Table of Contents
Definition / general | Major updates | WHO (2022) | Microscopic (histologic) images | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Rizkalla C, Tretiakova M. WHO classification. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bladderwhoisup.html. Accessed April 25th, 2024.
Definition / general
- The new WHO 2022 classification of urinary and male genital tumors (5th edition) replaces the previous WHO 2016 classification
- Diagnostic criteria, molecular correlates and nomenclature have been updated
Major updates
- 5th edition of WHO classification for bladder cancers is organized based on tumor lineage: urothelial, squamous and glandular tumors (Pathologica 2022;115:32)
- Exceptions for urachal, diverticular and urethral accessory gland tumors
- Separate chapters for neuroendocrine neoplasms, mesenchymal tumors, hematolymphoid malignancies, melanocytic tumors and metastatic tumors
- Genetic tumor syndromes of urinary and male genital tract are covered in dedicated chapter
- Histologic subtypes are now preferred over variants (Pathologica 2022;115:32)
- Standardized terminology: genetic alterations as variants, distinct morphologies as histologic patterns and significant morphologies as tumor subtypes
- All subtypes of urothelial carcinoma and those with divergent differentiation are classified as high grade tumors, regardless of bland morphology (e.g., microcystic / tubular, small or large nested)
- WHO 5th edition stresses reporting the presence and percentage(s) of different subtypes and divergent differentiation in urothelial carcinomas
- Papillary tumors are deemed high grade if containing ≥ 5% high grade component; < 5% is noted as low grade with < 5% high grade component, prompted by poor interobserver reproducibility (J Pathol Transl Med 2024;58:45, Pathologica 2022;115:32)
- The descriptor inverted is reserved for papillary tumors with almost exclusively inverted architecture
- Urothelial proliferation with undetermined malignant potential is no longer considered a distinct entity but rather an early low grade noninvasive papillary urothelial carcinoma or extension at the tumor edge / shoulder lesion (J Pathol Transl Med 2024;58:45, Pathologica 2022;115:32)
- Urothelial dysplasia no longer has a separate section; the term has been retained for preneoplastic lesions falling short of carcinoma in situ diagnosis (Pathologica 2022;115:32, J Pathol Transl Med 2024;58:45)
- Clear cell urothelial carcinoma was renamed clear cell urothelial carcinoma (glycogen rich) for clearer distinction from clear cell adenocarcinoma with Müllerian differentiation (Pathologica 2022;115:32)
- Signet ring / diffuse has been removed from plasmacytoid subtype terminology (Pathologica 2022;115:32)
- New edition advocates for pT1 tumor substaging via histoanatomical (tumor relative to muscularis mucosa and vascular plexus) or micrometric approach (measuring of invasive tumor component); however, it does not favor any specific methodology of subcategorization or tier system (Pathologica 2022;115:32)
- Predictors of immune checkpoint inhibitor response: PDL1 expression in tumor and host immune cells, tumor mutation burden and microsatellite instability / mismatch repair defect status (Mod Pathol 2018;31:623)
WHO (2022)
| Urothelial tumors | ICD-O | ICD-11 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8120/0 | 2F35 & XH5M82 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8121/0 | 2F35 & XH5A08 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8130/1 | 2F78 & XH5UU5 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8130/2 | 2C91.0 & XH12F0 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8130/2 | 2C91.0 & XH12F0 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8120/2 | 2C91.0 & XH5GH8 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
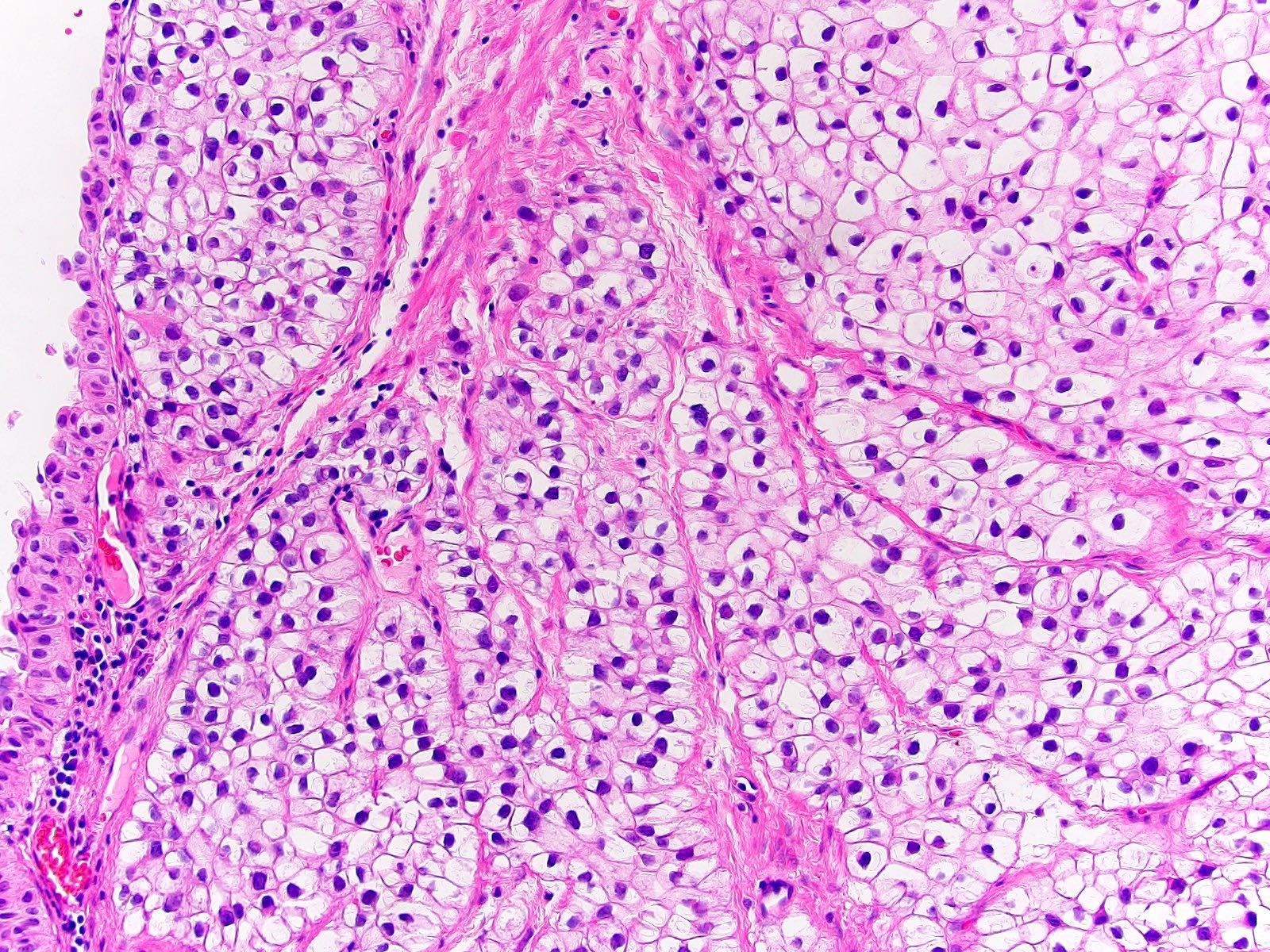
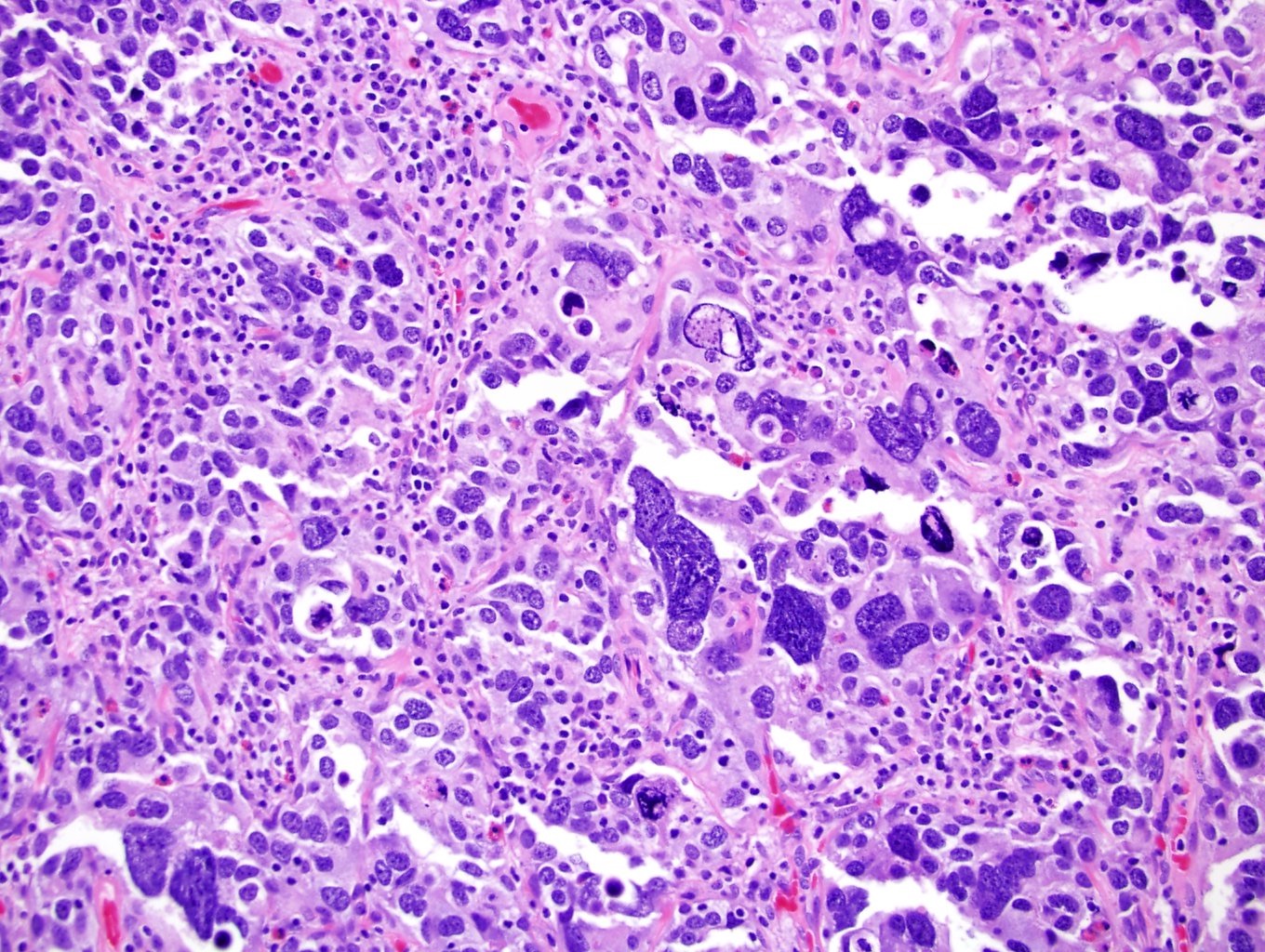
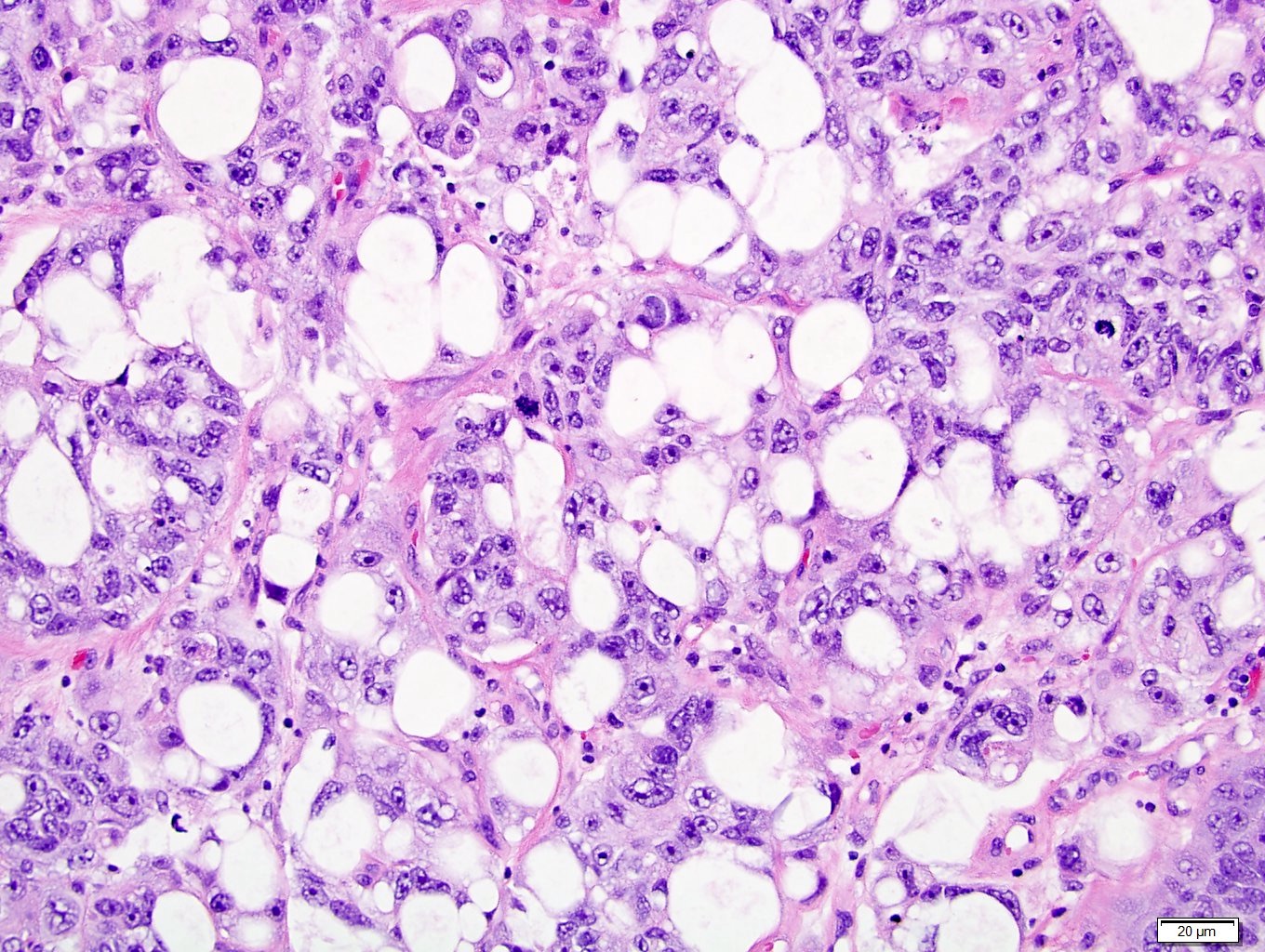
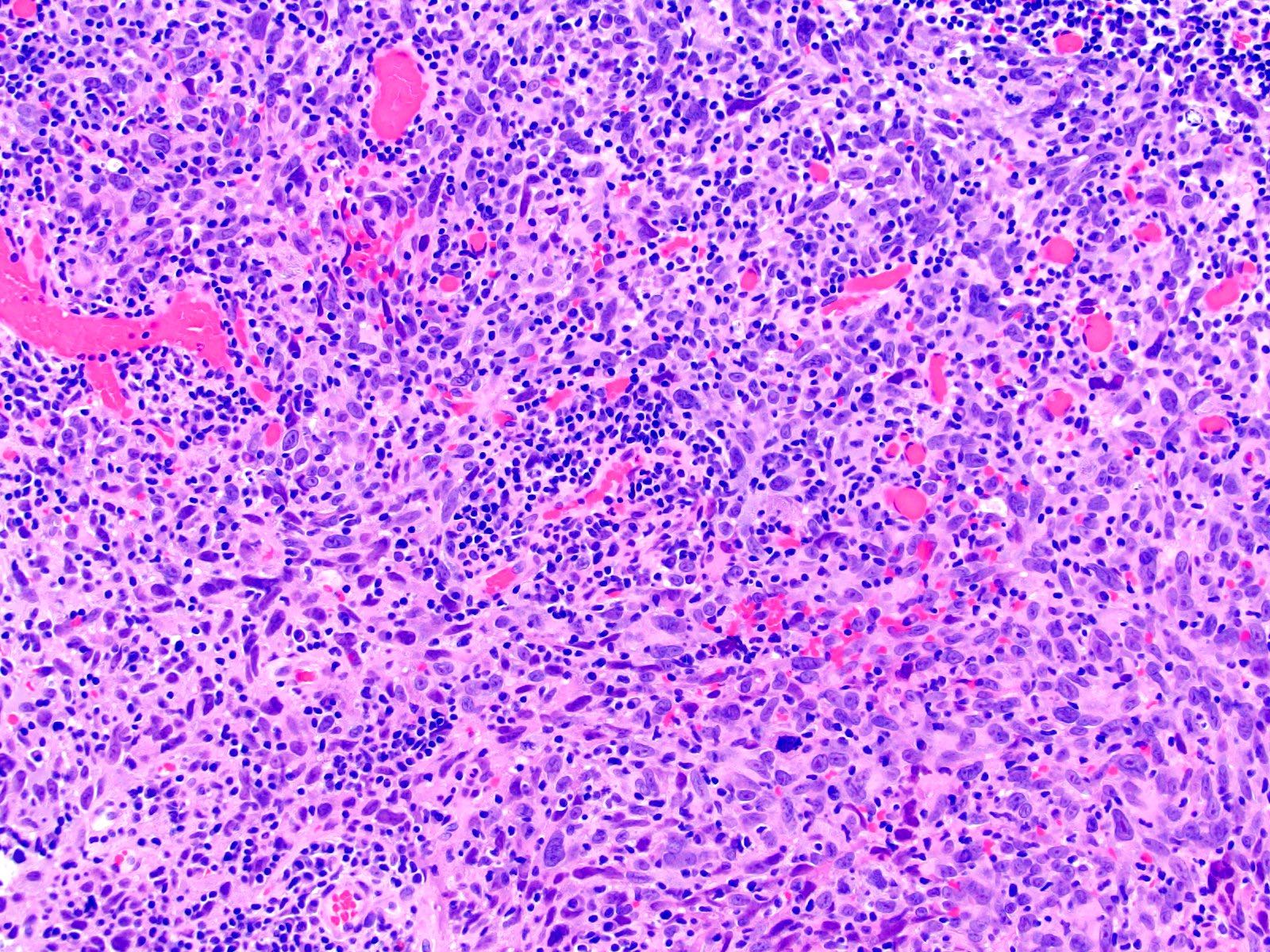
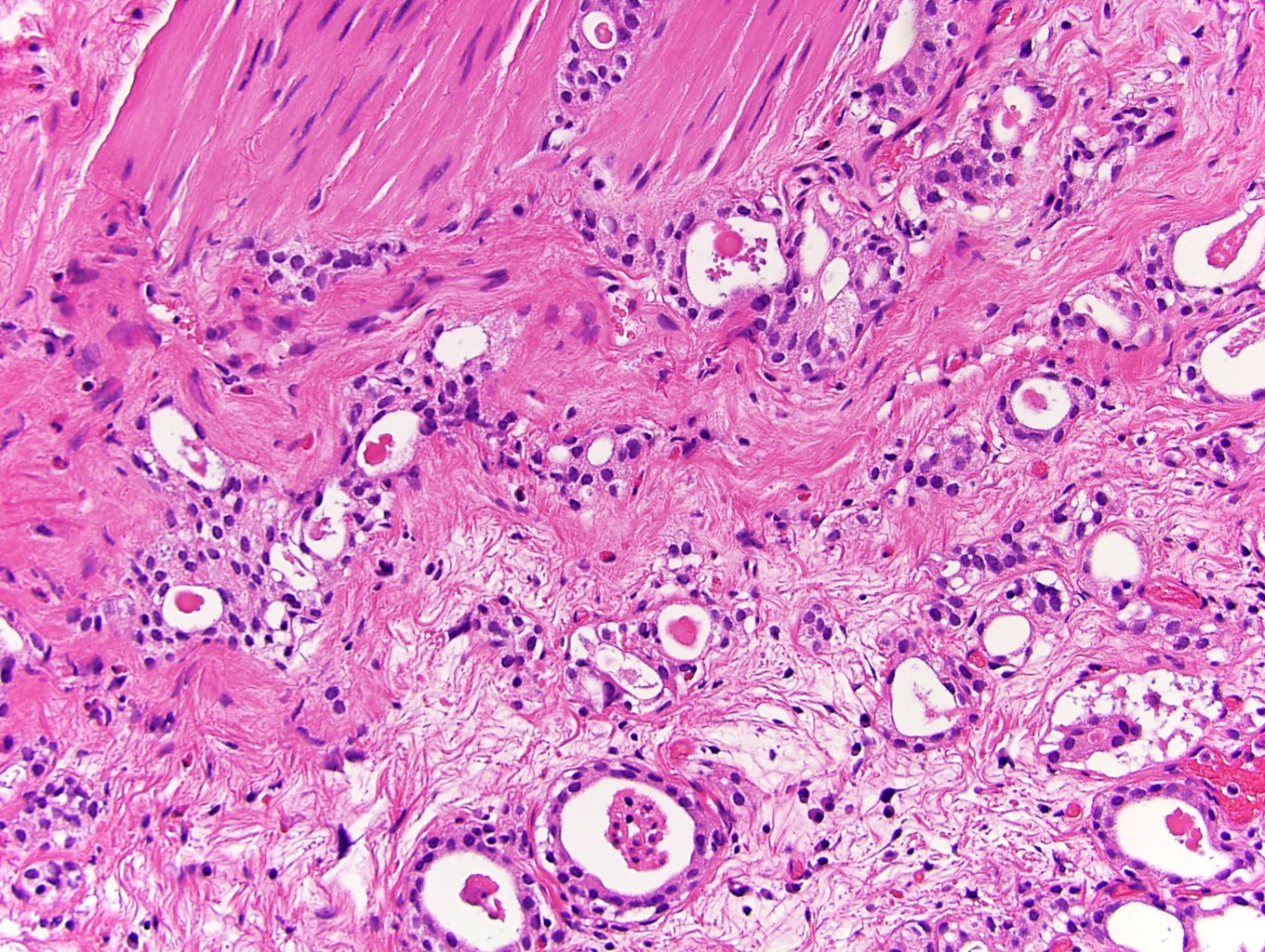
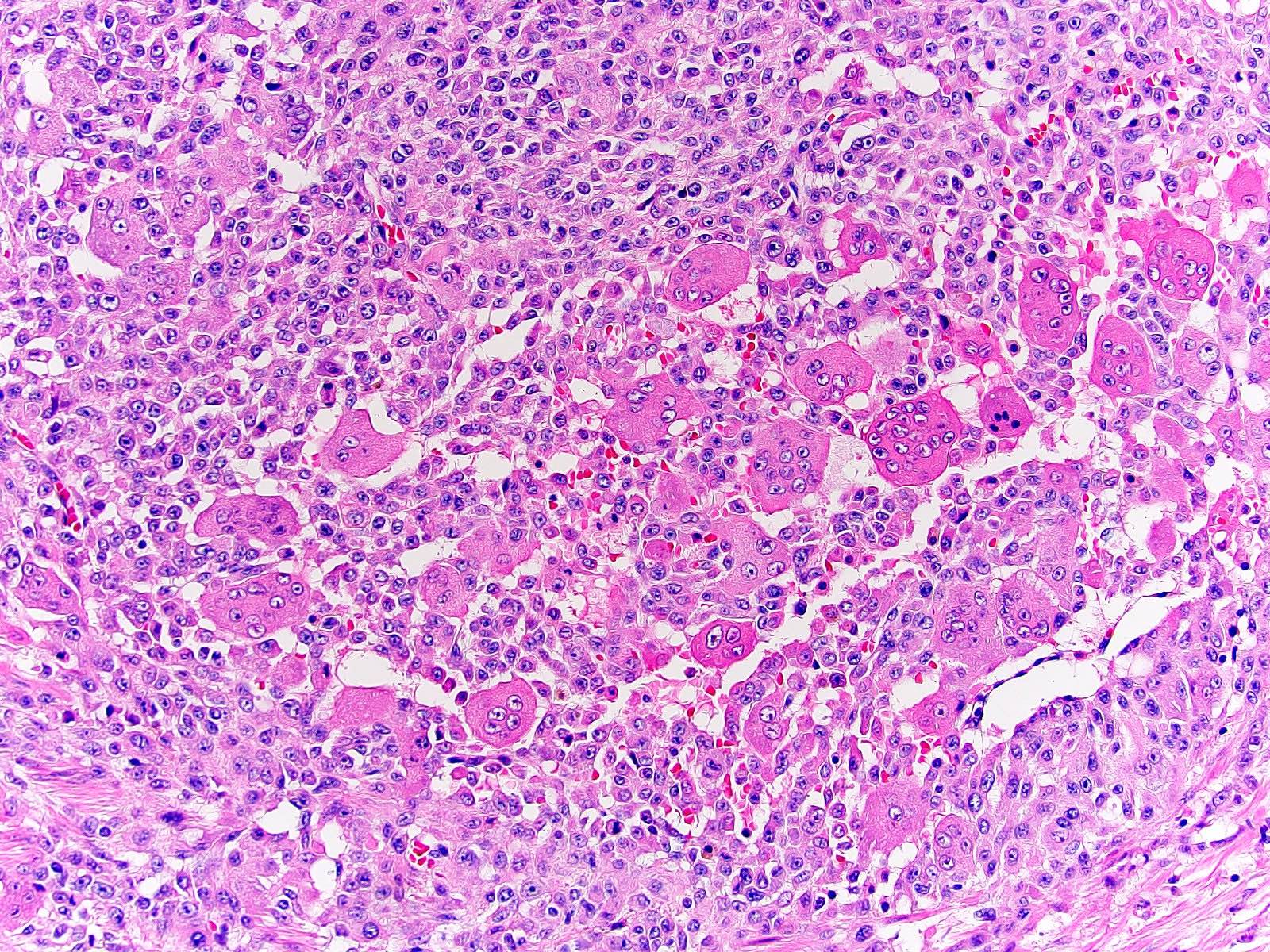
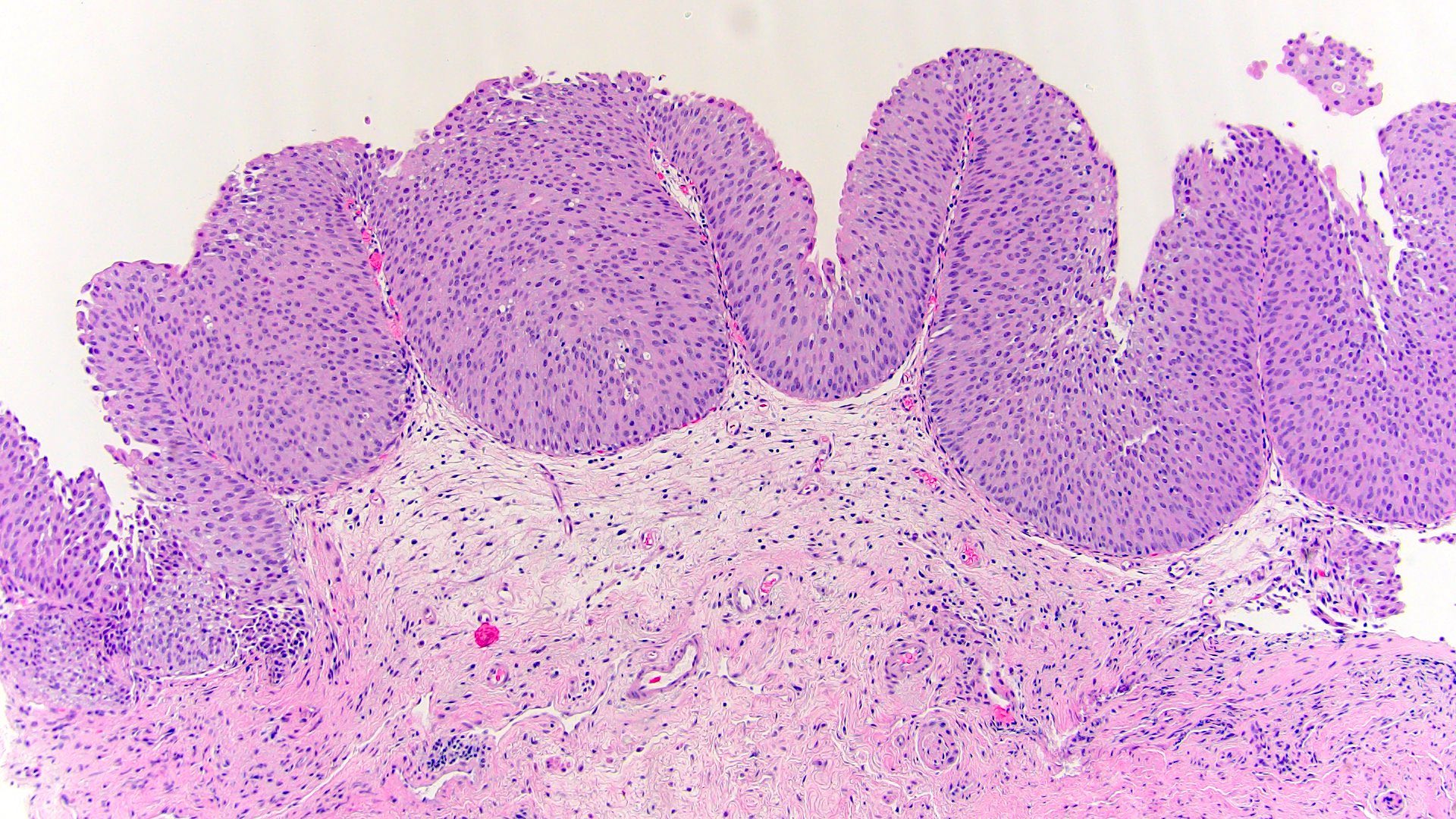
Microscopic (histologic) images
Additional references
- WHO Classification of Tumours Editorial Board: Urinary and Male Genital Tumours, 5th Edition, 2022, Virchows Arch 2014;465:199, Histopathology 2014;64:872, J Urol 2014;191:1693, World J Urol 2015;33:847, Hum Pathol 2016;47:20, Chin J Cancer Res 2016;28:107, J Clin Med 2020;9:138, Am J Surg Pathol 2020;44:1322, Adv Anat Pathol 2021;28:179, Eur Urol 2018;73:560, Surg Pathol Clin 2018;11:775, Am J Surg Pathol 2012;36:454, Adv Anat Pathol 2017;24:113
Board review style question #1
What is the cut off for a high grade component in diagnosing noninvasive high grade papillary urothelial carcinoma?
- 1%
- 5%
- 10%
- 25%
- 50%
Board review style answer #1
B. 5%. Papillary tumors are deemed high grade if they contain ≥ 5% high grade component; < 5% is noted as low grade with < 5% high grade component, prompted by poor interobserver reproducibility. Wide adoption of the 5% cut off would standardize reporting and improve interobserver agreement and tumor prognostication.
Comment Here
Reference: Bladder & urothelial tract - WHO classification
Comment Here
Reference: Bladder & urothelial tract - WHO classification
Board review style question #2
Board review style answer #2
A. Early low grade noninvasive papillary carcinoma. This lesion is composed of short, nonbranching papillae covered by mildly atypical urothelium that has cytological features similar to those of low grade noninvasive papillary carcinoma. This lesion is no longer considered a distinct entity and should be designated as a precursor or early low grade noninvasive papillary carcinoma. Answer B is incorrect given that the lesion is not entirely flat but rather has early papillary features (the term low grade dysplasia is used in the context of flat lesions which this is not). Answers C and E are incorrect because the lesion has atypical cytologic features similar to those of the neoplastic entity low grade noninvasive papillary carcinoma. Answer D is incorrect because it is the previous term that was used for these lesions and is no longer recommended.
Comment Here
Reference: Bladder & urothelial tract - WHO classification
Comment Here
Reference: Bladder & urothelial tract - WHO classification