Table of Contents
Definition / general | Essential features | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Radiology description | Case reports | Treatment | Clinical images | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Heyraty MP, Pezhouh MK. Anti-PD1 associated colitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colonAntiPD1.html. Accessed April 24th, 2024.
Definition / general
- Colitis is an immune related adverse event of anti-PD1 (nivolumab, pembrolizumab) and anti-PDL1 medications (atezolizumab, avelumab and durvalumab)
- PDL1 (programmed death ligand 1) and its receptor PD1 protect host cells from autoreactive T cells; monoclonal antibodies which block this interaction have been approved for treatment of several cancers (see PDL1 topic)
Essential features
- Colitis is an immune related side effect of anti-PD1 and anti-PDL1 therapy
- Often mild (diarrhea); very rarely severe (perforation) (Surg Case Rep 2017;3:94)
- 2 main histologic patterns of injury (Am J Surg Pathol 2017;41:643):
- Active colitis with neutrophilic crypt microabscesses, prominent crypt epithelial cell apoptosis and crypt atrophy / dropout (the most common pattern)
- Lymphocytic colitis-like pattern with surface injury
Epidemiology
- Incidence of 1.3 - 13.6% based on the specific agent, dose and combination of treatment for patients taking anti-PD1 and anti-PDL1 medication (BMJ 2018;360:k793, Front Pharmacol 2017;8:730, Oncoimmunology 2017;6:e1344805)
Sites
- Can affect the entire gastrointestinal tract and liver (Histopathology 2017;70:558, Mod Pathol 2018;31:965)
Pathophysiology
- Caused by immune dysregulation of the gastrointestinal mucosa (Cell 2020;182:655)
Clinical features
- Abdominal pain / cramping, diarrhea, urgency and rectal bleeding in severe form
Diagnosis
- Diagnosis of anti-PD1 colitis should be considered in patients who present with diarrhea or abdominal pain and have a history of treatment with anti-PD1 medication
- Further evaluation with endoscopy and biopsy could confirm the diagnosis
Radiology description
- Segmental / diffuse bowel wall thickening, mucosal hyperenhancement and diffuse or segmental peritoneal fat infiltration with mesenteric vessel engorgement (Eur J Cancer 2018;96:91, Eur Radiol 2021;31:8868)
Case reports
- 51 year old woman with colonic perforation after treatment with pembrolizumab (anti-PD1 inhibitor) for metastatic melanoma (Case Rep Gastrointest Med 2018;2018:3406437)
- 62 year old man with infliximab refractory severe nivolumab induced enterocolitis (Am J Case Rep 2018;19:360)
- 68 year old woman with anti-PD1 induced collagenous colitis (Melanoma Res 2016;26:308)
- 71 year old man with intestinal perforation after nivolumab immunotherapy for a malignant melanoma (Surg Case Rep 2017;3:94)
- 82 year old man with nivolumab associated colitis mimicking ulcerative colitis (Clin Gastroenterol Hepatol 2017;15:A35)
Treatment
- Withholding the immune check point inhibitor
- Most patients respond to corticosteroids
- In steroid refractory cases, tumor necrosis factor α (TNFα) blocking agents such as infliximab and vedolizumab can be used
- Reference: Practice Guideline Gastroenterology 2021;160:1384
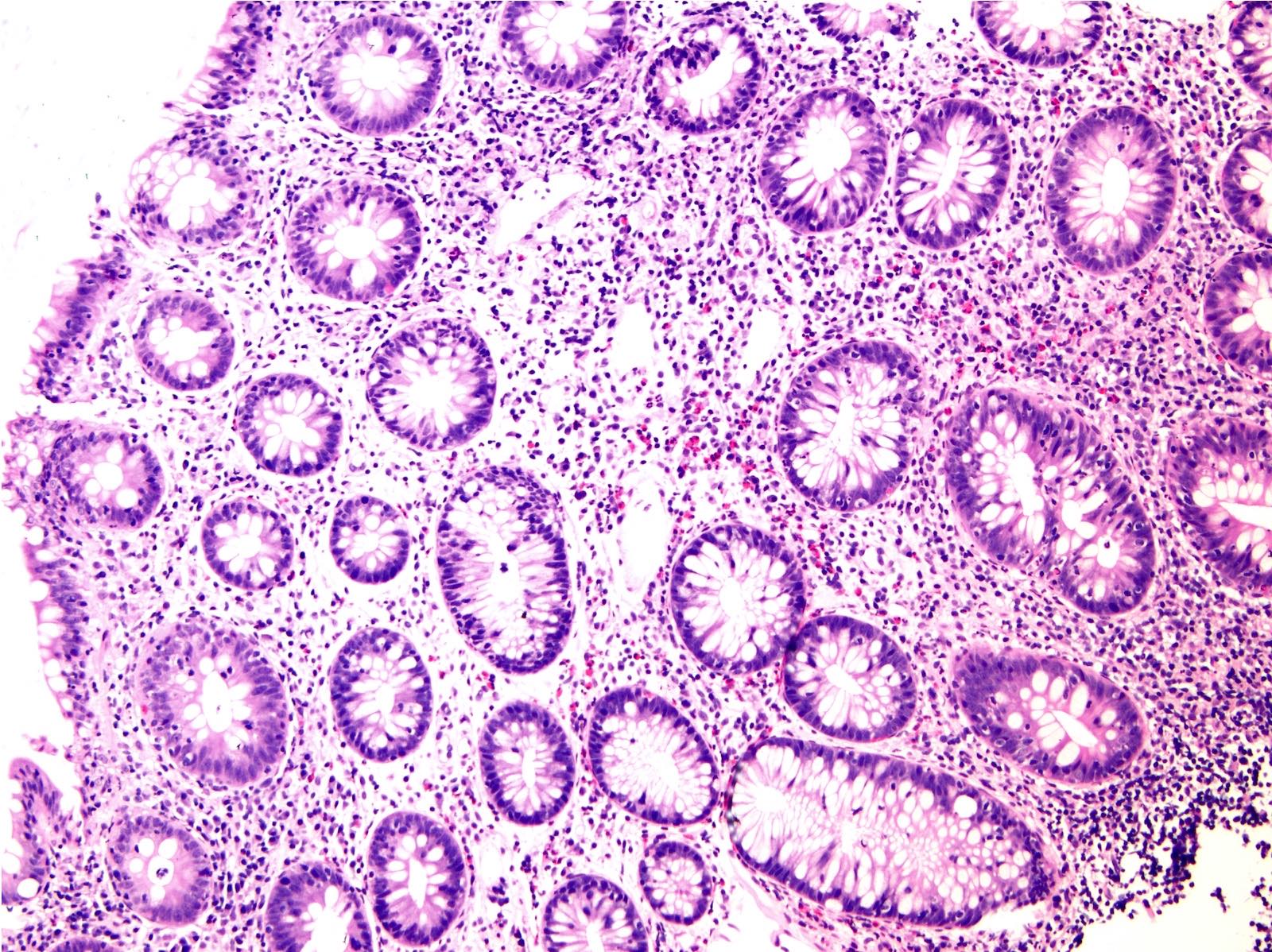
Microscopic (histologic) description
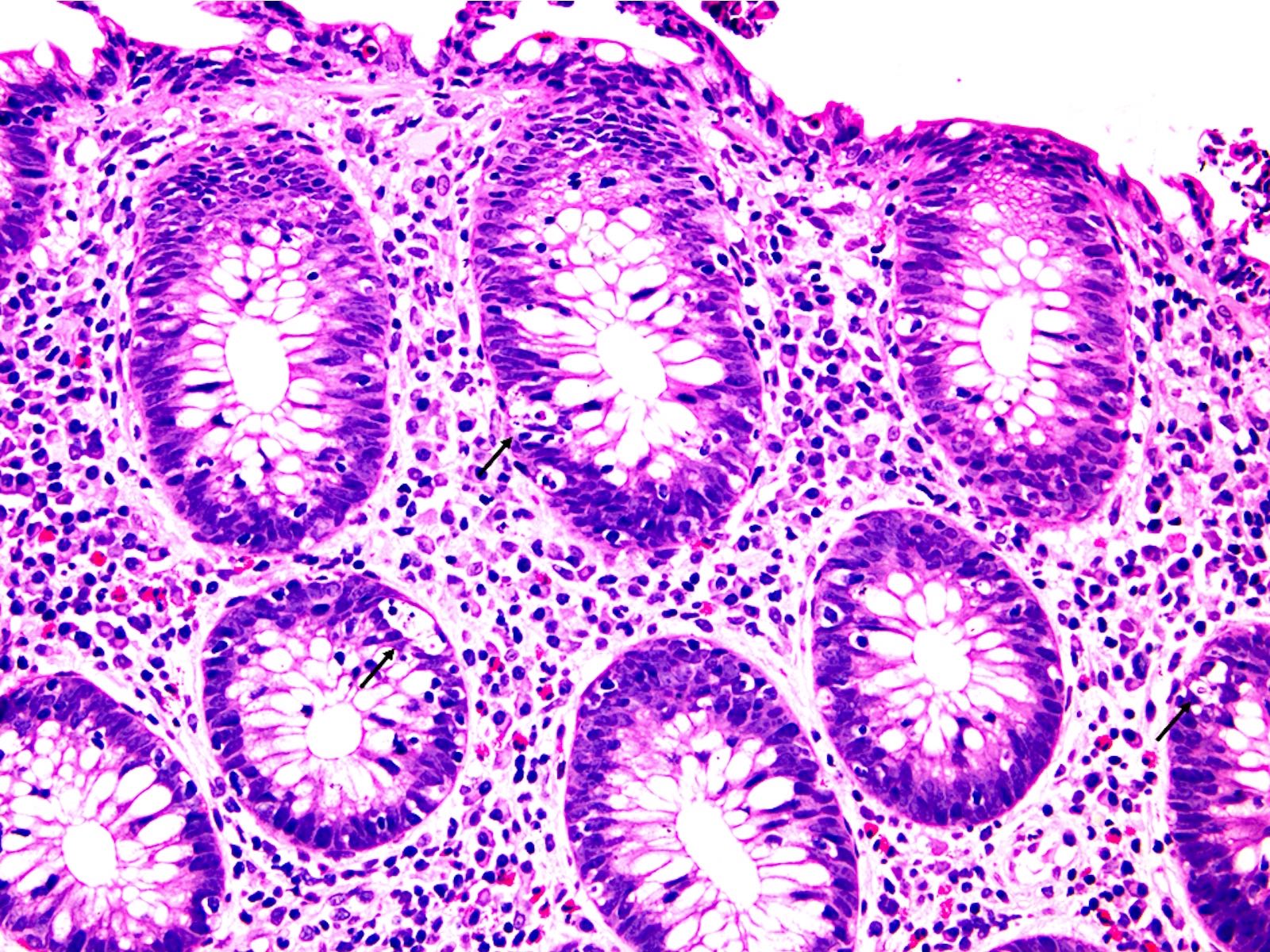
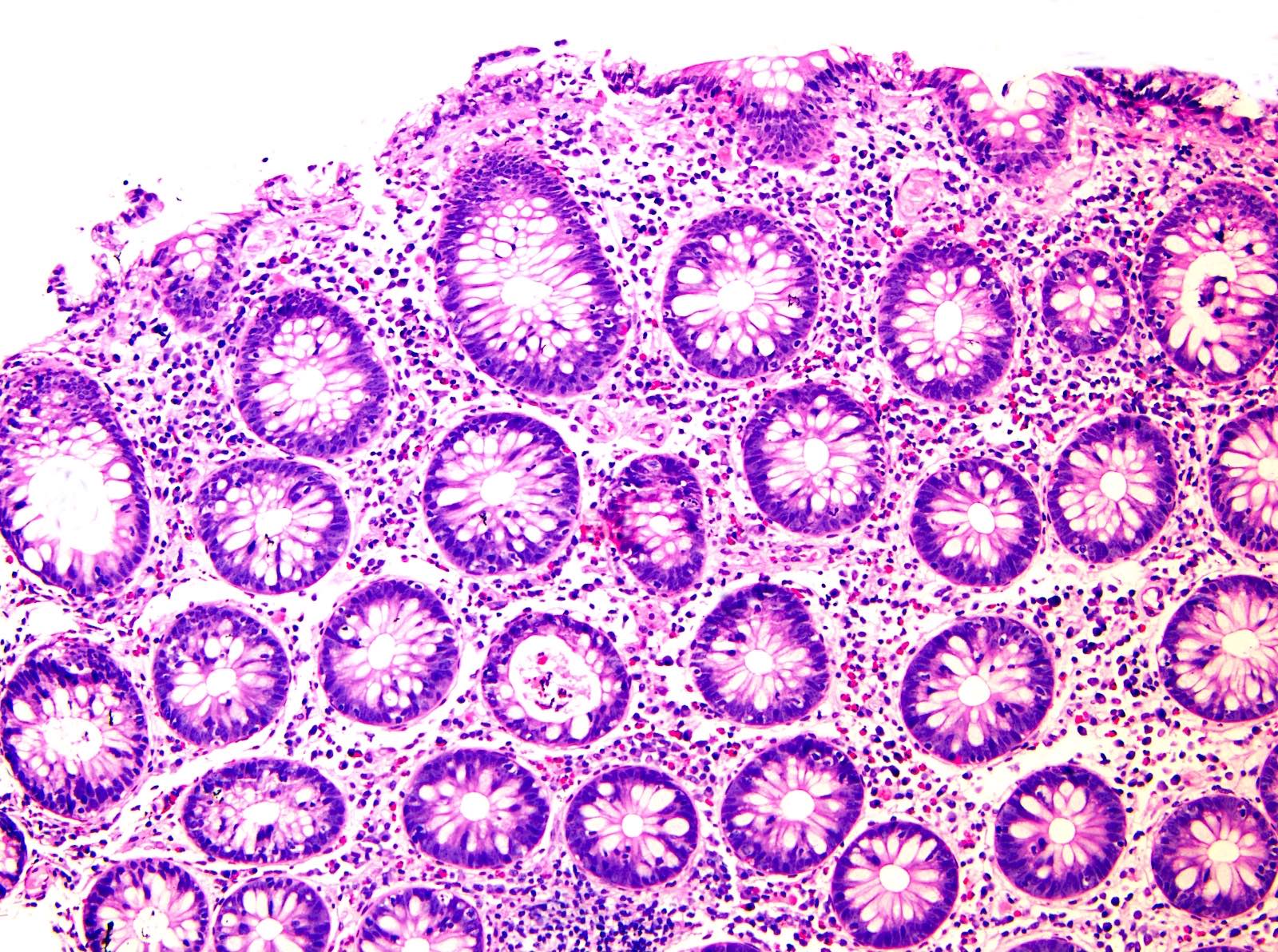
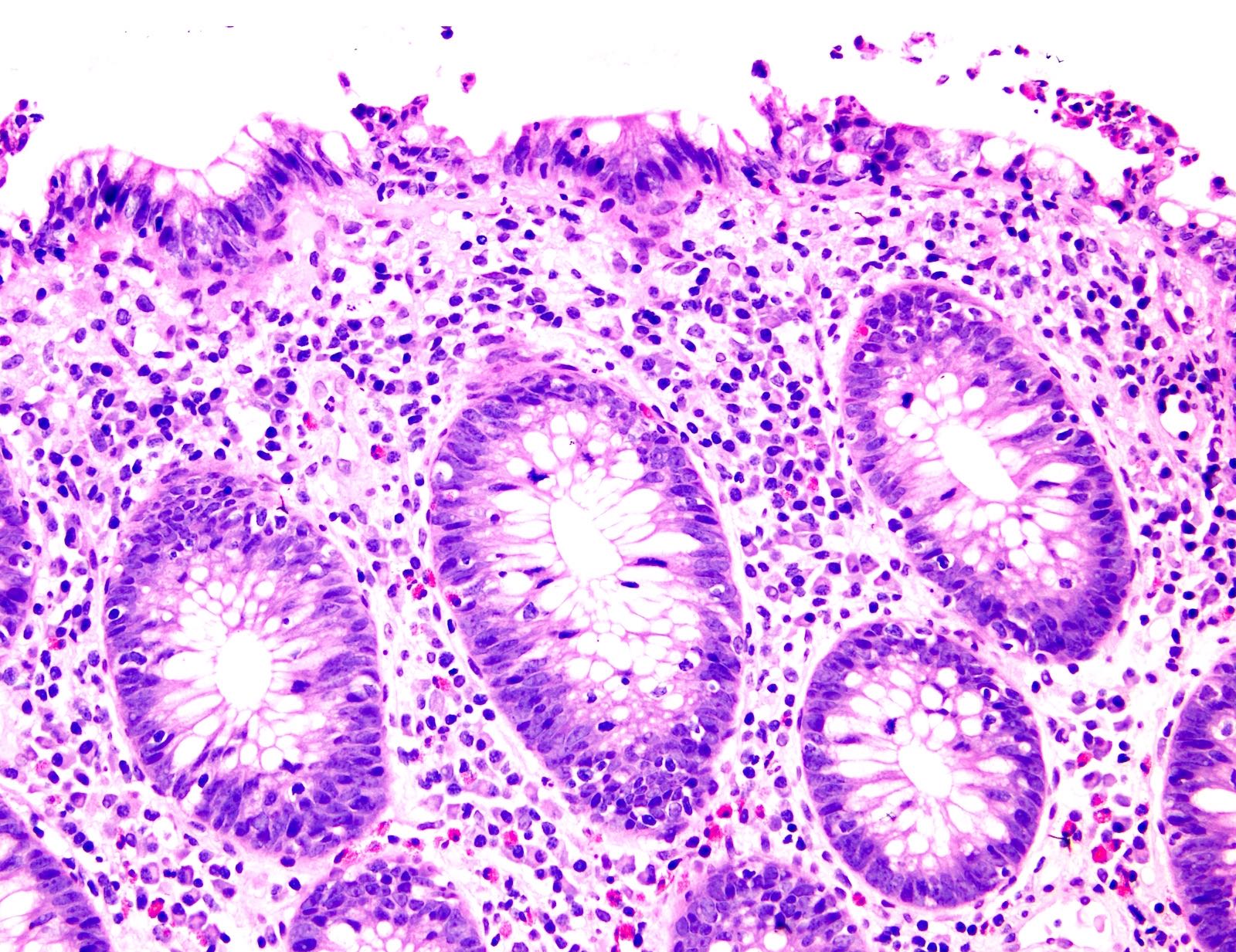
- Common patterns of injury (Am J Surg Pathol 2017;41:643, Histopathology 2021;78:532):
- Focal active colitis: neutrophilic crypt microabscesses or cryptitis with prominent crypt epithelial cell apoptosis, focal crypt atrophy / dropout
- Lymphocytic colitis-like pattern of injury
- Other histopathologic patterns include graft versus host disease-like or collagenous colitis patterns of injury (Histol Histopathol 2022;37:699)
- Anti-PD1 associated colitis rarely causes perforation
Microscopic (histologic) images
Negative stains
Sample pathology report
- Colon, biopsy:
- Colonic mucosa with lymphocytic colitis pattern of injury and mild focal active colitis (see comment)
- Comment: Patient’s history of advanced melanoma status post treatment with pembrolizumab is noted. The biopsies show a predominantly lymphocytic colitis pattern of injury with focal mild active colitis. No significant chronicity, no granuloma and no viral cytopathic effects are seen. Overall, these findings are most consistent with anti-PD1 associated colitis.
Differential diagnosis
- Other causes of active colitis with prominent apoptosis, such as infections (CMV colitis), acute graft versus host disease
- Inflammatory bowel disease:
- Basal plasmacytosis, less apoptosis, evidence of chronicity
- Chemotherapy induced colitis:
- Changes depend on the type of medication but may show similar histology; history is probably necessary for distinction
- Ipilimumab associated colitis:
- Lymphoplasmacytic expansion of lamina propria, increased apoptosis and intraepithelial lymphocytes, cryptitis and crypt elongation
- Somewhat similar histology; history is probably necessary for distinction
- Idelalisib associated colitis:
- Somewhat similar histology to anti-PD1 associated colitis; history is probably necessary for distinction (Am J Surg Pathol 2015;39:1661)
Board review style question #1
A 64 year old man with ulcerative colitis recently completed 3 cycles of pembrolizumab therapy for metastatic carcinoma. He underwent a colonoscopy with a biopsy for diarrhea. Which of the following features is key to differentiating anti-PD1 associated colitis from ulcerative colitis?
- Increased crypt epithelial apoptosis, lack of significant chronicity and absence of basal plasmacytosis
- Involvement of the rectum
- Presence of crypt abscesses
- Presence of erosions
Board review style answer #1
A. Increased crypt epithelial apoptosis, lack of significant chronicity and absence of basal plasmacytosis. Increased crypt epithelial apoptosis is most commonly seen in anti-PD1 colitis. On the other hand, presence of significant chronicity and basal plasmacytosis is more in favor of inflammatory bowel disease. Rectum involvement, crypt abscesses and erosions can be seen in both.
Comment Here
Reference: Anti-PD1 associated colitis
Comment Here
Reference: Anti-PD1 associated colitis
Board review style question #2
A 72 year old man with a history of melanoma recently received 3 cycles of nivolumab and developed abdominal pain and diarrhea. A colonoscopy was done which found erythema in the ascending and transverse colon. Histology is shown in the image above. What is the most likely diagnosis?
- Anti-PD1 associated colitis
- Collagenous colitis
- Diverticular associated colitis
- Severe ulcerative colitis
Board review style answer #2
A. Anti-PD1 associated colitis. Based on the history and findings of a mild focal active colitis and mild increase in intraepithelial lymphocytes, the most likely diagnosis is anti-PD1 colitis.
Comment Here
Reference: Anti-PD1 associated colitis
Comment Here
Reference: Anti-PD1 associated colitis