Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology images | Positive stains | Negative stains | Electron microscopy description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Multz R, Ahrendsen JT. Multiple sclerosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cnsmultiplesclerosis.html. Accessed April 19th, 2024.
Definition / general
- Chronic, inflammatory demyelinating disease that may involve any part of the central nervous system
- Lesions, known as plaques, are characterized by loss of myelin with relative axonal preservation, reactive gliosis and the presence of lymphocytes or macrophages
Essential features
- Most common immune mediated demyelinating disorder of the central nervous system and most common cause of nontrauma related neurologic disability in young adults
- Female predominant neurologic disorder consisting of episodic nervous system dysfunction and characteristic radiologic findings that demonstrate both dissemination in time (multiple episodes) and dissemination in space (multiple lesions seen on imaging)
Terminology
- Multiple sclerosis
- MS
ICD coding
- ICD-10: G35 - multiple sclerosis
Epidemiology
- Most frequent cause of nontrauma related permanent disability in young adults (Neurol Clin 2011;29:207)
- Female predominance with F:M = 2.3:1
- Mean age of onset: 28 - 31 years
- Risk factors:
- Genetics (HLA::DRB1)
- Presence of coexisting autoimmune disease
- Decreased sunlight exposure
- Low vitamin D levels
- Geographic location, with a higher latitude corresponding with a higher incidence of disease (Nature 2011;476:214)
- More recently, it has been posited that there may be an association between EBV infection and the development of MS (Science 2022;375:296)
Sites
- Can involve any site in the central nervous system (CNS), typically within the white matter but also involves the gray matter (Brain 2019;142:1858)
- Most common sites for MS plaques:
- Optic chiasm and tract (nearly always involved)
- Periventricular white matter
- Subcortical white matter
- Deep gray nuclei
- Periventricular areas of the brainstem, cerebellum and spinal cord
Pathophysiology
- Since the cause of MS is unknown, a detailed pathophysiologic pathway has not yet been established (see Etiology)
Etiology
- Cause of MS is unknown, though it is favored to be due to an autoimmune activation of lymphocytes (Arch Neurol 2004;61:1613)
Clinical features
- Patients present with one or more distinct episodes of CNS dysfunction and characteristic MRI findings (dissemination in time and space) (Lancet Neurol 2018;17:162, Nat Rev Dis Primers 2018;4:43)
- Relapsing remitting MS (RRMS)
- Most common subtype of MS
- Episodic neurologic deficits that may partially or fully resolve but are followed by additional relapses
- Primary progressive MS (PPMS)
- Nonepisodic progression of disease from the initial onset of symptoms
- Secondary progressive MS (SPMS)
- Typically follows RRMS, where the disease transitions from episodic to continued progression
- Acute Marburg MS
- Fulminant MS that is monophasic and rapidly progressive, usually leading to death within a year of symptom onset
- Often seen in children and young adults
- Tumefactive MS:
- Uncommon subtype of acute MS that presents as a mass-like lesion with a radiologic differential diagnosis that includes demyelination, infection or neoplasm
- Radiologically characterized by contrast enhancement often with unique open or incomplete ring
- Surgical biopsy (with intraoperative frozen section consultation) is sometimes performed to help resolve the differential diagnosis
Diagnosis
- MS is a clinical diagnosis, combining clinical history and physical exam findings with imaging findings
- 2017 McDonald criteria can be applied where there is clinical suspicion for MS (Lancet Neurol 2018;17:162)
- Evoked potentials and optical coherence tomography (OCT) can also be used to aid in diagnosis (Lancet Neurol 2006;5:853, Mult Scler 2014;20:1342)
Laboratory
- Lumbar puncture is not required for the diagnosis of MS but can test for the presence of oligoclonal IgG bands in the cerebrospinal fluid (CSF), which is supportive of MS
- E.g., if a patient is symptomatic with classic MRI findings showing dissemination in space but there is no known dissemination in time, oligoclonal bands can support a diagnosis of MS (Brain 2018;141:1075)
- Majority of cells in the CSF differential count are lymphocytes (specifically T cells) and the protein levels should be within the reference range (Neurology 2004;63:1966)
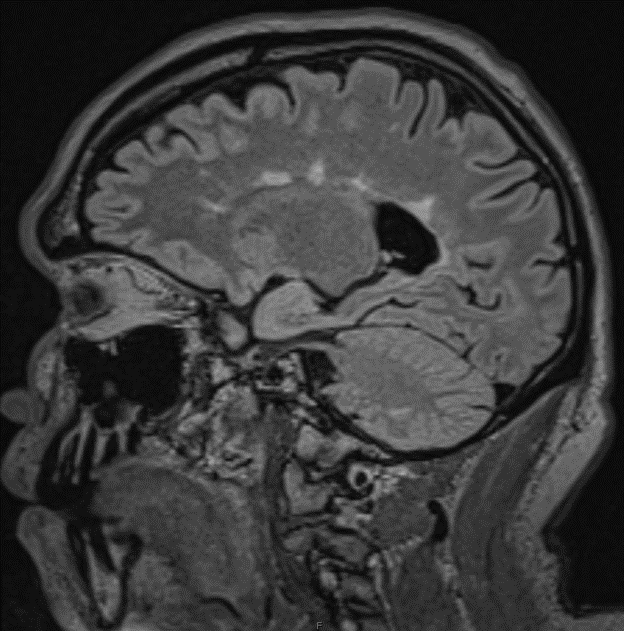
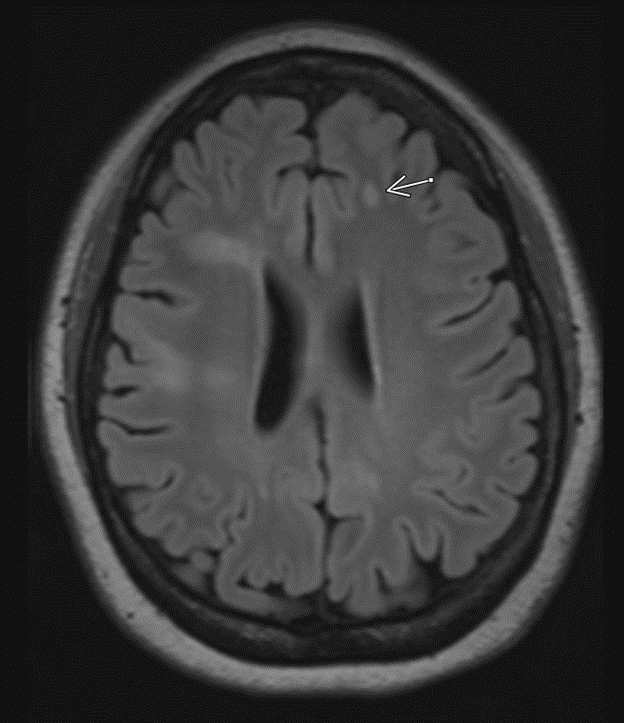
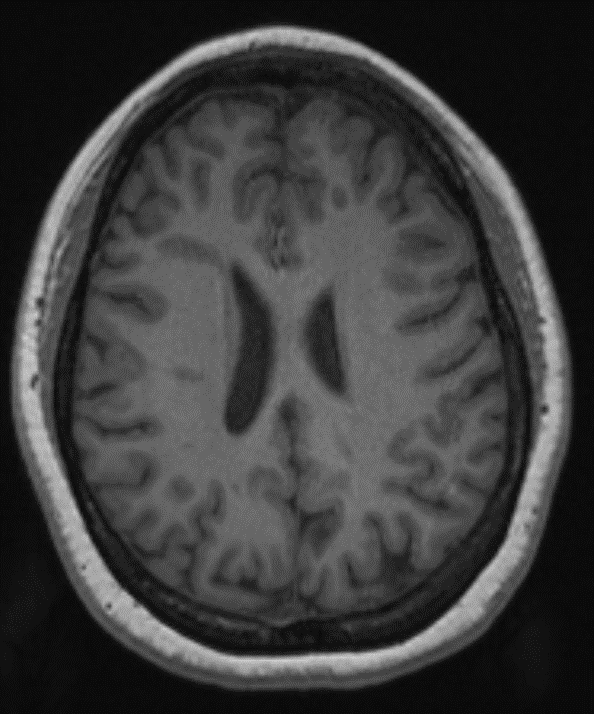
Radiology description
- MRI is the best imaging modality since CT findings can be nonspecific
- Best visualized on T2 / FLAIR sequences:
- Extends perpendicularly on sagittal view, known as Dawson fingers (Cold Spring Harb Perspect Med 2018;8:a028969)
- Enhancement is a nonspecific marker of disease activity
- Tumefactive MS will present as an incomplete / open ring enhancing lesion following contrast administration (Neurol Neuroimmunol Neuroinflamm 2019;6:e589)
- Persistent hypointensities on T1 weighted images are characteristic of chronic plaques and are referred to as black holes (Acta Neurol Scand 2010;122:1)
- Healing or fully healed plaques will convert from hypointense to isointense on T1 (Acta Neurol Scand 2010;122:1)
Radiology images
Prognostic factors
- There are no consistently reliable prognostic factors for MS and outcomes for MS patients cannot be accurately predicted
- Generally, patients with relapsing and remitting courses have a better prognosis than those with progressive forms of the disease (Brain 2006;129:584)
- Rate of cervical cord atrophy, bowel / bladder symptoms at disease onset and incomplete recovery from initial attack are associated with a worse prognosis (Arch Neurol 2006;63:1686)
- Pregnancy is thought to be protective, though disease can worsen in the initial postpartum period (Neurology 2017;89:563)
- Extent of MRI abnormalities does not necessarily correlate with disease severity or prognosis (Neurology 2006;66:1384)
Case reports
- 34 year old woman with acute onset left hemiparesis (Front Neurol 2022;13:891113)
- 36 year old man with blurred vision, vertigo, perioral numbness and confusion (CMAJ 2022;194:E776)
- 41 year old man with dysphagia, apraxia and ataxia (Neurol India 2022;70:1226)
- 47 year old woman with fatigue, blurry vision and numbness 3 weeks after recovering from SARS-CoV-2 infection (Cureus 2021;13:e19036)
Treatment
- Acute exacerbation / episode (Mult Scler 2020;26:1352458520924595)
- High dose glucocorticoids are the mainstay of treatment for an acute exacerbation
- Plasma exchange can be considered in patients with poor response
- Relapsing remitting MS (Mult Scler 2020;26:1352458520924595, Neurology 2018;90:777)
- Monoclonal antibodies (natalizumab, alemtuzumab, ocrelizumab, rituximab) are generally first line therapy
- Oral therapies including fumarates and S1P receptor modulators (siponimod, fingolimod) can be used in patients who do not wish to have or are unable to tolerate infusions / injectables
- Interferons and glatiramer acetate
- Secondary progressive MS
- Same treatment as for relapsing remitting MS, though generally ineffective
- Primary progressive MS
- Ocrelizumab is the only FDA approved drug that has been shown to slow the progression of disease in PPMS (N Engl J Med 2017;376:209)
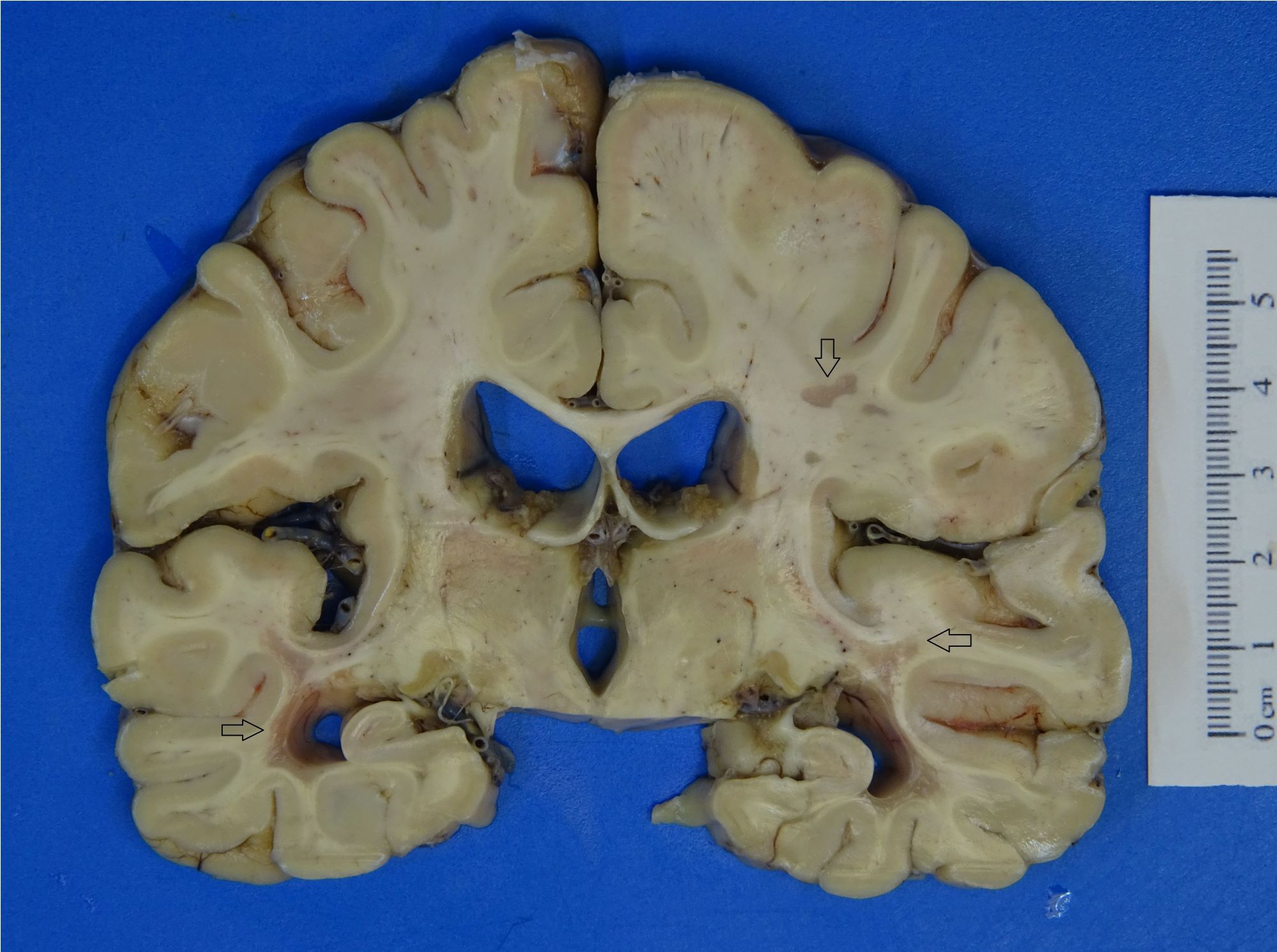
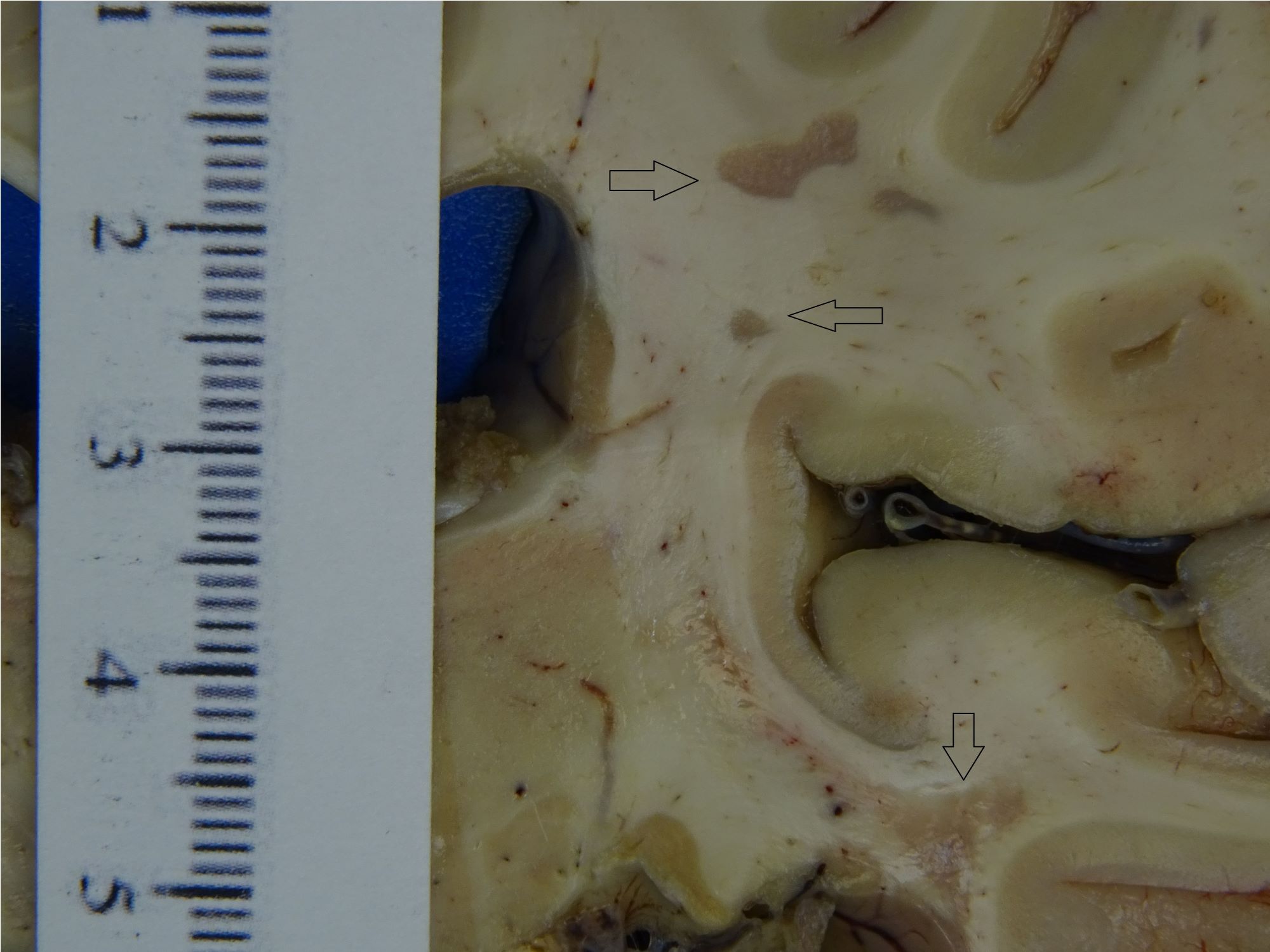
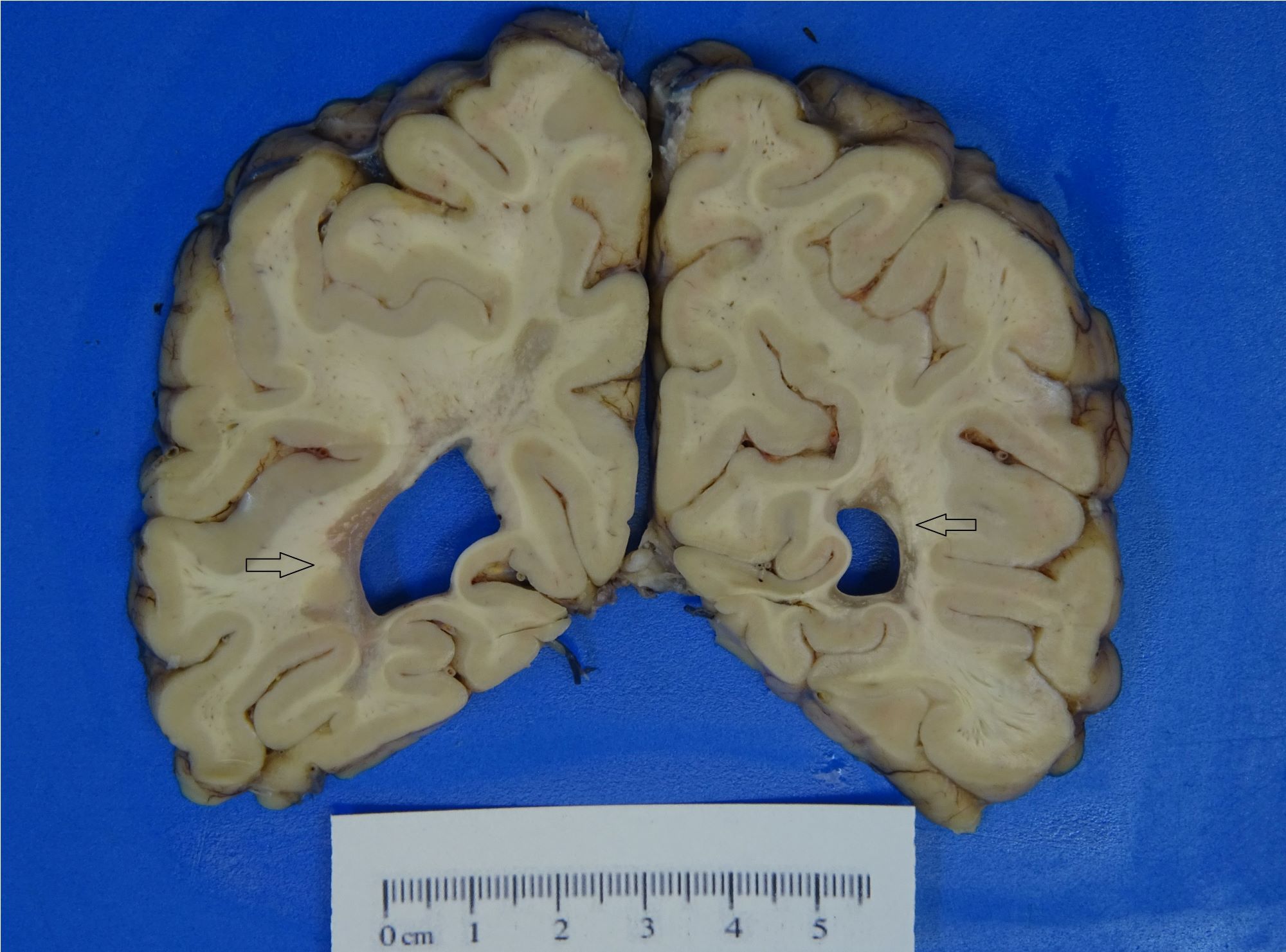
Gross description
- Chronic plaques tend to be rounded, tan-gray and variably sized with a sharp demarcation from the surrounding brain tissue
- More recent lesions will be tan-pink or tan-yellow with less sharply defined borders
- In the spinal cord, plaques will have a fanned out appearance with sharp borders and can potentially involve multiple adjacent signaling pathways (Pract Neurol 2016;16:279)
Gross images
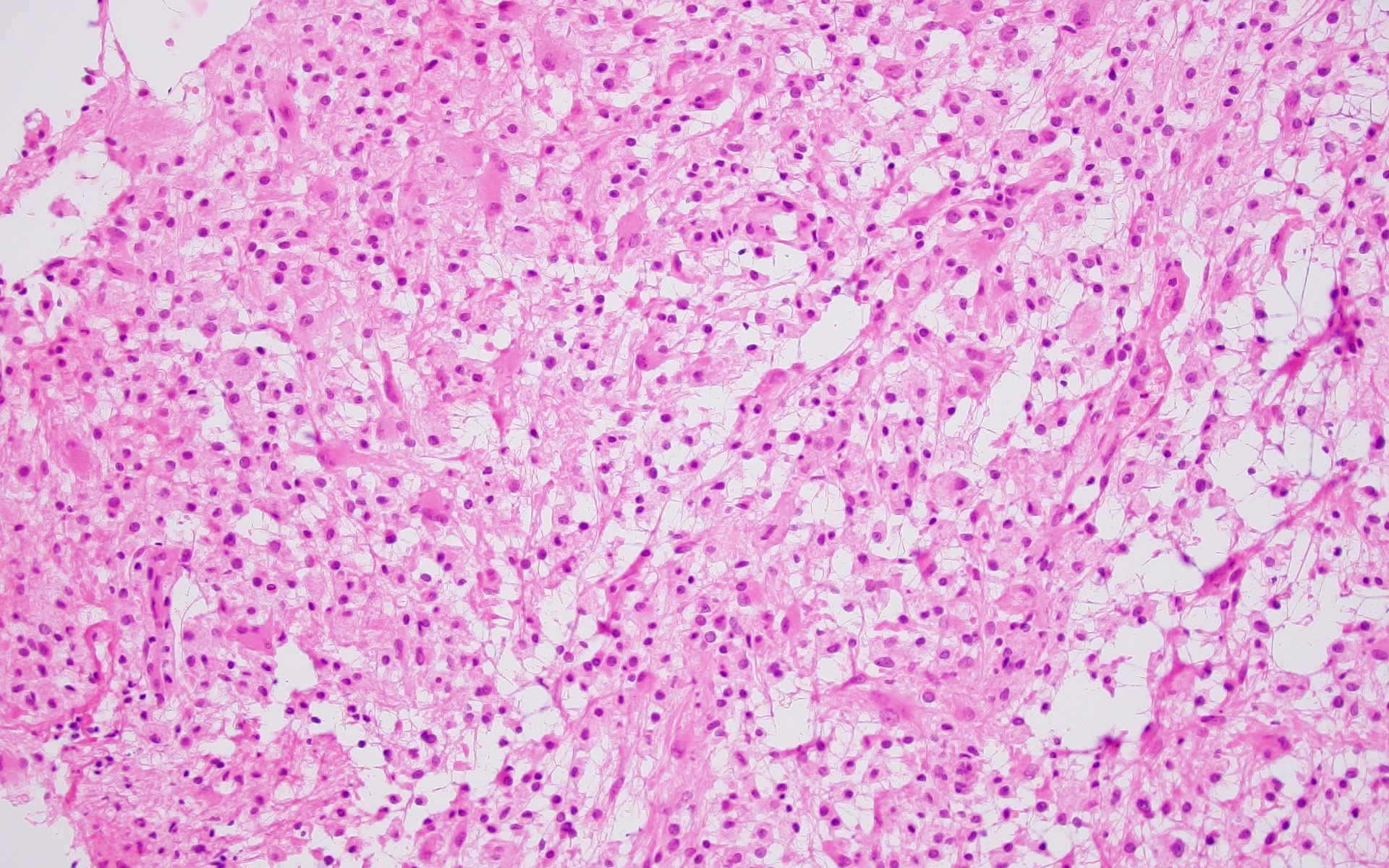
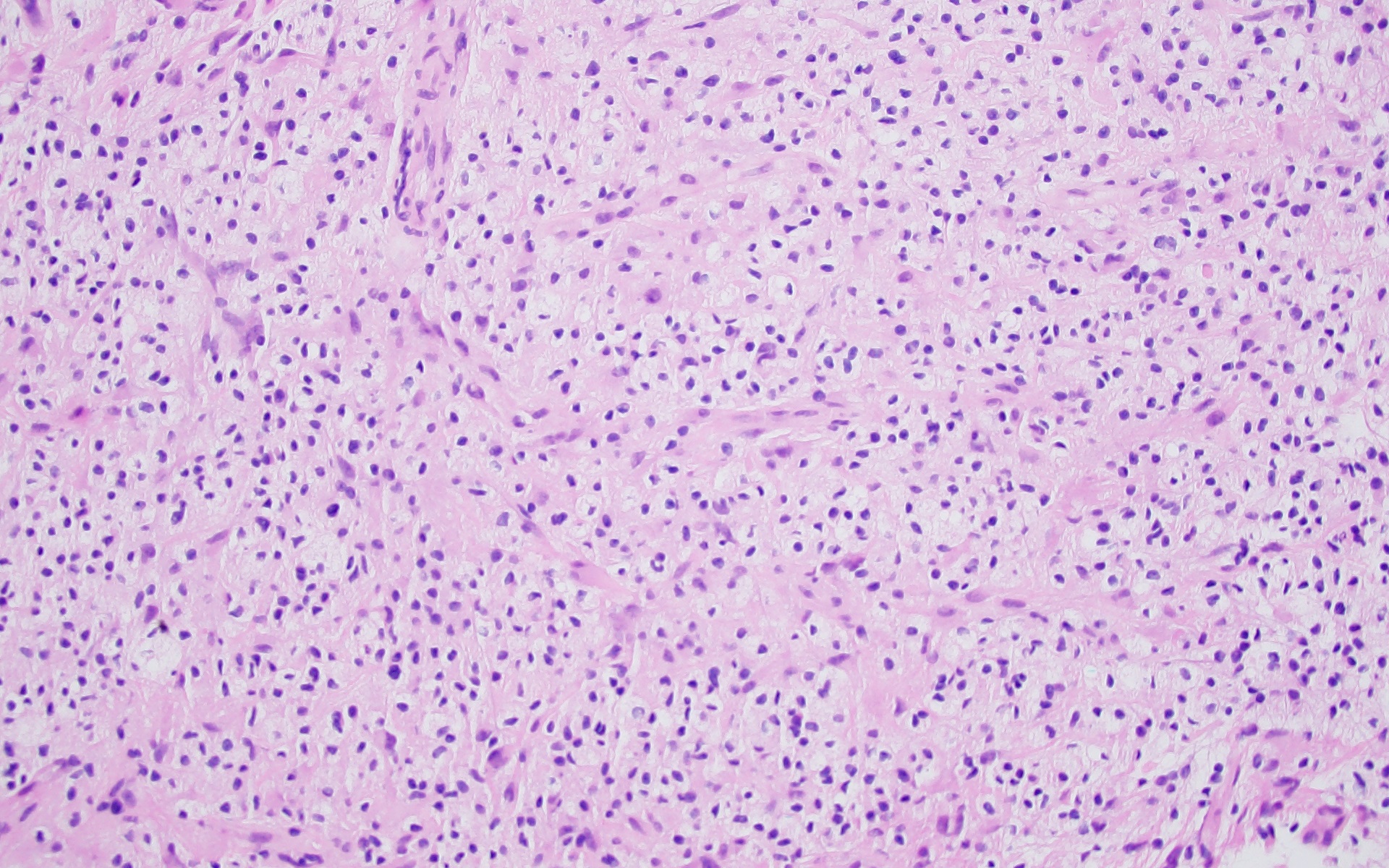
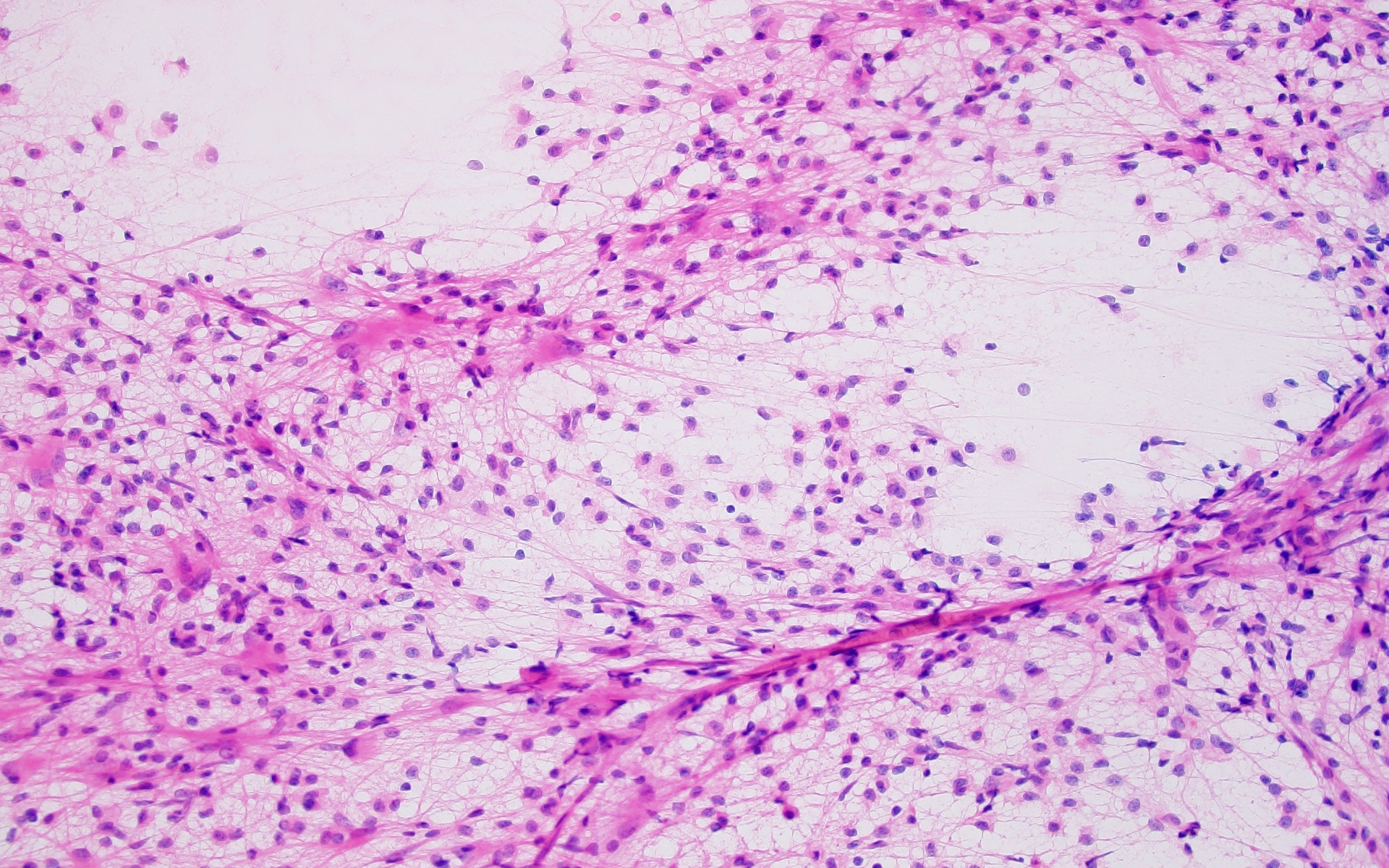
Frozen section description
- Typically only performed in cases of acute tumefactive MS, where there is radiologic suspicion for neoplasm or infection
- Findings are similar for any type of demyelinating disease:
- Sheets of foamy macrophages in a background of reactive gliosis
- Can be misdiagnosed as high grade glioma, especially since reactive atypia and mitotic can activity seen (Creutzfeldt cells)
- Cell populations will be more heterogeneous than neoplastic processes
- On permanent sections, there will be a sharp border between the area of interest and background brain tissue
- Reference: Acta Neuropathol 2017;133:13
Frozen section images
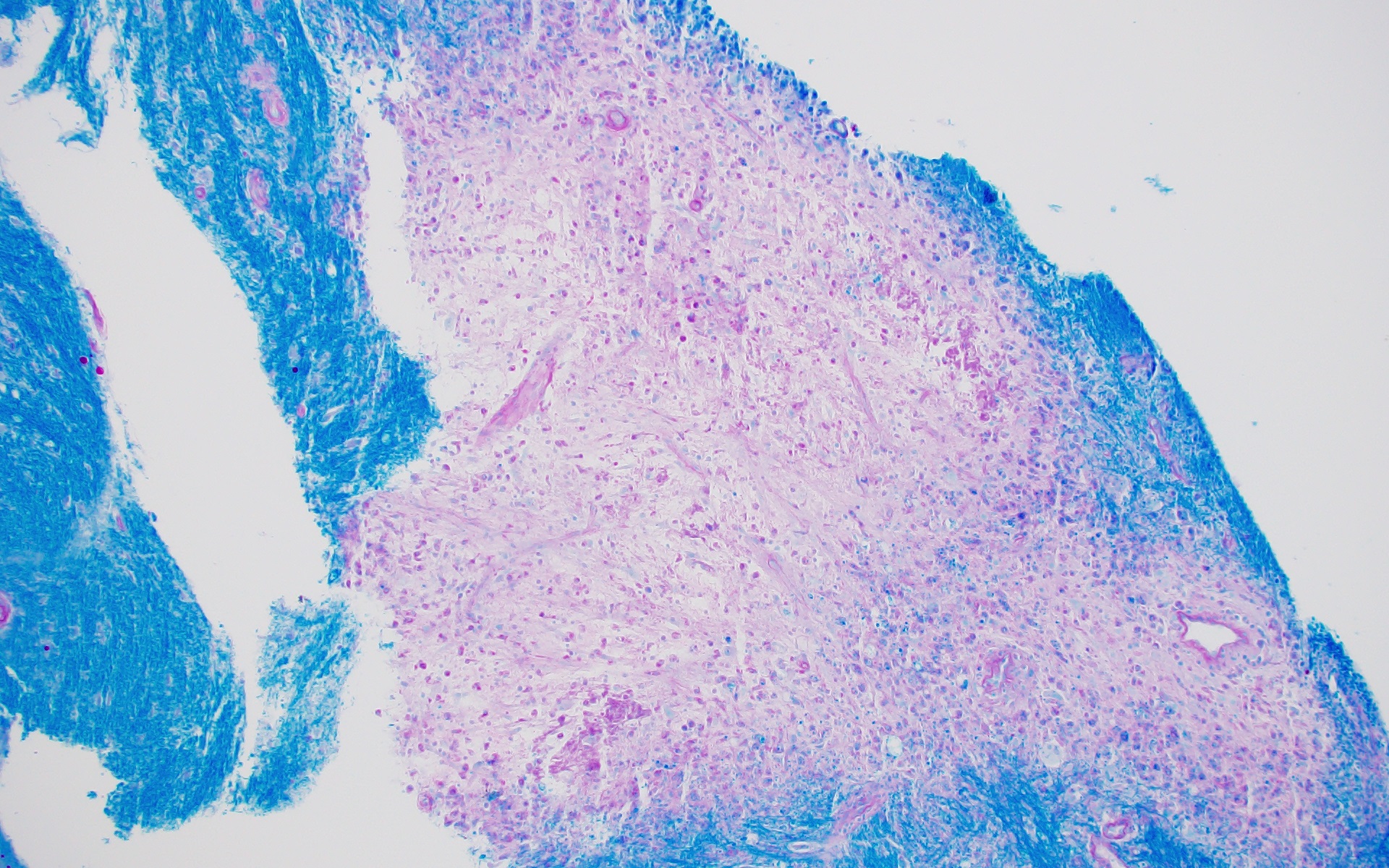
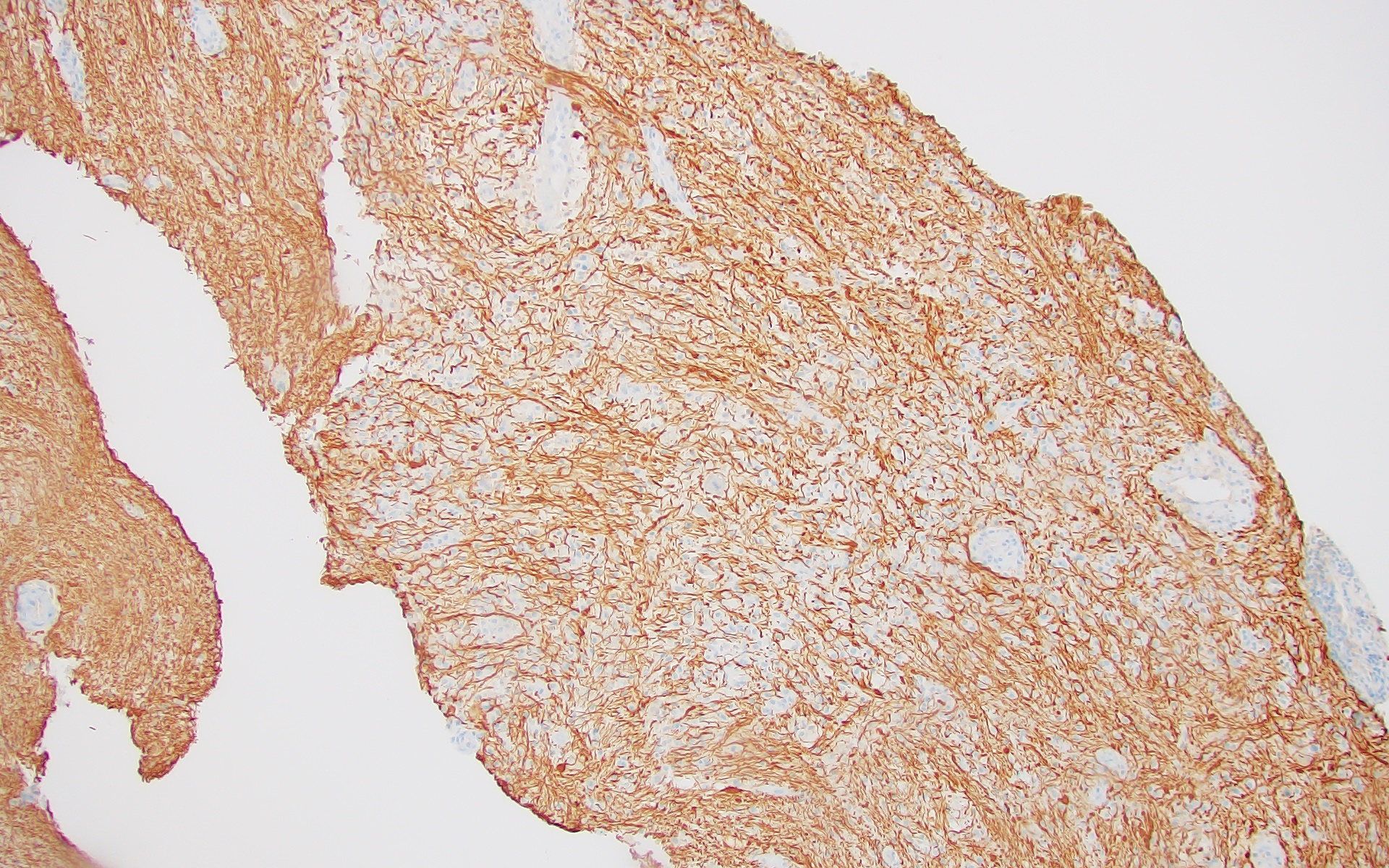
Microscopic (histologic) description
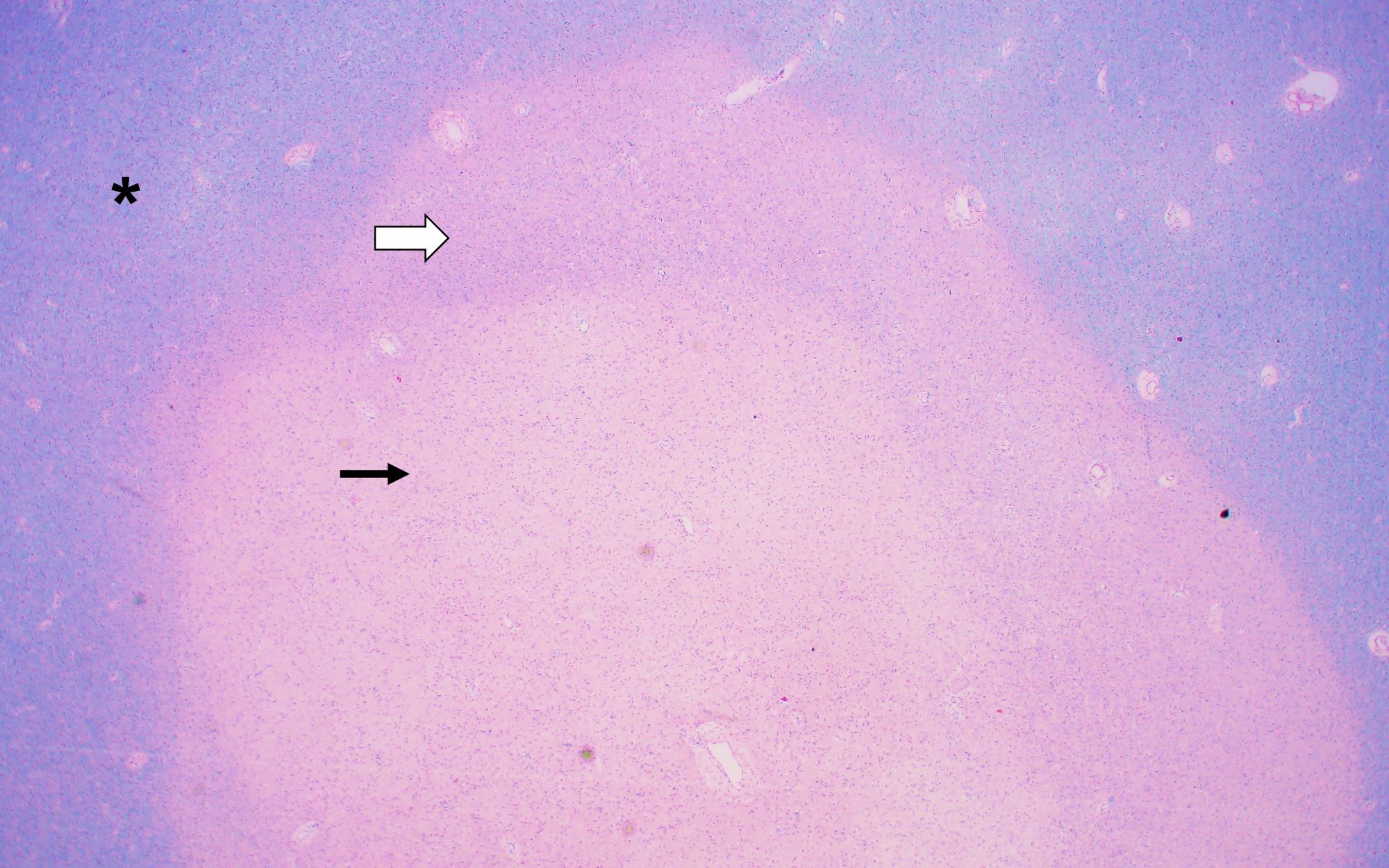
- Active MS plaque (Brain Pathol 2005;15:217):
- Prominent perivascular lymphoid infiltrates consisting predominantly of CD8+ T lymphocytes
- Parenchymal and perivascular macrophages, some with visible myelin globules on Luxol fast blue / periodic acid-Schiff stain (LFB / PAS)
- More specific for active demyelination than lymphocytes
- Preferential loss of myelin with relative axonal preservation and the formation of axonal spheroids (swellings)
- Reactive astrocytosis
- In the periphery of the plaque will see remyelination with thinner myelin sheaths than background axons
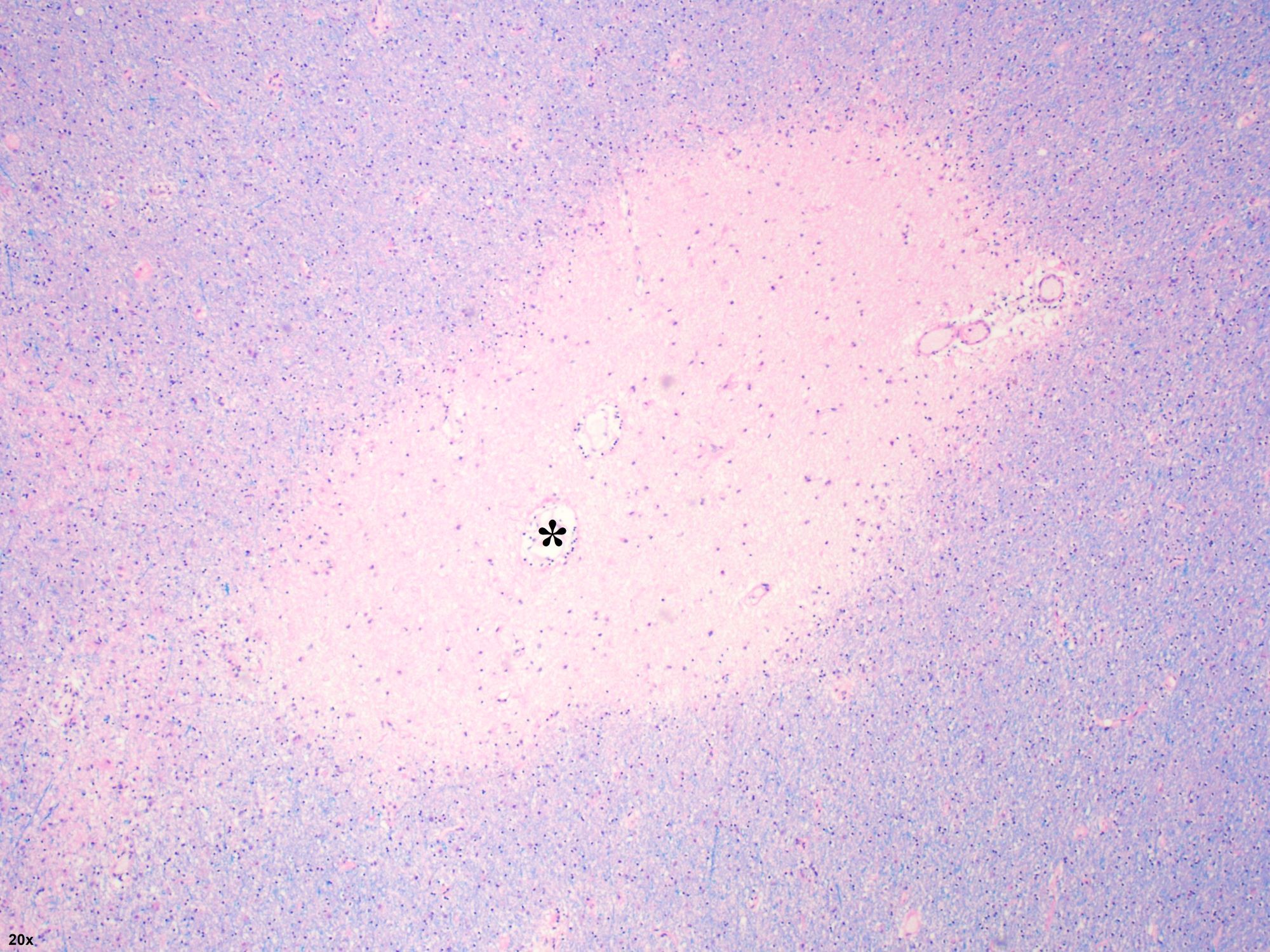
- Chronic / inactive MS plaque (Brain Pathol 2005;15:217):
- Relatively acellular lesions with near complete loss of myelin and sharp borders
- Should not see inflammation (or if present, rare lymphocytes) and will only see oligodendrocytes at the margin
- Reactive gliosis
- Baló concentric sclerosis (Neurol Sci 2004;25:S319):
- Rare histologic subtype of MS with concentric and alternating rings of demyelination and preserved myelin
- Areas of demyelination will show features similar to those of an active MS plaque
- Acute multiple sclerosis, Marburg type (Mult Scler 2015;21:485)
- Multiple, poorly defined plaques
- All plaques are active, with numerous macrophages, reactive astrogliosis and perivascular lymphocyte cuffs
- Sometimes edema or necrosis may be seen
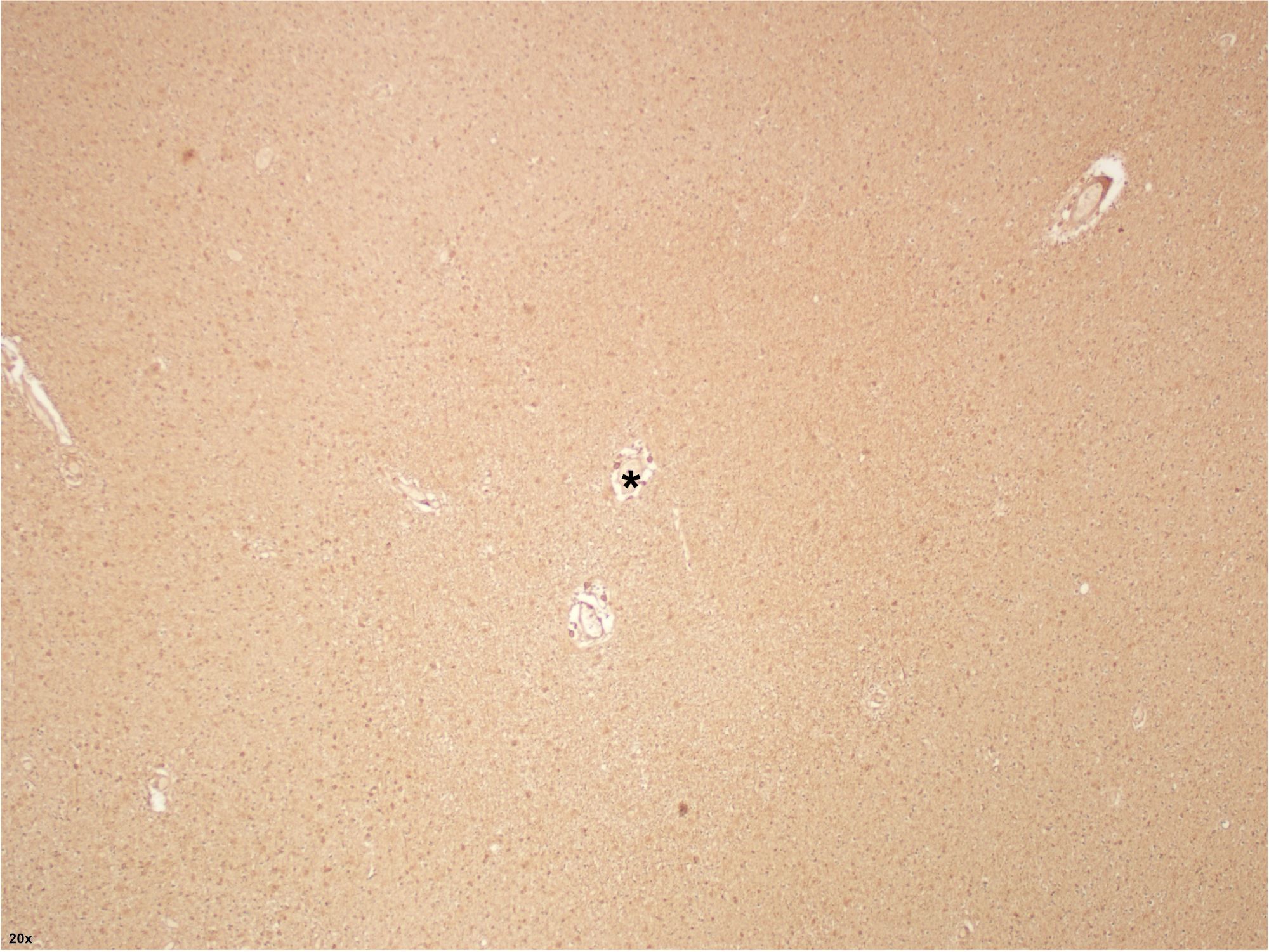
Microscopic (histologic) images
Cytology images
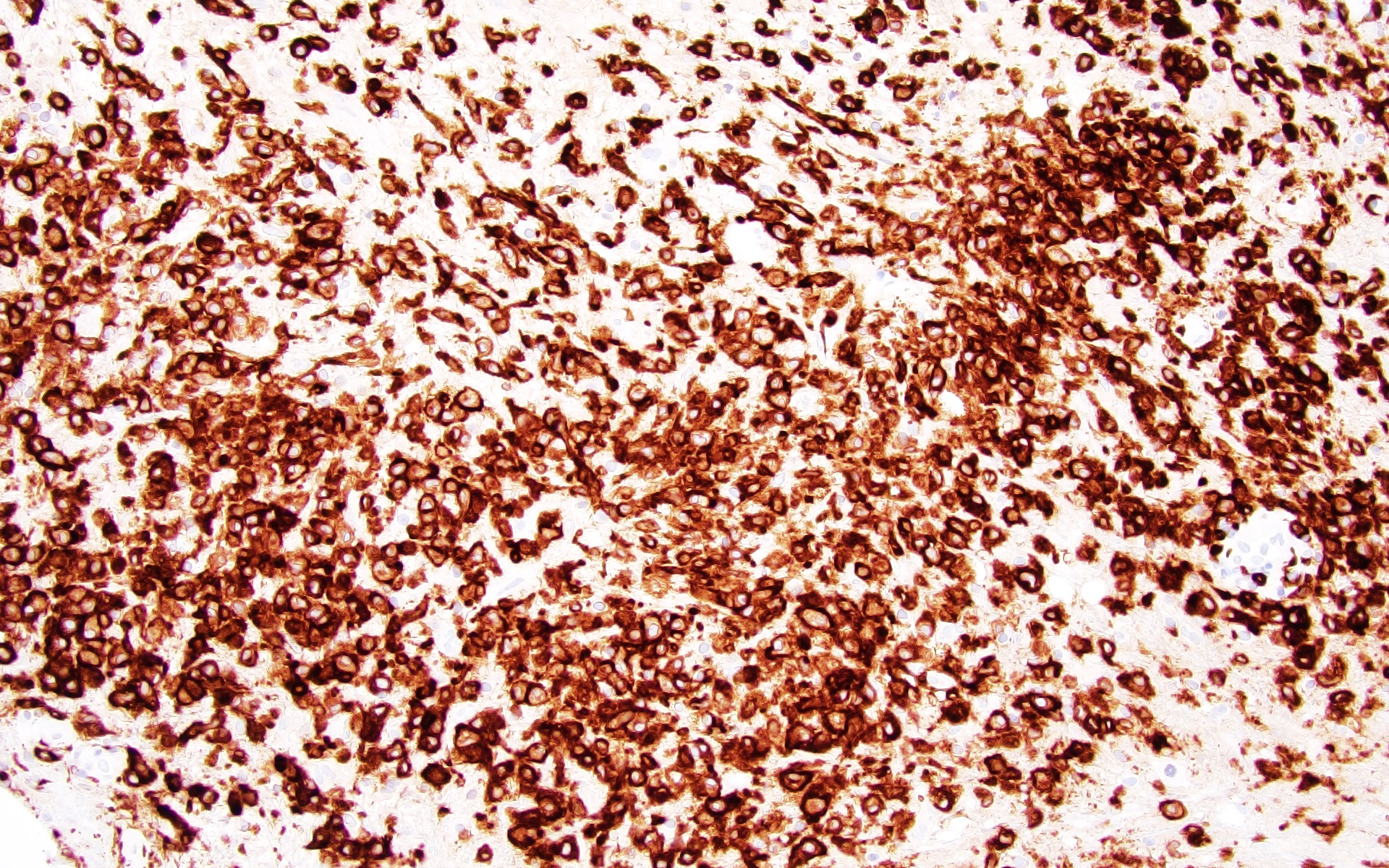
Positive stains
- Luxol fast blue (LFB):
- In active plaques, will highlight normal background myelin with complete loss of staining in the area of demyelination
- Border between demyelination and normal appearing white matter will be distinct but not as sharp as that of an inactive plaque
- In areas where remyelination has occurred, myelin will be present but less dense than the uninvolved white matter (shadow plaque)
- Highlights myelin globules within macrophages in areas of active demyelination
- In active plaques, will highlight normal background myelin with complete loss of staining in the area of demyelination
- CD68 or CD163 will highlight macrophages in areas of active demyelination
- Neurofilament or a silver stain will highlight relative axonal preservation and the presence of occasional axonal spheroids
- GFAP highlights reactive astrogliosis
- Ki67 may be elevated in active plaques
- CD3 will highlight perivascular T lymphocytes but is not necessary for diagnosis
- Reference: Acta Neuropathol 2017;133:13
Negative stains
- Viral stains (HIV, HSV, SV40, etc.)
- Markers of high grade glioma (IDH1 [R132H], p53, ATRX, etc.)
- There should not be a significant CD20+ B cell population
- Reference: Acta Neuropathol 2017;133:13
Electron microscopy description
- No longer used in routine clinical practice
- Active lesions will show lymphocytes entering the endothelium of blood vessels, axonal spheroids filled with mitochondria and neurofilaments, a vesicular network of degenerated myelin surrounding axons and myelin globules within macrophages
- Chronic lesions will show demyelinated axons or remyelinated axons with thinner myelin sheaths (N Engl J Med 2006;354:942)
Sample pathology report
- Brain lesion, left parietal lobe, biopsy:
- Reactive brain tissue with numerous macrophages and evidence of demyelination (see comment)
- Comment: The findings are suggestive of a demyelinating process. Given the radiologic impression of a mass-like lesion in the brain, tumefactive multiple sclerosis should be considered as a diagnostic consideration.
Differential diagnosis
- Cerebral infarction:
- Sheets of macrophages with engulfed myelin and evidence of demyelination (but primarily distributed along vascular territories)
- Loss of axons (as opposed to demyelination, in which axons are relatively spared)
- Other features of hypoxic ischemic injury are generally present
- Neuromyelitis optica (NMO):
- Formerly considered a variant of multiple sclerosis
- Predominantly involves the optic tract and spinal cord, sometimes extensively involving the gray matter
- Unique pathogenesis with antiaquaporin 4 antibodies
- Neutrophils present in areas of demyelination, which are absent in MS
- Prominent axonal loss and destruction of astrocytes
- Acute disseminated encephalomyelitis (ADEM):
- Marked T cell perivascular inflammation with local demyelination, however, will lack large plaque formation
- Often with history of recent viral illness or vaccination
- Self limited with rapid recovery and low probability of lasting neurologic sequelae
- Progressive multifocal leukoencephalopathy (PML):
- Clinical history of immunosuppression
- Multiple foci of demyelination with sheets of macrophages and minimal lymphoid infiltrates
- Unique plum colored viral inclusions in oligodendrocytes and bizarre appearing astrocytes
- Demonstration of JC viral (PCR assay on cerebrospinal fluid; SV40 immunostain on tissue sections)
- Note that MS patients treated with certain immunomodulatory agents (especially natalizumab) are at increased risk of developing PML (Front Neurol 2020;11:579438)
Additional references
Board review style question #1
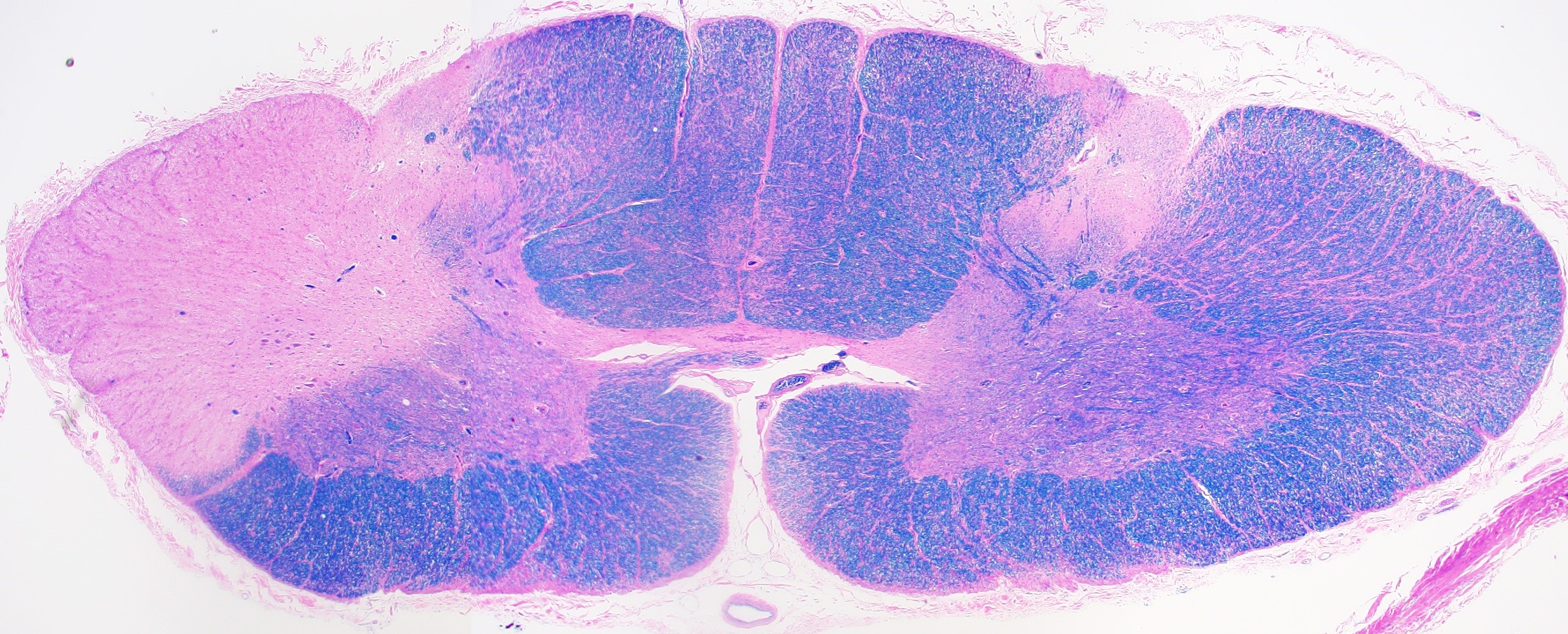
The pathologic features seen in this axial section of the spinal cord (H&E with Luxol fast blue [LFB]) taken at autopsy are most consistent with which of the following conditions?
- Amyotrophic lateral sclerosis
- Foix-Alajouanine syndrome
- Multiple sclerosis
- Subacute combined degeneration
- Tabes dorsalis
Board review style answer #1
C. Multiple sclerosis (MS). As shown in the image, there is asymmetric demyelination in random areas of the spinal cord in MS. Answer A is incorrect because amyotrophic lateral sclerosis shows symmetric degeneration of lateral corticospinal tracts. Answer B is incorrect because Foix-Alajouanine syndrome demonstrates myelopathy caused by dural arteriovenous malformation located in the spinal cord. Answer D is incorrect because subacute combined degeneration demonstrates relatively symmetric degeneration of both the lateral corticospinal tracts and the dorsal columns. Answer E is incorrect because tabes dorsalis shows symmetric degeneration of dorsal columns and dorsal nerve roots.
Comment Here
Reference: Multiple sclerosis
Comment Here
Reference: Multiple sclerosis
Board review style question #2
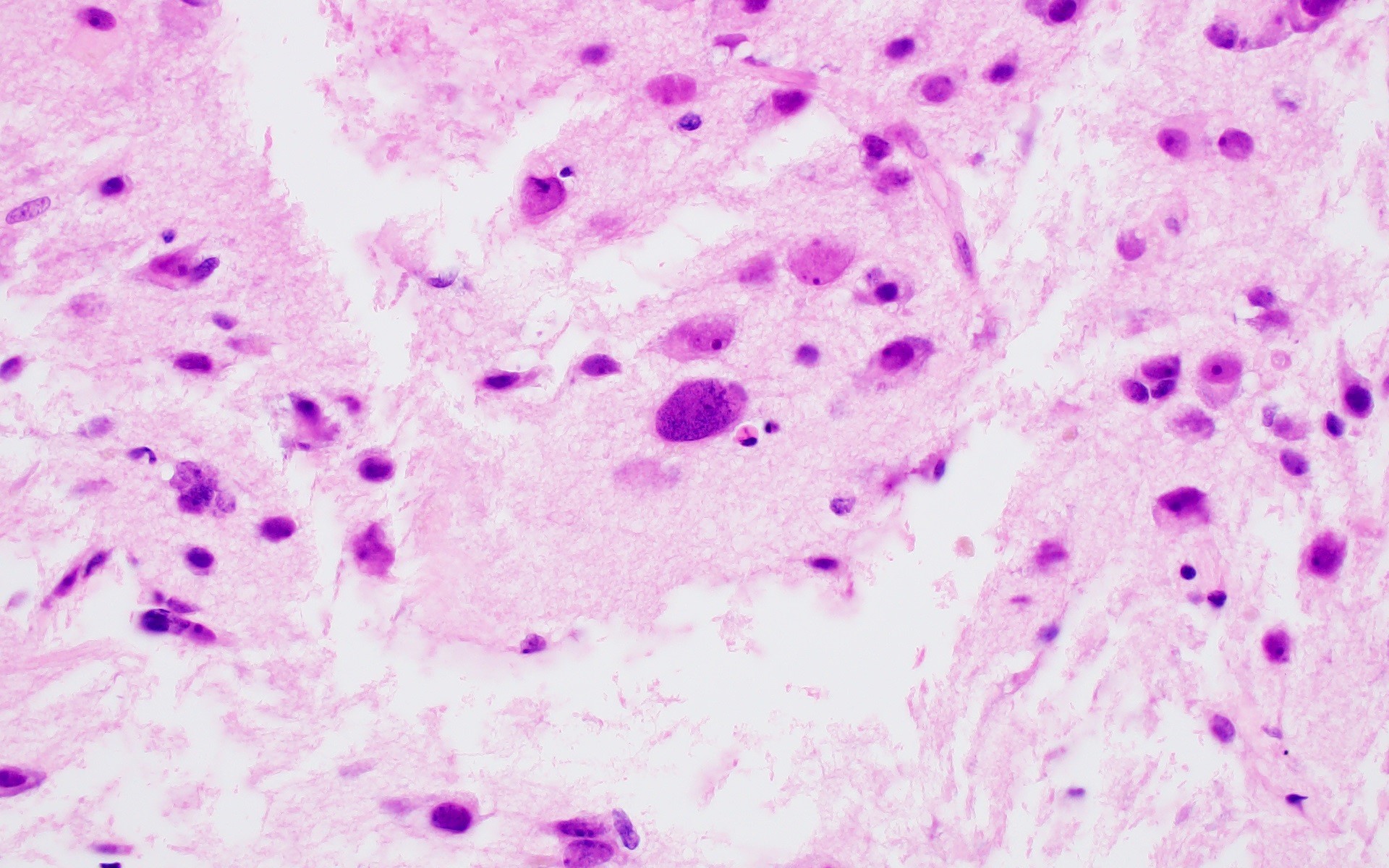
A 48 year old woman with multiple sclerosis treated with natalizumab develops numerous FLAIR signal abnormalities in the right centrum semiovale and left occipital lobe white matter. The patient deteriorated clinically and died 2 weeks after presentation. Brain autopsy was performed, revealing the microscopic features shown in the image above in areas of FLAIR signal abnormality. What is the most likely diagnosis?
- Active multiple sclerosis plaque
- Acute disseminated encephalomyeltis
- Infiltrating astrocytoma
- Progressive multifocal leukoenceophalopathy
- Toxoplasma encephalitis
Board review style answer #2
D. Progressive multifocal leukoencephalopathy (PML). The presence of macrophages, reactive gliosis, bizarre appearing astrocytes and plum colored oligodendroglial inclusions, along with the characteristic history described in the vignette, is most suggestive of PML. Active multiple sclerosis lesion is incorrect: active MS lesions are characterized by numerous macrophages and reactive gliosis; however, viral inclusions would not be seen in oligodendrocytes. Acute disseminated encephalomyelitis is incorrect: this is a monophasic demyelinating illness, distinct from multiple sclerosis and classically associated with recent viral infection or immunization; viral inclusions would not be seen in oligodendrocytes. Infiltrating astrocytoma is incorrect: while the atypical glial cells shown in the image might raise a concern for an infiltrating astrocytoma, the clinical history and imaging findings are not suggestive of a neoplastic process. Toxoplasma encephalitis is incorrect: Toxoplasma infection in the brain is characterized by necrotizing abscesses and the presence of parasites within pseudocysts (bradyzoites) or free parasites (tachyzoites).
Comment Here
Reference: Multiple sclerosis
Comment Here
Reference: Multiple sclerosis