Table of Contents
Definition / general | Essential features | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: France A, Lakis NS. Adamantinomatous craniopharyngioma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cnstumoradamcraniopharyngioma.html. Accessed April 24th, 2024.
Definition / general
- Adamantinomatous craniopharyngioma is a histologically benign, partially cystic epithelial neoplasm of the suprasellar or sellar region, resembling ameloblastoma or keratinizing and calcifying odontogenic cyst
Essential features
- Always WHO grade 1
- Tumor with palisading epithelium, wet keratin and stellate reticulum associated with surrounding gliosis and Rosenthal fibers
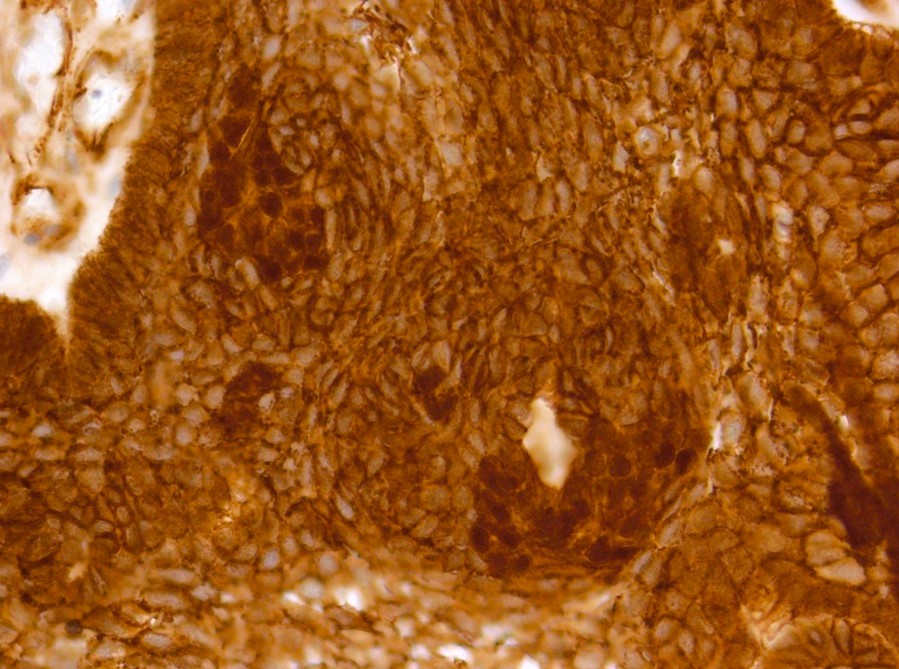
- Shows CTNNB1 mutations and aberrant nuclear expression of beta catenin in up to 95% of cases (Acta Neuropathol Commun 2016;4:20)
Epidemiology
- Incidence: low
- Age: bimodal, with peaks at 5 - 15 years and 45 - 60 years; rare neonatal and fetal cases have been reported (Nat Rev Dis Primers 2019;5:75)
- More common than papillary craniopharyngioma (even in adults)
- Incidence rates are similar in males and females and between Caucasians and African Americans (Neurosurg Focus 1997;3:e1)
Sites
- Suprasellar: frequently extends into neighboring structures
- Rarely intranasal, sphenoid sinus, cerebellopontine angle and pineal region
- Reference: J Neurol Surg Rep 2016;77:e121
Pathophysiology
- Possibly arises from neoplastic transformation of ectodermal derived epithelial cell remnants of Rathke pouch and the craniopharyngeal duct
- Misplaced odontogenic rests along pituitary stalk
- Reference: Childs Nerv Syst 2005;21:622
Clinical features
- Insidious, with a delay of approximately 1 - 2 years between initial symptoms and diagnosis (Orphanet J Rare Dis 2007;2:18)
- Visual disturbances are more frequently observed in children
- Endocrine deficiencies:
- Growth hormone (GH) > luteinizing hormone (LH) / follicle stimulating hormone (FSH) > adrenocorticotrophic hormone (ACTH) > thyroid stimulating hormone (TSH)
- Growth failure and delayed puberty in children
- Diabetes insipidus (> adults)
- Headache (most common, due to mass effect or hydrocephalus)
- Cognitive impairment and personality changes (about 50% of patients)
- Rare chemical meningitis with cyst rupture and spillage
Diagnosis
- Best diagnostic clue is preoperative imaging (Front Endocrinol (Lausanne) 2011;2:70)
- Usually extra-axial and suprasellar
- Multilobulated and multicystic lesions
- Variable in size, often > 5 cm
- Recurrences may be massive
- MRI:
- High signal intensity on T1 weighted images
- Heterogeneous enhancement
- Fluid levels consistent with cystic components
- CT:
- Better than MRI at showing calcifications
Laboratory
- Same for both types of craniopharyngiomas
- Full pituitary endocrine workup is usually mandatory (Front Endocrinol (Lausanne) 2011;2:70)
- Visual acuity and visual field assessment is also performed to show any deficits and rule out papilledema
Radiology description
- MRI:
- T1: solid regions are hypo- or isointense, cystic regions are hyperintense
- Strong heterogeneous enhancement
- Hyperintense on T2
- CT:
- 9Solid regions and cyst wall enhancement
- Calcifications visible (J Neurol Surg Rep 2016;77:e121)
Prognostic factors
- 5 year survival excellent (Front Endocrinol (Lausanne) 2011;2:70)
- Patients may be left with variable endocrinologic deficiencies
- Cystic recurrence common after incomplete excision
- Very rare malignant transformation
Case reports
- 26 year old man with malignant craniopharyngioma without radiation therapy (J Korean Neurosurg Soc 2017;60:108)
- 35 year old man with adamantinomatous craniopharyngioma (Int Med Case Rep J 2020;13:123)
- 52 year old man with craniopharyngioma presenting with severe hyponatremia, hyponatremia induced myopathy and panhypopituitarism (J Med Case Rep 2017;11:31)
Treatment
- Gross total excision or subtotal resection followed by radiation therapy (Front Endocrinol (Lausanne) 2011;2:70)
- Anatomic location, size, invasion of the nearby structures and the nature of the tumor determine surgical approach
- Most common indication for surgery is neurologic compromise from tumor mass effect
- In children, hypothalamic and endocrine dysfunction may develop before visual defects are noticed
- Radiotherapy is indicated for treatment of residual tumor or recurrence
Gross description
- Lobular and cystic tumor with calcifications
- Cysts with dark "motor oil" fluid composed of cholesterol and hemorrhage
- Irregular tumor interface with adjacent brain
- Can be densely adherent to brain
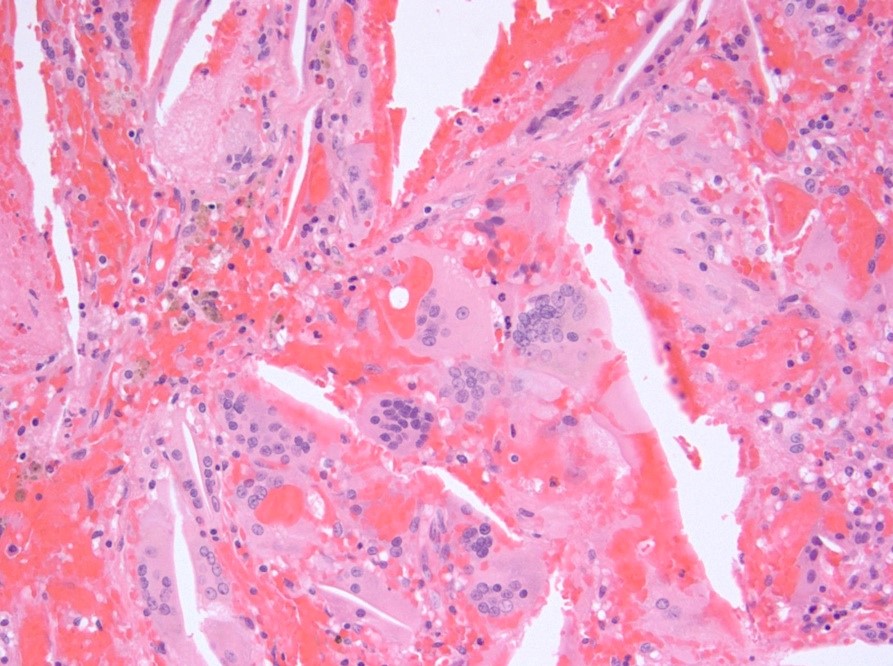
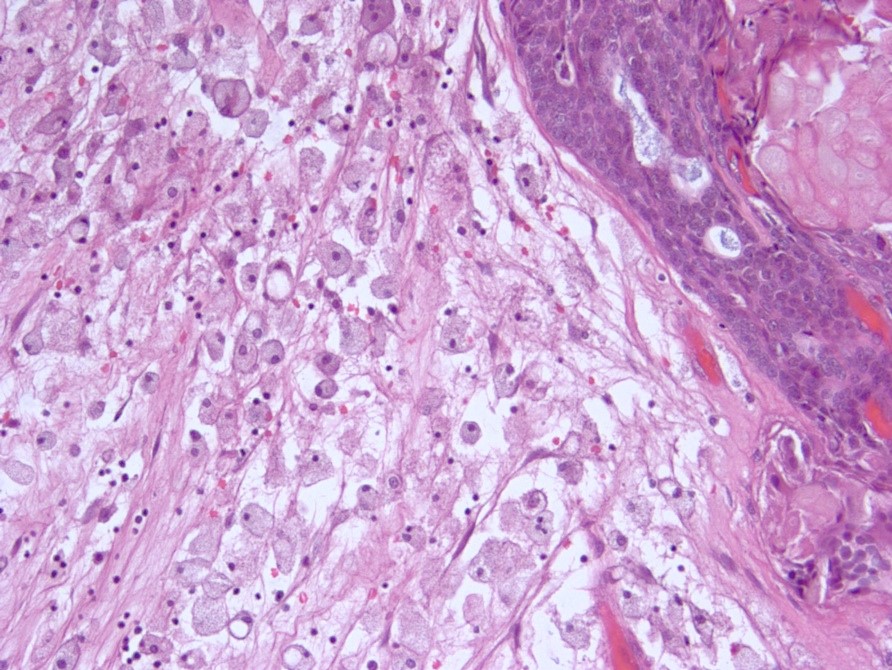
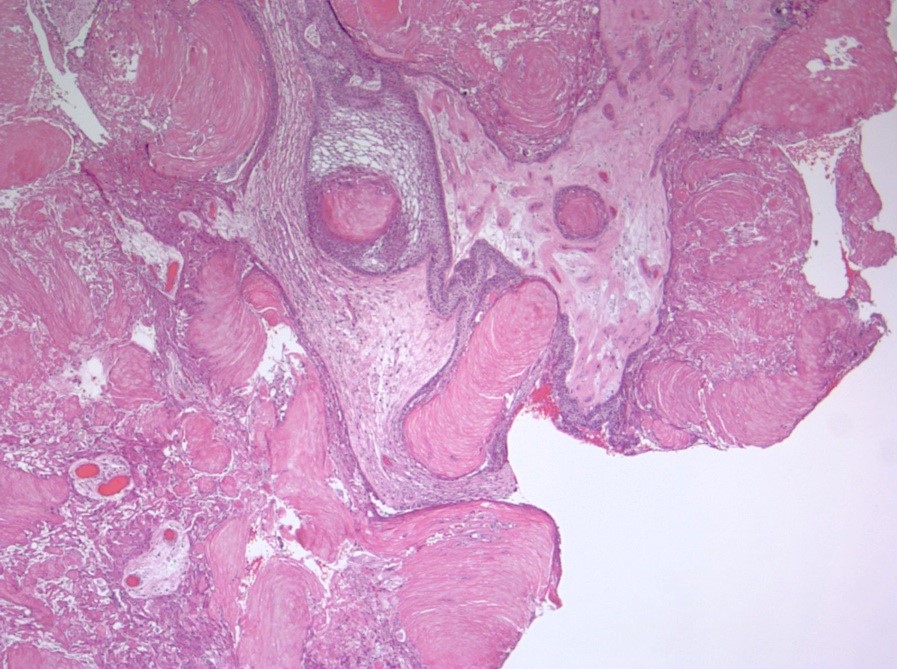
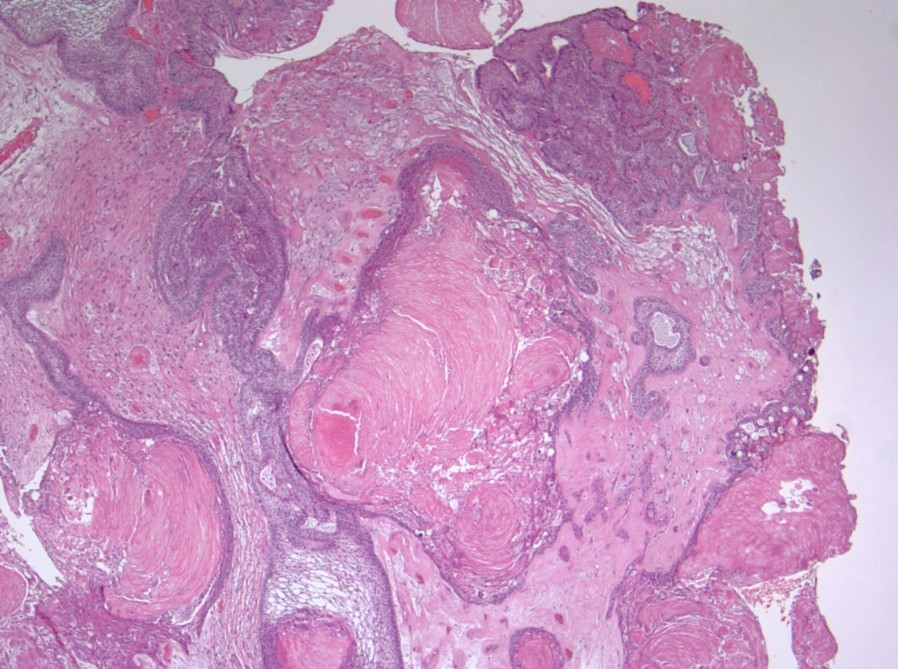
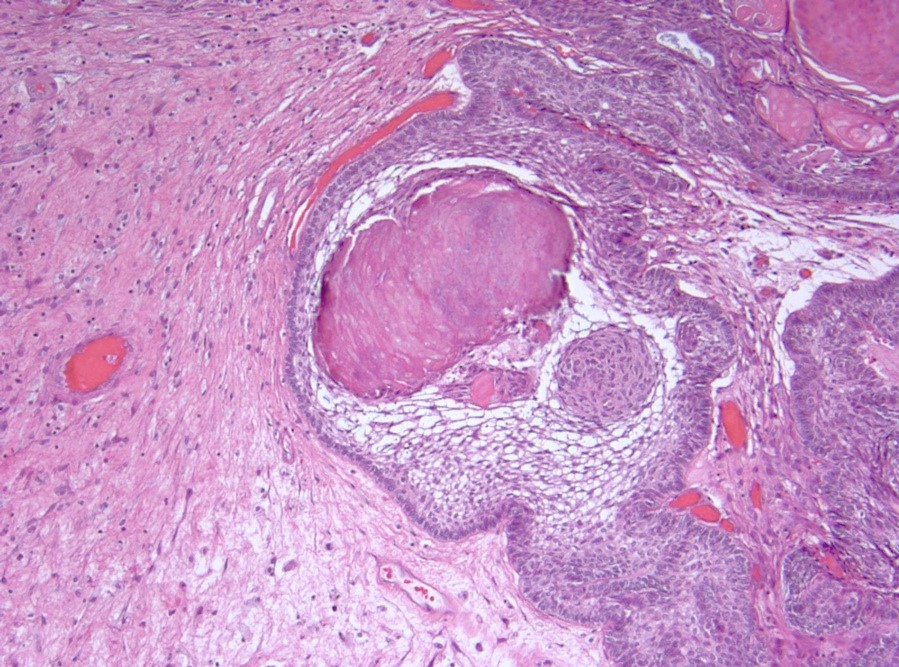
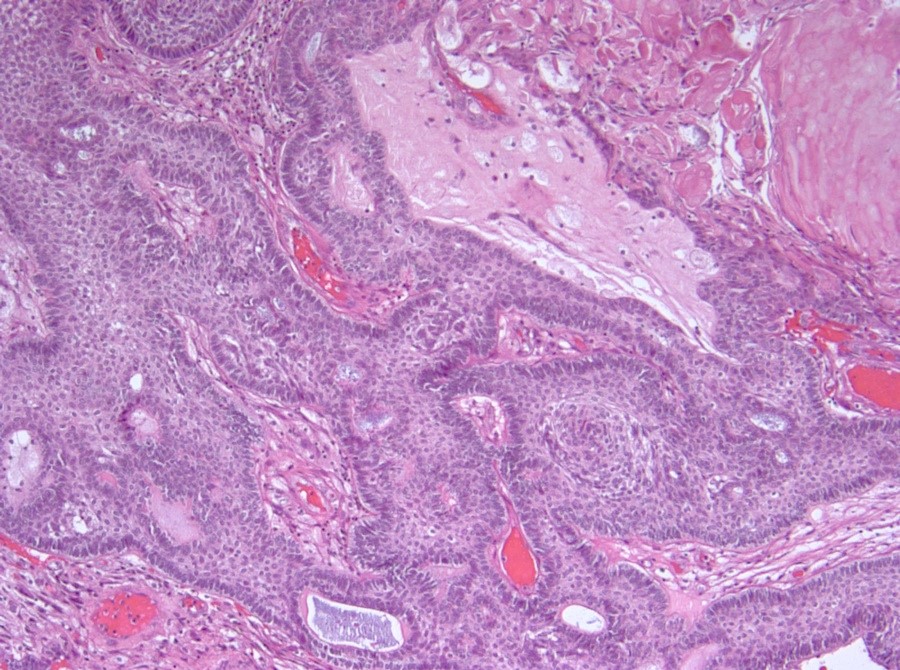
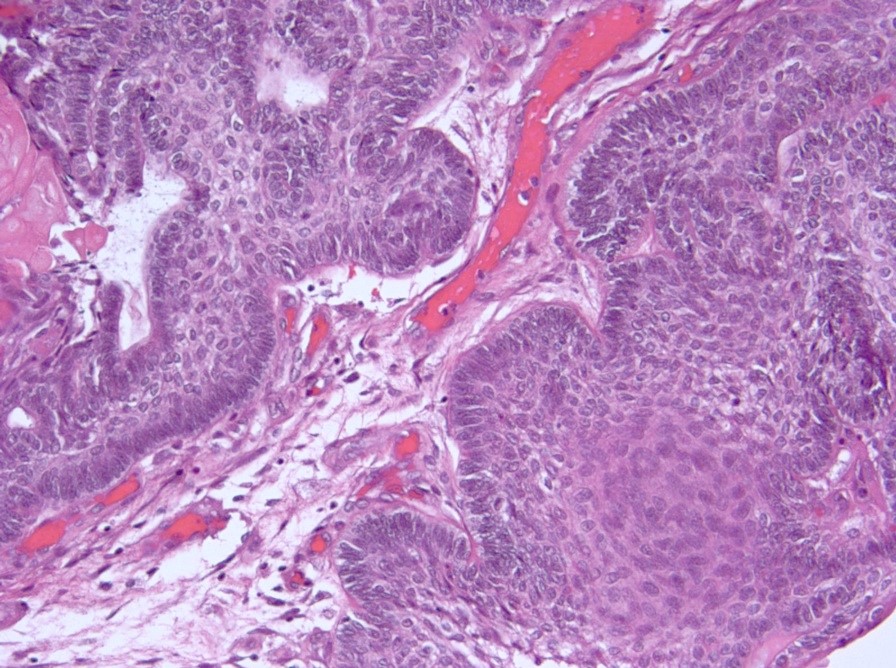
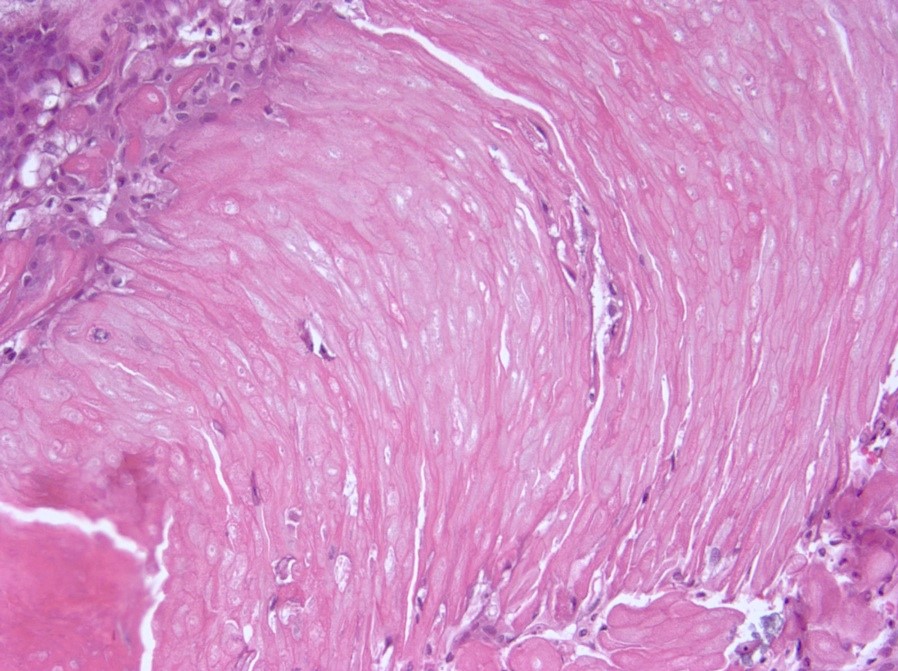
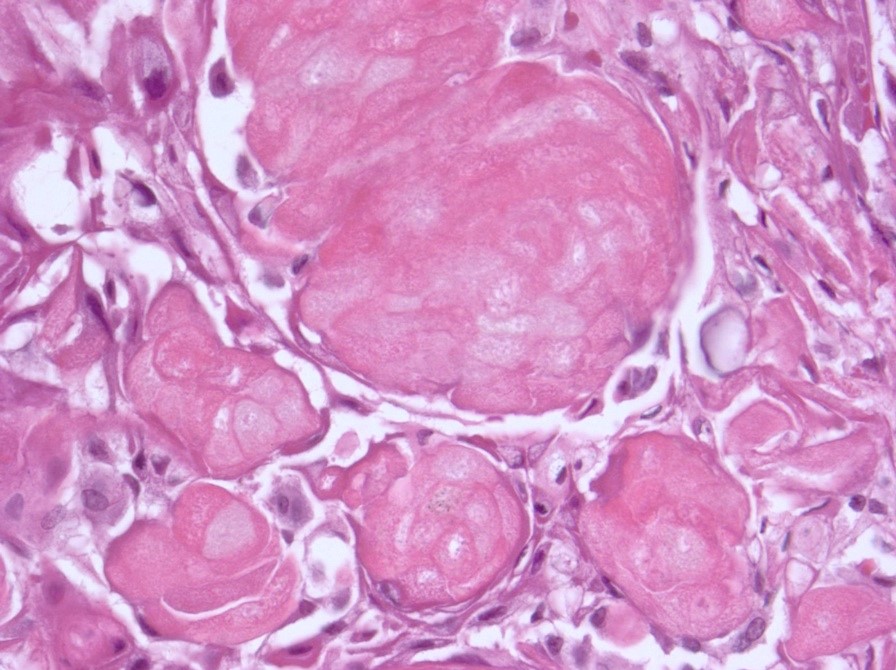
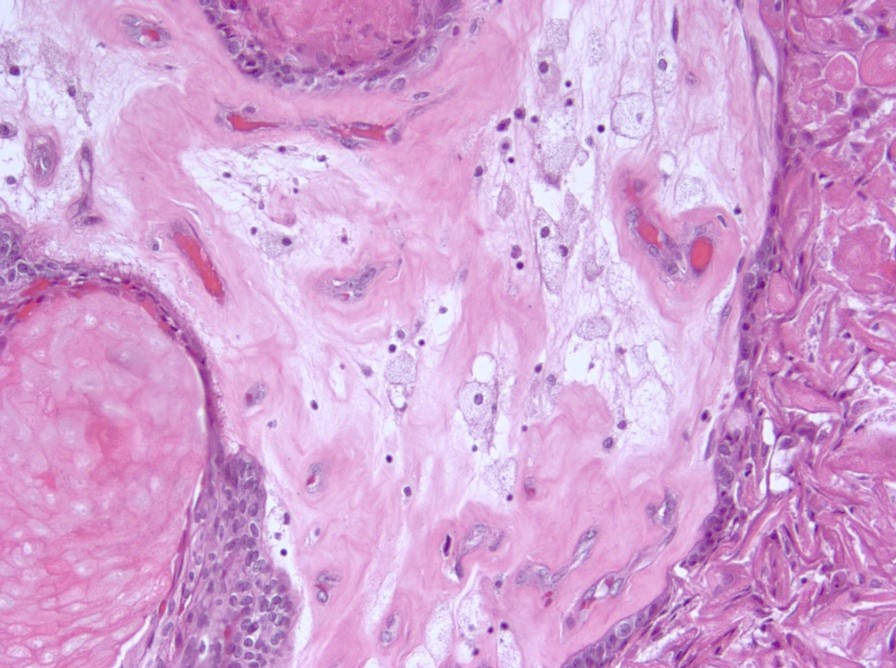
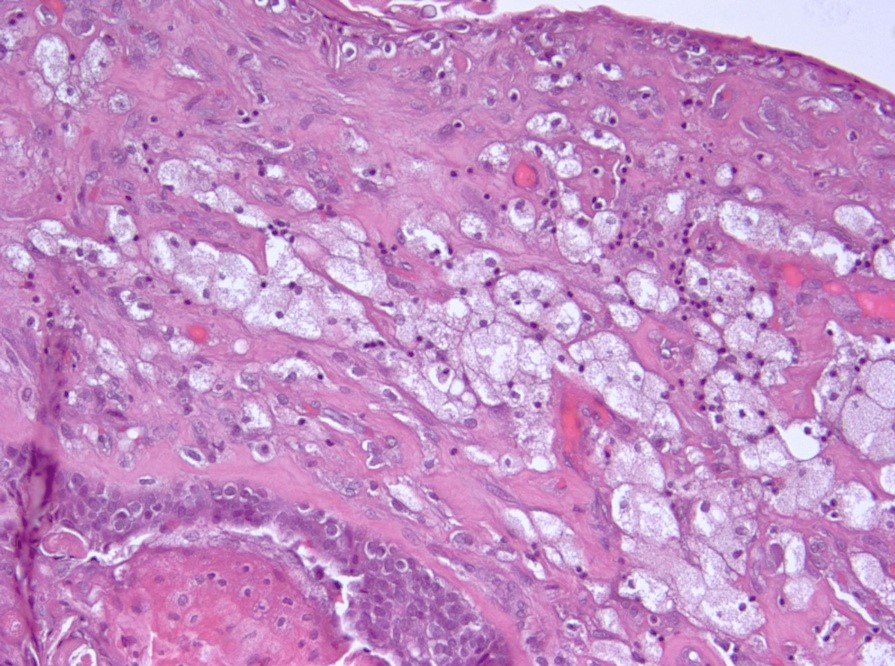
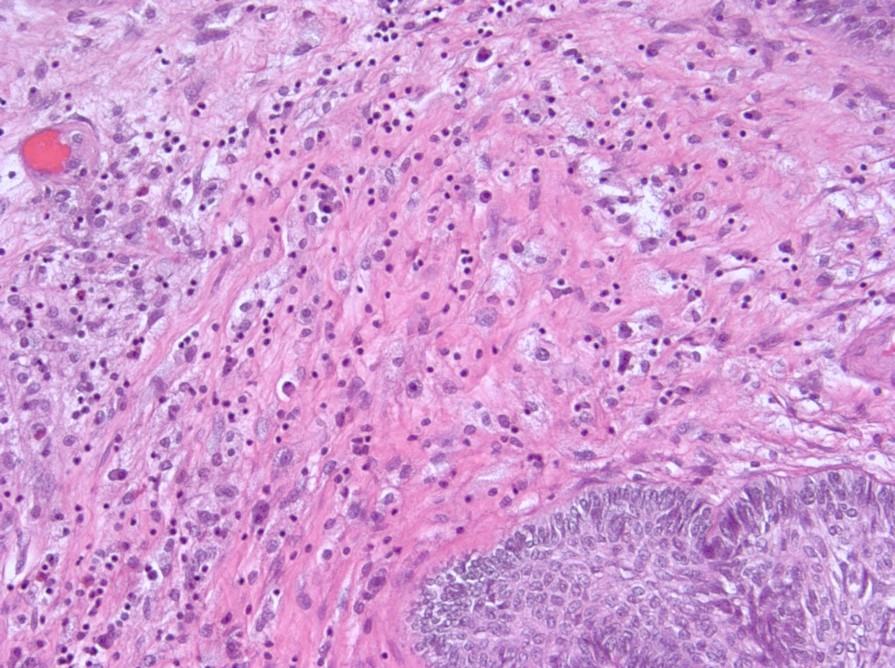
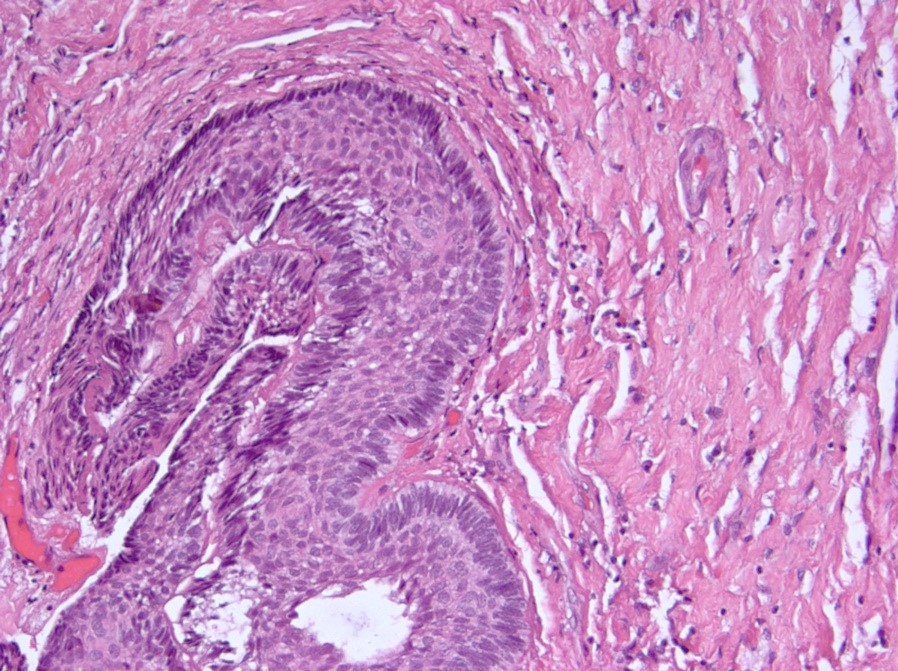
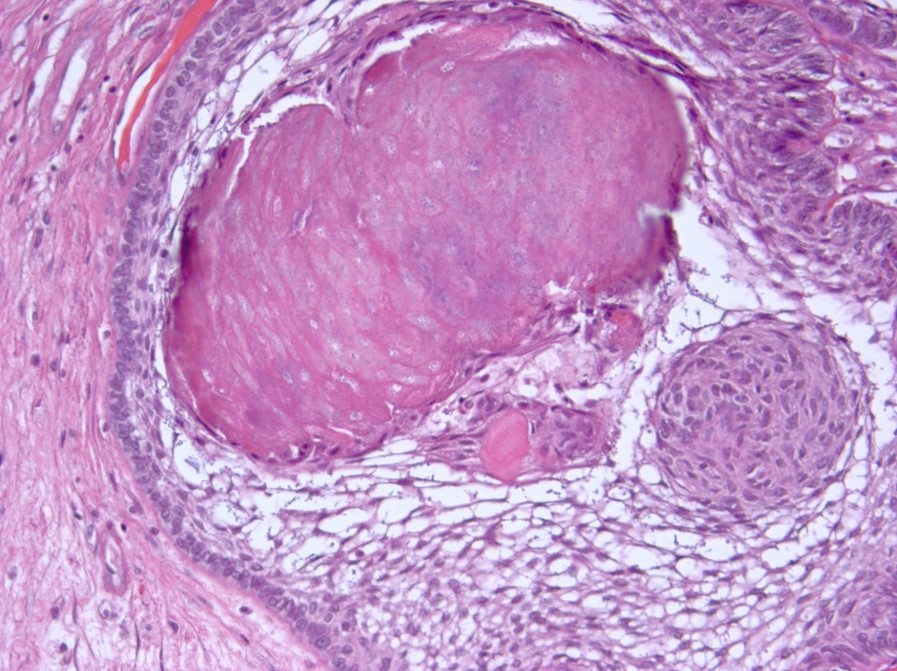
Microscopic (histologic) description
- May appear well circumscribed
- Cords, lobules, nodular whorls and trabeculae of well differentiated squamous epithelium bordered by palisading columnar epithelium
- Peripheral cells surround looser plumper cells called stellate reticulum
- Nodules of plump, anucleate squamous cells (ghost cells) and wet keratin
- Intralobular whorl-like formations (Int Med Case Rep J 2020;13:123)
- May have degenerative changes with cystic degeneration, calcifications and xanthogranulomatous reactions with giant cells
- Piloid gliosis and Rosenthal fibers in adjacent brain
- Rarely, melanin pigment
- Microscopic brain invasion common with tongues of tumor extending into hypothalamic parenchyma
Microscopic (histologic) images
Cytology description
- Cohesive clumps of well differentiated squamous epithelium (Int Med Case Rep J 2020;13:123)
- Nodules of anucleate squamous cells
- Macrophages, amorphous debris and calcifications
Positive stains
- CK7, CK8, CK19, pancytokeratin, CK5/6, EMA, CK14 (Int Med Case Rep J 2020;13:123)
- Beta catenin: in whorls, both intranuclear (translocated) and cytoplasmic
- Ki67 (low, usually concentrated along the peripheral palisading cells)
Negative stains
- Most cases are negative for mutant BRAF (V600E)
Molecular / cytogenetics description
- Activating mutations of the WNT pathway gene CTNNB1 encoding beta catenin in almost all cases
Sample pathology report
- Sellar / suprasellar region, suprasellar mass, endoscopic resection:
- Adamantinomatous craniopharyngioma (see synoptic report)
Differential diagnosis
- Epidermoid cyst:
- Uniloculate with thin layer of keratinizing squamous epithelium and keratohyalin granules
- Papillary craniopharyngioma:
- No palisading, no wet keratin, no calcifications, no "motor oil" cystic fluid, no xanthogranulomatous reaction
- Harbors a BRAF V600E mutation and is negative for beta catenin
- Pilocytic astrocytoma:
- Much greater cellularity than piloid gliosis, biphasic and may have eosinophilic granular bodies
- Rathke cleft cyst with squamous metaplasia:
- Intrasellar, squamous epithelium, as well as ciliated or mucus containing cells, no wet keratin, no calcifications
- Beta catenin negative nuclei
- Xanthogranuloma of sellar region:
- Sellar region cholesterol clefts, lymphoplasmacytic infiltrates, marked hemosiderin deposits, fibrosis, multinucleated giant cells around cholesterol clefts, eosinophilic granular necrotic debris and accumulation of macrophages, no true epithelium and may be associated with Rathke cleft cyst leakage / rupture / hemorrhage (Brain Pathol 2017;27:377)
Additional references
- Eur J Endocrinol 2016;174:R139, Clin Neuropathol 2003;22:229, J Egypt Natl Canc Inst 2015;27:139, J Neuropathol Exp Neurol 2017;76:126, AJNR Am J Neuroradiol 2015;36:E55, Neuropathol Appl Neurobiol 2015;41:733, eMedicine: Surgery for Craniopharyngiomas Treatment & Management [Accessed 26 April 2021], Radiopaedia: Craniopharyngioma [Accessed 26 April 2021], Radiopaedia: Craniopharyngioma - Papillary [Accessed 26 April 2021], Kleinschmidt-DeMasters: Diagnostic Pathology - Neuropathology, 2nd Edition, 2016
Board review style question #1
A 16 year old boy comes to the clinic because he has been experiencing headaches and vision disturbances. The headaches have worsened over this past year and also are associated with nausea. His head is imaged and a suprasellar mass with calcifications is identified. The mass is removed surgically and gross histological examination reveals the presence of cystic spaces that are filled with thick dark brown fluid. Which of the following is the most likely diagnosis?
- Adamantinomatous craniopharyngioma
- Epidermoid cyst
- Papillary craniopharyngioma
- Rathke cleft cyst
Board review style answer #1
Board review style question #2
A 13 year old girl is brought to the clinic because she has been experiencing headaches for the past 8 months. She also complains of visual difficulty. A physical exam reveals the presence of papilledema. The mass is removed surgically and gross histological examination reveals a diagnosis of adamantinomatous craniopharyngioma. Which of the following features is associated with this diagnosis?
- BRAF V600E mutation
- Lack of nuclear palisading
- Nodules of anucleate squamous cells
- WHO grade 2
Board review style answer #2