Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Horton R, Hagen CE. Ulcerative colitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colonuc.html. Accessed April 25th, 2024.
Definition / general
- Idiopathic chronic inflammatory disorder of the colon mucosa
- Generally starts in the rectum and extends proximally in a continuous pattern
Essential features
- Begins in the rectum and continues proximally in a continuous pattern to include up to the entire colon (pancolitis)
- Histologically characterized by active chronic colitis, with inflammation limited to mucosa / submucosa, absence of granulomas and absence of fissuring ulcers
- Complex multifactorial process involving an overwhelming T helper type 2-like immune response, leading to mucosal injury in response to gut microbial dysbiosis in genetically predisposed patients
- Risk of colorectal carcinoma, compared with the general population, is increased with duration of disease and severity of inflammation (Gastroenterol Hepatol (N Y) 2017;13:357)
ICD coding
- ICD-10: K51 - ulcerative colitis
Epidemiology
- Higher incidence (9 - 20/100,000 person years) and prevalence (156 - 291/100,000 people) in populations of North American and Northern European descent (Lancet 2012;380:1606)
- Incidence increased in industrialized countries and urban versus rural locations, suggestive of environmental triggers, such as improved sanitation, reduced exposure to childhood enteric infections and mucosal immune system maturation (Lancet 2012;380:1606)
- Bimodal age distribution with peaks at 15 - 30 years and 50 - 70 years (Lancet 2012;380:1606)
- Family history of inflammatory bowel disease, particularly that of a first degree relative (5.7 - 15.5%) and Ashkenazi Jewish descent (3 - 5x) show higher risk of disease development (Lancet 2012;380:1606)
- Gastrointestinal infections with Salmonella spp, Shigella spp and Campylobacter spp have twice the risk of developing ulcerative colitis postinfection (Lancet 2012;380:1606)
- M = F
- Former cigarette smoking is strong risk factor (Lancet 2017;389:1756)
Sites
- Almost always involves the rectum
- Continuous pattern of involvement proximally to include up to the entire colon (pancolitis)
- Rectal sparing can be seen, particularly after treatment (Lancet 2012;380:1606, Histopathology 2014;64:317, Am J Clin Pathol 2004;122:94)
- Patch of inflammation in the cecum, often involving the periappendiceal mucosa (cecal patch), can be present (Lancet 2012;380:1606, Histopathology 2014;64:317)
- Approximately 20% of patients will have inflammation in the terminal ileum (backwash ileitis)
- Typically present in patients with pancolitis (Am J Surg Pathol 2005;29:1472)
- Focally enhanced gastritis can be seen in approximately 20% of pediatric patients (Pathology 2017;49:808)
- Extraintestinal manifestations:
- Peripheral arthritis, seronegative
- Ankylosing spondylitis or sacroiliitis
- Erythema nodosum
- Pyoderma granulosum
- Primary sclerosing cholangitis (PSC)
Pathophysiology
- Not fully known but appears to be a complex multifactorial process involving an overwhelming T helper type 2-like immune response, leading to mucosal injury in response to gut microbial dysbiosis in genetically predisposed patients
- Proposed mechanisms include:
- Damage to the colonic epithelial barrier due to dysregulation of epithelial tight junctions, which provide a physical barrier between the immune cells and the luminal microbes, leads to increased permeability (Lancet 2012;380:1606)
- Colonic epithelium upregulation of antimicrobial peptides, known as beta defensins (Lancet 2012;380:1606)
- Disruption in the homeostatic balance of the mucosal immunity and the enteric nonpathogenic bacteria, resulting in the patient's aberrant immune response to the enteric commensal bacteria (Lancet 2012;380:1606, Front Microbiol 2018;9:2247)
- Increased number of colonic epithelium activated and mature dendritic cells with increased stimulatory capacity (Lancet 2012;380:1606)
- Increased expression of TLR4 by lamina propria cells and TLR4 polymorphism, which can alter susceptibility to enteric infections and tolerance to commensal bacteria (Lancet 2012;380:1606)
- Disruption in the homeostatic balance between regulatory and effector T cells, leading to a nonclassic natural killer T cell production of IL5 and IL13, which have cytotoxic effects on epithelial cells, mediating an atypical Th2 response
- IL13 can induce a positive feedback system on the natural killer T cells, leading to increased tissue injury (Lancet 2012;380:1606)
- Increase in proinflammatory cytokines, chemoattractants such as CXCL8 and adhesion molecules such as MadCAM1 recruit increased leukocytes to the colonic mucosa (Lancet 2012;380:1606)
- Other genetic risk loci include IL23 and IL10, JAK2 kinase pathway genes, hepatocyte nuclear factor 4α, CDH1 and laminin β1 (Lancet 2012;380:1606)
Etiology
- Idiopathic
Clinical features
- Clinical symptoms include bloody diarrhea, abdominal pain, mucus discharge, fecal urgency, tenesmus; in severe cases, symptoms may include weight loss, fever or colonic perforation (Mayo Clin Proc 2019;94:1357)
- Characterized by alternating periods of clinical relapse and remission
- At diagnosis, most patients have mild to moderate symptoms, with fewer than 10% having severe disease
- Patients presenting with severe disease are usually those diagnosed at young ages (15 - 30 years of age) or with simultaneous PSC (Lancet 2012;380:1606)
- 30 - 50% of patients will present with disease of the rectum or sigmoid colon and only approximately 20% of patients will present with pancolitis (Lancet 2012;380:1606)
- Appendectomy due to acute appendicitis before age 20 has been shown to be protective against ulcerative colitis (Lancet 2012;380:1606)
- Fulminant colitis, known as acute, clinically severe colitis involving the entire colon and requiring surgical resection, can be seen (Histopathology 2014;64:317)
- Toxic megacolon (marked colonic dilation with signs of systemic toxicity) can occur and requires surgical intervention (BMJ Case Rep 2018;2018:bcr2018227121)
- May have iron deficiency anemia
- Increased risk of hypercoagulability and thrombosis
- Disease severity via endoscopy is stratified as remission, mild, moderate or severe
- Numerous severity indices exist
- Goal of endoscopic remission following therapy
Diagnosis
- Correlation of clinical symptoms with endoscopic and histological examination
- Exclusion of other etiologies for colitis (infection, drug, etc.)
- Colonoscopy with biopsy is essential
- Endoscopic findings include erythema, loss of vascular pattern, granularity, friability and erosion / ulceration
- Often a sharp demarcation between inflammation and normal mucosa (Lancet 2017;389:1756)
- High definition colonoscopy or chromoendoscopy are preferred over traditional white light endoscopy due to higher sensitivity (93 - 97%) and specificity (93%) (Dig Endosc 2016;28:266, Histopathology 2015;66:37)
- Targeted biopsies of mucosal abnormalities and random biopsies at each segment of the colon help determine microscopic extent of disease (Gastroenterol Hepatol (N Y) 2017;13:357, Dig Endosc 2016;28:266)
- Esophagogastroduodenoscopy to rule out upper gastrointestinal tract involvement
Laboratory
- Overall nonspecific
- Markers of inflammation
- Erythrocyte sedimentation rate ≥ 30 mm/h
- C reactive protein > 8 mg/L
- Leukocytosis and thrombocytosis
- Antineutrophil cytoplasmic antibodies
- Fecal calprotectin > 50.0 mcg/g
- References: Pathologica 2021;113:39, Diagnostics (Basel) 2021;11:207
Radiology description
- Magnetic resonance imaging (MRI) and computed tomography (CT) may be useful in identifying bowel wall thickening and ahaustral colon but are not sensitive or specific for diagnosis of acute disease
- Plain upright abdominal Xray can be performed in patients with severe colitis to assess for toxic megacolon
- Mid transverse colon dilation > 5.5 cm (Lancet 2017;389:1756)
- Target or double halo sign can be seen in cases of advanced disease
Radiology images
Prognostic factors
- Colorectal carcinoma is the cause of death in an estimated 15% of inflammatory bowel disease patients; risk factors for developing colorectal carcinoma include:
- Duration of disease (increased risk of up to 2% after 10 years, 8% after 20 years and 18% after 30 years)
- Extent of disease, with pancolitis carrying the highest risk
- Simultaneous PSC, severity of colitis, psuedopolyps, family history of sporadic colorectal carcinoma and male sex
- Risk factors for aggressive or complicated disease include:
- Young age at onset, pancolitis, lack of endoscopic healing, deep ulcerations and high concentrations of antineutrophil cytoplasmic antibodies
- References: Lancet 2012;380:1606, Lancet 2017;389:1756
Case reports
- 14 year old girl with myositis as initial presentation of ulcerative colitis before gastrointestinal symptoms (Pediatr Gastroenterol Hepatol Nutr 2020;23:297)
- 26 year old pregnant woman with COVID-19 and acute severe ulcerative colitis (Inflamm Bowel Dis 2020;26:971)
- 39 year old woman with ulcerative colitis and a giant pyoderma gangrenosum (Medicine (Baltimore) 2020;99:e18795)
- 55 year old woman with appendiceal orifice inflammation in ulcerative colitis mimicking mucosa associated lymphoid tissue lymphoma in the cecum (Case Rep Gastrointest Med 2020;2020:8893604)
Treatment
- 5-aminosalicylate agents are first line therapy for mild to moderate disease
- Corticosteroids
- Patients with moderate to severe disease may require thiopurines or biologic agents (anti-TNF therapy or anti-integrin therapy) (Mayo Clin Proc 2019;94:1357)
- Patients with proctitis only may be treated with topical agents
- Colorectal carcinoma surveillance at 8 - 10 years after the onset of symptoms and fixed interval surveillance every 1 - 2 years afterward (Gastroenterol Hepatol (N Y) 2017;13:357)
- Surgery will eventually be required in 20 - 30% of patients with ulcerative colitis that has become refractory to medical management or who have developed dysplasia or colorectal carcinoma (Lancet 2012;380:1606)
- Total colectomy with ileal pouch - anal anastomosis is preferred surgical intervention
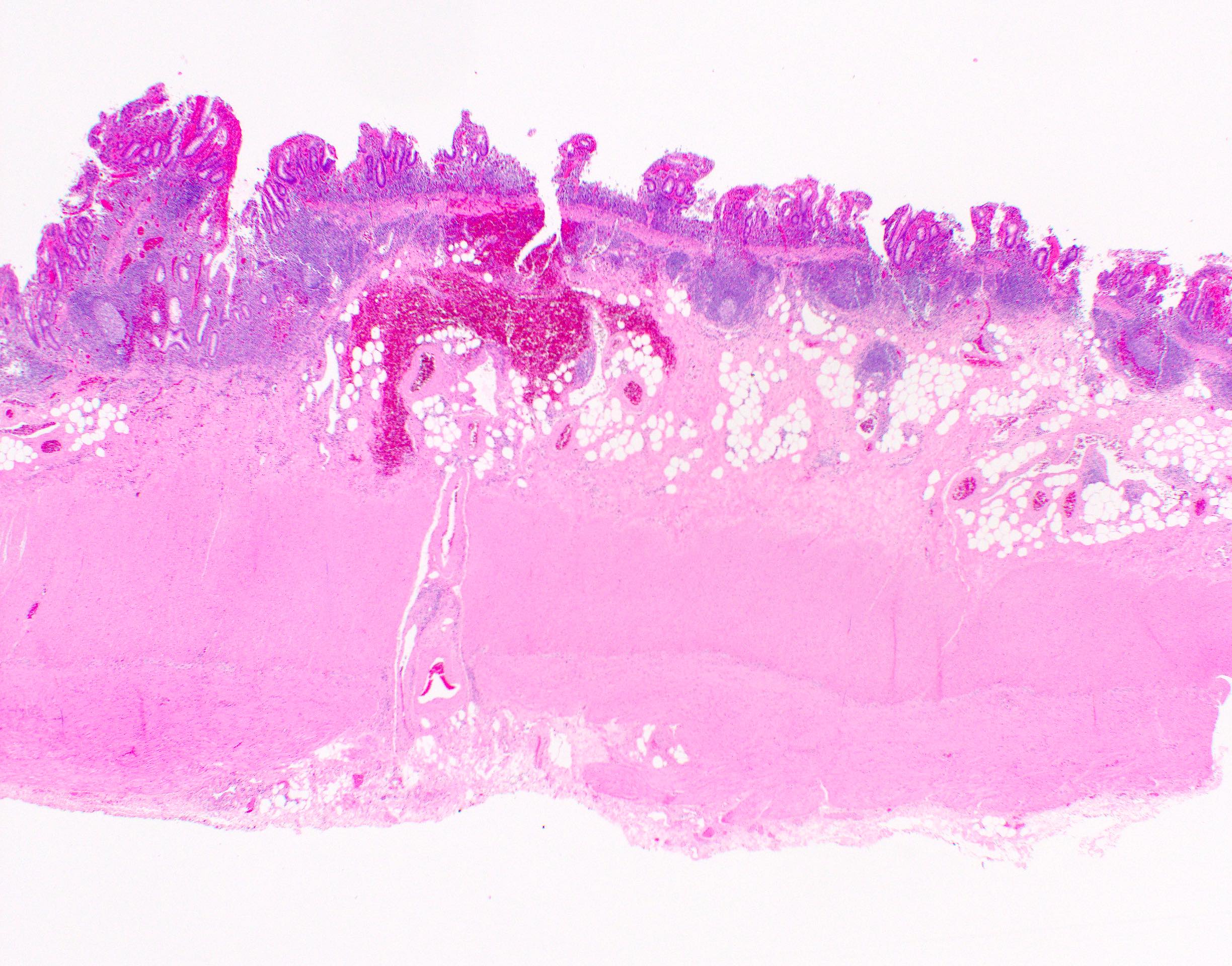
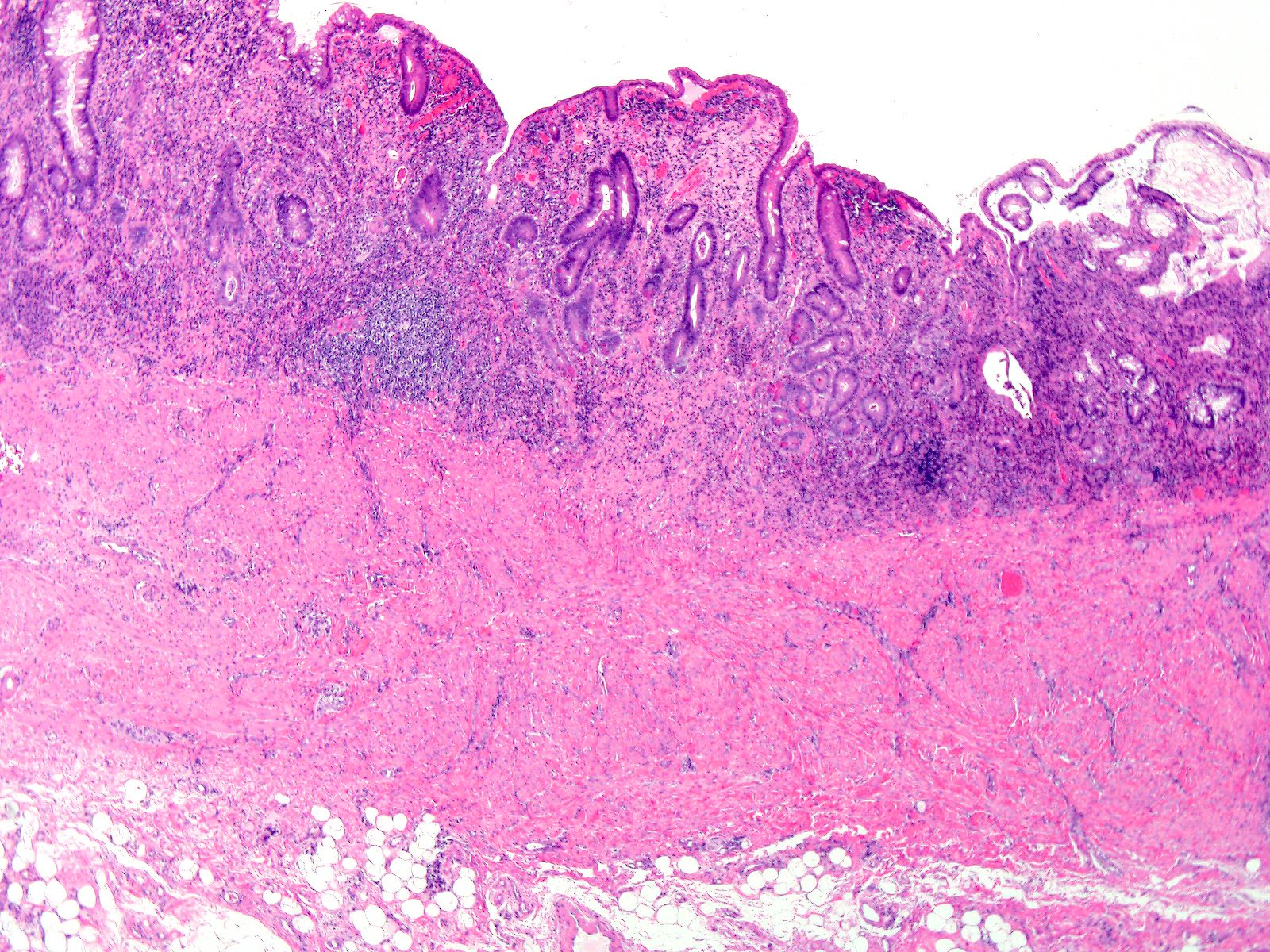
Gross description
- Findings generally progress in a continuous pattern from distal to proximal along the specimen
- Absence of skip lesions
- Mucosal erythema and granularity with superficial ulceration
- Usually no deep, fissuring ulceration
- Absence of strictures, fistulas and creeping fat
- Pseudopolyp formation due to ulceration with intervening areas of preserved mucosa
- Filiform polyposis is an exaggerated form of pseudopolyp formation and shows elongated, finger-like mucosal projection
- Toxic megacolon shows marked dilation and thinning of the colonic wall
- References: Virchows Arch 2014;464:511, Virchows Arch 2018;472:81
Gross images
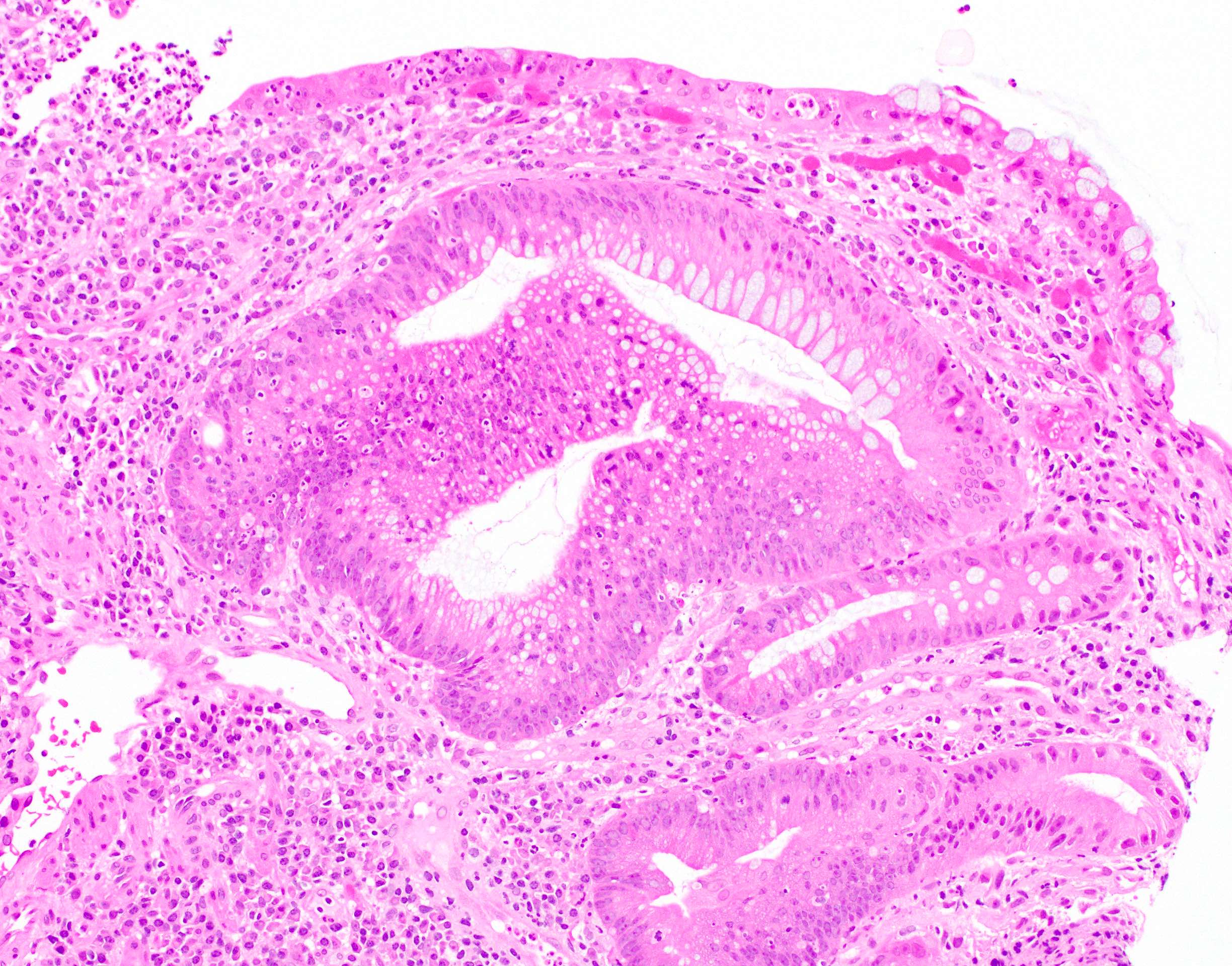
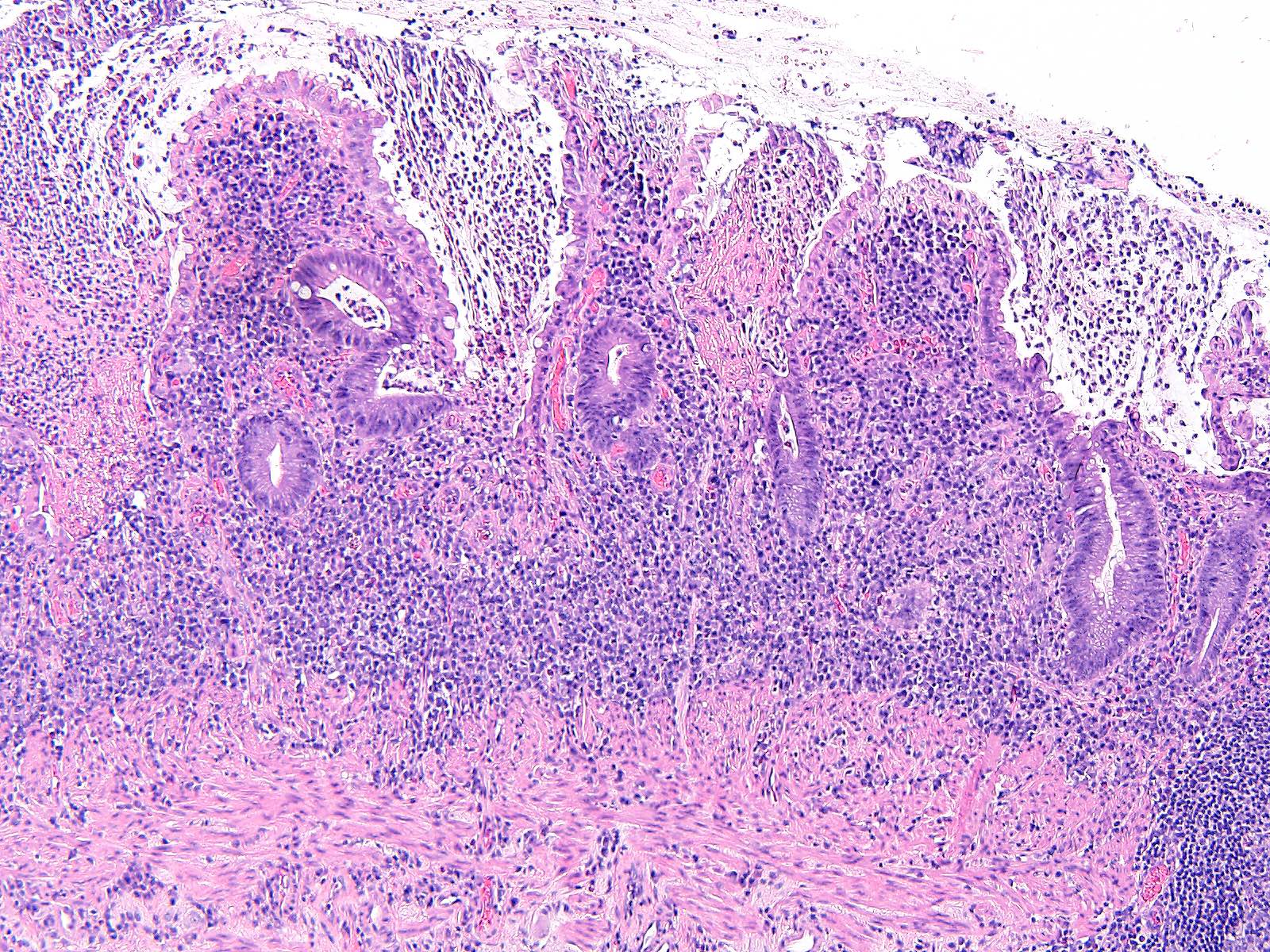
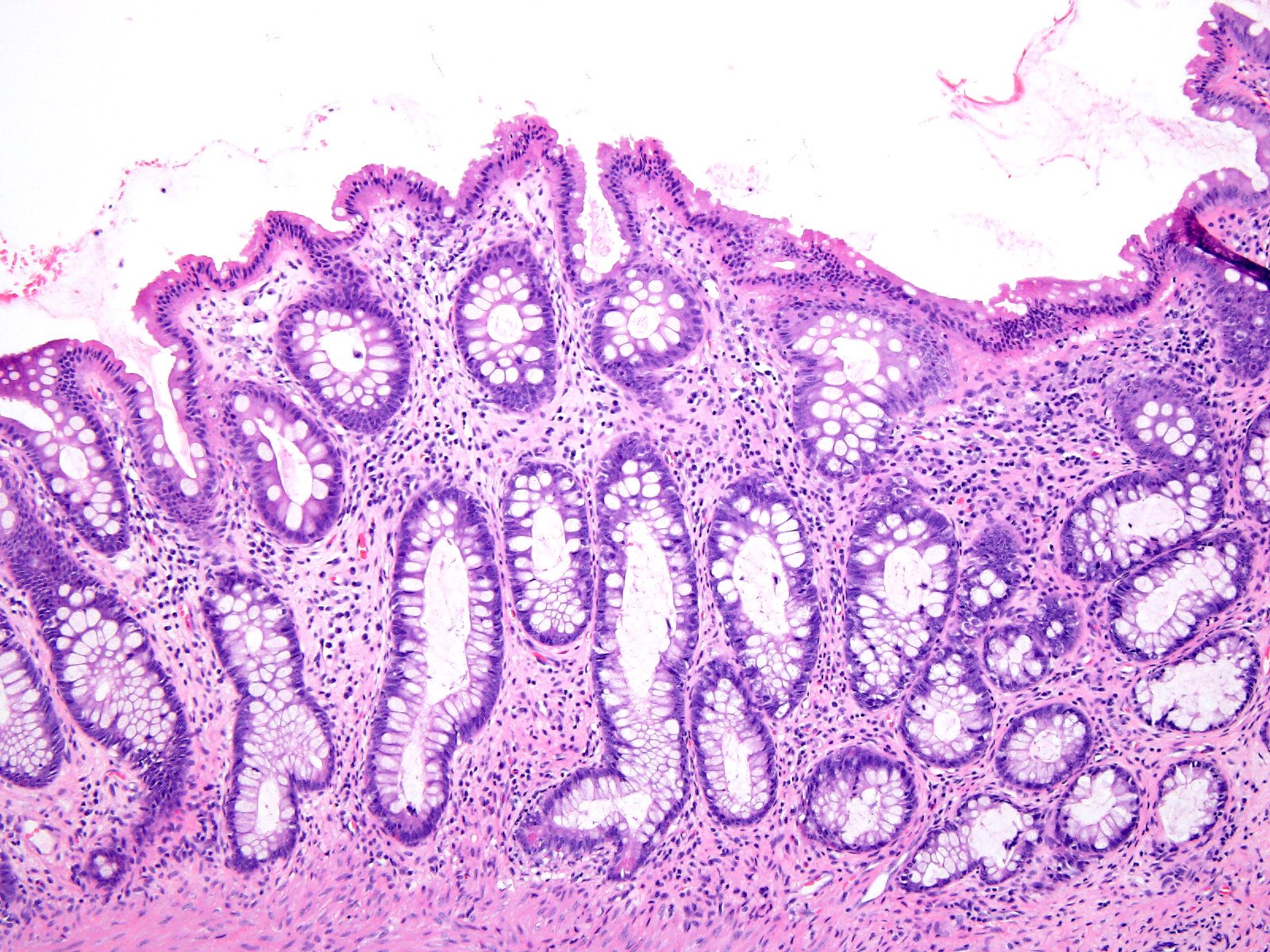
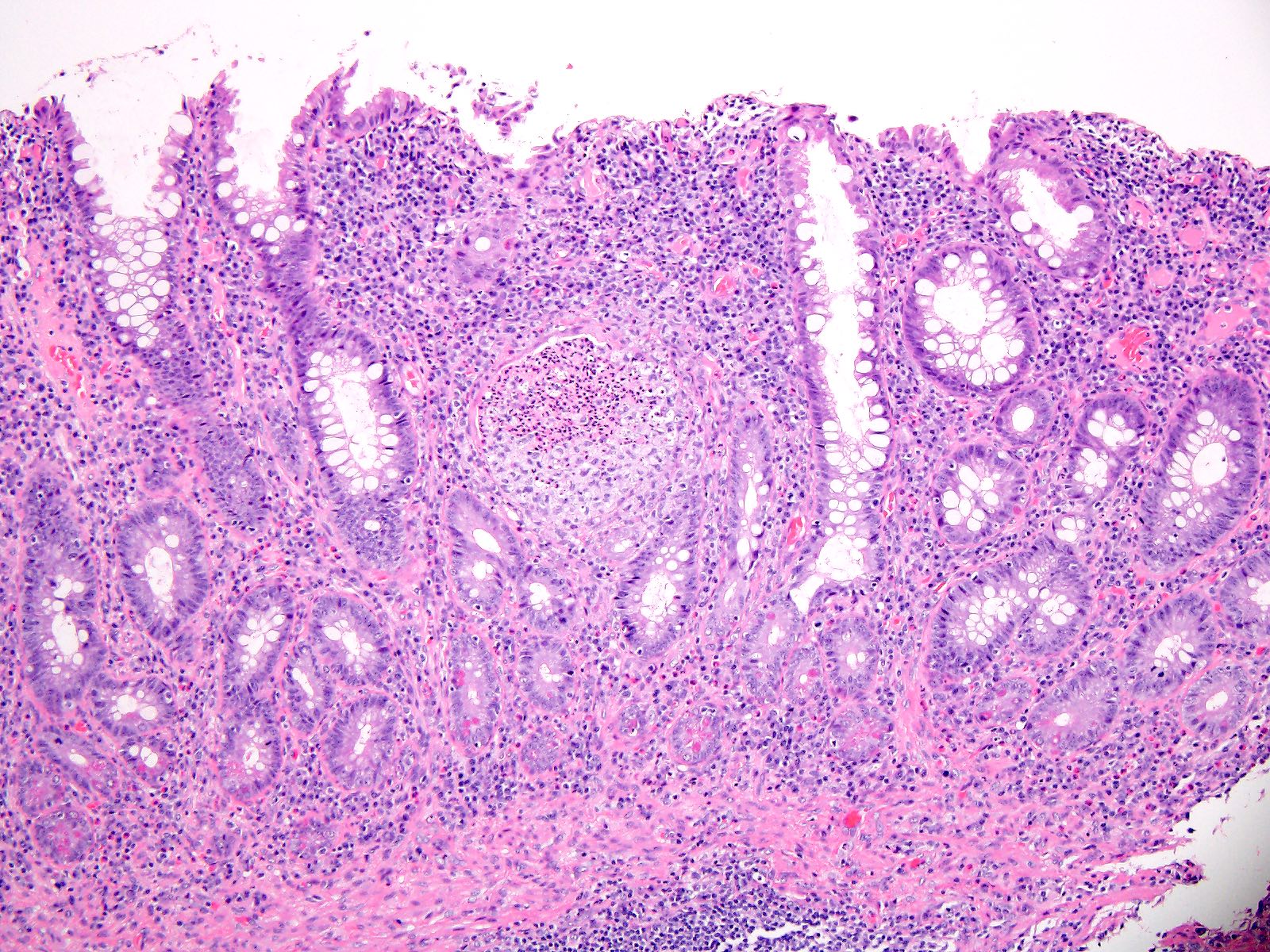
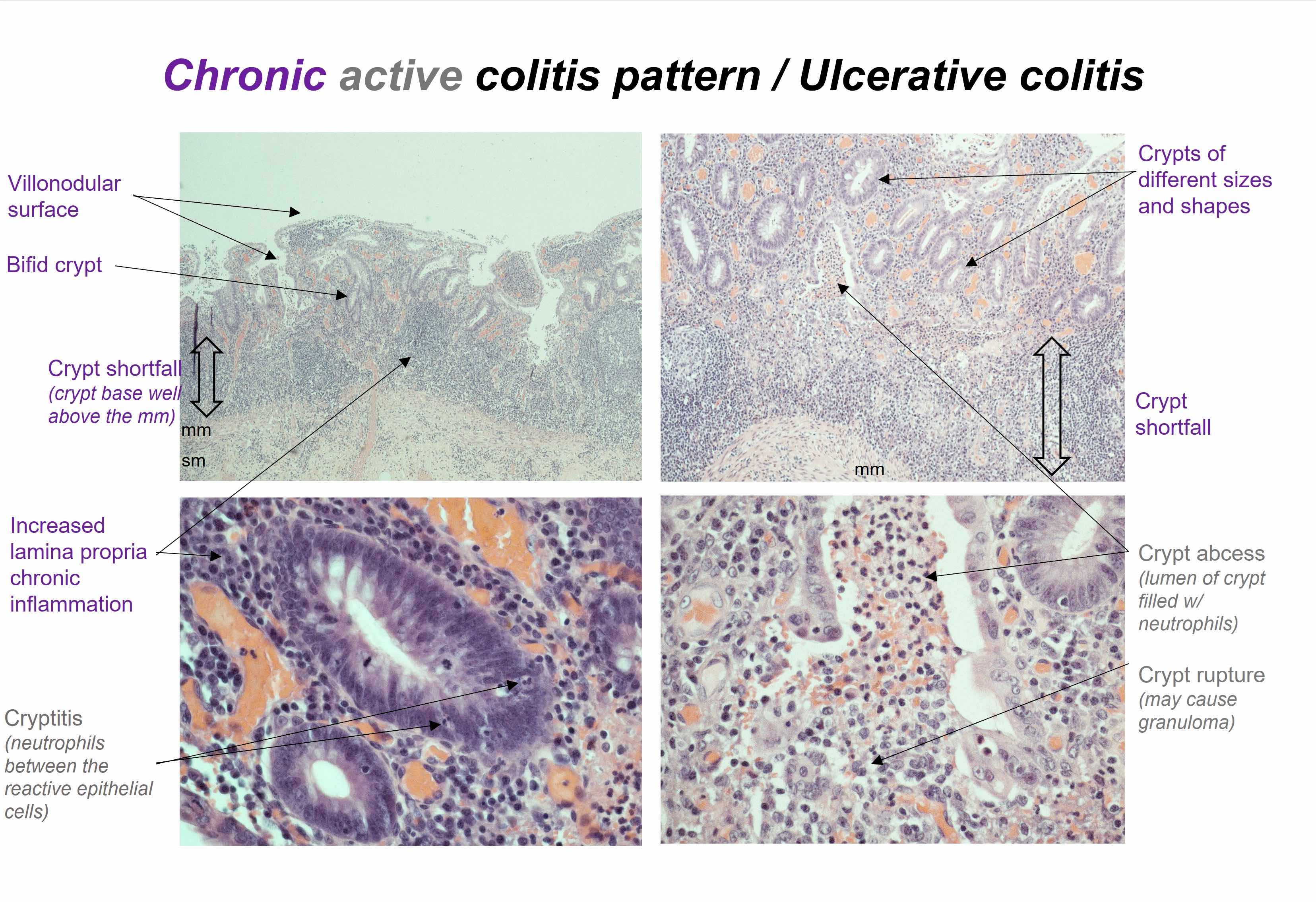
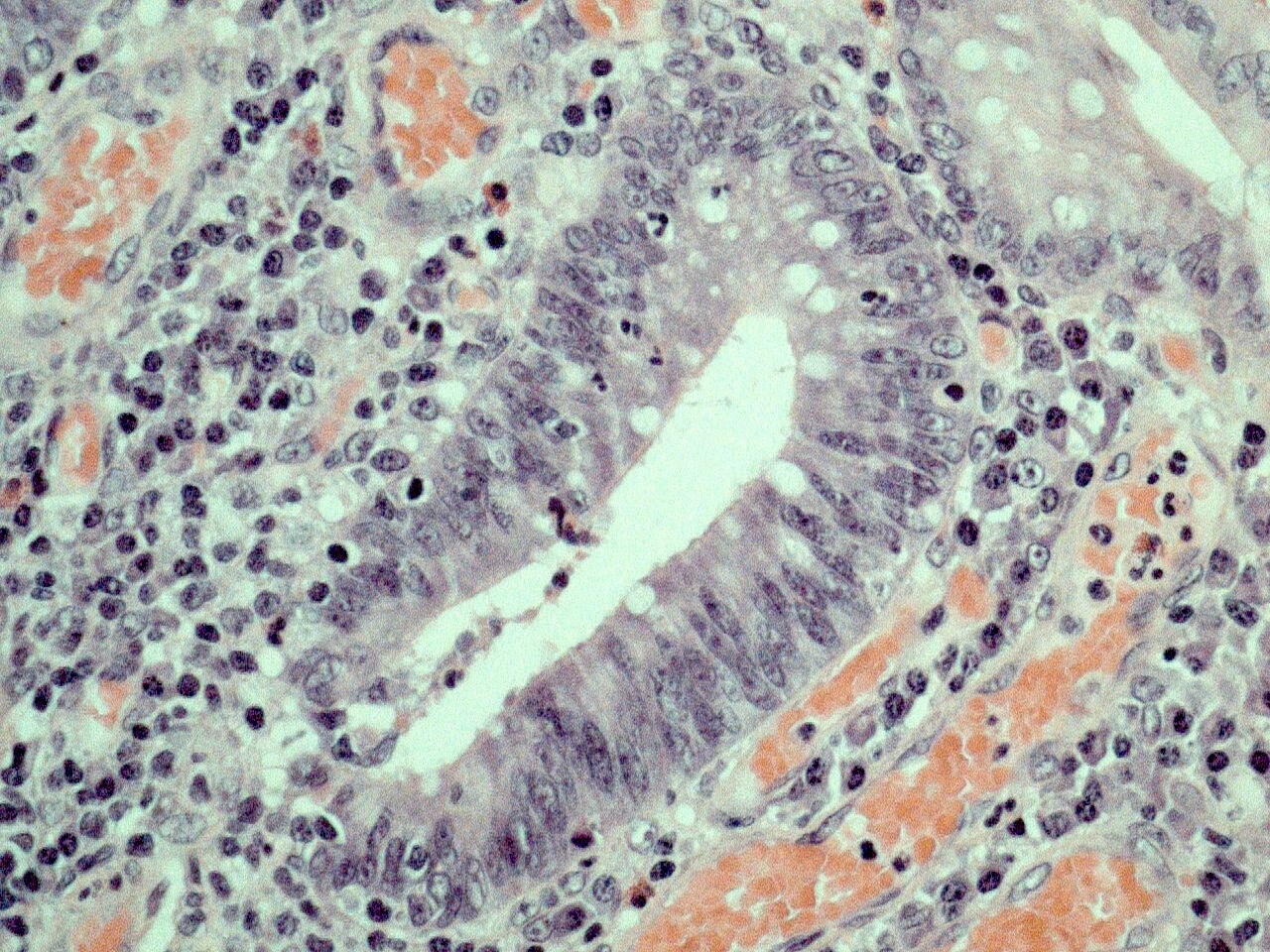
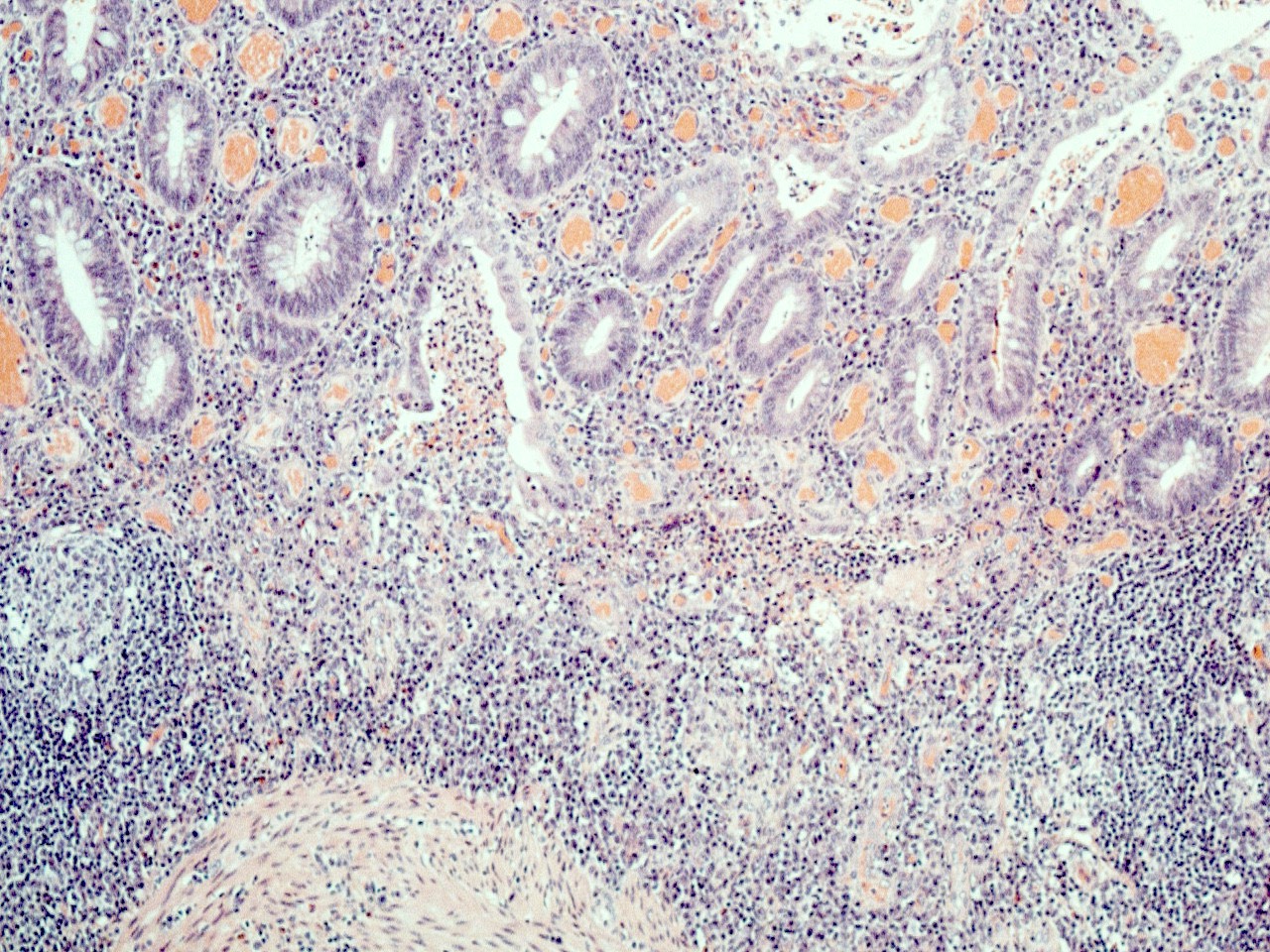
Microscopic (histologic) description
- Untreated disease characteristically shows active chronic colitis
- Features of chronicity include:
- Crypt architectural distortion including crypt atrophy, irregular spacing and size of crypts, crypt shortening and crypt branching
- Inflammatory expansion of the lamina propria with basal lymphoplasmacytosis
- Paneth cell metaplasia or hyperplasia
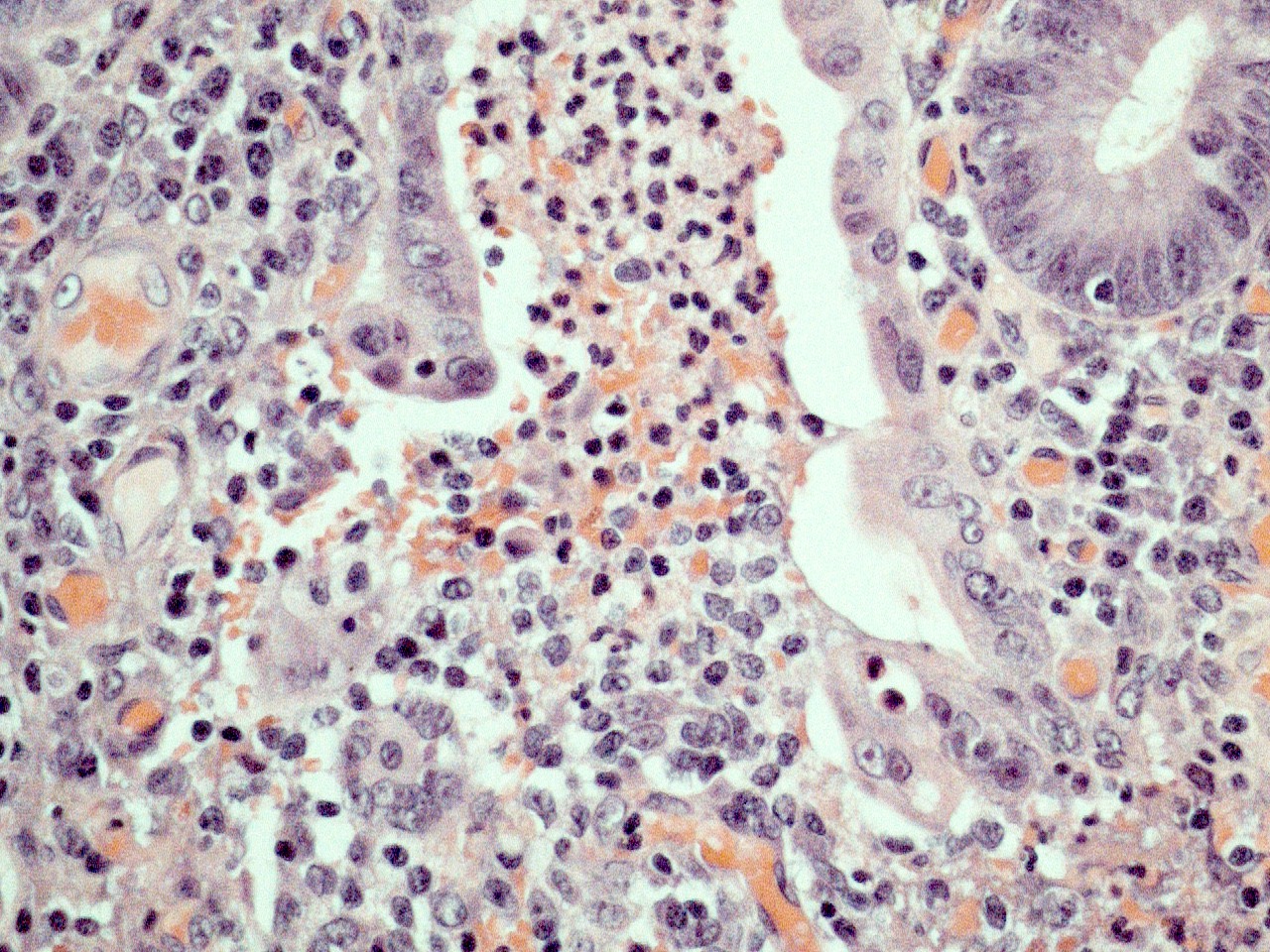
- Features of activity
- Neutrophilic inflammation with cryptitis, crypt abscess or ulceration
- Patients who have had symptoms for a short duration, longstanding disease or who have undergone therapy may have histological changes that may make microscopic diagnosis difficult (Histopathology 2014;64:317)
- Early / evolving cases may lack features of chronicity
- Treated cases may show chronic inactive (quiescent) colitis
- Superficial inflammation limited to mucosa / submucosa, with lack of transmural inflammation
- Lack of granulomas
- Crypt rupture granulomas may be noted
- Lack of fissuring ulcers
- Cases of fulminant ulcerative colitis may show fissuring ulcers and transmural inflammation (Am J Gastroenterol 2000;95:3184)
- Biopsies are limited in determining the depth of inflammation and the exact anatomical distribution of the inflammation (Histopathology 2014;64:317)
- Dysplasia (low or high grade) may be present, especially in patients with longstanding disease (Histopathology 2014;64:317)
- Activity is usually graded (Gastroenterology 2007;133:1099):
- Inactive: absence of neutrophils
- Mild: activity involving < 50% of the mucosa
- Moderate: activity involving > 50% of the mucosa; crypt abscesses usually seen at this grade
- Severe: presence of surface ulceration or erosion
- More complex grading systems, including Geboes and Robarts, exist but are not typically used in everyday practice (Gut 2000;47:404, Gut 2017;66:50)
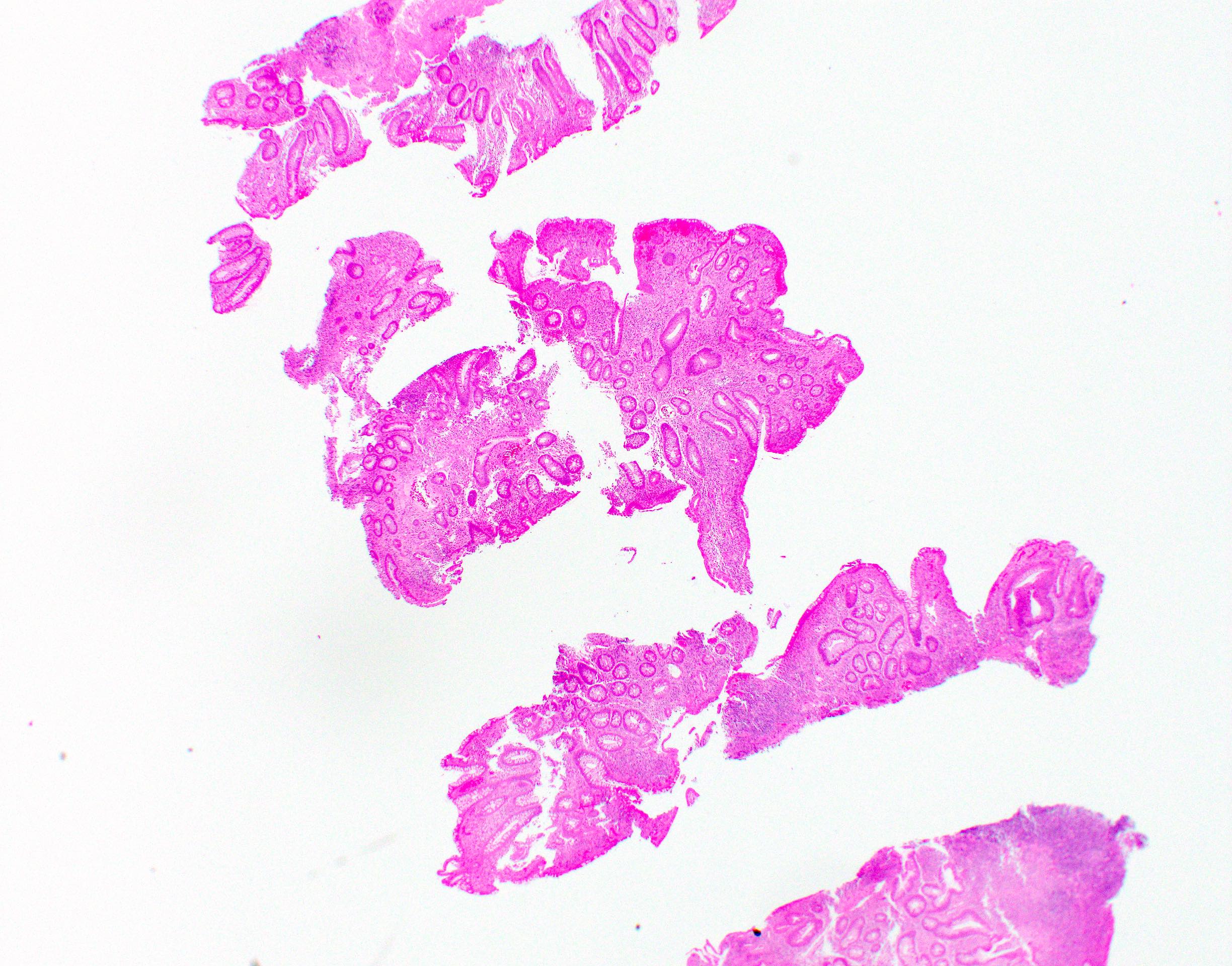
Microscopic (histologic) images
Negative stains
- CMV immunohistochemical stain
Molecular / cytogenetics description
- Association with major histocompatibility complex class 2 region near HLA-DRA
- DRB1*0103 HLA haplotype is associated with disease susceptibility and extensive disease, as well as higher risk of colectomy (Lancet 2012;380:1606)
Sample pathology report
- Colon, total colectomy:
- Severely active chronic colitis, compatible with ulcerative colitis; no dysplasia (see comment)
- Comment: Sections show continuous involvement of the colon by active chronic colitis. No transmural inflammation, deep fissuring ulcers or granulomas are seen. The findings are compatible with a diagnosis of ulcerative colitis.
- Colon, biopsy:
- Moderately active chronic colitis; no granulomas (see comment)
- Comment: The histologic features are compatible with idiopathic inflammatory bowel disease provided other etiologies have been excluded. Clinical correlation with distribution of disease is required to distinguish Crohn's disease from ulcerative colitis.
Differential diagnosis
- Crohn's disease:
- Transmural inflammation, skip lesions, fissuring ulcers, granulomas
- Fistulas or stricture formation
- Involvement of ileum or upper gastrointestinal tract more common
- Indeterminate colitis:
- Unable to make definitive diagnosis of ulcerative colitis versus Crohn's disease
- Segmental colitis associated with diverticulitis:
- Can have similar microscopic findings to ulcerative colitis but restricted to region of diverticulosis (typically sigmoid colon)
- Collagenous or lymphocytic colitis:
- Mucosal architectural distortion absent
- Acute inflammation absent or minimal
- Endoscopically normal colon
- Acute self limited colitis:
- Abundant superficial acute inflammation without features of chronicity
- CMV colitis:
- Identification of viral inclusions via H&E or immunohistochemistry
- CMV reactivation can be seen in ulcerative colitis patients, especially those receiving corticosteroid therapy (Mod Pathol 2019;32:1210)
- Diversion colitis:
- Mucosal atrophy with dense lymphoid aggregates
- May be difficult to assess concurrent background ulcerative colitis if patient known to have disease
Board review style question #1
Which of the following pathologic features, if present in a colectomy specimen, favors a diagnosis of ulcerative colitis over Crohn's disease?
- Fissuring ulcers
- Granulomas
- Inflammation limited to mucosa
- Skip lesions
Board review style answer #1
Board review style question #2
A 22 year old man reports to the emergency department complaining of abdominal pain and bloody diarrhea. He is diagnosed with fulminant colitis and requires colectomy. Histologic sections of the sigmoid colon are most consistent with which diagnosis?
- Acute infectious colitis
- Collagenous colitis
- Ischemic colitis
- Ulcerative colitis
Board review style answer #2