Table of Contents
Definition / general | Essential features | CPT coding | Sites | Ancillary testing | Procedure (FNA) | Limitations / disadvantages of FNA | Breast cytologic studies other than FNA | Case reports | Breast FNA C1 - C5 classification | Breast FNA Masood and Modified Masood classification | Cytology description of benign lesions | Cytology description of malignant lesions | Grading of malignant smears | Cytology images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Al Nemer AM. Cytology. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastcytology.html. Accessed April 19th, 2024.
Definition / general
- Refers mainly to fine needle aspiration cytology (FNA) and also includes cytologic examination of imprint, nipple discharge and ductal lavage
- Although largely replaced by core needle biopsy, FNA can increase the accuracy rate if both tests are combined, minimizing false negative results of core needle biopsy related to sampling issues, as more needle passes are performed in FNA (Diagn Cytopathol 2016;44:578)
- Nowadays, it is used as part of the triple approach (along with clinical and radiologic findings) to confirm a benign diagnosis, as a conjugate to core needle biopsy to enhance the accuracy rate, solo for palpable breast lesions in one step clinic, for lymph node assessment and for lesions difficult to access by core needle biopsy, like those near the chest wall
- Breast FNA is a safe, reliable, accurate, fast, cost saving, almost complication free method that can be performed without anesthesia
- Along with core needle biopsy, these tests replaced frozen sections and surgical biopsies for diagnosing breast lesions
- Breast FNA cytology doesn't give a definite diagnosis name to the lesion most of the time and also can't differentiate atypical ductal hyperplasia from low grade cancer or high grade in situ carcinoma from invasive cancer
Essential features
- Breast FNA can't differentiate atypical duct hyperplasia from low grade ductal carcinoma in situ or high grade ductal carcinoma in situ from invasive carcinoma
- It is a screening test; it doesn't usually provide a specific diagnosis name to the lesion but enhances the sensitivity of cancer detection if combined with core needle biopsy
- Biomarkers and other ancillary studies can be performed on cell block
- False negative result is frequent in special types of carcinoma, like lobular and tubular, and false positive diagnoses are seen with changes associated with lactation and therapy
CPT coding
- 10004: FNA without imaging guidance, each additional lesion
- 10005: FNA including ultrasound guidance, first lesion
- 10006: FNA including ultrasound guidance, each additional lesion
- 10007: FNA including fluoroscopic guidance, first lesion
- 10008: FNA including fluoroscopic guidance, each additional lesion
- 10009: FNA including CT guidance, first lesion
- 10010: FNA including CT guidance, each additional lesion
- 10011: FNA including MRI guidance, first lesion
- 10012: FNA including MRI guidance, each additional lesion
- 10021: FNA without imaging guidance, first lesion only
- 19000: Puncture aspiration of breast cyst
- 19001: Puncture aspiration of breast cyst, each additional cyst (used with 19000)
Sites
- Breast, lymph node
Ancillary testing
- Ancillary studies include biomarker testing in carcinoma cases, flow cytometry in lymphoma cases and molecular studies
- Biomarker testing on breast FNA
- Useful for patients who will undergo neoadjuvant therapy if core needle biopsy is not available
- Also, the American Society of Clinical Oncology / College of American Pathologists (ASCO / CAP) recommends evaluating the biomarkers on FNA obtained from foci of metastasis and local recurrence after treatment
- Same ASCO / CAP criteria that is used for tissue can be applied to cytology specimens, including the cold ischemia time (ideally less than an hour), as well as fixation time (6 - 72 hours) (College of American Pathologists: CAP QCDR Measure Formalin Fixation Time [Accessed 19 August 2021])
- Recommendation of CAP is to report the percentage of positive nuclei for ER and PR; minimum of 100 cells should be counted (Arch Pathol Lab Med 2010;134:907)
- FISH is more reliable than IHC for HER2 / neu
- HER2 gene amplification can be reliably detected in cytology specimen when air fixed or fixed with FISH fixative
- More interobserver discordance rate than the corresponding biomarker testing in histologic samples is attributed to the admixed inflammatory cells and mesothelial cells in body cavities; adding GATA3 or GCDFP-15 is recommended to enhance the accurate detection of tumor cells (Acta Cytol 2018;62:288)
- It is impossible to distinguish the positivity of markers in the invasive component from the in situ component
Procedure (FNA)
- Ideally performed by a trained radiologist under ultrasound or stereotactic guidance
- Direct smearing is the most common preparation method in FNA
- Both alcohol fixed and air dried are used
- Alternatives include cytospin preparation, thin layer preparation, cell block
Limitations / disadvantages of FNA
- Requires training, subjective in interpretation; the accuracy is influenced by both the quality of smear and the expertise of the reader
- Can't differentiate atypical duct hyperplasia from low grade ductal carcinoma in situ
- Can't differentiate high grade ductal carcinoma in situ from invasive carcinoma
- Doesn’t give a definite diagnosis name to the lesion most of the time
- Equivocal, false positive, false negative results
Breast cytologic studies other than FNA
- Cell block:
- Enhances the utility of FNA
- Ancillary studies including biomarkers can be done
- Diagnostic architectural features can be displayed
- Returned cell block from a Papanicolaou stained smear is also useful in difficult cases to interpret, e.g. if the morphology is obscured by blood (Diagn Cytopathol 2016;44:505)
- Nipple discharge cytology:
- Nipple discharge fluid commonly reflects hormonopathy, like dysthyroidism and hyperprolactinemia
- Papilloma is the most common breast lesion that presents with nipple discharge
- It has a weak association with cancer; increased if the discharge is bloody or associated with a mass
- Nipple discharge cytology has a low sensitivity (Ann Surg Oncol 2020 Nov 9 [Epub ahead of print], Diagnosis (Berl) 2020 Jun 26 [Epub ahead of print])
- Negative discharge: acellular or hypocellular, composed mainly of proteinaceous fluid and foamy cells; benign ductal epithelial or apocrine cells can be seen with no atypical features
- Ductal lavage cytology:
- Has a questionable utility in risk stratification of getting breast cancer in women with contralateral breast cancer or BRCA1 or BRCA2 mutation
- Imprints:
- Intraoperative imprint cytology of sentinel lymph node: limited sensitivity for micrometastasis
- Intraoperative imprint cytology for diagnosing breast carcinoma and evaluating margins: useful in combination with frozen section or alone
- Intraoperative imprint cytology to predict occult nipple involvement before performing nipple sparing mastectomy (Breast Cancer Res Treat 2015;153:557)
- Touch imprint cytology of core needle biopsy: to complement core needle biopsy, providing immediate cytologic diagnosis to the lesion (Geburtshilfe Frauenheilkd 2016;76:59)
Case reports
- 44 year old woman with positive FNA and negative excision (Int J Surg Case Rep 2016;25:132)
- 45 year old woman with silicone nipple discharge (Int J Surg Case Rep 2020;74:73)
- 47 year old woman with primary cystic type squamous cell carcinoma of the breast (Asian J Surg 2017;40:243)
- 48 year old woman with nodular faciitis of the breast diagnosed by FNA (BMJ Case Rep 2015;2015:bcr2015213076)
- 54 year old woman with metaplastic breast carcinoma (In Vivo 2017;31:737)
- 57 year old woman with Hodgkin lymphoma of the breast diagnosed by FNA (Case Rep Hematol 2019;2019:9256807
- 62 and 70 year old men with cytologic examination of nipple discharges revealed atypia and positive results (Diagn Cytopathol 2019;47:121)
- 74 year old man with ductal carcinoma in situ, diagnosed as atypia in nipple discharge cytology (Breast J 2002;8:112)
- 77 year old woman diagnosed with adenoid cystic carcinoma of the breast based on immunohistochemistry done on FNA (Diagn Cytopathol 2015;43:722)
- 86 year old woman with solid papillary carcinoma; cytologic findings of nipple discharge and FNA are described (Diagn Cytopathol 2020;48:53)
Breast FNA C1 - C5 classification
- In U.K. and Europe, numerical system of 5 points classification is used (C1 to C5)
- In U.S. and Canada, same system but without the numerical designation
- 5 categories: inadequate, benign, atypia favor benign, suspicious probably malignant and malignant
- Inadequate / C1:
- Smear is not interpretable or is undiagnostic
- Common causes include: low cellularity, obscured morphology due to blood, crushing artifact, poor fixation and degenerated cells
- No definite criteria for adequacy in breast FNA cytology
- MD Anderson Cancer Center Group proposed that 4 - 6 well visualized cell groups with 10 or more cells / flat sheets as an adequacy criteria (Cancer 1997;81:3)
- Samples that lack epithelial cells are considered inadequate in general
- If the lesion is suspected to be lipoma or fat necrosis, the absence of epithelial clusters doesn't indicate inadequacy
- Benign / C2:
- Benign epithelial clusters are seen with no atypia or malignant features
- Cellularity is usually not high; cells are seen in flat sheets, depicting fine chromatin, smooth nuclear membrane, low nuclear cytoplasmic (N/C) ratio, no pleomorphism
- Fatty fragments are commonly seen
- Bare nuclei of myoepithelial cells are easily seen
- Histiocytes and apocrine cells can be found
- In duct ectasia: inspissated material within macrophages and multinucleated giant cells
- Atypia / C3:
- Similar to the findings of benign category but with higher cellularity, slight crowdedness, 3 dimensional groups, nuclear enlargement and pleomorphism
- Common lesions encountered in this category: proliferative fibrocystic change with or without atypia, papillary lesions, lobular lesions including atypical lobular hyperplasia / lobular carcinoma in situ and some special types of breast carcinoma commonly missed in FNA, like lobular, tubular and cribriform
- Suspicious / C4:
- Highly atypical findings but insufficient to be called malignant
- Commonly encountered reasons: hypocellular or poorly preserved smear, the findings are focally seen in a benign background or the degree of atypia is more than the previously described in C3 category but not sufficient for C5 category
- Common lesions encountered in this category: atypical duct hyperplasia, low grade ductal carcinoma in situ, invasive carcinoma that wasn't adequately sampled and special types of carcinoma like lobular, tubular and cribriform
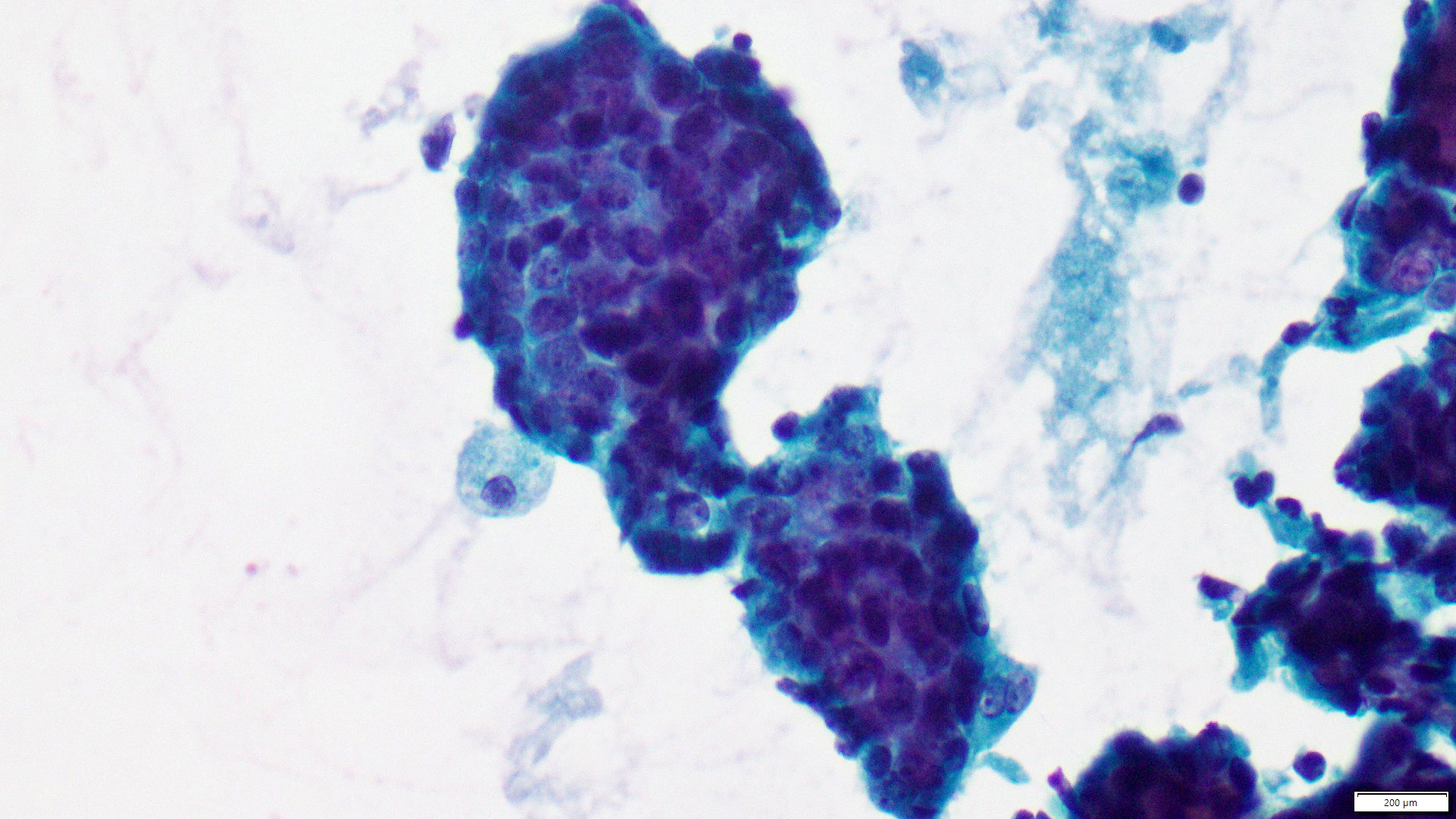
- Malignant / C5:
- Cellularity is usually high and the cytologic features are malignant (high N/C ratio, irregular nuclear contour, hyperchromasia, conspicuous nucleoli)
- Malignant cells are seen singly or in loose clusters
- Necrotic debris might be seen in background
- Some special types of carcinoma can be specifically recognized or suspected, like mucinous, medullary-like, papillary
Breast FNA Masood and Modified Masood classification
- Suggested scoring systems: Masood followed by the more reproducible Modified Masood Scoring System (Acta Cytol 2019;63:233)
- It is based on 6 morphologic features:
| Cell arrangement | Cell pleomorphism | Myoepithelial cells | Anisonucleosis | Nucleoli | Chromatin clumping | Score |
| Monolayer | No | Many | No | No | No | 1 |
| Nuclear overlapping | Mild | Moderate | Mild | Micronucleoli | Rare | 2 |
| Clustering | Moderate | Few | Moderate | Rare macronucleoli | Occasional | 3 |
| Discohesion | Marked | No | Marked | Mainly macronucleoli | Marked | 4 |
- Breast lesions are classified into 4 categories according to the given score:
| Breast lesion | Total score in Masood system | Total score in Modified Masood system |
| Nonproliferative breast disease | 6 - 10 | 6 - 8 |
| Proliferative breast disease with no atypia | 11 - 14 | 9 - 14 |
| Proliferative breast disease with atypia | 15 - 18 | 15 - 18 |
| Malignancy | 19 - 24 | 19 - 24 |
Cytology description of benign lesions
- Fibrocystic change:
- Cellularity is variable, commonly moderately cellular but can be paucicellular if fibrotic
- Epithelial cells are arranged in cohesive flat sheets, polarized to give honeycomb pattern
- Myoepithelial cells naked nuclei are seen in background and overlying the epithelial sheets
- With or without apocrine and foam cells, fat and stroma
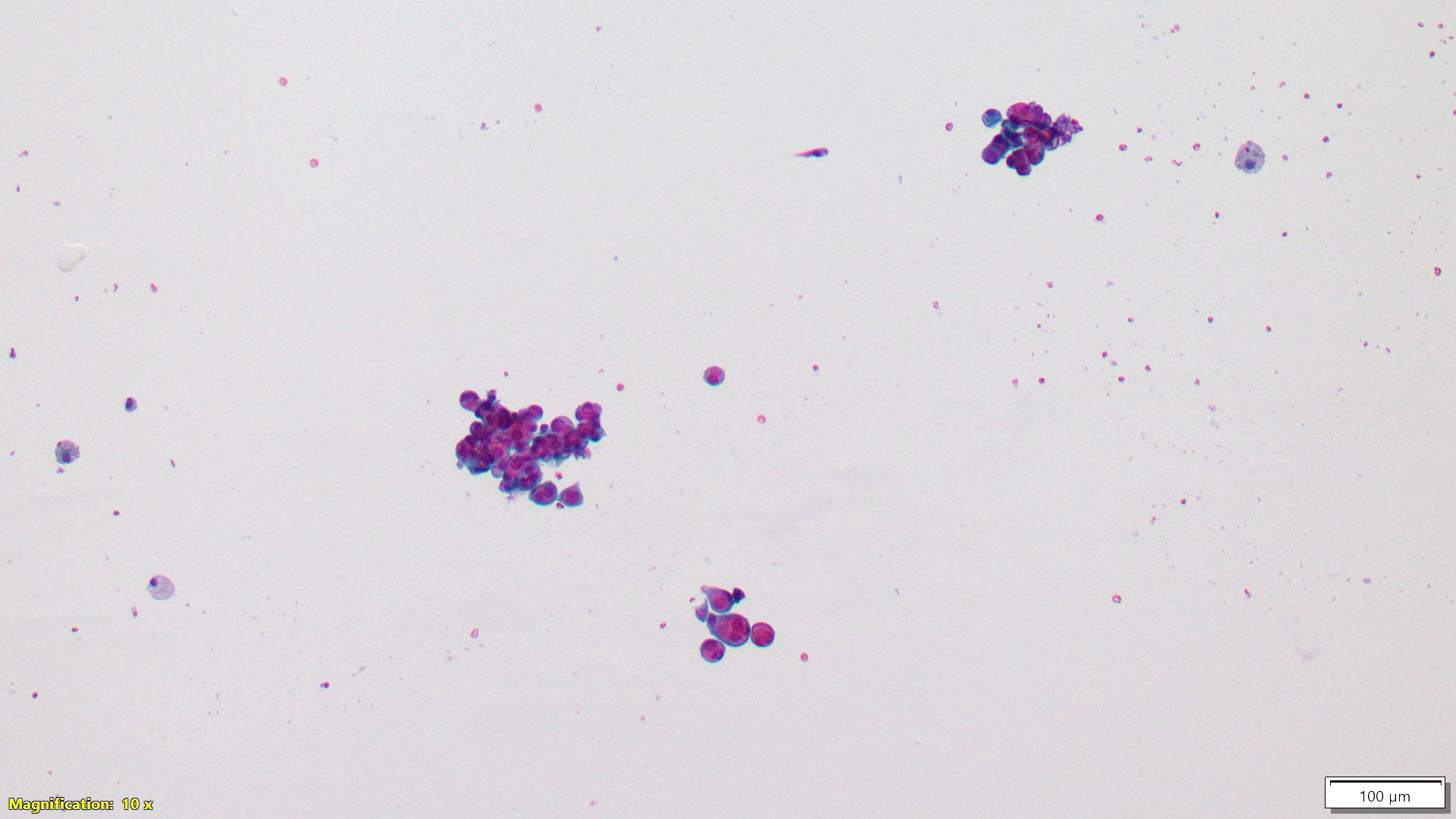
- Fibroadenoma:
- Moderately to highly cellular smear
- Sheets of cohesive epithelial cells that branch, giving the antler horn pattern
- Myoepithelial cells naked nuclei are numerous
- Stromal fragments can be seen
- Apocrine and foam cells: less likely than fibrocystic change
- If hypercellular stromal fragment is seen with atypia, the lesion is likely to be phyllodes tumor
- Adenomyoepithelioma:
- Moderately to highly cellular smear
- More chance to show crowded groups or 3 dimensional clusters than fibroadenoma
- Epithelial cells and myoepithelial cells are seen in variable proportions
- Myoepithelial cells can be seen as naked nuclei as in other lesions or take the form of comma shaped dark nuclei, spindle, epithelioid or plasmacytoid
- Epithelioid cells with intranuclear inclusion and intracytoplasmic vacuoles gives the characteristic soap bubble appearance (Cancer 2006;108:250)
- Papillary lesions (intraductal papilloma, etc):
- Difficult to segregate benign papilloma from well differentiated carcinoma in FNA
- Cellular smear, branching epithelial sheets like fibroadenoma or 3 dimensional clusters with or without stromal cores
- Columnar cells favor papilloma over fibroadenoma (Cancer 2003;99:156)
- Uniformity of cells favor malignancy and polymorphism favor benign papilloma
- Gynecomastia:
- Spectrum of pictures from overtly benign to fibroadenoma-like changes to worrisome morphology like nuclear molding, atypia, conspicuous nucleoli and inconspicuous myoepithelial cell component
Cytology description of malignant lesions
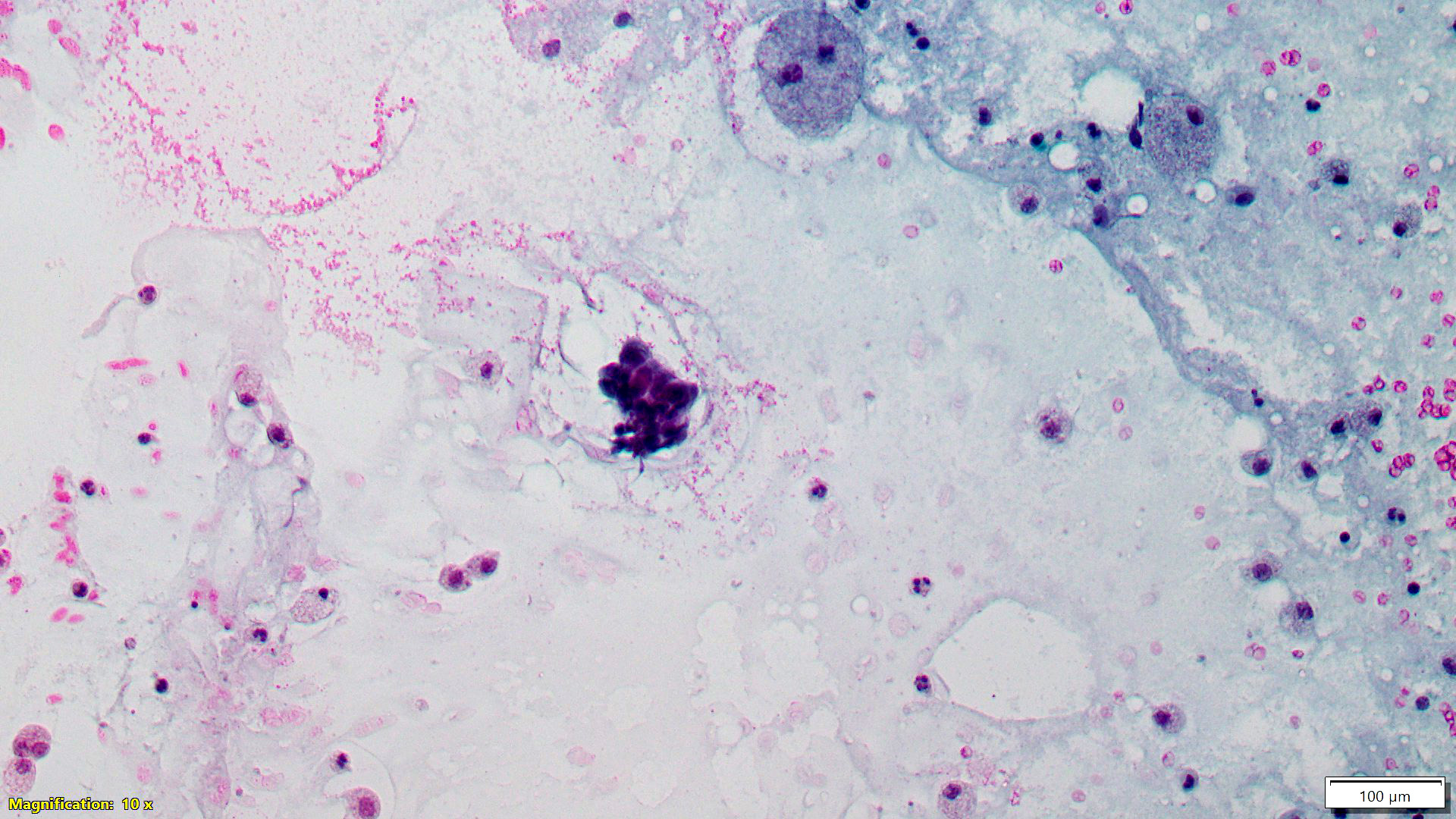
- Invasive breast carcinoma of no special type:
- Cellular smear
- Less cohesiveness with or without single epithelial cells scattered in background
- Epithelial sheets are crowded with 3 dimensional or syncytial pattern; might form acini
- No or minimal myoepithelial cells
- With or without tumor diathesis
- Lobular carcinoma:
- Can be missed as false negative due to the low cellularity and limited atypia
- Some cases resemble invasive carcinoma of no special type
- Cellularity is frequently low to moderate
- Cells are uniform, mildly atypical, dispersed in singles, linear cords or loose clusters
- Myoepithelial cells are absent
- Signet ring cells can be seen
Grading of malignant smears
- Not routinely done
- Mainly depends on nuclear grading due to the difficulty of assessing mitoses and tubular formation
- Robinson and McKee proposed a grading system that correlates well with the histologic grading, depending on 6 parameters: dissociation, nuclear size and margin, nucleoli, chromatin and uniformity of cells (Acta Cytol 1995;39:1257)
- Another proposed prognostic system is based on 3 characteristics: nuclear grade, architecture (discohesion) and background features (bare atypical epithelial cell nuclei); it is claimed to correlate well with histologic grading, lymph node status, positivity for HER2 / neu, p53 and Ki67 (Diagn Cytopathol 2006;34:542)
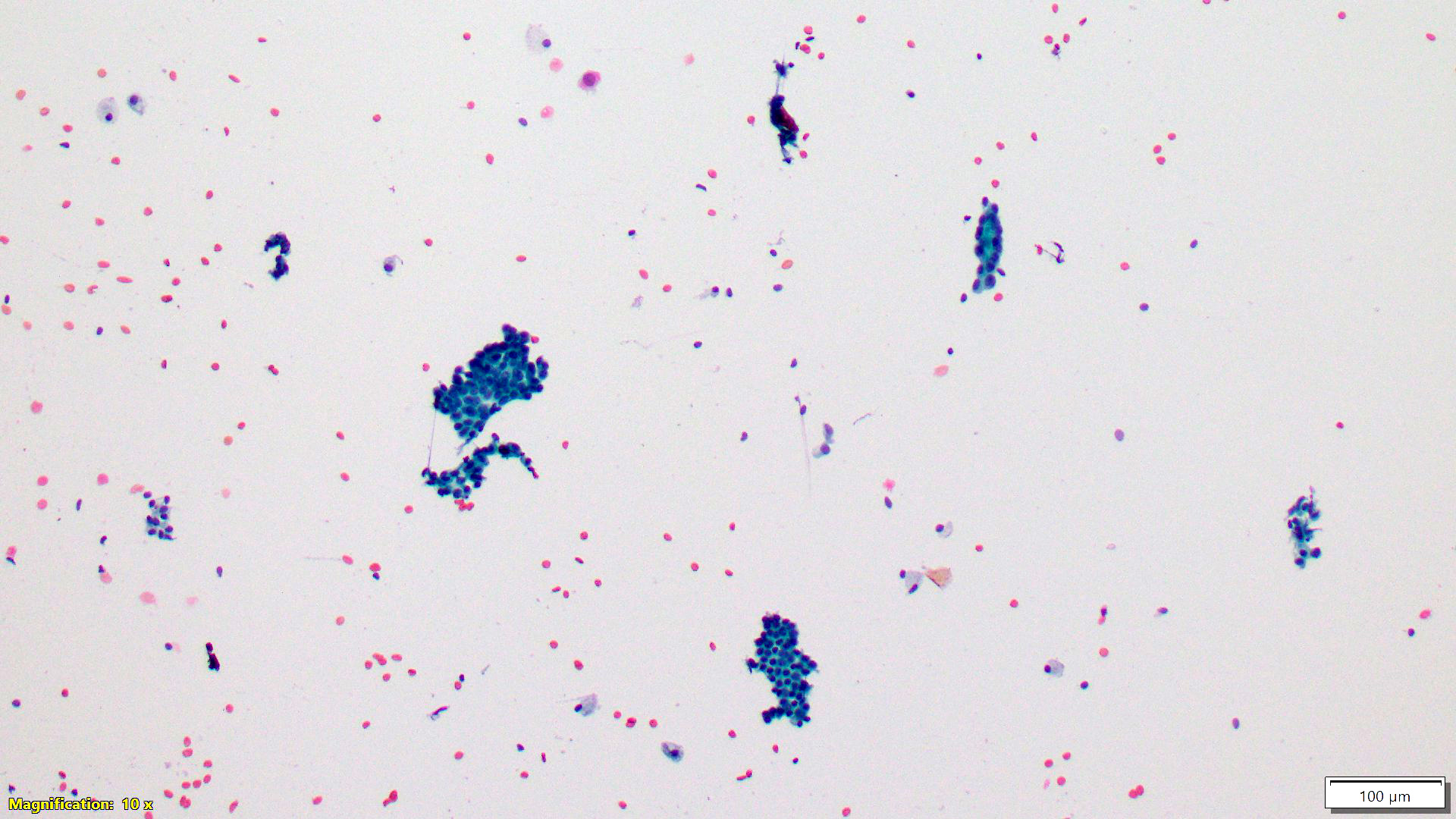
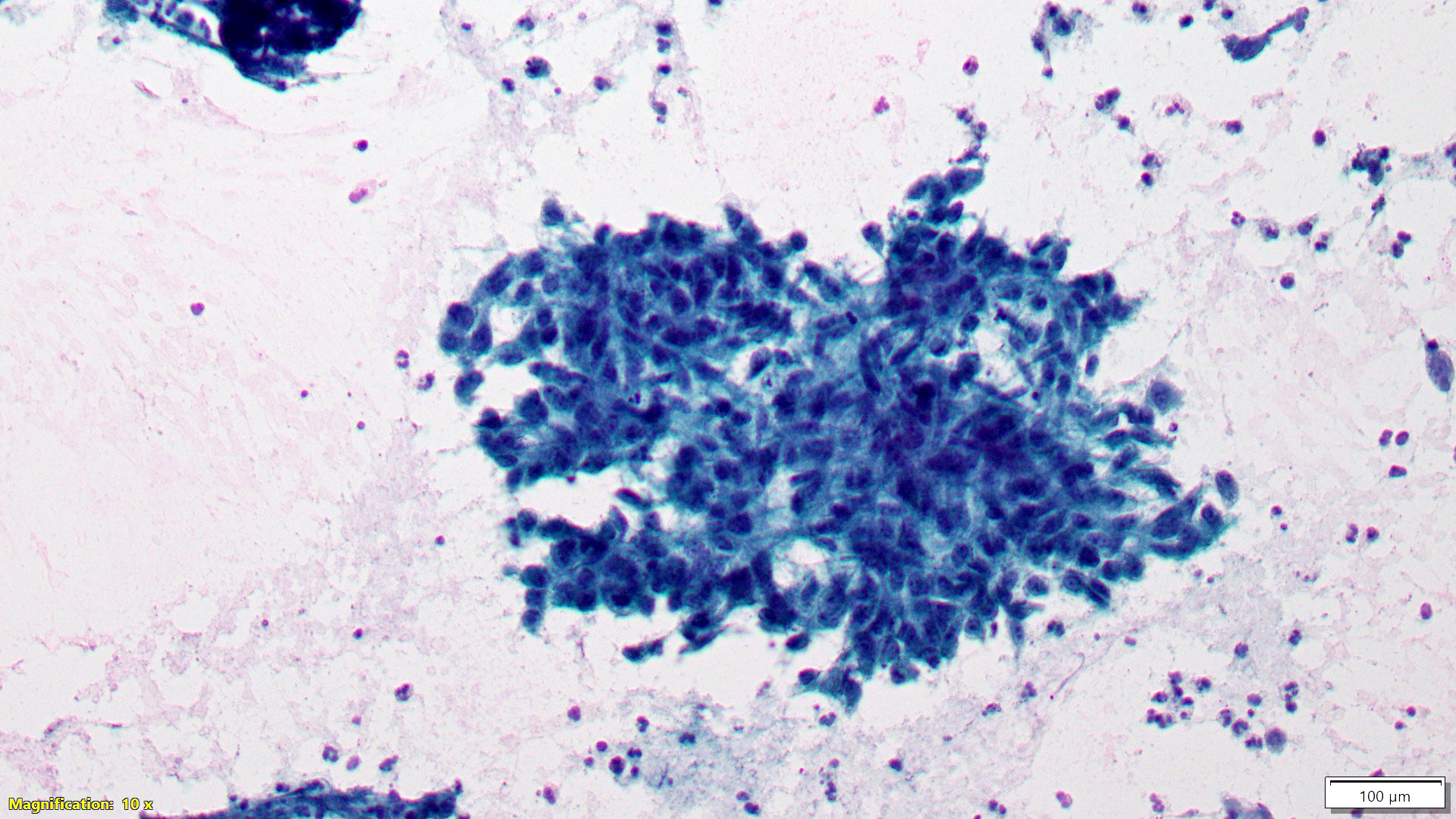
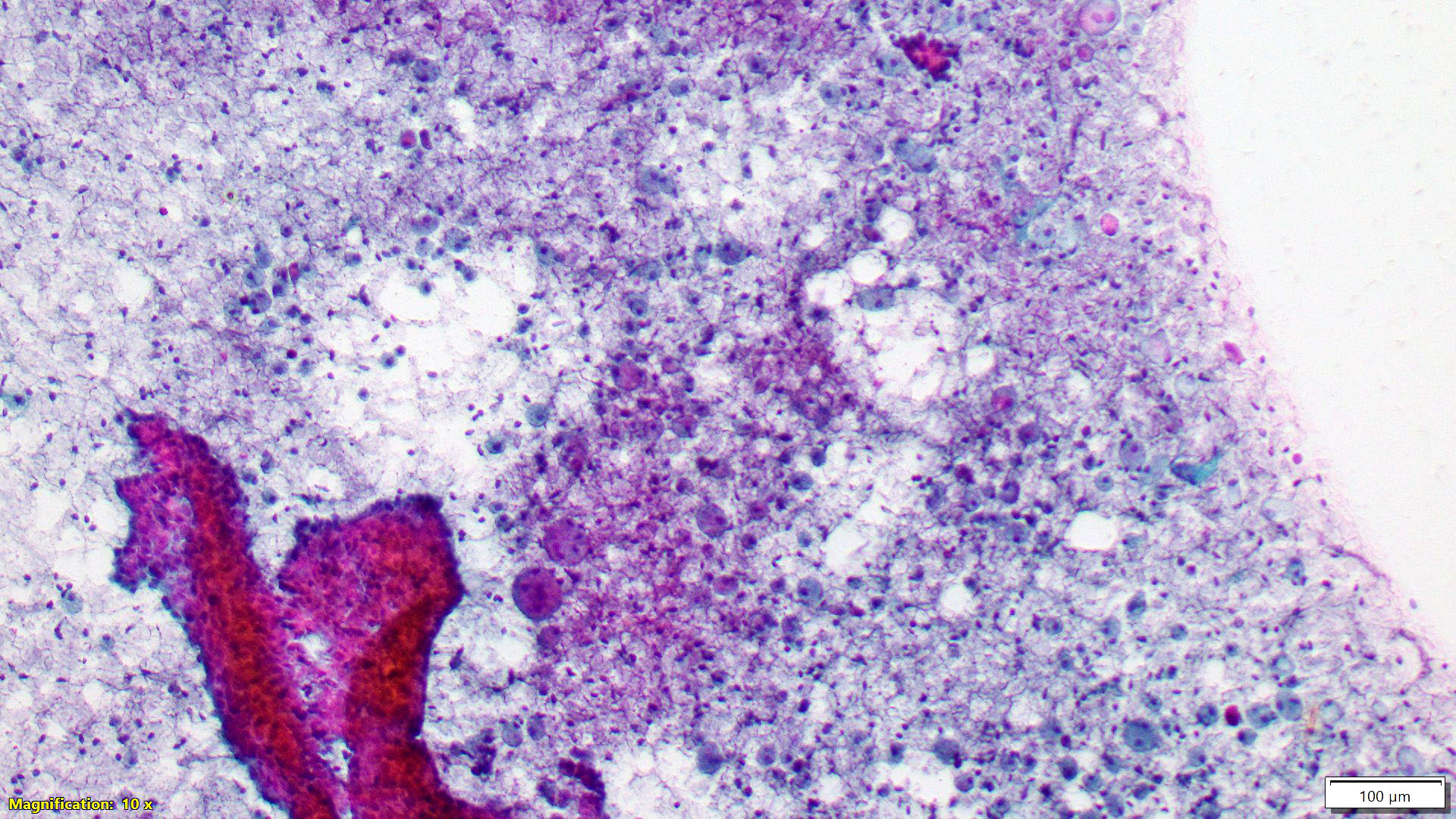
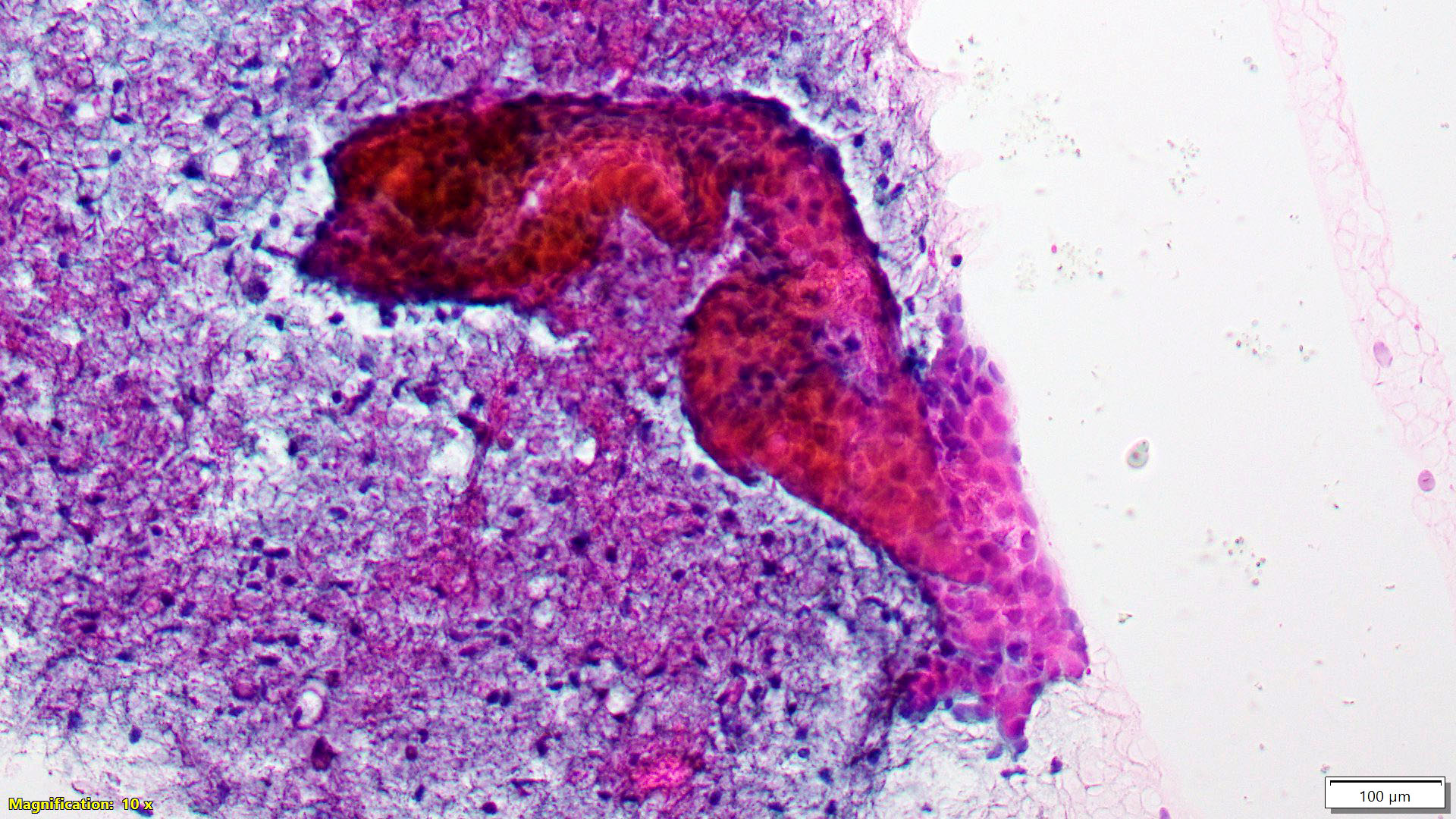
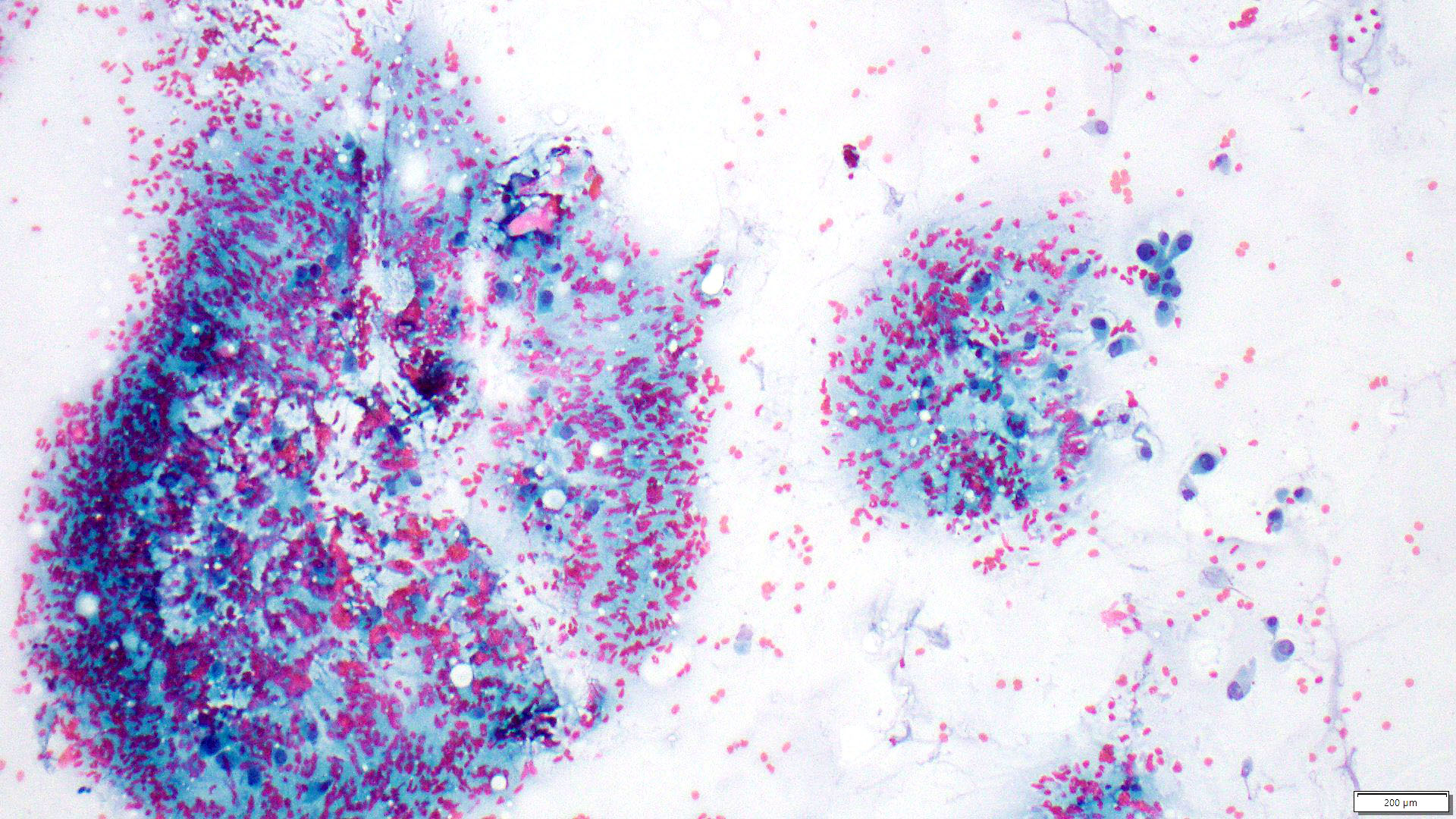
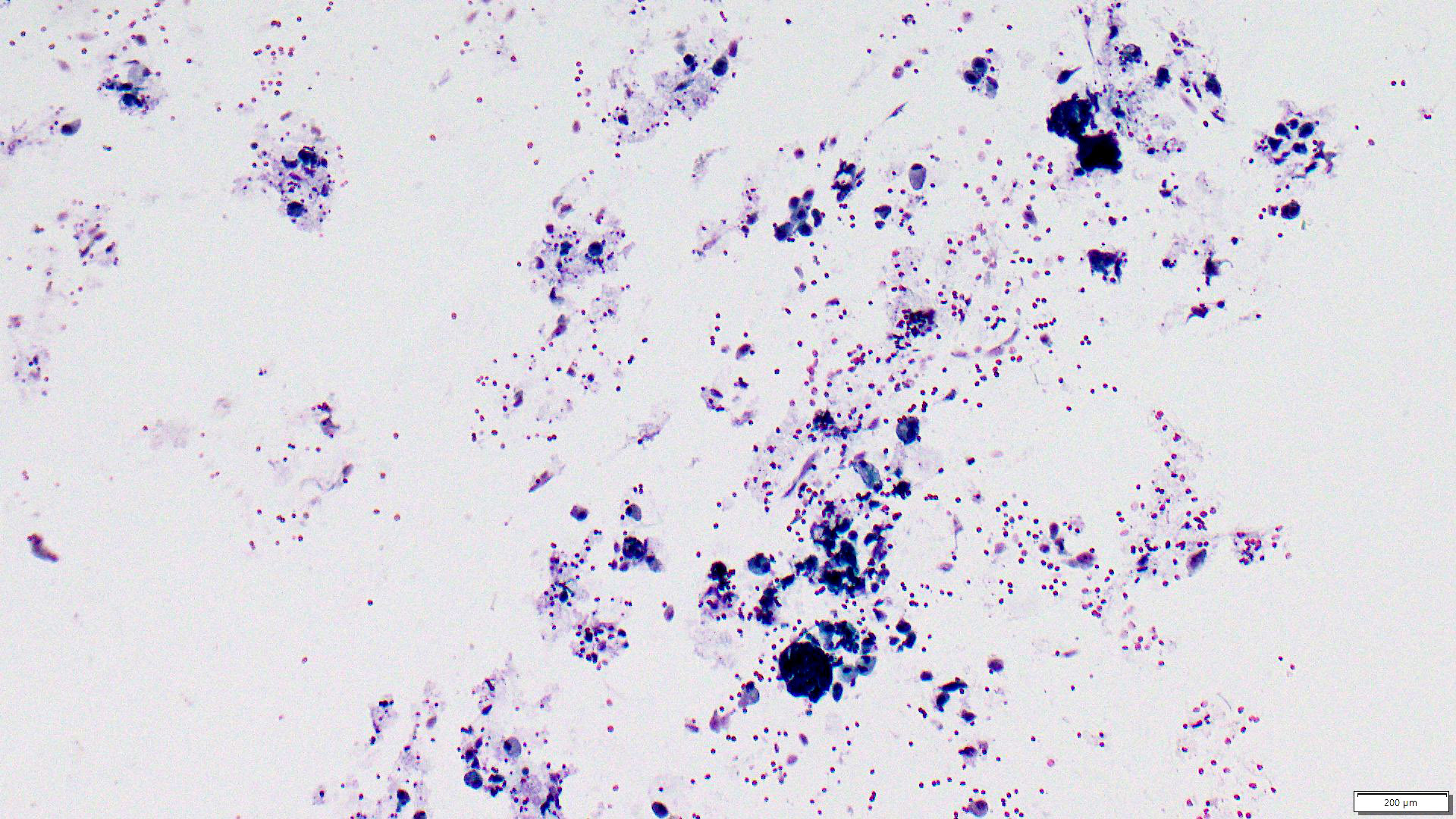
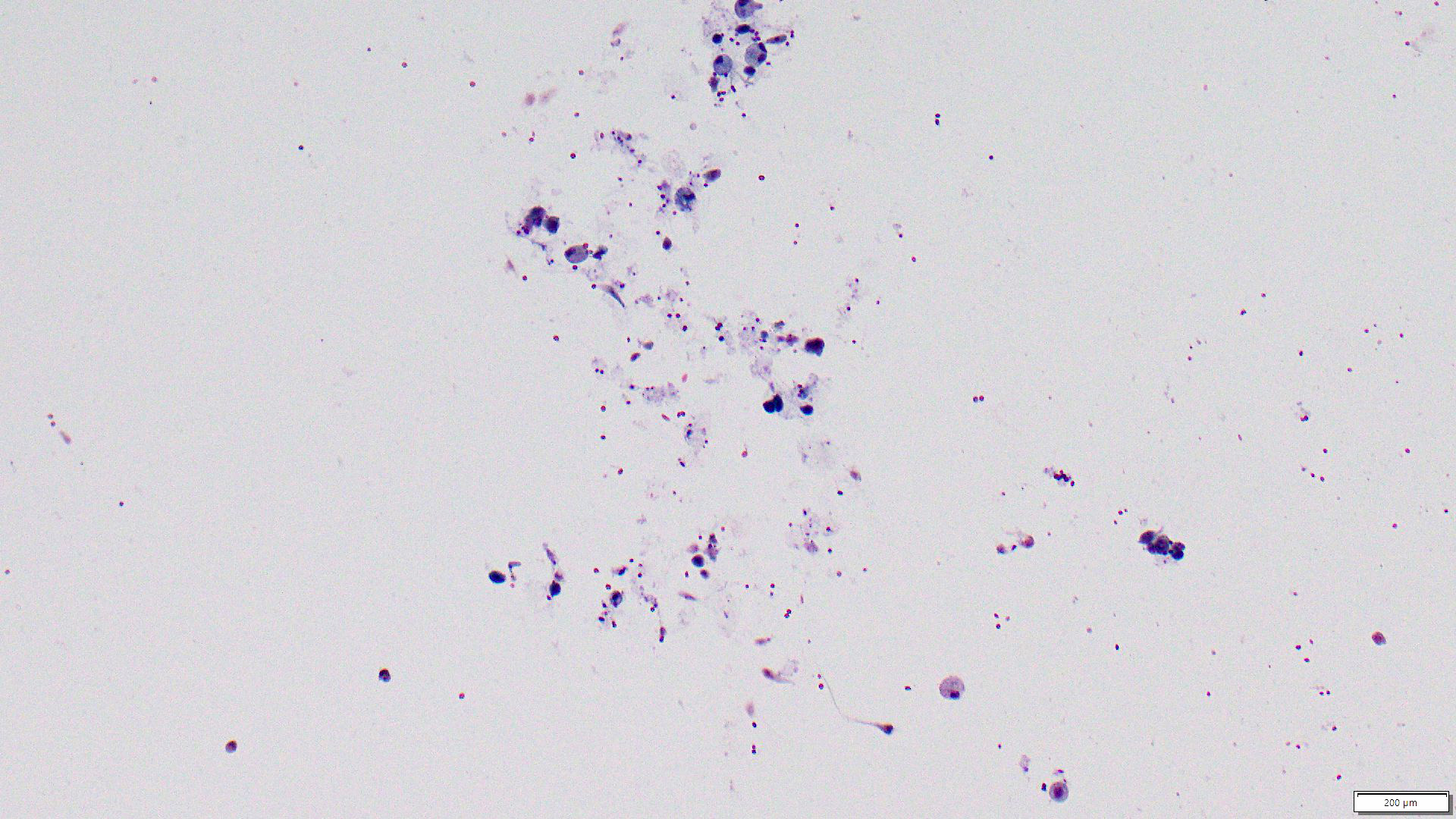
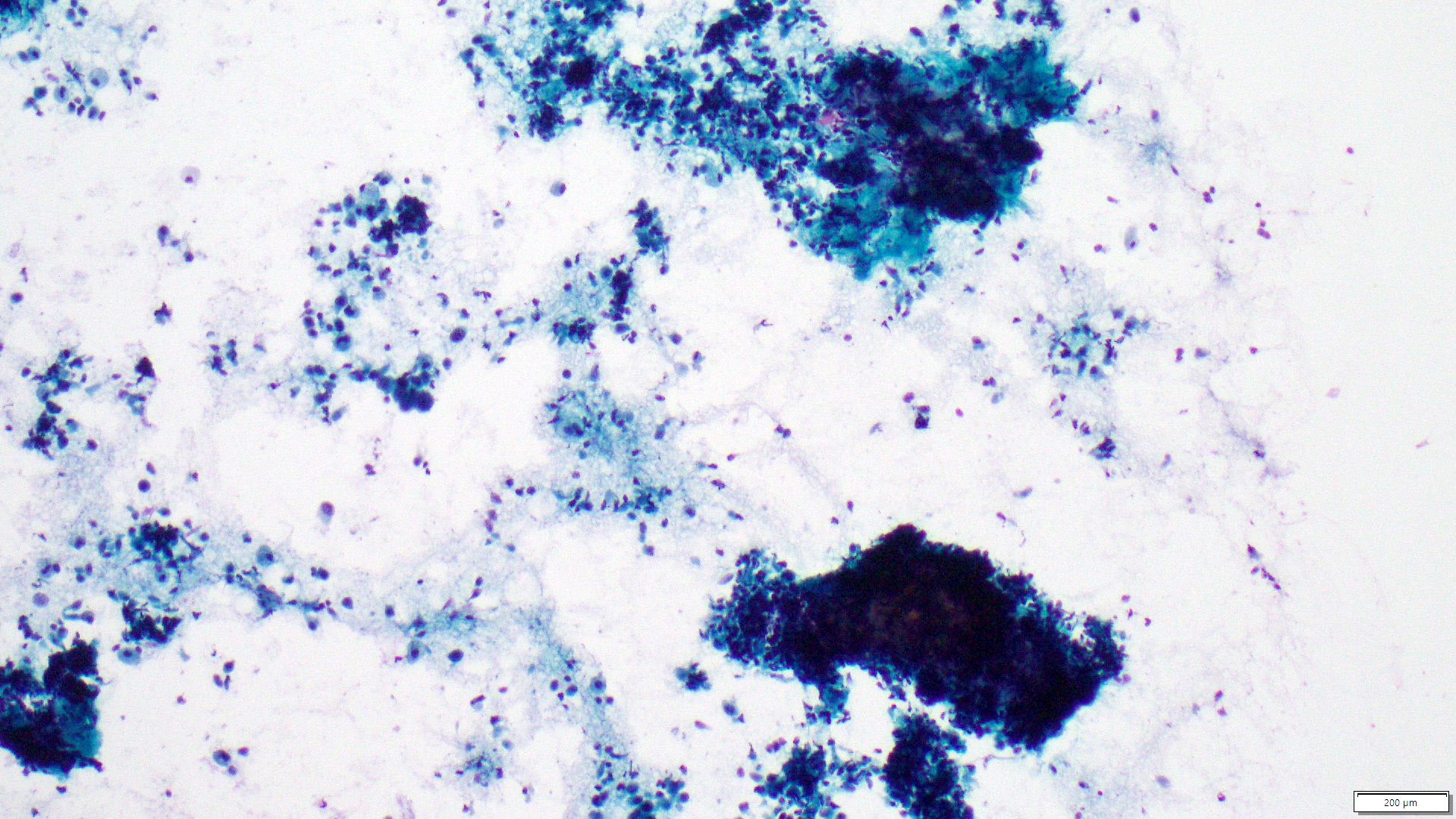
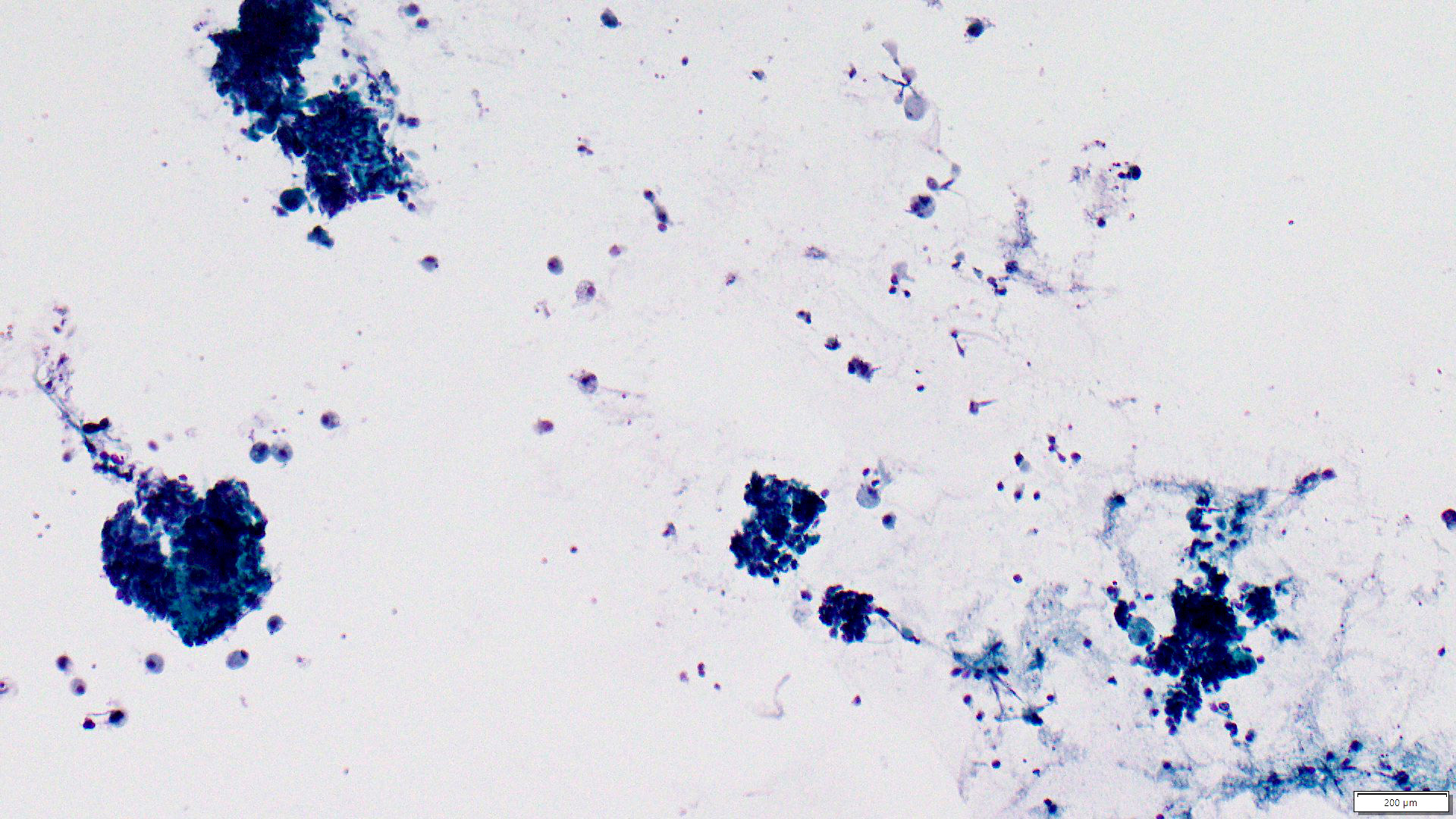
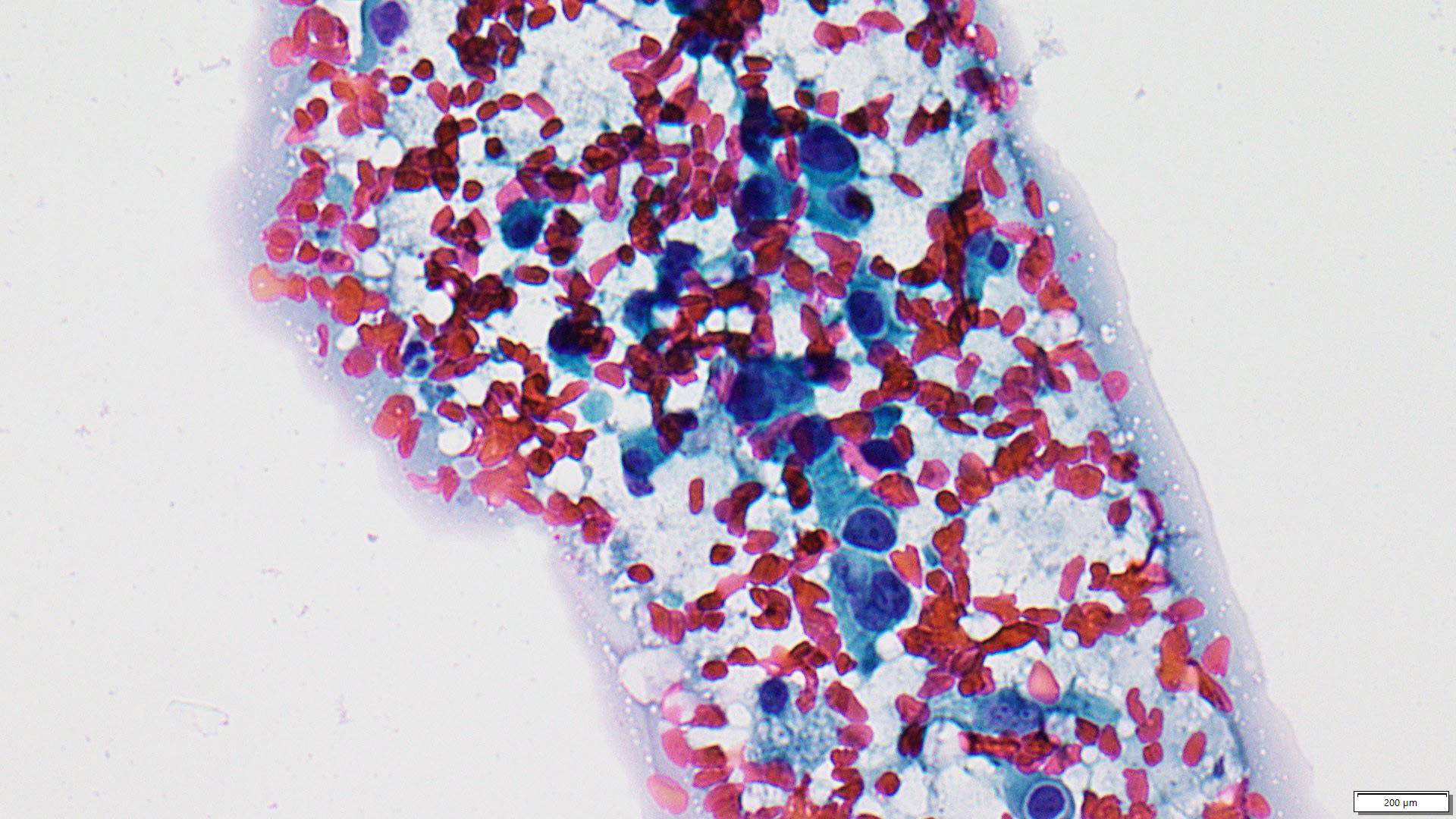
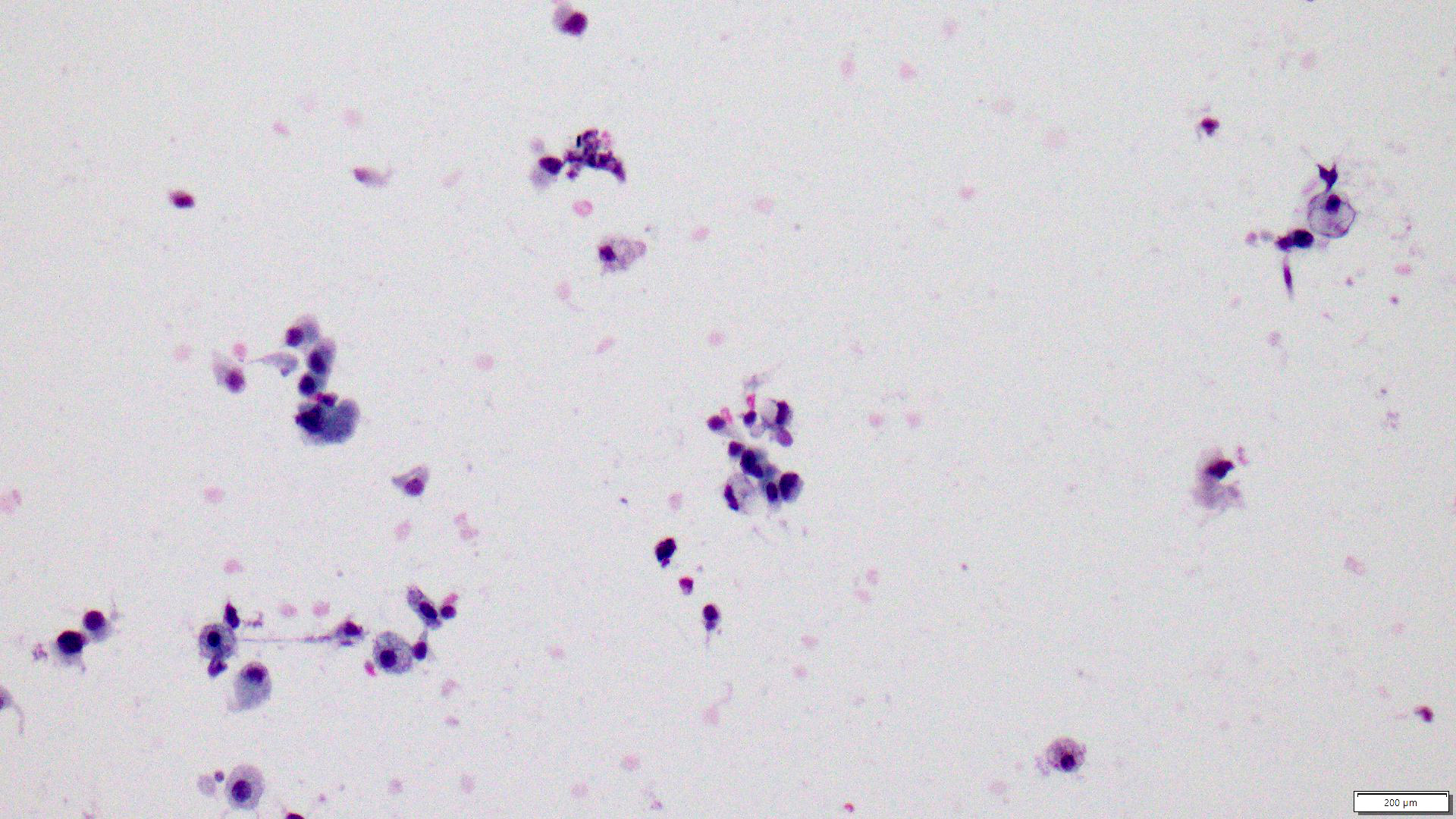
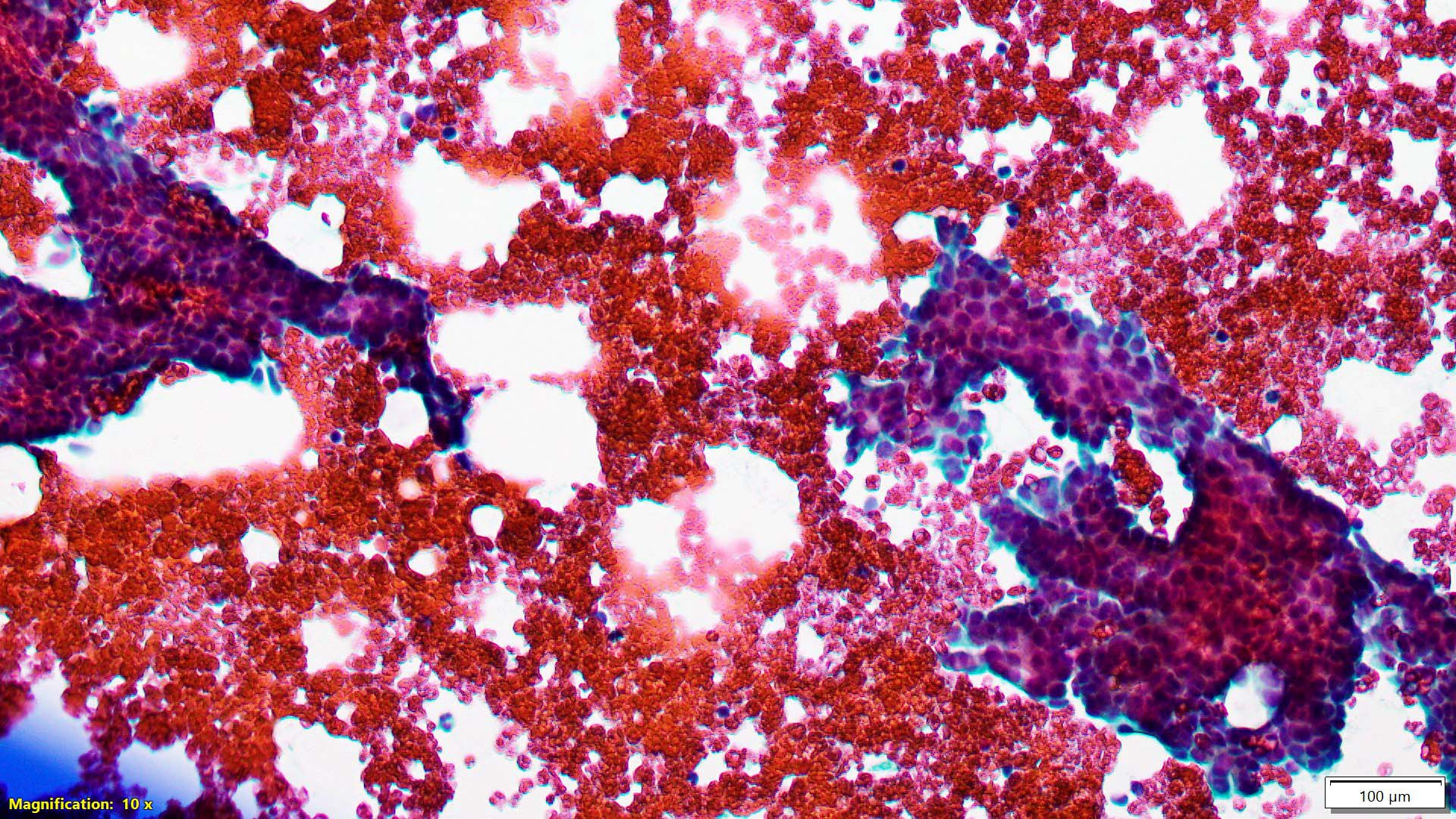
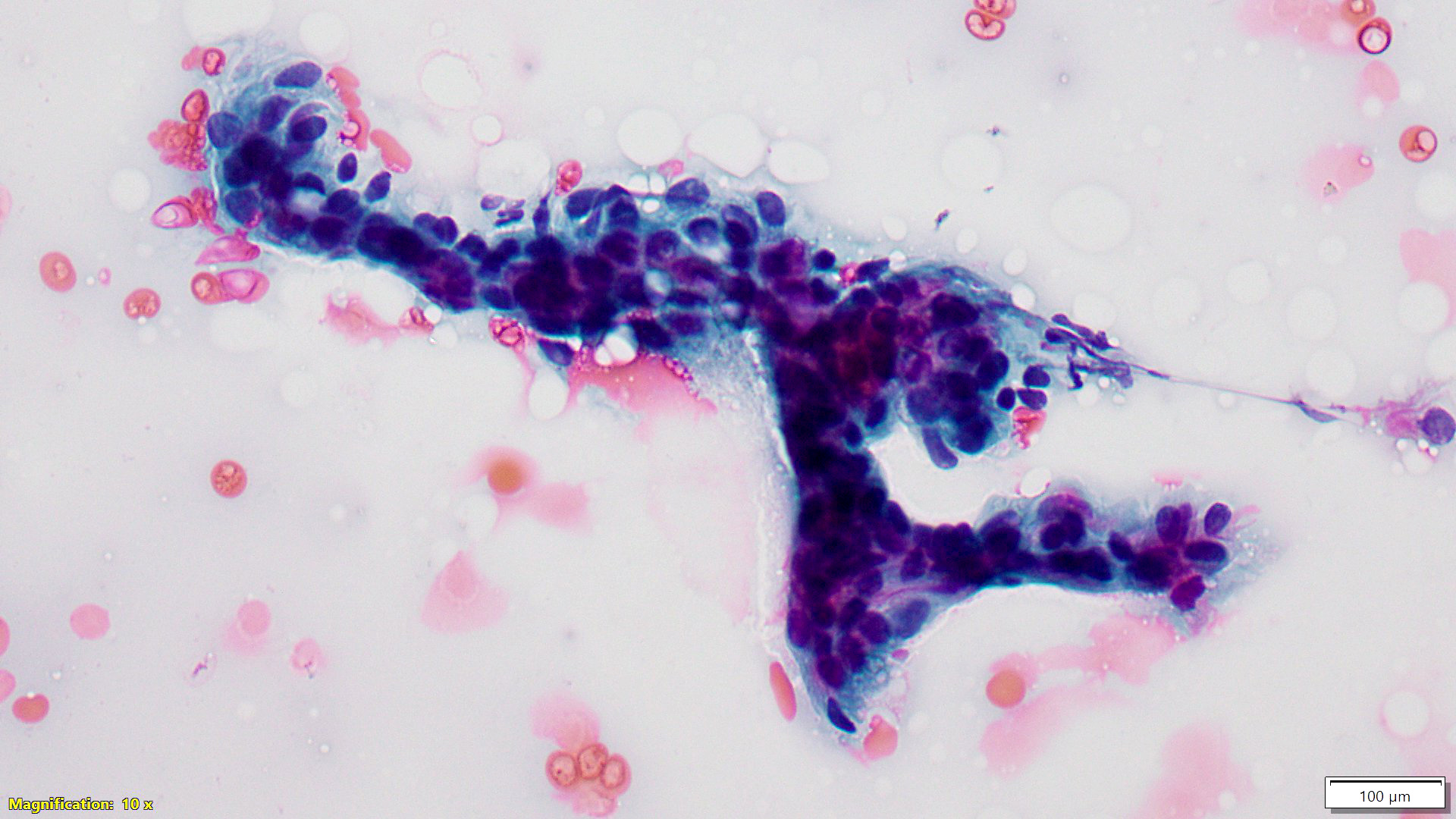
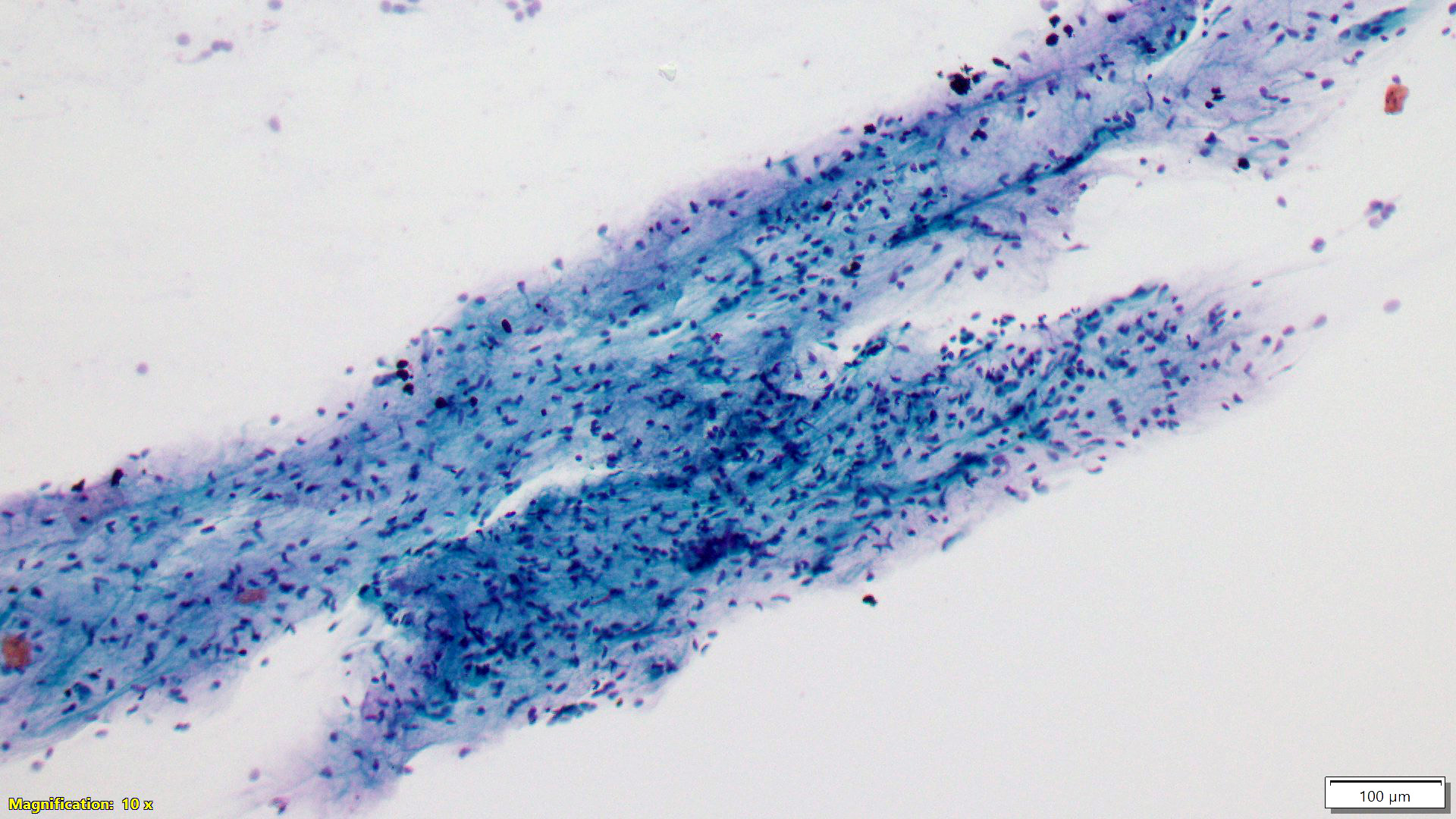
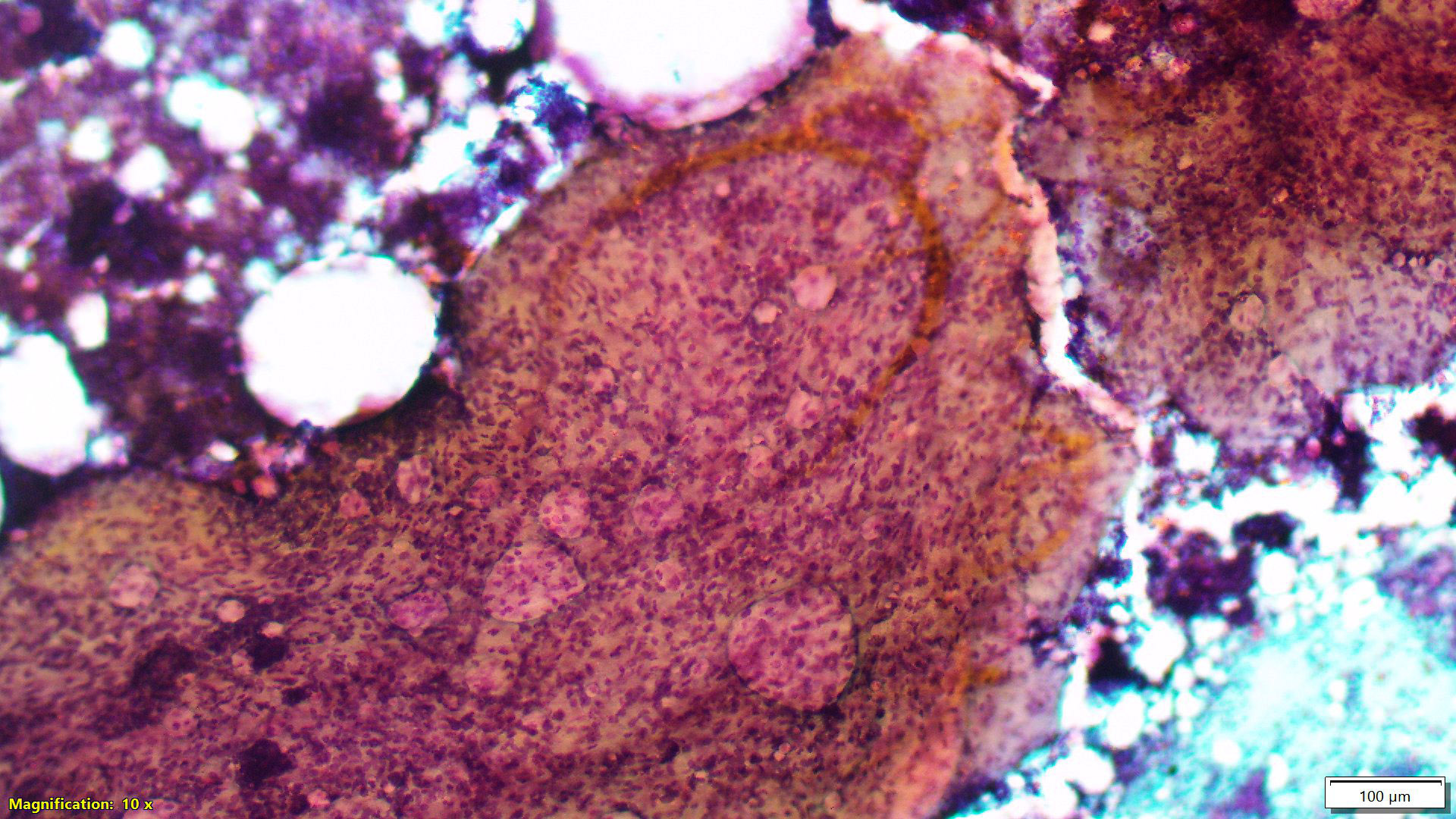
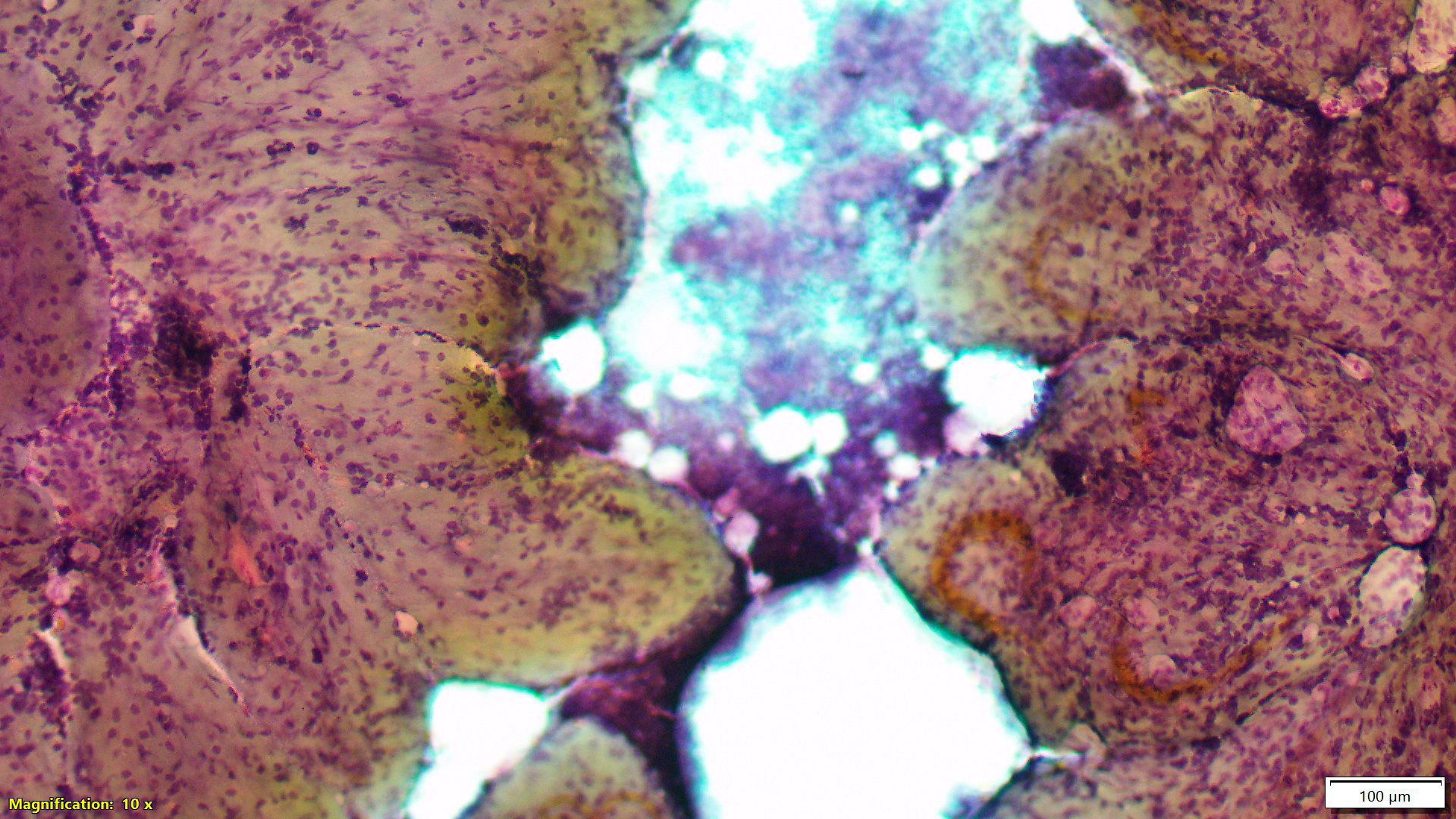
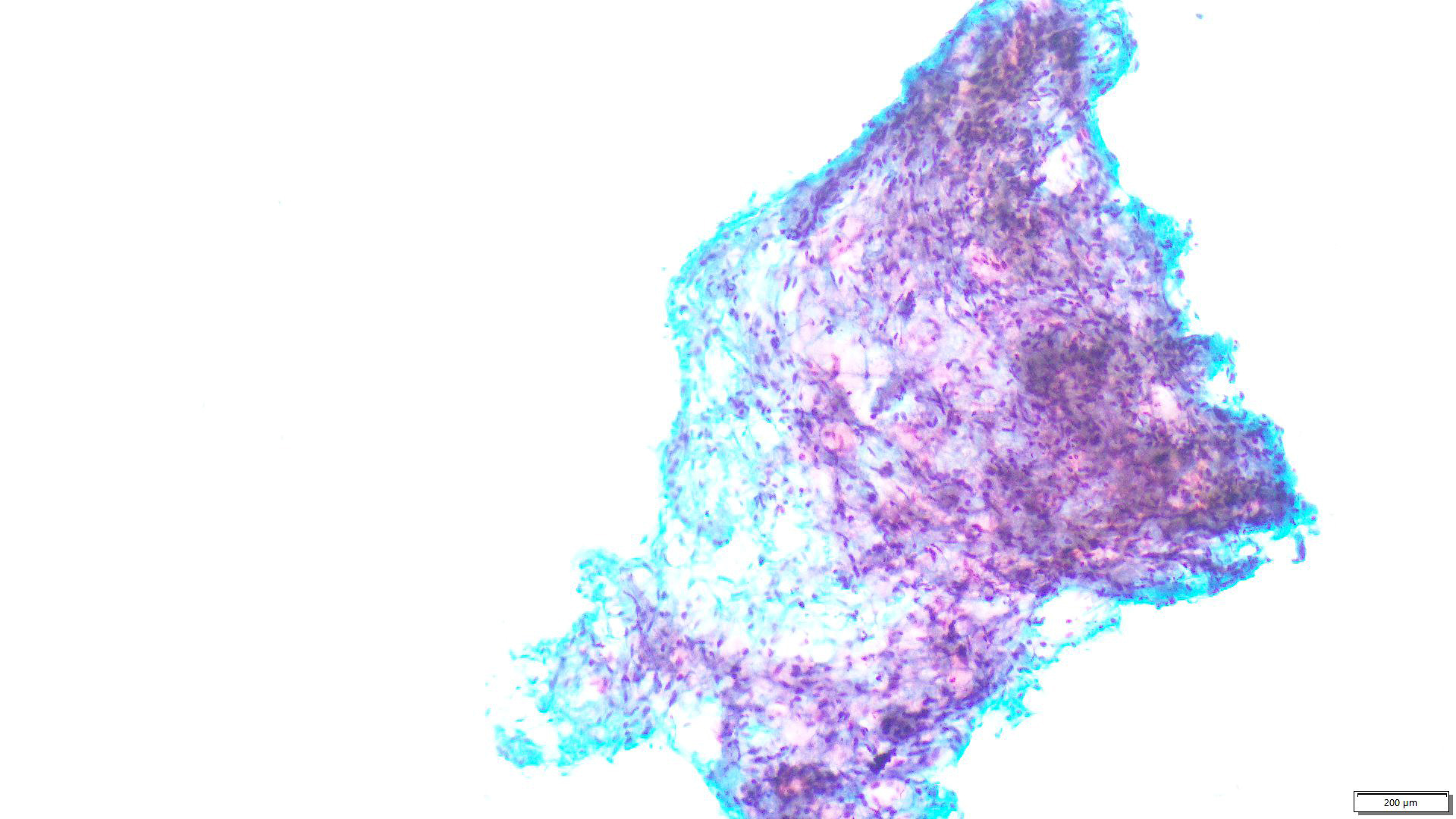
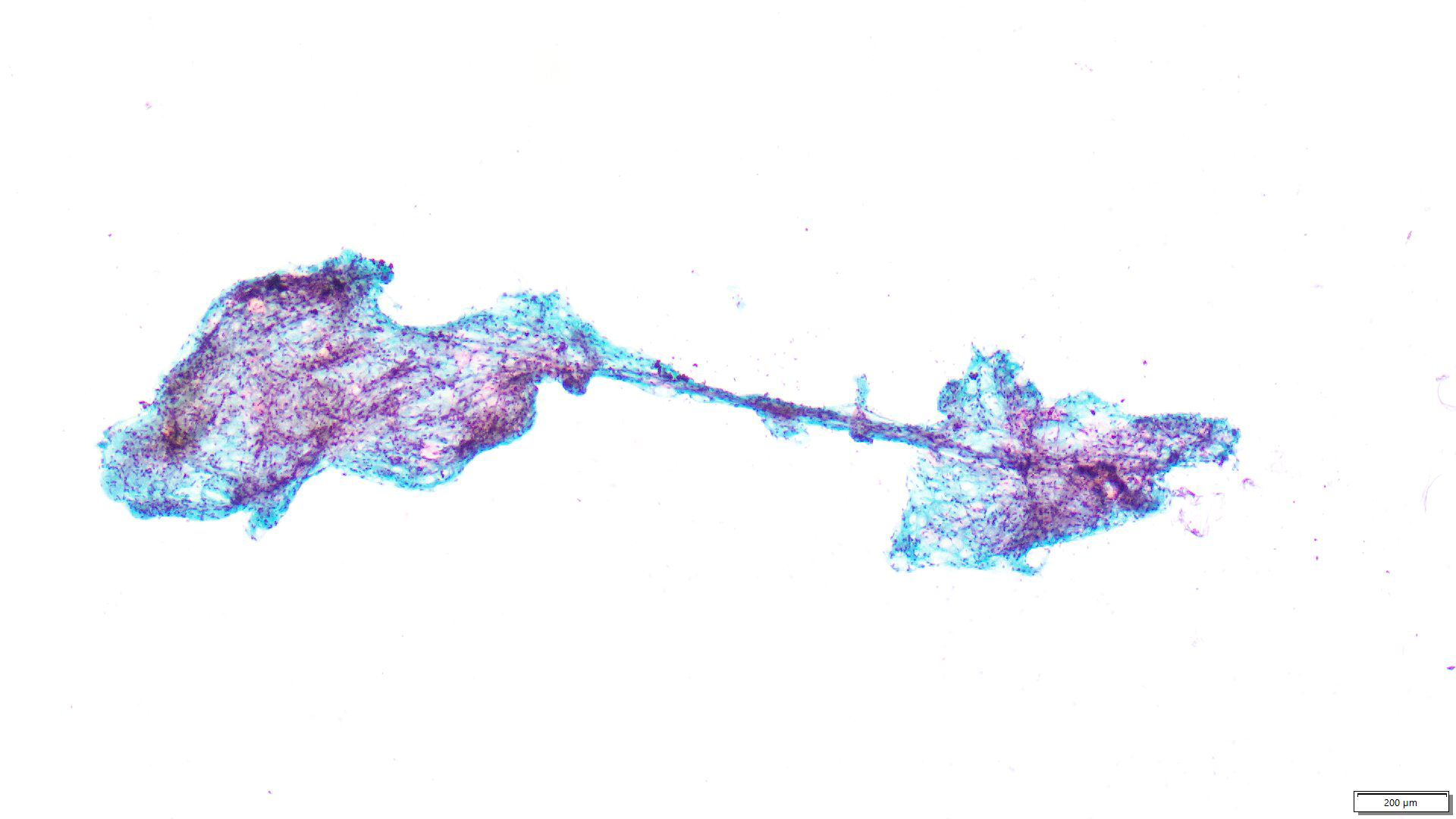
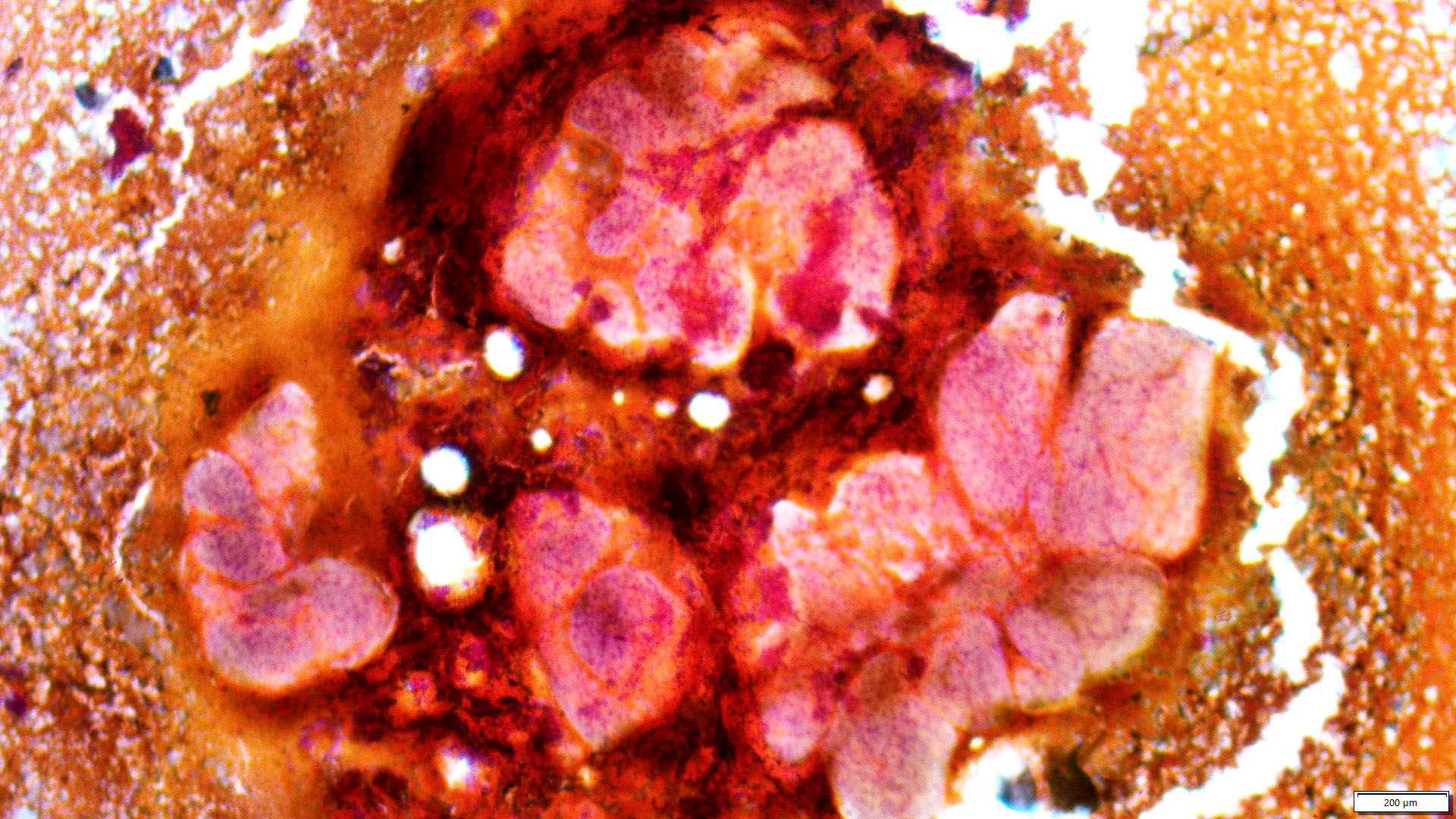
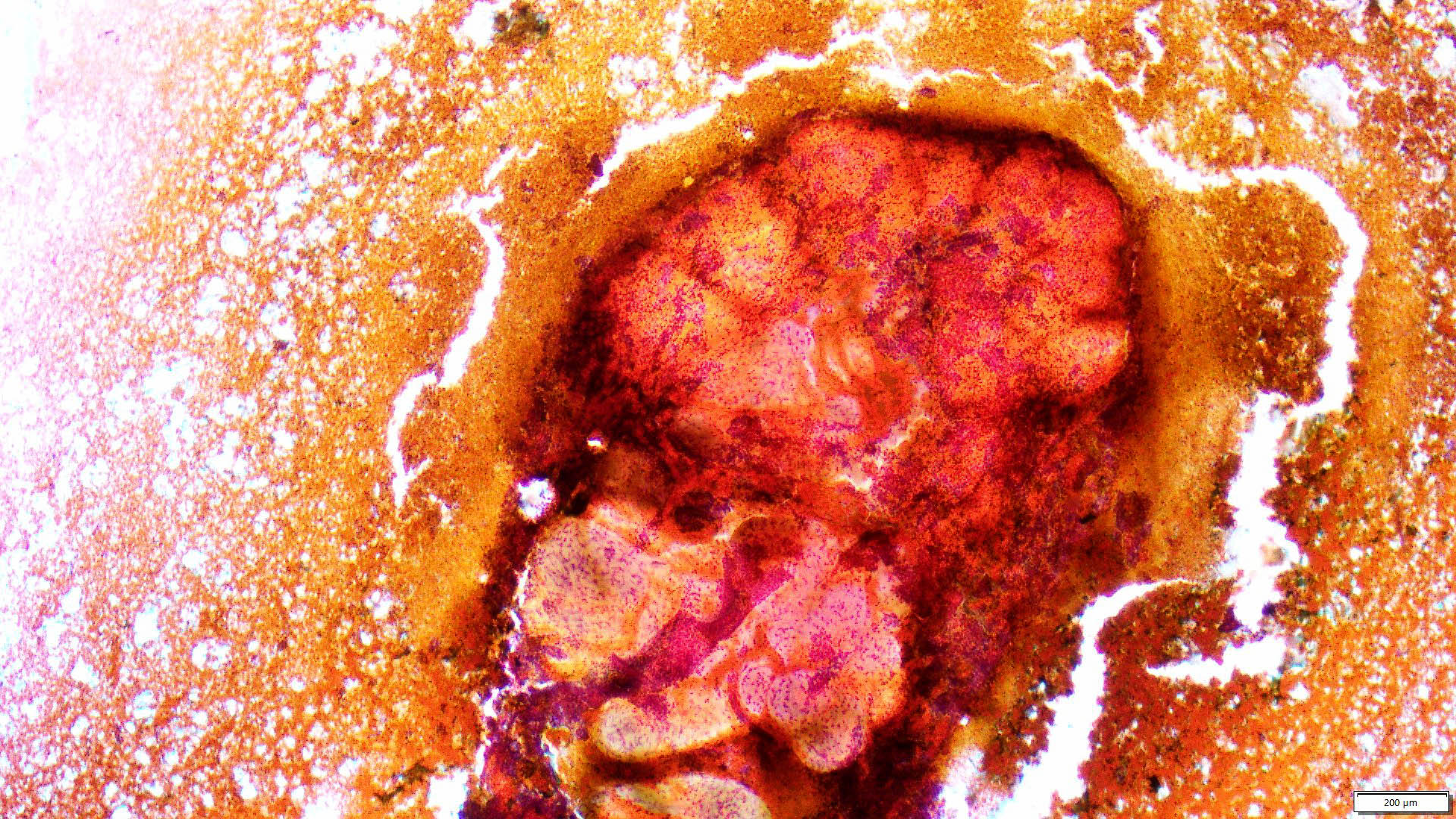
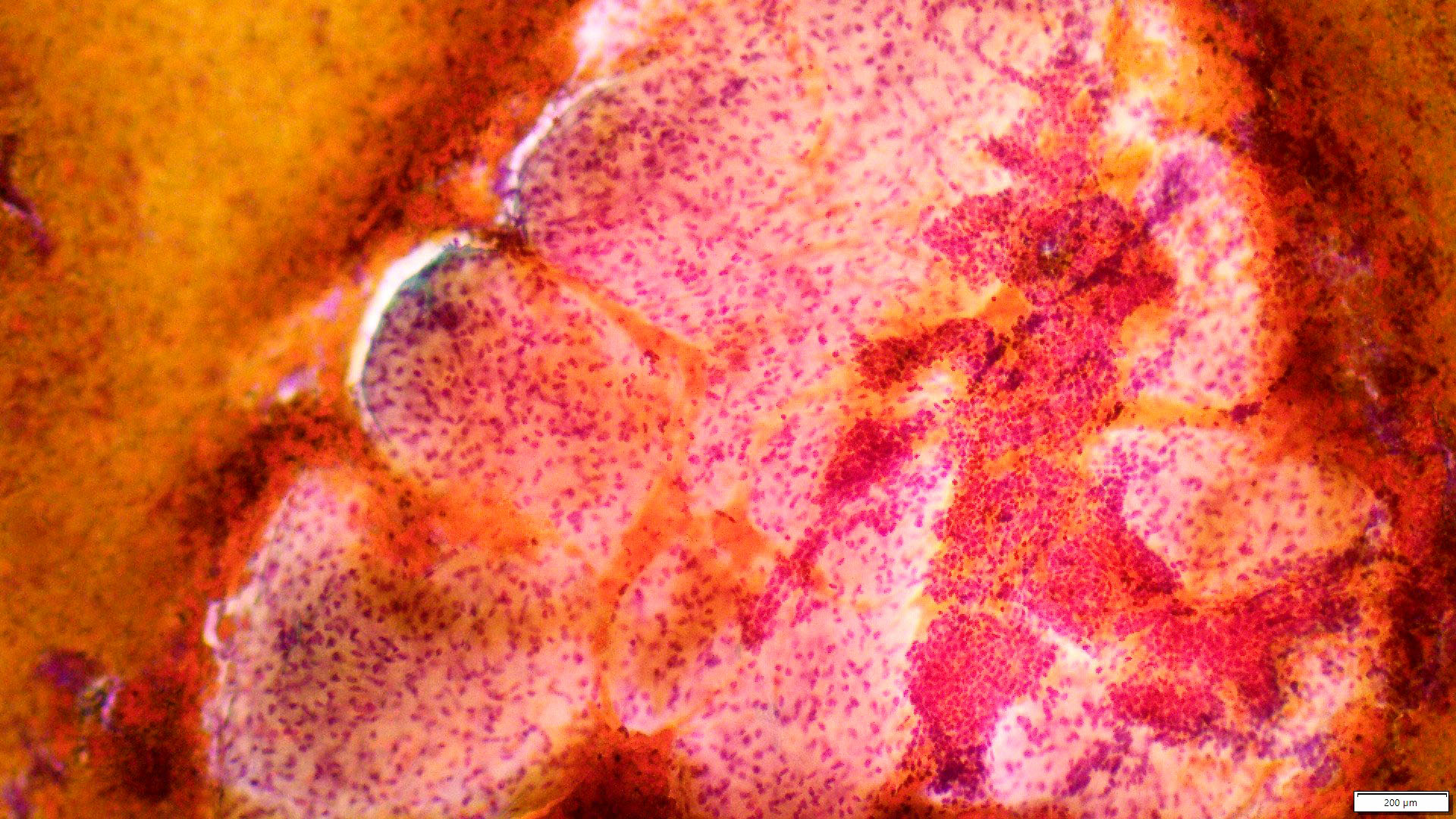
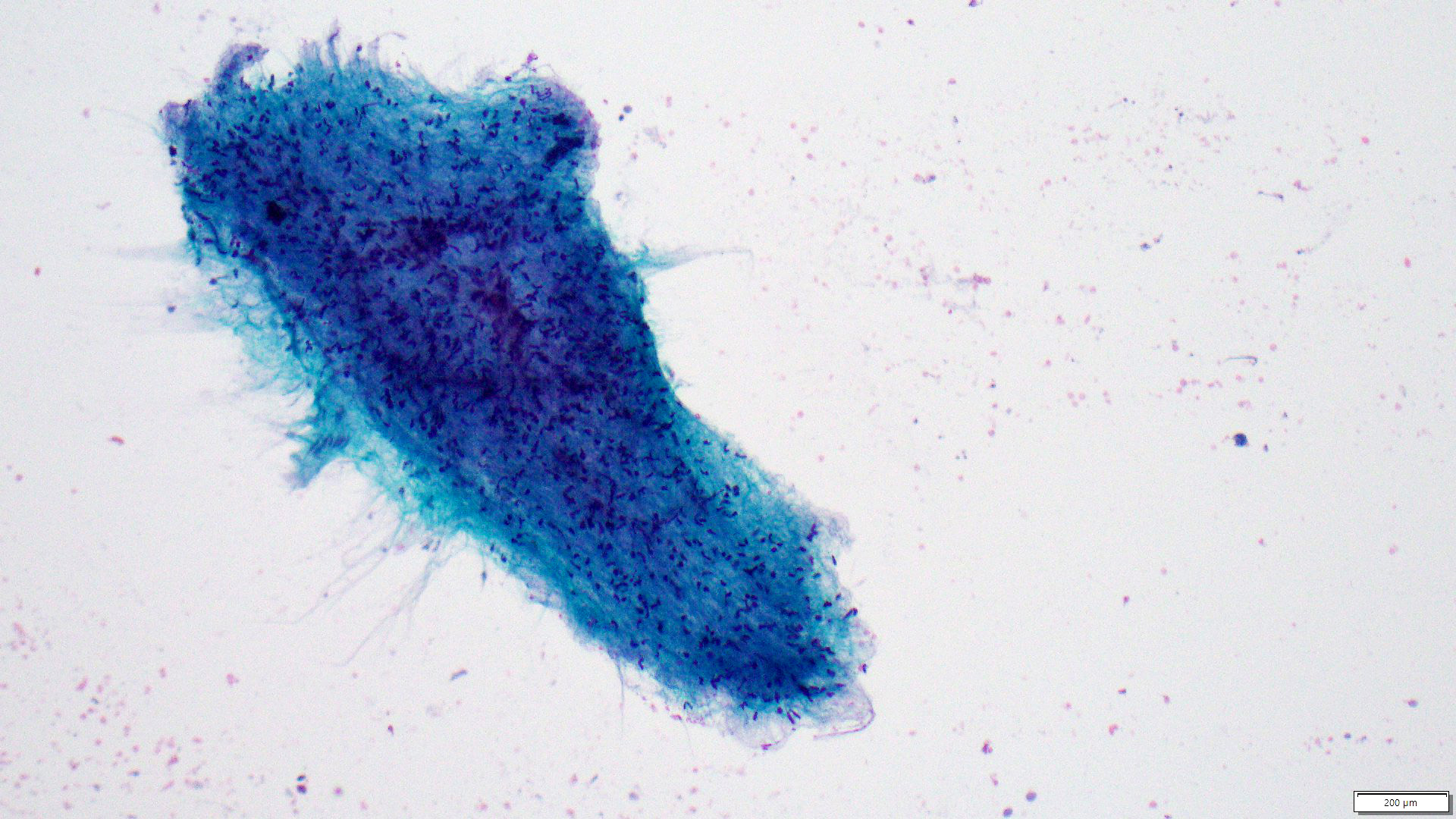
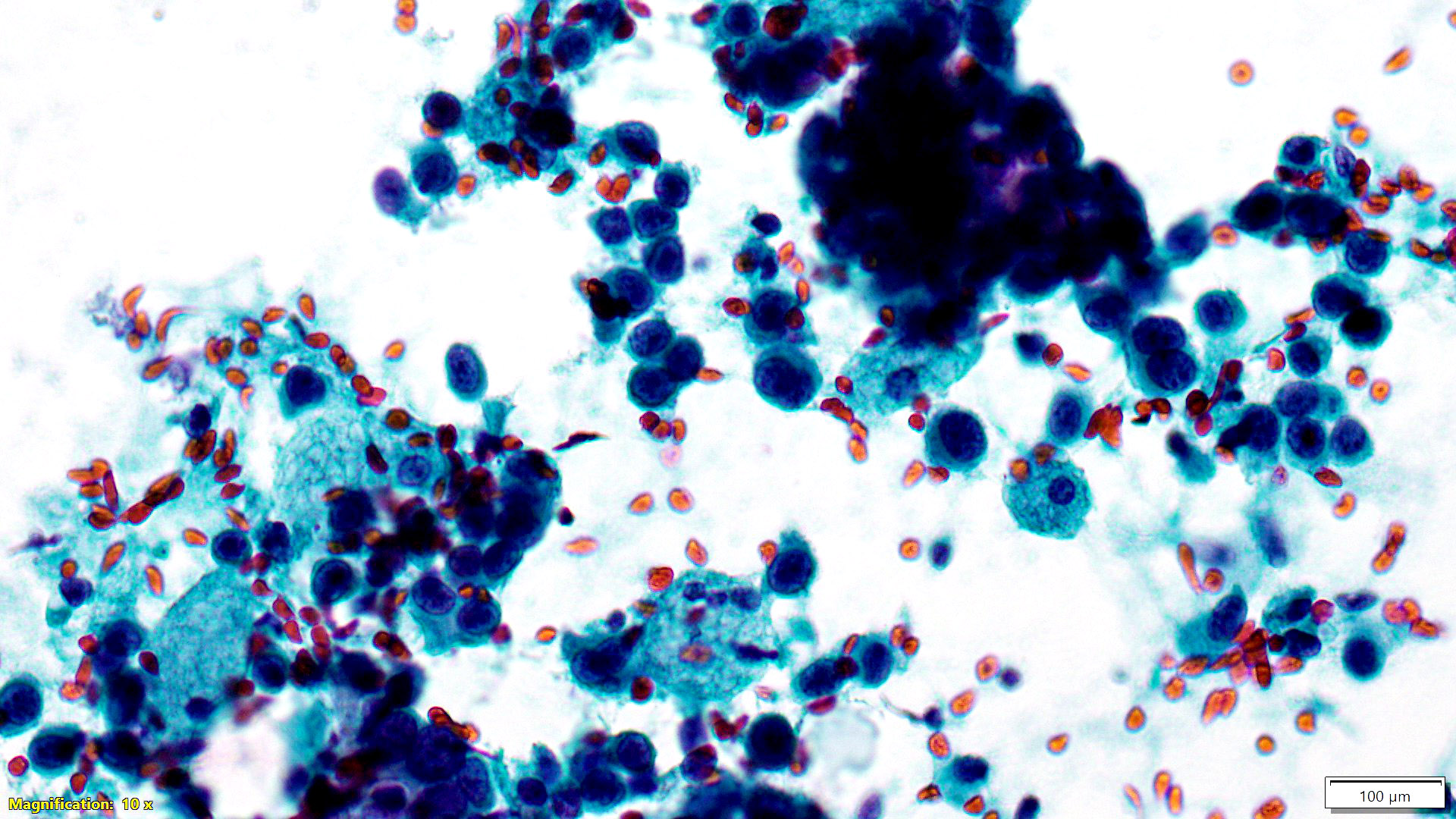
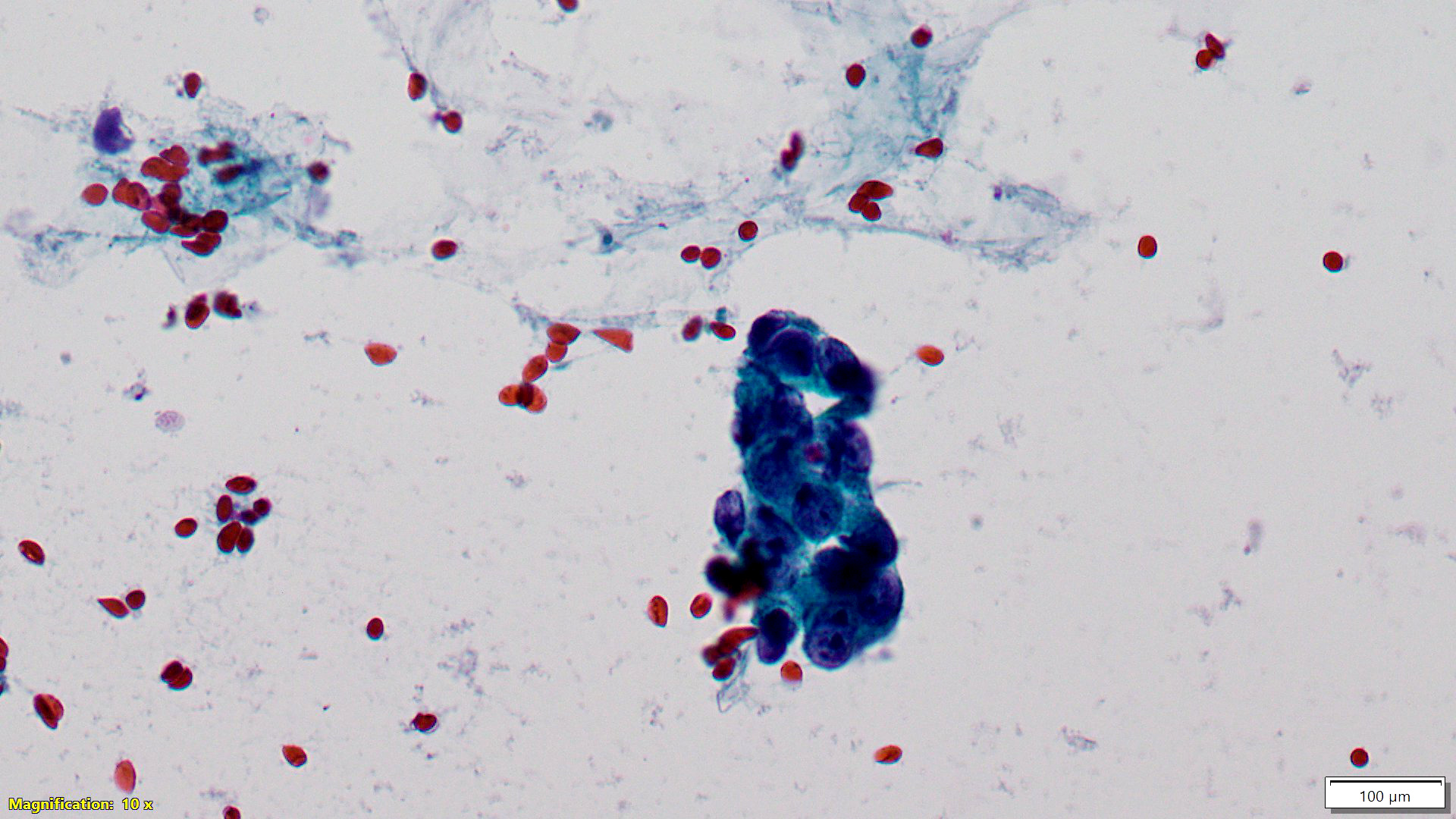
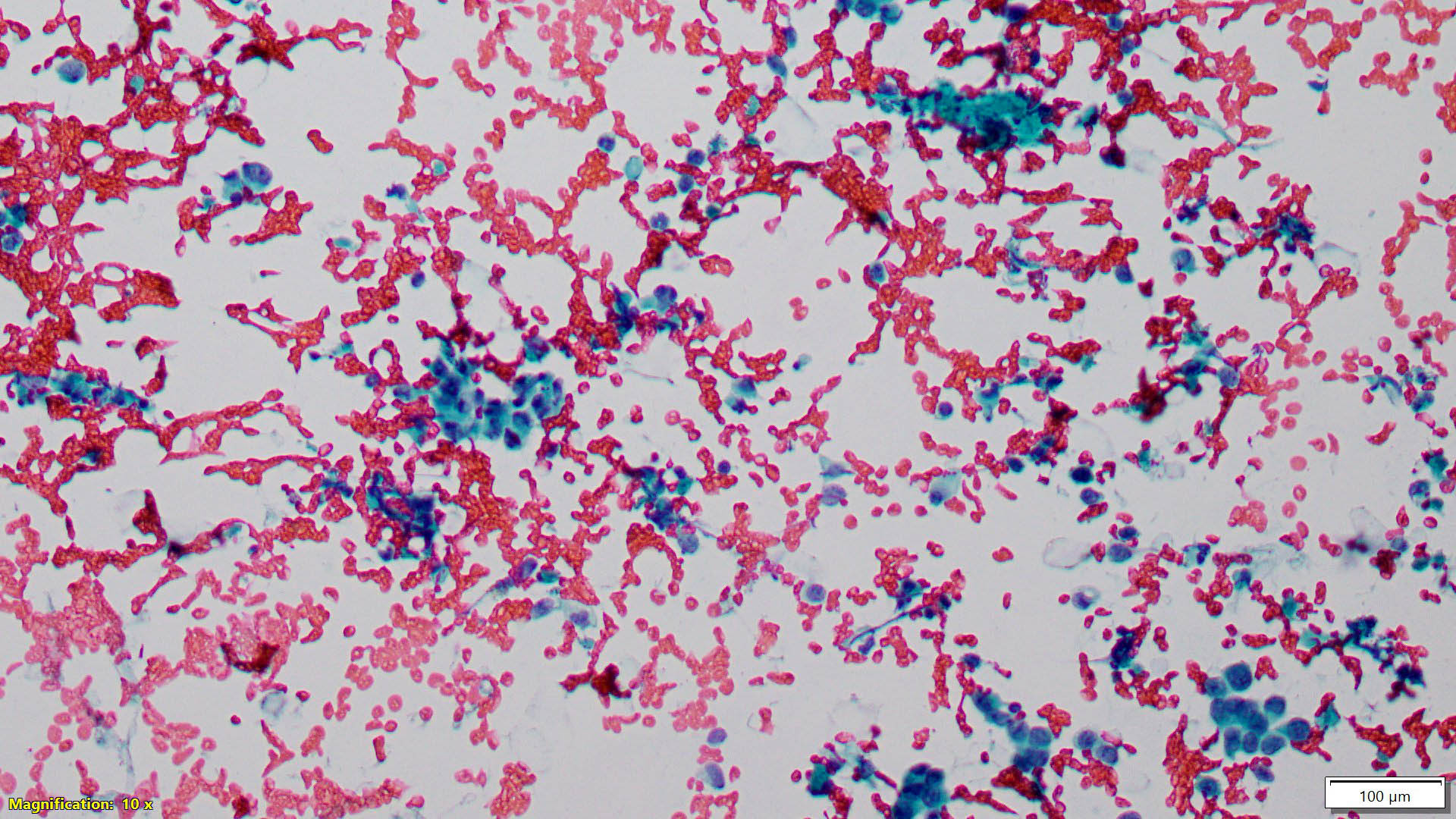
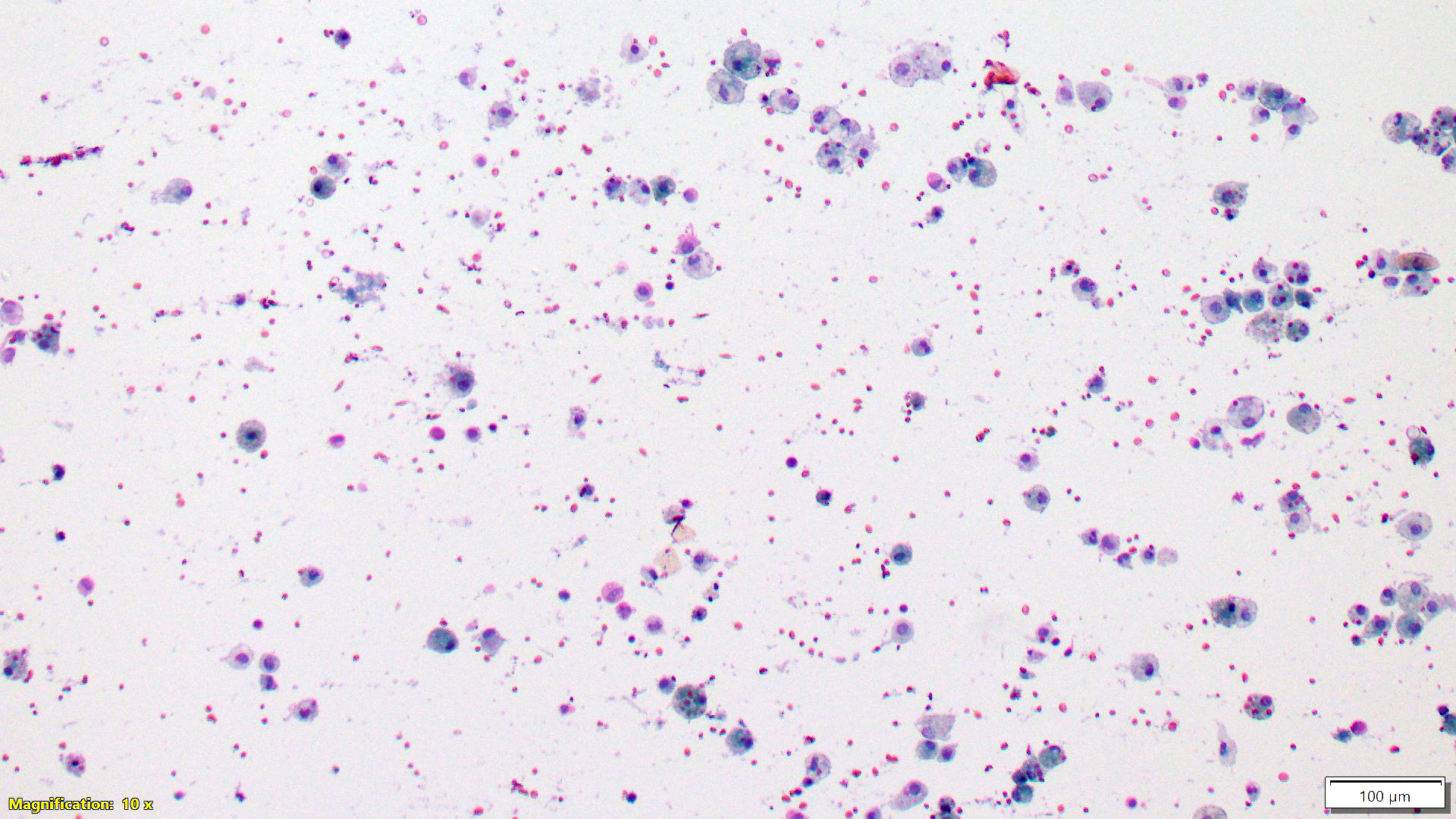
Cytology images
Contributed by Areej M. Al Nemer, M.D.
Sample pathology report
- Should state the category, followed by detailed explanation of the findings that justify the specified category
- If positive for malignancy, it is recommended to comment on the nuclear grade
- Examples:
- Left breast, FNA:
- Inadequate (C1)
- The smear shows only blood and rare degenerated cells.
- Right breast, FNA:
- Malignant (C5)
- Markedly hypercellular smear with single epithelial cells admixed with cohesive and discohesive clusters of malignant cells, depicting enlarged, highly pleomorphic nuclei, coarse chromatin, some prominent nucleoli, nuclear molding and occasional mitoses. Nuclear grade 3/3.
- Left breast, FNA:
Differential diagnosis
- False positive diagnosis:
- Poor fixation:
- Cellular enlargement and irregular chromatin
- Crush artifacts: hyperchromatic dissociated cells
- Ultrasound gel: contaminating the aspirate resembling necrotic debris
- Fibroadenoma:
- Cellular smear, mild pleomorphism, some discohesion, irregular clusters
- Hint: myoepithelial cells are easily seen
- Apocrine lesions:
- Might show atypia and discohesion
- Hint: no necrosis, admixture with benign ductal cells and macrophages, low N/C ratio
- Lactational changes / adenoma:
- Cellular smear, mild pleomorphism, enlarged hyperchromatic nuclei, prominent nucleoli, discohesion with fragile granular / vacuolated cytoplasm
- Myoepithelial cells are there but less conspicuous
- Background is dirty, with secretions that can be confused with necrosis by the nonexpert
- Clinical history of pregnancy, lactation or hormonal intake is helpful
- Proliferative fibrocystic change:
- Cellular smear with mild atypia
- Myoepithelial cells are plentiful
- Seroma:
- Cystic lesion that might follow breast conserving surgery
- Smear is usually hypocellular with a few degenerated cells
- Might show atypia with high N/C ratio and squamous metaplasia
- Treatment induced cellular change:
- Commonly hypocellular smear with scattered atypical, maybe enlarged epithelial cells
- Might show nuclear enlargement with prominent nucleolus, chromatin clearing, nuclear and cytoplasmic vacuolation
- Clinical data of prior therapy is crucial for accurate diagnosis
- Intramammary lymph node:
- Some activated lymphocytes might resemble lobular carcinoma
- Smear will show nodal polymorphic population of lymphocytes admixed with tangible body macrophages
- CD45+ and cytokeratin-
- Axillary lymph node:
- Sampling through apocrine glands, presence of benign intranodal epithelial inclusions, activated lymphocytes mimicking lobular carcinoma, granulomas, metastatic melanoma or carcinoma from other sites can cause false positive diagnosis
- Immunohistochemistry is helpful to resolve any ambiguity
- Poor fixation:
- False negative diagnosis:
- Sampling issues:
- In unguided biopsies and in small, fibrous, vascular or necrotic lesions
- Lobular carcinoma:
- Hypocellular to normocellular smear, minimal atypia
- Look for intracytoplasmic vacuoles (not diagnostic; seen in myoepithelial cells)
- Tubular carcinoma:
- Can be confused with radial scar, microglandular adenosis, tubular adenoma and fibroadenoma
- Clues: angulated clusters with one cell type with some nuclear atypia
- Sampling issues:
Additional references
Board review style question #1
Board review style answer #1
D. Negative. In nipple fluid cytology, the presence of epithelial cells is not mandatory to call it adequate.
Comment Here
Reference: Cytology
Comment Here
Reference: Cytology
Board review style question #2
Which of the following is correct regarding breast biomarker testing on cytologic specimen?
- Any positivity for hormonal receptors is counted as positive results
- Exact percentage of positivity is less accurate than the corresponding tissue assessment
- For HER2 / neu assessment, only immunohistochemistry can be performed on cytologic specimens
- It has similar interobserver discordance rate as in the tissue testing
Board review style answer #2
B. Exact percentage of positivity is less accurate than the corresponding tissue assessment. It is impossible to differentiate the malignant cells of the in situ component from the invasive component. For hormonal receptor positivity, the same cutoff point of 1% is used as in tissue.
Comment Here
Reference: Cytology
Comment Here
Reference: Cytology