Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Turashvili G. HPV associated cervical squamous cell carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cervixSCC.html. Accessed April 23rd, 2024.
Definition / general
- Invasive epithelial tumor composed of neoplastic cells with varying degrees of squamous differentiation
Essential features
- Most common type of cervical carcinoma
- Most cervical squamous cell carcinomas are associated with high risk human papillomavirus (HPV) and arise from a precursor lesion, high grade squamous intraepithelial lesion (HSIL)
- Predominantly associated with HPV 16 and HPV 18 (HPV 16 > HPV 18)
- More common in low resource countries and in women without adequate cytologic screening
- Variable morphology with several histologic variants described
ICD coding
Epidemiology
- Fourth most common type of cancer (15.1 per 100,000) and cause of cancer mortality (8.2 per 100,000) among women worldwide in 2018 (CA Cancer J Clin 2018;68:394)
- Most common type of cervical carcinoma (> 90% of cases)
- Most patients are 40 - 54 years old (Cancer Manag Res 2018;10:3177)
- Significant disparities in incidence and mortality between low resource countries versus high resource countries (CA Cancer J Clin 2018;68:394)
- Incidence varies from 100 per 100,000 in unscreened women to 1 - 5 per 100,000 in highly screened women
- ~75% decrease over the past 50 years in countries with cervical cancer screening programs (Cancer 2004;100:1035)
- ~76% of recent cases occur in countries without screening programs
- In high resource countries, more common in women who failed to receive screening or follow up (Cancer Epidemiol Biomarkers Prev 2012;21:1402)
Sites
- Most cases arise at the squamous columnar junction of the cervix
Pathophysiology
- High prevalence of HPV infection among adolescents and young women
- Most infections spontaneously regress (N Engl J Med 1998;338:423)
- Persistent infection with high risk HPV subtypes is necessary but not sufficient for developing HSIL and squamous cell carcinoma
- Most tumors are due to progression of a precursor lesion, HSIL
- Progression of HSIL is variable among women and may take decades
- Risk factors (see Etiology below) significantly increase risk of HPV persistence
- High risk HPV acts via E6 and E7 oncogenes (Biotech Histochem 2015;90:573, Ecancermedicalscience 2015;9:526)
- E6 binds to tumor suppressor p53, causing its proteolytic degradation and inactivation, p53 mediated DNA damage and apoptosis
- E7 binds to retinoblastoma gene (Rb), displacing transcription factors normally bound by Rb and the inactivating Rb mediated cell cycle regulation pathway
- Rb inactivation leads to overexpression of p16, a tumor suppressor gene involved in cell cycle regulation by inhibition of cyclin dependent kinases
- p16 immunohistochemistry is used as a surrogate marker for high risk HPV infection
- Usually spreads through cervical lymphatics to regional lymph nodes or via direct extension to vagina, uterus, parametrium, lower urinary tract, uterosacral ligaments; distant metastases may involve aortic and mediastinal lymph nodes, lungs, bones and adnexa
- HPV vaccination of women 16 - 23 years of age offers durable protection for at least 12 years; the Centers for Disease Control and Prevention (CDC) recommends HPV vaccination in 2 or 3 doses depending on age (EClinicalMedicine 2020;23:100401, CDC: HPV Vaccine Schedule and Dosing [Accessed 20 October 2023])
- 2 doses for children and adolescents of any gender ages 9 - 14 years
- 3 doses for adolescents and adults of any gender ages 15 - 26 years
Etiology
- Most cases are associated with persistent infection by high risk HPV subtypes such as 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68 and others (Lancet Oncol 2010;11:1048, Lancet 2002;359:1093)
- HPV 16 is the major causal agent for squamous cell carcinoma; this is in contrast to HPV 18, which is typically associated with endocervical adenocarcinoma
- ~5 - 7% of cases are HPV negative (BJOG 2015;122:119, Mod Pathol 2019;32:1189)
- Previous or concurrent history of HSIL (J Natl Cancer Inst 2011;103:368)
- Additional risk factors
- Younger age at first intercourse and higher lifetime number of sexual partners (Br J Cancer 2003;89:2078, Br J Cancer 2000;83:1565)
- Single contact with infected partner may result in infection and risk plateaus with many contacts (Sex Transm Dis 2000;27:438)
- Immunodeficiency, including human immunodeficiency virus (HIV) infection, transplantation and medications (J Natl Cancer Inst 2000;92:1500)
- Cigarette smoking for > 20 years (Br J Cancer 2003;89:2078, Br J Cancer 2000;83:1565, Cancer Causes Control 2002;13:839)
- Multiparity and early age at first birth (Br J Cancer 2003;89:2078, Lancet 2002;359:1093)
- Long term oral contraceptive use (Br J Cancer 2003;89:2078, Lancet 2003;361:1159)
- Chronic inflammation or concurrent sexually transmitted diseases, such as chlamydia
- Positive family history
- No circumcision in male partner (N Engl J Med 2002;346:1105)
Clinical features
- Abnormal cervical cytology in asymptomatic patients (Gynecol Oncol 1991;42:48)
- Cervical mass
- Vaginal bleeding or discharge
- Pain, urinary symptoms (ureteral obstruction leading to anuria or uremia, hematuria, frequency, vesicovaginal fistula), gastrointestinal symptoms (tenesmus, rectovaginal fistula), lymphedema in the lower extremities in advanced tumors
Diagnosis
- Histologic examination of biopsy or excisional material
Radiology description
- Only tumors that are at least stage IB can be identified radiologically (Radiology 2013;269:149)
- Magnetic resonance imaging (MRI) is the imaging modality of choice to assess the extent of primary tumor (Eur Radiol 2011;21:1102)
- Mass lesion with a high signal relative to the low signal of the cervical stroma
- Ultrasound examination may also be used
- Hypoechoic, heterogeneous mass, sometimes with increased vascularity on color Doppler
- Adenopathy and metastatic disease are best assessed with computed tomography (CT)
- Positron emission tomography (PET) may also be used to rule out metastases (J Natl Compr Canc Netw 2006;4:463)
Prognostic factors
- Tumor stage, patient age, depth of invasion, disease volume, lymphovascular invasion (Eur J Cancer 1998;34:2218, Semin Surg Oncol 1994;10:31, Cancer 1991;67:2776, J Clin Oncol 2007;25:2804)
- Overall 5 year disease free survival by tumor stage
- Stage IA: 95%
- Stages IB1 and IIA: 70 - 85%
- Stages IB2 and IIB: 50 - 70%
- Stage III: 30 - 50%
- Stage IV: 5 - 15%
- Better prognosis for lymphoepithelial and verrucous variants
- Worse prognosis with lower CD4+ cell counts in HIV seropositive patients (J Clin Oncol 2016;34:3749)
Case reports
- 29 year old woman with cervical verrucous carcinoma (J Adolesc Young Adult Oncol 2017;6:499)
- 37 year old woman with cervical squamous cell carcinoma combined with adenoid basal carcinoma (Diagn Cytopathol 2019;47:1051)
- 40 year old woman with cervical squamous cell carcinoma metastatic to the breast (Breast Dis 2022;41:407)
- 52 year old woman with cervical squamous cell carcinoma metastatic to the cerebellum presenting with pulmonary aspiration (BMJ Case Rep 2019;12:e229063)
- 53 year old woman with cervical squamous cell carcinoma metastatic to the pancreas (J Gastrointest Cancer 2023;54:300)
- 60 year old woman with papillary squamotransitional cell carcinoma (Clin Case Rep 2023;11:e7508)
- 64 year old woman with cervical squamous cell carcinoma metastatic to the orbital cavity (J Med Invest 2019;66:355)
Treatment
- Treatment follows the International Federation of Obstetrics and Gynecology (FIGO) and the National Comprehensive Cancer Network (NCCN) guidelines for cervical cancer according to stage (Int J Gynaecol Obstet 2019;147:279, NCCN: NCCN Guidelines [Accessed 20 October 2023])
- Conization or loop electrosurgical excision procedure (LEEP) for low stage (IA) tumors (Int J Gynecol Cancer 2014;24:113)
- Radical trachelectomy or radical hysterectomy with sentinel lymph node mapping or pelvic lymph node dissection with or without radiotherapy for higher stage tumors (J Natl Compr Canc Netw 2019;17:64)
- Radiotherapy and platinum based chemotherapy or pelvic exenteration for advanced tumors (J Natl Compr Canc Netw 2019;17:64)
Gross description
- Variable appearance and size (Gynecol Oncol 2023;176:147)
- Red, friable, indurated or ulcerated lesion or elevated granular area in early stage tumors
- Exophytic, papillary, polypoid, nodular or ulcerated mass
- Deeply invasive mass with infiltration into surrounding structures
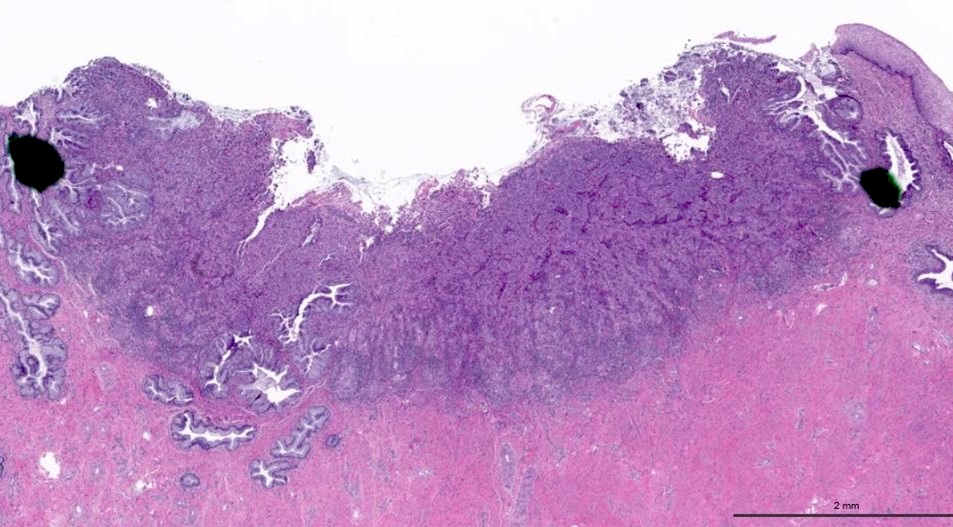
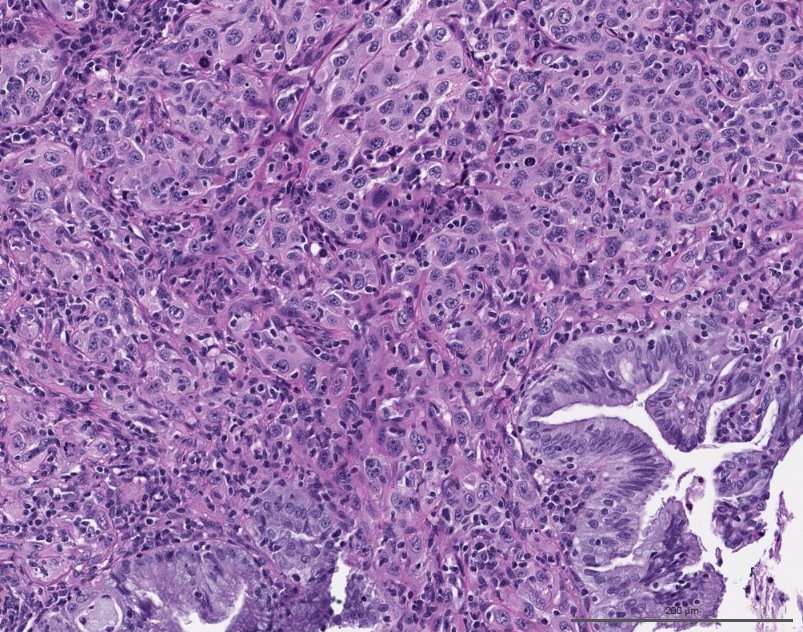
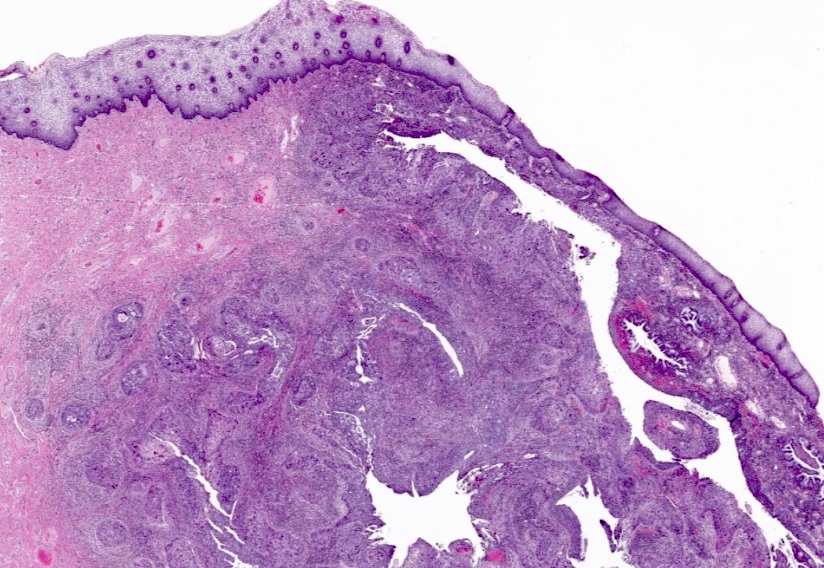
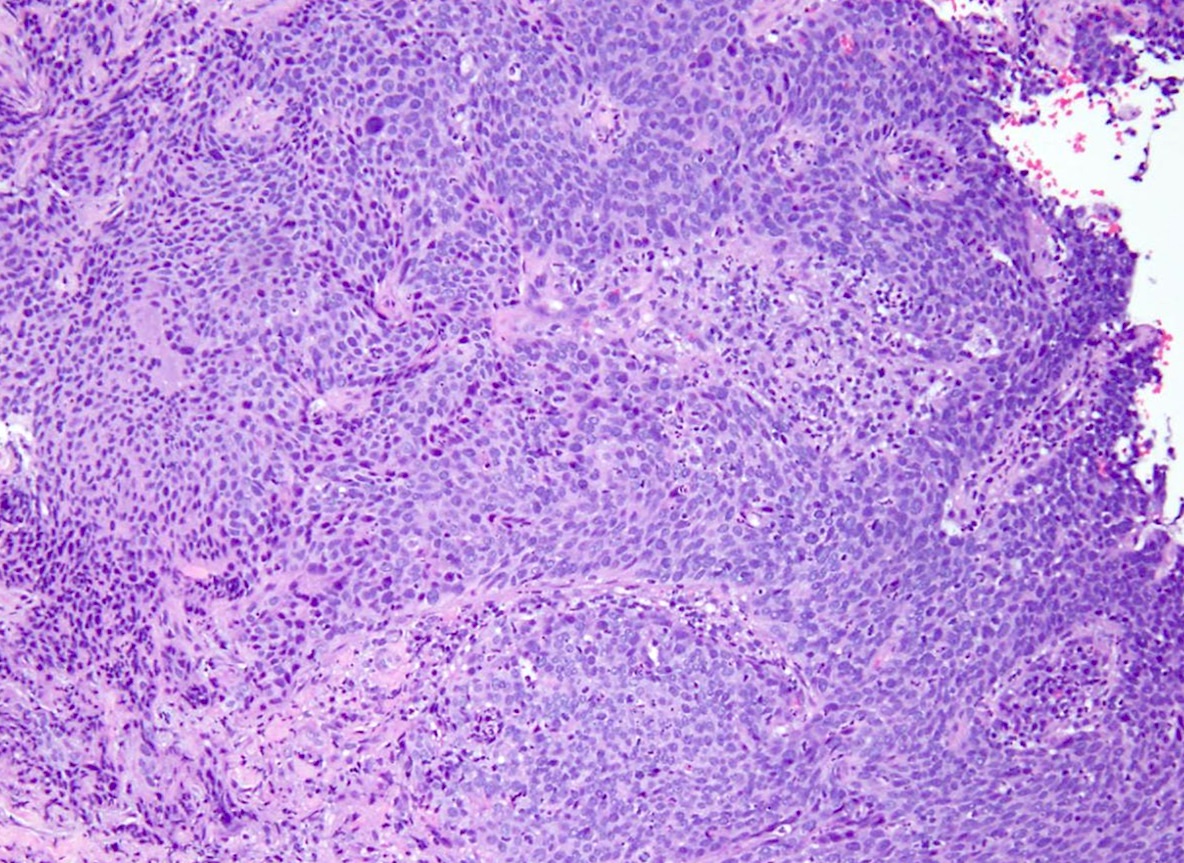
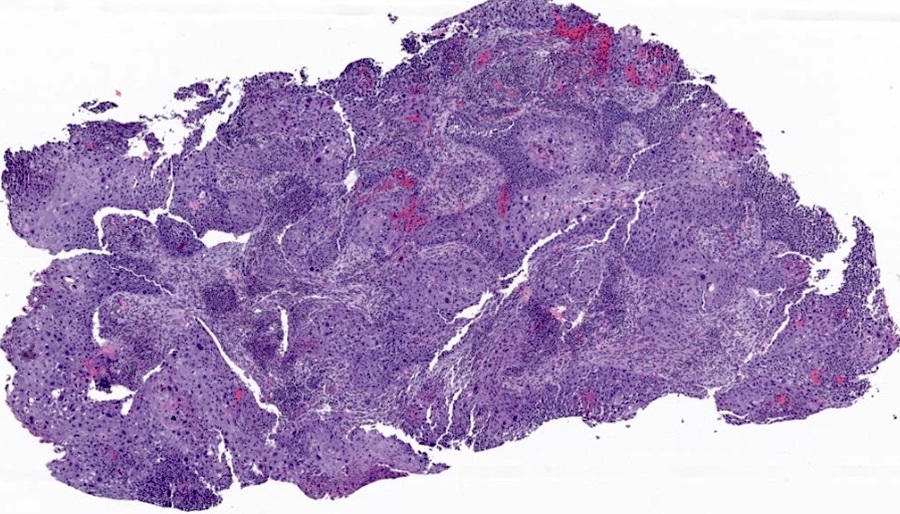
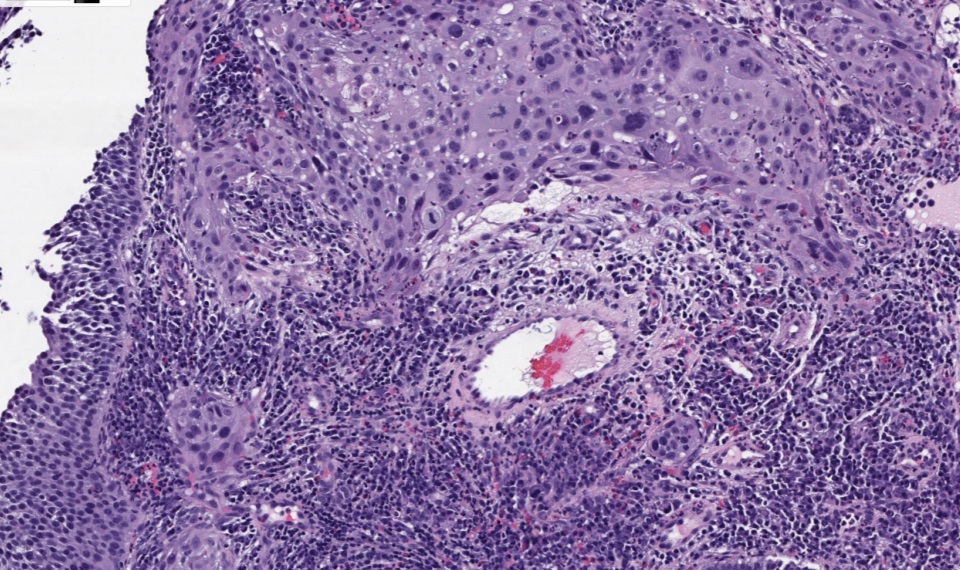
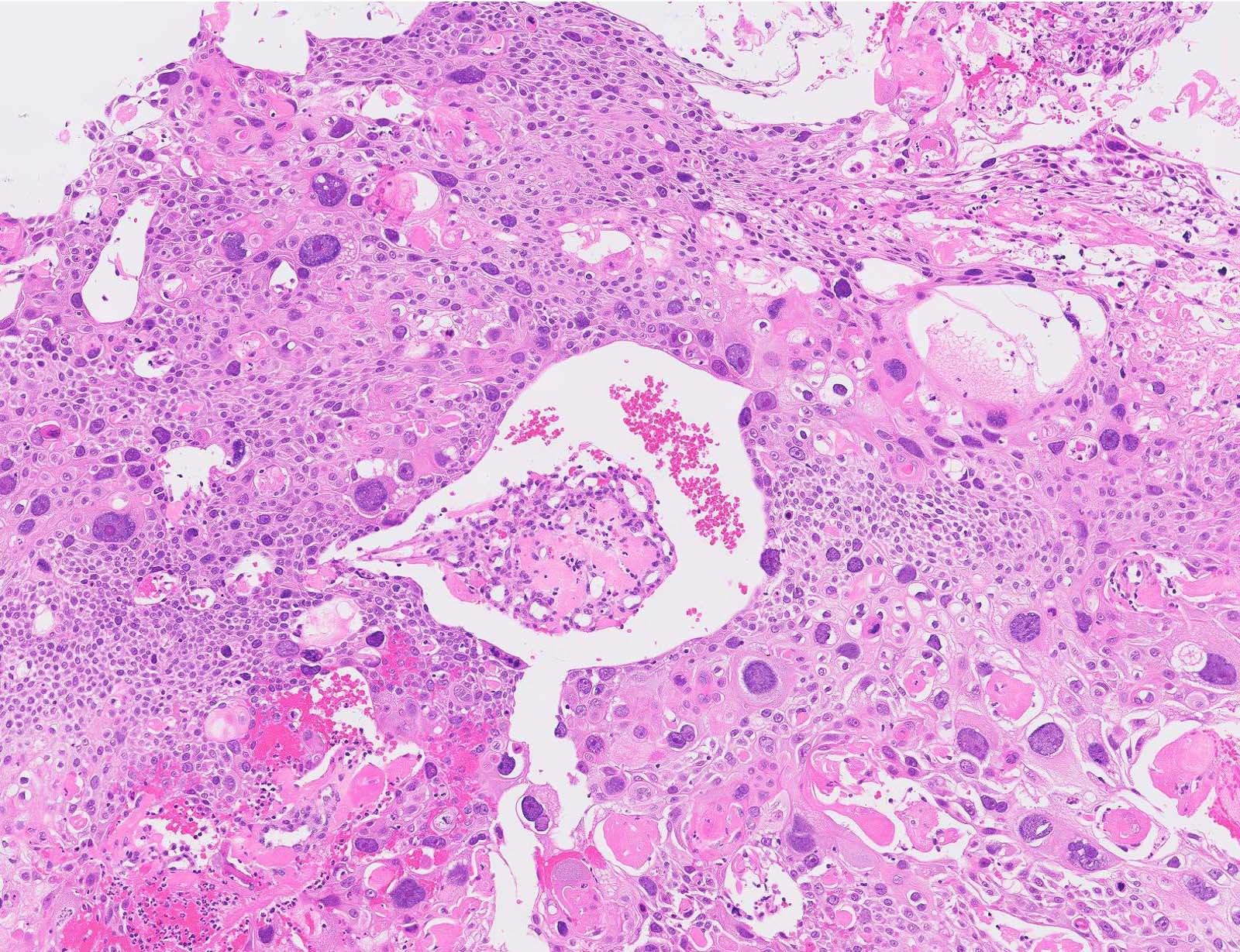
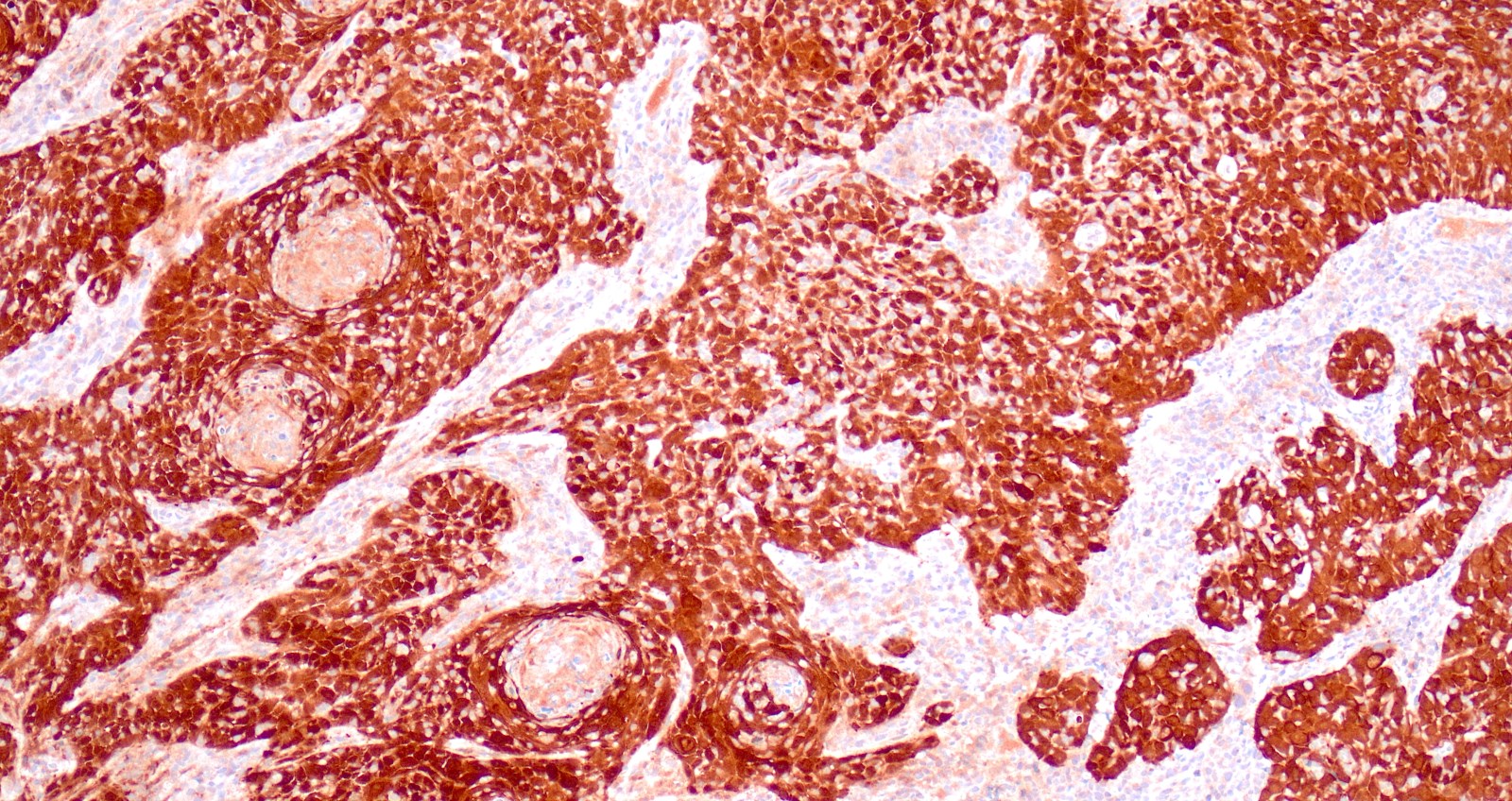
Microscopic (histologic) description
- Tumor cells infiltrating as irregular anastomosing nests or single cells within desmoplastic or inflammatory stroma
- Stromal loosening, desmoplasia or increased epithelial cell cytoplasmic eosinophilia in tumors with superficial stromal invasion
- Lymphovascular invasion may be present
- Grading is based on nuclear pleomorphism or differentiation and does not correlate with prognosis (J Pathol Clin Res 2018;4:81)
- Morphologic variants
- Keratinizing
- Keratin pearls, abundant keratohyaline granules and intercellular bridges
- Large, hyperchromatic nuclei with coarse chromatin and inconspicuous nucleoli
- Nonkeratinizing
- Polygonal cells forming sheets or nests
- Intercellular bridges but not keratin pearls
- Large nuclei with unevenly distributed, coarsely granular chromatin and one or multiple nucleoli
- Numerous mitoses
- Papillary (Int J Gynecol Pathol 2000;19:231)
- Thin or broad papillae with fibrovascular cores lined by multilayered epithelium with squamous differentiation resembling HSIL
- Stromal invasion may not be seen in superficial biopsies
- Basaloid (Adv Anat Pathol 2002;9:290, Am J Surg Pathol 1993;17:133)
- Well defined nests of immature basaloid cells (resembling the cells of HSIL) with peripheral palisading of pleomorphic, hyperchromatic nuclei, brisk mitoses and scant cytoplasm
- Geographical or comedo-like necrosis
- Focal keratinization but no keratin pearls
- Resembles basaloid squamous cell carcinomas at other sites usually exhibiting an aggressive behavior
- Warty (Am J Surg Pathol 1993;17:133)
- Warty surface and low power architecture resembling a condyloma or bowenoid lesion of the vulva
- Keratinization and koilocytic atypia may be seen
- Verrucous
- Very rare and poorly understood form of squamous cell carcinoma in the cervix
- Highly differentiated
- Exophytic growth with undulating, warty surface and hyper or parakeratotic and frond-like acanthotic squamous epithelium
- Broad based pushing invasion with bulbous epithelial pegs
- Abundant cytoplasm, minimal cytologic atypia and rare mitoses
- Absence of koilocytes
- Squamotransitional (Am J Surg Pathol 1997;21:915)
- Resembles squamotransitional carcinoma of the urinary bladder
- Papillae with fibrovascular cores lined by multilayered epithelium with transitional differentiation resembling HSIL
- May occur in a pure form or in association with squamous elements
- Not related to transitional cell metaplasia
- Lymphoepithelial-like carcinoma (Arch Pathol Lab Med 2002;126:1501, Arch Gynecol Obstet 2009;280:725)
- Resembles nasopharyngeal lymphoepithelial-like carcinoma
- Poorly defined nests of undifferentiated, discohesive squamous cells with uniform, vesicular nuclei, conspicuous nucleoli and moderate amounts of cytoplasm in a background of abundant lymphocytes
- Indistinct cell borders impart a syncytial-like appearance
- No evidence of keratinization and lack of intercellular bridges
- Associated with HPV, not Epstein-Barr virus (EBV)
- Spindled / sarcomatoid (J Cancer Res Ther 2008;4:39)
- Spindled cells with hyperchromatic nuclei, conspicuous nucleoli and brisk mitoses
- May be admixed with more conventional epithelioid areas
- Occasional osteoclast-like giant cells
- Necrosis may be present
- Keratinizing
- Rare findings are focal mucinous differentiation, pseudoglandular pattern due to acantholysis, amyloid, signet ring cells, melanin granules, HSIL-like growth pattern (Arch Pathol Lab Med 1993;117:199)
- There are no reliable morphologic criteria to distinguish between HPV associated and HPV independent subtypes (Mod Pathol 2019;32:1189)
- Depth of stromal invasion
- Measured from the focus of HSIL, from which it originated, to the deepest point of invasion
- If the invasive focus is not in continuity with the focus of dysplastic epithelium, measure the depth of invasion from the base of the nearest dysplastic crypt or surface epithelium to the deepest focus of invasion
- If there is no obvious epithelial origin, measure the depth of invasion from the base of the nearest surface epithelium (regardless of whether it is dysplastic or not) to the deepest focus of invasion
- If the tumor is exophytic and lacks conventional stromal invasion, measure the tumor thickness (from the surface to the deepest point of tumor) instead and clearly state it in the pathology report
- Horizontal extent is no longer used for the AJCC 9th version or FIGO 2018 staging
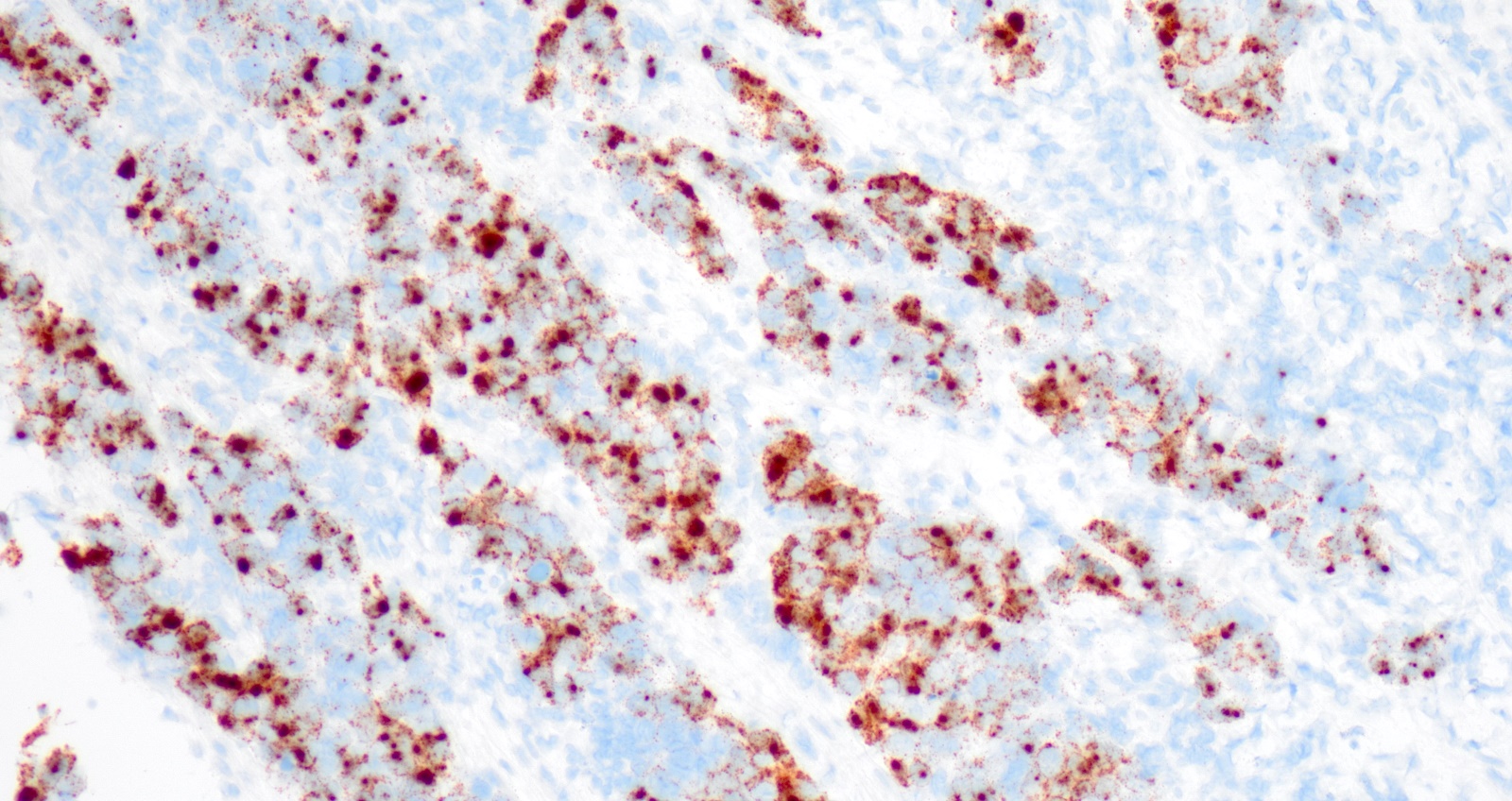
Microscopic (histologic) images
Contributed by Gulisa Turashvili, M.D., Ph.D., Jijgee Munkhdelger, M.D., Ph.D. and Andrey Bychkov, M.D., Ph.D.
Cytology description
- Adequacy criteria: adequate if abnormal cells are seen, irrespective of cellularity
- Cellular specimens, usually with background tumor diathesis (fresh or hemolyzed blood and necrotic cellular debris)
- Tumor diathesis may not be seen in tumors with < 5 mm depth of invasion or exophytic tumors (Acta Cytol 1997;41:781)
- Necrotic material at the periphery of cell groups (clinging diathesis) rather than in the background in liquid based preparations (Diagn Cytopathol 2002;26:1)
- Nonkeratinizing variants
- Crowded groups and syncytial fragments
- Large to medium sized nonkeratinized cells with high N:C ratio
- Round nuclei with irregular contours, coarse, irregularly distributed chromatin and macronucleoli
- Naked nuclei
- Scant, dense basophilic cytoplasm without keratinization
- Rare keratinized single cells may be seen
- Keratinizing squamous cell carcinoma
- Dispersed cells and less prominent background diathesis
- Markedly hyperchromatic nuclei with granular irregular chromatin and rare nucleoli
- Irregularly shaped keratinized cells with orangeophilic cytoplasm, often with squamous pearls
- Tadpole shaped cells with Herxheimer spirals and keratohyaline granules in cytoplasm
- Compared to adenocarcinoma, cells and nuclei are more irregular with denser cytoplasm, greater chromatin granularity and nuclear hyperchromasia
Cytology images
Positive stains
- Pancytokeratin
- p63
- p40
- CK5/6
- EMA
- p16: diffuse, block-like staining (except verrucous variant)
- PDL1: positive in ~80% of cases; reported as combined positive score (CPS) = (number of positive tumor cells, lymphocytes and macrophages / total number of tumor cells) x 100, cutoff point for positivity is ≥ 1% (Mod Pathol 2020;33:1182, Diagn Pathol 2017;12:45, Arch Pathol Lab Med 2019;143:330)
- CEA
- CK7 (in 66 - 87% of cases) (Mod Pathol 2000;13:962, Diagn Pathol 2017;12:18)
- RNA in situ hybridization for high risk human papillomavirus
Negative stains
- GATA3 (positive in ~33% of cases, usually weak and focal) (Am J Surg Pathol 2014;38:13, Am J Surg Pathol 2016;40:27)
- PAX8 (positive in ~25% of cases) (Am J Clin Pathol 2013;140:872)
- Inhibin, MEL-CAM, HPL (Am J Surg Pathol 2009;33:633)
- Napsin A
- HNF-1B (Diagn Pathol 2015;10:8)
- p53: rarely aberrant p53 expression
- CK20 (Appl Immunohistochem Mol Morphol 2011;19:10)
Electron microscopy description
- Well developed intracytoplasmic tonofilaments, desmosome tonofilament complexes and intercellular microvilli in well differentiated tumors, lost with decreasing differentiation
Molecular / cytogenetics description
- Mutations in PIK3CA are most frequent (37%); low frequency of KRAS mutations (Cancer 2013;119:3776)
- TP53 mutations in 16% of cases (J Transl Med 2014;12:255)
- Loss of heterozygosity (LOH) in multiple loci (1q, 3p, 3q, 6p, 6q, 11q, 17p, 18q) (Int J Cancer 2001;96:286, Genes Chromosomes Cancer 1999;26:346)
Sample pathology report
- Uterus with cervix, fallopian tubes and ovaries, radical hysterectomy and bilateral salpingo-oophorectomy:
- Squamous cell carcinoma, human papillomavirus associated (see synoptic report)
- Cervix
- Tumor size: 21 mm
- Depth of stromal invasion: 4 mm
- Lymphovascular space invasion: positive
- Margins: negative for carcinoma
- Endometrium: inactive
- Myometrium: leiomyomata
- Uterine serosa: negative for carcinoma
- Ovaries: negative for carcinoma
- Fallopian tubes: fimbriated, negative for carcinoma
Differential diagnosis
- HPV independent cervical squamous cell carcinoma:
- Morphologic features are similar to HPV associated squamous cell carcinoma
- Negative for p16 and RNA in situ hybridization for high risk human papillomavirus
- Clear cell carcinoma (versus squamous cell carcinoma with cytoplasmic clearing):
- Adenoid basal carcinoma:
- Deeply infiltrative nests of basaloid squamous cells with nuclear palisading and focal lumina, no desmoplastic stromal reaction
- Adenoid cystic carcinoma:
- Cribriform, solid and tubular growth patterns, luminal epithelial cells and basal cells, basement membrane-like material
- p63 positive in myoepithelial cells, positive for MYB::NFIB fusion
- Small cell neuroendocrine carcinoma (versus basaloid squamous cell carcinoma):
- Nests, cords, trabeculae and rosettes of small cells with scant cytoplasm, hyperchromatic nuclei with molding and crush artifact, brisk mitoses, apoptotic debris, geographic necrosis
- Positive for neuroendocrine markers
- Carcinosarcoma (versus sarcomatoid squamous cell carcinoma):
- Epithelioid trophoblastic tumor:
- Immature squamous metaplasia:
- Uniform cells lacking significant nuclear atypia
- Negative for p16
- Placental site nodule:
- HSIL involving endocervical glands:
- Well defined nests with smooth borders, preserved polarity of basal epithelial cells, no abrupt maturation at interface, no desmoplastic stromal reaction
Additional references
- Int J Gynaecol Obstet 2018;143:22, Mol Cancer 2005;4:38, J Clin Oncol 2019;37:1449, Adv Anat Pathol 2017;24:304, Cancer 2017;123:2404, Cancer 2017;123:2219, Eur J Surg Oncol 2015;41:1, Acta Cytol 2003;47:141, Gynecol Oncol 2005;97:716, Arch Gynecol Obstet 2008;277:175, Surg Pathol Clin 2022;15:369, WHO Classification of Tumours Editorial Board: Female Genital Tumours, 5th Edition, 2020, Int J Gynecol Pathol 2022;41:S64
Board review style question #1
Which of the following immunoprofiles would be expected in the cervical tumor shown above?
- Negative p63, p40, CK5/6, p16; positive CK18, napsin A, inhibin, HPL
- Positive CK5/6, p16, inhibin; negative p63, p40, CK18, napsin A, HPL
- Positive CK18, p16, p63, inhibin, HPL; negative napsin A, p40, CK5/6
- Positive p63, p40, CK5/6, p16; negative CK18, napsin A, inhibin, HPL
Board review style answer #1
D. Positive p63, p40, CK5/6, p16; negative CK18, napsin A, inhibin, HPL. This is an HPV associated cervical squamous cell carcinoma. The tumor is positive for p63, p40, CK5/6 and p16 and negative for CK18, napsin A, inhibin and HPL. Answer A is incorrect because all negative markers in this option should be positive and all positive ones should be negative in the immunoprofile of the tumor shown. Answer B is incorrect because p63 and p40 should be positive. Answer C is incorrect because CK18 and HPL should be positive and p40 and CK5/6 should be negative.
Comment Here
Reference: Squamous cell carcinoma and variants
Comment Here
Reference: Squamous cell carcinoma and variants
Board review style question #2
What are the most significant risk factors of cervical squamous cell carcinoma?
- HPV 16, history of HSIL, multiple sexual partners, multiparity, smoking, immunodeficiency
- HPV 16, history of HSIL, multiple sexual partners, nulliparity, smoking, immunodeficiency
- HPV 16, history of LSIL, multiple sexual partners, nulliparity, smoking, immunodeficiency
- HPV 18, history of LSIL, single sexual partner, multiparity, smoking, immunodeficiency
Board review style answer #2
A. HPV 16, history of HSIL, multiple sexual partners, multiparity, smoking, immunodeficiency. Risk factors of cervical squamous cell carcinoma include persistent high risk HPV infection, particularly HPV 16, history of HSIL, multiple sexual partners, multiparity, smoking and immunodeficiency. Answer B is incorrect because nulliparity is not a significant risk factor. Answer C is incorrect for the same reason in addition to LSIL not being a significant risk factor. Answer D is incorrect because cervical squamous cell carcinoma is associated with multiple sexual partners and more often HPV 16 rather than HPV 18.
Comment Here
Reference: Squamous cell carcinoma and variants
Comment Here
Reference: Squamous cell carcinoma and variants
Board review style question #3
Which of the following statements is true regarding squamous cell carcinoma of the cervix?
- Most cervical squamous cell carcinomas are associated with human papilloma virus (HPV) 18
- Nearly all cases of cervical squamous cell carcinoma are associated with high risk HPV and arise from a precursor lesion, high grade squamous intraepithelial lesion (HSIL)
- Poorly differentiated squamous cell carcinomas are associated with high risk HPV subtypes, while low risk HPV subtypes are more likely to cause well differentiated tumors
- Squamous cell carcinoma is the second most common type of cervical cancer following endocervical adenocarcinoma
Board review style answer #3
B. Nearly all cases of cervical squamous cell carcinoma are associated with high risk HPV and arise from a precursor lesion, HSIL. Answer A is incorrect because HPV 16 is more prevalent than HPV 18. Answer C is incorrect because HPV subtypes are not associated with tumor grade. Answer D is incorrect because cervical squamous cell carcinoma is the most common cervical cancer.
Comment Here
Reference: Squamous cell carcinoma and variants
Comment Here
Reference: Squamous cell carcinoma and variants