Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Shih P, Putnam NE. Shigella. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colonshigella.html. Accessed April 23rd, 2024.
Definition / general
- Infectious diarrhea and subsequent colitis caused by bacteria of the Shigella genus
- Shigella species are virulent, invasive, nonmotile, noncapsulated, facultatively anaerobic, gram negative rods (StatPearls: Shigella [Accessed 20 February 2023])
- 4 groups:
- S. dysenteriae
- S. flexneri
- S. boydii
- S. sonnei
Essential features
- Shigella are highly infective, virulent, invasive, gram negative rods
- Causes watery diarrhea associated with fever and abdominal pain, which may progress to dysentery (severe diarrhea with blood or mucus in stool) (Clin Lab Med 2015;35:225)
- Shigellosis is very common especially in the developing world and spreads via fecal oral route
- Shiga toxin released by S. dysenteriae is associated with more severe disease and may be complicated by hemolytic uremic syndrome
- Diagnosis is based on microbiological studies (culture and PCR); biopsy is not routinely performed
- Infection is self limited in most cases but can be severe in children and immunocompromised
- Antibiotic therapy is appropriate for moderate to severe disease or certain patient populations (StatPearls: Shigella [Accessed 20 February 2023])
- Antibiotic resistance is a growing problem (Clin Lab Med 2015;35:225)
Terminology
- Shigellosis and related terms are named after Dr. Kiyoshi Shiga, a Japanese physician and microbiologist who discovered the bacterium in 1897 and made contributions to understanding the disease (EcoSal Plus 2018;8:10.1128)
- Member of the Enterobacterales order and Enterobacteriaceae family and is closely related to and causes similar disease to enteroinvasive Escherichia coli
ICD coding
Epidemiology
- According to 2010 data, an estimated 188 million cases occur worldwide annually (Lancet 2018;391:801)
- Shigellosis is a leading cause of diarrheal death, with most deaths due to Shigella infection occurring in south Asia and sub-Saharan Africa
- Infection occurs from ingestion of bacteria through fecal contamination of food or water and is linked to poor hygiene and sanitation, overcrowding and lack of access to clean water
- The majority of cases occur in developing countries by serotype S. flexneri
- The United States has an incidence of ~450,000 cases annually, most by S. sonnei (StatPearls: Shigella [Accessed 20 February 2023])
- Infection in the U.S. often results from exposure / outbreak at daycare centers or institutional housing, is due to food borne transmission or in men who have sex with men
- Shigella is acquiring resistance to antimicrobial therapy
- Drug resistance to ciprofloxacin and azithromycin has been increasing in the U.S. since 2013 (CDC: 2019 Antibiotic Resistance Threats Report [Accessed 21 February 2023])
- A recent extensively drug resistant Shigella sonnei outbreak was detected in the United Kingdom between 2021 - 2022 (Lancet Infect Dis 2022;22:1503)
Sites
- Colon
Pathophysiology
- Shigella are resistant to gastric acid, allowing them to pass through the stomach into the intestine after ingestion
- Shigella bacterial cells invade M cells that are important for immune activation, are phagocytosed by macrophages which subsequently undergo apoptosis and lead to inflammation
- Once bacteria transverse the gut epithelium, they can invade enteric epithelial cells from the basolateral side and by spreading between adjacent cells (Curr Trop Med Rep 2014;1:81)
- Shigella can avoid immune recognition and destruction by escaping the phagocytic vacuole and replicating in the cytosol and by modifying its lipopolysaccharide structure
- Shigella can produce toxins that lead to enterocyte cell death and increased production of inflammatory cytokines and chemokines: Shigella enterotoxin 1 (ShET1), Shigella enterotoxin 2 (ShET2) and Shiga toxin 1 (stx1) (Curr Trop Med Rep 2014;1:81)
- Not all Shigella isolates produce Shiga toxin
- Inflammation exacerbates tissue destruction
- Less commonly, shigellosis can advance to extraintestinal disease, such as with S. dysenteriae serotype 1
- Hemolytic uremic syndrome can occur in patients infected with Shiga toxin producing Shigella strains, leading to hemolytic anemia, thrombocytopenia and acute kidney injury (J Health Popul Nutr 2012;30:257)
Etiology
- Humans are the only known natural reservoir for Shigella (StatPearls: Shigella [Accessed 20 February 2023])
- Shigellosis typically refers to invasive infection of the colon and rectum, as evidenced by severe inflammation, tissue necrosis and hemorrhage
- S. dysenteriae causes the most severe illness (Microbiol Spectr 2014;2:EHEC-0024-2013)
Clinical features
- Most patients suffer a self limited diarrhea associated with fever and abdominal pain
- Fever, nausea, vomiting, tenesmus
- Fractional stools (an increase in the number of stools with smaller volumes)
- May progress to bloody / mucoid diarrhea (dysentery)
- Without treatment, gastroenteritis lasts ~7 days in an immunocompetent patient
- Shedding may occur for up to 6 weeks (Mandell: Principles and Practice of Infectious Diseases, 6th Edition, 2004)
- Incubation period is 1 - 4 days (Clin Lab Med 2015;35:225)
- Complications include sepsis, perforation, toxic megacolon, hepatic dysfunction and toxic encephalopathy due to brain edema (Ekiri syndrome) (J Microbiol Immunol Infect 2012;45:147)
Diagnosis
- Traditionally, diagnosis was based on stool culture but cultures may be falsely negative as microorganisms are fastidious
- Culture is still useful to rule out other pathogens and for susceptibility testing
- Stool PCR panels for multiple organisms are faster and more sensitive than culture
- Endoscopy and biopsy are rarely performed (Pathologe 2022;43:16)
Prognostic factors
- Disease is more severe in children, elderly or immunocompromised (Emerg Infect Dis 2020;26:122)
- Shigella bacteremia is extremely rare in immunocompetent adults (Case Rep Gastrointest Med 2017;2017:7293281)
- S. dysenteriae is associated with more severe disease
- Antibiotic treatment reduces the length and severity of illness
Case reports
- 23 year old man who had sex with men post-Roux-en-Y gastric bypass presented with hepatic dysfunction and Shigella bacteremia (Case Rep Gastrointest Med 2017;2017:7293281)
- 40 year old immunocompetent man with Shigella bacteremia (Cureus 2021;13:e19778)
- 44 year old man presented with shigellemia after a renal transplant (J Infect Dev Ctries 2014;8:237)
- 45 year old HIV negative man who had sex with men with shigellosis associated encephalopathy (BMJ Case Rep 2018;2018:bcr2017222372)
Treatment
- Disease may be self limited
- Oral or intravenous hydration and electrolyte management are essential to replace losses
- Antidiarrheal medication is contraindicated as it delays clearance of microorganisms and prolongs symptoms (StatPearls: Shigella [Accessed 20 February 2023])
- Empiric fluoroquinolone is an acceptable therapy for adults and empiric azithromycin is acceptable for children (StatPearls: Shigella [Accessed 20 February 2023])
- Local antibiogram should be consulted prior to initiation of empiric therapy
- Antimicrobial susceptibility testing should be performed if feasible due to rising resistance
- Other antibiotic choices include cephalosporins, trimethoprim / sulfamethoxazole, ampicillin and amoxicillin
Gross description
- Involved mucosa is edematous, hemorrhagic, inflamed and ulcerated depending on the severity of infection
- Pseudomembranes may be present (Pathologe 2022;43:16)
Microscopic (histologic) description
- Biopsy is rarely performed
- No specific histologic findings for Shigella versus other infectious bacterial colitides (StatPearls: Infectious Colitis [Accessed 20 February 2023])
- Immunohistochemical staining for Shigella is not used
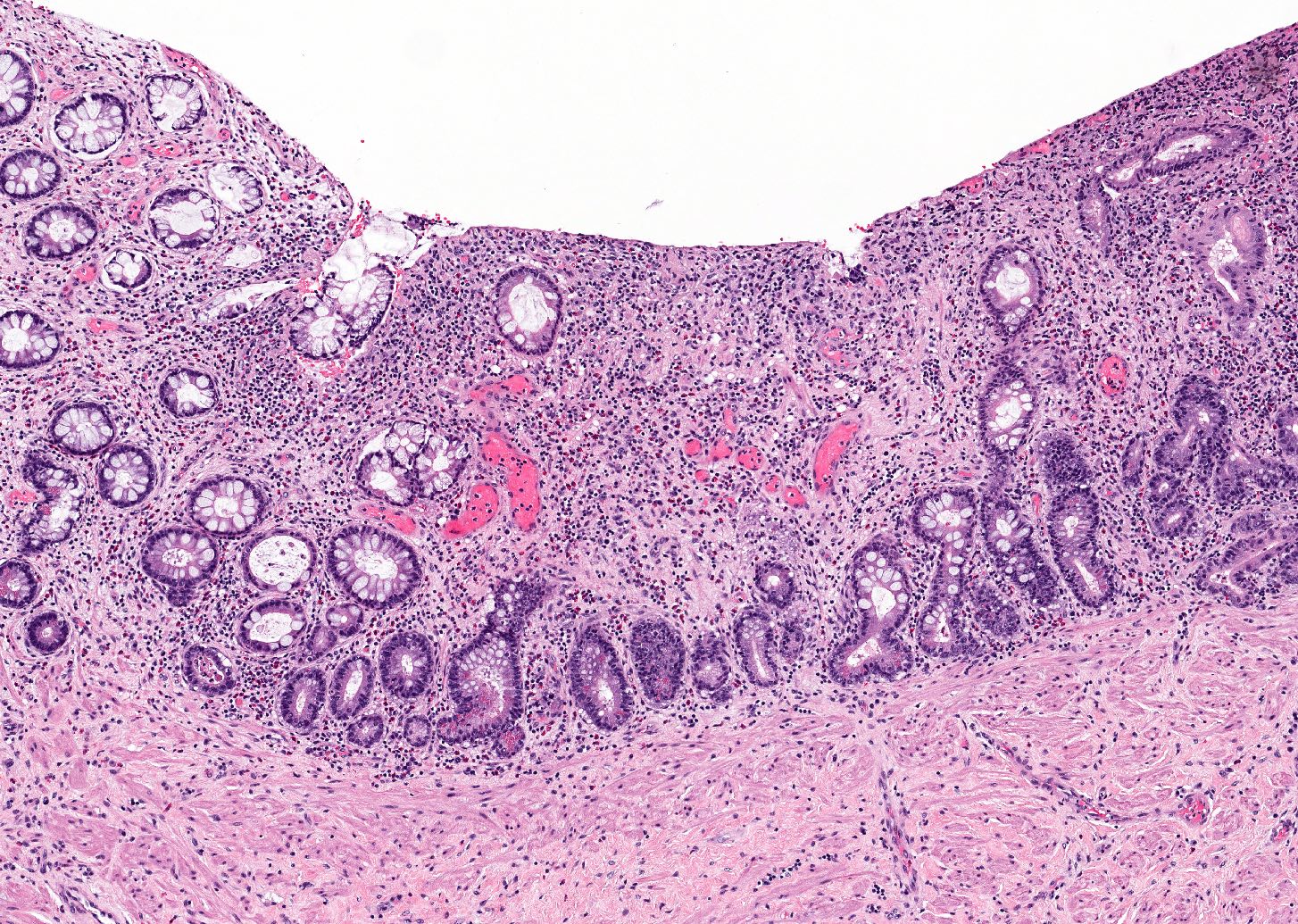
- If performed, colon biopsy in the acute phase shows a neutrophilic inflammatory infiltrate with cryptitis and crypt abscesses similar to active inflammatory bowel disease (Virchows Arch 2018;472:135)
- In the later phases of infection, there is an increase in other inflammatory cells, such as plasma cells and eosinophils (Pathologe 2022;43:16)
- Features of chronicity such as significant crypt architectural distortion and Paneth cell metaplasia are absent
Microscopic (histologic) images
Sample pathology report
- Colon, rectosigmoid, biopsy:
- Colon with pseudomembranous formation and active inflammation including cryptitis and crypt abscess (see comment)
- Comment: Features of chronicity are not seen. Negative for granuloma or viral cytopathic effects. The histologic findings are most in keeping with an infectious colitis. Inflammatory bowel disease is less likely. Correlation with clinical history, microbiological and serologic findings is recommended.
Differential diagnosis
- Definitive diagnosis based on histopathology is not possible; correlation with history and presentation, microbiological, serological, radiographic or endoscopic findings is essential
- Other infectious causes of colitis, including Escherichia coli, Campylobacter, nontyphoidal Salmonella, Clostridium difficile (Pathologe 2022;43:16)
- Acute inflammatory bowel disease:
- Granulomas are more specific to Crohn's disease; however, there is a large morphologic overlap
- Drug induced colitis:
- Many histologic patterns may overlap with Shigella colitis; however, increased intraepithelial apoptosis and the presence of pill fragments may be the clues to the diagnosis of drug induced colitis (Pathologica 2021;113:54)
- Some small molecule inhibitors (ending in "ib" such as idelalisib) and monoclonal antibodies (ending in "mab" such as ipilimumab / nivolumab) may cause diarrhea, with a histologic triad of active colitis, intraepithelial lymphocytosis and crypt epithelial cell apoptosis (often popcorn type) (Am J Surg Pathol 2015;39:1661, Histopathology 2021;78:532)
- Radiation enterocolitis:
- In the acute radiation colitis phase, the inflammatory infiltrate is eosinophilic rather than neutrophilic, as expected with the acute phase of Shigella infection; however, there is a large morphologic overlap
- Radiation atypia is seen only in radiation enterocolitis (Cancers (Basel) 2020;12:2571)
- Ischemic colitis:
- Features of acute ischemic colitis include superficial mucosal necrosis, crypt damage (withering) or loss and hyalinization of the lamina propria; acute cases may exhibit acute inflammatory exudate (pseudomembranes) on the mucosa, which can be indistinguishable based on histologic features (Pathologica 2021;113:54)
Additional references
Board review style question #1
An otherwise healthy 5 year old girl presents to the emergency department with fever, abdominal pain and bloody diarrhea. She has felt unwell for the past 2 days and subsequently developed an initially watery but then bloody diarrhea. She has had many small volume bloody stools. History reveals that she attends a daycare where other children have experienced similar symptoms. Mucous membranes are dry, however, electrolytes are within normal limits. She is given an oral rehydration solution and is discharged. If biopsy were performed, random sections of colon would demonstrate the histology shown above. What is the most likely diagnosis?
- Active inflammatory bowel disease
- Cytomegalovirus (CMV) infection
- Giardiasis
- Pinworm infection
- Shigellosis
Board review style answer #1
E. Shigellosis. The patient presents with acute gastroenteritis that has progressed to dysentery. An infectious etiology is suspected given the history; therefore, active inflammatory bowel disease is unlikely. CMV colitis is unlikely in an otherwise healthy child and viral nuclear and cytoplasmic inclusions would be seen on histopathology. The history of daycare exposure would be consistent with shigellosis, pinworm infection / enterobiasis or giardiasis. Of the choices listed, the dysenteric symptoms are most consistent with shigellosis; enterobiasis presents with pruritis and giardiasis presents with watery diarrhea. Histologic sections of giardiasis show minimal inflammation and organisms present on the mucosal surface (Virchows Arch 2018;472:135).
Comment Here
Reference: Shigella
Comment Here
Reference: Shigella
Board review style question #2
A 75 year old woman with relapsed refractory multiple myeloma undergoing stem cell transplant is seen in the emergency department presenting with fever, abdominal pain and bloody diarrhea. She is admitted and quickly develops hypotension, toxic megacolon and multiorgan failure. She is started on broad spectrum antibiotic therapy. A nucleic acid amplification test (NAAT) for the Clostridium difficile toxin gene is negative. Blood cultures are preliminarily positive for a gram negative bacillus. Stool cultures are pending. She is found to have an intestinal perforation on further imaging studies, then develops toxic encephalopathy. The decision is made to transition her to comfort care. An autopsy is performed and the findings above are seen in the colon. Which of the following is the most likely diagnosis?
- Clostridioides difficile infection
- CMV colitis
- Inflammatory bowel disease
- Ischemic colitis
- Shigellosis
Board review style answer #2
E. Shigellosis. The gross photograph shows the colonic mucosa covered in yellow-tan irregular plaques that coalesce in some areas. Pseudomembranous colitis is most commonly associated with Clostridioides difficile colitis. However, the nucleic acid amplification test for the C. difficile toxin gene is negative. In addition, the infection is rarely extraintestinal. Shigella associated colitis can form pseudomembranes and the fulminant disease exhibited in the case can be seen in immunocompromised patients. Ischemic colitis may also cause pseudomembranous colitis; however, the patient presented with infectious symptoms and sepsis. CMV pseudomembranous colitis is rare and has been reported; however, it would not fit with the blood culture positivity with gram negative rods (Dis Mon 2015;61:181). Inflammatory bowel disease also causes pseudomembranous colitis; however, it is unlikely in an older patient with the infectious clinical picture.
Comment Here
Reference: Shigella
Comment Here
Reference: Shigella