Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Yoshiki M. Squamous metaplasia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cervixmetaplasiasquamous.html. Accessed April 19th, 2024.
Definition / general
- Stratified squamous epithelium replacing preexisting mucin producing columnar epithelium
Essential features
- Stratified squamous epithelium replacing overlying preexisting endocervical glands in the stroma
- Absence of nuclear abnormalities and brisk mitotic activity
- Physiological change due to estrogenic milieu and vulnerable to HPV infection
- Mimic of high grade squamous intraepithelial lesion (HSIL) but immunohistochemically negative for p16
Terminology
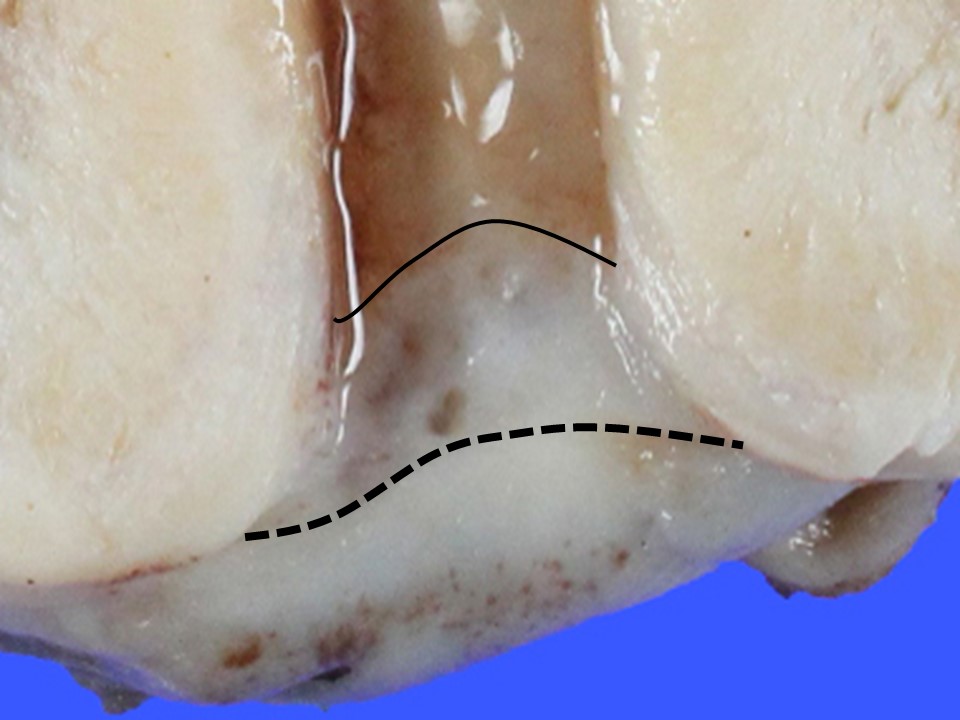
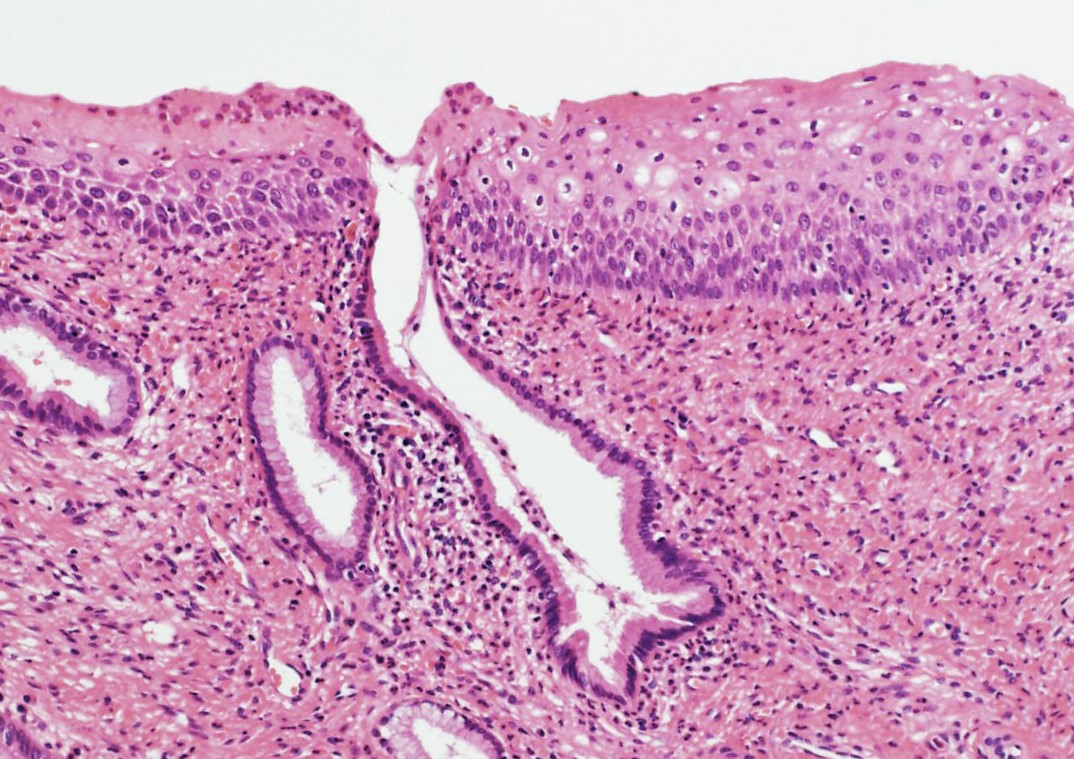
- Transformation zone defined as area of newly formed squamous epithelium
- Junction between squamous and columnar cervical epithelium is called squamocolumnar junction
- Transformation zone is defined as the area of newly formed squamous epithelium (between the original squamocolumnar junction and the functional / current squamocolumnar junction)
- Immature squamous metaplasia for those with incomplete squamous maturation
ICD coding
- ICD-11: GA15.Y - other specified acquired abnormalities of cervix uteri
Epidemiology
- Common among women of reproductive age
Sites
- External os of the cervical canal
- Adjacent to squamocolumnar junction (histologic external os)
Pathophysiology
- Direct extension of stratified squamous epithelium into the endocervix (squamous epithelialization) (Mills: Histology for Pathologists, 5th Edition, 2020)
- Arises in association with reserve cell hyperplasia adjacent to squamocolumnar junction (true metaplasia) (Mills: Histology for Pathologists, 5th Edition, 2020)
- Association with a discrete population of reserve cells at the squamocolumnar junction suggested (Proc Natl Acad Sci U S A 2012;109:10516)
Etiology
- Induced by estrogenic stimulation and vaginal acidic environment
Clinical features
- No clinical manifestation
- Found incidentally on biopsy, conization or hysterectomy specimen
- Recognized as transformation zone bordered by original and secondary squamocolumnar junction
Diagnosis
- Diagnosed by microscopic examination
- Can be identified on cytology (cervicovaginal smear)
Prognostic factors
- Nonneoplastic condition per se but vulnerable to human papillomavirus (HPV) infection
- Risk for high grade squamous intraepithelial lesion defined by maturation status of squamous metaplasia (Am J Surg Pathol 2013;37:1311)
Case reports
- 30 year old woman with melanin containing cells identified in the basal layer of squamous metaplasia (Indian J Pathol Microbiol 2004;47:22)
- 4 women with ectopic prostatic tissue in the uterine cervix in association with prominent squamous metaplasia (Am J Surg Pathol 2000;24:1224)
Treatment
- No need for treatment
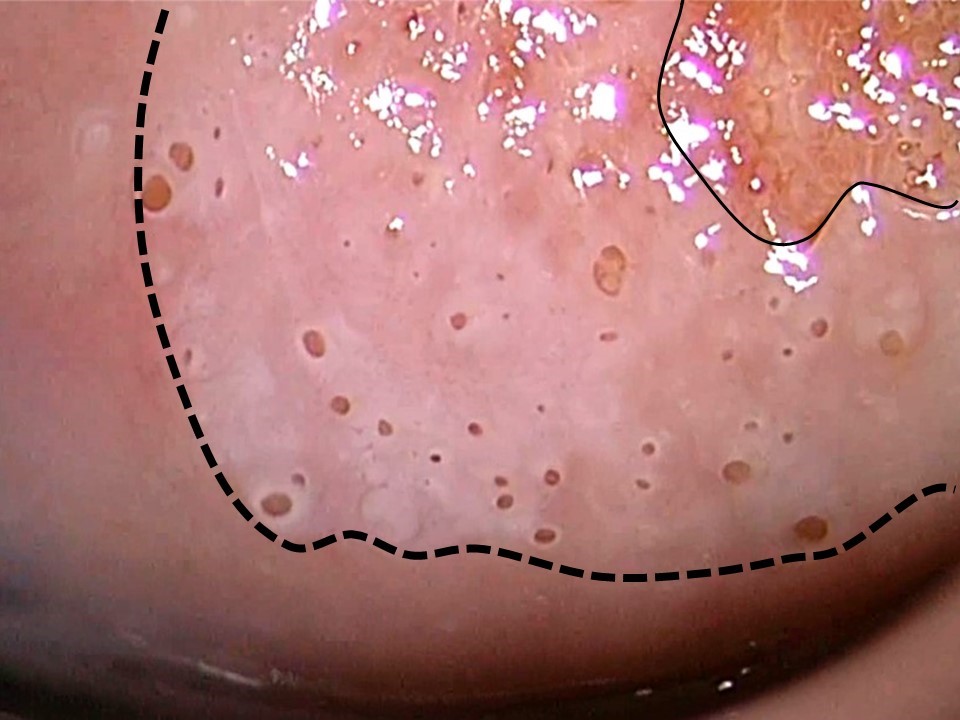
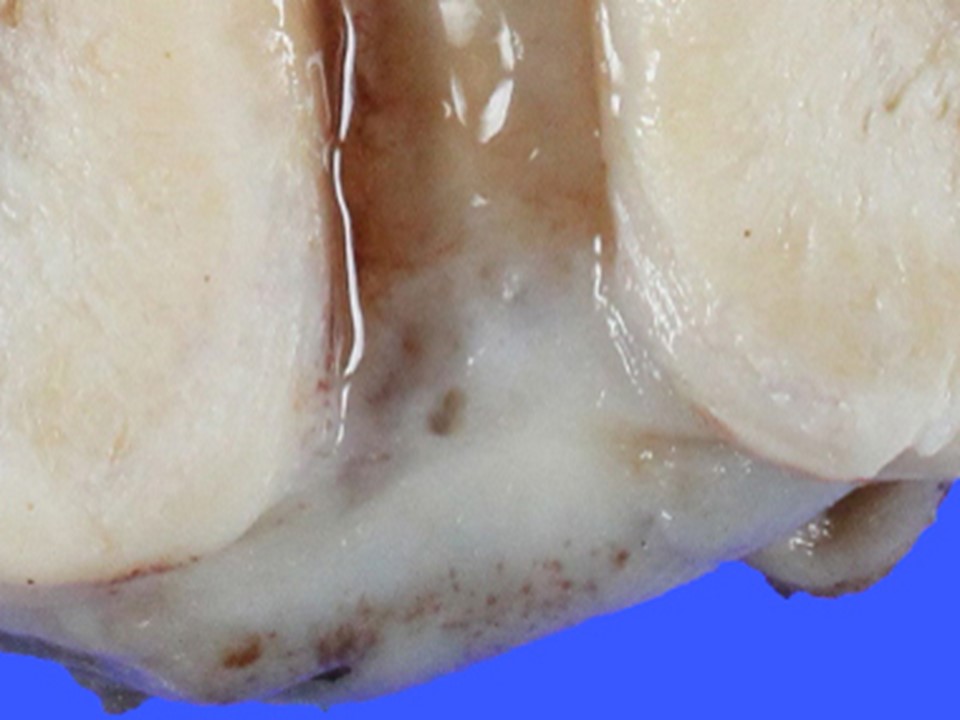
Gross description
- Whitish and rather translucent mucosa with opening of endocervical glands
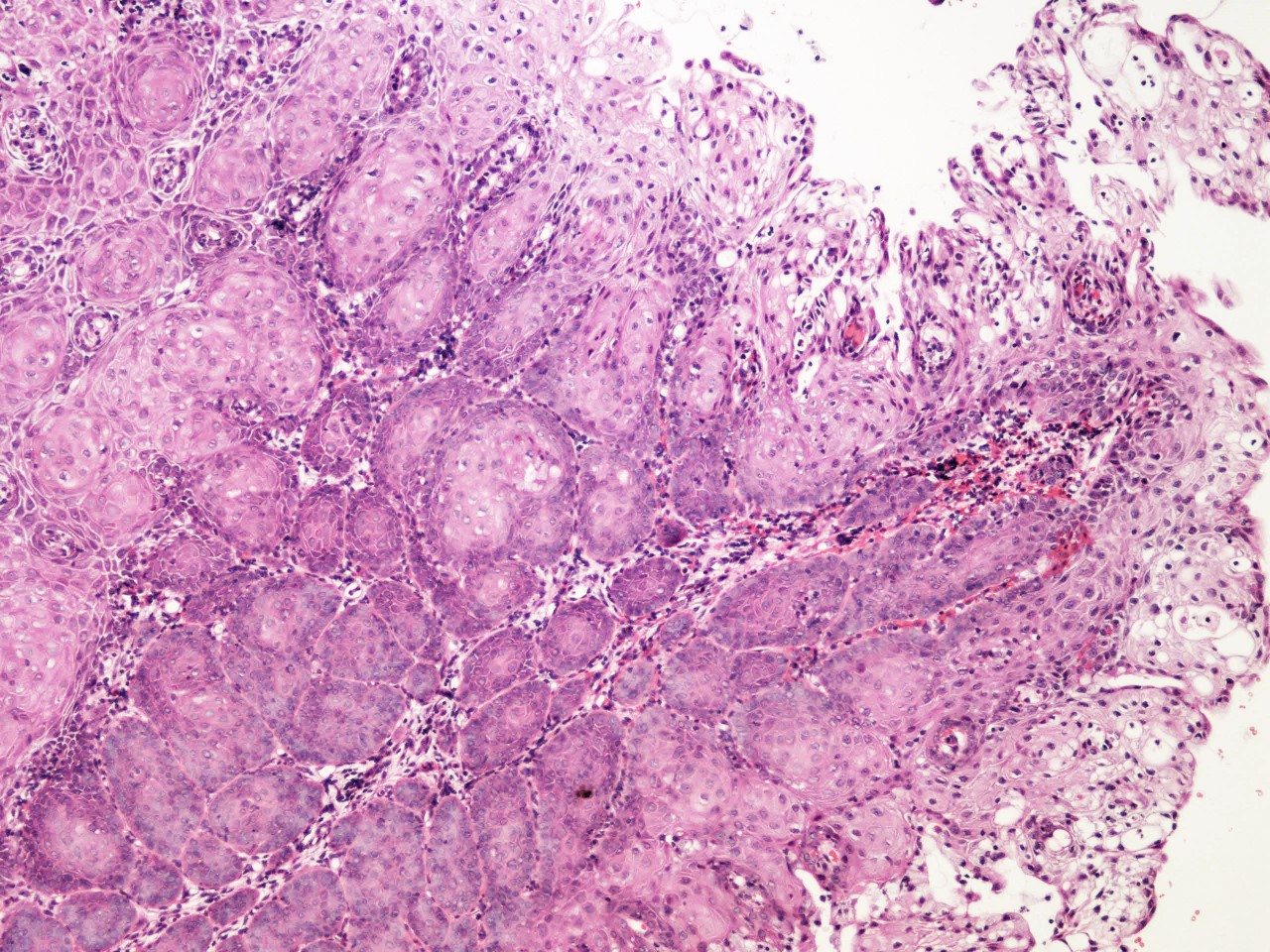
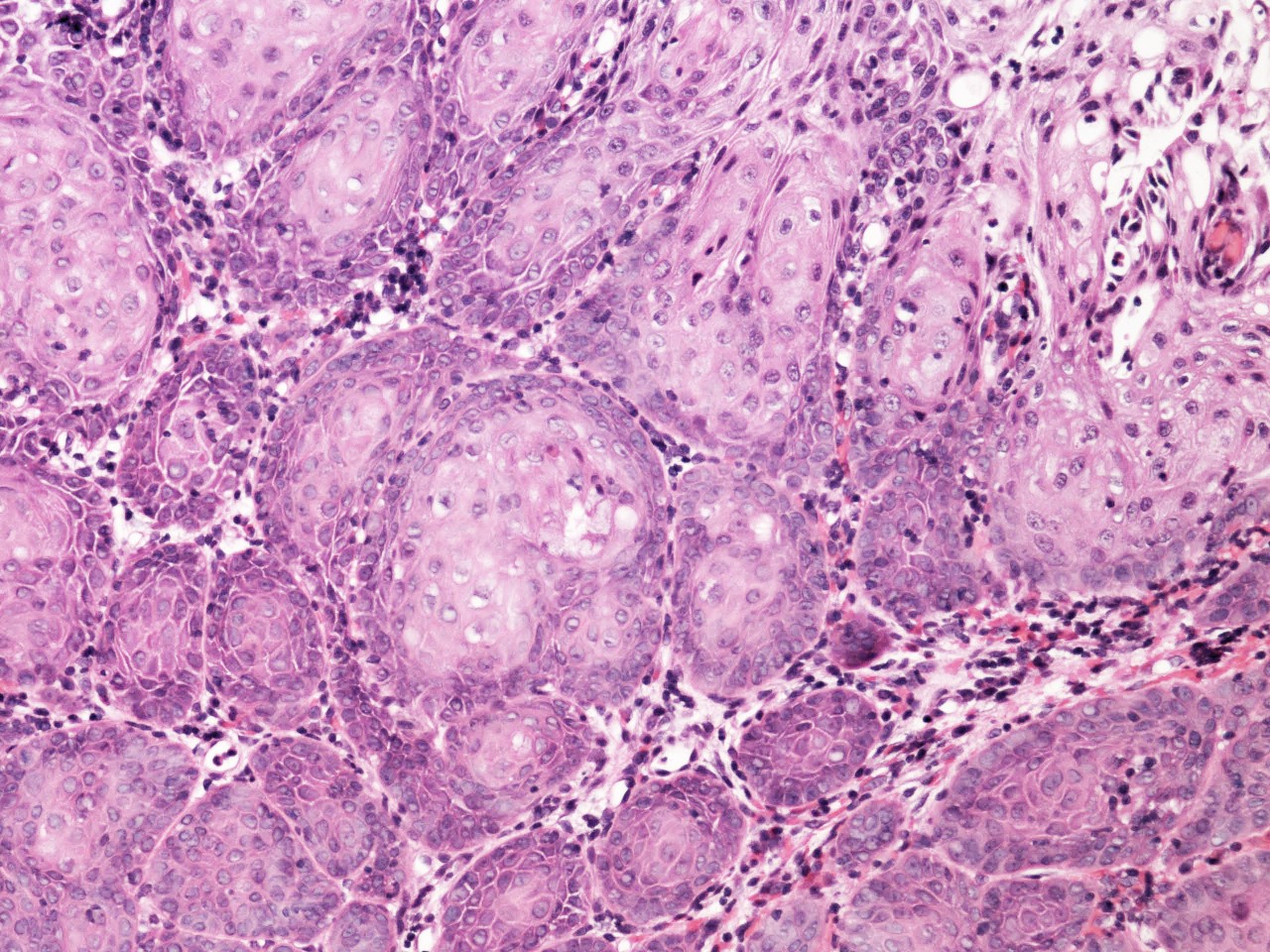
Microscopic (histologic) description
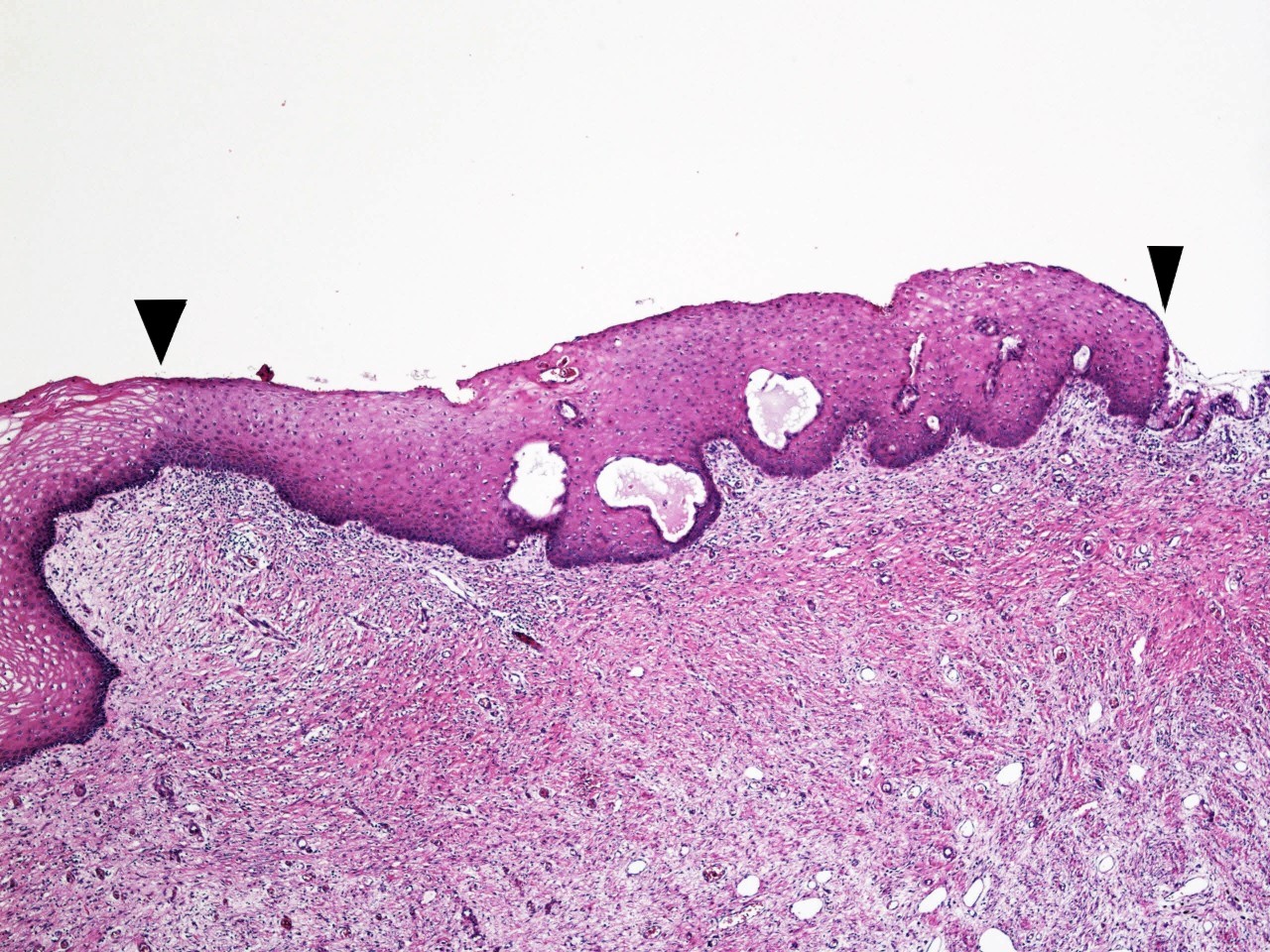
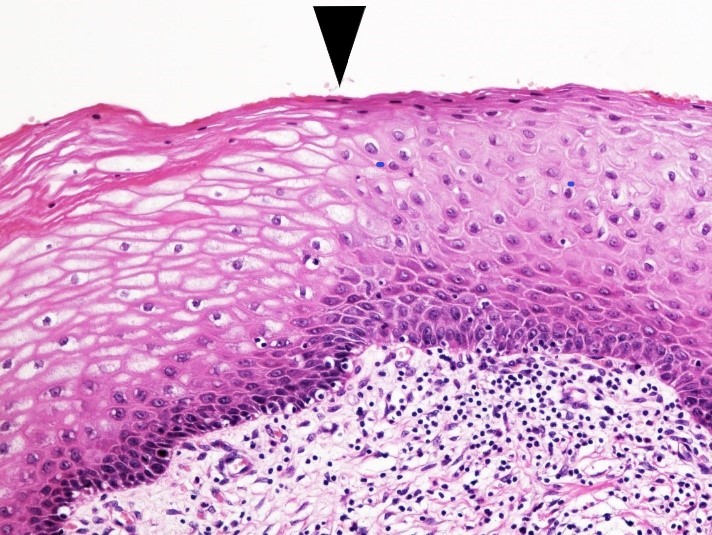
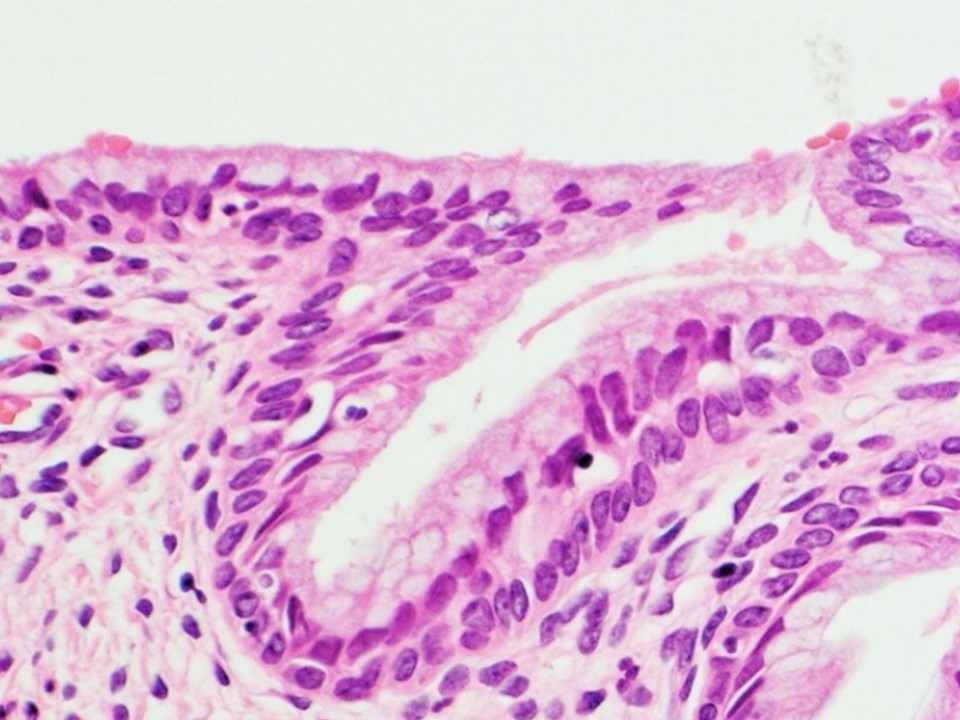
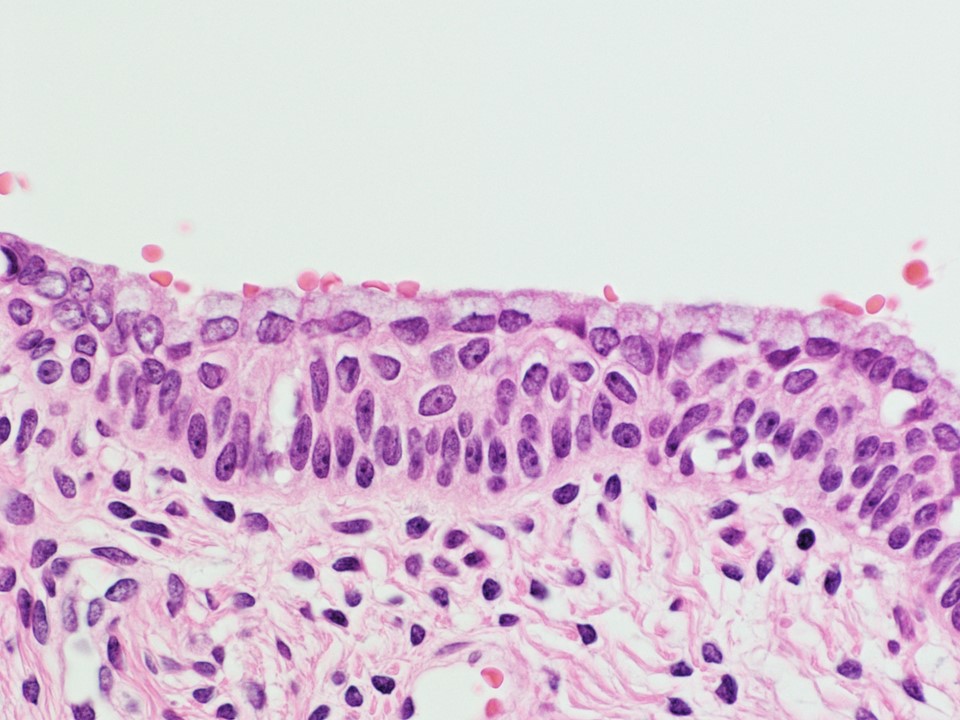
- Stratified epithelium with varying degrees of superficial squamous differentiation, divided into 2 forms, i.e., mature and immature forms (Mills: Histology for Pathologists, 5th Edition, 2020)
- Mature squamous metaplasia, showing superficial and intermediate cells with relatively abundant eosinophilic cytoplasm
- Immature squamous metaplasia, composed of polygonal cells with scant cytoplasm
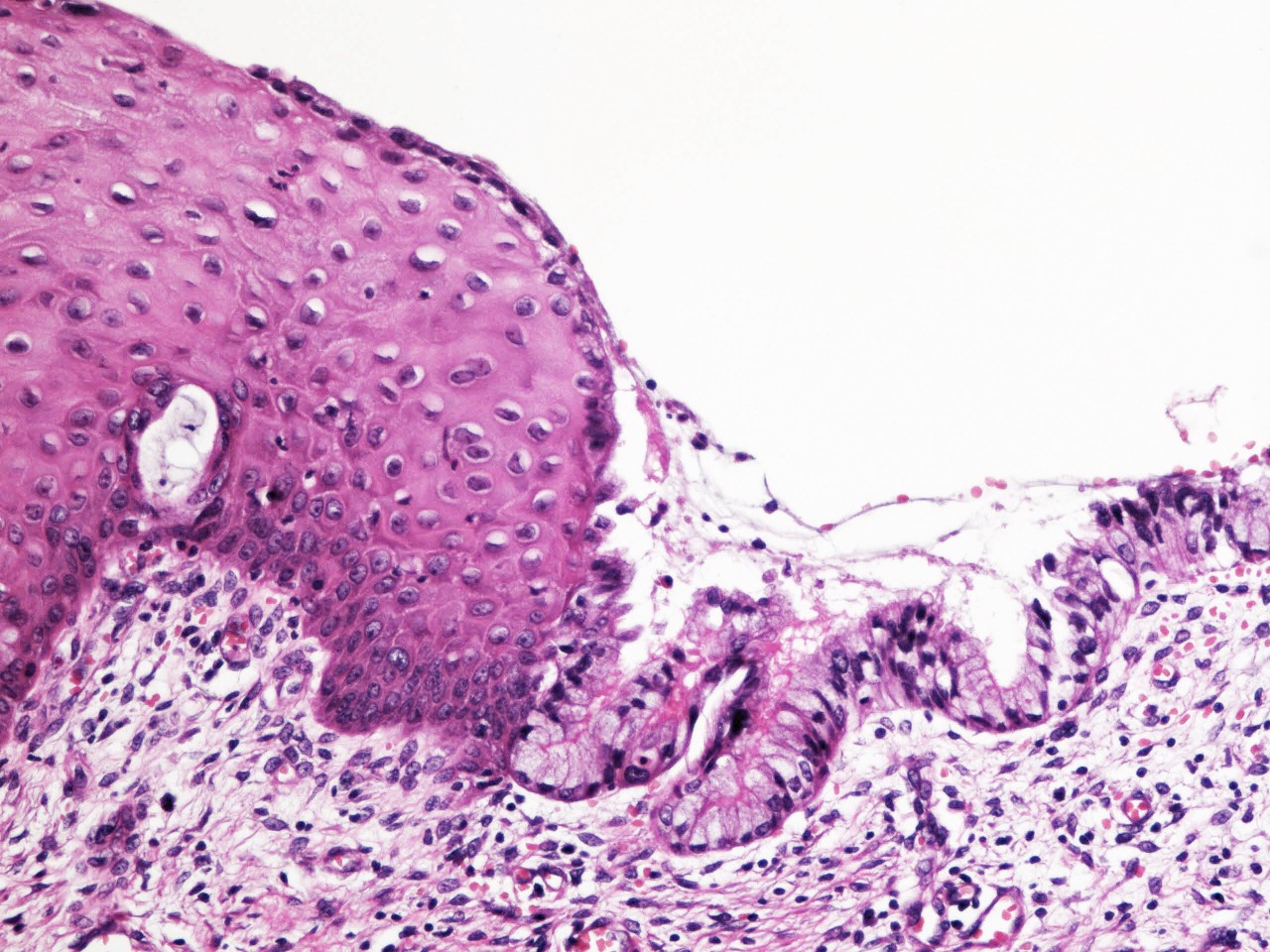
- Preexisting endocervical glands are usually colonized by metaplastic epithelium
- Metaplastic squamous epithelium usually grows beneath the pre-existing endocervical epithelium
- Single layer of mucin producing columnar or cuboidal cells may remain on the surface of the epithelium
- Occasional normal mitotic figures or nuclear enlargement in association with inflammation
- Significant heterogeneity in nuclear size and shape, hyperchromatism, nuclear overlapping and abnormal mitotic figures absent
Microscopic (histologic) images
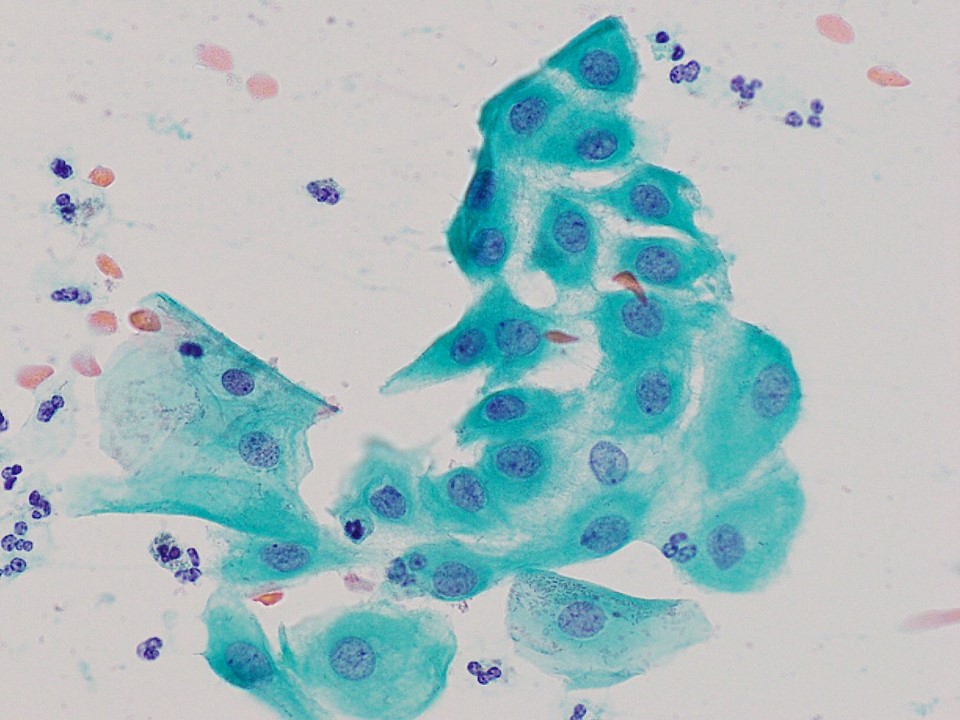
Cytology description
- Sheets of polygonal cells with high nuclear to cytoplasmic ratio (Cibas: Cytology - Diagnostic Principles and Clinical Correlates, 5th Edition, 2020)
- Homogeneity in nuclear size and shape
Positive stains
- p40, p63 (Adv Anat Pathol 2009;16:316)
- Cytokeratin 5/6 (can be focal and weak)
Negative stains
- p16 (can be focally positive with patchy distribution) (Adv Anat Pathol 2006;13:8)
- Ki67 (low labeling index) (Adv Anat Pathol 1999;6:177)
Sample pathology report
- Uterine cervix, biopsy:
- Squamous metaplasia, negative for intraepithelial lesion or malignancy (see comment)
- Comment: There is immature squamous epithelium composed of polygonal cells with homogeneity in nuclear size and shape adjacent to mucin producing columnar epithelium. Abnormal mitotic figures and significant nuclear hyperchromasia are absent. These features support the diagnosis of squamous metaplasia, although further examination may be considered if the previous cytology interpretation was HSIL or atypical squamous cells, cannot exclude HSIL (ASC-H).
- Uterine cervix, biopsy:
- Immature squamous metaplasia (see comment)
- Comment: Negative staining for p16 and low Ki67 labeling index exclude the diagnosis of HSIL.
Differential diagnosis
- High grade squamous intraepithelial lesion (HSIL):
- Low grade squamous intraepithelial lesion (LSIL) with metaplastic features:
- Stratified mucin producing intraepithelial lesion (SMILE):
- Mild to moderate nuclear abnormalities
- Cells with intracytoplasmic mucin throughout all epithelial layers
- Diffuse and strong staining for low molecular cytokeratin (i.e. CAM5.2)
- Negative or weak and focal immunoreactivity for p63 or p40
- Positive for p16 overexpression
- Atrophy:
- Thin epithelium composed of cells with scant cytoplasm
- Shows homogeneity in nuclear size and shape
- Transitional cell metaplasia:
- Resembles urothelium of the urinary tract
- Characterized by elongated cells with nuclear groove, arranged in perpendicular direction to basement membrane
- Regarded as a form of atrophy (postmenopausal squamous atypia)
- Squamous cell carcinoma:
- Confused with squamous metaplasia extending into preexisting endocervical glands
- Shows significant nuclear abnormalities
- Epithelial nests showing irregular border, distinguishable from outline of preexisting endocervical glands and desmoplastic stromal reaction
- May be associated with HSIL
- Positive for p16 overexpression
- Squamous metaplasia of endometrium (icthyosis):
- May be identified on endocervical biopsy or curettage
- Commonly associated with pyometra
- Endometrioid carcinoma with squamous differentiation:
- May be identified on endocervical biopsy or curettage, particularly in case of cervical stroma involvement
- Coexisting malignant glandular component contributory to exact diagnosis
Board review style question #1
Board review style answer #1
E. Vulnerable for HPV infection. Squamous metaplasia is a preferential site for high risk HPV infection and HPV related carcinogenesis and thus is a hot spot for developing squamous intraepithelial lesion (SIL) and squamous cell carcinoma. However, it is a physiologic condition and is not a precursor per se. Colposcopy can identify squamous metaplasia as transformation zone, which is a site for targeted biopsy in case of abnormal Pap smear. Transitional cell metaplasia is a mimic of squamous metaplasia and high grade SIL (HSIL) and is a form of atrophy. It should be kept in mind that squamous metaplasia, in particular its immature form, can be erroneously misinterpreted as HSIL. The p16 immunohistochemistry, a diagnostic tool for HPV related neoplastic condition including HSIL, can solve the problem since squamous metaplasia is negative for this particular maker.
Comment Here
Reference: Squamous metaplasia
Comment Here
Reference: Squamous metaplasia
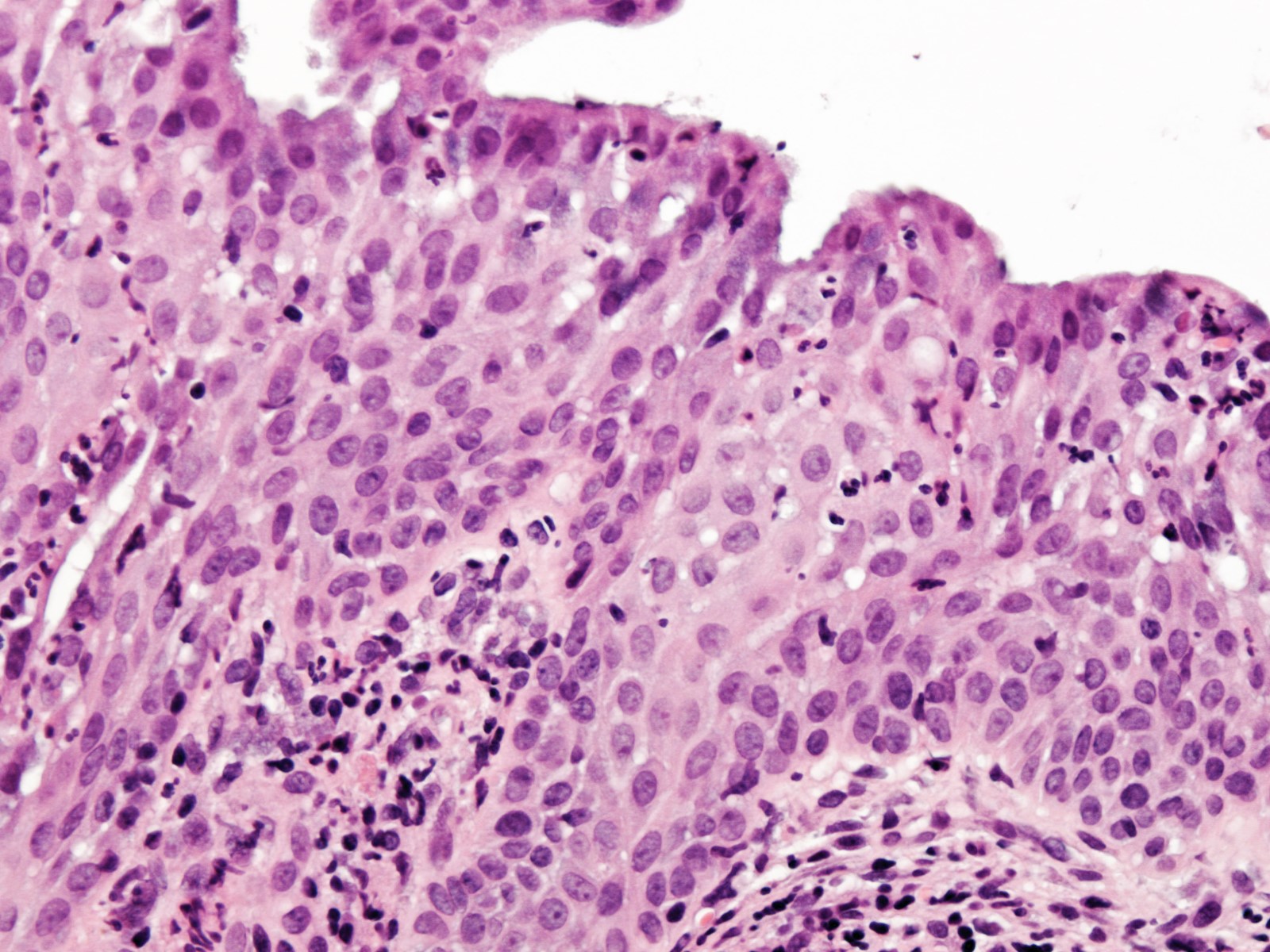
Board review style question #2
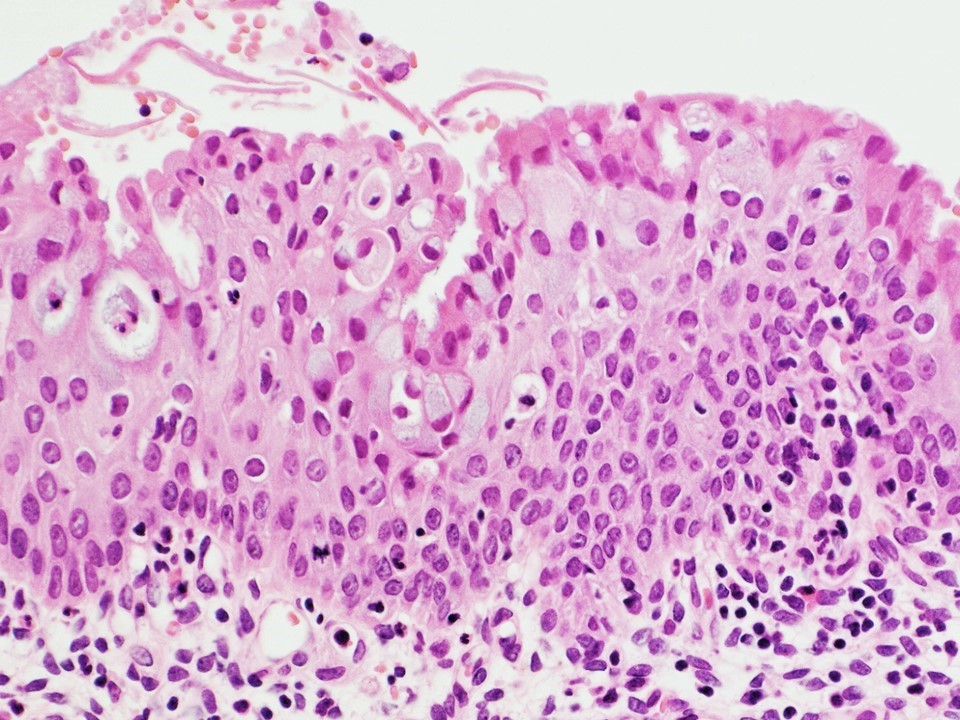
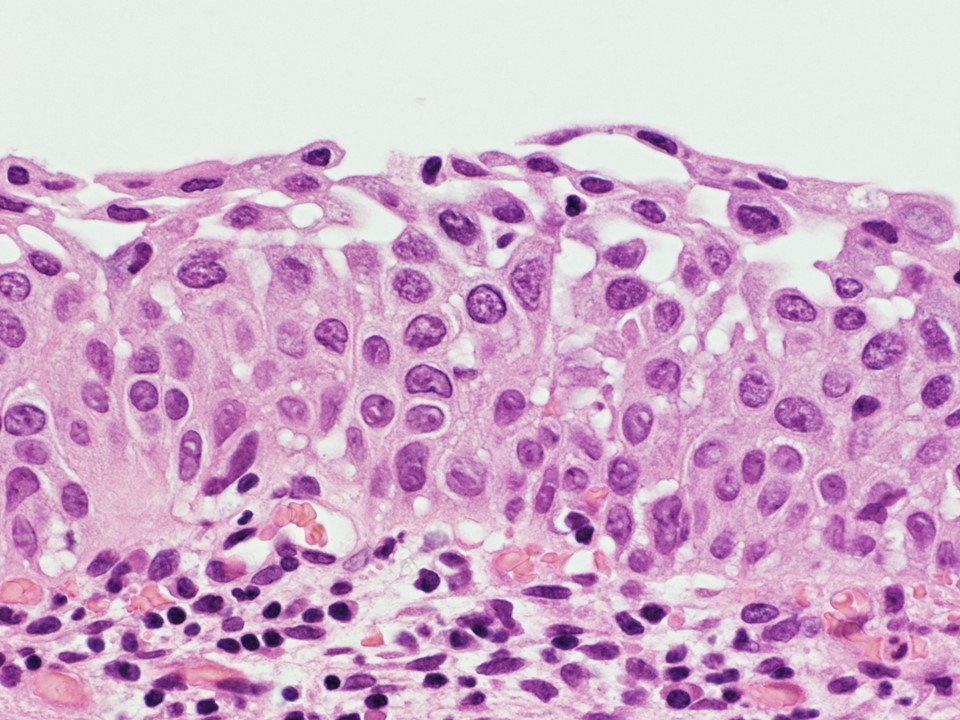
A 28 year old woman was referred to a gynecology clinic for colposcopy because of abnormal Pap smear, which was interpreted as atypical squamous cells, cannot exclude HSIL (ASC-H). The photomicrograph is obtained from one of the cervical biopsy specimens and shows
- Atrophy
- High grade squamous intraepithelial lesion (HSIL)
- Low grade squamous intraepithelial lesion (LSIL)
- Squamous metaplasia
- Transitional cell metaplasia
Board review style answer #2
D. Squamous metaplasia. The image illustrates squamous metaplasia composed of polygonal cells with scant cytoplasm. Nuclear morphology is homogenous in size and shape and nuclear hyperchromasia, coarse chromatin texture, nuclear overlapping and brisk mitotic activity are absent and thus HSIL is excluded. Absence of koilocytosis makes LSIL unlikely. Atrophy is also unlikely, considering patient age. Transitional cell metaplasia is a variant of atrophy, characterized by nuclear groove and elongated nuclei perpendicular to basement membrane, features inconsistent with the image under discussion.
Comment Here
Reference: Squamous metaplasia
Comment Here
Reference: Squamous metaplasia