Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Challa B, Yearsley MM. Diverticulosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colondiverticulosis.html. Accessed April 19th, 2024.
Definition / general
- Anatomic change in the colon characterized by outpouchings of mucosa and submucosa through the muscularis (Clin Geriatr Med 2021;37:141)
- Diverticulosis: presence of diverticula, regardless of symptoms
- Diverticular disease: clinically relevant symptomatic diverticulosis
Essential features
- Anatomic change in the colon characterized by outpouchings of mucosa and submucosa through the muscularis
- Diverticulosis can be asymptomatic or symptomatic
- Sigmoid colon / left colon, most common site (90%)
- Mucosa normal to markedly abnormal
- Expansion of lamina propria by lymphoplasmacytic infiltrate, lymphoglandular complexes, mucin depletion and focal Paneth cell metaplasia may be seen
- No rationale for treatment of asymptomatic colonic diverticulosis
Terminology
- Most colonic diverticula are false diverticula
- Mucosa and submucosa herniate through defect or weakness in muscularis layer and is covered by serosa
- True diverticula are uncommon
- Involves the outpouching of all layers of the intestinal wall (e.g., Meckel diverticulum) (Expert Rev Gastroenterol Hepatol 2018;12:683)
- Diverticulosis can be asymptomatic or symptomatic
- Symptomatic diverticulosis:
- Symptomatic uncomplicated diverticular disease (SUDD)
- Diverticulitis (acute, chronic or recurrent)
- Diverticular hemorrhage
- Segmental colitis associated with diverticulosis (SCAD)
- Diverticulitis: uncomplicated or complicated
- Complicated diverticulitis includes abscess, fistula, perforation, obstruction (Clin Geriatr Med 2021;37:141)
ICD coding
- ICD-10: K57.90 - diverticulosis of intestine, part unspecified, without perforation or abscess without bleeding
Epidemiology
- Highest incidence in Western world
- Prevalence increases with age
- > 75% people above 75 years of age
- < 50 years of age: more common in males
- 50 - 70 years of age: slightly more common in females
- > 70 years of age: significantly increased incidence in females (Expert Rev Gastroenterol Hepatol 2018;12:683)
- Left sided diverticula: more common in Western world
- Right sided diverticula: more common in Asia
- Diverticular bleeding 5 - 15%
- Usual source is right sided diverticula
- Possibly due to thinner wall on right side of colon, widened necks and domes of right sided diverticula
- Diverticulitis: in 4 - 15% of patients with diverticula
Sites
- Sigmoid colon / left colon, most common site (90%)
- Right sided colon (5 - 15%)
- Pancolonic involvement (2%) (Int J Colorectal Dis 2018;33:1299)
Pathophysiology
- Occurs in weaker portions of the colonic wall where vasa recta infiltrate the circular muscle layer
- Abnormal colonic motility → exaggerated segmental contractions → increased intraluminal pressure and separation of colonic lumen into chambers (Expert Rev Gastroenterol Hepatol 2018;12:683)
- Sigmoid colon, segment with smallest diameter and largest intraluminal pressure
- In diverticula, vasa recta are separated from intestinal lumen by a layer of mucosa alone
- Exposed to greater amount of injury and can lead to bleeding
Etiology
- Host of complex factors are implicated
- Altered colonic motility
- Visceral hypersensitivity
- Inflammation
- Genetic susceptibility
- Diet, tobacco use
- Medication
- Gut microbiome imbalances (Clin Geriatr Med 2021;37:141)
- Connective tissue disease, Marfan syndrome, Ehlers-Danlos and autosomal dominant polycystic kidney disease
- Can cause structural changes in intestinal walls
Clinical features
- Usually asymptomatic
- Abdominal pain, cramping, altered bowel functions, painless bleeding
- Resembles irritable bowel syndrome (IBS) (Dig Dis 2012;30:64, Curr Opin Gastroenterol 2019;35:27)
Diagnosis
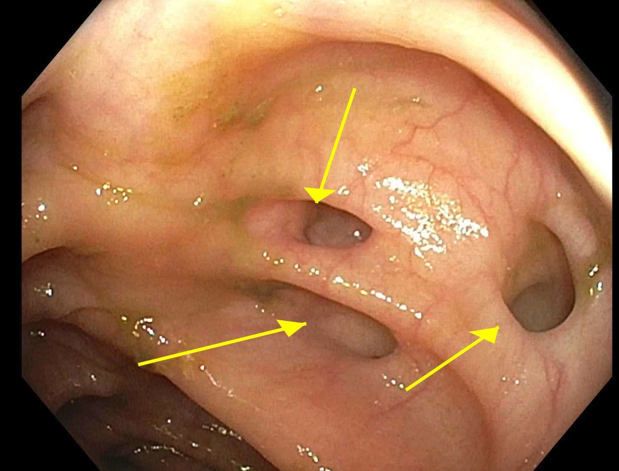
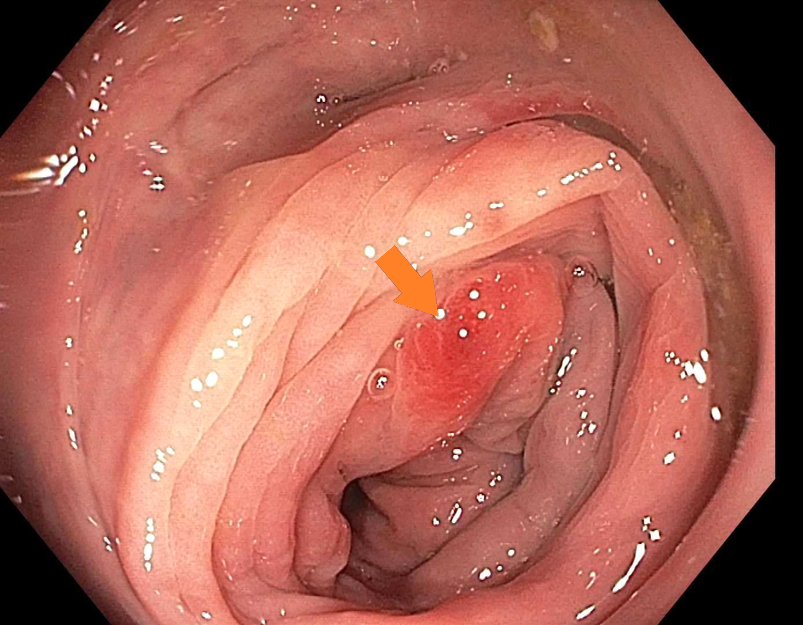
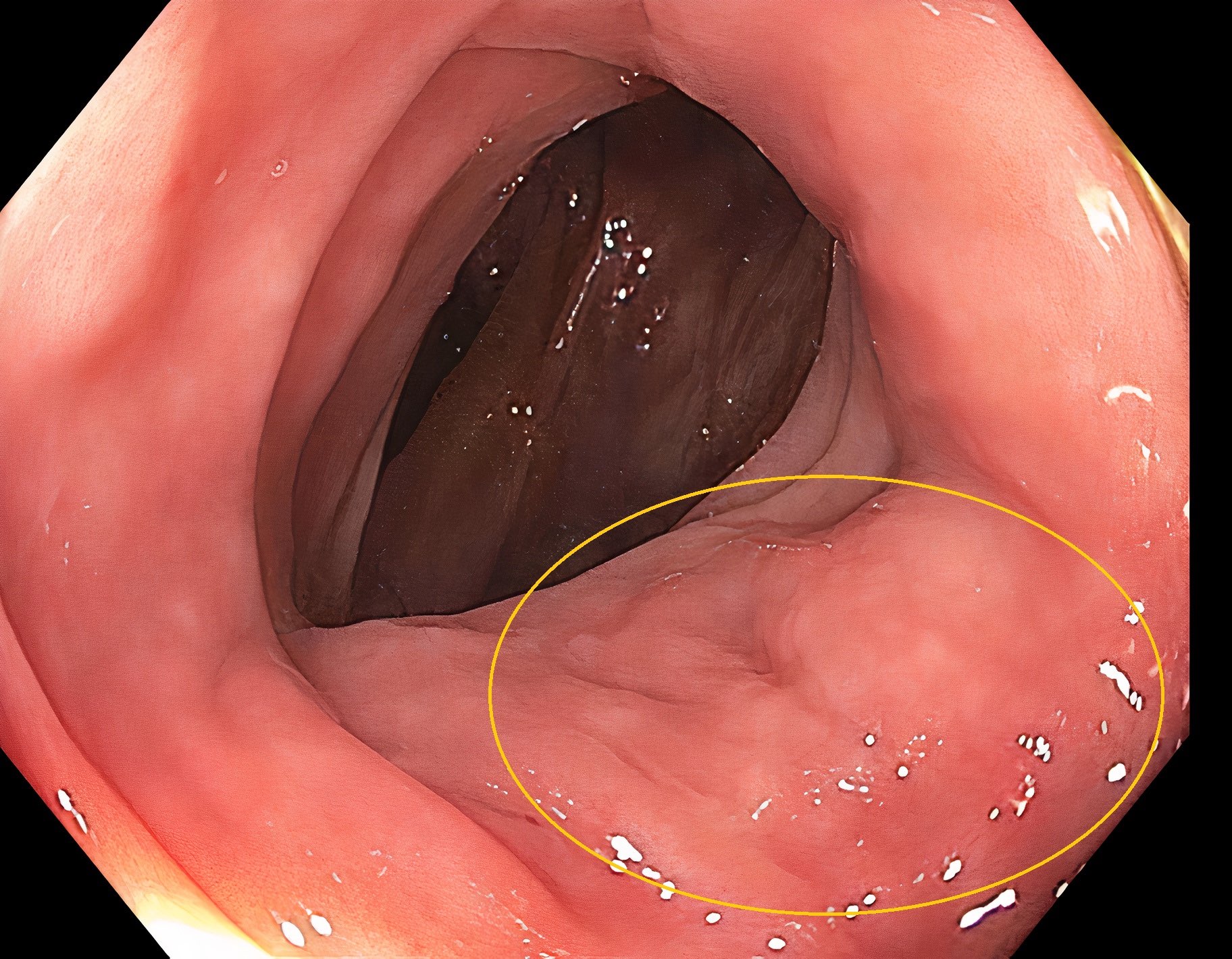
- Frequently is an incidental finding during colonoscopy
- Symptomatic patients, classic presenting symptoms and confirmation with radiology or via colonoscopy (Mayo Clin Proc 2016;91:1094)
- Colonoscopy or Xray following barium enema (StatPearls: Diverticulosis [Accessed 21 April 2022])
- Colonoscopy should be avoided in acute diverticulitis (Mayo Clin Proc 2016;91:1094)
Laboratory
- Fecal calprotectin measurement
- Calprotectin is a calcium and zinc binding protein; can be considered neutrophil specific
- Marker of gastrointestinal inflammation
- Can help in distinguishing IBS from diverticular disease (Expert Rev Gastroenterol Hepatol 2018;12:791)
- Increased white blood cell (WBC), erythrocyte sedimentation rate (ESR), C reactive protein (CRP) in diverticulitis
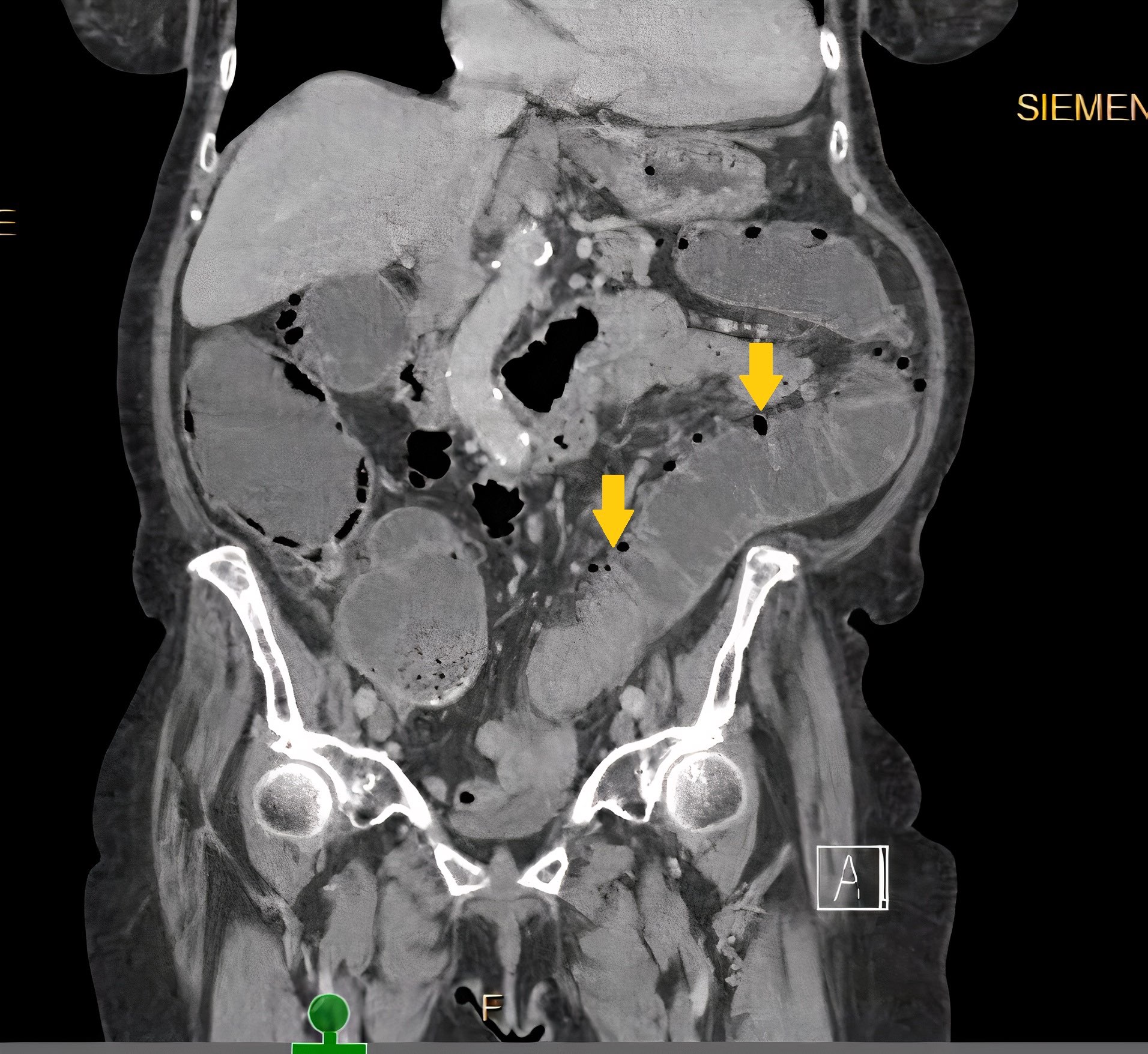
Radiology description
- Barium enema: barium filled outpouchings; can look similar to polyps
- Ultrasound: gas filled outpouchings
- CT: diverticula outlined by gas
- Intramural diverticula seen as a tiny focus of gas or contrast within the colonic wall (J Clin Gastroenterol 2004;38:S11)
- CT allows grading of severity and detection of complications (Br J Radiol 2020;93:20200670)
Radiology images
Prognostic factors
- Mortality rate in uncomplicated diverticulitis is negligible (StatPearls: Acute Diverticulitis [Accessed 21 April 2022])
- Complicated diverticulitis requiring surgery may lead to death in ~5% of patients
- Perforation of the bowel with resulting peritonitis, risk of death increases to 20%
Case reports
- 15 year old boy with dysmorphic features and learning disabilities presents with acute onset abdominal pain, nausea and vomiting (ACG Case Rep J 2019;6:1)
- 50 year old man with longstanding history of ulcerative colitis and severe diverticulosis on colonoscopy (Rev Esp Enferm Dig 2021;113:550)
- 68 year old man with lower gastrointestinal bleeding and arteriovenous malformations within jejunal diverticulosis (BMC Surg 2019;19:70)
- 83 year old woman with history of chronic abdominal pain is found to have partial midgut volvulus (Am J Case Rep 2021;22:e933180)
- 88 year old man presents with hematochezia and perianal pain (Cureus 2021;13:e14900)
Treatment
- No rationale for treatment of asymptomatic colonic diverticulosis (Pol Przegl Chir 2015;87:203, United European Gastroenterol J 2014;2:413)
- Symptomatic uncomplicated diverticular disease (SUDD)
- Dietary modifications to increase fiber, use of probiotics has been proposed (Neurogastroenterol Motil 2015;27:305)
- Antibiotics in acute complicated diverticulitis (Gastroenterology 2015;149:1944)
Clinical images
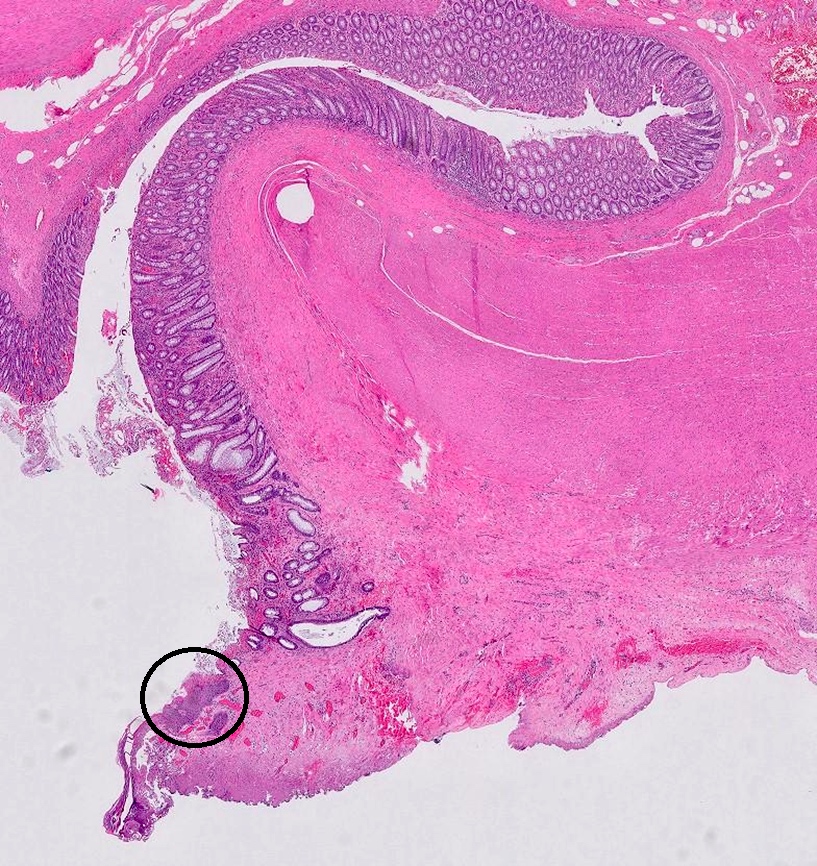
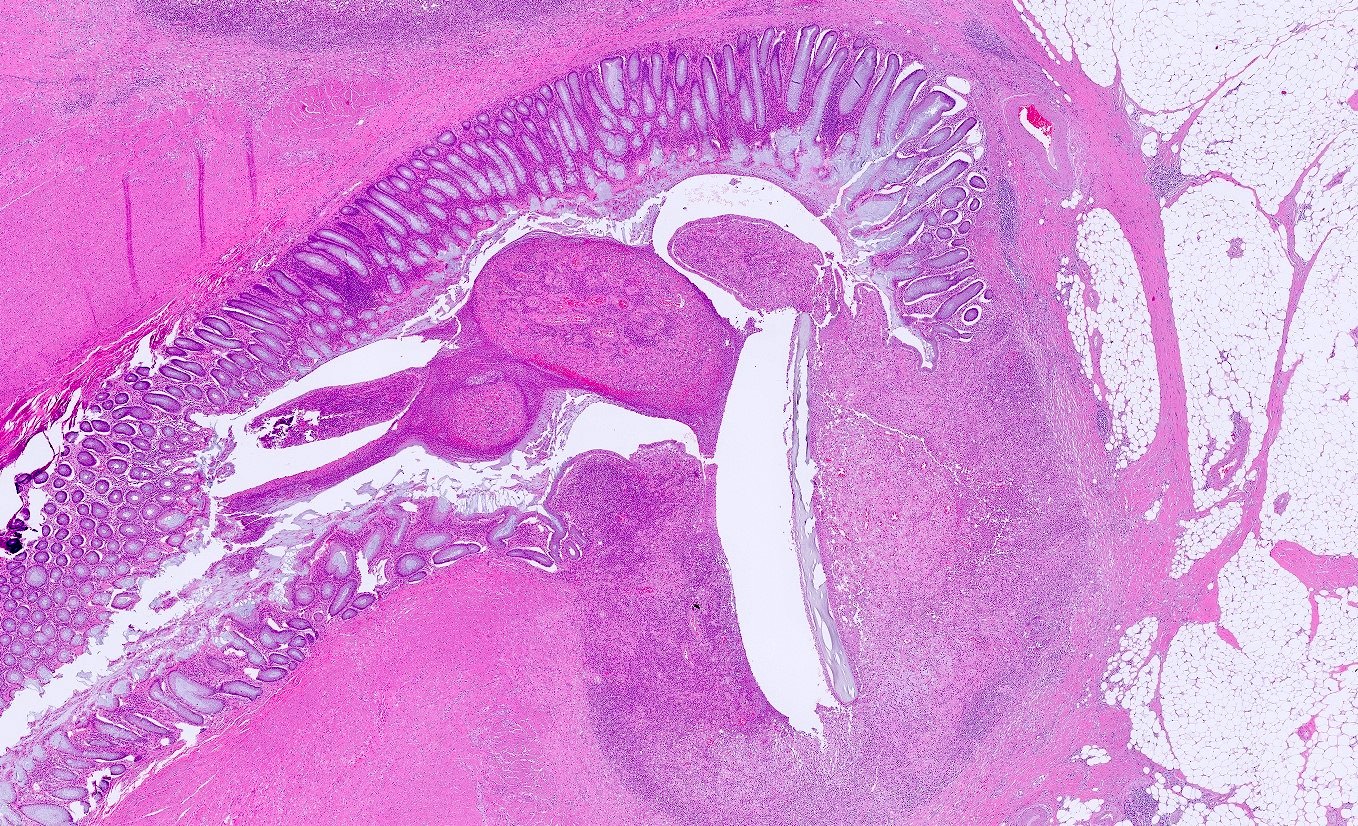
Gross description
- Specimen should be fixed and opened longitudinally for easy sampling of diverticula
- Usually, multiple flask shaped invaginations of colonic wall
- Wall thickening may be present (Surg Endosc 2011;25:2586)
- Narrowing of lumen, shortening of tenia and marked thickening of circular muscle layer may be present (J Clin Gastroenterol 2006;40:S108)
- If it extends deeply, perforation and serosal adhesions may be seen
Gross images
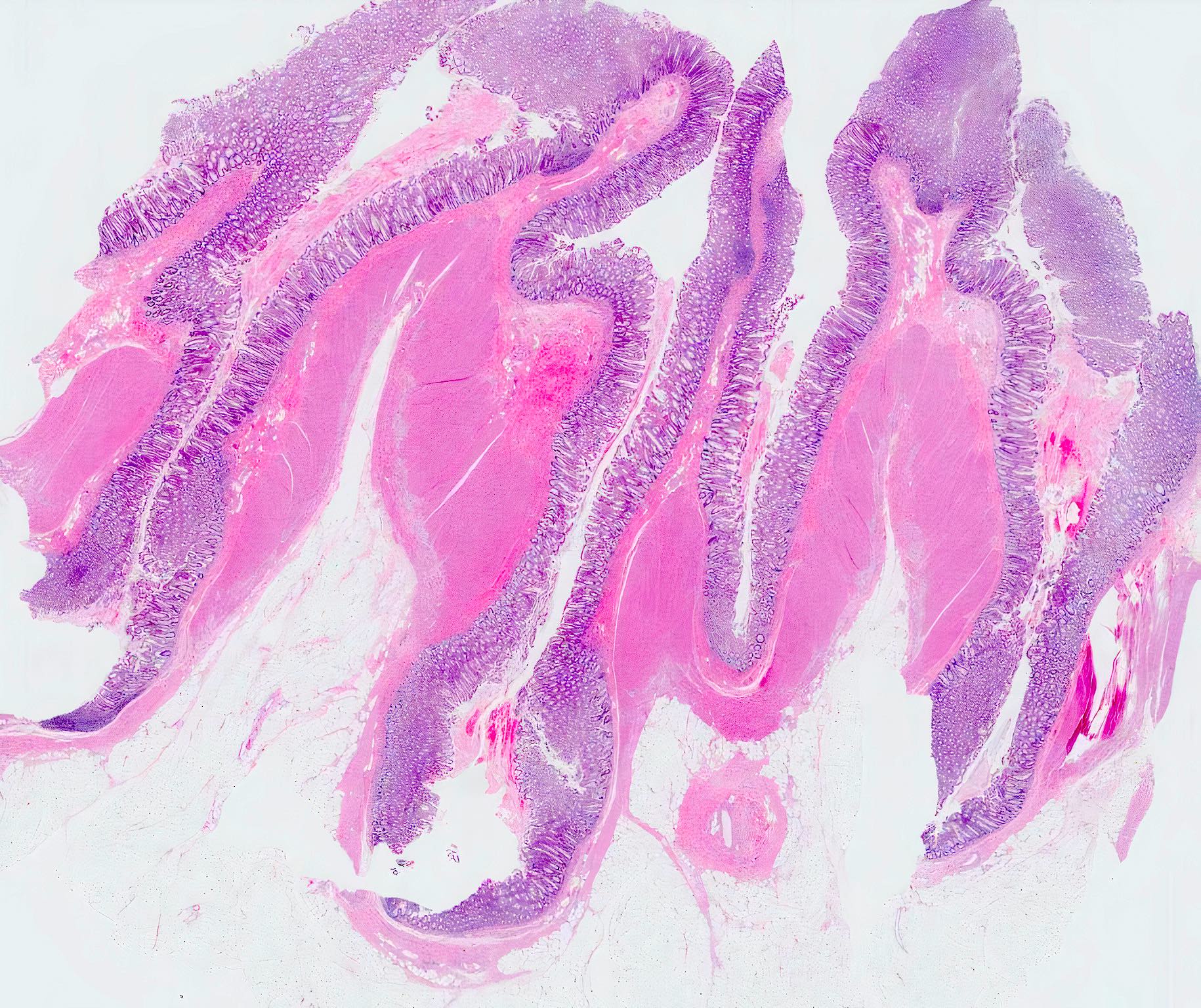
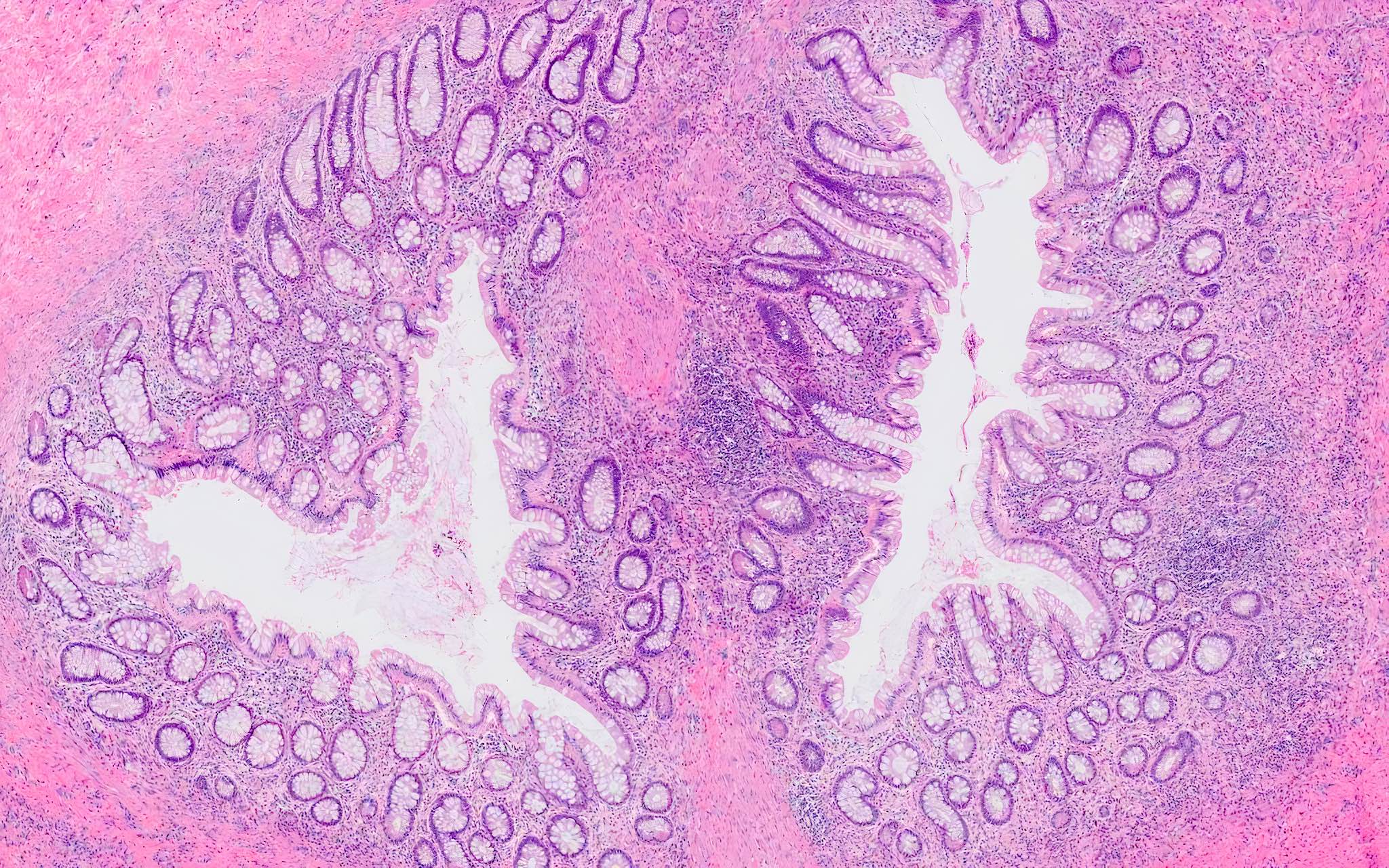
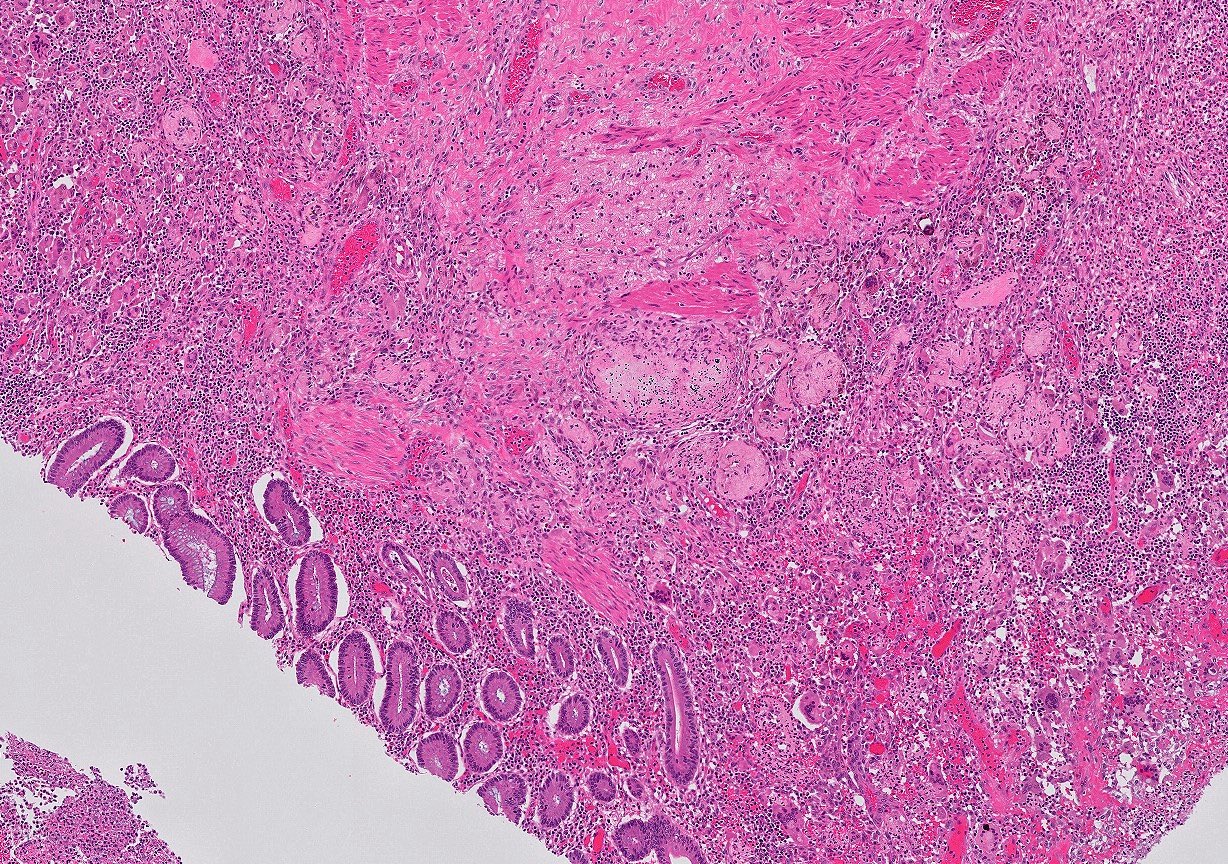
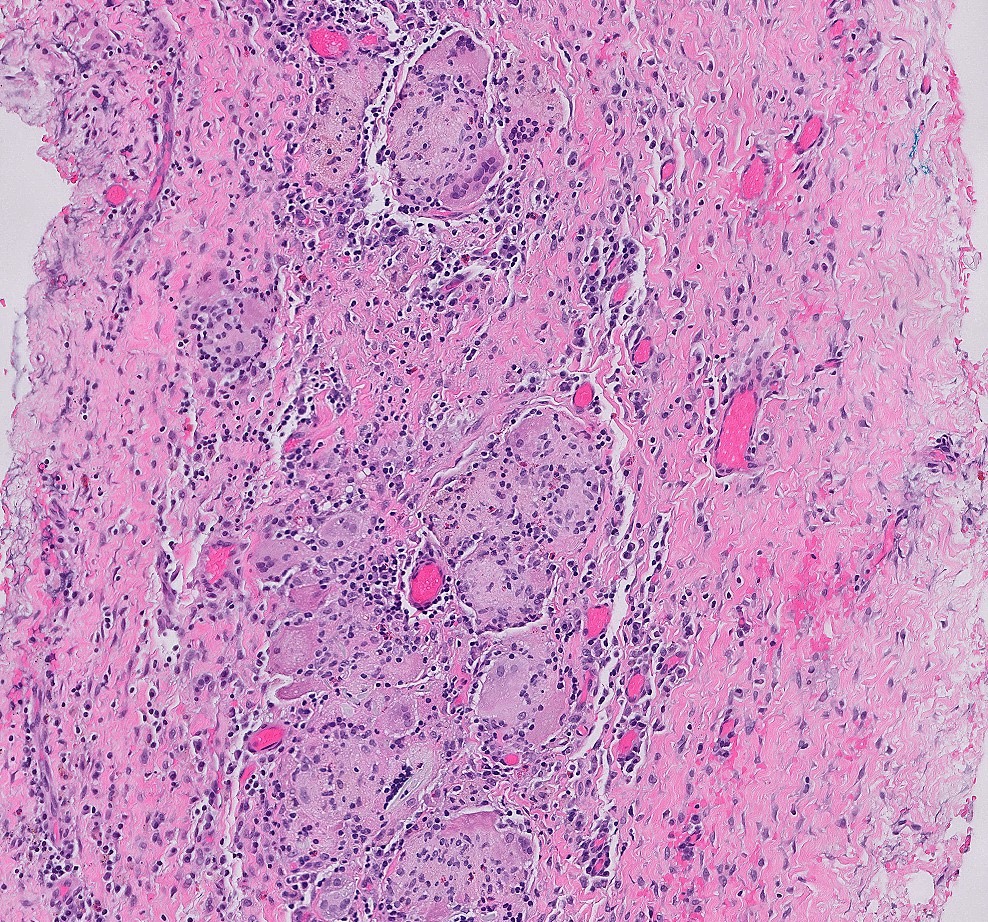
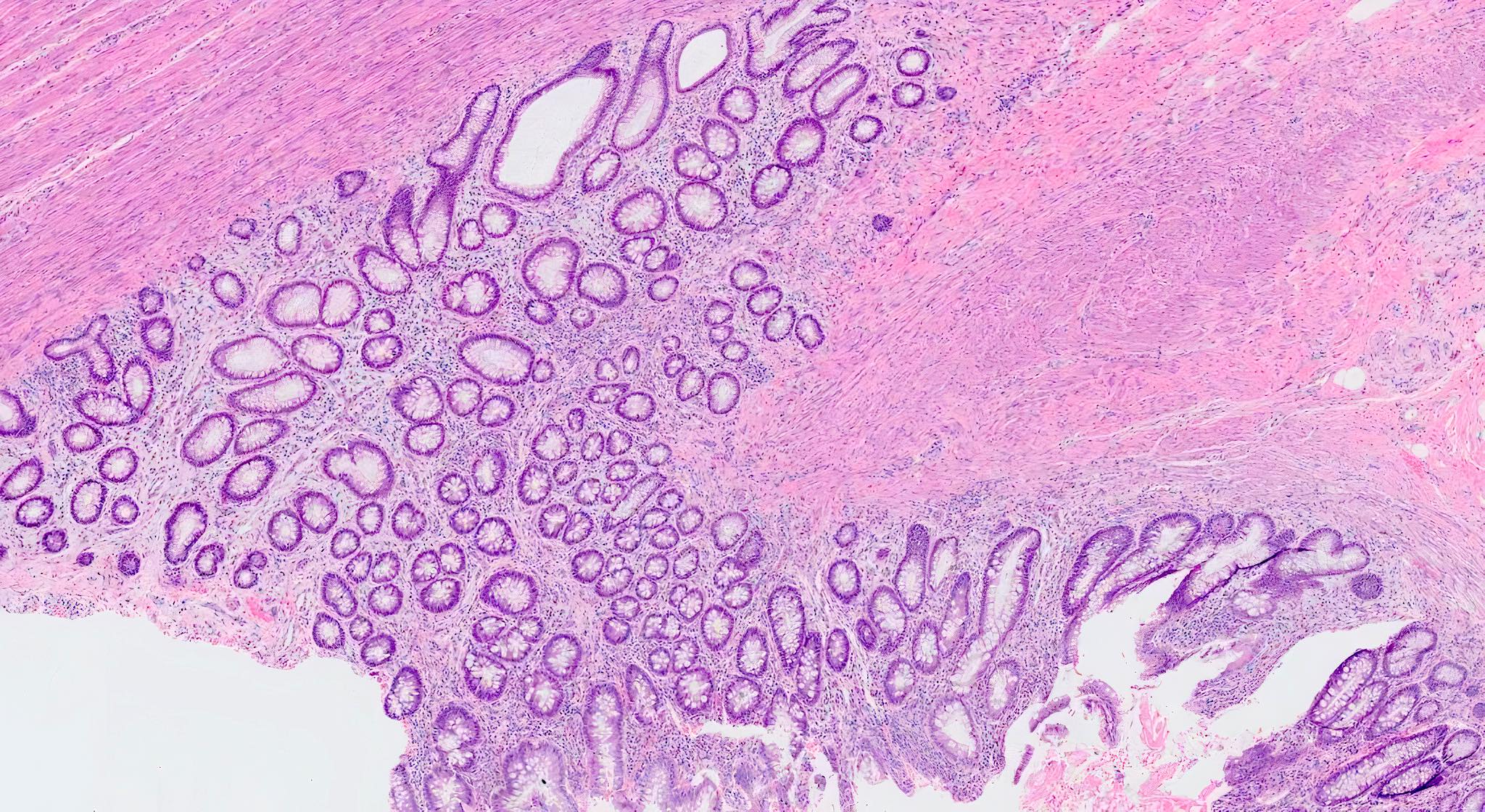
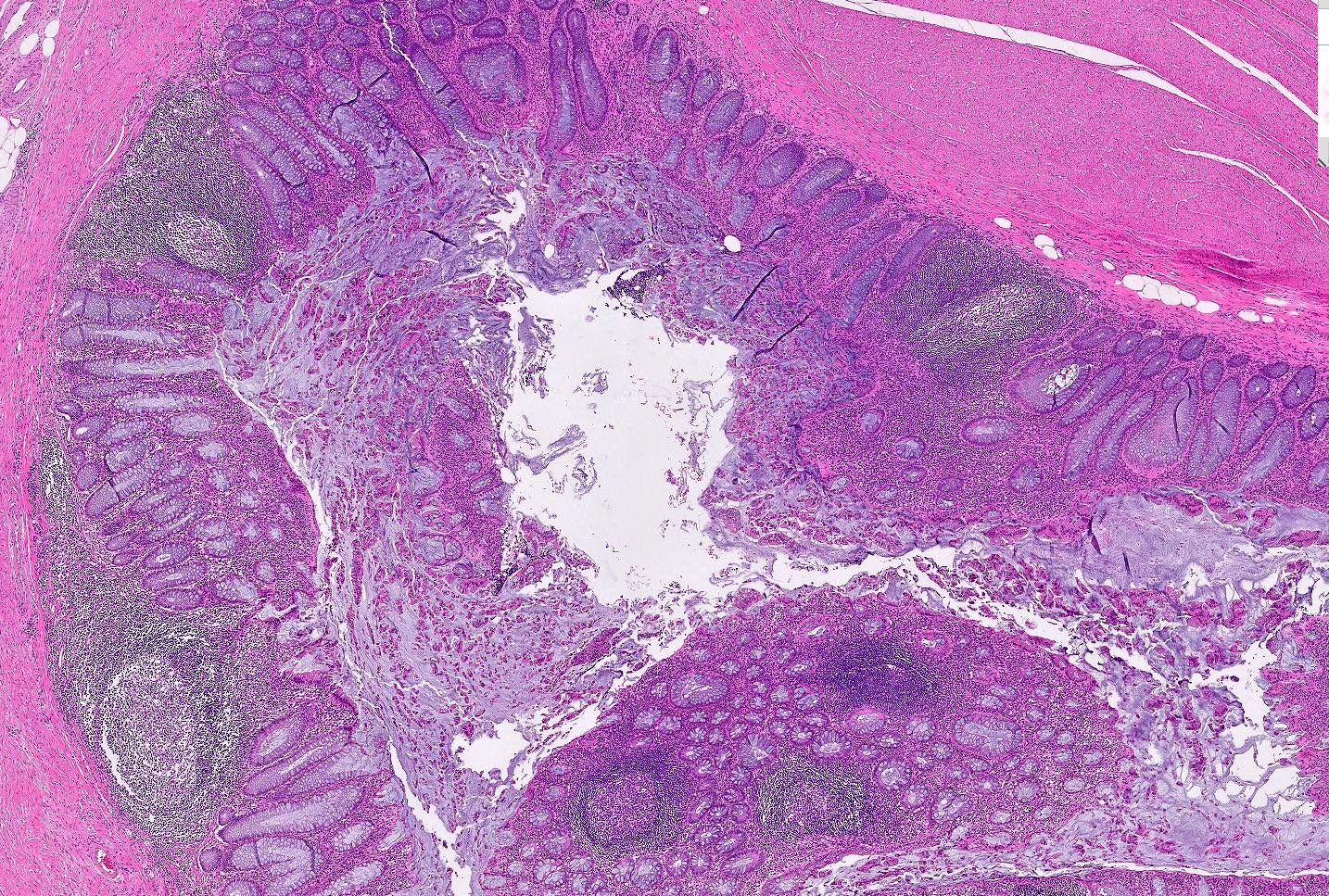
Microscopic (histologic) description
- Mucosa may be normal to markedly abnormal
- Expansion of lamina propria by lymphoplasmacytic infiltrate (more prominent in basal half)
- Lymphoglandular complexes, mucin depletion, focal Paneth cell metaplasia (in chronic cases) may be seen (J Clin Gastroenterol 2004;38:S11)
- Muscularis mucosa extends towards surface between elongated crypts
- Shortening of the affected bowel and hypertrophy of circular muscle layer (myochosis) leads to exaggerated mucosal folds (Am J Surg Pathol 1991;15:871)
- Some cases can show lamina propria fibrosis, crypt elongation on the tips of prominent mucosal folds, like mucosal prolapse syndrome in rectum and anus (J Clin Gastroenterol 2008;42:1137)
- Hemosiderin deposition in submucosa may be seen (StatPearls: Diverticulosis [Accessed 21 April 2022])
- Can mimic inflammatory bowel disease
- Hyperplasia of lymphoid aggregates is one of the earliest signs of diverticulitis
- Cryptitis, crypt abscesses, peridiverticular abscess and fistulas may be superimposed on this background in acute diverticulitis
- Tracking abscesses can spread longitudinally or circumferentially and can cause diverticular colitis
- Persistent localized inflammation can lead to phlegmon which is a thickened, firm segment of bowel wall that can lead to strictures and acute or subacute large bowel obstruction (Best Pract Res Clin Gastroenterol 2002;16:543)
Microscopic (histologic) images
Contributed by Bindu Challa, M.D. and Martha M. Yearsley, M.D.
Videos
Histopathology of diverticular disease
Whole slide image of case of diverticulosis with diverticulitis
Sample pathology report
- Colon, sigmoid, segmental resection:
- Diverticulosis
- Two lymph nodes, negative for tumor
- Colon, sigmoid, partial colectomy:
- Segment of colon with diverticulosis, diverticulitis and abscess formation
- Colon, total colectomy:
- Colonic diverticular disease with perforated diverticulum
Differential diagnosis
- Inflammatory bowel disease:
- Diverticular disease associated chronic active colitis can resemble ulcerative colitis
- Wall thickening, transmural lymphoid aggregates and granulomas can mimic Crohn's disease
- Solitary rectal ulcer syndrome and inflammatory cloacogenic polyp:
- Prominent mucosal folds / prolapsed folds adjacent to diverticula can mimic these conditions
- Angiodysplasia:
- Abnormal, tortuous, thin walled blood vessels in mucosa and submucosa
Additional references
Board review style question #1
Board review style answer #1
D. Sigmoid colon. Diverticulosis occurs most commonly in sigmoid colon in 90% of cases.
Comment Here
Reference: Diverticulosis
Comment Here
Reference: Diverticulosis
Board review style question #2
What is the laboratory test that can help distinguish irritable bowel syndrome from diverticular disease?
- Aspartate transaminase
- Fecal calprotectin
- Fecal lactoferrin
- Gamma glutamyl transferase
Board review style answer #2
B. Fecal calprotectin is a marker of gastrointestinal inflammation. Elevated fecal calprotectin favors diverticular disease and helps in distinguishing it from functional gastrointestinal disorders like irritable bowel syndrome.
Comment Here
Reference: Diverticulosis
Comment Here
Reference: Diverticulosis