Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Immunofluorescence images | Positive stains | Electron microscopy description | Electron microscopy images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Peng F, Zuckerman JE. IgG4 related disease. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneyigg4related.html. Accessed April 19th, 2024.
Definition / general
- A component of a systemic immune mediated fibroinflammatory condition which generally manifests in the kidney as an acute or chronic interstitial nephritis with lymphoplasmacytic inflammation containing increased IgG4+ plasma cells, tubulointerstitial immune complex deposits and frequently storiform fibrosis, which may be mass forming / tumor-like
- Varying degrees of glomerular involvement, predominantly membranous nephropathy, can also be seen
Essential features
- Usually chronic interstitial nephritis with dense lymphoplasmacytic inflammation with a predominance of IgG4+ plasma cells (hallmark)
- Some degree of fibrosis, usually storiform in character
- Generally associated with other systemic manifestations of IgG4 disease
- Good response to glucocorticoids
- Antineutrophil cytoplasmic antibody (ANCA) related disease has been excluded
Terminology
- Also has been called
- IgG4 related systemic disease
- IgG4 syndrome
- IgG4 associated disease
- IgG4 related sclerosing disease
- IgG4 related systemic sclerosing disease
- IgG4 related autoimmune disease
- IgG4+ multiorgan lymphoproliferative syndrome
- Hyper-IgG4 disease
- Systemic IgG4 related plasmacytic syndrome
- Systemic IgG4 related sclerosing syndrome
- Multifocal fibrosclerosis
- Multifocal idiopathic fibrosclerosis
ICD coding
Epidemiology
- Average ~65 years (range 20 - 80 years) (Am J Surg Pathol 2010;34:1812, Adv Chronic Kidney Dis 2017;24:94)
- Male predominance (3:1 - 7:1)
- Likely underestimated; 0.28 - 6 individuals/100,000 people (Japan) (Int J Rheumatol 2012;2012:358371)
Sites
- Affects almost any organ, including the pancreas, bile duct, lacrimal glands, salivary glands, central nervous system, thyroid, lungs, liver, gastrointestinal tract, kidney, prostate, retroperitoneum, arteries, lymph nodes, skin, breast (N Engl J Med 2012;366:539)
- Within the kidney / ureter
- Predominantly tubulointerstitial compartment
- Less frequently glomerulus (membranous nephropathy)
- Ureter (strictures / pseudotumor)
Pathophysiology
- Pathogenesis poorly understood
- Findings consistent with both an autoimmune disorder and an allergic disorder are present (Adv Anat Pathol 2010;17:303, Am J Surg Pathol 2006;30:1537)
- Follicular helper T cells and CD4+ cytotoxic T cell appears to be involved in the disease (J Allergy Clin Immunol 2016;138:825, Adv Chronic Kidney Dis 2017;24:94)
Etiology
- Unclear
- May be related to genetic background, bacterial infection and molecular mimicry, and autoimmune disease (World J Nephrol 2018;7:29)
Clinical features
- Acute or progressive kidney insufficiency in most patients (Nat Rev Nephrol 2015;11:599)
- May present as kidney mass lesion(s) resembling renal cell carcinoma
- May be multiple lesions
- Diffuse renal enlargement, sometimes bilateral, can occur
- Renal pelvis thickening alone can occur
- Ureteral stricture
- Multiple organs are affected in 60 - 90% of patients
- Lymphadenopathy is common
- Substantial weight loss (~9 - 14 kg) over months in patients with multiorgan disease
- Up to 90% with elevated serum IgG4 levels (Mod Pathol 2012;25:1181)
- ~50% have hypocomplementemia (low C3, C4 or CH50)
- Peripheral eosinophilia can be seen
Diagnosis
- 3 tiered diagnostic terminology (Mod Pathol 2012;25:1181)
- Histologically highly suggestive of IgG4 related disease
- Requires at least 2 of 3 histologic features:
- Dense lymphoplasmacytic infiltrate
- Fibrosis, usually storiform in character
- Obliterative phlebitis
- > 40% IgG4/IgG plasma cell ratio
- IgG4+ plasma cells/high power field > 30 in surgical specimen or > 10 in biopsy specimen
- Requires at least 2 of 3 histologic features:
- Probable histological features of IgG4 related disease
- Lacks the full histological spectrum or immunohistochemical profile associated with IgG4 related disease
- Usually only a single histopathological feature, typically a dense lymphoplasmacytic infiltrate and required numbers of IgG4+ cells
- Requires additional clinical, serological or radiological evidence to confirm the diagnosis of IgG4 related disease:
- Serum IgG4 > 135 mg/dl
- Other organ involvement, as demonstrated by radiological or pathological examination
- Or other evidence of IgG4 related disease
- Lacks the full histological spectrum or immunohistochemical profile associated with IgG4 related disease
- Insufficient histopathological evidence of IgG4 related disease
- Outside of 2 categories above
- Does not necessarily exclude the diagnosis of IgG4 related disease entirely
- May reflect sampling artifact, prior treatment or advanced fibrotic stage
- Histologically highly suggestive of IgG4 related disease
Laboratory
- Elevated total serum IgG or IgG4 levels (79 - 90% of patients) (Clin Exp Nephrol 2011;15:615, J Am Soc Nephrol 2011;22:1343)
- ~50% have hypocomplementemia with decreased C3 (42%) or C4 (46%) (J Am Soc Nephrol 2011;22:1343)
- Hypergammaglobulinemia
- Eosinophilia (33%)
Radiology description
- Single or multiple mass lesion(s) within the kidney (N Engl J Med 2012;366:539)
- Masses may extend into perinephric tissues
- Masses in other organs may be clue to diagnosis
Prognostic factors
- > 80% response rate with ~10% relapse rate has been achieved in a Japanese cohort (Arthritis Rheumatol 2015;67:1688)
- Elevation in serum IgG4 and IgE levels and an increased number of circulating eosinophils could predict IgG4 related disease relapses independently
- No consensus has been reached regarding patients at high risk of relapse
- Can recur in kidney allografts (Am J Transplant 2018;18:1799)
Case reports
- 28 year old man with recurrent IgG4 related tubulointerstitial nephritis concurrent with chronic active antibody mediated rejection (Am J Transplant 2018;18:1799)
- 40 year old man with IgG4 related membranous glomerulonephritis and generalized lymphadenopathy without pancreatitis (BMC Nephrol 2017;18:139)
- 56 year old man with a right renal mass suspected of being malignant (Case Rep Surg 2017;2017:9690218)
- 80 year old woman with IgG4 related inflammatory pseudotumor mimicking renal cell carcinoma (Oncol Lett 2016;11:3438)
- 81 year old man with IgG4 related tubulointerstitial nephritis and membranous glomerulonephritis during the clinical course of gastric cancer (Mod Rheumatol 2019;29:542)
Treatment
- Glucocorticoids (Arthritis Rheumatol 2015;67:1688)
- Rituximab may be appropriate if relapse or glucocorticoid treatment is contraindicated (Arthritis Rheumatol 2015;67:1688)
Gross description
- Resection specimens of the kidney may show masses / tumor-like lesions
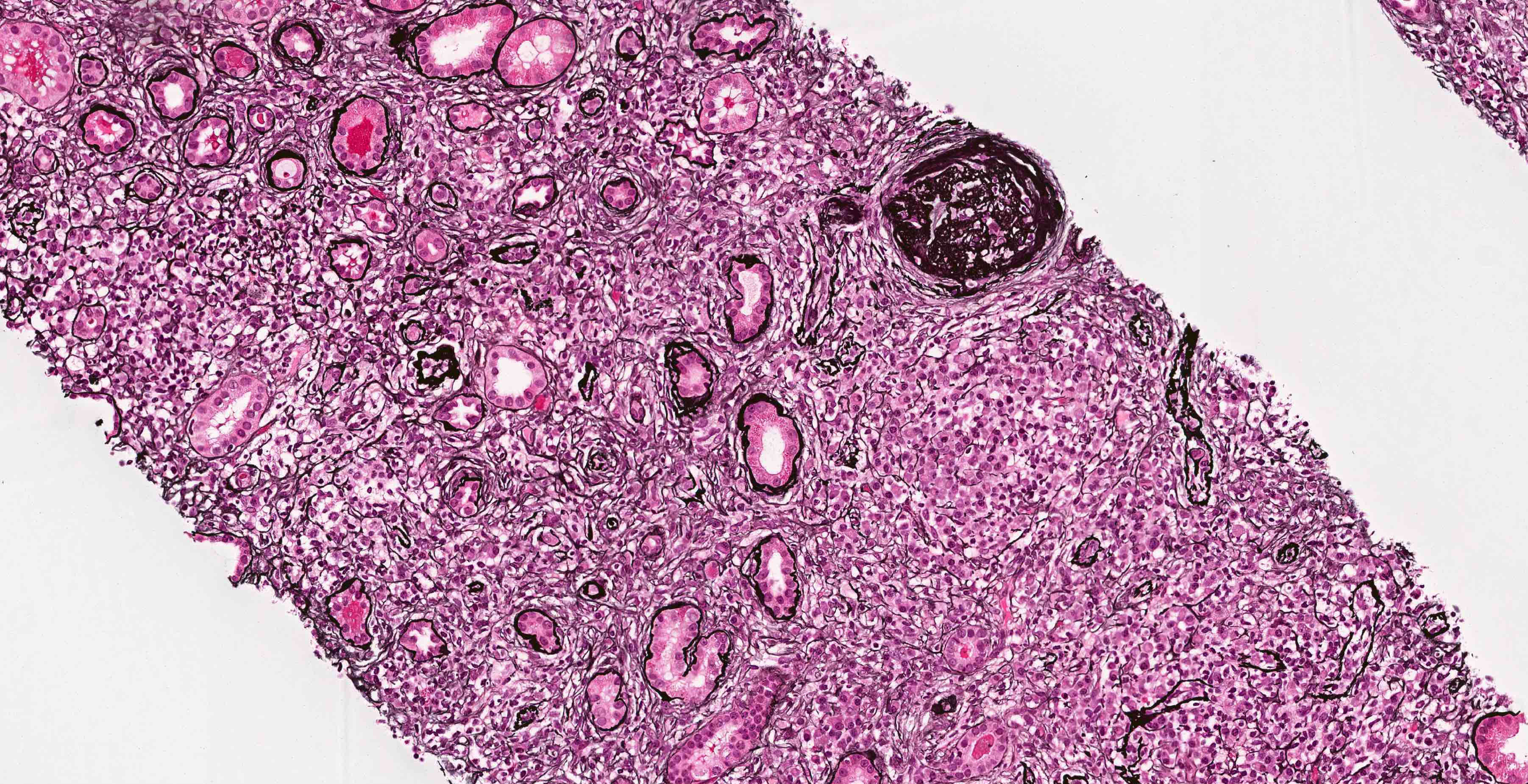
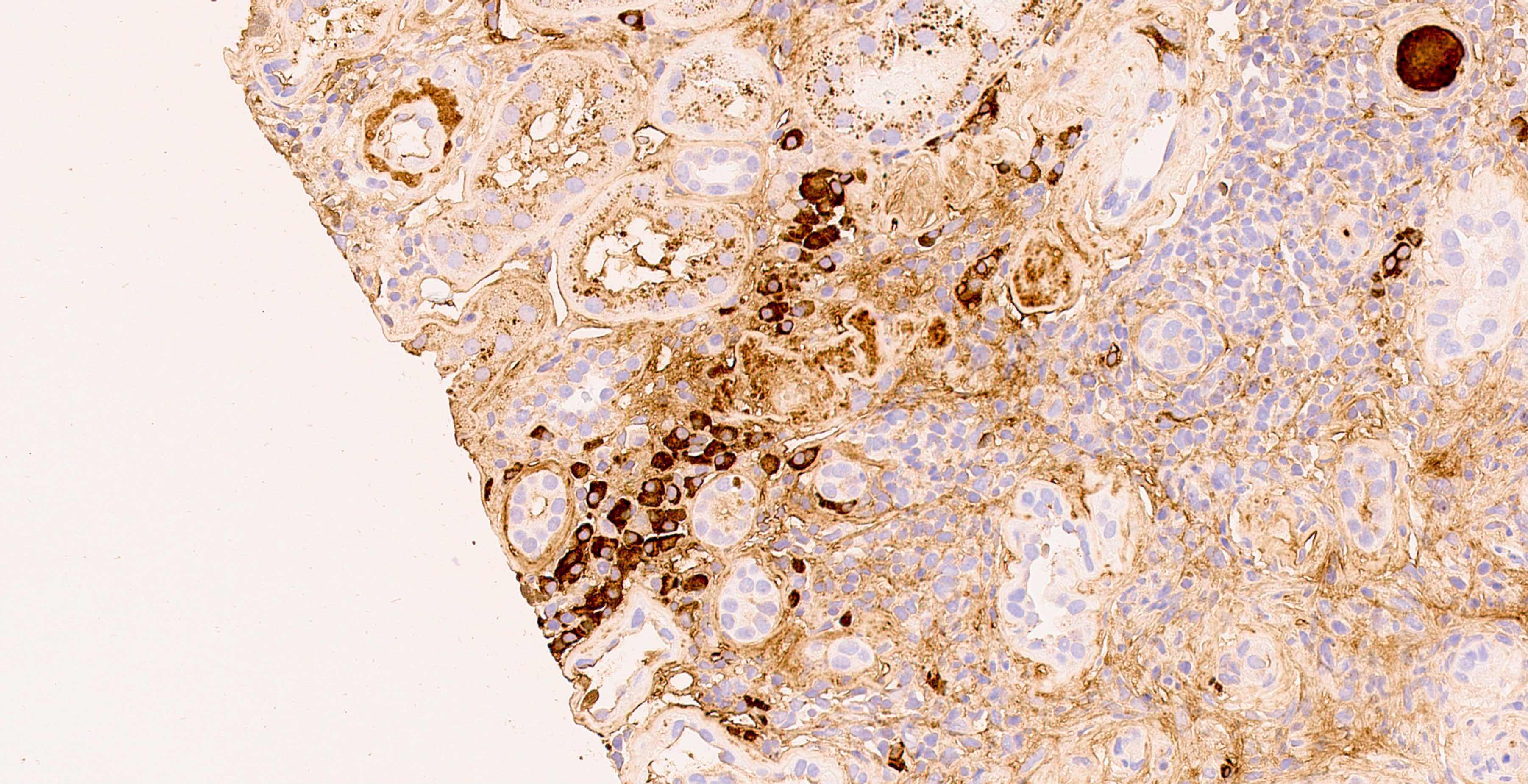
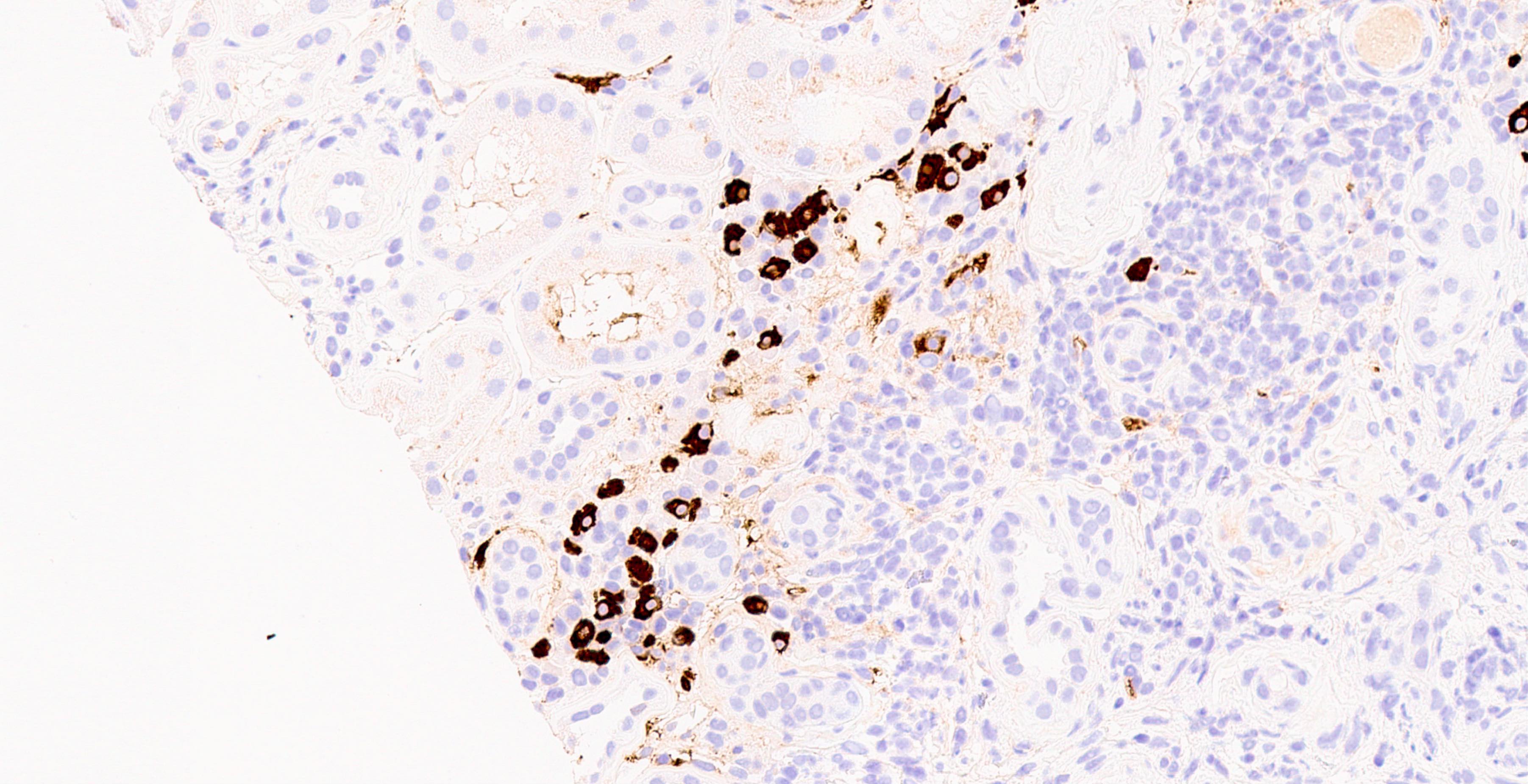
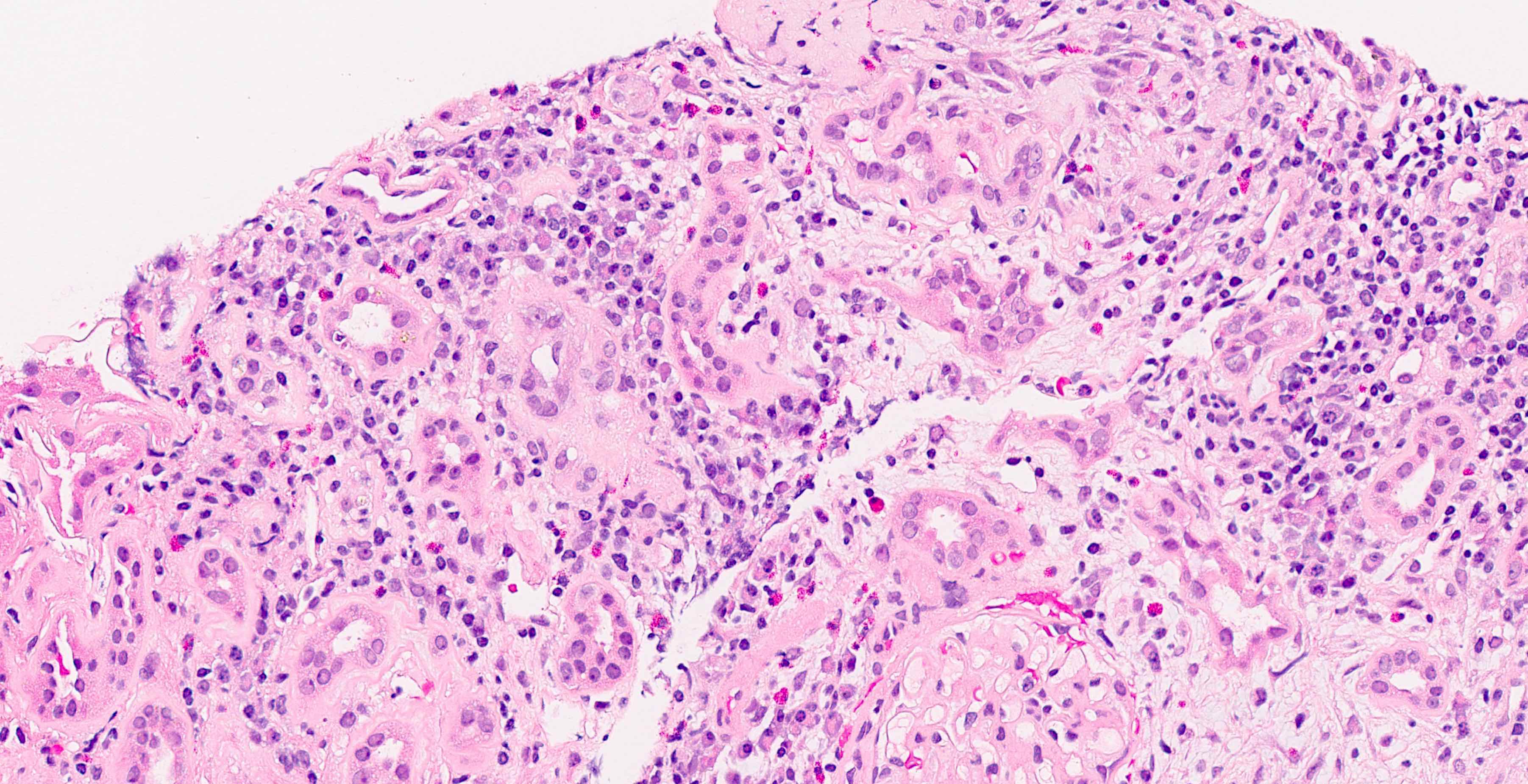
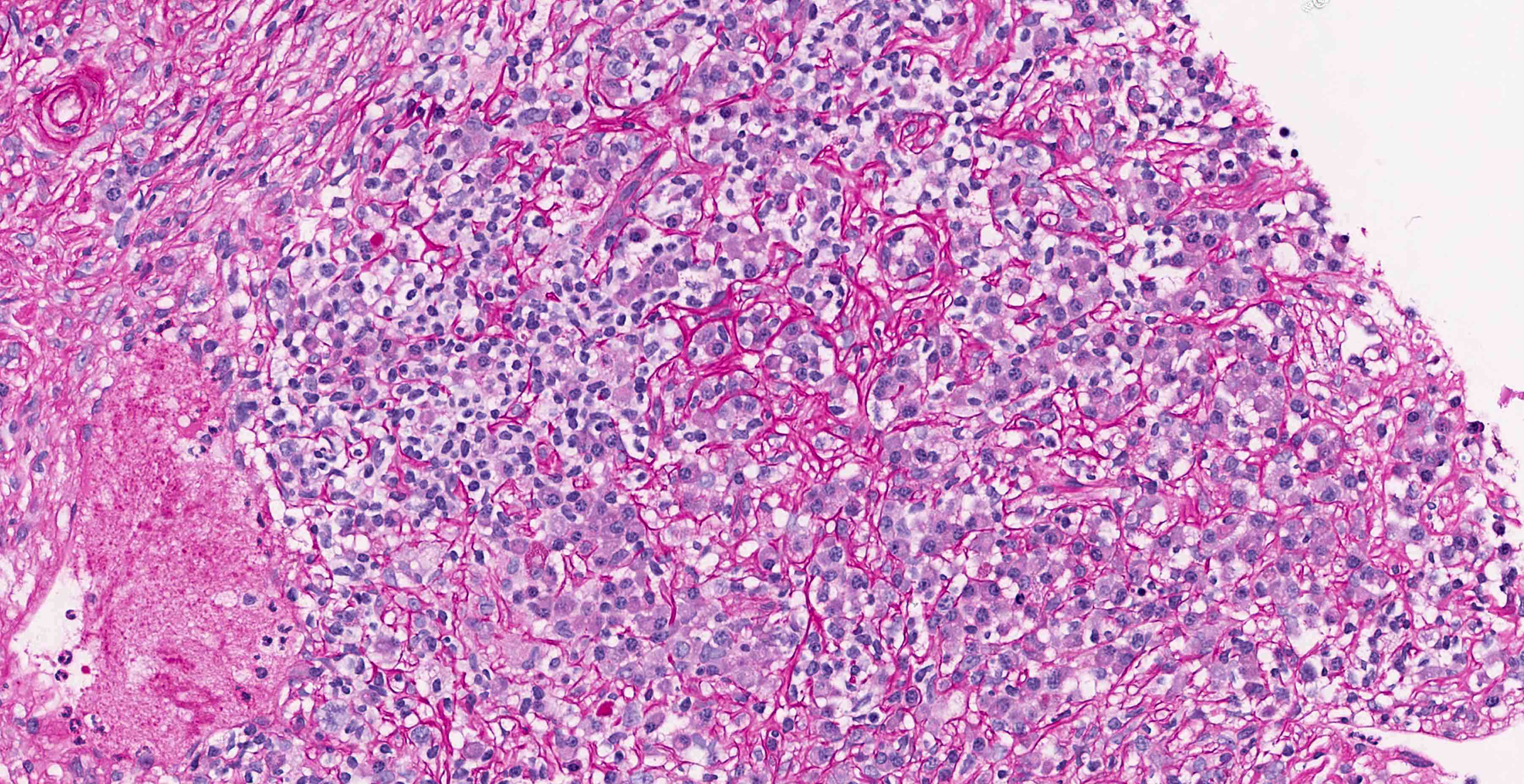
Microscopic (histologic) description
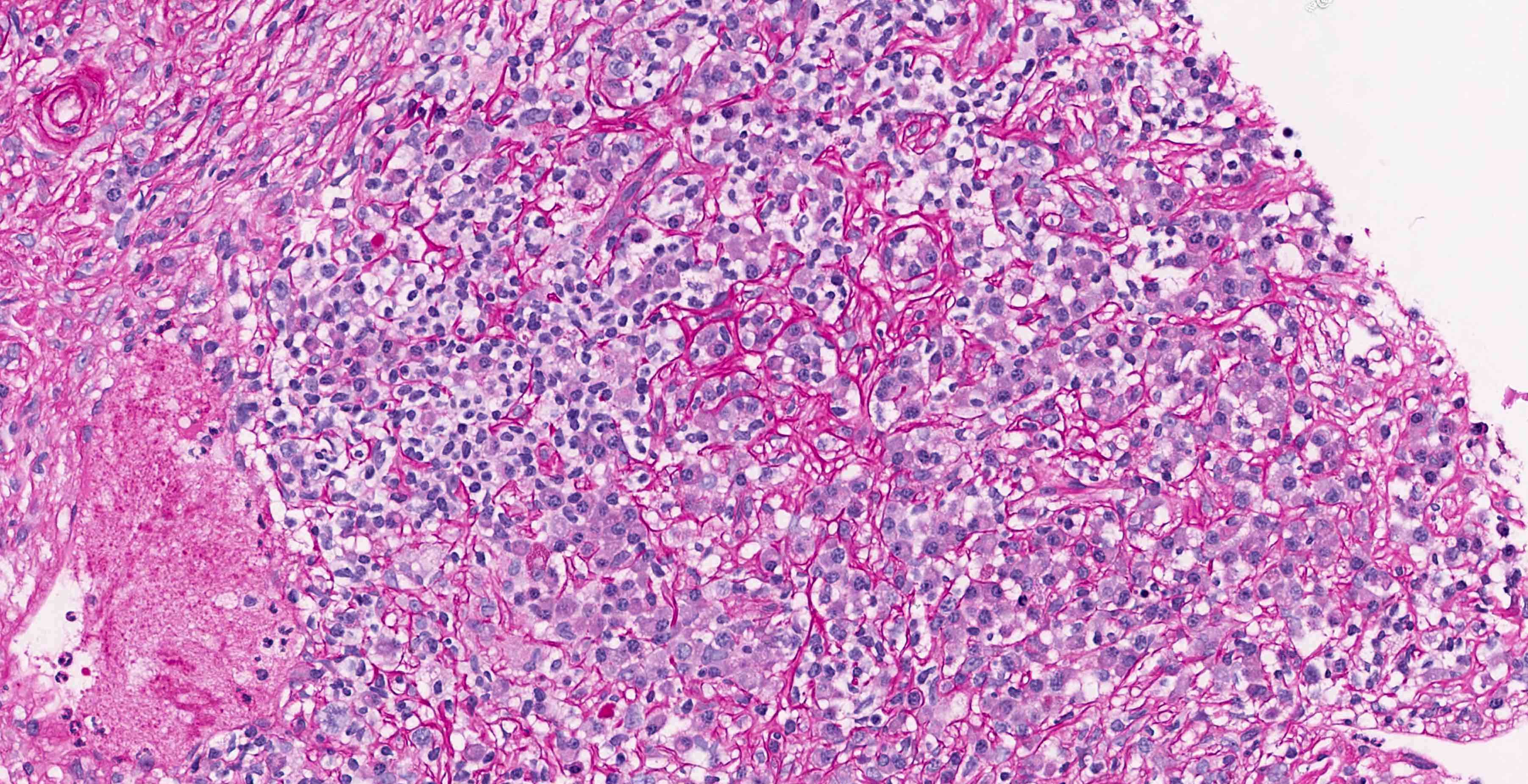
- Most cases show chronic interstitial nephritis with dense lymphoplasmacytic interstitial inflammation with prominent plasma cells (J Am Soc Nephrol 2011;22:1343)
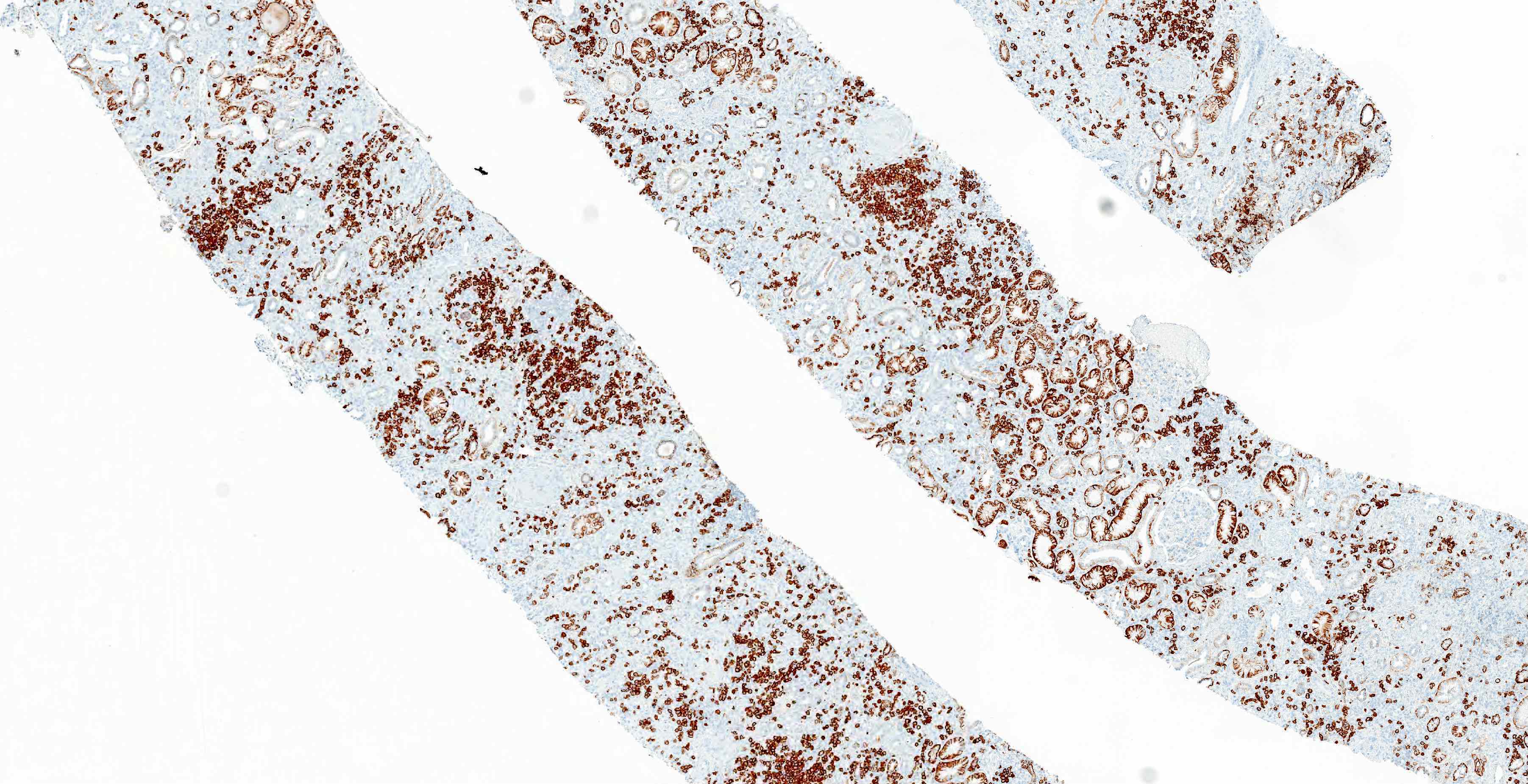
- Increased IgG4+ plasma cells
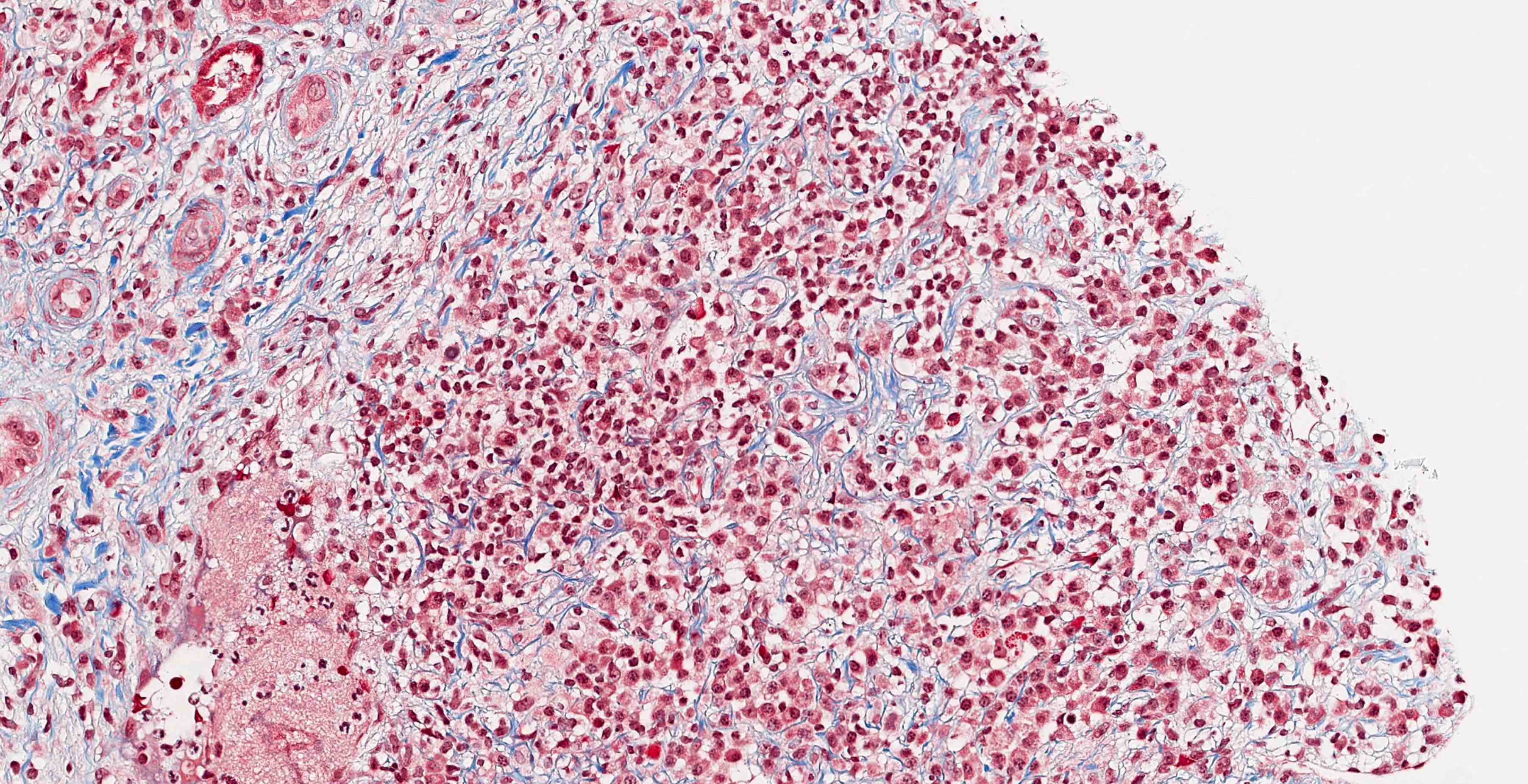
- Storiform fibrosis
- Often marked effacement of tubulointerstitial compartment
- Tubulitis may be present
- Tubular basement membrane deposits may be seen on trichrome stain
- Obliterative phlebitis usually not seen in kidney biopsies
- Rarely, injury pattern may resemble acute interstitial nephritis
- Glomeruli may show membranous pattern of injury (Nat Rev Nephrol 2015;11:599)
- True degree of interstitial fibrosis is difficult to estimate on biopsy alone
- Granulomatous inflammation or necrosis should not be present and excludes diagnosis of IgG4 disease
Microscopic (histologic) images
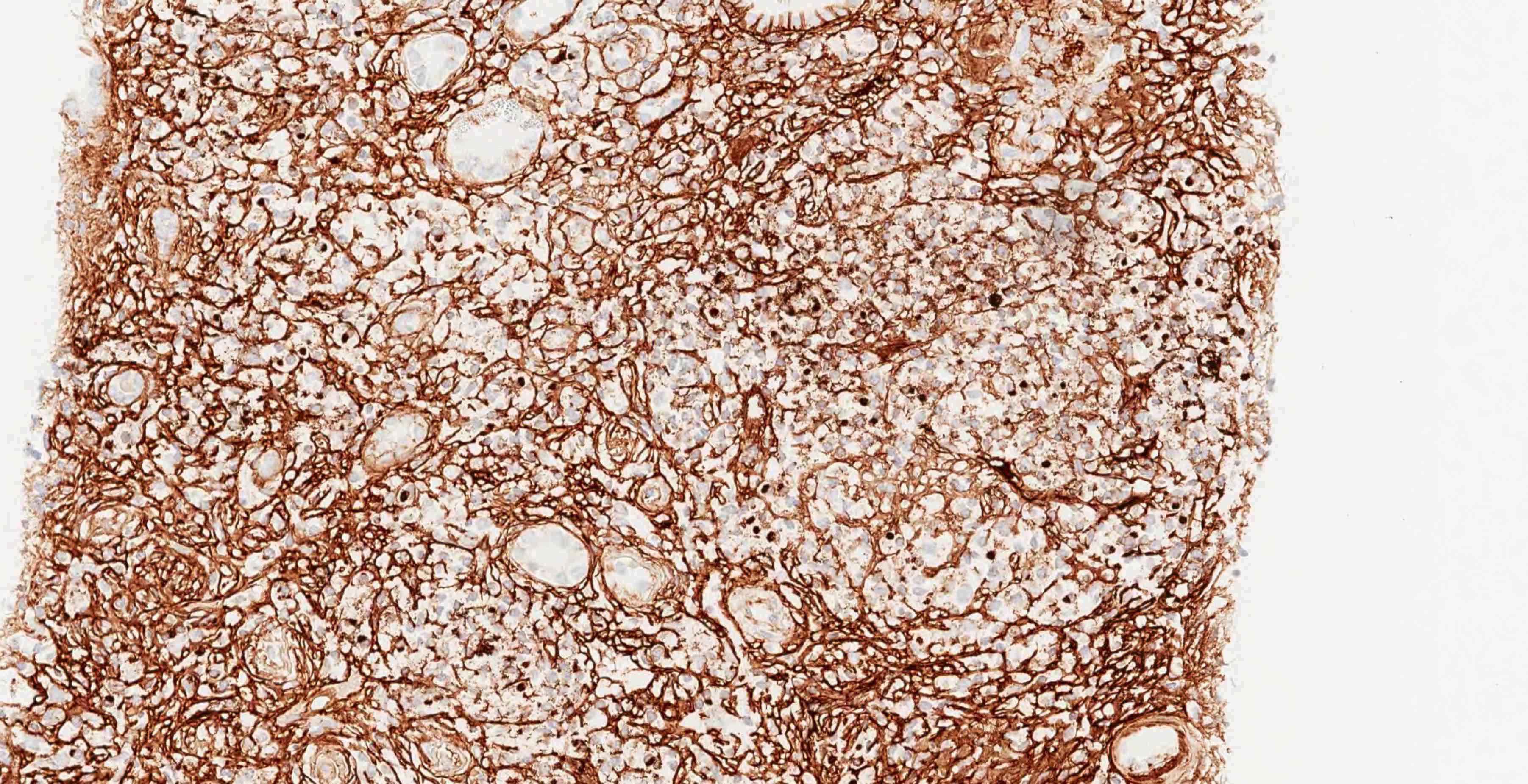
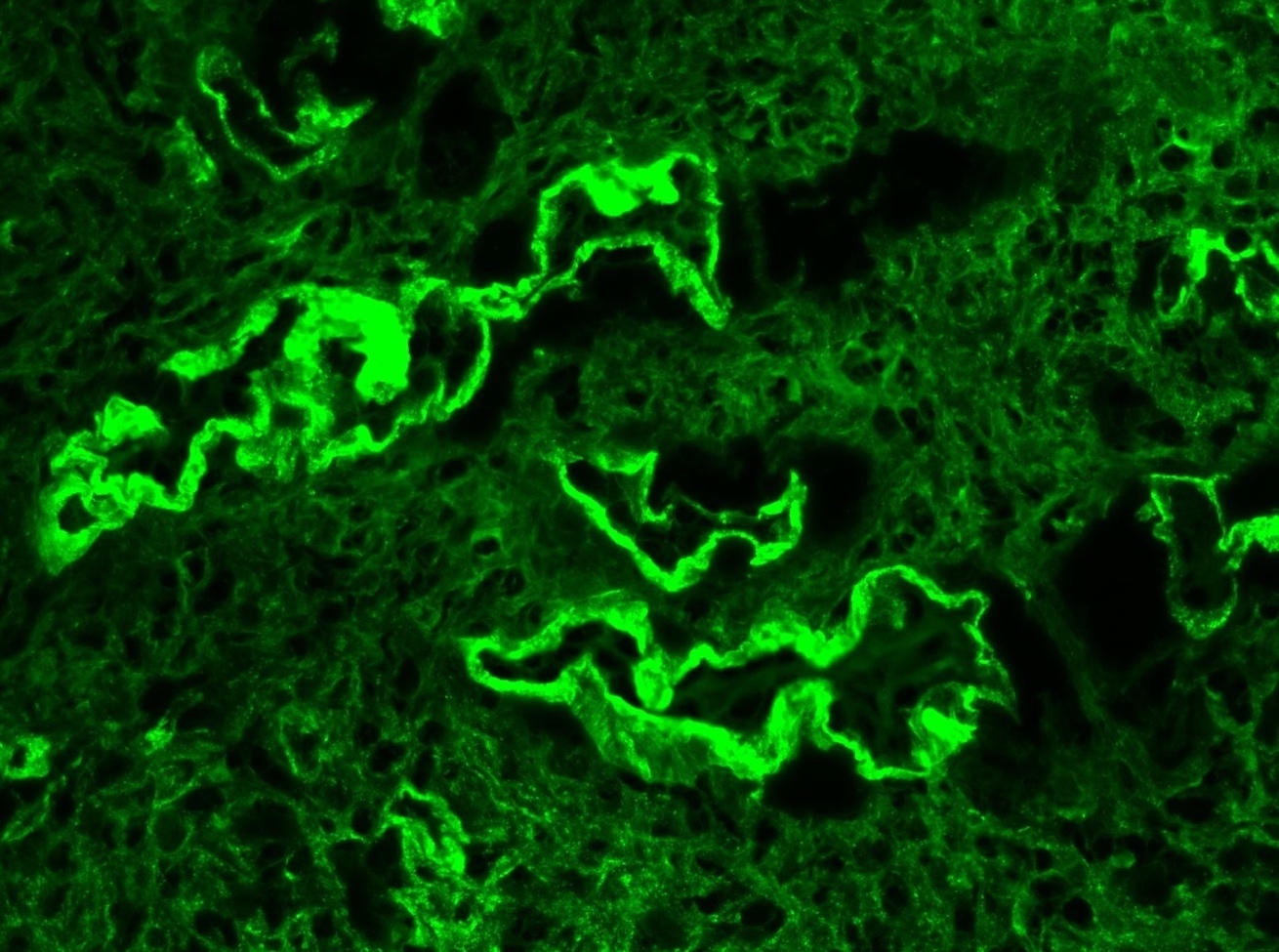
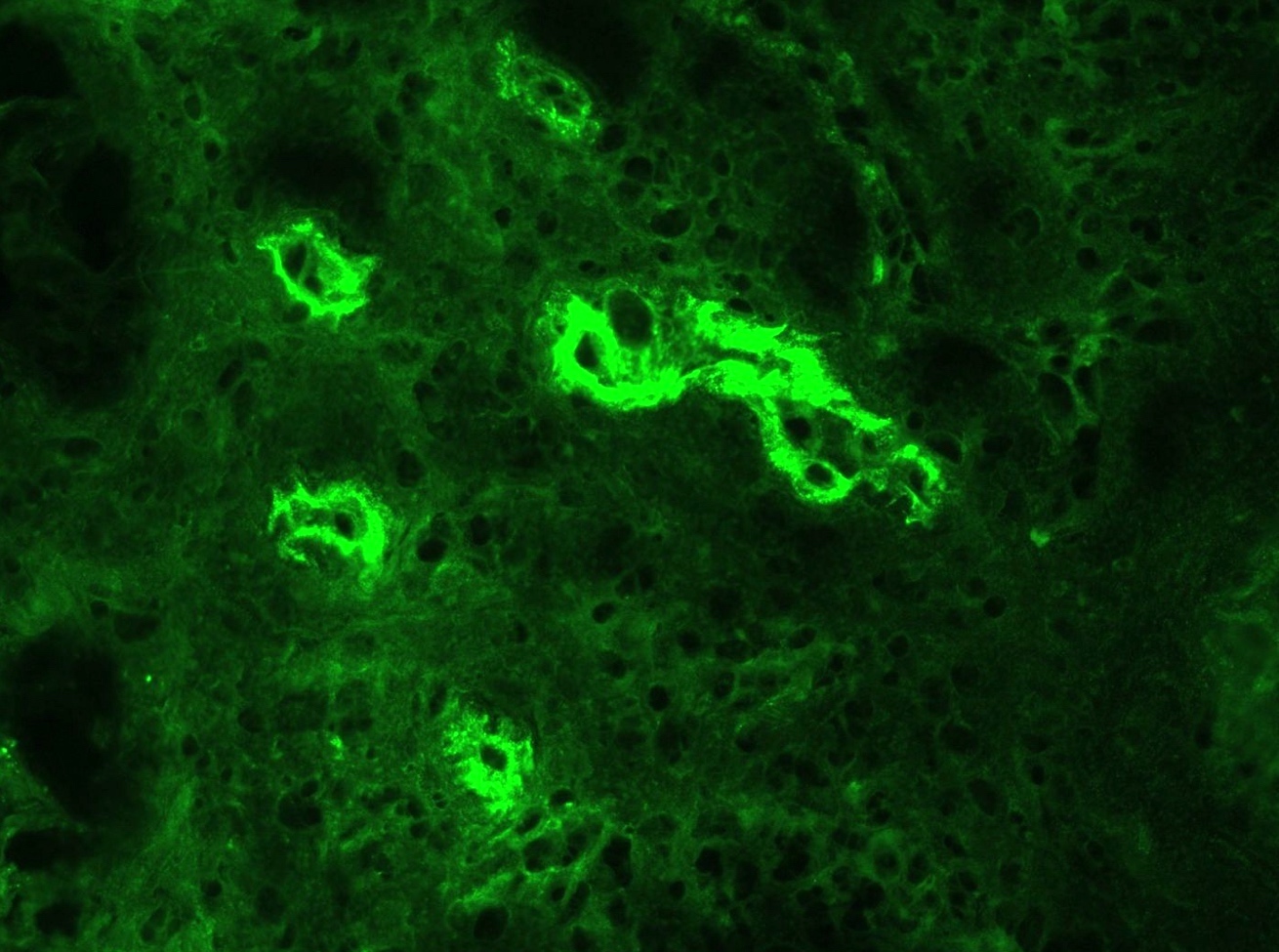
Immunofluorescence description
- Tubulointerstitium
- Granular tubular basement membrane deposits
- Majority show IgG (predominantly IgG4) (J Am Soc Nephrol 2011;22:1343)
- Both light chains
- C1q and IgM less common
- Tend to be concentrated in areas of fibrosis and may be absent in uninvolved areas
- Plasma cells may show staining with IgG and both light chains
- Quantification of IgG4 plasma cells is not recommended on immunofluorescence tissue
- Granular tubular basement membrane deposits
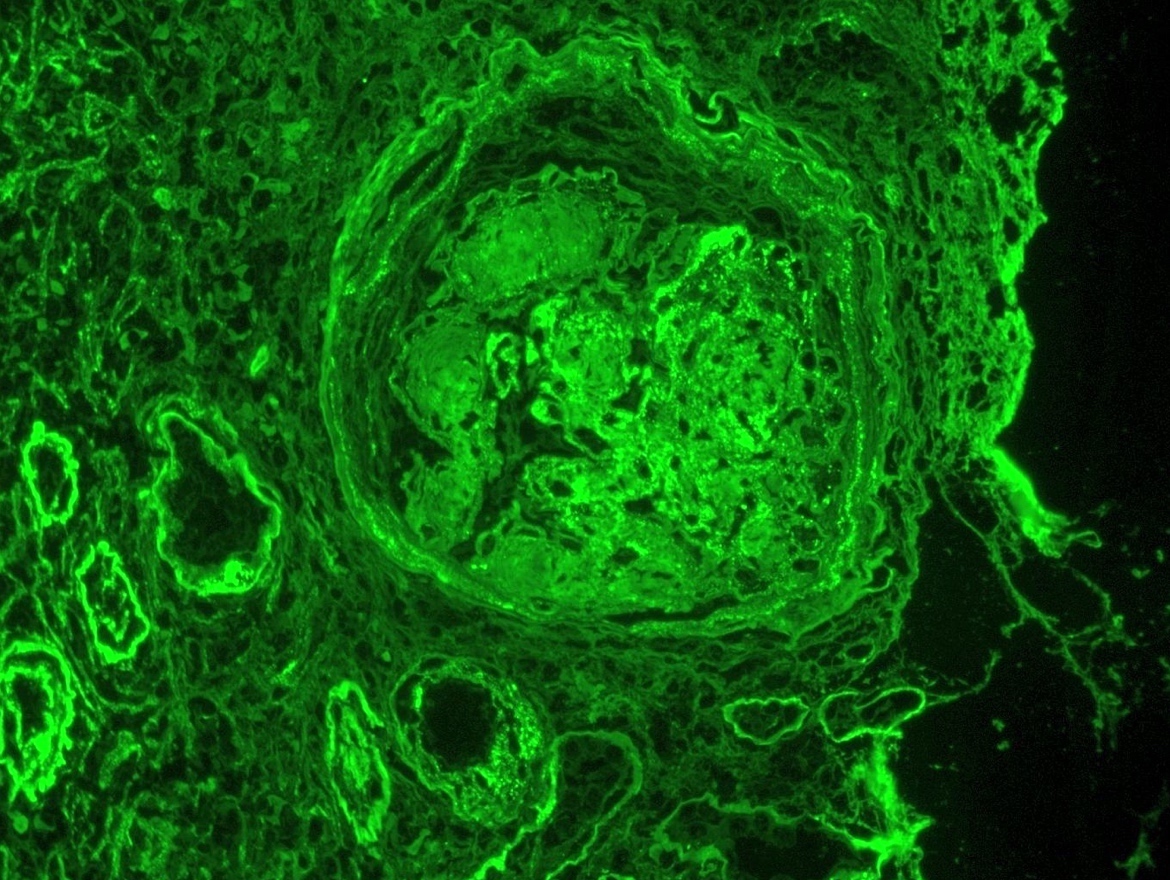
- Glomerulus
- If membranous glomerulopathy present: granular capillary loop staining
- IgG, C3 and light chain staining
- Some cases without membranous pattern may show granular mesangial staining
- Glomeruli may show negative staining if no membranous component
- Bowman capsule deposits may be seen (Adv Chronic Kidney Dis 2017;24:94)
- If membranous glomerulopathy present: granular capillary loop staining
Immunofluorescence images
Positive stains
- CD138 can highlight increased plasma cells
- IgG4 shows increased positivity in plasma cells (J Am Soc Nephrol 2011;22:1343)
- Jones methenamine silver (JMS), PAS and trichrome stains can highlight storiform fibrosis
- Jones methenamine silver (JMS) stain can highlight membrane capillary spike / pinhole pattern
- Trichrome can highlight tubular basement membrane and capillary deposits
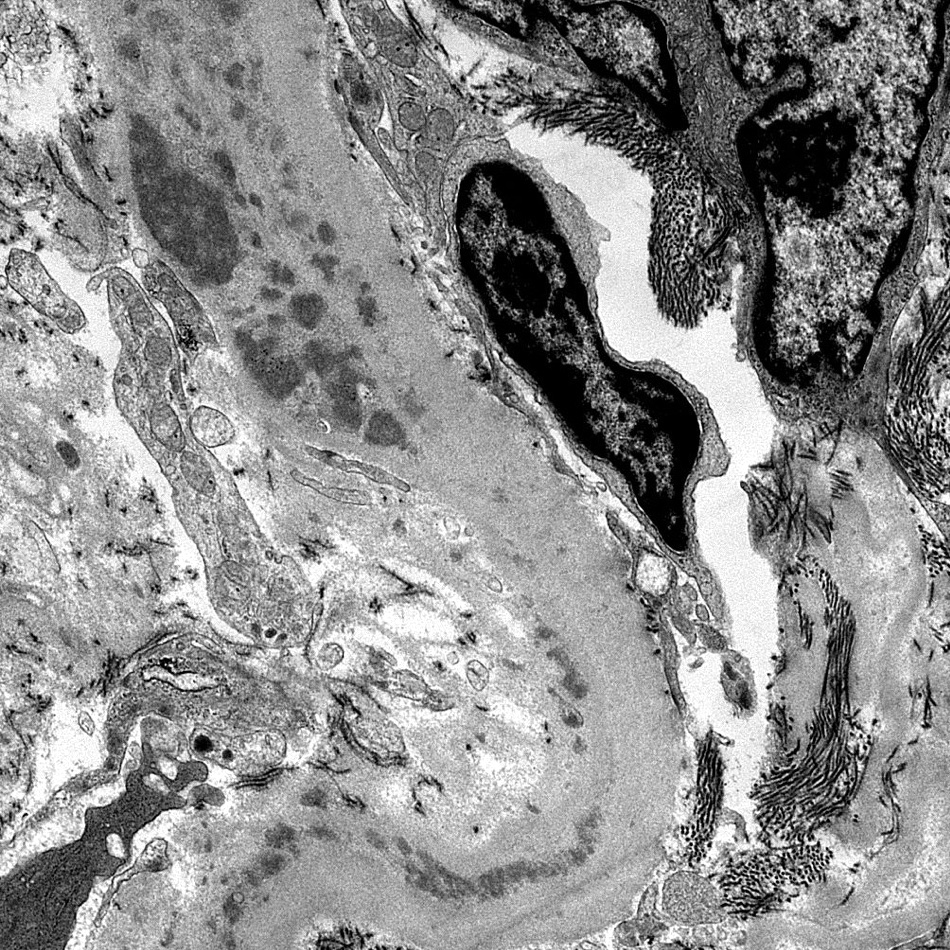
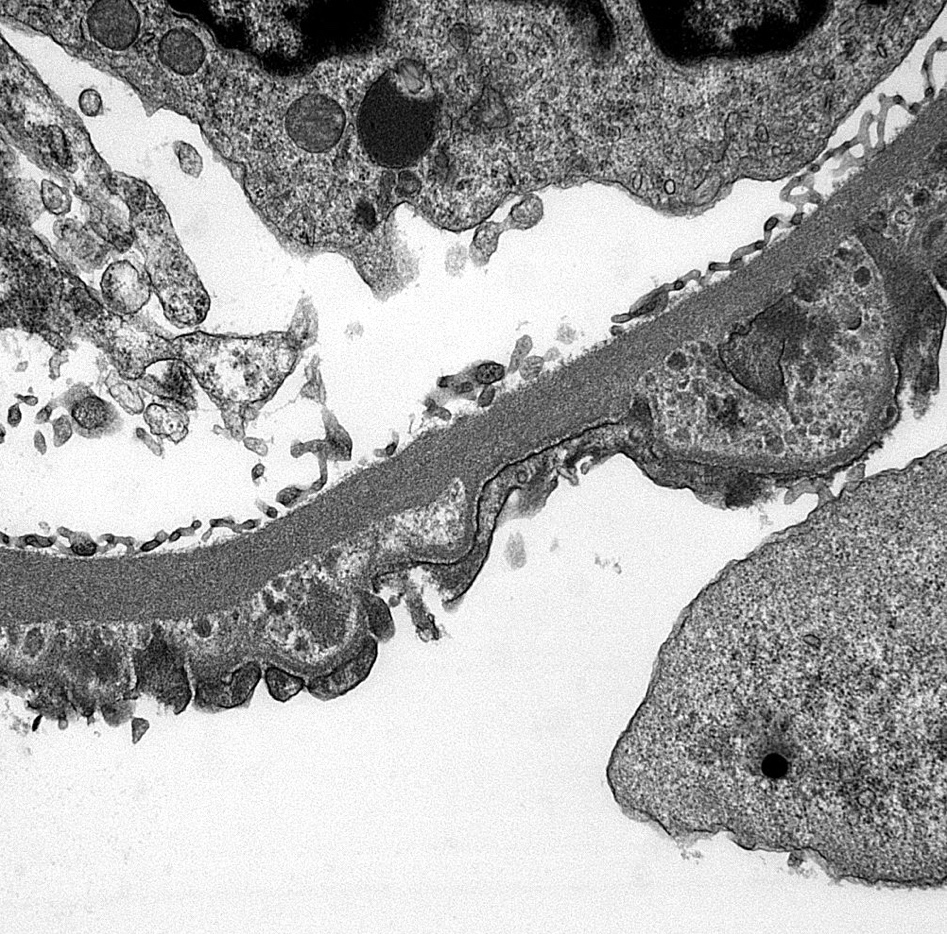
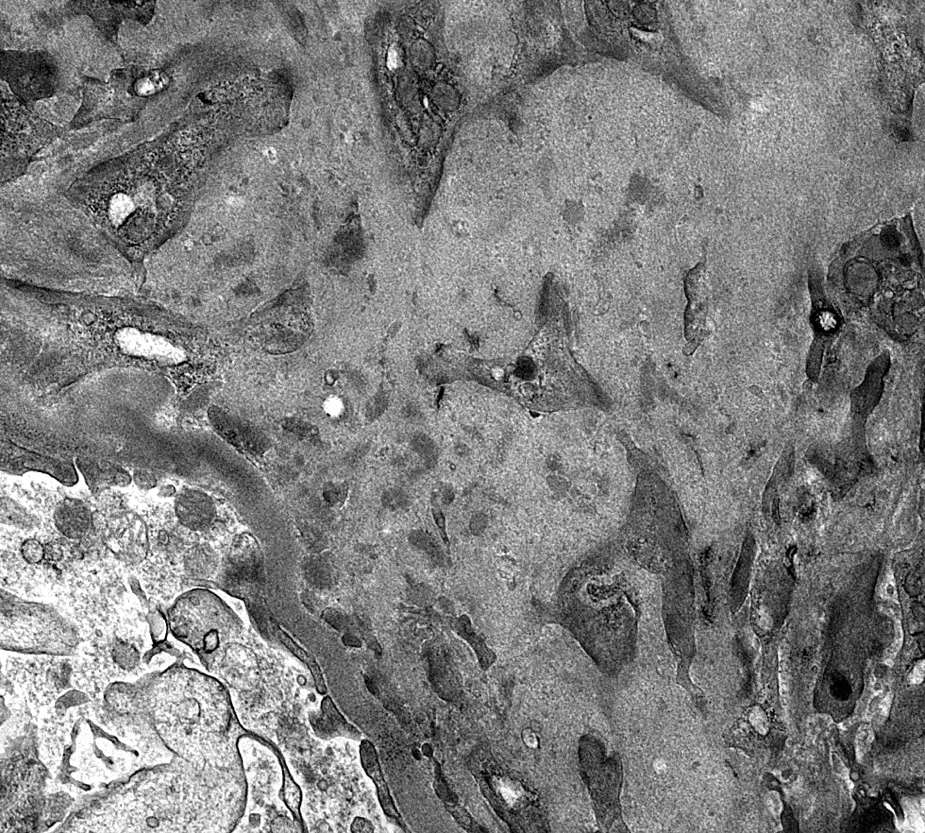
Electron microscopy description
- Electron dense deposits, without substructure, along tubular basement membranes
- Subepithelial deposits associated with glomerular basement membrane remodeling if membranous component present
- Identical to any other cause of membranous nephropathy pattern of injury
- May see increased interstitial type collagen bundles
- Some have proposed classification of fibrosis based on pattern of collagen bundles (Hum Pathol 2012;43:536)
Electron microscopy images
Sample pathology report
- Kidney, needle core biopsy:
- Chronic interstitial nephritis with increased IgG4 positive plasma cells and storiform fibrosis
- Membranous glomerulopathy
- Comment: The morphologic features in this biopsy including > 10 IgG4 positive plasma cells/high powered field and an IgG/IgG4 plasma cell ratio of > 40% are highly suggestive of IgG4 related tubulointerstitial nephritis. Correlation with serum IgG4 levels is recommended. ANCA related disease can also show increased IgG4 positive plasma cells and thus correlation with ANCA serologies is recommended. Membranous glomerulopathy can be a manifestation of IgG4 related renal disease; however, serological / clinical correlation is recommended to completely exclude other etiologies for membranous nephropathy (e.g. other systemic rheumatologic disease, chronic infections, malignancy and idiopathic / primary membranous nephropathy).
Differential diagnosis
- Sjögren syndrome related tubulointerstitial nephritis:
- Usually no tubular basement membrane deposits, no increased IgG4 plasma cells, no storiform fibrosis
- Interstitial inflammation associated with pauci-immune (ANCA associated) glomerulonephritis:
- May show increased IgG4 plasma cells
- Usually will show other features such as necrotizing / crescentic glomerulonephritis, vasculitis, medullary angiitis; no tubular basement membrane deposits
- Allergic / drug related acute or chronic interstitial nephritis:
- Usually no tubular basement membrane deposits; plasma cells usually not prominent
- No increased IgG4 plasma cells; no storiform fibrosis, may show increased eosinophils
- Chronic pyelonephritis:
- May show increased plasma cells
- No tubular basement membrane deposits, no increased IgG4+ plasma cells
- Lupus nephritis:
- May show active and chronic interstitial nephritis with tubular basement membrane deposits
- Usually glomerulonephritis is present
- Full house immunofluorescence staining (staining with all 3 Ig classes [IgG, IgA, IgM] and both complement proteins [C1q and C3])
- No increased IgG4+ plasma cells
- Clinical history and serologic findings can be characteristic
- Small B cell lymphomas (e.g. extranodal marginal zone):
- May show a chronic interstitial nephritis-like pattern with increased plasma cells
- May form mass lesion
- Should show numerous B cells with light chain restriction
- Diabetic nephropathy:
- May show increased interstitial IgG4+ plasma cells
- May be difficult to differentiate from true IgG4 tubulointerstitial nephritis
- IgG4 patients may have diabetes from autoimmune pancreatitis
- Multicentric Castleman and Erdheim-Chester disease:
- May show dense lymphoplasmacytic inflammation sometimes with increased IgG4+ plasma cells (Am J Kidney Dis 2017;69:e19)
- Other etiologies of membranous glomerulopathy:
- Clinical history for secondary causes and other markers for membranous etiologies can help differentiate (e.g. phospholipase A2 receptor, thrombospondin containing domain 7A (THSD7A), exostosin 1/2)
- Anti-brush border antibody disease / Anti-LRP2 nephropathy:
- Also has granular tubular basement membrane deposits and membranous pattern glomerulopathy
- Has less tubulointerstitial inflammation, fewer IgG4+ plasma cells, no storiform fibrosis and positive staining of TBM deposits for LRP2 / megalin
- Lacks systemic features of IgG4 related disease
Board review style question #1
Board review style answer #1
Board review style question #2
Which of the following renal lesions is most likely to be present in IgG4 related disease?
- Chronic tubulointerstitial nephritis
- Glomerular crescent formation
- Membranous glomerulonephritis
- Mesangial immune complex deposition
Board review style answer #2