Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Immunofluorescence images | Positive stains | Electron microscopy description | Electron microscopy images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Khan A, Minhas MK, Memon A. Acute postinfectious glomerulonephritis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneypoststrep.html. Accessed April 25th, 2024.
Definition / general
- Infection related glomerulonephritis (GN) encompasses the entities of postinfectious GN, IgA dominant (Staphylococcus associated) infection related glomerulonephritis, endocarditis associated glomerulonephritis and shunt nephritis
- Classic poststrep glomerulonephritis is usually seen in children and has a good prognosis; infection related glomerulonephritis in adults is mostly concurrent with infection and has a poorer outcome; these are more likely to be IgA and C3 codominant and humps are usually not seen on electron microscopy (Glomerular Dis 2021;1:82)
- Postinfectious glomerulonephritis is secondary to bacterial, viral, mycotic or parasitic infections (Dtsch Med Wochenschr 2020;145:240, Pediatr Clin North Am 2022;69:1051)
Essential features
- Poststreptococcal glomerulonephritis (PSGN) most frequently presents in children 1 - 2 weeks after a sore throat or 6 weeks after a skin infection (impetigo)
- It is characterized by diffuse exudative, hypercellular glomerulonephritis with prominent endocapillary hypercellularity and numerous neutrophils
- On immunofluorescence, appears as small, irregular, coarse granular (lumpy bumpy) deposits of polyclonal IgG and C3 along the glomerular capillary walls with scattered mesangial deposits
- On electron microscopy, has characteristic hump type large subepithelial deposits, occasional mesangial deposits and rare subendothelial deposits without significant glomerular basement membrane reaction
- It has an excellent prognosis, especially in children, with 95% completely recovering with conservative therapy within 6 - 8 weeks
- ~1% develop rapidly progressive glomerulonephritis and another 1 - 2% develop chronic glomerulonephritis
Terminology
- Acute postinfectious glomerulonephritis (APIGN)
- Poststreptococcal glomerulonephritis (PSGN)
ICD coding
Epidemiology
- Primarily affects children aged 3 - 12 years with a mean age of 6 - 8 years
- Uncommon in children younger than 3 years
- M:F = 2:1 (Pediatr Clin North Am 2022;69:1051)
- Adult cases are well documented (Medicine (Baltimore) 2008;87:21)
- It is rare in industrialized countries
- Incidence is also decreasing in developing countries mainly because of improvement in public health and frequent use of antibiotics (Front Med (Lausanne) 2018;5:327)
Sites
- Kidney glomeruli
Pathophysiology
- Immunological disease; representing a type II or type III hypersensitivity reaction
- Immune complexes containing the streptococcal antigen are formed
- Nephritis associated plasmin receptor (NAPlr) and streptococcal pyrogenic exotoxin B (SPeB) are the 2 common antigens associated with the pathogenesis of PSGN
- Staphylococcal antigen may function as a superantigen
- Immune complex deposition in glomeruli or in situ formation of the antigen antibody complex within the kidney glomeruli
- In situ immune complex formation is either due to a reaction against streptococcal antigens deposited in the glomerular basement membrane or due to an antibody reaction against glomerular components that crossreact with streptococcal antigen due to molecular mimicry (Paediatr Int Child Health 2017;37:240, Pediatr Rev 2015;36:3)
- Activation of the alternate complement pathway, resulting in hypocomplementemia, infiltration of the leukocytes and proliferation of the mesangial cells in the glomerulus, thus impairing the capillary perfusion and glomerular filtration rate (GFR)
- Reduction in GFR can lead to renal failure (oliguria or anuria), acid base imbalance, electrolyte abnormalities, volume overload, edema and hypertension
Etiology
- Mostly associated with nephritogenic strains of Streptococcus pyogenes (beta hemolytic strep group A)
- Other etiologies include staphylococci, malaria, toxoplasmosis, hepatitis B / C, HIV, varicella, spirochetes, meningococci and other bacteria (Clin J Am Soc Nephrol 2006;1:1179)
Clinical features
- Presentation, clinical course and outcomes of nonstreptococcal cases of APIGN are generally similar to those of PSGN
- A recent identifiable illness is usually present that precedes APIGN, though there is variability in presentation, with the majority of patients having had a preceding upper respiratory tract infection, scarlet fever, impetigo, gastroenteritis, cervical adenitis or no recalled illness (Pediatr Clin North Am 2019;66:59)
- Dark urine (brown, tea or cola colored) is often the first clinical manifestation of PSGN
- Periorbital edema, hypertension or in some cases, generalized edema
- Other features of circulatory congestion, such as dyspnea, may be present
- Nonspecific symptoms including general malaise, weakness and anorexia may also be present
Diagnosis
- Clinicopathological diagnosis
- Diagnosis is confirmed on renal biopsy with characteristic light microscopic features, immunofluorescence and electron microscopic findings
Laboratory
- Serological tests: antistreptolysin O (ASO), antihyaluronidase and DNase B together are highly sensitive to detect an immunological response to prior group A streptococcal infection
- Serum complement level (C3) is usually low due to its consumption in the inflammatory reaction
- Urine analysis
- Shows macroscopic or microscopic hematuria, RBC casts, mild proteinuria
- Only 5% of patients with PSGN have massive proteinuria that indicates nephrotic syndrome
- White blood cell casts, hyaline and cellular casts are usually present in the urine analysis
- Renal function tests: blood urea nitrogen (BUN) and serum creatinine typically elevate during the acute phase (Pediatr Nephrol 2011;26:165)
Prognostic factors
- PSGN has an excellent prognosis especially in children, with 95% completely recovering with conservative therapy within 6 - 8 weeks
- ~1% develop rapidly progressive glomerulonephritis and another 1 - 2% develop chronic glomerulonephritis (Pediatr Int 2001;43:364, Int J Mol Sci 2021;22:905)
- ~50% of the adult patients continue to have reduced renal function, hypertension or persistent proteinuria (J Am Soc Nephrol 2011;22:187)
Case reports
- 3 year old girl with IgA dominant postinfectious glomerulonephritis (IgA PIGN) presented with acute renal failure, edema, hypertension and heavy proteinuria (BMC Nephrol 2022;23:333)
- 4 year old boy who developed acute glomerulonephritis following pneumococcal bacteremia (Singapore Med J 2014;55:e69)
- 12 year old boy and 18 year old woman with atypical presentation of acute postinfectious glomerulonephritis and sickle cell disease (BMC Nephrol 2020;21:56)
- 32 year old woman diagnosed with postinfectious glomerulonephritis secondary to parvovirus B19 infection (Clin Nephrol 2016;85:238)
- 46 year old man with Granulicatella, a nutritionally variant Streptococcus (NVS) species, that developed infective endocarditis and glomerulonephritis (IDCases 2020;21:e00792)
- 74 year old diabetic woman that developed postinfectious glomerulonephritis with crescents (Cureus 2020;12:e11440)
Treatment
- Self limiting condition in the majority of cases and thus requires symptomatic treatment only
- Main aim is to control the complications of volume overload such as hypertension and edema, which are prominent during the acute phase of the disease
- Pharmacological therapy
- Antimicrobials
- Patients with evidence of a streptococcal infection should receive a course of antibiotic therapy; however, they may not prevent the development of PSGN
- Diuretics
- Loop diuretics increase urinary output and consequently improve cardiovascular congestion and hypertension
- Antihypertensive medications
- Blood pressure can be managed by restricting salt and fluid intake along with diuretics as needed
- In cases with uncontrolled blood pressure, the use of calcium channel blockers is recommended
- Use of angiotensin converting enzyme inhibitors (ACEI), angiotensin receptor blockers (ARBs) is recommended in patients with stable GFR and with near normal potassium levels
- Immunosuppressive therapy
- Steroids, immunosuppressive agents and plasmapheresis are not generally indicated
- However, patients with progressive renal failure or the presence of crescents on the renal biopsy may warrant the use of corticosteroids (Cureus 2018;10:e3150, J Pediatr 1981;98:403)
- Antimicrobials
- Dialysis
- Dialysis is only performed to manage the acid base balance, electrolyte abnormalities (especially hyperkalemia) and fluid management
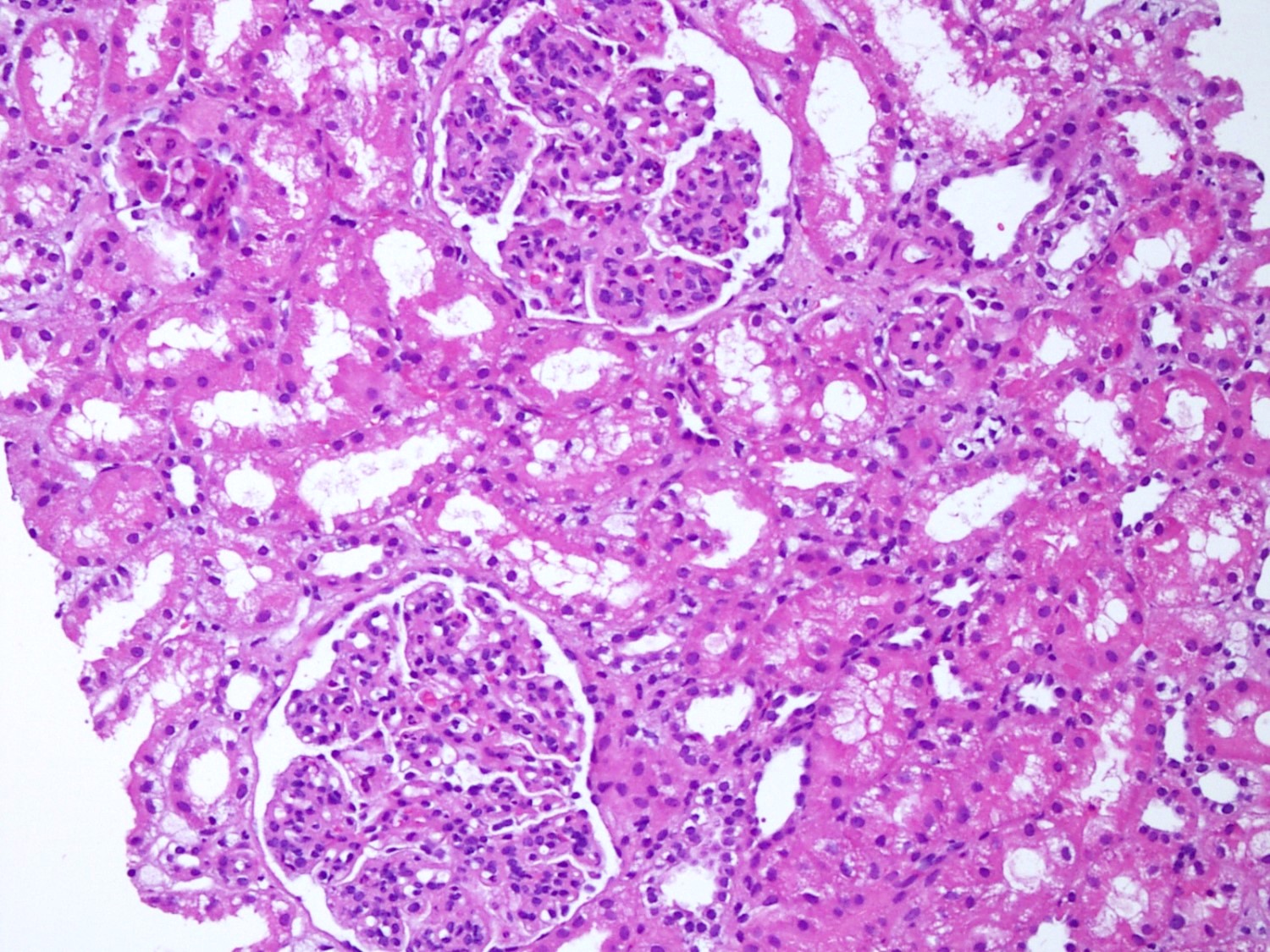
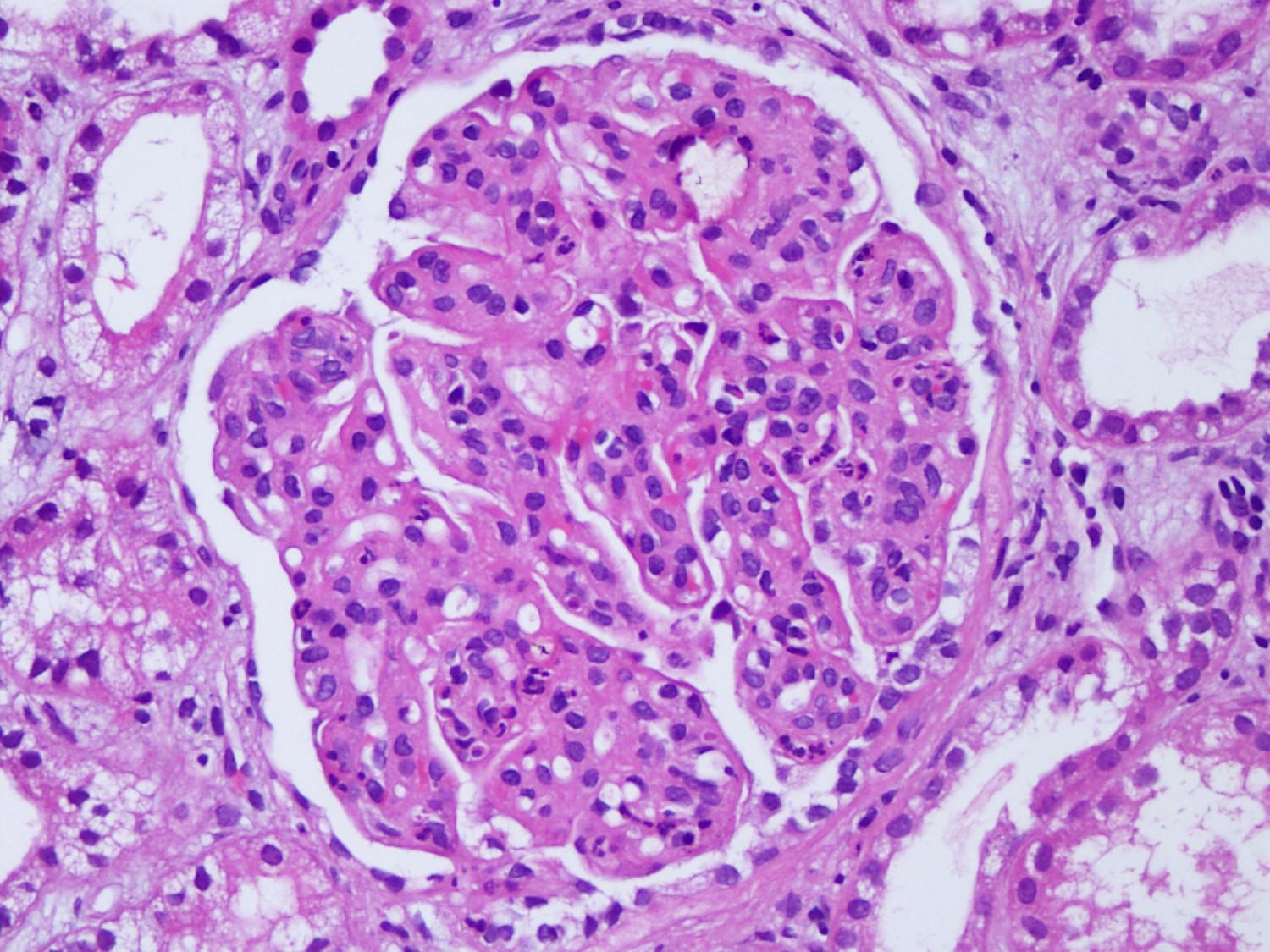
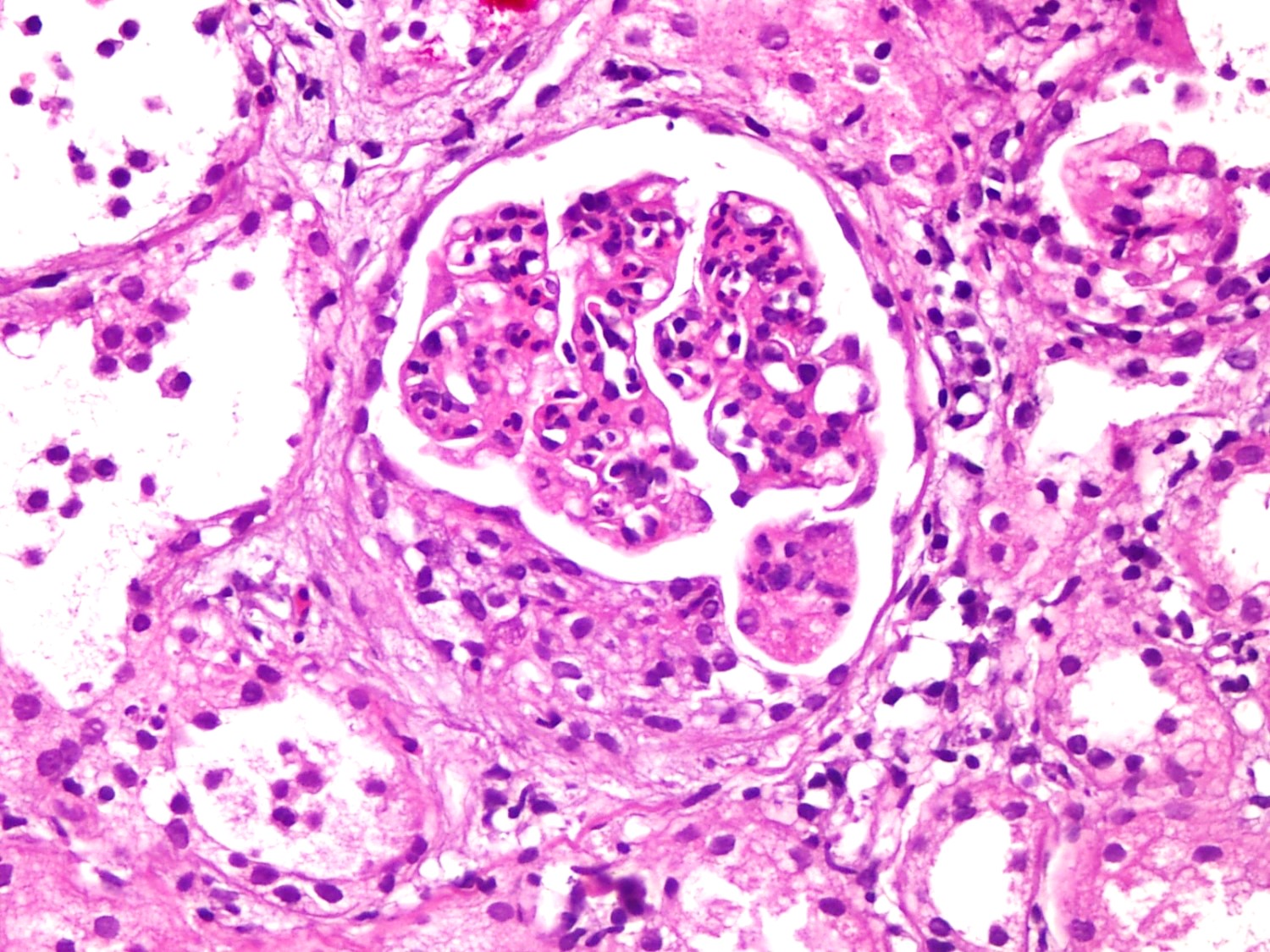
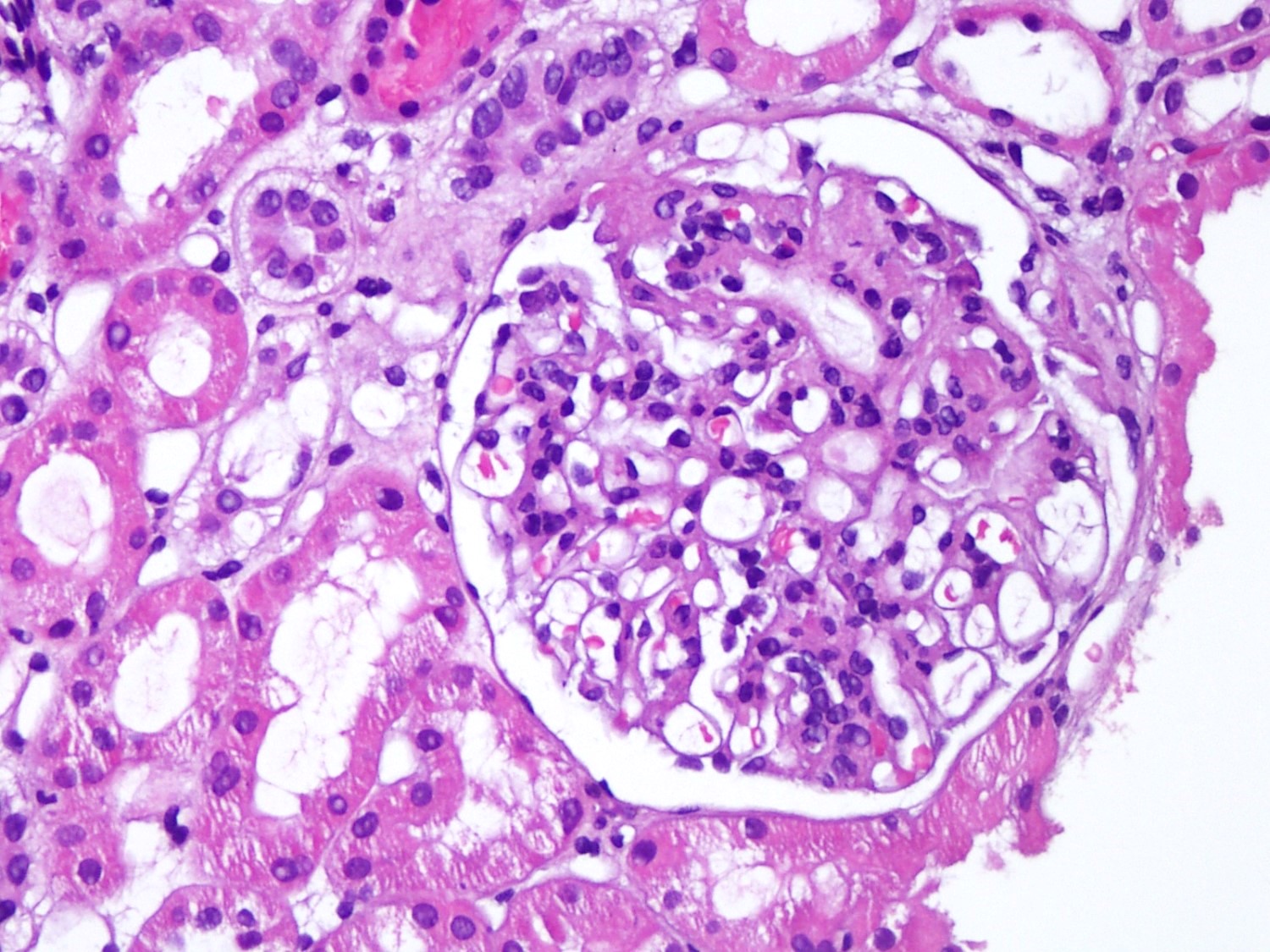
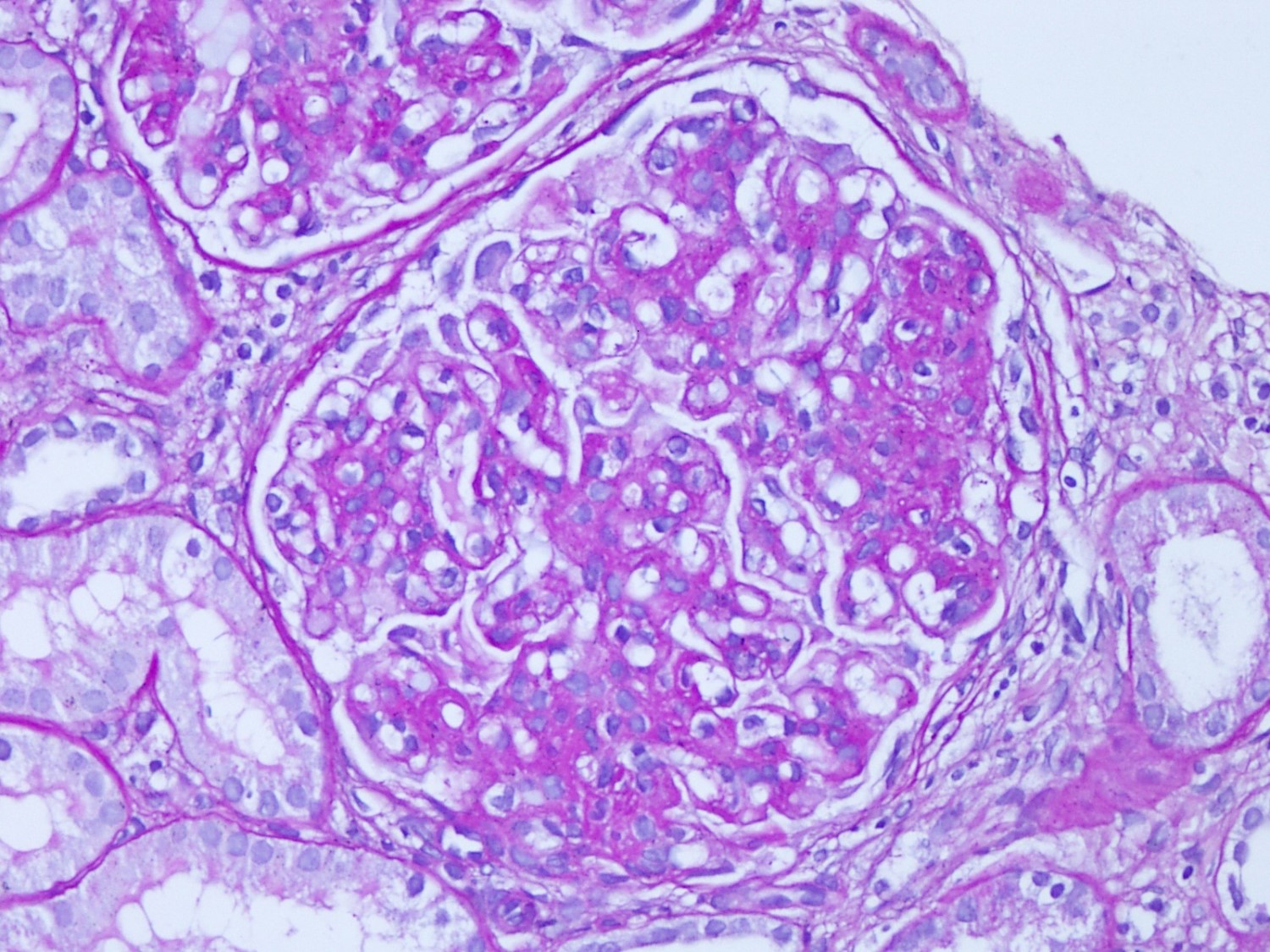
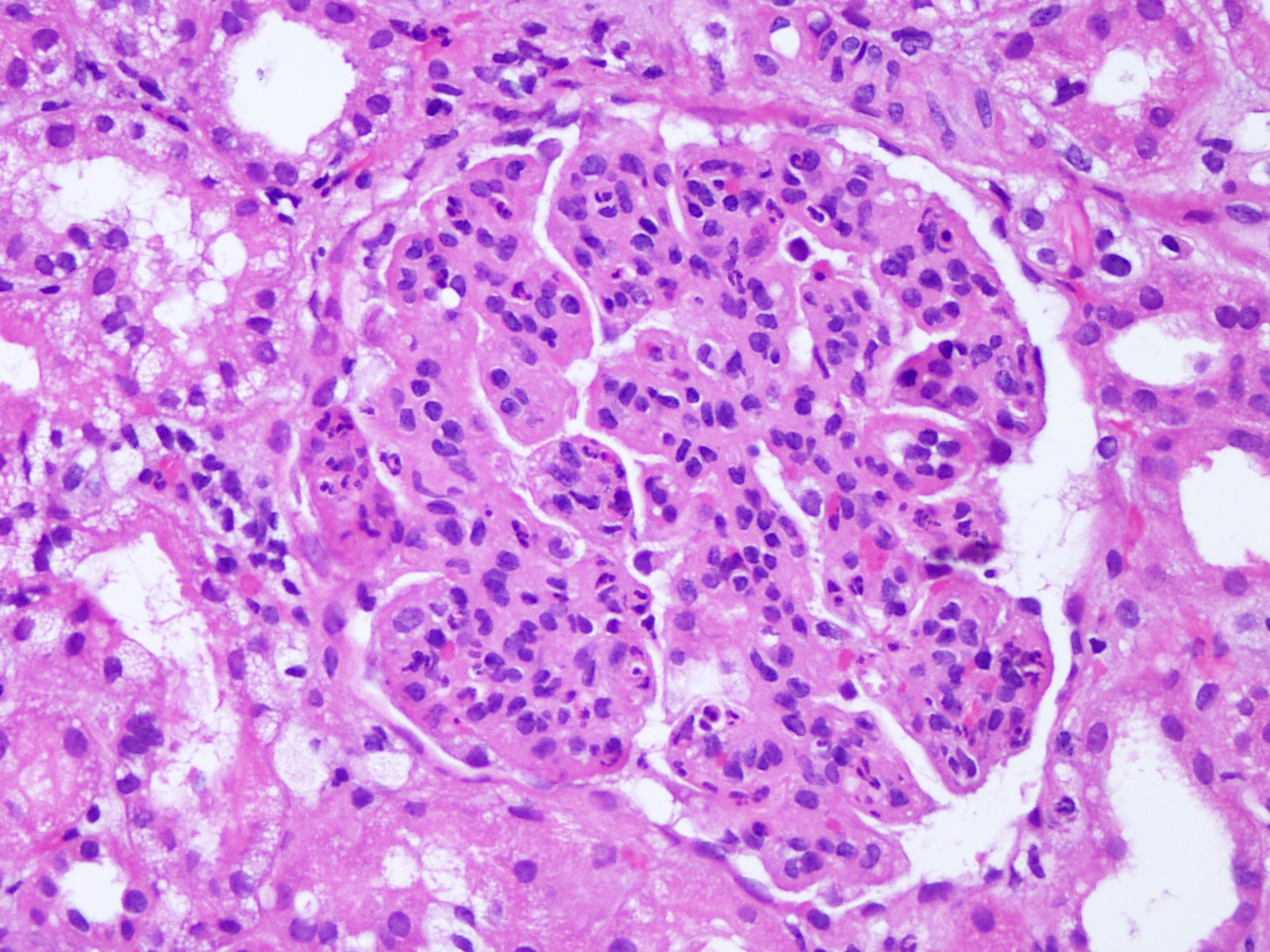
Microscopic (histologic) description
- Glomeruli are diffusely, segmentally or globally enlarged with endocapillary and mesangial hypercellularity resulting in a lobular configuration
- Neutrophilic (hence, exudative glomerulonephritis) and later mononuclear infiltration of glomeruli
- Proliferation of mesangial cells and endothelial cells with mesangial edema and inflammatory cells obstructing the capillary lumina
- Capillary basement membranes are of normal thickness
- Glomerular fibrinoid necrosis, microthrombosis and cellular crescents are rare but can be seen in the setting of rapidly progressive glomerulonephritis (RPGN) (Paediatr Int Child Health 2017;37:240)
- In the later stages of the disease, the glomerular lesions progressively lose neutrophils and the endocapillary hypercellularity evolves into pure mesangial hypercellularity
- Mild mesangial cellularity and matrix expansion may persist for several years, which eventually resolves to leave a normal appearing glomerulus
- Interstitial and tubular leukocyte infiltrate can be prominent
- Tubules contain red blood cells, sometimes mixed with eosinophilic cast-like material
- References: Jennette: Heptinstall's Pathology of the Kidney, 2 Volume Set Edition, 2014, Fogo: Diagnostic Atlas of Renal Pathology, 3rd Edition, 2016
Microscopic (histologic) images
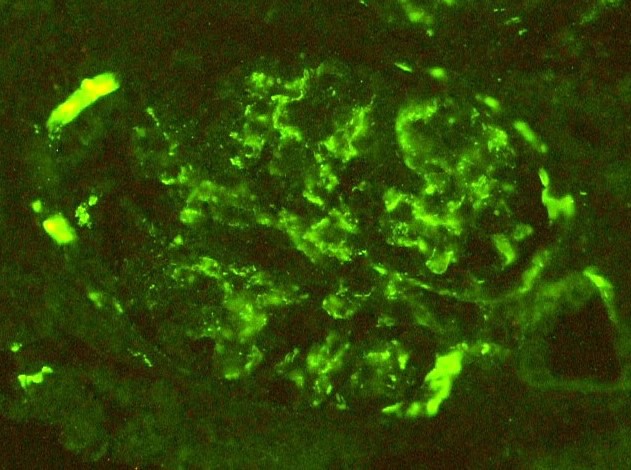
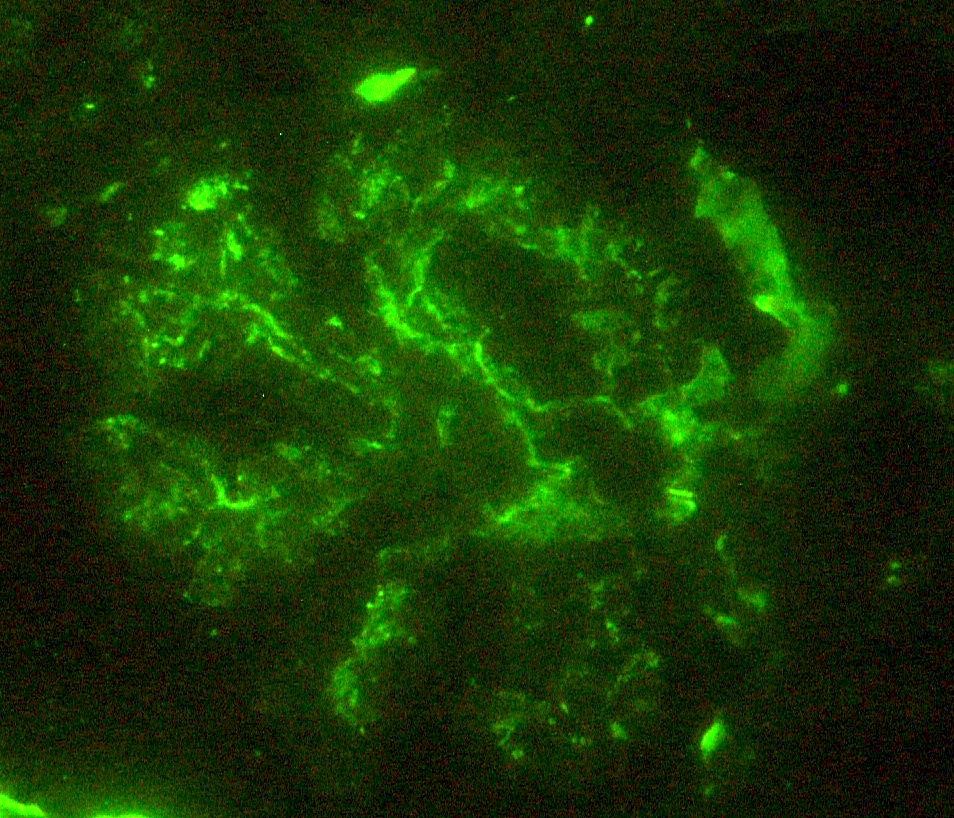
Immunofluorescence description
- Small, irregular, coarse granular (lumpy bumpy) deposits of polyclonal IgG and C3 along the glomerular capillary walls with scattered mesangial deposits
- IgM and IgA staining is absent or minimal except in cases caused by Staphylococcus infection where IgA may be predominant
- C1q or C4 are absent
- Properdin may be present
- Starry sky, garland and mesangial patterns are typically described for poststreptococcal glomerulonephritis
- References: Jennette: Heptinstall's Pathology of the Kidney, 2 Volume Set Edition, 2014, Fogo: Diagnostic Atlas of Renal Pathology, 3rd Edition, 2016
Immunofluorescence images
Positive stains
- PAS, Jones methenamine silver and trichrome are used to evaluate the morphology
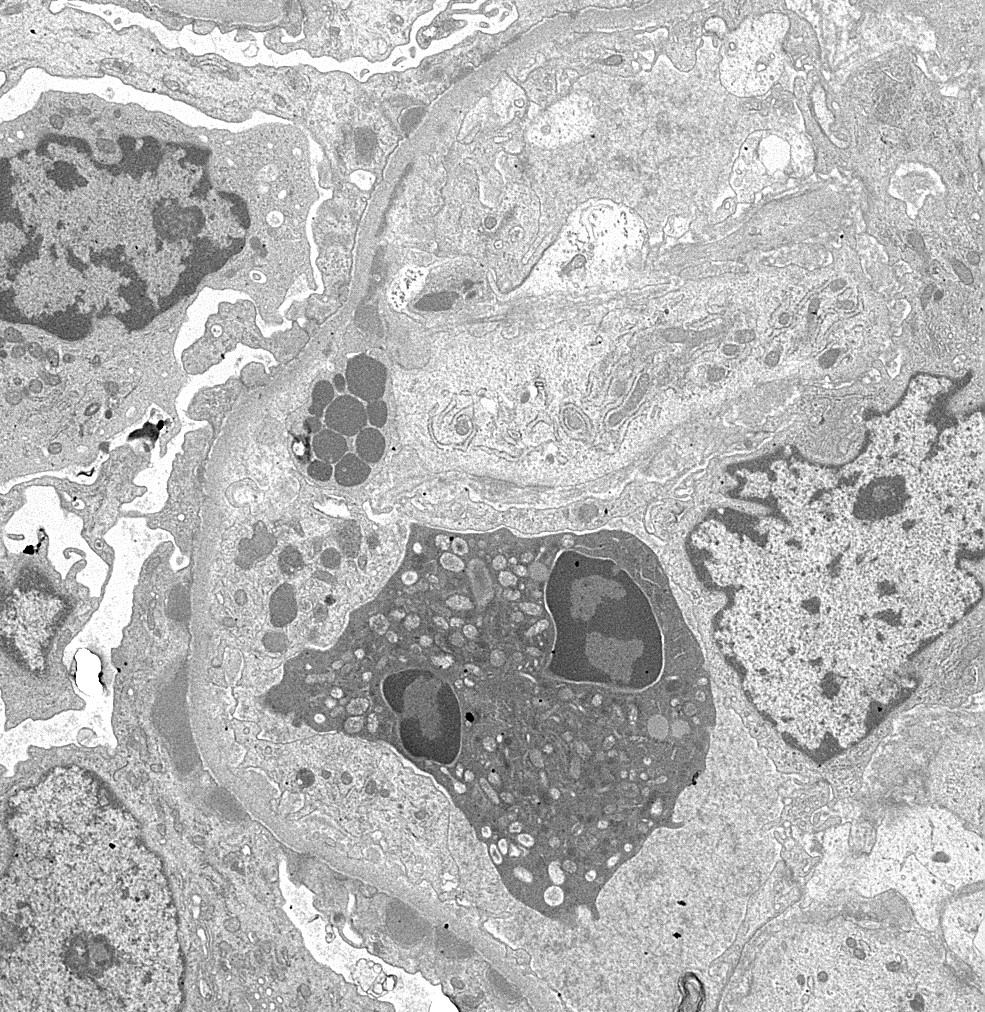
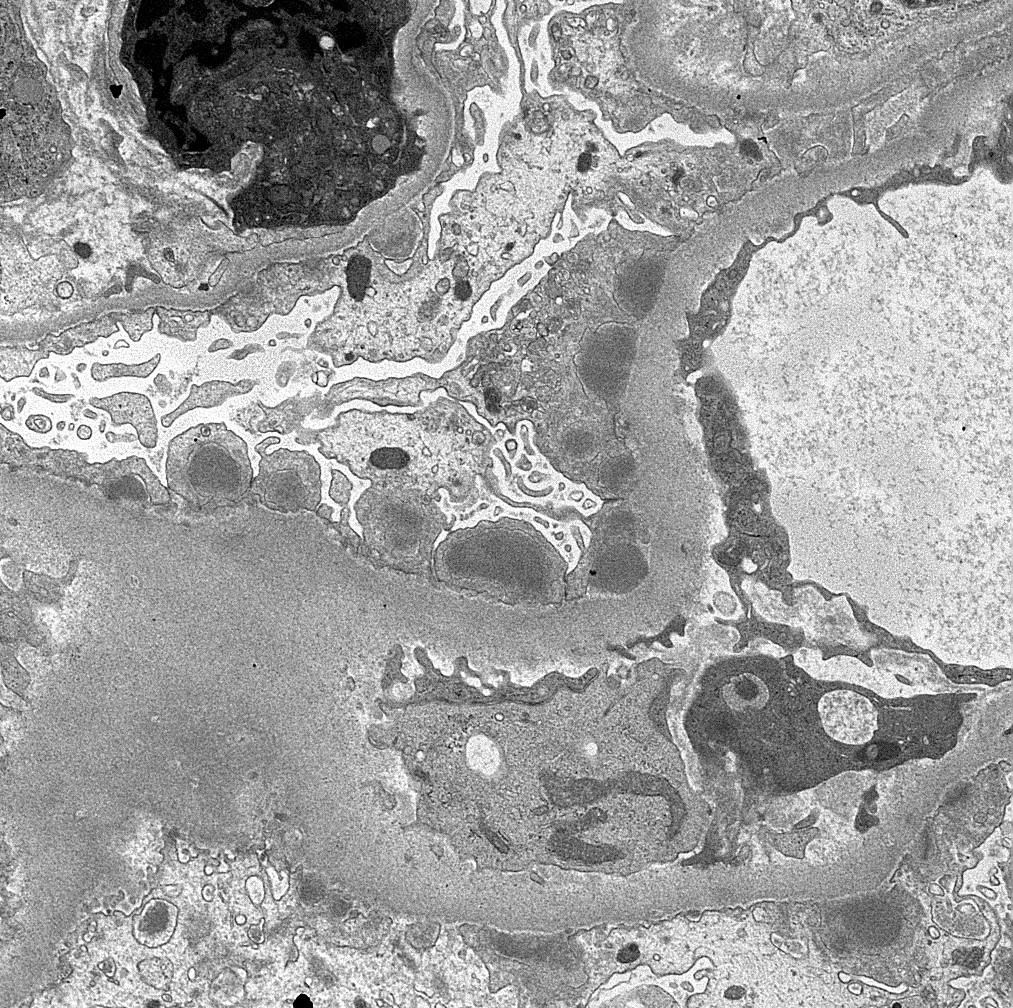
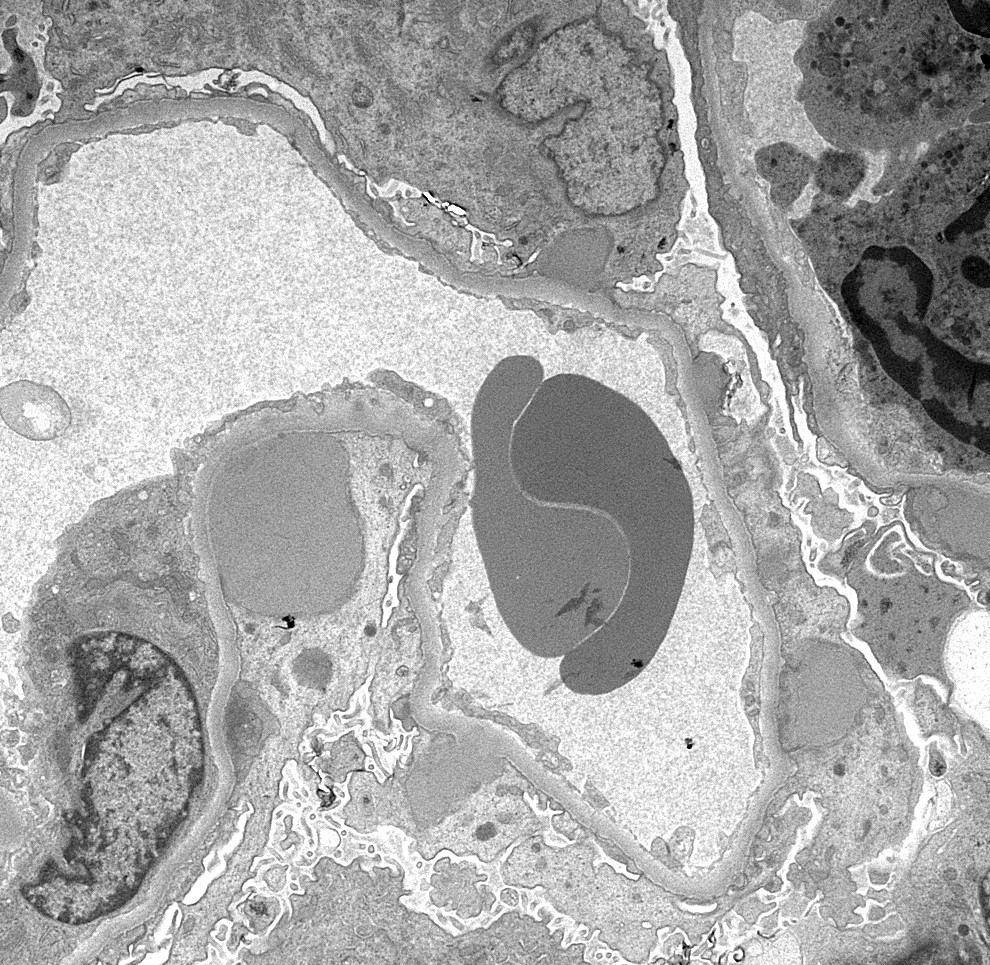
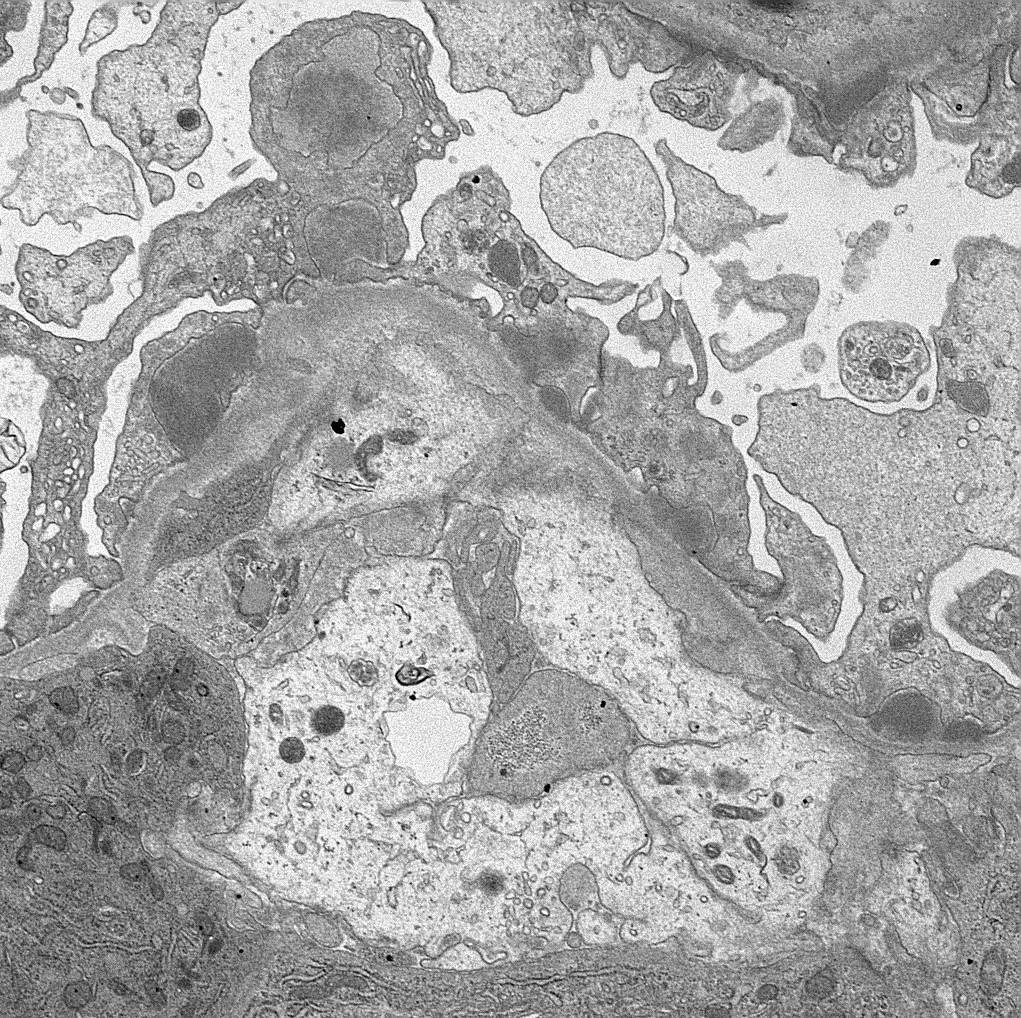
Electron microscopy description
- Endocapillary hypercellularity, frequent neutrophils in the glomerular tuft
- There may be occasional mesangial and small subendothelial deposits but the most consistent diagnostic change is hump type, large, subepithelial deposits without significant glomerular basement membrane reaction
- In chronic phase of the disease, mesangial deposits predominate, usually with less endocapillary proliferation
- References: Jennette: Heptinstall's Pathology of the Kidney, 2 Volume Set Edition, 2014, Fogo: Diagnostic Atlas of Renal Pathology, 3rd Edition, 2016
Electron microscopy images
Sample pathology report
- Right kidney, biopsy:
- Acute postinfectious glomerulonephritis
- Adequacy: adequate (2 cores with 80% cortex and 20% medulla)
- Microscopic description: 16 glomeruli are seen with one exhibiting global sclerosis and the rest showing diffuse, global mesangial and endocapillary hypercellularity with numerous neutrophils. The surrounding tubulointerstitium shows mild inflammation with no significant tubular atrophy or interstitial fibrosis. The vessels are unremarkable with no evidence of vasculitis.
- Immunofluorescence microscopy: IgG and C3 show coarse granular positivity in mesangium and along glomerular basement membrane.
- Electron microscopy: Prominent subepithelial hump type deposits with rare intramembranous and subendothelial deposits.
Differential diagnosis
- Lupus nephritis:
- Postinfectious glomerulonephritis may have dominant C3 positivity on immunofluorescence but there is usually absence of C1q deposits
- Lupus nephritis usually shows full house staining by immunofluorescence
- Tubuloreticular inclusions (reticular aggregates) in endothelial cells on electron microscopy
- C3 glomerulonephritis:
- More likely to have membranoproliferative glomerulonephritis (MPGN) pattern on histology
- Predominant C3 deposition with scant immunoglobulin on immunofluorescence
- Rare or no deposits on electron microscopy
- Not necessarily preceded by infection
- It has a poor outcome
- It is associated with complement alternative pathway dysregulation
- PIGN may be indistinguishable histologically from C3 glomerulonephritis (including exudative glomerulonephritis pattern and subepithelial humps by electron microscopy) and careful clinical correlation is required, especially if renal abnormalities do not resolve as expected
- Dense deposit disease:
- Membranoproliferative or mesangial proliferative features by light microscopy
- C3 only or C3 dominant deposits by immunofluorescence
- Characteristic dense deposits by electron microscopy
- IgA nephropathy:
- Lack of polymorphonuclear neutrophils, IgA dominant (or codominant) deposits and lambda > kappa on immunofluorescence and presence of mesangial and occasional subendothelial deposits on electron microscopy favors IgA nephropathy (Kidney Int Rep 2022;7:2462)
- In comparison, presence of polymorphonuclear neutrophils, dominant C3 and kappa > lambda on immunofluorescence, hump shaped deposits on electron microscopy favors IgA dominant postinfectious glomerulonephritis
- Staphylococcus infection associated glomerulonephritis (SAGN) often shows C3 > IgA, typically fewer focal segmental glomerulosclerosis (FSGS) lesions (if any) and more endocapillary hypercellularity as compared to IgA nephropathy (Nat Rev Nephrol 2020;16:32)
- IgA deposits in sclerotic glomeruli can be helpful in differentiating IgAN from IgA dominant infection related glomerulonephritis (Kidney Int Rep 2020;5:909)
- Cryoglobulinemic glomerulonephritis:
- Shows PAS+ cryoplugs on light microscopy
- Shows IgM dominance of deposits on immunofluorescence
- May have monoclonal component with either kappa or lambda staining on immunofluorescence
Board review style question #1
A 9 year old girl presented to the nephrology clinic with a history of hematuria and oliguria. She recently had a sore throat. On examination, bilateral pedal edema was noticed. Laboratory investigations included low complement levels and raised antistreptolysin O (ASO) titers. Renal biopsy was performed. Which characteristic electron microscopic finding would most likely be expected in this case?
- Effacement of foot processes
- Mesangial deposits
- Reticular aggregates
- Subendothelial deposits
- Subepithelial hump shaped deposits
Board review style answer #1
E. Subepithelial hump shaped deposits are characteristically seen in acute postinfectious glomerulonephritis. Answer A is incorrect as diffuse effacement of foot processes is seen in minimal change disease and variable effacement is seen in focal and segmental glomerulosclerosis. Answer B is incorrect as mesangial deposits are seen in IgA nephropathy and class I and II mesangial forms of lupus nephritis. Answer C is incorrect as reticular aggregates are classically seen in lupus nephritis. Answer D is incorrect as subendothelial deposits are seen in dense deposit disease and C3 glomerulopathy.
Comment Here
Reference: Acute postinfectious glomerulonephritis
Comment Here
Reference: Acute postinfectious glomerulonephritis
Board review style question #2
A 12 year old boy presented with history of a sore throat followed by hematuria. Renal biopsy revealed diffuse proliferative pattern and immunofluorescence showed coarse granular deposits in mesangium and along capillary loops for IgG and C3. Which serological test would support the diagnosis?
- Antidouble stranded DNA
- Anti-GBM antibodies
- Antimitochondrial antibodies
- Antinuclear antibodies
- Antistreptolysin O antibodies
Board review style answer #2
E. Antistreptolysin O antibodies. Evidence of preceding streptococcal infection is determined by measuring antistreptolysin titer (ASO). Answer A is incorrect as antidouble stranded DNA antibodies are high in lupus nephritis. Answer B is incorrect as anti-GBM antibodies are raised in good pasture syndrome (anti-GBM antibody disease). Answer C is incorrect as antimitochondrial antibodies are raised in some cases of lupus nephritis. Answer D is incorrect as antinuclear antibodies are also raised in lupus nephritis.
Comment Here
Reference: Acute postinfectious glomerulonephritis
Comment Here
Reference: Acute postinfectious glomerulonephritis