Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style question #1 | Board review style question #2 | Board review style answer #2Cite this page: Nisarga P, Gyure KA. Wernicke-Korsakoff syndrome. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cnswernickekorsakoff.html. Accessed April 25th, 2024.
Definition / general
- Acute and chronic neuropsychiatric condition secondary to thiamine (vitamin B1) deficiency
- Wernicke encephalopathy (WE): neuropsychiatric syndrome resulting from thiamine (vitamin B1) deficiency; short lived and severe condition
- Korsakoff syndrome (KS): a disproportionate impairment in memory relative to other features of cognition and secondary to thiamine deficiency
- Usually follows or accompanies Wernicke encephalopathy
- Chronic, long lasting and debilitating condition
Essential features
- Inability to utilize glucose due to deficiency of thiamine, a cofactor for 3 enzymatic processes
- Mammillary bodies and periventricular (third and fourth) regions are usually affected
- Neuropathological changes of Wernicke-Korsakoff syndrome (WKS) depend on age, stage and severity of the disease
Terminology
- Wernicke disease
- Wernicke-Korsakoff syndrome
- Wernicke encephalopathy
- Korsakoff psychosis
- Alcohol amnestic disorder
ICD coding
- ICD-10:
- E51 - thiamine deficiency
- E51.2 - Wernicke encephalopathy
- F10.26 - alcohol dependence with alcohol induced persisting amnestic disorder
- F10.26 - Wernicke-Korsakoff syndrome or psychosis (alcohol dependence)
- F10.96 - alcohol use, unspecified with alcohol induced persisting amnestic disorder
- F10.96 - Wernicke-Korsakoff syndrome or psychosis (alcohol use)
- F04 - amnestic disorder due to known physiological condition
- F04 - Wernicke-Korsakoff syndrome or psychosis (nonalcoholic)
- Korsakoff syndrome induced by other psychoactive substances (F13.26, F13.96, F19.16, F19.26, F19.96)
Epidemiology
- Prevalence of Wernicke encephalopathy:
- < 1 - 3% in autopsies of the general population (Metab Brain Dis 1995;10:17)
- Increases in cases of alcohol abuse and alcohol related death (12.5% and 29 - 59%, respectively) (J Neurol Sci 1982;56:233, S Afr Med J 1996;86:1110, Int J Legal Med 1991;104:209)
- Prevalence of Korsakoff syndrome depends on the management of Wernicke encephalopathy
- Approximately 80 - 90% of alcoholics with Wernicke encephalopathy developed Korsakoff syndrome (Victor: The Wernicke-Korsakoff Syndrome and Related Neurologic Disorders Due to Alcoholism and Malnutrition, Subsequent Edition, 1989)
- Factors predisposing to Wernicke encephalopathy:
- Inadequate nutrition: chronic alcoholism (developed countries), anorexia nervosa or other psychiatric disorders that affect nutrition (hyperemesis gravidarum, inadequate supplementation in total parenteral nutrition [TPN], unbalanced staple diet or prolonged starvation [especially with refeeding])
- Systemic diseases: gastrointestinal diseases, malignancy, AIDS
- Surgery or procedures: bariatric surgery, hemodialysis or peritoneal dialysis, chemotherapy and transplantation
Sites
- Wernicke encephalopathy: mammillary bodies, periventricular regions of thalamus (mediodorsal nucleus and medial pulvinar) and hypothalamus, periaqueductal gray matter (oculomotor nucleus), tectum and reticular formation (midbrain) and corpora quadrigemina and floor of the fourth ventricle (Alcohol Res Health 2003;27:134)
- Degeneration of superior cerebellar vermis associated with alcohol use and thiamine deficiency; may be seen with or without Wernicke-Korsakoff syndrome but more severe in Wernicke-Korsakoff (Alcohol Res Health 2003;27:134)
- Korsakoff syndrome: same distribution as that of Wernicke encephalopathy; most commonly involves mammillary bodies, mediodorsal nucleus of thalamus and medial pulvinar (wall of third ventricle) (Victor: The Wernicke-Korsakoff Syndrome and Related Neurologic Disorders Due to Alcoholism and Malnutrition, Subsequent Edition, 1989, AMA Arch Neurol Psychiatry 1956;76:585)
Pathophysiology
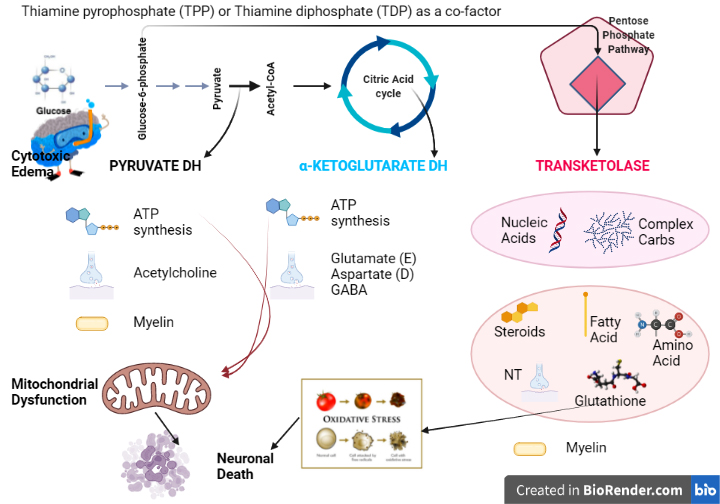
- Thiamine is a cofactor for enzymes involved in energy production and synthesis of biomolecules (see Diagrams / tables)
- Brain areas with high energy requirement or high thiamine turnover show characteristic lesions
- Mitochondrial dysfunction → decreased ATP → cell death (necrosis / apoptosis)
- Decreased glutathione → increased free radicals → oxidative stress
- Disturbances in carbohydrate metabolism leads to loss of osmotic gradients, resulting in intracellular fluid accumulation (cytotoxic edema) and eventual blood brain barrier breakdown (vasogenic edema)
- References: Alcohol Res Health 2003;27:134, Int J Biochem Cell Biol 2009;41:717
Etiology
- Wernicke encephalopathy: thiamine deficiency with or without magnesium deficiency (Lancet 1999;353:1768)
- Korsakoff syndrome: failure to treat Wernicke encephalopathy
Diagrams / tables
Clinical features
- Wernicke encephalopathy:
- Triad (seen in 16%); 19% of the patients have none of these symptoms
- Mental status abnormality (confusion) (34 - 82%)
- Ocular abnormalities (nystagmus or ophthalmoplegia) (15 - 29%)
- Ataxia (23 - 25%)
- Other symptoms: polyneuropathy (11%), hypotension, epileptic seizures, progressive hearing loss (Neuropsychol Rev 2012;22:170)
- Triad (seen in 16%); 19% of the patients have none of these symptoms
- Korsakoff syndrome: profound anterograde amnesia and temporally graded retrograde amnesia with confabulation
- Clinical course: reversible stages of Wernicke encephalopathy → failure to treat → Korsakoff syndrome or death
Diagnosis
- Mainly based on clinical and imaging findings
Laboratory
- Measurement of thiamine or its metabolites in blood / erythrocytes
- Red blood cell transketolase activity
- Reference: Jpn J Radiol 2020;38:809
Radiology description
- Acute Wernicke encephalopathy: bilateral, symmetric T2 and fluid attenuated inversion recovery (FLAIR) signal hyperintensities (figures 1 and 2)
- Chronic Wernicke-Korsakoff syndrome: structural volume deficits in thalamus and mammillary bodies (figure 3)
- Reference: Alcohol Alcohol 2009;44:155
Radiology images
Prognostic factors
- ~20% mortality rate (without treatment)
- ~80% of individuals who survive Wernicke encephalopathy will develop Korsakoff syndrome (without treatment)
- Reference: Victor: The Wernicke-Korsakoff Syndrome and Related Neurologic Disorders Due to Alcoholism and Malnutrition, Subsequent Edition, 1989
Case reports
- 28 year old woman, 45 days after childbirth, with recurrent vomiting during pregnancy and medical past of esophagectomy and partial gastrectomy, presented with Wernicke encephalopathy and catatonia (Neurology 2020;94:2378)
- 54 year old woman with extensive cognitive problems following acute Wernicke encephalopathy (Front Psychiatry 2014;5:59)
- 56 year old woman with schizophrenia developed Wernicke encephalopathy (Front Psychiatry 2021;12:657649)
Treatment
- Parenteral thiamine administration, given before or with intravenous glucose
Gross description
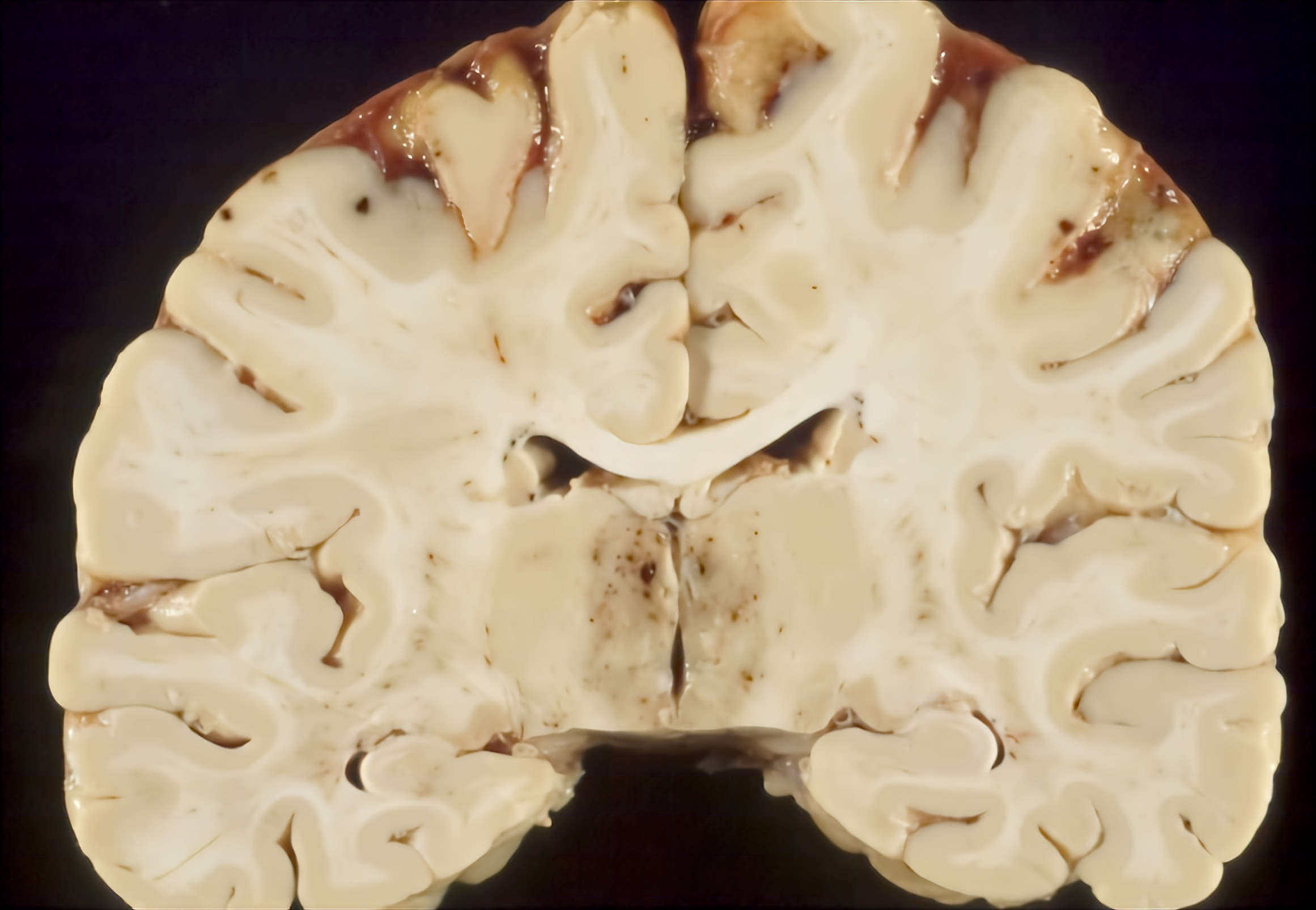
- Changes of Wernicke-Korsakoff syndrome depend on age, stage and severity of the disease
- Wernicke encephalopathy and Wernicke-Korsakoff syndrome are not distinguishable by gross or microscopic pathology
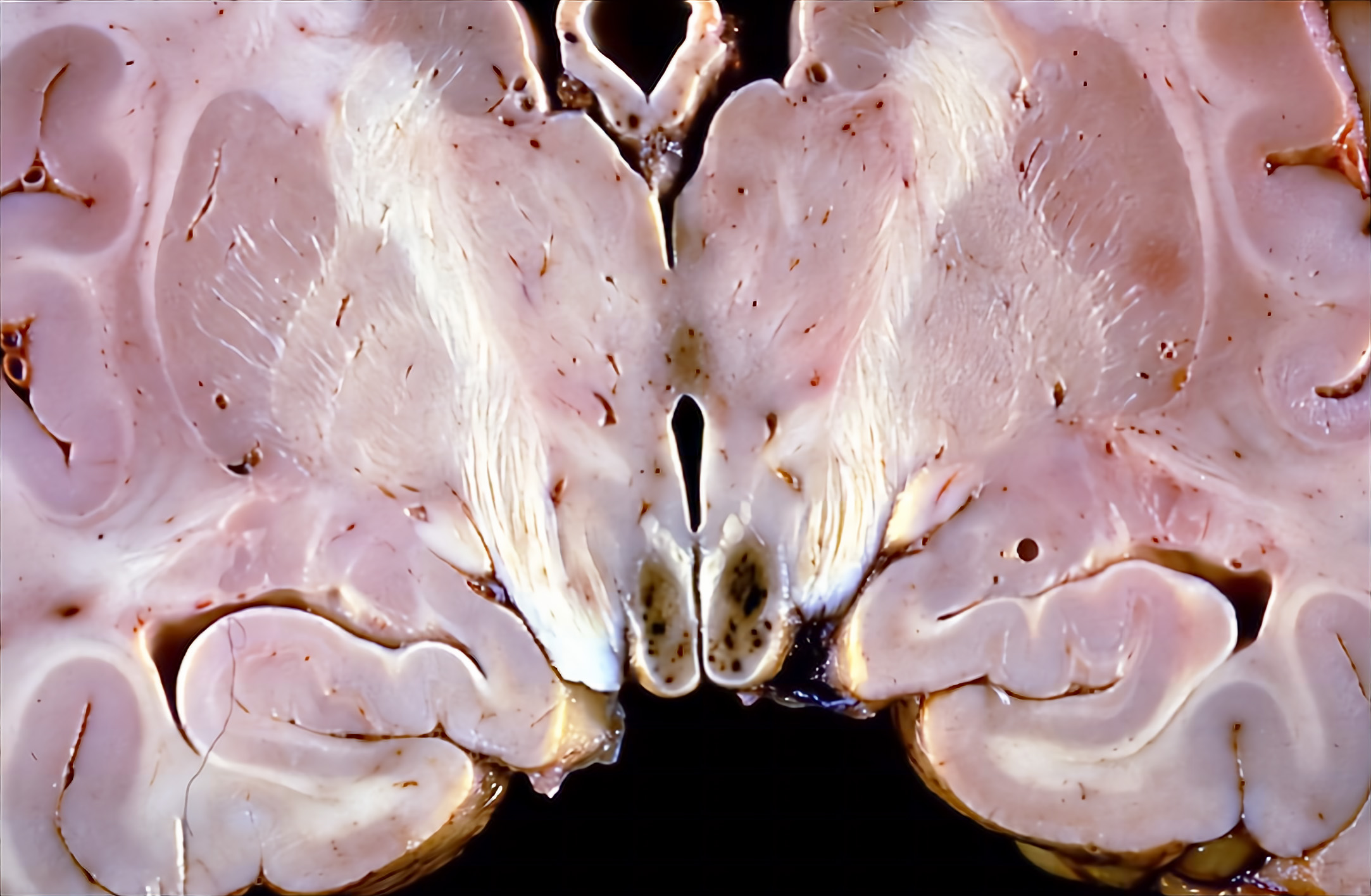
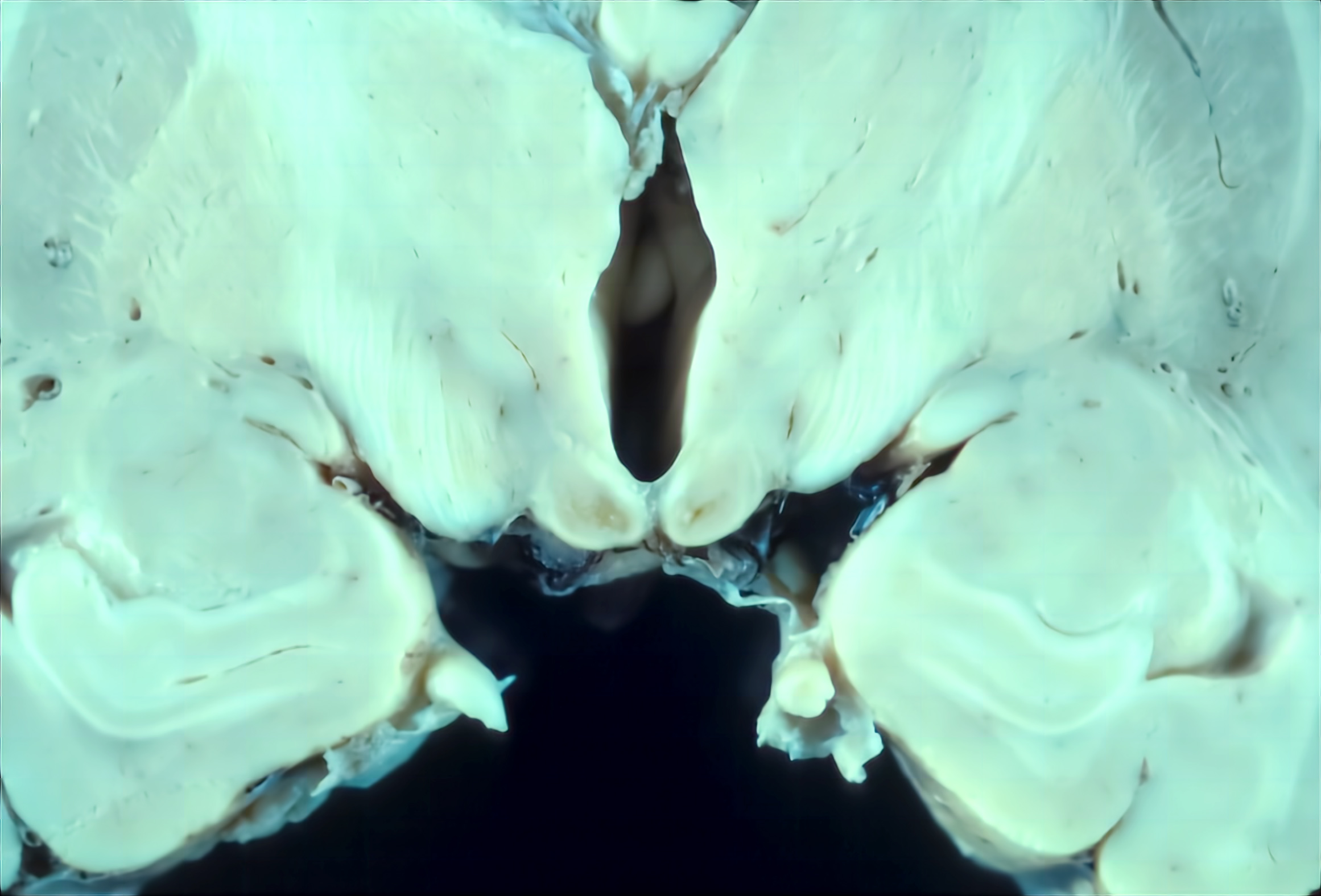
- Acute Wernicke encephalopathy:
- Petechial hemorrhages (and rarely necrosis) involving mammillary bodies and bilateral subcortical regions of periventricular (third and fourth) areas in affected structures
- 25% have normal appearing mammillary bodies
- Chronic Wernicke encephalopathy:
- Atrophy / shrinkage and brown-tan discoloration (hemosiderin) of mammillary bodies
- Unaffected band of tissue immediately adjacent to the ventricular system
- Widened third ventricle
- Atrophy of anterior / superior part of cerebellar vermis (lobes I - IV)
- References: Gray: Escourolle & Poirier's Manual of Basic Neuropathology, 5th Edition, 2013, Love: Greenfield's Neuropathology, 9th Edition, 2015
Gross images
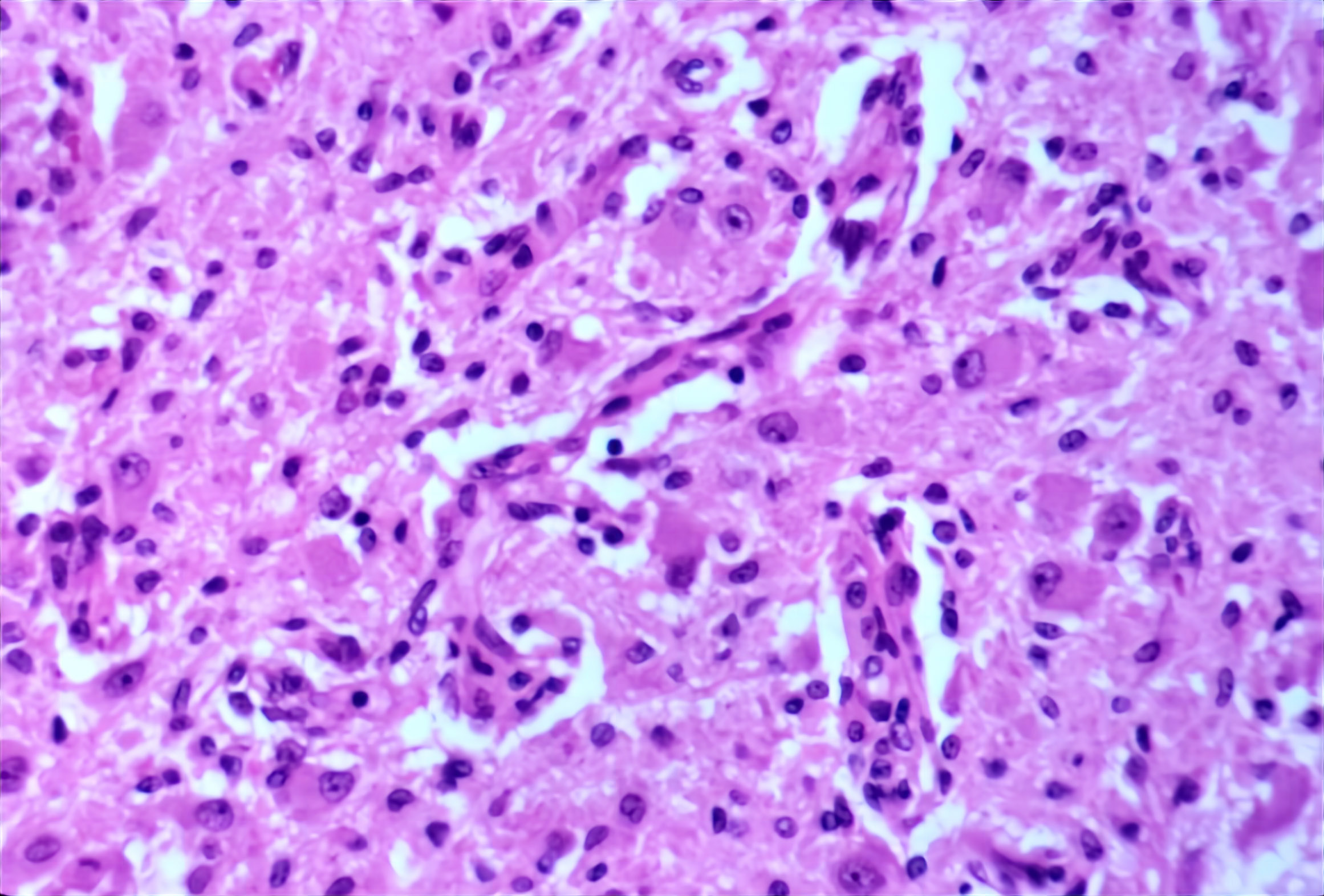
Microscopic (histologic) description
- Changes of Wernicke-Korsakoff syndrome depend on age, stage and severity of the disease
- Superimposed cases: acute Wernicke encephalopathy on chronic Wernicke encephalopathy
- Acute Wernicke encephalopathy:
- Edema
- Vascular changes:
- Hypertrophy or hyperplasia of endothelial cells (all vessel types)
- Fibrinoid degeneration / necrosis (arterioles)
- Earliest change is seen (1 - 2 days)
- Perivascular spaces may contain lipid laden macrophages
- Hemorrhagic areas reveal extravasated red blood cells and few hemosiderin laden macrophages
- Ball microhemorrhages
- Reactive gliosis (follows vascular changes)
- Neurons are usually spared
- Loss of myelin
- Absence of inflammatory reaction
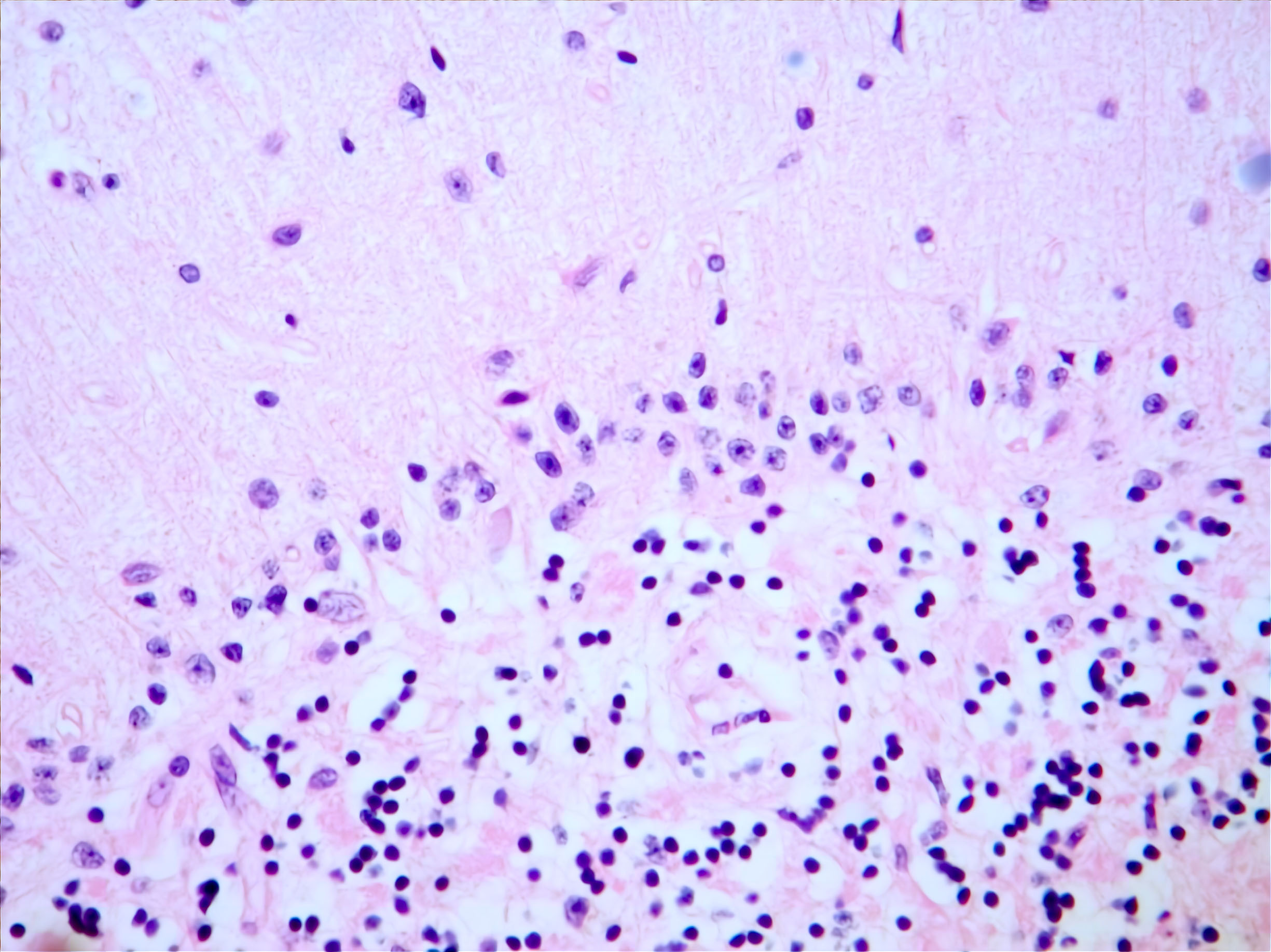
- Chronic Wernicke encephalopathy:
- Loss of native tissue (atrophy)
- Gliosis / astrocytosis
- Hemosiderin laden macrophages
- Mild neuronal loss to neuronal sparing
- Cerebellum
- Cortical degeneration of anterior / superior cerebellar vermis
- Patchy loss of Purkinje cells (decrease in 20 - 30% of mean cellular density) with Bergmann gliosis
- Thinning of molecular layer, atrophy / shrinkage
- Preserved granule cells
- Superimposed cases: acute Wernicke encephalopathy on chronic Wernicke encephalopathy
- Korsakoff psychosis:
- Findings similar to chronic Wernicke encephalopathy
- Mammillary bodies and medial dorsal thalamus are affected
- References: Gray: Escourolle & Poirier's Manual of Basic Neuropathology, 5th Edition, 2013, Love: Greenfield's Neuropathology, 9th Edition, 2015
Microscopic (histologic) images
Sample pathology report
- Brain, autopsy:
- History of thiamine deficiency with associated encephalopathy
- Mammillary body atrophy with relative preservation of neurons and gliosis consistent with Wernicke encephalopathy
Differential diagnosis
- Alcohol / drug intoxication:
- Alcohol abuse is one of the etiologies for Wernicke-Korsakoff syndrome
- Hyperactive delirium could be secondary to possible alcohol withdrawal symptoms
- Symmetric, hyperintense signal in the basal ganglia, especially the globus pallidus, on T1 weighted MR images
- Alcohol related brain injury - neuronal loss in superior frontal cortex, hypothalamus (supraoptic / paraventricular nuclei); cerebellum - superior vermis molecular layer atrophy, Purkinje cell loss, Bergmann gliosis
- Hepatic encephalopathy - affects globus pallidus (commonly), cerebellar dentate, diencephalon, brain stem; Alzheimer type II astrocytosis
- Bilateral paramedian thalamic infarcts:
- Infractions to the artery of Percheron (with or without midbrain involvement)
- Confusion, hypersomnolence, dysarthria, amnesia and ocular movement disorders
- Noninvasive imaging usually enough for diagnosis (CT, MRI, CT angiogram, MRA angiogram, PET and SPECT)
- Hypoxic ischemic damage / stroke:
- Noninvasive imaging usually enough for diagnosis (CT, MRI, CT angiogram, MRA angiogram, PET and SPECT)
- Circumscribed areas of pallor with red dead neurons (12 - 48 hours), macrophage infiltrate + cavitation of cortex (layers 2 - 6) + loss of axons (3 - 30 days) and circumscribed organized area of cavitation + scattered macrophages + residual glial tissue (months - years)
- Seizure disorders:
- Wernicke-Korsakoff syndrome can be associated with seizures
- Detailed personal and family history is essential
- Electroencephalography (EEG) is a biomarker for epilepsy
- Temporal lobe epilepsy - hippocampal sclerosis (classical hippocampal sclerosis [40%] to end folium sclerosis [25%]) (Noebels: Jasper's Basic Mechanisms of the Epilepsies, 4th Edition, 2012)
- Tumors - ganglioglioma, dysembryoplastic neuroepithelial tumors, anglocentric glioma, gangliocytoma, etc.
- Focal cortical dysplasia or cortical malformations
- Others: glial scar, vascular malformations, encephalitis (N Engl J Med 2017;377:1648)
- Concussion:
- Traumatically induced transient disturbance of brain function
- Diagnosis remains an exclusively clinical diagnosis based on history and exam findings
- Imaging modalities can be employed to rule out other injuries
- Neurodegeneration reported in mouse model (J Neurotrauma 1994;11:657)
- Using silver stain - modified Gallyas method described by Nadler and Evenson (Methods Enzymol 1983;103:393)
- Viral (herpes) encephalitis:
- Preceded by prodromal flu-like illness (including fever and headache) and manifests as superimposed behavioral changes, seizures, focal neurological signs and cognitive impairment
- MRI shows asymmetric high signal within the medial temporal lobes, insular cortex and orbitofrontal and cingulate cortex
- Perivascular lymphocytic cuffing, microglial nodules, neuronophagia, demyelination, ependymitis, gliosis
- Viral inclusions are rarely seen
- Intranuclear inclusions (Cowdry type A: herpes simplex, oligodendrocytic JC virus)
- Cytoplasmic inclusions (Negri bodies; rabies)
- Pathogen specific immunohistochemistry
- Neurodegenerative / demyelinating disease:
- Diagnosis remains an exclusively clinical diagnosis based on history, exam, laboratory and ancillary test findings
- Most reliable method to detect mild cognitive impairment is neuropsychological testing
- Includes diagnostic criteria to diagnose demyelinating disorders
- Multiple sclerosis - myelin loss + relative axonal sparing, macrophage infiltrate (activity), chronic inactive / active plaques
- Acute demyelinating encephalomyelitis - perivenular cuffs of myelin loss, perivascular macrophages
- Acute hemorrhagic leukoencephalitis - fibrinoid necrosis of postcapillary venules + hemorrhage (ring and ball), neutrophilic debris and fibrin exudates + ischemic changes
- Tumefactive demyelinating lesion - myelin loss + relative axonal sparing; macrophages, reactive astrocytosis, mitoses and variable perivascular / parenchymal lymphocytes
- Neoplasia:
- Clinical history, imaging and tissue biopsy is helpful to differentiate
Additional references
Board review style question #1
Which of the following pathological features is seen in acute Wernicke encephalopathy?
- Acute inflammation
- Alzheimer type II astrocytes
- Endothelial hyperplasia
- Geographic necrosis
- Granuloma
Board review style question #1
Board review style question #2
Board review style answer #2