Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Intraoperative frozen / smear cytology images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Barresi V. Schwannoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cnstumorschwannoma.html. Accessed April 25th, 2024.
Definition / general
- Schwannoma is a benign nerve sheath tumor composed of differentiated neoplastic Schwann cells
- Classified as CNS WHO grade 1
Essential features
- CNS primary tumor mostly occurring in the spine / spinal nerve roots (intradural, extramedullary) and vestibular division of the eighth cranial nerve within the cerebellopontine angle
- Multiple tumors in patients with neurofibromatosis type 2 (NF2, bilateral vestibular schwannomas) or schwannomatosis
- Excellent prognosis with nearly absent recurrence after gross total resection
- Malignant transformation is exceptionally rare
- Biphasic, encapsulated tumor composed of compact areas with spindle cells (Antoni A) and palisading nuclei (Verocay bodies) and loose microcystic areas with lipid laden macrophages (Antoni B)
Terminology
- Neurilemmoma (not recommended)
- Acoustic neuroma (not recommended)
ICD coding
- ICD-O: 9560/0 - schwannoma, NOS
- ICD-11: 2A02.3 & XH98Z3 - benign neoplasm of cranial nerves & schwannoma, NOS
Epidemiology
- Majority (90%) are solitary and sporadic
- May occur at any age but the peak incidence is between
- 55 and 75 years for vestibular schwannoma (Neurooncol Adv 2020;2:vdaa135)
- 65 and 75 years for spinal schwannomas (J Neurosurg Spine 2019 Dec 27 [Epub ahead of print])
- Younger (third decade of life) age at onset in patients with neurofibromatosis type 2 (Q J Med 1992;84:603)
- Vestibular schwannoma: most common nonmalignant nerve sheath tumor (75.7%) and third most common nonmalignant primary brain tumor (Neuro Oncol 2022;24:v1)
- Multiple schwannomas in patients with neurofibromatosis type 2 or schwannomatosis (Acta Neuropathol 2020;139:643, Genet Med 2022;24:1967)
- Bilateral vestibular schwannomas are typically seen in patients with neurofibromatosis type 2 (Genet Med 2022;24:1967)
Sites
- Most common sites in the CNS:
- Spine, where it is typically intradural and extramedullary
- Vestibular division of the eighth cranial nerve (Neuro Oncol 2022;24:v1)
Pathophysiology
- NF2 inactivating mutation (frameshift and nonsense) and loss of the remaining wild type allele on chromosome 22, in 50 - 75% of sporadic schwannomas (J Neurosurg 2018;128:911)
- Germline pathogenic NF2 mutation in schwannomas associated with neurofibromatosis type 2 (Genet Med 2022;24:1967)
- Germline mutations of either SMARCB1 or LZTR1 on chromosome 22, followed by a somatic mutation in NF2 along with the deletion of the other chromosome 22 in schwannomas associated with schwannomatosis (Neurology 2015;84:141, Clin Genet 2020;97:376, Genet Med 2022;24:1967)
Etiology
- Mostly unknown
- Previous irradiation (J Natl Cancer Inst 2002;94:1555)
- Association with neurofibromatosis type 2 and schwannomatosis (Genet Med 2022;24:1967)
Clinical features
- Symptoms depend on the anatomical site of the tumor:
- Tinnitus, unilateral sensorineural hearing loss, vertigo or disequilibrium in patients with vestibular schwannoma (J Neurosurg 2022 Dec 2 [Epub ahead of print])
- Sensory or motor symptoms in patients with spinal schwannoma
Diagnosis
- Based on imaging (CT, MRI) / biopsy / resection specimen
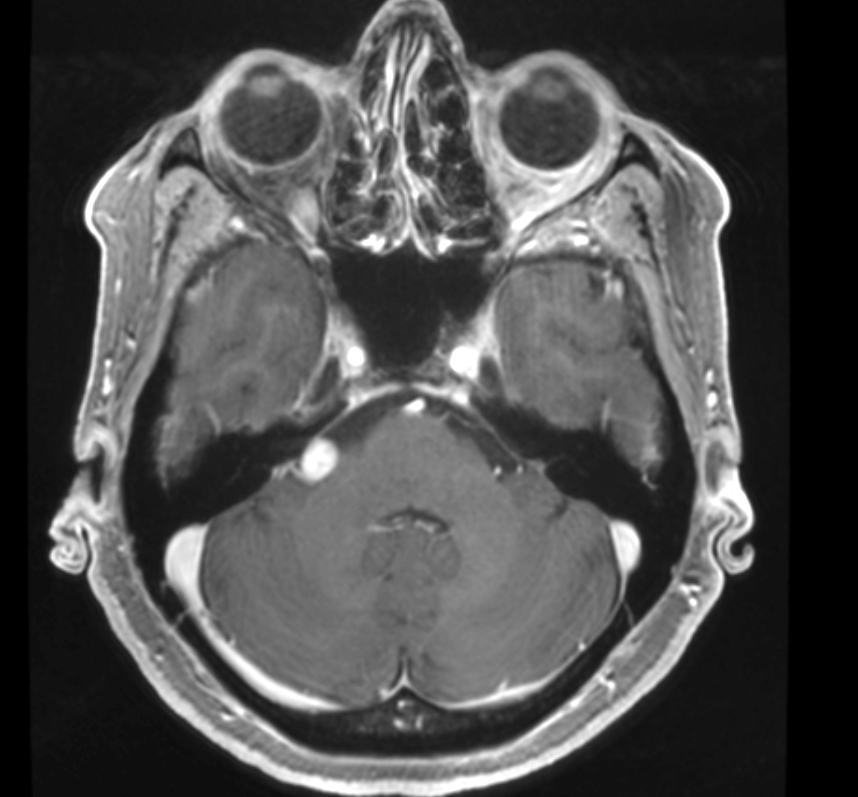
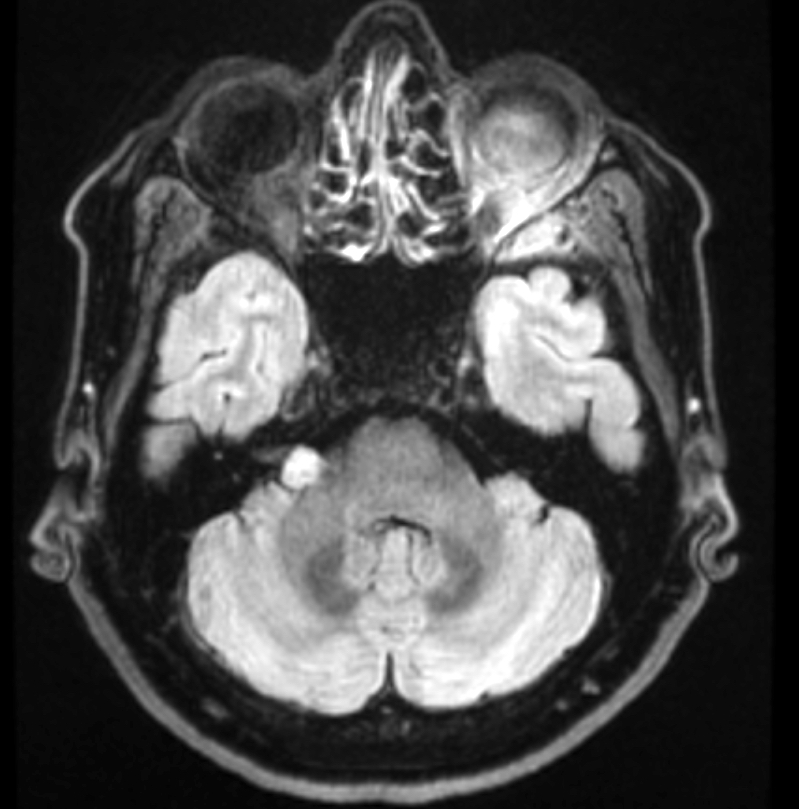
Radiology description
- Well circumscribed masses that displace adjacent structures without direct invasion
- On MRI, it may be
- Iso or hyperintense in T2 weighted images (Spine (Phila Pa 1976) 2017;42:E150)
- Hyperintense in fluid attenuated inversion recovery (FLAIR) images
- Heterogeneous or homogeneous enhancement in T1 weighted sequences (J Clin Imaging Sci 2017;7:38)
Radiology images
Prognostic factors
- Excellent prognosis with nearly absent recurrence after gross total resection (Otol Neurotol 2022;43:702)
- Regrowth after incomplete surgery is correlated with the volume of residual tumor (Laryngoscope 2016;126:1877)
- Malignant transformation is exceptionally rare and has been associated with irradiation and epithelioid subtype (Acta Neurochir (Wien) 2022;164:343, Skull Base 2010;20:381, Neurosurg Rev 2022;45:915, APMIS 2021;129:524, Am J Surg Pathol 2015;39:673)
Case reports
- 23 year old man with a large multicystic spinal lesion (BMJ Case Rep 2021;14:e242690)
- 48 year old man with a cervical spinal lesion (Asian J Neurosurg 2015;10:42)
- 53 year old woman with intramedullary lesion (Neurosurg Rev 2021;44:1833)
- 70 year old man with an intramedullary mass (Surg Neurol Int 2020;11:454)
Treatment
- Observation, radiosurgery, surgery or surgery followed by radiosurgery, depending on symptoms, tumor size and association with neurofibromatosis type 2 (Neurooncol Pract 2016;3:281)
- Bevacizumab is considered as an option in patients with neurofibromatosis type 2 (Neuro Oncol 2020;22:31)
Gross description
- Usually encapsulated, with a smooth surface
- Cut surfaces are firm, light tan and interrupted by white-yellow or hemorrhagic areas (Asian J Neurosurg 2015;10:42, Neurosurg Rev 2021;44:1833)
Gross images
Frozen section description
- Admixture of compact and loose areas, Verocay bodies and wavy / spindled nuclei with pointed ends are useful diagnostic clues in the differential diagnosis versus other spindle cell tumors (e.g., meningioma, ependymoma, sarcoma, solitary fibrous tumor) (Arch Pathol Lab Med 2007;131:1532)
- Additional features: hyalinized blood vessels, chronic inflammatory infiltrates along capsule, hemosiderin
- Additional clues:
- Differential diagnosis versus ependymoma: absence of fibrillary background and perivascular pseudorosettes
- Differential diagnosis versus meningioma: lack of psammoma bodies, whorls or epithelioid syncytia
- Differential diagnosis versus sarcoma: in malignant sarcomas, mitoses are more commonly encountered, nuclear atypia is more uniformly widespread and necrosis may be present (Arch Pathol Lab Med 2007;131:1532)
- Differential diagnosis versus solitary fibrous tumor: lack of staghorn vessels
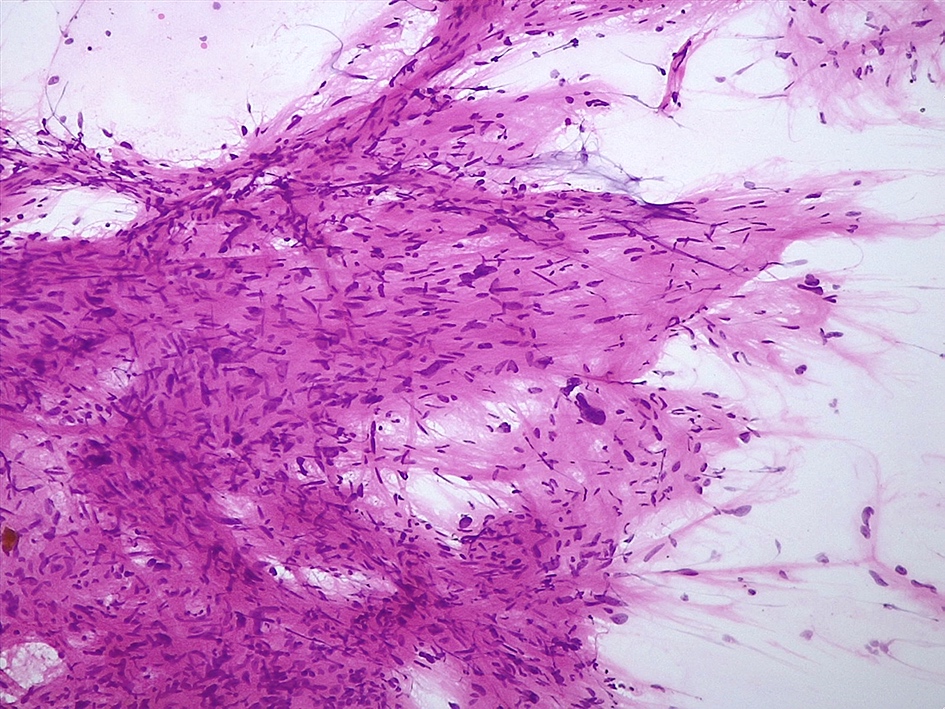
Intraoperative frozen / smear cytology images
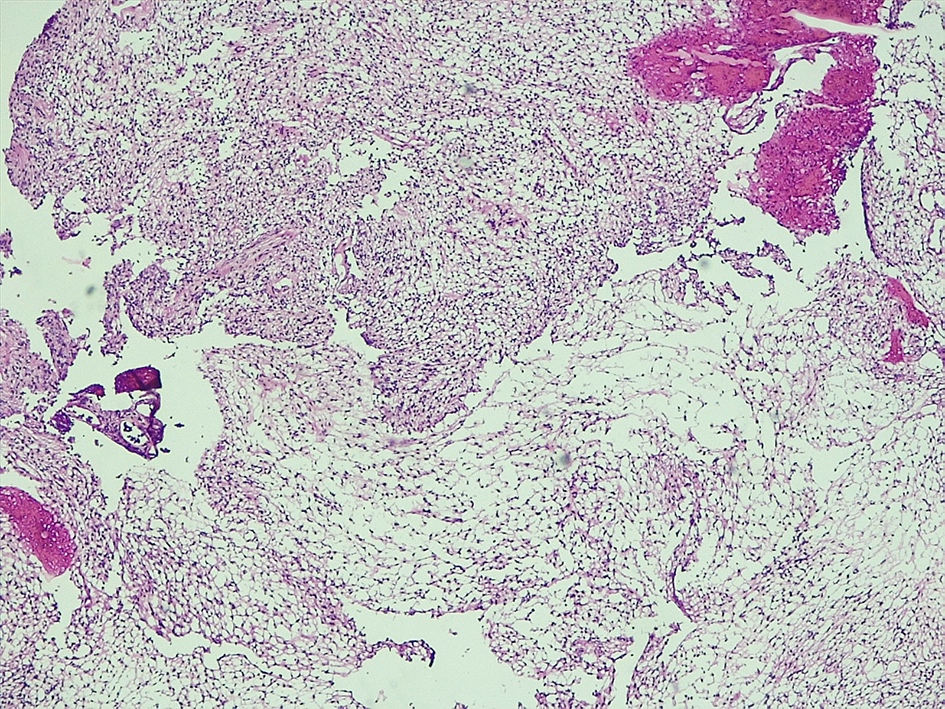
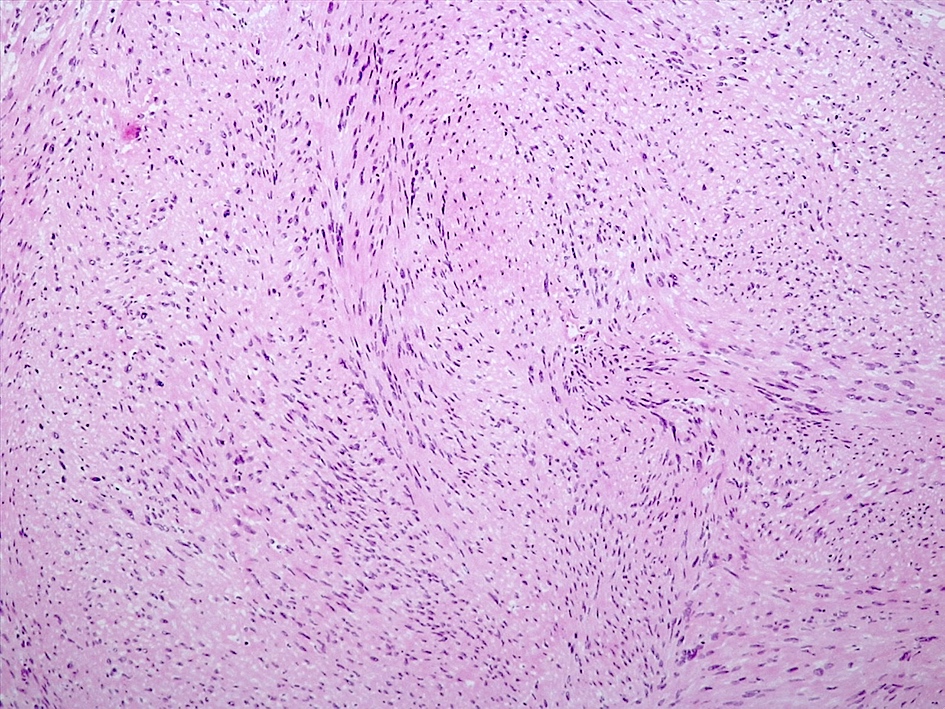
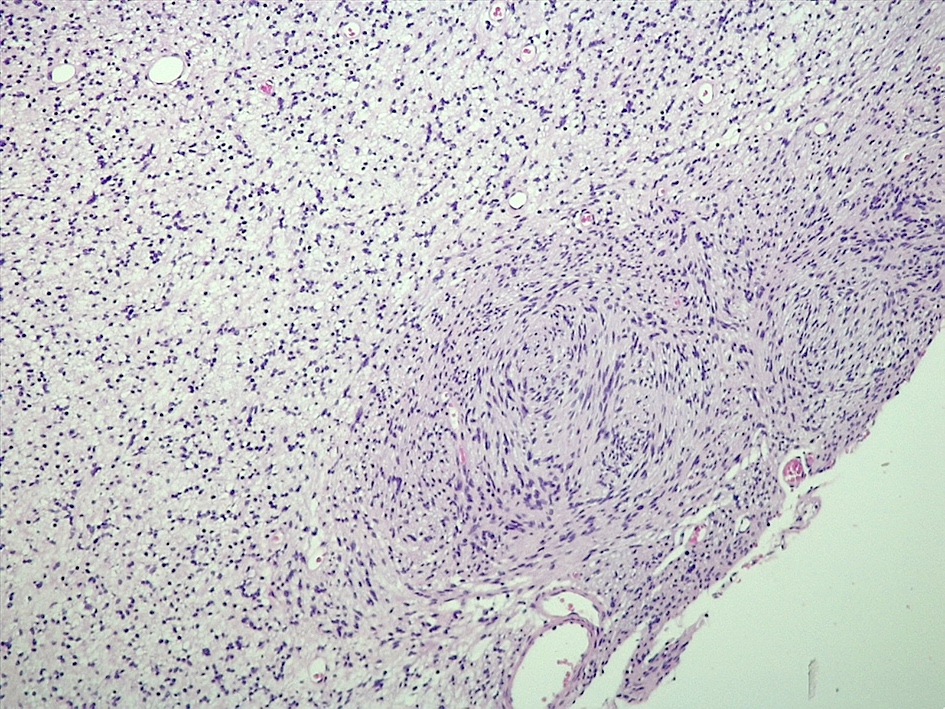
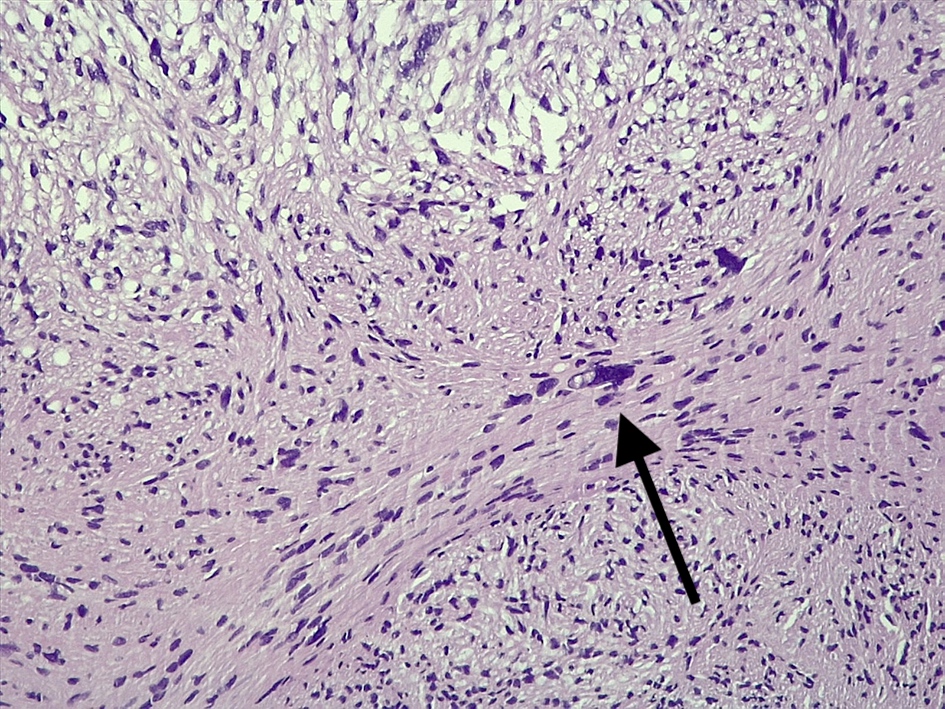
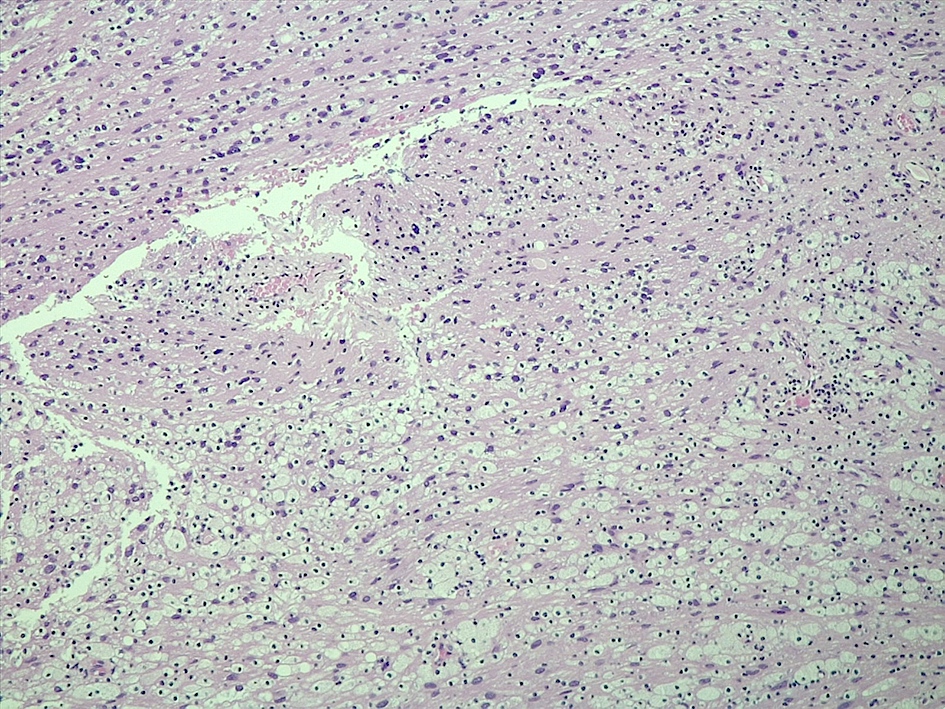
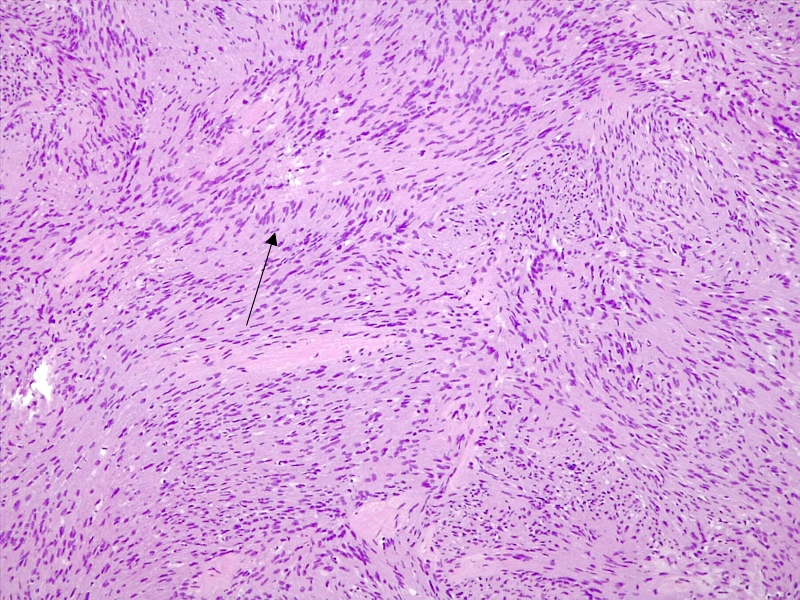
Microscopic (histologic) description
- Spindle cell tumo (usually biphasic) and composed of compact hypercellular areas (Antoni A tissue) showing nuclear palisading (Verocay bodies) and loose microcystic areas (Antoni B tissue) with collection of lipid laden histiocytes and thick walled hyalinized blood vessels (Surg Neurol Int 2020;11:454)
- Lymphoid aggregates maybe seen peripherally or in a subcapsular distribution
- Mitoses or focal degenerative atypia may be present
- Ancient subtype: characterized by scattered atypical or bizarre nuclei
- Cellular subtype: composed exclusively or predominantly by Antoni A tissue and devoid of Verocay bodies
- Mitoses may be more conspicuous; uncommon in the CNS (Clin Neurol Neurosurg 2009;111:467)
- Epithelioid subtype: characterized by epithelioid cells with amphophilic or eosinophilic cytoplasm and uniform round nuclei with inconspicuous nucleoli
Microscopic (histologic) images
Cytology description
- Cohesive lesion with sharp borders in squash preparation or smear and composed of cells with spindle nuclei (Cytopathology 2022;33:196, Cancer Cytopathol 2015;123:171)
- Fibrillary matrix lacking cotton wool look at low magnification
- Hemosiderin deposition may be present (Cytopathology 2022;33:196)
- Nuclear hyperchromasia and pleomorphism may be present
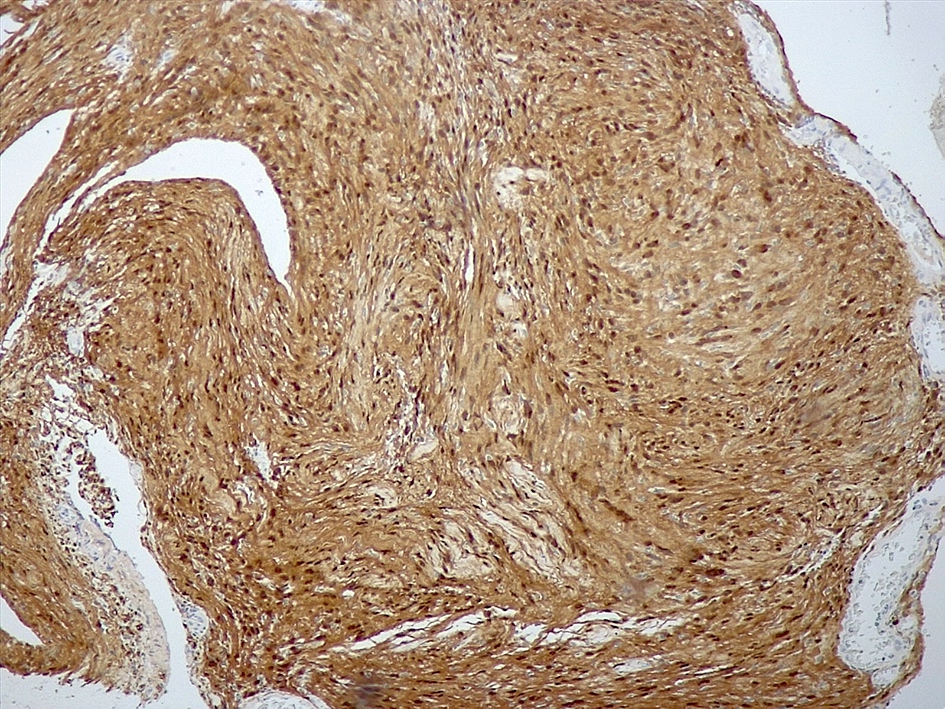
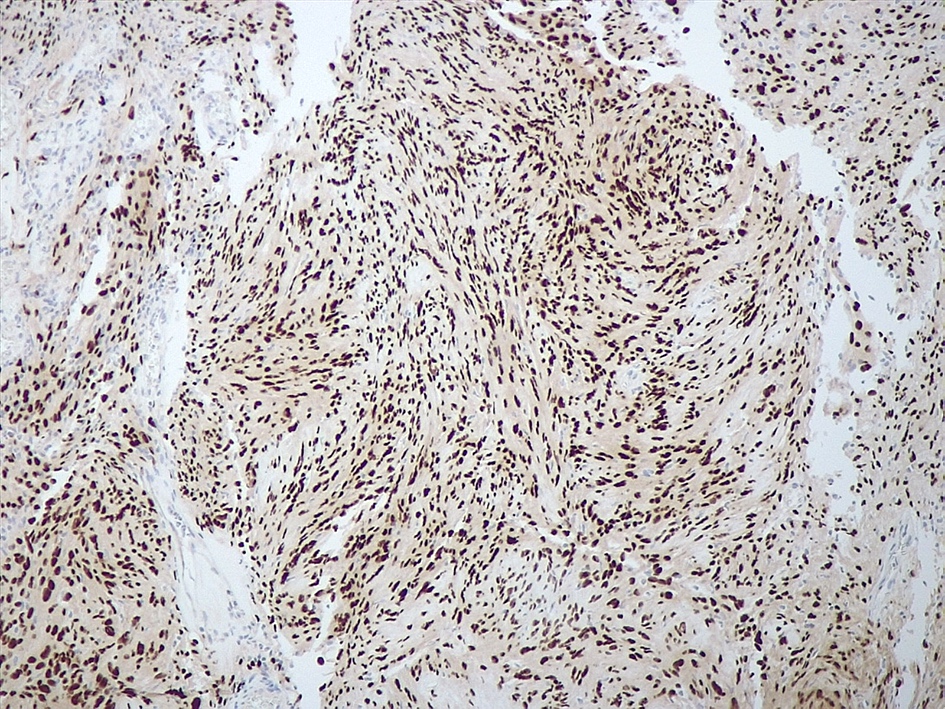
Positive stains
- Strong diffuse SOX10 (Am J Surg Pathol 2008;32:1291)
- Strong diffuse S100 (Appl Immunohistochem Mol Morphol 2012;20:445)
- Neurofilament stain demonstrates axons predominantly pushed to the periphery of the tumor
Negative stains
- EMA (95%) (J Neuropathol Exp Neurol 2017;76:289)
- Progesteron receptor (97%) (J Neuropathol Exp Neurol 2017;76:289)
- CD34 (87%) (J Neuropathol Exp Neurol 2017;76:289)
- STAT6 (J Neuropathol Exp Neurol 2017;76:289, Pathology 2014;46:389)
- SSTR2A (J Neuropathol Exp Neurol 2017;76:289)
- GFAP (J Neuropathol Exp Neurol 2017;76:289)
- CK AE1 / AE3 (J Neuropathol Exp Neurol 2017;76:289)
- MelanA (J Neuropathol Exp Neurol 2017;76:289)
- HMB45 (J Neuropathol Exp Neurol 2017;76:289)
Molecular / cytogenetics description
- NF2 inactivating mutation (frameshift and nonsense) and loss of the remaining wild type allele on chromosome 22 is frequent but not specific (J Neurosurg 2018;128:911)
- Distinct methylation pattern (Nat Genet 2016;48:1339, Acta Neuropathol 2016;131:877)
Sample pathology report
- Spine, tumor, resection:
- Schwannoma, CNS WHO grade 1 (see comment)
- Comment: Spindle cell tumor showing loose areas with lipid laden macrophages and compact areas with nuclear palisading.
Differential diagnosis
- Meningioma, fibrous subtype:
- Solitary fibrous tumor:
- Malignant peripheral nerve sheath tumor:
- Brisk mitotic activity and frequent necrosis
- Frequent necrosis
- Negative or patchy S100 and SOX10 staining
- Complete immunohistochemical loss of H3 p.K27me3 in 50 - 80% of cases
- Neurofibroma:
- Usually not encapsulated
- Presence of shredded carrot collagen bands
- Smaller cells
- Absence of a biphasic pattern
Board review style question #1
An intradural, extramedullary mass is found in the spine. Histological examination shows a tumor with compact areas composed of spindle cells alternating with loose areas with collection of lipid laden macrophages. What is the most likely diagnosis?
- Ependymoma
- Meningioma, fibrous subtype
- Schwannoma
- Solitary fibrous tumor
Board review style answer #1
C. Schwannoma. Fibrous meningioma may localize in the spine but it does not feature alternating compact and loose areas or lipid laden macrophages. Solitary fibrous tumor shows typical staghorn vessels, collagen fibers and neoplastic cells with oval nuclei. In spinal ependymoma, tumor cells have processes forming fibrillary areas around tumor vessels (pseudovascular rosettes) and they often dispose to form rosettes.
Comment Here
Reference: Schwannoma
Comment Here
Reference: Schwannoma
Board review style question #2
An extra-axial mass is found in the cerebellopontine angle. Histological examination shows a tumor with compact areas composed of spindle cells with nuclear palisading and scattered atypical nuclei and loose areas. No mitoses or necrosis are seen. At immunohistochemistry, tumor cells are extensively positive for SOX10 and S100 and negative for EMA, STAT6, GFAP. Which is the most likely diagnosis?
- Malignant peripheral nerve sheath tumor
- Meningioma, fibrous subtype
- Schwannoma, ancient subtype
- Solitary fibrous tumor
Board review style answer #2
C. Schwannoma, ancient subtype. Schwannoma is typically SOX10 and S100 positive and EMA, STAT6 and GFAP negative. Ancient subtype shows scattered atypical nuclei. Meningioma, fibrous subtype may be negative for EMA but it is negative for SOX10 or S100 staining. Solitary fibrous tumor is STAT6 positive and negative for SOX10. Malignant peripheral nerve sheath tumor is negative or has only patchy positivity for SOX10 and S100 and it shows brisk mitotic activity and mitoses.
Comment Here
Reference: Schwannoma
Comment Here
Reference: Schwannoma