Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Ahmed S, Haroon S. Tuberculosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colonTB.html. Accessed April 25th, 2024.
Definition / general
- Infectious disease of the colon or small intestine by acid fast bacilli, Mycobacterium tuberculosis
- Second leading infectious killer after COVID-19 (BMC Gastroenterol 2022;22:89)
- 10% of all cases of extrapulmonary tuberculosis are intestinal tuberculosis (BMC Gastroenterol 2022;22:89)
Essential features
- Infection occurs through ingestion of mycobacteria in sputum or infected milk, direct extension from adjacent infected lymph node or hematogenous spread
- Ileocecal region is the most common site
- Common symptoms include weight loss, anorexia, fever, abdominal pain, diarrhea, constipation and palpable mass
- Endoscopic findings comprise strictures, ulcers and mucosal hypertrophy
- Colonoscopic biopsies show granulomatous inflammation with caseous necrosis
- Special stain, culture or PCR is used to detect the organisms
- Treatment is with combination of antibiotics and more aggressive treatment is essential for multidrug resistant tuberculosis
- Surgery may be necessary to treat complications such as perforation, obstruction, fistula or bleeding
ICD coding
- ICD-11: 1B12.7 - tuberculosis of the digestive system
Epidemiology
- Worldwide (2021): 10.6 million cases of tuberculosis (TB) and 1.6 million deaths (WHO: Global Tuberculosis Report 2022 [Accessed 8 August 2023])
- TB incidence rate is estimated to have increased by 3.6% between 2020 and 2021 (WHO: Global Tuberculosis Report 2022 [Accessed 8 August 2023])
- United States (2022): 8,300 cases, rate of 2.5 per 100,000 (MMWR Morb Mortal Wkly Rep 2023;72:297)
- Gastrointestinal (GI) TB accounts for about 5% of all TB cases (BMC Gastroenterol 2019;19:106)
- GI TB is common in populations with low socioeconomic status; most of the cases occur in developing world (Southeast Asia, Africa, Eastern Europe, Latin and Central America) (BMC Gastroenterol 2022;22:89)
- Usually affects young to middle aged adults but all populations are at risk, with most cases occurring in females
- Abdominal TB embodies the sixth most frequent form of extrapulmonary TB, after the more common ones being, lymphatic, genitourinary, bone and joint, miliary and meningeal TB (J Lab Physicians 2009;1:56)
- Extrapulmonary TB is more common in immunocompromised patients
- ~15 - 25% cases with abdominal TB have concomitant pulmonary TB (World J Gastroenterol 2014;20:14831)
- Risk factors: HIV / AIDS, substance abuse, silicosis, diabetes mellitus, chronic kidney disease, poverty and malnutrition, old age, infancy, immunosuppressive therapy (Indian J Nephrol 2019;29:132)
- GI TB has also been associated with antitumor necrosis factor therapy in a patient who underwent solid organ transplantation (Indian J Nephrol 2019;29:132)
Sites
- Most common site is ileocecal region; 64% of patients with GI TB have ileocecal disease (World J Gastroenterol 2014;20:14831)
- Followed by jejunum and other colorectal sites
- Rectum and anus rarely involved, anus representing only 1% of abdominal TB (J Clin Tuberc Other Mycobact Dis 2018;12:1)
- Isolated colorectal involvement is uncommon; only 10.8% of abdominal GI TB (World J Gastroenterol 2014;20:14831)
Pathophysiology
- Most commonly, Mycobacterium bacilli enter the gastrointestinal tract through the ingestion of infected milk or sputum (World J Emerg Surg 2019;14:33)
- Second pathway is hematogenous spread from tubercular focus elsewhere in the body
- Ileocecum is a favored site in GI tract due to abundant lymphoid tissue
- Nonspore forming, obligate aerobic, catalase negative, nonmotile bacillus with high lipid and mycolic acid content of cell wall (World J Emerg Surg 2019;14:33)
- Cell mediated delayed type IV hypersensitivity reaction develops that helps to contain the bacteria
- Bacilli are phagocytosed by macrophages, phagolysosome blockage occurs, further replication and bacteremia develops leading to primary TB (J Clin Tuberc Other Mycobact Dis 2022;27:100300)
- Caseating granulomatous inflammation and tissue damage occurs
- Reactivation may occur when immune status is compromised
- 5 - 10% of immune competent patients develop active disease while 30% of the patients with HIV develop active disease (Emerg Microbes Infect 2016;5:e10)
Etiology
- Causative agent is Mycobacterium (M) tuberculosis
- Mycobacterium (M) tuberculosis complex includes M. tuberculosis, M. africanum, M. bovis, M. microti (Ig Sanita Pubbl 2020;76:59)
Clinical features
- Colon
- Chronic disease is usually present for months
- Most common symptoms include anorexia, fever, abdominal pain, diarrhea, constipation, abdominal distension and a palpable abdominal mass (BMC Gastroenterol 2022;22:89)
- Other symptoms may include night sweats, rectal bleeding and malabsorption
- Perforation, intestinal obstruction and lymphadenopathy may also occur in complicated cases (Saudi J Gastroenterol 2021;27:261)
- Small intestine
- Disease occasionally seen in less developed countries
- Small intestinal disease may be transmitted via contaminated milk
- Common symptoms encompass abdominal pain, malabsorption, strictures, perforation and fistula (BMC Gastroenterol 2022;22:89)
Diagnosis
- Gold standard diagnosis is demonstration of microorganisms with culture of Mycobacterium tuberculosis using intestinal mucosal tissue (BMC Gastroenterol 2022;22:89)
- Histopathological examination of the intestinal tissue, acid fast bacilli (AFB) staining and nucleic acid amplification tests (MMWR Morb Mortal Wkly Rep 1996;45:950)
- GI TB is a paucibacillary disease and acid fast bacilli may not be isolated from the clinical specimens
- Colonoscopic biopsies have 80% diagnostic accuracy (BMC Gastroenterol 2022;22:89)
Laboratory
- Blood tests help in detecting erythrocyte sedimentation rate (ESR) and anemia
- Gene Xpert MTB / RIF test detects acid fast bacillus and rifampicin resistance, polymerase chain reaction (PCR), multiplex PCR and immunological markers (BMC Gastroenterol 2022;22:89)
- One of the conventional tests used to detect TB is intestinal biopsy
Radiology description
- Cross sectional imaging with ultrasonography, multidetector CT and MRI play an important role in the diagnosis (World J Gastroenterol 2014;20:14831)
- CT scan is the modality of choice; it detects nodular mucosal thickening with loss of symmetry in the fold pattern, thickened omentum and peritoneum
- Mesenteric lymphadenopathy with necrotic lymph node can be associated with GI TB in children (World J Emerg Surg 2019;14:33)
- May see fissures, fistulae, sinus tracts, linear and transverse ulcers perpendicular to long axis or perforation (World J Gastroenterol 2014;20:14831)
- Obliteration of ileocecal angle with widely patent ileocecal valve
- Rapid emptying of cecum with passage of barium, from terminal ileum to the ascending colon (Stierlin sign) (Indian J Radiol Imaging 2016;26:161)
Prognostic factors
- Overall prognosis is not very good, owing to delayed diagnosis and usual occurrence in immunocompromised persons (Cureus 2021;13:e13058)
- Specifically untreated GI TB causes significant morbidity, leading to prolonged hospitalization and may require surgical intervention
- Poor prognosis is seen in cases of life threatening complications, such as intestinal stricture, obstruction, bleeding and perforation (Cureus 2021;13:e13058)
- HIV patients with low CD4 counts, other immunosuppressed states, elderly and the debilitated also tend to have a poorer prognosis
Case reports
- 37 year old Mexican man with history of heavy alcohol abuse and progressive diffuse abdominal pain (Cureus 2021;13:e13058)
- 47 year old man, originally from India, residing in Portugal for a year, presented to emergency with diarrhea and diffuse abdominal pain (Cureus 2022;14:e30600)
- 81 year old immunocompetent woman from a nonendemic area who developed intestinal TB (Eur J Gastroenterol Hepatol 2011;23:1074)
Treatment
- 2 months of 4 drug therapies (rifampicin, isoniazid, pyrazinamide, ethambutol) followed by 4 months of 2 drug therapies (rifampicin, isoniazid) (BMC Gastroenterol 2019;19:106)
- Drug resistant TB is defined as resistant to at least 1 first line drug, extensively drug resistant is resistant to isoniazid and rifampin, plus at least 1 of 3 injectable second line drugs (amikacin, kanamycin or capreomycin)
- WHO recommends directly observed therapy (DOT)
- CDC recommends expert consultation to treat drug resistant and extensively drug resistant TB
- Most common complication is perforation, which requires surgical intervention (Abdom Imaging 1999;24:32)
- Inflammatory cecal masses can mimic acute appendicitis, leading to surgery (Abdom Imaging 1999;24:32)
Gross description
- Ulcerative (most common, 60%), ulcerohypertrophic (30%) and hypertrophic (10%) forms are described (J Clin Tuberc Other Mycobact Dis 2018;12:1)
- Usually multiple superficial ulcers perpendicular to long axis of bowel; may see deep ulcers (J Clin Tuberc Other Mycobact Dis 2018;12:1)
- May see thickened mucosal folds, strictures, ulcers, inflammatory nodules; fistulas are rare
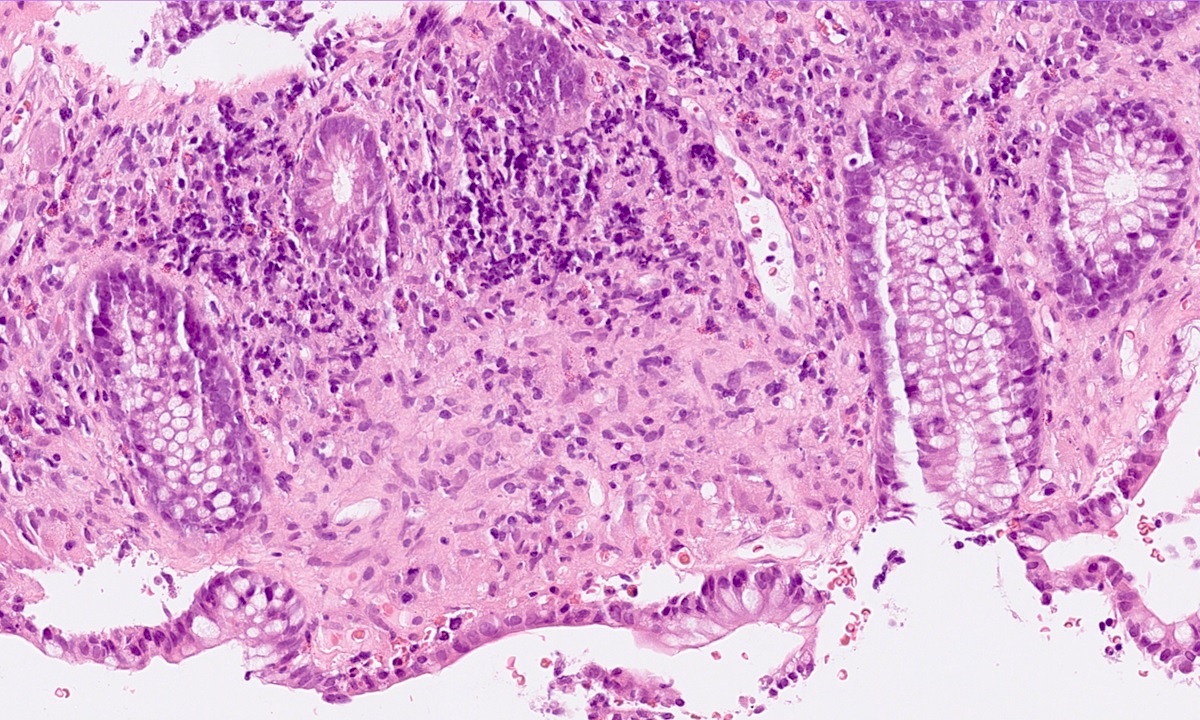
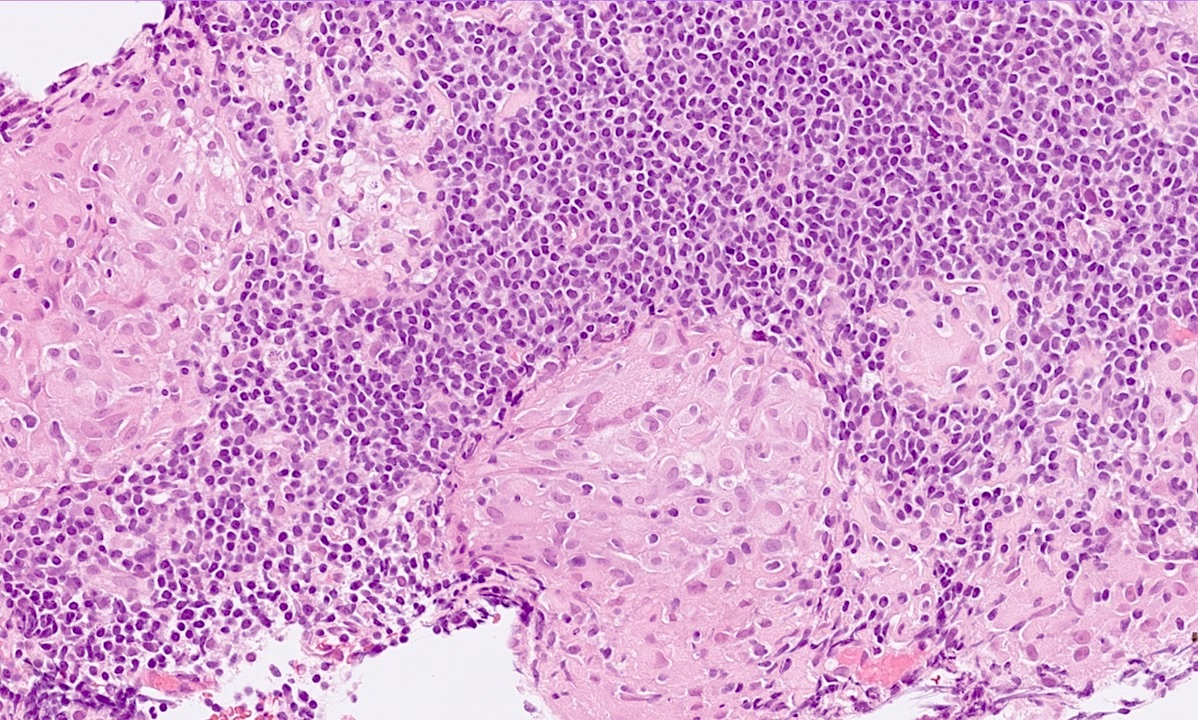
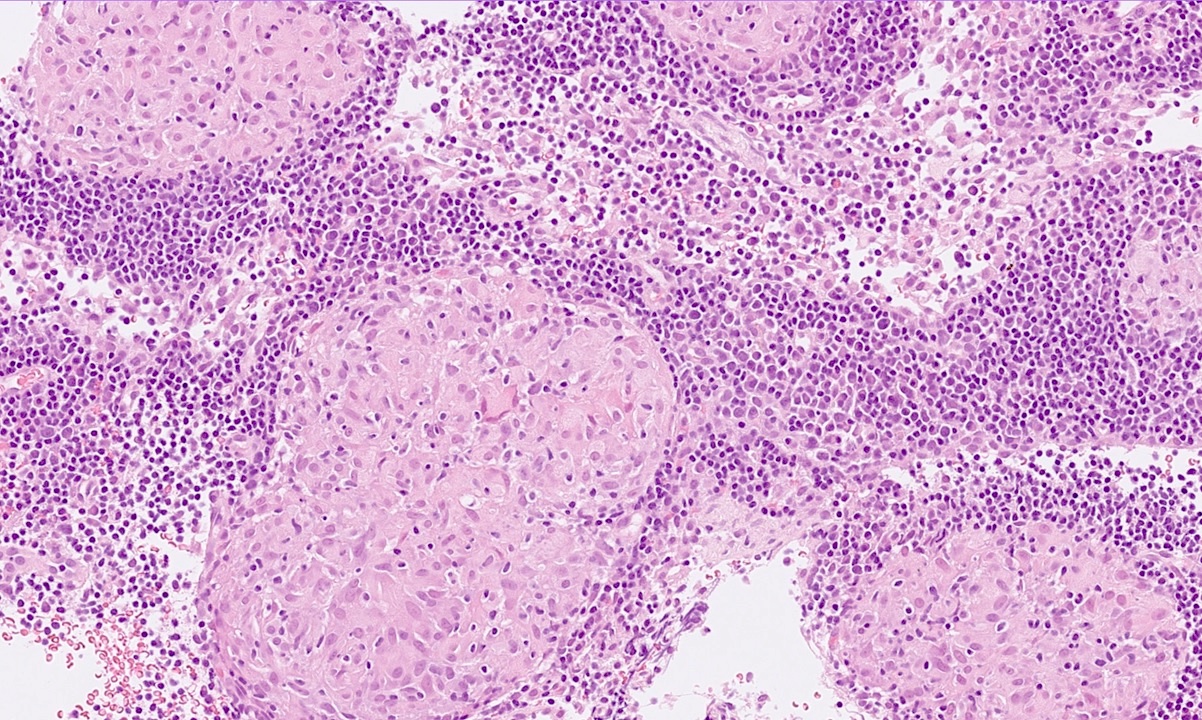
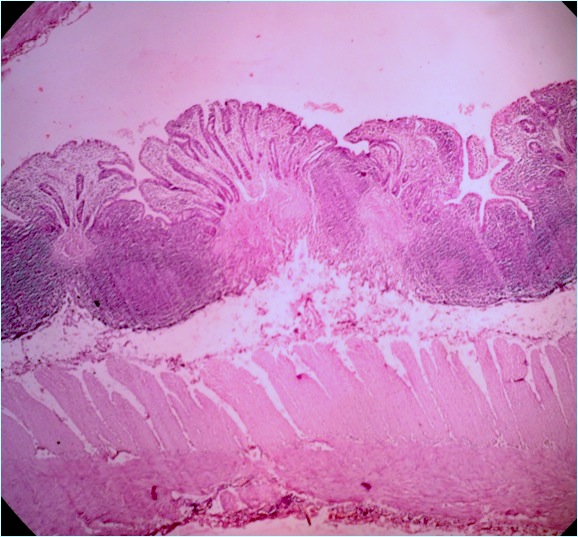
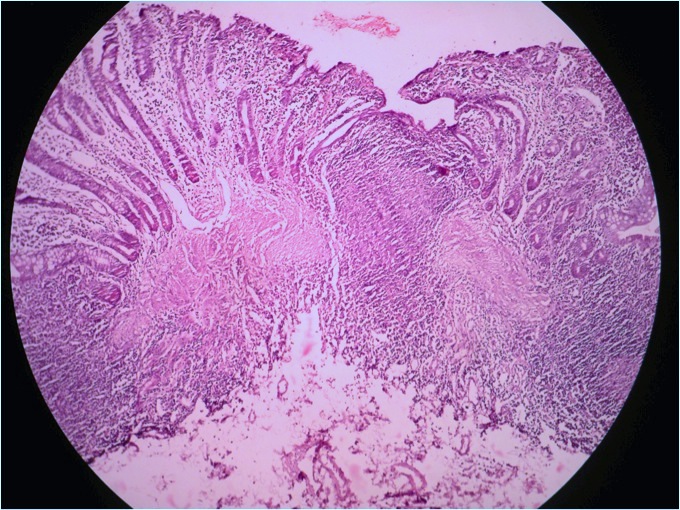
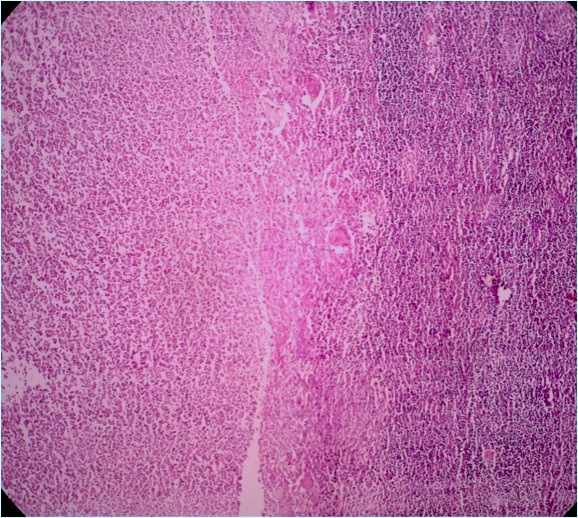
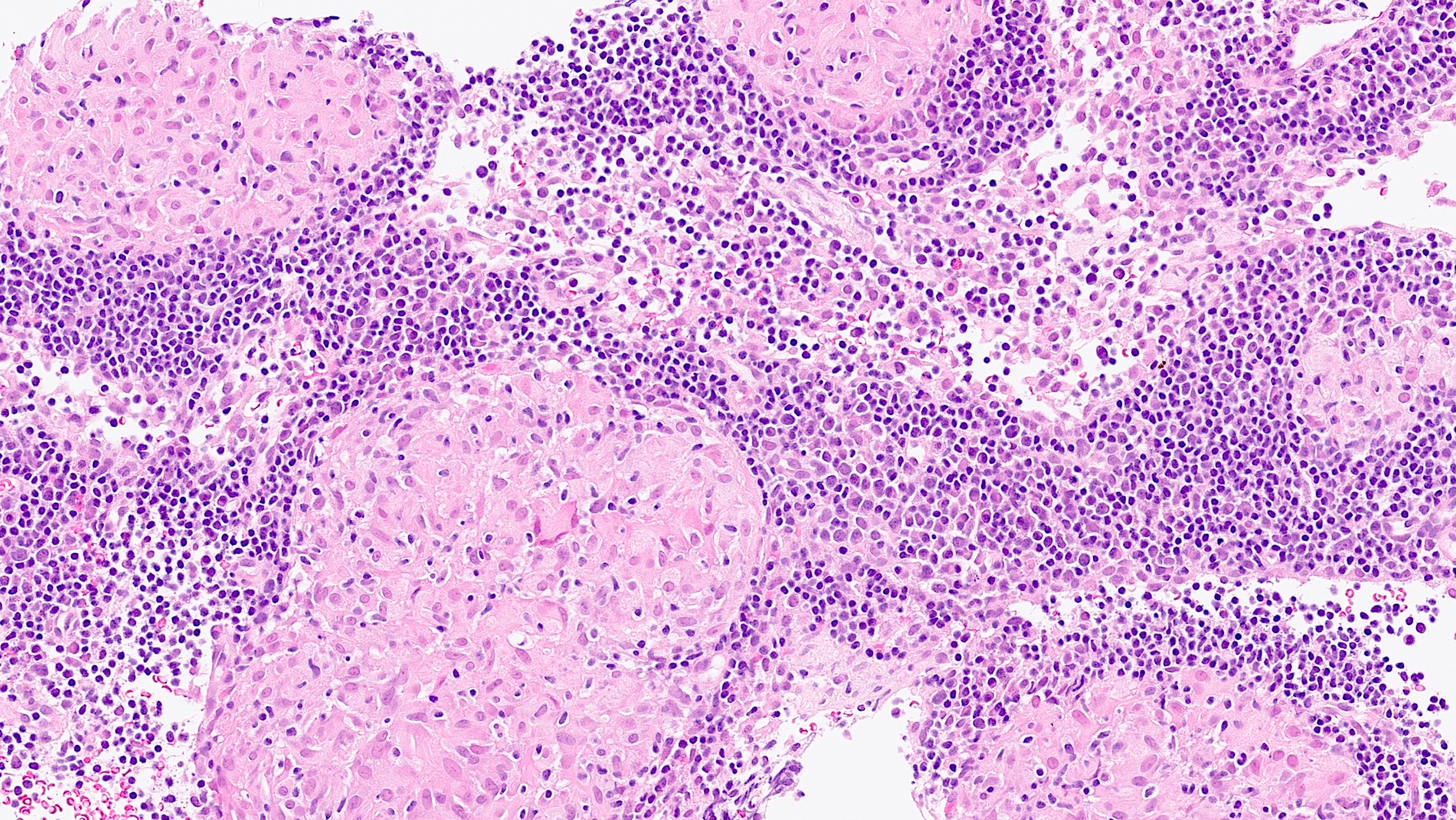
Microscopic (histologic) description
- Granulomas with caseating necrosis, conglomerate epithelioid histiocytes, cuff of lymphocytes, Langhans giant cells, aphthous to deep ulcers, with architectural distortion of normal colon mucosa (BMC Gastroenterol 2022;22:89)
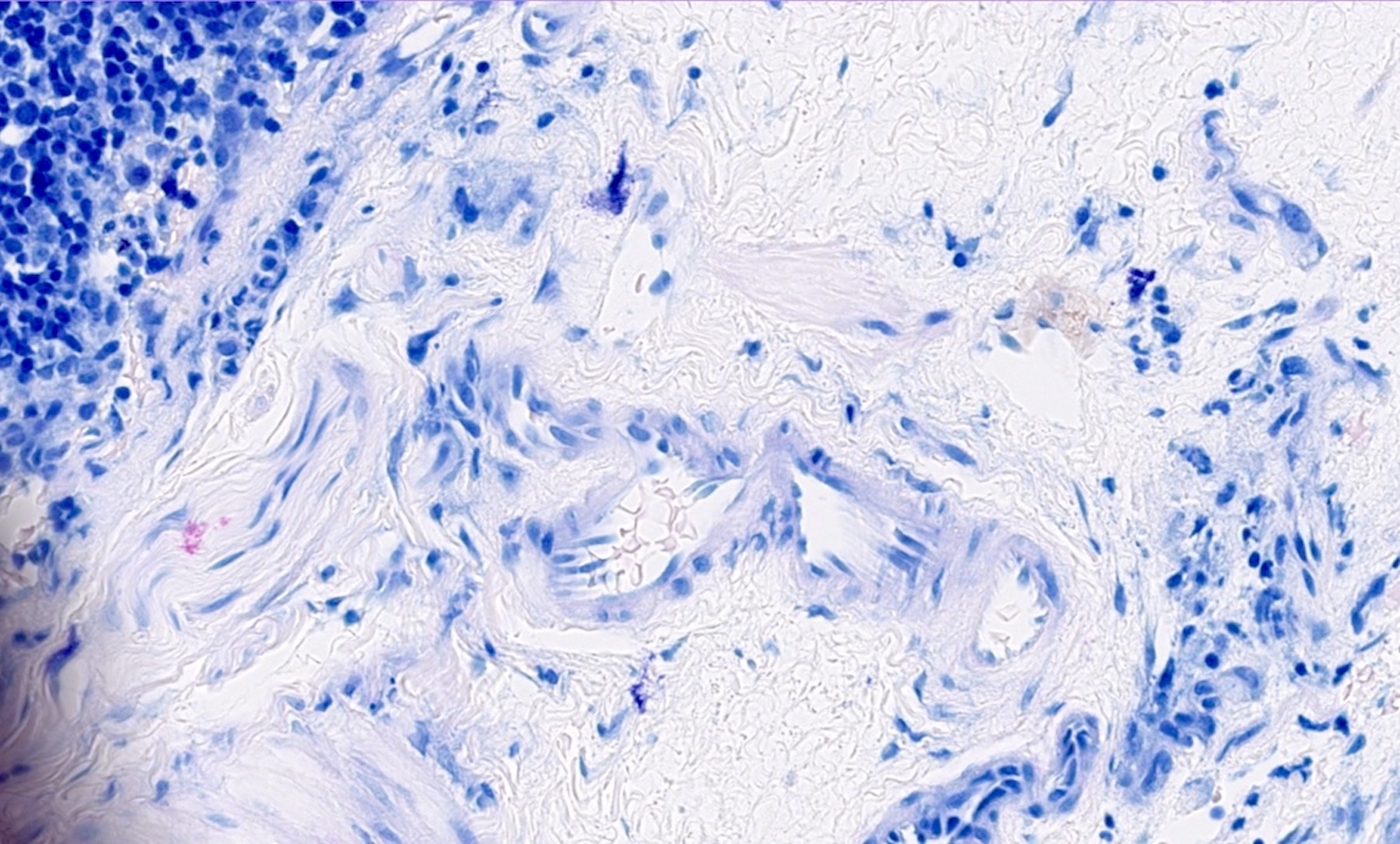
- AFB stains may highlight acid fast bacillus in necrotic areas and histiocytes
- Disproportionate submucosal inflammation (BMC Gastroenterol 2022;22:89)
- Hyalinization, fibrotic strictures and calcified granulomas within the lesions may occur in chronic cases (World J Gastroenterol 2014;20:14831)
- Destruction of muscularis propria, along with scarring in long term can be encountered
Microscopic (histologic) images
Positive stains
- There are 3 common acid fast staining methods: Ziehl-Neelsen (ZN) (hot), Kinyoun (cold) and auramine-rhodamine fluorochrome (Truant method)
- Bacteria stain bright red by the Ziehl-Neelsen / Kinyoun method
- Fluorochrome method is used by large laboratories that have a fluorescent (ultraviolet) microscope
- Finding a small acid fast bacillus in a ZN stained slide is a cumbersome procedure for a pathologist; therefore, an artificial intelligence based method can be used to detect microorganisms (Diagnostics (Basel) 2022;12:1484)
Molecular / cytogenetics description
- World Health Organization (WHO) has recommended the use of molecular nucleic acid amplification tests (NAATs) tests for TB detection as they are able to detect TB more accurately, particularly in patients with paucibacillary disease (J Clin Microbiol 2020;58:e01582)
- Gene Xpert / MTB and Gene Xpert / MDR are WHO endorsed tests (J Clin Microbiol 2020;58:e01582)
Videos
Endoscopy of TB of ascending colon
Sample pathology report
- Colon, biopsy:
- Colonic mucosa showing necrotizing granulomatous inflammation; Ziehl-Neelsen (ZN) stain is negative for AFB and periodic acid-Schiff with diastase (PASD) is negative for fungal elements (see comment)
- Comment: Correlation with clinical and microbiological culture findings is advised.
- Colon, resection:
- Colonic mucosa showing effacement of architecture with numerous caseating granulomatous inflammation and AFB positive bacilli
- Features are consistent with tuberculosis
- Resection margins are free of inflammation
- Total of 14 benign reactive lymph nodes recovered, none of which show granuloma
Differential diagnosis
- Crohn's disease:
- Linear and serpiginous ulcers
- Noncaseating granulomas
- No bacteria identified
- Intestinal sarcoidosis:
- Nonnecrotizing granulomas
- No bacteria identified
- Foreign body granuloma:
- Noncaseating foreign body type granulomas
- Foreign material identified
- No bacteria identified
- Intestinal malignancy:
- Atypical cells / adenocarcinoma glands seen
- No granuloma identified
- Yersiniosis:
- Neutrophilic infiltrate
- Suppurative granulomas
Additional references
Board review style question #1
A 45 year old HIV positive man has presented with abdominal pain, low grade fever and change in bowel habits. CT of the abdomen shows an ileocecal mass. Endoscopic biopsy is taken then processed into a histological slide as shown in the picture. Special stain Ziehl-Neelsen shows positive AFB. Which of the following is the likely diagnosis?
- Crohn's disease
- Fungal infection
- Sarcoidosis
- Tuberculosis
Board review style answer #1
D. Tuberculosis. Tuberculosis is the correct answer because caseating granulomas with positive AFB are seen in tuberculosis. Answer B is incorrect because fungi will stain by PASD and no AFB will be identified. Answer C is incorrect because with sarcoidosis, no caseous necrosis will be seen and no AFB will be present. Answer A is incorrect because no caseous necrosis will be seen and no AFB are identified. Also, typical fissures and lymphoid aggregates are seen in a beaded appearance.
Comment Here
Reference: Tuberculosis
Comment Here
Reference: Tuberculosis
Board review style question #2
A 66 year old woman was diagnosed with intestinal tuberculosis. She underwent a colonoscopic biopsy. Which one of the following types of necrosis will you see in her biopsy?
- Caseous
- Coagulative
- Fibrinoid
- Liquefactive
Board review style answer #2
A. Caseous. Caseous is the correct answer because it is seen in tuberculosis. Answer B is incorrect because coagulative necrosis is seen in myocardial infarction or renal infarction. Answer C is incorrect because fibrinoid necrosis is present in autoimmune diseases and in peptic ulcer. Answer D is incorrect because liquefactive necrosis is seen in the central nervous system, such as in brain infarcts or brain abscesses (Histopathology.guru: Types of Necrosis with Examples [Accessed 10 August 2023]).
Comment Here
Reference: Tuberculosis
Comment Here
Reference: Tuberculosis