Table of Contents
Definition / general | Essential features | Clinical features | Cryoprobe | Radiology description | Case reports | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosis | Board review style question #1 | Board review style answer #1Cite this page: Reisenbichler ES. Radiation therapy & cryoprobe. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastmalignanttreatmenteffectradiation.html. Accessed April 19th, 2024.
Definition / general
- Whole breast irradiation primarily occurs following breast conserving surgery for breast carcinoma
- Also patients with Hodgkin lymphoma receiving mediastinal radiation with secondary breast exposure to radiation
- Radiation can also be delivered intraoperatively to the surgical cavity after removing the tumor but prior to closing the wound
Essential features
- Effects of radiation on skin, such as changes in vascularity, pigmentation and fibrosis, may be induced acutely or as a latent reaction years after radiation (Clin Cosmet Investig Dermatol 2016;9:473)
- Increased risk of secondary radiation induced sarcomas, most commonly angiosarcoma, with an incidence of 0.03 - 0.2% and average latency period of 10 years (Cases J 2008;1:313) (see also Breast angiosarcoma)
- Radiation may induce cytologic changes in normal breast tissue that can mimic atrophy, recurrent carcinoma or sarcoma
Clinical features
- In acute stages, breast skin may become pink or red and peel, as with a sunburn, followed by thickening of the skin in later stages
- Firmness of the breast may result from fibrosis
- Lactation may still occur after pregnancy in at least 50% of women who have undergone prior radiation therapy, but production is reduced
- Lactation is unaffected in the contralateral, untreated breast (Expert Rev Anticancer Ther 2013;13:159)
- Radiation may induce bullous pemphigoid in the skin (Dermatol Online J 2016;22:13030)
- In patients undergoing immediate reconstructive surgery, volume loss and fat necrosis may occur due to postmastectomy radiation; however it has not resulted in higher rates of revision surgery in the radiated breast (Ann Plast Surg 2013;71:149)
Cryoprobe
- Cryoprobe: uses cryotherapy to makes nonpalpable carcinomas well defined and palpable by creating an ice ball, leading to removal of less tissue (Am J Surg 2006;192:462)
- Alters tumor morphology making it difficult to grade tumor, distinguish DCIS and invasive tumor, and identify angiolymphatic invasion or mitotic figures (Am J Clin Pathol 2007;128:239)
- Alternative to excision of fibroadenomas (Radiology 2005;234:63)
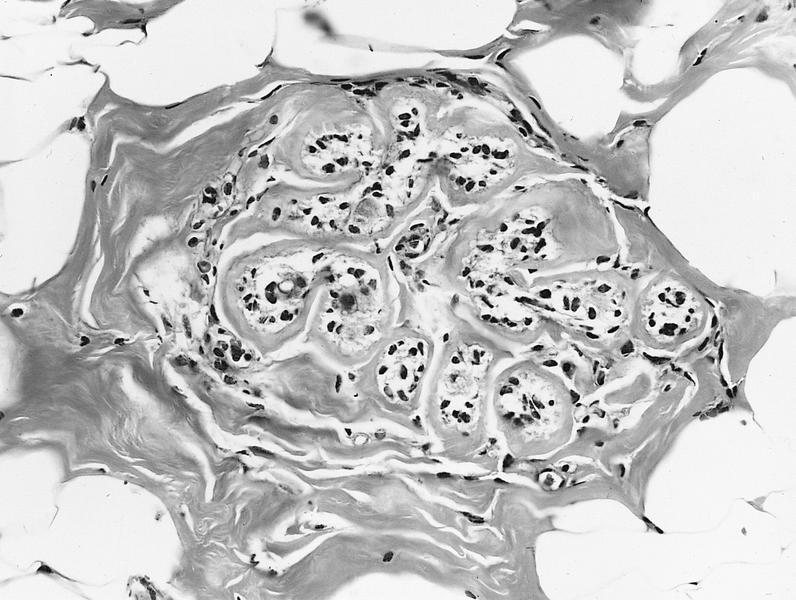
- Normal breast parenchyma in cryozone shows dense fibrosis, fat necrosis, xanthogranulomatous reaction, endovascular fibrosis and hemorrhage (Cryobiology 2007;55:44)
- Causes reduction in ER / PR receptors, but does not affect Ki67 staining or margin evaluation
Radiology description
- Mammographic changes following radiation therapy include increased breast density and skin thickening, both of which are more common following whole breast radiotherapy than with intraoperative radiotherapy (Eur J Surg Oncol 2014;40:163)
Case reports
- 57 year old woman with radiation induced morphea (J Med Case Rep 2008;2:136)
- 62 year old woman with radiation fibrosis imitating breast cancer recurrence (J Breast Health (2013) 2017;13:40)
- Two cases of papillary endothelial hyperplasia mimicking angiosarcoma after breast irradiation (Pathol Res Pract 2016;212:604)
- Series of 10 cases of postradiation angiosarcoma of the breast mimicking radiation dermatitis (J Cutan Pathol 2017;44:456)
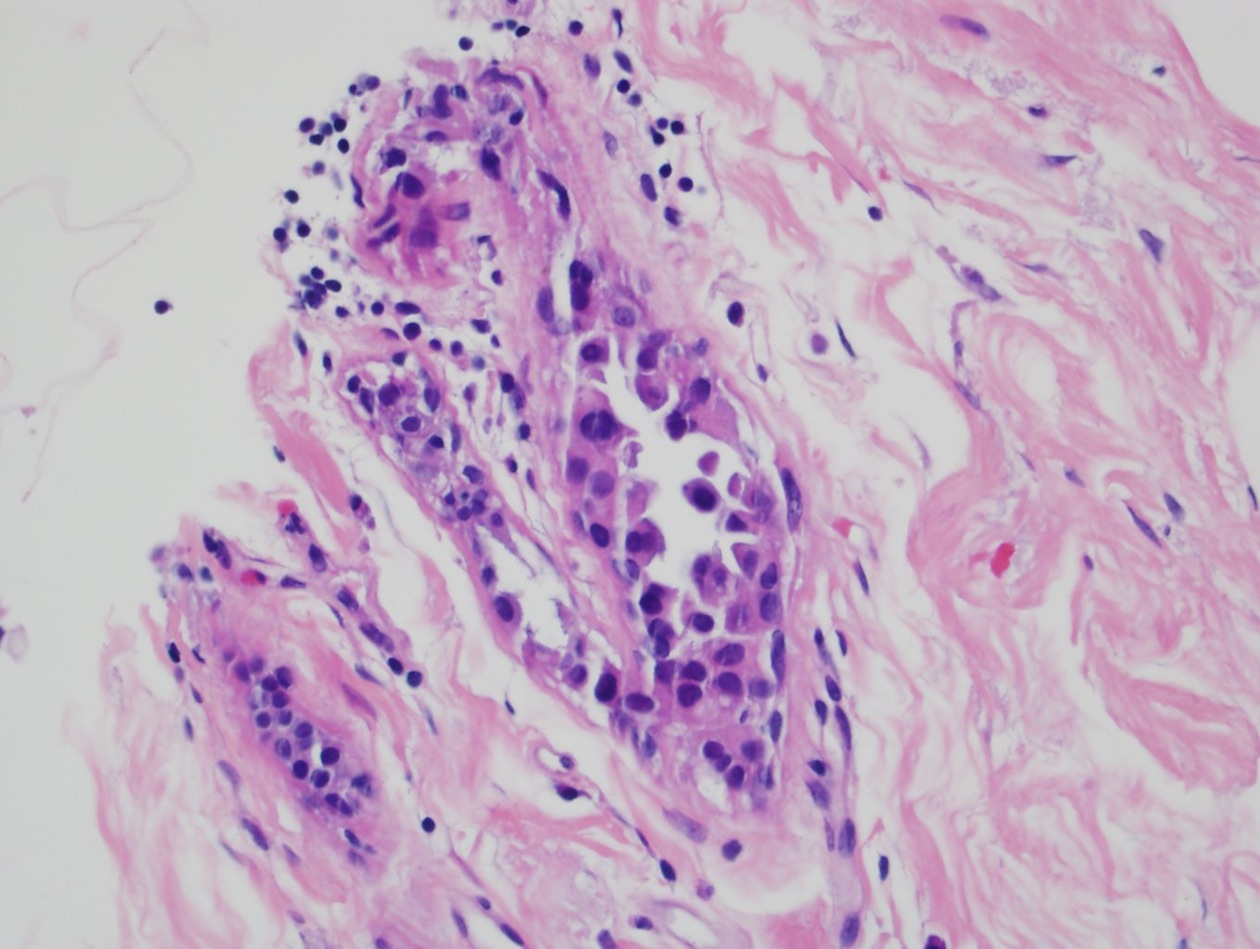
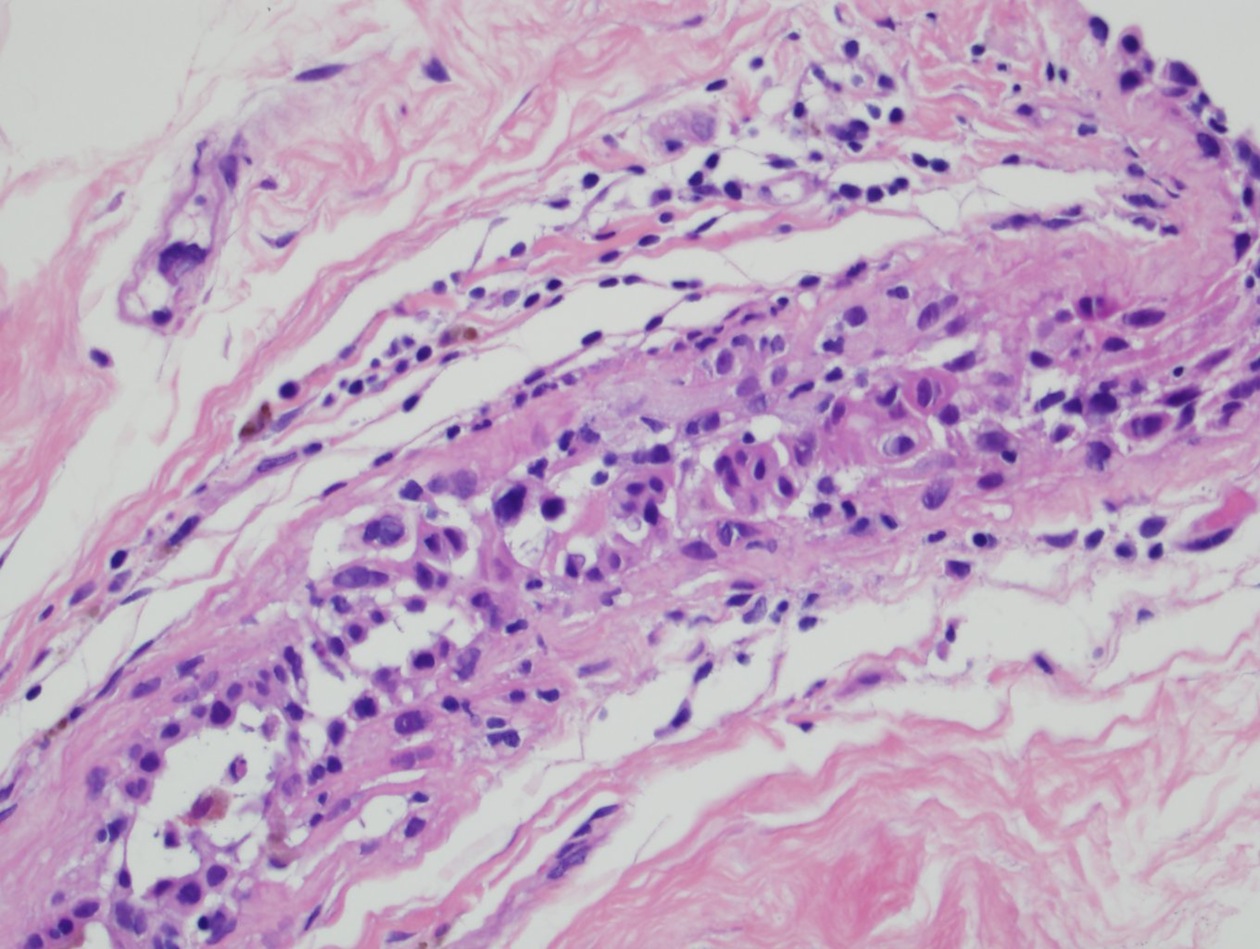
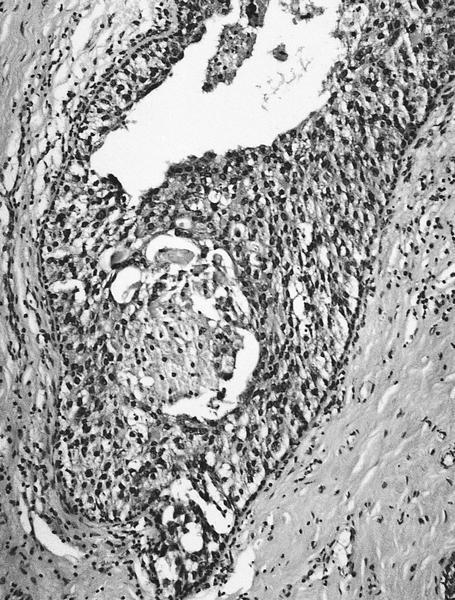
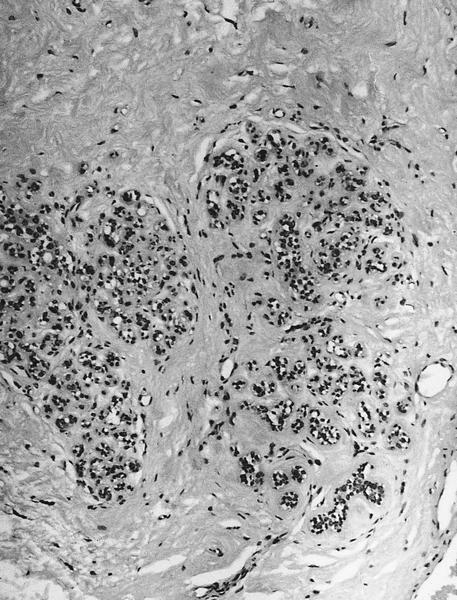
Microscopic (histologic) description
- Giant tumor cells with bizarre nuclear changes (J Clin Pathol 1990;43:152), naked nuclei and abnormal mitotic figures
- Extensive tumor necrosis demarcated by thick fibrous walls (when radiating tumor prior to surgery)
- Changes in nonneoplastic breast take place primarily in the terminal duct lobular unit and include atypia, lobular sclerosis and atrophy (may distort lobular architecture and obscure myoepithelial cells, Hum Pathol 1984;15:545)
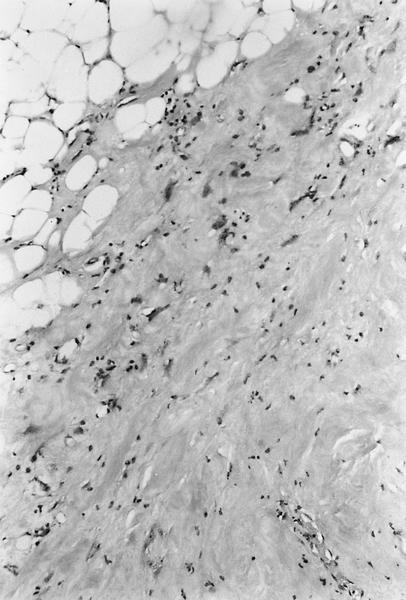
- Intimal thickening in small muscular arteries (Radiother Oncol 2009;92:477) and fat necrosis, but usually no mitotic activity or loss of polarity
- Epithelial atypia in larger ducts ranges from mild to severe but proliferation of the epithelium is generally seen only with mild cytologic atypia (Am J Surg Pathol 2004;28:47)
- Atypical stromal fibroblasts
- Changes do not regress over time (Am J Surg Pathol 2004;28:47)
Microscopic (histologic) images
AFIP images
Images hosted on other servers:
Differential diagnosis
- Recurrent carcinoma (invasive or in situ): cells should be keratin positive and demonstrate similar histologic grade and receptor profile as the previous carcinoma
- Atypical stromal fibroblasts will be keratin negative
- Cytologic atypia in a lobule secondary to radiation will typically not fill and distend lumina or demonstrate necrosis and mitotic activity (features suggestive of recurrent high grade DCIS)
- Sarcoma (radiation induced or primary): radiation induced sarcomas typically present as mass forming lesions rather than microscopic atypical stromal cells seen postradiation
- Primary sarcoma of the breast would likely be a component of a malignant phyllodes and therefore demonstrate other features of a fibroepithelial lesion
- Primary sarcoma of the breast would likely be a component of a malignant phyllodes and therefore demonstrate other features of a fibroepithelial lesion
Board review style question #1
- Which statement about distinguishing radiation induced changes in benign breast tissue from recurrent carcinoma is true?
- Cytologically atypical cells scattered in the stroma that are estrogen receptor and keratin positive likely represent fibroblasts with radiation induced atypia.
- If the radiation took place more than 10 years previously, any atypia must represent recurrent malignancy.
- Low grade cytologic atypia is not seen in benign lobules secondary to radiation effect.
- Necrosis in proliferative ductal epithelium with high grade cytologic atypia is indicative of carcinoma in situ.
- Proliferative epithelium with high grade cytologic atypia is commonly seen secondary to radiation effect.
Board review style answer #1
D. Radiation may induce cytologic atypia of any degree from low to high, but proliferation of epithelium takes place secondary to radiation generally with only low grade atypia. Necrosis, mitoses and proliferative epithelium with high grade atypia together are suggestive of carcinoma rather than radiation atypia. Changes secondary to radiation do not regress over time and can be seen for more than 10 years following radiation therapy. Atypical, postradiation stromal fibroblasts should not be keratin or estrogen receptor positive. This staining pattern is more in keeping with recurrent invasive carcinoma.
Comment Here
Reference: Radiation therapy & cryoprobe
Comment Here
Reference: Radiation therapy & cryoprobe