Table of Contents
Definition / general | Essential features | Terminology | Anatomy | Embryology | Physiology | Diagrams / tables | Clinical features | Laboratory | Radiology description | Radiology images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Videos | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Stringham N. Anatomy & histology-adrenal cortex, medulla & paraganglia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/adrenalglandcortex.html. Accessed April 20th, 2024.
Definition / general
- Adrenal cortex is the outer layer of the adrenal gland responsible for synthesizing and secreting mineralocorticoids, glucocorticoids and sex hormones; this steroid hormone secretion corresponds histologically to its 3 cellular layers: zona glomerulosa, zona fasciculata and zona reticularis
- Adrenal medulla is a neuroendocrine organ (paraganglia) composed of chromaffin cells, which secrete catecholamines; extra-adrenal paraganglia are aggregates of crest derived neuroendocrine cells that are dispersed throughout the body and are associated with autonomic function
Essential features
- Adrenal glands are paired endocrine organs that are comprised of 2 embryologically distinct layers (cortex and medulla) and are situated above the kidneys within the retroperitoneum
- Adrenal medulla is a neuroendocrine organ composed of chromaffin cells, which secrete catecholamines (norepinephrine and epinephrine) and originate from neural crest
- Adrenal cortex has 3 layers that are histologically and physiologically distinct, listed below from superficial to deep
- Zona glomerulosa: produces mineralocorticoids, specifically aldosterone, which increases sodium and water absorption and potassium secretion
- Zona fasciculata: produces glucocorticoids (cortisol) and some sex hormones
- Zona reticularis: produces estrogens and androgens, some glucocorticoids; this layer lies adjacent to the adrenal medulla
- Paraganglia are aggregates of neurosecretory chromaffin cells; extraadrenal paraganglia are dispersed throughout the body and are divided into the following 4 subgroups
- Chemoreceptor, intravagal, sympathetic and visceral - autonomic
Terminology
- Suprarenal glands
Anatomy
- Adrenal gland is composed of the inner medulla and outer cortex; each region is histologically, embryologically and physiologically distinct (StatPearls: Anatomy, Abdomen and Pelvis - Adrenal Glands (Suprarenal Glands) [Accessed 7 November 2023])
- Adrenal cortex
- Mesodermal origin
- Produces steroid hormones aldosterone, cortisol and sex hormones
- Adrenal medulla
- Neuroectodermal origin
- Produces catecholamines (epinephrine and norepinephrine)
- Adrenal cortex
- Adrenal gland is surrounded by a complete connective tissue capsule, which may merge with capsule of kidney (bilaterally) and the liver (on the right side)
- In cross section, adrenal cortex surrounds the medulla and comprises the majority of the tissue (~85%)
- Coronally, the right gland is pyramidal and the left is crescentic
- Axially, the right gland is V shaped with a medial limb that is larger than the lateral limb; the left gland is triangular
- Adrenal glands are retroperitoneal organs and are located atop the kidneys (i.e., suprarenal)
- Right gland is medial to the right lobe of the liver and posterior to the inferior vena cava
- Left gland is medial to the spleen, lateral to the aorta and posterior to the pancreatic tail
- Normal size range is 2 - 4 mm thick and 2 - 4 cm in length
- Normal weight is 4 - 6 grams each gland after dissection of fat
- Acute stress reduces lipid content and weight
- Prolonged stress induces hypertrophy and hyperplasia and increases weight
- Adrenal enlargement can result from endocrine disorders (e.g., Cushing syndrome, multiple endocrine neoplasia type 1 [MEN1], primary hyperaldosteronism, congenital adrenal hyperplasia) (Int J Endocrinol 2015:2015:192874)
- Neonatal gland is dark red-brown with no visible medullary tissue
- Arterial supply to the adrenal glands is by the aorta, inferior phrenic arteries and renal arteries via the superior, middle and inferior adrenal arteries; venous return is via the right adrenal vein to inferior vena cava and left adrenal vein to left renal vein
- 2 lymphatic plexuses are present, one just deep to the capsule and one within the medulla; these drain to the para-aortic and lateral aortic lymph nodes (Am J Anat 1966;119:359, UpToDate: Surgical Anatomy of the Adrenal Glands [Accessed 5 January 2024])
- Light and electron microscopy has shown that adrenal cortex in an adult is innervated by the autonomic nervous system; specifically postganglionic unmyelinated fibers to zona fasciculata (J Neural Transm Gen Sect 1991;84:75)
- Cells of the adrenal medulla are considered specialized sympathetic postganglionic neurons; however, instead of utilizing neurotransmitter, the medulla releases hormones thus functioning as a neuroendocrine transducer (Am J Pharm Educ 2007;71:78)
- Adrenal medulla receives sympathetic innervation from the greater splanchnic nerve; these preganglionic type B nerve fibers arise from the intermediolateral column of the lateral horn of the spinal cord at T5-T8 (StatPearls: Anatomy, Abdomen and Pelvis - Adrenal Glands (Suprarenal Glands) [Accessed 5 January 2024])
- Paraganglia (Treuting: Comparative Anatomy and Histology - A Mouse, Rat, and Human Atlas, 2nd Edition, 2017, Nosé: Diagnostic Pathology - Endocrine, 2nd Edition, 2019)
- Sympathetic paraganglia are situated along the paravertebral sympathetic chain and near nerves that supply organs of the pelvis and retroperitoneum
- Parasympathetic paraganglia are arranged along the glossopharyngeal and vagus nerves; these include the carotid and aortic bodies as well as the jugulotympanic, orbital, vagal, laryngeal paraganglia (head and neck paraganglia)
- Carotid body weight correlates with body weight and can be estimated using the equation, CBw = 0.29 x body weight + 3.0, where CBw is the combined weight of the bilateral carotid bodies
Embryology
- Adrenal medulla and cortex have different embryonic origins
- Adrenal medulla originates from neural crest and has large eosinophilic cells mixed with small nodules of primitive neuroblastic cells
- Adrenal cortex is derived from intermediate mesoderm; its earliest form, called the adrenal blastema or primordium, arises 4.5 weeks postconception
- At 6 weeks postconception, adrenal glands enlarge and pheochromoblasts migrate through the fetal cortex to form what will become medulla; at this point paraganglionic cells replicate and differentiate into chromaffin cells, which express chromogranin A and tyrosine hydroxylase
- At 8 weeks postconception, outer (definitive) cortex is distinct from inner (fetal) cortex and the organ becomes encapsulated; each gland weighs ~4 mg
- Fetal adrenal gland is relatively large and at week 20, is roughly the same size as the kidney
- However, after birth a decrease in androgen secretion promotes involution of the inner fetal cortex resulting in a weight decrease of ~50%
- Fetal cortex involution also results in a postnatal gland that is ~33% the size of the kidney
- Surrounding mesenchyme differentiates to form an outer adrenal cortex, which is later replaced and becomes adult cortex
- Extra-adrenal paraganglia of the head and neck develop in association with the arteries and cranial nerves of the ontogenetic gill arches
- References: Endocr Rev 2011;32:317, Clin Anat 2015;28:235, Gnepp: Diagnostic Surgical Pathology of the Head and Neck, 2nd Edition, 2009
Physiology
- Zona glomerulosa: produces mineralocorticoids (salt regulation)
- Mineralocorticoids act on the renal distal tubules of the kidney to increase sodium reuptake and promote potassium excretion
- Overall physiologic effect is increased water reabsorption and increased blood pressure
- Aldosterone accounts for ~90% of mineralocorticoid activity; others are 11-deoxycorticosterone and corticosterone
- Regulated by angiotensin II, potassium and adrenocorticotropic hormone (ACTH); also modulated by dopamine, atrial natriuretic peptide and other neuropeptides
- Zona fasciculata: produces glucocorticoids (sugar regulation)
- Release of cortisol raises blood glucose level
- Cortisol also regulates metabolism (increases gluconeogenesis), immune function (immunosuppression) and blood pressure (via regulation of vasoconstrictors and dilators)
- Cortisol is secreted in response to stress and by activation of the hypothalamic pituitary adrenal (HPA) axis; release is controlled by ACTH secretion from anterior pituitary, which is controlled by corticotropin releasing hormone (CRH) from the hypothalamus
- Biosynthesis of glucocorticoids is also influenced by catecholamines, neuropeptides and some cytokines (i.e., IL1, IL6, TNF)
- Zona reticularis: produces androgens (sex hormones)
- Primary products are dehydroepiandrosterone (DHEA), DHEA sulfate (DHEA-S) and androstenedione (testosterone precursor); some glucocorticoid production
- Precursors that require peripheral conversion to active sex steroids within the gonads or elsewhere; androgens are the main source of circulating testosterone in females
- Circulating DHEA-S is the best measure of adrenal androgen excess
- Regulation of adrenal cortex (Int J Mol Sci 2017;18:2150, Nephron Physiol 2014;128:26, Endocrinol Metab Clin North Am 1991;20:401)
- Hypothalamic corticotropin releasing hormone (CRH) stimulates release of ACTH from the anterior pituitary gland, which is transported in the blood to adrenal cortex; pituitary ACTH is the primary regulator of glucocorticoid and androgen synthesis; however, androgens are also controlled by other factors (e.g., adrenal blood supply and hormones)
- Negative feedback on HPA axis: cortisol and ACTH inhibit release of CRH; cortisol also inhibits secretion of ACTH
- Mineralocorticoid regulation: changes in blood volume affect renin - angiotensin system and stimulates secretion of aldosterone; potassium levels also affect aldosterone activity and subsequent acid base balance
- Medulla synthesizes and secretes catacholamines (20% epinephrine and 80% norepinephrine) and is the largest sympathetic paraganglion
- Dopamine is the precursor to catacholamines, which is combined with tyrosine to form norepinephrine
- Phenylethanolamine N methyltransferase (PNMT) is present in the adrenal medulla and can methylate norephinephrine to form epinephrine (Am J Physiol Regul Integr Comp Physiol 2004;287:R1007)
- Activity of the medulla is regulated via direct neural input
- Parasympathetic paraganglia function as chemoreceptors and are sensitive to changes in blood CO2, pH and oxygen; detection of these changes help to regulate respiration and circulation
- Carotid and aortic bodies can increase heart rate and elevate arterial blood pressure (sympathetic) or increase respiration depth, volume and rate (parasympathetic) (Treuting: Comparative Anatomy and Histology - A Mouse, Rat, and Human Atlas, 2nd Edition, 2017)
Diagrams / tables
Clinical features
- Primary aldosteronism, excessive aldosterone production from the adrenal gland, is the most common form of secondary arterial hypertension; alterations in the vascular compartment may underlie development of this condition (Front Endocrinol (Lausanne) 2022:13:995228)
- Adrenal pathologies can result in hypertension, such as in Cushing syndrome (excess cortisol); additionally, excess aldosterone can cause treatment resistant hypertension (Int J Mol Sci 2017;18:2150, Arch Endocrinol Metab 2017;61:305)
- Neoplasms of the adrenal medulla are referred to as pheochromocytomas whereas neoplasms of the paraganglia are termed paragangliomas
- Chemodectoma has been used for tumors of the chemoreceptor paraganglia
Laboratory
- Both core biopsy and fine needle aspirate (FNA) biopsy is useful for diagnosing metastatic carcinoma (Am J Clin Pathol 2012;137:124)
- Adrenal biopsy cannot distinguish normal adrenal cortex from adrenocortical adenoma or from sampling error (Am J Clin Pathol 2012;137:124)
- Primary function of adrenal biopsy is to evaluate adrenal metastasis
- Reference: Tickoo: Biopsy Interpretation of the Kidney & Adrenal Gland, 1st Edition, 2015
Radiology description
- On ultrasound, cortex is hypoechoic to medulla; medulla is echogenic
- T1 weighted: isodense to liver
- T2 weighted: brighter than fat and slightly brighter than liver
- Reference: Radiol Technol 2009;81:57
Radiology images
Gross description
- Normal size of adult adrenal glands is 2 - 4 mm thick and 2 - 4 cm in length
- Normal weight is 4 - 6 grams each gland after dissection of fat
- Acute stress reduces lipid content and weight
- Prolonged stress induces hypertrophy and hyperplasia and increases weight
- Adrenal enlargement can result from endocrine disorders (e.g., Cushing syndrome, multiple endocrine neoplasia type 1 [MEN1], primary hyperaldosteronism, congenital adrenal hyperplasia) (Int J Endocrinol 2015:2015:192874)
- Neonatal adrenal gland is dark red-brown with no distinct medullary tissue
- Adult adrenal gland is yellow due to its lipid content
Gross images
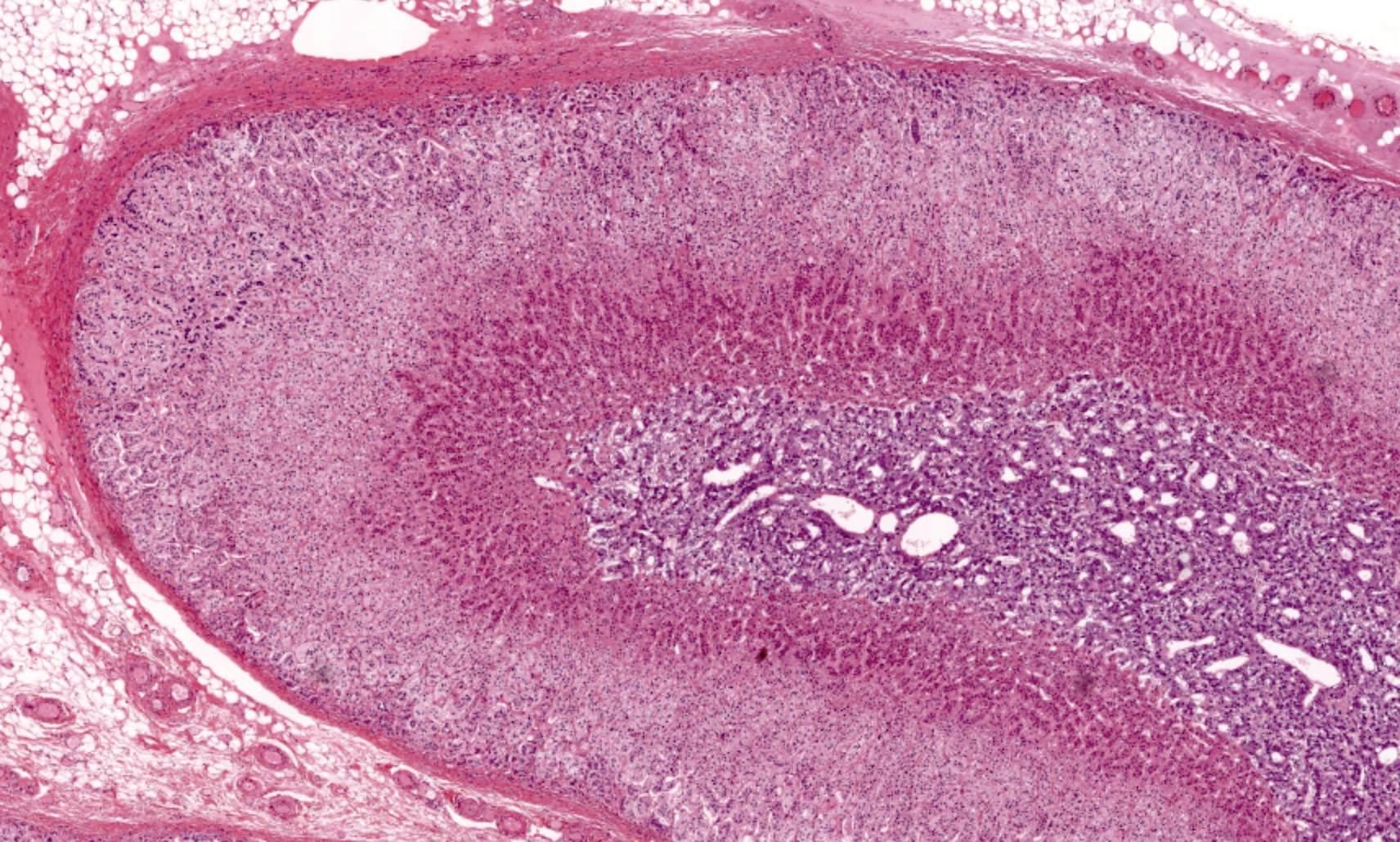
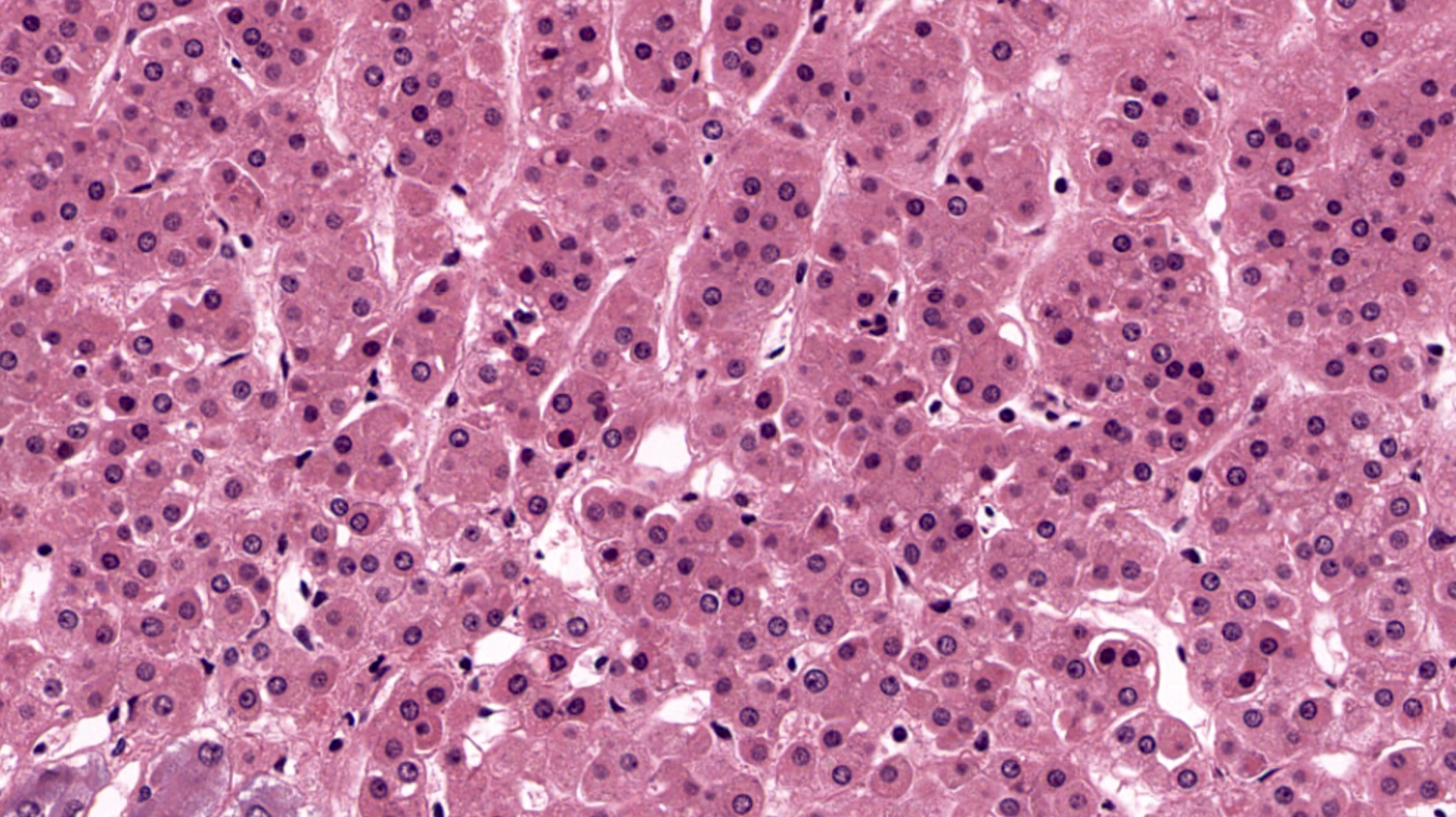
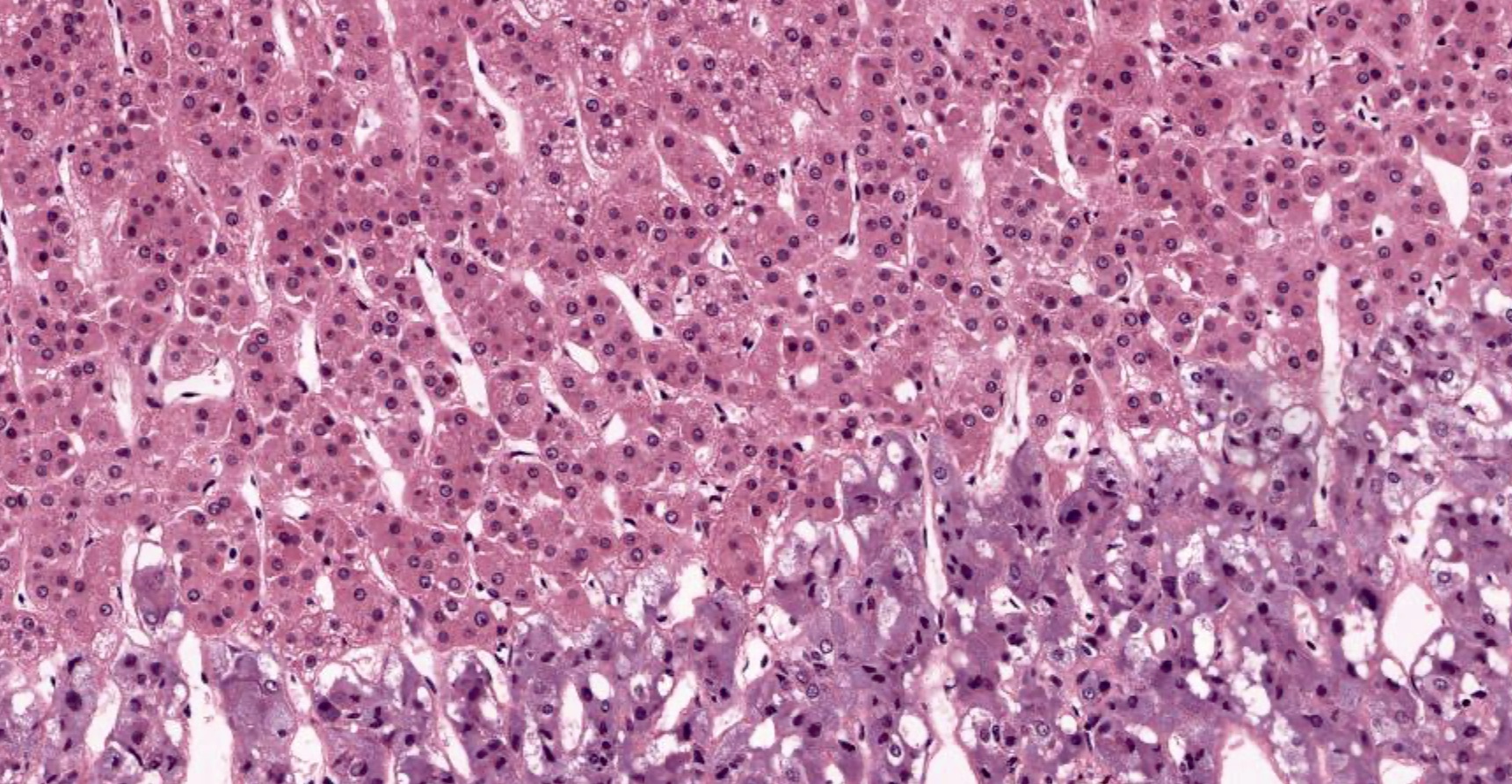
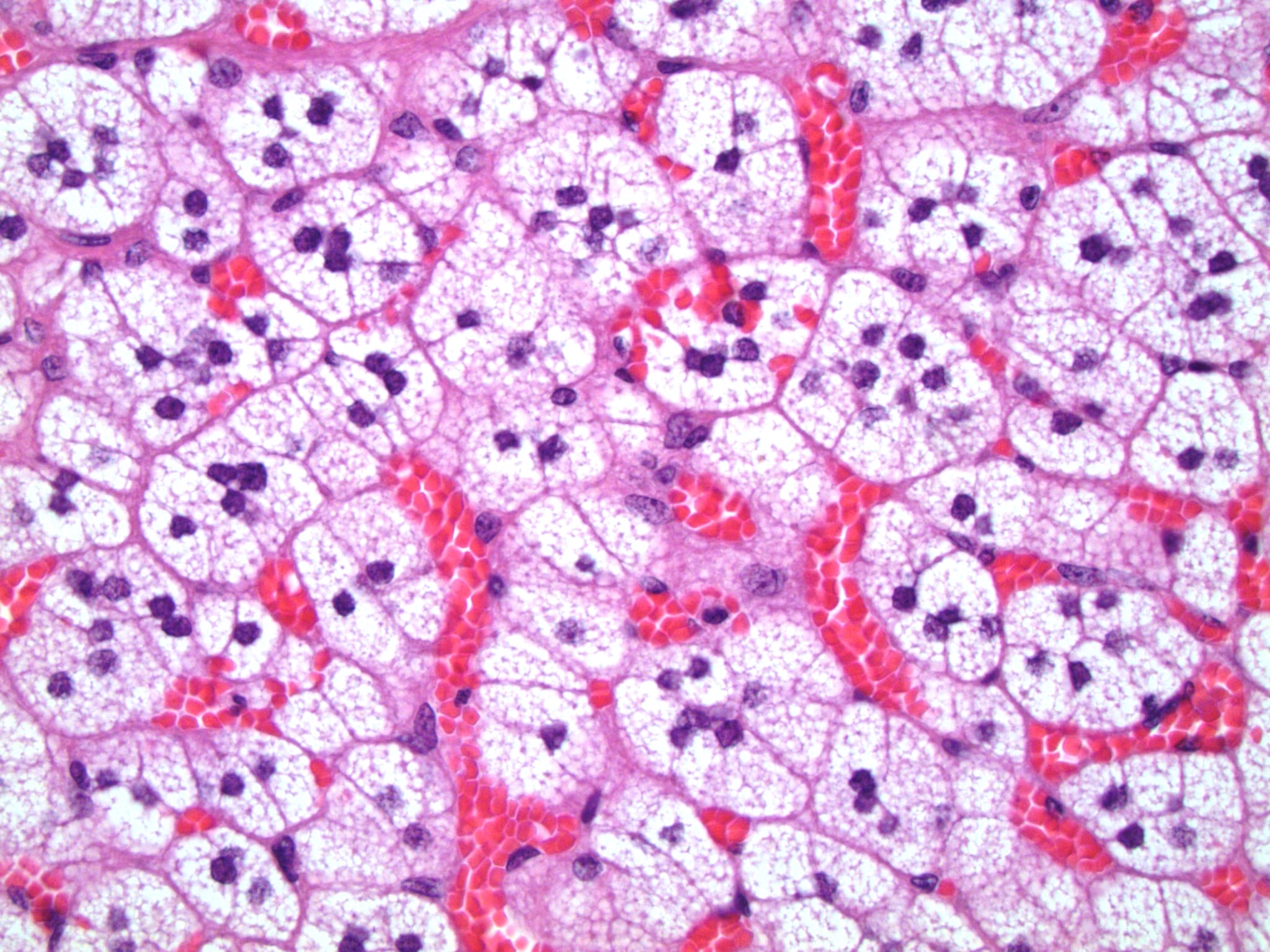
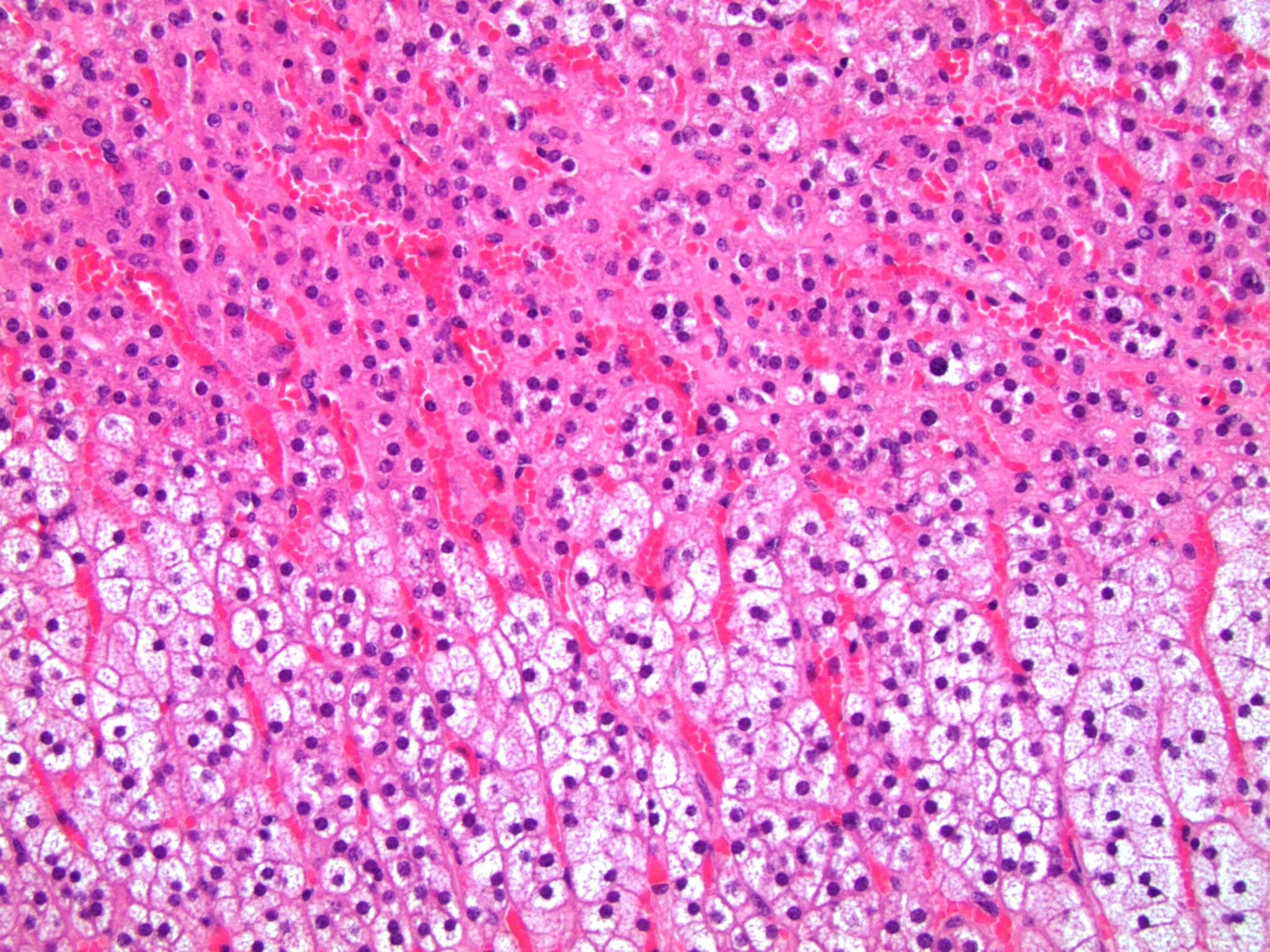
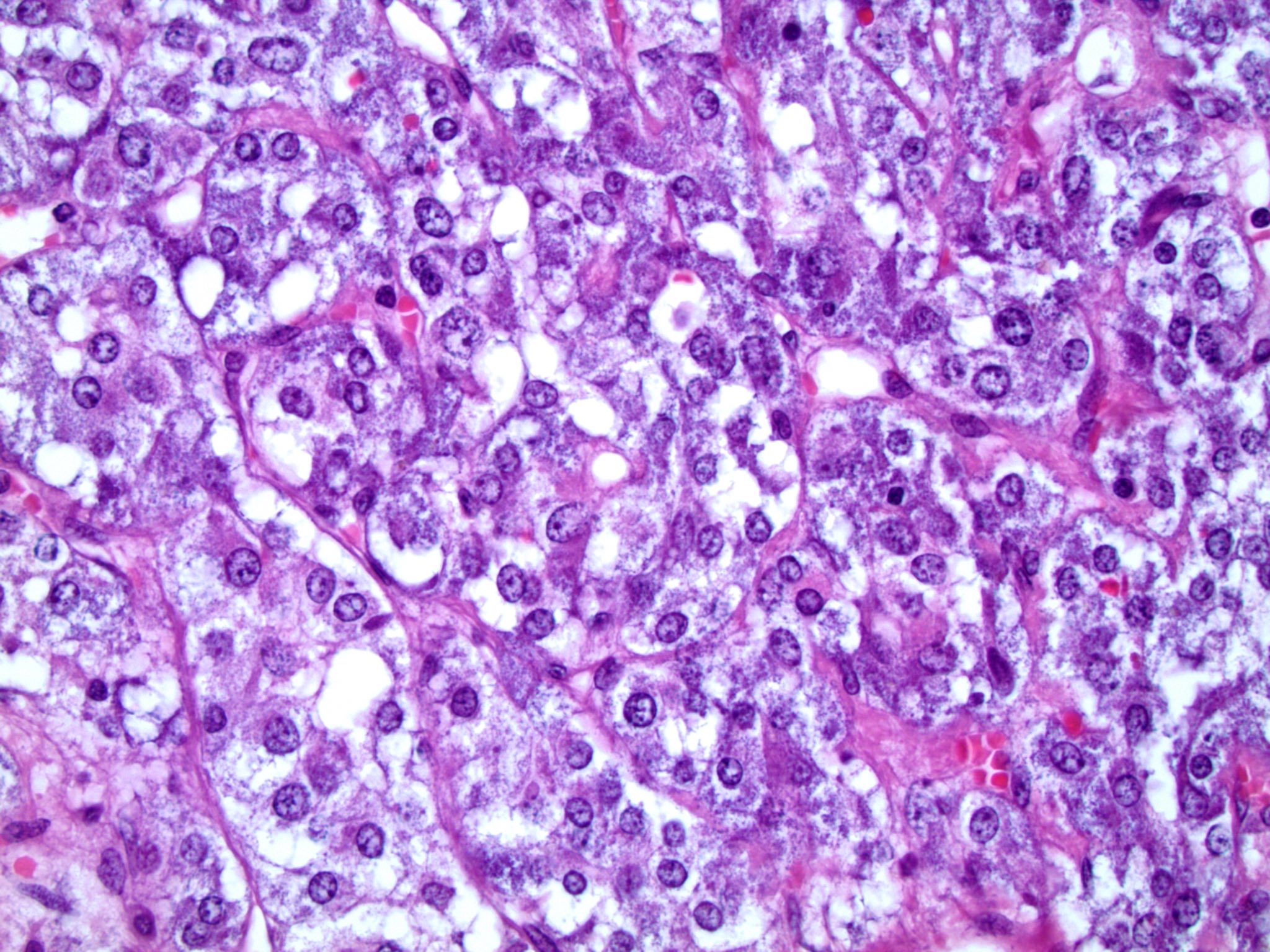
Microscopic (histologic) description
- Adrenal cortex has 3 zones that can be appreciated at the microscopic level
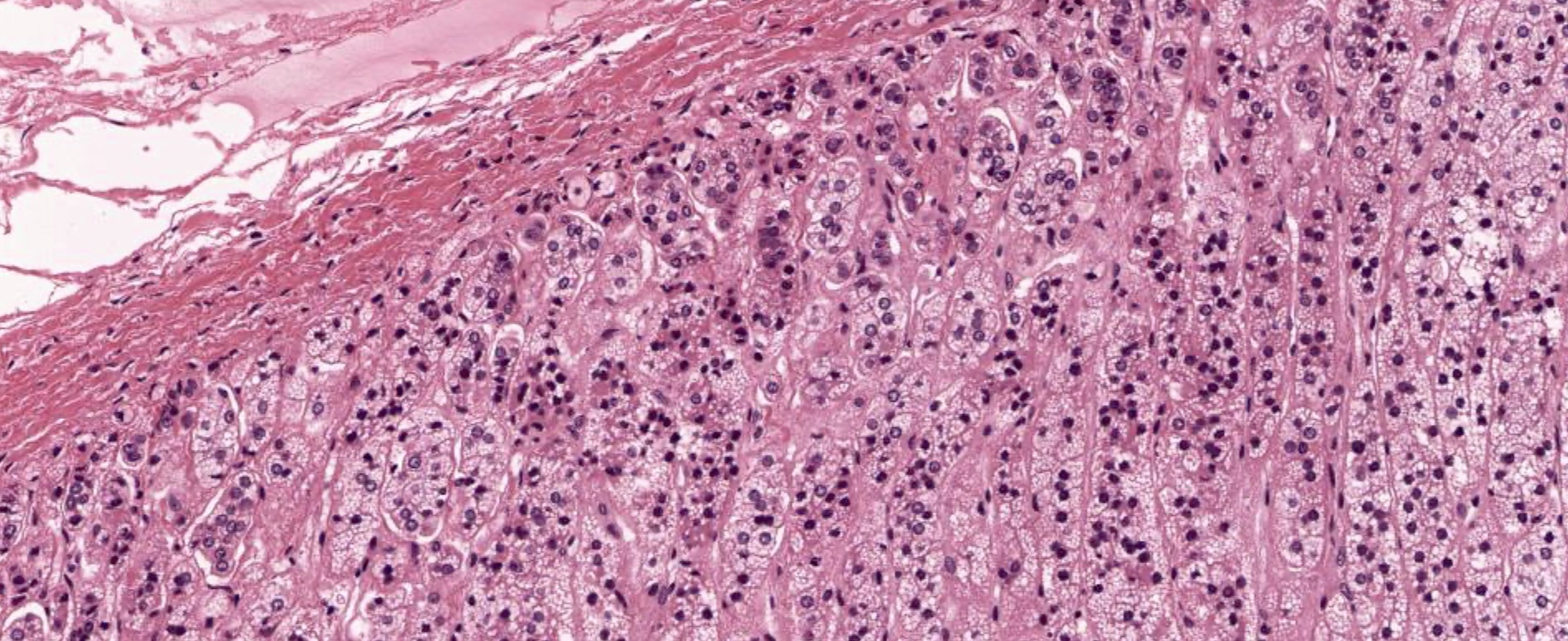
- Zona glomerulosa
- Outermost / superficial layer of cortex, just beneath the connective tissue capsule
- Well defined cells are arranged in small, round clusters
- Lipid poor with less cytoplasm than other cortical cells
- ~15% of cortical volume
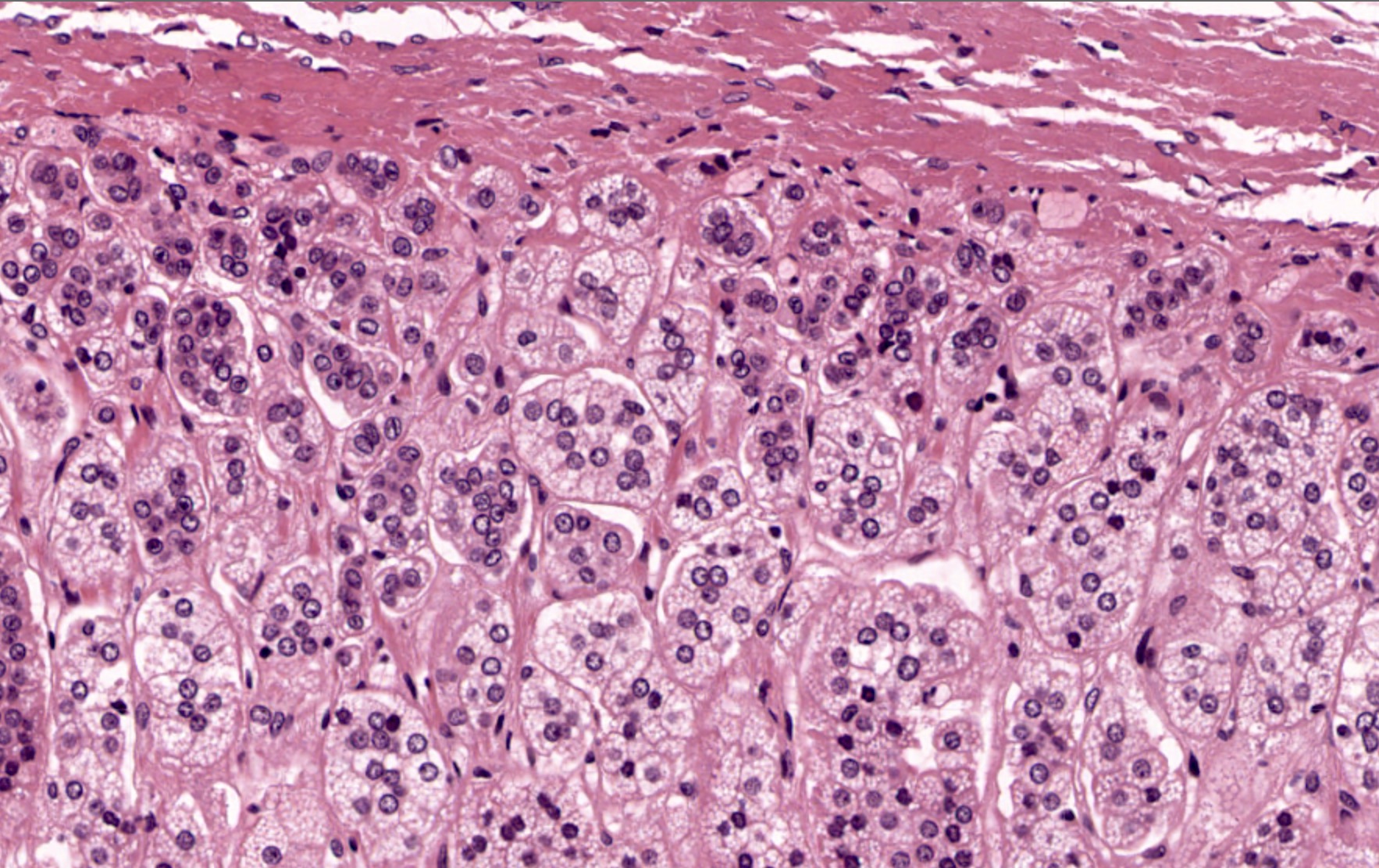
- Zona fasciculata
- Middle / intermediate layer of cortex
- Broad, lighter staining zone of large cells with distinct membranes; cells are arranged in cords 1 - 2 cells wide that run perpendicular to the surface of the gland
- Cytoplasm has numerous small lipid vacuoles, which may indent the central nucleus and give the cells a frothy appearance
- Largest layer of cortex; ~70 - 80% of cortical volume
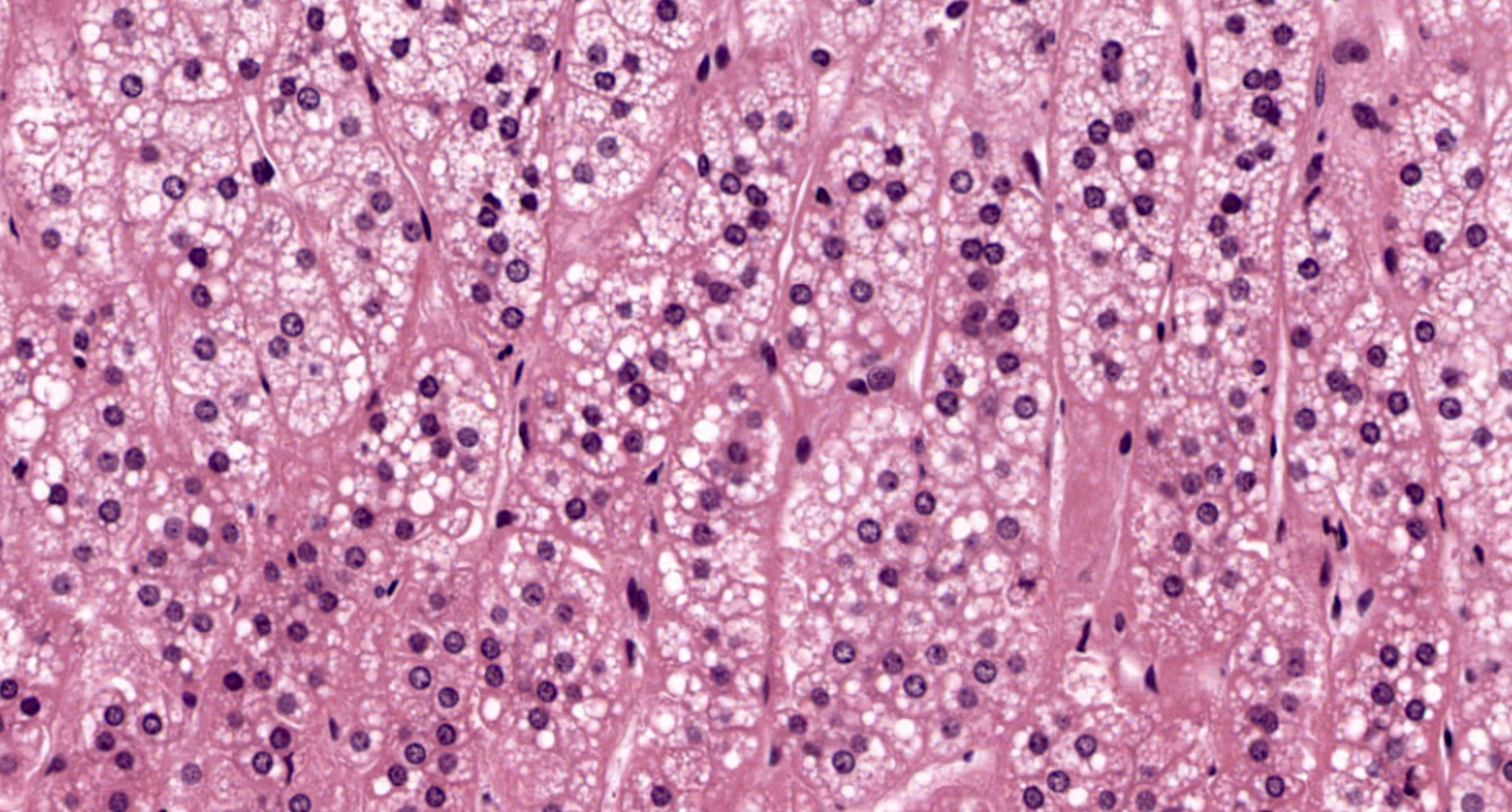
- Zona reticularis
- Innermost / deep layer of cortex; immediately adjacent to adrenal medulla
- Cells are arranged in a reticular (i.e., net-like) pattern of anastomosing cords; cells are smaller than those of the zona fasciculata
- Granular and eosinophilic cytoplasm with lipofuscin but very little lipid
- Thinner layer than zona glomerulosa or fasciculata; darkest staining layer of adrenal cortex
- Zona glomerulosa
- Adrenal cortex is richly vascularized tissue that shows abundant capillaries throughout, with capsular blood vessels, nerves and lymphatics penetrating the organ along connective tissue septa
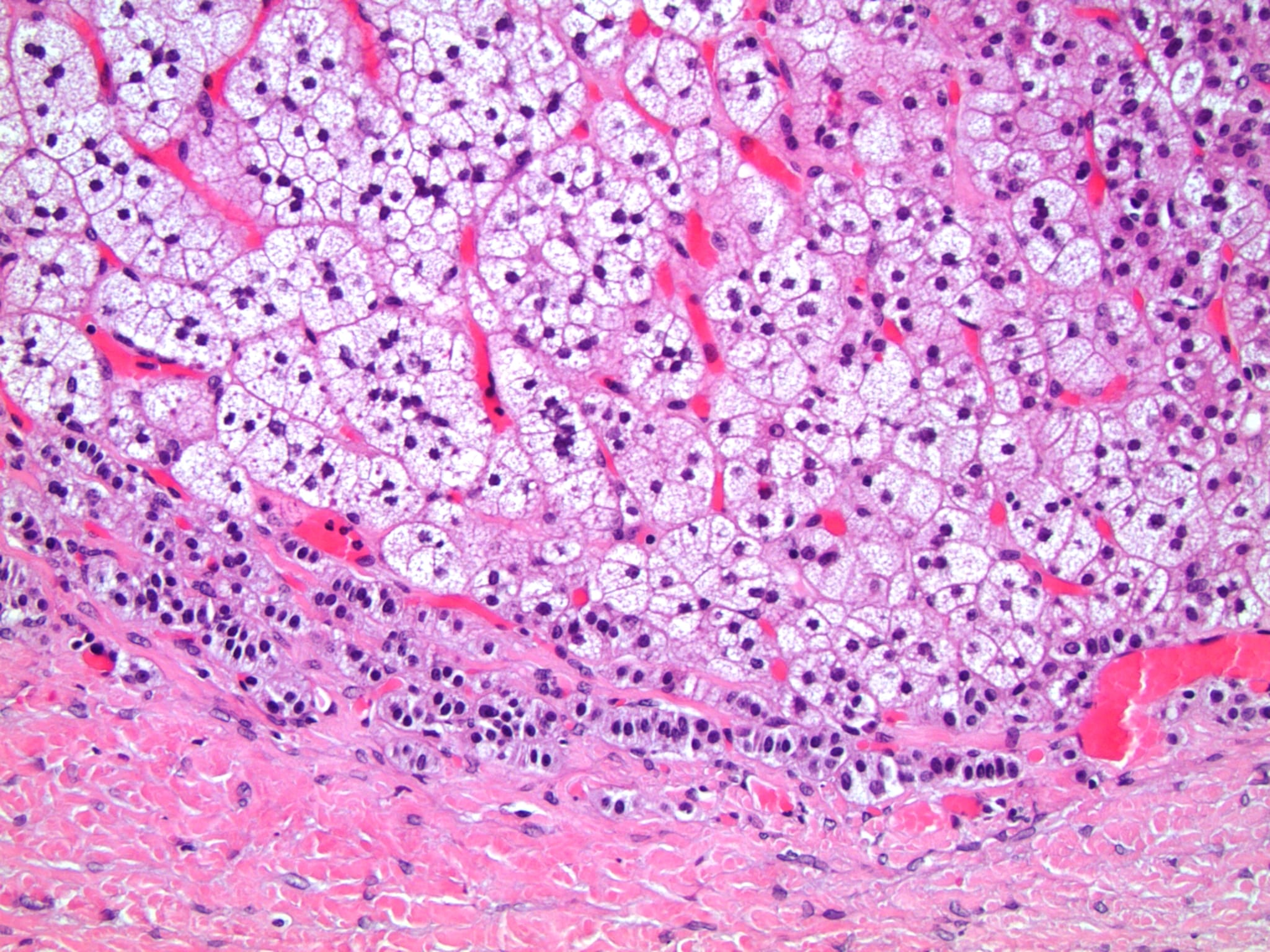
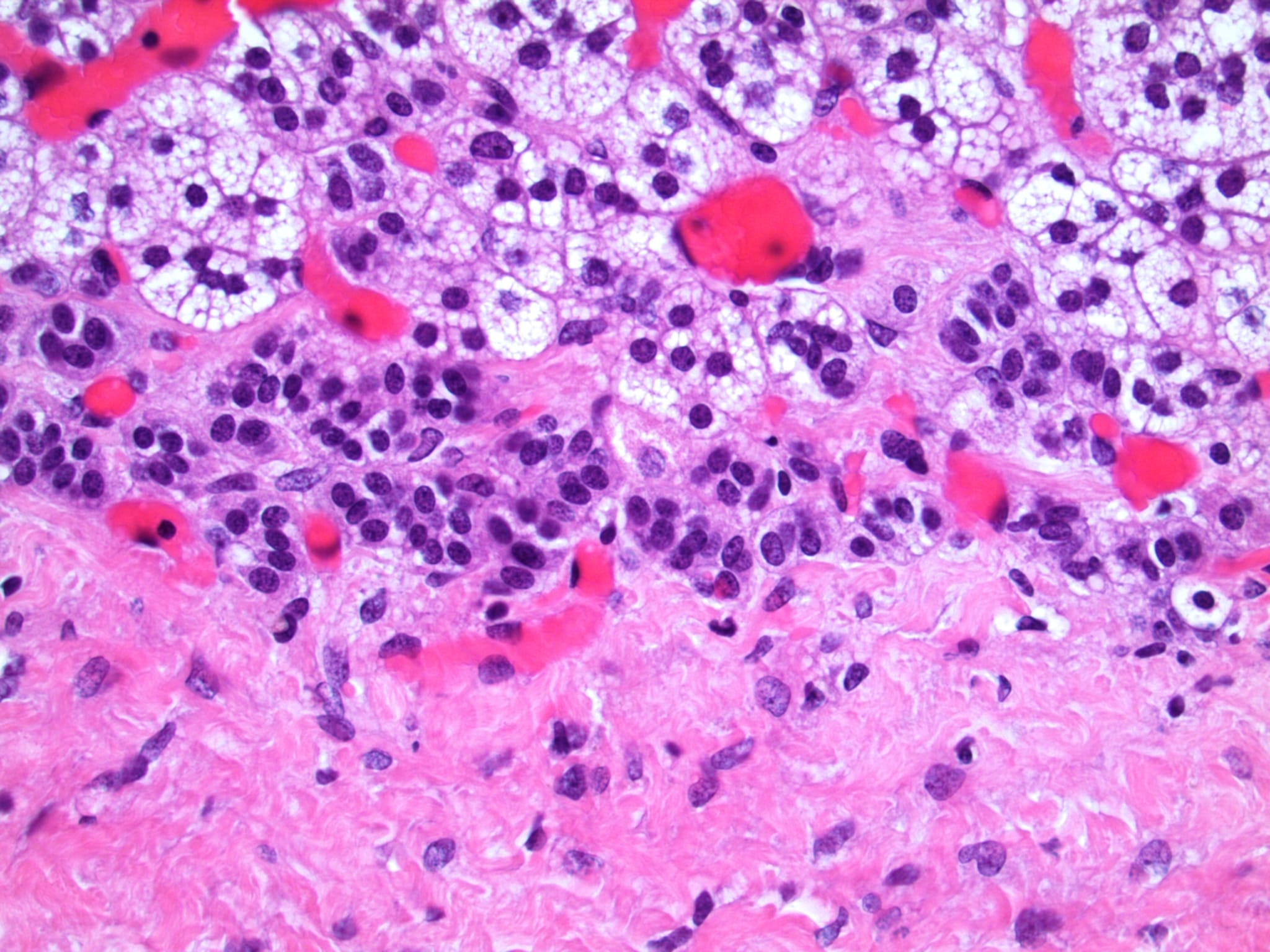
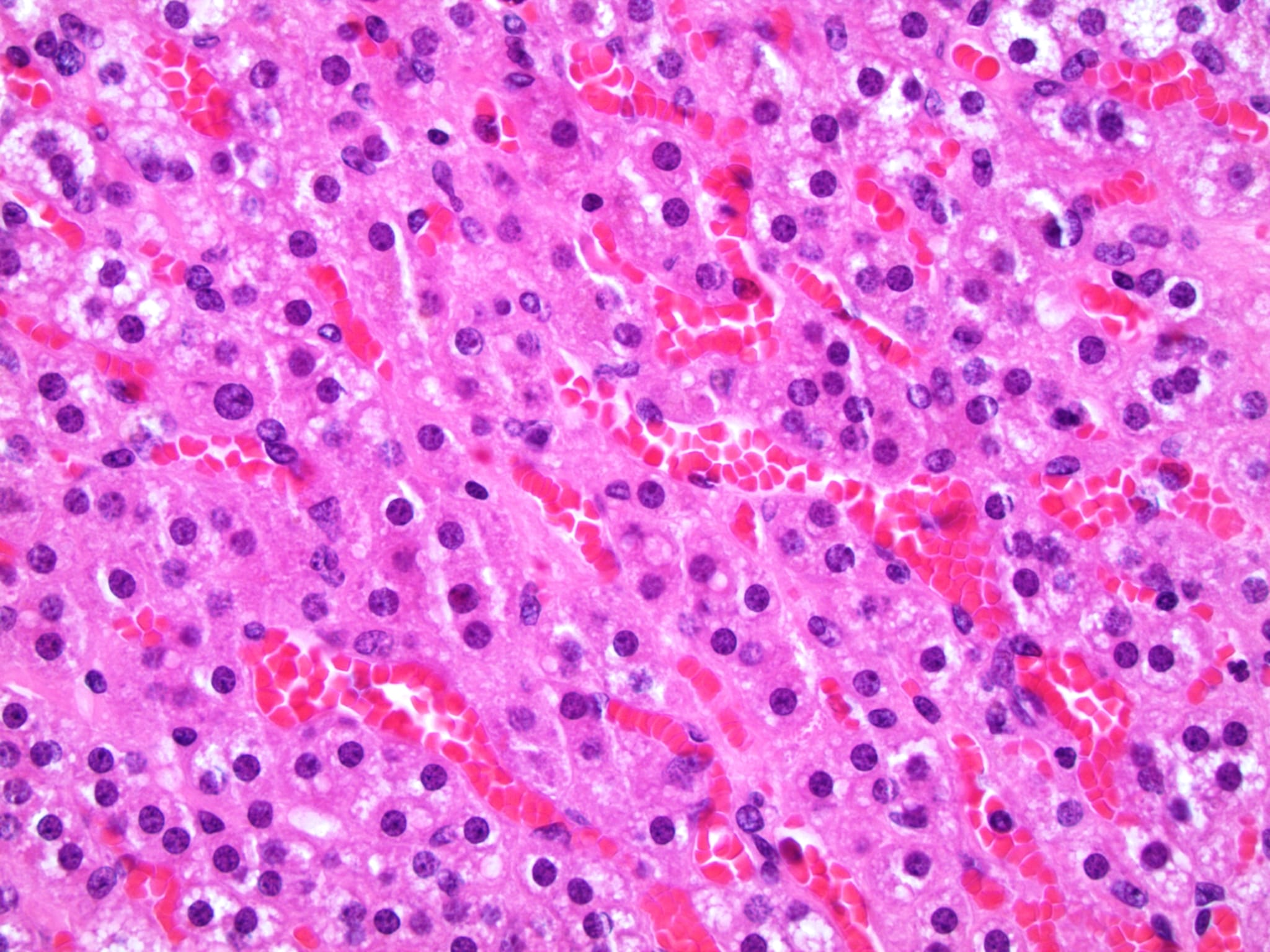
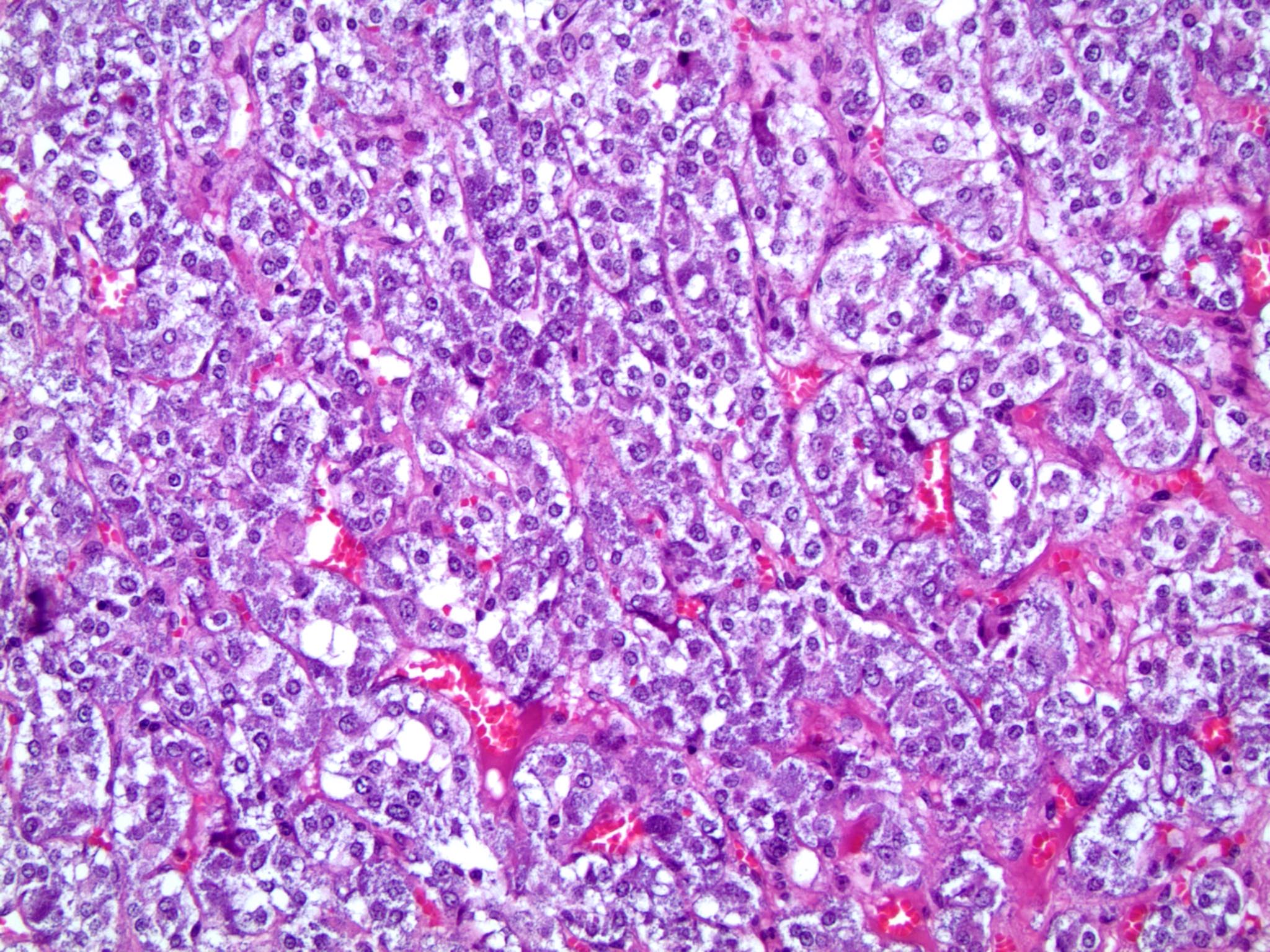
- Adrenal medulla is the innermost portion of the adrenal gland and is composed of chromaffin cells, sustentacular cells and occasional ganglion cells
- Chromaffin cells are large polygonal neuroendocrine cells that are arranged in nests and clusters around blood vessels throughout the adrenal medulla; they have abundant membrane bound granules and a basophilic cytoplasm and are the functional cell of the gland
- Chromaffin cells are named for the cellular granules that darken after exposure to chromium salts
- Sustentacular cells are spindle shaped support cells that are found in close proximity to chromaffin cells and are hypothesized to have glial functions (Front Endocrinol (Lausanne) 2020;11:79)
- Vasulature of the medulla includes venous channels, which drain blood from the cortical sinusoids and into the medullary vein
- Central adrenomedullary vein contains smooth muscle in the tunica media; most commonly one central vein drains each adrenal gland (Clin Anat 2014;27:1253)
- Chromaffin cells are large polygonal neuroendocrine cells that are arranged in nests and clusters around blood vessels throughout the adrenal medulla; they have abundant membrane bound granules and a basophilic cytoplasm and are the functional cell of the gland
- Paraganglia are composed primarily of chromaffin cells, which are polygonal neuroendocrine cells with basophilic cytoplasm and many membrane bound granules
- References: Erickson: Atlas of Endocrine Pathology, 1st Edition, 2014, StatPearls: Physiology, Adrenal Gland [Accessed 7 November 2023]
Microscopic (histologic) images
Contributed by Nicole Stringham, Ph.D. (source: University of Michigan virtual slide box) and Debra L. Zynger, M.D.
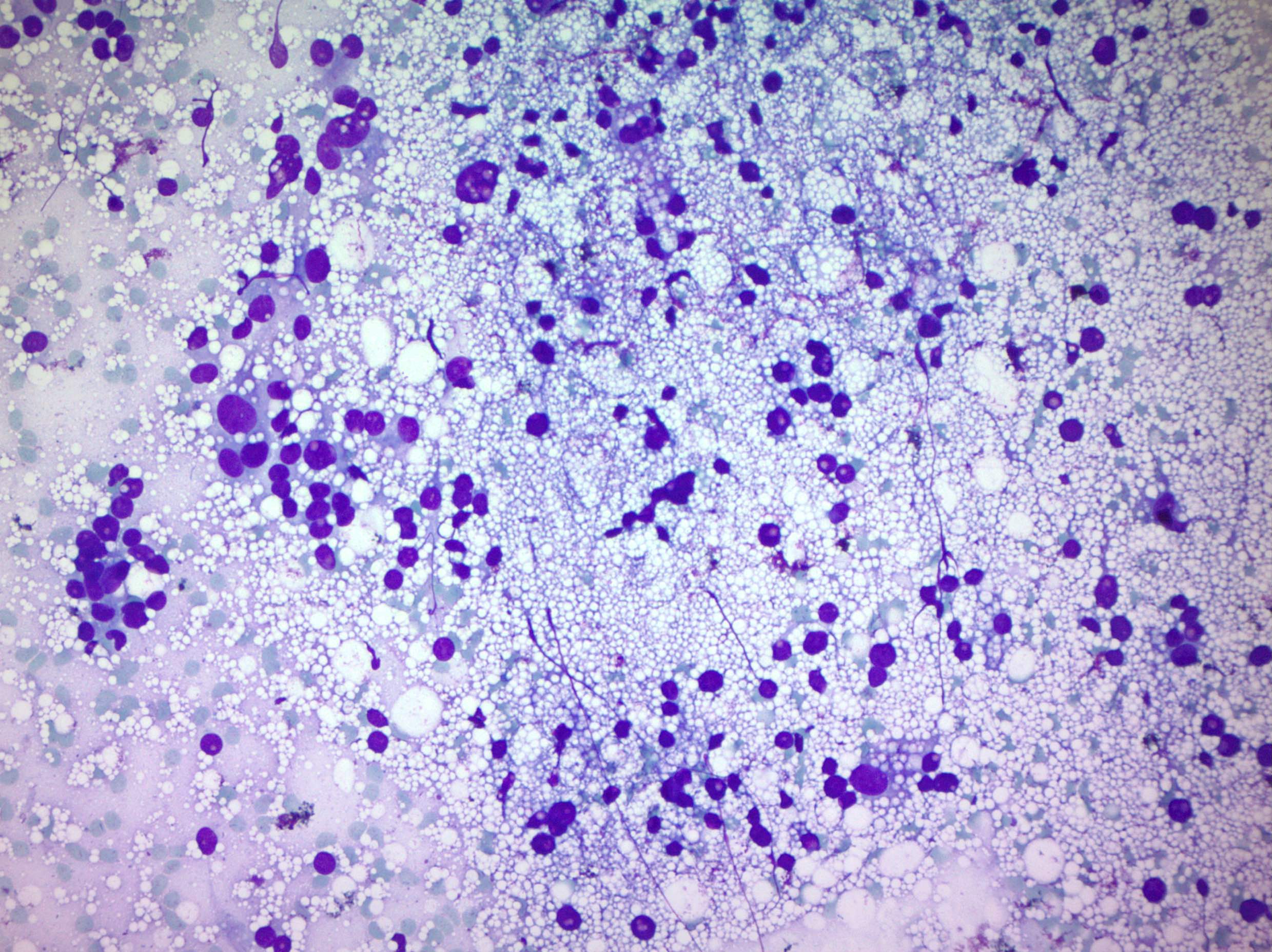
Cytology description
- FNA may contain naked nuclei of adrenal cortical cells that mimic small cell carcinoma (Mod Pathol 1991;4:594)
- FNA can be helpful for differentiating benign from malignant masses (97.6% accuracy) (Cytopathology 2000;11:302)
Positive stains
- Cortex
- Alpha inhibin, mainly confined to zona reticularis; alpha inhibin subunit has been suggested as a regulatory factor of adrenal androgen production in normal cortex showing less expression in zona fasciculata and even less within the zona glomerulosa (Endocr Res 1998;24:865, J Endocrinol 2000;165:223)
- Also positive in cortical hyperplasia, adenoma and carcinoma but may be helpful in distinguishing adrenal cortical carcinoma from pheochromocytoma and metastatic tumor (J Clin Pathol 1998;51:114)
- Useful in distinguishing cortical from medullary adrenal tumors; alpha inhibin is negative in adrenal medulla (Mod Pathol 2003;16:591)
- CD44 (J Clin Pathol 1998;51:52)
- MelanA, calretinin, BCL2, KIT (Mod Pathol 2003;16:591)
- D2, mainly in zona glomerulosa and reticularis, to a lesser extent in fasciculata (J Clin Endocrinol Metab 2004;89:4493)
- SF1, most reliable for confirmation of adrenal cortical origin of neoplasms (Endocr Pathol 2022;33:155)
- Low molecular weight cytokeratin, vimentin (Am J Pathol 1990;136:1077)
- Alpha inhibin, mainly confined to zona reticularis; alpha inhibin subunit has been suggested as a regulatory factor of adrenal androgen production in normal cortex showing less expression in zona fasciculata and even less within the zona glomerulosa (Endocr Res 1998;24:865, J Endocrinol 2000;165:223)
- Medulla
- Chromogranin, epinephrine, GATA3
- Synaptophysin, tyrosine hydroxylase
- S100, GFAP, vimentin (sustentacular cells) (Front Endocrinol (Lausanne) 2020:11:79)
- Paraganglia (Respir Med Case Rep 2020:31:101278)
- Synaptophysin, chromogranin
- S100 (sustentacular cells)
Negative stains
- Cortex: chromogranin, epinephrine, GATA3, S100 (Am J Surg Pathol 2010;34:423)
- Medulla: MelanA, inhibin, calretinin, SF1, keratin, vimentin
- CK7, CK20: not expressed in adrenal cortex or medulla
Electron microscopy description
- Zona glomerulosa: outer undifferentiated small cells and inner well differentiated larger elements with mitochondria and tubulolaminar cristae, abundant smooth endoplasmic reticulum and sparse lipid droplets
- Zona fasciculata: typical mitochondria with vesicular cristae, well developed smooth endoplasmic reticulum, prominent lipid droplets, occasional lipofuscin pigment granules that increase in number from superficial to deep, some lipid laden cells
- Zona reticularis: similar features to zona fasciculata but with more abundant lipofuscin pigment granules and sparse lipid droplets
- Medulla: chromaffin cells have many membrane bound granules; granule size varies from 100 to 350 nm (Acta Endocrinol (Buchar) 2018;14:272)
- Norepinephrine producing cells have granules that are larger, more electron dense and with a wide clear halo around the dense core
- Epinephrine producing cells have smaller, less electron dense granules, with a narrow halo surrounding a more homogenous core
Videos
Adrenal gland histology
Additional references
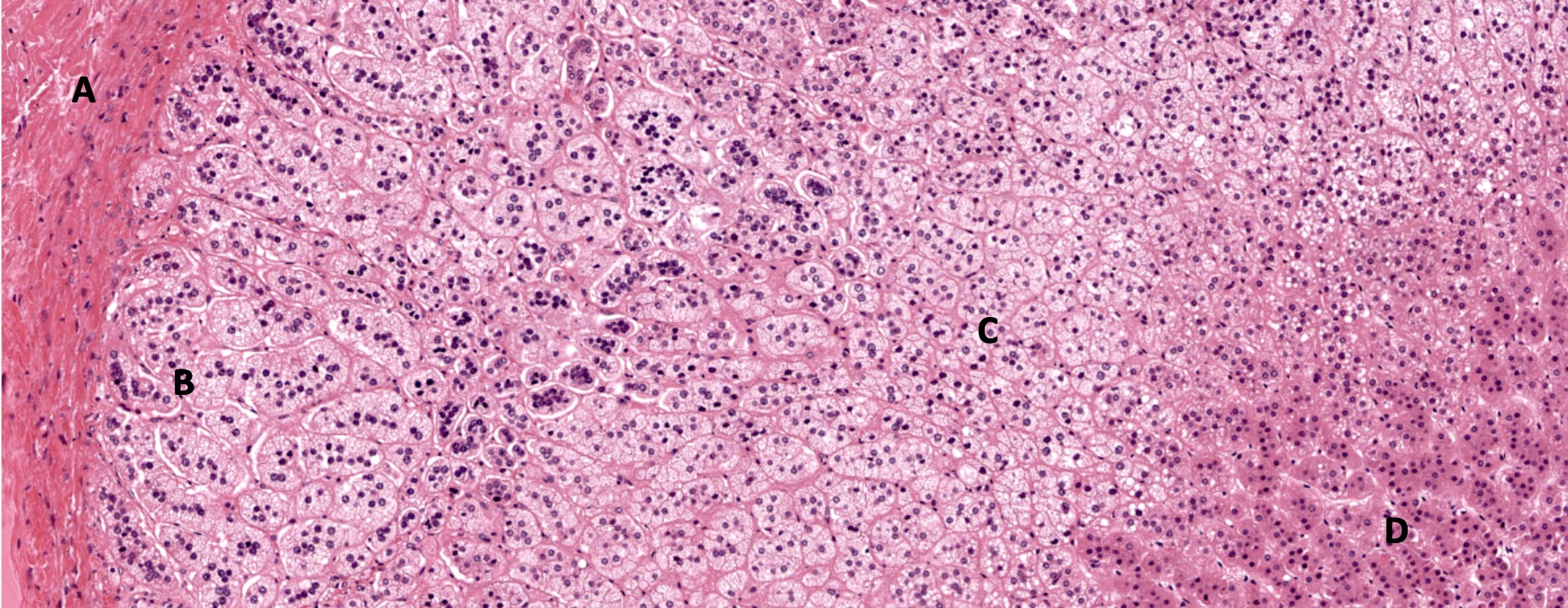
Board review style question #1
A 39 year old woman presents to clinic with persistent feelings of uncontrollable anxiety and reported weight gain. Upon examination she appears to have a fatty hump that is developing between her shoulders and several purple stretch marks on her abdomen. Her laboratory report shows elevated serum cortisol. Which cell type shown in the micro image above is most likely responsible for the increased serum cortisol seen in her laboratory report?
- A
- B
- C
- D
Board review style answer #1
C. Option C in the micro image labels cells of the zona fasciculata, which secrete glucocorticoids (i.e., cortisol) and may account for the serum hypercortisolism and clinical features described in this patient. Further workup could determine primary or secondary causes (e.g., Cushing disease). Answer A is incorrect because it is labeling the connective tissue capsule. Answer B is incorrect because these are cells of the zona glomerulosa, which secrete aldosterone. Answer D is incorrect because these are cells of the zona reticularis, which secrete androgens; these cells do secrete some glucocorticoids, however, the majority is secreted by the zona fasciculata.
Comment Here
Reference: Anatomy & histology-adrenal cortex, medulla & paraganglia
Comment Here
Reference: Anatomy & histology-adrenal cortex, medulla & paraganglia
Board review style question #2
A 59 year old patient has been referred to nephrology for suspected primary aldosteronism. They are experiencing peripheral fluid retention, high blood pressure and laboratory studies indicate mild hypokalemia. Radiological examination reveals a small tumor within the adrenal gland that is later determined to be benign. Which layer of adrenal gland was likely the location of tumor?
- Adrenal medulla
- Subcapsular lymphoid space
- Zona fasciculata
- Zona glomerulosa
- Zona reticularis
Board review style answer #2
D. Zona glomerulosa. Cells of zona glomerulosa are responsible for secretion of mineralocorticoids (i.e., aldosterone). A benign tumor within this layer of adrenal cortex could produce excess aldosterone and cause symptoms such as high blood pressure, fluid retention and hypokalemia. Answer A is incorrect because a tumor within the adrenal medulla (i.e., pheochromocytoma) would affect catecholamine production. Answer B is incorrect because although a tumor might extend into the subcapsular space, it would likely affect the most superficial layer of cortex. Answer C is incorrect because a tumor within the zona fasciculata would affect glucocorticoid production. Answer E is incorrect because a tumor within the zona reticularis would affect androgens, such as DHEA-S.
Comment Here
Reference: Anatomy & histology-adrenal cortex, medulla & paraganglia
Comment Here
Reference: Anatomy & histology-adrenal cortex, medulla & paraganglia