Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Pathophysiology | Clinical features | Diagnosis | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Chornenkyy Y, Pezhouh MK. Radiation enterocolitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colonradiationproctitis.html. Accessed April 19th, 2024.
Definition / general
- Radiation injury
Essential features
- Injury process that occurs as a result of radiation damage and can be classified as acute (< 6 months) or chronic (> 6 months)
- Acute injury findings include prominent eosinophils (cryptitis and crypt abscesses) and apoptosis; chronic injury findings result from damage to vasculature and include pronounced fibrosis and vascular changes (hyalinization and intimal thickening)
- Should be differentiated from mimickers, such as ischemia, inflammatory bowel disease, collagenous colitis and mucosal prolapse
ICD coding
- ICD-10: K52.9 - noninfective gastroenteritis and colitis, unspecified
Epidemiology
- Over 100,000 American patients annually receive therapeutic pelvic radiation for malignancies of prostate, anus, rectum, uterine cervix, endometrium, urinary bladder and rarely other sites
- Some acute radiation mucosal injury occurs in nearly all patients; most is self limited and medical management is effective in > 80% of symptomatic cases
- Approximately 5 - 15% of patients develop chronic radiation proctitis
- References: Gastroenterol Clin North Am 2013;42:913, Medicine (Baltimore) 2018;97:e13328
Pathophysiology
- Ionizing radiation damages proteins, lipid bilayer and DNA of rapidly proliferating cells
- Radiation changes are typically classified as acute (< 6 months) or chronic (> 6 months) (Curr Opin Support Palliat Care 2007;1:23)
- Acute radiation injury (< 6 months): presents within hours to days, often self limited, due to ionizing radiation damage to mucosa
- Chronic radiation injury (> 6 months): presents within months to years, due to damaged blood vessels:
- Endothelial damage causes vascular sclerosis with obliterative endarteritis of small vessels, leading to chronic ischemia and fibrosis
- Lack of perfusion causes fibrosis, ulcers, stenosis, strictures, fistulas, infection and bleeding
Clinical features
- Acute radiation injury: diarrhea, pain, tenesmus, hematochezia
- Chronic radiation injury: diarrhea, bleeding, pain secondary to stricture
- Risk factors for developing radiation proctitis include: higher radiation doses, less fractionation, thinner patients, the elderly, concurrent or subsequent chemotherapy, collagen vascular disease, hypertension and diabetes mellitus
- Radiation increases risk for secondary malignancies
- Endoscopic findings:
- Acute radiation proctitis shows edematous, dusky red rectal mucosa
- Chronic radiation proctitis shows mucosal atrophy, ectatic superficial capillaries and variable stenosis, strictures and fistulas
- References: Gastroenterol Clin North Am 2013;42:913, Medicine (Baltimore) 2018;97:e13328
Diagnosis
- Acute radiation proctitis: clinical disease, rarely biopsied
- Chronic radiation proctitis: typically biopsied; history is essential for diagnosis
Case reports
- 3 year old boy with neuroblastoma in the left adrenal gland, status postradiotherapy (Medicine (Baltimore) 2020;99:e20905)
- 54 year old man received surgery and chemotherapy for rectal cancer (Medicine (Baltimore) 2018;97:e13328)
- 58 year old woman had undergone surgery for cervical cancer approximately 21 years ago (JA Clin Rep 2019;5:20)
- 74 year old woman with metastatic uterine carcinosarcoma, pelvic radiation and radiation proctitis (GE Port J Gastroenterol 2019;26:128)
- 81 year old man with radiation proctitis (Therap Adv Gastroenterol 2013;6:69)
Treatment
- Acute radiation proctitis can be self limited or managed medically
- Chronic radiation proctitis medical, endoscopic and surgical options:
- Medical options: anti-inflammatory agents, antioxidants, formalin application and hyperbaric oxygen may improve bleeding related to chronic radiation proctitis (Dig Dis Sci 2018;63:2180, Support Care Cancer 2014;22:1715)
- Endoscopic options include argon plasma coagulation (Dig Dis Sci 2018;63:2180)
- Surgery is considered for severe or refractory cases (Dig Dis Sci 2018;63:2180)
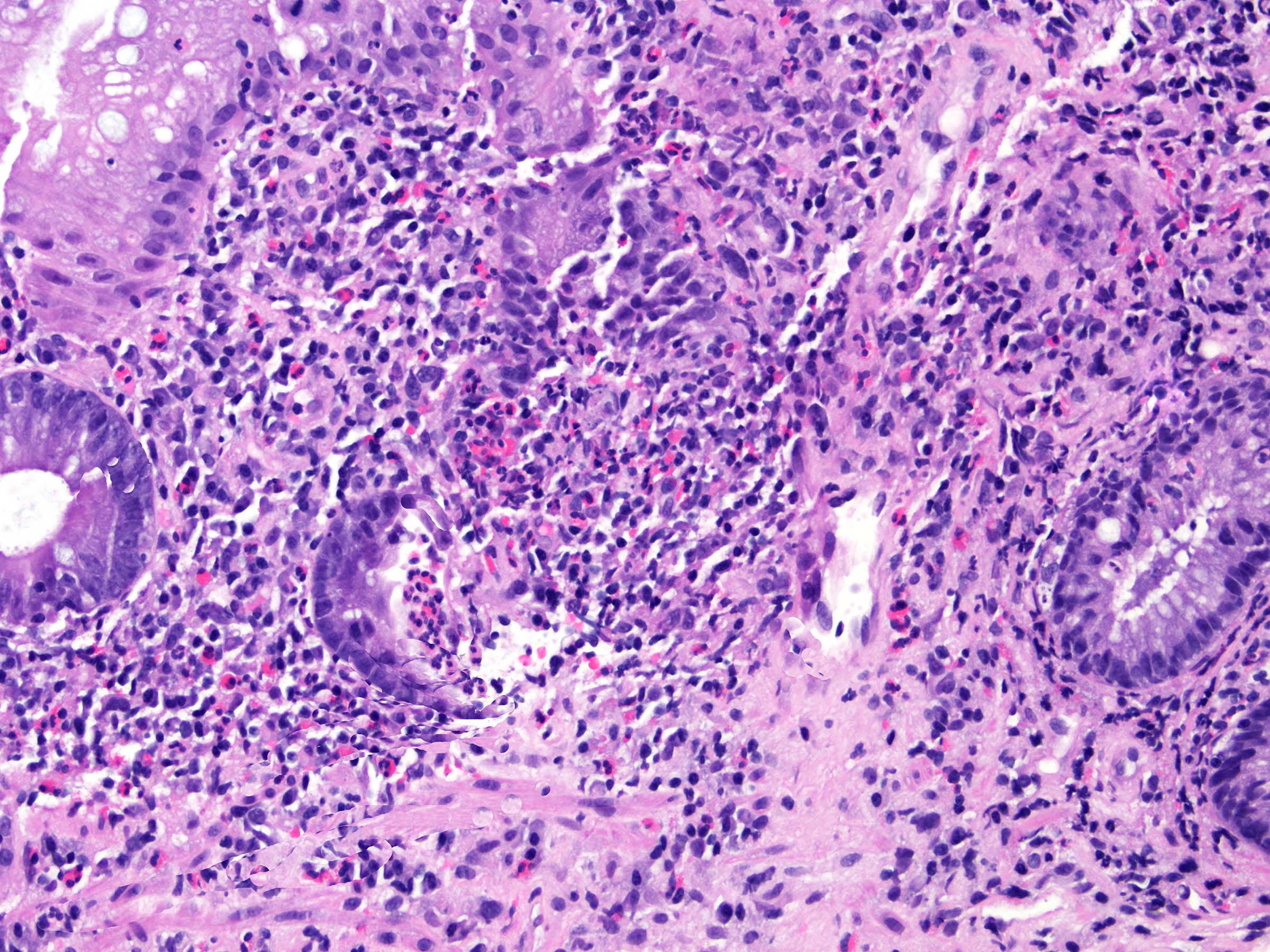
Microscopic (histologic) description
- Acute radiation colitis (< 6 months after radiation treatment):
- Epithelium can contain:
- Reduced mitotic activity
- Apoptosis
- Reduced goblet cell mucin
- Goblet cell swelling
- Degenerative changes
- Atypia (nuclear enlargement and malorientation)
- Inflammation
- Typically eosinophilic (characteristic)
- Lamina propria eosinophilic infiltration
- Eosinophilic cryptitis
- Eosinophilic crypt abscesses
- Typically eosinophilic (characteristic)
- Can be fibroblast proliferation in lamina propria (reactive changes to radiation)
- Epithelium can contain:
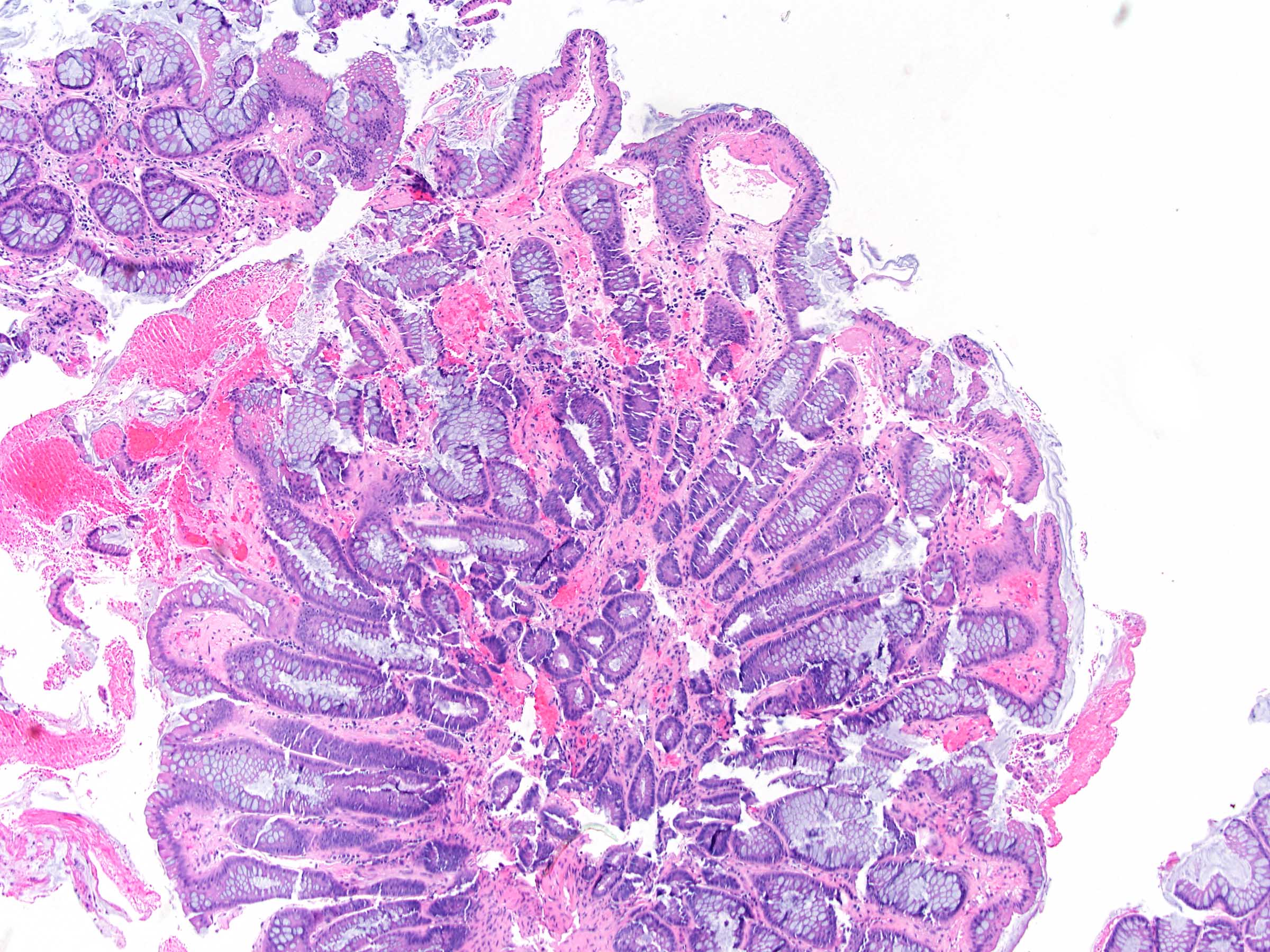
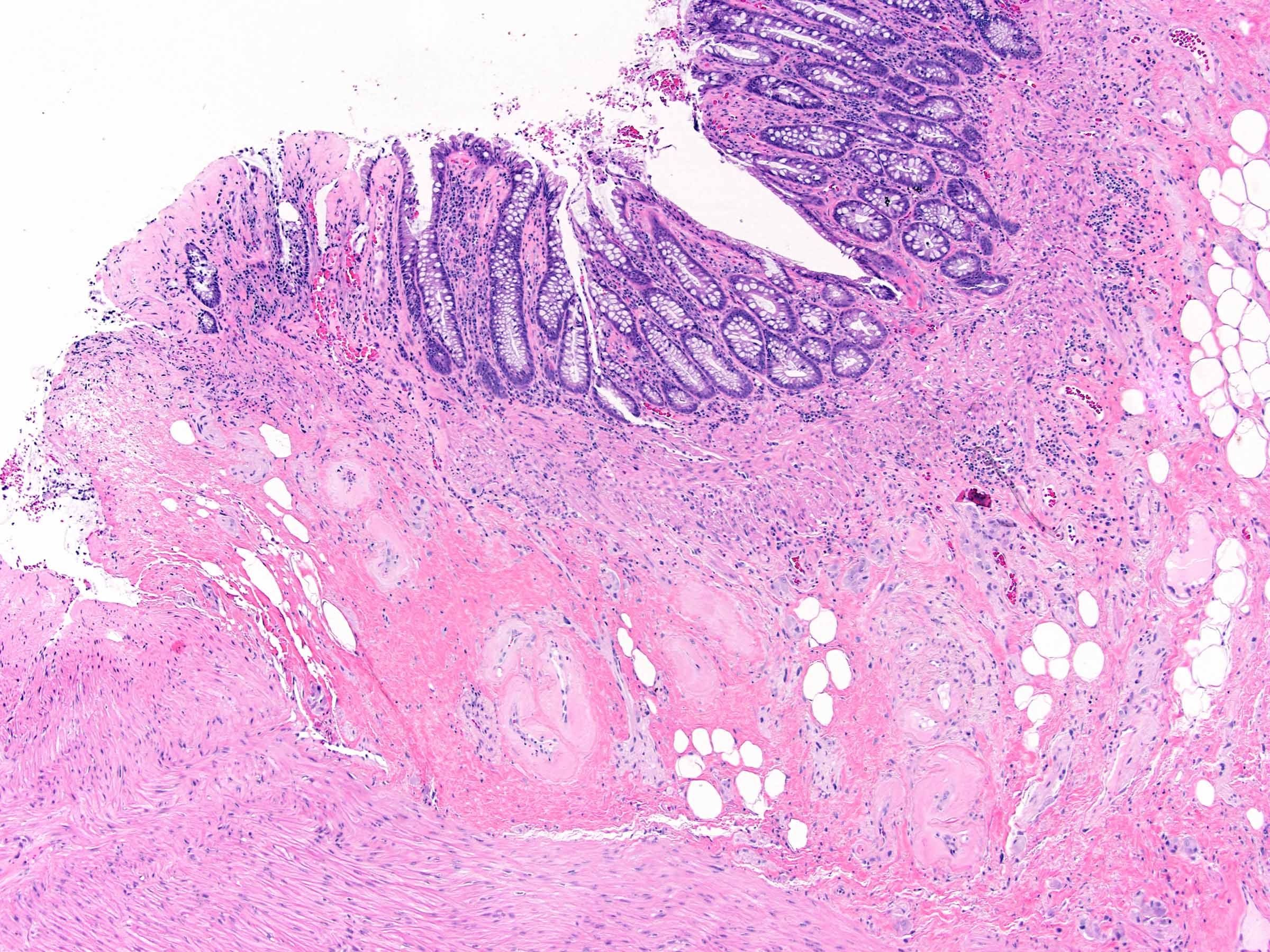
- Chronic radiation colitis (> 6 months after radiation treatment):
- Epithelium:
- Paneth cell metaplasia
- Ulceration
- Mild epithelial atypia
- Crypts:
- Architectural changes and atrophy
- Lamina propria:
- Fibrosis
- Mild chronic inflammation
- Atypical fibroblasts / stromal cells with enlarged hyperchromatic nuclei
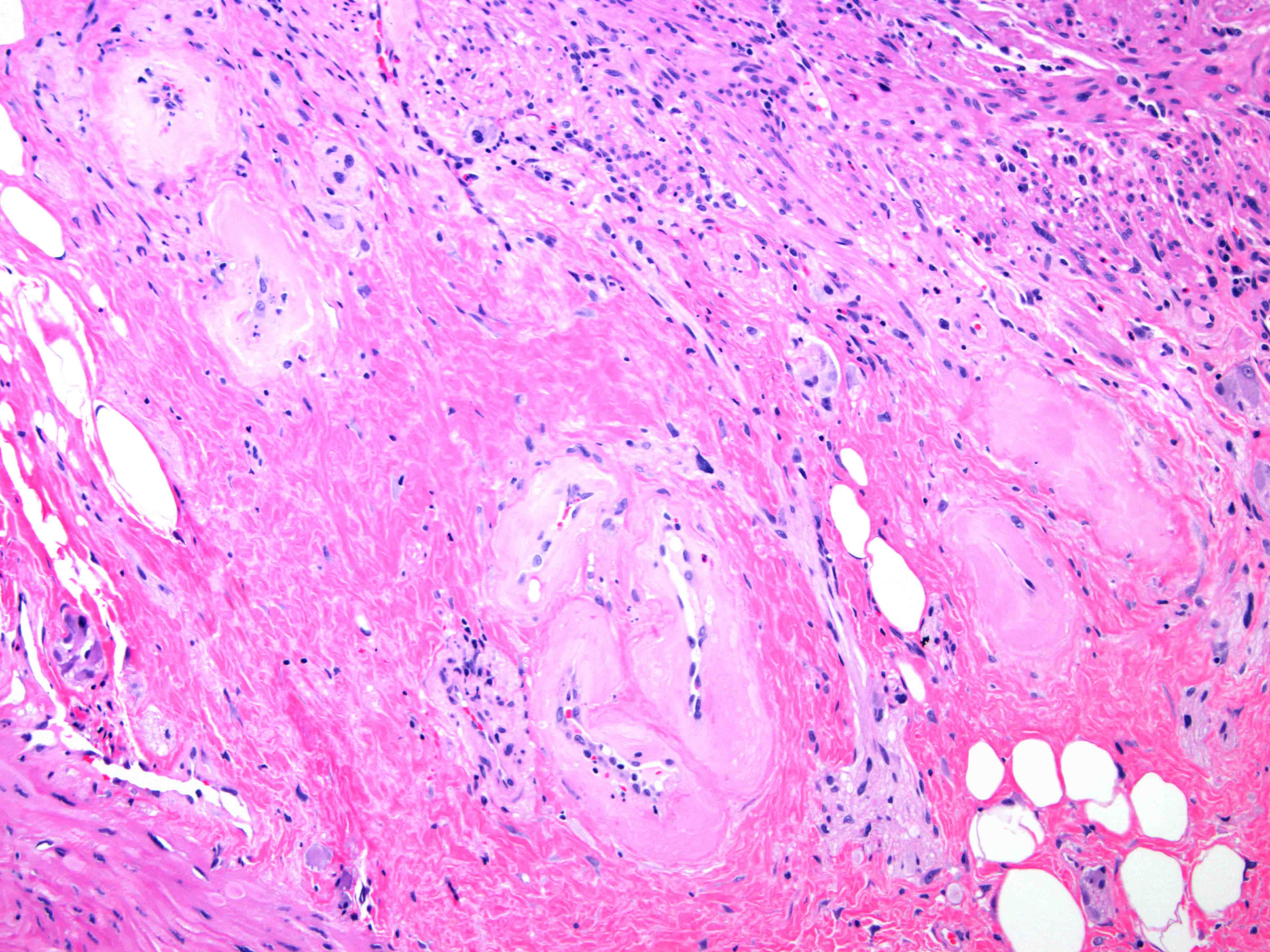
- Submucosa and deeper layers:
- Vasculature
- Hyalinization and fibrosis of vessel wall
- Intimal thickening
- Vascular ectasia or narrowing
- Thrombosis
- Endothelial cell atypia
- Vasculature
- Epithelium:
- Reference: Am J Surg Pathol 2002;26:498
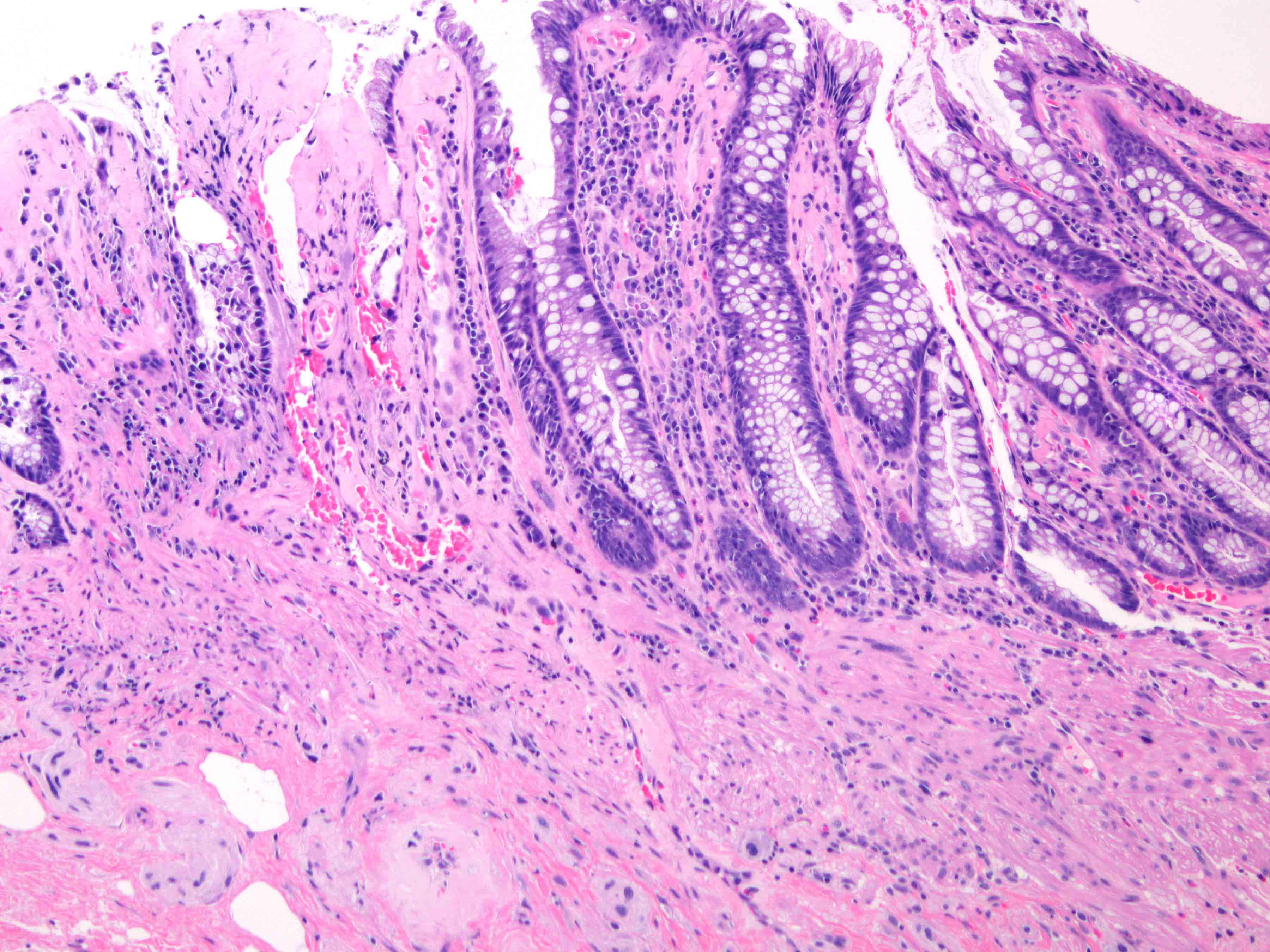
Microscopic (histologic) images
Sample pathology report
- Colon, biopsy:
- Colonic mucosa with lamina propria fibrosis and ectatic, hyalinized vessels consistent with mild chronic radiation associated colitis
Differential diagnosis
- Ischemia:
- Present: hyalinized lamina propria, withered regenerative crypts, possible coagulative necrosis, thrombi, little if any inflammation, hemosiderin laden macrophages
- Absent: eosinophilic inflammation, atypical fibroblasts / stromal cells with enlarged hyperchromatic nuclei and vascular changes (see Microscopic (histologic) description above for vasculature)
- Inflammatory bowel disease:
- Present: active chronic inflammation, including cryptitis, crypt abscesses with evidence of chronicity, such as glandular architectural distortion and increased basal lamina propria lymphoplasmacytosis
- Absent: atypical fibroblasts / stromal cells with enlarged hyperchromatic nuclei and vascular changes (see Microscopic (histologic) description above for vasculature)
- Collagenous colitis:
- Present: thick subepithelial table collagenous band
- Absent: atypical fibroblasts / stromal cells with enlarged hyperchromatic nuclei and vascular changes (see Microscopic (histologic) description above for vasculature) and submucosal fibrosis
- Mucosal prolapse:
- Present: telangiectatic vessels and fibromuscular hyperplasia, inflammation (typically noneosinophilic), erosion and ulceration
- Absent: eosinophilic inflammation, atypical fibroblasts / stromal cells with enlarged hyperchromatic nuclei and vascular changes (see Microscopic (histologic) description above for vasculature) and submucosal fibrosis
- Amyloidosis:
- Present: vessels with eosinophilic amorphous material that is Congo red positive
- Absent: eosinophilic inflammation, atypical fibroblasts / stromal cells with enlarged hyperchromatic nuclei and vascular changes (see Microscopic (histologic) description above for vasculature)
Additional references
Board review style question #1
A 76 year old woman with a history of cervical cancer status post stereotactic radiation presents 7 months later with spotty rectal bleeding. Colonoscopy reveals erythema, which is biopsied. Histology demonstrates lamina propria fibrosis and mild chronic inflammation; the epithelium shows focal mild crypt architectural distortion and ectatic vessels. No significant activity was found. What is the most appropriate diagnosis?
- Inflammatory bowel disease
- Ischemia
- Metastatic cervical cancer, direct extension
- Radiation colitis
Board review style answer #1
D. Radiation colitis. Chronic radiation colitis usually presents later than 6 months and has the following histological changes that are secondary to vascular damage: epithelium with Paneth cell metaplasia, ulceration, mild atypia, crypt architectural distortion, lamina propria fibrosis, mild chronic inflammation and atypical fibroblasts with enlarged nuclei. Vascular changes, such as hyalinization and fibrosis of vessel wall, intimal thickening, vascular ectasia and endothelial cell atypia, can be seen in the submucosa. Inflammatory bowel disease (answer A) presents with active chronic colitis pattern of injury. The absence of activity is not a typical feature of emerging inflammatory bowel disease. Although radiation can also induce ischemia (answer B), features of radiation should be absent (example: atypical fibroblasts and hyalinization of lamina propria). Direct extension of cervical cancer (answer C) would show squamous cell carcinoma invading submucosal. The endoscopic findings would also likely show luminal narrowing secondary to mass effect, rather than a small ulcer.
Comment Here
Reference: Radiation enterocolitis
Comment Here
Reference: Radiation enterocolitis
Board review style question #2
A 60 year old man with a prior history of prostate adenocarcinoma status postradiation 5 years ago presents with severe sigmoid colon stricture. The patient underwent a partial colonic resection and a section of the colonic wall is shown. What is the most likely diagnosis?
- Collagenous colitis
- Infection
- Mucosal prolapse
- Radiation colitis, acute
- Radiation colitis, chronic
Board review style answer #2
E. Radiation colitis, chronic. Chronic radiation colitis is expected at > 6 months postradiation therapy. Sections show ulcerations, mild epithelial atypia, architectural changes and atrophy. The lamina propria contains fibrosis, mild chronic inflammation and fibroblast atypia (enlarged hyperchromatic nuclei). The vasculature within submucosal and deeper layers contains hyalinization of vessel wall and intimal thickening. Vascular ectasia, narrowing and thrombosis can also be present. Collagenous colitis (answer A) typically presents with history of watery diarrhea and a > 10 μM subepithelial collagen table (collagenous band). Infection (bacterial) (answer B) will present with an acute clinical history (example: diarrhea and vomiting) after an inciting event (example: food consumption, travel). Acute colitis and granulomas can sometimes be seen. Viral infections (example: cytomegalovirus, Epstein-Barr virus) can occur in immunocompromised patients (example: HIV or transplant) and will contain atypical cells with nuclear changes. Mucosal prolapse (answer C) can present endoscopically as a polyp and contains ingrowth of thick muscle bundles that can mechanically squeeze ensnared epithelium. This is accompanied by variable inflammation, ulceration and reaction epithelial change. Acute radiation colitis (answer D) is expected at < 6 months postradiation therapy. The inflammation is typically eosinophilic (characteristic) with eosinophilic cryptitis, crypt abscesses and lamina propria eosinophilia. Sections demonstrate reduced mitotic activity, apoptosis, reduced goblet cell mucin, goblet cell swelling, degenerative changes and atypia (nuclear enlargement and malorientation).
Comment Here
Reference: Radiation enterocolitis
Comment Here
Reference: Radiation enterocolitis