Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Sites | Pathophysiology | Etiology | Hereditary renal cell tumors | Diagnosis | Radiology description | Prognostic factors | Treatment | Handling and staging guide | Gross description | Gross images | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | IHC panels | Differential diagnosis | Additional referencesCite this page: Andeen NK, Tretiakova M. Renal cell carcinoma overview. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneytumormalignantrcc.html. Accessed May 6th, 2024.
Definition / general
- Adult renal cell carcinoma (RCC)
Essential features
- Sixteenth most common cause of death from cancer worldwide; estimated 143,000 deaths from kidney cancer in 2012 (WHO 2016)
- See subtypes: Kidney tumor
Terminology
- Historic synonyms: nephrocellular carcinoma, Grawitz tumor, hypernephroma (due to perceived origin from adrenal gland)
Epidemiology
- Incidence: worldwide as of 2012, ninth most common cancer in men (214,000 cases) and fourteenth most common in women (124,000 cases) (WHO 2016)
- M:F = approximately 2:1
- Approximately 70% of new cases occur in countries with high socioeconomic development
- RCC incidence varies widely from region to region with the highest rates in the Czech Republic and North America
- In the United States, there are ~64,000 new cases and almost 14,000 deaths from RCC each year (CA Cancer J Clin 2017;67:7)
Sites
- Kidney
Pathophysiology
- Various molecular pathways
Etiology
- Risk factors: obesity, smoking, hypertension, acquired cystic kidney disease due to end stage renal disease, occupational exposure to trichloroethylene, treated neuroblastoma
- Genetic susceptibilities estimated to account for 2 - 4% (WHO 2016)
- Usually > 50 years old
Hereditary renal cell tumors
-
von Hippel-Lindau syndrome
- Autosomal dominant, due to germline mutation of VHL gene at chromosome 3p25
- Renal lesions: renal cysts and clear cell renal cell carcinoma
- Associated with bilateral or multiple renal cell carcinomas in 50% (eMedicine - Von Hippel-Lindau Syndrome)
- Other organs: hemangioblastomas of cerebellum and retina, cysts of pancreas, liver and kidney, clear cell tumors of other sites, papillary cystadenoma of epididymis, pheochromocytoma
- Due to activating mutation of MET oncogene at chromosome 7q31
- Autosomal dominant, late onset bilateral papillary renal tumors
- Autosomal dominant, familial
- Due to germline fumarate hydratase mutations
- Cutaneous or uterine leiomyomas
- Renal tumors are often papillary with characteristic large nucleus with a very prominent inclusion-like eosinophilic nucleolus (HLRCC)
- Autosomal dominant with incomplete penetrance
- Due to germline mutations in BHD gene at chromosome 17p112, which codes for folliculin
- Skin lesions: fibrofolliculomas, trichodiscomas, acrochordons
- Lung: cysts, spontaneous pneumothorax
- Renal tumors variable: oncocytoma, clear cell carcinoma and hybrid oncocytic / chromophobe tumor with areas of clear cells (Am J Surg Pathol 2002;26:1542)
- Mutations in TSC1 and TSC2 genes via an alternate pathway not involving VHL mutations (Mod Pathol 2002;15:205)
- Multiple, bilateral angiomyolipomas or epithelioid angiomyolipoma
Hereditary papillary renal cell carcinoma
Hereditary leiomyomatosis and renal cell carcinoma
Familial papillary thyroid carcinoma
Hyperparathyroidism-jaw tumor syndrome
Birt-Hogg-Dubé syndrome
Tuberous sclerosis
Constitutional chromosome 3 translocations
Diagnosis
- Image guided biopsy of solitary small renal masses may be utilized for treatment planning, since pathology cannot be predicted by clinical features (Am J Clin Pathol 2008;130:560, Hum Pathol. 2005;36:1309)
Radiology description
- "Classic" clinical features of costovertebral pain, palpable mass and hematuria are now present in only 10%
- Most tumors are detected incidentally due to increased use of imaging; historically were large (10 cm) at diagnosis
- "Great mimic" due to associated paraneoplastic syndromes of Cushing syndrome, gynecomastia, hypercalcemia, hypertension, leukemoid reaction, polycythemia, Stauffer syndrome (hepatomegaly with hepatic dysfunction), systemic amyloidosis, polyneuromyopathy
Prognostic factors
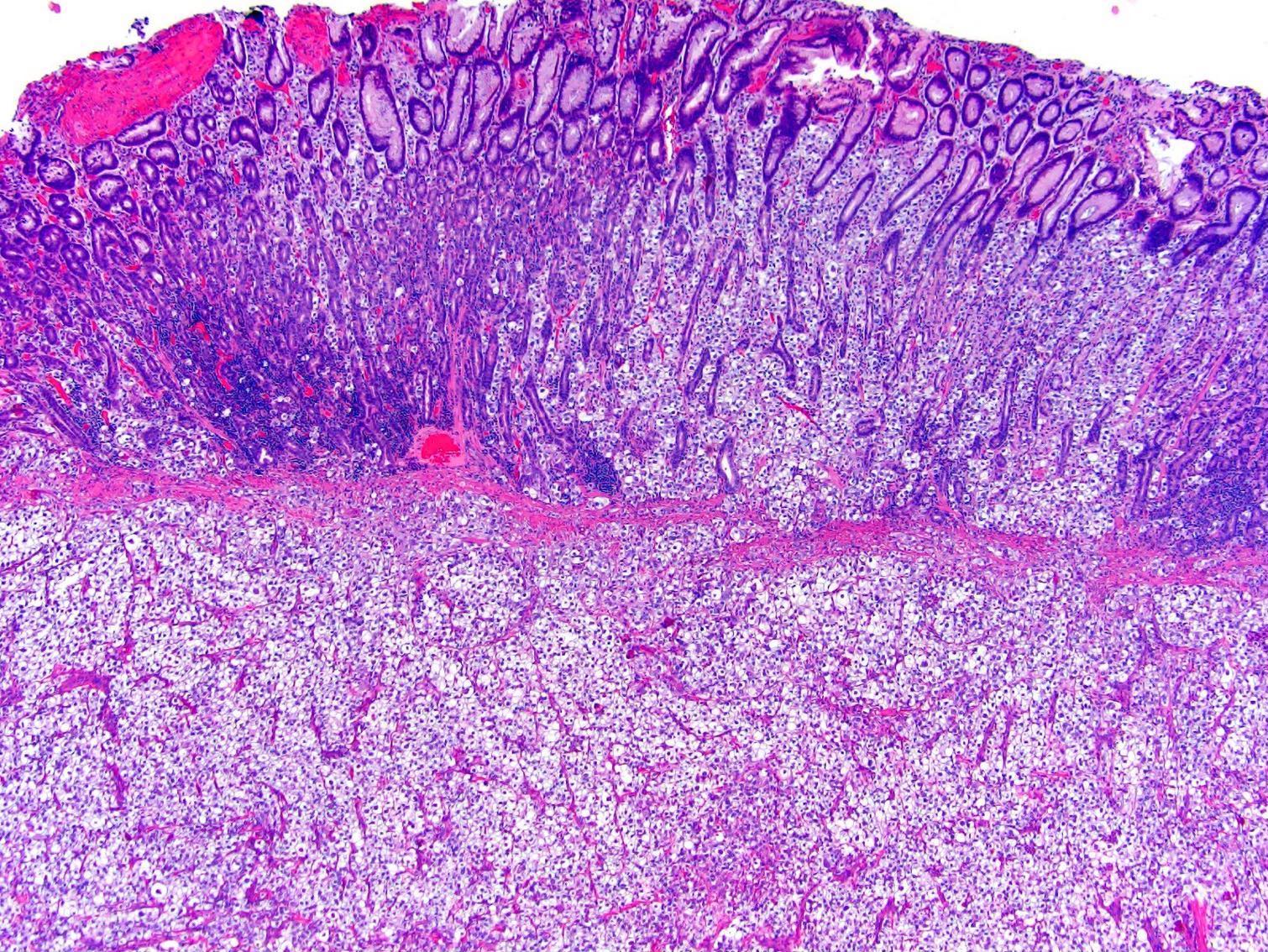
- WHO / International Society of Urologic Pathology (ISUP) Grading for Clear Cell and Papillary RCC:
- Grade 1: nucleoli inconspicuous or absent at 400x (objective magnification 40x)
- Grade 2: nucleoli prominent at 400x
- Grade 3: nucleoli prominent at 100x magnification
- Grade 4: extreme nuclear pleomorphism, multinucleated giant cells, sarcomatoid or rhabdoid change
- Staging
- Histologic subtype: Kidney tumor
Treatment
- Resection (partial or radical nephrectomy)
- Depends on subtype
- Chemotherapy and radiation traditionally considered ineffective; however, increasing use of interferon,cytokine IL2,antiangiogenic agents and immunotherapy (sorafenib, sunitinib, temsirolimus, everolimus, bevacizumab, pazopanib, nivolumab)
- 5 year survival: 68% (all histologic types and stages), varies from 60% - 80% in stage I versus 5% in stage IV, lower for renal pelvis carcinoma (51%) compared with RCC (70%)
Handling and staging guide
- Perinephric fat invasion: either the tumor touching the fat or extending as irregular tongues into the perinephric tissue, with or without desmoplasia
- Renal sinus invasion: when the tumor is in direct contact with the sinus fat or the loose connective tissue of the sinus, clearly beyond the renal parenchyma or if it involves any endothelium lined spaces within the renal sinus If uncertain, at least 3 blocks of the tumor renal sinus interface should be submitted
- Renal vein margin: margin is positive only when adherent tumor is visible microscopically at the actual margin If there is a submitted separately as “caval thrombus” take 2 or more sections to look for adherent caval wall tissue
- Uninvolved renal parenchyma: should be sampled, distant from tumor, for underlying renal disease
- Lymph nodes: should be sought but are found in < 10% of radical nephrectomy specimens
- Reference: Am J Surg Pathol 2013;37:1469
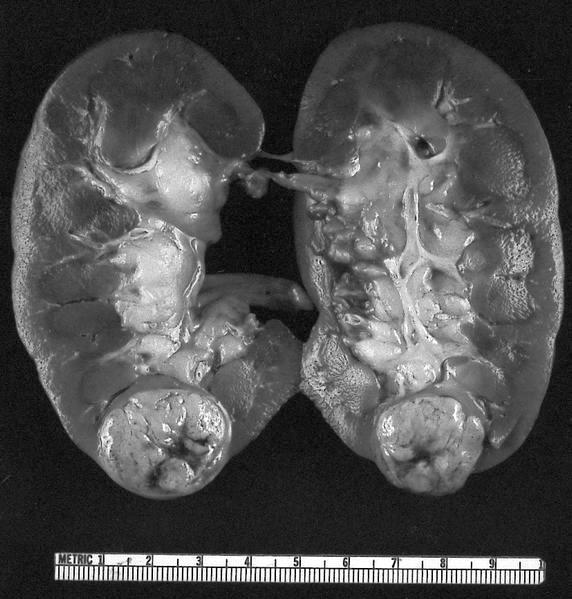
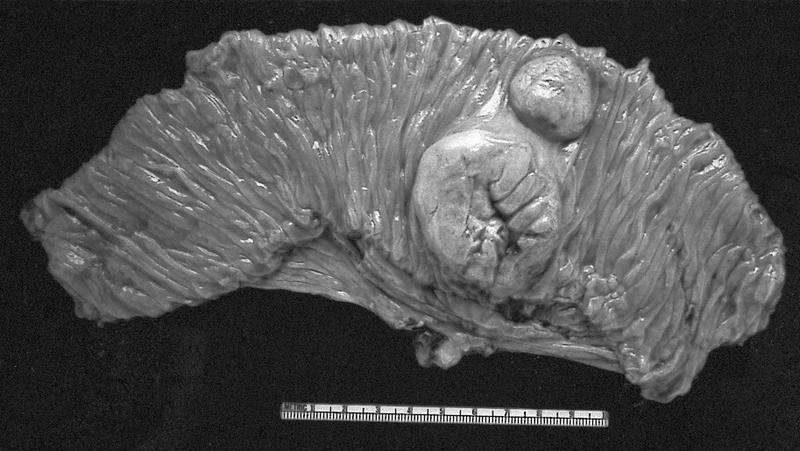
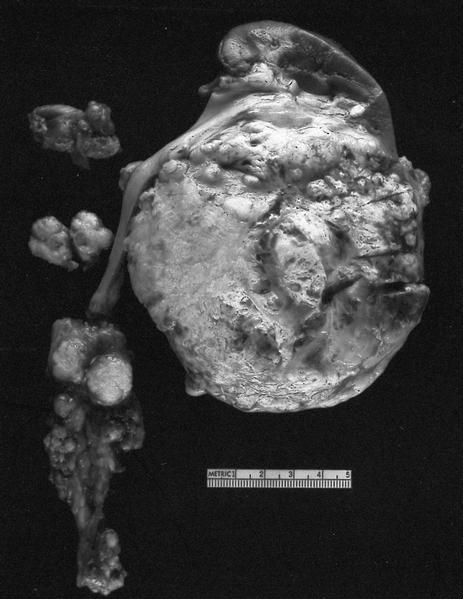
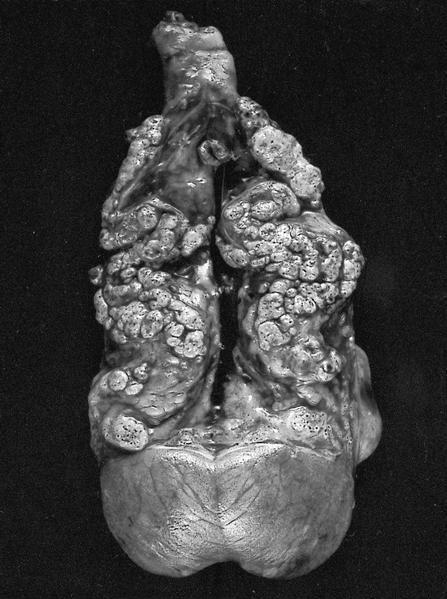
Gross description
- Well circumscribed, centered on cortex, may bulge / distort kidney contour
- Often extends into renal vein or vena cava
- Renal sinus invasion common in large tumors
- May have satellite nodules, often hemorrhage, necrosis, calcification and cystic change
Gross images
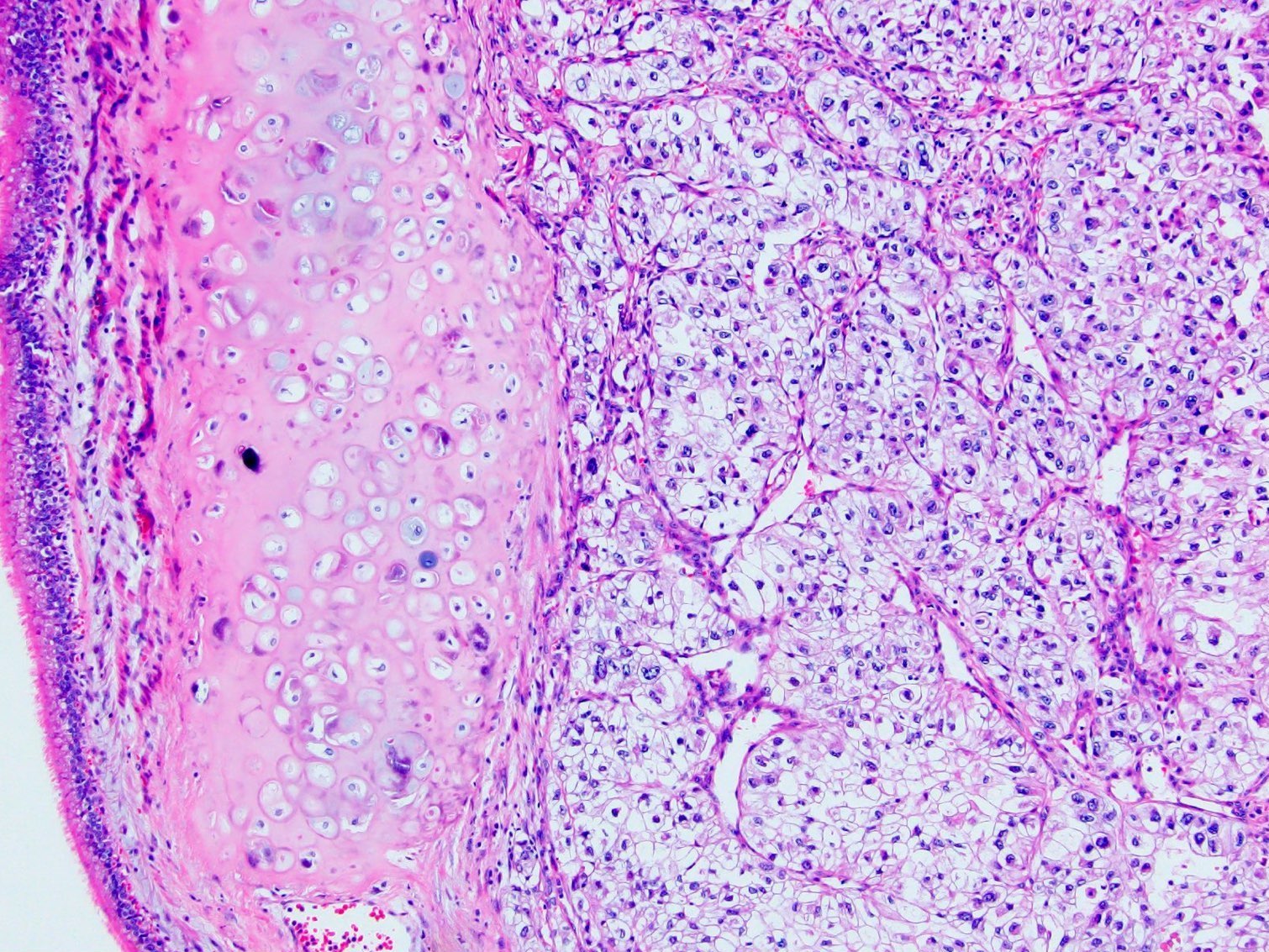
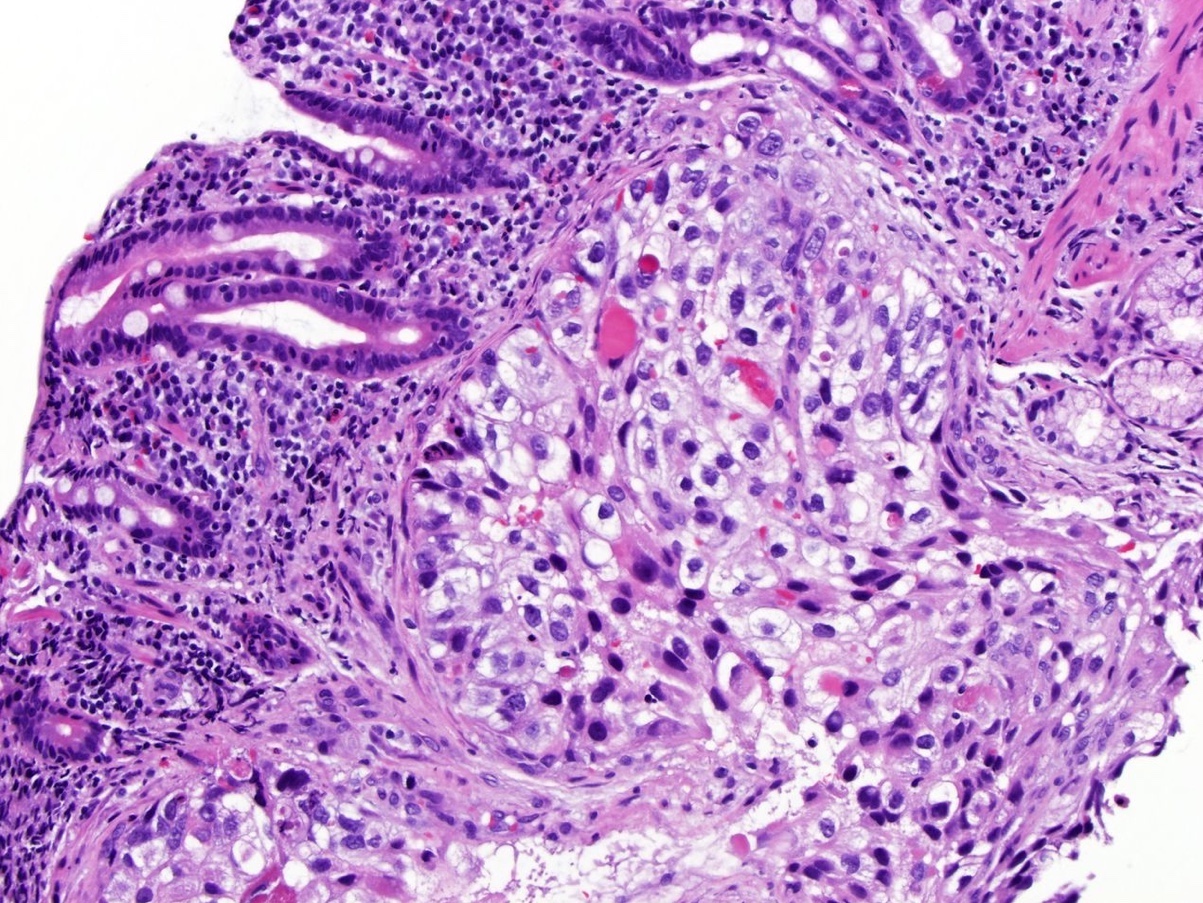
Microscopic (histologic) images
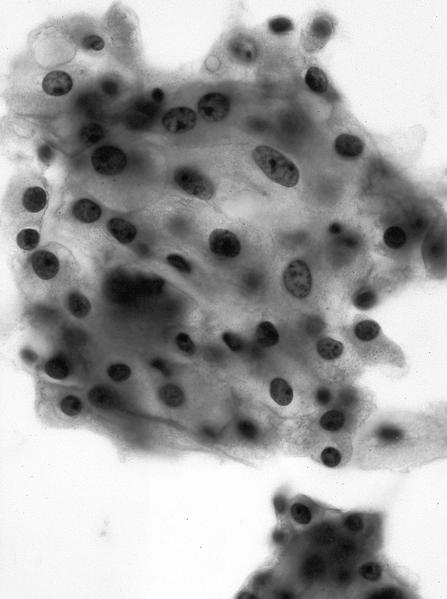
Cytology description
- Tumor cells have abundant cytoplasm that is vacuolated, fluffy or granular, usually with indistinct cell borders (chromophobe renal cell carcinoma has distinct borders)
- Tumor nuclei have variable atypia, irregular contours, haphazard orientation with abnormal chromatin, variably prominent nucleoli
- Renal tubular cells have well defined cell borders, homogenous cytoplasm, round, regular and orderly nuclei
- Important features to distinguish from other neoplasms include heterogeneous cell population, small cytoplasmic vacuoles and hemosiderin deposits (Arch Pathol Lab Med 2005;129:1017)
- High false positive rate for FNAs in one study (Arch Pathol Lab Med 2002;126:670)
Cytology images
Positive stains
Negative stains
- Generally CK20, inhibin (Mod Pathol 1998;11:1160), MelanA / MART1, calretinin, TTF1, CEA
IHC panels
| Hale | KIT | CK7 | S100A1 | VIM | CAIX | AMACR | SDH | TFE3 | |
| Chromophobe RCC | +++ | +++ | +++ | - | - | - | - | +++ | - |
| Clear cell RCC | - | - | - | - | +++ | +++ | - | +++ | - |
| Oncocytoma | - | +++ | rare | +++ | - | - | - | +++ | - |
| Papillary RCC | - | - | +++ | - | +++ | - | +++ | +++ | - |
| Translocation RCC | - | - | - | - | - | - | ++ | +++ | +++ |
| SDH deficient RCC | - | - | - | - | - | - | - | - | - |
References: Pathol Res Pract 2015;211:303, Ann Diagn Pathol 2020;44:151448, Am J Surg Pathol 2014;38:e6, Arch Pathol Lab Med 2019;143:1455, Transl Androl Urol 2019;8:S123, Hum Pathol 2020 Jul 13 [Epub ahead of print]
Differential diagnosis
Gross differential diagnosis
Multilocular cystic renal neoplasm of low malignant potential
Cystic clear cell papillary renal cell carcinoma
Clear cell renal cell carcinoma with cystic degeneration
Clear cell renal cell carcinoma originating in a benign cyst
Acquired cystic disease associated renal cell carcinoma
Tubulocystic renal cell carcinoma
Cystic nephroma (in adult)
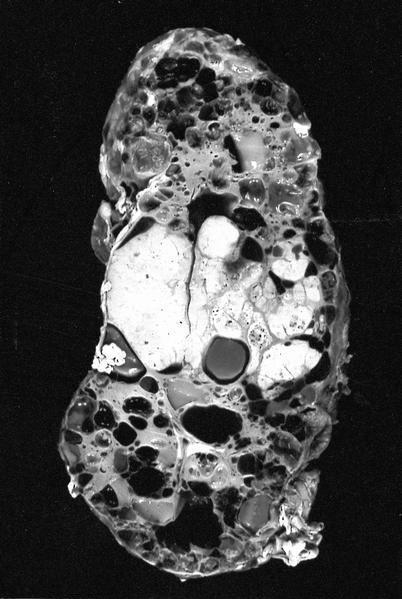
- Up to 15% of renal epithelial neoplasms are cystic on radiographic and gross examination; selected differential diagnoses are below (Urology 1986;28:145)
- Additional reference: Arch Pathol Lab Med 2012;136:400
Multilocular cystic renal neoplasm of low malignant potential
- "Neoplasm composed entirely of numerous cysts, the septa of which contain individual or groups of clear cells without expansile growth" (WHO 2016) clear cells have low grade nuclei (ISUP 1 or 2)
- Multicystic with no expansile growth / solid nodules
Cystic clear cell papillary renal cell carcinoma
- Linear arrangement of nuclei away from basal membrane
- Coexpression of CK7 & CAIX (cup shaped positivity)
Clear cell renal cell carcinoma with cystic degeneration
- An extensively cystic / necrotic tumor may still exhibit aggressive behavior even if only rare identifiable tumor cells (Am J Surg Pathol 2000;24:988)
- Hemorrhage, necrosis, thick irregular cyst wall, may be papillary / pseudopapillary, may have large areas of solid architecture or few residual tumor cells.
Clear cell renal cell carcinoma originating in a benign cyst
- Controversial - cases include multilocular renal cysts with renal cell carcinoma (Chang Gung Med J 2003;26:772, Int Braz J Urol 2006;32:187)
Acquired cystic disease associated renal cell carcinoma
- Most common kidney tumor in patients with end stage renal disease and acquired cystic disease
- Characterized by abundant calcium oxalate crystals and variable morphology: papillary, solid, eosinophilic and clear cell-like areas
Tubulocystic renal cell carcinoma
- Sponge-like, composed of small to intermediate size cysts
- Usually enlarged nuclei and ISUP grade 3 nucleoli
- Shares cytogenetic abnormalities with papillary RCC (trisomy 7 / 17)
Cystic nephroma (in adult)
- Multiloculated benign tumor with cysts lined by flat to hobnailed epithelial cells separated by fibrous septa containing paucicellular or ovarian-like stroma; no septal nodules of clear cells
- Part of a spectrum of renal epithelial and stromal tumors that includes mixed epithelial and stromal tumor (Am J Surg Pathol 2009;33:72, Am J Surg Pathol 2007;31:489)
Additional references