Table of Contents
Definition / general | Essential features | Sites | Pathophysiology | Clinical features | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosis | Board review style question #1 | Board review style answer #1Cite this page: Feely M, Gonzalez RS. Peutz-Jeghers syndrome. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colontumorPeutz.html. Accessed April 20th, 2024.
Definition / general
- Autosomal dominant polyposis syndrome with near complete penetrance characterized by hamartomatous gastrointestinal polyps and mucocutaneous melanin pigmentation
Essential features
- WHO diagnostic criteria: (a) three or more histologically confirmed Peutz-Jeghers polyps; or (b) any number of Peutz-Jeghers polyps with a family history of Peutz-Jeghers syndrome; or (c) characteristic prominent mucocutaneous pigmentation with a family history of Peutz-Jeghers syndrome; or (d) any number of PJ polyps and characteristic prominent mucocutaneous pigmentation
- Increased risk of GI and non-GI malignancies, with largest cohort putting the incidence at 23% (Clin Cancer Res 2006;12:3209)
- Associated GI malignancies include colorectal, small bowel and pancreatic adenocarcinomas
- Non-GI tumors include:
- Sex cord tumor with annular tubules (SCTAT) of the ovary
- Adenoma malignum of the cervix
- Sertoli cell tumor of the testis
- Breast carcinoma
Sites
- Polyps found throughout the GI tract but most commonly encountered in the small bowel
- Polyps also described in gallbladder, bladder and nasopharynx (Int J Colorectal Dis 2000;15:118)
Pathophysiology
- Almost all cases are linked to a germline mutation in LKB1 / STK11 at 19p13.3 (OMIM: Peutz-Jeghers Syndrome [Accessed 5 February 2021])
- Syndrome has high penetrance, with males and females equally affected (Nat Genet 1997;15:87)
Clinical features
- Mucocutaneous pigmented lesions are common and may be the first clue to an individual having Peutz-Jeghers syndrome; however, this pigmentation may fade over time
- Presenting symptoms commonly include GI bleeding, abdominal pain or intussusception
Case reports
- 43 year old man with Peutz-Jeghers syndrome, intussusception and malignant transformation of polyps (Oncol Lett 2015;10:1008)
Treatment
- Following baseline colonoscopic examination and evaluation of the small bowel, patients should have repeat studies every 1 - 3 years, depending on previous findings (Gut 2010;59:975)
- More frequent evaluation of the GI tract suggested after age 50, as most malignancies occur at that time
- Surveillance thought to detect sizeable GI polyps which may cause intussusception / obstruction or bleeding and also detect early stage carcinomas
Clinical images
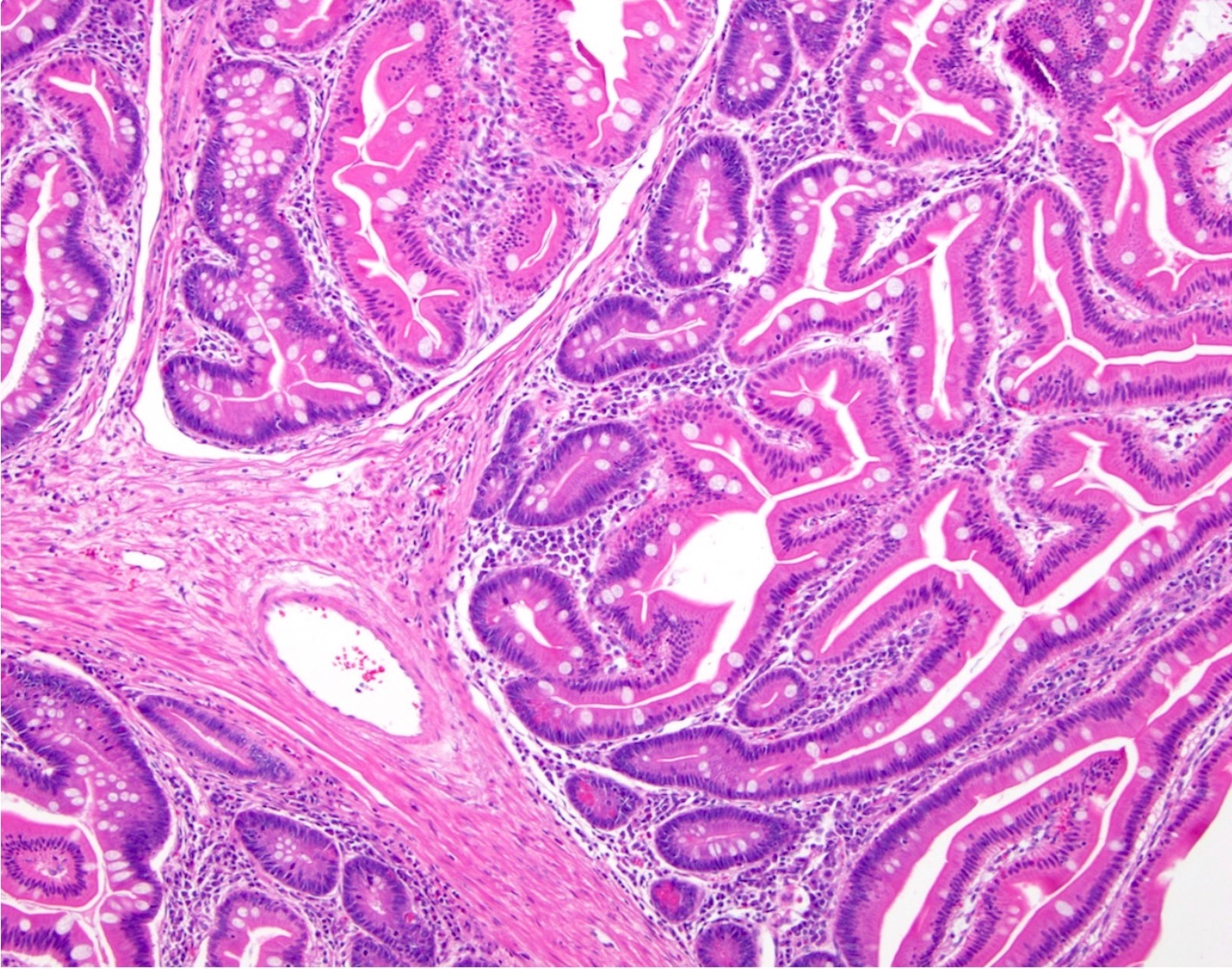
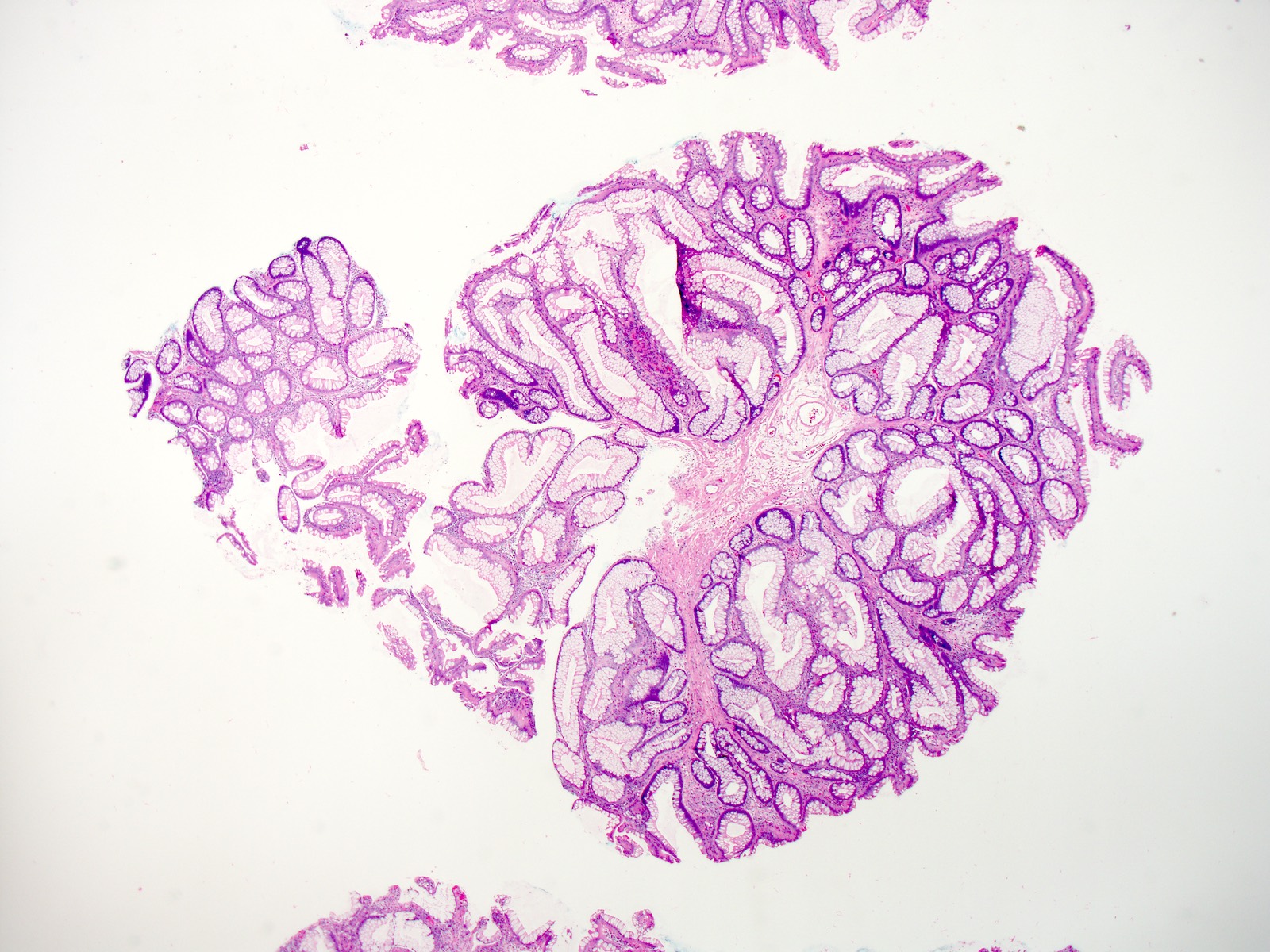
Microscopic (histologic) description
- Hamartomatous mucosal polyps with characteristic central core of branching smooth muscle associated with a mucosa native to site of origin
- Smaller polyps or those from the stomach and colon, may lack the prominent arborizing smooth muscle (Mod Pathol 2013;26:1235)
- Epithelial misplacement is not uncommon and is likely secondary to prolapse changes
- Dysplasia and adenocarcinoma can develop within polyps
Microscopic (histologic) images
Differential diagnosis
- Sporadic Peutz-Jeghers polyps:
- Histologically identical, although they are exceedingly rare, if they exist at all (Am J Surg Pathol 2007;31:1209)
- Juvenile polyps in the stomach:
- May resemble gastric Peutz-Jeghers polyps (Am J Surg Pathol 2010;34:1656)
Board review style question #1
Which of the following is true about Peutz-Jeghers syndrome?
- 1 Peutz-Jeghers polyp alone meets criteria to diagnose a patient with the syndrome
- Patients have essentially a 100% risk of developing malignancy
- Patients may develop mucocutaneous pigmentation
- Peutz-Jeghers polyps are most common in the colon
Board review style answer #1