Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Nisarga P, Gyure KA. Radiation injury. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cnsradiationinjury.html. Accessed April 25th, 2024.
Definition / general
- Radiation therapy is commonly used as adjuvant therapy for primary and secondary malignant CNS neoplasms
- Includes autonomic, cognitive and functional deficits
- Spectrum of toxic CNS effects is classified based on time of appearance of symptoms
- Histological features range from no obvious lesions to overt brain necrosis
Essential features
- Radiation injury mainly affects white matter
- Typically classified based on time of appearance of symptoms
- Late focal radiation injury: differential diagnosis includes recurrent / residual tumor
- Acute, early delayed and late (diffuse) radiation injury: clinical and radiological diagnosis
Terminology
- Radiation induced brain injury
- CNS lesions secondary to radiation injury are typically classified based on time of appearance of symptoms (see Diagrams / tables) (Radiat Res 2000;153:357)
- Acute radiation induced brain injury: days to weeks
- Early delayed radiation induced brain injury: weeks to 3 - 6 months
- Late radiation induced brain injury (focal and diffuse): > 3 - 6 months
- CNS lesions secondary to radiation injury are typically classified based on time of appearance of symptoms (see Diagrams / tables) (Radiat Res 2000;153:357)
- Treatment induced necrosis of brain (in neurooncology setting): also known as late radiation induced brain injury, focal type; includes chemoradiation or only radiation effects
- Necrotizing leukoencephalopathy: diffuse white matter injury following chemotherapy with or without radiation (AJNR Am J Neuroradiol 1991;12:45)
- Radiation induced brain cavernomas (Acta Biomed 2019;90:77)
- Radiation induced brain aneurysms (World Neurosurg 2020;135:339)
- Additional terminologies
- Pseudoprogression - transient, weeks to < 6 months
- Progressive disease - recurrent / residual disease status post therapy
- Pseudoresponse - frequently observed in high grade glioma patients treated with angiogenesis inhibitors (e.g.. bevacizumab) (Semin Neurol 2017;37:589)
ICD coding
- ICD-10: G93.89 - other specified disorders of brain
- Not well characterized
- Applicable to postradiation encephalopathy
Epidemiology
- Radiation therapy (adjuvant) for primary and secondary malignant CNS neoplasms
- Prevalence of late radiation induced brain injury
- Based on clinical and imaging features: 37 - 58% among survivors, with an overall prevalence of 14% (AJNR Am J Neuroradiol 1991;12:45)
- Based on histologic features: 4 - 5% (Int J Radiat Oncol Biol Phys 1981;7:243, Cancer 1975;36:1681)
Sites
- White matter in field of (or adjacent to) previous radiation therapy in primary and metastatic CNS neoplasms
- White matter of inferior temporal lobe and lower part of brain stem in nasopharyngeal carcinomas
- Based on site, radiation induced brain injuries are classified as (IntechOpen: Radiation Induced Brain Injury After Radiotherapy for Brain Tumor [Accessed 7 April 2023])
- Cerebral type
- Brain stem type
- Cerebellar type
- Mixed type
- Based on site, radiation induced brain injuries are classified as (IntechOpen: Radiation Induced Brain Injury After Radiotherapy for Brain Tumor [Accessed 7 April 2023])
Pathophysiology
- Acute radiation induced brain injury: disruption of blood brain barrier, edema and increased intracranial pressure (focal)
- Early delayed radiation induced brain injury: transient demyelination
- Late radiation induced brain injury (focal and diffuse): microvascular injury resulting in tissue hypoxia, demyelination and gliosis, white matter necrosis
- Experimental hypothesis
- Vascular hypothesis (late radiation injury)
- Radiation induced vascular changes: vessel wall thickening, vessel dilation and endothelial cell nuclear enlargement (dose dependent); capillary rarefaction
- Parenchymal / glial hypothesis
- Dynamic interaction between the 2 hypotheses
- Vascular hypothesis (late radiation injury)
- Pseudoprogression
- Not well understood (Neuro Oncol 2019;21:1118)
- Transient interruption of myelin synthesis secondary to radiation injury to oligodendrocytes could be a possible mechanism (Int J Mol Sci 2014;15:11832)
- Higher incidence in treated MGMT methylated glioblastoma (2 times) compared to the unmethylated tumors (J Clin Oncol 2008;26:2192)
- Reference: Front Oncol 2012;2:73
Etiology
- Unknown predisposing intrinsic factors (brain location treated, age, clinical status, tumor diagnosis and genetic susceptibility) (Neurooncol Adv 2020;2:vdaa057, Neuro Oncol 2019;21:1118)
- Partly identified extrinsic factors (dose / technique of the therapy) (Neurooncol Adv 2020;2:vdaa057, Neuro Oncol 2019;21:1118)
- Acute CNS syndrome is seen with > 30 Gy; white matter necrosis is seen with > 60 Gy
- Uncommon with modern radiation techniques (Front Oncol 2012;2:73)
- Late radiation injury (both focal and diffuse) is seen with the modern radiation techniques (Front Oncol 2012;2:73)
Clinical features
- Latency: 0 - 32 years (mean: 6 years)
- Clinical features are heterogeneous and difficult to predict
- Acute radiation induced brain injury: headache, fatigue and drowsiness
- Transient worsening of symptoms
- Early delayed radiation induced brain injury: generalized weakness, somnolence, attention deficits and short term memory loss
- Usually transient
- Late radiation induced brain injury: reflects damage to both hippocampal and nonhippocampal dependent domains (irreversible / progressive / fatal)
- Focal radiation injury: focal neurologic deficits and focal increase in intracranial pressure
- Indistinguishable from symptoms due to a mass of any kind
- Principal clinical differential diagnosis is recurrent / residual tumor (progressive disease)
- Diffuse radiation injury (cognitive impairment): decreased verbal memory, spatial memory, attention, problem solving ability and executional functions
- Can also have depression, anxiety and somatization
- Focal radiation injury: focal neurologic deficits and focal increase in intracranial pressure
- Advanced stages: dementia, stupor state, hallucinations and delusion
- Pseudoprogression
- Occurs in ~21 - 31% of malignant gliomas treated with radiation and chemotherapy
- Significant mass effect and clinical neurologic deficits (Semin Neurol 2017;37:589)
- Suggest a transient course with spontaneous recovery (Int J Mol Sci 2014;15:11832)
- References: IntechOpen: Radiation Induced Brain Injury After Radiotherapy for Brain Tumor [Accessed 7 April 2023], Front Oncol 2012;2:73, Neuro Oncol 2019;21:1118
Diagnosis
- Acute, early delayed and late (diffuse) radiation injury: clinical and radiological diagnosis
- Late (focal) radiation injury (diagnostic ambiguity)
- Clinically and radiographically overlap with recurrent / residual disease
- Histopathologic diagnosis depends on pathologist's experience and subjective impression
- Radiation necrosis versus recurrent / residual tumor
- Requires multidisciplinary approach (neuropathologist, neuroradiologist, radiation oncologist, neurosurgeon and neurooncologist) (J Neurooncol 2013;113:485)
- Reference: Neuro Oncol 2019;21:1118
Radiology description
- Late (focal) radiation injury
- CT: focal hypodensity, contrast enhancement, mass effect
- MRI: focal decreased signal on T1WI; focal hyperintensity on T2WI, contrast enhancement, mass effect
- Late (diffuse) radiation injury
- CT: diffuse white matter hypodensity, contrast enhancement, mass effect
- MRI: diffuse decreased white matter signal on T1WI; diffuse white matter hyperintensity on T2WI
- Pseudoprogression
- Represents a unique, transient, predominantly radiographic phenomenon encountered in patients with high grade glioma status post chemoradiation
- MRI - increase in abnormal nodular enhancement on T1 post contrast; increase in T2/FLAIR signal hyperintensities (suggestive of cerebral edema) (Semin Neurol 2017;37:589)
- Reference: AJNR Am J Neuroradiol 1991;12:45
Radiology images
Images hosted on other servers:
Prognostic factors
- Radiation necrosis and pseudoprogression without active tumor is associated with better prognosis (J Neurooncol 2013;113:485)
- Active malignant tumor portends poor prognosis (percentage treatment response has limited prognostic value) (J Neurooncol 2019;141:421)
- Increased Ki67 proliferation index is associated with worse prognosis
- See Etiology
Case reports
- 23 year old woman with remote history of low grade brainstem glioma, with delayed radiation induced stroke (Pediatr Neurol 2019;98:87)
- 37 year old man with radiation retinopathy after external beam irradiation for nasopharyngeal carcinoma (Pract Radiat Oncol 2018;8:366)
- 52 year old man with cystic radiation encephalopathy after radiotherapy treatment for nasopharyngeal carcinoma (BMC Neurol 2021;21:59)
- 59 year old man's autopsy revealing late delayed radiation injury following radiotherapy treatment at age 14 (Neuropathology 2019;39:106)
Treatment
- Symptomatic treatment
- Oral corticosteroids for symptomatic cases
- Resection with frozen section diagnosis
- No known medical therapy for cognitive impairment (Front Oncol 2012;2:73)
- Hippocampal avoidance strategies
- Stereotactic conformal radiotherapy
- Intensity modulated radiotherapy
- Proton beam therapy
- Potential therapies under investigation (IntechOpen: Radiation Induced Brain Injury After Radiotherapy for Brain Tumor [Accessed 7 April 2023], Neurooncol Adv 2020;2:vdaa057)
- Antiplatelet and anticoagulation
- Reactive oxygen species (ROS) scavengers
- Improving microcirculation: butylphthalide
- Neurogenesis: neural stem cell therapy
- Renin angiotensin system inhibitors
- Anti-VEGF antibody
- Hyperbaric oxygen treatment
- Exercise
- Small molecule compounds targeting p53 isoform Δ133p53α
- Peroxisomal proliferator activated receptor agonists
- Memantine
- Lithium
Gross description
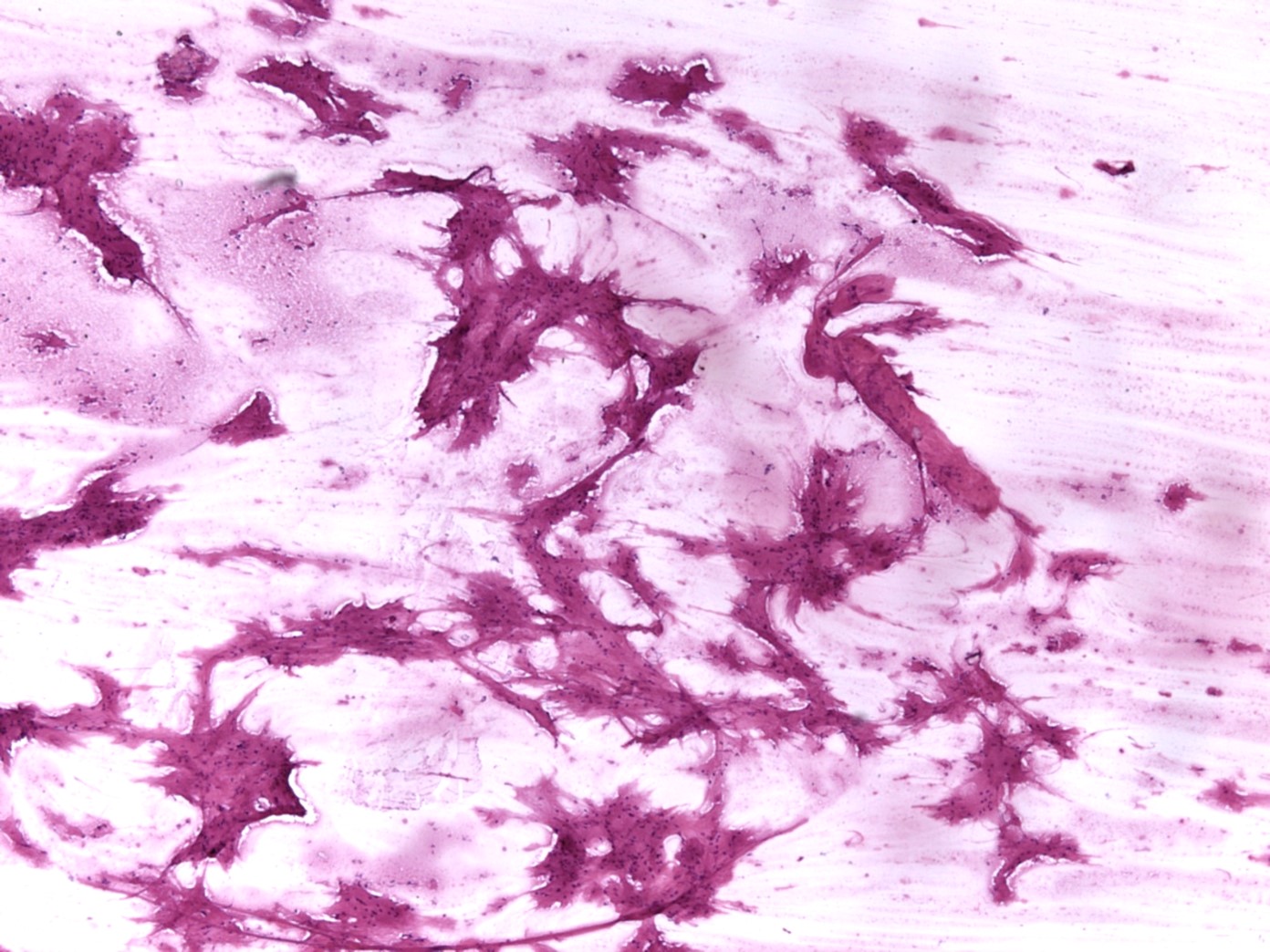
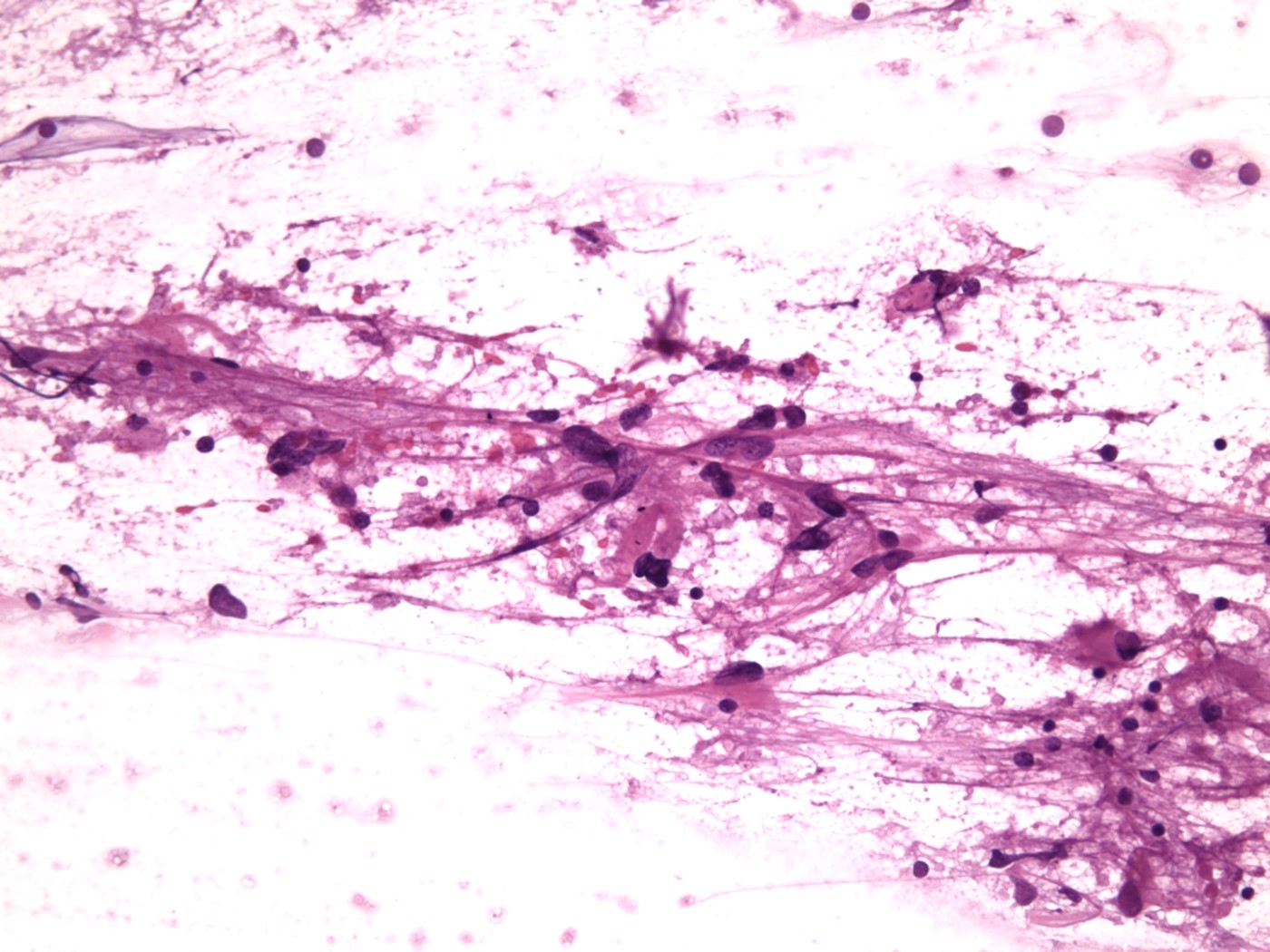
Frozen section description
- Gross: see Gross description
- Squash / smears: see Cytology description
- Microscopy
- Challenging to differentiate between postradiation effects (radiation induced atypia) and brain tumor (residual / recurrent)
- Experience improves accuracy
- Seek second opinion when unsure
- See Microscopic (histologic) description - focal late radiation injury; and see Differential diagnosis - focal late radiation induced brain injury (treatment induced necrosis) versus recurrent / residual tumor
Frozen section images
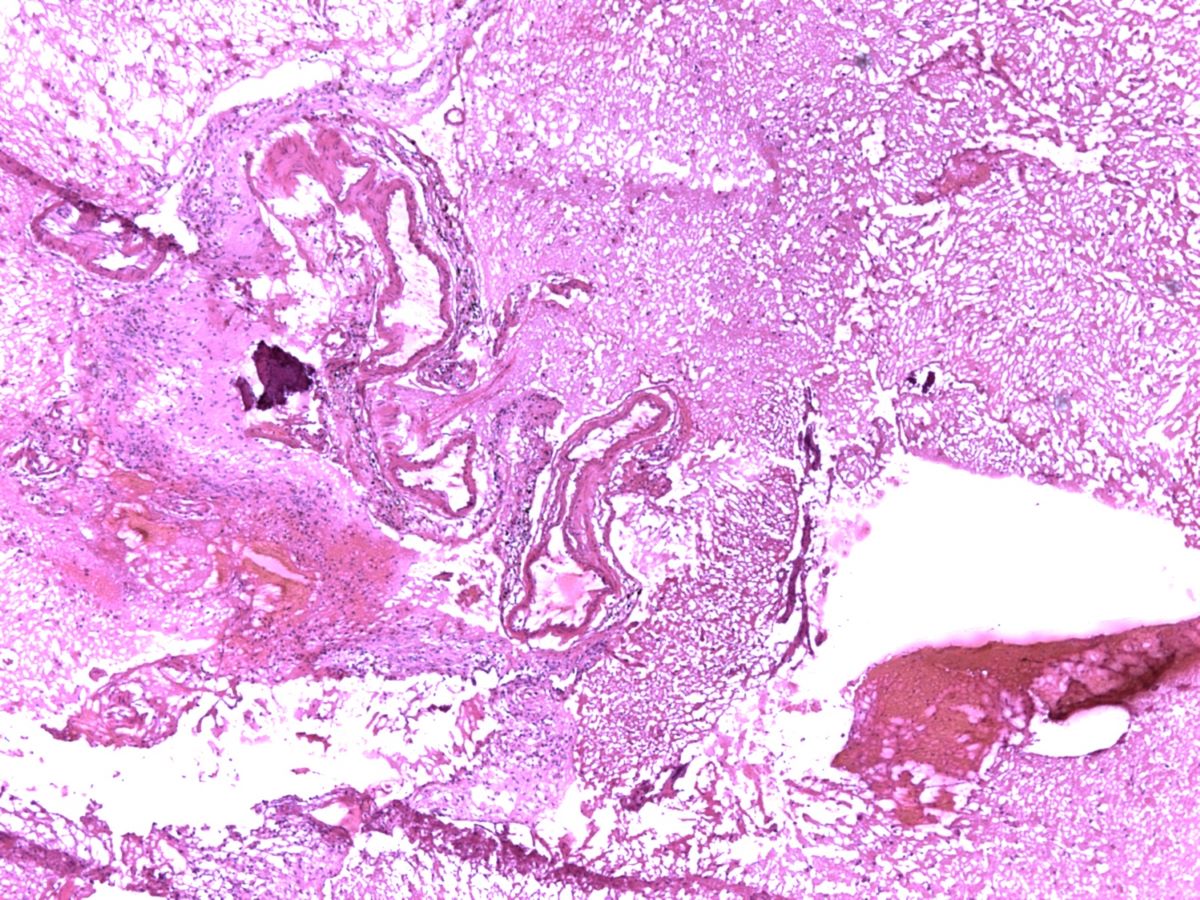
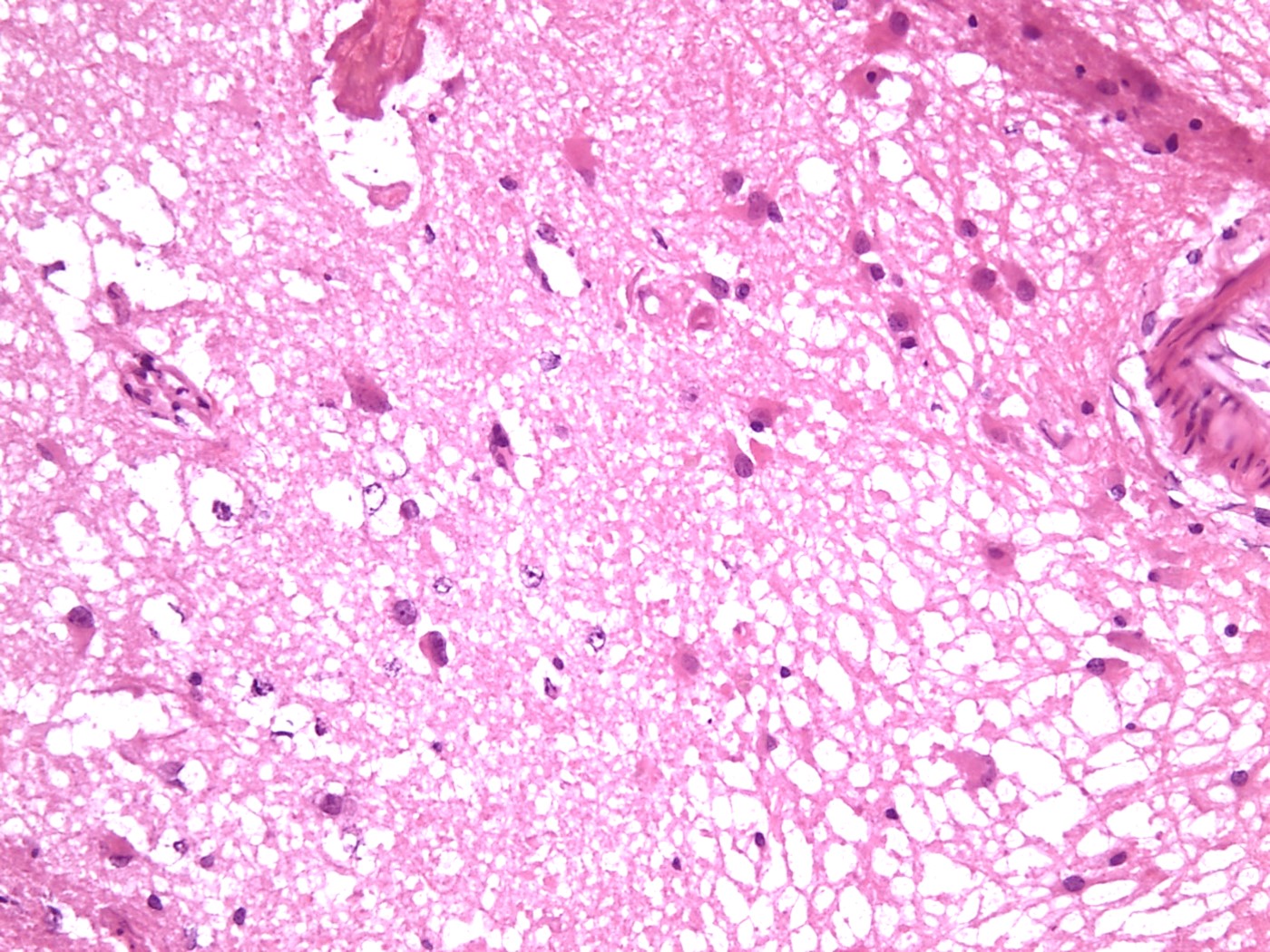
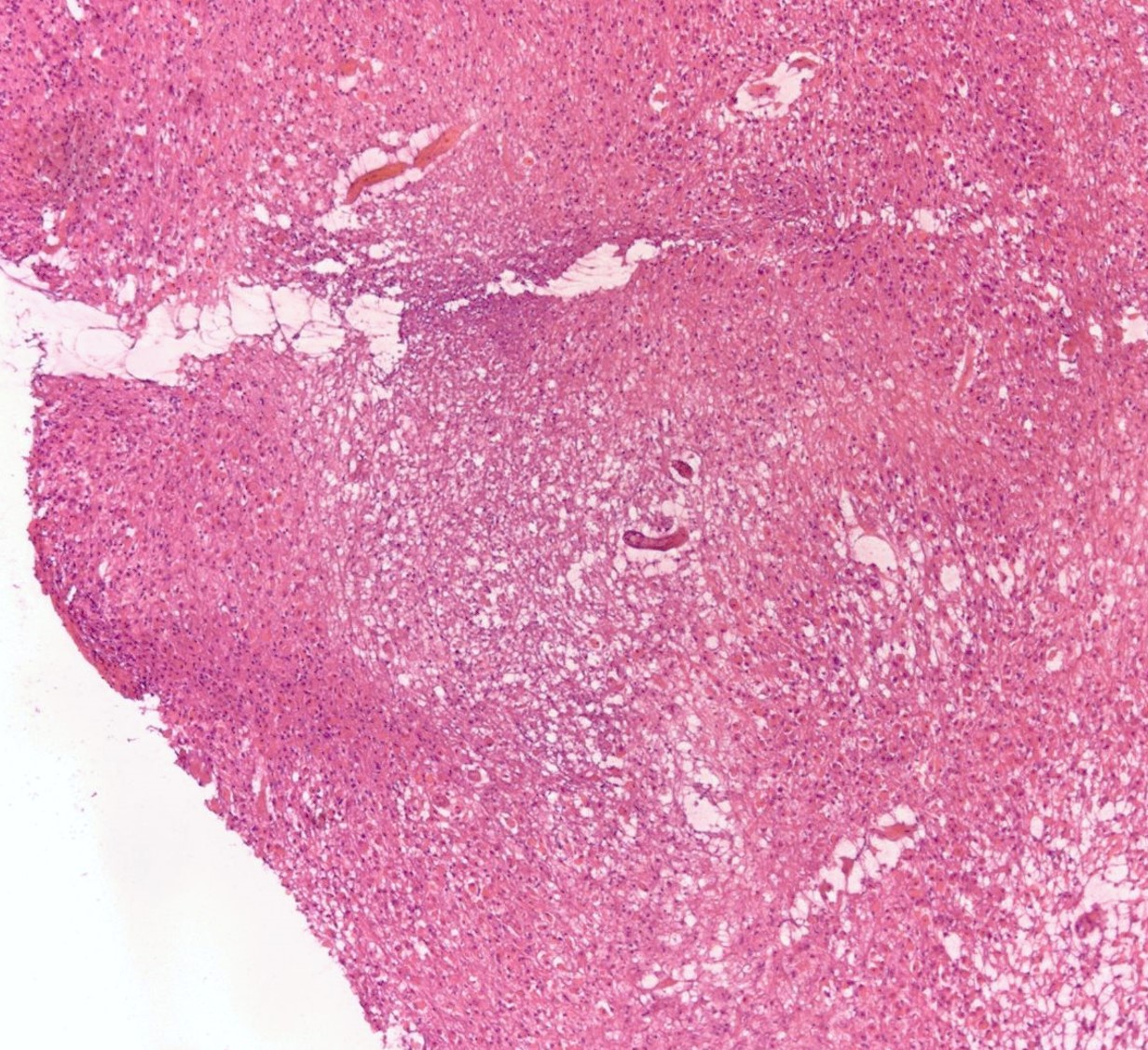
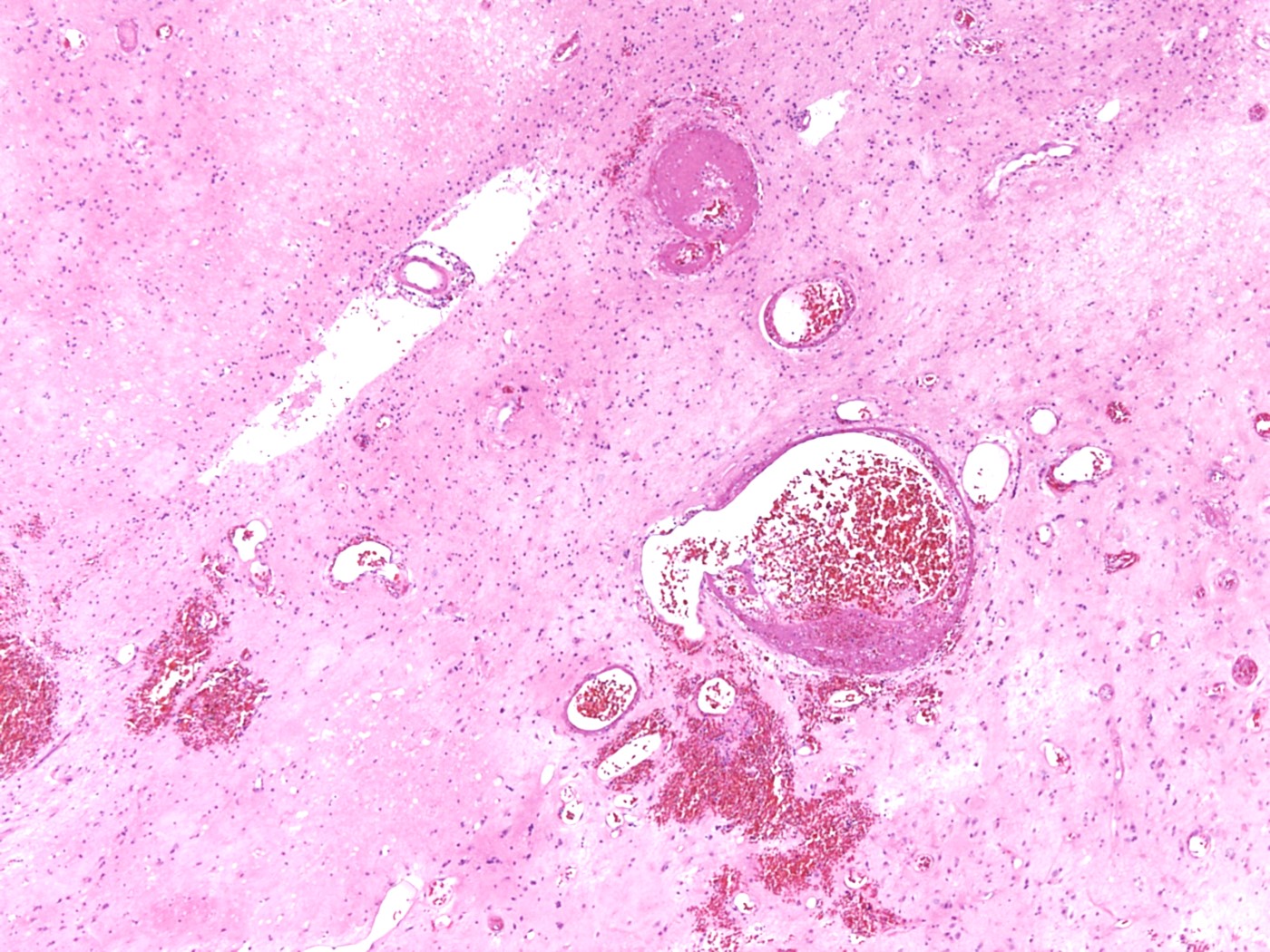
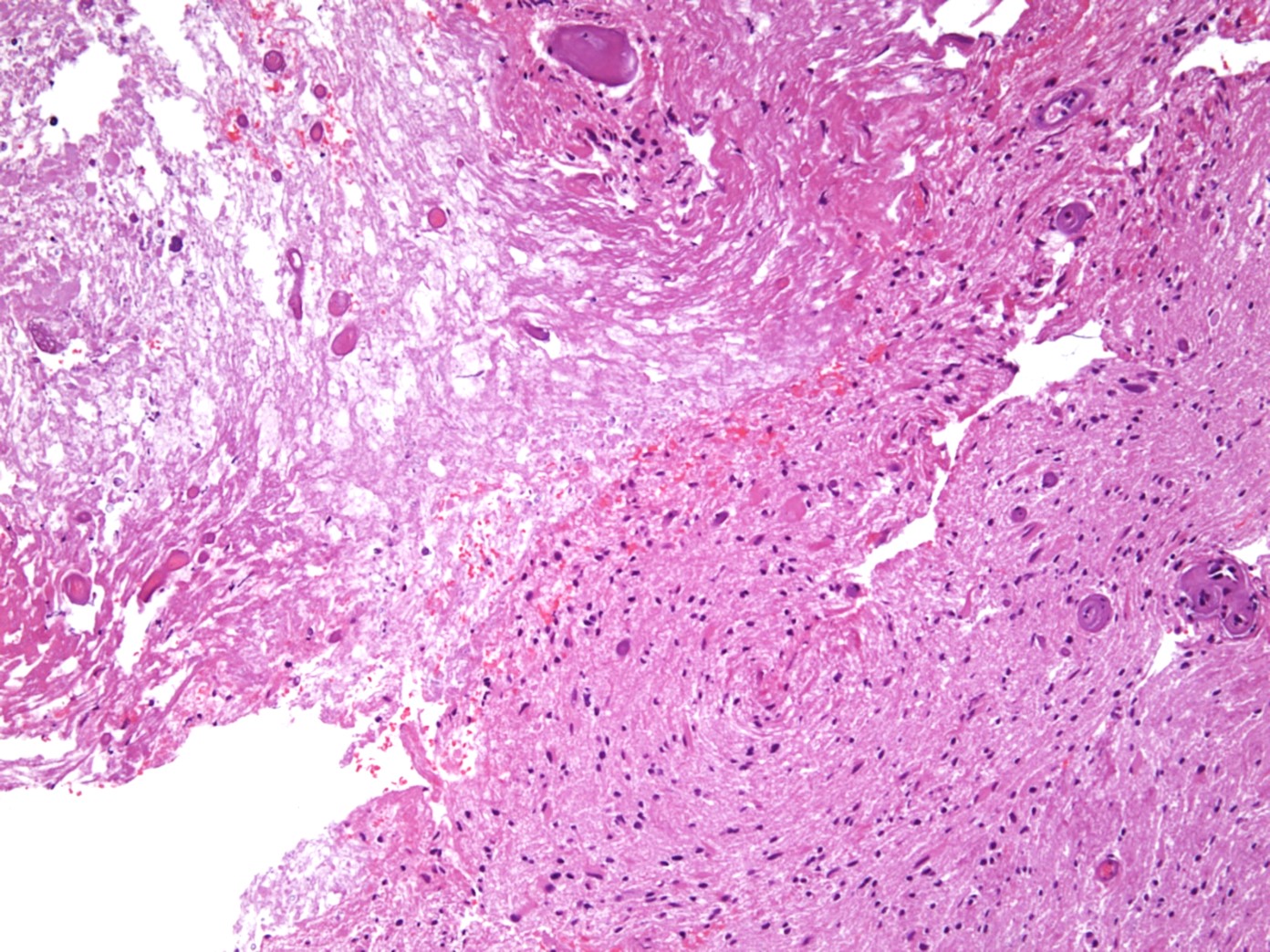
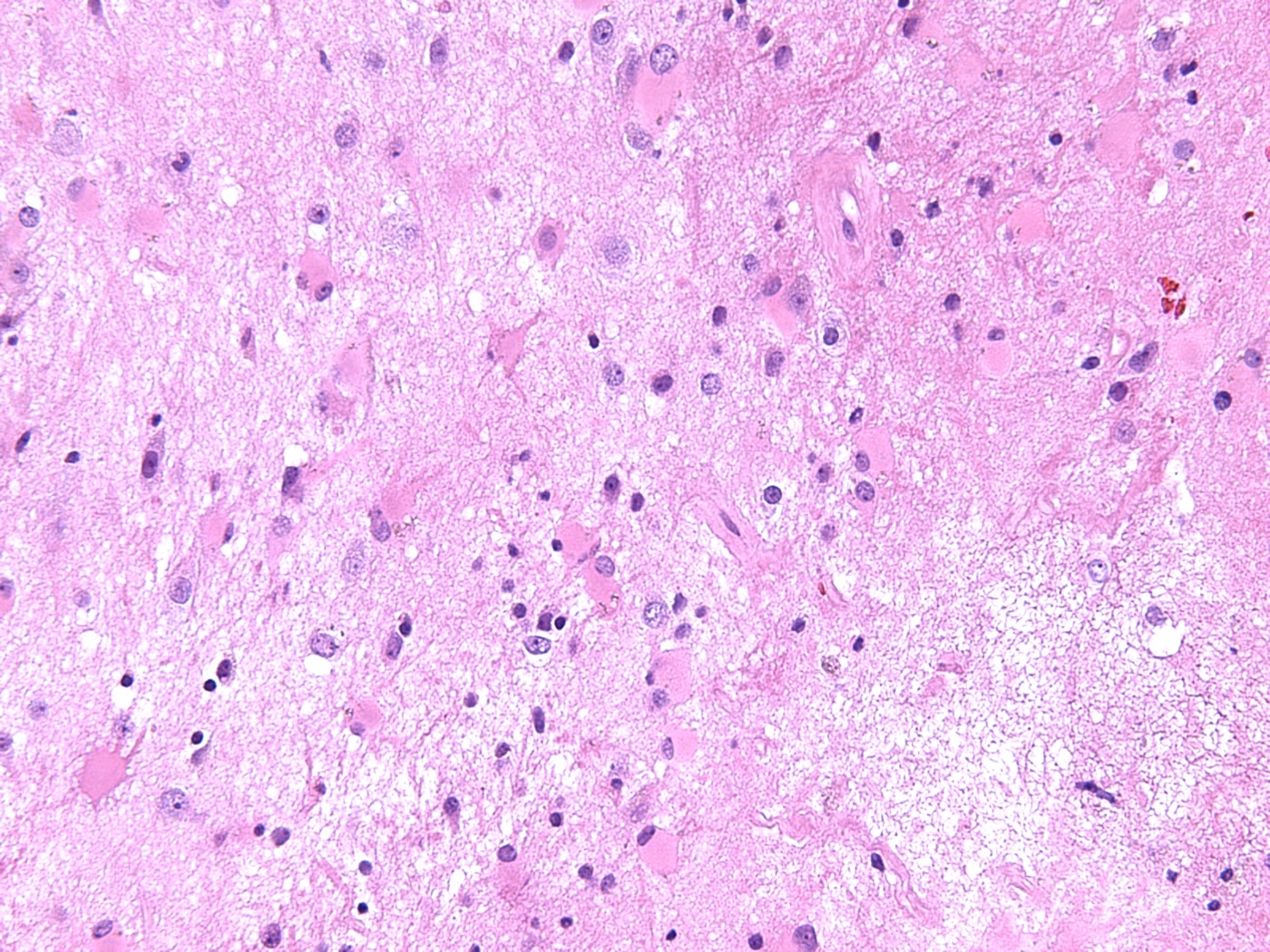
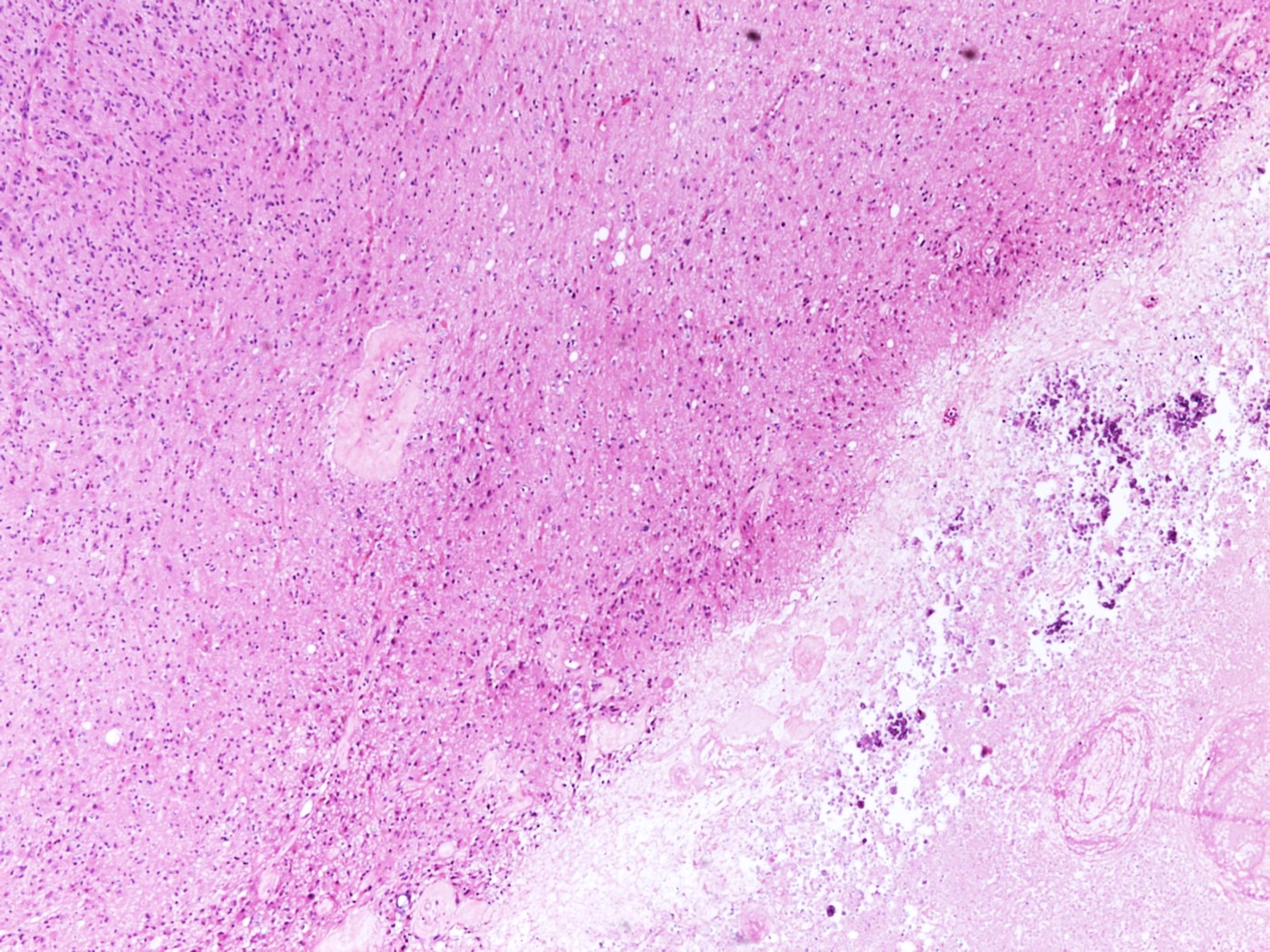
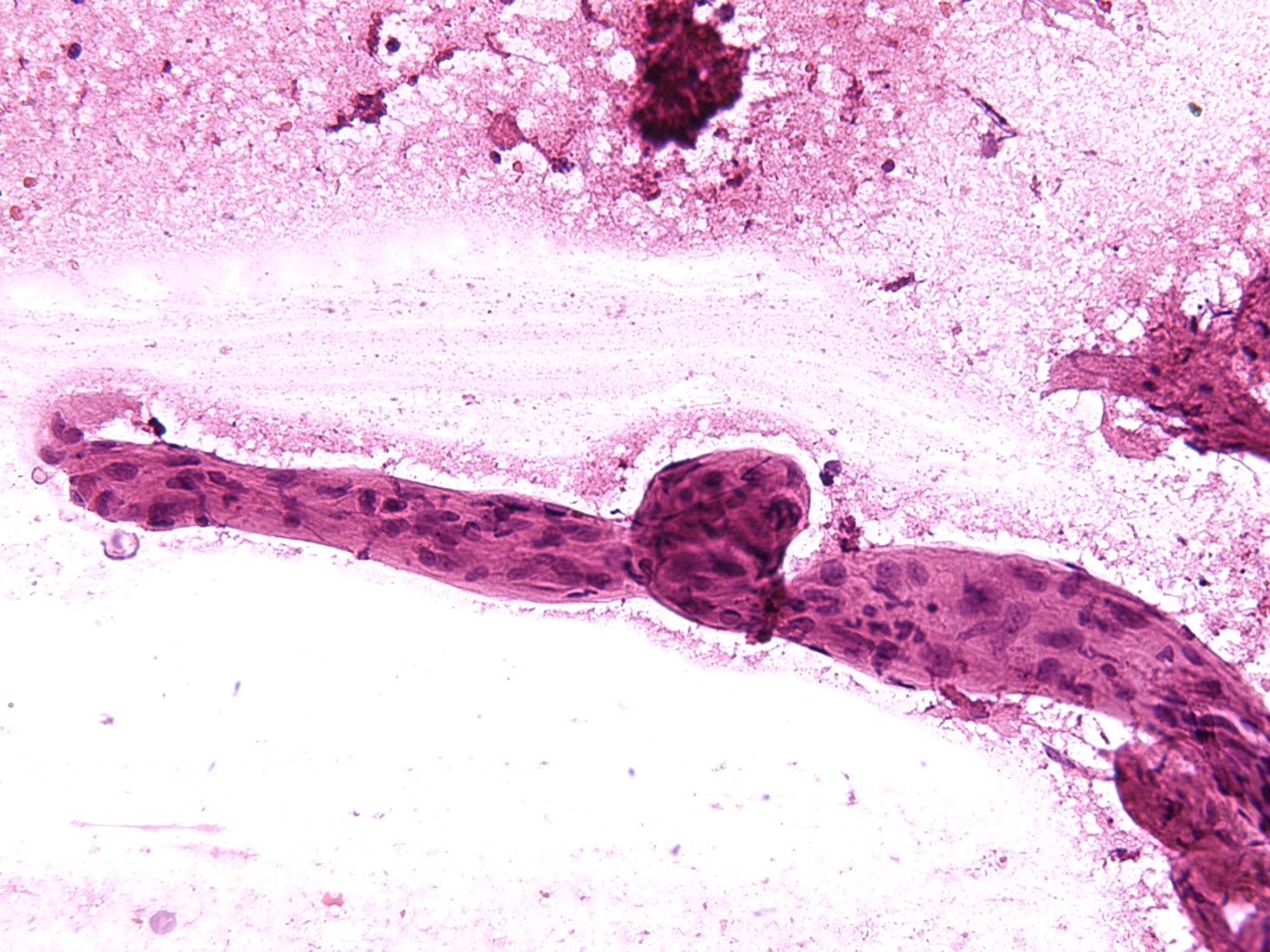
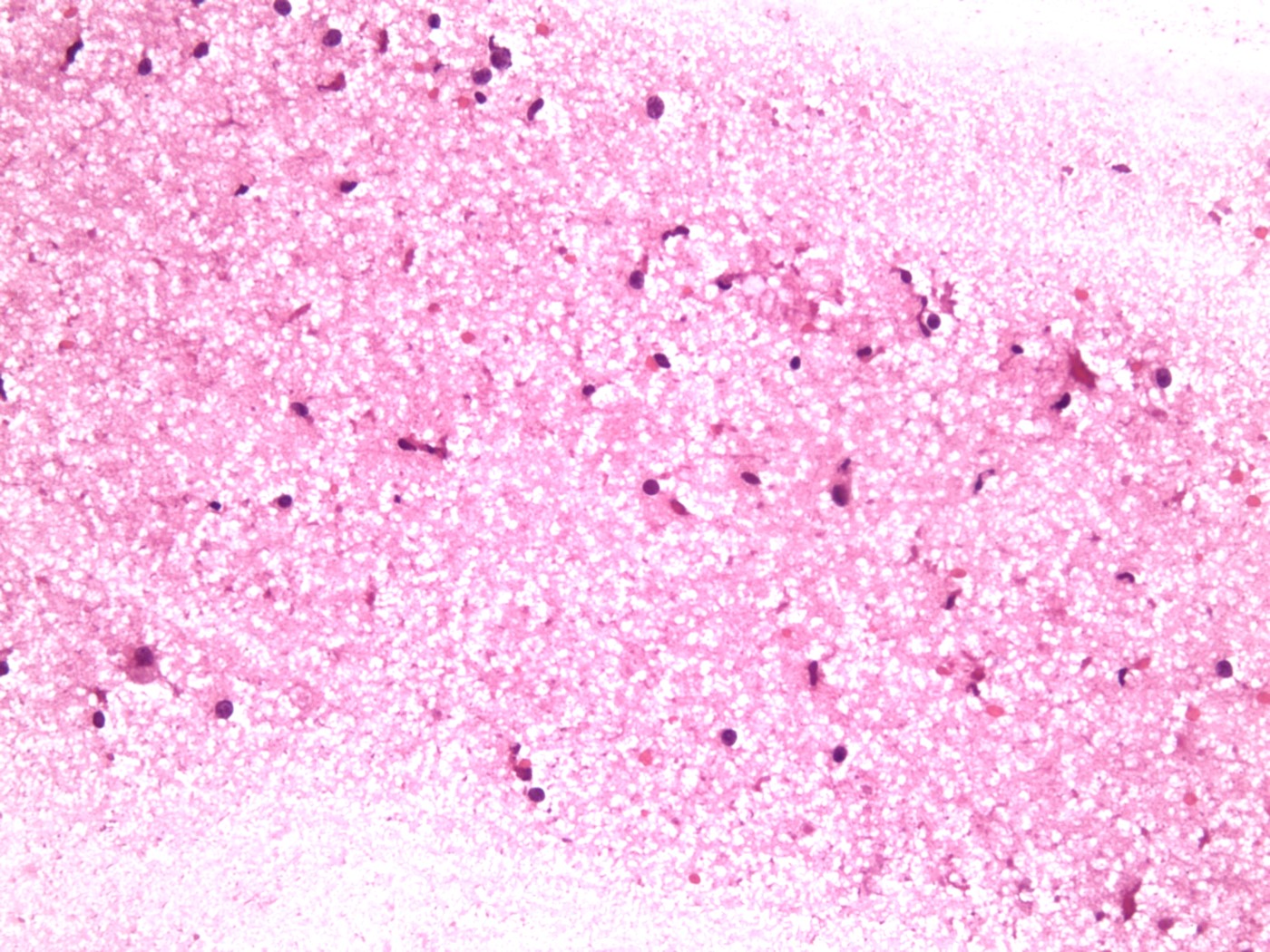
Microscopic (histologic) description
- Focal late radiation injury
- Hyalinization and fibrinoid necrosis of small arteries and arterioles (characteristic finding) and narrow lumens with endothelial proliferation
- White matter changes range from minimal changes to rarefaction of myelin and reactive gliosis to coagulative necrosis
- With or without perivascular mononuclear infiltrate
- Radiation induced cytologic atypia
- Diffuse late radiation injury
- Histopathologic diagnosis not indicated
- White matter changes similar to focal late radiation injury
- Pseudoprogression
- No established histopathological classification criteria for treatment necrosis or pseudoprogression (Neuro Oncol 2019;21:1118)
- Progressive disease
- Tumor cellularity depends on the treatment (radiation) response
- In practice, the most common histologic finding is radiation necrosis with active tumor (J Neurooncol 2019;141:347)
- References: AJNR Am J Neuroradiol 1991;12:45, IntechOpen: Radiation Induced Brain Injury After Radiotherapy for Brain Tumor [Accessed 7 April 2023]
Microscopic (histologic) images
Cytology description
Cytology images
Sample pathology report
- Brain, right temporal, resection:
- Changes consistent with radiation / chemotherapy effect
- No evidence of tumor
- Brain, left frontal, resection:
- Recurrent / residual glioblastoma with changes consistent with radiation / chemotherapy effect
Differential diagnosis
- Focal late radiation induced brain injury (treatment induced necrosis) versus recurrent / residual tumor:
- Clinical and radiological features similar
- Radiation necrosis
- Hyalinization and fibrinoid necrosis of small arteries and arterioles (characteristic finding) and endothelial proliferation
- Reactive gliosis to coagulative necrosis
- Perivascular mononuclear infiltrate may be present
- Recurrent / residual tumor
- Tumor cells should be differentiated from radiation induced atypia
- IDH1 (R132H) is useful in astrocytomas to differentiate from reactive astrocytes
- Ki67 could be helpful; no established cutoff value
- Molecular studies may be helpful (Strahlenther Onkol 2022;198:873, J Neurooncol 2013;113:485)
- Diffuse late radiation induced brain injury versus Alzheimer disease and dementia spectrum disorders:
- Clinically and radiologically different diseases
- Histopathologic diagnosis not required
- References: IntechOpen: Radiation Induced Brain Injury After Radiotherapy for Brain Tumor [Accessed 7 April 2023], Neurooncol Adv 2020;2:vdaa057, AJNR Am J Neuroradiol 1991;12:45
Board review style question #1
Intraoperative histopathologic evaluation is recommended in which of the following types of brain radiation injury?
- Acute radiation induced brain injury
- Early delayed radiation induced brain injury
- Early delayed and late focal radiation induced brain injury
- Late diffuse radiation induced brain injury
- Late focal radiation induced brain injury
Board review style answer #1
E. Late focal radiation induced brain injury. Late focal radiation injury can be confused with residual / recurrent tumor based on the imaging findings. Answers A - D are incorrect because they have imaging findings different from that of a tumor.
Comment Here
Reference: Radiation injury
Comment Here
Reference: Radiation injury
Board review style question #2
What is the characteristic histopathologic finding in focal (late) radiation induced brain injury?
- Coagulative necrosis with reactive gliosis
- Hyalinization and fibrinoid necrosis of small sized arteries
- Narrow vascular lumen with endothelial proliferation
- Perivascular mononuclear infiltrate
- Rarefaction of myelin
Board review style answer #2
B. Hyalinization and fibrinoid necrosis of small sized arteries. Answers A, C, D and E are incorrect because these findings are nonspecific for radiation injury and can be seen in other conditions.
Comment Here
Reference: Radiation injury
Comment Here
Reference: Radiation injury