Table of Contents
Definition / general | Essential features | Terminology | Physiology | Laboratory | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Videos | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Zhang L. Histology-joints. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/jointsnormalhistology.html. Accessed April 23rd, 2024.
Definition / general
- Articulations that allow bones to move relative to one another
Essential features
- Various types of joints but the synovial joint (diarthrosis) is what mainly concerns pathologists
- Synovial joint is composed of the articular cartilage (hyaline cartilage), articular capsule (synovial membrane and fibrous capsule) and in certain joints, other connective tissues (menisci, tendons and ligaments)
- Normal synovial joint contains a scant amount of synovial fluid
- Second most important type of joint is the amphiarthrosis, which consists of flattened attached disc of fibrocartilage between 2 subchondral plates of adjacent bones
- Functional joint depends on the normal function of all of its components
Terminology
- Classification based on degree of movement
- Synarthroses: immovable joints (e.g., skull sutures, the distal tibial fibular joint)
- Amphiarthroses: slightly movable joints (e.g., intervertebral joints, symphysis pubis)
- Diarthroses: freely movable joints (e.g., hip, knee)
- Classification based on type of connective tissue
- Fibrous joints (e.g., skull sutures)
- Cartilaginous joints (e.g., intervertebral joints, symphysis pubis)
- Synovial joints (e.g., hip, knee: the type of joint that we usually have in mind when speaking of joints in general
- Histologic varieties of cartilage
- Hyaline cartilage: most common composition of articular cartilage; also seen in growth plates
- Fibrocartilage: constitutes intraarticular structures (menisci, annuli fibrosis of the vertebrae) and occasionally articular cartilage and is also associated with entheses (tendinous and ligamentous insertions); compared with hyaline and elastic cartilage
- Elastic cartilage: not directly associated with joints
- Tidemark:
- Interface between calcified and noncalcified cartilage layers in areas exposed to either loading (joint) or pulling (insertion) (Acta Biol Hung 1984;35:271)
- In articular cartilage it appears with skeletal maturation; in other localizations it is age independent
Physiology
- Articulates the tubular bones of the extremities; there are varieties of synovial joints in regard to the kind of motion (e.g., hinge joints, pivot joints, ball and socket joints, etc.)
- Characterized by the presence of a joint space, which is closed off by a capsule that holds the bone ends together
- Capsule is lined by synovium
- Synovial recesses increase the joint space and allow a greater range of motion
- Normal synovial joint contains a scant amount of synovial fluid which lubricates the cartilaginous surface
- Articular cartilage, a specialized type of connective tissue, covers the area of functional contact between the opposed bone ends (within the joint capsule) and provides structural support, cushioning and gliding
- At its periphery, the articular cartilage fuses with the joint capsule and with the periosteum
- Normal articular cartilage is devoid of blood vessels, lymphatics and nerves; chondrocytes receive their nourishment by means of diffusion, mainly from the synovial fluid
- In some synovial joints, the articular space is divided, completely or incompletely, by a disk or by menisci
- Periphery of these intraarticular structures is continuous with the capsule
- Functional synovial joint depends on the normal function of all of its components
Laboratory
- Synovial fluid white blood cell (WBC) count and neutrophils percentages are used to aid in the diagnosis of joint infection
- Septic arthritis (native joint): WBC > 50 x 109/L and neutrophils > 50%
- Prosthetic joint infection: WBC > 1.7 x 109/L or neutrophils > 65%
- Negative Gram stain and culture cannot rule out joint infection due to low sensitivity
- Wet preparation and microscopy (in polarized light with an interference plate) is used to detect crystalline material:
- Monosodium urate monohydrate: needle shaped, negative birefringent
- Calcium pyrophosphate dehydrate: rod shaped, positive birefringent
Gross description
- Most commonly encountered joint specimens are hips and knees (from arthroplasty)
- Each component of the joint (including subarticular bone) should be described if possible
- Hip joint (specimen consists of a femoral head with or without femoral neck and fragmented labrum):
- Femoral head is round, the convex surface of which is lined by smooth and glistening hyaline cartilage
- At the periphery of articular cartilage there is thin and smooth synovium
- On cut section, the cartilage is yellow-white and ranges 2 - 3 mm in thickness
- In a middle age individual, the subarticular bone contains yellow (fatty) marrow
- Knee joint (specimen consists of fragments of soft tissue, articular, cortical and cancellous bone of the femoral condyles, tibial plateau and patella articular surfaces):
- Articular surfaces of the medial, lateral and patella femoral compartments are lined by smooth, glistening hyaline cartilage
- Synovium is thin and smooth
- Medial and lateral menisci are preserved
Microscopic (histologic) description
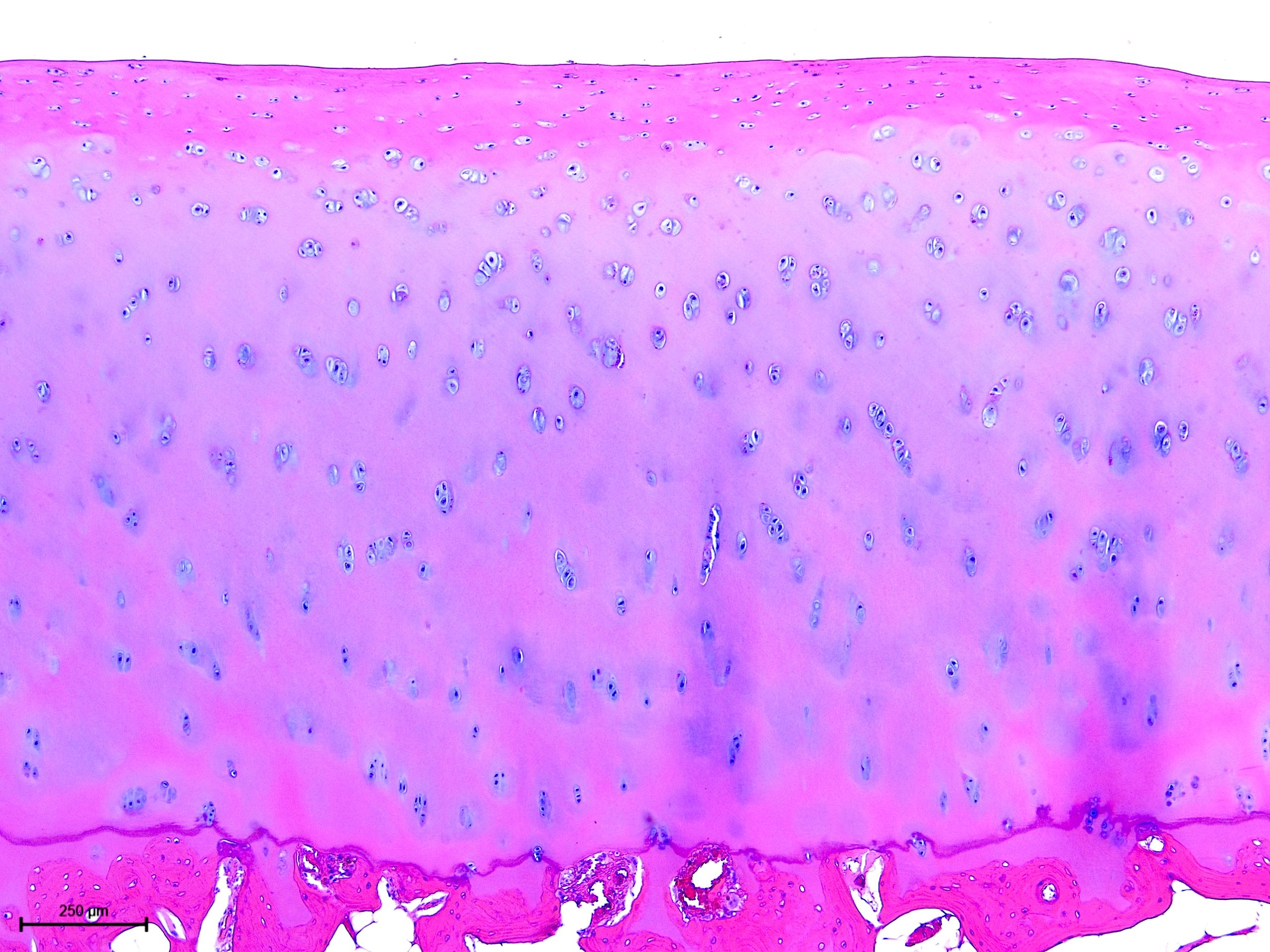
- Articular cartilage
- Hyaline: smooth, glistening; may be fibrous (e.g., temporomandibular and sternoclavicular joints)
- Composed of chondrocytes (1% of volume), matrix water (70 - 80% wet weight) and a matrix macromolecular framework (collagen [chiefly type II collagen], hydrophilic proteoglycans, decoran, aggrecan and other noncollagenous proteins and glycoproteins) (J Physiol 2006;574:643)
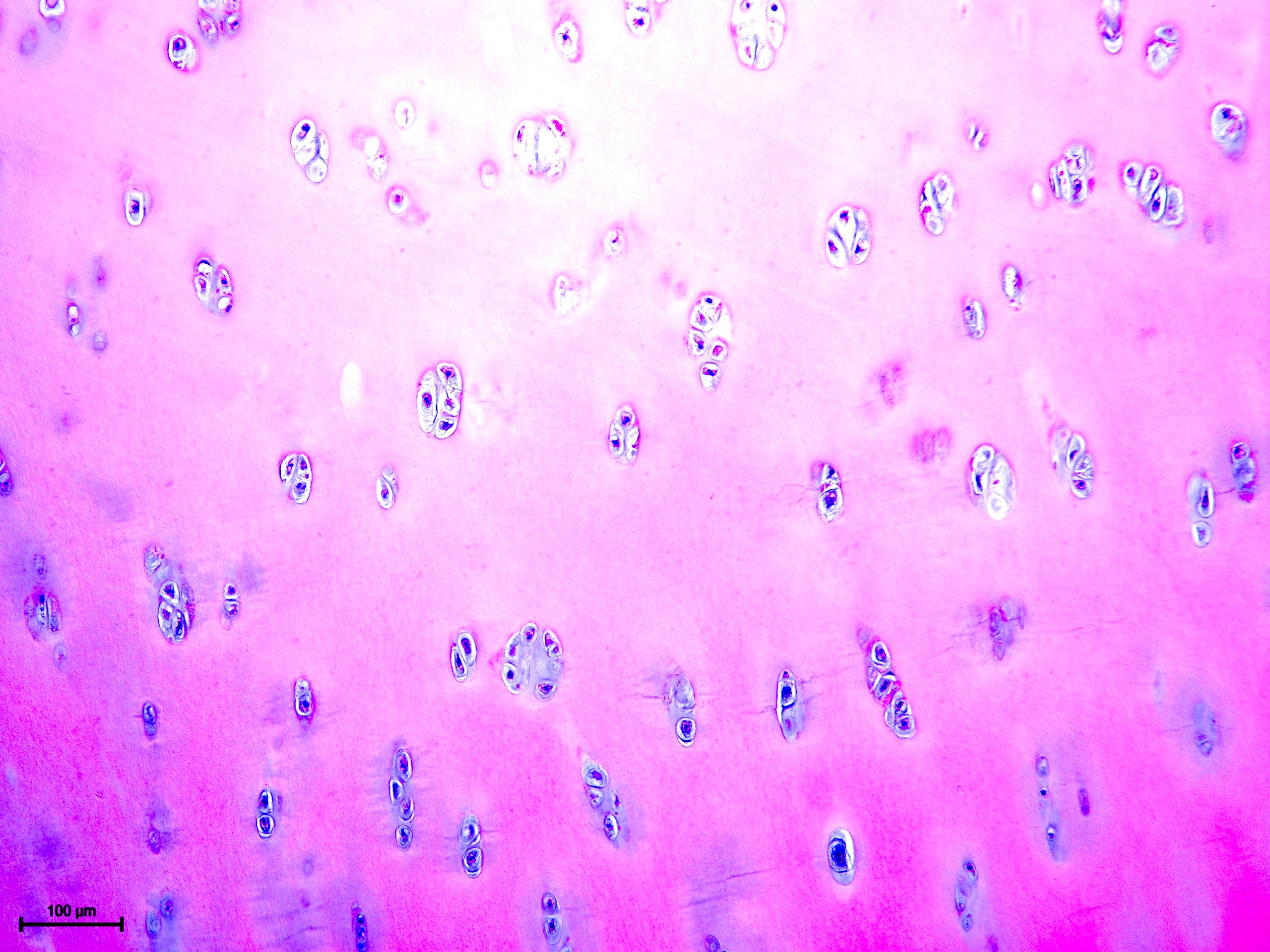
- Chondrocytes are dispersed within the extracellular matrix and reside in lacunae
- Chondrocytes have pyknotic nulei and lack abundant nuclear detail
- Clustering of chondrocytes (cloning) may be seen in degenerative and neoplastic conditions
- 4 zones (from superficial to deep): gliding (superficial) zone, transitional zone, radial zone and calcified zone (Instr Course Lect 1998;47:477)
- Chondrocytes are flattened near the surface and more rounded elsewhere
- Calcified zone stands out by virtue of calcification of its matrix; delineated from the broad radial zone by a wavy line (tidemark), along which the calcareous material is concentrated
- Calcified zone is anchored to a layer of dense osseous tissue (bony end plate), which seals off the marrow cavity
- Synovium
- Lines the remainder of the joint space
- 2 layers: a thin intimal layer (1 - 3 synoviocytes in depth) and a deeper subintimal layer (vascular loose connective tissue with foci of fat)
- Synovial fluid
- Clear and slightly yellow, viscid mucoid
- Chemical composition similar to plasma, supplemented with hyaluronans
- 200 - 300 cells/mm2 (synoviocytes, fibrochondrocytes, lymphocytes)
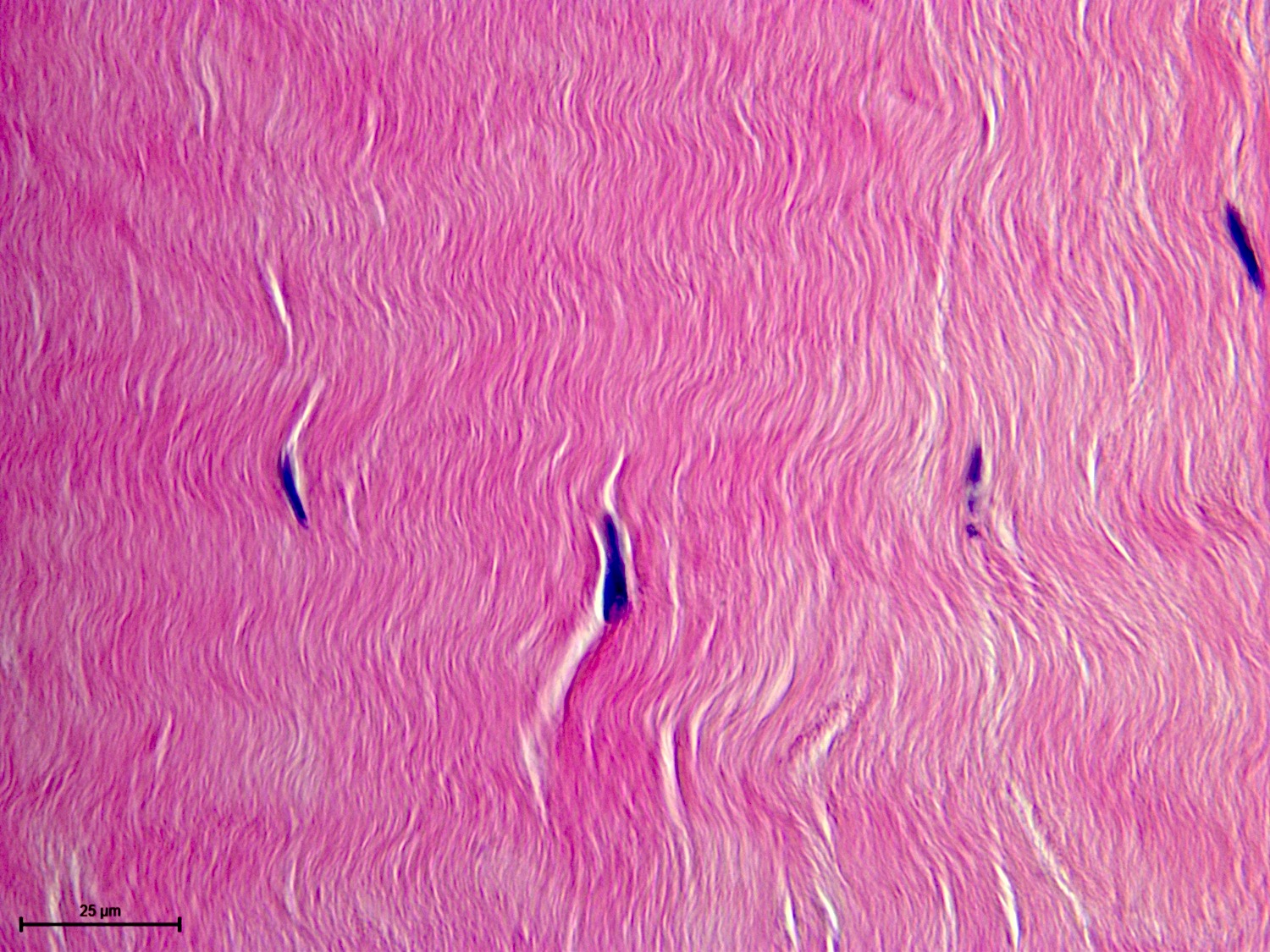
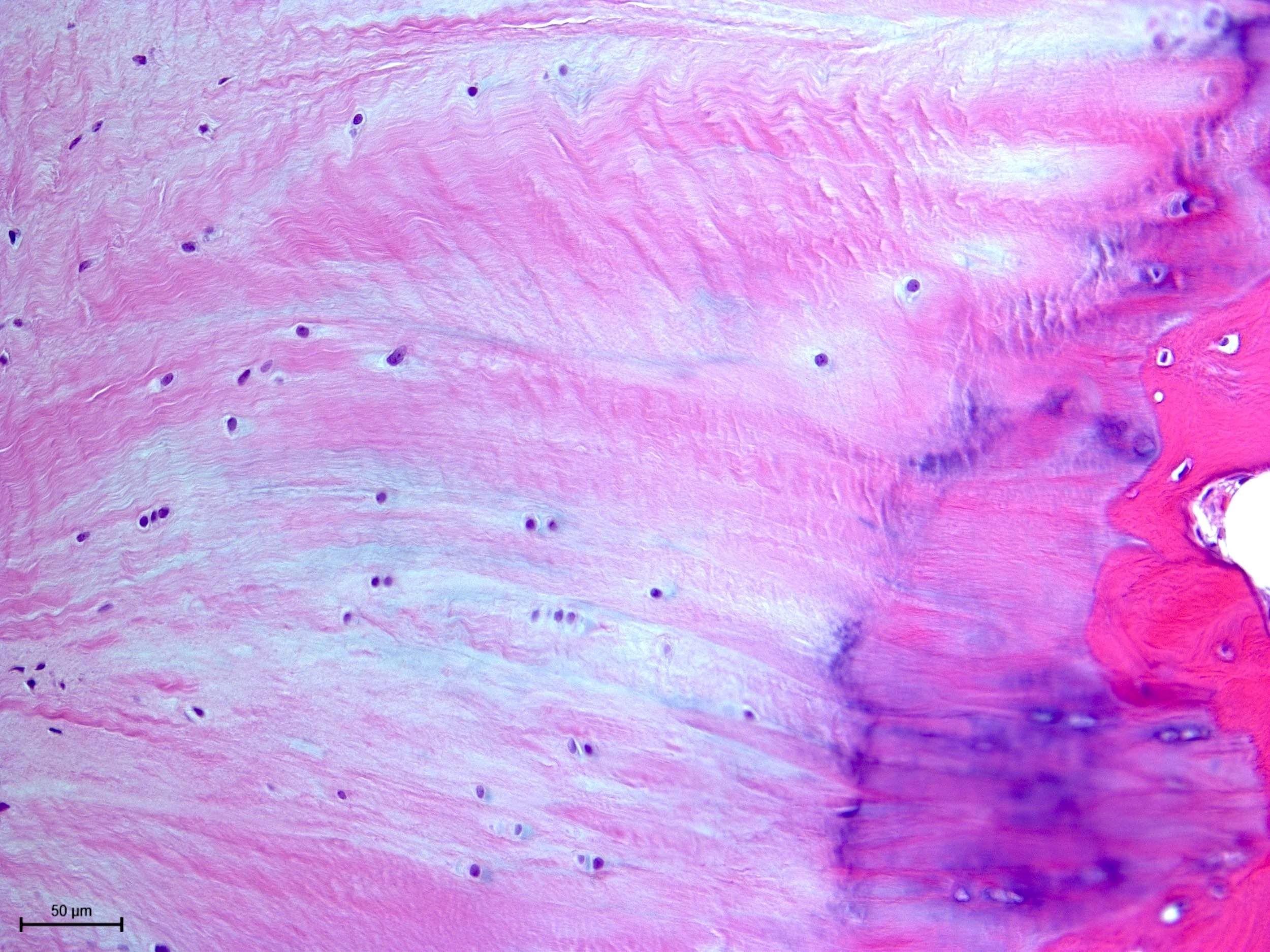
- Intraarticular and extracapsular structures
- May be incorporated into the joint capsule or form independent structures, poorly vascularized
- Ligament: bundles of collagen fibers (joined by proteoglycans) in an organized, hierarchical structure; connect bones to one another
- Tendon: similar histology to ligaments; connect muscles to bone
- Enthesis: the interface between bone and tendon / ligament
- In polarized light, individual collagen fibers can be seen passing from the fibrous tissue at right angle to the bony endplate (Sharpey fibers)
- Intermediary tissue may be fibrocartilage or hyaline cartilage
- Disk and meniscus: circular or semilunar collagenous connective tissue in certain joints (e.g., temporomandibular, knee)
Microscopic (histologic) images
Videos
Histology of the joint
Embryology, history and pathology of articular cartilage
Additional references
- Jaffe: Metabolic Degenerative and Inflammatory Diseases of Bones and Joints, 1972, Milgram: Radiologic and Histologic Pathology of Nontumorous Diseases of Bones and Joints, 1990, Klein: Non-Neoplastic Diseases of Bones and Joints (Atlas of Nontumor Pathology), 1st Edition, 2011, Young: Wheater's Functional Histology: A Text and Colour Atlas, 6th Edition, 2013
Board review style question #1
What are the articulating surfaces of the bone ends of synovial joints normally covered by?
- Elastic cartilage
- Fibrocartilage
- Hyaline cartilage
- No cartilage
Board review style answer #1
Board review style question #2
Chondrocytes generally have a limited proliferating capacity. The phenomenon shown in the microphotograph is most commonly seen in which scenario?
- 30 year old man presents with right knee pain and founded to have numerous loose bodies in the joint
- 60 year old woman presents with progressive bilateral hip pain with limited range of motion
- 25 year old man presents with an expansile, radiolucent mass in his proximal phalanx of left long finger, with no frank destructive radiological features
- 55 year old woman has had increasing epigastric pain for 10 years; imaging reveals a 12 cm exophytic, partially calcified rib mass
Board review style answer #2
B. 60 year old woman presents with progressive bilateral hip pain with limited range of motion. The clinical scenario is degenerative joint disease (osteoarthritis). Chondrocyte cloning can be seen in the other scenarios (A: synovial chondromatosis, C: enchondroma, D: chondrosarcoma) but they are far less common than degenerative joint disease.
Comment Here
Reference: Histology-joints
Comment Here
Reference: Histology-joints