Table of Contents
Definition / general | Essential features | Diagrams / tables | Indications for testing | Laboratory | Types of elements in urine | Automated urine analyzers | Urine reagent strips | Microscopic (histologic) images | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Shetty A. Urine crystals & microscopy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/chemistryurinecrystals.html. Accessed April 18th, 2024.
Definition / general
- Standard component of complete urinalysis
- One of the oldest laboratory tests in medicine is to look for abnormal microscopic constituents in urine (JAMA Netw Open 2020;3:e2013959)
Essential features
- Urine analysis is the third major diagnostic screening test in the clinical laboratory, only preceded by serum / plasma chemistry profiles and complete blood count analysis
- As sample collection is done by the patient, it is more likely to be susceptible to preanalytical issues
- Routine urine microscopic examination includes looking for cellular, formed elements and organisms
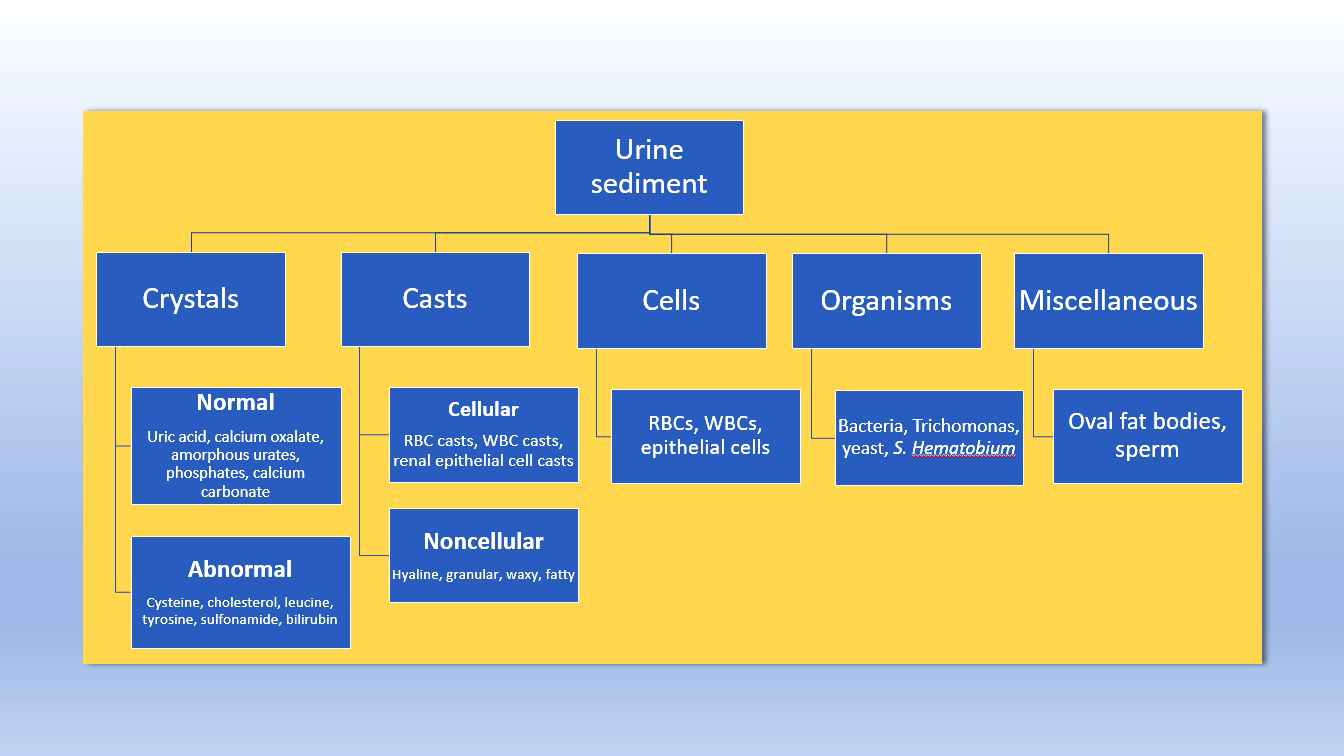
Diagrams / tables
Indications for testing
- Helps diagnose:
- Kidney disease
- Urinary tract infection
- Cancers of urinary tract
- Reactions to medicines
- Prostate infection
- Liver disease
- Yeast, viral, parasitic infections
Laboratory
- Specimen for testing:
- First void urine preferred in routine practice
- Midstream urine is the most appropriate sample, since contaminating elements, such as bacteria, analytes and formed particles, are minimized
- Collection instructions:
- Clean catch urine or midstream portions of first morning urine
- Samples should be collected in a wide mouthed, sterile container made of nonabsorbing materials, with no influence on any analyte
- Due to influence on the viability of bacteria, the use of soap or antiseptics while washing the genitalia is not recommended (Ann Biol Clin (Paris) 2018;76:609)
- Catheter urine sample for bacteriological study or culture in bed ridden patients or patients with obstruction of urinary tract
- For infants, a clean plastic bag can be attached around genitalia and left in place for some time for sample to be collected
- Volume required:
- 12 mL is the recommended urine volume for adult patients
- Range of 5 - 12 mL of urine is acceptable to examine the formed elements in urine
- Test protocol and acceptance of smaller urine specimens is determined by the individual laboratory
- Procedure:
- Centrifuge urine at 1,500 rpm for 10 minutes
- Resuspend sediment in 1 drop of urine an observe under microscope
- Examine first using low power and then high power
- Lower the condenser and minimize the light to view elements
- Possible interferences:
- Dietary intake, exercise
- Medications
- Increased time lag between sampling and analysis
- For urinalysis that cannot be performed within 2 hours of collection
- Lack of temperature control and lack of addition of a preservative to samples will lower the quality of urinary test results
- If testing by strip method, test can be performed within 24 hours if urine is refrigerated without preservatives (Biochem Med (Zagreb) 2014;24:89)
- For urinalysis that cannot be performed within 2 hours of collection
Types of elements in urine
- Urinary crystals:
- Crystals are formed in urine when it is supersaturated with certain minerals, which may be due to
- Increased excretion of these constituents
- Reduced urine volume, an alteration in urine pH
- A combination of the above factors
- Crystals can be seen in both healthy and disease states
- Crystals are formed in urine when it is supersaturated with certain minerals, which may be due to
| Normal crystals | |||
| Crystals | Ph of urine | Identification | Remarks |
| Uric acid | Acidic |
| Urate nephrolithiasis or acute urate nephropathy, gout and leukemia |
| Calcium oxalate | Acidic or alkaline |
| Dietary oxalate ingestion (spinach, tomato, cabbage and asparagus) and nephrolithiasis |
| Calcium phosphate | Alkaline |
| In rare cases, could be caused by hypoparathyroidism |
| Triple phosphate | Alkaline |
| In patients with struvite stones and in urinary tract infection with Proteus |
| Calcium carbonate | Alkaline |
| Normal |
| Ammonium biurate | Alkaline |
| Old or longstanding urine sample |
| Amorphous | Phosphates - seen in alkaline urine and soluble in acetic acid |
| Can be confused with degenerating cells |
| Abnormal crystals | |||
| Crystals | Ph of urine | Identification | Remarks |
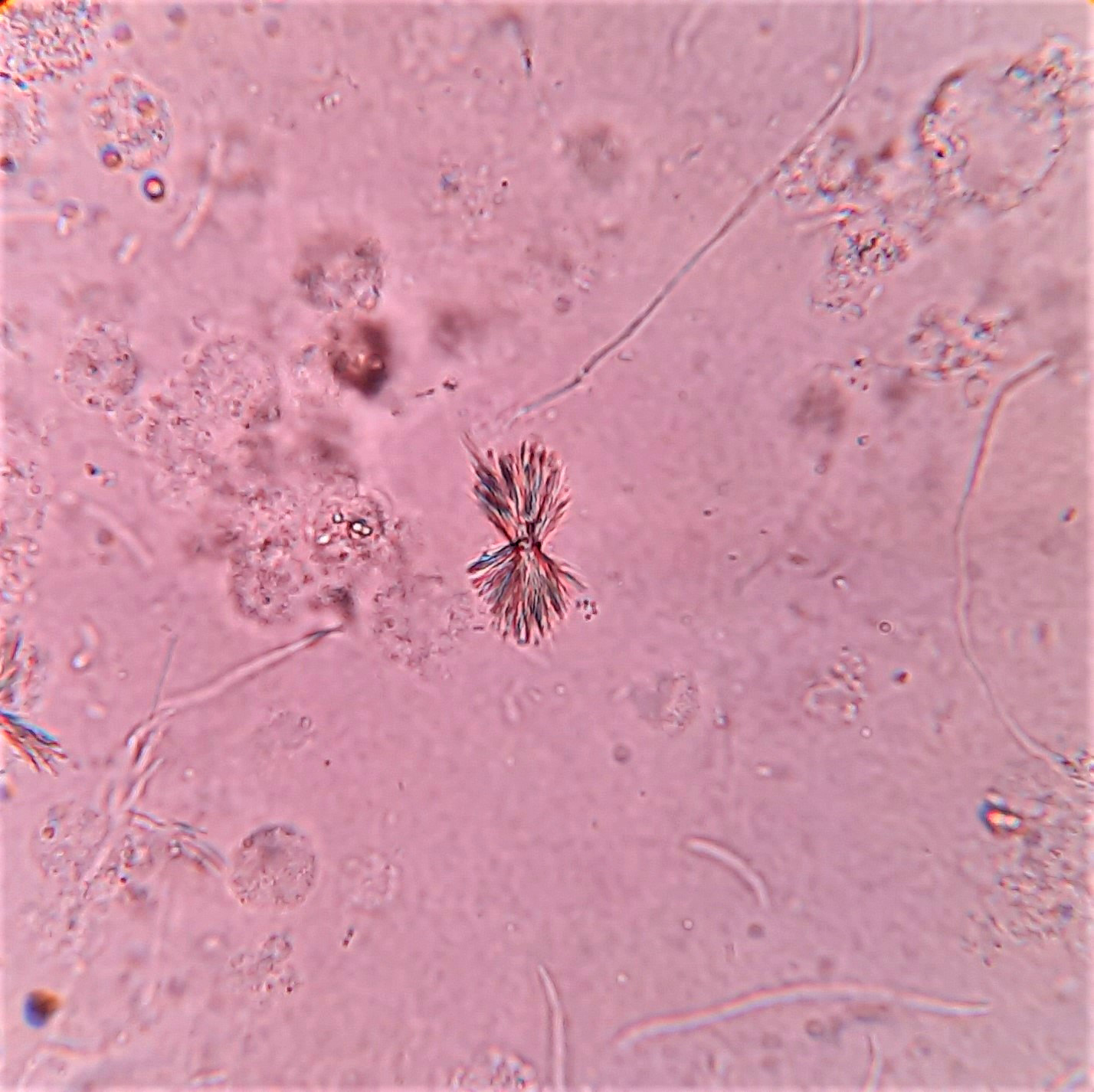
| Bilirubin | Acidic |
| Associated with increased conjugated bilirubin, severe liver disorders of obstructive cause |
| Cholesterol | Acidic |
| Nephrotic syndrome |
| Cysteine | Acidic |
| Genetic disease - cysteinuria (Nephrol Ther 2015;11:174) |
| Leucine | Acidic / neutral |
| Liver disorders with impaired amino acid metabolism |
| Tyrosine | Acidic / neutral |
| Liver disorders with impaired amino acid metabolism |
| Sulfonamide | Acidic / neutral |
| Drug related |
- Urinary casts:
- Casts are cylindrical, cigar shaped microscopic structures composed mainly of mucoprotein (Tamm-Horsfall mucoprotein, also known as uromodulin) that is secreted by epithelial cells lining the loops of Henle, the distal tubules and the collecting ducts
- As they are formed in the distal and collecting tubules, their presence in urine suggests renal parenchymal pathology
- Named depending on the predominant constituent
- Reported as number seen per low power field (10x objective)
| Noncellular casts | ||
| Type of cast | Appearance | Remarks |
| Hyaline |
| Seen normally (not associated with disease states); seen after strenuous exercise and with nonrenal diseases, such as dehydration (EJIFCC 2021;32:410) |
| Granular |
| Seen in acute glomerulonephritis and pyelonephritis; appears muddy brown in acute tubular necrosis |
| Waxy |
| Final stage of cast degeneration: indicates tubular injury of a more chronic nature than granular or cellular casts and is likely associated with low urine flow; always of pathologic significance (associated with end stage renal failure) |
| Fatty |
| Seen in nephrotic syndrome; may represent tubular degeneration |
| Cellular casts | ||||||||
| Type of cast | Appearance | Remarks | ||||||
| White blood cell (WBC) |
| |||||||
- Cells:
- Reported as the number of each type found per average high power field (HPF)
| Cell type | Description | Remarks | |||||||||
| Renal tubular epithelial |
| Tubular damage (like acute tubular necrosis) pyelonephritis, viral infection of kidney, allograft rejection and salicylate or heavy metal poisoning (Clin J Am Soc Nephrol 2010;5:402) | |||||||||
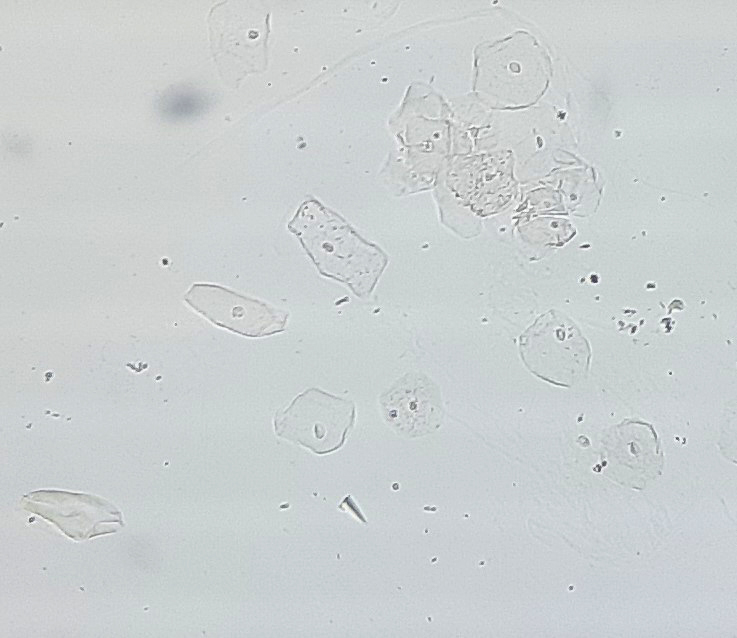
| Transitional epithelial |
| Seen after catheterization and in transitional cell carcinoma | |||||||||
| Squamous epithelial |
|
- Organisms:
| Organism | Description | Remarks | |||
| Bacteria |
| In a wet preparation, presence of bacteria should be reported only when urine is fresh; presence of only bacteria without pus cells indicates contamination with vaginal or skin flora | |||
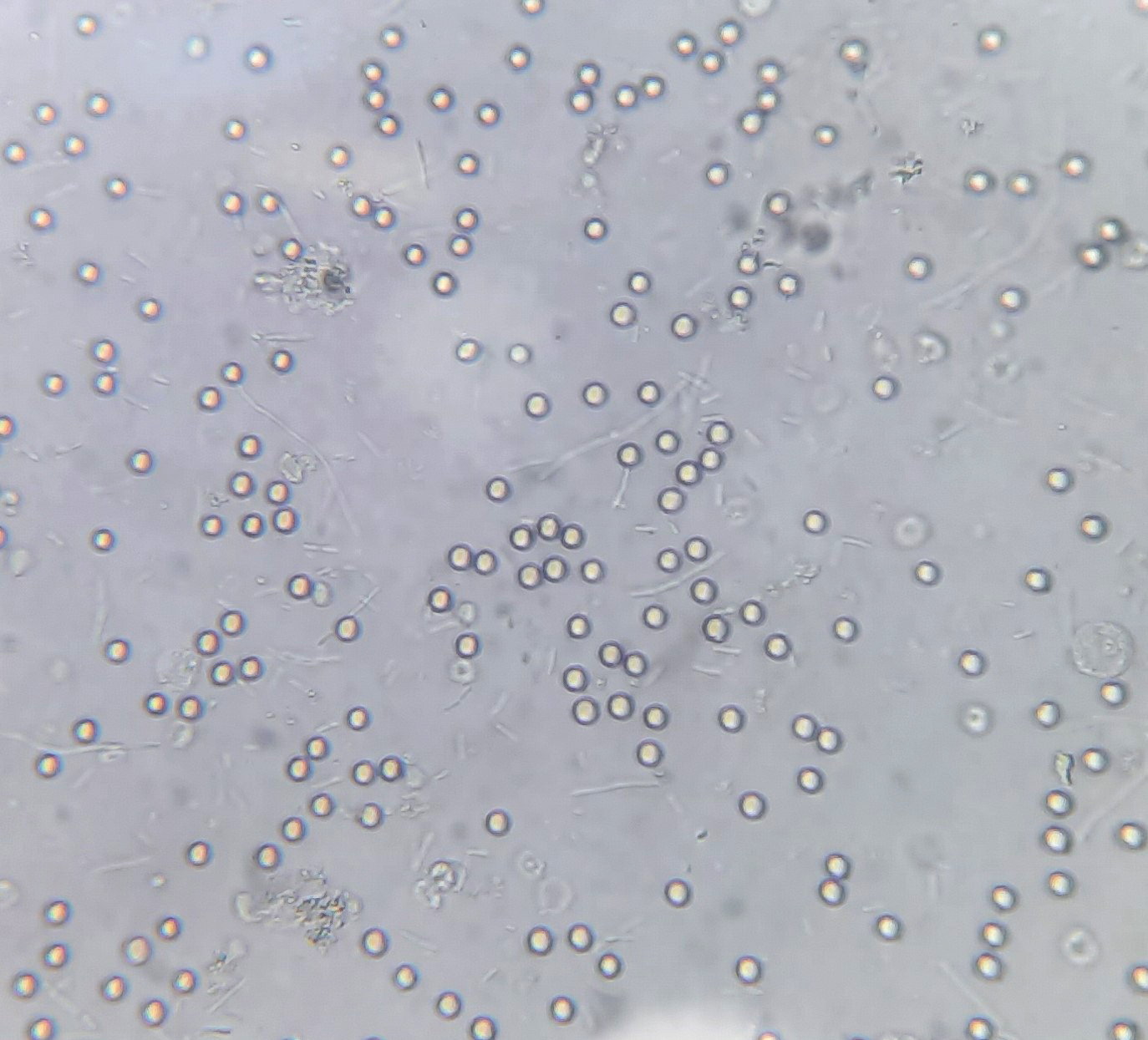
| Yeast cells |
| Seen in immunocompromised state, vaginal candidiasis or diabetes mellitus | |||
| Trichomonas vaginalis |
| Causes vaginitis in females and are thus contaminants in urine
Note: wet preparation of genital secretions or wet mount is the diagnostic method of choice (Sci Rep 2019;9:11074) | |||
| Schistosoma haematobium |
|
- Miscellaneous:
| Element | Description | Remarks |
| Sperm |
| Significant in infertility cases and sexual abuse
May be seen in males after a nocturnal emission or ejaculation Presence in the urine is of significance in the case of retrograde ejaculation |
Automated urine analyzers
- Automated urine analyzers enhance productivity and efficiency in the laboratories by increasing the reproducibility and throughput and reducing potential human errors
- Reduces the time and labor required to process urine samples
- Automated analyzers help standardize analysis so that laboratories can accurately recognize pathological elements in urine (Clin Chem Lab Med 2015;53:s1509)
- One study comparing 3 automated urine analyzers (Roche's Cobas 6500, Sysmex's UN3000-111b and Iris's iRICELL 3000) showed fairly good correlation among the 3 platforms and with manual microscopy (Pract Lab Med 2021;24:e00203)
- However, microscopic confirmation by experienced technologists is still necessary to avoid errors and definitively classify urine sediments, especially in pathologic specimen samples and images (particularly dysmorphic cells, bacteria, yeasts, casts and crystals)
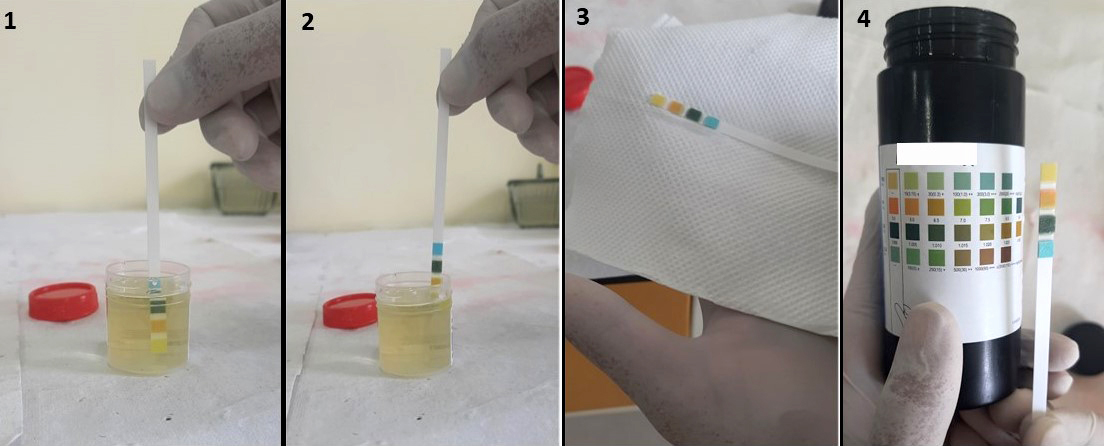
Urine reagent strips
- Urine strips are firm, plastic strips onto which several separate reagent areas are affixed
- Analytes detected can be ascorbic acid, glucose, bilirubin, ketone (acetoacetic acid), specific gravity, blood, pH, protein, urobilinogen, nitrite and leukocytes
- Reagent strips are packaged along with a drying agent in a plastic bottle with a twist off cap
- Each strip is stable and ready to use upon removal from the bottle
- Entire reagent strip is disposable
- Results are obtained by direct comparison of the test strip with the color blocks printed on the bottle label
- Procedure:
- Completely immerse reagent areas of the strip in fresh, well mixed urine
- While removing, touch the side of the strip against the rim of the urine container to remove excess urine
- Blot the lengthwise edge of the strip on an absorbent paper towel to further remove excess urine and avoid running over
- Compare each reagent area to its corresponding color blocks on the color chart and read at the times specified
- Proper read time is critical for optimal results
- Interpretation of microscopic findings can be correlated with strip findings for better interpretation
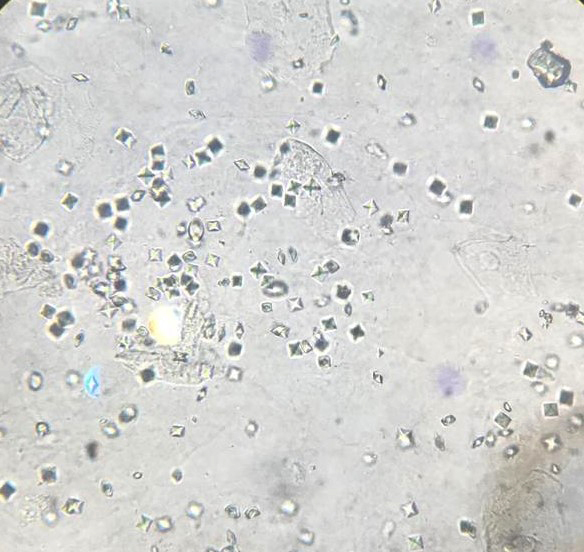
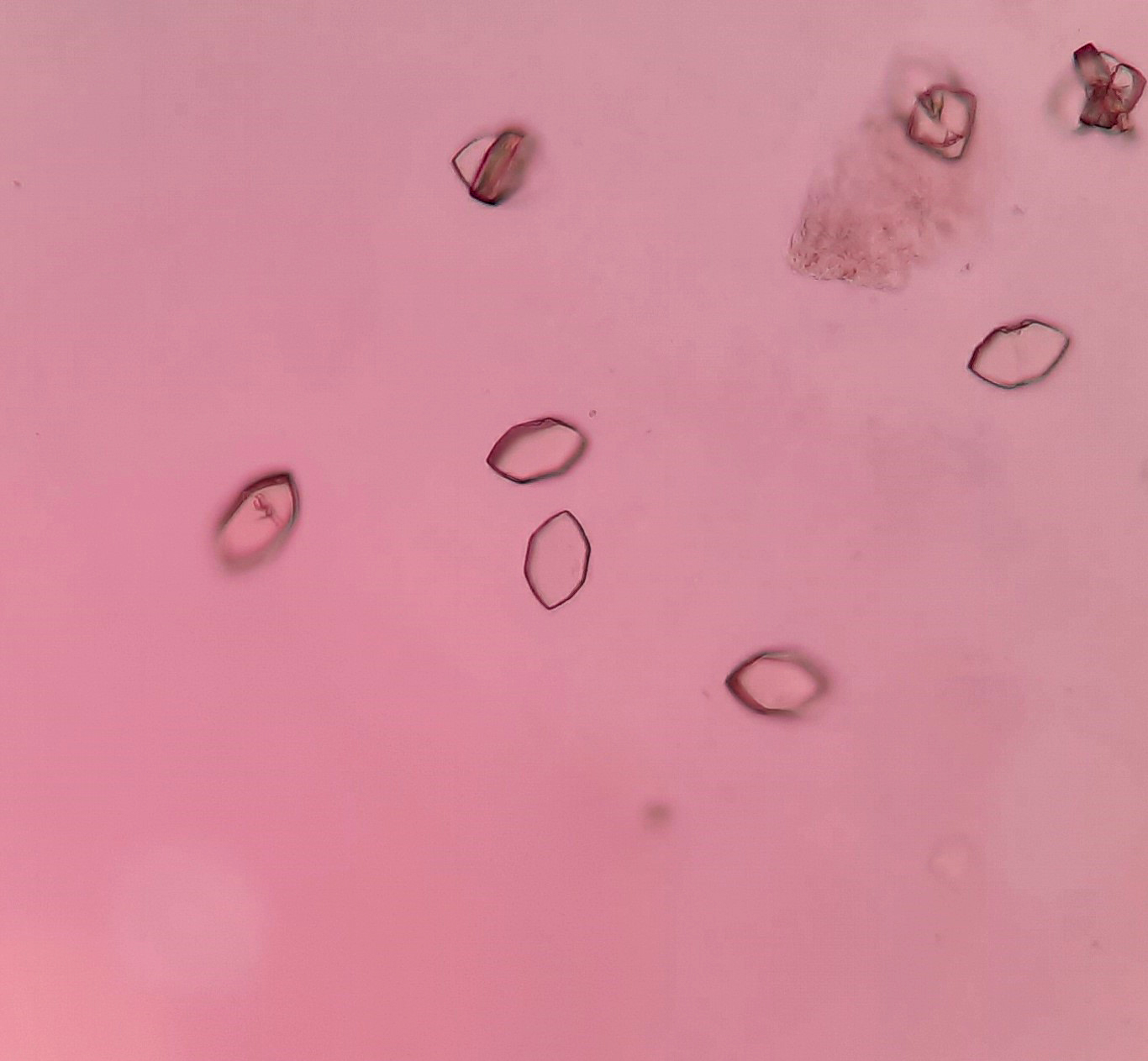
Microscopic (histologic) images
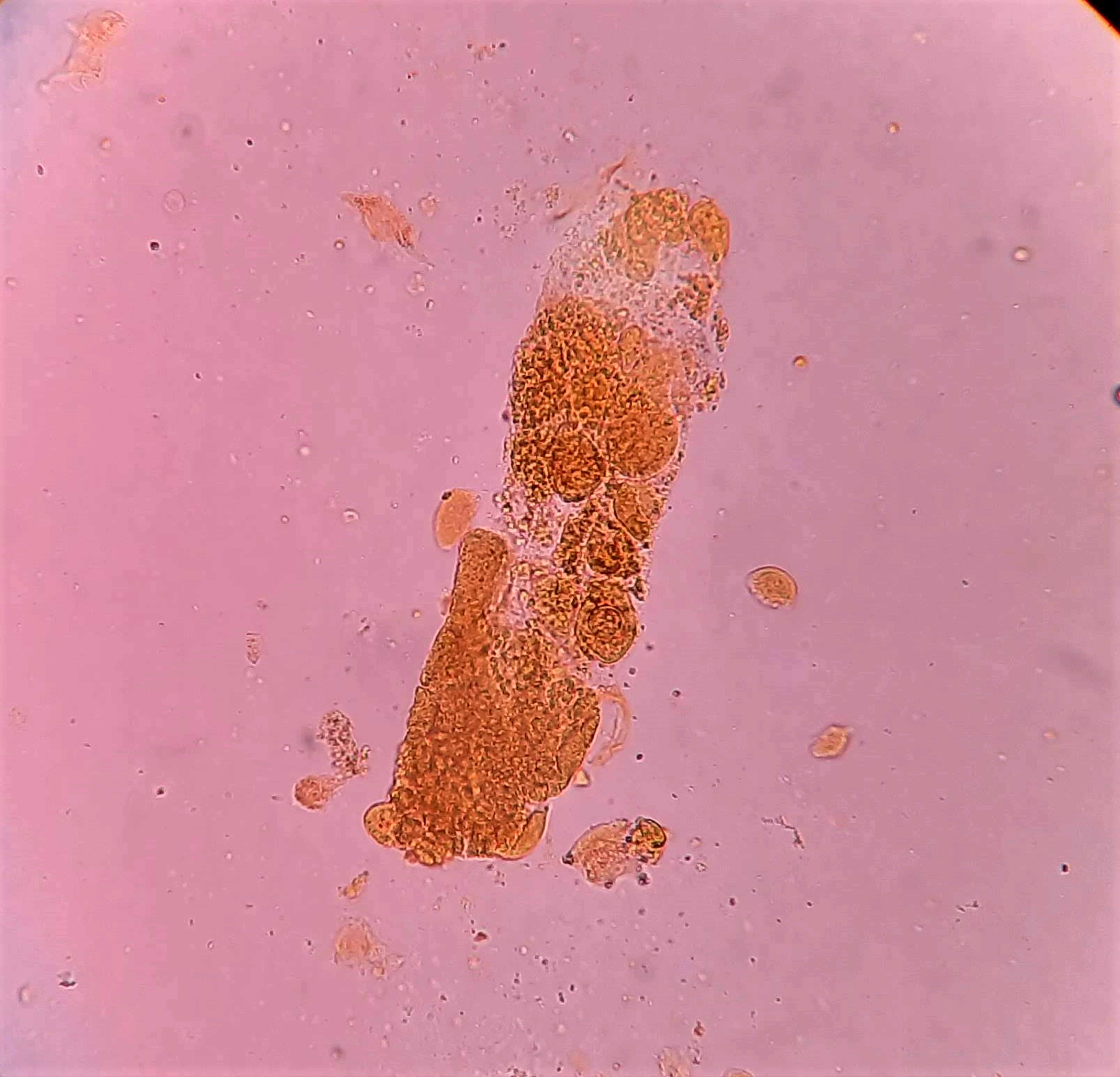
Board review style question #1
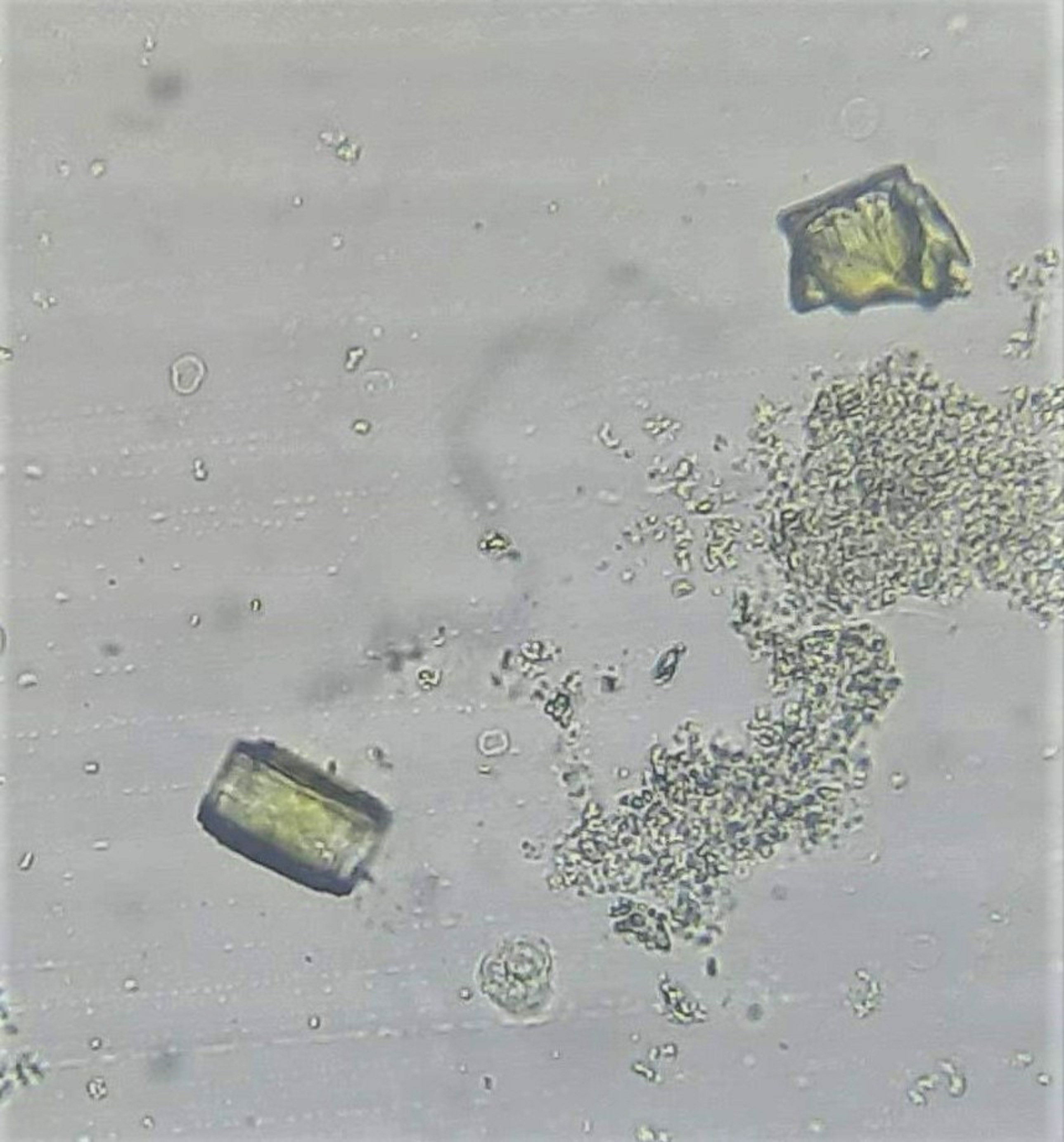
A urine sample from a 38 year old man with alcohol induced cirrhosis, ascites and jaundice is shown above. The appearance of the crystal is golden brown, with specific gravity = 1.015 and pH = 6.0. Identify the sediment finding (arrow)
- Cholesterol crystals
- Cysteine crystals
- Leucine crystals
- Tyrosine crystals
Board review style answer #1
C. Leucine crystals are seen in acidic urine. They appear as concentric circles with radial striations and are yellow-brown in color. They resemble a cross section of a tree trunk and are associated with liver disorder.
Comment Here
Reference: Urine crystals & microscopy
Comment Here
Reference: Urine crystals & microscopy
Board review style question #2
Which of the following types of urinary cast has serrated edges and is an indicator of end stage renal disease?
- Fatty cast
- Granular cast
- Waxy cast
- White blood cell (WBC) cast
Board review style answer #2
C. Waxy cast is seen in the setting of prolonged low urine flow.
Comment Here
Reference: Urine crystals & microscopy
Comment Here
Reference: Urine crystals & microscopy