Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Daniels E, Assarzadegan N. Traumatic neuroma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/gallbladdertraumaticneuroma.html. Accessed April 19th, 2024.
Definition / general
- Nonneoplastic, disorganized proliferation of normal nerve components at the site of previously damaged peripheral nerves
Essential features
- Commonly seen after gallbladder surgery (i.e., cholecystectomy)
- Usually asymptomatic but can present with obstructive jaundice and a solitary mass, mimicking malignancy
- Appears as firm, gray-white mass or multiple nodules at the nerve stump
- Histologically, appears as haphazard proliferation of normal nerve components
Terminology
- Amputation neuroma
ICD coding
Epidemiology
- Patients who have had prior gallbladder or biliary surgery
- No predilection for gender or age
- Found incidentally in up to 10% of autopsies with prior cholecystectomy (Am Surg 1999;65:47)
Sites
- Gallbladder
- Extrahepatic bile ducts
- Commonly seen in cystic duct stump
Pathophysiology
- Gallbladder or bile duct nerve fibers become damaged after procedures, inflammatory processes or trauma
- Proximal and distal stumps of nerves are not reapproximated or a distal nerve stump is not present (Goldblum: Enzinger and Weiss's Soft Tissue Tumors, 7th Edition, 2020)
- Proximal nerve stump attempts to regenerate resulting in disorganized proliferation of normal nerve components, including nerve fibers, Schwann cells and perineural cells arranged in fascicles
Etiology
- Presents after surgery or procedure (i.e., laparoscopic or open cholecystectomy, biliary surgery for cholangiocarcinoma, liver transplantation, gallbladder biopsy)
- Can arise without prior surgery (e.g., inflammation) (Acta Med Okayama 1996;50:273)
Clinical features
- Most are asymptomatic without any specific physical examination findings
- Can present with right upper quadrant pain, obstructive jaundice, ascending biliary cholangitis (upper abdominal pain, fever, jaundice) and mass (Ann Hepatobiliary Pancreat Surg 2019;23:282)
- Symptoms can present decades after the initial injury
Diagnosis
- Abdominal ultrasound (Abdom Imaging 2008;33:560)
- CT
- MRI
- Magnetic resonance cholangiopancreatography (MRCP)
- Endoscopic retrograde cholangiopancreatography (ERCP) / endoscopic ultrasound
Laboratory
- Normal liver transaminases, bilirubin and tumor markers
- If causing obstructive jaundice, may have elevated bilirubin
- Can have elevated CA19-9, raising concern for biliary malignancy (South Med J 2003;96:89)
- Leukocytosis, elevated bilirubin if associated with ascending cholangitis (Ann Hepatobiliary Pancreat Surg 2019;23:282)
Radiology description
- Abdominal ultrasound: mildly echogenic mass (Abdom Imaging 2008;33:560)
- Contrast enhanced CT: enhancing mass near bile ducts, can increase in size compared to prior exams
- T2 weighted MRI: high intensity nodule with low intensity capsule, dilatation of bile ducts
- T1 weighted MRI: homogenously enhanced nodule isointense to aorta
- Solitary mass or multiple nodules if nerve plexus is affected
- May see biliary structure with proximal dilatation of ducts
- Radiographically similar to cholangiocarcinoma, periampullary tumors, metastatic lymph nodes if at level of hilum (Int J Surg Case Rep 2017;39:123)
Radiology images
Prognostic factors
- Favorable prognosis
- Symptoms usually resolve after surgical resection
Case reports
- 41 year old man with acute cholangitis 10 years after open cholecystectomy (Ann Hepatobiliary Pancreat Surg 2019;23:282)
- 69 year old woman with hilar traumatic neuroma masquerading as Klatskin tumor (Trop Gastroenterol 2015;36:54)
- 72 year old man with traumatic neuroma of cystic duct mimicking duodenal subepithelial tumor (World J Clin Cases 2020;8:3821)
- 76 year old man with obstructive jaundice 1 year after cholecystectomy (Clin Case Rep 2021;9:e04619)
Treatment
- Surgical resection is curative
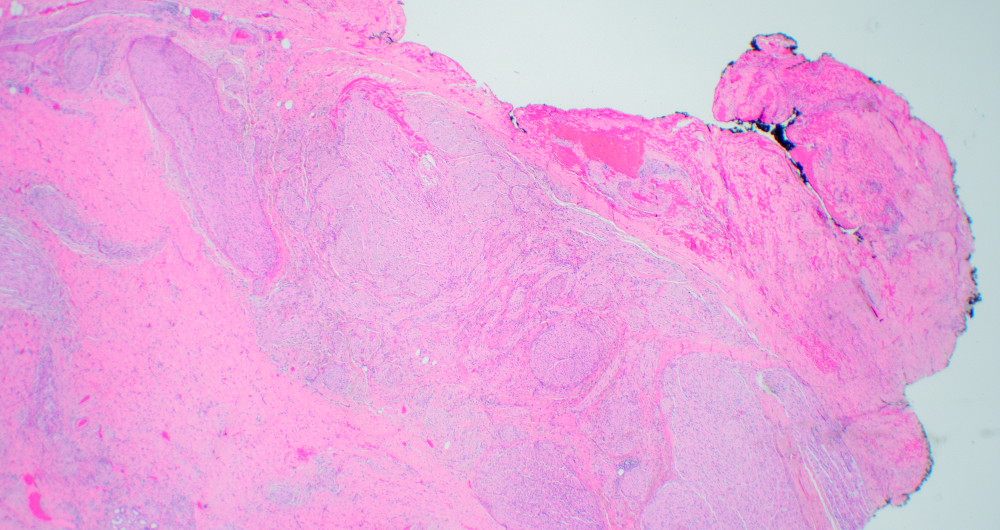
Gross description
- Circumscribed, firm gray-white rubbery mass (Goldblum: Enzinger and Weiss's Soft Tissue Tumors, 7th Edition, 2020)
- Solitary mass or multiple nodules if nerve plexus is affected
- < 5 cm in diameter
- Located at end of proximal nerve
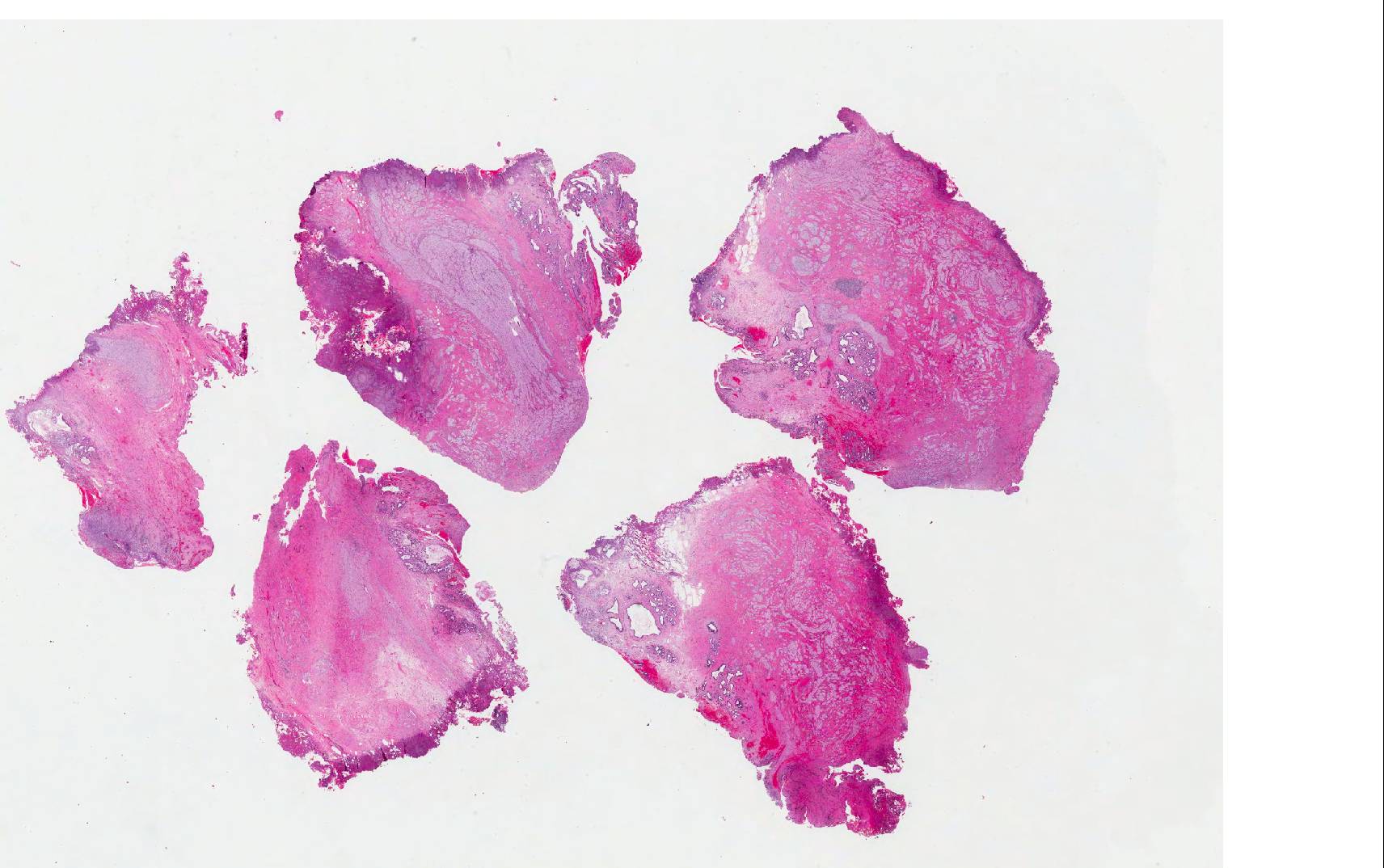
Gross images
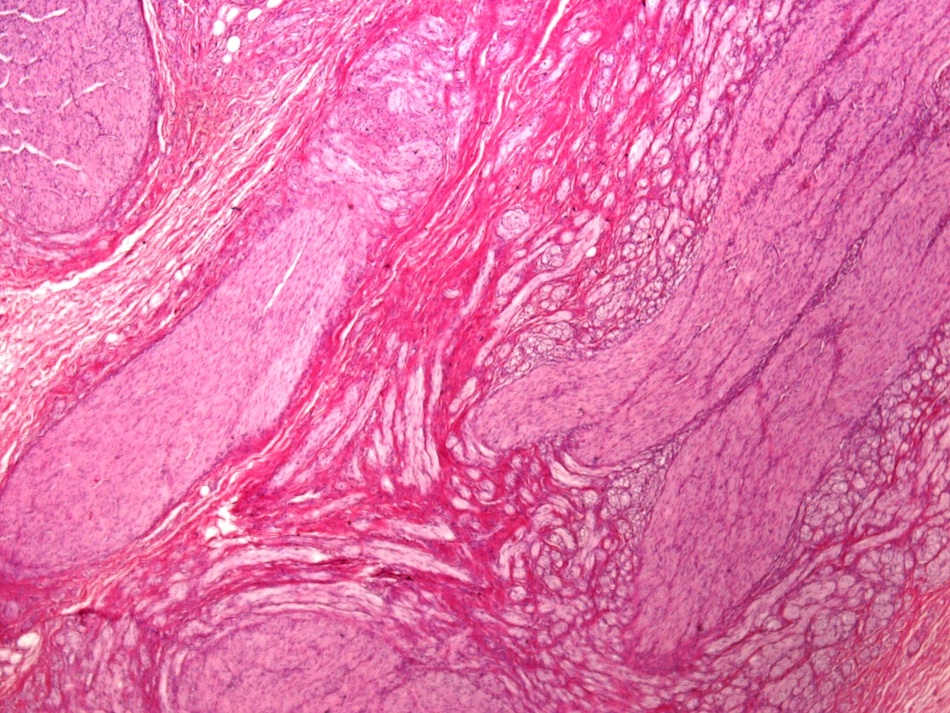
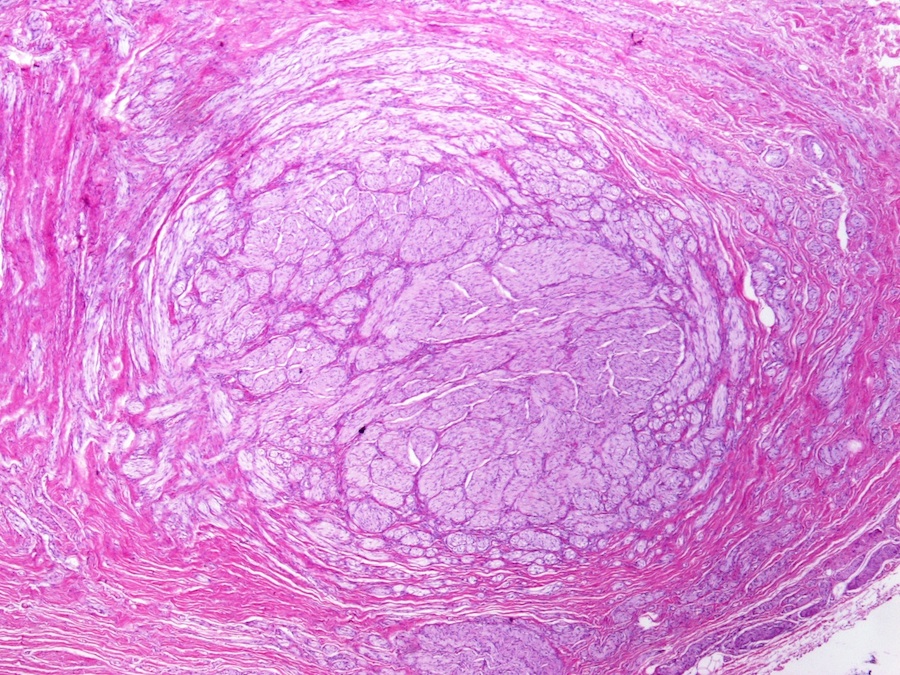
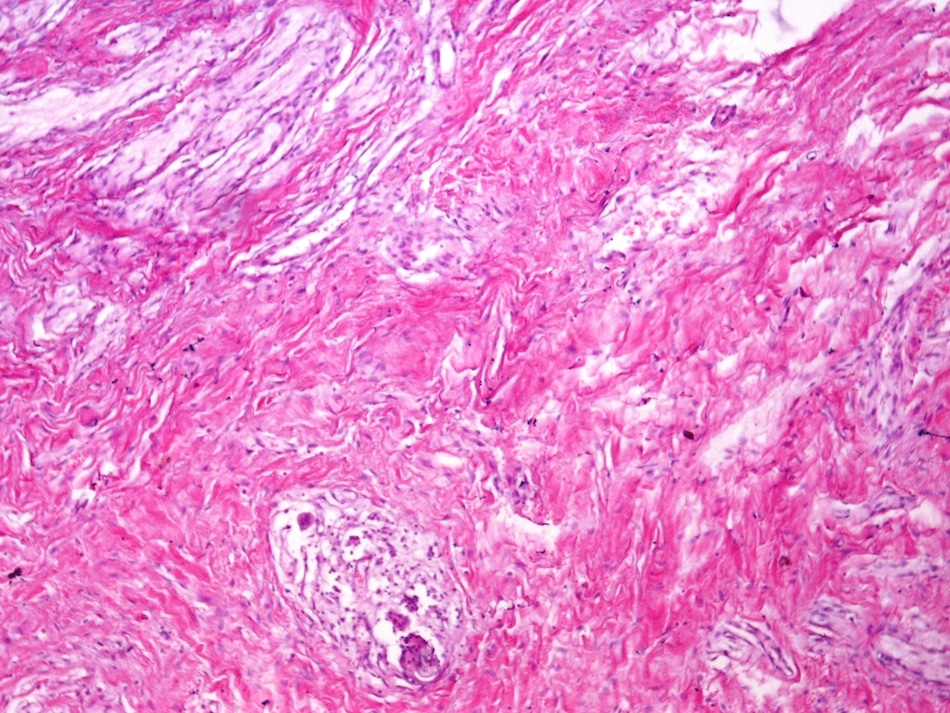
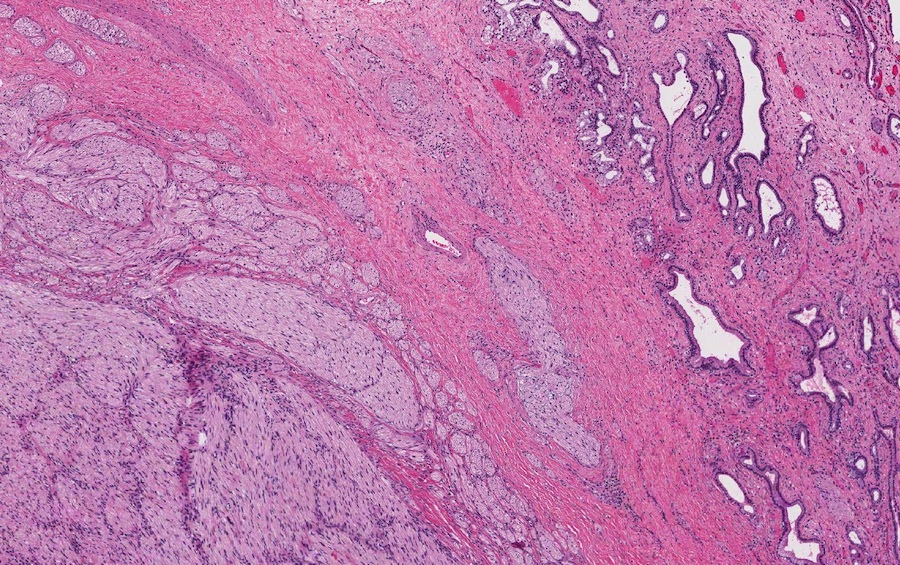
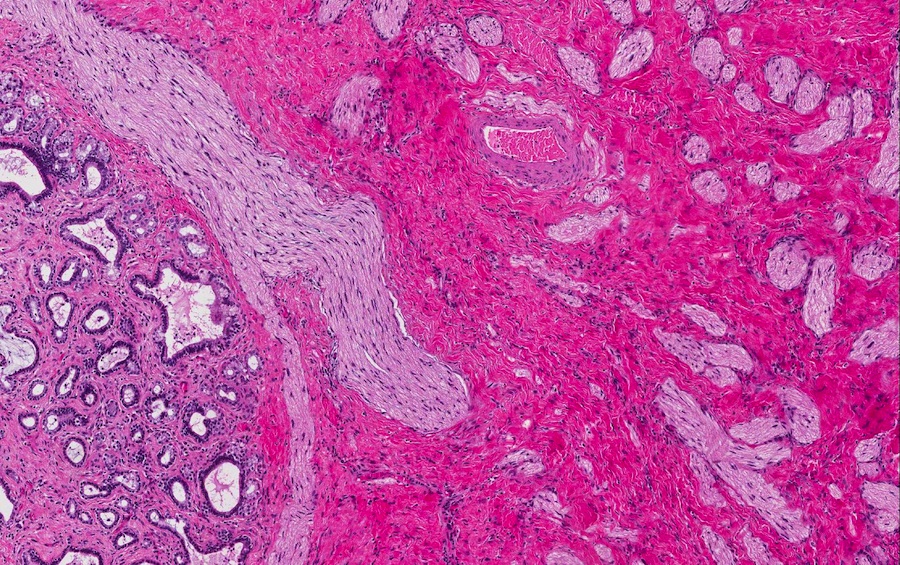
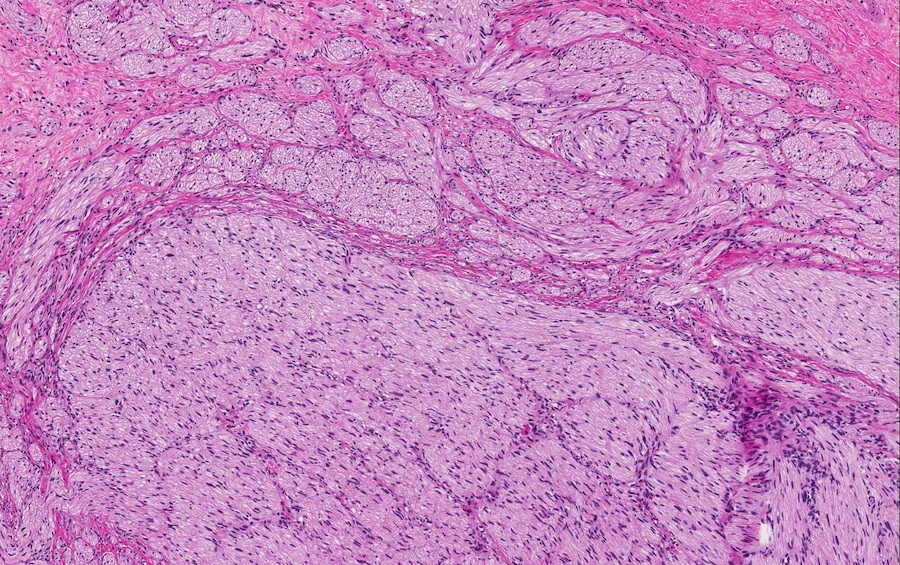
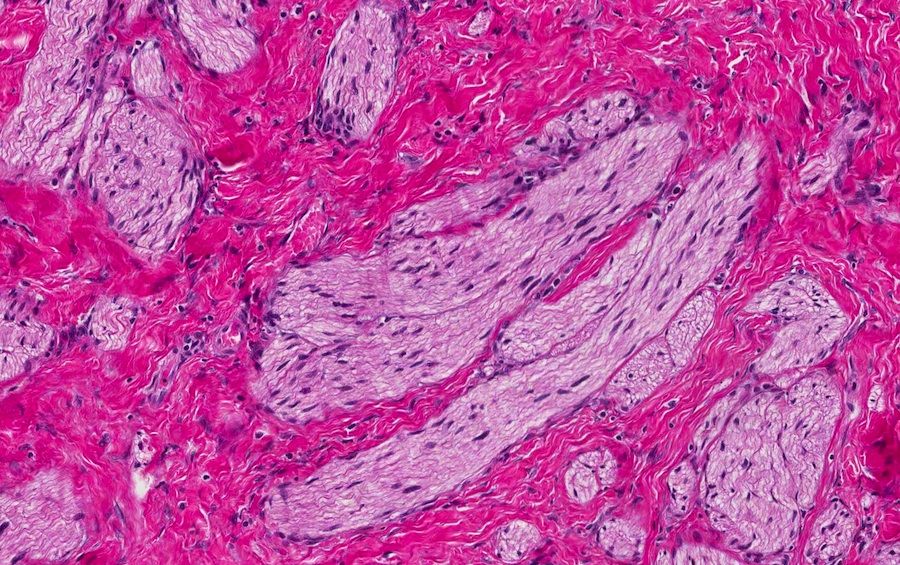
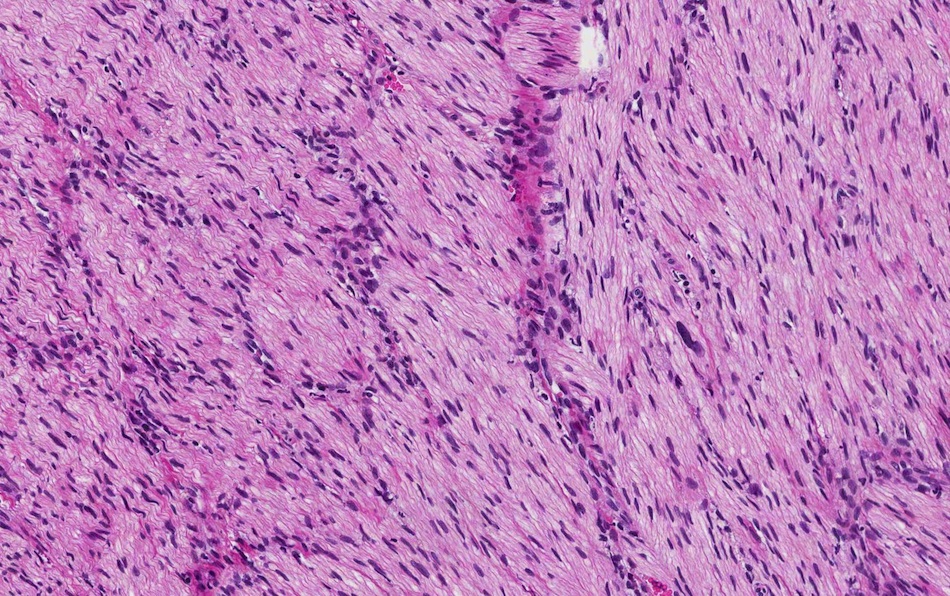
Microscopic (histologic) description
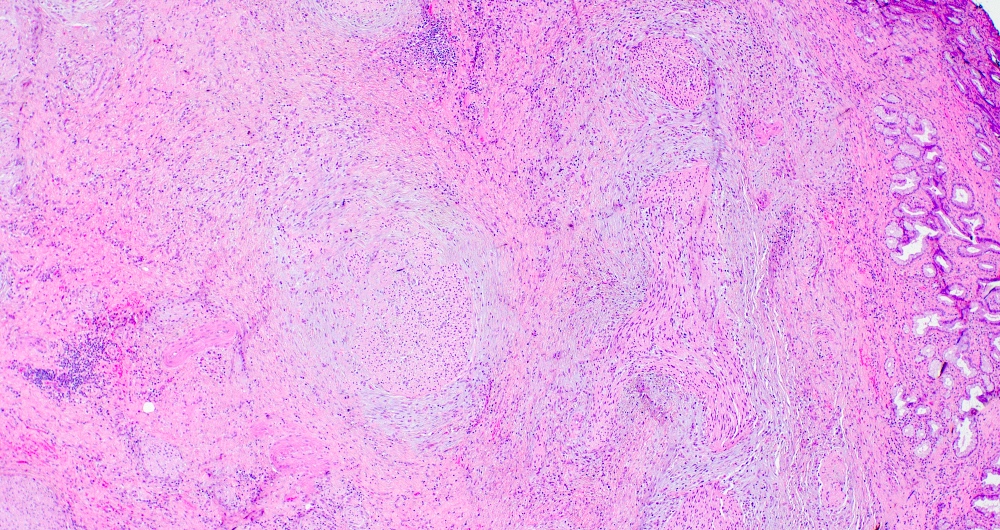
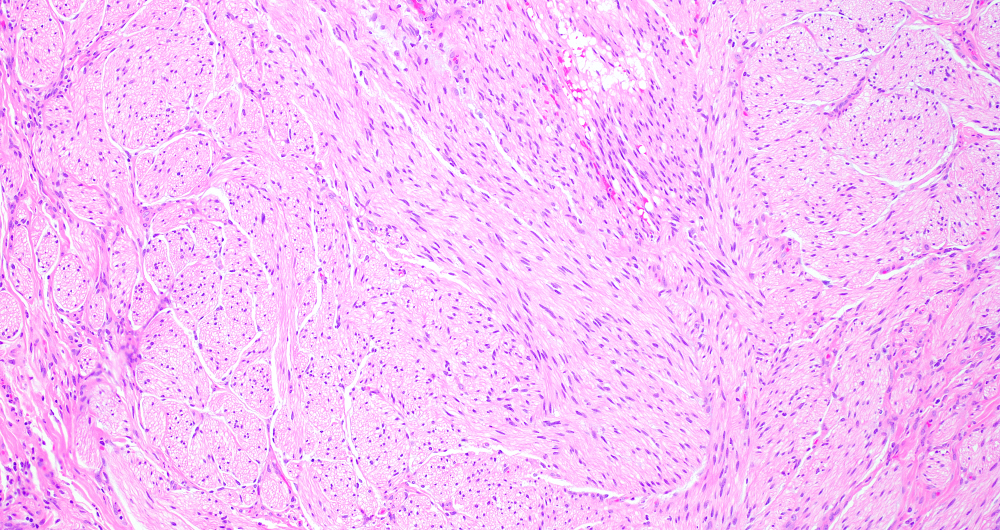
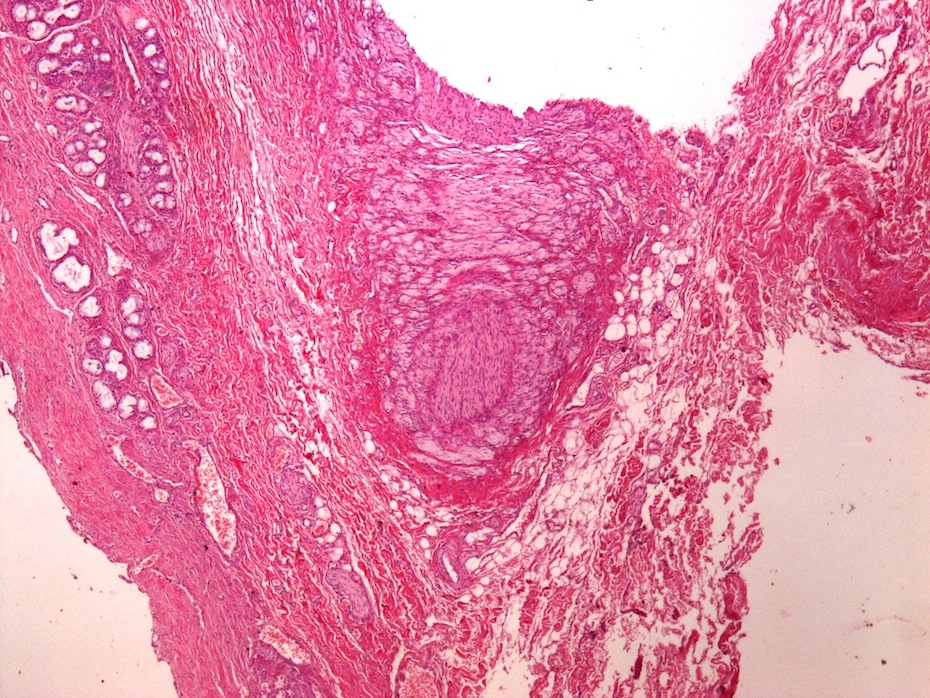
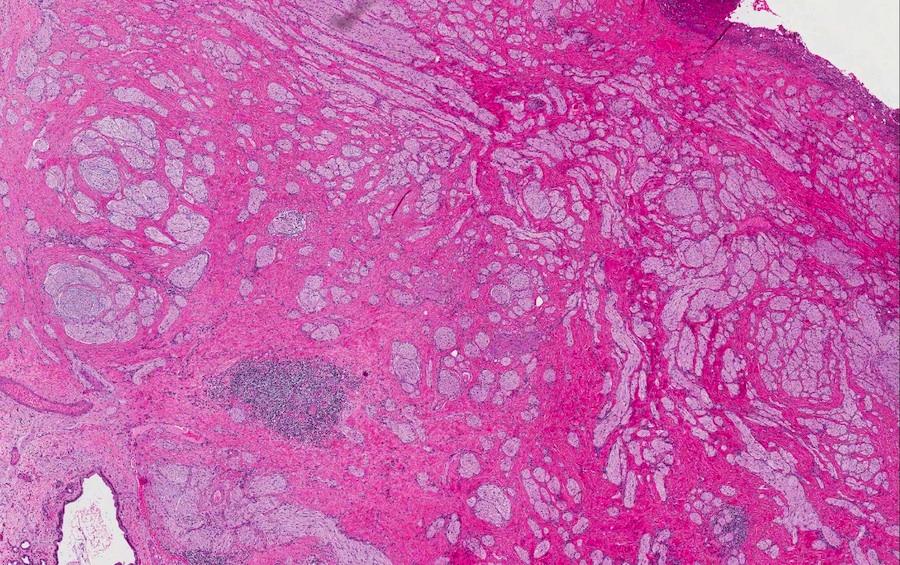
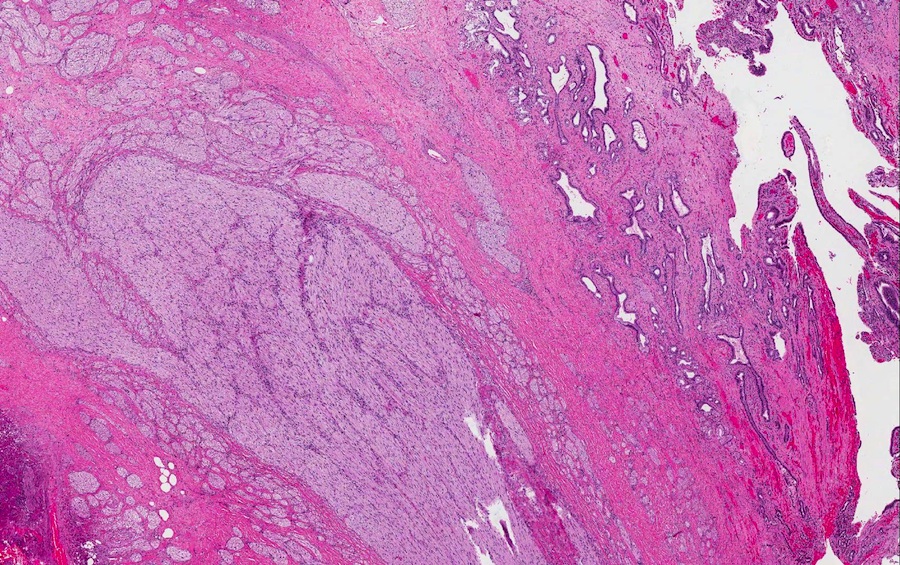
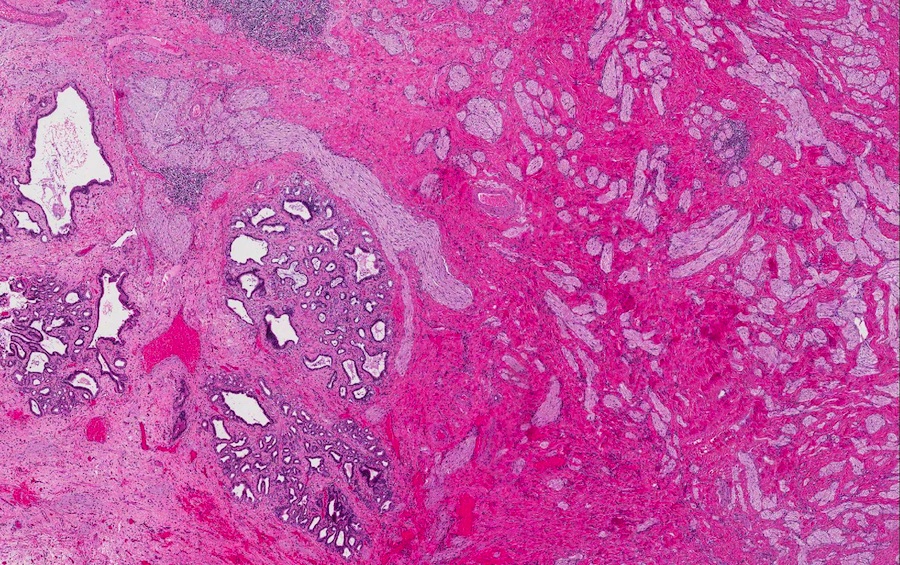
- Disordered proliferation of nerve fascicles composed of axons, surrounded by Schwann cells and perineural cells within collagenous stroma (Goldblum: Enzinger and Weiss's Soft Tissue Tumors, 7th Edition, 2020)
- Fascicles are less myelinated than normal nerve
- Collagenous stroma may demonstrate inflammatory or myxoid change if subjected to repeat trauma or infection
- Perineural fibrosis
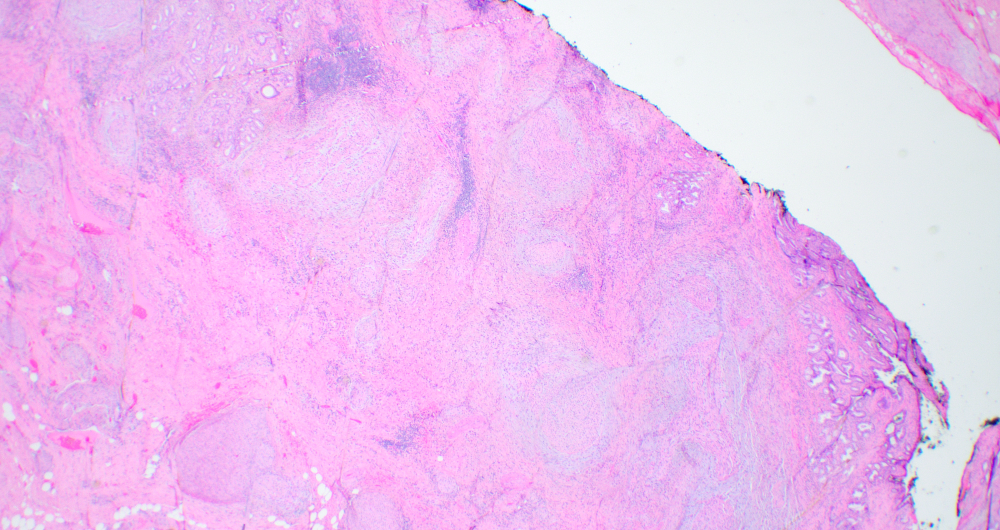
Microscopic (histologic) images
Contributed by Naziheh Assarzadegan, M.D., Saba Hassan, M.B.B.S. and Kristin Olson, M.D. (Case #329)
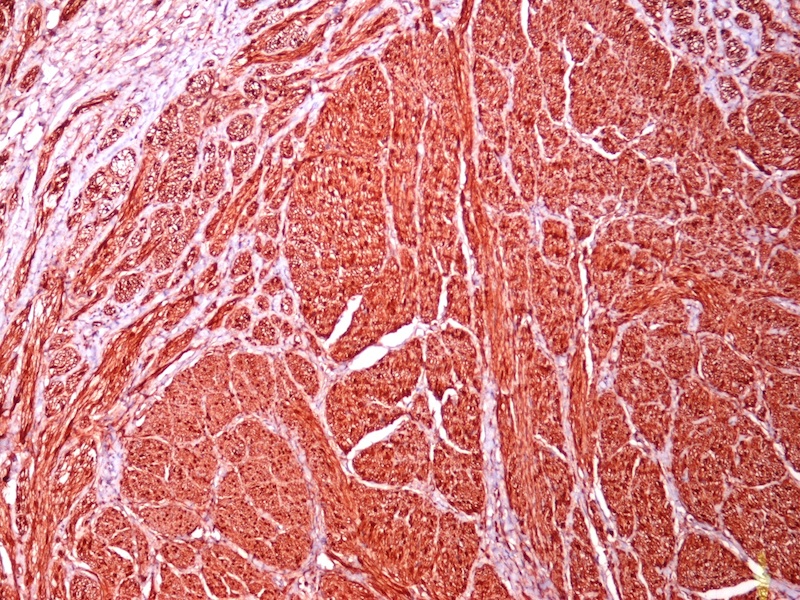
Positive stains
- EMA and GLUT1: perineural cells (Mod Pathol 2003;16:293)
- CD34: endoneurium
- S100: stains surrounding Schwann cells
Sample pathology report
- Bile duct, excision:
- Portion of bile duct with benign traumatic neuroma; no malignancy seen (see comment)
- Comment: The patient's history of obstructive jaundice, biliary stricture, perihilar mass and previous cholecystectomy is noted. Histological examination reveals a benign haphazard proliferation of nerve fascicles in the fibromuscular layer of the bile duct, features consistent with a postcholecystectomy traumatic neuroma. The lesion focally displays areas of nuclear palisading and we considered the possibility of a benign nerve sheath tumor such as plexiform schwannoma. However, the lesion lacks encapsulation and has interspersed, normal appearing nerves. Immunostains show that the lesional cells are immunoreactive with S100 protein and SOX10. Ki67 proliferation index is not increased. EMA highlights the perineurium. CD34 highlights the myofibroblasts. Traumatic neuromas are a rare, nonneoplastic cause of long distance bile duct stenosis and progressive jaundice; in particular, in patients with a history of cholecystectomy or surgical history in this abdominal region.
- References: Hepatogastroenterology 2004;51:39, Visc Med 2021;37:226
Differential diagnosis
- Cholangiocarcinoma:
- Both can present with biliary stricture and obstructive jaundice
- Composed of malignant glands, not normal components of peripheral nerve
- Schwannoma (Stanford University: Traumatic Neuroma [Accessed 5 May 2022]):
- No prior trauma or surgery
- Encapsulated
- Proliferation of Schwann cells and axons
- Rare axons, which are subcapsular
- Antoni A and Antoni B areas
- Verocay bodies
- Neurofibroma:
- No prior trauma or surgery
- Infiltrates into soft tissue
- Proliferation of Schwann cells and axons
- Rare axons
Additional references
Board review style question #1
Board review style answer #1
D. Traumatic neuroma. The lesion is composed of disorganized proliferation of nerve fascicles in a collagenous stroma and in the clinical context of cholecystectomy is in keeping with traumatic neuroma.
Comment Here
Reference: Traumatic neuroma
Comment Here
Reference: Traumatic neuroma
Board review style question #2
A patient with a history of cholecystectomy presents with a mass near the cystic duct stump. Histologic examination is consistent with a traumatic neuroma. Which of the following best describes the gross and microscopic findings in traumatic neuroma?
- Large, heterogeneous mass with fascicles of uniform spindle cells with frequent mitoses and areas of coagulative necrosis in vascularized, myxoid to collagenous stroma
- Well circumscribed, encapsulated, tan-gray mass with spindle cells arranged in biphasic hypercellular and hypocellular areas with diffuse staining of S100 and SOX10
- Well circumscribed, gray-white mass with haphazard proliferation of benign nerve fascicles
- Well circumscribed, nonencapsulated, tan-gray mass with haphazard spindle cells, mast cells, rare axons in shredded carrot collagenous stroma with hypocellular and myxoid areas
Board review style answer #2
C. Well circumscribed, gray-white mass with haphazard proliferation of benign nerve fascicles. Traumatic neuromas are benign lesions with haphazard proliferation of benign nerve fascicles. They usually occur after damage to peripheral nerves from surgery, trauma or inflammation. Choice A describes findings in malignant peripheral nerve sheath tumors. Choice B describes the findings in schwannoma. Choice D describes findings in neurofibromas.
Comment Here
Reference: Traumatic neuroma
Comment Here
Reference: Traumatic neuroma