Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Immunofluorescence description | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Suleman S, Qureshi MB, Ud Din N. Gout and gouty arthritis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/jointsgout.html. Accessed April 23rd, 2024.
Definition / general
- Gout is a metabolic disorder that affects joints, bones, skin and soft tissues
- Associated with hyperuricemia, which causes saturation of monosodium urate and eventual formation of crystals within tissue (Nat Rev Rheumatol 2020;16:380)
Essential features
- Gout is the most common inflammatory arthritis
- Monosodium urate crystals induce an acute neutrophil mediated inflammatory reaction in joint fluid, and a macrophage and giant cell reaction in other tissues
- Crystal induced inflammation leads to acute, severe, self limiting joint pain
- Can present as acute or chronic arthritis or tophaceous gout
- Recurrent arthropathy becomes destructive
- Risk of gout increases with age, obesity, hypertension and diuretic use (Arthritis Res Ther 2018;20:136)
Terminology
- Acute gout
- Gout attack
- Gout flare
- Podagra
- Chronic gout with tophi
- Chronic tophaceous gout
ICD coding
Epidemiology
- Variable incidence and prevalence between countries (Arthritis Rheumatol 2020;72:1916, Semin Arthritis Rheum 2021;51:121, GSC Biological and Pharmaceutical Sciences 2018;5:50)
- More common in men than women (4:1) (Nat Rev Rheumatol 2020;16:380)
- Women are usually affected after menopause
- Estradiol exhibits inhibitory action on urate crystal synthesis, making young women less susceptible
- Positive association with certain gene loci, conditions and comorbidities, including cardiovascular diseases like myocardial infarction, stroke and hypertension, chronic kidney disease, obesity, hypertriglyceridemia, depression, diabetes, etc. (Ann Rheum Dis 2019;78:1430, Int J Geriatr Psychiatry 2018;33:441, BMC Med 2017;15:123)
Sites
- Involves lower extremities: first metatarsophalangeal joint (most common), midfoot, ankle and knee (Best Pract Res Clin Rheumatol 2010;24:811)
- Late involvement of other joints including joints of upper extremities
- Axial joint involvement is less common
- Most common sites of deposition include periarticular soft tissue with involvement of bursae, tendons and ligaments
- Tophi commonly involve olecranon bursa and Achilles tendon
- Can affect other organs and viscera (BMC Musculoskelet Disord 2019;20:140)
- Skin ulceration can be present
Pathophysiology
- Core mechanism for pathogenesis of gout is an augmented serum level of uric acid following a reduced renal excretion (Int J Cardiol 2016;213:8)
- Uric acid is the end product of exogenous and endogenous purine
- Exogenous pool depends upon dietary intake, increased by foods like animal proteins
- Endogenous production of uric acid is mainly from the liver, intestines and other tissues, like muscles, kidneys and the vascular endothelium (Cardiorenal Med 2013;3:208)
- At physiologic pH, uric acid is a weak acid and exists mainly as urate, the salt of uric acid
- As urate concentration increases in blood, uric acid crystal formation increases
- When the level of uric acid becomes higher than 6.8 mg/dL, crystals of uric acid form as monosodium urate (MSU) (J Cardiol 2021;78:51)
- MSU crystals are needle shaped crystals, targeted for consumption by neutrophils and monocytes
- Inflammatory response is initiated via the release of interleukin 1 (IL1) and other cytokines, resulting in acute gout attack (RMD Open 2015;1:e000046)
- Neutrophils with the ingested crystals grow closer and form a tight packing
- This proceeds to cell death, presenting as tophaceous gout
- High sodium content of the crystals increases intracellular sodium concentrations
- To maintain iso-osmolarity, water enters the cell through aquaporins and induces cell swelling
- Water also dilutes potassium, which falls below a critical level for the induction of the inflammasome
- Activation of the inflammasome produces large amounts of interleukin 1β, resulting in chronic form
Etiology
- Gout is caused by hyperuricemia
- 10% of individuals with hyperuricemia develop gout
- High intake of protein and alcohol increase risk of development
- Hyperuricemia can be primary (90%), familial or sporadic, or secondary (10%)
- 90% cases of primary hyperuricemia are sporadic: caused by reduced renal excretion of uric acid
- Urate transporter dysfunctions cause urate transport disorders and hyperuricemia (Int J Mol Sci 2021;22:9221, Tohoku J Exp Med 2020;251:87)
- Dysfunction of ABCG2 exporter causes hyperuricemia due to both renal urate underexcretion and renal urate overload (Sci Rep 2014;4:3755)
- 10% of cases are familial: caused by inherited gene mutations like Lesch-Nyhan syndrome (J Cardiol 2021;78:51)
- Secondary causes include pre-existing acquired or genetic disease
- Hyperuricemia occurs due to increase in purine metabolism because of rapid cell turn over in diseases like psoriasis, myeloproliferative disorders and conditions like fasting, chemotherapy (Ann Rheum Dis 2015;74:1495, Clin Rheumatol 2001;20:288)
- Hyperuricemia may also occur due to decreased secretion of uric acid, as in renal failure
- Rare genetic disorders also cause high cell turn over and hyperuricemia, like certain glycogen storage diseases (Adv Skin Wound Care 2021;34:1)
Diagrams / tables
Clinical features
- Presents in 3 ways: acute gout, tophaceous gout and chronic arthropathy
- Acute gout:
- Intermittent: presents with swelling, intense pain and soreness around joints
- Asymptomatic period may occur between gout attacks (intercritical gout)
- Acute flares are characterized by warmth, swelling, redness and severe pain
- Pain tends to begin in the middle of the night or early morning
- Fever and constitutional features such as malaise due to release of cytokines (Nature 2006;440:237)
- Tophaceous gout:
- Untreated cases result in soft tissue deposits, called tophi
- Occurs almost 10 - 15 years after initial acute episode
- Chronic arthropathy:
- Recurrent gouty episodes result in chronic inflammatory arthropathy
- Can cause secondary osteoarthritis
- Phases of gout (progression):
- Stage 1: asymptomatic hyperuricemia
- Urate deposits directly contribute to organ damage
- Does not occur in everyone
- No evidence that treatment is warranted
- Stages 2 and 3: acute gout and intercritical periods
- Sufficient urate deposits develop around joints
- Release of crystals is triggered into joint space by trauma, causing acute attack
- During intercritical periods, crystals may be present at low level in the fluid
- Crystals are also present in the periarticular and synovial tissue, providing a nidus for future attacks
- Stage 4: advanced gout
- Crystal deposits continue to accumulate
- Patients develop chronically stiff and swollen joints
- Uncommon stage, avoidable with therapy (Cleve Clin J Med 2008;75:S5)
- Stage 1: asymptomatic hyperuricemia
Diagnosis
- Presence of MSU crystals in the joint fluid or tophus is the gold standard for the diagnosis of gout (Minerva Med 2007;98:759)
- Clinical, radiological and laboratory findings are helpful (Ann Intern Med 2017;166:27)
Laboratory
- Blood tests: leukocytosis with neutrophilia, raised erythrocyte sedimentation rate (ESR), C reactive protein (CRP) and cytokines (Immunol Invest 2016;45:383)
- Synovial fluid or bursal fluid analysis: tests include differential white cell count, examination of crystals under polarizing light microscopy
Radiology description
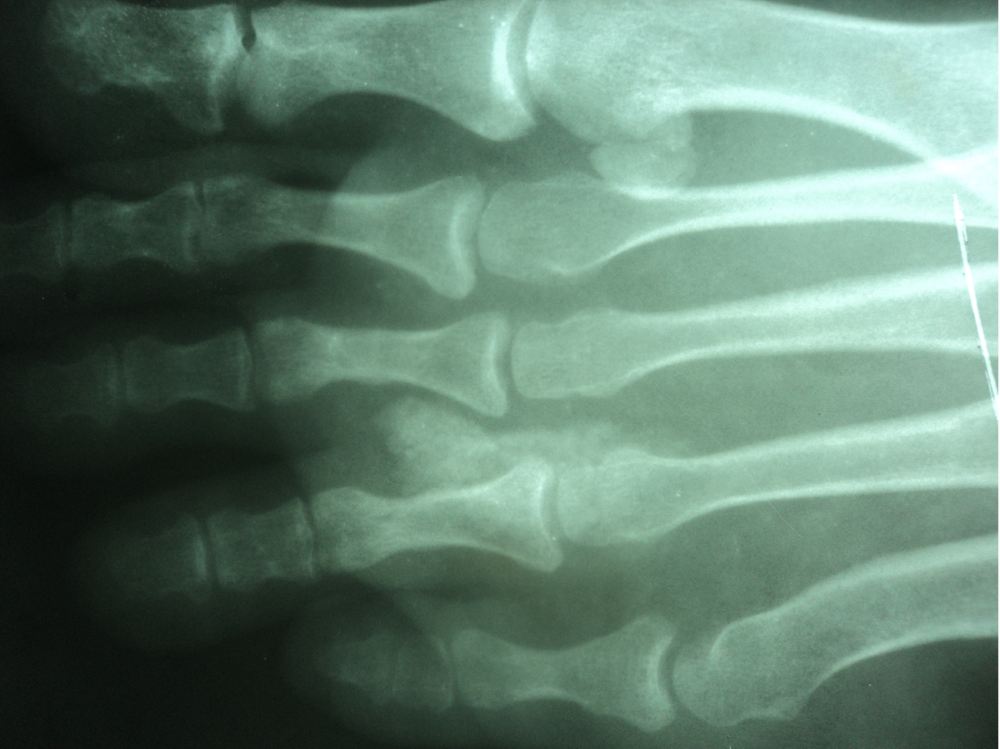
- Plain radiography:
- Joint effusion (earliest sign)
- Subcortical bone cysts, chondrocalcinosis (5%)
- Specific delicate bone erosions due to tophi occur with chronicity
- Punched out erosions with sclerotic margins (rat bite erosions)
- Punched out lytic lesions in bone
- Osteonecrosis
- Olecranon and prepatellar bursitis
- Hyperdense periarticular soft tissue swelling (Eur Radiol 2008;18:621)
- Ultrasonography:
- Hyperechoic linear density (double contour sign) overlying the surface of joint cartilage
- Tophaceous appearing deposits in joints or tendons, represented by an ovoid stippled signal (hyperechoic cloudy area) (Rheum Dis Clin North Am 2014;40:231, Ann Rheum Dis 2015;74:1868)
- Synovial thickening with irregular bands opposed to articular cartilage
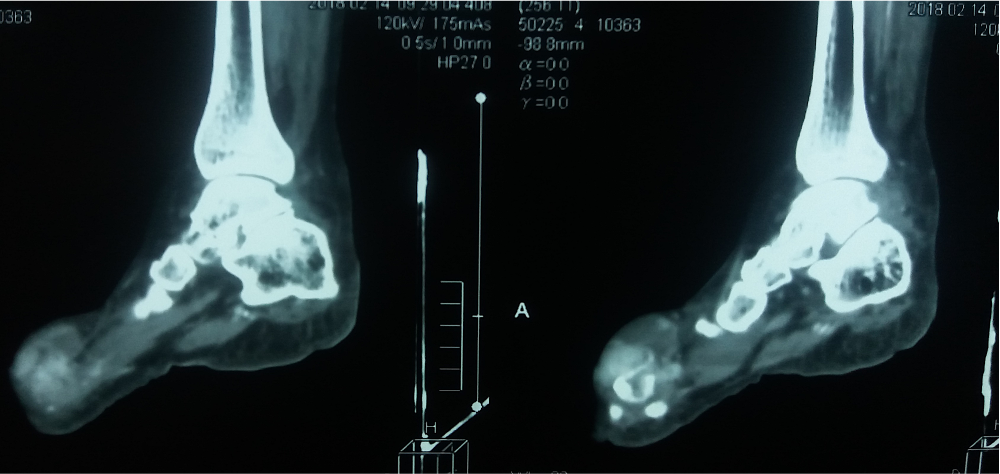
- Computed tomography (CT): same as plain radiographic findings
- Dual energy computed tomography (DECT):
- Tissue characterization and detection of urate is based on different attenuation of Xrays of variable energy in different tissues
- Only imaging technique that visualizes urate crystal depositions by their chemical composition
- Able to detect presence of dense urate crystal deposits even in small volumes
- Color coded images help in the clinical management of gout patients (Semin Arthritis Rheum 2014;43:662, Skeletal Radiol 2014;43:277)
- Magnetic resonance imaging (MRI):
- Tophi are isointense on T1
- Characteristically heterogeneously hypointense on T2
Prognostic factors
- Maori and Pacific ethnicity is recognized as a prognostic factor for more severe outcomes in gout (Clin Rheumatol 2013;32:247)
- Optimal medical control of gout and its comorbidities may improve prognosis (J Rheumatol 2005;32:1923)
- CRP levels > 30 mg/L and a lack of prophylaxis when starting urate lowering therapy (ULT) are prognostic factors for early gout flare reccurrence in patients starting ULT during an acute gout flare (Clin Rheumatol 2019;38:2233)
Case reports
- 48 year old man presented with patellar lesion (Skeletal Radiol 2020;49:1325)
- 53 year old man presented with white-yellow papules and plaques over his elbows, knees and arms (QJM 2016;109:811)
- 55 year old man presented with multiple asymptomatic nodules on hands, feet, soles and elbow joints (Dermatol Online J 2015;21:13030)
- 60 year old man presented with direct trauma to the right forearm and knee (Radiol Case Rep 2022;17:1180)
- 71 year old man, 71 year old woman and 74 year old woman presented with abnormal pancreatic contents (pseudocyst / mass) (Case Rep Rheumatol 2022;2022:3671627)
- 77 year old man presented with lumbar spine mass mimicking a spinal meningioma (Eur Spine J 2018;27:815)
Treatment
- Acute gout: nonsteroidal anti-inflammatory drugs (NSAIDs), colchicine, prednisolone or cytokine blocking agents (e.g., IL1 blockers) if refractory disease
- Long term treatment: urate lowering therapies include xanthine oxidase inhibitors (e.g., allopurinol or febuxostat), uricosuric drugs (e.g., probenecid) or uricase agents (e.g., pegloticase) (Lancet 2018;392:1403, Arthritis Rheumatol 2017;69:1903)
- Risk reduction strategies that work on causes of hyperuricemia: lifestyle modification including dietary changes, weight loss, reduction in alcohol intake and substitutions for medications that can promote hyperuricemia (Arthritis Rheum 2005;52:283)
- Prophylactic therapy includes use of colchicine prophylaxis for at least 3 - 6 months (Arthritis Rheumatol 2020;72:879)
- Low dose NSAIDs in patients who do not tolerate low dose colchicine (Naunyn Schmiedebergs Arch Pharmacol 1986;334:138)
- Symptomatic lesions of tophaceous gout may require surgical excision
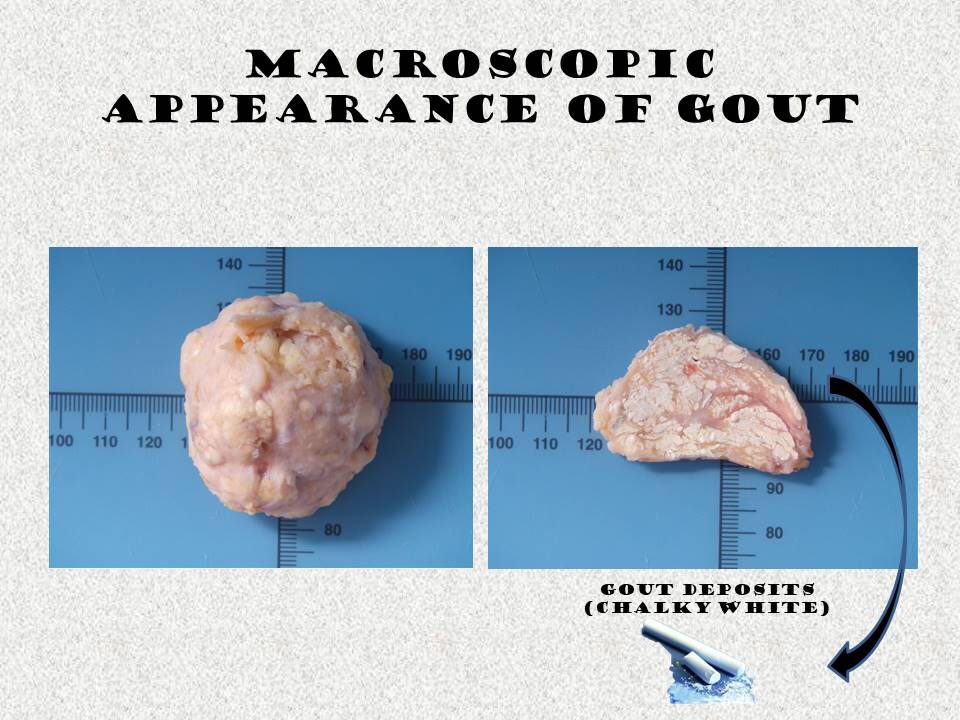
Gross description
- Specimens of patients with history of gout / gross suspicion for crystals should not be processed in formalin
- Uric acid crystals are water soluble and destroyed in routine formalin processing
- They require alcohol fixation and anhydrous processing for microscopic visualization (The University of Chicago: Gross Pathology Manual [Accessed 12 August 2022])
- If specimen is processed in formalin, chalky material should be removed from sample and scraped on slide for examination
- Small white flecks to large deposits of crystals that may appear white or tan and chalky or crumbly
- This appearance is associated with sugar icing, snow-like, powdery or toothpaste-like material
Gross images
Frozen section description
- Foreign brown feathery material in tissue surrounded by histiocytic reaction (JAAD Case Rep 2021;10:11, JBJS Case Connect 2020;10:e2000231)
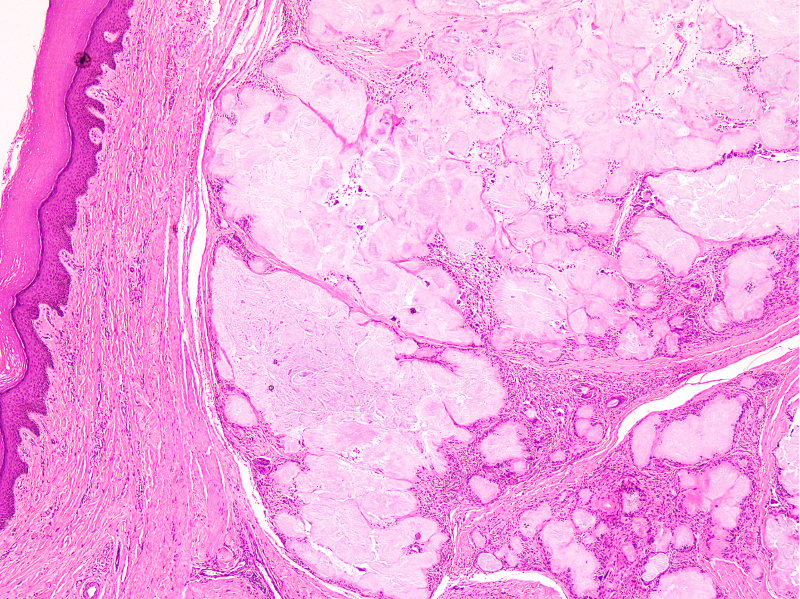
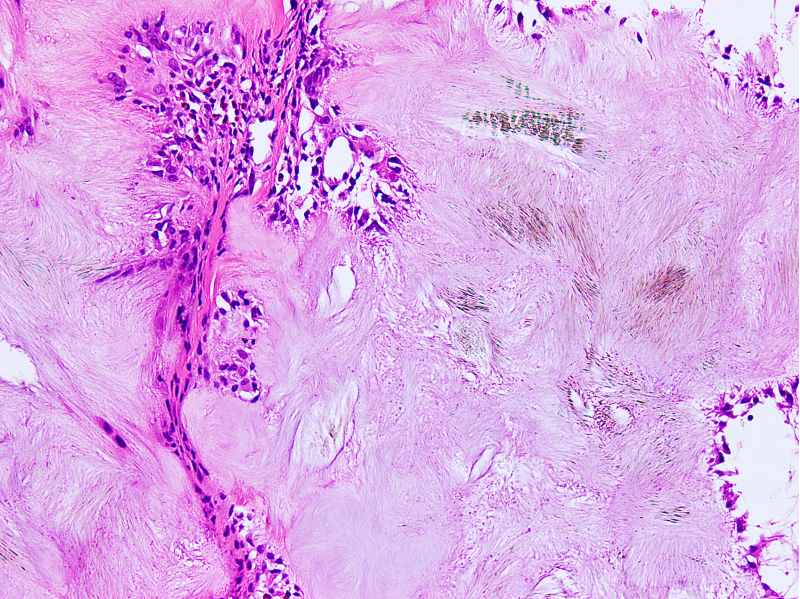
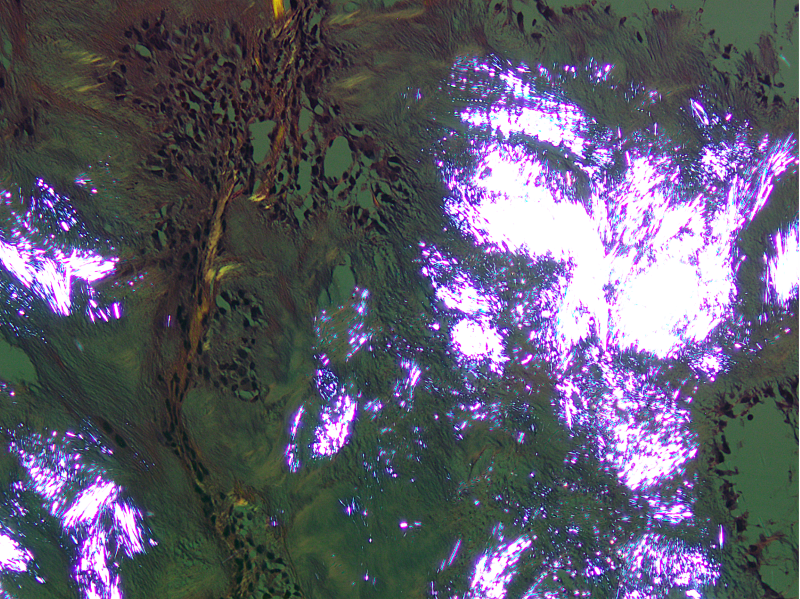
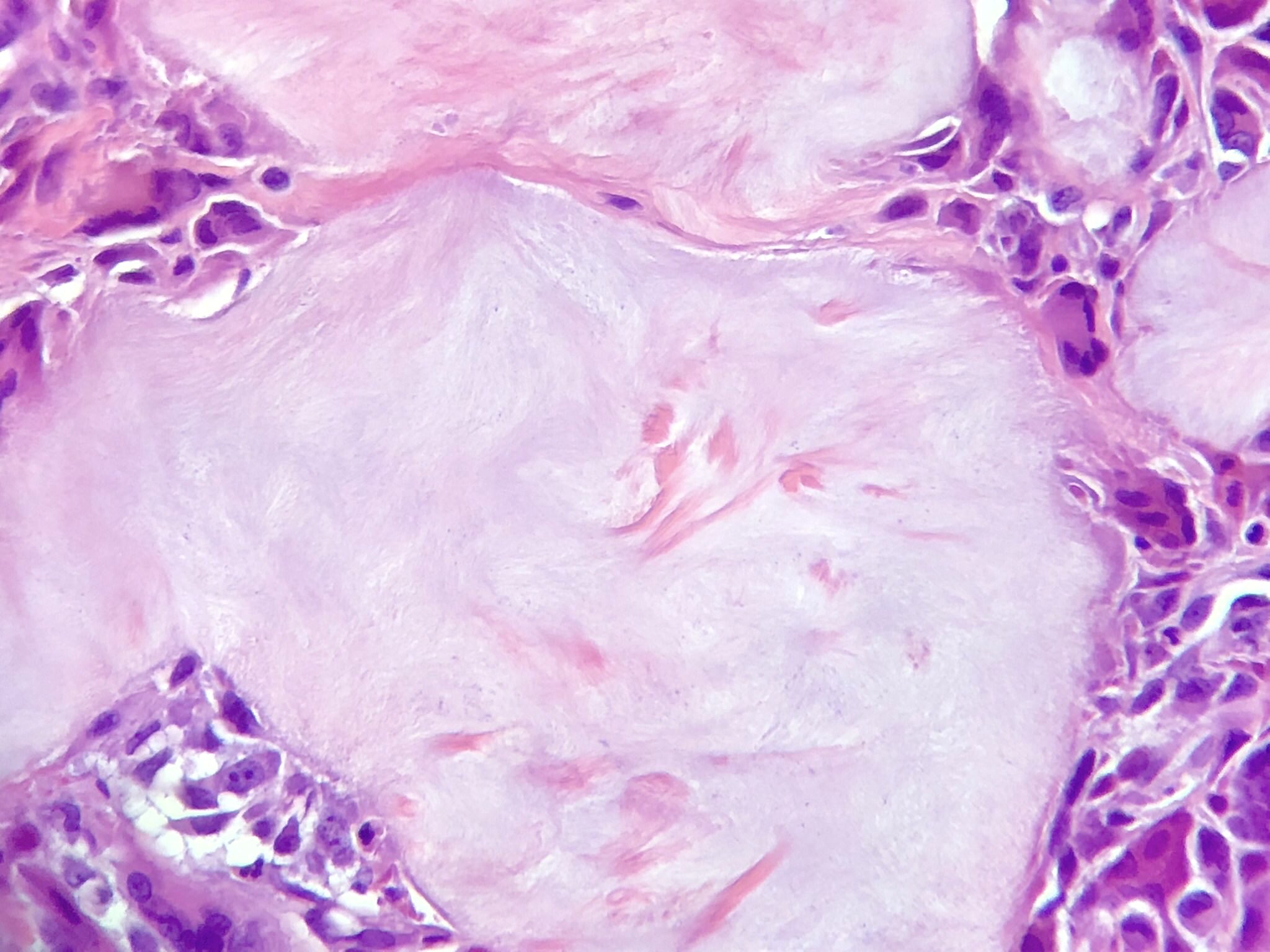
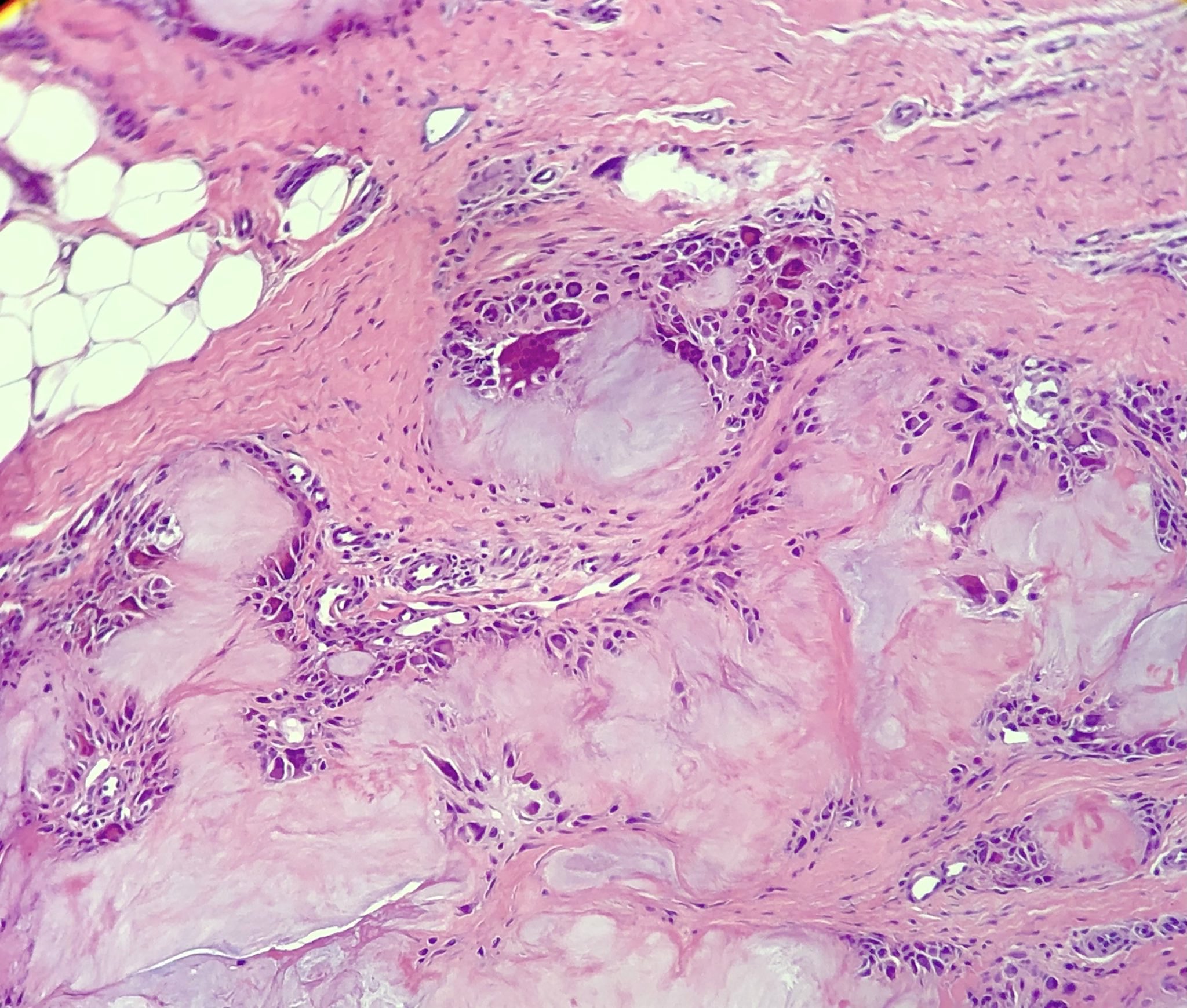
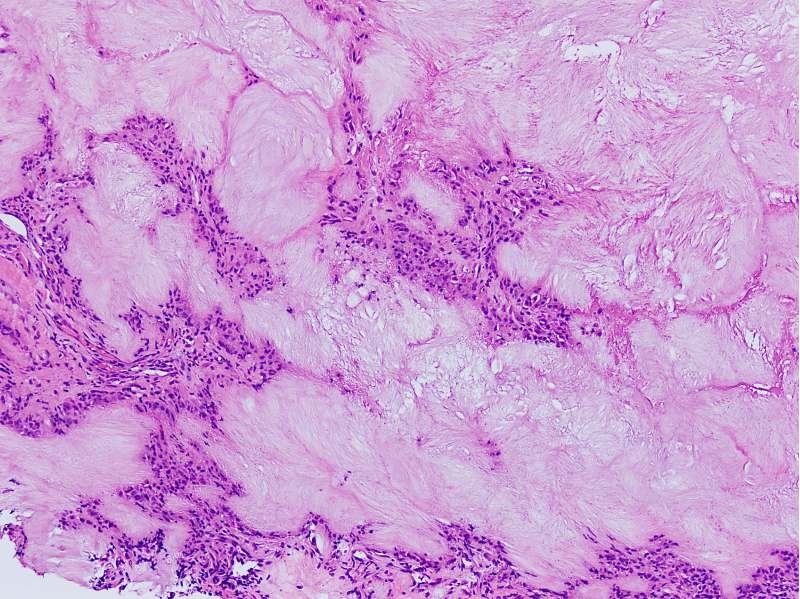
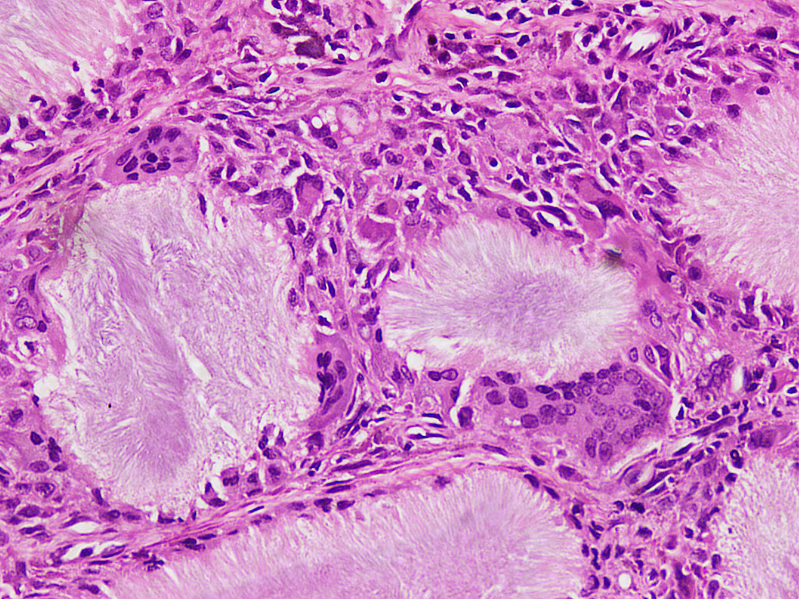
Microscopic (histologic) description
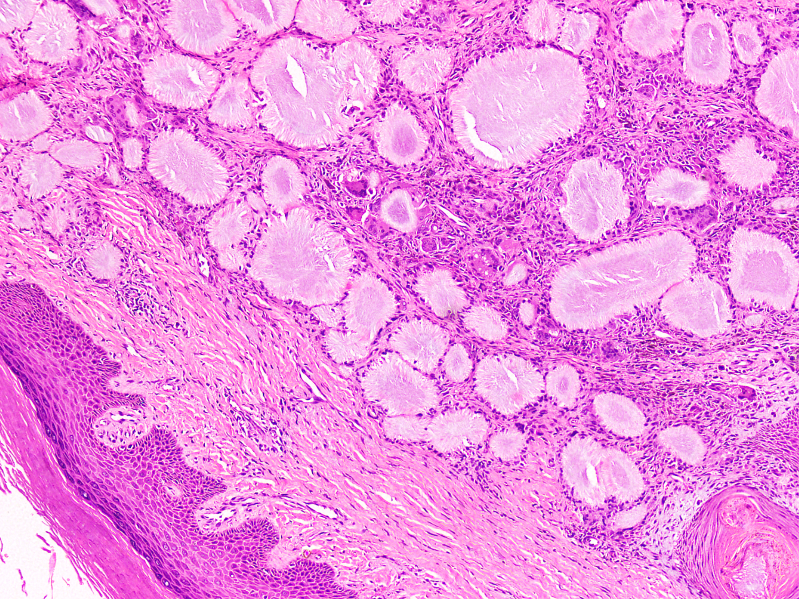
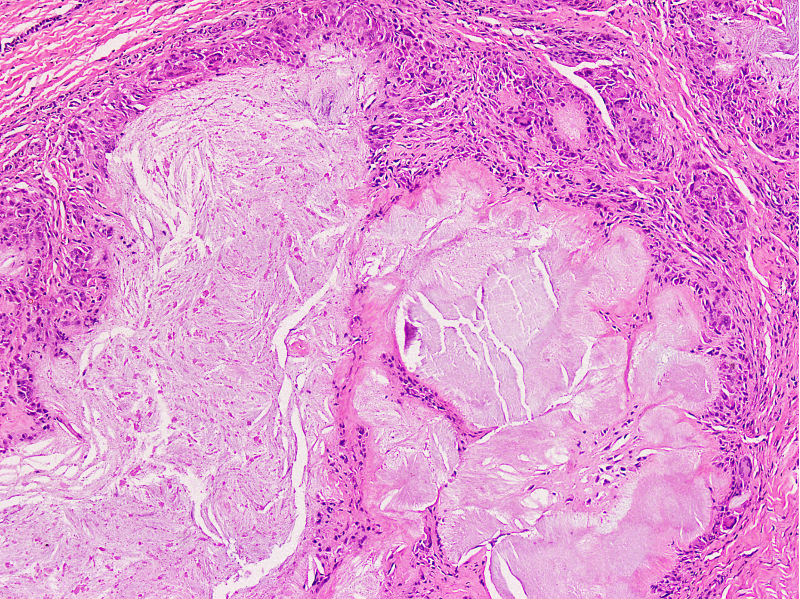
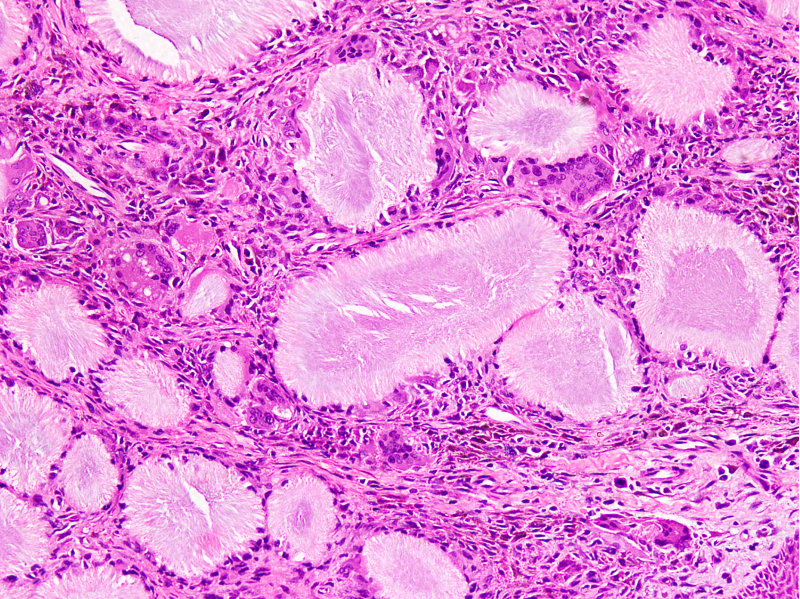
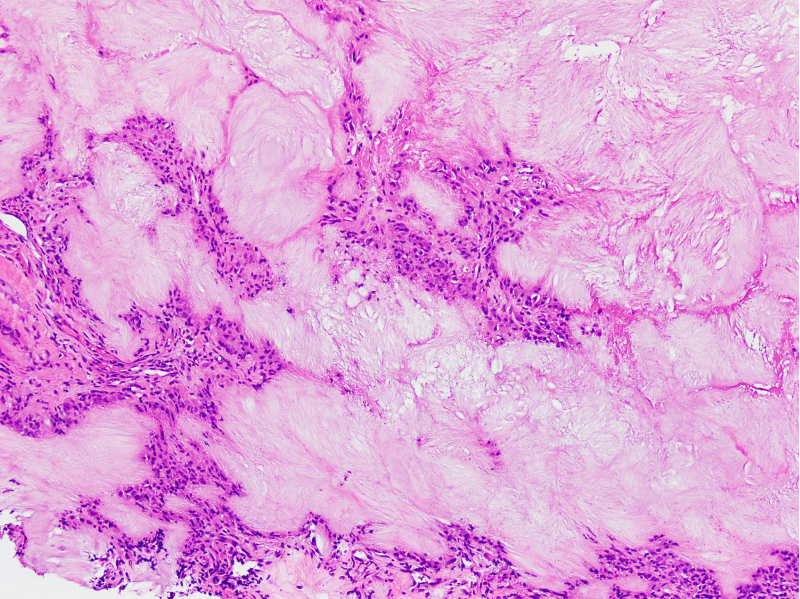
- Gout tophus:
- Nodular aggregates / granuloma-like appearance consisting of acellular, amorphous, pale eosinophilic material surrounded by palisading arrangement of histiocytes and multinucleated giant cells (Dermatol Online J 2015;21:13030)
- Feathery appearance in some deposits due to empty needle shaped spaces (Skeletal Radiol 2020;49:1325)
- Presence of monosodium urate crystals (MSU) is diagnostic
- Needle-like crystals that measure 5 - 25 micrometers in length
- Brightly anisotropic under polarized light
- Negative birefringence when examined with an interference plate in the light path (Otol Neurotol 2009;30:127)
- Crystals appear yellowish when aligned parallel to the plate axis
- Bluish appearance when alignment is across the direction of polarization
- Synovium changes:
- Affected synovium shows villous hyperplasia and synoviocyte hypertrophy and hyperplasia
- Typical chronic synovitis with mononuclear leukocyte infiltrate
- Urate crystals are also identified (Medicine (Baltimore) 1978;57:239)
- Bone and cartilage changes:
- MSU crystal deposition in bone is associated with cystic erosion, secondary cortical fracture, destruction of bony trabeculae, osteonecrosis and infiltration of trabecular spaces by chronic inflammatory cells
- Other changes include fibrotic bone marrow with proliferation of dilated capillaries, osteoclastic and osteoblastic activity and new bone formation (BMC Musculoskelet Disord 2019;20:140)
- Affected cartilage appears fibrillated, eroded and fissured
- Granulation tissue formation, fibrous replacement and chondronecrosis may occur (BMC Musculoskelet Disord 2019;20:140)
- Skin changes:
- Skin changes include calcification, fat necrosis, granulomatous dermatitis and hemosiderin deposition
- Thin epidermis, parakeratosis and hyperkeratosis
- Increased melanin pigment and pigment laden melanophages in superficial dermis
- Dermis shows dilated blood vessels, endothelial cell swelling and perivascular small mononuclear cell infiltrate (BMC Musculoskelet Disord 2019;20:140)
- Kidney changes:
- Light microscopy in gouty kidney shows diffuse thickening of glomerular capillary walls accompanied by spike formation and bubble-like appearance
- Tophaceous granuloma in interstitium, tubular atrophy, chronic interstitial nephritis and benign nephrosclerosis (Nephron 1986;44:361)
Microscopic (histologic) images
Cytology description
- Fine needle aspiration cytology (FNAC) of tophi is easier and less painful than synovial biopsy and joint fluid analysis
- Presence of MSU crystals in Papanicolaou stained smears is diagnostic
- Crystals appear as a mass of fuzzy, amorphous, granular or crystalline material
- Needle shaped crystals are arranged in sheaves and stacks, seen under polarized light
- Foamy histiocytes, multinucleated giant cells and acute and chronic inflammatory cells can be variably present (Acta Cytol 2006;50:101)
- Wet mount preparations from needle washings reveal long, thin, needle shaped crystals, singly and in clusters
- These crystals show strong, yellow, negative birefringence (Acta Cytol 2000;44:433)
- Synovial fluid wet preparation shows MSU crystals in tiny fragments of fibrin, cytoplasm of neutrophils and macrophages, or free in fluid
Cytology images
Immunofluorescence description
- Not required for diagnosis (J Am Geriatr Soc 1966;14:475)
Positive stains
- Not required for diagnosis
- CD68 positive macrophages surrounding crystals (Arthritis Rheum 2010;62:1549)
- Special stains: positive silver nitrate staining in the central crystalline core of tophus (Acta Derm Venereol 2013;93:189)
Negative stains
- Not required for diagnosis
Electron microscopy description
- Tophus: crystals are present in various arrangements: parallel to each other, interspersed with mature collagen fibers and thin fibrils, or haphazardly
- Background amorphous matrix
- Cells adjacent to the crystals have prominent rough endoplasmic reticulum and large lipid deposits
- Crystals are seen occasionally in small phagosomes of the cells (Hum Pathol 1973;4:265)
- Renal involvement: subepithelial dense deposits are observed
- Membranous nephropathy should be considered in patients with gout having moderate to severe proteinuria (Nephron 1986;44:361)
Molecular / cytogenetics description
- Genes involved in the renal urate transport system have been identified as cause of hyperuricemia and gout (Sci Rep 2018;8:3137)
- Genes for urate transporters include GLUT9, ABCG2, SLC22A12, SLC2A9, SLC17A1 and SLC17A3 (J Pers Med 2021;11:231, Nat Rev Rheumatol 2012;8:610, Hum Mol Genet 2009;18:R177)
- Genes encoding proteins that are involved in the NLRP3 (NOD, LRR and pyrin domain containing 3) inflammasome pathway are also involved in progression from hyperuricaemia to gout (Nat Rev Rheumatol 2018;14:341)
Molecular / cytogenetics images
Videos
Brilliant polarizable birefringent monosodium urate crystals
Sample pathology report
- Great toe, excisional biopsy:
- Histologic features are consistent with gout (see comment)
- Comment: Biopsy shows fibroadipose tissue exhibiting nodular aggregates and granulomatous appearance of acellular, amorphous, pale eosinophilic material surrounded by palisading arrangement of histiocytes and multinucleated giant cells. The eosinophilic material shows needle-like monosodium urate crystals, which exhibit negative birefringence under polarized light. Described features are consistent with gout. Gout is a metabolic condition associated with hyperuricemia. It can be primary (sporadic or familial) or secondary. Clinical and serological correlation with serum uric acid levels is recommended.
Differential diagnosis
- Pseudogout (calcium pyrophosphate crystal deposition disease [CPPD]):
- M = F
- Polarizable rhomboid shaped calcium pyrophosphate crystals show positive birefringence (Mod Pathol 2001;14:806)
- Response is more fibroblastic than histiocytic
- Calcium apatite deposition disease (CADD):
- Age range: 30 - 60 years
- Usually involves shoulder joint (Milwaukee shoulder in elderly)
- Radiology: fluffy, ill defined or well defined, homogenous calcifications
- Calcium apatite stains purple with Wright-Giemsa stain and red with Alizarin stain (Radiol Res Pract 2016;2016:4801474)
- Oxalate crystal disease:
- Associated with primary or secondary hyperoxaluria
- Typical joint involvement includes the proximal interphalangeal and metacarpophalangeal joints, knees, elbows and ankles
- Radiology shows calcification around joints and within tendon sheaths and soft tissue
- Calcium oxalate crystals occur in 2 forms: monohydrate (irregular squares or rods) and dihydrate (envelope-like shape)
- Positive birefringence under polarized light (Curr Rheumatol Rep 2013;15:340)
- Tumoral calcinosis:
- Usually affects younger age group in the first and second decades of life
- Most commonly occurs in elbows, hips and shoulders
- Subcutaneous calcified masses in the periarticular soft tissues
- Lobular to irregular deposits of amorphous calcium crystals (Arthritis Rheumatol 2020;72:1408)
- Rheumatoid arthritis:
- Affects small bones of adult women
- Presence of periarticular osteopenia and joint space narrowing helps differentiate rheumatoid disease from gout
- Proliferative synovitis with dense lymphoplasmacytic infiltrate
- Necrobiotic nodules, fibrosis and organizing fibrin (Semin Arthritis Rheum 2017;46:e15)
- Septic arthritis:
- Usually affects young adults and children
- Involves single joint
- Increased neutrophils and neutrophilic collections within tissue
- Osteoarthritis:
- Usually affects joints of weight bearing distribution
- Manifests after 50
- Necrotic chondrocytes with thinned and fragmented cartilage
- MSU crystals not seen
- Necrotizing granulomatous inflammation:
- Foreign body giant cell reaction:
- Bone graft material mimics gout appearance
- Eosinophilic material is more myxoid
- More sharply angulated deposition than in gout
Additional references
Board review style question #1
A 58 year old man presented with painful foot swelling. Biopsy showed skin covered fibroadipose and fibrocollagenous tissue with tan-white, chalky deposits. Histology showed nodular aggregates consisting of acellular, amorphous, pale eosinophilic material surrounded by palisading arrangement of histiocytes and multinucleated giant cells. The material showed needle-like crystals which appeared brightly anisotropic under polarized light. What is the most likely diagnosis?
- Calcium apatite deposition disease
- Calcium pyrophosphate crystal deposition disease
- Gout
- Rheumatoid arthritis
- Tumoral calcinosis
Board review style answer #1
Board review style question #2
Board review style answer #2