Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Mubeen A, Gopinath A. Serous tubal intraepithelial carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/fallopiantubesstic.html. Accessed April 25th, 2024.
Definition / general
- Lesion that is limited to the fallopian tube epithelium and a precursor to extrauterine (pelvic) high grade serous carcinoma
Essential features
- Confined to epithelium
- Histologic features: significant atypia, architectural alterations, high proliferative index and mutant pattern of p53 staining
- Important precursor lesion to recognize, as it is a criterion for assigning fallopian tube as primary site of high grade tubo-ovarian serous carcinoma irrespective of presence and size of ovarian and peritoneal disease (Histopathology 2015;67:331)
Terminology
- Various terms used to describe a spectrum of tubal epithelial alterations:
- Secretory cell outgrowths (SCOUTs): secretory cell expansion with variable ciliation (type 1 / tubal differentiation and type 2 / endometrioid differentiation), wild type p53 staining
- p53 signature: histologically normal epithelium (at least 12 cells) with mutant pattern p53 staining and low proliferation index (MIB1) (typically less than 10%)
- Serous tubal intraepithelial lesion (STIL): abnormal histology (high N/C but preserved polarity), mutant p53 and variable MIB1; STIL is regarded as a lesion of uncertain significance and diagnostic features fall short of STIC
- Serous tubal intraepithelial carcinoma (STIC): abnormal histology (high N/C, loss of polarity, lack of ciliated cells), mutant pattern p53 staining and high proliferation index (MIB1)
ICD coding
- ICD-10: N83.9 - fallopian tube disorder
Epidemiology
- Patients with hereditary BRCA mutation have a high risk of high grade serous carcinoma
- Incidence of STIC in risk reducing salpingo-oophorectomies in BRCA+ women is 5 - 8% (Gynecol Oncol 2006;100:58)
Sites
- Fallopian tube fimbria is the most common site of origin
Pathophysiology
- Secretory epithelium of fallopian tube is postulated as the cell of origin (Adv Anat Pathol 2010;17:293)
Clinical features
- Usually discovered incidentally during routine surgery or risk reducing prophylactic salpingo-oophorectomies
- May be seen adjacent to invasive carcinoma
- Reference: Gynecol Oncol 2017;146:69
Diagnosis
- Careful morphologic evaluation is key to the diagnosis; immunohistochemistry (p53 and MIB1) is only supportive
- Gross protocol (sectioning and extensively examining the fimbria [SEE-FIM]) influences ability to diagnose (Am J Surg Pathol 2006;30:230):
- Amputation and longitudinal sectioning of the infundibulum and fimbrial segment (distal 2 cm) allows maximal exposure of the tubal plicae; isthmus and ampulla are cut transversely at 2 - 3 mm intervals
- Entire fallopian tube should be submitted for evaluation in women with BRCA mutations or strong family history of ovarian carcinoma
- Extensively examine the fimbriated end
- Controversial role of multiple levels with 1 study finding no impact and another study reporting 25% missed with a single section (Am J Surg Pathol 2009;33:1878, Int J Gynecol Pathol 2013;32:353)
- STIC is staged as pathologic stage pT1
Case reports
- 48 year old woman with STIC in cervical smears (Diagn Cytopathol 2018;46:945)
- 51 year old postmenopausal woman with STIC and BRCA1 mutation (Jpn J Clin Oncol 2014;44:597)
- 55 year old woman with synchronous papillary serous carcinoma of ovary and endometrium and STIC (Indian J Pathol Microbiol 2017;60:125)
- 56 year old woman with incidental STIC (Case Rep Obstet Gynecol 2015;2015:760429)
- 58 year old woman with retroperitoneal high grade serous carcinoma and STIC (Diagn Pathol 2019;14:17)
Treatment
- No current consensus among gynecologic oncologists regarding appropriate management of incidental STIC
- Patients have been managed by surgical staging / peritoneal washings / chemotherapy or follow up without additional intervention
- Yield of surgical staging is low and short term clinical outcomes are favorable
- Individualized management is warranted until additional data become available (Int J Gynecol Cancer 2013;23:1603)
Gross description
- Not evident on gross examination
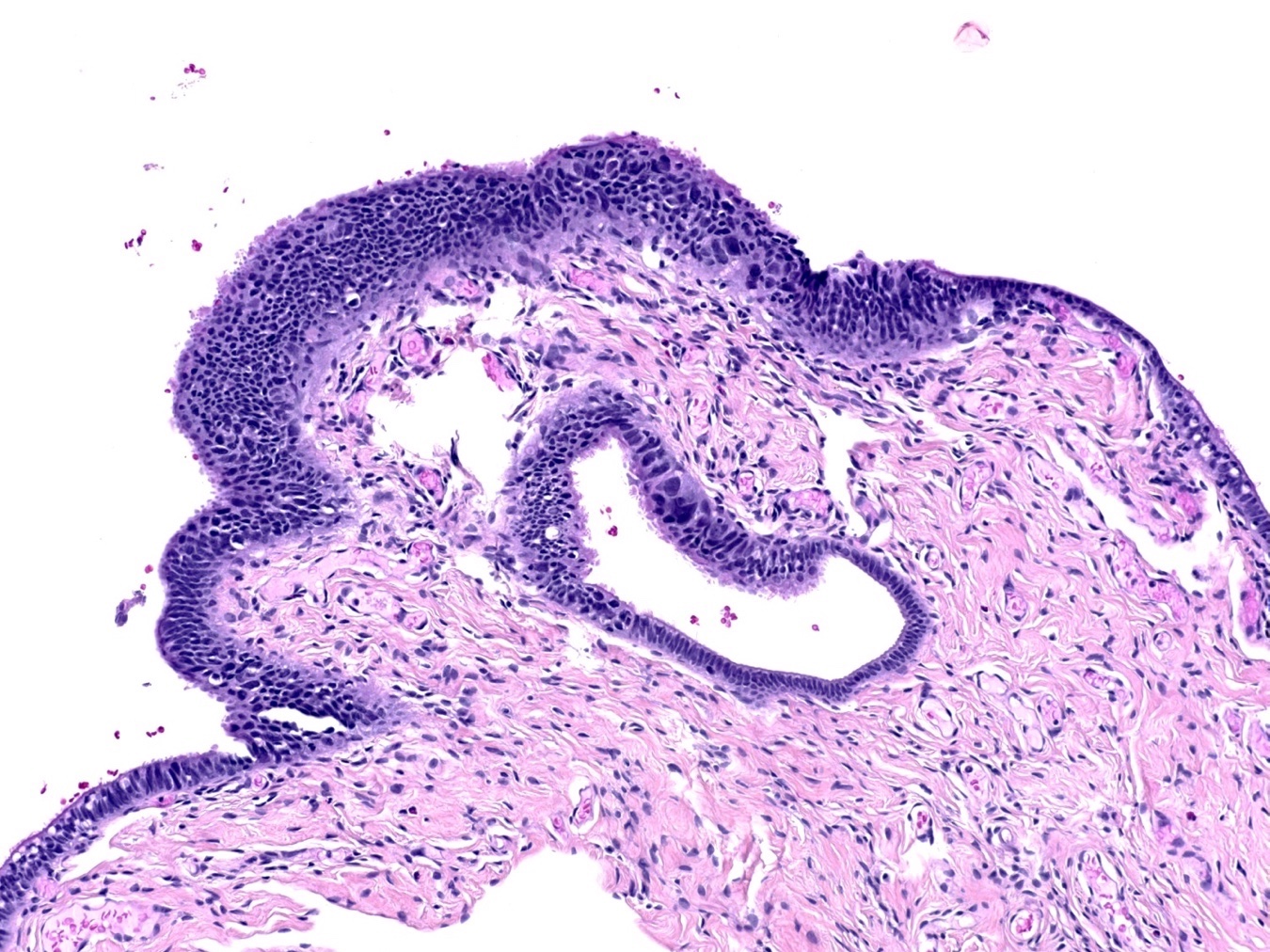
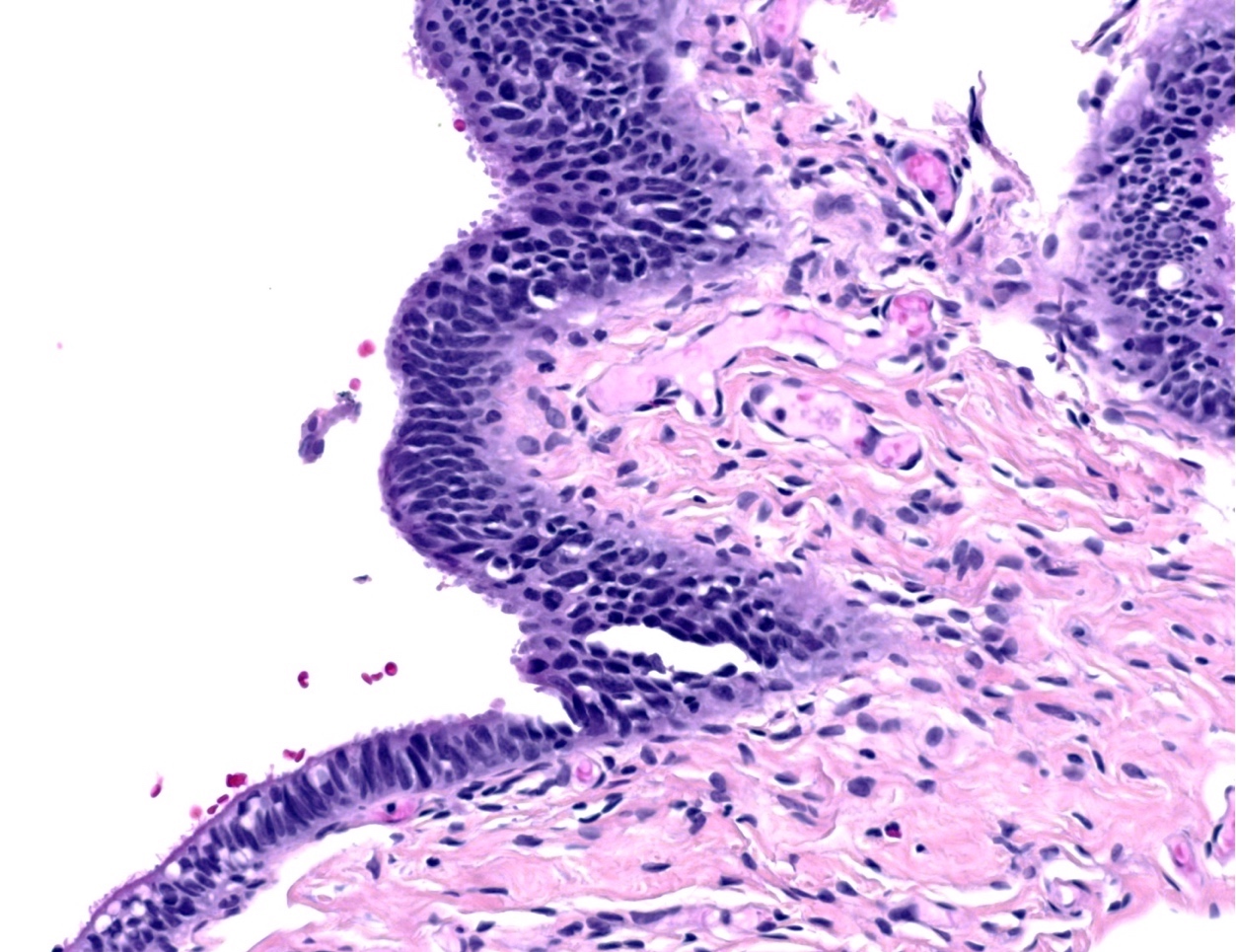
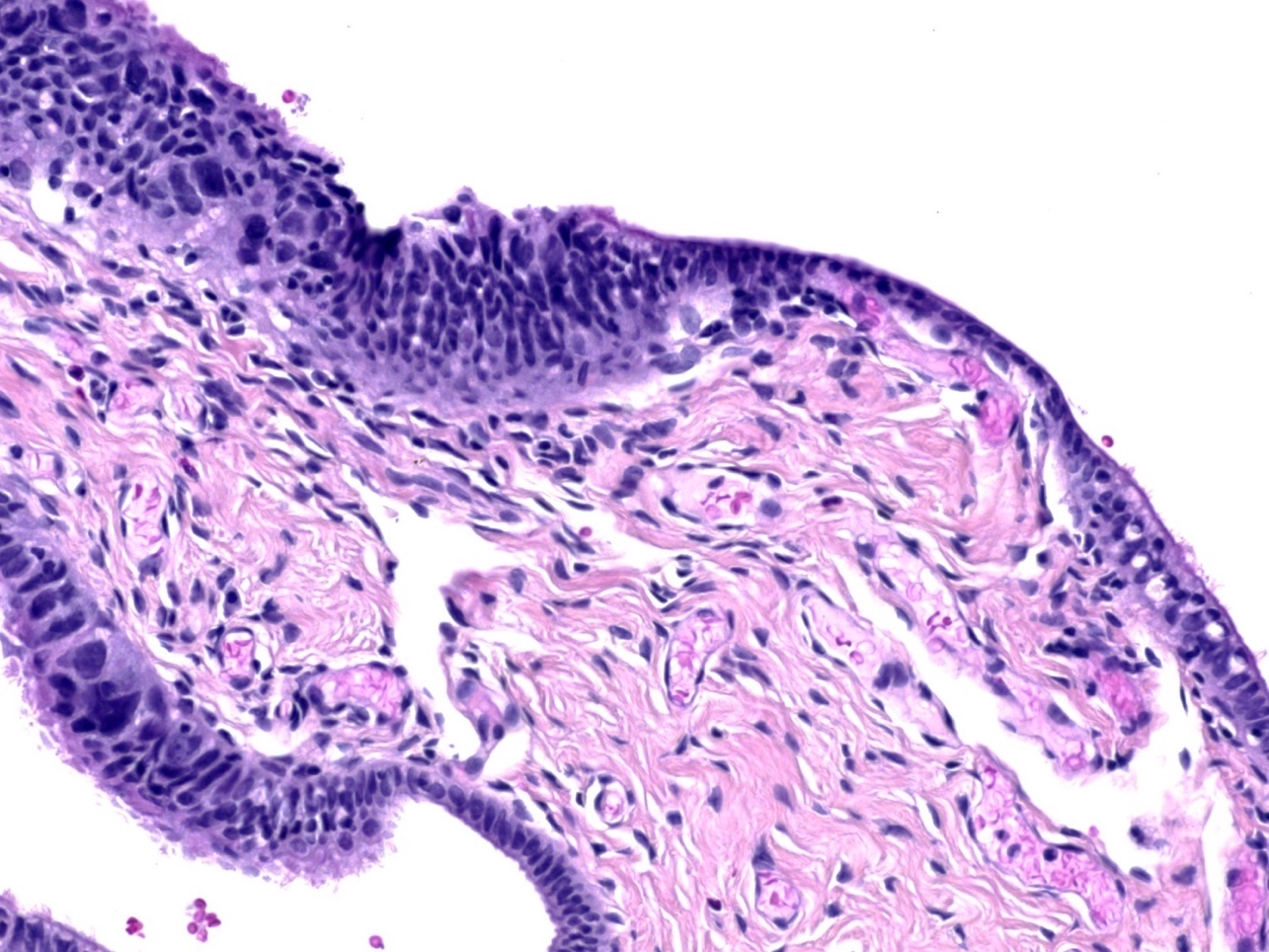
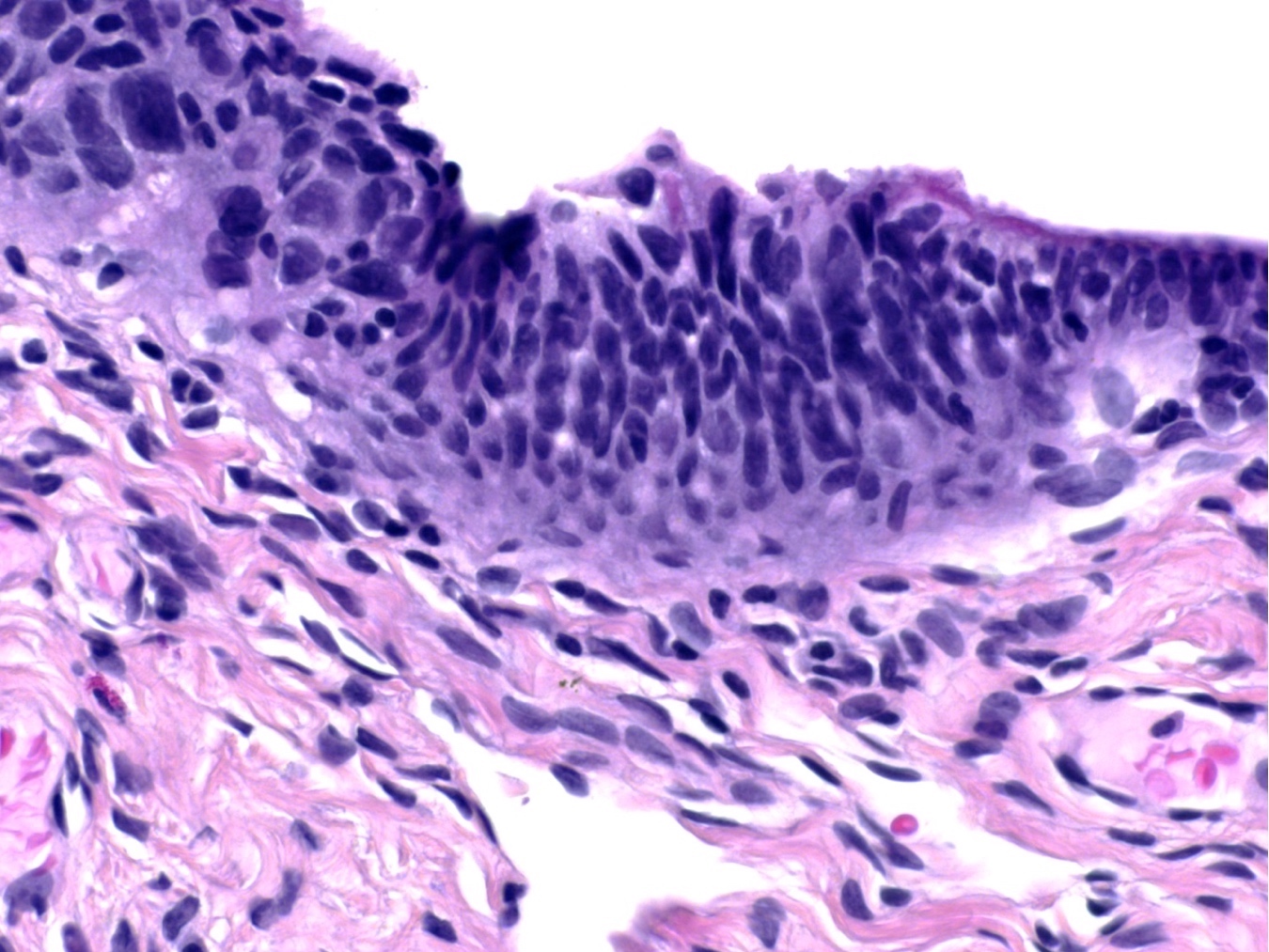
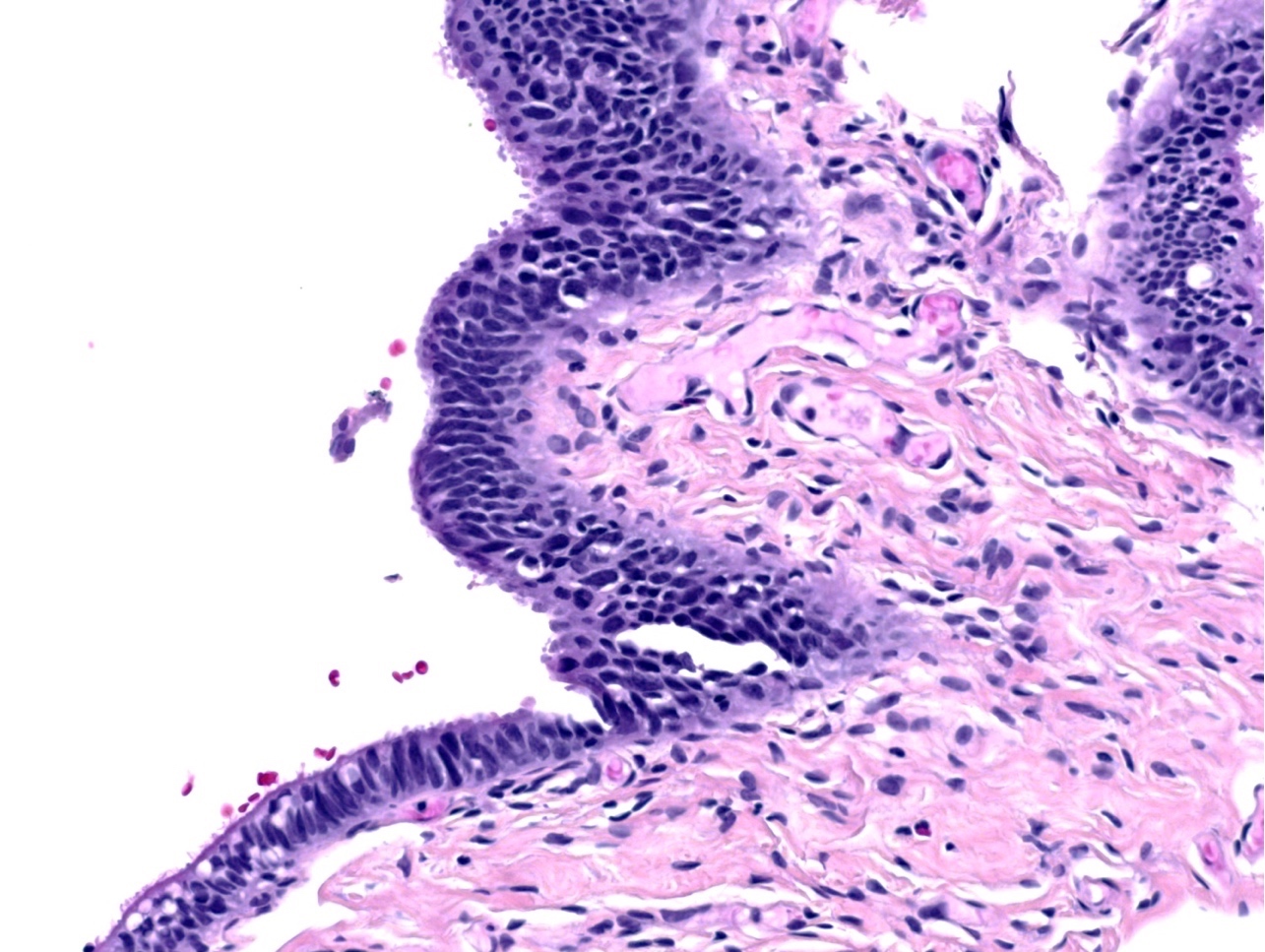
Microscopic (histologic) description
- Epithelial stratification
- Lack of ciliated cells (Mod Pathol 2017;30:710)
- High N/C ratio
- Nuclear pleomorphism, hyperchromasia, prominent nucleoli
- Loss of polarity (may be focal)
- Epithelial fractures (Adv Anat Pathol 2010;17:293)
- Exfoliation of small epithelial clusters
Microscopic (histologic) images
Virtual slides
Cytology description
- Brush cytology shows clusters of cells with haphazard pleomorphic nuclei, high N/C ratio and lack of cilia (Cancer Cytopathol 2019;127:192)
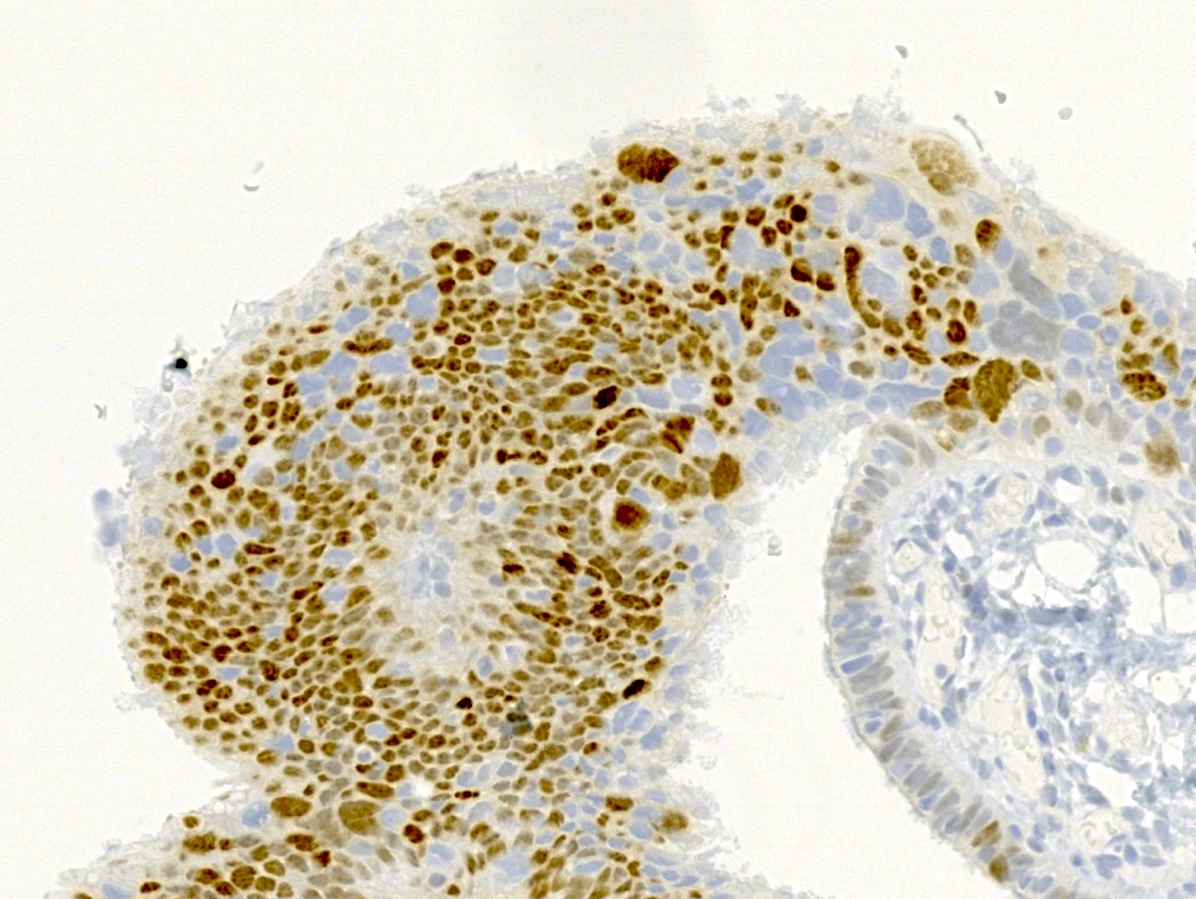
Positive stains
- p53: mutant pattern of staining (diffusely positive (nuclear), completely negative (null type) or less commonly, cytoplasmic staining)
- Ki67 / MIB index: high (suggested cutoff of 10%) (Am J Surg Pathol 2011;35:1766, Int J Gynecol Pathol 2012;31:243)
Sample pathology report
- Bilateral fallopian tubes, salpingectomy:
- Right fallopian tube with serous tubal intraepithelial carcinoma (see comment)
- Left fallopian tube with no pathologic change
- Comment: Immunostain for p53 is diffusely and strongly positive in the lesional cells. Ki67 index is > 10%.
Differential diagnosis
- p53 signature:
- Precursor lesion which shows normal histology with p53 mutant pattern of staining
- Transitional cell metaplasia:
- Uniform cells with nuclear grooves; p53 wild type (Am J Surg Pathol 2009;33:111)
- Florid epithelial hyperplasia and reactive atypia associated with acute salpingitis:
- Has a background of inflammation, retained polarity and presence of ciliated cells; p53 wild type
- Intramucosal fallopian tube metastasis from uterine serous carcinoma:
- May closely mimic STIC; usually WT1 negative (Am J Surg Pathol 2017;41:161)
Additional references
- Front Biosci (Elite Ed) 2011;3:625, Int J Gynecol Pathol 2010;29:310, Mod Pathol 2009;22:985, Curr Opin Obstet Gynecol 2007;19:3, Adv Anat Pathol 2006;13:1, CAP: Protocol for the Examination of Specimens from Patients with Primary Tumors of the Ovary, Fallopian Tube or Peritoneum [Accessed 5 January 2022]
Board review style question #1
Which fallopian tube lesion appears normal on histology but shows a mutant pattern of p53 immunostaining?
- p53 signature
- Reactive atypia
- Secretory cell outgrowth (SCOUT)
- Serous tubal intraepithelial carcinoma (STIC)
Board review style answer #1
Board review style question #2
The grossing protocol for examination of the fallopian tube to identify the diagnosis in the photomicrograph should
- Ensure complete evaluation of the fallopian tube in all cases
- Increase detection of precursor lesions in at risk women
- Require multistep levels in at risk women
- Require tangential sectioning of the infundibulum and fimbrial segment to allow maximal exposure
Board review style answer #2
B. Increase detection of precursor lesions in at risk women. Serous tubal intraepithelial carcinoma is shown in the photomicrograph.
Comment Here
Reference: Serous tubal intraepithelial carcinoma
Comment Here
Reference: Serous tubal intraepithelial carcinoma