Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Turashvili G. Adenocarcinoma in situ. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cervixAIS.html. Accessed April 25th, 2024.
Definition / general
- An intraepithelial lesion containing malignant appearing glandular epithelium that carries a significant risk of invasive adenocarcinoma if not treated
Essential features
- Neoplastic glandular precursor for invasive endocervical adenocarcinoma
- Variable histologic features based on adenocarcinoma in situ type
- Most adenocarcinoma in situ types are associated with high risk human papillomavirus (HPV)
- Negative p16 immunohistochemical staining may indicate a non HPV associated adenocarcinoma in situ type
Terminology
- Histology:
- Also known as high grade cervical glandular intraepithelial neoplasia (HG-CGIN); please note that this terminology is not recommended by the WHO classification
- Cytology (IARC: Cytopathology of the Uterine Cervix - Digital Atlas [Accessed 30 January 2020]):
- Endocervical adenocarcinoma in situ
- Atypical endocervical cells, favor neoplastic
- Atypical endocervical cells (not otherwise specified or specify)
ICD coding
- ICD-O: 8140/2 - adenocarcinoma in situ, NOS
- ICD-10: D06.0 - carcinoma in situ of endocervix
- ICD-11: 2E66.Y (XA7Z73) - other specified carcinoma in situ of cervix uteri (cervical canal)
Epidemiology
- Uncommon (1% of cervical noninvasive lesions versus 99% high grade squamous intraepithelial lesion (HSIL) in the SEER registry)
- Mean age 38 years, 10 - 15 years younger than invasive endocervical adenocarcinoma
- Coexists with high grade squamous intraepithelial lesion in at least 50% of cases (Int J Gynecol Pathol 2002;21:314)
- Declined incidence rates in young women (21 - 24 years of age) in US since introduction of HPV vaccine (Int J Cancer 2020;146:810)
Sites
- At or near transformation zone of cervix
Pathophysiology
- Arises from reserve cells with capacity to undergo columnar differentiation or from columnar epithelium (Int J Gynecol Pathol 2010;29:378)
- An interval of approximately 13 years between the average age of presentation of AIS (39 years) and the average age of presentation of invasive adenocarcinoma (52 years) has been documented; this interval is shorter than the one seen in squamous cervical lesions (Gynecol Oncol 1999;75:55)
Etiology
- HPV, most often types 16 and 18 (Gynecol Oncol 2010;117:297)
Clinical features
- Typically asymptomatic
- Most commonly abnormal cervical cytology with atypical endocervical glandular cells (Aust N Z J Obstet Gynaecol 2004;44:436)
- Rarely vaginal bleeding
Diagnosis
- Cytologic or histologic examination
Prognostic factors
- Excellent prognosis in most cases
- After conization, positive endocervical margins increase risk of residual or recurrent in-situ disease (19.4% with positive margins versus 2.6% with negative margins) and subsequent diagnosis of invasive adenocarcinoma (5.2% with positive margins versus 0.1% with negative margins) (Am J Obstet Gynecol 2009;200:182.e1)
- Rarely may involve endometrium or adnexa via pagetoid spread
Case reports
- 30 year old woman with prior HSIL on Pap smear (Case of the Week #202)
- 30 year old woman with atypical glandular cells on Pap smear with subsequent diagnosis of stratified mucin producing intraepithelial lesion (SMILE) and HSIL on biopsy (Virol J 2019;16:76)
- 36 year old woman with simultaneous squamous cell carcinoma in situ and adenocarcinoma in situ (Arch Gynecol Obstet 2010;281:527)
- 38 year old woman with endocervical adenocarcinoma in situ presenting in fundal endometrial polyp (Int J Gynecol Pathol 2015;34:228)
- Two cases of premenopausal women with normal Pap smears but adenocarcinoma in situ on cervical biopsy (J Reprod Med 2009;54:451)
- Two cases of gastric type adenocarcinoma in situ (Diagn Cytopathol 2017;45:842)
Treatment
- Management after cytologic diagnosis of adenocarcinoma in situ
- Referral to a qualified health care provider for medical follow up
- Colposcopy with endocervical sampling in all women
- Endometrial sampling in women aged ≥ 35 years or at risk for endometrial neoplasia (J Low Genit Tract Dis 2007;11:201)
- Management after histologic diagnosis of adenocarcinoma in situ
- Cold knife conization or hysterectomy
- Most patients can be successfully treated with conization and close follow up by colposcopy, cytology and HPV testing, provided the endocervical margin is negative
- Hysterectomy may be considered in women with positive endocervical margins or women not desirous of maintaining fertility
Gross description
- Typically incidental without distinctive gross appearance
- Rarely erythematous mucosa on colposcopy
- May be multifocal
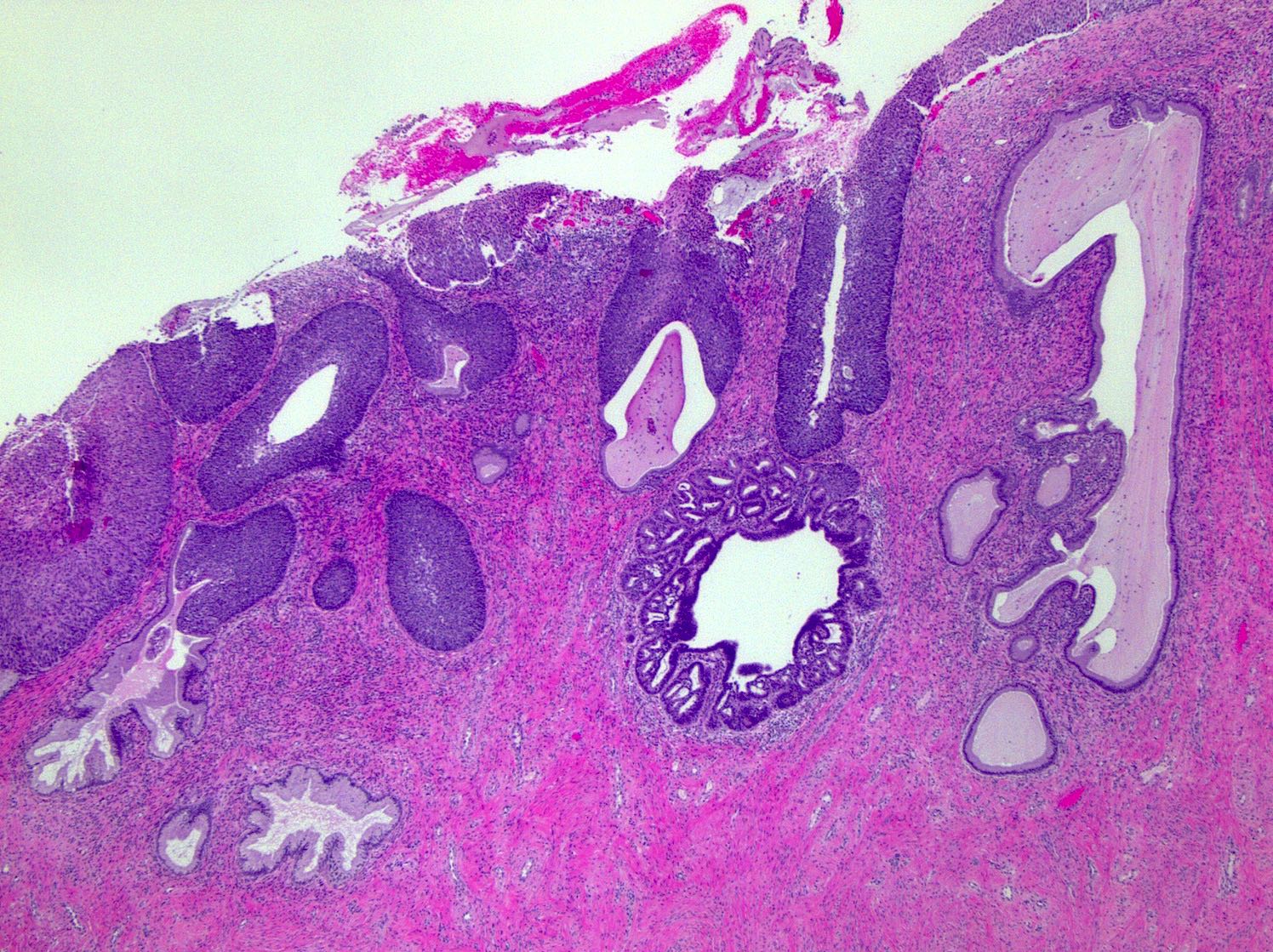
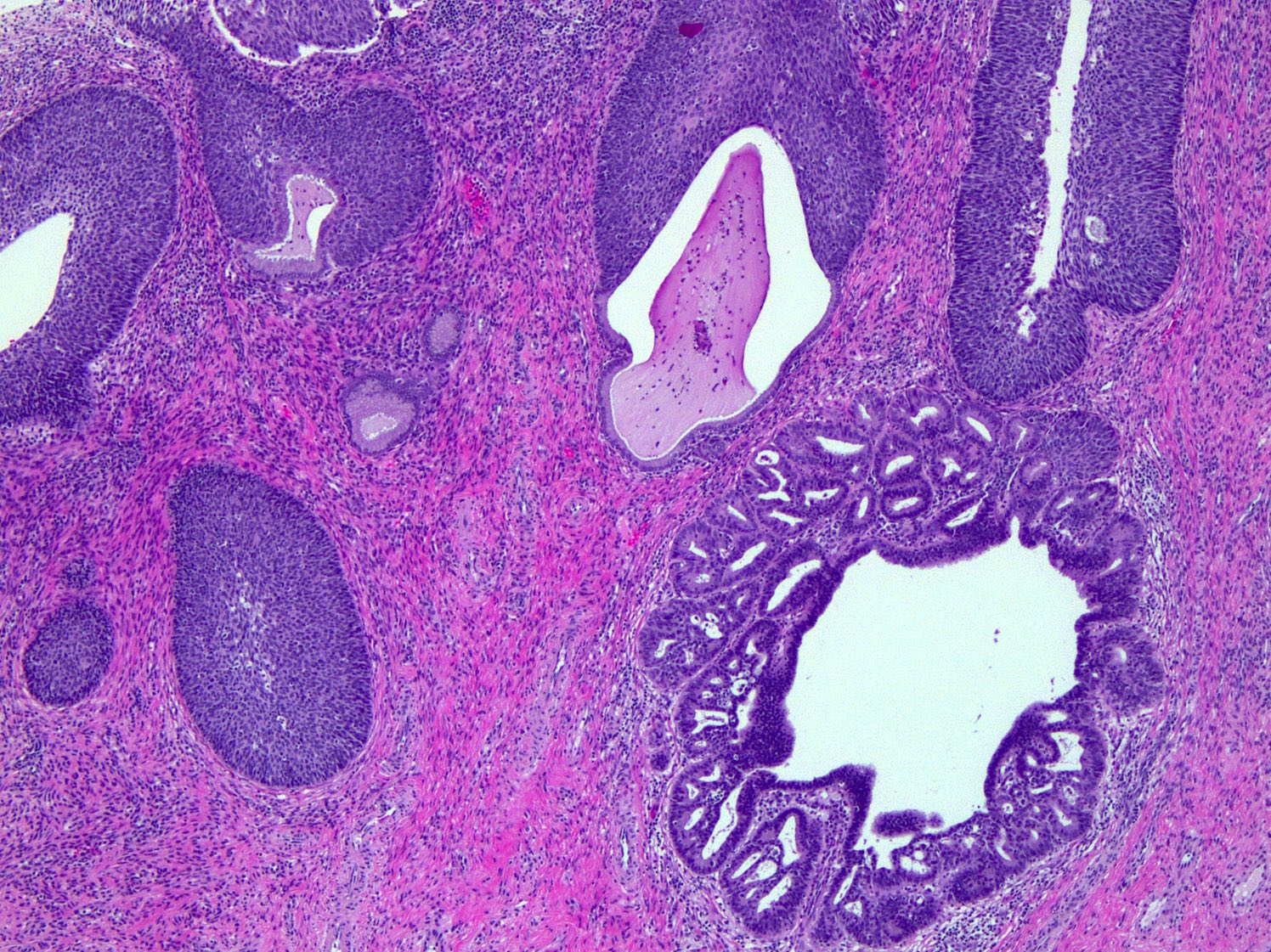
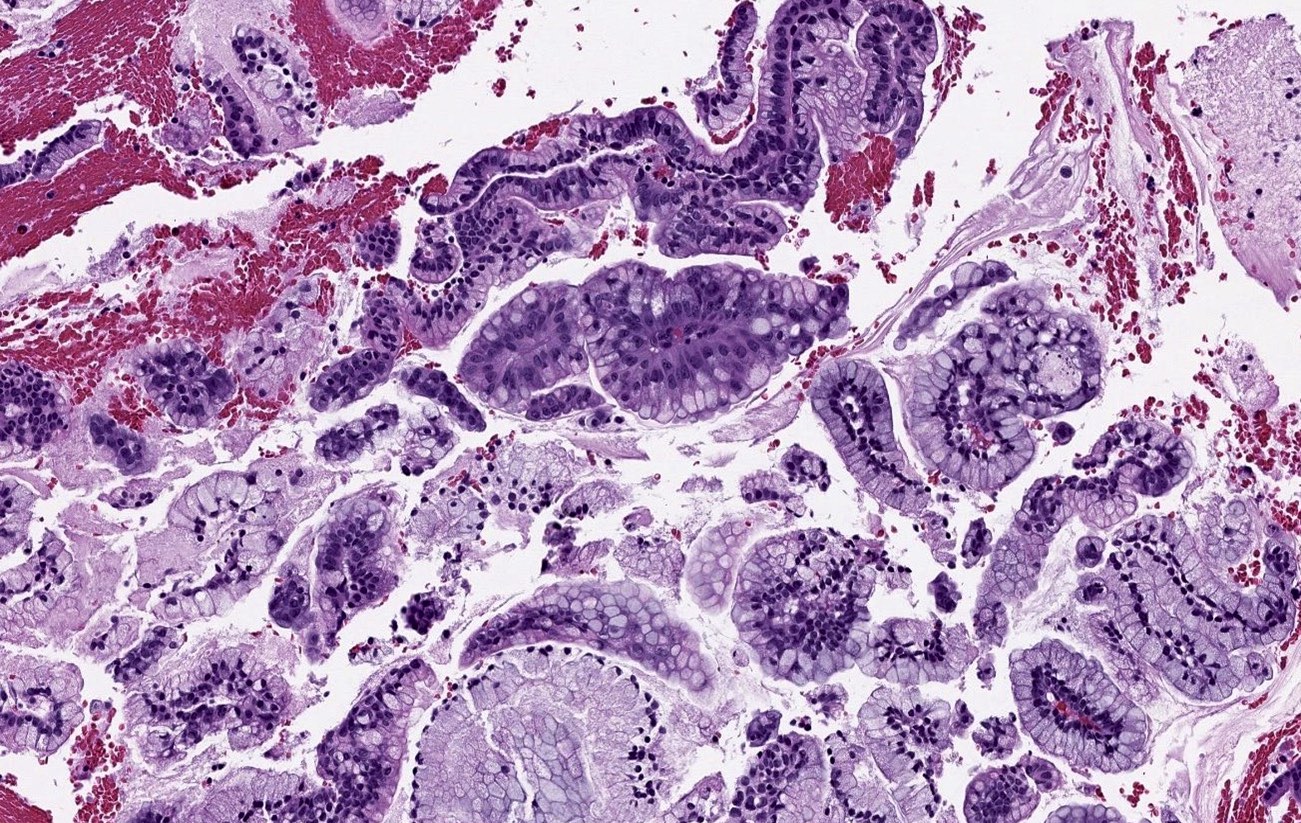
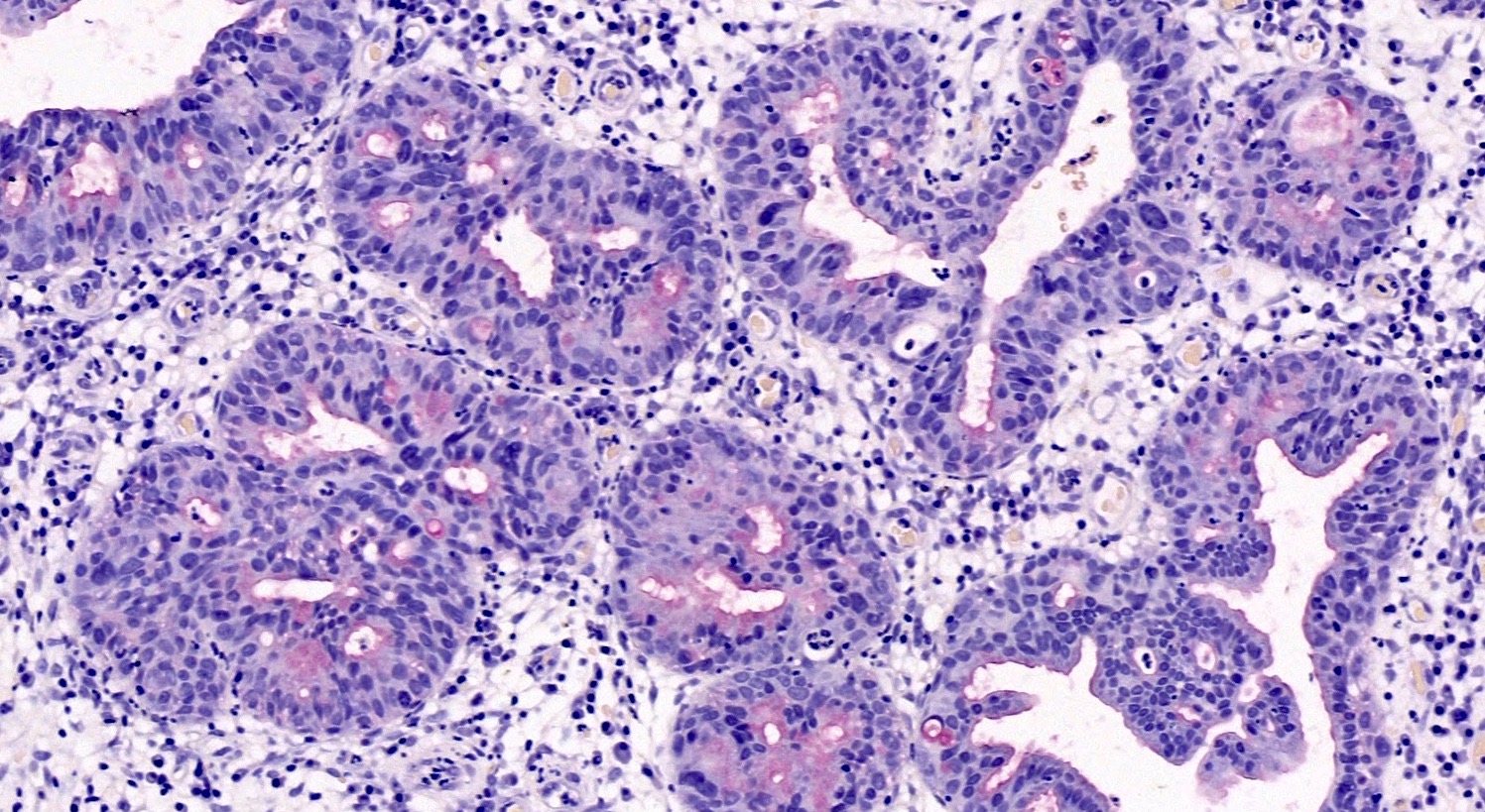
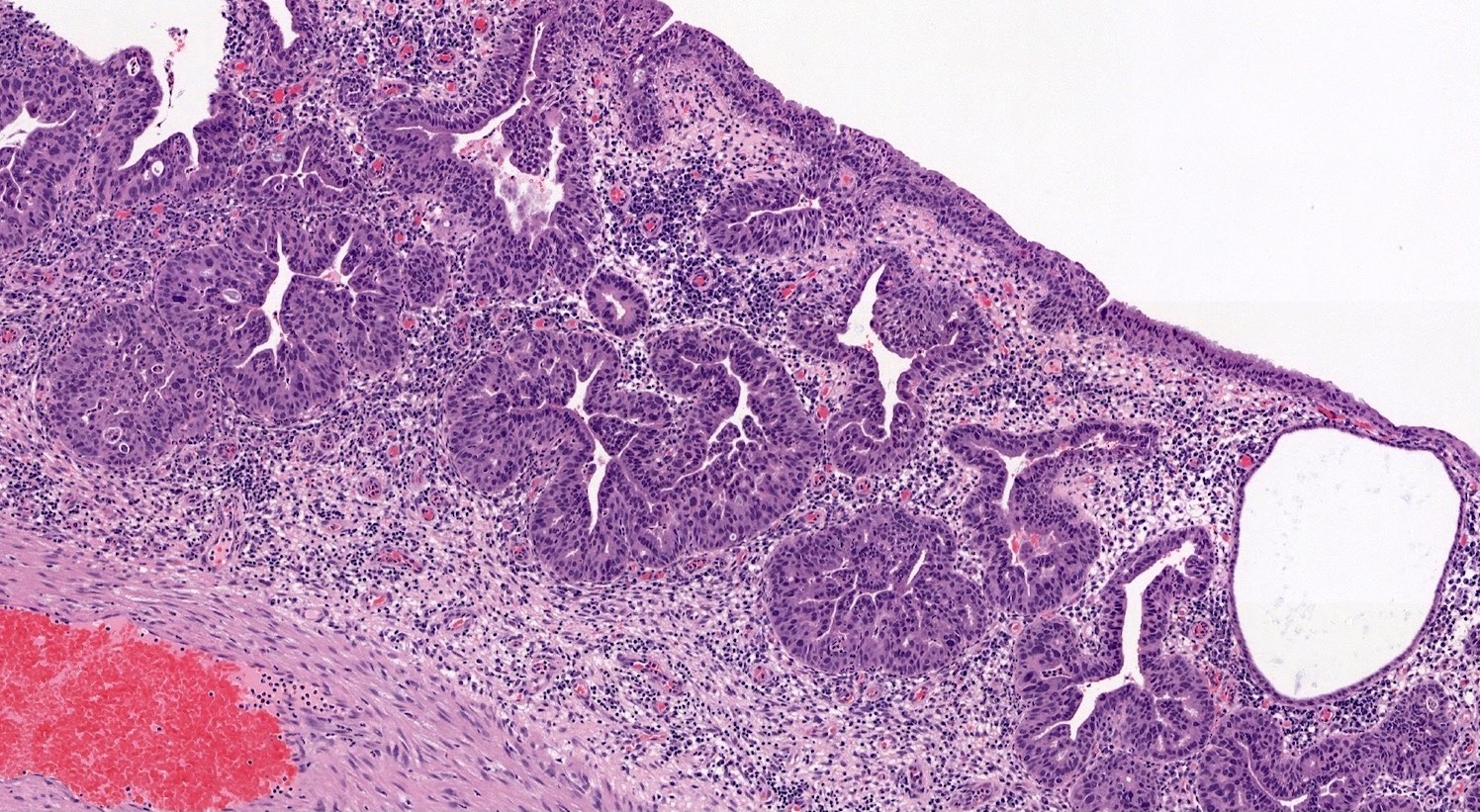
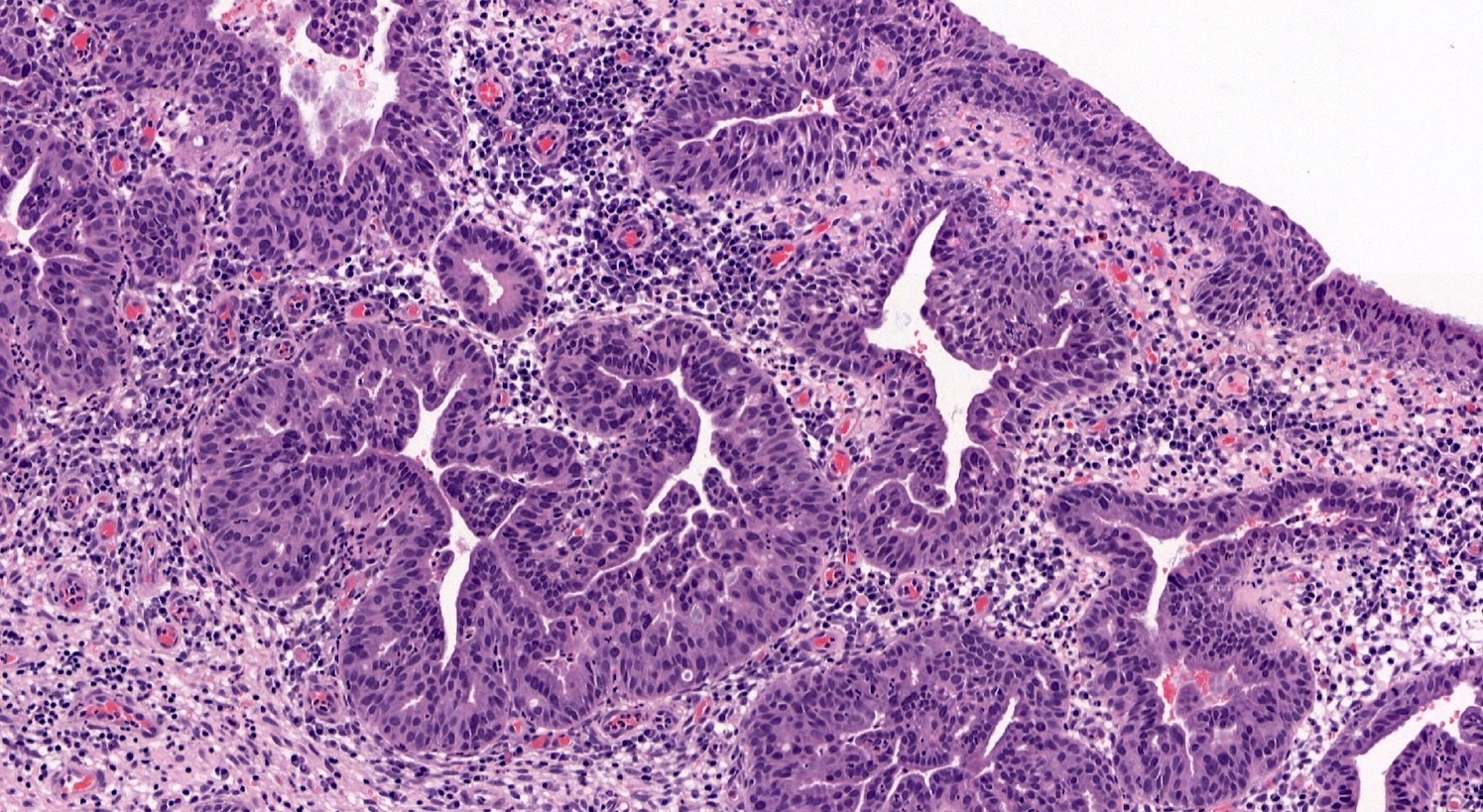
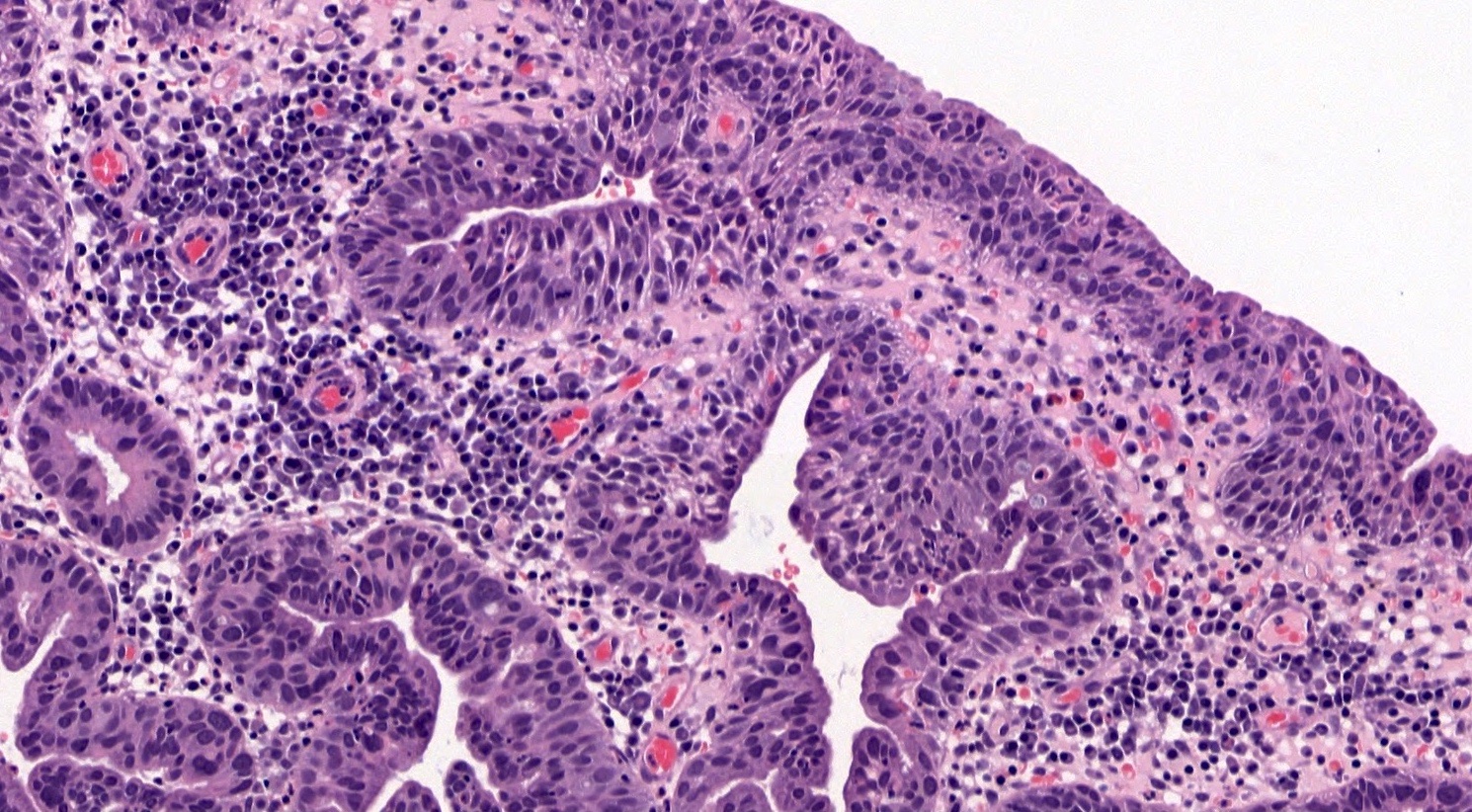
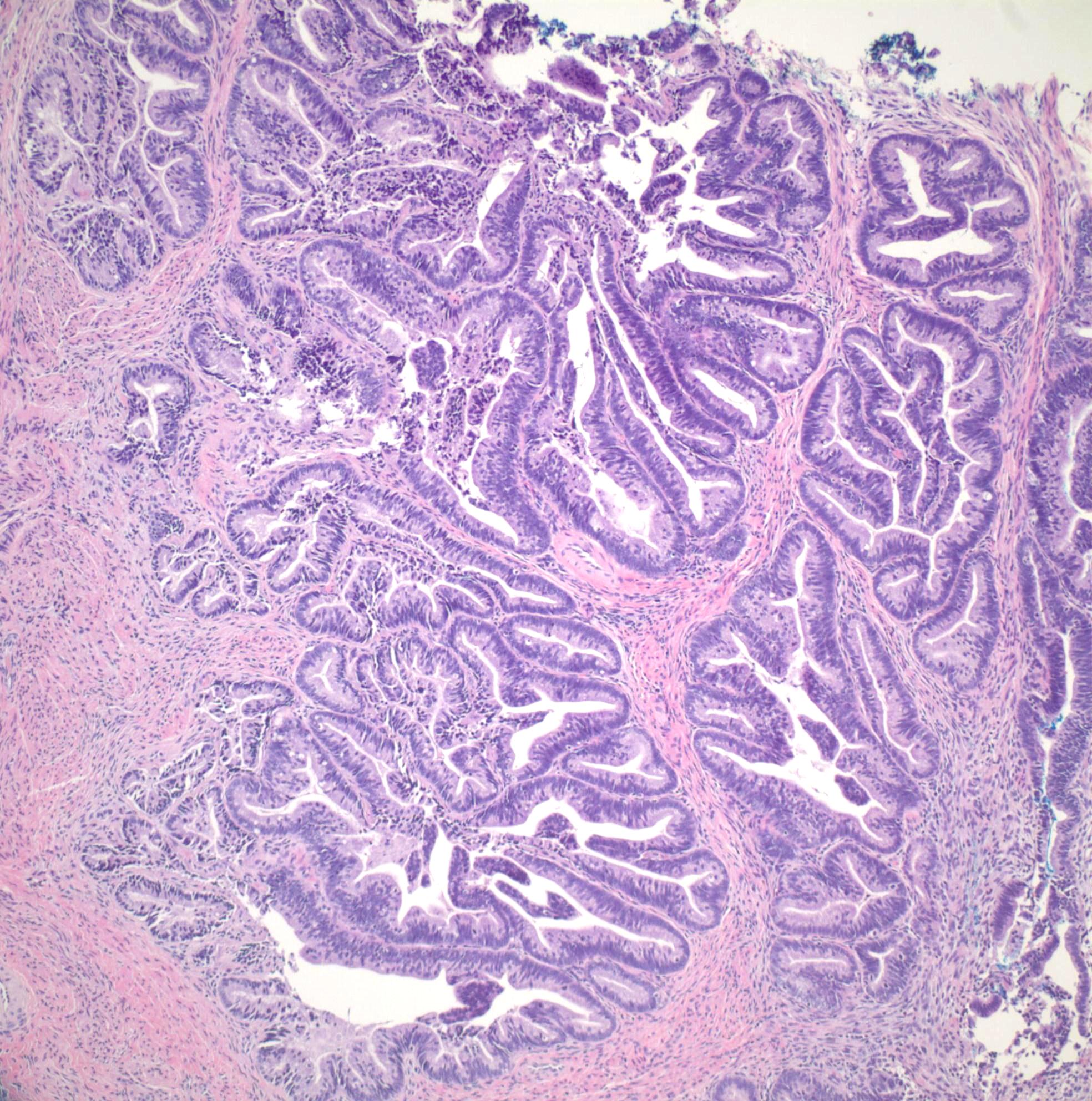
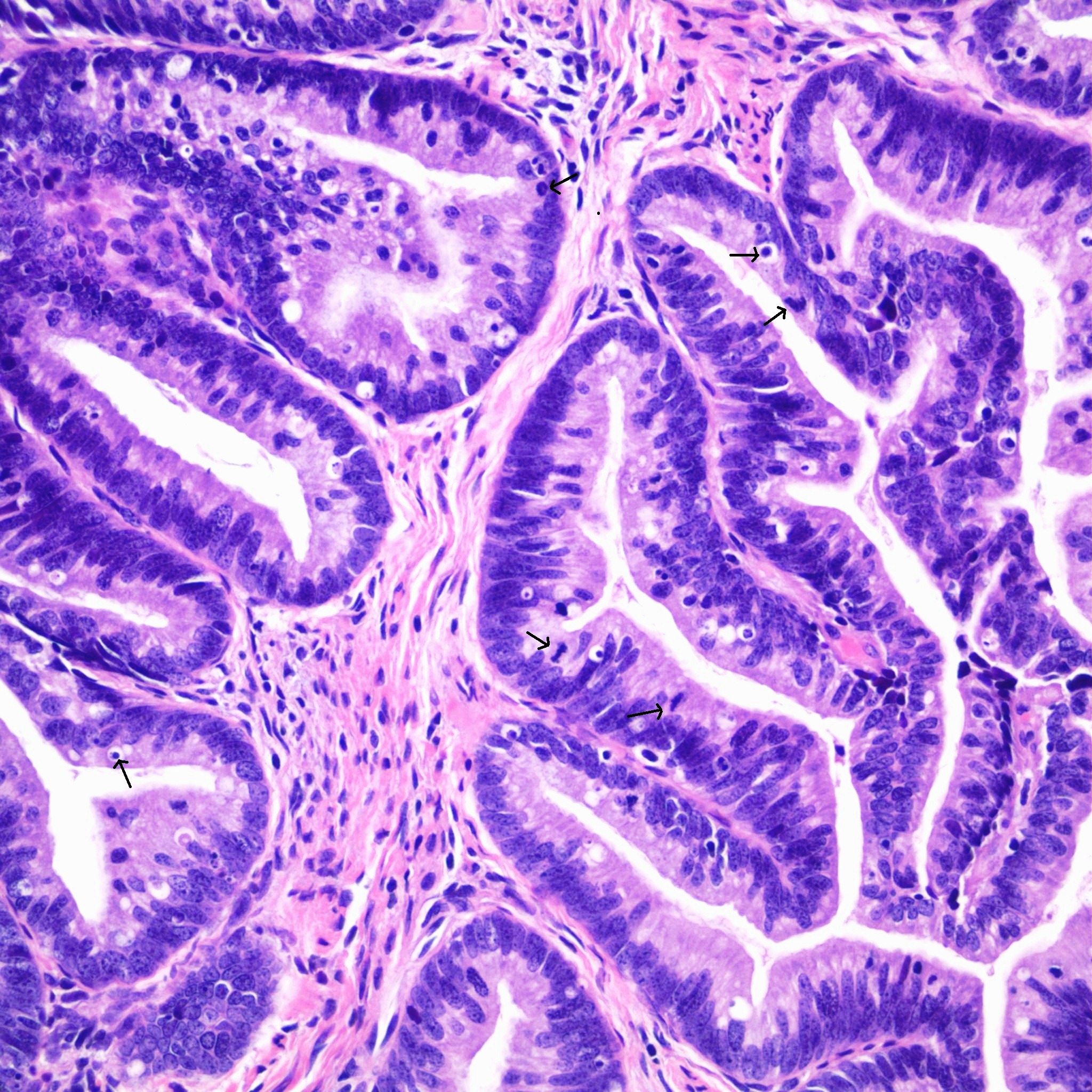
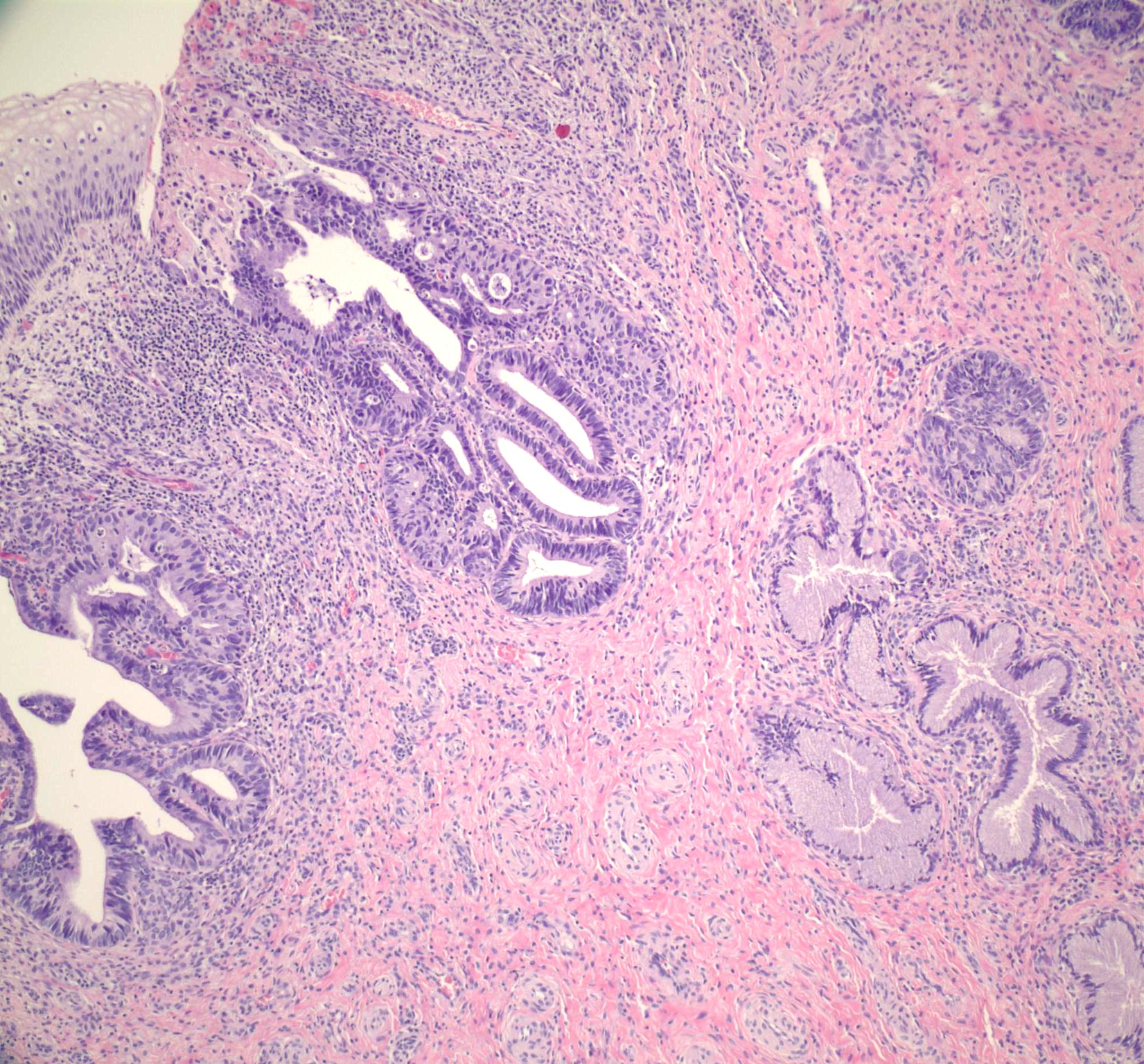
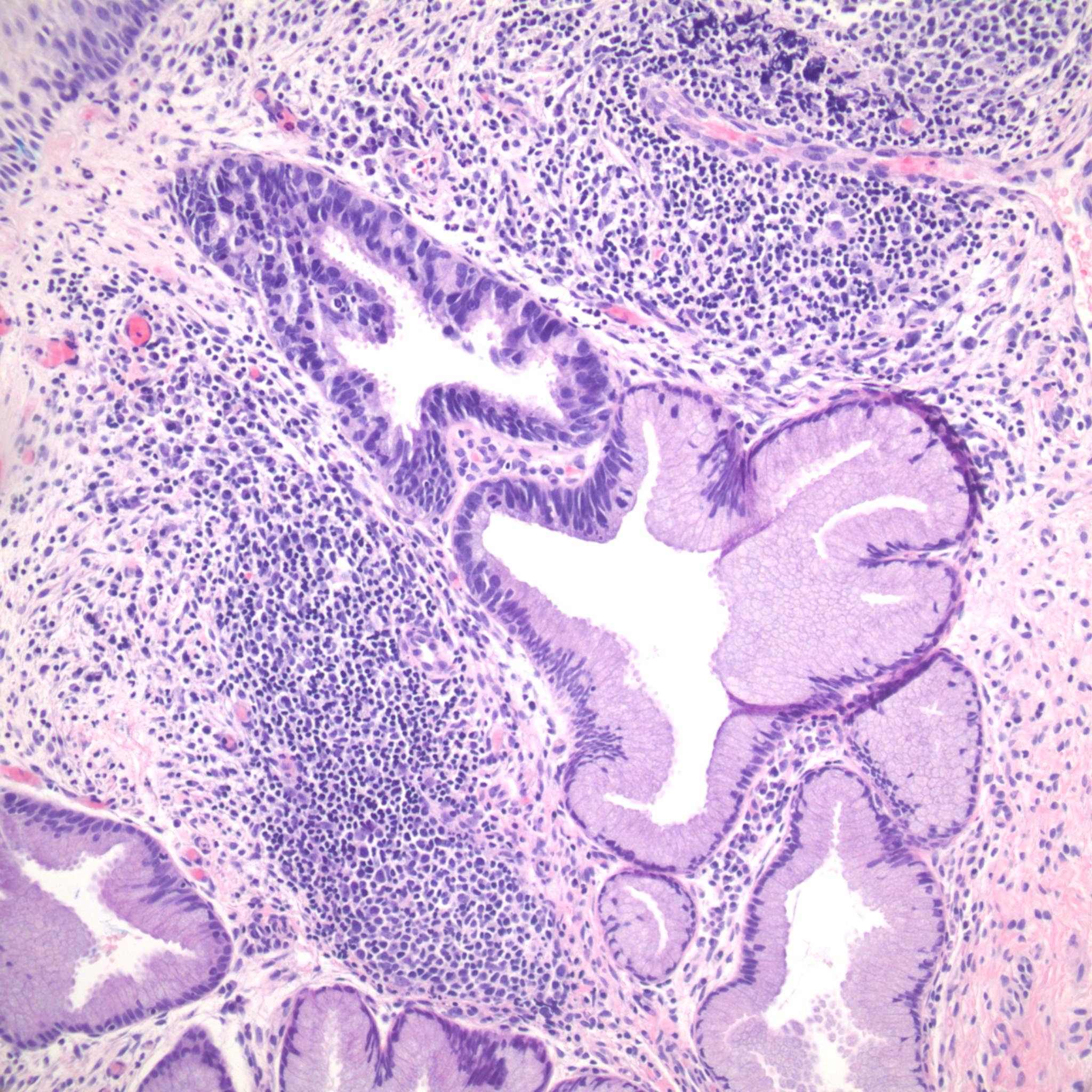
Microscopic (histologic) description
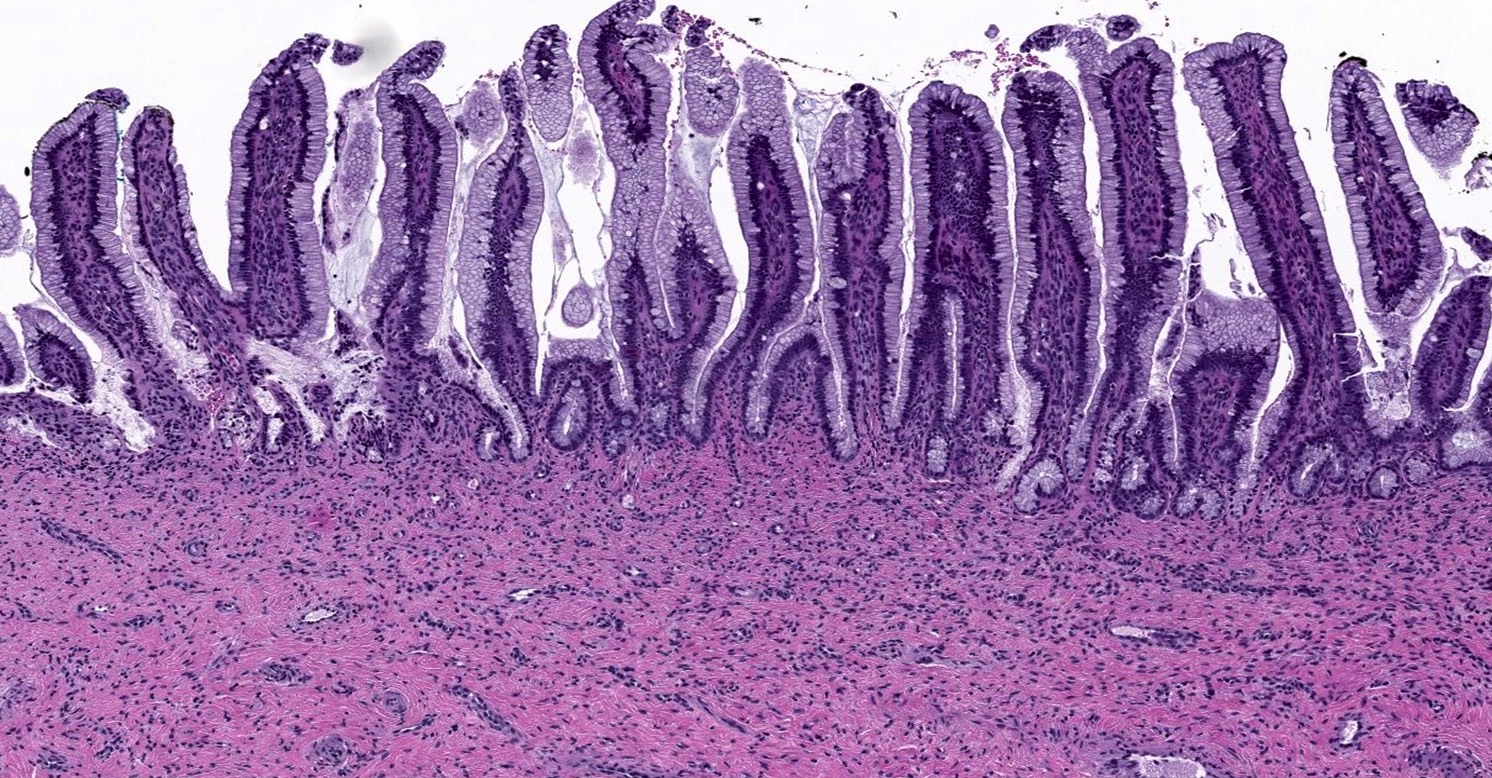
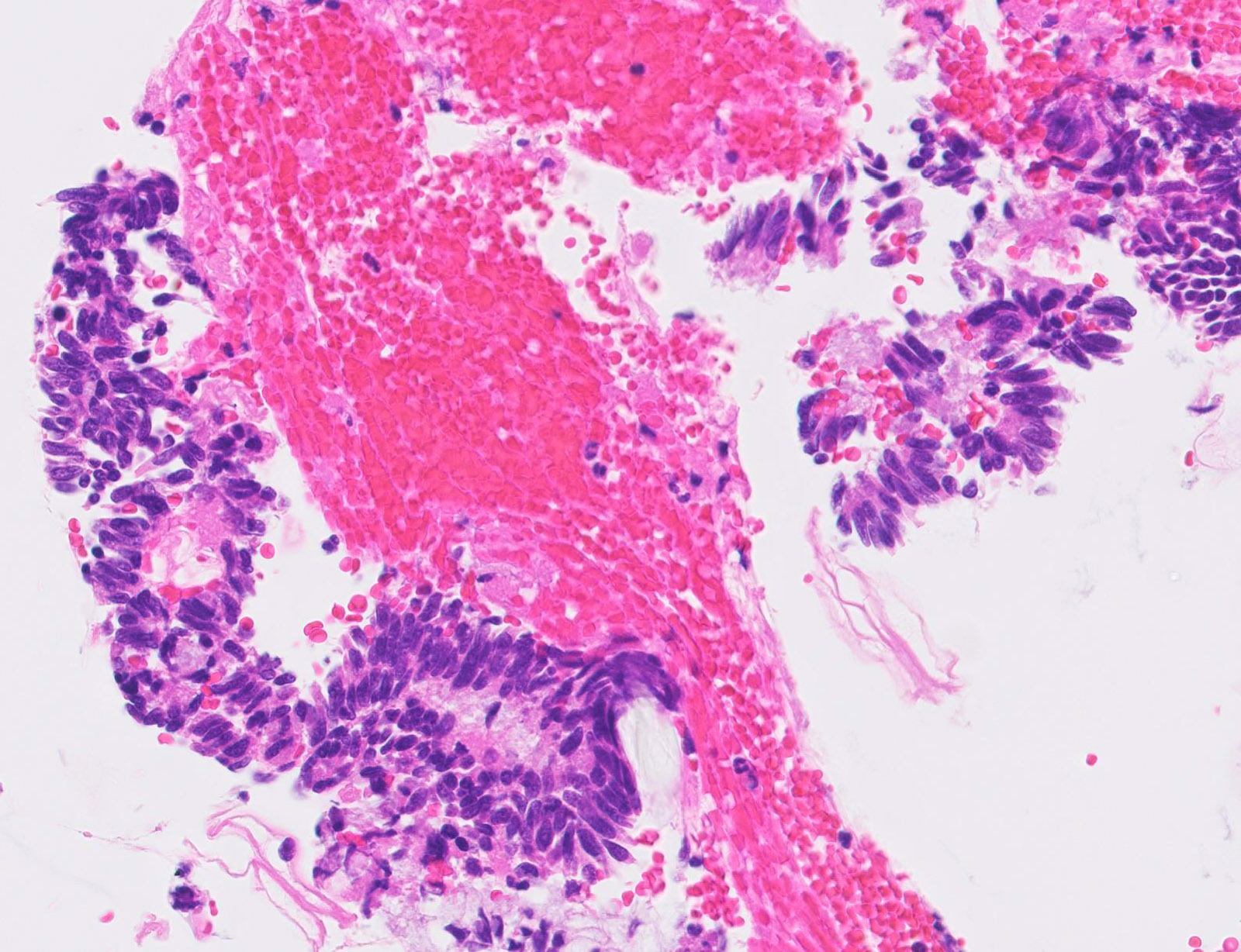
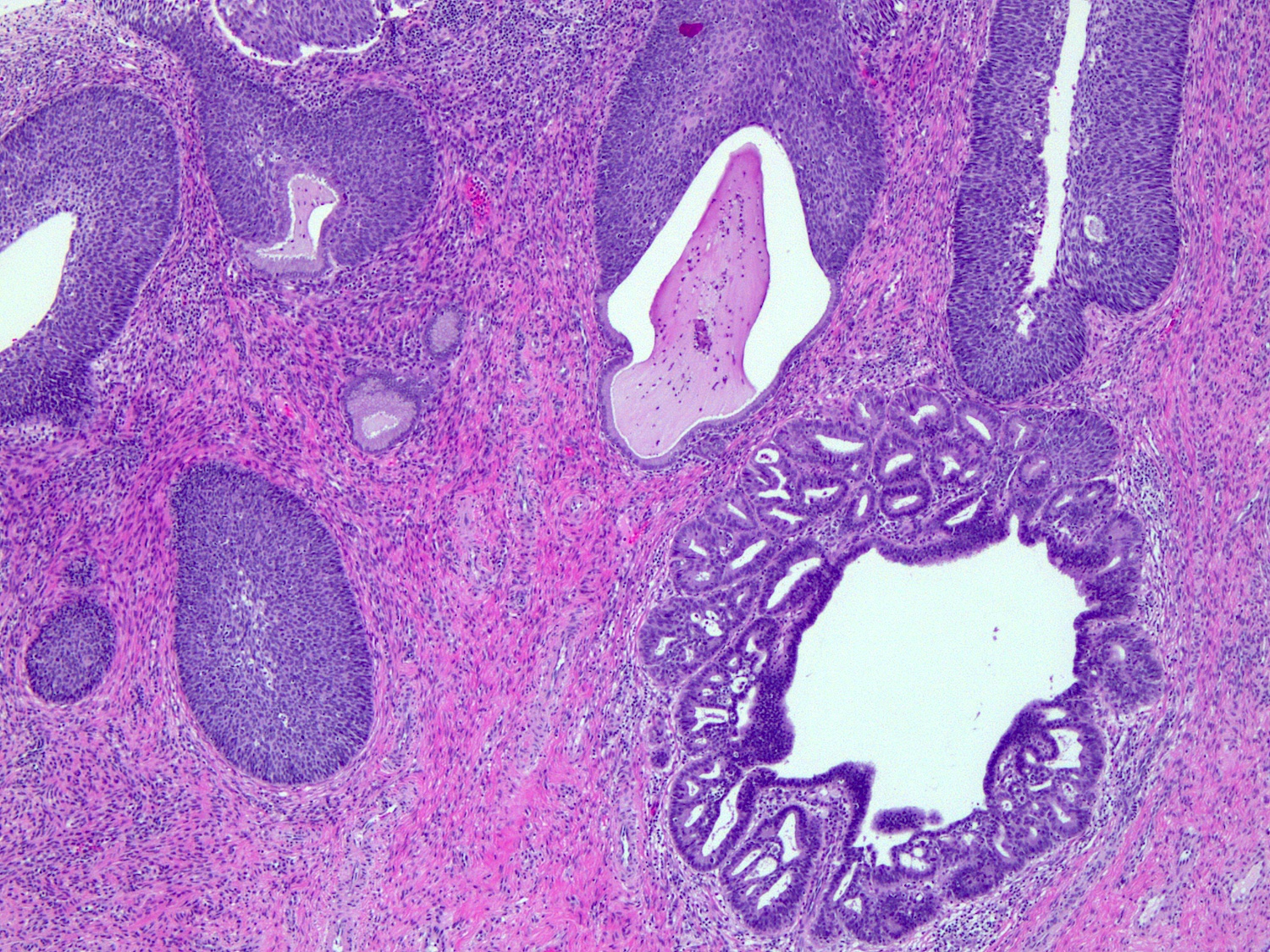
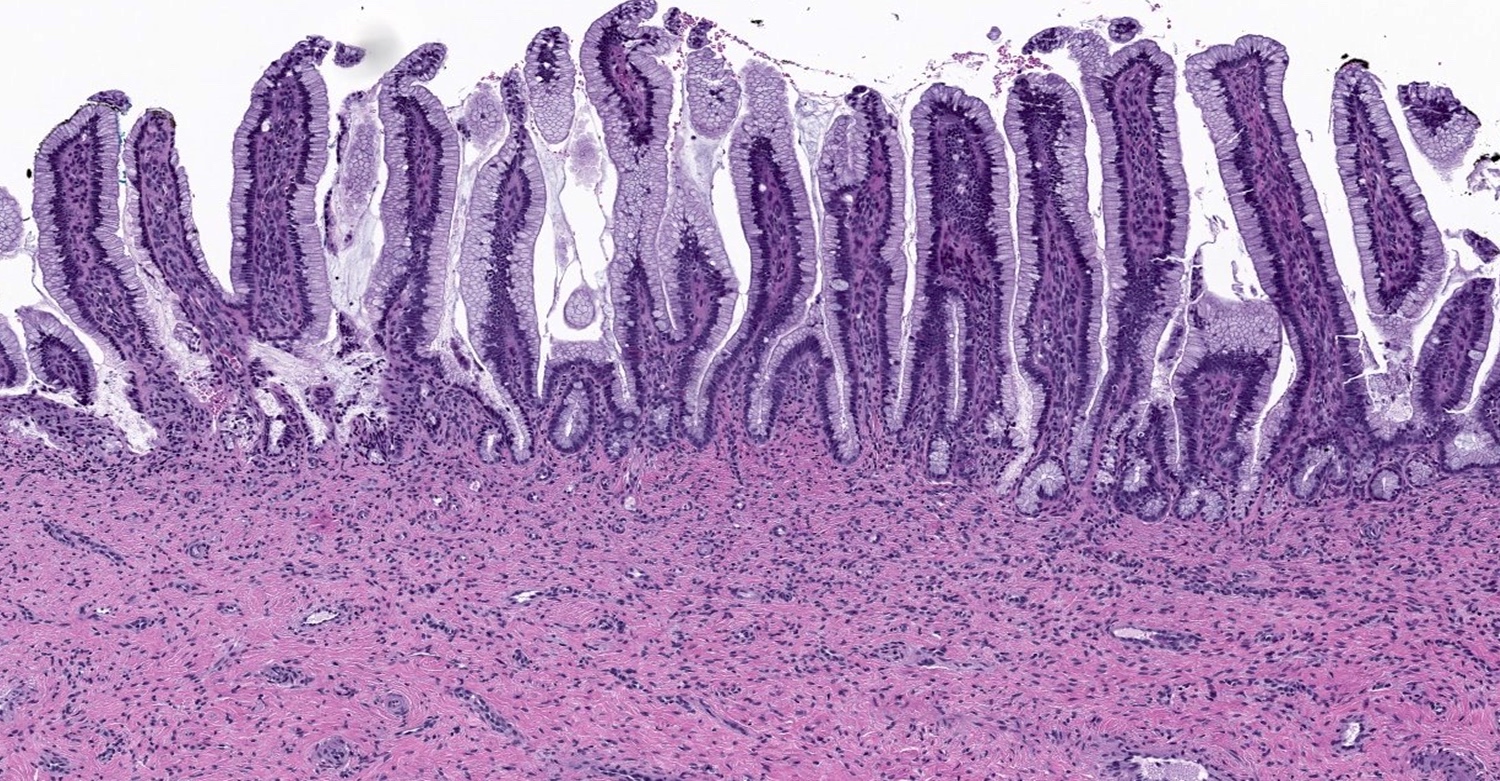
- Replacement of normal epithelium on the endocervical surface and in pre-existing endocervical glands with preservation of the normal endocervical architecture (comparison with the uninvolved cervix is often useful)
- Abrupt transition from normal to atypical epithelium from gland to gland and within individual glands
- Skip lesions are often seen
- Common partial gland involvement or surface epithelial involvement
- No desmoplastic stromal reaction and minimal inflammatory infiltrate
- Additional variable histologic features depending on type
- HPV related
- Usual (conventional) type
- Rarely cribriform or papillary intraglandular growth patterns
- Variable amounts of apical eosinophilic to mucinous cytoplasm
- Enlarged, fusiform, hyperchromatic, pseudostratified nuclei with irregular, coarse chromatin and occasionally with prominent nucleoli
- Frequent mitotic figures, often apical or “floating”
- Frequent apoptotic bodies
- Superficial forms show less nuclear enlargement and stratification with fewer apoptotic bodies and commonly occur in younger women (mean age 27 years)
- Intestinal type
- Commonly admixed with conventional subtype
- Frequent goblet cells
- Paneth and enteroendocrine cells may be present
- Few mitotic figures and apoptotic bodies
- Less commonly pancreatobiliary type epithelium
- Tubal type
- Apical eosinophilic cytoplasm and cilia
- Variable cytologic atypia and mitotic figures
- Important to rule out tubal metaplasia
- Stratified mucin producing intraepithelial lesion (SMILE)
- Variably pseudostratified epithelium
- Polyhedral to columnar cells with eosinophilic to mucinous cytoplasm
- Resembles HSIL on low power but the stratified neoplastic cells contain intracellular mucin in the form of discrete vacuoles or as cytoplasmic clearing throughout all cell layers
- Can be an isolated finding or more often found in association with HSIL or conventional adenocarcinoma in situ (Am J Surg Pathol 2000;24:1414)
- May be a form of adenosquamous carcinoma in situ
- Usual (conventional) type
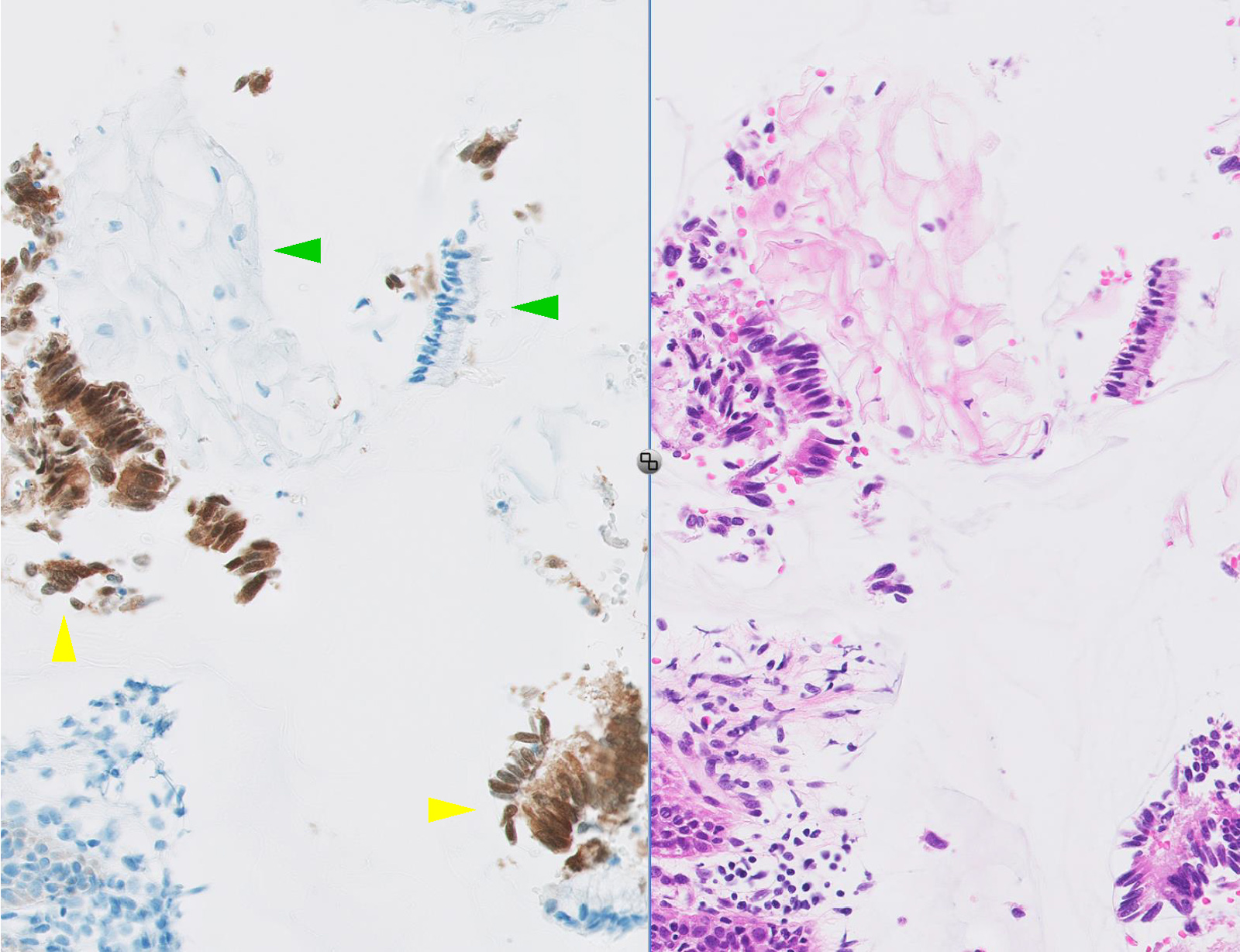
- HPV independent
- Gastric type (Am J Surg Pathol 2017;41:1023)
- Columnar cells with pale foamy to mucinous cytoplasm and prominent cytoplasmic borders
- Basally located nuclei
- Intestinal differentiation often seen
- Fewer mitotic figures and apoptotic bodies compared to HPV related adenocarcinoma in situ
- Gastric type (Am J Surg Pathol 2017;41:1023)
- HPV related
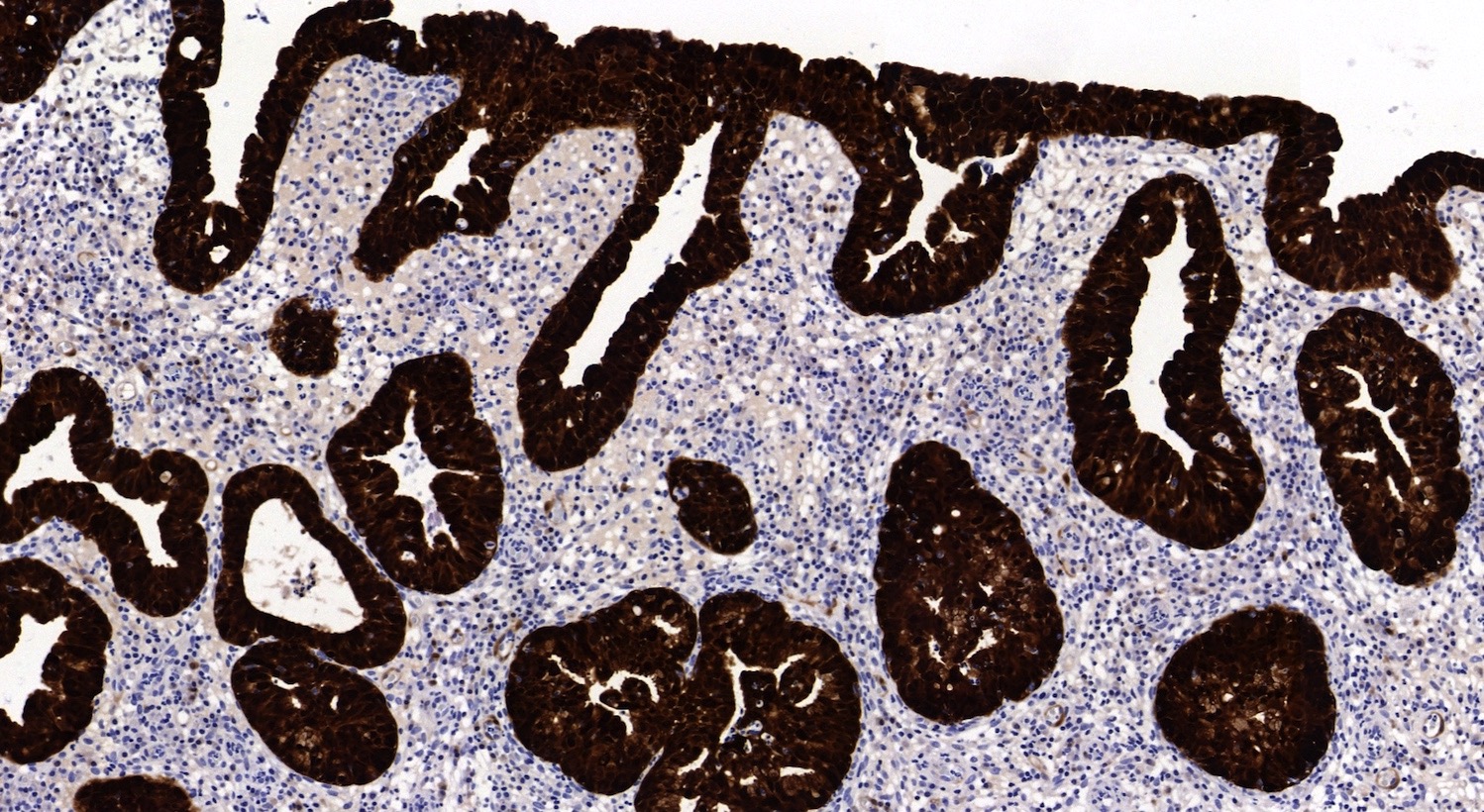
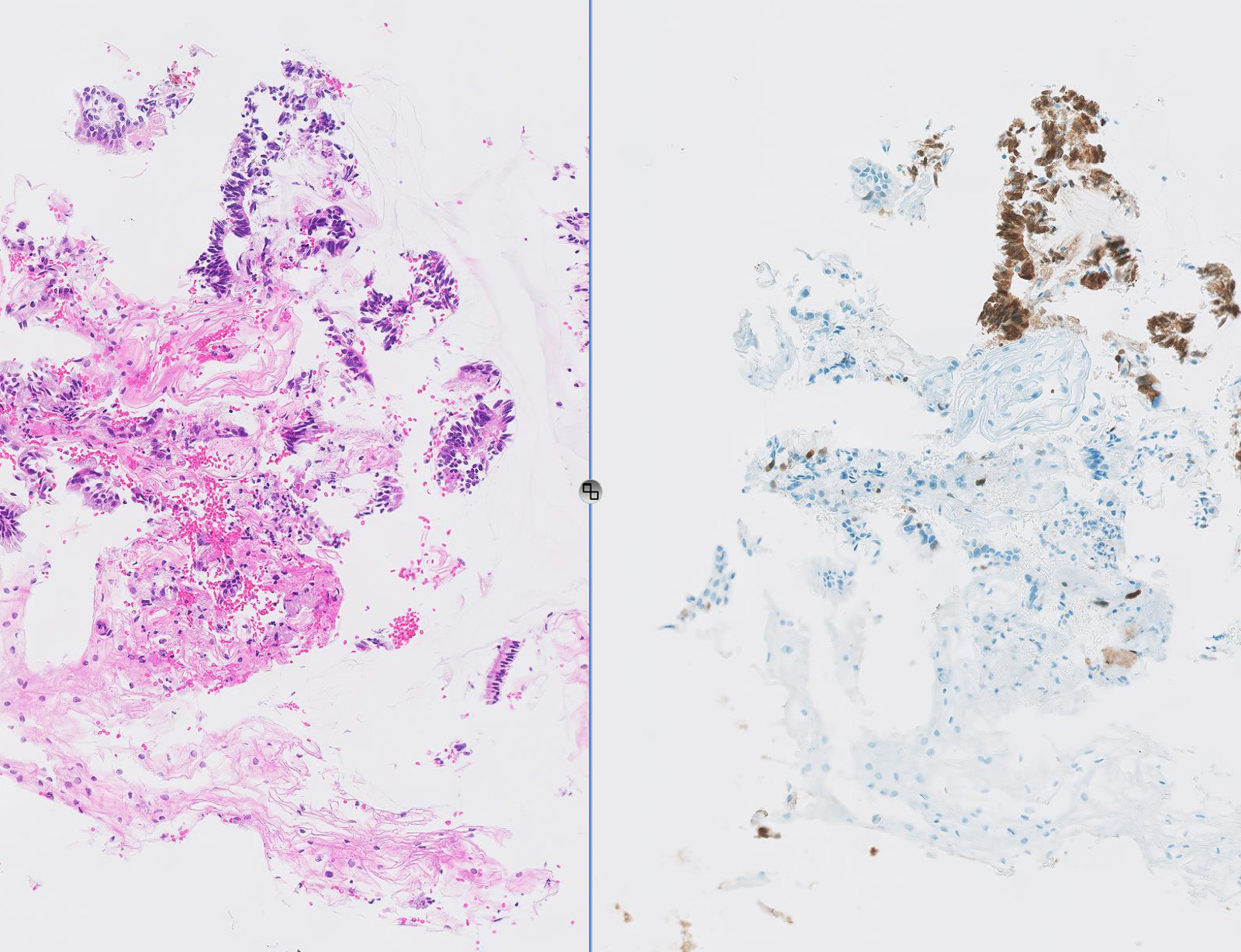
Microscopic (histologic) images
Contributed by Gulisa Turashvili, M.D., Ph.D., Seema Khutti, M.D., Jijgee Munkhdelger, M.D., Ph.D. and Andrey Bychkov, M.D., Ph.D.
Virtual slides
Cytology description
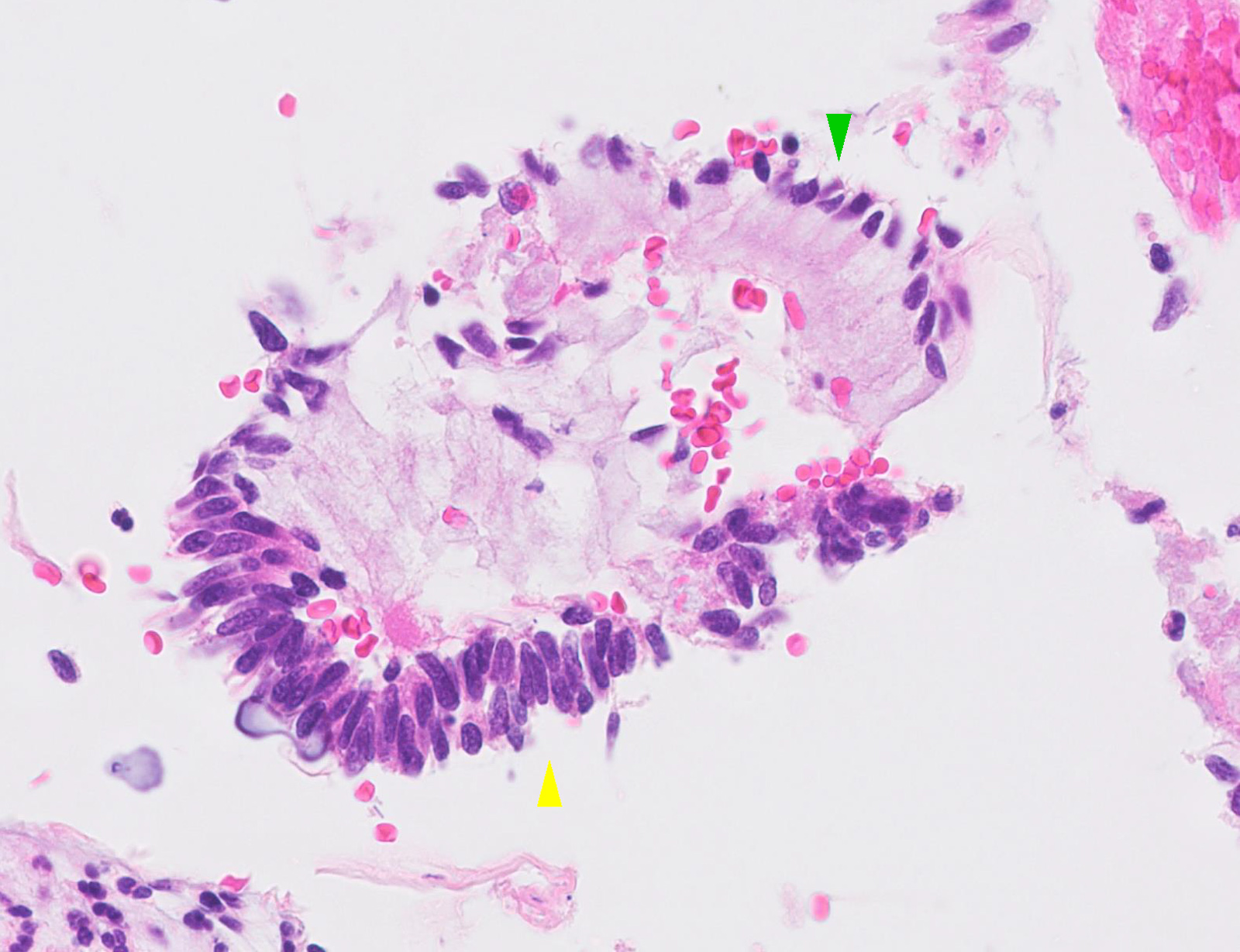
- General features
- Variable cellularity
- Background shows intact red blood cells
- Crowded sheets, strips and torn gland forms of crowded, overlapping nuclei with polarization perpendicular to circumferential or luminal axis
- Peripheral feathering of atypical cells may be seen due to polarization and wisps of cytoplasm
- Rosette-like structures may be seen
- Nuclei may bulge out from center of cytoplasm, imparting a snake egg appearance
- Nuclei
- Oval to elongated hyperchromatic nuclei with increased nuclear cytoplasmic ratio, mild pleomorphism and evenly dispersed chromatin
- Mitotic and apoptotic figures are difficult to appreciate
- Feathering and prominent nucleoli may be absent in SMILE (Acta Cytol 2016;60:225)
- Cytoplasm
- Variable cytoplasmic characteristics depending on stain and type of adenocarcinoma in situ
- Usually eosinophilic or cyanophilic
- Goblet cells may be present
- Liquid based cytology
- Clean background
- Sheets of atypical glandular cells are often smaller
- Peripheral feathering may be difficult to appreciate as it appears as peripheral knuckles
- Rosette-like structures may be difficult to appreciate
- Single cells and more strips with fish tail or bird tail appearance on SurePath preparations
- Subtle strips and smaller cells lacking cytoplasmic mucin may mimic endometrial cells
- Gastric type adenocarcinoma
- Clean background
- Single or crowded clusters of tumor cells with pale, foamy or vacuolated cytoplasm and well defined cytoplasmic borders (Int J Gynecol Pathol 2019;38:263)
Cytology images
Images hosted on other servers:
Atypical glandular cells
Positive stains
- p16: strong and diffuse block-like positivity in HPV related adenocarcinoma in situ types, patchy or negative staining in gastric type (rarely overexpressed)
- ProExTMC (aberrant S-phase induction): strong and diffuse positivity
- CEA: diffuse cytoplasmic positivity (especially conventional type)
- Ki67: high (usually > 75% in conventional type, variable in other types)
- P63: may be positive in basal portion of SMILE
- CDX2: positive in intestinal type
- HIK1083: positive in gastric type adenocarcinoma in situ (Virchows Arch 2016;469:351, Methods Mol Biol 2015;1249:213)
- Mucicarmine: positive (pink) intracytoplasmic staining in SMILE
Negative stains
Molecular / cytogenetics description
- Human papillomavirus detection (Int J Gynecol Pathol 2010;29:378)
- Positive by polymerase chain reaction or in situ hybridization in most adenocarcinoma in situ types
- Gastric and intestinal types are typically negative
Sample pathology report
- Cervix, cone biopsy:
- Endocervical adenocarcinoma in situ, HPV associated (usual type)
- All resection margins free of adenocarcinoma
Differential diagnosis
- Histology
- Cervical Arias-Stella reaction:
- History or pregnancy or hormonal therapy; usually focal, enlarged cells with abundant eosinophilic to vacuolated cytoplasm, preserved nuclear cytoplasmic ratio, enlarged hyperchromatic and irregular nuclei with variable chromatin and intranuclear cytoplasmic inclusions, hobnail cells, no mitotic figures or apoptotic bodies, ER / PR positive, Ki67 low, p16 negative
- Cervical endometriosis:
- Evidence of recent or remote hemorrhage, endometrial stroma, endometrioid glands with cuboidal to columnar eosinophilic cytoplasm and bland nuclei, variable mitoses in both glandular and stromal components
- Benign reactive endocervical glands:
- Lack abrupt transition to normal endocervical cells, often associated with inflammatory infiltrate, typically dispersed chromatin with prominent nucleoli, p16 negative or focally positive
- Mesonephric remnants:
- Microglandular hyperplasia:
- Smaller and more uniform glands with frequent subnuclear and supranuclear vacuoles, bland nuclei, no mitotic activity, associated with acute inflammation, no apoptotic bodies, variable mitoses
- Tubal metaplasia:
- Radiation and cautery effects:
- Enlarged nuclei with smudged chromatin, preserved nuclear cytoplasmic ratio, vacuolated cytoplasm, no pseudostratification, no apoptotic bodies or mitoses
-
Invasive adenocarcinoma:
- Infiltrating glands with irregular, haphazard or confluent growth with desmoplastic stromal reaction and extension beyond benign endocervical glands
- High grade squamous intraepithelial lesion (HSIL):
- Should be differentiated from SMILE, polygonal cells with intercellular bridges lacking intracytoplasmic mucin
- Cervical Arias-Stella reaction:
- Cytology
- Cervical Arias-Stella reaction:
- Endometriosis, directly sampled lower uterine segment or endometrial polyps:
- Strips, variably shaped glands or spheres that may be accompanied by plump stromal cells
- Background blood may mimic tumor diathesis
- p16 negative to focally positive
- Endometrium is also commonly found in post-trachelectomy samples (Cancer 2008;114:1, Diagn Cytopathol 2009;37:641)
- Benign reactive endocervical glands:
- Flat sheets, school of fish appearance, preserved nuclear cytoplasmic ratio, evenly dispersed chromatin with prominent nucleoli, p16 negative to focally positive
- Tubal metaplasia:
- Rare groups or strips, powdery or watery chromatin, no other patterns of adenocarcinoma in situ, no mitotic and apoptotic bodies, terminal bars and cilia are key diagnostic features, p16 focally or patchy positive
- Radiation atypia:
- Cells with bizarre sizes and shapes with vacuoles but preserved nuclear cytoplasmic ratio, p16 negative to focally positive
-
Invasive adenocarcinoma:
- Tumor diathesis in background which is variable depending on cytology preparation, more rounded vesicular nuclei with conspicuous nucleoli, nuclear pleomorphism and polarization may be lost
- High grade squamous intraepithelial lesion (HSIL):
- Peripheral flattening or rounding of hyperchromatic crowded groups of cells, larger cells compared to adenocarcinoma in situ arranged parallel to circumferential axis, lack of peripheral feathering
Additional references
- Histology: Arch Pathol Lab Med 2014;138:453, Surg Pathol Clin 2019;12:281, Pathology 2018;50:122, Am J Surg Pathol 2017;41:1023, Cancer Med 2017;6:416, Am J Surg Pathol 2013;37:625, Adv Anat Pathol 2013;20:227
- Cytology: Acta Cytol 2012;56:55, Diagn Cytopathol 2016;44:20, Acta Cytol 1996;40:1127, Acta Cytol 1998;42:16, Acta Cytol 2004;48:372, Diagn Cytopathol 2007;35:584, Cytopathology 2008;19:34, Diagn Cytopathol 2010 A;38:551, Arch Pathol Lab Med 2017;141:666
- Nayar: The Bethesda System for Reporting Cervical Cytology - Definitions, Criteria, and Explanatory Notes, 3rd Edition, 2015
Board review style question #1
Board review style answer #1
B. Block-like p16, high Ki67 index, focal ER. HPV related usual type adenocarcinoma in situ is characterized by diffuse, block-like staining for p16, high Ki67 index and negative or focal ER expression.
Comment Here
Reference: Adenocarcinoma in situ (AIS)
Comment Here
Reference: Adenocarcinoma in situ (AIS)
Board review style question #2
Board review style answer #2
C. Focal p16, variable Ki67, focal ER. Most cases of gastric type adenocarcinoma in situ are characterized by negative or focal staining for p16, variable Ki67 index and focal ER staining
.
Comment Here
Reference: Adenocarcinoma in situ (AIS)
Comment Here
Reference: Adenocarcinoma in situ (AIS)
Board review style question #3
- Which of the following cytologic features would be expected in a posttrachelectomy Pap smear from a 35 year old woman treated with trachelectomy for invasive endocervical adenocarcinoma?
- Atypical endocervical cells, favor neoplastic
- Atypical endometrial cells
- Tubular endometrial glands in a bloody background
- Atypical glandular cells, not otherwise specified
Board review style answer #3
C. Tubular endometrial glands in a bloody background. 33% of patients treated with trachelectomy for cervical cancer show endometrium on follow up Pap smears.
Comment Here
Reference: Adenocarcinoma in situ (AIS)
Comment Here
Reference: Adenocarcinoma in situ (AIS)