Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Sun L, Yin F. IBD associated. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colontumoribdassociated.html. Accessed April 20th, 2024.
Definition / general
- Colitis associated colorectal cancer (CAC) is a malignant epithelial tumor originating in the large bowel associated with longstanding inflammatory bowel disease (IBD)
Essential features
- Associated with longstanding inflammatory bowel disease
- Other risk factors: disease extent, longstanding anorectal fistula, pseudopolyposis and coexisting primary sclerosing cholangitis (PSC)
- Evenly distributed (left sided and right sided)
- Mucinous adenocarcinoma and signet ring cell adenocarcinoma are common in this setting
ICD coding
- No official coding established
Epidemiology
- Longstanding inflammatory bowel disease patients are at a higher risk of developing colitis associated colorectal cancer compared with the general population; the risks are higher along with longer duration of inflammatory bowel disease
- An inflammatory bowel disease patient with a first degree relative having colorectal adenocarcinoma has an eightfold increase in risk of developing colitis associated colorectal cancer (Clin Gastroenterol Hepatol 2019;17:1807)
- Among inflammatory bowel disease patients, the disease extent (> 50% of the colon), longstanding anorectal fistula, presence of pseudopolyposis and coexisting primary sclerosing cholangitis (PSC) determine higher risk of developing colitis associated colorectal cancer (Clin Colon Rectal Surg 2018;31:168)
Sites
- Colitis associated colorectal cancer is more evenly distributed across the colon, compared with sporadic colorectal adenocarcinoma which is located mainly distal to the splenic flexure (Clin Gastroenterol Hepatol 2006;4:335)
Pathophysiology
- Cytokines such as TNFα, IL1 and IL6 are involved in the promotion of colitis associated colorectal cancer in inflammatory bowel disease patients through chronic inflammation induced accumulation of reactive oxygen species, mutagenic DNA damage and activation of transcription factors such as NFκB and STAT3 (Curr Cancer Drug Targets 2011;11:451, Gastroenterology 2011;140:1807)
Etiology
- Longstanding inflammatory bowel disease (IBD), including Crohn’s disease (CD) and ulcerative colitis (UC)
Clinical features
- Similar to sporadic colorectal adenocarcinoma; hematochezia or rectal bleeding may be present
Diagnosis
- Clinical history of longstanding inflammatory bowel disease; endoscopic, histopathologic and radiographic findings
Radiology description
- Two different CT patterns are described:
- Type 1 tumor (47%): clearly visible soft tissue mass
- Type 2 tumor (53%): circumferential thickening of the colorectal wall with stenosis; significant association with the presence of signet ring cells (Abdom Imaging 2013;38:421)
Prognostic factors
- Risk factors: long duration of inflammatory bowel disease, degree of inflammation, disease extent (pancolitis or left sided colitis), longstanding anorectal fistula, pseudopolyposis, coexistenting primary sclerosing cholangitis
- Role of chemoprevention with 5-aminosalicylic acid derivatives (5-ASA) as a protecting factor has been controversial (Dig Dis 2012;30 Suppl 2:55)
Case reports
- 16 year old girl with synchronous colorectal neoplasms in ulcerative pancolitis of 6 years duration (BMJ Case Rep 2013;2013:bcr2013200172)
- 36 year old man with synchronous multifocal colorectal carcinoma after delayed diagnosis of ulcerative pancolitis (Pathol Res Pract 2008;204:905)
- 36 year old man with primary sclerosing cholangitis and inflammatory bowel disease developed two synchronous colitis associated colorectal cancers (World J Gastroenterol 2014;20:12657)
- 41 year old man with colitis associated colorectal cancer developing only 2 years after the first symptoms of ulcerative colitis (J Gastroenterol 2007;42:854)
- 51 year old man with Crohn’s disease developed a mucinous adenocarcinoma with signet ring cell carcinoma 3 years post resection of a sporadic adenocarcinoma (World J Surg Oncol 2013;11:295)
Treatment
- Prophylactic proctocolectomy in patients with primary sclerosing cholangitis and inflammatory bowel disease is still controversial (Gastrointest Cancer Res 2011;4:53)
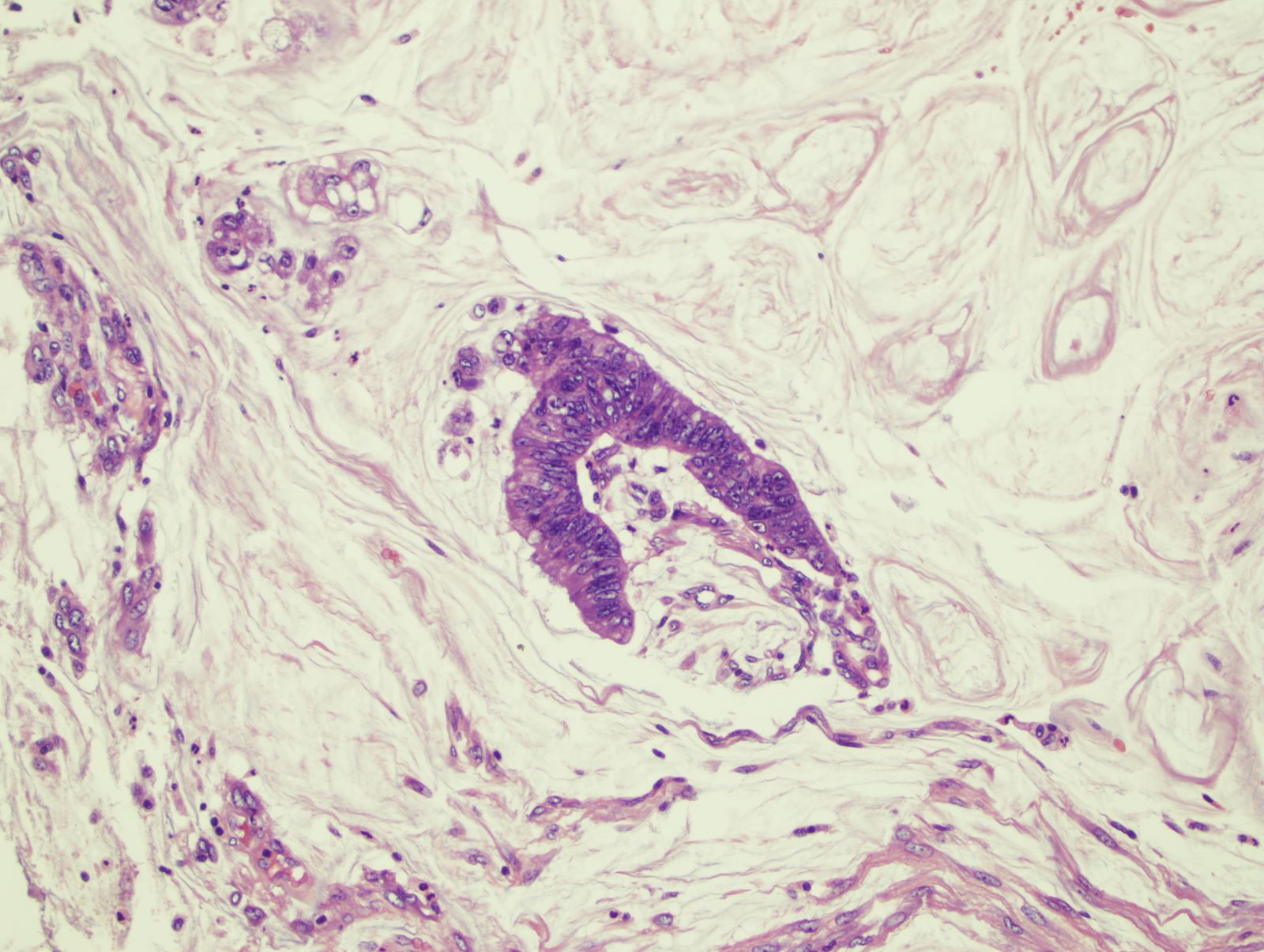
Microscopic (histologic) description
- Conventional adenocarcinoma most common
- One known histologic cancer variant in this setting is low grade tubuloglandular adenocarcinoma (Mod Pathol 2019;32:884)
- Mucinous carcinomas and signet ring cell adenocarcinomas are much more common in colitis associated colorectal cancer as compared with sporadic cases
- Rarely, other types of carcinoma may be seen, such as neuroendocrine carcinoma, mixed adenocarcinoma / squamous cell carcinoma, undifferentiated carcinoma and pure squamous cell carcinoma (Mod Pathol 1998;11:537, Can J Gastroenterol 2007;21:47)
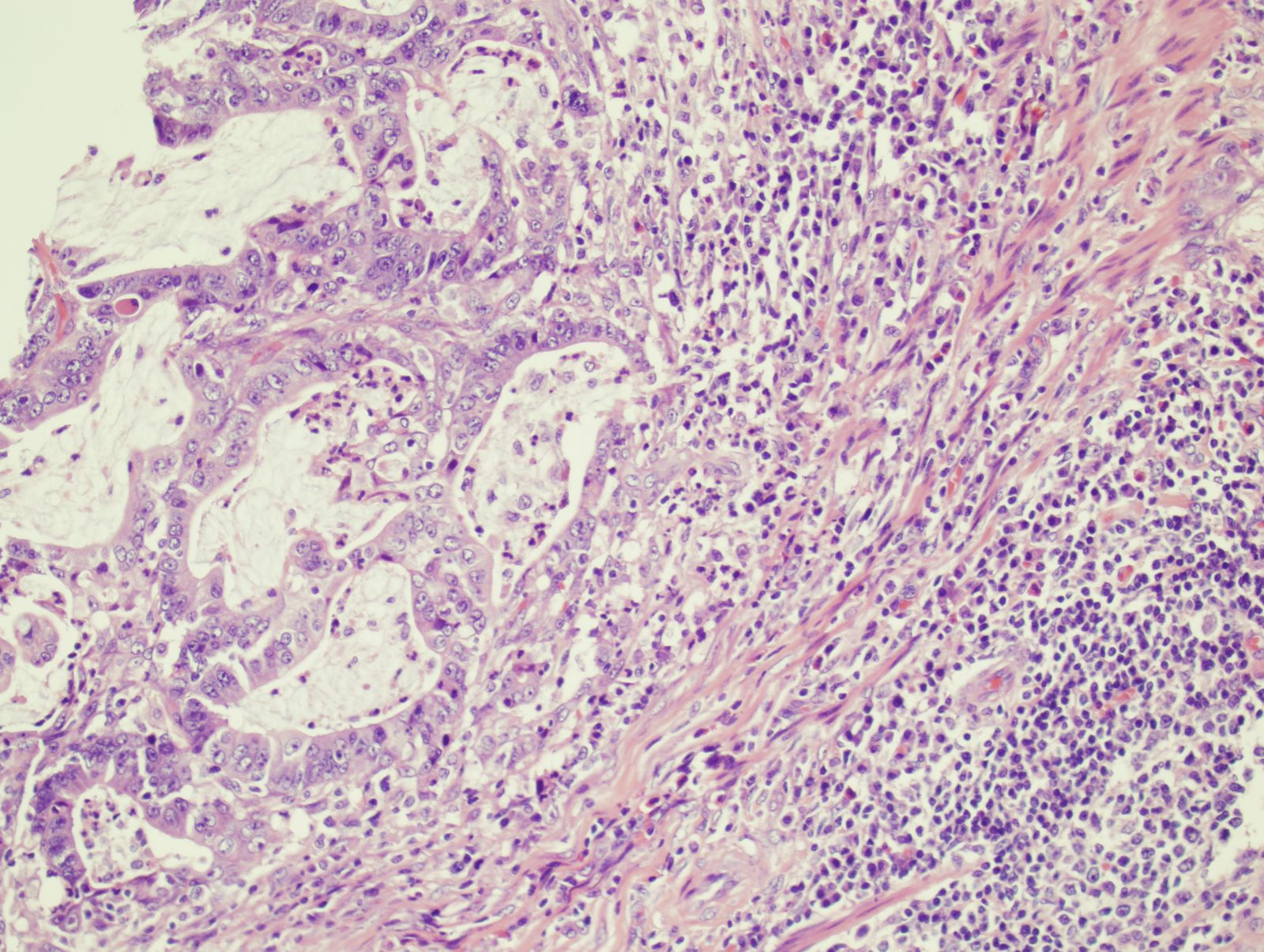
Microscopic (histologic) images
Positive stains
- CK20, CDX2
- AMACR positive in low grade dysplasia (96%), high grade dysplasia (80%) and adenocarcinoma (71%) (Am J Surg Pathol 2006;30:871)
- p53 (mutation as an early event in colitis associated colorectal cancer but a late event in sporadic colorectal adenocarcinoma) (Int J Mol Sci 2017;18:E1284)
Negative stains
- CK7 (similar to sporadic colorectal adenocarcinoma)
Molecular / cytogenetics description
- Mutation of TP53 occurs at earlier stage in inflammatory bowel disease associated dysplasia and is observed in 50 - 85% of colitis associated colorectal cancers
- KRAS and APC mutations are less frequently seen and occur at later stage in colitis associated colorectal cancer (Oncotarget 2017;8:22175)
- Mutations such as MLH1, RNF43, RPL22 and BRAF have been reported (Pathol Res Pract 2019;215:730)
- IDH1 R132 mutations more common in patients with Crohn’s disease but not ulcerative colitis
- MYC amplification more common in colitis associated colorectal cancer (Gastroenterology 2016;151:278)
Sample pathology report
- Colon, mass, biopsy:
- Adenocarcinoma, well differentiated, arising in a background of chronic active colitis with high grade dysplasia, consistent with colitis associated colorectal adenocarcinoma
Differential diagnosis
- Sporadic colorectal adenocarcinoma:
- Usually affects elderly population, single lesion
- Less likely to have mucinous or signet ring features
- No clinical history of long standing chronic colitis
Board review style question #1
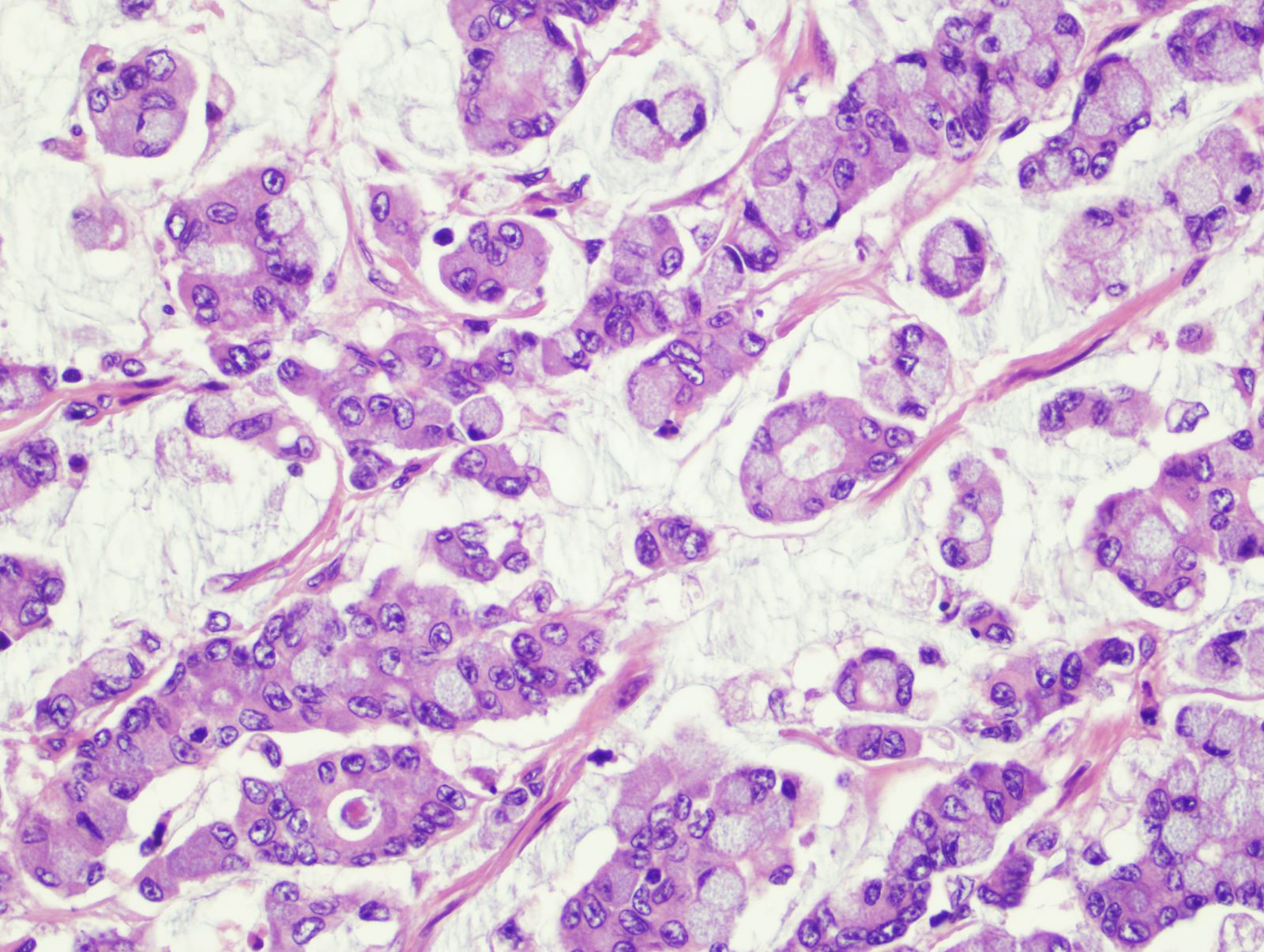
A 32 year old woman with Crohn’s disease presented with abdominal pain and hematochezia. The abdominal CT scan showed a segment of circumferential bowel wall thickening. Colonoscopy showed a stricture in the descending colon. A representative photomicrograph of the biopsy is shown. Which is the most likely diagnosis?
- Colorectal adenocarcinoma, NOS
- Metastatic breast lobular carcinoma
- Metastatic gastric signet ring cell carcinoma
- Signet ring cell carcinoma, colitis associated
Board review style answer #1
D. Signet ring cell carcinoma, colitis associated. The biopsy reveals signet ring cell carcinoma in a young patient with longstanding Crohn’s disease. This is a classic presentation of colitis associated colorectal cancer. Signet ring cell carcinoma and mucinous adenocarcinoma are more common in colitis associated colorectal cancer as compared with sporadic cases.
Comment Here
Reference: IBD associated carcinoma
Comment Here
Reference: IBD associated carcinoma
Board review style question #2
Which mutation often occurs at an early stage of colitis associated colorectal cancer?
- APC
- BRAF
- KRAS
- MLH1
- TP53
Board review style answer #2
E. TP53. TP53 mutation occurs early in colitis associated colorectal cancer but is a late event in sporadic colorectal adenocarcinoma. In contrast, APC mutation occurs early in sporadic colorectal adenocarcinoma but is very rare and usually a late event in colitis associated colorectal cancer.
Comment Here
Reference: IBD associated carcinoma
Comment Here
Reference: IBD associated carcinoma