Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Jones J, Maldonado L. Adenosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/vaginaladenosis.html. Accessed April 26th, 2024.
Definition / general
- First described in 1877 by von Preuschen, vaginal adenosis refers to the persistence of Müllerian glandular epithelium in the vagina after birth
Essential features
- Most noted for its association with diethylstilbestrol (DES) use during pregnancy by mothers of affected young women during the mid 1940s and 1950s; DES use was to prevent a threatened abortion (Reprod Toxicol 2011;31:151)
- Present in 35 - 90% after in utero exposure to diethylstilbestrol (100% have adenosis if diethylstilbestrol started before gestational week 8, 6% if started week 15 or later) (Goldblum: Rosai and Ackerman's Surgical Pathology, 11th Edition, 2017)
- Dethylstilbestrol adenosis is similar histologically to non-diethylstilbestrol adenosis
- Most common type is mucinous, with endocervical-like glands present; tuboendometrial glands can also be present (Mutter: Pathology of the Female Reproductive Tract, 3rd Edition, 2014)
- Women are at risk of neoplasia, including clear cell adenocarcinoma as well as squamous dysplasia (Am Fam Physician 2004;69:2395)
ICD coding
Epidemiology
- An estimated 5 to 10 million women in the United States received diethylstilbestrol during pregnancy (IARC Monogr Eval Carcinog Risks Hum 2012;100:1)
- Approximately 20 - 33% of women who were exposed in utero to diethylstilbestrol demonstrate gross structural changes in the cervix or vagina including vaginal adenosis (Obstet Gynecol Annu 1982;11:187, N Engl J Med 1975;292:334)
- Vaginal adenosis has also been reported in 2 - 10% of nonexposed females (Eur J Gynaecol Oncol 2001;22:260)
Sites
- Involves the upper third of the vagina (34% of diethylstilbestrol exposed cases), with the anterior wall more frequently involved than the posterior wall
- Middle third (9% of cases) and lower third (2% of cases) of the vagina may be involved
Pathophysiology
- Diethylstilbestrol causes irregularities in p63 gene expression, which determines whether Müllerian duct epithelium becomes uterine or vaginal cells and leads to vaginal adenosis
- Mouse model of diethylstilbestrol exposure demonstrates vaginal adenosis and structural changes similar to actual changes observed in women (Hum Pathol 1982;13:190)
- Pathophysiology of non-diethylstilbestrol related adenosis has not been determined conclusively; however, it may result from p63 gene expression changes in squamous epithelium or Müllerian remnants upon epithelial damage or from implantation of Müllerian derived columnar cells into vaginal lesions during menstruation
- Glandular proliferation in adenosis is regulated by estrogen (Rev Obstet Gynecol 2011;4:81)
Etiology
- Diethylstilbestrol is a synthetic nonsteroidal estrogen that profoundly affects the development of the vagina, uterus and fallopian tubes
- Today, in the post-diethylstilbestrol era, vaginal adenosis usually occurs in women exposed to other hormones, drugs, trauma, inflammation, vulvovaginal involvement by Stevens-Johnson syndrome or toxic epidermal necrolysis (SJS / TEN), laser, radiation or chemotherapy (5-fluorouracil) (Rev Obstet Gynecol 2011;4:81)
Clinical features
- Usually asymptomatic, although vaginal discharge or postcoital bleeding or dyspareunia have been reported (Mutter: Pathology of the Female Reproductive Tract, 3rd Edition, 2014)
- Vaginal mucosa displays red granular spots or patches and fails to stain with an iodine solution (Mutter: Pathology of the Female Reproductive Tract, 3rd Edition, 2014)
- Mosaicism and punctation are common findings during colposcopy (Obstet Gynecol 1978;52:457)
Diagnosis
- Lesions identified on physical examination
- Lesions can be identified on colposcopic examination as mosaicism and punctation (Obstet Gynecol 1978;52:457)
- Diagnosis confirmed on biopsy specimens with or without cytologic brushing of clinically suspicious lesions on colposcopy
Case reports
- 39 year old woman with long history of vaginal pain and bleeding as well as dyspareunia (BMC Cancer 2019;19:798)
- 40 year old woman with primary vaginal clear cell adenocarcinoma and Herlyn-Werner-Wunderlich syndrome without DES exposure (Int J Clin Exp Pathol 2020;13:2784)
- 47 year old woman with vaginal cystic appearing mucosa and exophytic mass in mid-vagina (Gynecol Oncol Rep 2020;34:100672)
- 11 cases of vaginal glandular lesions exhibiting gastric differentiation (Am J Surg Pathol 2018;42:958)
Treatment
- In symptomatic patients, treatment with CO2 laser, simple excision or unipolar cautery may be considered (Lasers Surg Med 1983;3:23)
- In patients with vulvovaginal involvement by Stevens-Johnson syndrome and toxic epidermal necrolysis, adenosis prevention includes intravaginal steroids and menstrual suppression ((luteinizing hormone releasing hormone [LHRH] agonists, combined oral contraceptives or progesterone only contraceptives) (Rev Obstet Gynecol 2011;4:81)
Clinical images
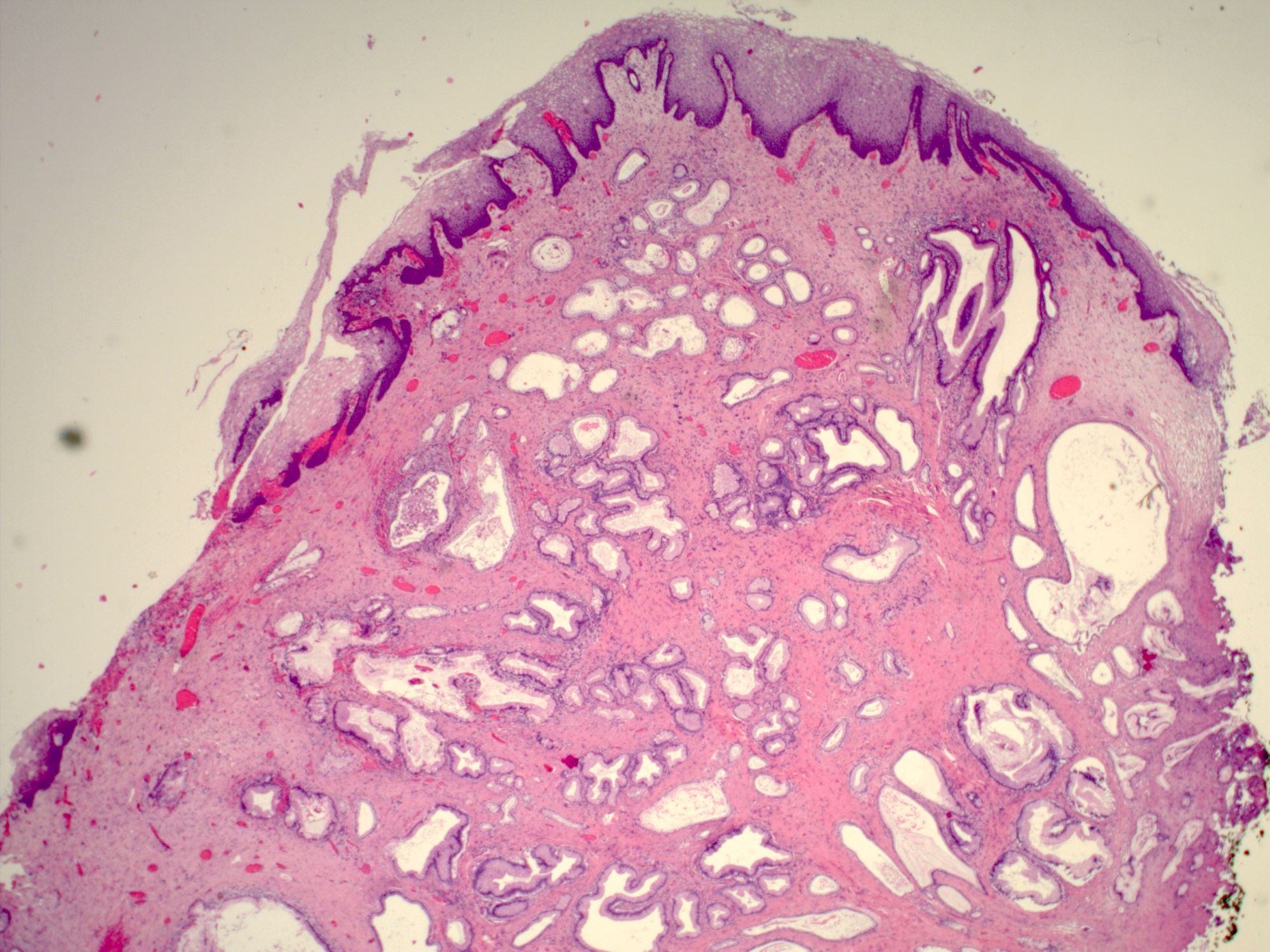
Gross description
- Vaginal mucosa displays cysts or red granular spots or patches
- In the setting of DES exposure, you may also find a flattened, shallow upper vagina with absent vaginal fornices around a hypoplastic cervix
- Menopause can cause involution of vaginal adenosis into the cervical canal as the upper vagina contracts in these patients (Case Rep Obstet Gynecol 2017;2017:9523853)
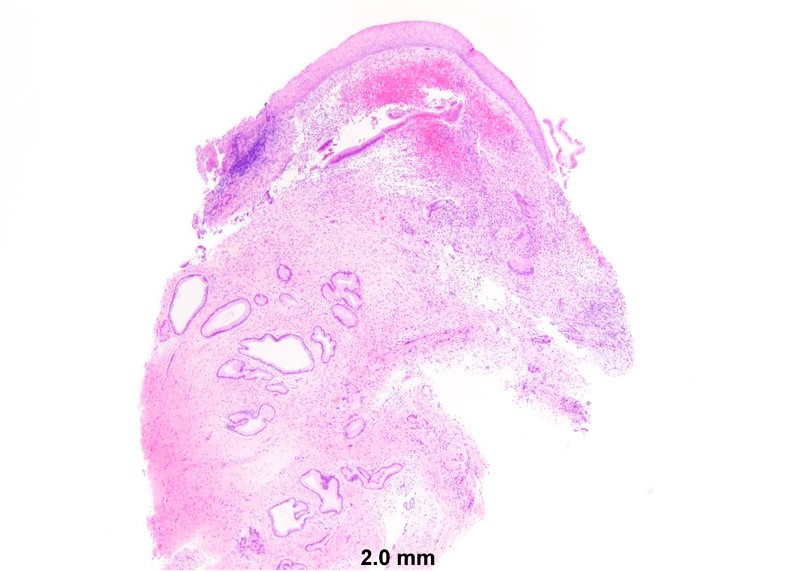
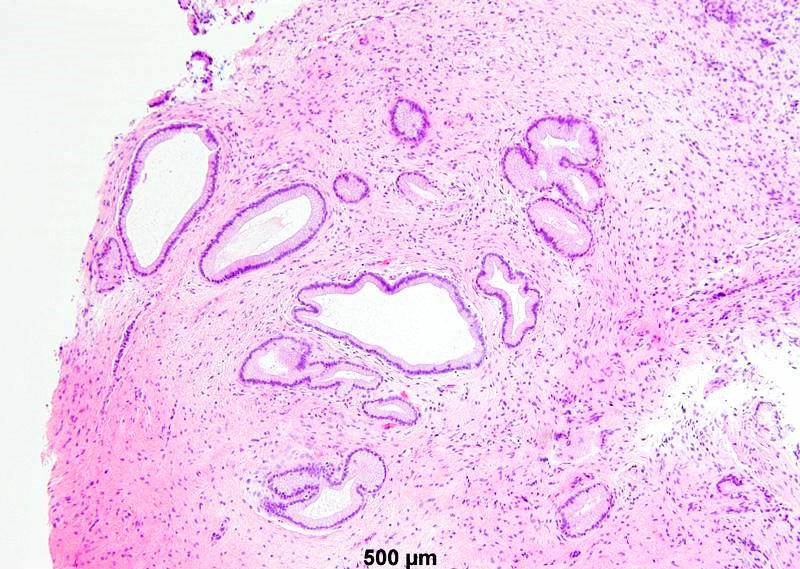
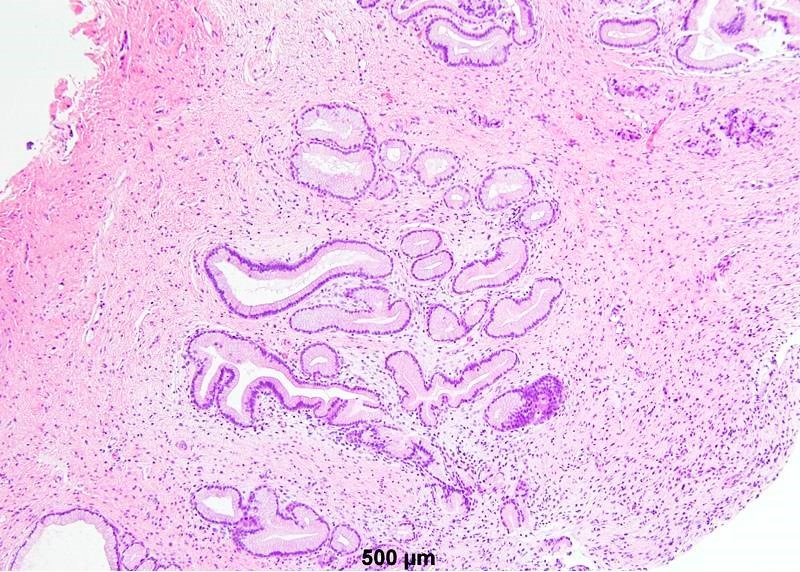
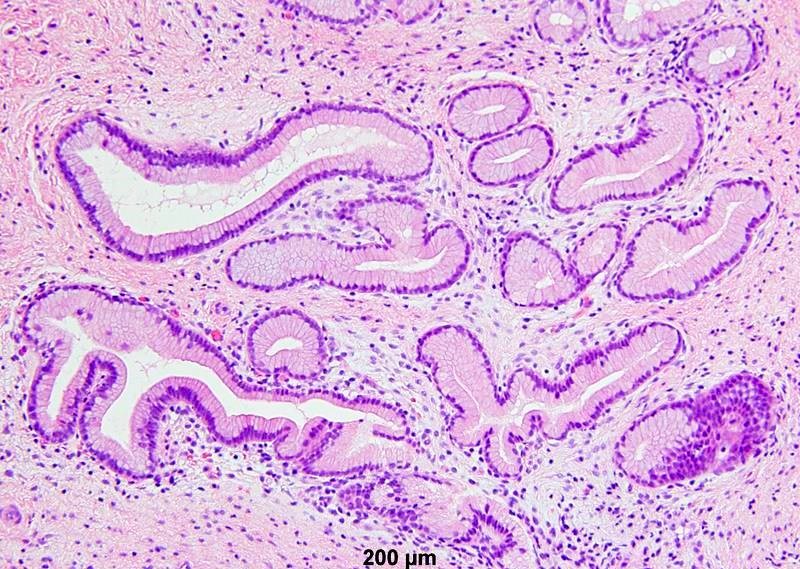
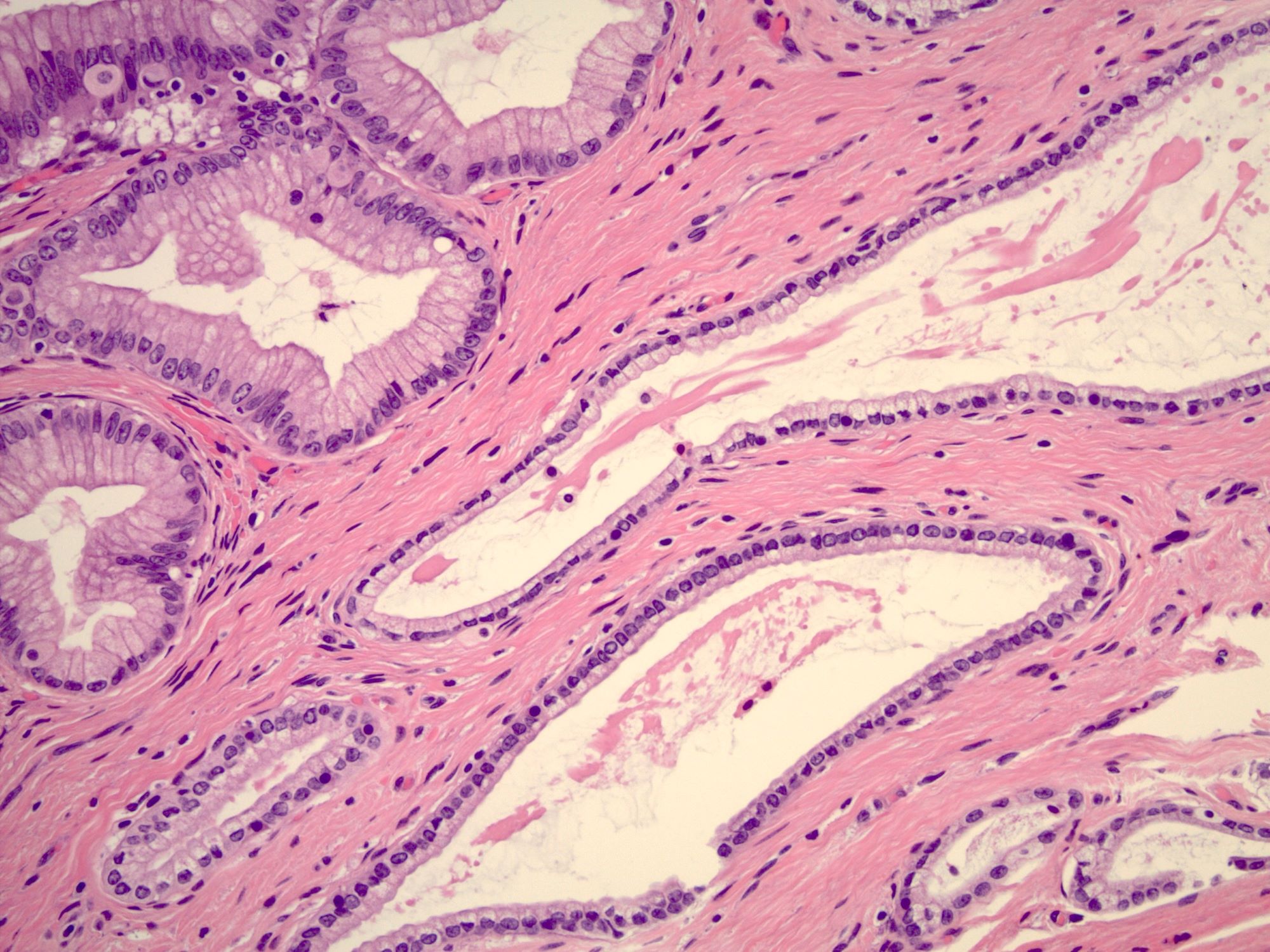
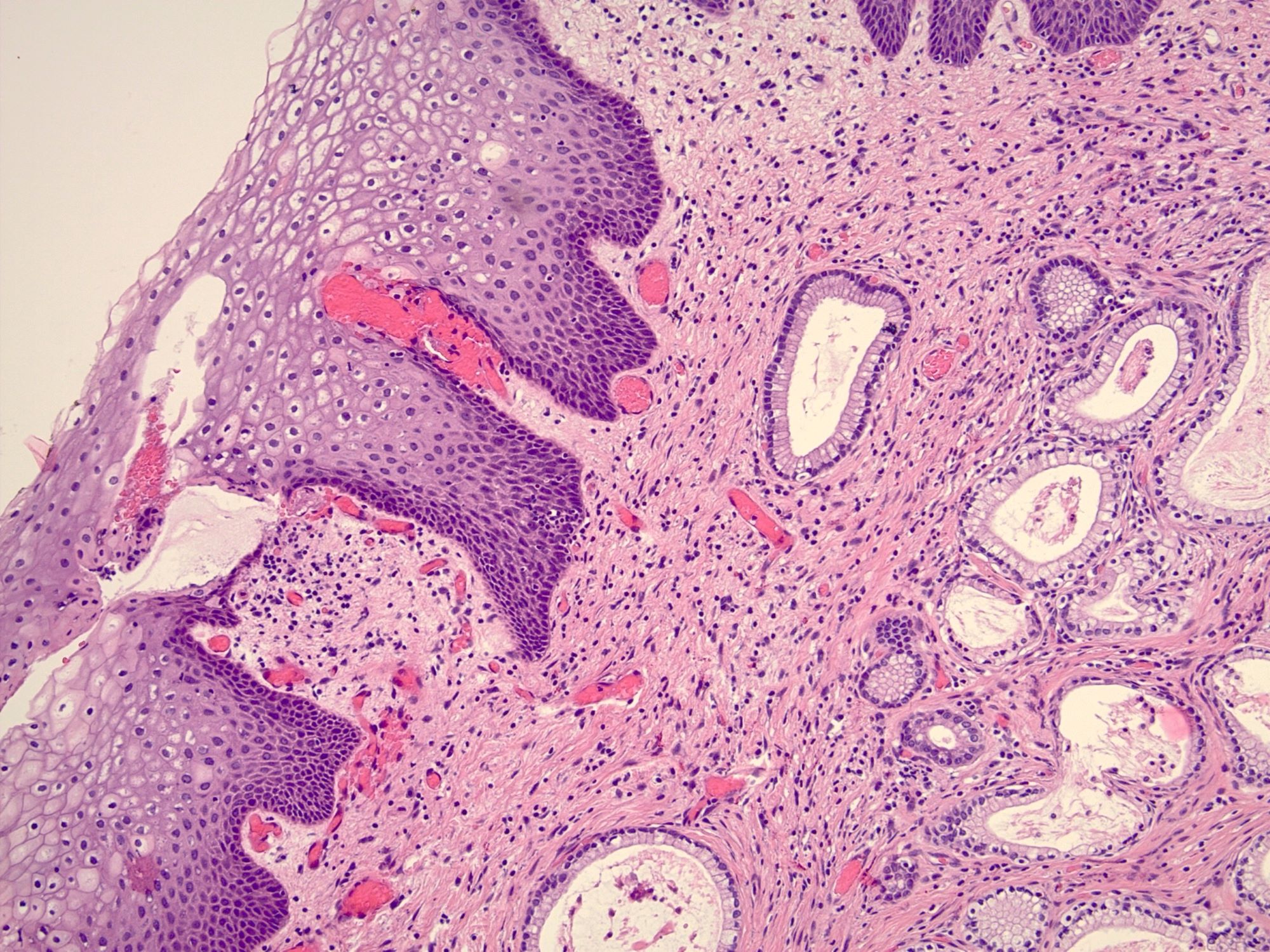
Microscopic (histologic) description
- 2 adult (differentiated) forms of adenosis have been described:
- Mucinous: most common type of adenosis (62% of biopsy specimens); characterized by mucinous columnar cells that resemble those of the normal endocervical mucosa
- Tuboendometrial: found in 21% of specimens; glands are lined by light and dark cells, often ciliated and resemble fallopian tube and endometrial gland cells
- Embryonic: glands composed of low columnar or cuboid cells
- Glands may be simple, complex, cystic or papillary and usually found in the lamina propria but also on the mucosal surface
- Cysts lined by a single layer of columnar mucinous cells may resemble cervical nabothian cysts
- Squamous metaplasia can be present and represents the process by which adenosis transforms and heals
- Rarely, intestinal metaplasia may be seen
- References: Mutter: Pathology of the Female Reproductive Tract, 3rd Edition, 2014, Kurman: Blaustein's Pathology of the Female Genital Tract, 6th Edition, 2011
Microscopic (histologic) images
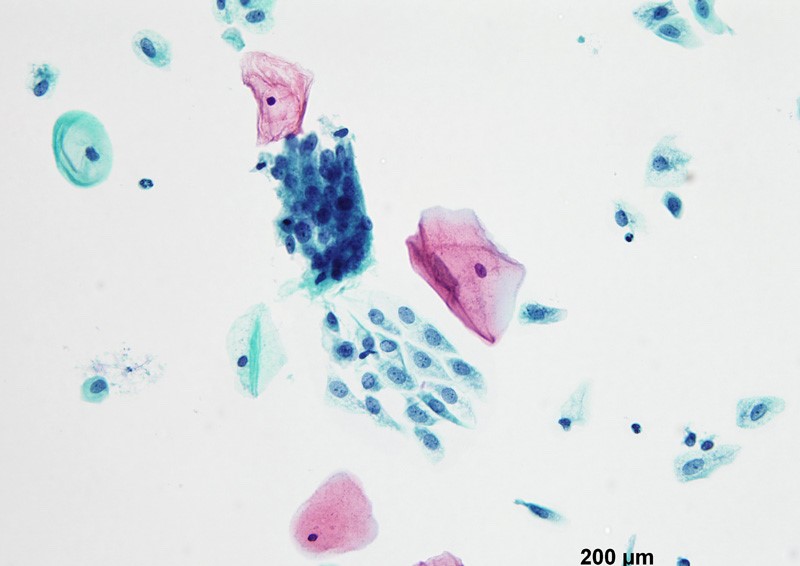
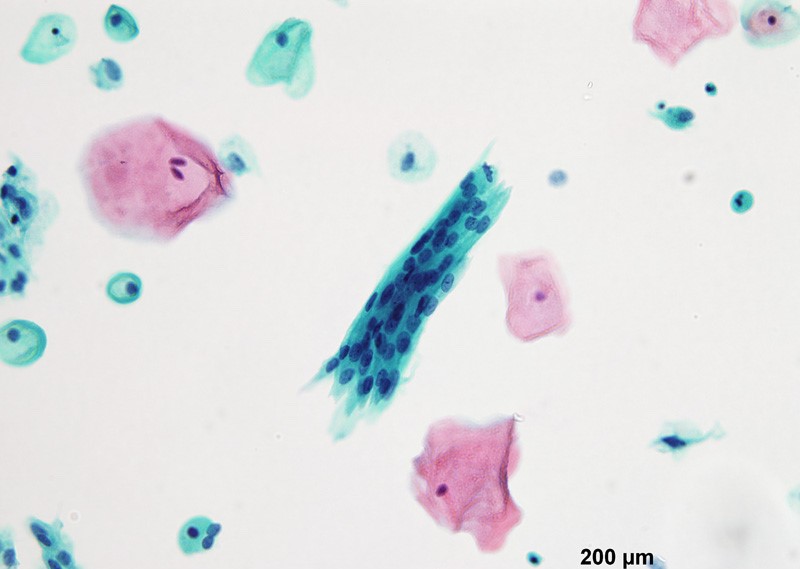
Cytology description
- Vaginal specimens are characterized by endocervical-like glandular cells or metaplastic squamous cells
- Endometrioid glandular cells can also occur
Videos
Vaginal adenosis diffuse, rare case
Sample pathology report
- Vagina, posterior wall, biopsy:
- Squamous mucosa with bland mucinous glands consistent with vaginal adenosis; negative for malignancy
Differential diagnosis
- Clear cell adenocarcinoma (vagina):
- May be confused with the glands of adenosis that undergo microglandular hyperplasia (small, uniform, crowded glands without mucin, nuclear pleomorphism and prominent nucleoli)
- Endometriosis:
- Presence of endometrial stroma with glands that much more closely resemble those of normal endometrium than the glands seen in adenosis
- CD10 is useful to confirm the presence of endometrial stroma
- Mesonephric (Wolffian) remnants:
- Mesonephric tubules are lined by nonciliated, nonmucinous cuboid cells with dense, eosinophilic luminal secretions; these remnants are surrounded by a loose fibrovascular stroma that may contain smooth muscle fibers
- Recurrent endometrial adenocarcinoma:
- Glandular cells in vaginal cytology Papanicolaou tests in patients with hysterectomy for endometrial adenocarcinoma (Diagn Cytopathol 2012;40:138)
Additional references
Board review style question #1
A 28 year old woman presents with persistent vaginal discharge and is found to have submucosal mucinous glands on a vaginal biopsy. What is the most likely scenario?
- Maternal grandmother's use of diethylstilbestrol (DES) caused in utero exposure for the patient’s mother
- Maternal use of DES caused in utero exposure for the patient
- The patient had prior treatment for bacterial vaginosis
- The patient had prior treatment for vaginal condyloma acuminata
- Use of DES by the patient
Board review style answer #1
D. The patient had prior treatment for vaginal condyloma acuminata. Vaginal application of 5-fluoruracil and vaginal CO2 laser therapy (common treatments for condyloma acuminata) are 2 known non-DES causes for vaginal adenosis. Answer C is incorrect because these are not common treatments for bacterial vaginosis. Answers A, B and E are incorrect because in utero exposure to diethylstilbestrol (DES) was the most common cause of vaginal adenosis for women born in the middle of the 20th century but DES exposure is not a concern in this patient who was born long after its discontinued use.
Comment Here
Reference: Vaginal adenosis
Comment Here
Reference: Vaginal adenosis
Board review style question #2
Which statement concerning vaginal adenosis is true?
- Inapparent on gross examination
- May be associated with microglandular hyperplasia
- Progresses to adenocarcinoma in a majority of the cases
- Usually manifests in prepubertal age
- Usually related to bacterial vaginosis
Board review style answer #2
B. May be associated with microglandular hyperplasia. Vaginal adenosis commonly appears as red nodules / red granular spots or patches and fails to stain with an iodine solution on colposcopy. Mosaicism and punctation are common findings during colposcopy. It commonly manifests as excessive mucous discharge in postpubertal age. Vaginal adenosis seldom progresses to cancer. Microglandular hyperplasia develops in foci of vaginal adenosis, especially after oral contraceptive use. Microglandular hyperplasia may be confused with clear cell adenocarcinoma (which is also diethylstilbestrol associated).
Comment Here
Reference: Vaginal adenosis
Comment Here
Reference: Vaginal adenosis