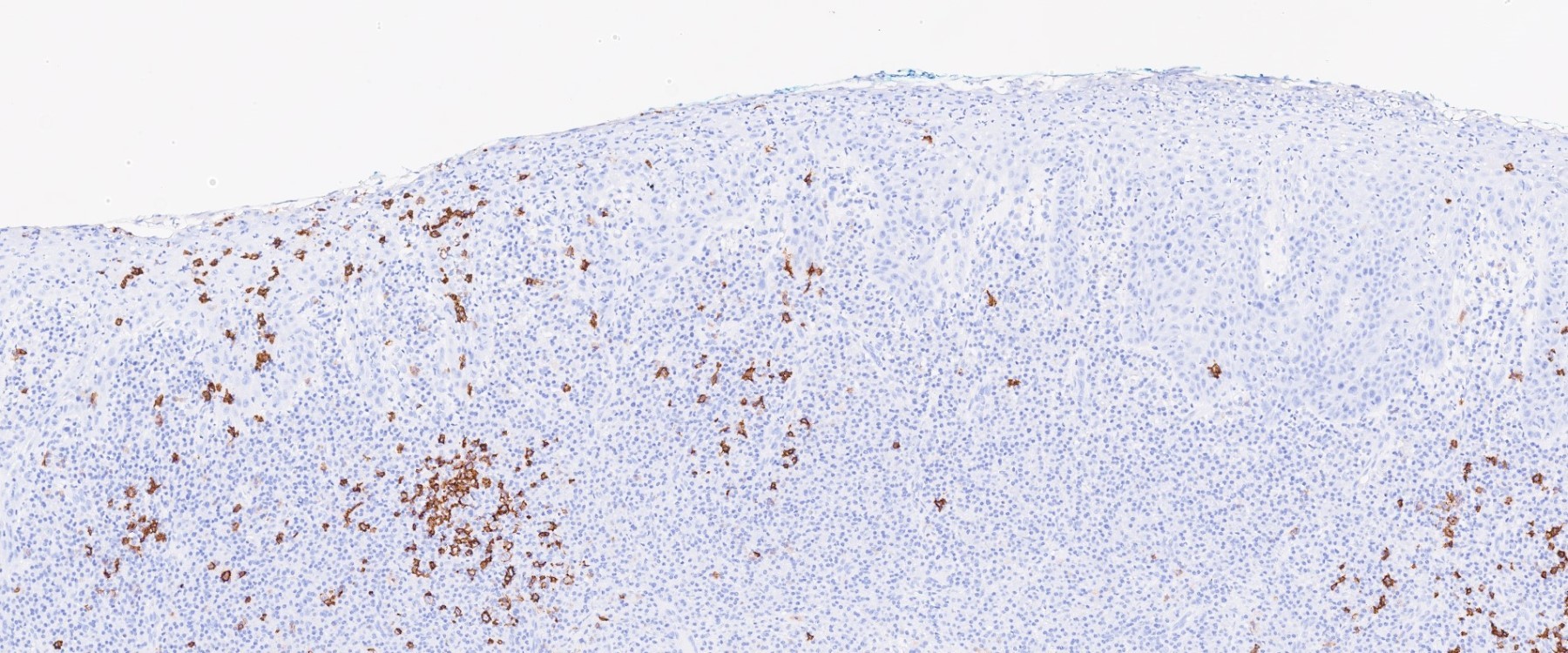
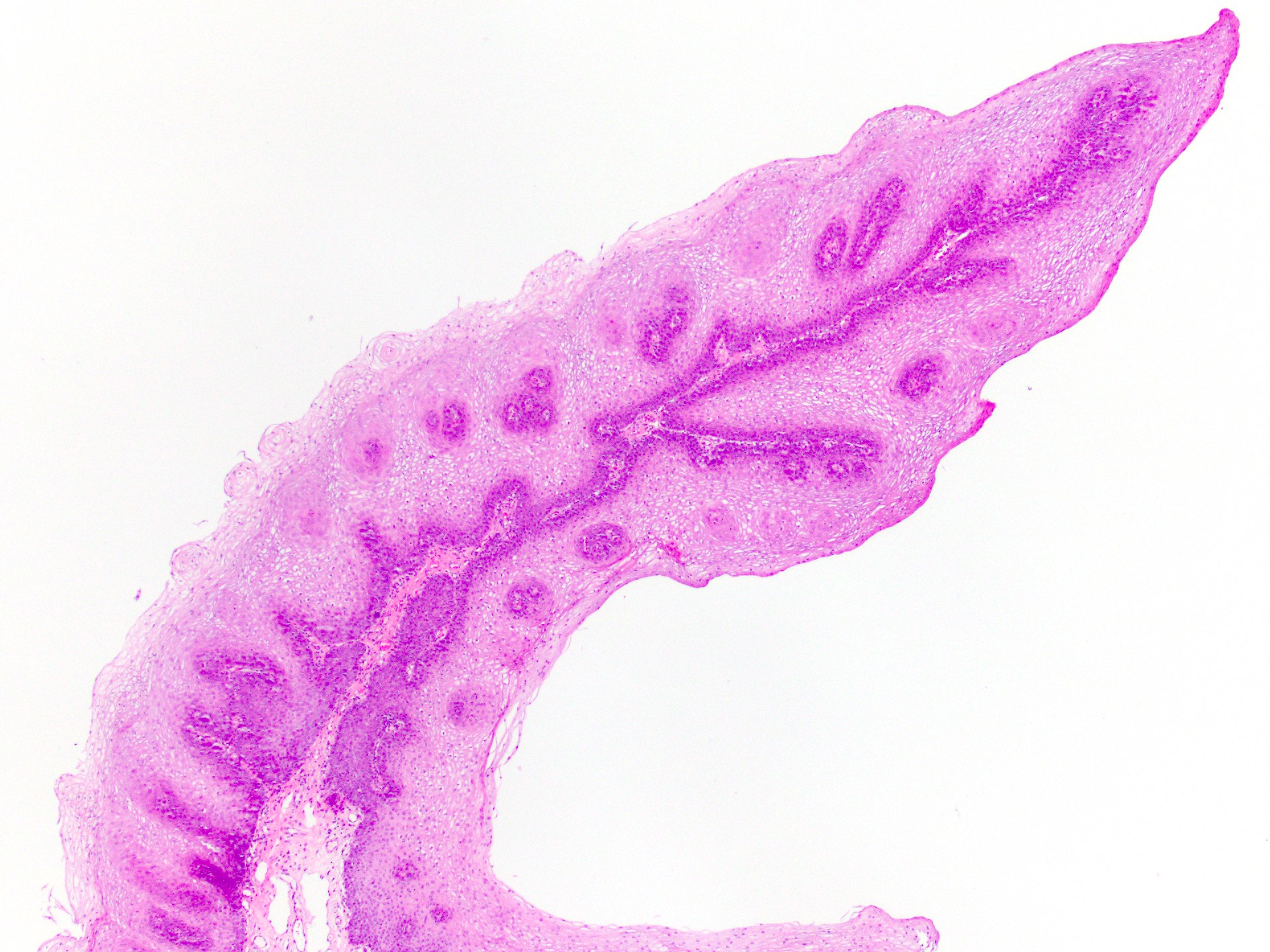
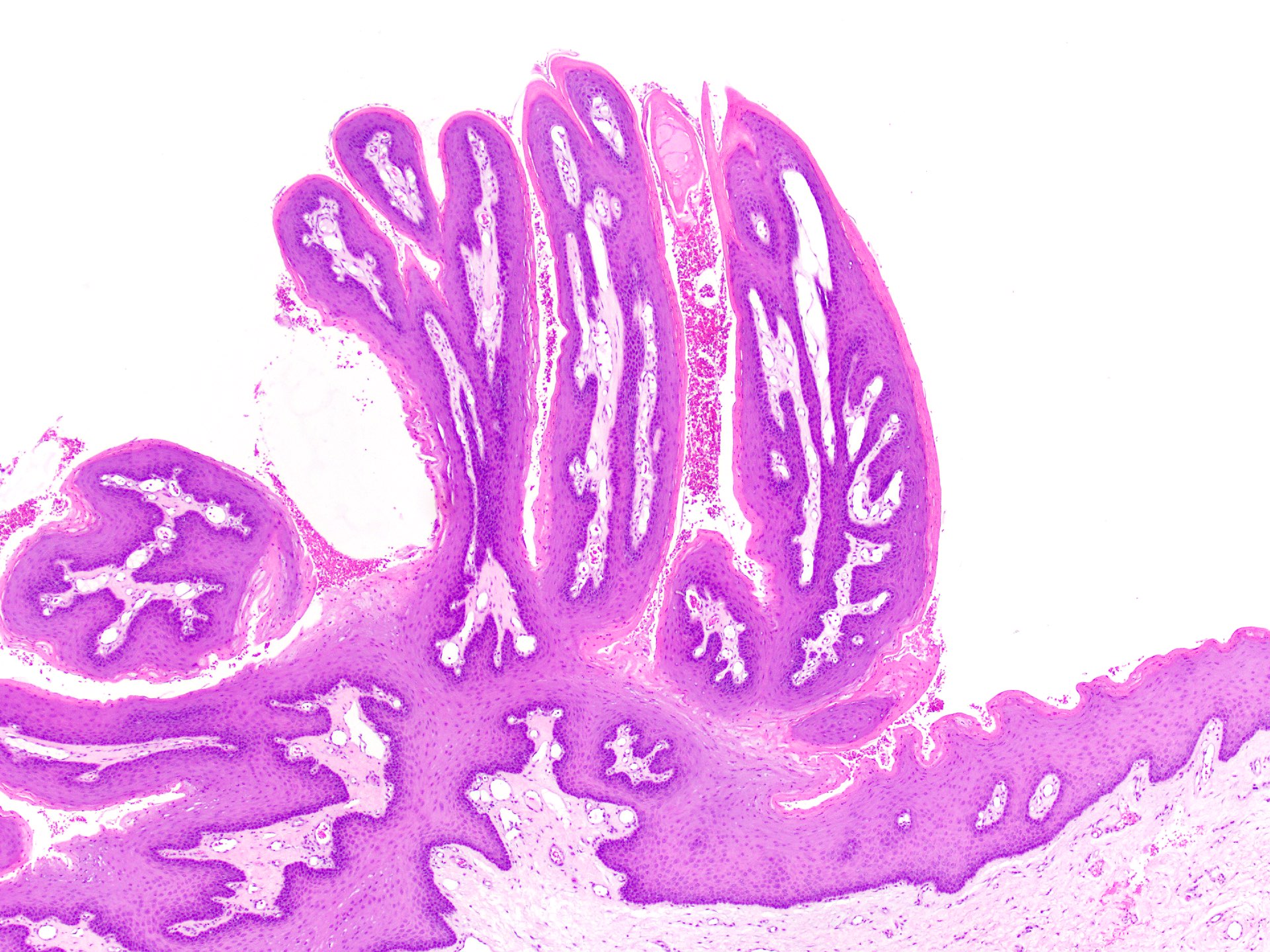
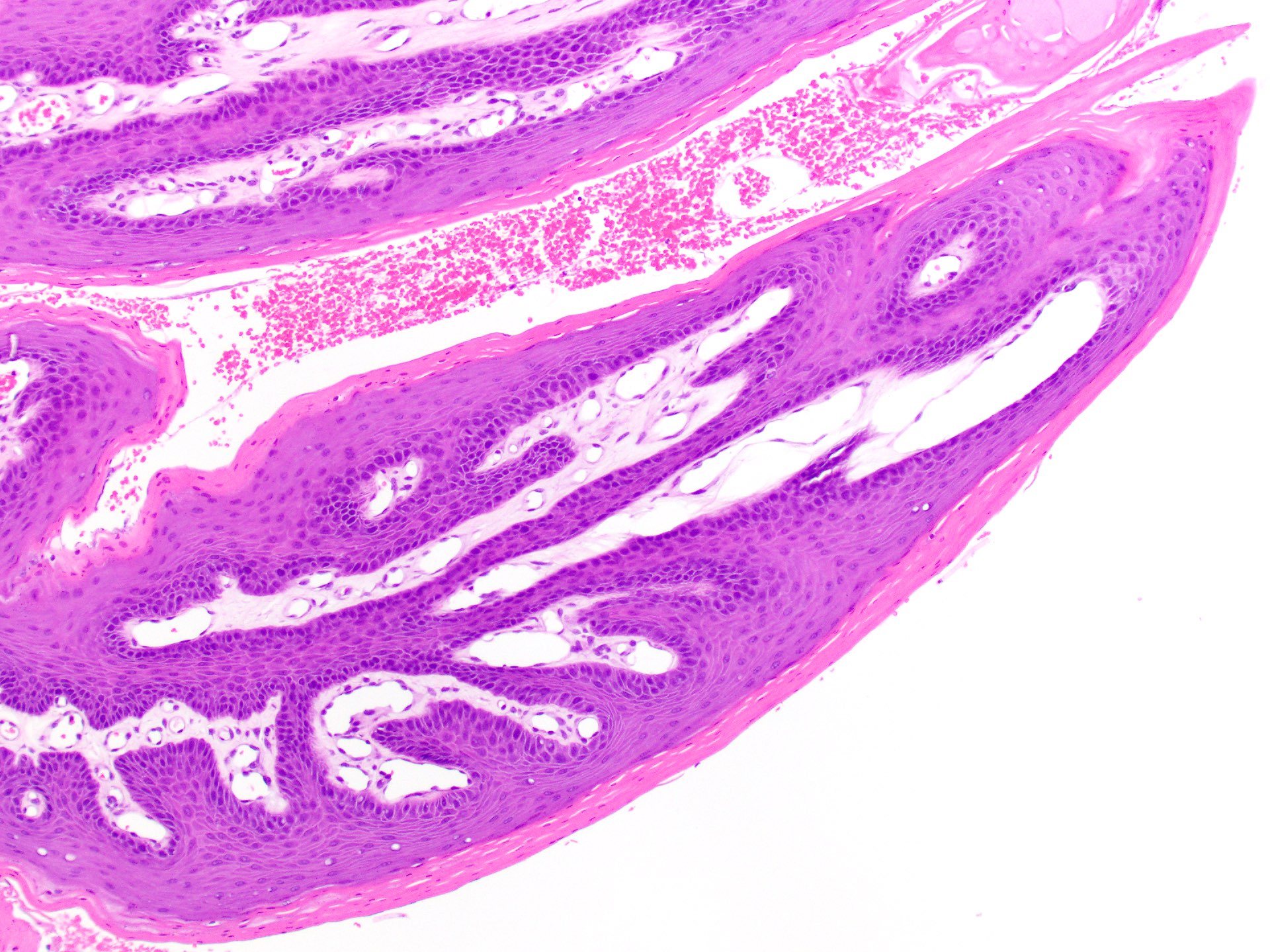
Microscopic (histologic) images
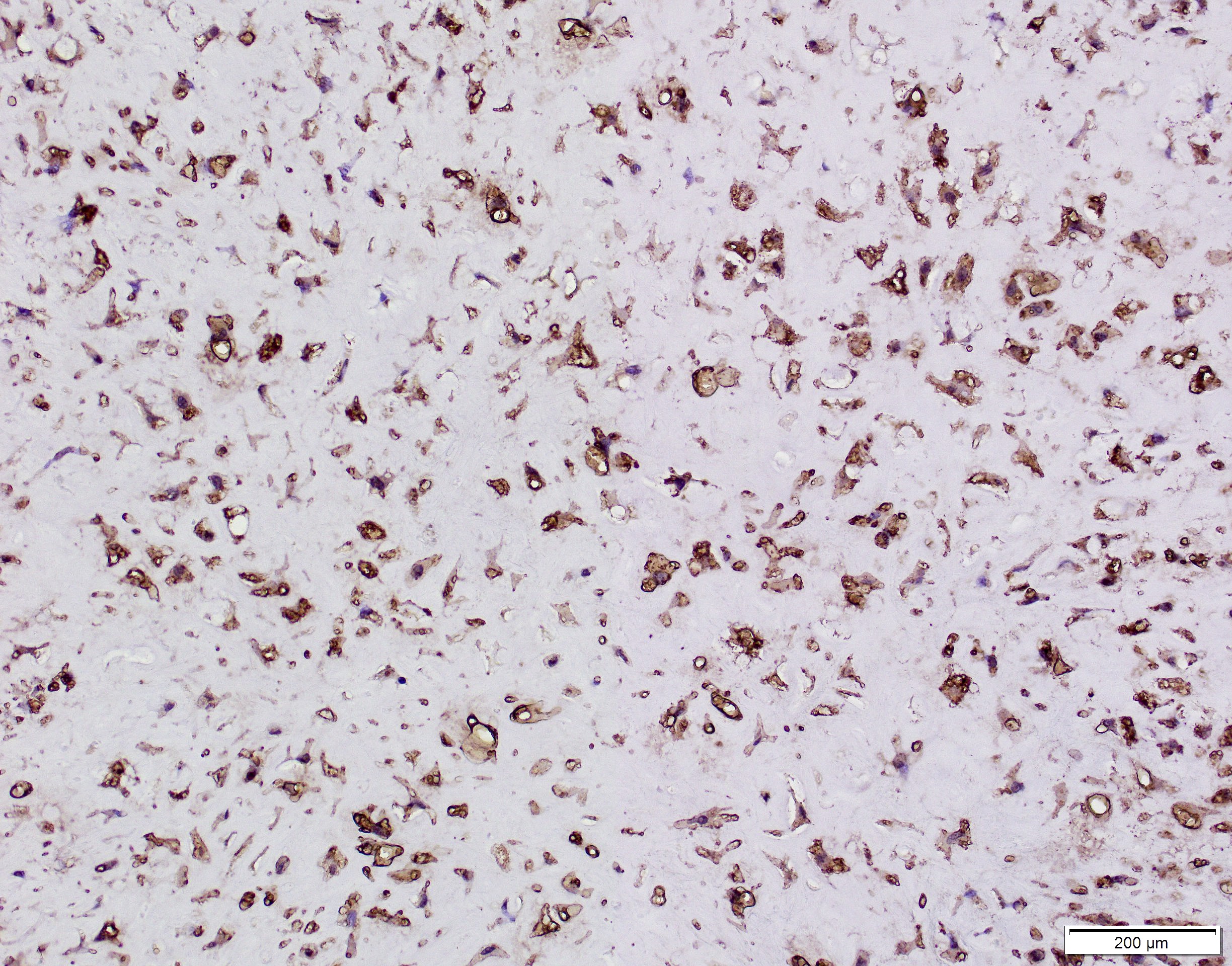
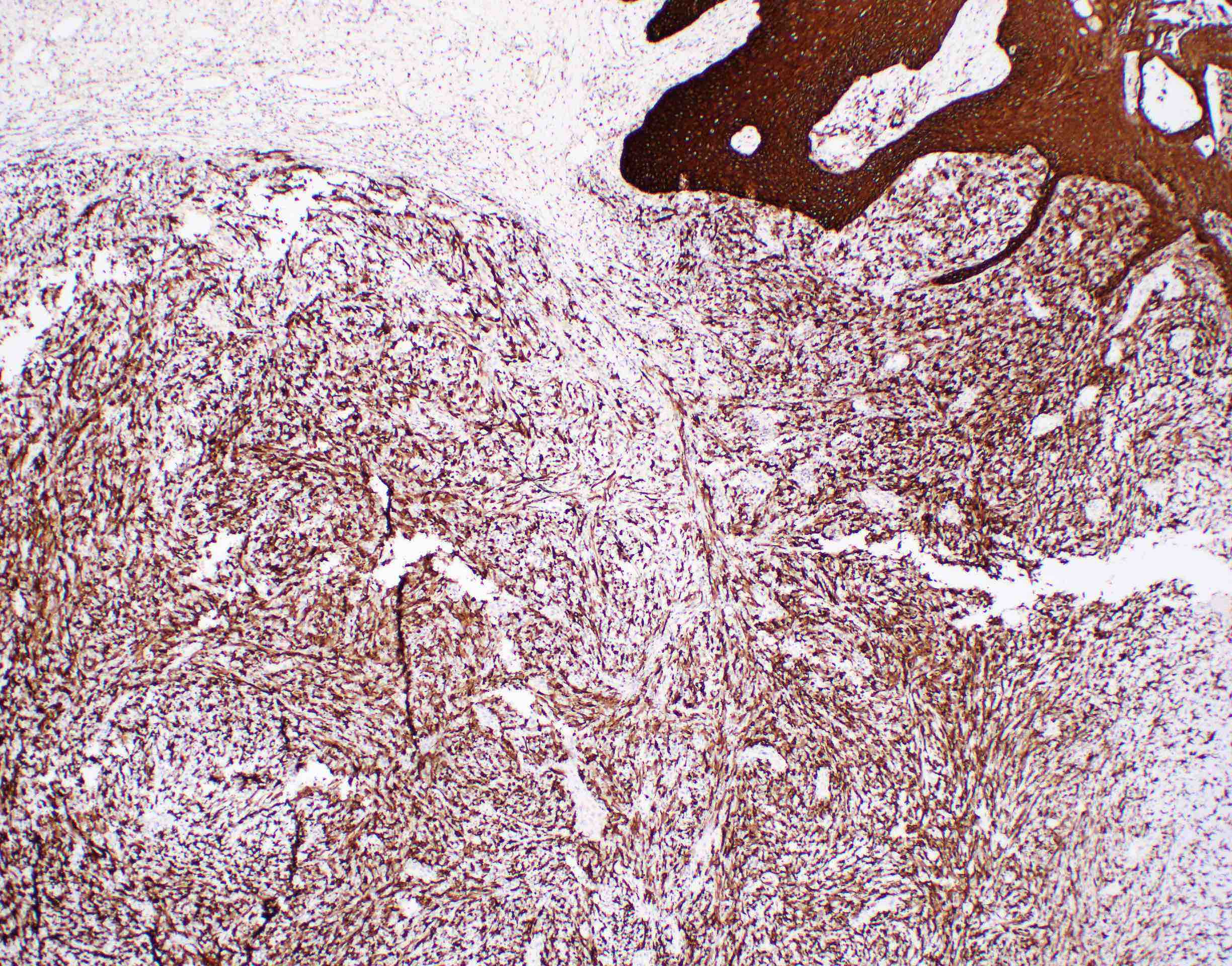
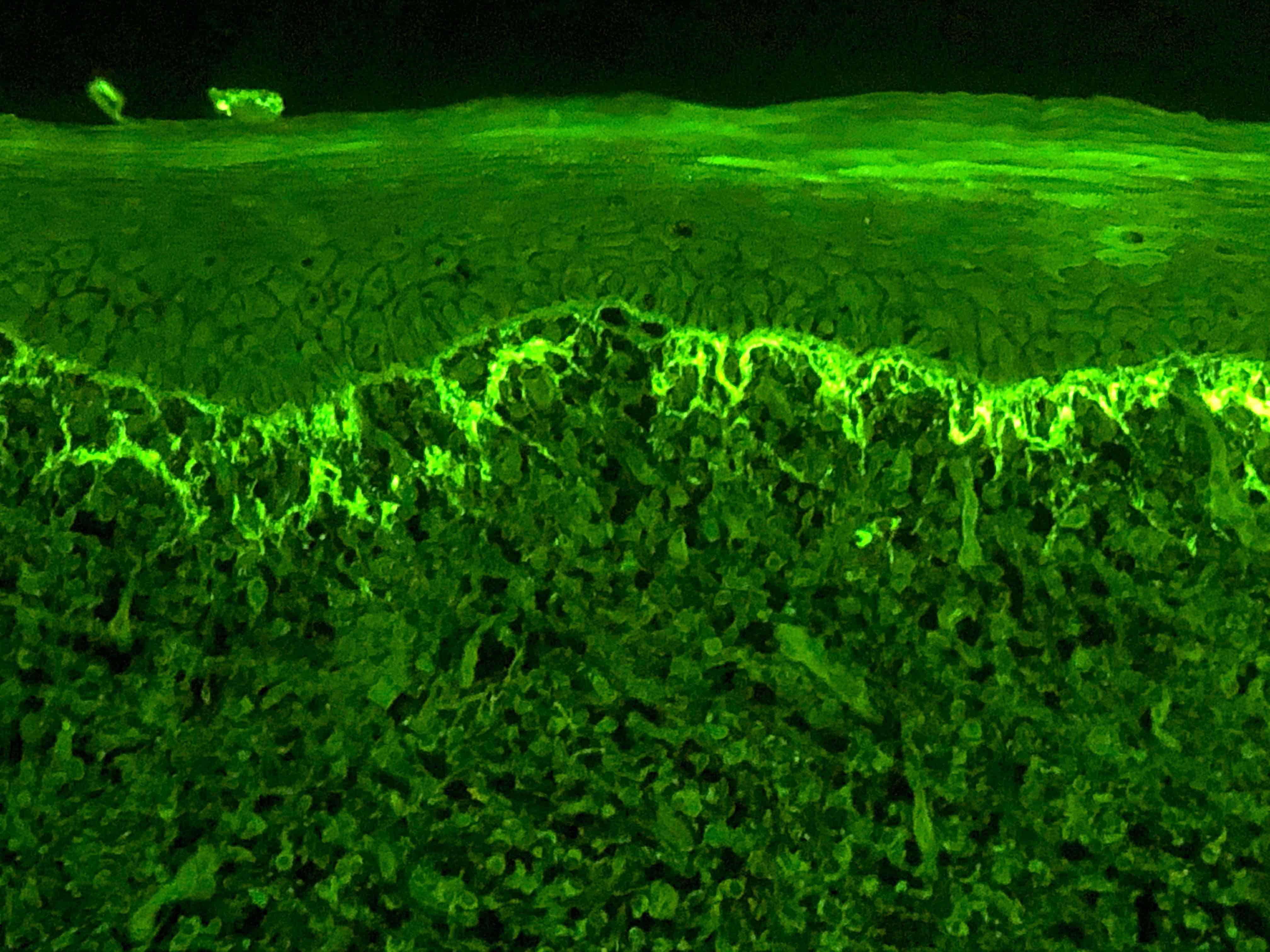
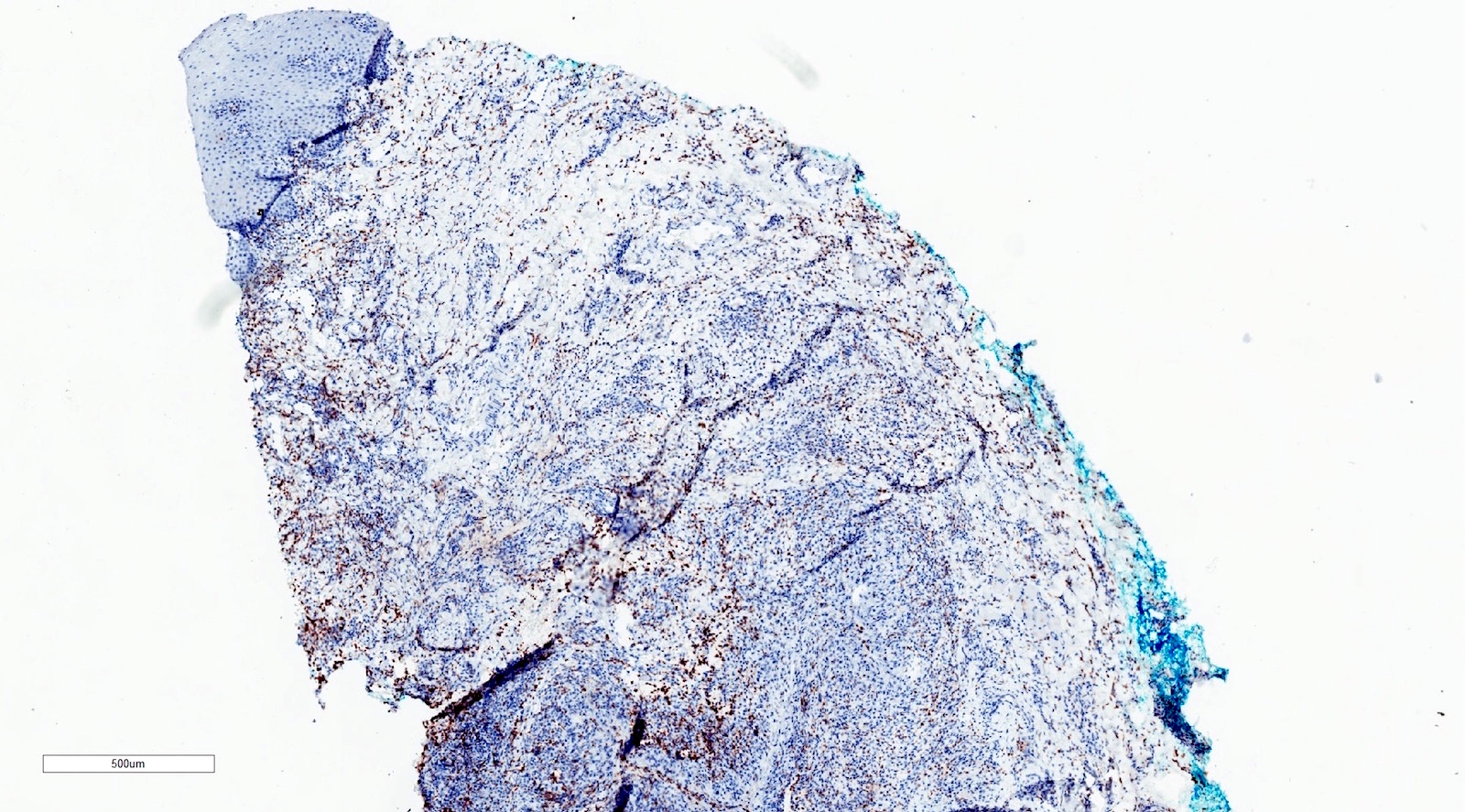
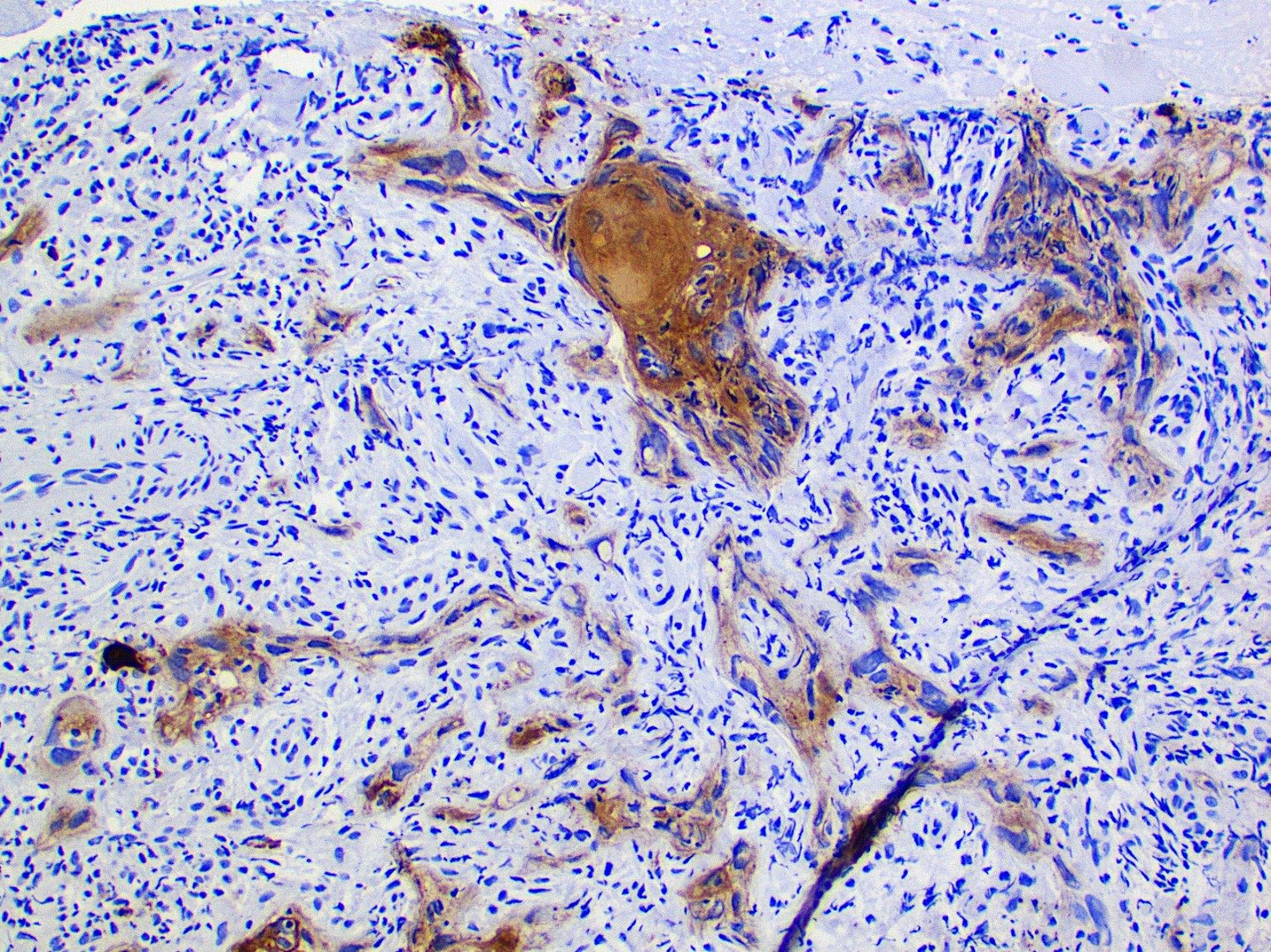
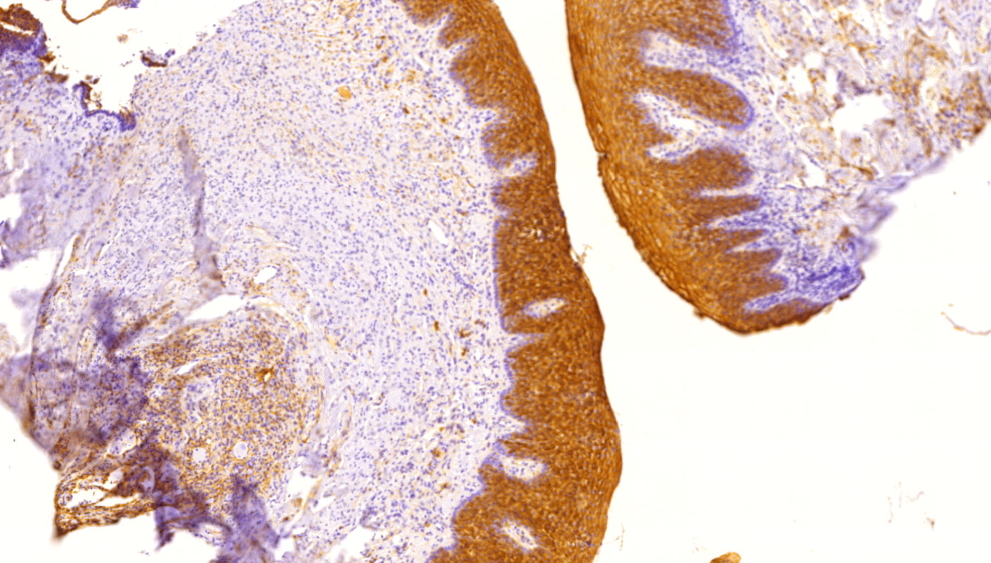
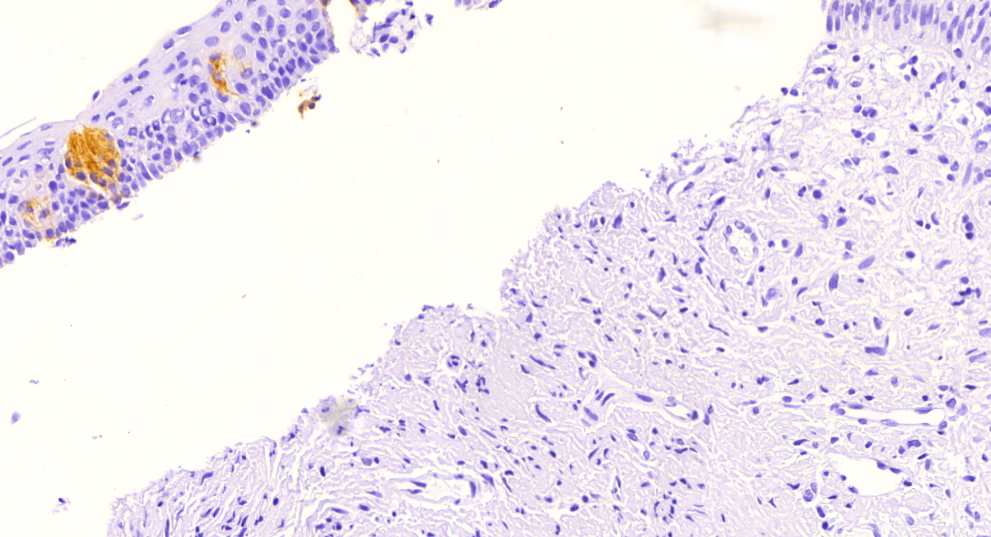
Positive stains
- p53 is variable; may have extreme (loss or gain) staining of surface epithelium or may be nonextreme (nonmutated)
- MDM2 coexpression may also be increased (Oral Oncol 2008;44:878)
- Ki67 and IMP3 may exhibit respective increased proliferation and expression within surface epithelium (Oral Maxillofac Surg 2022;26:587)
Negative stains
- SOX10, MelanA / MART1, MITF and HMB45
Sample pathology report
- Left lower lip, incisional biopsy:
- Actinic cheilitis (see comment)
- Comment: Actinic cheilitis is considered a premalignant condition. Long term monitoring is advised. Further, the patient should be cautioned against future unprotected sun exposure and smoking (if applicable) (Oral Surg Oral Med Oral Pathol Oral Radol and Endodontol 1999;88:181).
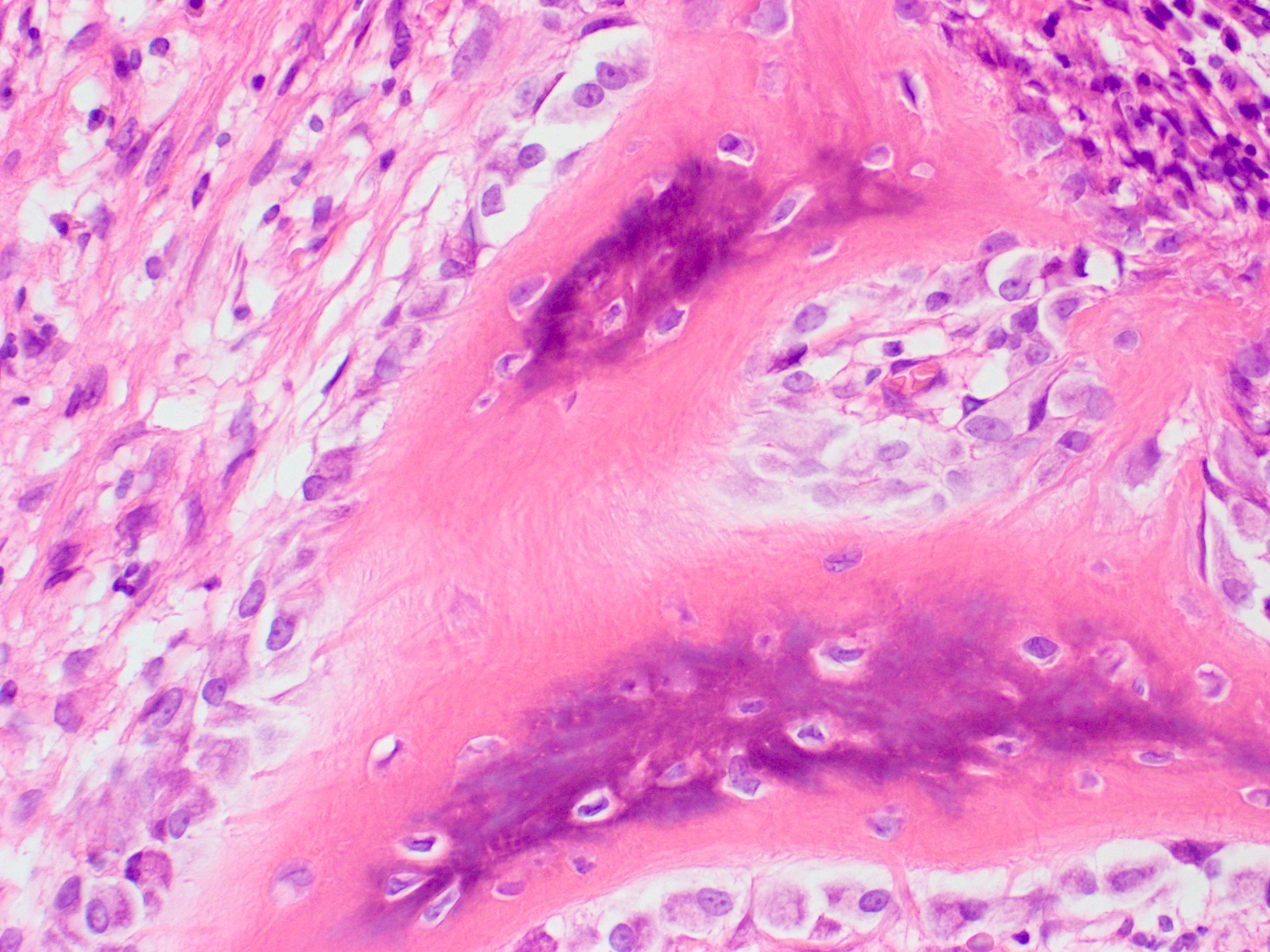
Differential diagnosis
- Squamous cell carcinoma:
- Invasive tumor islands are seen within the connective tissue
- Abnormal mitotic figures and keratin pearl formation may be seen
- Cheilitis glandularis:
- Inflammatory condition of the minor salivary glands and excretory duct dilation, particularly of the lower lip
- Nodular enlargement, reduced mobility and eversion of the affected lip(s) (J Am Dent Assoc 1989;118:317)
- Basal cell carcinoma:
- Nests of basaloid cells with peripheral palisading associated with a fibromyxoid stroma
- Basaloid cells have a high N:C ratio with hyperchromatic nuclei
- Nests of basaloid cells with peripheral palisading associated with a fibromyxoid stroma
- Herpes labialis:
- Intraepidermal blisters with acantholytic epithelium and solitary keratinocytes within the blister pouch
- Nuclei of the keratinocytes show nuclear changes, including margination of chromatin, multinucleation and nuclear inclusions
- Nuclear viral inclusions are small, pink deposits with a clear halo
- Initial clinical lesions appear as blisters that rupture and ulcerate
- The condition is self limiting and recurrences may occur
- Intraepidermal blisters with acantholytic epithelium and solitary keratinocytes within the blister pouch
Board review style question #1
A biopsy of the lower lip of a 65 year old man reveals high grade dysplastic change, solar elastosis and telangiectasia. Based on these findings, what is the most appropriate diagnosis?
- Actinic cheilitis
- Cheilitis glandularis
- Keratoacanthoma
- Squamous cell carcinoma
Board review style answer #1
A. Actinic cheilitis. High grade dysplasia in the context of solar elastosis and telangiectasias is consistent with actinic cheilitis. Answer B is incorrect because cheilitis glandularis appears as inflammation of the salivary glands and dilation of the excretory ducts. Answer C is incorrect because keratoacanthomas are nodular with a central keratin plug. Answer D is incorrect because squamous cell carcinomas appear as nests of atypical epithelial cells within the stroma that arise from the surface.
Comment Here
Reference: Actinic cheilitis
Comment Here
Reference: Actinic cheilitis
Board review style question #2
Board review style answer #2
A. Actinic cheilitis. This clinical image depicts blurring of the lower lip vermilion that is consistent with chronic solar damage. Answer B is incorrect because basal cell carcinoma often appears as ulcerated, nodular lesions with associated telangiectasias. Answer C is incorrect because cheilitis glandularis presents as nodular enlargement and eversion of the affected lip(s). Answer D is incorrect because melanoma (cutaneous) often exhibits irregular, pigmented areas.
Comment Here
Reference: Actinic cheilitis
Comment Here
Reference: Actinic cheilitis
Adenoid cystic carcinoma
Adenomatoid hyperplasia of minor glands
Table of Contents
Definition / general | Terminology | Epidemiology | Sites | Etiology | Clinical features | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Differential diagnosisDefinition / general
- Uncommon benign entity first described in 1971 (Oral Surg Oral Med Oral Pathol 1991;71:583)
Terminology
- Also called acinar adenomatoid hyperplasia (Barnes: Surgical Pathology of the Head and Neck, 3rd Edition, 2008 [p500])
Epidemiology
- Most cases reported in Caucasians, uncommon in Asians (Barnes: Surgical Pathology of the Head and Neck, 3rd Edition, 2008 [p500])
- Ages 9 to 79 years; 58% male (Oral Surg Oral Med Oral Pathol 1991;71:583)
Sites
- 80% on hard and soft palate
Etiology
- Chronic, local trauma (smokers, denture wearers) may be contributing factor (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995;79:482)
Clinical features
- Presents as painless, sessile swelling at junction of hard and soft palate; may mimic a salivary gland tumor (Barnes: Surgical Pathology of the Head and Neck, 3rd Edition, 2008 [p500])
Prognostic factors
- Does not appear to predispose to benign or malignant salivary gland neoplasia
Case reports
- 48 year old Asian man with painless swelling in palate (J Laryngol Otol 1996;110:167)
Treatment
- Excision is curative (Barnes: Surgical Pathology of the Head and Neck, 3rd Edition, 2008 [p500])
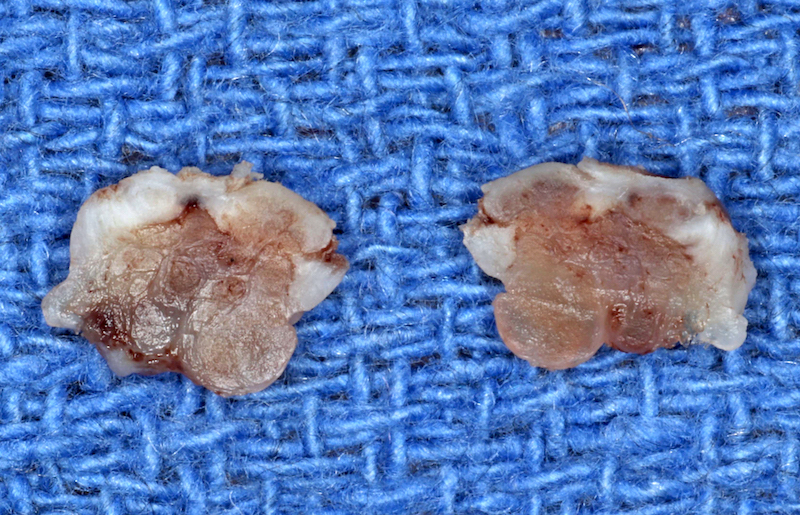
Gross description
- Localized swelling resembling a neoplasm, 0.5 - 2.7 cm
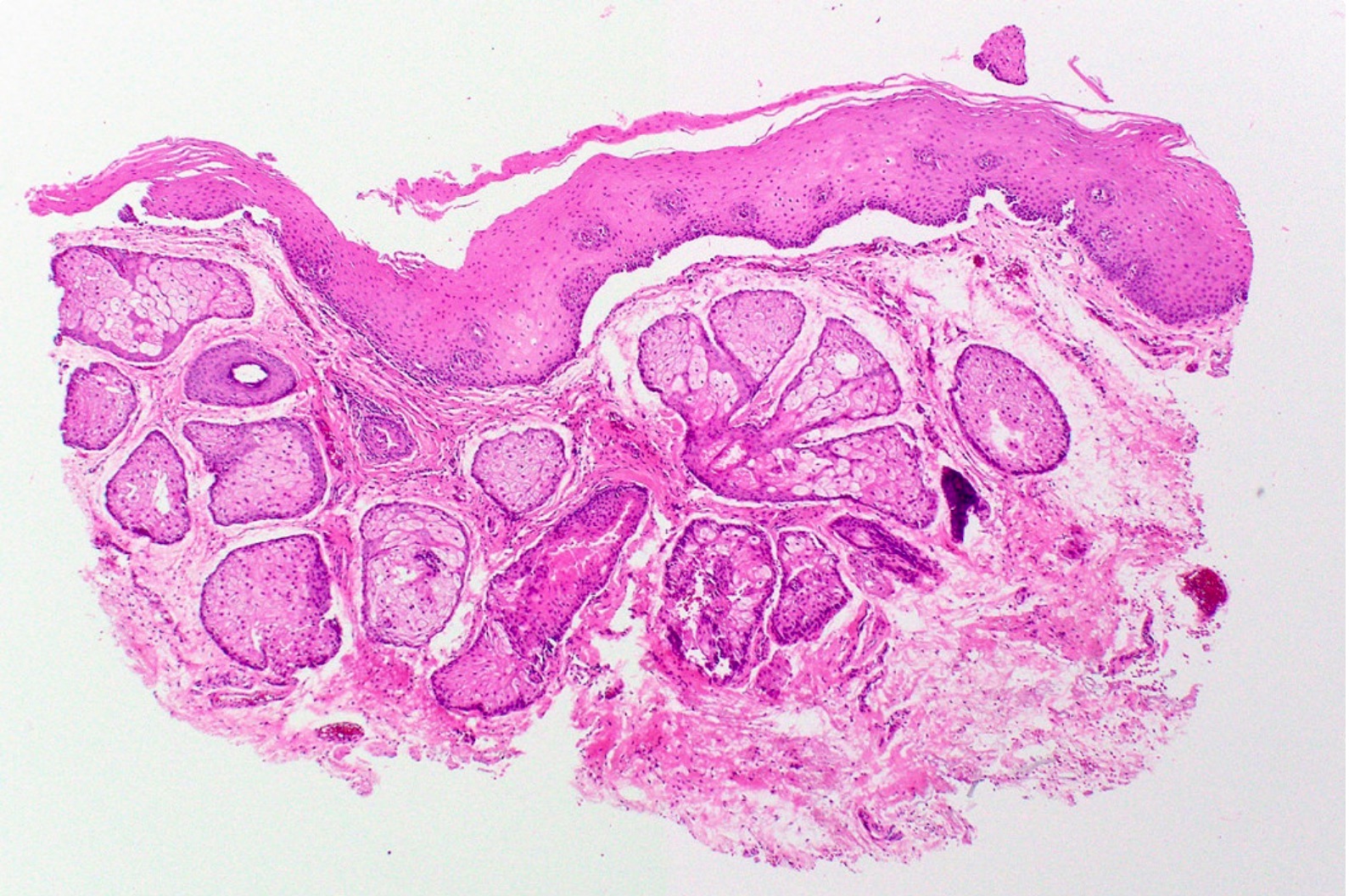
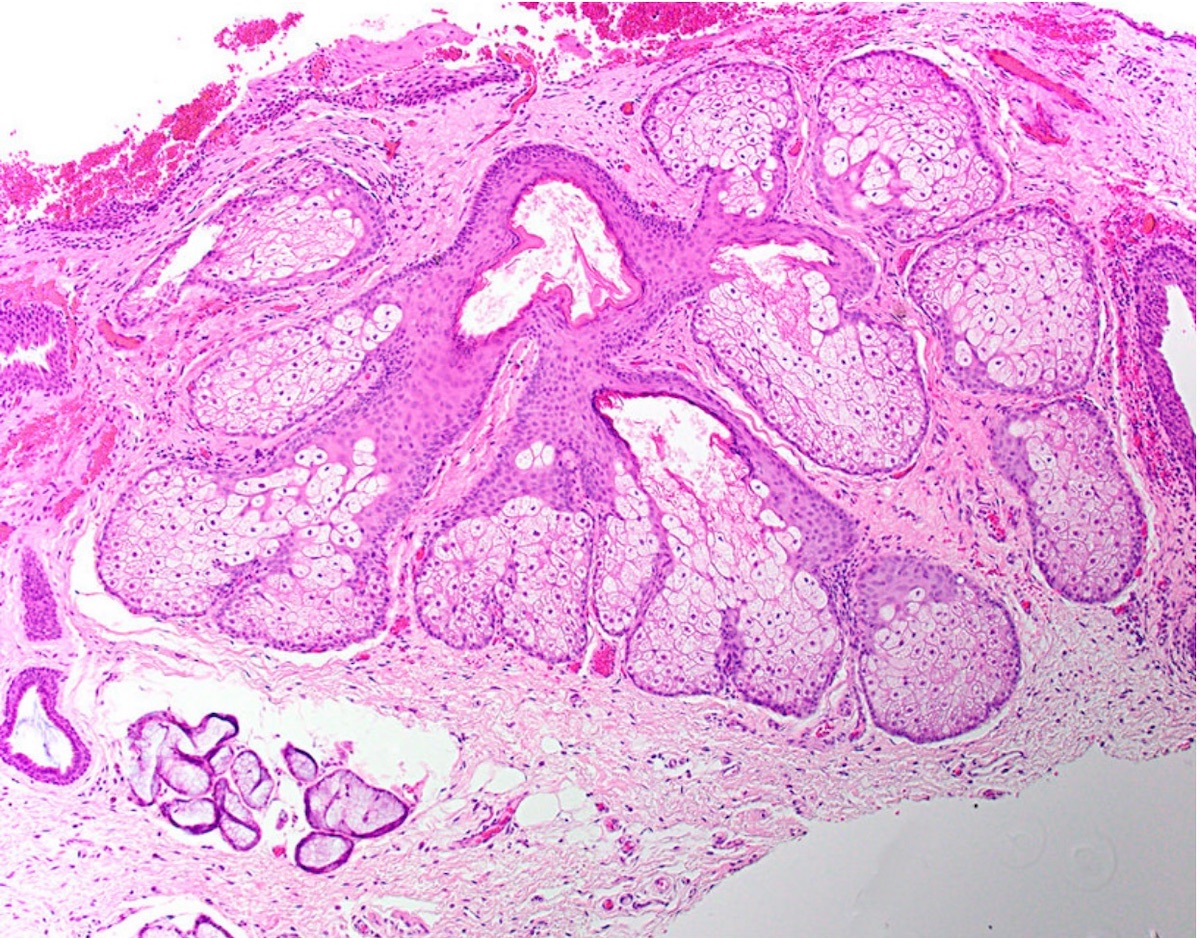
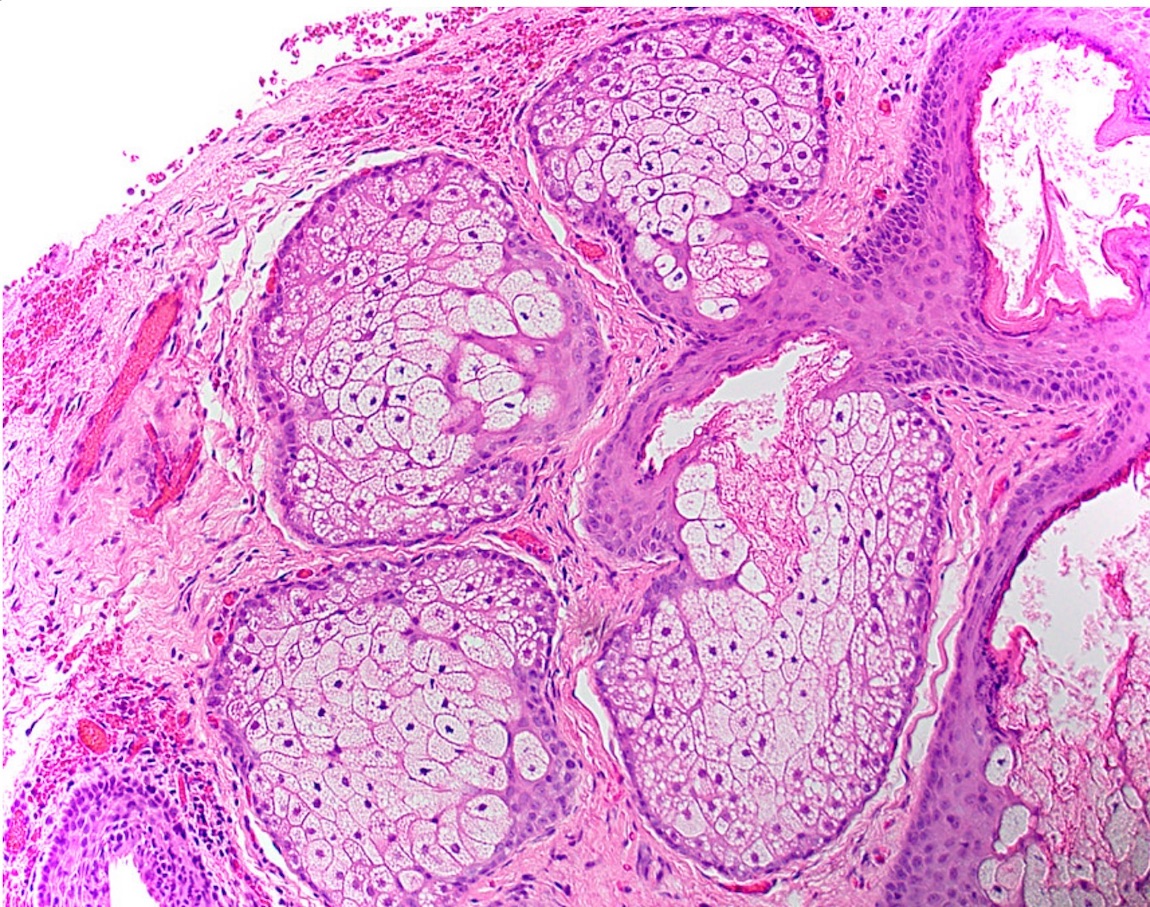
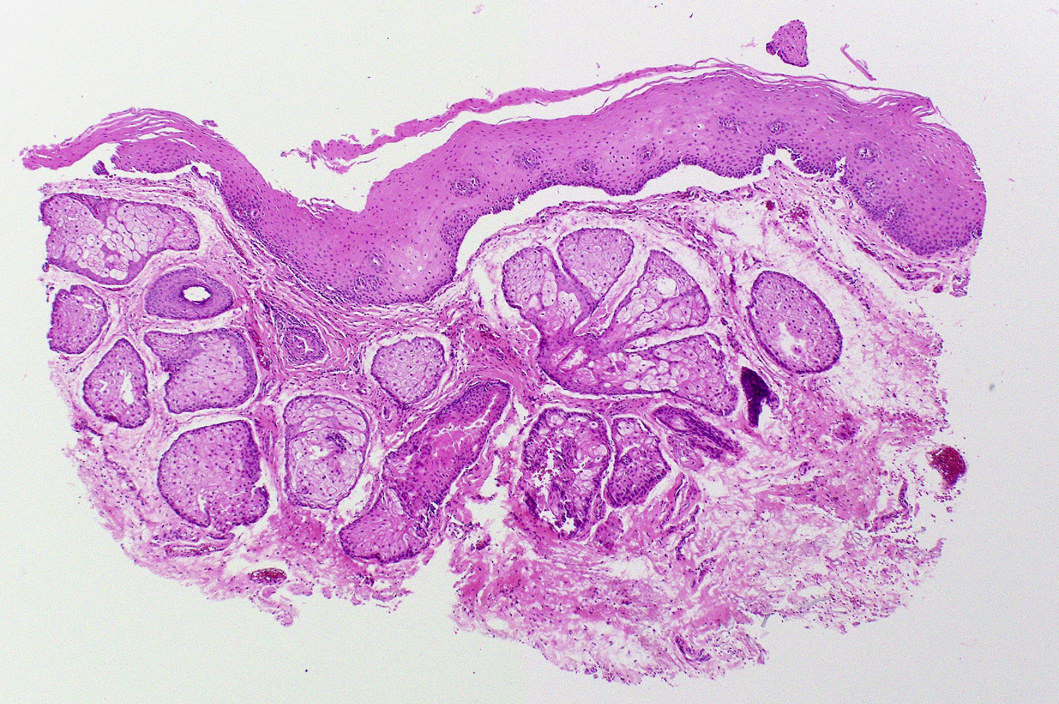
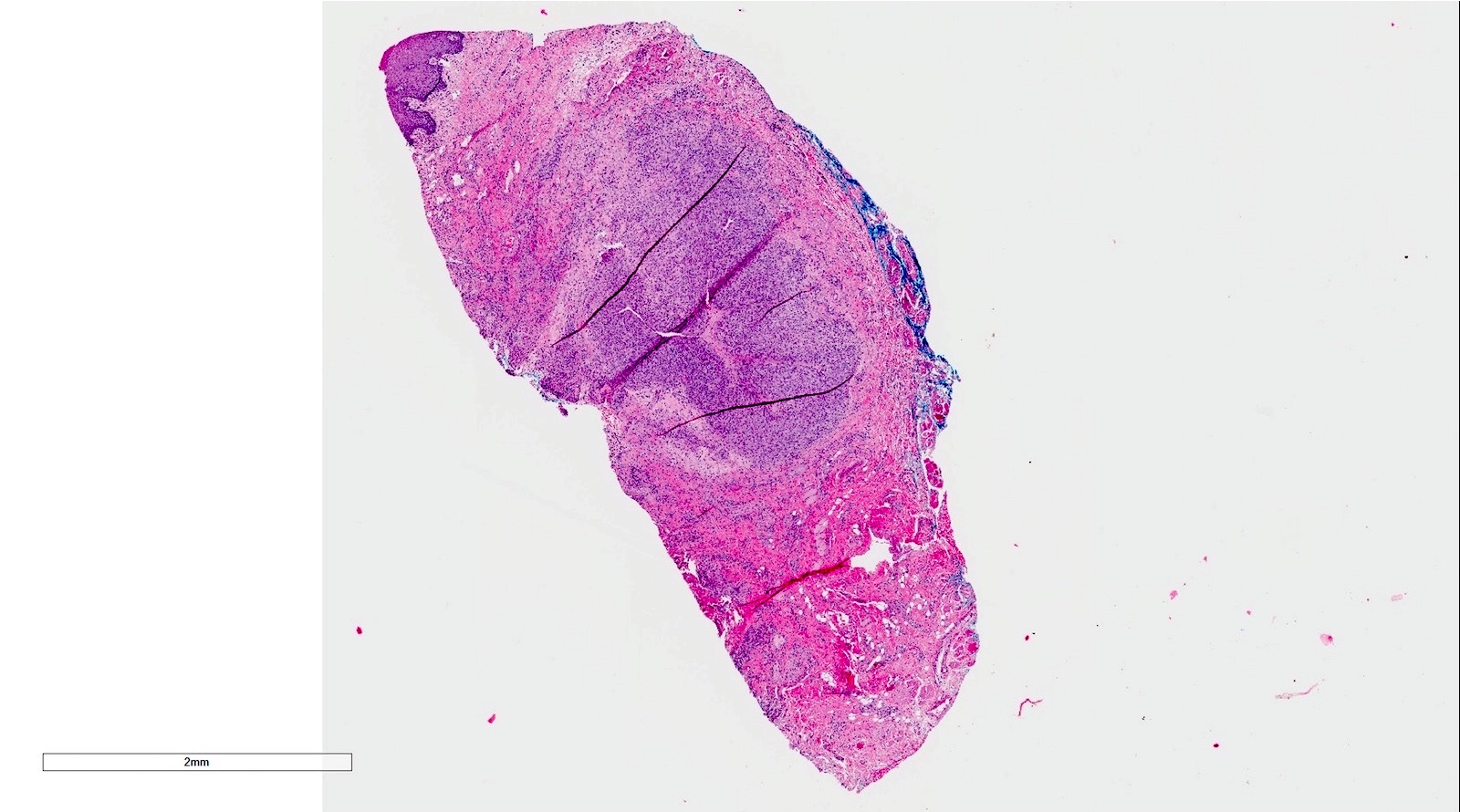
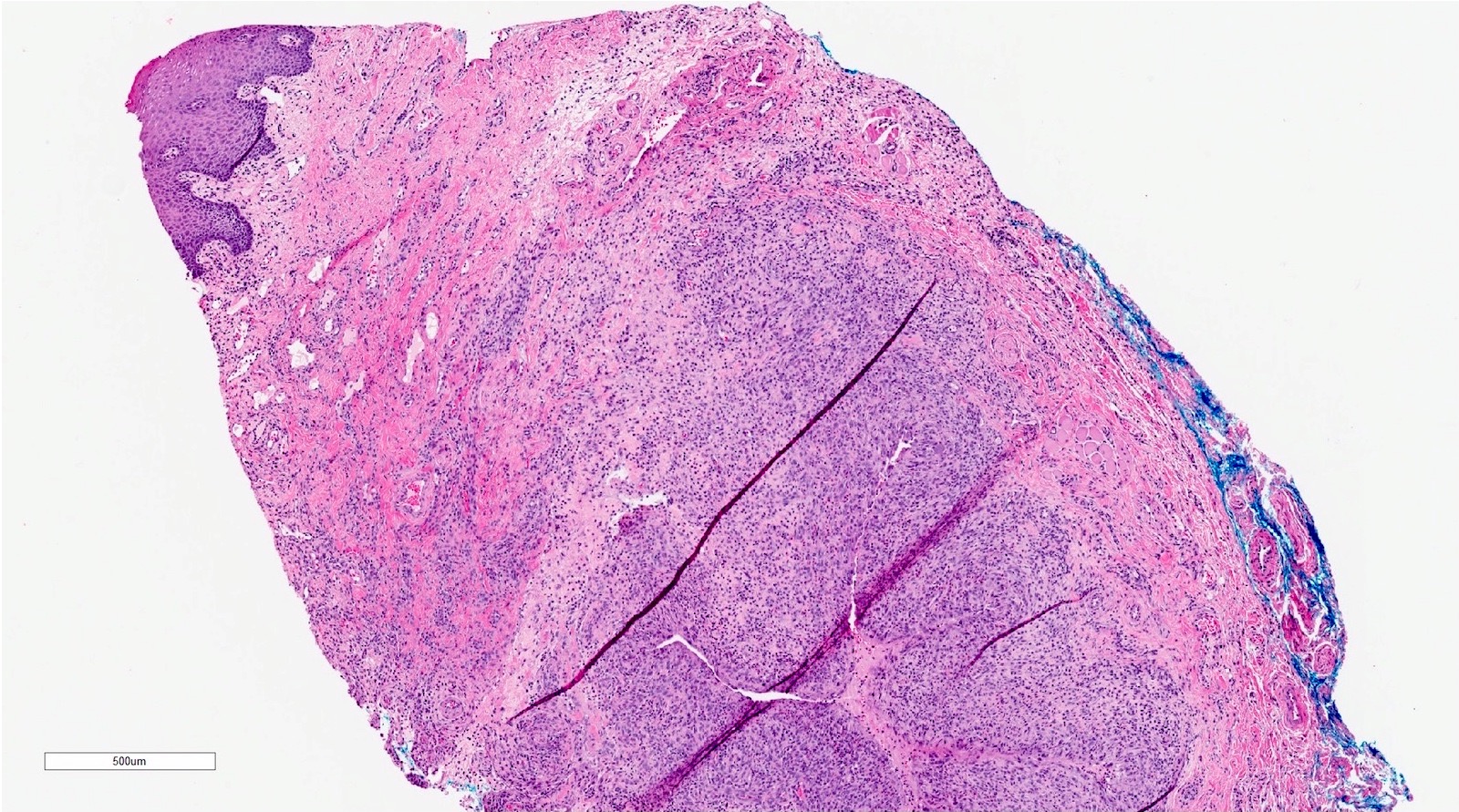
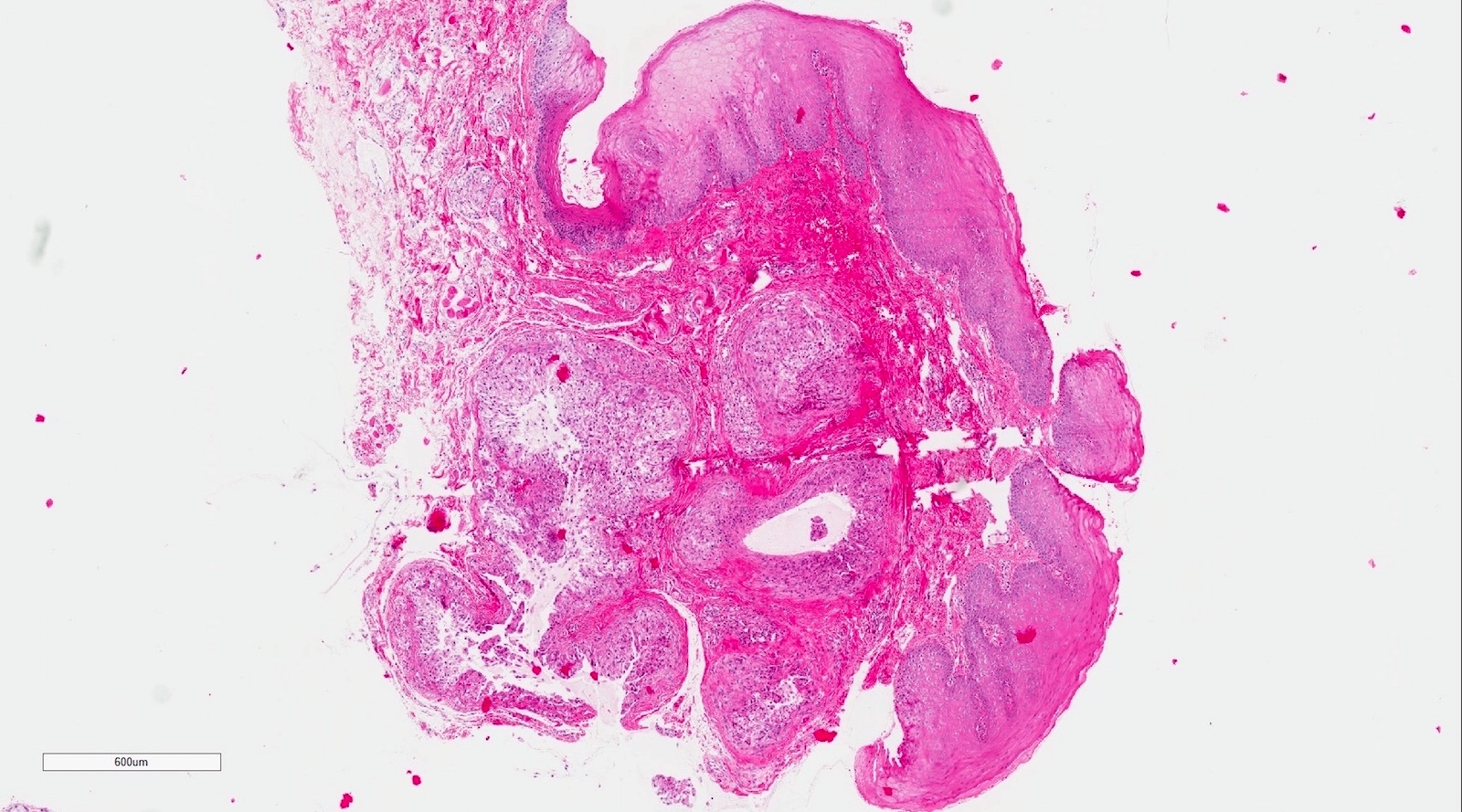
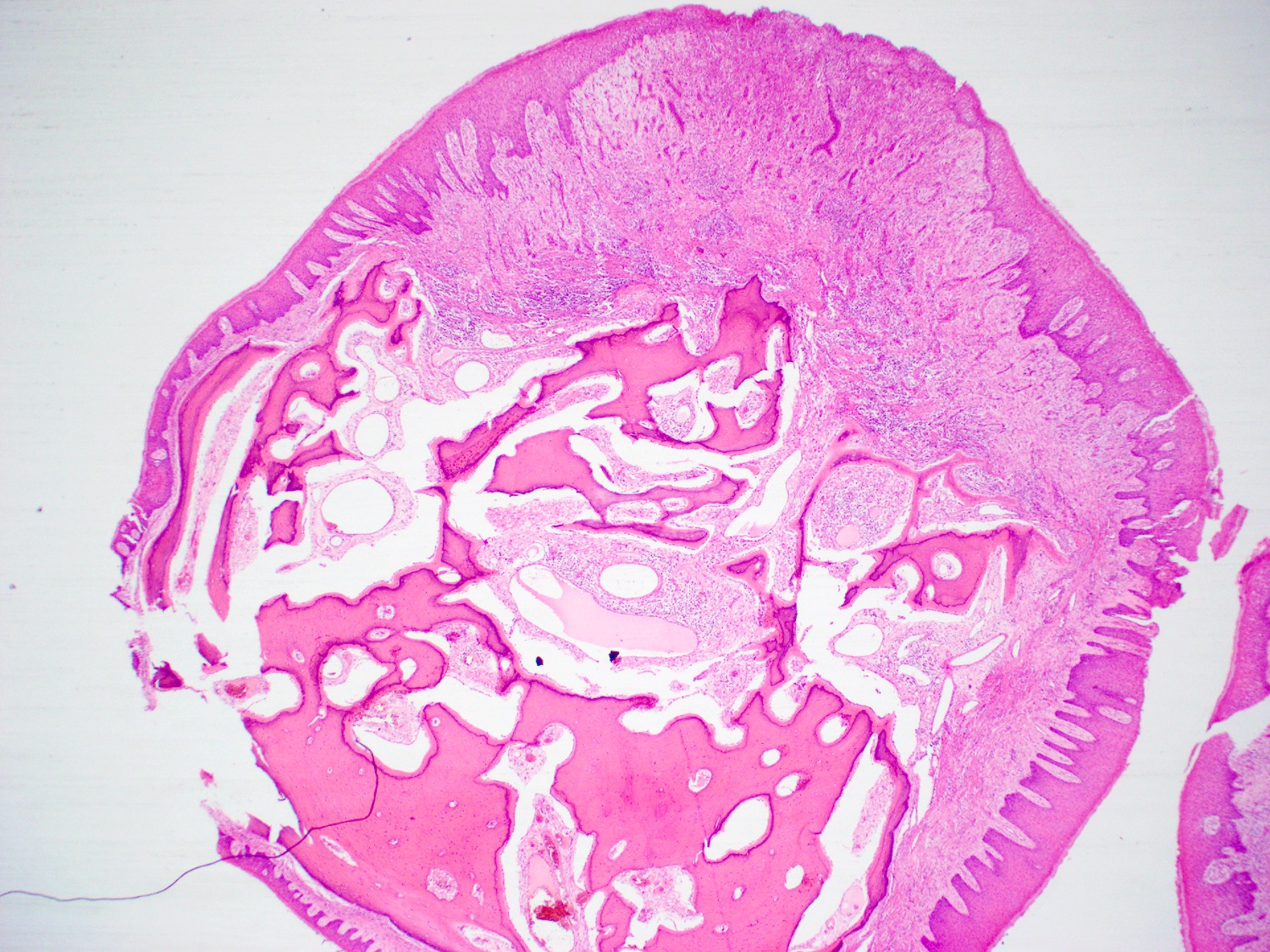
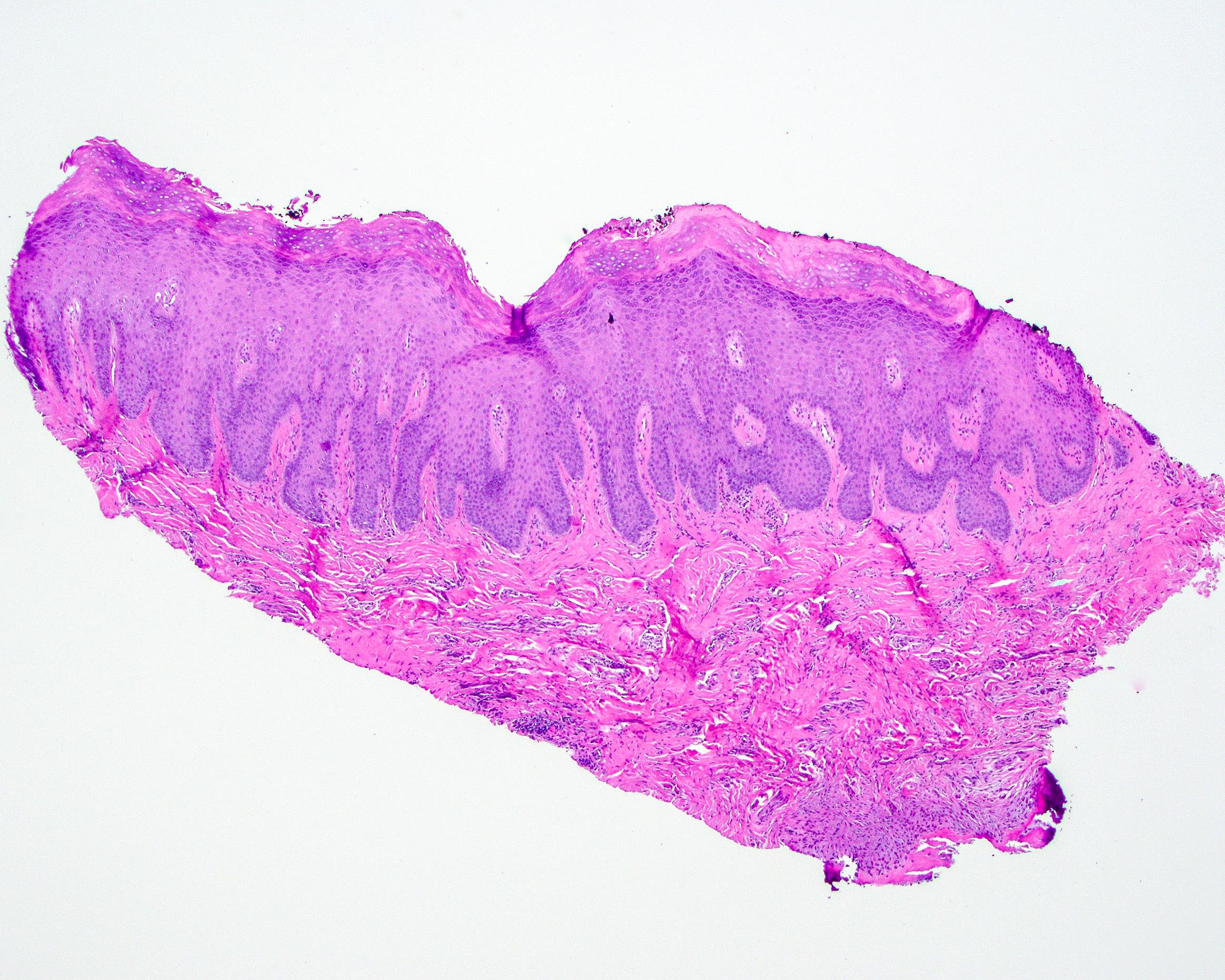
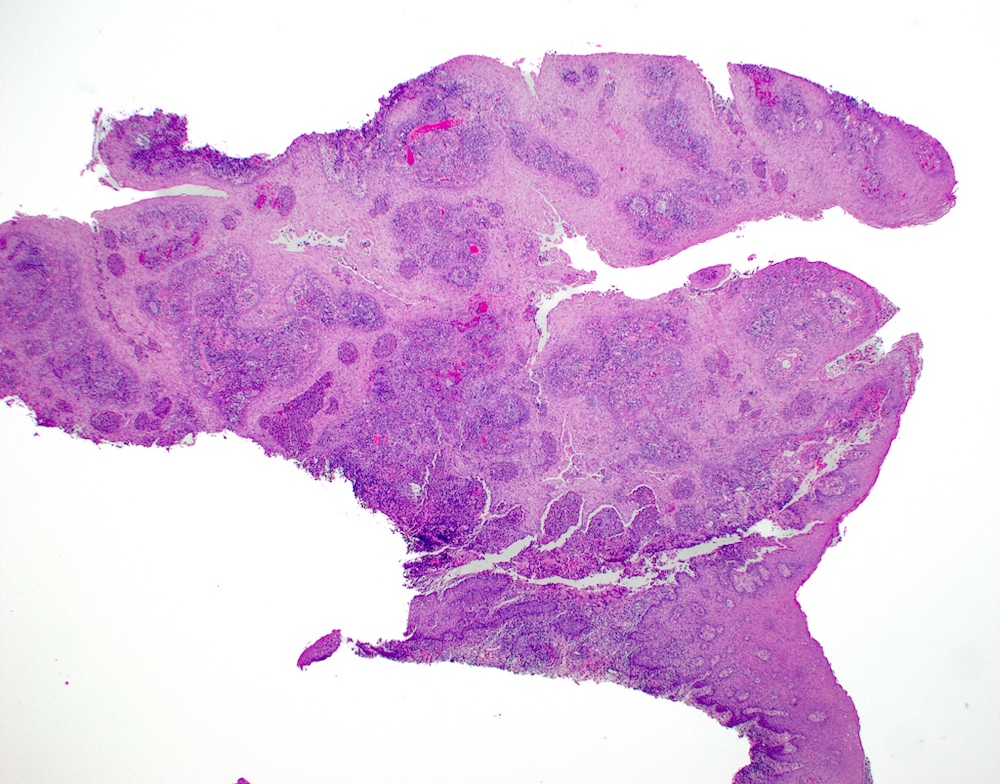
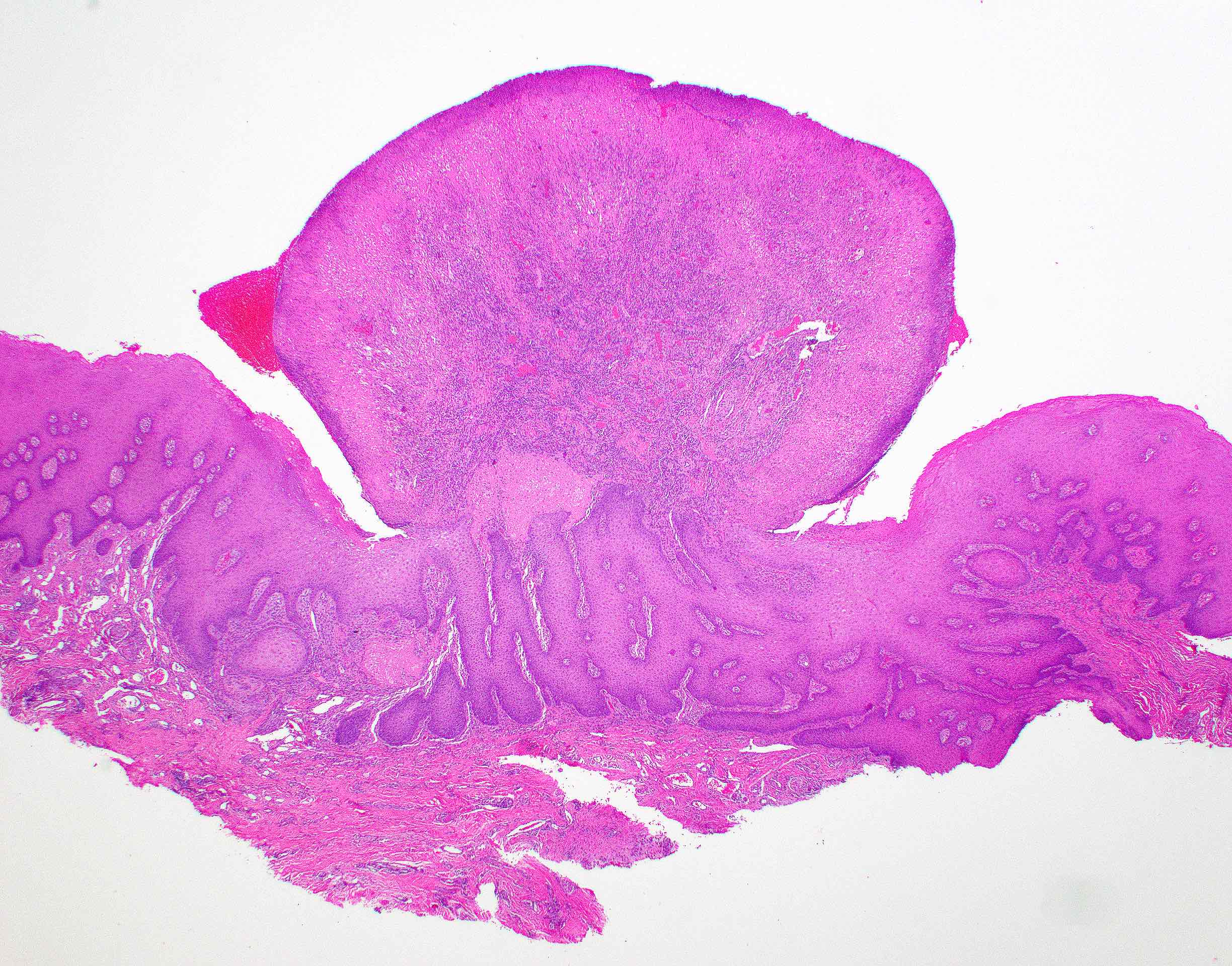
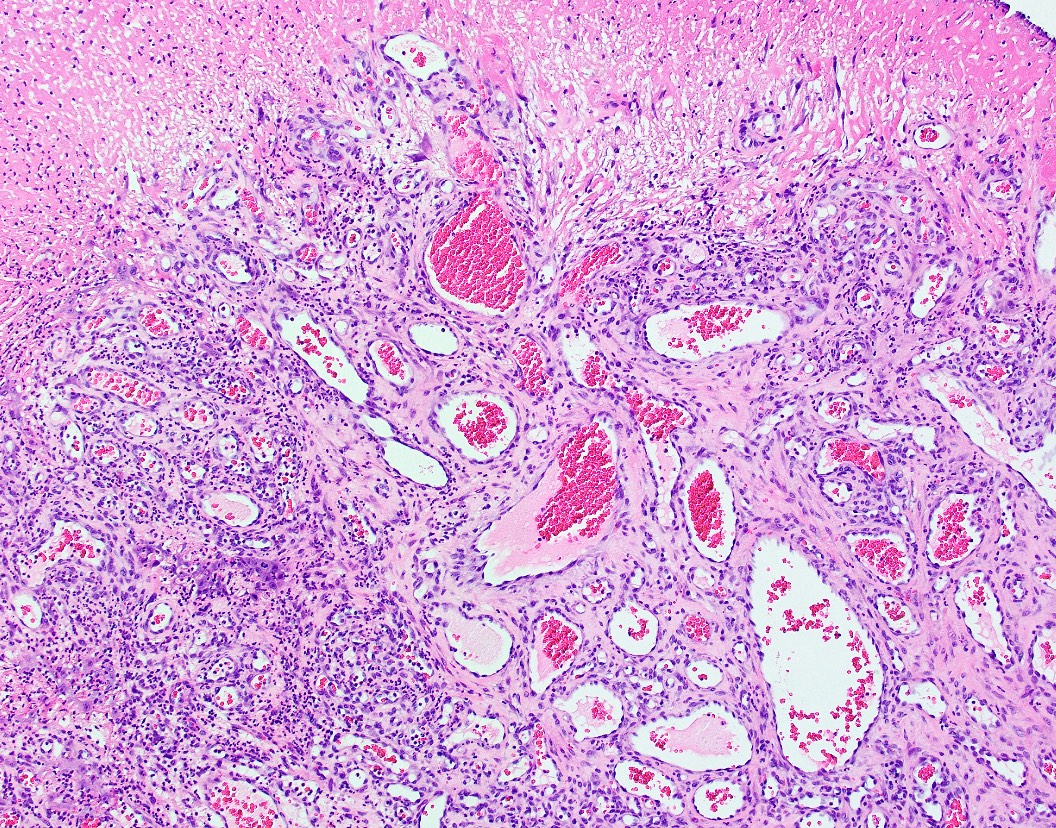
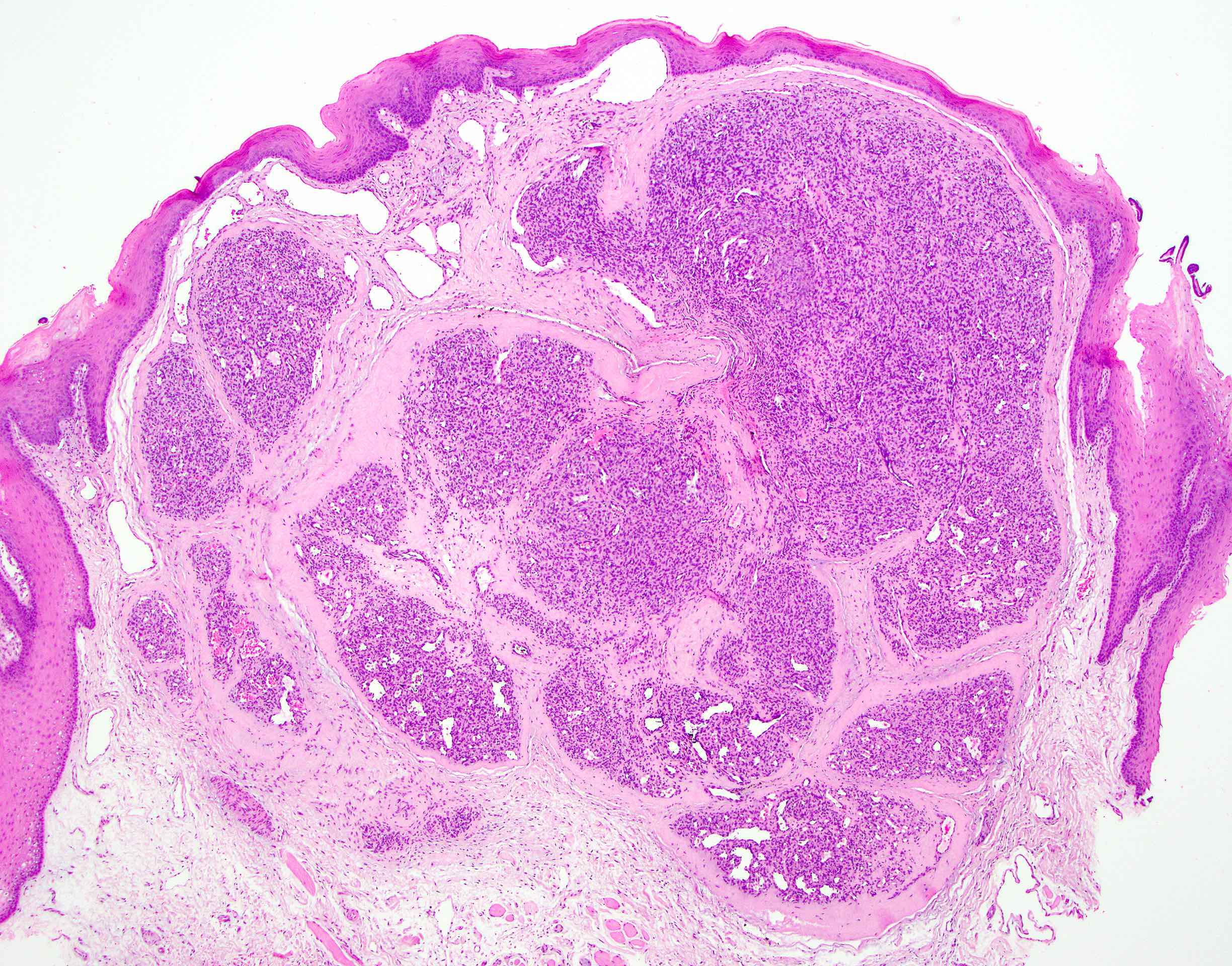
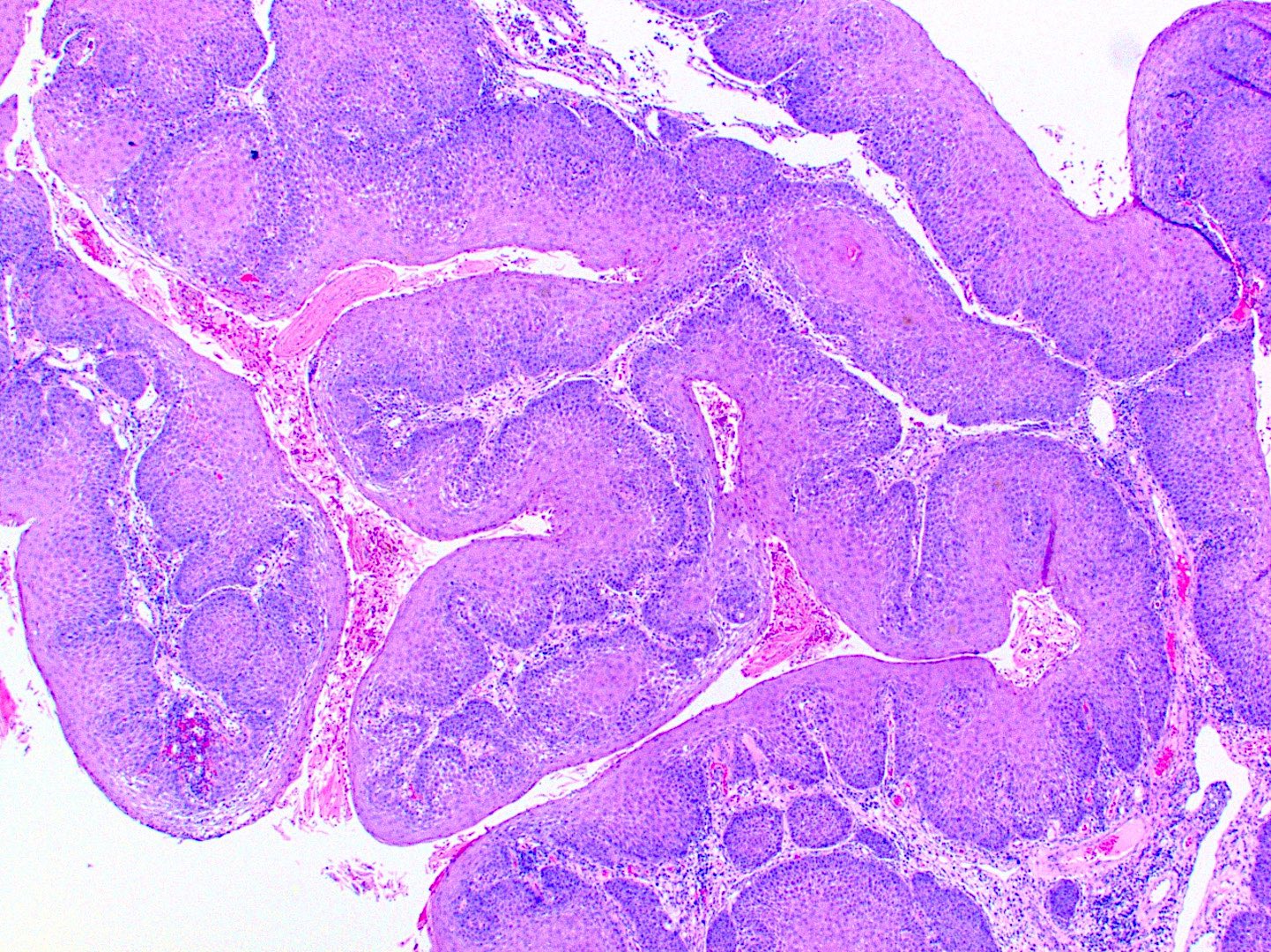
Microscopic (histologic) description
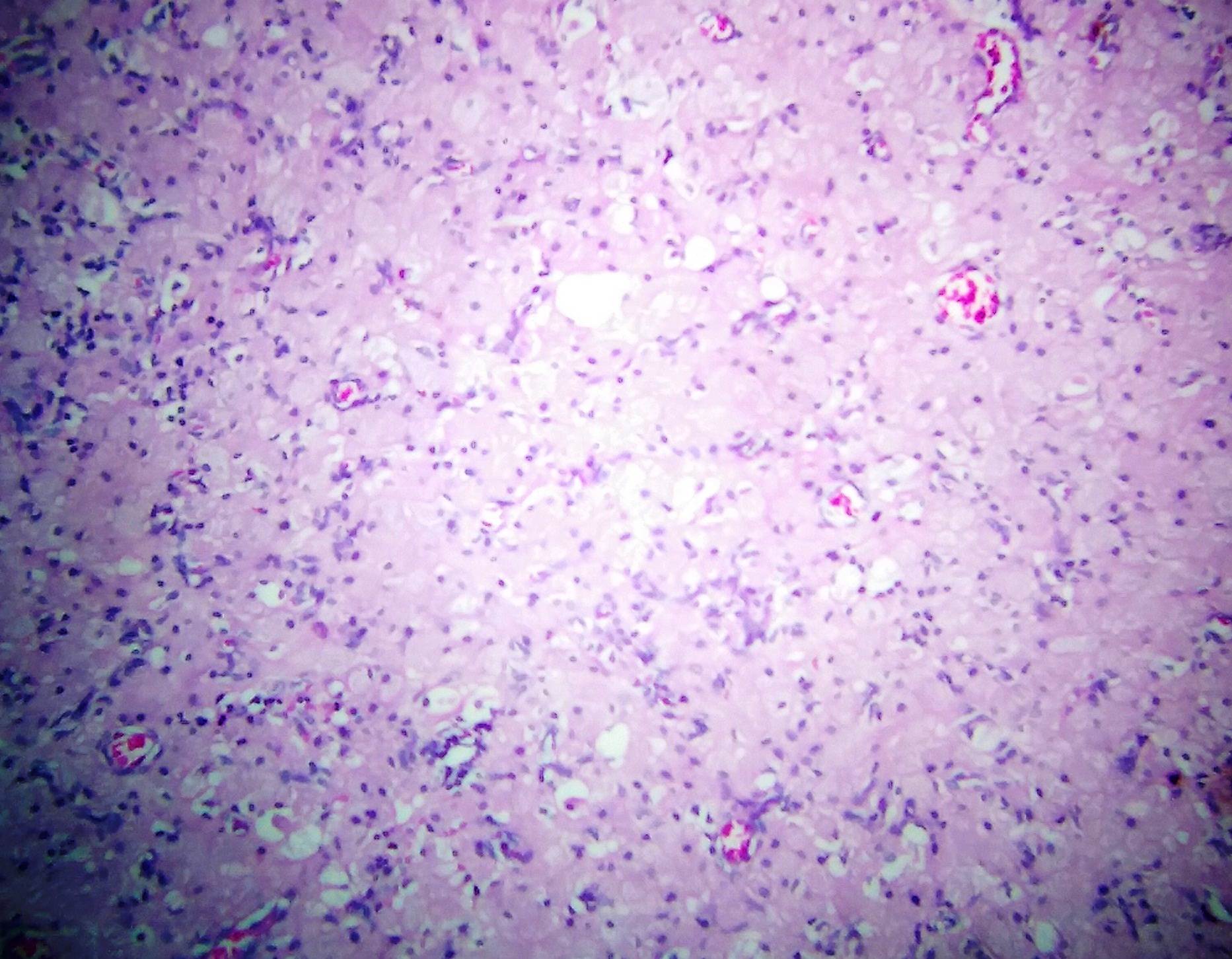
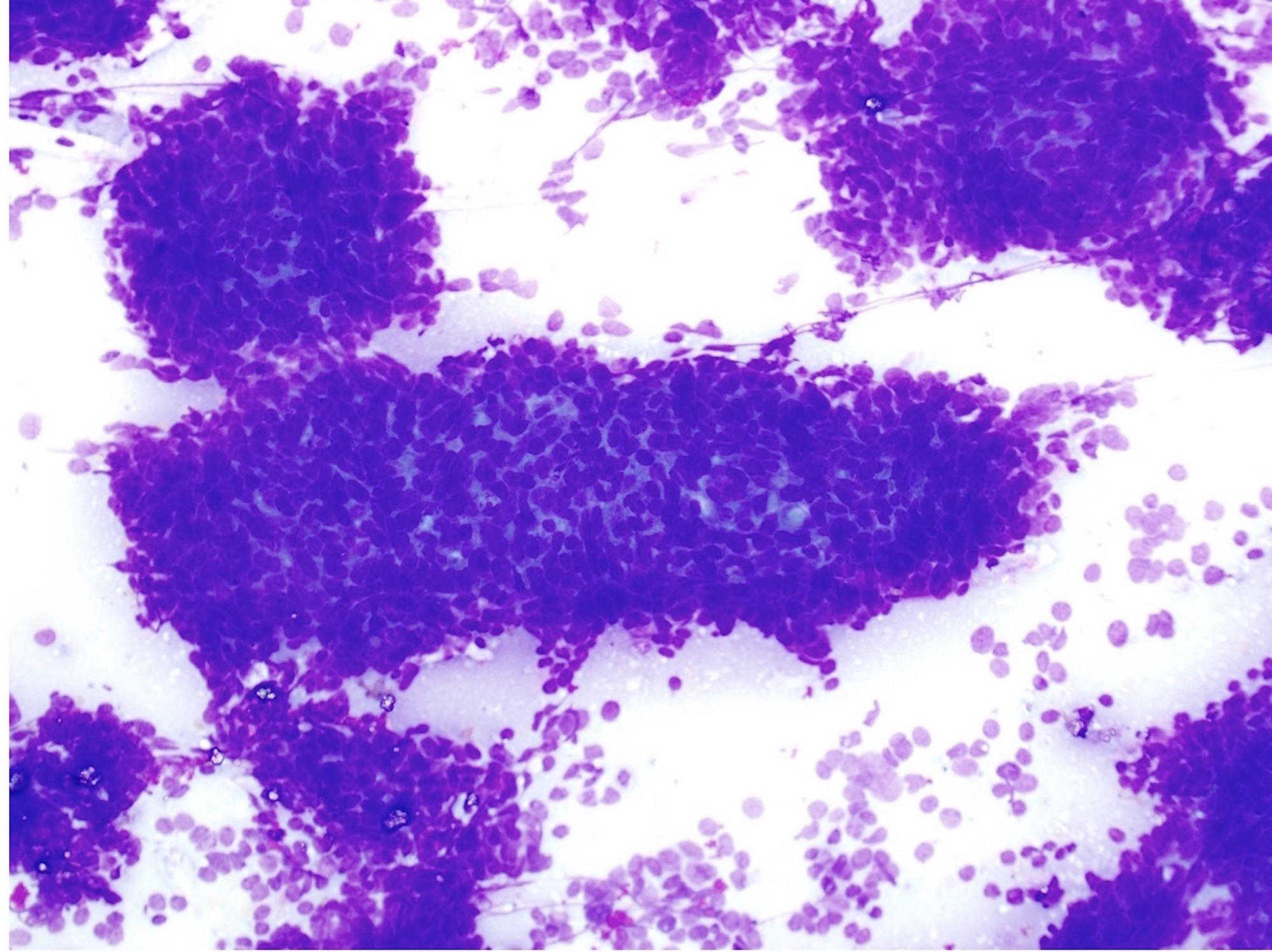
- Multiple aggregates, varying in size, of normal appearing mucous acini surrounded by fibrous connective tissue stroma
- Normal ductal structures
- Overlying palatal epithelium is usually normal but may have lichenoid reaction or pseudoepitheliomatous hyperplasia
- Occasionally, areas of interstitial mucous extravasation with associated inflammatory reaction (Barnes: Surgical Pathology of the Head and Neck, 3rd Edition, 2008 [p500]) but typically no significant inflammatory cell infiltrates (Oral Surg Oral Med Oral Pathol 1991;71:583)
Differential diagnosis
- Idiopathic hyperplasia of the sublingual gland or "pouting" sublingual glands is seen as an enlargement in the floor of the mouth in totally or partially edentulous patients; sublingual glands may be otherwise normal or show nonspecific chronic inflammation
Adult type rhabdomyoma
Amalgam tattoo
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Iatrogenic implantation of exogenous foreign material, specifically dental amalgam, into the tissues of the oral cavity
Essential features
- Deposition often occurs during oral procedures involving amalgam
- Gray, blue or black macule on clinical exam in the oral cavity
- Large black deposits or fine black granules in the connective tissue with affinity for reticulin fibers
Terminology
- Foreign body tattoo
ICD coding
- ICD-10: M79.5 - residual foreign body in soft tissue
Epidemiology
- Person with history of amalgam tooth restorations (dental fillings)
- Affects 3.3% of the U.S. adult population (Head Neck Pathol 2019;13:47)
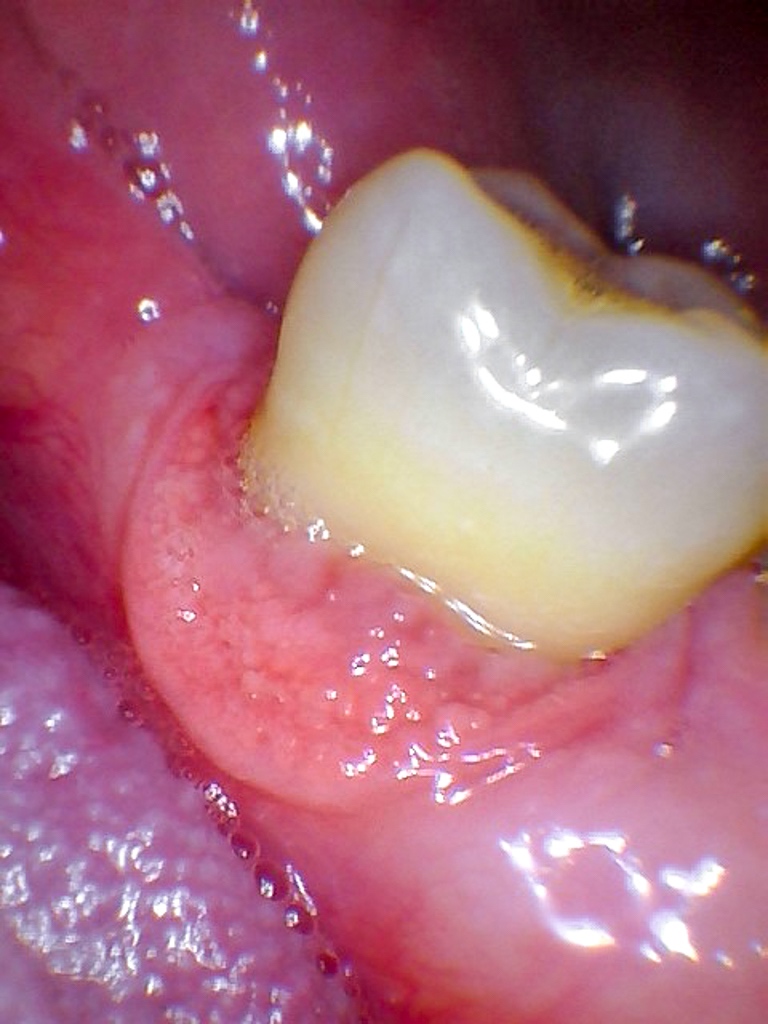
Sites
- Any location in the oral cavity, with gingiva and alveolar mucosa being the most common location due to proximity to the teeth
Pathophysiology
- Implantation of dental amalgam into oral mucosa
Etiology
- Implantation of dental amalgam can occur several ways, including contaminated mucosal abrasion during dental procedure, broken amalgam pieces in an extraction site and endodontic retrofill procedure (Neville: Oral and Maxillofacial Pathology, 4th Edition, 2015)
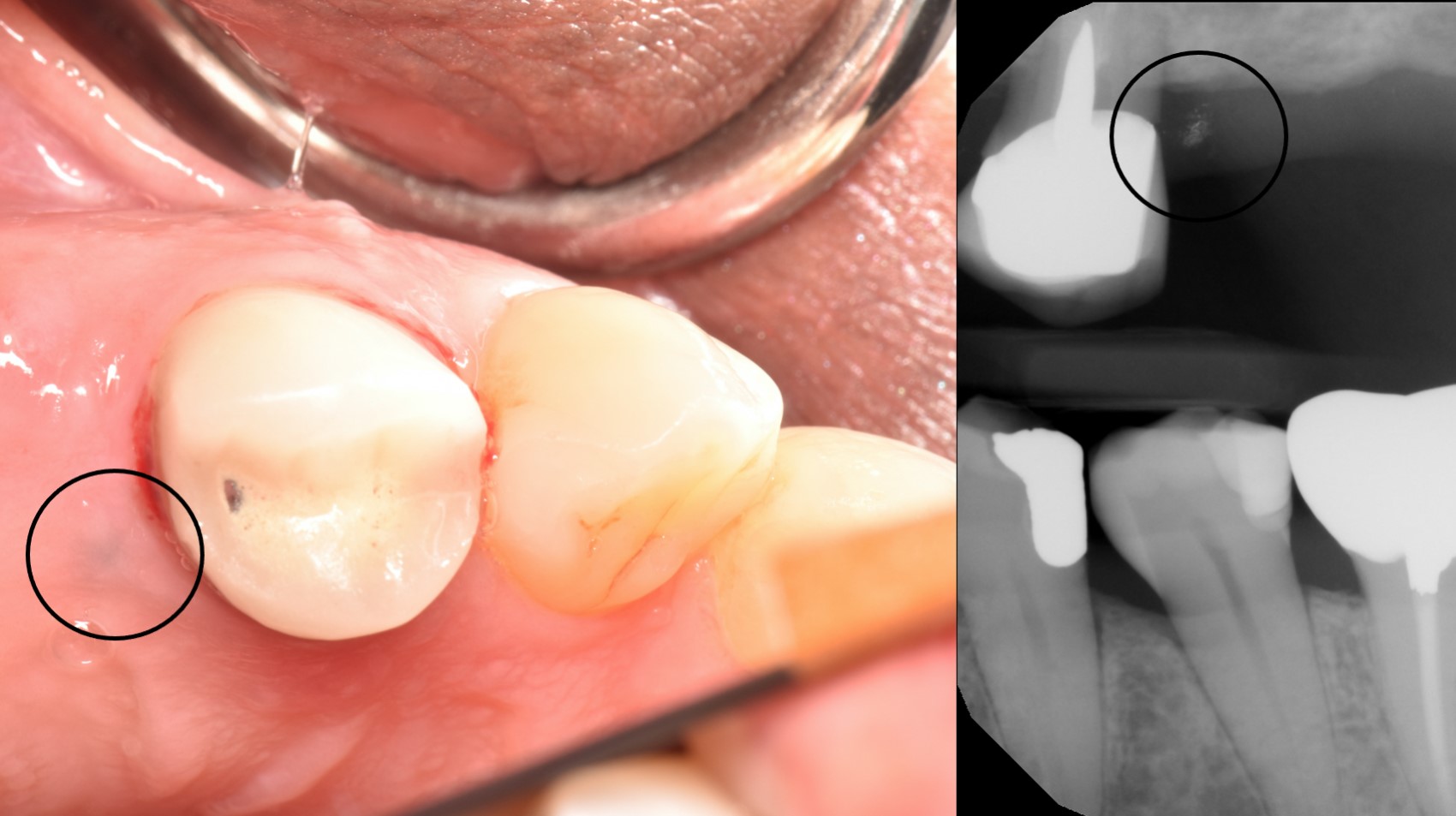
Clinical features
- Gray, blue or black macule that is rarely raised
- Multiple macules may occur
- Borders may be well defined, irregular or diffuse
- Enlargement can occur (Head Neck Pathol 2019;13:47)
- May be useful as a means for person identifications (J Forensic Odontostomatol 1991;9:17)
Diagnosis
- In some cases, the diagnosis may be presumed on clinical exam with corresponding historical information and radiographic features
- If the diagnosis cannot be made confidently on clinical exam, a biopsy is recommended for definitive diagnosis (Head Neck Pathol 2019;13:47)
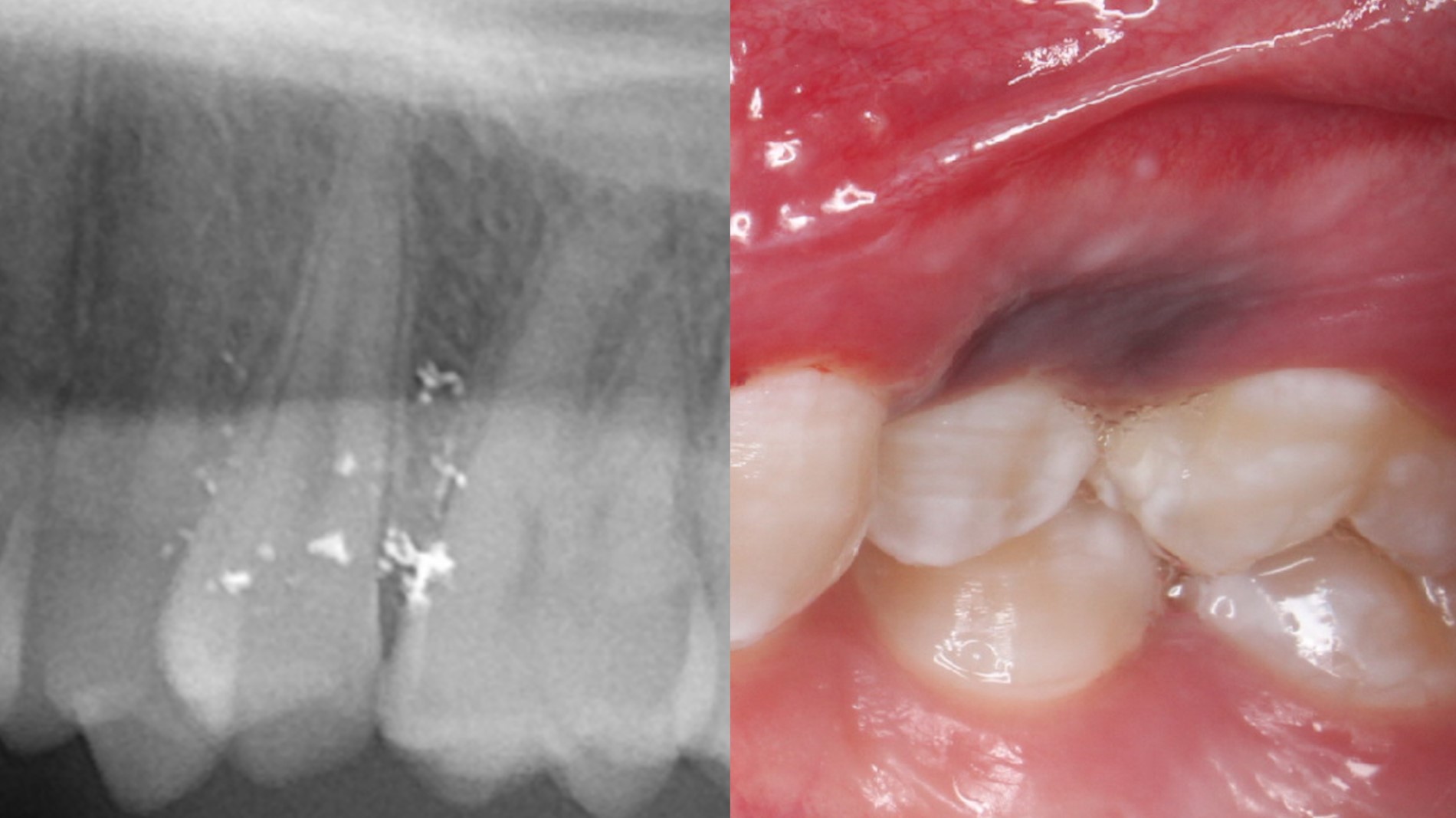
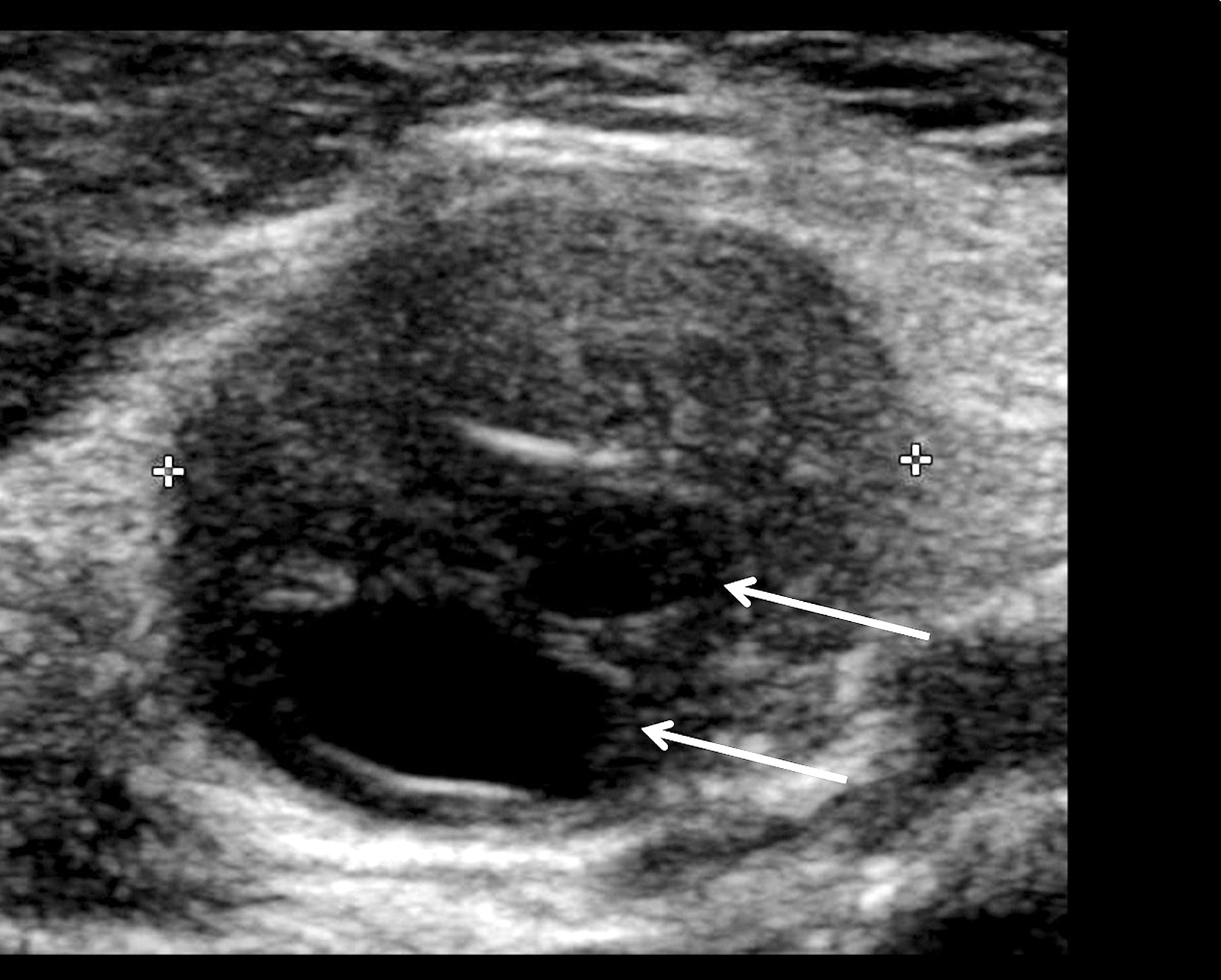
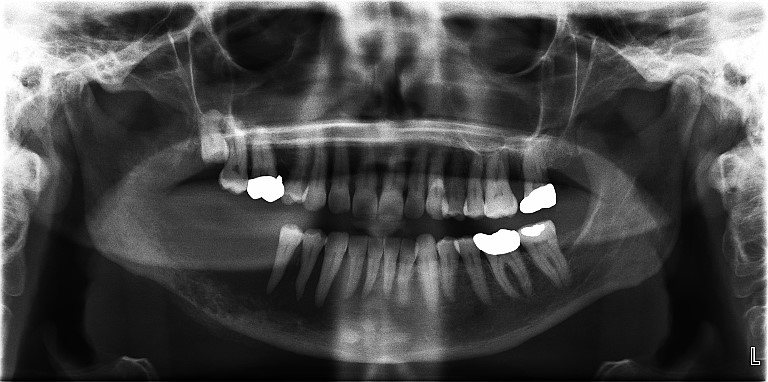
Radiology description
- Radiopaque fragments may be noted on radiographic exam if amalgam particles are large; however, this is not common
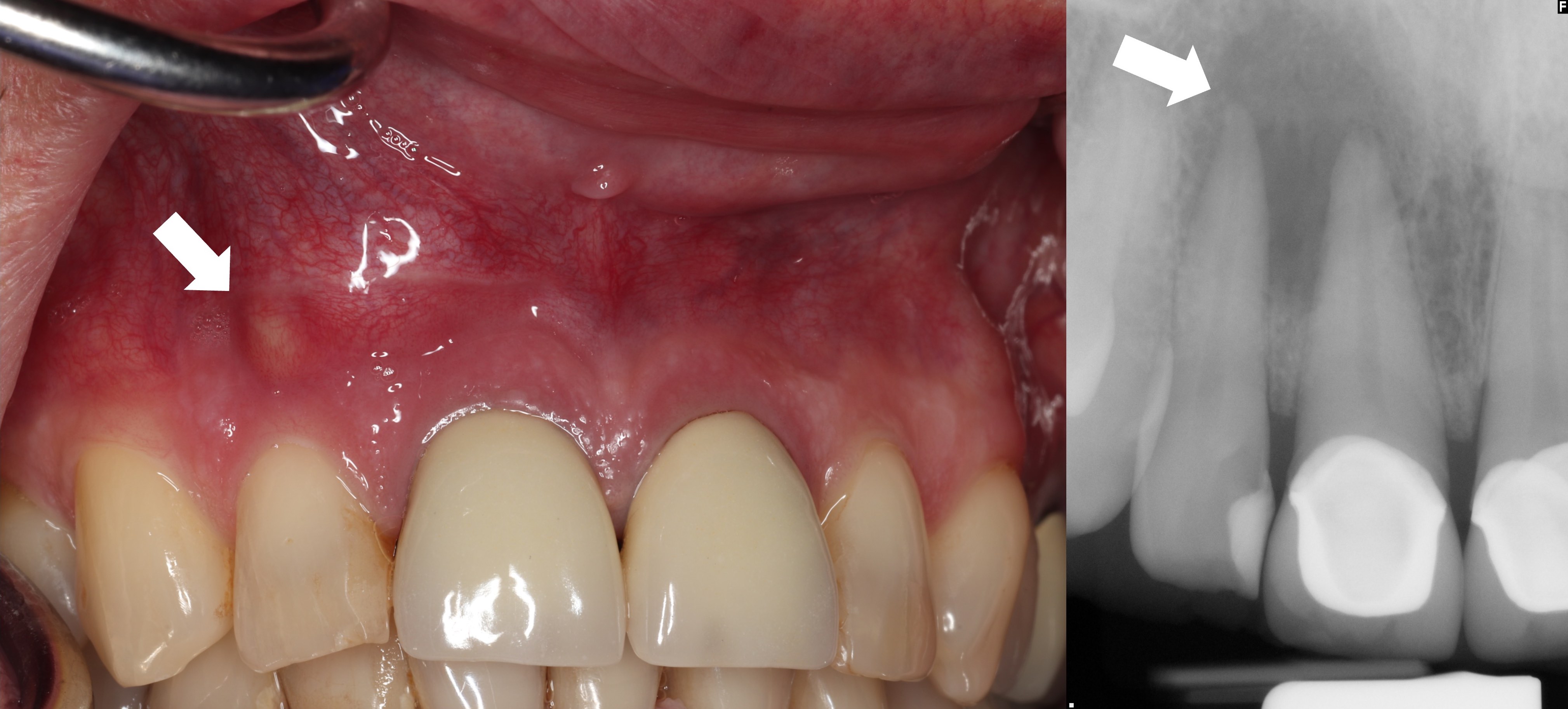
Radiology images
Prognostic factors
- Excellent prognosis
Case reports
- 38 year old woman with amalgam in mucoperiosteal flap from endodontic surgery (J Conserv Dent 2016;19:280)
- 49 year old woman with a brown-gray macule on the ventral tongue noted after dental restoration (N Engl J Med 2016;374:e21)
- 53 year old man with black macule on alveolar ridge and remote history of tooth extraction (Indian J Med Res 2018;148:240)
Treatment
- No treatment is needed once diagnosis is established
- Conservative surgical excision can be recommended for esthetic concerns, especially for the anterior maxilla (J Esthet Restor Dent 2020;32:770)
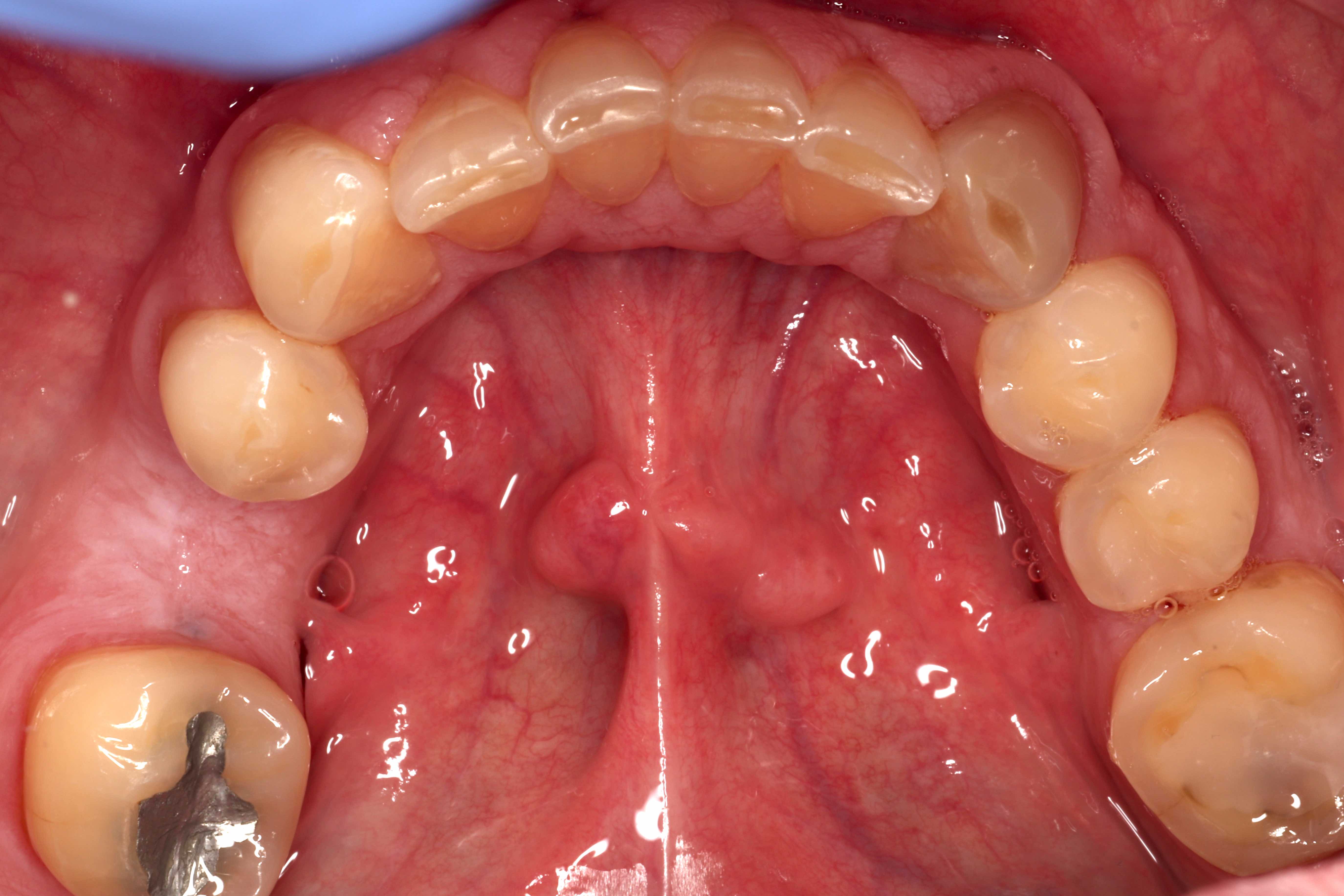
Clinical images
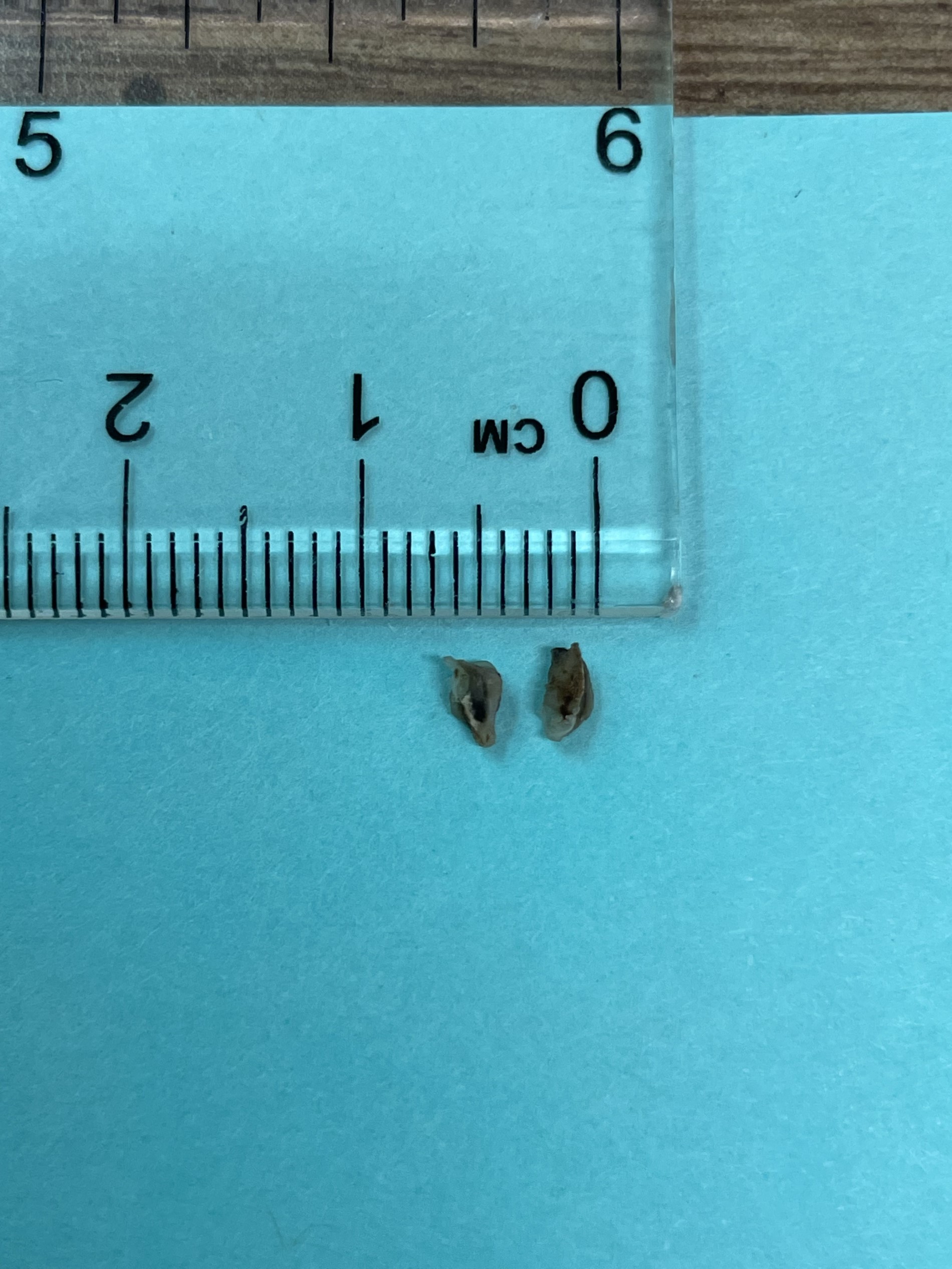
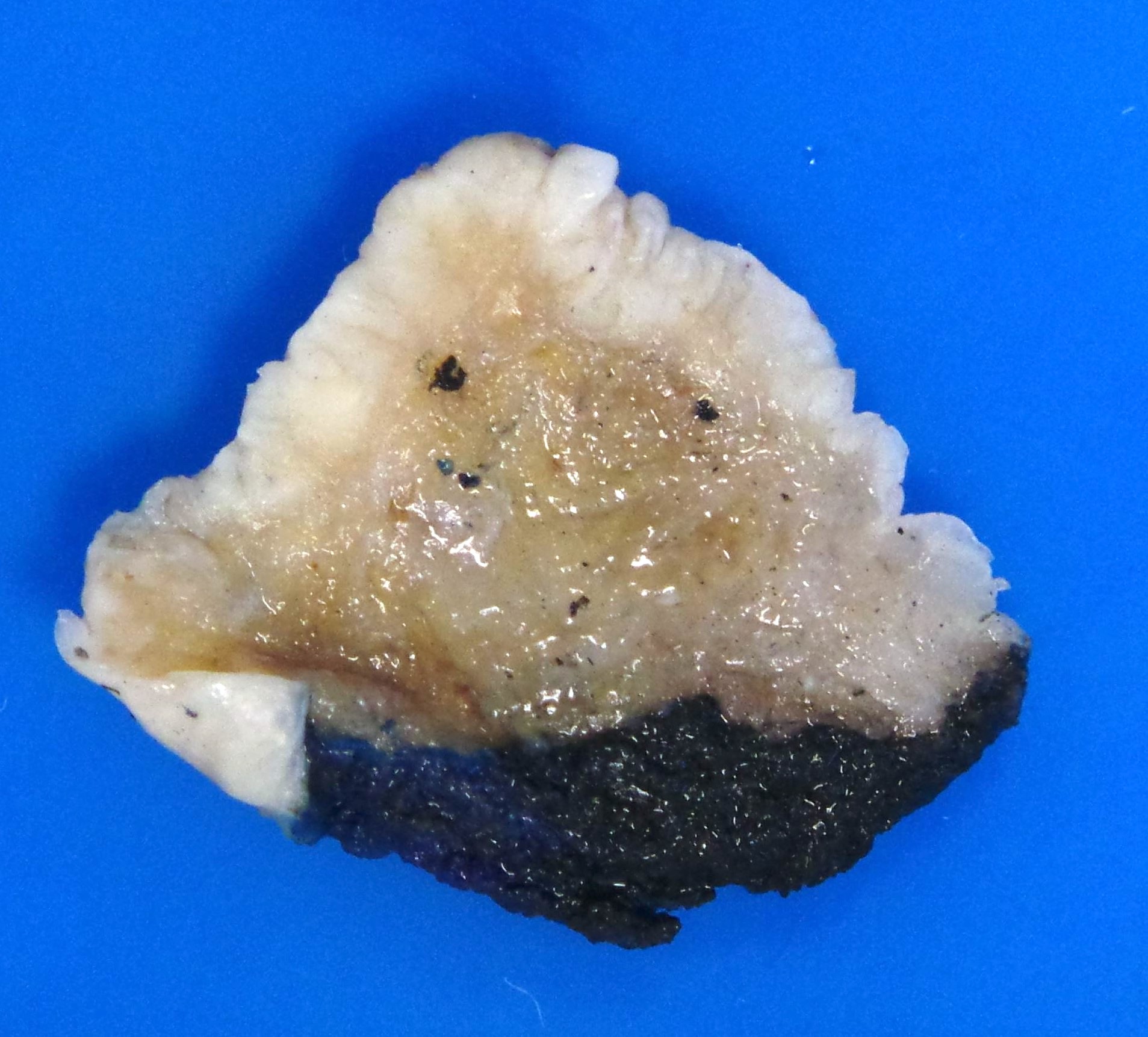
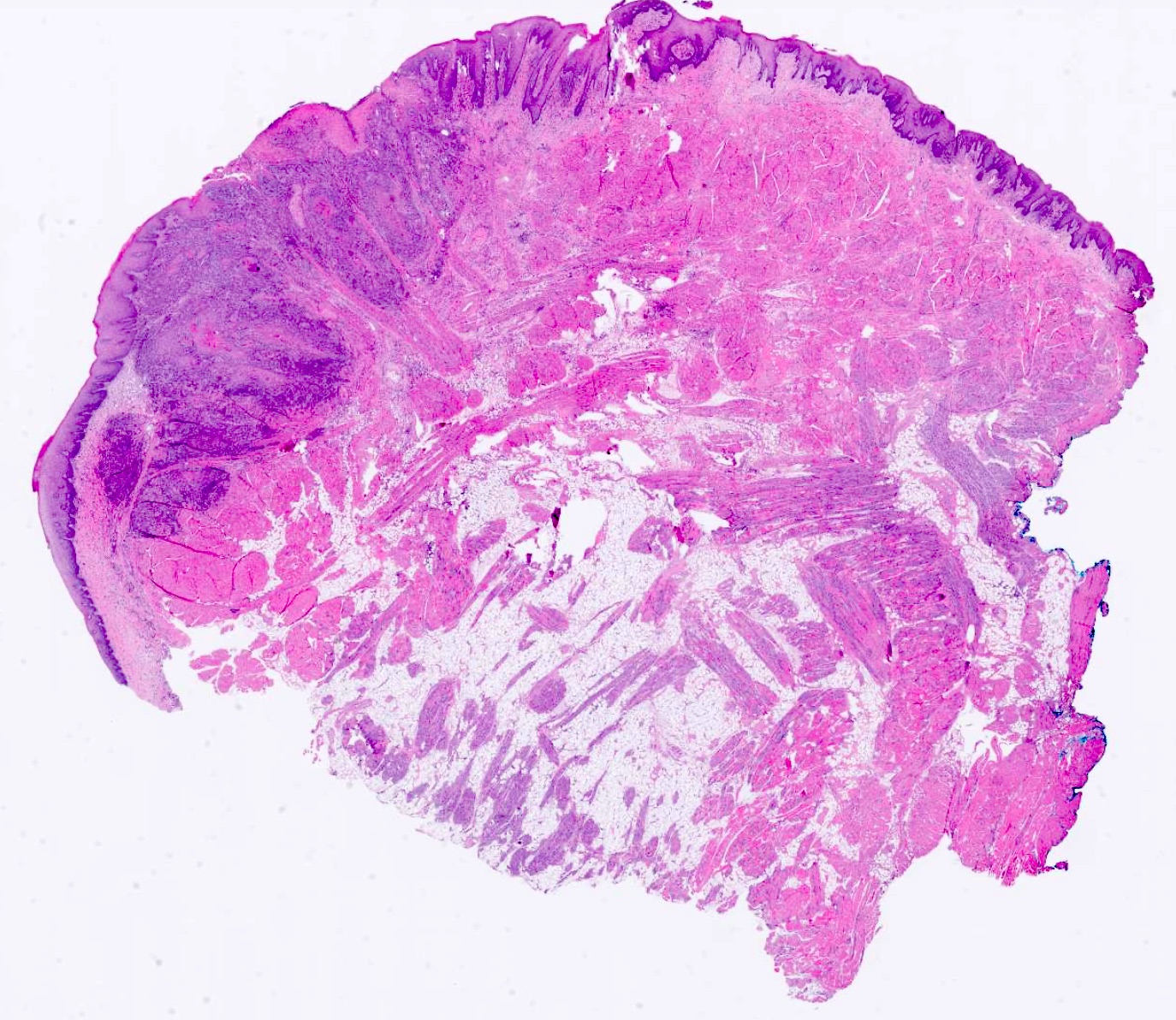
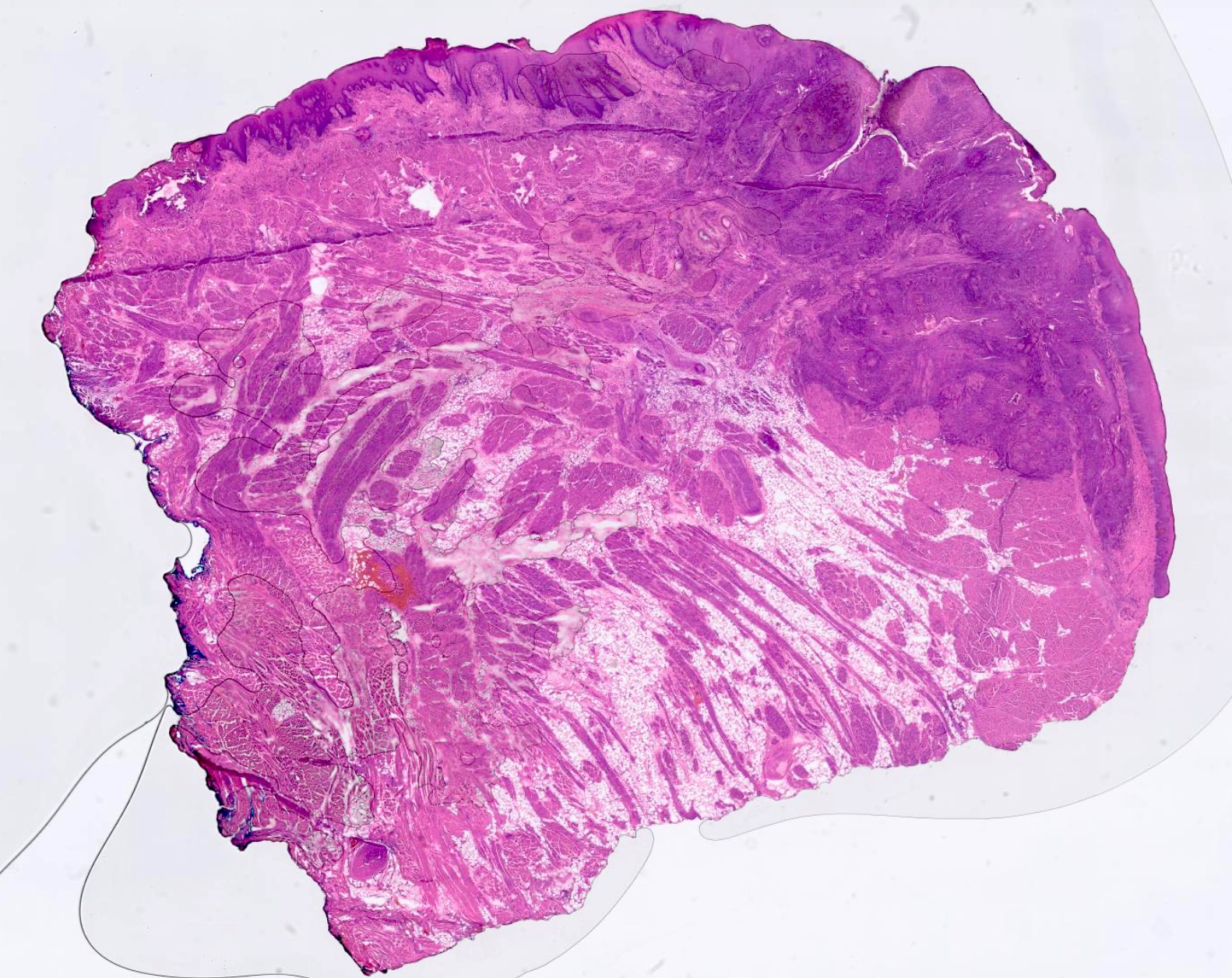
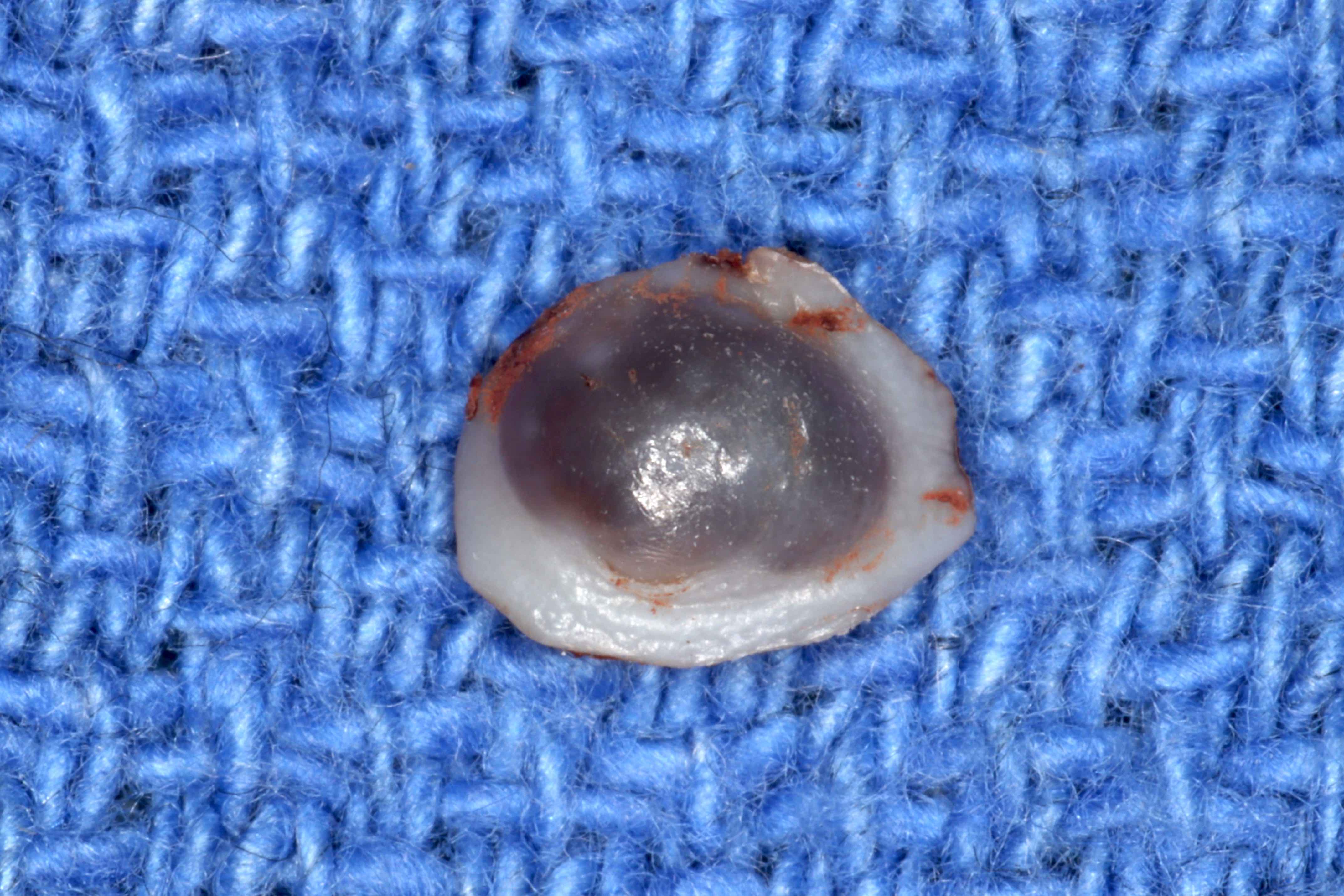
Gross description
- Well defined or diffuse black, gray or blue pigmentation in connective tissue on cross section
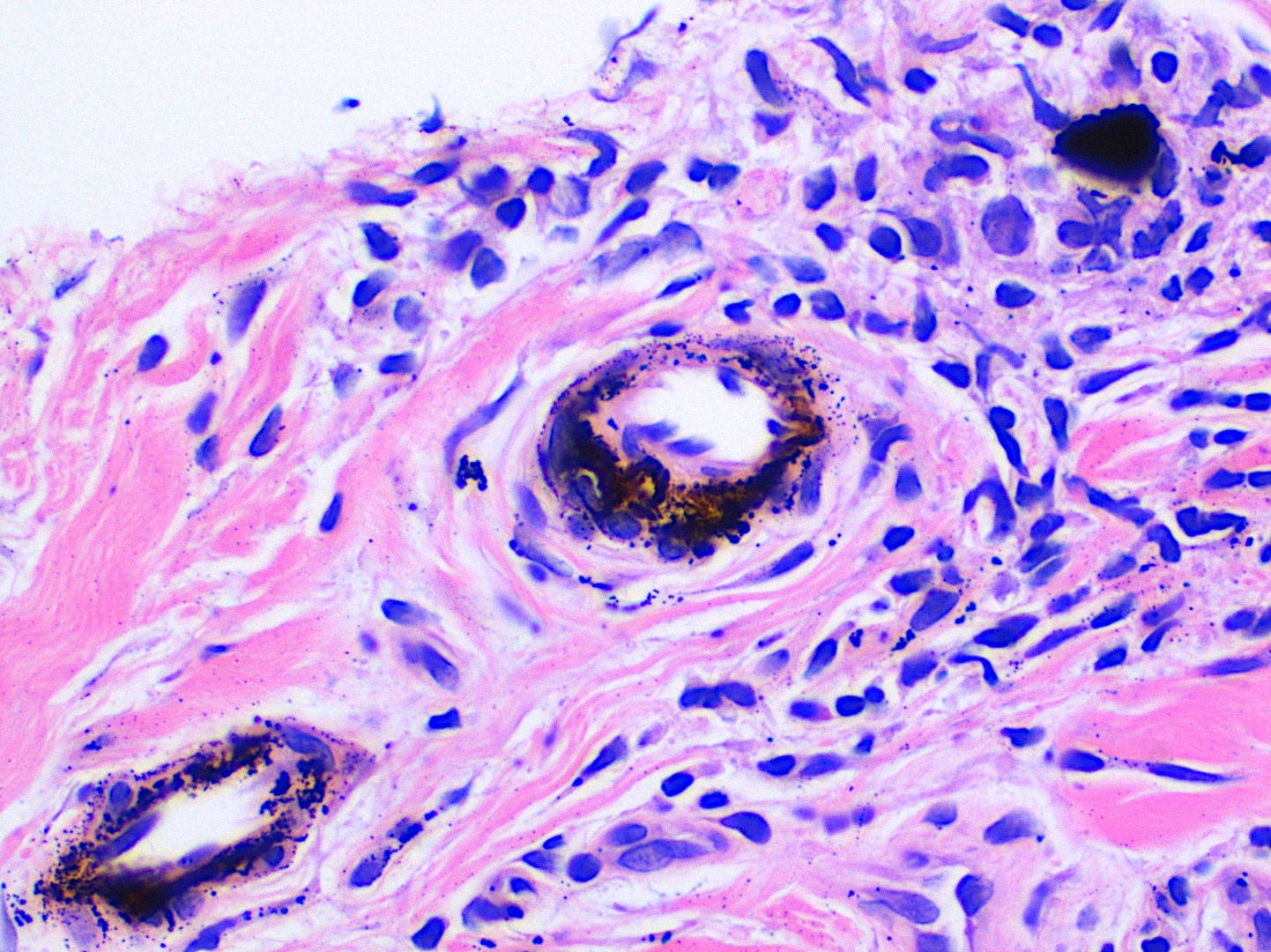
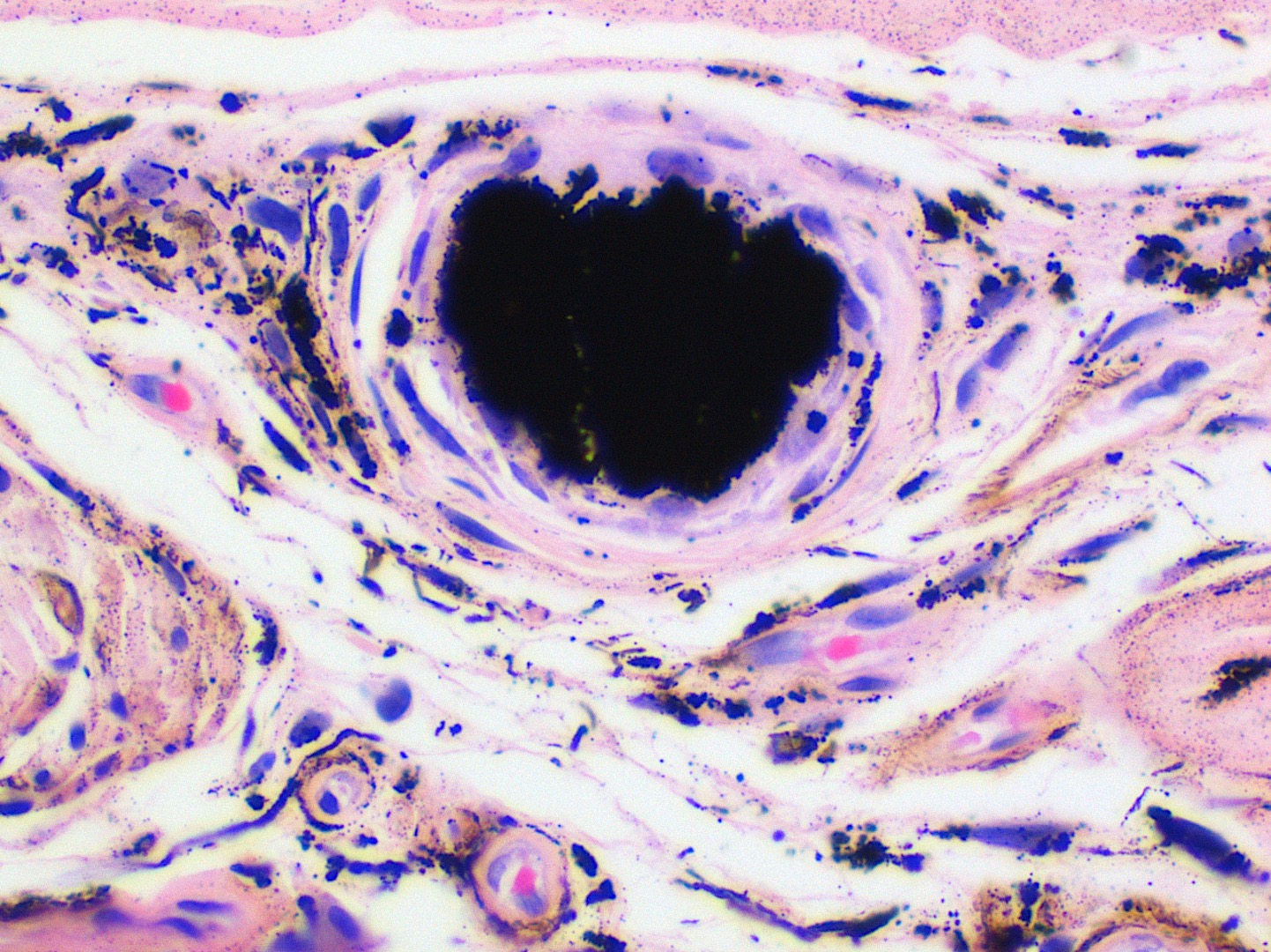
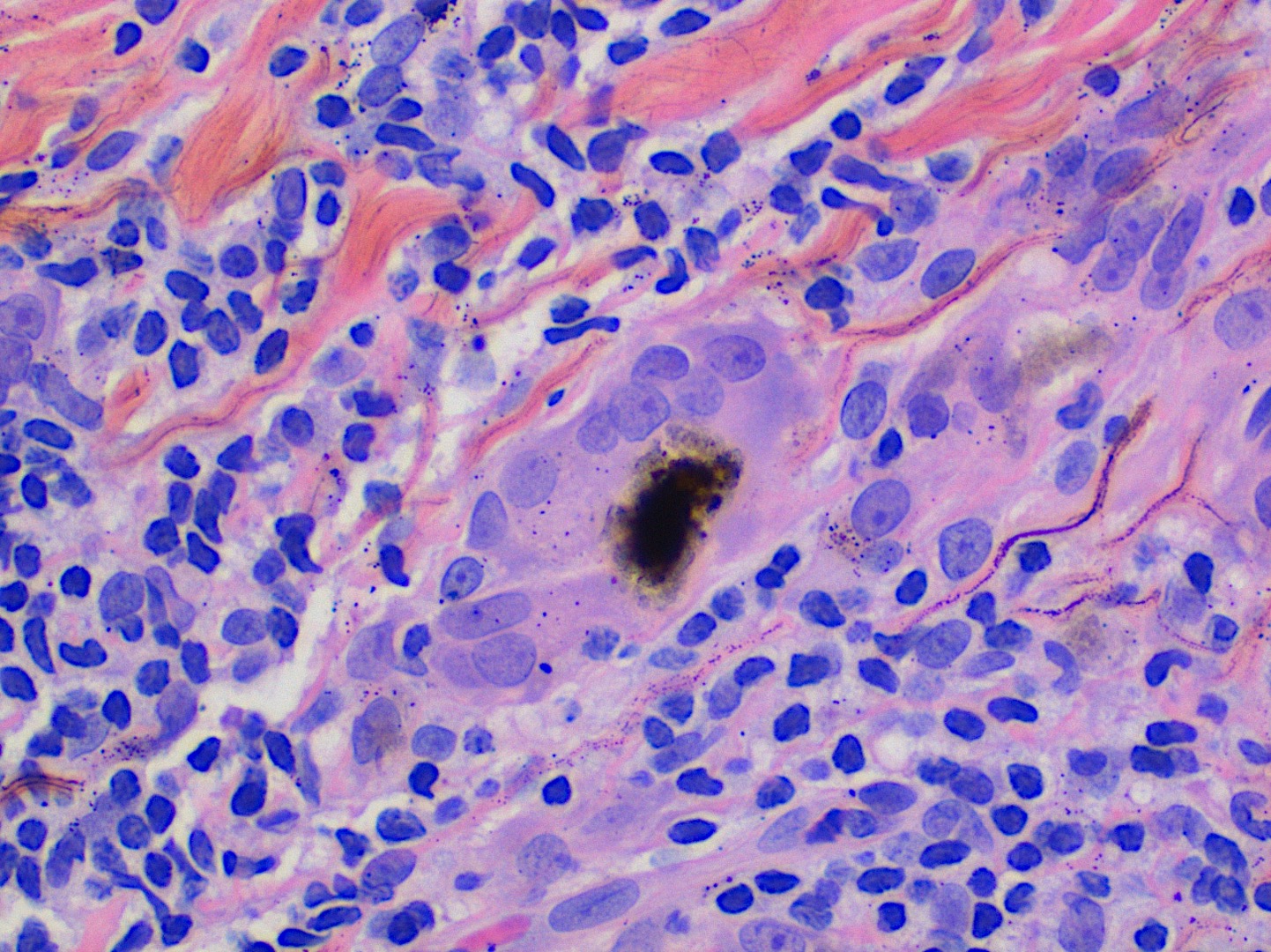
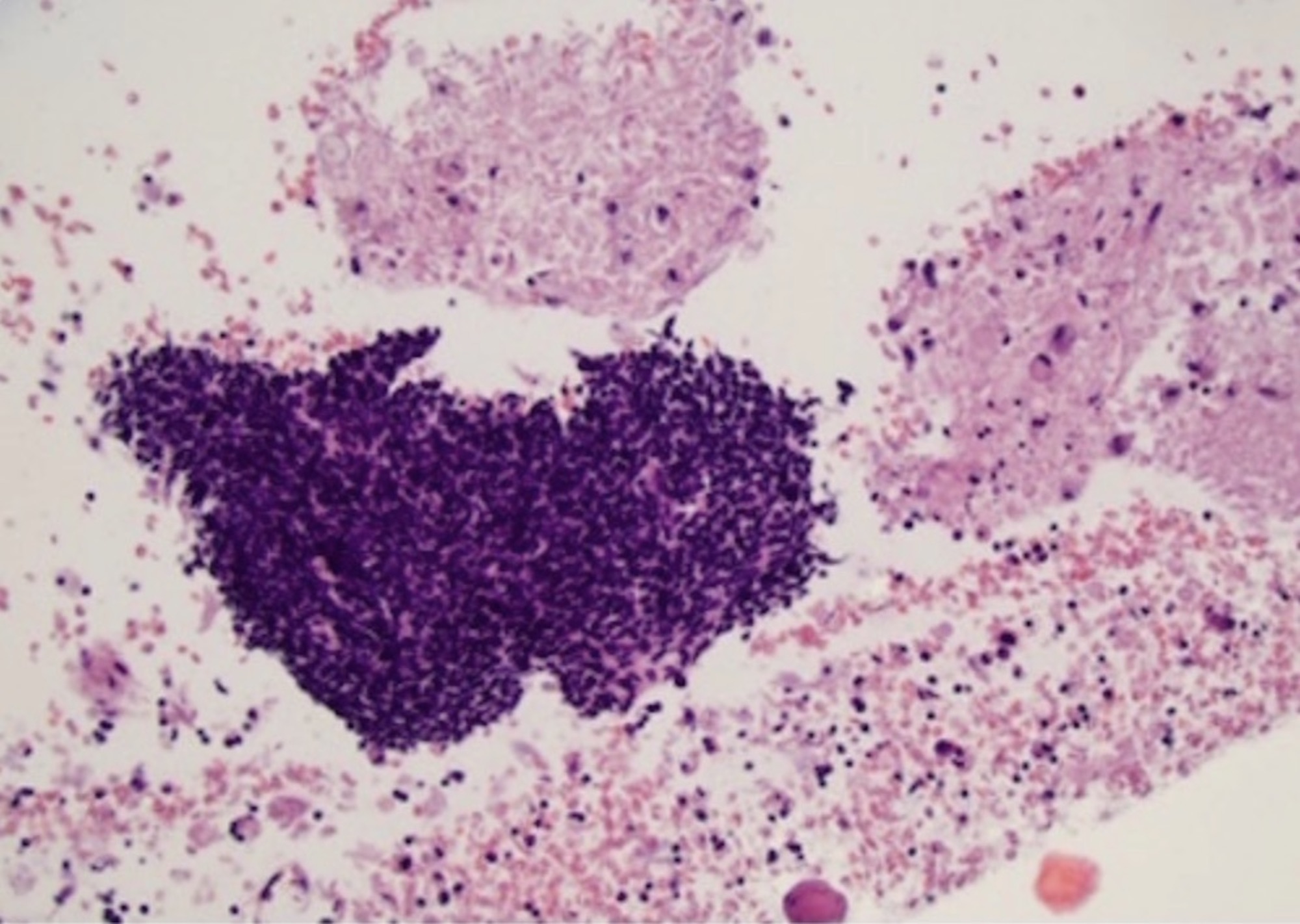
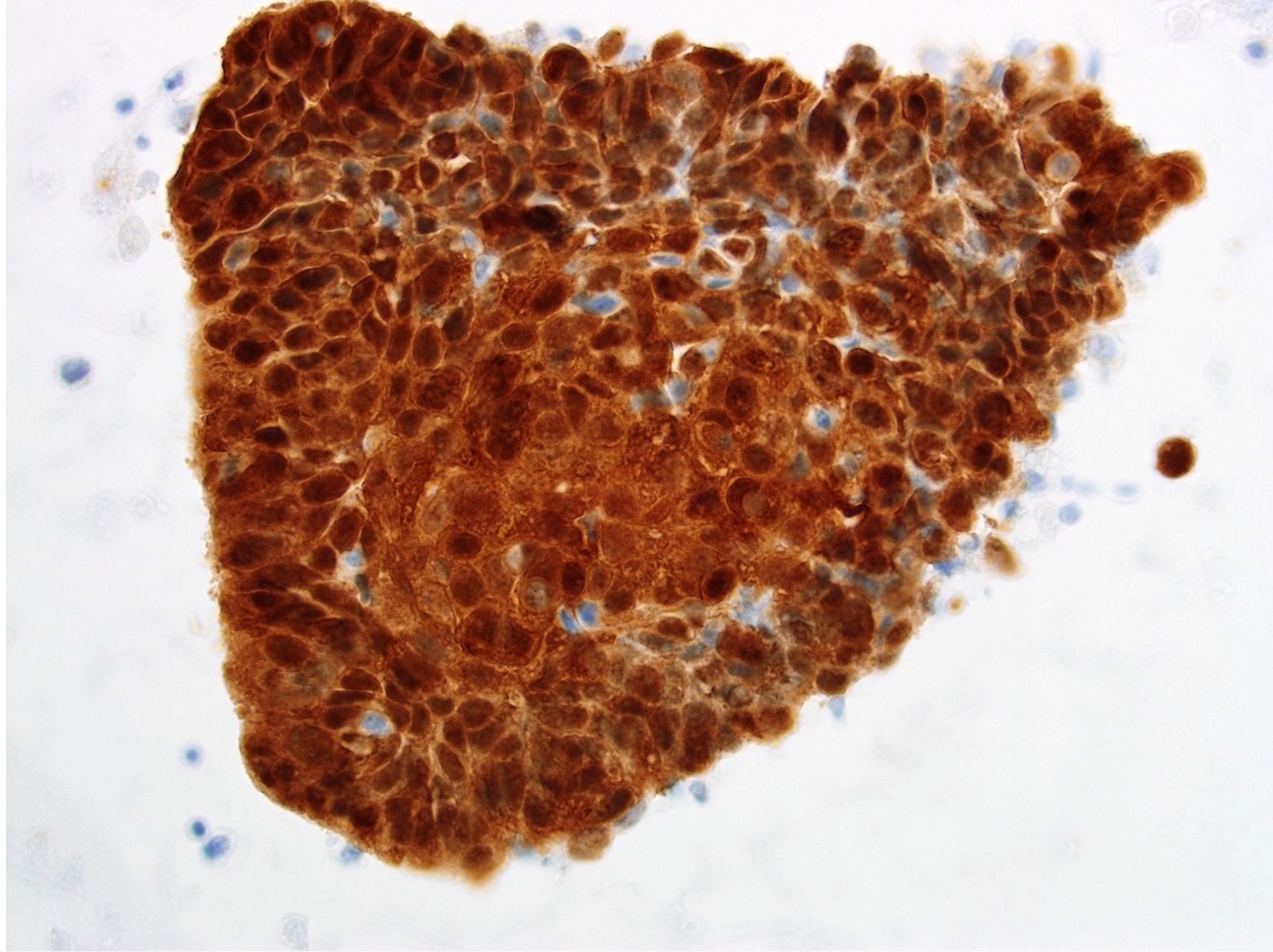
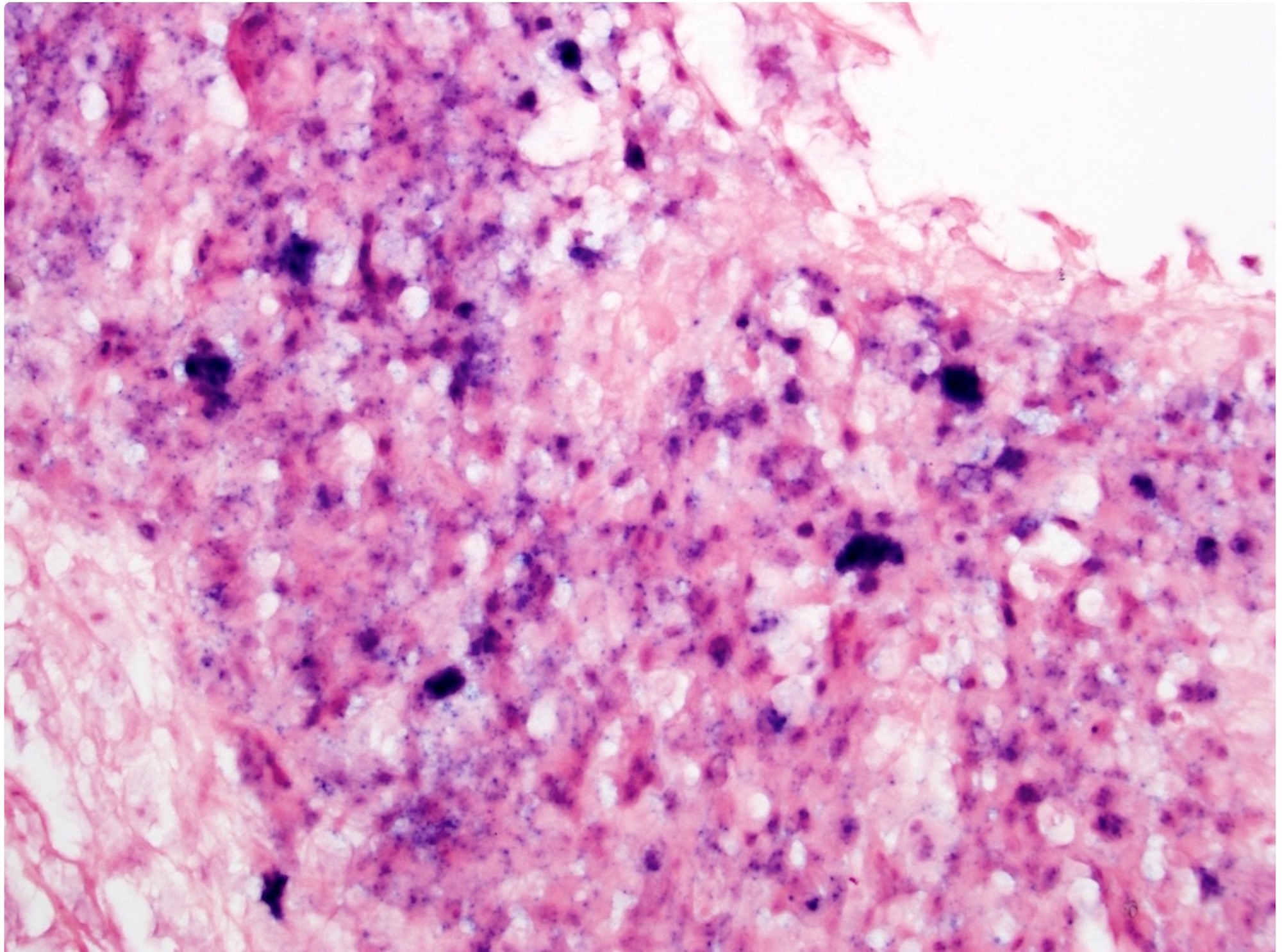
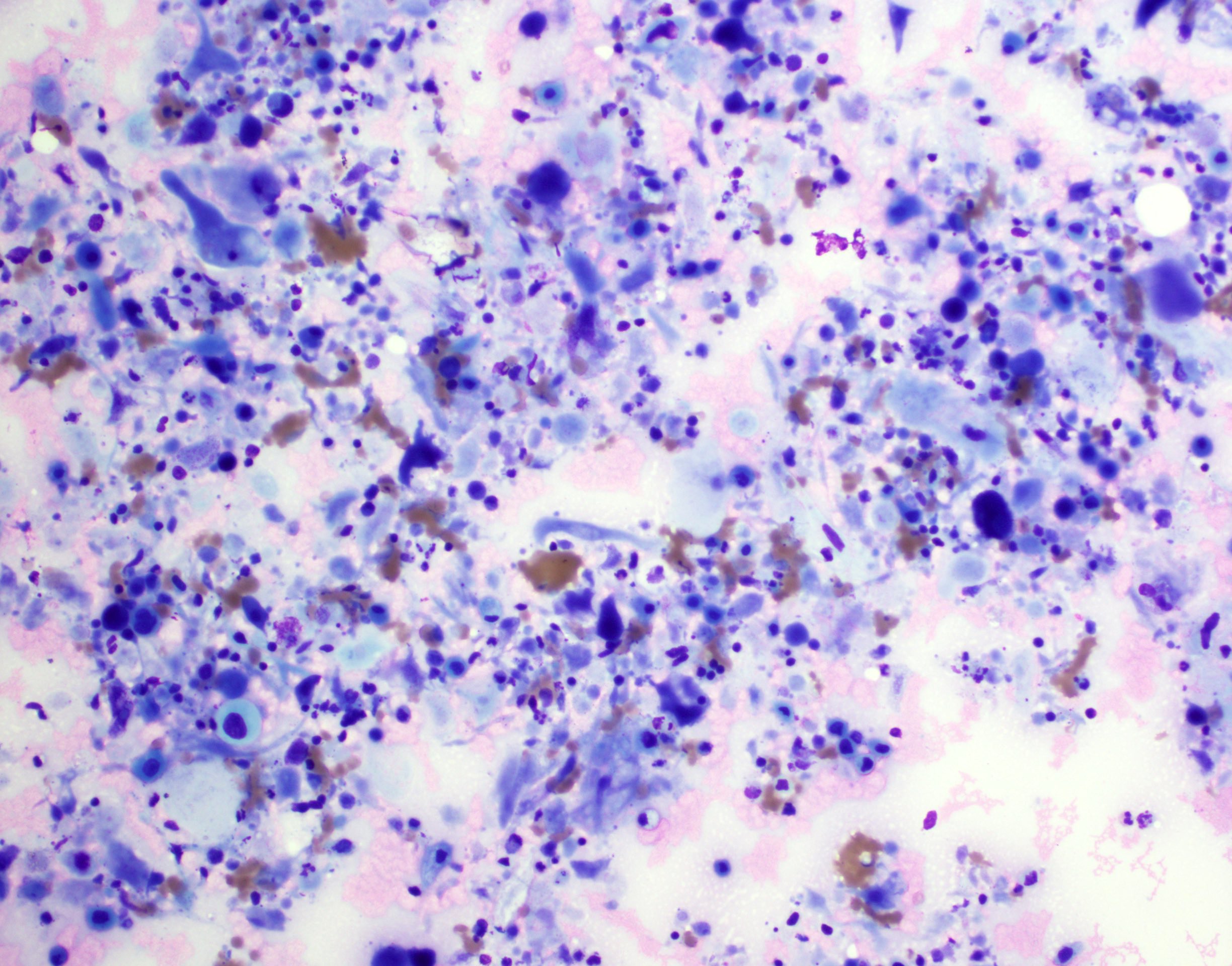
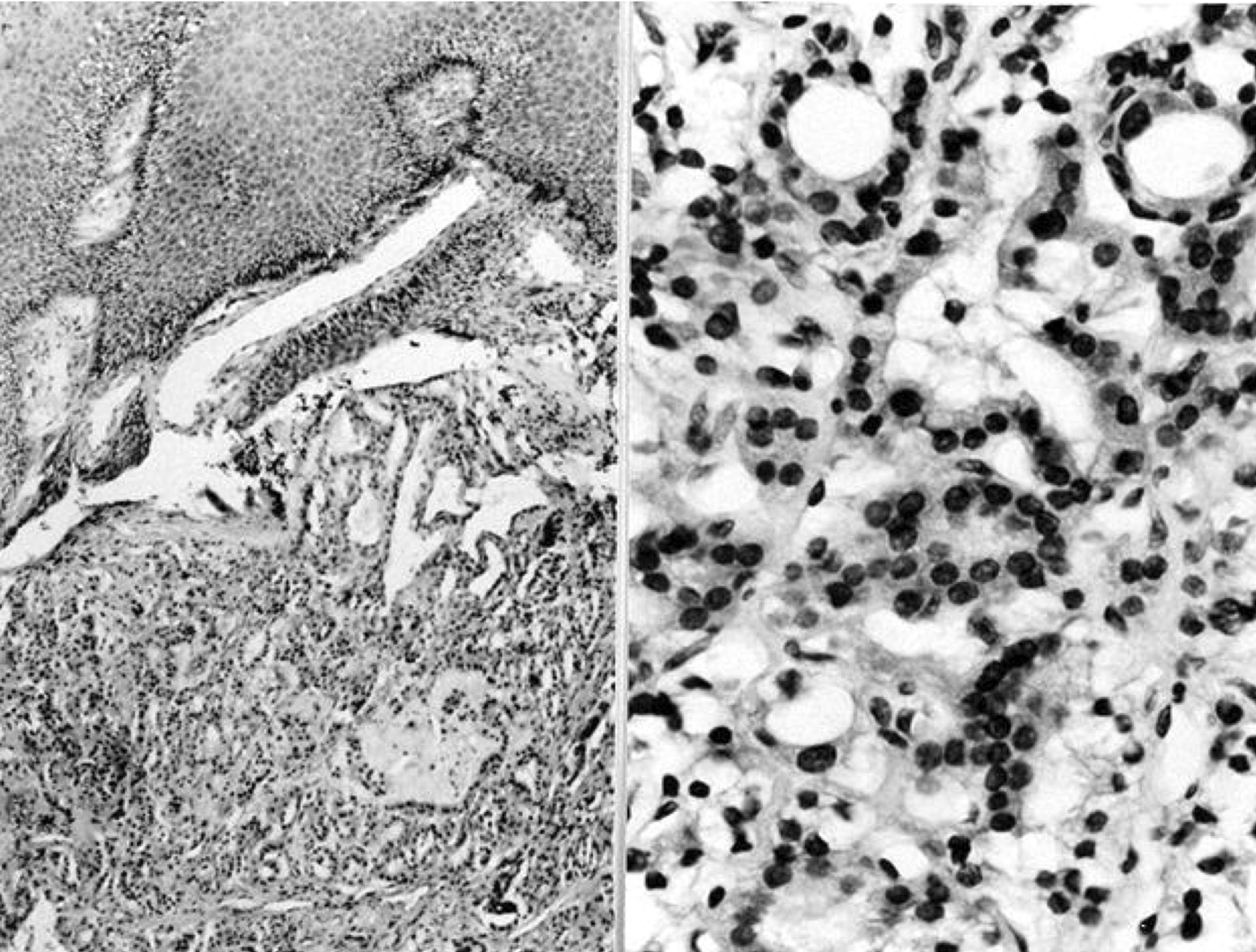
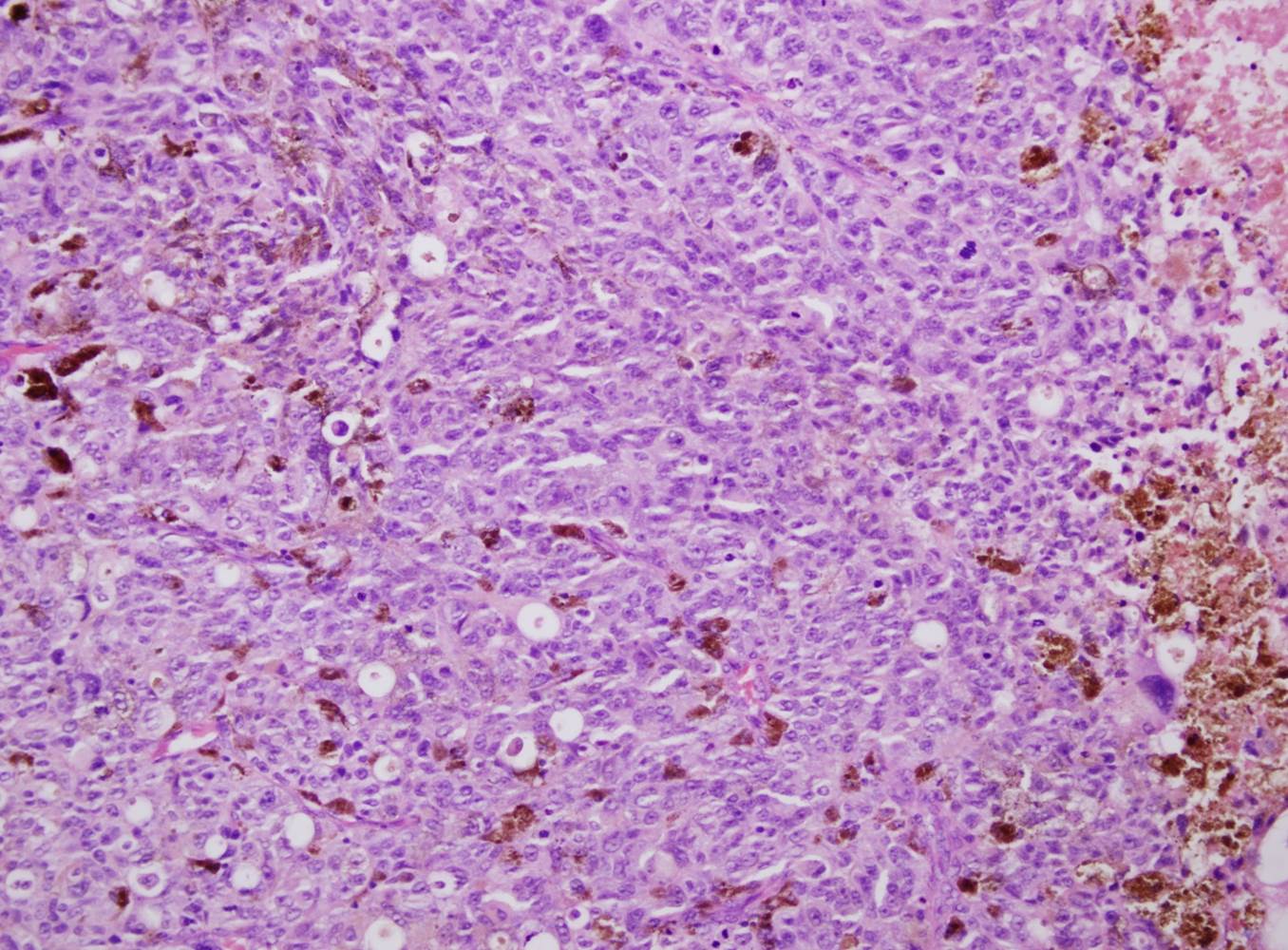
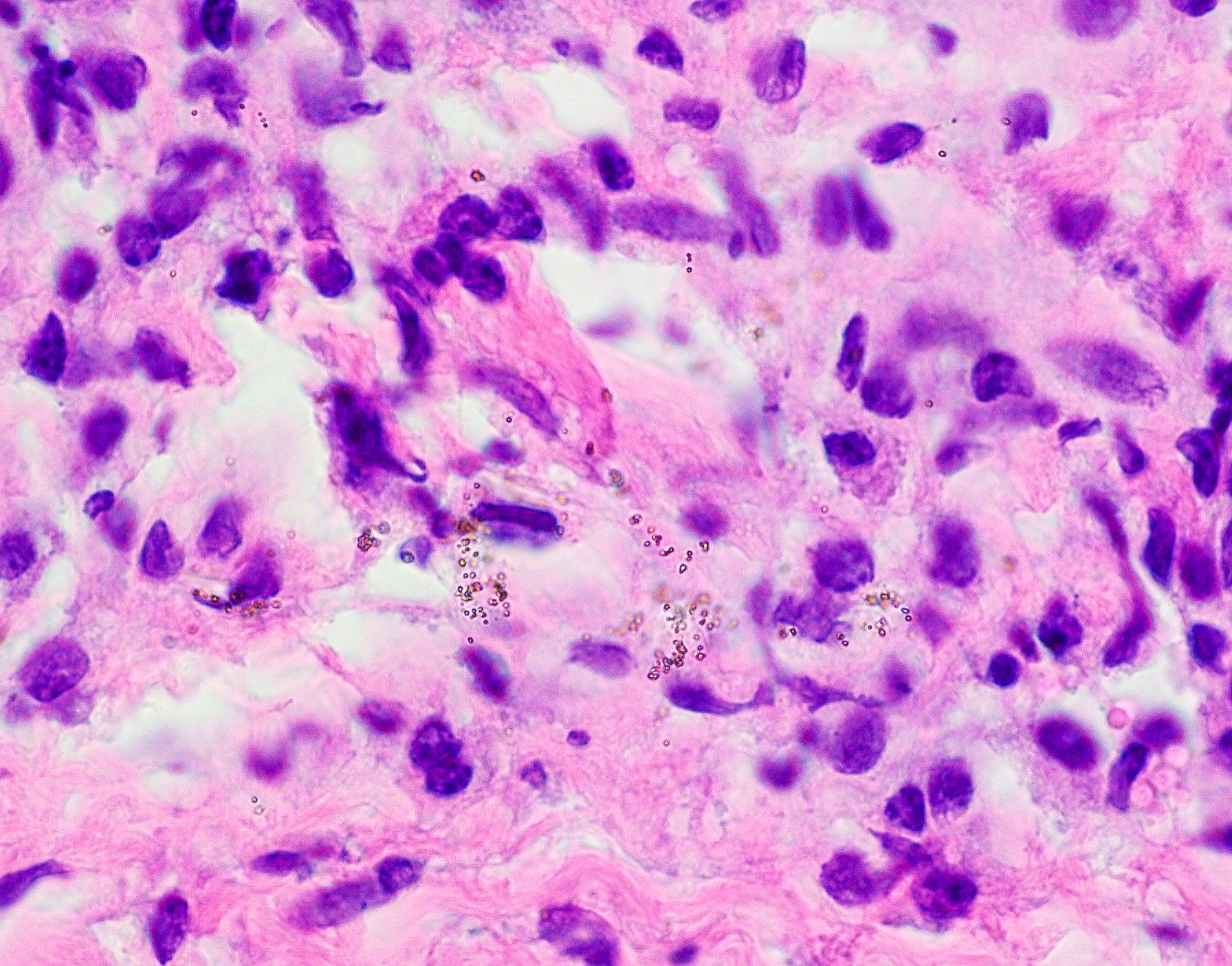
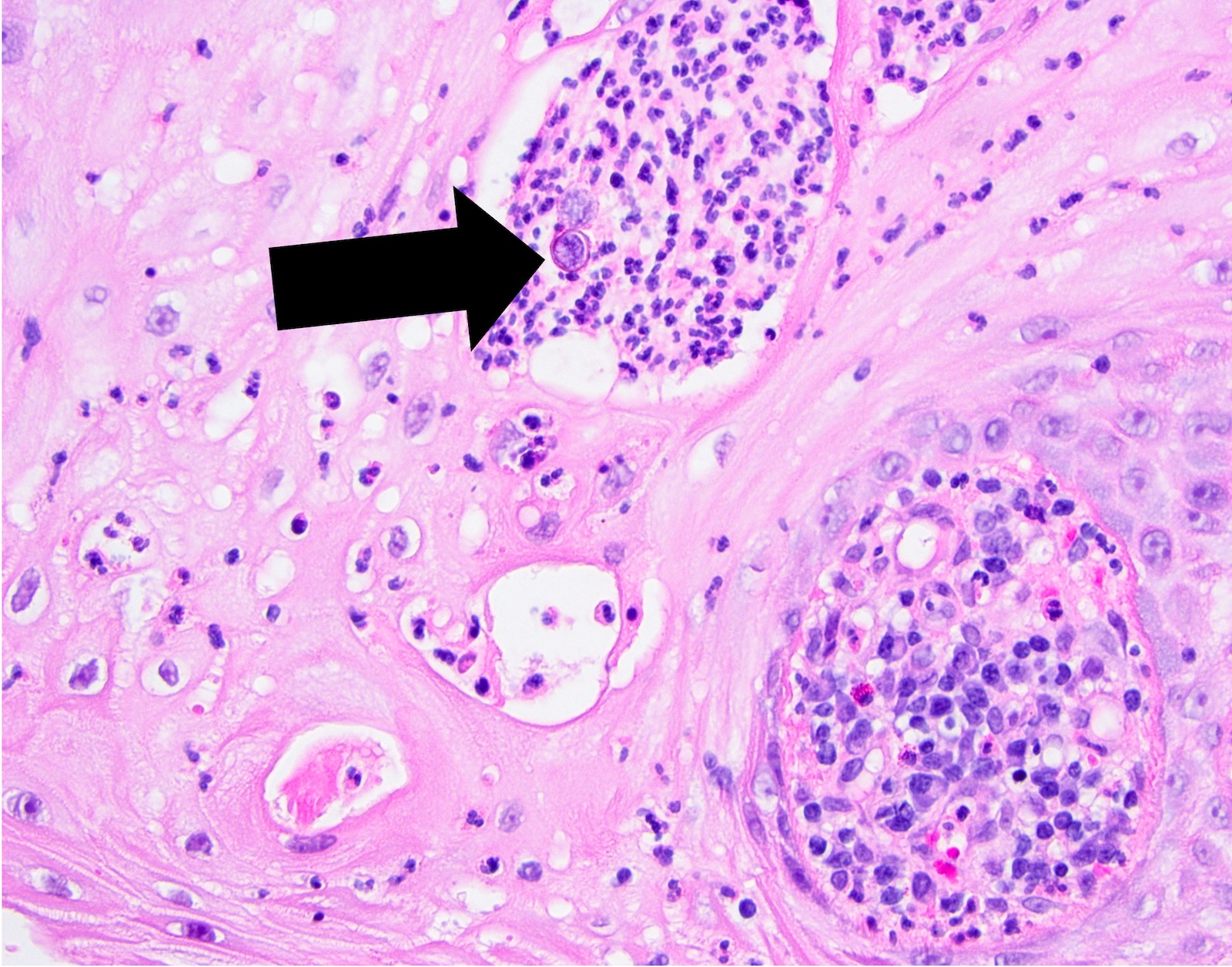
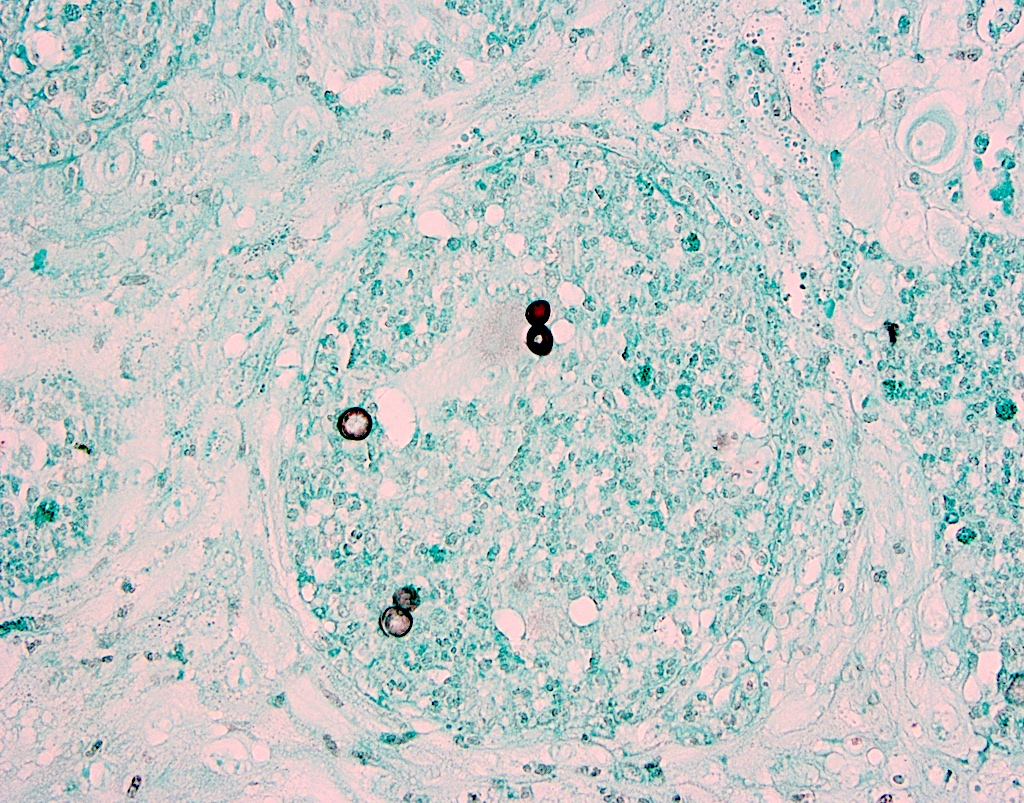
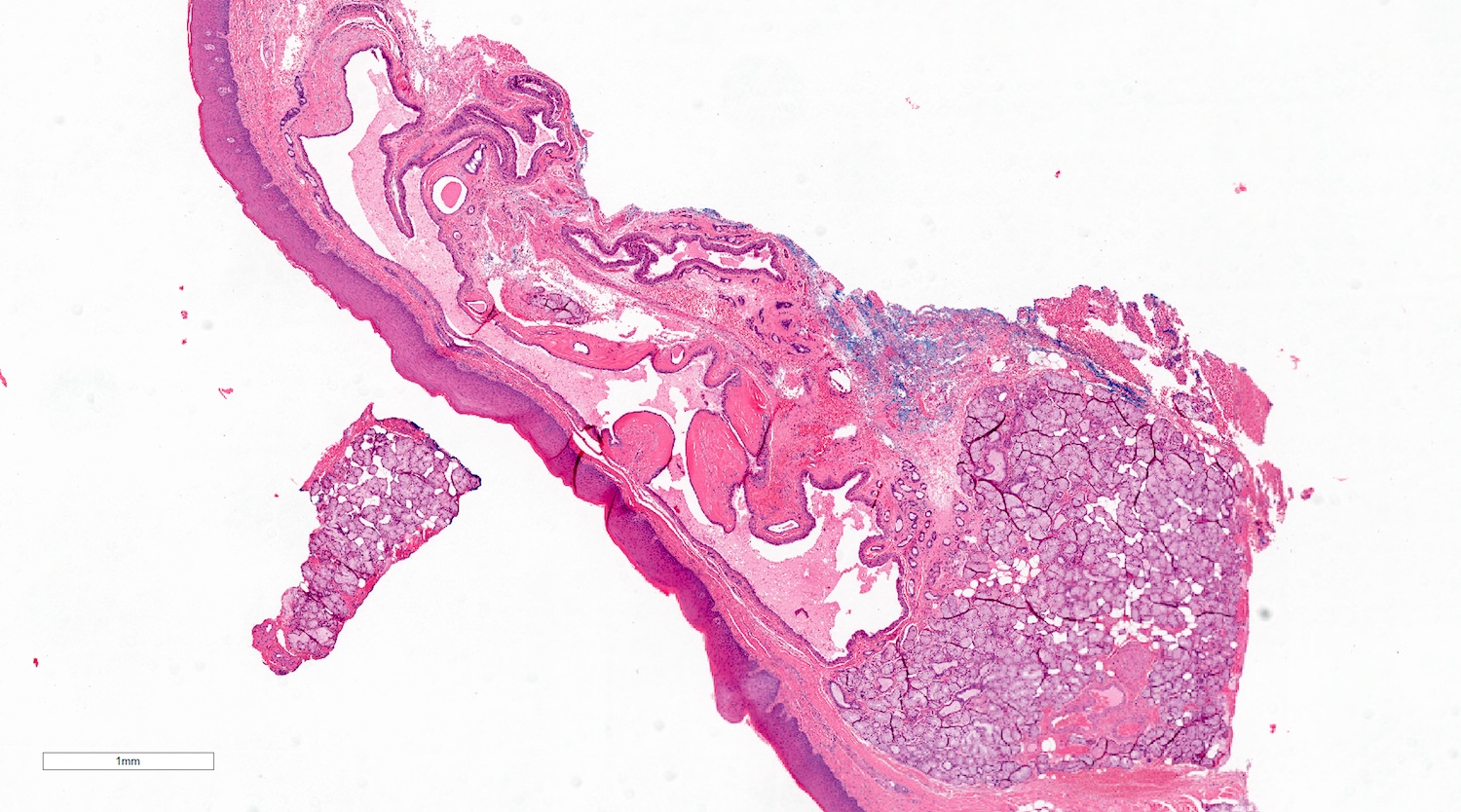
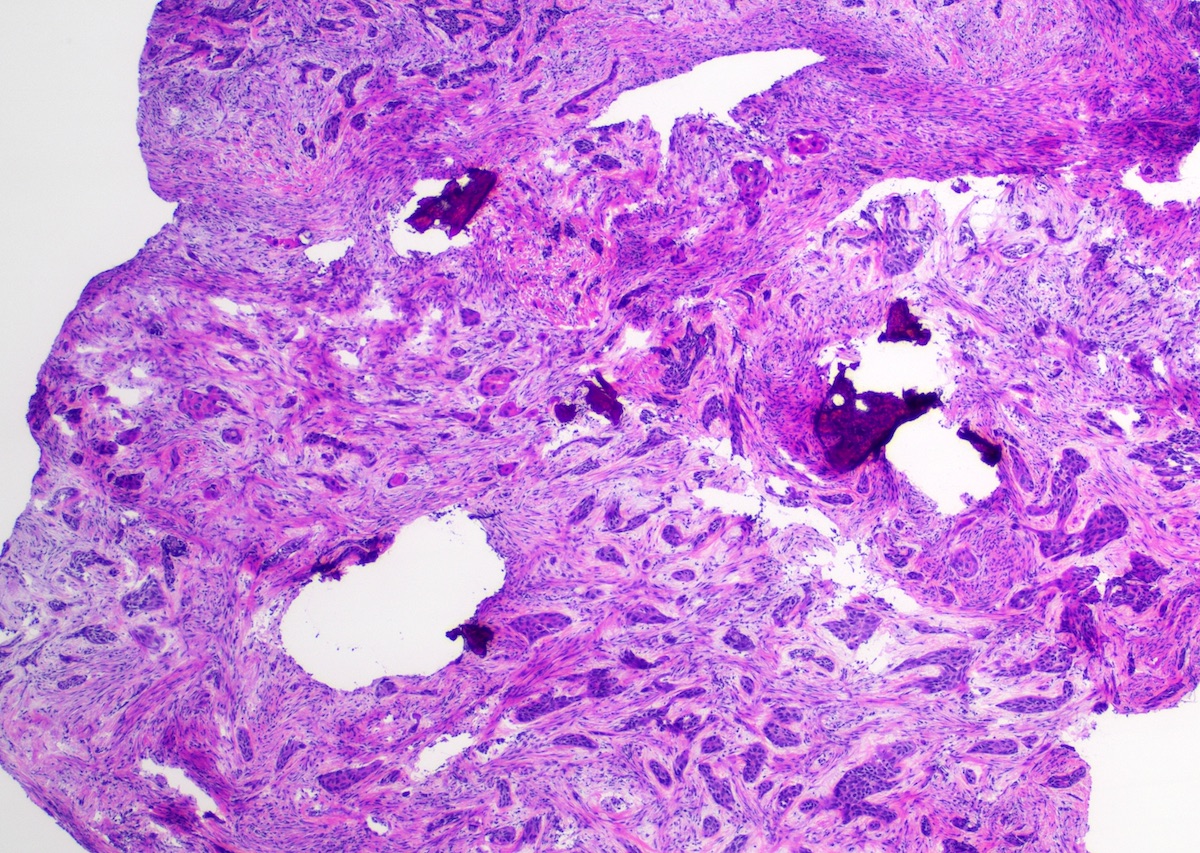
Microscopic (histologic) description
- Large black deposits of foreign material with or without a chronic inflammatory response in the connective tissue
- Fine black granules in the connective tissue; may demonstrate affinity for reticulin fibers (Head Neck Pathol 2019;13:47)
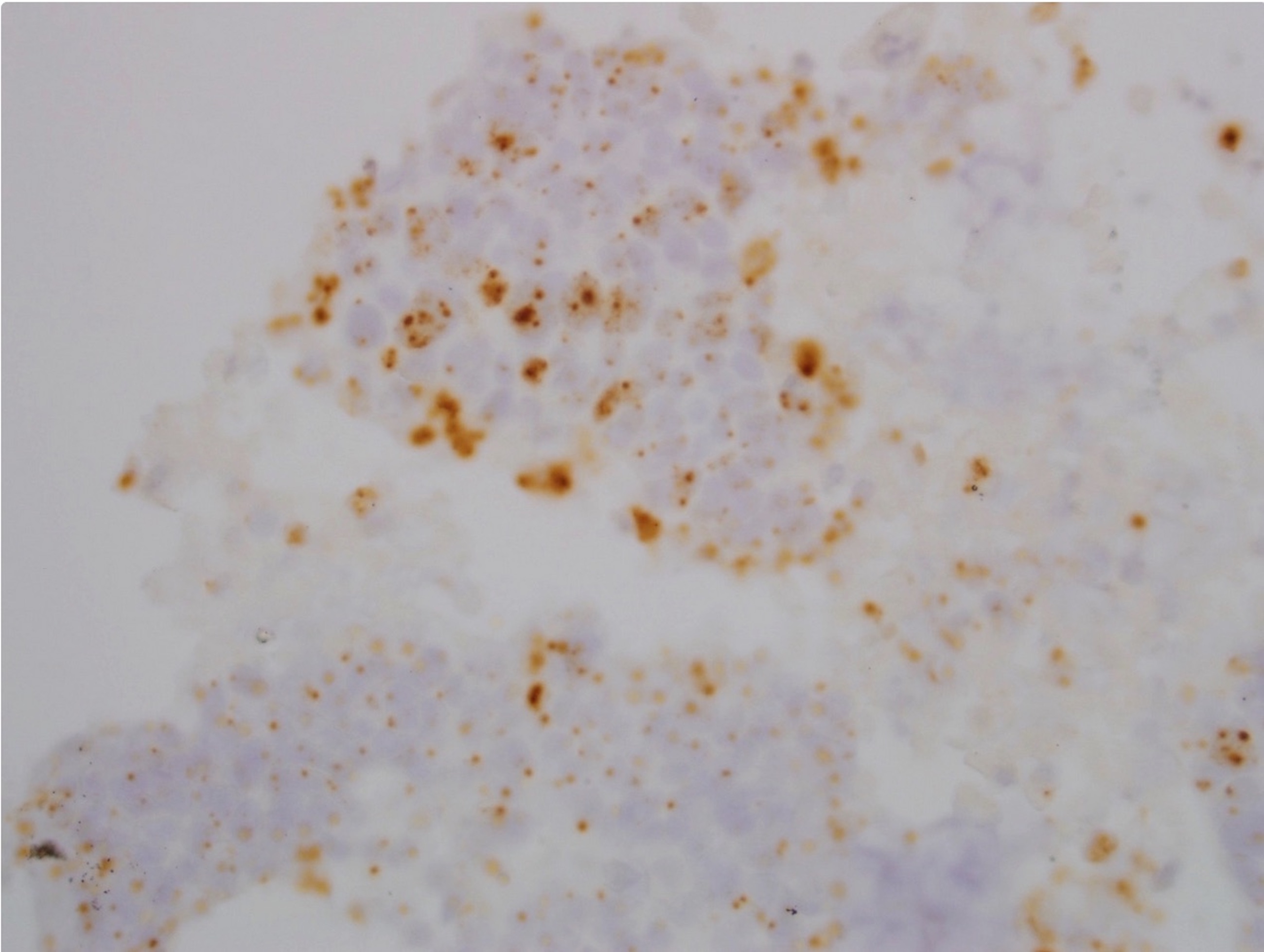
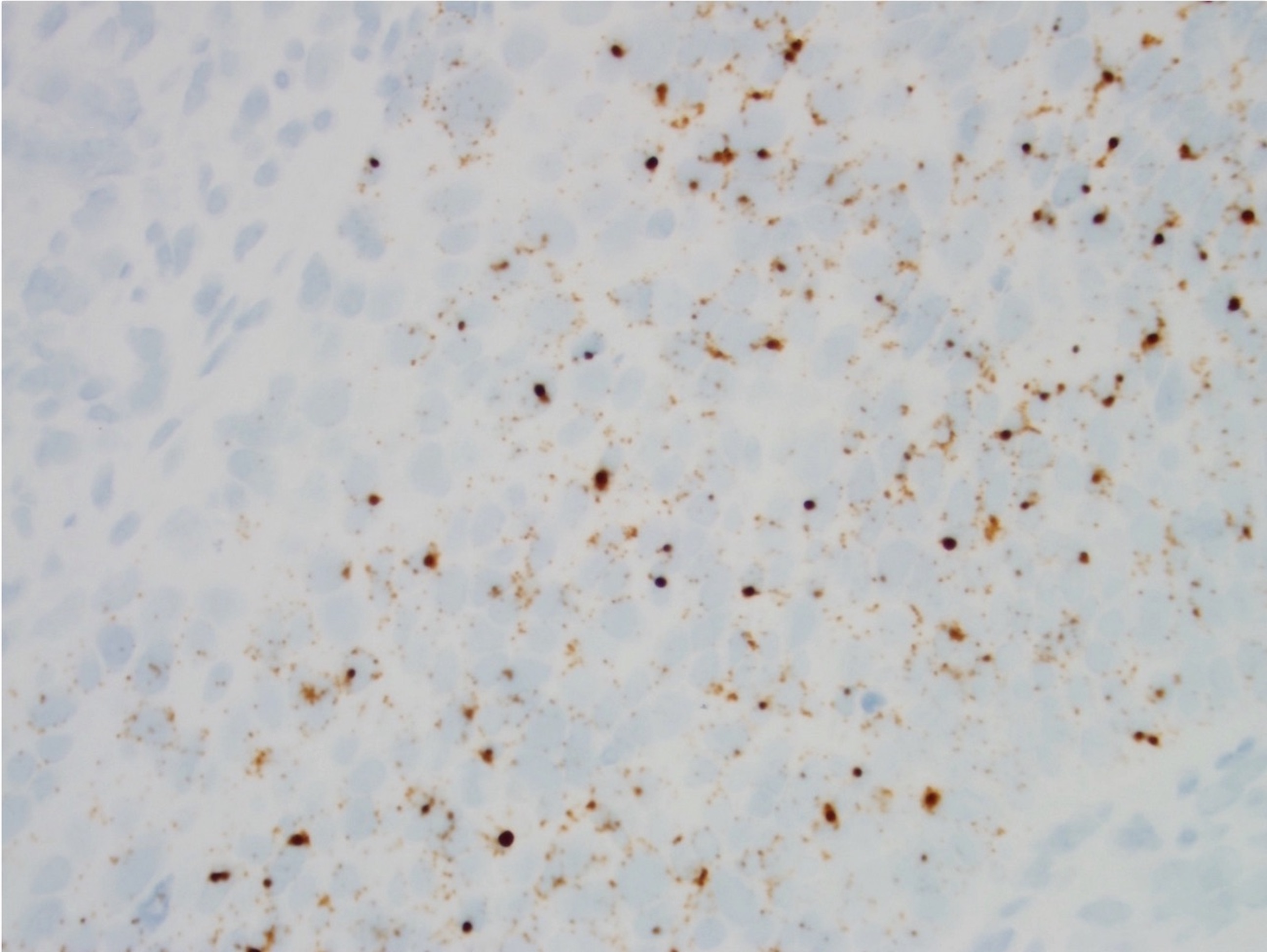
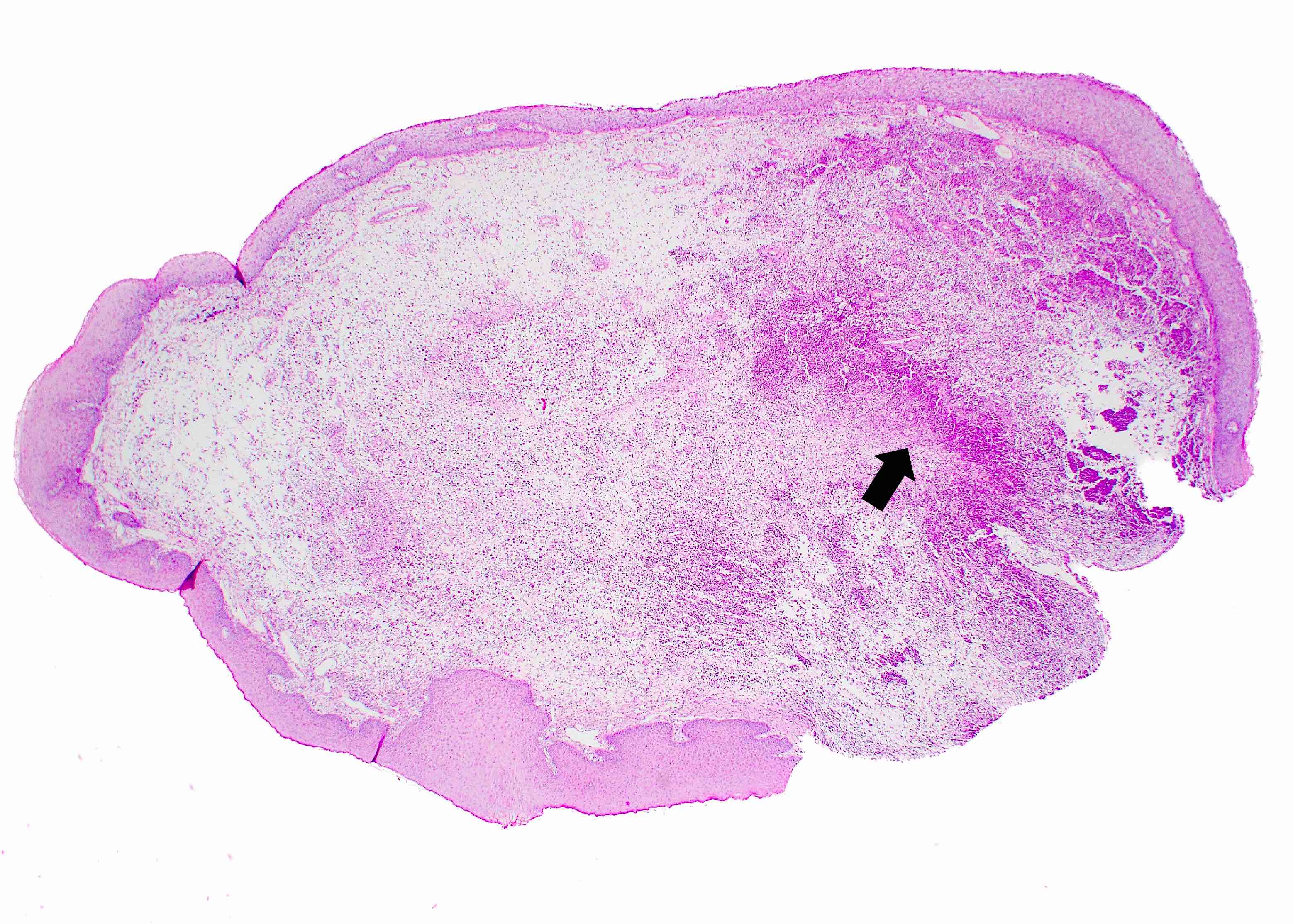
Microscopic (histologic) images
Sample pathology report
- Oral cavity, excisional biopsy:
- Foreign body tattoo (see comment)
- Comment: The histopathology and clinical information are consistent with an amalgam tattoo.
Differential diagnosis
- Oral melanotic macule:
- Increased melanin in basal cell layer of the epithelium with melanin incontinence in the superficial connective tissue
- Multifocal presentation may be seen in a systemic disease, such as Addison disease or Peutz-Jegher syndrome (Head Neck Pathol 2019;13:47)
- Foreign body tattoo or other exogenous material:
- Intentional tattoo pigment (shown above)
- Graphite from pencil (Dermatol Online J 2015;21:13030)
- Drug related discolorations:
- Depending on the drug, histopathology features mimic those of melanotic macule or brown-yellow granules in connective tissue (Head Neck Pathol 2019;13:47)
- Submucosal hemorrhage:
- Hemosiderin in the connective tissue from trauma
- Positive Prussian blue
Additional references
Board review style question #1
Board review style answer #1
A. Amalgam tattoo. Although all answer choices can result in pigmented macules in the oral cavity, amalgam is the only exogenous material. This foreign material has a particular affinity for reticulin fibers and can be seen around blood vessels.
Comment Here
Reference: Amalgam tattoo
Comment Here
Reference: Amalgam tattoo
Board review style question #2
What is the etiology of an amalgam tattoo from the oral cavity?
- Drug related discoloration
- Iatrogenic implantation of dental filling material
- Increased melanin production
- Trauma induced hemosiderin deposition
Board review style answer #2
B. Iatrogenic implantation of dental filling material. A dental professional may inadvertently implant amalgam, an exogenous foreign material, into the oral mucosa during a dental procedure.
Comment Here
Reference: Amalgam tattoo
Comment Here
Reference: Amalgam tattoo
Anatomy & histology
Table of Contents
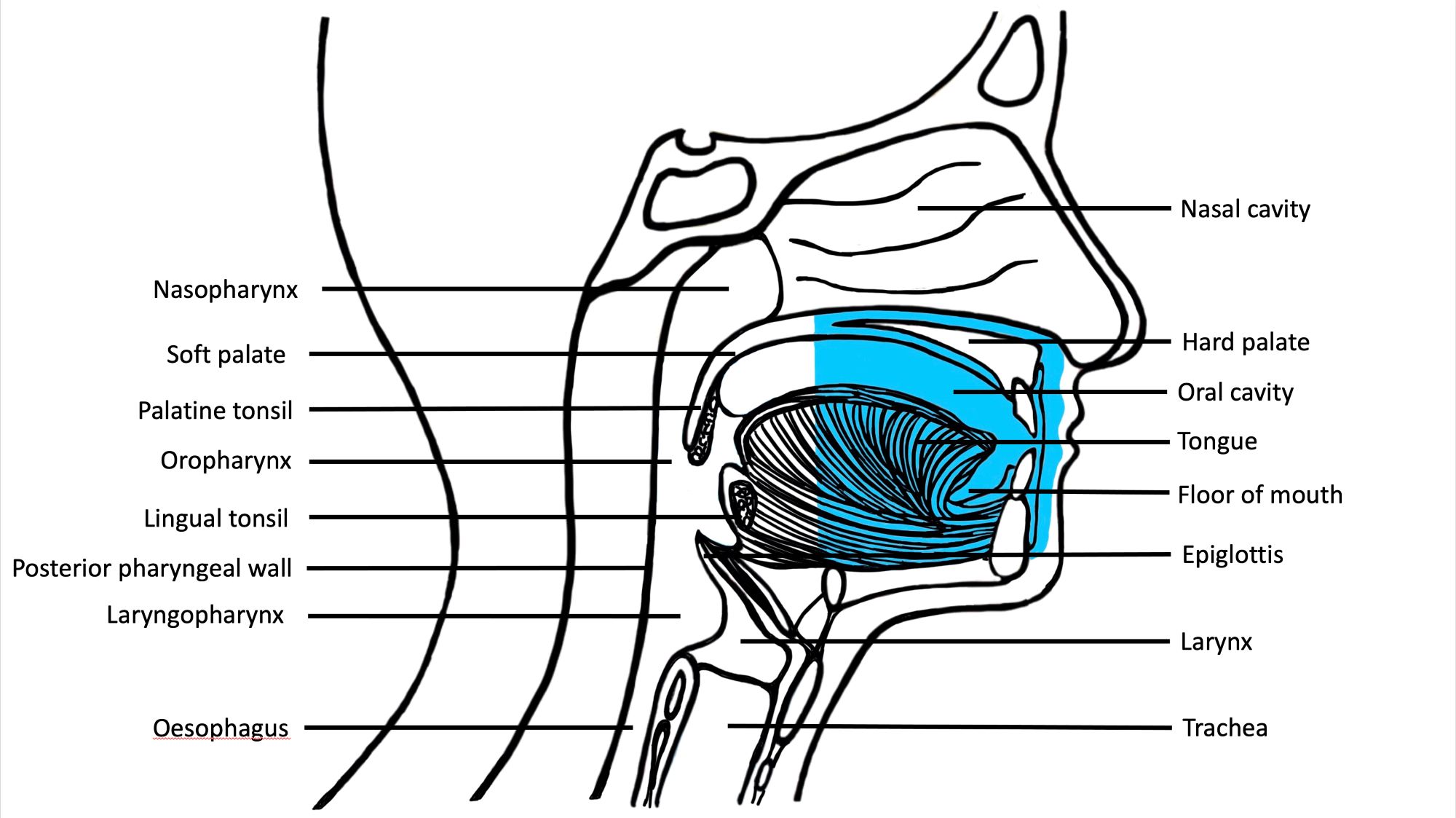
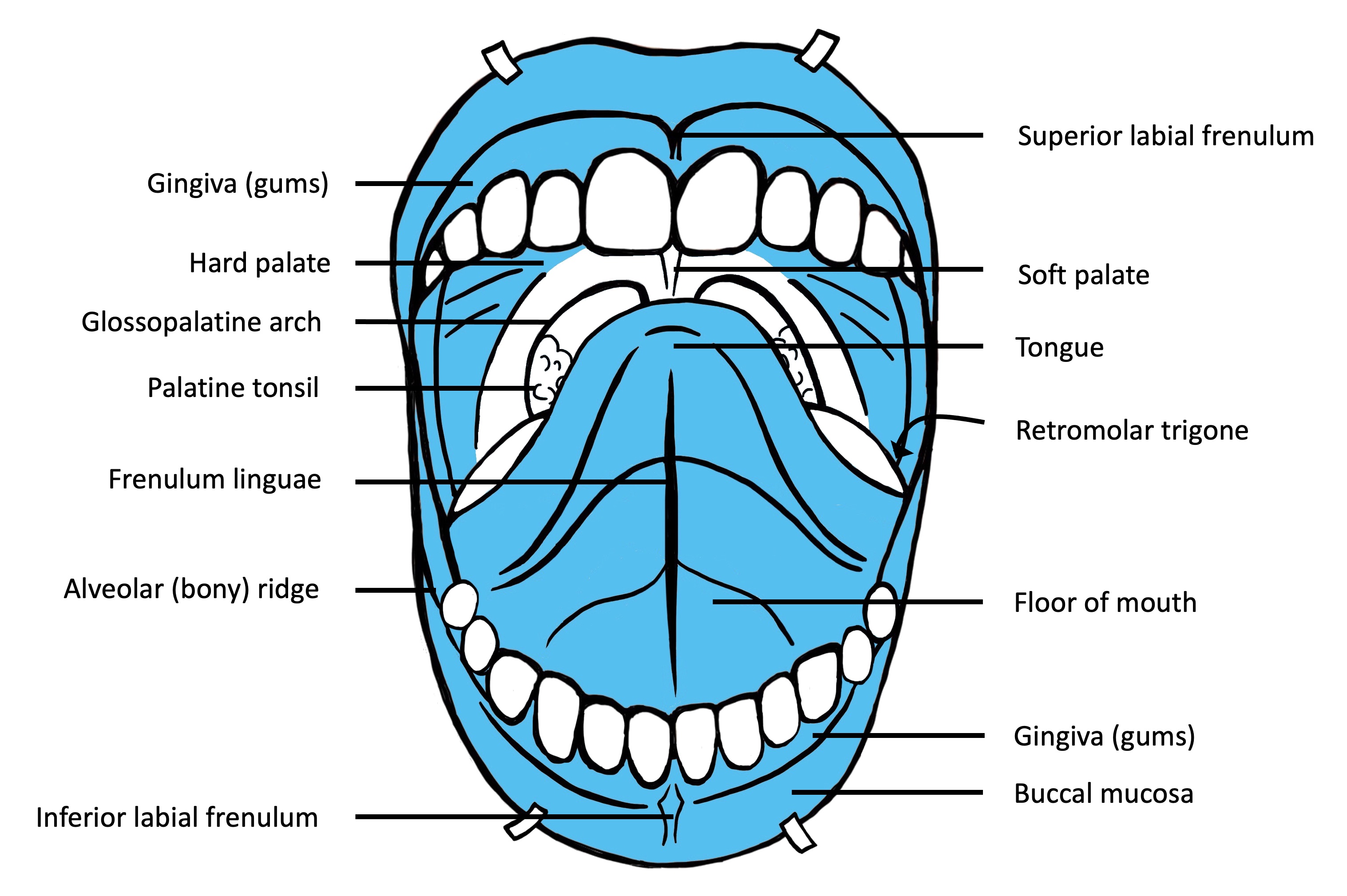
Anatomy | Juxtaoral organ of Chievitz | Histology-oral cavity | Histology-oropharynx | Drawings | Diagrams / tablesAnatomy
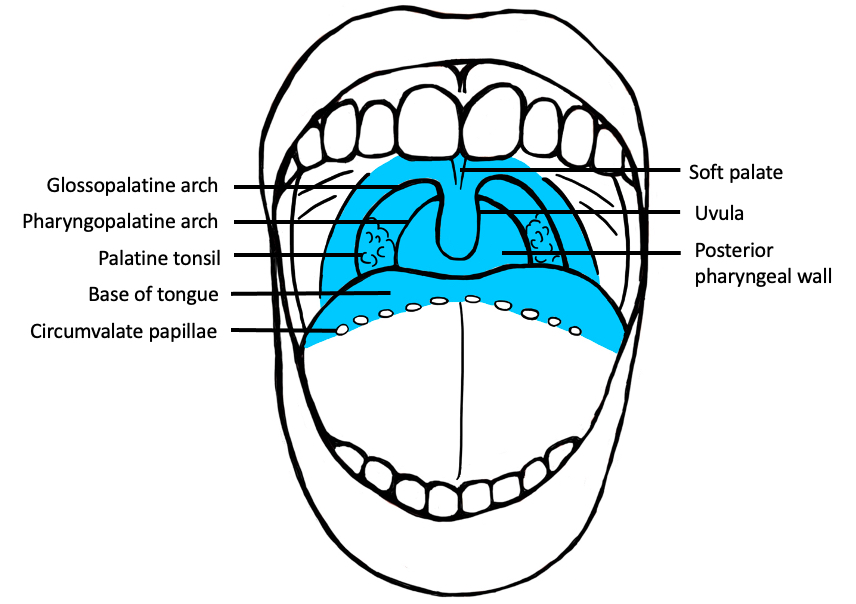
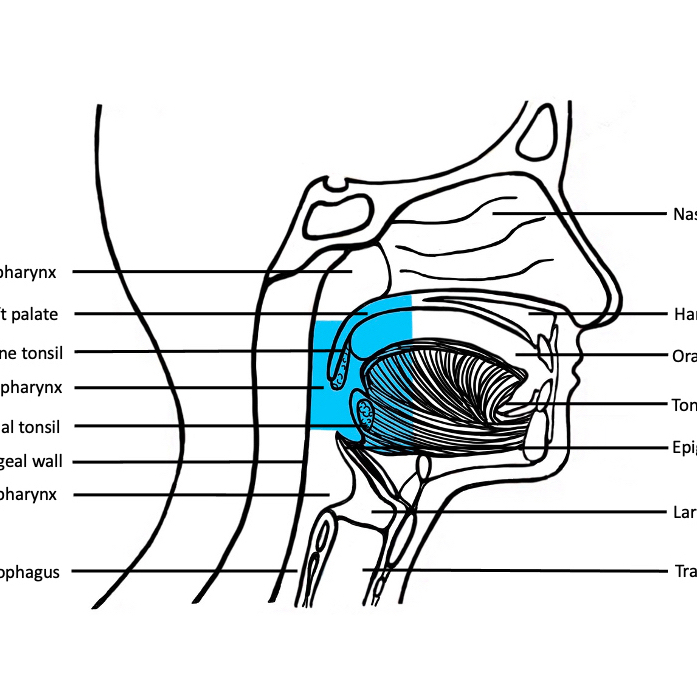
- Oral cavity extends anteriorly from vermilion junction of lips to junction of hard and soft palate above and to line of circumvallate papillae on dorsal tongue below; communicates freely with oropharynx posteriorly
- Oral cavity contains buccal mucosa, maxillary and mandibular arches, retromolar trigone, anterior two - thirds of tongue, floor of mouth and hard palate
- Dorsal tongue: villous, normally exposed surface; contains papillae and specialized taste receptors
- Ventral tongue: nonvillous, undersurface
- Anterior two - thirds of tongue (oral tongue): freely mobile portion of tongue that extends anteriorly from line of circumvallate papillae to undersurface of tongue at junction of floor of mouth; composed of skeletal muscle, includes 4 areas: tip, lateral borders, dorsum and undersurface (nonvillous ventral surface of tongue)
- Base of tongue (posterior one - third of tongue): bound anteriorly by circumvallate papillae, laterally by glossotonsillar sulci and posteriorly by epiglottis
- Buccal mucosa: all of membrane lining inner surface of cheeks and lips from line of contact of opposing lips to line of attachment of mucosa of alveolar ridge (upper and lower) and pterygomandibular raphe; contains ostia of main duct of parotid gland (Stenson duct)
- Floor of mouth: semilunar space of myelohyoid and hyoglossus muscles, extending from inner surface of lower alveolar ridge to undersurface of tongue; posterior boundary is base of anterior pillar of tonsil; divided into two sides by frenulum of tongue, contains ostia of submaxillary and sublingual salivary glands
- Gingiva: mucosa in area of teeth and palate; extends from labial sulcus and buccal sulcus to a cuff of tissue around each tooth
- Hard palate: forms roof of oral cavity; semilunar surface between upper alveolar ridge and mucous membrane covering palatine process of maxillary palatine bones; extends from inner surface of superior alveolar ridge to posterior edge of palatine bone
- Lip: begins at junction of vermilion border (mucocutaneous junction) with skin, includes only vermilion surface or that portion of lip that comes into contact with opposing lip; upper and lower lip are joined at commissures of mouth; external surface is skin and mucous membrane; internally contains orbicularis oris muscle, blood vessels, nerves, areolar tissue, fat and small labial glands; inner surface of lip is connected to gum in midline by frenulum, a mucous membrane fold
- Lower alveolar ridge: mucosa overlying alveolar process of mandible which extends from line of attachment of mucosa in lower gingivobuccal sulcus to line of free mucosa of floor of mouth; posteriorly extends to ascending ramus of mandible
- Retromolar gingiva (retromolar trigone): mucosa overlying ascending ramus of mandible from level of posterior surface of last molar tooth to apex superiorly, adjacent to tuberosity of maxilla
- Tonsillar area: anterior and posterior tonsillar pillars and tonsillar fossa
- Upper alveolar ridge: mucosa overlying alveolar process of maxilla which extends from line of attachment of mucosa in upper gingivobuccal sulcus to junction of hard palate; posterior margin is upper end of pterygopalatine arch
- Vermillion border: mucocutaneous junction of lip
Juxtaoral organ of Chievitz
- Not actually a congenital anomaly but normal occurring neuroepithelial structure called organ of Chievitz, Chievitz paraparotid organ, juxtaoral organ or epithelial nests
- Reported in 56% of adult autopsies without oral mucosal lesions
- Within intraoral sensory nerve
- May undergo nodular hyperplasia
- Located bilaterally in buccotemporal fascia on medial surface of mandible, near angle
- Rare examples of proliferative / hamartomatous masses of juxtaoral organ reported
- May be interpreted as squamous cell carcinoma, mucoepidermoid carcinoma or metastasis especially during frozen sections (Am J Surg Pathol 1979;3:147)
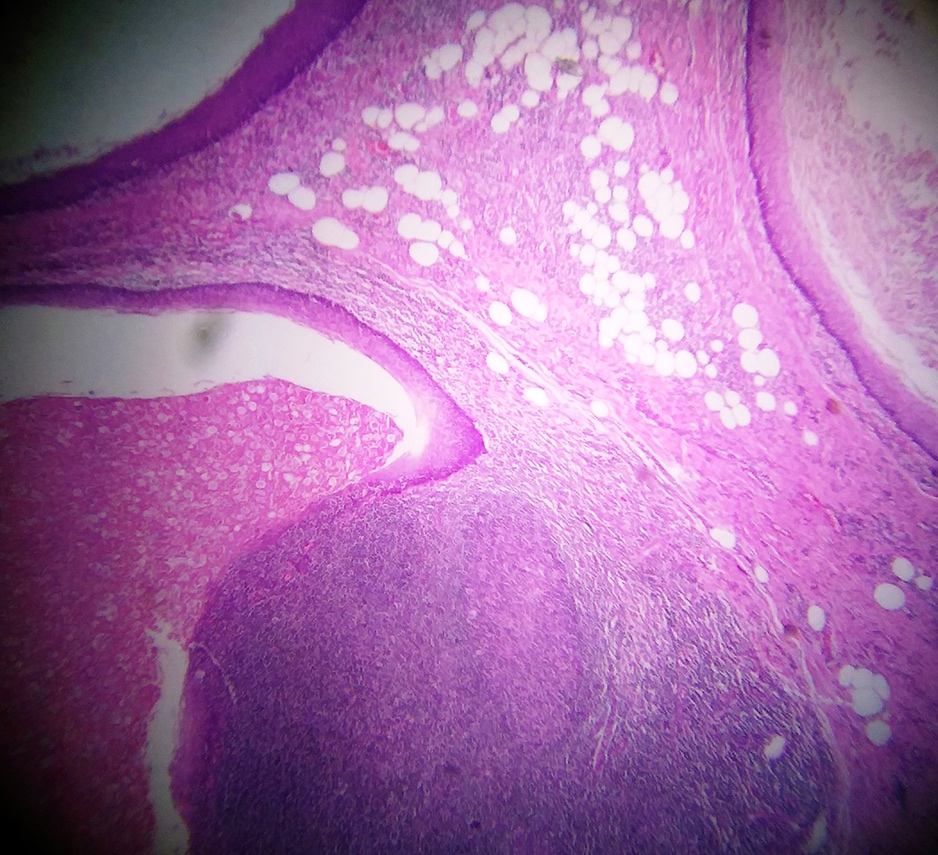
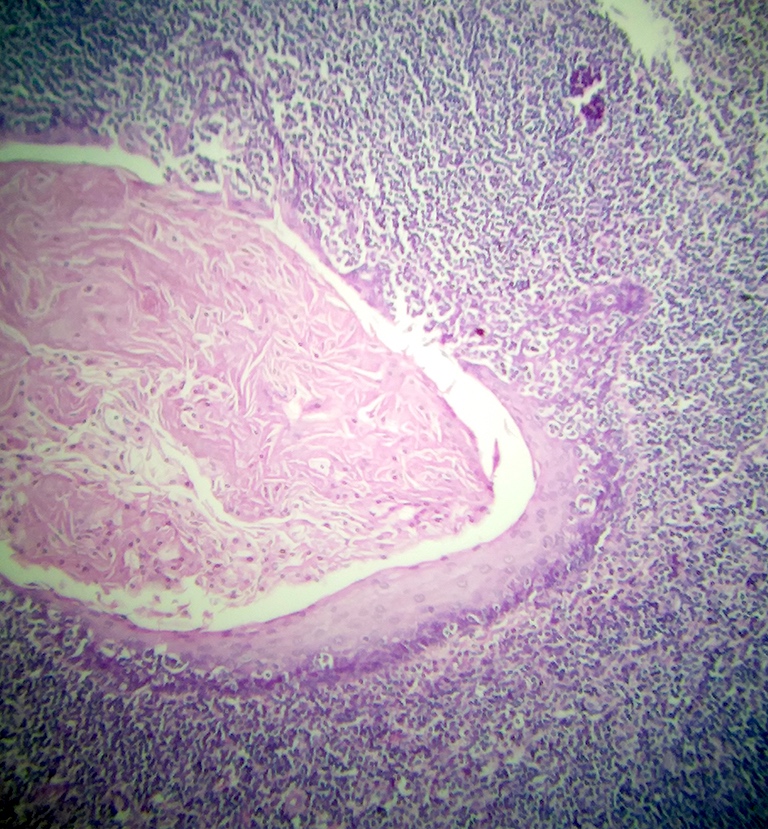
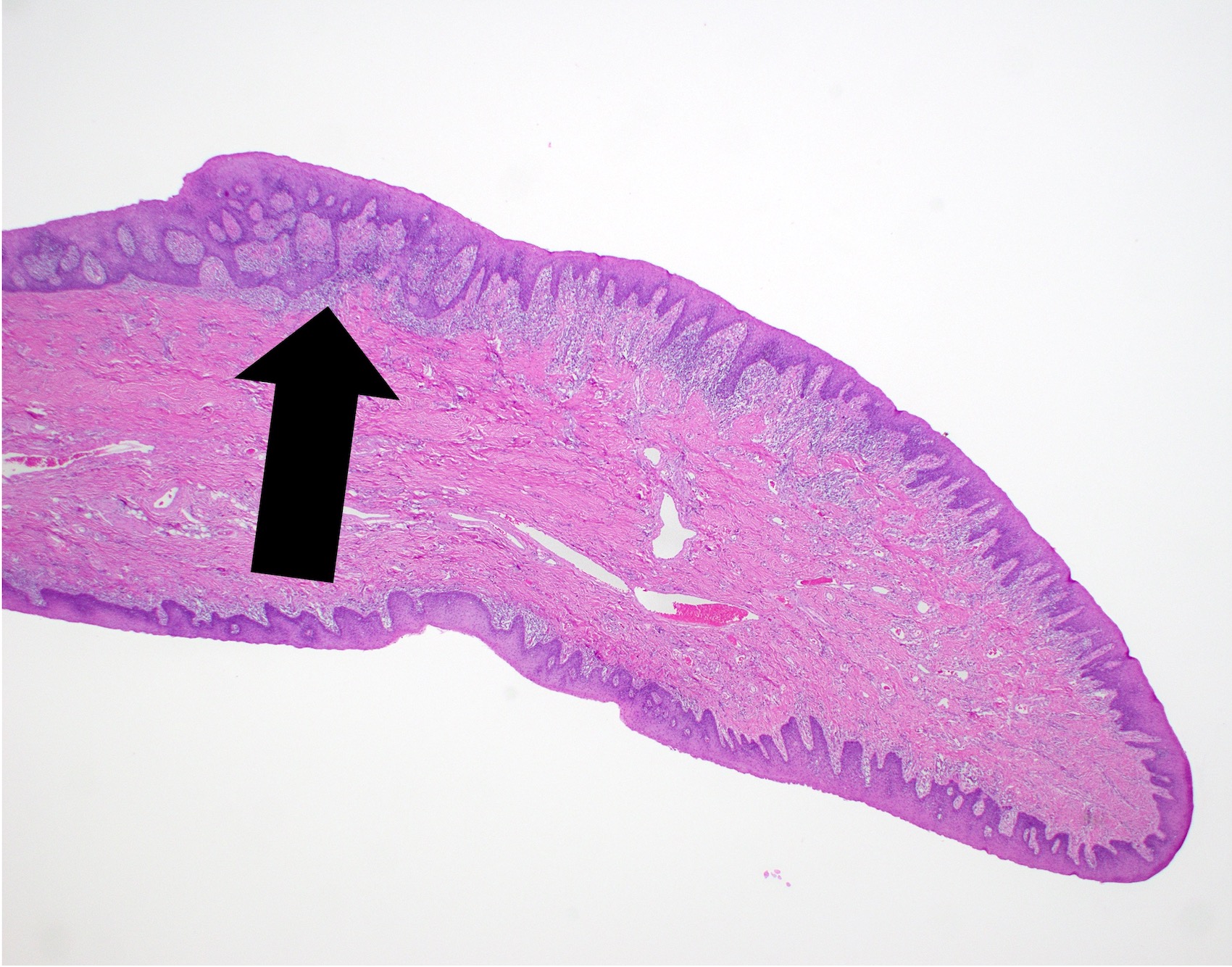
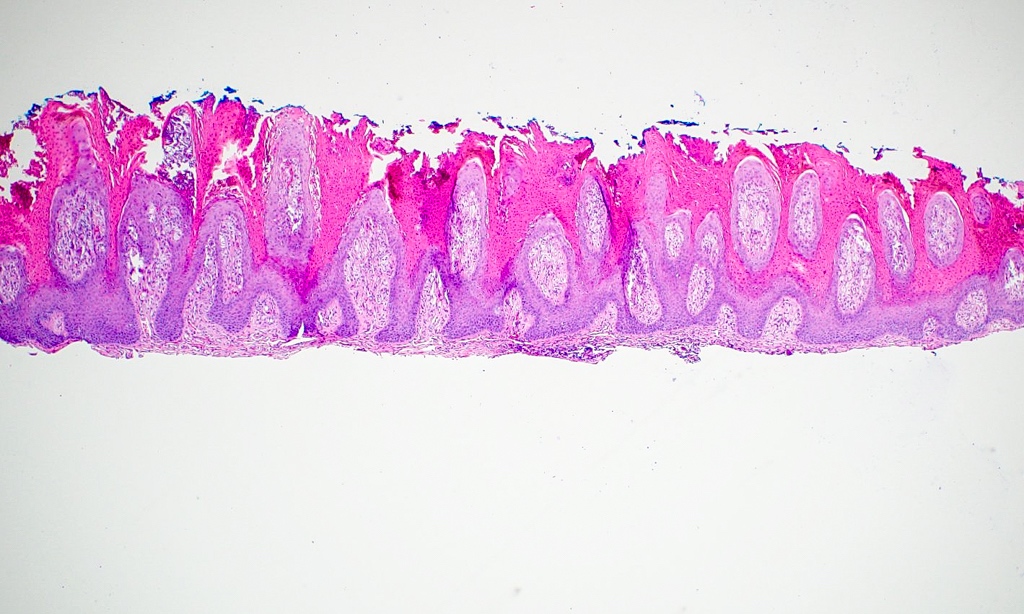
Microscopic (histologic) description
- Multilobulated nests of squamous-like epithelium without keratin formation, occasionally with lumen lined by cuboidal cells
- Associated with small nerves and resembling perineural invasion
Case reports
- Child with intraoral tumor (Int J Oral Maxillofac Surg 2003;32:101)
- 63 year old man with rare hamartomatous lesion (J Clin Pathol 2003;56:789)
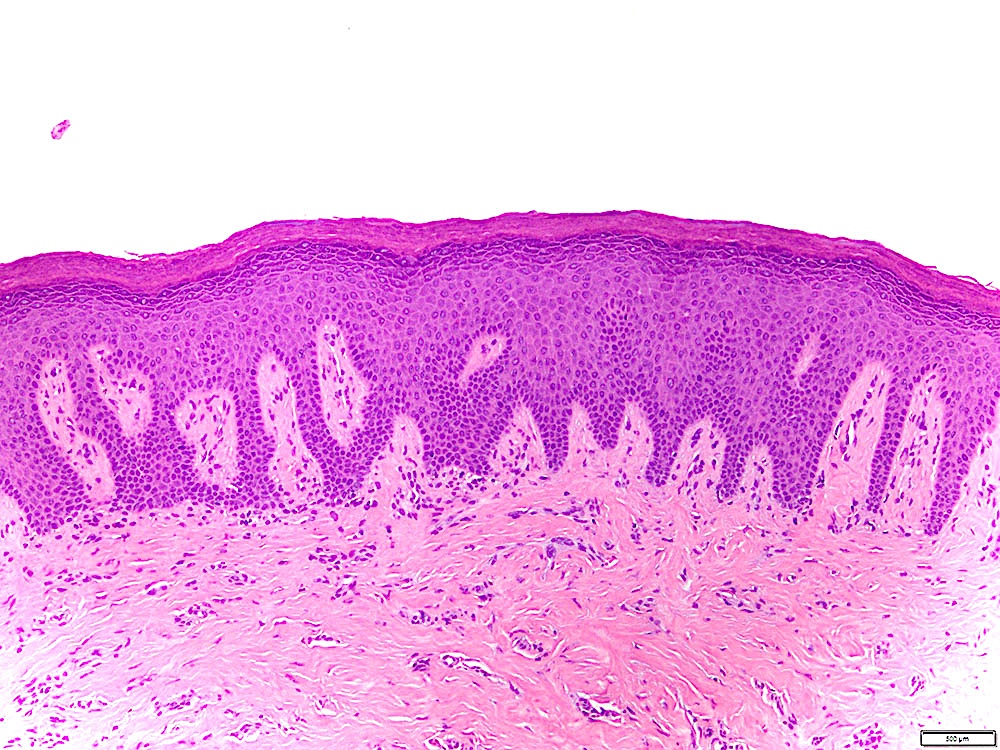
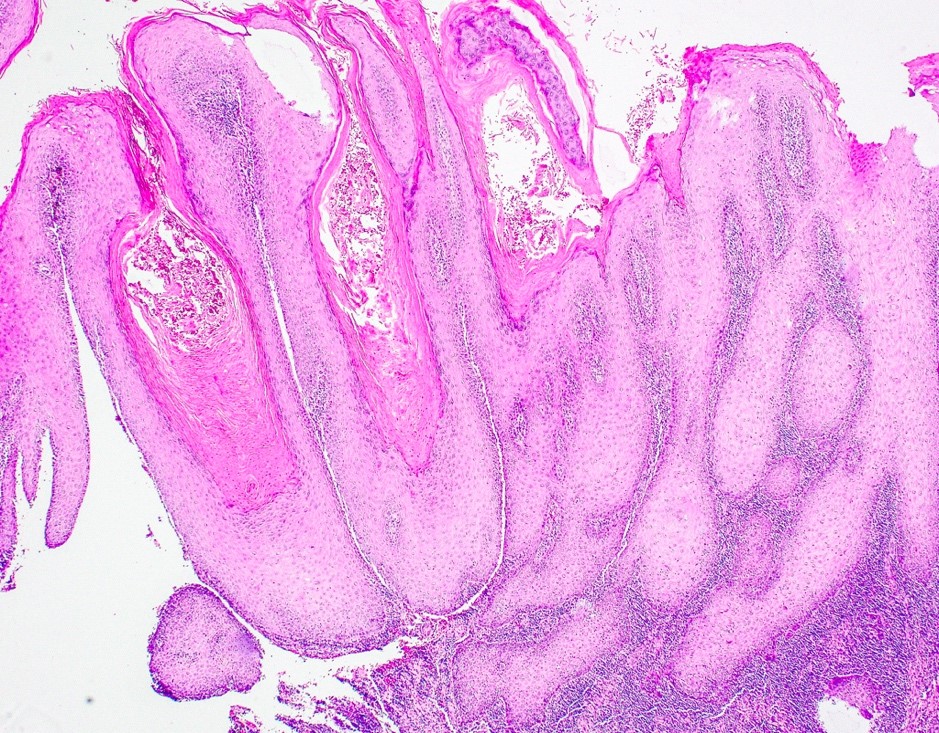
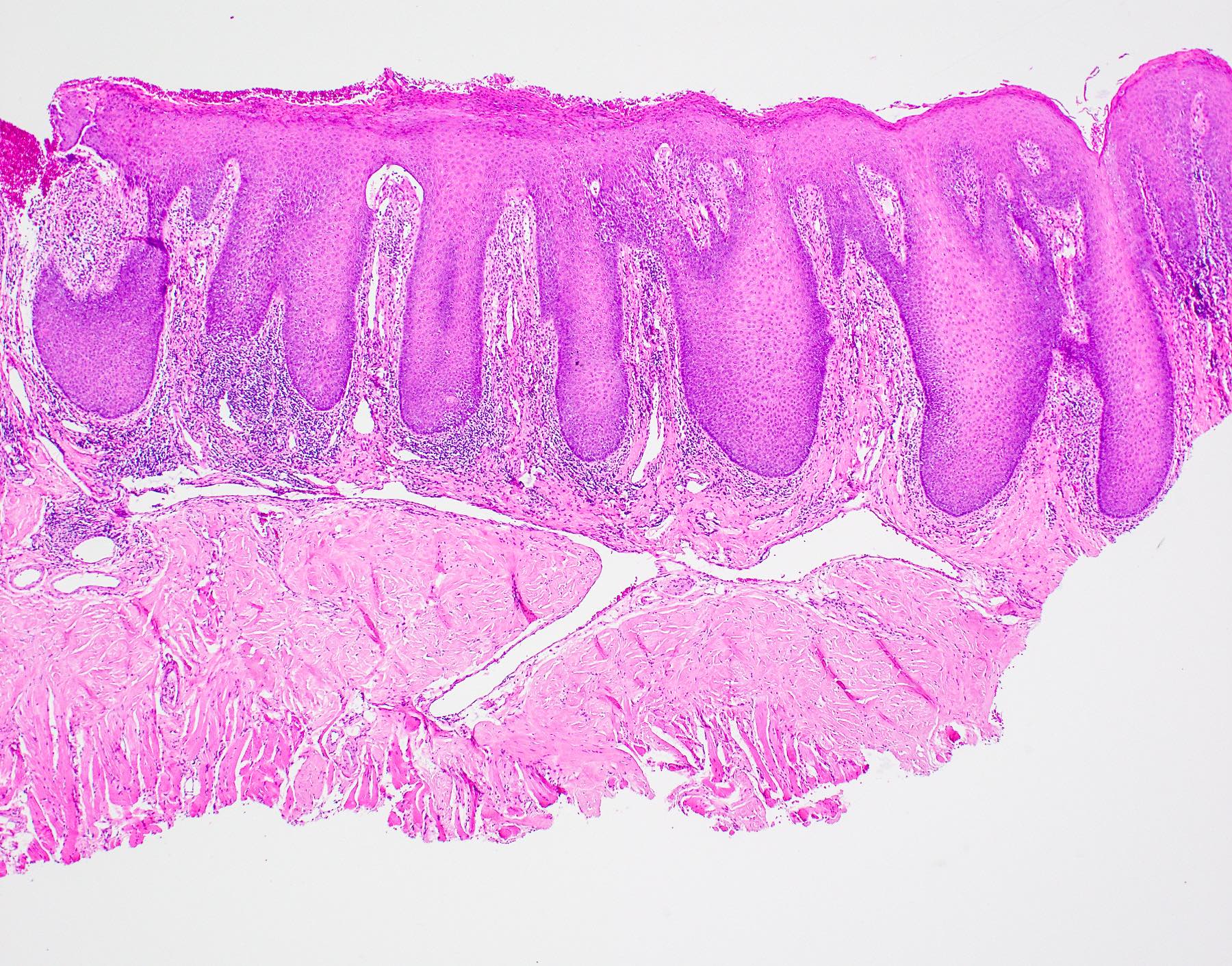
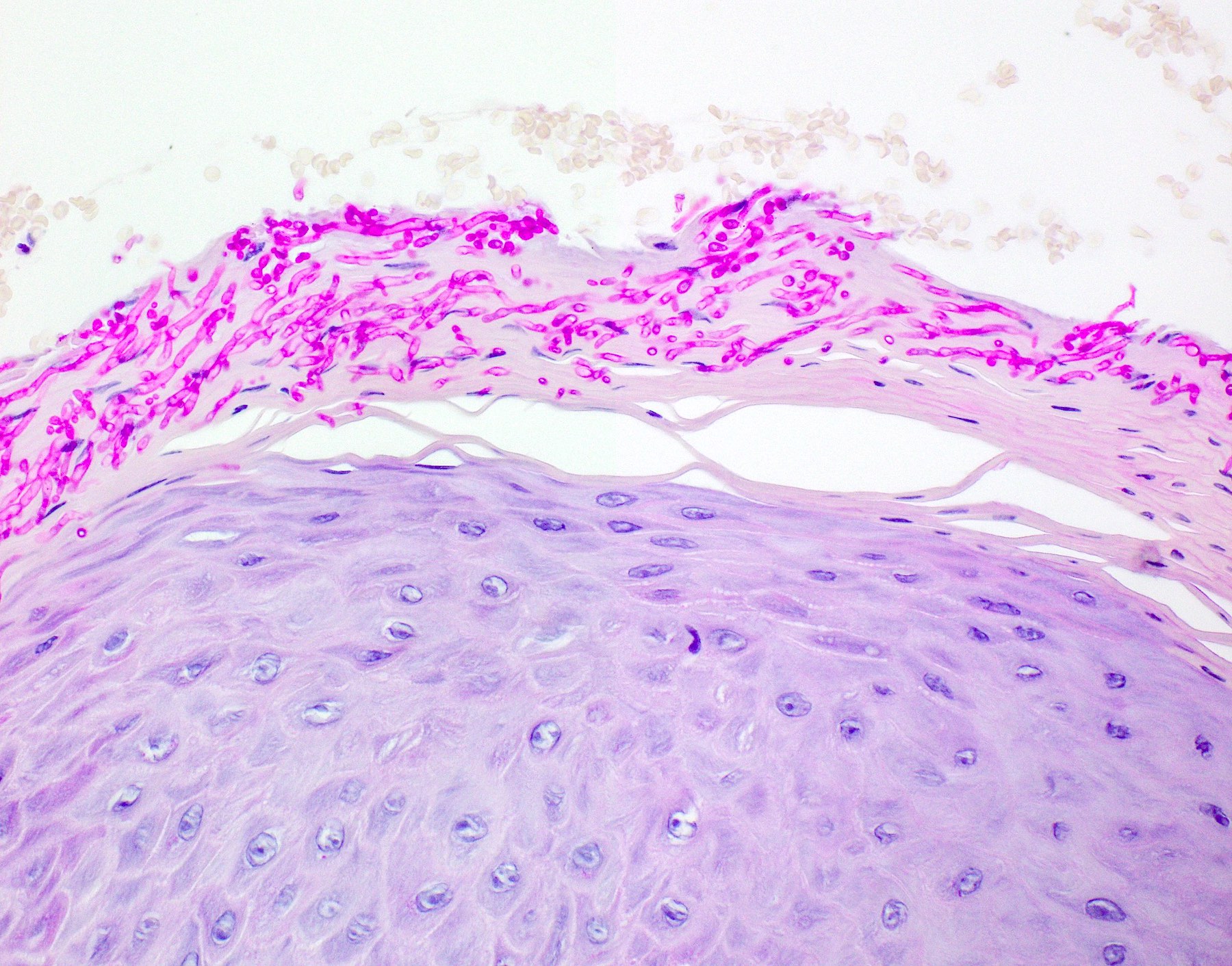
Histology-oral cavity
- Stratified squamous epithelium often with parakeratosis
- No hair follicles or sweat glands present
- Keratinization in areas most exposed to mastication (gingiva, hard palate, dorsum of tongue)
- Lamina propria contains loose connective tissue, mucous glands, serous minor salivary type glands
- Submucosa has dense collagenous fibrous tissue
- Oral tongue mucosa: modified keratinized squamous epithelium with small papillae; papillae can be filiform (majority, conical projections of keratinized epithelium), fungiform (rounded elevations, nonkeratinized), foliate (along sides of tongue) or cirucumvallate (at junction of anterior 2/3 and posterior 1/3 tongue, largest papillae)
- Taste buds: barrel shaped, lightly staining, intramucosal sensory receptors present in large numbers on circumvallate papillae and in lesser numbers elsewhere
- Intraepithelial nonkeratinocytes: melanocytes (basal), Merkel cells (basal), Langerhans cells (suprabasal) and lymphocytes occur in oral mucosa
- Ectopic sebaceous glands (Fordyce spots) increase with age in adults
- Tonsillectomy specimens frequently contain skeletal muscle (Hum Pathol 2000;31:813)
Immunostains
- Oral epithelium expresses cytokeratin 5 and 14, ABO blood group antigens
- Taste buds express low molecular weight keratins, such as CK18 and CAM5.2
Histology-oropharynx
[Pending]
Drawings
Diagrams / tables
Aphthous ulcers
Table of Contents
Definition / general | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) descriptionDefinition / general
- Also called canker sores
- Affect 40% in U.S.
- More common up to 20 years
- Painful, recurrent and familial
Case reports
- 26 year old HIV+ man with recurrent ulcer treated with laser therapy (Case Rep Med 2012;2012:695642)
Treatment
- Symptomatic
Clinical images
Gross description
- Single or multiple, shallow, hyperemic ulcerations covered by a thin exudate with hyperemic rim
Microscopic (histologic) description
- Initially mononuclear infiltrate, then neutrophilic infiltrate from secondary bacterial infection
Caliber persistent artery (pending)
[Pending]
Carcinoma cuniculatum (pending)
[Pending]
Choristoma
Table of Contents
Definition / general | Epidemiology | Sites | Clinical features | Radiology images | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosisDefinition / general
- Choristoma is a tumor-like mass consisting of normal cells in an abnormal location (J Oral Maxillofac Surg 2012;24:110)
- Hamartoma is a tumor-like malformation composed of mature normal cells in usual location but as a disorganized mass
Epidemiology
- Most cases occur in adults but may occur at all ages
- > 70% of lingual osseous and cartilaginous choristomas occur in females (Barnes: Surgical Pathology of the Head and Neck, 3rd Edition, 2008 [p822])
Sites
- 85% of osseous and cartilaginous choristomas occur on tongue (dorsal posterior third near foramen cecum)
Clinical features
- Firm, exophytic, asymptomatic nodule covered by intact oral mucosa
- Base may be sessile or pedunculated
Radiology images
Case reports
- Glial choristomas of palate in newborn / one month old (J Oral Pathol Med 1997;26:147)
- 5 year old boy with buccal osseous choristoma (Oral Oncology 2005;41:198)
- 73 year old woman with asymptomatic ventral tongue lesion (Gerodontology 2009;26:78)
Treatment
- Surgical excision
Gross description
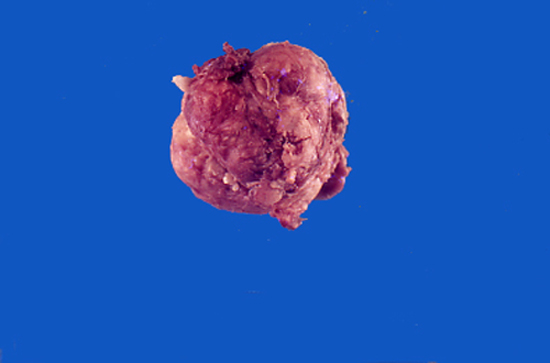
- Firm mass covered by oral mucosa, with smooth contour
- Usually < 1.0 cm; lesions > 2.0 cm warrant careful microscopic examination (Barnes: Surgical Pathology of the Head and Neck, 3rd Edition, 2008 [p822])
Gross images
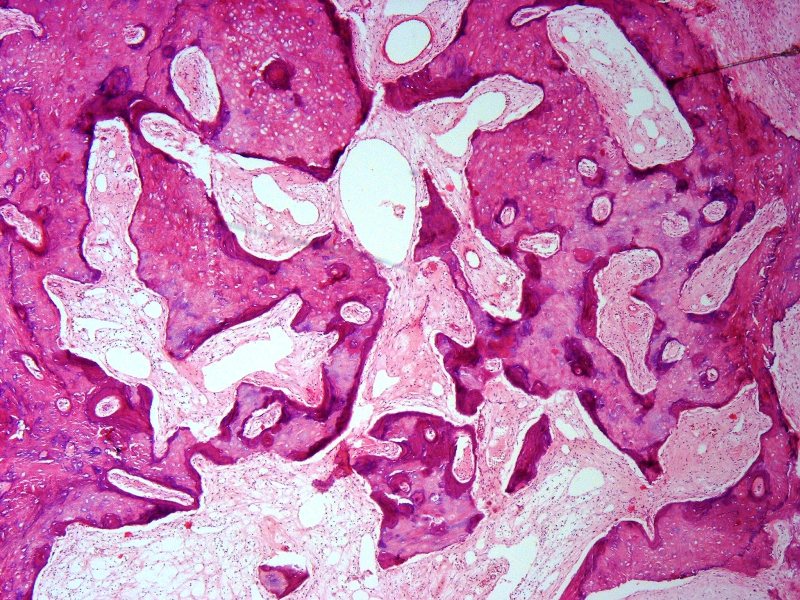
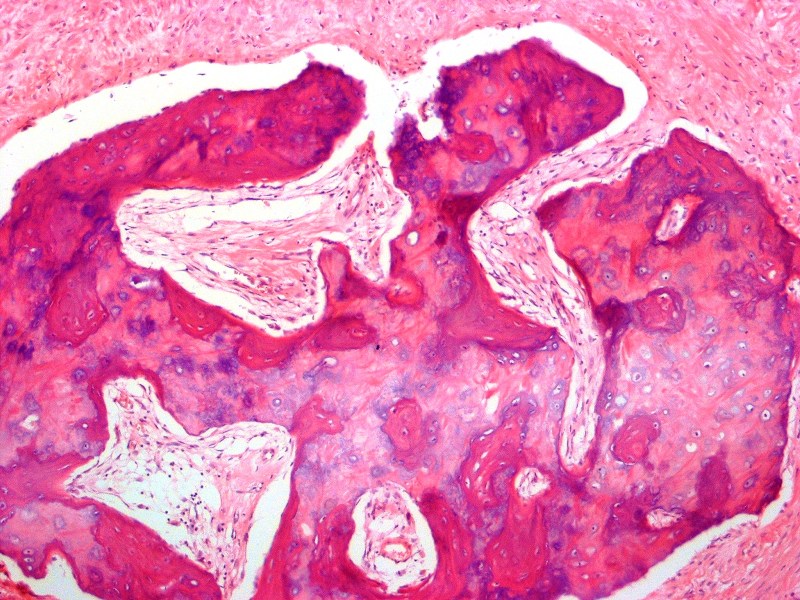
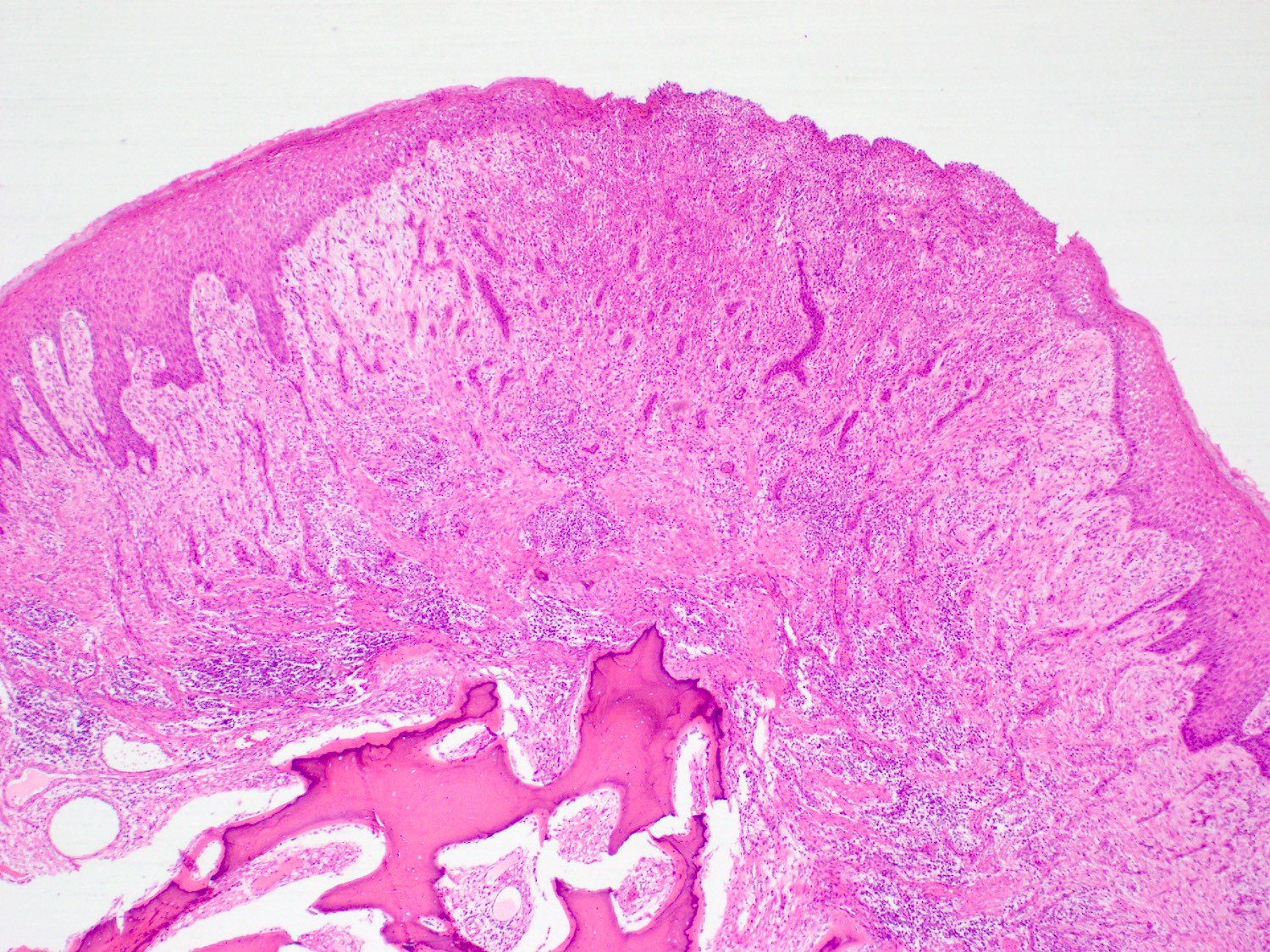
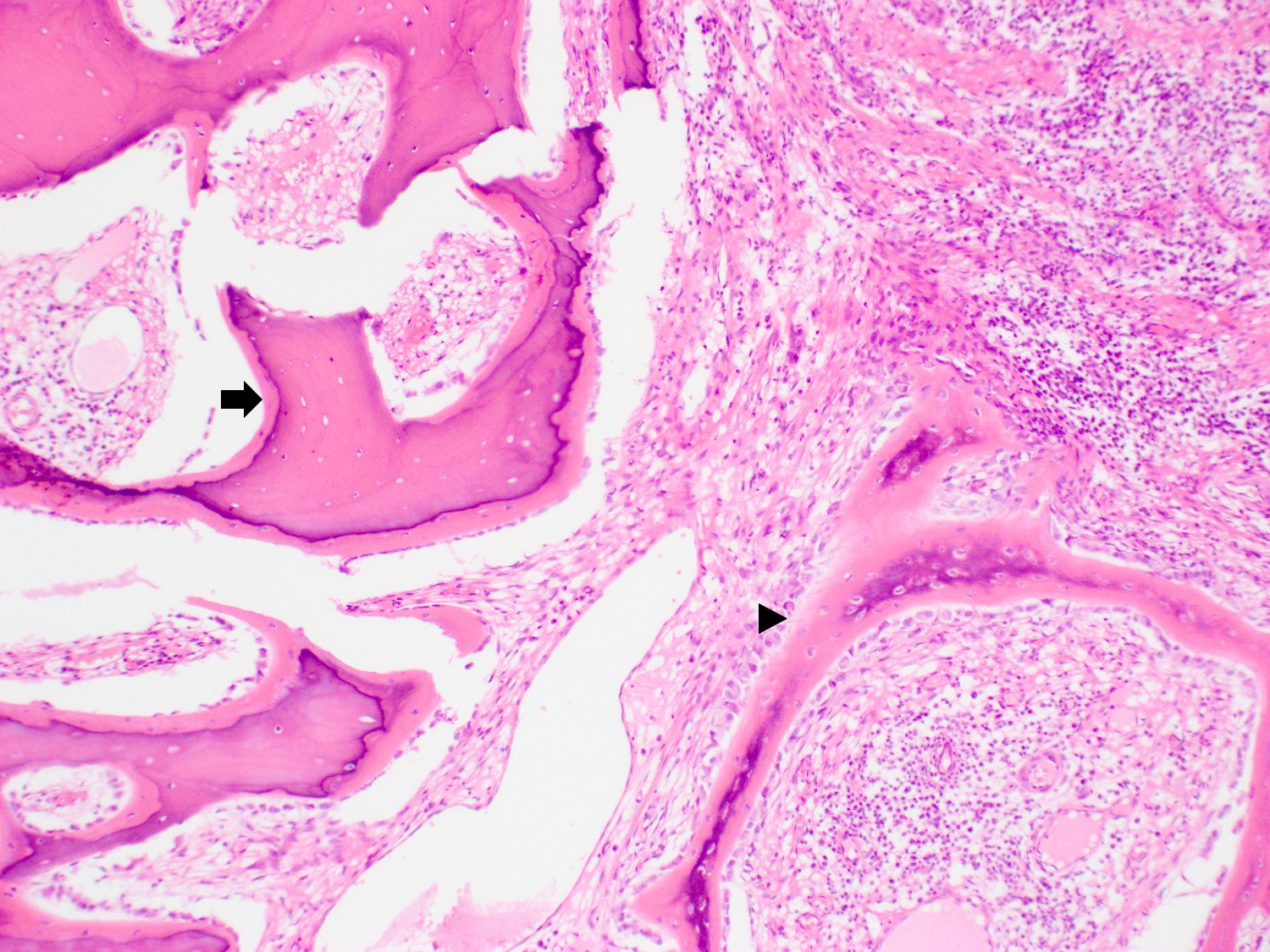
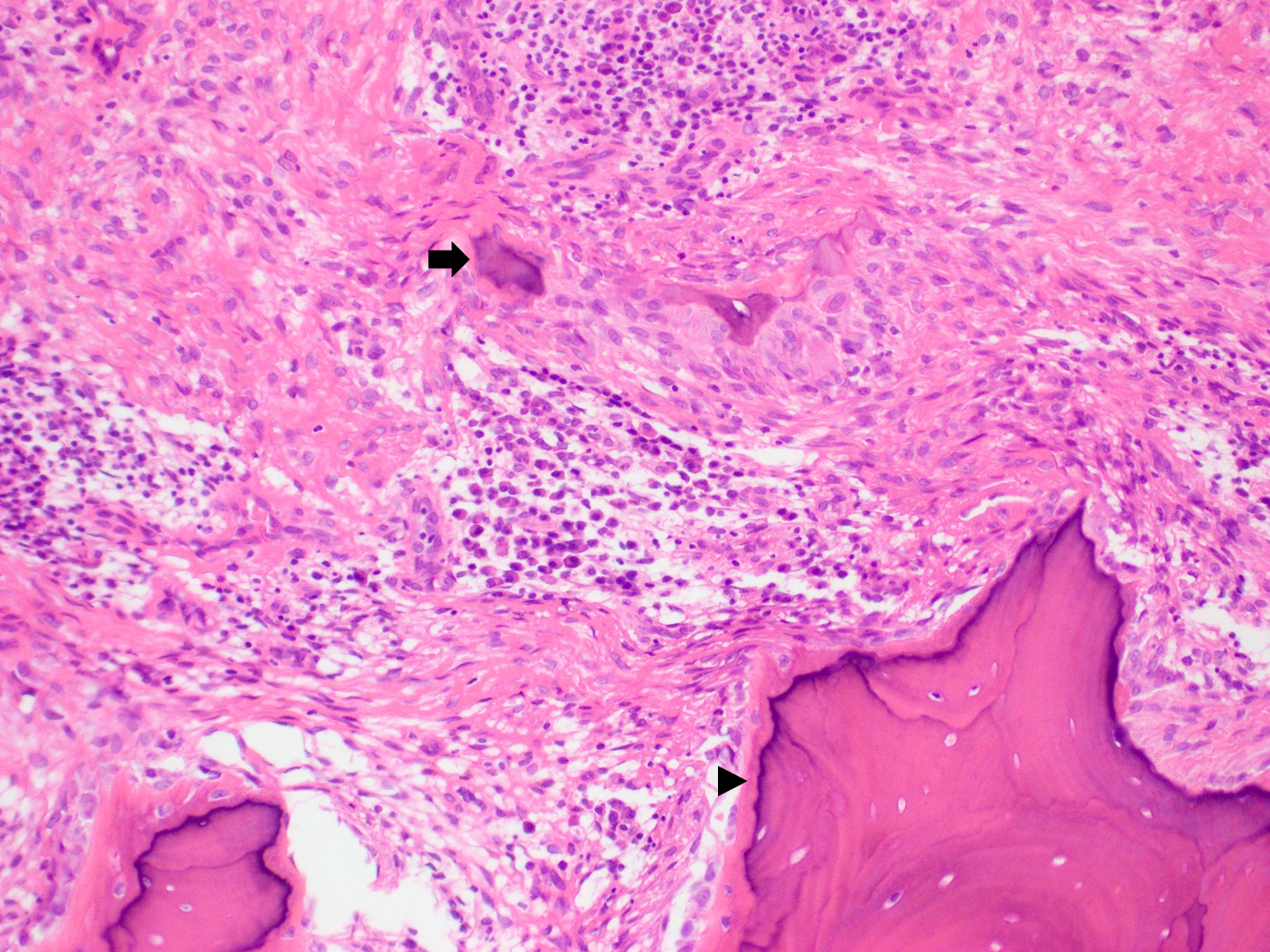
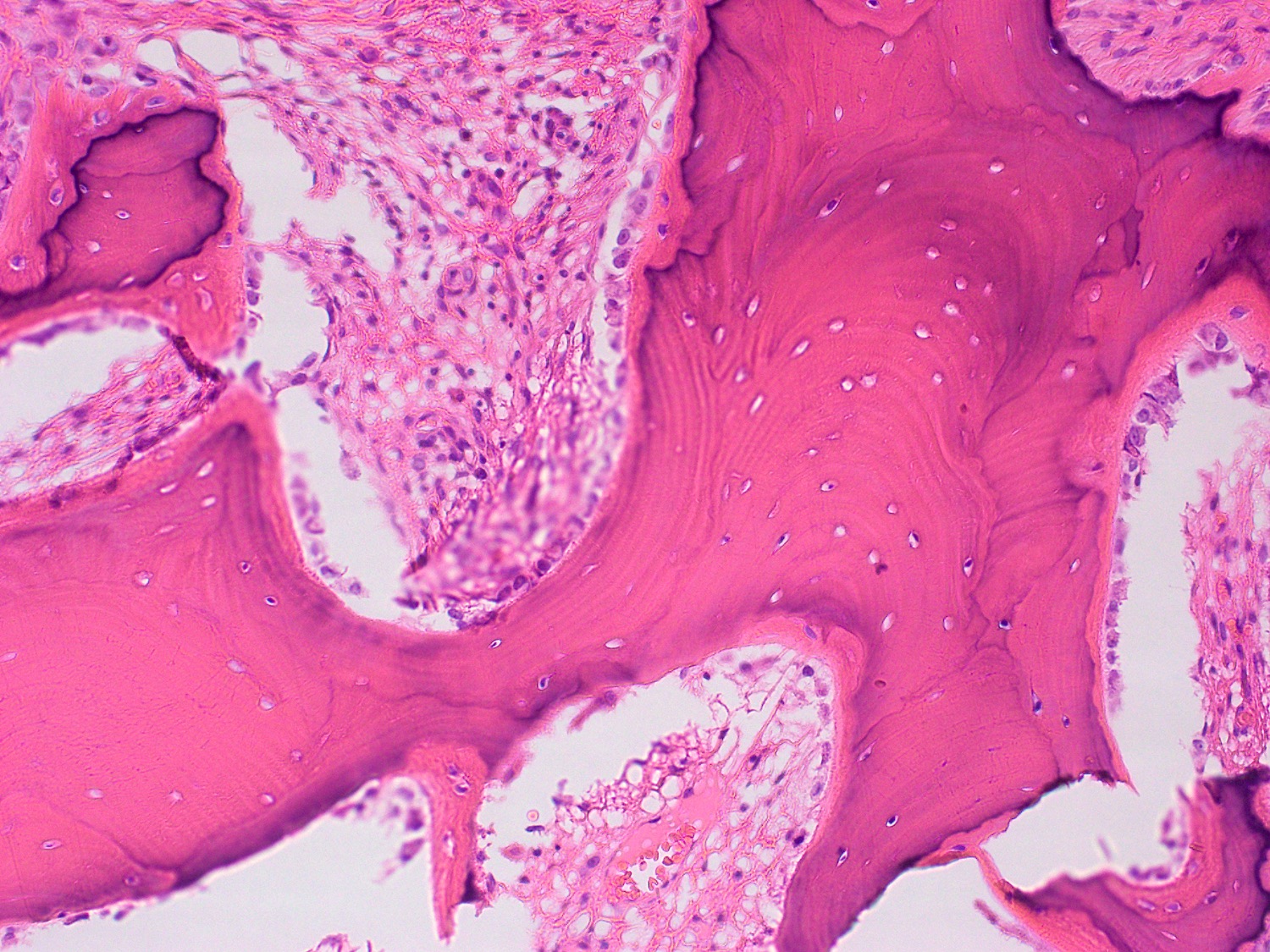
Microscopic (histologic) description
- Oral choristomas can be classified according to types of tissues they constitute (J Oral Maxillofac Surg 2012;24:110):
- Salivary gland choristoma
- Central
- Gingival
- Both have ectopic salivary gland tissue appearing as a raised tumor-like mass; must not have any connection with normal minor or major salivary glands
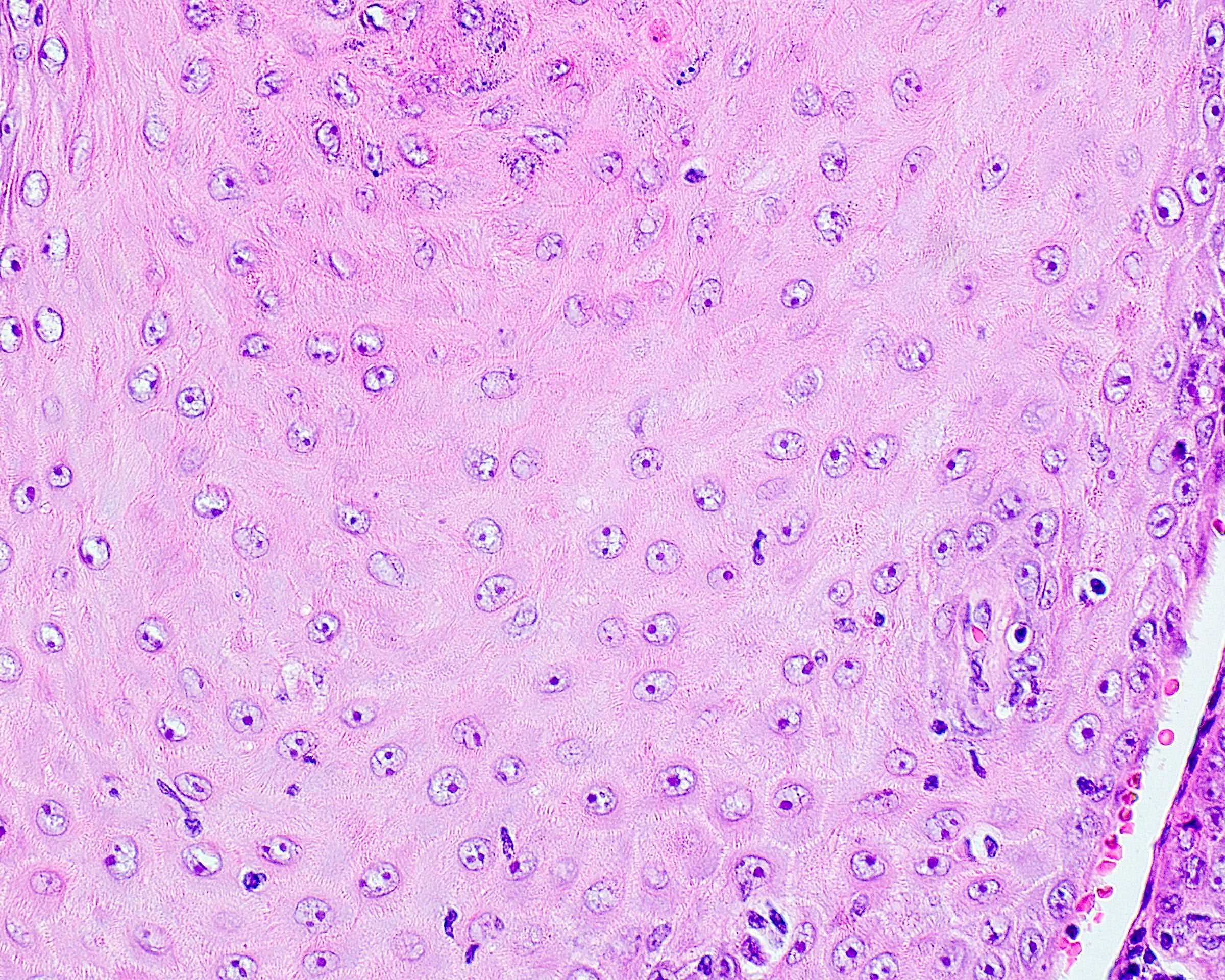
- Cartilagenous choristoma: composed of mature hyaline cartilage in fibrous tissue that resembles perichondrium; usually multilobulated; chondrocytes vary from small to large but lack atypia
- Osseous choristoma: composed of dense mature bone; osteocytes are compact and unremarkable; no prominent osteoblastic rimming; occasionally bone and cartilage are present in same lesion
- Lingual thyroid choristoma
- Lingual sebaceous choristoma
- Glial choristoma
- Gastric / respiratory mucosal choristoma
- Solid
- Cystic
- Salivary gland choristoma
Microscopic (histologic) images
Differential diagnosis
- Cartilaginous metaplasia:
- Usually occurs in soft tissue beneath ill fitting dentures, has diffuse deposits of calcium, scattered cartilaginous cells arranged in various stages of maturation in single or clustered foci
- Pleomorphic adenoma:
- May have osteocartilaginous foci
- Salivary gland tissue:
- Choristomas lack salivary gland ductal or myoepithelial components
Chronic ulcerative stomatitis (pending)
[Pending]
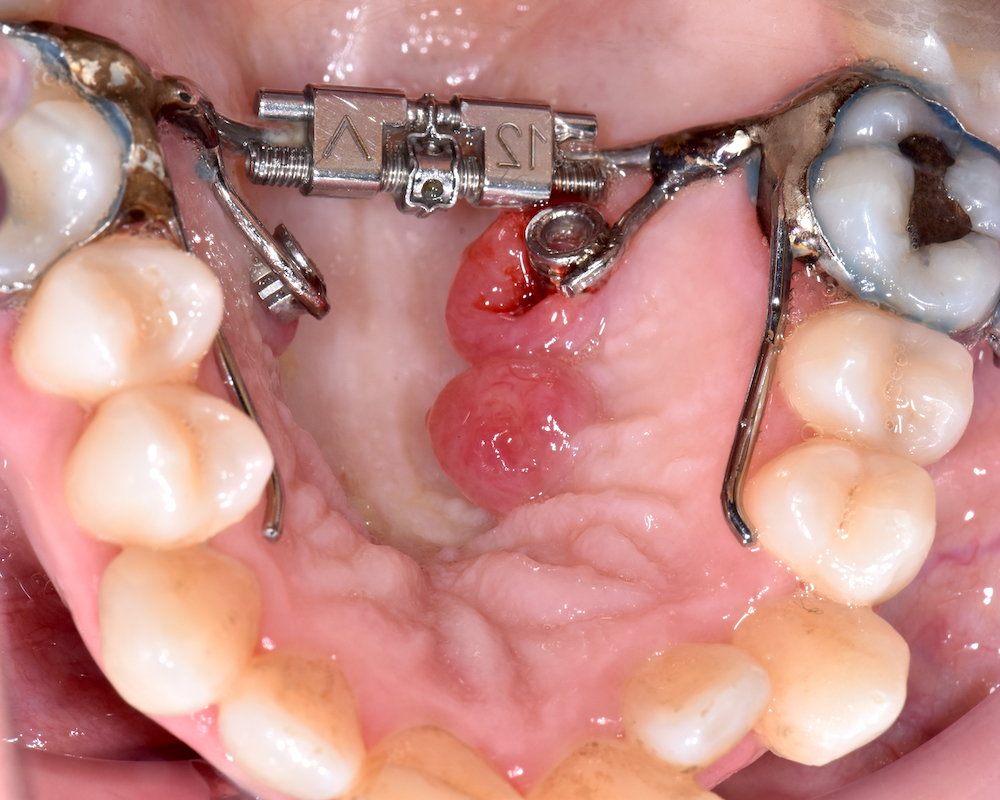
Congenital epulis of newborn
Table of Contents
Definition / general | Terminology | Sites | Case reports | Clinical images | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Differential diagnosis | Board review style question #1 | Board review style answer #1Definition / general
- Congenital granular cell tumor of alveolar mucosa of jaw in newborns
- 90% girls; 10% present as multiple lesions
- Doesn't recur, even if incompletely excised
- 0.5 - 2 cm soft, pedunculated mucosal mass
- Spontaneously regresses over first 8 months of life (Am J Surg Pathol 1981;5:37)
Terminology
- Congenital granular cell myoblastoma, granular cell epulis of infancy and granular cell fibroblastoma
Sites
- Exclusively on anterior alveolar ridge of maxilla and mandible, usually overlying future canine and lateral incisor teeth
Case reports
- Newborn girl with 2 cm tumor (Pediatrics 2001;107:E22)
- 2 day old girl with 4 x 2 cm exophytic growth (Pan Afr Med J 2012;12:105)
- 3 week old girl with spontaneous regression (J Med Case Rep 2010;4:331)
- 3 week old girl had a pedunculated lesion of the anterior maxillary alveolar process, which was excised (Case of the Month #524)
Clinical images
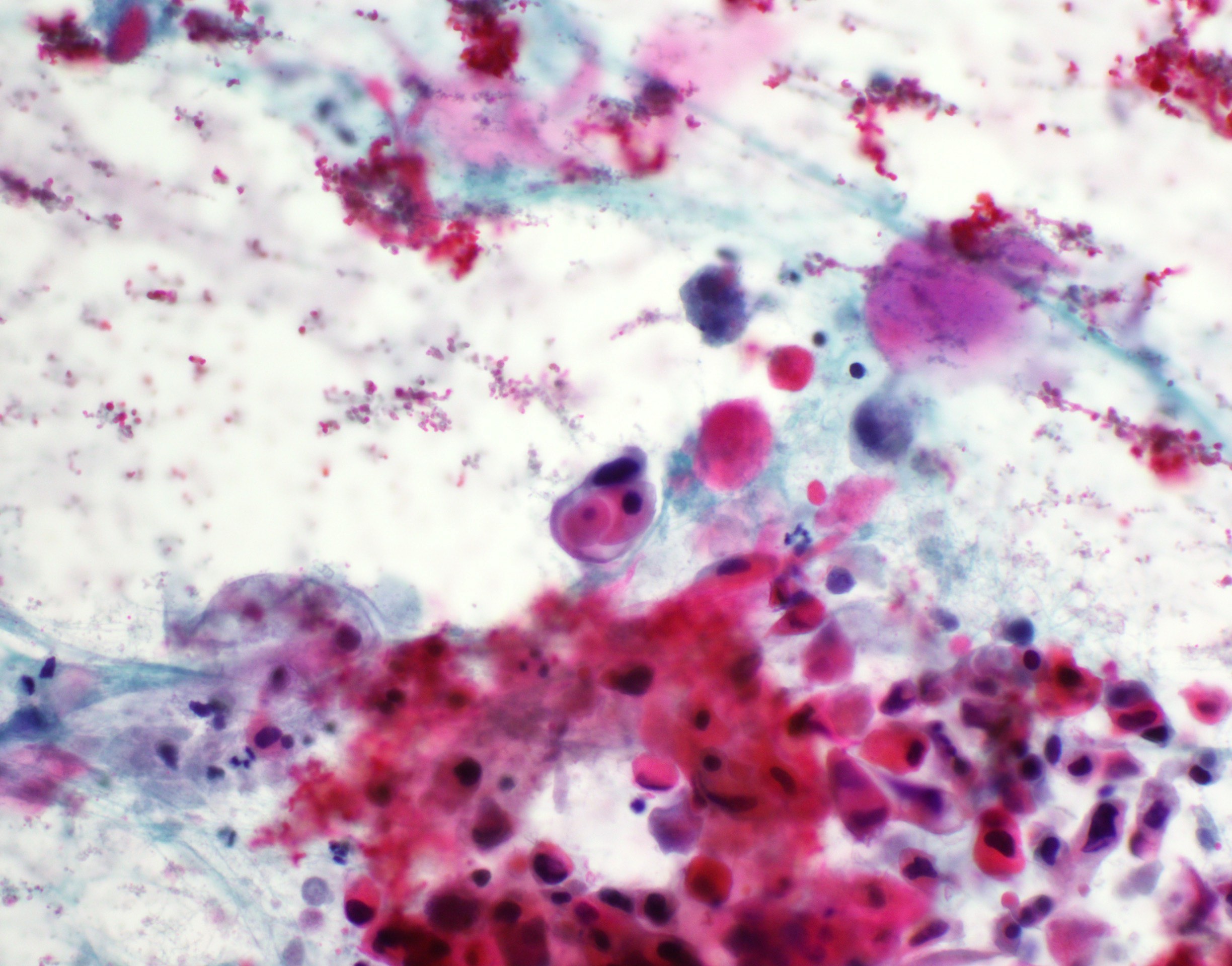
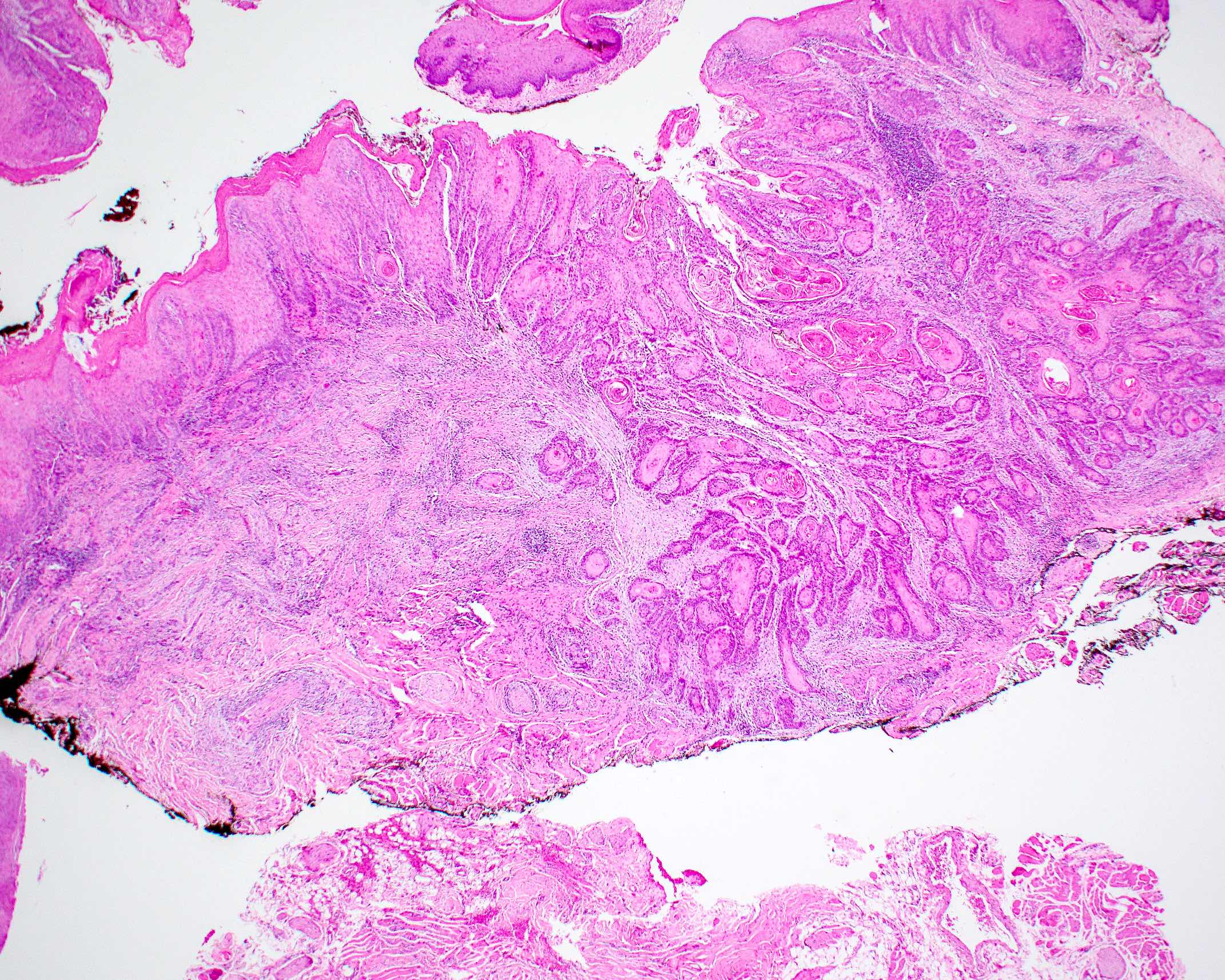
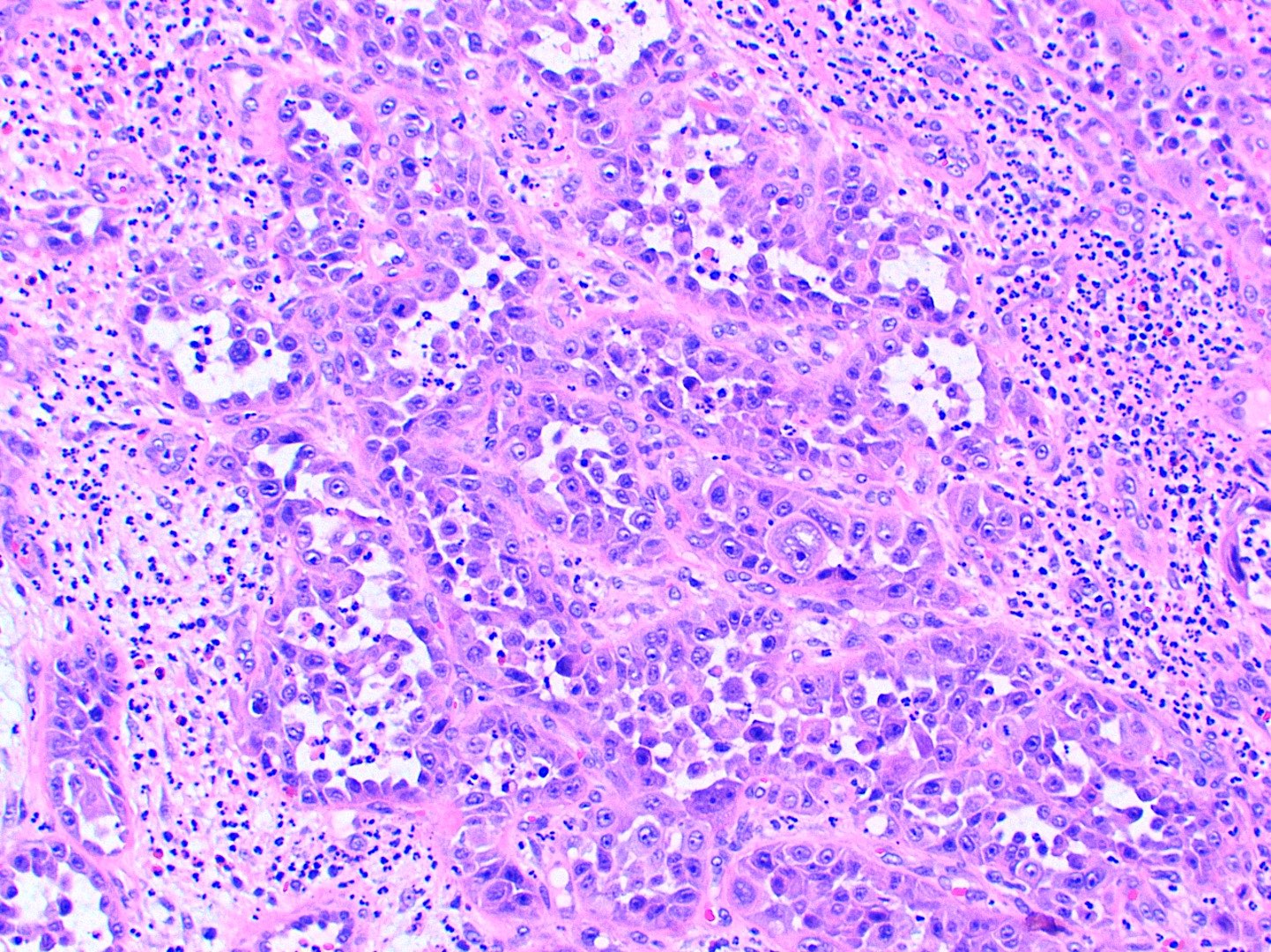
Microscopic (histologic) description
- Confluent to nodular submucosal growth of tumors composed of large polygonal cells with eosinophilic granular cytoplasm and small central nuclei
- Overlying epithelium is atrophic; does NOT show pseudoepitheliomatous hyperplasia (common with granular cell tumor of adults)
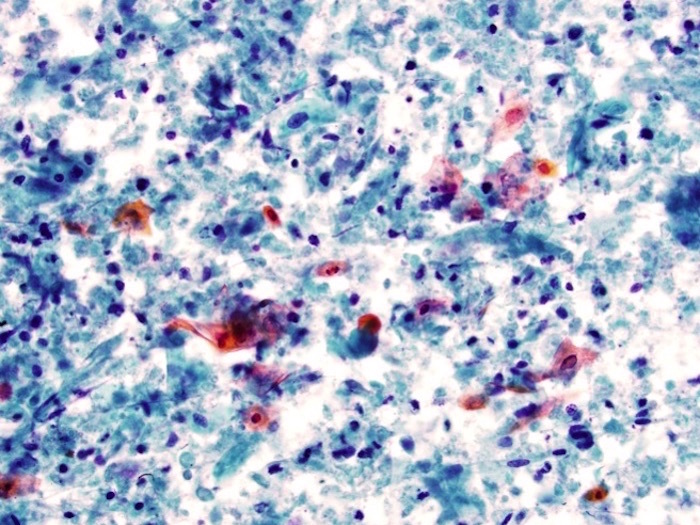
Microscopic (histologic) images
Contributed by Dhiraj B. Nikumbh, M.B.B.S., M.D. and Kelly Magliocca, D.D.S., M.P.H. (Case #524)
Images hosted on other servers:
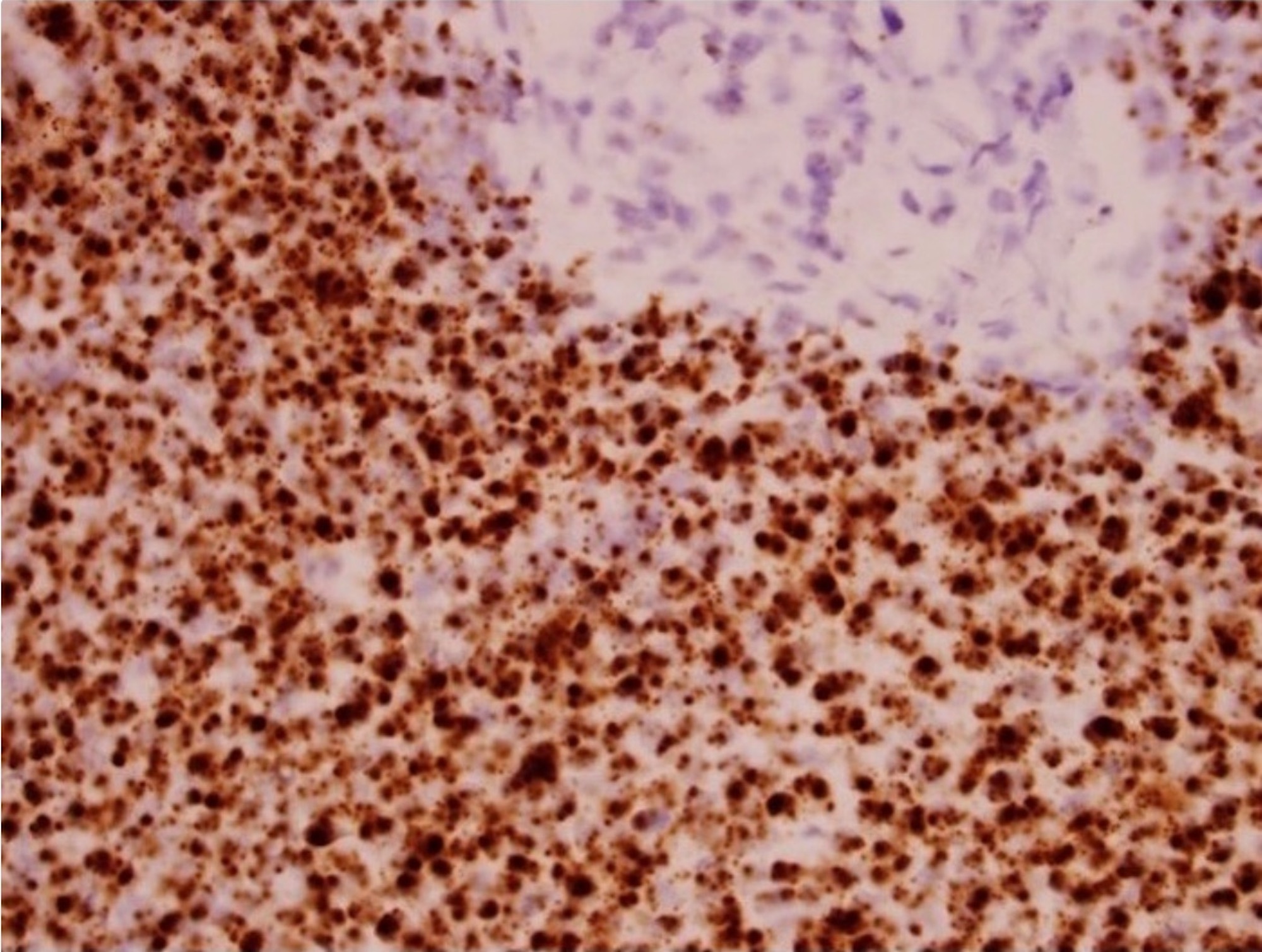
Positive stains
Differential diagnosis
- Granular cell tumor:
- Adults, infiltrates deep tissues, overlying epithelial hyperplasia
- S100+
- Verruciform xanthoma:
- Adults, overlying papillomatosis
Board review style question #1
Which of the following is a feature of congenital granular cell epulis?
- Clinical presentation at ages 5 - 15
- Detection within first trimester
- Female predilection
- Local recurrence after excision
- Pseudoepitheliomatous hyperplasia
Board review style answer #1
C. Female predilection. The characteristic presentation of CGCE is the presence of a solitary, soft pedunculated mass on the anterior maxillary alveolar ridge in a female infant. The female to male ratio is striking at nearly 8:1. Pseudoepitheliomatous hyperplasia is not present (the overlying epithelium is attenuated) and recurrence has not been reported (J Neonatal Surg 2015;4:17).
Comment Here
Reference: Topic name
Comment Here
Reference: Topic name
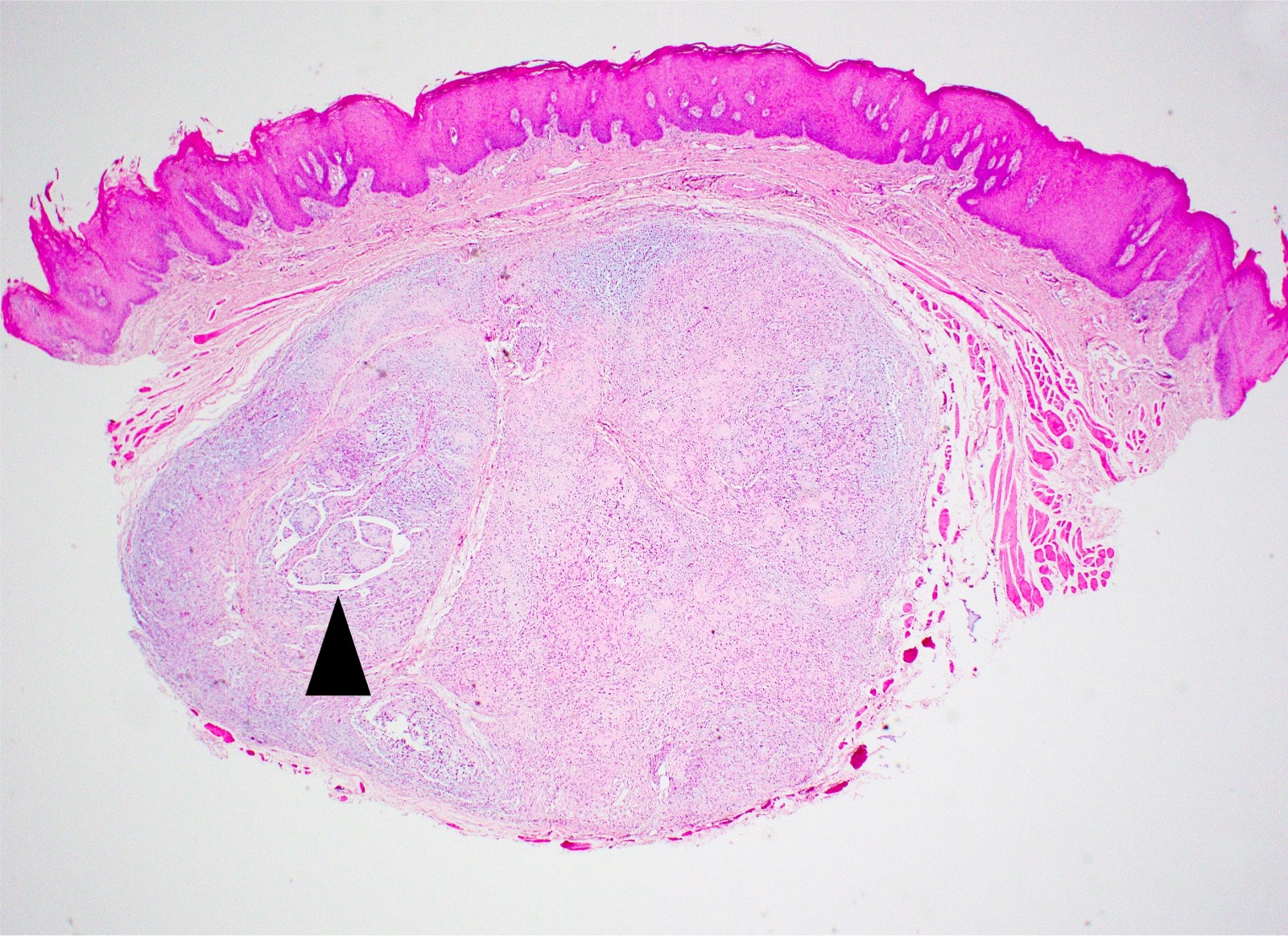
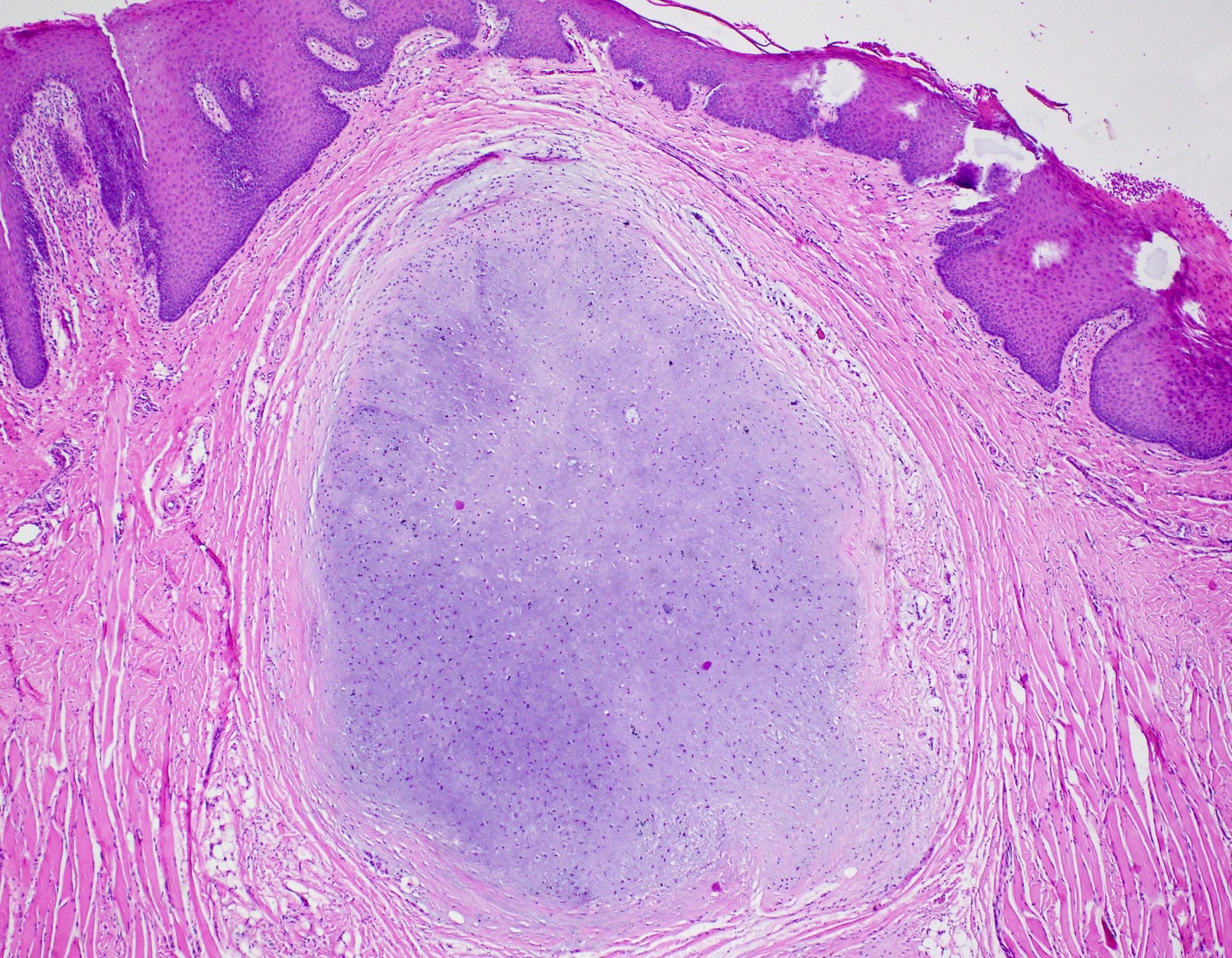
Dermoid / epidermoid cyst
Table of Contents
Definition / general | Case reports | Treatment | Clinical images | Gross images | Microscopic (histologic) description | Microscopic (histologic) imagesDefinition / general
- Midline in floor of mouth
- Present at birth but asymptomatic until inflamed
Case reports
- 11 year old boy with sublingual epidermoid cyst (J Med Case Rep 2007;1:87)
- 21 year old woman with sublingual dermoid cyst and difficulty in swallowing food (Case Rep Otolaryngol 2012;2012:634949)
- 25 year old man with epidermoid cyst presenting as large sublingual swelling (J Can Dent Assoc 2007;73:525)
Treatment
- Conservative surgical removal
Gross images
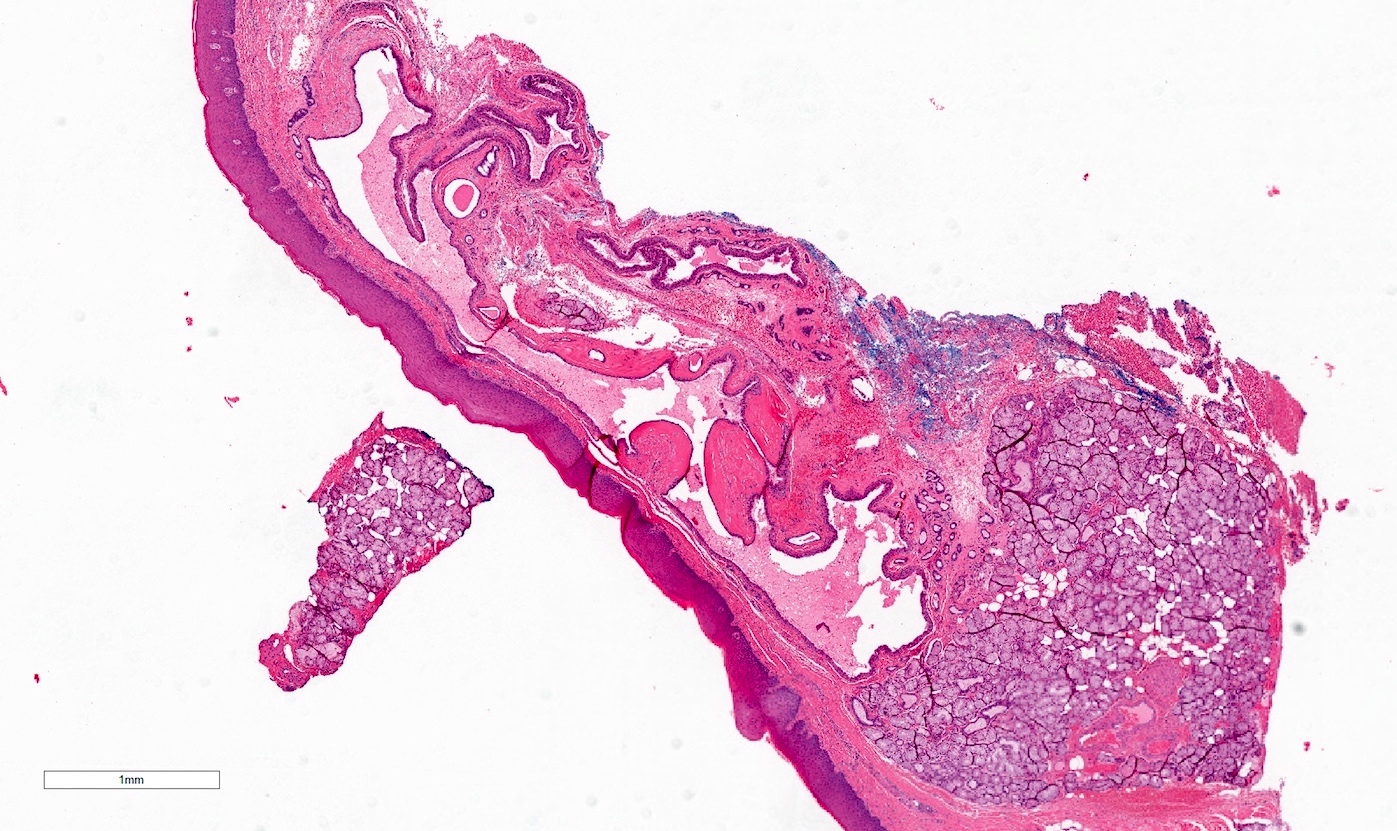
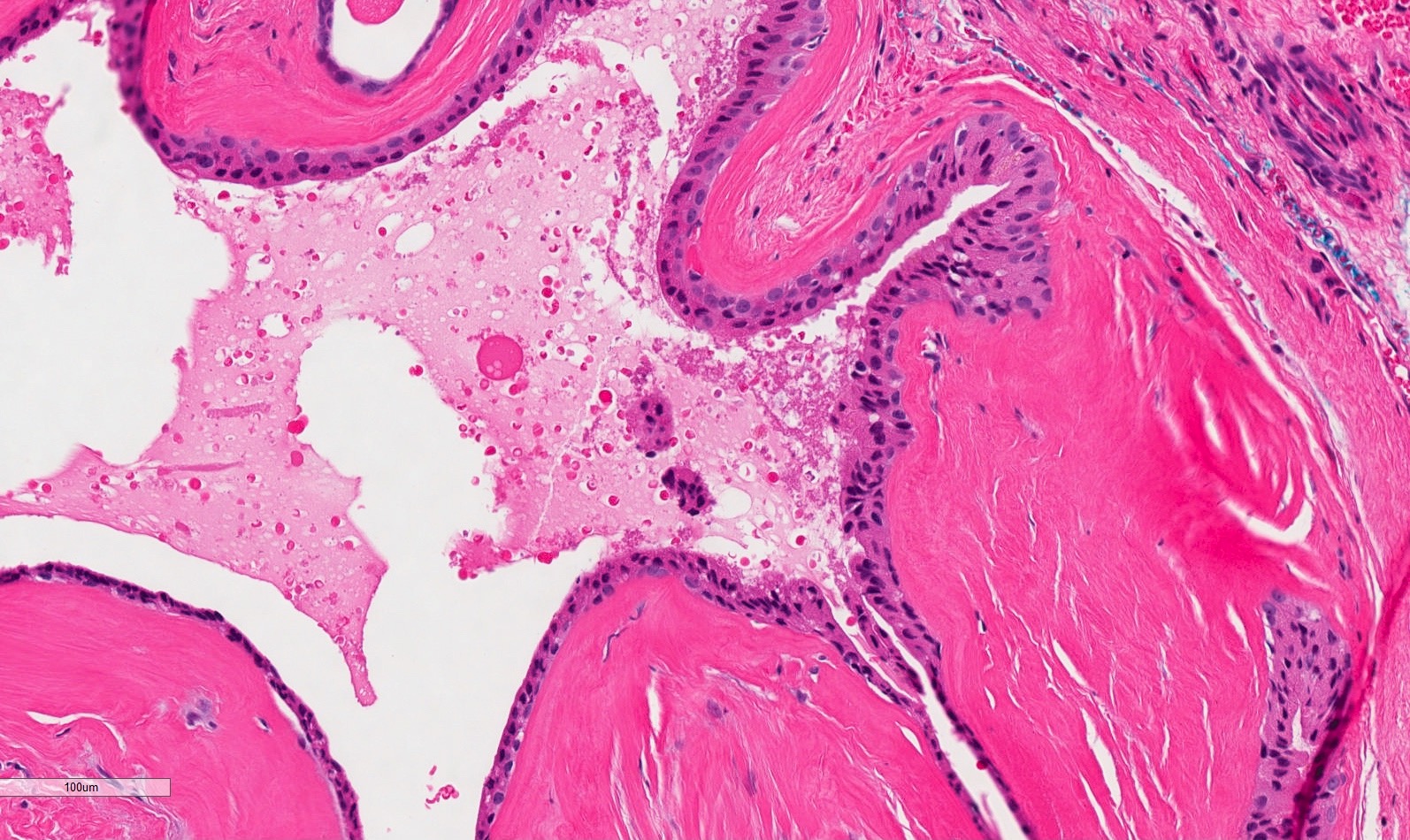
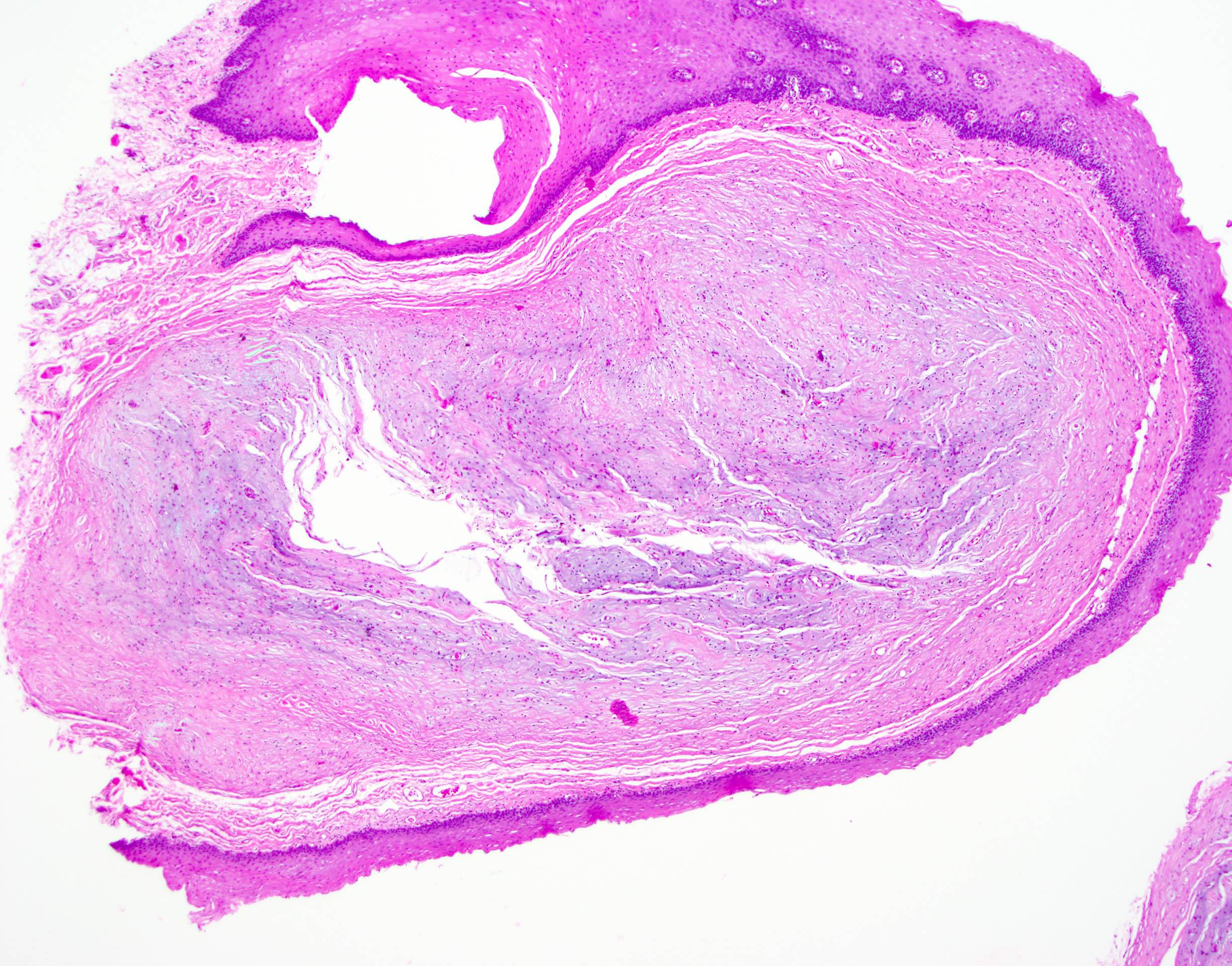
Microscopic (histologic) description
- Lined by squamous epithelium, contains skin adnexae if dermoid cyst
Microscopic (histologic) images
Duplication cyst
Table of Contents
Definition / general | Case reports | Treatment | Clinical images | Gross images | Microscopic (histologic) imagesDefinition / general
- Lined by indigenous mucosa of segment it is duplicating
Case reports
- Newborn with cyst containing gastrointestinal and respiratory epithelium (Arch Pathol Lab Med 1989;113:1301)
- Six infants with cysts of anterior tongue (Arch Otolaryngol Head Neck Surg 2001;127:1484)
- 7 year old girl with enteric duplication cyst of floor of mouth and base of tongue (Arch Pathol Lab Med 2000;124:614)
Treatment
- Excision; may recur if incompletely excised
Clinical images
Microscopic (histologic) images
Dysplasia
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Abnormal proliferation of oral epithelial squamous cells showing cytologic and architectural atypia; associated with risk of progression to squamous cell carcinoma
Essential features
- Oral epithelial dysplasia describes a spectrum of changes in the oral squamous mucosa, as it transforms from normal epithelium into a premalignant lesion with potential to develop invasive carcinoma (if not adequately treated)
- Various grading systems have been proposed to capture this spectrum of changes, to reduce inter / intraobserver variability and to guide patient management; the current widely used system is a 3 tier system, with some authors advocating for a binary system to increase reproducibility
- Clinical correlation and good communication with the surgeons / dentists is important in distinguishing dysplasia from mimics
Terminology
- Oral epithelial dysplasia (OED): histologically defined entity indicating premalignant changes in the epithelium
- Oral potentially malignant disorders (OPMD): clinically defined entities that may or may not show histologic features of dysplasia
- These include leukoplakia, erythroplakia, erythroleukoplakia, oral submucous fibrosis, oral dysplasia
ICD coding
Epidemiology
- Epidemiology for high grade dysplasia / carcinoma in situ is similar to oral squamous cell carcinoma (SCC) and includes:
- Gender: worldwide incidence higher among males than females
- Age: older adult population
- Geographic (IARC: Global Cancer Observatory [Accessed 28 February 2022])
- Higher incidence of oral cavity cancer in southern Asia, Melanesia; associated with areca / betel nut use
- High incidence also in Australia, eastern and western Europe; associated with smoking / tobacco use
- Certain oral potentially malignant disorders (OPMD) have specific predilection:
- Leukoplakia: middle aged men (> 40 years old)
- Proliferative verrucous leukoplakia: older (> 60 years old), women
- Oral submucous fibrosis: Asian, broad age range, affects both male and female with betel nut chewing habits
Sites
- Oral cavity
- Tongue: anterior two - thirds from circumvallate papillae to the junction at floor of mouth
- Floor of mouth: inner surface of lower alveolar ridge to ventral tongue
- Buccal: inner surface of cheek
- Labial: inner surface of lips
- Alveolar ridge: mucosa over the alveolar process of maxilla and mandible
- Retromolar trigone: mucosa over the ramus of the mandible, posterior to the last molar tooth
- Hard palate: area between the upper alveolar ridge extending to posterior edge of palatine bone (OED is rare on the hard palate)
- Higher risk of malignant transformation in tongue (lateral / ventral) and floor of mouth dysplastic lesions
Pathophysiology
- Progression of dysplasia to carcinoma is a stepwise event with accumulation of genetic changes with loss of heterozygosity, copy number variations, somatic mutations and hypermethylation leading to increasing severity of dysplasia and eventually to carcinoma
Etiology
- Causes are similar to those of oral squamous cell carcinoma
- Lifestyle factors:
- Smoking, tobacco use
- Areca nut chewing
- Excessive alcohol consumption
- Alcohol use has synergistic effect with smoking / areca nut chewing (Br J Cancer 2015;112:580, Eur J Cancer Prev 2010;19:431)
- Medical background:
- Autoimmune disorders
- Immunosuppressed state
- Genetic syndromes (Cancers (Basel) 2021;13:3696):
- Dyskeratosis congenita
- Bloom syndrome (congenital telangiectatic erythema)
- Xeroderma pigmentosum
- Fanconi anemia
- Nutritional deficiencies (Cancers (Basel) 2021;13:3696):
- Iron deficiency
- Vitamin A, B and C deficiencies
- HPV infection (HPV oncogenic type 16 and 18) (Anticancer Res 2010;30:3435, Mod Pathol 2017;30:1646, Mod Pathol 2013;26:1288):
- Prevalence of HPV in oral cavity SCC 4 - 6%
- Prevalence of HPV in OPMD and oral dysplasia reported 7 - 34%
Diagrams / tables
Clinical features
- Presentation can be variable, ranging from asymptomatic lesions to nonhealing ulcers
- Examination and detection require visual inspection and palpation for induration
- OED can present clinically as leukoplakia or erythroplakia (Head Neck Pathol 2019;13:423)
- Leukoplakia:
- Defined as white plaque of uncertain risk, provided that other known diseases / disorders with known cancer risk have been excluded
- Localized leukoplakia more common in men and can present as
- Homogeneous leukoplakia: uniform plaque, partially well delineated
- Nonhomogeneous leukoplakia: warty / verrucous appearance with nodular or red areas, higher risk of dysplasia and carcinoma
- Majority are keratosis of unknown significance but a proportion (40 - 46%) can show dysplasia, carcinoma in situ or invasive carcinoma at presentation (Oral Surg Oral Med Oral Pathol Oral Radiol 2014;118:713)
- Proliferative verrucous leukoplakia:
- Affects older women
- Presents as white plaque, verrucoid / warty keratotic surface and multifocal disease
- May demonstrate a ring around the collar appearance, extending along the marginal gingiva (J Periodontol 2021;92:273)
- Demonstrates a higher rate of malignant transformation
- Erythroplakia:
- Granular red plaque, painless (much less common than leukoplakia)
- More frequently associated with dysplasia, carcinoma in situ and invasive malignancy
- Oral submucous fibrosis:
- Mucosal pallor
- Palpable fibrous area
- Burning sensation
- Associated with areca nut chewing
- Leukoplakia:
Diagnosis
- Diagnosis is based on histological examination of biopsy specimen of the lesion
- Biopsies should aim to sample the most representative area with dysplasia / malignancy; e.g., thick white plaques, erythematous, indurated areas and adjacent to ulcer (J Can Dent Assoc 2008;74:283, J Can Dent Assoc 2012;78:c75)
- Biopsies of the lesion periphery can be useful in certain cases (e.g., verruciform lesions) as it allows for comparison with adjacent normal mucosa
- Large lesions may require multiple biopsy samples of heterogeneous area
- Types of biopsies (J Can Dent Assoc 2012;78:c75):
- Incisional biopsy
- Method of choice in examining representative area of tissue, especially where there is concern for malignancy
- Excisional biopsy
- Complete removal of a lesion is usually more appropriate for benign lesions
- Punch biopsy
- This technique can be used for incisional or excisional biopsy of a small lesion that is easy to access
- Laser technique
- Greater value in wound management over scalpel biopsy where wound closure is difficult or inappropriate
- Used for complete excision of lesions
- Avoid use during incisional biopsy to avoid cytologic alterations, which may interfere with diagnosis
- Incisional biopsy
Prognostic factors
- Presence of risk factors:
- Persisting lifestyle factors (smoking / tobacco, excess alcohol, areca nut) increases risk of recurrence / progression
- Precursor lesions:
- Nonhomogeneous leukoplakia, erythroleukoplakia and erythroplakia are associated with higher risk of dysplasia and transformation
- Multifocal disease increases risk of recurrence
- Incomplete resection increases risk of recurrence
- Size of the lesion (> 200 mm2) increases risk of malignant transformation (J Oral Pathol Med 2016;45:155)
- Location of lesion:
- Higher risk of malignant transformation in tongue and floor of mouth lesions (J Oral Pathol Med 2016;45:155, Cancer 2001;91:2148)
- Grade of dysplasia:
- Not all dysplastic lesions progress to invasive carcinoma
- Transformation rate (annual) reported at 12% with higher rates associated with higher grades of dysplasia (Head Neck 2009;31:1600, Head Neck 2020;42:539)
- Transformation rates over 15 year period:
- Low grade (mild) dysplasia ~6%,
- Moderate dysplasia ~18%,
- High grade (severe) dysplasia ~39% (Cancer Prev Res (Phila) 2013;6:822)
- Not all dysplastic lesions progress to invasive carcinoma
Case reports
- 18 year old man with right lateral tongue leukoplakia (Oral Oncol 2021;122:105565)
- 39 year old woman (no history of smoking or alcohol use), on treatment for rheumatoid arthritis, develops a right lateral tongue lesion (J Oral Pathol Med 2005;34:447)
- 46 year old man with a left buccal mucosa nodule of several years duration (Int J Surg Pathol 2014;22:248)
- 54 year old man, with myeloma treated with hematopoietic stem cell transplantation, develops diffuse white lesions of the buccal, tongue and palate mucosa (Spec Care Dentist 2019;39:51)
Treatment
- Surgical management is the treatment of choice
- Excision or laser ablation
- Does not completely eliminate the risk of recurrence or transformation; therefore, regular follow up is required
- Nonsurgical management
- Topical and systemic treatments (e.g., bleomycin, cyclooxygenase [COX] inhibitors, vitamin A and beta carotene) have been examined but show no benefit in reducing risk of recurrence or malignant transformation (Cochrane Database Syst Rev 2016;7:CD001829, Periodontol 2000 2019;80:126)
- Elimination of risk factors is essential to reduce the risk of recurrence
Clinical images
Gross description
- Identification of OED may be easier on excisions rather than small biopsies
- Mucosal resections can show ill defined, pale areas or plaque-like lesions with / without ulceration
- Thickened, verruciform appearance in lesions with verrucous hyperplasia
- OED is confined to surface mucosa
Frozen section description
- Dysplastic changes may be seen in mucosal margins of radical resections for oral squamous cell carcinoma (Cancer 2006;107:2792, Head Neck Oncol 2011;3:56)
- Frozen sections should not be performed for diagnosis of OED as it can compromise evaluation of grade and invasion
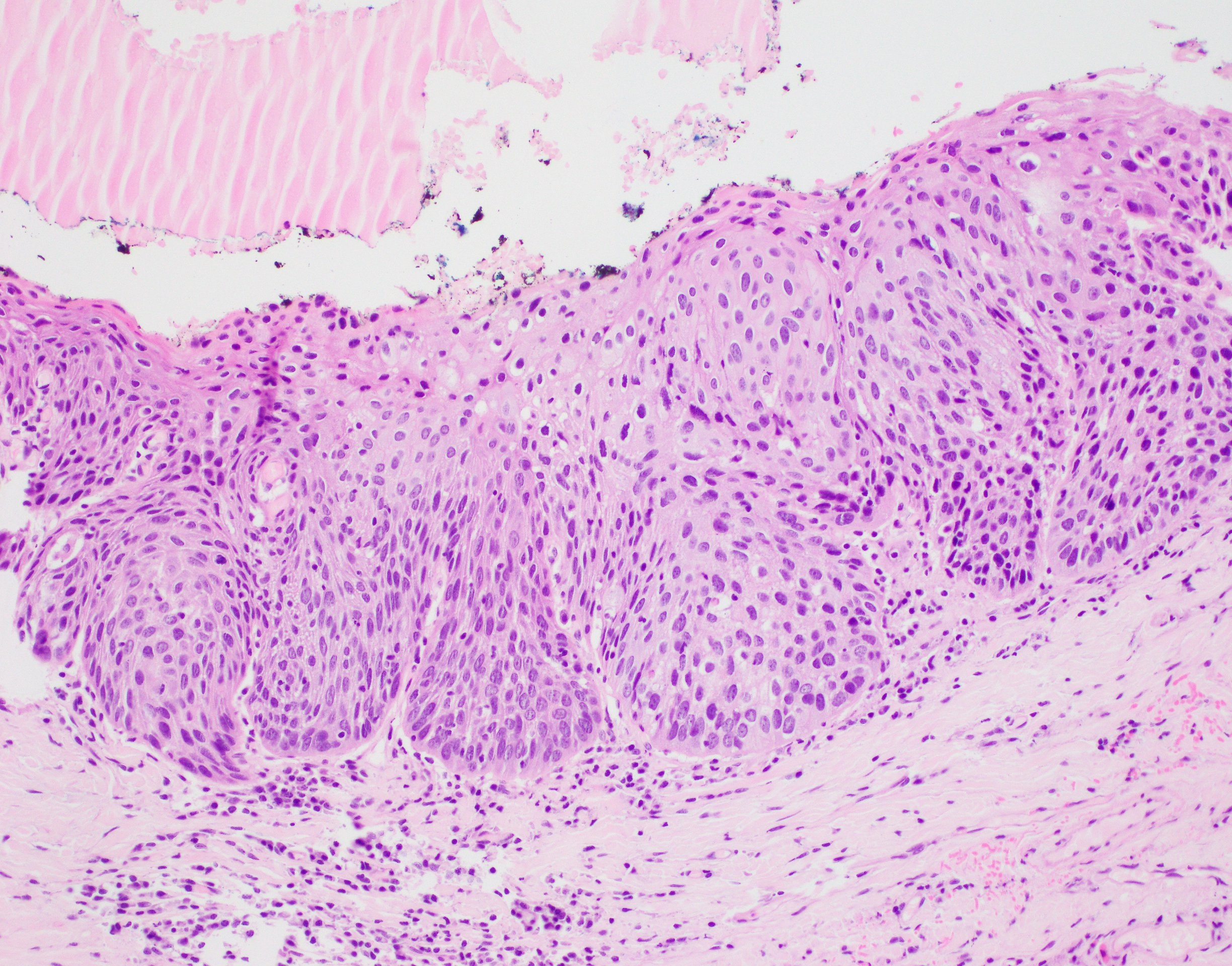
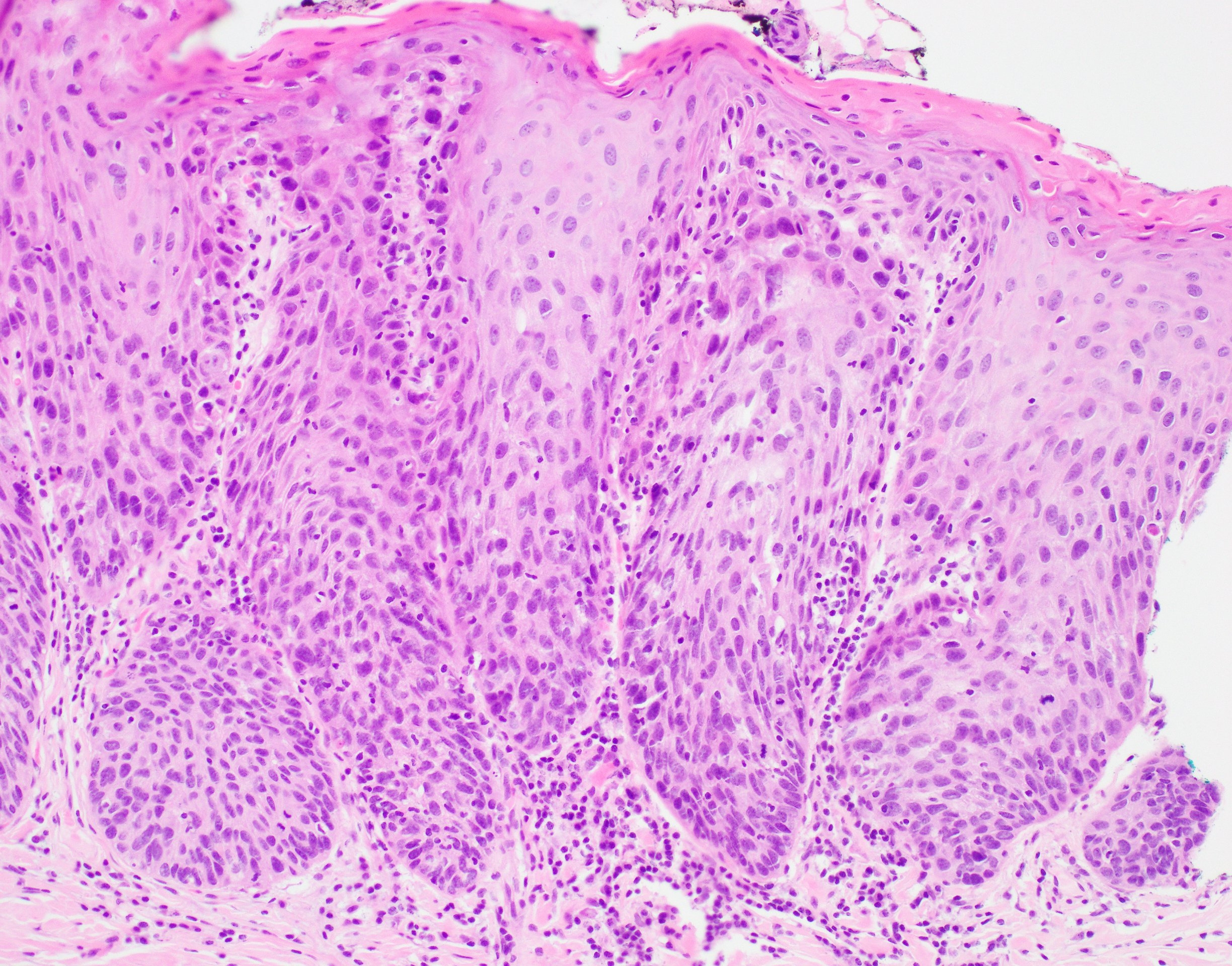
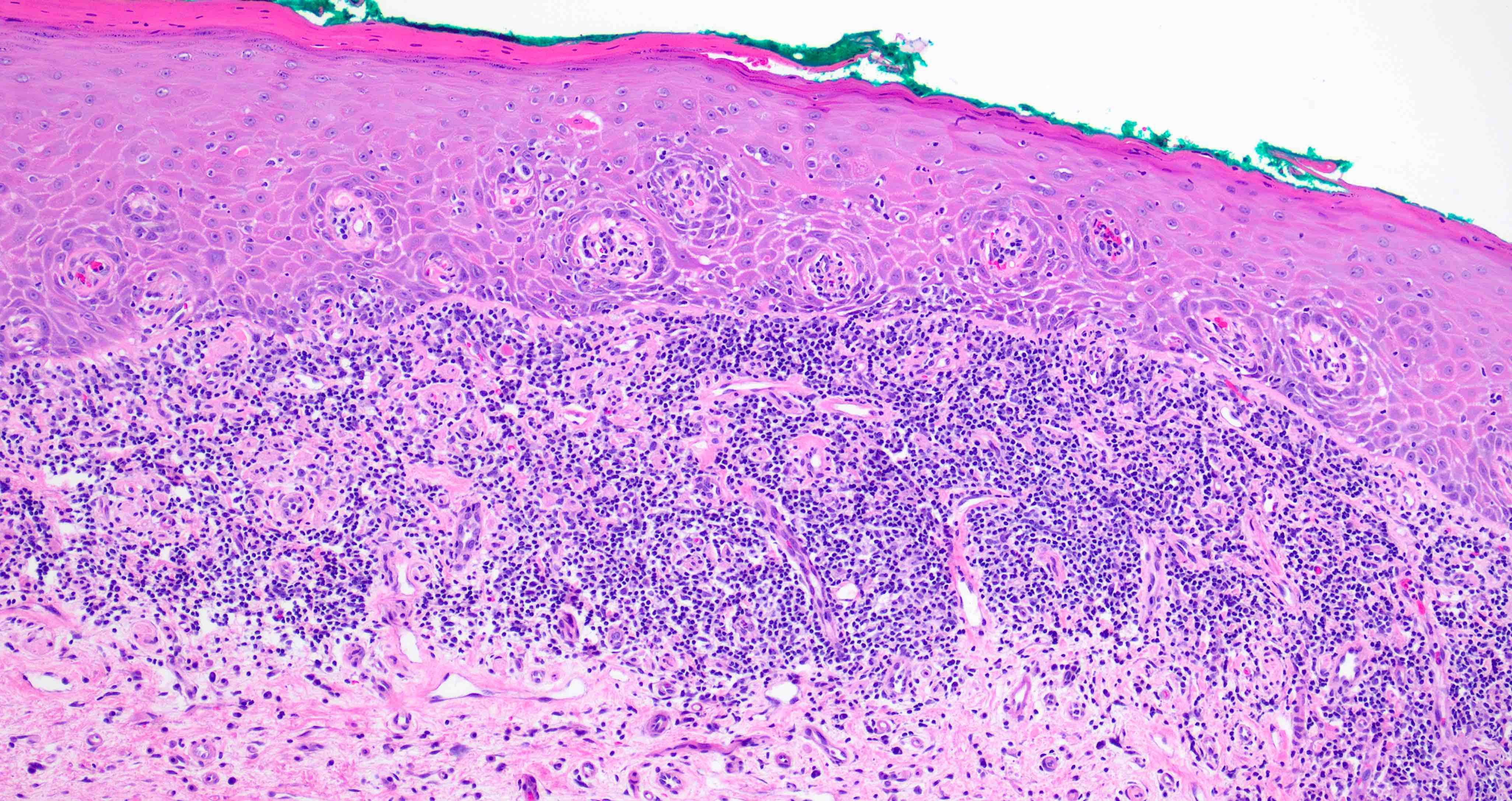
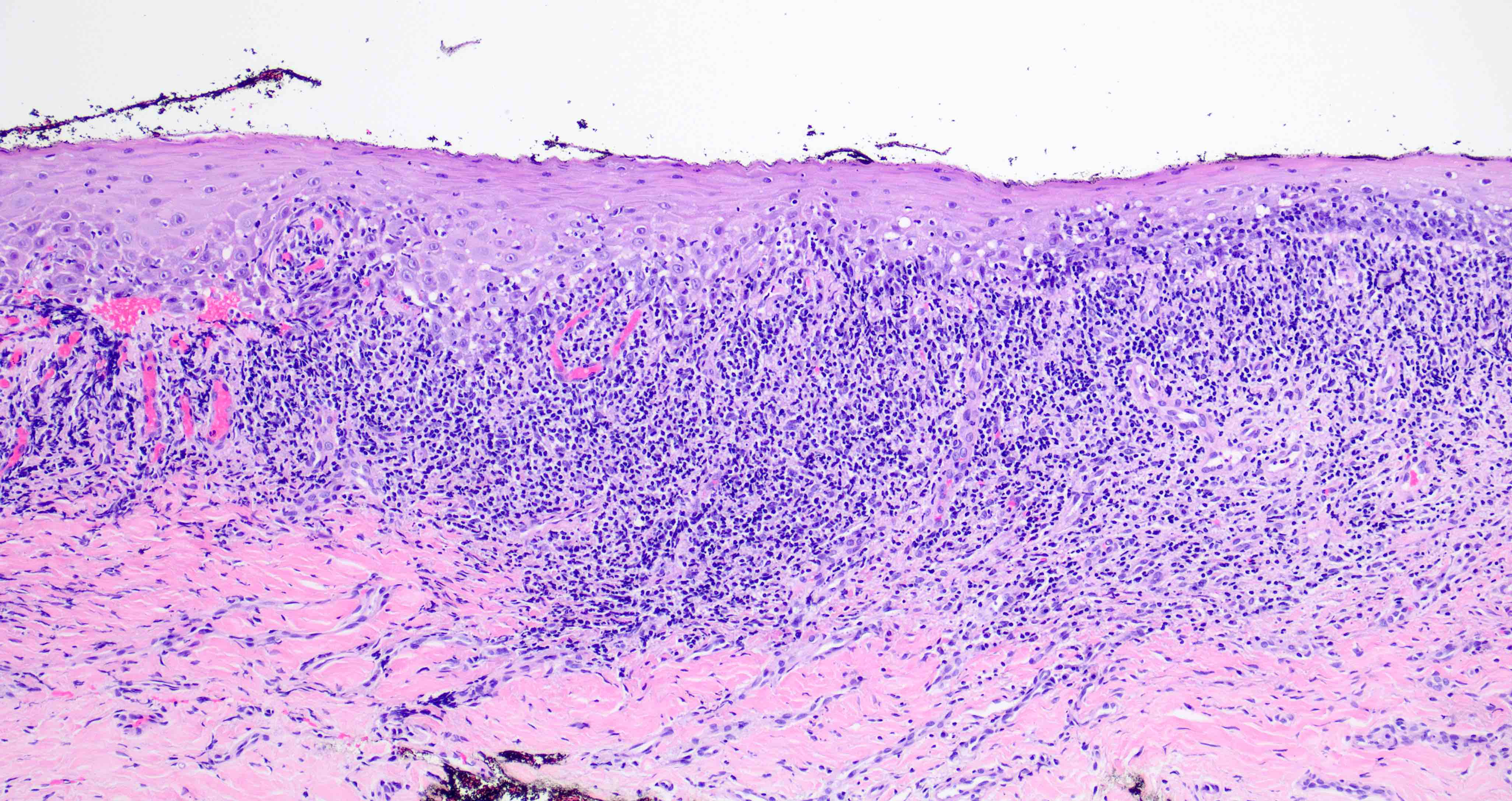
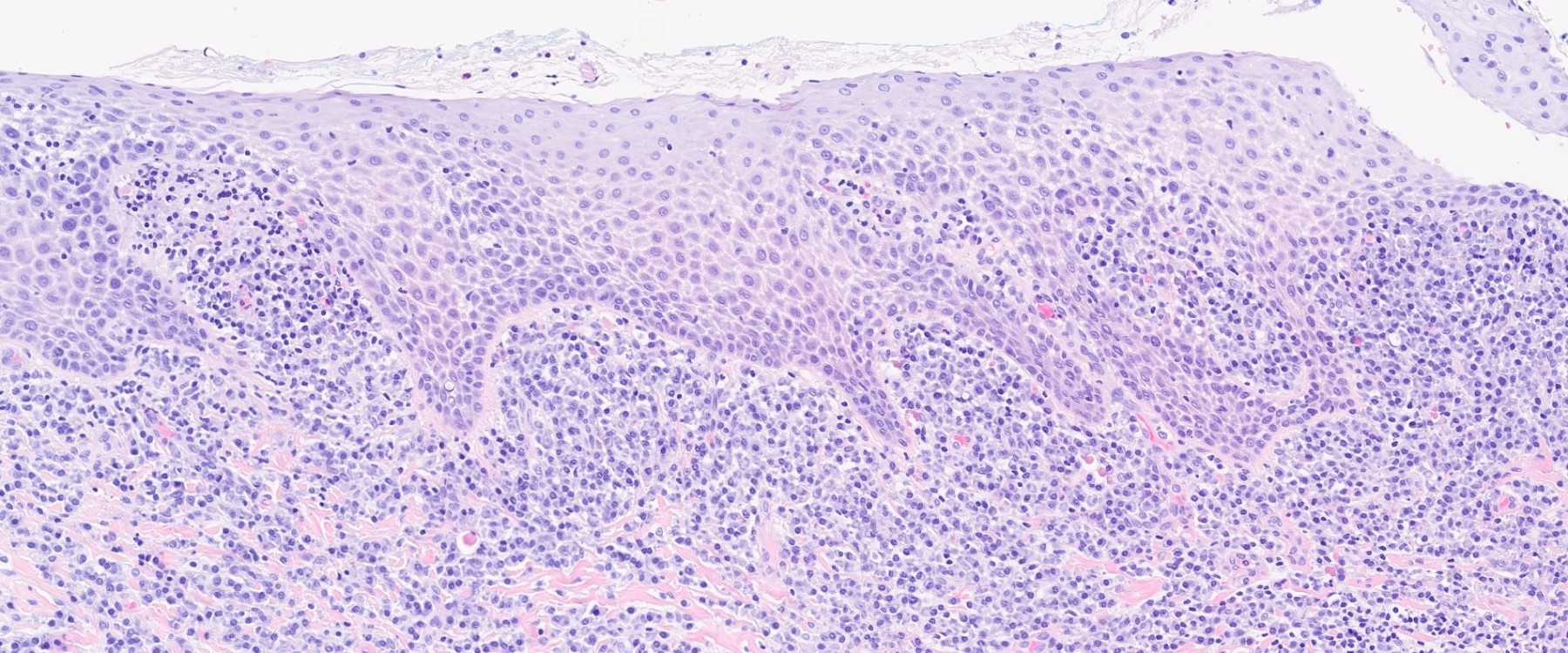
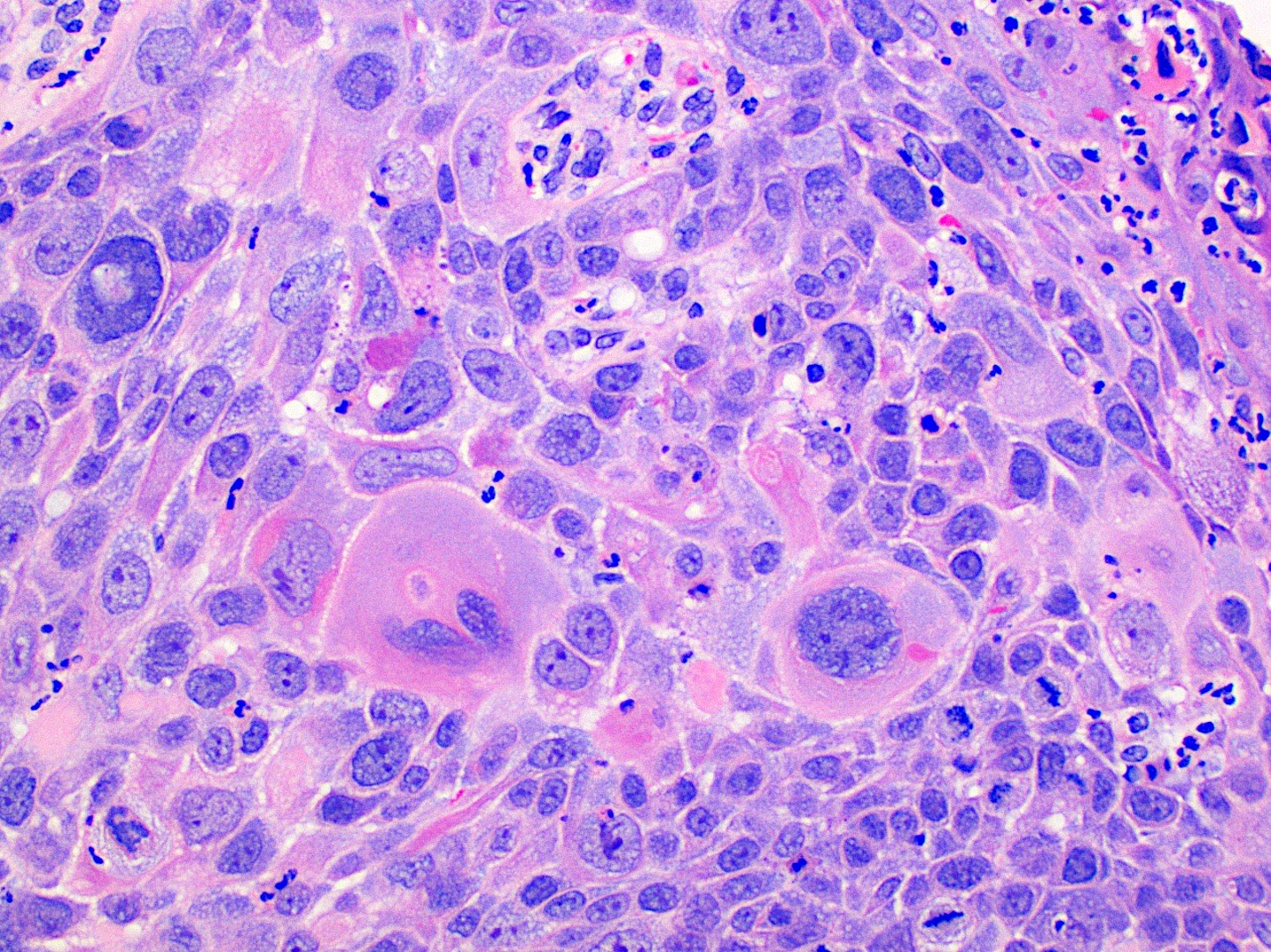
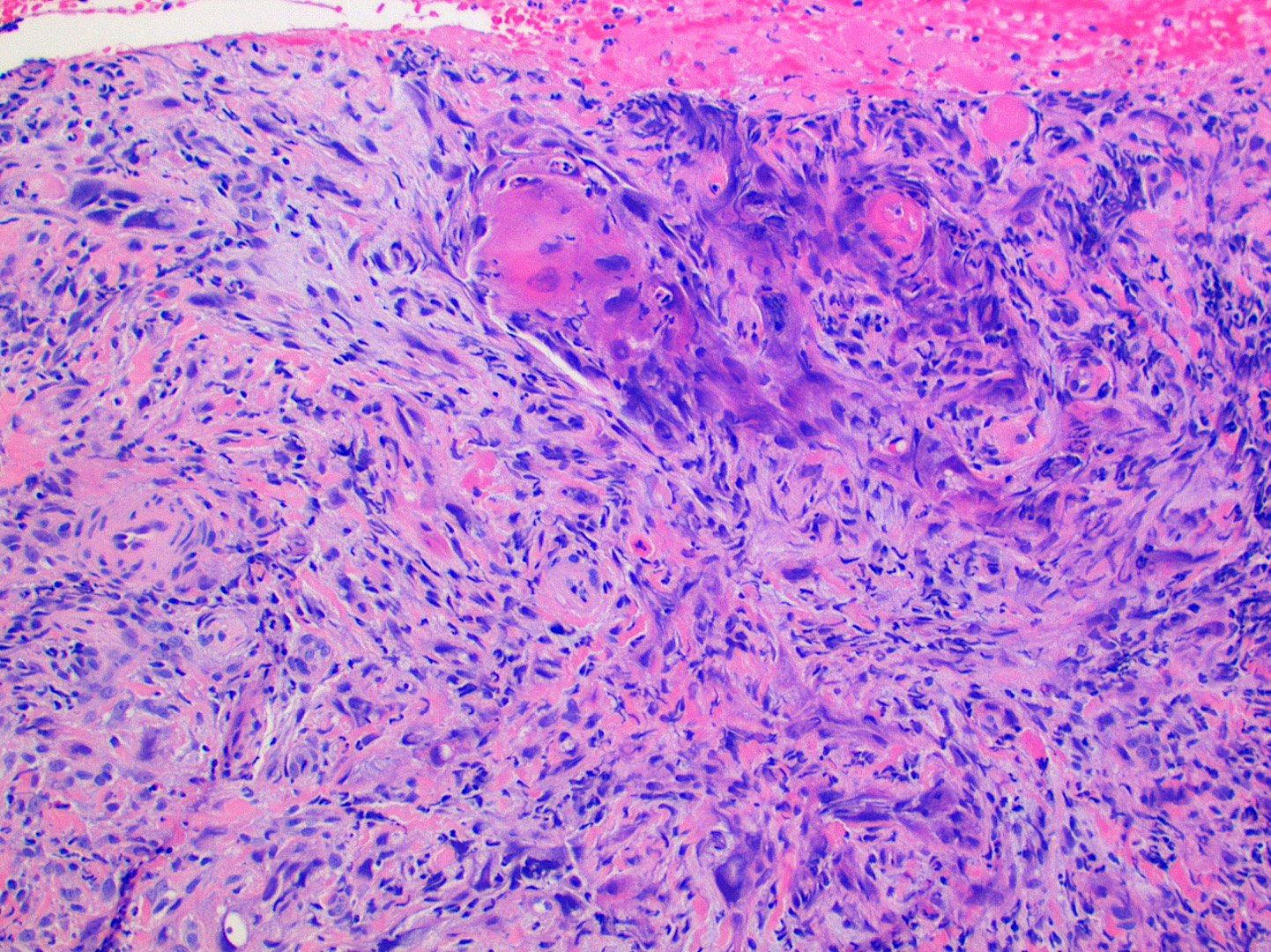
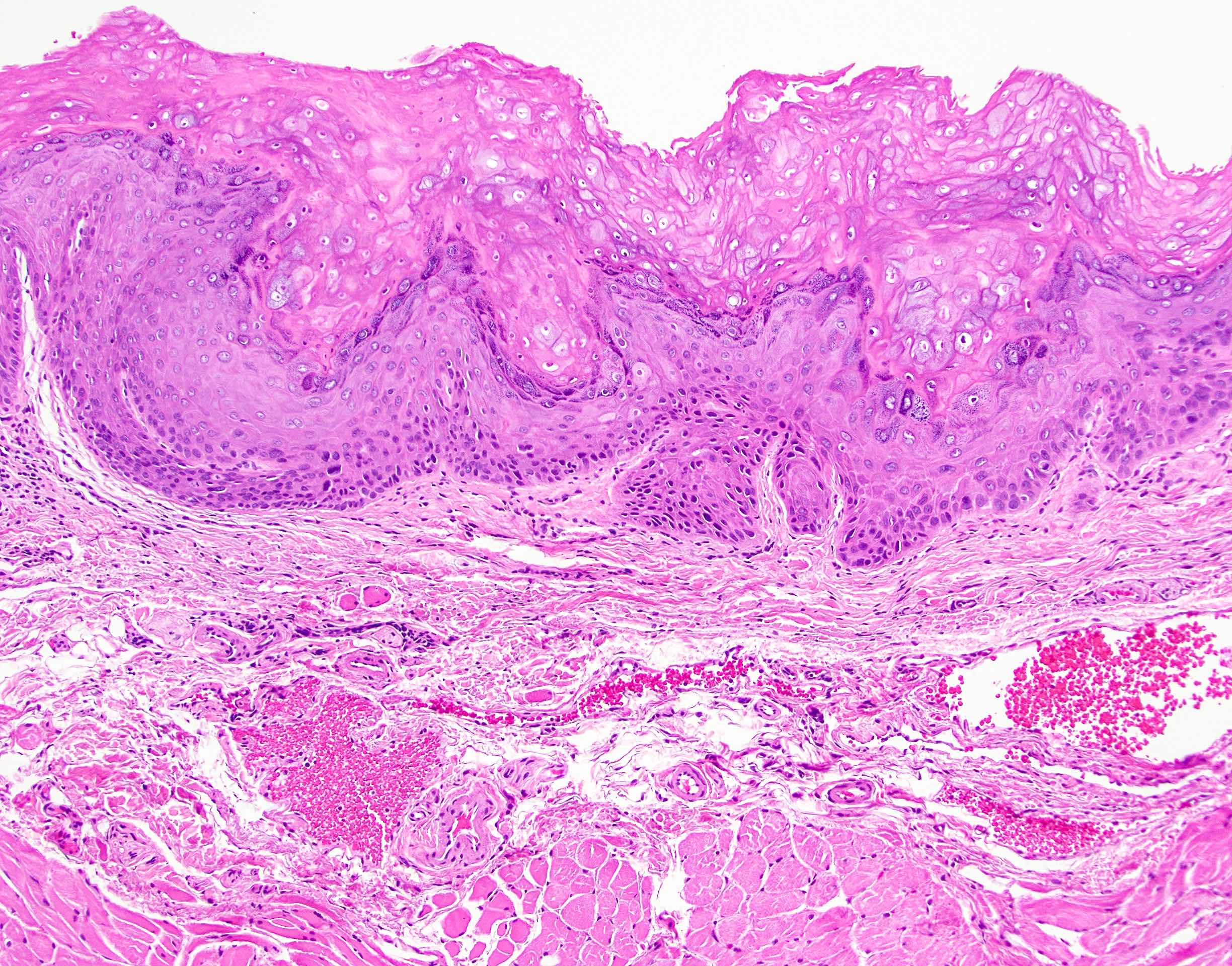
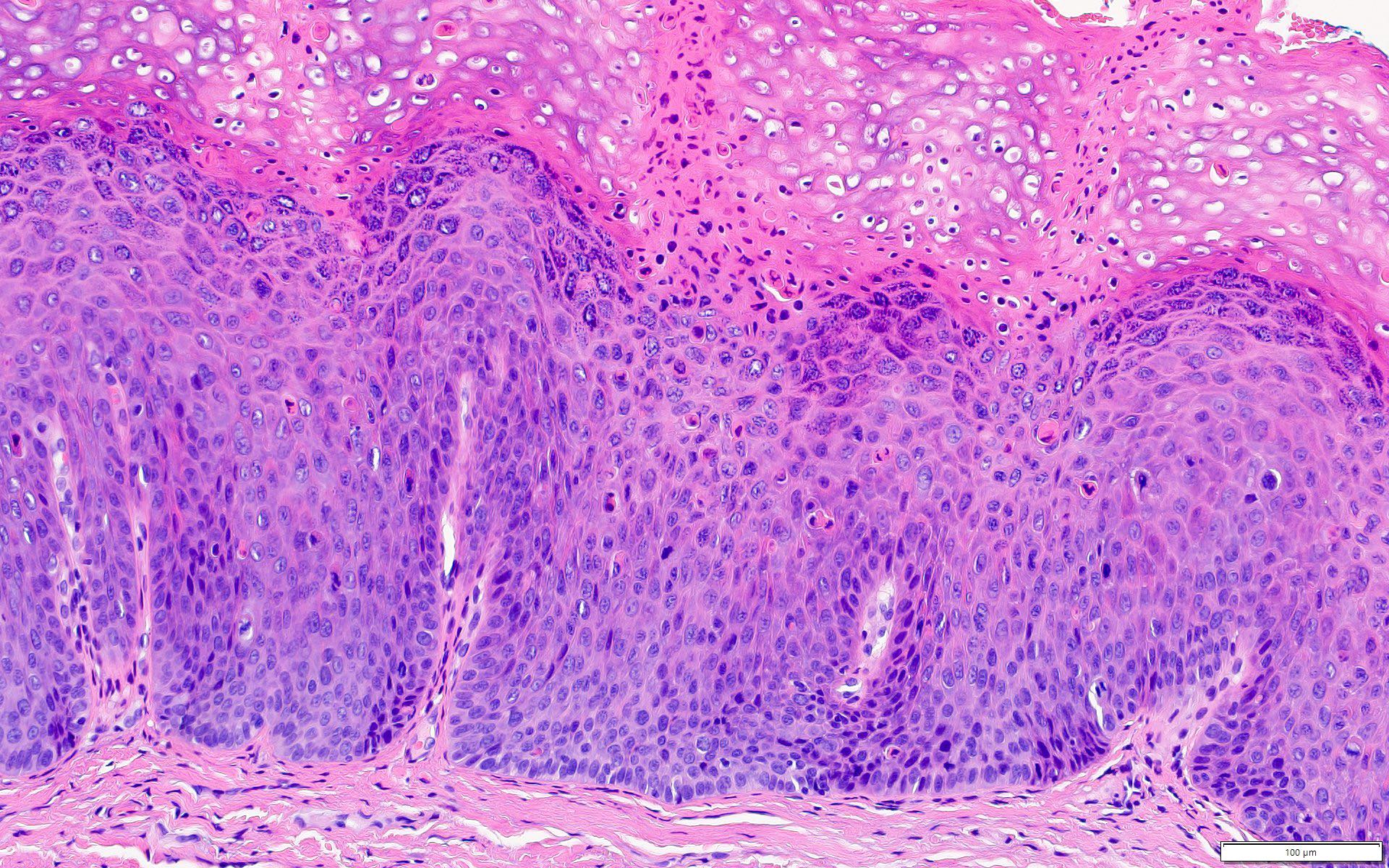
Microscopic (histologic) description
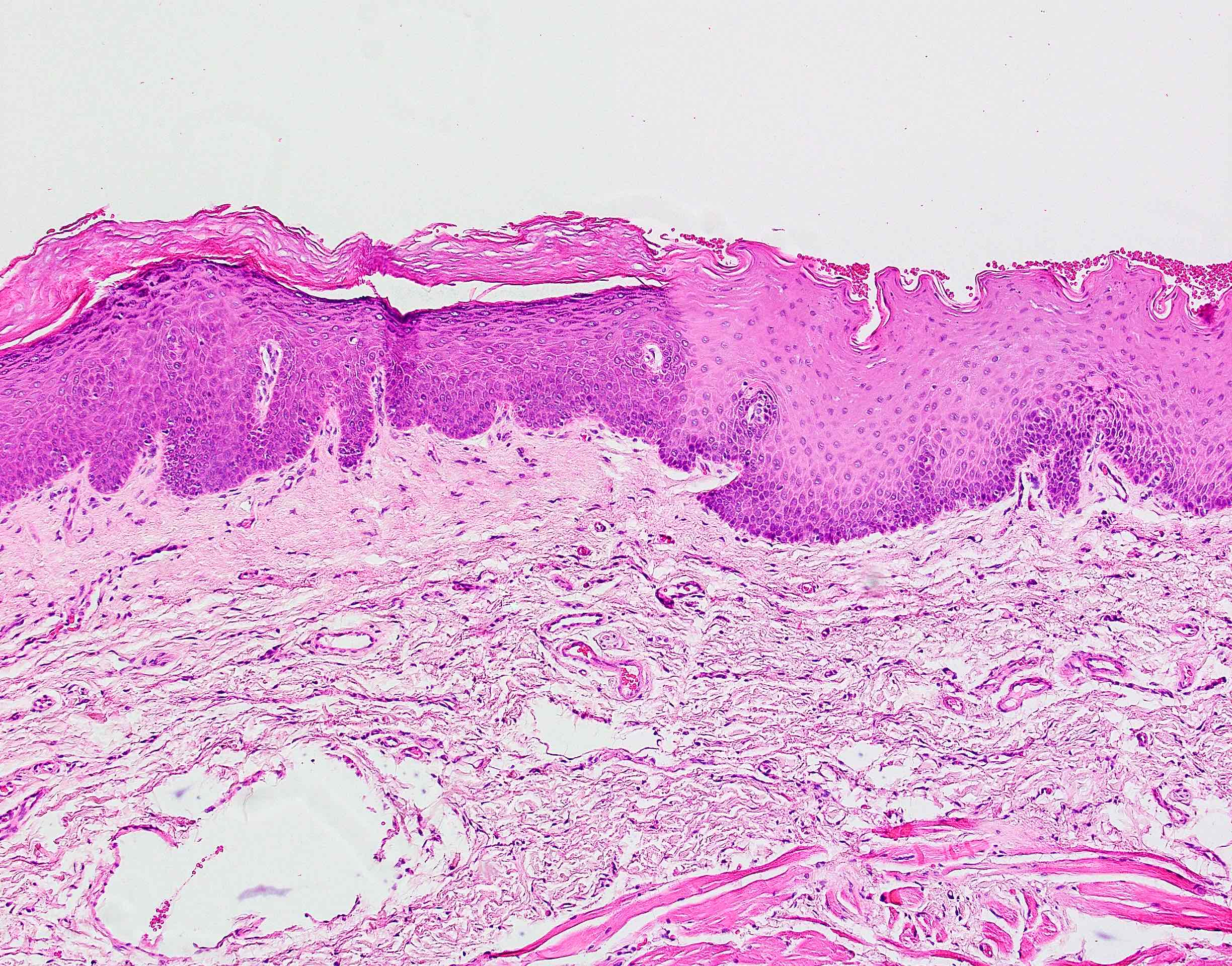
- Diagnostic criteria for epithelial dysplasia are divided into 2 types of features, architectural and cytological; various combinations of these features lead to a specific grade of dysplasia
- Dysplasia is divided into 3 grades of severity ranging from:
- Mild / low: atypia involves < one - third
- Moderate / intermediate: atypia involves one to two - thirds of the mucosal thickness
- Severe / high: atypia involves > two - thirds of the epithelial thickness
- However, the degree of cytologic atypia can increase the grade even if involving lower part of mucosa
- Carcinoma in situ is synonymous with severe dysplasia and involves full thickness of the oral mucosa
- Diagnostic criteria for epithelial dysplasia adapted from WHO Classification of Head and Neck Tumors, 2017:
- Architectural features:
- Basal hyperplasia and increased stratification
- Loss of epithelial cell cohesion
- Bulbous drop shaped rete ridges
- Confluence of the rete
- Keratin pearls within rete ridges
- Abnormal superficial mitotic figures
- Lack of maturation towards the surface
- Verrucous / papillary architecture
- Bulky epithelial hyperplasia
- Sharp demarcation from the adjacent inflamed or normal mucosa
- Extension of squamous atypia along minor salivary gland ducts
- Cytological features:
- Abnormal variation in cell size
- Abnormal variation in cell shape
- Dyskeratosis and glassy cytoplasm
- Abnormal variation in nuclear size
- Abnormal variation in nuclear shape
- Increased nuclear:cytoplasmic ratio
- Increased number of mitotic figures
- Atypical mitotic figures
- Premature keratinization in single cells
- Increased number and size of nucleoli
- Hyperchromasia
- Architectural features:
- Further additions to the architectural and cytologic criteria outlined in WHO have been proposed, including hyperkeratosis with epithelial atrophy (Head Neck Pathol 2019;13:423)
- Purpose of grading dysplasia is for risk stratification and to direct appropriate patient management (when considered together with other risk / prognostic factors)
- History of grading oral dysplasia (J Oral Biol Craniofac Res 2020;10:788):
- Smith and Pindborg 1969
- Use of standardized photographs for each criterion of dysplasia (total of 13 criteria) (J Oral Maxillofac Pathol 2015;19:198)
- Each criterion was graded as absent, slight and marked; then were assigned specific scores that were added to give a final epithelial atypia index
- This system was found to be tedious and time consuming
- Ljubljana classification 2003
- System proposed for classifying laryngeal dysplasia was also proposed for lesions of the oral cavity (J Craniomaxillofac Surg 2003;31:75)
- Initial 4 grade system: squamous hyperplasia, basal parabasal hyperplasia, atypical hyperplasia and carcinoma in situ (Histopathology 1999;34:226)
- Differences in interpretation of terminology for each grade led to variability in grading and difficulty in categorizing dysplasia in atrophic mucosa
- Brothwell 2003 (Community Dent Oral Epidemiol 2003;31:300)
- 5 tier system: no dysplasia, mild, moderate, severe and carcinoma in situ
- Diagnostic criteria for dysplasia based on 4 histologic features only: basal and parabasal hyperplasia, nuclear hyperchromasia, nuclear pleomorphism and bulbous retes
- WHO 2005
- Recognized 5 stages of precursor lesion: squamous hyperplasia, mild dysplasia, moderate dysplasia, severe dysplasia and carcinoma in situ
- Dysplasia was based on changes in architecture and cytology and the epithelium was divided into thirds in order to classify the lesion as mild, moderate or severe
- Binary system 2006
- Due to the variability in interpretation of each cytological / architectural dysplasia criterion (presence of and degree of change), it was proposed that a 2 tier classification would increase concordance (J Oral Pathol Med 2008;37:127, Oral Oncol 2006;42:987)
- WHO 2017
- Squamous hyperplasia and carcinoma in situ were removed (carcinoma in situ synonymous with high grade dysplasia in oral cavity), leaving a 3 tiered system
- WHO recommends consensus grading by more than 1 pathologist to enhance reproducibility
- Smith and Pindborg 1969
- HPV associated oral dysplasia (Mod Pathol 2017;30:1646, Mod Pathol 2013;26:1288)
- Predilection for tongue and floor of mouth location
- Associated with high risk HPV subtype 16
- Distinct histologic features include parakeratosis, epithelial hyperplasia, prominent karyorrhexis and apoptosis in all levels of the mucosa and conventional carcinoma in situ histology; koilocytes may be focal / few in number
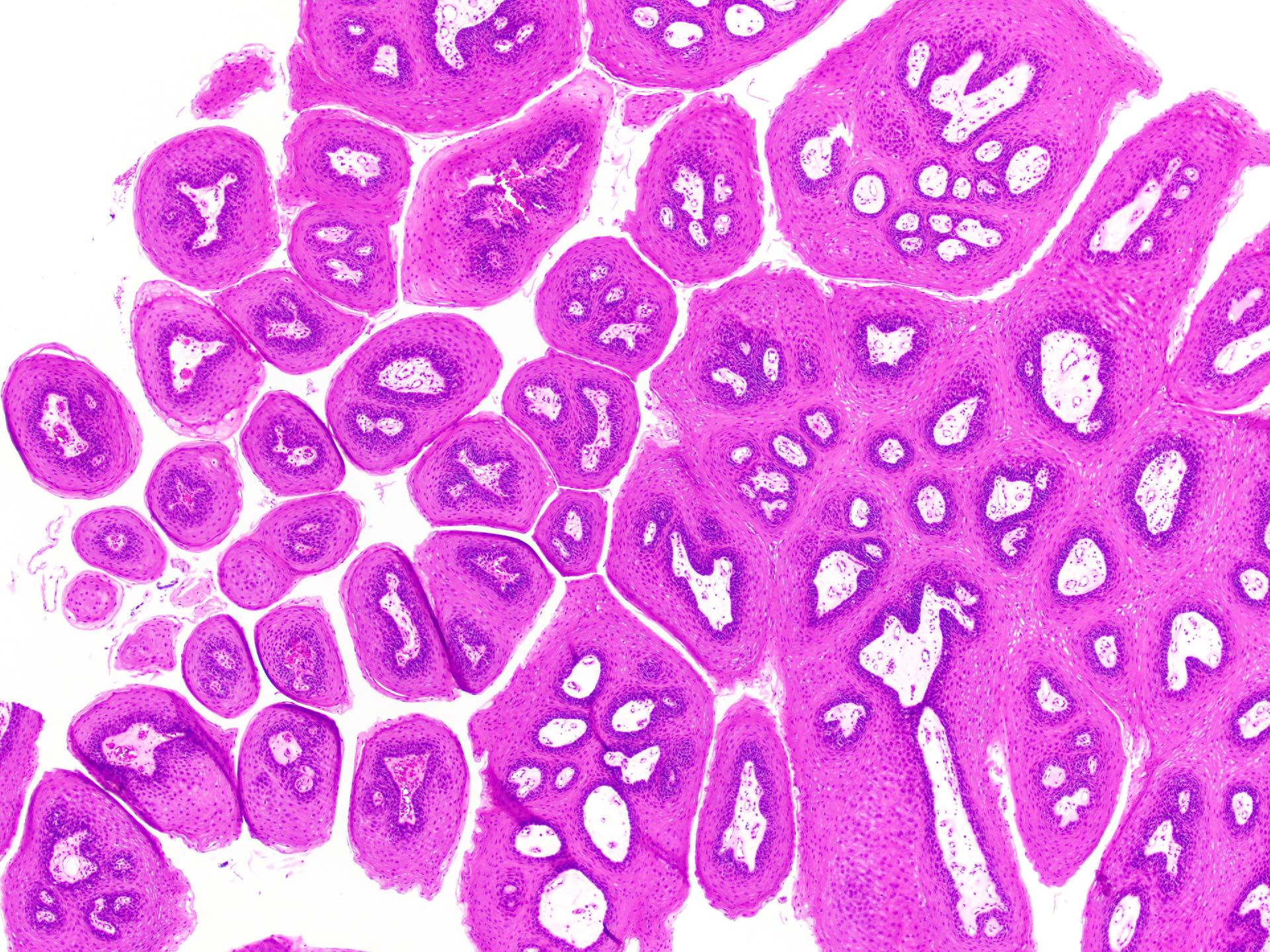
Microscopic (histologic) images
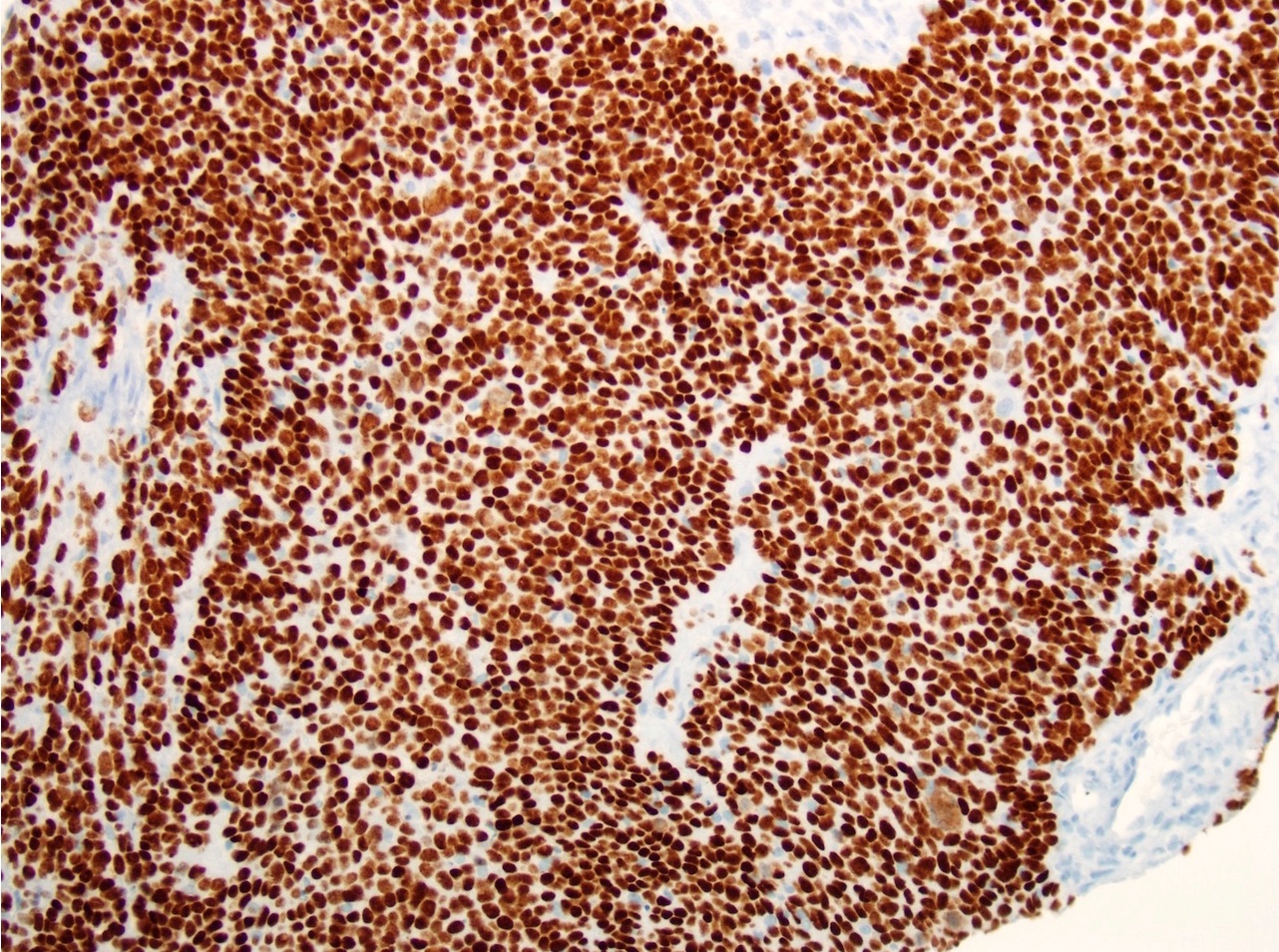
Positive stains
- While immunohistochemistry stains (p53, cyclin D1, Ki67, BCL2, EGFR) have been utilized in studying the progression of epithelial dysplasia and in an attempt to assess degree of dysplasia, the gold standard for diagnosis and grading of OED is based on routine histological examination (Anticancer Res 2008;28:2535, Int J Biol Markers 2007;22:132)
Molecular / cytogenetics description
- Loss of heterozygosity (LOH) (Cancer Prev Res (Phila) 2012;5:1081, Clin Cancer Res
2000;6:357)
- LOH at 3p and 9p associated with dysplasia with slight increase in relative risk of developing invasive cancer
- Increased risk of progression in the presence of LOH at other chromosomes including 4q, 8p, 11q, 13q and 17p
- LOH at 3p and 9p associated with dysplasia with slight increase in relative risk of developing invasive cancer
- Other molecular alterations detected in premalignant lesions include increased expression of EGFR, cyclin D1 amplification, loss of Rb and disruption / overexpression of p53 (J Oral Pathol Med 2009;38:737, J Oral Pathol Med 2021;50:632, Mod Pathol 2022;35:177)
Sample pathology report
- Lateral tongue, mucosal excision - stitch anterior:
- Low to high grade mucosal dysplasia (see comment)
- Comment: The entire specimen has been embedded and the sections studied through levels to show oral tongue mucosa with superficial skeletal muscle. There is a broad area of mucosal dysplastic changes ranging from low to high grade dysplasia. The latter is characterized by moderately thickened mucosa with atypical squamous cells involving almost full thickness of the epithelium. There is loss of polarity, increased nuclear size, hyperchromasia and pleomorphism with readily seen nucleoli. Suprabasal mitoses are noted including a few atypical forms. There is focal superficial excoriation and acute inflammation, with isolated fungal hyphae seen on dPAS stain. No invasive carcinoma is identified. The high grade dysplasia is 2 mm away from the closest peripheral margin, midline, while low grade dysplasia is seen focally at the anterior margin.
Differential diagnosis
- Clinical history is often useful to distinguish OED from mimics
- Traumatic / reactive keratoses:
- Clues to reactive keratosis: superficial changes, shredding keratin, shaggy parakeratosis, uniform cytologic atypia, balloon cells and intracellular edema
- Can show basal cell hyperchromasia and pleomorphism but usually less severe than true dysplasia
- Candida:
- Causes hyperplasia, parakeratosis, superficial neutrophilic infiltrate
- Fungal hyphae: PAS and PAS diastase
- Oral lichen planus (OLP):
- OLP tends to present as bilateral, multifocal, migrating / evolving lesions in contrast to an isolated, nonmigrating lesion of epithelial dysplasia
- Reactive atypia from lichenoid inflammation can be difficult to distinguish from mild dysplasia
- Look for classic features of OED: loss of polarity, drop shaped rete, mitoses, premature keratinization, sharp distinction from normal adjacent mucosa
- Lymphocyte predominant infiltrate versus mixed infiltrate in epithelial dysplasia with lichenoid features may be helpful
- In some situations, it may be impossible to differentiate between reactive atypia and true dysplasia
- Discussion with surgeon / dentist and recommend treatment or healing / resolution of inflammation before re-evaluation and rebiopsy, if clinically indicated
- Good communication with the clinician is important in ensuring appropriate patient management
Additional references
Board review style question #1
You receive a wedge biopsy from a 48 year old woman with a longstanding tongue lesion. Which of the following is true in relation to this histological finding?
- Ensure the entire specimen is embedded and examined with levels
- Following complete excision, the patient will no longer require any follow up
- Immunohistochemistry for p16 can be used to confirm diagnosis
- Presence of fungal hyphae will confirm the mucosal changes are reactive and are not dysplasia
Board review style answer #1
A. Ensure the entire specimen is embedded and examined with levels. Small mucosal biopsy / excisions should be entirely embedded and examined through levels to identify highest grade of dysplasia and the presence / absence of (micro) invasive disease.
Comment Here
Reference: Dysplasia
Comment Here
Reference: Dysplasia
Board review style question #2
Which of the following is the most favorable prognostic factor for oral epithelial dysplasia?
- 45 year old woman with recurrent lateral tongue erythroplakia
- Complete resection of low to intermediate grade dysplasia of lip buccal mucosa
- Floor of mouth dysplasia recurrence
- Multifocal intermediate to high grade dysplasia
- Tobacco chewing in patient with previous tongue cancer
Board review style answer #2
B. Complete resection of low to intermediate grade dysplasia of lip buccal mucosa. The most favorable prognostic factor is the complete resection of a low risk lesion in a lower risk site (compared with tongue and floor of mouth sites that have higher risk of malignant transformation).
Comment Here
Reference: Dysplasia
Comment Here
Reference: Dysplasia
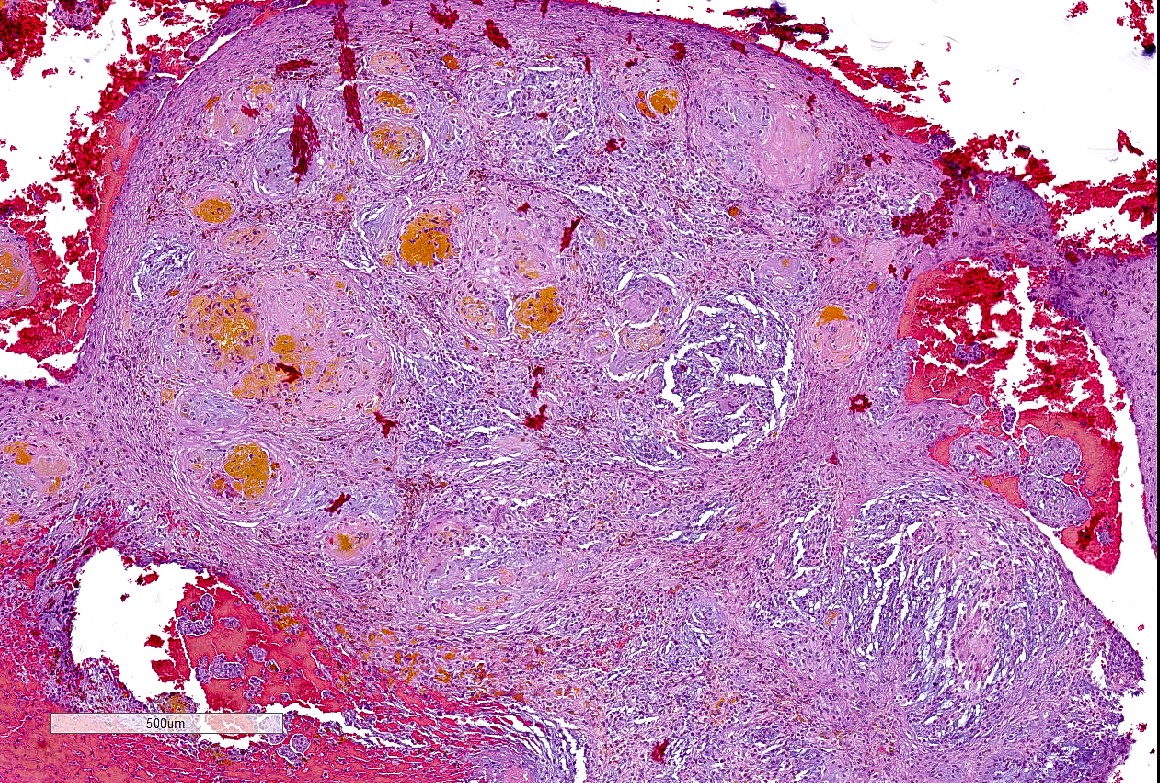
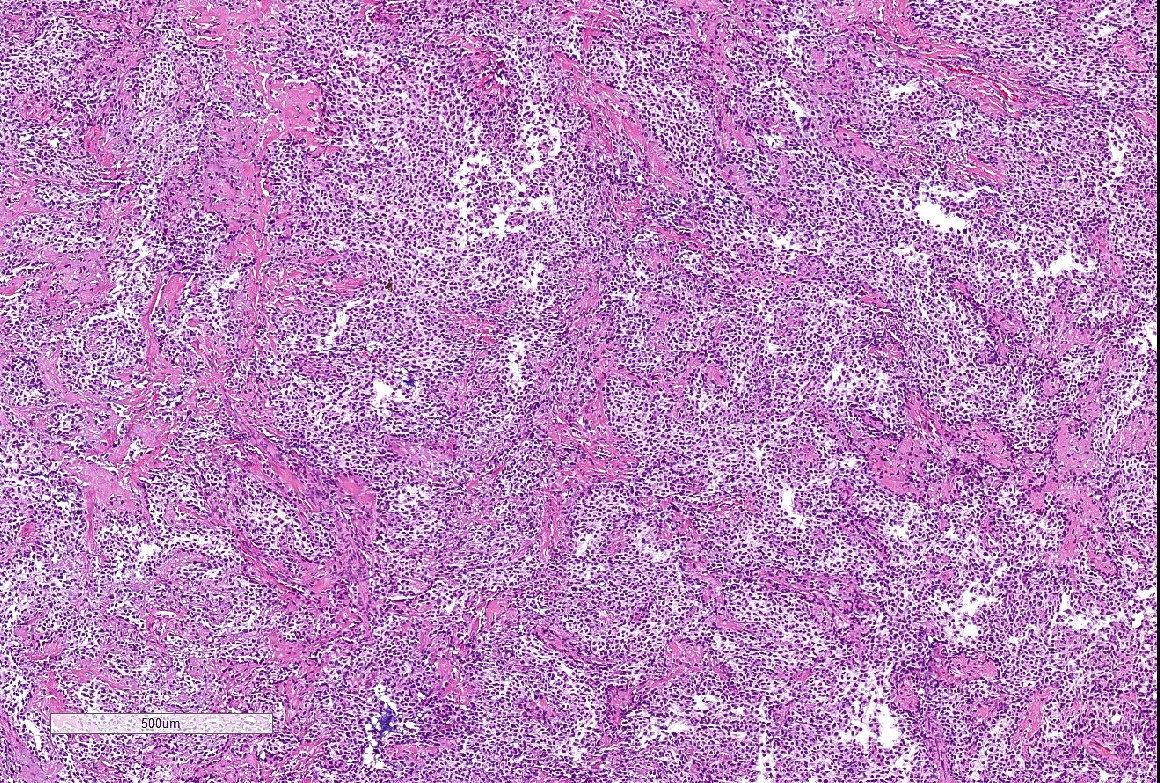
Ectomesenchymal chondromyxoid tumor
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Definition / general
- Rare, benign soft tissue tumor with striking predilection for the anterior dorsal tongue
- First named by Smith et al. in 1995 (Am J Surg Pathol 1995;19:519)
Essential features
- Most are found on the anterior dorsal tongue
- Fewer than 120 well documented cases have been reported
- Histopathologically demonstrates a well defined, often multilobulated tumor with ovoid, round, fusiform or polygonal cells within a sometimes myxoid, chondromyxoid or mucoid background
- Reticular arrangement of cells is often noted
- Characterized by RREB1::MRTFB (previously MKL2) fusion in 90% of cases (Am J Surg Pathol 2018;42:1297)
- Conservative excision recommended; < 10% have recurred
Terminology
- Ectomesenchymal chondromyxoid tumor of the anterior tongue (Am J Surg Pathol 1995;19:519)
ICD coding
- ICD-10: D10.1 - benign neoplasm of tongue
Epidemiology
- No sex predilection
- Average age ~40 years
- Age range is from 2.3 - 78 years (Cleft Palate Craniofac J 2022;59:932, Am J Surg Pathol 1995;19:519)
Sites
- Striking predilection for anterior dorsal tongue
- Rare cases reported in other oral locations
- Posterior tongue / base of tongue (Am J Surg Pathol 2018;42:1297, Cleft Palate Craniofac J 2022;59:932, Head Neck Pathol 2014;8:329, Oral Oncol 2017;67:192)
- Gingiva / anterior hard palate (Int J Oral Sci 2018;10:4, Oral Surg Oral Med Oral Pathol Oral Radiol 2012;114:154)
- Buccal mucosa (J Am Dent Assoc 2015;146:196)
- Mandible (Head Neck Pathol 2021;15:319)
- Cases with the same RREB1::MRTFB fusion and overlapping morphologic features have been noted in extraoral sites
- It is unclear whether these tumors are completely different entities or if they represent a variation of ectomesenchymal chondromyxoid tumor
- Mediastinum (Histopathology 2020;76:1023)
- Maxillo-ethmoidal angle, reported as a biphenotypic sinonasal sarcoma (Genes Chromosomes Cancer 2021;60:565)
- Oropharynx, reported as a biphenotypic oropharyngeal sarcoma (Genes Chromosomes Cancer 2018;57:203)
Etiology
- Currently considered as tumors of uncertain histogenesis by WHO classification
- Most authors support neural crest origin (Am J Surg Pathol 1995;19:519)
- Supported by the fact that the anterior tongue derives from the neural crest mesenchyme of the first branchial arch (Head Neck Pathol 2015;9:315)
- Pluripotency of the neural crest may explain the significant immunohistochemical variability (Oral Surg Oral Med Oral Pathol Oral Radiol 2021;132:4, Oral Oncol 2006;42:1026)
- Markers for undifferentiated embryonic stem cells (OCT 3/4, SOX2, Nanog, MAP2, CD105 mRNAs) have been found in ectomesenchymal chondromyxoid tumors (Oral Surg Oral Med Oral Pathol Oral Radiol 2013;115:233)
- Some authors cite potential link between ectomesenchymal chondromyxoid tumor and myoepithelioma of soft parts (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005;99:581, Histopathology 2016;69:607)
Clinical features
- Slow growing, usually asymptomatic, firm submucosal nodule on anterior dorsal tongue
- Purulent drainage noted in one case report (Anticancer Research 2010;30:4685)
- Tumor size ranges from 0.3 - 4.0 cm (Am J Surg Pathol 1995;19:519, Oral Oncol 2017;67:192)
- Pain is rarely noted (Advances in Oral and Maxillofacial Surgery 2021;1:100006)
Diagnosis
- Diagnosis is made on histopathological examination
Radiology description
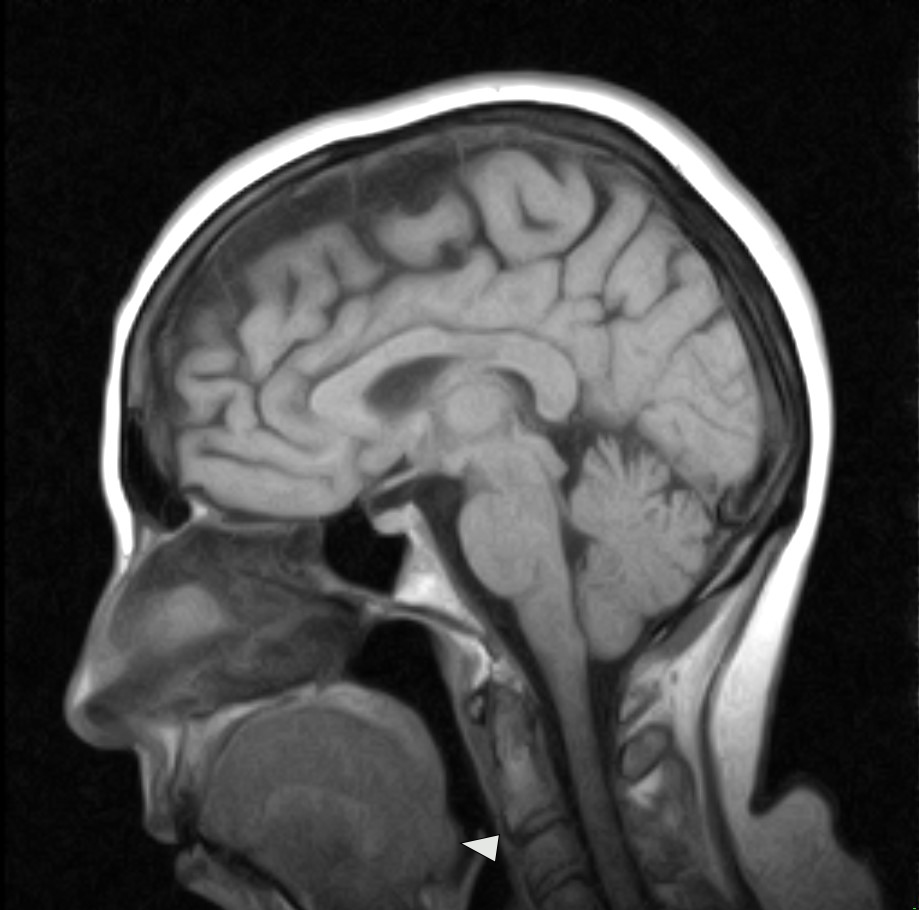
- Isointense signal or low intensity signal on T1 weighted MRI and hyperintense signal on T2 weighted MRI (Oral Surg Oral Med Oral Pathol Oral Radiol 2013;115:233, Oral Oncol 2017;67:192, BMJ Case Rep 2019;12:e231278)
- Case detailing CT scan without contrast shows cystic appearing lesion with hemorrhagic areas (Head Neck Pathol 2014;8:329)
Radiology images
Prognostic factors
- 5 cases (< 10% of reported cases with follow up information) are reported to have recurred (Am J Surg Pathol 2018;42:1297, Am J Surg Pathol 1995;19:519, Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;108:e20)
- Local re-excision appears curative (Oral Dis 2008;14:390)
Case reports
- 26 year old woman with slow growing nodule on the anterior dorsal tongue (Advances in Oral and Maxillofacial Surgery 2021;1:100006)
- 37 year old woman with expansile radiolucency in the body of the mandible (Head Neck Pathol 2021;15:319)
- 43 year old man with mass on posterior dorsal tongue (Head Neck Pathol 2014;8:329)
- 46 year old man with anterior dorsal tongue mass, present for 5 years (BMJ Case Rep 2019;12:e231278)
Treatment
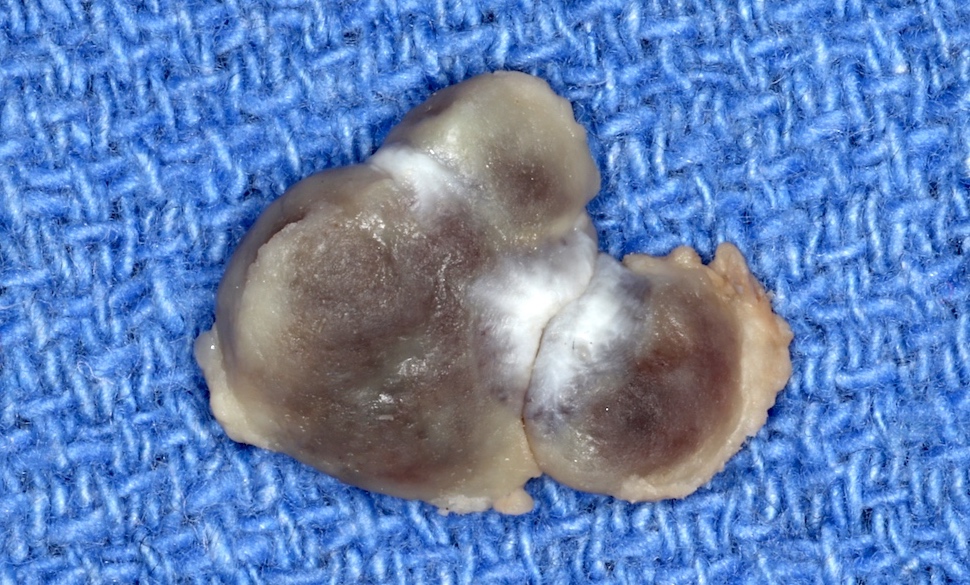
- Conservative surgical excision is recommended (Int J Surg Case Rep 2017;41:162, Oral Dis 2008;14:390)
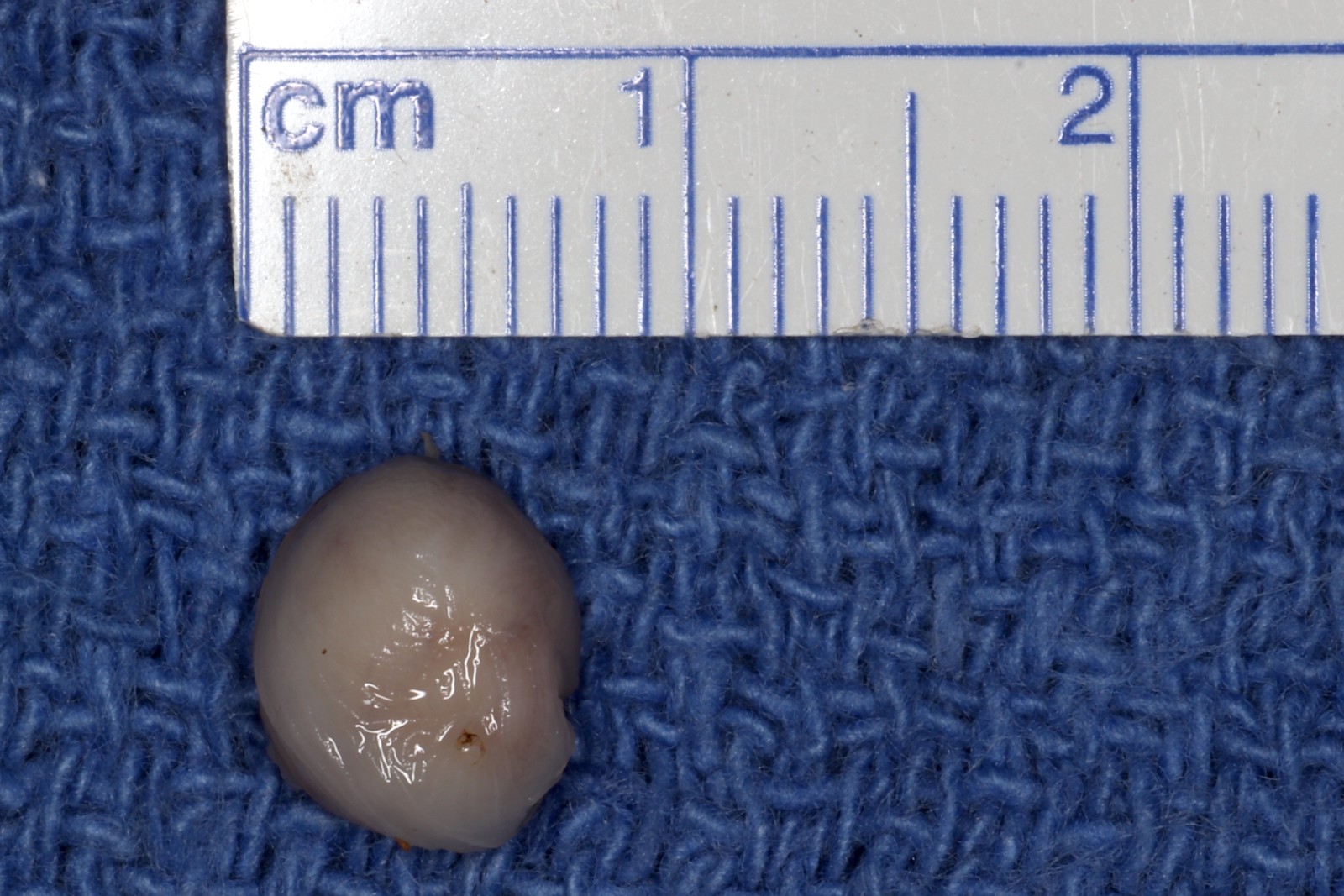
Gross description
- Firm, well defined tumor
- White, tan, yellow or gray in color (Am J Surg Pathol 1995;19:519, Acta Cytol 2010;54:82, Oral Surg Oral Med Oral Pathol Oral Radiol 2021;132:4)
- Cystic, gelatinous or hemorrhagic areas often are described (Virchows Arch 2003;442:302, Int J Surg Pathol 2016;24:586, Oral Surg Oral Med Oral Pathol Oral Radiol 2021;132:4)
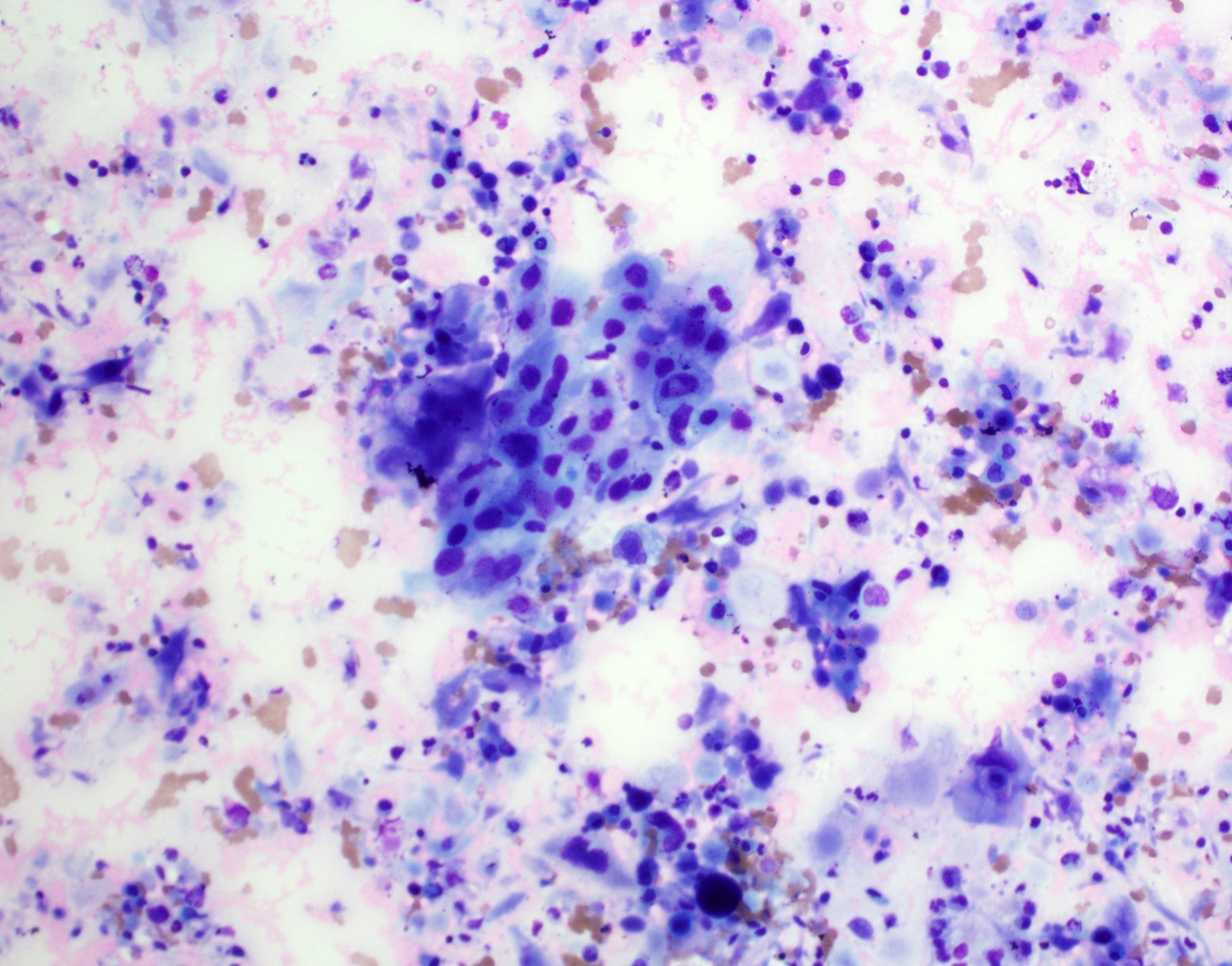
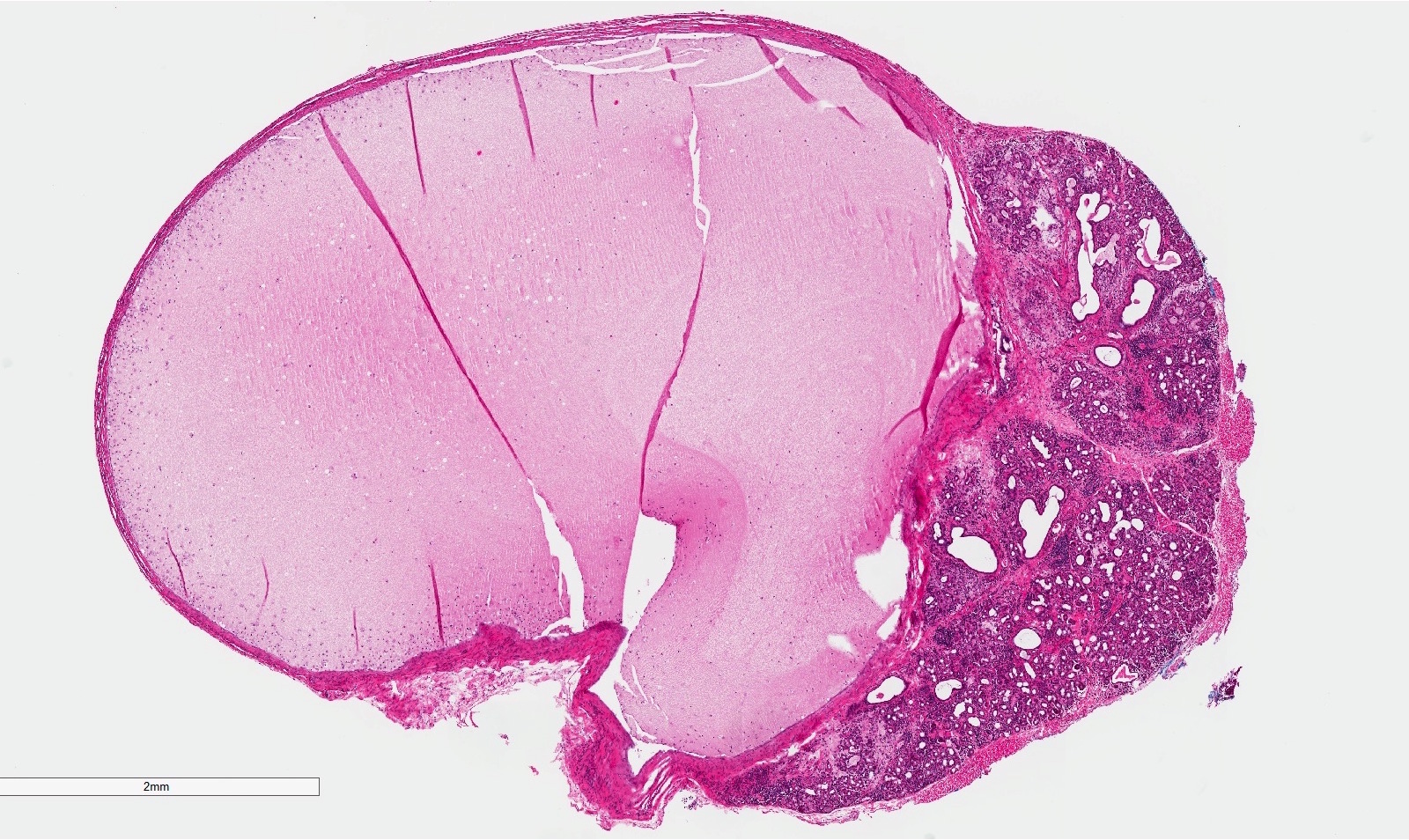
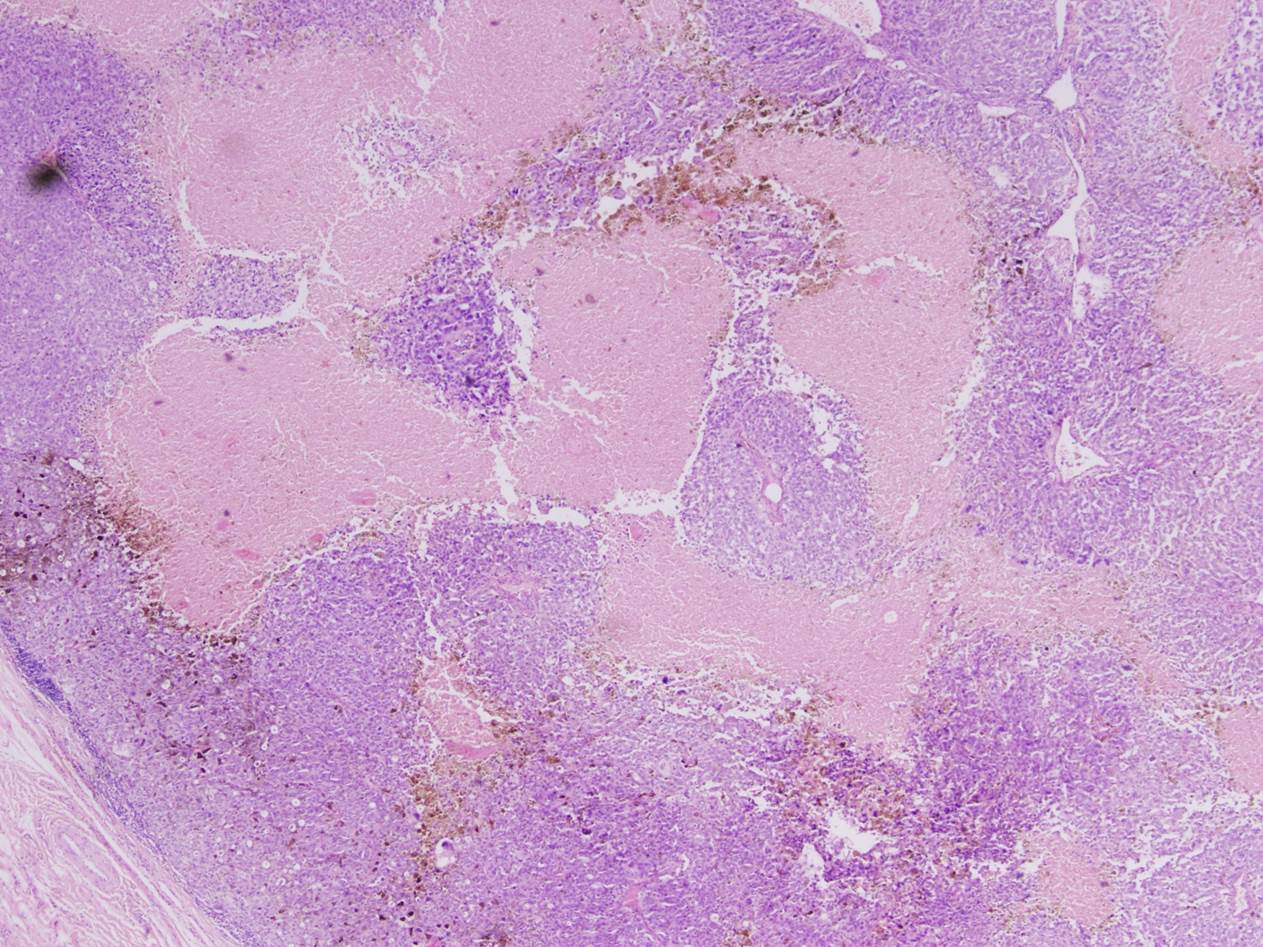
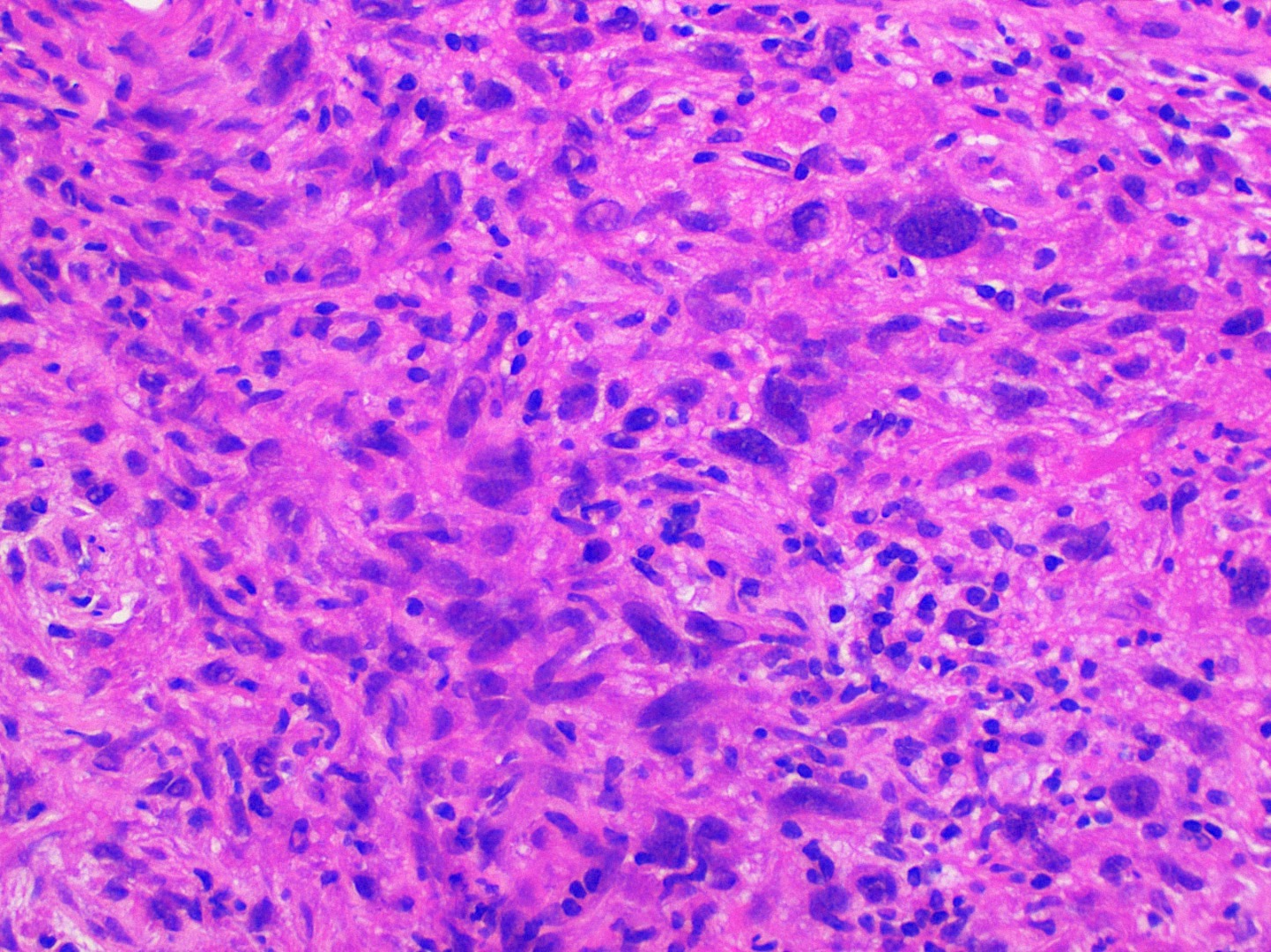
Microscopic (histologic) description
- Well demarcated tumor, often entrapped within skeletal muscle and frequently multilobulated (Am J Surg Pathol 2018;42:1297, Head Neck Pathol 2015;9:315)
- Stromal background may be hyalinized or demonstrate mucoid, myxoid or chondromyxoid areas
- Cords, strands or sheets of oval, round, fusiform or polygonal bland cells, sometimes arranged in a reticular / net-like or globoid pattern (Am J Surg Pathol 2018;42:1297)
- Myxoglobulosis-like changes have been noted (Virchows Arch 2003;442:302)
- May focally demonstrate fine calcifications, cellular atypia, necrosis, multinucleated giant cells (Am J Surg Pathol 2018;42:1297, Head Neck Pathol 2015;9:315, Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996;82:417)
- Cystic, slit-like spaces or hemorrhagic areas often noted (Head Neck Pathol 2014;8:329)
- Mitotic figures not seen (Head Neck Pathol 2015;9:315)
Microscopic (histologic) images
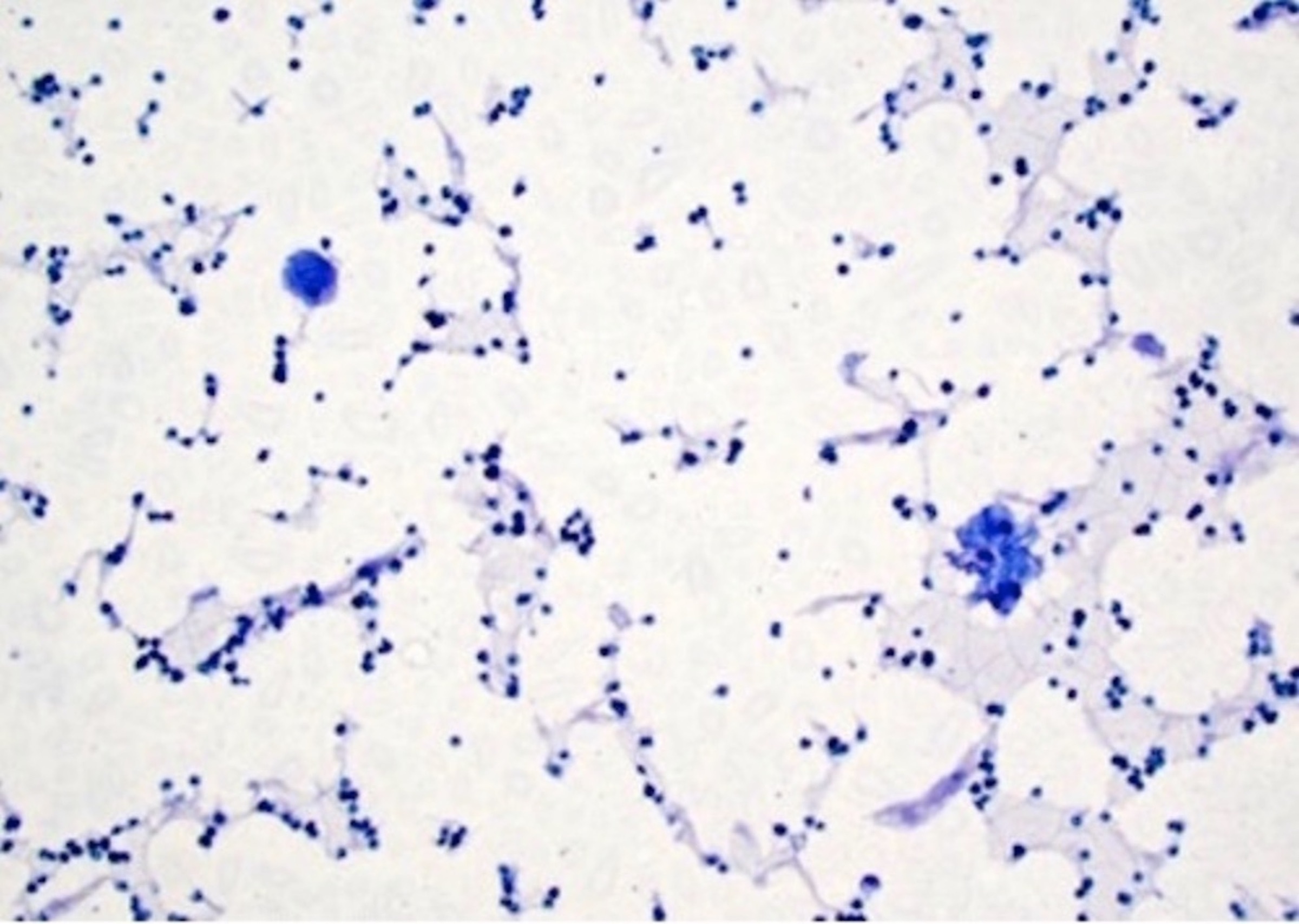
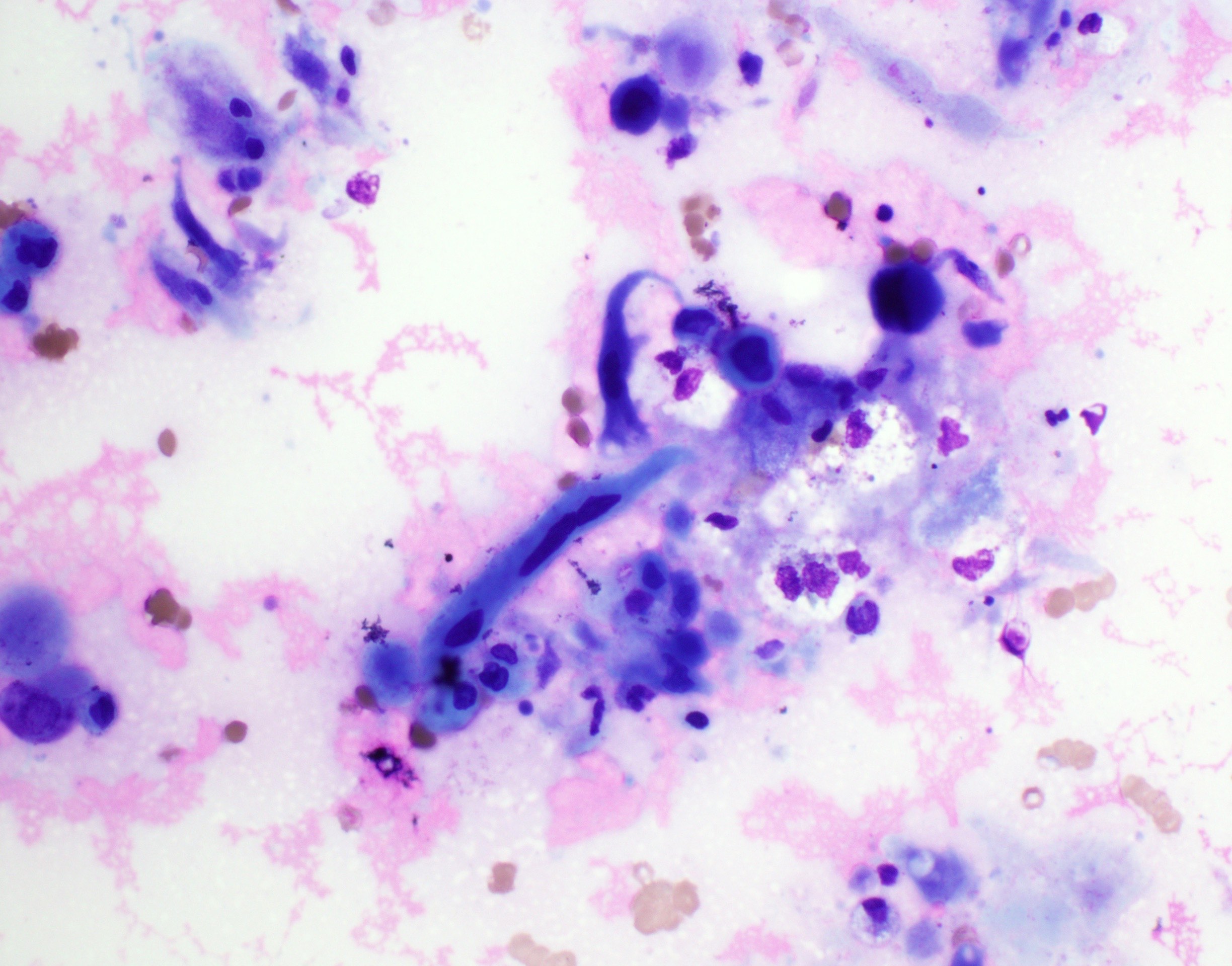
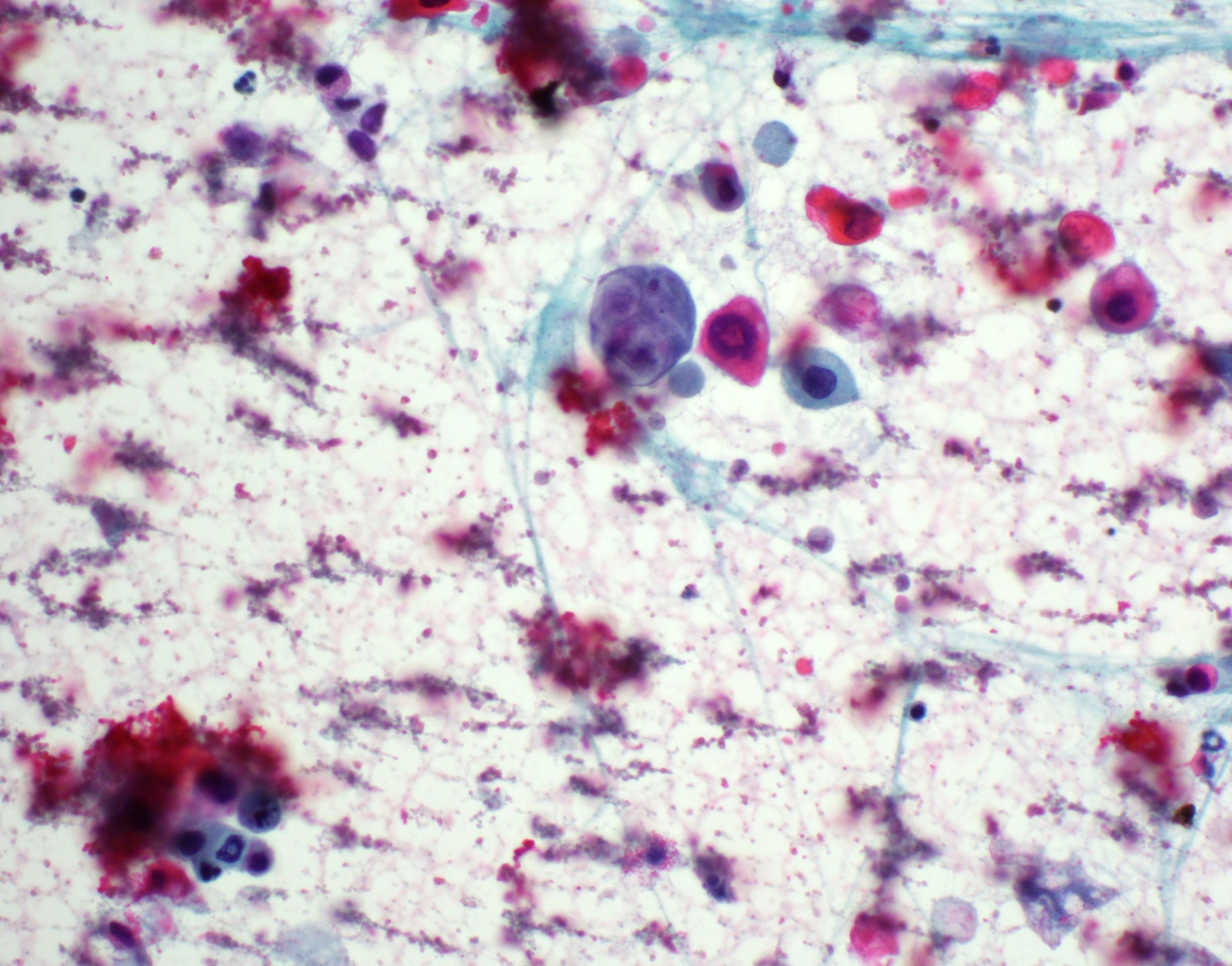
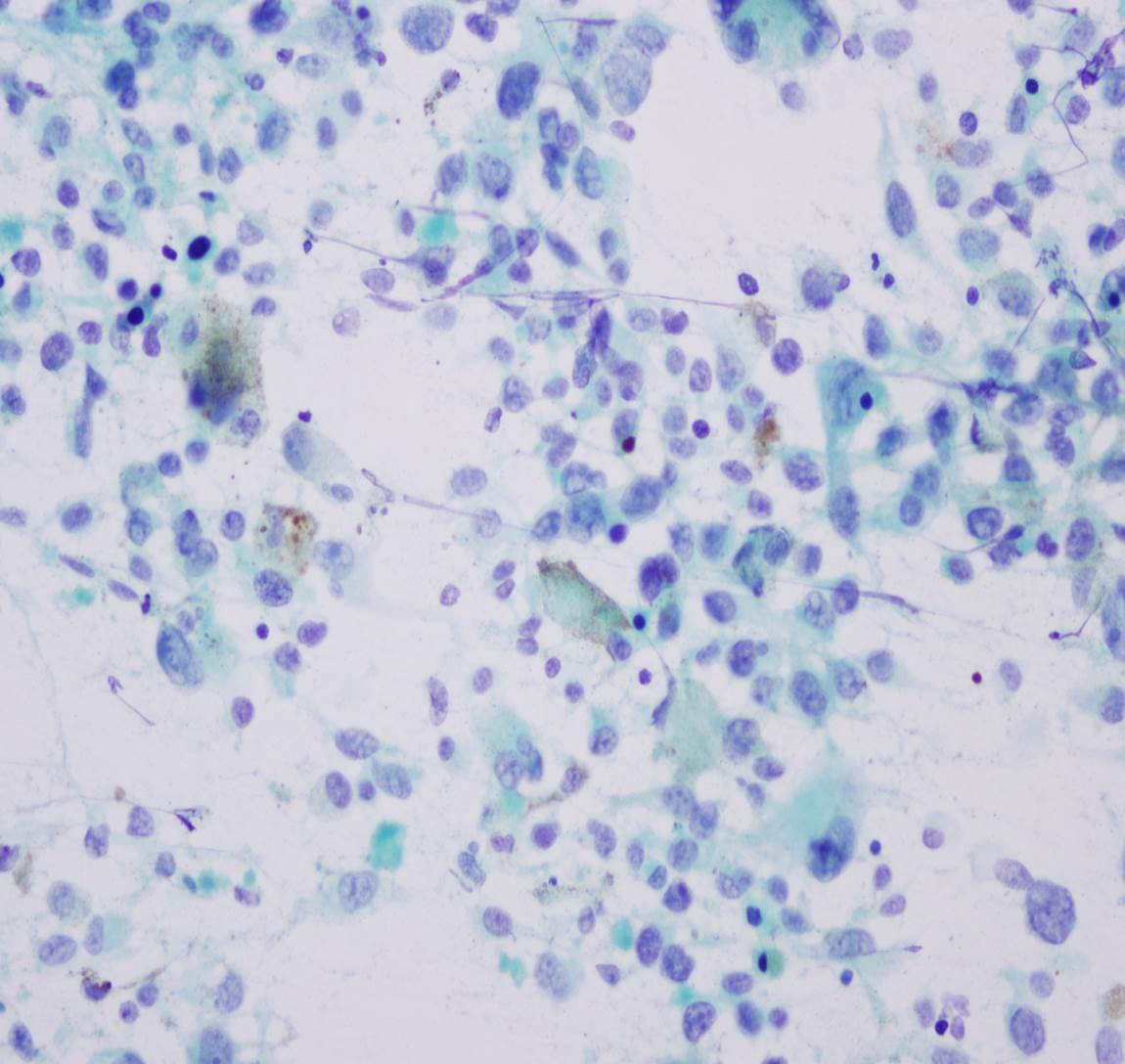
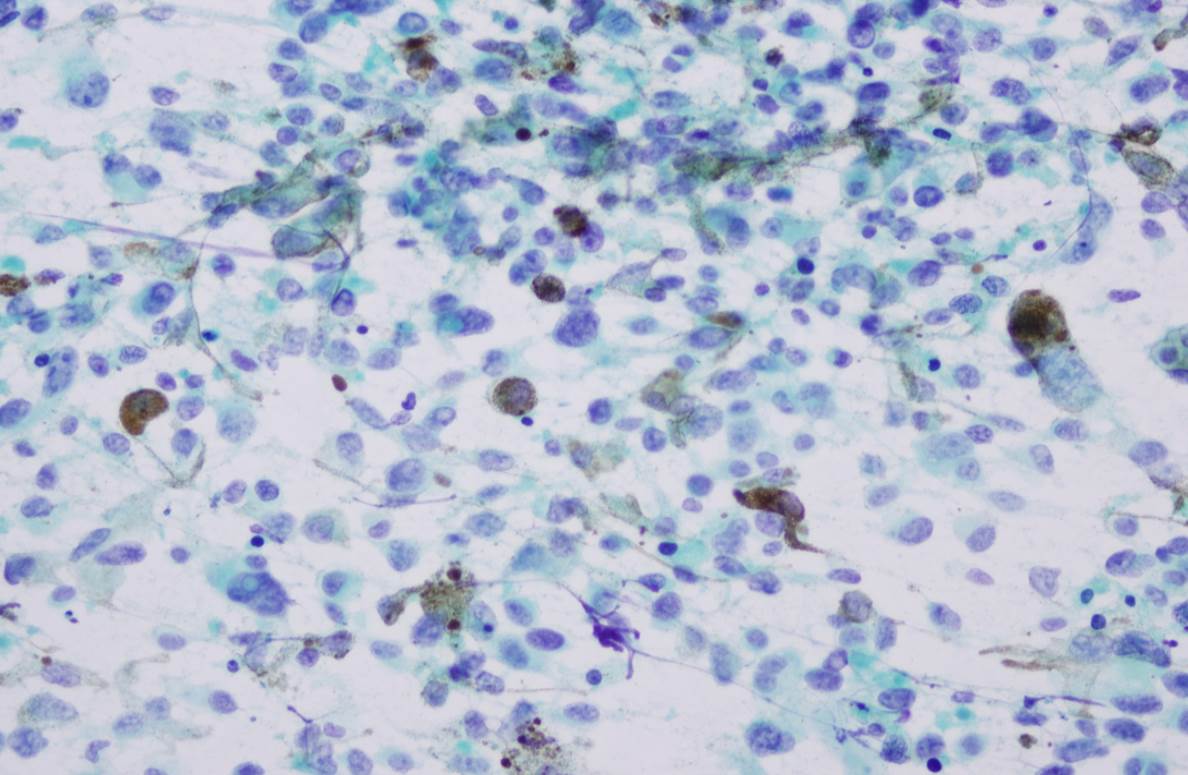
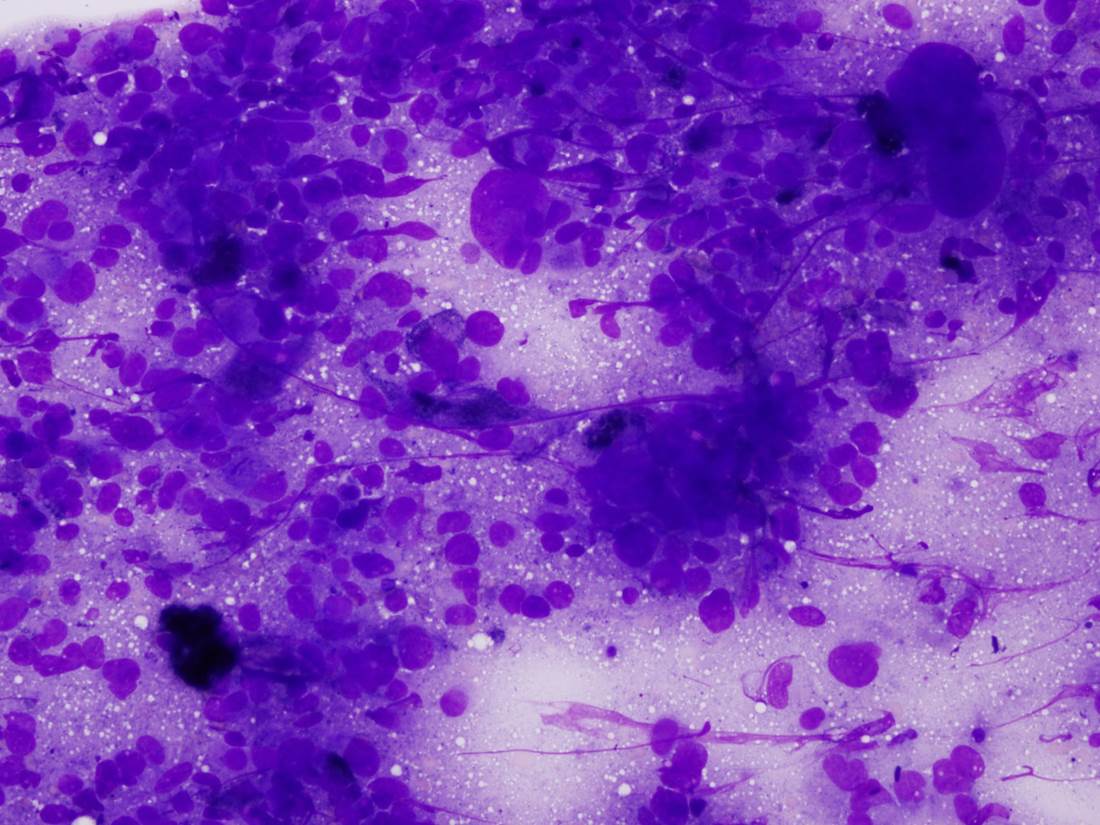
Cytology description
- Overlapping features with pleomorphic adenoma (Acta Cytol 2010;54:82, Oral Oncol 2003;39:83)
- Cellular, with abundant thick to myxoid fibrillary stromal elements (Acta Cytol 2010;54:82)
- Clusters of oval, spindled or polygonal cells with uniform nuclei (Acta Cytol 2010;54:82)
- Lacking mitotic figures (Acta Cytol 2010;54:82)
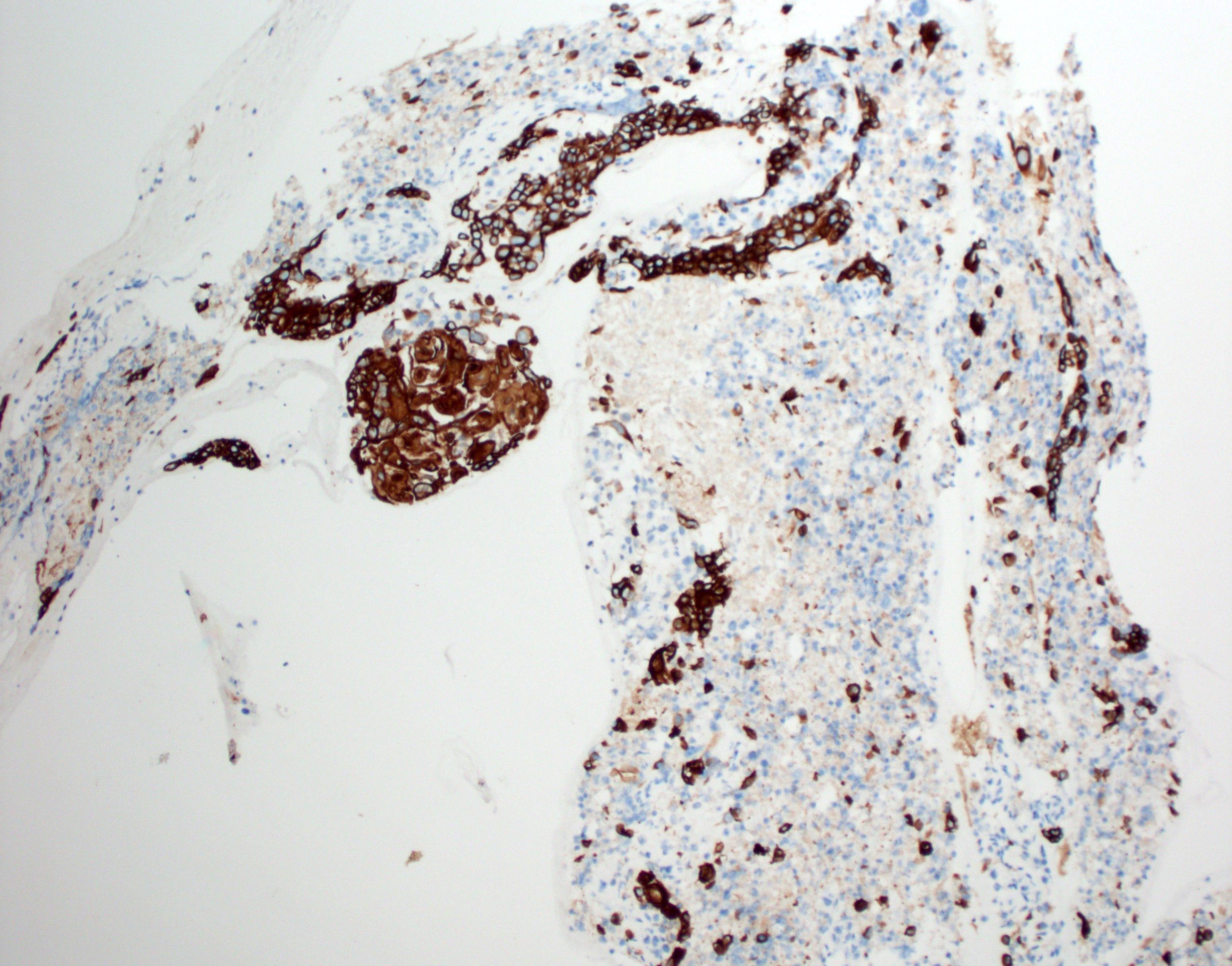
Positive stains
- Glial fibrillary acidic protein (GFAP) ~90% (Head Neck Pathol 2015;9:315)
- S100 protein > 90%
- CD56 and CD57 > 50% (Head Neck Pathol 2015;9:315)
- Authors often attribute the immunodiversity to the pluripotency of the neural crest origin
- Many other markers, such as SMA, p63, cytokeratin, desmin and SOX10, are positive in a subset (< 50%) (Head Neck Pathol 2015;9:315, Int J Surg Pathol 2016;24:586, Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010;110:e48)
Negative stains
- EMA typically negative
Electron microscopy description
- Electron microscopy is not specific (Int J Surg Pathol 2016;24:586)
- Lobulated, concave nuclei; well developed rough endoplasmic reticulum; intermediate filament bundles (Int J Surg Pathol 2016;24:586, Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996;82:417)
Molecular / cytogenetics description
- RREB1::MRTFB (previously MKL2) gene fusion (RNA sequencing and FISH) (Am J Surg Pathol 2018;42:1297)
- EWSR1::CREM fusion product found in 1/21 cases and 3/11 cases showed EWSR1 rearrangement on FISH (Am J Surg Pathol 2018;42:1297, Histopathology 2016;69:607)
- Unclear at this point whether EWSR1 rearranged ectomesenchymal chondromyxoid tumors represent a separate entity or part of the spectrum of ectomesenchymal chondromyxoid tumors
Molecular / cytogenetics images
Sample pathology report
- Anterior tongue, excision:
- Ectomesenchymal chondromyxoid tumor
Differential diagnosis
- Soft tissue myoepithelioma:
- Due to the overlapping morphologic, immunohistochemical and molecular findings (EWSR1 rearrangements), some authors note significant overlap or potential link between soft tissue myoepithelioma and ectomesenchymal chondromyxoid tumor (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005;99:581, Histopathology 2016;69:607)
- Pleomorphic adenoma / salivary myoepithelioma:
- Do not occur on the anterior dorsal tongue due to the lack of salivary glands in this area
- PLAG1 aberrations not found in ectomesenchymal chondromyxoid tumors (Histopathology 2016;69:607)
- Oral focal mucinosis:
- Stroma positive for PAS and Alcian blue (Head Neck Pathol 2015;9:315)
- Less cellular than ectomesenchymal chondromyxoid tumors
- Most commonly found on the gingiva
- Neurothekeoma:
- Positive with NKI / C3 (CD63), MITF (Head Neck Pathol 2015;9:315)
- Negative with S100, GFAP, CD57, cytokeratin (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996;82:417)
- Reticular perineurioma:
- EMA positive (Virchows Arch 2005;447:677)
- GLUT1 and claudin1 often positive
- Negative with S100, GFAP, CD57, cytokeratin
- Clinical differential diagnosis for a submucosal nodule on the dorsal tongue most often includes fibroma / fibrous hyperplasia, granular cell tumor or cartilaginous / osseous choristoma, all of which can easily be differentiated from an ectomesenchymal chondromyxoid tumor by biopsy
- GLI1 altered mesenchymal tumors:
- Both tumors have a propensity to oral tongue location, multilobulated to nodular growth pattern and immunopositivity of SMA, S100 and keratins
- GLI1 altered mesenchymal tumors have epithelioid morphology, arborizing capillary network and show GLI1 amplification or GLI1 translocation at molecular level (Am J Surg Pathol 2020;44:729)
Board review style question #1
Board review style answer #1
A. Ectomesenchymal chondromyxoid tumor. This tumor is well defined and comprised of ovoid cells set within a mucoid background.
B. While glomus tumors may show a similar morphology, the immunohistochemical profile is not compatible with glomus tumor.
C. While the dorsal tongue is a common location for granular cell tumor and S100 is positive, the morphology of the cells is inconsistent with granular cell tumor.
D. While the histomorphology is highly suggestive of pleomorphic adenoma, pleomorphic adenomas do not occur on the anterior dorsal tongue due to the lack of salivary glands in the area.
Comment Here
Reference: Ectomesenchymal chondromyxoid tumor
B. While glomus tumors may show a similar morphology, the immunohistochemical profile is not compatible with glomus tumor.
C. While the dorsal tongue is a common location for granular cell tumor and S100 is positive, the morphology of the cells is inconsistent with granular cell tumor.
D. While the histomorphology is highly suggestive of pleomorphic adenoma, pleomorphic adenomas do not occur on the anterior dorsal tongue due to the lack of salivary glands in the area.
Comment Here
Reference: Ectomesenchymal chondromyxoid tumor
Ephelis
Table of Contents
Definition / general | Case reports | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosisDefinition / general
- Also called freckle
- Solitary melanotic macules, usually of lower lip
- More common in women; associated with Peutz-Jeghers syndrome
Case reports
- 4 patients with labial melanotic macule (Dermatology 2012;224:209)
Clinical images
Microscopic (histologic) description
- Hyperpigmentation of basal layer with elongation of rete ridges
Differential diagnosis
- Melanoacanthoma:
- Melanocytes mixed with keratinocytes
- Melanosis:
- Pigmented patches in hard palate or gingiva
Erythema multiforme
Table of Contents
Definition / general | Case reports | Clinical images | Microscopic (histologic) descriptionDefinition / general
- Part of spectrum of reactive mucocutaneous disorders with maculopapular vesiculobulbous eruptions that includes erythema multiforme (EM - minor and major), Stevens-Johnson syndrome (SJS, if more mucosal involvement and epidermal necrosis) and toxic epidermal necrolysis (TEN)
- Due to cancer, collagen vascular disorder, drugs, infection
- Oral erythema multiforme: variant with only oral lesions and no skin involvement
Case reports
- 21 and 23 year old women with drug induced lip and oral ulcerations (J Oral Maxillofac Pathol 2012;16:145)
- 40 year old man with oral variant precipitated by alcohol (Indian J Otolaryngol Head Neck Surg 2011;63:9)
Clinical images
Microscopic (histologic) description
- Necrotic keratinocytes, spongiosis, basal layer liquefaction, dermal edema, perivascular or interface lymphocytes
Fordyce granules
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Ectopic sebaceous glands within oral cavity or on vermillion border of lips
Essential features
- Appear as yellow-white, asymptomatic 1 - 3 mm papules in the oral cavity or lip vermillion
- May be hyperplastic and nodular
- Neoplastic transformation very rare but reported (Oral Surg Oral Med Oral Pathol 1991;72:709, Head Neck 2016;38:E20, Case Rep Dent 2018;2018:3054931)
- Have been associated with Lynch and Muir-Torre syndromes (Gut 2005;54:1279, J Oral Pathol Med 2015;44:552)
- Present in ~80 - 90% of the population (Med Clin North Am 2014;98:1281)
Terminology
- Fordyce granules
- Fordyce spots
ICD coding
- ICD-10: Q38.6 - other congenital malformations of the mouth
Epidemiology
- No sex or racial predilection
- Often most prominent after puberty (Med Clin North Am 2014;98:1281)
- Hyperplastic examples have been associated with Lynch and Muir-Torre syndromes (Gut 2005;54:1279, J Oral Pathol Med 2015;44:552)
- Patients with high densities of Fordyce granules may have higher lipid profiles (Dent Res J (Isfahan) 2014;11:553)
Sites
- Buccal mucosa (often bilateral), upper lip vermilion border, mandibular retromolar pad and tonsillar areas
- Similar anomalies affect the areolae, glans penis and labia minora
Etiology
- Congenital
- Considered benign sebaceous hamartomas
Clinical features
- Yellow-white, asymptomatic, floral appearing 1 - 3 mm papules that remain constant throughout life
- May be hyperplastic and nodular
Diagnosis
- Diagnosed clinically
- Rarely may require biopsy for identification when hyperplastic or nodular
Treatment
- No treatment necessary unless for cosmetic reasons
Clinical images
Microscopic (histologic) description
- Similar to normal sebaceous glands of skin but lack hair follicles and almost always lack ductal communication with surface
- Parakeratotic stratified squamous epithelium overlies the sebaceous lobules
Microscopic (histologic) images
Positive stains
- Although associated with Lynch and Muir-Torre syndromes, which demonstrate defects in DNA mismatch repair (MMR) proteins leading to microsatellite instability, preservation of MMR proteins is noted upon immunostaining of Fordyce granules (Appl Immunohistochem Mol Morphol 2017;25:209)
Sample pathology report
- Left buccal mucosa, incision:
- Fordyce granules (see comment)
- Comment: Microscopic examination reveals parakeratotic stratified squamous epithelium overlying mesenchymal tissue. Within the mesenchymal stroma are numerous sebaceous gland lobules. Hair follicles are not appreciated.
Differential diagnosis
- Clinically diagnostic and doesn't have a differential diagnosis; often are not even biopsied but found only incidentally on pathology
- Usually noted on routine examination
Additional references
Board review style question #1
Which of the following is true about this oral mucosal entity?
- Immunohistochemistry is necessary to define this process
- It is found in higher frequency in those who have Lynch and Muir-Torre syndromes
- Neoplastic transformation occurs in the majority of cases
- This entity is most frequently found on the tongue
Board review style answer #1
B. It is found in higher frequency in those who have Lynch and Muir-Torre syndromes
Comment here
Reference: Fordyce granules
Comment here
Reference: Fordyce granules
Board review style question #2
A 43 year old female patient presents to the clinic for a routine head and neck cancer screening.
Upon examination, numerous yellow-white papules (approximately 1 - 3 mm in diameter) are present
along the upper lip vermillion border and on the right and left buccal mucosa. The patient states that
the spots are asymptomatic and thinks that they have always been there. Which is the most likely
diagnosis?
- Actinic cheilitis
- Fordyce granules
- Morsicatio buccarum
- Salivary gland hyperplasia
Board review style answer #2
Frictional keratosis (pending)
[Pending]
Geographic tongue
Table of Contents
Definition / general | Terminology | Epidemiology | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) imagesDefinition / general
- Inflammatory disorder characterized by asymptomatic erythematous patches with serpiginous borders
- Local loss of filiform papillae leads to ulcer-like lesions that rapidly change color and size
- Associated with common cold, work / home stress
- Associated with tongue fissures
Terminology
- Also called benign migratory glossitis, glossitis migrans
Epidemiology
- 1 - 2% of population, usually adults
Case reports
- 77 year old man and woman successfully treated with topical tacrolimus (J Dermatol Case Rep 2010;4:57)
Treatment
- Usually none in asympomatic patients
Clinical images
Gross description
- Erythematous flat zone on tongue dorsum due to loss of filiform papillae
Microscopic (histologic) description
- Acanthosis with neutrophils throughout epithelium and surface microabscesses, plus inflammatory infiltrate in lamina propria
- Resembles psoriasis
Giant cell fibroma
Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Benign fibrous proliferation of the oral cavity mucosa with distinct stellate fibroblasts
Essential features
- Fibrous nodule that most commonly presents on the gingiva and can have a papillary appearance
- Histologic features include large, plump stellate fibroblasts in the superficial connective tissue
- Treatment is conservative excision and recurrence is rare
ICD coding
Epidemiology
- 2 - 5% of all oral benign fibrous growths (Neville: Oral and Maxillofacial Pathology, 4th Edition, 2015)
- Increased frequency in (Case Rep Dent 2014;2014:864512):
- Patients' first to third decade
- Caucasians
Sites
- Most common location is the gingiva followed by the tongue, palate, buccal mucosa and lip (Oral Surg Oral Med Oral Pathol 1982;53:582)
Pathophysiology
- Fibrous proliferation generally considered to be reactive process (Braz J Otorhinolaryngol 2019;85:399, Case Rep Dent 2014;2014:864512)
- Giant cell fibroma shows limited growth potential, local recurrence would be considered exceptional and microscopic appearance is indistinguishable from nonneoplastic retrocuspid papilla; on balance, some authors have suggested the possibility that the lesion represents a neoplasm (Acta Histochem 2016;118:451, Head Neck Pathol 2019;13:71)
Etiology
- Unclear etiology but less likely to be associated with chronic mild trauma (Head Neck Pathol 2019;13:71)
Clinical features
- Dome shaped sessile or pedunculated fibrous nodule
- Surface may be smooth, pebbly, bosselated, nodular or papillary
- Most lesions are less than 1 cm in diameter (Head Neck Pathol 2019;13:71)
- Asymptomatic unless secondarily traumatized
Diagnosis
- Definitive diagnosis is made on histopathology
Prognostic factors
- Excellent prognosis and recurrence is rare
Case reports
- 7 year old boy with a pedunculated soft tissue nodule on the mandibular gingiva (J Oral Maxillofac Res 2013;4:e5)
- 19 year old man with a small growth on the tip of the tongue (Case Rep Dent 2014;2014:864512)
- 30 year old man with a growth on gingiva in the retromolar area (J Oral Maxillofac Pathol 2017;21:429)
- 40 year old man with a sessile mass of the buccal mucosa (J Dent Sci 2021;16:552)
Treatment
- Conservative surgical excision
Gross description
- Firm tan nodule with white cut surface
Microscopic (histologic) description
- Varying numbers of large, plump angular and stellate fibroblasts that may demonstrate multiple nuclei in the superficial connective tissue (Oral Surg Oral Med Oral Pathol 1974;37:374)
- Proliferation of collagen bundles
- Overlying surface epithelium with narrow and elongated epithelial rete ridges
- Absence of inflammation
Microscopic (histologic) images
Positive stains
Negative stains
Sample pathology report
- Oral cavity, excisional biopsy:
- Giant cell fibroma
Differential diagnosis
- Retrocuspid papillae (Head Neck Pathol 2019;13:71):
- Normal anatomic structure, therefore clinicopathologic correlation required
- Histopathologically identical to giant cell fibroma
- Oral squamous papilloma:
- Epithelial proliferation with koilocytes related to low risk human papillomavirus
- Verruciform xanthoma:
- Foam cells in the superficial connective tissue with overlying clefts of orange keratin
- Irritation fibroma:
- Reactive fibrous proliferation with chronic inflammation and without large stellate fibroblasts
- Other clinically noted common masses of the gingiva include pyogenic granuloma, peripheral ossifying fibroma and peripheral giant cell granuloma:
- Diagnosis made with histopathologic examination
Board review style question #1
A 30 year old patient presents with a 5 mm bosselated soft tissue mass on the mandibular gingiva. Histopathology shows a benign fibrous proliferation with stellate fibroblasts in the superficial connective tissue with no inflammation. There is no history of trauma. What is the diagnosis?
- Giant cell fibroma
- Irritation fibroma
- Papilloma
- Pyogenic granuloma
Board review style answer #1
A. Giant cell fibroma. All of the answer choices could be included on a clinical differential diagnosis of a gingival mass. Giant cell fibromas demonstrate stellate fibroblasts on microscopic exam. These lesions are not associated with trauma and do not routinely demonstrate inflammation unless secondarily traumatized.
Comment Here
Reference: Giant cell fibroma
Comment Here
Reference: Giant cell fibroma
Board review style question #2
Which of the following is true regarding giant cell fibromas of the oral cavity?
- Features of human papillomavirus in the epithelium
- History of repeated trauma to the site
- Majority of lesions are larger than 1 cm
- Stellate fibroblasts in the superficial connective tissue
Board review style answer #2
D. Stellate fibroblasts in the superficial connective tissue. Defining histologic feature of a giant cell fibroma is the presence of large, plump angular and stellate fibroblasts that may demonstrate multiple nuclei in the superficial connective tissue. These lesions generally have limited growth potential, are not associated with trauma and are not related to human papillomavirus.
Comment Here
Reference: Giant cell fibroma
Comment Here
Reference: Giant cell fibroma
Gingival hyperplasia
Table of Contents
Definition / generalDefinition / general
- Also called fibrous hyperplasia
- Associated with diphenylhydantoin (Dilantin) ingestion; also cyclosporine A, nifedipine and other drugs
- May require surgical excision
Granulomatous inflammation
Table of Contents
Definition / general | Case reports | Treatment | Clinical images | Microscopic (histologic) imagesDefinition / general
- Associated with chronic recurrent tonsillitis
- Usually benign course, no specific organism recovered
- Must rule out infectious causes (tuberculosis, tertiary syphilis, salmonella, mycotic granulomas), systemic causes (sarcoidosis, Crohn's, Granulomatosis with polyangiitis (Wegener's), eosinophilic granuloma), foreign body reaction, cholesterol granuloma
- Idiopathic orofacial granulomatosis: condition restricted to oral and maxillofacial region without any identifiable systemic granulomatous disease
Case reports
- 9 year old girl with idiopathic orofacial granulomatosis (J Oral Maxillofac Pathol 2012;16:432)
- 11 year old boy with idiopathic orofacial granulomatosis (J Indian Soc Periodontol 2012;16:469)
Treatment
- Individualized and often needs to change for each patient; includes corticosteroids or other drugs, gingivectomy
Clinical images
Microscopic (histologic) images
Grossing & features to report
Grossing
- At least one section per 1 cm of tumor for large tumors, including tumor center and periphery
- Submit entire tumor if can do so in 5 sections or less
- Resection margins
- Save intervening levels on biopsies for special stains
Features to Report
- Tumor histologic type and pattern
- Tumor size and location
- Tumor histologic grade
- Depth of invasion (not used for TNM staging)
- Pattern of invasion (noncohesive irregular cords, infiltrative single cells, well defined blunt pushing borders, thick rounded invasive cords)
- Tumor extension to adjacent structures
- Status of resection margins
- Vascular invasion
- Perineural invasion
- Lymph nodes: for each level, number obtained, number involved by tumor, size of nodal metastases and presence of extracapsular spread
- Dysplasia
- References: Mod Pathol 2000;13:1038
Measurements
- Endophytic tumors: measure perpendicularly from surface of invasive carcinoma to deepest area of involvement, using nontangential sections with a clearly recognizable surface component
- Exophytic tumors: measure tumor thickness from surface to deepest area
- Ulcerated tumors: measure from ulcer base to deepest area as well as from surface of most lateral extent of invasive carcinoma to deepest area
Hairy tongue
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Benign condition of the dorsal tongue characterized by elongation and often staining of the filiform papilla, imparting a hairy appearance
Essential features
- Marked elongation of the lingual filiform papillae
- Hairy appearance of the dorsal tongue
- Associated with cigarette use, electronic cigarette use, xerostomia, oxidizing mouthwashes, hyposalivation, radiation, older age, general debilitation, medication use, lack of coarse foods in diet and poor oral hygiene
Terminology
- Oral hairy tongue
- Black hairy tongue
- Foliate papillae hypertrophy
- Lingua villosa nigra
- Melanoglossia
- Similar to coated tongue
- Not to be confused with oral hairy leukoplakia, an unrelated entity
ICD coding
- ICD-10: K14.3 - hypertrophy of tongue papillae
Epidemiology
- Slight male predominance
- Prevalence varies from 0.6 - 11.3% of the general population (World J Gastroenterol 2014;20:10845)
Sites
- Dorsal tongue, often posterior midline area
Pathophysiology
- Elongation of filiform papillae due to decreased sloughing or increased production of keratin
Etiology
- Associated with cigarette use, electronic cigarette use, xerostomia, oxidizing mouthwashes, hyposalivation, radiation, older age, general debilitation, medication use, lack of coarse / crunchy foods in diet and poor oral hygiene (J Evid Based Dent Pract 2019;19:101318, World J Gastroenterol 2014;20:10845)
- Associated medications include bismuth, penicillin, chlorpromazine, ranitidine, tetracycline, linezolid, olanzapine, interferon, prednisolone (Head Neck Pathol 2019;13:47)
- Pigment often is caused by pigment producing bacteria or exogenous substances, such as food, medicines or tobacco
Clinical features
- Hair-like projections of the dorsal tongue (Head Neck Pathol 2019;13:47)
- Brown, black, green or yellow discoloration may be present
Diagnosis
- Diagnosis is made clinically; biopsy is not necessary
Prognostic factors
- Asymptomatic, although some patients may experience gagging sensation, malodor or foul taste
Case reports
- 54 year old woman smoker with hairy tongue occurring concurrently with respiratory infection (Cleve Clin J Med 2017;84:434)
- 56 year old white man with black hairy tongue associated with linezolid (J Med Case Rep 2013;7:46)
- 60 year old woman with hairy tongue after prednisolone use (Arch Rheumatol 2019;34:348)
- 63 year old man with amyotrophic lateral sclerosis and hairy tongue (J Int Soc Prev Community Dent 2016;6:80)
- 64 year old woman with hairy tongue associated with interferon therapy for hepatitis C (Ann Hepatol 2015;14:414)
Treatment
- Treatment is not urgent or immediately necessary
- Patients may seek treatment for foul breath, abnormal sensation
- Includes tongue scraping / brushing, elimination of offending / contributing agents (e.g. tobacco, medications), addition of crunchy / coarse foods to diet and oral hygiene improvement (Head Neck Pathol 2019;13:47)
Clinical images
Microscopic (histologic) description
- Markedly elongated filiform papillae with hair-like spires of keratin (World J Gastroenterol 2014;20:10845)
- Basophilic bacterial colonies often adhered to keratin surface
Microscopic (histologic) images
Molecular / cytogenetics description
- Negative in situ hybridization for Epstein-Barr virus (EBER); there is no association with EBV
Sample pathology report
- Dorsal tongue, incisional biopsy:
- Hyperkeratosis and elongation of filiform papillae (see comment)
- Comment: The histologic findings are compatible with hairy tongue.
Differential diagnosis
- Coated tongue:
- White, brown, black, yellow discoloration of the dorsal tongue without prominent elongation of the filiform papillae
- Oral hairy leukoplakia:
- Only included in differential diagnosis due to similarity of terminology
- Most often presents as furrowed white plaques on lateral tongue
- Associated with Epstein-Barr virus
- Positive upon in situ hybridization with EBER
Board review style question #1
Which of the following is true about hairy tongue, shown in the image?
- Hairy tongue is positive upon in situ hybridization for Epstein-Barr virus (EBER)
- Hairy tongue is strongly correlated with smoking and medication use
- Microscopic examination reveals eosinophilic condensation in a perinuclear arrangement in the superficial aspects of the epithelium
- Treatment varies based on the histologic grade
Board review style answer #1
B. Hairy tongue is strongly correlated with smoking and medication use
Comment Here
Reference: Hairy tongue
Comment Here
Reference: Hairy tongue
Board review style question #2
Board review style answer #2
Hereditary benign intraepithelial dyskeratosis (pending)
[Pending]
HPV associated
Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- An increasing subset of oropharyngeal carcinomas caused by high risk human papillomaviruses (HPV) (El-Naggar: WHO Classification of Head and Neck Tumours, 4th Edition, 2017)
Essential features
- Oropharyngeal squamous cell carcinoma caused by high risk HPV
- Mostly present as a cystic or solid neck mass, enlarged cervical lymph node, or rarely enlarged tonsil
- Variable squamous differentiation characterized by orangeophilic keratinized squamous cells in Papanicolaou stain
- p16 immunostain, a surrogate marker for high risk HPV, is considered positive when expressed in ≥ 70% of tumor cells with both nuclear and cytoplasmic staining; occasionally p16 is focal / patchy positive or negative
- High risk HPV can be detected by different methods such as RNA in situ hybridization
- High risk HPV testing can be performed on both primary or metastatic tumor
- No tumor grading
- Overall favorable prognosis despite early local lymph node metastasis (Cancer Epidemiol Biomarkers Prev 2019;28:1660)
- Rare cases associated with distant metastasis and poor prognosis
- HPV+ squamous cell carcinoma is associated with better prognosis than HPV- squamous cell carcinoma
Terminology
- Also known as HPV+ squamous cell carcinoma of oropharyngeal origin (El-Naggar: WHO Classification of Head and Neck Tumours, 4th Edition, 2017)
Epidemiology
- Affects both males and females, more common in white males, mostly younger than 65
- Incidence is growing rapidly (J Clin Oncol 2011;29:4294)
- U.S. incidence of oropharyngeal HPV+ squamous cell carcinoma is higher than the incidence of HPV- cases, 4.62 versus 1.82 per 100,000 (Cancer Epidemiol Biomarkers Prev 2019;28:1660)
- Patients are younger, predominantly Caucasians and higher socioeconomic status compered to HPV- squamous cell carcinoma
Sites
- Most common in oropharynx (tonsils, base of tongue and adenoids) and posterior pharyngeal wall
- Arise from the tonsillar crypts
Pathophysiology
- Etiologic agent is high risk HPV
- Arises from the tonsillar crypts
- Initial step is infection of the epithelial basal layer by HPV through microabrasions or trauma
- HPV double stranded DNA genome encodes oncoproteins such as Early genes E1, E2, E6 and E7 after integration into the host cell nucleus (J Dent Res 2015;94:1532)
- E1 and E2 genes activate viral replication
- E6 binds to p53 and inactivates tumor suppressor protein p53 and E7 binds to pRB and inactivates tumor suppressor protein pRB
- E6 and E7 expression promotes cellular proliferation and increases chance of malignancy (J Am Soc Cytopathol 2016;5:203)
Etiology
- Caused by high risk HPV, mostly commonly associated with HPV16 and HPV18 strains
- Also includes high risk HPV strains 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68, 82, as well as others (Cancer Epidemiol Biomarkers Prev 1996;5:567)
- Oral sexual contact is a major risk factor, but not alcohol or tobacco (smoking or chewing)
Clinical features
- Initial presentation in most cases is a neck mass or cervical lymphadenopathy
- Occasionally presents with a unilateral enlarged tonsil
- May have distant metastases to the lungs, mediastinal lymph nodes, brain, liver, bone, skin, duodenum (J Am Soc Cytopathol 2016;5:203)
Diagnosis
- Tissue findings in which morphology, along with nuclear and cytoplasmic expression of p16 in ≥ 70% of tumor cells or detection of high risk HPV in tumor cells, is required for the diagnosis
Radiology description
- Imaging findings, including ultrasound, such as enlargement, loss of the central fatty hilum, irregular cortical thickening, increased vascularity and loss of elongated shape are suspicious characteristics for metastatic HPV related squamous cell carcinoma; however, they are nonspecific
- Central necrosis appears as a cystic area within the node, demonstrating an anechoic, or completely black, echo texture enhanced through transmission (AJR Am J Roentgenol 2005;184:1691)
Prognostic factors
- Distant metastasis, although rare, is associated with poor prognosis
Case reports
- 18 year old woman with larynx tumor (Head Neck 2019;41:E59)
- 52 year old man with metastasis to the pleura (J Oral Maxillofac Surg 2018;76:2577)
- 61 year old man with solitary dural metastasis (Head Neck 2014;36:E103)
Treatment
- Resection of primary tumor with or without ipsilateral or bilateral neck dissection
- Radiation therapy or systemic therapy in cases with extranodal extension, positive margins or other high risk associated features such as pT3 or pT4 primary, one positive node > 3 cm or multiple positive nodes, nodal metastasis in levels IV or V, perineural invasion, vascular invasion and lymphatic invasion (National Comprehensive Cancer Network, J Am Soc Cytopathol 2016;5:203)
Microscopic (histologic) description
- Variable squamous differentiation including:
- Basaloid features with no squamous differentiation, most common pattern
- Focal keratinization
- Abundant keratinization
- Other morphology types:
- Nonkeratinizing squamous cell carcinoma with maturation
- Hybrid variant
- Keratinizing SCC
- Cystic / microcystic, ciliated
- Papillary SCC
- Adenosquamous SCC
- Spindle cell carcinoma (sarcomatoid)
- Undifferentiated SCC (Am J Surg Pathol 2015;39:1591)
- No tumor grade or differentiation status should be reported (CAP: Human Papillomavirus Testing in Head and Neck Carcinomas [Accessed 24 September 2019])
Microscopic (histologic) images
Cytology description
- Non / minimally keratinized squamous cell carcinoma, fragments of basaloid cells with high N/C ratio and hyperchromatic nuclei
- Fragments of cohesive malignant squamous cells with dense cytoplasm
- Variable squamous differentiation, tadpole, snake cells and squamous cells with orangeophilic cytoplasm in Papanicolaou stain and blue in Romanowsky stain, respectively
- Individual keratinized cells with marked pleomorphism
- Necrosis, cystic degeneration and macrophages, common
Cytology images
Positive stains
- p16 in ≥ 70% of tumor cells with both nuclear and cytoplasmic staining (Arch Pathol Lab Med 2018;142:559), a surrogate marker
- p40, p63, CK5/6
Molecular / cytogenetics description
- Positive for high risk HPV by hybrid captured II assay, DNA in situ hybridization, RNA in situ hybridization, PCR (J Am Soc Cytopathol 2016;5:203)
- EBER-
Molecular / cytogenetics images
Sample pathology report
- Lymph node, right level II, ultrasound guided fine needle aspiration:
- Metastatic HPV related squamous cell carcinoma (see comment)
- Comment: An immunostain for p16 is positive in 80% of the tumor cells. In situ hybridization for high risk HPV RNA is positive.
Differential diagnosis
- HPV- squamous cell carcinoma of oropharynx
- History of heavy alcohol consumption or chewing / smoking tobacco
- Shows higher degree of squamous differentiation in most cases
- p16-, high risk HPV-
- Metastatic squamous cell carcinoma of skin
- Older patients
- Shows higher degree of squamous differentiation in most cases
- p16-, high risk HPV-
- Lymphoepithelial cyst
- Overall less cellularity
- Unilateral and single cyst
- p16 focally positive, HPV-
- Nasopharyngeal carcinoma
- Presents as keratinizing squamous cell carcinoma or nonkeratinizing squamous cell carcinoma including basaloid squamous cell carcinoma and undifferentiated subtype (El-Naggar: WHO Classification of Head and Neck Tumours, 4th Edition, 2017)
- Syncytial growth pattern, vesicular nuclei with prominent central nucleoli and reactive lymphocytes in stroma
- Usually positive for Epstein-Barr virus (EBV) / Epstein-Barr encoded RNA (EBER)
- p16-, high risk HPV-
- Metastatic squamous cell carcinoma of lung
- Prior relevant clinical history
- Variable squamous differentiation
- p16-, HPV-
- Metastatic HPV related anogenital squamous cell carcinoma including uterine cervix
- Prior relevant clinical history
- Cytomorphologic overlap
- Also p16+ and high risk HPV+
- Adenoid cystic carcinoma, solid type
- Metastatic small cell carcinoma of the lung
- Chest imaging useful to differentiate these two entities
- Same morphology with small cell variant of oropharyngeal carcinoma
- CD56+, chromogranin+, synaptophysin+
- High risk HPV-
- Metastatic large cell neuroendocrine carcinoma
- Sheets and three dimensional fragments of cohesive cells with large pleomorphic nuclei and vesicular chromatin
- Mitoses, molding and necrosis common
- Neuroendocrine markers (chromogranin, synaptophysin, CD56)+, HPV-, p40-
Additional references
Board review style question #1
Board review style answer #1
E. 70% nuclear and cytoplasmic
Comment Here
Reference: HPV related oropharyngeal squamous cell carcinoma
Comment Here
Reference: HPV related oropharyngeal squamous cell carcinoma
Board review style question #2
- Which one of the following statements is true about HPV related oropharyngeal carcinoma?
- Extranodal extension has no impact on treatment
- Distant metastasis is very common
- High risk HPV testing can be performed on primary or metastatic tumor
- The prognosis is poor in most cases
- Tumor differentiation must be reported for all cases
Board review style answer #2
C. High risk HPV testing can be performed on primary or metastatic tumor
Comment Here
Reference: HPV related oropharyngeal squamous cell carcinoma
Comment Here
Reference: HPV related oropharyngeal squamous cell carcinoma
HPV independent
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- A subset of oropharyngeal squamous cell carcinomas that are not associated with high risk human papillomaviruses (HPV)
Essential features
- Squamous cell carcinoma involving the oropharynx
- Oropharynx includes the soft palate, uvula, palatine tonsils, posterior third (base) of the tongue and posterior wall of the pharynx
- Associated with smoking and alcohol
- Not associated with HPV
- Resembles squamous cell carcinoma (SCC) and its morphologic variants observed in other head and neck mucosal sites; can show surface dysplasia, keratinization and desmoplasia
Terminology
- Keratinizing squamous cell carcinoma
ICD coding
Epidemiology
- Age: mean 61 years (standard deviation 10.49) (Cancer 2019;125:761)
- M:F = 3.2:1 (Cancer 2019;125:761)
- Higher incidence in Indian subcontinent, French Polynesia, New Caledonia and Papua New Guinea, Eastern Europe, North America, Australia and Brazil
Sites
- Oropharynx
- Most commonly soft palate
- Arises in the surface mucosa and invades neighboring structures with metastases to draining regional nodes
Pathophysiology
- Invasive lesion is typically preceded by progressively severe dysplasia
- Chronic insult with abrogation of DNA repair mechanisms and mutations in tumor suppressor genes, such as gatekeeper p53 (J Oncol 2011;2011:603740)
Etiology
- Most commonly chewing or smoking tobacco, heavy alcohol use and poor oral hygiene (J Natl Cancer Inst 2008;100:407)
- Also reported in association with syphilis, other infections (bacterial, fungal or viral) and Fanconi anemia (Int J Epidemiol 1994;23:381, Sci Rep 2017;7:4036, Arch Otolaryngol Head Neck Surg 2003;129:106)
Diagrams / tables
Clinical features
- Presents as nonhealing mucosal ulcer identified by patient or clinician and confirmed with nasoendoscopy and biopsy
- Difficulty and pain while swallowing
- Metastasis to ipsilateral or bilateral neck nodes may rarely be the initial presenting feature
Diagnosis
- Clinical examination with biopsy of primary lesion
- Biopsy of primary lesion may require examination under anesthesia of the oropharynx
- Cytology of lymph node metastases followed by biopsy of the primary lesion identified on diagnostic CT and PET scan
Radiology description
- Primarily used for staging of nodal drainage sites and distant spread
- PET may identify primary lesion in the rare setting of neck nodal disease of unknown origin
Prognostic factors
- Overall survival at 3 years 57% (N Engl J Med 2010;363:24)
- Prognostic factors
- Clinical
- Tobacco use (N Engl J Med 2010;363:24)
- Overall patient health, comorbidity and lifestyle factors
- Women have worse overall survival and cancer specific survival than men (Expert Rev Anticancer Ther 2020;20:813)
- Histological
- Size
- Depth of invasion
- Perineural invasion (J Surg Oncol 2015;111:352, Head Neck 2019;41:3992)
- Worst pattern of invasion (Am J Surg Pathol 2005;29:167)
- Completeness of resection
- Lymph node involvement
- Extranodal extension
- Stage as per the AJCC 8th edition chapter 11 oropharynx (p16) and hypopharynx (AJCC: Cancer Staging Manual [Accessed 12 December 2020])
- Clinical
Case reports
- 49 year old man with a lymphoepithelial carcinoma in the soft palate and uvula (Head Neck Pathol 2011;5:327)
- 58 year old woman with a spindle cell carcinoma of the palatine tonsil (Am J Otolaryngol 2008;29:123)
- 65 year old man with a basaloid squamous cell carcinoma of the retromolar trigone (J Oral Maxillofac Pathol 2011;15:192)
Treatment
- Surgical resection of the primary along with ipsilateral or bilateral elective neck dissection (N Engl J Med 2015;373:521)
- Surgical resection can be through transoral robotic surgery (TORS)
- Adjuvant radiotherapy and platinum based chemotherapy
- Immune check point inhibitors have demonstrated response in 25 - 29% patients (Future Oncol 2020;16:1235)
Gross description
- Macroscopic appearance varies with the morphologic type
- Common conventional squamous cell carcinoma shows an ulceroproliferative mucosal lesion with a firm gray-white infiltrative surface
- Verrucous and papillary squamous cell carcinomas demonstrate prominent exophytic, finger-like projections
- Spindle cell carcinoma generally presents as a mucosal polypoid lesion
Gross images
Frozen section description
- Not routinely done
- Value with confirming clearance of margins of primary lesion
Microscopic (histologic) description
- Squamous cell carcinoma, conventional
- Most common and typical morphology of conventional keratinizing squamous cell carcinoma at any site
- Large polygonal malignant cells with intercellular bridges
- Cytoplasmic or extracellular eosinophilic keratin
- Dyskeratotic cells and squamous pearls
- Nuclear size, pleomorphism, hyperchromasia and mitoses increase with increasing grade
- Other morphological types
- Verrucous carcinoma
- Pronounced exophytic growth of well differentiated squamous epithelium
- Bulbous enlargement of the rete ridges with elephant foot appearance
- Broad pushing border
- Does not metastasize; good prognosis
- Carcinoma cuniculatum
- Well differentiated exophytic verruciform lesion with broad front of burrowing invasion
- Generally involves mucoperiosteal sites; rare in the oropharynx
- Papillary squamous cell carcinoma
- Well differentiated keratinocytes forming exophytic organized papillary structures with fibrovascular cores
- 70% of tumor must show papillary architecture
- Better prognosis than conventional squamous cell carcinoma
- Acantholytic squamous cell carcinoma (Head Neck Pathol 2012;6:438)
- Keratinocytes with loss of adhesion molecules appear "falling apart"
- May have pseudolumina mimicking glands or vessels but no mucin
- Adenosquamous carcinoma (Head Neck Pathol 2016;10:486)
- True glandular and squamous differentiation close but distinct and separate
- Poor prognosis with frequent metastases
- Basaloid squamous cell carcinoma (J Oral Maxillofac Pathol 2011;15:192)
- Cells with minimal cytoplasm
- Enlarged, angulated, hyperchromatic nuclei
- Basement membrane-like matrix
- Solid pattern with lobular configuration
- May have prominent peripheral palisading
- May have comedo type necrosis
- May have abrupt change to differentiated component
- Lymphoepithelial carcinoma (nonnasopharyngeal) (Head Neck Pathol 2011;5:327)
- Cohesive tumor nests of nonkeratinising epithelioid cells with prominent intermixed reactive lymphoplasmacytic infiltrate
- Present at high stage with metastases
- Spindle cell / sarcomatoid squamous cell carcinoma (Am J Otolaryngol 2008;29:123)
- Most commonly occurs postradiotherapy or as second primary
- Mesenchymal in appearance
- Atypical plump spindled cells arranged in fascicles or storiform pattern
- May have metaplastic or neoplastic cartilage or bone
- Verrucous carcinoma
Microscopic (histologic) images
Contributed by Ruta Gupta, M.B.B.S., M.D.
Cytology description
- Role of cytology only in investigation of regional or distant metastases
- Appearance depends on type and differentiation
- Conventional squamous cell carcinoma shows sheets and small clusters of large polygonal malignant cells with intercellular bridges and cytoplasmic or extracellular eosinophilic keratin
Cytology images
Positive stains
- Diffusely and strongly positive:
Negative stains
Molecular / cytogenetics description
- Negative for presence of high risk HPV DNA / RNA
- EBV ISH negative
Sample pathology report
- Right soft palate and uvula and bilateral neck dissection levels I - IV, excision:
- Moderately differentiated squamous cell carcinoma (T = 28 mm, pT2) arising on a background of carcinoma in situ (see comment)
- Comment: Extensive perineural involvement is present. Local excision complete, closest margin: anterior mucosal 3 mm away. Bilateral neck dissection shows 2/66 lymph nodes with metastatic squamous cell carcinoma. The larger involved node is present in the right neck, measures 25 mm and shows extranodal extension (pN3b). AJCC 8th Ed pT2pN3b group stage 4. The tumor cells lack immunostaining with p16 excluding an HPV related oropharyngeal squamous cell carcinoma. HPV negative oropharyngeal squamous cell carcinoma is frequently associated with smoking and alcohol and does not carry the good prognosis described in HPV related oropharyngeal squamous cell carcinoma.
Differential diagnosis
- HPV+ oropharyngeal squamous cell carcinoma:
- HPV related oral diseases: squamous papilloma, verruca vulgaris, condyloma acuminatum
- Usually low risk HPV+
- Nasopharyngeal carcinoma:
- Arising in the nasopharynx
- Usually EBV+
- Verrucous hyperplasia / proliferative verrucous leukoplakia:
- Exophytic growth only
- Mature keratinocytes with marked acanthosis
- Can be multifocal and widespread
- Squamous dysplasia:
- No invasive component
- Dysplastic keratinocytes with variable level of thickness involvement
Additional references
Board review style question #1
Board review style answer #1
Board review style question #2
Board review style answer #2
Infections-general
Table of Contents
Actinomycosis | Blastomycosis | Candidiasis (thrush) | Herpes simplex virus | Herpes simplex / zoster | Histoplasmosis | Infectious mononucleosis | Syphilis | Verruca vulgarisActinomycosis
Blastomycosis
Candidiasis (thrush)
Definition / general
Case reports
Clinical images
Images hosted on other servers:
Gross description
Microscopic (histologic) description
Microscopic (histologic) images
Images hosted on other servers:
- Normal flora that overgrows due to AIDS, antibiotics, diabetes, immunosuppression, neutropenia, xerostomia (Med Oral Patol Oral Cir Bucal 2013;18:e381)
Case reports
- 45 year old HIV+ man (Case Rep Dent 2011;2011:929616)
Clinical images
Images hosted on other servers:
Gross description
- Superficial curdy, gray-white membranes that easily wipe off (pseudomembranous candidiasis) or painful erosions (erythematous candidiasis)
Microscopic (histologic) description
- PAS+ hyphae within keratin layer in neutrophilic background; prominent inflammatory infiltrate along the lamina propria
Microscopic (histologic) images
Images hosted on other servers:
Herpes simplex virus
Definition / general
Gross description
Microscopic (histologic) description
- Also called cold sore
- Usually HSV1
- Lasts 3 - 4 weeks, then virus tracks along regional nerves and becomes dormant in trigeminal or other local ganglia
- Most infected adults have latent HSV1 that is activated by upper respiratory infection, excessive exposure to cold, wind, sun, allergies
- Acute herpetic gingivostomatitis:
- Rare, children 2 - 4 years with diffuse involvement of oral and pharyngeal mucosa, tongue, gingiva
- Fiery red mucosa and swelling with clusters of vesicles
- Recurrent herpetic stomatitis:
- Groups of 1 - 3 mm vesicles on the lips, nasal orifices, buccal mucosa
- Lesions heal in 7 - 10 days
- Tzanck test: microscopic examination of vesicle fluid shows giant cells, inclusions
Gross description
- Vesicles or bullae with clear serous fluid, painful shallow ulcers
Microscopic (histologic) description
- Intra and intercellular edema (acantholysis), intranuclear inclusions, multinucleate polykaryons (giant cells)
Herpes simplex / zoster
Histoplasmosis
Infectious mononucleosis
Definition / general
Microscopic (histologic) description
Microscopic (histologic) images
Images hosted on other servers:
Negative stains
- Acute pharyngitis and tonsillitis with gray-white exudate, lymphadenopathy in neck
- Due to Epstein-Barr virus infection
Microscopic (histologic) description
- Tonsil: reactive lymphoid hyperplasia (polymorphous transformed lymphocytes) with extensive immunoblastic proliferation in sheets and nodules, marked atypia resembling Reed-Sternberg cells (Am J Surg Pathol 1987;11:122)
Microscopic (histologic) images
Images hosted on other servers:
Negative stains
Syphilis
Verruca vulgaris
Inflammatory fibrous hyperplasia (pending)
A 56 year old man presents with a chief complaint of a bump inside the oral cavity. On clinical exam, a pink, smooth surfaced nodule is noted along the patient’s bite line. He states that the mass interferes with chewing and speaking. The microscopic appearance is pictured. What is the diagnosis?
A 61 year old woman presents with a solitary nodular mass of the oral buccal mucosa that has been present over 5 years with minimal change. Histopathological review of the mass reveals a fibrous mass containing collagen bundles interspersed with fibroblasts and blood vessels. Which of the following is true regarding this pathological entity?
Contributed by Ivan J. Stojanov, D.M.D., M.M.Sc.
Which of the following is true regarding leukoplakia without dysplasia?
A 54 year old woman presents to her dentist for a routine examination. Clinical examination reveals thin, interlacing white lines on the buccal mucosa. The lesions present bilaterally. The patient reports that the lesions are asymptomatic and that she had them for years. She reports that the lesions tend to wax and wane. What is the most likely diagnosis?
Images hosted on other servers:
CT scan:
MRI:
Radionuclide scan:
Angiography:
Oral examination of a patient reveals an asymmetric 4 mm red nodule at the dorsal tongue base. The patient is asymptomatic and was unaware of the finding. Biopsy of the lesion is shown. Which of the following is true regarding the diagnosis?
A patient presents with a focal collection of red papules on the posterior lateral tongue. Biopsy demonstrates a well defined aggregate of lymphocytes showing germinal center formation. An epithelial lined crypt containing keratin is seen in the central aspects of the lymphocytic nodule. What is the most likely diagnosis?
Cone beam computed tomography (CBCT) of the patient shown above demonstrates a well defined, nonexpansile radiolucency surrounding the root of the associated necrotic maxillary incisor. Biopsy shows a nodule of granulation tissue demonstrating dense accumulations of neutrophils at the base of the specimen. What is the most likely diagnosis?
Central giant cell granuloma:
Images hosted on other servers:
Contributed by Timothy Fielder, M.B.B.S., B.Med.Sci., Ruta Gupta, M.D. and Molly Housley Smith, D.M.D.
Contributed by Molly Housley Smith, D.M.D., Michael Piepgrass, D.M.D.,
John McGehee, D.M.D., Michael Menis, D.D.S. and Trent Clifton, D.M.D., M.D.
Contributed by Molly Housley Smith, D.M.D.
A 73 year old woman presents with multiple, asymptomatic white patches of the attached gingiva that have progressed over a few months. The lesions do not change pattern and do not migrate. Histopathologic examination reveals epithelium with a thickened, corrugated layer of orthokeratin devoid of overt cytologic dysplasia. What condition does this patient have?
Contributed by Brittany Camenisch, D.M.D., Nehal Almehmadi, B.D.S., Sana Naheed, B.D.S., Evan Lynch, M.D., Ph.D.,
Justin Kolasa, M.D., D.M.D., Molly Housley Smith, D.M.D. and Susanna Goggin, D.M.D.
The above mass is found on the gingiva. What is true regarding this diagnosis?
Contributed by Kathleen Higgins, D.D.S., M.S., Duane Schafer, D.D.S., M.S. and Sarah Glass, D.D.S.
Notes:
Notes:
Notes:
Notes:
A 2.4 cm primary gingival carcinoma was resected in continuity with the underlying posterior mandible. Which of the T category criteria in the 8th edition AJCC staging guide is satisfied by the examination of the microscopic sections above?
Notes:
Notes:
HPV unrelated (p16-) oropharyngeal and hypopharyngeal squamous cell carcinoma
Notes:
Notes:
Notes:
Inflammatory papillary hyperplasia
Table of Contents
Definition / general | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) imagesDefinition / general
- Common, usually involves palate or lingual mandibular gingiva
- Called palatal papillomatosis in palate
- Middle aged and older persons, 2/3 female
- Associated with ill fitting dentures or partial dentures (Braz Dent J 2009;20:243), wearing prostheses at night, poor oral hygiene; also candidiasis
- Not a premalignant condition
Treatment
- Removal of offending agent; proper fitting dentures
- Complete excision
Gross description
- Multiple red polyp-like projections, often under ill fitting dentures and usually in palate
Microscopic (histologic) description
- Exophytic mucosal epithelial hyperplasia, including pseudoepitheliomatous hyperplasia and submucosal fibrous hyperplasia
- Islands of hyperplastic squamous mucosa may appear in submucosa
- May have chronic inflammation of accessory salivary glands; no dysplasia
Irritation fibroma
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Fibrous nodule of oral cavity, often considered a reactive hyperplasia to trauma or local sources of irritation
Essential features
- Common reactive fibrous hyperplasia of oral cavity
- Typically affects buccal mucosa along the line of occlusion / bite line
- Conservative surgical excision is recommended and recurrences are rare
Terminology
- Irritation fibroma
- Oral fibroma
- Traumatic fibroma
- Focal fibrous hyperplasia
ICD coding
Epidemiology
- Any age, although most common in fifth and sixth decades (Iran J Otorhinolaryngol 2015;27:137)
- About twice as common in women
Sites
- Most common along the bite line on the buccal mucosa (may be bilateral)
- Also seen on the labial mucosa, tongue, palate and gingiva (Iran J Otorhinolaryngol 2015;27:137, Am Fam Physician 2007;75:509)
Pathophysiology
- Considered to be a reactive proliferation rather than a true neoplasm, although true fibrous neoplasms of unlimited growth potential are possible (Neville: Oral and Maxillofacial Pathology, 4th Edition, 2016)
Etiology
- Thought to be induced by recurrent local irritants of the oral cavity, which may include bite trauma, denture irritation, food impaction, poor oral hygiene, broken teeth or overhanging dental restorations (Iran J Otorhinolaryngol 2015;27:137)
Clinical features
- Smooth, round, flesh colored nodule (Am Fam Physician 2007;75:509)
- Asymptomatic unless painful due to bite trauma
- May be ulcerated or demonstrate a thickened white surface (hyperkeratosis)
- Often 1 - 2 cm in diameter (Indian J Dent Res 2018;29:61)
Diagnosis
- Definitive diagnosis is made upon histopathological review, although irritation fibromas may be highly suspected based on clinical features (Braz J Otorhinolaryngol 2019;85:399)
Prognostic factors
- Excellent prognosis with infrequent recurrence after conservative surgical excision
Case reports
- 23 year old man with dermoscopic features of oral fibroma (Skin Res Technol 2019;25:768)
- 53 year old man with oral fibroma of the tip of his tongue (Postepy Dermatol Alergol 2019;36:125)
Treatment
- Conservative surgical excision with removal of local irritants (J Indian Soc Periodontol 2017;21:258)
Clinical images
Gross description
- Tan or gray nodule of soft tissue with white cut surface
- Surface ulceration or thickened keratin surface may be present
Microscopic (histologic) description
- Nonencapsulated nodular mass
- Mass composed of fibrous connective tissue with collagen bundles interspersed with fibroblasts, blood vessels and scattered chronic inflammatory cells
- Overlying surface of squamous epithelium (J Oral Maxillofac Pathol 2015;19:330)
Microscopic (histologic) images
Positive stains
Sample pathology report
- Right buccal mucosa, excisional biopsy:
- Focal fibrous hyperplasia (irritation fibroma)
Differential diagnosis
- Clinical:
- Nodules of neural, muscular, lipomatous, vascular or salivary gland origins, as well as fibrous proliferations associated with embedded foreign material (e.g. dermal fillers); proper diagnosis is made upon histopathological review
- Multiple fibrous nodules may be associated with various syndromes (e.g. Cowden syndrome) (Cancers (Basel) 2019;11:844)
- Multiple endocrine neoplasia, type 2B (MEN 2B):
- Bilateral flesh colored nodules in the oral commissure regions or multiple nodules of the tip of the tongue are highly suggestive of MEN 2B (Head Neck Pathol 2017;11:364)
- Biopsy of the nodules reveals a diagnosis of mucosal neuroma
- Histopathological:
- Giant cell fibroma (which is of little consequence):
- Papillary surface architecture and plump, stellate shaped fibroblasts within the connective tissue (J Oral Maxillofac Pathol 2012;16:359)
- Giant cell fibroma (which is of little consequence):
Board review style question #1
A 56 year old man presents with a chief complaint of a bump inside the oral cavity. On clinical exam, a pink, smooth surfaced nodule is noted along the patient’s bite line. He states that the mass interferes with chewing and speaking. The microscopic appearance is pictured. What is the diagnosis?
- Irritation fibroma
- Lipoma
- Neurofibroma
- Pleomorphic adenoma
Board review style answer #1
A. Irritation fibroma. Although all of the entities listed fall under the clinical differential diagnosis list, the histology demonstrates a nodular mass of fibrous connective tissue with scattered fibroblasts, blood vessels and chronic inflammatory cells, which rules out all of the listed entities except irritation fibroma.
Comment Here
Reference: Irritation fibroma
Comment Here
Reference: Irritation fibroma
Board review style question #2
A 61 year old woman presents with a solitary nodular mass of the oral buccal mucosa that has been present over 5 years with minimal change. Histopathological review of the mass reveals a fibrous mass containing collagen bundles interspersed with fibroblasts and blood vessels. Which of the following is true regarding this pathological entity?
- Lesional tissue is positive upon immunohistochemistry with S100
- The patient should be evaluated for multiple endocrine neoplasia, type 2B
- This entity represents most likely represents a reactive hyperplasia rather than a true tumor
- Without surgical excision, this mass will continue to grow to enormous size
Board review style answer #2
C. This entity represents most likely represents a reactive hyperplasia rather than a true tumor. The pathological entity described is an irritation fibroma. Irritation fibromas are the most common oral reactive lesion. While irritation fibromas would be positive upon immunohistochemical staining with vimentin, they are negative with S100, SMA, CD34 and other soft tissue markers. MEN 2B should be considered in a patient with bilateral flesh colored nodules in the commissures of the mouth or multiple nodules of the tip of the tongue, although the biopsy results would reveal a mucosal neuroma rather than purely fibrous connective tissue. Because irritation fibrous are not considered true tumors, they often do not grow with unlimited potential. They most frequently measure 1 - 2 cm in diameter and may increase or decrease in size depending on local irritating factors.
Comment Here
Reference: Irritation fibroma
Comment Here
Reference: Irritation fibroma
Kaposi sarcoma
Leukoedema (pending)
[Pending]
Leukoplakia
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Hyperkeratotic (white) plaque / patch of mucosa exhibiting clonality and representing precursor lesion to squamous cell carcinoma
- Approximately 40% of leukoplakias exhibit keratinizing dysplasia (Oral Surg Oral Med Oral Pathol Oral Radiol 2014;118:713)
- Remaining exhibit hyperkeratosis / parakeratosis characterized genomically by KMT2C, TP53, TIAM1 or other mutations (Oral Dis 2019;25:1707)
- Term leukoplakia / leukoplakic also used descriptively in clinical setting to denote any white lesion without a readily apparent diagnosis
- Such use may skew understanding of leukoplakia biology / behavior due to preponderance of frictional / reactive keratoses in oral cavity, which are not always recognizable clinically but have no malignant potential (Head Neck Pathol 2019;13:423)
- Defined by WHO as a white plaque of questionable risk having excluded (other) known diseases or disorders that carry no increased risk for cancer (J Oral Pathol Med 2007;36:575)
- Leukoplakia may occur throughout the upper aerodigestive tract
Essential features
- Hyperkeratotic (white) plaque / patch of mucosa exhibiting clonality and representing precursor lesion to squamous cell carcinoma
- Approximately 40% of leukoplakias exhibit keratinizing dysplasia; the remainder are characterized by hyperkeratosis alone
- Annual malignant transformation rate is 3% and most strongly predicted by presence of dysplasia on biopsy; increasing duration, increasing size and nonhomogenous appearance also associated with malignant transformation
- Leukoplakia exhibiting hyperkeratosis that is not frictional / reactive exhibits a malignant transformation rate of approximately 5%, similar to that of mild epithelial dysplasia
- Histologic appearance of leukoplakia indistinguishable from proliferative (verrucous) leukoplakia and requires clinical correlation
- Surgical excision reduces risk of malignant transformation approximately 3 times
Terminology
- Leukoplasia, erythroleukoplakia, erythroplakia
ICD coding
- ICD-10: K13.21 - Leukoplakia of oral mucosa, including tongue
Epidemiology
- Worldwide prevalence approximately 0.5% (Oral Oncol 2003;39:770, Oral Oncol 2009;45:317)
- Characteristically a disease of older males (M:F = 3:1)
Sites
- May present on any mucosal surface
- Associated with highest incidences of malignant transformation when occurring on ventrolateral tongue or floor of mouth (Oral Oncol 2009;45:317)
Pathophysiology
- Leukoplakia exhibiting keratinizing dysplasia characterized by genomic alterations including TP53 mutations and loss of heterozygosity at 3p and 9p (Cancer Prev Res (Phila) 2012;5:1081)
- Leukoplakia exhibiting hyperkeratosis alone characterized by genomic alterations including KMT2C, TP53 and TIAM1 mutations (Oral Dis 2019;25:1707)
- Genetic progression model of head and neck cancer not well worked out, particularly with regards to early precursor lesions (Clin Cancer Res 2000;6:347)
Etiology
- Associated with smoking / smokeless tobacco, alcohol and areca nut (betel quid) use
- HPV associated with only a very small percentage of cases (Mod Pathol 2017;30:1646)
Clinical features
- Hyperkeratosis on mucosal sites not amenable to frictional / factitial trauma, particularly when sharply demarcated, considered clinically concerning (J Oral Maxillofac Surg 2017;75:723)
- Biopsy proven leukoplakia may clinically appear homogenous or nonhomogenous (Oral Oncol 2009;45:317)
- Homogenous leukoplakia: uniformly thin or thick hyperkeratosis, frequently sharply demarcated
- Nonhomogenous leukoplakia: irregular texture with fissuring, nodular / verrucous components or erythematous components (erythroleukoplakia)
- Proliferative (verrucous) leukoplakia: uncommon and significantly more aggressive (60 - 100% malignant transformation rate) disease characterized by multifocal oral mucosal involvement and a predilection for middle aged / elderly females with no / minimal history of tobacco or alcohol exposure (Oral Dis 2018;24:749)
- Best considered a separate disease on the basis of differing demographic / clinical presentation, biologic behavior and patient management considerations
Diagnosis
- Biopsy required for diagnosis and risk stratification
- Leukoplakia with dysplasia readily diagnosed on basis of conventional histopathologic features of epithelial dysplasia (Head Neck Pathol 2019;13:423)
- Leukoplakia without dysplasia requires clinicopathologic correlation and exclusion of frictional / factitial features as identified clinically or histopathologically
Prognostic factors
- Annual malignant transformation rate 3% (Oral Oncol 1998;34:270)
- Presence of epithelial dysplasia most significant risk factor for malignant transformation (Oral Oncol 2009;45:317, Mod Pathol 2017;30:S112)
- Severe epithelial dysplasia: 28.4% risk
- Moderate epithelial dysplasia: 22.5% risk
- Mild epithelial dysplasia: 5.7% risk
- Hyperkeratosis: 4.9% risk
- Reported overall malignant transformation rates of 0.36 - 34% difficult to interpret due to historical inclusion of frictional / reactive keratoses in leukoplakia cohorts and variability in followup duration (J Oral Pathol Med 2016;45:155)
- Length of duration, increasing size and nonhomogenous appearance associated with increased risk of malignant transformation
Case reports
- 21 year old man with amalgam associated leukoplakia (J Oral Sci 2016;58:445)
- 59 and 66 year old men with tongue leukoplakia and squamous cell carcinoma (Mol Med Rep 2017;16:6780)
- 75 year old man with tongue lesion (Cleve Clin J Med 2020;87:133)
Treatment
- Surgical excision results in 3 times reduction in risk of malignant transformation (Head Neck 2009;31:1600)
- Leukoplakia with high grade (moderate / severe) dysplasia should be excised whenever possible
- Close clinical observation may be appropriate for extensive leukoplakia or patients with comorbidities but otherwise appears to have a limited role when conservative surgical management is possible (J Oral Maxillofac Surg 2017;75:723)
Clinical images
Microscopic (histologic) description
- Leukoplakia with dysplasia exhibits characteristic architectural and cytological features of keratinizing dysplasia
- Features include hyperkeratosis / parakeratosis, epithelial atrophy or hyperplasia with bulbous rete ridges, basal cell hyperplasia with nuclear hyperchromasia or increased nuclear cytoplasmic ratio, variable suprabasal or atypical mitoses, dyskeratosis or glassy cytoplasm, dyscohesion
- Approximately 33% of dysplasias are characterized by an inflammatory infiltrate and should not be misdiagnosed as lichen planus (Oral Surg Oral Med Oral Pathol Oral Radiol 2014;117:511)
- Leukoplakia without dysplasia exhibits hyperkeratosis with no histologic features of a frictional / reactive process but is otherwise less well characterized
- Histologic features include (Head Neck Pathol 2019;13:423):
- Compact hyperkeratosis with hypergranulosis
- Subtle verrucoid architecture
- Epithelial atrophy or hyperplasia
- If the periphery of the leukoplakia is sampled, hyperkeratosis will appear sharply demarcated
- Histologic features include (Head Neck Pathol 2019;13:423):
- Some leukoplakias without dysplasia may exhibit prominent verrucous architecture and be reported as verrucous hyperplasia
Microscopic (histologic) images
Contributed by Ivan J. Stojanov, D.M.D., M.M.Sc.
Cytology description
- Currently limited role for cytology:
- Difficulty sampling adequate tissue in unanaesthetized patients
- Epithelial atypia, if present, difficult to classify as reactive or dysplastic in absence of architectural features
- Patterns of keratinization cannot be assessed
- Oral cavity sites readily amenable to incisional biopsy
Molecular / cytogenetics description
- See Pathophysiology
Molecular / cytogenetics images
Sample pathology report
- Mandible, gingiva, incisional biopsy:
- Hyperkeratosis, epithelial atrophy and mild chronic inflammation, not reactive (see comment)
- Comment: The hyperkeratosis exhibits no features of a frictional / reactive process and resembles the surface keratinization commonly seen in epithelial dysplasias. Cytologic atypia is minimal / absent in this specimen but leukoplakia without dysplasia (hyperkeratosis that is not reactive) has malignant transformation rates of approximately 5%, similar to that of leukoplakia with mild dysplasia. The findings are consistent with the clinically observed leukoplakia, which in approximately 60% of cases presents without dysplasia. If the clinical context is appropriate, proliferative (verrucous) leukoplakia may also be considered.
Differential diagnosis
- Benign alveolar ridge keratosis:
- Histologic features similar to lichen simplex chronicus
- Epithelial hyperplasia with verrucous / undulating surface and wedge shaped hypergranulosis
- Compact hyperkeratosis that tapers towards the edges and is not sharply demarcated
- Elongated rete ridges, occasionally confluent at tips
- No epithelial atypia
- Fibrosis and sparse chronic inflammation
- Chronic frictional / factitial keratosis:
- Shaggy / macerated parakeratosis with superficial bacterial colonization
- Epithelial hyperplasia with keratinocyte edema but no epithelial atypia
- Variable fibrosis, acute and chronic inflammation and leukocyte exocytosis
- Lichen planus / lichenoid mucositis:
- Squamatization / degeneration of the basal cell layer with Civatte bodies (dyskeratotic keratinocytes)
- Band-like lymphoplasmahistiocytic infiltrate in the superficial lamina propria with leukocyte exocytosis and spongiosis
- Proliferative (verrucous) leukoplakia:
- Characterized clinically by multifocal leukoplakia
- Gingival involvement common
- Predilection for middle aged / elderly females and with no / minimal tobacco or alcohol exposure
- Reason for this association is unclear
- Indistinguishable histologically from leukoplakia
- Verrucous epithelial architecture common but not necessarily present
- Characterized clinically by multifocal leukoplakia
Board review style question #1
Board review style answer #1
Board review style question #2
Which of the following is true regarding leukoplakia without dysplasia?
- It can be readily recognized by histologic features of a frictional / reactive process
- It can undergo malignant transformation
- It is usually associated with HPV infection
- It is diagnostic of proliferative (verrucous) leukoplakia
- It is rarely encountered in leukoplakia biopsies
Board review style answer #2
Lichen planus
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Immunofluorescence description | Immunofluorescence images | Positive stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Chronic, T cell mediated inflammatory mucocutaneous disorder of uncertain etiology and pathogenesis
- Characterized by relapses and remissions
Essential features
- Common oral mucosal disease with multifocal, bilateral and symmetrical involvement
- Characterized by white, lace-like lesions (Wickham striae) with or without atrophic or erosive areas
- Accurate identification is challenging and often requires clinicopathological correlation
- Histopathology is nonspecific but includes hyperkeratosis, interface mucositis, hydropic degeneration and apoptotic keratinocytes
- Direct immunofluorescence is nonspecific with a shaggy deposition of fibrinogen at the basement membrane zone
Terminology
- Lichen planus
ICD coding
Epidemiology
- Global oral lichen planus prevalence is 1.01% (Oral Dis 2021;27:813)
- Most commonly seen in middle aged adults (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;103:S25.e1)
- Rarely seen in pediatric populations (Pediatr Dermatol 2014;31:59)
- F > M (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;103:S25.e1)
- May be associated with hepatitis C (varies geographically) (Br J Dermatol 2004;151:1172)
Sites
- Intraoral
- Oral lichen planus is typically multifocal and bilateral with a symmetric distribution of lesions
- Most common site is buccal mucosa; oral lichen planus usually involves the buccal mucosa bilaterally
- May affect the gingiva, vestibule and labial mucosa; tongue involvement is uncommon (J Cancer Prev 2016;21:55)
- Extraoral
- Skin (flexor, wrists and forearms, dorsal hands, shins, presacral area), mucous membranes (oral mucosa, genitalia), hair, nails, esophagus (rare)
- 16% of oral lichen planus patients also have cutaneous involvement (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999;88:431)
Pathophysiology
- Unknown pathogenesis (Oral Surg Oral Med Oral Pathol Oral Radiol 2016;122:72)
Etiology
- Believed to be a T cell mediated chronic inflammatory oral mucosal disease of unknown etiology (J Oral Pathol Med 2010;39:729)
Clinical features
- Most common clinical patterns of oral lichen planus are the reticular and erosive forms (Head Neck Pathol 2020;14:192)
- Reticular pattern: characterized by thin, interlacing and white lines (Wickham striae); lesions typically wax and wane over weeks or months (Oral Maxillofac Surg Clin North Am 2013;25:93)
- Erosive pattern: characterized by atrophic and erythematous areas with central ulceration
- Other clinical patterns include atrophic, papular, plaque and bullous forms (Clin Dermatol 2016;34:495)
- Reactive pigmentation may be seen, particularly in persons of color (Oral Surg Oral Med Oral Pathol Oral Radiol 2016;122:332)
- Multiple forms may be seen in one patient; clinical forms represent the same disease process
- Worse symptoms / lesions tend to be in areas of trauma, chronic irritation, poor oral hygiene
Diagnosis
- Diagnosis is based on both clinical and histopathologic features (J Oral Pathol Med 2021;50:520)
- Histopathologic features of oral lichen planus may mimic numerous pathologic processes with an inflammatory infiltrate (Oral Surg Oral Med Oral Pathol Oral Radiol 2016;122:332)
- Adjunct direct immunofluorescence may be beneficial to differentiate oral lichen planus from conditions with similar histomorphology (e.g., chronic ulcerative stomatitis) or clinical features (e.g., mucous membrane pemphigoid and pemphigus vulgaris) (Oral Surg Oral Med Oral Pathol Oral Radiol 2016;122:332)
- Direct immunofluorescence does not distinguish lichen planus from oral dysplasia (Oral Surg Oral Med Oral Pathol Oral Radiol 2015;119:675)
Prognostic factors
- Oral lichen planus is characterized by relapses and remissions
- Uncertain malignant potential
- Small subset of patients with oral lichen planus (1.1%) develops oral squamous cell carcinoma (Oral Oncol 2017;68:92)
Case reports
- 8 year old boy with oral ulcerations (J Oral Maxillofac Pathol 2020;24:S128)
- 57 year old man with bilateral white lesions of the buccal mucosa (Head Neck Pathol 2020;14:192)
- 77 year old woman with desquamative gingivitis (Case Rep Dent 2019;2019:4659134)
Treatment
- Reticular oral lichen planus is often asymptomatic; no treatment is needed, although management includes monitoring patients at regular intervals to ensure the lesions are migrating or changing patterns
- Photographic documentation is beneficial (Head Neck Pathol 2019;13:423)
- Lesions that do not migrate are concerning for evolving oral dysplasia or contact related lichenoid lesions
- Erosive oral lichen planus is often bothersome due to open sores; typically managed with topical or systemic corticosteroids (Cochrane Database Syst Rev 2020;2:CD001168)
Clinical images
Gross description
- Nonspecific
- Often tan wedge of mucosa with white striations, papules, erosions or ulcerations
Microscopic (histologic) description
- 2003 modified WHO criteria may have more specificity than the 1978 WHO criteria (Int J Prev Med 2021;12:126, J Oral Pathol Med 2003;32:507):
- Orthokeratosis or parakeratosis
- Epithelial thickness varies, sawtooth rete ridges occasionally seen
- Colloid (civatte) bodies in the epithelium or superficial lamina propria
- Thin band of eosinophilic material in the basement membrane
- Well defined, band-like zone of cellular infiltration consisting mainly of lymphocytes and confined to the superficial lamina propria
- Liquefactive degeneration in the basal cell layer (hydropic degeneration)
- Absence of epithelial dysplasia
- Additional criteria proposed by Cheng et al. 2016 (Oral Surg Oral Med Oral Pathol Oral Radiol 2016;122:332):
- Band-like or patchy, predominantly lymphocytic infiltrate in the lamina propria that is confined to the interface of the epithelium and lamina propria
- Lymphocytic exocytosis
- Absence of epithelial dysplasia
- Absence of verrucous epithelial architectural changes
- Histopathologic features of oral lichen planus are nonspecific and should be correlated with clinical features (Oral Surg Oral Med Oral Pathol Oral Radiol 2016;122:332)
Microscopic (histologic) images
Immunofluorescence description
- Direct immunofluorescence is nonspecific
- IgG, IgA, IgM and complement (C3) are characteristically negative
- Shaggy, linear deposition of fibrinogen may be seen at the basement membrane zone
- Fibrinogen positivity at the basement membrane zone may also be seen in epithelial dysplasia and squamous cell carcinoma (Oral Surg Oral Med Oral Pathol Oral Radiol 2015;119:675)
- Colloid bodies may be positive for immunoglobulins
- Indirect immunofluorescence is negative
Positive stains
- PAS (colloid bodies)
Sample pathology report
- Buccal mucosa, incisional biopsy:
- Chronic interface mucositis and hyperparakeratosis (see comment)
- Comment: The histomorphology of interface mucositis combined with the clinical presentation of bilateral, migrating erosions with Wickham striae is most consistent with oral lichen planus.
Differential diagnosis
- Oral lichenoid drug reaction:
- Oral mucosal immunoinflammatory disorder characterized by erythematous plaques, vesiculation, ulceration or hyperkeratosis in response to a medication (Dermatol Ther 2010;23:251)
- Time range between initiation of medication and onset of reaction can vary widely
- Resembles oral lichen planus; mixed inflammation may extend into the deep lamina propria, may show perivascular inflammation
- Epithelium may have a greater number of colloid bodies (Int J Dermatol 2012;51:1199)
- Infiltrate may be more diffuse or mixed with plasma cells
- Indirect immunofluorescence may detect circulating antibodies directed to basal cells in a string of pearls pattern (Am J Dermatopathol 1982;4:155)
- Common implicated medications: nonsteroidal anti-inflammatory drugs, anticonvulsants, antihypertensives, antimalarials and antiretrovirals
- Oral lichenoid contact hypersensitivity reaction:
- Oral mucosal immunoinflammatory disorder characterized by erythematous plaques, vesiculation, ulceration or hyperkeratosis in response to a local agent (Oral Surg Oral Med Oral Pathol Oral Radiol 2017;123:559)
- May present with pain, burning sensation or itchiness (Oral Surg Oral Med Oral Pathol Oral Radiol 2017;123:559)
- Lichenoid interface mucositis; mixed inflammation may extend into the deep lamina propria, may show perivascular inflammation (Eur J Dermatol 2004;14:284)
- Common implicated agents: mouthwashes, foods, spices (particularly cinnamon), gloves, rubber dams and dental materials (Eur J Dermatol 2004;14:284)
- Chronic ulcerative stomatitis:
- Rare, autoimmune disorder that affects the oral mucosa (J Oral Pathol Med 2022;51:501)
- Patients develop autoantibodies against nuclear protein ΔNp63α (an isoform of p63) (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011;111:742)
- Clinically, lesions often respond to antimalarial medications and are less responsive to corticosteroid therapy than oral lichen planus (Oral Surg Oral Med Oral Pathol Oral Radiol 2016;122:332, Oral Dis 2008;14:383)
- Histopathological features may be indistinguishable from oral lichen planus; often demonstrates marked epithelial atrophy (Head Neck Pathol 2019;13:386)
- Direct immunofluorescence: specific antinuclear antibody (SES ANA) pattern; IgG antibodies present in the nuclei of basal and parabasal cells (Head Neck Pathol 2019;13:386)
- Oral graft versus host disease:
- Clinical and histopathological presentations are similar to oral lichen planus
- Develops as a result of allogeneic hematopoietic cell transplantation
- Lupus erythematosus:
- Oral involvement in ~25% of cases (Expert Rev Mol Diagn 2014;14:169)
- Majority of cases have cutaneous involvement or systemic inflammatory disease
- Histopathology resembles oral lichen planus; may have perivascular inflammation
- Direct immunofluorescence: linear band or continuous granular IgG, IgM, IgA or C3 at the basement membrane zone
- Proliferative verrucous leukoplakia:
- Multifocal, aggressive form of oral leukoplakia with a tendency to recur and undergo malignant transformation (Head Neck 2014;36:1662)
- Clinicopathological diagnosis (Head Neck Pathol 2021;15:572)
- Early lesions may mimic oral lichen planus clinically and microscopically
- Histopathology may have inflammatory infiltrate (Head Neck Pathol 2021;15:572)
- Oral lichen planus should lack a prominent corrugated architecture (Oral Surg Oral Med Oral Pathol Oral Radiol 2016;122:332)
- Evolving / early dysplasia:
- Clinical correlation is necessary to distinguish from oral lichen planus
- Oral dysplastic lesions may demonstrate lichenoid inflammatory infiltrate in superficial lamina propria
- Clinically, the lesion does not migrate or change patterns
- Foreign body gingivitis:
- White, progressing, verrucous / corrugated clinical lesions (mimicking proliferative verrucous leukoplakia) were recently found to be strongly associated with granules of embedded foreign material (Oral Surg Oral Med Oral Pathol Oral Radiol 2019;128:250)
- Similar histomorphology to oral lichen planus; however, inflammatory infiltrate is often mixed and patchy, containing minuscule granules of foreign material
- Silica is the most common element found in the embedded foreign material (Oral Surg Oral Med Oral Pathol Oral Radiol 2019;128:250)
Board review style question #1
A 54 year old woman presents to her dentist for a routine examination. Clinical examination reveals thin, interlacing white lines on the buccal mucosa. The lesions present bilaterally. The patient reports that the lesions are asymptomatic and that she had them for years. She reports that the lesions tend to wax and wane. What is the most likely diagnosis?
- Lichen planus
- Mucous membrane pemphigoid
- Oral candidiasis
- Pemphigus vulgaris
- Squamous cell carcinoma
Board review style answer #1
A. Lichen planus. The prevalence of oral lichen planus is 0.1% to 2.2%. The 2 most common clinical patterns of oral lichen planus are reticular and erosive. Reticular oral lichen planus is named because of its characteristic pattern of interlacing white lines (Wickham striae).
Comment Here
Reference: Lichen planus
Comment Here
Reference: Lichen planus
Board review style question #2
Which direct immunofluorescence finding is most supportive of oral lichen planus?
- IgG in the basal and parabasal epithelial nuclei
- Intracellular IgG deposition
- Linear IgG deposition at the basement membrane zone
- Shaggy, linear deposition of fibrinogen at the basement membrane zone
Board review style answer #2
D. Shaggy, linear deposition of fibrinogen at the basement membrane zone. Direct immunofluorescence studies may be necessary to differentiate oral lichen planus from autoimmune blistering diseases. Shaggy deposition of fibrinogen at the basement membrane zone and the absence of immunoglobulin is seen in oral lichen planus.
Comment Here
Reference: Lichen planus
Comment Here
Reference: Lichen planus
Lingual thyroid
Table of Contents
Definition / general | Epidemiology | Sites | Pathophysiology / etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Molecular / cytogenetics description | Videos | Differential diagnosisDefinition / general
- Developmental anomaly in which ectopic thyroid gland is located at the base of tongue
- Tongue is the most common site for total thyroid ectopia
- First reported by Hickman in 1869 (AMA Arch Otolaryngol 1953;57:60)
Epidemiology
- Prevalence in general population is 1 per 10,000 - 100,000 people (Endocr Pract 2016;22:343)
- Historically, thyroid tissue has been found in the tongue in 10% of autopsies (J Pathol 1970;102:239, Oral Surg Oral Med Oral Pathol 1972;34:781)
- F:M = 3 - 7:1
- Mean age at presentation is about 40 years, ranging from infancy to 83 years (Eur J Endocrinol 2011;165:375)
- Some studies report a bimodal age distribution, with peaks in 2nd and 4th decades (Br J Surg 1979;66:537)
Sites
- Most cases arise superficially or submucosally along the midline of base of the tongue between foramen cecum and epiglottis
- Sublingual types (body of the tongue) are rarer and may be suprahyoid, infrahyoid or at the level of the hyoid bone
Pathophysiology / etiology
- Failure of thyroid gland to descend from the foramen cecum to its normal prelaryngeal location
- Pathogenesis is unclear, but there are speculations that maternal antithyroid immunoglobulin may stop thyroid gland descent (Barnes: Surgical Pathology of the Head and Neck, 3rd Edition, 2008)
- Hypothyroidism is commonly seen in patients with lingual thyroid and some have hypothesized that lingual thyroid is a hyperplastic physiologic response by small thyroid remnants in the tongue to a low thyroid hormone level
- Mutation in the genes of thyroid specific transcription factors TTF1, TTF2 (FOXE1) and PAX8 might be involved in thyroid arrest in tongue, as was shown in animals (Nat Genet 1998;19:395); however, no mutation in known genes has so far been associated with the human ectopic thyroid
Clinical features
- Most lingual thyroids are asymptomatic
- Symptomatic lingual ectopia is often manifested in women during puberty, pregnancy or menstruation
- Most common symptoms are dysphagia, dyspnea and upper airway obstruction; other symptoms are foreign body sensation, pain, hemoptysis, dysphonia, snoring and sleep apnea (Endocr Pract 2016;22:343)
- In more than 75% of patients, orthotopic thyroid is absent (total migration failure) and lingual thyroid represents the only thyroid tissue; as a result, 70% of patients with symptomatic lingual thyroid are hypothyroid; hyperthyroidism is exceptionally rare (Int J Surg 2014;12:S3)
- Malignant neoplasms may arise in up to 1% of lingual thyroids; 50+ cases have been reported (J Clin Endocrinol Metab 2011;96:2684)
- Most are follicular carcinomas
- However, recent reports more often encounter papillary carcinomas, which probably reflects greater recognition of the follicular variant of papillary carcinoma (Nikiforov: Diagnostic Pathology and Molecular Genetics of the Thyroid, 2nd Edition, 2012)
Diagnosis
- Radionuclide scan with technetium or radioiodine
- CT, MRI and angiography are important for the preoperative assessment of patients
- FNA helps to differentiate benign from neoplastic conditions
- Incisional biopsy is discouraged due to risk of complications, e.g. infection, necrosis or hemorrhage (Wenig: Atlas of Head and Neck Pathology, 3rd Edition, 2015)
Laboratory
- Hypothyroidism (low T3 and T4, high TSH)
Radiology description
- MRI is useful in estimating extent of a lesion, because it can clearly distinguish thyroid tissue (low-intermediate T2 signal) from the tongue muscle (Hormones (Athens) 2011;10:261)
Radiology images
Images hosted on other servers:
CT scan:
MRI:
Radionuclide scan:
Angiography:
Prognostic factors
- Prognosis is good, since resection of lingual thyroid achieves significant improvement in patient symptoms with low rates of recurrence (Wenig: Atlas of Head and Neck Pathology, 3rd Edition, 2015)
Case reports
- 7 year old girl with Hashimoto thyroiditis in lingual thyroid (BMJ Case Rep 2013;2013:bcr2013200247)
- 12 year old girl with ectopic lingual thyroid (Case Rep Pediatr 2015;2015:252357)
- 12 year old boy with hyperfuctioning lingual thyroid (J Anaesthesiol Clin Pharmacol 2013;29:132)
- 15 year old girl with lingual thyroid and TSH secreting pituitary adenoma (Case Rep Endocrinol 2013;2013:570847)
- 24 year old woman with follicular adenoma of sublingual ectopic thyroid gland (J Med Case Rep 2014;8:270)
- 25 year old woman with fine needle aspiration diagnosis of hyperfunctioning ectopic thyroid (Acta Cytol 2005;49:228)
- 26 year old man with hemoptysis caused by ectopic lingual thyroid (Quant Imaging Med Surg 2015;5:480)
- 31 year old man with ectopic lingual goiter (Acta Otorhinolaryngol Ital 2013;33:343)
- 40 year old woman with lingual thyroid (Ann Maxillofac Surg 2015;5:104)
- 45 year old woman with dyspnea caused by lingual thyroid (N Engl J Med 2012;366:e15)
- 60 year old man with ectopic lingual thyroid with a multinodular goiter (Surgery 2013;153:294)
- 63 year old woman with differentiated thyroid carcinoma in lingual thyroid (Endocrine 2016;51:189)
Treatment
- Small lesions without symptoms usually require no therapy
- Nonsurgical treatment includes thyroid hormone and radioiodine ablation to induce tissue regression (Int J Surg 2014;12:S3)
- Major indications for surgical excision are airway obstruction and repeated significant hemorrhage
- Transoral robotic surgery (TORS) is the most advanced surgical technique (Thyroid 2013;23:466)
- Most patients with lingual thyroid have no other thyroid tissue and acute hypothyroidism may occur after surgical removal
- Autotransplantation of pieces of lingual thyroid into the neck soft tissues may be considered
Clinical images
Gross description
- Midline of base of tongue, usually between circumvallate papillae and epiglottis
- Dome shaped, soft to firm mass with smooth surface, rarely ulcerated
- Several mm to several cm in size (mean 2 - 3 cm)
- Red, smooth to lobulated to nodular, either well or ill defined on sectioning
Microscopic (histologic) description
- Thyroid tissue appears normal, with normofollicular and microfollicular patterns
- Follicular cells are benign in appearance, without nuclear features of papillary carcinoma
- Thyroid tissue usually grows between skeletal muscle and minor salivary glands of tongue, which may simulate tumor invasion
- Circumscribed and encapsulated arrangement is rare
- Diagnosis of primary thyroid carcinoma in a lingual site requires vascular invasion, unequivocal infiltration with desmoplastic response or metastasis in the absence of another primary site (Endocr Pathol 2002;13:353)
Microscopic (histologic) images
Cytology description
- Clusters of follicular cells and colloid, with usual hemorrhagic background (Acta Cytol 2005;49:228)
- Features of associated pathological conditions, e.g. inflammatory and neoplastic, if such are present (Cytopathology 2013;24:275)
Positive stains
- Immunophenotype of thyroid tissue: thyroglobulin, TTF1 in follicular cells and calcitonin in C cells (J Clin Endocrinol Metab 2012;97:951)
Molecular / cytogenetics description
- Mutations typical for thyroid cancer (BRAF V600E, NRAS, HRAS, KRAS) are absent in benign appearing ectopic thyroid tissue (Int J Surg Pathol 2015;23:170)
Videos
Ectopic thyroid in a 6 year old child
Differential diagnosis
- Lingual thyroglossal duct cyst
- Lymphoepithelial cyst of oral cavity
- Some tumors in oral cavity may mimic papillary thyroid carcinoma (Wenig: Atlas of Head and Neck Pathology, 3rd Edition, 2015)
- Cribriform adenocarcinoma of minor salivary glands of oral cavity: thyroglobulin-, TTF1-
- Low grade nasopharyngeal papillary adenocarcinoma: thyroglobulin-, TTF1+
Lingual tonsil
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Radiology images | Case reports | Treatment | Clinical images | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Collection of reactive submucosal lymphoid nodules situated on the dorsal or lateral aspects of the tongue base, which presents clinically as red papules or nodules
- One of the three sets of tonsils present within Waldeyer ring, along with the pharyngeal and palatine tonsils
Essential features
- Clinically presents as red papules or nodules posterior to the circumvallate papillae
- Often clinically diagnostic, although asymmetric, hyperplastic nodules may warrant biopsy to rule out lymphoma, HPV-positive squamous cell carcinoma, or other pathology
- Hyperplastic lingual tonsil is associated with obesity, obstructive sleep apnea, acid reflux disease, younger age, allergic rhinitis and smoking (Am J Rhinol Allergy 2020;34:87)
Terminology
- Hyperplastic lingual tonsil
- Hyperplastic lymphoid aggregates
- Lingual tonsillar hypertrophy
ICD coding
- ICD-10: J35.1 - hyperplastic lingual tonsil
Epidemiology
- Normal anatomical structure
- Hyperplastic lingual tonsils demonstrate higher incidence in younger patients (Am J Rhinol Allergy 2020;34:87)
- Associated with obesity, obstructive sleep apnea, laryngopharyngeal reflux, younger age, allergic rhinitis and smoking (Am J Rhinol Allergy 2020;34:87)
Sites
- Base of tongue, dorsal or lateral aspects, posterior to the circumvallate papillae
- Anterior to the epiglottis
Clinical features
- Red papules or nodules on the dorsal or lateral aspects of the base of the tongue
- Size ranges from a small papule to a large mass (Clin Otolaryngol 2017;42:144)
- Patients with hyperplastic lingual tonsils may present with dysphagia, chronic cough, voice changes, globus sensation, snoring, lingual tonsillitis or rarely airway compromise (Am J Rhinol Allergy 2020;34:87, Cureus 2020;12:e8309, BMJ Case Rep 2019;12:e229555)
- May contribute to the pathogenesis of acid reflux or obstructive sleep apnea in children who are obese (J Otolaryngol Head Neck Surg 2017;46:32)
- Hyperplastic lingual tonsils may cause difficulty in face mask ventilation or tracheal intubation (Clin Otolaryngol 2017;42:144, Anesthesiology 2010;112:746)
Diagnosis
- Diagnosis is made upon clinical features or awake endoscopy (Otolaryngol Head Neck Surg 2018;158:391)
- Biopsy rarely is indicated to rule out other pathological causes of submusocal masses (e.g. lymphoma)
- Head and neck computed tomography (CT), magnetic resonance imaging (MRI), skull lateral radiographs may prove useful in diagnosis and staging of lingual tonsil hypertrophy (Otolaryngol Head Neck Surg 2017;157:898)
Radiology description
- Head and neck computed tomography (CT), magnetic resonance imaging (MRI) and skull lateral radiographs demonstrate lingual tonsils at the level of the epiglottis on the tongue base (Otolaryngol Head Neck Surg 2017;157:898)
Case reports
- 17 year old girl and 26 and 30 year old women present with eosinophilic lingual tonsillitis following sublingual immunotherapy for allergic rhinitis (Clin Case Rep 2020;8:2211)
- 48 year old woman with lingual tonsil abscess contributing to rapidly progressing sore throat (BMJ Case Rep 2019;12:e229555)
- 70 year old woman with hyperplastic lingual tonsil leading to partial airway obstruction (Cureus 2020;12:e8309)
Treatment
- Nonsurgical medical management or surgical debulking / removal may be indicated in cases of hyperplastic lingual tonsil contributing to sleep apnea (Clin Otolaryngol 2017;42:144)
- Nonsurgical management most often entails treating symptoms of acid reflux to prevent inflammation of the tonsil tissue (Clin Otolaryngol 2017;42:144)
- Surgical debulking or removal includes a number of different techniques including sharp dissection, coblation, cryotherapy, laser ablation, suction diathermy, ultrasonographic coagulating dissection and bipolar radiofrequency plasma excision (JAMA Otolaryngol Head Neck Surg 2013;139:1032, Clin Otolaryngol 2017;42:144)
Clinical images
Microscopic (histologic) description
- Aggregates of benign lymphoid tissue, often with germinal center formation; germinal centers lack capsules and sinusoidal spaces
- May contain crypts lined by specialized keratinized stratified squamous epithelium (termed reticular epithelium) that invaginate from the surface; crypts are often filled with desquamated epithelial cells and bacteria, which may calcify
- Often surrounded by other normal structures of the tongue, including striated muscle, mucinous glands and serous glands
- Reference: Anat Histol Embryol 2005;34:27
Microscopic (histologic) images
Videos
Histology of the lingual tonsil
Lingual tonsillectomy for obstructive sleep apnea
Sample pathology report
- Tongue base, incisional biopsy:
- Hyperplastic lingual tonsil (see comment)
- Comment: Microscopic examination reveals surface stratified squamous epithelium and supporting connective tissue. The surface epithelium contains scattered taste buds and focally invaginates into the mesenchymal tissue forming deep crypts containing keratin flakes. Within the supporting connective tissue is a well defined area of lymphoid tissue. Germinal center formation is noted. Lobules of minor salivary glands and associated ductal structures are noted in the surrounding stroma.
Differential diagnosis
- Lymphoepithelial cyst:
- Often clinically presents as an opaque yellow-white nodule that easily ruptures upon manipulation
- Microscopically similar to lingual tonsil, although an enlarged cystic space is seen rather than an crypt-like invagination of surface epithelium (J Clin Exp Dent 2017;9:e1035)
- Human Papilloma Virus-Positive Squamous Cell Carcinoma (HPV-positive SCCa):
- Since HPV positive SCCa often originates deep within the tonsillar crypt epithelium, it may clinically present as an enlarged, smooth surfaced, red / pink nodule within the area of the lingual tonsils (Statpearls: Oropharyngeal Squamous Cell Carcinoma [Accessed 23 June 2021])
- Firm / indurated on palpation
- Typically larger in size when compared to the contralateral side of the tongue
- Microscopically, islands of epithelium arising from the tonsillar crypt epithelium are seen invading into the connective tissue in HPV-pos SCCa; P16ink4a or cytokeratin immunohistochemical markers may be used to highlight the invasive islands when dense inflammation obscures the presence of overt invasion
Additional references
Board review style question #1
Oral examination of a patient reveals an asymmetric 4 mm red nodule at the dorsal tongue base. The patient is asymptomatic and was unaware of the finding. Biopsy of the lesion is shown. Which of the following is true regarding the diagnosis?
- Diagnosis of this entity relies heavily on immunohistochemical findings
- Diagnosis represents reactive hyperplasia of a normal structure
- Significant clinical follow up is recommended, since malignant transformation occurs in the majority of patients with this finding
- This entity is more commonly found in older adults
Board review style answer #1
B. Diagnosis represents reactive hyperplasia of a normal structure
Comment Here
Reference: Lingual tonsil
Comment Here
Reference: Lingual tonsil
Board review style question #2
A patient presents with a focal collection of red papules on the posterior lateral tongue. Biopsy demonstrates a well defined aggregate of lymphocytes showing germinal center formation. An epithelial lined crypt containing keratin is seen in the central aspects of the lymphocytic nodule. What is the most likely diagnosis?
- Fibroma
- HPV related squamous cell carcinoma
- Lingual tonsil
- Lymphoma
Board review style answer #2
Low grade myofibroblastic sarcoma
Lymphoepithelial cyst
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Lymphoepithelial cysts are uncommon benign oral cavity cysts
Essential features
- Oral lymphoepithelial cysts are most common in the lateral tongue and floor of mouth
- Histologic features include a squamous epithelial lined cyst filled with keratin debris and stromal lymphoid tissue
- Treatment is conservative surgical excision with no recurrence
Terminology
- Oral lymphoepithelial cyst
- Intraoral lymphoepithelial cyst
- Benign lymphoepithelial cyst
ICD coding
Epidemiology
- < 1% of all lesions in oral cavity
- Occurs in adults
- Most common in fifth to sixth decade
- F > M (Head Neck Pathol 2021 Jun 29 [Epub ahead of print])
Sites
- Oral cavity (Head Neck Pathol 2021 Jun 29 [Epub ahead of print], J Oral Pathol Med 2020;49:219)
- Most common site: ventral and posterolateral tongue
- Second most common site: floor of mouth
- Other sites in the oral cavity: buccal mucosa, palate, tonsillar pillar, lip
Etiology
- Unknown:
- Leading theory: pseudocysts develop from obstruction of tonsil crypt of oral tonsil tissue (Oral Surg Oral Med Oral Pathol 1970;29:295)
- Another theory postulates traumatic implantation of epithelium into deeper tissues, forming cyst (Oral Surg Oral Med Oral Pathol 1963;16:1214)
- A third theory postulates lymphoid tissue with ectopic foci of entrapped glandular epithelium (Oral Surg Oral Med Oral Pathol 1966;21:120)
- Oral lymphoepithelial cyst is not associated with human immunodeficiency virus (HIV), unlike a subset of lymphoepithelial cysts of the major salivary glands
Clinical features
- Small, white-yellow submucosal nodule
- < 1 cm
- Often painless and asymptomatic
- References: Head Neck Pathol 2021 Jun 29 [Epub ahead of print], J Oral Pathol Med 2020;49:219
Diagnosis
- Combination of clinical and histologic findings
Prognostic factors
- Good prognosis
- No recurrence after excision
Case reports
- 21 year old man with lymphoepithelial cyst in the palatine tonsil (Int J Clin Exp Pathol 2015;8:4264)
- 42 year old woman with multiple lymphoepithelial cysts (Indian J Pathol Microbiol 2013;56:473)
- 55 and 57 year old women with oral lymphoepithelial cysts (Bull Tokyo Dent Coll 2012;53:17)
Treatment
- Conservative surgical excision
Clinical images
Gross description
- Cystic structure, well demarcated, filled with yellowish keratin-like material
Microscopic (histologic) description
- Well circumscribed cyst lined by parakeratinized stratified squamous epithelium with lymphoid stroma
- May have connection to overlying epithelium but not always identified
- Other cyst linings: nonkeratinized squamous epithelium, respiratory metaplasia or ciliated pseudostratified epithelium (or any combination)
- Cyst contents: predominantly keratin debris, amorphous eosinophilic material and inflammatory cells
- Lymphoid stroma may or may not have germinal centers
- Rarely subgemmal neurogenous plaques have been reported near the cyst (Head Neck Pathol 2021 Jun 29 [Epub ahead of print], J Oral Pathol Med 2020;49:219)
Microscopic (histologic) images
Positive stains
- Cyst lining: p40+
- Lymphoid stroma: CD20+ cells predominant, rare CD3+ (J Oral Pathol Med 2020;49:219)
Sample pathology report
- Floor of mouth, biopsy:
- Oral lymphoepithelial cyst
Differential diagnosis
- Epidermal inclusion cyst (epidermoid cyst):
- Squamous lined cyst without lymphoid stroma
- Sebaceous cyst:
- Squamous lined cyst with adnexal structures, lacking lymphoid stroma
- Fordyce granules:
- Clusters of sebaceous glands
- Sialolith:
- Calcified material with surrounding ductal epithelium (with squamous metaplasia)
- Mucocele:
- Pseudocyst filled with mucin, lined by histiocytes and lymphocytes
- Foreign body reaction:
- Numerous multinucleated giant cells with poorly formed granulomas with foreign material
- Squamous cell carcinoma:
- Invasive proliferation of squamous nests
Board review style question #1
Board review style answer #1
Board review style question #2
Which of the following is seen in the stroma surrounding the cyst lining of a lymphoepithelial cyst?
- Collagen
- Lymphoid tissue
- Mucin
- Sebaceous glands
- Seromucinous glands
Board review style answer #2
Median rhomboid glossitis
Table of Contents
Definition / general | Terminology | Epidemiology | Clinical features | Treatment | Clinical images | Microscopic (histologic) descriptionDefinition / general
- Inflammation or beefy red tongue associated with deficiency states
- Due to atrophy of tongue papillae, thinning of mucosa and exposure of underlying vasculature
Terminology
- Also called central papillary atrophy, posterior lingual papillary atrophy
Epidemiology
- 1% population, usually males, ages 30 - 50 years
Clinical features
- Usually a clinical diagnosis
- Causes: pernicious anemia (vitamin B12 deficiency), deficiency of riboflavin, niacin or pyridoxine; sprue, iron deficiency anemia; also associated with jagged teeth, ill fitting dentures, rarely syphilis, burns and ingestion of corrosive chemicals
- Susceptible to recurring or chronic atrophic candidiasis
- Plummer-Vinson / Paterson-Kelly syndrome: iron deficiency anemia, glossitis and esophageal webs
- Median rhomboid glossitis: red patch, usually 2 - 3 cm long, in posterior midline dorsal tongue just anterior to V shaped grouping of circumvallate papillae with loss of papillae or taste buds; associated with candidiasis and diabetes mellitus (Eur J Dent 2011;5:367)
Treatment
- Usually none
- Antifungal therapy to reduce clinical erythema of candidiasis
Microscopic (histologic) description
- Atrophic stratified squamous epithelium overlying moderately fibrosed stroma with chronic inflammation
- Also chronic candida infection with associated pseudoepitheliomatous hyperplasia
Melanotic neuroectodermal tumor of infancy (pending)
[Pending]
Melanotic pigmentation
Definition / general
- Associated with Addison disease, fibrous dysplasia of bone (Albright syndrome), hemochromatosis, Peutz-Jeghers syndrome
- Oral mucosal pigmented lesions are divided into 2 groups:
- Melanin associated lesions - racial pigmentation, syndrome associated, melanotic macules, melanocytic nevi, melanoma
- Nonmelanin associated lesions - blood related pigmentations, metallic pigmentation
Clinical / microscopic (histologic) images
Melkersson-Rosenthal syndrome
Table of Contents
Definition / general | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosisDefinition / general
- Rare neurological disorder characterized by orofacial swelling (usually of upper lip), peripheral facial nerve paralysis and plicated tongue
- No known cause; onset in childhood or early adolescence
- After recurrent attacks, swelling may persist and eventually become permanent
- Lips become hard, cracked and fissured with a reddish brown discoloration
- Cheilitis granulomatosa: may be a variant, sometimes considered to be a monosymptomatic form of Melkersson-Rosenthal syndrome
Case reports
- 14 year old girl with monosymptomatic form of Melkersson-Rosenthal syndrome (Rom J Morphol Embryol 2012;53:851)
- 30 year old man with Down syndrome (Dermatol Online J 2012;18:7)
Treatment
- Symptomatic
Microscopic (histologic) description
- Granulomatous inflammation of lip stroma
Microscopic (histologic) images
Differential diagnosis
Mucocele
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Reactive lesion to mucus extravasation that attracts muciphages without any epithelial lining
Essential features
- Mucus extravasation into the surrounding tissue secondary to salivary gland duct trauma
- Pseudocyst with epithelioid macrophages (muciphages) forming the periphery
- Found on oral mucosal sites with minor salivary glands or sublingual gland
- May recur if feeding salivary gland is not also removed
Terminology
- Mucus extravasation phenomenon
- Ranula (if on the floor of mouth arising from the sublingual gland)
- Plunging ranula (if the mucin dissects through the mylohyoid muscle to involve the cervical area)
- Mucus escape reaction
- Not to be confused with salivary duct cyst / salivary retention cyst / mucus retention cyst / mucus duct cyst / sialocyst
ICD coding
- ICD-10: K11.6 - mucocele of salivary gland
Epidemiology
- No gender predilection (J Oral Maxillofac Surg 2011;69:1086)
- Reported in patients of all ages but more common before the third decade due to association with trauma to oral mucosa containing salivary glands (J Oral Maxillofac Surg 2011;69:1086)
Sites
- Lower labial mucosa > floor of the mouth > ventral tongue > buccal mucosa (J Oral Maxillofac Surg 2011;69:1086)
- Superficial mucoceles are most common at the soft palate, retromolar pad and buccal mucosa (J Oral Maxillofac Surg 2011;69:1086)
- Very rare at the upper labial mucosa as it is difficult to traumatize that site; neoplastic minor salivary gland lesions should be considered (J Oral Maxillofac Surg 2011;69:1086)
Pathophysiology
- Local mechanical trauma, such as biting that injures a salivary gland excretory duct (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;95:467)
- When the duct is severed, mucus escapes into the adjacent tissue (J Oral Maxillofac Surg 2008;66:2050)
- Extravasated mucin attracts macrophages that attempt to phagocytose the foreign material (Acta Histochem 2014;116:40)
- Not associated with primary obstruction of a salivary gland excretory duct, which will lead to mucus retention within a salivary duct cyst (J Oral Maxillofac Surg 2007;65:855)
Etiology
- Trauma to salivary gland excretory duct (Laryngoscope 1988;98:296)
Clinical features
- Dome shaped, sessile nodule measuring a few millimeters to several centimeters (especially ranula) in diameter (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;95:467)
- Fluctuant to palpation but painless, some may feel firmer (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;95:467)
- Blue tinge due to the Tyndall effect (J Oral Maxillofac Surg 2008;66:2050)
- Waxes and wanes over time; patient may report “popping” of lesion, may also resolve spontaneously (Laryngoscope 1988;98:296)
- Superficial mucoceles are associated with hyposalivation and lichenoid lesions such as oral lichen planus, lichenoid drug reaction and chronic graft versus host disease (J Oral Maxillofac Surg 2011;69:1086)
Diagnosis
- Based on patient reported history and clinical examination with definitive diagnosis made by histopathologic evaluation under light microscopy
Prognostic factors
- Benign with good prognosis
Case reports
- 11 month old boy with a 3 month history of difficulty suckling and lower labial mucosal nodule (Case Rep Dent 2014;2014:723130)
- 9 year old boy with a nail-biting habit and deep anterior overbite with a recurrent vesicle at the lower labial mucosa (BMJ Case Rep 2016;2016:bcr2016216354)
- 9 year old boy with a history of local trauma resulting in an enlarging left lower lip swelling (J Pharm Bioallied Sci 2015;7:S731)
- 35 year old woman with complicated medical history presenting with an upper labial mucosal nodule (Braz Dent J 2017;28:405)
Treatment
- Excision along with the feeding salivary gland is curative
- Iatrogenic intraoperative damage to neighboring salivary gland parenchyma may contribute to recurrence
- Removal of the sublingual gland with marsupialization of Wharton's duct can reduce the risk of recurrence for large ranulas (J Oral Maxillofac Surg 2008;66:2050)
- Laser ablation, superpotent topical corticosteroids and gamma-linolenic acid have been reported to be effective in isolated case reports for superficial mucoceles (J Oral Maxillofac Surg 2007;65:855)
Gross description
- Nodular mass resembling gelatinous material if removed intact (Acta Histochem 2014;116:40)
Microscopic (histologic) description
- If removed intact
- Pseudocyst cavity containing mucin, abundant epithelioid foamy histiocytes (muciphages), neutrophils and granulation tissue (Acta Histochem 2014;116:40)
- If removed ruptured
- Fragments of granulation tissue containing epithelioid foamy histiocytes (muciphages) and neutrophils, may see mucinous material (Acta Histochem 2014;116:40)
- Removed salivary gland parenchyma showing obstructive changes
- Acinar atrophy, ductal dilatation with periductal hyalinization, interstitial lymphoplasmacytic infiltrate and interstitial fibrosis at late stage (J Oral Maxillofac Surg 2008;66:2050)
- May see ruptured feeding salivary duct with squamous metaplasia (J Oral Maxillofac Surg 2008;66:2050)
- Long standing lesions organize into fibrosis resembling a fibroepithelial polyp (Acta Histochem 2014;116:40)
- No epithelial cyst lining, may see overlying surface oral mucosa with variable atrophy in superficial mucoceles (J Oral Maxillofac Surg 2011;69:1086)
Microscopic (histologic) images
Positive stains
- Note: stains typically not needed to make the diagnosis
- CD68
- PAS-D
- Mucicarmine
- Alcian blue
Negative stains
Sample pathology report
- Right lower labial mucosa, excision:
- Mucous extravasation phenomenon (mucocele)
- Minor salivary gland parenchyma showing chronic sialoadenitis
Differential diagnosis
- Salivary duct cyst / salivary retention cyst / mucus retention cyst / mucus duct cyst / sialocyst:
- True salivary gland duct epithelial lining that may show an oncocytic bilayer or squamous metaplasia
- Mucoepidermoid carcinoma
- 3 populations of atypical cells (mucous, intermediate, epidermoid) invading the surrounding stroma
- Autoimmune sialadenitis (Sjögren syndrome)
- Minimal obstructive changes such as salivary gland duct dilation and the lymphocytic inflammation is not periductal
- Glandular odontogenic cyst
- True epithelial cystic lining with goblet cells, no extravasated mucin and this lesion is not within the orofacial soft tissues
- Oral focal mucinosis
- No mucin and instead is a well localized non encapsulated collection of myxomatous connective tissue in the stroma
Additional references
Board review style question #1
Board review style answer #1
Board review style question #2
- Among the choices below, what is the most common site to find an oral cavity mucocele?
- Gingiva
- Intrabony, within the maxillary or mandibular bone
- Labial commissure
- Parotid gland
- Upper labial mucosa
Board review style answer #2
Mucoepidermoid carcinoma
Multifocal epithelial hyperplasia
Table of Contents
Definition / general | Case reports | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) imagesDefinition / general
- Also called Heck disease
- Discrete, recurrent papillary lesions on oral mucosa in Native American and Inuit children, associated with HPV 1, 13, 32 (Eur J Dermatol 2011;21:396)
Case reports
- 7 year old girl with HPV 32 related disease (J Maxillofac Oral Surg 2011;10:357)
Clinical images
Gross description
- Well circumscribed, sessile and pale elevation of buccal mucosa
Microscopic (histologic) description
- Balloon cells in Malpighian layers, localized areas of mucosal epithelial hyperplasia with marked acanthosis and parakeratosis
Microscopic (histologic) images
Nasolabial cyst
Table of Contents
Definition / general | Terminology | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Prognosis and treatment | Radiology description | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Immunohistochemistry & special stains | Electron microscopy description | Differential diagnosisDefinition / general
- A rare, developmental non-odontogenic cyst that occurs in the soft tissues of the upper lip lateral to midline
Terminology
- Klestadt cyst
- Nasal alveolar cyst
- Nasoalveolar cyst
- Nasal wing cyst
- Nasal vestibule cyst
- Mucoid cyst of the nose
Epidemiology
- Rare, represents:
- < 1% of jaw cysts
- 2.5% of non-odontogenic cysts
- Adults, peak prevalence in fourth and fifth decades
- 3:1 predilection for women
Sites
- Nasolabial region of the facial soft tissues
- Does not involve the underlying bone, therefore nasoalveolar cyst is a misnomer
Etiology
- Unsettled, but two main theories:
- First suggests remnants of the embryonic nasolacrimal ridge, duct or rod as origin
- Support for this theory is the immunohistochemical protein expression pattern which is very similar to the physiologic pattern of normal nasolacrimal duct epithelium
- Second theory, now less favored:
- Suggests entrapped epithelial remnants along fusion line of medial nasal, lateral nasal and maxillary processes as an origin
Clinical features
- Benign, slow growing cystic mass usually less than 3 cm in size
- Usually asymptomatic, rarely nasal obstruction or reports of pain if infected
- Most common patient concern is swelling
- Mass effect results in distention of nasolabial fold and elevation of the ala of the nose, extraorally
- Presentation could result in clinical differential diagnosis of odontogenic infection
- Intraorally, obliterates the mucolabial fold
- 10% of cysts are bilateral
Diagnosis
- Diagnosis dependent of clinical, radiologic and pathologic correlation
Prognosis and treatment
- Malignant transformation has never been reported
Radiology description
- On CT, will appear as ovoid, well circumscribed lesion, distortion of the affected nasolabial area / base of the nose
- Aside from subtle surface saucerization of bone, bone changes are not identified with this soft tissue cyst
Case reports
- 45 year old woman with Klestadt cyst visualized with radiographic contrast medium (J Clin Diagn Res 2014;8:ZD33)
- 54 year old woman with nasolabial cyst (Head Neck Pathol 2013;7:155)
- 69 year old woman with bilateral nasolabial cysts (J Oral Maxillofac Pathol 2013;17:443)
Treatment
- Surgical excision, performed intraorally, is most common
- Transnasal marsupialization has also been performed
Clinical images
Gross description
- Rubbery, smooth surfaced mass, ballotable soft tissue cyst
- Sectioning reveals cystic and fibrous areas, without internal surface papillary projections
Microscopic (histologic) description
- Histologic examination often reveals lining of multilayered or pseudostratified, cuboidal to columnar epithelium
- Presence of true 'ciliated' epithelium has been described but there is a question whether true cilia remains
- Other combinations possible:
- Bilayered epithelium with a cuboidal basal layer and a columnar luminal layer that contains interspersed scattered mucinous goblet cells
- Both stratified squamous and cuboidal epithelium
- Cuboidal epithelial lining only
- A minority exhibit pseudostratified columnar, stratified squamous and cuboidal epithelium together
- Scattered interspersed luminal goblet cells are common
- Focal squamous metaplasia or apocrine changes may be present
- Cyst wall is composed of hypocellular fibrous connective tissue and may include skeletal muscle
- Inflammation may be present if a history of secondary infection
Microscopic (histologic) images
Immunohistochemistry & special stains
Electron microscopy description
- Bilayered structure of the lining epithelium with cuboidal basal layer and columnar luminal cells and mucous (goblet) cells
- Nonmucous luminal cells frequently feature prominent rough endoplasmic reticulum and numerous submembranous secretory granules, some with electron dense cores
- Microvilli decorated with glycocalix, but no true cilia present, which is in keeping with the newer literature
Differential diagnosis
- Cyst of the incisive papilla:
- Soft tissue cyst with similar histologic features to nasolabial cyst, but distinguished by anatomic site
- Cyst of the incisive papillae occurs within the soft tissue of the anterior hard palate only and shows no communication with the upper lip or nasal area
- Cystic salivary gland neoplasms (benign or malignant) could show overlapping features with nasolabial cyst, particularly on small biopsies:
- Mucoepidermoid carcinoma
- Mammary analogue secretory carcinoma
- Pleomorphic adenoma
- Cystadenoma
- Dilated salivary duct due to obstruction:
- Soft tissue cystic proliferation, typically associated with inflammation in fibrous connective tissue wall
- Epidermal inclusion cyst:
- Soft tissue cyst distinguished from nasolabial cyst by keratinizing epithelium
- Glandular odontogenic cyst:
- Is an intraosseous cyst
- If bony cortical perforation has occurred, then a sampling of the 'soft tissue' component of the cyst lining will create a diagnostic dilemma
- Hidrocystoma:
- Soft tissue cyst of the skin, usually occurring in the periorbital region. Thin, uniform lining, usually 2 cell layers
- Nasopalatine duct cyst:
- Is an intraosseous cyst with histologic features similar to nasolabial cyst
- If bony cortical perforation has occurred, then a sampling of the 'soft tissue' component of the cyst lining will create a diagnostic dilemma
- Contents of incisive foramen typically identified in the surgically resected specimen (peripheral nerve, cartilaginous rests, vascular channels)
Necrotizing sialometaplasia
Nicotine stomatitis (pending)
[Pending]
Oral focal mucinosis (pending)
[Pending]
Oral hairy leukoplakia
Table of Contents
Definition / general | Microscopic (histologic) description | Electron microscopy descriptionDefinition / general
- White, confluent patches of fluffy (hairy) mucosa, bilateral, along lateral tongue
- Associated with HIV+ patients (AIDS may appear within 2 - 3 years) but actually due to EBV infection
Microscopic (histologic) description
- Hyperkeratotic oral mucosa due to piling of keratotic squamous epithelium
- Cowdry type A intranuclear inclusions
- Balloon cells with margination of chromatin (nuclear beading); EBV present in clear cells of spinous layer
- Variable koilocytosis, superimposed Candida infection, without inflammatory response
Electron microscopy description
- Herpes type virions
Oral mucosal melanoma
Table of Contents
Definition / general | Prognostic factors | Case reports | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Differential diagnosis | Board review style question #1 | Board review style answer #1Definition / general
- Rare; annual incidence of 1.2 cases per 10 million; more common in Japanese, black Africans, Native Americans and Hispanics
- Median age 61 years, 78% men
- Differs from cutaneous melanoma due to lack of association with sun damage, family history or atypical nevi and difference in prognostic factors
- Nodal and distant metastases are common
- References: Am J Surg Pathol 2001;25:782, Am J Surg Pathol 2002;26:883
Prognostic factors
- Extremely poor prognosis, with median survival 2 - 3 years; some lower grade tumors without vascular invasion had median survival of 8 years
- Poor prognostic factors: vascular invasion, polymorphous tumor cell population and necrosis
- No prognostic value: tumor thickness, ulceration and level of invasion
Case reports
- 17 year old girl with tender lesion of hard palate (Arch Pathol Lab Med 2002;126:1110)
- 47 year old man with tumor after low dose radiation therapy for lichen planus (Arch Pathol Lab Med 1985;109:290)
- 71 year old man with multiple firm left submandibular swellings for two months (Case #419)
Gross description
- Mucosa covering maxillary bone (62%), labial mucosa (13%) and lower gingiva (8%)
- Usually flat, erythematous or pigmented, less commonly presents as a mass
Microscopic (histologic) description
- Mean 3 mm thick; pigmented or frequently amelanotic; morphology includes epithelioid, fusiform and polymorphous cells
- Some tumor giant cells in almost all cases; 90% have associated melanoma in situ; usually mitotic figures
- Frequent ulceration, necrosis, vascular invasion and perineural invasion; may have desmoplastic features, particularly if lower lip
Microscopic (histologic) images
Positive stains
- S100 (97%), tyrosinase / T311 (94%), MelanA / Mart1 / A103 (85%), microphthalmia associated transcription factor / MITF (D5, 74%) and HMB45 (71%)
- Desmoplastic melanoma: S100, tyrosinase
Negative stains
Differential diagnosis
- Amelanotic melanomas:
- Large cell lymphoma, poorly differentiated carcinoma
Board review style question #1
What do primary mucosal melanoma and cutaneous melanoma have in common?
- Both commonly have BRAF mutations
- Both use the same staging criteria
- Sun exposure is a risk factor for both
- They have a similar prognosis
- They have the same immunohistochemical profile
Board review style answer #1
E. They have the same immunohistochemical profiles. Primary mucosal melanomas share histologic and immunohistochemical features with cutaneous melanomas but differ in terms of risk factors, aggressiveness, molecular profiles and staging criteria.
Comment Here
Reference: Melanoma
Comment Here
Reference: Melanoma
Oral mucosal neuroma (pending)
[Pending]
Oral submucosal fibrosis
Table of Contents
Definition / general | Sites | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosisDefinition / general
- Mainly in India and Pakistan due to smokeless tobacco / chewing of betel quid
- Reactive but risk factor for squamous cell carcinoma
- Early lesions show blanching, mottled, marble-like appearance; later fibrous bands lead to stiffness, restricting ability to open mouth (trismus)
Sites
- Buccal mucosa, lips, retromolar areas, soft palate
Case reports
- 10 year old boy and 12 year old girl (J Indian Soc Pedod Prev Dent 2012;30:85)
- 38 year old man with successful reconstruction using skin graft in buccal mucosa (Case Rep Dent 2012;2012:628301)
Treatment
- None, irreversible once it develops
- Cessation of quid chewing reduces risk of oral cancer but fibrosis is not altered
Clinical images
Microscopic (histologic) description
- Subepithelial fibrosis, chronic inflammation, often with eosinophils, hyalinization and loss of vascularity
- Overlying epithelium is atrophic or hyperplastic and hyperkeratotic
Differential diagnosis
- Amyloidosis
Oropharnygeal neuroendocrine carcinoma (pending)
[Pending]
Paraneoplastic pemphigus (pending)
[Pending]
Parulis
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Localized collection of acute inflammation and edematous granulation tissue on the gingiva, which represents the intraoral opening of a draining odontogenic (dental) infection
Essential features
- Reactive soft tissue swelling of the gingiva
- By definition, must be associated with draining dental abscess / infection (periapical or periodontal fistula)
- Similar to pyogenic granuloma but contains linear tracks or accumulations of neutrophils
- Must treat the source of infection, since surgical removal of the parulis alone likely will lead to recurrence
Terminology
- Gum boil
- Dental fistulous tract / dental fistula
- Dental abscess with sinus tract
ICD coding
- ICD-10: K04.6 - periapical abscess with sinus
Sites
- Exclusively occurs on the gingiva; attached or unattached gingiva
Etiology
- Associated with dental infection
- Pulpal necrosis, abscess (Eur Endod J 2020;5:54)
- Infection associated with an untreated dental cavity
- Infection surrounding dental implant, embedded foreign material or other oral prosthesis
Clinical features
- Smooth and sometimes lobulated exophytic polypoid lesion on the gingiva
- Yellow, red or pink (when fibrosed) in color (Case Rep Dent 2018;2018:4850901)
- Often fluctuant
- Light pressure may reveal drainage of purulent exudate
Diagnosis
- Diagnosis is most often made upon clinical evaluation of fluctuant / draining gingival nodule associated with adjacent dental infection; histopathologic confirmation is useful but may not be needed
- Pulpal necrosis is evaluated with electric pulp testing or thermal evaluation in combination with radiographic correlation
- Intraoral sinus track can be traced with gutta percha to help confirm etiologic origin (J Clin Diagn Res 2013;7:2392)
Radiology description
- Parulides may be accompanied by an ill or well defined radiolucency at or around the apex of a nonvital tooth (Eur Endod J 2020;5:54)
Case reports
- 40 year old woman with multiple parulides (intraoral draining sinus tracts) all associated with a single necrotic tooth (J Clin Diagn Res 2013;7:2392)
- 53 year old woman with parulis forming around dental implant (J Oral Implantol 2016;42:505)
- 59 year old man presents with a large exophytic mass of the gingiva adjacent to a necrotic tooth (Case Rep Dent 2018;2018:4850901)
Treatment
- While the gingival nodule may be removed surgically, the nodule will recur without effective treatment of the underlying associated infection (e.g., root canal therapy, dental extraction, etc.) (Eur Endod J 2020;5:54)
- Antibiotics not indicated unless systemic spread is present (Fertil Steril 1986;45:75)
Clinical images
Gross description
- Tan / gray / brown nodule that often collapses upon sectioning and contains yellow exudate
Microscopic (histologic) description
- Nodule or collapsed nodule surfaced by keratinized squamous epithelium and comprised of edematous granulation tissue (World J Clin Cases 2015;3:779)
- Collections or linear tracts of neutrophils are present and often extend to the base of the specimen
Microscopic (histologic) images
Videos
Etiology and treatment of a dental fistulous tract / parulis
Tracing a dental fistulous tract with gutta percha
Sample pathology report
- Gingiva, excisional biopsy:
- Granulation tissue with linear tracts of neutrophils (see comment)
- Comment: When combined with the clinical information, the histomorphology is compatible with a parulis (draining fistulous tract).
Differential diagnosis
- Histopathologic:
- Pyogenic granuloma:
- May be histopathologically identical / similar, although parulis tends to demonstrate dense accumulations or linear tracts of neutrophils that may extend to the base of the specimen
- Clinical correlation is vital in the differentiation of the two entities
- Distinguishing pyogenic granuloma from parulis is essential for appropriate treatment
- Local excision of the polypoid lesion is sufficient for pyogenic granuloma
- Parulides require treatment of the underlying infection to prevent recurrence
- Pyogenic granuloma:
- Clinical:
- Clinical differential diagnosis for a red, yellow or pink nodule on the gingiva is exhaustive and may include pyogenic granuloma, peripheral giant cell granuloma, peripheral ossifying fibroma, peripheral odontogenic fibroma, localized accumulation of dermal filler, metastatic disease or other malignant or benign tumors (Head Neck Pathol 2019;13:4, World J Clin Cases 2015;3:779, Head Neck Pathol 2013;7:241)
- Identification of a soft tissue gingival nodule, in combination with underlying dental infection, favors diagnosis of parulis
- Excisional biopsy may be used to confirm diagnosis
- Clinical differential diagnosis for a red, yellow or pink nodule on the gingiva is exhaustive and may include pyogenic granuloma, peripheral giant cell granuloma, peripheral ossifying fibroma, peripheral odontogenic fibroma, localized accumulation of dermal filler, metastatic disease or other malignant or benign tumors (Head Neck Pathol 2019;13:4, World J Clin Cases 2015;3:779, Head Neck Pathol 2013;7:241)
Additional references
Board review style question #1
Cone beam computed tomography (CBCT) of the patient shown above demonstrates a well defined, nonexpansile radiolucency surrounding the root of the associated necrotic maxillary incisor. Biopsy shows a nodule of granulation tissue demonstrating dense accumulations of neutrophils at the base of the specimen. What is the most likely diagnosis?
- Foreign body granuloma due to dermal filler
- Leukoplakia
- Parulis
- Pyogenic granuloma
Board review style answer #1
C. Parulis. The main distractor for this gingival nodule comprised of inflamed granulation tissue is a pyogenic granuloma; however, the description of dense accumulations of neutrophils at the base of the specimen favors a parulis, a soft tissue mass representing the intraoral opening of a draining odontogenic (dental) infection. Although both entities are benign, differentiating the two entities is important, as treatment modalities are different.
Although accumulations of dermal filler may present as a yellow nodule in the oral cavity, dermal filler accumulates under unattached mucosa rather than attached gingiva. Past medical history regarding previous cosmetic injections may also aid in excluding this entity from the differential diagnosis.
Leukoplakia is a flat, white patch of the oral cavity and does not clinically present as a nodule or histopathologically as granulation tissue.
Comment Here
Reference: Parulis
Although accumulations of dermal filler may present as a yellow nodule in the oral cavity, dermal filler accumulates under unattached mucosa rather than attached gingiva. Past medical history regarding previous cosmetic injections may also aid in excluding this entity from the differential diagnosis.
Leukoplakia is a flat, white patch of the oral cavity and does not clinically present as a nodule or histopathologically as granulation tissue.
Comment Here
Reference: Parulis
Board review style question #2
Board review style answer #2
A. Parulis. The main distractor for this gingival nodule comprised of inflamed granulation tissue is a pyogenic granuloma; however, the presence of dense accumulations of neutrophils at the base of the specimen favors a parulis, a soft tissue mass representing the intraoral opening of a draining odontogenic (dental) infection. Although both entities are benign, differentiating the two entities is important, as treatment modalities are different.
Peripheral giant cell granulomas contain osteoclast type giant cells, not appreciated within the present biopsy.
Peripheral ossifying fibromas contain focal to large islands of vital bone, not appreciated within this biopsy.
Comment Here
Reference: Parulis
Peripheral giant cell granulomas contain osteoclast type giant cells, not appreciated within the present biopsy.
Peripheral ossifying fibromas contain focal to large islands of vital bone, not appreciated within this biopsy.
Comment Here
Reference: Parulis
Pemphigoid
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology / etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Immunofluorescence images | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Definition / general
- Chronic, immune mediated, subepithelial blistering disease that predominantly affects mucous membranes
- Autoantibodies directed at components of the basement membrane zone
Essential features
- Second most common immune mediated, subepithelial blistering disease, after bullous pemphigoid (J Invest Dermatol 2016;136:2495)
- Most often presents in the oral cavity
- Autoimmune (IgG, IgA or C3) attack of hemidesmosomes / basement membrane zone
- May affect the oral cavity, conjunctiva, subglottis, larynx, nose, esophagus, penis, vulva, anal mucosa or skin
Terminology
- Mucous membrane pemphigoid
- Benign mucous membrane pemphigoid (BMMP)
- Cicatricial pemphigoid
- Mucosal pemphigoid
ICD coding
- ICD-10: L12.1 - benign mucous membrane pemphigoid
Epidemiology
- Wide age range; predilection for middle aged to older adults
- Slight female predominance
Sites
- Affects the oral cavity (96.7%), conjunctiva (42.2%), subglottis, larynx, nose, esophagus, skin or anogenital regions (27.9%) (J Eur Acad Dermatol Venereol 2016;30:72)
- Oral cavity is the most commonly affected site
- Gingiva > buccal mucosa > palate > alveolar ridge > tongue > lower lip
Pathophysiology / etiology
- Likely an autoantibody induced and complement mediated sequestration of leukocytes (predominantly neutrophils) with release of cytokines and leukocyte enzymes leading to detachment of epithelium at the basement membrane zone (Br J Oral Maxillofac Surg 2008;46:358)
- Combination of IgG (94.6%), C3 (85.8%) or IgA (16.5%) autoantibodies directed against epithelial basement membrane zone components BP180, BP230, alpha 6 integrin, beta 4 integrin or laminin 332 (laminin-5) (J Eur Acad Dermatol Venereol 2016;30:72, Acta Derm Venereol 2004;84:381)
- BP180 is the most frequently affected target, in ~75% (Br J Dermatol 2006;154:90)
- Oral only subset: α6 integrin target antigen (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998;85:37)
- Ocular only subset: β4 integrin (J Invest Dermatol 2006;126:2631)
- Mechanism that links the binding of autoantibodies to the basement membrane zone and the subsequent scarring process is unknown (Clin Dermatol 2012;30:34)
- Association with HLA-DQB1*0301 (Br J Dermatol 2001;145:805, Br J Dermatol 2001;145:406, Br J Oral Maxillofac Surg 2008;46:358)
- Emerging association with anti-PDL1 medications (Front Med (Lausanne) 2018;5:268, J Immunother 2019;42:359, J Eur Acad Dermatol Venereol 2019 Oct 29 [Epub ahead of print], Br J Dermatol 2018;179:993)
Clinical features
- General: erythematous or ulcerated mucous membranes +/- blood blister formation (+ Nikolsky sign); periodic episodes leading to potential scarring (Br J Oral Maxillofac Surg 2008;46:358)
- Ocular: scarring on the conjunctiva may produce a symblepharon or blindness
- Oropharynx: dyspnea, hoarseness
- Esophagus: difficulty swallowing or bleeding; stenosis
- Nose: nosebleeds
- Skin: rare; vesicles / bullae
- Laryngeal involvement can lead to airway loss
Diagnosis
- Diagnosis made on routine H&E histological examination and biopsy for direct immunofluorescence
- Direct immunofluorescence is gold standard for diagnosis
- Cases may be followed with indirect immunofluorescence, immunoblotting or enzyme-linked immunosorbent assay (ELISA) testing
- 2015 consensus group created a disease area index table to standardize diagnosis (J Am Acad Dermatol 2015;72:168)
Laboratory
- IgG autoantibodies against basement membrane zone components (BP180, BP230, alpha 6 integrin, beta 4 integrin or laminin 332) detected
- IgG titers correlate with disease severity (Br J Dermatol 1999;140:645)
- Laminin-332 is detected in up to 20% of patients (J Invest Dermatol 2001;116:348, Br J Dermatol 2019;180:149)
Prognostic factors
- Detection of both IgG and IgA autoantibodies associated with more severe disease (Br J Dermatol 1998;138:602)
- Laminin-332 is associated with more severe disease and solid organ tumors in up to 30% (J Invest Dermatol 2001;116:348, Br J Dermatol 2019;180:149)
Case reports
- 58 year old man presents with painful mouth sores, cutaneous blisters, paronychia and onychomadesis (BMC Dermatol 2019;19:3)
- 83 year old patient presenting with oral blisters and erosions after taking pembrolizumab (Front Med (Lausanne) 2018;5:268)
Treatment
- Mild-to-moderate disease:
- Topical therapies, including betamethasone, fluticasone propionate or clobetasol propionate
- Dapsone (Br J Oral Maxillofac Surg 2008;46:358) or sulfapyridine
- Moderate-to-severe disease:
- Mycophenolate mofetil, azathioprine, sulfa drug or prednisolone
- Severe, recalcitrant disease:
- Pulsed IV cyclophosphamide, IV immunoglobulin and rituximab (Clin Exp Dermatol 2019;44:732)
- Rituximab (anti-CD20 therapy) in combination with conventional immunosuppressive therapy leads to more rapid and sustained disease control with fewer potential adverse events (J Am Acad Dermatol 2016;74:835)
- Encourage excellent oral hygiene habits and regular ophthalmologic examinations
Clinical images
Gross description
- Thin wedge of white-tan surface epithelium with underlying tan-brown connective tissue
- Epithelium occasionally separated from underlying connective tissue
Microscopic (histologic) description
- Surface epithelium cleanly detached from the underlying connective tissue at the point of the basement membrane zone
- Superficial lamina propria contains a variable amount of inflammation that may contain lymphocytes, eosinophils and neutrophils (Br J Oral Maxillofac Surg 2008;46:358)
- Aggregates of erythrocytes may be present in area of bullae formation
Microscopic (histologic) images
Immunofluorescence description
- Direct immunofluorescence (DIF): linear deposits of IgG, IgA or C3 along the basement membrane zone (Br J Oral Maxillofac Surg 2008;46:358)
- Indirect immunofluorescence (IIF): IgG autoantibodies against the basement membrane zone with known target antigens including BP180, BP230, alpha 6 integrin, beta 4 integrin or laminin 332 (laminin-5)
Videos
Clinical, histology, laboratory findings with discussion on pathophysiology
Sample pathology report
- Buccal gingiva, incisional biopsy:
- Subepithelial vesiculo-erosive condition consistent with benign mucous membrane pemphigoid (see comment)
- Comment: On H&E, there is a clean separation of the superficial stratified squamous epithelium from the underlying connective tissue at the layer of the basement membrane zone. On direct immunofluorescence, a shaggy and linear deposition of IgG, C3 and IgA is present in the basement membrane zone.
Differential diagnosis
- Bullous pemphigoid (BP)
- Most common immune mediated, subepithelial blistering disease
- Widespread skin lesions
- Persistent mucosal lesions are not seen
- Propensity to scar is less frequent
- Infrequent in the oral cavity
- Pemphigus vulgaris
- Autoimmune bullous disease directed against desmosomes
- Skin lesions heal without scarring
- Buccal mucosa > palate > tongue > labial mucosa > gingiva
- Suprabasilar clefting with acantholysis
- Direct immunofluorescence shows intracellular IgG and C3 staining
- Enzyme-linked immunosorbent assay demonstrates antibodies directed against desmoglein 1 and 3
- Paraneoplastic pemphigus
- Autoimmune blistering condition that indicates an underlying benign or malignant disease
- Patient may be unwell at time of diagnosis
- Intraepidermal-acantholytic bullae
- Direct immunofluorescence may demonstrate intracellular or basement membrane zone IgG and C3 staining
- Immunoblotting reveals antibodies to desmoglein 3 (Dsg3), BP230, envoplakin, plectin, periplakin or epiplakin
- Erosive lichen planus
- T-cell mediated autoimmune disease
- Interface mucositis with Civatte bodies
- Subepithelial band of lymphocytes
- Direct immunofluorescence shaggy fibrin deposition at basement membrane zone
- Epidermolysis bullosa acquisita
- Immune mediated, subepithelial blistering condition
- Differentiate using salt split testing or enzyme-linked immunosorbent assay
- Enzyme-linked immunosorbent assay detects antibodies against type VII collagen
- Antibodies bind to the connective tissue floor of the bullae in epidermolysis bullosa acquista rather than the roof of the bullae as seen in metalloproteinases
- Lichen planus pemphigoides
- Generally younger
- Lichenoid lesions along with bullae
- Also has lichenoid characteristics
- Similar direct immunofluorescence with IgG, C3 or IgA+ at basement membrane zone
- Bullous lichen planus
- Least common variant of oral lichen planus
- Extremely rare
- Demonstrates clinical features similar to lichen planus and lichen planus pemphigoides; vesicles or bullae on pre-existing lichen planus lesions
- Histopathologic and immunofluorescent antibody studies are similar to lichen planus
- Angina bullosa hemorrhagica
- Often traumatic in nature
- Blood filled blisters on the soft palate
- Can be a mimicker on H&E
- Direct immunofluorescence is usually negative (Dermatol Reports 2014;6:5282)
- Erythema multiforme
- Self limiting blistering condition
- Lesions typically last 2 - 4 weeks
- Triggers may include infections (HSV, mycoplasma) or medications
- May demonstrate target lesions on the skin
- Lichenoid infiltrate in basement membrane zone
- Epithelium is edematous and spongiotic with necrosis of basal and suprabasal epithelial cells (intraepithelial and subepithelial bullae formation)
- Direct immunofluorescence shows diffuse granular staining of C3 in basement membrane zone
Board review style question #1
- Which is true about this entity (biopsied from the oral cavity)?
- Affected patients are often young, in the second to third decades of life
- Gingiva is the most commonly affected location
- Patients demonstrate significant ulceration and blistering of mucous membranes without subsequent scarring
- This entity mimics erosive lichen planus on direct immunofluorescence
Board review style answer #1
B. Gingiva is the most commonly affected location. This is mucous membrane pemphigoid.
Comment Here
Reference: Mucous membrane pemphigoid
Comment Here
Reference: Mucous membrane pemphigoid
Board review style question #2
- Which of the follow target antigens is not associated with mucous membrane pemphigoid?
- BP180
- BP230
- Desmoglein 1
- Laminin-332
- α6 integrin
Board review style answer #2
Board review style question #3
- Which target antigen is associated with malignancy in up to 30% of mucous membrane pemphigoid cases?
- BP 180
- BP 230
- Desmoglein 3
- Laminin-332
- Type VII collagen
Board review style answer #3
Pemphigus vulgaris
Table of Contents
Definition / general | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) imagesDefinition / general
- Autoimmune disease with antigen antibody complexes at desmosomes; produces vesicles and bullae prone to rupture, leaving erosions covered with exudate
Case reports
- 36 year old woman with gingival pemphigus vulgaris preceding cutaneous lesion (J Indian Soc Periodontol 2012;16:588)
- 52 year old woman with lesion presenting as gingival involvement (Indian Dermatol Online J 2012;3:202)
Treatment
- Steroids
Clinical images
Microscopic (histologic) description
- Intraepithelial blister with acantholysis and chronic inflammation
Peripheral giant cell granuloma
Table of Contents
Definition / general | Terminology | Epidemiology | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosisDefinition / general
- Reactive gingival mass resembling pyogenic granuloma, which pushes teeth aside and may erode alveolar bone or involve periodontal membrane
- Arises from periodontal ligament enclosing root of tooth
- Central giant cell granuloma: similar to peripheral giant cell granuloma but multiloculated
Terminology
- Also called giant cell epulis, giant cell reparative granuloma, osteoclastoma, myeloid epulis
Epidemiology
- Usually women, 30s to 50s, although may involve children or elderly patients without teeth
Case reports
- 22 year old woman with lesion in maxillary anterior region (Contemp Clin Dent 2012;3:S118)
- 53 year old man, 57 and 81 year old women with lesion in same location as edentulous mandible (Eur J Dent 2010;4:329)
Central giant cell granuloma:
- 15 year old girl with lesion mimicking adenomatoid odontogenic tumor (Contemp Clin Dent 2011;2:249)
Treatment
- Excision with curettage of base of lesion extending into adjacent periodontal membrane
- Recurs if not completely excised or source of irritation not removed (10% recurrence rate)
Clinical images
Images hosted on other servers:
Gross description
- Nodular, pedunculated, inflammatory lesion up to 1.5 cm that protrudes from gingiva at site of chronic inflammation
- Covered by gingival mucosa or ulcerated
Microscopic (histologic) description
- Nonencapsulated aggregates of foreign body giant cells and fibroangiomatous stroma with hemorrhage, hemosiderin, acute and chronic inflammatory cells
- Alveolar bone often expanded in edentulous patients, leading to superficial bone loss with peripheral cuffing
- Variable mitotic activity
Microscopic (histologic) images
Differential diagnosis
Peripheral ossifying fibroma
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Reactive gingival proliferation characterized by spindle cell proliferation with calcification or ossification
Essential features
- Reactive gingival lesion; thought to be associated with chronic irritation
- Spindle cell proliferation with calcification or ossification within gingival connective tissue
Terminology
- Other terms include peripheral cementifying fibroma, peripheral cemento-ossifying fibroma, ossifying fibrous epulis, calcifying fibrous epulis (J Indian Soc Periodontol 2014;18:527)
- Should not be confused with odontogenic / central bone tumors, such as ossifying fibroma and cemento-ossifying fibroma
ICD coding
Epidemiology
- More common in females (F:M = ~2:1) (Oral Surg Oral Med Oral Pathol 1987;63:452, Med Oral Patol Oral Cir Bucal 2022;27:e460, J Indian Soc Periodontol 2015;19:83, Pediatr Dent 2001;23:245)
- Second to fourth decades (children and young adults) (Oral Surg Oral Med Oral Pathol 1987;63:452, Med Oral Patol Oral Cir Bucal 2022;27:e460, Br J Oral Maxillofac Surg 2019;57:1081)
- Can occur at any age, reports range from 2 months to 87 years (Oral Surg Oral Med Oral Pathol Oral Radiol 2020;130:e74, Med Oral Patol Oral Cir Bucal 2022;27:e460)
- ~5% of oral hyperplastic lesions (Braz J Otorhinolaryngol 2019;85:399, Indian J Dent Res 2018;29:61, Acta Odontol Latinoam 2015;28:103)
- ~20% of gingival hyperplastic lesions (Quintessence Int 2007;38:103, J Oral Pathol Med 2010;39:631)
Sites
- Arise exclusively on the gingiva
- Maxilla more common than mandible (Oral Surg Oral Med Oral Pathol 1987;63:452, Pediatr Dent 2001;23:245)
- ~67% in incisor cuspid region (Oral Surg Oral Med Oral Pathol 1987;63:452, Med Oral Patol Oral Cir Bucal 2022;27:e460, J Indian Soc Periodontol 2015;19:83)
Pathophysiology
- Unknown, likely a reaction to chronic irritation (J Indian Soc Periodontol 2015;19:83)
- Hormonal influence has been proposed since the lesion is common in adolescents and young women (Niger Med J 2011;52:35)
- However, lesional cells do not express estrogen or progesterone receptors (ER / PR) (J Oral Sci 2010;52:95)
Etiology
- Associated with chronic irritation, poor dentition and dental prosthetics, especially if poorly fitted (J Indian Soc Periodontol 2015;19:83)
- Thought to arise from the periodontal ligament (Ann Diagn Pathol 2020;46:151510)
Clinical features
- Slow growing nodule with a mean time to presentation of 16 months (Med Oral Patol Oral Cir Bucal 2022;27:e460)
- Generally painless or causing mild discomfort (J Indian Soc Periodontol 2015;19:83)
- May ulcerate (Oral Surg Oral Med Oral Pathol 1987;63:452)
- Indolent clinical course but in some cases, the size and location may interfere with normal oral function, displace teeth and distort local anatomy (Int J Surg Case Rep 2021;84:106127, Ann Maxillofac Surg 2016;6:300, Head Neck Pathol 2013;7:356)
- Recurrence in ~15% despite surgical excision (Oral Surg Oral Med Oral Pathol 1987;63:452, Br J Oral Maxillofac Surg 2019;57:1081, J Indian Soc Periodontol 2015;19:83)
- Multifocal disease is rare (Indian J Dent Res 2014;25:220)
Diagnosis
- Difficult to distinguish clinically from other entities (pyogenic granuloma, oral irritation fibroma, giant cell fibroma, peripheral giant cell granuloma, metastatic lesions)
- Readily diagnosed histologically with high interobserver concordance (Med Oral Patol Oral Cir Bucal 2022;27:e460)
Radiology description
- May show irregular radiopacity due to calcification / ossification or show mild alveolar bone resorption (Dentomaxillofac Radiol 2007;36:180, Med Oral Patol Oral Cir Bucal 2022;27:e460, Head Neck Pathol 2013;7:356)
Prognostic factors
- Benign but may recur
- Recurrence is more likely if offending irritant is not removed (J Indian Soc Periodontol 2015;19:83)
Case reports
- 2 month old girl with peripheral ossifying fibroma (Oral Surg Oral Med Oral Pathol Oral Radiol 2020;130:e74)
- 24 year old man with multifocal disease (Indian J Dent Res 2014;25:220)
- 25 year old woman with 4 cm tumor interfering with oral function (Int J Surg Case Rep 2021;84:106127)
Treatment
- Surgical excision (J Indian Soc Periodontol 2015;19:83)
- Removal of irritants including plaque / calculus or poorly fitted prosthetics (J Indian Soc Periodontol 2015;19:83)
Clinical images
Gross description
- Exophytic mass that may be sessile or pedunculated (Med Oral Patol Oral Cir Bucal 2022;27:e460, J Indian Soc Periodontol 2015;19:83)
- Mean size of < 2 cm but sizes up to 10 cm have been reported (Med Oral Patol Oral Cir Bucal 2022;27:e460, J Indian Soc Periodontol 2015;19:83, Ann Maxillofac Surg 2016;6:300)
Microscopic (histologic) description
- Variably cellular fibroblastic spindle cell proliferation in subepithelial connective tissue in variably collagenous background (J Indian Soc Periodontol 2015;19:83)
- Collagen deposition is more prominent in the deep aspect (J Indian Soc Periodontol 2015;19:83)
- Dystrophic calcification, lamellar or woven bone formation is essential for diagnosis (J Indian Soc Periodontol 2015;19:83)
- Overlying hyperplastic epithelium with hyperkeratosis (J Indian Soc Periodontol 2015;19:83)
- Surface epithelium may be ulcerated (J Indian Soc Periodontol 2015;19:83, Oral Surg Oral Med Oral Pathol 1987;63:452)
- Background contains variable chronic inflammatory infiltrate, predominantly lymphoplasmacytic and proliferating small capillary sized vessels (J Indian Soc Periodontol 2015;19:83, Med Oral Patol Oral Cir Bucal 2022;27:e460)
Microscopic (histologic) images
Contributed by Timothy Fielder, M.B.B.S., B.Med.Sci., Ruta Gupta, M.D. and Molly Housley Smith, D.M.D.
Positive stains
- Not used in routine diagnosis
- SMA in 73% (Br J Oral Maxillofac Surg 2019;57:1081)
- CD68 in 54% (Br J Oral Maxillofac Surg 2019;57:1081)
- SATB2 in 100% (Head Neck Pathol 2022;16:339, Ann Diagn Pathol 2020;46:151510)
- Positive for osteoblastic / cementoblastic proteins RUNX2, BMP2, CAP in one study and osterix (OSX) in another (J Oral Pathol Med 2015;44:628, Braz Oral Res 2017;31:e53)
Negative stains
Sample pathology report
- Gingiva, excision:
- Peripheral ossifying fibroma (see comment)
- Comment: Sections include oral squamous mucosa with underlying connective tissues and show features of a peripheral ossifying fibroma. The mucosa shows focal ulceration with organizing granulation tissue. The submucosal tissues show a well demarcated but unencapsulated lesion composed of areas of fibrosis and metaplastic ossification. There is no dysplasia or malignancy.
Differential diagnosis
- Oral irritation fibroma:
- Clinically difficult to distinguish
- Histologically lacks calcification or bone formation
- Peripheral giant cell granuloma:
- Clinically difficult to distinguish
- Stromal multinucleated giant cells are seen on histology
- Pyogenic granuloma:
- Clinically difficult to distinguish
- Lobulated vascular proliferation on histology
- Giant cell fibroma:
- Clinically difficult to distinguish
- Lacks bone formation
Board review style question #1
Which of the following is true regarding peripheral ossifying fibroma?
- It is a reactive gingival proliferation thought to occur in response to irritation or trauma
- It is histologically characterized by lobulated growth of capillary sized vessels with a central feeder vessel
- It is molecularly characterized by recurrent internal tandem duplication of BCOR
- It is most common in males over 50
Board review style answer #1
A. It is a reactive gingival proliferation thought to occur in response to irritation or trauma
Comment Here
Reference: Peripheral ossifying fibroma
Comment Here
Reference: Peripheral ossifying fibroma
Board review style question #2
Board review style answer #2
Plasma cell gingivitis
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Immunofluorescence description | Immunofluorescence images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Plasma cell gingivitis (PCG) is a rare, idiopathic, nonneoplastic plasma cell proliferative disorder of the gingiva
Essential features
- Plasma cell gingivitis is a distinctive pattern of gingival inflammation of unknown etiology
- Inflammatory infiltrate is dense and composed predominantly of nonneoplastic plasma cells
- The most common clinical presentation is diffuse erythema and oedema of the gingiva
- While this condition is widely considered to be idiopathic, hypersensitivity reactions to various types of antigens including flavoring agents, spices, mouthwash, tobacco, alcohol, chewing gum, candy and medications have been previously proposed in the literature (J Periodontol 1971;42:709, CDS Rev 1995;88:22, Br Dent J 1990;168:115, Oral Surg Oral Med Oral Pathol 1992;73:690, SADJ 2008;63:394)
- Therapeutic strategies are based mainly on symptom control and removal of the offending substance
- Surgical intervention has proven successful in severe cases (BMJ Case Rep 2015;2015:bcr2014207013, Int J Surg Case Rep 2022;93:106998)
Terminology
- Atypical gingivostomatitis
- Idiopathic gingivitis / gingivostomatitis
- Allergic gingivitis / gingivostomatitis
- Plasma cell gingivitis / gingivostomatitis
Epidemiology
- Based on limited data in the literature, the average age of onset is 45 years and there is a higher prevalence in males (J Clin Med 2021;10:830)
Sites
- This condition typically affects the gingiva but additional sites of involvement may be seen, including lips, tongue and larynx
Pathophysiology
- There is a diffuse and dense infiltrate of polyclonal plasma cells in the superficial lamina propria
- Plasma cells show no cytological atypia
- No nodular architecture is seen
- The overlying squamous epithelium is hyperplastic but there is no disruption of normal architecture
- Plasma cells show no affinity for vasculature
- References: J Clin Med 2021;10:830, J Indian Soc Periodontol 2022;26:434
Etiology
- Unclear
- This condition may arise in the context of a hypersensitivity reaction to environmental antigens
- Previously reported antigens include flavoring agents, spices, mouthwash, tobacco, alcohol, chewing gum, candy and medications
- On follow up of cases in the literature there is no increased rate of myeloma, monoclonal gammopathy of undetermined significance (MGUS) or amyloid
- Due to the rarity of the condition and relatively small number of cases in the literature, it is not possible to classify the full extent of this condition and confirm if this is a purely localized phenomenon or if infiltration exists elsewhere
- References: J Clin Med 2021;10:830, J Indian Soc Periodontol 2022;26:434
Diagrams / tables
Image moved to Clinical images
Clinical features
- This condition most commonly presents as diffuse swelling and redness of the gingiva
- Tenderness and bleeding have been frequently reported
- Ulceration is rare and several case reports have described alveolar bone loss (BMJ Case Rep 2015;2015:bcr2014207013, J Oral Maxillofac Pathol 2021;25:S54, J Indian Soc Periodontol 2013;17:527)
Diagnosis
- Diagnosis is made by clinicopathological correlation
- Clinical history of antigen exposure
- Characteristic clinical features of erythema and swelling of the gingiva
- Biopsy of the gingiva, which classically shows a diffuse benign infiltrate of plasma cells in the subepithelial space with no light chain restriction
- References: J Clin Med 2021;10:830, J Indian Soc Periodontol 2022;26:434
Laboratory
Not applicable
Radiology description
Not applicable
Radiology images
No information provided
Prognostic factors
- Type of offending stimulus
- Extent of stimulus exposure
- Condition may resolve following removal of offending stimulus
- On follow up of cases in the literature there is no increased incidence of myeloma, MGUS or amyloid
- References: J Clin Med 2021;10:830, J Indian Soc Periodontol 2022;26:434
Case reports
- 17 year old girl with severe alveolar bone loss related to herbal toothpaste (J Indian Soc Periodontol 2013;17:527)
- 18 year old man with cheilitis that was managed by gingivectomy (Case Rep Dent 2019;2019:2939126)
- 38 year old woman mistakenly treated as aggressive periodontitis (Int J Surg Case Rep 2022;93:106998)
- 42 year old man presenting with severe alveolar bone loss, which was managed by surgical intervention (BMJ Case Rep 2015;2015:bcr2014207013)
- 64 year old man treated with photobiomodulation with no evidence of recurrence after 5 years (Case Rep Dent 2022;2022:2992656)
Treatment
- Treatment is based mainly on symptom control and removal of the offending agent
- Patients are advised to keep a complete dietary history and avoid potential allergens
- Allergy testing and elimination diet may prove helpful
- Other strategies including topical and systemic immunosuppressive therapies, antibiotics, radiation and tissue destruction by liquid nitrogen, carbon dioxide laser and electrocoagulation have had variable results in the literature
- Surgical treatments including gingivectomy may be effective in severe cases
- References: J Clin Med 2021;10:830, J Indian Soc Periodontol 2022;26:434
Gross description
Not applicable
Gross images
Not applicable
Frozen section description
Not applicable
Frozen section images
Not applicable
Microscopic (histologic) description
- Diagnostic criteria: nonneoplastic proliferation of predominantly plasma cells
- Histology shows hyperplastic and spongiotic squamous epithelium
- Ulceration may rarely be seen
- The juxtaepithelial tissues contain a dense inflammatory infiltrate rich in mature plasma cells
- Granulomatous inflammation, blister formation and vasculitis are absent
- References: J Clin Med 2021;10:830, J Indian Soc Periodontol 2022;26:434
Microscopic (histologic) images
Virtual slides
Not applicable
Cytology description
Not applicable
Cytology images
Not applicable
Immunofluorescence description
Not applicable
Immunofluorescence images
Not applicable
Negative stains
Electron microscopy description
Not applicable
Electron microscopy images
Not applicable
Molecular / cytogenetics description
Not applicable
Molecular / cytogenetics images
Not applicable
Videos
Not applicable
Sample pathology report
- Gingiva, biopsy:
- Plasma cell gingivitis (see comment)
- Hyperplastic and spongiotic squamous epithelium
- Dense and diffuse proliferation of mature plasma cells in the superficial lamina propria, in close juxtaposition with the squamous epithelium.
- Kappa and Lambda immunohistochemistry or ISH shows a polyclonal plasma cell population.
- Plasma cells are negative for CD56.
- Relevant negative findings: No granulomas, spirochete infection, vasculitis or blister formation.
- Comment: The differentials include an allergic or hypersensitivity phenomenon (plasma cell gingivitis), response to medication or other agents (lichenoid reaction) and a nonspecific reaction to injury. Of these, plasma cell gingivitis is felt the most likely. Does the clinical impression support this interpretation?
Differential diagnosis
- Multiple myeloma:
- Clonal plasma cell population and 70% of cases are positive with CD56
- Solitary plasmacytoma:
- Clonal plasma cell population
- Chronic hyperplastic gingivitis:
- Absence of diffuse plasma cell infiltrate
- Granulomatous gingivitis:
- Absence of diffuse plasma cell infiltrate
- Granulomas are present
- Spirochete infection
Additional references
Board review style question #1
Board review style answer #1
B. CD20-, CD138+, CD56-. Plasma cell gingivitis is gingival inflammation composed predominantly of a population of nonneoplastic plasma cells. These cells show polyclonal pattern of staining with Kappa and Lambda. CD138 would be positive in both nonneoplastic and neoplastic plasma cell populations. Answer A is incorrect because CD20 and CD68 are negative in plasma cells. CD20 is a B cell marker which is retained on mature B cells until plasma cell differentiation so is not expressed by mature plasma cells. CD68 highlights histiocytes which would be positive in granulomatous gingivitis. Answer C is incorrect because CD56 is positive in 70% of neoplastic plasma cells and negative in nonneoplastic plasma cells. Answer D is incorrect because in a normal or reactive plasma cell population, the ratio of Kappa to Lambda light chains is approximately 2:1. Immunoglobulins from a neoplastic (clonal) plasma cell population contain either Kappa or Lambda light chains. Light chain restriction or monoclonality can therefore be used to distinguish between reactive / nonneoplastic and neoplastic plasma cell proliferations.
Comment Here
Reference: Plasma cell gingivitis
Comment Here
Reference: Plasma cell gingivitis
Board review style question #2
Which antibodies could be used to highlight the plasma cells in plasma cell gingivitis?
- CD20 and CD3
- CD56
- Cyclin D1
- MUM1 / IRF4 and CD138
Board review style answer #2
D. MUM1 / IRF4 and CD138 are positive in both neoplastic and nonneoplastic plasma cells populations. Answers B and C are incorrect because CD56 and cyclin D1 are expressed in neoplastic plasma cells. Overexpression of cyclin D1 by either translocation t(111;14) (most common) or gene amplification is a well recognized oncogenic event in both mantle cell lymphoma and myeloma (Indian J Med Paediatr Oncol 2013;34:283). CD56 is positive in 70% of neoplastic plasma cells and is usually negative in nonneoplastic plasma cells (Histopathology 2004;44:375). Answer A is incorrect because CD20 and CD3 are usually negative in plasma cells. CD20 is a B cell marker which is retained on mature B cells until plasma cell differentiation so is not expressed by mature plasma cells. CD3 is a T cell marker and is typically not expressed by B cells and plasma cells or their neoplastic counterparts.
Comment Here
Reference: Plasma cell gingivitis
Comment Here
Reference: Plasma cell gingivitis
Plasma cell gingivitis (pending)
[Pending]
Pleomorphic adenoma
Polymorphous adenocarcinoma
Primary mucosal CD30 positive T cell lymphoproliferative disorder (pending)
[Pending]
Proliferative verrucous leukoplakia (PVL)
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- An oral potentially malignant disorder that shows slow growing, persistent and often multifocal proliferations of white, verruciform lesions of the oral cavity, particularly the gingiva
Essential features
- Diagnosis requires clinical - pathologic correlation
- Shows high rates (~50%) of recurrence and progression to squamous cell carcinoma (Head Neck Pathol 2021;15:572, Cancers (Basel) 2021;13:4085)
- Older women are most affected
Terminology
- Leukoplakia: white patch of the mucous membrane that is not clinically diagnostic
- Verrucous hyperplasia: a term used by Shear and Pindborg in 1980 for lesions having a histopathologic pattern similar to the bulky hyperkeratotic epithelial proliferation seen in proliferative verrucous leukoplakia and appearing histopathologically and clinically similar to verrucous carcinoma (Cancer 1980;46:1855)
ICD coding
- ICD-10: K13.21 - leukoplakia of oral mucosa
Epidemiology
- Middle aged to older women are most affected (Cancers (Basel) 2021;13:4085)
Sites
- Any oral site
- Gingiva / alveolar ridge mucosa is the most common site for hyperkeratotic PVL lesions and for malignant transformation of PVL lesions (Cancers (Basel) 2021;13:4085)
Pathophysiology
- Little is known about the molecular pathways and biologic factors associated with PVL (Head Neck Pathol 2021;15:572)
Etiology
- Etiology is unknown
- Tobacco and alcohol do not appear to be significant etiologic factors, as seen in other oral precursor lesions (Cancers (Basel) 2021;13:4085)
Clinical features
- Clinical criteria proposed by Villa et al. in 2018 (Oral Dis 2018;24:749):
- White, hyperkeratotic lesions that are smooth, fissured, verrucous or erythematous with or without ulcers
- Multifocal, noncontinuous lesions or a single, large lesion > 4 cm involving 1 site or a single, large lesion > 3 cm involving continuous sites
- Lesions that progress, expand in size or develop multifocality over time
- White / keratotic lesions of the gingiva that often demonstrate a ring around the collar appearance, where the lesion appears to follow the marginal gingiva around the tooth (Head Neck Pathol 2021;15:572)
Diagnosis
- Diagnosis is made upon clinical examination; however, biopsy is required to determine transformation of hyperkeratotic lesions into cytologic dysplasia or carcinoma
- Biopsy from uninflamed and nonulcerated sites is recommended (Head Neck Pathol 2021;15:572)
Prognostic factors
- Women have a 3 times higher risk of developing oral squamous cell carcinoma in PVL compared to men with PVL (Cancers (Basel) 2021;13:4085)
Case reports
- 38 year old man with carcinomatous transformation in a setting of PVL (J Indian Soc Periodontol 2017;21:499)
- 60 year old man presented with multifocal white patches (Contemp Clin Dent 2013;4:258)
- 84 year old woman treated with high dose rate brachytherapy (Cureus 2021;13:e15696)
Treatment
- There is no current treatment for PVL; however, management includes the following:
- Close clinical follow up (every 3 - 6 months) (Oral Dis 2018;24:749)
- Lesions should be photographed at each clinical visit and photographs should be submitted to the pathologist along with any biopsy specimens (Oral Dis 2018;24:749)
- Biopsies are taken periodically, particularly when lesions have changed character (e.g., increased significantly in size, become nodular, exophytic, indurated or more verrucoid) or when destruction of adjacent structures or tooth mobility is noticed
- Early detection and patient education is critical to management
- Early success with laser assisted photodynamic therapy has been reported (Photodiagnosis Photodyn Ther 2022;39:103002)
- Although no standard of care exists for treatment, cases of PVL with cytologic dysplasia or those diagnosed as bulky hyperkeratotic epithelial proliferation (with or without suspicion for invasion) are generally excised with conservative, assured margins when clinically feasible
Clinical images
Contributed by Molly Housley Smith, D.M.D., Michael Piepgrass, D.M.D.,
John McGehee, D.M.D., Michael Menis, D.D.S. and Trent Clifton, D.M.D., M.D.
Gross description
- White lesions demonstrate well demarcated borders, contrasting with adjacent tan, unaffected mucosa
- Pebbled, papillary, verrucoid or sometimes smooth surface texture
Microscopic (histologic) description
- Microscopic features may be subtle; clinical correlation or photographs are vital to diagnosis
- The following histopathologic categories of proliferative verrucous leukoplakia are taken directly from the Consensus Guideline by Thompson et al., 2021 (Head Neck Pathol 2021;15:572, see table)
- Corrugated ortho(para)hyperkeratotic lesion, not reactive
- Disproportionate orthokeratosis
- Orthokeratosis that is > half of adjacent epithelial thickness
- Troughs and crests of keratosis or epithelium, i.e., corrugation
- Wave-like undulation commonly seen in sentinel lesions
- Prominent crests or spikes in clinically worrisome lesions (formerly Christmas tree keratosis)
- Minor subgroup in this category shows flat, dense, markedly thickened orthokeratin with atrophic underlying spinous layer (proliferative leukoplakia)
- Usually prominent granular layer
- Skip segments of ortho and parahyperkeratosis
- Absent to scant acute surface inflammation
- Loss of rete pegs or atrophic epithelium for site
- Sharp demarcation / abrupt transitions
- Architectural distortion is greater than cytologic atypia
- Disproportionate orthokeratosis
- Bulky hyperkeratotic epithelial proliferation, not reactive
- Amplified bulkiness of the epithelial proliferation that accounts for the lesion's thickness rather than keratosis (usually orthokeratosis)
- Bulbous rete pegs that sometimes coalesce to appear confluent, with architectural abnormalities overshadowing cytologic findings
- Separation artifact between epithelium and stroma
- Lichenoid inflammation at advancing epithelial front is sometimes present
- Consider risky sites in order: gingiva > soft palate > floor of mouth > buccal > tongue
- Suspicious for or squamous cell carcinoma
- Voluminous squamous epithelial proliferation with acanthotic endophytic appearing columns with complex folding and invaginations that is > 3 - 4 times the adjacent uninvolved epithelial thickness
- Thick, clubby, bulbous, blunt, downwardly directed rete peg projections:
- May or may not extend below level of adjacent epithelium and often lacking classical invasion or extension below adjacent epithelium
- Basement membrane is often intact
- Intraepithelial microabscesses, sometimes with keratin pearls
- Increased intraepithelial eosinophils
- Muscle abutment / displacement
- Parakeratotic crypting
- Occasional church spire hyperkeratosis in some
- Focal dysplasia may be present but is usually limited
- Corrugated ortho(para)hyperkeratotic lesion, not reactive
Microscopic (histologic) images
Contributed by Molly Housley Smith, D.M.D.
Sample pathology report
- Gingiva, biopsy:
- Corrugated hyperorthokeratosis and chronic mucositis (see comment)
- Comment: When combined with the clinical description and photographs, the histomorphology is compatible with proliferative verrucous leukoplakia.
Differential diagnosis
- Lichen planus / lichenoid reaction:
- Histopathologic features
- Degeneration of the epithelium at the stromal - epithelial junction with blurring of the basal cells with the superficial lamina propria
- Band of lymphocytes within the superficial lamina propria (although lichenoid reactions often have plasma cells, histiocytes or eosinophils as well)
- Sawtooth rete ridges or atrophy
- Degenerated keratinocytes, termed Civatte, colloid or hyaline bodies
- Parakeratosis or minimal to absent orthokeratosis
- Ulceration or subepithelial separation may be present
- Cytologic dysplasia is absent
- Because lichen planus may show overlapping histopathologic features with PVL, diagnosis requires clinical - pathologic correlation (Head Neck Pathol 2021;15:572)
- Lichen planus and medication related lichenoid reactions should migrate or change patterns; although contact related reactions (e.g., due to an adjacent amalgam restoration) may remain in one place, the lesion should not progress and should ameliorate upon elimination of the adjacent irritant
- May be painful, particularly when eating acidic foods
- May show lace-like striations, papules, plaques, ulcerations / erosions or erythema
- Should respond to steroid therapy (although medication related lichenoid reactions may be recalcitrant)
- Histopathologic features
- Foreign body gingivitis with hyperkeratotic lesions:
- Recently, white, progressing, verrucous clinical lesions (mimicking PVL) were found to be strongly associated with granules of embedded foreign material (Oral Surg Oral Med Oral Pathol Oral Radiol 2019;128:250)
- Silica is the most common element found in the embedded foreign material (Oral Surg Oral Med Oral Pathol Oral Radiol 2019;128:250)
- It is uncertain whether this embedded foreign material plays a role in the pathogenesis of PVL or if it represents a separate disease process
- Alveolar ridge keratosis:
- White plaque without erythema or ulceration, present on the edentulous alveolar ridge or the retromolar pad
- Clinically exhibits fading margins rather than well demarcated margins seen in PVL (Head Neck Pathol 2021;15:572)
- White lesions that extend off the alveolar ridge are more concerning
- Histopathologically demonstrates a corrugated layer of orthokeratin but has elongated rete ridges and the inflammatory component is insignificant
- Fibrous stroma is often densely fibrotic
- Traumatic hyperkeratosis (morsicatio):
- Lesions that arise from chronic biting, nibbling or rubbing of the area
- Often arise on the buccal mucosa or lateral tongue along the line of occlusion
- Patients may or may not be aware of the biting habit
- Clinically, lesions are white and often demonstrate a shaggy or shredded surface texture; the lesions blend in with the surrounding mucosa
- Microscopic examination shows thickened parakeratin, often with bacterial surface colonies, areas of plasma / serum pooling, edema within the keratinocytes and thickening of the spinous cell layer; scattered inflammatory cells are seen within the underlying connective tissue
- Tobacco pouch keratosis:
- Mucosal alterations due to habitual use of chewing tobacco or snuff
- Clinically, the mucosa is thickened and fissured with a white-gray sheen
- Histopathologic examination reveals thickening of the spinous cell layer, basilar hyperplasia and a thickened layer of edematous ortho or parakeratin which forms epithelial peaks or chevrons; a dense band of eosinophilic hyalinization may be seen in the superficial lamina propria with use of wet snuff
- Epithelial dysplasia / unifocal leukoplakia, not attributable to PVL:
- M > F
- Associated with tobacco and alcohol use (Cancers (Basel) 2021;13:4085)
- Histopathologically shows bulbous or teardrop shaped rete ridges with variable degree of pleomorphism, hyperchromasia, hypercellularity, increased and abnormal mitotic figures, increased nuclear size and individual cell keratinization
Board review style question #1
A 73 year old woman presents with multiple, asymptomatic white patches of the attached gingiva that have progressed over a few months. The lesions do not change pattern and do not migrate. Histopathologic examination reveals epithelium with a thickened, corrugated layer of orthokeratin devoid of overt cytologic dysplasia. What condition does this patient have?
- Alveolar ridge keratosis
- Proliferative verrucous leukoplakia
- Squamous cell carcinoma
- Tobacco pouch keratosis
Board review style answer #1
Board review style question #2
Which of the following is true of the condition proliferative verrucous leukoplakia?
- Chewing tobacco is a common etiologic factor
- Males are most frequently affected
- Microscopic examination of the associated white lesions shows frank cytologic dysplasia during early stages
- Patients demonstrate a ~50% risk of developing oral squamous cell carcinoma
Board review style answer #2
D. Patients demonstrate a ~50% risk of developing oral squamous cell carcinoma
Comment Here
Reference: Proliferative verrucous leukoplakia
Comment Here
Reference: Proliferative verrucous leukoplakia
Pseudoepitheliomatous hyperplasia
Table of Contents
Definition / general | Essential features | Terminology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Definition / general
- Histopathological pattern characterized by the benign, reactive elongation of the epithelial rete ridges, which deceivingly may mimic squamous cell carcinoma
- Seen in a variety of conditions / tumors, namely granular cell tumor, candidiasis (median rhomboid glossitis, chronic hyperplastic candidiasis), necrotizing sialometaplasia, blastomycosis, granulomatosis with polyangiitis, etc. (Oral Dis 2020;26:573)
Essential features
- Microscopic pattern rather than a distinct diagnosis
- Benign hyperplasia of the epithelial rete ridges
- May be misdiagnosed as squamous cell carcinoma
- Seen in a wide variety of infectious, inflammatory, traumatic and neoplastic conditions (Am J Dermatopathol 2012;34:165)
Terminology
- Pathologists often use the acronym PEH
- Pseudocarcinomatous hyperplasia
Sites
- Not site specific; site predilection depends on the primary diagnosis
- Oral granular cell tumors most commonly occur on the dorsal tongue, necrotizing sialometaplasia is most commonly on the hard palate and median rhomboid glossitis occurs on the posterior dorsal tongue at the midline (Oral Dis 2020;26:573)
Pathophysiology
- Unknown
- Possible role of transforming growth factor alpha (TGF alpha) in PEH development via autocrine growth effect or by blocking downregulation of epidermal growth factor receptor (EGFR) (Ann Diagn Pathol 2003;7:73, Am J Dermatopathol 2012;34:165)
Etiology
- Reported in a variety of conditions / tumors
- Granular cell tumor (Oral Dis 2020;26:573)
- Candidiasis (median rhomboid glossitis, chronic hyperplastic candidiasis) (J Int Oral Health 2015;7:148)
- Reactive proliferations, such as epulis fissuratum (J Int Oral Health 2015;7:148)
- Necrotizing sialometaplasia (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;89:600)
- Deep chronic infections, such as blastomycosis (Am J Dermatopathol 2011;33:112)
- Granulomatosis with polyangiitis (Intractable Rare Dis Res 2022;11:93)
- Oral submucous fibrosis (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;106:556)
- Melanocytic nevi (Int J Oral Maxillofac Surg 2002;31:330)
- Melanoma (J Cutan Pathol 2000;27:153)
Clinical features
- Clinical appearance dictated by the condition / background setting in which PEH is found
- For example, PEH in chronic hyperplastic candidiasis may manifest as a well demarcated plaque
- Granular cell tumors present as dome shaped, often yellow nodules (Am J Dermatopathol 2011;33:112)
Diagnosis
- Biopsy with clinicopathologic correlation, sometimes with review of multiple levels (Am J Dermatopathol 2011;33:112)
- Diagnosis of PEH is made with significant caution, as atypical epithelial processes (e.g., verrucous carcinoma, proliferative verrucous leukoplakia, squamous cell carcinoma) may imitate PEH
- Misdiagnosis of PEH as squamous cell carcinoma may lead to radical surgery or surgery related morbidity (J Cutan Aesthet Surg 2014;7:232)
- Double reporting or obtaining a second opinion aids in preventing misdiagnosis of PEH for squamous cell carcinoma and vice versa (Eur Arch Otorhinolaryngol 2014;271:847)
- Special stains may be necessary to diagnose infections
Prognostic factors
- Prognosis dictated by primary diagnosis
Case reports
- 27 year old woman with PEH in necrotizing sialometaplasia (Dermatol Online J 2020;26:13030)
- 32 year old man with granulomatosis with polyangiitis of the gingiva showing PEH on biopsy (Intractable Rare Dis Res 2022;11:93)
- 44 year old white man with granular cell tumor showing PEH (BMC Res Notes 2017;10:14)
- 62 year old man with PEH in an intramucosal nevus (Int J Oral Maxillofac Surg 2002;31:330)
Treatment
- Depends on primary diagnosis
Clinical images
Gross description
- Depends on the underlying diagnosis (e.g., granular cell tumor, blastomycosis, etc.) but in general, thickening of the epithelium is noted
- Tan, although may be pigmented if overlying a nevus or melanoma (Am J Dermatopathol 2011;33:112)
Microscopic (histologic) description
- Thick elongation of the overlying epithelium with bulbous or sometimes jagged / sharp, interconnecting rete ridges (Am J Dermatopathol 2011;33:112)
- May exhibit keratin pearl formation: concentric layers of keratinocytes with central keratinization (Am J Dermatopathol 2011;33:112)
- Lacks significant nuclear atypia; although mitotic figures may be seen, they are not numerous or atypical (Am J Dermatopathol 2011;33:112)
- Awareness of microscopic features seen in conditions / tumors associated with PEH is paramount for proper diagnosis
- Prominent leukocytic exocytosis or extravasated red blood cells should alert the pathologist to look for infection (candidiasis, blastomycosis, etc.) or granulomatosis with polyangiitis (Am J Dermatopathol 2011;33:112)
- Replacement of underlying fibrous stroma with sheets of pale, basophilic, plump granular cells suggests that the overlying epithelial proliferation is likely associated with granular cell tumor
- Connection with metaplastic salivary ducts and presence of spilled mucin suggests necrotizing sialometaplasia
- Underlying stromal fibrosis may be seen in oral submucous fibrosis (in a patient who uses betel quid) or in median rhomboid glossitis, as the posterior dorsal tongue is a region that tends to exhibit prominent fibrosis of the stroma
Microscopic (histologic) images
Positive stains
- Usually not utilized for diagnosis as clinicopathologic correlation is often the most valuable
- Special stains PAS or GMS may highlight the underlying infectious process
- p53 reportedly positive only in basilar portion of epithelium (differentiated keratinocytes not stained) (Am J Dermatopathol 2011;33:112, Arch Pathol Lab Med 2005;129:1032, Cancer 1994;73:2317)
Videos
PEH in excision of skin lesion
Definition, causes and histologic appearance of PEH
PEH in granular cell tumor
Sample pathology report
- Dorsal tongue, incisional biopsy:
- Hyperparakeratosis, epithelial hyperplasia and superficial candidal colonization (see comment)
- Comment: The microscopic pattern of epithelial hyperplasia is suggestive of pseudoepitheliomatous hyperplasia, likely caused by the presence of candidiasis. If lesional tissue persists after adequate antifungal therapy, however, rebiopsy is recommended in order to rule out atypical epithelial processes that may mimic pseudoepitheliomatous hyperplasia.
Differential diagnosis
- Squamous cell carcinoma (SCC):
- May be difficult to differentiate from PEH on small biopsies or without supplemental clinical information
- Demonstrates significant cellular atypia and increased / abnormal mitotic figures
- Frankly invasive islands that lack surrounding basement membrane
- May show perineural, lymphovascular, skeletal muscle or ductal invasion
- p53 reportedly positive throughout full thickness in SCCs as opposed to in PEH, where it highlights only the basilar portion (Arch Pathol Lab Med 2005;129:1032, Am J Dermatopathol 2011;33:112)
- In cases with secondary candidiasis, repeat biopsy after antifungal therapy may aid in determining a more definitive diagnosis
- Verrucous carcinoma:
- May be difficult to differentiate from PEH on small biopsies or without supplemental clinical information
- Church spire-like or papillary hyperkeratosis with deep keratin clefting
- Broad, bulbous, plunging rete ridges that demonstrate pushing encroachment on muscle or other deep submucosal structures, below the level of intact normal epithelium (Head Neck Pathol 2021;15:572)
- Persists despite antifungal therapy
- In cases with secondary candidiasis, repeat biopsy after antifungal therapy may aid in determining a more definitive diagnosis
- Bulky hyperkeratotic epithelial proliferation in proliferative verrucous leukoplakia (PVL) (Head Neck Pathol 2021;15:572):
- May be difficult to differentiate from PEH on small biopsies or without supplemental clinical information
- Generalized thickened epithelium
- Bulbous rete pegs that sometimes coalesce
- Lichenoid inflammation may be present
- High risk of progression into malignancy if untreated
- Associated with multifocal lesions
- Persists despite antifungal therapy
- High risk sites in order: gingiva > soft palate > floor of mouth > buccal > tongue
Board review style question #1
Board review style answer #1
A. Pseudoepitheliomatous hyperplasia. When combined with the clinical information / photograph, the overall diagnosis of this case is median rhomboid glossitis, which is a particular diagnosis made in a patient with a red patch on the middle portion of the posterior dorsal tongue. The epithelium often shows elongated, bulbous shaped rete ridges (pseudoepitheliomatous hyperplasia) and superficial candidal colonization, as highlighted here by a PAS stain. Answer B is incorrect because the epithelium does not show significant atypia or detached islands of invasive epithelium. Answer C is incorrect because there are no salivary ducts pictured above; however, squamous ductal metaplasia may be seen in association with pseudoepitheliomatous hyperplasia in a setting of necrotizing sialometaplasia, a condition most often diagnosed on the hard palate. Answer D is incorrect because although the epithelium is bulbous and hyperplasic, a prominent verrucoid surface architecture and keratin clefting are not identified.
Comment Here
Reference: Pseudoepitheliomatous hyperplasia
Comment Here
Reference: Pseudoepitheliomatous hyperplasia
Board review style question #2
Board review style answer #2
B. Granular cell tumor with overlying pseudoepitheliomatous hyperplasia (PEH). Microscopic sections show a dome shaped mass of pale, basophilic, plump granular cells surfaced by hyperkeratotic and hyperplastic epithelium. Although the rete ridges are significantly proliferative and demonstrate keratin pearls, overt cytologic atypia is not appreciated. This proliferative pattern of the epithelium is termed pseudoepitheliomatous hyperplasia and is known to be associated with granular cell tumors. Answer A is incorrect because although there is a thickened layer of parakeratin, this answer choice ignores the replacement of the fibrous stroma by plump granular cells. Answer C, a common pitfall in the diagnosis of this tumor, is incorrect because although the epithelium is proliferative, prominent cytologic atypia is not appreciated. The pathologist must be keen in recognizing the underlying replacement of the fibrous stroma with plump granular cells and must know that granular cell tumors characteristically show PEH in many cases. Answer D is incorrect because verrucous carcinoma would show keratin clefting and prominent, bulbous, plunging rete ridges that push into the underlying muscle.
Comment Here
Reference: Pseudoepitheliomatous hyperplasia
Comment Here
Reference: Pseudoepitheliomatous hyperplasia
Board review style question #3
Board review style answer #3
A. Blastomycosis with pseudoepitheliomatous hyperplasia. Blastomycosis is one of the conditions that characteristically shows pseudoepitheliomatous hyperplasia (PEH) in which the epithelium is thickened and forms elongated and anastomosing rete ridges. Answer D is incorrect because although blastomycosis has often been misdiagnosed as squamous cell carcinoma (SCC) due to this prominent PEH, neutrophilic abscesses throughout the epithelium should prompt the pathologist into getting infectious stains, such as the GMS shown above. The GMS stain highlights the thick walled blastomycosis organisms, which show broad based budding. SCC is a common pitfall in the diagnosis of blastomycosis but is incorrect because fungal stains are negative for deep organisms in SCC. Answer B is incorrect because granulomatosis with polyangiitis (GPA) also demonstrates dense inflammation and PEH; however, GPA has evidence of vasculitis and a lack of deep fungal organisms. Answer C is incorrect because pyogenic granulomas can also show dense inflammation and some degree of PEH; however, the epithelium is often not this prolific and microorganisms would not be present on GMS staining.
Comment Here
Reference: Pseudoepitheliomatous hyperplasia
Comment Here
Reference: Pseudoepitheliomatous hyperplasia
Pyogenic granuloma
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Benign and often reactive vascular proliferation of the oral mucosa, most commonly found on the gingiva
Essential features
- Benign red / vascular soft tissue proliferation, most commonly found on the anterior maxillary gingiva
- Associated with poor oral hygiene, chronic trauma, pregnancy, medications
- Form of capillary hemangioma that is most often considered reactive and may demonstrate a lobular architecture histopathologically
- May demonstrate rapid growth and clinically mimic malignancy (Clin Case Rep 2018;6:690, Case Rep Dent 2021;2021:5575896)
- Constitutes 3.8 - 7% of oral biopsy diagnoses (J Oral Maxillofac Surg 2010;68:2185)
Terminology
- Lobular capillary hemangioma, subtype
- Pregnancy tumor
- Epulis gravidarum / granuloma gravidarum: pyogenic granuloma occurring in a setting of pregnancy
- Epulis granulomatosum: pyogenic granuloma located in an extraction socket
ICD coding
Epidemiology
- Large age range; most common in the second and third decades of life (J Oral Maxillofac Surg 2010;68:2185, Oral Maxillofac Surg 2012;16:305)
- Female predilection (J Oral Maxillofac Surg 2010;68:2185, Pathol Int 2005;55:391, Oral Maxillofac Surg 2012;16:305)
Sites
- Gingiva affected most often (maxillary anterior) (J Oral Maxillofac Surg 2010;68:2185, Head Neck Pathol 2019;13:4)
- May also affect lips, buccal mucosa, tongue or palate
Pathophysiology
- Largely unknown, although in pregnancy, estrogen enhances vascular endothelial growth factor (VEGF) production in macrophages, likely contributing to the development of pyogenic granulomas (J Dermatol Sci 2005;38:1)
- Also in pregnancy, progesterone may function as an immunosuppressant in gingiva, preventing an acute inflammatory reaction against oral bacteria and resulting in proliferative gingival inflammation (J Clin Periodontol 1991;18:262)
- Increased estrogen and progesterone in pregnancy increases concentrations of Prevotella intermedia in the subgingival biofilm, decreases the host response to the bacteria and increases the vascular permeability and infiltration of fluids into the gingival tissues, contributing to formation of pyogenic granulomas (J Appl Oral Sci 2013;21:215)
- 2018 International Society for the Study of Vascular Anomalies (ISSVA) Classification of Vascular Anomalies lists BRAF, RAS and GNA14 as causal genes for the lobular capillary hemangioma (pyogenic granuloma) (ISSVA: ISSVA Classification for Vascular Anomalies [Accessed 11 August 2021])
Etiology
- Associated with chronic irritation (J Oral Maxillofac Surg 2010;68:2185, Head Neck Pathol 2019;13:4)
- Poor oral hygiene
- Ill fitting oral appliances or overhang margins of dental restorations
- Persistent bite trauma
- May be seen in patients with drug induced gingival overgrowth from use of calcium channel blockers, calcineurin inhibitors, antiseizure medications or anticancer medications (e.g. TNF alpha antagonists, BRAF inhibitors, tyrosine kinase inhibitors, epidermal growth factor receptor inhibitors, mTOR inhibitors, taxanes, pyrimidine analogs) (Case Rep Dent 2021;2021:5575896, Pediatr Transplant 2020;e13947)
Clinical features
- Smooth or lobulated exophytic mass
- Ranges from red / pink to deep red / blue / purple in color (Head Neck Pathol 2019;13:4)
- Frequently ulcerated or crusted (Pathol Int 2005;55:391)
- Often pedunculated, although the lobular capillary hemangioma variant is more commonly sessile (Pathol Int 2005;55:391)
- May bleed easily upon gentle manipulation
- May exhibit rapid growth (Case Rep Dent 2021;2021:5575896)
- 1 mm to several centimeters in diameter
- Lesions tend to become more fibrotic / pink / rubbery over time and with elimination of irritating factors (termed sclerosed pyogenic granuloma or inflammatory fibrous hyperplasia) (J Oral Maxillofac Surg 2010;68:2185)
Diagnosis
- Made upon histopathological examination of the excisional specimen
Prognostic factors
- Good prognosis with low recurrence rate (8.2%) (J Oral Maxillofac Surg 2010;68:2185)
Case reports
- 15 and 26 year old women with large, progressive pyogenic granulomas (Clin Case Rep 2018;6:690)
- 51 year old woman with pyogenic granuloma treated with diode laser (Saudi Med J 2016;37:1395)
- 57 year old man taking amlodipine with rapid development of an epulis granulomatosum (Case Rep Dent 2021;2021:5575896)
Treatment
- Conservative excision, extending to periosteum, with subsequent histopathologic examination (J Oral Maxillofac Surg 2010;68:2185, Neville: Oral and Maxillofacial Pathology, 4th Edition, 2015)
- Elimination of precipitating factors
- Granuloma gravidarum (pyogenic granuloma) should be excised after pregnancy, unless significant esthetic or functional concerns are present (J Appl Oral Sci 2013;21:215)
- In pregnancy, pyogenic granulomas may spontaneously regress after removal of local irritants or after childbirth (J Appl Oral Sci 2013;21:215)
Clinical images
Contributed by Brittany Camenisch, D.M.D., Nehal Almehmadi, B.D.S., Sana Naheed, B.D.S., Evan Lynch, M.D., Ph.D.,
Justin Kolasa, M.D., D.M.D., Molly Housley Smith, D.M.D. and Susanna Goggin, D.M.D.
Gross description
- Tan / brown mass, often pedunculated or lobulated
- May demonstrate hemorrhagic foci on cut surface (Case Rep Dent 2016;2016:1323798)
- Often exhibits ulcerated surface
Gross images
Microscopic (histologic) description
- Highly vascularized proliferation of granulation tissue (J Oral Maxillofac Surg 2010;68:2185)
- Often demonstrates surface ulceration and a subacute inflammatory cell infiltrate comprised of neutrophils, lymphocytes and plasma cells
- May demonstrate a lobular arrangement of capillary vessels and proliferating endothelial cells delineated by fibrous septae (termed lobular capillary hemangioma)
- May be pedunculated
- May show brisk mitotic rate (up to 10 mitotic figures per high power field); however, lacks pleomorphism (Ann Diagn Pathol 2020;46:151506)
Microscopic (histologic) images
Positive stains
- Immunohistochemistry is not routinely performed; however, CD34, CD31, erythroblast transformation specific related gene (ERG), alpha smooth muscle actin (SMA) and muscle specific actin (MSA) highlight the prominent vasculature throughout the mass
- WT1 (Ann Diagn Pathol 2020;46:151506)
Negative stains
Videos
Histopathology of pyogenic granuloma
Clinical and etiologic features
Sample pathology report
- Gingiva, excision:
- Pyogenic granuloma
Differential diagnosis
- Peripheral ossifying fibroma:
- May be clinically identical
- Only on the gingiva / alveolar ridge
- Differentiated based on histopathologic examination
- Peripheral ossifying fibroma demonstrates the presence of bone, at least focally, within the mesenchymal stroma
- Peripheral giant cell granuloma:
- May be clinically identical
- Only on the gingiva / alveolar ridge
- Differentiated based on histopathologic examination
- Presence of osteoclast type multinucleated giant cells
- Parulis:
- May be clinically identical, although may express red-yellow fluid on palpation
- Associated with an adjacent nonvital tooth or inflamed periodontal pocket
- Can be traced using gutta percha to reveal the inflammatory origin
- Differentiated based on histopathologic examination
- Accumulations of neutrophils arranged in a linear fashion
- Metastatic disease:
- May be clinically identical
- Differentiated based on histopathologic examination
- Gingival squamous cell carcinoma:
- May be clinically identical, although often demonstrates a granular or papillary surface architecture (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;107:92)
- Differentiated based on histopathologic examination
- Invasive islands of squamous epithelium arising from surface
- Spongiotic gingival hyperplasia / localized juvenile spongiotic gingival hyperplasia:
- Papillary / pebbly surface architecture
- Recalcitrant to oral hygiene measures
- < 1 cm in size (J Cutan Pathol 2019;46:839)
- Traditionally localized, although multifocal examples have been noted
- Histopathologic examination reveals papillary proliferation of spongiotic, nonkeratinized squamous epithelium with elongation of rete ridges, intermixed capillary vessels and neutrophilic exocytosis
- Angiosarcoma:
- Rare in the oral cavity (Int J Oral Maxillofac Surg 2014;43:917)
- Differentiated based on histopathologic examination
- Infiltrative
- May demonstrate rounded, polygonal or spindled cells, often with an epithelioid morphology (Lancet Oncol 2010;11:983)
- Brisk mitotic rate with atypical mitotic figures or pleomorphism
- Forms vascular sinusoids and less clearly defined vascular spaces (Lancet Oncol 2010;11:983)
- May demonstrate keratin or EMA positivity
- Kaposi sarcoma:
- Often multifocal or associated with diffuse violaceous gingival enlargement (JAMA Dermatol 2019;155:370)
- Associated with AIDS (JAMA Dermatol 2019;155:370)
- Differentiated based on histopathologic examination
- HHV8 positive
Additional references
Board review style question #1
The above mass is found on the gingiva. What is true regarding this diagnosis?
- This entity is more commonly found in pregnant women
- This entity is more commonly found in men
- This entity is more commonly found in patients who are taking long term steroids
- No treatment is indicated for this particular entity; clinical diagnosis is sufficient
Board review style answer #1
Board review style question #2
Board review style answer #2
Pyostomatitis vegetans (pending)
[Pending]
Salivary duct cyst
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Reactive lesion to salivary gland duct obstruction and buildup of trapped mucin within
Essential features
- Mucus trapped within lumen secondary to salivary gland duct obstruction
- Severe obstruction can lead to squamous or oncocytic metaplasia of duct epithelial bilayer
- Found on oral mucosal sites with minor salivary glands or parotid gland
- May become secondarily infected around sialolith, which acts as a nidus
Terminology
- Salivary retention cyst
- Mucus retention cyst
- Mucus duct cyst
- Sialocyst
- Reactive oncocytoid cyst (if epithelial lining has oncocytic metaplasia)
- Not to be confused with mucocele / mucus extravasation phenomenon / ranula / plunging rannula / mucus escape reaction
ICD coding
- ICD-10: K11.8 - other diseases of salivary glands
Epidemiology
- M = F (Arch Otolaryngol Head Neck Surg 1987;113:51)
- Some reports have found a slight female predilection (Arch Otolaryngol Head Neck Surg 1987;113:51)
- Adults with median age of 56 years from 177 cases (Head Neck Pathol 2017;11:469)
- Rarer than the oral cavity mucocele (Pediatr Dermatol 2008;25:308)
Sites
- Minor salivary glands of the floor of mouth, vestibule (mucobuccal fold), buccal mucosa, upper labial mucosa (Head Neck Pathol 2017;11:469)
- Parotid is the most commonly associated major salivary gland (J Oral Sci 2001;43:9)
- Rare in the lower lip (Pediatr Dermatol 2008;25:308)
Pathophysiology
- Salivary duct occlusion leading to reactive ductal ectasia (Diagn Cytopathol 2015;43:495)
- True developmental cyst with epithelial lining unlike the oral cavity mucocele (Head Neck Pathol 2017;11:469)
Etiology
- May be associated with sialoliths, mucus plugs, postoperative or postinflammatory stricture (J Oral Sci 2001;43:9)
- Distal obstruction of a salivary duct leads to retention of secretion within the duct (Diagn Cytopathol 2015;43:495)
Clinical features
- Dome shaped, sessile, slow growing but asymptomatic nodule (Oral Surg Oral Med Oral Pathol 1984;58:692)
- 1 - 3 cm but have been reported to grow up to 10 cm (J Oral Sci 2001;43:9)
- Fluctuant to palpation but usually painless, some may feel firmer especially if a sialolith is present (Oral Surg Oral Med Oral Pathol 1964;18:191)
- Mucus or pus may be expressed from dilated ductal orifices when palpated if secondarily infected (Oral Surg Oral Med Oral Pathol 1984;58:692)
- Blue tinge due to Tyndall effect
- Do not typically wax and wane over time (Arch Otolaryngol Head Neck Surg 1987;113:51)
Diagnosis
- Based on patient reported history and clinical examination, definitive diagnosis made by histopathologic evaluation under light microscopy
Prognostic factors
- Benign with good prognosis
Case reports
- 15 year old boy with a 3 month history of a left lower labial mucosa swelling (J Oral Maxillofac Pathol 2014;18:S151)
- 30 year old man with a left submandibular swelling only noticeable on swallowing and nose blowing (J Laryngol Otol. 2000;114:305)
- 56 year old man with an obstructive mass at the vallecula (Arch Otolaryngol Head Neck Surg 1989;115:1254)
- 63 year old man presenting with an enlarging left preauricular swelling (J Clin Imaging Sci 2013;3:3)
- 78 year old man with a firm swelling at the left upper labial mucosal (Indian J Pathol Microbiol 2013;56:163)
Treatment
- Complete excision along with the feeding minor salivary gland is curative (Arch Otolaryngol Head Neck Surg 1987;113:51)
- Iatrogenic intraoperative damage to neighboring salivary gland parenchyma may contribute to the development of postoperative mucocele (Oral Surg Oral Med Oral Pathol 1964;18:191)
- Partial or total removal of feeding major salivary glands may be required (Pediatr Dermatol 2008;25:308)
- Chlorhexidine mouth rinse or oral antibiotics for secondarily infected salivary duct cysts (Oral Surg Oral Med Oral Pathol 1984;58:692)
- Sialagogues may decrease the risk of salivary stasis within dilated ducts by stimulating salivary flow
Clinical images
Gross description
- Nodular mass with soft texture
Microscopic (histologic) description
- Mucoid secretion surrounded by a bilayer of cuboidal or columnar stratified salivary duct epithelium (Oral Surg Oral Med Oral Pathol 1964;18:191)
- Cyst lining may have papillary folds into the lumen (Head Neck Pathol 2017;11:469)
- May have squamous or oncocytic metaplasia of cyst lining, especially with more severe obstruction (Oral Surg Oral Med Oral Pathol 1964;18:191)
- Sialolith and bacteria causing secondary infection may be present among the submitted tissue (Head Neck Pathol 2017;11:469)
- Feeding salivary gland, if included, has obstructive changes with variable ductal dilation, lymphocytic infiltrate with periductal pattern and fibrosis (Oral Surg Oral Med Oral Pathol 1984;58:692)
Microscopic (histologic) images
Positive stains
Negative stains
Sample pathology report
- Right upper labial mucosa, exision:
- Salivary duct cyst (mucus retention cyst)
- Minor salivary gland parenchyma showing chronic sialoadenitis
Differential diagnosis
- Mucocele/mucus extravasation phenomenon/ranula/plunging rannula/mucus escape reaction
- There is no true salivary gland duct epithelial lining and instead this is mimicked by epithelioid macrophages (muciphages) at the periphery of the extravasated mucin
- Warthin tumor (papillary cystadenoma lymphomatosum)
- Lymphoid stroma in the cyst wall and multiple papillary infoldings with a bilayer of columnar and oncocytic epithelial lining
- Papillary cystadenoma
- The lining epithelium has an adenomatous proliferation forming multilayered plaques of columnar or oncocytic salivary duct lining with papillary infoldings
- Gingival cyst of the adult
- These occur only on the gingiva which has no minor salivary glands
Board review style question #1
Board review style answer #1
Board review style question #2
-
Among the choices below, what is the most common site for a salivary duct cyst?
- Dorsal tongue
- Gingiva
- Intrabony
- Maxillary sinus
- Parotid gland
Board review style answer #2
SCC-general
Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Squamous cell carcinoma (SCC) is a malignant neoplasm that arises from the mucosal epithelium of the oral cavity and shows variable squamous differentiation
Essential features
- Most common cancer of the oral cavity, with a variable clinical appearance and a predilection for the ventrolateral tongue
- Associated with tobacco, alcohol and betel quid
- Malignancy of squamous cells with varying degrees of keratinization
ICD coding
- ICD-10: C00 - C14 - malignant neoplasms of lip, oral cavity and pharynx
Epidemiology
- > 90% of cancers in the oral cavity are SCC
- Globally, the highest rates are seen in Melanesia and South Central Asia; it is the leading cause of cancer related death for men in India (CA Cancer J Clin 2021;71:209)
- For the United States, the American Cancer Society estimates ~58,000 new cases of oral and oropharyngeal cancers in 2024 with 12,230 deaths (American Cancer Society: Key Statistics for Oral Cavity and Oropharyngeal Cancers [Accessed 2 February 2024])
- M > F
- Average age is 63
- Can occur in younger patients, especially in the setting of dyskeratosis congenita or Fanconi anemia (J Pediatr Hematol Oncol 2019;41:501, Head Neck Pathol 2021;15:1099)
Sites
- Can occur at any oral mucosal site (mucosal lip, buccal mucosa, alveolar ridge, floor of the mouth, hard palate, mobile tongue)
- Classic high risk locations are ventrolateral tongue and floor of mouth
- Patients can develop second primaries, synchronous or metachronous, with field cancerization as a probable hypothesis (Head Neck 2020;42:1848, Oral Oncol 2015;51:643)
- Proliferative (verrucous) leukoplakia lesions have a high risk of malignant transformation, especially in locations such as the gingiva (Head Neck Pathol 2021;15:572)
- Spread typically occurs via the lymphatic system to cervical lymph nodes
Pathophysiology
- Multifactorial with accumulation of genetic alterations
- Loss of function of TP53 mutations and CDKN2A inactivation are frequently seen (Nature 2015;517:576)
- Oral potentially malignant disorders, many of which harbor some degree of epithelial dysplasia, are associated with a risk of malignant progression (Head Neck Pathol 2019;13:423)
Etiology
- Tobacco (Int J Cancer 2008;122:155)
- Alcohol (Lancet Oncol 2021;22:1071)
- Significantly higher risk with synergistic consumption of alcohol and tobacco (Clin Oral Investig 2019;23:2849)
- Betel quid, gutka, pan masala (Curr Oncol Rep 2019;21:53)
- Smokeless tobacco products (Nicotine Tob Res 2019;21:1162)
- Ultraviolet (UV) radiation for lip squamous cell carcinoma (Laryngoscope 2018;128:84)
- High risk human papillomavirus (HPV) is strongly associated with oropharyngeal squamous cell carcinoma; in contrast, 4.4% of oral squamous cell carcinoma cases are associated with high risk HPV (Braz J Otorhinolaryngol 2021;87:346)
- Controversy regarding oral lichen planus and malignant transformation is unresolved (Oral Surg Oral Med Oral Pathol Oral Radiol 2016;122:332)
- Due to confounding variables, chronic mechanical irritation has not been established as an independent risk factor (Bosn J Basic Med Sci 2021;21:647)
Clinical features
- Varied clinical presentation, including exophytic, endophytic, white (leukoplakia), red (erythroplakia), nonhealing ulceration
- May be preceded by or associated with an oral, potentially malignant disorder
- Clinical factors associated with malignancy include nonhomogenous leukoplakia, erythroplakia, induration, deep ulceration, exophytic component and pain (Oral Surg Oral Med Oral Pathol Oral Radiol 2020;130:264)
- Patient factors associated with malignant transformation include heavy tobacco smoking (> 20 pack years), heavy alcohol consumption (> 14 drinks/week for women and 21 drinks/week in men), immunosuppression (Head Neck 2021;43:3552)
- Firm, fixed, nontender cervical lymph nodes may indicate regional spread
Diagnosis
- U.S. Preventive Services Task Force concludes that for primary care providers, current evidence is insufficient to assess balance of benefits and harms of oral cancer screening in asymptomatic adults (Ann Intern Med 2014;160:55)
- Visual and tactile exams of the oral cavity are often performed by oral health care providers and otolaryngologists
- Immediate tissue biopsy with histopathologic examination for definitive diagnosis (J Am Dent Assoc 2017;148:712)
- 48.4% of cases are regional at diagnosis (NIH: Oral Cavity and Pharynx Stage Distribution of SEER Incidence Cases, 2011-2020 [Accessed 2 February 2024])
Radiology description
- Invasive, advanced tumors may be detected on dental radiographs as destruction of underlying bone producing an ill defined radiolucency
- Positron emission tomography (PET), computed tomography (CT) and magnetic resonance imaging (MRI) can be used to determine the presence and extent of disease
- Carcinomas arising in the jaw bones without a mucosal origin are primary intraosseous squamous cell carcinoma and are not discussed here (Head Neck Pathol 2021;15:608)
Prognostic factors
- 5 year survival rate of 68.5% (NIH: Cancer Stat Facts - Oral Cavity and Pharynx Cancer [Accessed 2 February 2024])
- Depth of invasion (DOI) and extranodal extension (ENE) were added to the AJCC staging 8th edition and are associated with upstaging (Oral Oncol 2018;85:82)
- Bone invasion is correlated with a worse prognosis (and invasion through cortical bone into medullary bone provides the tumor with AJCC stage T4a) (Arch Pathol Lab Med 2019;143:439)
- Noncohesive pattern of invasion is an adverse prognostic factor (Arch Pathol Lab Med 2019;143:439)
- Perineural invasion is associated with poor disease specific survival (J Oral Pathol Med 2020;49:994)
- Lymphovascular invasion may serve as a prognostic predictor of metastasis (Oral Surg Oral Med Oral Pathol Oral Radiol 2021;131:319)
- Margin of < 1 mm is associated with increased risk of local recurrence (JAMA Otolaryngol Head Neck Surg 2017;143:1166)
Case reports
- 28 year old woman with asymptomatic tumor of the left mandibular gingiva and Fanconi anemia (Case Rep Dent 2021;2021:5571649)
- 63 year old man with pain and swelling on the right lower jaw (Head Neck Pathol 2021;15:1313)
- 66 year old woman with fungating ulcerative mass on the left lateral tongue (Head Neck Pathol 2017;11:552)
- 70 year old woman with ulcerated mass on the lateral border of the tongue (Head Neck Pathol 2018;12:580)
Treatment
- Early staged lesions are often treated with surgery
- Patients with early stage cancer may benefit from elective neck dissection (N Engl J Med 2015;373:521)
- Moderate staged lesions are often treated with surgery, radiation therapy or chemotherapy
- Patients with recurrent or metastatic head and neck cancer may benefit from immunotherapeutic agents (J Immunother Cancer 2019;7:184)
Clinical images
Gross description
- Site of involvement, tumor laterality and operative procedure should be communicated from the surgeon (Arch Pathol Lab Med 2019;143:439)
- Gross examination of a specimen may not entirely reflect microscopic tumor extent, as dysplasia, ulceration or inflammation may appear as tumor on macroscopic examination (Arch Pathol Lab Med 2019;143:439)
- White infiltrating tumor on cross section
Gross images
Frozen section description
- Frozen section analysis can be used to evaluate tumor diagnosis and margin status
- Results are highly specific but only moderately sensitive when compared with final margins (Laryngoscope 2000;110:1773)
Frozen section images
Microscopic (histologic) description
- Dysplastic stratified squamous epithelium that extends through the basement membrane and into the underlying fibrous connective tissue without attachment to the surface
- Malignant epithelial cells show eosinophilic cytoplasm, hyperchromatic nuclei, pleomorphism, mitotic activity, individual cell keratinization and intercellular bridging
- Superficial or microinvasion can be used to describe the earliest moment of invasion
- Malignant epithelium can invade fibrous connective tissue in islands, cords or individual cells
- Keratin pearls of round, eosinophilic, concentric layers of keratin can be seen and are associated with well differentiated tumors
- 3 histologic grades for conventional squamous cell carcinoma include well, moderately and poorly differentiated based on amount of keratinization, mitotic activity, cellular and nuclear pleomorphism, pattern of invasion and host response (Arch Pathol Lab Med 2019;143:439)
- Histologic variants are listed below (Arch Pathol Lab Med 2019;143:439)
- Verrucous squamous cell carcinoma
- Papillary squamous cell carcinoma
- Exophytic growth demonstrating multiple, thin keratinized papillary projections with fibrovascular cores or rounded, bulbous projections with nonkeratinized epithelium
- Malignant epithelial cells show an increased N:C ratio, prominent nucleoli and mitotic figures
- Obvious invasive components uncommon (Ann Diagn Pathol 2013;17:18)
- Spindle cell squamous cell carcinoma
- Also called sarcomatoid
- Monoclonal, evolving from conventional squamous carcinoma with dedifferentiation (Head Neck Pathol 2010;4:265)
- Often polypoid configuration on biopsy; tumor may be ulcerated
- Overlying epithelium may show carcinoma in situ or dysplasia with elongation and spindling of the basal epithelial cells
- Nest of moderately or poorly differentiated conventional squamous cell carcinoma may be intricately mixed sarcomatoid component
- High mitotic count with bizarre, atypical mitotic figures
- Dense and eosinophilic cytoplasm
- Cells can be arranged in various patterns with variable amount of intervening matrix, which can mimic mesenchymal malignancies
- Metaplastic mesenchymal elements such as bone or cartilage not identified
- Carcinoma cuniculatum
- Well differentiated squamous epithelium with minimal to no cytologic atypia
- Unique deeply infiltrative, large sized, branching, keratin filled cavities, resembling rabbit burrows (Head Neck Pathol 2022;16:213)
- Lymphocytic infiltrate surrounding epithelial tunnels and intraepithelial neutrophilic microabscesses
- Basaloid squamous cell carcinoma
- Lobules, nests or cribriform patterns of small basaloid cells with peripheral palisading and a thick basement membrane
- Cells have minimal cytoplasm, are moderately pleomorphic with hyperchromatic nuclei and often abruptly transition to squamous epithelium
- Single cell necrosis and comedonecrosis are common; often contiguous with carcinoma in situ in surface epithelium
- Frequent mitotic activity, stroma is often hyalinized or myxoid; variable pseudoglandular spaces resembling adenoid cystic carcinoma
- Rarely has a spindle cell component (Arch Pathol Lab Med 1995;119:181)
- Acantholytic squamous cell carcinoma
- Pseudoglandular structures, dyskeratotic cells and prominent acantholysis within tumor islands (Head Neck Pathol 2022;16:388)
- Adenosquamous cell carcinoma
- Distinct squamous and glandular differentiation in close proximity with blending and intermixing
- Typically presents as a superficial squamous cell carcinoma transitioning to a deeper adenocarcinoma (Head Neck Pathol 2018;12:576)
- Lymphoepithelial carcinoma
- Undifferentiated squamous cell carcinoma associated with a prominent, nonneoplastic lymphoplasmacytic cell infiltrate (Head Neck Pathol 2020;14:1001)
- Definitive squamous differentiation may be present but is usually limited, while a basaloid morphology can be identified (Head Neck Pathol 2012;6:445)
- Epstein-Barr virus (EBV) associated
- Morphologically indistinguishable from undifferentiated nasopharyngeal carcinoma (Head Neck Pathol 2020;14:1001)
- Although more often seen in salivary gland neoplasms and odontogenic tumors, oral squamous cell carcinoma may rarely show clear cell change (Cureus 2022;14:e25057)
- American Joint Committee on Cancer (AJCC) 8th edition is currently used for staging (see Staging - oral cavity)
- College of American Pathologists (CAP) protocol including TNM (CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Lip and Oral Cavity [Accessed 2 February 2024])
- Data set elements: operative procedure, specimens submitted, tumor dimensions, histologic tumor type, histologic tumor grade, pattern of invasive front, bone invasion, perineural invasion, lymphovascular invasion, margin status, pathologic staging (Arch Pathol Lab Med 2019;143:439)
Microscopic (histologic) images
Contributed by Kathleen Higgins, D.D.S., M.S., Duane Schafer, D.D.S., M.S. and Sarah Glass, D.D.S.
Cytology description
- Cytology is not routinely recommended for evaluation of intraoral lesions suspicious for malignancy (J Am Dent Assoc 2017;148:712)
- Fine needle aspiration can identify regional spread to cervical lymph nodes
Positive stains
- Cytokeratin stains are positive: AE1 / AE3, CK5/6, p63, p40 (Arch Pathol Lab Med 2019;143:439)
- This can be helpful to support epithelial origin in poorly differentiated tumors
Negative stains
- Pathologists should not routinely perform high risk HPV testing on patients with nonoropharyngeal primary head and neck tumors (Arch Pathol Lab Med 2018;142:559)
Molecular / cytogenetics description
- Due to advances in targeted therapy, some centers are evaluating the mutational profiles of tumors (Nat Rev Dis Primers 2020;6:92)
Sample pathology report
- Right lateral tongue, incisional biopsy:
- Squamous cell carcinoma, well differentiated (see comment)
- Comment: Tumor islands are present at all surgical margins. Depth of invasion is at least 3 mm. Perineural and lymphovascular invasion are identified.
Differential diagnosis
- Pseudoepitheliomatous hyperplasia (Arch Otolaryngol Head Neck Surg 2003;129:127):
- Benign lesions in the oral cavity, such as granular cell tumor, may show pseudoepitheliomatous hyperplasia of the overlying squamous mucosa
- Granular cell tumors are S100 positive and occur on the dorsal tongue, an uncommon location for oral squamous cell carcinoma
- Mucoepidermoid carcinoma:
- May be difficult to distinguish high grade mucoepidermoid carcinoma from squamous cell carcinoma, adenosquamous variant
- High grade tumors may show predominantly squamous and intermediate cells with infrequent mucous cells
- Basaloid salivary gland tumors (Semin Diagn Pathol 2022;39:17):
- Oral malignant melanoma:
- Epithelioid sarcoma (Ann Otol Rhinol Laryngol 2021;130:416):
- Epithelioid sarcoma may express epithelial markers but most importantly does not express INI1
- Angiosarcoma (Head Face Med 2008;4:17):
- May be difficult to distinguish angiosarcoma from squamous cell carcinoma, acantholytic variant
- Expresses endothelial cell markers such as FLI1
- Metastatic squamous cell carcinoma to the oral cavity:
- Metastases may involve the soft tissue or bone
- First manifestation of disease in 25 - 30% of patients (Head Neck Pathol 2022;16:802)
- Histopathology is variable
- Patient history can be helpful, especially the ability to compare histopathology of known primary with current specimen
- Overlying mucosa uninvolved with lack of overt surface dysplasia
- Neuroepithelial structures, including the juxtaoral organ of Chievitz:
- Avoid misinterpretation as carcinoma showing neural invasion (Head Neck Pathol 2020;14:876)
- Located lingual to the mandible, buccal to the mandible and within the posterior tongue
- Smalls islands of squamoid epithelium in close association with small nerves or the taste buds
- Absence of keratinization, cytological atypia and mitotic activity
Additional references
Board review style question #1
Board review style answer #1
D. Squamous cell carcinoma. The histopathologic image shows well differentiated malignant squamous cells that have broken through the basement membrane and are invading the underlying connective tissue. Answer A is incorrect because the proliferation of abnormal squamous cells is not confined to the epithelium as seen in epithelial dysplasia. Answer B is incorrect because granular cells are not present in the connective tissue. Granular cell tumors may show pseudoepitheliomatous hyperplasia, which can be mistaken for squamous cell carcinoma. Answer C is incorrect because mucous cells and intermediate cells are not seen.
Comment Here
Reference: SCC-general
Comment Here
Reference: SCC-general
Board review style question #2
Which oral squamous cell carcinoma histologic variant is the most likely to show minimal to no cytologic atypia?
- Adenosquamous cell carcinoma
- Basaloid squamous cell carcinoma
- Carcinoma cuniculatum
- Spindle cell squamous cell carcinoma
Board review style answer #2
C. Carcinoma cuniculatum. This histologic variant shows minimal to no cytologic atypia. Architecturally, the tumor is described as resembling rabbit burrows. Answer B is incorrect because basaloid squamous cell carcinoma frequently demonstrates mitotic activity, pleomorphic nuclei and single cell necrosis. Answer D is incorrect because spindle cell squamous cell carcinoma frequently demonstrates bizarre, atypical mitotic figures. Answer A is incorrect because adenosquamous cell carcinoma typically displays classic features of both squamous cell carcinoma and adenocarcinoma.
Comment Here
Reference: SCC-general
Comment Here
Reference: SCC-general
Schwannoma
Smokeless tobacco keratosis
Table of Contents
Definition / general | Gross description | Microscopic (histologic) description | Differential diagnosisDefinition / general
- Occurs in users of smokeless tobacco (snuff) or tobacco chewers
- Severity related to length of exposure and tobacco brand
- Reversible with cessation of use (Arch Pathol Lab Med 2004;128:e17)
Gross description
- Filmy, gray-white opalescence at areas of contact with tobacco
Microscopic (histologic) description
- Parakeratosis or hyperorthokeratosis with parakeratin spires ("chevrons"), acanthosis, mild chronic inflammation and PAS+ marked hyalin deposition resembling amyloid
Differential diagnosis
- Hyalinosis cutis et mucosae:
- Deposition begins around vessels, eccrine glands and epithelial-stromal interface, then fills entire dermis of all oral mucosa, tongue, pharynx, larynx and vocal cords
Spongiotic gingival hyperplasia (pending)
[Pending]
Squamous papilloma
Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Common, small, benign intraoral squamoproliferation
- Most common papillary lesion of oral cavity
Essential features
- Common, small (< 1.0 cm), benign intraoral squamoproliferation
- Associated with HPV 6 and 11 in approximately 50% of cases
- Commonly involves soft palate, tongue, lips, tonsils
- Excisional biopsy curative with recurrences rare; no known association with oral or oropharyngeal squamous cell carcinoma
- Squamous cell papilloma represents WHO 4th edition head and neck preferred nomenclature; however, in practice, squamous papilloma is commonly used
ICD coding
Epidemiology
- Most frequently seen in third to fifth decades (Oral Surg Oral Med Oral Pathol 1980;49:419)
- Can occur at any age
- No gender predilection
Sites
- Soft palate / uvula, tongue, lips, gingiva most common intraoral sites (Semin Diagn Pathol 2015;32:3)
- Also may occur in oropharynx, larynx
Etiology
- Approximately 50% associated with HPV 6 and 11 (Eur Arch Otorhinolaryngol 2017;274:3477)
- Not associated with high risk HPV infection
- Remaining cases may represent persistence of papillary epithelial architecture following viral clearance or may represent nonspecific epithelial alteration
- No evidence of clonality
Clinical features
- Majority < 1.0 cm in size and do not show persistent growth
- In setting of immunosuppression, may be larger, multifocal, less obviously papillary, more aggressive clinically (J Oral Maxillofac Surg 2018;76:128)
Diagnosis
- Frequently suspected clinically on basis of papillary appearance
- Excisional biopsy necessary for diagnosis
Prognostic factors
- Recurrence rate minimal and related to incomplete excision
- Since mucosal HPV infections may persist for 1 - 2 years, patient may be at mildly elevated risk for additional squamous papillomas (Lancet 2013;382:877)
- Dypslasia infrequently encountered in squamous papillomas; generally not considered premalignant condition
- No known association with oral or oropharyngeal squamous cell carcinoma
Case reports
- 5 year old girl with recurrent palate papilloma (Niger J Clin Pract 2018;21:1674)
- 10 year old girl with hard palate mass (Int J Clin Pediatr Dent 2018;11:244)
- 14 year old boy with hard palate mass (Indian J Dent 2014;5:211)
- 21 year old man with uvula lesion causing sore throat (Malays Fam Physician 2019;14:74)
- 43 year old man with lesion causing airway obstruction during conscious sedation (Anesth Prog 2017;64:168)
Treatment
- Excisional biopsy
Clinical images
Gross description
- Papillary (cauliflower-like) and exophytic, tan-white lesion
Microscopic (histologic) description
- Papillary proliferation of stratified squamous epithelium with variable hyperkeratosis or parakeratosis (Oral Surg Oral Med Oral Pathol 1980;49:419)
- Hyperplasia and mitotic activity restricted to basal / parabasal layers
- Retention of cellular polarity and normal maturation in suprabasal layers
- Papillary (finger-like) projections exhibit prominent fibrovascular cores
- Hyalinization at tips of cores may be seen occasionally
- Often pedunculated but may be sessile
- Koilocytes rare / absent
- No endophytic component
- Secondarily traumatized squamous papillomas may show spongiosis, leukocyte exocytosis and absence of surface keratinization
- Dysplasia in squamous papilloma characterized by cytologic abnormalities typical for epithelial dysplasia
Microscopic (histologic) images
Molecular / cytogenetics description
- HPV ISH not routinely performed for diagnosis
Sample pathology report
- Right soft palate, mucosa, excision:
- Squamous papilloma
Differential diagnosis
- Verruca vulgaris:
- Hyperkeratosis with marked hypergranulosis including large keratohyaline granules
- Axial inclination of rete ridges
- Rarely pedunculated and attached to underlying epithelium by narrow stalk
- Relatively uncommon in oral cavity
- Condyloma acuminatum:
- More significant epithelial hyperplasia
- Bulbous rete ridges, blunted tips of individual papillae
- Koilocytes always seen
- Relatively uncommon in oral cavity and clinical correlation beneficial
- Giant cell fibroma:
- Nodular proliferation of densely collagenous fibrovascular tissue
- Lage stellate and occasionally multinucleated fibroblasts present, particularly in superficial lamina propria
- Surface epithelium thinly keratinized and frequently papillary
- Rete ridges often elongated and occasionally anastamosing
- Verrucous hyperplasia:
- Verrucous epithelial architecture with surface keratosis representing dysplastic phenotype
- Epithelial dysplasia may or may not be present
- Epithelium often atrophic but may be hyperplastic
- Hyperkeratosis / parakeratosis and verrucous architecture often sharply demarcated
- No true fibrovascular cores
- May or may not be seen in setting of proliferative (verrucous) leukoplakia
- Verrucous carcinoma:
- Generally indolent histopathologic variant of squamous cell carcinoma
- Verrucous architecture with prominent hyperkeratosis / parakeratosis
- Endophytic growth pattern involving deep lamina propria or skeletal muscle in the absence of frank invasion
- Minimal to modest epithelial atypia / dysplasia
- Focal epithelial hyperplasia (Heck disease):
- Often multifocal
- Epithelial hyperplasia with subtle to absent papillary features
- Mitosoid bodies characteristic: karyorrhectic cells with fragmented chromatin
- Inflammatory papillary hyperplasia:
- Reactive condition exclusively seen in denture wearers or mouth breathers
- Generally presents as diffuse involvement of hard palatal mucosa
- Nodular / papillary proliferation of fibrovascular tissue
- Variable lymphoplasmacytic infiltrate
- Epithelium exhibits leukocyte exocytosis and spongiosis
- Pseudoepitheliomatous hyperplasia may be present
Board review style question #1
Board review style answer #1
Board review style question #2
Which is the most common papillary lesion in the oral cavity?
- Condyloma acuminatum
- Squamous cell papilloma
- Verruca vulgaris
- Verrucous hyperplasia
Board review style answer #2
Stafne defect (pending)
[Pending]
Staging features
Table of Contents
Measurement of tumor metastasis | Isolated tumor cells | Extranodal extension | TNM descriptors | Staging terminology | Additional TNM descriptorsMeasurement of tumor metastasis
- Cross sectional diameter of the largest lymph node metastasis (not the lymph node itself) is measured in the gross specimen at the time of macroscopic examination or if necessary, on the histologic slide at the time of microscopic examination (AJCC: Cancer Staging [Accessed 20 September 2018], CAP: Protocol for the Examination of Specimens From Patients With Cancers of the Pharynx [Accessed 20 September 2018])
- Measurement of the metastatic focus in the lymph nodes is based on the largest metastatic deposit size, which may include matted or fused lymph nodes
Isolated tumor cells
- Isolated tumor cells (ITCs) are single cells or small clusters of cells ≤ 0.2 mm in greatest dimension
- While the generic recommendation is that lymph nodes with ITCs found by histologic examination, immunohistochemistry or nonmorphologic techniques (e.g. flow cytometry, DNA analysis, PCR amplification of a specific tumor marker), be classified as pN0 or pM0, evidence for the validity of this practice in head and neck squamous cell carcinoma and other histologic subtypes is lacking
- In fact, rare studies relevant to head and neck sites indicate that isolated tumor cells may actually be a poor prognosticator in terms of local control
Extranodal extension
- AJCC 8th edition introduces the use of extranodal extension (ENE) in subcategorizing the "N" category for metastatic cancer to neck nodes
- Effect of ENE on prognosis in head and neck cancers is profound, except for those tumors associated with high risk HPV
- Pathological ENE also must be clearly defined as extension of metastatic tumor (tumor present within the confines of the lymph node and extending through the lymph node capsule into the surrounding connective tissue, with or without associated stromal reaction)
- Histopathologic designations for ENE are as follows (Amin: AJCC Cancer Staging Manual, 8th Edition, 2018):
- ENEn (none)
- ENEmi (microscopic ENE ≤ 2 mm)
- ENEma (ENE > 2 mm or gross ENE)
- ENEmi and ENEma are used to define pathological ENE nodal status
- ENEmi versus ENEn will affect current nodal staging but data collection is recommended to allow standardization of data collection and future analysis (AJCC: Cancer Staging [Accessed 20 September 2018])
- ENE does not appear to be as prognostically relevant for HPV mediated / p16+ and nasopharyngeal cancers
- While it may be recorded, it is not required under AJCC 8th edition guidelines
- However, ENE is still required for pN categorization of HPV unrelated (p16-) squamous cell carcinoma and hypopharyngeal carcinomas
TNM descriptors
- By AJCC / UICC convention, the designation "T" refers to a primary tumor that has not been previously treated
- "p" symbol refers to the pathologic classification of the TNM, as opposed to the clinical classification and based on clinical stage information supplemented / modified by operative findings and gross and microscopic evaluation of the resected specimens
- pT entails a resection of the primary tumor or biopsy adequate to evaluate the highest pT category
- pN entails removal of nodes adequate to validate lymph node metastasis and pM implies microscopic examination of distant lesions
- Clinical classification (cTNM) is usually carried out by the referring physician before treatment during initial evaluation of the patient or when pathologic classification is not possible
- Pathologic staging is usually performed after surgical resection of the primary tumor
- Pathologic staging depends on pathologic documentation of the anatomic extent of disease, whether or not the primary tumor has been completely removed
- If a biopsied tumor is not resected for any reason (e.g. when technically unfeasible) and if the highest T and N categories or the M1 category of the tumor can be confirmed microscopically, the criteria for pathologic classification and staging have been satisfied without total removal of the primary cancer
Staging terminology
- Additional change in AJCC 8th edition is the elimination of the pT0 category for all oral cavity, skin, larynx, HPV- oropharynx, hypopharynx and sinus
- This change affects cases where a cervical lymph node has metastatic squamous cell carcinoma but no primary tumor is identified despite thorough history, examination and available imaging studies
- Assigning these cases to a specific head and neck site is not possible
- Previous editions of TNM staging included a pT0 category in each of these disease sites
- However, it is seldom used and if it is, the cancer could not be assigned to a stage group
- Therefore, for the 8th edition, the expert panel eliminated the pT0 category from the head and neck staging systems
- Use of HPV+ or EBV+ pharyngeal "pT0" (AJCC: Cancer Staging [Accessed 20 September 2018], CAP: Protocol for the Examination of Specimens From Patients With Cancers of the Pharynx [Accessed 20 September 2018]):
- Risk of regional (cervical neck) nodal spread from cancers of the pharynx is high
- Majority of metastatic carcinomas to the cervical lymph nodes take origin from a head and neck primary carcinoma
- Most common histologic type of carcinoma to metastasize to cervical neck lymph nodes is squamous cell carcinoma
- Cervical nodal metastases may occur in the setting of an unknown primary carcinoma referred to as metastatic cervical carcinoma with an unknown primary
- As per AJCC 8th edition guidelines, 3 separate approaches are employed to stage patients who present with an occult primary tumor
- Primary T category is described as pT0 and the pN category is designated according to the respective anatomic site based on Epstein-Barr virus (EBV) and HPV status:
- Patients with EBV related cervical adenopathy use the pN classification of nasopharynx
- Patients with HPV mediated (positive) cervical adenopathy use the pN classification of HPV mediated / p16+ oropharyngeal cancer
- All other patients with EBV unrelated and HPV unrelated cervical adenopathy use the generic pN classification used for the other head and neck sites and for unknown primary
Additional TNM descriptors
- For identification of special cases of TNM or pTNM classifications, the "m" suffix and "y" and "r" prefixes are used; although they do not affect the stage grouping, they indicate cases needing separate analysis
- "m" suffix indicates the presence of multiple primary tumors in a single site and is recorded in parentheses: pT(m)NM
- "y" prefix indicates those cases in which classification is performed during or following initial multimodality therapy (i.e. neoadjuvant chemotherapy, radiation therapy or both chemotherapy and radiation therapy)
- cTNM or pTNM category is identified by a "y" prefix
- ycTNM or ypTNM categorizes the extent of tumor actually present at the time of that examination
- "y" categorization is not an estimate of tumor prior to multimodality therapy (i.e. before initiation of neoadjuvant therapy)
- "r" prefix indicates a recurrent tumor when staged after a documented disease free interval and is identified by the "r" prefix: rTNM
Staging-mucosal melanoma
Table of Contents
Definition / general | Primary tumor (T) | Regional lymph nodes (N) | Distant metastasis (M) | Anatomic stage / prognostic groupsDefinition / general
- This staging is appropriate for all Head and Neck sites. It is still PENDING for the AJCC 8th Edition.
Primary tumor (T)
Regional lymph nodes (N)
- NX: regional lymph nodes cannot be assessed
- N0: no regional lymph node metastases
- N1: regional lymph node metastases present
Distant metastasis (M)
- M0: no distant metastasis
- M1: distant metastasis
Anatomic stage / prognostic groups
| III: | T3 | N0 | M0 | ||||
| IVA: | T4a | N0 | M0 | or | T3 - 4a | N1 | M0 |
| IVB: | T4b | any N | M0 | ||||
| IVC: | any T | any N | M1 |
Staging-oral cavity
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Primary tumor (pT) | Pathological regional lymph nodes (pN) | Distant metastasis (M) | AJCC prognostic stage grouping for oral cavity | Registry data collection variables | Histologic grade | Histopathologic type | Diagrams / tables | Microscopic (histologic) images | Board review style question #1 | Board review style answer #1Definition / general
- Staging of definitive resections for carcinoma (squamous cell carcinoma, neuroendocrine carcinoma and minor salivary gland carcinoma) of the oral cavity should use this system (AJCC: Cancer Staging [Accessed 21 September 2018], CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Lip and Oral Cavity [Accessed 29 December 2020])
- Oral cavity extends from the portion of the lip that contacts the opposed lip (wet mucosa) to the junction of the hard and soft palate above to the line of circumvallate papillae below and to the anterior tonsillar pillars laterally (AJCC: Cancer Staging [Accessed 21 September 2018], CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Lip and Oral Cavity [Accessed 29 December 2020])
- Staging system name "oral cavity" reflects the focus on all of oral cavity, which includes mucosa of lip but not the external (dry) lip
- External lip, including the dry vermillion border, has a more similar embryologic origin to skin and its etiology, which is based on ultraviolet exposure (AJCC: Cancer Staging [Accessed 21 September 2018], CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Lip and Oral Cavity [Accessed 29 December 2020])
- Staging protocols, such as those of CAP, are to document procedure, tumor site, tumor laterality, tumor focality, tumor size, histologic type, histologic grade where applicable, margin status, lymphovascular invasion, perineural invasion, regional lymph node findings and summarize these pathologic findings using TNM system (CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Lip and Oral Cavity [Accessed 29 December 2020])
- See also Head and neck staging features
Essential features
- AJCC 7th edition staging was sunset on December 31, 2017; as of January 1, 2018, use of the 8th edition is mandatory
- 2 key significant alterations in the 8th edition for lip and oral cavity are the incorporation of depth of invasion (DOI) into T stage and extranodal extension (ENE) into N stage
- In essence, DOI increases the T category by 1 for each 5 mm of tumor depth (until ≥ 10 mm)
- Similarly, pathologic ENE+ will increase the nodal category by 1 (AJCC: Cancer Staging [Accessed 21 September 2018], CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Lip and Oral Cavity [Accessed 29 December 2020])
- Use of the CAP protocol is not required for recurrent tumors or for metastatic tumors that are resected at a different time than the primary tumor
- Use of this protocol is also not required for pathology reviews performed at a second institution (i.e. secondary consultation, second opinion or review of outside case at second institution) (CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Lip and Oral Cavity [Accessed 29 December 2020])
- Carcinomas of minor salivary glands of the upper aerodigestive tract site, including the oral cavity, are staged according to schemes corresponding to the anatomic site of occurrence
- There is no currently accepted staging for central (primary intraosseous) salivary gland tumors (CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Lip and Oral Cavity [Accessed 29 December 2020])
- Reporting of surgical margins for carcinomas of the minor salivary glands should follow those used for squamous cell carcinoma of oral cavity (CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Lip and Oral Cavity [Accessed 29 December 2020])
- CAP oral cavity staging protocol: CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Lip and Oral Cavity [Accessed 29 December 2020]
- Alternatively for providers practicing in different geographic regions, there may be interest in the International Collaboration on Cancer Reporting (ICCR) guidelines: ICCR: Carcinomas of the Oral Cavity (TNM8) [Accessed 29 December 2020]
Terminology
- Anatomic boundaries and primary site(s): the oral cavity extends from the portion of the lip that contacts the opposed lip (wet mucosa) to the junction of the hard and soft palate above, to the line of circumvallate papillae below and to the anterior tonsillar pillars laterally; it is additionally divided into multiple specific sites listed below (AJCC: Cancer Staging [Accessed 21 September 2018], CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Lip and Oral Cavity [Accessed 29 December 2020], see figure 1 in Diagrams / tables)
- Mucosal lip:
- Begins at the junction of the wet and dry mucosa of the lip (the anterior border of the portion of the lip that comes into contact with the opposed lip) and extends posteriorly into the oral cavity to the attached gingiva of the alveolar ridge
- Dry vermilion lip and vermilion border are staged using the chapter on cutaneous carcinoma of the head and neck; this is a change from past AJCC editions where the dry vermilion was included in the lip and oral cavity chapter
- Buccal mucosa:
- Includes all the mucous membrane lining of the inner surface of the cheeks and lips from the line of contact of the opposing lips to the line of attachment of mucosa of the alveolar ridge (upper and lower) and pterygomandibular raphe
- Lower alveolar ridge:
- Refers to the mucosa overlying the alveolar process of the mandible, which extends from the line of attachment of mucosa in the lower gingivobuccal sulcus to the line of attachment of free mucosa of the floor of the mouth
- Posteriorly, it extends to the ascending ramus of the mandible
- Upper alveolar ridge:
- Refers to the mucosa overlying the alveolar process of the maxilla, which extends from the line of attachment of mucosa in the upper gingivobuccal sulcus to the junction of the hard palate
- Its posterior margin is the upper end of the pterygopalatine arch
- Retromolar gingiva (retromolar trigone):
- Attached mucosa overlying the ascending ramus of the mandible from the level of the posterior surface of the last lower molar tooth to the apex superiorly, adjacent to the tuberosity of the maxilla
- Floor of the mouth:
- Crescentic surface overlying the mylohyoid and hyoglossus muscles, extending from the inner surface of the lower alveolar ridge to the undersurface of the tongue
- Its posterior boundary is the base of the anterior pillar of the tonsil
- It is divided into 2 sides by the frenulum of the tongue and harbors the ostia of the submandibular and sublingual salivary glands
- Hard palate:
- Semilunar area between the upper alveolar ridge and the mucous membrane covering the palatine process of the maxillary palatine bones
- It extends from the inner surface of the superior alveolar ridge to the posterior edge of the palatine bone
- Anterior two - thirds of the tongue (oral tongue):
- Freely mobile portion of the tongue that extends anteriorly from the line of circumvallate papillae to the undersurface of the tongue at the junction with the floor of the mouth
- It is composed of 4 areas: the tip, the lateral borders, the dorsum and the undersurface (nonvillous ventral surface of the tongue)
- Undersurface of the tongue is considered a separate category by the World Health Organization (WHO)
- Mucosal lip:
- Tumor thickness (TT) versus depth of invasion (DOI) (AJCC: Cancer Staging [Accessed 21 September 2018], CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Lip and Oral Cavity [Accessed 29 December 2020]):
- Tumor thickness is usually measured from the mucosal surface of the tumor to the deepest point of tissue invasion in a perpendicular fashion with a measuring instrument
- DOI is measured from the basement membrane of an adjacent normal to the deepest point of invasion of the tumor
- DOI assesses the invasiveness of a carcinoma, regardless of any exophytic component
- It is measured by first finding the "horizon" of the basement membrane of the adjacent squamous mucosa
- Perpendicular "plumb line" is established from this horizon to the deepest point of tumor invasion, which represents DOI
- DOI is recorded in millimeters
- See figures 2A and 2B in Microscopic (histologic) images
- Extrinsic tongue muscle (ETM) invasion (AJCC: Cancer Staging [Accessed 21 September 2018], CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Lip and Oral Cavity [Accessed 29 December 2020]):
- No longer used as a component of pT4 staging because this is a feature of DOI
- No longer a staging criterion for T4 designation in oral cavity because depth of invasion supersedes it and extrinsic muscle invasion is difficult to assess (both clinically and pathologically)
- Surgical margins (AJCC: Cancer Staging [Accessed 21 September 2018], CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Lip and Oral Cavity [Accessed 29 December 2020]):
- Definition of a positive margin is somewhat controversial given the varied results from prior studies
- However, overall, several studies support the definition of a positive margin to be invasive carcinoma or carcinoma in situ / high grade dysplasia present at margins (microscopic cut through of tumor)
- Furthermore, reporting of surgical margins should also include information regarding the distance of invasive carcinoma, carcinoma in situ or high grade dysplasia (moderate to severe) from the surgical margin
- Tumor bed versus specimen margins:
- Regarding what actually represents the relevant margin status, it becomes increasingly clear that margins obtained from the main resection specimen are of more reliable prognostic value
- Clinical value of tumor bed margins (i.e. margins taken separately) is often undermined by their uncertain origin with respect to the main resection, infrequent orientation as to the new margin surface and fragmentation
- Nonetheless, tumor bed margin status is still utilized in various practice settings for patient management
- However, the challenge for pathologists is to arrive at a "final" margin status, integrating both tumor bed and specimen margin status
- As it is in multipart resections, the pathologist's ability to confidently establish the relationship between the main resected specimen and additional, separately submitted parts and to assess the adequacy of excision is compromised
- To optimize reporting, both specimen margin and tumor bed margin status should thus be reported separately
- "Final" margin status then becomes a multidisciplinary integration of these findings
- For instance, in cases with differing margin statuses (i.e. resection specimen margin positive, corresponding tumor bed margin negative), the small size and lack of orientation of the tumor bed margin may preclude a reliable conversion to final negative margin
- Conversely, in some cases the tumor bed specimen (e.g. revision of margin) may be a reliable indicator of a true final margin
- This is a judgment call that requires close interaction between the surgeon and pathologist but generally, the following basic requirements are met:
- Tumor bed margins are quite large (i.e. thick enough to be readily processed as radial margins and large enough to match the corresponding aspect of the main specimen margin)
- Are oriented as to the new true margin surface (by ink or stitch)
- Physical relationship between the main resection specimen and additional tumor bed margins is confirmed by pathologist and surgeon (usually through unequivocal labeling and even fitting the tumor bed margin to the main specimen)
- In such a case, the tumor bed margin could be considered a final margin
- Regarding what actually represents the relevant margin status, it becomes increasingly clear that margins obtained from the main resection specimen are of more reliable prognostic value
- Worst pattern of invasion (WPOI) (AJCC: Cancer Staging [Accessed 21 September 2018], CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Lip and Oral Cavity [Accessed 29 December 2020]):
- Validated outcome predictor for oral cavity squamous carcinoma patients in multivariate analysis
- To simplify prognostication and enhance adaptation, the only cutpoint recommended for assessment is whether or not WPOI-5 is present
- WPOI-5 is defined as tumor dispersion of ≥ 1 mm between tumor satellites
- Tumor dispersion is assessed at the advancing tumor edge
- To some, WPOI can be viewed as redundant and only optional for reporting purposes, as extratumoral perineural invasion or extratumoral lymphovascular invasion also count as WPOI-5
ICD coding
- C00.3: Mucosa of upper lip
- C00.4: Mucosa of lower lip
- C00.5: Mucosa of lip, NOS
- C00.8: Overlapping lesion of lip
- C00.9: Lip, NOS
- C02.0: Dorsal surface of tongue, NOS
- C02.1: Border of tongue
- C02.2: Ventral surface of tongue, NOS
- C02.3: Anterior 2/3 of tongue, NOS
- C02.8: Overlapping lesion of tongue
- C02.9: Tongue, NOS
- C03.0: Upper gum
- C03.1: Lower gum
- C03.9: Gum, NOS
- C04.0: Anterior floor of mouth
- C04.1: Lateral floor of mouth
- C04.8: Overlapping lesion of floor of mouth
- C04.9: Floor of mouth, NOS
- C05.0: Hard palate
- C05.8: Overlapping lesion of palate
- C05.9: Palate, NOS
- C06.0: Cheek mucosa
- C06.1: Vestibule of mouth
- C06.2: Retromolar area
- C06.8: Overlapping lesion of other and unspecified parts of mouth
- C06.9: Mouth, NOS
Primary tumor (pT)
- TX: Primary tumor cannot be assessed
- Tis: Carcinoma in situ
- T1: Tumor ≤ 2 cm with depth of invasion (DOI)* ≤ 5 mm
- T2: Tumor ≤ 2 cm with DOI* > 5 mm and ≤ 10 mm or tumor > 2 cm and ≤ 4 cm with DOI* ≤ 10 mm
- T3: Tumor > 2 cm and ≤ 4 cm with DOI* > 10 mm or tumor > 4 cm with DOI* ≤ 10 mm or any tumor
- T4: Moderately advanced or very advanced local disease
- T4a: Moderately advanced disease
- Tumor > 4 cm with DOI* > 10 mm or
- Tumor invades adjacent structures only (e.g. through cortical bone of the mandible or maxilla or involves the maxillary sinus or skin of the face)
- T4b: Very advanced disease
- Tumor invades masticator space, pterygoid plates or skull base or encases the internal carotid artery
- T4a: Moderately advanced disease
Notes:
- *DOI is depth of invasion and not tumor thickness, see above Terminology section for definition
- Superficial erosion of bone / tooth socket alone by a gingival primary is not sufficient to classify a tumor as T4
Pathological regional lymph nodes (pN)
- NX: Regional lymph nodes cannot be assessed
- N0: No regional lymph node metastasis
- N1: Metastasis in a single ipsilateral lymph node, ≤ 3 cm in greatest dimension and extranodal extension (ENE)-
- N2: Metastasis in a single ipsilateral lymph node, ≤ 3 cm in greatest dimension and ENE+ or > 3 cm but ≤ 6 cm in greatest dimension and ENE-; or metastases in multiple ipsilateral lymph nodes, none > 6 cm in greatest dimension and ENE-; or in bilateral or contralateral lymph nodes(s), none > 6 cm in greatest dimension and ENE-
- N2a: Metastasis in either
- Single ipsilateral lymph node that is ≤ 3 cm and ENE+ or
- Single ipsilateral lymph node that is > 3 cm but ≤ 6 cm in greatest dimension and ENE-
- N2b: Metastasis in multiple ipsilateral lymph nodes, none > 6 cm in greatest dimension and ENE-
- N2c: Metastasis in bilateral or contralateral lymph node(s), none > 6 cm in greatest dimension and ENE-
- N2a: Metastasis in either
- N3: Metastasis in a lymph node > 6 cm in greatest dimension and ENE-; or in a single ipsilateral node > 3 cm in greatest dimension and ENE+; or multiple ipsilateral, contralateral or bilateral nodes, any with ENE+; or a single contralateral node of any size and ENE+
- N3a: Metastasis in a lymph node that is > 6 cm in greatest dimension and ENE-
- N3b: Metastasis in either
- Single ipsilateral lymph node, > 3 cm and ENE+ or
- Multiple ipsilateral, contralateral or bilateral lymph nodes, any with ENE+ or
- Single contralateral lymph node of any size and ENE+
Notes:
- Designation of "U" or "L" may be used for any N category to indicate metastasis above the lower border of the cricoid (U) or below the lower border of the cricoid (L)
- Per AJCC 8th edition, for pN, a selective neck dissection ordinarly will include 10+ lymph nodes and a comprehensive neck dissection (radical or modified radical neck dissection) ordinarily will include 15+ lymph nodes
- Negative pathologic examination of a smaller number of nodes still mandates a pN0 designation
- Midline nodes are considered ipsilateral nodes
Distant metastasis (M)
- M0: No distant metastasis
- M1: Distant metastasis
Notes:
- Metastasis found on imaging is considered cM1
- Biopsy proven metastasis is considered pM1
AJCC prognostic stage grouping for oral cavity
| Stage 0: | Tis | N0 | M0 |
| Stage I: | T1 | N0 | M0 |
| Stage II: | T2 | N0 | M0 |
| Stage III: | T3 | N0 | M0 |
| T1 - 3 | N1 | M0 | |
| Stage IVA: | T4a | N0 - 1 | M0 |
| T1 - 4a | N2 | M0 | |
| Stage IVB: | Any T | N3 | M0 |
| T4b | Any N | M0 | |
| Stage IVC: | Any T | Any N | M1 |
Registry data collection variables
- Extranodal extension (ENE) clinical (present versus absent)
- ENE pathological (present versus absent)
- Extent of microscopic ENE (distance of extension from the native lymph node capsule to the farthest point of invasion in extranodal tissue)
- Perineural invasion
- Lymphovascular invasion
- p16 / HPV status
- Performance status
- Tobacco use and pack year
- Alcohol use
- Depression diagnosis
- Depth of invasion (mm)
- Margin status (grossly involved, microscopic involvement)
- Distance of tumor (or moderate / severe dysplasia) from closest margin
- Distance of moderate / severe dysplasia from closest margin
- Worst pattern of invasion - 5
Histologic grade
- Gx: Cannot be assessed
- G1: Well differentiated
- G2: Moderately differentiated
- G3: Poorly differentiated
Notes:
- For histologic types of carcinomas that are amenable to grading, 3 histologic grades are suggested, as shown below (AJCC: Cancer Staging [Accessed 21 September 2018], CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Lip and Oral Cavity [Accessed 29 December 2020])
- For conventional squamous cell carcinoma, histologic grading as a whole does not perform well as a prognosticator
- Nonetheless, it should be recorded when applicable, as it is a basic tumor characteristic
- Selecting either the most prevalent grade or the highest grade for this synoptic protocol is acceptable
- Variants of squamous cell carcinoma (i.e. verrucous, basaloid, etc.) have an intrinsic biologic potential and currently do not appear to require grading
- Histologic (microscopic) grading of salivary gland carcinomas has been shown to be an independent predictor of behavior and plays a role in optimizing therapy
- However, most salivary gland carcinoma types have an intrinsic biologic behavior and attempted application of a universal grading scheme is merely a crude surrogate
- Thus a generic grading scheme is no longer recommended for salivary gland carcinomas
- Carcinoma types for which grading systems exist and are relevant are incorporated into histologic type
- 3 major categories that are amenable to grading include adenoid cystic carcinoma, mucoepidermoid carcinoma and adenocarcinoma, not otherwise specified
- In some carcinomas, histologic grading may be based on growth pattern, such as in adenoid cystic carcinoma, for which a histologic high grade variant has been recognized based on the percentage of solid growth
- Those adenoid cystic carcinomas showing ≥ 30% of solid growth pattern are considered to be histologically high grade carcinomas
- Histologic grading of mucoepidermoid carcinoma includes a combination of growth pattern characteristics (e.g. cystic, solid, neurotropism) and cytomorphologic findings (e.g. anaplasia, mitoses, necrosis)
- Adenocarcinomas, not otherwise specified do not have a formalized grading scheme and are graded intuitively based on cytomorphologic features
Histopathologic type
- Carcinoma of the oral cavity
- Squamous cell carcinoma (conventional)
- Verrucous squamous cell carcinoma
- Papillary squamous cell carcinoma
- Spindle cell squamous cell carcinoma
- Acantholytic squamous cell carcinoma
- Lymphoepithelial carcinoma
- Basaloid squamous carcinoma
- Adenosquamous carcinoma
- Carcinoma cuniculatum
- Carcinoma of minor salivary gland
- Acinic cell
- Adenoid cystic
- Adenocarcinoma, NOS
- Basal cell adenocarcinoma
- Carcinoma ex pleomorphic adenoma
- Carcinoma type cannot be determined
- Carcinosarcoma
- Clear cell adenocarcinoma
- Cystadenocarcinoma
- Epithelial myoepithelial carcinoma
- Mammary analogue secretory carcinoma
- Mucoepidermoid carcinoma
- Mucinous carcinoma
- Myoepithelial carcinoma
- Oncocytic carcinoma
- Polymorphous adenocarcinoma
- Salivary duct carcinoma
- Neuroendocrine carcinoma
- Well differentiated neuroendocrine carcinoma (typical carcinoid tumor)
- Moderately differentiated neuroendocrine carcinoma (atypical carcinoid tumor)
- Poorly differentiated neuroendocrine carcinoma, small cell type
- Poorly differentiated neuroendocrine carcinoma, large cell type
- Combined (or composite) neuroendocrine carcinoma (specify types)
- Carcinoma type cannot be determined
- Mucosal melanoma
Board review style question #1
A 2.4 cm primary gingival carcinoma was resected in continuity with the underlying posterior mandible. Which of the T category criteria in the 8th edition AJCC staging guide is satisfied by the examination of the microscopic sections above?
- T1 by depth of invasion
- T2 by depth of invasion
- T3 by mandibular medullary bone invasion
- T4 by mandibular medullary bone invasion
Board review style answer #1
D. T4 by mandibular medullary bone invasion
Comment Here
Reference: Pathologic TNM staging of lip & oral cavity, AJCC 8th edition
Comment Here
Reference: Pathologic TNM staging of lip & oral cavity, AJCC 8th edition
Staging-oropharynx & hypopharynx
Table of Contents
See also | Definition / general | Essential features | Terminology | Staging anatomy | Surgical margins | ICD coding | HPV mediated oropharyngeal primary squamous cell carcinoma (pT) | HPV mediated regional lymph nodes (pN) | AJCC clinical prognostic stage grouping for HPV mediated oropharyngeal squamous cell carcinoma | p16- oropharynx primary tumor (pT) | p16- hypopharynx primary tumor (pT) | p16- oropharynx and hypopharynx pathologic regional lymph nodes (pN) | Distant metastasis (pM) | AJCC clinical prognostic stage grouping for HPV unrelated oropharyngeal and hypopharyngeal squamous cell carcinoma | Registry data collection variables | Histologic grade | Histopathologic type | Diagrams / tables | Board review style question #1 | Board review style answer #1See also
Definition / general
- AJCC 8th edition staging has introduced a separate staging system for HPV mediated (p16+) squamous cell carcinomas of the oropharynx and HPV unrelated (p16-) squamous cell carcinoma of the oropharynx (AJCC: Cancer Staging [Accessed 20 September 2018], CAP: Protocol for the Examination of Specimens From Patients With Cancers of the Pharynx [Accessed 20 September 2018])
- Testing with p16 immunohistochemistry is mandatory for all oropharyngeal squamous carcinomas but not for hypopharyngeal cancers
- If p16 testing is not performed on oropharyngeal carcinoma, that case is staged according to the system for p16- cancers
- AJCC level of evidence: II
- Cancers staged using the oropharynx (p16-) and hypopharynx staging system include
- p16- squamous cancers of the oropharynx
- Oropharyngeal cancers without a p16 immunostain performed
- All cancers of the hypopharynx
- Minor gland salivary cancers of the oropharynx and hypopharynx
- Neuroendocrine carcinoma of the oropharynx and hypopharynx
- Cancers staged using the oropharynx (p16+) staging system include
- HPV related squamous cell carcinoma of the oropharynx
- Note: p16 immunohistochemistry assessment is necessary only for squamous carcinomas
- Unknown primary (T0) with nodal positive disease should be staged using this section if a node is p16+ / HPV+ and no primary site is identified
- HPV related squamous cell carcinoma of the oropharynx
- Staging protocols, such as those of CAP, are to document procedure, tumor site, tumor laterality, tumor focality, tumor size, histologic type, histologic grade where applicable, margin status, lymphovascular invasion, perineural invasion, regional lymph node findings and summarize these pathologic findings using TNM system (CAP: Protocol for the Examination of Specimens From Patients With Cancers of the Pharynx [Accessed 20 September 2018])
Essential features
- AJCC 7th edition staging was sunset on December 31, 2017; as of January 1, 2018, use of the 8th edition is mandatory
- Use of the CAP protocol is not required for recurrent tumors or for metastatic tumors that are resected at a different time than the primary tumor
- Use of this protocol is also not required for pathology reviews performed at a second institution (i.e. secondary consultation, second opinion or review of outside case at second institution) (CAP: Protocol for the Examination of Specimens From Patients With Cancers of the Pharynx [Accessed 20 September 2018])
- Alternatively for providers practicing in different geographic regions, there may be interest in the International Collaboration on Cancer Reporting (ICCR) guidelines:
Terminology
- Synonyms for HPV mediated oropharyngeal carcinoma:
- HPV+ oropharyngeal carcinoma
- p16+ oropharyngeal carcinoma
- Nonkeratinizing oropharyngeal squamous cell carcinoma
Staging anatomy
- Anatomic boundaries and primary site(s) of the pharynx: divided into 3 parts including the oropharynx, nasopharynx and hypopharynx
- Oropharynx (see figure 1 in Diagrams / tables) (CAP: Protocol for the Examination of Specimens From Patients With Cancers of the Pharynx [Accessed 20 September 2018]):
- Portion of the continuity of the pharynx extending from the plane of the superior surface of the soft palate to the superior surface of the hyoid bone or floor of the vallecula
- Contents include:
- Soft palate
- Palatine tonsils
- Anterior and posterior tonsillar pillars
- Tonsillar fossa and tonsillar (faucial) pillars
- Uvula
- Base of tongue, including the lingual tonsils
- Vallecular
- Posterior oropharyngeal wall
- Nasopharynx (see figure 1 in Diagrams / tables) (CAP: Protocol for the Examination of Specimens From Patients With Cancers of the Pharynx [Accessed 20 September 2018]):
- Situated behind the nasal cavity and above the soft palate; it begins anteriorly at the posterior choana and extends along the plane of the airway to the level of the free border of the soft palate
- Contents include:
- Nasopharyngeal tonsils (adenoids) lie along the posterior and lateral of the nasopharynx
- Orifice of Eustachian tube lies along the lateral aspects of the nasopharyngeal wall
- Fossa of Rosenmüller
- Hypopharynx (see figure 1 in Diagrams / tables) (CAP: Protocol for the Examination of Specimens From Patients With Cancers of the Pharynx [Accessed 20 September 2018]):
- Portion of the pharynx extending from the plane of the superior border of the hyoid bone (or floor of the vallecula) to the plane corresponding to the lower border of the cricoid cartilage
- Contents include:
- Pyriform sinus (right and left): represents part of the hypopharynx which expands bilaterally and forward around the sides of the larynx and lies between the larynx and the thyroid cartilage
- Lateral and posterior hypopharyngeal walls
- Postcricoid region extending from the level of the arytenoid cartilage and connecting folds to the inferior border of the cricoid cartilage; it connects the 2 piriform sinuses, thereby forming the anterior wall of the hypopharynx
- Waldeyer ring:
- Formed by a ring or group of extranodal lymphoid tissues about the upper end of the pharynx (see figure 2 in Diagrams / tables) which consists of the:
- Palatine tonsils
- Pharyngeal tonsils (adenoids)
- Base of tongue / lingual tonsils
- Adjacent submucosal lymphatics
- Formed by a ring or group of extranodal lymphoid tissues about the upper end of the pharynx (see figure 2 in Diagrams / tables) which consists of the:
Surgical margins
- Historically, documentation of margin status for many oropharyngeal and hypopharyngeal tumors was not possible, as they were not oncologically resected but rather treated with chemotherapy and radiation
- With the advent of transoral robotic and laser surgery, however, intact resections have become increasingly common
- Limited evidence suggests that at the very minimum, a positive margin consists of invasive carcinoma present at the inked margin
- Akin to other sites, there is no standard definition of a "close" margin and definitions have ranged from 2 - 5 mm
- Despite the paucity of data, in keeping with other sites, the distance from the nearest margin should be recorded
- For hypopharyngeal and HPV- oropharyngeal tumors, in situ disease and high grade dysplasia is plausible and if present at a margin, the margin is considered positive in line with other sites
- When such lesions are identified in pharyngeal sites, they usually occur in association with an invasive carcinoma
- In this setting, the same criteria detailed in the oral cavity and laryngeal protocols apply (see CAP: Protocol for the Examination of Specimens from Patients With Cancers of the Lip and Oral Cavity [Accessed 20 September 2018] and CAP: Protocol for the Examination of Specimens From Patients With Cancers of the Larynx [Accessed 20 September 2018])
- For HPV+ oropharyngeal carcinoma, in situ disease for practical purposes is nonexistent, likely given its derivation from the specialized "lymphoepithelium" of tonsillar crypt; this has resulted in the elimination of pTis staging (AJCC: Cancer Staging [Accessed 20 September 2018])
ICD coding
- C01.9: Base of tongue, NOS
- C02.4: Lingual tonsil
- C05.1: Soft palate, NOS
- C05.2: Uvula
- C09.0: Tonsillar fossa
- C09.1: Tonsillar pillar
- C09.8: Overlapping lesion of tonsil
- C09.9: Tonsil, NOS
- C10.0: Vallecula
- C10.2: Lateral wall of oropharynx
- C10.3: Posterior pharyngeal wall
- C10.8: Overlapping lesion of oropharynx
- C10.9: Oropharynx, NOS
- C11.1: Pharyngeal tonsils
- C12.9: Pyriform sinus
- C13.0: Postcricoid region
- C13.1: Hypopharyngeal aspect of aryepiglottic fold
- C13.2: Posterior wall of hypopharynx
- C13.8: Overlapping lesion of hypopharynx
- C13.9: Hypopharynx, NOS
HPV mediated oropharyngeal primary squamous cell carcinoma (pT)
- pT0: no primary identified
- pT1: tumor ≤ 2 cm in greatest dimension
- pT2: tumor > 2 cm but ≤ 4 cm in greatest dimension
- pT3: tumor > 4 cm in greatest dimension or extension to lingual surface of epiglottis
- pT4: tumor of any size invading adjacent organ(s), such as larynx, extrinsic muscle of tongue, medial pterygoid, hard palate or mandible
Notes:
- Mucosal extension to lingual surface of epiglottis from primary tumor of the base of tongue and vallecular does not constitute invasion of the larynx
HPV mediated regional lymph nodes (pN)
- pNX: regional lymph nodes cannot be assessed
- pN0: no regional lymph node metastasis
- pN1: metastasis in ≤ 4 lymph nodes
- pN2: metastasis in > 4 lymph nodes
Notes:
- Per AJCC 8th edition, for pN, a selective neck dissection ordinarily will include 10+ lymph nodes and a comprehensive neck dissection (radical or modified radical neck dissection) ordinarily will include 15+ lymph nodes
- Negative pathologic examination of a smaller number of nodes still mandates a pN0 designation
AJCC clinical prognostic stage grouping for HPV mediated oropharyngeal squamous cell carcinoma
| Stage I: | T0 - 2 | N0 - 1 | M0 |
| Stage II: | T0 - 2 | N2 | M0 |
| T3 - 4 | N0 - 1 | M0 | |
| Stage III: | T3 - 4 | N2 | M0 |
| Stage IV: | Any T | Any N | M1 |
HPV unrelated (p16-) oropharyngeal and hypopharyngeal squamous cell carcinoma
p16- oropharynx primary tumor (pT)
- pTX: primary tumor cannot be assessed
- pTis: carcinoma in situ
- pT1: tumor ≤ 2 cm in greatest dimension
- pT2: tumor > 2 cm but ≤ 4 cm in greatest dimension
- pT3: tumor > 4 cm in greatest dimension or extension to lingual surface of epiglottis
- pT4a: tumor of any size invading adjacent organ(s), such as larynx, extrinsic muscle of tongue, medial pterygoid, hard palate or mandible
- pT4b: tumor of any size invading adjacent organ(s), such as lateral pterygoid muscle, pterygoid plates, lateral nasopharynx, skull base or encases carotid artery
Notes:
- Mucosal extension to lingual surface of epiglottis from primary tumor of the base of tongue and vallecular does not constitute invasion of the larynx
p16- hypopharynx primary tumor (pT)
- pTX: primary tumor cannot be assessed
- pTis: carcinoma in situ
- pT1: tumor limited to one subsite of hypopharynx or ≤ 2 cm in greatest dimension
- pT2: tumor invades > 1 subsite of hypopharynx or an adjacent site or tumor > 2 cm but ≤ 4 cm in greatest dimension without fixation of hemilarynx
- pT3: tumor > 4 cm in greatest dimension or with fixation of hemilarynx or extension to esophageal mucosa
- pT4a: tumor of any size invading thyroid / cricoid cartilage, hyoid bone, thyroid gland, esophageal muscle or central compartment soft tissue (central compartment soft tissue includes prelaryngeal strap muscles and subcutaneous fat)
- pT4b: tumor of any size invading prevertebral fascia, encases carotid artery or involves mediastinal structures
p16- oropharynx and hypopharynx pathologic regional lymph nodes (pN)
- pNX: regional lymph nodes cannot be assessed
- pN0: no regional lymph node metastasis
- pN1: metastasis in a single ipsilateral lymph node, ≤ 3 cm and extranodal extension (ENE)-
- pN2: metastasis in a single ipsilateral lymph node, ≤ 3 cm in greatest dimension and ENE+; or > 3 cm but ≤ 6 cm in greatest dimension and ENE-; or metastases in multiple ipsilateral lymph nodes, none > 6 cm in greatest dimension and ENE-; or in bilateral or contralateral lymph node(s), none > 6 cm in greatest dimension and ENE-
- pN2a: metastasis in either
- Single ipsilateral lymph node that is ≤ 3 cm and ENE+ or
- Single ipsilateral lymph node that is > 3 cm but ≤ 6 cm in greatest dimension and ENE-
- pN2b: metastasis in multiple ipsilateral lymph nodes, none > 6 cm in greatest dimension and ENE-
- pN2c: metastasis in bilateral or contralateral lymph node(s), none > 6 cm in greatest dimension and ENE-
- pN2a: metastasis in either
- pN3: metastasis in a lymph node > 6 cm in greatest dimension and ENE-; or in a single ipsilateral node > 3 cm in greatest dimension and ENE+; or multiple ipsilateral, contralateral or bilateral nodes, any with ENE+; or a single contralateral node of any size and ENE+
- pN3a: metastasis in a lymph node that is > 6 cm in greatest dimension and ENE-
- pN3b: metastasis in either
- Single ipsilateral lymph node, > 3 cm and ENE+ or
- Multiple ipsilateral, contralateral or bilateral lymph nodes, any with ENE+ or
- Single contralateral lymph node of any size and ENE+
Notes:
- Designation of "U" or "L" may be used for any N category to indicate metastasis above the lower border of the cricoid (U) or below the lower border of the cricoid (L)
- Per AJCC 8th edition, for pN, a selective neck dissection ordinarily will include 10+ lymph nodes and a comprehensive neck dissection (radical or modified radical neck dissection) ordinarily will include 15+ lymph nodes
- Negative pathologic examination of a smaller number of nodes still mandates a pN0 designation
- Midline nodes are considered ipsilateral nodes
Distant metastasis (pM)
- pM0: no distant metastasis
- pM1: distant metastasis
Registry data collection variables
- ENE clinical (present versus absent)
- ENE pathological (present versus absent)
- Extent of microscopic ENE (distance of extension from the native lymph node capsule to the farthest point of invasion in extranodal tissue)
- Perineural invasion
- Lymphovascular invasion
- p16 / HPV status
- Performance status
- Tobacco use and pack year
- Alcohol use
- Depression diagnosis
Histologic grade
- GX: cannot be assessed
- G1: well differentiated
- G2: moderately differentiated
- G3: poorly differentiated
Notes:
- No grading system exists for HPV mediated oropharyngeal carcinoma
- For histologic types of carcinomas that are amenable to grading, 3 histologic grades are suggested, as shown below
- For conventional squamous cell carcinoma, histologic grading as a whole does not perform well as a prognosticator
- Nonetheless, it should be recorded when applicable, as it is a basic tumor characteristic
- Selecting either the most prevalent grade or the highest grade for this synoptic protocol is acceptable
- Variants of squamous cell carcinoma (i.e. verrucous, basaloid, etc.) have an intrinsic biologic potential and currently do not appear to require grading
- Histologic (microscopic) grading of salivary gland carcinomas has been shown to be an independent predictor of behavior and plays a role in optimizing therapy
- However, most salivary gland carcinoma types have an intrinsic biologic behavior and attempted application of a universal grading scheme is merely a crude surrogate
- Thus a generic grading scheme is no longer recommended for salivary gland carcinomas
- Carcinoma types for which grading systems exist and are relevant are incorporated into histologic type
- 3 major categories that are amenable to grading include adenoid cystic carcinoma, mucoepidermoid carcinoma and adenocarcinoma, not otherwise specified
- In some carcinomas, histologic grading may be based on growth pattern, such as in adenoid cystic carcinoma, for which a histologic high grade variant has been recognized based on the percentage of solid growth
- Those adenoid cystic carcinomas showing ≥ 30% of solid growth pattern are considered to be histologically high grade carcinomas
- Histologic grading of mucoepidermoid carcinoma includes a combination of growth pattern characteristics (e.g. cystic, solid, neurotropism) and cytomorphologic findings (e.g. anaplasia, mitoses, necrosis)
- Adenocarcinomas, not otherwise specified, do not have a formalized grading scheme and are graded intuitively based on cytomorphologic features
Histopathologic type
- Carcinoma of the oropharynx and hypopharynx
- Squamous cell carcinoma
- Human papillomavirus (HPV) mediated (positive) squamous cell carcinoma (oropharynx only)*
- HPV unrelated (negative) squamous cell carcinoma (oropharynx and hypopharynx)*
* Modification based on separation of HPV mediated (positive) and HPV unrelated (negative) oropharyngeal squamous cell carcinoma in the AJCC 8th edition and WHO 4th edition
- Variants of squamous cell carcinoma
- Keratinizing
- Nonkeratininizing
- Acantholytic squamous cell carcinoma
- Adenosquamous carcinoma
- Basaloid squamous cell carcinoma
- Papillary squamous cell carcinoma
- Spindle cell squamous cell carcinoma
- Verrucous squamous cell carcinoma
- Lymphoepithelial carcinoma
- Squamous cell carcinoma
- Carcinoma of minor salivary gland
- Acinic cell carcinoma
- Adenoid cystic carcinoma
- Adenocarcinoma, NOS
- Basal cell adenocarcinoma
- Carcinoma ex pleomorphic adenoma
- Carcinoma type cannot be determined
- Carcinosarcoma
- Clear cell adenocarcinoma
- Cystadenocarcinoma
- Epithelial myoepithelial carcinoma
- Mammary analogue secretory carcinoma
- Mucoepidermoid carcinoma
- Mucinous carcinoma
- Myoepithelial carcinoma
- Oncocytic carcinoma
- Polymorphous adenocarcinoma
- Salivary duct carcinoma
- Neuroendocrine carcinoma
- Small cell neuroendocrine carcinoma, HPV-
- Small cell neuroendocrine carcinoma, HPV+
- Large cell neuroendocrine carcinoma, HPV-
- Large cell neuroendocrine carcinoma, HPV+
Diagrams / tables
Board review style question #1
With respect to HPV mediated oropharyngeal squamous cell carcinoma, which of the following is not a recognized pT stage under AJCC 8th edition?
- pTis
- pT0
- pT1
- pT2
- pT3
Board review style answer #1
Subgemmal neurogenous plaque
Table of Contents
Definition / general | Essential features | Terminology | Sites | Case reports | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Differential diagnosis | Board review style question #1 | Board review style answer #1Definition / general
- Normal neural structure associated with taste buds
Essential features
- Generally asymptomatic but may present as white or red patches, hyperplastic nodules, ulcers or complaints of a burning sensation
Terminology
- Also called the subepithelial nerve plexus of taste buds
Sites
- Posterior third of the lateral tongue
Case reports
- 69 year old woman with small indurated lesion on the lateral border of tongue (Case of the Week #445)
Microscopic (histologic) description
Shows a biphasic pattern:
- Superficial part of the lesion
- Contains elongated and wavy spindle cells running in parallel to the epithelium
- Can contain varying amounts of collagen
- May have an inflammatory infiltrate and lymphoid follicles
- Deeper part of the lesion
- Contains small nerve fascicles and scattered ganglion cells
Microscopic (histologic) images
Positive stains
Differential diagnosis
- Neural neoplasms such as neurofibroma or neuroma
- Invasive squamous cell carcinoma, when squamous islands present
Board review style question #1
Which of the following is true of subgemmal neurogenous plaque?
A. They can be located anywhere in the head and neck
B. They are aggressive lesions that typically recur after excision
C. They are normal neural structures associated with taste buds
D. They arise in response to trauma
A. They can be located anywhere in the head and neck
B. They are aggressive lesions that typically recur after excision
C. They are normal neural structures associated with taste buds
D. They arise in response to trauma
Board review style answer #1
C. They are normal neural structures associated with taste buds
Comment Here
Reference: Subgemmal neurogenous plaque
Comment Here
Reference: Subgemmal neurogenous plaque
Tonsillitis (pending)
A patient presents with a white lesion on the hard palate. Microscopic examination shows a well defined proliferation of stratified squamous epithelium forming exophytic papillary fronds. The epithelium is covered by a thickened layer of dense orthokeratin, which forms church spires and hypergranulosis and koilocytosis are appreciated. The rete ridges demonstrate prominent inward cupping. What is the diagnosis?
Contributed by Molly Housley Smith, D.M.D. and Kelly Magliocca, D.D.S., M.P.H.
A patient presents with a white and red exophytic granular growth on the alveolar ridge. Microscopic examination shows church spire-like keratin peaks, keratin plugging and bulbous shaped, hyperplastic rete ridges that push downward and abut underlying bone. What is the diagnosis?
Contributed by Molly Housley Smith, D.M.D.
A patient presents with a brown patch on the buccal mucosa. Which of the following is true regarding oral melanoacanthomas?
Oral potentially malignant disorders and oral epithelial dysplasia
Papillomas
Tumors of uncertain histogenesis
Soft tissue and neural tumors
Oral mucosal melanoma
Salivary type tumors
Hematolymphoid tumors
ICD-O note: The first four digits indicate the specific histological term. The fifth digit after the slash (/) is the behavior code, which indicates whether a tumor is malignant, benign, in situ or uncertain (whether benign or malignant) (WHO: International Classification of Diseases for Oncology, 3rd Edition (ICD-O-3)) Back to top
Find related Pathology books: head & neck/endocrine
Transient lingual papillitis (pending)
[Pending]
Traumatic ulceration with stroma eosinophilia (TUGSE)
Table of Contents
Definition / general | Terminology | Case reports | Clinical images | Microscopic (histologic) description | Microscopic (histologic) imagesDefinition / general
- Resembles carcinoma clinically
- Presumed due to crush injury of tongue muscle
Terminology
- Also called ulcerative eosinophilic granuloma, Riga-Fede disease, traumatic granuloma
Case reports
- 6 month old boy with traumatic lingual ulceration (Ital J Pediatr 2012;38:20)
- 70 year old woman with Riga-Fede-like disease (Indian J Dermatol 2010;55:92)
Clinical images
Microscopic (histologic) description
- Eosinophils and other inflammatory cells in submucosa, mucosa, salivary glands
- Dilated vessels often present
Varix / varicosities / varices
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Oral varicosities are tortuous and aberrantly dilated venous structures that most often present on the lips and ventral tongue of older individuals
- They represent a developmental anomaly of unknown etiology with minimal clinical implications
Essential features
- Abnormally dilated venous structures
- The most common oral mucosal lesion in older adults (J Dent Res Dent Clin Dent Prospects 2019;13:24)
- Most often found under the tongue and around the lips / labial mucosa
Terminology
- Varicosity / varicosities
- Varix
- Varices
- Caviar tongue
- Phlebectasia linguae
Epidemiology
- Older individuals (67% of patients are > 60 years) (Clin Dermatol 2016;34:458)
Sites
- Sublingual varices are most common
- May also be found on skin of lip, labial mucosa or buccal mucosa
Etiology
- Unknown etiology
- Loosely associated risk factors include smoking, cardiovascular disease (e.g. hypertension), female gender, denture wearing, chronic liver disease and old age (Clin Dermatol 2016;34:458, Folia Morphol (Warsz) 2019;78:325, Medicine (Baltimore) 2019;98:e16987, Saudi Med J 2015;36:310, BMC Oral Health 2015;15:78)
Clinical features
- Presents as a chain of compressible blue-purple nodules on either side of the lingual frenum or as a single elevated or flat submucosal nodule in other locations
- May be firm when thrombosed
- Ventral tongue is the most common site, although also found on labial mucosa, skin of lip, buccal mucosa or other rare oral sites
- Painless and often inconsequential (Gerodontology 2015;32:82)
Diagnosis
- Diagnosis often is made on clinical presentation, especially when in the sublingual location; biopsy often is not required
- Diascopy may prove useful in differential diagnosis, as varicosities demonstrate blanching (Gerodontology 2015;32:82)
- A single varicosity may be diagnosed upon histologic examination when the presentation is not clinically diagnostic
Radiology description
- Occasionally, oral varicosities may demonstrate small opacifications on radiographic imaging due to phlebolith formation within a thrombus (Gerodontology 2015;32:82)
Prognostic factors
- Varicosities are of little clinical consequence
- Patients have a good prognosis, although rare cases may be associated with bleeding (Medicine (Baltimore) 2019;98:e16987)
Case reports
- 42 year old woman with bleeding varicosity at base of tongue in association with liver cirrhosis (Medicine (Baltimore) 2019;98:e16987)
- 60 year old white woman with oral varicosity treated with sclerotherapy (Med Oral Patol Oral Cir Bucal 2006;11:E44)
- 62 year old woman with lingual varicosities visualized via dermoscopy / mucoscopy (Dermatol Pract Concept 2018;8:54)
Treatment
- Varicosities generally are not treated unless thrombosed or displeasing to the patient in form or function
- In such cases, conservative surgical excision or sclerotherapy is sufficient (Med Oral Patol Oral Cir Bucal 2018;23:e180)
- Safe and effective treatment has been performed with diode and Nd:YAG lasers (J Contemp Dent Pract 2015;16:723)
Clinical images
Gross description
- Tan surface with raised or flat blue-purple-black ovoid structure, which may be firm or depressible
- Cut surface shows dilated or collapsed vascular space that may demonstrate luminal accumulation of brown erythrocytes
Microscopic (histologic) description
- 1 - 3 tortuous, enlarged venous structures lined by a thin layer of endothelium (Gerodontology 2015;32:82)
- Thrombosis or organizing thrombosis is often present, which is depicted by concentric layers of erythrocytes and platelets, referred to as lines of Zahn
- Aggregates of granulation tissue may also be present during formation
- Concentric rings of eosinophilic calcifications may be present within the lumen
Microscopic (histologic) images
Negative stains
Sample pathology report
- Lower lip, excision:
- Vascular anomaly consistent with varicosity
Differential diagnosis
- Sublingual varicosities are clinically diagnostic and do not require biopsy
- Clinical differential diagnosis for a single, blue oral varix may include the following:
- Hemangioma:
- An abnormal collection of more than 3 dilated vessels, seen on light microscopy
- Congenital
- Often GLUT1 positive (Oral Dis 2007;13:51)
- Vascular leiomyoma (angioleiomyoma):
- Histopathologic examination reveals a well defined proliferation of smooth muscle emanating from vascular walls
- Positive for alpha smooth muscle actin
- Salivary tumors / reactive processes, differentiated upon biopsy:
- Amalgam tattoo:
- May demonstrate opacification on radiograph
- Flat, blue-black pigmentation
- Histopathologic examination reveals foreign particles within connective tissue
- Melanocytic nevus (especially blue nevus):
- Histopathologic examination reveals focal collection of melanocytes
- Melanoma:
- Often irregular borders
- Histopathologic examination reveals abnormal increase in melanocytes
- Most common on the maxillary gingiva and hard palate
- Focal melanosis / melanocytic macule:
- Flat, never raised
- Focal accumulation of melanin without increase in melanocytes, seen on light microscopy
- Hemangioma:
Additional references
Board review style question #1
Board review style answer #1
Board review style question #2
Board review style answer #2
Verruca vulgaris
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Benign epithelial proliferation of squamous mucosa
- Associated with human papilloma virus (HPV) types 2 and 4
Essential features
- Associated with low risk strains of HPV
- Mostly found on the skin but uncommonly may be seen in the oral cavity
- Similar to cutaneous lesions both histopathologically and microscopically (Dent Clin North Am 2014;58:385)
- Histopathological features include exophytic epithelial growth with prominent hyperkeratosis, inward cupping of the rete pegs, koilocytes and hypergranulosis within the superficial epithelial aspects
Terminology
- Oral wart
- Common wart
ICD coding
- ICD-10:
Epidemiology
- M > F (J Oral Pathol Med 1993;22:113)
- Wide age range, although more frequent in younger populations
Sites
- Lips, palate, anterior tongue most common but can affect any intraoral location
- 50% affect the hard palate in Venezuelan population (J Oral Pathol Med 1993;22:113)
Pathophysiology
- HPV is thought to gain access to epithelial cells via microabrasion or trauma (Head Neck Pathol 2019;13:80, Rev Med Virol 2015;25:2)
- Virus infects the basilar epithelial stem cells via endocytosis
- Cell division occurs during wound / trauma repair, populating the basal cell layer with transiently amplifying cells with HPV genomes
- There is slow division of the infected basal stem cells with little or no viral gene expression within the basal layer (Rev Med Virol 2015;25:2)
- Transformation of verruca vulgaris to HPV related squamous cell carcinoma is not possible since low risk HPV strains lack oncogenic properties (Rev Med Virol 2015;25:2)
Etiology
- Associated with HPV types 2 and 4 (Head Neck Pathol 2019;13:80, Dent Clin North Am 2014;58:385, Atlas Oral Maxillofac Surg Clin North Am 2017;25:163, J Oral Pathol Med 1993;22:113)
- Types 1, 26, 27 and 57 have also been implicated (Head Neck Pathol 2019;13:80, Dent Clin North Am 2014;58:385)
- Autoinoculation from cutaneous lesions is the most common route of transmission (J Cutan Med Surg 2017;21:251, Head Neck Pathol 2019;13:80)
- Thumb sucking, biting fingers / fingernails
Clinical features
- Similar to cutaneous counterpart (Head Neck Pathol 2019;13:80)
- Asymptomatic, well delineated, often white papule or nodule with a papillary or pebbled surface
- Sessile or pedunculated
- May demonstrate a keratin horn
- Most are single lesions but multiple may occur (Atlas Oral Maxillofac Surg Clin North Am 2017;25:163)
- < 1 cm in diameter (Head Neck Pathol 2019;13:80)
Diagnosis
- Histopathologic examination of excisional specimen
- Presence of HPV has been detected via immunohistochemical staining, electron microscopy, in situ hybridization and polymerase chain reaction studies; however, these studies are unnecessary for diagnosis (J Oral Pathol Med 1993;22:113)
Prognostic factors
- Good prognosis
- Rare recurrence attributed to incomplete removal of lesional tissue (Dent Clin North Am 2014;58:385)
Case reports
- 9 year old boy presented with oral verruca vulgaris and extensive cutaneous involvement (Int J Clin Pediatr Dent 2011;4:65)
- 18 year old man presented with verruca vulgaris lesions on the fingers and lips (J Cutan Med Surg 2017;21:251)
Treatment
- Excision (via surgery, cryosurgery or electrosurgery)
- Spontaneous regression has been reported (Dent Clin North Am 2014;58:385)
Clinical images
Gross description
- White, exophytic, papillary growth
Microscopic (histologic) description
- Similar to cutaneous counterpart (Head Neck Pathol 2019;13:80)
- Prominent surface keratinization (often orthokeratin with superficial parakeratin tufts)
- Inward cupping of the rete pegs
- Exophytic / papillary fronds which form church spire-like peaks
- Hypergranulosis with coarse keratohyalin granules and potential eosinophilic intranuclear viral inclusions within the granular cell layer
- Koilocytosis within the superficial epithelial layers
Microscopic (histologic) images
Videos
Verruca vulgaris versus seborrheic keratosis pathology
Sample pathology report
- Hard palate, excisional biopsy:
- Verruca vulgaris (see comment)
- Comment: Microscopic examination reveals a well defined proliferation of keratinized stratified squamous epithelium forming papillary projections above the surrounding mucosa. The epithelium is covered by a dense and thickened layer of orthokeratin. Prominent granular cells and koilocytes are noted. Cytologic atypia is not appreciated.
Differential diagnosis
- Oral squamous papilloma:
- Clinically identical to verruca vulgaris
- HPV types 6, 11
- Lack the prominent hypergranulosis and koilocytosis in the superficial epithelial layers
- Variable keratinization (Head Neck Pathol 2019;13:80)
- Condyloma acuminatum:
- HPV types 6, 11, 16, 18
- Labial mucosa, soft palate, lingual frenum
- Often demonstrates a fleshy, broad based clinical appearance
- Bulbous rete pegs and blunted papillary projections
- Multifocal epithelial hyperplasia (Heck disease):
- HPV types 13, 32
- Multiple / generalized, often coalescing, sessile lesions (Head Neck Pathol 2019;13:80)
- Exhibits mitosoid bodies
- Higher frequency in Inuit and Indian populations of North, Central and South America, Greenland and North Canada, as well as in descendants of Khoisan in South Africa (J Oral Pathol Med 2013;42:435)
- Living in crowded, unhygienic environmental conditions is a risk factor (Dent Clin North Am 2014;58:385)
- Verruciform xanthoma:
- Similar clinically, although may have a yellow hue
- Demonstrates foamy xanthoma cells within papillary projections
- More likely to occur on gingiva (Head Neck Pathol 2019;13:80)
- Inward cupping of the rete pegs is not apparent
- Proliferative verrucous leukoplakia:
- May be confused with verruca vulgaris on small, incisional biopsies
- Patients with verrucous leukoplakia often demonstrate multiple, flattened or slightly raised, well demarcated white plaques
- Often affects marginal gingiva
- Also demonstrates prominent granular cell layer and church spire keratin peaks
- Inward cupping of the rete pegs is not apparent
- Verrucous carcinoma:
- Not associated with HPV
- Rete ridges show downward, pushing growth
- Inward cupping of the rete pegs is not apparent
Additional references
Board review style question #1
Board review style answer #1
C. Verruca vulgaris. The microscopic images show a well circumscribed, papillary epithelial proliferation with inward cupping of the rete ridges, prominent koilocytosis and prominent keratohyaline granules, which are all features of verruca vulgaris. Answers A and B are incorrect because condyloma acuminatum and squamous papilloma both lack prominent hypergranulosis while condyloma acuminatum exhibits broad, blunted papillary projections rather than the thin, hyperkeratotic projections seen above. Answer D is incorrect because verrucous carcinoma demonstrates broad, pushing rete ridges and lacks circumscription.
Comment Here
Reference: Verruca vulgaris
Comment Here
Reference: Verruca vulgaris
Board review style question #2
A patient presents with a white lesion on the hard palate. Microscopic examination shows a well defined proliferation of stratified squamous epithelium forming exophytic papillary fronds. The epithelium is covered by a thickened layer of dense orthokeratin, which forms church spires and hypergranulosis and koilocytosis are appreciated. The rete ridges demonstrate prominent inward cupping. What is the diagnosis?
- Condyloma acuminatum
- Proliferative verrucous leukoplakia
- Verruca vulgaris
- Verrucous carcinoma
Board review style answer #2
C. Verruca vulgaris. Verruca vulgaris is characterized by a papillary epithelial proliferation with hypergranulosis, inward cupping of the rete ridges and koilocytosis, as described in the question. Answer A is incorrect because condyloma acuminata are not bright white clinically and lack prominent hypergranulosis. Answer B is incorrect because proliferative verrucous leukoplakia may look very similar to verruca vulgaris on small biopsies but proliferative verrucous leukoplakia is not well circumscribed clinically and not isolated. Additionally, proliferative verrucous leukoplakia does not show circumscription and inward cupping of the rete ridges histopathologically. Answer D is incorrect because verrucous carcinoma is traditionally larger clinically and demonstrates a pushing pattern of invasion without circumscription.
Comment Here
Reference: Verruca vulgaris
Comment Here
Reference: Verruca vulgaris
Verruciform xanthoma
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Definition / general
- Uncommon, reactive, histiocytic lesion of the oral cavity, first described in 1971 by Dr. Shafer (Oral Surg Oral Med Oral Pathol 1971;31:784)
Essential features
- Often misdiagnosed clinically and presents as a verrucoid or papillary mass, most commonly on the gingiva (Head Neck Pathol 2020;14:742)
- Characterized histologically by aggregates of foamy histiocytes / xanthoma cells within connective tissue papillae of papillary epithelium
- Frequently seen within a background setting of chronic inflammation or trauma
Terminology
- Verruciform xanthoma (VX)
ICD coding
- ICD-10: K13.4 - granuloma and granuloma-like lesions of the oral mucosa (including verruciform xanthoma)
Epidemiology
- Age range: 9 - 94 years, mean of 61 years (Head Neck Pathol 2020;14:742)
- M:F ratio is almost equal
Sites
- ~70% on masticatory mucosa (gingiva and hard palate); less common oral sites: buccal mucosa, tongue, vestibule, lip, floor of mouth (Head Neck Pathol 2020;14:742)
- May also occur on skin or anogenital mucosa
Pathophysiology
- Uncertain pathogenesis; MCP1 / CCR2 mediated recruitment of foamy macrophages in connective tissue papillae and lysosomal engulfment of epithelial lipids by MRS1 bearing macrophages under regulation of T lymphocytes may be essential in formation of VX (Oral Dis 2008;14:150)
- Necrosis of foamy macrophages and macrophage dependent debris may help perpetuate the lesion (Oral Dis 2008;14:150)
- Not related to human papillomavirus (Med Oral Patol Oral Cir Bucal 2018;23:e429)
Etiology
- May be initiated by trauma, inflammation or altered immunological response (Head Neck Pathol 2020;14:742)
- Has been seen in background setting of inflammatory conditions, such as lichen planus, graft versus host disease, oral submucous fibrosis (Case Rep Dent 2018;2018:1615086, Support Care Cancer 2021;29:79, J Oral Maxillofac Pathol 2019;23:43)
- Tobacco, mechanical stimuli, periodontal pathogens, alcohol, food sensitizing or allergic agents, dental materials, medications may trigger epithelial damage (Oral Dis 2008;14:150)
- Also has been seen within epithelial dysplasia / carcinoma in situ (J Oral Maxillofac Surg 1989;47:398)
Clinical features
- Slow growing, asymptomatic, often solitary, well demarcated plaques or masses with papillary, granular or verrucoid surface architecture
- May be white, yellow, pink or red in color (Head Neck Pathol 2020;14:742)
- Often < 1.5 cm
Diagnosis
- Biopsy with histopathological examination
Case reports
- 45 year old patient with VX of floor of mouth clinically mimicking malignancy (BMJ Case Rep 2015;2015:bcr2014209216)
- 47 year old man with chronic graft versus host disease presents with multiple VX lesions of the oral cavity (BMC Res Notes 2017;10:631)
- 52 year old man with oral submucous fibrosis presents with VX of maxillary gingiva (J Oral Maxillofac Pathol 2019;23:43)
- 56 year old woman with oral lichen planus presents with VX of tongue (Case Rep Dent 2018;2018:1615086)
Treatment
- Conservative excision is usually curative
- In a large series of 212 cases, only 3 cases were listed as recurrences (Head Neck Pathol 2020;14:742)
- In another large study of 429 cases, a 12% recurrence rate was noted (Med Oral Patol Oral Cir Bucal 2018;23:e429)
Clinical images
Gross description
- Raised, granular or verrucoid mass
Microscopic (histologic) description
- Accumulations of lipid laden, foamy macrophages within connective tissue papillae of papillary epithelial projections
- Papillary or verrucoid surface architecture covered by a thickened layer of orange parakeratin with keratin filled clefts between papillary projections (Med Oral Patol Oral Cir Bucal 2018;23:e429)
- Neutrophilic exocytosis may be present
- Lacks cytologic atypia
- Variable inflammation within the underlying connective tissue
Microscopic (histologic) images
Contributed by Molly Housley Smith, D.M.D. and Kelly Magliocca, D.D.S., M.P.H.
Videos
VX of skin, histology
Clinical description of VX
Sample pathology report
- Gingiva, excision:
- Verruciform xanthoma (see comment)
- Comment: The microscopic features show a well circumscribed papillary proliferation of epithelium covered by a thickened verrucoid parakeratin exhibiting neutrophilic exocytosis. Notably, the connective tissue papillae in between acanthotic rete ridges contain accumulations of foamy macrophages. Cytologic atypia is not appreciated. A chronic inflammatory cell infiltrate, consisting predominantly of lymphocytes, is appreciated within the superficial lamina propria.
Differential diagnosis
- Squamous papilloma:
- Well circumscribed papillary proliferation of squamous epithelium, often with converging rete ridges
- Lacks collections of lipid laden foamy macrophages in connective tissue papillae (Head Neck Pathol 2020;14:742)
- Associated with HPV (6 and 11 most commonly)
- Verruca vulgaris:
- Well circumscribed papillary / verrucoid proliferation of squamous epithelium, often with converging rete ridges, koilocytes and hypergranulosis
- Associated with HPV (2 and 4 most commonly)
- Lacks collections of lipid laden foamy macrophages in connective tissue papillae
- Proliferative verrucous leukoplakia / verrucous hyperplasia:
- Characterized clinically by multifocal white plaques with well defined margins that often progress
- Often affects marginal gingiva
- Histopathologically demonstrates verrucoid hyperkeratosis, sometimes with keratin plugging / clefting and sharp clonal margins
- Lacks circumscription
- Lacks collections of lipid laden foamy macrophages in connective tissue papillae
- Verrucous carcinoma:
- Atypical verrucoid hyperplasia of squamous epithelium with downward pushing margins and keratin clefting
- Lacks circumscription
- Lacks collections of lipid laden foamy macrophages in connective tissue papillae
Additional references
Board review style question #1
Board review style answer #1
C. Verruciform xanthoma. Answers A, B and D are incorrect because while papillomas, verrucous carcinomas and verruca vulgaris all may be solitary and show a verrucoid architecture, only verruciform xanthoma shows the characteristic aggregates of lipid laden macrophages within the connective tissue papillae.
Comment Here
Reference: Verruciform xanthoma
Comment Here
Reference: Verruciform xanthoma
Verrucous carcinoma
Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Definition / general
- Locally invasive, nonmetastasizing, highly differentiated, exophytic variant of squamous cell carcinoma
Essential features
- 2 - 12% of all oral carcinomas (Int J Oncol 2016;49:59)
- M > F; sixth to seventh decades of life
- May occur at any oral or pharyngeal site, although the oral cavity (tongue, buccal mucosa, alveolar mucosa) is the most common site
- Characterized by slow growing, verrucoid / cauliflower-like exophytic growth
- Elongated and bulbous rete ridges exhibiting a pushing margin below the level of intact, uninvolved surface epithelium; church spire peaks of keratin, keratin clefting and bland cytology
Terminology
- Use of historic term Ackerman tumor not recommended by 5th edition of the World Health Organization
ICD coding
- ICD-10: C00 - C14 - malignant neoplasm of lip, oral cavity and pharynx
Epidemiology
- 2 - 12% of all oral carcinomas (Int J Oncol 2016;49:59)
- M > F
- Sixth to seventh decades of life; mean age at diagnosis: 69.5 years (1973 - 2012) (Laryngoscope 2018;128:393)
Sites
- Oral tongue, alveolar ridge and buccal mucosa are the most common sites (Laryngoscope 2018;128:393, Int J Oncol 2016;49:59)
Pathophysiology
- Multistep process involving genetic alterations / predisposition and environmental influences (Int J Oncol 2016;49:59)
- Several biomarkers have been studied / identified; however, DAMTS12, COL4A1, COL4A2, INHBA, MMP1, SEROINE1, TGFBI and HLF are all genes that are expressed differently in oral verrucous carcinoma when compared to traditional oral squamous cell carcinoma, suggesting future therapeutic potential (Int J Clin Exp Med 2014;7:1845, Int J Oncol 2016;49:59)
Etiology
- Proliferative verrucous leukoplakia (PVL) is a known risk factor (Cancers (Basel) 2021;13:4085)
- 29.5% prevalence of developing verrucous carcinoma in patients with proliferative verrucous leukoplakia (Cancers (Basel) 2021;13:4085)
- Associations (synergistic or independent) with tobacco use, areca nut chewing, chronic inflammation, alcohol consumption, antioxidant deficient diet and oral microbiota (Int J Oncol 2016;49:59)
- Controversial association with HPV in older literature; no conclusive association has been proven (Int J Oncol 2016;49:59, Arch Otolaryngol Head Neck Surg 1993;119:1299, Pathobiology 2008;75:257, Tumour Biol 2011;32:409, Radiat Res 1970;41:375)
- No transcriptionally active high risk HPV has been identified (Hum Pathol 2013;44:2385)
Clinical features
- Exophytic, papillary or verrucoid mass
- Slow growth
- Locoregional metastasis and or bone involvement suggests transformation (or component) of conventional invasive squamous cell carcinoma (Int J Oncol 2016;49:59)
Diagnosis
- Along with supportive histopathology, diagnosis may incorporate one or more elements such as patient history, symptoms, clinical examination and imaging
Prognostic factors
- Nodal disease is found in 1.6% of cases and likely can be attributed to transformation into traditional invasive squamous cell carcinoma (Laryngoscope 2018;128:393)
- 2, 5 and 10 year survival rates are 83%, 64% and 42%, respectively (Laryngoscope 2018;128:393)
- Recurrence rate is high if incompletely excised
Case reports
- 14 year old boy with xeroderma pigmentosum presented with verrucous carcinoma on the tip of the tongue (Cureus 2022;14:e31706)
- 30 year old gutka chewer and 60 year old patient with an areca nut and tobacco chewing habit both presented with white verrucoid lesions of the oral cavity (Contemp Clin Dent 2016;7:391)
- 56 year old man with verrucous carcinoma treated successfully with topical 5-aminolevulinic acid mediated photodynamic therapy (J Oral Pathol Med 2005;34:253)
- 67 year old woman presented with a slowly growing, white verrucoid lesion on the maxillary alveolar ridge (Case Rep Oncol Med 2012;2012:190272)
Treatment
- Surgical removal with adequate margins is preferred treatment (Contemp Clin Dent 2012;3:60, Int J Oncol 2016;49:59)
- Chemotherapy and radiation have questionable effectiveness due to poor response and anaplastic transformation (Int J Oncol 2016;49:59, Laryngoscope 2017;127:1334)
Clinical images
Gross description
- White / tan
- Exophytic, papillary, fungating, cauliflower-like growth (J Maxillofac Oral Surg 2011;10:148)
- May bluntly invade adjacent soft tissue
Microscopic (histologic) description
- Poor interobserver agreement among pathologists (Head Neck Pathol 2020;14:156)
- Lack of consistency with terminology for verrucoid lesions creates confusion for clinicians (Head Neck Pathol 2020;14:156)
- Well differentiated / cytologically bland, hyperplastic squamous epithelium
- Broad, bulbous, plunging rete ridges that demonstrate pushing encroachment on muscle or other deep submucosal structures, below the level of intact normal epithelium (Head Neck Pathol 2021;15:572)
- Church spire-like or papillary hyperkeratosis with deep keratin clefting
- Intact basement membrane (Contemp Clin Dent 2016;7:391)
- Minimal cytologic atypia
- Inward cupping of the rete pegs is not apparent
Microscopic (histologic) images
Videos
Verrucous carcinoma
Cutaneous verrucous carcinoma
Sample pathology report
- Right buccal mucosa, biopsy:
- Verrucous carcinoma (see comment)
- Comment: Microscopic examination reveals atypical superficial stratified squamous epithelium overlying fibrous connective tissue. The epithelium exhibits a significantly thickened layer of orthokeratin that forms prominent church spire-like peaks. The rete ridges are bulbous and elongated, forming a broad, pushing margin that abuts skeletal muscle. Prominent keratin clefting / plugging is apparent. The underlying connective tissue contains a dense mixed inflammatory cell infiltrate immediately subjacent to the epithelial proliferation.
Differential diagnosis
- Oral squamous papilloma:
- May be difficult to differentiate from verrucous carcinoma on small, incisional or fragmented biopsies
- Caution is advised when making a diagnosis of papilloma on incisional or fragmented biopsies or when the lesion is not well circumscribed or symmetrical
- Limited growth potential, often small
- Papillary, finger-like projections with fibrovascular connective tissue cores
- Often pedunculated but may be sessile
- Well defined margins
- Lacks endophytic growth pattern
- Lacks prominent hypergranulosis
- Variable keratinization (Head Neck Pathol 2019;13:80)
- May be difficult to differentiate from verrucous carcinoma on small, incisional or fragmented biopsies
- Condyloma acuminatum:
- Labial mucosa, soft palate, lingual frenum
- Often demonstrates a fleshy, broad based clinical appearance but should demonstrate circumscription and symmetry
- Bulbous rete pegs and blunted papillary projections
- Exophytic; lacks broad, pushing, endophytic growth pattern
- Pseudoepitheliomatous hyperplasia:
- Associated with chronic candidiasis and granular cell tumor
- Extreme caution is recommended in diagnosing pseudoepitheliomatous hyperplasia, as secondary candidal colonization may be seen on atypical epithelial processes (e.g., verrucous carcinoma)
- Excision or rebiopsy of lesional tissue remaining after antifungal therapy may be recommended
- Lacks prominent exophytic growth pattern and endophytic pushing margin into bone or skeletal muscle
- Verruciform xanthoma:
- May demonstrate similar clinical characteristics, although may have yellow hue
- Demonstrates foamy xanthoma cells within papillary projections
- Proliferative verrucous leukoplakia / verrucous leukoplakia:
- Characterized by multifocal white plaques with well defined margins
- High transformation rate into verrucous carcinoma or squamous cell carcinoma
- Very similar histology to the bulky hyperkeratotic epithelial proliferation category of proliferative verrucous leukoplakia proposed by Thompson et al. in 2021 (Head Neck Pathol 2021;15:572)
- Verruciform, church spire-like keratin peaks, prominent endophytic growth with bulbous, hyperplastic rete ridges and keratin plugging
- Lacks the pushing architectural pattern
- Squamous cell carcinoma:
- Squamous cell carcinoma (SCCa) may arise within verrucous carcinoma
- Overt evidence of connective tissue invasion lacking intact basement membrane; SCCa shows infiltrative nests of epithelium and may invade into or around nerves, blood vessels or salivary glands
- SCCa may also infiltrate into skeletal muscle bundles, as opposed to verrucous carcinoma, which only pushes into the skeletal muscle
- Carcinoma cuniculatum and papillary squamous cell carcinoma in particular may be confused with verrucous carcinoma
- Carcinoma cuniculatum demonstrates deep burrowing of the epithelium with keratin filled crypts (J Clin Diagn Res 2017;11:ZD37)
- Papillary SCCa likely is confusing based on its name
- Papillary SCCa demonstrates a papillary or filiform architecture (like verrucous carcinoma) but lacks prominent surface keratinization and cytologically exhibits malignant epithelium
Additional references
Board review style question #1
Board review style answer #1
D. Verrucous carcinoma. The microscopic image shows a broad, verrucoid / papillary epithelial proliferation with prominent church spire hyperkeratosis on top of hyperplastic, pushing rete ridges. These findings are consistent with verrucous carcinoma. Answers A, B and C are incorrect because condyloma acuminatum, squamous papilloma and verruca vulgaris all may demonstrate exophytic papillary projections; however, all 3 of these entities should demonstrate some degree of circumscription (perhaps inward cupping rate ridges) and symmetry. Most importantly, these 3 entities should lack pushing, infiltrative rete ridges.
Comment Here
Reference: Verrucous carcinoma
Comment Here
Reference: Verrucous carcinoma
Board review style question #2
A patient presents with a white and red exophytic granular growth on the alveolar ridge. Microscopic examination shows church spire-like keratin peaks, keratin plugging and bulbous shaped, hyperplastic rete ridges that push downward and abut underlying bone. What is the diagnosis?
- Condyloma acuminatum
- Squamous papilloma
- Verruca vulgaris
- Verrucous carcinoma
Board review style answer #2
D. Verrucous carcinoma. Church spire-like keratin peaks, keratin plugging and bulbous shaped, hyperplastic rete ridges that push downward and abut underlying bone are all features of verrucous carcinoma. Answers A, B and C are incorrect because condyloma acuminatum, squamous papilloma and verruca vulgaris all may demonstrate exophytic papillary projections; however, all 3 of these entities should demonstrate some degree of circumscription (perhaps inward cupping rate ridges) and symmetry. Most importantly, these 3 entities should lack pushing, infiltrative rete ridges. Additionally, the clinical image shows a large, broad based lesion lacking symmetry. Clinically, condyloma acuminatum, squamous papilloma and verruca vulgaris show circumscription and symmetry.
Comment Here
Reference: Verrucous carcinoma
Comment Here
Reference: Verrucous carcinoma
White sponge nevus (pending)
[Pending]
WHO classification-oral cavity & oropharynx
Table of Contents
Definition / general | Major updates | WHO (2022) - oral cavity and mobile tongue tumors | WHO (2022) - oropharyngeal tumors (base of tongue, tonsils, adenoids) | Diagrams / tables | Microscopic (histologic) images | Additional references | Board review style question #1 | Board review style answer #1Definition / general
- WHO classification of tumors of the oral cavity and mobile tongue tumors and oropharynx (base of tongue, tonsils, adenoids)
- Currently on 5th edition, published in 2022
Major updates
- Oral cavity and mobile tongue tumors
- Added a section on nonneoplastic lesions, including necrotizing sialometaplasia, multifocal epithelial hyperplasia and melanoacanthoma
- Epithelial tumors were reorganized with alterations and significant expansions made in diagnosis of oral potentially malignant disorders and oral epithelial dysplasia, namely adding the concept of architectural dysplasia and better defining features of proliferative verrucous leukoplakia (PVL)
- Human papillomavirus (HPV) associated dysplasia was added to the classification as a separate entity with discussion of incomplete data existing on p16 as an adequate surrogate marker for HPV infection in the oral cavity
- Carcinoma cuniculatum and verrucous carcinoma are now listed separately as subtypes of oral squamous cell carcinoma based on distinctive clinical presentation as well as histopathological appearances and behavior
- RREB1::MRTFB gene fusion was added to ectomesenchymal chondromyxoid tumor
- Sections on soft tissue and neural tumors, oral mucosal melanoma, salivary gland tumors and hematolymphoid tumors are removed from the oral cavity section and inserted into chapters dedicated to those tumor categories
- Oropharyngeal tumors (base of tongue, tonsils, adenoids)
- Draws the clear distinction of oropharyngeal squamous cell from squamous cell carcinoma of the oral cavity, larynx, nasopharynx and sinonasal tract, emphasizing the critical role of p16 / HPV testing in routine practice
- Section on tonsillar hamartomas has been added
- To reduce redundancy, sections on salivary gland, neuroendocrine tumors and lymphoid malignancies have been removed from this chapter and inserted into other chapters
- Reference: Head Neck Pathol 2022;16:54
WHO (2022) - oral cavity and mobile tongue tumors
| Nonneoplastic lesions | ICD-O | ICD-11 |
| DA04 | ||
| 1E82.0 | ||
| 2E90.3
| ||
| Epithelial tumors | ||
| ||
| 8052/0 | 2E90.3 & XH50T2 | |
| ||
| 8077/0, 8077/2 | ||
| DA01.00 | ||
| DA02.2 | ||
| ||
| 8071/3 | 2B6E.0 | |
| 8051/3 | 2B66.0 & XH5PM0 | |
| 8071/3 | 2B6E.0
| |
| Tumors of uncertain histogenesis | ||
| KC23 | ||
| 9580/0, 9580/3 | 2E90.1 | |
| 8982/0 | ||
| 9363/0 | 2D42 & XH6C72
| |
| Hematolymphoid proliferations and neoplasia | ||
WHO (2022) - oropharyngeal tumors (base of tongue, tonsils, adenoids)
| Benign oropharyngeal lesions | ICD-O | ICD-11 |
| DB35.3
| |
| Epithelial tumors | ||
| 8085/3 | 2B6A.0 & XH0EJ7 | |
| 8086/3 | 2B6A.0 & XA4J67 & XH4CR9 |
Diagrams / tables
None
Microscopic (histologic) images
Contributed by Molly Housley Smith, D.M.D.
Additional references
Board review style question #1
A patient presents with a brown patch on the buccal mucosa. Which of the following is true regarding oral melanoacanthomas?
- They are frequently very painful
- They are more common in males
- They occur more frequently in patients with lower natural levels of skin pigmentation
- They often present as a rapidly growing pigmented lesion
Board review style answer #1
D. They often present as a rapidly growing pigmented lesion. Melanoacanthomas often present as rapidly growing, smooth, sometimes mildly raised, pigmentated zones involving any area of the oral mucosa. Answer C is incorrect because melanoacanthomas are more often found in patients with higher natural levels of skin pigmentation. Answer B is incorrect because melanoacanthomas more commonly affect females. Answer A is incorrect because they are often asymptomatic or show mild symptoms, such as itching or burning.
Comment Here
Reference: WHO classification-oral cavity & oropharynx
Comment Here
Reference: WHO classification-oral cavity & oropharynx
WHO classification-oral cavity & oropharynx
Table of Contents
Definition / general | WHO (2017) - Oral cavity | WHO (2017) - Oropharynx | Additional referencesDefinition / general
- WHO classification of tumors of the oropharynx (base of tongue, tonsils, adenoids)
- Currently on 4th edition, published in 2017
WHO (2017) - Oral cavity
Oral potentially malignant disorders and oral epithelial dysplasia
- Oral potentially malignant disorders - general (pending)
- Oral epithelial dysplasia
- Proliferative verrucous leukoplakia
Papillomas
Tumors of uncertain histogenesis
Soft tissue and neural tumors
- Granular cell tumor
- Rhabdomyoma
- Lymphangioma
- Hemangioma
- Schwannoma
- Neurofibroma
- Kaposi sarcoma
- Myofibroblastic sarcoma
Oral mucosal melanoma
Salivary type tumors
Hematolymphoid tumors
- CD30 positive T cell lymphoproliferative disorder
- Plasmablastic lymphoma
- Langerhans cell histiocytosis
- Extramedullary myeloid sarcoma
WHO (2017) - Oropharynx
-
Squamous cell carcinoma ICD-O
- See also Salivary glands chapter
- Pleomorphic adenoma8940/0
- Adenoid cystic carcinoma8200/3
- Polymorphous adenocarcinoma8525/3
Salivary gland tumors ICD-O
Hematolymphoid tumors ICD-O
ICD-O note: The first four digits indicate the specific histological term. The fifth digit after the slash (/) is the behavior code, which indicates whether a tumor is malignant, benign, in situ or uncertain (whether benign or malignant) (WHO: International Classification of Diseases for Oncology, 3rd Edition (ICD-O-3))
Additional references
Recent Oral cavity & oropharynx Pathology books
Find related Pathology books: head & neck/endocrine