Table of Contents
Definition / general | Essential features | Indications for biopsy | Contraindications | ICD coding | Planning the biopsy | Types of bone biopsy | Advantages and disadvantages | Diagnosis | Radiology description | Radiology images | Clinical images | Special specimen handling requirements | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Alexiev BA. Biopsy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bonebiopsy.html. Accessed April 23rd, 2024.
Definition / general
- Procedure in which bone samples are removed with a special biopsy needle or obtained during surgery to find out if cancer or other abnormal cells are present
- Involves the outer layers of bone, unlike a bone marrow biopsy, which involves the innermost part of the bone
Essential features
- Bone biopsies aim to facilitate definitive pathological diagnoses while minimizing complications, limiting potential tumor seeding and avoiding interference with subsequent therapies (Medicine (Baltimore) 2018;97:e11567)
- There are 3 types of bone biopsies: open (surgical) biopsy, core needle biopsy and fine needle aspiration biopsy
- Biopsy of a suspected primary bone neoplasm must yield enough tissue to permit complete histopathological evaluation, including grading
- Core needle biopsy is the most common type of needle biopsy used for bone tumors
Indications for biopsy
- Biopsy is the most critical first step in determining treatment strategy and outcomes in the management of musculoskeletal lesions (Medicine (Baltimore) 2018;97:e11567)
- Bone biopsy is indicated in the following circumstances (Eur J Radiol 2013;82:2092, Oper Orthop Traumatol 2012;24:403):
- Whenever there is significant doubt regarding the diagnosis of a benign or malignant lesion
- When the histologic distinction among possible diagnoses could alter the planned course of treatment
- Histopathologic evaluation of tumor entity and grading
- Planning of definitive tumor resection and initiation of neoadjuvant therapeutic regimen
- Obtaining unfixed, fresh frozen tumor samples for molecular / genetic analyses or tumor tissue bank
- Bone biopsy is also important for diagnosis of nonneoplastic bone disease, including infection and bone turnover disorders, among others (the diagnostic yield may vary, however)
Contraindications
- Bone biopsy is contraindicated in the following circumstances (Oper Orthop Traumatol 2012;24:403):
- Hemorrhagic diathesis
- Tumor is only accessible with a surgical approach leading to a significant damage of the surrounding tissue
- High probability of tumor cell contamination with incisional biopsy
- Poor physical status
- Poor therapeutic compliance
ICD coding
- Possible ICD-10 codes include but may not be limited to
- M86.171 - other acute osteomyelitis, right ankle and foot
- M86.172 - other acute osteomyelitis, left ankle and foot
- M86.671 - other chronic osteomyelitis, right ankle and foot
- M86.672 - other chronic osteomyelitis, left ankle and foot
- C40.31 - malignant neoplasm of short bones of right lower limb
- C40.32 - malignant neoplasm of short bones of left lower limb
- D16.31 - benign neoplasm of short bones of right lower limb
- D16.32 - benign neoplasm of short bones of left lower limb
- D49.2 - neoplasm of unspecified behavior of bone, soft tissue and skin
Planning the biopsy
- Biopsy must be carefully planned to ensure that adequate diagnostic tissue is obtained without compromising the oncologic outcome (Eur J Radiol 2013;82:2092)
- Biopsies should take place after the completion of staging studies; the surgeon, radiologist and pathologist should review these studies in detail so that each member of the team is fully apprised of the diagnostic considerations
- Site, approach and method selected for biopsy are intimately connected to the planned operative procedure; therefore, the biopsy should generally be performed at the hospital where definitive surgery will be carried out
- Biopsy of a suspected primary neoplasm must yield enough tissue to permit complete histopathological evaluation, including grading
- Biopsy must be performed such that the entire biopsy tract can be easily excised during later definitive surgery
- Careful hemostasis is mandatory; a hematoma may permit the spread of tumor cells into adjacent compartments, compromise the possibility of limb salvage and increase the likelihood of a wound infection
Types of bone biopsy
- Open (surgical) biopsy (Arch Orthop Trauma Surg 1979;94:71)
- Can be categorized as either incisional (the tumor capsule is intentionally violated as part of the procedure and a portion of the mass or lesion is removed) or excisional (the entire tumor is removed)
- Incisional biopsy is generally recommended for suspected benign lesions that can be treated definitively at the time of biopsy or in cases where greater volumes of tissue may be required than can be obtained with a needle biopsy in order to perform special staining or molecular diagnostics
- Incisional biopsies are also often performed when a needle biopsy result is nondiagnostic; for incisional biopsies, the incision and dissection tract are planned such that they can be excised during the definitive limb salvage procedure
- Excisional biopsy may be performed through the reactive zone that surrounds the tumor (termed marginal excision) or with a cuff of healthy tissue (primary wide excision)
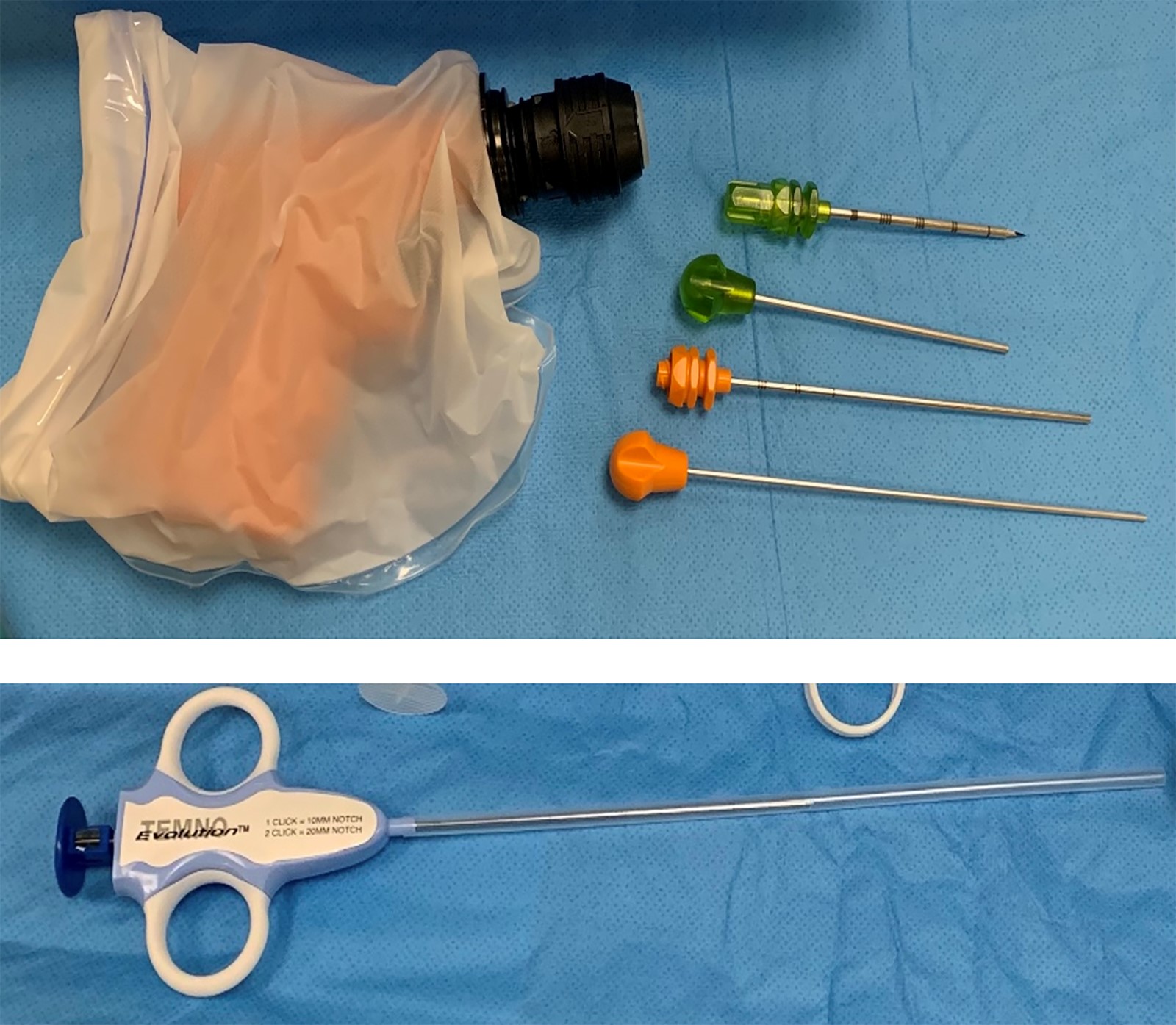
- Core needle biopsy (Clin Orthop Relat Res 2010;468:2992, Medicine (Baltimore) 2018;97:e11567, Eur J Surg Oncol 2001;27:668, Eur J Radiol 2013;82:2092)
- Uses a large needle to remove a cylinder of tissue
- The most common type of needle biopsy used for bone tumors
- It is a safe, reliable and accurate procedure and yields diagnostic information in a high proportion of patients (Radiology 2008;248:962)
- Fine needle aspiration (FNA) biopsy (Clin Orthop Relat Res 2010;468:2992, Medicine (Baltimore) 2018;97:e11567, Eur J Surg Oncol 2001;27:668, Eur J Radiol 2013;82:2092)
- Uses a very thin needle on the end of a syringe to obtain a small amount of fluid and some cells from the tumor
- It is a safe, reliable and accurate procedure and yields diagnostic information in a high proportion of patients (Radiology 2008;248:962)
Advantages and disadvantages
- Open (surgical) biopsy has historically been the diagnostic standard (Medicine (Baltimore) 2018;97:e11567)
- Provides large volumes of tissue sample, which facilitates accurate histological analyses and more precise estimates of patient prognoses
- Biopsy associated complications involve hematoma, infection and neurapraxia
- Biopsy procedure may spread tumor cells to surrounding tissue and therefore increase the risk of local recurrence
- It is imperative that the biopsy tract be placed within the planned resection margins prior to planning of future treatment involving surgical resection and radiation
- Core needle biopsy is increasingly accepted for the diagnosis of bone tumors (Clin Orthop Relat Res 2010;468:2992, Medicine (Baltimore) 2018;97:e11567)
- Yields diagnostic results comparable to open biopsy when determining malignancy and grade in bone tumors
- Advantages over open biopsy include time, cost and reduced morbidity
- Higher diagnostic accuracy than FNA in all aspects, such as determining the nature of the tumor, establishing the histologic type and grade and achieving a specific diagnosis (Arch Pathol Lab Med 2004;128:759)
- Fine needle aspiration (FNA) biopsy (Arch Pathol Lab Med 2004;128:759, Eur J Radiol 2013;82:2092, Clin Orthop Relat Res 2010;468:2992)
- An excellent method to confirm metastatic disease in bone and to document tumor recurrence
- It is also suitable for diagnosis of infection; although identification of a specific organism in chronic osteomyelitis may be difficult using any method
- This type of biopsy is less likely to be helpful for bone tumors, as the smaller needle might not be able to penetrate the bone and may not remove enough of a sample for testing
- FNA is usually insufficient for making a primary diagnosis of a bone tumor because it lacks tissue architecture and can only rarely provide information regarding tumor grade
Diagnosis
- Correlation with clinical and radiologic characteristics is critical; therefore, to achieve an accurate diagnosis, it requires a high level of skill from both the radiologist and the pathologist
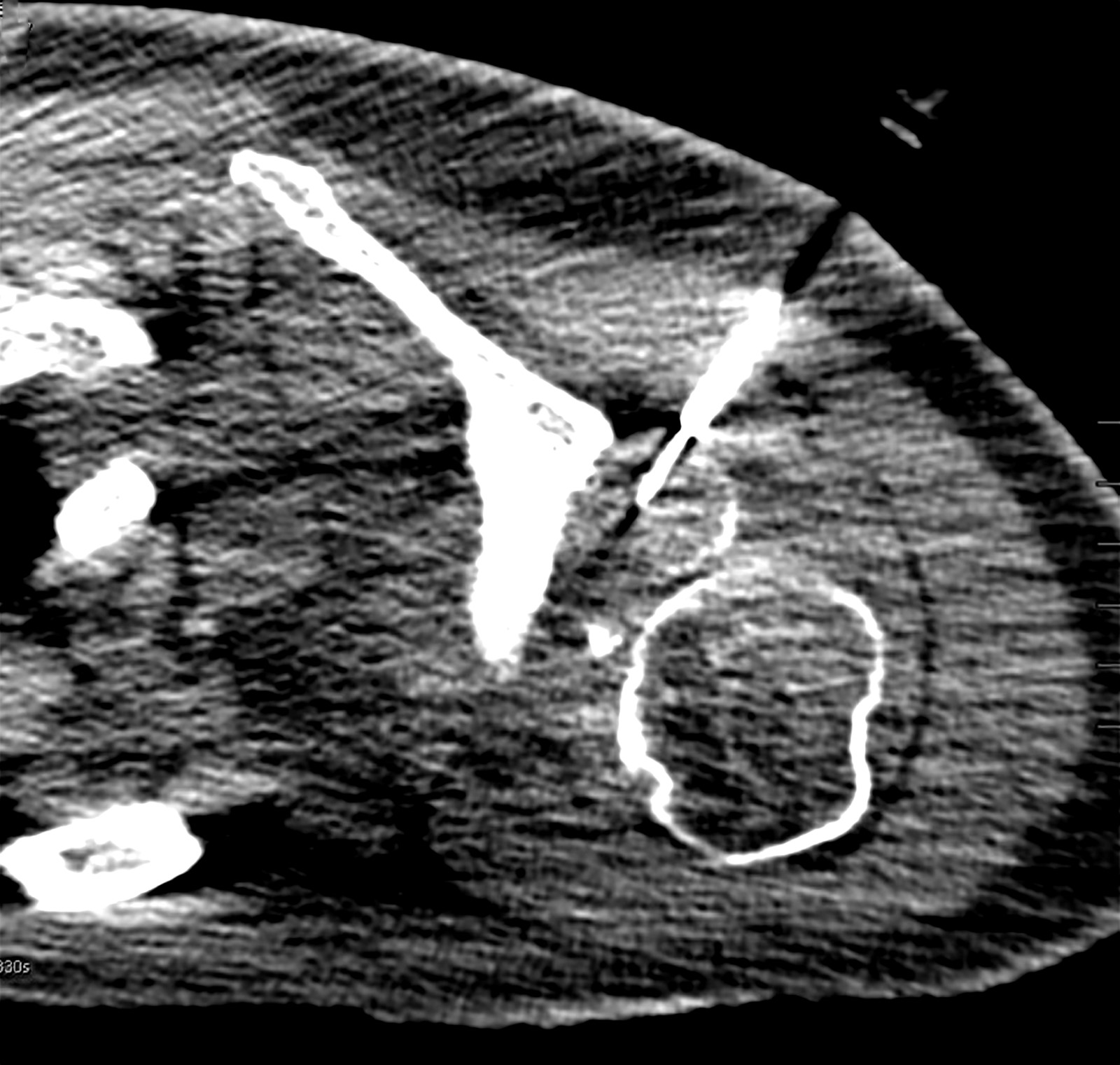
Radiology description
- Prebiopsy imaging (EFORT Open Rev 2017;2:51)
- Although initial referral imaging may be adequate for determining whether a biopsy is needed, imaging may have to be repeated if the whole lesion has not been imaged or in the case of malignant disease and the whole bone has not been imaged
- For bone sarcomata, MRI is the technique of choice; this will provide additional information regarding the type of biopsy to consider (in order to supply sufficient tissue for the pathologist), the approach and the appropriate part of the lesion to target
- MRI will also define areas which need to be avoided, such as the neurovascular bundle; the team will also be able to decide which imaging technique to use for guidance of the biopsy itself
- In cases where an additional lesion is discovered within the bone that does not have the typical appearance of a skip metastasis, the second lesion may also require biopsy
- MRI is also critical in defining whether there is local joint involvement
- Growth dynamics are best assessed via PET CT for systemic screening and assessment of local metabolic activity of a tumor
- Core biopsy with image guidance (i.e., fluoroscopy, ultrasound, CT or MRI) (EFORT Open Rev 2017;2:51)
- Provides the opportunity to selectively biopsy specific areas of the tumor
- CT is the most versatile of the imaging techniques, although relatively time consuming
- Almost any part of the body can be biopsied safely with CT guidance and specific areas of tumor can be targeted for biopsy
- Obtaining a minimum of 3 specimens in bone lesions optimizes diagnostic yield (Radiology 2008;248:962)
- Multiple biopsies are often needed and even then, may not yield a definitive diagnosis
- Diagnostic yield is lower for sclerotic bone lesions than for lytic lesions
- Onsite adequacy assessment of touch preparations is an accurate, simple and fast method for obtaining sufficient material for a complete diagnostic workup
Special specimen handling requirements
- Smears are air dried for Diff-Quik stain or fixed in 95% acidified alcohol for Papanicolaou stain (Cancer Cytopathol 2014;122:851, J Am Soc Cytopathol 2020;9:322)
- Tissue fragments retrieved from FNA biopsy are fixed in 10% buffered formalin and embedded in paraffin for cell blocks and hematoxylin eosin stained sections
- Core biopsy specimens are immediately placed in 10% saline buffered formalin, embedded in paraffin and sectioned for hematoxylin eosin staining (Pathol Res Pract 2022;231:153777)
- Decalcification to adequately process the biopsy
- Specialized immunocytochemical studies for diagnosis
- Molecular analysis on formalin fixed paraffin embedded (FFPE) or frozen tissue (cryopreserved at -70 °C)
- Cytologic imprinting for fluorescence in situ hybridization (FISH) studies (alcohol fixed and air dried)
- Tissue sample, fluid aspirate or swab should be sent for microbial culture if osteomyelitis is in the differential diagnosis
- If lymphoma is suspected, the hematopathologist should be alerted ahead of time for proper tissue handling
- Samples should be collected in saline and sent to the laboratory where they can be triaged to flow cytometry, cytogenetic and molecular studies
Board review style question #1
Which of the following is true about core needle biopsy (CNB)?
- CNB is usually insufficient for making a primary diagnosis of a bone tumor
- For each biopsy, a minimum of 1 core is obtained
- Lower diagnostic accuracy than FNA in all aspects, including determining the nature of the tumor, establishing the histologic type and grade and achieving a specific diagnosis
- Diagnostic yield is higher for sclerotic bone lesions than for lytic lesions
- Yields diagnostic results comparable to open biopsy for determining malignancy and grade in bone tumors
Board review style answer #1
E. Yields diagnostic results comparable to open biopsy for determining malignancy and grade in bone tumors. CNB is usually sufficient for making a primary diagnosis of a bone tumor. It has higher diagnostic accuracy than FNA in all aspects, including determining the nature of the tumor, establishing the histologic type and grade and achieving a specific diagnosis. For each biopsy, a minimum of 3 cores are obtained. The diagnostic yield is lower for sclerotic bone lesions than for lytic lesions.
Comment Here
Reference: Bone biopsy
Comment Here
Reference: Bone biopsy
Board review style question #2
Which of the following is true about open (surgical) biopsy?
- It is unimportant that the biopsy tract be placed within the planned resection margins prior to future treatment planning involving surgical resection and radiation
- Lower diagnostic accuracy than fine needle aspiration biopsy
- Open biopsy is not associated with increased risk for local recurrence
- Provides large volumes of tissue sample, which facilitates accurate histological analyses and more precise estimates of patient prognoses
- There are no contraindications for open biopsy
Board review style answer #2
D. Provides large volumes of tissue sample, which facilitates accurate histological analyses and more precise estimates of patient prognoses. Open biopsy is associated with increased risk for local recurrence. It has higher diagnostic accuracy than FNA in all aspects, including determining the nature of the tumor, establishing the histologic type and grade and achieving a specific diagnosis. Open biopsy is contraindicated in the following circumstances: hemorrhagic diathesis, high probability of tumor cell contamination, poor physical status and poor therapeutic compliance. It is imperative that the biopsy tract be placed within the planned resection margins prior to future treatment planning involving surgical resection and radiation.
Comment Here
Reference: Bone biopsy
Comment Here
Reference: Bone biopsy