Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Puzyrenko A, Jorns JM, Philip J, Salih Z. Filariasis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastfilariasis.html. Accessed April 17th, 2024.
Definition / general
- Lymphatic filariasis is caused by a chronic mosquito borne parasitic infection that involves the lymphatic vessels and lymph nodes of a human host (Trends Parasitol 2017;33:83)
Essential features
- Lymphatic filariasis is transmitted by mosquito bite
- Infection is caused by the migration of filaria larvae into lymph nodes and lymphatic obstruction
Terminology
- Elephantiasis
- Bancroftian filariasis
ICD coding
- ICD-10:
- ICD-11:
Epidemiology
- Lymphatic filariasis is a human parasitic infection (animal reservoirs are of minor epidemiologic importance or absent)
- Lymphatic filariasis affects over 120 million people in 73 countries
- Endemic in Central Africa, Southeast Asia, the Western Pacific, South America and the Caribbean (Nurs Clin North Am 2019;54:181)
- In the USA, Charleston, South Carolina was the last known place with lymphatic filariasis; the infection was eradicated in the USA in the early 20th century (CDC: Lymphatic Filariasis [Accessed 18 October 2021])
- M:F = 10:1 (Asian Pac J Trop Med 2011;4:581)
Sites
- Inguinal (femoral) lymph nodes and lower extremities are most commonly involved but can also occur in the arms, breasts and genitalia (Clin Microbiol Rev 1998;11:366)
- Microfilariae have been reported in multiple aspiration sites, cervicovaginal smears, urine, bronchial washings and effusions (Acta Cytol 1983;27:432, Diagn Cytopathol 2011;39:8)
Pathophysiology
- Bite from an infected mosquito introduces third stage infective filarial larvae onto the human skin
- They penetrate into the bite wound to reach the lymphatics where they reside and develop into adults
- Adult females give birth to numerous microfilariae (Asian Pac J Trop Med 2011;4:581)
- Intact adult worms produce minimal tissue reaction but can cause lymphatic obstruction leading to lymphedema (peau d'orange skin - mimics malignancy)
- Disrupted lymphatic drainage increases the susceptibility to repeated infections, most commonly streptococcal and fungal infections
- Acute and chronic inflammation lead to fibrosis, hyperpigmentation and hyperkeratosis (Microcirculation 2013;20:349)
- Degenerating / dying worms provoke an inflammatory reaction in the tissue, forming a mass with eosinophilic and granulomatous inflammation
- Life cycle continues as microfilariae actively move through lymph and blood channels and are ingested by mosquitoes during a blood meal
- After ingestion, the microfilariae develop into an infective larvae inside the mosquito through a 3 stage process
- Third stage infective larvae migrate through the mosquito's proboscis and can infect another human when the mosquito takes a blood meal
Etiology
- 3 species of nematode (roundworm) parasites cause lymphatic filariasis in humans (Trends Parasitol 2017;33:83):
- Wuchereria bancrofti is the most common cause of infections worldwide (accounting for > 90% of cases)
- Brugia malayi and Brugia timori can be the causative organisms in Asia
- Infection is transmitted by mosquito vectors (Culex, Anopheles, Aedes and Mansonia species)
- Humans are the definitive host
Clinical features
- May be asymptomatic
- Incubation period is variable and can be 8 - 16 months
- Breast (local) (Asian Pac J Trop Med 2011;4:581)
- Unilateral, nontender swelling, commonly in the upper outer quadrant
- May be mobile from quadrant to quadrant and mimic fibroadenoma
- May be filarial abscess
- May be associated with enlarged lymph nodes and simulate breast carcinoma
- Overlying skin has induration, hyperpigmentation, dilated veins
- Systemic (filariatic fever) (Korean J Parasitol 2008;46:119)
- Headache, fever, chills and general malaise
- Vaginal bleeding is common; lymphedema is common at late stages
Diagnosis
- Standard method to diagnose active infection is microscopic blood smear examination; sensitivity can be increased by concentration techniques
- Peripheral blood smear (preferably taken after 8 p.m. and stained with either Giemsa or H&E stain) (Asian Pac J Trop Med 2011;4:581)
- PCR (detection parasite antigen)
- Serologic enzyme immunoassay test (detection of antifilarial IgG1 and IgG4)
- Imaging with CT, MRI and ultrasonography (Filaria J 2003;2:3)
- Histologic evaluation of surgically removed tissue
Laboratory
- Antifilarial IgG1 and IgG4 antibody in peripheral blood by enzyme linked immunoassay (ELISA)
- DNA sequencing and nucleic acid amplification by PCR
- In chronic cases with lymphedema, lab tests are usually negative
- Reference: CDC: Lymphatic Filariasis [Accessed 24 February 2021]
Radiology description
- Real time ultrasound may show the movement of echogenic particles ("filarial dance") (Filaria J 2003;2:3)
Radiology images
Images hosted on other servers:
Prognostic factors
- Chronic lymphedema is irreversible (Korean J Parasitol 2008;46:119)
- Good prognosis if recognized and treated early
Case reports
- 21 year old woman with swelling and pain in both breasts (Med J Armed Forces India 2015;71:S240)
- 55 year old woman with a nontender palpable mass in the right axilla (Breast Care (Basel) 2012;7:487)
- 59 year old woman with a nodule in the right breast (Indian J Pathol Microbiol 2008;51:85)
- 69 year old woman presenting for a baseline mammography (Radiology 2002;222:515)
- Woman with breast mass (Arch Pathol Lab Med 1987;111:757)
- Microfilariae of Wuchereria bancrofti identified in a cervicovaginal smear (Acta Cytol 1998;42:840)
- Microfilaria in cervicovaginal smear (Cytopathology 2005;16:156, J Obstet Gynaecol 2004;24:843)
- Vaginal parasitosis (Acta Cytol 1987;31:866)
Treatment
- Medical treatments
- Diethylcarbamazine (DEC) is recommended as potential monotherapy (Trends Parasitol 2017;33:83)
- Single combined dose of ivermectin, albendazole and DEC resulted in clearance of microfilaria in 96% of affected patients for up to 3 years (currently recommended by the WHO as triple therapy) (Clin Infect Dis 2020;71:e68)
- Surgical treatment may be an option (J Cutan Med Surg 2018;22:611)
- Chronic management
- Skin hygiene, regular washing with soap and water, using compressive bandages, cold / heat therapy, antibiotic and antifungal creams to prevent flares of lymphangitis (PLoS Negl Trop Dis 2015;9:e0004171)
Clinical images
Gross description
- Adult worm
- Long, cylindrical, slender and smooth with rounded ends
- White in color and almost transparent
- Females: 8 - 10 cm; males: 2 - 3 cm
- Microfilaria (miniature adult)
- Retains the egg membrane as a sheath
- Often considered as an advanced embryo (Magill: Hunter's Tropical Medicine and Emerging Infectious Diseases, 9th Edition, 2013)
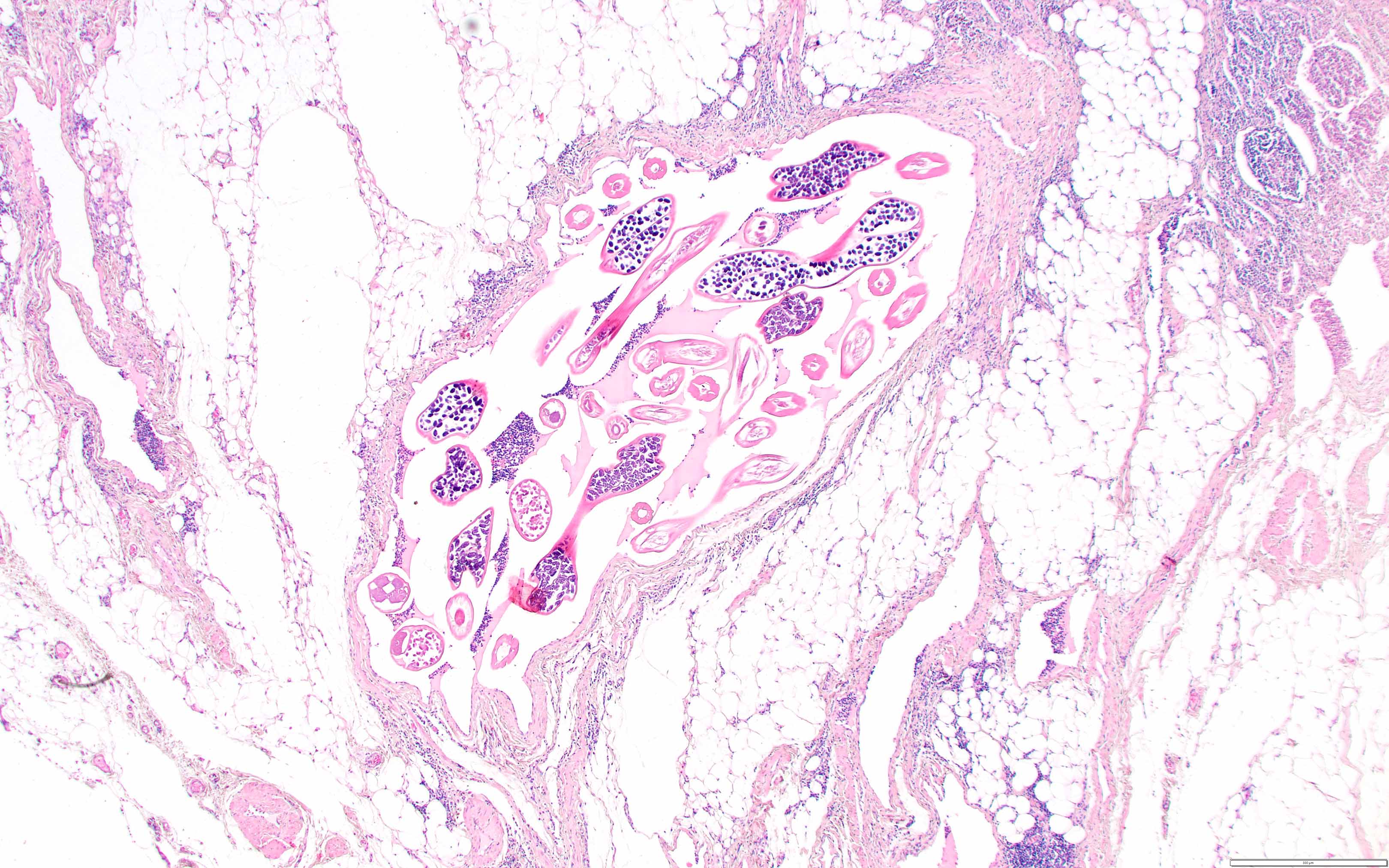
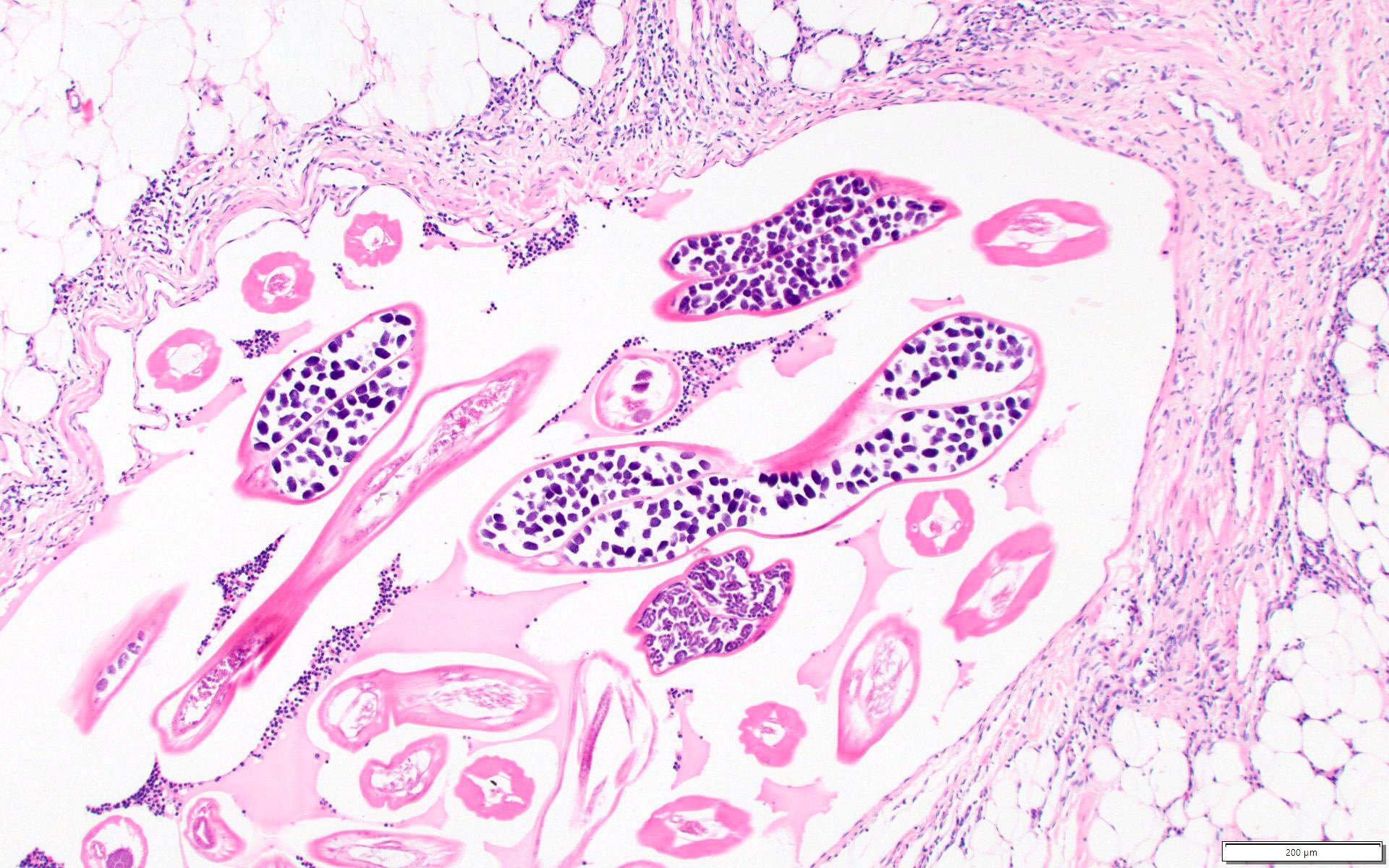
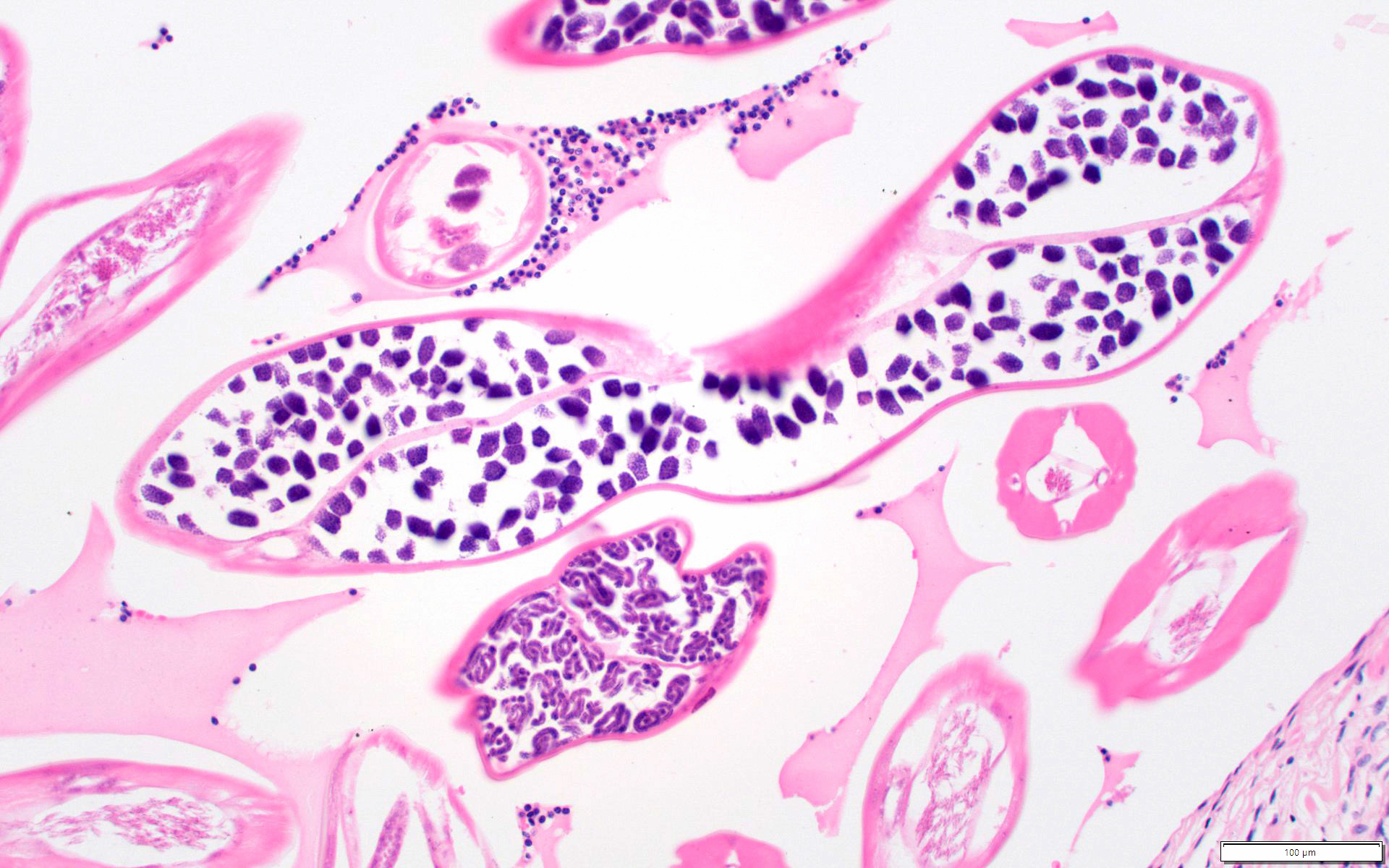
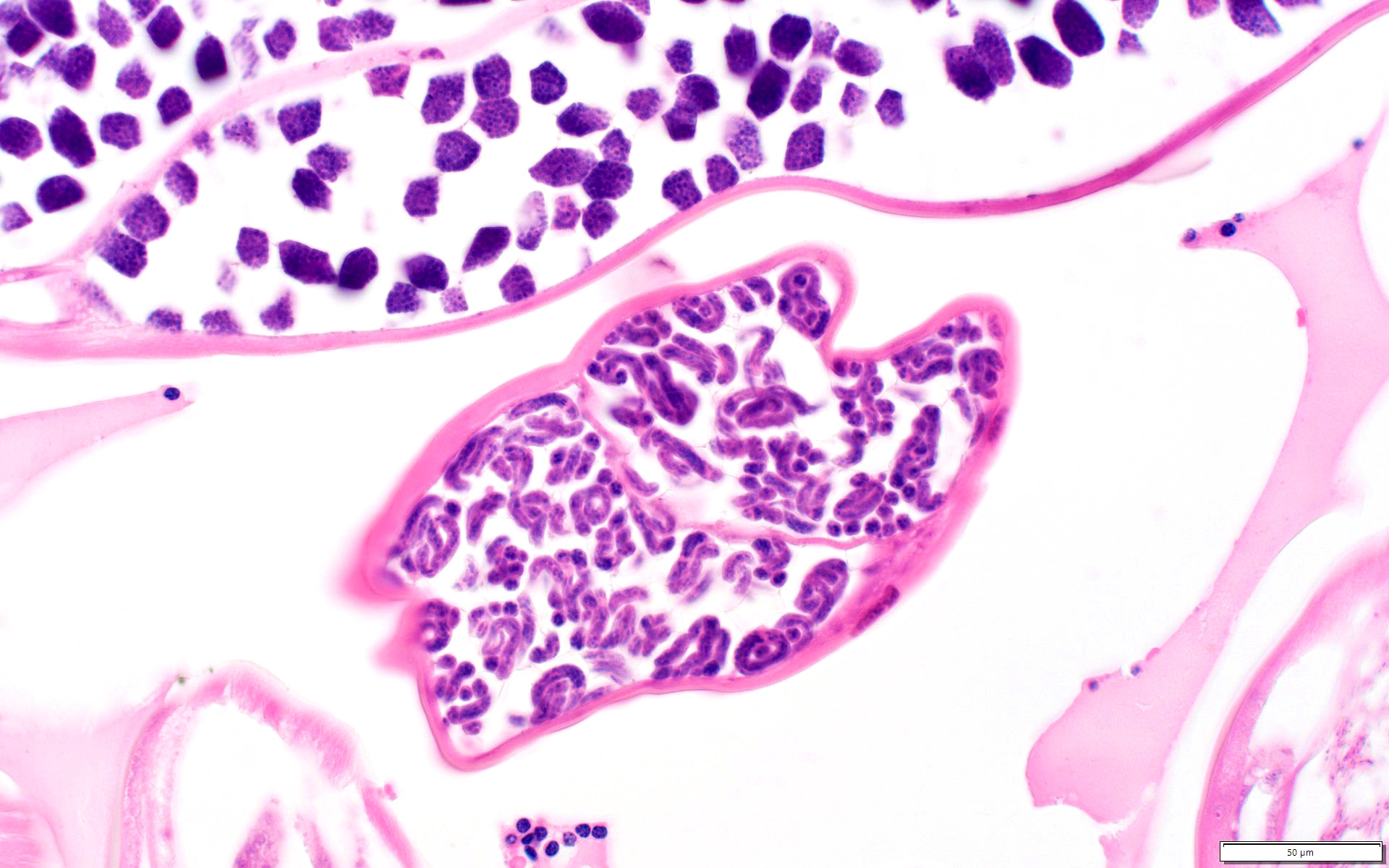
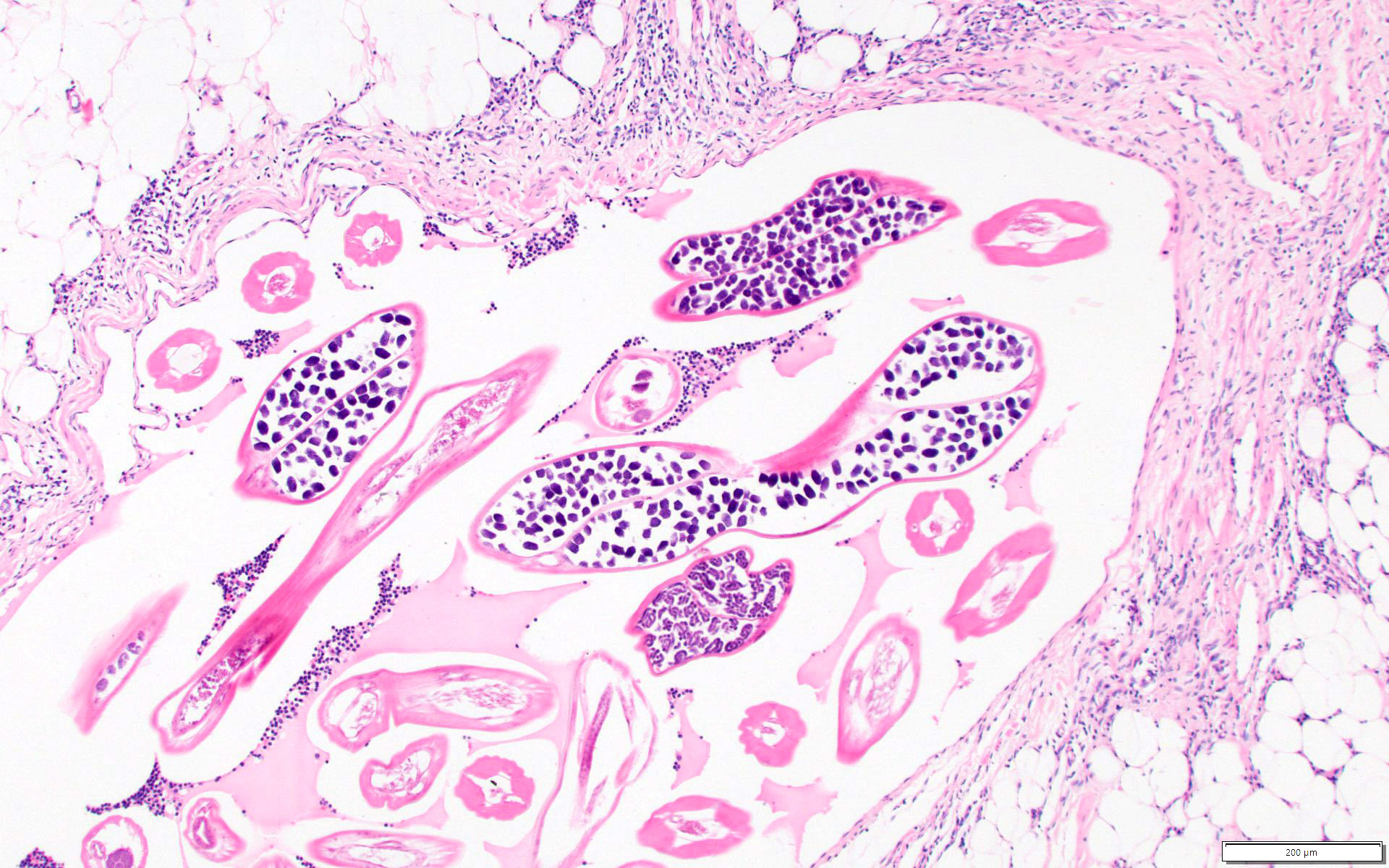
Microscopic (histologic) description
- Microfilariae are the diagnostic form
- Intact adult filariae in lymph nodes are pathognomonic; may see dead filariae with surrounding granulomatous inflammation and calcifications (Clin Microbiol Rev 1998;11:366)
- Eggs may be seen
- Background shows increased eosinophils, neutrophils, plasma cells, macrophages and even granulomas with lymphatic vessel dilatation and fibrosis
- Microfilarial morphology is better appreciated with a Giemsa stain
- Presence or absence of a sheath and the pattern of nuclei in their tail are the main features used to distinguish the various species
- Microfilariae of Wuchereria bancrofti are sheathed with no nuclei in the tip of the tail
Microscopic (histologic) images
Cytology description
- Microfilaria may appear as coiled structures with visible nuclei (Diagn Cytopathol 2011;39:8)
- Fragments of adult worms may be present
Positive stains
- Filaria are visible on Giemsa stain
Videos
"Filarial dance"
BMJ Case Rep 2019;12:e229956
Sample pathology report
- Left breast, excisional biopsy:
- Foreign body reaction to larval organisms showing a granulomatous inflammation with longitudinal calcified corpuscles, consistent with filariasis
Differential diagnosis
- Granulomatous mastitis:
- Shows well formed granulomas within lobules or adjacent to ducts
- May show giant cells and chronic inflammation
- Microabscesses may be present with lipid vacuoles
- Bacterial or fungal lymphadenitis:
- Presence of bacteria on Gram or silver stain
- Presence of fungal forms on silver stain
- Cysticercosis:
- Caused by larval cysts of the tapeworm Taenia solium
- Larvae with similar stroma but contain a scolex, hooks and surrounding fluid filled "bladder"
- Clinically presents with multiple lesions
- Breast carcinoma:
- Poorly defined palpable mass or area of thickening
- Neoplastic epithelial proliferation with variable architecture, including glandular, cribriform, cords, trabeculae, papillae or solid growth
- Fibroadenoma:
- Painless, slowly growing, mobile, well defined, palpable mass
- Calcifications may be present and appear as a cluster
- Admixed benign glandular and stromal elements
- Wuchereria bancrofti (1):
- Sheath, no nuclei in the tip of the tail
- Brugia malayi (2):
- Sheath, 2 distinct nuclei in the tip of the tail
- Loa loa (3):
- Sheath, nuclei extending to the tip of the tail
- Onchocerca volvulus (4):
- No sheath, no nuclei in the tip of the tail
- Mansonella perstans (5):
- No sheath, nuclei extending to the tip of the tail
- Mansonella ozzardi (6):
- No sheath, no nuclei in the tip of the tail
- Mansonella streptocerca (7):
- No sheath, nuclei extending to the tip of the tail
Additional references
Board review style question #1
A 37 year old woman presents with a nodule in her left breast associated with enlarged axillary lymph nodes. The nodule is surgically removed and shows the image above on review. What histological finding is most specific for lymphatic filariasis of the breast?
- Adult worm with eggs in lymph node
- Chronic lymphangitis with fibrosis
- Eosinophilic lymphadenitis
- Granulomatous lymphadenitis with calcifications
- Lymphatic vessel dilatation
Board review style answer #1
A. Adult worm with eggs in lymph node
Lymphatic filariasis of the breast due to Wuchereria and Brugia can show chronic lymphangitis with lymphatic vessel dilatation, eosinophilic lymphadenitis and granulomatous inflammation; however, these are not specific for filariasis and can be often seen due to other conditions. A key histologic feature supportive of filariasis is the presence of adult worms in lymph nodes.
Comment Here
Reference: Filariasis
Lymphatic filariasis of the breast due to Wuchereria and Brugia can show chronic lymphangitis with lymphatic vessel dilatation, eosinophilic lymphadenitis and granulomatous inflammation; however, these are not specific for filariasis and can be often seen due to other conditions. A key histologic feature supportive of filariasis is the presence of adult worms in lymph nodes.
Comment Here
Reference: Filariasis