Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Immunofluorescence images | Positive stains | Electron microscopy description | Electron microscopy images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Lee CM, Zuckerman JE. Scleroderma renal disease. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneysclerodermarenaldisease.html. Accessed April 25th, 2024.
Definition / general
- Scleroderma is a multi-organ disease distinguished by vasculopathy and excess fibrosis (Rheumatology (Oxford) 2019;58:2099)
- Scleroderma associated renal vasculopathy is often clinically insignificant but rarely manifests as scleroderma renal crisis, a thrombotic microangiopathic process which leads to renal ischemia, acute hypertension and rapidly deteriorating renal function (Lancet 2017;390:1685)
Essential features
- Scleroderma associated renal disease is a spectrum of small arterial and arteriolar vasculopathy ranging from mild fibrointimal thickening to thrombotic microangiopathy (Am J Kidney Dis 2016;67:e19)
- Scleroderma related thrombotic microangiopathy is characterized by mucoid intimal edema, onion skin-like intimal proliferation, fibrinoid necrosis and thrombosis
- Glomerular changes include ischemic collapse and endothelial swelling and thrombosis, acutely and basement membrane duplication, chronically
- Ischemic injury to tubules results in acute tubular injury or necrosis and eventually, interstitial fibrosis and tubular atrophy
Terminology
- Scleroderma is also called systemic sclerosis
- Scleroderma renal crisis is a clinical diagnosis that is encompassed by the pathological diagnosis scleroderma associated renal disease or scleroderma renal disease
ICD coding
Epidemiology
- Scleroderma
- Affects 1:10,000 people globally (Semin Immunopathol 2015;37:443)
- Prevalence varies by geographic location (J Rheumatol 2014;41:1040):
- 200 - 260 cases per million in the U.S. and Australia (Arthritis Rheum 2003;48:2246)
- 20 - 50 cases per million in Asia (Arch Dermatol Res 1991;283:366)
- 100 - 200 cases per million in Europe (Rheumatology (Oxford) 2004;43:1129)
- Women 30 - 50 years of age are most commonly affected (Am J Kidney Dis 2016;67:e19)
- Renal disease is observed clinically in up to 50% of scleroderma patients, usually those with diffuse cutaneous scleroderma (Medicine (Baltimore) 1974;53:1, Am J Kidney Dis 2016;67:e19)
- Scleroderma renal crisis (Nat Rev Nephrol 2016;12:678):
- A rare complication occurring in 2.4 - 15% of diffuse cutaneous scleroderma patients and 2% of limited cutaneous scleroderma patients (Ann Rheum Dis 2015;74:1124, QJM 2007;100:485)
- More commonly seen in the early stages (< 4 years after onset) of diffuse cutaneous scleroderma (Ann Rheum Dis 2008;67:110)
- > 80% of patients in scleroderma renal crisis have diffuse cutaneous scleroderma (Ann Rheum Dis 2008;67:110)
- Incidence is decreasing as a result of effective monitoring
Sites
- Diffuse versus limited cutaneous systemic sclerosis (Lancet 2017;390:1685)
- Determined by extent of skin involvement
- Diffuse cutaneous systemic sclerosis affects proximal sites
- Limited cutaneous systemic sclerosis affects skin distal to elbows or knees with or without face and neck involvement
- Scleroderma involves multiple organ systems (Lancet 2017;390:1685)
- Pulmonary fibrosis, pulmonary arterial hypertension
- Gastrointestinal symptoms, intestinal pseudo-obstruction, gastric antral vascular ectasia
- Cardiac fibrosis
- Renal vasculopathy, scleroderma renal crisis
- Digital vasculopathy
- Scleroderma renal disease (J Rheumatol 2014;41:1040)
- Small arteries and arterioles (interlobular and arcuate arteries) are primarily and most significantly affected
- Glomeruli may be affected by thrombotic microangiopathy
- Glomeruli and tubules may also be secondarily affected by ischemic sequelae of severe vascular injury
Pathophysiology
- Scleroderma
- Disease mediated by vasculopathy, immune activation and inflammation and excess fibrosis in response to injury (Rheumatology (Oxford) 2019;58:2099)
- Scleroderma renal crisis
- Endothelial injury or activation by unclear mechanism leads to intimal proliferation, increased permeability and edema (Rheumatology (Oxford) 2019;58:2099)
- Vascular narrowing and hyperreactivity contribute to decreased renal perfusion and ischemic injury (J Rheumatol 2014;41:1040)
- Decreased renal perfusion activates the renin-angiotensin-aldosterone system which can result in accelerated hypertension and progressive renal injury (Int J Rheumatol 2010;2010:543704)
- Increased vascular permeability allows blood components to interact with extravascular connective tissue which can turn on the coagulation cascade and lead to vascular thrombosis as well as injury to adjacent connective tissue and stromal proliferation (Int J Rheumatol 2010;2010:543704)
- Other precipitating factors (J Rheumatol 2014;41:1040)
- Decreased intravascular volume (sepsis, dehydration, congestive heart failure)
- Nephrotoxic drugs (nonsteroidal antiinflammatory drugs, cocaine, cyclosporine, corticosteroids)
Etiology
- Etiology of scleroderma renal vasculopathy and specifically, scleroderma renal crisis is unknown (Nat Rev Nephrol 2016;12:678)
- Pathogenesis of the vasculopathy may be immune mediated (Int J Rheumatol 2010;2010:543704)
- Cellular and humoral immune activation is described in scleroderma
- Specific autoantibodies are associated with scleroderma renal crisis
- Anti-RNA polymerase III is strongly associated with diffuse systemic sclerosis and scleroderma renal crisis (Arthritis Rheumatol 2016;68:2778)
- Scleroderma renal crisis develops in one third of patients with anti-RNA polymerase III autoantibody and scleroderma (Ann Intern Med 1993;119:1005)
- 85% of patients with scleroderma renal crisis are found to have anti-endothelial cell antibodies, which can cause endothelial cell apoptosis (Ann Rheum Dis 2010;69:319)
- Endothelin and its receptors (endothelin receptors A and B) are overexpressed in the glomeruli, tubules and vessels of patients in scleroderma renal crisis (Hum Pathol 2011;42:95)
Clinical features
- Isolated reduced glomerular filtration rate, reduced renal functional reserve, microalbuminuria and proteinuria (Int J Rheumatol 2010;2010:538589)
- Scleroderma renal crisis
- Acute onset of moderate to marked hypertension
- At least one sign of acute decline in renal function (increase in serum creatinine, proteinuria or hematuria) (Rheumatology (Oxford) 2019;58:2099)
- Sometimes hypertensive encephalopathy and retinopathy
- 90% of scleroderma renal crisis cases present with a blood pressure > 150/90 mm Hg (J Rheumatol 2014;41:1040)
- Scleroderma renal crisis can be the presenting manifestation (Nat Rev Nephrol 2016;12:678)
- 10% of scleroderma renal crisis cases occur without significant hypertension (Ann Rheum Dis 2008;67:110)
- Several diseases associated with scleroderma (Kidney Blood Press Res 2018;43:682, Int J Rheumatol 2010;2010:543704):
- Renal artery stenosis
- Antiphospholipid associated nephropathy
- Myeloperoxidase antineutrophil cytoplasmic antibody (MPO-ANCA) associated glomerulonephritis and vasculitis
Diagnosis
- Acute onset of hypertension with evidence of renal failure in a patient with scleroderma
- Thrombotic microangiopathy of small renal arteries and arterioles, including interlobular and arcuate vessels and glomerular capillaries
Laboratory
- No laboratory parameter is predictive of scleroderma renal crisis (Nat Rev Nephrol 2016;12:678)
- Antinuclear antibody is positive in 90% of scleroderma renal crisis cases (Am J Kidney Dis 2016;67:e19)
- Anti-RNA polymerase III is present in 33% of cases (Medicine (Baltimore) 2013;92:1)
- Anticentromere antibodies are usually not detected (J Rheumatol 2014;41:1040)
- Elevated serum creatinine (J Rheumatol 2014;41:1040)
- Urinalysis frequently shows proteinuria and hematuria (J Rheumatol 2014;41:1040)
- If present, thrombocytopenia is usually moderate with a platelet count > 50,000/mm3 (J Rheumatol 2014;41:1040)
- Evidence of intravascular hemolysis may be present, such as increased schistocytes on peripheral blood smear and decreased haptoglobin (J Rheumatol 2014;41:1040)
Prognostic factors
- Scleroderma renal crisis has high mortality (30 - 40% at 5 years) and low survival (65% 5 year survival) despite monitoring and appropriate therapy (QJM 2007;100:485)
- Normotensive scleroderma renal crisis has a particularly unfavorable prognosis (Lancet 2017;390:1685, Hum Pathol 2009;40:332)
- Clinical factors of poor prognosis (J Rheumatol 2014;41:1040)
- Male gender
- Older age
- Congestive heart failure
- Serum creatinine level > 3 mg/dl at the initiation of treatment
- Difficulty controlling blood pressure beyond 3 days
- ACE inhibitor use prior to the onset of scleroderma renal crisis is associated with poor prognosis
- Patients who survive the first year of scleroderma renal crisis without requiring dialysis have a good long term outcome (J Rheumatol 2014;41:1040)
- Features of severe vascular injury, vascular thrombosis and fibrinoid change, as well as subsequent ischemic changes (glomerular ischemic collapse and acute tubular necrosis) are predictive of poor outcome (Int J Rheumatol 2010;2010:543704, Hum Pathol 2009;40:332)
- Peritubular C4d deposits may indicate a worse prognosis (Hum Pathol 2009;40:332)
- Predictive risk factors for development of scleroderma renal crisis in scleroderma patients include (Nat Rev Nephrol 2016;12:678, J Rheumatol 2014;41:1040):
- Diffuse and rapid skin involvement
- Disease duration of < 4 years
- New onset anemia
- Cardiac events
- Systemic inflammatory features
- Anti-RNA polymerase III antibodies
- Moderate to high doses of gluocorticoids (> 15 mg/day) with or without other nephrotoxic drugs (calcineurin inhibitors, antithymocyte globulin, etc.) can increase risk (Nat Rev Nephrol 2016;12:678)
Case reports
- 21 year old man with history of mixed connective tissue disease presented with acute renal failure and accelerated hypertension (Saudi J Kidney Dis Transpl 2014;25:844)
- 40 year old woman with renal failure, hypertension and microangiopathic hemolytic anemia treated with eculizumab (Case Rep Nephrol 2018;2018:6051083)
- 60 year old woman with Sjögren syndrome and cutaneous vasculitis presented with hypertension, elevated serum creatinine and mild thrombocytopenia (Clin Exp Rheumatol 2015;33:S171)
- 69 year old man with limited cutaneous systemic sclerosis presented in hypertensive crisis with anti-RNA polymerase III autoantibodies (Mod Rheumatol 2018;28:369)
- 70 year old woman with hypertension, elevated serum creatinine and serologies positive for antinuclear antibodies and myeloperoxidase antibodies (J Investig Med High Impact Case Rep 2018;6:2324709618785188)
Treatment
- High dose ACE inhibitors are first line therapy (Nat Rev Nephrol 2016;12:678, Ann Rheum Dis 2017;76:1327)
- Additional antihypertensives that can be used in case of refractory hypertension include dihydropyridine calcium channel blockers, diuretics, clonidine, nitrates or other vasodilators, prazosin (Nat Rev Nephrol 2016;12:678, J Rheumatol 2014;41:1040)
- Beta blockers should not be used as they can provoke Raynaud phenomenon
- ET1 receptor antagonists (ERAs) as a standard therapy in addition to antihypertensive drugs are being evaluated (Nat Rev Nephrol 2016;12:678)
- Scleroderma related end stage renal disease can be managed with either dialysis or kidney transplantation (Nat Rev Nephrol 2016;12:678)
- Plasma exchange as a therapy for scleroderma associated microangiopathic hemolytic anemia is controversial (Rheumatology (Oxford) 2019;58:2099, J Rheumatol 2014;41:1040)
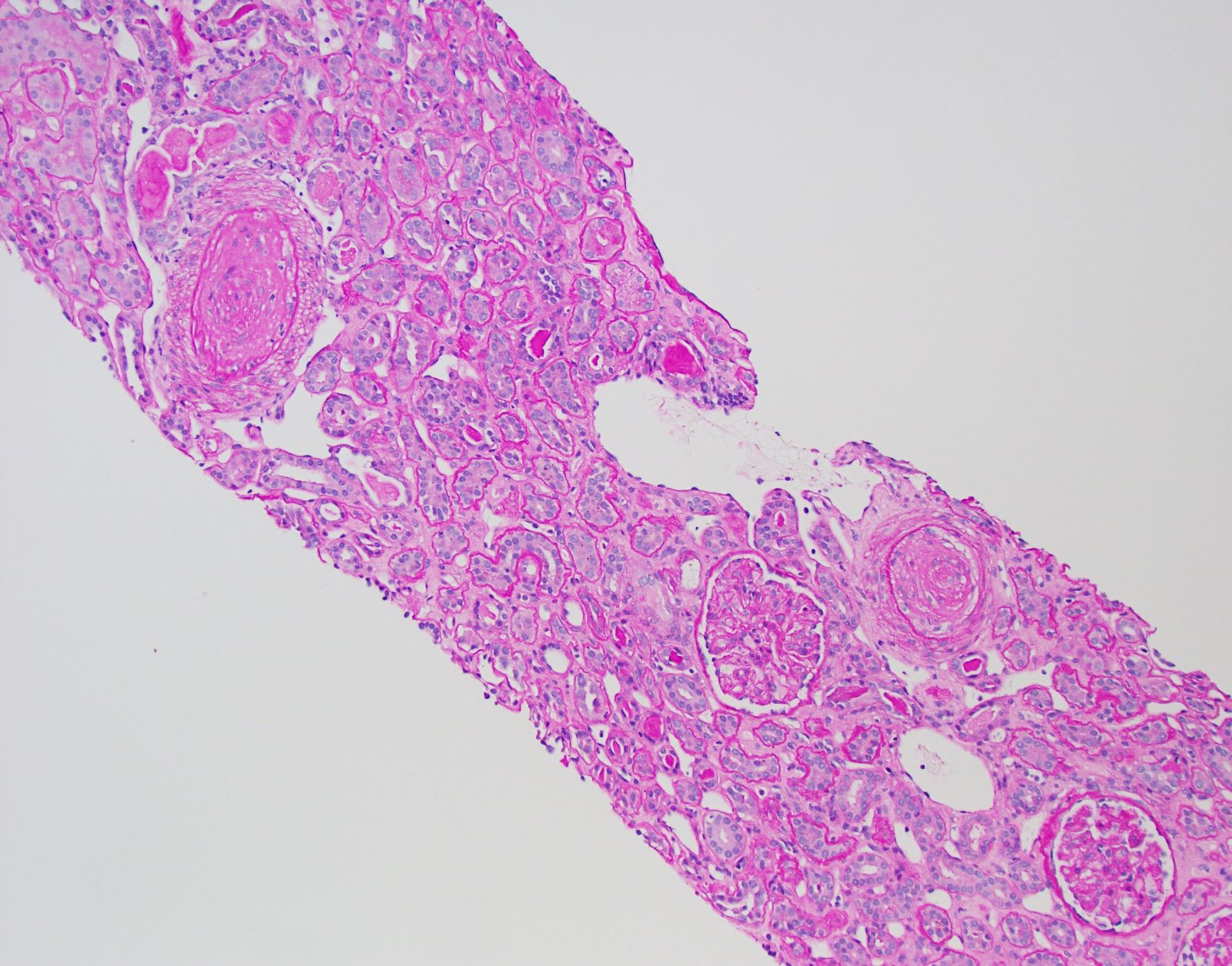
Microscopic (histologic) description
- Renal pathology findings in scleroderma patients without scleroderma renal crisis:
- Fibrointimal thickening of arteries (arteriosclerosis) (Int J Rheumatol 2010;2010:543704)
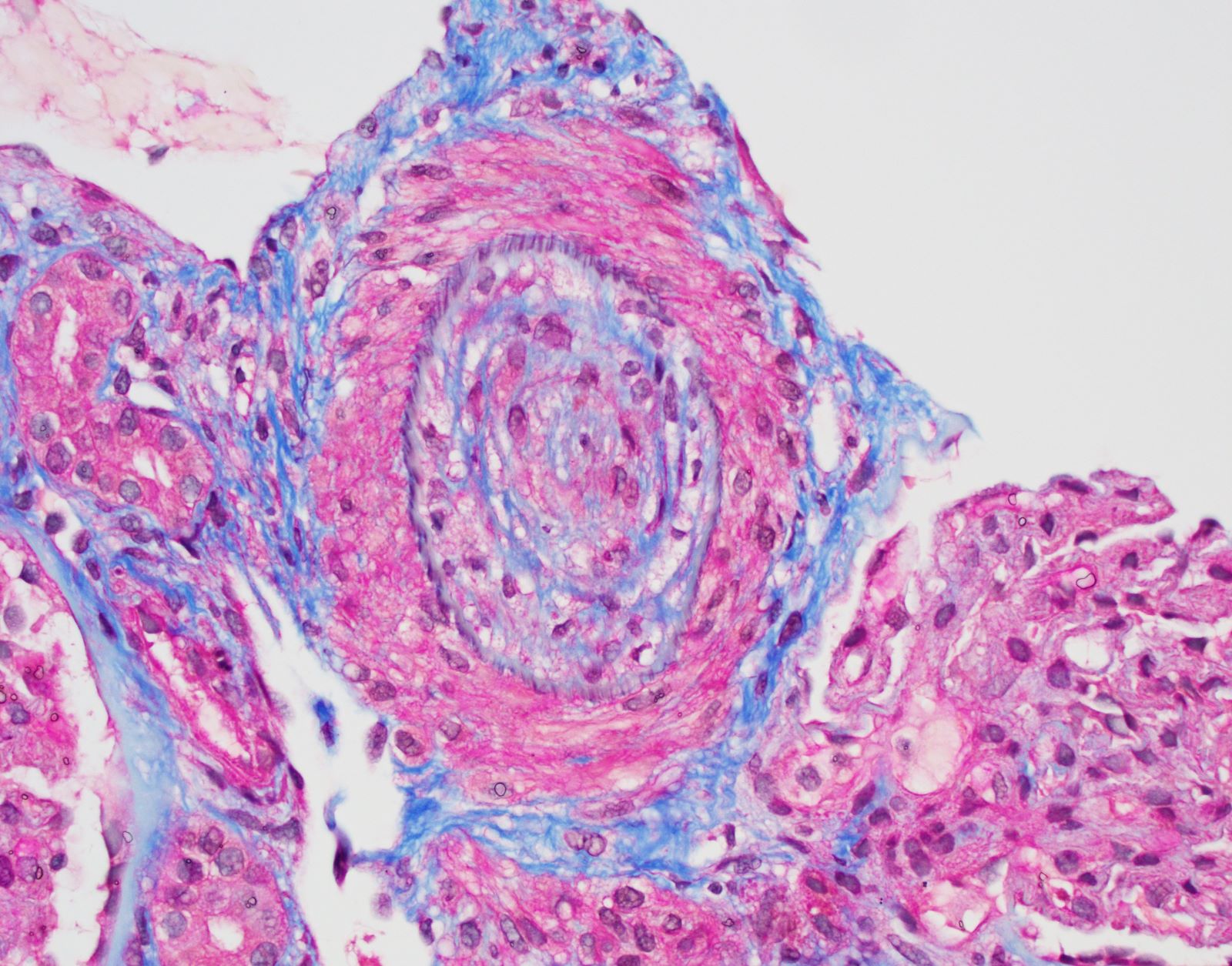
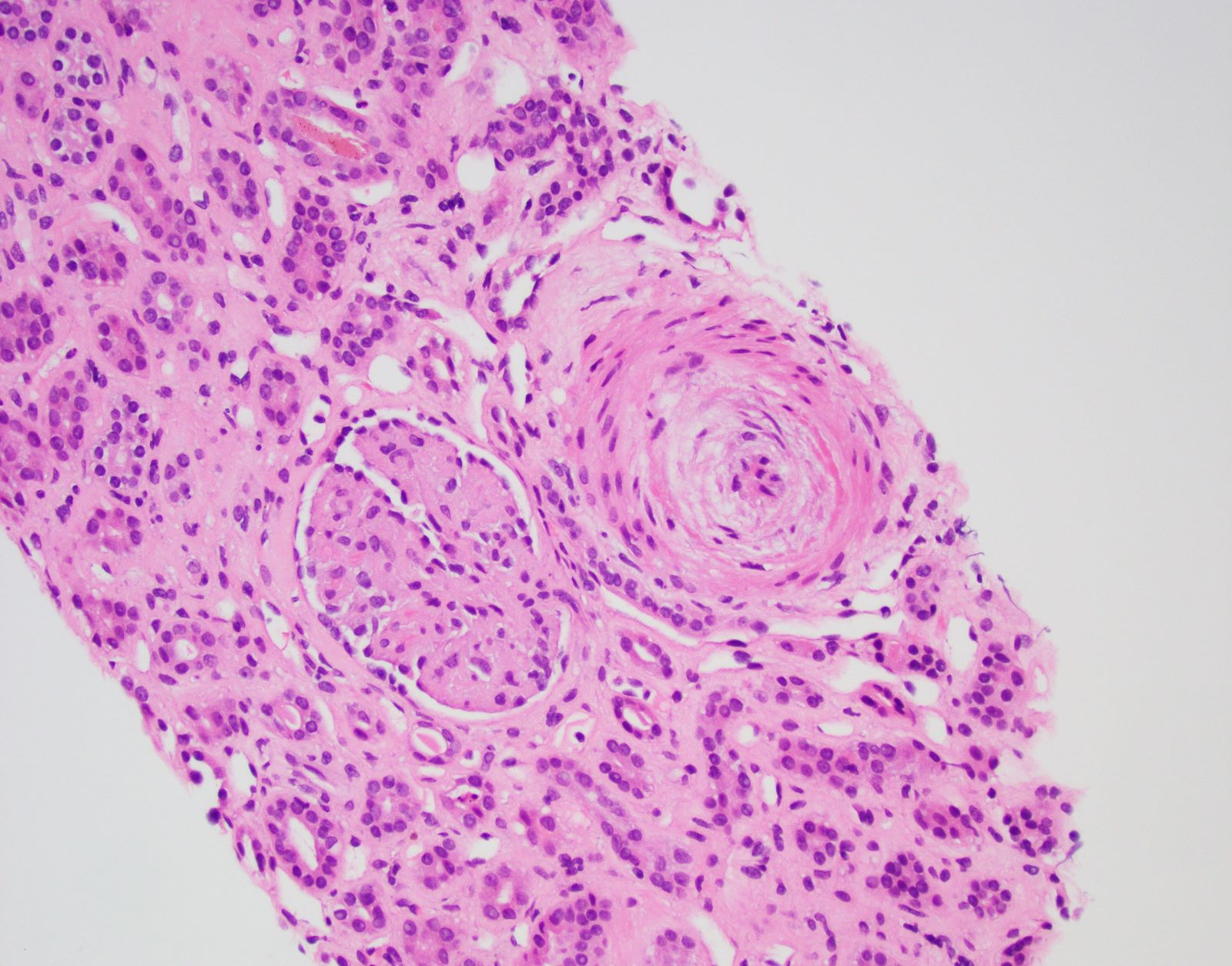
- Scleroderma renal crisis (Int J Rheumatol 2010;2010:543704, Am J Kidney Dis 2016;67:e19):
- Arterial / arteriolar injury
- Acute / early
- Endothelial swelling
- Intimal mucoid change
- Fibrin thrombi within arteries / arterioles or glomeruli
- Subacute to chronic
- Concentric intimal proliferation (onion skinning) and narrowing of the lumen
- Fibrointimal sclerosis
- Acute / early
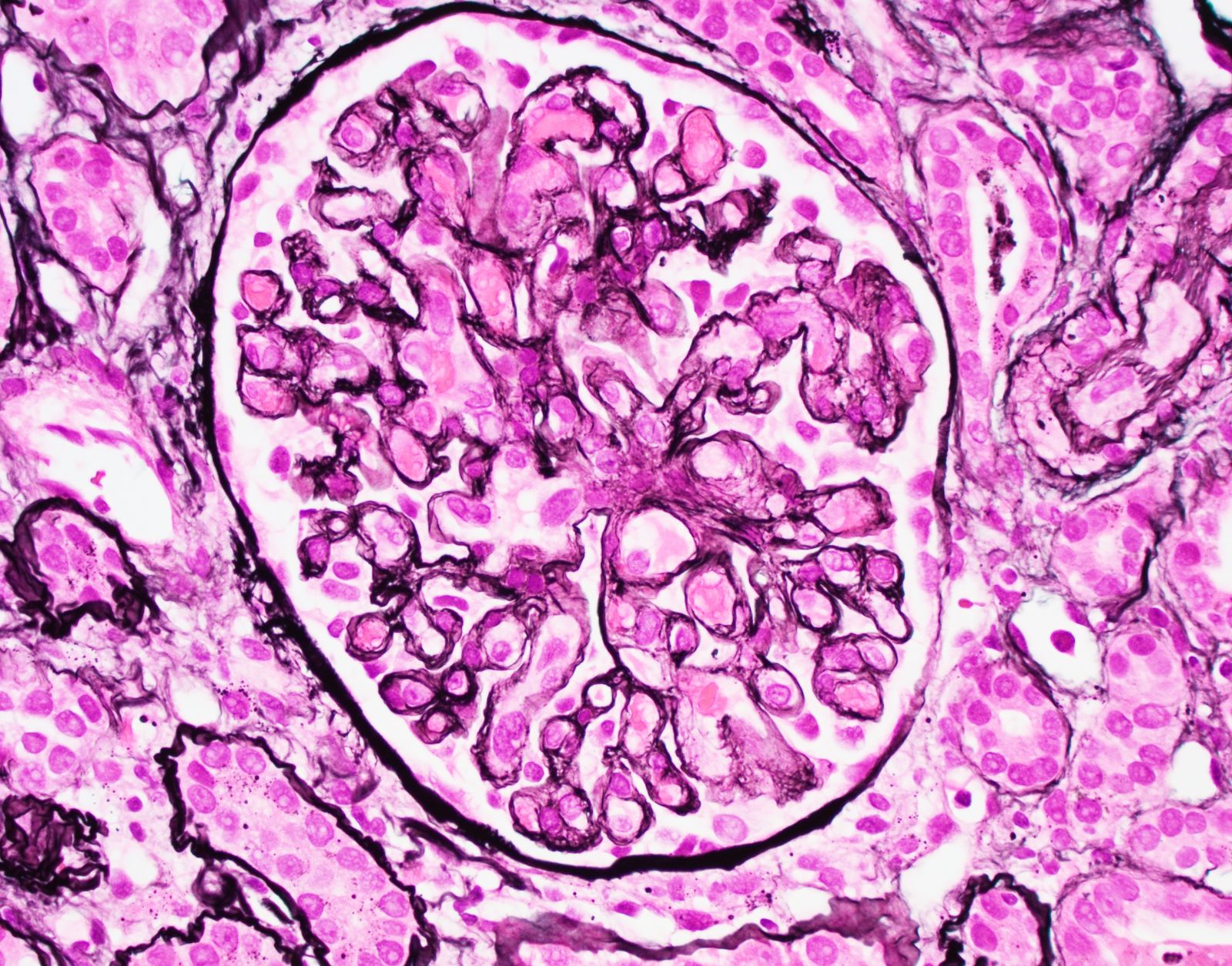
- Glomeruli
- Acute
- Ischemic corrugation
- Endothelial swelling
- Mesangiolysis
- Glomerular capillary thrombosis
- Chronic
- Glomerular basement membrane duplication and glomerulosclerosis
- Acute
- Tubulointerstitium
- Ischemic effect on tubules is acutely seen as acute tubular injury or necrosis
- Ongoing injury can result in tubular atrophy and interstitial fibrosis
- Mild interstitial lymphohistiocytic inflammatory infiltrate may be present
- Arterial / arteriolar injury
Microscopic (histologic) images
Immunofluorescence description
- Fibrinogen staining is in areas of vascular or glomerular thrombosis (Int J Rheumatol 2010;2010:543704, Am J Kidney Dis 2016;67:e19)
- Peritubular C4d deposits may suggest antibody mediated injury and indicate a worse prognosis as staining appears to be increased in patients who died or had irreversible loss of renal function (Hum Pathol 2009;40:332)
- Negative staining for immunoglobulins within glomeruli
Immunofluorescence images
Positive stains
- Trichrome can highlight fibrin thrombi and interstitial fibrosis
- Jones silver highlights onion skin change and glomerular double contours
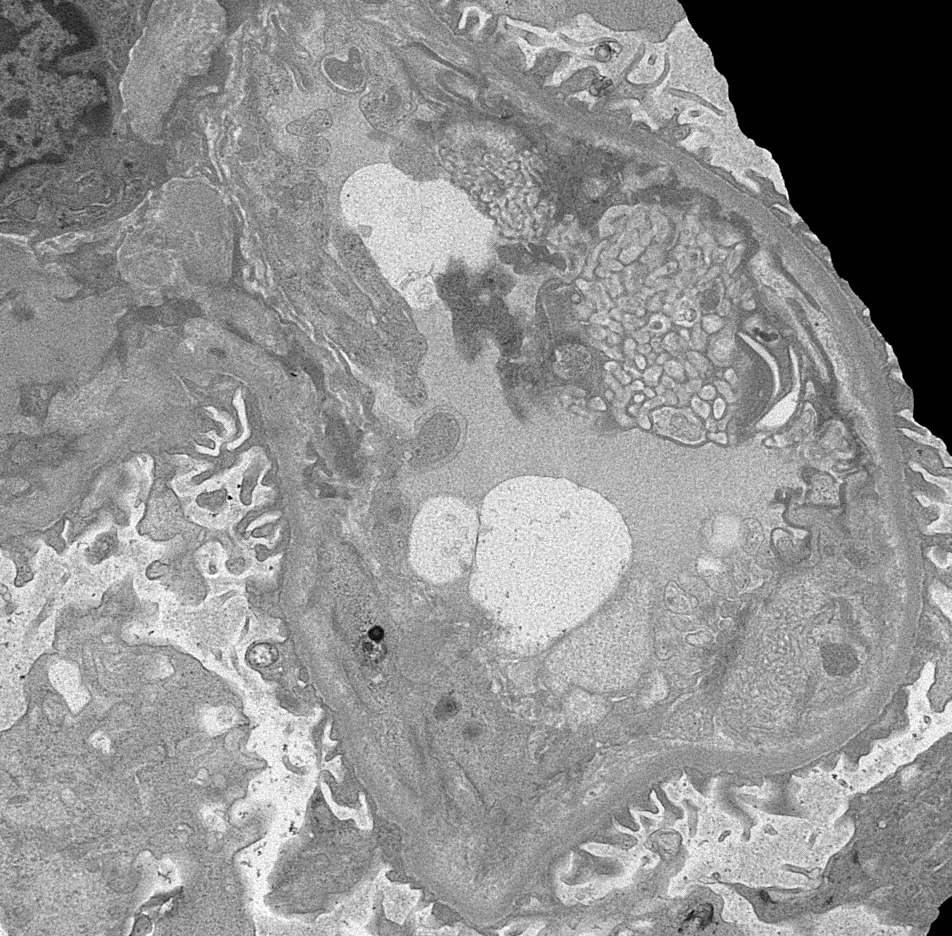
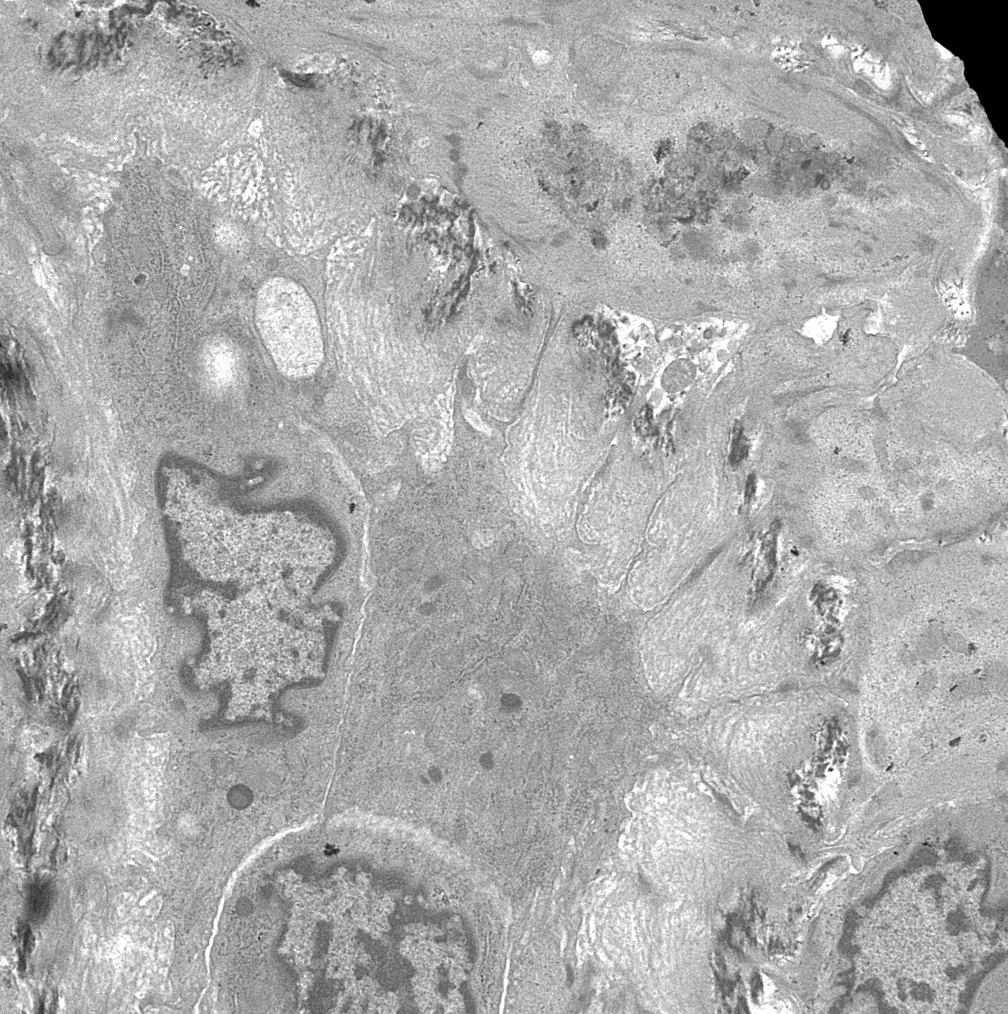
Electron microscopy description
- Endothelial cell injury (Int J Rheumatol 2010;2010:543704, Am J Kidney Dis 2016;67:e19)
- Swollen endothelial cells
- Expansion of subendothelial space within glomeruli with interporision of lucent material and cell processes
- Platelet aggregates and fibrin tactoids in areas of thrombosis
- Glomerular basement membrane duplication can be seen in cases of chronic injury
- Swollen endothelial cells within vessels
- Subendothelial edema and basement membrane remodeling within vessels
Electron microscopy images
Sample pathology report
- Left kidney, native, needle core biopsy:
- Diffuse active chronic thrombotic microangiopathy (TMA), arterial predominant, consistent with scleroderma associated renal disease (see comment)
- Comment: While the marked arterial changes are highly consistent with scleroderma associated renal disease, the differential diagnosis for these findings includes any potential cause of thrombotic microangiopathy (e.g. TTP, HUS, complement associated TMA, antiphospholipid antibody syndrome, drug toxicity, infection, etc.).
Differential diagnosis
- The main differential diagnoses include other renal diseases that cause thrombotic microangiopathy:
- Scleroderma renal crisis generally shows vascular > glomerular involvement
- No specific morphologic features can reliably distinguish underlying etiologies for thrombotic microangiopathy on renal biopsy alone
- Differential diagnosis for thrombotic microangiopathy on renal biopsy includes:
- Thrombotic thrombocytopenic purpura:
- Low ADAMTS13 levels (Int J Rheumatol 2010;2010:543704, Nat Rev Nephrol 2016;12:678, J Rheumatol 2014;41:1040)
- Complement mediated thrombotic microangiopathy (atypical hemolytic uremic syndrome):
- Genetic or acquired abnormalities in alternative complement cascade may be present
- Hemolytic uremic syndrome associated with E. coli enterocolitis
- Viral infections (e.g. HIV)
- Antiphospholipid antibody syndrome
- Many medications (e.g. quinine, gemcitabine and cyclosporin) (Rheumatology (Oxford) 2019;58:2099)
- Malignancy
- Illicit drugs (e.g. cocaine)
- Metabolism mediated thrombotic microangiopathy, such as disorders of intracellular vitamin B12 metabolism (Rheumatology (Oxford) 2019;58:2099)
- Thrombotic thrombocytopenic purpura:
- The differential diagnosis in a renal allograft would include other entities:
- Antibody mediated rejection
- Calcineurin inhibitor toxicity
- Infection and other less common allograft related abnormalities (Int J Rheumatol 2010;2010:543704)
Board review style question #1
Board review style answer #1
E. Thrombotic microangiopathy of small arteries and arterioles
Comment Here
Reference: Scleroderma renal disease
Comment Here
Reference: Scleroderma renal disease
Board review style question #2
Which of the following is true about scleroderma renal crisis?
- Associated with low ADAMTS13 levels
- Can present with normal or only mildly elevated blood pressure
- Evidence of acute renal failure is not required for diagnosis
- Microangiopathic hemolytic anemia is seen in all cases
- More commonly seen in patients with limited rather than diffuse cutaneous systemic sclerosis
Board review style answer #2
B. Can present with normal or only mildly elevated blood pressure
Comment Here
Reference: Scleroderma renal disease
Comment Here
Reference: Scleroderma renal disease