Table of Contents
Definition / general | Granules | Clinical features | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy images | Additional referencesCite this page: Luca DC. Neutrophil maturation. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bonemarrowneutrophilmaturation.html. Accessed April 16th, 2024.
Definition / general
- The myeloid - monocytic lineage predominates in the bone marrow (50 - 70% of nucleated cells), which produces 1 - 2 x 109 granulocytes/kg/day
- Proliferation driven by multiple factors including G-CSF, especially adjacent to bony trabeculae and blood vessels
- Progresses from myeloid stem cell to myeloblast to promyelocyte to neutrophilic myelocyte to neutrophilic metamyelocyte to neutrophilic band to segmented neutrophil (polymorphonuclear neutrophil - PMN)
- Maturation is characterized by decreasing N/C ratio and increasing granule production and nuclear segmentation
- Immature forms are usually paratrabecular or perivascular; exceptions are after bone marrow transplantation, cytokine administration or chemotherapy
- Mature granulocytes pass through the bone marrow sinus wall, through endothelial cell cytoplasm and into the circulation
- Less mature cells are not released into the circulation under homeostatic conditions
- Present in the blood for only a few hours (circulating or marginated pools) before they egress into tissues
- Granulopoiesis is inhibited (negative feedback) by mature granulocytes and the bone marrow microenvironment
- Granulopoiesis can increase tenfold in patients with sustained infections or other inflammatory conditions
Granules
- Primary granules: large, round, red pink, electron dense; contain myeloperoxidase, elastase, lysozyme, cathepsin G and acid hydrolases; also called azurophilic (stains sky blue with azure stains used in the past); these granules are formed in promyelocytes (Blood 1979;53:179)
- Secondary (specific) granules: smaller, electron lucent (clear), cause characteristic cytoplasmic color in Wright stained preparations; contain lactoferrin and lysozyme; these granules are formed in myelocytes
- Also tertiary (contain gelatinase) and even quaternary (represented by secretory vesicles probably formed via endocytosis)
Clinical features
- Variations: brisk neutrophilia (30 x 109/L or 30,000/μL) at birth at high altitude, lower counts in black patients than in other populations, age related (newborn: 7,000 - 28,000/μL; infant: 2,500 - 10,000; child: 1,500 - 8,000; adult: 1,500 - 7,000)
- Causes of neutrophilia: constitutional (hereditary neutrophilia, familial cold urticaria, leukocyte adhesion deficiency) and acquired (bacterial infections, chronic Epstein-Barr virus infection, cytokine therapy, eosinophilia myalgia syndrome)
- Causes of neutropenia: constitutional (Fanconi anemia, cyclic neutropenia, Kostmann syndrome, Chédiak-Higashi syndrome) and acquired (drug induced neutropenia, acquired aplastic anemia, megaloblastic anemia)
Microscopic (histologic) description
- Myeloblast: 15 - 20 microns, round / oval; usually scant basophilic cytoplasm with no perinuclear halo; may contain Auer rods (due to fusion of azurophilic granules) or delicate azurophilic granules; round / oval nuclei with occasional indentations or clefts; one or more nucleoli; finely reticulated chromatin; N/C ratio is 80 - 85%
- Type I myeloblast: no granules in cytoplasm
- Type II myeloblast: up to 15 - 20 delicate granules in cytoplasm
- Type III myeloblast: more than 15 - 20 cytoplasmic granules but otherwise has features of a blast cell
- Promyelocyte: 10 - 20 microns; increased basophilic cytoplasm (compared to blasts) with primary coarse red purple, azurophilic granules; large, round / oval nucleus with red blue and fine to slightly condensed chromatin; 1 - 2 nucleoli; N/C ratio is 75 - 85%
- Myelocyte: 10 - 18 microns; round / oval with abundant pink cytoplasm with prominent red purple azurophilic (primary) granules and numerous fine, lilac and specific (neutrophilic) secondary granules; round / oval to slightly indented nucleus with red blue and slightly condensed chromatin; usually no nucleolus; N/C ratio is 50 - 65%
- Metamyelocyte: 10 - 16 microns; moderate pink or colorless cytoplasm with occasional red purple azurophilic (primary) granules and variable fine, lilac and specific (neutrophilic) secondary granules; indented nucleus with light blue purple and granular chromatin; no nucleolus; N/C ratio is 40 - 50%
- Band: 10 - 15 microns; abundant pink cytoplasm with many fine, lilac and neutrophilic (secondary) granules and possibly a few red purple azurophilic (primary) granules; nucleus is indented to more than half the distance from the farthest nuclear margin; elongated and horseshoe shaped nucleus; if lobulated, the bridge or isthmus between the lobes must be wide enough to have two distinct parallel dark margins with light nuclear chromatin in between; has blue purple and clumped granular chromatin; no nucleolus; N/C ratio is 33 - 40%
- Neutrophil: 10 - 15 microns; abundant pink cytoplasm with many fine, lilac and neutrophilic (specific or secondary) granules; lobulated (segmented) nucleus with 2 - 5 lobes, connected by a thin filament of chromatin; the filament is so narrow that there is no visible chromatin between the two sides; filaments may be difficult to visualize due to folding or twisting of nucleus; in other areas, the chromatin is dense with no nucleolus; N/C ratio is 33%
- Classify cell with folded nucleus as neutrophil if:
- Margins of two adjacent lobes are completely separated
- Width of either of the two adjacent lobes markedly narrows or converges towards the junction of the lobes (making it possible for there to be a hidden filament)
- The nucleus is so extensively folded that one cannot determine if a filament is present
- Classify cell with folded nucleus as band if:
- Elongated band form crosses over itself without any evidence of constriction to a filament
- Only the distal tip of the nucleus is slightly bent upon itself
- The hidden area in the fold between two adjacent lobes is so small and the lobe width is so thick that it is unlikely that a thin filament is present
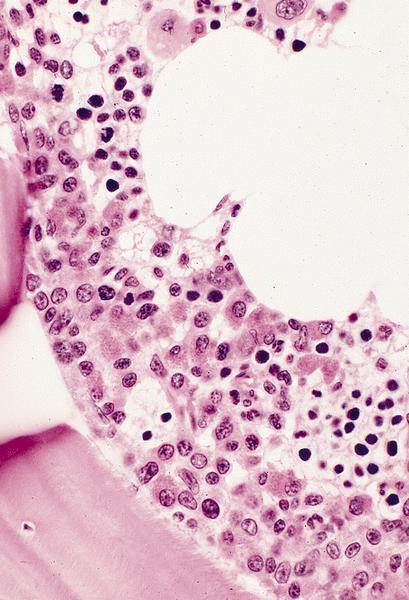
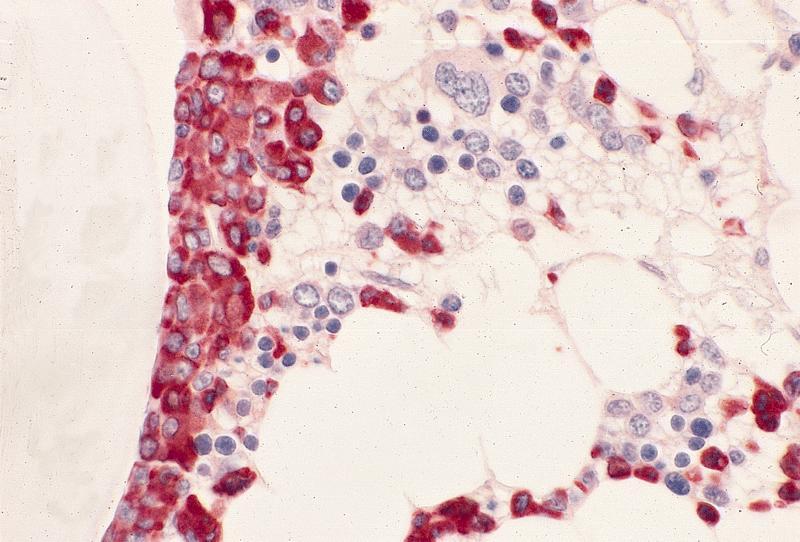
Microscopic (histologic) images
AFIP images
Images hosted on other servers:
Positive stains
- Neutrophils (may also stain other precursors): CD10, CD11b, CD11c, CD12, CD13, CD14 (weak - 30%), CD15, CD15s, CD15u, CD16a, CD16b, CD17, CD18, CD24, CD29 (low), CD30, CD31, CD32, CD33 (low), CD35, CD37 (low), CD43, CD45RO, CD47, CD47R (weak), CD48 (weak), CD49e, CD62L, CD63 (weak), CD64, CD65s, CD66a, CD66b, CD66c, CD66d, CD66e, CD68, CD69, CD83, CD84, CD85F, CD85M, CD87, CD88, CD89, CD92, CD93, CD97, CD101, CD107a, CD107b (weak), CD114, CD116, CD128a, CD128b, CD132, CD139, CD141, CD148, CD156a, CD157 and CD170
Additional references