Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Immunofluorescence images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Genetics | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Sisk A. Renal amyloidosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneyamyloidosis.html. Accessed April 24th, 2024.
Definition / general
- A group of insoluble proteins organized into beta pleated sheets, which deposit within extracellular spaces of a variety of tissues leading to organ dysfunction and disease
- Renal involvement largely consists of AL, AA, ALECT2 and rare hereditary types such as ATTR (transthyretin) amyloidosis (BMC Nephrol 2022;23:144)
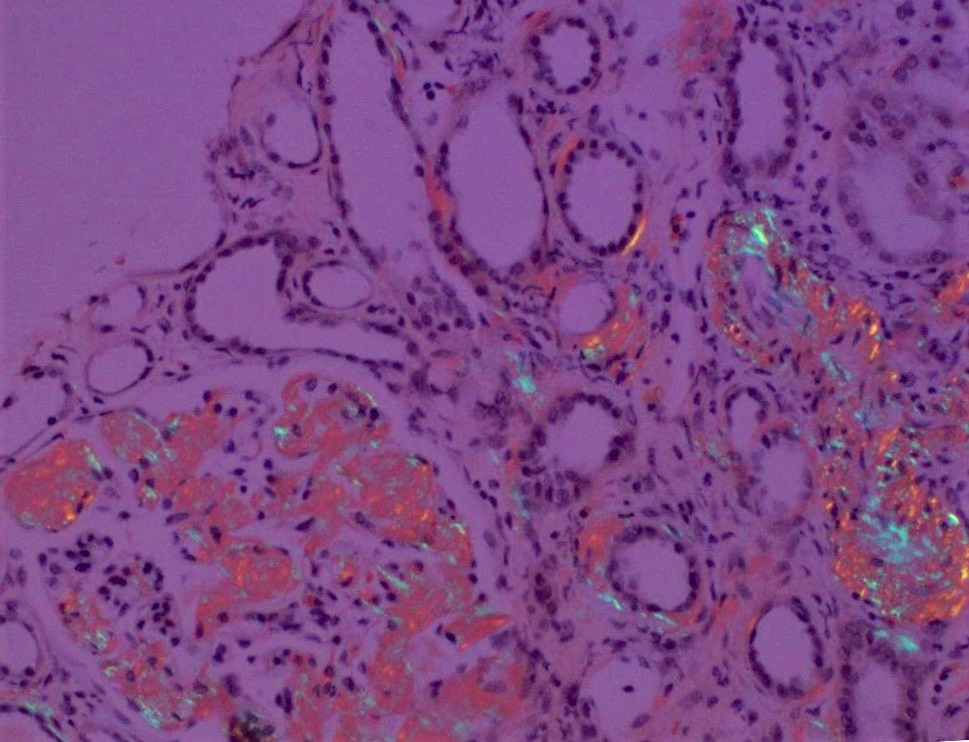
- Amyloid deposits show similar morphology (irrespective of type) and display orangeophilic staining with Congo red and apple green birefringence under polarization
Essential features
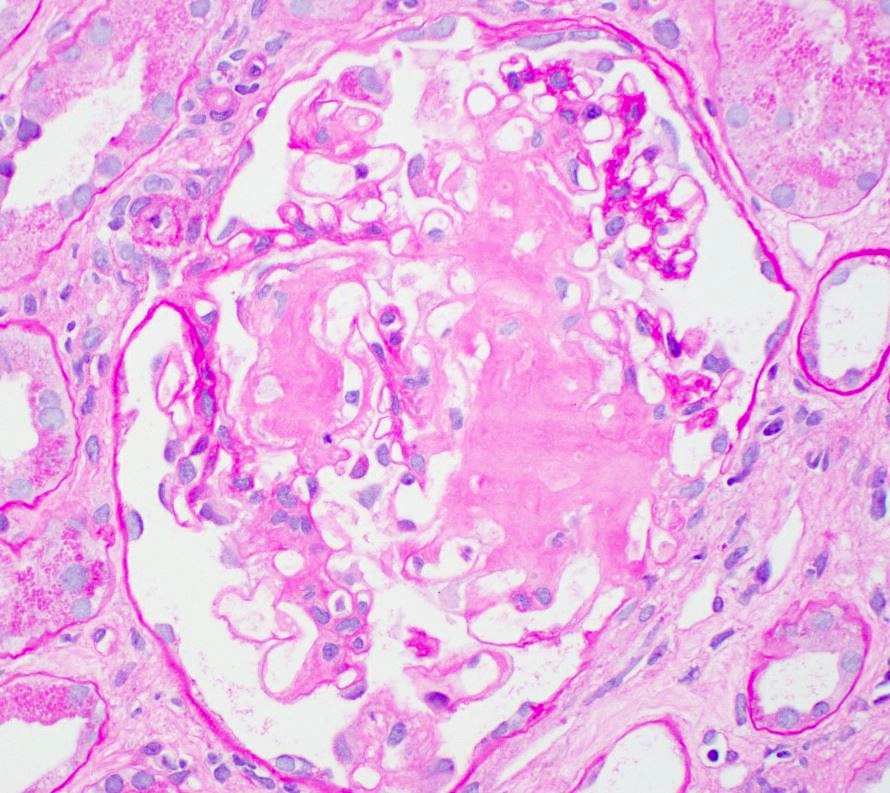
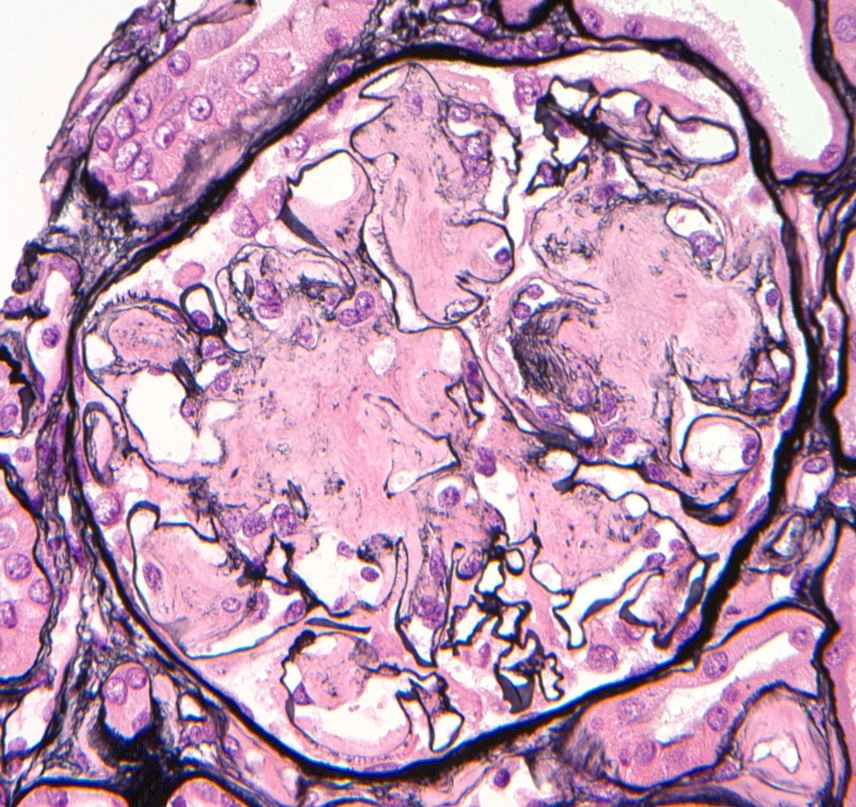
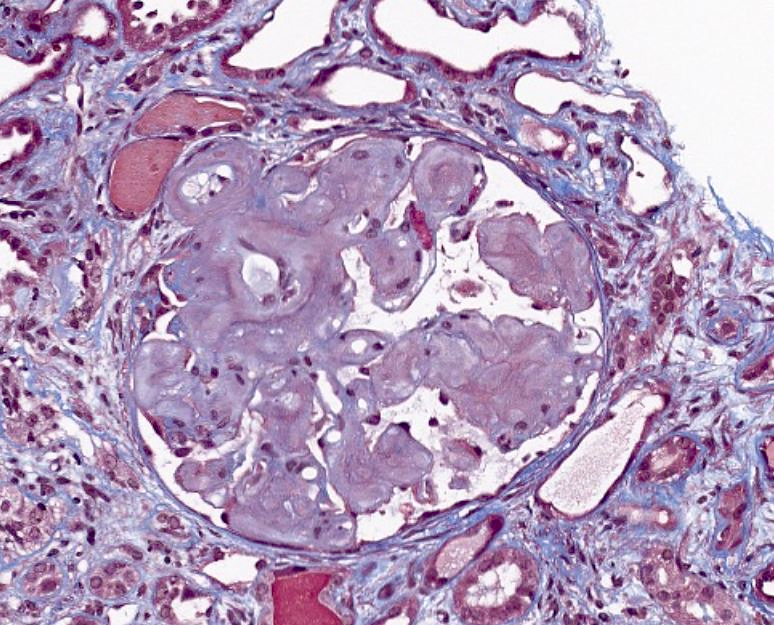
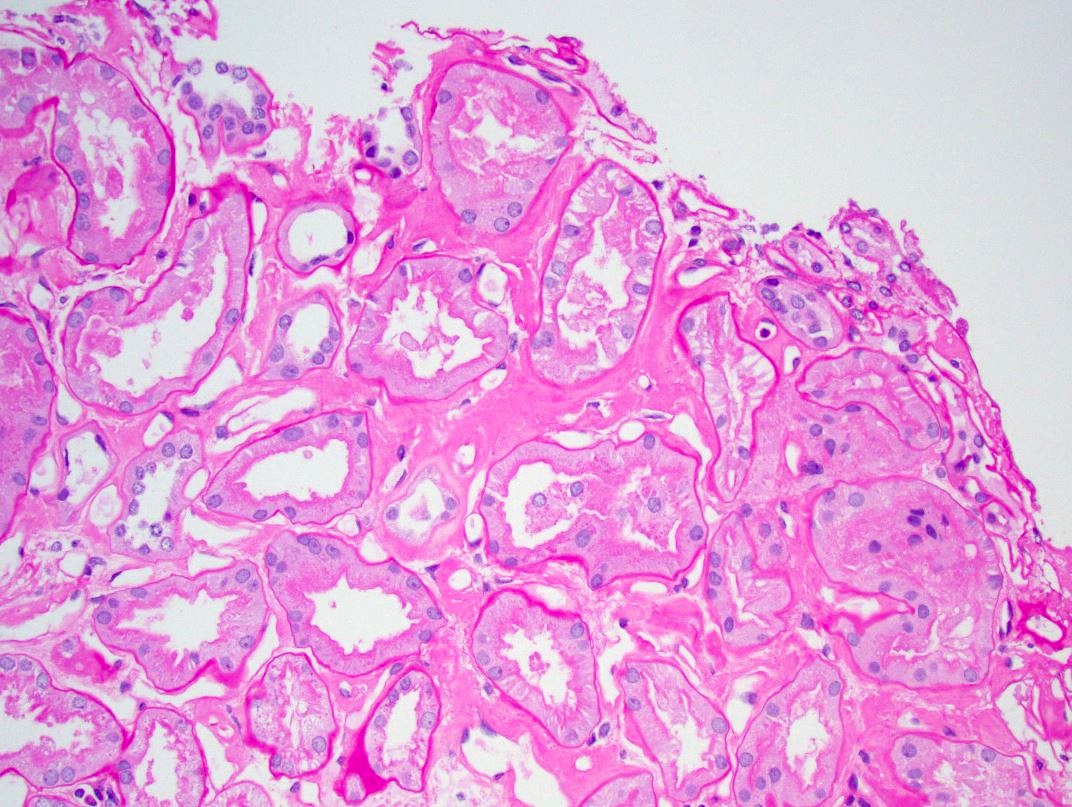
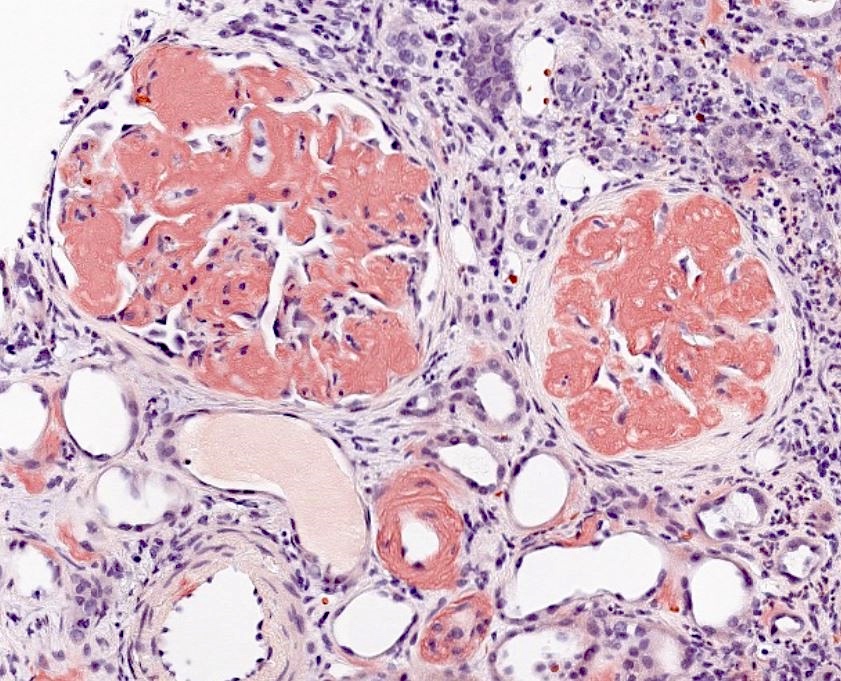
- Deposition of acellular, eosinophilic material within glomeruli, tubulointerstitium and vessel walls; this is negative on Jones silver, pale on PAS / H&E and blue-gray on trichrome
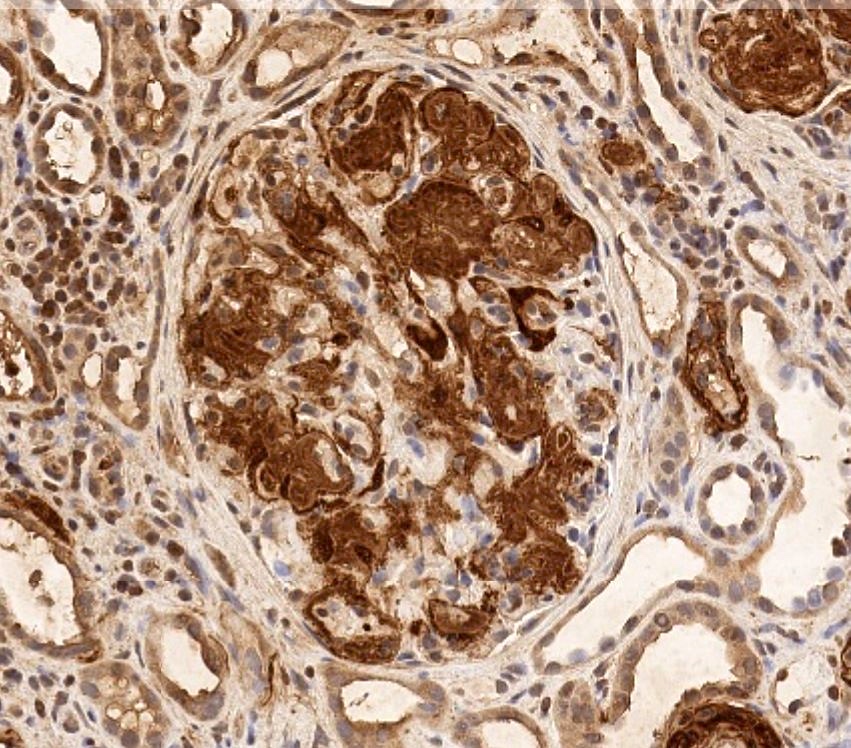
- Immunofluorescence and immunohistochemistry findings can be helpful in determining amyloid type
- Laser dissection of amyloid, followed by tandem mass spectrometry analysis, is the gold standard for definitive amyloid typing
- Treatment options rely on accurate typing of amyloid (Kidney Int 2015;87:516)
ICD coding
Epidemiology
- Dependent on the amyloid type
- AL type:
- Primary amyloidosis is most commonly seen in people over the age of 50
- Most common type in the United States
- Caused by a monoclonal gammopathy of light chains (AH - heavy chains and mixed AH / AL types are much rarer)
- Most frequently associated with lambda light chains
- Related to both monoclonal gammopathy of undetermined significance (MGUS) and multiple myeloma
- AA type:
- Secondary amyloidosis characterized by serum amyloid A protein
- More common in developing countries
- Associated with prolonged inflammatory states including rheumatoid arthritis and other connective tissue disorders, infections, IV drug use, inflammatory bowel disease and paraneoplastic syndromes
- ALECT2 type:
- Leukocyte cell derived chemotaxin 2 associated amyloidosis
- Kidney is the most common organ involved, followed by the liver
- Initial reports indicated that Mexican Americans are preferentially affected but new reports document different ethnicities including Middle Eastern, Indian / Punjabi and Chinese populations (Nephrol Dial Transplant 2018;33:241, J Investig Med 2022;70:348)
- Hereditary types:
- Rare group of diseases involving mutations in a number of genes
- Autosomal dominant with variable penetrance
- Most common type is transthyretin (prealbumin) amyloidosis (ATTR), may be wild type but renal involvement is nearly always hereditary due to Val30Met mutations (Nephron 2022 Mar 18 [Epub ahead of print])
- Fibrinogen alpha chain (AFIB) followed by apolipoprotein A1 (AapoA1) are the next 2 (rarely seen) types (Amyloid 2022 May 3 [Epub ahead of print])
Sites
- Growing number of amyloid protein types, involving various organ systems and tissues, with relatively few involving the kidney specifically
- All components of the kidney may be involved (glomerular, tubular basement membranes and casts, interstitium, vessels)
Pathophysiology
- Specific causes are dependent on amyloid type
- Polypeptides become misfolded, usually into beta sheet secondary structures, where beta strands are oriented perpendicular to the long axis of the fiber
- These misfolded proteins have a propensity for aggregation and deposition within various organs and tissues (including vessels and nerves), causing damage (StatPearls: Amyloidosis [Accessed 8 June 2022])
Etiology
- Dependent on amyloid type
- Monoclonal protein (AL), chronic infection / inflammation (AA), specific populations with unknown cause (ALECT2), hereditary (ATTR, AApol1)
Clinical features
- Varies with type of amyloidosis and component of kidney affected
- Glomerular involvement presents with nephrotic range proteinuria and nephrotic syndrome, which may present suddenly
- Often with AL and AA type amyloidosis
- Tubulointerstitial predominant involvement will present with slow progressive renal failure and less proteinuria
- Often seen with ALECT2 amyloidosis
- Rarely, rapidly progressive renal failure and nephrotic syndrome in the setting of amyloid induced crescentic glomerulonephritis
- Most often with AA type amyloidosis (Indian J Nephrol 2020;30:352)
- Acute renal failure may be seen in the setting of amyloid cast nephropathy
- Glomerular involvement presents with nephrotic range proteinuria and nephrotic syndrome, which may present suddenly
Diagnosis
- May be suspected clinically
- Visualization of the characteristic amyloid deposits, as seen on special stains
- Confirmation with Congo red staining and polarization of amyloid showing typical apple green birefringence
- Thicker tissue sections (8 - 10 microns) are helpful in visualizing the polarized deposits
- Immunohistochemistry stains are available including serum amyloid A, transthyretin and antiserum amyloid P (SAP)
- Immunofluorescence microscopy to determine light or heavy chain restriction
- Electron microscopy findings with characteristic fibrillary deposits
- Amyloid type can be confirmed with mass spectrometry based proteomics
Laboratory
- Serum and urine protein electrophoresis with immunofixation
- Serum free light chain elevation
Prognostic factors
- Unfavorable factors (J Res Med Sci 2014;19:644, Blood 2003;101:827, J Clin Oncol 2016;34:2037):
- Dialysis requirement
- Massive proteinuria
- Renal failure at presentation
- Severe hypoalbuminemia
- Coexisting multiple myeloma
- Heavy organ involvement
- IgM related monoclonal protein
Case reports
- 31 year old woman presents with proteinuria during her second pregnancy (Clin Res Cardiol 2020;109:1438)
- 56 year old man with longstanding Crohn's disease presents with nephrotic syndrome (Ochsner J 2021;21:291)
- 60 year old Caucasian woman with 8 weeks of lower extremity edema, renal failure and a 10 cm kidney mass (Kidney Int Rep 2019;4:882)
Treatment
- Treatment based on amyloid type, underlying cause of disease and symptoms
- Dialysis and kidney transplant in end stage kidney disease
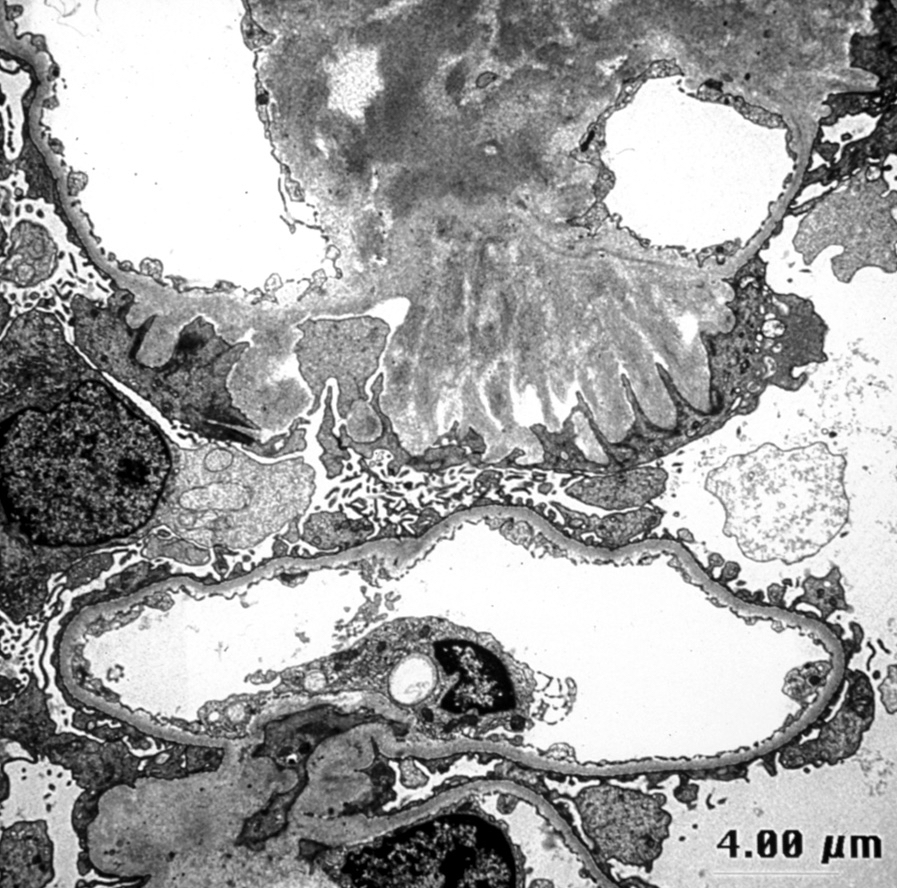
Microscopic (histologic) description
- Pale eosinophilic, amorphous and extracellular material on H&E and PAS stains, typically silver negative and gray-blue on trichrome
- Amyloid involving glomerular basement membranes may show long perpendicular spikes
Microscopic (histologic) images
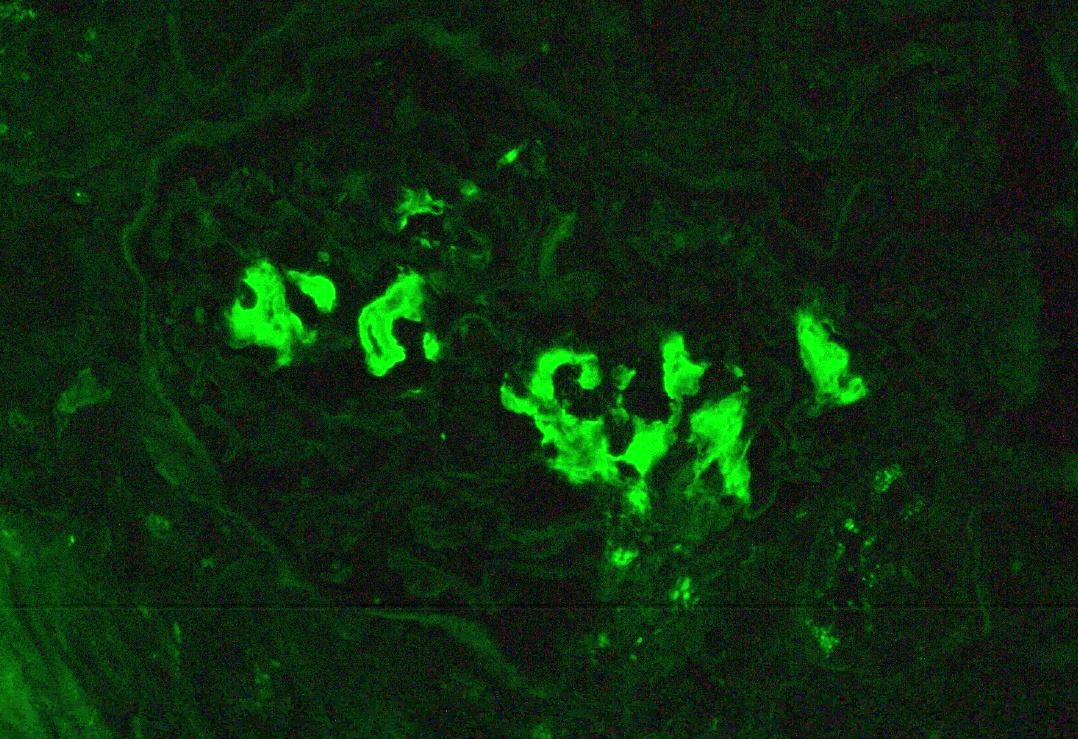
Immunofluorescence description
- Light chain and heavy chain restriction may be seen within amyloid
Positive stains
Negative stains
- Jones silver: does not typically stain amyloid
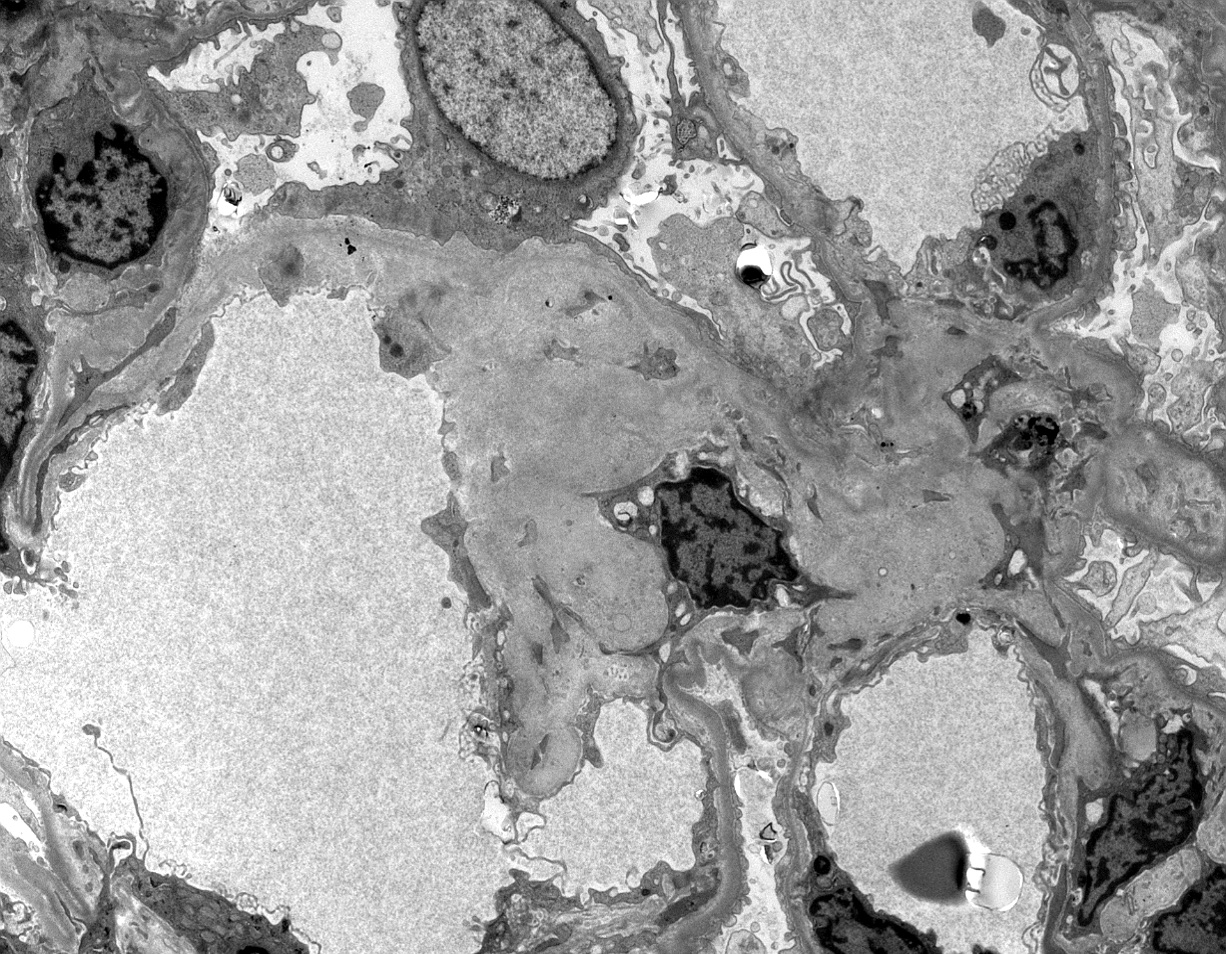
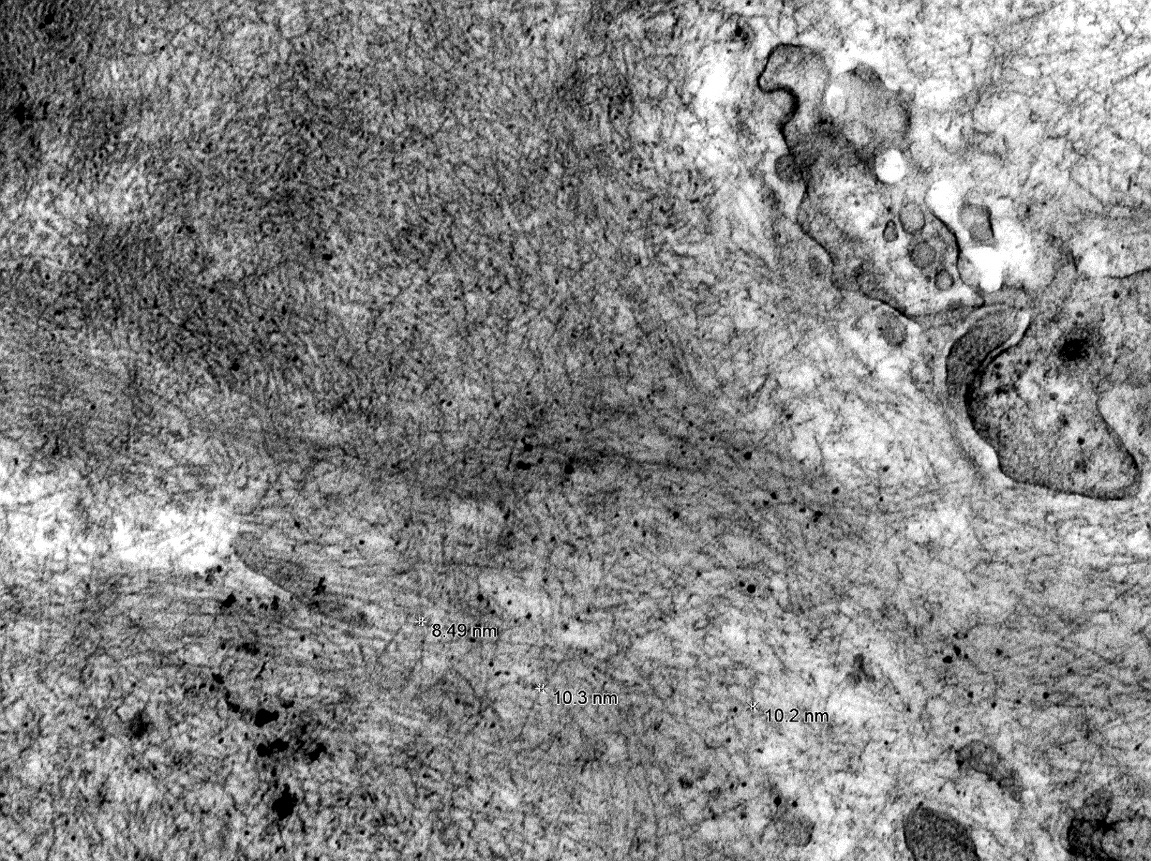
Electron microscopy description
- Randomly arranged, nonbranching fibrils with a variable thickness, close to 10 nm
Electron microscopy images
Genetics
- Mostly acquired with rare inherited forms
- Hereditary forms
- All show an autosomal dominant inheritance
- Transthyretin gene mutation most common - Val30Met seen with renal involvement (Nephron 2022 Mar 18 [Epub ahead of print])
- Other gene mutations include fibrinogen alpha chain, apolipoprotein A1 and A2
Sample pathology report
- Kidney, native, core biopsy:
- Amyloidosis, lambda restricted (AL type), predominantly glomerular
- No significant interstitial fibrosis / tubular atrophy
- Congo red stain confirms amyloid deposits
Differential diagnosis
- Fibrillary glomerulonephritis:
- Immunotactoid glomerulonephritis:
- Extremely rare, microtubules of 20 - 50 nm
- Diabetic nephropathy:
- Strong mesangial silver stain, no well formed fibrils
Board review style question #1
Board review style answer #1
Board review style question #2
Which of the following is the typical presentation for ALECT2 amyloidosis?
- Microscopic hematuria
- Nephrotic syndrome and renal failure
- Slow decline in renal function
- Sudden nephrotic range proteinuria
Board review style answer #2