Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Liu Q. Acute appendicitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/appendixacuteappendicitis.html. Accessed April 24th, 2024.
Definition / general
- Acute inflammation of the vermiform appendix not attributable to distinct inflammatory disorders, such as idiopathic inflammatory bowel disease
- Existence of chronic appendicitis is disputed; may represent recurrent acute appendicitis
Essential features
- Disease of the young; most typically presents in children and adolescents (10 - 19 years), although no age group is exempt (Ulus Travma Acil Cerrahi Derg 2010;16:38)
- Male > female (Ulus Travma Acil Cerrahi Derg 2010;16:38)
- Pathogenesis includes obstruction of appendiceal orifice and subsequent bacterial infection
- Most common symptom is periumbilical pain radiating to the right lower quadrant
- Histological findings include variable acute inflammation with predominance of neutrophils involving some or all layers of the appendiceal wall
Terminology
- Acute suppurative appendicitis
- Acute gangrenous appendicitis
ICD coding
- ICD-10:
- K35 - acute appendicitis
- K35.2 - acute appendicitis with generalized peritonitis
- K35.3 - acute appendicitis with localized peritonitis
- K35.30 - acute appendicitis with localized peritonitis, without perforation or gangrene
- K35.31 - acute appendicitis with localized peritonitis and gangrene, without perforation
- K35.32 - acute appendicitis with perforation and localized peritonitis, without abscess
- K35.33 - acute appendicitis with perforation and localized peritonitis, with abscess
- K35.8 - other and unspecified acute appendicitis
- K35 - acute appendicitis
Epidemiology
- Incidence is approximately 233/100,000 people
- M > F; lifetime incidence of 8.6% for men and 6.7% for women
- Approximately 300,000 hospital visits yearly in the United States for appendicitis related issues (StatPearls: Appendicitis [Accessed 2 September 2021])
Sites
- Appendix
Pathophysiology
- Obstruction of appendiceal orifice leads to an increase in intraluminal and intramural pressure, resulting in small vessel occlusion and lymphatic stasis
- Wall of the appendix becomes ischemic and necrotic
- Bacterial infection then occurs in the obstructed appendix
- Aerobic organisms predominant in early appendicitis and mixed aerobes and anaerobes later in the course
- Commonly identified bacteria associated with acute appendicitis include Escherichia coli, Peptostreptococcus, Bacteroides and Pseudomonas (StatPearls: Appendicitis [Accessed 2 September 2021])
- Aerobic organisms predominant in early appendicitis and mixed aerobes and anaerobes later in the course
- If left untreated, acute appendicitis can progress to mural necrosis and perforation, local abscess formation and peritonitis
Etiology
- Obstruction of the appendiceal lumen followed by bacterial infection
- Can be from an appendicolith or some other mechanical etiologies
- Appendiceal tumors (benign or malignant)
- Intestinal parasites
- Hypertrophied lymphatic tissue
- Diverticulosis (Orv Hetil 2018;159:768)
- Vascular compromise (World J Emerg Surg 2017;12:38)
- Primary infection
- Hypersensitivity reaction (JAMA Pediatr 2018;172:943)
- Trauma (Ann Surg 1991;214:61)
Clinical features
- Main symptom is abdominal pain
- Initially colicky, periumbilical abdominal pain, classically dull and poorly localized
- Pain later migrates and localizes to right lower quadrant, typically sharp and well localized
- Other symptoms can include nausea, vomiting (typically after the pain, not preceding it), anorexia, diarrhea or constipation and fever
- In severe cases, patients can show features of sepsis, being tachycardic and hypotensive
- On examination:
- There may be rebound tenderness and percussion pain over McBurney point (located 3.8 to 5.7 cm over the right anterior iliac spine, in line with the umbilicus) and guarding (especially if the appendix is perforated)
- Other specific signs that may be found include:
- Rovsing sign: palpation of the left lower quadrant of a patient’s abdomen increases the pain felt in the right lower quadrant
- Psoas sign: right iliac fossa pain with extension of the right hip
- Obturator sign: pain with internal rotation of the right hip
- Atypical location of the appendix may cause atypical manifestations:
- Atypical locations include inguinal canal, femoral canal, subhepatic, retrocecal, intraperitoneal abdominal midline and left side in situs inversus or intestinal malrotation patients (Pol J Radiol 2016;81:583)
- Retrocecal appendix may cause atypical manifestations, mimicking pathology in the right flank and hypochondrium, such as acute cholecystitis, diverticulitis, acute gastroenteritis, ureter colic and acute pyelonephritis (J Comput Assist Tomogr 2006;30:772)
Diagnosis
- Based on clinical presentation, physical examination, laboratory testing and radiologic findings (World J Emerg Surg 2020;15:27)
- Emergency department physicians must refrain from giving patients any pain medication until the surgeon has seen the patient; analgesics can mask the peritoneal signs and lead to a delay in diagnosis or even a ruptured appendix
Laboratory
- Elevated white blood cells (WBC) with or without a left shift or bandemia is classically present but up to 33% of patients with acute appendicitis will present with a normal WBC count
- Elevated C reactive protein, elevated erythrocyte sedimentation rate (ESR)
- There are usually ketones found in the urine (Am J Emerg Med 2013;31:1560)
- HIV positive patients may lack or have minimal granulocytosis (Am J Surg 1991;162:9)
Radiology description
- CT scan has greater than 95% accuracy for the diagnosis of appendicitis and is used with increasing frequency (Gastroenterol Clin North Am 2018;47:667, AJR Am J Roentgenol 2018;211:901, AJR Am J Roentgenol 2018;211:W140)
- Characteristic CT findings include appendiceal mural thickening and enhancement, luminal dilation and periappendiceal inflammatory changes, including fat stranding, fluid and phlegmon, presence of appendiceal perforation, free peritoneal fluid, abscess, fascial thickening and changes in the adjacent bowel wall, including mass effect on the cecum, presence of appendicoliths and lymphadenopathy (Gastroenterol Clin North Am 2018;47:667, AJR Am J Roentgenol 2018;211:901, AJR Am J Roentgenol 2018;211:W140)
- CT findings of retrocecal appendicitis include an inflamed appendix located in the posterolateral aspect of the ascending colon, an abscess in the retrocolic space, paracolic gutter and subhepatic space and retroperitoneal extension of inflammation associated with thickening of the lateroconal and Gerota fascia and the ascending colon (J Comput Assist Tomogr 2006;30:772)
Radiology images
Prognostic factors
- If diagnosed and treated early (within 24 - 48 hours), the prognosis is excellent
- Cases that present with advanced abscesses, sepsis and peritonitis may have a more prolonged and complicated course
- Reference: Open Access Emerg Med 2021;13:265
Case reports
- 37 year old man with no past medical history presented to the emergency department with vague abdominal pain as well as 12 days of cyclical fever (Clin Pract Cases Emerg Med 2021;5:66)
- 36 year old slightly obese man presented with pain in the lower abdomen for 24 hours, followed by nausea, vomiting and mild fever (World J Clin Cases 2014;2:391)
- 43 year old man who had undergone an appendectomy 10 years previously with acute onset of abdominal pain (Cases J 2010;3:14)
- 64 year old woman, seamstress, presented with abdominal pain; plain radiography and CT scan showed metal density, suggesting a foreign body in the lower right abdomen (Int J Surg Case Rep 2020;72:499)
- 66 year old man who had undergone bilateral blepharoplasty 3 days earlier was admitted with a 24 hour history of increasing right lower quadrant pain accompanied by nausea, vomiting and anorexia (J Surg Case Rep 2020;2020:rjaa173)
Treatment
- While in the emergency department, the patient must be kept nil per os (NPO) and hydrated intravenously with crystalloid
- Antibiotics should be administered intravenously as per the surgeon
- Appendectomy is the gold standard treatment
- Laparoscopic appendectomy is preferred over the open approach
- When there is a known abscess from a perforated appendix, may require a percutaneous drainage procedure, usually done by interventional radiologist
- Laparoscopic appendectomy to be performed at a later date
- Several studies promote the treatment of uncomplicated appendicitis solely with antibiotics and avoiding surgery (J Pediatr Surg 2019;54:1365, Eur J Pediatr Surg 2019;29:53)
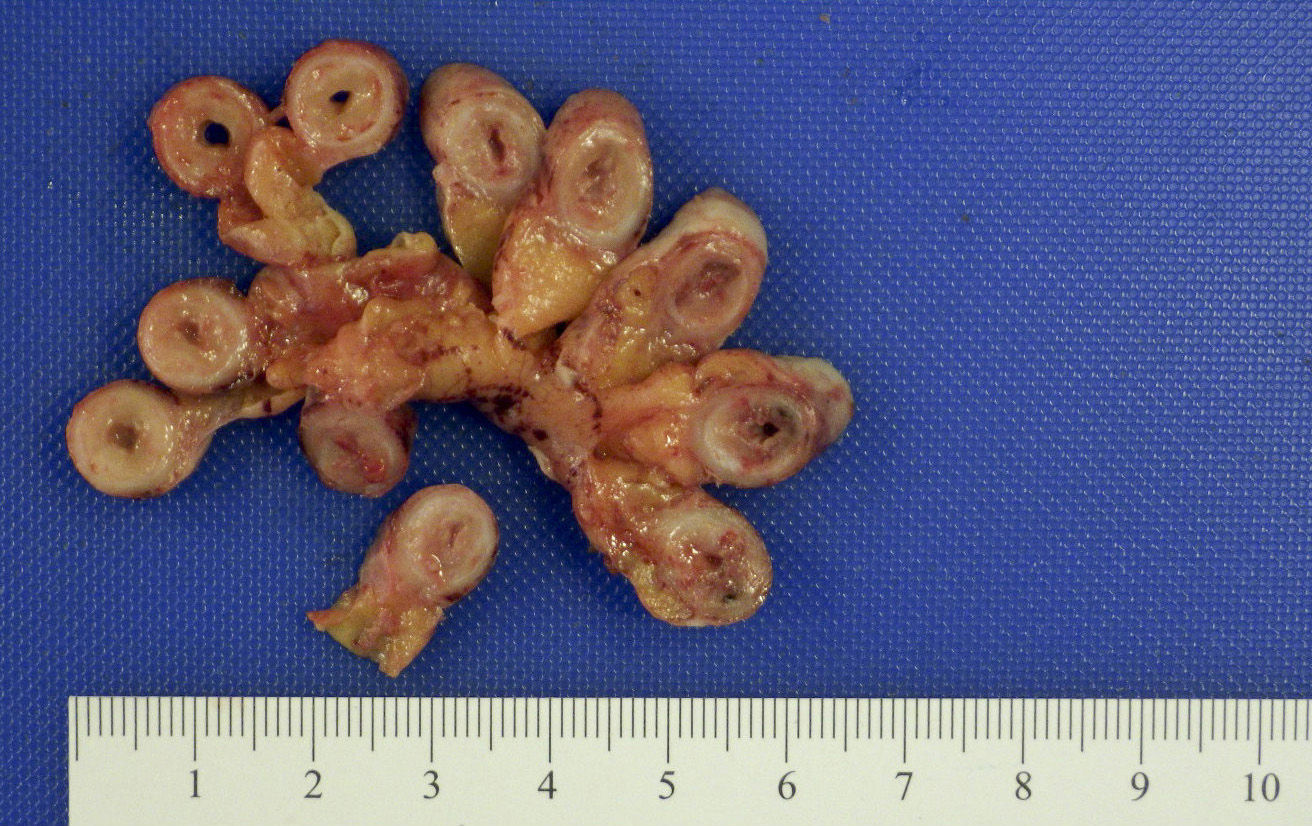
Gross description
- Gross and microscopic extent of inflammation may not correlate
- Inflammation may involve entire appendix or only a segment
- Appendix may appear grossly normal when inflammation is limited to the mucosa and submucosa
- Appendix appears swollen and erythematous when inflammation extends into the muscularis propria
- When the serosa is affected, a purulent exudate appears
- Cut surface may show hyperemia or intraluminal or intramural abscess
- Appendiceal wall may be completely necrotic in gangrenous appendicitis (J Pediatr Surg 2019;54:718)
- Perforation in severe cases
Gross images
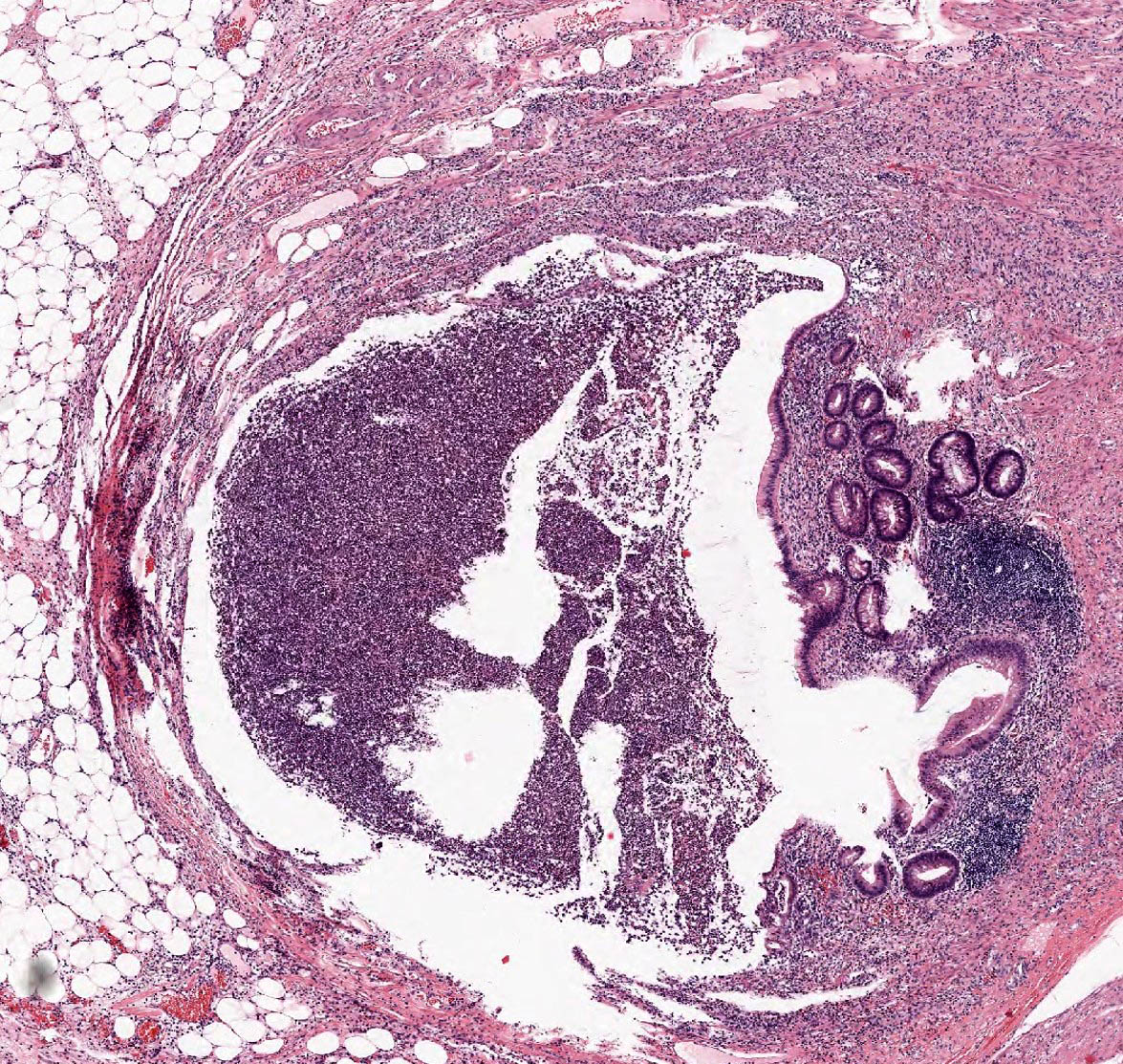
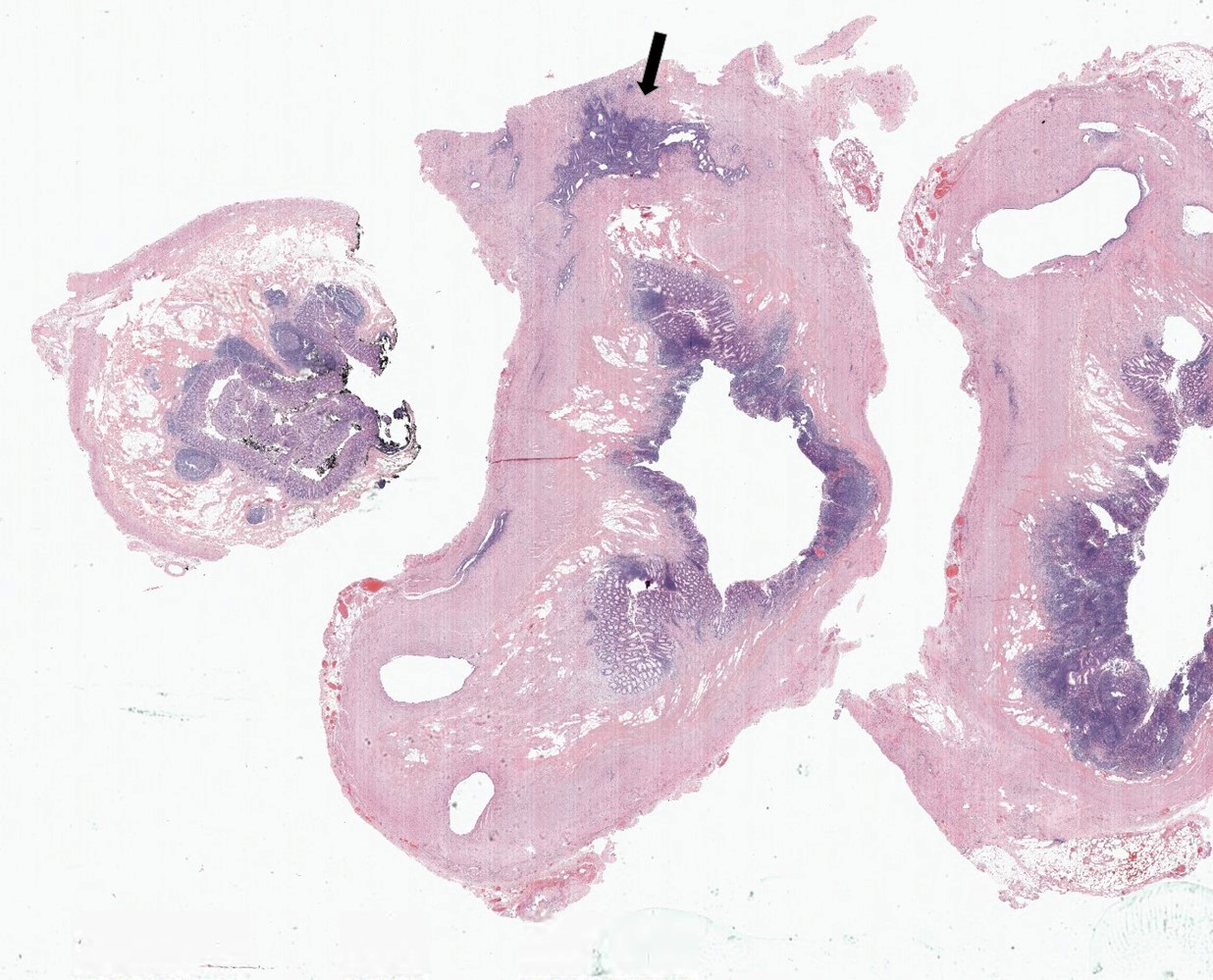
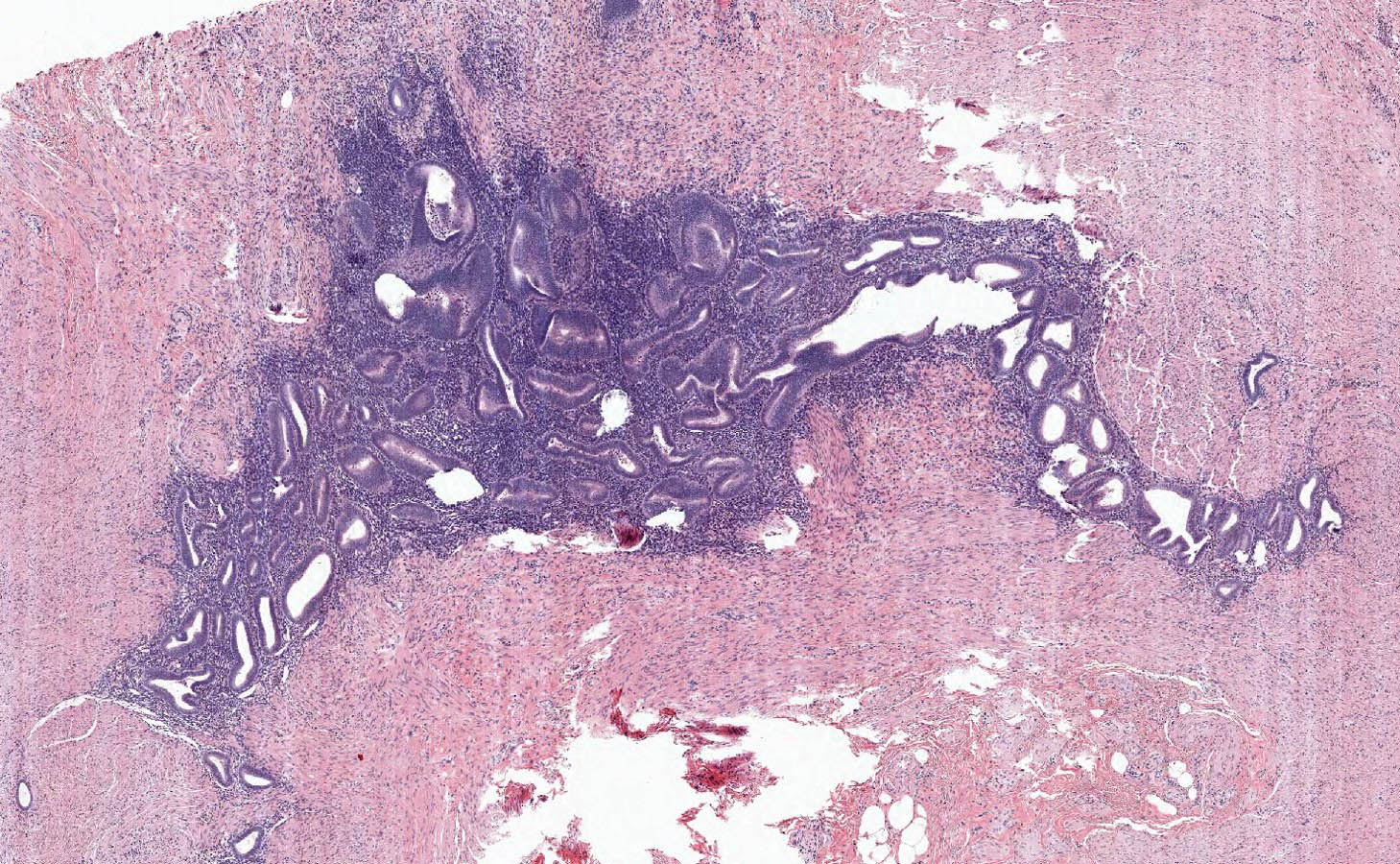
Microscopic (histologic) description
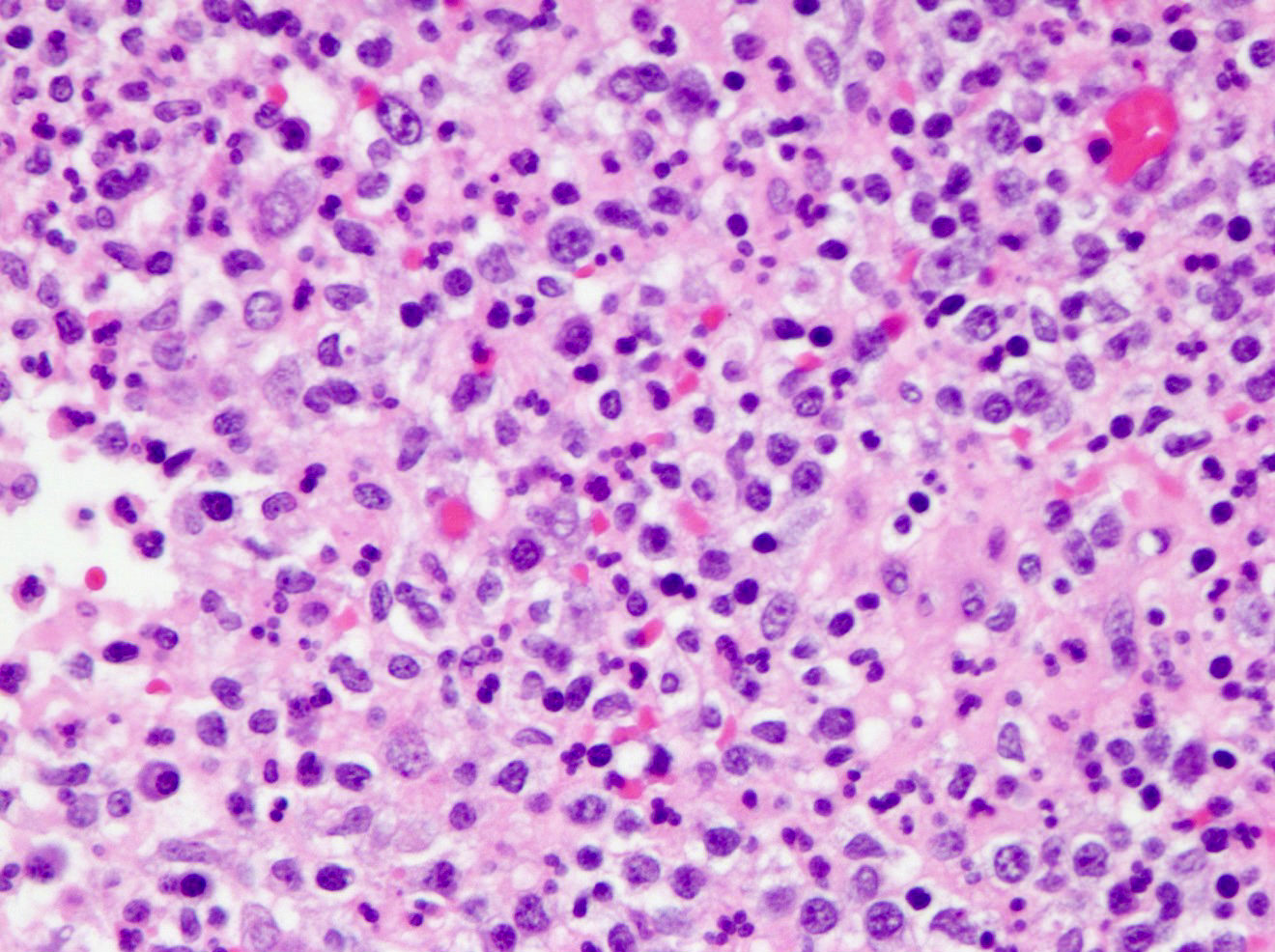
- Variable acute inflammation with predominance of neutrophils; involves some or all layers of the appendiceal wall
- Process may be divided into acute focal, acute suppurative, gangrenous and perforative
- Early lesions display mucosal erosions and scattered crypt abscesses
- Later, the inflammation extends into the lamina propria and collections of neutrophils are also seen in the lumen
- Mural necrosis in gangrenous appendicitis
- Process may be divided into acute focal, acute suppurative, gangrenous and perforative
- Periappendiceal inflammation alone (found in 1 - 5% of appendices resected for clinically acute appendicitis) suggests extraappendicular cause for symptoms
- Majority is attributable to salpingitis
- Gonococcal salpingitis (Pediatrics 1976;58:287)
- Chlamydial salpingitis (Surg Gynecol Obstet 1985;160:304)
- Appendiceal diverticulosis
- Majority is attributable to salpingitis
- Incidental tumors may be found (i.e. well differentiated neuroendocrine tumor)
Microscopic (histologic) images
Sample pathology report
- Appendix, appendectomy:
- Acute suppurative appendicitis and periappendicitis
Differential diagnosis
- Idiopathic inflammatory bowel disease is the most important pathologic differential diagnosis
- Ulcerative appendicitis (ulcerative colitis involving the appendix):
- Typically present in patients with pancolitis but also common as a skip lesion or in patients with left sided or rectal disease (Can J Gastroenterol 2001;15:201)
- Same histological changes as those seen in ulcerative colitis, including mucosal based active chronic inflammation
- Distinction from acute appendicitis mainly relies on clinical history
- Expression of prominent S100 protein reactive dendritic cells, MAC387 positive dendritic cells and upregulated HLA class II antigens in ulcerative appendicitis (Hum Pathol 1997;28:297)
- Ulcerative appendicitis (ulcerative colitis involving the appendix):
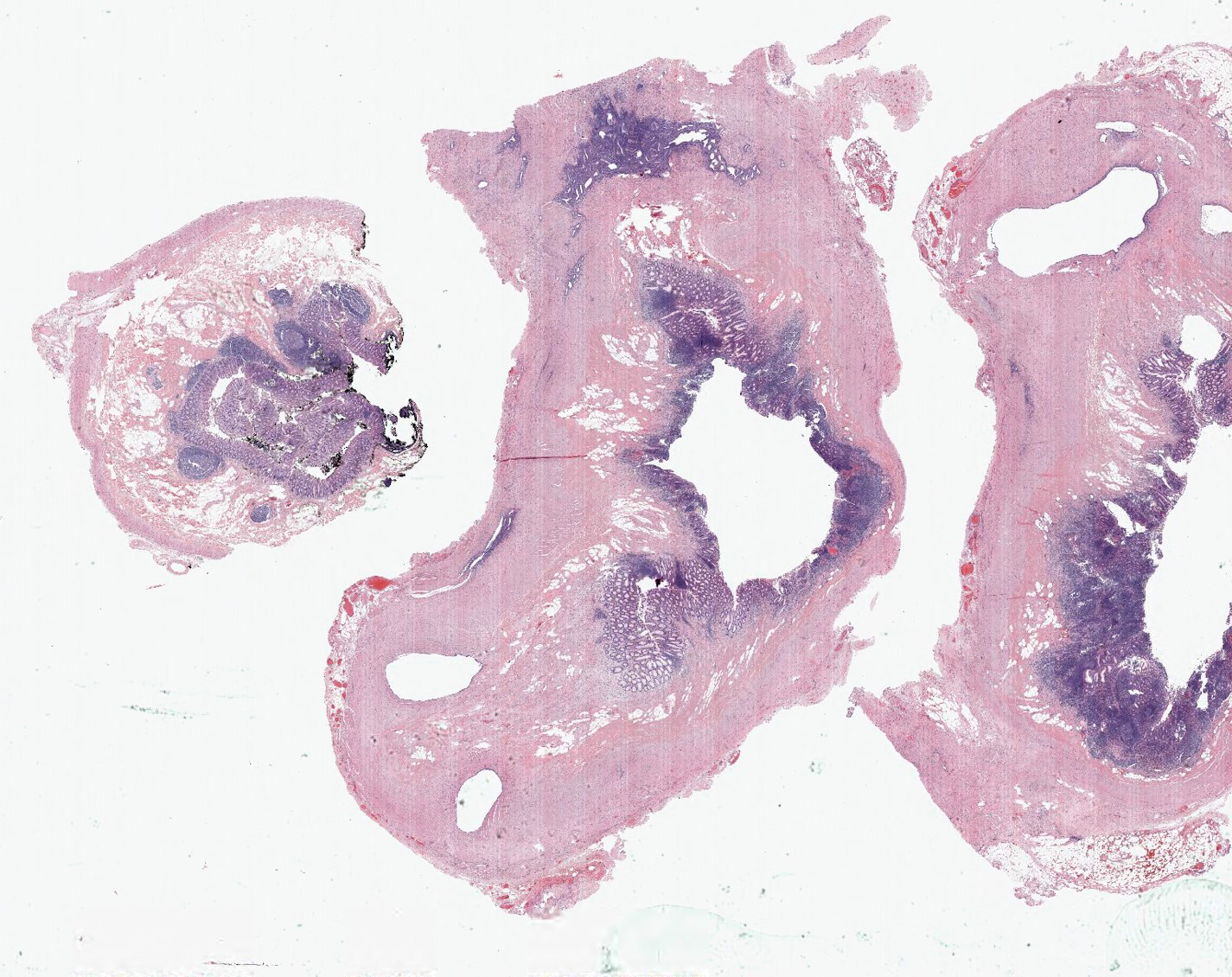
- Appendiceal endometriosis:
- Typically has a nonspecific presentation; pain may wax and wane with the menstrual cycle
- Most often affects the serosa or muscularis propria and is accompanied by abundant fibrosis and adhesions
- Microscopically, consists of endometrial type glands and stroma associated hemosiderin deposition and a fibroblastic response (Afr Health Sci 2008;8:196)
- Appendiceal deciduosis:
- Found in the appendix of pregnant women
- Present with typical signs and symptoms of acute appendicitis
- Microscopically, lacks glands and consists only of large polyhedral cells arranged in sheets in the serosa or outer muscularis propria
- Large cells are positive for vimentin and may show desmin or smooth muscle actin positivity; they are negative for cytokeratin, CEA, EMA and S100 immunostaining
- Appendiceal diverticulosis:
- Congenital (true) or acquired (false) (incidence 0.014% and 1.9%, respectively) (Hum Pathol 2008;39:1823)
- Occurs in relatively older age group (Surg Today 2012;42:363)
- Symptoms mimic acute appendicitis; higher risk of perforation than acute appendicitis (Surg Today 2012;42:363)
- Often associated with higher risk of neoplasm, especially neuroendocrine tumor and mucinous neoplasms (Int J Surg Case Rep 2017;33:31)
Additional references
Board review style question #1
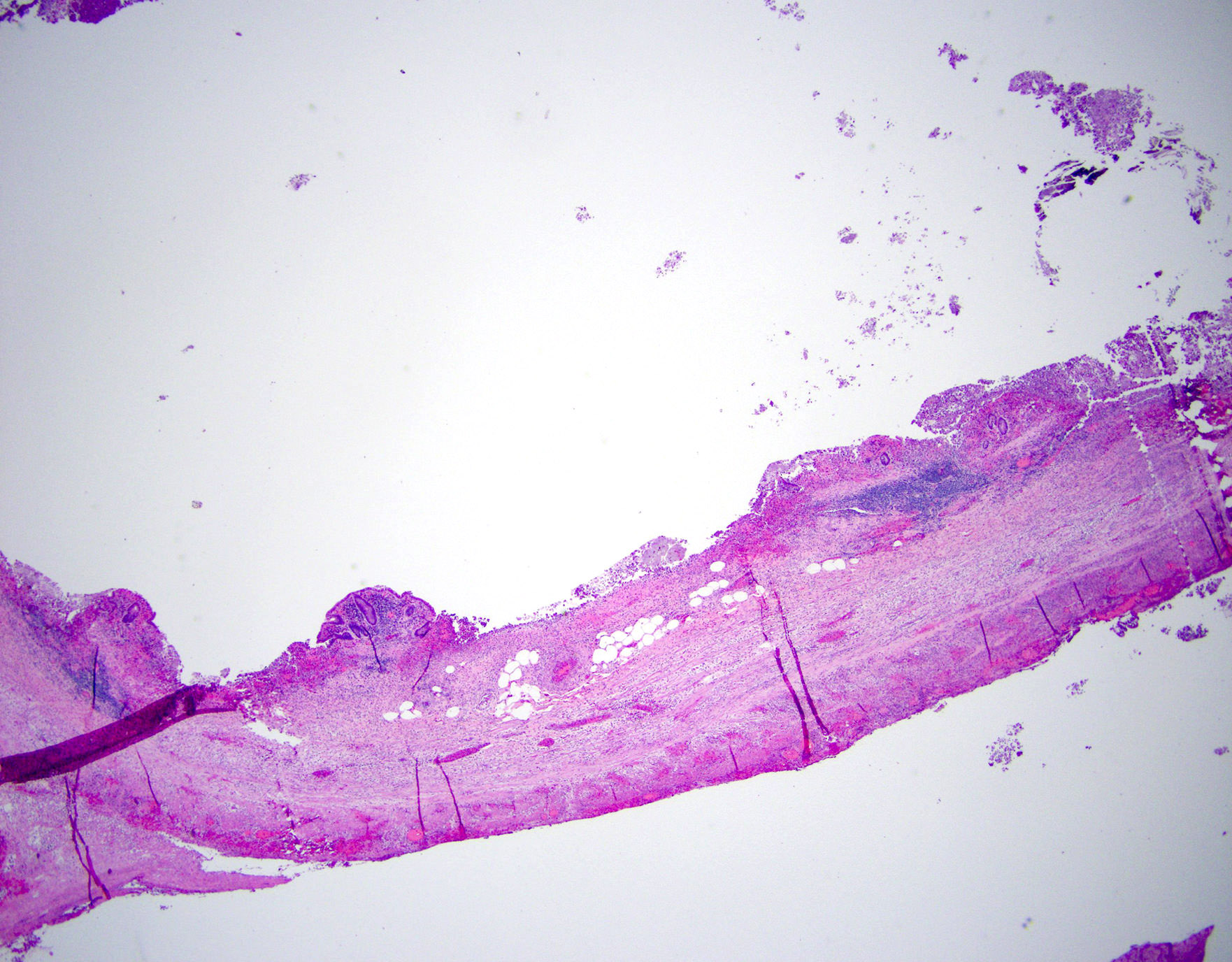
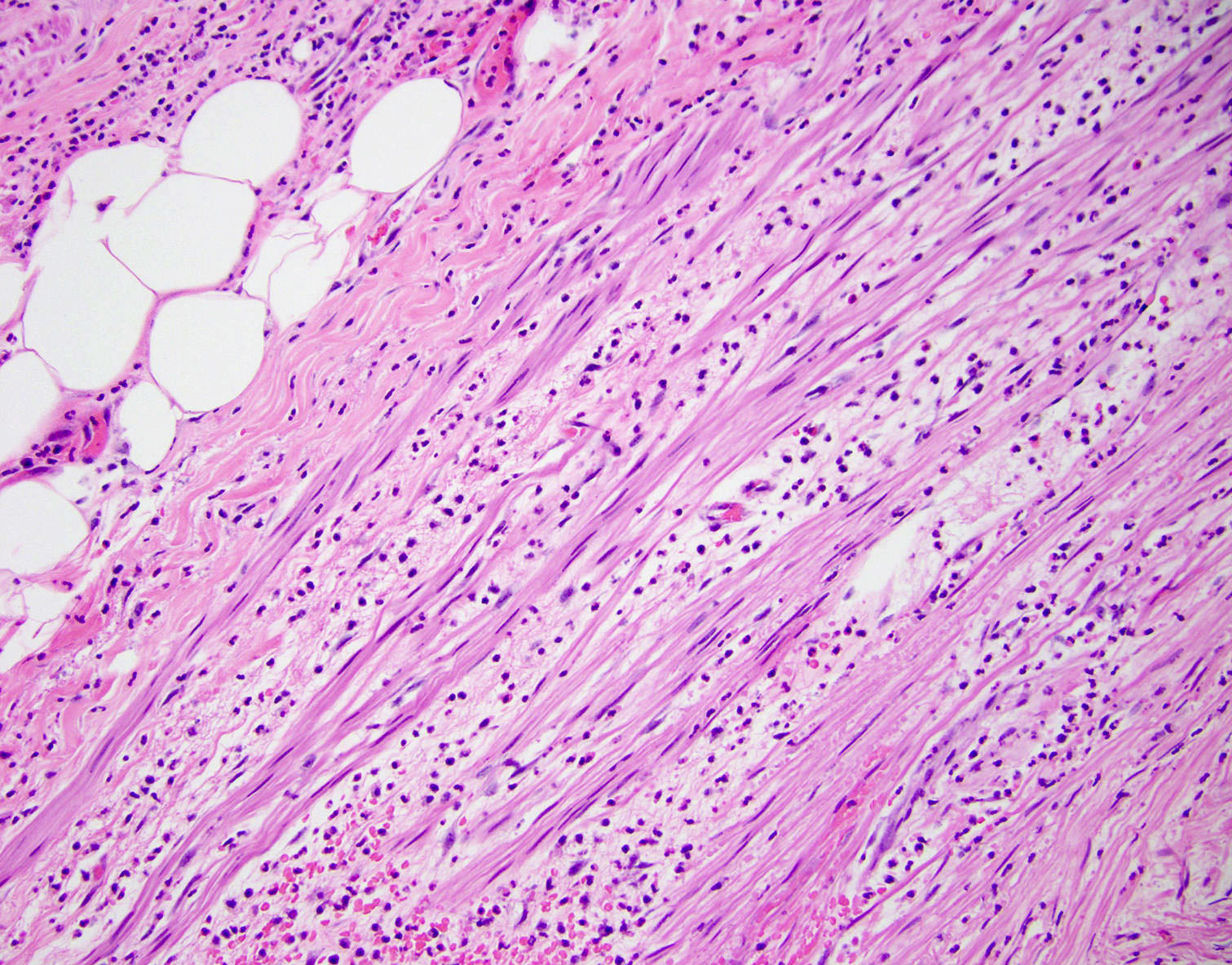
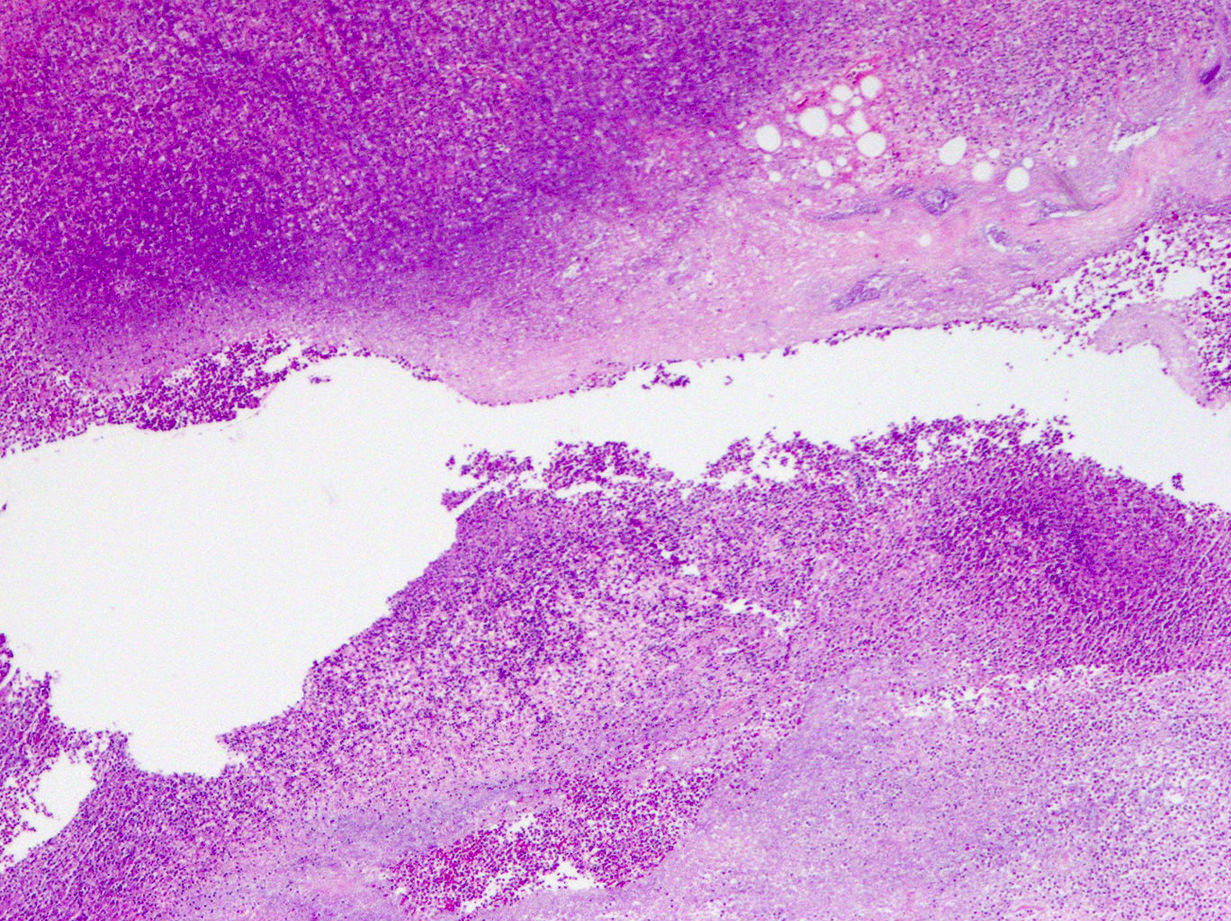
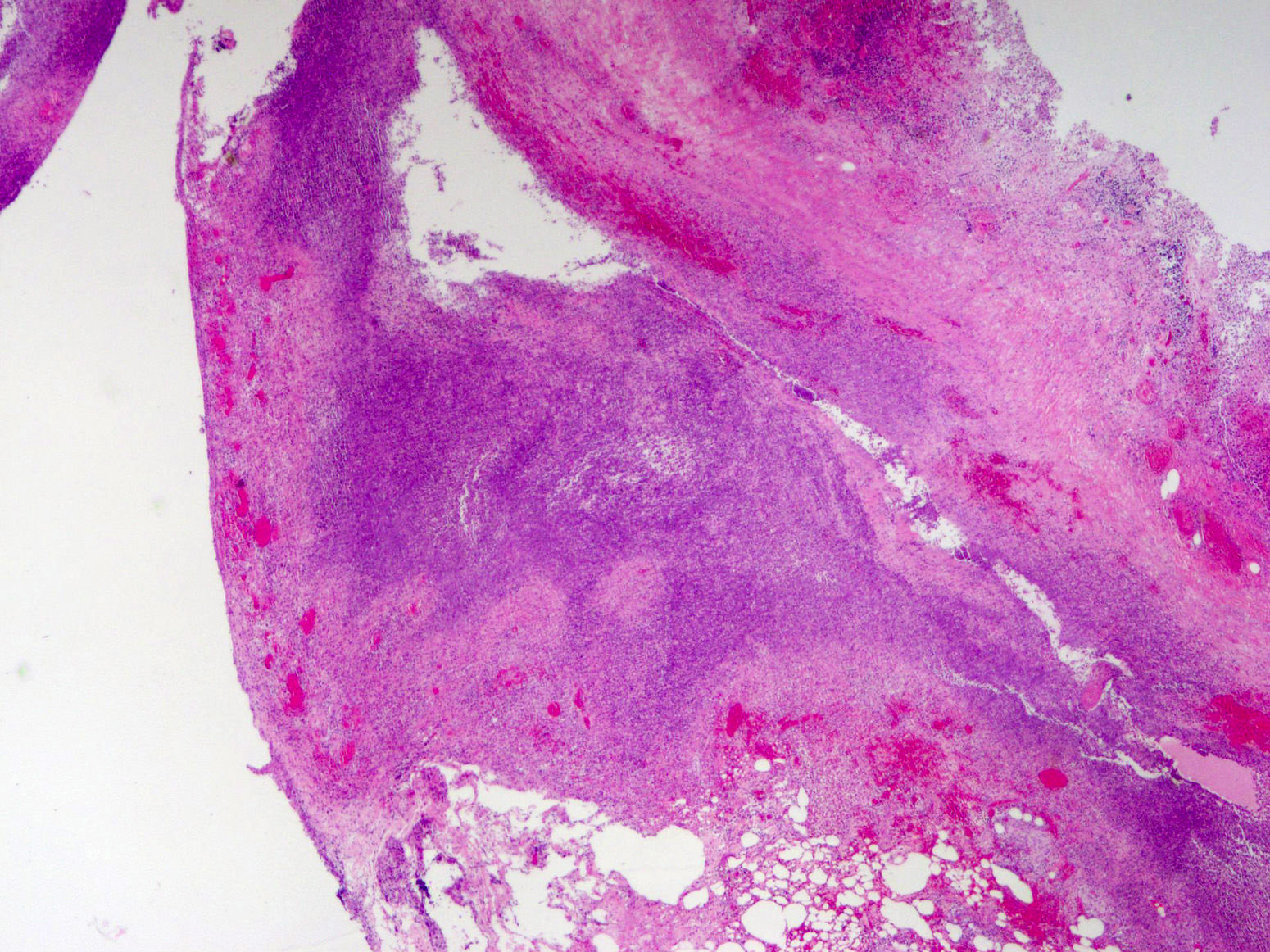
A 40 year old caucasian man presented into the emergency room with right lower quadrant pain associated with vomiting, abdominal tenderness, fever and moderate leukocytosis. Acute appendicitis was suspected and he underwent an appendectomy. His appendix was sent to pathology for histological evaluation. The H&E images are shown above. Which of the following is the most likely diagnosis?
- Appendiceal diverticulitis
- Appendiceal endometriosis
- Interval appendicitis
- Low grade appendiceal mucinous neoplasm
Board review style answer #1
Board review style question #2
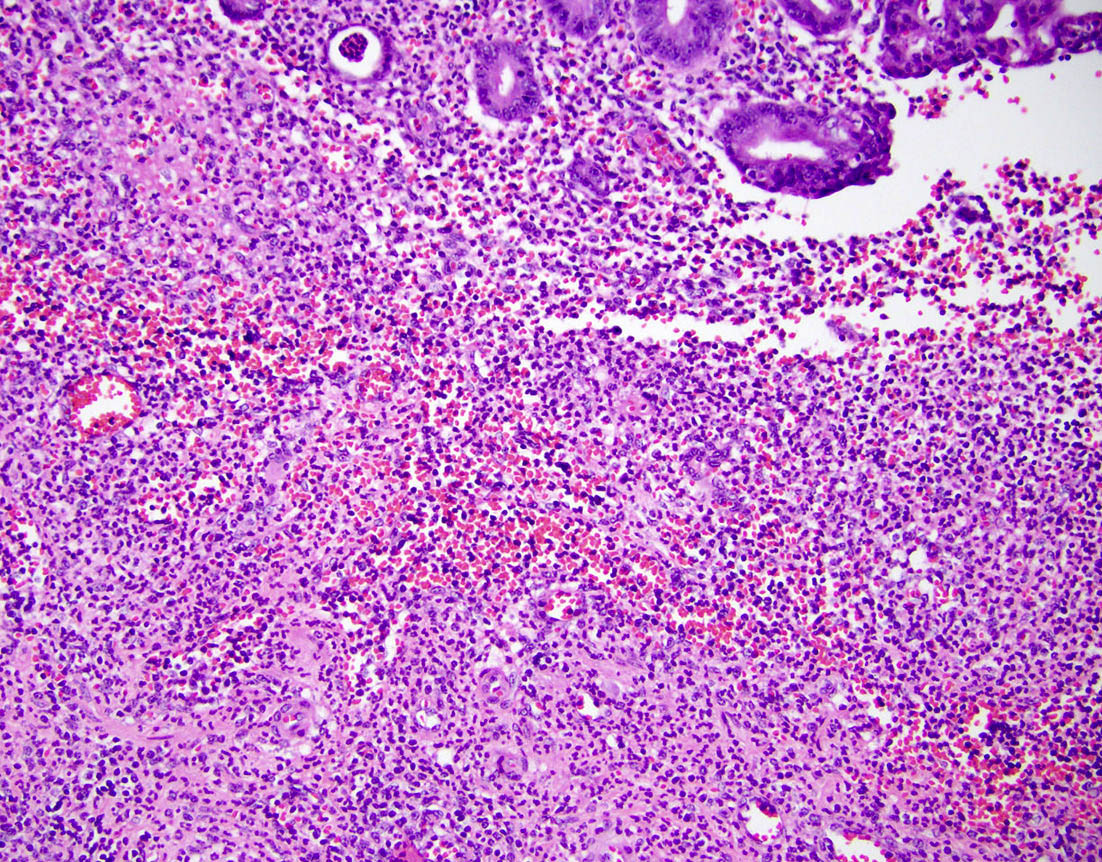
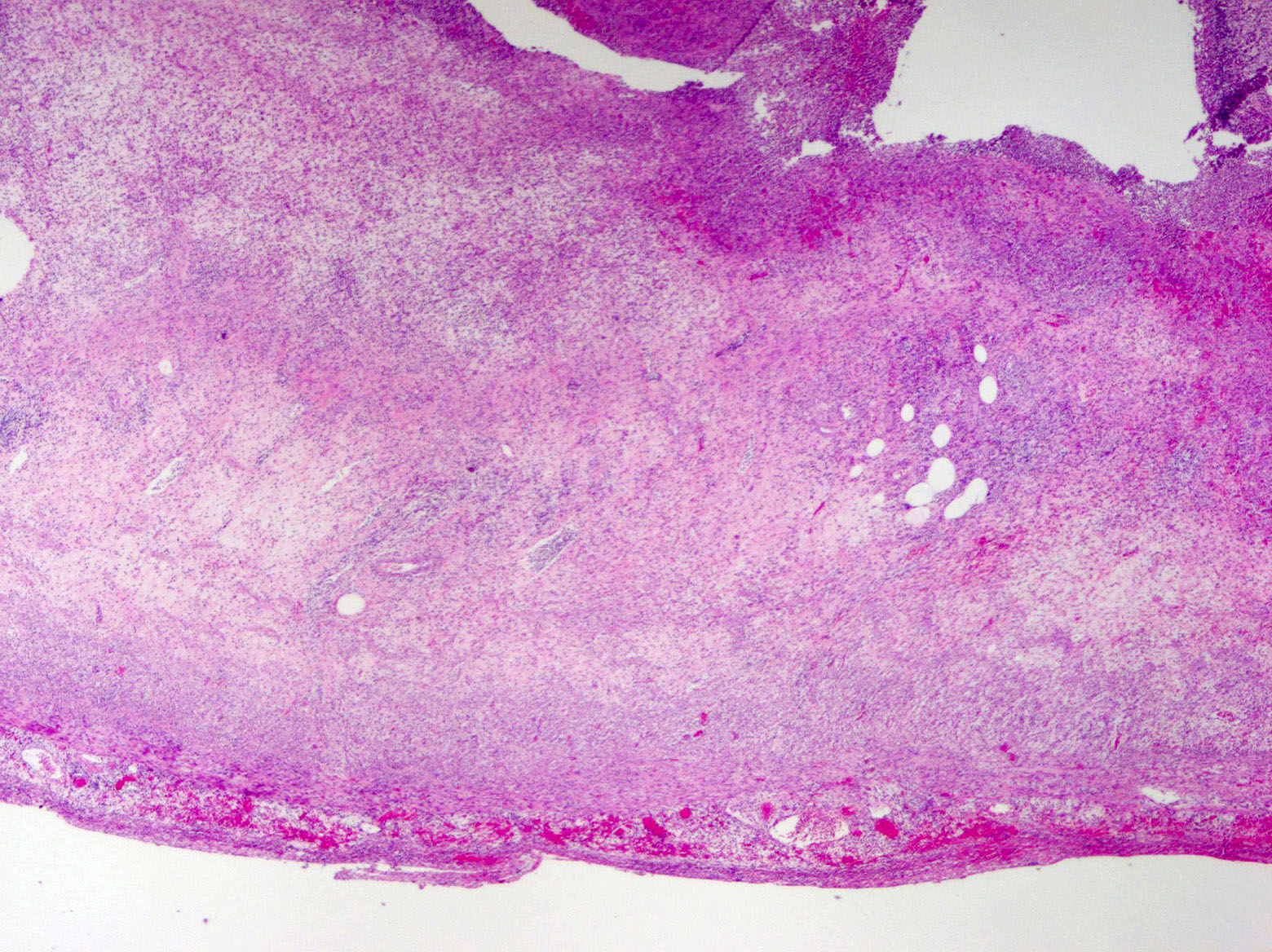
A 35 year old woman presented with localized right lower quadrant abdominal pain for 1 day. She also presented with nausea, vomiting, menorrhagia and dizziness. She reported that she was actively menstruating and that these symptoms typically occurred monthly with menstruation but had been particularly severe in that month. CT scan showed thick walled appendix consistent with acute appendicitis. She underwent an appendectomy. The H&E images are shown above. Which of the following is the most likely diagnosis?
- Acute appendicitis
- Appendiceal diverticulitis
- Appendiceal endometriosis
- Interval appendicitis
Board review style answer #2