Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Cite this page: Dunn ALJ, Gonzalez RS. Inflammatory polyp. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colontumorinflammatory.html. Accessed April 19th, 2024.
Definition / general
- Generic term for nonneoplastic mixture of epithelial and stromal components admixed with inflammatory cells
- Often related to inflammatory bowel disease (Crohn's disease or ulcerative colitis), anastomosis, ischemic colitis or infection
Essential features
- Nonneoplastic colon polyp composed of inflamed mucosa
- Typically shows surface erosion with surrounding granulation tissue and epithelial distortion
Terminology
- Inflammatory polyp as a diagnosis is generally used to describe small foci of nonspecifically inflamed colonic mucosa or inflammatory pseudopolyps
- Inflammatory polyp as a category includes several subtypes, including:
- Inflammatory cap polyp
- Inflammatory fibroid polyp
- Inflammatory myoglandular polyp
- Prolapse associated polyps
ICD coding
- ICD-10: K51.4 - inflammatory polyps of colon
Epidemiology
- Typically second and third decades for inflammatory bowel disease; incidence range of 10 - 20% in ulcerative colitis patients (World J Gastroenterol 2017;23:1541)
- May occur in older patients with peripheral vascular disease
Sites
- Can arise anywhere in the colon, especially at the ileocecal region in Crohn’s disease
- May form at anastomotic sites
Pathophysiology
- Believed to be secondary to repeated bouts of intense inflammation
- Formation of inflammatory polyps may be related to increases in C reactive protein, C4 and procollagen III peptide (World J Gastroenterol 2003;9:619)
Clinical features
- Sporadic inflammatory polyps are usually incidental at colonoscopy
- May present with intussusception or obstructive symptoms
- Presence of pseudopolyps in inflammatory bowel disease may represent recent flare, although lesions are found in active or dormant disease (World J Gastroenterol 2017;23:1541)
- Also may be related to arthropathy or other extracolonic symptoms (Lancet 1969;2:555)
Case reports
- 28 year old woman with pseudosarcomatous changes in inflammatory polyp (Korean J Gastrointest Endosc 2007;35:51)
- 47 year old man with intussusception due to 3 cm inflammatory polyp (Asian J Surg 2005;28:58)
- 62 year old man with inflammatory polyp due to Kirschner wire (Intern Med 2014;53:699)
- 74 year old man with inflammatory polyp with osseous metaplasia (Gastroenterology Res 2012;5:74)
- Patient with inflammatory polyp containing schistosomiasis (bilharzial polyp) (J Clin Gastroenterol 1983;5:169)
Treatment
- Typically treated endoscopically via polypectomy
- Examples related to inflammatory bowel disease may improve with infliximab (J Crohns Colitis 2010;4:707)
- Argon plasma coagulation or ablation for bleeding control
- Surgical resection if profuse bleeding, obstruction or intussusception
Gross description
- Usually sessile and less than 3 cm
- May be pedunculated or filiform
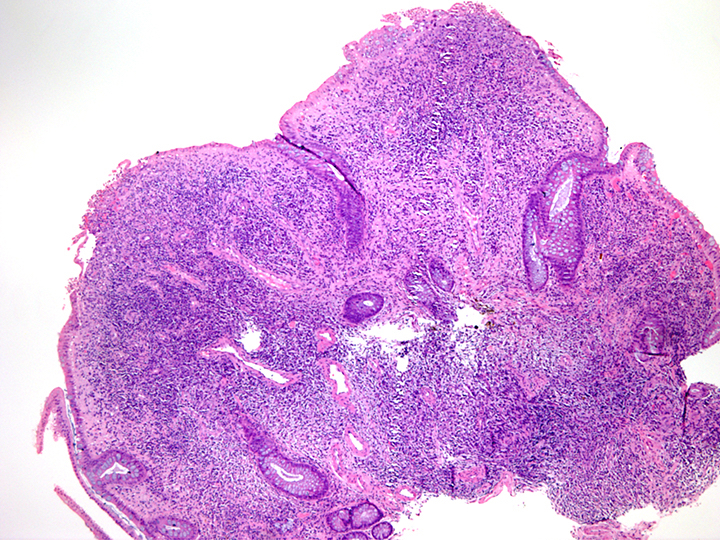
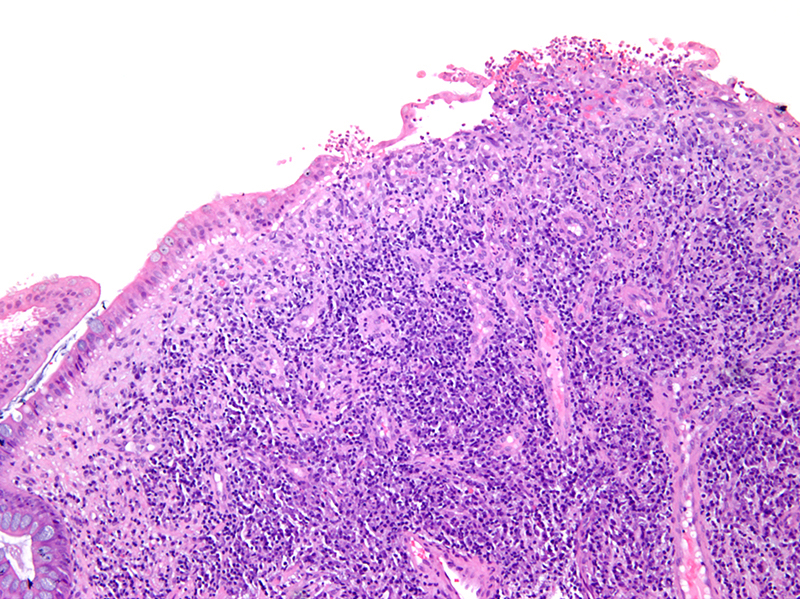
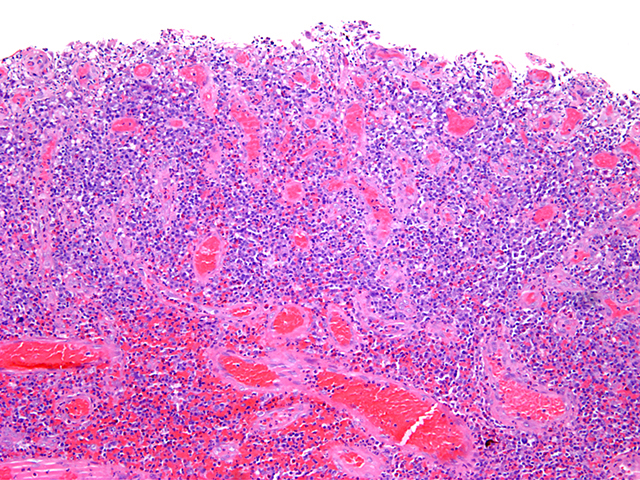
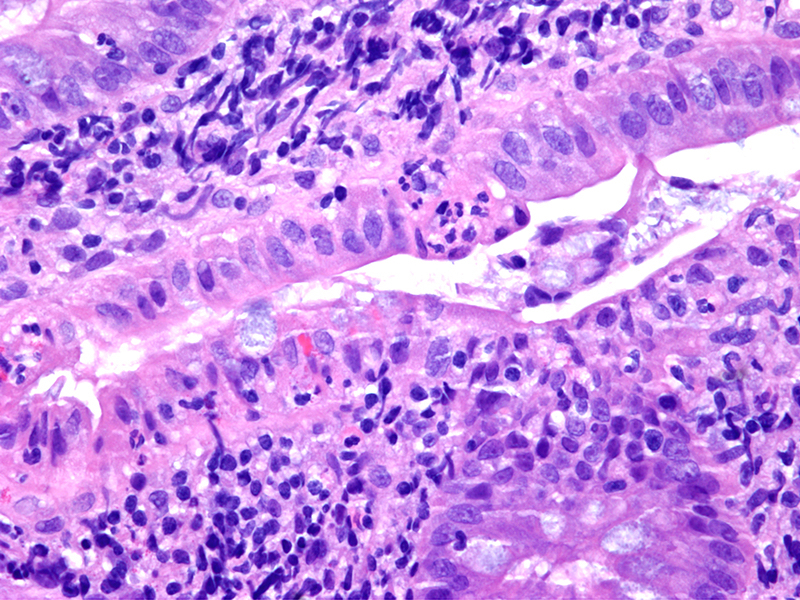
Microscopic (histologic) description
- Often consists of normal colonic mucosa in a polypoid configuration, with increased inflammation (expanded lamina propria and crypt abscesses or cryptitis)
- Epithelium can show various degrees of surface erosion, crypt distortion / dilation or hyperplasia, along with reactive nuclear features within the mucosal epithelial cells
- May consist entirely of granulation tissue (abundant thin walled and dilated vessels surrounded by mixed neutrophilic and lymphoplasmacytic inflammation)
- Reactive stromal cells may be markedly pleomorphic and mimic sarcoma
- Cases associated with inflammatory bowel disease may rarely show epithelial dysplasia
Microscopic (histologic) images
Negative stains
- S100, cytokeratin (reactive stromal cells), CMV
Molecular / cytogenetics description
- Usually no abnormalities
Videos
Inflammatory polyp on colonoscopy
Sample pathology report
- Sigmoid colon, polypectomy:
- Inflammatory polyp
Differential diagnosis
- Juvenile polyp:
- Large cystically dilated glands; wide histologic overlap and the distinction is of little importance in adult patients
- Pyogenic granuloma:
- Lobular arrangement of capillaries within edematous stroma (Ann Diagn Pathol 2005;9:106)
Board review style question #1
Which of the following is not a typical feature of colonic inflammatory polyps?
- Crypt distortion / branching
- Granulation tissue changes
- Microsatellite instability
- Surface mucosal erosion
Board review style answer #1
C. Microsatellite instability. Inflammatory polyps are a benign process with various degrees of mucosal erosion, increased vascular density similar to granulation tissue and architectural changes.
Comment here
Reference: Inflammatory polyp
Comment here
Reference: Inflammatory polyp